User login
Transcatheter mitral valve-in-valve implantation advantageous in failed bioprosthetic valves
PARIS – Transcatheter mitral valve-in-valve procedures in patients with a failed bioprosthetic mitral valve provide superior clinical results, compared with valve-in-ring implantations, according to the latest data from the VIVID registry.
“Obviously, these results have numerous implications for the interventional community: for surgeons, who employ bioprostheses and rings, and for the cardiovascular industry that designs transcatheter strategies for mitral valve and ring implantations,” Dr. Danny Dvir said in presenting the VIVID update at the annual congress of the European Association of Percutaneous Cardiovascular Interventio
Bioprosthetic rather than mechanical valves are increasingly popular in open-heart valve replacement operations because they avoid the need for lifelong oral anticoagulation. But over time bioprosthetic valves often fail. And that event creates a need for a high-risk, repeat open surgery or a far less invasive transcatheter valve replacement.
Lots of data are available regarding the effectiveness and limitations of transcatheter aortic valve-in-valve procedures in patients with failed bioprosthetic aortic valves, including a previous report from the VIVID (Valve-in-Valve International Data registry) by Dr. Dvir and coworkers (JAMA 2014;312:162-70). However, very little data exist about the effectiveness of mitral valve-in-valve and valve-in-ring procedures, noted Dr. Dvir of St. Paul’s Hospital and the University of British Columbia, Vancouver.
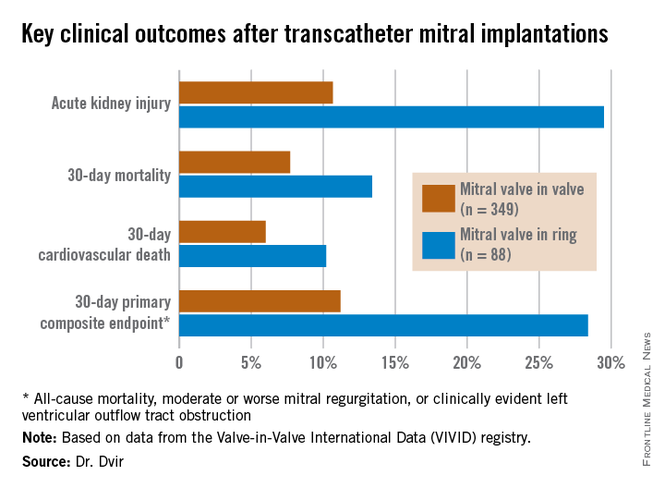
The VIVID registry is drawn from 94 sites on six continents. Dr. Dvir presented an analysis of 437 transcatheter mitral implantations in patients with failed bioprosthetic valves. The study population consisted of 349 patients with mitral valve-in-valve (VIV) and 88 with valve-in-ring (VIR) procedures.
The average Society of Thoracic Surgeons (STS) score was 12.9. “This is one of the highest-risk groups of patients that you’ll ever see,” the cardiologist commented.
Mitral regurgitation was the mechanism of bioprosthetic valve failure in 45% of cases, stenosis in 23%, and a combination of the two in the remainder. The median time from placement of the initial bioprosthetic valve to the transcatheter VIV or VIR procedure was 9 years.
Transcatheter access for the mitral VIV or VIR was transapical in 79% of cases, directly through the left atrium in 2.5%, and by the increasingly popular transseptal route in the remainder. The median follow-up post procedure was 408 days.
Mitral VIV procedures looked significantly better from the standpoint of procedural characteristics. Moderate or severe mitral regurgitation was present at the conclusion of the procedure in 2.6% of patients undergoing mitral VIV, compared with 14.8% who had a VIR procedure.
“We were a bit shocked to see that difference between the two groups,” Dr. Dvir said.
Implantation of a small surgical valve of 25 mm or less was the major independent predictor of having an elevated gradient post procedure, with an adjusted odds ratio of 3.7.
In addition, the mean valve area was 1.99 cm2 in the VIV group vs. 2.33 cm2 in the VIR group. Postinflation was employed in 3.2% of the VIV group, compared with 22.7% of the VIR group. Left ventricular outflow tract obstruction – a potentially fatal complication – occurred in 2.6% of the mitral VIV group and was significantly more common at 8% in the VIR group.
Mitral VIR procedures were associated with markedly worse clinical outcomes. Highlighting the 11.2% rate of the 30-day primary composite endpoint in the mitral VIV group, Dr. Dvir commented, “I must say, I think that is a very reasonable number given that we’re talking about a very high–risk group of patients. For this group of patients having a very high STS score, reaching good results in 30 days in the mitral valve-in-valve group is a good signal for the regulatory groups and for the community that this is a good procedure.”
In contrast, the 28.4% rate of the composite endpoint in the VIR group “is a big disappointment; almost one-third of patients undergoing mitral valve in ring experience the composite adverse event endpoint at 30 days. There is an issue there,” he added.
Dr. Dvir reported having no relevant financial conflicts.
PARIS – Transcatheter mitral valve-in-valve procedures in patients with a failed bioprosthetic mitral valve provide superior clinical results, compared with valve-in-ring implantations, according to the latest data from the VIVID registry.
“Obviously, these results have numerous implications for the interventional community: for surgeons, who employ bioprostheses and rings, and for the cardiovascular industry that designs transcatheter strategies for mitral valve and ring implantations,” Dr. Danny Dvir said in presenting the VIVID update at the annual congress of the European Association of Percutaneous Cardiovascular Interventio
Bioprosthetic rather than mechanical valves are increasingly popular in open-heart valve replacement operations because they avoid the need for lifelong oral anticoagulation. But over time bioprosthetic valves often fail. And that event creates a need for a high-risk, repeat open surgery or a far less invasive transcatheter valve replacement.
Lots of data are available regarding the effectiveness and limitations of transcatheter aortic valve-in-valve procedures in patients with failed bioprosthetic aortic valves, including a previous report from the VIVID (Valve-in-Valve International Data registry) by Dr. Dvir and coworkers (JAMA 2014;312:162-70). However, very little data exist about the effectiveness of mitral valve-in-valve and valve-in-ring procedures, noted Dr. Dvir of St. Paul’s Hospital and the University of British Columbia, Vancouver.
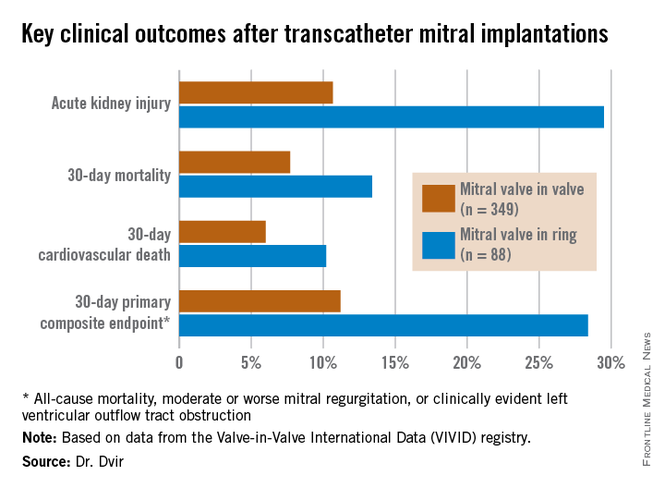
The VIVID registry is drawn from 94 sites on six continents. Dr. Dvir presented an analysis of 437 transcatheter mitral implantations in patients with failed bioprosthetic valves. The study population consisted of 349 patients with mitral valve-in-valve (VIV) and 88 with valve-in-ring (VIR) procedures.
The average Society of Thoracic Surgeons (STS) score was 12.9. “This is one of the highest-risk groups of patients that you’ll ever see,” the cardiologist commented.
Mitral regurgitation was the mechanism of bioprosthetic valve failure in 45% of cases, stenosis in 23%, and a combination of the two in the remainder. The median time from placement of the initial bioprosthetic valve to the transcatheter VIV or VIR procedure was 9 years.
Transcatheter access for the mitral VIV or VIR was transapical in 79% of cases, directly through the left atrium in 2.5%, and by the increasingly popular transseptal route in the remainder. The median follow-up post procedure was 408 days.
Mitral VIV procedures looked significantly better from the standpoint of procedural characteristics. Moderate or severe mitral regurgitation was present at the conclusion of the procedure in 2.6% of patients undergoing mitral VIV, compared with 14.8% who had a VIR procedure.
“We were a bit shocked to see that difference between the two groups,” Dr. Dvir said.
Implantation of a small surgical valve of 25 mm or less was the major independent predictor of having an elevated gradient post procedure, with an adjusted odds ratio of 3.7.
In addition, the mean valve area was 1.99 cm2 in the VIV group vs. 2.33 cm2 in the VIR group. Postinflation was employed in 3.2% of the VIV group, compared with 22.7% of the VIR group. Left ventricular outflow tract obstruction – a potentially fatal complication – occurred in 2.6% of the mitral VIV group and was significantly more common at 8% in the VIR group.
Mitral VIR procedures were associated with markedly worse clinical outcomes. Highlighting the 11.2% rate of the 30-day primary composite endpoint in the mitral VIV group, Dr. Dvir commented, “I must say, I think that is a very reasonable number given that we’re talking about a very high–risk group of patients. For this group of patients having a very high STS score, reaching good results in 30 days in the mitral valve-in-valve group is a good signal for the regulatory groups and for the community that this is a good procedure.”
In contrast, the 28.4% rate of the composite endpoint in the VIR group “is a big disappointment; almost one-third of patients undergoing mitral valve in ring experience the composite adverse event endpoint at 30 days. There is an issue there,” he added.
Dr. Dvir reported having no relevant financial conflicts.
PARIS – Transcatheter mitral valve-in-valve procedures in patients with a failed bioprosthetic mitral valve provide superior clinical results, compared with valve-in-ring implantations, according to the latest data from the VIVID registry.
“Obviously, these results have numerous implications for the interventional community: for surgeons, who employ bioprostheses and rings, and for the cardiovascular industry that designs transcatheter strategies for mitral valve and ring implantations,” Dr. Danny Dvir said in presenting the VIVID update at the annual congress of the European Association of Percutaneous Cardiovascular Interventio
Bioprosthetic rather than mechanical valves are increasingly popular in open-heart valve replacement operations because they avoid the need for lifelong oral anticoagulation. But over time bioprosthetic valves often fail. And that event creates a need for a high-risk, repeat open surgery or a far less invasive transcatheter valve replacement.
Lots of data are available regarding the effectiveness and limitations of transcatheter aortic valve-in-valve procedures in patients with failed bioprosthetic aortic valves, including a previous report from the VIVID (Valve-in-Valve International Data registry) by Dr. Dvir and coworkers (JAMA 2014;312:162-70). However, very little data exist about the effectiveness of mitral valve-in-valve and valve-in-ring procedures, noted Dr. Dvir of St. Paul’s Hospital and the University of British Columbia, Vancouver.
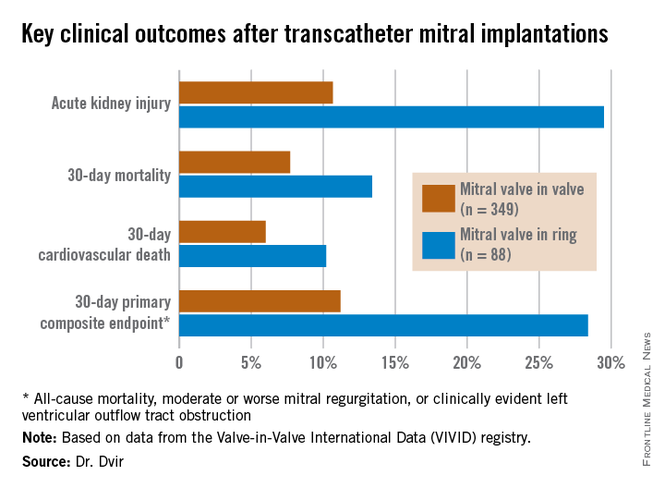
The VIVID registry is drawn from 94 sites on six continents. Dr. Dvir presented an analysis of 437 transcatheter mitral implantations in patients with failed bioprosthetic valves. The study population consisted of 349 patients with mitral valve-in-valve (VIV) and 88 with valve-in-ring (VIR) procedures.
The average Society of Thoracic Surgeons (STS) score was 12.9. “This is one of the highest-risk groups of patients that you’ll ever see,” the cardiologist commented.
Mitral regurgitation was the mechanism of bioprosthetic valve failure in 45% of cases, stenosis in 23%, and a combination of the two in the remainder. The median time from placement of the initial bioprosthetic valve to the transcatheter VIV or VIR procedure was 9 years.
Transcatheter access for the mitral VIV or VIR was transapical in 79% of cases, directly through the left atrium in 2.5%, and by the increasingly popular transseptal route in the remainder. The median follow-up post procedure was 408 days.
Mitral VIV procedures looked significantly better from the standpoint of procedural characteristics. Moderate or severe mitral regurgitation was present at the conclusion of the procedure in 2.6% of patients undergoing mitral VIV, compared with 14.8% who had a VIR procedure.
“We were a bit shocked to see that difference between the two groups,” Dr. Dvir said.
Implantation of a small surgical valve of 25 mm or less was the major independent predictor of having an elevated gradient post procedure, with an adjusted odds ratio of 3.7.
In addition, the mean valve area was 1.99 cm2 in the VIV group vs. 2.33 cm2 in the VIR group. Postinflation was employed in 3.2% of the VIV group, compared with 22.7% of the VIR group. Left ventricular outflow tract obstruction – a potentially fatal complication – occurred in 2.6% of the mitral VIV group and was significantly more common at 8% in the VIR group.
Mitral VIR procedures were associated with markedly worse clinical outcomes. Highlighting the 11.2% rate of the 30-day primary composite endpoint in the mitral VIV group, Dr. Dvir commented, “I must say, I think that is a very reasonable number given that we’re talking about a very high–risk group of patients. For this group of patients having a very high STS score, reaching good results in 30 days in the mitral valve-in-valve group is a good signal for the regulatory groups and for the community that this is a good procedure.”
In contrast, the 28.4% rate of the composite endpoint in the VIR group “is a big disappointment; almost one-third of patients undergoing mitral valve in ring experience the composite adverse event endpoint at 30 days. There is an issue there,” he added.
Dr. Dvir reported having no relevant financial conflicts.
AT EuroPCR 2015
Key clinical point: Transcatheter mitral valve-in-valve procedures for very high surgical risk patients with a failed bioprosthetic valve yield far superior outcomes, compared with mitral valve-in-ring procedures.
Major finding: The 30-day composite adverse outcome rate comprised of death, moderate or severe mitral regurgitation, or clinically evident left ventricular outflow tract obstruction occurred in 11.2% of patients who underwent a transcatheter mitral valve-in-valve procedure, compared with 28.4% of those with a transcatheter valve-in-ring procedure.
Data source: The ongoing VIVID registry includes patients on six continents undergoing transcatheter implantation of aortic, mitral, and/or tricuspid valves after failure of an earlier bioprosthetic valve.
Disclosures: The presenter reported having no relevant financial conflicts.
IHC: Acupuncture deflates migraine
VALENCIA, SPAIN – Acupuncture is as effective as standard pharmacotherapy for migraine prophylaxis, according to a randomized, clinical trial. Forty-four percent of patients in the acupuncture group were deemed treatment responders based upon at least a 50% reduction in headache days per month at 4 months of follow-up, compared with baseline, Dr. Giulia Giannini reported at the International Headache Congress.
The responder rate in the prophylactic pharmacotherapy group was similar at 38%. However, it must be noted that half of the migraineurs assigned to the medication group dropped out of the study for various reasons – No. 1 being treatment side effects – and in this study the responder rate was based upon patients who made it to the 4-month mark, noted Dr. Giannini of the University of Bologna (Italy).
The study included 85 patients, none of whom had been on prophylactic medication during the previous 3 months. They were randomized to a series of 12 acupuncture sessions or to whatever conventional prophylactic drug the physician and patient agreed was most appropriate.
Eight of 42 patients in the acupuncture group and 21 of 43 controls discontinued the study.
Among the study completers in the acupuncture group, migraine frequency dropped from 9.26 headache days per month at baseline to 6 days per month at 4 months. The group on prophylactic pharmacotherapy improved from 7.95 to 6.24 headache days per month.
These results are consistent with the findings of several published clinical trials comparing acupuncture with prophylactic antimigraine drugs, including one in which acupuncture proved more effective than valproic acid (Minerva Anestesiol. 2013;79:634-42). The published data prompted a Cochrane systematic review which concluded that acupuncture is at least as effective as prophylactic drug therapy, has fewer adverse effects, and should be considered a legitimate treatment option (Cochrane Database Syst. Rev. 2009 [doi:10.1002/14651858.CD001218.pub2]). Dr. Giannini noted at the meeting sponsored by the International Headache Society and the American Headache Society.
No serious adverse events occurred in either study arm.
The study was funded by the Emilia-Romagna (Italy) Department of Health. Dr. Giannini reported having no financial conflicts.
VALENCIA, SPAIN – Acupuncture is as effective as standard pharmacotherapy for migraine prophylaxis, according to a randomized, clinical trial. Forty-four percent of patients in the acupuncture group were deemed treatment responders based upon at least a 50% reduction in headache days per month at 4 months of follow-up, compared with baseline, Dr. Giulia Giannini reported at the International Headache Congress.
The responder rate in the prophylactic pharmacotherapy group was similar at 38%. However, it must be noted that half of the migraineurs assigned to the medication group dropped out of the study for various reasons – No. 1 being treatment side effects – and in this study the responder rate was based upon patients who made it to the 4-month mark, noted Dr. Giannini of the University of Bologna (Italy).
The study included 85 patients, none of whom had been on prophylactic medication during the previous 3 months. They were randomized to a series of 12 acupuncture sessions or to whatever conventional prophylactic drug the physician and patient agreed was most appropriate.
Eight of 42 patients in the acupuncture group and 21 of 43 controls discontinued the study.
Among the study completers in the acupuncture group, migraine frequency dropped from 9.26 headache days per month at baseline to 6 days per month at 4 months. The group on prophylactic pharmacotherapy improved from 7.95 to 6.24 headache days per month.
These results are consistent with the findings of several published clinical trials comparing acupuncture with prophylactic antimigraine drugs, including one in which acupuncture proved more effective than valproic acid (Minerva Anestesiol. 2013;79:634-42). The published data prompted a Cochrane systematic review which concluded that acupuncture is at least as effective as prophylactic drug therapy, has fewer adverse effects, and should be considered a legitimate treatment option (Cochrane Database Syst. Rev. 2009 [doi:10.1002/14651858.CD001218.pub2]). Dr. Giannini noted at the meeting sponsored by the International Headache Society and the American Headache Society.
No serious adverse events occurred in either study arm.
The study was funded by the Emilia-Romagna (Italy) Department of Health. Dr. Giannini reported having no financial conflicts.
VALENCIA, SPAIN – Acupuncture is as effective as standard pharmacotherapy for migraine prophylaxis, according to a randomized, clinical trial. Forty-four percent of patients in the acupuncture group were deemed treatment responders based upon at least a 50% reduction in headache days per month at 4 months of follow-up, compared with baseline, Dr. Giulia Giannini reported at the International Headache Congress.
The responder rate in the prophylactic pharmacotherapy group was similar at 38%. However, it must be noted that half of the migraineurs assigned to the medication group dropped out of the study for various reasons – No. 1 being treatment side effects – and in this study the responder rate was based upon patients who made it to the 4-month mark, noted Dr. Giannini of the University of Bologna (Italy).
The study included 85 patients, none of whom had been on prophylactic medication during the previous 3 months. They were randomized to a series of 12 acupuncture sessions or to whatever conventional prophylactic drug the physician and patient agreed was most appropriate.
Eight of 42 patients in the acupuncture group and 21 of 43 controls discontinued the study.
Among the study completers in the acupuncture group, migraine frequency dropped from 9.26 headache days per month at baseline to 6 days per month at 4 months. The group on prophylactic pharmacotherapy improved from 7.95 to 6.24 headache days per month.
These results are consistent with the findings of several published clinical trials comparing acupuncture with prophylactic antimigraine drugs, including one in which acupuncture proved more effective than valproic acid (Minerva Anestesiol. 2013;79:634-42). The published data prompted a Cochrane systematic review which concluded that acupuncture is at least as effective as prophylactic drug therapy, has fewer adverse effects, and should be considered a legitimate treatment option (Cochrane Database Syst. Rev. 2009 [doi:10.1002/14651858.CD001218.pub2]). Dr. Giannini noted at the meeting sponsored by the International Headache Society and the American Headache Society.
No serious adverse events occurred in either study arm.
The study was funded by the Emilia-Romagna (Italy) Department of Health. Dr. Giannini reported having no financial conflicts.
AT IHC 2015
Key clinical point: Acupuncture is at least as effective for migraine prophylaxis as standard preventive medications.
Major finding: Forty-four percent of migraine patients who completed 12 sessions of acupuncture had at least a 50% reduction in headache days per month at 4 months of follow-up, similar to the 38% rate in patients randomized to prophylactic medication.
Data source: This was a prospective, unblinded, randomized trial involving 85 migraineurs.
Disclosures: The study was funded by the Emilia-Romagna (Italy) Department of Health. The presenter reported having no financial conflicts.
WCD: Six new technologies will change dermatology practice
VANCOUVER – Six developments – daylight photodynamic therapy, body sculpting, better laser treatments for tattoo removal, marketing of home-use fractionated lasers for skin rejuvenation, novel lasers for vascular malformations, and light-based multiphoton microscopy as an alternative to conventional histopathology – will have significant impact upon dermatologic practice, Dr. Christopher B. Zachary predicted in a keynote address at the World Congress of Dermatology.
Savvy patients will increasingly be asking their dermatologists about them, added Dr. Zachary, professor and chair of the department of dermatology at the University of California, Irvine.
Several of these advances fall within cosmetic dermatology, a field he vigorously defended. Showing before-and-after facial photos of a middle-aged woman who appeared 10-15 years younger following skin resurfacing with an ablative laser, Dr. Zachary asserted, “You can dramatically change people’s lives with this therapy.
“When this lady’s at work, she’s surrounded by younger women who want her job. So, this therapy has social and economic benefits,” he said. “I know that some of you in the audience might think that aesthetics is sort of a Cinderella sister to mainstream dermatology, but it’s important. We’re going to live longer, hopefully, and we want to look good – because in this culture, that’s important.”
• Daylight photodynamic therapy. Developed in Scandinavia as a field therapy for photodamaged skin and precancerous skin conditions, daylight PDT delivers continuous, low-level activation of protoporphyrin IX rather than the faster activation achieved with pulsed dye laser or other artificial light sources.
The big advantage of daylight PDT is that it’s essentially pain free. In contrast, most patients find traditional PDT so unpleasant they are reluctant to return for a second session. Moreover, natural daylight is actually a better light source, in Dr. Zachary’s view, because daylight includes all the relevant absorption wavelengths, including those in the red spectrum that allow for deeper penetration into the skin.
Daylight PDT is quite popular throughout Europe, and it’s sure to catch on here, according to Dr. Zachary, who has published research confirming its safety and efficacy (Lasers Surg. Med. 2015;47:168-72). Because patients receive their daylight therapy at home, it saves time for the patient, physician, and clinic. Plus, physicians avoid the need for expensive equipment, he noted.
Dr. Zachary offered a tip based upon his daylight PDT experience: Because aminolevulinic acid (ALA) is poorly absorbed on the arms and legs, he often pretreats those target areas with a superficial fractional ablative laser to a depth of 20 microns.
“It enhances ALA uptake tremendously,” the dermatologist said.
He also finds daylight PDT to be an excellent therapy for patients with severe, drug-resistant acne. The only difference is they get 4 hours of daylight exposure ALA incubation instead of the 2.5 hours used in field therapy for photodamaged skin. The result is a robust acute PDT reaction, reliably followed by a significant reduction in inflammatory and comedonal acne lesions. Dr. Zachary typically treats at 2- to 3-week intervals and finds fewer and fewer new lesions appear between consecutive treatments.
“This is, to me, a great therapy. But I’ll tell you, these patients come in after the first 2 weeks and say, ‘I’m never going to have this procedure again, ever.’ Then 2 weeks later they call and ask, ‘When can I have my next treatment session?’ Because they actually get phenomenal results,” according to Dr. Zachary.
• Body sculpting. Physicians should expect hard scientific evidence of benefit from the device companies before investing large sums in the purchase of new noninvasive body-sculpting devices. Cryolipolysis is the leading technology in this regard, and for good reason. Careful studies have confirmed that bulk cooling of the fat can provide safe, effective, and long-lasting fat removal. The treatment is relatively painless, and the results are predictable, Dr. Zachary noted.
New studies have demonstrated encouraging outcomes with bulk heating devices, including 1,060-nm infrared laser systems.
“I will tell you that whether you cool or heat fat for a long period actually doesn’t make much difference,” he explained. “In either case, you’re inducing a delayed-onset panniculitis. There are no immediate histologic changes. The low-level panniculitic process is evident histologically at day 14 or so post treatment; with an apoptotic response and gradual fat reduction over the next 2 months.”
Other recent useful developments in body sculpting, albeit for treatment of smaller areas, include the Food and Drug Administration’s approval of ATX-101 for reduction of preplatysmal excess submental fat, or the double chin, and the use of botulinum toxin injections for facial contouring. An example of the latter is botulinum toxin injections to reduce the size of large masseter muscles in order to change the facial shape and reduce the common problem of nighttime teeth grinding known as bruxism, he continued.
• Novel laser therapies for tattoo removal. The new picosecond pulse lasers are what everyone in laser medicine is talking about. “I think this is definitely the pico epoch,” Dr. Zachary declared.
Twenty years in development, these picosecond lasers produce faster results and more complete clearing of tattoos than obtainable with Q-switched nanosecond lasers. The results are particularly impressive when addressing the traditionally challenging green and blue pigments.
Other noteworthy developments in laser tattoo removal include the so-called R20 technique developed by Dr. Dora Kossida and Dr. R. Rox Anderson of Harvard Medical School, Boston, and coworkers (J. Am. Acad. Dermatol. 2012;66:271-7) and the use of topical perfluorodecalin. The R20 technique allows for four treatment passes per session rather than just one pass. However, it’s impractically time consuming, because the passes have to be spaced 20 minutes apart.
Physicians at the Laser and Skin Surgery Center of New York have refined the R20 technique by showing that applying perfluorodecalin speeds resolution of the laser-induced immediate whitening reaction. This effectively turns the R20 technique into R0 (Lasers Surg. Med. 2013;45:76-80).
• Home-use fractionated lasers for skin rejuvenation. The skin rejuvenation lasers that dermatologists use in their offices are being miniaturized and made available for home self-treatment. Do they work?
“Some do,” according to Dr. Zachary. “If you use them frequently – once or twice a week for an entire year – they’ll probably give you the same benefit as with the traditional in-office treatments. Histologically, they cause a similar tissue injury.”
A host of handheld ultrasound devices for home-use skin rejuvenation are coming soon as well, he added.
• Laser treatment of vascular malformations. There is a growing sense among experts that the 595-nm pulsed dye laser, the traditional workhorse in treating port wine stains, is not necessarily the best tool for the job. Utilization of alternative wavelengths may be a better way to prevent lesion recurrences. The long-pulsed Nd:YAG 1,065-nm laser and 755-nm alexandrite laser appear advantageous in this regard. But so too could those wavelengths that target deoxygenated hemoglobin.
• Multiphoton microscopy. At the University of California, Irvine’s Beckman Laser Institute, Dr. Zachary and coworkers are using laser-scanning microscopy to achieve submicron-resolution three-dimensional in vivo images of skin lesions. They have found it compares favorably to standard histopathology of processed biopsy specimens for basal cell carcinoma (JAMA Dermatol. April 24, 2015 [doi:10.1001/jamadermatol.2015.0453]).
In other studies, they have compared in vivo multiphoton microscopy to standard histopathology for melanocytic nevi and melanomas. “In some ways, there is better detail than with H&E staining,” according to the dermatologist.
Will this novel in vivo imaging method replace conventional histopathology? Quite possibly, but not for many years to come, Dr. Zachary cautioned.
”I think what’s going to happen is it will take a whole generation of people to understand this. We’ll have to miniaturize these devices, which currently are very large, and put them into clinics so we can look at tens of thousands of lesions before we feel confident about replacing conventional histopathology with noninvasive imaging,” he predicted.
Dr. Zachary reported serving as a consultant to and receiving honoraria and/or equipment loans from Amway, Solta, Valeant, Cynosure, Sciton, and Zeltiq.
VANCOUVER – Six developments – daylight photodynamic therapy, body sculpting, better laser treatments for tattoo removal, marketing of home-use fractionated lasers for skin rejuvenation, novel lasers for vascular malformations, and light-based multiphoton microscopy as an alternative to conventional histopathology – will have significant impact upon dermatologic practice, Dr. Christopher B. Zachary predicted in a keynote address at the World Congress of Dermatology.
Savvy patients will increasingly be asking their dermatologists about them, added Dr. Zachary, professor and chair of the department of dermatology at the University of California, Irvine.
Several of these advances fall within cosmetic dermatology, a field he vigorously defended. Showing before-and-after facial photos of a middle-aged woman who appeared 10-15 years younger following skin resurfacing with an ablative laser, Dr. Zachary asserted, “You can dramatically change people’s lives with this therapy.
“When this lady’s at work, she’s surrounded by younger women who want her job. So, this therapy has social and economic benefits,” he said. “I know that some of you in the audience might think that aesthetics is sort of a Cinderella sister to mainstream dermatology, but it’s important. We’re going to live longer, hopefully, and we want to look good – because in this culture, that’s important.”
• Daylight photodynamic therapy. Developed in Scandinavia as a field therapy for photodamaged skin and precancerous skin conditions, daylight PDT delivers continuous, low-level activation of protoporphyrin IX rather than the faster activation achieved with pulsed dye laser or other artificial light sources.
The big advantage of daylight PDT is that it’s essentially pain free. In contrast, most patients find traditional PDT so unpleasant they are reluctant to return for a second session. Moreover, natural daylight is actually a better light source, in Dr. Zachary’s view, because daylight includes all the relevant absorption wavelengths, including those in the red spectrum that allow for deeper penetration into the skin.
Daylight PDT is quite popular throughout Europe, and it’s sure to catch on here, according to Dr. Zachary, who has published research confirming its safety and efficacy (Lasers Surg. Med. 2015;47:168-72). Because patients receive their daylight therapy at home, it saves time for the patient, physician, and clinic. Plus, physicians avoid the need for expensive equipment, he noted.
Dr. Zachary offered a tip based upon his daylight PDT experience: Because aminolevulinic acid (ALA) is poorly absorbed on the arms and legs, he often pretreats those target areas with a superficial fractional ablative laser to a depth of 20 microns.
“It enhances ALA uptake tremendously,” the dermatologist said.
He also finds daylight PDT to be an excellent therapy for patients with severe, drug-resistant acne. The only difference is they get 4 hours of daylight exposure ALA incubation instead of the 2.5 hours used in field therapy for photodamaged skin. The result is a robust acute PDT reaction, reliably followed by a significant reduction in inflammatory and comedonal acne lesions. Dr. Zachary typically treats at 2- to 3-week intervals and finds fewer and fewer new lesions appear between consecutive treatments.
“This is, to me, a great therapy. But I’ll tell you, these patients come in after the first 2 weeks and say, ‘I’m never going to have this procedure again, ever.’ Then 2 weeks later they call and ask, ‘When can I have my next treatment session?’ Because they actually get phenomenal results,” according to Dr. Zachary.
• Body sculpting. Physicians should expect hard scientific evidence of benefit from the device companies before investing large sums in the purchase of new noninvasive body-sculpting devices. Cryolipolysis is the leading technology in this regard, and for good reason. Careful studies have confirmed that bulk cooling of the fat can provide safe, effective, and long-lasting fat removal. The treatment is relatively painless, and the results are predictable, Dr. Zachary noted.
New studies have demonstrated encouraging outcomes with bulk heating devices, including 1,060-nm infrared laser systems.
“I will tell you that whether you cool or heat fat for a long period actually doesn’t make much difference,” he explained. “In either case, you’re inducing a delayed-onset panniculitis. There are no immediate histologic changes. The low-level panniculitic process is evident histologically at day 14 or so post treatment; with an apoptotic response and gradual fat reduction over the next 2 months.”
Other recent useful developments in body sculpting, albeit for treatment of smaller areas, include the Food and Drug Administration’s approval of ATX-101 for reduction of preplatysmal excess submental fat, or the double chin, and the use of botulinum toxin injections for facial contouring. An example of the latter is botulinum toxin injections to reduce the size of large masseter muscles in order to change the facial shape and reduce the common problem of nighttime teeth grinding known as bruxism, he continued.
• Novel laser therapies for tattoo removal. The new picosecond pulse lasers are what everyone in laser medicine is talking about. “I think this is definitely the pico epoch,” Dr. Zachary declared.
Twenty years in development, these picosecond lasers produce faster results and more complete clearing of tattoos than obtainable with Q-switched nanosecond lasers. The results are particularly impressive when addressing the traditionally challenging green and blue pigments.
Other noteworthy developments in laser tattoo removal include the so-called R20 technique developed by Dr. Dora Kossida and Dr. R. Rox Anderson of Harvard Medical School, Boston, and coworkers (J. Am. Acad. Dermatol. 2012;66:271-7) and the use of topical perfluorodecalin. The R20 technique allows for four treatment passes per session rather than just one pass. However, it’s impractically time consuming, because the passes have to be spaced 20 minutes apart.
Physicians at the Laser and Skin Surgery Center of New York have refined the R20 technique by showing that applying perfluorodecalin speeds resolution of the laser-induced immediate whitening reaction. This effectively turns the R20 technique into R0 (Lasers Surg. Med. 2013;45:76-80).
• Home-use fractionated lasers for skin rejuvenation. The skin rejuvenation lasers that dermatologists use in their offices are being miniaturized and made available for home self-treatment. Do they work?
“Some do,” according to Dr. Zachary. “If you use them frequently – once or twice a week for an entire year – they’ll probably give you the same benefit as with the traditional in-office treatments. Histologically, they cause a similar tissue injury.”
A host of handheld ultrasound devices for home-use skin rejuvenation are coming soon as well, he added.
• Laser treatment of vascular malformations. There is a growing sense among experts that the 595-nm pulsed dye laser, the traditional workhorse in treating port wine stains, is not necessarily the best tool for the job. Utilization of alternative wavelengths may be a better way to prevent lesion recurrences. The long-pulsed Nd:YAG 1,065-nm laser and 755-nm alexandrite laser appear advantageous in this regard. But so too could those wavelengths that target deoxygenated hemoglobin.
• Multiphoton microscopy. At the University of California, Irvine’s Beckman Laser Institute, Dr. Zachary and coworkers are using laser-scanning microscopy to achieve submicron-resolution three-dimensional in vivo images of skin lesions. They have found it compares favorably to standard histopathology of processed biopsy specimens for basal cell carcinoma (JAMA Dermatol. April 24, 2015 [doi:10.1001/jamadermatol.2015.0453]).
In other studies, they have compared in vivo multiphoton microscopy to standard histopathology for melanocytic nevi and melanomas. “In some ways, there is better detail than with H&E staining,” according to the dermatologist.
Will this novel in vivo imaging method replace conventional histopathology? Quite possibly, but not for many years to come, Dr. Zachary cautioned.
”I think what’s going to happen is it will take a whole generation of people to understand this. We’ll have to miniaturize these devices, which currently are very large, and put them into clinics so we can look at tens of thousands of lesions before we feel confident about replacing conventional histopathology with noninvasive imaging,” he predicted.
Dr. Zachary reported serving as a consultant to and receiving honoraria and/or equipment loans from Amway, Solta, Valeant, Cynosure, Sciton, and Zeltiq.
VANCOUVER – Six developments – daylight photodynamic therapy, body sculpting, better laser treatments for tattoo removal, marketing of home-use fractionated lasers for skin rejuvenation, novel lasers for vascular malformations, and light-based multiphoton microscopy as an alternative to conventional histopathology – will have significant impact upon dermatologic practice, Dr. Christopher B. Zachary predicted in a keynote address at the World Congress of Dermatology.
Savvy patients will increasingly be asking their dermatologists about them, added Dr. Zachary, professor and chair of the department of dermatology at the University of California, Irvine.
Several of these advances fall within cosmetic dermatology, a field he vigorously defended. Showing before-and-after facial photos of a middle-aged woman who appeared 10-15 years younger following skin resurfacing with an ablative laser, Dr. Zachary asserted, “You can dramatically change people’s lives with this therapy.
“When this lady’s at work, she’s surrounded by younger women who want her job. So, this therapy has social and economic benefits,” he said. “I know that some of you in the audience might think that aesthetics is sort of a Cinderella sister to mainstream dermatology, but it’s important. We’re going to live longer, hopefully, and we want to look good – because in this culture, that’s important.”
• Daylight photodynamic therapy. Developed in Scandinavia as a field therapy for photodamaged skin and precancerous skin conditions, daylight PDT delivers continuous, low-level activation of protoporphyrin IX rather than the faster activation achieved with pulsed dye laser or other artificial light sources.
The big advantage of daylight PDT is that it’s essentially pain free. In contrast, most patients find traditional PDT so unpleasant they are reluctant to return for a second session. Moreover, natural daylight is actually a better light source, in Dr. Zachary’s view, because daylight includes all the relevant absorption wavelengths, including those in the red spectrum that allow for deeper penetration into the skin.
Daylight PDT is quite popular throughout Europe, and it’s sure to catch on here, according to Dr. Zachary, who has published research confirming its safety and efficacy (Lasers Surg. Med. 2015;47:168-72). Because patients receive their daylight therapy at home, it saves time for the patient, physician, and clinic. Plus, physicians avoid the need for expensive equipment, he noted.
Dr. Zachary offered a tip based upon his daylight PDT experience: Because aminolevulinic acid (ALA) is poorly absorbed on the arms and legs, he often pretreats those target areas with a superficial fractional ablative laser to a depth of 20 microns.
“It enhances ALA uptake tremendously,” the dermatologist said.
He also finds daylight PDT to be an excellent therapy for patients with severe, drug-resistant acne. The only difference is they get 4 hours of daylight exposure ALA incubation instead of the 2.5 hours used in field therapy for photodamaged skin. The result is a robust acute PDT reaction, reliably followed by a significant reduction in inflammatory and comedonal acne lesions. Dr. Zachary typically treats at 2- to 3-week intervals and finds fewer and fewer new lesions appear between consecutive treatments.
“This is, to me, a great therapy. But I’ll tell you, these patients come in after the first 2 weeks and say, ‘I’m never going to have this procedure again, ever.’ Then 2 weeks later they call and ask, ‘When can I have my next treatment session?’ Because they actually get phenomenal results,” according to Dr. Zachary.
• Body sculpting. Physicians should expect hard scientific evidence of benefit from the device companies before investing large sums in the purchase of new noninvasive body-sculpting devices. Cryolipolysis is the leading technology in this regard, and for good reason. Careful studies have confirmed that bulk cooling of the fat can provide safe, effective, and long-lasting fat removal. The treatment is relatively painless, and the results are predictable, Dr. Zachary noted.
New studies have demonstrated encouraging outcomes with bulk heating devices, including 1,060-nm infrared laser systems.
“I will tell you that whether you cool or heat fat for a long period actually doesn’t make much difference,” he explained. “In either case, you’re inducing a delayed-onset panniculitis. There are no immediate histologic changes. The low-level panniculitic process is evident histologically at day 14 or so post treatment; with an apoptotic response and gradual fat reduction over the next 2 months.”
Other recent useful developments in body sculpting, albeit for treatment of smaller areas, include the Food and Drug Administration’s approval of ATX-101 for reduction of preplatysmal excess submental fat, or the double chin, and the use of botulinum toxin injections for facial contouring. An example of the latter is botulinum toxin injections to reduce the size of large masseter muscles in order to change the facial shape and reduce the common problem of nighttime teeth grinding known as bruxism, he continued.
• Novel laser therapies for tattoo removal. The new picosecond pulse lasers are what everyone in laser medicine is talking about. “I think this is definitely the pico epoch,” Dr. Zachary declared.
Twenty years in development, these picosecond lasers produce faster results and more complete clearing of tattoos than obtainable with Q-switched nanosecond lasers. The results are particularly impressive when addressing the traditionally challenging green and blue pigments.
Other noteworthy developments in laser tattoo removal include the so-called R20 technique developed by Dr. Dora Kossida and Dr. R. Rox Anderson of Harvard Medical School, Boston, and coworkers (J. Am. Acad. Dermatol. 2012;66:271-7) and the use of topical perfluorodecalin. The R20 technique allows for four treatment passes per session rather than just one pass. However, it’s impractically time consuming, because the passes have to be spaced 20 minutes apart.
Physicians at the Laser and Skin Surgery Center of New York have refined the R20 technique by showing that applying perfluorodecalin speeds resolution of the laser-induced immediate whitening reaction. This effectively turns the R20 technique into R0 (Lasers Surg. Med. 2013;45:76-80).
• Home-use fractionated lasers for skin rejuvenation. The skin rejuvenation lasers that dermatologists use in their offices are being miniaturized and made available for home self-treatment. Do they work?
“Some do,” according to Dr. Zachary. “If you use them frequently – once or twice a week for an entire year – they’ll probably give you the same benefit as with the traditional in-office treatments. Histologically, they cause a similar tissue injury.”
A host of handheld ultrasound devices for home-use skin rejuvenation are coming soon as well, he added.
• Laser treatment of vascular malformations. There is a growing sense among experts that the 595-nm pulsed dye laser, the traditional workhorse in treating port wine stains, is not necessarily the best tool for the job. Utilization of alternative wavelengths may be a better way to prevent lesion recurrences. The long-pulsed Nd:YAG 1,065-nm laser and 755-nm alexandrite laser appear advantageous in this regard. But so too could those wavelengths that target deoxygenated hemoglobin.
• Multiphoton microscopy. At the University of California, Irvine’s Beckman Laser Institute, Dr. Zachary and coworkers are using laser-scanning microscopy to achieve submicron-resolution three-dimensional in vivo images of skin lesions. They have found it compares favorably to standard histopathology of processed biopsy specimens for basal cell carcinoma (JAMA Dermatol. April 24, 2015 [doi:10.1001/jamadermatol.2015.0453]).
In other studies, they have compared in vivo multiphoton microscopy to standard histopathology for melanocytic nevi and melanomas. “In some ways, there is better detail than with H&E staining,” according to the dermatologist.
Will this novel in vivo imaging method replace conventional histopathology? Quite possibly, but not for many years to come, Dr. Zachary cautioned.
”I think what’s going to happen is it will take a whole generation of people to understand this. We’ll have to miniaturize these devices, which currently are very large, and put them into clinics so we can look at tens of thousands of lesions before we feel confident about replacing conventional histopathology with noninvasive imaging,” he predicted.
Dr. Zachary reported serving as a consultant to and receiving honoraria and/or equipment loans from Amway, Solta, Valeant, Cynosure, Sciton, and Zeltiq.
EXPERT ANALYSIS FROM WCD 2015
EUROPCR: New technology shows early promise for transcatheter tricuspid valve repair
PARIS – Early highly preliminary results from the first-in-human study of percutaneous repair of a failing tricuspid valve indicate that the transcatheter procedure appears safe, durable, and effective – at least through the first 6 months.
“Even though the one-grade reduction of tricuspid regurgitation on color Doppler flow imaging is modest, the impact in terms of clinical improvement seems very encouraging and warrants pursuing this innovative technique,” Dr. Jean-Michel Juliard said in presenting the early findings at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The three-country, prospective, single-arm study is aimed at winning European regulatory approval for 4tech Cardio’s TriCinch System. The study includes 24 patients with severe functional tricuspid regurgitation. Dr. Juliard, a cardiologist at Bichat Hospital in Paris, presented 6-month follow-up data on two patients and 3-month follow-up for a third.
First, a bit about the procedure. It’s conducted under general anesthesia and relies upon transesophageal and intracardiac echocardiographic guidance. The objectives are to reduce the effective cross-sectional valve area by diminishing the septo-lateral dimension of the tricuspid annulus diameter, restore tricuspid valve leaflet coaptation, and relieve symptoms.
The 4tech delivery system consists of two parts. To begin, a guidewire is placed in the right coronary artery, a 24-French sheath is introduced via the right femoral vein, and an exchange guidewire is positioned in the right ventricular apex. The first part of the delivery system is then inserted in order to place an anchor on the tricuspid valve annulus in the vicinity of the antero-posterior commissure.
“This is probably the most difficult part of the whole procedure,” according to Dr. Juliard. “It is done using intracoronary and transesophageal echo guidance.”
Once the anchor is well positioned, the second part of the system is advanced, locked into the first part, and tension is applied under echocardiographic control in order to implant a nitinol self-expanding stent in the inferior vena cava. As soon as traction is applied, the tricuspid regurgitation decreases. Once the correction process is completed, the TriCinch delivery system and venous introducers are removed. For study purposes, dosing of diuretics remained unchanged post procedure.
In the first 6 months, the tricuspid septo-lateral distance improved from 52 to 42 mm in one patient and from 45 to 40 mm in another. A third patient had improvement from 43 to 34 mm at 3 months of follow-up.
In terms of clinical improvement, two patients went from New York Heart Association functional class III to class II, and another went from class III to class I. Six-minute walk distance increased from a baseline of 320 m to 367 m at 6 months of follow-up in one patient and from 400 m to 750 m in another, with a 3-month improvement from 160 to 280 m in the third patient.
Serial imaging studies showed device stability over time, with no migration and no stent thrombosis.
In response to an audience question, Dr. Juliard conceded that at this early stage in the development of the procedure, the placebo effect can’t be ruled out as a possible explanation for the observed strong clinical improvement despite what he conceded was “very modest” reduction in tricuspid regurgitation. Time will tell.
“I hope it is not a placebo effect, but as we maintain the same dose of diuretics, it does seem that the patients feel better,” he added.
The rationale for developing a transcatheter solution to functional tricuspid regurgitation, especially one that’s compatible with concomitant transcatheter mitral valve procedures, as the TriCinch System is intended to be, lies in the wealth of evidence that tricuspid regurgitation is associated with increased mortality, substantial morbidity, and severely impaired quality of life due to the need for repeated hospitalizations. Surgery for patients with tricuspid regurgitation is often extremely high risk because affected patients typically have right ventricular dysfunction, pulmonary hypertension, and/or previous valve surgery.
The ongoing study is funded by 4tech Cardio. Dr. Juliard reported having no financial conflicts.
PARIS – Early highly preliminary results from the first-in-human study of percutaneous repair of a failing tricuspid valve indicate that the transcatheter procedure appears safe, durable, and effective – at least through the first 6 months.
“Even though the one-grade reduction of tricuspid regurgitation on color Doppler flow imaging is modest, the impact in terms of clinical improvement seems very encouraging and warrants pursuing this innovative technique,” Dr. Jean-Michel Juliard said in presenting the early findings at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The three-country, prospective, single-arm study is aimed at winning European regulatory approval for 4tech Cardio’s TriCinch System. The study includes 24 patients with severe functional tricuspid regurgitation. Dr. Juliard, a cardiologist at Bichat Hospital in Paris, presented 6-month follow-up data on two patients and 3-month follow-up for a third.
First, a bit about the procedure. It’s conducted under general anesthesia and relies upon transesophageal and intracardiac echocardiographic guidance. The objectives are to reduce the effective cross-sectional valve area by diminishing the septo-lateral dimension of the tricuspid annulus diameter, restore tricuspid valve leaflet coaptation, and relieve symptoms.
The 4tech delivery system consists of two parts. To begin, a guidewire is placed in the right coronary artery, a 24-French sheath is introduced via the right femoral vein, and an exchange guidewire is positioned in the right ventricular apex. The first part of the delivery system is then inserted in order to place an anchor on the tricuspid valve annulus in the vicinity of the antero-posterior commissure.
“This is probably the most difficult part of the whole procedure,” according to Dr. Juliard. “It is done using intracoronary and transesophageal echo guidance.”
Once the anchor is well positioned, the second part of the system is advanced, locked into the first part, and tension is applied under echocardiographic control in order to implant a nitinol self-expanding stent in the inferior vena cava. As soon as traction is applied, the tricuspid regurgitation decreases. Once the correction process is completed, the TriCinch delivery system and venous introducers are removed. For study purposes, dosing of diuretics remained unchanged post procedure.
In the first 6 months, the tricuspid septo-lateral distance improved from 52 to 42 mm in one patient and from 45 to 40 mm in another. A third patient had improvement from 43 to 34 mm at 3 months of follow-up.
In terms of clinical improvement, two patients went from New York Heart Association functional class III to class II, and another went from class III to class I. Six-minute walk distance increased from a baseline of 320 m to 367 m at 6 months of follow-up in one patient and from 400 m to 750 m in another, with a 3-month improvement from 160 to 280 m in the third patient.
Serial imaging studies showed device stability over time, with no migration and no stent thrombosis.
In response to an audience question, Dr. Juliard conceded that at this early stage in the development of the procedure, the placebo effect can’t be ruled out as a possible explanation for the observed strong clinical improvement despite what he conceded was “very modest” reduction in tricuspid regurgitation. Time will tell.
“I hope it is not a placebo effect, but as we maintain the same dose of diuretics, it does seem that the patients feel better,” he added.
The rationale for developing a transcatheter solution to functional tricuspid regurgitation, especially one that’s compatible with concomitant transcatheter mitral valve procedures, as the TriCinch System is intended to be, lies in the wealth of evidence that tricuspid regurgitation is associated with increased mortality, substantial morbidity, and severely impaired quality of life due to the need for repeated hospitalizations. Surgery for patients with tricuspid regurgitation is often extremely high risk because affected patients typically have right ventricular dysfunction, pulmonary hypertension, and/or previous valve surgery.
The ongoing study is funded by 4tech Cardio. Dr. Juliard reported having no financial conflicts.
PARIS – Early highly preliminary results from the first-in-human study of percutaneous repair of a failing tricuspid valve indicate that the transcatheter procedure appears safe, durable, and effective – at least through the first 6 months.
“Even though the one-grade reduction of tricuspid regurgitation on color Doppler flow imaging is modest, the impact in terms of clinical improvement seems very encouraging and warrants pursuing this innovative technique,” Dr. Jean-Michel Juliard said in presenting the early findings at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The three-country, prospective, single-arm study is aimed at winning European regulatory approval for 4tech Cardio’s TriCinch System. The study includes 24 patients with severe functional tricuspid regurgitation. Dr. Juliard, a cardiologist at Bichat Hospital in Paris, presented 6-month follow-up data on two patients and 3-month follow-up for a third.
First, a bit about the procedure. It’s conducted under general anesthesia and relies upon transesophageal and intracardiac echocardiographic guidance. The objectives are to reduce the effective cross-sectional valve area by diminishing the septo-lateral dimension of the tricuspid annulus diameter, restore tricuspid valve leaflet coaptation, and relieve symptoms.
The 4tech delivery system consists of two parts. To begin, a guidewire is placed in the right coronary artery, a 24-French sheath is introduced via the right femoral vein, and an exchange guidewire is positioned in the right ventricular apex. The first part of the delivery system is then inserted in order to place an anchor on the tricuspid valve annulus in the vicinity of the antero-posterior commissure.
“This is probably the most difficult part of the whole procedure,” according to Dr. Juliard. “It is done using intracoronary and transesophageal echo guidance.”
Once the anchor is well positioned, the second part of the system is advanced, locked into the first part, and tension is applied under echocardiographic control in order to implant a nitinol self-expanding stent in the inferior vena cava. As soon as traction is applied, the tricuspid regurgitation decreases. Once the correction process is completed, the TriCinch delivery system and venous introducers are removed. For study purposes, dosing of diuretics remained unchanged post procedure.
In the first 6 months, the tricuspid septo-lateral distance improved from 52 to 42 mm in one patient and from 45 to 40 mm in another. A third patient had improvement from 43 to 34 mm at 3 months of follow-up.
In terms of clinical improvement, two patients went from New York Heart Association functional class III to class II, and another went from class III to class I. Six-minute walk distance increased from a baseline of 320 m to 367 m at 6 months of follow-up in one patient and from 400 m to 750 m in another, with a 3-month improvement from 160 to 280 m in the third patient.
Serial imaging studies showed device stability over time, with no migration and no stent thrombosis.
In response to an audience question, Dr. Juliard conceded that at this early stage in the development of the procedure, the placebo effect can’t be ruled out as a possible explanation for the observed strong clinical improvement despite what he conceded was “very modest” reduction in tricuspid regurgitation. Time will tell.
“I hope it is not a placebo effect, but as we maintain the same dose of diuretics, it does seem that the patients feel better,” he added.
The rationale for developing a transcatheter solution to functional tricuspid regurgitation, especially one that’s compatible with concomitant transcatheter mitral valve procedures, as the TriCinch System is intended to be, lies in the wealth of evidence that tricuspid regurgitation is associated with increased mortality, substantial morbidity, and severely impaired quality of life due to the need for repeated hospitalizations. Surgery for patients with tricuspid regurgitation is often extremely high risk because affected patients typically have right ventricular dysfunction, pulmonary hypertension, and/or previous valve surgery.
The ongoing study is funded by 4tech Cardio. Dr. Juliard reported having no financial conflicts.
AT EUROPCR 2015
Key clinical point: A novel technology for transcatheter repair of a failing tricuspid valve shows early promise of safety and efficacy.
Major finding: At 3-6 months of follow-up, the first three participants in a first-in-human study of percutaneous tricuspid valve repair show substantial clinical benefits.
Data source: This is a prospective, three-center, nonrandomized, single-arm study of a novel percutaneous therapy in 24 patients with severe functional tricuspid regurgitation.
Disclosures: This ongoing study is funded by 4tech Cardio. The presenter reported having no financial conflicts.
A Call to Action on Metabolic Syndrome and Pediatric Psoriasis
VANCOUVER – Dermatologists and primary care physicians working collaboratively have a golden opportunity to improve the long-term health of pediatric psoriasis patients by addressing their predisposition to components of the metabolic syndrome, Dr. Amy S. Paller declared at the World Congress of Dermatology.
“I think we as dermatologists should be in touch with the primary care doctors of every one of our children with psoriasis. Together, we should be thinking about whether the child has metabolic issues and working jointly to most effectively counsel and evaluate these children for their potential risk for these metabolic disorders,” said Dr. Paller, professor and chair of the department of dermatology and professor of pediatrics at Northwestern University, Chicago.
Pediatric psoriasis is commonly associated with other comorbid conditions in addition to metabolic disorders. But the metabolic syndrome has recently become the focus of increasing attention given that cardiovascular disease is the No. 1 cause of death in the United States, and it appears that children with psoriasis may be getting a jump start on the atherosclerotic process.
By now, it’s well established that plaque psoriasis in adults is strongly associated with increased risks of diabetes, obesity, dyslipidemia, the metabolic syndrome, and cardiovascular disease. Mounting evidence indicates children and adolescents with psoriasis face the same risks.
Everyone knows how difficult it can be to make the long-term lifestyle changes that reverse obesity and its related metabolic disorders. But dermatologists, pediatricians, and family physicians have some leverage when it comes to pediatric psoriasis.
“Think about the fact that 30% of children with psoriasis have a first-degree relative with psoriasis, usually a parent. I think we need to think about counseling young adults with psoriasis early on, especially if that adult is overweight or obese, about the need for adopting a healthy lifestyle. If they do that, it’s not just for themselves but for their children, and we just might prevent pediatric psoriasis in that family or temper its severity through that healthy lifestyle intervention,” Dr. Paller continued.
The hope is that effectively addressing the metabolic comorbidities of pediatric psoriasis will modulate and improve the skin disease; in other words, that weight loss could improve psoriasis. As yet, however, that’s just a hope, as there is no persuasive supporting evidence.
“We’re looking towards ongoing adult trials to give us some clues about whether that’s the case,” she said.
Evidence for comorbidities
Some of the key evidence regarding the metabolic comorbidities of pediatric psoriasis comes from a landmark German epidemiologic study involving 33,981 pediatric psoriasis patients. The prevalence of psoriasis in German youth rose linearly from 0.12% at age 1 year to 1.2% at age 18. Pediatric psoriasis patients had significantly higher rates of diabetes, hyperlipidemia, obesity, and hypertension than did nonpsoriatic controls (Br. J. Dermatol. 2010;162:633-6).
A Kaiser Permanente study of nearly 711,000 youths aged 2-19 years showed that those who were overweight were 2.8-fold more likely than normal-weight youth to have severe or widespread psoriasis, while those who were moderately obese were at 2.9-fold increased risk and extremely obese youth were at 4.2-fold increased risk. Among adolescents, having psoriasis was associated with significantly higher mean total and LDL cholesterol, triglycerides, and alanine aminotransferase levels (J. Pediatr. 2011;159:577-83).
Recent evidence suggests that even before increased levels of LDL cholesterol and triglycerides are apparent in children with psoriasis, abnormalities in lipid function are present and may potentially serve as a novel marker for early cardiovascular risk. Dr. Paller cited a study presented by Dr. Wynnis L. Tom of Rady Children’s Hospital, San Diego, at the 2015 annual meeting of the Society for Investigative Dermatology. The case-control study included 50 children with psoriasis and 50 matched controls with a mean age of 13 years.
Like other investigators, Dr. Tom found that the psoriatic children had higher waist/hip ratios and more insulin resistance. While fasting lipid levels didn’t differ between the two groups, the psoriasis patients had significantly higher levels of atherogenic apolipoprotein B, fewer of the particularly cardioprotective large-size HDL particles, and reduced HDL efflux capacity. Stay tuned regarding these potential early markers, Dr. Paller advised.
She was lead author of a 409-patient international study that showed the risks of obesity and a high waist circumference rise with greater severity of pediatric psoriasis. Children with severe psoriasis were at 4.92-fold increased risk of obesity, compared with controls, while even those with mild psoriasis were at 3.6-fold increased risk (JAMA Dermatol. 2013;149:166-76).
Which comes first?
The question arises: Which comes first in children, the excess adiposity or the psoriasis? Dr. Paller said that although the final word isn’t in, she and her coworkers found in a pilot study of 27 overweight or obese children with psoriasis that excess adiposity typically came first. Moreover, among the roughly one-half of children with a family history of obesity, onset of psoriasis occurred a full 3 years earlier than in those without a positive family history (JAMA Dermatol. 2014;150:573-4).
In another small study, this by investigators at Tufts University, Boston, 6 of 20 children with psoriasis (30%) met criteria for the metabolic syndrome, compared with just 1 of 20 matched nonpsoriatic controls (Pediatr. Dermatol. 2013;30:700-5).
Dr. Paller said that if dermatologists and primary care physicians are to successfully collaborate in tackling the comorbid metabolic disorders associated with pediatric psoriasis, a prerequisite is that dermatologists are going to have to do a better job of educating their primary care colleagues about the skin disease as manifest in children.
“I think it’s very important that pediatricians are aware that psoriasis is a risk factor for metabolic syndrome. But pediatric psoriasis is often misdiagnosed by primary care physicians who mistake it for eczema or tinea infection or contact dermatitis,” according to the pediatric dermatologist.
In one eye-catching Australian study, she noted, a mere 9% of patients with pediatric psoriasis were correctly diagnosed before referral to a dermatologist (Australas. J. Dermatol. 2012;53:98-105).
Pediatric psoriasis: not just skin deep
In addition to the increased risk of metabolic disorders faced by pediatric psoriasis patients, other common comorbidities include depression, anxiety disorders, impaired self-esteem and quality of life, arthritis, and Crohn’s disease, Dr. Paller observed.
• Quality of life. “The quality of life impact of psoriasis is profound. It’s a highly visible disorder, which affects the development of self-esteem and social relationships,” Dr. Paller said.
Investigators at Texas A&M University applied the Pediatric Quality of Life Inventory Version 4.0 to 208 patients aged 2-17 years with moderate to severe psoriasis and compared the results to published data on children with arthritis, asthma, diabetes, and psychiatric disorders. Health-related quality of life turned out to be more impaired in the psoriasis patients than in those with diabetes. The quality-of-life impairment associated with pediatric psoriasis was comparable to that of having asthma or arthritis, albeit not as severe as for pediatric psychiatric disorders (Eur. J. Pediatr. 2012;171:485-92).
• Psychiatric disorders. A study of more than 7,400 pediatric psoriasis patients concluded they had an adjusted 25% increased risk of developing depression, compared with psoriasis-free controls, as well as a 32% increased risk of anxiety disorders and a 55% greater risk of bipolar disorder (J. Am. Acad. Dermatol. 2012;67:651-7.e2).
• Psoriatic arthritis. An estimated 1 in 10 U.S. children with psoriasis report having arthritis, often classified as juvenile idiopathic arthritis (JAMA Dermatol. 2013;149:1180-5).
• Crohn’s disease. A large German epidemiologic study concluded that psoriasis was associated with a 3.69-fold increased risk of Crohn’s disease. There was no increased risk of ulcerative colitis (Br. J. Dermatol. 2010;162:633-6).
Dr. Paller reported receiving research grants from Amgen and Leo and serving as a consultant to AbbVie.
VANCOUVER – Dermatologists and primary care physicians working collaboratively have a golden opportunity to improve the long-term health of pediatric psoriasis patients by addressing their predisposition to components of the metabolic syndrome, Dr. Amy S. Paller declared at the World Congress of Dermatology.
“I think we as dermatologists should be in touch with the primary care doctors of every one of our children with psoriasis. Together, we should be thinking about whether the child has metabolic issues and working jointly to most effectively counsel and evaluate these children for their potential risk for these metabolic disorders,” said Dr. Paller, professor and chair of the department of dermatology and professor of pediatrics at Northwestern University, Chicago.
Pediatric psoriasis is commonly associated with other comorbid conditions in addition to metabolic disorders. But the metabolic syndrome has recently become the focus of increasing attention given that cardiovascular disease is the No. 1 cause of death in the United States, and it appears that children with psoriasis may be getting a jump start on the atherosclerotic process.
By now, it’s well established that plaque psoriasis in adults is strongly associated with increased risks of diabetes, obesity, dyslipidemia, the metabolic syndrome, and cardiovascular disease. Mounting evidence indicates children and adolescents with psoriasis face the same risks.
Everyone knows how difficult it can be to make the long-term lifestyle changes that reverse obesity and its related metabolic disorders. But dermatologists, pediatricians, and family physicians have some leverage when it comes to pediatric psoriasis.
“Think about the fact that 30% of children with psoriasis have a first-degree relative with psoriasis, usually a parent. I think we need to think about counseling young adults with psoriasis early on, especially if that adult is overweight or obese, about the need for adopting a healthy lifestyle. If they do that, it’s not just for themselves but for their children, and we just might prevent pediatric psoriasis in that family or temper its severity through that healthy lifestyle intervention,” Dr. Paller continued.
The hope is that effectively addressing the metabolic comorbidities of pediatric psoriasis will modulate and improve the skin disease; in other words, that weight loss could improve psoriasis. As yet, however, that’s just a hope, as there is no persuasive supporting evidence.
“We’re looking towards ongoing adult trials to give us some clues about whether that’s the case,” she said.
Evidence for comorbidities
Some of the key evidence regarding the metabolic comorbidities of pediatric psoriasis comes from a landmark German epidemiologic study involving 33,981 pediatric psoriasis patients. The prevalence of psoriasis in German youth rose linearly from 0.12% at age 1 year to 1.2% at age 18. Pediatric psoriasis patients had significantly higher rates of diabetes, hyperlipidemia, obesity, and hypertension than did nonpsoriatic controls (Br. J. Dermatol. 2010;162:633-6).
A Kaiser Permanente study of nearly 711,000 youths aged 2-19 years showed that those who were overweight were 2.8-fold more likely than normal-weight youth to have severe or widespread psoriasis, while those who were moderately obese were at 2.9-fold increased risk and extremely obese youth were at 4.2-fold increased risk. Among adolescents, having psoriasis was associated with significantly higher mean total and LDL cholesterol, triglycerides, and alanine aminotransferase levels (J. Pediatr. 2011;159:577-83).
Recent evidence suggests that even before increased levels of LDL cholesterol and triglycerides are apparent in children with psoriasis, abnormalities in lipid function are present and may potentially serve as a novel marker for early cardiovascular risk. Dr. Paller cited a study presented by Dr. Wynnis L. Tom of Rady Children’s Hospital, San Diego, at the 2015 annual meeting of the Society for Investigative Dermatology. The case-control study included 50 children with psoriasis and 50 matched controls with a mean age of 13 years.
Like other investigators, Dr. Tom found that the psoriatic children had higher waist/hip ratios and more insulin resistance. While fasting lipid levels didn’t differ between the two groups, the psoriasis patients had significantly higher levels of atherogenic apolipoprotein B, fewer of the particularly cardioprotective large-size HDL particles, and reduced HDL efflux capacity. Stay tuned regarding these potential early markers, Dr. Paller advised.
She was lead author of a 409-patient international study that showed the risks of obesity and a high waist circumference rise with greater severity of pediatric psoriasis. Children with severe psoriasis were at 4.92-fold increased risk of obesity, compared with controls, while even those with mild psoriasis were at 3.6-fold increased risk (JAMA Dermatol. 2013;149:166-76).
Which comes first?
The question arises: Which comes first in children, the excess adiposity or the psoriasis? Dr. Paller said that although the final word isn’t in, she and her coworkers found in a pilot study of 27 overweight or obese children with psoriasis that excess adiposity typically came first. Moreover, among the roughly one-half of children with a family history of obesity, onset of psoriasis occurred a full 3 years earlier than in those without a positive family history (JAMA Dermatol. 2014;150:573-4).
In another small study, this by investigators at Tufts University, Boston, 6 of 20 children with psoriasis (30%) met criteria for the metabolic syndrome, compared with just 1 of 20 matched nonpsoriatic controls (Pediatr. Dermatol. 2013;30:700-5).
Dr. Paller said that if dermatologists and primary care physicians are to successfully collaborate in tackling the comorbid metabolic disorders associated with pediatric psoriasis, a prerequisite is that dermatologists are going to have to do a better job of educating their primary care colleagues about the skin disease as manifest in children.
“I think it’s very important that pediatricians are aware that psoriasis is a risk factor for metabolic syndrome. But pediatric psoriasis is often misdiagnosed by primary care physicians who mistake it for eczema or tinea infection or contact dermatitis,” according to the pediatric dermatologist.
In one eye-catching Australian study, she noted, a mere 9% of patients with pediatric psoriasis were correctly diagnosed before referral to a dermatologist (Australas. J. Dermatol. 2012;53:98-105).
Pediatric psoriasis: not just skin deep
In addition to the increased risk of metabolic disorders faced by pediatric psoriasis patients, other common comorbidities include depression, anxiety disorders, impaired self-esteem and quality of life, arthritis, and Crohn’s disease, Dr. Paller observed.
• Quality of life. “The quality of life impact of psoriasis is profound. It’s a highly visible disorder, which affects the development of self-esteem and social relationships,” Dr. Paller said.
Investigators at Texas A&M University applied the Pediatric Quality of Life Inventory Version 4.0 to 208 patients aged 2-17 years with moderate to severe psoriasis and compared the results to published data on children with arthritis, asthma, diabetes, and psychiatric disorders. Health-related quality of life turned out to be more impaired in the psoriasis patients than in those with diabetes. The quality-of-life impairment associated with pediatric psoriasis was comparable to that of having asthma or arthritis, albeit not as severe as for pediatric psychiatric disorders (Eur. J. Pediatr. 2012;171:485-92).
• Psychiatric disorders. A study of more than 7,400 pediatric psoriasis patients concluded they had an adjusted 25% increased risk of developing depression, compared with psoriasis-free controls, as well as a 32% increased risk of anxiety disorders and a 55% greater risk of bipolar disorder (J. Am. Acad. Dermatol. 2012;67:651-7.e2).
• Psoriatic arthritis. An estimated 1 in 10 U.S. children with psoriasis report having arthritis, often classified as juvenile idiopathic arthritis (JAMA Dermatol. 2013;149:1180-5).
• Crohn’s disease. A large German epidemiologic study concluded that psoriasis was associated with a 3.69-fold increased risk of Crohn’s disease. There was no increased risk of ulcerative colitis (Br. J. Dermatol. 2010;162:633-6).
Dr. Paller reported receiving research grants from Amgen and Leo and serving as a consultant to AbbVie.
VANCOUVER – Dermatologists and primary care physicians working collaboratively have a golden opportunity to improve the long-term health of pediatric psoriasis patients by addressing their predisposition to components of the metabolic syndrome, Dr. Amy S. Paller declared at the World Congress of Dermatology.
“I think we as dermatologists should be in touch with the primary care doctors of every one of our children with psoriasis. Together, we should be thinking about whether the child has metabolic issues and working jointly to most effectively counsel and evaluate these children for their potential risk for these metabolic disorders,” said Dr. Paller, professor and chair of the department of dermatology and professor of pediatrics at Northwestern University, Chicago.
Pediatric psoriasis is commonly associated with other comorbid conditions in addition to metabolic disorders. But the metabolic syndrome has recently become the focus of increasing attention given that cardiovascular disease is the No. 1 cause of death in the United States, and it appears that children with psoriasis may be getting a jump start on the atherosclerotic process.
By now, it’s well established that plaque psoriasis in adults is strongly associated with increased risks of diabetes, obesity, dyslipidemia, the metabolic syndrome, and cardiovascular disease. Mounting evidence indicates children and adolescents with psoriasis face the same risks.
Everyone knows how difficult it can be to make the long-term lifestyle changes that reverse obesity and its related metabolic disorders. But dermatologists, pediatricians, and family physicians have some leverage when it comes to pediatric psoriasis.
“Think about the fact that 30% of children with psoriasis have a first-degree relative with psoriasis, usually a parent. I think we need to think about counseling young adults with psoriasis early on, especially if that adult is overweight or obese, about the need for adopting a healthy lifestyle. If they do that, it’s not just for themselves but for their children, and we just might prevent pediatric psoriasis in that family or temper its severity through that healthy lifestyle intervention,” Dr. Paller continued.
The hope is that effectively addressing the metabolic comorbidities of pediatric psoriasis will modulate and improve the skin disease; in other words, that weight loss could improve psoriasis. As yet, however, that’s just a hope, as there is no persuasive supporting evidence.
“We’re looking towards ongoing adult trials to give us some clues about whether that’s the case,” she said.
Evidence for comorbidities
Some of the key evidence regarding the metabolic comorbidities of pediatric psoriasis comes from a landmark German epidemiologic study involving 33,981 pediatric psoriasis patients. The prevalence of psoriasis in German youth rose linearly from 0.12% at age 1 year to 1.2% at age 18. Pediatric psoriasis patients had significantly higher rates of diabetes, hyperlipidemia, obesity, and hypertension than did nonpsoriatic controls (Br. J. Dermatol. 2010;162:633-6).
A Kaiser Permanente study of nearly 711,000 youths aged 2-19 years showed that those who were overweight were 2.8-fold more likely than normal-weight youth to have severe or widespread psoriasis, while those who were moderately obese were at 2.9-fold increased risk and extremely obese youth were at 4.2-fold increased risk. Among adolescents, having psoriasis was associated with significantly higher mean total and LDL cholesterol, triglycerides, and alanine aminotransferase levels (J. Pediatr. 2011;159:577-83).
Recent evidence suggests that even before increased levels of LDL cholesterol and triglycerides are apparent in children with psoriasis, abnormalities in lipid function are present and may potentially serve as a novel marker for early cardiovascular risk. Dr. Paller cited a study presented by Dr. Wynnis L. Tom of Rady Children’s Hospital, San Diego, at the 2015 annual meeting of the Society for Investigative Dermatology. The case-control study included 50 children with psoriasis and 50 matched controls with a mean age of 13 years.
Like other investigators, Dr. Tom found that the psoriatic children had higher waist/hip ratios and more insulin resistance. While fasting lipid levels didn’t differ between the two groups, the psoriasis patients had significantly higher levels of atherogenic apolipoprotein B, fewer of the particularly cardioprotective large-size HDL particles, and reduced HDL efflux capacity. Stay tuned regarding these potential early markers, Dr. Paller advised.
She was lead author of a 409-patient international study that showed the risks of obesity and a high waist circumference rise with greater severity of pediatric psoriasis. Children with severe psoriasis were at 4.92-fold increased risk of obesity, compared with controls, while even those with mild psoriasis were at 3.6-fold increased risk (JAMA Dermatol. 2013;149:166-76).
Which comes first?
The question arises: Which comes first in children, the excess adiposity or the psoriasis? Dr. Paller said that although the final word isn’t in, she and her coworkers found in a pilot study of 27 overweight or obese children with psoriasis that excess adiposity typically came first. Moreover, among the roughly one-half of children with a family history of obesity, onset of psoriasis occurred a full 3 years earlier than in those without a positive family history (JAMA Dermatol. 2014;150:573-4).
In another small study, this by investigators at Tufts University, Boston, 6 of 20 children with psoriasis (30%) met criteria for the metabolic syndrome, compared with just 1 of 20 matched nonpsoriatic controls (Pediatr. Dermatol. 2013;30:700-5).
Dr. Paller said that if dermatologists and primary care physicians are to successfully collaborate in tackling the comorbid metabolic disorders associated with pediatric psoriasis, a prerequisite is that dermatologists are going to have to do a better job of educating their primary care colleagues about the skin disease as manifest in children.
“I think it’s very important that pediatricians are aware that psoriasis is a risk factor for metabolic syndrome. But pediatric psoriasis is often misdiagnosed by primary care physicians who mistake it for eczema or tinea infection or contact dermatitis,” according to the pediatric dermatologist.
In one eye-catching Australian study, she noted, a mere 9% of patients with pediatric psoriasis were correctly diagnosed before referral to a dermatologist (Australas. J. Dermatol. 2012;53:98-105).
Pediatric psoriasis: not just skin deep
In addition to the increased risk of metabolic disorders faced by pediatric psoriasis patients, other common comorbidities include depression, anxiety disorders, impaired self-esteem and quality of life, arthritis, and Crohn’s disease, Dr. Paller observed.
• Quality of life. “The quality of life impact of psoriasis is profound. It’s a highly visible disorder, which affects the development of self-esteem and social relationships,” Dr. Paller said.
Investigators at Texas A&M University applied the Pediatric Quality of Life Inventory Version 4.0 to 208 patients aged 2-17 years with moderate to severe psoriasis and compared the results to published data on children with arthritis, asthma, diabetes, and psychiatric disorders. Health-related quality of life turned out to be more impaired in the psoriasis patients than in those with diabetes. The quality-of-life impairment associated with pediatric psoriasis was comparable to that of having asthma or arthritis, albeit not as severe as for pediatric psychiatric disorders (Eur. J. Pediatr. 2012;171:485-92).
• Psychiatric disorders. A study of more than 7,400 pediatric psoriasis patients concluded they had an adjusted 25% increased risk of developing depression, compared with psoriasis-free controls, as well as a 32% increased risk of anxiety disorders and a 55% greater risk of bipolar disorder (J. Am. Acad. Dermatol. 2012;67:651-7.e2).
• Psoriatic arthritis. An estimated 1 in 10 U.S. children with psoriasis report having arthritis, often classified as juvenile idiopathic arthritis (JAMA Dermatol. 2013;149:1180-5).
• Crohn’s disease. A large German epidemiologic study concluded that psoriasis was associated with a 3.69-fold increased risk of Crohn’s disease. There was no increased risk of ulcerative colitis (Br. J. Dermatol. 2010;162:633-6).
Dr. Paller reported receiving research grants from Amgen and Leo and serving as a consultant to AbbVie.
EXPERT ANALYSIS FROM WCD 2015
A call to action on metabolic syndrome and pediatric psoriasis
VANCOUVER – Dermatologists and primary care physicians working collaboratively have a golden opportunity to improve the long-term health of pediatric psoriasis patients by addressing their predisposition to components of the metabolic syndrome, Dr. Amy S. Paller declared at the World Congress of Dermatology.
“I think we as dermatologists should be in touch with the primary care doctors of every one of our children with psoriasis. Together, we should be thinking about whether the child has metabolic issues and working jointly to most effectively counsel and evaluate these children for their potential risk for these metabolic disorders,” said Dr. Paller, professor and chair of the department of dermatology and professor of pediatrics at Northwestern University, Chicago.
Pediatric psoriasis is commonly associated with other comorbid conditions in addition to metabolic disorders. But the metabolic syndrome has recently become the focus of increasing attention given that cardiovascular disease is the No. 1 cause of death in the United States, and it appears that children with psoriasis may be getting a jump start on the atherosclerotic process.
By now, it’s well established that plaque psoriasis in adults is strongly associated with increased risks of diabetes, obesity, dyslipidemia, the metabolic syndrome, and cardiovascular disease. Mounting evidence indicates children and adolescents with psoriasis face the same risks.
Everyone knows how difficult it can be to make the long-term lifestyle changes that reverse obesity and its related metabolic disorders. But dermatologists, pediatricians, and family physicians have some leverage when it comes to pediatric psoriasis.
“Think about the fact that 30% of children with psoriasis have a first-degree relative with psoriasis, usually a parent. I think we need to think about counseling young adults with psoriasis early on, especially if that adult is overweight or obese, about the need for adopting a healthy lifestyle. If they do that, it’s not just for themselves but for their children, and we just might prevent pediatric psoriasis in that family or temper its severity through that healthy lifestyle intervention,” Dr. Paller continued.
The hope is that effectively addressing the metabolic comorbidities of pediatric psoriasis will modulate and improve the skin disease; in other words, that weight loss could improve psoriasis. As yet, however, that’s just a hope, as there is no persuasive supporting evidence.
“We’re looking towards ongoing adult trials to give us some clues about whether that’s the case,” she said.
Evidence for comorbidities
Some of the key evidence regarding the metabolic comorbidities of pediatric psoriasis comes from a landmark German epidemiologic study involving 33,981 pediatric psoriasis patients. The prevalence of psoriasis in German youth rose linearly from 0.12% at age 1 year to 1.2% at age 18. Pediatric psoriasis patients had significantly higher rates of diabetes, hyperlipidemia, obesity, and hypertension than did nonpsoriatic controls (Br. J. Dermatol. 2010;162:633-6).
A Kaiser Permanente study of nearly 711,000 youths aged 2-19 years showed that those who were overweight were 2.8-fold more likely than normal-weight youth to have severe or widespread psoriasis, while those who were moderately obese were at 2.9-fold increased risk and extremely obese youth were at 4.2-fold increased risk. Among adolescents, having psoriasis was associated with significantly higher mean total and LDL cholesterol, triglycerides, and alanine aminotransferase levels (J. Pediatr. 2011;159:577-83).
Recent evidence suggests that even before increased levels of LDL cholesterol and triglycerides are apparent in children with psoriasis, abnormalities in lipid function are present and may potentially serve as a novel marker for early cardiovascular risk. Dr. Paller cited a study presented by Dr. Wynnis L. Tom of Rady Children’s Hospital, San Diego, at the 2015 annual meeting of the Society for Investigative Dermatology. The case-control study included 50 children with psoriasis and 50 matched controls with a mean age of 13 years.
Like other investigators, Dr. Tom found that the psoriatic children had higher waist/hip ratios and more insulin resistance. While fasting lipid levels didn’t differ between the two groups, the psoriasis patients had significantly higher levels of atherogenic apolipoprotein B, fewer of the particularly cardioprotective large-size HDL particles, and reduced HDL efflux capacity. Stay tuned regarding these potential early markers, Dr. Paller advised.
She was lead author of a 409-patient international study that showed the risks of obesity and a high waist circumference rise with greater severity of pediatric psoriasis. Children with severe psoriasis were at 4.92-fold increased risk of obesity, compared with controls, while even those with mild psoriasis were at 3.6-fold increased risk (JAMA Dermatol. 2013;149:166-76).
Which comes first?
The question arises: Which comes first in children, the excess adiposity or the psoriasis? Dr. Paller said that although the final word isn’t in, she and her coworkers found in a pilot study of 27 overweight or obese children with psoriasis that excess adiposity typically came first. Moreover, among the roughly one-half of children with a family history of obesity, onset of psoriasis occurred a full 3 years earlier than in those without a positive family history (JAMA Dermatol. 2014;150:573-4).
In another small study, this by investigators at Tufts University, Boston, 6 of 20 children with psoriasis (30%) met criteria for the metabolic syndrome, compared with just 1 of 20 matched nonpsoriatic controls (Pediatr. Dermatol. 2013;30:700-5).
Dr. Paller said that if dermatologists and primary care physicians are to successfully collaborate in tackling the comorbid metabolic disorders associated with pediatric psoriasis, a prerequisite is that dermatologists are going to have to do a better job of educating their primary care colleagues about the skin disease as manifest in children.
“I think it’s very important that pediatricians are aware that psoriasis is a risk factor for metabolic syndrome. But pediatric psoriasis is often misdiagnosed by primary care physicians who mistake it for eczema or tinea infection or contact dermatitis,” according to the pediatric dermatologist.
In one eye-catching Australian study, she noted, a mere 9% of patients with pediatric psoriasis were correctly diagnosed before referral to a dermatologist (Australas. J. Dermatol. 2012;53:98-105).
Pediatric psoriasis: not just skin deep
In addition to the increased risk of metabolic disorders faced by pediatric psoriasis patients, other common comorbidities include depression, anxiety disorders, impaired self-esteem and quality of life, arthritis, and Crohn’s disease, Dr. Paller observed.
• Quality of life. “The quality of life impact of psoriasis is profound. It’s a highly visible disorder, which affects the development of self-esteem and social relationships,” Dr. Paller said.
Investigators at Texas A&M University applied the Pediatric Quality of Life Inventory Version 4.0 to 208 patients aged 2-17 years with moderate to severe psoriasis and compared the results to published data on children with arthritis, asthma, diabetes, and psychiatric disorders. Health-related quality of life turned out to be more impaired in the psoriasis patients than in those with diabetes. The quality-of-life impairment associated with pediatric psoriasis was comparable to that of having asthma or arthritis, albeit not as severe as for pediatric psychiatric disorders (Eur. J. Pediatr. 2012;171:485-92).
• Psychiatric disorders. A study of more than 7,400 pediatric psoriasis patients concluded they had an adjusted 25% increased risk of developing depression, compared with psoriasis-free controls, as well as a 32% increased risk of anxiety disorders and a 55% greater risk of bipolar disorder (J. Am. Acad. Dermatol. 2012;67:651-7.e2).
• Psoriatic arthritis. An estimated 1 in 10 U.S. children with psoriasis report having arthritis, often classified as juvenile idiopathic arthritis (JAMA Dermatol. 2013;149:1180-5).
• Crohn’s disease. A large German epidemiologic study concluded that psoriasis was associated with a 3.69-fold increased risk of Crohn’s disease. There was no increased risk of ulcerative colitis (Br. J. Dermatol. 2010;162:633-6).
Dr. Paller reported receiving research grants from Amgen and Leo and serving as a consultant to AbbVie.
VANCOUVER – Dermatologists and primary care physicians working collaboratively have a golden opportunity to improve the long-term health of pediatric psoriasis patients by addressing their predisposition to components of the metabolic syndrome, Dr. Amy S. Paller declared at the World Congress of Dermatology.
“I think we as dermatologists should be in touch with the primary care doctors of every one of our children with psoriasis. Together, we should be thinking about whether the child has metabolic issues and working jointly to most effectively counsel and evaluate these children for their potential risk for these metabolic disorders,” said Dr. Paller, professor and chair of the department of dermatology and professor of pediatrics at Northwestern University, Chicago.
Pediatric psoriasis is commonly associated with other comorbid conditions in addition to metabolic disorders. But the metabolic syndrome has recently become the focus of increasing attention given that cardiovascular disease is the No. 1 cause of death in the United States, and it appears that children with psoriasis may be getting a jump start on the atherosclerotic process.
By now, it’s well established that plaque psoriasis in adults is strongly associated with increased risks of diabetes, obesity, dyslipidemia, the metabolic syndrome, and cardiovascular disease. Mounting evidence indicates children and adolescents with psoriasis face the same risks.
Everyone knows how difficult it can be to make the long-term lifestyle changes that reverse obesity and its related metabolic disorders. But dermatologists, pediatricians, and family physicians have some leverage when it comes to pediatric psoriasis.
“Think about the fact that 30% of children with psoriasis have a first-degree relative with psoriasis, usually a parent. I think we need to think about counseling young adults with psoriasis early on, especially if that adult is overweight or obese, about the need for adopting a healthy lifestyle. If they do that, it’s not just for themselves but for their children, and we just might prevent pediatric psoriasis in that family or temper its severity through that healthy lifestyle intervention,” Dr. Paller continued.
The hope is that effectively addressing the metabolic comorbidities of pediatric psoriasis will modulate and improve the skin disease; in other words, that weight loss could improve psoriasis. As yet, however, that’s just a hope, as there is no persuasive supporting evidence.
“We’re looking towards ongoing adult trials to give us some clues about whether that’s the case,” she said.
Evidence for comorbidities
Some of the key evidence regarding the metabolic comorbidities of pediatric psoriasis comes from a landmark German epidemiologic study involving 33,981 pediatric psoriasis patients. The prevalence of psoriasis in German youth rose linearly from 0.12% at age 1 year to 1.2% at age 18. Pediatric psoriasis patients had significantly higher rates of diabetes, hyperlipidemia, obesity, and hypertension than did nonpsoriatic controls (Br. J. Dermatol. 2010;162:633-6).
A Kaiser Permanente study of nearly 711,000 youths aged 2-19 years showed that those who were overweight were 2.8-fold more likely than normal-weight youth to have severe or widespread psoriasis, while those who were moderately obese were at 2.9-fold increased risk and extremely obese youth were at 4.2-fold increased risk. Among adolescents, having psoriasis was associated with significantly higher mean total and LDL cholesterol, triglycerides, and alanine aminotransferase levels (J. Pediatr. 2011;159:577-83).
Recent evidence suggests that even before increased levels of LDL cholesterol and triglycerides are apparent in children with psoriasis, abnormalities in lipid function are present and may potentially serve as a novel marker for early cardiovascular risk. Dr. Paller cited a study presented by Dr. Wynnis L. Tom of Rady Children’s Hospital, San Diego, at the 2015 annual meeting of the Society for Investigative Dermatology. The case-control study included 50 children with psoriasis and 50 matched controls with a mean age of 13 years.
Like other investigators, Dr. Tom found that the psoriatic children had higher waist/hip ratios and more insulin resistance. While fasting lipid levels didn’t differ between the two groups, the psoriasis patients had significantly higher levels of atherogenic apolipoprotein B, fewer of the particularly cardioprotective large-size HDL particles, and reduced HDL efflux capacity. Stay tuned regarding these potential early markers, Dr. Paller advised.
She was lead author of a 409-patient international study that showed the risks of obesity and a high waist circumference rise with greater severity of pediatric psoriasis. Children with severe psoriasis were at 4.92-fold increased risk of obesity, compared with controls, while even those with mild psoriasis were at 3.6-fold increased risk (JAMA Dermatol. 2013;149:166-76).
Which comes first?
The question arises: Which comes first in children, the excess adiposity or the psoriasis? Dr. Paller said that although the final word isn’t in, she and her coworkers found in a pilot study of 27 overweight or obese children with psoriasis that excess adiposity typically came first. Moreover, among the roughly one-half of children with a family history of obesity, onset of psoriasis occurred a full 3 years earlier than in those without a positive family history (JAMA Dermatol. 2014;150:573-4).
In another small study, this by investigators at Tufts University, Boston, 6 of 20 children with psoriasis (30%) met criteria for the metabolic syndrome, compared with just 1 of 20 matched nonpsoriatic controls (Pediatr. Dermatol. 2013;30:700-5).
Dr. Paller said that if dermatologists and primary care physicians are to successfully collaborate in tackling the comorbid metabolic disorders associated with pediatric psoriasis, a prerequisite is that dermatologists are going to have to do a better job of educating their primary care colleagues about the skin disease as manifest in children.
“I think it’s very important that pediatricians are aware that psoriasis is a risk factor for metabolic syndrome. But pediatric psoriasis is often misdiagnosed by primary care physicians who mistake it for eczema or tinea infection or contact dermatitis,” according to the pediatric dermatologist.
In one eye-catching Australian study, she noted, a mere 9% of patients with pediatric psoriasis were correctly diagnosed before referral to a dermatologist (Australas. J. Dermatol. 2012;53:98-105).
Pediatric psoriasis: not just skin deep
In addition to the increased risk of metabolic disorders faced by pediatric psoriasis patients, other common comorbidities include depression, anxiety disorders, impaired self-esteem and quality of life, arthritis, and Crohn’s disease, Dr. Paller observed.
• Quality of life. “The quality of life impact of psoriasis is profound. It’s a highly visible disorder, which affects the development of self-esteem and social relationships,” Dr. Paller said.
Investigators at Texas A&M University applied the Pediatric Quality of Life Inventory Version 4.0 to 208 patients aged 2-17 years with moderate to severe psoriasis and compared the results to published data on children with arthritis, asthma, diabetes, and psychiatric disorders. Health-related quality of life turned out to be more impaired in the psoriasis patients than in those with diabetes. The quality-of-life impairment associated with pediatric psoriasis was comparable to that of having asthma or arthritis, albeit not as severe as for pediatric psychiatric disorders (Eur. J. Pediatr. 2012;171:485-92).
• Psychiatric disorders. A study of more than 7,400 pediatric psoriasis patients concluded they had an adjusted 25% increased risk of developing depression, compared with psoriasis-free controls, as well as a 32% increased risk of anxiety disorders and a 55% greater risk of bipolar disorder (J. Am. Acad. Dermatol. 2012;67:651-7.e2).
• Psoriatic arthritis. An estimated 1 in 10 U.S. children with psoriasis report having arthritis, often classified as juvenile idiopathic arthritis (JAMA Dermatol. 2013;149:1180-5).
• Crohn’s disease. A large German epidemiologic study concluded that psoriasis was associated with a 3.69-fold increased risk of Crohn’s disease. There was no increased risk of ulcerative colitis (Br. J. Dermatol. 2010;162:633-6).
Dr. Paller reported receiving research grants from Amgen and Leo and serving as a consultant to AbbVie.
VANCOUVER – Dermatologists and primary care physicians working collaboratively have a golden opportunity to improve the long-term health of pediatric psoriasis patients by addressing their predisposition to components of the metabolic syndrome, Dr. Amy S. Paller declared at the World Congress of Dermatology.
“I think we as dermatologists should be in touch with the primary care doctors of every one of our children with psoriasis. Together, we should be thinking about whether the child has metabolic issues and working jointly to most effectively counsel and evaluate these children for their potential risk for these metabolic disorders,” said Dr. Paller, professor and chair of the department of dermatology and professor of pediatrics at Northwestern University, Chicago.
Pediatric psoriasis is commonly associated with other comorbid conditions in addition to metabolic disorders. But the metabolic syndrome has recently become the focus of increasing attention given that cardiovascular disease is the No. 1 cause of death in the United States, and it appears that children with psoriasis may be getting a jump start on the atherosclerotic process.
By now, it’s well established that plaque psoriasis in adults is strongly associated with increased risks of diabetes, obesity, dyslipidemia, the metabolic syndrome, and cardiovascular disease. Mounting evidence indicates children and adolescents with psoriasis face the same risks.
Everyone knows how difficult it can be to make the long-term lifestyle changes that reverse obesity and its related metabolic disorders. But dermatologists, pediatricians, and family physicians have some leverage when it comes to pediatric psoriasis.
“Think about the fact that 30% of children with psoriasis have a first-degree relative with psoriasis, usually a parent. I think we need to think about counseling young adults with psoriasis early on, especially if that adult is overweight or obese, about the need for adopting a healthy lifestyle. If they do that, it’s not just for themselves but for their children, and we just might prevent pediatric psoriasis in that family or temper its severity through that healthy lifestyle intervention,” Dr. Paller continued.
The hope is that effectively addressing the metabolic comorbidities of pediatric psoriasis will modulate and improve the skin disease; in other words, that weight loss could improve psoriasis. As yet, however, that’s just a hope, as there is no persuasive supporting evidence.
“We’re looking towards ongoing adult trials to give us some clues about whether that’s the case,” she said.
Evidence for comorbidities
Some of the key evidence regarding the metabolic comorbidities of pediatric psoriasis comes from a landmark German epidemiologic study involving 33,981 pediatric psoriasis patients. The prevalence of psoriasis in German youth rose linearly from 0.12% at age 1 year to 1.2% at age 18. Pediatric psoriasis patients had significantly higher rates of diabetes, hyperlipidemia, obesity, and hypertension than did nonpsoriatic controls (Br. J. Dermatol. 2010;162:633-6).
A Kaiser Permanente study of nearly 711,000 youths aged 2-19 years showed that those who were overweight were 2.8-fold more likely than normal-weight youth to have severe or widespread psoriasis, while those who were moderately obese were at 2.9-fold increased risk and extremely obese youth were at 4.2-fold increased risk. Among adolescents, having psoriasis was associated with significantly higher mean total and LDL cholesterol, triglycerides, and alanine aminotransferase levels (J. Pediatr. 2011;159:577-83).
Recent evidence suggests that even before increased levels of LDL cholesterol and triglycerides are apparent in children with psoriasis, abnormalities in lipid function are present and may potentially serve as a novel marker for early cardiovascular risk. Dr. Paller cited a study presented by Dr. Wynnis L. Tom of Rady Children’s Hospital, San Diego, at the 2015 annual meeting of the Society for Investigative Dermatology. The case-control study included 50 children with psoriasis and 50 matched controls with a mean age of 13 years.
Like other investigators, Dr. Tom found that the psoriatic children had higher waist/hip ratios and more insulin resistance. While fasting lipid levels didn’t differ between the two groups, the psoriasis patients had significantly higher levels of atherogenic apolipoprotein B, fewer of the particularly cardioprotective large-size HDL particles, and reduced HDL efflux capacity. Stay tuned regarding these potential early markers, Dr. Paller advised.
She was lead author of a 409-patient international study that showed the risks of obesity and a high waist circumference rise with greater severity of pediatric psoriasis. Children with severe psoriasis were at 4.92-fold increased risk of obesity, compared with controls, while even those with mild psoriasis were at 3.6-fold increased risk (JAMA Dermatol. 2013;149:166-76).
Which comes first?
The question arises: Which comes first in children, the excess adiposity or the psoriasis? Dr. Paller said that although the final word isn’t in, she and her coworkers found in a pilot study of 27 overweight or obese children with psoriasis that excess adiposity typically came first. Moreover, among the roughly one-half of children with a family history of obesity, onset of psoriasis occurred a full 3 years earlier than in those without a positive family history (JAMA Dermatol. 2014;150:573-4).
In another small study, this by investigators at Tufts University, Boston, 6 of 20 children with psoriasis (30%) met criteria for the metabolic syndrome, compared with just 1 of 20 matched nonpsoriatic controls (Pediatr. Dermatol. 2013;30:700-5).
Dr. Paller said that if dermatologists and primary care physicians are to successfully collaborate in tackling the comorbid metabolic disorders associated with pediatric psoriasis, a prerequisite is that dermatologists are going to have to do a better job of educating their primary care colleagues about the skin disease as manifest in children.
“I think it’s very important that pediatricians are aware that psoriasis is a risk factor for metabolic syndrome. But pediatric psoriasis is often misdiagnosed by primary care physicians who mistake it for eczema or tinea infection or contact dermatitis,” according to the pediatric dermatologist.
In one eye-catching Australian study, she noted, a mere 9% of patients with pediatric psoriasis were correctly diagnosed before referral to a dermatologist (Australas. J. Dermatol. 2012;53:98-105).
Pediatric psoriasis: not just skin deep
In addition to the increased risk of metabolic disorders faced by pediatric psoriasis patients, other common comorbidities include depression, anxiety disorders, impaired self-esteem and quality of life, arthritis, and Crohn’s disease, Dr. Paller observed.
• Quality of life. “The quality of life impact of psoriasis is profound. It’s a highly visible disorder, which affects the development of self-esteem and social relationships,” Dr. Paller said.
Investigators at Texas A&M University applied the Pediatric Quality of Life Inventory Version 4.0 to 208 patients aged 2-17 years with moderate to severe psoriasis and compared the results to published data on children with arthritis, asthma, diabetes, and psychiatric disorders. Health-related quality of life turned out to be more impaired in the psoriasis patients than in those with diabetes. The quality-of-life impairment associated with pediatric psoriasis was comparable to that of having asthma or arthritis, albeit not as severe as for pediatric psychiatric disorders (Eur. J. Pediatr. 2012;171:485-92).
• Psychiatric disorders. A study of more than 7,400 pediatric psoriasis patients concluded they had an adjusted 25% increased risk of developing depression, compared with psoriasis-free controls, as well as a 32% increased risk of anxiety disorders and a 55% greater risk of bipolar disorder (J. Am. Acad. Dermatol. 2012;67:651-7.e2).
• Psoriatic arthritis. An estimated 1 in 10 U.S. children with psoriasis report having arthritis, often classified as juvenile idiopathic arthritis (JAMA Dermatol. 2013;149:1180-5).
• Crohn’s disease. A large German epidemiologic study concluded that psoriasis was associated with a 3.69-fold increased risk of Crohn’s disease. There was no increased risk of ulcerative colitis (Br. J. Dermatol. 2010;162:633-6).
Dr. Paller reported receiving research grants from Amgen and Leo and serving as a consultant to AbbVie.
EXPERT ANALYSIS FROM WCD 2015
ZEUS: Second-generation DES with 30 days DAPT best in bleeding-risk patients
PARIS – The use of a second-generation zotarolimus-eluting coronary stent rather than a bare metal stent in conjunction with 30 days of dual antiplatelet therapy (DAPT) in patients deemed at high bleeding risk results in lower 1-year rates of major adverse cardiovascular events and stent thrombosis, according to a prespecified analysis of the ZEUS trial presented at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
Asked if the ZEUS results mean it’s time to take bare-metal stents (BMS) out of the cupboard and get rid of them, the study presenter, Dr. Marco Valgimigli, replied “I did so already.”
ZEUS (Zotarolimus-Eluting Endeavor Sprint Stent in Uncertain DES Candidates Study) was an open-label, prospective study in which 1,606 patients undergoing urgent or emergent percutaneous coronary intervention were randomized to a thin-strut BMS or the zotarolimus-eluting Endeavor Sprint stent, a second-generation hydrophilic polymer-based device that, uniquely, elutes 100% of the drug within the first 2 weeks. All participants were placed on an intended 30-day regimen of DAPT. The study was conducted in four European countries, explained Dr. Valgimigli of Erasmus University in Rotterdam.
This prespecified analysis focused on the 828 patients with one or more factors placing them at high bleeding risk, since the use of a drug-eluting stent (DES) with a 30-day DAPT protocol hadn’t been adequately studied in that setting, the cardiologist noted.
High bleeding risk was defined by one or more of the following: age greater than 80, being on oral anticoagulation therapy, a prior bleeding event, need for corticosteroid or NSAID therapy, known anemia, or a bleeding diathesis; 47% of study participants had more than one of these criteria.
The primary study endpoint was the composite of all-cause mortality, acute MI, or target vessel revascularization through 1 year of follow-up. The rate was 29% in the BMS group, compared with 22.6% in the DES group, for a highly significant 26% relative risk reduction.
The zotarolimus-eluting stent group also fared significantly better in terms of stent thrombosis and the other prespecified secondary endpoints.
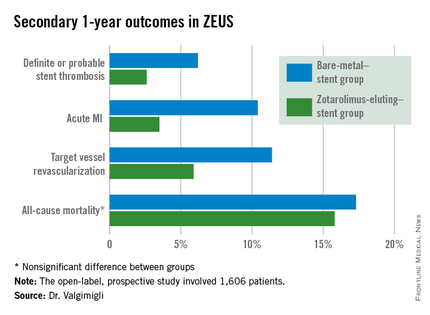
Asked how the ZEUS findings have affected his own clinical practice, Dr. Valgimigli replied, “My stent of choice in patients at high bleeding risk is a second-generation DES. Since there aren’t data showing a specific second-generation DES is preferable, basically whatever I have I implant.”
He sticks to the 30-day DAPT regimen featured in the ZEUS protocol except under specific circumstances, which were allowed under the protocol. One involves staged PCI procedures, in which case the 30 days of DAPT begins after the last stent is implanted, even though the patient has been on DAPT in the interim. The other circumstance where he goes beyond 30 days of DAPT in a patient on a second-generation DES is if an ischemic event occurs down the road: “That patient is put back on DAPT and left there,” he said.
In response to another question, Dr. Valgimigli said he doesn’t believe the lower stent thrombosis rate seen in the Endeavor Sprint group in ZEUS is unique to that stent.
“If you look at any BMS versus DES study, taking the first-generation DES out of the picture, it’s quite clear that the second-generation DES are much safer than a BMS,” according to the cardiologist.
The ZEUS study was sponsored by the University of Ferrara (Italy) and funded by Medtronic. Dr. Valgimigli serves as a consultant to and/or on speakers’ bureaus for Medtronic and more than half a dozen other pharmaceutical and medical devices companies.
PARIS – The use of a second-generation zotarolimus-eluting coronary stent rather than a bare metal stent in conjunction with 30 days of dual antiplatelet therapy (DAPT) in patients deemed at high bleeding risk results in lower 1-year rates of major adverse cardiovascular events and stent thrombosis, according to a prespecified analysis of the ZEUS trial presented at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
Asked if the ZEUS results mean it’s time to take bare-metal stents (BMS) out of the cupboard and get rid of them, the study presenter, Dr. Marco Valgimigli, replied “I did so already.”
ZEUS (Zotarolimus-Eluting Endeavor Sprint Stent in Uncertain DES Candidates Study) was an open-label, prospective study in which 1,606 patients undergoing urgent or emergent percutaneous coronary intervention were randomized to a thin-strut BMS or the zotarolimus-eluting Endeavor Sprint stent, a second-generation hydrophilic polymer-based device that, uniquely, elutes 100% of the drug within the first 2 weeks. All participants were placed on an intended 30-day regimen of DAPT. The study was conducted in four European countries, explained Dr. Valgimigli of Erasmus University in Rotterdam.
This prespecified analysis focused on the 828 patients with one or more factors placing them at high bleeding risk, since the use of a drug-eluting stent (DES) with a 30-day DAPT protocol hadn’t been adequately studied in that setting, the cardiologist noted.
High bleeding risk was defined by one or more of the following: age greater than 80, being on oral anticoagulation therapy, a prior bleeding event, need for corticosteroid or NSAID therapy, known anemia, or a bleeding diathesis; 47% of study participants had more than one of these criteria.
The primary study endpoint was the composite of all-cause mortality, acute MI, or target vessel revascularization through 1 year of follow-up. The rate was 29% in the BMS group, compared with 22.6% in the DES group, for a highly significant 26% relative risk reduction.
The zotarolimus-eluting stent group also fared significantly better in terms of stent thrombosis and the other prespecified secondary endpoints.
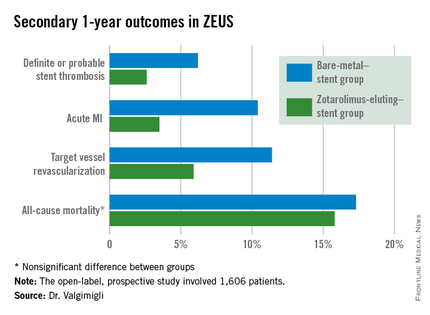
Asked how the ZEUS findings have affected his own clinical practice, Dr. Valgimigli replied, “My stent of choice in patients at high bleeding risk is a second-generation DES. Since there aren’t data showing a specific second-generation DES is preferable, basically whatever I have I implant.”
He sticks to the 30-day DAPT regimen featured in the ZEUS protocol except under specific circumstances, which were allowed under the protocol. One involves staged PCI procedures, in which case the 30 days of DAPT begins after the last stent is implanted, even though the patient has been on DAPT in the interim. The other circumstance where he goes beyond 30 days of DAPT in a patient on a second-generation DES is if an ischemic event occurs down the road: “That patient is put back on DAPT and left there,” he said.
In response to another question, Dr. Valgimigli said he doesn’t believe the lower stent thrombosis rate seen in the Endeavor Sprint group in ZEUS is unique to that stent.
“If you look at any BMS versus DES study, taking the first-generation DES out of the picture, it’s quite clear that the second-generation DES are much safer than a BMS,” according to the cardiologist.
The ZEUS study was sponsored by the University of Ferrara (Italy) and funded by Medtronic. Dr. Valgimigli serves as a consultant to and/or on speakers’ bureaus for Medtronic and more than half a dozen other pharmaceutical and medical devices companies.
PARIS – The use of a second-generation zotarolimus-eluting coronary stent rather than a bare metal stent in conjunction with 30 days of dual antiplatelet therapy (DAPT) in patients deemed at high bleeding risk results in lower 1-year rates of major adverse cardiovascular events and stent thrombosis, according to a prespecified analysis of the ZEUS trial presented at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
Asked if the ZEUS results mean it’s time to take bare-metal stents (BMS) out of the cupboard and get rid of them, the study presenter, Dr. Marco Valgimigli, replied “I did so already.”
ZEUS (Zotarolimus-Eluting Endeavor Sprint Stent in Uncertain DES Candidates Study) was an open-label, prospective study in which 1,606 patients undergoing urgent or emergent percutaneous coronary intervention were randomized to a thin-strut BMS or the zotarolimus-eluting Endeavor Sprint stent, a second-generation hydrophilic polymer-based device that, uniquely, elutes 100% of the drug within the first 2 weeks. All participants were placed on an intended 30-day regimen of DAPT. The study was conducted in four European countries, explained Dr. Valgimigli of Erasmus University in Rotterdam.
This prespecified analysis focused on the 828 patients with one or more factors placing them at high bleeding risk, since the use of a drug-eluting stent (DES) with a 30-day DAPT protocol hadn’t been adequately studied in that setting, the cardiologist noted.
High bleeding risk was defined by one or more of the following: age greater than 80, being on oral anticoagulation therapy, a prior bleeding event, need for corticosteroid or NSAID therapy, known anemia, or a bleeding diathesis; 47% of study participants had more than one of these criteria.
The primary study endpoint was the composite of all-cause mortality, acute MI, or target vessel revascularization through 1 year of follow-up. The rate was 29% in the BMS group, compared with 22.6% in the DES group, for a highly significant 26% relative risk reduction.
The zotarolimus-eluting stent group also fared significantly better in terms of stent thrombosis and the other prespecified secondary endpoints.
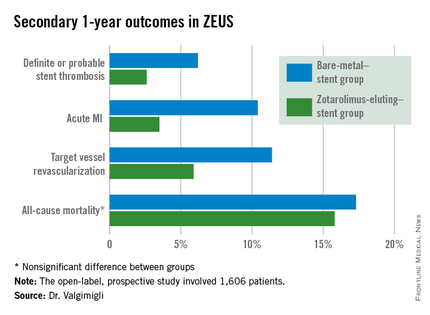
Asked how the ZEUS findings have affected his own clinical practice, Dr. Valgimigli replied, “My stent of choice in patients at high bleeding risk is a second-generation DES. Since there aren’t data showing a specific second-generation DES is preferable, basically whatever I have I implant.”
He sticks to the 30-day DAPT regimen featured in the ZEUS protocol except under specific circumstances, which were allowed under the protocol. One involves staged PCI procedures, in which case the 30 days of DAPT begins after the last stent is implanted, even though the patient has been on DAPT in the interim. The other circumstance where he goes beyond 30 days of DAPT in a patient on a second-generation DES is if an ischemic event occurs down the road: “That patient is put back on DAPT and left there,” he said.
In response to another question, Dr. Valgimigli said he doesn’t believe the lower stent thrombosis rate seen in the Endeavor Sprint group in ZEUS is unique to that stent.
“If you look at any BMS versus DES study, taking the first-generation DES out of the picture, it’s quite clear that the second-generation DES are much safer than a BMS,” according to the cardiologist.
The ZEUS study was sponsored by the University of Ferrara (Italy) and funded by Medtronic. Dr. Valgimigli serves as a consultant to and/or on speakers’ bureaus for Medtronic and more than half a dozen other pharmaceutical and medical devices companies.
AT EUROPCR 2015
Key clinical point: High bleeding risk patients fare significantly better with a second-generation drug-eluting stent and 30 days of dual antiplatelet therapy than with a bare-metal stent.
Major finding: The 1-year incidence of major adverse cardiovascular events was 29.6% in high bleeding risk patients who received a bare-metal stent and 22.6% in those who got a second-generation zotarolimus-eluting stent with 30 days of dual antiplatelet therapy.
Data source: This was a prespecified analysis of 828 high bleeding risk patients randomized to a bare-metal stent or a second-generation zotarolimus-eluting stent in conjunction with 30 days of DAPT and then followed prospectively for 1 year.
Disclosures: The ZEUS study was sponsored by the University of Ferrara (Italy) and funded by Medtronic. The presenter serves as a consultant and/or on speakers’ bureaus for Medtronic and more than half a dozen other pharmaceutical and medical devices companies.
WCD: Pramocaine Is a Common Contact Sensitizer
VANCOUVER – Pramocaine, a topical anesthetic long used in many OTC anti-itch preparations, turns out to itself be a common cause of contact sensitization, Dr. Mariam Abbas reported at the World Congress of Dermatology.
Pramocaine, also known as pramoxine, is an ingredient in Gold Bond cream, some forms of calamine lotion, hemorrhoid relief products, and other OTC antipruritic agents. It’s not available in commercial patch test kits, so Dr. Abbas created a test material comprised of 2% pramocaine in petrolatum.
Seven of 232 patients (3%) referred to a university patch test clinic and who underwent testing to pramocaine along with recognized contact sensitizers showed a clear positive response to pramocaine at 96 hours. The reactions were clinically relevant, according to Dr. Abbas of the University of Alberta, Edmonton.
That 3% positive rate is in the range of published figures for such well-known problem contact sensitizers as neomycin, thiuram mix, and Balsam of Peru.
Dr. Mariam Abbas reported having no financial conflicts regarding this study, conducted free of commercial support.
VANCOUVER – Pramocaine, a topical anesthetic long used in many OTC anti-itch preparations, turns out to itself be a common cause of contact sensitization, Dr. Mariam Abbas reported at the World Congress of Dermatology.
Pramocaine, also known as pramoxine, is an ingredient in Gold Bond cream, some forms of calamine lotion, hemorrhoid relief products, and other OTC antipruritic agents. It’s not available in commercial patch test kits, so Dr. Abbas created a test material comprised of 2% pramocaine in petrolatum.
Seven of 232 patients (3%) referred to a university patch test clinic and who underwent testing to pramocaine along with recognized contact sensitizers showed a clear positive response to pramocaine at 96 hours. The reactions were clinically relevant, according to Dr. Abbas of the University of Alberta, Edmonton.
That 3% positive rate is in the range of published figures for such well-known problem contact sensitizers as neomycin, thiuram mix, and Balsam of Peru.
Dr. Mariam Abbas reported having no financial conflicts regarding this study, conducted free of commercial support.
VANCOUVER – Pramocaine, a topical anesthetic long used in many OTC anti-itch preparations, turns out to itself be a common cause of contact sensitization, Dr. Mariam Abbas reported at the World Congress of Dermatology.
Pramocaine, also known as pramoxine, is an ingredient in Gold Bond cream, some forms of calamine lotion, hemorrhoid relief products, and other OTC antipruritic agents. It’s not available in commercial patch test kits, so Dr. Abbas created a test material comprised of 2% pramocaine in petrolatum.
Seven of 232 patients (3%) referred to a university patch test clinic and who underwent testing to pramocaine along with recognized contact sensitizers showed a clear positive response to pramocaine at 96 hours. The reactions were clinically relevant, according to Dr. Abbas of the University of Alberta, Edmonton.
That 3% positive rate is in the range of published figures for such well-known problem contact sensitizers as neomycin, thiuram mix, and Balsam of Peru.
Dr. Mariam Abbas reported having no financial conflicts regarding this study, conducted free of commercial support.
AT WCD 2015
WCD: Pramocaine is a common contact sensitizer
VANCOUVER – Pramocaine, a topical anesthetic long used in many OTC anti-itch preparations, turns out to itself be a common cause of contact sensitization, Dr. Mariam Abbas reported at the World Congress of Dermatology.
Pramocaine, also known as pramoxine, is an ingredient in Gold Bond cream, some forms of calamine lotion, hemorrhoid relief products, and other OTC antipruritic agents. It’s not available in commercial patch test kits, so Dr. Abbas created a test material comprised of 2% pramocaine in petrolatum.
Seven of 232 patients (3%) referred to a university patch test clinic and who underwent testing to pramocaine along with recognized contact sensitizers showed a clear positive response to pramocaine at 96 hours. The reactions were clinically relevant, according to Dr. Abbas of the University of Alberta, Edmonton.
That 3% positive rate is in the range of published figures for such well-known problem contact sensitizers as neomycin, thiuram mix, and Balsam of Peru.
Dr. Mariam Abbas reported having no financial conflicts regarding this study, conducted free of commercial support.
VANCOUVER – Pramocaine, a topical anesthetic long used in many OTC anti-itch preparations, turns out to itself be a common cause of contact sensitization, Dr. Mariam Abbas reported at the World Congress of Dermatology.
Pramocaine, also known as pramoxine, is an ingredient in Gold Bond cream, some forms of calamine lotion, hemorrhoid relief products, and other OTC antipruritic agents. It’s not available in commercial patch test kits, so Dr. Abbas created a test material comprised of 2% pramocaine in petrolatum.
Seven of 232 patients (3%) referred to a university patch test clinic and who underwent testing to pramocaine along with recognized contact sensitizers showed a clear positive response to pramocaine at 96 hours. The reactions were clinically relevant, according to Dr. Abbas of the University of Alberta, Edmonton.
That 3% positive rate is in the range of published figures for such well-known problem contact sensitizers as neomycin, thiuram mix, and Balsam of Peru.
Dr. Mariam Abbas reported having no financial conflicts regarding this study, conducted free of commercial support.
VANCOUVER – Pramocaine, a topical anesthetic long used in many OTC anti-itch preparations, turns out to itself be a common cause of contact sensitization, Dr. Mariam Abbas reported at the World Congress of Dermatology.
Pramocaine, also known as pramoxine, is an ingredient in Gold Bond cream, some forms of calamine lotion, hemorrhoid relief products, and other OTC antipruritic agents. It’s not available in commercial patch test kits, so Dr. Abbas created a test material comprised of 2% pramocaine in petrolatum.
Seven of 232 patients (3%) referred to a university patch test clinic and who underwent testing to pramocaine along with recognized contact sensitizers showed a clear positive response to pramocaine at 96 hours. The reactions were clinically relevant, according to Dr. Abbas of the University of Alberta, Edmonton.
That 3% positive rate is in the range of published figures for such well-known problem contact sensitizers as neomycin, thiuram mix, and Balsam of Peru.
Dr. Mariam Abbas reported having no financial conflicts regarding this study, conducted free of commercial support.
AT WCD 2015
Key clinical point: Pramocaine, a topical anesthetic that’s an ingredient in many widely used OTC anti-itch products, turns out to be a common cause of contact sensitization.
Major finding: Seven of 232 patients (3%) referred to a patch test clinic showed a clinically relevant positive test to pramocaine.
Data source: A prospective study of 232 patients referred to a patch test clinic.
Disclosures: Dr. Mariam Abbas reported having no financial conflicts regarding this study, conducted free of commercial support.
Bivalirudin in STEMI has low real-world stent thrombosis rate
PARIS – Antithrombotic therapy with bivalirudin for primary percutaneous coronary intervention in patients with ST-elevation myocardial infarction may have been unfairly tarnished as having a high stent thrombosis rate, according to a large, prospective, observational cohort study.
A new analysis from the Swedish Coronary Angiography and Angioplasty Registry (SCAAR) showed similarly low stent thrombosis rates within 30 days following primary PCI for STEMI regardless of whether the antithrombotic regimen involved bivalirudin (Angiomax), heparin only, or a glycoprotein IIb/IIIa inhibitor, Dr. Per Grimfjard reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The SCAAR analysis captured all STEMI patients undergoing primary PCI in Sweden from 2007 through mid-2014. These data reflect real-world interventional practice in Sweden and elsewhere, where bivalirudin is typically administered in a prolonged infusion to protect against early stent thrombosis. In contrast, the randomized trials that linked bivalirudin to high stent thrombosis rates featured protocols in which the drug was stopped immediately after the procedure, noted Dr. Grimfjard, an interventional cardiologist at Uppsala (Sweden) University.
“These are nationwide Swedish numbers, and they are complete. We think the numbers are reassuring in that respect,” he said.
Session chair Dr. Andreas Baumbach said the Swedish data are consistent with his own experience in using bivalirudin in primary PCI for STEMI.
“The headline last year was that bivalirudin has a high stent thrombosis rate. It made the newspapers everywhere. But we never saw that, and we always thought that the difference might be in how we used the drug. There’s a new headline now, that this high stent thrombosis rate is not seen in clinical practice. The practice differs from the randomized trials, and the outcomes differ as well,” observed Dr. Baumbach, professor of interventional cardiology at the University of Bristol (England).
In SCAAR, the 30-day rate of definite, angiographically proven stent thrombosis was 0.84% in 16,860 bivalirudin-treated patients, 0.94% in 3,182 who got heparin only, and 0.83% in 11,216 glycoprotein IIb/IIIa inhibitor recipients. These numeric differences weren’t statistically significant.
All-cause mortality 1 year post-PCI was 9.1% in patients with no stent thrombosis, 16.1% in those who experienced stent thrombosis within 1 day post PCI, and 23.0% in those whose stent thrombosis occurred on days 2-30. Dr. Grimfjard speculated that the explanation for the numerically higher 1-year all-cause mortality rate in patients whose stent thrombosis occurred on days 2-30 as opposed to day 0-1 is probably that they were more likely to have left the hospital when stent thrombosis occurred. That would translate to a longer time to repeat revascularization, hence a larger MI, more heart failure and arrhythmia, and thus a higher long-term risk of death.
Several audience members commented that they weren’t sure what to make of the observational Swedish data because of the looming presence of several potential confounders. For one, clinical practice trends changed considerably during the 7-year time frame of the study, as evidenced by the fact that the use of drug-eluting stents was far more common in bivalirudin-treated patients than in the glycoprotein IIb/IIIa inhibitor group. Also, Swedish cardiologists who put their STEMI patients on bivalirudin were more likely to utilize the more modern radial artery access in performing primary PCI; their practice may have differed from their colleagues’ in other, unrecorded ways as well, it was noted.
Dr. Grimfjard reported having no financial conflicts regarding the study, which was conducted free of commercial support.
PARIS – Antithrombotic therapy with bivalirudin for primary percutaneous coronary intervention in patients with ST-elevation myocardial infarction may have been unfairly tarnished as having a high stent thrombosis rate, according to a large, prospective, observational cohort study.
A new analysis from the Swedish Coronary Angiography and Angioplasty Registry (SCAAR) showed similarly low stent thrombosis rates within 30 days following primary PCI for STEMI regardless of whether the antithrombotic regimen involved bivalirudin (Angiomax), heparin only, or a glycoprotein IIb/IIIa inhibitor, Dr. Per Grimfjard reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The SCAAR analysis captured all STEMI patients undergoing primary PCI in Sweden from 2007 through mid-2014. These data reflect real-world interventional practice in Sweden and elsewhere, where bivalirudin is typically administered in a prolonged infusion to protect against early stent thrombosis. In contrast, the randomized trials that linked bivalirudin to high stent thrombosis rates featured protocols in which the drug was stopped immediately after the procedure, noted Dr. Grimfjard, an interventional cardiologist at Uppsala (Sweden) University.
“These are nationwide Swedish numbers, and they are complete. We think the numbers are reassuring in that respect,” he said.
Session chair Dr. Andreas Baumbach said the Swedish data are consistent with his own experience in using bivalirudin in primary PCI for STEMI.
“The headline last year was that bivalirudin has a high stent thrombosis rate. It made the newspapers everywhere. But we never saw that, and we always thought that the difference might be in how we used the drug. There’s a new headline now, that this high stent thrombosis rate is not seen in clinical practice. The practice differs from the randomized trials, and the outcomes differ as well,” observed Dr. Baumbach, professor of interventional cardiology at the University of Bristol (England).
In SCAAR, the 30-day rate of definite, angiographically proven stent thrombosis was 0.84% in 16,860 bivalirudin-treated patients, 0.94% in 3,182 who got heparin only, and 0.83% in 11,216 glycoprotein IIb/IIIa inhibitor recipients. These numeric differences weren’t statistically significant.
All-cause mortality 1 year post-PCI was 9.1% in patients with no stent thrombosis, 16.1% in those who experienced stent thrombosis within 1 day post PCI, and 23.0% in those whose stent thrombosis occurred on days 2-30. Dr. Grimfjard speculated that the explanation for the numerically higher 1-year all-cause mortality rate in patients whose stent thrombosis occurred on days 2-30 as opposed to day 0-1 is probably that they were more likely to have left the hospital when stent thrombosis occurred. That would translate to a longer time to repeat revascularization, hence a larger MI, more heart failure and arrhythmia, and thus a higher long-term risk of death.
Several audience members commented that they weren’t sure what to make of the observational Swedish data because of the looming presence of several potential confounders. For one, clinical practice trends changed considerably during the 7-year time frame of the study, as evidenced by the fact that the use of drug-eluting stents was far more common in bivalirudin-treated patients than in the glycoprotein IIb/IIIa inhibitor group. Also, Swedish cardiologists who put their STEMI patients on bivalirudin were more likely to utilize the more modern radial artery access in performing primary PCI; their practice may have differed from their colleagues’ in other, unrecorded ways as well, it was noted.
Dr. Grimfjard reported having no financial conflicts regarding the study, which was conducted free of commercial support.
PARIS – Antithrombotic therapy with bivalirudin for primary percutaneous coronary intervention in patients with ST-elevation myocardial infarction may have been unfairly tarnished as having a high stent thrombosis rate, according to a large, prospective, observational cohort study.
A new analysis from the Swedish Coronary Angiography and Angioplasty Registry (SCAAR) showed similarly low stent thrombosis rates within 30 days following primary PCI for STEMI regardless of whether the antithrombotic regimen involved bivalirudin (Angiomax), heparin only, or a glycoprotein IIb/IIIa inhibitor, Dr. Per Grimfjard reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The SCAAR analysis captured all STEMI patients undergoing primary PCI in Sweden from 2007 through mid-2014. These data reflect real-world interventional practice in Sweden and elsewhere, where bivalirudin is typically administered in a prolonged infusion to protect against early stent thrombosis. In contrast, the randomized trials that linked bivalirudin to high stent thrombosis rates featured protocols in which the drug was stopped immediately after the procedure, noted Dr. Grimfjard, an interventional cardiologist at Uppsala (Sweden) University.
“These are nationwide Swedish numbers, and they are complete. We think the numbers are reassuring in that respect,” he said.
Session chair Dr. Andreas Baumbach said the Swedish data are consistent with his own experience in using bivalirudin in primary PCI for STEMI.
“The headline last year was that bivalirudin has a high stent thrombosis rate. It made the newspapers everywhere. But we never saw that, and we always thought that the difference might be in how we used the drug. There’s a new headline now, that this high stent thrombosis rate is not seen in clinical practice. The practice differs from the randomized trials, and the outcomes differ as well,” observed Dr. Baumbach, professor of interventional cardiology at the University of Bristol (England).
In SCAAR, the 30-day rate of definite, angiographically proven stent thrombosis was 0.84% in 16,860 bivalirudin-treated patients, 0.94% in 3,182 who got heparin only, and 0.83% in 11,216 glycoprotein IIb/IIIa inhibitor recipients. These numeric differences weren’t statistically significant.
All-cause mortality 1 year post-PCI was 9.1% in patients with no stent thrombosis, 16.1% in those who experienced stent thrombosis within 1 day post PCI, and 23.0% in those whose stent thrombosis occurred on days 2-30. Dr. Grimfjard speculated that the explanation for the numerically higher 1-year all-cause mortality rate in patients whose stent thrombosis occurred on days 2-30 as opposed to day 0-1 is probably that they were more likely to have left the hospital when stent thrombosis occurred. That would translate to a longer time to repeat revascularization, hence a larger MI, more heart failure and arrhythmia, and thus a higher long-term risk of death.
Several audience members commented that they weren’t sure what to make of the observational Swedish data because of the looming presence of several potential confounders. For one, clinical practice trends changed considerably during the 7-year time frame of the study, as evidenced by the fact that the use of drug-eluting stents was far more common in bivalirudin-treated patients than in the glycoprotein IIb/IIIa inhibitor group. Also, Swedish cardiologists who put their STEMI patients on bivalirudin were more likely to utilize the more modern radial artery access in performing primary PCI; their practice may have differed from their colleagues’ in other, unrecorded ways as well, it was noted.
Dr. Grimfjard reported having no financial conflicts regarding the study, which was conducted free of commercial support.
AT EUROPCR 2015
Key clinical point: The 30-day incidence of stent thrombosis following primary PCI in a large, real-world STEMI population was reassuringly low regardless of the antithrombotic regimen.
Major finding: The stent thrombosis rate within 30 days after primary PCI for STEMI was 0.84% in patients who received bivalirudin for antithrombotic therapy, 0.94% with heparin only, and 0.83% with a glycoprotein IIb/IIIa inhibitor in this real-world nationwide Swedish registry.
Data source: A prospective observational cohort study which included all patients who underwent primary PCI for STEMI in Sweden during 2007-2014.
Disclosures: The presenter reported having no financial conflicts regarding the study, which was conducted free of commercial support.