User login
Head and Neck Cancer: Should Patients Get PEG Access Prior to Therapy? VA pilot study could help clinicians make better-informed decisions to head off malnutrition
Research conducted at the US Department of Veterans Affairs (VA) could offer crucial insight into the hotly debated question of whether patients with head and neck cancer should have access to percutaneous endoscopic gastrostomy (PEG) before they develop malnutrition.
While no definitive conclusions can be drawn until a complete study is performed, early findings of a pilot trial are intriguing, said advanced practice oncology dietitian Katherine Petersen, MS, RDN, CSO, of the Phoenix VA Health Care System, who spoke in an interview with Federal Practitioner and at the annual meeting of the Association of VA Hematology/Oncology.
So far, the 12 patients with head and neck cancer who agreed to the placement of prophylactic feeding tubes prior to chemoradiation have had worse outcomes in some areas compared to the 9 patients who had tubes inserted when clinically indicated and the 12 who didn't need feeding tubes.
Petersen cautioned that the study is small and underpowered at this point. Still, she noted, "We're seeing a hint of exactly the opposite of what I expected. Those who get a tube prophylactically are doing worse than those who are getting it reactively or not at all, If that's the case, that's a really important outcome."
As Petersen explained, the placement of PEG feeding tubes is a hot topic in head and neck cancer care. Malnutrition affects about 80% of these patients and can contribute to mortality, raising the question of whether they should have access to feeding tubes placed prior to treatment in case enteral nutrition is needed.
In some patients with head and neck cancer, malnutrition may arise when tumors block food intake or prevent patients from swallowing. "But in my clinical experience, most often it's from the adverse effects of radiation and chemotherapy. Radiation creates burns inside their throat that make it hard to swallow. Or they have taste changes or really dry mouth," Petersen said.
"On top of these problems, chemotherapy can cause nausea and vomiting," she said. Placing feeding tube access may seem like a smart strategy to head off malnutrition as soon as it occurs. But, as Petersen noted, feeding tube use can lead to dependency as patients lose their ability to swallow. "There's a theory that if we give people feeding tubes, they'll go with the easier route of using a feeding tube and not keep swallowing. Then those swallowing muscles would weaken, and patients would end up permanently on a feeding tube."
In 2020, a retrospective VA study linked feeding tube dependence to lower overall survival in head and neck cancer patients. There are also risks to feeding tube placement, such as infection, pain, leakage, and inflammation.
But what if feeding tube valves are inserted prophylactically so they can be used for nutrition if needed? "We just haven't had any prospective studies to get to the heart of the matter and answer the question," she said. "It's hard to recruit. How do you convince somebody to randomly be assigned to have a hole poked in their stomach?"
For the new pilot study, researchers in Phoenix decided not to randomize patients. Instead, they asked them whether they'd accept the placement of feeding tube valves on a prophylactic basis.
Thirty-six veterans enrolled in 3 years, 33% of those were eligible. Twelve have died, 1 withdrew, and 2 were lost to follow-up.
Those in the prophylactic group had worse physical function and muscle strength over time, while those who received feeding tubes when needed had more adverse events.
Why might some outcomes be worse for patients who chose the prophylactic approach? "The answer is unclear," Petersen said. "Although one possibility is that those patients had higher-risk tumors and were more clued into their own risk."
"The goal now is to get funding for an expanded, multicenter study within the VA," Petersen said. The big question that she hopes to answer is: Does a prophylactic approach work? "Does it make a difference for patients in terms of how quickly they go back to living a full, meaningful life and be able to do all the things that they normally would do?"
A complete study would likely last 7 years, but helpful results may come earlier. "We are starting to see significant differences in terms of our main outcomes of physical function," Petersen said. "We only need 1 to 2 years of data for each patient to get to the heart of that."
The study is not funded, and Petersen reported no disclosures.
Research conducted at the US Department of Veterans Affairs (VA) could offer crucial insight into the hotly debated question of whether patients with head and neck cancer should have access to percutaneous endoscopic gastrostomy (PEG) before they develop malnutrition.
While no definitive conclusions can be drawn until a complete study is performed, early findings of a pilot trial are intriguing, said advanced practice oncology dietitian Katherine Petersen, MS, RDN, CSO, of the Phoenix VA Health Care System, who spoke in an interview with Federal Practitioner and at the annual meeting of the Association of VA Hematology/Oncology.
So far, the 12 patients with head and neck cancer who agreed to the placement of prophylactic feeding tubes prior to chemoradiation have had worse outcomes in some areas compared to the 9 patients who had tubes inserted when clinically indicated and the 12 who didn't need feeding tubes.
Petersen cautioned that the study is small and underpowered at this point. Still, she noted, "We're seeing a hint of exactly the opposite of what I expected. Those who get a tube prophylactically are doing worse than those who are getting it reactively or not at all, If that's the case, that's a really important outcome."
As Petersen explained, the placement of PEG feeding tubes is a hot topic in head and neck cancer care. Malnutrition affects about 80% of these patients and can contribute to mortality, raising the question of whether they should have access to feeding tubes placed prior to treatment in case enteral nutrition is needed.
In some patients with head and neck cancer, malnutrition may arise when tumors block food intake or prevent patients from swallowing. "But in my clinical experience, most often it's from the adverse effects of radiation and chemotherapy. Radiation creates burns inside their throat that make it hard to swallow. Or they have taste changes or really dry mouth," Petersen said.
"On top of these problems, chemotherapy can cause nausea and vomiting," she said. Placing feeding tube access may seem like a smart strategy to head off malnutrition as soon as it occurs. But, as Petersen noted, feeding tube use can lead to dependency as patients lose their ability to swallow. "There's a theory that if we give people feeding tubes, they'll go with the easier route of using a feeding tube and not keep swallowing. Then those swallowing muscles would weaken, and patients would end up permanently on a feeding tube."
In 2020, a retrospective VA study linked feeding tube dependence to lower overall survival in head and neck cancer patients. There are also risks to feeding tube placement, such as infection, pain, leakage, and inflammation.
But what if feeding tube valves are inserted prophylactically so they can be used for nutrition if needed? "We just haven't had any prospective studies to get to the heart of the matter and answer the question," she said. "It's hard to recruit. How do you convince somebody to randomly be assigned to have a hole poked in their stomach?"
For the new pilot study, researchers in Phoenix decided not to randomize patients. Instead, they asked them whether they'd accept the placement of feeding tube valves on a prophylactic basis.
Thirty-six veterans enrolled in 3 years, 33% of those were eligible. Twelve have died, 1 withdrew, and 2 were lost to follow-up.
Those in the prophylactic group had worse physical function and muscle strength over time, while those who received feeding tubes when needed had more adverse events.
Why might some outcomes be worse for patients who chose the prophylactic approach? "The answer is unclear," Petersen said. "Although one possibility is that those patients had higher-risk tumors and were more clued into their own risk."
"The goal now is to get funding for an expanded, multicenter study within the VA," Petersen said. The big question that she hopes to answer is: Does a prophylactic approach work? "Does it make a difference for patients in terms of how quickly they go back to living a full, meaningful life and be able to do all the things that they normally would do?"
A complete study would likely last 7 years, but helpful results may come earlier. "We are starting to see significant differences in terms of our main outcomes of physical function," Petersen said. "We only need 1 to 2 years of data for each patient to get to the heart of that."
The study is not funded, and Petersen reported no disclosures.
Research conducted at the US Department of Veterans Affairs (VA) could offer crucial insight into the hotly debated question of whether patients with head and neck cancer should have access to percutaneous endoscopic gastrostomy (PEG) before they develop malnutrition.
While no definitive conclusions can be drawn until a complete study is performed, early findings of a pilot trial are intriguing, said advanced practice oncology dietitian Katherine Petersen, MS, RDN, CSO, of the Phoenix VA Health Care System, who spoke in an interview with Federal Practitioner and at the annual meeting of the Association of VA Hematology/Oncology.
So far, the 12 patients with head and neck cancer who agreed to the placement of prophylactic feeding tubes prior to chemoradiation have had worse outcomes in some areas compared to the 9 patients who had tubes inserted when clinically indicated and the 12 who didn't need feeding tubes.
Petersen cautioned that the study is small and underpowered at this point. Still, she noted, "We're seeing a hint of exactly the opposite of what I expected. Those who get a tube prophylactically are doing worse than those who are getting it reactively or not at all, If that's the case, that's a really important outcome."
As Petersen explained, the placement of PEG feeding tubes is a hot topic in head and neck cancer care. Malnutrition affects about 80% of these patients and can contribute to mortality, raising the question of whether they should have access to feeding tubes placed prior to treatment in case enteral nutrition is needed.
In some patients with head and neck cancer, malnutrition may arise when tumors block food intake or prevent patients from swallowing. "But in my clinical experience, most often it's from the adverse effects of radiation and chemotherapy. Radiation creates burns inside their throat that make it hard to swallow. Or they have taste changes or really dry mouth," Petersen said.
"On top of these problems, chemotherapy can cause nausea and vomiting," she said. Placing feeding tube access may seem like a smart strategy to head off malnutrition as soon as it occurs. But, as Petersen noted, feeding tube use can lead to dependency as patients lose their ability to swallow. "There's a theory that if we give people feeding tubes, they'll go with the easier route of using a feeding tube and not keep swallowing. Then those swallowing muscles would weaken, and patients would end up permanently on a feeding tube."
In 2020, a retrospective VA study linked feeding tube dependence to lower overall survival in head and neck cancer patients. There are also risks to feeding tube placement, such as infection, pain, leakage, and inflammation.
But what if feeding tube valves are inserted prophylactically so they can be used for nutrition if needed? "We just haven't had any prospective studies to get to the heart of the matter and answer the question," she said. "It's hard to recruit. How do you convince somebody to randomly be assigned to have a hole poked in their stomach?"
For the new pilot study, researchers in Phoenix decided not to randomize patients. Instead, they asked them whether they'd accept the placement of feeding tube valves on a prophylactic basis.
Thirty-six veterans enrolled in 3 years, 33% of those were eligible. Twelve have died, 1 withdrew, and 2 were lost to follow-up.
Those in the prophylactic group had worse physical function and muscle strength over time, while those who received feeding tubes when needed had more adverse events.
Why might some outcomes be worse for patients who chose the prophylactic approach? "The answer is unclear," Petersen said. "Although one possibility is that those patients had higher-risk tumors and were more clued into their own risk."
"The goal now is to get funding for an expanded, multicenter study within the VA," Petersen said. The big question that she hopes to answer is: Does a prophylactic approach work? "Does it make a difference for patients in terms of how quickly they go back to living a full, meaningful life and be able to do all the things that they normally would do?"
A complete study would likely last 7 years, but helpful results may come earlier. "We are starting to see significant differences in terms of our main outcomes of physical function," Petersen said. "We only need 1 to 2 years of data for each patient to get to the heart of that."
The study is not funded, and Petersen reported no disclosures.
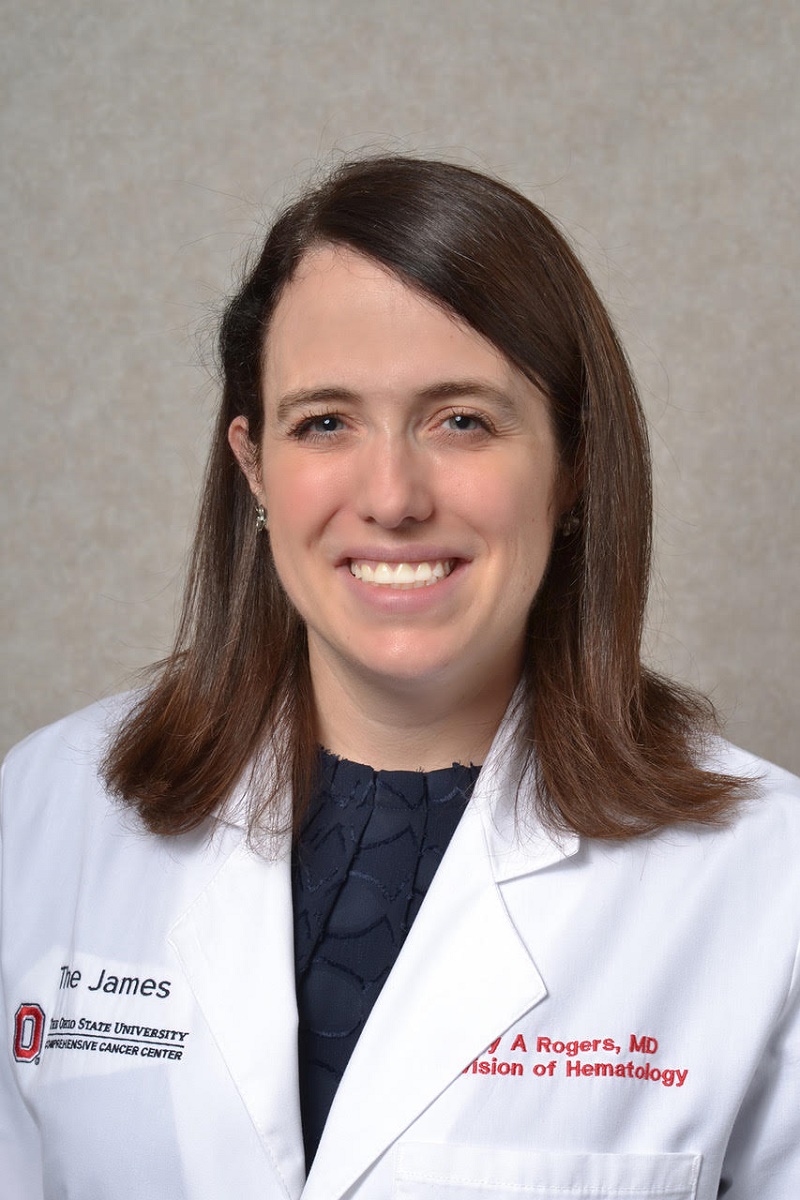
Dr. Rogers’ Neighborhood: Guinea Pigs and Groundbreaking Cancer Care
Sometimes, however, Dr. Rogers’ guinea pigs pay visits to her workplace. Every Halloween, she dresses them up and shows off their photos to just about everyone. Patients, coworkers, and even random people in the elevator get glimpses of the furry pair, who pose as dinosaurs, bats, aquarium shrimp, sharks, spiders, and bumblebees.
“Being in the hospital is not funny, but guinea pigs dressed up for Halloween is incredibly funny,” Dr. Rogers said. “They make a lot of people smile.”
For physician-scientist Dr. Rogers, a native of suburban Chicago, quality of life for patients is a priority, even when she’s not trying to entertain them and lift their spirits.
The field of hematology “is trying to figure out not only what’s biologically effective for disease, but also what might be best for people living with the condition,” she said. “This is especially true in terms of patient preference for a treatment you complete vs an ongoing or continuous treatment. I really like this idea of having more attention paid to what matters to patients, which the field of medicine sometimes forgets.”
In an interview, Dr. Rogers spoke about the appeal of storytelling in medicine, advances in treatment for CLL and hairy cell leukemia, and the challenges of college football loyalty.
How did you get drawn to medicine?
Ever since I was a kid, I thought, “Oh, I really want to be a doctor. That sounds fun.” At its core, medicine blends things I really like: science, helping people with a problem, and storytelling.
The practice of medicine is a lot about stories — talking to people, figuring out what they’re telling you about what’s going on, then explaining what you know in a way that makes sense to them.
What changes have you seen in leukemia care during your career?
The biggest change is the move from chemotherapies to targeted agents. When I first did a fellowship here at Ohio State, we had studies of ibrutinib, the first-in-class covalent Bruton tyrosine kinase (BTK) inhibitor. We’d see patients who’d been on chemotherapy for the past 10 or 15 years, and then they got in a clinical trial. Ibrutinib worked better than any of the chemotherapy, and they felt better and had fewer side effects.
Now, chemoimmunotherapy is not recommended for CLL, and you can see the impact of targeted agents on the lives of patients. Instead of telling people they need to put aside work and personal plans to take intensive chemotherapy for 6 months, you say: “You’ve got to come to some more appointments to make sure the treatment is going well, and you don’t have too many side effects. But you can expect to continue to work full-time and go to your niece’s wedding out of state or whatever else you want to do.”
What are you most excited about working on?
I’m the principal investigator of a study combining obinutuzumab, ibrutinib, and venetoclax for a fixed duration, a defined treatment course of a little over a year. I just reported the median progression-free survival for phase 2 at the European Hematology Association meeting this spring. It was over 7 years for both patients who had prior treatment and those who hadn’t.
The idea that people could take a year of treatment and get a huge benefit after completing it is quite important. The regimen has gone into phase 3 testing, and we’re now trying to understand the impact in terms of which patients got longer responses or which didn’t.
What are some challenges that remain in CLL?
There are still patients whose CLL becomes resistant to our two most commonly used classes of agents: BTK inhibitors and the BLC2 inhibitor, venetoclax. There are some more BCL2 inhibitors in development, but venetoclax is the only one currently approved.
I am also principal investigator on another study that added venetoclax to ibrutinib when resistance mutations developed that would predict ultimate resistance to ibrutinib. The median progression-free survival in that study was 40.7 months, whereas the expectation with venetoclax alone is 24 months. So, it really improved the amount of time people were in remission. This study is ongoing.
We’ve just started a phase 2 study to have patients take pirtobrutinib, a noncovalent BTK inhibitor, in combination with venetoclax in cases where CLL has become resistant to a covalent BTK inhibitor. Patients will take this combination for about a year and a half.
It’s been really exciting to see the impact of some of these combinations both as first-line CLL treatment and in CLL that’s become resistant. But trying to understand what predicts response is a harder thing. I wish I knew the answers for what causes this synergy between those two classes of drugs.
You also specialize in hairy cell leukemia. Could you talk about what it is?
CLL is the most prevalent adult leukemia in the Western world, whereas hairy cell leukemia is very rare. It’s a slow-growing B-cell cancer that got its name because under the microscope, the cells have hairy projections on them.
It had a survival of only about 2-4 years before the development of purine analogs. After a course of pentostatin or cladribine (2-chlordeoxyadenosine), some people never need treatment again in our natural lifespan.
But some patients don’t benefit from purine analogs, either because they have a devastating infection that makes them unsuitable or for another reason. Or they end up needing treatment every 2-3 years, which isn’t something you want to do for 30 years of someone’s lifespan.
What are some challenges in hairy cell leukemia?
It’s a rare condition, so it can be hard to do a really large clinical trial. A lot of physicians think that the prognosis is good and miss out on an opportunity for better treatment and to generate new knowledge.
Also, some people perceive that it’s not actually a problem for people living with it. Cladribine and pentostatin are not terrible chemotherapies, and most people tolerate them very well. But we can make treatment for hairy cell more effective and more tolerable for our patients if we put more effort into researching it.
I’ve heard that you’re a big college football fan. How do you balance your history as a University of Michigan medical school alum with your work for archrival Ohio State?
I went to Northwestern for undergrad, as did several people in my family. So, I usually just claim Northwestern is my football affiliation. It doesn’t inspire much vitriol if you cheer for Northwestern!
And I understand that you live with a pair of guinea pigs. Do tell.
I adopted guinea pigs as pets in medical school. They’re cute and friendly, and they make all this noise for you when you come home.
Once, one of my clinic patients said, “I don’t want to be your guinea pig.” I thought, “you should be so lucky.” They have quite a lifestyle: They’ve trained me to bring them vegetables, they nap most of the time, and they have a play space, a guinea pig playground.
I thought I liked the guinea pigs more than they liked me. But last fall, I was gone for about 10 days. When I got back, I’d never heard them make so much noise. They were extremely happy to see me. Then for the next 48 hours, one would randomly start whistling for me to come over. I thought, “oh, these things do like me a little bit.”
Dr. Rogers disclosed receiving research funding from Genentech, AbbVie, Novartis, and AstraZeneca and consulting/advisory relationships with AstraZeneca, AbbVie, Genentech, Janssen, Pharmacyclics, BeiGene, Loxo@Lilly, and Alpine Immune Sciences.
A version of this article first appeared on Medscape.com.
Sometimes, however, Dr. Rogers’ guinea pigs pay visits to her workplace. Every Halloween, she dresses them up and shows off their photos to just about everyone. Patients, coworkers, and even random people in the elevator get glimpses of the furry pair, who pose as dinosaurs, bats, aquarium shrimp, sharks, spiders, and bumblebees.
“Being in the hospital is not funny, but guinea pigs dressed up for Halloween is incredibly funny,” Dr. Rogers said. “They make a lot of people smile.”
For physician-scientist Dr. Rogers, a native of suburban Chicago, quality of life for patients is a priority, even when she’s not trying to entertain them and lift their spirits.
The field of hematology “is trying to figure out not only what’s biologically effective for disease, but also what might be best for people living with the condition,” she said. “This is especially true in terms of patient preference for a treatment you complete vs an ongoing or continuous treatment. I really like this idea of having more attention paid to what matters to patients, which the field of medicine sometimes forgets.”
In an interview, Dr. Rogers spoke about the appeal of storytelling in medicine, advances in treatment for CLL and hairy cell leukemia, and the challenges of college football loyalty.
How did you get drawn to medicine?
Ever since I was a kid, I thought, “Oh, I really want to be a doctor. That sounds fun.” At its core, medicine blends things I really like: science, helping people with a problem, and storytelling.
The practice of medicine is a lot about stories — talking to people, figuring out what they’re telling you about what’s going on, then explaining what you know in a way that makes sense to them.
What changes have you seen in leukemia care during your career?
The biggest change is the move from chemotherapies to targeted agents. When I first did a fellowship here at Ohio State, we had studies of ibrutinib, the first-in-class covalent Bruton tyrosine kinase (BTK) inhibitor. We’d see patients who’d been on chemotherapy for the past 10 or 15 years, and then they got in a clinical trial. Ibrutinib worked better than any of the chemotherapy, and they felt better and had fewer side effects.
Now, chemoimmunotherapy is not recommended for CLL, and you can see the impact of targeted agents on the lives of patients. Instead of telling people they need to put aside work and personal plans to take intensive chemotherapy for 6 months, you say: “You’ve got to come to some more appointments to make sure the treatment is going well, and you don’t have too many side effects. But you can expect to continue to work full-time and go to your niece’s wedding out of state or whatever else you want to do.”
What are you most excited about working on?
I’m the principal investigator of a study combining obinutuzumab, ibrutinib, and venetoclax for a fixed duration, a defined treatment course of a little over a year. I just reported the median progression-free survival for phase 2 at the European Hematology Association meeting this spring. It was over 7 years for both patients who had prior treatment and those who hadn’t.
The idea that people could take a year of treatment and get a huge benefit after completing it is quite important. The regimen has gone into phase 3 testing, and we’re now trying to understand the impact in terms of which patients got longer responses or which didn’t.
What are some challenges that remain in CLL?
There are still patients whose CLL becomes resistant to our two most commonly used classes of agents: BTK inhibitors and the BLC2 inhibitor, venetoclax. There are some more BCL2 inhibitors in development, but venetoclax is the only one currently approved.
I am also principal investigator on another study that added venetoclax to ibrutinib when resistance mutations developed that would predict ultimate resistance to ibrutinib. The median progression-free survival in that study was 40.7 months, whereas the expectation with venetoclax alone is 24 months. So, it really improved the amount of time people were in remission. This study is ongoing.
We’ve just started a phase 2 study to have patients take pirtobrutinib, a noncovalent BTK inhibitor, in combination with venetoclax in cases where CLL has become resistant to a covalent BTK inhibitor. Patients will take this combination for about a year and a half.
It’s been really exciting to see the impact of some of these combinations both as first-line CLL treatment and in CLL that’s become resistant. But trying to understand what predicts response is a harder thing. I wish I knew the answers for what causes this synergy between those two classes of drugs.
You also specialize in hairy cell leukemia. Could you talk about what it is?
CLL is the most prevalent adult leukemia in the Western world, whereas hairy cell leukemia is very rare. It’s a slow-growing B-cell cancer that got its name because under the microscope, the cells have hairy projections on them.
It had a survival of only about 2-4 years before the development of purine analogs. After a course of pentostatin or cladribine (2-chlordeoxyadenosine), some people never need treatment again in our natural lifespan.
But some patients don’t benefit from purine analogs, either because they have a devastating infection that makes them unsuitable or for another reason. Or they end up needing treatment every 2-3 years, which isn’t something you want to do for 30 years of someone’s lifespan.
What are some challenges in hairy cell leukemia?
It’s a rare condition, so it can be hard to do a really large clinical trial. A lot of physicians think that the prognosis is good and miss out on an opportunity for better treatment and to generate new knowledge.
Also, some people perceive that it’s not actually a problem for people living with it. Cladribine and pentostatin are not terrible chemotherapies, and most people tolerate them very well. But we can make treatment for hairy cell more effective and more tolerable for our patients if we put more effort into researching it.
I’ve heard that you’re a big college football fan. How do you balance your history as a University of Michigan medical school alum with your work for archrival Ohio State?
I went to Northwestern for undergrad, as did several people in my family. So, I usually just claim Northwestern is my football affiliation. It doesn’t inspire much vitriol if you cheer for Northwestern!
And I understand that you live with a pair of guinea pigs. Do tell.
I adopted guinea pigs as pets in medical school. They’re cute and friendly, and they make all this noise for you when you come home.
Once, one of my clinic patients said, “I don’t want to be your guinea pig.” I thought, “you should be so lucky.” They have quite a lifestyle: They’ve trained me to bring them vegetables, they nap most of the time, and they have a play space, a guinea pig playground.
I thought I liked the guinea pigs more than they liked me. But last fall, I was gone for about 10 days. When I got back, I’d never heard them make so much noise. They were extremely happy to see me. Then for the next 48 hours, one would randomly start whistling for me to come over. I thought, “oh, these things do like me a little bit.”
Dr. Rogers disclosed receiving research funding from Genentech, AbbVie, Novartis, and AstraZeneca and consulting/advisory relationships with AstraZeneca, AbbVie, Genentech, Janssen, Pharmacyclics, BeiGene, Loxo@Lilly, and Alpine Immune Sciences.
A version of this article first appeared on Medscape.com.
Sometimes, however, Dr. Rogers’ guinea pigs pay visits to her workplace. Every Halloween, she dresses them up and shows off their photos to just about everyone. Patients, coworkers, and even random people in the elevator get glimpses of the furry pair, who pose as dinosaurs, bats, aquarium shrimp, sharks, spiders, and bumblebees.
“Being in the hospital is not funny, but guinea pigs dressed up for Halloween is incredibly funny,” Dr. Rogers said. “They make a lot of people smile.”
For physician-scientist Dr. Rogers, a native of suburban Chicago, quality of life for patients is a priority, even when she’s not trying to entertain them and lift their spirits.
The field of hematology “is trying to figure out not only what’s biologically effective for disease, but also what might be best for people living with the condition,” she said. “This is especially true in terms of patient preference for a treatment you complete vs an ongoing or continuous treatment. I really like this idea of having more attention paid to what matters to patients, which the field of medicine sometimes forgets.”
In an interview, Dr. Rogers spoke about the appeal of storytelling in medicine, advances in treatment for CLL and hairy cell leukemia, and the challenges of college football loyalty.
How did you get drawn to medicine?
Ever since I was a kid, I thought, “Oh, I really want to be a doctor. That sounds fun.” At its core, medicine blends things I really like: science, helping people with a problem, and storytelling.
The practice of medicine is a lot about stories — talking to people, figuring out what they’re telling you about what’s going on, then explaining what you know in a way that makes sense to them.
What changes have you seen in leukemia care during your career?
The biggest change is the move from chemotherapies to targeted agents. When I first did a fellowship here at Ohio State, we had studies of ibrutinib, the first-in-class covalent Bruton tyrosine kinase (BTK) inhibitor. We’d see patients who’d been on chemotherapy for the past 10 or 15 years, and then they got in a clinical trial. Ibrutinib worked better than any of the chemotherapy, and they felt better and had fewer side effects.
Now, chemoimmunotherapy is not recommended for CLL, and you can see the impact of targeted agents on the lives of patients. Instead of telling people they need to put aside work and personal plans to take intensive chemotherapy for 6 months, you say: “You’ve got to come to some more appointments to make sure the treatment is going well, and you don’t have too many side effects. But you can expect to continue to work full-time and go to your niece’s wedding out of state or whatever else you want to do.”
What are you most excited about working on?
I’m the principal investigator of a study combining obinutuzumab, ibrutinib, and venetoclax for a fixed duration, a defined treatment course of a little over a year. I just reported the median progression-free survival for phase 2 at the European Hematology Association meeting this spring. It was over 7 years for both patients who had prior treatment and those who hadn’t.
The idea that people could take a year of treatment and get a huge benefit after completing it is quite important. The regimen has gone into phase 3 testing, and we’re now trying to understand the impact in terms of which patients got longer responses or which didn’t.
What are some challenges that remain in CLL?
There are still patients whose CLL becomes resistant to our two most commonly used classes of agents: BTK inhibitors and the BLC2 inhibitor, venetoclax. There are some more BCL2 inhibitors in development, but venetoclax is the only one currently approved.
I am also principal investigator on another study that added venetoclax to ibrutinib when resistance mutations developed that would predict ultimate resistance to ibrutinib. The median progression-free survival in that study was 40.7 months, whereas the expectation with venetoclax alone is 24 months. So, it really improved the amount of time people were in remission. This study is ongoing.
We’ve just started a phase 2 study to have patients take pirtobrutinib, a noncovalent BTK inhibitor, in combination with venetoclax in cases where CLL has become resistant to a covalent BTK inhibitor. Patients will take this combination for about a year and a half.
It’s been really exciting to see the impact of some of these combinations both as first-line CLL treatment and in CLL that’s become resistant. But trying to understand what predicts response is a harder thing. I wish I knew the answers for what causes this synergy between those two classes of drugs.
You also specialize in hairy cell leukemia. Could you talk about what it is?
CLL is the most prevalent adult leukemia in the Western world, whereas hairy cell leukemia is very rare. It’s a slow-growing B-cell cancer that got its name because under the microscope, the cells have hairy projections on them.
It had a survival of only about 2-4 years before the development of purine analogs. After a course of pentostatin or cladribine (2-chlordeoxyadenosine), some people never need treatment again in our natural lifespan.
But some patients don’t benefit from purine analogs, either because they have a devastating infection that makes them unsuitable or for another reason. Or they end up needing treatment every 2-3 years, which isn’t something you want to do for 30 years of someone’s lifespan.
What are some challenges in hairy cell leukemia?
It’s a rare condition, so it can be hard to do a really large clinical trial. A lot of physicians think that the prognosis is good and miss out on an opportunity for better treatment and to generate new knowledge.
Also, some people perceive that it’s not actually a problem for people living with it. Cladribine and pentostatin are not terrible chemotherapies, and most people tolerate them very well. But we can make treatment for hairy cell more effective and more tolerable for our patients if we put more effort into researching it.
I’ve heard that you’re a big college football fan. How do you balance your history as a University of Michigan medical school alum with your work for archrival Ohio State?
I went to Northwestern for undergrad, as did several people in my family. So, I usually just claim Northwestern is my football affiliation. It doesn’t inspire much vitriol if you cheer for Northwestern!
And I understand that you live with a pair of guinea pigs. Do tell.
I adopted guinea pigs as pets in medical school. They’re cute and friendly, and they make all this noise for you when you come home.
Once, one of my clinic patients said, “I don’t want to be your guinea pig.” I thought, “you should be so lucky.” They have quite a lifestyle: They’ve trained me to bring them vegetables, they nap most of the time, and they have a play space, a guinea pig playground.
I thought I liked the guinea pigs more than they liked me. But last fall, I was gone for about 10 days. When I got back, I’d never heard them make so much noise. They were extremely happy to see me. Then for the next 48 hours, one would randomly start whistling for me to come over. I thought, “oh, these things do like me a little bit.”
Dr. Rogers disclosed receiving research funding from Genentech, AbbVie, Novartis, and AstraZeneca and consulting/advisory relationships with AstraZeneca, AbbVie, Genentech, Janssen, Pharmacyclics, BeiGene, Loxo@Lilly, and Alpine Immune Sciences.
A version of this article first appeared on Medscape.com.
Who’s an Anesthesiologist? Turf War Sparks Trademark Dispute
The turf war between two types of anesthesia providers is escalating:
At issue: Who can be called an anesthesiologist?
In its complaint, filed in June 2024 with the US Trademark Trial and Appeal Board, the 54,000-member physician society seeks to deny the nurse group the registration of its trademark. If ASA wins, it could sue AANA in federal court.
AANA denied the physicians’ allegations in its recent response to the complaint.
The dispute between the two associations comes at a time when physicians are facing challenges from providers such as nurse practitioners and physician assistants who seek new titles and more autonomy in medical decision-making.
A Controversial Name Change
In 2021, the 61,000-member AANA changed its name from the American Association of Nurse Anesthetists, saying the change “clarifies” the role of its members.
The ASA declared it was “gravely concerned” by the name change, which “confuses patients and creates discord in the care setting, ultimately risking patient safety.
“ ’Anesthesiologist’ has always been used to differentiate physicians trained in the science and study of anesthesiology from nonphysicians, including nurse anesthetists,” the physicians’ group said in a news release.
Chicago Intellectual Property Attorney Laura M. Schaefer, who represents AANA, told this news organization that certified registered nurse anesthetists (CRNAs) — “also known as nurse anesthesiologists or nurse anesthetists — have a 150-year track record of administering safe, effective anesthesia to patients in need of care. Not only are CRNAs highly trained and capable, they also use the exact same techniques to provide anesthesia as other anesthesiology professionals.”
Ms. Schaefer declined to comment further, and ASA declined to comment at all, citing pending litigation.
The scope of practice of nurse anesthetists has long been disputed. In mid-September, California health officials clarified what nurse anesthetists can do on the job after complaints about lack of oversight, The Modesto Bee reported.
According to nursing education site NurseJournal.org, CRNAs and anesthesiologists “perform many of the same duties,” although CRNAs are in more demand. Also, the site says some states require CRNAs to be supervised by anesthesiologists.
“It is possible that scope of practice debates are increasing in prominence due to the increase in demand for healthcare services, coupled with workforce shortages in certain areas,” Alice Chen, PhD, MBA, vice dean for research at the USC Sol Price School of Public Policy in Los Angeles, told this news organization. “For example, during COVID, the federal government temporarily expanded scope of practice to help address healthcare needs.”
She added her group’s research has shown that despite the large stakes perceived by both sides of the debate, changes in practice behavior were actually quite small in states that allowed CRNAs to practice without supervision.
“In fact, we found only modest reduction in anesthesiologist billing for supervision, and we did not find an increase in the supply of anesthesia care,” she noted.
Trademark law specialists told this news organization that they couldn’t predict which way the board will rule. However, they noted potential weaknesses of the ASA’s case.
Rebecca Tushnet, JD, a professor at Harvard Law School, Cambridge, Massachusetts, explained that a trademark “can’t misrepresent those goods or services in a way that deceives consumers.” However, if insurers, doctors, and hospitals are considered the “consumers” — and not patients — “then confusion is probably less likely because they will have relevant expertise to distinguish among groups.”
Christine Farley, JD, LLM, JSD, professor at American University Washington College of Law, said attacking the AANA’s trademark as deceptive may be one of the ASA’s strongest arguments. The suggestion, she said, is that “nurse anesthesiologist” is an oxymoron, like “jumbo shrimp.”
On the other hand, she said it’s not clear that people will miss the word “nurse” in AANA’s name and say, “ ’Well, obviously these people are doctors.’ So that that’s an uphill battle.”
What happens now? The Trademark Trial and Appeal Board will decide whether AANA’s trademark application should be granted or denied, said Kayla Jimenez, JD, a San Diego trademark attorney and adjunct law professor at the University of San Diego. The entire process can take 2-3 years, she said.
The board “cannot award attorneys’ fees or force a party to stop using a trademark,” she said. “You would have to go file a lawsuit in federal court if that is your endgame.” Also, she said, the board’s ultimate decision can be appealed in federal court.
Eric Goldman, JD, MBA, associate dean for research and professor at Santa Clara University School of Law, Santa Clara, California, doesn’t expect the trademark case will spell the end of this dispute.
“ASA is signaling that it will challenge AANA’s use of the term in multiple battlegrounds,” he said. “I see this as a move by ASA to contest AANA in every potentially relevant venue, even if neither side can score a knockout blow in the Trademark Trial and Appeal Board.”
Dr. Chen, Ms. Farley, Ms. Jimenez, and Mr. Goldman had no disclosures.
A version of this article appeared on Medscape.com.
The turf war between two types of anesthesia providers is escalating:
At issue: Who can be called an anesthesiologist?
In its complaint, filed in June 2024 with the US Trademark Trial and Appeal Board, the 54,000-member physician society seeks to deny the nurse group the registration of its trademark. If ASA wins, it could sue AANA in federal court.
AANA denied the physicians’ allegations in its recent response to the complaint.
The dispute between the two associations comes at a time when physicians are facing challenges from providers such as nurse practitioners and physician assistants who seek new titles and more autonomy in medical decision-making.
A Controversial Name Change
In 2021, the 61,000-member AANA changed its name from the American Association of Nurse Anesthetists, saying the change “clarifies” the role of its members.
The ASA declared it was “gravely concerned” by the name change, which “confuses patients and creates discord in the care setting, ultimately risking patient safety.
“ ’Anesthesiologist’ has always been used to differentiate physicians trained in the science and study of anesthesiology from nonphysicians, including nurse anesthetists,” the physicians’ group said in a news release.
Chicago Intellectual Property Attorney Laura M. Schaefer, who represents AANA, told this news organization that certified registered nurse anesthetists (CRNAs) — “also known as nurse anesthesiologists or nurse anesthetists — have a 150-year track record of administering safe, effective anesthesia to patients in need of care. Not only are CRNAs highly trained and capable, they also use the exact same techniques to provide anesthesia as other anesthesiology professionals.”
Ms. Schaefer declined to comment further, and ASA declined to comment at all, citing pending litigation.
The scope of practice of nurse anesthetists has long been disputed. In mid-September, California health officials clarified what nurse anesthetists can do on the job after complaints about lack of oversight, The Modesto Bee reported.
According to nursing education site NurseJournal.org, CRNAs and anesthesiologists “perform many of the same duties,” although CRNAs are in more demand. Also, the site says some states require CRNAs to be supervised by anesthesiologists.
“It is possible that scope of practice debates are increasing in prominence due to the increase in demand for healthcare services, coupled with workforce shortages in certain areas,” Alice Chen, PhD, MBA, vice dean for research at the USC Sol Price School of Public Policy in Los Angeles, told this news organization. “For example, during COVID, the federal government temporarily expanded scope of practice to help address healthcare needs.”
She added her group’s research has shown that despite the large stakes perceived by both sides of the debate, changes in practice behavior were actually quite small in states that allowed CRNAs to practice without supervision.
“In fact, we found only modest reduction in anesthesiologist billing for supervision, and we did not find an increase in the supply of anesthesia care,” she noted.
Trademark law specialists told this news organization that they couldn’t predict which way the board will rule. However, they noted potential weaknesses of the ASA’s case.
Rebecca Tushnet, JD, a professor at Harvard Law School, Cambridge, Massachusetts, explained that a trademark “can’t misrepresent those goods or services in a way that deceives consumers.” However, if insurers, doctors, and hospitals are considered the “consumers” — and not patients — “then confusion is probably less likely because they will have relevant expertise to distinguish among groups.”
Christine Farley, JD, LLM, JSD, professor at American University Washington College of Law, said attacking the AANA’s trademark as deceptive may be one of the ASA’s strongest arguments. The suggestion, she said, is that “nurse anesthesiologist” is an oxymoron, like “jumbo shrimp.”
On the other hand, she said it’s not clear that people will miss the word “nurse” in AANA’s name and say, “ ’Well, obviously these people are doctors.’ So that that’s an uphill battle.”
What happens now? The Trademark Trial and Appeal Board will decide whether AANA’s trademark application should be granted or denied, said Kayla Jimenez, JD, a San Diego trademark attorney and adjunct law professor at the University of San Diego. The entire process can take 2-3 years, she said.
The board “cannot award attorneys’ fees or force a party to stop using a trademark,” she said. “You would have to go file a lawsuit in federal court if that is your endgame.” Also, she said, the board’s ultimate decision can be appealed in federal court.
Eric Goldman, JD, MBA, associate dean for research and professor at Santa Clara University School of Law, Santa Clara, California, doesn’t expect the trademark case will spell the end of this dispute.
“ASA is signaling that it will challenge AANA’s use of the term in multiple battlegrounds,” he said. “I see this as a move by ASA to contest AANA in every potentially relevant venue, even if neither side can score a knockout blow in the Trademark Trial and Appeal Board.”
Dr. Chen, Ms. Farley, Ms. Jimenez, and Mr. Goldman had no disclosures.
A version of this article appeared on Medscape.com.
The turf war between two types of anesthesia providers is escalating:
At issue: Who can be called an anesthesiologist?
In its complaint, filed in June 2024 with the US Trademark Trial and Appeal Board, the 54,000-member physician society seeks to deny the nurse group the registration of its trademark. If ASA wins, it could sue AANA in federal court.
AANA denied the physicians’ allegations in its recent response to the complaint.
The dispute between the two associations comes at a time when physicians are facing challenges from providers such as nurse practitioners and physician assistants who seek new titles and more autonomy in medical decision-making.
A Controversial Name Change
In 2021, the 61,000-member AANA changed its name from the American Association of Nurse Anesthetists, saying the change “clarifies” the role of its members.
The ASA declared it was “gravely concerned” by the name change, which “confuses patients and creates discord in the care setting, ultimately risking patient safety.
“ ’Anesthesiologist’ has always been used to differentiate physicians trained in the science and study of anesthesiology from nonphysicians, including nurse anesthetists,” the physicians’ group said in a news release.
Chicago Intellectual Property Attorney Laura M. Schaefer, who represents AANA, told this news organization that certified registered nurse anesthetists (CRNAs) — “also known as nurse anesthesiologists or nurse anesthetists — have a 150-year track record of administering safe, effective anesthesia to patients in need of care. Not only are CRNAs highly trained and capable, they also use the exact same techniques to provide anesthesia as other anesthesiology professionals.”
Ms. Schaefer declined to comment further, and ASA declined to comment at all, citing pending litigation.
The scope of practice of nurse anesthetists has long been disputed. In mid-September, California health officials clarified what nurse anesthetists can do on the job after complaints about lack of oversight, The Modesto Bee reported.
According to nursing education site NurseJournal.org, CRNAs and anesthesiologists “perform many of the same duties,” although CRNAs are in more demand. Also, the site says some states require CRNAs to be supervised by anesthesiologists.
“It is possible that scope of practice debates are increasing in prominence due to the increase in demand for healthcare services, coupled with workforce shortages in certain areas,” Alice Chen, PhD, MBA, vice dean for research at the USC Sol Price School of Public Policy in Los Angeles, told this news organization. “For example, during COVID, the federal government temporarily expanded scope of practice to help address healthcare needs.”
She added her group’s research has shown that despite the large stakes perceived by both sides of the debate, changes in practice behavior were actually quite small in states that allowed CRNAs to practice without supervision.
“In fact, we found only modest reduction in anesthesiologist billing for supervision, and we did not find an increase in the supply of anesthesia care,” she noted.
Trademark law specialists told this news organization that they couldn’t predict which way the board will rule. However, they noted potential weaknesses of the ASA’s case.
Rebecca Tushnet, JD, a professor at Harvard Law School, Cambridge, Massachusetts, explained that a trademark “can’t misrepresent those goods or services in a way that deceives consumers.” However, if insurers, doctors, and hospitals are considered the “consumers” — and not patients — “then confusion is probably less likely because they will have relevant expertise to distinguish among groups.”
Christine Farley, JD, LLM, JSD, professor at American University Washington College of Law, said attacking the AANA’s trademark as deceptive may be one of the ASA’s strongest arguments. The suggestion, she said, is that “nurse anesthesiologist” is an oxymoron, like “jumbo shrimp.”
On the other hand, she said it’s not clear that people will miss the word “nurse” in AANA’s name and say, “ ’Well, obviously these people are doctors.’ So that that’s an uphill battle.”
What happens now? The Trademark Trial and Appeal Board will decide whether AANA’s trademark application should be granted or denied, said Kayla Jimenez, JD, a San Diego trademark attorney and adjunct law professor at the University of San Diego. The entire process can take 2-3 years, she said.
The board “cannot award attorneys’ fees or force a party to stop using a trademark,” she said. “You would have to go file a lawsuit in federal court if that is your endgame.” Also, she said, the board’s ultimate decision can be appealed in federal court.
Eric Goldman, JD, MBA, associate dean for research and professor at Santa Clara University School of Law, Santa Clara, California, doesn’t expect the trademark case will spell the end of this dispute.
“ASA is signaling that it will challenge AANA’s use of the term in multiple battlegrounds,” he said. “I see this as a move by ASA to contest AANA in every potentially relevant venue, even if neither side can score a knockout blow in the Trademark Trial and Appeal Board.”
Dr. Chen, Ms. Farley, Ms. Jimenez, and Mr. Goldman had no disclosures.
A version of this article appeared on Medscape.com.
Trial Looks at Early Use of Mycophenolate to Reduce Flares, Nephritis
Early use of mycophenolate mofetil (MMF), a drug used to dampen the immune system in organ transplant recipients, may reduce the risk for severe flares in patients with newly diagnosed systemic lupus erythematosus (SLE), according to results from a randomized, open-label, observer-blinded clinical trial.
In interviews, two SLE specialists who were not involved with the study said the research is preliminary but promising. However, another specialist criticized the paper’s reliance on unusual doses of prednisone and MMF, saying it “puts people on a treatment regimen that nobody ever uses.”
The Lupus Foundation of America estimates that about 16,000 people in the United States are diagnosed with lupus each year. “Our current treatment paradigm is to go pretty slowly and start treatment for new-onset, mild SLE with glucocorticoids, if necessary, and hydroxychloroquine,” said Karen H. Costenbader, MD, MPH, of Harvard Medical School and Harvard School of Public Health, Boston, Massachusetts.
Stronger immunosuppressive agents may be added as patients progress, she said.
Off-label use of MMF, which is approved by the Food and Drug Administration only for patients with certain organ transplants, may be appropriate in some cases, she said. “There is a big push to start immunosuppressives earlier, but we currently would reserve mycophenolate for those with severe manifestations — lupus nephritis; vasculitis; or lung, brain, or heart inflammation.”
In the trial, adult patients who received oral prednisone (starting at 0.5 mg/kg per day) and hydroxychloroquine sulfate (5 mg/kg per day) plus MMF (500 mg twice daily) for 96 weeks were less likely to develop severe flares than those who took the regimen without MMF (relative risk [RR], 0.39; 95% CI, 0.17-0.87; P = .01). Severe flares occurred in 10.8% of the MMF group (7 of 65 patients) and in 27.7% of the control group (18 of 65), Yijun You, MD, of Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China, and colleagues reported in JAMA Network Open.
Patients in the MMF group also had 89% lower risk for lupus nephritis than those in the control group (RR, 0.11; 95% CI, 0.01-0.85; P = .008), with kidney involvement occurring in 1.5% (1 of 65) vs 13.8% (9 of 65).
During 2018-2021, researchers recruited 130 patients in China aged 18-65 years with newly diagnosed SLE, a high titer of anti–double-stranded DNA (dsDNA) antibodies, and no major organ involvement (mean age, 34.5 years; 86.2% women). Patients’ initial 0.5–mg/kg per day prednisone dose was maintained for 4 weeks, then tapered by 5.0 mg every 2 weeks, and when the dose had been reduced to 20.0 mg/day, it was tapered by 5 mg every month and then gradually to 0.1-0.2 mg/kg per day. If patients had severe flares, they stopped taking MMF. (The study authors did not respond to requests for comment on the study.)
‘A Treatment Regimen That Nobody Ever Uses’
While Dr. Costenbader called the study “very interesting” and said “every person diagnosing or taking care of patients with lupus should be familiar” with it, she noted that the prednisone doses were high. “I am wondering why they used quite so much glucocorticoid for everyone. This may have masked some of the MMF effect and biased toward the null. They also used a low dose of MMF and did not ramp it up as we would normally to a full dose. That being said, it is remarkable that it was well-tolerated and resulted in better outcomes over the period of the trial.”
Daniel J. Wallace, MD, of Cedars-Sinai Medical Center, Los Angeles, California, and the University of California, Los Angeles, also highlighted the high doses of prednisone and low doses of MMF. “It’s a useless paper that puts people on a treatment regimen that nobody ever uses,” he said.
The rates of mild to moderate flares were similar between the control and intervention groups (38.5% vs 36.9%, respectively; RR, 0.96; P = .90). This finding is surprising, said Judith A. James, MD, PhD, executive vice president, chief medical officer, and head of the rheumatology clinic and Arthritis and Clinical Immunology Research Program at the Oklahoma Medical Research Foundation in Oklahoma City and also the Associate Vice Provost of Clinical & Translational Science, professor of medicine, and George Lynn Cross Research Professor at the University of Oklahoma Health Sciences Center in Oklahoma City. “It may be that mild flares have a different mechanism or are caused by noninflammatory endotypes that don’t respond to MMF.”
Dr. Costenbader noted that a risk-benefit analysis will need to be done to take the risks of MMF into account. “However, every time that a person flares or is not in lupus low-disease activity state, potentially permanent organ damage is done and the patient suffers,” she said. “Preventing lupus nephritis de novo was also seen — nine cases potentially prevented — and that is also really interesting. It would be amazing if we could completely avoid that life-threatening complication.”
MMF can cause miscarriage and boost the risk for birth defects, and the manufacturer says it can lower the effectiveness of birth control pills. It can also boost the risk for some cancers such as lymphoma and increase the risk for infections.
Surprisingly, the number of adverse events in the control and intervention groups were similar (35.4% vs 46.2%, respectively; RR, 1.30; 95% CI, 0.86-1.99; P = .20). They included infection (30.8% vs 33.8%, respectively; P = .70) and gastrointestinal tract events (16.9% for both; P > .99).
“There were overall pretty similar rates of side effects, but maybe this was because MMF dose was pretty low in the treated group, or the glucocorticoid dose was not so low in both groups,” Dr. Costenbader said. She also noted that “the risk of malignancy with MMF is longer term than this study. It may not show up for 5-10 or even more years, but we know it exists. Infections are also increased with MMF — some of which can be avoided with vaccines for COVID, pneumonia, influenza, shingles, etc. MMF also causes gastrointestinal intolerance, and people often are not able to take it because of nausea, vomiting, diarrhea, and elevated liver function tests.”
Dr. James said the infection rates “may be due to the higher doses of steroids patients in both groups are on for several months at the beginning of the study.”
A total of 12 patients in the MMF group discontinued the intervention for various reasons, and 6 were lost to follow-up. In the control group, 20 discontinued the intervention and two were lost to follow-up. However, all 130 patients in the trial were included in the primary and secondary outcome analyses.
Should clinicians consider prescribing MMF to patients with new-onset SLE? “We usually wait until later when there are indications of more severe disease, but here they started it from the time of diagnosis if the patient was anti-dsDNA positive. Given insurance restrictions in this country, we would be unlikely to be able to do that for many patients,” Dr. Costenbader said. “They likely also overtreated a lot of patients who didn’t need it. Due to our lack of more specific biomarkers and precision medicine for lupus, we do currently undertreat a lot of patients, as this study highlights, as well as overtreat others.”
How Much Might Cost Factor Into Treatment Decisions?
The study did not examine cost. Prednisone and hydroxychloroquine sulfate are inexpensive, but Dr. James said MMF can cost about $450 a month at the study dosage. However, “the average hospitalization without an ICU [intensive care unit] visit for an SLE patient is about $15,000-$20,000. If you can avoid one hospitalization, you can pay for nearly 4 years of MMF. More importantly, from a financial perspective, if you can convert a severe lupus patient to a mild/moderate lupus patient, then the annual costs of lupus decrease nearly by half, from about $52,000 per year to $25,000 per year.”
The study authors noted various limitations such as the small number of subjects, the need for a longer trial “to determine the advantages and disadvantages of early application of MMF,” and the fact that all subjects were Asian. The authors also called for confirmation via a double-blind, placebo-controlled study.
The study was funded by grants to the authors by the National Natural Science Foundation of China, Shanghai Rising-Star Program, Natural Science Foundation of Shanghai, Five-Year National Key R&D Program, and Ruijin–Zhongmei Huadong Lupus Funding. The authors had no disclosures. Dr. Costenbader disclosed consulting/research collaboration relationships with AstraZeneca, Amgen, Biogen, Bristol-Myers Squibb, GSK, Merck, Gilead, and Cabaletta. Dr. James and Dr. Wallace had no disclosures.
A version of this article first appeared on Medscape.com.
Early use of mycophenolate mofetil (MMF), a drug used to dampen the immune system in organ transplant recipients, may reduce the risk for severe flares in patients with newly diagnosed systemic lupus erythematosus (SLE), according to results from a randomized, open-label, observer-blinded clinical trial.
In interviews, two SLE specialists who were not involved with the study said the research is preliminary but promising. However, another specialist criticized the paper’s reliance on unusual doses of prednisone and MMF, saying it “puts people on a treatment regimen that nobody ever uses.”
The Lupus Foundation of America estimates that about 16,000 people in the United States are diagnosed with lupus each year. “Our current treatment paradigm is to go pretty slowly and start treatment for new-onset, mild SLE with glucocorticoids, if necessary, and hydroxychloroquine,” said Karen H. Costenbader, MD, MPH, of Harvard Medical School and Harvard School of Public Health, Boston, Massachusetts.
Stronger immunosuppressive agents may be added as patients progress, she said.
Off-label use of MMF, which is approved by the Food and Drug Administration only for patients with certain organ transplants, may be appropriate in some cases, she said. “There is a big push to start immunosuppressives earlier, but we currently would reserve mycophenolate for those with severe manifestations — lupus nephritis; vasculitis; or lung, brain, or heart inflammation.”
In the trial, adult patients who received oral prednisone (starting at 0.5 mg/kg per day) and hydroxychloroquine sulfate (5 mg/kg per day) plus MMF (500 mg twice daily) for 96 weeks were less likely to develop severe flares than those who took the regimen without MMF (relative risk [RR], 0.39; 95% CI, 0.17-0.87; P = .01). Severe flares occurred in 10.8% of the MMF group (7 of 65 patients) and in 27.7% of the control group (18 of 65), Yijun You, MD, of Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China, and colleagues reported in JAMA Network Open.
Patients in the MMF group also had 89% lower risk for lupus nephritis than those in the control group (RR, 0.11; 95% CI, 0.01-0.85; P = .008), with kidney involvement occurring in 1.5% (1 of 65) vs 13.8% (9 of 65).
During 2018-2021, researchers recruited 130 patients in China aged 18-65 years with newly diagnosed SLE, a high titer of anti–double-stranded DNA (dsDNA) antibodies, and no major organ involvement (mean age, 34.5 years; 86.2% women). Patients’ initial 0.5–mg/kg per day prednisone dose was maintained for 4 weeks, then tapered by 5.0 mg every 2 weeks, and when the dose had been reduced to 20.0 mg/day, it was tapered by 5 mg every month and then gradually to 0.1-0.2 mg/kg per day. If patients had severe flares, they stopped taking MMF. (The study authors did not respond to requests for comment on the study.)
‘A Treatment Regimen That Nobody Ever Uses’
While Dr. Costenbader called the study “very interesting” and said “every person diagnosing or taking care of patients with lupus should be familiar” with it, she noted that the prednisone doses were high. “I am wondering why they used quite so much glucocorticoid for everyone. This may have masked some of the MMF effect and biased toward the null. They also used a low dose of MMF and did not ramp it up as we would normally to a full dose. That being said, it is remarkable that it was well-tolerated and resulted in better outcomes over the period of the trial.”
Daniel J. Wallace, MD, of Cedars-Sinai Medical Center, Los Angeles, California, and the University of California, Los Angeles, also highlighted the high doses of prednisone and low doses of MMF. “It’s a useless paper that puts people on a treatment regimen that nobody ever uses,” he said.
The rates of mild to moderate flares were similar between the control and intervention groups (38.5% vs 36.9%, respectively; RR, 0.96; P = .90). This finding is surprising, said Judith A. James, MD, PhD, executive vice president, chief medical officer, and head of the rheumatology clinic and Arthritis and Clinical Immunology Research Program at the Oklahoma Medical Research Foundation in Oklahoma City and also the Associate Vice Provost of Clinical & Translational Science, professor of medicine, and George Lynn Cross Research Professor at the University of Oklahoma Health Sciences Center in Oklahoma City. “It may be that mild flares have a different mechanism or are caused by noninflammatory endotypes that don’t respond to MMF.”
Dr. Costenbader noted that a risk-benefit analysis will need to be done to take the risks of MMF into account. “However, every time that a person flares or is not in lupus low-disease activity state, potentially permanent organ damage is done and the patient suffers,” she said. “Preventing lupus nephritis de novo was also seen — nine cases potentially prevented — and that is also really interesting. It would be amazing if we could completely avoid that life-threatening complication.”
MMF can cause miscarriage and boost the risk for birth defects, and the manufacturer says it can lower the effectiveness of birth control pills. It can also boost the risk for some cancers such as lymphoma and increase the risk for infections.
Surprisingly, the number of adverse events in the control and intervention groups were similar (35.4% vs 46.2%, respectively; RR, 1.30; 95% CI, 0.86-1.99; P = .20). They included infection (30.8% vs 33.8%, respectively; P = .70) and gastrointestinal tract events (16.9% for both; P > .99).
“There were overall pretty similar rates of side effects, but maybe this was because MMF dose was pretty low in the treated group, or the glucocorticoid dose was not so low in both groups,” Dr. Costenbader said. She also noted that “the risk of malignancy with MMF is longer term than this study. It may not show up for 5-10 or even more years, but we know it exists. Infections are also increased with MMF — some of which can be avoided with vaccines for COVID, pneumonia, influenza, shingles, etc. MMF also causes gastrointestinal intolerance, and people often are not able to take it because of nausea, vomiting, diarrhea, and elevated liver function tests.”
Dr. James said the infection rates “may be due to the higher doses of steroids patients in both groups are on for several months at the beginning of the study.”
A total of 12 patients in the MMF group discontinued the intervention for various reasons, and 6 were lost to follow-up. In the control group, 20 discontinued the intervention and two were lost to follow-up. However, all 130 patients in the trial were included in the primary and secondary outcome analyses.
Should clinicians consider prescribing MMF to patients with new-onset SLE? “We usually wait until later when there are indications of more severe disease, but here they started it from the time of diagnosis if the patient was anti-dsDNA positive. Given insurance restrictions in this country, we would be unlikely to be able to do that for many patients,” Dr. Costenbader said. “They likely also overtreated a lot of patients who didn’t need it. Due to our lack of more specific biomarkers and precision medicine for lupus, we do currently undertreat a lot of patients, as this study highlights, as well as overtreat others.”
How Much Might Cost Factor Into Treatment Decisions?
The study did not examine cost. Prednisone and hydroxychloroquine sulfate are inexpensive, but Dr. James said MMF can cost about $450 a month at the study dosage. However, “the average hospitalization without an ICU [intensive care unit] visit for an SLE patient is about $15,000-$20,000. If you can avoid one hospitalization, you can pay for nearly 4 years of MMF. More importantly, from a financial perspective, if you can convert a severe lupus patient to a mild/moderate lupus patient, then the annual costs of lupus decrease nearly by half, from about $52,000 per year to $25,000 per year.”
The study authors noted various limitations such as the small number of subjects, the need for a longer trial “to determine the advantages and disadvantages of early application of MMF,” and the fact that all subjects were Asian. The authors also called for confirmation via a double-blind, placebo-controlled study.
The study was funded by grants to the authors by the National Natural Science Foundation of China, Shanghai Rising-Star Program, Natural Science Foundation of Shanghai, Five-Year National Key R&D Program, and Ruijin–Zhongmei Huadong Lupus Funding. The authors had no disclosures. Dr. Costenbader disclosed consulting/research collaboration relationships with AstraZeneca, Amgen, Biogen, Bristol-Myers Squibb, GSK, Merck, Gilead, and Cabaletta. Dr. James and Dr. Wallace had no disclosures.
A version of this article first appeared on Medscape.com.
Early use of mycophenolate mofetil (MMF), a drug used to dampen the immune system in organ transplant recipients, may reduce the risk for severe flares in patients with newly diagnosed systemic lupus erythematosus (SLE), according to results from a randomized, open-label, observer-blinded clinical trial.
In interviews, two SLE specialists who were not involved with the study said the research is preliminary but promising. However, another specialist criticized the paper’s reliance on unusual doses of prednisone and MMF, saying it “puts people on a treatment regimen that nobody ever uses.”
The Lupus Foundation of America estimates that about 16,000 people in the United States are diagnosed with lupus each year. “Our current treatment paradigm is to go pretty slowly and start treatment for new-onset, mild SLE with glucocorticoids, if necessary, and hydroxychloroquine,” said Karen H. Costenbader, MD, MPH, of Harvard Medical School and Harvard School of Public Health, Boston, Massachusetts.
Stronger immunosuppressive agents may be added as patients progress, she said.
Off-label use of MMF, which is approved by the Food and Drug Administration only for patients with certain organ transplants, may be appropriate in some cases, she said. “There is a big push to start immunosuppressives earlier, but we currently would reserve mycophenolate for those with severe manifestations — lupus nephritis; vasculitis; or lung, brain, or heart inflammation.”
In the trial, adult patients who received oral prednisone (starting at 0.5 mg/kg per day) and hydroxychloroquine sulfate (5 mg/kg per day) plus MMF (500 mg twice daily) for 96 weeks were less likely to develop severe flares than those who took the regimen without MMF (relative risk [RR], 0.39; 95% CI, 0.17-0.87; P = .01). Severe flares occurred in 10.8% of the MMF group (7 of 65 patients) and in 27.7% of the control group (18 of 65), Yijun You, MD, of Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China, and colleagues reported in JAMA Network Open.
Patients in the MMF group also had 89% lower risk for lupus nephritis than those in the control group (RR, 0.11; 95% CI, 0.01-0.85; P = .008), with kidney involvement occurring in 1.5% (1 of 65) vs 13.8% (9 of 65).
During 2018-2021, researchers recruited 130 patients in China aged 18-65 years with newly diagnosed SLE, a high titer of anti–double-stranded DNA (dsDNA) antibodies, and no major organ involvement (mean age, 34.5 years; 86.2% women). Patients’ initial 0.5–mg/kg per day prednisone dose was maintained for 4 weeks, then tapered by 5.0 mg every 2 weeks, and when the dose had been reduced to 20.0 mg/day, it was tapered by 5 mg every month and then gradually to 0.1-0.2 mg/kg per day. If patients had severe flares, they stopped taking MMF. (The study authors did not respond to requests for comment on the study.)
‘A Treatment Regimen That Nobody Ever Uses’
While Dr. Costenbader called the study “very interesting” and said “every person diagnosing or taking care of patients with lupus should be familiar” with it, she noted that the prednisone doses were high. “I am wondering why they used quite so much glucocorticoid for everyone. This may have masked some of the MMF effect and biased toward the null. They also used a low dose of MMF and did not ramp it up as we would normally to a full dose. That being said, it is remarkable that it was well-tolerated and resulted in better outcomes over the period of the trial.”
Daniel J. Wallace, MD, of Cedars-Sinai Medical Center, Los Angeles, California, and the University of California, Los Angeles, also highlighted the high doses of prednisone and low doses of MMF. “It’s a useless paper that puts people on a treatment regimen that nobody ever uses,” he said.
The rates of mild to moderate flares were similar between the control and intervention groups (38.5% vs 36.9%, respectively; RR, 0.96; P = .90). This finding is surprising, said Judith A. James, MD, PhD, executive vice president, chief medical officer, and head of the rheumatology clinic and Arthritis and Clinical Immunology Research Program at the Oklahoma Medical Research Foundation in Oklahoma City and also the Associate Vice Provost of Clinical & Translational Science, professor of medicine, and George Lynn Cross Research Professor at the University of Oklahoma Health Sciences Center in Oklahoma City. “It may be that mild flares have a different mechanism or are caused by noninflammatory endotypes that don’t respond to MMF.”
Dr. Costenbader noted that a risk-benefit analysis will need to be done to take the risks of MMF into account. “However, every time that a person flares or is not in lupus low-disease activity state, potentially permanent organ damage is done and the patient suffers,” she said. “Preventing lupus nephritis de novo was also seen — nine cases potentially prevented — and that is also really interesting. It would be amazing if we could completely avoid that life-threatening complication.”
MMF can cause miscarriage and boost the risk for birth defects, and the manufacturer says it can lower the effectiveness of birth control pills. It can also boost the risk for some cancers such as lymphoma and increase the risk for infections.
Surprisingly, the number of adverse events in the control and intervention groups were similar (35.4% vs 46.2%, respectively; RR, 1.30; 95% CI, 0.86-1.99; P = .20). They included infection (30.8% vs 33.8%, respectively; P = .70) and gastrointestinal tract events (16.9% for both; P > .99).
“There were overall pretty similar rates of side effects, but maybe this was because MMF dose was pretty low in the treated group, or the glucocorticoid dose was not so low in both groups,” Dr. Costenbader said. She also noted that “the risk of malignancy with MMF is longer term than this study. It may not show up for 5-10 or even more years, but we know it exists. Infections are also increased with MMF — some of which can be avoided with vaccines for COVID, pneumonia, influenza, shingles, etc. MMF also causes gastrointestinal intolerance, and people often are not able to take it because of nausea, vomiting, diarrhea, and elevated liver function tests.”
Dr. James said the infection rates “may be due to the higher doses of steroids patients in both groups are on for several months at the beginning of the study.”
A total of 12 patients in the MMF group discontinued the intervention for various reasons, and 6 were lost to follow-up. In the control group, 20 discontinued the intervention and two were lost to follow-up. However, all 130 patients in the trial were included in the primary and secondary outcome analyses.
Should clinicians consider prescribing MMF to patients with new-onset SLE? “We usually wait until later when there are indications of more severe disease, but here they started it from the time of diagnosis if the patient was anti-dsDNA positive. Given insurance restrictions in this country, we would be unlikely to be able to do that for many patients,” Dr. Costenbader said. “They likely also overtreated a lot of patients who didn’t need it. Due to our lack of more specific biomarkers and precision medicine for lupus, we do currently undertreat a lot of patients, as this study highlights, as well as overtreat others.”
How Much Might Cost Factor Into Treatment Decisions?
The study did not examine cost. Prednisone and hydroxychloroquine sulfate are inexpensive, but Dr. James said MMF can cost about $450 a month at the study dosage. However, “the average hospitalization without an ICU [intensive care unit] visit for an SLE patient is about $15,000-$20,000. If you can avoid one hospitalization, you can pay for nearly 4 years of MMF. More importantly, from a financial perspective, if you can convert a severe lupus patient to a mild/moderate lupus patient, then the annual costs of lupus decrease nearly by half, from about $52,000 per year to $25,000 per year.”
The study authors noted various limitations such as the small number of subjects, the need for a longer trial “to determine the advantages and disadvantages of early application of MMF,” and the fact that all subjects were Asian. The authors also called for confirmation via a double-blind, placebo-controlled study.
The study was funded by grants to the authors by the National Natural Science Foundation of China, Shanghai Rising-Star Program, Natural Science Foundation of Shanghai, Five-Year National Key R&D Program, and Ruijin–Zhongmei Huadong Lupus Funding. The authors had no disclosures. Dr. Costenbader disclosed consulting/research collaboration relationships with AstraZeneca, Amgen, Biogen, Bristol-Myers Squibb, GSK, Merck, Gilead, and Cabaletta. Dr. James and Dr. Wallace had no disclosures.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Transgender Women and Prostate Cancer: It’s Complicated
The Veterans Health Administration (VHA) provides care for about 10,000 transgender women, and clinicians must understand their distinctive needs for prostate cancer screening, a urologist told cancer specialists during a presentation at the 2024 annual meeting of the Association of VA Hematology/Oncology in Atlanta.
Even if they’ve undergone gender reassignment surgery, “all transgender women still have a prostate, so therefore they remain at risk of prostate cancer and could still be considered for prostate cancer screening,” said Farnoosh Nik-Ahd, MD, a resident physician at the University of California San Francisco. However, “clinicians and patients may not be aware of prostate cancer risk, so that they may not think [of screening] transgender women.”
Nik-Ahd also noted another complication: The results of prostate screening tests may be misleading in this population.
Transgender women were born biologically male but now identify as female. These individuals may have undergone gender reassignment surgery to remove male genitalia, but the procedures do not remove the prostate. They also might be taking estrogen therapy. “Prostate cancer is a hormonally driven cancer, and the exact impact of gender-affirming hormones on prostate cancer risk and development is unknown,” Nik-Ahd said.
In a 2023 study in JAMA, Nik-Ahd and colleagues identified 155 cases of prostate cancer in transgender women within the VHA (about 14 cases per year) from 2000 to 2022. Of these patients, 116 had never used estrogen, while 17 had used it previously and 22 used it at diagnosis.
The median age of patients was 61 years, 88% identified as White, and the median prostate-specific antigen (PSA) was 6.8 ng/mL. “Given estimates of 10,000 transgender women in the US Department of Veterans Affairs, 33 cases per year would be expected. Instead, only about 14 per year were observed,” the researchers wrote. “Lower rates may stem from less PSA screening owing to barriers including lack of prostate cancer risk awareness or stigma, the suppressive effects of estrogen on prostate cancer development, or prostate cancers being missed in transgender women because of misinterpretation of ‘normal’ PSA levels among those receiving gender-affirming hormone therapies.”
In the presentation, Nik-Ahd said, “PSA density, which is a marker of prostate cancer aggressiveness, was highest in transgender women who were actively on estrogen.”
She noted, “the existing thyrotropin reference ranges, which is what we use to interpret PSA values, are all based on data from cisgender men.” The ranges would be expected to be far lower in transgender women who are taking estrogen, potentially throwing off screening tests, she said, and “ultimately missing clinically significant prostate cancer.”
In the larger picture, there are no specific guidelines about PSA screening in transgender women, she said.
A recent study published in JAMA by Nik-Ahd and colleagues examined PSA levels in 210 transgender women (mean age 60 years) treated within the VHA from 2000 to 2023. All were aged 40 to 80 years, had received estrogen for at least 6 months (mean duration 4.7 years), and didn’t have prostate cancer diagnoses.
“Median (IQR) PSA was 0.02 (0-0.2) ng/mL and the 95th percentile value was 0.6 ng/mL,” the report found. “PSAs were undetectable in 36% of patients (23% and 49% of PSAs in patients without and with orchiectomy, respectively).”
The researchers write that “the historic cut point of 4 ng/mL, often used as a threshold for further evaluation, is likely far too high a threshold for this population.”
Nik-Ahd noted, “clinicians should interpret PSA values in transgender women on estrogen with extreme caution. In this population, normal might actually not be normal, and a value that is considered normal might be very abnormal for somebody who is on estrogen. If you're unsure of whether a PSA value is appropriate for a transgender woman on estrogen, refer that patient to a urologist so they can undergo further evaluation.”
Farnoosh Nik-Ahd discloses consulting for Janssen.
The Veterans Health Administration (VHA) provides care for about 10,000 transgender women, and clinicians must understand their distinctive needs for prostate cancer screening, a urologist told cancer specialists during a presentation at the 2024 annual meeting of the Association of VA Hematology/Oncology in Atlanta.
Even if they’ve undergone gender reassignment surgery, “all transgender women still have a prostate, so therefore they remain at risk of prostate cancer and could still be considered for prostate cancer screening,” said Farnoosh Nik-Ahd, MD, a resident physician at the University of California San Francisco. However, “clinicians and patients may not be aware of prostate cancer risk, so that they may not think [of screening] transgender women.”
Nik-Ahd also noted another complication: The results of prostate screening tests may be misleading in this population.
Transgender women were born biologically male but now identify as female. These individuals may have undergone gender reassignment surgery to remove male genitalia, but the procedures do not remove the prostate. They also might be taking estrogen therapy. “Prostate cancer is a hormonally driven cancer, and the exact impact of gender-affirming hormones on prostate cancer risk and development is unknown,” Nik-Ahd said.
In a 2023 study in JAMA, Nik-Ahd and colleagues identified 155 cases of prostate cancer in transgender women within the VHA (about 14 cases per year) from 2000 to 2022. Of these patients, 116 had never used estrogen, while 17 had used it previously and 22 used it at diagnosis.
The median age of patients was 61 years, 88% identified as White, and the median prostate-specific antigen (PSA) was 6.8 ng/mL. “Given estimates of 10,000 transgender women in the US Department of Veterans Affairs, 33 cases per year would be expected. Instead, only about 14 per year were observed,” the researchers wrote. “Lower rates may stem from less PSA screening owing to barriers including lack of prostate cancer risk awareness or stigma, the suppressive effects of estrogen on prostate cancer development, or prostate cancers being missed in transgender women because of misinterpretation of ‘normal’ PSA levels among those receiving gender-affirming hormone therapies.”
In the presentation, Nik-Ahd said, “PSA density, which is a marker of prostate cancer aggressiveness, was highest in transgender women who were actively on estrogen.”
She noted, “the existing thyrotropin reference ranges, which is what we use to interpret PSA values, are all based on data from cisgender men.” The ranges would be expected to be far lower in transgender women who are taking estrogen, potentially throwing off screening tests, she said, and “ultimately missing clinically significant prostate cancer.”
In the larger picture, there are no specific guidelines about PSA screening in transgender women, she said.
A recent study published in JAMA by Nik-Ahd and colleagues examined PSA levels in 210 transgender women (mean age 60 years) treated within the VHA from 2000 to 2023. All were aged 40 to 80 years, had received estrogen for at least 6 months (mean duration 4.7 years), and didn’t have prostate cancer diagnoses.
“Median (IQR) PSA was 0.02 (0-0.2) ng/mL and the 95th percentile value was 0.6 ng/mL,” the report found. “PSAs were undetectable in 36% of patients (23% and 49% of PSAs in patients without and with orchiectomy, respectively).”
The researchers write that “the historic cut point of 4 ng/mL, often used as a threshold for further evaluation, is likely far too high a threshold for this population.”
Nik-Ahd noted, “clinicians should interpret PSA values in transgender women on estrogen with extreme caution. In this population, normal might actually not be normal, and a value that is considered normal might be very abnormal for somebody who is on estrogen. If you're unsure of whether a PSA value is appropriate for a transgender woman on estrogen, refer that patient to a urologist so they can undergo further evaluation.”
Farnoosh Nik-Ahd discloses consulting for Janssen.
The Veterans Health Administration (VHA) provides care for about 10,000 transgender women, and clinicians must understand their distinctive needs for prostate cancer screening, a urologist told cancer specialists during a presentation at the 2024 annual meeting of the Association of VA Hematology/Oncology in Atlanta.
Even if they’ve undergone gender reassignment surgery, “all transgender women still have a prostate, so therefore they remain at risk of prostate cancer and could still be considered for prostate cancer screening,” said Farnoosh Nik-Ahd, MD, a resident physician at the University of California San Francisco. However, “clinicians and patients may not be aware of prostate cancer risk, so that they may not think [of screening] transgender women.”
Nik-Ahd also noted another complication: The results of prostate screening tests may be misleading in this population.
Transgender women were born biologically male but now identify as female. These individuals may have undergone gender reassignment surgery to remove male genitalia, but the procedures do not remove the prostate. They also might be taking estrogen therapy. “Prostate cancer is a hormonally driven cancer, and the exact impact of gender-affirming hormones on prostate cancer risk and development is unknown,” Nik-Ahd said.
In a 2023 study in JAMA, Nik-Ahd and colleagues identified 155 cases of prostate cancer in transgender women within the VHA (about 14 cases per year) from 2000 to 2022. Of these patients, 116 had never used estrogen, while 17 had used it previously and 22 used it at diagnosis.
The median age of patients was 61 years, 88% identified as White, and the median prostate-specific antigen (PSA) was 6.8 ng/mL. “Given estimates of 10,000 transgender women in the US Department of Veterans Affairs, 33 cases per year would be expected. Instead, only about 14 per year were observed,” the researchers wrote. “Lower rates may stem from less PSA screening owing to barriers including lack of prostate cancer risk awareness or stigma, the suppressive effects of estrogen on prostate cancer development, or prostate cancers being missed in transgender women because of misinterpretation of ‘normal’ PSA levels among those receiving gender-affirming hormone therapies.”
In the presentation, Nik-Ahd said, “PSA density, which is a marker of prostate cancer aggressiveness, was highest in transgender women who were actively on estrogen.”
She noted, “the existing thyrotropin reference ranges, which is what we use to interpret PSA values, are all based on data from cisgender men.” The ranges would be expected to be far lower in transgender women who are taking estrogen, potentially throwing off screening tests, she said, and “ultimately missing clinically significant prostate cancer.”
In the larger picture, there are no specific guidelines about PSA screening in transgender women, she said.
A recent study published in JAMA by Nik-Ahd and colleagues examined PSA levels in 210 transgender women (mean age 60 years) treated within the VHA from 2000 to 2023. All were aged 40 to 80 years, had received estrogen for at least 6 months (mean duration 4.7 years), and didn’t have prostate cancer diagnoses.
“Median (IQR) PSA was 0.02 (0-0.2) ng/mL and the 95th percentile value was 0.6 ng/mL,” the report found. “PSAs were undetectable in 36% of patients (23% and 49% of PSAs in patients without and with orchiectomy, respectively).”
The researchers write that “the historic cut point of 4 ng/mL, often used as a threshold for further evaluation, is likely far too high a threshold for this population.”
Nik-Ahd noted, “clinicians should interpret PSA values in transgender women on estrogen with extreme caution. In this population, normal might actually not be normal, and a value that is considered normal might be very abnormal for somebody who is on estrogen. If you're unsure of whether a PSA value is appropriate for a transgender woman on estrogen, refer that patient to a urologist so they can undergo further evaluation.”
Farnoosh Nik-Ahd discloses consulting for Janssen.
No Matched Sibling Donor? Sickle Cell Experts Debate Next-Best Option
“If there is an indication for intervention, for a curative therapy, in the absence of a matched sibling donor, gene therapy is the first choice,” Jaap-Jan Boelens, MD, PhD, of Memorial Sloan Kettering Cancer Center, New York City, argued in a presentation at the annual meeting of the Society of Hematologic Oncology (SOHO) in Houston.
“In the registries, alternative transplant outcomes are pretty poor, although there is some encouraging data coming up. The time is not there yet when this is the [best] choice.”
But Adetola Kassim, MBBS, of Vanderbilt University Medical Center in Nashville, Tennessee, said patients with sickle cell disease (SCD) who don’t qualify for a matched sibling donor transplant can still have good transplant options. And the results can be impressive.
“Once you’re engrafted, and you don’t lose your graft, the effect in transplant is lifelong,” he said. When it comes to long-lasting effects, he added, “we’re not sure yet about gene therapy.”
As Dr. Kassim noted, SCD continues to take a huge toll.
“Median survival for patients with sickle cell anemia remains stuck in the fifth decade of life with no change in 25 years,” he said. Heart, lung, and kidney complications account for 50% of identifiable causes of death, followed by about 26% attributed to cardiovascular disease, he said. “The question here is about which therapy can impact the most debilitating complication in children, which is stroke, and improve survival in adults with progressive organ dysfunction.”
Dr. Boelens said there are “huge barriers” to stem cell transplant in SCD because only 15% of patients eligible for the treatment have a matched related donor, and only 10% have a matched related or unrelated donor.
“There’s also a lack of financial and psychosocial support in many of the families. There is also parental refusal because of the mortality risk, and there’s also physician refusal because hematologists aren’t always in the same hospitals as the transplant programs.”
Dr. Boelens highlighted a 2019 study of data from 2008-2017 that found outcomes in unmatched donor transplantations are “not great,” with higher risk for mortality and graft failure.
As an alternative, he said, two gene therapies, both gene “additions,” are now approved by the US Food and Drug Administration (FDA). They are exagamglogene autotemcel (exa-cel, Casgevy) and betibeglogene autotemcel (LentiGlobin, Zynteglo). There’s also a gene “correction” option in the works, but it’s not yet ready for prime time, he said.
In the two approved gene therapy treatments, stem cells are removed from the patient, modified/manufactured in an outside facility, and then engrafted.
The advantages of gene therapy include no need to find a donor or worry about graft resistance, and there’s no need for immunosuppression, he said. However, the process takes a long time, there’s limited long-term data, and there’s a risk for loss of fertility and other chemotherapy-related adverse effects.
For his part, Dr. Kassim noted how several groups are excluded from the strong outcomes in matched sibling donor stem-cell transplants: Children with strokes and no eligible donors, others without eligible donors, and adults with severe disease and organ dysfunction who are typically excluded.
“We need transplants with less toxicity and alternative donors,” he said. Another challenge: “How do we decrease graft failure without increasing transplant-related mortality?”
Researchers are exploring several strategies to adjust drug therapy during conditioning, Dr. Kassim said, and he led a promising phase II study that explored one approach. The results of that study were recently published in the journal Blood. Graft failures were very low in both adults and children, he said, and 2-year survival among 70 patients was 94.8%. The five deaths were related to infection.
The evidence about the various strategies shows that “virtually all SCD patients, except those with severe heart, lung, or kidney disease” can benefit from a curative transplant, Dr. Kassim said.
Dr. Boelens had no disclosures. Disclosures for Dr. Kassim were not provided, but he recently reported no disclosures in a report about transplants in SCD.
A version of this article appeared on Medscape.com.
“If there is an indication for intervention, for a curative therapy, in the absence of a matched sibling donor, gene therapy is the first choice,” Jaap-Jan Boelens, MD, PhD, of Memorial Sloan Kettering Cancer Center, New York City, argued in a presentation at the annual meeting of the Society of Hematologic Oncology (SOHO) in Houston.
“In the registries, alternative transplant outcomes are pretty poor, although there is some encouraging data coming up. The time is not there yet when this is the [best] choice.”
But Adetola Kassim, MBBS, of Vanderbilt University Medical Center in Nashville, Tennessee, said patients with sickle cell disease (SCD) who don’t qualify for a matched sibling donor transplant can still have good transplant options. And the results can be impressive.
“Once you’re engrafted, and you don’t lose your graft, the effect in transplant is lifelong,” he said. When it comes to long-lasting effects, he added, “we’re not sure yet about gene therapy.”
As Dr. Kassim noted, SCD continues to take a huge toll.
“Median survival for patients with sickle cell anemia remains stuck in the fifth decade of life with no change in 25 years,” he said. Heart, lung, and kidney complications account for 50% of identifiable causes of death, followed by about 26% attributed to cardiovascular disease, he said. “The question here is about which therapy can impact the most debilitating complication in children, which is stroke, and improve survival in adults with progressive organ dysfunction.”
Dr. Boelens said there are “huge barriers” to stem cell transplant in SCD because only 15% of patients eligible for the treatment have a matched related donor, and only 10% have a matched related or unrelated donor.
“There’s also a lack of financial and psychosocial support in many of the families. There is also parental refusal because of the mortality risk, and there’s also physician refusal because hematologists aren’t always in the same hospitals as the transplant programs.”
Dr. Boelens highlighted a 2019 study of data from 2008-2017 that found outcomes in unmatched donor transplantations are “not great,” with higher risk for mortality and graft failure.
As an alternative, he said, two gene therapies, both gene “additions,” are now approved by the US Food and Drug Administration (FDA). They are exagamglogene autotemcel (exa-cel, Casgevy) and betibeglogene autotemcel (LentiGlobin, Zynteglo). There’s also a gene “correction” option in the works, but it’s not yet ready for prime time, he said.
In the two approved gene therapy treatments, stem cells are removed from the patient, modified/manufactured in an outside facility, and then engrafted.
The advantages of gene therapy include no need to find a donor or worry about graft resistance, and there’s no need for immunosuppression, he said. However, the process takes a long time, there’s limited long-term data, and there’s a risk for loss of fertility and other chemotherapy-related adverse effects.
For his part, Dr. Kassim noted how several groups are excluded from the strong outcomes in matched sibling donor stem-cell transplants: Children with strokes and no eligible donors, others without eligible donors, and adults with severe disease and organ dysfunction who are typically excluded.
“We need transplants with less toxicity and alternative donors,” he said. Another challenge: “How do we decrease graft failure without increasing transplant-related mortality?”
Researchers are exploring several strategies to adjust drug therapy during conditioning, Dr. Kassim said, and he led a promising phase II study that explored one approach. The results of that study were recently published in the journal Blood. Graft failures were very low in both adults and children, he said, and 2-year survival among 70 patients was 94.8%. The five deaths were related to infection.
The evidence about the various strategies shows that “virtually all SCD patients, except those with severe heart, lung, or kidney disease” can benefit from a curative transplant, Dr. Kassim said.
Dr. Boelens had no disclosures. Disclosures for Dr. Kassim were not provided, but he recently reported no disclosures in a report about transplants in SCD.
A version of this article appeared on Medscape.com.
“If there is an indication for intervention, for a curative therapy, in the absence of a matched sibling donor, gene therapy is the first choice,” Jaap-Jan Boelens, MD, PhD, of Memorial Sloan Kettering Cancer Center, New York City, argued in a presentation at the annual meeting of the Society of Hematologic Oncology (SOHO) in Houston.
“In the registries, alternative transplant outcomes are pretty poor, although there is some encouraging data coming up. The time is not there yet when this is the [best] choice.”
But Adetola Kassim, MBBS, of Vanderbilt University Medical Center in Nashville, Tennessee, said patients with sickle cell disease (SCD) who don’t qualify for a matched sibling donor transplant can still have good transplant options. And the results can be impressive.
“Once you’re engrafted, and you don’t lose your graft, the effect in transplant is lifelong,” he said. When it comes to long-lasting effects, he added, “we’re not sure yet about gene therapy.”
As Dr. Kassim noted, SCD continues to take a huge toll.
“Median survival for patients with sickle cell anemia remains stuck in the fifth decade of life with no change in 25 years,” he said. Heart, lung, and kidney complications account for 50% of identifiable causes of death, followed by about 26% attributed to cardiovascular disease, he said. “The question here is about which therapy can impact the most debilitating complication in children, which is stroke, and improve survival in adults with progressive organ dysfunction.”
Dr. Boelens said there are “huge barriers” to stem cell transplant in SCD because only 15% of patients eligible for the treatment have a matched related donor, and only 10% have a matched related or unrelated donor.
“There’s also a lack of financial and psychosocial support in many of the families. There is also parental refusal because of the mortality risk, and there’s also physician refusal because hematologists aren’t always in the same hospitals as the transplant programs.”
Dr. Boelens highlighted a 2019 study of data from 2008-2017 that found outcomes in unmatched donor transplantations are “not great,” with higher risk for mortality and graft failure.
As an alternative, he said, two gene therapies, both gene “additions,” are now approved by the US Food and Drug Administration (FDA). They are exagamglogene autotemcel (exa-cel, Casgevy) and betibeglogene autotemcel (LentiGlobin, Zynteglo). There’s also a gene “correction” option in the works, but it’s not yet ready for prime time, he said.
In the two approved gene therapy treatments, stem cells are removed from the patient, modified/manufactured in an outside facility, and then engrafted.
The advantages of gene therapy include no need to find a donor or worry about graft resistance, and there’s no need for immunosuppression, he said. However, the process takes a long time, there’s limited long-term data, and there’s a risk for loss of fertility and other chemotherapy-related adverse effects.
For his part, Dr. Kassim noted how several groups are excluded from the strong outcomes in matched sibling donor stem-cell transplants: Children with strokes and no eligible donors, others without eligible donors, and adults with severe disease and organ dysfunction who are typically excluded.
“We need transplants with less toxicity and alternative donors,” he said. Another challenge: “How do we decrease graft failure without increasing transplant-related mortality?”
Researchers are exploring several strategies to adjust drug therapy during conditioning, Dr. Kassim said, and he led a promising phase II study that explored one approach. The results of that study were recently published in the journal Blood. Graft failures were very low in both adults and children, he said, and 2-year survival among 70 patients was 94.8%. The five deaths were related to infection.
The evidence about the various strategies shows that “virtually all SCD patients, except those with severe heart, lung, or kidney disease” can benefit from a curative transplant, Dr. Kassim said.
Dr. Boelens had no disclosures. Disclosures for Dr. Kassim were not provided, but he recently reported no disclosures in a report about transplants in SCD.
A version of this article appeared on Medscape.com.
FROM SOHO 2024
Treatment Options in MCL: What Are the Best Practices?
In the frontline setting, findings suggest that regimens should differ significantly on the basis of whether patients are older or younger, whereas more data are needed to understand whether treatment can overcome poor prognoses in patients with TP53 mutations, lymphoma specialist Nina Wagner-Johnston, MD, of Johns Hopkins University School of Medicine, Baltimore, said in a presentation at the annual meeting of the Society of Hematologic Oncology (SOHO) 2024 in Houston, Texas.
On the relapsed/refractory front, patients need better options after treatment with Bruton tyrosine kinase inhibitors or chimeric antigen receptor (CAR) T-cell therapy, Krish Patel, MD, a lymphoma specialist with Swedish Cancer Institute in Seattle, said in an adjoining presentation. Fortunately, he said, some treatments are showing early promise.
Here’s a closer look at the presentations by Dr. Wagner-Johnston and Dr. Patel.
Frontline MCL: Age Helps Determine Best Approach
“For older and less fit patients, the standard approach has typically been bendamustine (Bendeka, Treanda) and rituximab (Rituxan), and the median progression-free survival is about 4 years, with overall survival not reached at a median 5 years of follow-up,” Dr. Wagner-Johnston said.
Low doses of the chemotherapy drug cytarabine have been added to the bendamustine-rituximab regimen, with encouraging results, she said. “Certainly there’s more toxicity associated even with lower doses, but those data look fairly promising.”
For younger and fit patients, “the standard of care approach has been to administer intensive chemoimmunotherapy that contains high-dose cytarabine, and then that’s typically followed with an autologous stem cell transplant,” she said. A 2016 study reported median progression-free survival of 8.5 years and median overall survival of 12.7 years.
Now, second-generation Bruton tyrosine kinase inhibitors “look very promising” in the frontline setting, Dr. Wagner-Johnston said.
The road has been rocky, however. The SHINE trial of more than 500 patients aged over 65 found that adding ibrutinib to bendamustine-rituximab improved progression-free survival. “However, progression-free survival did not [connect] to an overall survival benefit, and that’s likely due to the toxicity seen with ibrutinib,” she said.
“It’s not surprising to many of you that ibrutinib has been removed from the FDA label for mantle cell lymphoma,” she said. However, “second-generation [Bruton tyrosine kinase inhibitors] are known to be associated with less toxicity and potentially increased potency.”
What about Bruton tyrosine kinase inhibitors in younger and fitter patients? The TRIANGLE trial demonstrated their benefit, Dr. Wagner-Johnston said, linking ibrutinib to improvement in progression-free survival.
However, “it’s really too early to evaluate the statistical significance for overall survival.” And while the study looks at therapy without stem cell transplant, she believes it’s too early to know whether that’s a good option.
Dr. Wagner-Johnston tackled another topic: Can Bruton tyrosine kinase inhibitors overcome the poor prognosis seen with MCL with TP53 mutation? For now, the limitations of research makes it “hard to know,” she said, although early results of the BOVen trial are promising.
Relapsed/Refractory MCL: Better Options Are Still Needed
In his presentation, Dr. Patel spoke about therapy in patients with MCL and relapsed/refractory disease. “We know that outcomes for patients who progress on covalent [Bruton tyrosine kinase inhibitors] is really dismal,” he said. “This has been shown by multiple groups now across the globe.”
Noncovalent Bruton tyrosine kinase inhibitors are now an option, he noted. “We do understand that they work for some patients, and it can be quite useful, but even noncovalent [Bruton tyrosine kinase inhibitors] themselves are susceptible to resistance mutations. We’ve seen that in the [chronic lymphocytic leukemia] world.”
Dr. Patel asked the audience, “Why not just give everybody CAR T-cells, post-[Bruton tyrosine kinase inhibitors]? You get a CAR T-cell! You get a CAR T-cell! Everybody gets one.”
However, he noted, “Unfortunately, mantle cell lymphoma patients experience the worst high-grade toxicity when receiving CD19[-targeted] CAR T-cells.”
Are there better options? At the moment, “really, really early data” suggest benefits from molecular glues and degraders, novel inhibitors, antibody-drug conjugates, novel CAR T-cells, and bispecific antibodies, Dr. Patel said.
“All of these tools are in clinical trials, and hopefully some of them will help,” he said.
Disclosures were not provided. Dr. Wagner-Johnston recently disclosed advisory committee/board of directors’ relationships with ADC Therapeutics, Regeneron, Calibr, and Verastem. Dr. Patel recently disclosed ties with a long list of pharmaceutical companies, including AbbVie, AstraZeneca, BeiGene, Bristol Myers Squibb, Genentech, Janssen, Merck, and others.
A version of this article first appeared on Medscape.com.
In the frontline setting, findings suggest that regimens should differ significantly on the basis of whether patients are older or younger, whereas more data are needed to understand whether treatment can overcome poor prognoses in patients with TP53 mutations, lymphoma specialist Nina Wagner-Johnston, MD, of Johns Hopkins University School of Medicine, Baltimore, said in a presentation at the annual meeting of the Society of Hematologic Oncology (SOHO) 2024 in Houston, Texas.
On the relapsed/refractory front, patients need better options after treatment with Bruton tyrosine kinase inhibitors or chimeric antigen receptor (CAR) T-cell therapy, Krish Patel, MD, a lymphoma specialist with Swedish Cancer Institute in Seattle, said in an adjoining presentation. Fortunately, he said, some treatments are showing early promise.
Here’s a closer look at the presentations by Dr. Wagner-Johnston and Dr. Patel.
Frontline MCL: Age Helps Determine Best Approach
“For older and less fit patients, the standard approach has typically been bendamustine (Bendeka, Treanda) and rituximab (Rituxan), and the median progression-free survival is about 4 years, with overall survival not reached at a median 5 years of follow-up,” Dr. Wagner-Johnston said.
Low doses of the chemotherapy drug cytarabine have been added to the bendamustine-rituximab regimen, with encouraging results, she said. “Certainly there’s more toxicity associated even with lower doses, but those data look fairly promising.”
For younger and fit patients, “the standard of care approach has been to administer intensive chemoimmunotherapy that contains high-dose cytarabine, and then that’s typically followed with an autologous stem cell transplant,” she said. A 2016 study reported median progression-free survival of 8.5 years and median overall survival of 12.7 years.
Now, second-generation Bruton tyrosine kinase inhibitors “look very promising” in the frontline setting, Dr. Wagner-Johnston said.
The road has been rocky, however. The SHINE trial of more than 500 patients aged over 65 found that adding ibrutinib to bendamustine-rituximab improved progression-free survival. “However, progression-free survival did not [connect] to an overall survival benefit, and that’s likely due to the toxicity seen with ibrutinib,” she said.
“It’s not surprising to many of you that ibrutinib has been removed from the FDA label for mantle cell lymphoma,” she said. However, “second-generation [Bruton tyrosine kinase inhibitors] are known to be associated with less toxicity and potentially increased potency.”
What about Bruton tyrosine kinase inhibitors in younger and fitter patients? The TRIANGLE trial demonstrated their benefit, Dr. Wagner-Johnston said, linking ibrutinib to improvement in progression-free survival.
However, “it’s really too early to evaluate the statistical significance for overall survival.” And while the study looks at therapy without stem cell transplant, she believes it’s too early to know whether that’s a good option.
Dr. Wagner-Johnston tackled another topic: Can Bruton tyrosine kinase inhibitors overcome the poor prognosis seen with MCL with TP53 mutation? For now, the limitations of research makes it “hard to know,” she said, although early results of the BOVen trial are promising.
Relapsed/Refractory MCL: Better Options Are Still Needed
In his presentation, Dr. Patel spoke about therapy in patients with MCL and relapsed/refractory disease. “We know that outcomes for patients who progress on covalent [Bruton tyrosine kinase inhibitors] is really dismal,” he said. “This has been shown by multiple groups now across the globe.”
Noncovalent Bruton tyrosine kinase inhibitors are now an option, he noted. “We do understand that they work for some patients, and it can be quite useful, but even noncovalent [Bruton tyrosine kinase inhibitors] themselves are susceptible to resistance mutations. We’ve seen that in the [chronic lymphocytic leukemia] world.”
Dr. Patel asked the audience, “Why not just give everybody CAR T-cells, post-[Bruton tyrosine kinase inhibitors]? You get a CAR T-cell! You get a CAR T-cell! Everybody gets one.”
However, he noted, “Unfortunately, mantle cell lymphoma patients experience the worst high-grade toxicity when receiving CD19[-targeted] CAR T-cells.”
Are there better options? At the moment, “really, really early data” suggest benefits from molecular glues and degraders, novel inhibitors, antibody-drug conjugates, novel CAR T-cells, and bispecific antibodies, Dr. Patel said.
“All of these tools are in clinical trials, and hopefully some of them will help,” he said.
Disclosures were not provided. Dr. Wagner-Johnston recently disclosed advisory committee/board of directors’ relationships with ADC Therapeutics, Regeneron, Calibr, and Verastem. Dr. Patel recently disclosed ties with a long list of pharmaceutical companies, including AbbVie, AstraZeneca, BeiGene, Bristol Myers Squibb, Genentech, Janssen, Merck, and others.
A version of this article first appeared on Medscape.com.
In the frontline setting, findings suggest that regimens should differ significantly on the basis of whether patients are older or younger, whereas more data are needed to understand whether treatment can overcome poor prognoses in patients with TP53 mutations, lymphoma specialist Nina Wagner-Johnston, MD, of Johns Hopkins University School of Medicine, Baltimore, said in a presentation at the annual meeting of the Society of Hematologic Oncology (SOHO) 2024 in Houston, Texas.
On the relapsed/refractory front, patients need better options after treatment with Bruton tyrosine kinase inhibitors or chimeric antigen receptor (CAR) T-cell therapy, Krish Patel, MD, a lymphoma specialist with Swedish Cancer Institute in Seattle, said in an adjoining presentation. Fortunately, he said, some treatments are showing early promise.
Here’s a closer look at the presentations by Dr. Wagner-Johnston and Dr. Patel.
Frontline MCL: Age Helps Determine Best Approach
“For older and less fit patients, the standard approach has typically been bendamustine (Bendeka, Treanda) and rituximab (Rituxan), and the median progression-free survival is about 4 years, with overall survival not reached at a median 5 years of follow-up,” Dr. Wagner-Johnston said.
Low doses of the chemotherapy drug cytarabine have been added to the bendamustine-rituximab regimen, with encouraging results, she said. “Certainly there’s more toxicity associated even with lower doses, but those data look fairly promising.”
For younger and fit patients, “the standard of care approach has been to administer intensive chemoimmunotherapy that contains high-dose cytarabine, and then that’s typically followed with an autologous stem cell transplant,” she said. A 2016 study reported median progression-free survival of 8.5 years and median overall survival of 12.7 years.
Now, second-generation Bruton tyrosine kinase inhibitors “look very promising” in the frontline setting, Dr. Wagner-Johnston said.
The road has been rocky, however. The SHINE trial of more than 500 patients aged over 65 found that adding ibrutinib to bendamustine-rituximab improved progression-free survival. “However, progression-free survival did not [connect] to an overall survival benefit, and that’s likely due to the toxicity seen with ibrutinib,” she said.
“It’s not surprising to many of you that ibrutinib has been removed from the FDA label for mantle cell lymphoma,” she said. However, “second-generation [Bruton tyrosine kinase inhibitors] are known to be associated with less toxicity and potentially increased potency.”
What about Bruton tyrosine kinase inhibitors in younger and fitter patients? The TRIANGLE trial demonstrated their benefit, Dr. Wagner-Johnston said, linking ibrutinib to improvement in progression-free survival.
However, “it’s really too early to evaluate the statistical significance for overall survival.” And while the study looks at therapy without stem cell transplant, she believes it’s too early to know whether that’s a good option.
Dr. Wagner-Johnston tackled another topic: Can Bruton tyrosine kinase inhibitors overcome the poor prognosis seen with MCL with TP53 mutation? For now, the limitations of research makes it “hard to know,” she said, although early results of the BOVen trial are promising.
Relapsed/Refractory MCL: Better Options Are Still Needed
In his presentation, Dr. Patel spoke about therapy in patients with MCL and relapsed/refractory disease. “We know that outcomes for patients who progress on covalent [Bruton tyrosine kinase inhibitors] is really dismal,” he said. “This has been shown by multiple groups now across the globe.”
Noncovalent Bruton tyrosine kinase inhibitors are now an option, he noted. “We do understand that they work for some patients, and it can be quite useful, but even noncovalent [Bruton tyrosine kinase inhibitors] themselves are susceptible to resistance mutations. We’ve seen that in the [chronic lymphocytic leukemia] world.”
Dr. Patel asked the audience, “Why not just give everybody CAR T-cells, post-[Bruton tyrosine kinase inhibitors]? You get a CAR T-cell! You get a CAR T-cell! Everybody gets one.”
However, he noted, “Unfortunately, mantle cell lymphoma patients experience the worst high-grade toxicity when receiving CD19[-targeted] CAR T-cells.”
Are there better options? At the moment, “really, really early data” suggest benefits from molecular glues and degraders, novel inhibitors, antibody-drug conjugates, novel CAR T-cells, and bispecific antibodies, Dr. Patel said.
“All of these tools are in clinical trials, and hopefully some of them will help,” he said.
Disclosures were not provided. Dr. Wagner-Johnston recently disclosed advisory committee/board of directors’ relationships with ADC Therapeutics, Regeneron, Calibr, and Verastem. Dr. Patel recently disclosed ties with a long list of pharmaceutical companies, including AbbVie, AstraZeneca, BeiGene, Bristol Myers Squibb, Genentech, Janssen, Merck, and others.
A version of this article first appeared on Medscape.com.
FROM SOHO 2024
Debate: Should Patients With CLL Take Breaks From Targeted Therapies?
At the annual meeting of the Society of Hematologic Oncology, two hematologist-oncologists — Inhye Ahn, MD, of Dana-Farber Cancer Institute in Boston, Massachusetts, and Kerry A. Rogers, MD, of Ohio State University in Columbus — faced off in a debate. Ahn said the drugs can indeed be discontinued, while Rogers argued against stopping the medications.
“When I talk to my own patient about standard of care options in CLL, I use the analogy of a marathon and a sprint,” Dr. Ahn said. A marathon refers to continuous treatment with Bruton’s kinase inhibitors given daily for years, while the sprint refers to the combination of venetoclax with an anti-CD20 monoclonal antibody given over 12 cycles for the frontline regimen and 2 years for refractory CLL.
“I tell them these are both considered very efficacious regimens and well tolerated, one is by IV [the venetoclax regimen] and the other isn’t [Bruton’s kinase inhibitors], and they have different toxicity profile. I ask them what would you do? The most common question that I get from my patient is, ‘why would anyone do a marathon?’ ”
It’s not solely the length of treatment that’s important, Dr. Ahn said, as toxicities from the long-term use of Bruton’s kinase inhibitors build up over time and can lead to hypertension, arrhythmia, and sudden cardiac death.
In addition, she said, infections can occur, as well as hampered vaccine response, an important risk in the era of the COVID-19 pandemic. The cost of the drugs is high and adds up over time, and continuous use can boost resistance.
Is there a way to turn the marathon of Bruton’s kinase inhibitor use into a sprint without hurting patients? The answer is yes, through temporary discontinuation, Dr. Ahn said, although she cautioned that early cessation could lead to disease flare. “We dipped into our own database of 84 CLL patients treated with ibrutinib, and our conclusion was that temporary dose interruption or dose reduction did not impact progression-free survival”
Moving forward, she said, “more research is needed to define the optimal regimen that would lead to treatment cessation, the optimal patient population, who would benefit most from the cessation strategy, treatment duration, and how we define success.” For her part, Dr. Rogers argued that the continuous use of Bruton’s kinase inhibitors is “really the most effective treatment we have in CLL.”
It’s clear that “responses deepen with continued treatment,” Dr. Rogers said, noting that remission times grow over years of treatment. She highlighted a 2022 study of patients with CLL who took ibrutinib that found complete remission or complete remission with incomplete hematologic recovery was 7% at 12 months and 34% at 7 years. When patients quit taking the drugs, “you don’t get to maximize your patient’s response to this treatment.”
Dr. Rogers also noted that the RESONATE-2 trial found that ibrutinib is linked to the longest median progression-free survival of any CLL treatment at 8.9 years. “That really struck me a very effective initial therapy.”
Indeed, “when you’re offering someone initial therapy with a Bruton’s kinase inhibitor as a continuous treatment strategy, you can tell people that they can expect a normal lifespan with this approach. That’s extremely important when you’re talking to patients about whether they might want to alter their leukemia treatment.”
Finally, she noted that discontinuation of ibrutinib was linked to shorter survival in early research. “This was the first suggestion that discontinuation is not good.”
Dr. Rogers said that discontinuing the drugs is sometimes necessary because of adverse events, but patients can “certainly switch to a more tolerable Bruton’s kinase inhibitor. With the options available today, that should be a strategy that’s considered.”
Audience members at the debate were invited to respond to a live online survey about whether Bruton’s kinase inhibitors can be discontinued. Among 49 respondents, most (52.3%) said no, 42.8% said yes, and the rest were undecided/other.
Disclosures for the speakers were not provided. Dr. Ahn disclosed consulting for BeiGene and AstraZeneca. Dr. Rogers disclosed receiving research funding from Genentech, AbbVie, Janssen, and Novartis; consulting for AstraZeneca, BeiGene, Janssen, Pharmacyclics, AbbVie, Genentech, and LOXO@Lilly; and receiving travel funding from AstraZeneca.
A version of this article appeared on Medscape.com.
At the annual meeting of the Society of Hematologic Oncology, two hematologist-oncologists — Inhye Ahn, MD, of Dana-Farber Cancer Institute in Boston, Massachusetts, and Kerry A. Rogers, MD, of Ohio State University in Columbus — faced off in a debate. Ahn said the drugs can indeed be discontinued, while Rogers argued against stopping the medications.
“When I talk to my own patient about standard of care options in CLL, I use the analogy of a marathon and a sprint,” Dr. Ahn said. A marathon refers to continuous treatment with Bruton’s kinase inhibitors given daily for years, while the sprint refers to the combination of venetoclax with an anti-CD20 monoclonal antibody given over 12 cycles for the frontline regimen and 2 years for refractory CLL.
“I tell them these are both considered very efficacious regimens and well tolerated, one is by IV [the venetoclax regimen] and the other isn’t [Bruton’s kinase inhibitors], and they have different toxicity profile. I ask them what would you do? The most common question that I get from my patient is, ‘why would anyone do a marathon?’ ”
It’s not solely the length of treatment that’s important, Dr. Ahn said, as toxicities from the long-term use of Bruton’s kinase inhibitors build up over time and can lead to hypertension, arrhythmia, and sudden cardiac death.
In addition, she said, infections can occur, as well as hampered vaccine response, an important risk in the era of the COVID-19 pandemic. The cost of the drugs is high and adds up over time, and continuous use can boost resistance.
Is there a way to turn the marathon of Bruton’s kinase inhibitor use into a sprint without hurting patients? The answer is yes, through temporary discontinuation, Dr. Ahn said, although she cautioned that early cessation could lead to disease flare. “We dipped into our own database of 84 CLL patients treated with ibrutinib, and our conclusion was that temporary dose interruption or dose reduction did not impact progression-free survival”
Moving forward, she said, “more research is needed to define the optimal regimen that would lead to treatment cessation, the optimal patient population, who would benefit most from the cessation strategy, treatment duration, and how we define success.” For her part, Dr. Rogers argued that the continuous use of Bruton’s kinase inhibitors is “really the most effective treatment we have in CLL.”
It’s clear that “responses deepen with continued treatment,” Dr. Rogers said, noting that remission times grow over years of treatment. She highlighted a 2022 study of patients with CLL who took ibrutinib that found complete remission or complete remission with incomplete hematologic recovery was 7% at 12 months and 34% at 7 years. When patients quit taking the drugs, “you don’t get to maximize your patient’s response to this treatment.”
Dr. Rogers also noted that the RESONATE-2 trial found that ibrutinib is linked to the longest median progression-free survival of any CLL treatment at 8.9 years. “That really struck me a very effective initial therapy.”
Indeed, “when you’re offering someone initial therapy with a Bruton’s kinase inhibitor as a continuous treatment strategy, you can tell people that they can expect a normal lifespan with this approach. That’s extremely important when you’re talking to patients about whether they might want to alter their leukemia treatment.”
Finally, she noted that discontinuation of ibrutinib was linked to shorter survival in early research. “This was the first suggestion that discontinuation is not good.”
Dr. Rogers said that discontinuing the drugs is sometimes necessary because of adverse events, but patients can “certainly switch to a more tolerable Bruton’s kinase inhibitor. With the options available today, that should be a strategy that’s considered.”
Audience members at the debate were invited to respond to a live online survey about whether Bruton’s kinase inhibitors can be discontinued. Among 49 respondents, most (52.3%) said no, 42.8% said yes, and the rest were undecided/other.
Disclosures for the speakers were not provided. Dr. Ahn disclosed consulting for BeiGene and AstraZeneca. Dr. Rogers disclosed receiving research funding from Genentech, AbbVie, Janssen, and Novartis; consulting for AstraZeneca, BeiGene, Janssen, Pharmacyclics, AbbVie, Genentech, and LOXO@Lilly; and receiving travel funding from AstraZeneca.
A version of this article appeared on Medscape.com.
At the annual meeting of the Society of Hematologic Oncology, two hematologist-oncologists — Inhye Ahn, MD, of Dana-Farber Cancer Institute in Boston, Massachusetts, and Kerry A. Rogers, MD, of Ohio State University in Columbus — faced off in a debate. Ahn said the drugs can indeed be discontinued, while Rogers argued against stopping the medications.
“When I talk to my own patient about standard of care options in CLL, I use the analogy of a marathon and a sprint,” Dr. Ahn said. A marathon refers to continuous treatment with Bruton’s kinase inhibitors given daily for years, while the sprint refers to the combination of venetoclax with an anti-CD20 monoclonal antibody given over 12 cycles for the frontline regimen and 2 years for refractory CLL.
“I tell them these are both considered very efficacious regimens and well tolerated, one is by IV [the venetoclax regimen] and the other isn’t [Bruton’s kinase inhibitors], and they have different toxicity profile. I ask them what would you do? The most common question that I get from my patient is, ‘why would anyone do a marathon?’ ”
It’s not solely the length of treatment that’s important, Dr. Ahn said, as toxicities from the long-term use of Bruton’s kinase inhibitors build up over time and can lead to hypertension, arrhythmia, and sudden cardiac death.
In addition, she said, infections can occur, as well as hampered vaccine response, an important risk in the era of the COVID-19 pandemic. The cost of the drugs is high and adds up over time, and continuous use can boost resistance.
Is there a way to turn the marathon of Bruton’s kinase inhibitor use into a sprint without hurting patients? The answer is yes, through temporary discontinuation, Dr. Ahn said, although she cautioned that early cessation could lead to disease flare. “We dipped into our own database of 84 CLL patients treated with ibrutinib, and our conclusion was that temporary dose interruption or dose reduction did not impact progression-free survival”
Moving forward, she said, “more research is needed to define the optimal regimen that would lead to treatment cessation, the optimal patient population, who would benefit most from the cessation strategy, treatment duration, and how we define success.” For her part, Dr. Rogers argued that the continuous use of Bruton’s kinase inhibitors is “really the most effective treatment we have in CLL.”
It’s clear that “responses deepen with continued treatment,” Dr. Rogers said, noting that remission times grow over years of treatment. She highlighted a 2022 study of patients with CLL who took ibrutinib that found complete remission or complete remission with incomplete hematologic recovery was 7% at 12 months and 34% at 7 years. When patients quit taking the drugs, “you don’t get to maximize your patient’s response to this treatment.”
Dr. Rogers also noted that the RESONATE-2 trial found that ibrutinib is linked to the longest median progression-free survival of any CLL treatment at 8.9 years. “That really struck me a very effective initial therapy.”
Indeed, “when you’re offering someone initial therapy with a Bruton’s kinase inhibitor as a continuous treatment strategy, you can tell people that they can expect a normal lifespan with this approach. That’s extremely important when you’re talking to patients about whether they might want to alter their leukemia treatment.”
Finally, she noted that discontinuation of ibrutinib was linked to shorter survival in early research. “This was the first suggestion that discontinuation is not good.”
Dr. Rogers said that discontinuing the drugs is sometimes necessary because of adverse events, but patients can “certainly switch to a more tolerable Bruton’s kinase inhibitor. With the options available today, that should be a strategy that’s considered.”
Audience members at the debate were invited to respond to a live online survey about whether Bruton’s kinase inhibitors can be discontinued. Among 49 respondents, most (52.3%) said no, 42.8% said yes, and the rest were undecided/other.
Disclosures for the speakers were not provided. Dr. Ahn disclosed consulting for BeiGene and AstraZeneca. Dr. Rogers disclosed receiving research funding from Genentech, AbbVie, Janssen, and Novartis; consulting for AstraZeneca, BeiGene, Janssen, Pharmacyclics, AbbVie, Genentech, and LOXO@Lilly; and receiving travel funding from AstraZeneca.
A version of this article appeared on Medscape.com.
FROM SOHO 2024
Could Aspirin Avert Bad Outcomes in Leukemia?
A new analysis hints that there may be a benefit from aspirin for hospitalized patients with leukemia. In a preliminary study, researchers found that aspirin users had much lower odds of intracranial bleeding, deep vein thrombosis, in-hospital mortality, and septic stroke.
Aspirin users also spent less time in the hospital and had less costly care.
No one is suggesting that clinicians give aspirin to hospitalized patients with leukemia when the drug is not otherwise indicated. However, the findings, released at the Society of Hematologic Oncology (SOHO 2024) meeting in Houston, do indicate that more research is warranted, study lead author Jayalekshmi Jayakumar, MD, of the Brooklyn Hospital Center in New York City, said in a presentation.
“We hope our study can act as background for further prospective and experimental studies to explore this association,” she said. “If we can establish causation, then aspirin has a potential to be a thromboprophylactic agent to enhance outcomes and reduce resource utilization among leukemia hospitalizations.”
Dr. Jayakumar noted that previous research has suggested aspirin may help prevent deep vein thrombosis in patients with breast and pancreatic cancer. And in blood cancer, animal research has suggested that aspirin may “promote apoptosis in leukemia cells and decrease the spread of leukemia cells through platelet inhibition,” she said.
However, “we do not have any prospective or retrospective studies to establish causation or to see if this actually has some value within the clinical practice,” she noted.
Dr. Jayakumar stated that new study aims to detect whether aspirin may be beneficial in leukemia. She and her colleagues retrospectively tracked 1,663,149 US hospitalizations of patients with leukemia from 2016 to 2020 via the National Inpatient Sample. Of those patients, 11.2% used aspirin, although the data didn’t say whether they started it during hospitalization, and dosages were not reported. Aspirin users were older (mean age, 74.53 years vs 64.83 years in nonusers).
After adjustment for confounders, aspirin users had lower odds of several conditions than nonusers:
- Epistaxis (odds ratio [OR], 0.63; 95% CI, 0.55-0.72; P < .001)
- Hemoptysis (OR, 0.71; 95% CI, 0.61-0.82; P < .001)
- Intracranial bleed (OR, 0.74; 95% CI, 0.64-0.85; P < .001)
- Deep vein thrombosis (OR, 0.72; 95% CI, 0.66-0.78; P < .001)
- In-hospital mortality (OR, 0.54; 95% CI, 0.50-0.58; P < .001)
- Sepsis (OR, 0.71; 95% CI, 0.68-0.75; P < .001)
- Septic shock (OR, 0.55; 95% CI, 0.50-0.60; P < .001)
There was no association reported for gastrointestinal bleeding, a possible side effect of aspirin use, or tumor lysis syndrome. Aspirin users also had a shorter typical stay (−2.8 days) and lower typical hospital charges ($40,719).
“We also found that aspirin users had a slightly reduced risk of minor bleeding and infection compared to non–aspirin users,” Dr. Jayakumar said.
In an interview, Dr. Jayakumar noted that the study is retrospective and declined to speculate on why aspirin may have benefits or why it may have the seemingly contradictory effect of reducing both blood clots and bleeding.
Aspirin is one of the least expensive drugs in existence.
In an interview, Richard M. Stone, MD, oncologist at Dana-Farber Cancer Institute in Boston, who’s familiar with the study findings but didn’t take part in the research, said the findings are “totally counterintuitive.”
“It doesn’t mean they should be rejected, but they should be highly scrutinized,” he said.
Dr. Stone added that bleeding is a major risk in leukemia due to low platelet counts, although platelet transplants can be helpful, and patients rarely die of bleeding. Thrombosis is also a problem in leukemia, he said, and it’s being increasingly recognized as a risk in acute myeloid leukemia.
No funding was reported. Dr. Jayakumar and Dr. Stone had no disclosures.
A version of this article appeared on Medscape.com.
A new analysis hints that there may be a benefit from aspirin for hospitalized patients with leukemia. In a preliminary study, researchers found that aspirin users had much lower odds of intracranial bleeding, deep vein thrombosis, in-hospital mortality, and septic stroke.
Aspirin users also spent less time in the hospital and had less costly care.
No one is suggesting that clinicians give aspirin to hospitalized patients with leukemia when the drug is not otherwise indicated. However, the findings, released at the Society of Hematologic Oncology (SOHO 2024) meeting in Houston, do indicate that more research is warranted, study lead author Jayalekshmi Jayakumar, MD, of the Brooklyn Hospital Center in New York City, said in a presentation.
“We hope our study can act as background for further prospective and experimental studies to explore this association,” she said. “If we can establish causation, then aspirin has a potential to be a thromboprophylactic agent to enhance outcomes and reduce resource utilization among leukemia hospitalizations.”
Dr. Jayakumar noted that previous research has suggested aspirin may help prevent deep vein thrombosis in patients with breast and pancreatic cancer. And in blood cancer, animal research has suggested that aspirin may “promote apoptosis in leukemia cells and decrease the spread of leukemia cells through platelet inhibition,” she said.
However, “we do not have any prospective or retrospective studies to establish causation or to see if this actually has some value within the clinical practice,” she noted.
Dr. Jayakumar stated that new study aims to detect whether aspirin may be beneficial in leukemia. She and her colleagues retrospectively tracked 1,663,149 US hospitalizations of patients with leukemia from 2016 to 2020 via the National Inpatient Sample. Of those patients, 11.2% used aspirin, although the data didn’t say whether they started it during hospitalization, and dosages were not reported. Aspirin users were older (mean age, 74.53 years vs 64.83 years in nonusers).
After adjustment for confounders, aspirin users had lower odds of several conditions than nonusers:
- Epistaxis (odds ratio [OR], 0.63; 95% CI, 0.55-0.72; P < .001)
- Hemoptysis (OR, 0.71; 95% CI, 0.61-0.82; P < .001)
- Intracranial bleed (OR, 0.74; 95% CI, 0.64-0.85; P < .001)
- Deep vein thrombosis (OR, 0.72; 95% CI, 0.66-0.78; P < .001)
- In-hospital mortality (OR, 0.54; 95% CI, 0.50-0.58; P < .001)
- Sepsis (OR, 0.71; 95% CI, 0.68-0.75; P < .001)
- Septic shock (OR, 0.55; 95% CI, 0.50-0.60; P < .001)
There was no association reported for gastrointestinal bleeding, a possible side effect of aspirin use, or tumor lysis syndrome. Aspirin users also had a shorter typical stay (−2.8 days) and lower typical hospital charges ($40,719).
“We also found that aspirin users had a slightly reduced risk of minor bleeding and infection compared to non–aspirin users,” Dr. Jayakumar said.
In an interview, Dr. Jayakumar noted that the study is retrospective and declined to speculate on why aspirin may have benefits or why it may have the seemingly contradictory effect of reducing both blood clots and bleeding.
Aspirin is one of the least expensive drugs in existence.
In an interview, Richard M. Stone, MD, oncologist at Dana-Farber Cancer Institute in Boston, who’s familiar with the study findings but didn’t take part in the research, said the findings are “totally counterintuitive.”
“It doesn’t mean they should be rejected, but they should be highly scrutinized,” he said.
Dr. Stone added that bleeding is a major risk in leukemia due to low platelet counts, although platelet transplants can be helpful, and patients rarely die of bleeding. Thrombosis is also a problem in leukemia, he said, and it’s being increasingly recognized as a risk in acute myeloid leukemia.
No funding was reported. Dr. Jayakumar and Dr. Stone had no disclosures.
A version of this article appeared on Medscape.com.
A new analysis hints that there may be a benefit from aspirin for hospitalized patients with leukemia. In a preliminary study, researchers found that aspirin users had much lower odds of intracranial bleeding, deep vein thrombosis, in-hospital mortality, and septic stroke.
Aspirin users also spent less time in the hospital and had less costly care.
No one is suggesting that clinicians give aspirin to hospitalized patients with leukemia when the drug is not otherwise indicated. However, the findings, released at the Society of Hematologic Oncology (SOHO 2024) meeting in Houston, do indicate that more research is warranted, study lead author Jayalekshmi Jayakumar, MD, of the Brooklyn Hospital Center in New York City, said in a presentation.
“We hope our study can act as background for further prospective and experimental studies to explore this association,” she said. “If we can establish causation, then aspirin has a potential to be a thromboprophylactic agent to enhance outcomes and reduce resource utilization among leukemia hospitalizations.”
Dr. Jayakumar noted that previous research has suggested aspirin may help prevent deep vein thrombosis in patients with breast and pancreatic cancer. And in blood cancer, animal research has suggested that aspirin may “promote apoptosis in leukemia cells and decrease the spread of leukemia cells through platelet inhibition,” she said.
However, “we do not have any prospective or retrospective studies to establish causation or to see if this actually has some value within the clinical practice,” she noted.
Dr. Jayakumar stated that new study aims to detect whether aspirin may be beneficial in leukemia. She and her colleagues retrospectively tracked 1,663,149 US hospitalizations of patients with leukemia from 2016 to 2020 via the National Inpatient Sample. Of those patients, 11.2% used aspirin, although the data didn’t say whether they started it during hospitalization, and dosages were not reported. Aspirin users were older (mean age, 74.53 years vs 64.83 years in nonusers).
After adjustment for confounders, aspirin users had lower odds of several conditions than nonusers:
- Epistaxis (odds ratio [OR], 0.63; 95% CI, 0.55-0.72; P < .001)
- Hemoptysis (OR, 0.71; 95% CI, 0.61-0.82; P < .001)
- Intracranial bleed (OR, 0.74; 95% CI, 0.64-0.85; P < .001)
- Deep vein thrombosis (OR, 0.72; 95% CI, 0.66-0.78; P < .001)
- In-hospital mortality (OR, 0.54; 95% CI, 0.50-0.58; P < .001)
- Sepsis (OR, 0.71; 95% CI, 0.68-0.75; P < .001)
- Septic shock (OR, 0.55; 95% CI, 0.50-0.60; P < .001)
There was no association reported for gastrointestinal bleeding, a possible side effect of aspirin use, or tumor lysis syndrome. Aspirin users also had a shorter typical stay (−2.8 days) and lower typical hospital charges ($40,719).
“We also found that aspirin users had a slightly reduced risk of minor bleeding and infection compared to non–aspirin users,” Dr. Jayakumar said.
In an interview, Dr. Jayakumar noted that the study is retrospective and declined to speculate on why aspirin may have benefits or why it may have the seemingly contradictory effect of reducing both blood clots and bleeding.
Aspirin is one of the least expensive drugs in existence.
In an interview, Richard M. Stone, MD, oncologist at Dana-Farber Cancer Institute in Boston, who’s familiar with the study findings but didn’t take part in the research, said the findings are “totally counterintuitive.”
“It doesn’t mean they should be rejected, but they should be highly scrutinized,” he said.
Dr. Stone added that bleeding is a major risk in leukemia due to low platelet counts, although platelet transplants can be helpful, and patients rarely die of bleeding. Thrombosis is also a problem in leukemia, he said, and it’s being increasingly recognized as a risk in acute myeloid leukemia.
No funding was reported. Dr. Jayakumar and Dr. Stone had no disclosures.
A version of this article appeared on Medscape.com.
FROM SOHO 2024
Wait, a Health Worker Surplus? Workforce Report Projects Big Surprises
A surprising new report by the Mercer consulting firm projects that the American healthcare workforce will face a small shortfall in 2028 — a shortage of less than 1% of all employees.
Mercer’s projections are rosier than federal workforce projections, which paint a grimmer picture of impending shortages.
“The labor market is a little more stabilized right now, and most healthcare systems are seeing less turnover,” Dan Lezotte, PhD, a partner with Mercer, said in an interview. But he noted “critical shortages” are still expected in some areas.
Mercer last projected workforce numbers in a 2020-2021 report released during the height of the COVID-19 pandemic. Now, “the labor market is drastically different,” Dr. Lezotte said. Health workforce shortages and surpluses have long varied significantly by region across the country.
The report forecasts a small surplus of physicians in 2028 but not in states such as California, New York, and Texas. The upper Midwest states will largely see doctor surpluses while Southern states face shortages. Some states with general physician surpluses may still experience shortages of specialists.
A surplus of nearly 30,000 registered nurses is expected, but New York, New Jersey, and Connecticut are projected to have a combined shortage of 16,000 nurses.
Overall, the report projects a shortage of more than 100,000 healthcare workers nationally by 2028. That’s less than 1% of the entire healthcare workforce of 18.6 million expected by then.
The report also predicts a shortage of nurse practitioners, especially in California and New York, and a shortage of 73,000 nursing assistants, especially in California, New York, and Texas.
“Healthcare systems are having the most difficulty hiring and hanging on to those workers who are supposed to take up the load off physicians and nurses,” Dr. Lezotte said. “They’re competing not only with other healthcare systems but with other industries like Amazon warehouses or McDonald’s in California paying $20 an hour. Healthcare was a little slow to keep up with that. In a lot of healthcare systems, that’s their biggest headache right now.”
On the other hand, the report projects a national surplus of 48,000 home health/personal care aides.
That surprised Bianca K. Frogner, PhD, director of the Center for Health Workforce Studies at the University of Washington, Seattle.
“We are seeing increasing movement of investments toward moving patients out of skilled nursing facilities and keeping them in the home and community, which requires many more home health aides,” Dr. Frogner said. “Given such high turnover in this occupation, it’s hard to know if the surplus is really a surplus or if they will quickly be employed.”
Dr. Frogner receives grants and contracts from not-for-profit entities to investigate issues related to the health workforce.
Dr. Lezotte said the report’s findings are based on data from sources such as public and private databases and job postings. According to the report, “projections were made up to 2028 based on historical data up to 2023,” and “supply projections were derived using a linear autoregressive model based on historical supply within each occupation and geography.”
It’s not clear why some states like New York are expected to have huge shortages, but migration might be a factor, along with a lack of nearby nursing schools, Dr. Lezotte said.
As for shortages, Dr. Lezotte said healthcare systems will have to understand their local workforce situation and adapt. “They’ll need to be more proactive about their employee value proposition” via competitive pay and benefits Flexibility regarding scheduling is also important.
“They’re going to have to figure out how to up their game,” he said.
What about states with surpluses? They might be target-rich environments for states facing shortages, he said.
Positive Outlook Not Shared by Other Researchers
Other workforce projections conflict with Mercer’s, according to Jean Moore, DrPH, and Gaetano Forte, MS, director and assistant director of the Center for Health Workforce Studies, School of Public Health, University at Albany, New York.
The National Center for Health Workforce Analysis projects a 10% shortage of registered nurses and a 13% shortage of physicians in 2031. The agency didn’t make projections for home health aides because that workforce is in flux.
Why are Mercer’s projections so different? Dr. Lezotte said other projections assume that equity efforts will bring healthcare to everyone who needs it. The report assumes this won’t happen, he said. As a result, it expects there will be fewer patients who need to be served by workers.
Other projections expect a shortage of 300,000 registered nurses by 2035, Mr. Forte said. But the number of nurse practitioners in New York is growing quickly, Dr. Moore said.
Dr. Moore said it’s difficult to interpret Mercer’s findings because the company doesn’t provide enough information about its methodology.
“At some level, it’s not particularly useful regarding what the next steps are,” she said. “Projections should make you think about what you should do to change and improve, to create more of what you need.”
The Center for Health Workforce Studies at the University of Albany has provided consulting services to multiple companies that provide healthcare workforce projections. It has no relationship with Mercer.
A version of this article first appeared on Medscape.com.
A surprising new report by the Mercer consulting firm projects that the American healthcare workforce will face a small shortfall in 2028 — a shortage of less than 1% of all employees.
Mercer’s projections are rosier than federal workforce projections, which paint a grimmer picture of impending shortages.
“The labor market is a little more stabilized right now, and most healthcare systems are seeing less turnover,” Dan Lezotte, PhD, a partner with Mercer, said in an interview. But he noted “critical shortages” are still expected in some areas.
Mercer last projected workforce numbers in a 2020-2021 report released during the height of the COVID-19 pandemic. Now, “the labor market is drastically different,” Dr. Lezotte said. Health workforce shortages and surpluses have long varied significantly by region across the country.
The report forecasts a small surplus of physicians in 2028 but not in states such as California, New York, and Texas. The upper Midwest states will largely see doctor surpluses while Southern states face shortages. Some states with general physician surpluses may still experience shortages of specialists.
A surplus of nearly 30,000 registered nurses is expected, but New York, New Jersey, and Connecticut are projected to have a combined shortage of 16,000 nurses.
Overall, the report projects a shortage of more than 100,000 healthcare workers nationally by 2028. That’s less than 1% of the entire healthcare workforce of 18.6 million expected by then.
The report also predicts a shortage of nurse practitioners, especially in California and New York, and a shortage of 73,000 nursing assistants, especially in California, New York, and Texas.
“Healthcare systems are having the most difficulty hiring and hanging on to those workers who are supposed to take up the load off physicians and nurses,” Dr. Lezotte said. “They’re competing not only with other healthcare systems but with other industries like Amazon warehouses or McDonald’s in California paying $20 an hour. Healthcare was a little slow to keep up with that. In a lot of healthcare systems, that’s their biggest headache right now.”
On the other hand, the report projects a national surplus of 48,000 home health/personal care aides.
That surprised Bianca K. Frogner, PhD, director of the Center for Health Workforce Studies at the University of Washington, Seattle.
“We are seeing increasing movement of investments toward moving patients out of skilled nursing facilities and keeping them in the home and community, which requires many more home health aides,” Dr. Frogner said. “Given such high turnover in this occupation, it’s hard to know if the surplus is really a surplus or if they will quickly be employed.”
Dr. Frogner receives grants and contracts from not-for-profit entities to investigate issues related to the health workforce.
Dr. Lezotte said the report’s findings are based on data from sources such as public and private databases and job postings. According to the report, “projections were made up to 2028 based on historical data up to 2023,” and “supply projections were derived using a linear autoregressive model based on historical supply within each occupation and geography.”
It’s not clear why some states like New York are expected to have huge shortages, but migration might be a factor, along with a lack of nearby nursing schools, Dr. Lezotte said.
As for shortages, Dr. Lezotte said healthcare systems will have to understand their local workforce situation and adapt. “They’ll need to be more proactive about their employee value proposition” via competitive pay and benefits Flexibility regarding scheduling is also important.
“They’re going to have to figure out how to up their game,” he said.
What about states with surpluses? They might be target-rich environments for states facing shortages, he said.
Positive Outlook Not Shared by Other Researchers
Other workforce projections conflict with Mercer’s, according to Jean Moore, DrPH, and Gaetano Forte, MS, director and assistant director of the Center for Health Workforce Studies, School of Public Health, University at Albany, New York.
The National Center for Health Workforce Analysis projects a 10% shortage of registered nurses and a 13% shortage of physicians in 2031. The agency didn’t make projections for home health aides because that workforce is in flux.
Why are Mercer’s projections so different? Dr. Lezotte said other projections assume that equity efforts will bring healthcare to everyone who needs it. The report assumes this won’t happen, he said. As a result, it expects there will be fewer patients who need to be served by workers.
Other projections expect a shortage of 300,000 registered nurses by 2035, Mr. Forte said. But the number of nurse practitioners in New York is growing quickly, Dr. Moore said.
Dr. Moore said it’s difficult to interpret Mercer’s findings because the company doesn’t provide enough information about its methodology.
“At some level, it’s not particularly useful regarding what the next steps are,” she said. “Projections should make you think about what you should do to change and improve, to create more of what you need.”
The Center for Health Workforce Studies at the University of Albany has provided consulting services to multiple companies that provide healthcare workforce projections. It has no relationship with Mercer.
A version of this article first appeared on Medscape.com.
A surprising new report by the Mercer consulting firm projects that the American healthcare workforce will face a small shortfall in 2028 — a shortage of less than 1% of all employees.
Mercer’s projections are rosier than federal workforce projections, which paint a grimmer picture of impending shortages.
“The labor market is a little more stabilized right now, and most healthcare systems are seeing less turnover,” Dan Lezotte, PhD, a partner with Mercer, said in an interview. But he noted “critical shortages” are still expected in some areas.
Mercer last projected workforce numbers in a 2020-2021 report released during the height of the COVID-19 pandemic. Now, “the labor market is drastically different,” Dr. Lezotte said. Health workforce shortages and surpluses have long varied significantly by region across the country.
The report forecasts a small surplus of physicians in 2028 but not in states such as California, New York, and Texas. The upper Midwest states will largely see doctor surpluses while Southern states face shortages. Some states with general physician surpluses may still experience shortages of specialists.
A surplus of nearly 30,000 registered nurses is expected, but New York, New Jersey, and Connecticut are projected to have a combined shortage of 16,000 nurses.
Overall, the report projects a shortage of more than 100,000 healthcare workers nationally by 2028. That’s less than 1% of the entire healthcare workforce of 18.6 million expected by then.
The report also predicts a shortage of nurse practitioners, especially in California and New York, and a shortage of 73,000 nursing assistants, especially in California, New York, and Texas.
“Healthcare systems are having the most difficulty hiring and hanging on to those workers who are supposed to take up the load off physicians and nurses,” Dr. Lezotte said. “They’re competing not only with other healthcare systems but with other industries like Amazon warehouses or McDonald’s in California paying $20 an hour. Healthcare was a little slow to keep up with that. In a lot of healthcare systems, that’s their biggest headache right now.”
On the other hand, the report projects a national surplus of 48,000 home health/personal care aides.
That surprised Bianca K. Frogner, PhD, director of the Center for Health Workforce Studies at the University of Washington, Seattle.
“We are seeing increasing movement of investments toward moving patients out of skilled nursing facilities and keeping them in the home and community, which requires many more home health aides,” Dr. Frogner said. “Given such high turnover in this occupation, it’s hard to know if the surplus is really a surplus or if they will quickly be employed.”
Dr. Frogner receives grants and contracts from not-for-profit entities to investigate issues related to the health workforce.
Dr. Lezotte said the report’s findings are based on data from sources such as public and private databases and job postings. According to the report, “projections were made up to 2028 based on historical data up to 2023,” and “supply projections were derived using a linear autoregressive model based on historical supply within each occupation and geography.”
It’s not clear why some states like New York are expected to have huge shortages, but migration might be a factor, along with a lack of nearby nursing schools, Dr. Lezotte said.
As for shortages, Dr. Lezotte said healthcare systems will have to understand their local workforce situation and adapt. “They’ll need to be more proactive about their employee value proposition” via competitive pay and benefits Flexibility regarding scheduling is also important.
“They’re going to have to figure out how to up their game,” he said.
What about states with surpluses? They might be target-rich environments for states facing shortages, he said.
Positive Outlook Not Shared by Other Researchers
Other workforce projections conflict with Mercer’s, according to Jean Moore, DrPH, and Gaetano Forte, MS, director and assistant director of the Center for Health Workforce Studies, School of Public Health, University at Albany, New York.
The National Center for Health Workforce Analysis projects a 10% shortage of registered nurses and a 13% shortage of physicians in 2031. The agency didn’t make projections for home health aides because that workforce is in flux.
Why are Mercer’s projections so different? Dr. Lezotte said other projections assume that equity efforts will bring healthcare to everyone who needs it. The report assumes this won’t happen, he said. As a result, it expects there will be fewer patients who need to be served by workers.
Other projections expect a shortage of 300,000 registered nurses by 2035, Mr. Forte said. But the number of nurse practitioners in New York is growing quickly, Dr. Moore said.
Dr. Moore said it’s difficult to interpret Mercer’s findings because the company doesn’t provide enough information about its methodology.
“At some level, it’s not particularly useful regarding what the next steps are,” she said. “Projections should make you think about what you should do to change and improve, to create more of what you need.”
The Center for Health Workforce Studies at the University of Albany has provided consulting services to multiple companies that provide healthcare workforce projections. It has no relationship with Mercer.
A version of this article first appeared on Medscape.com.