User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
How much would you bet on a diagnosis?
“You have psoriasis,” I say all the time. I mean it when I say it, of course. But I don’t always to the same degree. Sometimes I’m trying to say, “You probably have psoriasis.” Other times I mean, “You most definitely have psoriasis.” I rarely use those terms though.
One 36-year-old man with a flaky scalp and scaly elbows wasn’t satisfied with my assessment. His dad has psoriasis. So does his older brother. He was in to see me to find out if he had psoriasis too. “Probably” was what I gave him. He pushed back, “What percent chance?” That’s a good question — must be an engineer. I’m unsure.
With the exception of the poker players, our species is notoriously bad at probabilities. We’re wired to notice the significance of events, but terrible at understanding their likelihood. This is salient in lottery ticket holders and some NFL offensive coordinators who persist despite very long odds of things working out. It’s also reflected in the language we use. Rarely do we say, there’s a sixty percent chance something will happen. Rather, we say, “it’s likely.” There are two problems here. One, we often misjudge the actual probability of something occurring and two, the terms we use are subjective and differences in interpretation can lead to misunderstandings.
Let’s take a look. A 55-year-old man with a chronic eczematous rash on his trunk and extremities is getting worse despite dupilumab. He recently had night sweats. Do you think he has atopic dermatitis or cutaneous T-cell lymphoma? If you had to place a $100 bet, would you change your answer? Immanuel Kant thinks you would. In his “Critique of Pure Reason,” the German philosopher proposes that betting helps clarify the mind, an antidote to brashness. The example Kant uses is of a physician who observes a patient and concludes he has phthisis (tuberculosis), but we really don’t know if the physician is confident. Kant proposes that if he had to bet on his conclusion, then we’d have insight into just how convinced he is of phthisis. So, what’s your bet?
If you’re a bad poker player, then you might bet he has cutaneous T-cell lymphoma. However, not having any additional information, the smart call is atopic dermatitis, which has a base rate 1000-fold higher than CTCL. It is therefore more probable to be eczema even in a case that worsens despite dupilumab or with recent night sweats, both of which could be a result of common variables such as weather and COVID. Failure to account for the base rate is a mistake we physicians sometimes make. Economists rarely do. Try to think like one before answering a likelihood question.
If you think about it, “probably” means something different even to me, depending on the situation. I might say I’ll probably go to Montana this summer and I’ll probably retire at 65. The actual likelihoods might be 95% and 70%. That’s a big difference. What about between probably and likely? Or possibly and maybe? Do they mean the same to you as to the person you’re speaking with? For much of the work we do, precise likelihoods aren’t critical. Yet, it can be important in decision making and in discussing probabilities, such as the risk of hepatitis on terbinafine or of melanoma recurrence after Mohs.
I told my patient “I say about a 70% chance you have psoriasis. I could do a biopsy today to confirm.” He thought for a second and asked, “What is the chance it’s psoriasis if the biopsy shows it?” “Eighty six percent,” I replied.
Seemed like a good bet to me.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X. Write to him at dermnews@mdedge.com.
“You have psoriasis,” I say all the time. I mean it when I say it, of course. But I don’t always to the same degree. Sometimes I’m trying to say, “You probably have psoriasis.” Other times I mean, “You most definitely have psoriasis.” I rarely use those terms though.
One 36-year-old man with a flaky scalp and scaly elbows wasn’t satisfied with my assessment. His dad has psoriasis. So does his older brother. He was in to see me to find out if he had psoriasis too. “Probably” was what I gave him. He pushed back, “What percent chance?” That’s a good question — must be an engineer. I’m unsure.
With the exception of the poker players, our species is notoriously bad at probabilities. We’re wired to notice the significance of events, but terrible at understanding their likelihood. This is salient in lottery ticket holders and some NFL offensive coordinators who persist despite very long odds of things working out. It’s also reflected in the language we use. Rarely do we say, there’s a sixty percent chance something will happen. Rather, we say, “it’s likely.” There are two problems here. One, we often misjudge the actual probability of something occurring and two, the terms we use are subjective and differences in interpretation can lead to misunderstandings.
Let’s take a look. A 55-year-old man with a chronic eczematous rash on his trunk and extremities is getting worse despite dupilumab. He recently had night sweats. Do you think he has atopic dermatitis or cutaneous T-cell lymphoma? If you had to place a $100 bet, would you change your answer? Immanuel Kant thinks you would. In his “Critique of Pure Reason,” the German philosopher proposes that betting helps clarify the mind, an antidote to brashness. The example Kant uses is of a physician who observes a patient and concludes he has phthisis (tuberculosis), but we really don’t know if the physician is confident. Kant proposes that if he had to bet on his conclusion, then we’d have insight into just how convinced he is of phthisis. So, what’s your bet?
If you’re a bad poker player, then you might bet he has cutaneous T-cell lymphoma. However, not having any additional information, the smart call is atopic dermatitis, which has a base rate 1000-fold higher than CTCL. It is therefore more probable to be eczema even in a case that worsens despite dupilumab or with recent night sweats, both of which could be a result of common variables such as weather and COVID. Failure to account for the base rate is a mistake we physicians sometimes make. Economists rarely do. Try to think like one before answering a likelihood question.
If you think about it, “probably” means something different even to me, depending on the situation. I might say I’ll probably go to Montana this summer and I’ll probably retire at 65. The actual likelihoods might be 95% and 70%. That’s a big difference. What about between probably and likely? Or possibly and maybe? Do they mean the same to you as to the person you’re speaking with? For much of the work we do, precise likelihoods aren’t critical. Yet, it can be important in decision making and in discussing probabilities, such as the risk of hepatitis on terbinafine or of melanoma recurrence after Mohs.
I told my patient “I say about a 70% chance you have psoriasis. I could do a biopsy today to confirm.” He thought for a second and asked, “What is the chance it’s psoriasis if the biopsy shows it?” “Eighty six percent,” I replied.
Seemed like a good bet to me.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X. Write to him at dermnews@mdedge.com.
“You have psoriasis,” I say all the time. I mean it when I say it, of course. But I don’t always to the same degree. Sometimes I’m trying to say, “You probably have psoriasis.” Other times I mean, “You most definitely have psoriasis.” I rarely use those terms though.
One 36-year-old man with a flaky scalp and scaly elbows wasn’t satisfied with my assessment. His dad has psoriasis. So does his older brother. He was in to see me to find out if he had psoriasis too. “Probably” was what I gave him. He pushed back, “What percent chance?” That’s a good question — must be an engineer. I’m unsure.
With the exception of the poker players, our species is notoriously bad at probabilities. We’re wired to notice the significance of events, but terrible at understanding their likelihood. This is salient in lottery ticket holders and some NFL offensive coordinators who persist despite very long odds of things working out. It’s also reflected in the language we use. Rarely do we say, there’s a sixty percent chance something will happen. Rather, we say, “it’s likely.” There are two problems here. One, we often misjudge the actual probability of something occurring and two, the terms we use are subjective and differences in interpretation can lead to misunderstandings.
Let’s take a look. A 55-year-old man with a chronic eczematous rash on his trunk and extremities is getting worse despite dupilumab. He recently had night sweats. Do you think he has atopic dermatitis or cutaneous T-cell lymphoma? If you had to place a $100 bet, would you change your answer? Immanuel Kant thinks you would. In his “Critique of Pure Reason,” the German philosopher proposes that betting helps clarify the mind, an antidote to brashness. The example Kant uses is of a physician who observes a patient and concludes he has phthisis (tuberculosis), but we really don’t know if the physician is confident. Kant proposes that if he had to bet on his conclusion, then we’d have insight into just how convinced he is of phthisis. So, what’s your bet?
If you’re a bad poker player, then you might bet he has cutaneous T-cell lymphoma. However, not having any additional information, the smart call is atopic dermatitis, which has a base rate 1000-fold higher than CTCL. It is therefore more probable to be eczema even in a case that worsens despite dupilumab or with recent night sweats, both of which could be a result of common variables such as weather and COVID. Failure to account for the base rate is a mistake we physicians sometimes make. Economists rarely do. Try to think like one before answering a likelihood question.
If you think about it, “probably” means something different even to me, depending on the situation. I might say I’ll probably go to Montana this summer and I’ll probably retire at 65. The actual likelihoods might be 95% and 70%. That’s a big difference. What about between probably and likely? Or possibly and maybe? Do they mean the same to you as to the person you’re speaking with? For much of the work we do, precise likelihoods aren’t critical. Yet, it can be important in decision making and in discussing probabilities, such as the risk of hepatitis on terbinafine or of melanoma recurrence after Mohs.
I told my patient “I say about a 70% chance you have psoriasis. I could do a biopsy today to confirm.” He thought for a second and asked, “What is the chance it’s psoriasis if the biopsy shows it?” “Eighty six percent,” I replied.
Seemed like a good bet to me.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X. Write to him at dermnews@mdedge.com.
Public Citizen seeks stronger warning for Botox, related products
.
The nonprofit watchdog group successfully petitioned the FDA in 2008 to require a warning for Botox and related products regarding the risk of distant spread of the toxin. In its latest petition to the agency, it says that the injectables need additional warnings about the possibility of iatrogenic botulism with initial and repeated doses and that individuals who contract the condition may need botulinum antitoxin to avert temporary muscle paralysis, hospitalization, and death.
The current warning does not contain any information about the potential need for antitoxin and downplays the need for giving antitoxin in the settings of excessive dosing, accidental injection, and oral ingestion, said Public Citizen.
“Our petition is based on clear postmarketing evidence that refutes industry propaganda claiming that Botox and related drugs are ‘always safe’ and that no ‘definitive’ cases of botulism have occurred with recommended doses,” Azza AbuDagga, PhD, health services researcher at Public Citizen’s Health Research Group, said in a statement.
Public Citizen said that using data from the FDA’s Adverse Event Reporting System (FAERS), it found 5414 reports of serious outcomes from botulinum toxin products from January 1989 through March 2021. Almost 22% involved cosmetic indications and about 78% involved therapeutic indications.
Of the 5414 reports, 121 (2%) specified botulism as an adverse reaction; 89 involved therapeutic uses of a botulinum toxin products, and 32 involved cosmetic uses. Many of those 121 reports involved doses within the recommended range for the indication, according to Public Citizen.
The group is also asking the FDA to remove what it calls misleading promotional statements in the labeling of Botox and Botox Cosmetic and from the medication guides for those products. The labels state that there have been “no definitive serious adverse event reports of distant spread of toxin effect” with either the cosmetic use or for use in treating chronic migraine, severe underarm sweating, blepharospasm, or strabismus. These statements do not appear in similar labeling in other countries, such as Canada and the United Kingdom, said Public Citizen.
“The FDA needs to implement our two requested actions quickly to warn the public in unambiguous terms about the risk of botulism associated with the use of Botox and related drugs,” Dr. AbuDagga said in the Public Citizen statement. “This will allow health care professionals and patients to make more informed decisions about the benefit-risk profile of these widely used drugs.”
The Public Citizen petition would apply to all seven approved botulinum toxin biological products: abobotulinumtoxinA (Dysport), daxibotulinumtoxinA-lanm (Daxxify), incobotulinumtoxinA (Xeomin), onabotulinumtoxinA (Botox, Botox Cosmetic), prabotulinumtoxinA-xvfs (Jeuveau) and rimabotulinumtoxinB (Myobloc).
An FDA spokesperson said the agency is reviewing the citizen petition, and that generally the agency does not comment on pending petitions. “When we respond to the petition, we will respond directly to the petitioner and post the response in the designated agency docket,” the spokesperson told this news organization. At press time, Botox manufacturer AbbVie had not responded to a request for a comment.
Botulinum toxin is the most-used product for nonsurgical cosmetic procedures, according to the International Society of Aesthetic Plastic Surgery (ISAPS). The ISAPS reported that there were more than 7 million botulinum toxin procedures performed by plastic surgeons worldwide in 2021.
The American Society of Plastic Surgery reported that its members performed 4.4 million Botox procedures in 2020, while the American Society of Dermatologic Surgery (ASDS) said its members performed 2.3 million wrinkle-relaxing procedures in 2019, a 60% increase since 2012.
.
The nonprofit watchdog group successfully petitioned the FDA in 2008 to require a warning for Botox and related products regarding the risk of distant spread of the toxin. In its latest petition to the agency, it says that the injectables need additional warnings about the possibility of iatrogenic botulism with initial and repeated doses and that individuals who contract the condition may need botulinum antitoxin to avert temporary muscle paralysis, hospitalization, and death.
The current warning does not contain any information about the potential need for antitoxin and downplays the need for giving antitoxin in the settings of excessive dosing, accidental injection, and oral ingestion, said Public Citizen.
“Our petition is based on clear postmarketing evidence that refutes industry propaganda claiming that Botox and related drugs are ‘always safe’ and that no ‘definitive’ cases of botulism have occurred with recommended doses,” Azza AbuDagga, PhD, health services researcher at Public Citizen’s Health Research Group, said in a statement.
Public Citizen said that using data from the FDA’s Adverse Event Reporting System (FAERS), it found 5414 reports of serious outcomes from botulinum toxin products from January 1989 through March 2021. Almost 22% involved cosmetic indications and about 78% involved therapeutic indications.
Of the 5414 reports, 121 (2%) specified botulism as an adverse reaction; 89 involved therapeutic uses of a botulinum toxin products, and 32 involved cosmetic uses. Many of those 121 reports involved doses within the recommended range for the indication, according to Public Citizen.
The group is also asking the FDA to remove what it calls misleading promotional statements in the labeling of Botox and Botox Cosmetic and from the medication guides for those products. The labels state that there have been “no definitive serious adverse event reports of distant spread of toxin effect” with either the cosmetic use or for use in treating chronic migraine, severe underarm sweating, blepharospasm, or strabismus. These statements do not appear in similar labeling in other countries, such as Canada and the United Kingdom, said Public Citizen.
“The FDA needs to implement our two requested actions quickly to warn the public in unambiguous terms about the risk of botulism associated with the use of Botox and related drugs,” Dr. AbuDagga said in the Public Citizen statement. “This will allow health care professionals and patients to make more informed decisions about the benefit-risk profile of these widely used drugs.”
The Public Citizen petition would apply to all seven approved botulinum toxin biological products: abobotulinumtoxinA (Dysport), daxibotulinumtoxinA-lanm (Daxxify), incobotulinumtoxinA (Xeomin), onabotulinumtoxinA (Botox, Botox Cosmetic), prabotulinumtoxinA-xvfs (Jeuveau) and rimabotulinumtoxinB (Myobloc).
An FDA spokesperson said the agency is reviewing the citizen petition, and that generally the agency does not comment on pending petitions. “When we respond to the petition, we will respond directly to the petitioner and post the response in the designated agency docket,” the spokesperson told this news organization. At press time, Botox manufacturer AbbVie had not responded to a request for a comment.
Botulinum toxin is the most-used product for nonsurgical cosmetic procedures, according to the International Society of Aesthetic Plastic Surgery (ISAPS). The ISAPS reported that there were more than 7 million botulinum toxin procedures performed by plastic surgeons worldwide in 2021.
The American Society of Plastic Surgery reported that its members performed 4.4 million Botox procedures in 2020, while the American Society of Dermatologic Surgery (ASDS) said its members performed 2.3 million wrinkle-relaxing procedures in 2019, a 60% increase since 2012.
.
The nonprofit watchdog group successfully petitioned the FDA in 2008 to require a warning for Botox and related products regarding the risk of distant spread of the toxin. In its latest petition to the agency, it says that the injectables need additional warnings about the possibility of iatrogenic botulism with initial and repeated doses and that individuals who contract the condition may need botulinum antitoxin to avert temporary muscle paralysis, hospitalization, and death.
The current warning does not contain any information about the potential need for antitoxin and downplays the need for giving antitoxin in the settings of excessive dosing, accidental injection, and oral ingestion, said Public Citizen.
“Our petition is based on clear postmarketing evidence that refutes industry propaganda claiming that Botox and related drugs are ‘always safe’ and that no ‘definitive’ cases of botulism have occurred with recommended doses,” Azza AbuDagga, PhD, health services researcher at Public Citizen’s Health Research Group, said in a statement.
Public Citizen said that using data from the FDA’s Adverse Event Reporting System (FAERS), it found 5414 reports of serious outcomes from botulinum toxin products from January 1989 through March 2021. Almost 22% involved cosmetic indications and about 78% involved therapeutic indications.
Of the 5414 reports, 121 (2%) specified botulism as an adverse reaction; 89 involved therapeutic uses of a botulinum toxin products, and 32 involved cosmetic uses. Many of those 121 reports involved doses within the recommended range for the indication, according to Public Citizen.
The group is also asking the FDA to remove what it calls misleading promotional statements in the labeling of Botox and Botox Cosmetic and from the medication guides for those products. The labels state that there have been “no definitive serious adverse event reports of distant spread of toxin effect” with either the cosmetic use or for use in treating chronic migraine, severe underarm sweating, blepharospasm, or strabismus. These statements do not appear in similar labeling in other countries, such as Canada and the United Kingdom, said Public Citizen.
“The FDA needs to implement our two requested actions quickly to warn the public in unambiguous terms about the risk of botulism associated with the use of Botox and related drugs,” Dr. AbuDagga said in the Public Citizen statement. “This will allow health care professionals and patients to make more informed decisions about the benefit-risk profile of these widely used drugs.”
The Public Citizen petition would apply to all seven approved botulinum toxin biological products: abobotulinumtoxinA (Dysport), daxibotulinumtoxinA-lanm (Daxxify), incobotulinumtoxinA (Xeomin), onabotulinumtoxinA (Botox, Botox Cosmetic), prabotulinumtoxinA-xvfs (Jeuveau) and rimabotulinumtoxinB (Myobloc).
An FDA spokesperson said the agency is reviewing the citizen petition, and that generally the agency does not comment on pending petitions. “When we respond to the petition, we will respond directly to the petitioner and post the response in the designated agency docket,” the spokesperson told this news organization. At press time, Botox manufacturer AbbVie had not responded to a request for a comment.
Botulinum toxin is the most-used product for nonsurgical cosmetic procedures, according to the International Society of Aesthetic Plastic Surgery (ISAPS). The ISAPS reported that there were more than 7 million botulinum toxin procedures performed by plastic surgeons worldwide in 2021.
The American Society of Plastic Surgery reported that its members performed 4.4 million Botox procedures in 2020, while the American Society of Dermatologic Surgery (ASDS) said its members performed 2.3 million wrinkle-relaxing procedures in 2019, a 60% increase since 2012.
What Makes Patients Vulnerable to Delusions of Parasitosis?
, reported researchers in a small retrospective case-control study.
Delusions of parasitosis (DOP) affects mostly middle-aged women and has associations with renal failure and some medications, wrote corresponding author Colleen Reisz, MD, a dermatologist with the department of internal medicine at the University of Missouri–Kansas City School of Medicine, and her coauthors. The study was published online December 15, 2023, in the Journal of the American Academy of Dermatology.
“We hypothesize that vulnerability to DOP emerges when multiple factors combine, such as age, sex, medications, and changes in [drug] clearance capacity,” Dr. Reisz and her coauthors wrote. “Changes in health care, such as the dramatic increase in stimulant prescriptions and alternatives to opioids in pain management, may be contributing to off target drug effects on the brain.”
To test their hypothesis, the researchers conducted a case-control study of biometric and pharmaceutical data from 34 patients with DOP which they compared to an age-matched control group of 53 women presenting with a dermatitis above the clavicle from a general dermatology practice between 2012 and 2020. They de-identified the data and performed statistical analysis on variables that included biometric data and intake of pharmaceuticals and nutraceuticals. Polypharmacy was defined as five or more drugs.
Of the 34 patients with DOP, 27 were women with a mean age of 58 years and 7 were men with a mean age of 60 years. Dr. Reisz and her colleagues observed statistical significance between cases and controls in terms of polypharmacy (P = .011), attention-deficit/hyperactivity disorder medications (P < .001), selective serotonin reuptake inhibitors (P = .005), opioids (P = .003), and gabapentin (P = .003).
In other findings, half of DOP cases presented with samples of perceived parasitic material, and four associated the perceived infestation with a single emotion-laden event. This prompted the researchers “to consider that DOP may share mechanisms with fear conditioning and extinction,” they wrote. “Fear conditioning refers to the process of memory acquisition and extinction. This process is essential for survival and has been studied in posttraumatic stress disorder.”
They acknowledged certain limitations of the study, including its retrospective single-center design and the lack of control for factors such as socioeconomic background and level of education.
“Patients with DOP should undergo detailed drug histories and examination of clearance profiles, especially renal function,” the researchers concluded.
Evan A. Rieder, MD, a New York City–based dermatologist and psychiatrist who was asked to comment on the study, said that delusional infestation is one of the most difficult medical conditions to treat and study.
“Though the numbers of cases in this research letter are small, they are instructive in demonstrating a high burden of polypharmacy including psychostimulants, opioids, and SSRIs in such patients,” he told this news organization. “Dermatologists should be performing detailed drug histories, obtaining comprehensive lab work, and considering the effects of medications — both illicit and prescribed — on clinical presentations. While in many cases, delusional patients refuse to consent to psychopharmacologic medications (or treatment in general), the elimination or decrease in dose of certain problematic medications may be helpful in and of themselves.”
The researchers reported having no financial disclosures. Dr. Rieder disclosed that he is a consultant for AbbVie, L’Oréal, Pierre Fabre, Procter & Gamble, and Unilever.
, reported researchers in a small retrospective case-control study.
Delusions of parasitosis (DOP) affects mostly middle-aged women and has associations with renal failure and some medications, wrote corresponding author Colleen Reisz, MD, a dermatologist with the department of internal medicine at the University of Missouri–Kansas City School of Medicine, and her coauthors. The study was published online December 15, 2023, in the Journal of the American Academy of Dermatology.
“We hypothesize that vulnerability to DOP emerges when multiple factors combine, such as age, sex, medications, and changes in [drug] clearance capacity,” Dr. Reisz and her coauthors wrote. “Changes in health care, such as the dramatic increase in stimulant prescriptions and alternatives to opioids in pain management, may be contributing to off target drug effects on the brain.”
To test their hypothesis, the researchers conducted a case-control study of biometric and pharmaceutical data from 34 patients with DOP which they compared to an age-matched control group of 53 women presenting with a dermatitis above the clavicle from a general dermatology practice between 2012 and 2020. They de-identified the data and performed statistical analysis on variables that included biometric data and intake of pharmaceuticals and nutraceuticals. Polypharmacy was defined as five or more drugs.
Of the 34 patients with DOP, 27 were women with a mean age of 58 years and 7 were men with a mean age of 60 years. Dr. Reisz and her colleagues observed statistical significance between cases and controls in terms of polypharmacy (P = .011), attention-deficit/hyperactivity disorder medications (P < .001), selective serotonin reuptake inhibitors (P = .005), opioids (P = .003), and gabapentin (P = .003).
In other findings, half of DOP cases presented with samples of perceived parasitic material, and four associated the perceived infestation with a single emotion-laden event. This prompted the researchers “to consider that DOP may share mechanisms with fear conditioning and extinction,” they wrote. “Fear conditioning refers to the process of memory acquisition and extinction. This process is essential for survival and has been studied in posttraumatic stress disorder.”
They acknowledged certain limitations of the study, including its retrospective single-center design and the lack of control for factors such as socioeconomic background and level of education.
“Patients with DOP should undergo detailed drug histories and examination of clearance profiles, especially renal function,” the researchers concluded.
Evan A. Rieder, MD, a New York City–based dermatologist and psychiatrist who was asked to comment on the study, said that delusional infestation is one of the most difficult medical conditions to treat and study.
“Though the numbers of cases in this research letter are small, they are instructive in demonstrating a high burden of polypharmacy including psychostimulants, opioids, and SSRIs in such patients,” he told this news organization. “Dermatologists should be performing detailed drug histories, obtaining comprehensive lab work, and considering the effects of medications — both illicit and prescribed — on clinical presentations. While in many cases, delusional patients refuse to consent to psychopharmacologic medications (or treatment in general), the elimination or decrease in dose of certain problematic medications may be helpful in and of themselves.”
The researchers reported having no financial disclosures. Dr. Rieder disclosed that he is a consultant for AbbVie, L’Oréal, Pierre Fabre, Procter & Gamble, and Unilever.
, reported researchers in a small retrospective case-control study.
Delusions of parasitosis (DOP) affects mostly middle-aged women and has associations with renal failure and some medications, wrote corresponding author Colleen Reisz, MD, a dermatologist with the department of internal medicine at the University of Missouri–Kansas City School of Medicine, and her coauthors. The study was published online December 15, 2023, in the Journal of the American Academy of Dermatology.
“We hypothesize that vulnerability to DOP emerges when multiple factors combine, such as age, sex, medications, and changes in [drug] clearance capacity,” Dr. Reisz and her coauthors wrote. “Changes in health care, such as the dramatic increase in stimulant prescriptions and alternatives to opioids in pain management, may be contributing to off target drug effects on the brain.”
To test their hypothesis, the researchers conducted a case-control study of biometric and pharmaceutical data from 34 patients with DOP which they compared to an age-matched control group of 53 women presenting with a dermatitis above the clavicle from a general dermatology practice between 2012 and 2020. They de-identified the data and performed statistical analysis on variables that included biometric data and intake of pharmaceuticals and nutraceuticals. Polypharmacy was defined as five or more drugs.
Of the 34 patients with DOP, 27 were women with a mean age of 58 years and 7 were men with a mean age of 60 years. Dr. Reisz and her colleagues observed statistical significance between cases and controls in terms of polypharmacy (P = .011), attention-deficit/hyperactivity disorder medications (P < .001), selective serotonin reuptake inhibitors (P = .005), opioids (P = .003), and gabapentin (P = .003).
In other findings, half of DOP cases presented with samples of perceived parasitic material, and four associated the perceived infestation with a single emotion-laden event. This prompted the researchers “to consider that DOP may share mechanisms with fear conditioning and extinction,” they wrote. “Fear conditioning refers to the process of memory acquisition and extinction. This process is essential for survival and has been studied in posttraumatic stress disorder.”
They acknowledged certain limitations of the study, including its retrospective single-center design and the lack of control for factors such as socioeconomic background and level of education.
“Patients with DOP should undergo detailed drug histories and examination of clearance profiles, especially renal function,” the researchers concluded.
Evan A. Rieder, MD, a New York City–based dermatologist and psychiatrist who was asked to comment on the study, said that delusional infestation is one of the most difficult medical conditions to treat and study.
“Though the numbers of cases in this research letter are small, they are instructive in demonstrating a high burden of polypharmacy including psychostimulants, opioids, and SSRIs in such patients,” he told this news organization. “Dermatologists should be performing detailed drug histories, obtaining comprehensive lab work, and considering the effects of medications — both illicit and prescribed — on clinical presentations. While in many cases, delusional patients refuse to consent to psychopharmacologic medications (or treatment in general), the elimination or decrease in dose of certain problematic medications may be helpful in and of themselves.”
The researchers reported having no financial disclosures. Dr. Rieder disclosed that he is a consultant for AbbVie, L’Oréal, Pierre Fabre, Procter & Gamble, and Unilever.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Is It Time to Air Grievances?
‘Twas the night before Festivus and all through the house, everyone was griping.
In case you’ve only been watching Friends reruns lately, Festivus is a holiday that originated 25 years ago in the last season of Seinfeld. George’s father created it as an alternative to Christmas hype. In addition to an aluminum pole, the holiday features the annual airing of grievances, when one is encouraged to voice complaints. Aluminum poles haven’t replaced Christmas trees, but the spirit of Festivus is still with us in the widespread airing of grievances in 2023.
Complaining isn’t just a post-pandemic problem. Hector spends quite a bit of time complaining about Paris in the Iliad. That was a few pandemics ago. And repining is ubiquitous in literature — as human as walking on two limbs it seems. Ostensibly, we complain to effect change: Something is wrong and we expect it to be different. But that’s not the whole story. No one believes the weather will improve or the Patriots will play better because we complain about them. So why do we bother?
Even if nothing changes on the outside, it does seem to alter our internal state, serving a healthy psychological function. Putting to words what is aggravating can have the same benefit of deep breathing. We describe it as “getting something off our chest” because that’s what it feels like. We feel unburdened just by saying it out loud. Think about the last time you complained: Cranky staff, prior auths, Medicare, disrespectful patients, many of your colleagues will nod in agreement, validating your feelings and making you feel less isolated.
There are also maladaptive reasons for whining. It’s obviously an elementary way to get attention or to remove responsibility. It can also be a political weapon (office politics included). It’s such a potent way to connect that it’s used to build alliances and clout. “Washington is doing a great job,” said no candidate ever. No, if you want to get people on your side, find something irritating and complain to everyone how annoying it is. This solidifies “us” versus “them,” which can harm organizations and families alike.
Yet, eliminating all complaints is neither feasible, nor probably advisable. You could try to make your office a complaint-free zone, but the likely result would be to push any griping to the remote corners where you can no longer hear them. These criticisms might have uncovered missed opportunities, identify problems, and even improve cohesion if done in a safe and transparent setting. If they are left unaddressed or if the underlying culture isn’t sound, then they can propagate and lead to factions that harm productivity.
Griping is as much part of the holiday season as jingle bells and jelly donuts. I don’t believe complaining is up now because people were grumpier in 2023. Rather I think people just craved connection more than ever. So join in: Traffic after the time change, Tesla service, (super) late patients, prior auths, perioral dermatitis, post-COVID telogen effluvium.
I feel better.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X (formerly Twitter). Write to him at dermnews@mdedge.com.
‘Twas the night before Festivus and all through the house, everyone was griping.
In case you’ve only been watching Friends reruns lately, Festivus is a holiday that originated 25 years ago in the last season of Seinfeld. George’s father created it as an alternative to Christmas hype. In addition to an aluminum pole, the holiday features the annual airing of grievances, when one is encouraged to voice complaints. Aluminum poles haven’t replaced Christmas trees, but the spirit of Festivus is still with us in the widespread airing of grievances in 2023.
Complaining isn’t just a post-pandemic problem. Hector spends quite a bit of time complaining about Paris in the Iliad. That was a few pandemics ago. And repining is ubiquitous in literature — as human as walking on two limbs it seems. Ostensibly, we complain to effect change: Something is wrong and we expect it to be different. But that’s not the whole story. No one believes the weather will improve or the Patriots will play better because we complain about them. So why do we bother?
Even if nothing changes on the outside, it does seem to alter our internal state, serving a healthy psychological function. Putting to words what is aggravating can have the same benefit of deep breathing. We describe it as “getting something off our chest” because that’s what it feels like. We feel unburdened just by saying it out loud. Think about the last time you complained: Cranky staff, prior auths, Medicare, disrespectful patients, many of your colleagues will nod in agreement, validating your feelings and making you feel less isolated.
There are also maladaptive reasons for whining. It’s obviously an elementary way to get attention or to remove responsibility. It can also be a political weapon (office politics included). It’s such a potent way to connect that it’s used to build alliances and clout. “Washington is doing a great job,” said no candidate ever. No, if you want to get people on your side, find something irritating and complain to everyone how annoying it is. This solidifies “us” versus “them,” which can harm organizations and families alike.
Yet, eliminating all complaints is neither feasible, nor probably advisable. You could try to make your office a complaint-free zone, but the likely result would be to push any griping to the remote corners where you can no longer hear them. These criticisms might have uncovered missed opportunities, identify problems, and even improve cohesion if done in a safe and transparent setting. If they are left unaddressed or if the underlying culture isn’t sound, then they can propagate and lead to factions that harm productivity.
Griping is as much part of the holiday season as jingle bells and jelly donuts. I don’t believe complaining is up now because people were grumpier in 2023. Rather I think people just craved connection more than ever. So join in: Traffic after the time change, Tesla service, (super) late patients, prior auths, perioral dermatitis, post-COVID telogen effluvium.
I feel better.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X (formerly Twitter). Write to him at dermnews@mdedge.com.
‘Twas the night before Festivus and all through the house, everyone was griping.
In case you’ve only been watching Friends reruns lately, Festivus is a holiday that originated 25 years ago in the last season of Seinfeld. George’s father created it as an alternative to Christmas hype. In addition to an aluminum pole, the holiday features the annual airing of grievances, when one is encouraged to voice complaints. Aluminum poles haven’t replaced Christmas trees, but the spirit of Festivus is still with us in the widespread airing of grievances in 2023.
Complaining isn’t just a post-pandemic problem. Hector spends quite a bit of time complaining about Paris in the Iliad. That was a few pandemics ago. And repining is ubiquitous in literature — as human as walking on two limbs it seems. Ostensibly, we complain to effect change: Something is wrong and we expect it to be different. But that’s not the whole story. No one believes the weather will improve or the Patriots will play better because we complain about them. So why do we bother?
Even if nothing changes on the outside, it does seem to alter our internal state, serving a healthy psychological function. Putting to words what is aggravating can have the same benefit of deep breathing. We describe it as “getting something off our chest” because that’s what it feels like. We feel unburdened just by saying it out loud. Think about the last time you complained: Cranky staff, prior auths, Medicare, disrespectful patients, many of your colleagues will nod in agreement, validating your feelings and making you feel less isolated.
There are also maladaptive reasons for whining. It’s obviously an elementary way to get attention or to remove responsibility. It can also be a political weapon (office politics included). It’s such a potent way to connect that it’s used to build alliances and clout. “Washington is doing a great job,” said no candidate ever. No, if you want to get people on your side, find something irritating and complain to everyone how annoying it is. This solidifies “us” versus “them,” which can harm organizations and families alike.
Yet, eliminating all complaints is neither feasible, nor probably advisable. You could try to make your office a complaint-free zone, but the likely result would be to push any griping to the remote corners where you can no longer hear them. These criticisms might have uncovered missed opportunities, identify problems, and even improve cohesion if done in a safe and transparent setting. If they are left unaddressed or if the underlying culture isn’t sound, then they can propagate and lead to factions that harm productivity.
Griping is as much part of the holiday season as jingle bells and jelly donuts. I don’t believe complaining is up now because people were grumpier in 2023. Rather I think people just craved connection more than ever. So join in: Traffic after the time change, Tesla service, (super) late patients, prior auths, perioral dermatitis, post-COVID telogen effluvium.
I feel better.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X (formerly Twitter). Write to him at dermnews@mdedge.com.
Electronic Health Records — Recent Survey Results
I have been writing about electronic health records since the mid-1990s. While the basic concept has always been sound, I have always been (and continue to be) a critic of its implementation, which I have compared to the work of the Underpants Gnomes from the television show South Park.
You may recall that Phase One of the Gnomes’ grand scheme was to collect underpants, and Phase Three was to reap enormous profits. Unfortunately, they never quite figured out Phase Two.
EHR’s problems have run a similar course, ever since George W. Bush introduced the EHR Incentive Program (later renamed the Promoting Interoperability Program) in 2000. “By computerizing health records,” the president said, “we can avoid dangerous medical mistakes, reduce costs, and improve care.” That was the ultimate goal — Phase Three, if you will — but nearly a quarter-century later, we are still struggling with Phase Two.
According to the results of a recent survey by this news organization, progress has been made, but issues with usability, reliability, and patient privacy remain.
surveys, respectively. But 56% of them continue to worry about harmful effects from incorrect or misdirected information as a result of inputs from multiple sources, and the rapid turnover of staff that is doing the inputting. Many doctors worry about the potential for incorrect medications and “rule out” diagnoses getting embedded in some patients’ records and undermining future care.
The lack of information sharing among different EHR systems has been the technology’s greatest unmet promise, according to the survey. A lack of interoperability was cited as the most common reason for switching EHR systems. Other reasons included difficulties in clinical documentation and extracting data for quality reporting, as well as the inability to merge inpatient and outpatient records.
A clear majority (72%) felt EHR systems are getting easier to use. The recent decrease in government mandates has freed vendors to work on improving ease of documentation and information retrieval. The incorporation of virtual assistants and other artificial intelligence–based features (as I discussed in two recent columns) have also contributed to improved overall usability. Some newer applications even allow users to build workarounds to compensate for inherent deficiencies in the system.
Physicians tended to be most praiseworthy of functions related to electronic prescribing and retrieval of individual patient data. They felt that much more improvement was needed in helpful prompt features, internal messaging, and communications from patients.
The survey found that 38% of physicians “always” or “often” copy and paste information in patient charts, with another 37% doing so “occasionally.” Noting some of the problems inherent in copy and paste, such as note bloat, internal inconsistencies, error propagation, and documentation in the wrong patient chart, the survey authors suggest that EHR developers could help by shifting away from timelines that appear as one long note. They could also add functionality to allow new information to be displayed as updates on a digital chart.
Improvement is also needed in the way the EHR affects patient interactions, according to the survey results. Physicians are still often forced to click to a different screen to find lab results, another for current medications, and still another for past notes, all while trying to communicate with the patient. Such issues are likely to decrease in the next few years as doctors gain the ability to give voice commands to AI-based system add-ons to obtain this information.
Security concerns seem to be decreasing. In this year’s survey, nearly half of all physicians voiced no EHR privacy problems or concerns, even though a recent review of medical literature concluded that security risks remain meaningful. Those who did have privacy concerns were mostly worried about hackers and other unauthorized access to patient information.
The survey found that around 40% of EHR systems are not using patient portals to post lab results, diagnoses and procedure notes, or prescriptions. However, other physicians complained that their systems were too prompt in posting results, so that patients often received them before the doctor did. This is certainly another area where improvement at both extremes is necessary.
Other areas in which physicians saw a need for improvement were in system reliability, user training, and ongoing customer service. And among the dwindling ranks of physicians with no EHR experience, the most common reasons given for refusing to invest in an EHR system were affordability and interference with the doctor-patient relationship.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
I have been writing about electronic health records since the mid-1990s. While the basic concept has always been sound, I have always been (and continue to be) a critic of its implementation, which I have compared to the work of the Underpants Gnomes from the television show South Park.
You may recall that Phase One of the Gnomes’ grand scheme was to collect underpants, and Phase Three was to reap enormous profits. Unfortunately, they never quite figured out Phase Two.
EHR’s problems have run a similar course, ever since George W. Bush introduced the EHR Incentive Program (later renamed the Promoting Interoperability Program) in 2000. “By computerizing health records,” the president said, “we can avoid dangerous medical mistakes, reduce costs, and improve care.” That was the ultimate goal — Phase Three, if you will — but nearly a quarter-century later, we are still struggling with Phase Two.
According to the results of a recent survey by this news organization, progress has been made, but issues with usability, reliability, and patient privacy remain.
surveys, respectively. But 56% of them continue to worry about harmful effects from incorrect or misdirected information as a result of inputs from multiple sources, and the rapid turnover of staff that is doing the inputting. Many doctors worry about the potential for incorrect medications and “rule out” diagnoses getting embedded in some patients’ records and undermining future care.
The lack of information sharing among different EHR systems has been the technology’s greatest unmet promise, according to the survey. A lack of interoperability was cited as the most common reason for switching EHR systems. Other reasons included difficulties in clinical documentation and extracting data for quality reporting, as well as the inability to merge inpatient and outpatient records.
A clear majority (72%) felt EHR systems are getting easier to use. The recent decrease in government mandates has freed vendors to work on improving ease of documentation and information retrieval. The incorporation of virtual assistants and other artificial intelligence–based features (as I discussed in two recent columns) have also contributed to improved overall usability. Some newer applications even allow users to build workarounds to compensate for inherent deficiencies in the system.
Physicians tended to be most praiseworthy of functions related to electronic prescribing and retrieval of individual patient data. They felt that much more improvement was needed in helpful prompt features, internal messaging, and communications from patients.
The survey found that 38% of physicians “always” or “often” copy and paste information in patient charts, with another 37% doing so “occasionally.” Noting some of the problems inherent in copy and paste, such as note bloat, internal inconsistencies, error propagation, and documentation in the wrong patient chart, the survey authors suggest that EHR developers could help by shifting away from timelines that appear as one long note. They could also add functionality to allow new information to be displayed as updates on a digital chart.
Improvement is also needed in the way the EHR affects patient interactions, according to the survey results. Physicians are still often forced to click to a different screen to find lab results, another for current medications, and still another for past notes, all while trying to communicate with the patient. Such issues are likely to decrease in the next few years as doctors gain the ability to give voice commands to AI-based system add-ons to obtain this information.
Security concerns seem to be decreasing. In this year’s survey, nearly half of all physicians voiced no EHR privacy problems or concerns, even though a recent review of medical literature concluded that security risks remain meaningful. Those who did have privacy concerns were mostly worried about hackers and other unauthorized access to patient information.
The survey found that around 40% of EHR systems are not using patient portals to post lab results, diagnoses and procedure notes, or prescriptions. However, other physicians complained that their systems were too prompt in posting results, so that patients often received them before the doctor did. This is certainly another area where improvement at both extremes is necessary.
Other areas in which physicians saw a need for improvement were in system reliability, user training, and ongoing customer service. And among the dwindling ranks of physicians with no EHR experience, the most common reasons given for refusing to invest in an EHR system were affordability and interference with the doctor-patient relationship.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
I have been writing about electronic health records since the mid-1990s. While the basic concept has always been sound, I have always been (and continue to be) a critic of its implementation, which I have compared to the work of the Underpants Gnomes from the television show South Park.
You may recall that Phase One of the Gnomes’ grand scheme was to collect underpants, and Phase Three was to reap enormous profits. Unfortunately, they never quite figured out Phase Two.
EHR’s problems have run a similar course, ever since George W. Bush introduced the EHR Incentive Program (later renamed the Promoting Interoperability Program) in 2000. “By computerizing health records,” the president said, “we can avoid dangerous medical mistakes, reduce costs, and improve care.” That was the ultimate goal — Phase Three, if you will — but nearly a quarter-century later, we are still struggling with Phase Two.
According to the results of a recent survey by this news organization, progress has been made, but issues with usability, reliability, and patient privacy remain.
surveys, respectively. But 56% of them continue to worry about harmful effects from incorrect or misdirected information as a result of inputs from multiple sources, and the rapid turnover of staff that is doing the inputting. Many doctors worry about the potential for incorrect medications and “rule out” diagnoses getting embedded in some patients’ records and undermining future care.
The lack of information sharing among different EHR systems has been the technology’s greatest unmet promise, according to the survey. A lack of interoperability was cited as the most common reason for switching EHR systems. Other reasons included difficulties in clinical documentation and extracting data for quality reporting, as well as the inability to merge inpatient and outpatient records.
A clear majority (72%) felt EHR systems are getting easier to use. The recent decrease in government mandates has freed vendors to work on improving ease of documentation and information retrieval. The incorporation of virtual assistants and other artificial intelligence–based features (as I discussed in two recent columns) have also contributed to improved overall usability. Some newer applications even allow users to build workarounds to compensate for inherent deficiencies in the system.
Physicians tended to be most praiseworthy of functions related to electronic prescribing and retrieval of individual patient data. They felt that much more improvement was needed in helpful prompt features, internal messaging, and communications from patients.
The survey found that 38% of physicians “always” or “often” copy and paste information in patient charts, with another 37% doing so “occasionally.” Noting some of the problems inherent in copy and paste, such as note bloat, internal inconsistencies, error propagation, and documentation in the wrong patient chart, the survey authors suggest that EHR developers could help by shifting away from timelines that appear as one long note. They could also add functionality to allow new information to be displayed as updates on a digital chart.
Improvement is also needed in the way the EHR affects patient interactions, according to the survey results. Physicians are still often forced to click to a different screen to find lab results, another for current medications, and still another for past notes, all while trying to communicate with the patient. Such issues are likely to decrease in the next few years as doctors gain the ability to give voice commands to AI-based system add-ons to obtain this information.
Security concerns seem to be decreasing. In this year’s survey, nearly half of all physicians voiced no EHR privacy problems or concerns, even though a recent review of medical literature concluded that security risks remain meaningful. Those who did have privacy concerns were mostly worried about hackers and other unauthorized access to patient information.
The survey found that around 40% of EHR systems are not using patient portals to post lab results, diagnoses and procedure notes, or prescriptions. However, other physicians complained that their systems were too prompt in posting results, so that patients often received them before the doctor did. This is certainly another area where improvement at both extremes is necessary.
Other areas in which physicians saw a need for improvement were in system reliability, user training, and ongoing customer service. And among the dwindling ranks of physicians with no EHR experience, the most common reasons given for refusing to invest in an EHR system were affordability and interference with the doctor-patient relationship.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
Headache after drinking red wine? This could be why
This transcript has been edited for clarity.
Robert Louis Stevenson famously said, “Wine is bottled poetry.” And I think it works quite well. I’ve had wines that are simple, elegant, and unpretentious like Emily Dickinson, and passionate and mysterious like Pablo Neruda. And I’ve had wines that are more analogous to the limerick you might read scrawled on a rest-stop bathroom wall. Those ones give me headaches.
– and apparently it’s not just the alcohol.
Headaches are common, and headaches after drinking alcohol are particularly common. An interesting epidemiologic phenomenon, not yet adequately explained, is why red wine is associated with more headache than other forms of alcohol. There have been many studies fingering many suspects, from sulfites to tannins to various phenolic compounds, but none have really provided a concrete explanation for what might be going on.
A new hypothesis came to the fore on Nov. 20 in the journal Scientific Reports:
To understand the idea, first a reminder of what happens when you drink alcohol, physiologically.
Alcohol is metabolized by the enzyme alcohol dehydrogenase in the gut and then in the liver. That turns it into acetaldehyde, a toxic metabolite. In most of us, aldehyde dehydrogenase (ALDH) quickly metabolizes acetaldehyde to the inert acetate, which can be safely excreted.
I say “most of us” because some populations, particularly those with East Asian ancestry, have a mutation in the ALDH gene which can lead to accumulation of toxic acetaldehyde with alcohol consumption – leading to facial flushing, nausea, and headache.
We can also inhibit the enzyme medically. That’s what the drug disulfiram, also known as Antabuse, does. It doesn’t prevent you from wanting to drink; it makes the consequences of drinking incredibly aversive.
The researchers focused in on the aldehyde dehydrogenase enzyme and conducted a screening study. Are there any compounds in red wine that naturally inhibit ALDH?
The results pointed squarely at quercetin, and particularly its metabolite quercetin glucuronide, which, at 20 micromolar concentrations, inhibited about 80% of ALDH activity.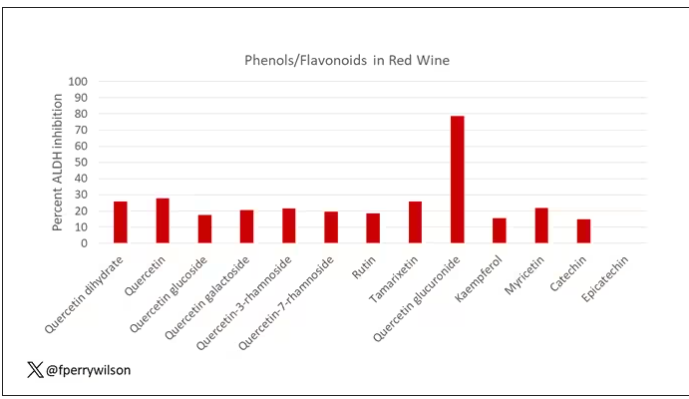
Quercetin is a flavonoid – a compound that gives color to a variety of vegetables and fruits, including grapes. In a test tube, it is an antioxidant, which is enough evidence to spawn a small quercetin-as-supplement industry, but there is no convincing evidence that it is medically useful. The authors then examined the concentration of quercetin glucuronide to achieve various inhibitions of ALDH, as you can see in this graph here.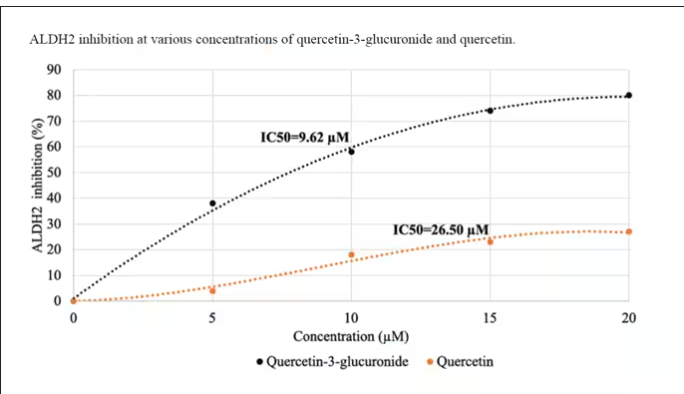
By about 10 micromolar, we see a decent amount of inhibition. Disulfiram is about 10 times more potent than that, but then again, you don’t drink three glasses of disulfiram with Thanksgiving dinner.
This is where this study stops. But it obviously tells us very little about what might be happening in the human body. For that, we need to ask the question: Can we get our quercetin levels to 10 micromolar? Is that remotely achievable?
Let’s start with how much quercetin there is in red wine. Like all things wine, it varies, but this study examining Australian wines found mean concentrations of 11 mg/L. The highest value I saw was close to 50 mg/L.
So let’s do some math. To make the numbers easy, let’s say you drank a liter of Australian wine, taking in 50 mg of quercetin glucuronide.
How much of that gets into your bloodstream? Some studies suggest a bioavailability of less than 1%, which basically means none and should probably put the quercetin hypothesis to bed. But there is some variation here too; it seems to depend on the form of quercetin you ingest.
Let’s say all 50 mg gets into your bloodstream. What blood concentration would that lead to? Well, I’ll keep the stoichiometry in the graphics and just say that if we assume that the volume of distribution of the compound is restricted to plasma alone, then you could achieve similar concentrations to what was done in petri dishes during this study.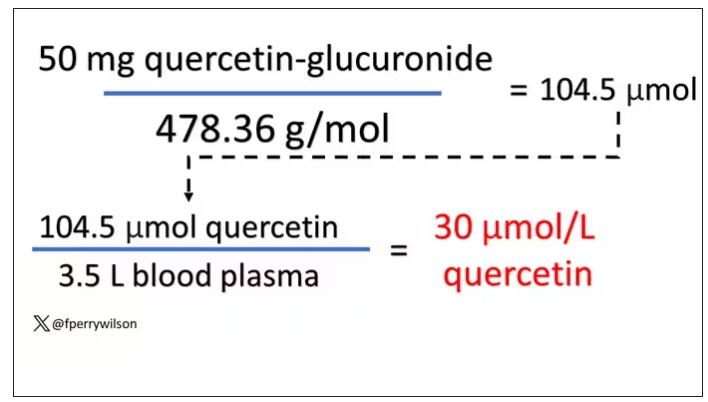
Of course, if quercetin is really the culprit behind red wine headache, I have some questions: Why aren’t the Amazon reviews of quercetin supplements chock full of warnings not to take them with alcohol? And other foods have way higher quercetin concentration than wine, but you don’t hear people warning not to take your red onions with alcohol, or your capers, or lingonberries.
There’s some more work to be done here – most importantly, some human studies. Let’s give people wine with different amounts of quercetin and see what happens. Sign me up. Seriously.
As for Thanksgiving, it’s worth noting that cranberries have a lot of quercetin in them. So between the cranberry sauce, the Beaujolais, and your uncle ranting about the contrails again, the probability of headache is pretty darn high. Stay safe out there, and Happy Thanksgiving.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Robert Louis Stevenson famously said, “Wine is bottled poetry.” And I think it works quite well. I’ve had wines that are simple, elegant, and unpretentious like Emily Dickinson, and passionate and mysterious like Pablo Neruda. And I’ve had wines that are more analogous to the limerick you might read scrawled on a rest-stop bathroom wall. Those ones give me headaches.
– and apparently it’s not just the alcohol.
Headaches are common, and headaches after drinking alcohol are particularly common. An interesting epidemiologic phenomenon, not yet adequately explained, is why red wine is associated with more headache than other forms of alcohol. There have been many studies fingering many suspects, from sulfites to tannins to various phenolic compounds, but none have really provided a concrete explanation for what might be going on.
A new hypothesis came to the fore on Nov. 20 in the journal Scientific Reports:
To understand the idea, first a reminder of what happens when you drink alcohol, physiologically.
Alcohol is metabolized by the enzyme alcohol dehydrogenase in the gut and then in the liver. That turns it into acetaldehyde, a toxic metabolite. In most of us, aldehyde dehydrogenase (ALDH) quickly metabolizes acetaldehyde to the inert acetate, which can be safely excreted.
I say “most of us” because some populations, particularly those with East Asian ancestry, have a mutation in the ALDH gene which can lead to accumulation of toxic acetaldehyde with alcohol consumption – leading to facial flushing, nausea, and headache.
We can also inhibit the enzyme medically. That’s what the drug disulfiram, also known as Antabuse, does. It doesn’t prevent you from wanting to drink; it makes the consequences of drinking incredibly aversive.
The researchers focused in on the aldehyde dehydrogenase enzyme and conducted a screening study. Are there any compounds in red wine that naturally inhibit ALDH?
The results pointed squarely at quercetin, and particularly its metabolite quercetin glucuronide, which, at 20 micromolar concentrations, inhibited about 80% of ALDH activity.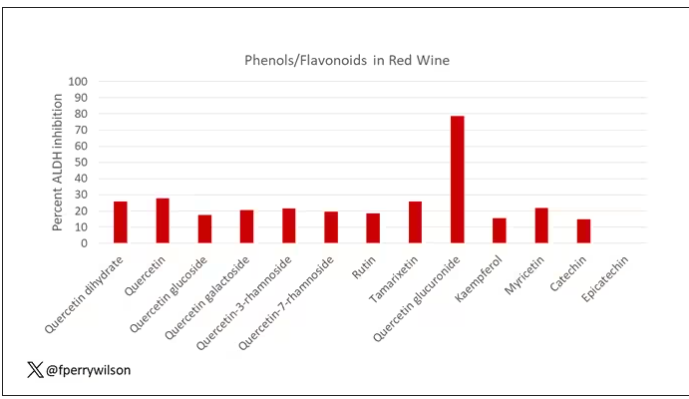
Quercetin is a flavonoid – a compound that gives color to a variety of vegetables and fruits, including grapes. In a test tube, it is an antioxidant, which is enough evidence to spawn a small quercetin-as-supplement industry, but there is no convincing evidence that it is medically useful. The authors then examined the concentration of quercetin glucuronide to achieve various inhibitions of ALDH, as you can see in this graph here.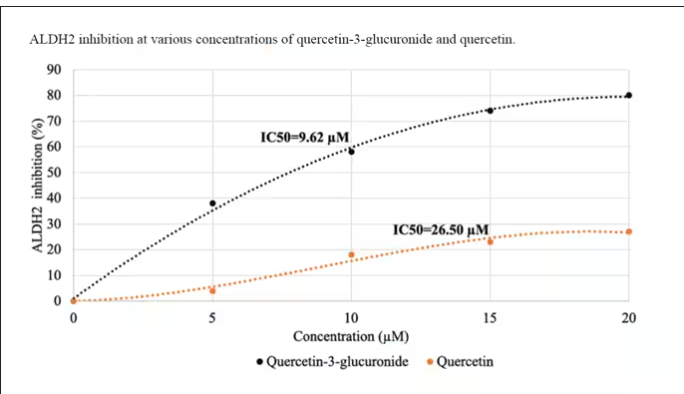
By about 10 micromolar, we see a decent amount of inhibition. Disulfiram is about 10 times more potent than that, but then again, you don’t drink three glasses of disulfiram with Thanksgiving dinner.
This is where this study stops. But it obviously tells us very little about what might be happening in the human body. For that, we need to ask the question: Can we get our quercetin levels to 10 micromolar? Is that remotely achievable?
Let’s start with how much quercetin there is in red wine. Like all things wine, it varies, but this study examining Australian wines found mean concentrations of 11 mg/L. The highest value I saw was close to 50 mg/L.
So let’s do some math. To make the numbers easy, let’s say you drank a liter of Australian wine, taking in 50 mg of quercetin glucuronide.
How much of that gets into your bloodstream? Some studies suggest a bioavailability of less than 1%, which basically means none and should probably put the quercetin hypothesis to bed. But there is some variation here too; it seems to depend on the form of quercetin you ingest.
Let’s say all 50 mg gets into your bloodstream. What blood concentration would that lead to? Well, I’ll keep the stoichiometry in the graphics and just say that if we assume that the volume of distribution of the compound is restricted to plasma alone, then you could achieve similar concentrations to what was done in petri dishes during this study.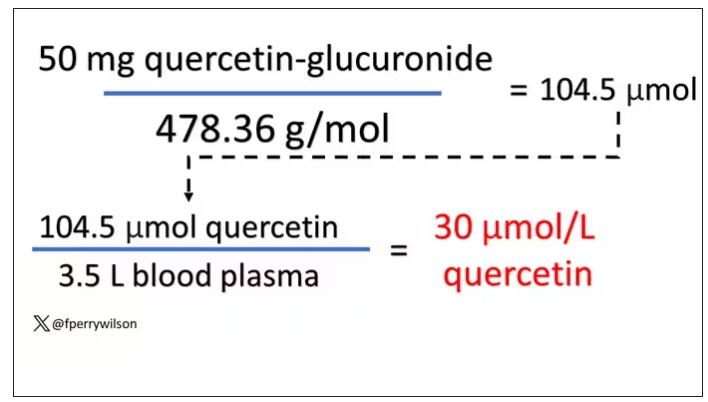
Of course, if quercetin is really the culprit behind red wine headache, I have some questions: Why aren’t the Amazon reviews of quercetin supplements chock full of warnings not to take them with alcohol? And other foods have way higher quercetin concentration than wine, but you don’t hear people warning not to take your red onions with alcohol, or your capers, or lingonberries.
There’s some more work to be done here – most importantly, some human studies. Let’s give people wine with different amounts of quercetin and see what happens. Sign me up. Seriously.
As for Thanksgiving, it’s worth noting that cranberries have a lot of quercetin in them. So between the cranberry sauce, the Beaujolais, and your uncle ranting about the contrails again, the probability of headache is pretty darn high. Stay safe out there, and Happy Thanksgiving.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Robert Louis Stevenson famously said, “Wine is bottled poetry.” And I think it works quite well. I’ve had wines that are simple, elegant, and unpretentious like Emily Dickinson, and passionate and mysterious like Pablo Neruda. And I’ve had wines that are more analogous to the limerick you might read scrawled on a rest-stop bathroom wall. Those ones give me headaches.
– and apparently it’s not just the alcohol.
Headaches are common, and headaches after drinking alcohol are particularly common. An interesting epidemiologic phenomenon, not yet adequately explained, is why red wine is associated with more headache than other forms of alcohol. There have been many studies fingering many suspects, from sulfites to tannins to various phenolic compounds, but none have really provided a concrete explanation for what might be going on.
A new hypothesis came to the fore on Nov. 20 in the journal Scientific Reports:
To understand the idea, first a reminder of what happens when you drink alcohol, physiologically.
Alcohol is metabolized by the enzyme alcohol dehydrogenase in the gut and then in the liver. That turns it into acetaldehyde, a toxic metabolite. In most of us, aldehyde dehydrogenase (ALDH) quickly metabolizes acetaldehyde to the inert acetate, which can be safely excreted.
I say “most of us” because some populations, particularly those with East Asian ancestry, have a mutation in the ALDH gene which can lead to accumulation of toxic acetaldehyde with alcohol consumption – leading to facial flushing, nausea, and headache.
We can also inhibit the enzyme medically. That’s what the drug disulfiram, also known as Antabuse, does. It doesn’t prevent you from wanting to drink; it makes the consequences of drinking incredibly aversive.
The researchers focused in on the aldehyde dehydrogenase enzyme and conducted a screening study. Are there any compounds in red wine that naturally inhibit ALDH?
The results pointed squarely at quercetin, and particularly its metabolite quercetin glucuronide, which, at 20 micromolar concentrations, inhibited about 80% of ALDH activity.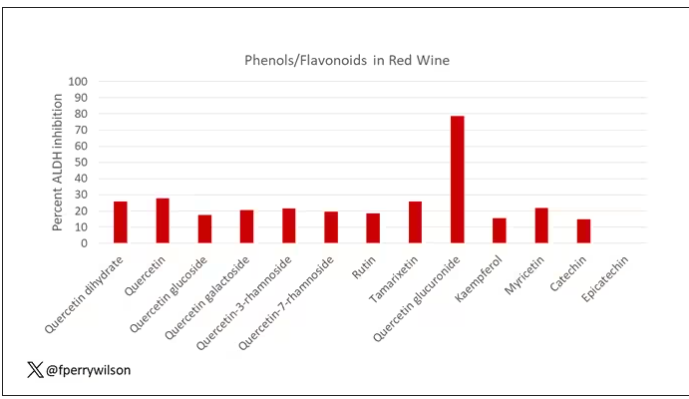
Quercetin is a flavonoid – a compound that gives color to a variety of vegetables and fruits, including grapes. In a test tube, it is an antioxidant, which is enough evidence to spawn a small quercetin-as-supplement industry, but there is no convincing evidence that it is medically useful. The authors then examined the concentration of quercetin glucuronide to achieve various inhibitions of ALDH, as you can see in this graph here.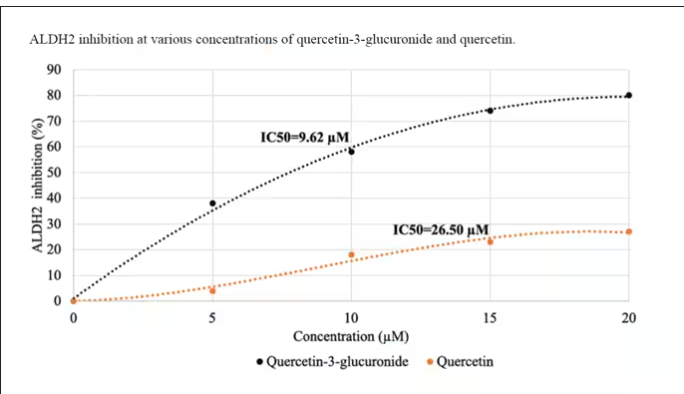
By about 10 micromolar, we see a decent amount of inhibition. Disulfiram is about 10 times more potent than that, but then again, you don’t drink three glasses of disulfiram with Thanksgiving dinner.
This is where this study stops. But it obviously tells us very little about what might be happening in the human body. For that, we need to ask the question: Can we get our quercetin levels to 10 micromolar? Is that remotely achievable?
Let’s start with how much quercetin there is in red wine. Like all things wine, it varies, but this study examining Australian wines found mean concentrations of 11 mg/L. The highest value I saw was close to 50 mg/L.
So let’s do some math. To make the numbers easy, let’s say you drank a liter of Australian wine, taking in 50 mg of quercetin glucuronide.
How much of that gets into your bloodstream? Some studies suggest a bioavailability of less than 1%, which basically means none and should probably put the quercetin hypothesis to bed. But there is some variation here too; it seems to depend on the form of quercetin you ingest.
Let’s say all 50 mg gets into your bloodstream. What blood concentration would that lead to? Well, I’ll keep the stoichiometry in the graphics and just say that if we assume that the volume of distribution of the compound is restricted to plasma alone, then you could achieve similar concentrations to what was done in petri dishes during this study.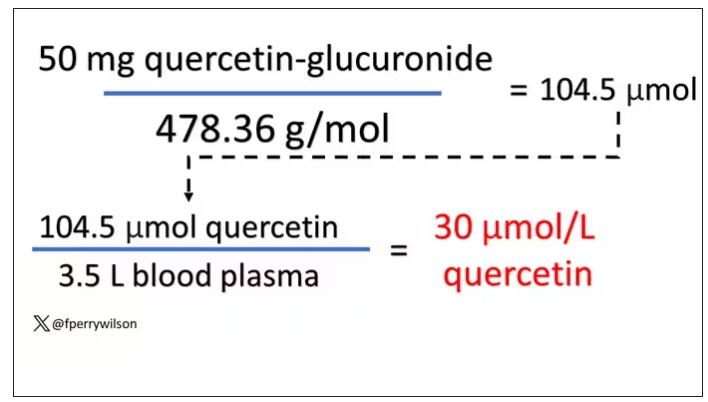
Of course, if quercetin is really the culprit behind red wine headache, I have some questions: Why aren’t the Amazon reviews of quercetin supplements chock full of warnings not to take them with alcohol? And other foods have way higher quercetin concentration than wine, but you don’t hear people warning not to take your red onions with alcohol, or your capers, or lingonberries.
There’s some more work to be done here – most importantly, some human studies. Let’s give people wine with different amounts of quercetin and see what happens. Sign me up. Seriously.
As for Thanksgiving, it’s worth noting that cranberries have a lot of quercetin in them. So between the cranberry sauce, the Beaujolais, and your uncle ranting about the contrails again, the probability of headache is pretty darn high. Stay safe out there, and Happy Thanksgiving.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
UHC accused of using AI to skirt doctors’ orders, deny claims
.
In a class action suit filed in Minnesota district court, the attorneys for the families of two deceased UHC Medicare Advantage plan policyholders say that the company uses the technology to systematically deny skilled nursing facility (SNF) claims and shirk its responsibility to adhere to Medicare’s coverage determination standards.
The case raises ethical and legal questions about whether AI can replace or supplement human tasks and interactions, particularly in a field as complex as health care. California-based public advocacy firm Clarkson Law filed a similar complaint against Cigna earlier this year and has previously sued tech giants Google and ChatGPT creator OpenAI for harvesting Internet users’ data to train their AI systems.
Clarkson Law represents the plaintiffs and says that the policyholders had to pay thousands in out-of-pocket costs or forgo the recommended postacute care owing to UHC’s faulty AI model, nH Predict. The tool has a 90% error rate, says the lawsuit, as evidenced by the number of claims that are reversed following review by a medical professional. Still, just 0.2% of policyholders appeal the denials.
nH Predict was created by naviHealth and was acquired by UnitedHealth Group, UHC’s parent company, in 2020. In a statement to Bloomberg Law, a spokesperson for naviHealth said that the lawsuit has no merit and the model was not used for making coverage determinations.
According to the complaint, nH Predict determines the appropriate amount of SNF, home health, or rehabilitation services a patient requires on the basis of the diagnosis, age, and living situation. The model compares the patient with its database of 6 million patients and estimates the ideal length of stay and target discharge date, “pinpointing the precise moment when [UHC] will cut off payment for a patient’s treatment.”
The lawsuit says that employees are instructed to strictly adhere to the AI model’s predictions, and those who do not are disciplined and terminated, even when additional care for the patient is warranted. Employees are told that the generated reports contain proprietary information and that they cannot share them with physicians and patients who inquire about extending care.
“Every patient is entitled to a nuanced evaluation of their health care needs,” Zarrina Ozari, senior associate at Clarkson Law, said in a prepared statement. “By replacing licensed practitioners with unchecked AI, UHC is telling its patients that they are completely interchangeable with one another and undervaluing the expertise of the physicians devoted to key elements of care.”
According to the complaint, Gene Lokken fell in May 2022 and fractured his leg and ankle. After a 1-month SNF stay, the 91-year-old man’s doctor ordered physical therapy. However, the insurer said Mr. Lokken was safe to be discharged home two and a half weeks later, conflicting with a physical therapist’s notes that indicated he still had paralyzed and weak muscles. The insurer denied Mr. Lokken’s appeal. He remained in the facility for another year until his death, paying about $150,000 in out-of-pocket expenses, according to the lawsuit.
Another patient, Dale H. Tetzloff, initially spent just 20 days in a SNF for stroke rehabilitation before UHC denied coverage. An appeal later extended the stay to 40 days, short of the 100 days recommended by his physician. Requests for further extensions were unsuccessful, and Mr. Tetzloff ultimately paid about $70,000 in out-of-pocket expenses over the next 10 months, according to the complaint.
New federal rules prohibit Medicare Advantage plans from relying on an algorithm or software to make medically necessary determinations instead of an individual’s specific circumstances. Any medical necessity denial must be “reviewed by a physician or other appropriate health care professional with expertise in the field of medicine or health care that is appropriate for the service at issue.”
Clarkson is demanding a jury trial and has asked the court to certify the case as a federal class action, which could open the suit to any U.S. resident who purchased a UHC Medicare Advantage plan in the past 4 years.
A version of this article appeared on Medscape.com.
.
In a class action suit filed in Minnesota district court, the attorneys for the families of two deceased UHC Medicare Advantage plan policyholders say that the company uses the technology to systematically deny skilled nursing facility (SNF) claims and shirk its responsibility to adhere to Medicare’s coverage determination standards.
The case raises ethical and legal questions about whether AI can replace or supplement human tasks and interactions, particularly in a field as complex as health care. California-based public advocacy firm Clarkson Law filed a similar complaint against Cigna earlier this year and has previously sued tech giants Google and ChatGPT creator OpenAI for harvesting Internet users’ data to train their AI systems.
Clarkson Law represents the plaintiffs and says that the policyholders had to pay thousands in out-of-pocket costs or forgo the recommended postacute care owing to UHC’s faulty AI model, nH Predict. The tool has a 90% error rate, says the lawsuit, as evidenced by the number of claims that are reversed following review by a medical professional. Still, just 0.2% of policyholders appeal the denials.
nH Predict was created by naviHealth and was acquired by UnitedHealth Group, UHC’s parent company, in 2020. In a statement to Bloomberg Law, a spokesperson for naviHealth said that the lawsuit has no merit and the model was not used for making coverage determinations.
According to the complaint, nH Predict determines the appropriate amount of SNF, home health, or rehabilitation services a patient requires on the basis of the diagnosis, age, and living situation. The model compares the patient with its database of 6 million patients and estimates the ideal length of stay and target discharge date, “pinpointing the precise moment when [UHC] will cut off payment for a patient’s treatment.”
The lawsuit says that employees are instructed to strictly adhere to the AI model’s predictions, and those who do not are disciplined and terminated, even when additional care for the patient is warranted. Employees are told that the generated reports contain proprietary information and that they cannot share them with physicians and patients who inquire about extending care.
“Every patient is entitled to a nuanced evaluation of their health care needs,” Zarrina Ozari, senior associate at Clarkson Law, said in a prepared statement. “By replacing licensed practitioners with unchecked AI, UHC is telling its patients that they are completely interchangeable with one another and undervaluing the expertise of the physicians devoted to key elements of care.”
According to the complaint, Gene Lokken fell in May 2022 and fractured his leg and ankle. After a 1-month SNF stay, the 91-year-old man’s doctor ordered physical therapy. However, the insurer said Mr. Lokken was safe to be discharged home two and a half weeks later, conflicting with a physical therapist’s notes that indicated he still had paralyzed and weak muscles. The insurer denied Mr. Lokken’s appeal. He remained in the facility for another year until his death, paying about $150,000 in out-of-pocket expenses, according to the lawsuit.
Another patient, Dale H. Tetzloff, initially spent just 20 days in a SNF for stroke rehabilitation before UHC denied coverage. An appeal later extended the stay to 40 days, short of the 100 days recommended by his physician. Requests for further extensions were unsuccessful, and Mr. Tetzloff ultimately paid about $70,000 in out-of-pocket expenses over the next 10 months, according to the complaint.
New federal rules prohibit Medicare Advantage plans from relying on an algorithm or software to make medically necessary determinations instead of an individual’s specific circumstances. Any medical necessity denial must be “reviewed by a physician or other appropriate health care professional with expertise in the field of medicine or health care that is appropriate for the service at issue.”
Clarkson is demanding a jury trial and has asked the court to certify the case as a federal class action, which could open the suit to any U.S. resident who purchased a UHC Medicare Advantage plan in the past 4 years.
A version of this article appeared on Medscape.com.
.
In a class action suit filed in Minnesota district court, the attorneys for the families of two deceased UHC Medicare Advantage plan policyholders say that the company uses the technology to systematically deny skilled nursing facility (SNF) claims and shirk its responsibility to adhere to Medicare’s coverage determination standards.
The case raises ethical and legal questions about whether AI can replace or supplement human tasks and interactions, particularly in a field as complex as health care. California-based public advocacy firm Clarkson Law filed a similar complaint against Cigna earlier this year and has previously sued tech giants Google and ChatGPT creator OpenAI for harvesting Internet users’ data to train their AI systems.
Clarkson Law represents the plaintiffs and says that the policyholders had to pay thousands in out-of-pocket costs or forgo the recommended postacute care owing to UHC’s faulty AI model, nH Predict. The tool has a 90% error rate, says the lawsuit, as evidenced by the number of claims that are reversed following review by a medical professional. Still, just 0.2% of policyholders appeal the denials.
nH Predict was created by naviHealth and was acquired by UnitedHealth Group, UHC’s parent company, in 2020. In a statement to Bloomberg Law, a spokesperson for naviHealth said that the lawsuit has no merit and the model was not used for making coverage determinations.
According to the complaint, nH Predict determines the appropriate amount of SNF, home health, or rehabilitation services a patient requires on the basis of the diagnosis, age, and living situation. The model compares the patient with its database of 6 million patients and estimates the ideal length of stay and target discharge date, “pinpointing the precise moment when [UHC] will cut off payment for a patient’s treatment.”
The lawsuit says that employees are instructed to strictly adhere to the AI model’s predictions, and those who do not are disciplined and terminated, even when additional care for the patient is warranted. Employees are told that the generated reports contain proprietary information and that they cannot share them with physicians and patients who inquire about extending care.
“Every patient is entitled to a nuanced evaluation of their health care needs,” Zarrina Ozari, senior associate at Clarkson Law, said in a prepared statement. “By replacing licensed practitioners with unchecked AI, UHC is telling its patients that they are completely interchangeable with one another and undervaluing the expertise of the physicians devoted to key elements of care.”
According to the complaint, Gene Lokken fell in May 2022 and fractured his leg and ankle. After a 1-month SNF stay, the 91-year-old man’s doctor ordered physical therapy. However, the insurer said Mr. Lokken was safe to be discharged home two and a half weeks later, conflicting with a physical therapist’s notes that indicated he still had paralyzed and weak muscles. The insurer denied Mr. Lokken’s appeal. He remained in the facility for another year until his death, paying about $150,000 in out-of-pocket expenses, according to the lawsuit.
Another patient, Dale H. Tetzloff, initially spent just 20 days in a SNF for stroke rehabilitation before UHC denied coverage. An appeal later extended the stay to 40 days, short of the 100 days recommended by his physician. Requests for further extensions were unsuccessful, and Mr. Tetzloff ultimately paid about $70,000 in out-of-pocket expenses over the next 10 months, according to the complaint.
New federal rules prohibit Medicare Advantage plans from relying on an algorithm or software to make medically necessary determinations instead of an individual’s specific circumstances. Any medical necessity denial must be “reviewed by a physician or other appropriate health care professional with expertise in the field of medicine or health care that is appropriate for the service at issue.”
Clarkson is demanding a jury trial and has asked the court to certify the case as a federal class action, which could open the suit to any U.S. resident who purchased a UHC Medicare Advantage plan in the past 4 years.
A version of this article appeared on Medscape.com.
Before signing an offer letter: Read this
You’ve just received an offer letter from that job you interviewed for. Sometimes you want to let the employer know right away how interested you are. The verbiage says the letter isn’t “binding.” So you eagerly sign on the dotted line. Everything looks great ... until it isn’t.
Attorney Ericka Adler, JD, LLM, a partner at Roetzel & Andress, a Chicago-based law firm that represents physicians and health care professionals nationwide, described her client who was in this predicament. The physician, a dermatologist, left a practice where she had been employed because she had received an “amazing” offer letter that included promises about her new work location, staffing, equipment, and hours. She signed and immediately gave notice to her previous employer.
“When she received the actual employment contract, none of those details from the offer letter – which is also called a letter of intent [LOI] – were included,” Ms. Adler told this news organization. The physician wanted to have the details from the LOI formally spelled out in the contract, but the employer refused.
“Basically, they said, ‘This is our standard contract and you’ll just have to trust us that we’ll keep our word. We meant what we said in the LOI, but we cannot include those details in the actual agreement because everyone has the same form of agreement.’ “ The physician decided to sign the contract and accept the position.
She contacted Ms. Adler after she had been at her new position for a month. “She had received none of the things they had promised her in the LOI,” Ms. Adler reported. “She lacked the NP and PA support, she lacked the equipment, she didn’t have enough exam rooms. As soon as she started, someone with whom she was sharing call coverage left, and she was expected to take over. The LOI had a cap on the amount of call she would be required to take, but that verbiage didn’t make it into the contract.”
Ms. Adler tried to address this issue with the employer. “We couldn’t say they had literally breached the agreement, but we did list the things that were mentioned in the LOI but on which they hadn’t delivered. We asked them to fix the issue within 10 days.”
The employer argued “that they didn’t have to fulfill anything that wasn’t spelled out in the contract, even if it was in the LOI. In fact, the contract specified clearly that the signed employment agreement was the only agreement and replaced any previous written or oral agreements between the parties.”
The dermatologist ultimately left the new position. “She might have been able to have a legal claim against the employer for breach or perhaps ‘detrimental reliance’ – meaning, she might have argued that she had been financially harmed due to the false promises made to her. But it would have been difficult and expensive for her to litigate the issue,” said Ms. Adler.
“It also didn’t seem like the physician could remain in the job and develop a positive work relationship with the employer, given that she felt betrayed and misled, and didn’t like the terms of employment, which didn’t match her needs or expectations,” said Ms. Adler.
She added that “most employers are not as unscrupulous and dishonest as this one was. But some employers do play on the fact that younger doctors – especially residents and fellows – tend to be trusting or feel they don’t have negotiation power. They’re often excited to get an offer and sign it without a second thought.”
That’s why she advises physicians to “review the terms of the LOI carefully and make sure you’re comfortable with them before signing it; but know that the real contract to negotiate will be the actual Employment Agreement.”
She also advises physicians not to give notice at their current place of employment until they’ve signed the final contract with the new employer.
On the same page?
Anu Murthy, JD, an attorney and associate contract review specialist at Contract Diagnostics, explained that the LOI is a document that the candidate receives after an interview but before a full contract. Sometimes, the LOI is preceded by a verbal or e-mailed offer, which is less formal.
“An LOI is sometimes called a Term Sheet or Memorandum of Understanding,“ Ms. Murthy told this news organization. “Typically, it lays out key provisions, such as compensation, initial term of the contract, location, and recruitment incentives.” Sometimes it includes mention of staffing, call schedule, malpractice, noncompete covenants, and other components of the position.
Justin Nabity, founder and CEO of Physicians Thrive, a physician financial advisory group, said that LOIs are “a way for employers to gauge a prospective employee’s level of interest.”
The employer “doesn’t want to send a contract with a lot of details before determining whether the candidate is really serious about the position, so the offer letter doesn’t show the whole picture,” Mr. Nabity told this news organization.
Dennis Hursh, managing partner of Physician Agreements Health Law, a Pennsylvania-based law firm that represents physicians, agreed.
“Another way of putting it is that the employer wants to see whether the prospective employee is on the same page. The LOI will typically include some key components that will later appear in a more complete and formal contract, together with other topics and details. Agreeing to those key components signals that indeed you and the employer are in accord,” said Mr. Hursh.
But are you really on the same page with your prospective employer? And if you seem to be on the same page, and you sign the LOI, is that a guarantee that the employer will honor its terms?
Not necessarily, according to the experts. In fact, many LOIs contain some verbiage stating that the letter isn’t binding, which can be confusing. Others suggest that it is binding, but the candidate doesn’t realize that the letter isn’t a formal contract and that the contract may contain details not included in the LOI or may omit details mentioned in the LOI, as happened to Ms. Adler’s unfortunate client.
“One of the pitfalls I see is that doctors sign the LOI without recognizing whether it’s binding or nonbinding,” Ms. Murthy said. “If it’s binding, it creates a legal obligation on your part and could preclude you from further negotiation once you see the contract and feel you’d like to negotiate some of its terms.”
Binding letters are typically offered to candidates after some back-and-forth between the parties, and important terms have been agreed to, which can happen either verbally or via e-mail. Once these agreements have been reached, they’re summarized in a “binding” letter before being extended into a full contract.
“But even if you’ve agreed on the terms verbally, it’s still important to have someone more experienced review the offer letter before signing it,” Ms. Murthy said. “It’s important to understand the ‘legalese’ and what your rights and obligations are before agreeing to anything.”
And certainly, if you receive a binding LOI, you shouldn’t sign anything until you’re sure you’re comfortable with its contents and have more details.
Are “nonbinding” LOIs really not binding?
Even if the LOI is nonbinding, that doesn’t necessarily mean you can sign it and expect to negotiate later. “I see people tripped up when they sign the LOI, thinking they’ll negotiate later,” said Mr. Hursh. “They may not like the terms – for example, they think the compensation is too low – and they figure they’ll work it out at the contract stage, because the LOI is ‘not legally binding.’ “
But because the candidate signed the LOI, “the employer is under the impression that the compensation was acceptable, so now you’ve tied your hands – and the hands of any attorney you may consult down the road – to negotiate those terms.”
Mr. Hursh said he is often consulted by physicians who signed the contract “to get the ball rolling,” thinking that the LOI was “just a meaningless bureaucratic paper.” They need to understand “that the employer wants to make sure they’re in agreement on the basic points before getting into the details,” he said. “Large hospitals with in-house counsel may not want to use their legal department’s valuable time in redrafting terms they thought were acceptable to the candidate, and most practices don’t want to pay a lawyer to draft an LOI and then come back and say, ‘Actually, the physician wants more compensation.’ “
Mr. Nabity summarized: “The LOI is essentially a negotiation tactic to take some of the cards out of the hands of the doctor and commit him or her to something they’re not ready to commit to.” Employers may be playing on the sense of pressure and candidate’s fear that the job will slip through their fingers if they wait too long to sign. “But it’s better to wait longer at this stage before signing even a nonbinding LOI,” he said.
What to do before signing
So how should physicians relate to the LOI? Mr. Nabity advises “working through the details of the offer letter first, going through it carefully and identifying areas of concern, bearing in mind that employers never begin with their best offer.”
He pointed out that physicians “rarely know their value and usually don’t know how to work through the dynamics of compensation, call schedules, additional incentives, bonuses, and productivity,” so they need to be informed about these areas before signing anything.
Ms. Murthy recommended “going back and saying [to the prospective employer], ‘Thank you, but I need time to consider and evaluate this offer.’ Then, do some due diligence.”
At that point, you can hire an attorney to go over the offer, educate yourself about compensation benchmarks and what your worth actually is, or consult another trained professional or more experienced individual who can review the LOI before you sign it.
That’s what Dominique Cleveland, MD, a Texas-based ob.gyn., did when she received an LOI 5 years ago.
“The offer letter from the group practice contained a statement that the group wanted me to come on board, what the salary would be, and the time frame that would be covered in the contract,” she told this news organization. “It mentioned benefits and incentives and relocation, but it was only a short document – maybe one or two pages long.”
At the time that she received her LOI, Dr. Cleveland was completing her residency. She consulted experienced faculty members from her institution to find out whether the terms laid out in the LOI “were the norm and were reasonable.” She was “fairly certain” that the salary was low and this was confirmed by the faculty members she talked to. “So I felt comfortable asking for more [compensation],” she said.
The employer was receptive to her proposed changes, which were included in the more detailed contract that followed. “I can’t say there were any surprises per se in the contract because I had negotiated my salary after receiving the offer letter,” she said. She accepted the position and has been working there ever since.
Dr. Cleveland advises physicians “not to make a decision without speaking to someone who’s experienced and can help you compare what’s out there.”
She also encourages physicians to ask for what they want, whether it’s compensation or something else, such as call schedule or vacation time, without being afraid. “I’m a firm believer that you won’t know what you can get if you don’t ask for it,” she said.
Negotiation tips
Mr. Nabity recommended not agreeing to any terms until you are ready to enter into negotiation, recognizing that negotiation is an “art” that requires skill and training. “Either get trained in negotiation, perhaps taking courses to advocate for yourself – which is rare, and most doctors aren’t likely to do this – or go to a trained advocate, such as a lawyer, who can do so on your behalf.”
You might share your concerns with the person who interviewed you, with the person whose name is on the LOI, or with the recruiter who can advocate on your behalf, Ms. Murthy said. “You can reach out to the recruiter and say, ‘I really appreciate the opportunity, but there are some things in the offer letter I’d like to continue discussing.’ “
When you’re ready to negotiate, be sure to assemble all of your “asks” in a single document rather than going back to the prospective employer with “multiple individual questions multiple times,” Ms. Murthy advised. It’s more efficient and the employer or recruiter will appreciate that.
She also advised couching your request in language that expresses your appreciation for the offer and stating that you would like the agreement to serve the best interests of both parties. “Use open-ended language like that, and ask if it’s all right for you to send back some questions, ask for clarification, or share concerns.”
Most employers “will be fine with that,” Ms. Murthy said. “Most won’t say, ‘This is it, take it or leave it.’ If they do, that’s a red flag for you to reconsider whether you really want to work for this particular employer.”
Mr. Hursh suggested that if you choose to sign the LOI immediately, so as to rapidly let the prospective employer know of your interest, “you should add some type of qualification such as, ‘I’m signing this to express my interest, but accepting the position will be dependent upon a more thorough review of compensation benchmarks,’ for example.”
Mr. Nabity agreed: “You can add a handwritten note to the signed LOI expressing that you’re eager to move forward and proceed with the position, but it shouldn’t be construed as accepting the terms of the LOI until you’ve seen the full contract.
“Remember, health care can’t exist without doctors,” Mr. Nabity said. “Doctors are the star players and should go into the negotiation process recognizing their true worth.”
A version of this article appeared on Medscape.com.
You’ve just received an offer letter from that job you interviewed for. Sometimes you want to let the employer know right away how interested you are. The verbiage says the letter isn’t “binding.” So you eagerly sign on the dotted line. Everything looks great ... until it isn’t.
Attorney Ericka Adler, JD, LLM, a partner at Roetzel & Andress, a Chicago-based law firm that represents physicians and health care professionals nationwide, described her client who was in this predicament. The physician, a dermatologist, left a practice where she had been employed because she had received an “amazing” offer letter that included promises about her new work location, staffing, equipment, and hours. She signed and immediately gave notice to her previous employer.
“When she received the actual employment contract, none of those details from the offer letter – which is also called a letter of intent [LOI] – were included,” Ms. Adler told this news organization. The physician wanted to have the details from the LOI formally spelled out in the contract, but the employer refused.
“Basically, they said, ‘This is our standard contract and you’ll just have to trust us that we’ll keep our word. We meant what we said in the LOI, but we cannot include those details in the actual agreement because everyone has the same form of agreement.’ “ The physician decided to sign the contract and accept the position.
She contacted Ms. Adler after she had been at her new position for a month. “She had received none of the things they had promised her in the LOI,” Ms. Adler reported. “She lacked the NP and PA support, she lacked the equipment, she didn’t have enough exam rooms. As soon as she started, someone with whom she was sharing call coverage left, and she was expected to take over. The LOI had a cap on the amount of call she would be required to take, but that verbiage didn’t make it into the contract.”
Ms. Adler tried to address this issue with the employer. “We couldn’t say they had literally breached the agreement, but we did list the things that were mentioned in the LOI but on which they hadn’t delivered. We asked them to fix the issue within 10 days.”
The employer argued “that they didn’t have to fulfill anything that wasn’t spelled out in the contract, even if it was in the LOI. In fact, the contract specified clearly that the signed employment agreement was the only agreement and replaced any previous written or oral agreements between the parties.”
The dermatologist ultimately left the new position. “She might have been able to have a legal claim against the employer for breach or perhaps ‘detrimental reliance’ – meaning, she might have argued that she had been financially harmed due to the false promises made to her. But it would have been difficult and expensive for her to litigate the issue,” said Ms. Adler.
“It also didn’t seem like the physician could remain in the job and develop a positive work relationship with the employer, given that she felt betrayed and misled, and didn’t like the terms of employment, which didn’t match her needs or expectations,” said Ms. Adler.
She added that “most employers are not as unscrupulous and dishonest as this one was. But some employers do play on the fact that younger doctors – especially residents and fellows – tend to be trusting or feel they don’t have negotiation power. They’re often excited to get an offer and sign it without a second thought.”
That’s why she advises physicians to “review the terms of the LOI carefully and make sure you’re comfortable with them before signing it; but know that the real contract to negotiate will be the actual Employment Agreement.”
She also advises physicians not to give notice at their current place of employment until they’ve signed the final contract with the new employer.
On the same page?
Anu Murthy, JD, an attorney and associate contract review specialist at Contract Diagnostics, explained that the LOI is a document that the candidate receives after an interview but before a full contract. Sometimes, the LOI is preceded by a verbal or e-mailed offer, which is less formal.
“An LOI is sometimes called a Term Sheet or Memorandum of Understanding,“ Ms. Murthy told this news organization. “Typically, it lays out key provisions, such as compensation, initial term of the contract, location, and recruitment incentives.” Sometimes it includes mention of staffing, call schedule, malpractice, noncompete covenants, and other components of the position.
Justin Nabity, founder and CEO of Physicians Thrive, a physician financial advisory group, said that LOIs are “a way for employers to gauge a prospective employee’s level of interest.”
The employer “doesn’t want to send a contract with a lot of details before determining whether the candidate is really serious about the position, so the offer letter doesn’t show the whole picture,” Mr. Nabity told this news organization.
Dennis Hursh, managing partner of Physician Agreements Health Law, a Pennsylvania-based law firm that represents physicians, agreed.
“Another way of putting it is that the employer wants to see whether the prospective employee is on the same page. The LOI will typically include some key components that will later appear in a more complete and formal contract, together with other topics and details. Agreeing to those key components signals that indeed you and the employer are in accord,” said Mr. Hursh.
But are you really on the same page with your prospective employer? And if you seem to be on the same page, and you sign the LOI, is that a guarantee that the employer will honor its terms?
Not necessarily, according to the experts. In fact, many LOIs contain some verbiage stating that the letter isn’t binding, which can be confusing. Others suggest that it is binding, but the candidate doesn’t realize that the letter isn’t a formal contract and that the contract may contain details not included in the LOI or may omit details mentioned in the LOI, as happened to Ms. Adler’s unfortunate client.
“One of the pitfalls I see is that doctors sign the LOI without recognizing whether it’s binding or nonbinding,” Ms. Murthy said. “If it’s binding, it creates a legal obligation on your part and could preclude you from further negotiation once you see the contract and feel you’d like to negotiate some of its terms.”
Binding letters are typically offered to candidates after some back-and-forth between the parties, and important terms have been agreed to, which can happen either verbally or via e-mail. Once these agreements have been reached, they’re summarized in a “binding” letter before being extended into a full contract.
“But even if you’ve agreed on the terms verbally, it’s still important to have someone more experienced review the offer letter before signing it,” Ms. Murthy said. “It’s important to understand the ‘legalese’ and what your rights and obligations are before agreeing to anything.”
And certainly, if you receive a binding LOI, you shouldn’t sign anything until you’re sure you’re comfortable with its contents and have more details.
Are “nonbinding” LOIs really not binding?
Even if the LOI is nonbinding, that doesn’t necessarily mean you can sign it and expect to negotiate later. “I see people tripped up when they sign the LOI, thinking they’ll negotiate later,” said Mr. Hursh. “They may not like the terms – for example, they think the compensation is too low – and they figure they’ll work it out at the contract stage, because the LOI is ‘not legally binding.’ “
But because the candidate signed the LOI, “the employer is under the impression that the compensation was acceptable, so now you’ve tied your hands – and the hands of any attorney you may consult down the road – to negotiate those terms.”
Mr. Hursh said he is often consulted by physicians who signed the contract “to get the ball rolling,” thinking that the LOI was “just a meaningless bureaucratic paper.” They need to understand “that the employer wants to make sure they’re in agreement on the basic points before getting into the details,” he said. “Large hospitals with in-house counsel may not want to use their legal department’s valuable time in redrafting terms they thought were acceptable to the candidate, and most practices don’t want to pay a lawyer to draft an LOI and then come back and say, ‘Actually, the physician wants more compensation.’ “
Mr. Nabity summarized: “The LOI is essentially a negotiation tactic to take some of the cards out of the hands of the doctor and commit him or her to something they’re not ready to commit to.” Employers may be playing on the sense of pressure and candidate’s fear that the job will slip through their fingers if they wait too long to sign. “But it’s better to wait longer at this stage before signing even a nonbinding LOI,” he said.
What to do before signing
So how should physicians relate to the LOI? Mr. Nabity advises “working through the details of the offer letter first, going through it carefully and identifying areas of concern, bearing in mind that employers never begin with their best offer.”
He pointed out that physicians “rarely know their value and usually don’t know how to work through the dynamics of compensation, call schedules, additional incentives, bonuses, and productivity,” so they need to be informed about these areas before signing anything.
Ms. Murthy recommended “going back and saying [to the prospective employer], ‘Thank you, but I need time to consider and evaluate this offer.’ Then, do some due diligence.”
At that point, you can hire an attorney to go over the offer, educate yourself about compensation benchmarks and what your worth actually is, or consult another trained professional or more experienced individual who can review the LOI before you sign it.
That’s what Dominique Cleveland, MD, a Texas-based ob.gyn., did when she received an LOI 5 years ago.
“The offer letter from the group practice contained a statement that the group wanted me to come on board, what the salary would be, and the time frame that would be covered in the contract,” she told this news organization. “It mentioned benefits and incentives and relocation, but it was only a short document – maybe one or two pages long.”
At the time that she received her LOI, Dr. Cleveland was completing her residency. She consulted experienced faculty members from her institution to find out whether the terms laid out in the LOI “were the norm and were reasonable.” She was “fairly certain” that the salary was low and this was confirmed by the faculty members she talked to. “So I felt comfortable asking for more [compensation],” she said.
The employer was receptive to her proposed changes, which were included in the more detailed contract that followed. “I can’t say there were any surprises per se in the contract because I had negotiated my salary after receiving the offer letter,” she said. She accepted the position and has been working there ever since.
Dr. Cleveland advises physicians “not to make a decision without speaking to someone who’s experienced and can help you compare what’s out there.”
She also encourages physicians to ask for what they want, whether it’s compensation or something else, such as call schedule or vacation time, without being afraid. “I’m a firm believer that you won’t know what you can get if you don’t ask for it,” she said.
Negotiation tips
Mr. Nabity recommended not agreeing to any terms until you are ready to enter into negotiation, recognizing that negotiation is an “art” that requires skill and training. “Either get trained in negotiation, perhaps taking courses to advocate for yourself – which is rare, and most doctors aren’t likely to do this – or go to a trained advocate, such as a lawyer, who can do so on your behalf.”
You might share your concerns with the person who interviewed you, with the person whose name is on the LOI, or with the recruiter who can advocate on your behalf, Ms. Murthy said. “You can reach out to the recruiter and say, ‘I really appreciate the opportunity, but there are some things in the offer letter I’d like to continue discussing.’ “
When you’re ready to negotiate, be sure to assemble all of your “asks” in a single document rather than going back to the prospective employer with “multiple individual questions multiple times,” Ms. Murthy advised. It’s more efficient and the employer or recruiter will appreciate that.
She also advised couching your request in language that expresses your appreciation for the offer and stating that you would like the agreement to serve the best interests of both parties. “Use open-ended language like that, and ask if it’s all right for you to send back some questions, ask for clarification, or share concerns.”
Most employers “will be fine with that,” Ms. Murthy said. “Most won’t say, ‘This is it, take it or leave it.’ If they do, that’s a red flag for you to reconsider whether you really want to work for this particular employer.”
Mr. Hursh suggested that if you choose to sign the LOI immediately, so as to rapidly let the prospective employer know of your interest, “you should add some type of qualification such as, ‘I’m signing this to express my interest, but accepting the position will be dependent upon a more thorough review of compensation benchmarks,’ for example.”
Mr. Nabity agreed: “You can add a handwritten note to the signed LOI expressing that you’re eager to move forward and proceed with the position, but it shouldn’t be construed as accepting the terms of the LOI until you’ve seen the full contract.
“Remember, health care can’t exist without doctors,” Mr. Nabity said. “Doctors are the star players and should go into the negotiation process recognizing their true worth.”
A version of this article appeared on Medscape.com.
You’ve just received an offer letter from that job you interviewed for. Sometimes you want to let the employer know right away how interested you are. The verbiage says the letter isn’t “binding.” So you eagerly sign on the dotted line. Everything looks great ... until it isn’t.
Attorney Ericka Adler, JD, LLM, a partner at Roetzel & Andress, a Chicago-based law firm that represents physicians and health care professionals nationwide, described her client who was in this predicament. The physician, a dermatologist, left a practice where she had been employed because she had received an “amazing” offer letter that included promises about her new work location, staffing, equipment, and hours. She signed and immediately gave notice to her previous employer.
“When she received the actual employment contract, none of those details from the offer letter – which is also called a letter of intent [LOI] – were included,” Ms. Adler told this news organization. The physician wanted to have the details from the LOI formally spelled out in the contract, but the employer refused.
“Basically, they said, ‘This is our standard contract and you’ll just have to trust us that we’ll keep our word. We meant what we said in the LOI, but we cannot include those details in the actual agreement because everyone has the same form of agreement.’ “ The physician decided to sign the contract and accept the position.
She contacted Ms. Adler after she had been at her new position for a month. “She had received none of the things they had promised her in the LOI,” Ms. Adler reported. “She lacked the NP and PA support, she lacked the equipment, she didn’t have enough exam rooms. As soon as she started, someone with whom she was sharing call coverage left, and she was expected to take over. The LOI had a cap on the amount of call she would be required to take, but that verbiage didn’t make it into the contract.”
Ms. Adler tried to address this issue with the employer. “We couldn’t say they had literally breached the agreement, but we did list the things that were mentioned in the LOI but on which they hadn’t delivered. We asked them to fix the issue within 10 days.”
The employer argued “that they didn’t have to fulfill anything that wasn’t spelled out in the contract, even if it was in the LOI. In fact, the contract specified clearly that the signed employment agreement was the only agreement and replaced any previous written or oral agreements between the parties.”
The dermatologist ultimately left the new position. “She might have been able to have a legal claim against the employer for breach or perhaps ‘detrimental reliance’ – meaning, she might have argued that she had been financially harmed due to the false promises made to her. But it would have been difficult and expensive for her to litigate the issue,” said Ms. Adler.
“It also didn’t seem like the physician could remain in the job and develop a positive work relationship with the employer, given that she felt betrayed and misled, and didn’t like the terms of employment, which didn’t match her needs or expectations,” said Ms. Adler.
She added that “most employers are not as unscrupulous and dishonest as this one was. But some employers do play on the fact that younger doctors – especially residents and fellows – tend to be trusting or feel they don’t have negotiation power. They’re often excited to get an offer and sign it without a second thought.”
That’s why she advises physicians to “review the terms of the LOI carefully and make sure you’re comfortable with them before signing it; but know that the real contract to negotiate will be the actual Employment Agreement.”
She also advises physicians not to give notice at their current place of employment until they’ve signed the final contract with the new employer.
On the same page?
Anu Murthy, JD, an attorney and associate contract review specialist at Contract Diagnostics, explained that the LOI is a document that the candidate receives after an interview but before a full contract. Sometimes, the LOI is preceded by a verbal or e-mailed offer, which is less formal.
“An LOI is sometimes called a Term Sheet or Memorandum of Understanding,“ Ms. Murthy told this news organization. “Typically, it lays out key provisions, such as compensation, initial term of the contract, location, and recruitment incentives.” Sometimes it includes mention of staffing, call schedule, malpractice, noncompete covenants, and other components of the position.
Justin Nabity, founder and CEO of Physicians Thrive, a physician financial advisory group, said that LOIs are “a way for employers to gauge a prospective employee’s level of interest.”
The employer “doesn’t want to send a contract with a lot of details before determining whether the candidate is really serious about the position, so the offer letter doesn’t show the whole picture,” Mr. Nabity told this news organization.
Dennis Hursh, managing partner of Physician Agreements Health Law, a Pennsylvania-based law firm that represents physicians, agreed.
“Another way of putting it is that the employer wants to see whether the prospective employee is on the same page. The LOI will typically include some key components that will later appear in a more complete and formal contract, together with other topics and details. Agreeing to those key components signals that indeed you and the employer are in accord,” said Mr. Hursh.
But are you really on the same page with your prospective employer? And if you seem to be on the same page, and you sign the LOI, is that a guarantee that the employer will honor its terms?
Not necessarily, according to the experts. In fact, many LOIs contain some verbiage stating that the letter isn’t binding, which can be confusing. Others suggest that it is binding, but the candidate doesn’t realize that the letter isn’t a formal contract and that the contract may contain details not included in the LOI or may omit details mentioned in the LOI, as happened to Ms. Adler’s unfortunate client.
“One of the pitfalls I see is that doctors sign the LOI without recognizing whether it’s binding or nonbinding,” Ms. Murthy said. “If it’s binding, it creates a legal obligation on your part and could preclude you from further negotiation once you see the contract and feel you’d like to negotiate some of its terms.”
Binding letters are typically offered to candidates after some back-and-forth between the parties, and important terms have been agreed to, which can happen either verbally or via e-mail. Once these agreements have been reached, they’re summarized in a “binding” letter before being extended into a full contract.
“But even if you’ve agreed on the terms verbally, it’s still important to have someone more experienced review the offer letter before signing it,” Ms. Murthy said. “It’s important to understand the ‘legalese’ and what your rights and obligations are before agreeing to anything.”
And certainly, if you receive a binding LOI, you shouldn’t sign anything until you’re sure you’re comfortable with its contents and have more details.
Are “nonbinding” LOIs really not binding?
Even if the LOI is nonbinding, that doesn’t necessarily mean you can sign it and expect to negotiate later. “I see people tripped up when they sign the LOI, thinking they’ll negotiate later,” said Mr. Hursh. “They may not like the terms – for example, they think the compensation is too low – and they figure they’ll work it out at the contract stage, because the LOI is ‘not legally binding.’ “
But because the candidate signed the LOI, “the employer is under the impression that the compensation was acceptable, so now you’ve tied your hands – and the hands of any attorney you may consult down the road – to negotiate those terms.”
Mr. Hursh said he is often consulted by physicians who signed the contract “to get the ball rolling,” thinking that the LOI was “just a meaningless bureaucratic paper.” They need to understand “that the employer wants to make sure they’re in agreement on the basic points before getting into the details,” he said. “Large hospitals with in-house counsel may not want to use their legal department’s valuable time in redrafting terms they thought were acceptable to the candidate, and most practices don’t want to pay a lawyer to draft an LOI and then come back and say, ‘Actually, the physician wants more compensation.’ “
Mr. Nabity summarized: “The LOI is essentially a negotiation tactic to take some of the cards out of the hands of the doctor and commit him or her to something they’re not ready to commit to.” Employers may be playing on the sense of pressure and candidate’s fear that the job will slip through their fingers if they wait too long to sign. “But it’s better to wait longer at this stage before signing even a nonbinding LOI,” he said.
What to do before signing
So how should physicians relate to the LOI? Mr. Nabity advises “working through the details of the offer letter first, going through it carefully and identifying areas of concern, bearing in mind that employers never begin with their best offer.”
He pointed out that physicians “rarely know their value and usually don’t know how to work through the dynamics of compensation, call schedules, additional incentives, bonuses, and productivity,” so they need to be informed about these areas before signing anything.
Ms. Murthy recommended “going back and saying [to the prospective employer], ‘Thank you, but I need time to consider and evaluate this offer.’ Then, do some due diligence.”
At that point, you can hire an attorney to go over the offer, educate yourself about compensation benchmarks and what your worth actually is, or consult another trained professional or more experienced individual who can review the LOI before you sign it.
That’s what Dominique Cleveland, MD, a Texas-based ob.gyn., did when she received an LOI 5 years ago.
“The offer letter from the group practice contained a statement that the group wanted me to come on board, what the salary would be, and the time frame that would be covered in the contract,” she told this news organization. “It mentioned benefits and incentives and relocation, but it was only a short document – maybe one or two pages long.”
At the time that she received her LOI, Dr. Cleveland was completing her residency. She consulted experienced faculty members from her institution to find out whether the terms laid out in the LOI “were the norm and were reasonable.” She was “fairly certain” that the salary was low and this was confirmed by the faculty members she talked to. “So I felt comfortable asking for more [compensation],” she said.
The employer was receptive to her proposed changes, which were included in the more detailed contract that followed. “I can’t say there were any surprises per se in the contract because I had negotiated my salary after receiving the offer letter,” she said. She accepted the position and has been working there ever since.
Dr. Cleveland advises physicians “not to make a decision without speaking to someone who’s experienced and can help you compare what’s out there.”
She also encourages physicians to ask for what they want, whether it’s compensation or something else, such as call schedule or vacation time, without being afraid. “I’m a firm believer that you won’t know what you can get if you don’t ask for it,” she said.
Negotiation tips
Mr. Nabity recommended not agreeing to any terms until you are ready to enter into negotiation, recognizing that negotiation is an “art” that requires skill and training. “Either get trained in negotiation, perhaps taking courses to advocate for yourself – which is rare, and most doctors aren’t likely to do this – or go to a trained advocate, such as a lawyer, who can do so on your behalf.”
You might share your concerns with the person who interviewed you, with the person whose name is on the LOI, or with the recruiter who can advocate on your behalf, Ms. Murthy said. “You can reach out to the recruiter and say, ‘I really appreciate the opportunity, but there are some things in the offer letter I’d like to continue discussing.’ “
When you’re ready to negotiate, be sure to assemble all of your “asks” in a single document rather than going back to the prospective employer with “multiple individual questions multiple times,” Ms. Murthy advised. It’s more efficient and the employer or recruiter will appreciate that.
She also advised couching your request in language that expresses your appreciation for the offer and stating that you would like the agreement to serve the best interests of both parties. “Use open-ended language like that, and ask if it’s all right for you to send back some questions, ask for clarification, or share concerns.”
Most employers “will be fine with that,” Ms. Murthy said. “Most won’t say, ‘This is it, take it or leave it.’ If they do, that’s a red flag for you to reconsider whether you really want to work for this particular employer.”
Mr. Hursh suggested that if you choose to sign the LOI immediately, so as to rapidly let the prospective employer know of your interest, “you should add some type of qualification such as, ‘I’m signing this to express my interest, but accepting the position will be dependent upon a more thorough review of compensation benchmarks,’ for example.”
Mr. Nabity agreed: “You can add a handwritten note to the signed LOI expressing that you’re eager to move forward and proceed with the position, but it shouldn’t be construed as accepting the terms of the LOI until you’ve seen the full contract.
“Remember, health care can’t exist without doctors,” Mr. Nabity said. “Doctors are the star players and should go into the negotiation process recognizing their true worth.”
A version of this article appeared on Medscape.com.
Life in the woods
“I went to the woods because I wished to live deliberately, to front only the essential facts of life, and see if I could not learn what it had to teach.” – Henry David Thoreau
I have many patients like Maxine. Tall, with a shock of white hair. Old, but still in charge. When you try to make eye contact, she looks right through you. First with her left eye. Then her right. Her face is inscrutable. What’s she thinking? Unlike many of my patients, however, this Maxine was a llama. Every morning my daughter and I tried to coax her into moving as we leaned on the cold steel gate that kept her in her pasture. We were visiting family in October and chose to stay on a working New England farm. The kids will love the animals, we thought, and we’ll appreciate the extra bedrooms.
Airbnb helped us find this charming fiber-farm in Rhode Island where they raise Leicester Longwool sheep, a historic breed that once roamed George Washington’s pastures, along with a few goats, ducks, chickens, and Maxine. It’s situated deep in the woods, which were yellow, orange, and red that week. As it happens, we were just a short drive due south of Walden Pond where Henry David Thoreau spent 2 years, 2 months and 2 days escaping “overcivilization” nearly 175 years ago. Hoisting our overweight bags over the uneven granite stone steps when we arrived, I realized this was going to be more like the Thoreau experiment than I intended. The farmhouse dated to the 1790s. There were wide, creaky floorboards, low ceilings, one staircase to the bedrooms (which could have aptly been called a ladder) and loads of book-laden shelves. Instructions posted in the kitchen warned that the heat is tricky to regulate – a redundant admonition as we watched our 3-year-old putting on her socks and shoes as she got into bed.
Now, if you’ve ever been on vacation with little kids, you know that it’s basically just childcare in a novel location. After barricading the staircase with luggage and unplugging lamps from their dicey outlets we set out to feed the chickens and try to pet a sheep. Walking the perimeter of the farm we saw stone walls that needed mending and stumbled across two ancient cemeteries, one had been for family, the other for slaves. I wondered how many farmers and weavers and menders had walked this trail with their kids over the generations.
The next morning, we learned that roosters do not in fact crow at dawn, they crow before dawn (which could also aptly be called nighttime). There were no commutes or late patients here. But there was work to be done. Chickens don’t care that it’s Sunday. It downpoured. Watching the sheep from the kitchen as I sipped my coffee, they didn’t seem to mind. Nor did our farmer hosts who trudged past them in tall boots, just as they had every other day of their farmer lives.
By the fifth day, we had fallen into the rhythms of the homestead. We cracked the blue, green, and brown eggs that our hosts placed outside our door in the early hours and made omelets that were as orange as the foliage. We finally learned to adjust the heat so we neither got chilblains nor had to open the windows and strip naked to cool down. The sky was a brilliant blue that last morning and Sloan ran around trying to catch leaves as they blew off the trees. She had no objective. No counting. No contest. Just chasing leaves as they fell. It was the ultimate atelic activity, done just for doing it. I joined her and found I was no better at this than a 3-year-old.
We might all benefit from a little time in the woods.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
“I went to the woods because I wished to live deliberately, to front only the essential facts of life, and see if I could not learn what it had to teach.” – Henry David Thoreau
I have many patients like Maxine. Tall, with a shock of white hair. Old, but still in charge. When you try to make eye contact, she looks right through you. First with her left eye. Then her right. Her face is inscrutable. What’s she thinking? Unlike many of my patients, however, this Maxine was a llama. Every morning my daughter and I tried to coax her into moving as we leaned on the cold steel gate that kept her in her pasture. We were visiting family in October and chose to stay on a working New England farm. The kids will love the animals, we thought, and we’ll appreciate the extra bedrooms.
Airbnb helped us find this charming fiber-farm in Rhode Island where they raise Leicester Longwool sheep, a historic breed that once roamed George Washington’s pastures, along with a few goats, ducks, chickens, and Maxine. It’s situated deep in the woods, which were yellow, orange, and red that week. As it happens, we were just a short drive due south of Walden Pond where Henry David Thoreau spent 2 years, 2 months and 2 days escaping “overcivilization” nearly 175 years ago. Hoisting our overweight bags over the uneven granite stone steps when we arrived, I realized this was going to be more like the Thoreau experiment than I intended. The farmhouse dated to the 1790s. There were wide, creaky floorboards, low ceilings, one staircase to the bedrooms (which could have aptly been called a ladder) and loads of book-laden shelves. Instructions posted in the kitchen warned that the heat is tricky to regulate – a redundant admonition as we watched our 3-year-old putting on her socks and shoes as she got into bed.
Now, if you’ve ever been on vacation with little kids, you know that it’s basically just childcare in a novel location. After barricading the staircase with luggage and unplugging lamps from their dicey outlets we set out to feed the chickens and try to pet a sheep. Walking the perimeter of the farm we saw stone walls that needed mending and stumbled across two ancient cemeteries, one had been for family, the other for slaves. I wondered how many farmers and weavers and menders had walked this trail with their kids over the generations.
The next morning, we learned that roosters do not in fact crow at dawn, they crow before dawn (which could also aptly be called nighttime). There were no commutes or late patients here. But there was work to be done. Chickens don’t care that it’s Sunday. It downpoured. Watching the sheep from the kitchen as I sipped my coffee, they didn’t seem to mind. Nor did our farmer hosts who trudged past them in tall boots, just as they had every other day of their farmer lives.
By the fifth day, we had fallen into the rhythms of the homestead. We cracked the blue, green, and brown eggs that our hosts placed outside our door in the early hours and made omelets that were as orange as the foliage. We finally learned to adjust the heat so we neither got chilblains nor had to open the windows and strip naked to cool down. The sky was a brilliant blue that last morning and Sloan ran around trying to catch leaves as they blew off the trees. She had no objective. No counting. No contest. Just chasing leaves as they fell. It was the ultimate atelic activity, done just for doing it. I joined her and found I was no better at this than a 3-year-old.
We might all benefit from a little time in the woods.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
“I went to the woods because I wished to live deliberately, to front only the essential facts of life, and see if I could not learn what it had to teach.” – Henry David Thoreau
I have many patients like Maxine. Tall, with a shock of white hair. Old, but still in charge. When you try to make eye contact, she looks right through you. First with her left eye. Then her right. Her face is inscrutable. What’s she thinking? Unlike many of my patients, however, this Maxine was a llama. Every morning my daughter and I tried to coax her into moving as we leaned on the cold steel gate that kept her in her pasture. We were visiting family in October and chose to stay on a working New England farm. The kids will love the animals, we thought, and we’ll appreciate the extra bedrooms.
Airbnb helped us find this charming fiber-farm in Rhode Island where they raise Leicester Longwool sheep, a historic breed that once roamed George Washington’s pastures, along with a few goats, ducks, chickens, and Maxine. It’s situated deep in the woods, which were yellow, orange, and red that week. As it happens, we were just a short drive due south of Walden Pond where Henry David Thoreau spent 2 years, 2 months and 2 days escaping “overcivilization” nearly 175 years ago. Hoisting our overweight bags over the uneven granite stone steps when we arrived, I realized this was going to be more like the Thoreau experiment than I intended. The farmhouse dated to the 1790s. There were wide, creaky floorboards, low ceilings, one staircase to the bedrooms (which could have aptly been called a ladder) and loads of book-laden shelves. Instructions posted in the kitchen warned that the heat is tricky to regulate – a redundant admonition as we watched our 3-year-old putting on her socks and shoes as she got into bed.
Now, if you’ve ever been on vacation with little kids, you know that it’s basically just childcare in a novel location. After barricading the staircase with luggage and unplugging lamps from their dicey outlets we set out to feed the chickens and try to pet a sheep. Walking the perimeter of the farm we saw stone walls that needed mending and stumbled across two ancient cemeteries, one had been for family, the other for slaves. I wondered how many farmers and weavers and menders had walked this trail with their kids over the generations.
The next morning, we learned that roosters do not in fact crow at dawn, they crow before dawn (which could also aptly be called nighttime). There were no commutes or late patients here. But there was work to be done. Chickens don’t care that it’s Sunday. It downpoured. Watching the sheep from the kitchen as I sipped my coffee, they didn’t seem to mind. Nor did our farmer hosts who trudged past them in tall boots, just as they had every other day of their farmer lives.
By the fifth day, we had fallen into the rhythms of the homestead. We cracked the blue, green, and brown eggs that our hosts placed outside our door in the early hours and made omelets that were as orange as the foliage. We finally learned to adjust the heat so we neither got chilblains nor had to open the windows and strip naked to cool down. The sky was a brilliant blue that last morning and Sloan ran around trying to catch leaves as they blew off the trees. She had no objective. No counting. No contest. Just chasing leaves as they fell. It was the ultimate atelic activity, done just for doing it. I joined her and found I was no better at this than a 3-year-old.
We might all benefit from a little time in the woods.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
How to develop a patient referral program
Here is how old I am: When I graduated from medical school in 1977, marketing was prohibited. It was the legal profession that challenged the ban on advertising by professionals, leading to a landmark Supreme Court decision (Bates v State Bar of Arizona, 1977), which opened the door to marketing in the legal and medical professions.
Since then, Strategies range from the basic Internet website through postings on the major social media sites, and occasionally to larger-budget campaigns involving local radio, television, or billboard advertising.
All these methods are effective, to varying degrees; but nothing provides as much benefit – relative to its comparatively low cost – as the original marketing tool, word-of-mouth patient referrals. According to one survey, a clear majority of Americans still consider word-of-mouth recommendations to be the most influential element driving purchase decisions. Of course, some of your new patients already come from such referrals; but you can get a lot more by actively encouraging your existing patients to sing your praises, rather than waiting for them to do it on their own.
Soliciting current patients for referrals does take a little planning, structure, and a basic understanding of exactly how patient referral programs work. When executed correctly, a patient referral program can add substantial growth to your practice at minimal cost.
Your first step, as with any new project, should be to identify your goals: Clearly define what kind of patients you are looking to attract. Do you want more patients for cosmetic procedures, medical treatment, skin cancer screenings, a specific diagnosis (such as psoriasis), or a general mix? Design your announcements, brochures, and other literature (more on that in a minute) with those goals in mind.
Next, identify any applicable federal or state laws that dictate what you can and cannot legally do to encourage such referrals. It might be tempting, for example, to offer discounts on future services for successful referrals; but some medical groups frown on it, some states prohibit it, and the Federal Anti-Kickback Statute makes it illegal to pay anyone to refer Medicare or Medicaid patients to you if you file a claim for your services. In my experience, most patients are happy to recommend someone whom they believe provides excellent care to a friend or relative without any sort of monetary incentive; but if you plan to offer a material reward of any kind, run it by your attorney first.
Once your legal ducks are in order, make patients aware that you are accepting new patients and would welcome referrals by posting notices to that effect around your office and on your website and social media pages. Outline exactly what sort of patients (based on your goals, above) you are looking for, how to refer someone, whom to contact, and what kind of information is needed. Make it clear why existing patients should refer someone to your practice. Remind them of your specialized training, advanced technology, and patient-focused approach to health care. Highlight the benefits of the program and encourage your patients to participate.
Before implementation, you will need to educate your employees about the referral program and its benefits. All staff members should understand the program and be able to answer basic questions about it from patients or referring professionals. Encourage staffers to actively promote the program during patient interactions.
Then, start making some decisions. How, specifically, will you be requesting referrals in the office? Many physicians are not comfortable asking patients themselves. If you are going to let your assistants or receptionists do it, you will need to write a script for them to follow. An example of a basic script might be, “If you are happy with the care you are receiving here, we would love for you to tell your friends and family about us.” Your staff can then hand out cards, brochures, or both to reinforce the message, and perhaps send a follow-up email to remind them.
A referral system isn’t worth the effort if you don’t know whether it is working. Establish a system to track and monitor referrals. This could be as simple as a spreadsheet or purchasing a more sophisticated software program. Ensure that you can accurately identify and credit the referring patients for their referrals.
Make sure to thank referring patients with a thank-you note or email. Expressing gratitude will encourage continued participation in the program.
A successful referral program does not happen overnight. It relies on providing exceptional patient care and building strong relationships with your existing patients. By implementing such a program, you can leverage the satisfaction and loyalty of your patients to attract new patients and grow your private practice.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
Here is how old I am: When I graduated from medical school in 1977, marketing was prohibited. It was the legal profession that challenged the ban on advertising by professionals, leading to a landmark Supreme Court decision (Bates v State Bar of Arizona, 1977), which opened the door to marketing in the legal and medical professions.
Since then, Strategies range from the basic Internet website through postings on the major social media sites, and occasionally to larger-budget campaigns involving local radio, television, or billboard advertising.
All these methods are effective, to varying degrees; but nothing provides as much benefit – relative to its comparatively low cost – as the original marketing tool, word-of-mouth patient referrals. According to one survey, a clear majority of Americans still consider word-of-mouth recommendations to be the most influential element driving purchase decisions. Of course, some of your new patients already come from such referrals; but you can get a lot more by actively encouraging your existing patients to sing your praises, rather than waiting for them to do it on their own.
Soliciting current patients for referrals does take a little planning, structure, and a basic understanding of exactly how patient referral programs work. When executed correctly, a patient referral program can add substantial growth to your practice at minimal cost.
Your first step, as with any new project, should be to identify your goals: Clearly define what kind of patients you are looking to attract. Do you want more patients for cosmetic procedures, medical treatment, skin cancer screenings, a specific diagnosis (such as psoriasis), or a general mix? Design your announcements, brochures, and other literature (more on that in a minute) with those goals in mind.
Next, identify any applicable federal or state laws that dictate what you can and cannot legally do to encourage such referrals. It might be tempting, for example, to offer discounts on future services for successful referrals; but some medical groups frown on it, some states prohibit it, and the Federal Anti-Kickback Statute makes it illegal to pay anyone to refer Medicare or Medicaid patients to you if you file a claim for your services. In my experience, most patients are happy to recommend someone whom they believe provides excellent care to a friend or relative without any sort of monetary incentive; but if you plan to offer a material reward of any kind, run it by your attorney first.
Once your legal ducks are in order, make patients aware that you are accepting new patients and would welcome referrals by posting notices to that effect around your office and on your website and social media pages. Outline exactly what sort of patients (based on your goals, above) you are looking for, how to refer someone, whom to contact, and what kind of information is needed. Make it clear why existing patients should refer someone to your practice. Remind them of your specialized training, advanced technology, and patient-focused approach to health care. Highlight the benefits of the program and encourage your patients to participate.
Before implementation, you will need to educate your employees about the referral program and its benefits. All staff members should understand the program and be able to answer basic questions about it from patients or referring professionals. Encourage staffers to actively promote the program during patient interactions.
Then, start making some decisions. How, specifically, will you be requesting referrals in the office? Many physicians are not comfortable asking patients themselves. If you are going to let your assistants or receptionists do it, you will need to write a script for them to follow. An example of a basic script might be, “If you are happy with the care you are receiving here, we would love for you to tell your friends and family about us.” Your staff can then hand out cards, brochures, or both to reinforce the message, and perhaps send a follow-up email to remind them.
A referral system isn’t worth the effort if you don’t know whether it is working. Establish a system to track and monitor referrals. This could be as simple as a spreadsheet or purchasing a more sophisticated software program. Ensure that you can accurately identify and credit the referring patients for their referrals.
Make sure to thank referring patients with a thank-you note or email. Expressing gratitude will encourage continued participation in the program.
A successful referral program does not happen overnight. It relies on providing exceptional patient care and building strong relationships with your existing patients. By implementing such a program, you can leverage the satisfaction and loyalty of your patients to attract new patients and grow your private practice.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
Here is how old I am: When I graduated from medical school in 1977, marketing was prohibited. It was the legal profession that challenged the ban on advertising by professionals, leading to a landmark Supreme Court decision (Bates v State Bar of Arizona, 1977), which opened the door to marketing in the legal and medical professions.
Since then, Strategies range from the basic Internet website through postings on the major social media sites, and occasionally to larger-budget campaigns involving local radio, television, or billboard advertising.
All these methods are effective, to varying degrees; but nothing provides as much benefit – relative to its comparatively low cost – as the original marketing tool, word-of-mouth patient referrals. According to one survey, a clear majority of Americans still consider word-of-mouth recommendations to be the most influential element driving purchase decisions. Of course, some of your new patients already come from such referrals; but you can get a lot more by actively encouraging your existing patients to sing your praises, rather than waiting for them to do it on their own.
Soliciting current patients for referrals does take a little planning, structure, and a basic understanding of exactly how patient referral programs work. When executed correctly, a patient referral program can add substantial growth to your practice at minimal cost.
Your first step, as with any new project, should be to identify your goals: Clearly define what kind of patients you are looking to attract. Do you want more patients for cosmetic procedures, medical treatment, skin cancer screenings, a specific diagnosis (such as psoriasis), or a general mix? Design your announcements, brochures, and other literature (more on that in a minute) with those goals in mind.
Next, identify any applicable federal or state laws that dictate what you can and cannot legally do to encourage such referrals. It might be tempting, for example, to offer discounts on future services for successful referrals; but some medical groups frown on it, some states prohibit it, and the Federal Anti-Kickback Statute makes it illegal to pay anyone to refer Medicare or Medicaid patients to you if you file a claim for your services. In my experience, most patients are happy to recommend someone whom they believe provides excellent care to a friend or relative without any sort of monetary incentive; but if you plan to offer a material reward of any kind, run it by your attorney first.
Once your legal ducks are in order, make patients aware that you are accepting new patients and would welcome referrals by posting notices to that effect around your office and on your website and social media pages. Outline exactly what sort of patients (based on your goals, above) you are looking for, how to refer someone, whom to contact, and what kind of information is needed. Make it clear why existing patients should refer someone to your practice. Remind them of your specialized training, advanced technology, and patient-focused approach to health care. Highlight the benefits of the program and encourage your patients to participate.
Before implementation, you will need to educate your employees about the referral program and its benefits. All staff members should understand the program and be able to answer basic questions about it from patients or referring professionals. Encourage staffers to actively promote the program during patient interactions.
Then, start making some decisions. How, specifically, will you be requesting referrals in the office? Many physicians are not comfortable asking patients themselves. If you are going to let your assistants or receptionists do it, you will need to write a script for them to follow. An example of a basic script might be, “If you are happy with the care you are receiving here, we would love for you to tell your friends and family about us.” Your staff can then hand out cards, brochures, or both to reinforce the message, and perhaps send a follow-up email to remind them.
A referral system isn’t worth the effort if you don’t know whether it is working. Establish a system to track and monitor referrals. This could be as simple as a spreadsheet or purchasing a more sophisticated software program. Ensure that you can accurately identify and credit the referring patients for their referrals.
Make sure to thank referring patients with a thank-you note or email. Expressing gratitude will encourage continued participation in the program.
A successful referral program does not happen overnight. It relies on providing exceptional patient care and building strong relationships with your existing patients. By implementing such a program, you can leverage the satisfaction and loyalty of your patients to attract new patients and grow your private practice.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.









