User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
Nicotine patch may be an effective precision therapy for select epilepsies
NEW ORLEANS – according to research presented at the annual meeting of the American Epilepsy Society. Of four epilepsy patients at one center who received nicotine-patch treatment, three had a good clinical response, one of whom became seizure free.
“We confirm that, in select patients, treatment with a nicotine patch ... can be an effective precision therapy for epilepsy. We propose consideration of nicotine-patch treatment in refractory patients with known cholinergic nicotine receptor subunit variants, especially those with a clinical history consistent with autosomal dominant nocturnal frontal lobe epilepsy (ADNFLE),” said Jordana Fox, DO, and Alison Dolce, MD, both with the University of Texas Southwestern Medical Center in Dallas.
Gene variants in CHRAn4,CHRNA2, and CHRNB2 can cause ADNFLE. Preclinical and n-of-1 studies have suggested that nicotine may be a precision treatment for ADNFLE.
Dr. Fox and Dr. Dolce reviewed next-generation sequencing epilepsy panels from patients seen at Children’s Medical Center, Dallas, during 2011-2015 to identify patients with nAChR gene variants (CHNRA4, CHRNA2, CHRNB2, and CHRNA7). They reviewed patients’ medical and laboratory records, including genetic variant details and treatment history, and focused on patients who underwent a trial of nicotine-patch treatment.
Of the 21 patients who had nAChR gene variants, 4 tried treatment with a nicotine patch, either 7 mg or 14 mg. The patients who received nicotine-patch treatment had genetic variants in CHRNA4, CHRNB2, and CHRNA2. Three of the patients who tried nicotine-patch treatment had a greater than 50% reduction in seizures, whereas one had no treatment response.
“One patient became seizure free and is now treated with the nicotine patch as monotherapy,” Dr. Fox said.
The patient with complete resolution of seizures had a heterozygous disease–causing mutation in CHRNB2. This patient had nocturnal focal seizures, normal neuroimaging, and had been receiving treatment with oxcarbazepine and zonisamide.
The review identified four patients with nAChR gene variants and the ADNFLE phenotype who have not been treated with nicotine. Further phenotype-genotype characterizations and preclinical studies will help neurologists understand the mechanisms of these complex gene variants.
The researchers received no funding for the study and had no relevant financial disclosures.
SOURCE: Fox J et al. AES 2018, Abstract 1.230.
NEW ORLEANS – according to research presented at the annual meeting of the American Epilepsy Society. Of four epilepsy patients at one center who received nicotine-patch treatment, three had a good clinical response, one of whom became seizure free.
“We confirm that, in select patients, treatment with a nicotine patch ... can be an effective precision therapy for epilepsy. We propose consideration of nicotine-patch treatment in refractory patients with known cholinergic nicotine receptor subunit variants, especially those with a clinical history consistent with autosomal dominant nocturnal frontal lobe epilepsy (ADNFLE),” said Jordana Fox, DO, and Alison Dolce, MD, both with the University of Texas Southwestern Medical Center in Dallas.
Gene variants in CHRAn4,CHRNA2, and CHRNB2 can cause ADNFLE. Preclinical and n-of-1 studies have suggested that nicotine may be a precision treatment for ADNFLE.
Dr. Fox and Dr. Dolce reviewed next-generation sequencing epilepsy panels from patients seen at Children’s Medical Center, Dallas, during 2011-2015 to identify patients with nAChR gene variants (CHNRA4, CHRNA2, CHRNB2, and CHRNA7). They reviewed patients’ medical and laboratory records, including genetic variant details and treatment history, and focused on patients who underwent a trial of nicotine-patch treatment.
Of the 21 patients who had nAChR gene variants, 4 tried treatment with a nicotine patch, either 7 mg or 14 mg. The patients who received nicotine-patch treatment had genetic variants in CHRNA4, CHRNB2, and CHRNA2. Three of the patients who tried nicotine-patch treatment had a greater than 50% reduction in seizures, whereas one had no treatment response.
“One patient became seizure free and is now treated with the nicotine patch as monotherapy,” Dr. Fox said.
The patient with complete resolution of seizures had a heterozygous disease–causing mutation in CHRNB2. This patient had nocturnal focal seizures, normal neuroimaging, and had been receiving treatment with oxcarbazepine and zonisamide.
The review identified four patients with nAChR gene variants and the ADNFLE phenotype who have not been treated with nicotine. Further phenotype-genotype characterizations and preclinical studies will help neurologists understand the mechanisms of these complex gene variants.
The researchers received no funding for the study and had no relevant financial disclosures.
SOURCE: Fox J et al. AES 2018, Abstract 1.230.
NEW ORLEANS – according to research presented at the annual meeting of the American Epilepsy Society. Of four epilepsy patients at one center who received nicotine-patch treatment, three had a good clinical response, one of whom became seizure free.
“We confirm that, in select patients, treatment with a nicotine patch ... can be an effective precision therapy for epilepsy. We propose consideration of nicotine-patch treatment in refractory patients with known cholinergic nicotine receptor subunit variants, especially those with a clinical history consistent with autosomal dominant nocturnal frontal lobe epilepsy (ADNFLE),” said Jordana Fox, DO, and Alison Dolce, MD, both with the University of Texas Southwestern Medical Center in Dallas.
Gene variants in CHRAn4,CHRNA2, and CHRNB2 can cause ADNFLE. Preclinical and n-of-1 studies have suggested that nicotine may be a precision treatment for ADNFLE.
Dr. Fox and Dr. Dolce reviewed next-generation sequencing epilepsy panels from patients seen at Children’s Medical Center, Dallas, during 2011-2015 to identify patients with nAChR gene variants (CHNRA4, CHRNA2, CHRNB2, and CHRNA7). They reviewed patients’ medical and laboratory records, including genetic variant details and treatment history, and focused on patients who underwent a trial of nicotine-patch treatment.
Of the 21 patients who had nAChR gene variants, 4 tried treatment with a nicotine patch, either 7 mg or 14 mg. The patients who received nicotine-patch treatment had genetic variants in CHRNA4, CHRNB2, and CHRNA2. Three of the patients who tried nicotine-patch treatment had a greater than 50% reduction in seizures, whereas one had no treatment response.
“One patient became seizure free and is now treated with the nicotine patch as monotherapy,” Dr. Fox said.
The patient with complete resolution of seizures had a heterozygous disease–causing mutation in CHRNB2. This patient had nocturnal focal seizures, normal neuroimaging, and had been receiving treatment with oxcarbazepine and zonisamide.
The review identified four patients with nAChR gene variants and the ADNFLE phenotype who have not been treated with nicotine. Further phenotype-genotype characterizations and preclinical studies will help neurologists understand the mechanisms of these complex gene variants.
The researchers received no funding for the study and had no relevant financial disclosures.
SOURCE: Fox J et al. AES 2018, Abstract 1.230.
REPORTING FROM AES 2018
Key clinical point: In select patients with epilepsy, nicotine may be an effective precision therapy.
Major finding: Of four patients who received nicotine-patch treatment at one center, three had a good clinical response, one of whom became seizure free.
Study details: Single-center chart review of 21 patients with gene variants in subunits of the nicotinic acetylcholine receptor.
Disclosures: The researchers received no funding for the study and had no relevant financial disclosures.
Source: Fox J et al. AES 2018, Abstract 1.230.
Common AEDs confer modestly increased risk of major congenital malformations
NEW ORLEANS – The most commonly used antiepileptic drugs modestly increased the risk of major congenital malformations among prenatally exposed infants in the MONEAD study.
Malformations occurred among 5% of pregnancies exposed to the medications – higher than the 2% background rate – but this was still much lower than the 9%-10% rate associated with valproate.
Overall, however, the message of the Maternal Outcomes and Neurodevelopmental Effects of Antiepileptic (MONEAD) study is quite reassuring, Kimford J. Meador, MD, said at the annual meeting of the American Epilepsy Society. MONEAD is an ongoing, prospective study to determine both maternal outcomes and long-term childhood neurodevelopmental outcomes associated with the use of antiepileptic drugs (AEDs) during pregnancy.
“The rate of malformations was higher than I thought it would be, and higher than the 2% background rate, but it’s still a modest increase and most babies are born completely normal,” Dr. Meador, professor of neurology and neurosciences at Stanford (Calif.) University, said in an interview. “I think the news here is good, and it’s especially reassuring when you put it in the context that, 60 years ago, there were laws that women with epilepsy couldn’t get married, and some states even had laws to sterilize women. I think that’s absurd when most infants born to these women are without malformations and the risk of miscarriage is very low.”
Another positive finding, he said, is that valproate use among pregnant women is now practically nonexistent. Only 1 of 351 pregnant women with epilepsy and just 2 of a comparator group of 109 nonpregnant women with epilepsy were taking it. That’s great news, said Dr. Meador, who also initiated the NEAD (Neurodevelopmental Effects of Antiepileptic Drugs) study in the early 2000s. NEAD determined the drug’s serious teratogenic potential.
In addition to the cohorts of pregnant and nonpregnant women with epilepsy, 105 healthy pregnant women enrolled in the MONEAD study. Women will be monitored during pregnancy and postpartum to measure maternal outcomes and their children will be monitored from birth through age 6 years to measure their health and developmental outcomes.
The study has six primary outcomes, three for the women and three for their children.
- Determine if women with epilepsy have increased seizures during pregnancy and delineate the contributing factors.
- Determine if C-section rate is increased in women with epilepsy and delineate contributing factors.
- Determine if women with epilepsy have an increased risk for depression during pregnancy and the postpartum period and characterize risk factors.
- Determine the long-term effects of in utero AED exposure on verbal intellectual abilities and other neurobehavioral outcomes.
- Determine if small-for-gestational age and other adverse neonatal outcomes are increased.
- Determine if breastfeeding when taking AEDs impairs the child’s ultimate verbal and other cognitive outcomes.
Rates of miscarriage and neonatal malformations were not primary study outcomes, but the descriptive data were collected and are of high interest, Dr. Meador said.
At baseline, all the women had a mean age of about 30 years. Most (75%) were on monotherapy, 20% were on polytherapy, and the rest were not taking an AED. About 60% had focal epilepsy, 31% had generalized epilepsy, and the remainder had an unclassified seizure disorder. Three subjects had multiple seizure types. The most commonly used AEDs were lamotrigine and levetiracetam (both about 30%); 4% were taking zonisamide, 4% carbamazepine, and 4% oxcarbazepine. Topiramate was being used for 2% of the pregnant woman and 5% of the nonpregnant woman. The combination of lamotrigine and levetiracetam was used for 9.0% of pregnant and 5.5% of nonpregnant women, and other polytherapies in 12.0% of the pregnant and 14.0% of the nonpregnant woman. About 4% of the pregnant and 1% of the nonpregnant women were not taking any AED.
There were 10 (2.8%) spontaneous miscarriages among the pregnant women with epilepsy and none among the healthy pregnant women. Spontaneous miscarriages weren’t associated with acute seizures, and there were no major congenital malformations reported among them. There were also two elective abortions among the pregnant women with epilepsy.
There were 18 major congenital malformations among the pregnant woman with epilepsy (5%). A total of 14 were among pregnancies exposed to monotherapy, 3 were in polytherapy-exposed pregnancies, and 1 was in the group not taking any AEDs.
The malformations were:
- Carbamazepine (one case) – hydronephrosis.
- Gabapentin (one case) – inguinal hernia.
- Lamotrigine (five cases) – aortic coarctation, cryptorchidism, hydronephrosis, pectus excavatum, and morning glory syndrome (a funnel-shaped optic nerve disc associated with impaired visual acuity).
- Levetiracetam (five cases) – atrial septal defect, buried penis syndrome, cryptorchidism, hypoplastic aortic valve, ventricular septal defect.
- Topiramate (one case) – ventricular septal defect.
- Zonisamide (one case) – inguinal hernia, absent pinna.
- Lamotrigine plus clonazepam (one case) – cardiomyopathy.
- Lamotrigine plus levetiracetam (one case) – microcephaly, myelomeningocele, Chiari II malformation.
- Levetiracetam plus phenobarbital (one case) – bilateral inguinal hernia.
MONEAD is funded by the National Institutes of Health; Dr. Meador reported no financial disclosures.
SOURCE: Meador KJ et al. AES 2018, Abstract 3.231.
NEW ORLEANS – The most commonly used antiepileptic drugs modestly increased the risk of major congenital malformations among prenatally exposed infants in the MONEAD study.
Malformations occurred among 5% of pregnancies exposed to the medications – higher than the 2% background rate – but this was still much lower than the 9%-10% rate associated with valproate.
Overall, however, the message of the Maternal Outcomes and Neurodevelopmental Effects of Antiepileptic (MONEAD) study is quite reassuring, Kimford J. Meador, MD, said at the annual meeting of the American Epilepsy Society. MONEAD is an ongoing, prospective study to determine both maternal outcomes and long-term childhood neurodevelopmental outcomes associated with the use of antiepileptic drugs (AEDs) during pregnancy.
“The rate of malformations was higher than I thought it would be, and higher than the 2% background rate, but it’s still a modest increase and most babies are born completely normal,” Dr. Meador, professor of neurology and neurosciences at Stanford (Calif.) University, said in an interview. “I think the news here is good, and it’s especially reassuring when you put it in the context that, 60 years ago, there were laws that women with epilepsy couldn’t get married, and some states even had laws to sterilize women. I think that’s absurd when most infants born to these women are without malformations and the risk of miscarriage is very low.”
Another positive finding, he said, is that valproate use among pregnant women is now practically nonexistent. Only 1 of 351 pregnant women with epilepsy and just 2 of a comparator group of 109 nonpregnant women with epilepsy were taking it. That’s great news, said Dr. Meador, who also initiated the NEAD (Neurodevelopmental Effects of Antiepileptic Drugs) study in the early 2000s. NEAD determined the drug’s serious teratogenic potential.
In addition to the cohorts of pregnant and nonpregnant women with epilepsy, 105 healthy pregnant women enrolled in the MONEAD study. Women will be monitored during pregnancy and postpartum to measure maternal outcomes and their children will be monitored from birth through age 6 years to measure their health and developmental outcomes.
The study has six primary outcomes, three for the women and three for their children.
- Determine if women with epilepsy have increased seizures during pregnancy and delineate the contributing factors.
- Determine if C-section rate is increased in women with epilepsy and delineate contributing factors.
- Determine if women with epilepsy have an increased risk for depression during pregnancy and the postpartum period and characterize risk factors.
- Determine the long-term effects of in utero AED exposure on verbal intellectual abilities and other neurobehavioral outcomes.
- Determine if small-for-gestational age and other adverse neonatal outcomes are increased.
- Determine if breastfeeding when taking AEDs impairs the child’s ultimate verbal and other cognitive outcomes.
Rates of miscarriage and neonatal malformations were not primary study outcomes, but the descriptive data were collected and are of high interest, Dr. Meador said.
At baseline, all the women had a mean age of about 30 years. Most (75%) were on monotherapy, 20% were on polytherapy, and the rest were not taking an AED. About 60% had focal epilepsy, 31% had generalized epilepsy, and the remainder had an unclassified seizure disorder. Three subjects had multiple seizure types. The most commonly used AEDs were lamotrigine and levetiracetam (both about 30%); 4% were taking zonisamide, 4% carbamazepine, and 4% oxcarbazepine. Topiramate was being used for 2% of the pregnant woman and 5% of the nonpregnant woman. The combination of lamotrigine and levetiracetam was used for 9.0% of pregnant and 5.5% of nonpregnant women, and other polytherapies in 12.0% of the pregnant and 14.0% of the nonpregnant woman. About 4% of the pregnant and 1% of the nonpregnant women were not taking any AED.
There were 10 (2.8%) spontaneous miscarriages among the pregnant women with epilepsy and none among the healthy pregnant women. Spontaneous miscarriages weren’t associated with acute seizures, and there were no major congenital malformations reported among them. There were also two elective abortions among the pregnant women with epilepsy.
There were 18 major congenital malformations among the pregnant woman with epilepsy (5%). A total of 14 were among pregnancies exposed to monotherapy, 3 were in polytherapy-exposed pregnancies, and 1 was in the group not taking any AEDs.
The malformations were:
- Carbamazepine (one case) – hydronephrosis.
- Gabapentin (one case) – inguinal hernia.
- Lamotrigine (five cases) – aortic coarctation, cryptorchidism, hydronephrosis, pectus excavatum, and morning glory syndrome (a funnel-shaped optic nerve disc associated with impaired visual acuity).
- Levetiracetam (five cases) – atrial septal defect, buried penis syndrome, cryptorchidism, hypoplastic aortic valve, ventricular septal defect.
- Topiramate (one case) – ventricular septal defect.
- Zonisamide (one case) – inguinal hernia, absent pinna.
- Lamotrigine plus clonazepam (one case) – cardiomyopathy.
- Lamotrigine plus levetiracetam (one case) – microcephaly, myelomeningocele, Chiari II malformation.
- Levetiracetam plus phenobarbital (one case) – bilateral inguinal hernia.
MONEAD is funded by the National Institutes of Health; Dr. Meador reported no financial disclosures.
SOURCE: Meador KJ et al. AES 2018, Abstract 3.231.
NEW ORLEANS – The most commonly used antiepileptic drugs modestly increased the risk of major congenital malformations among prenatally exposed infants in the MONEAD study.
Malformations occurred among 5% of pregnancies exposed to the medications – higher than the 2% background rate – but this was still much lower than the 9%-10% rate associated with valproate.
Overall, however, the message of the Maternal Outcomes and Neurodevelopmental Effects of Antiepileptic (MONEAD) study is quite reassuring, Kimford J. Meador, MD, said at the annual meeting of the American Epilepsy Society. MONEAD is an ongoing, prospective study to determine both maternal outcomes and long-term childhood neurodevelopmental outcomes associated with the use of antiepileptic drugs (AEDs) during pregnancy.
“The rate of malformations was higher than I thought it would be, and higher than the 2% background rate, but it’s still a modest increase and most babies are born completely normal,” Dr. Meador, professor of neurology and neurosciences at Stanford (Calif.) University, said in an interview. “I think the news here is good, and it’s especially reassuring when you put it in the context that, 60 years ago, there were laws that women with epilepsy couldn’t get married, and some states even had laws to sterilize women. I think that’s absurd when most infants born to these women are without malformations and the risk of miscarriage is very low.”
Another positive finding, he said, is that valproate use among pregnant women is now practically nonexistent. Only 1 of 351 pregnant women with epilepsy and just 2 of a comparator group of 109 nonpregnant women with epilepsy were taking it. That’s great news, said Dr. Meador, who also initiated the NEAD (Neurodevelopmental Effects of Antiepileptic Drugs) study in the early 2000s. NEAD determined the drug’s serious teratogenic potential.
In addition to the cohorts of pregnant and nonpregnant women with epilepsy, 105 healthy pregnant women enrolled in the MONEAD study. Women will be monitored during pregnancy and postpartum to measure maternal outcomes and their children will be monitored from birth through age 6 years to measure their health and developmental outcomes.
The study has six primary outcomes, three for the women and three for their children.
- Determine if women with epilepsy have increased seizures during pregnancy and delineate the contributing factors.
- Determine if C-section rate is increased in women with epilepsy and delineate contributing factors.
- Determine if women with epilepsy have an increased risk for depression during pregnancy and the postpartum period and characterize risk factors.
- Determine the long-term effects of in utero AED exposure on verbal intellectual abilities and other neurobehavioral outcomes.
- Determine if small-for-gestational age and other adverse neonatal outcomes are increased.
- Determine if breastfeeding when taking AEDs impairs the child’s ultimate verbal and other cognitive outcomes.
Rates of miscarriage and neonatal malformations were not primary study outcomes, but the descriptive data were collected and are of high interest, Dr. Meador said.
At baseline, all the women had a mean age of about 30 years. Most (75%) were on monotherapy, 20% were on polytherapy, and the rest were not taking an AED. About 60% had focal epilepsy, 31% had generalized epilepsy, and the remainder had an unclassified seizure disorder. Three subjects had multiple seizure types. The most commonly used AEDs were lamotrigine and levetiracetam (both about 30%); 4% were taking zonisamide, 4% carbamazepine, and 4% oxcarbazepine. Topiramate was being used for 2% of the pregnant woman and 5% of the nonpregnant woman. The combination of lamotrigine and levetiracetam was used for 9.0% of pregnant and 5.5% of nonpregnant women, and other polytherapies in 12.0% of the pregnant and 14.0% of the nonpregnant woman. About 4% of the pregnant and 1% of the nonpregnant women were not taking any AED.
There were 10 (2.8%) spontaneous miscarriages among the pregnant women with epilepsy and none among the healthy pregnant women. Spontaneous miscarriages weren’t associated with acute seizures, and there were no major congenital malformations reported among them. There were also two elective abortions among the pregnant women with epilepsy.
There were 18 major congenital malformations among the pregnant woman with epilepsy (5%). A total of 14 were among pregnancies exposed to monotherapy, 3 were in polytherapy-exposed pregnancies, and 1 was in the group not taking any AEDs.
The malformations were:
- Carbamazepine (one case) – hydronephrosis.
- Gabapentin (one case) – inguinal hernia.
- Lamotrigine (five cases) – aortic coarctation, cryptorchidism, hydronephrosis, pectus excavatum, and morning glory syndrome (a funnel-shaped optic nerve disc associated with impaired visual acuity).
- Levetiracetam (five cases) – atrial septal defect, buried penis syndrome, cryptorchidism, hypoplastic aortic valve, ventricular septal defect.
- Topiramate (one case) – ventricular septal defect.
- Zonisamide (one case) – inguinal hernia, absent pinna.
- Lamotrigine plus clonazepam (one case) – cardiomyopathy.
- Lamotrigine plus levetiracetam (one case) – microcephaly, myelomeningocele, Chiari II malformation.
- Levetiracetam plus phenobarbital (one case) – bilateral inguinal hernia.
MONEAD is funded by the National Institutes of Health; Dr. Meador reported no financial disclosures.
SOURCE: Meador KJ et al. AES 2018, Abstract 3.231.
REPORTING FROM AES 2018
Key clinical point:
Major finding: The malformation rate was 5% in exposed pregnancies.
Study details: The MONEAD study comprised 351 pregnant women with epilepsy, 109 nonpregnant women with epilepsy, and 105 healthy pregnant women.
Disclosures: The National Institutes of Health funded the study; Dr. Meador reported no financial disclosures.
Source: Meador KJ et al. AES 2018, Abstract 3.231.
Breastfeeding with MS: Good for mom, too
BERLIN – In the changing multiple sclerosis landscape, more women are having babies, and more are asking questions. With these women, what’s the best way to address the complicated interplay among pregnancy, relapse risk, breastfeeding, and medication resumption? A starting point is to recognize that “women with MS are very different today than they were 25 years ago,” said Annette Langer-Gould, MD, PhD. Not only have diagnostic criteria changed but also highly effective treatments now exist that were not available when the first pregnancy cohorts were studied, she pointed out, speaking at the annual congress of the European Committee on Treatment and Research in Multiple Sclerosis.
The existing literature, said Dr. Langer-Gould, has addressed one controversy: “Most women with MS can have normal pregnancies – and breastfeed – without incurring harm,” though it’s true that severe rebound relapses are possible if natalizumab (Tysabri) or fingolimod (Gilenya) are stopped before pregnancy. In any case, new small-molecule MS medications need to be stopped during pregnancy and breastfeeding, she pointed out. “We didn’t have to worry about that too much when we only had injectables and monoclonal antibodies because they were larger and didn’t cross the placenta.”
Since the 1980s, the conversation about pregnancy and MS has moved from asking “Is pregnancy bad for women with MS?” to the current MS landscape, in which sicker women are able to become pregnant, Dr. Langer-Gould said, adding that how women with MS fare through pregnancy and in the postpartum period is changing over time as well. She and her colleagues’ experience with pregnancy in a cohort of women with MS in the Kaiser Permanente care system, where she is a clinical neurologist and regional research lead, revealed a relapse rate of 8.4%. “So it was pretty rare for a woman to have a relapse during pregnancy,” Dr. Langer-Gould said.
Most women with MS who become pregnant, whether their care is received in a referral center or is community based, are now doing so while on a disease-modifying therapy (DMT), Dr. Langer-Gould said. On these highly effective treatments, “women who were too sick to get pregnant are now well controlled and having babies.”
As more women with MS become pregnant, more conversations about breastfeeding will inevitably crop up, she said. And the discussion about breastfeeding has now begun to acknowledge the “strong benefits to mom and the baby of not just breastfeeding, but longer breastfeeding,” as well.
“Because of this baby-friendly push in a lot of hospitals in the United States, where they’re trying to encourage all women to breastfeed,” a full 87% of women breastfed their infants at least some of the time, and over a third of women (35%) breastfed exclusively for at least 2 months, Dr. Langer-Gould said.
“There’s no one clear explanation of why the women seem to be healthier and doing better through pregnancy as a group, but it’s probably a combination of having milder disease, breastfeeding more, and they’ve got better controlled disease before pregnancy,” she said.
At least eight studies to date have examined the relationship between postpartum MS relapses and breastfeeding, Dr. Langer-Gould said.
“The thing to take away ... is that, even though we’ve studied this many, many times, no one can show that it’s harmful,” she said. For mothers who want to breastfeed, “you can support them in the breastfeeding choice, because they are not going to have more severe disease because of that.”
Whether breastfeeding is exclusive or not has not always been tracked in studies of childbearing women with MS, but when it was captured in the data, exclusive breastfeeding has exerted a protective effect, with about a 50% reduction in risk for postpartum relapse seen in one study (JAMA Neurol. 2015 Oct;72[10]:1132-8).
There is a hormonal rationale for exclusive breastfeeding exerting a protective effect on MS: With exclusive breastfeeding comes more frequent, intense suckling, with more profound elevations in prolactin, and larger drops in follicle-stimulating hormone, luteinizing hormone, progesterone, and estradiol. All these hormonal changes work together to produce more prolonged amenorrhea and anovulation, Dr. Langer-Gould said, with potentially beneficial immunologic effects.
When other, more general maternal and infant health benefits of breastfeeding also are taken into account, there’s strong evidence for the benefits of breastfeeding for women with MS whose medication profile allows them to breastfeed, she said.
However, the “treatment” effect of exclusive breastfeeding is only effective until the infant starts taking regular supplemental feedings, including the introduction of table food at around 6 months of age. “Once regular supplemental feedings are introduced, relapses return,” Dr. Langer-Gould said.
There is some suggestion that, in women without MS, prolonged breastfeeding may be associated with reduced risk of MS. In the MS Sunshine study, breastfeeding for 15 months or longer decreased the risk of later MS by 23%-53% (Nutrients. 2018 Feb 27;10[3]:268). The investigators, led by Dr. Langer-Gould, summed the total months of breastfeeding across all children, so that the 15-month threshold could be reached by breastfeeding one child for 15 months, or three children for 5 months each. “It’s a single study; I wouldn’t make too much out of it,” Dr. Langer-Gould said.
Open questions still remain, she said: “So far, no one has been able to demonstrate a clear beneficial effect in reducing the risk of postpartum relapse if they resume their DMT early in the postpartum period.” Dr. Langer-Gould noted that the literature in this area is hampered by heterogeneity and by the fact that newer, more highly active DMTs have not been well studied.
Also, the link between postpartum relapses and long-term prognosis is not completely delineated. Indirect evidence, she said, points to a postpartum relapse as being “overall, a low-impact event.”
Dr. Langer-Gould reported that she has been the site principal investigator for clinical trials sponsored by Roche and Biogen.
SOURCE: Langer-Gould A. ECTRIMS 2018, Abstract 5.
BERLIN – In the changing multiple sclerosis landscape, more women are having babies, and more are asking questions. With these women, what’s the best way to address the complicated interplay among pregnancy, relapse risk, breastfeeding, and medication resumption? A starting point is to recognize that “women with MS are very different today than they were 25 years ago,” said Annette Langer-Gould, MD, PhD. Not only have diagnostic criteria changed but also highly effective treatments now exist that were not available when the first pregnancy cohorts were studied, she pointed out, speaking at the annual congress of the European Committee on Treatment and Research in Multiple Sclerosis.
The existing literature, said Dr. Langer-Gould, has addressed one controversy: “Most women with MS can have normal pregnancies – and breastfeed – without incurring harm,” though it’s true that severe rebound relapses are possible if natalizumab (Tysabri) or fingolimod (Gilenya) are stopped before pregnancy. In any case, new small-molecule MS medications need to be stopped during pregnancy and breastfeeding, she pointed out. “We didn’t have to worry about that too much when we only had injectables and monoclonal antibodies because they were larger and didn’t cross the placenta.”
Since the 1980s, the conversation about pregnancy and MS has moved from asking “Is pregnancy bad for women with MS?” to the current MS landscape, in which sicker women are able to become pregnant, Dr. Langer-Gould said, adding that how women with MS fare through pregnancy and in the postpartum period is changing over time as well. She and her colleagues’ experience with pregnancy in a cohort of women with MS in the Kaiser Permanente care system, where she is a clinical neurologist and regional research lead, revealed a relapse rate of 8.4%. “So it was pretty rare for a woman to have a relapse during pregnancy,” Dr. Langer-Gould said.
Most women with MS who become pregnant, whether their care is received in a referral center or is community based, are now doing so while on a disease-modifying therapy (DMT), Dr. Langer-Gould said. On these highly effective treatments, “women who were too sick to get pregnant are now well controlled and having babies.”
As more women with MS become pregnant, more conversations about breastfeeding will inevitably crop up, she said. And the discussion about breastfeeding has now begun to acknowledge the “strong benefits to mom and the baby of not just breastfeeding, but longer breastfeeding,” as well.
“Because of this baby-friendly push in a lot of hospitals in the United States, where they’re trying to encourage all women to breastfeed,” a full 87% of women breastfed their infants at least some of the time, and over a third of women (35%) breastfed exclusively for at least 2 months, Dr. Langer-Gould said.
“There’s no one clear explanation of why the women seem to be healthier and doing better through pregnancy as a group, but it’s probably a combination of having milder disease, breastfeeding more, and they’ve got better controlled disease before pregnancy,” she said.
At least eight studies to date have examined the relationship between postpartum MS relapses and breastfeeding, Dr. Langer-Gould said.
“The thing to take away ... is that, even though we’ve studied this many, many times, no one can show that it’s harmful,” she said. For mothers who want to breastfeed, “you can support them in the breastfeeding choice, because they are not going to have more severe disease because of that.”
Whether breastfeeding is exclusive or not has not always been tracked in studies of childbearing women with MS, but when it was captured in the data, exclusive breastfeeding has exerted a protective effect, with about a 50% reduction in risk for postpartum relapse seen in one study (JAMA Neurol. 2015 Oct;72[10]:1132-8).
There is a hormonal rationale for exclusive breastfeeding exerting a protective effect on MS: With exclusive breastfeeding comes more frequent, intense suckling, with more profound elevations in prolactin, and larger drops in follicle-stimulating hormone, luteinizing hormone, progesterone, and estradiol. All these hormonal changes work together to produce more prolonged amenorrhea and anovulation, Dr. Langer-Gould said, with potentially beneficial immunologic effects.
When other, more general maternal and infant health benefits of breastfeeding also are taken into account, there’s strong evidence for the benefits of breastfeeding for women with MS whose medication profile allows them to breastfeed, she said.
However, the “treatment” effect of exclusive breastfeeding is only effective until the infant starts taking regular supplemental feedings, including the introduction of table food at around 6 months of age. “Once regular supplemental feedings are introduced, relapses return,” Dr. Langer-Gould said.
There is some suggestion that, in women without MS, prolonged breastfeeding may be associated with reduced risk of MS. In the MS Sunshine study, breastfeeding for 15 months or longer decreased the risk of later MS by 23%-53% (Nutrients. 2018 Feb 27;10[3]:268). The investigators, led by Dr. Langer-Gould, summed the total months of breastfeeding across all children, so that the 15-month threshold could be reached by breastfeeding one child for 15 months, or three children for 5 months each. “It’s a single study; I wouldn’t make too much out of it,” Dr. Langer-Gould said.
Open questions still remain, she said: “So far, no one has been able to demonstrate a clear beneficial effect in reducing the risk of postpartum relapse if they resume their DMT early in the postpartum period.” Dr. Langer-Gould noted that the literature in this area is hampered by heterogeneity and by the fact that newer, more highly active DMTs have not been well studied.
Also, the link between postpartum relapses and long-term prognosis is not completely delineated. Indirect evidence, she said, points to a postpartum relapse as being “overall, a low-impact event.”
Dr. Langer-Gould reported that she has been the site principal investigator for clinical trials sponsored by Roche and Biogen.
SOURCE: Langer-Gould A. ECTRIMS 2018, Abstract 5.
BERLIN – In the changing multiple sclerosis landscape, more women are having babies, and more are asking questions. With these women, what’s the best way to address the complicated interplay among pregnancy, relapse risk, breastfeeding, and medication resumption? A starting point is to recognize that “women with MS are very different today than they were 25 years ago,” said Annette Langer-Gould, MD, PhD. Not only have diagnostic criteria changed but also highly effective treatments now exist that were not available when the first pregnancy cohorts were studied, she pointed out, speaking at the annual congress of the European Committee on Treatment and Research in Multiple Sclerosis.
The existing literature, said Dr. Langer-Gould, has addressed one controversy: “Most women with MS can have normal pregnancies – and breastfeed – without incurring harm,” though it’s true that severe rebound relapses are possible if natalizumab (Tysabri) or fingolimod (Gilenya) are stopped before pregnancy. In any case, new small-molecule MS medications need to be stopped during pregnancy and breastfeeding, she pointed out. “We didn’t have to worry about that too much when we only had injectables and monoclonal antibodies because they were larger and didn’t cross the placenta.”
Since the 1980s, the conversation about pregnancy and MS has moved from asking “Is pregnancy bad for women with MS?” to the current MS landscape, in which sicker women are able to become pregnant, Dr. Langer-Gould said, adding that how women with MS fare through pregnancy and in the postpartum period is changing over time as well. She and her colleagues’ experience with pregnancy in a cohort of women with MS in the Kaiser Permanente care system, where she is a clinical neurologist and regional research lead, revealed a relapse rate of 8.4%. “So it was pretty rare for a woman to have a relapse during pregnancy,” Dr. Langer-Gould said.
Most women with MS who become pregnant, whether their care is received in a referral center or is community based, are now doing so while on a disease-modifying therapy (DMT), Dr. Langer-Gould said. On these highly effective treatments, “women who were too sick to get pregnant are now well controlled and having babies.”
As more women with MS become pregnant, more conversations about breastfeeding will inevitably crop up, she said. And the discussion about breastfeeding has now begun to acknowledge the “strong benefits to mom and the baby of not just breastfeeding, but longer breastfeeding,” as well.
“Because of this baby-friendly push in a lot of hospitals in the United States, where they’re trying to encourage all women to breastfeed,” a full 87% of women breastfed their infants at least some of the time, and over a third of women (35%) breastfed exclusively for at least 2 months, Dr. Langer-Gould said.
“There’s no one clear explanation of why the women seem to be healthier and doing better through pregnancy as a group, but it’s probably a combination of having milder disease, breastfeeding more, and they’ve got better controlled disease before pregnancy,” she said.
At least eight studies to date have examined the relationship between postpartum MS relapses and breastfeeding, Dr. Langer-Gould said.
“The thing to take away ... is that, even though we’ve studied this many, many times, no one can show that it’s harmful,” she said. For mothers who want to breastfeed, “you can support them in the breastfeeding choice, because they are not going to have more severe disease because of that.”
Whether breastfeeding is exclusive or not has not always been tracked in studies of childbearing women with MS, but when it was captured in the data, exclusive breastfeeding has exerted a protective effect, with about a 50% reduction in risk for postpartum relapse seen in one study (JAMA Neurol. 2015 Oct;72[10]:1132-8).
There is a hormonal rationale for exclusive breastfeeding exerting a protective effect on MS: With exclusive breastfeeding comes more frequent, intense suckling, with more profound elevations in prolactin, and larger drops in follicle-stimulating hormone, luteinizing hormone, progesterone, and estradiol. All these hormonal changes work together to produce more prolonged amenorrhea and anovulation, Dr. Langer-Gould said, with potentially beneficial immunologic effects.
When other, more general maternal and infant health benefits of breastfeeding also are taken into account, there’s strong evidence for the benefits of breastfeeding for women with MS whose medication profile allows them to breastfeed, she said.
However, the “treatment” effect of exclusive breastfeeding is only effective until the infant starts taking regular supplemental feedings, including the introduction of table food at around 6 months of age. “Once regular supplemental feedings are introduced, relapses return,” Dr. Langer-Gould said.
There is some suggestion that, in women without MS, prolonged breastfeeding may be associated with reduced risk of MS. In the MS Sunshine study, breastfeeding for 15 months or longer decreased the risk of later MS by 23%-53% (Nutrients. 2018 Feb 27;10[3]:268). The investigators, led by Dr. Langer-Gould, summed the total months of breastfeeding across all children, so that the 15-month threshold could be reached by breastfeeding one child for 15 months, or three children for 5 months each. “It’s a single study; I wouldn’t make too much out of it,” Dr. Langer-Gould said.
Open questions still remain, she said: “So far, no one has been able to demonstrate a clear beneficial effect in reducing the risk of postpartum relapse if they resume their DMT early in the postpartum period.” Dr. Langer-Gould noted that the literature in this area is hampered by heterogeneity and by the fact that newer, more highly active DMTs have not been well studied.
Also, the link between postpartum relapses and long-term prognosis is not completely delineated. Indirect evidence, she said, points to a postpartum relapse as being “overall, a low-impact event.”
Dr. Langer-Gould reported that she has been the site principal investigator for clinical trials sponsored by Roche and Biogen.
SOURCE: Langer-Gould A. ECTRIMS 2018, Abstract 5.
REPORTING FROM ECTRIMS 2018
Redo carotid endarterectomy is more risky than previously estimated
NEW YORK – It is well known that reoperative carotid endarterectomy can be technically challenging because of the scarring left from the initial procedure, but an analysis of a large database presented at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation also revealed that the risk of complications, particularly stroke, is greater.
When “redo” carotid endarterectomies were compared with the index primary procedure collected in the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database, the odds ratio for stroke was several times greater (odds ratio, 3.71; P = .002) on univariate analysis, reported Jeffrey J. Siracuse, MD, associate professor of surgery and radiology at Boston University.
Previous single-center reports of redo endarterectomies “showed terrific results, really no perioperative stroke or morbidity, but this is older data from a different era,” said Dr. Siracuse, who undertook this study to determine whether “real-world” data would tell a different story.
In this study, 75,943 primary carotid endarterectomies and 140 redo procedures were identified in the ACS NSQIP database and compared. The redo population had a significantly higher incidence of end-stage renal disease (3.6% vs. 1.1%; P = .004), but history of stroke, whether with deficit (20.8% vs. 15.4%) or without (11.5% vs. 9.1%), was numerically higher among those undergoing a primary procedure even though these differences did not reach statistical significance. Baseline demographics and comorbidities were otherwise similar.
Presumably because of the difficulty of recanalizing scarred tissue, the mean procedure time for redos was longer than that for the primary procedures (137 vs. 49 minutes; P less than .001), but there were no significant differences in the rate of surgical site infections (0.7% vs. 0.3%; P = .482), return to the operating room (3.6% vs. 4%; P = .853), or 30-day readmissions (2.1% vs. 6.9%; P = .810) for the redo and index procedures, respectively.
Although perioperative MI rates were higher in the redo group (2.1%) than in the primary endarterectomy group (0.9%), this difference did not reach statistical significance (P = .125). However, a multivariate analysis associated redo carotid endarterectomy procedures with a nearly threefold increase in risk of a composite of major adverse cardiovascular events when compared on a multivariate analysis (OR, 2.76; P = .007), Dr. Siracuse reported.
For the surgeons considering a redo carotid endarterectomy, these data “inform a risk-benefit analysis,” according to Dr. Siracuse, but he also said that redo procedures still should be considered a viable strategy when considered in the context of other options.
Presenting a case he performed just prior to the VEITHsymposium, Dr. Siracuse displayed CT images that showed internal and common carotids with more than 75% stenosis in an 80-year-old women 7 years after a primary carotid endarterectomy. The tight stenoses and the evidence of substantial intra-arterial debris were concerns, but a decision to perform a redo endarterectomy was reached after other options, including stenting, were considered.
“She did great. She went home and has had no more symptoms,” Dr. Siracuse reported. “The point is you still have to take these [potential redo endarterectomies] on a case-by case basis.”
Dr. Siracuse reported he had no financial relationships relevant to this study.
NEW YORK – It is well known that reoperative carotid endarterectomy can be technically challenging because of the scarring left from the initial procedure, but an analysis of a large database presented at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation also revealed that the risk of complications, particularly stroke, is greater.
When “redo” carotid endarterectomies were compared with the index primary procedure collected in the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database, the odds ratio for stroke was several times greater (odds ratio, 3.71; P = .002) on univariate analysis, reported Jeffrey J. Siracuse, MD, associate professor of surgery and radiology at Boston University.
Previous single-center reports of redo endarterectomies “showed terrific results, really no perioperative stroke or morbidity, but this is older data from a different era,” said Dr. Siracuse, who undertook this study to determine whether “real-world” data would tell a different story.
In this study, 75,943 primary carotid endarterectomies and 140 redo procedures were identified in the ACS NSQIP database and compared. The redo population had a significantly higher incidence of end-stage renal disease (3.6% vs. 1.1%; P = .004), but history of stroke, whether with deficit (20.8% vs. 15.4%) or without (11.5% vs. 9.1%), was numerically higher among those undergoing a primary procedure even though these differences did not reach statistical significance. Baseline demographics and comorbidities were otherwise similar.
Presumably because of the difficulty of recanalizing scarred tissue, the mean procedure time for redos was longer than that for the primary procedures (137 vs. 49 minutes; P less than .001), but there were no significant differences in the rate of surgical site infections (0.7% vs. 0.3%; P = .482), return to the operating room (3.6% vs. 4%; P = .853), or 30-day readmissions (2.1% vs. 6.9%; P = .810) for the redo and index procedures, respectively.
Although perioperative MI rates were higher in the redo group (2.1%) than in the primary endarterectomy group (0.9%), this difference did not reach statistical significance (P = .125). However, a multivariate analysis associated redo carotid endarterectomy procedures with a nearly threefold increase in risk of a composite of major adverse cardiovascular events when compared on a multivariate analysis (OR, 2.76; P = .007), Dr. Siracuse reported.
For the surgeons considering a redo carotid endarterectomy, these data “inform a risk-benefit analysis,” according to Dr. Siracuse, but he also said that redo procedures still should be considered a viable strategy when considered in the context of other options.
Presenting a case he performed just prior to the VEITHsymposium, Dr. Siracuse displayed CT images that showed internal and common carotids with more than 75% stenosis in an 80-year-old women 7 years after a primary carotid endarterectomy. The tight stenoses and the evidence of substantial intra-arterial debris were concerns, but a decision to perform a redo endarterectomy was reached after other options, including stenting, were considered.
“She did great. She went home and has had no more symptoms,” Dr. Siracuse reported. “The point is you still have to take these [potential redo endarterectomies] on a case-by case basis.”
Dr. Siracuse reported he had no financial relationships relevant to this study.
NEW YORK – It is well known that reoperative carotid endarterectomy can be technically challenging because of the scarring left from the initial procedure, but an analysis of a large database presented at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation also revealed that the risk of complications, particularly stroke, is greater.
When “redo” carotid endarterectomies were compared with the index primary procedure collected in the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database, the odds ratio for stroke was several times greater (odds ratio, 3.71; P = .002) on univariate analysis, reported Jeffrey J. Siracuse, MD, associate professor of surgery and radiology at Boston University.
Previous single-center reports of redo endarterectomies “showed terrific results, really no perioperative stroke or morbidity, but this is older data from a different era,” said Dr. Siracuse, who undertook this study to determine whether “real-world” data would tell a different story.
In this study, 75,943 primary carotid endarterectomies and 140 redo procedures were identified in the ACS NSQIP database and compared. The redo population had a significantly higher incidence of end-stage renal disease (3.6% vs. 1.1%; P = .004), but history of stroke, whether with deficit (20.8% vs. 15.4%) or without (11.5% vs. 9.1%), was numerically higher among those undergoing a primary procedure even though these differences did not reach statistical significance. Baseline demographics and comorbidities were otherwise similar.
Presumably because of the difficulty of recanalizing scarred tissue, the mean procedure time for redos was longer than that for the primary procedures (137 vs. 49 minutes; P less than .001), but there were no significant differences in the rate of surgical site infections (0.7% vs. 0.3%; P = .482), return to the operating room (3.6% vs. 4%; P = .853), or 30-day readmissions (2.1% vs. 6.9%; P = .810) for the redo and index procedures, respectively.
Although perioperative MI rates were higher in the redo group (2.1%) than in the primary endarterectomy group (0.9%), this difference did not reach statistical significance (P = .125). However, a multivariate analysis associated redo carotid endarterectomy procedures with a nearly threefold increase in risk of a composite of major adverse cardiovascular events when compared on a multivariate analysis (OR, 2.76; P = .007), Dr. Siracuse reported.
For the surgeons considering a redo carotid endarterectomy, these data “inform a risk-benefit analysis,” according to Dr. Siracuse, but he also said that redo procedures still should be considered a viable strategy when considered in the context of other options.
Presenting a case he performed just prior to the VEITHsymposium, Dr. Siracuse displayed CT images that showed internal and common carotids with more than 75% stenosis in an 80-year-old women 7 years after a primary carotid endarterectomy. The tight stenoses and the evidence of substantial intra-arterial debris were concerns, but a decision to perform a redo endarterectomy was reached after other options, including stenting, were considered.
“She did great. She went home and has had no more symptoms,” Dr. Siracuse reported. “The point is you still have to take these [potential redo endarterectomies] on a case-by case basis.”
Dr. Siracuse reported he had no financial relationships relevant to this study.
REPORTING FROM VEITHSYMPOSIUM
Key clinical point:
Major finding: The odds ratio for stroke is 3.71 times higher (P = .002) with redo than with primary carotid endarterectomy.
Study details: Multivariate retrospective database analysis.
Disclosures: Dr. Siracuse reported he had no financial relationships relevant to this study.
Fewer insured may have helped slow health spending growth in 2017
Health care spending as a percentage of gross domestic product remained relatively stable in 2017, despite a slowdown in the growth of spending.
Total health care spending in the United States was $3.5 trillion in 2017, an increase of 3.9% from 2016, according to data released Dec. 6 by the Centers for Medicare & Medicaid Services.
The growth rate was down from that of 2016 (4.8%) but similar to growth rates experienced during 2008-2013, according to the research article in Health Affairs.
“The slower growth in health care spending in 2017 resulted primarily from slower growth in hospital care, physician and clinical services, and retail prescription drugs, with residual use and intensity of these goods and services contributing substantially to the trend,” Anne B. Martin, an economist in the CMS Office of the Actuary’s National Health Statistics Group, and her colleagues wrote.
The report notes that slower growth in the use and intensity of health care goods and services in 2017 “may have been affected by slower growth in overall health insurance enrollment, as the insured share of the population fell from 91.1% in 2016 to 90.9% in 2017.”
Spending on hospital care increased 4.6% to $1.1 trillion in 2017 and accounted for 33% of total health care spending; however, growth was slower than in the previous year (5.6%). Ms. Martin and her colleagues noted that growth in outpatient visits slowed while growth in inpatient days increased at about the same rate and prices in hospital care grew in 2017 to 1.7% from 1.2% in the previous year.
Spending on physician and clinical services grew 4.2% in 2017 to $694.3 billion and accounted for 20% of total health care spending. The growth rate is down from the previous year (5.6%) and a recent peak of 6% in 2015.
“Although spending growth for both physician services and clinical services slowed in 2017, the growth rate for the latter (5.0%) continued to out pace the rate for the former (3.9%), as spending for most types of outpatient care centers contributed to the stronger growth in spending for clinical services,” Ms. Martin and her colleagues reported.
They attributed the slowdown to non-price factors, such as slower growth in the use and intensity of physician and clinical services, although price growth for physician and clinical services increased 0.4% in 2017, up from 0.2% in 2016.
Spending on retail prescription drugs grew 0.4% in 2017 to $333.4 billion and accounted for 10% of total national health spending. It is the slowest growth rate increase since 2012, a year that saw a number of blockbuster drugs lose patent protection. This was down from a growth rate of 2.3% in 2016 and down from recent rates of 12.4% in 2014 and 8.9% in 2015.
“Slower growth in non-price factors, such as the use and mix of retail prescription drugs – and, to a lesser extent, in retail prescription drug prices – contributed to the slower overall growth in retail prescription drug spending in 2017,” according to the authors. Key factors included slower growth in the number of prescriptions dispensed, the continued shift to lower-cost generics, and slower growth in the volume of high-cost drugs, particularly those used to treat hepatitis C. Price decreases in generics and lower increases for existing brand-name drugs also contributed to the lower spending growth in 2017.
Ms. Martin and her colleagues highlighted the slower growth rate in the number of prescriptions (1.8% in 2017, down from 2.3% in 2016) “resulted in large part from a decline in the number of prescriptions dispensed for drugs used to treat pain.”
Medicare spending, which represents 20% of all national health care spending in 2017 ($705.9 billion), grew 4.2%, a slight decline from the 4.3% growth in 2016. Enrollment growth slowed slightly to 2.5% in 2017 from 2.7% in the previous year, while in the same time frame, per-enrollee expenditures increased slightly to 1.7% from 1.6%. Slower growth in fee-for-service Medicare spending was offset by faster growth in spending by Medicare private health plans.
Medicaid spending reached $581.9 billion (17% of national health care spending), and the growth rate slowed for the third straight year, increasing 2.9% in 2017 versus 4.2% in 2016. The slower growth “was influenced by a deceleration in enrollment growth and a reduction in the Medicaid net cost of health insurance as the federal government recovered payments from managed care organizations based on their favorable prior-period experience,” the authors stated. Enrollment growth has been decelerating following a peak of growth of 11.9% in 2014 because of states that elected to expand Medicaid eligibility, which was followed by 3 years of slower growth rates of 4.9%, 3.0% and 2.0% in 2015, 2016, and 2017, respectively. Per-enrollee spending also slowed to 0.9% growth in 2017 from a rate of 1.2% in 2016, attributed to “the decline in government administration and the net cost of insurance.”
SOURCE: Martin A et al. Health Aff. 2018. doi: 10.1377/hlthaff.2018.05085.
Health care spending as a percentage of gross domestic product remained relatively stable in 2017, despite a slowdown in the growth of spending.
Total health care spending in the United States was $3.5 trillion in 2017, an increase of 3.9% from 2016, according to data released Dec. 6 by the Centers for Medicare & Medicaid Services.
The growth rate was down from that of 2016 (4.8%) but similar to growth rates experienced during 2008-2013, according to the research article in Health Affairs.
“The slower growth in health care spending in 2017 resulted primarily from slower growth in hospital care, physician and clinical services, and retail prescription drugs, with residual use and intensity of these goods and services contributing substantially to the trend,” Anne B. Martin, an economist in the CMS Office of the Actuary’s National Health Statistics Group, and her colleagues wrote.
The report notes that slower growth in the use and intensity of health care goods and services in 2017 “may have been affected by slower growth in overall health insurance enrollment, as the insured share of the population fell from 91.1% in 2016 to 90.9% in 2017.”
Spending on hospital care increased 4.6% to $1.1 trillion in 2017 and accounted for 33% of total health care spending; however, growth was slower than in the previous year (5.6%). Ms. Martin and her colleagues noted that growth in outpatient visits slowed while growth in inpatient days increased at about the same rate and prices in hospital care grew in 2017 to 1.7% from 1.2% in the previous year.
Spending on physician and clinical services grew 4.2% in 2017 to $694.3 billion and accounted for 20% of total health care spending. The growth rate is down from the previous year (5.6%) and a recent peak of 6% in 2015.
“Although spending growth for both physician services and clinical services slowed in 2017, the growth rate for the latter (5.0%) continued to out pace the rate for the former (3.9%), as spending for most types of outpatient care centers contributed to the stronger growth in spending for clinical services,” Ms. Martin and her colleagues reported.
They attributed the slowdown to non-price factors, such as slower growth in the use and intensity of physician and clinical services, although price growth for physician and clinical services increased 0.4% in 2017, up from 0.2% in 2016.
Spending on retail prescription drugs grew 0.4% in 2017 to $333.4 billion and accounted for 10% of total national health spending. It is the slowest growth rate increase since 2012, a year that saw a number of blockbuster drugs lose patent protection. This was down from a growth rate of 2.3% in 2016 and down from recent rates of 12.4% in 2014 and 8.9% in 2015.
“Slower growth in non-price factors, such as the use and mix of retail prescription drugs – and, to a lesser extent, in retail prescription drug prices – contributed to the slower overall growth in retail prescription drug spending in 2017,” according to the authors. Key factors included slower growth in the number of prescriptions dispensed, the continued shift to lower-cost generics, and slower growth in the volume of high-cost drugs, particularly those used to treat hepatitis C. Price decreases in generics and lower increases for existing brand-name drugs also contributed to the lower spending growth in 2017.
Ms. Martin and her colleagues highlighted the slower growth rate in the number of prescriptions (1.8% in 2017, down from 2.3% in 2016) “resulted in large part from a decline in the number of prescriptions dispensed for drugs used to treat pain.”
Medicare spending, which represents 20% of all national health care spending in 2017 ($705.9 billion), grew 4.2%, a slight decline from the 4.3% growth in 2016. Enrollment growth slowed slightly to 2.5% in 2017 from 2.7% in the previous year, while in the same time frame, per-enrollee expenditures increased slightly to 1.7% from 1.6%. Slower growth in fee-for-service Medicare spending was offset by faster growth in spending by Medicare private health plans.
Medicaid spending reached $581.9 billion (17% of national health care spending), and the growth rate slowed for the third straight year, increasing 2.9% in 2017 versus 4.2% in 2016. The slower growth “was influenced by a deceleration in enrollment growth and a reduction in the Medicaid net cost of health insurance as the federal government recovered payments from managed care organizations based on their favorable prior-period experience,” the authors stated. Enrollment growth has been decelerating following a peak of growth of 11.9% in 2014 because of states that elected to expand Medicaid eligibility, which was followed by 3 years of slower growth rates of 4.9%, 3.0% and 2.0% in 2015, 2016, and 2017, respectively. Per-enrollee spending also slowed to 0.9% growth in 2017 from a rate of 1.2% in 2016, attributed to “the decline in government administration and the net cost of insurance.”
SOURCE: Martin A et al. Health Aff. 2018. doi: 10.1377/hlthaff.2018.05085.
Health care spending as a percentage of gross domestic product remained relatively stable in 2017, despite a slowdown in the growth of spending.
Total health care spending in the United States was $3.5 trillion in 2017, an increase of 3.9% from 2016, according to data released Dec. 6 by the Centers for Medicare & Medicaid Services.
The growth rate was down from that of 2016 (4.8%) but similar to growth rates experienced during 2008-2013, according to the research article in Health Affairs.
“The slower growth in health care spending in 2017 resulted primarily from slower growth in hospital care, physician and clinical services, and retail prescription drugs, with residual use and intensity of these goods and services contributing substantially to the trend,” Anne B. Martin, an economist in the CMS Office of the Actuary’s National Health Statistics Group, and her colleagues wrote.
The report notes that slower growth in the use and intensity of health care goods and services in 2017 “may have been affected by slower growth in overall health insurance enrollment, as the insured share of the population fell from 91.1% in 2016 to 90.9% in 2017.”
Spending on hospital care increased 4.6% to $1.1 trillion in 2017 and accounted for 33% of total health care spending; however, growth was slower than in the previous year (5.6%). Ms. Martin and her colleagues noted that growth in outpatient visits slowed while growth in inpatient days increased at about the same rate and prices in hospital care grew in 2017 to 1.7% from 1.2% in the previous year.
Spending on physician and clinical services grew 4.2% in 2017 to $694.3 billion and accounted for 20% of total health care spending. The growth rate is down from the previous year (5.6%) and a recent peak of 6% in 2015.
“Although spending growth for both physician services and clinical services slowed in 2017, the growth rate for the latter (5.0%) continued to out pace the rate for the former (3.9%), as spending for most types of outpatient care centers contributed to the stronger growth in spending for clinical services,” Ms. Martin and her colleagues reported.
They attributed the slowdown to non-price factors, such as slower growth in the use and intensity of physician and clinical services, although price growth for physician and clinical services increased 0.4% in 2017, up from 0.2% in 2016.
Spending on retail prescription drugs grew 0.4% in 2017 to $333.4 billion and accounted for 10% of total national health spending. It is the slowest growth rate increase since 2012, a year that saw a number of blockbuster drugs lose patent protection. This was down from a growth rate of 2.3% in 2016 and down from recent rates of 12.4% in 2014 and 8.9% in 2015.
“Slower growth in non-price factors, such as the use and mix of retail prescription drugs – and, to a lesser extent, in retail prescription drug prices – contributed to the slower overall growth in retail prescription drug spending in 2017,” according to the authors. Key factors included slower growth in the number of prescriptions dispensed, the continued shift to lower-cost generics, and slower growth in the volume of high-cost drugs, particularly those used to treat hepatitis C. Price decreases in generics and lower increases for existing brand-name drugs also contributed to the lower spending growth in 2017.
Ms. Martin and her colleagues highlighted the slower growth rate in the number of prescriptions (1.8% in 2017, down from 2.3% in 2016) “resulted in large part from a decline in the number of prescriptions dispensed for drugs used to treat pain.”
Medicare spending, which represents 20% of all national health care spending in 2017 ($705.9 billion), grew 4.2%, a slight decline from the 4.3% growth in 2016. Enrollment growth slowed slightly to 2.5% in 2017 from 2.7% in the previous year, while in the same time frame, per-enrollee expenditures increased slightly to 1.7% from 1.6%. Slower growth in fee-for-service Medicare spending was offset by faster growth in spending by Medicare private health plans.
Medicaid spending reached $581.9 billion (17% of national health care spending), and the growth rate slowed for the third straight year, increasing 2.9% in 2017 versus 4.2% in 2016. The slower growth “was influenced by a deceleration in enrollment growth and a reduction in the Medicaid net cost of health insurance as the federal government recovered payments from managed care organizations based on their favorable prior-period experience,” the authors stated. Enrollment growth has been decelerating following a peak of growth of 11.9% in 2014 because of states that elected to expand Medicaid eligibility, which was followed by 3 years of slower growth rates of 4.9%, 3.0% and 2.0% in 2015, 2016, and 2017, respectively. Per-enrollee spending also slowed to 0.9% growth in 2017 from a rate of 1.2% in 2016, attributed to “the decline in government administration and the net cost of insurance.”
SOURCE: Martin A et al. Health Aff. 2018. doi: 10.1377/hlthaff.2018.05085.
FROM HEALTH AFFAIRS
Key clinical point: National health care spending growth slowed to 3.9% in 2017.
Major finding: The $3.5 trillion in national health care spending represents 17.9% of GDP.
Study details: Annual analysis of national health expenditures conducted by federal actuaries.
Disclosures: Analysis conducted by the Centers for Medicaid & Medicare Services Office of the Actuary; the authors have no relevant financial conflicts of interest.
Source: Martin A et al. Health Affairs. 2018. doi: 10.1377/hlthaff.2018.05085.
Thrombectomy shows efficacy for basilar artery strokes
MONTREAL – A randomized trial designed to definitively test the efficacy of mechanical thrombectomy for treating acute ischemic strokes caused by basilar artery occlusion fell victim to slow recruitment and crossovers that muddied the intention-to-treat results, but the per-protocol and as-treated analyses both showed that thrombectomy was superior to best medical therapy in a multicenter, randomized study with 131 Chinese patients.
“Our findings should be considered in the context of the best evidence currently available, and progressive loss of equipoise for endovascular therapy for severe, large-vessel occlusion strokes,” Raul G. Nogueira, MD, said at the World Stroke Congress. “This was not a perfect trial, but it’s the best data we have, by far, at least for now” on the value of mechanical thrombectomy for treating acute ischemic stroke caused by a basilar artery occlusion, added Dr. Nogueira, professor of neurology and director of the neuroendovascular service at Emory University, Atlanta.
In the study’s per-protocol analysis, which considered patients who received their randomized treatment, the study’s primary endpoint of a modified Rankin Scale (mRS) score of 0-3 at 90 days after treatment was 44% in 63 patients who underwent thrombectomy and 26% in 51 patients randomized to best medical therapy who remained on that regimen, a statistically significant difference, Dr. Nogueira reported. In the as-treated analysis, which considered all enrolled patients based on the treatment they actually received regardless of randomization group, 77 patients treated with thrombectomy had a 47% rate of achieving the primary outcome, compared with 24% of 54 controls, also a statistically significant difference.
In contrast, the prespecified primary analysis for the study, the intention-to-treat analysis that considered patients based on their randomization assignment regardless of the treatment they actually received, showed that after 90 days the rate of patients with a mRS score of 0-3 was 42% in 66 thrombectomy patients and 32% among 65 controls, a difference that was not significant; this is a finding that, from a purist’s standpoint, makes the trial’s result neutral. The per-protocol and as-treated analyses were also prespecified steps in the study’s design, but not primary endpoints.
Despite the shortcoming for the primary analysis, Dr. Nogueira said that he found the per-protocol and as-treated findings very persuasive. “I personally could not randomize these patients” in the future to not receive mechanical thrombectomy, he confessed from the podium.
The BEST trial randomized 131 patients at any of 28 Chinese sites between April 2015 and September 2017. Patients had to enter within 8 hours of stroke onset. The original trial design called for enrolling 344 patients, but the steering committee decided in 2017 to prematurely stop the study because of a progressive drop in enrollment of patients, and “excessive” crossovers from the control arm to thrombectomy, a total of 14 patients. During the final month of the trial, 6 of 10 patients assigned by randomization to receive best medical care instead underwent thrombectomy. “At that point, we pretty much had to stop,” Dr. Nogueira said. Enrolled patients averaged about 65 years old, about 90% had a basilar artery occlusion and about 10% a vertebral artery occlusion, about 30% received intravenous alteplase, and the median National Institutes of Health Stroke Scale score at entry was about 30.
The major adverse effect from thrombectomy seen in the study was symptomatic intracranial hemorrhage, which occurred in 5 of the 77 patients (6%) actually treated with thrombectomy, compared with none of the 54 patients not treated with thrombectomy. This modest rate of intracranial hemorrhages was “not unexpected,” Dr. Nogueira noted.
Acute ischemic strokes caused by a basilar artery occlusion are relatively uncommon, accounting for about 1% of all acute ischemic strokes and 5%-10% of acute ischemic strokes caused by occlusion of a proximal intracranial artery. But when these strokes occur, they are a “neurological catastrophe,” Dr. Nogueira said, causing severe disability or mortality in about 70% of patients.
BEST had no commercial funding. Dr. Nogueira reported no disclosures.
SOURCE: Nogueira RG et al. Int J Stroke. 2018;13(2_suppl):227, Abstract 978.
MONTREAL – A randomized trial designed to definitively test the efficacy of mechanical thrombectomy for treating acute ischemic strokes caused by basilar artery occlusion fell victim to slow recruitment and crossovers that muddied the intention-to-treat results, but the per-protocol and as-treated analyses both showed that thrombectomy was superior to best medical therapy in a multicenter, randomized study with 131 Chinese patients.
“Our findings should be considered in the context of the best evidence currently available, and progressive loss of equipoise for endovascular therapy for severe, large-vessel occlusion strokes,” Raul G. Nogueira, MD, said at the World Stroke Congress. “This was not a perfect trial, but it’s the best data we have, by far, at least for now” on the value of mechanical thrombectomy for treating acute ischemic stroke caused by a basilar artery occlusion, added Dr. Nogueira, professor of neurology and director of the neuroendovascular service at Emory University, Atlanta.
In the study’s per-protocol analysis, which considered patients who received their randomized treatment, the study’s primary endpoint of a modified Rankin Scale (mRS) score of 0-3 at 90 days after treatment was 44% in 63 patients who underwent thrombectomy and 26% in 51 patients randomized to best medical therapy who remained on that regimen, a statistically significant difference, Dr. Nogueira reported. In the as-treated analysis, which considered all enrolled patients based on the treatment they actually received regardless of randomization group, 77 patients treated with thrombectomy had a 47% rate of achieving the primary outcome, compared with 24% of 54 controls, also a statistically significant difference.
In contrast, the prespecified primary analysis for the study, the intention-to-treat analysis that considered patients based on their randomization assignment regardless of the treatment they actually received, showed that after 90 days the rate of patients with a mRS score of 0-3 was 42% in 66 thrombectomy patients and 32% among 65 controls, a difference that was not significant; this is a finding that, from a purist’s standpoint, makes the trial’s result neutral. The per-protocol and as-treated analyses were also prespecified steps in the study’s design, but not primary endpoints.
Despite the shortcoming for the primary analysis, Dr. Nogueira said that he found the per-protocol and as-treated findings very persuasive. “I personally could not randomize these patients” in the future to not receive mechanical thrombectomy, he confessed from the podium.
The BEST trial randomized 131 patients at any of 28 Chinese sites between April 2015 and September 2017. Patients had to enter within 8 hours of stroke onset. The original trial design called for enrolling 344 patients, but the steering committee decided in 2017 to prematurely stop the study because of a progressive drop in enrollment of patients, and “excessive” crossovers from the control arm to thrombectomy, a total of 14 patients. During the final month of the trial, 6 of 10 patients assigned by randomization to receive best medical care instead underwent thrombectomy. “At that point, we pretty much had to stop,” Dr. Nogueira said. Enrolled patients averaged about 65 years old, about 90% had a basilar artery occlusion and about 10% a vertebral artery occlusion, about 30% received intravenous alteplase, and the median National Institutes of Health Stroke Scale score at entry was about 30.
The major adverse effect from thrombectomy seen in the study was symptomatic intracranial hemorrhage, which occurred in 5 of the 77 patients (6%) actually treated with thrombectomy, compared with none of the 54 patients not treated with thrombectomy. This modest rate of intracranial hemorrhages was “not unexpected,” Dr. Nogueira noted.
Acute ischemic strokes caused by a basilar artery occlusion are relatively uncommon, accounting for about 1% of all acute ischemic strokes and 5%-10% of acute ischemic strokes caused by occlusion of a proximal intracranial artery. But when these strokes occur, they are a “neurological catastrophe,” Dr. Nogueira said, causing severe disability or mortality in about 70% of patients.
BEST had no commercial funding. Dr. Nogueira reported no disclosures.
SOURCE: Nogueira RG et al. Int J Stroke. 2018;13(2_suppl):227, Abstract 978.
MONTREAL – A randomized trial designed to definitively test the efficacy of mechanical thrombectomy for treating acute ischemic strokes caused by basilar artery occlusion fell victim to slow recruitment and crossovers that muddied the intention-to-treat results, but the per-protocol and as-treated analyses both showed that thrombectomy was superior to best medical therapy in a multicenter, randomized study with 131 Chinese patients.
“Our findings should be considered in the context of the best evidence currently available, and progressive loss of equipoise for endovascular therapy for severe, large-vessel occlusion strokes,” Raul G. Nogueira, MD, said at the World Stroke Congress. “This was not a perfect trial, but it’s the best data we have, by far, at least for now” on the value of mechanical thrombectomy for treating acute ischemic stroke caused by a basilar artery occlusion, added Dr. Nogueira, professor of neurology and director of the neuroendovascular service at Emory University, Atlanta.
In the study’s per-protocol analysis, which considered patients who received their randomized treatment, the study’s primary endpoint of a modified Rankin Scale (mRS) score of 0-3 at 90 days after treatment was 44% in 63 patients who underwent thrombectomy and 26% in 51 patients randomized to best medical therapy who remained on that regimen, a statistically significant difference, Dr. Nogueira reported. In the as-treated analysis, which considered all enrolled patients based on the treatment they actually received regardless of randomization group, 77 patients treated with thrombectomy had a 47% rate of achieving the primary outcome, compared with 24% of 54 controls, also a statistically significant difference.
In contrast, the prespecified primary analysis for the study, the intention-to-treat analysis that considered patients based on their randomization assignment regardless of the treatment they actually received, showed that after 90 days the rate of patients with a mRS score of 0-3 was 42% in 66 thrombectomy patients and 32% among 65 controls, a difference that was not significant; this is a finding that, from a purist’s standpoint, makes the trial’s result neutral. The per-protocol and as-treated analyses were also prespecified steps in the study’s design, but not primary endpoints.
Despite the shortcoming for the primary analysis, Dr. Nogueira said that he found the per-protocol and as-treated findings very persuasive. “I personally could not randomize these patients” in the future to not receive mechanical thrombectomy, he confessed from the podium.
The BEST trial randomized 131 patients at any of 28 Chinese sites between April 2015 and September 2017. Patients had to enter within 8 hours of stroke onset. The original trial design called for enrolling 344 patients, but the steering committee decided in 2017 to prematurely stop the study because of a progressive drop in enrollment of patients, and “excessive” crossovers from the control arm to thrombectomy, a total of 14 patients. During the final month of the trial, 6 of 10 patients assigned by randomization to receive best medical care instead underwent thrombectomy. “At that point, we pretty much had to stop,” Dr. Nogueira said. Enrolled patients averaged about 65 years old, about 90% had a basilar artery occlusion and about 10% a vertebral artery occlusion, about 30% received intravenous alteplase, and the median National Institutes of Health Stroke Scale score at entry was about 30.
The major adverse effect from thrombectomy seen in the study was symptomatic intracranial hemorrhage, which occurred in 5 of the 77 patients (6%) actually treated with thrombectomy, compared with none of the 54 patients not treated with thrombectomy. This modest rate of intracranial hemorrhages was “not unexpected,” Dr. Nogueira noted.
Acute ischemic strokes caused by a basilar artery occlusion are relatively uncommon, accounting for about 1% of all acute ischemic strokes and 5%-10% of acute ischemic strokes caused by occlusion of a proximal intracranial artery. But when these strokes occur, they are a “neurological catastrophe,” Dr. Nogueira said, causing severe disability or mortality in about 70% of patients.
BEST had no commercial funding. Dr. Nogueira reported no disclosures.
SOURCE: Nogueira RG et al. Int J Stroke. 2018;13(2_suppl):227, Abstract 978.
REPORTING FROM THE WORLD STROKE CONGRESS
Key clinical point:
Major finding: In the as-treated analysis, thrombectomy produced a 47% rate of modified Rankin Scale scores of 0-3 after 90 days, compared with 24% in controls.
Study details: BEST, a multicenter, randomized trial with 131 Chinese patients.
Disclosures: BEST had no commercial funding. Dr. Nogueira reported no disclosures.
Source: Nogueira RG et al. Int J Stroke. 2018;13(2_suppl):227, Abstract 978.
Acute stroke thrombolysis worked safely despite GI bleed or malignancy
CHICAGO – A recent history of GI bleeding or malignancy may not be a valid contraindication to thrombolytic therapy in patients with an acute ischemic stroke, based on a review of outcomes from more than 40,000 U.S. stroke patients.
The analysis showed that, among 40,396 U.S. patients who had an acute ischemic stroke during 2009-2015 and received timely treatment with alteplase, “we did not find statistically significant increased rates of in-hospital mortality or bleeding” in the small number of patients who received alteplase (Activase) despite a recent GI bleed or diagnosed GI malignancy, Taku Inohara, MD, said at the American Heart Association scientific sessions. The 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke deemed thrombolytic therapy with alteplase in these types of patients contraindicated, based on consensus expert opinion (Stroke. 2018 March;49[3]:e66-e110).
“Further study is needed to evaluate the safety of recombinant tissue–type plasminogen activator [alteplase] in this specific population,” suggested Dr. Inohara, a cardiologist and research fellow at Duke University, Durham, N.C.
His analysis used data collected by the Get With the Guidelines–Stroke program, a voluntary quality promotion and improvement program that during 2009-2015 included records for more than 633,000 U.S. stroke patients that could be linked with records kept by the Centers for Medicare & Medicaid Services. From this database, 40,396 patients (6%) treated with alteplase within 4.5 hours of stroke onset were identified. The alteplase-treated patients included 93 with a diagnosis code during the prior year for a GI malignancy and 43 with a diagnostic code within the prior 21 days for a GI bleed.
Dr. Inohara and his associates determined patients’ mortality during their stroke hospitalization, as well as several measures of functional recovery at hospital discharge and thrombolysis-related complications. For each of these endpoints, the rate among patients with a GI malignancy, a GI bleed, or the rate among a combined group of both patients showed no statistically significant differences, compared with the more than 40,000 other patients without a GI complication after adjustment for several demographic and clinical between-group differences. However, Dr. Inohara cautioned that residual or unmeasured confounding may exist that distorts these findings. The rate of in-hospital mortality, the prespecified primary endpoint for the analysis, was 10% among patients with either type of GI complication and 9% in those without. The rate of serious thrombolysis-related complications was 7% in the patients with GI disease and 9% in those without.
In a separate analysis of the complete database of more than 633,000 patients, Dr. Inohara and his associates found 148 patients who had either a GI bleed or malignancy and otherwise qualified for thrombolytic therapy but did not receive this treatment. This meant that overall, in this large U.S. experience, 136 of 284 (48%) acute ischemic stroke patients who qualified for thrombolysis but had a GI complication nonetheless received thrombolysis. Further analysis showed that the patients not treated with thrombolysis had at admission an average National Institutes of Health Stroke Scale score of 11, compared with an average score of 14 among patients who received thrombolysis.
This apparent selection for thrombolytic treatment of patients with more severe strokes “may have overestimated risk in the patients with GI disease,” Dr. Inohara said.
Dr. Inohara reported receiving research funding from Boston Scientific.
SOURCE: Inohara T et al. Circulation. 2018 Nov 6;138[suppl 1], Abstract 12291.
CHICAGO – A recent history of GI bleeding or malignancy may not be a valid contraindication to thrombolytic therapy in patients with an acute ischemic stroke, based on a review of outcomes from more than 40,000 U.S. stroke patients.
The analysis showed that, among 40,396 U.S. patients who had an acute ischemic stroke during 2009-2015 and received timely treatment with alteplase, “we did not find statistically significant increased rates of in-hospital mortality or bleeding” in the small number of patients who received alteplase (Activase) despite a recent GI bleed or diagnosed GI malignancy, Taku Inohara, MD, said at the American Heart Association scientific sessions. The 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke deemed thrombolytic therapy with alteplase in these types of patients contraindicated, based on consensus expert opinion (Stroke. 2018 March;49[3]:e66-e110).
“Further study is needed to evaluate the safety of recombinant tissue–type plasminogen activator [alteplase] in this specific population,” suggested Dr. Inohara, a cardiologist and research fellow at Duke University, Durham, N.C.
His analysis used data collected by the Get With the Guidelines–Stroke program, a voluntary quality promotion and improvement program that during 2009-2015 included records for more than 633,000 U.S. stroke patients that could be linked with records kept by the Centers for Medicare & Medicaid Services. From this database, 40,396 patients (6%) treated with alteplase within 4.5 hours of stroke onset were identified. The alteplase-treated patients included 93 with a diagnosis code during the prior year for a GI malignancy and 43 with a diagnostic code within the prior 21 days for a GI bleed.
Dr. Inohara and his associates determined patients’ mortality during their stroke hospitalization, as well as several measures of functional recovery at hospital discharge and thrombolysis-related complications. For each of these endpoints, the rate among patients with a GI malignancy, a GI bleed, or the rate among a combined group of both patients showed no statistically significant differences, compared with the more than 40,000 other patients without a GI complication after adjustment for several demographic and clinical between-group differences. However, Dr. Inohara cautioned that residual or unmeasured confounding may exist that distorts these findings. The rate of in-hospital mortality, the prespecified primary endpoint for the analysis, was 10% among patients with either type of GI complication and 9% in those without. The rate of serious thrombolysis-related complications was 7% in the patients with GI disease and 9% in those without.
In a separate analysis of the complete database of more than 633,000 patients, Dr. Inohara and his associates found 148 patients who had either a GI bleed or malignancy and otherwise qualified for thrombolytic therapy but did not receive this treatment. This meant that overall, in this large U.S. experience, 136 of 284 (48%) acute ischemic stroke patients who qualified for thrombolysis but had a GI complication nonetheless received thrombolysis. Further analysis showed that the patients not treated with thrombolysis had at admission an average National Institutes of Health Stroke Scale score of 11, compared with an average score of 14 among patients who received thrombolysis.
This apparent selection for thrombolytic treatment of patients with more severe strokes “may have overestimated risk in the patients with GI disease,” Dr. Inohara said.
Dr. Inohara reported receiving research funding from Boston Scientific.
SOURCE: Inohara T et al. Circulation. 2018 Nov 6;138[suppl 1], Abstract 12291.
CHICAGO – A recent history of GI bleeding or malignancy may not be a valid contraindication to thrombolytic therapy in patients with an acute ischemic stroke, based on a review of outcomes from more than 40,000 U.S. stroke patients.
The analysis showed that, among 40,396 U.S. patients who had an acute ischemic stroke during 2009-2015 and received timely treatment with alteplase, “we did not find statistically significant increased rates of in-hospital mortality or bleeding” in the small number of patients who received alteplase (Activase) despite a recent GI bleed or diagnosed GI malignancy, Taku Inohara, MD, said at the American Heart Association scientific sessions. The 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke deemed thrombolytic therapy with alteplase in these types of patients contraindicated, based on consensus expert opinion (Stroke. 2018 March;49[3]:e66-e110).
“Further study is needed to evaluate the safety of recombinant tissue–type plasminogen activator [alteplase] in this specific population,” suggested Dr. Inohara, a cardiologist and research fellow at Duke University, Durham, N.C.
His analysis used data collected by the Get With the Guidelines–Stroke program, a voluntary quality promotion and improvement program that during 2009-2015 included records for more than 633,000 U.S. stroke patients that could be linked with records kept by the Centers for Medicare & Medicaid Services. From this database, 40,396 patients (6%) treated with alteplase within 4.5 hours of stroke onset were identified. The alteplase-treated patients included 93 with a diagnosis code during the prior year for a GI malignancy and 43 with a diagnostic code within the prior 21 days for a GI bleed.
Dr. Inohara and his associates determined patients’ mortality during their stroke hospitalization, as well as several measures of functional recovery at hospital discharge and thrombolysis-related complications. For each of these endpoints, the rate among patients with a GI malignancy, a GI bleed, or the rate among a combined group of both patients showed no statistically significant differences, compared with the more than 40,000 other patients without a GI complication after adjustment for several demographic and clinical between-group differences. However, Dr. Inohara cautioned that residual or unmeasured confounding may exist that distorts these findings. The rate of in-hospital mortality, the prespecified primary endpoint for the analysis, was 10% among patients with either type of GI complication and 9% in those without. The rate of serious thrombolysis-related complications was 7% in the patients with GI disease and 9% in those without.
In a separate analysis of the complete database of more than 633,000 patients, Dr. Inohara and his associates found 148 patients who had either a GI bleed or malignancy and otherwise qualified for thrombolytic therapy but did not receive this treatment. This meant that overall, in this large U.S. experience, 136 of 284 (48%) acute ischemic stroke patients who qualified for thrombolysis but had a GI complication nonetheless received thrombolysis. Further analysis showed that the patients not treated with thrombolysis had at admission an average National Institutes of Health Stroke Scale score of 11, compared with an average score of 14 among patients who received thrombolysis.
This apparent selection for thrombolytic treatment of patients with more severe strokes “may have overestimated risk in the patients with GI disease,” Dr. Inohara said.
Dr. Inohara reported receiving research funding from Boston Scientific.
SOURCE: Inohara T et al. Circulation. 2018 Nov 6;138[suppl 1], Abstract 12291.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point:
Major finding: In-hospital mortality after thrombolysis was 10% in those with a GI bleed or malignancy and 9% in those without.
Study details: A review of Medicare records for 40,396 acute ischemic stroke patients treated with thrombolysis during 2009-2015.
Disclosures: Dr. Inohara reported receiving research funding from Boston Scientific.
Source: Inohara T et al. Circulation. 2018 Nov 6;138[suppl 1], Abstract A12291.
Carol Bernstein: Burnout or depression?
Dr. Bernstein is a professor at NYU Langone in New York City and has been a guest on the MDedge Psychcast.
Apple Podcasts
Google Podcasts
Dr. Bernstein is a professor at NYU Langone in New York City and has been a guest on the MDedge Psychcast.
Apple Podcasts
Google Podcasts
Dr. Bernstein is a professor at NYU Langone in New York City and has been a guest on the MDedge Psychcast.
Apple Podcasts
Google Podcasts
New strategy for less computer time
Also today, diuretics are linked to diabetic amputations in type 2 diabetes, pausing direct acting oral anticoagulants show favorable outcomes for atrial fibrillation, and while therapy has matured for patients with HCV, there are still issues with access.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, diuretics are linked to diabetic amputations in type 2 diabetes, pausing direct acting oral anticoagulants show favorable outcomes for atrial fibrillation, and while therapy has matured for patients with HCV, there are still issues with access.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, diuretics are linked to diabetic amputations in type 2 diabetes, pausing direct acting oral anticoagulants show favorable outcomes for atrial fibrillation, and while therapy has matured for patients with HCV, there are still issues with access.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Action on HealthCare.gov picked up during week 5
Activity during week 5 of open enrollment on HealthCare.gov was up by more than 50% over the previous week, but the total number of plans selected for the 2019 coverage year remains lower than it was last year, according to the Centers for Medicare & Medicaid Services.
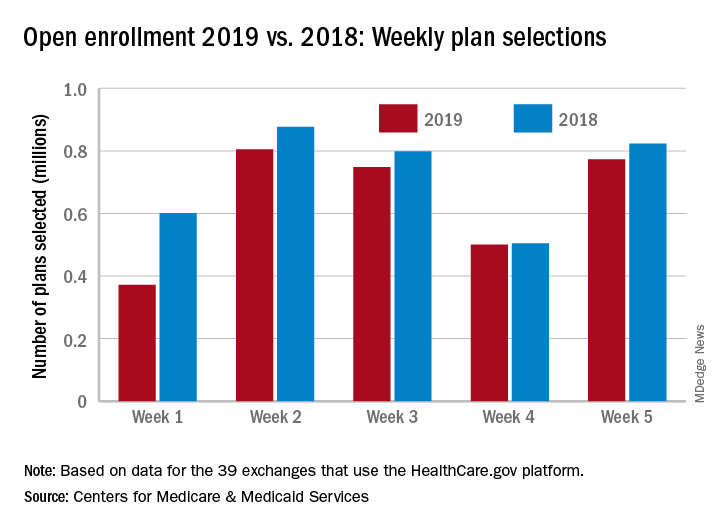
The 773,000 plans selected during week 5 (Nov. 25 – Dec. 1) of the 2019 open enrollment season were an increase of 54% over week 4, CMS data show for the 39 states that use the HealthCare.gov platform, with the cumulative total now at 3.2 million. By comparison, week-5 selections in last year’s open enrollment totaled 823,000, and the cumulative figure was 3.6 million.
The deadline for applying for 2019 coverage on HealthCare.gov is Dec. 15.
Activity during week 5 of open enrollment on HealthCare.gov was up by more than 50% over the previous week, but the total number of plans selected for the 2019 coverage year remains lower than it was last year, according to the Centers for Medicare & Medicaid Services.
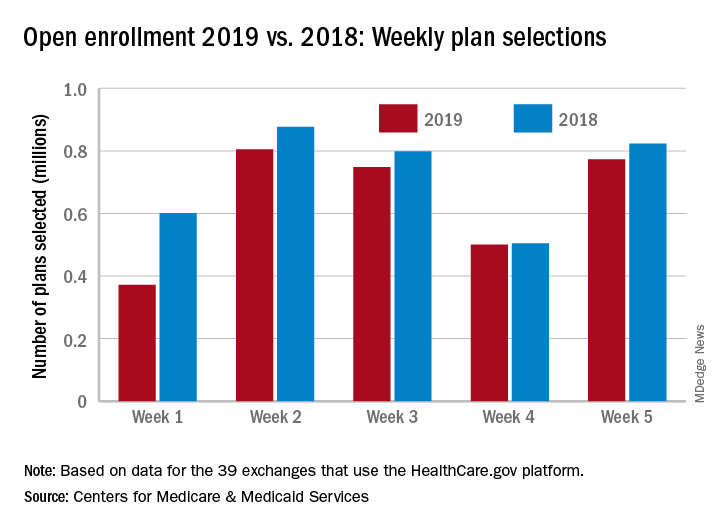
The 773,000 plans selected during week 5 (Nov. 25 – Dec. 1) of the 2019 open enrollment season were an increase of 54% over week 4, CMS data show for the 39 states that use the HealthCare.gov platform, with the cumulative total now at 3.2 million. By comparison, week-5 selections in last year’s open enrollment totaled 823,000, and the cumulative figure was 3.6 million.
The deadline for applying for 2019 coverage on HealthCare.gov is Dec. 15.
Activity during week 5 of open enrollment on HealthCare.gov was up by more than 50% over the previous week, but the total number of plans selected for the 2019 coverage year remains lower than it was last year, according to the Centers for Medicare & Medicaid Services.
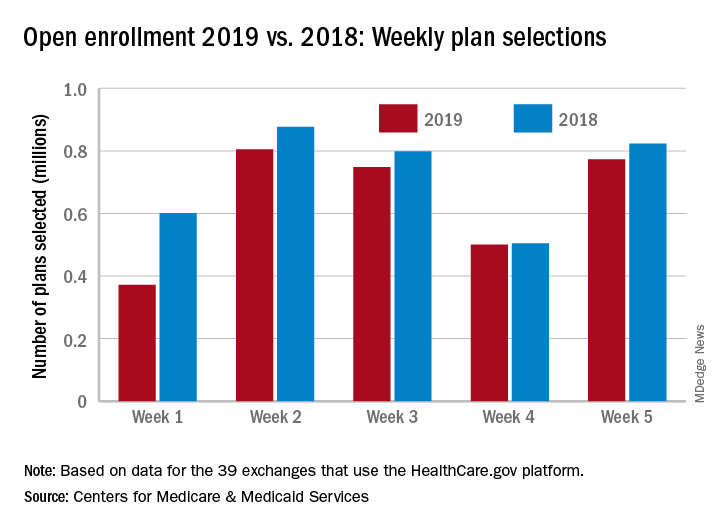
The 773,000 plans selected during week 5 (Nov. 25 – Dec. 1) of the 2019 open enrollment season were an increase of 54% over week 4, CMS data show for the 39 states that use the HealthCare.gov platform, with the cumulative total now at 3.2 million. By comparison, week-5 selections in last year’s open enrollment totaled 823,000, and the cumulative figure was 3.6 million.
The deadline for applying for 2019 coverage on HealthCare.gov is Dec. 15.