User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
One weird trick to fight burnout
“Here and now is what counts. So, let’s go to work!” –Walter Orthmann, 100 years old
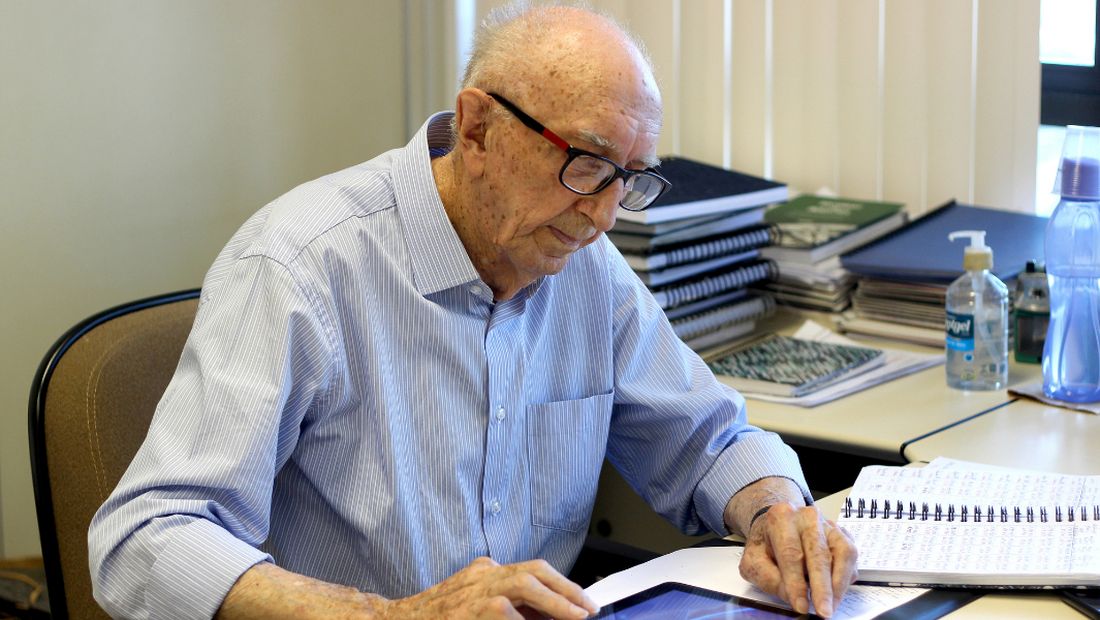
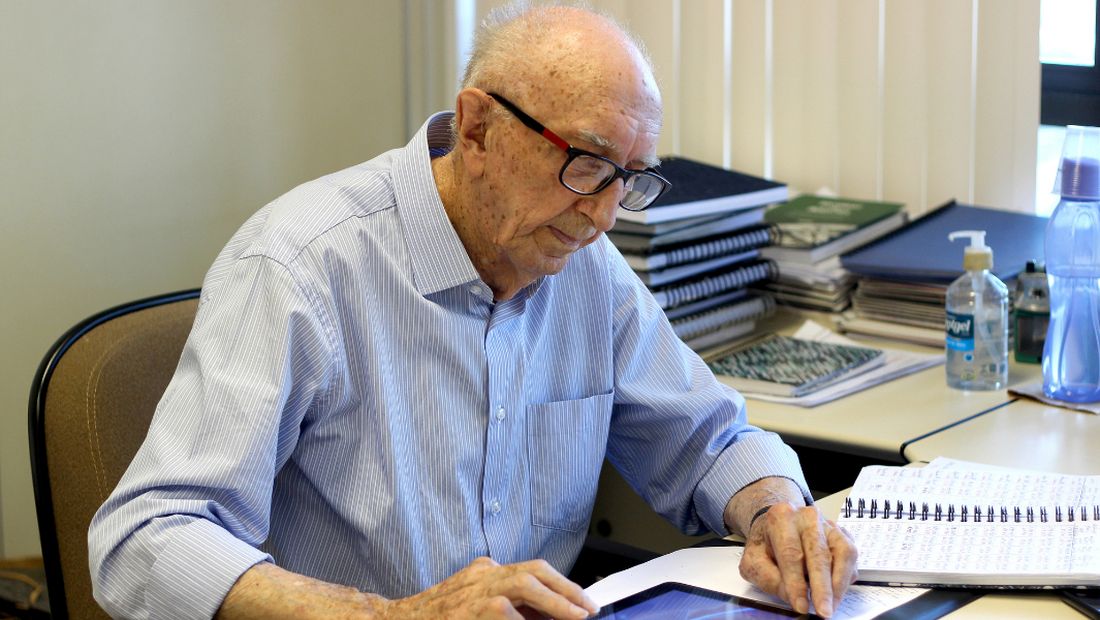
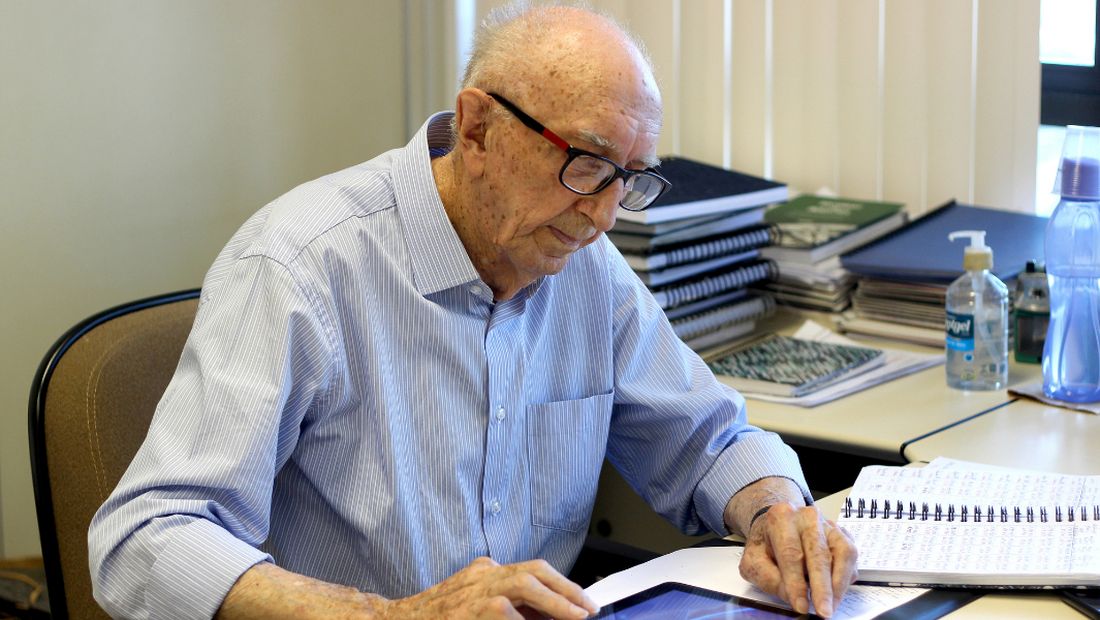
How long before you retire? If you know the answer in exact years, months, and days, you aren’t alone. For many good reasons, we doctors are more likely to be counting down the years until we retire rather than counting up the years since we started working. For me, if I’m to break the Guinness World Record, I have 69 more years, 3 months and 6 days left to go. That would surpass the current achievement for the longest career at one company, Mr. Walter Orthmann, who has been sitting at the same desk for 84 years. At 100 years old, Mr. Orthmann still shows up every Monday morning, as bright eyed and bushy tailed as a young squirrel. I’ll be 119 when I break his streak, which would also put me past Anthony Mancinelli, a New York barber who at 107 years of age was still brushing off his chair for the next customer. Unbelievable, I know! I wonder, what’s the one weird trick these guys are doing that keeps them going?
Of course, the job itself matters. Some jobs, like being a police officer, aren’t suitable for old people. Or are they? Officer L.C. “Buckshot” Smith was still keeping streets safe from his patrol car at 91 years old. After a bit of searching, I found pretty much any job you can think of has a very long-lasting Energizer Bunny story: A female surgeon who was operating at 90 years old, a 100-year-old rheumatologist who was still teaching at University of California, San Francisco, and a 105-year-old Japanese physician who was still seeing patients. There are plenty of geriatric lawyers, nurses, land surveyors, accountants, judges, you name it. So it seems it’s not the work, but the worker that matters. Why do some older workers recharge daily and carry on while many younger ones say the daily grind is burning them out? What makes the Greatest Generation so great?
We all know colleagues who hung up their white coats early. In my medical group, it’s often financially feasible to retire at 58 and many have chosen that option. Yet, we have loads of Partner Emeritus docs in their 70’s who still log on to EPIC and pitch in everyday.
“So, how do you keep going?” I asked my 105-year-old patient who still walks and manages his affairs. “Just stay healthy,” he advised. A circular argument, yet he’s right. You must both be lucky and also choose to be active mentally and physically. Mr. Mancinelli, who was barbering full time at 107 years old, had no aches and pains and all his teeth. He pruned his own bushes. The data are crystal clear that physical activity adds not only years of life, but also improves cognitive capabilities during those years.
As for beating burnout, it seems the one trick that these ultraworkers do is to focus only on the present. Mr. Orthmann’s pithy advice as quoted by NPR is, “You need to get busy with the present, not the past or the future.” These centenarian employees also frame their work not as stressful but rather as their daily series of problems to be solved.
When I asked my super-geriatric patient how he sleeps so well, he said, “I never worry when I get into bed, I just shut my eyes and sleep. I’ll think about tomorrow when I wake up.” Now if I can do that about 25,000 more times, I’ll have the record.
Dr. Jeff Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com
“Here and now is what counts. So, let’s go to work!” –Walter Orthmann, 100 years old
How long before you retire? If you know the answer in exact years, months, and days, you aren’t alone. For many good reasons, we doctors are more likely to be counting down the years until we retire rather than counting up the years since we started working. For me, if I’m to break the Guinness World Record, I have 69 more years, 3 months and 6 days left to go. That would surpass the current achievement for the longest career at one company, Mr. Walter Orthmann, who has been sitting at the same desk for 84 years. At 100 years old, Mr. Orthmann still shows up every Monday morning, as bright eyed and bushy tailed as a young squirrel. I’ll be 119 when I break his streak, which would also put me past Anthony Mancinelli, a New York barber who at 107 years of age was still brushing off his chair for the next customer. Unbelievable, I know! I wonder, what’s the one weird trick these guys are doing that keeps them going?
Of course, the job itself matters. Some jobs, like being a police officer, aren’t suitable for old people. Or are they? Officer L.C. “Buckshot” Smith was still keeping streets safe from his patrol car at 91 years old. After a bit of searching, I found pretty much any job you can think of has a very long-lasting Energizer Bunny story: A female surgeon who was operating at 90 years old, a 100-year-old rheumatologist who was still teaching at University of California, San Francisco, and a 105-year-old Japanese physician who was still seeing patients. There are plenty of geriatric lawyers, nurses, land surveyors, accountants, judges, you name it. So it seems it’s not the work, but the worker that matters. Why do some older workers recharge daily and carry on while many younger ones say the daily grind is burning them out? What makes the Greatest Generation so great?
We all know colleagues who hung up their white coats early. In my medical group, it’s often financially feasible to retire at 58 and many have chosen that option. Yet, we have loads of Partner Emeritus docs in their 70’s who still log on to EPIC and pitch in everyday.
“So, how do you keep going?” I asked my 105-year-old patient who still walks and manages his affairs. “Just stay healthy,” he advised. A circular argument, yet he’s right. You must both be lucky and also choose to be active mentally and physically. Mr. Mancinelli, who was barbering full time at 107 years old, had no aches and pains and all his teeth. He pruned his own bushes. The data are crystal clear that physical activity adds not only years of life, but also improves cognitive capabilities during those years.
As for beating burnout, it seems the one trick that these ultraworkers do is to focus only on the present. Mr. Orthmann’s pithy advice as quoted by NPR is, “You need to get busy with the present, not the past or the future.” These centenarian employees also frame their work not as stressful but rather as their daily series of problems to be solved.
When I asked my super-geriatric patient how he sleeps so well, he said, “I never worry when I get into bed, I just shut my eyes and sleep. I’ll think about tomorrow when I wake up.” Now if I can do that about 25,000 more times, I’ll have the record.
Dr. Jeff Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com
“Here and now is what counts. So, let’s go to work!” –Walter Orthmann, 100 years old
How long before you retire? If you know the answer in exact years, months, and days, you aren’t alone. For many good reasons, we doctors are more likely to be counting down the years until we retire rather than counting up the years since we started working. For me, if I’m to break the Guinness World Record, I have 69 more years, 3 months and 6 days left to go. That would surpass the current achievement for the longest career at one company, Mr. Walter Orthmann, who has been sitting at the same desk for 84 years. At 100 years old, Mr. Orthmann still shows up every Monday morning, as bright eyed and bushy tailed as a young squirrel. I’ll be 119 when I break his streak, which would also put me past Anthony Mancinelli, a New York barber who at 107 years of age was still brushing off his chair for the next customer. Unbelievable, I know! I wonder, what’s the one weird trick these guys are doing that keeps them going?
Of course, the job itself matters. Some jobs, like being a police officer, aren’t suitable for old people. Or are they? Officer L.C. “Buckshot” Smith was still keeping streets safe from his patrol car at 91 years old. After a bit of searching, I found pretty much any job you can think of has a very long-lasting Energizer Bunny story: A female surgeon who was operating at 90 years old, a 100-year-old rheumatologist who was still teaching at University of California, San Francisco, and a 105-year-old Japanese physician who was still seeing patients. There are plenty of geriatric lawyers, nurses, land surveyors, accountants, judges, you name it. So it seems it’s not the work, but the worker that matters. Why do some older workers recharge daily and carry on while many younger ones say the daily grind is burning them out? What makes the Greatest Generation so great?
We all know colleagues who hung up their white coats early. In my medical group, it’s often financially feasible to retire at 58 and many have chosen that option. Yet, we have loads of Partner Emeritus docs in their 70’s who still log on to EPIC and pitch in everyday.
“So, how do you keep going?” I asked my 105-year-old patient who still walks and manages his affairs. “Just stay healthy,” he advised. A circular argument, yet he’s right. You must both be lucky and also choose to be active mentally and physically. Mr. Mancinelli, who was barbering full time at 107 years old, had no aches and pains and all his teeth. He pruned his own bushes. The data are crystal clear that physical activity adds not only years of life, but also improves cognitive capabilities during those years.
As for beating burnout, it seems the one trick that these ultraworkers do is to focus only on the present. Mr. Orthmann’s pithy advice as quoted by NPR is, “You need to get busy with the present, not the past or the future.” These centenarian employees also frame their work not as stressful but rather as their daily series of problems to be solved.
When I asked my super-geriatric patient how he sleeps so well, he said, “I never worry when I get into bed, I just shut my eyes and sleep. I’ll think about tomorrow when I wake up.” Now if I can do that about 25,000 more times, I’ll have the record.
Dr. Jeff Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com
Lost keys, missed appointments: The struggle of treating executive dysfunction
Maybe you know some of these patients: They may come late or not show up at all. They may have little to say and minimize their difficulties, often because they are ashamed of how much effort it takes to meet ordinary obligations. They may struggle to complete assignments, fail classes, or lose jobs. And being in the right place at the right time can feel monumental to them: They forget appointments, double book themselves, or sometimes sleep through important events.
It’s not just appointments. They lose their keys and valuables, forget to pay bills, and may not answer calls, texts, or emails. Their voicemail may be full and people are often frustrated with them. These are all characteristics of executive dysfunction, which together can make the routine responsibilities of life very difficult.
Treatments include stimulants, and because of their potential for abuse, these medications are more strictly regulated when it comes to prescribing. The FDA does not allow them to be phoned into a pharmacy or refills to be added to prescriptions. Patients must wait until right before they are due to run out to get the next prescription, and this can present a problem if the patient travels or takes long vacations.
And although it is not the patient’s fault that stimulants can’t be ordered with refills, this adds to the burden of treating patients who take them. It’s hard to imagine that these restrictions on stimulants and opiates (but not on benzodiazepines) do much to deter abuse or diversion.
I trained at a time when ADD and ADHD were disorders of childhood, and as an adult psychiatrist, I was not exposed to patients on these medications. Occasionally, a stimulant was prescribed in a low dose to help activate a very depressed patient, but it was thought that children outgrow issues of attention and focus, and I have never felt fully confident in the more nuanced use of these medications with adults. Most of the patients I now treat with ADD have come to me on stable doses of the medications or at least with a history that directs care.
With others, the tip-off to look for the disorder is their disorganization in the absence of a substance use or active mood disorder. Medications help, sometimes remarkably, yet patients still struggle with organization and planning, and sometimes I find myself frustrated when patients forget their appointments or the issues around prescribing stimulants become time-consuming.
David W. Goodman, MD, director of the Adult Attention Deficit Center of Maryland, Lutherville, currently treats hundreds of patients with ADD and has written and spoken extensively about treating this disorder in adults.
“There are three things that make it difficult to manage patients with ADD,” Dr. Goodman noted, referring specifically to administrative issues. “You can’t write for refills, but with e-prescribing you can write a sequence of prescriptions with ‘fill-after’ dates. Or some patients are able to get a 90-day supply from mail-order pharmacies. Still, it’s a hassle if the patient moves around, as college students often do, and there are inventory shortages when some pharmacies can’t get the medications.”
“The second issue,” he adds, “is that it’s the nature of this disorder that patients struggle with organizational issues. Yelling at someone with ADD to pay attention is like yelling at a blind person not to run into furniture when they are in a new room. They go through life with people being impatient that they can’t do the things an ordinary person can do easily.”
Finally, Dr. Goodman noted that the clinicians who treat patients with ADD may have counter-transference issues.
“You have to understand that this is a disability and be sympathetic to it. They often have comorbid disorders, including personality disorders, and this can all bleed over to cause frustrations in their care. Psychiatrists who treat patients with ADD need to know they can deal with them compassionately.”
“I am occasionally contacted by patients who already have an ADHD diagnosis and are on stimulants, and who seem like they just want to get their prescriptions filled and aren’t interested in working on their issues,” says Douglas Beech, MD, a psychiatrist in private practice in Worthington, Ohio. “The doctor in this situation can feel like they are functioning as a sort of drug dealer. There are logistical matters that are structurally inherent in trying to assist these patients, from both a regulatory perspective and from a functional perspective. Dr. Beech feels that it’s helpful to acknowledge these issues when seeing patients with ADHD, so that he is prepared when problems do arise.
“It can almost feel cruel to charge a patient for a “no-show,” when difficulty keeping appointments may be a symptom of their illness, Dr. Beech adds. But he does believe it’s important to apply any fee policy equitably to all patients. “I don’t apply the ‘missed appointment’ policy differently to a person with an ADHD diagnosis versus any other diagnosis.” Though for their first missed appointment, he does give patients a “mulligan.”
“I don’t charge, but it puts both patient and doctor on notice,” he says.
And when his patients do miss an appointment, he offers to send a reminder for the next time, which is he says is effective. “With electronic messaging, this is a quick and easy way to prevent missed appointments and the complications that arise with prescriptions and rescheduling,” says Dr. Beech.
Dr. Goodman speaks about manging a large caseload of patients, many of whom have organizational issues.
“I have a full-time office manager who handles a lot of the logistics of scheduling and prescribing. Patients are sent multiple reminders, and I charge a nominal administrative fee if prescriptions need to be sent outside of appointments. This is not to make money, but to encourage patients to consider the administrative time.”
“I charge for appointments that are not canceled 48 hours in advance, and for patients who have missed appointments, a credit card is kept on file,” he says.
In a practice similar to Dr. Beech, Dr. Goodman notes that he shows some flexibility for new patients when they miss an appointment the first time. “By the second time, they know this is the policy. Having ADHD can be financially costly.”
He notes that about 10% of his patients, roughly one a day, cancel late or don’t show up for scheduled appointments: “We keep a waitlist, and if someone cancels before the appointment, we can often fill the time with another patient in need on our waitlist.”
Dr. Goodman noted repeatedly that the clinician needs to be able to empathize with the patient’s condition and how they suffer. “This is not something people choose to have. The trap is that people think that if you’re successful you can’t have ADHD, and that’s not true. Often people with this condition work harder, are brighter, and find ways to compensate.”
If a practice is set up to accommodate the needs of patients with attention and organizational issues, treating them can be very gratifying. In settings without administrative support, the psychiatrist needs to stay cognizant of this invisible disability and the frustration that may come with this disorder, not just for the patient, but also for the family, friends, and employers, and even for the psychiatrist.
Dr. Dinah Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, Baltimore. Dr. Miller has no conflicts of interest.
A version of this article first appeared on Medscape.com.
Maybe you know some of these patients: They may come late or not show up at all. They may have little to say and minimize their difficulties, often because they are ashamed of how much effort it takes to meet ordinary obligations. They may struggle to complete assignments, fail classes, or lose jobs. And being in the right place at the right time can feel monumental to them: They forget appointments, double book themselves, or sometimes sleep through important events.
It’s not just appointments. They lose their keys and valuables, forget to pay bills, and may not answer calls, texts, or emails. Their voicemail may be full and people are often frustrated with them. These are all characteristics of executive dysfunction, which together can make the routine responsibilities of life very difficult.
Treatments include stimulants, and because of their potential for abuse, these medications are more strictly regulated when it comes to prescribing. The FDA does not allow them to be phoned into a pharmacy or refills to be added to prescriptions. Patients must wait until right before they are due to run out to get the next prescription, and this can present a problem if the patient travels or takes long vacations.
And although it is not the patient’s fault that stimulants can’t be ordered with refills, this adds to the burden of treating patients who take them. It’s hard to imagine that these restrictions on stimulants and opiates (but not on benzodiazepines) do much to deter abuse or diversion.
I trained at a time when ADD and ADHD were disorders of childhood, and as an adult psychiatrist, I was not exposed to patients on these medications. Occasionally, a stimulant was prescribed in a low dose to help activate a very depressed patient, but it was thought that children outgrow issues of attention and focus, and I have never felt fully confident in the more nuanced use of these medications with adults. Most of the patients I now treat with ADD have come to me on stable doses of the medications or at least with a history that directs care.
With others, the tip-off to look for the disorder is their disorganization in the absence of a substance use or active mood disorder. Medications help, sometimes remarkably, yet patients still struggle with organization and planning, and sometimes I find myself frustrated when patients forget their appointments or the issues around prescribing stimulants become time-consuming.
David W. Goodman, MD, director of the Adult Attention Deficit Center of Maryland, Lutherville, currently treats hundreds of patients with ADD and has written and spoken extensively about treating this disorder in adults.
“There are three things that make it difficult to manage patients with ADD,” Dr. Goodman noted, referring specifically to administrative issues. “You can’t write for refills, but with e-prescribing you can write a sequence of prescriptions with ‘fill-after’ dates. Or some patients are able to get a 90-day supply from mail-order pharmacies. Still, it’s a hassle if the patient moves around, as college students often do, and there are inventory shortages when some pharmacies can’t get the medications.”
“The second issue,” he adds, “is that it’s the nature of this disorder that patients struggle with organizational issues. Yelling at someone with ADD to pay attention is like yelling at a blind person not to run into furniture when they are in a new room. They go through life with people being impatient that they can’t do the things an ordinary person can do easily.”
Finally, Dr. Goodman noted that the clinicians who treat patients with ADD may have counter-transference issues.
“You have to understand that this is a disability and be sympathetic to it. They often have comorbid disorders, including personality disorders, and this can all bleed over to cause frustrations in their care. Psychiatrists who treat patients with ADD need to know they can deal with them compassionately.”
“I am occasionally contacted by patients who already have an ADHD diagnosis and are on stimulants, and who seem like they just want to get their prescriptions filled and aren’t interested in working on their issues,” says Douglas Beech, MD, a psychiatrist in private practice in Worthington, Ohio. “The doctor in this situation can feel like they are functioning as a sort of drug dealer. There are logistical matters that are structurally inherent in trying to assist these patients, from both a regulatory perspective and from a functional perspective. Dr. Beech feels that it’s helpful to acknowledge these issues when seeing patients with ADHD, so that he is prepared when problems do arise.
“It can almost feel cruel to charge a patient for a “no-show,” when difficulty keeping appointments may be a symptom of their illness, Dr. Beech adds. But he does believe it’s important to apply any fee policy equitably to all patients. “I don’t apply the ‘missed appointment’ policy differently to a person with an ADHD diagnosis versus any other diagnosis.” Though for their first missed appointment, he does give patients a “mulligan.”
“I don’t charge, but it puts both patient and doctor on notice,” he says.
And when his patients do miss an appointment, he offers to send a reminder for the next time, which is he says is effective. “With electronic messaging, this is a quick and easy way to prevent missed appointments and the complications that arise with prescriptions and rescheduling,” says Dr. Beech.
Dr. Goodman speaks about manging a large caseload of patients, many of whom have organizational issues.
“I have a full-time office manager who handles a lot of the logistics of scheduling and prescribing. Patients are sent multiple reminders, and I charge a nominal administrative fee if prescriptions need to be sent outside of appointments. This is not to make money, but to encourage patients to consider the administrative time.”
“I charge for appointments that are not canceled 48 hours in advance, and for patients who have missed appointments, a credit card is kept on file,” he says.
In a practice similar to Dr. Beech, Dr. Goodman notes that he shows some flexibility for new patients when they miss an appointment the first time. “By the second time, they know this is the policy. Having ADHD can be financially costly.”
He notes that about 10% of his patients, roughly one a day, cancel late or don’t show up for scheduled appointments: “We keep a waitlist, and if someone cancels before the appointment, we can often fill the time with another patient in need on our waitlist.”
Dr. Goodman noted repeatedly that the clinician needs to be able to empathize with the patient’s condition and how they suffer. “This is not something people choose to have. The trap is that people think that if you’re successful you can’t have ADHD, and that’s not true. Often people with this condition work harder, are brighter, and find ways to compensate.”
If a practice is set up to accommodate the needs of patients with attention and organizational issues, treating them can be very gratifying. In settings without administrative support, the psychiatrist needs to stay cognizant of this invisible disability and the frustration that may come with this disorder, not just for the patient, but also for the family, friends, and employers, and even for the psychiatrist.
Dr. Dinah Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, Baltimore. Dr. Miller has no conflicts of interest.
A version of this article first appeared on Medscape.com.
Maybe you know some of these patients: They may come late or not show up at all. They may have little to say and minimize their difficulties, often because they are ashamed of how much effort it takes to meet ordinary obligations. They may struggle to complete assignments, fail classes, or lose jobs. And being in the right place at the right time can feel monumental to them: They forget appointments, double book themselves, or sometimes sleep through important events.
It’s not just appointments. They lose their keys and valuables, forget to pay bills, and may not answer calls, texts, or emails. Their voicemail may be full and people are often frustrated with them. These are all characteristics of executive dysfunction, which together can make the routine responsibilities of life very difficult.
Treatments include stimulants, and because of their potential for abuse, these medications are more strictly regulated when it comes to prescribing. The FDA does not allow them to be phoned into a pharmacy or refills to be added to prescriptions. Patients must wait until right before they are due to run out to get the next prescription, and this can present a problem if the patient travels or takes long vacations.
And although it is not the patient’s fault that stimulants can’t be ordered with refills, this adds to the burden of treating patients who take them. It’s hard to imagine that these restrictions on stimulants and opiates (but not on benzodiazepines) do much to deter abuse or diversion.
I trained at a time when ADD and ADHD were disorders of childhood, and as an adult psychiatrist, I was not exposed to patients on these medications. Occasionally, a stimulant was prescribed in a low dose to help activate a very depressed patient, but it was thought that children outgrow issues of attention and focus, and I have never felt fully confident in the more nuanced use of these medications with adults. Most of the patients I now treat with ADD have come to me on stable doses of the medications or at least with a history that directs care.
With others, the tip-off to look for the disorder is their disorganization in the absence of a substance use or active mood disorder. Medications help, sometimes remarkably, yet patients still struggle with organization and planning, and sometimes I find myself frustrated when patients forget their appointments or the issues around prescribing stimulants become time-consuming.
David W. Goodman, MD, director of the Adult Attention Deficit Center of Maryland, Lutherville, currently treats hundreds of patients with ADD and has written and spoken extensively about treating this disorder in adults.
“There are three things that make it difficult to manage patients with ADD,” Dr. Goodman noted, referring specifically to administrative issues. “You can’t write for refills, but with e-prescribing you can write a sequence of prescriptions with ‘fill-after’ dates. Or some patients are able to get a 90-day supply from mail-order pharmacies. Still, it’s a hassle if the patient moves around, as college students often do, and there are inventory shortages when some pharmacies can’t get the medications.”
“The second issue,” he adds, “is that it’s the nature of this disorder that patients struggle with organizational issues. Yelling at someone with ADD to pay attention is like yelling at a blind person not to run into furniture when they are in a new room. They go through life with people being impatient that they can’t do the things an ordinary person can do easily.”
Finally, Dr. Goodman noted that the clinicians who treat patients with ADD may have counter-transference issues.
“You have to understand that this is a disability and be sympathetic to it. They often have comorbid disorders, including personality disorders, and this can all bleed over to cause frustrations in their care. Psychiatrists who treat patients with ADD need to know they can deal with them compassionately.”
“I am occasionally contacted by patients who already have an ADHD diagnosis and are on stimulants, and who seem like they just want to get their prescriptions filled and aren’t interested in working on their issues,” says Douglas Beech, MD, a psychiatrist in private practice in Worthington, Ohio. “The doctor in this situation can feel like they are functioning as a sort of drug dealer. There are logistical matters that are structurally inherent in trying to assist these patients, from both a regulatory perspective and from a functional perspective. Dr. Beech feels that it’s helpful to acknowledge these issues when seeing patients with ADHD, so that he is prepared when problems do arise.
“It can almost feel cruel to charge a patient for a “no-show,” when difficulty keeping appointments may be a symptom of their illness, Dr. Beech adds. But he does believe it’s important to apply any fee policy equitably to all patients. “I don’t apply the ‘missed appointment’ policy differently to a person with an ADHD diagnosis versus any other diagnosis.” Though for their first missed appointment, he does give patients a “mulligan.”
“I don’t charge, but it puts both patient and doctor on notice,” he says.
And when his patients do miss an appointment, he offers to send a reminder for the next time, which is he says is effective. “With electronic messaging, this is a quick and easy way to prevent missed appointments and the complications that arise with prescriptions and rescheduling,” says Dr. Beech.
Dr. Goodman speaks about manging a large caseload of patients, many of whom have organizational issues.
“I have a full-time office manager who handles a lot of the logistics of scheduling and prescribing. Patients are sent multiple reminders, and I charge a nominal administrative fee if prescriptions need to be sent outside of appointments. This is not to make money, but to encourage patients to consider the administrative time.”
“I charge for appointments that are not canceled 48 hours in advance, and for patients who have missed appointments, a credit card is kept on file,” he says.
In a practice similar to Dr. Beech, Dr. Goodman notes that he shows some flexibility for new patients when they miss an appointment the first time. “By the second time, they know this is the policy. Having ADHD can be financially costly.”
He notes that about 10% of his patients, roughly one a day, cancel late or don’t show up for scheduled appointments: “We keep a waitlist, and if someone cancels before the appointment, we can often fill the time with another patient in need on our waitlist.”
Dr. Goodman noted repeatedly that the clinician needs to be able to empathize with the patient’s condition and how they suffer. “This is not something people choose to have. The trap is that people think that if you’re successful you can’t have ADHD, and that’s not true. Often people with this condition work harder, are brighter, and find ways to compensate.”
If a practice is set up to accommodate the needs of patients with attention and organizational issues, treating them can be very gratifying. In settings without administrative support, the psychiatrist needs to stay cognizant of this invisible disability and the frustration that may come with this disorder, not just for the patient, but also for the family, friends, and employers, and even for the psychiatrist.
Dr. Dinah Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, Baltimore. Dr. Miller has no conflicts of interest.
A version of this article first appeared on Medscape.com.
Omicron breakthrough cases boost protection, studies say
two preprint studies show.
The University of Washington, Seattle, working with Vir Biotechnology of San Francisco, looked at blood samples of vaccinated people who had breakthrough cases of Delta or Omicron and compared the samples with three other groups: people who caught COVID and were later vaccinated, vaccinated people who were never infected, and people who were infected and never vaccinated.
The vaccinated people who had a breakthrough case of Omicron produced antibodies that helped protect against coronavirus variants, whereas unvaccinated people who caught Omicron didn’t produce as many antibodies, the study showed.
BioNTech, the German biotechnology company, found that people who’d been double and triple vaccinated and then became infected with Omicron had a better B-cell response than people who’d gotten a booster shot but had not been infected.
The University of Washington research team also came up with similar findings about B cells.
The findings don’t mean people should deliberately try to become infected with COVID, said Alexandra Walls, PhD, one of the University of Washington scientists, according to Business Standard.
But the study does indicate “that we are at the point where we may want to consider having a different vaccine to boost people,” said David Veesler, PhD, of the University of Washington team.
“We should think about breakthrough infections as essentially equivalent to another dose of vaccine,” John Wherry, PhD, a professor and director of the Institute for Immunology at the University of Pennsylvania, Philadelphia, told Business Standard. Dr. Wherry was not involved in the studies but reviewed the BioNTech study.
A version of this article first appeared on WebMD.com.
two preprint studies show.
The University of Washington, Seattle, working with Vir Biotechnology of San Francisco, looked at blood samples of vaccinated people who had breakthrough cases of Delta or Omicron and compared the samples with three other groups: people who caught COVID and were later vaccinated, vaccinated people who were never infected, and people who were infected and never vaccinated.
The vaccinated people who had a breakthrough case of Omicron produced antibodies that helped protect against coronavirus variants, whereas unvaccinated people who caught Omicron didn’t produce as many antibodies, the study showed.
BioNTech, the German biotechnology company, found that people who’d been double and triple vaccinated and then became infected with Omicron had a better B-cell response than people who’d gotten a booster shot but had not been infected.
The University of Washington research team also came up with similar findings about B cells.
The findings don’t mean people should deliberately try to become infected with COVID, said Alexandra Walls, PhD, one of the University of Washington scientists, according to Business Standard.
But the study does indicate “that we are at the point where we may want to consider having a different vaccine to boost people,” said David Veesler, PhD, of the University of Washington team.
“We should think about breakthrough infections as essentially equivalent to another dose of vaccine,” John Wherry, PhD, a professor and director of the Institute for Immunology at the University of Pennsylvania, Philadelphia, told Business Standard. Dr. Wherry was not involved in the studies but reviewed the BioNTech study.
A version of this article first appeared on WebMD.com.
two preprint studies show.
The University of Washington, Seattle, working with Vir Biotechnology of San Francisco, looked at blood samples of vaccinated people who had breakthrough cases of Delta or Omicron and compared the samples with three other groups: people who caught COVID and were later vaccinated, vaccinated people who were never infected, and people who were infected and never vaccinated.
The vaccinated people who had a breakthrough case of Omicron produced antibodies that helped protect against coronavirus variants, whereas unvaccinated people who caught Omicron didn’t produce as many antibodies, the study showed.
BioNTech, the German biotechnology company, found that people who’d been double and triple vaccinated and then became infected with Omicron had a better B-cell response than people who’d gotten a booster shot but had not been infected.
The University of Washington research team also came up with similar findings about B cells.
The findings don’t mean people should deliberately try to become infected with COVID, said Alexandra Walls, PhD, one of the University of Washington scientists, according to Business Standard.
But the study does indicate “that we are at the point where we may want to consider having a different vaccine to boost people,” said David Veesler, PhD, of the University of Washington team.
“We should think about breakthrough infections as essentially equivalent to another dose of vaccine,” John Wherry, PhD, a professor and director of the Institute for Immunology at the University of Pennsylvania, Philadelphia, told Business Standard. Dr. Wherry was not involved in the studies but reviewed the BioNTech study.
A version of this article first appeared on WebMD.com.
Student loan forgiveness plans exclude physicians
In the run up to the midterm elections in November, President Biden has warmed to student loan forgiveness. However, before even being proposed,
What was the plan?
During the 2020 election, student loan forgiveness was a hot topic as the COVID epidemic raged. The CARES Act has placed all federal student loans in forbearance, with no payments made and the interest rate set to 0% to prevent further accrual. While this was tremendously useful to 45 million borrowers around the country (including the author), nothing material was done to deal with the loans.
The Biden Administration’s approach at that time was multi-tiered and chaotic. Plans were put forward that either expanded Public Service Loan Forgiveness (PSLF) or capped it. Plans were put forward that either extended free undergraduate or severely limited it through Pell Grants. Unfortunately, that duality continues today, with current plans not having a clear goal or a target group of beneficiaries.
Necessary CARES Act extensions
The Biden Administration has attempted repeatedly to turn the student loan apparatus back on, restarting payments en masse. However, each time, they are beset by challenges, ranging from repeat COVID spikes to servicer withdrawals or macroeconomic indicators of a recession.
At each step, the administration has had little choice but to extend the CARES Act forbearance, lest they suffer retribution for hastily resuming payments for 45 million borrowers without the apparatus to do so. Two years ago, the major federal servicers laid off hundreds, if not thousands, of staffers responsible for payment processing, accounting, customer care, and taxation. Hiring, training, and staffing these positions is nontrivial.
The administration has been out of step with servicers such that three of the largest have chosen not to renew their contracts: Navient, MyFedLoan, and Granite State Management and Resources. This has left 15 million borrowers in the lurch, not knowing who their servicer is – and, even worse, losing track of qualifying payments toward programs like PSLF.
Avenues of forgiveness
There are two major pathways to forgiveness. It is widely believed that the executive branch has the authority to broadly forgive student loans under executive order and managed through the U.S. Department of Education.
The alternative is through congressional action, voting on forgiveness as an economic stimulus plan. There is little appetite in Congress for forgiveness, and prominent congresspeople like Senator Warren and Senator Schumer have both pushed the executive branch for forgiveness in recognition of this.
What has been proposed?
First, it’s important to state that as headline-grabbing as it is to see that $50,000 of forgiveness has been proposed, the reality is that President Biden has repeatedly stated that he will not be in favor of that level of forgiveness. Instead, the number most commonly being discussed is $10,000. This would represent an unprecedented amount of support, alleviating 35% of borrowers of all student debt.
The impact of proposed forgiveness plans for physicians
For the medical community, sadly, this doesn’t represent a significant amount of forgiveness. At graduation, the average MD has $203,000 in debt, and the average DO has $258,000 in debt. These numbers grow during residency for years before any meaningful payments are made.
Further weakening forgiveness plans for physicians has been two caps proposed by the administration in recent days. The first is an income cap of $125,000. While this would maintain forgiveness for nearly all residents and fellows, this would exclude nearly every practicing physician. The alternative to an income cap is specific exclusion of certain careers seen to be high-earning: doctors and lawyers.
The bottom line
Physicians are unlikely to be included in any forgiveness plans being proposed recently by the Biden Administration. If they are considered, it will be for exclusion from any forgiveness offered.
For physicians no longer eligible for PSLF, this exclusion needs to be considered in managing the student loan debt associated with becoming a doctor.
Dr. Palmer is a part-time instructor, department of pediatrics, Harvard Medical School, Boston, and staff physician, department of medical critical care, Boston Children’s Hospital. He disclosed that he serves as director for Panacea Financial.
A version of this article first appeared on Medscape.com.
In the run up to the midterm elections in November, President Biden has warmed to student loan forgiveness. However, before even being proposed,
What was the plan?
During the 2020 election, student loan forgiveness was a hot topic as the COVID epidemic raged. The CARES Act has placed all federal student loans in forbearance, with no payments made and the interest rate set to 0% to prevent further accrual. While this was tremendously useful to 45 million borrowers around the country (including the author), nothing material was done to deal with the loans.
The Biden Administration’s approach at that time was multi-tiered and chaotic. Plans were put forward that either expanded Public Service Loan Forgiveness (PSLF) or capped it. Plans were put forward that either extended free undergraduate or severely limited it through Pell Grants. Unfortunately, that duality continues today, with current plans not having a clear goal or a target group of beneficiaries.
Necessary CARES Act extensions
The Biden Administration has attempted repeatedly to turn the student loan apparatus back on, restarting payments en masse. However, each time, they are beset by challenges, ranging from repeat COVID spikes to servicer withdrawals or macroeconomic indicators of a recession.
At each step, the administration has had little choice but to extend the CARES Act forbearance, lest they suffer retribution for hastily resuming payments for 45 million borrowers without the apparatus to do so. Two years ago, the major federal servicers laid off hundreds, if not thousands, of staffers responsible for payment processing, accounting, customer care, and taxation. Hiring, training, and staffing these positions is nontrivial.
The administration has been out of step with servicers such that three of the largest have chosen not to renew their contracts: Navient, MyFedLoan, and Granite State Management and Resources. This has left 15 million borrowers in the lurch, not knowing who their servicer is – and, even worse, losing track of qualifying payments toward programs like PSLF.
Avenues of forgiveness
There are two major pathways to forgiveness. It is widely believed that the executive branch has the authority to broadly forgive student loans under executive order and managed through the U.S. Department of Education.
The alternative is through congressional action, voting on forgiveness as an economic stimulus plan. There is little appetite in Congress for forgiveness, and prominent congresspeople like Senator Warren and Senator Schumer have both pushed the executive branch for forgiveness in recognition of this.
What has been proposed?
First, it’s important to state that as headline-grabbing as it is to see that $50,000 of forgiveness has been proposed, the reality is that President Biden has repeatedly stated that he will not be in favor of that level of forgiveness. Instead, the number most commonly being discussed is $10,000. This would represent an unprecedented amount of support, alleviating 35% of borrowers of all student debt.
The impact of proposed forgiveness plans for physicians
For the medical community, sadly, this doesn’t represent a significant amount of forgiveness. At graduation, the average MD has $203,000 in debt, and the average DO has $258,000 in debt. These numbers grow during residency for years before any meaningful payments are made.
Further weakening forgiveness plans for physicians has been two caps proposed by the administration in recent days. The first is an income cap of $125,000. While this would maintain forgiveness for nearly all residents and fellows, this would exclude nearly every practicing physician. The alternative to an income cap is specific exclusion of certain careers seen to be high-earning: doctors and lawyers.
The bottom line
Physicians are unlikely to be included in any forgiveness plans being proposed recently by the Biden Administration. If they are considered, it will be for exclusion from any forgiveness offered.
For physicians no longer eligible for PSLF, this exclusion needs to be considered in managing the student loan debt associated with becoming a doctor.
Dr. Palmer is a part-time instructor, department of pediatrics, Harvard Medical School, Boston, and staff physician, department of medical critical care, Boston Children’s Hospital. He disclosed that he serves as director for Panacea Financial.
A version of this article first appeared on Medscape.com.
In the run up to the midterm elections in November, President Biden has warmed to student loan forgiveness. However, before even being proposed,
What was the plan?
During the 2020 election, student loan forgiveness was a hot topic as the COVID epidemic raged. The CARES Act has placed all federal student loans in forbearance, with no payments made and the interest rate set to 0% to prevent further accrual. While this was tremendously useful to 45 million borrowers around the country (including the author), nothing material was done to deal with the loans.
The Biden Administration’s approach at that time was multi-tiered and chaotic. Plans were put forward that either expanded Public Service Loan Forgiveness (PSLF) or capped it. Plans were put forward that either extended free undergraduate or severely limited it through Pell Grants. Unfortunately, that duality continues today, with current plans not having a clear goal or a target group of beneficiaries.
Necessary CARES Act extensions
The Biden Administration has attempted repeatedly to turn the student loan apparatus back on, restarting payments en masse. However, each time, they are beset by challenges, ranging from repeat COVID spikes to servicer withdrawals or macroeconomic indicators of a recession.
At each step, the administration has had little choice but to extend the CARES Act forbearance, lest they suffer retribution for hastily resuming payments for 45 million borrowers without the apparatus to do so. Two years ago, the major federal servicers laid off hundreds, if not thousands, of staffers responsible for payment processing, accounting, customer care, and taxation. Hiring, training, and staffing these positions is nontrivial.
The administration has been out of step with servicers such that three of the largest have chosen not to renew their contracts: Navient, MyFedLoan, and Granite State Management and Resources. This has left 15 million borrowers in the lurch, not knowing who their servicer is – and, even worse, losing track of qualifying payments toward programs like PSLF.
Avenues of forgiveness
There are two major pathways to forgiveness. It is widely believed that the executive branch has the authority to broadly forgive student loans under executive order and managed through the U.S. Department of Education.
The alternative is through congressional action, voting on forgiveness as an economic stimulus plan. There is little appetite in Congress for forgiveness, and prominent congresspeople like Senator Warren and Senator Schumer have both pushed the executive branch for forgiveness in recognition of this.
What has been proposed?
First, it’s important to state that as headline-grabbing as it is to see that $50,000 of forgiveness has been proposed, the reality is that President Biden has repeatedly stated that he will not be in favor of that level of forgiveness. Instead, the number most commonly being discussed is $10,000. This would represent an unprecedented amount of support, alleviating 35% of borrowers of all student debt.
The impact of proposed forgiveness plans for physicians
For the medical community, sadly, this doesn’t represent a significant amount of forgiveness. At graduation, the average MD has $203,000 in debt, and the average DO has $258,000 in debt. These numbers grow during residency for years before any meaningful payments are made.
Further weakening forgiveness plans for physicians has been two caps proposed by the administration in recent days. The first is an income cap of $125,000. While this would maintain forgiveness for nearly all residents and fellows, this would exclude nearly every practicing physician. The alternative to an income cap is specific exclusion of certain careers seen to be high-earning: doctors and lawyers.
The bottom line
Physicians are unlikely to be included in any forgiveness plans being proposed recently by the Biden Administration. If they are considered, it will be for exclusion from any forgiveness offered.
For physicians no longer eligible for PSLF, this exclusion needs to be considered in managing the student loan debt associated with becoming a doctor.
Dr. Palmer is a part-time instructor, department of pediatrics, Harvard Medical School, Boston, and staff physician, department of medical critical care, Boston Children’s Hospital. He disclosed that he serves as director for Panacea Financial.
A version of this article first appeared on Medscape.com.
Why do clinical trials still underrepresent minority groups?
It’s no secret that, for decades, the participants in clinical trials for new drugs and medical devices haven’t accurately represented the diverse groups of patients the drugs and devices were designed for.
In a recently published draft guidance, the Food and Drug Administration recommended that companies in charge of running these trials should submit a proposal to the agency that would address how they plan to enroll more “clinically relevant populations” and historically underrepresented racial and ethnic groups.
It’s an issue that the U.S. has been trying to fix for years. In 1993, the NIH Revitalization Act was passed into law. It mandated the appropriate inclusion of women and racial minorities in all National Institutes of Health–funded research.
Since then, the FDA has put out plans that encourage trial sponsors to recruit more diverse enrollees, offering strategies and best practices rather than establishing requirements or quotas that companies would be forced to meet. Despite its efforts to encourage inclusion, people of color continue to be largely underrepresented in clinical trials.
Experts aren’t just calling for trial cohorts to reflect U.S. census data. Rather, the demographics of participants should match those of the diagnosis being studied. An analysis of 24 clinical trials of cardiovascular drugs, for example, found that Black Americans made up 2.9% of trial participants, compared with 83.1% for White people. Given that cardiovascular diseases affect Black Americans at almost the same rate as Whites (23.5% and 23.7%, respectively) – and keeping in mind that Black Americans make up 13.4% of the population and White people represent 76.3% – the degree of underrepresentation is glaring.
One commonly cited reason for this lack of representation is that people of color, especially Black Americans, have lingering feelings of mistrust toward the medical field. The U.S.-run Tuskegee study – during which researchers documented the natural progression of syphilis in hundreds of Black men who were kept from life-saving treatment – is, justifiably, often named as a notable source of that suspicion.
But blaming the disproportionately low numbers of Black participants in clinical trials on medical mistrust is an easy answer to a much more complicated issue, said cardiologist Clyde Yancy, MD, who also serves as the vice dean for diversity and inclusion at Northwestern University’s Feinberg School of Medicine, Chicago.
“We need to not put the onus on the back of the patient cohort, and say they are the problem,” Dr. Yancy said, adding that many trials add financial barriers and don’t provide proper transportation for participants who may live farther away.
The diversity of the study team itself – the institutions, researchers, and recruiters – also contributes to a lack of diversity in the participant pool. When considering all of these factors, “you begin to understand the complexity and the multidimensionality of why we have underrepresentation,” said Dr. Yancy. “So I would not promulgate the notion that this is simply because patients don’t trust the system.”
Soumya Niranjan, PhD, worked as a study coordinator at the Tulane Cancer Center in New Orleans, La., where she recruited patients for a prostate cancer study. After researching the impact of clinicians’ biases on the recruitment of racial and ethnic minorities in oncology trials, she found that some recruiters view patients of color as less promising participants.
“Who ends up being approached for a clinical trial is based on a preset rubric that one has in mind about a patient who may be eligible for a cancer study,” said Dr. Niranjan. “There is a characterization of, ‘we want to make sure this patient is compliant, that they will be a good historian and seem responsible.’ ... Our study showed that it kind of fell along racial lines.”
In her study, published in the journal Cancer in 2020, Dr. Niranjan wrote that researchers sometimes “perceived racial minority groups to have low knowledge of cancer clinical trials. This was considered to be a hindrance while explaining cancer clinical trials in the face of limited provider time during a clinical encounter.”
Some researchers believed minority participants, especially Black women, would be less likely to file study protocols. Others said people of color are more likely to be selfish.
She quoted one research investigator as saying Black people are less knowledgeable.
“African Americans I think have less knowledge,” the unnamed researcher said. “We take a little bit more time to explain to African American [sic]. I think ... they have more questions because we know they are not more knowledgeable so I think it takes time. They have a lot of questions.”
Progress over the years
The FDA’s recent draft builds upon a guidance from 2016, which already recommended that trial teams submit an inclusion plan to the agency at the earliest phase of development. While the recent announcement is another step in the right direction, it may not be substantial enough.
“There’s always an enrollment plan,” Dr. Niranjan said. “But those enrollment plans are not enforced. So if it’s not enforced, what does that look like?”
In an emailed statement to this news organization, Lola Fashoyin-Aje, MD, the deputy director of the FDA Oncology Center of Excellence’s division to expand diversity, emphasized that the draft guidance does not require anything, but that the agency “expect[s] sponsors will follow FDA’s recommendations as described in the draft guidance.”
Without requirements, it’s up to the sponsor to make the effort to enroll people with varied racial and ethnic backgrounds. During the development of the COVID-19 vaccine, Moderna announced that the company would slow the trial’s enrollment to ensure minority groups were properly represented.
Not every sponsor is as motivated to make this a concerted effort, and some simply don’t have the funds to allocate to strengthening the enrollment process.
“There’s so much red tape and paperwork to get the funding for a clinical trial,” said Julie Silver, MD, professor of physical medicine and rehabilitation at Harvard Medical School, Boston, who studies workforce diversity and inclusion. “Even when people are equitably included, the amount of funding they have to do the trial might not be enough to do an analysis that shows potential differences.”
Whether the FDA will enforce enrollment plans in the future remains an open question; however, Dr. Yancy said the most effective way to do this would be through incentives, rather than penalties.
According to Dr. Fashoyin-Aje, the FDA and sponsors “will learn from these submissions and over time, whether and how these diversity plans lead to meaningful changes in clinical trial representation will need to be assessed, including whether additional steps need to be taken.”
A version of this article first appeared on Medscape.com.
It’s no secret that, for decades, the participants in clinical trials for new drugs and medical devices haven’t accurately represented the diverse groups of patients the drugs and devices were designed for.
In a recently published draft guidance, the Food and Drug Administration recommended that companies in charge of running these trials should submit a proposal to the agency that would address how they plan to enroll more “clinically relevant populations” and historically underrepresented racial and ethnic groups.
It’s an issue that the U.S. has been trying to fix for years. In 1993, the NIH Revitalization Act was passed into law. It mandated the appropriate inclusion of women and racial minorities in all National Institutes of Health–funded research.
Since then, the FDA has put out plans that encourage trial sponsors to recruit more diverse enrollees, offering strategies and best practices rather than establishing requirements or quotas that companies would be forced to meet. Despite its efforts to encourage inclusion, people of color continue to be largely underrepresented in clinical trials.
Experts aren’t just calling for trial cohorts to reflect U.S. census data. Rather, the demographics of participants should match those of the diagnosis being studied. An analysis of 24 clinical trials of cardiovascular drugs, for example, found that Black Americans made up 2.9% of trial participants, compared with 83.1% for White people. Given that cardiovascular diseases affect Black Americans at almost the same rate as Whites (23.5% and 23.7%, respectively) – and keeping in mind that Black Americans make up 13.4% of the population and White people represent 76.3% – the degree of underrepresentation is glaring.
One commonly cited reason for this lack of representation is that people of color, especially Black Americans, have lingering feelings of mistrust toward the medical field. The U.S.-run Tuskegee study – during which researchers documented the natural progression of syphilis in hundreds of Black men who were kept from life-saving treatment – is, justifiably, often named as a notable source of that suspicion.
But blaming the disproportionately low numbers of Black participants in clinical trials on medical mistrust is an easy answer to a much more complicated issue, said cardiologist Clyde Yancy, MD, who also serves as the vice dean for diversity and inclusion at Northwestern University’s Feinberg School of Medicine, Chicago.
“We need to not put the onus on the back of the patient cohort, and say they are the problem,” Dr. Yancy said, adding that many trials add financial barriers and don’t provide proper transportation for participants who may live farther away.
The diversity of the study team itself – the institutions, researchers, and recruiters – also contributes to a lack of diversity in the participant pool. When considering all of these factors, “you begin to understand the complexity and the multidimensionality of why we have underrepresentation,” said Dr. Yancy. “So I would not promulgate the notion that this is simply because patients don’t trust the system.”
Soumya Niranjan, PhD, worked as a study coordinator at the Tulane Cancer Center in New Orleans, La., where she recruited patients for a prostate cancer study. After researching the impact of clinicians’ biases on the recruitment of racial and ethnic minorities in oncology trials, she found that some recruiters view patients of color as less promising participants.
“Who ends up being approached for a clinical trial is based on a preset rubric that one has in mind about a patient who may be eligible for a cancer study,” said Dr. Niranjan. “There is a characterization of, ‘we want to make sure this patient is compliant, that they will be a good historian and seem responsible.’ ... Our study showed that it kind of fell along racial lines.”
In her study, published in the journal Cancer in 2020, Dr. Niranjan wrote that researchers sometimes “perceived racial minority groups to have low knowledge of cancer clinical trials. This was considered to be a hindrance while explaining cancer clinical trials in the face of limited provider time during a clinical encounter.”
Some researchers believed minority participants, especially Black women, would be less likely to file study protocols. Others said people of color are more likely to be selfish.
She quoted one research investigator as saying Black people are less knowledgeable.
“African Americans I think have less knowledge,” the unnamed researcher said. “We take a little bit more time to explain to African American [sic]. I think ... they have more questions because we know they are not more knowledgeable so I think it takes time. They have a lot of questions.”
Progress over the years
The FDA’s recent draft builds upon a guidance from 2016, which already recommended that trial teams submit an inclusion plan to the agency at the earliest phase of development. While the recent announcement is another step in the right direction, it may not be substantial enough.
“There’s always an enrollment plan,” Dr. Niranjan said. “But those enrollment plans are not enforced. So if it’s not enforced, what does that look like?”
In an emailed statement to this news organization, Lola Fashoyin-Aje, MD, the deputy director of the FDA Oncology Center of Excellence’s division to expand diversity, emphasized that the draft guidance does not require anything, but that the agency “expect[s] sponsors will follow FDA’s recommendations as described in the draft guidance.”
Without requirements, it’s up to the sponsor to make the effort to enroll people with varied racial and ethnic backgrounds. During the development of the COVID-19 vaccine, Moderna announced that the company would slow the trial’s enrollment to ensure minority groups were properly represented.
Not every sponsor is as motivated to make this a concerted effort, and some simply don’t have the funds to allocate to strengthening the enrollment process.
“There’s so much red tape and paperwork to get the funding for a clinical trial,” said Julie Silver, MD, professor of physical medicine and rehabilitation at Harvard Medical School, Boston, who studies workforce diversity and inclusion. “Even when people are equitably included, the amount of funding they have to do the trial might not be enough to do an analysis that shows potential differences.”
Whether the FDA will enforce enrollment plans in the future remains an open question; however, Dr. Yancy said the most effective way to do this would be through incentives, rather than penalties.
According to Dr. Fashoyin-Aje, the FDA and sponsors “will learn from these submissions and over time, whether and how these diversity plans lead to meaningful changes in clinical trial representation will need to be assessed, including whether additional steps need to be taken.”
A version of this article first appeared on Medscape.com.
It’s no secret that, for decades, the participants in clinical trials for new drugs and medical devices haven’t accurately represented the diverse groups of patients the drugs and devices were designed for.
In a recently published draft guidance, the Food and Drug Administration recommended that companies in charge of running these trials should submit a proposal to the agency that would address how they plan to enroll more “clinically relevant populations” and historically underrepresented racial and ethnic groups.
It’s an issue that the U.S. has been trying to fix for years. In 1993, the NIH Revitalization Act was passed into law. It mandated the appropriate inclusion of women and racial minorities in all National Institutes of Health–funded research.
Since then, the FDA has put out plans that encourage trial sponsors to recruit more diverse enrollees, offering strategies and best practices rather than establishing requirements or quotas that companies would be forced to meet. Despite its efforts to encourage inclusion, people of color continue to be largely underrepresented in clinical trials.
Experts aren’t just calling for trial cohorts to reflect U.S. census data. Rather, the demographics of participants should match those of the diagnosis being studied. An analysis of 24 clinical trials of cardiovascular drugs, for example, found that Black Americans made up 2.9% of trial participants, compared with 83.1% for White people. Given that cardiovascular diseases affect Black Americans at almost the same rate as Whites (23.5% and 23.7%, respectively) – and keeping in mind that Black Americans make up 13.4% of the population and White people represent 76.3% – the degree of underrepresentation is glaring.
One commonly cited reason for this lack of representation is that people of color, especially Black Americans, have lingering feelings of mistrust toward the medical field. The U.S.-run Tuskegee study – during which researchers documented the natural progression of syphilis in hundreds of Black men who were kept from life-saving treatment – is, justifiably, often named as a notable source of that suspicion.
But blaming the disproportionately low numbers of Black participants in clinical trials on medical mistrust is an easy answer to a much more complicated issue, said cardiologist Clyde Yancy, MD, who also serves as the vice dean for diversity and inclusion at Northwestern University’s Feinberg School of Medicine, Chicago.
“We need to not put the onus on the back of the patient cohort, and say they are the problem,” Dr. Yancy said, adding that many trials add financial barriers and don’t provide proper transportation for participants who may live farther away.
The diversity of the study team itself – the institutions, researchers, and recruiters – also contributes to a lack of diversity in the participant pool. When considering all of these factors, “you begin to understand the complexity and the multidimensionality of why we have underrepresentation,” said Dr. Yancy. “So I would not promulgate the notion that this is simply because patients don’t trust the system.”
Soumya Niranjan, PhD, worked as a study coordinator at the Tulane Cancer Center in New Orleans, La., where she recruited patients for a prostate cancer study. After researching the impact of clinicians’ biases on the recruitment of racial and ethnic minorities in oncology trials, she found that some recruiters view patients of color as less promising participants.
“Who ends up being approached for a clinical trial is based on a preset rubric that one has in mind about a patient who may be eligible for a cancer study,” said Dr. Niranjan. “There is a characterization of, ‘we want to make sure this patient is compliant, that they will be a good historian and seem responsible.’ ... Our study showed that it kind of fell along racial lines.”
In her study, published in the journal Cancer in 2020, Dr. Niranjan wrote that researchers sometimes “perceived racial minority groups to have low knowledge of cancer clinical trials. This was considered to be a hindrance while explaining cancer clinical trials in the face of limited provider time during a clinical encounter.”
Some researchers believed minority participants, especially Black women, would be less likely to file study protocols. Others said people of color are more likely to be selfish.
She quoted one research investigator as saying Black people are less knowledgeable.
“African Americans I think have less knowledge,” the unnamed researcher said. “We take a little bit more time to explain to African American [sic]. I think ... they have more questions because we know they are not more knowledgeable so I think it takes time. They have a lot of questions.”
Progress over the years
The FDA’s recent draft builds upon a guidance from 2016, which already recommended that trial teams submit an inclusion plan to the agency at the earliest phase of development. While the recent announcement is another step in the right direction, it may not be substantial enough.
“There’s always an enrollment plan,” Dr. Niranjan said. “But those enrollment plans are not enforced. So if it’s not enforced, what does that look like?”
In an emailed statement to this news organization, Lola Fashoyin-Aje, MD, the deputy director of the FDA Oncology Center of Excellence’s division to expand diversity, emphasized that the draft guidance does not require anything, but that the agency “expect[s] sponsors will follow FDA’s recommendations as described in the draft guidance.”
Without requirements, it’s up to the sponsor to make the effort to enroll people with varied racial and ethnic backgrounds. During the development of the COVID-19 vaccine, Moderna announced that the company would slow the trial’s enrollment to ensure minority groups were properly represented.
Not every sponsor is as motivated to make this a concerted effort, and some simply don’t have the funds to allocate to strengthening the enrollment process.
“There’s so much red tape and paperwork to get the funding for a clinical trial,” said Julie Silver, MD, professor of physical medicine and rehabilitation at Harvard Medical School, Boston, who studies workforce diversity and inclusion. “Even when people are equitably included, the amount of funding they have to do the trial might not be enough to do an analysis that shows potential differences.”
Whether the FDA will enforce enrollment plans in the future remains an open question; however, Dr. Yancy said the most effective way to do this would be through incentives, rather than penalties.
According to Dr. Fashoyin-Aje, the FDA and sponsors “will learn from these submissions and over time, whether and how these diversity plans lead to meaningful changes in clinical trial representation will need to be assessed, including whether additional steps need to be taken.”
A version of this article first appeared on Medscape.com.
Advancing digital health care past pandemic-driven telemedicine
COVID-19 forced consumers to adopt digital and virtual platforms to receive medical care, and more than 2 years after the start of the pandemic, it doesn’t appear that that will change.
“During the pandemic we witnessed a very steep rise in the utilization of digital health care transactions. And as we have now witnessed a plateau, we see that digital health care transactions have not fallen back to the way things were prepandemic,” said Bart M. Demaerschalk, MD, professor and chair of cerebrovascular diseases for digital health research at the Mayo Clinic in Phoenix, Ariz. “At Mayo Clinic and other health care organizations, approximately 20% ... of the composite care is occurring by digital means.”
Dr. Demaerschalk was among a panel representing retail and traditional health care organizations at the American Telemedicine Association conference in Boston.
The pandemic created this new reality, and health care leaders are now trying to make the most of all digital tools. Marcus Osborne, former senior vice president at Walmart Health, said that to progress, the health care industry needs to move beyond the conception of a world in which consumers interact with care providers via one-off in-person or digital experiences.
“What we’re actually seeing in other sectors and in life in general is that the world is not multichannel. The world is omnichannel,” Mr. Osborne said. Under an omnichannel paradigm, provider organizations integrate multiple digital and in-person health delivery methods, making it possible to “create whole new experiences for consumers that no one channel could deliver,” he added.
Creagh Milford, DO, vice president and head of enterprise virtual care at CVS Health, agreed and added that “the retail footprint will evolve” from offering separate physical and virtual care experiences to a “blended” experience.
To move in this direction, health care leaders need to “stop talking about the site of care so much,” said Christopher McCann, MBChB, CEO and cofounder of the health IT firm Current Health. Instead of “fixating” on either brick-and-mortar or digital experiences, leaders should meet “the consumer where they are and deliver what is the most appropriate care to that consumer in the most appropriate setting,” Dr. McCann said.
Three key digital technology strategies
In addition to supporting an omnichannel experience, the panelists pointed out that traditional and retail health care providers can make the most of digital technologies in a few different ways.
One is by helping consumers manage innovation. With venture capital investments in digital technologies at an all-time high, the health care industry is drowning in innovation, <r/ Osborne pointed out.
“So on one hand, we have been blessed with this eruption of innovation. On the other hand – and I’m saying this as a consumer – it [doesn’t] really matter. I’m overwhelmed, and I think the market is overwhelmed,” Mr. Osborne said. “So if we’re overwhelmed, it means we’re not going to leverage that innovation as effectively as we should.” The challenge, then, is to find a way to “not get overwhelmed by the sheer force of innovations occurring” and to instead leverage these new technologies to drive real transformation in our health care system.
To meet this challenge, health care organizations will have to provide consumers with “some guidance as to how to tailor that journey,” Dr. Demaerschalk said. “It’s the responsibility of all of us to be creating that tailored and individual guidance for our patients.” By doing so, health care organizations ultimately can help consumers feel less overwhelmed.
Another strategy is to ensure that the use of technology promotes health equity. Mr. Osborne pointed out that events such as the pandemic and George Floyd’s murder have resulted in a “much more robust conversation around the need to address health inequities in America. I’ve also heard a lot of people say they believe that digital health solutions are the answer.”
As such, health care organizations need to ensure that digital innovations are leveraged to “fundamentally address the inequities that we’re facing today and support the care of all Americans,” Mr. Osborne noted.
To move in this direction, leaders need to address one glaring gap: “We talk all the time about fancy technology, like artificial intelligence. Most of my clients, they’re just trying to get basic Internet access at home,” Dr. McCann said. “So, there’s a technology challenge we first have to solve.”
Once this hurdle is overcome, however, digital technologies could pay off in spades, especially for consumers who struggle to access in-person services because they live 2 or 3 hours away from the hospital, are working two jobs, and have child care responsibilities, Dr. McCann noted.
Health care must also address staffing issues, said the panelists. Leaders need to create new career paths for clinicians as digital care delivery becomes more prominent.
Some health care organizations have already discovered that using digital technologies to support hospital-at-home programs can also enhance the work lives of clinicians.
When working in hospital-at-home programs, clinicians can “deliver care in the way that they have always wanted to but have never been able to within an acute inpatient facility. They’re able to go into patients’ homes and spend an hour with them, actually develop a proper relationship and look at social determinants of health and medications and do things in a way they’ve never been able to do before. And that has dramatically reduced rates of burnout,” Dr. McCann said.
While these strategies will help organizations support “this exciting digital ecosystem,” health care technology innovators need to “really study the costs and the health outcomes related to these digital health transactions in order to move the entire field and the science forward,” Dr. Demaerschalk concluded.
A version of this article first appeared on Medscape.com.
COVID-19 forced consumers to adopt digital and virtual platforms to receive medical care, and more than 2 years after the start of the pandemic, it doesn’t appear that that will change.
“During the pandemic we witnessed a very steep rise in the utilization of digital health care transactions. And as we have now witnessed a plateau, we see that digital health care transactions have not fallen back to the way things were prepandemic,” said Bart M. Demaerschalk, MD, professor and chair of cerebrovascular diseases for digital health research at the Mayo Clinic in Phoenix, Ariz. “At Mayo Clinic and other health care organizations, approximately 20% ... of the composite care is occurring by digital means.”
Dr. Demaerschalk was among a panel representing retail and traditional health care organizations at the American Telemedicine Association conference in Boston.
The pandemic created this new reality, and health care leaders are now trying to make the most of all digital tools. Marcus Osborne, former senior vice president at Walmart Health, said that to progress, the health care industry needs to move beyond the conception of a world in which consumers interact with care providers via one-off in-person or digital experiences.
“What we’re actually seeing in other sectors and in life in general is that the world is not multichannel. The world is omnichannel,” Mr. Osborne said. Under an omnichannel paradigm, provider organizations integrate multiple digital and in-person health delivery methods, making it possible to “create whole new experiences for consumers that no one channel could deliver,” he added.
Creagh Milford, DO, vice president and head of enterprise virtual care at CVS Health, agreed and added that “the retail footprint will evolve” from offering separate physical and virtual care experiences to a “blended” experience.
To move in this direction, health care leaders need to “stop talking about the site of care so much,” said Christopher McCann, MBChB, CEO and cofounder of the health IT firm Current Health. Instead of “fixating” on either brick-and-mortar or digital experiences, leaders should meet “the consumer where they are and deliver what is the most appropriate care to that consumer in the most appropriate setting,” Dr. McCann said.
Three key digital technology strategies
In addition to supporting an omnichannel experience, the panelists pointed out that traditional and retail health care providers can make the most of digital technologies in a few different ways.
One is by helping consumers manage innovation. With venture capital investments in digital technologies at an all-time high, the health care industry is drowning in innovation, <r/ Osborne pointed out.
“So on one hand, we have been blessed with this eruption of innovation. On the other hand – and I’m saying this as a consumer – it [doesn’t] really matter. I’m overwhelmed, and I think the market is overwhelmed,” Mr. Osborne said. “So if we’re overwhelmed, it means we’re not going to leverage that innovation as effectively as we should.” The challenge, then, is to find a way to “not get overwhelmed by the sheer force of innovations occurring” and to instead leverage these new technologies to drive real transformation in our health care system.
To meet this challenge, health care organizations will have to provide consumers with “some guidance as to how to tailor that journey,” Dr. Demaerschalk said. “It’s the responsibility of all of us to be creating that tailored and individual guidance for our patients.” By doing so, health care organizations ultimately can help consumers feel less overwhelmed.
Another strategy is to ensure that the use of technology promotes health equity. Mr. Osborne pointed out that events such as the pandemic and George Floyd’s murder have resulted in a “much more robust conversation around the need to address health inequities in America. I’ve also heard a lot of people say they believe that digital health solutions are the answer.”
As such, health care organizations need to ensure that digital innovations are leveraged to “fundamentally address the inequities that we’re facing today and support the care of all Americans,” Mr. Osborne noted.
To move in this direction, leaders need to address one glaring gap: “We talk all the time about fancy technology, like artificial intelligence. Most of my clients, they’re just trying to get basic Internet access at home,” Dr. McCann said. “So, there’s a technology challenge we first have to solve.”
Once this hurdle is overcome, however, digital technologies could pay off in spades, especially for consumers who struggle to access in-person services because they live 2 or 3 hours away from the hospital, are working two jobs, and have child care responsibilities, Dr. McCann noted.
Health care must also address staffing issues, said the panelists. Leaders need to create new career paths for clinicians as digital care delivery becomes more prominent.
Some health care organizations have already discovered that using digital technologies to support hospital-at-home programs can also enhance the work lives of clinicians.
When working in hospital-at-home programs, clinicians can “deliver care in the way that they have always wanted to but have never been able to within an acute inpatient facility. They’re able to go into patients’ homes and spend an hour with them, actually develop a proper relationship and look at social determinants of health and medications and do things in a way they’ve never been able to do before. And that has dramatically reduced rates of burnout,” Dr. McCann said.
While these strategies will help organizations support “this exciting digital ecosystem,” health care technology innovators need to “really study the costs and the health outcomes related to these digital health transactions in order to move the entire field and the science forward,” Dr. Demaerschalk concluded.
A version of this article first appeared on Medscape.com.
COVID-19 forced consumers to adopt digital and virtual platforms to receive medical care, and more than 2 years after the start of the pandemic, it doesn’t appear that that will change.
“During the pandemic we witnessed a very steep rise in the utilization of digital health care transactions. And as we have now witnessed a plateau, we see that digital health care transactions have not fallen back to the way things were prepandemic,” said Bart M. Demaerschalk, MD, professor and chair of cerebrovascular diseases for digital health research at the Mayo Clinic in Phoenix, Ariz. “At Mayo Clinic and other health care organizations, approximately 20% ... of the composite care is occurring by digital means.”
Dr. Demaerschalk was among a panel representing retail and traditional health care organizations at the American Telemedicine Association conference in Boston.
The pandemic created this new reality, and health care leaders are now trying to make the most of all digital tools. Marcus Osborne, former senior vice president at Walmart Health, said that to progress, the health care industry needs to move beyond the conception of a world in which consumers interact with care providers via one-off in-person or digital experiences.
“What we’re actually seeing in other sectors and in life in general is that the world is not multichannel. The world is omnichannel,” Mr. Osborne said. Under an omnichannel paradigm, provider organizations integrate multiple digital and in-person health delivery methods, making it possible to “create whole new experiences for consumers that no one channel could deliver,” he added.
Creagh Milford, DO, vice president and head of enterprise virtual care at CVS Health, agreed and added that “the retail footprint will evolve” from offering separate physical and virtual care experiences to a “blended” experience.
To move in this direction, health care leaders need to “stop talking about the site of care so much,” said Christopher McCann, MBChB, CEO and cofounder of the health IT firm Current Health. Instead of “fixating” on either brick-and-mortar or digital experiences, leaders should meet “the consumer where they are and deliver what is the most appropriate care to that consumer in the most appropriate setting,” Dr. McCann said.
Three key digital technology strategies
In addition to supporting an omnichannel experience, the panelists pointed out that traditional and retail health care providers can make the most of digital technologies in a few different ways.
One is by helping consumers manage innovation. With venture capital investments in digital technologies at an all-time high, the health care industry is drowning in innovation, <r/ Osborne pointed out.
“So on one hand, we have been blessed with this eruption of innovation. On the other hand – and I’m saying this as a consumer – it [doesn’t] really matter. I’m overwhelmed, and I think the market is overwhelmed,” Mr. Osborne said. “So if we’re overwhelmed, it means we’re not going to leverage that innovation as effectively as we should.” The challenge, then, is to find a way to “not get overwhelmed by the sheer force of innovations occurring” and to instead leverage these new technologies to drive real transformation in our health care system.
To meet this challenge, health care organizations will have to provide consumers with “some guidance as to how to tailor that journey,” Dr. Demaerschalk said. “It’s the responsibility of all of us to be creating that tailored and individual guidance for our patients.” By doing so, health care organizations ultimately can help consumers feel less overwhelmed.
Another strategy is to ensure that the use of technology promotes health equity. Mr. Osborne pointed out that events such as the pandemic and George Floyd’s murder have resulted in a “much more robust conversation around the need to address health inequities in America. I’ve also heard a lot of people say they believe that digital health solutions are the answer.”
As such, health care organizations need to ensure that digital innovations are leveraged to “fundamentally address the inequities that we’re facing today and support the care of all Americans,” Mr. Osborne noted.
To move in this direction, leaders need to address one glaring gap: “We talk all the time about fancy technology, like artificial intelligence. Most of my clients, they’re just trying to get basic Internet access at home,” Dr. McCann said. “So, there’s a technology challenge we first have to solve.”
Once this hurdle is overcome, however, digital technologies could pay off in spades, especially for consumers who struggle to access in-person services because they live 2 or 3 hours away from the hospital, are working two jobs, and have child care responsibilities, Dr. McCann noted.
Health care must also address staffing issues, said the panelists. Leaders need to create new career paths for clinicians as digital care delivery becomes more prominent.
Some health care organizations have already discovered that using digital technologies to support hospital-at-home programs can also enhance the work lives of clinicians.
When working in hospital-at-home programs, clinicians can “deliver care in the way that they have always wanted to but have never been able to within an acute inpatient facility. They’re able to go into patients’ homes and spend an hour with them, actually develop a proper relationship and look at social determinants of health and medications and do things in a way they’ve never been able to do before. And that has dramatically reduced rates of burnout,” Dr. McCann said.
While these strategies will help organizations support “this exciting digital ecosystem,” health care technology innovators need to “really study the costs and the health outcomes related to these digital health transactions in order to move the entire field and the science forward,” Dr. Demaerschalk concluded.
A version of this article first appeared on Medscape.com.
FROM ATA 2022
Administrative hassle hacks: Strategies to curb physician stress
The American Medical Association estimates that physician burnout costs the country $4.6 billion annually, and that doesn’t include the cost for nurses and other clinicians. In addition, physicians note too many bureaucratic tasks as a main contributor to their daily stress.
Such revelations have prompted many in the health care industry to focus on clinician burnout, including a panel at the recent American Telemedicine Association annual conference in Boston.
Not surprisingly, the discussion quickly turned to the COVID-19 pandemic, commonly cited as an event that has exacerbated existing clinician burnout and caused what has become known as the “great resignation.”
Peter Yellowlees, MBBS, MD, professor of psychiatry and chief wellness officer at the University of California, Davis, said his health system has experienced a lot of its nursing staff resigning or moving to other employment, particularly from intensive care units and the emergency department.
“We actually haven’t had too many physicians go, but I have a funny feeling we’re going to see that over the next year or so because I think a lot of people have just put their head down during the pandemic and they’ve worked themselves hard,” he said. “They’re now sort of putting their heads up above the wall,” and could realize that they want a change.
In his role as the wellness officer at the academic medical center, Dr. Yellowlees is proactively addressing burnout among the organization’s 14,000 employees. For example, during the pandemic, he developed a peer responder program. Under this initiative, 600 staff members received training in “psychological first aid,” essentially utilizing staff to become therapists for peers.
For example, if a clinician is struggling emotionally while dealing with a patient who has had significant trauma, a peer responder could talk with the clinician, helping him or her to better deal with the situation.
Marlene McDermott, senior director of therapy services at Array Behavioral Care, a national telepsychiatry provider with offices in New Jersey and Illinois, noted that her organization also addresses burnout by creating opportunities for peer-to-peer support.
“We’ve got hundreds of clinicians and we’ll take 10 to 15 of them, put them in small treatment teams and they have a live chat, a one-off virtual meeting with each other to vent and to ask clinical questions. It’s all clinicians, there’s no administrative staff in there,” Ms. McDermott said. The clinicians have found value in these meetings, as they can share their concerns as well as “silly images or quotes, just to keep things light at times. That’s made a big difference.”
Retraining, technology can help curb administrative burdens
In addition to providing peer support, both Dr. Yellowlees and Ms. McDermott are addressing the significant administrative burden that plagues physicians.
This burden is especially onerous for physicians in the United States, according to a study that compared the number of keystrokes required to produce clinical notes among physicians in several countries.
“What [the study] discovered was that the American notes were three to five times longer than the notes of the Australian or U.K. physicians. I’ve worked in all three countries and I can promise you there’s no difference in the quality of the doctors across those places,” Dr. Yellowlees said.
To address this issue, Dr. Yellowlees is training physicians to reduce the length of their clinical documentation.
“I am trying to retrain physicians who for many years have been trained to be defensive in their documentation – to write absurd amounts just to justify billing,” Dr. Yellowlees said. “We are trying to go back in some respects to the way that we used to write notes 20 years ago ... so much shorter. This is a huge retraining exercise but it’s an exercise that is essential.”
Ms. McDermott also is tackling the administrative burden at her organization.
“We are trying to make the workflow as efficient as possible, doing some asynchronous work where consumers are completing information before a session ... so clinicians are essentially reconciling information instead of gathering all nonpertinent information. They can just work at the top of the license and not be burdened by some of the questions that don’t directly affect treatment,” Ms. McDermott noted.
Encouraging and training physicians in concurrent documentation also can help reduce administrative burden.
“Being proficient at remaining in session and documenting as much as you can during a session can help. So that at the end, you’re pressing the button, closing the encounter and you’ve finished documenting,” Ms. McDermott said. “It’s definitely possible to do that without losing the connection with the patient.”
To accomplish this, physicians need to leverage touch-typing – the practice of typing without looking at the keyboard. Fortunately, telehealth makes this mode of documentation easily achievable. Consider the following: During an online session, clinicians can place the patient’s picture “right underneath the camera and make it small. And then you type with the note floating behind it. So you’re actually staring at the note and the person all at the same time,” Ms. McDermott said.
The continued uptake of telehealth in general could also reduce stress for physicians, added Dr. Yellowlees.
“One of the interesting things about that is just how much time we save the physicians because it actually takes quite a lot of time to room patients,” Dr. Yellowlees concluded. “We are now doing about 20% of all our outpatient visits in all disciplines by video. We were higher than that midway through COVID. I’m hoping we’ll go back to being higher than that.”
A version of this article first appeared on Medscape.com.
The American Medical Association estimates that physician burnout costs the country $4.6 billion annually, and that doesn’t include the cost for nurses and other clinicians. In addition, physicians note too many bureaucratic tasks as a main contributor to their daily stress.
Such revelations have prompted many in the health care industry to focus on clinician burnout, including a panel at the recent American Telemedicine Association annual conference in Boston.
Not surprisingly, the discussion quickly turned to the COVID-19 pandemic, commonly cited as an event that has exacerbated existing clinician burnout and caused what has become known as the “great resignation.”
Peter Yellowlees, MBBS, MD, professor of psychiatry and chief wellness officer at the University of California, Davis, said his health system has experienced a lot of its nursing staff resigning or moving to other employment, particularly from intensive care units and the emergency department.
“We actually haven’t had too many physicians go, but I have a funny feeling we’re going to see that over the next year or so because I think a lot of people have just put their head down during the pandemic and they’ve worked themselves hard,” he said. “They’re now sort of putting their heads up above the wall,” and could realize that they want a change.
In his role as the wellness officer at the academic medical center, Dr. Yellowlees is proactively addressing burnout among the organization’s 14,000 employees. For example, during the pandemic, he developed a peer responder program. Under this initiative, 600 staff members received training in “psychological first aid,” essentially utilizing staff to become therapists for peers.
For example, if a clinician is struggling emotionally while dealing with a patient who has had significant trauma, a peer responder could talk with the clinician, helping him or her to better deal with the situation.
Marlene McDermott, senior director of therapy services at Array Behavioral Care, a national telepsychiatry provider with offices in New Jersey and Illinois, noted that her organization also addresses burnout by creating opportunities for peer-to-peer support.
“We’ve got hundreds of clinicians and we’ll take 10 to 15 of them, put them in small treatment teams and they have a live chat, a one-off virtual meeting with each other to vent and to ask clinical questions. It’s all clinicians, there’s no administrative staff in there,” Ms. McDermott said. The clinicians have found value in these meetings, as they can share their concerns as well as “silly images or quotes, just to keep things light at times. That’s made a big difference.”
Retraining, technology can help curb administrative burdens
In addition to providing peer support, both Dr. Yellowlees and Ms. McDermott are addressing the significant administrative burden that plagues physicians.
This burden is especially onerous for physicians in the United States, according to a study that compared the number of keystrokes required to produce clinical notes among physicians in several countries.
“What [the study] discovered was that the American notes were three to five times longer than the notes of the Australian or U.K. physicians. I’ve worked in all three countries and I can promise you there’s no difference in the quality of the doctors across those places,” Dr. Yellowlees said.
To address this issue, Dr. Yellowlees is training physicians to reduce the length of their clinical documentation.
“I am trying to retrain physicians who for many years have been trained to be defensive in their documentation – to write absurd amounts just to justify billing,” Dr. Yellowlees said. “We are trying to go back in some respects to the way that we used to write notes 20 years ago ... so much shorter. This is a huge retraining exercise but it’s an exercise that is essential.”
Ms. McDermott also is tackling the administrative burden at her organization.
“We are trying to make the workflow as efficient as possible, doing some asynchronous work where consumers are completing information before a session ... so clinicians are essentially reconciling information instead of gathering all nonpertinent information. They can just work at the top of the license and not be burdened by some of the questions that don’t directly affect treatment,” Ms. McDermott noted.
Encouraging and training physicians in concurrent documentation also can help reduce administrative burden.
“Being proficient at remaining in session and documenting as much as you can during a session can help. So that at the end, you’re pressing the button, closing the encounter and you’ve finished documenting,” Ms. McDermott said. “It’s definitely possible to do that without losing the connection with the patient.”
To accomplish this, physicians need to leverage touch-typing – the practice of typing without looking at the keyboard. Fortunately, telehealth makes this mode of documentation easily achievable. Consider the following: During an online session, clinicians can place the patient’s picture “right underneath the camera and make it small. And then you type with the note floating behind it. So you’re actually staring at the note and the person all at the same time,” Ms. McDermott said.
The continued uptake of telehealth in general could also reduce stress for physicians, added Dr. Yellowlees.
“One of the interesting things about that is just how much time we save the physicians because it actually takes quite a lot of time to room patients,” Dr. Yellowlees concluded. “We are now doing about 20% of all our outpatient visits in all disciplines by video. We were higher than that midway through COVID. I’m hoping we’ll go back to being higher than that.”
A version of this article first appeared on Medscape.com.
The American Medical Association estimates that physician burnout costs the country $4.6 billion annually, and that doesn’t include the cost for nurses and other clinicians. In addition, physicians note too many bureaucratic tasks as a main contributor to their daily stress.
Such revelations have prompted many in the health care industry to focus on clinician burnout, including a panel at the recent American Telemedicine Association annual conference in Boston.
Not surprisingly, the discussion quickly turned to the COVID-19 pandemic, commonly cited as an event that has exacerbated existing clinician burnout and caused what has become known as the “great resignation.”
Peter Yellowlees, MBBS, MD, professor of psychiatry and chief wellness officer at the University of California, Davis, said his health system has experienced a lot of its nursing staff resigning or moving to other employment, particularly from intensive care units and the emergency department.
“We actually haven’t had too many physicians go, but I have a funny feeling we’re going to see that over the next year or so because I think a lot of people have just put their head down during the pandemic and they’ve worked themselves hard,” he said. “They’re now sort of putting their heads up above the wall,” and could realize that they want a change.
In his role as the wellness officer at the academic medical center, Dr. Yellowlees is proactively addressing burnout among the organization’s 14,000 employees. For example, during the pandemic, he developed a peer responder program. Under this initiative, 600 staff members received training in “psychological first aid,” essentially utilizing staff to become therapists for peers.
For example, if a clinician is struggling emotionally while dealing with a patient who has had significant trauma, a peer responder could talk with the clinician, helping him or her to better deal with the situation.
Marlene McDermott, senior director of therapy services at Array Behavioral Care, a national telepsychiatry provider with offices in New Jersey and Illinois, noted that her organization also addresses burnout by creating opportunities for peer-to-peer support.
“We’ve got hundreds of clinicians and we’ll take 10 to 15 of them, put them in small treatment teams and they have a live chat, a one-off virtual meeting with each other to vent and to ask clinical questions. It’s all clinicians, there’s no administrative staff in there,” Ms. McDermott said. The clinicians have found value in these meetings, as they can share their concerns as well as “silly images or quotes, just to keep things light at times. That’s made a big difference.”
Retraining, technology can help curb administrative burdens
In addition to providing peer support, both Dr. Yellowlees and Ms. McDermott are addressing the significant administrative burden that plagues physicians.
This burden is especially onerous for physicians in the United States, according to a study that compared the number of keystrokes required to produce clinical notes among physicians in several countries.
“What [the study] discovered was that the American notes were three to five times longer than the notes of the Australian or U.K. physicians. I’ve worked in all three countries and I can promise you there’s no difference in the quality of the doctors across those places,” Dr. Yellowlees said.
To address this issue, Dr. Yellowlees is training physicians to reduce the length of their clinical documentation.
“I am trying to retrain physicians who for many years have been trained to be defensive in their documentation – to write absurd amounts just to justify billing,” Dr. Yellowlees said. “We are trying to go back in some respects to the way that we used to write notes 20 years ago ... so much shorter. This is a huge retraining exercise but it’s an exercise that is essential.”
Ms. McDermott also is tackling the administrative burden at her organization.
“We are trying to make the workflow as efficient as possible, doing some asynchronous work where consumers are completing information before a session ... so clinicians are essentially reconciling information instead of gathering all nonpertinent information. They can just work at the top of the license and not be burdened by some of the questions that don’t directly affect treatment,” Ms. McDermott noted.
Encouraging and training physicians in concurrent documentation also can help reduce administrative burden.
“Being proficient at remaining in session and documenting as much as you can during a session can help. So that at the end, you’re pressing the button, closing the encounter and you’ve finished documenting,” Ms. McDermott said. “It’s definitely possible to do that without losing the connection with the patient.”
To accomplish this, physicians need to leverage touch-typing – the practice of typing without looking at the keyboard. Fortunately, telehealth makes this mode of documentation easily achievable. Consider the following: During an online session, clinicians can place the patient’s picture “right underneath the camera and make it small. And then you type with the note floating behind it. So you’re actually staring at the note and the person all at the same time,” Ms. McDermott said.
The continued uptake of telehealth in general could also reduce stress for physicians, added Dr. Yellowlees.
“One of the interesting things about that is just how much time we save the physicians because it actually takes quite a lot of time to room patients,” Dr. Yellowlees concluded. “We are now doing about 20% of all our outpatient visits in all disciplines by video. We were higher than that midway through COVID. I’m hoping we’ll go back to being higher than that.”
A version of this article first appeared on Medscape.com.
Spell it out: Writing out common medical terms boosts patient understanding, says study
MI. HTN. hx. Although these abbreviations might make it easier for physicians and other health care professionals to create and consume clinical documentation, the shorthand confuses patients, according to a study published in JAMA Network Open.
Researchers, who conducted clinical trials at three hospitals, found that expansion of 10 common medical abbreviations and acronyms in patient health records significantly increased overall comprehension.
Corresponding author Lisa Grossman Liu, PhD, MD, of Columbia University, New York, told this news organization that “comprehension of abbreviations was much lower than we expected and much lower than the clinicians who participated in this study expected.”
This discovery is particularly relevant in this era of digital care, where providers are now communicating with patients electronically more than ever before – and are required by rules emanating from the 21st Century Cures Act to provide online access to electronic health records.
Using elongated terms
Although the study found that expansion of medical abbreviations and acronyms can improve patient understanding, identifying all of the medical abbreviations that exist is difficult because the terms vary by specialty and geography. The fact that many abbreviations and acronyms have multiple meanings complicates matters even more. For example, the abbreviation PA has 128 possible meanings, Dr. Grossman Liu pointed out.
Technology, fortunately, has advanced in the last few years and is on the cusp of providing a solution. Artificial intelligence systems could help to develop large compendiums of abbreviations and acronyms and then machine learning could elongate the words.
“We’re almost to the point where we have these automated systems that can actually expand abbreviations pretty well and with a great degree of accuracy and ... where those can actually be used in medicine to help with patient communication,” Dr. Grossman Liu said.
Such intervention, however, is not a cure-all.
“There are abbreviations that are really hard to understand even after you expand them, such as MI for myocardial infarction, which is really a tough term all around. It means heart attack. So even if you tell patients, MI means myocardial infarction, they’re still not going to understand it,” Dr. Grossman Liu said.
On the flip side, patients are likely to understand some abbreviations such as hrs, which stands for hours, without elongating the words.
Moving from in-person to online communication
A look at the evolution of clinical documentation explains how this abbreviation problem came to fruition. Prior to this digital age where providers communicate with patients through portals, secure messaging, and other electronic methods, patients and providers would talk face to face. Now, however, electronic written communication is becoming the norm.
“We are not only seeing direct written communication through things like messaging systems or email, but also patients are now reading their medical records online and you can consider that as a form of communication,” Dr. Grossman Liu said. “It’s really interesting that the electronic health record itself has essentially become a medium for communication between patients and providers when previously it was only a way for providers to communicate with themselves and document patient care. So, clinicians use abbreviations because they aren’t intending for patients to see the records.”
Requiring physicians to use complete words in clinical documentation now that electronic records are relied on for patient communication, however, is not a practical solution.
“Abbreviations are so commonly used because they are more efficient to read and more efficient to write. We really shouldn’t be putting the onus on providers to spell out all the abbreviations in their notes. That’s realistically not going to work, because it compromises clinical efficiency,” Dr. Grossman Liu said.
While physicians should not be forced to use complete words in documentation, they should be wary of patients’ unfamiliarity with abbreviations as they communicate in person.
“I use terms like ED constantly when I talk to patients, and it turns out that only 67% of patients understand what you’re talking about when you say ED in reference to the emergency department. So it’s important to be mindful of that,” Dr. Grossman Liu concluded.
A version of this article first appeared on Medscape.com.
MI. HTN. hx. Although these abbreviations might make it easier for physicians and other health care professionals to create and consume clinical documentation, the shorthand confuses patients, according to a study published in JAMA Network Open.
Researchers, who conducted clinical trials at three hospitals, found that expansion of 10 common medical abbreviations and acronyms in patient health records significantly increased overall comprehension.
Corresponding author Lisa Grossman Liu, PhD, MD, of Columbia University, New York, told this news organization that “comprehension of abbreviations was much lower than we expected and much lower than the clinicians who participated in this study expected.”
This discovery is particularly relevant in this era of digital care, where providers are now communicating with patients electronically more than ever before – and are required by rules emanating from the 21st Century Cures Act to provide online access to electronic health records.
Using elongated terms
Although the study found that expansion of medical abbreviations and acronyms can improve patient understanding, identifying all of the medical abbreviations that exist is difficult because the terms vary by specialty and geography. The fact that many abbreviations and acronyms have multiple meanings complicates matters even more. For example, the abbreviation PA has 128 possible meanings, Dr. Grossman Liu pointed out.
Technology, fortunately, has advanced in the last few years and is on the cusp of providing a solution. Artificial intelligence systems could help to develop large compendiums of abbreviations and acronyms and then machine learning could elongate the words.
“We’re almost to the point where we have these automated systems that can actually expand abbreviations pretty well and with a great degree of accuracy and ... where those can actually be used in medicine to help with patient communication,” Dr. Grossman Liu said.
Such intervention, however, is not a cure-all.
“There are abbreviations that are really hard to understand even after you expand them, such as MI for myocardial infarction, which is really a tough term all around. It means heart attack. So even if you tell patients, MI means myocardial infarction, they’re still not going to understand it,” Dr. Grossman Liu said.
On the flip side, patients are likely to understand some abbreviations such as hrs, which stands for hours, without elongating the words.
Moving from in-person to online communication
A look at the evolution of clinical documentation explains how this abbreviation problem came to fruition. Prior to this digital age where providers communicate with patients through portals, secure messaging, and other electronic methods, patients and providers would talk face to face. Now, however, electronic written communication is becoming the norm.
“We are not only seeing direct written communication through things like messaging systems or email, but also patients are now reading their medical records online and you can consider that as a form of communication,” Dr. Grossman Liu said. “It’s really interesting that the electronic health record itself has essentially become a medium for communication between patients and providers when previously it was only a way for providers to communicate with themselves and document patient care. So, clinicians use abbreviations because they aren’t intending for patients to see the records.”
Requiring physicians to use complete words in clinical documentation now that electronic records are relied on for patient communication, however, is not a practical solution.
“Abbreviations are so commonly used because they are more efficient to read and more efficient to write. We really shouldn’t be putting the onus on providers to spell out all the abbreviations in their notes. That’s realistically not going to work, because it compromises clinical efficiency,” Dr. Grossman Liu said.
While physicians should not be forced to use complete words in documentation, they should be wary of patients’ unfamiliarity with abbreviations as they communicate in person.
“I use terms like ED constantly when I talk to patients, and it turns out that only 67% of patients understand what you’re talking about when you say ED in reference to the emergency department. So it’s important to be mindful of that,” Dr. Grossman Liu concluded.
A version of this article first appeared on Medscape.com.
MI. HTN. hx. Although these abbreviations might make it easier for physicians and other health care professionals to create and consume clinical documentation, the shorthand confuses patients, according to a study published in JAMA Network Open.
Researchers, who conducted clinical trials at three hospitals, found that expansion of 10 common medical abbreviations and acronyms in patient health records significantly increased overall comprehension.
Corresponding author Lisa Grossman Liu, PhD, MD, of Columbia University, New York, told this news organization that “comprehension of abbreviations was much lower than we expected and much lower than the clinicians who participated in this study expected.”
This discovery is particularly relevant in this era of digital care, where providers are now communicating with patients electronically more than ever before – and are required by rules emanating from the 21st Century Cures Act to provide online access to electronic health records.
Using elongated terms
Although the study found that expansion of medical abbreviations and acronyms can improve patient understanding, identifying all of the medical abbreviations that exist is difficult because the terms vary by specialty and geography. The fact that many abbreviations and acronyms have multiple meanings complicates matters even more. For example, the abbreviation PA has 128 possible meanings, Dr. Grossman Liu pointed out.
Technology, fortunately, has advanced in the last few years and is on the cusp of providing a solution. Artificial intelligence systems could help to develop large compendiums of abbreviations and acronyms and then machine learning could elongate the words.
“We’re almost to the point where we have these automated systems that can actually expand abbreviations pretty well and with a great degree of accuracy and ... where those can actually be used in medicine to help with patient communication,” Dr. Grossman Liu said.
Such intervention, however, is not a cure-all.
“There are abbreviations that are really hard to understand even after you expand them, such as MI for myocardial infarction, which is really a tough term all around. It means heart attack. So even if you tell patients, MI means myocardial infarction, they’re still not going to understand it,” Dr. Grossman Liu said.
On the flip side, patients are likely to understand some abbreviations such as hrs, which stands for hours, without elongating the words.
Moving from in-person to online communication
A look at the evolution of clinical documentation explains how this abbreviation problem came to fruition. Prior to this digital age where providers communicate with patients through portals, secure messaging, and other electronic methods, patients and providers would talk face to face. Now, however, electronic written communication is becoming the norm.
“We are not only seeing direct written communication through things like messaging systems or email, but also patients are now reading their medical records online and you can consider that as a form of communication,” Dr. Grossman Liu said. “It’s really interesting that the electronic health record itself has essentially become a medium for communication between patients and providers when previously it was only a way for providers to communicate with themselves and document patient care. So, clinicians use abbreviations because they aren’t intending for patients to see the records.”
Requiring physicians to use complete words in clinical documentation now that electronic records are relied on for patient communication, however, is not a practical solution.
“Abbreviations are so commonly used because they are more efficient to read and more efficient to write. We really shouldn’t be putting the onus on providers to spell out all the abbreviations in their notes. That’s realistically not going to work, because it compromises clinical efficiency,” Dr. Grossman Liu said.
While physicians should not be forced to use complete words in documentation, they should be wary of patients’ unfamiliarity with abbreviations as they communicate in person.
“I use terms like ED constantly when I talk to patients, and it turns out that only 67% of patients understand what you’re talking about when you say ED in reference to the emergency department. So it’s important to be mindful of that,” Dr. Grossman Liu concluded.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
COVID drove telehealth forward in high gear: Now what?
Before the pandemic hit in 2019, Pooja Aysola, MD, considered herself lucky because she could tap into telehealth for neurology consults in her work as an emergency department physician.
“We would wheel in a computer screen with a neurologist on board every time we had a suspected stroke patient. And I was able to talk directly to the neurologist about my patient’s symptoms. And it was great,” Dr. Aysola said.
The pandemic, however, prompted the need for telehealth in many situations beyond specialty care. As such, investment exploded over the past few years.
“We’re seeing telehealth across all specialties ... more than half of clinicians are now saying that they do believe that virtual visits will surpass in-person visits for primary care needs,” said Dr. Aysola, who also serves as senior director, clinical operations at Wheel, a Texas-based telehealth company.
Dr. Aysola spoke during an American Telemedicine Association conference panel addressing how COVID prompted an uptick in telehealth investment and utilization and how such virtual care is likely to evolve moving forward.
Nathaniel Lacktman, a partner at law firm Foley & Lardner, agreed with Dr. Aysola’s assessment of the market.
“The appetite for virtual care has become voracious,” said Mr. Lacktman, who chairs the firm’s telemedicine and digital health team. “It reminds me in some ways of taking my kids out to dinner and saying, ‘Try this new food.’ They’re like, ‘No, I won’t like it.’ They finally get a little taste and they’re like, ‘This is amazing.’”
While there is no doubt that stakeholders – from innovators to investors to providers to patients – will want more than just a taste of telehealth in the future, panelists addressed if this undeniable demand for virtual care was simply a short-term response to the pandemic or if there is a long-term desire to fundamentally change how care is delivered.
Expanding on the pandemic-driven ‘sandbox’
While the uptick in telehealth investment and utilization is not expected to continue at such jarring rates in the future, the panelists pointed out that innovation will proceed but perhaps at a different pace.
“The last 3 years have been a sandbox during which the industry was able to experiment,” said Mr. Lacktman. “What we’re going to see more of even post pandemic is building upon that experimental sandbox and creating models that aren’t just high growth and really quick but that are sustainable and meaningful.”
As such, patients and providers won’t be looking for telehealth to simply provide access to care but to provide a full scope of services while also improving quality.
Rachel Stillman, vice president of 7wireVentures, a Chicago-based venture capital firm, also expects interest in telehealth to continue but at a less frenetic pace. In 2021, the industry witnessed nearly $31 billion of venture financing directed towards digital health companies, she said.
“Now, Q1 2022 has had a little bit of a slower start. But with that said, we still have invested $6 billion in early stage companies. So ... we’re seeing some initial signs perhaps of – I don’t want to call it a slowdown – but increased discipline,” Ms. Stillman said.
Start-up companies will need to carefully position themselves for success in this post pandemic environment. “Ultimately, it really goes down to making sure your fundamentals are strong ... and having a really compelling [return on investment] case for your health plan, your self-insured employer, your health system, or your ultimate buyer,” Ms. Stillman said.
Two models are coming into play as innovation continues, she added. One is a traditional care delivery model whereby a start-up organization is building their own provider network specialized for the conditions or patient populations they are serving.
“Conversely, there are new entrants that are thinking about how they can leverage their insightful and strong technology foundations and platforms for existing provider networks that could benefit from a telemedicine partner,” Ms. Stillman pointed out.
Dr. Aysola added that companies are moving forward strategically to achieve post pandemic success. Some telehealth start-ups, for instance, are “capturing some of the low-hanging fruit, the simple UTIs, the really easy things to treat,” Dr. Aysola said.
Others are addressing the clinician’s experience. “Over 50% of clinicians have thought about leaving their jobs at some point during the pandemic. And so it’s becoming really clear that focusing on the clinician and the clinician’s needs are just imperative to [creating a] winning model post-pandemic,” Dr. Aysola said.
Adapting to the new normal
Health care provider organizations also need to adjust to post pandemic realities. “We work with a number of hospital systems, and it’s astounding how slow they are compared to the start-ups because there’s a lot more constituents; there’s bureaucracy,” Mr. Lacktman said. As a result, “the hospitals are in a more uncomfortable position post pandemic than the start-ups.”
To move forward successfully, these organizations, which are typically risk averse, need to create alignment among legal, compliance, and clinical leaders, Mr. Lacktman advised.
One of the first decisions that these teams need to make is whether they should proceed on their own or enter into a partnership with a start-up or pursue a merger and acquisition. In addition, some health systems, hospitals, and health plans are even opting to establish their own venture funds.
“Building your own venture fund or even investing ... in companies directly or in other venture funds [are strategies] that health systems might be able to leverage both to accelerate partnerships and also really be on top of key trends,” Ms. Stillman said.
No matter how health care systems invest in and implement telemedicine technologies, though, the need to move quickly is paramount.
Traditional health care systems “don’t always have the luxury of time. Things have to be done pretty quickly in order to remain competitive,” Dr. Aysola concluded. “We’ve found that companies can launch a virtual care offering in a matter of weeks. When in reality, if a traditional health care system were to try to launch it on their own, it could take upwards of 15 months.”
A version of this article first appeared on Medscape.com.
Before the pandemic hit in 2019, Pooja Aysola, MD, considered herself lucky because she could tap into telehealth for neurology consults in her work as an emergency department physician.
“We would wheel in a computer screen with a neurologist on board every time we had a suspected stroke patient. And I was able to talk directly to the neurologist about my patient’s symptoms. And it was great,” Dr. Aysola said.
The pandemic, however, prompted the need for telehealth in many situations beyond specialty care. As such, investment exploded over the past few years.
“We’re seeing telehealth across all specialties ... more than half of clinicians are now saying that they do believe that virtual visits will surpass in-person visits for primary care needs,” said Dr. Aysola, who also serves as senior director, clinical operations at Wheel, a Texas-based telehealth company.
Dr. Aysola spoke during an American Telemedicine Association conference panel addressing how COVID prompted an uptick in telehealth investment and utilization and how such virtual care is likely to evolve moving forward.
Nathaniel Lacktman, a partner at law firm Foley & Lardner, agreed with Dr. Aysola’s assessment of the market.
“The appetite for virtual care has become voracious,” said Mr. Lacktman, who chairs the firm’s telemedicine and digital health team. “It reminds me in some ways of taking my kids out to dinner and saying, ‘Try this new food.’ They’re like, ‘No, I won’t like it.’ They finally get a little taste and they’re like, ‘This is amazing.’”
While there is no doubt that stakeholders – from innovators to investors to providers to patients – will want more than just a taste of telehealth in the future, panelists addressed if this undeniable demand for virtual care was simply a short-term response to the pandemic or if there is a long-term desire to fundamentally change how care is delivered.
Expanding on the pandemic-driven ‘sandbox’
While the uptick in telehealth investment and utilization is not expected to continue at such jarring rates in the future, the panelists pointed out that innovation will proceed but perhaps at a different pace.
“The last 3 years have been a sandbox during which the industry was able to experiment,” said Mr. Lacktman. “What we’re going to see more of even post pandemic is building upon that experimental sandbox and creating models that aren’t just high growth and really quick but that are sustainable and meaningful.”
As such, patients and providers won’t be looking for telehealth to simply provide access to care but to provide a full scope of services while also improving quality.
Rachel Stillman, vice president of 7wireVentures, a Chicago-based venture capital firm, also expects interest in telehealth to continue but at a less frenetic pace. In 2021, the industry witnessed nearly $31 billion of venture financing directed towards digital health companies, she said.
“Now, Q1 2022 has had a little bit of a slower start. But with that said, we still have invested $6 billion in early stage companies. So ... we’re seeing some initial signs perhaps of – I don’t want to call it a slowdown – but increased discipline,” Ms. Stillman said.
Start-up companies will need to carefully position themselves for success in this post pandemic environment. “Ultimately, it really goes down to making sure your fundamentals are strong ... and having a really compelling [return on investment] case for your health plan, your self-insured employer, your health system, or your ultimate buyer,” Ms. Stillman said.
Two models are coming into play as innovation continues, she added. One is a traditional care delivery model whereby a start-up organization is building their own provider network specialized for the conditions or patient populations they are serving.
“Conversely, there are new entrants that are thinking about how they can leverage their insightful and strong technology foundations and platforms for existing provider networks that could benefit from a telemedicine partner,” Ms. Stillman pointed out.
Dr. Aysola added that companies are moving forward strategically to achieve post pandemic success. Some telehealth start-ups, for instance, are “capturing some of the low-hanging fruit, the simple UTIs, the really easy things to treat,” Dr. Aysola said.
Others are addressing the clinician’s experience. “Over 50% of clinicians have thought about leaving their jobs at some point during the pandemic. And so it’s becoming really clear that focusing on the clinician and the clinician’s needs are just imperative to [creating a] winning model post-pandemic,” Dr. Aysola said.
Adapting to the new normal
Health care provider organizations also need to adjust to post pandemic realities. “We work with a number of hospital systems, and it’s astounding how slow they are compared to the start-ups because there’s a lot more constituents; there’s bureaucracy,” Mr. Lacktman said. As a result, “the hospitals are in a more uncomfortable position post pandemic than the start-ups.”
To move forward successfully, these organizations, which are typically risk averse, need to create alignment among legal, compliance, and clinical leaders, Mr. Lacktman advised.
One of the first decisions that these teams need to make is whether they should proceed on their own or enter into a partnership with a start-up or pursue a merger and acquisition. In addition, some health systems, hospitals, and health plans are even opting to establish their own venture funds.
“Building your own venture fund or even investing ... in companies directly or in other venture funds [are strategies] that health systems might be able to leverage both to accelerate partnerships and also really be on top of key trends,” Ms. Stillman said.
No matter how health care systems invest in and implement telemedicine technologies, though, the need to move quickly is paramount.
Traditional health care systems “don’t always have the luxury of time. Things have to be done pretty quickly in order to remain competitive,” Dr. Aysola concluded. “We’ve found that companies can launch a virtual care offering in a matter of weeks. When in reality, if a traditional health care system were to try to launch it on their own, it could take upwards of 15 months.”
A version of this article first appeared on Medscape.com.
Before the pandemic hit in 2019, Pooja Aysola, MD, considered herself lucky because she could tap into telehealth for neurology consults in her work as an emergency department physician.
“We would wheel in a computer screen with a neurologist on board every time we had a suspected stroke patient. And I was able to talk directly to the neurologist about my patient’s symptoms. And it was great,” Dr. Aysola said.
The pandemic, however, prompted the need for telehealth in many situations beyond specialty care. As such, investment exploded over the past few years.
“We’re seeing telehealth across all specialties ... more than half of clinicians are now saying that they do believe that virtual visits will surpass in-person visits for primary care needs,” said Dr. Aysola, who also serves as senior director, clinical operations at Wheel, a Texas-based telehealth company.
Dr. Aysola spoke during an American Telemedicine Association conference panel addressing how COVID prompted an uptick in telehealth investment and utilization and how such virtual care is likely to evolve moving forward.
Nathaniel Lacktman, a partner at law firm Foley & Lardner, agreed with Dr. Aysola’s assessment of the market.
“The appetite for virtual care has become voracious,” said Mr. Lacktman, who chairs the firm’s telemedicine and digital health team. “It reminds me in some ways of taking my kids out to dinner and saying, ‘Try this new food.’ They’re like, ‘No, I won’t like it.’ They finally get a little taste and they’re like, ‘This is amazing.’”
While there is no doubt that stakeholders – from innovators to investors to providers to patients – will want more than just a taste of telehealth in the future, panelists addressed if this undeniable demand for virtual care was simply a short-term response to the pandemic or if there is a long-term desire to fundamentally change how care is delivered.
Expanding on the pandemic-driven ‘sandbox’
While the uptick in telehealth investment and utilization is not expected to continue at such jarring rates in the future, the panelists pointed out that innovation will proceed but perhaps at a different pace.
“The last 3 years have been a sandbox during which the industry was able to experiment,” said Mr. Lacktman. “What we’re going to see more of even post pandemic is building upon that experimental sandbox and creating models that aren’t just high growth and really quick but that are sustainable and meaningful.”
As such, patients and providers won’t be looking for telehealth to simply provide access to care but to provide a full scope of services while also improving quality.
Rachel Stillman, vice president of 7wireVentures, a Chicago-based venture capital firm, also expects interest in telehealth to continue but at a less frenetic pace. In 2021, the industry witnessed nearly $31 billion of venture financing directed towards digital health companies, she said.
“Now, Q1 2022 has had a little bit of a slower start. But with that said, we still have invested $6 billion in early stage companies. So ... we’re seeing some initial signs perhaps of – I don’t want to call it a slowdown – but increased discipline,” Ms. Stillman said.
Start-up companies will need to carefully position themselves for success in this post pandemic environment. “Ultimately, it really goes down to making sure your fundamentals are strong ... and having a really compelling [return on investment] case for your health plan, your self-insured employer, your health system, or your ultimate buyer,” Ms. Stillman said.
Two models are coming into play as innovation continues, she added. One is a traditional care delivery model whereby a start-up organization is building their own provider network specialized for the conditions or patient populations they are serving.
“Conversely, there are new entrants that are thinking about how they can leverage their insightful and strong technology foundations and platforms for existing provider networks that could benefit from a telemedicine partner,” Ms. Stillman pointed out.
Dr. Aysola added that companies are moving forward strategically to achieve post pandemic success. Some telehealth start-ups, for instance, are “capturing some of the low-hanging fruit, the simple UTIs, the really easy things to treat,” Dr. Aysola said.
Others are addressing the clinician’s experience. “Over 50% of clinicians have thought about leaving their jobs at some point during the pandemic. And so it’s becoming really clear that focusing on the clinician and the clinician’s needs are just imperative to [creating a] winning model post-pandemic,” Dr. Aysola said.
Adapting to the new normal
Health care provider organizations also need to adjust to post pandemic realities. “We work with a number of hospital systems, and it’s astounding how slow they are compared to the start-ups because there’s a lot more constituents; there’s bureaucracy,” Mr. Lacktman said. As a result, “the hospitals are in a more uncomfortable position post pandemic than the start-ups.”
To move forward successfully, these organizations, which are typically risk averse, need to create alignment among legal, compliance, and clinical leaders, Mr. Lacktman advised.
One of the first decisions that these teams need to make is whether they should proceed on their own or enter into a partnership with a start-up or pursue a merger and acquisition. In addition, some health systems, hospitals, and health plans are even opting to establish their own venture funds.
“Building your own venture fund or even investing ... in companies directly or in other venture funds [are strategies] that health systems might be able to leverage both to accelerate partnerships and also really be on top of key trends,” Ms. Stillman said.
No matter how health care systems invest in and implement telemedicine technologies, though, the need to move quickly is paramount.
Traditional health care systems “don’t always have the luxury of time. Things have to be done pretty quickly in order to remain competitive,” Dr. Aysola concluded. “We’ve found that companies can launch a virtual care offering in a matter of weeks. When in reality, if a traditional health care system were to try to launch it on their own, it could take upwards of 15 months.”
A version of this article first appeared on Medscape.com.
Four mental health trajectories in youth: Predicting persistent psychopathology
A study that tracked psychopathology in 13,000 children and adolescents found that
Investigators also found a strong correlation between new incidence of high psychopathology and externalizing problems such as hyperactivity. “It is of paramount importance to identify factors that distinguish those with persisting problems and escalating trajectories so that resources can be appropriately directed,” wrote the authors of the study published online in JAMA Network Open.
Recent studies have shown that concurrent and sequential comorbidity of psychiatric disorders are very common in adult populations, lead author Colm Healy, PhD, a postdoctoral researcher for psychiatry with the University of Medicine and Health Sciences, Ireland, said in an interview.
The speculation is that this occurs in early life when psychiatry symptoms experience high fluidity. “This presents a complex scenario to model, where young people’s mental health appears to shift and change across development. Few investigations to date have had the data available to examine these trajectories over the full range of child development,” said Dr. Healy.
He and his colleagues attempted to map the profiles and trajectories of psychopathology in children and adolescents, using latent profile transition analysis (LPTA), a person-centered method, to assess comorbidity and movement in the various phases of childhood development.
“The idea behind person-centered methods such as LTPA is that it identifies unobserved subgroups of participants who respond similarly to specific variables – in this case responses to a broad measure of psychopathology,” explained Dr. Healy.
The study included 7,507 children from the child sample (ages 3, 5, and 9 years) and 6,039 children from the adolescent sample (ages 9, 13, and 17 or 18 years). Data analysis took place from October 2020 to September 2021.
Dr. Healy and colleagues in a supplementary investigation compared cohorts at age 9 years to look for sex and generational differences.
Four developmental profiles
Researchers identified 4 distinct developmental profies for person-centered psychopathological trajectories: no psychopathology (incidence range, 60%-70%), high psychopathology (incidence range, 3%-5%), externalizing problems (incidence range, 15%-25%), and internalizing problems (incidence range, 7%-12%).
Internalizing problems reflect issues with peers and emotional problems whereas externalizing problems more closely associate with hyperactivity and conduct.
Less than 5% of the youth studied experienced persistent symptoms. However, 48.6% in the child cohort and 44.1% in the adolescent cohort moved into one of the 3 psychopathology profiles (high psychopathology, externalizing, internalizing problems) at some point in development.
The spread of trajectories was more diverse in the child cohort, said Dr. Healy. “Children ebbed and flowed between the different profiles over time with a large proportion falling into one of the psychopathology categories and then switching between these profiles.” Switching was also evident in the adolescent cohort but to a lesser extent, he said.
Externalizing problems link to high psychopathology
Rates of remittance were higher among individuals in both cohorts for internalizing problems, compared with externalizing problems.
It’s possible that for some of these young people, internalizing problems are a reaction to environmental stressors such as bullying,” said Dr. Healy. “When that stress is relieved, the internalizing problems may dissipate.”
In a clinically relevant finding, children with externalizing problems (age 5, 129 [61.3%] and age 9, 95 [74.3%]) were more likely to present with new incidents of high psychopathology. This was also true in the adolescent group (age 13, 129 [91.1%] and age 17, 146 [89.9%]).
This suggests that a proportion of youth with externalizing problems have an escalating trajectory of psychopathology. “Thus, it may be possible to distinguish those with an escalating trajectory from a stable or remitting trajectory. The specific distinguishing factors require further investigation, but it has been observed before that some of those reporting externalizing problems in early life continue to have difficulties into later life,” noted Dr. Healy.
A combination of environmental or biological factors may explain this escalation, which could respond to early intervention, he said.
Overall, few children in the study transitioned directly from no psychopathology to high psychopathology.
Differences between boys, girls
In both cohorts, investigators noticed significant differences between the sexes.
Boys in childhood made up a larger proportion of the three psychopathology profiles. But by late adolescence, girls made up a larger proportion of the internalizing profile whereas boys made up a larger proportion of the externalizing profile. “These differences were in line with our expectations,” said Dr. Healy.
Trajectories also differed among boys and girls. In childhood, girls had a higher percentage of de-escalating trajectories relative to boys. “More girls than boys in the psychopathology profiles switched to a non or less severe profile. In adolescence, differences in trajectories were less obvious, with the exception that girls were more likely than boys to transition to internalizing problems from all of the other profiles at age 17,” said Dr. Healy.
Most young people who experience psychopathology will eventually see an improvement in symptoms, noted Dr. Healy. Next steps are to identify markers that distinguish individuals with persistent trajectories from remitting trajectories at the different phases of development, he said.
Study draws mixed reviews
Clinical psychiatrists not involved in the study had varying reactions to the results.
“This study is notable for its data-driven and powerful illustration of how childhood and adolescence are dynamic periods during which psychiatric symptoms can emerge and evolve,” said Sunny X. Tang, MD, a psychiatrist and an assistant professor at the Institute of Behavioral Science and the Feinstein Institutes for Medical Research, Manhasset, New York.
The clinical call for action is for person-centered mental health screening to be a routine part of pediatric and adolescent primary care or school-based services, noted Dr. Tang.
Paul S. Nestadt, MD, an assistant professor and public mental health researcher at Johns Hopkins University, Baltimore, did not think the study would have a significant impact on clinical practice.
He noted that Dr. Healy and coauthors found that some children stayed true to type, but many fluctuated between the four profile groups. The finding that fluctuation occurred more frequently in younger children is not surprising “and is consistent with what we know about the ‘moving targets’ that make diagnosing children so difficult,” said Dr. Nestadt.
“It would have been helpful to have identified clinical indicators of likely persistence in psychopathology, but the measure employed here did not allow that. It is also frustrating to not have any information on treatment, such that we cannot know whether the children who shifted to ‘no psychopathology’ did so because of treatment or spontaneously,” he added.
Victor M. Fornari, MD, MS, director of the Division of Child & Adolescent Psychiatry at The Zucker Hillside Hospital and Cohen’s Children’s Medical Center, New York, said the study is an important contribution to understanding the development of psychopathology during childhood.
“Generally, it is felt that nearly one in five youth will meet criteria for at least one psychiatric disorder by the age of 18. It is well known that externalizing disorders like ADHD manifest earlier in childhood and that depression often manifests later in adolescence,” he said.
No disclosures were reported.
A study that tracked psychopathology in 13,000 children and adolescents found that
Investigators also found a strong correlation between new incidence of high psychopathology and externalizing problems such as hyperactivity. “It is of paramount importance to identify factors that distinguish those with persisting problems and escalating trajectories so that resources can be appropriately directed,” wrote the authors of the study published online in JAMA Network Open.
Recent studies have shown that concurrent and sequential comorbidity of psychiatric disorders are very common in adult populations, lead author Colm Healy, PhD, a postdoctoral researcher for psychiatry with the University of Medicine and Health Sciences, Ireland, said in an interview.
The speculation is that this occurs in early life when psychiatry symptoms experience high fluidity. “This presents a complex scenario to model, where young people’s mental health appears to shift and change across development. Few investigations to date have had the data available to examine these trajectories over the full range of child development,” said Dr. Healy.
He and his colleagues attempted to map the profiles and trajectories of psychopathology in children and adolescents, using latent profile transition analysis (LPTA), a person-centered method, to assess comorbidity and movement in the various phases of childhood development.
“The idea behind person-centered methods such as LTPA is that it identifies unobserved subgroups of participants who respond similarly to specific variables – in this case responses to a broad measure of psychopathology,” explained Dr. Healy.
The study included 7,507 children from the child sample (ages 3, 5, and 9 years) and 6,039 children from the adolescent sample (ages 9, 13, and 17 or 18 years). Data analysis took place from October 2020 to September 2021.
Dr. Healy and colleagues in a supplementary investigation compared cohorts at age 9 years to look for sex and generational differences.
Four developmental profiles
Researchers identified 4 distinct developmental profies for person-centered psychopathological trajectories: no psychopathology (incidence range, 60%-70%), high psychopathology (incidence range, 3%-5%), externalizing problems (incidence range, 15%-25%), and internalizing problems (incidence range, 7%-12%).
Internalizing problems reflect issues with peers and emotional problems whereas externalizing problems more closely associate with hyperactivity and conduct.
Less than 5% of the youth studied experienced persistent symptoms. However, 48.6% in the child cohort and 44.1% in the adolescent cohort moved into one of the 3 psychopathology profiles (high psychopathology, externalizing, internalizing problems) at some point in development.
The spread of trajectories was more diverse in the child cohort, said Dr. Healy. “Children ebbed and flowed between the different profiles over time with a large proportion falling into one of the psychopathology categories and then switching between these profiles.” Switching was also evident in the adolescent cohort but to a lesser extent, he said.
Externalizing problems link to high psychopathology
Rates of remittance were higher among individuals in both cohorts for internalizing problems, compared with externalizing problems.
It’s possible that for some of these young people, internalizing problems are a reaction to environmental stressors such as bullying,” said Dr. Healy. “When that stress is relieved, the internalizing problems may dissipate.”
In a clinically relevant finding, children with externalizing problems (age 5, 129 [61.3%] and age 9, 95 [74.3%]) were more likely to present with new incidents of high psychopathology. This was also true in the adolescent group (age 13, 129 [91.1%] and age 17, 146 [89.9%]).
This suggests that a proportion of youth with externalizing problems have an escalating trajectory of psychopathology. “Thus, it may be possible to distinguish those with an escalating trajectory from a stable or remitting trajectory. The specific distinguishing factors require further investigation, but it has been observed before that some of those reporting externalizing problems in early life continue to have difficulties into later life,” noted Dr. Healy.
A combination of environmental or biological factors may explain this escalation, which could respond to early intervention, he said.
Overall, few children in the study transitioned directly from no psychopathology to high psychopathology.
Differences between boys, girls
In both cohorts, investigators noticed significant differences between the sexes.
Boys in childhood made up a larger proportion of the three psychopathology profiles. But by late adolescence, girls made up a larger proportion of the internalizing profile whereas boys made up a larger proportion of the externalizing profile. “These differences were in line with our expectations,” said Dr. Healy.
Trajectories also differed among boys and girls. In childhood, girls had a higher percentage of de-escalating trajectories relative to boys. “More girls than boys in the psychopathology profiles switched to a non or less severe profile. In adolescence, differences in trajectories were less obvious, with the exception that girls were more likely than boys to transition to internalizing problems from all of the other profiles at age 17,” said Dr. Healy.
Most young people who experience psychopathology will eventually see an improvement in symptoms, noted Dr. Healy. Next steps are to identify markers that distinguish individuals with persistent trajectories from remitting trajectories at the different phases of development, he said.
Study draws mixed reviews
Clinical psychiatrists not involved in the study had varying reactions to the results.
“This study is notable for its data-driven and powerful illustration of how childhood and adolescence are dynamic periods during which psychiatric symptoms can emerge and evolve,” said Sunny X. Tang, MD, a psychiatrist and an assistant professor at the Institute of Behavioral Science and the Feinstein Institutes for Medical Research, Manhasset, New York.
The clinical call for action is for person-centered mental health screening to be a routine part of pediatric and adolescent primary care or school-based services, noted Dr. Tang.
Paul S. Nestadt, MD, an assistant professor and public mental health researcher at Johns Hopkins University, Baltimore, did not think the study would have a significant impact on clinical practice.
He noted that Dr. Healy and coauthors found that some children stayed true to type, but many fluctuated between the four profile groups. The finding that fluctuation occurred more frequently in younger children is not surprising “and is consistent with what we know about the ‘moving targets’ that make diagnosing children so difficult,” said Dr. Nestadt.
“It would have been helpful to have identified clinical indicators of likely persistence in psychopathology, but the measure employed here did not allow that. It is also frustrating to not have any information on treatment, such that we cannot know whether the children who shifted to ‘no psychopathology’ did so because of treatment or spontaneously,” he added.
Victor M. Fornari, MD, MS, director of the Division of Child & Adolescent Psychiatry at The Zucker Hillside Hospital and Cohen’s Children’s Medical Center, New York, said the study is an important contribution to understanding the development of psychopathology during childhood.
“Generally, it is felt that nearly one in five youth will meet criteria for at least one psychiatric disorder by the age of 18. It is well known that externalizing disorders like ADHD manifest earlier in childhood and that depression often manifests later in adolescence,” he said.
No disclosures were reported.
A study that tracked psychopathology in 13,000 children and adolescents found that
Investigators also found a strong correlation between new incidence of high psychopathology and externalizing problems such as hyperactivity. “It is of paramount importance to identify factors that distinguish those with persisting problems and escalating trajectories so that resources can be appropriately directed,” wrote the authors of the study published online in JAMA Network Open.
Recent studies have shown that concurrent and sequential comorbidity of psychiatric disorders are very common in adult populations, lead author Colm Healy, PhD, a postdoctoral researcher for psychiatry with the University of Medicine and Health Sciences, Ireland, said in an interview.
The speculation is that this occurs in early life when psychiatry symptoms experience high fluidity. “This presents a complex scenario to model, where young people’s mental health appears to shift and change across development. Few investigations to date have had the data available to examine these trajectories over the full range of child development,” said Dr. Healy.
He and his colleagues attempted to map the profiles and trajectories of psychopathology in children and adolescents, using latent profile transition analysis (LPTA), a person-centered method, to assess comorbidity and movement in the various phases of childhood development.
“The idea behind person-centered methods such as LTPA is that it identifies unobserved subgroups of participants who respond similarly to specific variables – in this case responses to a broad measure of psychopathology,” explained Dr. Healy.
The study included 7,507 children from the child sample (ages 3, 5, and 9 years) and 6,039 children from the adolescent sample (ages 9, 13, and 17 or 18 years). Data analysis took place from October 2020 to September 2021.
Dr. Healy and colleagues in a supplementary investigation compared cohorts at age 9 years to look for sex and generational differences.
Four developmental profiles
Researchers identified 4 distinct developmental profies for person-centered psychopathological trajectories: no psychopathology (incidence range, 60%-70%), high psychopathology (incidence range, 3%-5%), externalizing problems (incidence range, 15%-25%), and internalizing problems (incidence range, 7%-12%).
Internalizing problems reflect issues with peers and emotional problems whereas externalizing problems more closely associate with hyperactivity and conduct.
Less than 5% of the youth studied experienced persistent symptoms. However, 48.6% in the child cohort and 44.1% in the adolescent cohort moved into one of the 3 psychopathology profiles (high psychopathology, externalizing, internalizing problems) at some point in development.
The spread of trajectories was more diverse in the child cohort, said Dr. Healy. “Children ebbed and flowed between the different profiles over time with a large proportion falling into one of the psychopathology categories and then switching between these profiles.” Switching was also evident in the adolescent cohort but to a lesser extent, he said.
Externalizing problems link to high psychopathology
Rates of remittance were higher among individuals in both cohorts for internalizing problems, compared with externalizing problems.
It’s possible that for some of these young people, internalizing problems are a reaction to environmental stressors such as bullying,” said Dr. Healy. “When that stress is relieved, the internalizing problems may dissipate.”
In a clinically relevant finding, children with externalizing problems (age 5, 129 [61.3%] and age 9, 95 [74.3%]) were more likely to present with new incidents of high psychopathology. This was also true in the adolescent group (age 13, 129 [91.1%] and age 17, 146 [89.9%]).
This suggests that a proportion of youth with externalizing problems have an escalating trajectory of psychopathology. “Thus, it may be possible to distinguish those with an escalating trajectory from a stable or remitting trajectory. The specific distinguishing factors require further investigation, but it has been observed before that some of those reporting externalizing problems in early life continue to have difficulties into later life,” noted Dr. Healy.
A combination of environmental or biological factors may explain this escalation, which could respond to early intervention, he said.
Overall, few children in the study transitioned directly from no psychopathology to high psychopathology.
Differences between boys, girls
In both cohorts, investigators noticed significant differences between the sexes.
Boys in childhood made up a larger proportion of the three psychopathology profiles. But by late adolescence, girls made up a larger proportion of the internalizing profile whereas boys made up a larger proportion of the externalizing profile. “These differences were in line with our expectations,” said Dr. Healy.
Trajectories also differed among boys and girls. In childhood, girls had a higher percentage of de-escalating trajectories relative to boys. “More girls than boys in the psychopathology profiles switched to a non or less severe profile. In adolescence, differences in trajectories were less obvious, with the exception that girls were more likely than boys to transition to internalizing problems from all of the other profiles at age 17,” said Dr. Healy.
Most young people who experience psychopathology will eventually see an improvement in symptoms, noted Dr. Healy. Next steps are to identify markers that distinguish individuals with persistent trajectories from remitting trajectories at the different phases of development, he said.
Study draws mixed reviews
Clinical psychiatrists not involved in the study had varying reactions to the results.
“This study is notable for its data-driven and powerful illustration of how childhood and adolescence are dynamic periods during which psychiatric symptoms can emerge and evolve,” said Sunny X. Tang, MD, a psychiatrist and an assistant professor at the Institute of Behavioral Science and the Feinstein Institutes for Medical Research, Manhasset, New York.
The clinical call for action is for person-centered mental health screening to be a routine part of pediatric and adolescent primary care or school-based services, noted Dr. Tang.
Paul S. Nestadt, MD, an assistant professor and public mental health researcher at Johns Hopkins University, Baltimore, did not think the study would have a significant impact on clinical practice.
He noted that Dr. Healy and coauthors found that some children stayed true to type, but many fluctuated between the four profile groups. The finding that fluctuation occurred more frequently in younger children is not surprising “and is consistent with what we know about the ‘moving targets’ that make diagnosing children so difficult,” said Dr. Nestadt.
“It would have been helpful to have identified clinical indicators of likely persistence in psychopathology, but the measure employed here did not allow that. It is also frustrating to not have any information on treatment, such that we cannot know whether the children who shifted to ‘no psychopathology’ did so because of treatment or spontaneously,” he added.
Victor M. Fornari, MD, MS, director of the Division of Child & Adolescent Psychiatry at The Zucker Hillside Hospital and Cohen’s Children’s Medical Center, New York, said the study is an important contribution to understanding the development of psychopathology during childhood.
“Generally, it is felt that nearly one in five youth will meet criteria for at least one psychiatric disorder by the age of 18. It is well known that externalizing disorders like ADHD manifest earlier in childhood and that depression often manifests later in adolescence,” he said.
No disclosures were reported.
FROM JAMA NETWORK OPEN








