User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Neuropsychiatric risks of COVID-19: New data
The neuropsychiatric ramifications of severe COVID-19 infection appear to be no different than for other severe acute respiratory infections (SARI).
This suggests that disease severity, rather than pathogen, is the most relevant factor in new-onset neuropsychiatric illness, the investigators note.
The risk of new-onset neuropsychological illness after severe COVID-19 infection are “substantial, but similar to those after other severe respiratory infections,” study investigator Peter Watkinson, MD, Nuffield Department of Clinical Neurosciences, University of Oxford, and John Radcliffe Hospital, Oxford, England, told this news organization.
The study was published online in JAMA Psychiatry.
Significant mental health burden
Research has shown a significant burden of neuropsychological illness after severe COVID-19 infection. However, it’s unclear how this risk compares to SARI.
To investigate, Dr. Watkinson and colleagues evaluated electronic health record data on more than 8.3 million adults, including 16,679 (0.02%) who survived a hospital admission for SARI and 32,525 (0.03%) who survived a hospital stay for COVID-19.
Compared with the remaining population, risks of new anxiety disorder, dementia, psychotic disorder, depression, and bipolar disorder diagnoses were significantly and similarly increased in adults surviving hospitalization for either COVID-19 or SARI.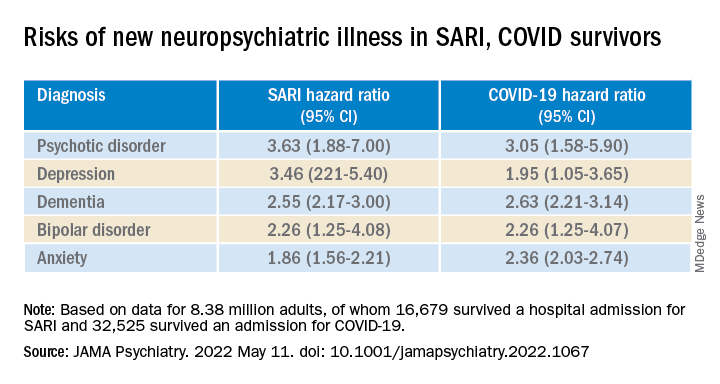
Compared with the wider population, survivors of severe SARI or COVID-19 were also at increased risk of starting treatment with antidepressants, hypnotics/anxiolytics, or antipsychotics.
When comparing survivors of SARI hospitalization to survivors of COVID-19 hospitalization, no significant differences were observed in the postdischarge rates of new-onset anxiety disorder, dementia, depression, or bipolar affective disorder.
The SARI and COVID groups also did not differ in terms of their postdischarge risks of antidepressant or hypnotic/anxiolytic use, but the COVID survivors had a 20% lower risk of starting an antipsychotic.
“In this cohort study, SARI were found to be associated with significant postacute neuropsychiatric morbidity, for which COVID-19 is not distinctly different,” Dr. Watkinson and colleagues write.
“These results may help refine our understanding of the post–severe COVID-19 phenotype and may inform post-discharge support for patients requiring hospital-based and intensive care for SARI regardless of causative pathogen,” they write.
Caveats, cautionary notes
Kevin McConway, PhD, emeritus professor of applied statistics at the Open University in Milton Keynes, England, described the study as “impressive.” However, he pointed out that the study’s observational design is a limitation.
“One can never be absolutely certain about the interpretation of findings of an observational study. What the research can’t tell us is what caused the increased psychiatric risks for people hospitalized with COVID-19 or some other serious respiratory disease,” Dr. McConway said.
“It can’t tell us what might happen in the future, when, we all hope, many fewer are being hospitalized with COVID-19 than was the case in those first two waves, and the current backlog of provision of some health services has decreased,” he added.
“So we can’t just say that, in general, serious COVID-19 has much the same neuropsychiatric consequences as other very serious respiratory illness. Maybe it does, maybe it doesn’t,” Dr. McConway cautioned.
Max Taquet, PhD, with the University of Oxford, noted that the study is limited to hospitalized adult patients, leaving open the question of risk in nonhospitalized individuals – which is the overwhelming majority of patients with COVID-19 – or in children.
Whether the neuropsychiatric risks have remained the same since the emergence of the Omicron variant also remains “an open question since all patients in this study were diagnosed before July 2021,” Dr. Taquet said in statement.
The study was funded by the Wellcome Trust, the John Fell Oxford University Press Research Fund, the Oxford Wellcome Institutional Strategic Support Fund and Cancer Research UK, through the Cancer Research UK Oxford Centre. Dr. Watkinson disclosed grants from the National Institute for Health Research and Sensyne Health outside the submitted work; and serving as chief medical officer for Sensyne Health prior to this work, as well as holding shares in the company. Dr. McConway is a trustee of the UK Science Media Centre and a member of its advisory committee. His comments were provided in his capacity as an independent professional statistician. Dr. Taquet has worked on similar studies trying to identify, quantify, and specify the neurological and psychiatric consequences of COVID-19.
A version of this article first appeared on Medscape.com.
The neuropsychiatric ramifications of severe COVID-19 infection appear to be no different than for other severe acute respiratory infections (SARI).
This suggests that disease severity, rather than pathogen, is the most relevant factor in new-onset neuropsychiatric illness, the investigators note.
The risk of new-onset neuropsychological illness after severe COVID-19 infection are “substantial, but similar to those after other severe respiratory infections,” study investigator Peter Watkinson, MD, Nuffield Department of Clinical Neurosciences, University of Oxford, and John Radcliffe Hospital, Oxford, England, told this news organization.
The study was published online in JAMA Psychiatry.
Significant mental health burden
Research has shown a significant burden of neuropsychological illness after severe COVID-19 infection. However, it’s unclear how this risk compares to SARI.
To investigate, Dr. Watkinson and colleagues evaluated electronic health record data on more than 8.3 million adults, including 16,679 (0.02%) who survived a hospital admission for SARI and 32,525 (0.03%) who survived a hospital stay for COVID-19.
Compared with the remaining population, risks of new anxiety disorder, dementia, psychotic disorder, depression, and bipolar disorder diagnoses were significantly and similarly increased in adults surviving hospitalization for either COVID-19 or SARI.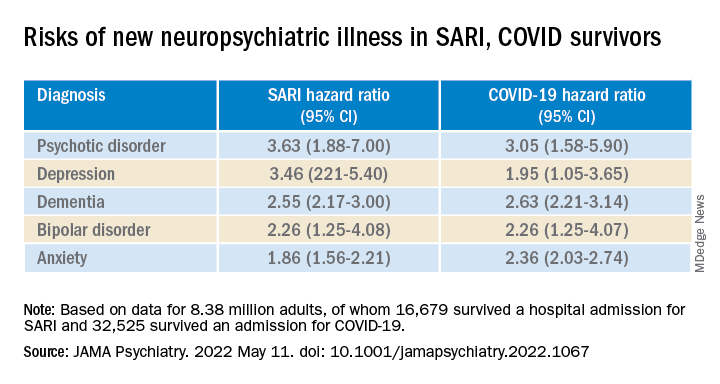
Compared with the wider population, survivors of severe SARI or COVID-19 were also at increased risk of starting treatment with antidepressants, hypnotics/anxiolytics, or antipsychotics.
When comparing survivors of SARI hospitalization to survivors of COVID-19 hospitalization, no significant differences were observed in the postdischarge rates of new-onset anxiety disorder, dementia, depression, or bipolar affective disorder.
The SARI and COVID groups also did not differ in terms of their postdischarge risks of antidepressant or hypnotic/anxiolytic use, but the COVID survivors had a 20% lower risk of starting an antipsychotic.
“In this cohort study, SARI were found to be associated with significant postacute neuropsychiatric morbidity, for which COVID-19 is not distinctly different,” Dr. Watkinson and colleagues write.
“These results may help refine our understanding of the post–severe COVID-19 phenotype and may inform post-discharge support for patients requiring hospital-based and intensive care for SARI regardless of causative pathogen,” they write.
Caveats, cautionary notes
Kevin McConway, PhD, emeritus professor of applied statistics at the Open University in Milton Keynes, England, described the study as “impressive.” However, he pointed out that the study’s observational design is a limitation.
“One can never be absolutely certain about the interpretation of findings of an observational study. What the research can’t tell us is what caused the increased psychiatric risks for people hospitalized with COVID-19 or some other serious respiratory disease,” Dr. McConway said.
“It can’t tell us what might happen in the future, when, we all hope, many fewer are being hospitalized with COVID-19 than was the case in those first two waves, and the current backlog of provision of some health services has decreased,” he added.
“So we can’t just say that, in general, serious COVID-19 has much the same neuropsychiatric consequences as other very serious respiratory illness. Maybe it does, maybe it doesn’t,” Dr. McConway cautioned.
Max Taquet, PhD, with the University of Oxford, noted that the study is limited to hospitalized adult patients, leaving open the question of risk in nonhospitalized individuals – which is the overwhelming majority of patients with COVID-19 – or in children.
Whether the neuropsychiatric risks have remained the same since the emergence of the Omicron variant also remains “an open question since all patients in this study were diagnosed before July 2021,” Dr. Taquet said in statement.
The study was funded by the Wellcome Trust, the John Fell Oxford University Press Research Fund, the Oxford Wellcome Institutional Strategic Support Fund and Cancer Research UK, through the Cancer Research UK Oxford Centre. Dr. Watkinson disclosed grants from the National Institute for Health Research and Sensyne Health outside the submitted work; and serving as chief medical officer for Sensyne Health prior to this work, as well as holding shares in the company. Dr. McConway is a trustee of the UK Science Media Centre and a member of its advisory committee. His comments were provided in his capacity as an independent professional statistician. Dr. Taquet has worked on similar studies trying to identify, quantify, and specify the neurological and psychiatric consequences of COVID-19.
A version of this article first appeared on Medscape.com.
The neuropsychiatric ramifications of severe COVID-19 infection appear to be no different than for other severe acute respiratory infections (SARI).
This suggests that disease severity, rather than pathogen, is the most relevant factor in new-onset neuropsychiatric illness, the investigators note.
The risk of new-onset neuropsychological illness after severe COVID-19 infection are “substantial, but similar to those after other severe respiratory infections,” study investigator Peter Watkinson, MD, Nuffield Department of Clinical Neurosciences, University of Oxford, and John Radcliffe Hospital, Oxford, England, told this news organization.
The study was published online in JAMA Psychiatry.
Significant mental health burden
Research has shown a significant burden of neuropsychological illness after severe COVID-19 infection. However, it’s unclear how this risk compares to SARI.
To investigate, Dr. Watkinson and colleagues evaluated electronic health record data on more than 8.3 million adults, including 16,679 (0.02%) who survived a hospital admission for SARI and 32,525 (0.03%) who survived a hospital stay for COVID-19.
Compared with the remaining population, risks of new anxiety disorder, dementia, psychotic disorder, depression, and bipolar disorder diagnoses were significantly and similarly increased in adults surviving hospitalization for either COVID-19 or SARI.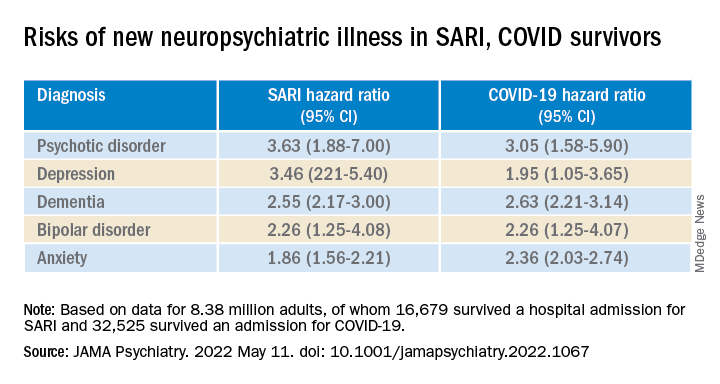
Compared with the wider population, survivors of severe SARI or COVID-19 were also at increased risk of starting treatment with antidepressants, hypnotics/anxiolytics, or antipsychotics.
When comparing survivors of SARI hospitalization to survivors of COVID-19 hospitalization, no significant differences were observed in the postdischarge rates of new-onset anxiety disorder, dementia, depression, or bipolar affective disorder.
The SARI and COVID groups also did not differ in terms of their postdischarge risks of antidepressant or hypnotic/anxiolytic use, but the COVID survivors had a 20% lower risk of starting an antipsychotic.
“In this cohort study, SARI were found to be associated with significant postacute neuropsychiatric morbidity, for which COVID-19 is not distinctly different,” Dr. Watkinson and colleagues write.
“These results may help refine our understanding of the post–severe COVID-19 phenotype and may inform post-discharge support for patients requiring hospital-based and intensive care for SARI regardless of causative pathogen,” they write.
Caveats, cautionary notes
Kevin McConway, PhD, emeritus professor of applied statistics at the Open University in Milton Keynes, England, described the study as “impressive.” However, he pointed out that the study’s observational design is a limitation.
“One can never be absolutely certain about the interpretation of findings of an observational study. What the research can’t tell us is what caused the increased psychiatric risks for people hospitalized with COVID-19 or some other serious respiratory disease,” Dr. McConway said.
“It can’t tell us what might happen in the future, when, we all hope, many fewer are being hospitalized with COVID-19 than was the case in those first two waves, and the current backlog of provision of some health services has decreased,” he added.
“So we can’t just say that, in general, serious COVID-19 has much the same neuropsychiatric consequences as other very serious respiratory illness. Maybe it does, maybe it doesn’t,” Dr. McConway cautioned.
Max Taquet, PhD, with the University of Oxford, noted that the study is limited to hospitalized adult patients, leaving open the question of risk in nonhospitalized individuals – which is the overwhelming majority of patients with COVID-19 – or in children.
Whether the neuropsychiatric risks have remained the same since the emergence of the Omicron variant also remains “an open question since all patients in this study were diagnosed before July 2021,” Dr. Taquet said in statement.
The study was funded by the Wellcome Trust, the John Fell Oxford University Press Research Fund, the Oxford Wellcome Institutional Strategic Support Fund and Cancer Research UK, through the Cancer Research UK Oxford Centre. Dr. Watkinson disclosed grants from the National Institute for Health Research and Sensyne Health outside the submitted work; and serving as chief medical officer for Sensyne Health prior to this work, as well as holding shares in the company. Dr. McConway is a trustee of the UK Science Media Centre and a member of its advisory committee. His comments were provided in his capacity as an independent professional statistician. Dr. Taquet has worked on similar studies trying to identify, quantify, and specify the neurological and psychiatric consequences of COVID-19.
A version of this article first appeared on Medscape.com.
Clozapine and cancer risk in schizophrenia patients: New data
Long-term treatment with clozapine is associated with a small but significant risk of hematological malignancies in individuals with schizophrenia, new research shows.
The study was published online in The Lancet Psychiatry.
An unresolved issue
Clozapine is more effective than other antipsychotics for managing symptoms and suicidal behavior in schizophrenia, with the lowest mortality, compared with other antipsychotics, but its use is restricted in many countries, the researchers note.
Reports of nine deaths associated with clozapine use – eight due to agranulocytosis and one due to leukemia – in southwestern Finland in 1975 resulted in worldwide withdrawal of the drug. In 1990, clozapine was relaunched with stipulations for strict blood count control. The cumulative incidence of clozapine-induced agranulocytosis or severe neutropenia is estimated at about 0.9%.
Several small studies from Australia, Denmark, and the United States, and a large pharmacovigilance study, suggest that clozapine treatment might be associated with an increased risk of hematological malignancies.
“Previous studies have suggested a possible risk of hematological malignancies associated with clozapine, but due to methodological issues, the question had remained unsettled,” said Dr. Tiihonen.
Finland has among the highest rates of clozapine use in the world, where 20% of schizophrenia cases are treated with the drug. In most other countries, clozapine use is less than half of that, in Finland largely because of agranulocytosis concerns.
To examine the risk of hematological malignancies associated with long-term use of clozapine and other antipsychotics, the investigators conducted a large prospective case-control and cohort study that used data from Finnish national registers and included all patients with schizophrenia.
“Unlike previous studies, we employed prospectively gathered data from a nationwide cohort [including all patients with schizophrenia], had a long follow-up time, and studied the dose-response of the risk of hematological malignancies,” Dr. Tiihonen noted.
The nested case-control study was constructed by individually matching cases of lymphoid and hematopoietic tissue malignancy and pairing them with up to 10 matched controls with schizophrenia but without cancer.
Inclusion criteria were restricted to malignancies diagnosed on a histological basis. Individuals outside the ages of 18-85 years were excluded, as were those with a previous malignancy. Analyses were done using conditional logistic regression adjusted for comorbid conditions.
Patient education, vigilant monitoring
The case-control analysis was based on 516 patients with a first-time diagnosis of lymphoid and hematopoietic tissue malignancy from 2000-2017 and diagnosed after first diagnosis of schizophrenia.
Of these, 102 patients were excluded because of a diagnosis with no histological basis, five were excluded because of age, and 34 for a previous malignancy, resulting in 375 patients with malignancies matched with 10 controls for a total of 3,743 study participants.
Of the 375 patients with hematological malignancies (305 had lymphoma, 42 leukemia, 22 myeloma, six unspecified) in 2000-2017, 208 (55%) were men and 167 (45%) were women. Ethnicity data were not available.
Compared with non-use of clozapine, clozapine use was associated with increased odds of hematological malignancies in a dose-response manner (adjusted odds ratio, 3.35; 95% confidence interval, 2.22-5.05] for ≥ 5,000 defined daily dose cumulative exposure (P < .0001).
Exposure to other antipsychotic medications was not associated with increased odds of hematological malignancies. A complementary analysis showed that the clozapine-related risk increase was specific to hematological malignancies only.
Over 17 years follow-up of the base cohort, 37 deaths occurred due to hematological malignancy among patients exposed to clozapine in 26 patients with ongoing use at the time they were diagnosed with malignancy and in 11 patients who did not use clozapine at the exact time of their cancer diagnosis. Only three deaths occurred due to agranulocytosis, the investigators report.
The use of a nationwide registry for the study makes it “unlikely” that there were any undiagnosed/unreported malignancies, the researchers note. This, plus the “robust dose-response finding, and additional analysis showing no substantial difference in odds of other cancers between users of clozapine versus other antipsychotics suggest the association is causal, and not attributable to surveillance bias,” they write.
These findings, the investigators note, suggest patients taking clozapine and their caregivers need to be educated about the signs of hematological malignancies. Furthermore, they call for mental health providers to be “vigilant” in monitoring for potential signs and symptoms of hematological malignancy in patients taking the drug.
A ‘vital’ medication
Commenting on the findings, Stephen Marder, MD, professor of psychiatry and biobehavioral sciences and vice chair of the department of psychiatry at UCLA, noted the link between clozapine and agranulocytosis.
“Clozapine has been previously associated with agranulocytosis. Over the years that seemed to be the main concern of clinicians. The monitoring system for agranulocytosis has been a burden on the system and for patients, but not really a significant cause for concern with the safety of the drug,” said Dr. Marder, who is also director of the VISN 22 Mental Illness Research, Education and Clinical Center for the Department of Veterans Affairs and director of the section on psychosis at the UCLA Neuropsychiatric Institute.
In fact, he noted recent research, including studies from this group that used large databases from Finland, which showed that clozapine was actually associated with a lower mortality risk than other antipsychotics.
The fact that the study showed prolonged use of clozapine at high doses was associated with a “very small” risk of hematological abnormalities does not undermine its standing as “the most effective antipsychotic [that is] associated with a lower risk of death,” said Dr. Marder.
“On the other hand,” he added, “it does suggest that clinicians should tell patients about it and, when they review the blood monitoring, they look at things beyond the neutrophil count” that may suggest malignancy.
“Clozapine has a vital role as the most effective antipsychotic drug and the only drug that has an indication for treatment-resistant schizophrenia and schizophrenia associated with suicidality,” said Dr. Marder.
The study was funded by the Finnish Ministry of Social Affairs and Health through the developmental fund for Niuvanniemi Hospital and by the Academy of Finland. Dr. Tiihonen and Dr. Marder have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Long-term treatment with clozapine is associated with a small but significant risk of hematological malignancies in individuals with schizophrenia, new research shows.
The study was published online in The Lancet Psychiatry.
An unresolved issue
Clozapine is more effective than other antipsychotics for managing symptoms and suicidal behavior in schizophrenia, with the lowest mortality, compared with other antipsychotics, but its use is restricted in many countries, the researchers note.
Reports of nine deaths associated with clozapine use – eight due to agranulocytosis and one due to leukemia – in southwestern Finland in 1975 resulted in worldwide withdrawal of the drug. In 1990, clozapine was relaunched with stipulations for strict blood count control. The cumulative incidence of clozapine-induced agranulocytosis or severe neutropenia is estimated at about 0.9%.
Several small studies from Australia, Denmark, and the United States, and a large pharmacovigilance study, suggest that clozapine treatment might be associated with an increased risk of hematological malignancies.
“Previous studies have suggested a possible risk of hematological malignancies associated with clozapine, but due to methodological issues, the question had remained unsettled,” said Dr. Tiihonen.
Finland has among the highest rates of clozapine use in the world, where 20% of schizophrenia cases are treated with the drug. In most other countries, clozapine use is less than half of that, in Finland largely because of agranulocytosis concerns.
To examine the risk of hematological malignancies associated with long-term use of clozapine and other antipsychotics, the investigators conducted a large prospective case-control and cohort study that used data from Finnish national registers and included all patients with schizophrenia.
“Unlike previous studies, we employed prospectively gathered data from a nationwide cohort [including all patients with schizophrenia], had a long follow-up time, and studied the dose-response of the risk of hematological malignancies,” Dr. Tiihonen noted.
The nested case-control study was constructed by individually matching cases of lymphoid and hematopoietic tissue malignancy and pairing them with up to 10 matched controls with schizophrenia but without cancer.
Inclusion criteria were restricted to malignancies diagnosed on a histological basis. Individuals outside the ages of 18-85 years were excluded, as were those with a previous malignancy. Analyses were done using conditional logistic regression adjusted for comorbid conditions.
Patient education, vigilant monitoring
The case-control analysis was based on 516 patients with a first-time diagnosis of lymphoid and hematopoietic tissue malignancy from 2000-2017 and diagnosed after first diagnosis of schizophrenia.
Of these, 102 patients were excluded because of a diagnosis with no histological basis, five were excluded because of age, and 34 for a previous malignancy, resulting in 375 patients with malignancies matched with 10 controls for a total of 3,743 study participants.
Of the 375 patients with hematological malignancies (305 had lymphoma, 42 leukemia, 22 myeloma, six unspecified) in 2000-2017, 208 (55%) were men and 167 (45%) were women. Ethnicity data were not available.
Compared with non-use of clozapine, clozapine use was associated with increased odds of hematological malignancies in a dose-response manner (adjusted odds ratio, 3.35; 95% confidence interval, 2.22-5.05] for ≥ 5,000 defined daily dose cumulative exposure (P < .0001).
Exposure to other antipsychotic medications was not associated with increased odds of hematological malignancies. A complementary analysis showed that the clozapine-related risk increase was specific to hematological malignancies only.
Over 17 years follow-up of the base cohort, 37 deaths occurred due to hematological malignancy among patients exposed to clozapine in 26 patients with ongoing use at the time they were diagnosed with malignancy and in 11 patients who did not use clozapine at the exact time of their cancer diagnosis. Only three deaths occurred due to agranulocytosis, the investigators report.
The use of a nationwide registry for the study makes it “unlikely” that there were any undiagnosed/unreported malignancies, the researchers note. This, plus the “robust dose-response finding, and additional analysis showing no substantial difference in odds of other cancers between users of clozapine versus other antipsychotics suggest the association is causal, and not attributable to surveillance bias,” they write.
These findings, the investigators note, suggest patients taking clozapine and their caregivers need to be educated about the signs of hematological malignancies. Furthermore, they call for mental health providers to be “vigilant” in monitoring for potential signs and symptoms of hematological malignancy in patients taking the drug.
A ‘vital’ medication
Commenting on the findings, Stephen Marder, MD, professor of psychiatry and biobehavioral sciences and vice chair of the department of psychiatry at UCLA, noted the link between clozapine and agranulocytosis.
“Clozapine has been previously associated with agranulocytosis. Over the years that seemed to be the main concern of clinicians. The monitoring system for agranulocytosis has been a burden on the system and for patients, but not really a significant cause for concern with the safety of the drug,” said Dr. Marder, who is also director of the VISN 22 Mental Illness Research, Education and Clinical Center for the Department of Veterans Affairs and director of the section on psychosis at the UCLA Neuropsychiatric Institute.
In fact, he noted recent research, including studies from this group that used large databases from Finland, which showed that clozapine was actually associated with a lower mortality risk than other antipsychotics.
The fact that the study showed prolonged use of clozapine at high doses was associated with a “very small” risk of hematological abnormalities does not undermine its standing as “the most effective antipsychotic [that is] associated with a lower risk of death,” said Dr. Marder.
“On the other hand,” he added, “it does suggest that clinicians should tell patients about it and, when they review the blood monitoring, they look at things beyond the neutrophil count” that may suggest malignancy.
“Clozapine has a vital role as the most effective antipsychotic drug and the only drug that has an indication for treatment-resistant schizophrenia and schizophrenia associated with suicidality,” said Dr. Marder.
The study was funded by the Finnish Ministry of Social Affairs and Health through the developmental fund for Niuvanniemi Hospital and by the Academy of Finland. Dr. Tiihonen and Dr. Marder have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Long-term treatment with clozapine is associated with a small but significant risk of hematological malignancies in individuals with schizophrenia, new research shows.
The study was published online in The Lancet Psychiatry.
An unresolved issue
Clozapine is more effective than other antipsychotics for managing symptoms and suicidal behavior in schizophrenia, with the lowest mortality, compared with other antipsychotics, but its use is restricted in many countries, the researchers note.
Reports of nine deaths associated with clozapine use – eight due to agranulocytosis and one due to leukemia – in southwestern Finland in 1975 resulted in worldwide withdrawal of the drug. In 1990, clozapine was relaunched with stipulations for strict blood count control. The cumulative incidence of clozapine-induced agranulocytosis or severe neutropenia is estimated at about 0.9%.
Several small studies from Australia, Denmark, and the United States, and a large pharmacovigilance study, suggest that clozapine treatment might be associated with an increased risk of hematological malignancies.
“Previous studies have suggested a possible risk of hematological malignancies associated with clozapine, but due to methodological issues, the question had remained unsettled,” said Dr. Tiihonen.
Finland has among the highest rates of clozapine use in the world, where 20% of schizophrenia cases are treated with the drug. In most other countries, clozapine use is less than half of that, in Finland largely because of agranulocytosis concerns.
To examine the risk of hematological malignancies associated with long-term use of clozapine and other antipsychotics, the investigators conducted a large prospective case-control and cohort study that used data from Finnish national registers and included all patients with schizophrenia.
“Unlike previous studies, we employed prospectively gathered data from a nationwide cohort [including all patients with schizophrenia], had a long follow-up time, and studied the dose-response of the risk of hematological malignancies,” Dr. Tiihonen noted.
The nested case-control study was constructed by individually matching cases of lymphoid and hematopoietic tissue malignancy and pairing them with up to 10 matched controls with schizophrenia but without cancer.
Inclusion criteria were restricted to malignancies diagnosed on a histological basis. Individuals outside the ages of 18-85 years were excluded, as were those with a previous malignancy. Analyses were done using conditional logistic regression adjusted for comorbid conditions.
Patient education, vigilant monitoring
The case-control analysis was based on 516 patients with a first-time diagnosis of lymphoid and hematopoietic tissue malignancy from 2000-2017 and diagnosed after first diagnosis of schizophrenia.
Of these, 102 patients were excluded because of a diagnosis with no histological basis, five were excluded because of age, and 34 for a previous malignancy, resulting in 375 patients with malignancies matched with 10 controls for a total of 3,743 study participants.
Of the 375 patients with hematological malignancies (305 had lymphoma, 42 leukemia, 22 myeloma, six unspecified) in 2000-2017, 208 (55%) were men and 167 (45%) were women. Ethnicity data were not available.
Compared with non-use of clozapine, clozapine use was associated with increased odds of hematological malignancies in a dose-response manner (adjusted odds ratio, 3.35; 95% confidence interval, 2.22-5.05] for ≥ 5,000 defined daily dose cumulative exposure (P < .0001).
Exposure to other antipsychotic medications was not associated with increased odds of hematological malignancies. A complementary analysis showed that the clozapine-related risk increase was specific to hematological malignancies only.
Over 17 years follow-up of the base cohort, 37 deaths occurred due to hematological malignancy among patients exposed to clozapine in 26 patients with ongoing use at the time they were diagnosed with malignancy and in 11 patients who did not use clozapine at the exact time of their cancer diagnosis. Only three deaths occurred due to agranulocytosis, the investigators report.
The use of a nationwide registry for the study makes it “unlikely” that there were any undiagnosed/unreported malignancies, the researchers note. This, plus the “robust dose-response finding, and additional analysis showing no substantial difference in odds of other cancers between users of clozapine versus other antipsychotics suggest the association is causal, and not attributable to surveillance bias,” they write.
These findings, the investigators note, suggest patients taking clozapine and their caregivers need to be educated about the signs of hematological malignancies. Furthermore, they call for mental health providers to be “vigilant” in monitoring for potential signs and symptoms of hematological malignancy in patients taking the drug.
A ‘vital’ medication
Commenting on the findings, Stephen Marder, MD, professor of psychiatry and biobehavioral sciences and vice chair of the department of psychiatry at UCLA, noted the link between clozapine and agranulocytosis.
“Clozapine has been previously associated with agranulocytosis. Over the years that seemed to be the main concern of clinicians. The monitoring system for agranulocytosis has been a burden on the system and for patients, but not really a significant cause for concern with the safety of the drug,” said Dr. Marder, who is also director of the VISN 22 Mental Illness Research, Education and Clinical Center for the Department of Veterans Affairs and director of the section on psychosis at the UCLA Neuropsychiatric Institute.
In fact, he noted recent research, including studies from this group that used large databases from Finland, which showed that clozapine was actually associated with a lower mortality risk than other antipsychotics.
The fact that the study showed prolonged use of clozapine at high doses was associated with a “very small” risk of hematological abnormalities does not undermine its standing as “the most effective antipsychotic [that is] associated with a lower risk of death,” said Dr. Marder.
“On the other hand,” he added, “it does suggest that clinicians should tell patients about it and, when they review the blood monitoring, they look at things beyond the neutrophil count” that may suggest malignancy.
“Clozapine has a vital role as the most effective antipsychotic drug and the only drug that has an indication for treatment-resistant schizophrenia and schizophrenia associated with suicidality,” said Dr. Marder.
The study was funded by the Finnish Ministry of Social Affairs and Health through the developmental fund for Niuvanniemi Hospital and by the Academy of Finland. Dr. Tiihonen and Dr. Marder have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE LANCET PSYCHIATRY
New data support electroconvulsive therapy for severe depression
Advocates and users of electroconvulsive therapy (ECT) have received further scientific backing:
The patient cohort comprised 27,231 men and 40,096 women who had been treated as inpatients. The average age was 45.1 years (range: 18-103 years), and 4,982 patients received ECT. The primary endpoint was death by suicide within 365 days of hospital discharge. The secondary endpoints were death not by suicide and total mortality. The cause-specific hazard ratio (csHR) was calculated for patients with ECT, compared with patients without ECT.
In the propensity score-weighted analysis, ECT was linked to a significantly reduced suicide risk (csHR: 0.53; 95% confidence interval, 0.31-0.92). According to the calculations, ECT was associated with a significantly decreased total mortality risk (hazard ratio, 0.75; 95% CI, 0.58-0.97). However, this was not the case for death from causes other than suicide.
The authors, led by Tyler S. Kaster, PhD, a psychiatrist at Temerty Centre for Therapeutic Brain Intervention, Centre for Addiction and Mental Health, Toronto, concluded that this study underlines the importance of ECT, in particular for people with severe depression.
A well-tested therapy
ECT has been used for decades as a substantial tool for the treatment of patients with severe mental illnesses. Over the past 15 years, new methods for the treatment of severely depressed patients have been tested, such as vagus nerve stimulation, transcranial magnetic stimulation, and intranasal administration of esketamine. However, in a recent review paper in the New England Journal of Medicine, American psychiatrists Randall T. Espinoza, MD, MPH, University of California, Los Angeles, and Charles H. Kellner, MD, University of South Carolina, Charleston, reported that none of these therapies had proven to be an indisputable substitute for ECT for people with severe depression.
Significant clinical benefits
According to these American psychiatrists, the benefit of ECT has been proven many times, and several studies demonstrate the effect on the risk for suicide. Moreover, quality of life is improved, and the rate of new hospital admissions is lowered. ECT can rapidly improve depressive, psychotic, and catatonic symptoms and reduce suicidal urges for certain patient groups.
Studies on ECT involving patients with treatment-refractory depression have shown response rates of 60%-80% and pooled remission rates of 50%-60%. High response rates for ECT have even been reported for patients with psychotic depression or catatonia. In one study that recruited patients with treatment-refractory schizophrenia, the ECT efficacy rates were between 40% and 70%. In some Asian countries, schizophrenia is the main indication for ECT.
Good safety profile
Overall, the psychiatrists consider ECT to be a safe and tolerable therapy. The estimated death rate is around 2.1 deaths per 100,000 treatments. The most common complications are acute cardiopulmonary events, which are estimated to occur in less than 1% of treatments. Rare serious adverse events linked to ECT are arrhythmias, shortness of breath, aspiration, and prolonged seizures. The common but mild side effects are headaches, jaw pain, myalgia, nausea, and vomiting after the procedure, as well as fatigue.
Concerns regarding cognitive impairment still represent an obstacle for the use of ECT. However, in today’s practice, ECT leads to fewer cognitive side effects than previous treatments. The authors stated that it is not possible to predict how an individual patient will be affected, but most patients have only mild or moderate cognitive side effects that generally abate days to weeks after an ECT course has ended.
However, retrograde amnesia linked to ECT can last over a year. In rare cases, acute confusion or delirium can develop that requires interruption or discontinuation of treatment. No indications of structural brain damage after ECT have been detected in neuropathological testing. A Danish cohort study involving 168,015 patients with depression, of whom 3.1% had at least one ECT treatment, did not find a link between ECT with a mean period of almost 5 years and increased onset of dementia.
Bad reputation
Dr. Espinoza and Dr. Kellner criticized the fact that, despite its proven efficacy and safety, ECT is used too little. This judgment is nothing new. Psychiatrists have been complaining for years that this procedure is used too little, including Eric Slade, MD, from the University of Baltimore, in 2017 and German professors Andreas Fallgatter, MD, and Urban Wiesing, MD, PhD, in 2018. Dr. Wiesing and Dr. Fallgatter attribute the low level of use to the fact that ECT is labor-intensive, compared with pharmacotherapy.
Another reason is clearly the bad reputation of this method. However, ECT’s poor image, which has only increased over time, is not a convincing argument to forego today’s ECT as a treatment for patients with severe mental illnesses. According to Dr. Fallgatter and Dr. Wiesing, even the risk of misuse of this method is “not a sufficient argument for categorical refusal, rather for caution at best.” They argued that otherwise, “modern medicine would have to renounce many more therapies.”
This article was translated from Univadis Germany.
Advocates and users of electroconvulsive therapy (ECT) have received further scientific backing:
The patient cohort comprised 27,231 men and 40,096 women who had been treated as inpatients. The average age was 45.1 years (range: 18-103 years), and 4,982 patients received ECT. The primary endpoint was death by suicide within 365 days of hospital discharge. The secondary endpoints were death not by suicide and total mortality. The cause-specific hazard ratio (csHR) was calculated for patients with ECT, compared with patients without ECT.
In the propensity score-weighted analysis, ECT was linked to a significantly reduced suicide risk (csHR: 0.53; 95% confidence interval, 0.31-0.92). According to the calculations, ECT was associated with a significantly decreased total mortality risk (hazard ratio, 0.75; 95% CI, 0.58-0.97). However, this was not the case for death from causes other than suicide.
The authors, led by Tyler S. Kaster, PhD, a psychiatrist at Temerty Centre for Therapeutic Brain Intervention, Centre for Addiction and Mental Health, Toronto, concluded that this study underlines the importance of ECT, in particular for people with severe depression.
A well-tested therapy
ECT has been used for decades as a substantial tool for the treatment of patients with severe mental illnesses. Over the past 15 years, new methods for the treatment of severely depressed patients have been tested, such as vagus nerve stimulation, transcranial magnetic stimulation, and intranasal administration of esketamine. However, in a recent review paper in the New England Journal of Medicine, American psychiatrists Randall T. Espinoza, MD, MPH, University of California, Los Angeles, and Charles H. Kellner, MD, University of South Carolina, Charleston, reported that none of these therapies had proven to be an indisputable substitute for ECT for people with severe depression.
Significant clinical benefits
According to these American psychiatrists, the benefit of ECT has been proven many times, and several studies demonstrate the effect on the risk for suicide. Moreover, quality of life is improved, and the rate of new hospital admissions is lowered. ECT can rapidly improve depressive, psychotic, and catatonic symptoms and reduce suicidal urges for certain patient groups.
Studies on ECT involving patients with treatment-refractory depression have shown response rates of 60%-80% and pooled remission rates of 50%-60%. High response rates for ECT have even been reported for patients with psychotic depression or catatonia. In one study that recruited patients with treatment-refractory schizophrenia, the ECT efficacy rates were between 40% and 70%. In some Asian countries, schizophrenia is the main indication for ECT.
Good safety profile
Overall, the psychiatrists consider ECT to be a safe and tolerable therapy. The estimated death rate is around 2.1 deaths per 100,000 treatments. The most common complications are acute cardiopulmonary events, which are estimated to occur in less than 1% of treatments. Rare serious adverse events linked to ECT are arrhythmias, shortness of breath, aspiration, and prolonged seizures. The common but mild side effects are headaches, jaw pain, myalgia, nausea, and vomiting after the procedure, as well as fatigue.
Concerns regarding cognitive impairment still represent an obstacle for the use of ECT. However, in today’s practice, ECT leads to fewer cognitive side effects than previous treatments. The authors stated that it is not possible to predict how an individual patient will be affected, but most patients have only mild or moderate cognitive side effects that generally abate days to weeks after an ECT course has ended.
However, retrograde amnesia linked to ECT can last over a year. In rare cases, acute confusion or delirium can develop that requires interruption or discontinuation of treatment. No indications of structural brain damage after ECT have been detected in neuropathological testing. A Danish cohort study involving 168,015 patients with depression, of whom 3.1% had at least one ECT treatment, did not find a link between ECT with a mean period of almost 5 years and increased onset of dementia.
Bad reputation
Dr. Espinoza and Dr. Kellner criticized the fact that, despite its proven efficacy and safety, ECT is used too little. This judgment is nothing new. Psychiatrists have been complaining for years that this procedure is used too little, including Eric Slade, MD, from the University of Baltimore, in 2017 and German professors Andreas Fallgatter, MD, and Urban Wiesing, MD, PhD, in 2018. Dr. Wiesing and Dr. Fallgatter attribute the low level of use to the fact that ECT is labor-intensive, compared with pharmacotherapy.
Another reason is clearly the bad reputation of this method. However, ECT’s poor image, which has only increased over time, is not a convincing argument to forego today’s ECT as a treatment for patients with severe mental illnesses. According to Dr. Fallgatter and Dr. Wiesing, even the risk of misuse of this method is “not a sufficient argument for categorical refusal, rather for caution at best.” They argued that otherwise, “modern medicine would have to renounce many more therapies.”
This article was translated from Univadis Germany.
Advocates and users of electroconvulsive therapy (ECT) have received further scientific backing:
The patient cohort comprised 27,231 men and 40,096 women who had been treated as inpatients. The average age was 45.1 years (range: 18-103 years), and 4,982 patients received ECT. The primary endpoint was death by suicide within 365 days of hospital discharge. The secondary endpoints were death not by suicide and total mortality. The cause-specific hazard ratio (csHR) was calculated for patients with ECT, compared with patients without ECT.
In the propensity score-weighted analysis, ECT was linked to a significantly reduced suicide risk (csHR: 0.53; 95% confidence interval, 0.31-0.92). According to the calculations, ECT was associated with a significantly decreased total mortality risk (hazard ratio, 0.75; 95% CI, 0.58-0.97). However, this was not the case for death from causes other than suicide.
The authors, led by Tyler S. Kaster, PhD, a psychiatrist at Temerty Centre for Therapeutic Brain Intervention, Centre for Addiction and Mental Health, Toronto, concluded that this study underlines the importance of ECT, in particular for people with severe depression.
A well-tested therapy
ECT has been used for decades as a substantial tool for the treatment of patients with severe mental illnesses. Over the past 15 years, new methods for the treatment of severely depressed patients have been tested, such as vagus nerve stimulation, transcranial magnetic stimulation, and intranasal administration of esketamine. However, in a recent review paper in the New England Journal of Medicine, American psychiatrists Randall T. Espinoza, MD, MPH, University of California, Los Angeles, and Charles H. Kellner, MD, University of South Carolina, Charleston, reported that none of these therapies had proven to be an indisputable substitute for ECT for people with severe depression.
Significant clinical benefits
According to these American psychiatrists, the benefit of ECT has been proven many times, and several studies demonstrate the effect on the risk for suicide. Moreover, quality of life is improved, and the rate of new hospital admissions is lowered. ECT can rapidly improve depressive, psychotic, and catatonic symptoms and reduce suicidal urges for certain patient groups.
Studies on ECT involving patients with treatment-refractory depression have shown response rates of 60%-80% and pooled remission rates of 50%-60%. High response rates for ECT have even been reported for patients with psychotic depression or catatonia. In one study that recruited patients with treatment-refractory schizophrenia, the ECT efficacy rates were between 40% and 70%. In some Asian countries, schizophrenia is the main indication for ECT.
Good safety profile
Overall, the psychiatrists consider ECT to be a safe and tolerable therapy. The estimated death rate is around 2.1 deaths per 100,000 treatments. The most common complications are acute cardiopulmonary events, which are estimated to occur in less than 1% of treatments. Rare serious adverse events linked to ECT are arrhythmias, shortness of breath, aspiration, and prolonged seizures. The common but mild side effects are headaches, jaw pain, myalgia, nausea, and vomiting after the procedure, as well as fatigue.
Concerns regarding cognitive impairment still represent an obstacle for the use of ECT. However, in today’s practice, ECT leads to fewer cognitive side effects than previous treatments. The authors stated that it is not possible to predict how an individual patient will be affected, but most patients have only mild or moderate cognitive side effects that generally abate days to weeks after an ECT course has ended.
However, retrograde amnesia linked to ECT can last over a year. In rare cases, acute confusion or delirium can develop that requires interruption or discontinuation of treatment. No indications of structural brain damage after ECT have been detected in neuropathological testing. A Danish cohort study involving 168,015 patients with depression, of whom 3.1% had at least one ECT treatment, did not find a link between ECT with a mean period of almost 5 years and increased onset of dementia.
Bad reputation
Dr. Espinoza and Dr. Kellner criticized the fact that, despite its proven efficacy and safety, ECT is used too little. This judgment is nothing new. Psychiatrists have been complaining for years that this procedure is used too little, including Eric Slade, MD, from the University of Baltimore, in 2017 and German professors Andreas Fallgatter, MD, and Urban Wiesing, MD, PhD, in 2018. Dr. Wiesing and Dr. Fallgatter attribute the low level of use to the fact that ECT is labor-intensive, compared with pharmacotherapy.
Another reason is clearly the bad reputation of this method. However, ECT’s poor image, which has only increased over time, is not a convincing argument to forego today’s ECT as a treatment for patients with severe mental illnesses. According to Dr. Fallgatter and Dr. Wiesing, even the risk of misuse of this method is “not a sufficient argument for categorical refusal, rather for caution at best.” They argued that otherwise, “modern medicine would have to renounce many more therapies.”
This article was translated from Univadis Germany.
FROM THE LANCET PSYCHIATRY
Most COVID-19 survivors return to work within 2 years
The burden of persistent COVID-19 symptoms appeared to improve over time, but a higher percentage of former patients reported poor health, compared with the general population. This suggests that some patients need more time to completely recover from COVID-19, wrote the authors of the new study, which was published in The Lancet Respiratory Medicine. Previous research has shown that the health effects of COVID-19 last for up to a year, but data from longer-term studies are limited, said Lixue Huang, MD, of Capital Medical University, Beijing, one of the study authors, and colleagues.
Methods and results
In the new study, the researchers reviewed data from 1,192 adult patients who were discharged from the hospital after surviving COVID-19 between Jan. 7, 2020, and May 29, 2020. The researchers measured the participants’ health outcomes at 6 months, 12 months, and 2 years after their onset of symptoms. A community-based dataset of 3,383 adults with no history of COVID-19 served as controls to measure the recovery of the COVID-19 patients. The median age of the patients at the time of hospital discharge was 57 years, and 46% were women. The median follow-up time after the onset of symptoms was 185 days, 349 days, and 685 days for the 6-month, 12-month, and 2-year visits, respectively. The researchers measured health outcomes using a 6-min walking distance (6MWD) test, laboratory tests, and questionnaires about symptoms, mental health, health-related quality of life, returning to work, and health care use since leaving the hospital.
Overall, the proportion of COVID-19 survivors with at least one symptom decreased from 68% at 6 months to 55% at 2 years (P < .0001). The most frequent symptoms were fatigue and muscle weakness, reported by approximately one-third of the patients (31%); sleep problems also were reported by 31% of the patients.
The proportion of individuals with poor results on the 6MWD decreased continuously over time, not only in COVID-19 survivors overall, but also in three subgroups of varying initial disease severity. Of the 494 survivors who reported working before becoming ill, 438 (89%) had returned to their original jobs 2 years later. The most common reasons for not returning to work were decreased physical function, unwillingness to return, and unemployment, the researchers noted.
However, at 2 years, COVID-19 survivors reported more pain and discomfort, as well as more anxiety and depression, compared with the controls (23% vs. 5% and 12% vs. 5%, respectively).
In addition, significantly more survivors who needed high levels of respiratory support while hospitalized had lung diffusion impairment (65%), reduced residual volume (62%), and total lung capacity (39%), compared with matched controls (36%, 20%, and 6%, respectively) at 2 years.
Long-COVID concerns
Approximately half of the survivors had symptoms of long COVID at 2 years. These individuals were more likely to report pain or discomfort or anxiety or depression, as well as mobility problems, compared to survivors without long COVID. Participants with long-COVID symptoms were more than twice as likely to have an outpatient clinic visit (odds ratio, 2.82), and not quite twice as likely to be rehospitalized (OR, 1.64).
“We found that [health-related quality of life], exercise capacity, and mental health continued to improve throughout the 2 years regardless of initial disease severity, but about half still had symptomatic sequelae at 2 years,” the researchers wrote in their paper.
Findings can inform doctor-patient discussions
“We are increasingly recognizing that the health effects of COVID-19 may persist beyond acute illness, therefore this is a timely study to assess the long-term impact of COVID-19 with a long follow-up period,” said Suman Pal, MD, an internal medicine physician at the University of New Mexico, Albuquerque, in an interview.
The findings are consistent with the existing literature, said Dr. Pal, who was not involved in the study. The data from the study “can help clinicians have discussions regarding expected recovery and long-term prognosis for patients with COVID-19,” he noted.
What patients should know is that “studies such as this can help COVID-19 survivors understand and monitor persistent symptoms they may experience, and bring them to the attention of their clinicians,” said Dr. Pal.
However, “As a single-center study with high attrition of subjects during the study period, the findings may not be generalizable,” Dr. Pal emphasized. “Larger-scale studies and patient registries distributed over different geographical areas and time periods will help obtain a better understanding of the nature and prevalence of long COVID,” he said.
The study findings were limited by several factors, including the lack of formerly hospitalized controls with respiratory infections other than COVID-19 to determine which outcomes are COVID-19 specific, the researchers noted. Other limitations included the use of data from only patients at a single center, and from the early stages of the pandemic, as well as the use of self-reports for comorbidities and health outcomes, they said.
However, the results represent the longest-known published longitudinal follow-up of patients who recovered from acute COVID-19, the researchers emphasized. Study strengths included the large sample size, longitudinal design, and long-term follow-up with non-COVID controls to determine outcomes. The researchers noted their plans to conduct annual follow-ups in the current study population. They added that more research is needed to explore rehabilitation programs to promote recovery for COVID-19 survivors and to reduce the effects of long COVID.
The study was supported by the Chinese Academy of Medical Sciences, National Natural Science Foundation of China, National Key Research and Development Program of China, National Administration of Traditional Chinese Medicine, Major Projects of National Science and Technology on New Drug Creation and Development of Pulmonary Tuberculosis, China Evergrande Group, Jack Ma Foundation, Sino Biopharmaceutical, Ping An Insurance (Group), and New Sunshine Charity Foundation. The researchers and Dr. Pal had no financial conflicts to disclose.
This article was updated on 5/16/2022.
The burden of persistent COVID-19 symptoms appeared to improve over time, but a higher percentage of former patients reported poor health, compared with the general population. This suggests that some patients need more time to completely recover from COVID-19, wrote the authors of the new study, which was published in The Lancet Respiratory Medicine. Previous research has shown that the health effects of COVID-19 last for up to a year, but data from longer-term studies are limited, said Lixue Huang, MD, of Capital Medical University, Beijing, one of the study authors, and colleagues.
Methods and results
In the new study, the researchers reviewed data from 1,192 adult patients who were discharged from the hospital after surviving COVID-19 between Jan. 7, 2020, and May 29, 2020. The researchers measured the participants’ health outcomes at 6 months, 12 months, and 2 years after their onset of symptoms. A community-based dataset of 3,383 adults with no history of COVID-19 served as controls to measure the recovery of the COVID-19 patients. The median age of the patients at the time of hospital discharge was 57 years, and 46% were women. The median follow-up time after the onset of symptoms was 185 days, 349 days, and 685 days for the 6-month, 12-month, and 2-year visits, respectively. The researchers measured health outcomes using a 6-min walking distance (6MWD) test, laboratory tests, and questionnaires about symptoms, mental health, health-related quality of life, returning to work, and health care use since leaving the hospital.
Overall, the proportion of COVID-19 survivors with at least one symptom decreased from 68% at 6 months to 55% at 2 years (P < .0001). The most frequent symptoms were fatigue and muscle weakness, reported by approximately one-third of the patients (31%); sleep problems also were reported by 31% of the patients.
The proportion of individuals with poor results on the 6MWD decreased continuously over time, not only in COVID-19 survivors overall, but also in three subgroups of varying initial disease severity. Of the 494 survivors who reported working before becoming ill, 438 (89%) had returned to their original jobs 2 years later. The most common reasons for not returning to work were decreased physical function, unwillingness to return, and unemployment, the researchers noted.
However, at 2 years, COVID-19 survivors reported more pain and discomfort, as well as more anxiety and depression, compared with the controls (23% vs. 5% and 12% vs. 5%, respectively).
In addition, significantly more survivors who needed high levels of respiratory support while hospitalized had lung diffusion impairment (65%), reduced residual volume (62%), and total lung capacity (39%), compared with matched controls (36%, 20%, and 6%, respectively) at 2 years.
Long-COVID concerns
Approximately half of the survivors had symptoms of long COVID at 2 years. These individuals were more likely to report pain or discomfort or anxiety or depression, as well as mobility problems, compared to survivors without long COVID. Participants with long-COVID symptoms were more than twice as likely to have an outpatient clinic visit (odds ratio, 2.82), and not quite twice as likely to be rehospitalized (OR, 1.64).
“We found that [health-related quality of life], exercise capacity, and mental health continued to improve throughout the 2 years regardless of initial disease severity, but about half still had symptomatic sequelae at 2 years,” the researchers wrote in their paper.
Findings can inform doctor-patient discussions
“We are increasingly recognizing that the health effects of COVID-19 may persist beyond acute illness, therefore this is a timely study to assess the long-term impact of COVID-19 with a long follow-up period,” said Suman Pal, MD, an internal medicine physician at the University of New Mexico, Albuquerque, in an interview.
The findings are consistent with the existing literature, said Dr. Pal, who was not involved in the study. The data from the study “can help clinicians have discussions regarding expected recovery and long-term prognosis for patients with COVID-19,” he noted.
What patients should know is that “studies such as this can help COVID-19 survivors understand and monitor persistent symptoms they may experience, and bring them to the attention of their clinicians,” said Dr. Pal.
However, “As a single-center study with high attrition of subjects during the study period, the findings may not be generalizable,” Dr. Pal emphasized. “Larger-scale studies and patient registries distributed over different geographical areas and time periods will help obtain a better understanding of the nature and prevalence of long COVID,” he said.
The study findings were limited by several factors, including the lack of formerly hospitalized controls with respiratory infections other than COVID-19 to determine which outcomes are COVID-19 specific, the researchers noted. Other limitations included the use of data from only patients at a single center, and from the early stages of the pandemic, as well as the use of self-reports for comorbidities and health outcomes, they said.
However, the results represent the longest-known published longitudinal follow-up of patients who recovered from acute COVID-19, the researchers emphasized. Study strengths included the large sample size, longitudinal design, and long-term follow-up with non-COVID controls to determine outcomes. The researchers noted their plans to conduct annual follow-ups in the current study population. They added that more research is needed to explore rehabilitation programs to promote recovery for COVID-19 survivors and to reduce the effects of long COVID.
The study was supported by the Chinese Academy of Medical Sciences, National Natural Science Foundation of China, National Key Research and Development Program of China, National Administration of Traditional Chinese Medicine, Major Projects of National Science and Technology on New Drug Creation and Development of Pulmonary Tuberculosis, China Evergrande Group, Jack Ma Foundation, Sino Biopharmaceutical, Ping An Insurance (Group), and New Sunshine Charity Foundation. The researchers and Dr. Pal had no financial conflicts to disclose.
This article was updated on 5/16/2022.
The burden of persistent COVID-19 symptoms appeared to improve over time, but a higher percentage of former patients reported poor health, compared with the general population. This suggests that some patients need more time to completely recover from COVID-19, wrote the authors of the new study, which was published in The Lancet Respiratory Medicine. Previous research has shown that the health effects of COVID-19 last for up to a year, but data from longer-term studies are limited, said Lixue Huang, MD, of Capital Medical University, Beijing, one of the study authors, and colleagues.
Methods and results
In the new study, the researchers reviewed data from 1,192 adult patients who were discharged from the hospital after surviving COVID-19 between Jan. 7, 2020, and May 29, 2020. The researchers measured the participants’ health outcomes at 6 months, 12 months, and 2 years after their onset of symptoms. A community-based dataset of 3,383 adults with no history of COVID-19 served as controls to measure the recovery of the COVID-19 patients. The median age of the patients at the time of hospital discharge was 57 years, and 46% were women. The median follow-up time after the onset of symptoms was 185 days, 349 days, and 685 days for the 6-month, 12-month, and 2-year visits, respectively. The researchers measured health outcomes using a 6-min walking distance (6MWD) test, laboratory tests, and questionnaires about symptoms, mental health, health-related quality of life, returning to work, and health care use since leaving the hospital.
Overall, the proportion of COVID-19 survivors with at least one symptom decreased from 68% at 6 months to 55% at 2 years (P < .0001). The most frequent symptoms were fatigue and muscle weakness, reported by approximately one-third of the patients (31%); sleep problems also were reported by 31% of the patients.
The proportion of individuals with poor results on the 6MWD decreased continuously over time, not only in COVID-19 survivors overall, but also in three subgroups of varying initial disease severity. Of the 494 survivors who reported working before becoming ill, 438 (89%) had returned to their original jobs 2 years later. The most common reasons for not returning to work were decreased physical function, unwillingness to return, and unemployment, the researchers noted.
However, at 2 years, COVID-19 survivors reported more pain and discomfort, as well as more anxiety and depression, compared with the controls (23% vs. 5% and 12% vs. 5%, respectively).
In addition, significantly more survivors who needed high levels of respiratory support while hospitalized had lung diffusion impairment (65%), reduced residual volume (62%), and total lung capacity (39%), compared with matched controls (36%, 20%, and 6%, respectively) at 2 years.
Long-COVID concerns
Approximately half of the survivors had symptoms of long COVID at 2 years. These individuals were more likely to report pain or discomfort or anxiety or depression, as well as mobility problems, compared to survivors without long COVID. Participants with long-COVID symptoms were more than twice as likely to have an outpatient clinic visit (odds ratio, 2.82), and not quite twice as likely to be rehospitalized (OR, 1.64).
“We found that [health-related quality of life], exercise capacity, and mental health continued to improve throughout the 2 years regardless of initial disease severity, but about half still had symptomatic sequelae at 2 years,” the researchers wrote in their paper.
Findings can inform doctor-patient discussions
“We are increasingly recognizing that the health effects of COVID-19 may persist beyond acute illness, therefore this is a timely study to assess the long-term impact of COVID-19 with a long follow-up period,” said Suman Pal, MD, an internal medicine physician at the University of New Mexico, Albuquerque, in an interview.
The findings are consistent with the existing literature, said Dr. Pal, who was not involved in the study. The data from the study “can help clinicians have discussions regarding expected recovery and long-term prognosis for patients with COVID-19,” he noted.
What patients should know is that “studies such as this can help COVID-19 survivors understand and monitor persistent symptoms they may experience, and bring them to the attention of their clinicians,” said Dr. Pal.
However, “As a single-center study with high attrition of subjects during the study period, the findings may not be generalizable,” Dr. Pal emphasized. “Larger-scale studies and patient registries distributed over different geographical areas and time periods will help obtain a better understanding of the nature and prevalence of long COVID,” he said.
The study findings were limited by several factors, including the lack of formerly hospitalized controls with respiratory infections other than COVID-19 to determine which outcomes are COVID-19 specific, the researchers noted. Other limitations included the use of data from only patients at a single center, and from the early stages of the pandemic, as well as the use of self-reports for comorbidities and health outcomes, they said.
However, the results represent the longest-known published longitudinal follow-up of patients who recovered from acute COVID-19, the researchers emphasized. Study strengths included the large sample size, longitudinal design, and long-term follow-up with non-COVID controls to determine outcomes. The researchers noted their plans to conduct annual follow-ups in the current study population. They added that more research is needed to explore rehabilitation programs to promote recovery for COVID-19 survivors and to reduce the effects of long COVID.
The study was supported by the Chinese Academy of Medical Sciences, National Natural Science Foundation of China, National Key Research and Development Program of China, National Administration of Traditional Chinese Medicine, Major Projects of National Science and Technology on New Drug Creation and Development of Pulmonary Tuberculosis, China Evergrande Group, Jack Ma Foundation, Sino Biopharmaceutical, Ping An Insurance (Group), and New Sunshine Charity Foundation. The researchers and Dr. Pal had no financial conflicts to disclose.
This article was updated on 5/16/2022.
FROM THE LANCET RESPIRATORY MEDICINE
‘Goodie bag’ pill mill doctor sentenced to 2 decades in prison
A Pennsylvania-based internist was sentenced to 20 years in prison by a federal judge on May 10 for running a prescription “pill mill” from his medical practice.
Since May 2005, Andrew Berkowitz, MD, 62, of Huntington Valley, Pa., was president and CEO of A+ Pain Management, a clinic in the Philadelphia area, according to his LinkedIn profile.
Prosecutors said patients, no matter their complaint, would leave Dr. Berkowitz’s offices with “goodie bags” filled with a selection of drugs. A typical haul included topical analgesics, such as Relyyt and/or lidocaine; muscle relaxants, including chlorzoxazone and/or cyclobenzaprine; anti-inflammatories, such as celecoxib and/or fenoprofen; and schedule IV substances, including tramadol, eszopiclone, and quazepam.
The practice was registered in Pennsylvania as a nonpharmacy dispensing site, allowing Dr. Berkowitz to bill insurers for the drugs, according to The Pennsylvania Record, a journal covering Pennsylvania’s legal system. Dr. Berkowitz also prescribed oxycodone for “pill seeking” patients, who gave him their tacit approval of submitting claims to their insurance providers, which included Medicare, Aetna, and others, for the items in the goodie bag.
In addition, Dr. Berkowitz fraudulently billed insurers for medically unnecessary physical therapy, acupuncture, and chiropractic adjustments, as well as for treatments that were never provided, according to federal officials.
According to the Department of Justice, Dr. Berkowitz collected more than $4,000 per bag from insurers. From 2015 to 2018, prosecutors estimate that Dr. Berkowitz took in more than $4 million in fraudulent proceeds from his scheme.
The pill mill came to the attention of federal authorities after Blue Cross investigators forwarded to the FBI several complaints it had received about Dr. Berkowitz. In 2017, the FBI sent a cooperating witness to Dr. Berkowitz’s clinic. The undercover patient received a prescription for oxycodone, Motrin, and Flexeril and paid $185, according to The Record.
After being indicted in 2019, Dr. Berkowitz pleaded guilty in January 2020 to 19 counts of health care fraud and to 23 counts of distributing oxycodone outside the course of professional practice and without a legitimate medical purpose.
On May 10, he was sentenced to 20 years in prison, followed by 5 years of supervised release. In addition, he was ordered to pay a $40,000 fine and almost $4 million in restitution. As a result of civil False Claims Act liability for false claims submitted to Medicare, he is also obligated to pay approximately $1.8 million and is subject to a permanent prohibition on prescribing, distributing, or dispensing controlled substances.
Dr. Berkowitz’s actions were deemed especially egregious in light of the opioid epidemic.
“Doctors are supposed to treat illness, not feed it,” said Jacqueline Maguire, special agent in charge of the FBI’s Philadelphia division. “Andrew Berkowitz prescribed patients unnecessary pills and handed out opioids to addicts.” Jennifer Arbittier Williams, acting U.S. Attorney, added upon announcing the sentence, “Doctors who dare engage in health care fraud and drug diversion, two drivers of the opioid epidemic ravaging our communities, should heed this sentence as a warning that they will be held responsible, criminally and financially.”
A version of this article first appeared on Medscape.com.
A Pennsylvania-based internist was sentenced to 20 years in prison by a federal judge on May 10 for running a prescription “pill mill” from his medical practice.
Since May 2005, Andrew Berkowitz, MD, 62, of Huntington Valley, Pa., was president and CEO of A+ Pain Management, a clinic in the Philadelphia area, according to his LinkedIn profile.
Prosecutors said patients, no matter their complaint, would leave Dr. Berkowitz’s offices with “goodie bags” filled with a selection of drugs. A typical haul included topical analgesics, such as Relyyt and/or lidocaine; muscle relaxants, including chlorzoxazone and/or cyclobenzaprine; anti-inflammatories, such as celecoxib and/or fenoprofen; and schedule IV substances, including tramadol, eszopiclone, and quazepam.
The practice was registered in Pennsylvania as a nonpharmacy dispensing site, allowing Dr. Berkowitz to bill insurers for the drugs, according to The Pennsylvania Record, a journal covering Pennsylvania’s legal system. Dr. Berkowitz also prescribed oxycodone for “pill seeking” patients, who gave him their tacit approval of submitting claims to their insurance providers, which included Medicare, Aetna, and others, for the items in the goodie bag.
In addition, Dr. Berkowitz fraudulently billed insurers for medically unnecessary physical therapy, acupuncture, and chiropractic adjustments, as well as for treatments that were never provided, according to federal officials.
According to the Department of Justice, Dr. Berkowitz collected more than $4,000 per bag from insurers. From 2015 to 2018, prosecutors estimate that Dr. Berkowitz took in more than $4 million in fraudulent proceeds from his scheme.
The pill mill came to the attention of federal authorities after Blue Cross investigators forwarded to the FBI several complaints it had received about Dr. Berkowitz. In 2017, the FBI sent a cooperating witness to Dr. Berkowitz’s clinic. The undercover patient received a prescription for oxycodone, Motrin, and Flexeril and paid $185, according to The Record.
After being indicted in 2019, Dr. Berkowitz pleaded guilty in January 2020 to 19 counts of health care fraud and to 23 counts of distributing oxycodone outside the course of professional practice and without a legitimate medical purpose.
On May 10, he was sentenced to 20 years in prison, followed by 5 years of supervised release. In addition, he was ordered to pay a $40,000 fine and almost $4 million in restitution. As a result of civil False Claims Act liability for false claims submitted to Medicare, he is also obligated to pay approximately $1.8 million and is subject to a permanent prohibition on prescribing, distributing, or dispensing controlled substances.
Dr. Berkowitz’s actions were deemed especially egregious in light of the opioid epidemic.
“Doctors are supposed to treat illness, not feed it,” said Jacqueline Maguire, special agent in charge of the FBI’s Philadelphia division. “Andrew Berkowitz prescribed patients unnecessary pills and handed out opioids to addicts.” Jennifer Arbittier Williams, acting U.S. Attorney, added upon announcing the sentence, “Doctors who dare engage in health care fraud and drug diversion, two drivers of the opioid epidemic ravaging our communities, should heed this sentence as a warning that they will be held responsible, criminally and financially.”
A version of this article first appeared on Medscape.com.
A Pennsylvania-based internist was sentenced to 20 years in prison by a federal judge on May 10 for running a prescription “pill mill” from his medical practice.
Since May 2005, Andrew Berkowitz, MD, 62, of Huntington Valley, Pa., was president and CEO of A+ Pain Management, a clinic in the Philadelphia area, according to his LinkedIn profile.
Prosecutors said patients, no matter their complaint, would leave Dr. Berkowitz’s offices with “goodie bags” filled with a selection of drugs. A typical haul included topical analgesics, such as Relyyt and/or lidocaine; muscle relaxants, including chlorzoxazone and/or cyclobenzaprine; anti-inflammatories, such as celecoxib and/or fenoprofen; and schedule IV substances, including tramadol, eszopiclone, and quazepam.
The practice was registered in Pennsylvania as a nonpharmacy dispensing site, allowing Dr. Berkowitz to bill insurers for the drugs, according to The Pennsylvania Record, a journal covering Pennsylvania’s legal system. Dr. Berkowitz also prescribed oxycodone for “pill seeking” patients, who gave him their tacit approval of submitting claims to their insurance providers, which included Medicare, Aetna, and others, for the items in the goodie bag.
In addition, Dr. Berkowitz fraudulently billed insurers for medically unnecessary physical therapy, acupuncture, and chiropractic adjustments, as well as for treatments that were never provided, according to federal officials.
According to the Department of Justice, Dr. Berkowitz collected more than $4,000 per bag from insurers. From 2015 to 2018, prosecutors estimate that Dr. Berkowitz took in more than $4 million in fraudulent proceeds from his scheme.
The pill mill came to the attention of federal authorities after Blue Cross investigators forwarded to the FBI several complaints it had received about Dr. Berkowitz. In 2017, the FBI sent a cooperating witness to Dr. Berkowitz’s clinic. The undercover patient received a prescription for oxycodone, Motrin, and Flexeril and paid $185, according to The Record.
After being indicted in 2019, Dr. Berkowitz pleaded guilty in January 2020 to 19 counts of health care fraud and to 23 counts of distributing oxycodone outside the course of professional practice and without a legitimate medical purpose.
On May 10, he was sentenced to 20 years in prison, followed by 5 years of supervised release. In addition, he was ordered to pay a $40,000 fine and almost $4 million in restitution. As a result of civil False Claims Act liability for false claims submitted to Medicare, he is also obligated to pay approximately $1.8 million and is subject to a permanent prohibition on prescribing, distributing, or dispensing controlled substances.
Dr. Berkowitz’s actions were deemed especially egregious in light of the opioid epidemic.
“Doctors are supposed to treat illness, not feed it,” said Jacqueline Maguire, special agent in charge of the FBI’s Philadelphia division. “Andrew Berkowitz prescribed patients unnecessary pills and handed out opioids to addicts.” Jennifer Arbittier Williams, acting U.S. Attorney, added upon announcing the sentence, “Doctors who dare engage in health care fraud and drug diversion, two drivers of the opioid epidemic ravaging our communities, should heed this sentence as a warning that they will be held responsible, criminally and financially.”
A version of this article first appeared on Medscape.com.
ED staff speak out about workplace violence, ask for mitigation
WASHINGTON – Speaker after speaker, veteran emergency department physicians and nurses approached the podium for a May 4 press conference on the U.S. Capitol lawn across from the East Senate steps to describe violent incidents – being bitten, punched, slapped, kicked, choked, spat on, threatened – that they have both observed and have been subject to while working in EDs.
The press conference was cosponsored by the American College of Emergency Physicians and the Emergency Nurses Association, which have partnered since 2019 on the No Silence on ED Violence campaign.
The numbers confirm their experience. A 2018 poll of 3,500 ED physicians nationwide, which was conducted by Marketing General and was reported at ACEP’s annual meeting, found that nearly half of respondents had been assaulted at work; 27% of them were injured from the assault. Nurses, who spend more time with patients, may face even higher rates.
Incidence was reported to be increasing in 2018, and that was before the social and psychological upheavals imposed by the COVID pandemic caused assaults on staff in the hospital to go up an estimated 200%-300%.
But what really grated was that more than 95% of such cases, mostly perpetrated by patients, were never prosecuted, said Jennifer Casaletto, MD, FACEP, a North Carolina emergency physician and president of the state’s ACEP chapter. “Hospital and law enforcement see violence as just part of the job in our EDs.”
It’s no secret that workplace violence is increasing, Dr. Casaletto said. Four weeks ago, she stitched up the face of a charge nurse who had been assaulted. The nurse didn’t report the incident because she didn’t believe anything would change.
“Listening to my colleagues, I know the terror they have felt in the moment – for themselves, their colleagues, their patients. I know that raw fear of being attacked, and the complex emotions that follow. I’ve been hit, bit, and punched and watched colleagues getting choked.”
Dr. Casaletto was present in the ED when an out-of-control patient clubbed a nurse with an IV pole as she tried to close the doors to other patients’ rooms. “Instinctively, I pulled my stethoscope from around my neck, hoping I wouldn’t be strangled with it.”
Tennessee emergency nurse Todd Haines, MSN, RN, AEMT, CEN, said he has stepped in to help pull patients off coworkers. “I’ve seen some staff so severely injured they could not return to the bedside. I’ve been verbally threatened. My family has been threatened by patients and their families,” he reported. “We’ve all seen it. And COVID has made some people even meaner. They just lose their minds, and ED staff take the brunt of their aggression. But then to report these incidents and hear: ‘It’s just part of your job,’ well, it’s not part of my job.”
Mr. Haines spent 10 years in law enforcement with a sheriff’s department in middle Tennessee and was on its special tactical response team before becoming an ED nurse. He said he saw many more verbal and physical assaults in 11 years in the ED than during his police career.
“I love emergency nursing at the bedside, but it got to the point where I took the first chance to leave the bedside. And I’m not alone. Other nurses are leaving in droves.” Mr. Haines now has a job directing a trauma program, and he volunteers on policy issues for the Tennessee ENA. But he worries about the toll of this violence on the ED workforce, with so many professionals already mulling over leaving the field because of job stress and burnout.
“We have to do something to keep experienced hospital emergency staff at the bedside.”
What’s the answer?
Also speaking at the press conference was Senator Tammy Baldwin (D-Wis.), who pledged to introduce the Workplace Violence Prevention for Health Care and Social Services Workers Act, which passed the House in April. This bill would direct the Occupational Health and Safety Administration to issue a standard requiring employers in health care and social services to develop and implement workplace violence prevention plans. It would cover a variety of health facilities but not doctor’s offices or home-based services.
An interim final standard would be due within a year of enactment, with a final version to follow. Covered employers would have 6 months to develop and implement their own comprehensive workplace violence prevention plans, with the meaningful participation of direct care employees, tailored for and specific to the conditions and hazards of their facility, informed by past violent incidents, and subject to the size and complexity of the setting.
The plan would also name an individual responsible for its implementation, would include staff training and education, and would require facilities to track incidents and prohibit retaliation against employees who reported incidents of workplace violence.
On Wednesday, Sen. Baldwin called for unanimous consent on the Senate floor to fast-track this bill, but that was opposed by Senator Mike Braun (R-Ind.). She will soon introduce legislation similar to HR 1195, which the House passed.
“This bill will provide long overdue protections and safety standards,” she said. It will ensure that workplaces adopt proven protection techniques, such as those in OSHA’s 2015 guideline for preventing health care workplace violence. The American Hospital Association opposed the House bill on the grounds that hospitals have already implemented policies and programs specifically tailored to address workplace violence, so the OSHA standards required by the bill are not warranted.
Another speaker at the press conference, Aisha Terry, MD, MPH, FACEP, an emergency physician for George Washington University and Veterans Affairs in Washington, D.C., and current vice president of ACEP, described an incident that occurred when she was at work. A patient punched the nurse caring for him in the face, knocking her unconscious to the floor. “I’ll never forget that sound,” Dr. Terry said. “To this day, it has impacted her career. She hasn’t known what to do.”
Many people don’t realize how bad workplace violence really is, Dr. Terry added. “You assume you can serve as the safety net of this country, taking care of patients in the context of the pandemic, and feel safe – and not have to worry about your own safety. It’s past due that we put an end to this.”
Biggest win
Mr. Haines called the workplace violence bill a game changer for ED professionals, now and into the future. “We’re not going to totally eliminate violence in the emergency department. That is part of our business. But this legislation will support us and give a safer environment for us to do the work we love,” he said.
“The biggest win for this legislation is that it will create a supportive, nonretaliatory environment. It will give us as nurses a structured way to report things.” And, when these incidents do get reported, staff will get the help they need, Mr. Haines said. “The legislation will help show the importance of implementing systems and processes in emergency settings to address the risks and hazards that makes us all vulnerable to violence.”
No relevant financial relationships have been disclosed.
A version of this article first appeared on Medscape.com.
WASHINGTON – Speaker after speaker, veteran emergency department physicians and nurses approached the podium for a May 4 press conference on the U.S. Capitol lawn across from the East Senate steps to describe violent incidents – being bitten, punched, slapped, kicked, choked, spat on, threatened – that they have both observed and have been subject to while working in EDs.
The press conference was cosponsored by the American College of Emergency Physicians and the Emergency Nurses Association, which have partnered since 2019 on the No Silence on ED Violence campaign.
The numbers confirm their experience. A 2018 poll of 3,500 ED physicians nationwide, which was conducted by Marketing General and was reported at ACEP’s annual meeting, found that nearly half of respondents had been assaulted at work; 27% of them were injured from the assault. Nurses, who spend more time with patients, may face even higher rates.
Incidence was reported to be increasing in 2018, and that was before the social and psychological upheavals imposed by the COVID pandemic caused assaults on staff in the hospital to go up an estimated 200%-300%.
But what really grated was that more than 95% of such cases, mostly perpetrated by patients, were never prosecuted, said Jennifer Casaletto, MD, FACEP, a North Carolina emergency physician and president of the state’s ACEP chapter. “Hospital and law enforcement see violence as just part of the job in our EDs.”
It’s no secret that workplace violence is increasing, Dr. Casaletto said. Four weeks ago, she stitched up the face of a charge nurse who had been assaulted. The nurse didn’t report the incident because she didn’t believe anything would change.
“Listening to my colleagues, I know the terror they have felt in the moment – for themselves, their colleagues, their patients. I know that raw fear of being attacked, and the complex emotions that follow. I’ve been hit, bit, and punched and watched colleagues getting choked.”
Dr. Casaletto was present in the ED when an out-of-control patient clubbed a nurse with an IV pole as she tried to close the doors to other patients’ rooms. “Instinctively, I pulled my stethoscope from around my neck, hoping I wouldn’t be strangled with it.”
Tennessee emergency nurse Todd Haines, MSN, RN, AEMT, CEN, said he has stepped in to help pull patients off coworkers. “I’ve seen some staff so severely injured they could not return to the bedside. I’ve been verbally threatened. My family has been threatened by patients and their families,” he reported. “We’ve all seen it. And COVID has made some people even meaner. They just lose their minds, and ED staff take the brunt of their aggression. But then to report these incidents and hear: ‘It’s just part of your job,’ well, it’s not part of my job.”
Mr. Haines spent 10 years in law enforcement with a sheriff’s department in middle Tennessee and was on its special tactical response team before becoming an ED nurse. He said he saw many more verbal and physical assaults in 11 years in the ED than during his police career.
“I love emergency nursing at the bedside, but it got to the point where I took the first chance to leave the bedside. And I’m not alone. Other nurses are leaving in droves.” Mr. Haines now has a job directing a trauma program, and he volunteers on policy issues for the Tennessee ENA. But he worries about the toll of this violence on the ED workforce, with so many professionals already mulling over leaving the field because of job stress and burnout.
“We have to do something to keep experienced hospital emergency staff at the bedside.”
What’s the answer?
Also speaking at the press conference was Senator Tammy Baldwin (D-Wis.), who pledged to introduce the Workplace Violence Prevention for Health Care and Social Services Workers Act, which passed the House in April. This bill would direct the Occupational Health and Safety Administration to issue a standard requiring employers in health care and social services to develop and implement workplace violence prevention plans. It would cover a variety of health facilities but not doctor’s offices or home-based services.
An interim final standard would be due within a year of enactment, with a final version to follow. Covered employers would have 6 months to develop and implement their own comprehensive workplace violence prevention plans, with the meaningful participation of direct care employees, tailored for and specific to the conditions and hazards of their facility, informed by past violent incidents, and subject to the size and complexity of the setting.
The plan would also name an individual responsible for its implementation, would include staff training and education, and would require facilities to track incidents and prohibit retaliation against employees who reported incidents of workplace violence.
On Wednesday, Sen. Baldwin called for unanimous consent on the Senate floor to fast-track this bill, but that was opposed by Senator Mike Braun (R-Ind.). She will soon introduce legislation similar to HR 1195, which the House passed.
“This bill will provide long overdue protections and safety standards,” she said. It will ensure that workplaces adopt proven protection techniques, such as those in OSHA’s 2015 guideline for preventing health care workplace violence. The American Hospital Association opposed the House bill on the grounds that hospitals have already implemented policies and programs specifically tailored to address workplace violence, so the OSHA standards required by the bill are not warranted.
Another speaker at the press conference, Aisha Terry, MD, MPH, FACEP, an emergency physician for George Washington University and Veterans Affairs in Washington, D.C., and current vice president of ACEP, described an incident that occurred when she was at work. A patient punched the nurse caring for him in the face, knocking her unconscious to the floor. “I’ll never forget that sound,” Dr. Terry said. “To this day, it has impacted her career. She hasn’t known what to do.”
Many people don’t realize how bad workplace violence really is, Dr. Terry added. “You assume you can serve as the safety net of this country, taking care of patients in the context of the pandemic, and feel safe – and not have to worry about your own safety. It’s past due that we put an end to this.”
Biggest win
Mr. Haines called the workplace violence bill a game changer for ED professionals, now and into the future. “We’re not going to totally eliminate violence in the emergency department. That is part of our business. But this legislation will support us and give a safer environment for us to do the work we love,” he said.
“The biggest win for this legislation is that it will create a supportive, nonretaliatory environment. It will give us as nurses a structured way to report things.” And, when these incidents do get reported, staff will get the help they need, Mr. Haines said. “The legislation will help show the importance of implementing systems and processes in emergency settings to address the risks and hazards that makes us all vulnerable to violence.”
No relevant financial relationships have been disclosed.
A version of this article first appeared on Medscape.com.
WASHINGTON – Speaker after speaker, veteran emergency department physicians and nurses approached the podium for a May 4 press conference on the U.S. Capitol lawn across from the East Senate steps to describe violent incidents – being bitten, punched, slapped, kicked, choked, spat on, threatened – that they have both observed and have been subject to while working in EDs.
The press conference was cosponsored by the American College of Emergency Physicians and the Emergency Nurses Association, which have partnered since 2019 on the No Silence on ED Violence campaign.
The numbers confirm their experience. A 2018 poll of 3,500 ED physicians nationwide, which was conducted by Marketing General and was reported at ACEP’s annual meeting, found that nearly half of respondents had been assaulted at work; 27% of them were injured from the assault. Nurses, who spend more time with patients, may face even higher rates.
Incidence was reported to be increasing in 2018, and that was before the social and psychological upheavals imposed by the COVID pandemic caused assaults on staff in the hospital to go up an estimated 200%-300%.
But what really grated was that more than 95% of such cases, mostly perpetrated by patients, were never prosecuted, said Jennifer Casaletto, MD, FACEP, a North Carolina emergency physician and president of the state’s ACEP chapter. “Hospital and law enforcement see violence as just part of the job in our EDs.”
It’s no secret that workplace violence is increasing, Dr. Casaletto said. Four weeks ago, she stitched up the face of a charge nurse who had been assaulted. The nurse didn’t report the incident because she didn’t believe anything would change.
“Listening to my colleagues, I know the terror they have felt in the moment – for themselves, their colleagues, their patients. I know that raw fear of being attacked, and the complex emotions that follow. I’ve been hit, bit, and punched and watched colleagues getting choked.”
Dr. Casaletto was present in the ED when an out-of-control patient clubbed a nurse with an IV pole as she tried to close the doors to other patients’ rooms. “Instinctively, I pulled my stethoscope from around my neck, hoping I wouldn’t be strangled with it.”
Tennessee emergency nurse Todd Haines, MSN, RN, AEMT, CEN, said he has stepped in to help pull patients off coworkers. “I’ve seen some staff so severely injured they could not return to the bedside. I’ve been verbally threatened. My family has been threatened by patients and their families,” he reported. “We’ve all seen it. And COVID has made some people even meaner. They just lose their minds, and ED staff take the brunt of their aggression. But then to report these incidents and hear: ‘It’s just part of your job,’ well, it’s not part of my job.”
Mr. Haines spent 10 years in law enforcement with a sheriff’s department in middle Tennessee and was on its special tactical response team before becoming an ED nurse. He said he saw many more verbal and physical assaults in 11 years in the ED than during his police career.
“I love emergency nursing at the bedside, but it got to the point where I took the first chance to leave the bedside. And I’m not alone. Other nurses are leaving in droves.” Mr. Haines now has a job directing a trauma program, and he volunteers on policy issues for the Tennessee ENA. But he worries about the toll of this violence on the ED workforce, with so many professionals already mulling over leaving the field because of job stress and burnout.
“We have to do something to keep experienced hospital emergency staff at the bedside.”
What’s the answer?
Also speaking at the press conference was Senator Tammy Baldwin (D-Wis.), who pledged to introduce the Workplace Violence Prevention for Health Care and Social Services Workers Act, which passed the House in April. This bill would direct the Occupational Health and Safety Administration to issue a standard requiring employers in health care and social services to develop and implement workplace violence prevention plans. It would cover a variety of health facilities but not doctor’s offices or home-based services.
An interim final standard would be due within a year of enactment, with a final version to follow. Covered employers would have 6 months to develop and implement their own comprehensive workplace violence prevention plans, with the meaningful participation of direct care employees, tailored for and specific to the conditions and hazards of their facility, informed by past violent incidents, and subject to the size and complexity of the setting.
The plan would also name an individual responsible for its implementation, would include staff training and education, and would require facilities to track incidents and prohibit retaliation against employees who reported incidents of workplace violence.
On Wednesday, Sen. Baldwin called for unanimous consent on the Senate floor to fast-track this bill, but that was opposed by Senator Mike Braun (R-Ind.). She will soon introduce legislation similar to HR 1195, which the House passed.
“This bill will provide long overdue protections and safety standards,” she said. It will ensure that workplaces adopt proven protection techniques, such as those in OSHA’s 2015 guideline for preventing health care workplace violence. The American Hospital Association opposed the House bill on the grounds that hospitals have already implemented policies and programs specifically tailored to address workplace violence, so the OSHA standards required by the bill are not warranted.
Another speaker at the press conference, Aisha Terry, MD, MPH, FACEP, an emergency physician for George Washington University and Veterans Affairs in Washington, D.C., and current vice president of ACEP, described an incident that occurred when she was at work. A patient punched the nurse caring for him in the face, knocking her unconscious to the floor. “I’ll never forget that sound,” Dr. Terry said. “To this day, it has impacted her career. She hasn’t known what to do.”
Many people don’t realize how bad workplace violence really is, Dr. Terry added. “You assume you can serve as the safety net of this country, taking care of patients in the context of the pandemic, and feel safe – and not have to worry about your own safety. It’s past due that we put an end to this.”
Biggest win
Mr. Haines called the workplace violence bill a game changer for ED professionals, now and into the future. “We’re not going to totally eliminate violence in the emergency department. That is part of our business. But this legislation will support us and give a safer environment for us to do the work we love,” he said.
“The biggest win for this legislation is that it will create a supportive, nonretaliatory environment. It will give us as nurses a structured way to report things.” And, when these incidents do get reported, staff will get the help they need, Mr. Haines said. “The legislation will help show the importance of implementing systems and processes in emergency settings to address the risks and hazards that makes us all vulnerable to violence.”
No relevant financial relationships have been disclosed.
A version of this article first appeared on Medscape.com.
Does noninvasive brain stimulation augment CBT for depression?
Results of a multicenter, placebo-controlled randomized clinical trials showed adjunctive transcranial direct current stimulation (tDCS) was not superior to sham-tDCS plus CBT or CBT alone.
“Combining these interventions does not lead to added value. This is an example where negative findings guide the way of future studies. What we learned is that we might change things in a few dimensions,” study investigator Malek Bajbouj, MD, Charité University Hospital, Berlin, told this news organization.
The study was published online in JAMA Psychiatry.
Urgent need for better treatment
MDD affects 10% of the global population. However, up to 30% of patients have an inadequate response to standard treatment of CBT, pharmacotherapy, or a combination of the two, highlighting the need to develop more effective therapeutic strategies, the investigators note.
A noninvasive approach, tDCS, in healthy populations, has been shown to enhance cognitive function in brain regions that are also relevant for CBT. Specifically, the investigators point out that tDCS can “positively modulate neuronal activity in prefrontal structures central for affective and cognitive processes,” including emotion regulation, cognitive control working memory, and learning.
Based on this early data, the investigators conducted a randomized, placebo-controlled trial to determine whether tDCS combined with CBT might have clinically relevant synergistic effects.
The multicenter study included adults aged 20-65 years with a single or recurrent depressive episode who were either not receiving medication or receiving a stable regimen of selective serotonin reuptake inhibitors (SSRIs) or mirtazapine (Remeron).
A total of 148 participants (89 women, 59 men) with a mean age of 41 years were randomly assigned to receive CBT alone (n = 53), CBT+ tDCS (n = 48) or CBT + sham tDCS (n = 47).
Participants attended a 6-week group intervention of 12 sessions of CBT. If assigned, tDCS was applied simultaneously. Active tDCS included stimulation with an intensity of 2 milliamps for 30 minutes.
The study’s primary outcome was the change in Montgomery-Åsberg Depression Rating Scale (MADRS) from baseline to post treatment in the intention-to-treat sample. A total of 126 patients completed the study.
At baseline, the average MADRS score was 23.0. In each of the study groups, MADRS scores were reduced by a mean of 6.5 points (95% confidence interval, 3.82-9.14 points). The Cohen d value was -0.90 (95% CI, -1.43 to -0.50), indicating a significant effect over time, the researchers report. However, they add that “there was not significant effect of group and no significant interaction of group x time, indicating the estimated additive effects were not statistically significant.”
Results suggest that more research is needed to optimize treatment synchronization to achieve synergies between noninvasive brain stimulation and psychotherapeutic interventions.
Beauty and promise
Commenting on the findings, Mark George, MD, director of the Medical University of South Carolina Center for Advanced Imaging Research and the Brain Stimulation Laboratory, Charleston, described the study as “a really good effort by a great group of researchers.”
It’s unclear, he added, why tDCS failed to augment CBT. “It may be about the nongeneralizability of tDCS to complex functions, it may be that they didn’t get the dose right, or it might be due to a placebo response,” he speculated.
Furthermore, “tDCS is the most simple form of brain stimulation. The beauty and promise of tDCS is that it is so inexpensive and safe,” Dr. George added.
If proven effective, tDCS could potentially be used at home and rolled out as a frontline therapy for depression, he added. “Everybody wants the technology to work as an antidepressant, since it could have a very big positive public health impact,” said Dr. George.
Referring to previous research showing tDCS’ ability to improve specific brain functions in healthy controls, Dr. George noted that the potential of tDCS may be limited to augmenting specific brain functions such as memory but not more complex behaviors like depression.
However, Dr. George believes a more plausible explanation is that the optimal dose for tDCS has not yet been determined.
With other types of neuromodulation, such as electroconvulsive therapy, “we know that we’re in the brain with the right dose. But for tDCS, we don’t know that, and we’ve got to figure that out before it’s ever really going to make it [as a treatment],” he said.
“There have been great advances through the years in the field of brain stimulation and the treatment of depression. But rates of depression and suicide are continuing to grow, and we have not yet made a significant dent in treatment, in part because these technologies require equipment, [and] they’re expensive. So when we figure out tDCS, it will be a very important piece of our toolkit – a real game changer,” Dr. George added.
A version of this article first appeared on Medscape.com.
Results of a multicenter, placebo-controlled randomized clinical trials showed adjunctive transcranial direct current stimulation (tDCS) was not superior to sham-tDCS plus CBT or CBT alone.
“Combining these interventions does not lead to added value. This is an example where negative findings guide the way of future studies. What we learned is that we might change things in a few dimensions,” study investigator Malek Bajbouj, MD, Charité University Hospital, Berlin, told this news organization.
The study was published online in JAMA Psychiatry.
Urgent need for better treatment
MDD affects 10% of the global population. However, up to 30% of patients have an inadequate response to standard treatment of CBT, pharmacotherapy, or a combination of the two, highlighting the need to develop more effective therapeutic strategies, the investigators note.
A noninvasive approach, tDCS, in healthy populations, has been shown to enhance cognitive function in brain regions that are also relevant for CBT. Specifically, the investigators point out that tDCS can “positively modulate neuronal activity in prefrontal structures central for affective and cognitive processes,” including emotion regulation, cognitive control working memory, and learning.
Based on this early data, the investigators conducted a randomized, placebo-controlled trial to determine whether tDCS combined with CBT might have clinically relevant synergistic effects.
The multicenter study included adults aged 20-65 years with a single or recurrent depressive episode who were either not receiving medication or receiving a stable regimen of selective serotonin reuptake inhibitors (SSRIs) or mirtazapine (Remeron).
A total of 148 participants (89 women, 59 men) with a mean age of 41 years were randomly assigned to receive CBT alone (n = 53), CBT+ tDCS (n = 48) or CBT + sham tDCS (n = 47).
Participants attended a 6-week group intervention of 12 sessions of CBT. If assigned, tDCS was applied simultaneously. Active tDCS included stimulation with an intensity of 2 milliamps for 30 minutes.
The study’s primary outcome was the change in Montgomery-Åsberg Depression Rating Scale (MADRS) from baseline to post treatment in the intention-to-treat sample. A total of 126 patients completed the study.
At baseline, the average MADRS score was 23.0. In each of the study groups, MADRS scores were reduced by a mean of 6.5 points (95% confidence interval, 3.82-9.14 points). The Cohen d value was -0.90 (95% CI, -1.43 to -0.50), indicating a significant effect over time, the researchers report. However, they add that “there was not significant effect of group and no significant interaction of group x time, indicating the estimated additive effects were not statistically significant.”
Results suggest that more research is needed to optimize treatment synchronization to achieve synergies between noninvasive brain stimulation and psychotherapeutic interventions.
Beauty and promise
Commenting on the findings, Mark George, MD, director of the Medical University of South Carolina Center for Advanced Imaging Research and the Brain Stimulation Laboratory, Charleston, described the study as “a really good effort by a great group of researchers.”
It’s unclear, he added, why tDCS failed to augment CBT. “It may be about the nongeneralizability of tDCS to complex functions, it may be that they didn’t get the dose right, or it might be due to a placebo response,” he speculated.
Furthermore, “tDCS is the most simple form of brain stimulation. The beauty and promise of tDCS is that it is so inexpensive and safe,” Dr. George added.
If proven effective, tDCS could potentially be used at home and rolled out as a frontline therapy for depression, he added. “Everybody wants the technology to work as an antidepressant, since it could have a very big positive public health impact,” said Dr. George.
Referring to previous research showing tDCS’ ability to improve specific brain functions in healthy controls, Dr. George noted that the potential of tDCS may be limited to augmenting specific brain functions such as memory but not more complex behaviors like depression.
However, Dr. George believes a more plausible explanation is that the optimal dose for tDCS has not yet been determined.
With other types of neuromodulation, such as electroconvulsive therapy, “we know that we’re in the brain with the right dose. But for tDCS, we don’t know that, and we’ve got to figure that out before it’s ever really going to make it [as a treatment],” he said.
“There have been great advances through the years in the field of brain stimulation and the treatment of depression. But rates of depression and suicide are continuing to grow, and we have not yet made a significant dent in treatment, in part because these technologies require equipment, [and] they’re expensive. So when we figure out tDCS, it will be a very important piece of our toolkit – a real game changer,” Dr. George added.
A version of this article first appeared on Medscape.com.
Results of a multicenter, placebo-controlled randomized clinical trials showed adjunctive transcranial direct current stimulation (tDCS) was not superior to sham-tDCS plus CBT or CBT alone.
“Combining these interventions does not lead to added value. This is an example where negative findings guide the way of future studies. What we learned is that we might change things in a few dimensions,” study investigator Malek Bajbouj, MD, Charité University Hospital, Berlin, told this news organization.
The study was published online in JAMA Psychiatry.
Urgent need for better treatment
MDD affects 10% of the global population. However, up to 30% of patients have an inadequate response to standard treatment of CBT, pharmacotherapy, or a combination of the two, highlighting the need to develop more effective therapeutic strategies, the investigators note.
A noninvasive approach, tDCS, in healthy populations, has been shown to enhance cognitive function in brain regions that are also relevant for CBT. Specifically, the investigators point out that tDCS can “positively modulate neuronal activity in prefrontal structures central for affective and cognitive processes,” including emotion regulation, cognitive control working memory, and learning.
Based on this early data, the investigators conducted a randomized, placebo-controlled trial to determine whether tDCS combined with CBT might have clinically relevant synergistic effects.
The multicenter study included adults aged 20-65 years with a single or recurrent depressive episode who were either not receiving medication or receiving a stable regimen of selective serotonin reuptake inhibitors (SSRIs) or mirtazapine (Remeron).
A total of 148 participants (89 women, 59 men) with a mean age of 41 years were randomly assigned to receive CBT alone (n = 53), CBT+ tDCS (n = 48) or CBT + sham tDCS (n = 47).
Participants attended a 6-week group intervention of 12 sessions of CBT. If assigned, tDCS was applied simultaneously. Active tDCS included stimulation with an intensity of 2 milliamps for 30 minutes.
The study’s primary outcome was the change in Montgomery-Åsberg Depression Rating Scale (MADRS) from baseline to post treatment in the intention-to-treat sample. A total of 126 patients completed the study.
At baseline, the average MADRS score was 23.0. In each of the study groups, MADRS scores were reduced by a mean of 6.5 points (95% confidence interval, 3.82-9.14 points). The Cohen d value was -0.90 (95% CI, -1.43 to -0.50), indicating a significant effect over time, the researchers report. However, they add that “there was not significant effect of group and no significant interaction of group x time, indicating the estimated additive effects were not statistically significant.”
Results suggest that more research is needed to optimize treatment synchronization to achieve synergies between noninvasive brain stimulation and psychotherapeutic interventions.
Beauty and promise
Commenting on the findings, Mark George, MD, director of the Medical University of South Carolina Center for Advanced Imaging Research and the Brain Stimulation Laboratory, Charleston, described the study as “a really good effort by a great group of researchers.”
It’s unclear, he added, why tDCS failed to augment CBT. “It may be about the nongeneralizability of tDCS to complex functions, it may be that they didn’t get the dose right, or it might be due to a placebo response,” he speculated.
Furthermore, “tDCS is the most simple form of brain stimulation. The beauty and promise of tDCS is that it is so inexpensive and safe,” Dr. George added.
If proven effective, tDCS could potentially be used at home and rolled out as a frontline therapy for depression, he added. “Everybody wants the technology to work as an antidepressant, since it could have a very big positive public health impact,” said Dr. George.
Referring to previous research showing tDCS’ ability to improve specific brain functions in healthy controls, Dr. George noted that the potential of tDCS may be limited to augmenting specific brain functions such as memory but not more complex behaviors like depression.
However, Dr. George believes a more plausible explanation is that the optimal dose for tDCS has not yet been determined.
With other types of neuromodulation, such as electroconvulsive therapy, “we know that we’re in the brain with the right dose. But for tDCS, we don’t know that, and we’ve got to figure that out before it’s ever really going to make it [as a treatment],” he said.
“There have been great advances through the years in the field of brain stimulation and the treatment of depression. But rates of depression and suicide are continuing to grow, and we have not yet made a significant dent in treatment, in part because these technologies require equipment, [and] they’re expensive. So when we figure out tDCS, it will be a very important piece of our toolkit – a real game changer,” Dr. George added.
A version of this article first appeared on Medscape.com.
FROM JAMA PSYCHIATRY
Neurology, psychiatry studies overlook sex as a variable
A large percentage of studies in neurology and psychiatry over the past decade have failed to account for differences between the sexes, according to a team of Canadian researchers.
“Despite the fact there are papers that are using males and females in the studies, they’re not using the males and females in the way that would optimally find the possibility of sex differences,” lead author Liisa A.M. Galea, PhD, told this news organization. Dr. Galea is a professor and distinguished scholar at the Djavad Mowafaghian Center for Brain Health at the University of British Columbia in Vancouver.
The study was published online in Nature Communications.
Optimal design uncommon
Differences in how neurologic and psychiatric diseases affect men and women have been well documented. Women, for example, are more susceptible to severe stroke, and men are more prone to cognitive decline with schizophrenia. With Alzheimer’s disease, women typically have more severe cognitive defects.
The researchers surveyed 3,193 papers that included a multitude of studies. Although most of the papers reported studies that included both sexes, only 19% of surveyed studies used what Dr. Galea called an optimal design for the discovery of sex differences. “What I mean by ‘optimally’ is the design of the experiments and the analysis of sex as a variable,” she said. And in 2019, only 5% of the studies used sex as a variable for determining differences between the sexes, the study found.
In the current research, two authors read the methods and results of each study described in each paper, Dr. Galea said. The readers noted whether the paper reported the study sample size and whether the studies used a balanced design. The surveyed journals include Nature Neuroscience, Neuron, Journal of Neuroscience, Molecular Psychiatry, Biological Psychiatry, and Neuropsychopharmacology.
‘Not much is changing’
“I had a suspicion that this was happening,” Dr. Galea said. “I didn’t know that it’s so bad, to be fair.” The “good news story,” she said, is that more papers considered sex as a factor in the later years surveyed. In 2019, more than 95% of papers across both disciplines reported participants’ sex, compared with about 70% in 2009. However, less than 20% of the papers in all study years reported studies that used sex optimally to determine differences between the sexes.
“The other thing that shocked me,” Dr. Galea said, “was that even despite the fact that we saw this increase in the number of papers that were using males and females, we didn’t see the sort of corresponding increase in those that were using ‘optimal design’ or ‘optimal analysis,’ ” Dr. Galea said. In 2009, 14% of papers used optimal design and 2% used optimal analysis for determining sex differences. By 2019, those percentages were 19% and 5%, respectively.
But even the papers that used both sexes had shortcomings, the study found. Just over one-third of these papers (34.5%) didn’t use a balanced design. Just over one-quarter (25.9%) didn’t identify the sample size, a shortcoming that marked 18% of these studies in 2009 and 33% in 2019. Fifteen percent of papers examined included studies that used both sexes inconsistently.
“That matters, because other studies have found that about 20% of papers are doing some kind of analysis with sex, but we had a suspicion that a lot of studies would include sex as a covariate,” Dr. Galea said. “Essentially what that does is, you remove that variable from the data. So, any statistical variation due to sex is then gone.
“The problem with that,” she added, “is you’re not actually looking to see if there’s an influence of sex; you’re removing it.”
Dr. Galea noted that this study points to a need for funding agencies to demand that researchers meet their mandates on sex- and gender-based analysis. “Despite the mandates, not much is really changing as far as the analysis or design of experiments, and we need to figure out how to change that,” she said. “We need to figure out how to get researchers more interested to use the power of studying sex differences.”
‘Not surprising, but disappointing’
Vladimir Hachinski, MD, professor of neurology and epidemiology at Western University in London, Ont., and former editor in chief of Stroke, told this news organization that women have almost twice the life risk of developing dementia, are at higher risk of stroke below age 35 years, and have more severe strokes and higher rates of disability at any age.
Commenting on the current study, Dr. Hachinski said, “It’s not surprising, but it’s disappointing, because we’ve known the difference for a long time.” He added, “The paper is very important because we were not aware that it was that bad.”
Dr. Hachinski also stated, “This paper needs a lot of reading. It’s a great resource, and it should be highlighted as one of those things that needs to be addressed, because it matters.”
The study was funded by a Natural Sciences and Engineering Research Council of Canada grant and by the British Columbia Women’s Foundation. Dr. Galea and Hachinski had no relevant disclosures.
A version of this article first appeared on Medscape.com.
A large percentage of studies in neurology and psychiatry over the past decade have failed to account for differences between the sexes, according to a team of Canadian researchers.
“Despite the fact there are papers that are using males and females in the studies, they’re not using the males and females in the way that would optimally find the possibility of sex differences,” lead author Liisa A.M. Galea, PhD, told this news organization. Dr. Galea is a professor and distinguished scholar at the Djavad Mowafaghian Center for Brain Health at the University of British Columbia in Vancouver.
The study was published online in Nature Communications.
Optimal design uncommon
Differences in how neurologic and psychiatric diseases affect men and women have been well documented. Women, for example, are more susceptible to severe stroke, and men are more prone to cognitive decline with schizophrenia. With Alzheimer’s disease, women typically have more severe cognitive defects.
The researchers surveyed 3,193 papers that included a multitude of studies. Although most of the papers reported studies that included both sexes, only 19% of surveyed studies used what Dr. Galea called an optimal design for the discovery of sex differences. “What I mean by ‘optimally’ is the design of the experiments and the analysis of sex as a variable,” she said. And in 2019, only 5% of the studies used sex as a variable for determining differences between the sexes, the study found.
In the current research, two authors read the methods and results of each study described in each paper, Dr. Galea said. The readers noted whether the paper reported the study sample size and whether the studies used a balanced design. The surveyed journals include Nature Neuroscience, Neuron, Journal of Neuroscience, Molecular Psychiatry, Biological Psychiatry, and Neuropsychopharmacology.
‘Not much is changing’
“I had a suspicion that this was happening,” Dr. Galea said. “I didn’t know that it’s so bad, to be fair.” The “good news story,” she said, is that more papers considered sex as a factor in the later years surveyed. In 2019, more than 95% of papers across both disciplines reported participants’ sex, compared with about 70% in 2009. However, less than 20% of the papers in all study years reported studies that used sex optimally to determine differences between the sexes.
“The other thing that shocked me,” Dr. Galea said, “was that even despite the fact that we saw this increase in the number of papers that were using males and females, we didn’t see the sort of corresponding increase in those that were using ‘optimal design’ or ‘optimal analysis,’ ” Dr. Galea said. In 2009, 14% of papers used optimal design and 2% used optimal analysis for determining sex differences. By 2019, those percentages were 19% and 5%, respectively.
But even the papers that used both sexes had shortcomings, the study found. Just over one-third of these papers (34.5%) didn’t use a balanced design. Just over one-quarter (25.9%) didn’t identify the sample size, a shortcoming that marked 18% of these studies in 2009 and 33% in 2019. Fifteen percent of papers examined included studies that used both sexes inconsistently.
“That matters, because other studies have found that about 20% of papers are doing some kind of analysis with sex, but we had a suspicion that a lot of studies would include sex as a covariate,” Dr. Galea said. “Essentially what that does is, you remove that variable from the data. So, any statistical variation due to sex is then gone.
“The problem with that,” she added, “is you’re not actually looking to see if there’s an influence of sex; you’re removing it.”
Dr. Galea noted that this study points to a need for funding agencies to demand that researchers meet their mandates on sex- and gender-based analysis. “Despite the mandates, not much is really changing as far as the analysis or design of experiments, and we need to figure out how to change that,” she said. “We need to figure out how to get researchers more interested to use the power of studying sex differences.”
‘Not surprising, but disappointing’
Vladimir Hachinski, MD, professor of neurology and epidemiology at Western University in London, Ont., and former editor in chief of Stroke, told this news organization that women have almost twice the life risk of developing dementia, are at higher risk of stroke below age 35 years, and have more severe strokes and higher rates of disability at any age.
Commenting on the current study, Dr. Hachinski said, “It’s not surprising, but it’s disappointing, because we’ve known the difference for a long time.” He added, “The paper is very important because we were not aware that it was that bad.”
Dr. Hachinski also stated, “This paper needs a lot of reading. It’s a great resource, and it should be highlighted as one of those things that needs to be addressed, because it matters.”
The study was funded by a Natural Sciences and Engineering Research Council of Canada grant and by the British Columbia Women’s Foundation. Dr. Galea and Hachinski had no relevant disclosures.
A version of this article first appeared on Medscape.com.
A large percentage of studies in neurology and psychiatry over the past decade have failed to account for differences between the sexes, according to a team of Canadian researchers.
“Despite the fact there are papers that are using males and females in the studies, they’re not using the males and females in the way that would optimally find the possibility of sex differences,” lead author Liisa A.M. Galea, PhD, told this news organization. Dr. Galea is a professor and distinguished scholar at the Djavad Mowafaghian Center for Brain Health at the University of British Columbia in Vancouver.
The study was published online in Nature Communications.
Optimal design uncommon
Differences in how neurologic and psychiatric diseases affect men and women have been well documented. Women, for example, are more susceptible to severe stroke, and men are more prone to cognitive decline with schizophrenia. With Alzheimer’s disease, women typically have more severe cognitive defects.
The researchers surveyed 3,193 papers that included a multitude of studies. Although most of the papers reported studies that included both sexes, only 19% of surveyed studies used what Dr. Galea called an optimal design for the discovery of sex differences. “What I mean by ‘optimally’ is the design of the experiments and the analysis of sex as a variable,” she said. And in 2019, only 5% of the studies used sex as a variable for determining differences between the sexes, the study found.
In the current research, two authors read the methods and results of each study described in each paper, Dr. Galea said. The readers noted whether the paper reported the study sample size and whether the studies used a balanced design. The surveyed journals include Nature Neuroscience, Neuron, Journal of Neuroscience, Molecular Psychiatry, Biological Psychiatry, and Neuropsychopharmacology.
‘Not much is changing’
“I had a suspicion that this was happening,” Dr. Galea said. “I didn’t know that it’s so bad, to be fair.” The “good news story,” she said, is that more papers considered sex as a factor in the later years surveyed. In 2019, more than 95% of papers across both disciplines reported participants’ sex, compared with about 70% in 2009. However, less than 20% of the papers in all study years reported studies that used sex optimally to determine differences between the sexes.
“The other thing that shocked me,” Dr. Galea said, “was that even despite the fact that we saw this increase in the number of papers that were using males and females, we didn’t see the sort of corresponding increase in those that were using ‘optimal design’ or ‘optimal analysis,’ ” Dr. Galea said. In 2009, 14% of papers used optimal design and 2% used optimal analysis for determining sex differences. By 2019, those percentages were 19% and 5%, respectively.
But even the papers that used both sexes had shortcomings, the study found. Just over one-third of these papers (34.5%) didn’t use a balanced design. Just over one-quarter (25.9%) didn’t identify the sample size, a shortcoming that marked 18% of these studies in 2009 and 33% in 2019. Fifteen percent of papers examined included studies that used both sexes inconsistently.
“That matters, because other studies have found that about 20% of papers are doing some kind of analysis with sex, but we had a suspicion that a lot of studies would include sex as a covariate,” Dr. Galea said. “Essentially what that does is, you remove that variable from the data. So, any statistical variation due to sex is then gone.
“The problem with that,” she added, “is you’re not actually looking to see if there’s an influence of sex; you’re removing it.”
Dr. Galea noted that this study points to a need for funding agencies to demand that researchers meet their mandates on sex- and gender-based analysis. “Despite the mandates, not much is really changing as far as the analysis or design of experiments, and we need to figure out how to change that,” she said. “We need to figure out how to get researchers more interested to use the power of studying sex differences.”
‘Not surprising, but disappointing’
Vladimir Hachinski, MD, professor of neurology and epidemiology at Western University in London, Ont., and former editor in chief of Stroke, told this news organization that women have almost twice the life risk of developing dementia, are at higher risk of stroke below age 35 years, and have more severe strokes and higher rates of disability at any age.
Commenting on the current study, Dr. Hachinski said, “It’s not surprising, but it’s disappointing, because we’ve known the difference for a long time.” He added, “The paper is very important because we were not aware that it was that bad.”
Dr. Hachinski also stated, “This paper needs a lot of reading. It’s a great resource, and it should be highlighted as one of those things that needs to be addressed, because it matters.”
The study was funded by a Natural Sciences and Engineering Research Council of Canada grant and by the British Columbia Women’s Foundation. Dr. Galea and Hachinski had no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM NATURE COMMUNICATIONS
Do psychotropic meds raise or lower COVID risk in psych patients?
Investigators found that second-generation antipsychotics were associated with a 48% lower risk of COVID-19, while valproic acid was associated with a 39% increased risk of the disease.
“Exposures to several psychotropic medications were associated with risk of COVID-19 infection among inpatients with serious mental illness; decreased risk was observed with the use of second generation antipsychotics, with paliperidone use associated with the largest effect size. Valproic acid use was associated with an increased risk of infection,” the investigators, led by Katlyn Nemani, MD, at NYU Langone Medical Center, New York, write.
The study was published online in JAMA Network Open.
Vulnerable population
Patients with serious mental illness are particularly vulnerable to COVID-19. Several psychotropic medications have been identified as potential therapeutic agents to prevent or treat COVID-19, but they have not been systematically studied in this patient population.
The researchers analyzed data from 1,958 adults who were continuously hospitalized with serious mental illness from March 8 to July 1, 2020. The mean age was 51.4 years, and 1,442 (74%) were men.
A total of 969 patients (49.5%) had laboratory-confirmed COVID-19 while hospitalized, and 38 (3.9%) died – a mortality rate four times higher than estimates from the general population in New York during the same time frame, the researchers note.
“This finding is consistent with prior studies that have found increased rates of infection in congregate settings and increased mortality after infection among patients with serious mental illness,” the investigators write.
The use of second-generation antipsychotic medications, as a class, was associated with a lower likelihood of COVID-19 (odds ratio, 0.62; 95% confidence interval, 0.45-0.86), while the use of mood stabilizers was associated with increased likelihood of infection (OR, 1.23; 95% CI, 1.03-1.47).
In a multivariable model of individual medications, use of the long-acting atypical antipsychotic paliperidone was associated with a lower odds of infection (OR, 0.59; 95% CI, 0.41-0.84), and use of valproic acid was associated with increased odds of infection (OR, 1.39; 95% CI, 1.10-1.76).
Valproic acid downregulates angiotensin-converting enzyme 2 in endothelial cells, which may impair immune function and contribute to poor outcomes for patients with COVID-19, the researchers say.
The use of clozapine was associated with reduced odds of COVID-related death (unadjusted OR, 0.25; 95% CI, 0.10-0.62; fully adjusted OR, 0.43; 95% CI, 0.17-1.12).
“Although there have been concerns about clozapine use during the pandemic as a risk factor for pneumonia and potential toxic effects during acute infection, clozapine use was not associated with an increased risk of COVID-19 infection or death in the present study. In fact, unadjusted estimates suggested a significant protective association,” the investigators write.
However, they note, data on clozapine and COVID-19 have been mixed.
Two prior studies of health record data showed an increased risk of COVID-19 associated with clozapine treatment, while a study that was limited to inpatients found a lower risk of infection and a lower risk of symptomatic disease in association with clozapine use.
The researchers also found a lower mortality risk in patients taking antidepressants; there were no COVID-related deaths among patients taking escitalopram, venlafaxine, bupropion, or fluvoxamine.
Although the association was not statistically significant, this observation is in line with larger studies that showed reduced risk of adverse outcomes associated with antidepressant use, the researchers note.
A matter of debate
In an accompanying commentary, Benedetta Vai, PhD, and Mario Gennaro Mazza, MD, with IRCCS San Raffaele Scientific Institute, Milan, point out that the link between psychopharmacologic compounds, in particular antipsychotics, and severe COVID-19 outcomes remains “a matter of debate, with inconsistent findings between studies.”
They note further research is needed to determine whether the protective role of second-generation antipsychotics on risk of COVID-19 is mediated by an immune effect or by the direct antiviral properties of these molecules.
The study had no specific funding. Dr. Nemani, Dr. Vai, and Dr. Mazza have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators found that second-generation antipsychotics were associated with a 48% lower risk of COVID-19, while valproic acid was associated with a 39% increased risk of the disease.
“Exposures to several psychotropic medications were associated with risk of COVID-19 infection among inpatients with serious mental illness; decreased risk was observed with the use of second generation antipsychotics, with paliperidone use associated with the largest effect size. Valproic acid use was associated with an increased risk of infection,” the investigators, led by Katlyn Nemani, MD, at NYU Langone Medical Center, New York, write.
The study was published online in JAMA Network Open.
Vulnerable population
Patients with serious mental illness are particularly vulnerable to COVID-19. Several psychotropic medications have been identified as potential therapeutic agents to prevent or treat COVID-19, but they have not been systematically studied in this patient population.
The researchers analyzed data from 1,958 adults who were continuously hospitalized with serious mental illness from March 8 to July 1, 2020. The mean age was 51.4 years, and 1,442 (74%) were men.
A total of 969 patients (49.5%) had laboratory-confirmed COVID-19 while hospitalized, and 38 (3.9%) died – a mortality rate four times higher than estimates from the general population in New York during the same time frame, the researchers note.
“This finding is consistent with prior studies that have found increased rates of infection in congregate settings and increased mortality after infection among patients with serious mental illness,” the investigators write.
The use of second-generation antipsychotic medications, as a class, was associated with a lower likelihood of COVID-19 (odds ratio, 0.62; 95% confidence interval, 0.45-0.86), while the use of mood stabilizers was associated with increased likelihood of infection (OR, 1.23; 95% CI, 1.03-1.47).
In a multivariable model of individual medications, use of the long-acting atypical antipsychotic paliperidone was associated with a lower odds of infection (OR, 0.59; 95% CI, 0.41-0.84), and use of valproic acid was associated with increased odds of infection (OR, 1.39; 95% CI, 1.10-1.76).
Valproic acid downregulates angiotensin-converting enzyme 2 in endothelial cells, which may impair immune function and contribute to poor outcomes for patients with COVID-19, the researchers say.
The use of clozapine was associated with reduced odds of COVID-related death (unadjusted OR, 0.25; 95% CI, 0.10-0.62; fully adjusted OR, 0.43; 95% CI, 0.17-1.12).
“Although there have been concerns about clozapine use during the pandemic as a risk factor for pneumonia and potential toxic effects during acute infection, clozapine use was not associated with an increased risk of COVID-19 infection or death in the present study. In fact, unadjusted estimates suggested a significant protective association,” the investigators write.
However, they note, data on clozapine and COVID-19 have been mixed.
Two prior studies of health record data showed an increased risk of COVID-19 associated with clozapine treatment, while a study that was limited to inpatients found a lower risk of infection and a lower risk of symptomatic disease in association with clozapine use.
The researchers also found a lower mortality risk in patients taking antidepressants; there were no COVID-related deaths among patients taking escitalopram, venlafaxine, bupropion, or fluvoxamine.
Although the association was not statistically significant, this observation is in line with larger studies that showed reduced risk of adverse outcomes associated with antidepressant use, the researchers note.
A matter of debate
In an accompanying commentary, Benedetta Vai, PhD, and Mario Gennaro Mazza, MD, with IRCCS San Raffaele Scientific Institute, Milan, point out that the link between psychopharmacologic compounds, in particular antipsychotics, and severe COVID-19 outcomes remains “a matter of debate, with inconsistent findings between studies.”
They note further research is needed to determine whether the protective role of second-generation antipsychotics on risk of COVID-19 is mediated by an immune effect or by the direct antiviral properties of these molecules.
The study had no specific funding. Dr. Nemani, Dr. Vai, and Dr. Mazza have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators found that second-generation antipsychotics were associated with a 48% lower risk of COVID-19, while valproic acid was associated with a 39% increased risk of the disease.
“Exposures to several psychotropic medications were associated with risk of COVID-19 infection among inpatients with serious mental illness; decreased risk was observed with the use of second generation antipsychotics, with paliperidone use associated with the largest effect size. Valproic acid use was associated with an increased risk of infection,” the investigators, led by Katlyn Nemani, MD, at NYU Langone Medical Center, New York, write.
The study was published online in JAMA Network Open.
Vulnerable population
Patients with serious mental illness are particularly vulnerable to COVID-19. Several psychotropic medications have been identified as potential therapeutic agents to prevent or treat COVID-19, but they have not been systematically studied in this patient population.
The researchers analyzed data from 1,958 adults who were continuously hospitalized with serious mental illness from March 8 to July 1, 2020. The mean age was 51.4 years, and 1,442 (74%) were men.
A total of 969 patients (49.5%) had laboratory-confirmed COVID-19 while hospitalized, and 38 (3.9%) died – a mortality rate four times higher than estimates from the general population in New York during the same time frame, the researchers note.
“This finding is consistent with prior studies that have found increased rates of infection in congregate settings and increased mortality after infection among patients with serious mental illness,” the investigators write.
The use of second-generation antipsychotic medications, as a class, was associated with a lower likelihood of COVID-19 (odds ratio, 0.62; 95% confidence interval, 0.45-0.86), while the use of mood stabilizers was associated with increased likelihood of infection (OR, 1.23; 95% CI, 1.03-1.47).
In a multivariable model of individual medications, use of the long-acting atypical antipsychotic paliperidone was associated with a lower odds of infection (OR, 0.59; 95% CI, 0.41-0.84), and use of valproic acid was associated with increased odds of infection (OR, 1.39; 95% CI, 1.10-1.76).
Valproic acid downregulates angiotensin-converting enzyme 2 in endothelial cells, which may impair immune function and contribute to poor outcomes for patients with COVID-19, the researchers say.
The use of clozapine was associated with reduced odds of COVID-related death (unadjusted OR, 0.25; 95% CI, 0.10-0.62; fully adjusted OR, 0.43; 95% CI, 0.17-1.12).
“Although there have been concerns about clozapine use during the pandemic as a risk factor for pneumonia and potential toxic effects during acute infection, clozapine use was not associated with an increased risk of COVID-19 infection or death in the present study. In fact, unadjusted estimates suggested a significant protective association,” the investigators write.
However, they note, data on clozapine and COVID-19 have been mixed.
Two prior studies of health record data showed an increased risk of COVID-19 associated with clozapine treatment, while a study that was limited to inpatients found a lower risk of infection and a lower risk of symptomatic disease in association with clozapine use.
The researchers also found a lower mortality risk in patients taking antidepressants; there were no COVID-related deaths among patients taking escitalopram, venlafaxine, bupropion, or fluvoxamine.
Although the association was not statistically significant, this observation is in line with larger studies that showed reduced risk of adverse outcomes associated with antidepressant use, the researchers note.
A matter of debate
In an accompanying commentary, Benedetta Vai, PhD, and Mario Gennaro Mazza, MD, with IRCCS San Raffaele Scientific Institute, Milan, point out that the link between psychopharmacologic compounds, in particular antipsychotics, and severe COVID-19 outcomes remains “a matter of debate, with inconsistent findings between studies.”
They note further research is needed to determine whether the protective role of second-generation antipsychotics on risk of COVID-19 is mediated by an immune effect or by the direct antiviral properties of these molecules.
The study had no specific funding. Dr. Nemani, Dr. Vai, and Dr. Mazza have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
TikTok challenge hits Taco Bell right in its ‘Stuft Nacho’
Losing weight for TikTok: Taco Bell edition
There are many reasons why a person would want to lose weight. Too numerous to list. Losing weight to improve your health, however, doesn’t bring in a few hundred thousand TikTok subscribers. Losing weight to convince Taco Bell to bring back an obscure menu item, on the other hand ...
Chris Sandberg, a 37-year-old man from San Francisco, has struggled with his weight for years, losing and gaining hundreds of pounds in an endless cycle of feast and famine. In an unrelated development, at the start of the pandemic he also started making videos on TikTok. As the pandemic wore on, he realized that his excess weight put him at increased risk for severe COVID, as well as other chronic diseases, and he resolved to lose weight. He decided to turn his weight-loss journey into a TikTok challenge but, as we said, losing weight for its own sake isn’t enough for the almighty algorithm. He needed a different goal, preferably something offbeat and a little silly.
Back in 2013, Taco Bell introduced the Grilled Stuft Nacho, “a flour tortilla, shaped like a nacho, stuffed with beef, cheesy jalapeño sauce, sour cream and crunchy red strips,” according to its website. Mr. Sandberg discovered the item in 2015 and instantly fell in love, purchasing one every day for a week. After that first week, however, he discovered, to his horror, that the Grilled Stuft Nacho had been discontinued.
That loss haunted him for years, until inspiration struck in 2021. He pledged to work out every day on TikTok until Taco Bell brought back the Grilled Stuft Nacho. A bit incongruous, exercising for notoriously unhealthy fast food, but that’s kind of the point. He began the challenge on Jan. 4, 2021, and has continued it every day since, nearly 500 days. Over that time, he’s lost 87 pounds (from 275 at the start to under 190) and currently has 450,000 TikTok subscribers.
A year into the challenge, a local Taco Bell made Mr. Sandberg his beloved Grilled Stuft Nacho, but since the challenge was to exercise until Taco Bell brings the item back to all its restaurants, not just for him, the great journey continues. And we admire him for it. In fact, he’s inspired us: We will write a LOTME every week until it receives a Pulitzer Prize. This is important journalism we do here. Don’t deny it!
Episode XIX: COVID strikes back
So what’s next for COVID? Is Disney going to turn it into a series? Can it support a spin-off? Did James Cameron really buy the movie rights? Can it compete against the NFL in the all-important 18-34 demographic? When are Star Wars characters going to get involved?
COVID’s motivations and negotiations are pretty much a mystery to us, but we can answer that last question. They already are involved. Well, one of them anyway.
The Chinese government has been enforcing a COVID lockdown in Shanghai for over a month now, but authorities had started letting people out of their homes for short periods of time. A recent push to bring down transmission, however, has made residents increasingly frustrated and argumentative, according to Reuters.
A now-unavailable video, which Reuters could not verify, surfaced on Chinese social media showing police in hazmat suits arguing with people who were being told that they were going to be quarantined because a neighbor had tested positive.
That’s when the Force kicks in, and this next bit comes directly from the Reuters report: “This is so that we can thoroughly remove any positive cases,” one of the officers is heard saying. “Stop asking me why, there is no why.”
There is no why? Does that remind you of someone? Someone short and green, with an odd syntax? That’s right. Clearly, Yoda it is. Yoda is alive and working for the Chinese government in Shanghai. You read it here first.
Your coffee may be guilty of sexual discrimination
How do you take your coffee? Espresso, drip, instant, or brewed from a regular old coffee machine? Well, a recent study published in Open Heart suggests that gender and brewing method can alter your coffee’s effect on cholesterol levels.
Besides caffeine, coffee beans have naturally occurring chemicals such as diterpenes, cafestol, and kahweol that raise cholesterol levels in the blood. And then there are the various brewing methods, which are going to release different amounts of chemicals from the beans. According to Consumer Reports, an ounce of espresso has 63 mg of caffeine and an ounce of regular coffee has 12-16 mg. That’s a bit deceiving, though, since no one ever drinks an ounce of regular coffee, so figure 96-128 mg of caffeine for an 8-ounce cup. That’s enough to make anyone’s heart race.
Data from 21,083 participants in the seventh survey of the Tromsø Study who were aged 40 and older showed that women drank a mean of 3.8 cups per day while men drank 4.9 cups. Drinking six or more cups of plunger-brewed coffee was associated with increased cholesterol in both genders, but drinking three to five cups of espresso was significantly associated with high cholesterol in men only. Having six or more cups of filtered coffee daily raised cholesterol in women, but instant coffee increased cholesterol levels in both genders, regardless of how many cups they drank.
People all over the planet drink coffee, some of us like our lives depend on it. Since “coffee is the most frequently consumed central stimulant worldwide,” the investigators said, “even small health effects can have considerable health consequences.”
We’ll drink to that.
Have you ever dreamed of having a clone?
When will science grace us with the ability to clone ourselves? It sounds like a dream come true. Our clones can do the stuff that we don’t want to do, like sit in on that 3-hour meeting or do our grocery shopping – really just all the boring stuff we don’t want to do.
In 1996, when a sheep named Dolly became the first mammal cloned successfully, people thought it was the start of an amazing cloning era, but, alas, we haven’t made it to cloning humans yet, as LiveScience discovered when it took a look at the subject.
The idea of cloning was quite exciting for science, as people looked forward to eradicating genetic diseases and birth defects. Research done in 1999, however, countered those hopes by suggesting that cloning might increase birth defects.
So why do you think we haven’t advanced to truly cloning humans? Ethics? Time and effort? Technological barriers? “Human cloning is a particularly dramatic action, and was one of the topics that helped launch American bioethics,” Hank Greely, professor of law and genetics at Stanford (Calif.) University, told LiveScience.
What if the clones turned evil and were bent on destroying the world?
We might imagine a clone of ourselves being completely identical to us in our thoughts, actions, and physical looks. However, that’s not necessarily true; a clone would be its own person even if it looks exactly like you.
So what do the professionals think? Is it worth giving human cloning a shot? Are there benefits? Mr. Greely said that “there are none that we should be willing to consider.”
The dream of having a clone to help your son with his math homework may have gone down the drain, but maybe it’s best not to open doors that could lead to drastic changes in our world.
Losing weight for TikTok: Taco Bell edition
There are many reasons why a person would want to lose weight. Too numerous to list. Losing weight to improve your health, however, doesn’t bring in a few hundred thousand TikTok subscribers. Losing weight to convince Taco Bell to bring back an obscure menu item, on the other hand ...
Chris Sandberg, a 37-year-old man from San Francisco, has struggled with his weight for years, losing and gaining hundreds of pounds in an endless cycle of feast and famine. In an unrelated development, at the start of the pandemic he also started making videos on TikTok. As the pandemic wore on, he realized that his excess weight put him at increased risk for severe COVID, as well as other chronic diseases, and he resolved to lose weight. He decided to turn his weight-loss journey into a TikTok challenge but, as we said, losing weight for its own sake isn’t enough for the almighty algorithm. He needed a different goal, preferably something offbeat and a little silly.
Back in 2013, Taco Bell introduced the Grilled Stuft Nacho, “a flour tortilla, shaped like a nacho, stuffed with beef, cheesy jalapeño sauce, sour cream and crunchy red strips,” according to its website. Mr. Sandberg discovered the item in 2015 and instantly fell in love, purchasing one every day for a week. After that first week, however, he discovered, to his horror, that the Grilled Stuft Nacho had been discontinued.
That loss haunted him for years, until inspiration struck in 2021. He pledged to work out every day on TikTok until Taco Bell brought back the Grilled Stuft Nacho. A bit incongruous, exercising for notoriously unhealthy fast food, but that’s kind of the point. He began the challenge on Jan. 4, 2021, and has continued it every day since, nearly 500 days. Over that time, he’s lost 87 pounds (from 275 at the start to under 190) and currently has 450,000 TikTok subscribers.
A year into the challenge, a local Taco Bell made Mr. Sandberg his beloved Grilled Stuft Nacho, but since the challenge was to exercise until Taco Bell brings the item back to all its restaurants, not just for him, the great journey continues. And we admire him for it. In fact, he’s inspired us: We will write a LOTME every week until it receives a Pulitzer Prize. This is important journalism we do here. Don’t deny it!
Episode XIX: COVID strikes back
So what’s next for COVID? Is Disney going to turn it into a series? Can it support a spin-off? Did James Cameron really buy the movie rights? Can it compete against the NFL in the all-important 18-34 demographic? When are Star Wars characters going to get involved?
COVID’s motivations and negotiations are pretty much a mystery to us, but we can answer that last question. They already are involved. Well, one of them anyway.
The Chinese government has been enforcing a COVID lockdown in Shanghai for over a month now, but authorities had started letting people out of their homes for short periods of time. A recent push to bring down transmission, however, has made residents increasingly frustrated and argumentative, according to Reuters.
A now-unavailable video, which Reuters could not verify, surfaced on Chinese social media showing police in hazmat suits arguing with people who were being told that they were going to be quarantined because a neighbor had tested positive.
That’s when the Force kicks in, and this next bit comes directly from the Reuters report: “This is so that we can thoroughly remove any positive cases,” one of the officers is heard saying. “Stop asking me why, there is no why.”
There is no why? Does that remind you of someone? Someone short and green, with an odd syntax? That’s right. Clearly, Yoda it is. Yoda is alive and working for the Chinese government in Shanghai. You read it here first.
Your coffee may be guilty of sexual discrimination
How do you take your coffee? Espresso, drip, instant, or brewed from a regular old coffee machine? Well, a recent study published in Open Heart suggests that gender and brewing method can alter your coffee’s effect on cholesterol levels.
Besides caffeine, coffee beans have naturally occurring chemicals such as diterpenes, cafestol, and kahweol that raise cholesterol levels in the blood. And then there are the various brewing methods, which are going to release different amounts of chemicals from the beans. According to Consumer Reports, an ounce of espresso has 63 mg of caffeine and an ounce of regular coffee has 12-16 mg. That’s a bit deceiving, though, since no one ever drinks an ounce of regular coffee, so figure 96-128 mg of caffeine for an 8-ounce cup. That’s enough to make anyone’s heart race.
Data from 21,083 participants in the seventh survey of the Tromsø Study who were aged 40 and older showed that women drank a mean of 3.8 cups per day while men drank 4.9 cups. Drinking six or more cups of plunger-brewed coffee was associated with increased cholesterol in both genders, but drinking three to five cups of espresso was significantly associated with high cholesterol in men only. Having six or more cups of filtered coffee daily raised cholesterol in women, but instant coffee increased cholesterol levels in both genders, regardless of how many cups they drank.
People all over the planet drink coffee, some of us like our lives depend on it. Since “coffee is the most frequently consumed central stimulant worldwide,” the investigators said, “even small health effects can have considerable health consequences.”
We’ll drink to that.
Have you ever dreamed of having a clone?
When will science grace us with the ability to clone ourselves? It sounds like a dream come true. Our clones can do the stuff that we don’t want to do, like sit in on that 3-hour meeting or do our grocery shopping – really just all the boring stuff we don’t want to do.
In 1996, when a sheep named Dolly became the first mammal cloned successfully, people thought it was the start of an amazing cloning era, but, alas, we haven’t made it to cloning humans yet, as LiveScience discovered when it took a look at the subject.
The idea of cloning was quite exciting for science, as people looked forward to eradicating genetic diseases and birth defects. Research done in 1999, however, countered those hopes by suggesting that cloning might increase birth defects.
So why do you think we haven’t advanced to truly cloning humans? Ethics? Time and effort? Technological barriers? “Human cloning is a particularly dramatic action, and was one of the topics that helped launch American bioethics,” Hank Greely, professor of law and genetics at Stanford (Calif.) University, told LiveScience.
What if the clones turned evil and were bent on destroying the world?
We might imagine a clone of ourselves being completely identical to us in our thoughts, actions, and physical looks. However, that’s not necessarily true; a clone would be its own person even if it looks exactly like you.
So what do the professionals think? Is it worth giving human cloning a shot? Are there benefits? Mr. Greely said that “there are none that we should be willing to consider.”
The dream of having a clone to help your son with his math homework may have gone down the drain, but maybe it’s best not to open doors that could lead to drastic changes in our world.
Losing weight for TikTok: Taco Bell edition
There are many reasons why a person would want to lose weight. Too numerous to list. Losing weight to improve your health, however, doesn’t bring in a few hundred thousand TikTok subscribers. Losing weight to convince Taco Bell to bring back an obscure menu item, on the other hand ...
Chris Sandberg, a 37-year-old man from San Francisco, has struggled with his weight for years, losing and gaining hundreds of pounds in an endless cycle of feast and famine. In an unrelated development, at the start of the pandemic he also started making videos on TikTok. As the pandemic wore on, he realized that his excess weight put him at increased risk for severe COVID, as well as other chronic diseases, and he resolved to lose weight. He decided to turn his weight-loss journey into a TikTok challenge but, as we said, losing weight for its own sake isn’t enough for the almighty algorithm. He needed a different goal, preferably something offbeat and a little silly.
Back in 2013, Taco Bell introduced the Grilled Stuft Nacho, “a flour tortilla, shaped like a nacho, stuffed with beef, cheesy jalapeño sauce, sour cream and crunchy red strips,” according to its website. Mr. Sandberg discovered the item in 2015 and instantly fell in love, purchasing one every day for a week. After that first week, however, he discovered, to his horror, that the Grilled Stuft Nacho had been discontinued.
That loss haunted him for years, until inspiration struck in 2021. He pledged to work out every day on TikTok until Taco Bell brought back the Grilled Stuft Nacho. A bit incongruous, exercising for notoriously unhealthy fast food, but that’s kind of the point. He began the challenge on Jan. 4, 2021, and has continued it every day since, nearly 500 days. Over that time, he’s lost 87 pounds (from 275 at the start to under 190) and currently has 450,000 TikTok subscribers.
A year into the challenge, a local Taco Bell made Mr. Sandberg his beloved Grilled Stuft Nacho, but since the challenge was to exercise until Taco Bell brings the item back to all its restaurants, not just for him, the great journey continues. And we admire him for it. In fact, he’s inspired us: We will write a LOTME every week until it receives a Pulitzer Prize. This is important journalism we do here. Don’t deny it!
Episode XIX: COVID strikes back
So what’s next for COVID? Is Disney going to turn it into a series? Can it support a spin-off? Did James Cameron really buy the movie rights? Can it compete against the NFL in the all-important 18-34 demographic? When are Star Wars characters going to get involved?
COVID’s motivations and negotiations are pretty much a mystery to us, but we can answer that last question. They already are involved. Well, one of them anyway.
The Chinese government has been enforcing a COVID lockdown in Shanghai for over a month now, but authorities had started letting people out of their homes for short periods of time. A recent push to bring down transmission, however, has made residents increasingly frustrated and argumentative, according to Reuters.
A now-unavailable video, which Reuters could not verify, surfaced on Chinese social media showing police in hazmat suits arguing with people who were being told that they were going to be quarantined because a neighbor had tested positive.
That’s when the Force kicks in, and this next bit comes directly from the Reuters report: “This is so that we can thoroughly remove any positive cases,” one of the officers is heard saying. “Stop asking me why, there is no why.”
There is no why? Does that remind you of someone? Someone short and green, with an odd syntax? That’s right. Clearly, Yoda it is. Yoda is alive and working for the Chinese government in Shanghai. You read it here first.
Your coffee may be guilty of sexual discrimination
How do you take your coffee? Espresso, drip, instant, or brewed from a regular old coffee machine? Well, a recent study published in Open Heart suggests that gender and brewing method can alter your coffee’s effect on cholesterol levels.
Besides caffeine, coffee beans have naturally occurring chemicals such as diterpenes, cafestol, and kahweol that raise cholesterol levels in the blood. And then there are the various brewing methods, which are going to release different amounts of chemicals from the beans. According to Consumer Reports, an ounce of espresso has 63 mg of caffeine and an ounce of regular coffee has 12-16 mg. That’s a bit deceiving, though, since no one ever drinks an ounce of regular coffee, so figure 96-128 mg of caffeine for an 8-ounce cup. That’s enough to make anyone’s heart race.
Data from 21,083 participants in the seventh survey of the Tromsø Study who were aged 40 and older showed that women drank a mean of 3.8 cups per day while men drank 4.9 cups. Drinking six or more cups of plunger-brewed coffee was associated with increased cholesterol in both genders, but drinking three to five cups of espresso was significantly associated with high cholesterol in men only. Having six or more cups of filtered coffee daily raised cholesterol in women, but instant coffee increased cholesterol levels in both genders, regardless of how many cups they drank.
People all over the planet drink coffee, some of us like our lives depend on it. Since “coffee is the most frequently consumed central stimulant worldwide,” the investigators said, “even small health effects can have considerable health consequences.”
We’ll drink to that.
Have you ever dreamed of having a clone?
When will science grace us with the ability to clone ourselves? It sounds like a dream come true. Our clones can do the stuff that we don’t want to do, like sit in on that 3-hour meeting or do our grocery shopping – really just all the boring stuff we don’t want to do.
In 1996, when a sheep named Dolly became the first mammal cloned successfully, people thought it was the start of an amazing cloning era, but, alas, we haven’t made it to cloning humans yet, as LiveScience discovered when it took a look at the subject.
The idea of cloning was quite exciting for science, as people looked forward to eradicating genetic diseases and birth defects. Research done in 1999, however, countered those hopes by suggesting that cloning might increase birth defects.
So why do you think we haven’t advanced to truly cloning humans? Ethics? Time and effort? Technological barriers? “Human cloning is a particularly dramatic action, and was one of the topics that helped launch American bioethics,” Hank Greely, professor of law and genetics at Stanford (Calif.) University, told LiveScience.
What if the clones turned evil and were bent on destroying the world?
We might imagine a clone of ourselves being completely identical to us in our thoughts, actions, and physical looks. However, that’s not necessarily true; a clone would be its own person even if it looks exactly like you.
So what do the professionals think? Is it worth giving human cloning a shot? Are there benefits? Mr. Greely said that “there are none that we should be willing to consider.”
The dream of having a clone to help your son with his math homework may have gone down the drain, but maybe it’s best not to open doors that could lead to drastic changes in our world.



















