User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Synthetic chemical in consumer products linked to early death, study says
Daily exposure to phthalates, which are synthetic chemicals founds in many consumer products, may lead to hundreds of thousands of early deaths each year among older adults in the United States, according to a new study published Oct. 12, 2021, in the peer-reviewed journal Environmental Pollution.
The chemicals are found in hundreds of types of products, including children’s toys, food storage containers, makeup, perfume, and shampoo. In the study, those with the highest levels of phthalates had a greater risk of death from any cause, especially heart disease.
“This study adds to the growing database on the impact of plastics on the human body and bolsters public health and business cases for reducing or eliminating the use of plastics,” Leonardo Trasande, MD, the lead author and a professor of environmental medicine and population health at New York University Langone Health, told CNN.
Dr. Trasande and colleagues measured the urine concentration of phthalates in more than 5,000 adults aged 55-64 and compared the levels with the risk of early death over an average of 10 years. The research team controlled for preexisting heart diseases, diabetes, cancer, poor eating habits, physical activity, body mass, and other known hormone disruptors such as bisphenol A, or BPA, an industrial chemical that’s been used since the 1950s to make certain plastics and resins, according to the Mayo Clinic
The research team found that phthalates could contribute to 91,000-107,000 premature deaths per year in the United States. These early deaths could cost the nation $40 billion to $47 billion each year in lost economic productivity.
Phthalates interrupt the body’s endocrine system and hormone production. Previous studies have found that the chemicals are linked with developmental, reproductive, and immune system problems, according to NYU Langone Health. They’ve also been linked with asthma, childhood obesity, heart issues, and cancer.
“These chemicals have a rap sheet,” Dr. Trasande told CNN. “And the fact of the matter is that when you look at the entire body of evidence, it provides a haunting pattern of concern.”
Phthalates are often called “everywhere chemicals” because they are so common, CNN reported. Also called “plasticizers,” they are added to products to make them more durable, including PVC plumbing, vinyl flooring, medical tubing, garden hoses, food packaging, detergents, clothing, furniture, and automotive materials.
People are often exposed when they breathe contaminated air or consume food that comes into contact with the chemical, according to the Centers for Disease Control and Prevention. Children may be exposed by touching plastic items and putting their hands in their mouth.
Dr. Trasande told CNN that it’s possible to lessen exposure to phthalates and other endocrine disruptors such as BPA by using unscented lotions, laundry detergents, and cleaning supplies, as well as substituting glass, stainless steel, ceramic, and wood for plastic food storage.
“First, avoid plastics as much as you can. Never put plastic containers in the microwave or dishwasher, where the heat can break down the linings so they might be absorbed more readily,” he said. “In addition, cooking at home and reducing your use of processed foods can reduce the levels of the chemical exposures you come in contact with.”
A version of this article first appeared on WebMD.com.
Daily exposure to phthalates, which are synthetic chemicals founds in many consumer products, may lead to hundreds of thousands of early deaths each year among older adults in the United States, according to a new study published Oct. 12, 2021, in the peer-reviewed journal Environmental Pollution.
The chemicals are found in hundreds of types of products, including children’s toys, food storage containers, makeup, perfume, and shampoo. In the study, those with the highest levels of phthalates had a greater risk of death from any cause, especially heart disease.
“This study adds to the growing database on the impact of plastics on the human body and bolsters public health and business cases for reducing or eliminating the use of plastics,” Leonardo Trasande, MD, the lead author and a professor of environmental medicine and population health at New York University Langone Health, told CNN.
Dr. Trasande and colleagues measured the urine concentration of phthalates in more than 5,000 adults aged 55-64 and compared the levels with the risk of early death over an average of 10 years. The research team controlled for preexisting heart diseases, diabetes, cancer, poor eating habits, physical activity, body mass, and other known hormone disruptors such as bisphenol A, or BPA, an industrial chemical that’s been used since the 1950s to make certain plastics and resins, according to the Mayo Clinic
The research team found that phthalates could contribute to 91,000-107,000 premature deaths per year in the United States. These early deaths could cost the nation $40 billion to $47 billion each year in lost economic productivity.
Phthalates interrupt the body’s endocrine system and hormone production. Previous studies have found that the chemicals are linked with developmental, reproductive, and immune system problems, according to NYU Langone Health. They’ve also been linked with asthma, childhood obesity, heart issues, and cancer.
“These chemicals have a rap sheet,” Dr. Trasande told CNN. “And the fact of the matter is that when you look at the entire body of evidence, it provides a haunting pattern of concern.”
Phthalates are often called “everywhere chemicals” because they are so common, CNN reported. Also called “plasticizers,” they are added to products to make them more durable, including PVC plumbing, vinyl flooring, medical tubing, garden hoses, food packaging, detergents, clothing, furniture, and automotive materials.
People are often exposed when they breathe contaminated air or consume food that comes into contact with the chemical, according to the Centers for Disease Control and Prevention. Children may be exposed by touching plastic items and putting their hands in their mouth.
Dr. Trasande told CNN that it’s possible to lessen exposure to phthalates and other endocrine disruptors such as BPA by using unscented lotions, laundry detergents, and cleaning supplies, as well as substituting glass, stainless steel, ceramic, and wood for plastic food storage.
“First, avoid plastics as much as you can. Never put plastic containers in the microwave or dishwasher, where the heat can break down the linings so they might be absorbed more readily,” he said. “In addition, cooking at home and reducing your use of processed foods can reduce the levels of the chemical exposures you come in contact with.”
A version of this article first appeared on WebMD.com.
Daily exposure to phthalates, which are synthetic chemicals founds in many consumer products, may lead to hundreds of thousands of early deaths each year among older adults in the United States, according to a new study published Oct. 12, 2021, in the peer-reviewed journal Environmental Pollution.
The chemicals are found in hundreds of types of products, including children’s toys, food storage containers, makeup, perfume, and shampoo. In the study, those with the highest levels of phthalates had a greater risk of death from any cause, especially heart disease.
“This study adds to the growing database on the impact of plastics on the human body and bolsters public health and business cases for reducing or eliminating the use of plastics,” Leonardo Trasande, MD, the lead author and a professor of environmental medicine and population health at New York University Langone Health, told CNN.
Dr. Trasande and colleagues measured the urine concentration of phthalates in more than 5,000 adults aged 55-64 and compared the levels with the risk of early death over an average of 10 years. The research team controlled for preexisting heart diseases, diabetes, cancer, poor eating habits, physical activity, body mass, and other known hormone disruptors such as bisphenol A, or BPA, an industrial chemical that’s been used since the 1950s to make certain plastics and resins, according to the Mayo Clinic
The research team found that phthalates could contribute to 91,000-107,000 premature deaths per year in the United States. These early deaths could cost the nation $40 billion to $47 billion each year in lost economic productivity.
Phthalates interrupt the body’s endocrine system and hormone production. Previous studies have found that the chemicals are linked with developmental, reproductive, and immune system problems, according to NYU Langone Health. They’ve also been linked with asthma, childhood obesity, heart issues, and cancer.
“These chemicals have a rap sheet,” Dr. Trasande told CNN. “And the fact of the matter is that when you look at the entire body of evidence, it provides a haunting pattern of concern.”
Phthalates are often called “everywhere chemicals” because they are so common, CNN reported. Also called “plasticizers,” they are added to products to make them more durable, including PVC plumbing, vinyl flooring, medical tubing, garden hoses, food packaging, detergents, clothing, furniture, and automotive materials.
People are often exposed when they breathe contaminated air or consume food that comes into contact with the chemical, according to the Centers for Disease Control and Prevention. Children may be exposed by touching plastic items and putting their hands in their mouth.
Dr. Trasande told CNN that it’s possible to lessen exposure to phthalates and other endocrine disruptors such as BPA by using unscented lotions, laundry detergents, and cleaning supplies, as well as substituting glass, stainless steel, ceramic, and wood for plastic food storage.
“First, avoid plastics as much as you can. Never put plastic containers in the microwave or dishwasher, where the heat can break down the linings so they might be absorbed more readily,” he said. “In addition, cooking at home and reducing your use of processed foods can reduce the levels of the chemical exposures you come in contact with.”
A version of this article first appeared on WebMD.com.
Anxiety, depression symptoms rose and fell with new COVID cases
Anxiety and depression symptoms increased in adults last winter as COVID-19 surged in the United States but declined in the spring as COVID activity approached its nadir, according to an analysis from the Centers for Disease Control and Prevention.
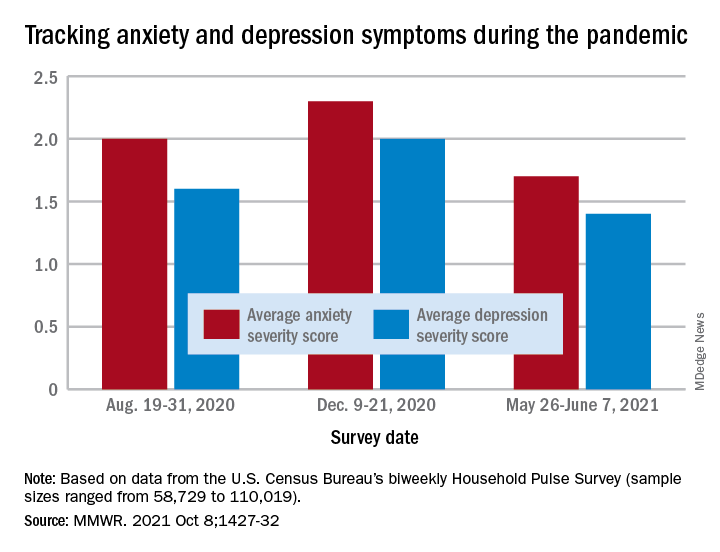
“The relative increases and decreases in frequency of reported symptoms of anxiety and depression at both the national and state levels mirrored the national weekly number of new COVID-19 cases during the same period,” Haomiao Jia, PhD, and associates wrote in the Morbidity and Mortality Weekly Report.
In a national survey conducted Aug. 19-31, 2020, the average anxiety severity score was 2.0 and the average depression score was 1.6 among adults in all 50 states. Those scores rose to 2.3 (+13.0%) and 2.0 (+14.8%), respectively, by Dec. 9-21, but then fell to 1.7 (–26.8%) and 1.4 (–24.8%) during the survey conducted from May 26 to June 7, 2021, the investigators reported.
Despite that decrease in the spring, however, “the frequency of symptoms ... in June 2021 remained elevated compared with estimates from” 2019, said Dr. Jia of Columbia University, New York, and associates. Data from the National Health Interview Survey put the prepandemic severity scores at 0.63 for anxiety and 0.51 for depression.
Weekly symptom frequency in the Household Pulse Survey, which began in April 2020, was assessed with the four-item Patient Health Questionnaire, which includes two questions on anxiety and two on depression. Each answer scored on a scale from 0 (no symptoms at all) to 3 (symptoms nearly every day), making a total of 6 possible for each severity score, they explained. Sample sizes for the biweekly surveys ranged from 58,729 to 110,019.
Among the states, there was something of a pattern involving the drop in scores during the fall and the rise over the winter and spring months. “States with larger increases in severity scores during August–December 2020 also tended to have larger decreases during January–June 2021,” the researchers noted.
That group includes Minnesota, Mississippi, South Dakota, and Utah for anxiety and Idaho, Michigan, Minnesota, and Wisconsin for depression, the survey data show.
Florida and New York had the smallest increases in depression and anxiety scores, respectively, from August to December, and New York had the smallest decrease in both anxiety and depression from January to June, Dr. Jia and associates said.
“ during national emergencies. The observed differences in severity score magnitude and peaks across states in this study indicate that these efforts are important at both the national and state levels,” they wrote.
Anxiety and depression symptoms increased in adults last winter as COVID-19 surged in the United States but declined in the spring as COVID activity approached its nadir, according to an analysis from the Centers for Disease Control and Prevention.
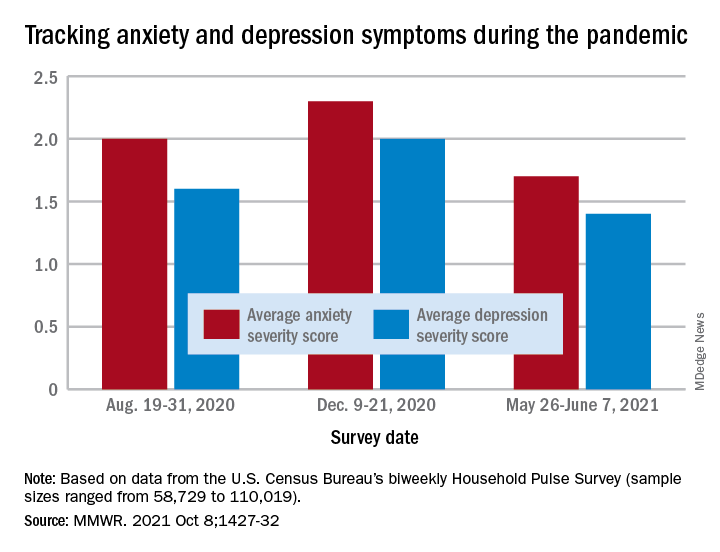
“The relative increases and decreases in frequency of reported symptoms of anxiety and depression at both the national and state levels mirrored the national weekly number of new COVID-19 cases during the same period,” Haomiao Jia, PhD, and associates wrote in the Morbidity and Mortality Weekly Report.
In a national survey conducted Aug. 19-31, 2020, the average anxiety severity score was 2.0 and the average depression score was 1.6 among adults in all 50 states. Those scores rose to 2.3 (+13.0%) and 2.0 (+14.8%), respectively, by Dec. 9-21, but then fell to 1.7 (–26.8%) and 1.4 (–24.8%) during the survey conducted from May 26 to June 7, 2021, the investigators reported.
Despite that decrease in the spring, however, “the frequency of symptoms ... in June 2021 remained elevated compared with estimates from” 2019, said Dr. Jia of Columbia University, New York, and associates. Data from the National Health Interview Survey put the prepandemic severity scores at 0.63 for anxiety and 0.51 for depression.
Weekly symptom frequency in the Household Pulse Survey, which began in April 2020, was assessed with the four-item Patient Health Questionnaire, which includes two questions on anxiety and two on depression. Each answer scored on a scale from 0 (no symptoms at all) to 3 (symptoms nearly every day), making a total of 6 possible for each severity score, they explained. Sample sizes for the biweekly surveys ranged from 58,729 to 110,019.
Among the states, there was something of a pattern involving the drop in scores during the fall and the rise over the winter and spring months. “States with larger increases in severity scores during August–December 2020 also tended to have larger decreases during January–June 2021,” the researchers noted.
That group includes Minnesota, Mississippi, South Dakota, and Utah for anxiety and Idaho, Michigan, Minnesota, and Wisconsin for depression, the survey data show.
Florida and New York had the smallest increases in depression and anxiety scores, respectively, from August to December, and New York had the smallest decrease in both anxiety and depression from January to June, Dr. Jia and associates said.
“ during national emergencies. The observed differences in severity score magnitude and peaks across states in this study indicate that these efforts are important at both the national and state levels,” they wrote.
Anxiety and depression symptoms increased in adults last winter as COVID-19 surged in the United States but declined in the spring as COVID activity approached its nadir, according to an analysis from the Centers for Disease Control and Prevention.
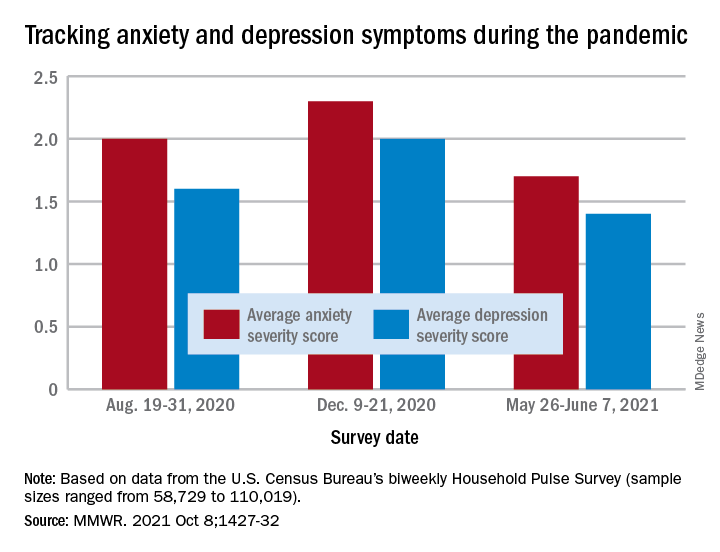
“The relative increases and decreases in frequency of reported symptoms of anxiety and depression at both the national and state levels mirrored the national weekly number of new COVID-19 cases during the same period,” Haomiao Jia, PhD, and associates wrote in the Morbidity and Mortality Weekly Report.
In a national survey conducted Aug. 19-31, 2020, the average anxiety severity score was 2.0 and the average depression score was 1.6 among adults in all 50 states. Those scores rose to 2.3 (+13.0%) and 2.0 (+14.8%), respectively, by Dec. 9-21, but then fell to 1.7 (–26.8%) and 1.4 (–24.8%) during the survey conducted from May 26 to June 7, 2021, the investigators reported.
Despite that decrease in the spring, however, “the frequency of symptoms ... in June 2021 remained elevated compared with estimates from” 2019, said Dr. Jia of Columbia University, New York, and associates. Data from the National Health Interview Survey put the prepandemic severity scores at 0.63 for anxiety and 0.51 for depression.
Weekly symptom frequency in the Household Pulse Survey, which began in April 2020, was assessed with the four-item Patient Health Questionnaire, which includes two questions on anxiety and two on depression. Each answer scored on a scale from 0 (no symptoms at all) to 3 (symptoms nearly every day), making a total of 6 possible for each severity score, they explained. Sample sizes for the biweekly surveys ranged from 58,729 to 110,019.
Among the states, there was something of a pattern involving the drop in scores during the fall and the rise over the winter and spring months. “States with larger increases in severity scores during August–December 2020 also tended to have larger decreases during January–June 2021,” the researchers noted.
That group includes Minnesota, Mississippi, South Dakota, and Utah for anxiety and Idaho, Michigan, Minnesota, and Wisconsin for depression, the survey data show.
Florida and New York had the smallest increases in depression and anxiety scores, respectively, from August to December, and New York had the smallest decrease in both anxiety and depression from January to June, Dr. Jia and associates said.
“ during national emergencies. The observed differences in severity score magnitude and peaks across states in this study indicate that these efforts are important at both the national and state levels,” they wrote.
FROM THE MMWR
Alleged on-the-job violence, racism, prompts psych workers to head to D.C.
A dozen workers from a psychiatric hospital near Seattle flew to Washington, D.C. to picket the National Association for Behavioral Healthcare’s annual meeting in an effort to get their employer to meet demands for a safer work environment, better staffing, and the hiring of security professionals.
They are also demanding that their employer, Cascade Behavioral Health Hospital, a private psychiatric facility owned by Acadia Healthcare and located in Tukwila, Washington, address what they call “racist harassment” by managers who have allegedly told many workers, who are primarily people of color, that they are going to be “filtered out,” Alazar Yirgu, a mental health technician at the facility, told this news organization.
The workers have been conducting a “safety strike” to protest working conditions at Cascade since early August. The protest in Tukwila began after a dozen or more workers were hurt in an August 1 incident during which they had attempted to restrain a violent patient.
“We’ve been out there for 2 months, and we will continue until our voice is heard,” said Mr. Yirgu, who was hospitalized as a result of the August patient outburst that he said has left him unable to work since the incident.
On Oct. 7, Mr. Yirgu and coworkers brought the protest to Washington, D.C., in a continued effort to voice their need for adequate personal protective equipment, increased staffing, and the hiring of security personnel.
“Any health care professional should not be fearful to do their job, because once they are in that state of mind, once they are fearful for themselves, then they are not doing their jobs; they are preoccupied with their fears,” said Mr. Yirgu, who has worked as a technician for 6 years.
Unsafe patient load
The workers reacted quickly after the August 1 patient outburst because there have been multiple previous incidents, Mr. Yirgu said.
In a 2019 news story by the Seattle Times, the newspaper reported there had been 65 assaults on patients or staff at Cascade from 2016 to 2018, resulting in concussions and broken bones in some instances.
Mr. Yirgu said that more recently, a patient broke a second story window, jumped to the ground, and ran off.
At the facility, workers are often assigned to as many as a dozen or more patients, he said, noting that at other psychiatric institutions, he’s cared for a maximum of five patients at once.
The Tukwila police have pushed back against the workers’ description of the incident in which Mr. Yirgu was injured, and Cascade Behavioral Health has aggressively defended its facility.
According to Mr. Yirgu, the expletive-spewing patient was clearly a danger to himself and others – especially after he stole a key card that would give him access to the entire facility, including the kitchen where knives were stored.
When more than a dozen staff answered the unit’s “Code Gray,” they were unable to subdue or restrain him. Mr. Yirgu ended up on the floor underneath the patient after the patient had jumped off a table.
As the incident unfolded, several workers called the police, who initially refused to go to the facility, saying that a new law prevented them from assisting with the restraint if there was no assault.
The Tukwila Police Department report shows that officers finally did go to the facility and determined that “a crime had not been committed based on the information presented to them, that there was no imminent threat of bodily harm, and that there was no legal grounds or authority for them to assist medical staff with physically restraining a patient.”
Cascade pushes back
A Service Employees International Union (SEIU) report shows about 70 workers refused to come in to work after the incident and began picketing outside the facility.
Cascade called it an illegal strike because the protesters had not given 10-days’ notice, as required by federal law, and moved to terminate those who participated. The local SEIU chapter, 1199NW, suggested the workers call their walkout a “safety strike,” because it was organized primarily to protest working conditions.
Meanwhile Cascade, which has erected a large fence so that no one in the facility can see the protesters, has said the strike is primarily about ongoing contract negotiations with the facility’s nurses and its union.
“The Union has been trying to apply unfair – and in some cases we believe unlawful – external pressures to this process, including picketing, work stoppages, smear campaigns, and false accusations,” Cascade CEO Christopher West wrote on the company’s website in mid-August.
He said the facility had “ample personal protective equipment” and that the “well-being and safety of our patients and staff always have been and will be our key priorities.”
In response to a request for comment, Cascade said in an emailed statement that physical confrontations had decreased by almost 50% and elopements (unauthorized leaving of the facility) by 80% from 2018 to 2021.
Cascade spokesperson Gretchen Hommrich said in the statement that the workers it has terminated “were let go for cause in violation to their employment agreement” and said the company still aimed to negotiate a new agreement with the union.
The “efforts outside of the bargaining process serve no productive purpose and have only brought harm to the residents they claim to serve,” said Ms. Hommrich.
‘Safety is the sole purpose’
Mr. Yirgu said it was outrageous to suggest workers were picketing over contract negotiations. “Safety is the sole purpose of this strike,” he said.
He noted that his patient care goal is to have a lot of one-on-one time with his patients, helping them navigate back to the outside world. The facility is supposed to be a safe place, Mr. Yirgu added. Violence inside the facility traumatizes the patients and may worsen their condition and delay their progress, he said.
“If I can’t keep them safe, there’s no way I’m going to be able to see them eye-to-eye when I told them I’d keep them safe and then they’re not anymore,” said Mr. Yirgu.
So far, 22 workers have been “terminated,” meaning they received a termination notice, have been taken off the work schedule by the employer, or otherwise been informed that the employer has deemed them to be separated, the SEIU reports. The organization has filed unfair labor practice (ULPs) for all 22.
A version of this article first appeared on Medscape.com.
A dozen workers from a psychiatric hospital near Seattle flew to Washington, D.C. to picket the National Association for Behavioral Healthcare’s annual meeting in an effort to get their employer to meet demands for a safer work environment, better staffing, and the hiring of security professionals.
They are also demanding that their employer, Cascade Behavioral Health Hospital, a private psychiatric facility owned by Acadia Healthcare and located in Tukwila, Washington, address what they call “racist harassment” by managers who have allegedly told many workers, who are primarily people of color, that they are going to be “filtered out,” Alazar Yirgu, a mental health technician at the facility, told this news organization.
The workers have been conducting a “safety strike” to protest working conditions at Cascade since early August. The protest in Tukwila began after a dozen or more workers were hurt in an August 1 incident during which they had attempted to restrain a violent patient.
“We’ve been out there for 2 months, and we will continue until our voice is heard,” said Mr. Yirgu, who was hospitalized as a result of the August patient outburst that he said has left him unable to work since the incident.
On Oct. 7, Mr. Yirgu and coworkers brought the protest to Washington, D.C., in a continued effort to voice their need for adequate personal protective equipment, increased staffing, and the hiring of security personnel.
“Any health care professional should not be fearful to do their job, because once they are in that state of mind, once they are fearful for themselves, then they are not doing their jobs; they are preoccupied with their fears,” said Mr. Yirgu, who has worked as a technician for 6 years.
Unsafe patient load
The workers reacted quickly after the August 1 patient outburst because there have been multiple previous incidents, Mr. Yirgu said.
In a 2019 news story by the Seattle Times, the newspaper reported there had been 65 assaults on patients or staff at Cascade from 2016 to 2018, resulting in concussions and broken bones in some instances.
Mr. Yirgu said that more recently, a patient broke a second story window, jumped to the ground, and ran off.
At the facility, workers are often assigned to as many as a dozen or more patients, he said, noting that at other psychiatric institutions, he’s cared for a maximum of five patients at once.
The Tukwila police have pushed back against the workers’ description of the incident in which Mr. Yirgu was injured, and Cascade Behavioral Health has aggressively defended its facility.
According to Mr. Yirgu, the expletive-spewing patient was clearly a danger to himself and others – especially after he stole a key card that would give him access to the entire facility, including the kitchen where knives were stored.
When more than a dozen staff answered the unit’s “Code Gray,” they were unable to subdue or restrain him. Mr. Yirgu ended up on the floor underneath the patient after the patient had jumped off a table.
As the incident unfolded, several workers called the police, who initially refused to go to the facility, saying that a new law prevented them from assisting with the restraint if there was no assault.
The Tukwila Police Department report shows that officers finally did go to the facility and determined that “a crime had not been committed based on the information presented to them, that there was no imminent threat of bodily harm, and that there was no legal grounds or authority for them to assist medical staff with physically restraining a patient.”
Cascade pushes back
A Service Employees International Union (SEIU) report shows about 70 workers refused to come in to work after the incident and began picketing outside the facility.
Cascade called it an illegal strike because the protesters had not given 10-days’ notice, as required by federal law, and moved to terminate those who participated. The local SEIU chapter, 1199NW, suggested the workers call their walkout a “safety strike,” because it was organized primarily to protest working conditions.
Meanwhile Cascade, which has erected a large fence so that no one in the facility can see the protesters, has said the strike is primarily about ongoing contract negotiations with the facility’s nurses and its union.
“The Union has been trying to apply unfair – and in some cases we believe unlawful – external pressures to this process, including picketing, work stoppages, smear campaigns, and false accusations,” Cascade CEO Christopher West wrote on the company’s website in mid-August.
He said the facility had “ample personal protective equipment” and that the “well-being and safety of our patients and staff always have been and will be our key priorities.”
In response to a request for comment, Cascade said in an emailed statement that physical confrontations had decreased by almost 50% and elopements (unauthorized leaving of the facility) by 80% from 2018 to 2021.
Cascade spokesperson Gretchen Hommrich said in the statement that the workers it has terminated “were let go for cause in violation to their employment agreement” and said the company still aimed to negotiate a new agreement with the union.
The “efforts outside of the bargaining process serve no productive purpose and have only brought harm to the residents they claim to serve,” said Ms. Hommrich.
‘Safety is the sole purpose’
Mr. Yirgu said it was outrageous to suggest workers were picketing over contract negotiations. “Safety is the sole purpose of this strike,” he said.
He noted that his patient care goal is to have a lot of one-on-one time with his patients, helping them navigate back to the outside world. The facility is supposed to be a safe place, Mr. Yirgu added. Violence inside the facility traumatizes the patients and may worsen their condition and delay their progress, he said.
“If I can’t keep them safe, there’s no way I’m going to be able to see them eye-to-eye when I told them I’d keep them safe and then they’re not anymore,” said Mr. Yirgu.
So far, 22 workers have been “terminated,” meaning they received a termination notice, have been taken off the work schedule by the employer, or otherwise been informed that the employer has deemed them to be separated, the SEIU reports. The organization has filed unfair labor practice (ULPs) for all 22.
A version of this article first appeared on Medscape.com.
A dozen workers from a psychiatric hospital near Seattle flew to Washington, D.C. to picket the National Association for Behavioral Healthcare’s annual meeting in an effort to get their employer to meet demands for a safer work environment, better staffing, and the hiring of security professionals.
They are also demanding that their employer, Cascade Behavioral Health Hospital, a private psychiatric facility owned by Acadia Healthcare and located in Tukwila, Washington, address what they call “racist harassment” by managers who have allegedly told many workers, who are primarily people of color, that they are going to be “filtered out,” Alazar Yirgu, a mental health technician at the facility, told this news organization.
The workers have been conducting a “safety strike” to protest working conditions at Cascade since early August. The protest in Tukwila began after a dozen or more workers were hurt in an August 1 incident during which they had attempted to restrain a violent patient.
“We’ve been out there for 2 months, and we will continue until our voice is heard,” said Mr. Yirgu, who was hospitalized as a result of the August patient outburst that he said has left him unable to work since the incident.
On Oct. 7, Mr. Yirgu and coworkers brought the protest to Washington, D.C., in a continued effort to voice their need for adequate personal protective equipment, increased staffing, and the hiring of security personnel.
“Any health care professional should not be fearful to do their job, because once they are in that state of mind, once they are fearful for themselves, then they are not doing their jobs; they are preoccupied with their fears,” said Mr. Yirgu, who has worked as a technician for 6 years.
Unsafe patient load
The workers reacted quickly after the August 1 patient outburst because there have been multiple previous incidents, Mr. Yirgu said.
In a 2019 news story by the Seattle Times, the newspaper reported there had been 65 assaults on patients or staff at Cascade from 2016 to 2018, resulting in concussions and broken bones in some instances.
Mr. Yirgu said that more recently, a patient broke a second story window, jumped to the ground, and ran off.
At the facility, workers are often assigned to as many as a dozen or more patients, he said, noting that at other psychiatric institutions, he’s cared for a maximum of five patients at once.
The Tukwila police have pushed back against the workers’ description of the incident in which Mr. Yirgu was injured, and Cascade Behavioral Health has aggressively defended its facility.
According to Mr. Yirgu, the expletive-spewing patient was clearly a danger to himself and others – especially after he stole a key card that would give him access to the entire facility, including the kitchen where knives were stored.
When more than a dozen staff answered the unit’s “Code Gray,” they were unable to subdue or restrain him. Mr. Yirgu ended up on the floor underneath the patient after the patient had jumped off a table.
As the incident unfolded, several workers called the police, who initially refused to go to the facility, saying that a new law prevented them from assisting with the restraint if there was no assault.
The Tukwila Police Department report shows that officers finally did go to the facility and determined that “a crime had not been committed based on the information presented to them, that there was no imminent threat of bodily harm, and that there was no legal grounds or authority for them to assist medical staff with physically restraining a patient.”
Cascade pushes back
A Service Employees International Union (SEIU) report shows about 70 workers refused to come in to work after the incident and began picketing outside the facility.
Cascade called it an illegal strike because the protesters had not given 10-days’ notice, as required by federal law, and moved to terminate those who participated. The local SEIU chapter, 1199NW, suggested the workers call their walkout a “safety strike,” because it was organized primarily to protest working conditions.
Meanwhile Cascade, which has erected a large fence so that no one in the facility can see the protesters, has said the strike is primarily about ongoing contract negotiations with the facility’s nurses and its union.
“The Union has been trying to apply unfair – and in some cases we believe unlawful – external pressures to this process, including picketing, work stoppages, smear campaigns, and false accusations,” Cascade CEO Christopher West wrote on the company’s website in mid-August.
He said the facility had “ample personal protective equipment” and that the “well-being and safety of our patients and staff always have been and will be our key priorities.”
In response to a request for comment, Cascade said in an emailed statement that physical confrontations had decreased by almost 50% and elopements (unauthorized leaving of the facility) by 80% from 2018 to 2021.
Cascade spokesperson Gretchen Hommrich said in the statement that the workers it has terminated “were let go for cause in violation to their employment agreement” and said the company still aimed to negotiate a new agreement with the union.
The “efforts outside of the bargaining process serve no productive purpose and have only brought harm to the residents they claim to serve,” said Ms. Hommrich.
‘Safety is the sole purpose’
Mr. Yirgu said it was outrageous to suggest workers were picketing over contract negotiations. “Safety is the sole purpose of this strike,” he said.
He noted that his patient care goal is to have a lot of one-on-one time with his patients, helping them navigate back to the outside world. The facility is supposed to be a safe place, Mr. Yirgu added. Violence inside the facility traumatizes the patients and may worsen their condition and delay their progress, he said.
“If I can’t keep them safe, there’s no way I’m going to be able to see them eye-to-eye when I told them I’d keep them safe and then they’re not anymore,” said Mr. Yirgu.
So far, 22 workers have been “terminated,” meaning they received a termination notice, have been taken off the work schedule by the employer, or otherwise been informed that the employer has deemed them to be separated, the SEIU reports. The organization has filed unfair labor practice (ULPs) for all 22.
A version of this article first appeared on Medscape.com.
Staff education cuts psychotropic drug use in long-term care
The effect of the intervention was transient, possibly because of high staff turnover, according to the investigators in the new randomized, controlled trial.
The findings were presented by Ulla Aalto, MD, PhD, during a session at the European Geriatric Medicine Society annual congress, a hybrid live and online meeting.
There was a significant reduction in the use of psychotropic agents at 6 months in long-term care wards where the nursing staff had undergone a short training session on drug therapy for older patients, but there was no improvement in wards that were randomly assigned to serve as controls, Dr. Aalto, from Helsinki Hospital, reported during the session.
“Future research would be investigating how we could maintain the positive effects that were gained at 6 months but not seen any more at 1 year, and how to implement the good practice in nursing homes by this kind of staff training,” she said.
Heavy drug use
Psychotropic medications are widely used in long-term care settings, but their indiscriminate use or use of the wrong drug for the wrong patient can be harmful. Inappropriate drug use in long-term care settings is also associated with higher costs, Dr. Aalto said.
To see whether a staff-training intervention could reduce drugs use and lower costs, the investigators conducted a randomized clinical trial in assisted living facilities in Helsinki in 2011, with a total of 227 patients 65 years and older.
Long-term care wards were randomly assigned to either an intervention for nursing staff consisting of two 4-hour sessions on good drug-therapy practice for older adults, or to serve as controls (10 wards in each group).
Drug use and costs were monitored at both 6 and 12 months after randomization. Psychotropic drugs included antipsychotics, antidepressants, anxiolytics, and hypnotics as classified by the World Health Organization. For the purposes of comparison, actual doses were counted and converted into relative proportions of defined daily doses.
The baseline characteristics of patients in each group were generally similar, with a mean age of around 83 years. In each study arm, nearly two-thirds of patients were on at least one psychotropic drug, and of this group, a third had been prescribed 2 or more psychotropic agents.
Nearly half of the patients were on at least one antipsychotic agent and/or antidepressant.
Short-term benefit
As noted before, in the wards randomized to staff training, there was a significant reduction in use of all psychotropics from baseline at 6 months after randomization (P = .045), but there was no change among the control wards.
By 12 months, however, the differences between the intervention and control arms narrowed, and drug use in the intervention arm was no longer significantly lower over baseline.
Drugs costs significantly decreased in the intervention group at 6 months (P = .027) and were numerically but not statistically lower over baseline at 12 months.
In contrast, drug costs in the control arm were numerically (but not statistically) higher at both 6 and 12 months of follow-up.
Annual drug costs in the intervention group decreased by mean of 12.3 euros ($14.22) whereas costs in the control group increased by a mean of 20.6 euros ($23.81).
“This quite light and feasible intervention succeeded in reducing overall defined daily doses of psychotropics in the short term,” Dr. Aalto said.
The waning of the intervention’s effect on drug use and costs may be caused partly by the high employee turnover rate in long-term care facilities and to the dilution effect, she said, referring to a form of judgment bias in which people tend to devalue diagnostic information when other, nondiagnostic information is also available.
Randomized design
In the question-and-answer session following her presentation, audience member Jesper Ryg, MD, PhD from Odense (Denmark) University Hospital and the University of Southern Denmark, also in Odense, commented: “It’s a great study, doing a [randomized, controlled trial] on deprescribing, we need more of those.”
“But what we know now is that a lot of studies show it is possible to deprescribe and get less drugs, but do we have any clinical data? Does this deprescribing lead to less falls, did it lead to lower mortality?” he asked.
Dr. Aalto replied that, in an earlier report from this study, investigators showed that harmful medication use was reduced and negative outcomes were reduced.
Another audience member asked why nursing staff were the target of the intervention, given that physicians do the actual drug prescribing.
Dr. Aalto responded: “It is the physician of course who prescribes, but in nursing homes and long-term care, nursing staff is there all the time, and the physicians are kind of consultants who just come there once in a while, so it’s important that the nurses also know about these harmful medications and can bring them to the doctor when he or she arrives there.”
Dr. Aalto and Dr. Ryg had no disclosures.
The effect of the intervention was transient, possibly because of high staff turnover, according to the investigators in the new randomized, controlled trial.
The findings were presented by Ulla Aalto, MD, PhD, during a session at the European Geriatric Medicine Society annual congress, a hybrid live and online meeting.
There was a significant reduction in the use of psychotropic agents at 6 months in long-term care wards where the nursing staff had undergone a short training session on drug therapy for older patients, but there was no improvement in wards that were randomly assigned to serve as controls, Dr. Aalto, from Helsinki Hospital, reported during the session.
“Future research would be investigating how we could maintain the positive effects that were gained at 6 months but not seen any more at 1 year, and how to implement the good practice in nursing homes by this kind of staff training,” she said.
Heavy drug use
Psychotropic medications are widely used in long-term care settings, but their indiscriminate use or use of the wrong drug for the wrong patient can be harmful. Inappropriate drug use in long-term care settings is also associated with higher costs, Dr. Aalto said.
To see whether a staff-training intervention could reduce drugs use and lower costs, the investigators conducted a randomized clinical trial in assisted living facilities in Helsinki in 2011, with a total of 227 patients 65 years and older.
Long-term care wards were randomly assigned to either an intervention for nursing staff consisting of two 4-hour sessions on good drug-therapy practice for older adults, or to serve as controls (10 wards in each group).
Drug use and costs were monitored at both 6 and 12 months after randomization. Psychotropic drugs included antipsychotics, antidepressants, anxiolytics, and hypnotics as classified by the World Health Organization. For the purposes of comparison, actual doses were counted and converted into relative proportions of defined daily doses.
The baseline characteristics of patients in each group were generally similar, with a mean age of around 83 years. In each study arm, nearly two-thirds of patients were on at least one psychotropic drug, and of this group, a third had been prescribed 2 or more psychotropic agents.
Nearly half of the patients were on at least one antipsychotic agent and/or antidepressant.
Short-term benefit
As noted before, in the wards randomized to staff training, there was a significant reduction in use of all psychotropics from baseline at 6 months after randomization (P = .045), but there was no change among the control wards.
By 12 months, however, the differences between the intervention and control arms narrowed, and drug use in the intervention arm was no longer significantly lower over baseline.
Drugs costs significantly decreased in the intervention group at 6 months (P = .027) and were numerically but not statistically lower over baseline at 12 months.
In contrast, drug costs in the control arm were numerically (but not statistically) higher at both 6 and 12 months of follow-up.
Annual drug costs in the intervention group decreased by mean of 12.3 euros ($14.22) whereas costs in the control group increased by a mean of 20.6 euros ($23.81).
“This quite light and feasible intervention succeeded in reducing overall defined daily doses of psychotropics in the short term,” Dr. Aalto said.
The waning of the intervention’s effect on drug use and costs may be caused partly by the high employee turnover rate in long-term care facilities and to the dilution effect, she said, referring to a form of judgment bias in which people tend to devalue diagnostic information when other, nondiagnostic information is also available.
Randomized design
In the question-and-answer session following her presentation, audience member Jesper Ryg, MD, PhD from Odense (Denmark) University Hospital and the University of Southern Denmark, also in Odense, commented: “It’s a great study, doing a [randomized, controlled trial] on deprescribing, we need more of those.”
“But what we know now is that a lot of studies show it is possible to deprescribe and get less drugs, but do we have any clinical data? Does this deprescribing lead to less falls, did it lead to lower mortality?” he asked.
Dr. Aalto replied that, in an earlier report from this study, investigators showed that harmful medication use was reduced and negative outcomes were reduced.
Another audience member asked why nursing staff were the target of the intervention, given that physicians do the actual drug prescribing.
Dr. Aalto responded: “It is the physician of course who prescribes, but in nursing homes and long-term care, nursing staff is there all the time, and the physicians are kind of consultants who just come there once in a while, so it’s important that the nurses also know about these harmful medications and can bring them to the doctor when he or she arrives there.”
Dr. Aalto and Dr. Ryg had no disclosures.
The effect of the intervention was transient, possibly because of high staff turnover, according to the investigators in the new randomized, controlled trial.
The findings were presented by Ulla Aalto, MD, PhD, during a session at the European Geriatric Medicine Society annual congress, a hybrid live and online meeting.
There was a significant reduction in the use of psychotropic agents at 6 months in long-term care wards where the nursing staff had undergone a short training session on drug therapy for older patients, but there was no improvement in wards that were randomly assigned to serve as controls, Dr. Aalto, from Helsinki Hospital, reported during the session.
“Future research would be investigating how we could maintain the positive effects that were gained at 6 months but not seen any more at 1 year, and how to implement the good practice in nursing homes by this kind of staff training,” she said.
Heavy drug use
Psychotropic medications are widely used in long-term care settings, but their indiscriminate use or use of the wrong drug for the wrong patient can be harmful. Inappropriate drug use in long-term care settings is also associated with higher costs, Dr. Aalto said.
To see whether a staff-training intervention could reduce drugs use and lower costs, the investigators conducted a randomized clinical trial in assisted living facilities in Helsinki in 2011, with a total of 227 patients 65 years and older.
Long-term care wards were randomly assigned to either an intervention for nursing staff consisting of two 4-hour sessions on good drug-therapy practice for older adults, or to serve as controls (10 wards in each group).
Drug use and costs were monitored at both 6 and 12 months after randomization. Psychotropic drugs included antipsychotics, antidepressants, anxiolytics, and hypnotics as classified by the World Health Organization. For the purposes of comparison, actual doses were counted and converted into relative proportions of defined daily doses.
The baseline characteristics of patients in each group were generally similar, with a mean age of around 83 years. In each study arm, nearly two-thirds of patients were on at least one psychotropic drug, and of this group, a third had been prescribed 2 or more psychotropic agents.
Nearly half of the patients were on at least one antipsychotic agent and/or antidepressant.
Short-term benefit
As noted before, in the wards randomized to staff training, there was a significant reduction in use of all psychotropics from baseline at 6 months after randomization (P = .045), but there was no change among the control wards.
By 12 months, however, the differences between the intervention and control arms narrowed, and drug use in the intervention arm was no longer significantly lower over baseline.
Drugs costs significantly decreased in the intervention group at 6 months (P = .027) and were numerically but not statistically lower over baseline at 12 months.
In contrast, drug costs in the control arm were numerically (but not statistically) higher at both 6 and 12 months of follow-up.
Annual drug costs in the intervention group decreased by mean of 12.3 euros ($14.22) whereas costs in the control group increased by a mean of 20.6 euros ($23.81).
“This quite light and feasible intervention succeeded in reducing overall defined daily doses of psychotropics in the short term,” Dr. Aalto said.
The waning of the intervention’s effect on drug use and costs may be caused partly by the high employee turnover rate in long-term care facilities and to the dilution effect, she said, referring to a form of judgment bias in which people tend to devalue diagnostic information when other, nondiagnostic information is also available.
Randomized design
In the question-and-answer session following her presentation, audience member Jesper Ryg, MD, PhD from Odense (Denmark) University Hospital and the University of Southern Denmark, also in Odense, commented: “It’s a great study, doing a [randomized, controlled trial] on deprescribing, we need more of those.”
“But what we know now is that a lot of studies show it is possible to deprescribe and get less drugs, but do we have any clinical data? Does this deprescribing lead to less falls, did it lead to lower mortality?” he asked.
Dr. Aalto replied that, in an earlier report from this study, investigators showed that harmful medication use was reduced and negative outcomes were reduced.
Another audience member asked why nursing staff were the target of the intervention, given that physicians do the actual drug prescribing.
Dr. Aalto responded: “It is the physician of course who prescribes, but in nursing homes and long-term care, nursing staff is there all the time, and the physicians are kind of consultants who just come there once in a while, so it’s important that the nurses also know about these harmful medications and can bring them to the doctor when he or she arrives there.”
Dr. Aalto and Dr. Ryg had no disclosures.
FROM EUGMS 2021
Family violence patterns change during pandemic
Among adolescents treated for injuries caused by family-member violence, the proportion of incidents that involved illegal drugs or weapons more than doubled during the pandemic, and incidents that involved alcohol nearly doubled, according to data presented October 10 at the American Academy of Pediatrics 2021 National Conference.
“The COVID-19 pandemic amplified risk factors known to increase family interpersonal violence, such as increased need for parental supervision, parental stress, financial hardship, poor mental health, and isolation,” said investigator Mattea Miller, an MD candidate at the Johns Hopkins University School of Medicine, Baltimore.
To examine the issue, she and her colleagues “sought to characterize the prevalence and circumstances of adolescent injuries resulting from family interpersonal violence,” Ms. Miller told this news organization.
Their retrospective analysis involved children 10 to 15 years of age seen before or during the pandemic in the emergency department at Johns Hopkins Children’s Center for injuries that resulted from a violent incident with a family member.
Of the 819 incidents of violence-related injuries seen during the study period – the prepandemic ran from Jan. 1, 2019 to March 29, 2020, and the pandemic period ran from March 30, 2020, the date a stay-at-home order was first issued in Maryland, to Dec. 31, 2020 – 448 (54.7%) involved a family member. The proportion of such injuries was similar before and during the pandemic (54.6% vs. 54.9%; P = .99).
Most (83.9%) of these incidents occurred at home, 76.6% involved a parent or guardian, and 66.7% involved the youth being transported to the hospital by police.
It is surprising that families accounted for such a high level of violence involving adolescents, said Christopher S. Greeley, MD, MS, chief of the division of public health pediatrics at Texas Children’s Hospital and professor of pediatrics at Baylor College of Medicine, Houston, who was not involved in the research.
“The most common source of child physical abuse in younger children – infants and toddlers – [is the] parents,” who account for about 75% of cases, “but to see that amount of violence in adolescents was unexpected,” he told this news organization.
Patients in the study cohort were more likely to be Black than the hospital’s overall emergency-department population (84.4% vs. 60.0%), and more likely to be covered by public insurance (71.2% vs. 60.0%).
In the study cohort, 54.0% of the patients were female.
“We were surprised to see that 8% of visits did not have a referral to a social worker” – 92% of patients in the study cohort received a social work consult during their visit to the emergency department – and that number “did not vary during the COVID-19 pandemic,” Ms. Miller said. The pandemic exacerbated the types of stresses that social workers can help address, so “this potentially represents a gap in care that is important to address,” she added.
Increase in use of alcohol, drugs, weapons
The most significant increases from the prepandemic period to the pandemic period were in incidents that involved alcohol (10.0% vs. 18.8%; P ≤ .001), illegal drugs (6.5% vs. 14.9%; P ≤ .001), and weapons, most often a knife (10.7% vs. 23.8%; P ≤ .001).
“An obvious potential explanation for the increase in alcohol, drug, and weapons [involvement] would be the mental health impact of the pandemic in conjunction with the economic stressors that some families may be feeling,” Dr. Greeley said. Teachers are the most common reporters of child abuse, so it’s possible that reports of violence decreased when schools switched to remote learning. But with most schools back to in-person learning, data have not yet shown a surge in reporting, he noted.
The “epidemiology of family violence may be impacted by increased time at home, disruptions in school and family routines, exacerbations in mental health conditions, and financial stresses common during the pandemic,” said senior study investigator Leticia Ryan, MD, MPH, director of research in pediatrics at Johns Hopkins Medicine.
And research has shown increases in the use of alcohol and illegal drugs during the pandemic, she noted.
“As we transition to postpandemic life, it will be important to identify at-risk adolescents and families and provide supports,” Dr. Ryan told this news organization. “The emergency department is an appropriate setting to intervene with youth who have experienced family violence and initiate preventive strategies to avoid future violence.”
Among the strategies to identify and intervene for at-risk patients is the CRAFFT substance use screening tool. Furthermore, “case management, involvement of child protection services, and linkage with relevant support services may all be appropriate, depending on circumstances,” Ms. Miller added.
“Exposure to family violence at a young age increases the likelihood that a child will be exposed to additional violence or become a perpetrator of violence in the future, continuing a cycle of violence,” Ms. Miller explained. “Given that studies of adolescent violence often focus on peer violence, a better understanding of the epidemiology of violence-related injuries resulting from family violence is needed to better inform the development of more comprehensive prevention strategies.”
This study did not note any external funding. Ms. Miller, Dr. Greeley, and Dr. Ryan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Among adolescents treated for injuries caused by family-member violence, the proportion of incidents that involved illegal drugs or weapons more than doubled during the pandemic, and incidents that involved alcohol nearly doubled, according to data presented October 10 at the American Academy of Pediatrics 2021 National Conference.
“The COVID-19 pandemic amplified risk factors known to increase family interpersonal violence, such as increased need for parental supervision, parental stress, financial hardship, poor mental health, and isolation,” said investigator Mattea Miller, an MD candidate at the Johns Hopkins University School of Medicine, Baltimore.
To examine the issue, she and her colleagues “sought to characterize the prevalence and circumstances of adolescent injuries resulting from family interpersonal violence,” Ms. Miller told this news organization.
Their retrospective analysis involved children 10 to 15 years of age seen before or during the pandemic in the emergency department at Johns Hopkins Children’s Center for injuries that resulted from a violent incident with a family member.
Of the 819 incidents of violence-related injuries seen during the study period – the prepandemic ran from Jan. 1, 2019 to March 29, 2020, and the pandemic period ran from March 30, 2020, the date a stay-at-home order was first issued in Maryland, to Dec. 31, 2020 – 448 (54.7%) involved a family member. The proportion of such injuries was similar before and during the pandemic (54.6% vs. 54.9%; P = .99).
Most (83.9%) of these incidents occurred at home, 76.6% involved a parent or guardian, and 66.7% involved the youth being transported to the hospital by police.
It is surprising that families accounted for such a high level of violence involving adolescents, said Christopher S. Greeley, MD, MS, chief of the division of public health pediatrics at Texas Children’s Hospital and professor of pediatrics at Baylor College of Medicine, Houston, who was not involved in the research.
“The most common source of child physical abuse in younger children – infants and toddlers – [is the] parents,” who account for about 75% of cases, “but to see that amount of violence in adolescents was unexpected,” he told this news organization.
Patients in the study cohort were more likely to be Black than the hospital’s overall emergency-department population (84.4% vs. 60.0%), and more likely to be covered by public insurance (71.2% vs. 60.0%).
In the study cohort, 54.0% of the patients were female.
“We were surprised to see that 8% of visits did not have a referral to a social worker” – 92% of patients in the study cohort received a social work consult during their visit to the emergency department – and that number “did not vary during the COVID-19 pandemic,” Ms. Miller said. The pandemic exacerbated the types of stresses that social workers can help address, so “this potentially represents a gap in care that is important to address,” she added.
Increase in use of alcohol, drugs, weapons
The most significant increases from the prepandemic period to the pandemic period were in incidents that involved alcohol (10.0% vs. 18.8%; P ≤ .001), illegal drugs (6.5% vs. 14.9%; P ≤ .001), and weapons, most often a knife (10.7% vs. 23.8%; P ≤ .001).
“An obvious potential explanation for the increase in alcohol, drug, and weapons [involvement] would be the mental health impact of the pandemic in conjunction with the economic stressors that some families may be feeling,” Dr. Greeley said. Teachers are the most common reporters of child abuse, so it’s possible that reports of violence decreased when schools switched to remote learning. But with most schools back to in-person learning, data have not yet shown a surge in reporting, he noted.
The “epidemiology of family violence may be impacted by increased time at home, disruptions in school and family routines, exacerbations in mental health conditions, and financial stresses common during the pandemic,” said senior study investigator Leticia Ryan, MD, MPH, director of research in pediatrics at Johns Hopkins Medicine.
And research has shown increases in the use of alcohol and illegal drugs during the pandemic, she noted.
“As we transition to postpandemic life, it will be important to identify at-risk adolescents and families and provide supports,” Dr. Ryan told this news organization. “The emergency department is an appropriate setting to intervene with youth who have experienced family violence and initiate preventive strategies to avoid future violence.”
Among the strategies to identify and intervene for at-risk patients is the CRAFFT substance use screening tool. Furthermore, “case management, involvement of child protection services, and linkage with relevant support services may all be appropriate, depending on circumstances,” Ms. Miller added.
“Exposure to family violence at a young age increases the likelihood that a child will be exposed to additional violence or become a perpetrator of violence in the future, continuing a cycle of violence,” Ms. Miller explained. “Given that studies of adolescent violence often focus on peer violence, a better understanding of the epidemiology of violence-related injuries resulting from family violence is needed to better inform the development of more comprehensive prevention strategies.”
This study did not note any external funding. Ms. Miller, Dr. Greeley, and Dr. Ryan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Among adolescents treated for injuries caused by family-member violence, the proportion of incidents that involved illegal drugs or weapons more than doubled during the pandemic, and incidents that involved alcohol nearly doubled, according to data presented October 10 at the American Academy of Pediatrics 2021 National Conference.
“The COVID-19 pandemic amplified risk factors known to increase family interpersonal violence, such as increased need for parental supervision, parental stress, financial hardship, poor mental health, and isolation,” said investigator Mattea Miller, an MD candidate at the Johns Hopkins University School of Medicine, Baltimore.
To examine the issue, she and her colleagues “sought to characterize the prevalence and circumstances of adolescent injuries resulting from family interpersonal violence,” Ms. Miller told this news organization.
Their retrospective analysis involved children 10 to 15 years of age seen before or during the pandemic in the emergency department at Johns Hopkins Children’s Center for injuries that resulted from a violent incident with a family member.
Of the 819 incidents of violence-related injuries seen during the study period – the prepandemic ran from Jan. 1, 2019 to March 29, 2020, and the pandemic period ran from March 30, 2020, the date a stay-at-home order was first issued in Maryland, to Dec. 31, 2020 – 448 (54.7%) involved a family member. The proportion of such injuries was similar before and during the pandemic (54.6% vs. 54.9%; P = .99).
Most (83.9%) of these incidents occurred at home, 76.6% involved a parent or guardian, and 66.7% involved the youth being transported to the hospital by police.
It is surprising that families accounted for such a high level of violence involving adolescents, said Christopher S. Greeley, MD, MS, chief of the division of public health pediatrics at Texas Children’s Hospital and professor of pediatrics at Baylor College of Medicine, Houston, who was not involved in the research.
“The most common source of child physical abuse in younger children – infants and toddlers – [is the] parents,” who account for about 75% of cases, “but to see that amount of violence in adolescents was unexpected,” he told this news organization.
Patients in the study cohort were more likely to be Black than the hospital’s overall emergency-department population (84.4% vs. 60.0%), and more likely to be covered by public insurance (71.2% vs. 60.0%).
In the study cohort, 54.0% of the patients were female.
“We were surprised to see that 8% of visits did not have a referral to a social worker” – 92% of patients in the study cohort received a social work consult during their visit to the emergency department – and that number “did not vary during the COVID-19 pandemic,” Ms. Miller said. The pandemic exacerbated the types of stresses that social workers can help address, so “this potentially represents a gap in care that is important to address,” she added.
Increase in use of alcohol, drugs, weapons
The most significant increases from the prepandemic period to the pandemic period were in incidents that involved alcohol (10.0% vs. 18.8%; P ≤ .001), illegal drugs (6.5% vs. 14.9%; P ≤ .001), and weapons, most often a knife (10.7% vs. 23.8%; P ≤ .001).
“An obvious potential explanation for the increase in alcohol, drug, and weapons [involvement] would be the mental health impact of the pandemic in conjunction with the economic stressors that some families may be feeling,” Dr. Greeley said. Teachers are the most common reporters of child abuse, so it’s possible that reports of violence decreased when schools switched to remote learning. But with most schools back to in-person learning, data have not yet shown a surge in reporting, he noted.
The “epidemiology of family violence may be impacted by increased time at home, disruptions in school and family routines, exacerbations in mental health conditions, and financial stresses common during the pandemic,” said senior study investigator Leticia Ryan, MD, MPH, director of research in pediatrics at Johns Hopkins Medicine.
And research has shown increases in the use of alcohol and illegal drugs during the pandemic, she noted.
“As we transition to postpandemic life, it will be important to identify at-risk adolescents and families and provide supports,” Dr. Ryan told this news organization. “The emergency department is an appropriate setting to intervene with youth who have experienced family violence and initiate preventive strategies to avoid future violence.”
Among the strategies to identify and intervene for at-risk patients is the CRAFFT substance use screening tool. Furthermore, “case management, involvement of child protection services, and linkage with relevant support services may all be appropriate, depending on circumstances,” Ms. Miller added.
“Exposure to family violence at a young age increases the likelihood that a child will be exposed to additional violence or become a perpetrator of violence in the future, continuing a cycle of violence,” Ms. Miller explained. “Given that studies of adolescent violence often focus on peer violence, a better understanding of the epidemiology of violence-related injuries resulting from family violence is needed to better inform the development of more comprehensive prevention strategies.”
This study did not note any external funding. Ms. Miller, Dr. Greeley, and Dr. Ryan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Merck seeks FDA authorization for antiviral COVID-19 pill
, an experimental antiviral COVID-19 treatment.
If the FDA grants authorization, the drug would be the first oral antiviral treatment for COVID-19. The capsule, made by Merck and Ridgeback Biotherapeutics, is intended to treat mild to moderate COVID-19 in adults who are at risk of having severe COVID-19 or hospitalization.
“The extraordinary impact of this pandemic demands that we move with unprecedented urgency, and that is what our teams have done by submitting this application for molnupiravir to the FDA within 10 days of receiving the data,” Robert Davis, CEO and president of Merck, said in a statement. On Oct. 1, Merck and Ridgeback released interim data from its phase III clinical trial, which showed that molnupiravir reduced the risk of hospitalization or death by about 50%. About 7% of patients who received the drug were hospitalized within 30 days in the study, as compared with 14% of patients who took a placebo, the company said.
No deaths were reported in the group that received the drug, as compared with eight deaths in the group that received the placebo. None of the trial participants had been vaccinated.
“Medicines and vaccines are both essential to our collective efforts,” Mr. Davis said. “We look forward to working with the FDA on its review of our application, and to working with other regulatory agencies as we do everything we can to bring molnupiravir to patients around the world as quickly as possible.”
Merck has been producing molnupiravir in anticipation of the clinical trial results and FDA authorization. The company expects to produce 10 million courses of treatment by the end of the year, with more expected for 2022.
In June, Merck signed an agreement with the United States to supply 1.7 million courses of molnupiravir once the FDA authorizes the drug. The company has agreed to advance purchase agreements with other countries as well.
Earlier in the year, Merck also announced voluntary licensing agreements with several generics manufacturers in India to provide molnupiravir to more than 100 low- and middle-income countries after approval from local regulatory agencies.
Data from the company’s late-stage clinical trial has not yet been peer-reviewed or published.
Last week, Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said the clinical trial results were “very encouraging” but noted that the FDA should closely scrutinize the drug, CNN reported.
“It is very important that this now must go through the usual process of careful examination of the data by the Food and Drug Administration, both for effectiveness but also for safety, because whenever you introduce a new compound, safety is very important,” Dr. Fauci said, adding that vaccines remain “our best tools against COVID-19.”
A version of this article firsts appeared on WebMD.com.
, an experimental antiviral COVID-19 treatment.
If the FDA grants authorization, the drug would be the first oral antiviral treatment for COVID-19. The capsule, made by Merck and Ridgeback Biotherapeutics, is intended to treat mild to moderate COVID-19 in adults who are at risk of having severe COVID-19 or hospitalization.
“The extraordinary impact of this pandemic demands that we move with unprecedented urgency, and that is what our teams have done by submitting this application for molnupiravir to the FDA within 10 days of receiving the data,” Robert Davis, CEO and president of Merck, said in a statement. On Oct. 1, Merck and Ridgeback released interim data from its phase III clinical trial, which showed that molnupiravir reduced the risk of hospitalization or death by about 50%. About 7% of patients who received the drug were hospitalized within 30 days in the study, as compared with 14% of patients who took a placebo, the company said.
No deaths were reported in the group that received the drug, as compared with eight deaths in the group that received the placebo. None of the trial participants had been vaccinated.
“Medicines and vaccines are both essential to our collective efforts,” Mr. Davis said. “We look forward to working with the FDA on its review of our application, and to working with other regulatory agencies as we do everything we can to bring molnupiravir to patients around the world as quickly as possible.”
Merck has been producing molnupiravir in anticipation of the clinical trial results and FDA authorization. The company expects to produce 10 million courses of treatment by the end of the year, with more expected for 2022.
In June, Merck signed an agreement with the United States to supply 1.7 million courses of molnupiravir once the FDA authorizes the drug. The company has agreed to advance purchase agreements with other countries as well.
Earlier in the year, Merck also announced voluntary licensing agreements with several generics manufacturers in India to provide molnupiravir to more than 100 low- and middle-income countries after approval from local regulatory agencies.
Data from the company’s late-stage clinical trial has not yet been peer-reviewed or published.
Last week, Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said the clinical trial results were “very encouraging” but noted that the FDA should closely scrutinize the drug, CNN reported.
“It is very important that this now must go through the usual process of careful examination of the data by the Food and Drug Administration, both for effectiveness but also for safety, because whenever you introduce a new compound, safety is very important,” Dr. Fauci said, adding that vaccines remain “our best tools against COVID-19.”
A version of this article firsts appeared on WebMD.com.
, an experimental antiviral COVID-19 treatment.
If the FDA grants authorization, the drug would be the first oral antiviral treatment for COVID-19. The capsule, made by Merck and Ridgeback Biotherapeutics, is intended to treat mild to moderate COVID-19 in adults who are at risk of having severe COVID-19 or hospitalization.
“The extraordinary impact of this pandemic demands that we move with unprecedented urgency, and that is what our teams have done by submitting this application for molnupiravir to the FDA within 10 days of receiving the data,” Robert Davis, CEO and president of Merck, said in a statement. On Oct. 1, Merck and Ridgeback released interim data from its phase III clinical trial, which showed that molnupiravir reduced the risk of hospitalization or death by about 50%. About 7% of patients who received the drug were hospitalized within 30 days in the study, as compared with 14% of patients who took a placebo, the company said.
No deaths were reported in the group that received the drug, as compared with eight deaths in the group that received the placebo. None of the trial participants had been vaccinated.
“Medicines and vaccines are both essential to our collective efforts,” Mr. Davis said. “We look forward to working with the FDA on its review of our application, and to working with other regulatory agencies as we do everything we can to bring molnupiravir to patients around the world as quickly as possible.”
Merck has been producing molnupiravir in anticipation of the clinical trial results and FDA authorization. The company expects to produce 10 million courses of treatment by the end of the year, with more expected for 2022.
In June, Merck signed an agreement with the United States to supply 1.7 million courses of molnupiravir once the FDA authorizes the drug. The company has agreed to advance purchase agreements with other countries as well.
Earlier in the year, Merck also announced voluntary licensing agreements with several generics manufacturers in India to provide molnupiravir to more than 100 low- and middle-income countries after approval from local regulatory agencies.
Data from the company’s late-stage clinical trial has not yet been peer-reviewed or published.
Last week, Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said the clinical trial results were “very encouraging” but noted that the FDA should closely scrutinize the drug, CNN reported.
“It is very important that this now must go through the usual process of careful examination of the data by the Food and Drug Administration, both for effectiveness but also for safety, because whenever you introduce a new compound, safety is very important,” Dr. Fauci said, adding that vaccines remain “our best tools against COVID-19.”
A version of this article firsts appeared on WebMD.com.
Steroid a promising short-term treatment option for major depression?
Study results of an experimental agent that improves symptoms of major depression and boosts quality of life in as little as 3 days suggest it may be an effective short-term treatment option.
Phase 3 results of a randomized, placebo-controlled trial compared zuranolone, an neuroactive steroid that binds to both synaptic and extra-synaptic GABA-A receptors, to placebo in patients with major depressive disorder (MDD). Overall, 30% of participants were already taking antidepressants.
Investigators found the drug was associated with a significant improvement in depression scores versus placebo, with benefit observed as early as day 3. This was accompanied by improved function and well-being.
, said study presenter Colville Brown, MD, Sage Therapeutics, Cambridge, Mass.
“These data continue to support the development of zuranolone as a potential 14-day short course treatment for major depressive disorder episodes.”
The findings were presented at the virtual congress of the European College of Neuropsychopharmacology.
High placebo response
However, despite being significant, the drug’s benefit was only slightly higher than that of placebo, raising questions about the study design and the true performance of the drug.
Dr. Brown explained that patients with MDD were randomized to oral zuranolone 50 mg or placebo once daily for 14 days, with dose reductions to 40 mg or matching placebo permitted in case of perceived intolerance.
Patients were assessed at baseline and day 15 via the 17-item Hamilton Rating Scale for Depression (HAMD-17) before entering a 28-day follow-up period off the study drug.
Among the 268 participants who received zuranolone, 90.3% completed the study, compared with 87.4% of 269 patients in the placebo group.
The mean age of participants was 40 years. Women made up 69.4% of those who received zuranolone and 61.7% assigned to placebo.
The mean HAMD-17 score at baseline was 26.8 and 26.9 in the zuranolone and placebo groups, respectively. Dr. Brown noted that 29.5% of patients in the zuranolone group and 30.1% of those assigned to placebo were taking antidepressants at baseline.
The study’s primary endpoint was met, with patients taking the study drug experiencing a significantly greater reduction in HAMD-17 scores from baseline to day 15 versus those given placebo, at 14.1 versus 12.3 points (P = .0141).
Dr. Brown highlighted that the difference in reduction in HAMD-17 scores between the zuranolone and placebo groups was already significant at day 3 (P < .0001), and again at day 8 (P < .0001) and day 12 (P < .001).
At day 3, response rates on the HAMD-17 were significantly higher among zuranolone-treated patients than among those given placebo, at 29.3% versus 16.3% (P < .001). However, the differences on day 15 and on day 42 were no longer significant.
A similar effect was seen for HAMD-17 remissions, which were seen in 7.6% of zuranolone-treated patients and 2.3% of those given placebo at day 3 (P < .01), rising to 29.8% versus 27.1% at day 15, and 30.8% versus 29.6% at day 42, and neither difference was significant.
Dr. Brown also showed that, at all time points during the treatment and follow-up periods, improvements in response rates in Global Improvement on the Clinical Global Impression scale favored zuranolone.
On the SF-36v2 quality of life questionnaire, improvements again favored zuranolone on all domains, although the difference between active treatment and placebo was significant only for vitality on day 15, at 12.8 versus 9.7 points (P < .05).
Treatment-emergent adverse events were more common with zuranolone, with 60.1% of patients experiencing at least one event of any grade versus 44.6% with placebo. However, severe events were seen in only 3.0% versus 1.1% of patients, and serious adverse events were recorded in only two patients (0.7%) in both groups.
The most common adverse events were somnolence, dizziness, headache, sedation, and diarrhea, with no increase in suicidal ideation or withdrawal. Dr. Brown noted that there was “no change in the safety signal” between patients with or without prior antidepressant therapy.
From the audience, Marie-Josée Filteau, MD, department of psychiatry, Laval University, Quebec, drew attention to the similarity in the improvement in HAMD-17 scores between the zuranolone and placebo groups, asking: “How is that compelling?”
Dr. Brown replied that “what they are excited about is that change from baseline with zuranolone,” adding: “You do see it in the placebo group as well, and ... this isn’t new to psychiatry.
“This is a heterogeneous disease, and remember this [study] was conducted during COVID, so patients were being seen with clinic visits during COVID.
“What impact did that have? The placebo is not really placebo” in this case.
More effective than results suggest?
Approached for comment by this news organization, Maurizio Fava, MD, executive vice chair, department of psychiatry, and executive director, Clinical Trials Network and Institute, Massachusetts General Hospital, Boston, noted there are several issues with the trial.
Because of those, the drug “is likely to be much more efficacious than it looks because it achieved statistical significance despite an extremely high placebo response,” he said
“Whenever your change on placebo is greater than 10 points on the HAMD, you have an excessive response ... and a very, very low chance of detecting a signal,” he said.
Dr. Fava said that another issue was including patients who were either on or off antidepressants, which meant the population was not sufficiently homogenous.
Another “flaw” was to assume that the placebo effect would be “transient” and deteriorate over time, whereas the results showed the opposite.
Nevertheless, “it’s a positive study because of the sample size ... that provides further evidence for the antidepressant activity of zuranolone” and the drug was “well tolerated.”
Dr. Fava expects zuranolone “will make it to the market,” as an indication from the Food and Drug Administration is likely, “but if you’re asking me: Is the drug as effective as shown in their studies? It’s probably much more effective.”
The study was funded by Sage Therapeutics and Biogen. Dr. Brown is an employee of Sage Therapeutics. Lead investigator Anita Clayton, MD, University of Virginia, Charlottesville, has reported relationships with Dario Bioscience, Janssen, Praxis Precision Medicines, Relmada Therapeutics, Sage Therapeutics, Fabre-Kramer, MindCure, Ovoca Bio, PureTech Health, S1 Biopharma, Vella Bioscience, WCG MedAvante-ProPhase, Ballantine Books/Random House, Guilford Publications, Euthymics, and Mediflix.
A version of this article first appeared on Medscape.com.
Study results of an experimental agent that improves symptoms of major depression and boosts quality of life in as little as 3 days suggest it may be an effective short-term treatment option.
Phase 3 results of a randomized, placebo-controlled trial compared zuranolone, an neuroactive steroid that binds to both synaptic and extra-synaptic GABA-A receptors, to placebo in patients with major depressive disorder (MDD). Overall, 30% of participants were already taking antidepressants.
Investigators found the drug was associated with a significant improvement in depression scores versus placebo, with benefit observed as early as day 3. This was accompanied by improved function and well-being.
, said study presenter Colville Brown, MD, Sage Therapeutics, Cambridge, Mass.
“These data continue to support the development of zuranolone as a potential 14-day short course treatment for major depressive disorder episodes.”
The findings were presented at the virtual congress of the European College of Neuropsychopharmacology.
High placebo response
However, despite being significant, the drug’s benefit was only slightly higher than that of placebo, raising questions about the study design and the true performance of the drug.
Dr. Brown explained that patients with MDD were randomized to oral zuranolone 50 mg or placebo once daily for 14 days, with dose reductions to 40 mg or matching placebo permitted in case of perceived intolerance.
Patients were assessed at baseline and day 15 via the 17-item Hamilton Rating Scale for Depression (HAMD-17) before entering a 28-day follow-up period off the study drug.
Among the 268 participants who received zuranolone, 90.3% completed the study, compared with 87.4% of 269 patients in the placebo group.
The mean age of participants was 40 years. Women made up 69.4% of those who received zuranolone and 61.7% assigned to placebo.
The mean HAMD-17 score at baseline was 26.8 and 26.9 in the zuranolone and placebo groups, respectively. Dr. Brown noted that 29.5% of patients in the zuranolone group and 30.1% of those assigned to placebo were taking antidepressants at baseline.
The study’s primary endpoint was met, with patients taking the study drug experiencing a significantly greater reduction in HAMD-17 scores from baseline to day 15 versus those given placebo, at 14.1 versus 12.3 points (P = .0141).
Dr. Brown highlighted that the difference in reduction in HAMD-17 scores between the zuranolone and placebo groups was already significant at day 3 (P < .0001), and again at day 8 (P < .0001) and day 12 (P < .001).
At day 3, response rates on the HAMD-17 were significantly higher among zuranolone-treated patients than among those given placebo, at 29.3% versus 16.3% (P < .001). However, the differences on day 15 and on day 42 were no longer significant.
A similar effect was seen for HAMD-17 remissions, which were seen in 7.6% of zuranolone-treated patients and 2.3% of those given placebo at day 3 (P < .01), rising to 29.8% versus 27.1% at day 15, and 30.8% versus 29.6% at day 42, and neither difference was significant.
Dr. Brown also showed that, at all time points during the treatment and follow-up periods, improvements in response rates in Global Improvement on the Clinical Global Impression scale favored zuranolone.
On the SF-36v2 quality of life questionnaire, improvements again favored zuranolone on all domains, although the difference between active treatment and placebo was significant only for vitality on day 15, at 12.8 versus 9.7 points (P < .05).
Treatment-emergent adverse events were more common with zuranolone, with 60.1% of patients experiencing at least one event of any grade versus 44.6% with placebo. However, severe events were seen in only 3.0% versus 1.1% of patients, and serious adverse events were recorded in only two patients (0.7%) in both groups.
The most common adverse events were somnolence, dizziness, headache, sedation, and diarrhea, with no increase in suicidal ideation or withdrawal. Dr. Brown noted that there was “no change in the safety signal” between patients with or without prior antidepressant therapy.
From the audience, Marie-Josée Filteau, MD, department of psychiatry, Laval University, Quebec, drew attention to the similarity in the improvement in HAMD-17 scores between the zuranolone and placebo groups, asking: “How is that compelling?”
Dr. Brown replied that “what they are excited about is that change from baseline with zuranolone,” adding: “You do see it in the placebo group as well, and ... this isn’t new to psychiatry.
“This is a heterogeneous disease, and remember this [study] was conducted during COVID, so patients were being seen with clinic visits during COVID.
“What impact did that have? The placebo is not really placebo” in this case.
More effective than results suggest?
Approached for comment by this news organization, Maurizio Fava, MD, executive vice chair, department of psychiatry, and executive director, Clinical Trials Network and Institute, Massachusetts General Hospital, Boston, noted there are several issues with the trial.
Because of those, the drug “is likely to be much more efficacious than it looks because it achieved statistical significance despite an extremely high placebo response,” he said
“Whenever your change on placebo is greater than 10 points on the HAMD, you have an excessive response ... and a very, very low chance of detecting a signal,” he said.
Dr. Fava said that another issue was including patients who were either on or off antidepressants, which meant the population was not sufficiently homogenous.
Another “flaw” was to assume that the placebo effect would be “transient” and deteriorate over time, whereas the results showed the opposite.
Nevertheless, “it’s a positive study because of the sample size ... that provides further evidence for the antidepressant activity of zuranolone” and the drug was “well tolerated.”
Dr. Fava expects zuranolone “will make it to the market,” as an indication from the Food and Drug Administration is likely, “but if you’re asking me: Is the drug as effective as shown in their studies? It’s probably much more effective.”
The study was funded by Sage Therapeutics and Biogen. Dr. Brown is an employee of Sage Therapeutics. Lead investigator Anita Clayton, MD, University of Virginia, Charlottesville, has reported relationships with Dario Bioscience, Janssen, Praxis Precision Medicines, Relmada Therapeutics, Sage Therapeutics, Fabre-Kramer, MindCure, Ovoca Bio, PureTech Health, S1 Biopharma, Vella Bioscience, WCG MedAvante-ProPhase, Ballantine Books/Random House, Guilford Publications, Euthymics, and Mediflix.
A version of this article first appeared on Medscape.com.
Study results of an experimental agent that improves symptoms of major depression and boosts quality of life in as little as 3 days suggest it may be an effective short-term treatment option.
Phase 3 results of a randomized, placebo-controlled trial compared zuranolone, an neuroactive steroid that binds to both synaptic and extra-synaptic GABA-A receptors, to placebo in patients with major depressive disorder (MDD). Overall, 30% of participants were already taking antidepressants.
Investigators found the drug was associated with a significant improvement in depression scores versus placebo, with benefit observed as early as day 3. This was accompanied by improved function and well-being.
, said study presenter Colville Brown, MD, Sage Therapeutics, Cambridge, Mass.
“These data continue to support the development of zuranolone as a potential 14-day short course treatment for major depressive disorder episodes.”
The findings were presented at the virtual congress of the European College of Neuropsychopharmacology.
High placebo response
However, despite being significant, the drug’s benefit was only slightly higher than that of placebo, raising questions about the study design and the true performance of the drug.
Dr. Brown explained that patients with MDD were randomized to oral zuranolone 50 mg or placebo once daily for 14 days, with dose reductions to 40 mg or matching placebo permitted in case of perceived intolerance.
Patients were assessed at baseline and day 15 via the 17-item Hamilton Rating Scale for Depression (HAMD-17) before entering a 28-day follow-up period off the study drug.
Among the 268 participants who received zuranolone, 90.3% completed the study, compared with 87.4% of 269 patients in the placebo group.
The mean age of participants was 40 years. Women made up 69.4% of those who received zuranolone and 61.7% assigned to placebo.
The mean HAMD-17 score at baseline was 26.8 and 26.9 in the zuranolone and placebo groups, respectively. Dr. Brown noted that 29.5% of patients in the zuranolone group and 30.1% of those assigned to placebo were taking antidepressants at baseline.
The study’s primary endpoint was met, with patients taking the study drug experiencing a significantly greater reduction in HAMD-17 scores from baseline to day 15 versus those given placebo, at 14.1 versus 12.3 points (P = .0141).
Dr. Brown highlighted that the difference in reduction in HAMD-17 scores between the zuranolone and placebo groups was already significant at day 3 (P < .0001), and again at day 8 (P < .0001) and day 12 (P < .001).
At day 3, response rates on the HAMD-17 were significantly higher among zuranolone-treated patients than among those given placebo, at 29.3% versus 16.3% (P < .001). However, the differences on day 15 and on day 42 were no longer significant.
A similar effect was seen for HAMD-17 remissions, which were seen in 7.6% of zuranolone-treated patients and 2.3% of those given placebo at day 3 (P < .01), rising to 29.8% versus 27.1% at day 15, and 30.8% versus 29.6% at day 42, and neither difference was significant.
Dr. Brown also showed that, at all time points during the treatment and follow-up periods, improvements in response rates in Global Improvement on the Clinical Global Impression scale favored zuranolone.
On the SF-36v2 quality of life questionnaire, improvements again favored zuranolone on all domains, although the difference between active treatment and placebo was significant only for vitality on day 15, at 12.8 versus 9.7 points (P < .05).
Treatment-emergent adverse events were more common with zuranolone, with 60.1% of patients experiencing at least one event of any grade versus 44.6% with placebo. However, severe events were seen in only 3.0% versus 1.1% of patients, and serious adverse events were recorded in only two patients (0.7%) in both groups.
The most common adverse events were somnolence, dizziness, headache, sedation, and diarrhea, with no increase in suicidal ideation or withdrawal. Dr. Brown noted that there was “no change in the safety signal” between patients with or without prior antidepressant therapy.
From the audience, Marie-Josée Filteau, MD, department of psychiatry, Laval University, Quebec, drew attention to the similarity in the improvement in HAMD-17 scores between the zuranolone and placebo groups, asking: “How is that compelling?”
Dr. Brown replied that “what they are excited about is that change from baseline with zuranolone,” adding: “You do see it in the placebo group as well, and ... this isn’t new to psychiatry.
“This is a heterogeneous disease, and remember this [study] was conducted during COVID, so patients were being seen with clinic visits during COVID.
“What impact did that have? The placebo is not really placebo” in this case.
More effective than results suggest?
Approached for comment by this news organization, Maurizio Fava, MD, executive vice chair, department of psychiatry, and executive director, Clinical Trials Network and Institute, Massachusetts General Hospital, Boston, noted there are several issues with the trial.
Because of those, the drug “is likely to be much more efficacious than it looks because it achieved statistical significance despite an extremely high placebo response,” he said
“Whenever your change on placebo is greater than 10 points on the HAMD, you have an excessive response ... and a very, very low chance of detecting a signal,” he said.
Dr. Fava said that another issue was including patients who were either on or off antidepressants, which meant the population was not sufficiently homogenous.
Another “flaw” was to assume that the placebo effect would be “transient” and deteriorate over time, whereas the results showed the opposite.
Nevertheless, “it’s a positive study because of the sample size ... that provides further evidence for the antidepressant activity of zuranolone” and the drug was “well tolerated.”
Dr. Fava expects zuranolone “will make it to the market,” as an indication from the Food and Drug Administration is likely, “but if you’re asking me: Is the drug as effective as shown in their studies? It’s probably much more effective.”
The study was funded by Sage Therapeutics and Biogen. Dr. Brown is an employee of Sage Therapeutics. Lead investigator Anita Clayton, MD, University of Virginia, Charlottesville, has reported relationships with Dario Bioscience, Janssen, Praxis Precision Medicines, Relmada Therapeutics, Sage Therapeutics, Fabre-Kramer, MindCure, Ovoca Bio, PureTech Health, S1 Biopharma, Vella Bioscience, WCG MedAvante-ProPhase, Ballantine Books/Random House, Guilford Publications, Euthymics, and Mediflix.
A version of this article first appeared on Medscape.com.
FROM ECNP 2021
Psychiatrists shift stance on gender dysphoria, recommend therapy
A new position statement from the Royal Australian and New Zealand College of Psychiatrists (RANZCP) stresses the importance of a mental health evaluation for people with gender dysphoria – in particular for children and adolescents – before any firm decisions are made on whether to prescribe hormonal treatments to transition, or perform surgeries, often referred to as “gender-affirming care.”
“There is a paucity of quality evidence on the outcomes of those presenting with gender dysphoria. In particular, there is a need for better evidence in relation to outcomes for children and young people,” the guidance states.
Because gender dysphoria “is associated with significant distress ... each case should be assessed by a mental health professional, which will frequently be a psychiatrist, with the person at the center of care. It is important the psychological state and context in which gender dysphoria has arisen is explored to assess the most appropriate treatment,” it adds.
The move by the psychiatry body represents a big shift in the landscape regarding recommendations for the treatment of gender dysphoria in Australia and New Zealand.
Asked to explain the new RANZCP position, Philip Morris, MBBS, FRANZCP, said: “The College acknowledged the complexity of the issues and the legitimacy of different approaches.”
Exploration of a patient’s reasons for identifying as transgender is essential, he said in an interview, especially when it comes to young people.
“There may be other reasons for doing it, and we need to look for those, identify them and treat them. This needs to be done before initiating hormones and changing the whole physical nature of the child,” he said.
“A cautious psychotherapy-first approach makes sense. If we can do that with adolescents, then we will take a big step in the right direction,” stressed Dr. Morris, who is president of the National Association of Practising Psychiatrists in Australia.
Keira Bell case and Scandinavian stance lead to more open discussion
The rapid rise in gender dysphoria among adolescents in the Western world, referred to as “rapid-onset” or “late-onset” gender dysphoria, has seen a huge increase in the number of natal girls presenting and created frenzied debate that has intensified worldwide in the last 12 months about how to best treat youth with gender dysphoria.
Concerns have arisen that some transgender identification is due to social contagion, and there is a growing number of “detransitioners” – people who identified as transgender, transitioned to the opposite gender, but then regretted their decision, changed their minds, and “detransitioned” back to their birth sex. If they have had hormone therapy, and in some cases surgery, they are left with irreversible changes to their bodies.
As a result, Scandinavian countries, most notably Finland, once eager advocates of the gender-affirmative approach, have pulled back and issued new treatment guidelines in 2020 stating that psychotherapy, rather than gender reassignment, should be the first line of treatment for gender-dysphoric youth.
This, along with a landmark High Court decision in the U.K. regarding the use of puberty-blocking drugs for children with gender dysphoria, brought by detransitioner Keira Bell, which was recently overturned by the Appeal Court, but which Ms. Bell now says she will take to the Supreme Court, has led to a considerable shift in the conversation around treating transgender adolescents with hormonal therapy, says Dr. Morris.
“This [has moved from] ... a topic that could previously not be talked about freely to one that we can discuss more openly now. This is a big improvement. Previously, everyone thought it was all settled, but it’s not, certainly not from a medical angle,” he states.
At odds with prior Australian recommendations
The RANZCP had previously endorsed the standard guidelines of the Royal Children’s Hospital (RCH) Melbourne, followed by most gender-identity services in Australia and similar guidance from New Zealand, which both recommend gender-affirming care.
“Increasing evidence demonstrates that with supportive, gender-affirming care during childhood and adolescence, harms can be ameliorated and mental health and well-being outcomes can be significantly improved,” state the RCH guidelines.
But in 2019, RANZCP removed its endorsement of the RCH guidelines and started a consultation, which resulted in the new position statement.
However, Ken Pang, MD, of the Murdoch Children’s Research Institute in Melbourne and an author of the RCH guidelines, says the key recommendations of the new RANZCP position statement are consistent with their own guidelines.
The former note “the need for a skilled mental health clinician in providing comprehensive exploration of a child or adolescent’s biopsychosocial context,” Dr. Pang says.
However, it’s difficult not to see the contrast in stance when the new RANZCP statement maintains: “Research on gender dysphoria is still emerging. There are polarized views and mixed evidence regarding treatment options for people presenting with gender identity concerns, especially children and young people.”
Dr. Pang says the RCH guidelines do, however, recognize the need for further research in the field.
“I look forward to being able to incorporate such research, including from our own Trans20 study, into future revisions of our guidelines,” he told this news organization.
Watch your backs with affirmative therapy: Will there be a compromise?
Dr. Morris says there will obviously be cases where “the child might transition with a medical intervention, but that wouldn’t be the first step.”
And yet, he adds, “There are those who push the pro-trans view that everyone should be allowed to transition, and the doctors are only technicians that provide hormones with no questions asked.”
But from a doctor’s perspective, clinicians will still be held responsible in medical and legal terms for the treatments given, he stressed.
“I don’t think they will ever not be accountable for that. They will always need to determine in their own mind whether their actions have positive value that outweigh any disadvantages,” Dr. Morris continues.
The RANZCP statement does, in fact, stress just this.
All health care professionals need to “be aware of ethical and medicolegal dilemmas” pertaining to affirmative therapy, it indicates. “Psychiatrists should practice within the relevant laws and accepted professional standards in relation to assessing capacity and obtaining consent...”
Dr. Morris hopes there will ultimately be many more checks and balances in place and that courts and clinicians will need to step back and not assume every child who seeks to transition is doing it as a result of pure gender dysphoria.
He predicts that things will end in a compromise.
“In my view, this compromise will treat children with respect and approach them like any other patient that presents with a condition that requires proper assessment and treatment.”
“In the end, some cases will be transitioned, but there will be fewer than [are] transitioned at the moment,” he predicts.
Dr. Morris has reported no relevant financial relationships. Dr. Pang is a member of the Australian Professional Association for Trans Health and its research committee.
A version of this article first appeared on Medscape.com.
A new position statement from the Royal Australian and New Zealand College of Psychiatrists (RANZCP) stresses the importance of a mental health evaluation for people with gender dysphoria – in particular for children and adolescents – before any firm decisions are made on whether to prescribe hormonal treatments to transition, or perform surgeries, often referred to as “gender-affirming care.”
“There is a paucity of quality evidence on the outcomes of those presenting with gender dysphoria. In particular, there is a need for better evidence in relation to outcomes for children and young people,” the guidance states.
Because gender dysphoria “is associated with significant distress ... each case should be assessed by a mental health professional, which will frequently be a psychiatrist, with the person at the center of care. It is important the psychological state and context in which gender dysphoria has arisen is explored to assess the most appropriate treatment,” it adds.
The move by the psychiatry body represents a big shift in the landscape regarding recommendations for the treatment of gender dysphoria in Australia and New Zealand.
Asked to explain the new RANZCP position, Philip Morris, MBBS, FRANZCP, said: “The College acknowledged the complexity of the issues and the legitimacy of different approaches.”
Exploration of a patient’s reasons for identifying as transgender is essential, he said in an interview, especially when it comes to young people.
“There may be other reasons for doing it, and we need to look for those, identify them and treat them. This needs to be done before initiating hormones and changing the whole physical nature of the child,” he said.
“A cautious psychotherapy-first approach makes sense. If we can do that with adolescents, then we will take a big step in the right direction,” stressed Dr. Morris, who is president of the National Association of Practising Psychiatrists in Australia.
Keira Bell case and Scandinavian stance lead to more open discussion
The rapid rise in gender dysphoria among adolescents in the Western world, referred to as “rapid-onset” or “late-onset” gender dysphoria, has seen a huge increase in the number of natal girls presenting and created frenzied debate that has intensified worldwide in the last 12 months about how to best treat youth with gender dysphoria.
Concerns have arisen that some transgender identification is due to social contagion, and there is a growing number of “detransitioners” – people who identified as transgender, transitioned to the opposite gender, but then regretted their decision, changed their minds, and “detransitioned” back to their birth sex. If they have had hormone therapy, and in some cases surgery, they are left with irreversible changes to their bodies.
As a result, Scandinavian countries, most notably Finland, once eager advocates of the gender-affirmative approach, have pulled back and issued new treatment guidelines in 2020 stating that psychotherapy, rather than gender reassignment, should be the first line of treatment for gender-dysphoric youth.
This, along with a landmark High Court decision in the U.K. regarding the use of puberty-blocking drugs for children with gender dysphoria, brought by detransitioner Keira Bell, which was recently overturned by the Appeal Court, but which Ms. Bell now says she will take to the Supreme Court, has led to a considerable shift in the conversation around treating transgender adolescents with hormonal therapy, says Dr. Morris.
“This [has moved from] ... a topic that could previously not be talked about freely to one that we can discuss more openly now. This is a big improvement. Previously, everyone thought it was all settled, but it’s not, certainly not from a medical angle,” he states.
At odds with prior Australian recommendations
The RANZCP had previously endorsed the standard guidelines of the Royal Children’s Hospital (RCH) Melbourne, followed by most gender-identity services in Australia and similar guidance from New Zealand, which both recommend gender-affirming care.
“Increasing evidence demonstrates that with supportive, gender-affirming care during childhood and adolescence, harms can be ameliorated and mental health and well-being outcomes can be significantly improved,” state the RCH guidelines.
But in 2019, RANZCP removed its endorsement of the RCH guidelines and started a consultation, which resulted in the new position statement.
However, Ken Pang, MD, of the Murdoch Children’s Research Institute in Melbourne and an author of the RCH guidelines, says the key recommendations of the new RANZCP position statement are consistent with their own guidelines.
The former note “the need for a skilled mental health clinician in providing comprehensive exploration of a child or adolescent’s biopsychosocial context,” Dr. Pang says.
However, it’s difficult not to see the contrast in stance when the new RANZCP statement maintains: “Research on gender dysphoria is still emerging. There are polarized views and mixed evidence regarding treatment options for people presenting with gender identity concerns, especially children and young people.”
Dr. Pang says the RCH guidelines do, however, recognize the need for further research in the field.
“I look forward to being able to incorporate such research, including from our own Trans20 study, into future revisions of our guidelines,” he told this news organization.
Watch your backs with affirmative therapy: Will there be a compromise?
Dr. Morris says there will obviously be cases where “the child might transition with a medical intervention, but that wouldn’t be the first step.”
And yet, he adds, “There are those who push the pro-trans view that everyone should be allowed to transition, and the doctors are only technicians that provide hormones with no questions asked.”
But from a doctor’s perspective, clinicians will still be held responsible in medical and legal terms for the treatments given, he stressed.
“I don’t think they will ever not be accountable for that. They will always need to determine in their own mind whether their actions have positive value that outweigh any disadvantages,” Dr. Morris continues.
The RANZCP statement does, in fact, stress just this.
All health care professionals need to “be aware of ethical and medicolegal dilemmas” pertaining to affirmative therapy, it indicates. “Psychiatrists should practice within the relevant laws and accepted professional standards in relation to assessing capacity and obtaining consent...”
Dr. Morris hopes there will ultimately be many more checks and balances in place and that courts and clinicians will need to step back and not assume every child who seeks to transition is doing it as a result of pure gender dysphoria.
He predicts that things will end in a compromise.
“In my view, this compromise will treat children with respect and approach them like any other patient that presents with a condition that requires proper assessment and treatment.”
“In the end, some cases will be transitioned, but there will be fewer than [are] transitioned at the moment,” he predicts.
Dr. Morris has reported no relevant financial relationships. Dr. Pang is a member of the Australian Professional Association for Trans Health and its research committee.
A version of this article first appeared on Medscape.com.
A new position statement from the Royal Australian and New Zealand College of Psychiatrists (RANZCP) stresses the importance of a mental health evaluation for people with gender dysphoria – in particular for children and adolescents – before any firm decisions are made on whether to prescribe hormonal treatments to transition, or perform surgeries, often referred to as “gender-affirming care.”
“There is a paucity of quality evidence on the outcomes of those presenting with gender dysphoria. In particular, there is a need for better evidence in relation to outcomes for children and young people,” the guidance states.
Because gender dysphoria “is associated with significant distress ... each case should be assessed by a mental health professional, which will frequently be a psychiatrist, with the person at the center of care. It is important the psychological state and context in which gender dysphoria has arisen is explored to assess the most appropriate treatment,” it adds.
The move by the psychiatry body represents a big shift in the landscape regarding recommendations for the treatment of gender dysphoria in Australia and New Zealand.
Asked to explain the new RANZCP position, Philip Morris, MBBS, FRANZCP, said: “The College acknowledged the complexity of the issues and the legitimacy of different approaches.”
Exploration of a patient’s reasons for identifying as transgender is essential, he said in an interview, especially when it comes to young people.
“There may be other reasons for doing it, and we need to look for those, identify them and treat them. This needs to be done before initiating hormones and changing the whole physical nature of the child,” he said.
“A cautious psychotherapy-first approach makes sense. If we can do that with adolescents, then we will take a big step in the right direction,” stressed Dr. Morris, who is president of the National Association of Practising Psychiatrists in Australia.
Keira Bell case and Scandinavian stance lead to more open discussion
The rapid rise in gender dysphoria among adolescents in the Western world, referred to as “rapid-onset” or “late-onset” gender dysphoria, has seen a huge increase in the number of natal girls presenting and created frenzied debate that has intensified worldwide in the last 12 months about how to best treat youth with gender dysphoria.
Concerns have arisen that some transgender identification is due to social contagion, and there is a growing number of “detransitioners” – people who identified as transgender, transitioned to the opposite gender, but then regretted their decision, changed their minds, and “detransitioned” back to their birth sex. If they have had hormone therapy, and in some cases surgery, they are left with irreversible changes to their bodies.
As a result, Scandinavian countries, most notably Finland, once eager advocates of the gender-affirmative approach, have pulled back and issued new treatment guidelines in 2020 stating that psychotherapy, rather than gender reassignment, should be the first line of treatment for gender-dysphoric youth.
This, along with a landmark High Court decision in the U.K. regarding the use of puberty-blocking drugs for children with gender dysphoria, brought by detransitioner Keira Bell, which was recently overturned by the Appeal Court, but which Ms. Bell now says she will take to the Supreme Court, has led to a considerable shift in the conversation around treating transgender adolescents with hormonal therapy, says Dr. Morris.
“This [has moved from] ... a topic that could previously not be talked about freely to one that we can discuss more openly now. This is a big improvement. Previously, everyone thought it was all settled, but it’s not, certainly not from a medical angle,” he states.
At odds with prior Australian recommendations
The RANZCP had previously endorsed the standard guidelines of the Royal Children’s Hospital (RCH) Melbourne, followed by most gender-identity services in Australia and similar guidance from New Zealand, which both recommend gender-affirming care.
“Increasing evidence demonstrates that with supportive, gender-affirming care during childhood and adolescence, harms can be ameliorated and mental health and well-being outcomes can be significantly improved,” state the RCH guidelines.
But in 2019, RANZCP removed its endorsement of the RCH guidelines and started a consultation, which resulted in the new position statement.
However, Ken Pang, MD, of the Murdoch Children’s Research Institute in Melbourne and an author of the RCH guidelines, says the key recommendations of the new RANZCP position statement are consistent with their own guidelines.
The former note “the need for a skilled mental health clinician in providing comprehensive exploration of a child or adolescent’s biopsychosocial context,” Dr. Pang says.
However, it’s difficult not to see the contrast in stance when the new RANZCP statement maintains: “Research on gender dysphoria is still emerging. There are polarized views and mixed evidence regarding treatment options for people presenting with gender identity concerns, especially children and young people.”
Dr. Pang says the RCH guidelines do, however, recognize the need for further research in the field.
“I look forward to being able to incorporate such research, including from our own Trans20 study, into future revisions of our guidelines,” he told this news organization.
Watch your backs with affirmative therapy: Will there be a compromise?
Dr. Morris says there will obviously be cases where “the child might transition with a medical intervention, but that wouldn’t be the first step.”
And yet, he adds, “There are those who push the pro-trans view that everyone should be allowed to transition, and the doctors are only technicians that provide hormones with no questions asked.”
But from a doctor’s perspective, clinicians will still be held responsible in medical and legal terms for the treatments given, he stressed.
“I don’t think they will ever not be accountable for that. They will always need to determine in their own mind whether their actions have positive value that outweigh any disadvantages,” Dr. Morris continues.
The RANZCP statement does, in fact, stress just this.
All health care professionals need to “be aware of ethical and medicolegal dilemmas” pertaining to affirmative therapy, it indicates. “Psychiatrists should practice within the relevant laws and accepted professional standards in relation to assessing capacity and obtaining consent...”
Dr. Morris hopes there will ultimately be many more checks and balances in place and that courts and clinicians will need to step back and not assume every child who seeks to transition is doing it as a result of pure gender dysphoria.
He predicts that things will end in a compromise.
“In my view, this compromise will treat children with respect and approach them like any other patient that presents with a condition that requires proper assessment and treatment.”
“In the end, some cases will be transitioned, but there will be fewer than [are] transitioned at the moment,” he predicts.
Dr. Morris has reported no relevant financial relationships. Dr. Pang is a member of the Australian Professional Association for Trans Health and its research committee.
A version of this article first appeared on Medscape.com.
Retraining the brain may eliminate chronic back pain
Psychological therapy that changes an individual’s beliefs about pain not only provides lasting chronic pain relief but also alters brain regions related to pain generation, new research shows.
In the first randomized controlled test of pain-reprocessing therapy (PRT), two-thirds of patients with chronic back pain (CBP) who received 4 weeks of PRT were pain free or nearly pain free afterward – and for most patients, relief was maintained for 1 year, the researchers found.
“Primary chronic back pain can be dramatically reduced or even eliminated by psychological treatment focused on changing how threatening we perceive the pain to be,” first author Yoni Ashar, PhD, department of psychiatry, Weill Cornell Medicine, New York, said in an interview.
“ given that large reductions in pain have rarely been observed in studies that tested psychological therapies for chronic back pain.
The study was published online Sept. 29, 2021, in JAMA Psychiatry.
Rethinking pain
CBP is a leading cause of disability, and treatment is often ineffective. In about 85% of cases of primary CBP, a definitive cause of the pain can’t be identified. In these cases, fear, avoidance, and beliefs that pain indicates injury may contribute to ongoing CBP.
PRT educates patients about the role of the brain in generating chronic pain; helps them reappraise their pain as they engage in movements that they had been afraid to undertake; and helps them address emotions that may exacerbate pain.
The study included 151 adults (54% women; mean age, 41 years) who had primary CBP of low to moderate severity (mean pain intensity, 4 of 10) for an average of 10 years.
A total of 50 participants were randomly allocated to undergo PRT (one telehealth session with a physician and eight PRT sessions over 4 weeks), 51 to receive placebo (subcutaneous saline injection in the back), and 50 to continue their routine, usual ongoing care.
Large group differences in pain were observed after treatment. The mean pain score was 1.18 in the PRT group, 2.84 in the placebo group, and 3.13 in the usual-care group. Hedges’ g was –1.14 for PRT versus placebo and –1.74 for PRT versus usual care (P < .001).
Two-thirds (66%) of adults in the PRT group were pain free or nearly pain free following treatment (pain-intensity score of 0 or 1 out of 10), compared with 20% of those in the placebo group and 10% of those who received usual care.
Treatment effects were maintained at 1-year follow-up. The mean pain score was 1.51 in the PRT group, 2.79 in the placebo group, and 3.00 in the usual-care group. Neither age nor sex moderated the effect of PRT on pain intensity.
Retraining the brain
The researchers said the effects of PRT on pain were mediated by lessening the belief that pain indicates tissue damage. Of note, PRT also reduced experimentally evoked back pain and spontaneous pain during functional MRI, with large effect sizes.
“The idea is that by thinking about the pain as safe rather than threatening, patients can alter the brain networks reinforcing the pain, and neutralize it,” Dr. Ashar said in a news release.
The authors noted that study participants were relatively well educated and active. The participants reported having longstanding low to moderate pain and disability at baseline.
The physician and therapists were experts in delivering PRT. Future studies should test generalizability to other patient populations, therapists, and treatment contexts.
“Our clinical experience shows that PRT is effective for other primary chronic pain conditions as well,” said Dr. Ashar, including primary knee pain and tension headache.
Restoring function
Commenting on the findings, Shaheen E. Lakhan, MD, PhD, neurologist and pain specialist in Newton, Mass., said he has long experience using psychological approaches to address pain, with good results.
“Imagine telling a person suffering from decades of chronic pain that your pain is all in your head. I’ve done that for years as a board-certified pain physician managing only the most severe and debilitating forms of pain. When used to ground brain retraining, I could ultimately restore function to people living with chronic pain,” Dr. Lakhan said.
“The statement is true – the brain ultimately processes signals from throughout the body, forms the perception of pain, and links it to emotional brain centers, among others. Pain is an important survival mechanism so that when your body is at threat of injury, you protect yourself from further damage and withdraw. The problem lies when pain outlasts its welcome and chronifies,” said Dr. Lakhan, senior vice president of research and development of Click Therapeutics in Boston.
The investigators in this study “eloquently prove” that with 4 weeks of PRT, patients can learn that chronic pain is largely a “brain-generated false alarm and that constantly affirming this truth can actually reduce or eliminate it,” Dr. Lakhan said.
“Further, the brain areas implicated with pain are calmed after going through the therapy to both resting pain and pain induced by extending the back,” he noted.
“Pain-reprocessing therapy can improve the lives of chronic [pain patients] who have low to moderate levels of pain and disability; however, much work needs to be done to make this scalable and universally available and covered by insurers as a treatment modality,” Dr. Lakhan added.
He cautioned that he has not seen therapies such as this work when there is significant depression, withdrawal, or lack of control over one’s situation such that one behaves in a helpless manner – “a terrible state of mind called learned helplessness.”
The study was funded by the National Institutes of Health, the National Center for Advancing Translational Sciences, the Radiological Society of North America, the German Research Foundation, the Psychophysiologic Disorders Association, the Foundation for the Study of the Therapeutic Encounter, and community donations. Dr. Ashar received grants from the National Institutes of Health during the conduct of the study and personal fees from UnitedHealth Group, Lin Health, Pain Reprocessing Therapy Center, and Mental Health Partners of Boulder County outside the submitted work. Dr. Lakhan disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Psychological therapy that changes an individual’s beliefs about pain not only provides lasting chronic pain relief but also alters brain regions related to pain generation, new research shows.
In the first randomized controlled test of pain-reprocessing therapy (PRT), two-thirds of patients with chronic back pain (CBP) who received 4 weeks of PRT were pain free or nearly pain free afterward – and for most patients, relief was maintained for 1 year, the researchers found.
“Primary chronic back pain can be dramatically reduced or even eliminated by psychological treatment focused on changing how threatening we perceive the pain to be,” first author Yoni Ashar, PhD, department of psychiatry, Weill Cornell Medicine, New York, said in an interview.
“ given that large reductions in pain have rarely been observed in studies that tested psychological therapies for chronic back pain.
The study was published online Sept. 29, 2021, in JAMA Psychiatry.
Rethinking pain
CBP is a leading cause of disability, and treatment is often ineffective. In about 85% of cases of primary CBP, a definitive cause of the pain can’t be identified. In these cases, fear, avoidance, and beliefs that pain indicates injury may contribute to ongoing CBP.
PRT educates patients about the role of the brain in generating chronic pain; helps them reappraise their pain as they engage in movements that they had been afraid to undertake; and helps them address emotions that may exacerbate pain.
The study included 151 adults (54% women; mean age, 41 years) who had primary CBP of low to moderate severity (mean pain intensity, 4 of 10) for an average of 10 years.
A total of 50 participants were randomly allocated to undergo PRT (one telehealth session with a physician and eight PRT sessions over 4 weeks), 51 to receive placebo (subcutaneous saline injection in the back), and 50 to continue their routine, usual ongoing care.
Large group differences in pain were observed after treatment. The mean pain score was 1.18 in the PRT group, 2.84 in the placebo group, and 3.13 in the usual-care group. Hedges’ g was –1.14 for PRT versus placebo and –1.74 for PRT versus usual care (P < .001).
Two-thirds (66%) of adults in the PRT group were pain free or nearly pain free following treatment (pain-intensity score of 0 or 1 out of 10), compared with 20% of those in the placebo group and 10% of those who received usual care.
Treatment effects were maintained at 1-year follow-up. The mean pain score was 1.51 in the PRT group, 2.79 in the placebo group, and 3.00 in the usual-care group. Neither age nor sex moderated the effect of PRT on pain intensity.
Retraining the brain
The researchers said the effects of PRT on pain were mediated by lessening the belief that pain indicates tissue damage. Of note, PRT also reduced experimentally evoked back pain and spontaneous pain during functional MRI, with large effect sizes.
“The idea is that by thinking about the pain as safe rather than threatening, patients can alter the brain networks reinforcing the pain, and neutralize it,” Dr. Ashar said in a news release.
The authors noted that study participants were relatively well educated and active. The participants reported having longstanding low to moderate pain and disability at baseline.
The physician and therapists were experts in delivering PRT. Future studies should test generalizability to other patient populations, therapists, and treatment contexts.
“Our clinical experience shows that PRT is effective for other primary chronic pain conditions as well,” said Dr. Ashar, including primary knee pain and tension headache.
Restoring function
Commenting on the findings, Shaheen E. Lakhan, MD, PhD, neurologist and pain specialist in Newton, Mass., said he has long experience using psychological approaches to address pain, with good results.
“Imagine telling a person suffering from decades of chronic pain that your pain is all in your head. I’ve done that for years as a board-certified pain physician managing only the most severe and debilitating forms of pain. When used to ground brain retraining, I could ultimately restore function to people living with chronic pain,” Dr. Lakhan said.
“The statement is true – the brain ultimately processes signals from throughout the body, forms the perception of pain, and links it to emotional brain centers, among others. Pain is an important survival mechanism so that when your body is at threat of injury, you protect yourself from further damage and withdraw. The problem lies when pain outlasts its welcome and chronifies,” said Dr. Lakhan, senior vice president of research and development of Click Therapeutics in Boston.
The investigators in this study “eloquently prove” that with 4 weeks of PRT, patients can learn that chronic pain is largely a “brain-generated false alarm and that constantly affirming this truth can actually reduce or eliminate it,” Dr. Lakhan said.
“Further, the brain areas implicated with pain are calmed after going through the therapy to both resting pain and pain induced by extending the back,” he noted.
“Pain-reprocessing therapy can improve the lives of chronic [pain patients] who have low to moderate levels of pain and disability; however, much work needs to be done to make this scalable and universally available and covered by insurers as a treatment modality,” Dr. Lakhan added.
He cautioned that he has not seen therapies such as this work when there is significant depression, withdrawal, or lack of control over one’s situation such that one behaves in a helpless manner – “a terrible state of mind called learned helplessness.”
The study was funded by the National Institutes of Health, the National Center for Advancing Translational Sciences, the Radiological Society of North America, the German Research Foundation, the Psychophysiologic Disorders Association, the Foundation for the Study of the Therapeutic Encounter, and community donations. Dr. Ashar received grants from the National Institutes of Health during the conduct of the study and personal fees from UnitedHealth Group, Lin Health, Pain Reprocessing Therapy Center, and Mental Health Partners of Boulder County outside the submitted work. Dr. Lakhan disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Psychological therapy that changes an individual’s beliefs about pain not only provides lasting chronic pain relief but also alters brain regions related to pain generation, new research shows.
In the first randomized controlled test of pain-reprocessing therapy (PRT), two-thirds of patients with chronic back pain (CBP) who received 4 weeks of PRT were pain free or nearly pain free afterward – and for most patients, relief was maintained for 1 year, the researchers found.
“Primary chronic back pain can be dramatically reduced or even eliminated by psychological treatment focused on changing how threatening we perceive the pain to be,” first author Yoni Ashar, PhD, department of psychiatry, Weill Cornell Medicine, New York, said in an interview.
“ given that large reductions in pain have rarely been observed in studies that tested psychological therapies for chronic back pain.
The study was published online Sept. 29, 2021, in JAMA Psychiatry.
Rethinking pain
CBP is a leading cause of disability, and treatment is often ineffective. In about 85% of cases of primary CBP, a definitive cause of the pain can’t be identified. In these cases, fear, avoidance, and beliefs that pain indicates injury may contribute to ongoing CBP.
PRT educates patients about the role of the brain in generating chronic pain; helps them reappraise their pain as they engage in movements that they had been afraid to undertake; and helps them address emotions that may exacerbate pain.
The study included 151 adults (54% women; mean age, 41 years) who had primary CBP of low to moderate severity (mean pain intensity, 4 of 10) for an average of 10 years.
A total of 50 participants were randomly allocated to undergo PRT (one telehealth session with a physician and eight PRT sessions over 4 weeks), 51 to receive placebo (subcutaneous saline injection in the back), and 50 to continue their routine, usual ongoing care.
Large group differences in pain were observed after treatment. The mean pain score was 1.18 in the PRT group, 2.84 in the placebo group, and 3.13 in the usual-care group. Hedges’ g was –1.14 for PRT versus placebo and –1.74 for PRT versus usual care (P < .001).
Two-thirds (66%) of adults in the PRT group were pain free or nearly pain free following treatment (pain-intensity score of 0 or 1 out of 10), compared with 20% of those in the placebo group and 10% of those who received usual care.
Treatment effects were maintained at 1-year follow-up. The mean pain score was 1.51 in the PRT group, 2.79 in the placebo group, and 3.00 in the usual-care group. Neither age nor sex moderated the effect of PRT on pain intensity.
Retraining the brain
The researchers said the effects of PRT on pain were mediated by lessening the belief that pain indicates tissue damage. Of note, PRT also reduced experimentally evoked back pain and spontaneous pain during functional MRI, with large effect sizes.
“The idea is that by thinking about the pain as safe rather than threatening, patients can alter the brain networks reinforcing the pain, and neutralize it,” Dr. Ashar said in a news release.
The authors noted that study participants were relatively well educated and active. The participants reported having longstanding low to moderate pain and disability at baseline.
The physician and therapists were experts in delivering PRT. Future studies should test generalizability to other patient populations, therapists, and treatment contexts.
“Our clinical experience shows that PRT is effective for other primary chronic pain conditions as well,” said Dr. Ashar, including primary knee pain and tension headache.
Restoring function
Commenting on the findings, Shaheen E. Lakhan, MD, PhD, neurologist and pain specialist in Newton, Mass., said he has long experience using psychological approaches to address pain, with good results.
“Imagine telling a person suffering from decades of chronic pain that your pain is all in your head. I’ve done that for years as a board-certified pain physician managing only the most severe and debilitating forms of pain. When used to ground brain retraining, I could ultimately restore function to people living with chronic pain,” Dr. Lakhan said.
“The statement is true – the brain ultimately processes signals from throughout the body, forms the perception of pain, and links it to emotional brain centers, among others. Pain is an important survival mechanism so that when your body is at threat of injury, you protect yourself from further damage and withdraw. The problem lies when pain outlasts its welcome and chronifies,” said Dr. Lakhan, senior vice president of research and development of Click Therapeutics in Boston.
The investigators in this study “eloquently prove” that with 4 weeks of PRT, patients can learn that chronic pain is largely a “brain-generated false alarm and that constantly affirming this truth can actually reduce or eliminate it,” Dr. Lakhan said.
“Further, the brain areas implicated with pain are calmed after going through the therapy to both resting pain and pain induced by extending the back,” he noted.
“Pain-reprocessing therapy can improve the lives of chronic [pain patients] who have low to moderate levels of pain and disability; however, much work needs to be done to make this scalable and universally available and covered by insurers as a treatment modality,” Dr. Lakhan added.
He cautioned that he has not seen therapies such as this work when there is significant depression, withdrawal, or lack of control over one’s situation such that one behaves in a helpless manner – “a terrible state of mind called learned helplessness.”
The study was funded by the National Institutes of Health, the National Center for Advancing Translational Sciences, the Radiological Society of North America, the German Research Foundation, the Psychophysiologic Disorders Association, the Foundation for the Study of the Therapeutic Encounter, and community donations. Dr. Ashar received grants from the National Institutes of Health during the conduct of the study and personal fees from UnitedHealth Group, Lin Health, Pain Reprocessing Therapy Center, and Mental Health Partners of Boulder County outside the submitted work. Dr. Lakhan disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Depression rates up threefold since start of COVID-19
A year into the COVID-19 pandemic, the share of the U.S. adult population reporting symptoms of elevated depression had more than tripled from prepandemic levels and worsened significantly since restrictions went into effect, a study of more than 1,000 adults surveyed at the start of the pandemic and 1 year into it has reported.
The study also found that younger adults, people with lower incomes and savings, unmarried people, and those exposed to multiple stress factors were most vulnerable to elevated levels of depression through the first year of the pandemic.
“The pandemic has been an ongoing exposure,” lead author Catherine K. Ettman, a PhD candidate at Brown University, Providence, R.I., said in an interview. “Mental health is sensitive to economic and social conditions. While living conditions have improved for some people over the last 12 months, the pandemic has been disruptive to life and economic well-being for many,” said Ms. Ettman, who is also chief of staff and director of strategic initiatives in the office of the dean at Boston University. Her study was published in Lancet Regional Health – Americas.
Ms. Ettman and coauthors reported that 32.8% (95% confidence interval, 29.1%-36.8%) of surveyed adults had elevated depressive symptoms in 2021, compared with 27.8% (95% CI, 24.9%-30.9%) in the early months of the pandemic in 2020 (P = .0016). That compares with a rate of 8.5% before the pandemic, a figure based on a prepandemic sample of 5,065 patients from the National Health and Nutrition Examination Survey reported previously by Ms. Ettman and associates.
“The COVID-19 pandemic and its economic consequences have displaced social networks, created ongoing stressors, and reduced access to the resources that protect mental health,” Ms. Ettman said.
Four groups most affected
In this latest research, a longitudinal panel study of a nationally representative group of U.S. adults, the researchers surveyed participants in March and April 2020 (n = 1,414) and the same group again in March and April 2021 (n = 1,161). The participants completed the Patient Health Questionnaire–9 (PHQ-9) and were enrolled in the COVID-19 and Life Stressors Impact on Mental Health and Well-Being study.
The study found that elevated depressive symptoms were most prevalent in four groups:
- Younger patients, with 43.9% of patients aged 18-39 years self-reporting elevated depressive symptoms, compared with 32.4% of those aged 40-59, and 19.1% of patients aged 60 and older.
- People with lower incomes, with 58.1% of people making $19,999 or less reporting elevated symptoms, compared with 41.3% of those making $20,000-$44,999, 31.4% of people making $45,000-$74,999, and 14.1% of those making $75,000 or more.
- People with less than $5,000 in family savings, with a rate of 51.1%, compared with 24.2% of those with more than that.
- People never married, with a rate of 39.8% versus 37.7% of those living with a partner; 31.5% widowed, divorced, or separated; and 18.3% married.
The study also found correlations between the number of self-reported stressors and elevated depression symptoms: a rate of 51.1% in people with four or more stressors; 25.8% in those with two or three stressors; and 17% in people with one or no stressors.
Among the groups reporting the lowest rates of depressive symptoms in 2021 were people making more than $75,000 a year; those with one or no COVID-19 stressors; and non-Hispanic Asian persons.
“Stressors such as difficulties finding childcare, difficulties paying for housing, and job loss were associated with greater depression 12 months into the COVID-19 pandemic,” Ms. Ettman said. “Efforts to address stressors and improve access to childcare, housing, employment, and fair wages can improve mental health.”
The duration of the pandemic is another explanation for the significant rise in depressive symptoms, senior author Sandro Galea, MD, MPH, DrPH, said in an interview. Dr. Galea added. “Unlike acute traumatic events, the COVID-19 pandemic has been ongoing.”
He said clinicians, public health officials, and policy makers need to be aware of the impact COVID-19 has had on mental health. “We can take steps as a society to treat and prevent depression and create conditions that allow all populations to be healthy,” said Dr. Galea, who is dean and a professor of family medicine at Boston University.
Age of sample cited as limitation
The study builds on existing evidence linking depression trends and the COVID-19 pandemic, David Puder, MD, a medical director at Loma Linda (Calif.) University, said in an interview. However, he noted it had some limitations. “The age range is only 18 and older, so we don’t get to see what is happening with a highly impacted group of students who have not been able to go to school and be with their friends during COVID,” said Dr. Puder, who also hosts the podcast “Psychiatry & Psychotherapy.” “Further, the PHQ-9 is often a screening tool for depression and is not best used for changes in mental health over time.”
At the same time, Dr. Puder said, one of the study’s strengths was that it showed how depressive symptoms increased during the COVID lockdown. “It shows certain groups are at higher risk, including those with less financial resources and those with higher amounts of stress,” Dr. Puder said.
Ms. Ettman, Dr. Galea, and Dr. Puder reported no relevant disclosures.
A year into the COVID-19 pandemic, the share of the U.S. adult population reporting symptoms of elevated depression had more than tripled from prepandemic levels and worsened significantly since restrictions went into effect, a study of more than 1,000 adults surveyed at the start of the pandemic and 1 year into it has reported.
The study also found that younger adults, people with lower incomes and savings, unmarried people, and those exposed to multiple stress factors were most vulnerable to elevated levels of depression through the first year of the pandemic.
“The pandemic has been an ongoing exposure,” lead author Catherine K. Ettman, a PhD candidate at Brown University, Providence, R.I., said in an interview. “Mental health is sensitive to economic and social conditions. While living conditions have improved for some people over the last 12 months, the pandemic has been disruptive to life and economic well-being for many,” said Ms. Ettman, who is also chief of staff and director of strategic initiatives in the office of the dean at Boston University. Her study was published in Lancet Regional Health – Americas.
Ms. Ettman and coauthors reported that 32.8% (95% confidence interval, 29.1%-36.8%) of surveyed adults had elevated depressive symptoms in 2021, compared with 27.8% (95% CI, 24.9%-30.9%) in the early months of the pandemic in 2020 (P = .0016). That compares with a rate of 8.5% before the pandemic, a figure based on a prepandemic sample of 5,065 patients from the National Health and Nutrition Examination Survey reported previously by Ms. Ettman and associates.
“The COVID-19 pandemic and its economic consequences have displaced social networks, created ongoing stressors, and reduced access to the resources that protect mental health,” Ms. Ettman said.
Four groups most affected
In this latest research, a longitudinal panel study of a nationally representative group of U.S. adults, the researchers surveyed participants in March and April 2020 (n = 1,414) and the same group again in March and April 2021 (n = 1,161). The participants completed the Patient Health Questionnaire–9 (PHQ-9) and were enrolled in the COVID-19 and Life Stressors Impact on Mental Health and Well-Being study.
The study found that elevated depressive symptoms were most prevalent in four groups:
- Younger patients, with 43.9% of patients aged 18-39 years self-reporting elevated depressive symptoms, compared with 32.4% of those aged 40-59, and 19.1% of patients aged 60 and older.
- People with lower incomes, with 58.1% of people making $19,999 or less reporting elevated symptoms, compared with 41.3% of those making $20,000-$44,999, 31.4% of people making $45,000-$74,999, and 14.1% of those making $75,000 or more.
- People with less than $5,000 in family savings, with a rate of 51.1%, compared with 24.2% of those with more than that.
- People never married, with a rate of 39.8% versus 37.7% of those living with a partner; 31.5% widowed, divorced, or separated; and 18.3% married.
The study also found correlations between the number of self-reported stressors and elevated depression symptoms: a rate of 51.1% in people with four or more stressors; 25.8% in those with two or three stressors; and 17% in people with one or no stressors.
Among the groups reporting the lowest rates of depressive symptoms in 2021 were people making more than $75,000 a year; those with one or no COVID-19 stressors; and non-Hispanic Asian persons.
“Stressors such as difficulties finding childcare, difficulties paying for housing, and job loss were associated with greater depression 12 months into the COVID-19 pandemic,” Ms. Ettman said. “Efforts to address stressors and improve access to childcare, housing, employment, and fair wages can improve mental health.”
The duration of the pandemic is another explanation for the significant rise in depressive symptoms, senior author Sandro Galea, MD, MPH, DrPH, said in an interview. Dr. Galea added. “Unlike acute traumatic events, the COVID-19 pandemic has been ongoing.”
He said clinicians, public health officials, and policy makers need to be aware of the impact COVID-19 has had on mental health. “We can take steps as a society to treat and prevent depression and create conditions that allow all populations to be healthy,” said Dr. Galea, who is dean and a professor of family medicine at Boston University.
Age of sample cited as limitation
The study builds on existing evidence linking depression trends and the COVID-19 pandemic, David Puder, MD, a medical director at Loma Linda (Calif.) University, said in an interview. However, he noted it had some limitations. “The age range is only 18 and older, so we don’t get to see what is happening with a highly impacted group of students who have not been able to go to school and be with their friends during COVID,” said Dr. Puder, who also hosts the podcast “Psychiatry & Psychotherapy.” “Further, the PHQ-9 is often a screening tool for depression and is not best used for changes in mental health over time.”
At the same time, Dr. Puder said, one of the study’s strengths was that it showed how depressive symptoms increased during the COVID lockdown. “It shows certain groups are at higher risk, including those with less financial resources and those with higher amounts of stress,” Dr. Puder said.
Ms. Ettman, Dr. Galea, and Dr. Puder reported no relevant disclosures.
A year into the COVID-19 pandemic, the share of the U.S. adult population reporting symptoms of elevated depression had more than tripled from prepandemic levels and worsened significantly since restrictions went into effect, a study of more than 1,000 adults surveyed at the start of the pandemic and 1 year into it has reported.
The study also found that younger adults, people with lower incomes and savings, unmarried people, and those exposed to multiple stress factors were most vulnerable to elevated levels of depression through the first year of the pandemic.
“The pandemic has been an ongoing exposure,” lead author Catherine K. Ettman, a PhD candidate at Brown University, Providence, R.I., said in an interview. “Mental health is sensitive to economic and social conditions. While living conditions have improved for some people over the last 12 months, the pandemic has been disruptive to life and economic well-being for many,” said Ms. Ettman, who is also chief of staff and director of strategic initiatives in the office of the dean at Boston University. Her study was published in Lancet Regional Health – Americas.
Ms. Ettman and coauthors reported that 32.8% (95% confidence interval, 29.1%-36.8%) of surveyed adults had elevated depressive symptoms in 2021, compared with 27.8% (95% CI, 24.9%-30.9%) in the early months of the pandemic in 2020 (P = .0016). That compares with a rate of 8.5% before the pandemic, a figure based on a prepandemic sample of 5,065 patients from the National Health and Nutrition Examination Survey reported previously by Ms. Ettman and associates.
“The COVID-19 pandemic and its economic consequences have displaced social networks, created ongoing stressors, and reduced access to the resources that protect mental health,” Ms. Ettman said.
Four groups most affected
In this latest research, a longitudinal panel study of a nationally representative group of U.S. adults, the researchers surveyed participants in March and April 2020 (n = 1,414) and the same group again in March and April 2021 (n = 1,161). The participants completed the Patient Health Questionnaire–9 (PHQ-9) and were enrolled in the COVID-19 and Life Stressors Impact on Mental Health and Well-Being study.
The study found that elevated depressive symptoms were most prevalent in four groups:
- Younger patients, with 43.9% of patients aged 18-39 years self-reporting elevated depressive symptoms, compared with 32.4% of those aged 40-59, and 19.1% of patients aged 60 and older.
- People with lower incomes, with 58.1% of people making $19,999 or less reporting elevated symptoms, compared with 41.3% of those making $20,000-$44,999, 31.4% of people making $45,000-$74,999, and 14.1% of those making $75,000 or more.
- People with less than $5,000 in family savings, with a rate of 51.1%, compared with 24.2% of those with more than that.
- People never married, with a rate of 39.8% versus 37.7% of those living with a partner; 31.5% widowed, divorced, or separated; and 18.3% married.
The study also found correlations between the number of self-reported stressors and elevated depression symptoms: a rate of 51.1% in people with four or more stressors; 25.8% in those with two or three stressors; and 17% in people with one or no stressors.
Among the groups reporting the lowest rates of depressive symptoms in 2021 were people making more than $75,000 a year; those with one or no COVID-19 stressors; and non-Hispanic Asian persons.
“Stressors such as difficulties finding childcare, difficulties paying for housing, and job loss were associated with greater depression 12 months into the COVID-19 pandemic,” Ms. Ettman said. “Efforts to address stressors and improve access to childcare, housing, employment, and fair wages can improve mental health.”
The duration of the pandemic is another explanation for the significant rise in depressive symptoms, senior author Sandro Galea, MD, MPH, DrPH, said in an interview. Dr. Galea added. “Unlike acute traumatic events, the COVID-19 pandemic has been ongoing.”
He said clinicians, public health officials, and policy makers need to be aware of the impact COVID-19 has had on mental health. “We can take steps as a society to treat and prevent depression and create conditions that allow all populations to be healthy,” said Dr. Galea, who is dean and a professor of family medicine at Boston University.
Age of sample cited as limitation
The study builds on existing evidence linking depression trends and the COVID-19 pandemic, David Puder, MD, a medical director at Loma Linda (Calif.) University, said in an interview. However, he noted it had some limitations. “The age range is only 18 and older, so we don’t get to see what is happening with a highly impacted group of students who have not been able to go to school and be with their friends during COVID,” said Dr. Puder, who also hosts the podcast “Psychiatry & Psychotherapy.” “Further, the PHQ-9 is often a screening tool for depression and is not best used for changes in mental health over time.”
At the same time, Dr. Puder said, one of the study’s strengths was that it showed how depressive symptoms increased during the COVID lockdown. “It shows certain groups are at higher risk, including those with less financial resources and those with higher amounts of stress,” Dr. Puder said.
Ms. Ettman, Dr. Galea, and Dr. Puder reported no relevant disclosures.
FROM LANCET REGIONAL HEALTH – AMERICAS








