User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Neuropsychiatry affects pediatric OCD treatment
Treatment of pediatric obsessive-compulsive disorder (OCD) has evolved in recent years, with more attention given to some of the neuropsychiatric underpinnings of the condition and how they can affect treatment response.
At the Focus on Neuropsychiatry 2021 meeting, Jeffrey Strawn, MD, outlined some of the neuropsychiatry affecting disease and potential mechanisms to help control obsessions and behaviors, and how they may fit with some therapeutic regimens.
Dr. Strawn discussed the psychological construct of cognitive control, which can provide patients an “out” from the cycle of obsession/fear/worry and compulsion/avoidance. In the face of distress, compulsion and avoidance lead to relief, which reinforces the obsession/fear/worry; this in turn leads to more distress.
“We have an escape door for this circuit” in the form of cognitive control, said Dr. Strawn, who is an associate professor of pediatrics at Cincinnati Children’s Hospital Medical Center.
Cognitive control is linked to insight, which can in turn increase adaptive behaviors that help the patient resist the compulsion. Patients won’t eliminate distress, but they can be helped to make it more tolerable. Therapists can then help them move toward goal-directed thoughts and behaviors. Cognitive control is associated with several neural networks, but Dr. Strawn focused on two: the frontoparietal network, associated with top-down regulation; and the cingular-opercular network. Both of these are engaged during cognitive control processes, and play a role inhibitory control and error monitoring.
Dr. Strawn discussed a recent study that explored the neurofunctional basis of treatment. It compared the effects of a stress management therapy and cognitive-behavioral therapy (CBT) in children and adults with OCD at 6 and 12 weeks. The study found similar symptom reductions in both adults and adolescents in both intervention groups.
Before initiating treatment, the researchers conducted functional MRI scans of participants while conducting an incentive flanker task, which reveals brain activity in response to cognitive control and reward processing.
A larger therapeutic response was found in the CBT group among patients who had a larger pretreatment activation within the right temporal lobe and rostral anterior cingulate cortex during cognitive control, as well as those with more activation within the medial prefrontal, orbitofrontal, lateral prefrontal, and amygdala regions during reward processing. On the other hand, within the stress management therapy group, treatment responses were better among those who had lower pretreatment activation among overlapping regions.
“There was a difference in terms of the neurofunctional predictors of treatment response. One of the key regions is the medial prefrontal cortex as well as the rostral anterior cingulate,” said Dr. Strawn, at the meeting presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
On the neuropharmacology side, numerous medications have been approved for OCD. Dr. Strawn highlighted some studies to illustrate general OCD treatment concepts. That included the 2004 Pediatric OCD Treatment Study, which was one of the only trials to compare placebo with an SSRI, CBT, and the combination of SSRI and CBT. It showed the best results with combination therapy, and the difference appeared early in the treatment course.
That study had aggressive dosing, which led to some issues with sertraline tolerability. Dr. Strawn showed results of a study at his institution which showed that the drug levels of pediatric patients treated with sertraline depended on CYP2C19 metabolism, which affects overall exposure and peak dose concentration. In pediatric populations, some SSRIs clear more slowly and can have high peak concentrations. SSRIs have more side effects than serotonin and norepinephrine reuptake inhibitors in both anxiety disorders and OCD. A key difference between the two is that SSRI treatment is associated with greater frequency of activation, which is difficult to define, but includes restlessness and agitation and insomnia in the beginning stages of treatment.
SSRIs also lead to improvement early in the course of treatment, which was shown in a meta-analysis of nine trials. However, the same study showed that clomipramine is associated with a faster and greater magnitude of improvement, compared with SSRIs, even when the latter are dosed aggressively.
Clomipramine is a potent inhibitor of both serotonin and norepinephrine reuptake. It is recommended to monitor clomipramine levels in pediatric OCD patients, and Dr. Strawn suggested that monitoring should include both the parent drug and its primary metabolite, norclomipramine. At a given dose, there can be a great deal of variation in drug level. The clomipramine/norclomipramine ratio can provide information about the patient’s metabolic state, as well as drug adherence.
Dr. Strawn noted that peak levels occur around 1-3 hours after the dose, “and we really do want at least a 12-hour trough level.” EKGs should be performed at baseline and after any titration of clomipramine dose.
He also discussed pediatric OCD patients with OCD and tics. About one-third of Tourette syndrome patients experience OCD at some point. Tics often improve, whereas OCD more often persists. Tics that co-occur with OCD are associated with a lesser response to SSRI treatment, but not CBT treatment. Similarly, patients with hoarding tendencies are about one-third less likely to respond to SSRIs, CBT, or combination therapy.
Dr. Strawn discussed the concept of accommodation, in which family members cope with a patient’s behavior by altering routines to minimize distress and impairment. This may take the form of facilitating rituals, providing reassurance about a patient’s fears, acquiescing to demands, reducing the child’s day-to-day responsibilities, or helping the child complete tasks. Such actions are well intentioned, but they undermine cognitive control, negatively reinforce symptom engagement, and are associated with functional impairment. Reassurance is the most important behavior, occurring in more than half of patients, and it’s measurable. Parental involvement with rituals is also a concern. “This is associated with higher levels of child OCD severity, as well as parental psychopathology, and lower family cohesion. So
New developments in neurobiology and neuropsychology have changed the view of exposure. The old model emphasized the child’s fear rating as an index of corrective learning. The idea was that habituation would decrease anxiety and distress from future exposures. The new model revolves around inhibitory learning theory, which focuses on the variability of distress and aims to increase tolerance of distress. Another goal is to develop new, non-threat associations.
Finally, Dr. Strawn pointed out predictors of poor outcomes in pediatric OCD, including factors such as compulsion severity, oppositional behavior, frequent handwashing, functional impairment, lack of insight, externalizing symptoms, and possibly hoarding. Problematic family characteristics include higher levels of accommodation, parental anxiety, low family cohesion, and high levels of conflict. “The last three really represent a very concerning triad of family behaviors that may necessitate specific family work in order to facilitate the recovery of the pediatric patient,” Dr. Strawn said.
During the question-and-answer session after the talk, Dr. Strawn was asked whether there might be an inflammatory component to OCD, and whether pediatric autoimmune neuropsychiatric disorders associated with streptococcus (PANDAS) might be a prodromal condition. He noted that some studies have shown a relationship, but results have been mixed, with lots of heterogeneity within the studied populations. To be suspicious that a patient had OCD resulting from PANDAS would require a high threshold, including an acute onset of symptoms. “This is a situation also where I would tend to involve consultation with some other specialties, including neurology. And obviously there would be follow-up in terms of the general workup,” he said.
Dr. Strawn has received research funding from Allergan, Otsuka, and Myriad Genetics. He has consulted for Myriad Genetics, and is a speaker for CMEology and the Neuroscience Education Institute.
Treatment of pediatric obsessive-compulsive disorder (OCD) has evolved in recent years, with more attention given to some of the neuropsychiatric underpinnings of the condition and how they can affect treatment response.
At the Focus on Neuropsychiatry 2021 meeting, Jeffrey Strawn, MD, outlined some of the neuropsychiatry affecting disease and potential mechanisms to help control obsessions and behaviors, and how they may fit with some therapeutic regimens.
Dr. Strawn discussed the psychological construct of cognitive control, which can provide patients an “out” from the cycle of obsession/fear/worry and compulsion/avoidance. In the face of distress, compulsion and avoidance lead to relief, which reinforces the obsession/fear/worry; this in turn leads to more distress.
“We have an escape door for this circuit” in the form of cognitive control, said Dr. Strawn, who is an associate professor of pediatrics at Cincinnati Children’s Hospital Medical Center.
Cognitive control is linked to insight, which can in turn increase adaptive behaviors that help the patient resist the compulsion. Patients won’t eliminate distress, but they can be helped to make it more tolerable. Therapists can then help them move toward goal-directed thoughts and behaviors. Cognitive control is associated with several neural networks, but Dr. Strawn focused on two: the frontoparietal network, associated with top-down regulation; and the cingular-opercular network. Both of these are engaged during cognitive control processes, and play a role inhibitory control and error monitoring.
Dr. Strawn discussed a recent study that explored the neurofunctional basis of treatment. It compared the effects of a stress management therapy and cognitive-behavioral therapy (CBT) in children and adults with OCD at 6 and 12 weeks. The study found similar symptom reductions in both adults and adolescents in both intervention groups.
Before initiating treatment, the researchers conducted functional MRI scans of participants while conducting an incentive flanker task, which reveals brain activity in response to cognitive control and reward processing.
A larger therapeutic response was found in the CBT group among patients who had a larger pretreatment activation within the right temporal lobe and rostral anterior cingulate cortex during cognitive control, as well as those with more activation within the medial prefrontal, orbitofrontal, lateral prefrontal, and amygdala regions during reward processing. On the other hand, within the stress management therapy group, treatment responses were better among those who had lower pretreatment activation among overlapping regions.
“There was a difference in terms of the neurofunctional predictors of treatment response. One of the key regions is the medial prefrontal cortex as well as the rostral anterior cingulate,” said Dr. Strawn, at the meeting presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
On the neuropharmacology side, numerous medications have been approved for OCD. Dr. Strawn highlighted some studies to illustrate general OCD treatment concepts. That included the 2004 Pediatric OCD Treatment Study, which was one of the only trials to compare placebo with an SSRI, CBT, and the combination of SSRI and CBT. It showed the best results with combination therapy, and the difference appeared early in the treatment course.
That study had aggressive dosing, which led to some issues with sertraline tolerability. Dr. Strawn showed results of a study at his institution which showed that the drug levels of pediatric patients treated with sertraline depended on CYP2C19 metabolism, which affects overall exposure and peak dose concentration. In pediatric populations, some SSRIs clear more slowly and can have high peak concentrations. SSRIs have more side effects than serotonin and norepinephrine reuptake inhibitors in both anxiety disorders and OCD. A key difference between the two is that SSRI treatment is associated with greater frequency of activation, which is difficult to define, but includes restlessness and agitation and insomnia in the beginning stages of treatment.
SSRIs also lead to improvement early in the course of treatment, which was shown in a meta-analysis of nine trials. However, the same study showed that clomipramine is associated with a faster and greater magnitude of improvement, compared with SSRIs, even when the latter are dosed aggressively.
Clomipramine is a potent inhibitor of both serotonin and norepinephrine reuptake. It is recommended to monitor clomipramine levels in pediatric OCD patients, and Dr. Strawn suggested that monitoring should include both the parent drug and its primary metabolite, norclomipramine. At a given dose, there can be a great deal of variation in drug level. The clomipramine/norclomipramine ratio can provide information about the patient’s metabolic state, as well as drug adherence.
Dr. Strawn noted that peak levels occur around 1-3 hours after the dose, “and we really do want at least a 12-hour trough level.” EKGs should be performed at baseline and after any titration of clomipramine dose.
He also discussed pediatric OCD patients with OCD and tics. About one-third of Tourette syndrome patients experience OCD at some point. Tics often improve, whereas OCD more often persists. Tics that co-occur with OCD are associated with a lesser response to SSRI treatment, but not CBT treatment. Similarly, patients with hoarding tendencies are about one-third less likely to respond to SSRIs, CBT, or combination therapy.
Dr. Strawn discussed the concept of accommodation, in which family members cope with a patient’s behavior by altering routines to minimize distress and impairment. This may take the form of facilitating rituals, providing reassurance about a patient’s fears, acquiescing to demands, reducing the child’s day-to-day responsibilities, or helping the child complete tasks. Such actions are well intentioned, but they undermine cognitive control, negatively reinforce symptom engagement, and are associated with functional impairment. Reassurance is the most important behavior, occurring in more than half of patients, and it’s measurable. Parental involvement with rituals is also a concern. “This is associated with higher levels of child OCD severity, as well as parental psychopathology, and lower family cohesion. So
New developments in neurobiology and neuropsychology have changed the view of exposure. The old model emphasized the child’s fear rating as an index of corrective learning. The idea was that habituation would decrease anxiety and distress from future exposures. The new model revolves around inhibitory learning theory, which focuses on the variability of distress and aims to increase tolerance of distress. Another goal is to develop new, non-threat associations.
Finally, Dr. Strawn pointed out predictors of poor outcomes in pediatric OCD, including factors such as compulsion severity, oppositional behavior, frequent handwashing, functional impairment, lack of insight, externalizing symptoms, and possibly hoarding. Problematic family characteristics include higher levels of accommodation, parental anxiety, low family cohesion, and high levels of conflict. “The last three really represent a very concerning triad of family behaviors that may necessitate specific family work in order to facilitate the recovery of the pediatric patient,” Dr. Strawn said.
During the question-and-answer session after the talk, Dr. Strawn was asked whether there might be an inflammatory component to OCD, and whether pediatric autoimmune neuropsychiatric disorders associated with streptococcus (PANDAS) might be a prodromal condition. He noted that some studies have shown a relationship, but results have been mixed, with lots of heterogeneity within the studied populations. To be suspicious that a patient had OCD resulting from PANDAS would require a high threshold, including an acute onset of symptoms. “This is a situation also where I would tend to involve consultation with some other specialties, including neurology. And obviously there would be follow-up in terms of the general workup,” he said.
Dr. Strawn has received research funding from Allergan, Otsuka, and Myriad Genetics. He has consulted for Myriad Genetics, and is a speaker for CMEology and the Neuroscience Education Institute.
Treatment of pediatric obsessive-compulsive disorder (OCD) has evolved in recent years, with more attention given to some of the neuropsychiatric underpinnings of the condition and how they can affect treatment response.
At the Focus on Neuropsychiatry 2021 meeting, Jeffrey Strawn, MD, outlined some of the neuropsychiatry affecting disease and potential mechanisms to help control obsessions and behaviors, and how they may fit with some therapeutic regimens.
Dr. Strawn discussed the psychological construct of cognitive control, which can provide patients an “out” from the cycle of obsession/fear/worry and compulsion/avoidance. In the face of distress, compulsion and avoidance lead to relief, which reinforces the obsession/fear/worry; this in turn leads to more distress.
“We have an escape door for this circuit” in the form of cognitive control, said Dr. Strawn, who is an associate professor of pediatrics at Cincinnati Children’s Hospital Medical Center.
Cognitive control is linked to insight, which can in turn increase adaptive behaviors that help the patient resist the compulsion. Patients won’t eliminate distress, but they can be helped to make it more tolerable. Therapists can then help them move toward goal-directed thoughts and behaviors. Cognitive control is associated with several neural networks, but Dr. Strawn focused on two: the frontoparietal network, associated with top-down regulation; and the cingular-opercular network. Both of these are engaged during cognitive control processes, and play a role inhibitory control and error monitoring.
Dr. Strawn discussed a recent study that explored the neurofunctional basis of treatment. It compared the effects of a stress management therapy and cognitive-behavioral therapy (CBT) in children and adults with OCD at 6 and 12 weeks. The study found similar symptom reductions in both adults and adolescents in both intervention groups.
Before initiating treatment, the researchers conducted functional MRI scans of participants while conducting an incentive flanker task, which reveals brain activity in response to cognitive control and reward processing.
A larger therapeutic response was found in the CBT group among patients who had a larger pretreatment activation within the right temporal lobe and rostral anterior cingulate cortex during cognitive control, as well as those with more activation within the medial prefrontal, orbitofrontal, lateral prefrontal, and amygdala regions during reward processing. On the other hand, within the stress management therapy group, treatment responses were better among those who had lower pretreatment activation among overlapping regions.
“There was a difference in terms of the neurofunctional predictors of treatment response. One of the key regions is the medial prefrontal cortex as well as the rostral anterior cingulate,” said Dr. Strawn, at the meeting presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
On the neuropharmacology side, numerous medications have been approved for OCD. Dr. Strawn highlighted some studies to illustrate general OCD treatment concepts. That included the 2004 Pediatric OCD Treatment Study, which was one of the only trials to compare placebo with an SSRI, CBT, and the combination of SSRI and CBT. It showed the best results with combination therapy, and the difference appeared early in the treatment course.
That study had aggressive dosing, which led to some issues with sertraline tolerability. Dr. Strawn showed results of a study at his institution which showed that the drug levels of pediatric patients treated with sertraline depended on CYP2C19 metabolism, which affects overall exposure and peak dose concentration. In pediatric populations, some SSRIs clear more slowly and can have high peak concentrations. SSRIs have more side effects than serotonin and norepinephrine reuptake inhibitors in both anxiety disorders and OCD. A key difference between the two is that SSRI treatment is associated with greater frequency of activation, which is difficult to define, but includes restlessness and agitation and insomnia in the beginning stages of treatment.
SSRIs also lead to improvement early in the course of treatment, which was shown in a meta-analysis of nine trials. However, the same study showed that clomipramine is associated with a faster and greater magnitude of improvement, compared with SSRIs, even when the latter are dosed aggressively.
Clomipramine is a potent inhibitor of both serotonin and norepinephrine reuptake. It is recommended to monitor clomipramine levels in pediatric OCD patients, and Dr. Strawn suggested that monitoring should include both the parent drug and its primary metabolite, norclomipramine. At a given dose, there can be a great deal of variation in drug level. The clomipramine/norclomipramine ratio can provide information about the patient’s metabolic state, as well as drug adherence.
Dr. Strawn noted that peak levels occur around 1-3 hours after the dose, “and we really do want at least a 12-hour trough level.” EKGs should be performed at baseline and after any titration of clomipramine dose.
He also discussed pediatric OCD patients with OCD and tics. About one-third of Tourette syndrome patients experience OCD at some point. Tics often improve, whereas OCD more often persists. Tics that co-occur with OCD are associated with a lesser response to SSRI treatment, but not CBT treatment. Similarly, patients with hoarding tendencies are about one-third less likely to respond to SSRIs, CBT, or combination therapy.
Dr. Strawn discussed the concept of accommodation, in which family members cope with a patient’s behavior by altering routines to minimize distress and impairment. This may take the form of facilitating rituals, providing reassurance about a patient’s fears, acquiescing to demands, reducing the child’s day-to-day responsibilities, or helping the child complete tasks. Such actions are well intentioned, but they undermine cognitive control, negatively reinforce symptom engagement, and are associated with functional impairment. Reassurance is the most important behavior, occurring in more than half of patients, and it’s measurable. Parental involvement with rituals is also a concern. “This is associated with higher levels of child OCD severity, as well as parental psychopathology, and lower family cohesion. So
New developments in neurobiology and neuropsychology have changed the view of exposure. The old model emphasized the child’s fear rating as an index of corrective learning. The idea was that habituation would decrease anxiety and distress from future exposures. The new model revolves around inhibitory learning theory, which focuses on the variability of distress and aims to increase tolerance of distress. Another goal is to develop new, non-threat associations.
Finally, Dr. Strawn pointed out predictors of poor outcomes in pediatric OCD, including factors such as compulsion severity, oppositional behavior, frequent handwashing, functional impairment, lack of insight, externalizing symptoms, and possibly hoarding. Problematic family characteristics include higher levels of accommodation, parental anxiety, low family cohesion, and high levels of conflict. “The last three really represent a very concerning triad of family behaviors that may necessitate specific family work in order to facilitate the recovery of the pediatric patient,” Dr. Strawn said.
During the question-and-answer session after the talk, Dr. Strawn was asked whether there might be an inflammatory component to OCD, and whether pediatric autoimmune neuropsychiatric disorders associated with streptococcus (PANDAS) might be a prodromal condition. He noted that some studies have shown a relationship, but results have been mixed, with lots of heterogeneity within the studied populations. To be suspicious that a patient had OCD resulting from PANDAS would require a high threshold, including an acute onset of symptoms. “This is a situation also where I would tend to involve consultation with some other specialties, including neurology. And obviously there would be follow-up in terms of the general workup,” he said.
Dr. Strawn has received research funding from Allergan, Otsuka, and Myriad Genetics. He has consulted for Myriad Genetics, and is a speaker for CMEology and the Neuroscience Education Institute.
FROM FOCUS ON NEUROPSYCHIATRY 2021
EDs saw more benzodiazepine overdoses, but fewer patients overall, in 2020
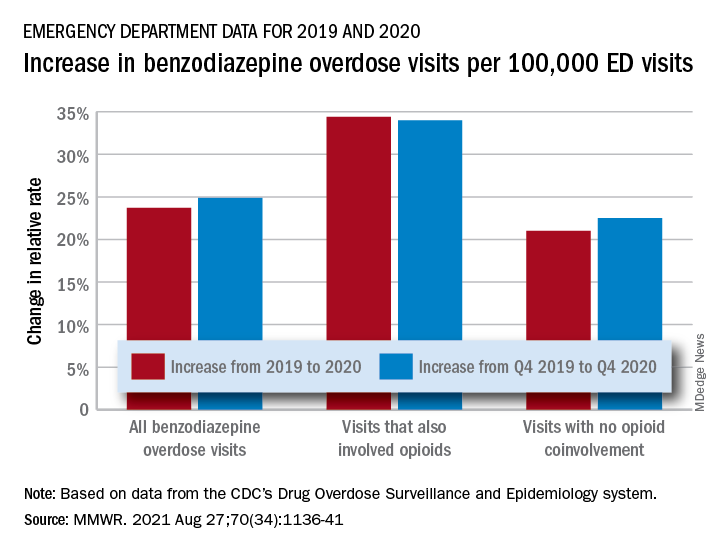
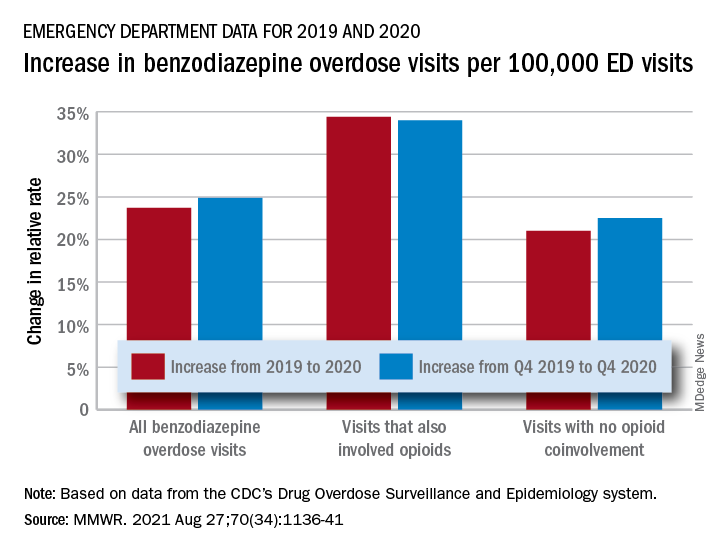
In a year when emergency department visits dropped by almost 18%, visits for benzodiazepine overdoses did the opposite, according to a report from the Centers for Disease Control and Prevention.
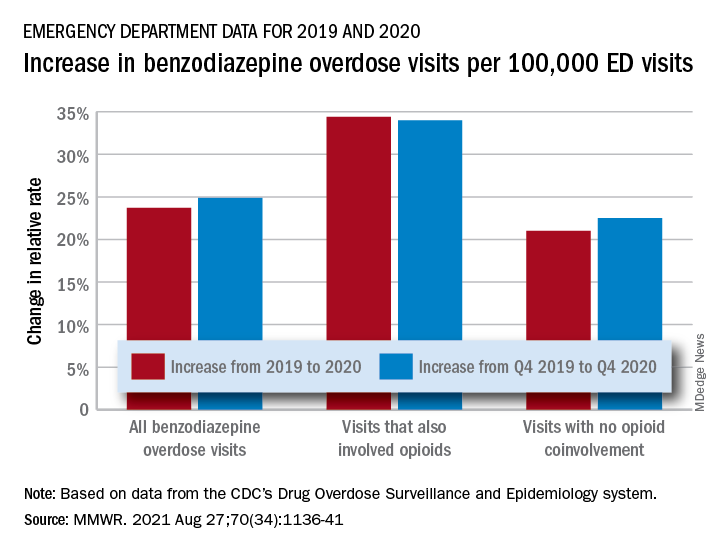
The actual increase in the number of overdose visits for benzodiazepine overdoses was quite small – from 15,547 in 2019 to 15,830 in 2020 (1.8%) – but the 11 million fewer ED visits magnified its effect, Stephen Liu, PhD, and associates said in the Morbidity and Mortality Weekly Report.
The rate of benzodiazepine overdose visits to all visits increased by 23.7% from 2019 (24.22 per 100,000 ED visits) to 2020 (29.97 per 100,000), with the larger share going to those involving opioids, which were up by 34.4%, compared with overdose visits not involving opioids (21.0%), the investigators said, based on data reported by 32 states and the District of Columbia to the CDC’s Drug Overdose Surveillance and Epidemiology system. All of the rate changes are statistically significant.
The number of overdose visits without opioid coinvolvement actually dropped, from 2019 (12,276) to 2020 (12,218), but not by enough to offset the decline in total visits, noted Dr. Liu, of the CDC’s National Center for Injury Prevention and Control and associates.
The number of deaths from benzodiazepine overdose, on the other hand, did not drop in 2020. Those data, coming from 23 states participating in the CDC’s State Unintentional Drug Overdose Reporting System, were available only for the first half of the year.
In those 6 months, The first quarter of 2020 also showed an increase, but exact numbers were not provided in the report. Overdose deaths rose by 22% for prescription forms of benzodiazepine and 520% for illicit forms in Q2 of 2020, compared with 2019, the researchers said.
Almost all of the benzodiazepine deaths (93%) in the first half of 2020 also involved opioids, mostly in the form of illicitly manufactured fentanyls (67% of all deaths). Between Q2 of 2019 and Q2 of 2020, involvement of illicit fentanyls in benzodiazepine overdose deaths increased from almost 57% to 71%, Dr. Liu and associates reported.
“Despite progress in reducing coprescribing [of opioids and benzodiazepines] before 2019, this study suggests a reversal in the decline in benzodiazepine deaths from 2017 to 2019, driven in part by increasing involvement of [illicitly manufactured fentanyls] in benzodiazepine deaths and influxes of illicit benzodiazepines,” they wrote.
In a year when emergency department visits dropped by almost 18%, visits for benzodiazepine overdoses did the opposite, according to a report from the Centers for Disease Control and Prevention.
The actual increase in the number of overdose visits for benzodiazepine overdoses was quite small – from 15,547 in 2019 to 15,830 in 2020 (1.8%) – but the 11 million fewer ED visits magnified its effect, Stephen Liu, PhD, and associates said in the Morbidity and Mortality Weekly Report.
The rate of benzodiazepine overdose visits to all visits increased by 23.7% from 2019 (24.22 per 100,000 ED visits) to 2020 (29.97 per 100,000), with the larger share going to those involving opioids, which were up by 34.4%, compared with overdose visits not involving opioids (21.0%), the investigators said, based on data reported by 32 states and the District of Columbia to the CDC’s Drug Overdose Surveillance and Epidemiology system. All of the rate changes are statistically significant.
The number of overdose visits without opioid coinvolvement actually dropped, from 2019 (12,276) to 2020 (12,218), but not by enough to offset the decline in total visits, noted Dr. Liu, of the CDC’s National Center for Injury Prevention and Control and associates.
The number of deaths from benzodiazepine overdose, on the other hand, did not drop in 2020. Those data, coming from 23 states participating in the CDC’s State Unintentional Drug Overdose Reporting System, were available only for the first half of the year.
In those 6 months, The first quarter of 2020 also showed an increase, but exact numbers were not provided in the report. Overdose deaths rose by 22% for prescription forms of benzodiazepine and 520% for illicit forms in Q2 of 2020, compared with 2019, the researchers said.
Almost all of the benzodiazepine deaths (93%) in the first half of 2020 also involved opioids, mostly in the form of illicitly manufactured fentanyls (67% of all deaths). Between Q2 of 2019 and Q2 of 2020, involvement of illicit fentanyls in benzodiazepine overdose deaths increased from almost 57% to 71%, Dr. Liu and associates reported.
“Despite progress in reducing coprescribing [of opioids and benzodiazepines] before 2019, this study suggests a reversal in the decline in benzodiazepine deaths from 2017 to 2019, driven in part by increasing involvement of [illicitly manufactured fentanyls] in benzodiazepine deaths and influxes of illicit benzodiazepines,” they wrote.
In a year when emergency department visits dropped by almost 18%, visits for benzodiazepine overdoses did the opposite, according to a report from the Centers for Disease Control and Prevention.
The actual increase in the number of overdose visits for benzodiazepine overdoses was quite small – from 15,547 in 2019 to 15,830 in 2020 (1.8%) – but the 11 million fewer ED visits magnified its effect, Stephen Liu, PhD, and associates said in the Morbidity and Mortality Weekly Report.
The rate of benzodiazepine overdose visits to all visits increased by 23.7% from 2019 (24.22 per 100,000 ED visits) to 2020 (29.97 per 100,000), with the larger share going to those involving opioids, which were up by 34.4%, compared with overdose visits not involving opioids (21.0%), the investigators said, based on data reported by 32 states and the District of Columbia to the CDC’s Drug Overdose Surveillance and Epidemiology system. All of the rate changes are statistically significant.
The number of overdose visits without opioid coinvolvement actually dropped, from 2019 (12,276) to 2020 (12,218), but not by enough to offset the decline in total visits, noted Dr. Liu, of the CDC’s National Center for Injury Prevention and Control and associates.
The number of deaths from benzodiazepine overdose, on the other hand, did not drop in 2020. Those data, coming from 23 states participating in the CDC’s State Unintentional Drug Overdose Reporting System, were available only for the first half of the year.
In those 6 months, The first quarter of 2020 also showed an increase, but exact numbers were not provided in the report. Overdose deaths rose by 22% for prescription forms of benzodiazepine and 520% for illicit forms in Q2 of 2020, compared with 2019, the researchers said.
Almost all of the benzodiazepine deaths (93%) in the first half of 2020 also involved opioids, mostly in the form of illicitly manufactured fentanyls (67% of all deaths). Between Q2 of 2019 and Q2 of 2020, involvement of illicit fentanyls in benzodiazepine overdose deaths increased from almost 57% to 71%, Dr. Liu and associates reported.
“Despite progress in reducing coprescribing [of opioids and benzodiazepines] before 2019, this study suggests a reversal in the decline in benzodiazepine deaths from 2017 to 2019, driven in part by increasing involvement of [illicitly manufactured fentanyls] in benzodiazepine deaths and influxes of illicit benzodiazepines,” they wrote.
FROM MMWR
Number of global deaths by suicide increased over 30 years
The overall global number of deaths by suicide increased by almost 20,000 during the past 30 years, new research shows.
The increase occurred despite a significant decrease in age-specific suicide rates from 1990 through 2019, according to data from the Global Burden of Disease Study 2019.
Population growth, population aging, and changes in population age structure may explain the increase in number of suicide deaths, the investigators note.
“As suicide rates are highest among the elderly (70 years or above) for both genders in almost all regions of the world, the rapidly aging population globally will pose huge challenges for the reduction in the number of suicide deaths in the future,” write the researchers, led by Paul Siu Fai Yip, PhD, of the HKJC Center for Suicide Research and Prevention, University of Hong Kong, China.
The findings were published online Aug. 16 in Injury Prevention.
Global public health concern
Around the world, approximately 800,000 individuals die by suicide each year, while many others attempt suicide. Yet suicide has not received the same level of attention as other global public health concerns, such as HIV/AIDS and cancer, the investigators write.
They examined data from the Global Burden of Disease Study 2019 to assess how demographic and epidemiologic factors contributed to the number of suicide deaths during the past 30 years.
The researchers also analyzed relationships between population growth, population age structure, income level, and gender- and age-specific suicide rates.
The Global Burden of Disease Study 2019 includes information from 204 countries about 369 diseases and injuries by age and gender. The dataset also includes population estimates for each year by location, age group, and gender.
In their analysis, the investigators looked at changes in suicide rates and the number of suicide deaths from 1990 to 2019 by gender and age group in the four income level regions defined by the World Bank. These categories include low-income, lower-middle–income, upper-middle–income, and high-income regions.
Number of deaths versus suicide rates
The number of deaths was 738,799 in 1990 and 758,696 in 2019.
The largest increase in deaths occurred in the lower-middle–income region, where the number of suicide deaths increased by 72,550 (from 232,340 to 304,890).
Population growth (300,942; 1,512.5%) was the major contributor to the overall increase in total number of suicide deaths. The second largest contributor was population age structure (189,512; 952.4%).
However, the effects of these factors were offset to a large extent by the effect of reduction in overall suicide rates (−470,556; −2,364.9%).
Interestingly, the overall suicide rate per 100,000 population decreased from 13.8 in 1990 to 9.8 in 2019.
The upper-middle–income region had the largest decline (−6.25 per 100,000), and the high-income region had the smallest decline (−1.77 per 100,000). Suicide rates also decreased in lower-middle–income (−2.51 per 100,000) and low-income regions (−1.96 per 100,000).
Reasons for the declines across all regions “have yet to be determined,” write the investigators. International efforts coordinated by the United Nations and World Health Organization likely contributed to these declines, they add.
‘Imbalance of resources’
The overall reduction in suicide rate of −4.01 per 100,000 “was mainly due” to reduction in age-specific suicide rates (−6.09; 152%), the researchers report.
This effect was partly offset, however, by the effect of the changing population age structure (2.08; −52%). In the high-income–level region, for example, the reduction in age-specific suicide rate (−3.83; 216.3%) was greater than the increase resulting from the change in population age structure (2.06; −116.3%).
“The overall contribution of population age structure mainly came from the 45-64 (565.2%) and 65+ (528.7%) age groups,” the investigators write. “This effect was observed in middle-income– as well as high-income–level regions, reflecting the global effect of population aging.”
They add that world populations will “experience pronounced and historically unprecedented aging in the coming decades” because of increasing life expectancy and declining fertility.
Men, but not women, had a notable increase in total number of suicide deaths. The significant effect of male population growth (177,128; 890.2% vs. 123,814; 622.3% for women) and male population age structure (120,186; 604.0% vs. 69,325; 348.4%) were the main factors that explained this increase, the investigators note.
However, from 1990 to 2019, the overall suicide rate per 100,000 men decreased from 16.6 to 13.5 (–3.09). The decline in overall suicide rate was even greater for women, from 11.0 to 6.1 (–4.91).
This finding was particularly notable in the upper-middle–income region (–8.12 women vs. –4.37 men per 100,000).
“This study highlighted the considerable imbalance of the resources in carrying out suicide prevention work, especially in low-income and middle-income countries,” the investigators write.
“It is time to revisit this situation to ensure that sufficient resources can be redeployed globally to meet the future challenges,” they add.
The study was funded by a Humanities and Social Sciences Prestigious Fellowship, which Dr. Yip received. He declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The overall global number of deaths by suicide increased by almost 20,000 during the past 30 years, new research shows.
The increase occurred despite a significant decrease in age-specific suicide rates from 1990 through 2019, according to data from the Global Burden of Disease Study 2019.
Population growth, population aging, and changes in population age structure may explain the increase in number of suicide deaths, the investigators note.
“As suicide rates are highest among the elderly (70 years or above) for both genders in almost all regions of the world, the rapidly aging population globally will pose huge challenges for the reduction in the number of suicide deaths in the future,” write the researchers, led by Paul Siu Fai Yip, PhD, of the HKJC Center for Suicide Research and Prevention, University of Hong Kong, China.
The findings were published online Aug. 16 in Injury Prevention.
Global public health concern
Around the world, approximately 800,000 individuals die by suicide each year, while many others attempt suicide. Yet suicide has not received the same level of attention as other global public health concerns, such as HIV/AIDS and cancer, the investigators write.
They examined data from the Global Burden of Disease Study 2019 to assess how demographic and epidemiologic factors contributed to the number of suicide deaths during the past 30 years.
The researchers also analyzed relationships between population growth, population age structure, income level, and gender- and age-specific suicide rates.
The Global Burden of Disease Study 2019 includes information from 204 countries about 369 diseases and injuries by age and gender. The dataset also includes population estimates for each year by location, age group, and gender.
In their analysis, the investigators looked at changes in suicide rates and the number of suicide deaths from 1990 to 2019 by gender and age group in the four income level regions defined by the World Bank. These categories include low-income, lower-middle–income, upper-middle–income, and high-income regions.
Number of deaths versus suicide rates
The number of deaths was 738,799 in 1990 and 758,696 in 2019.
The largest increase in deaths occurred in the lower-middle–income region, where the number of suicide deaths increased by 72,550 (from 232,340 to 304,890).
Population growth (300,942; 1,512.5%) was the major contributor to the overall increase in total number of suicide deaths. The second largest contributor was population age structure (189,512; 952.4%).
However, the effects of these factors were offset to a large extent by the effect of reduction in overall suicide rates (−470,556; −2,364.9%).
Interestingly, the overall suicide rate per 100,000 population decreased from 13.8 in 1990 to 9.8 in 2019.
The upper-middle–income region had the largest decline (−6.25 per 100,000), and the high-income region had the smallest decline (−1.77 per 100,000). Suicide rates also decreased in lower-middle–income (−2.51 per 100,000) and low-income regions (−1.96 per 100,000).
Reasons for the declines across all regions “have yet to be determined,” write the investigators. International efforts coordinated by the United Nations and World Health Organization likely contributed to these declines, they add.
‘Imbalance of resources’
The overall reduction in suicide rate of −4.01 per 100,000 “was mainly due” to reduction in age-specific suicide rates (−6.09; 152%), the researchers report.
This effect was partly offset, however, by the effect of the changing population age structure (2.08; −52%). In the high-income–level region, for example, the reduction in age-specific suicide rate (−3.83; 216.3%) was greater than the increase resulting from the change in population age structure (2.06; −116.3%).
“The overall contribution of population age structure mainly came from the 45-64 (565.2%) and 65+ (528.7%) age groups,” the investigators write. “This effect was observed in middle-income– as well as high-income–level regions, reflecting the global effect of population aging.”
They add that world populations will “experience pronounced and historically unprecedented aging in the coming decades” because of increasing life expectancy and declining fertility.
Men, but not women, had a notable increase in total number of suicide deaths. The significant effect of male population growth (177,128; 890.2% vs. 123,814; 622.3% for women) and male population age structure (120,186; 604.0% vs. 69,325; 348.4%) were the main factors that explained this increase, the investigators note.
However, from 1990 to 2019, the overall suicide rate per 100,000 men decreased from 16.6 to 13.5 (–3.09). The decline in overall suicide rate was even greater for women, from 11.0 to 6.1 (–4.91).
This finding was particularly notable in the upper-middle–income region (–8.12 women vs. –4.37 men per 100,000).
“This study highlighted the considerable imbalance of the resources in carrying out suicide prevention work, especially in low-income and middle-income countries,” the investigators write.
“It is time to revisit this situation to ensure that sufficient resources can be redeployed globally to meet the future challenges,” they add.
The study was funded by a Humanities and Social Sciences Prestigious Fellowship, which Dr. Yip received. He declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The overall global number of deaths by suicide increased by almost 20,000 during the past 30 years, new research shows.
The increase occurred despite a significant decrease in age-specific suicide rates from 1990 through 2019, according to data from the Global Burden of Disease Study 2019.
Population growth, population aging, and changes in population age structure may explain the increase in number of suicide deaths, the investigators note.
“As suicide rates are highest among the elderly (70 years or above) for both genders in almost all regions of the world, the rapidly aging population globally will pose huge challenges for the reduction in the number of suicide deaths in the future,” write the researchers, led by Paul Siu Fai Yip, PhD, of the HKJC Center for Suicide Research and Prevention, University of Hong Kong, China.
The findings were published online Aug. 16 in Injury Prevention.
Global public health concern
Around the world, approximately 800,000 individuals die by suicide each year, while many others attempt suicide. Yet suicide has not received the same level of attention as other global public health concerns, such as HIV/AIDS and cancer, the investigators write.
They examined data from the Global Burden of Disease Study 2019 to assess how demographic and epidemiologic factors contributed to the number of suicide deaths during the past 30 years.
The researchers also analyzed relationships between population growth, population age structure, income level, and gender- and age-specific suicide rates.
The Global Burden of Disease Study 2019 includes information from 204 countries about 369 diseases and injuries by age and gender. The dataset also includes population estimates for each year by location, age group, and gender.
In their analysis, the investigators looked at changes in suicide rates and the number of suicide deaths from 1990 to 2019 by gender and age group in the four income level regions defined by the World Bank. These categories include low-income, lower-middle–income, upper-middle–income, and high-income regions.
Number of deaths versus suicide rates
The number of deaths was 738,799 in 1990 and 758,696 in 2019.
The largest increase in deaths occurred in the lower-middle–income region, where the number of suicide deaths increased by 72,550 (from 232,340 to 304,890).
Population growth (300,942; 1,512.5%) was the major contributor to the overall increase in total number of suicide deaths. The second largest contributor was population age structure (189,512; 952.4%).
However, the effects of these factors were offset to a large extent by the effect of reduction in overall suicide rates (−470,556; −2,364.9%).
Interestingly, the overall suicide rate per 100,000 population decreased from 13.8 in 1990 to 9.8 in 2019.
The upper-middle–income region had the largest decline (−6.25 per 100,000), and the high-income region had the smallest decline (−1.77 per 100,000). Suicide rates also decreased in lower-middle–income (−2.51 per 100,000) and low-income regions (−1.96 per 100,000).
Reasons for the declines across all regions “have yet to be determined,” write the investigators. International efforts coordinated by the United Nations and World Health Organization likely contributed to these declines, they add.
‘Imbalance of resources’
The overall reduction in suicide rate of −4.01 per 100,000 “was mainly due” to reduction in age-specific suicide rates (−6.09; 152%), the researchers report.
This effect was partly offset, however, by the effect of the changing population age structure (2.08; −52%). In the high-income–level region, for example, the reduction in age-specific suicide rate (−3.83; 216.3%) was greater than the increase resulting from the change in population age structure (2.06; −116.3%).
“The overall contribution of population age structure mainly came from the 45-64 (565.2%) and 65+ (528.7%) age groups,” the investigators write. “This effect was observed in middle-income– as well as high-income–level regions, reflecting the global effect of population aging.”
They add that world populations will “experience pronounced and historically unprecedented aging in the coming decades” because of increasing life expectancy and declining fertility.
Men, but not women, had a notable increase in total number of suicide deaths. The significant effect of male population growth (177,128; 890.2% vs. 123,814; 622.3% for women) and male population age structure (120,186; 604.0% vs. 69,325; 348.4%) were the main factors that explained this increase, the investigators note.
However, from 1990 to 2019, the overall suicide rate per 100,000 men decreased from 16.6 to 13.5 (–3.09). The decline in overall suicide rate was even greater for women, from 11.0 to 6.1 (–4.91).
This finding was particularly notable in the upper-middle–income region (–8.12 women vs. –4.37 men per 100,000).
“This study highlighted the considerable imbalance of the resources in carrying out suicide prevention work, especially in low-income and middle-income countries,” the investigators write.
“It is time to revisit this situation to ensure that sufficient resources can be redeployed globally to meet the future challenges,” they add.
The study was funded by a Humanities and Social Sciences Prestigious Fellowship, which Dr. Yip received. He declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Report urges complete residency overhaul
from the Graduate Medical Education Review Committee (UGRC) of the Coalition for Physician Accountability.
The 275-page report presents preliminary findings that were released in April 2021 and a long list of stakeholder comments. According to the report, the coalition will meet soon to discuss the final recommendations and consider next steps toward implementation.
The UGRC includes representatives of national medical organizations, medical schools, and residency programs. Among the organizations that participated in the report’s creation are the American Medical Association, the National Board of Medical Examiners, the American Osteopathic Association, the National Board of Osteopathic Medical Examiners, the Educational Commission for Foreign Medical Graduates, and the Association of American Medical Colleges.
The report identifies a list of challenges that affect the transition of medical students into residency programs and beyond. They include:
- Too much focus on finding and filling residency positions instead of “assuring learner competence and readiness for residency training”
- Inattention to assuring congruence between applicant goals and program missions
- Overreliance on licensure exam scores rather than “valid, trustworthy measures of students’ competence and clinical abilities”
- Increasing financial costs to students
- Individual and systemic biases in the UME-GME transition, as well as inequities related to international medical graduates
Seeking a common framework for competence
Overall, the report calls for increased standardization of how students are evaluated in medical school and how residency programs evaluate students. Less reliance should be placed on the numerical scores of the U.S. Medical Licensing Examination (USMLE), the report says, and more attention should be paid to the direct observation of student performance in clinical situations. In addition, the various organizations involved in the UME-GME transition process are asked to work better together.
To develop better methods of evaluating medical students and residents, UME and GME educators should jointly define and implement a common framework and set of competencies to apply to learners across the UME-GME transition, the report suggests.
While emphasizing the need for a broader student assessment framework, the report says, USMLE scores should also continue to be used in judging residency applicants. “Assessment information should be shared in residency applications and a postmatch learner handover. Licensing examinations should be used for their intended purpose to ensure requisite competence.”
Among the committee’s three dozen recommendations are the following:
- The Centers for Medicare & Medicaid Services should change the GME funding structure so that the initial residency period is calculated starting with the second year of postgraduate training. This change would allow residents to reconsider their career choices. Currently, if a resident decides to switch to another program or specialty after beginning training, the hospital may not receive full GME funding, so may be less likely to approve the change.
- Residency programs should improve recruitment practices to increase specialty-specific diversity of residents. Medical educators should also receive additional training regarding antiracism, avoiding bias, and ensuring equity.
- The self-reported demographic information of applicants to residency programs should be measured and shared with stakeholders, including the programs and medical schools, to promote equity. “A residency program that finds bias in its selection process could go back in real time to find qualified applicants who may have been missed, potentially improving outcomes,” the report notes.
- An interactive database of GME program and specialty track information should be created and made available to all applicants, medical schools, and residency programs at no cost to applicants. “Applicants and their advisors should be able to sort the information according to demographic and educational features that may significantly impact the likelihood of matching at a program.”
Less than half of applicants get in-depth reviews
The 2020 National Resident Matching Program Program Director Survey found that only 49% of applications received in-depth review. In light of this, the report suggests that the application system be updated to use modern information technology, including discrete fields for key data to expedite application reviews.
Many applications have been discarded because of various filters used to block consideration of certain applications. The report suggests that new filters be designed to ensure that each detects meaningful differences among applicants and promotes review based on mission alignment and likelihood of success in a program. Filters should be improved to decrease the likelihood of random exclusions of qualified applicants.
Specialty-specific, just-in-time training for all incoming first-year residents is also suggested to support the transition from the role of student to a physician ready to assume increased responsibility for patient care. In addition, the report urges adequate time be allowed between medical school graduation and residency to enable new residents to relocate and find homes.
The report also calls for a standardized process in the United States for initial licensing of doctors at entrance to residency in order to streamline the process of credentialing for both residency training and continuing practice.
Osteopathic students’ dilemma
To promote equitable treatment of applicants regardless of licensure examination requirements, comparable exams with different scales (COMLEX-USA and USMLE) should be reported within the electronic application system in a single field, the report said.
Osteopathic students, who make up 25% of U.S. medical students, must take the COMLEX-USA exam, but residency programs may filter them out if they don’t also take the USMLE exam. Thus, many osteopathic students take both exams, incurring extra time, cost, and stress.
The UGRC recommends creating a combined field in the electronic residency application service that normalizes the scores between the two exams. Residency programs could then filter applications based only on the single normalized score.
This approach makes sense from the viewpoint that it would reduce the pressure on osteopathic students to take the USMLE, Bryan Carmody, MD, an outspoken critic of various current training policies, said in an interview. But it could also have serious disadvantages.
For one thing, only osteopathic students can take the COMLEX-USA exam, he noted. If they don’t like their score, they can then take the USMLE test to get a higher score – an option that allopathic students don’t have. It’s not clear that they’d be prevented from doing this under the UGRC recommendation.
Second, he said, osteopathic students, on average, don’t do as well as allopathic students on the UMSLE exam. If they only take the COMLEX-USA test, they’re competing against other students who don’t do as well on tests as allopathic students do. If their scores were normalized with those of the USMLE test takers, they’d gain an unfair advantage against students who can only take the USMLE, including international medical graduates.
Although Dr. Carmody admitted that osteopathic students face a harder challenge than allopathic students in matching to residency programs, he said that the UGRC approach to the licensing exams might actually penalize them further. As a result of the scores of the two exams being averaged, residency program directors might discount the scores of all osteopathic students.
A version of this article first appeared on Medscape.com.
from the Graduate Medical Education Review Committee (UGRC) of the Coalition for Physician Accountability.
The 275-page report presents preliminary findings that were released in April 2021 and a long list of stakeholder comments. According to the report, the coalition will meet soon to discuss the final recommendations and consider next steps toward implementation.
The UGRC includes representatives of national medical organizations, medical schools, and residency programs. Among the organizations that participated in the report’s creation are the American Medical Association, the National Board of Medical Examiners, the American Osteopathic Association, the National Board of Osteopathic Medical Examiners, the Educational Commission for Foreign Medical Graduates, and the Association of American Medical Colleges.
The report identifies a list of challenges that affect the transition of medical students into residency programs and beyond. They include:
- Too much focus on finding and filling residency positions instead of “assuring learner competence and readiness for residency training”
- Inattention to assuring congruence between applicant goals and program missions
- Overreliance on licensure exam scores rather than “valid, trustworthy measures of students’ competence and clinical abilities”
- Increasing financial costs to students
- Individual and systemic biases in the UME-GME transition, as well as inequities related to international medical graduates
Seeking a common framework for competence
Overall, the report calls for increased standardization of how students are evaluated in medical school and how residency programs evaluate students. Less reliance should be placed on the numerical scores of the U.S. Medical Licensing Examination (USMLE), the report says, and more attention should be paid to the direct observation of student performance in clinical situations. In addition, the various organizations involved in the UME-GME transition process are asked to work better together.
To develop better methods of evaluating medical students and residents, UME and GME educators should jointly define and implement a common framework and set of competencies to apply to learners across the UME-GME transition, the report suggests.
While emphasizing the need for a broader student assessment framework, the report says, USMLE scores should also continue to be used in judging residency applicants. “Assessment information should be shared in residency applications and a postmatch learner handover. Licensing examinations should be used for their intended purpose to ensure requisite competence.”
Among the committee’s three dozen recommendations are the following:
- The Centers for Medicare & Medicaid Services should change the GME funding structure so that the initial residency period is calculated starting with the second year of postgraduate training. This change would allow residents to reconsider their career choices. Currently, if a resident decides to switch to another program or specialty after beginning training, the hospital may not receive full GME funding, so may be less likely to approve the change.
- Residency programs should improve recruitment practices to increase specialty-specific diversity of residents. Medical educators should also receive additional training regarding antiracism, avoiding bias, and ensuring equity.
- The self-reported demographic information of applicants to residency programs should be measured and shared with stakeholders, including the programs and medical schools, to promote equity. “A residency program that finds bias in its selection process could go back in real time to find qualified applicants who may have been missed, potentially improving outcomes,” the report notes.
- An interactive database of GME program and specialty track information should be created and made available to all applicants, medical schools, and residency programs at no cost to applicants. “Applicants and their advisors should be able to sort the information according to demographic and educational features that may significantly impact the likelihood of matching at a program.”
Less than half of applicants get in-depth reviews
The 2020 National Resident Matching Program Program Director Survey found that only 49% of applications received in-depth review. In light of this, the report suggests that the application system be updated to use modern information technology, including discrete fields for key data to expedite application reviews.
Many applications have been discarded because of various filters used to block consideration of certain applications. The report suggests that new filters be designed to ensure that each detects meaningful differences among applicants and promotes review based on mission alignment and likelihood of success in a program. Filters should be improved to decrease the likelihood of random exclusions of qualified applicants.
Specialty-specific, just-in-time training for all incoming first-year residents is also suggested to support the transition from the role of student to a physician ready to assume increased responsibility for patient care. In addition, the report urges adequate time be allowed between medical school graduation and residency to enable new residents to relocate and find homes.
The report also calls for a standardized process in the United States for initial licensing of doctors at entrance to residency in order to streamline the process of credentialing for both residency training and continuing practice.
Osteopathic students’ dilemma
To promote equitable treatment of applicants regardless of licensure examination requirements, comparable exams with different scales (COMLEX-USA and USMLE) should be reported within the electronic application system in a single field, the report said.
Osteopathic students, who make up 25% of U.S. medical students, must take the COMLEX-USA exam, but residency programs may filter them out if they don’t also take the USMLE exam. Thus, many osteopathic students take both exams, incurring extra time, cost, and stress.
The UGRC recommends creating a combined field in the electronic residency application service that normalizes the scores between the two exams. Residency programs could then filter applications based only on the single normalized score.
This approach makes sense from the viewpoint that it would reduce the pressure on osteopathic students to take the USMLE, Bryan Carmody, MD, an outspoken critic of various current training policies, said in an interview. But it could also have serious disadvantages.
For one thing, only osteopathic students can take the COMLEX-USA exam, he noted. If they don’t like their score, they can then take the USMLE test to get a higher score – an option that allopathic students don’t have. It’s not clear that they’d be prevented from doing this under the UGRC recommendation.
Second, he said, osteopathic students, on average, don’t do as well as allopathic students on the UMSLE exam. If they only take the COMLEX-USA test, they’re competing against other students who don’t do as well on tests as allopathic students do. If their scores were normalized with those of the USMLE test takers, they’d gain an unfair advantage against students who can only take the USMLE, including international medical graduates.
Although Dr. Carmody admitted that osteopathic students face a harder challenge than allopathic students in matching to residency programs, he said that the UGRC approach to the licensing exams might actually penalize them further. As a result of the scores of the two exams being averaged, residency program directors might discount the scores of all osteopathic students.
A version of this article first appeared on Medscape.com.
from the Graduate Medical Education Review Committee (UGRC) of the Coalition for Physician Accountability.
The 275-page report presents preliminary findings that were released in April 2021 and a long list of stakeholder comments. According to the report, the coalition will meet soon to discuss the final recommendations and consider next steps toward implementation.
The UGRC includes representatives of national medical organizations, medical schools, and residency programs. Among the organizations that participated in the report’s creation are the American Medical Association, the National Board of Medical Examiners, the American Osteopathic Association, the National Board of Osteopathic Medical Examiners, the Educational Commission for Foreign Medical Graduates, and the Association of American Medical Colleges.
The report identifies a list of challenges that affect the transition of medical students into residency programs and beyond. They include:
- Too much focus on finding and filling residency positions instead of “assuring learner competence and readiness for residency training”
- Inattention to assuring congruence between applicant goals and program missions
- Overreliance on licensure exam scores rather than “valid, trustworthy measures of students’ competence and clinical abilities”
- Increasing financial costs to students
- Individual and systemic biases in the UME-GME transition, as well as inequities related to international medical graduates
Seeking a common framework for competence
Overall, the report calls for increased standardization of how students are evaluated in medical school and how residency programs evaluate students. Less reliance should be placed on the numerical scores of the U.S. Medical Licensing Examination (USMLE), the report says, and more attention should be paid to the direct observation of student performance in clinical situations. In addition, the various organizations involved in the UME-GME transition process are asked to work better together.
To develop better methods of evaluating medical students and residents, UME and GME educators should jointly define and implement a common framework and set of competencies to apply to learners across the UME-GME transition, the report suggests.
While emphasizing the need for a broader student assessment framework, the report says, USMLE scores should also continue to be used in judging residency applicants. “Assessment information should be shared in residency applications and a postmatch learner handover. Licensing examinations should be used for their intended purpose to ensure requisite competence.”
Among the committee’s three dozen recommendations are the following:
- The Centers for Medicare & Medicaid Services should change the GME funding structure so that the initial residency period is calculated starting with the second year of postgraduate training. This change would allow residents to reconsider their career choices. Currently, if a resident decides to switch to another program or specialty after beginning training, the hospital may not receive full GME funding, so may be less likely to approve the change.
- Residency programs should improve recruitment practices to increase specialty-specific diversity of residents. Medical educators should also receive additional training regarding antiracism, avoiding bias, and ensuring equity.
- The self-reported demographic information of applicants to residency programs should be measured and shared with stakeholders, including the programs and medical schools, to promote equity. “A residency program that finds bias in its selection process could go back in real time to find qualified applicants who may have been missed, potentially improving outcomes,” the report notes.
- An interactive database of GME program and specialty track information should be created and made available to all applicants, medical schools, and residency programs at no cost to applicants. “Applicants and their advisors should be able to sort the information according to demographic and educational features that may significantly impact the likelihood of matching at a program.”
Less than half of applicants get in-depth reviews
The 2020 National Resident Matching Program Program Director Survey found that only 49% of applications received in-depth review. In light of this, the report suggests that the application system be updated to use modern information technology, including discrete fields for key data to expedite application reviews.
Many applications have been discarded because of various filters used to block consideration of certain applications. The report suggests that new filters be designed to ensure that each detects meaningful differences among applicants and promotes review based on mission alignment and likelihood of success in a program. Filters should be improved to decrease the likelihood of random exclusions of qualified applicants.
Specialty-specific, just-in-time training for all incoming first-year residents is also suggested to support the transition from the role of student to a physician ready to assume increased responsibility for patient care. In addition, the report urges adequate time be allowed between medical school graduation and residency to enable new residents to relocate and find homes.
The report also calls for a standardized process in the United States for initial licensing of doctors at entrance to residency in order to streamline the process of credentialing for both residency training and continuing practice.
Osteopathic students’ dilemma
To promote equitable treatment of applicants regardless of licensure examination requirements, comparable exams with different scales (COMLEX-USA and USMLE) should be reported within the electronic application system in a single field, the report said.
Osteopathic students, who make up 25% of U.S. medical students, must take the COMLEX-USA exam, but residency programs may filter them out if they don’t also take the USMLE exam. Thus, many osteopathic students take both exams, incurring extra time, cost, and stress.
The UGRC recommends creating a combined field in the electronic residency application service that normalizes the scores between the two exams. Residency programs could then filter applications based only on the single normalized score.
This approach makes sense from the viewpoint that it would reduce the pressure on osteopathic students to take the USMLE, Bryan Carmody, MD, an outspoken critic of various current training policies, said in an interview. But it could also have serious disadvantages.
For one thing, only osteopathic students can take the COMLEX-USA exam, he noted. If they don’t like their score, they can then take the USMLE test to get a higher score – an option that allopathic students don’t have. It’s not clear that they’d be prevented from doing this under the UGRC recommendation.
Second, he said, osteopathic students, on average, don’t do as well as allopathic students on the UMSLE exam. If they only take the COMLEX-USA test, they’re competing against other students who don’t do as well on tests as allopathic students do. If their scores were normalized with those of the USMLE test takers, they’d gain an unfair advantage against students who can only take the USMLE, including international medical graduates.
Although Dr. Carmody admitted that osteopathic students face a harder challenge than allopathic students in matching to residency programs, he said that the UGRC approach to the licensing exams might actually penalize them further. As a result of the scores of the two exams being averaged, residency program directors might discount the scores of all osteopathic students.
A version of this article first appeared on Medscape.com.
Self-described ‘assassin,’ now doctor, indicted for 1M illegal opioid doses
A according to the U.S. Department of Justice. The substances include oxycodone and morphine.
Adrian Dexter Talbot, MD, 55, of Slidell, La., is also charged with maintaining a medical clinic for the purpose of illegally distributing controlled substances, per the indictment.
Because the opioid prescriptions were filled using beneficiaries’ health insurance, Dr. Talbot is also charged with defrauding Medicare, Medicaid, and Blue Cross and Blue Shield of Louisiana of more than $5.1 million.
When contacted by this news organization for comment on the case via Twitter, Dr. Talbot or a representative responded with a link to his self-published book on Amazon. In his author bio, Dr. Talbot refers to himself as “a former assassin,” “retired military commander,” and “leader of the Medellin Cartel’s New York operations at the age of 16.” The Medellin Cartel is a notorious drug distribution empire.
Dr. Talbot is listed as the author of another book on Google Books detailing his time as a “former teenage assassin” and leader of the cartel, told as he struggles with early onset Alzheimer’s.
Dr. Talbot could spend decades in prison
According to the National Institute on Drug Abuse, 444 residents of the Bayou State lost their lives because of an opioid-related drug overdose in 2018. During that year, the state’s health care providers wrote more than 79.4 opioid prescriptions for every 100 persons, which puts the state in the top five in the United States in 2018, when the average U.S. rate was 51.4 prescriptions per 100 persons.
Charged with one count each of conspiracy to unlawfully distribute and dispense controlled substances and maintaining drug-involved premises and conspiracy to commit health care fraud, Dr. Talbot is also charged with four counts of unlawfully distributing and dispensing controlled substances. He is scheduled for a federal court appearance on September 10.
In addition to presigning prescriptions for individuals he didn’t meet or examine, federal officials allege Dr. Talbot hired another health care provider to similarly presign prescriptions for people who weren’t examined at a medical practice in Slidell, where Dr. Talbot was employed. The DOJ says Dr. Talbot took a full-time job in Pineville, La., and presigned prescriptions while no longer physically present at the Slidell clinic.
A speaker’s bio for Dr. Talbot indicates he worked as chief of medical services for the Alexandria Veterans Affairs Health Care System in Pineville.
According to the DOJ’s indictment, Dr. Talbot was aware that patients were filling the prescriptions that were provided outside the scope of professional practice and not for a legitimate medical purpose. This is what triggered the DOJ’s fraudulent billing claim.
Dr. Talbot faces a maximum penalty of 10 years for conspiracy to commit health care fraud and 20 years each for the other counts, if convicted.
Dr. Talbot was candidate for local coroner
In February 2015, Dr. Talbot announced his candidacy for coroner for St. Tammany Parish, about an hour’s drive south of New Orleans, reported the Times Picayune. The seat was open because the previous coroner had resigned and ultimately pleaded guilty to a federal corruption charge.
The Times Picayune reported at the time that Dr. Talbot was a U.S. Navy veteran, in addition to serving as medical director and a primary care physician at the Medical Care Center in Slidell. Among the services provided to his patients were evaluations and treatment for substance use and mental health disorders, according to a press release issued by Dr. Talbot’s campaign.
Dr. Talbot’s medical license was issued in 1999 and inactive as of 2017, per the Louisiana State Board of Medical Examiners.
Louisiana expects $325M in multistate settlement with opioid companies
Louisiana is a party to a multistate and multijurisdictional lawsuit where the state is expected to receive more than $325 million in a settlement reached with drug distributors Cardinal, McKesson, and AmerisourceBergen, and drug manufacturer Johnson & Johnson, reported the Louisiana Illuminator in July. The total settlement may reach $26 billion dollars.
The Associated Press reported in July that there have been at least $40 billion in completed or proposed settlements, penalties, and fines between governments as a result of the opioid epidemic since 2007.
That total doesn’t include a proposed settlement involving members of the Sackler family, who own Purdue Pharmaceuticals, which manufactured and marketed the opioid painkiller OxyContin. The Sackler family have agreed to pay approximately $4.3 billion and surrender ownership of their bankrupt company, reported NPR. The family’s proposed settlement is part of a deal involving Purdue Pharmaceuticals worth more than $10 billion, reported Reuters.
In 2020, there were more than 81,000 drug overdose deaths, the highest number recorded in a 12-month period, per the U.S. Centers for Disease Control and Prevention. Fentanyl, an illicitly manufactured synthetic opioid, was the lead driver of those deaths.
A version of this article first appeared on Medscape.com.
A according to the U.S. Department of Justice. The substances include oxycodone and morphine.
Adrian Dexter Talbot, MD, 55, of Slidell, La., is also charged with maintaining a medical clinic for the purpose of illegally distributing controlled substances, per the indictment.
Because the opioid prescriptions were filled using beneficiaries’ health insurance, Dr. Talbot is also charged with defrauding Medicare, Medicaid, and Blue Cross and Blue Shield of Louisiana of more than $5.1 million.
When contacted by this news organization for comment on the case via Twitter, Dr. Talbot or a representative responded with a link to his self-published book on Amazon. In his author bio, Dr. Talbot refers to himself as “a former assassin,” “retired military commander,” and “leader of the Medellin Cartel’s New York operations at the age of 16.” The Medellin Cartel is a notorious drug distribution empire.
Dr. Talbot is listed as the author of another book on Google Books detailing his time as a “former teenage assassin” and leader of the cartel, told as he struggles with early onset Alzheimer’s.
Dr. Talbot could spend decades in prison
According to the National Institute on Drug Abuse, 444 residents of the Bayou State lost their lives because of an opioid-related drug overdose in 2018. During that year, the state’s health care providers wrote more than 79.4 opioid prescriptions for every 100 persons, which puts the state in the top five in the United States in 2018, when the average U.S. rate was 51.4 prescriptions per 100 persons.
Charged with one count each of conspiracy to unlawfully distribute and dispense controlled substances and maintaining drug-involved premises and conspiracy to commit health care fraud, Dr. Talbot is also charged with four counts of unlawfully distributing and dispensing controlled substances. He is scheduled for a federal court appearance on September 10.
In addition to presigning prescriptions for individuals he didn’t meet or examine, federal officials allege Dr. Talbot hired another health care provider to similarly presign prescriptions for people who weren’t examined at a medical practice in Slidell, where Dr. Talbot was employed. The DOJ says Dr. Talbot took a full-time job in Pineville, La., and presigned prescriptions while no longer physically present at the Slidell clinic.
A speaker’s bio for Dr. Talbot indicates he worked as chief of medical services for the Alexandria Veterans Affairs Health Care System in Pineville.
According to the DOJ’s indictment, Dr. Talbot was aware that patients were filling the prescriptions that were provided outside the scope of professional practice and not for a legitimate medical purpose. This is what triggered the DOJ’s fraudulent billing claim.
Dr. Talbot faces a maximum penalty of 10 years for conspiracy to commit health care fraud and 20 years each for the other counts, if convicted.
Dr. Talbot was candidate for local coroner
In February 2015, Dr. Talbot announced his candidacy for coroner for St. Tammany Parish, about an hour’s drive south of New Orleans, reported the Times Picayune. The seat was open because the previous coroner had resigned and ultimately pleaded guilty to a federal corruption charge.
The Times Picayune reported at the time that Dr. Talbot was a U.S. Navy veteran, in addition to serving as medical director and a primary care physician at the Medical Care Center in Slidell. Among the services provided to his patients were evaluations and treatment for substance use and mental health disorders, according to a press release issued by Dr. Talbot’s campaign.
Dr. Talbot’s medical license was issued in 1999 and inactive as of 2017, per the Louisiana State Board of Medical Examiners.
Louisiana expects $325M in multistate settlement with opioid companies
Louisiana is a party to a multistate and multijurisdictional lawsuit where the state is expected to receive more than $325 million in a settlement reached with drug distributors Cardinal, McKesson, and AmerisourceBergen, and drug manufacturer Johnson & Johnson, reported the Louisiana Illuminator in July. The total settlement may reach $26 billion dollars.
The Associated Press reported in July that there have been at least $40 billion in completed or proposed settlements, penalties, and fines between governments as a result of the opioid epidemic since 2007.
That total doesn’t include a proposed settlement involving members of the Sackler family, who own Purdue Pharmaceuticals, which manufactured and marketed the opioid painkiller OxyContin. The Sackler family have agreed to pay approximately $4.3 billion and surrender ownership of their bankrupt company, reported NPR. The family’s proposed settlement is part of a deal involving Purdue Pharmaceuticals worth more than $10 billion, reported Reuters.
In 2020, there were more than 81,000 drug overdose deaths, the highest number recorded in a 12-month period, per the U.S. Centers for Disease Control and Prevention. Fentanyl, an illicitly manufactured synthetic opioid, was the lead driver of those deaths.
A version of this article first appeared on Medscape.com.
A according to the U.S. Department of Justice. The substances include oxycodone and morphine.
Adrian Dexter Talbot, MD, 55, of Slidell, La., is also charged with maintaining a medical clinic for the purpose of illegally distributing controlled substances, per the indictment.
Because the opioid prescriptions were filled using beneficiaries’ health insurance, Dr. Talbot is also charged with defrauding Medicare, Medicaid, and Blue Cross and Blue Shield of Louisiana of more than $5.1 million.
When contacted by this news organization for comment on the case via Twitter, Dr. Talbot or a representative responded with a link to his self-published book on Amazon. In his author bio, Dr. Talbot refers to himself as “a former assassin,” “retired military commander,” and “leader of the Medellin Cartel’s New York operations at the age of 16.” The Medellin Cartel is a notorious drug distribution empire.
Dr. Talbot is listed as the author of another book on Google Books detailing his time as a “former teenage assassin” and leader of the cartel, told as he struggles with early onset Alzheimer’s.
Dr. Talbot could spend decades in prison
According to the National Institute on Drug Abuse, 444 residents of the Bayou State lost their lives because of an opioid-related drug overdose in 2018. During that year, the state’s health care providers wrote more than 79.4 opioid prescriptions for every 100 persons, which puts the state in the top five in the United States in 2018, when the average U.S. rate was 51.4 prescriptions per 100 persons.
Charged with one count each of conspiracy to unlawfully distribute and dispense controlled substances and maintaining drug-involved premises and conspiracy to commit health care fraud, Dr. Talbot is also charged with four counts of unlawfully distributing and dispensing controlled substances. He is scheduled for a federal court appearance on September 10.
In addition to presigning prescriptions for individuals he didn’t meet or examine, federal officials allege Dr. Talbot hired another health care provider to similarly presign prescriptions for people who weren’t examined at a medical practice in Slidell, where Dr. Talbot was employed. The DOJ says Dr. Talbot took a full-time job in Pineville, La., and presigned prescriptions while no longer physically present at the Slidell clinic.
A speaker’s bio for Dr. Talbot indicates he worked as chief of medical services for the Alexandria Veterans Affairs Health Care System in Pineville.
According to the DOJ’s indictment, Dr. Talbot was aware that patients were filling the prescriptions that were provided outside the scope of professional practice and not for a legitimate medical purpose. This is what triggered the DOJ’s fraudulent billing claim.
Dr. Talbot faces a maximum penalty of 10 years for conspiracy to commit health care fraud and 20 years each for the other counts, if convicted.
Dr. Talbot was candidate for local coroner
In February 2015, Dr. Talbot announced his candidacy for coroner for St. Tammany Parish, about an hour’s drive south of New Orleans, reported the Times Picayune. The seat was open because the previous coroner had resigned and ultimately pleaded guilty to a federal corruption charge.
The Times Picayune reported at the time that Dr. Talbot was a U.S. Navy veteran, in addition to serving as medical director and a primary care physician at the Medical Care Center in Slidell. Among the services provided to his patients were evaluations and treatment for substance use and mental health disorders, according to a press release issued by Dr. Talbot’s campaign.
Dr. Talbot’s medical license was issued in 1999 and inactive as of 2017, per the Louisiana State Board of Medical Examiners.
Louisiana expects $325M in multistate settlement with opioid companies
Louisiana is a party to a multistate and multijurisdictional lawsuit where the state is expected to receive more than $325 million in a settlement reached with drug distributors Cardinal, McKesson, and AmerisourceBergen, and drug manufacturer Johnson & Johnson, reported the Louisiana Illuminator in July. The total settlement may reach $26 billion dollars.
The Associated Press reported in July that there have been at least $40 billion in completed or proposed settlements, penalties, and fines between governments as a result of the opioid epidemic since 2007.
That total doesn’t include a proposed settlement involving members of the Sackler family, who own Purdue Pharmaceuticals, which manufactured and marketed the opioid painkiller OxyContin. The Sackler family have agreed to pay approximately $4.3 billion and surrender ownership of their bankrupt company, reported NPR. The family’s proposed settlement is part of a deal involving Purdue Pharmaceuticals worth more than $10 billion, reported Reuters.
In 2020, there were more than 81,000 drug overdose deaths, the highest number recorded in a 12-month period, per the U.S. Centers for Disease Control and Prevention. Fentanyl, an illicitly manufactured synthetic opioid, was the lead driver of those deaths.
A version of this article first appeared on Medscape.com.
CDC panel unanimously backs Pfizer vax, fortifying FDA approval
An independent expert panel within the Centers for Disease Control and Prevention (CDC) has studied the potential benefits and risks of the Pfizer-BioNTech COVID-19 vaccine and voted unanimously to recommend the shots for all Americans ages 16 and older.
The vaccine was fully approved by the U.S. Food and Drug Administration (FDA) last week.
The inoculation is still available to teens ages 12 to 15 under an emergency use authorization from the FDA.
ACIP now sends its recommendation to the CDC Director Rochelle Walensky, MD, for her sign off.
After reviewing the evidence behind the vaccine, panel member Sarah Long, MD, a professor of pediatrics at Drexel University College of Medicine, Philadelphia, said she couldn’t recall another instance where panelists had so much data on which to base their recommendation.
“This vaccine is worthy of the trust of the American people,” she said.
Doctors across the country use vaccines in line with the recommendations made by the ACIP. Their approval typically means that private and government insurers will cover the cost of the shots. In the case of the COVID-19 vaccines, the government is already picking up the tab.
Few surprises
The panel’s independent review of the vaccine’s effectiveness from nine studies held few surprises.
They found the Pfizer vaccine prevented a COVID infection with symptoms about 90%–92% of the time, at least for the first 4 months after the second shot. Protection against hospitalization and death was even higher.
The vaccine was about 89% effective at preventing a COVID infection without symptoms, according to a pooled estimate of five studies.
The data included in the review was updated only through March 13 of this year, however, and does not reflect the impact of further waning of immunity or the impact of the Delta variant.
In making their recommendation, the panel got an update on the safety of the vaccines, which have now been used in the United States for about 9 months.
The rate of anaphylaxis has settled at around five cases for every million shots given, according to the ACIP’s review of the evidence.
Cases of myocarditis and pericarditis were more common after getting a Pfizer-BioNTech vaccine than would be expected to happen naturally in the general population, but the risk was still very rare, and elevated primarily for men younger than age 30.
Out of 17 million second doses of Pfizer-BioNTech vaccines in the United States, there have been 327 confirmed cases of myocarditis reported to the Vaccine Adverse Event Reporting System in people who are younger than age 30. The average hospital stay for a myocarditis cases is 1 to 2 days.
So far, no one in the United States diagnosed with myocarditis after vaccination has died.
What’s more, the risk of myocarditis after vaccination was dwarfed by the risk of myocarditis after a COVID infection. The risk of myocarditis after a COVID infection was 6 to 34 times higher than the risk after receiving an mRNA vaccine.
About 11% of people who get the vaccine experience a serious reaction to the shot, compared with about 3% in the placebo group. Serious reactions were defined as pain; swelling or redness at the injection site that interferes with activity; needing to visit the hospital or ER for pain; tissue necrosis, or having skin slough off; high fever; vomiting that requires hydration; persistent diarrhea; severe headache; or muscle pain/severe joint pain.
“Safe and effective”
After hearing a presentation on the state of the pandemic in the US, some panel members were struck and shaken that 38% of Americans who are eligible are still not fully vaccinated.
Pablo Sanchez, MD, a pediatrician at Nationwide Children’s Hospital in Columbus, Ohio, said, “We’re doing an abysmal job vaccinating the American people. The message has to go out that the vaccines are safe and effective.”
A version of this story first appeared on Medscape.com.
An independent expert panel within the Centers for Disease Control and Prevention (CDC) has studied the potential benefits and risks of the Pfizer-BioNTech COVID-19 vaccine and voted unanimously to recommend the shots for all Americans ages 16 and older.
The vaccine was fully approved by the U.S. Food and Drug Administration (FDA) last week.
The inoculation is still available to teens ages 12 to 15 under an emergency use authorization from the FDA.
ACIP now sends its recommendation to the CDC Director Rochelle Walensky, MD, for her sign off.
After reviewing the evidence behind the vaccine, panel member Sarah Long, MD, a professor of pediatrics at Drexel University College of Medicine, Philadelphia, said she couldn’t recall another instance where panelists had so much data on which to base their recommendation.
“This vaccine is worthy of the trust of the American people,” she said.
Doctors across the country use vaccines in line with the recommendations made by the ACIP. Their approval typically means that private and government insurers will cover the cost of the shots. In the case of the COVID-19 vaccines, the government is already picking up the tab.
Few surprises
The panel’s independent review of the vaccine’s effectiveness from nine studies held few surprises.
They found the Pfizer vaccine prevented a COVID infection with symptoms about 90%–92% of the time, at least for the first 4 months after the second shot. Protection against hospitalization and death was even higher.
The vaccine was about 89% effective at preventing a COVID infection without symptoms, according to a pooled estimate of five studies.
The data included in the review was updated only through March 13 of this year, however, and does not reflect the impact of further waning of immunity or the impact of the Delta variant.
In making their recommendation, the panel got an update on the safety of the vaccines, which have now been used in the United States for about 9 months.
The rate of anaphylaxis has settled at around five cases for every million shots given, according to the ACIP’s review of the evidence.
Cases of myocarditis and pericarditis were more common after getting a Pfizer-BioNTech vaccine than would be expected to happen naturally in the general population, but the risk was still very rare, and elevated primarily for men younger than age 30.
Out of 17 million second doses of Pfizer-BioNTech vaccines in the United States, there have been 327 confirmed cases of myocarditis reported to the Vaccine Adverse Event Reporting System in people who are younger than age 30. The average hospital stay for a myocarditis cases is 1 to 2 days.
So far, no one in the United States diagnosed with myocarditis after vaccination has died.
What’s more, the risk of myocarditis after vaccination was dwarfed by the risk of myocarditis after a COVID infection. The risk of myocarditis after a COVID infection was 6 to 34 times higher than the risk after receiving an mRNA vaccine.
About 11% of people who get the vaccine experience a serious reaction to the shot, compared with about 3% in the placebo group. Serious reactions were defined as pain; swelling or redness at the injection site that interferes with activity; needing to visit the hospital or ER for pain; tissue necrosis, or having skin slough off; high fever; vomiting that requires hydration; persistent diarrhea; severe headache; or muscle pain/severe joint pain.
“Safe and effective”
After hearing a presentation on the state of the pandemic in the US, some panel members were struck and shaken that 38% of Americans who are eligible are still not fully vaccinated.
Pablo Sanchez, MD, a pediatrician at Nationwide Children’s Hospital in Columbus, Ohio, said, “We’re doing an abysmal job vaccinating the American people. The message has to go out that the vaccines are safe and effective.”
A version of this story first appeared on Medscape.com.
An independent expert panel within the Centers for Disease Control and Prevention (CDC) has studied the potential benefits and risks of the Pfizer-BioNTech COVID-19 vaccine and voted unanimously to recommend the shots for all Americans ages 16 and older.
The vaccine was fully approved by the U.S. Food and Drug Administration (FDA) last week.
The inoculation is still available to teens ages 12 to 15 under an emergency use authorization from the FDA.
ACIP now sends its recommendation to the CDC Director Rochelle Walensky, MD, for her sign off.
After reviewing the evidence behind the vaccine, panel member Sarah Long, MD, a professor of pediatrics at Drexel University College of Medicine, Philadelphia, said she couldn’t recall another instance where panelists had so much data on which to base their recommendation.
“This vaccine is worthy of the trust of the American people,” she said.
Doctors across the country use vaccines in line with the recommendations made by the ACIP. Their approval typically means that private and government insurers will cover the cost of the shots. In the case of the COVID-19 vaccines, the government is already picking up the tab.
Few surprises
The panel’s independent review of the vaccine’s effectiveness from nine studies held few surprises.
They found the Pfizer vaccine prevented a COVID infection with symptoms about 90%–92% of the time, at least for the first 4 months after the second shot. Protection against hospitalization and death was even higher.
The vaccine was about 89% effective at preventing a COVID infection without symptoms, according to a pooled estimate of five studies.
The data included in the review was updated only through March 13 of this year, however, and does not reflect the impact of further waning of immunity or the impact of the Delta variant.
In making their recommendation, the panel got an update on the safety of the vaccines, which have now been used in the United States for about 9 months.
The rate of anaphylaxis has settled at around five cases for every million shots given, according to the ACIP’s review of the evidence.
Cases of myocarditis and pericarditis were more common after getting a Pfizer-BioNTech vaccine than would be expected to happen naturally in the general population, but the risk was still very rare, and elevated primarily for men younger than age 30.
Out of 17 million second doses of Pfizer-BioNTech vaccines in the United States, there have been 327 confirmed cases of myocarditis reported to the Vaccine Adverse Event Reporting System in people who are younger than age 30. The average hospital stay for a myocarditis cases is 1 to 2 days.
So far, no one in the United States diagnosed with myocarditis after vaccination has died.
What’s more, the risk of myocarditis after vaccination was dwarfed by the risk of myocarditis after a COVID infection. The risk of myocarditis after a COVID infection was 6 to 34 times higher than the risk after receiving an mRNA vaccine.
About 11% of people who get the vaccine experience a serious reaction to the shot, compared with about 3% in the placebo group. Serious reactions were defined as pain; swelling or redness at the injection site that interferes with activity; needing to visit the hospital or ER for pain; tissue necrosis, or having skin slough off; high fever; vomiting that requires hydration; persistent diarrhea; severe headache; or muscle pain/severe joint pain.
“Safe and effective”
After hearing a presentation on the state of the pandemic in the US, some panel members were struck and shaken that 38% of Americans who are eligible are still not fully vaccinated.
Pablo Sanchez, MD, a pediatrician at Nationwide Children’s Hospital in Columbus, Ohio, said, “We’re doing an abysmal job vaccinating the American people. The message has to go out that the vaccines are safe and effective.”
A version of this story first appeared on Medscape.com.
Antidepressant helps prevent hospitalization in COVID patients: Study
A handful of studies have suggested that for newly infected COVID-19 patients, risk for serious illness may be reduced with a short course of fluvoxamine (Luvox), a decades-old pill typically prescribed for depression or obsessive-compulsive disorder (OCD). But those were small studies involving just a few hundred people.
This week, researchers reported promising data from a large, randomized phase 3 trial that enrolled COVID-19 patients from 11 sites in Brazil. In this study, in which 1,472 people were assigned to receive either a 10-day course of fluvoxamine or placebo pills, the antidepressant cut emergency department and hospital admissions by 29%.
Findings from the new study, which have not yet been peer reviewed, were published August 23 in MedRxiv.
Around the globe, particularly in countries without access to vaccines, “treatment options that are cheap and available and supported by good-quality evidence are the only hope we’ve got to reduce mortality within high-risk populations,” said Edward Mills, PhD, professor in the department of health research methods, evidence, and impact, McMaster University, Hamilton, Ont.
The new findings came from TOGETHER, a large platform trial coordinated by Dr. Mills and colleagues to evaluate the use of fluvoxamine and other repurposed drug candidates for symptomatic, high-risk, adult outpatients with confirmed cases of COVID-19.
The trial’s adaptive format allows multiple agents to be added and tested alongside placebo in a single master protocol – similar to the United Kingdom’s Recovery trial, which found that the common steroid dexamethasone could reduce deaths among hospitalized COVID-19 patients.
In platform trials, treatment arms can be dropped for futility, as was the case with hydroxychloroquine and lopinavir-ritonavir, neither of which did better than placebo at preventing hospitalization in an earlier TOGETHER trial analysis.
Study details
In the newly reported analysis, patients were randomly assigned to receive fluvoxamine or placebo between January and August 2021. Participants took fluvoxamine 100 mg twice daily for 10 days. By comparison, the U.S. Food and Drug Administration recommends a maximum daily dose of 300 mg of fluvoxamine for patients with OCD; full psychiatric benefits occur after 6 weeks.
For the primary outcome, the investigators assessed whether the conditions of patients with COVID worsened over a 28-day period so as to require either hospitalization or observation in the emergency department for more than 6 hours. In the placebo group, 108 of 733 patients’ conditions deteriorated to this extent (14.7%); by contrast, only 77 of 739 patients in the fluvoxamine group (10.4%) met these primary criteria – a relative risk reduction of 29%.
The treatment effect was greater (34%) in the per protocol analysis of participants who completed their course of pills.
The investigators also collected data on vital signs, including temperature and oxygen saturation, as well as adverse events reported at clinic visits or through video conferencing, phone calls, or social media applications. Side effects were mild, most commonly nausea and fatigue, and did not differ significantly between active treatment and control groups, Dr. Mills said in an interview.
Amid scores of studies evaluating repurposed drugs for COVID-19, the data on fluvoxamine are “looking much more favorable than anyone could have guessed – at least anyone in infectious disease,” said Paul Sax, MD, clinical director of the Division of Infectious Diseases at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School, Boston.
The new TOGETHER trial results augment supportive data published in JAMA last November from a phase 2 randomized trial that was small but “very well done,” Dr. Sax told this news organization.
Those results got a boost from a subsequent study of 65 racetrack workers who chose to take fluvoxamine during a COVID-19 outbreak in the San Francisco Bay area. Forty-eight persons opted against taking the drug. In this small, nonrandomized study, “the people who chose to be treated with fluvoxamine were sicker [at baseline] than the people who didn’t go on it, and yet the [treated group] ended up better,” said Dr. Sax, who discussed accumulating data on the use of fluvoxamine for COVID-19 in a recent New England Journal of Medicine blog post.
Anti-inflammatory effect?
After reviewing the new findings, Frank Domino, MD, professor of family medicine and community health at the University of Massachusetts, Worcester, said he would encourage patients with high-risk COVID-19 to consider taking fluvoxamine to lower their risk of being hospitalized. “But I would make it clear this was not a ‘cure,’ “ he said, “and we are unsure how it helps.”
At this point, U.S. treatment guidelines do not recommend fluvoxamine as the standard of care for nonhospitalized COVID-19 patients, but the National Institutes of Health is “very aware of the data,” Dr. Sax told this news organization.
Fluvoxamine is a selective serotonin reuptake inhibitor (SSRI) – a class of drugs that includes the more commonly prescribed antidepressant fluoxetine (Prozac). If prescribed off-label to COVID-19 patients, fluvoxamine should not be used within 2 weeks of starting treatment with other SSRI or monoamine oxidase inhibitor antidepressants and should be used with caution with other QT-interval prolonging medications, Dr. Sax said.
In addition, fluvoxamine can enhance the effect of antiplatelet and anticoagulant drugs, potentially triggering bleeding.
On the basis of in vitro and mouse studies of fluvoxamine, “we think it has an anti-inflammatory effect,” said child psychiatrist Angela Reiersen, MD, of Washington University, St. Louis, who came up with the idea for testing fluvoxamine in last year’s phase 2 trial and coauthored a recent article describing the drug’s potential mechanisms of action in COVID-19.
She and other researchers believe fluvoxamine’s anti-inflammatory effects derive from the molecule’s binding to the sigma-1 receptor in the endoplasmic reticulum, which regulates cellular responses to stress and infection.
Fluvoxamine also inhibits the activation of platelets. “In COVID-19, there does seem to be a problem with hyperactivation of platelets and excessive blood clots forming, so it is possible this could be another mechanism where it might be helping,” Dr. Reiersen said.
If sigma-1 activation turns out to be the main mechanism underlying fluvoxamine’s benefits in COVID-19, other sigma-1 agonists, such as fluoxetine, may also help. In a retrospective analysis of thousands of adults hospitalized for COVID-19 in France early in the pandemic, those who were taking antidepressants had a 44% lower risk for intubation or death.
And in a study under review, researchers at Stanford (Calif.) University and the University of California, San Francisco, analyzed electronic health records to explore a potential link between fluoxetine use and COVID outcomes among more than 80,000 patients from over 80 institutions across the United States. Other research suggests that antipsychotics could also have protective effects for patients with COVID-19.
Long COVID, long-term challenges
On the basis of its potential mechanisms of action, fluvoxamine may be able to prevent or treat long COVID, Dr. Reiersen said. That possibility will be assessed among other secondary endpoints in two ongoing studies of repurposed drugs: the NIH’s ACTIV-6, and the University of Minnesota’s COVID-OUT, an at-home trial of ivermectin, metformin, and fluvoxamine.
Dr. Reiersen and Washington University colleagues are also analyzing longer-term outcomes of participants in their own phase 3 trial of fluvoxamine (Stop COVID 2), which was discontinued when enrollment slowed to a trickle during the U.S. vaccine rollout. Logistical hurdles and scant funding have greatly hampered efforts to test the use of off-patent drugs for COVID-19 outpatients during the pandemic.
U.S. efforts face other obstacles as well. Elsewhere in the world – including Brazil, where the TOGETHER trial was run – vaccines are scarce, and there are no monoclonal antibodies.
“People have a great sense of community duty, and they’re participating in the trials,” Dr. Mills said. “You’re in a much more political environment in the U.S. on these outpatient trials.”
The TOGETHER trial was funded by Fast Grants and the Rainwater Foundation. Dr. Reiersen is an inventor on a patent application related to methods of treating COVID-19, which was filed by Washington University, St. Louis. Dr. Mills, Dr. Domino, and Dr. Sax report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A handful of studies have suggested that for newly infected COVID-19 patients, risk for serious illness may be reduced with a short course of fluvoxamine (Luvox), a decades-old pill typically prescribed for depression or obsessive-compulsive disorder (OCD). But those were small studies involving just a few hundred people.
This week, researchers reported promising data from a large, randomized phase 3 trial that enrolled COVID-19 patients from 11 sites in Brazil. In this study, in which 1,472 people were assigned to receive either a 10-day course of fluvoxamine or placebo pills, the antidepressant cut emergency department and hospital admissions by 29%.
Findings from the new study, which have not yet been peer reviewed, were published August 23 in MedRxiv.
Around the globe, particularly in countries without access to vaccines, “treatment options that are cheap and available and supported by good-quality evidence are the only hope we’ve got to reduce mortality within high-risk populations,” said Edward Mills, PhD, professor in the department of health research methods, evidence, and impact, McMaster University, Hamilton, Ont.
The new findings came from TOGETHER, a large platform trial coordinated by Dr. Mills and colleagues to evaluate the use of fluvoxamine and other repurposed drug candidates for symptomatic, high-risk, adult outpatients with confirmed cases of COVID-19.
The trial’s adaptive format allows multiple agents to be added and tested alongside placebo in a single master protocol – similar to the United Kingdom’s Recovery trial, which found that the common steroid dexamethasone could reduce deaths among hospitalized COVID-19 patients.
In platform trials, treatment arms can be dropped for futility, as was the case with hydroxychloroquine and lopinavir-ritonavir, neither of which did better than placebo at preventing hospitalization in an earlier TOGETHER trial analysis.
Study details
In the newly reported analysis, patients were randomly assigned to receive fluvoxamine or placebo between January and August 2021. Participants took fluvoxamine 100 mg twice daily for 10 days. By comparison, the U.S. Food and Drug Administration recommends a maximum daily dose of 300 mg of fluvoxamine for patients with OCD; full psychiatric benefits occur after 6 weeks.
For the primary outcome, the investigators assessed whether the conditions of patients with COVID worsened over a 28-day period so as to require either hospitalization or observation in the emergency department for more than 6 hours. In the placebo group, 108 of 733 patients’ conditions deteriorated to this extent (14.7%); by contrast, only 77 of 739 patients in the fluvoxamine group (10.4%) met these primary criteria – a relative risk reduction of 29%.
The treatment effect was greater (34%) in the per protocol analysis of participants who completed their course of pills.
The investigators also collected data on vital signs, including temperature and oxygen saturation, as well as adverse events reported at clinic visits or through video conferencing, phone calls, or social media applications. Side effects were mild, most commonly nausea and fatigue, and did not differ significantly between active treatment and control groups, Dr. Mills said in an interview.
Amid scores of studies evaluating repurposed drugs for COVID-19, the data on fluvoxamine are “looking much more favorable than anyone could have guessed – at least anyone in infectious disease,” said Paul Sax, MD, clinical director of the Division of Infectious Diseases at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School, Boston.
The new TOGETHER trial results augment supportive data published in JAMA last November from a phase 2 randomized trial that was small but “very well done,” Dr. Sax told this news organization.
Those results got a boost from a subsequent study of 65 racetrack workers who chose to take fluvoxamine during a COVID-19 outbreak in the San Francisco Bay area. Forty-eight persons opted against taking the drug. In this small, nonrandomized study, “the people who chose to be treated with fluvoxamine were sicker [at baseline] than the people who didn’t go on it, and yet the [treated group] ended up better,” said Dr. Sax, who discussed accumulating data on the use of fluvoxamine for COVID-19 in a recent New England Journal of Medicine blog post.
Anti-inflammatory effect?
After reviewing the new findings, Frank Domino, MD, professor of family medicine and community health at the University of Massachusetts, Worcester, said he would encourage patients with high-risk COVID-19 to consider taking fluvoxamine to lower their risk of being hospitalized. “But I would make it clear this was not a ‘cure,’ “ he said, “and we are unsure how it helps.”
At this point, U.S. treatment guidelines do not recommend fluvoxamine as the standard of care for nonhospitalized COVID-19 patients, but the National Institutes of Health is “very aware of the data,” Dr. Sax told this news organization.
Fluvoxamine is a selective serotonin reuptake inhibitor (SSRI) – a class of drugs that includes the more commonly prescribed antidepressant fluoxetine (Prozac). If prescribed off-label to COVID-19 patients, fluvoxamine should not be used within 2 weeks of starting treatment with other SSRI or monoamine oxidase inhibitor antidepressants and should be used with caution with other QT-interval prolonging medications, Dr. Sax said.
In addition, fluvoxamine can enhance the effect of antiplatelet and anticoagulant drugs, potentially triggering bleeding.
On the basis of in vitro and mouse studies of fluvoxamine, “we think it has an anti-inflammatory effect,” said child psychiatrist Angela Reiersen, MD, of Washington University, St. Louis, who came up with the idea for testing fluvoxamine in last year’s phase 2 trial and coauthored a recent article describing the drug’s potential mechanisms of action in COVID-19.
She and other researchers believe fluvoxamine’s anti-inflammatory effects derive from the molecule’s binding to the sigma-1 receptor in the endoplasmic reticulum, which regulates cellular responses to stress and infection.
Fluvoxamine also inhibits the activation of platelets. “In COVID-19, there does seem to be a problem with hyperactivation of platelets and excessive blood clots forming, so it is possible this could be another mechanism where it might be helping,” Dr. Reiersen said.
If sigma-1 activation turns out to be the main mechanism underlying fluvoxamine’s benefits in COVID-19, other sigma-1 agonists, such as fluoxetine, may also help. In a retrospective analysis of thousands of adults hospitalized for COVID-19 in France early in the pandemic, those who were taking antidepressants had a 44% lower risk for intubation or death.
And in a study under review, researchers at Stanford (Calif.) University and the University of California, San Francisco, analyzed electronic health records to explore a potential link between fluoxetine use and COVID outcomes among more than 80,000 patients from over 80 institutions across the United States. Other research suggests that antipsychotics could also have protective effects for patients with COVID-19.
Long COVID, long-term challenges
On the basis of its potential mechanisms of action, fluvoxamine may be able to prevent or treat long COVID, Dr. Reiersen said. That possibility will be assessed among other secondary endpoints in two ongoing studies of repurposed drugs: the NIH’s ACTIV-6, and the University of Minnesota’s COVID-OUT, an at-home trial of ivermectin, metformin, and fluvoxamine.
Dr. Reiersen and Washington University colleagues are also analyzing longer-term outcomes of participants in their own phase 3 trial of fluvoxamine (Stop COVID 2), which was discontinued when enrollment slowed to a trickle during the U.S. vaccine rollout. Logistical hurdles and scant funding have greatly hampered efforts to test the use of off-patent drugs for COVID-19 outpatients during the pandemic.
U.S. efforts face other obstacles as well. Elsewhere in the world – including Brazil, where the TOGETHER trial was run – vaccines are scarce, and there are no monoclonal antibodies.
“People have a great sense of community duty, and they’re participating in the trials,” Dr. Mills said. “You’re in a much more political environment in the U.S. on these outpatient trials.”
The TOGETHER trial was funded by Fast Grants and the Rainwater Foundation. Dr. Reiersen is an inventor on a patent application related to methods of treating COVID-19, which was filed by Washington University, St. Louis. Dr. Mills, Dr. Domino, and Dr. Sax report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A handful of studies have suggested that for newly infected COVID-19 patients, risk for serious illness may be reduced with a short course of fluvoxamine (Luvox), a decades-old pill typically prescribed for depression or obsessive-compulsive disorder (OCD). But those were small studies involving just a few hundred people.
This week, researchers reported promising data from a large, randomized phase 3 trial that enrolled COVID-19 patients from 11 sites in Brazil. In this study, in which 1,472 people were assigned to receive either a 10-day course of fluvoxamine or placebo pills, the antidepressant cut emergency department and hospital admissions by 29%.
Findings from the new study, which have not yet been peer reviewed, were published August 23 in MedRxiv.
Around the globe, particularly in countries without access to vaccines, “treatment options that are cheap and available and supported by good-quality evidence are the only hope we’ve got to reduce mortality within high-risk populations,” said Edward Mills, PhD, professor in the department of health research methods, evidence, and impact, McMaster University, Hamilton, Ont.
The new findings came from TOGETHER, a large platform trial coordinated by Dr. Mills and colleagues to evaluate the use of fluvoxamine and other repurposed drug candidates for symptomatic, high-risk, adult outpatients with confirmed cases of COVID-19.
The trial’s adaptive format allows multiple agents to be added and tested alongside placebo in a single master protocol – similar to the United Kingdom’s Recovery trial, which found that the common steroid dexamethasone could reduce deaths among hospitalized COVID-19 patients.
In platform trials, treatment arms can be dropped for futility, as was the case with hydroxychloroquine and lopinavir-ritonavir, neither of which did better than placebo at preventing hospitalization in an earlier TOGETHER trial analysis.
Study details
In the newly reported analysis, patients were randomly assigned to receive fluvoxamine or placebo between January and August 2021. Participants took fluvoxamine 100 mg twice daily for 10 days. By comparison, the U.S. Food and Drug Administration recommends a maximum daily dose of 300 mg of fluvoxamine for patients with OCD; full psychiatric benefits occur after 6 weeks.
For the primary outcome, the investigators assessed whether the conditions of patients with COVID worsened over a 28-day period so as to require either hospitalization or observation in the emergency department for more than 6 hours. In the placebo group, 108 of 733 patients’ conditions deteriorated to this extent (14.7%); by contrast, only 77 of 739 patients in the fluvoxamine group (10.4%) met these primary criteria – a relative risk reduction of 29%.
The treatment effect was greater (34%) in the per protocol analysis of participants who completed their course of pills.
The investigators also collected data on vital signs, including temperature and oxygen saturation, as well as adverse events reported at clinic visits or through video conferencing, phone calls, or social media applications. Side effects were mild, most commonly nausea and fatigue, and did not differ significantly between active treatment and control groups, Dr. Mills said in an interview.
Amid scores of studies evaluating repurposed drugs for COVID-19, the data on fluvoxamine are “looking much more favorable than anyone could have guessed – at least anyone in infectious disease,” said Paul Sax, MD, clinical director of the Division of Infectious Diseases at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School, Boston.
The new TOGETHER trial results augment supportive data published in JAMA last November from a phase 2 randomized trial that was small but “very well done,” Dr. Sax told this news organization.
Those results got a boost from a subsequent study of 65 racetrack workers who chose to take fluvoxamine during a COVID-19 outbreak in the San Francisco Bay area. Forty-eight persons opted against taking the drug. In this small, nonrandomized study, “the people who chose to be treated with fluvoxamine were sicker [at baseline] than the people who didn’t go on it, and yet the [treated group] ended up better,” said Dr. Sax, who discussed accumulating data on the use of fluvoxamine for COVID-19 in a recent New England Journal of Medicine blog post.
Anti-inflammatory effect?
After reviewing the new findings, Frank Domino, MD, professor of family medicine and community health at the University of Massachusetts, Worcester, said he would encourage patients with high-risk COVID-19 to consider taking fluvoxamine to lower their risk of being hospitalized. “But I would make it clear this was not a ‘cure,’ “ he said, “and we are unsure how it helps.”
At this point, U.S. treatment guidelines do not recommend fluvoxamine as the standard of care for nonhospitalized COVID-19 patients, but the National Institutes of Health is “very aware of the data,” Dr. Sax told this news organization.
Fluvoxamine is a selective serotonin reuptake inhibitor (SSRI) – a class of drugs that includes the more commonly prescribed antidepressant fluoxetine (Prozac). If prescribed off-label to COVID-19 patients, fluvoxamine should not be used within 2 weeks of starting treatment with other SSRI or monoamine oxidase inhibitor antidepressants and should be used with caution with other QT-interval prolonging medications, Dr. Sax said.
In addition, fluvoxamine can enhance the effect of antiplatelet and anticoagulant drugs, potentially triggering bleeding.
On the basis of in vitro and mouse studies of fluvoxamine, “we think it has an anti-inflammatory effect,” said child psychiatrist Angela Reiersen, MD, of Washington University, St. Louis, who came up with the idea for testing fluvoxamine in last year’s phase 2 trial and coauthored a recent article describing the drug’s potential mechanisms of action in COVID-19.
She and other researchers believe fluvoxamine’s anti-inflammatory effects derive from the molecule’s binding to the sigma-1 receptor in the endoplasmic reticulum, which regulates cellular responses to stress and infection.
Fluvoxamine also inhibits the activation of platelets. “In COVID-19, there does seem to be a problem with hyperactivation of platelets and excessive blood clots forming, so it is possible this could be another mechanism where it might be helping,” Dr. Reiersen said.
If sigma-1 activation turns out to be the main mechanism underlying fluvoxamine’s benefits in COVID-19, other sigma-1 agonists, such as fluoxetine, may also help. In a retrospective analysis of thousands of adults hospitalized for COVID-19 in France early in the pandemic, those who were taking antidepressants had a 44% lower risk for intubation or death.
And in a study under review, researchers at Stanford (Calif.) University and the University of California, San Francisco, analyzed electronic health records to explore a potential link between fluoxetine use and COVID outcomes among more than 80,000 patients from over 80 institutions across the United States. Other research suggests that antipsychotics could also have protective effects for patients with COVID-19.
Long COVID, long-term challenges
On the basis of its potential mechanisms of action, fluvoxamine may be able to prevent or treat long COVID, Dr. Reiersen said. That possibility will be assessed among other secondary endpoints in two ongoing studies of repurposed drugs: the NIH’s ACTIV-6, and the University of Minnesota’s COVID-OUT, an at-home trial of ivermectin, metformin, and fluvoxamine.
Dr. Reiersen and Washington University colleagues are also analyzing longer-term outcomes of participants in their own phase 3 trial of fluvoxamine (Stop COVID 2), which was discontinued when enrollment slowed to a trickle during the U.S. vaccine rollout. Logistical hurdles and scant funding have greatly hampered efforts to test the use of off-patent drugs for COVID-19 outpatients during the pandemic.
U.S. efforts face other obstacles as well. Elsewhere in the world – including Brazil, where the TOGETHER trial was run – vaccines are scarce, and there are no monoclonal antibodies.
“People have a great sense of community duty, and they’re participating in the trials,” Dr. Mills said. “You’re in a much more political environment in the U.S. on these outpatient trials.”
The TOGETHER trial was funded by Fast Grants and the Rainwater Foundation. Dr. Reiersen is an inventor on a patent application related to methods of treating COVID-19, which was filed by Washington University, St. Louis. Dr. Mills, Dr. Domino, and Dr. Sax report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Four police suicides in the aftermath of the Capitol siege: What can we learn?
Officer Scott Davis is a passionate man who thinks and talks quickly. As a member of the Special Events Team for Montgomery County, Maryland, he was already staging in Rockville, outside of Washington, D.C., when the call came in last Jan. 6 to move their unit to the U.S. Capitol.

“It was surreal,” said Mr. Davis. “There were people from all different groups at the Capitol that day. Many people were trying to get out, but others surrounded us. They called us ‘human race traitors.’ And then I heard someone say, ‘It’s good you brought your shields, we’ll carry your bodies out on them.’”
Mr. Davis described hours of mayhem during which he was hit with bear spray, a brick, a chair, and a metal rod. One of the members of Mr. Davis’ unit remains on leave with a head injury nearly 9 months after the siege.
“It went on for 3 hours, but it felt like 15 minutes. Then, all of a sudden, it was over.”
For the members of law enforcement at the Capitol that day, the repercussions are still being felt, perhaps most notably in the case of the four officers who subsequently died of suicide. Three of the officers were with the Metropolitan Police Department of the District of Columbia and one worked for the Capitol Police Department.
Police officers are subjected to traumas on a regular basis and often placed in circumstances where their lives are in danger. Yet four suicides within a short time – all connected to a single event – is particularly shocking and tragic, even more so for how little attention it has garnered to date.
What contributes to the high rate of suicide among officers?
Scott Silverii, PhD, a former police officer and author of Broken and Blue: A Policeman’s Guide to Health, Hope, and Healing, commented that he “wouldn’t be surprised if there are more suicides to come.” This stems not only from the experiences of that day but also the elevated risk for suicide that law enforcement officers already experienced prior to the Capitol riots. Suicide remains a rare event, with a national all-population average of 13.9 per 100,000 citizens. But as Dr. Silverii noted, more officers die by suicide each year than are killed in the line of duty.
“Suicide is a big part of police culture – officers are doers and fixers, and it is seen as being more honorable to take yourself out of the equation than it is to ask for help,” he said. “Most officers come in with past pain, and this is a situation where they are being overwhelmed and under-respected. At the same time, police culture is a closed culture, and it is not friendly to researchers.”
Another contributor is the frequency with which law enforcement officers are exposed to trauma, according to Vernon Herron, Director of Officer Safety and Wellness for the Baltimore City Police.
Mr. Herron said, citing the psychiatric and addiction issues that officers commonly experience.
Protecting the protectors
Mr. Herron and others are working to address these problems head-on.
“We are trying to identify employees exposed to trauma and to offer counseling and intervention,” he said, “Otherwise, everything else will fall short.”
Yet implementing such measures is no easy task, given the lack of a central oversight organization for law enforcement, said Sheldon Greenberg, PhD, a former police officer and professor of management in the School of Education at Johns Hopkins University, Baltimore.
“In the United States there is no such thing as ‘The Police.’ There is no one in a position to set policy, standards, or training mandates nationally,” he said. “There are approximately 18,000 police and sheriff departments in the country, and many of them are small. No one can compel law enforcement agencies to implement officer wellness and suicide prevention programs, make counseling available to officers, or train supervisors and peers to identify suicide ideation.”
Dr. Greenberg said a further barrier to helping police officers considering self-harm is posed by the fact that even if they do seek out counseling, there is no guarantee that it will remain confidential.
“Support personnel have an obligation to report an officer who is thinking about committing suicide,” he said. “Many officers are concerned about this lack of confidentiality and that they may be branded if they seek help.”
Although Dr. Greenberg said many police officers are self-professed “action junkies,” even their unusually high capacity for stress is often tested by the realities of the job.
“Increasing demands for service, shortages of personnel, misinformation about police, COVID-19, talk about restructuring policing with little concrete direction, increased exposure to violence, greater numbers of vulnerable people, and more take a toll over time,” he lamented. “In addition, we are in a recruiting crisis in law enforcement, and there are no standards to ensure the quality of psychological screening provided to applicants. Many officers will go through their entire career and never be screened again. We know little about the stresses and strains that officers bring to the job.”
After the siege
It is not clear how many police officers were present at the Capitol on Jan. 6. During the chaos of the day, reinforcements to the Capitol Police Department arrived from Washington D.C., Maryland, and Virginia, but no official numbers on responders were obtained; Mr. Davis thought it was likely that there were at least 1,000 law enforcement officers present. Those who did respond sustained an estimated 100 injuries, including an officer who died the next day. Of the officers who died by suicide, one died 3 days after, another died 9 days later, and two more died in July – numbers that contradict the notion that this is some coincidence. Officer Alexander Kettering, a colleague of Mr. Davis who has been with Montgomery County Police for 15 years, was among those tasked with protecting the Capitol on Jan. 6. The chaos, violence, and destruction of the day has stuck with him and continues to occupy his thoughts.
“I had a front-row seat to the whole thing. It was overwhelming, and I’ve never seen people this angry,” said Mr. Kettering. “There were people up on the veranda and on the scaffolding set up for the inauguration. They were smashing windows and throwing things into the crowd. It was insane. There were decent people coming up to us and saying they would pray for us, then others calling us traitors, telling us to stand down and join them.”
In the aftermath of the Capitol siege, Mr. Kettering watched in dismay as the narrative of the day’s events began to warp.
“At first there was a consensus that what happened was so wrong, and then the politics took over. People were saying it wasn’t as bad as the media said, that it really wasn’t that violent and those speaking out are traitors or political operatives. I relive it every day, and it’s hard to escape, even in casual conversation.”
He added that the days’ events were compounded by the already heightened tensions surrounding the national debate around policing.
“It’s been 18 months of stress, of anti-police movements, and there is a fine line between addressing police brutality and being anti-police,” Mr. Kettering said, noting that the aforementioned issues have all contributed to the ongoing struggles his fellow officers are experiencing.
“It’s not a thing for cops to talk about how an event affected them,” he said. “A lot of officers have just shut down. People have careers and pensions to protect, and every time we stop a motorist, something could go wrong, even if we do everything right. There are mixed signals: They tell us, ‘Defend but don’t defend.’”
His colleague, Mr. Davis, said that officers “need more support from politicians,” noting that he felt particularly insulted by a comment made by a Montgomery County public official who accused the officers present at the Capitol of racism. “And finally, we feel a little betrayed by the public.”
More questions than answers from the Capitol’s day of chaos
What about the events of Jan. 6 led to the suicides of four law enforcement officers and what can be done to prevent more deaths in the future? There are the individual factors of each man’s personal history, circumstances, and vulnerabilities, including the sense of being personally endangered, witnessing trauma, and direct injury – one officer who died of suicide had sustained a head injury that day.
We don’t know if the officers went into the event with preexisting mental illness or addiction or if the day’s events precipitated psychiatric episodes. And with all the partisan anger surrounding the presidential election, we don’t know if each officer’s political beliefs amplified his distress over what occurred in a social media climate where police are being faulted by all sides.
When multiple suicides occur in a community, there is always concern about a “copycat” phenomena. These concerns are made more difficult to address, however, given the police culture of taboo and stigma associated with getting professional help, difficulty accessing care, and career repercussions for speaking openly about suicidal thoughts and mental health issues.
Finally, there is the current political agenda that leaves officers feeling unsupported, fearful of negative outcomes, and unappreciated. The Capitol siege in particular embodied a great deal of national distress and confusion over basic issues of truth, justice, and perceptions of reality in our polarized society.
Can we move to a place where those who enforce laws have easy access to treatment, free from stigma? Can we encourage a culture that does not tolerate brutality or racism, while also refusing to label all police as bad and lending support to their mission? Can we be more attuned to the repercussions of circumstances where officers are witnesses to trauma, are endangered themselves, and would benefit from acknowledgment of their distress?
Time will tell if our anti-police pendulum swings back. In the meantime, these four suicides among people defending our country remain tragically overlooked.
Dinah Miller, MD, is coauthor of Committed: The Battle Over Involuntary Psychiatric Care (Johns Hopkins University Press, 2016). She has a private practice in Baltimore and is an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University. A version of this article first appeared on Medscape.com.
Officer Scott Davis is a passionate man who thinks and talks quickly. As a member of the Special Events Team for Montgomery County, Maryland, he was already staging in Rockville, outside of Washington, D.C., when the call came in last Jan. 6 to move their unit to the U.S. Capitol.

“It was surreal,” said Mr. Davis. “There were people from all different groups at the Capitol that day. Many people were trying to get out, but others surrounded us. They called us ‘human race traitors.’ And then I heard someone say, ‘It’s good you brought your shields, we’ll carry your bodies out on them.’”
Mr. Davis described hours of mayhem during which he was hit with bear spray, a brick, a chair, and a metal rod. One of the members of Mr. Davis’ unit remains on leave with a head injury nearly 9 months after the siege.
“It went on for 3 hours, but it felt like 15 minutes. Then, all of a sudden, it was over.”
For the members of law enforcement at the Capitol that day, the repercussions are still being felt, perhaps most notably in the case of the four officers who subsequently died of suicide. Three of the officers were with the Metropolitan Police Department of the District of Columbia and one worked for the Capitol Police Department.
Police officers are subjected to traumas on a regular basis and often placed in circumstances where their lives are in danger. Yet four suicides within a short time – all connected to a single event – is particularly shocking and tragic, even more so for how little attention it has garnered to date.
What contributes to the high rate of suicide among officers?
Scott Silverii, PhD, a former police officer and author of Broken and Blue: A Policeman’s Guide to Health, Hope, and Healing, commented that he “wouldn’t be surprised if there are more suicides to come.” This stems not only from the experiences of that day but also the elevated risk for suicide that law enforcement officers already experienced prior to the Capitol riots. Suicide remains a rare event, with a national all-population average of 13.9 per 100,000 citizens. But as Dr. Silverii noted, more officers die by suicide each year than are killed in the line of duty.
“Suicide is a big part of police culture – officers are doers and fixers, and it is seen as being more honorable to take yourself out of the equation than it is to ask for help,” he said. “Most officers come in with past pain, and this is a situation where they are being overwhelmed and under-respected. At the same time, police culture is a closed culture, and it is not friendly to researchers.”
Another contributor is the frequency with which law enforcement officers are exposed to trauma, according to Vernon Herron, Director of Officer Safety and Wellness for the Baltimore City Police.
Mr. Herron said, citing the psychiatric and addiction issues that officers commonly experience.
Protecting the protectors
Mr. Herron and others are working to address these problems head-on.
“We are trying to identify employees exposed to trauma and to offer counseling and intervention,” he said, “Otherwise, everything else will fall short.”
Yet implementing such measures is no easy task, given the lack of a central oversight organization for law enforcement, said Sheldon Greenberg, PhD, a former police officer and professor of management in the School of Education at Johns Hopkins University, Baltimore.
“In the United States there is no such thing as ‘The Police.’ There is no one in a position to set policy, standards, or training mandates nationally,” he said. “There are approximately 18,000 police and sheriff departments in the country, and many of them are small. No one can compel law enforcement agencies to implement officer wellness and suicide prevention programs, make counseling available to officers, or train supervisors and peers to identify suicide ideation.”
Dr. Greenberg said a further barrier to helping police officers considering self-harm is posed by the fact that even if they do seek out counseling, there is no guarantee that it will remain confidential.
“Support personnel have an obligation to report an officer who is thinking about committing suicide,” he said. “Many officers are concerned about this lack of confidentiality and that they may be branded if they seek help.”
Although Dr. Greenberg said many police officers are self-professed “action junkies,” even their unusually high capacity for stress is often tested by the realities of the job.
“Increasing demands for service, shortages of personnel, misinformation about police, COVID-19, talk about restructuring policing with little concrete direction, increased exposure to violence, greater numbers of vulnerable people, and more take a toll over time,” he lamented. “In addition, we are in a recruiting crisis in law enforcement, and there are no standards to ensure the quality of psychological screening provided to applicants. Many officers will go through their entire career and never be screened again. We know little about the stresses and strains that officers bring to the job.”
After the siege
It is not clear how many police officers were present at the Capitol on Jan. 6. During the chaos of the day, reinforcements to the Capitol Police Department arrived from Washington D.C., Maryland, and Virginia, but no official numbers on responders were obtained; Mr. Davis thought it was likely that there were at least 1,000 law enforcement officers present. Those who did respond sustained an estimated 100 injuries, including an officer who died the next day. Of the officers who died by suicide, one died 3 days after, another died 9 days later, and two more died in July – numbers that contradict the notion that this is some coincidence. Officer Alexander Kettering, a colleague of Mr. Davis who has been with Montgomery County Police for 15 years, was among those tasked with protecting the Capitol on Jan. 6. The chaos, violence, and destruction of the day has stuck with him and continues to occupy his thoughts.
“I had a front-row seat to the whole thing. It was overwhelming, and I’ve never seen people this angry,” said Mr. Kettering. “There were people up on the veranda and on the scaffolding set up for the inauguration. They were smashing windows and throwing things into the crowd. It was insane. There were decent people coming up to us and saying they would pray for us, then others calling us traitors, telling us to stand down and join them.”
In the aftermath of the Capitol siege, Mr. Kettering watched in dismay as the narrative of the day’s events began to warp.
“At first there was a consensus that what happened was so wrong, and then the politics took over. People were saying it wasn’t as bad as the media said, that it really wasn’t that violent and those speaking out are traitors or political operatives. I relive it every day, and it’s hard to escape, even in casual conversation.”
He added that the days’ events were compounded by the already heightened tensions surrounding the national debate around policing.
“It’s been 18 months of stress, of anti-police movements, and there is a fine line between addressing police brutality and being anti-police,” Mr. Kettering said, noting that the aforementioned issues have all contributed to the ongoing struggles his fellow officers are experiencing.
“It’s not a thing for cops to talk about how an event affected them,” he said. “A lot of officers have just shut down. People have careers and pensions to protect, and every time we stop a motorist, something could go wrong, even if we do everything right. There are mixed signals: They tell us, ‘Defend but don’t defend.’”
His colleague, Mr. Davis, said that officers “need more support from politicians,” noting that he felt particularly insulted by a comment made by a Montgomery County public official who accused the officers present at the Capitol of racism. “And finally, we feel a little betrayed by the public.”
More questions than answers from the Capitol’s day of chaos
What about the events of Jan. 6 led to the suicides of four law enforcement officers and what can be done to prevent more deaths in the future? There are the individual factors of each man’s personal history, circumstances, and vulnerabilities, including the sense of being personally endangered, witnessing trauma, and direct injury – one officer who died of suicide had sustained a head injury that day.
We don’t know if the officers went into the event with preexisting mental illness or addiction or if the day’s events precipitated psychiatric episodes. And with all the partisan anger surrounding the presidential election, we don’t know if each officer’s political beliefs amplified his distress over what occurred in a social media climate where police are being faulted by all sides.
When multiple suicides occur in a community, there is always concern about a “copycat” phenomena. These concerns are made more difficult to address, however, given the police culture of taboo and stigma associated with getting professional help, difficulty accessing care, and career repercussions for speaking openly about suicidal thoughts and mental health issues.
Finally, there is the current political agenda that leaves officers feeling unsupported, fearful of negative outcomes, and unappreciated. The Capitol siege in particular embodied a great deal of national distress and confusion over basic issues of truth, justice, and perceptions of reality in our polarized society.
Can we move to a place where those who enforce laws have easy access to treatment, free from stigma? Can we encourage a culture that does not tolerate brutality or racism, while also refusing to label all police as bad and lending support to their mission? Can we be more attuned to the repercussions of circumstances where officers are witnesses to trauma, are endangered themselves, and would benefit from acknowledgment of their distress?
Time will tell if our anti-police pendulum swings back. In the meantime, these four suicides among people defending our country remain tragically overlooked.
Dinah Miller, MD, is coauthor of Committed: The Battle Over Involuntary Psychiatric Care (Johns Hopkins University Press, 2016). She has a private practice in Baltimore and is an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University. A version of this article first appeared on Medscape.com.
Officer Scott Davis is a passionate man who thinks and talks quickly. As a member of the Special Events Team for Montgomery County, Maryland, he was already staging in Rockville, outside of Washington, D.C., when the call came in last Jan. 6 to move their unit to the U.S. Capitol.

“It was surreal,” said Mr. Davis. “There were people from all different groups at the Capitol that day. Many people were trying to get out, but others surrounded us. They called us ‘human race traitors.’ And then I heard someone say, ‘It’s good you brought your shields, we’ll carry your bodies out on them.’”
Mr. Davis described hours of mayhem during which he was hit with bear spray, a brick, a chair, and a metal rod. One of the members of Mr. Davis’ unit remains on leave with a head injury nearly 9 months after the siege.
“It went on for 3 hours, but it felt like 15 minutes. Then, all of a sudden, it was over.”
For the members of law enforcement at the Capitol that day, the repercussions are still being felt, perhaps most notably in the case of the four officers who subsequently died of suicide. Three of the officers were with the Metropolitan Police Department of the District of Columbia and one worked for the Capitol Police Department.
Police officers are subjected to traumas on a regular basis and often placed in circumstances where their lives are in danger. Yet four suicides within a short time – all connected to a single event – is particularly shocking and tragic, even more so for how little attention it has garnered to date.
What contributes to the high rate of suicide among officers?
Scott Silverii, PhD, a former police officer and author of Broken and Blue: A Policeman’s Guide to Health, Hope, and Healing, commented that he “wouldn’t be surprised if there are more suicides to come.” This stems not only from the experiences of that day but also the elevated risk for suicide that law enforcement officers already experienced prior to the Capitol riots. Suicide remains a rare event, with a national all-population average of 13.9 per 100,000 citizens. But as Dr. Silverii noted, more officers die by suicide each year than are killed in the line of duty.
“Suicide is a big part of police culture – officers are doers and fixers, and it is seen as being more honorable to take yourself out of the equation than it is to ask for help,” he said. “Most officers come in with past pain, and this is a situation where they are being overwhelmed and under-respected. At the same time, police culture is a closed culture, and it is not friendly to researchers.”
Another contributor is the frequency with which law enforcement officers are exposed to trauma, according to Vernon Herron, Director of Officer Safety and Wellness for the Baltimore City Police.
Mr. Herron said, citing the psychiatric and addiction issues that officers commonly experience.
Protecting the protectors
Mr. Herron and others are working to address these problems head-on.
“We are trying to identify employees exposed to trauma and to offer counseling and intervention,” he said, “Otherwise, everything else will fall short.”
Yet implementing such measures is no easy task, given the lack of a central oversight organization for law enforcement, said Sheldon Greenberg, PhD, a former police officer and professor of management in the School of Education at Johns Hopkins University, Baltimore.
“In the United States there is no such thing as ‘The Police.’ There is no one in a position to set policy, standards, or training mandates nationally,” he said. “There are approximately 18,000 police and sheriff departments in the country, and many of them are small. No one can compel law enforcement agencies to implement officer wellness and suicide prevention programs, make counseling available to officers, or train supervisors and peers to identify suicide ideation.”
Dr. Greenberg said a further barrier to helping police officers considering self-harm is posed by the fact that even if they do seek out counseling, there is no guarantee that it will remain confidential.
“Support personnel have an obligation to report an officer who is thinking about committing suicide,” he said. “Many officers are concerned about this lack of confidentiality and that they may be branded if they seek help.”
Although Dr. Greenberg said many police officers are self-professed “action junkies,” even their unusually high capacity for stress is often tested by the realities of the job.
“Increasing demands for service, shortages of personnel, misinformation about police, COVID-19, talk about restructuring policing with little concrete direction, increased exposure to violence, greater numbers of vulnerable people, and more take a toll over time,” he lamented. “In addition, we are in a recruiting crisis in law enforcement, and there are no standards to ensure the quality of psychological screening provided to applicants. Many officers will go through their entire career and never be screened again. We know little about the stresses and strains that officers bring to the job.”
After the siege
It is not clear how many police officers were present at the Capitol on Jan. 6. During the chaos of the day, reinforcements to the Capitol Police Department arrived from Washington D.C., Maryland, and Virginia, but no official numbers on responders were obtained; Mr. Davis thought it was likely that there were at least 1,000 law enforcement officers present. Those who did respond sustained an estimated 100 injuries, including an officer who died the next day. Of the officers who died by suicide, one died 3 days after, another died 9 days later, and two more died in July – numbers that contradict the notion that this is some coincidence. Officer Alexander Kettering, a colleague of Mr. Davis who has been with Montgomery County Police for 15 years, was among those tasked with protecting the Capitol on Jan. 6. The chaos, violence, and destruction of the day has stuck with him and continues to occupy his thoughts.
“I had a front-row seat to the whole thing. It was overwhelming, and I’ve never seen people this angry,” said Mr. Kettering. “There were people up on the veranda and on the scaffolding set up for the inauguration. They were smashing windows and throwing things into the crowd. It was insane. There were decent people coming up to us and saying they would pray for us, then others calling us traitors, telling us to stand down and join them.”
In the aftermath of the Capitol siege, Mr. Kettering watched in dismay as the narrative of the day’s events began to warp.
“At first there was a consensus that what happened was so wrong, and then the politics took over. People were saying it wasn’t as bad as the media said, that it really wasn’t that violent and those speaking out are traitors or political operatives. I relive it every day, and it’s hard to escape, even in casual conversation.”
He added that the days’ events were compounded by the already heightened tensions surrounding the national debate around policing.
“It’s been 18 months of stress, of anti-police movements, and there is a fine line between addressing police brutality and being anti-police,” Mr. Kettering said, noting that the aforementioned issues have all contributed to the ongoing struggles his fellow officers are experiencing.
“It’s not a thing for cops to talk about how an event affected them,” he said. “A lot of officers have just shut down. People have careers and pensions to protect, and every time we stop a motorist, something could go wrong, even if we do everything right. There are mixed signals: They tell us, ‘Defend but don’t defend.’”
His colleague, Mr. Davis, said that officers “need more support from politicians,” noting that he felt particularly insulted by a comment made by a Montgomery County public official who accused the officers present at the Capitol of racism. “And finally, we feel a little betrayed by the public.”
More questions than answers from the Capitol’s day of chaos
What about the events of Jan. 6 led to the suicides of four law enforcement officers and what can be done to prevent more deaths in the future? There are the individual factors of each man’s personal history, circumstances, and vulnerabilities, including the sense of being personally endangered, witnessing trauma, and direct injury – one officer who died of suicide had sustained a head injury that day.
We don’t know if the officers went into the event with preexisting mental illness or addiction or if the day’s events precipitated psychiatric episodes. And with all the partisan anger surrounding the presidential election, we don’t know if each officer’s political beliefs amplified his distress over what occurred in a social media climate where police are being faulted by all sides.
When multiple suicides occur in a community, there is always concern about a “copycat” phenomena. These concerns are made more difficult to address, however, given the police culture of taboo and stigma associated with getting professional help, difficulty accessing care, and career repercussions for speaking openly about suicidal thoughts and mental health issues.
Finally, there is the current political agenda that leaves officers feeling unsupported, fearful of negative outcomes, and unappreciated. The Capitol siege in particular embodied a great deal of national distress and confusion over basic issues of truth, justice, and perceptions of reality in our polarized society.
Can we move to a place where those who enforce laws have easy access to treatment, free from stigma? Can we encourage a culture that does not tolerate brutality or racism, while also refusing to label all police as bad and lending support to their mission? Can we be more attuned to the repercussions of circumstances where officers are witnesses to trauma, are endangered themselves, and would benefit from acknowledgment of their distress?
Time will tell if our anti-police pendulum swings back. In the meantime, these four suicides among people defending our country remain tragically overlooked.
Dinah Miller, MD, is coauthor of Committed: The Battle Over Involuntary Psychiatric Care (Johns Hopkins University Press, 2016). She has a private practice in Baltimore and is an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University. A version of this article first appeared on Medscape.com.
The secret I’ll take to my grave: Doc reveals
An internist will never forget the dark secret his patient revealed during a routine visit – or the grim aftermath.
The patient, who had a progressive, incurable neurological condition, confided that he planned to kill himself. The patient intended to conceal the true manner and make the death look natural.
“[He planned to do it] very carefully at home so no one would know,” said the internist, who remains anonymous. “[He shared] the methods he would use.”
Perhaps more shocking than the patient’s confession was the physician’s response.
“He did not require my help to do what he planned, and I did not try to stop him,” said the internist. “I reported his death as ‘natural causes’ and never told anyone.”
An ob.gyn., for instance, wrote about struggling with whether to tell a father that his newborn baby was not his genetic child. The newborn had a blood type that made it impossible for the father to be biologically related to the infant, the anonymous doctor wrote.
“I told the wife who then informed me she had a lover,” the ob.gyn. said. “I never told the husband.”
It’s uncertain whether carrying the burden of such hidden knowledge affected the physicians involved in these cases. However, in general, secrets can weigh heavily on the minds of those who keep them and can contribute to stress, said Malia Mason, PhD, a psychologist and dean of research at Columbia Business School in New York. Holding onto secrets can cause depression and anxiety, research shows. The more often people think about the secret, the greater the impact, according to a recent study coauthored by Dr. Mason.
“Keeping a secret diminishes well-being,” Dr. Mason said. “It makes people feel socially distant. It lowers relationship satisfaction, and it leads people to feel inauthentic. The reason that secrets do this is because people think about them all the time. The more you think about it, the more you see these consequences.”
Feelings that stem from a secret depend on the content. The more immoral a secret is thought to be, the more people feel ashamed, according to a 2021 analysis of thousands of secrets, reported by Michael L. Slepian, PhD, and Alex Koch, PhD. However, secrets more related to a person’s profession are often internalized differently, the study found. The more a secret fell higher on the profession/goal-oriented dimension, the more people felt they had insight into the secret, according to the analysis. For example, having clear thinking about the secret and/or knowing how to handle it.
“The more shame participants felt from their secret, the more they indicated the secret hurt their well-being,” Dr. Slepian and Dr. Koch wrote in the study. “The more insight participants felt they had into their secret, the less they indicated the secret hurt their well-being.”
Suspicious deaths exposed after investigations
The internist’s account of keeping his patient’s suicide a secret raises many questions, such as how the patient masked his manner of death. The internist did not share any more details about the incident.
Suicides are among the most challenging manners of deaths to certify, according to James Gill, MD, a pathologist and president of the National Association of Medical Examiners. Death investigators must demonstrate intent, meaning the individuals caused the injury to intentionally harm themselves. Fewer than half of people who die by suicide leave a note, Dr. Gill said, so investigators can’t rely on the absence or the presence of a note in making their determination.
A decedent who had cancer or a severe neurological disorder presents further challenges, said Dr. Gill, who serves as chief medical examiner for the state of Connecticut.
“These [deaths] may not be unexpected and may not be reported to the medical examiner/coroner,” Dr. Gill said. “If there is no suspicion and the treating doctor is willing to sign the death certificate, the death will not come under the jurisdiction of the medical examiner.”
Dr. Gill recalled a death his colleague once investigated that appeared to be natural but emerged as something else after a deeper look.
A woman with metastatic breast cancer was about to be discharged from a hospital into hospice the next morning. The night before, she had a “going away” party with friends who came to visit her in the hospital. Shortly after the friends left, the woman was found dead. Because of her condition, she could have died at any time, Dr. Gill said, but she also had a history of depression and hospital staff were suspicious. The death was reported to the medical examiner’s office.
Toxicology testing found markedly elevated concentrations of phenytoin and pentobarbital, neither of which were prescribed during her hospital stay. Dr. Gill said it turned out that the woman and her friends worked at a veterinarian’s office, and the medication they used to euthanize dogs was a combination of phenytoin and pentobarbital.
“The death was certified as a homicide because of the direct actions of another, but a reasonable argument could be made for suicide,” Dr. Gill said.
In a similar case reported in the journal Science & Justice, a 64-year-old cardiologist was found lifeless by his wife after he collapsed near the stairs of his home. Next to his body was a bottle of whiskey and two cups, one that appeared to be used for the alcohol and one with a yellowish liquid smelling of honey. The wife reported that her husband always drank whiskey with honey before bed. The death was initially classified as natural, but after vehement protest by the family, a forensic autopsy was performed.
Prior to the autopsy, death investigators learned the decedent, who was a well-known and successful practitioner in his community, had Parkinson’s disease. At times, he could not sign his prescriptions because of the increasing tremor in his hands, according to the case study. Investigators learned the patient’s mother had also suffered from Parkinson’s, and that her son had witnessed her decline.
The autopsy revealed only nonspecific lesions such as acute stasis of the viscera, moderate pulmonary and cerebral edema, and moderate generalized atheromatosis. Histological examinations did not yield any unusual findings.
An analysis of the beverage containers detected pentobarbital in the yellowish syrup residue of the second cup. Testing of the doctor’s peripheral blood revealed the presence of a metabolite of pentobarbital, ethanol, and traces of phenobarbital. In addition, a urine analysis showed the presence of venlafaxine, an antidepressant, as well as the benzophenone of lorazepam, a sedating benzodiazepine, and metoclopramide, an antiemetic.
Lead author C. Brandt-Casadevall, MD, and colleagues wrote that the levels were clearly compatible with a scenario of a pentobarbital overdose with a lethal outcome.
“... It is obvious that the victim attempted to hide his suicide from his family circle,” Dr. Brandt-Casadevall and colleagues wrote. “Thus, we obtained no evidence indicating that he might have spoken at any point of putting an end to his life. There was no written note. The victim did not wait to be alone at home. Instead, he committed his act in a routine situation: his wife was watching television late at night and he was upstairs, presumably going to sleep. Thus, he had one to two hours at his disposal, and he ingested a very fast-acting drug which would make any attempt at reanimation impossible, even after a brief period of time. This may have induced the physician in charge to believe that the cause of death was cardiac origin, a likely hypothesis given the age of the victim.”
What to do when a terminally ill patient talks suicide
When a terminally ill patient expresses the desire to end his or her life, it’s important to understand that desire is often a result of existential suffering, a sense of hopelessness, and lack of social support, said Lynn A. Jansen, PhD, a bioethicist at the University of Arizona in Tucson.
“The duty of beneficence requires that physicians attempt to provide the support and care that is needed,” said Dr. Jansen. “Here, interdisciplinary teamwork is important and should be utilized. Physicians should refer patients to professionals, such as social workers, pastoral care, psychologists, etc., who are better able to address these issues.”
The rate of desire for a hastened death among terminally ill patients ranges from 17% to 45%, depending on the population studied and how the desire is evaluated, according to an analysis in the Primary Care Companion to the Journal of Clinical Psychiatry. In one study, 14% of about 130 palliative care patients with cancer had a strong desire to quicken the dying process.
In addition, patients with neurologic disorders have a significantly higher suicide rate than that of those without neurologic disorders, a recent JAMA study found. About 1 in 150 patients diagnosed with a neurological disorder dies by suicide, the analysis determined.
A tricky point to remember is that a desire by a terminally ill patient to hasten his or her death by suicide should not be taken by itself to indicate depression, Dr. Jansen noted.
“In principle, such patients can make an autonomous decision to end their lives,” she said. “However, the expression of such a desire is very often associated with depression and forms of suffering that can be effectively addressed by the health care team.”
Physicians can also explore other avenues with the patient such as palliative care or making sure adequate pain relief is available, added Robert Klitzman, MD, professor of psychiatry and academic director of the master of science in bioethics program at Columbia University, New York.
“If they are saying it’s because they are distressed, ethically, a doctor can and should find ways to decrease their distress,” he said.
Of course, those who practice in the U.S. jurisdictions that have physician-assisted-dying laws have different legal and ethical elements to consider. Physicians in these areas have no ethical duty to participate in the process, Dr. Jansen said, but they have a duty to refer patients who express a desire to pursue physician aid-in-dying to another provider who can assist them.
Physician aid-in-dying laws vary somewhat so it’s important that physicians in these areas be aware of their specific statute, Dr. Klitzman said. California, Colorado, Hawaii, Maine, New Jersey, New Mexico, Oregon, Vermont, Washington, and the District of Columbia have these laws.
“In these states, if a terminally ill patient says they don’t want to live anymore, a physician would first decide if this is a result of depression or if it’s a request for physician aid-in-dying,” he said. “Even then, in most cases, the patient would be evaluated by not one, but two different health professionals at two different points. We want to see if it is a consistent decision that the person has made that they want physician aid-in-dying, and not just that they’ve had a bad day or a setback in their treatment.”
In the case of the internist who told no one of his patient’s suicide plan, Dr. Klitzman said he would have dug deeper into the patient’s mindset.
“Not knowing anything about the patient or the doctor, I would have responded differently,” he said. “I think a physician should address why a patient feels that way. They may feel their pain is unbearable, and we potentially offer more pain relief. Maybe the patient shows evidence of having depression, which may be treatable [with medication]. The patient would then feel better and be able to spend quality time with family and loved ones, make sure their affairs are in order, and have a chance to say goodbye.”
A version of this article first appeared on Medscape.com.
An internist will never forget the dark secret his patient revealed during a routine visit – or the grim aftermath.
The patient, who had a progressive, incurable neurological condition, confided that he planned to kill himself. The patient intended to conceal the true manner and make the death look natural.
“[He planned to do it] very carefully at home so no one would know,” said the internist, who remains anonymous. “[He shared] the methods he would use.”
Perhaps more shocking than the patient’s confession was the physician’s response.
“He did not require my help to do what he planned, and I did not try to stop him,” said the internist. “I reported his death as ‘natural causes’ and never told anyone.”
An ob.gyn., for instance, wrote about struggling with whether to tell a father that his newborn baby was not his genetic child. The newborn had a blood type that made it impossible for the father to be biologically related to the infant, the anonymous doctor wrote.
“I told the wife who then informed me she had a lover,” the ob.gyn. said. “I never told the husband.”
It’s uncertain whether carrying the burden of such hidden knowledge affected the physicians involved in these cases. However, in general, secrets can weigh heavily on the minds of those who keep them and can contribute to stress, said Malia Mason, PhD, a psychologist and dean of research at Columbia Business School in New York. Holding onto secrets can cause depression and anxiety, research shows. The more often people think about the secret, the greater the impact, according to a recent study coauthored by Dr. Mason.
“Keeping a secret diminishes well-being,” Dr. Mason said. “It makes people feel socially distant. It lowers relationship satisfaction, and it leads people to feel inauthentic. The reason that secrets do this is because people think about them all the time. The more you think about it, the more you see these consequences.”
Feelings that stem from a secret depend on the content. The more immoral a secret is thought to be, the more people feel ashamed, according to a 2021 analysis of thousands of secrets, reported by Michael L. Slepian, PhD, and Alex Koch, PhD. However, secrets more related to a person’s profession are often internalized differently, the study found. The more a secret fell higher on the profession/goal-oriented dimension, the more people felt they had insight into the secret, according to the analysis. For example, having clear thinking about the secret and/or knowing how to handle it.
“The more shame participants felt from their secret, the more they indicated the secret hurt their well-being,” Dr. Slepian and Dr. Koch wrote in the study. “The more insight participants felt they had into their secret, the less they indicated the secret hurt their well-being.”
Suspicious deaths exposed after investigations
The internist’s account of keeping his patient’s suicide a secret raises many questions, such as how the patient masked his manner of death. The internist did not share any more details about the incident.
Suicides are among the most challenging manners of deaths to certify, according to James Gill, MD, a pathologist and president of the National Association of Medical Examiners. Death investigators must demonstrate intent, meaning the individuals caused the injury to intentionally harm themselves. Fewer than half of people who die by suicide leave a note, Dr. Gill said, so investigators can’t rely on the absence or the presence of a note in making their determination.
A decedent who had cancer or a severe neurological disorder presents further challenges, said Dr. Gill, who serves as chief medical examiner for the state of Connecticut.
“These [deaths] may not be unexpected and may not be reported to the medical examiner/coroner,” Dr. Gill said. “If there is no suspicion and the treating doctor is willing to sign the death certificate, the death will not come under the jurisdiction of the medical examiner.”
Dr. Gill recalled a death his colleague once investigated that appeared to be natural but emerged as something else after a deeper look.
A woman with metastatic breast cancer was about to be discharged from a hospital into hospice the next morning. The night before, she had a “going away” party with friends who came to visit her in the hospital. Shortly after the friends left, the woman was found dead. Because of her condition, she could have died at any time, Dr. Gill said, but she also had a history of depression and hospital staff were suspicious. The death was reported to the medical examiner’s office.
Toxicology testing found markedly elevated concentrations of phenytoin and pentobarbital, neither of which were prescribed during her hospital stay. Dr. Gill said it turned out that the woman and her friends worked at a veterinarian’s office, and the medication they used to euthanize dogs was a combination of phenytoin and pentobarbital.
“The death was certified as a homicide because of the direct actions of another, but a reasonable argument could be made for suicide,” Dr. Gill said.
In a similar case reported in the journal Science & Justice, a 64-year-old cardiologist was found lifeless by his wife after he collapsed near the stairs of his home. Next to his body was a bottle of whiskey and two cups, one that appeared to be used for the alcohol and one with a yellowish liquid smelling of honey. The wife reported that her husband always drank whiskey with honey before bed. The death was initially classified as natural, but after vehement protest by the family, a forensic autopsy was performed.
Prior to the autopsy, death investigators learned the decedent, who was a well-known and successful practitioner in his community, had Parkinson’s disease. At times, he could not sign his prescriptions because of the increasing tremor in his hands, according to the case study. Investigators learned the patient’s mother had also suffered from Parkinson’s, and that her son had witnessed her decline.
The autopsy revealed only nonspecific lesions such as acute stasis of the viscera, moderate pulmonary and cerebral edema, and moderate generalized atheromatosis. Histological examinations did not yield any unusual findings.
An analysis of the beverage containers detected pentobarbital in the yellowish syrup residue of the second cup. Testing of the doctor’s peripheral blood revealed the presence of a metabolite of pentobarbital, ethanol, and traces of phenobarbital. In addition, a urine analysis showed the presence of venlafaxine, an antidepressant, as well as the benzophenone of lorazepam, a sedating benzodiazepine, and metoclopramide, an antiemetic.
Lead author C. Brandt-Casadevall, MD, and colleagues wrote that the levels were clearly compatible with a scenario of a pentobarbital overdose with a lethal outcome.
“... It is obvious that the victim attempted to hide his suicide from his family circle,” Dr. Brandt-Casadevall and colleagues wrote. “Thus, we obtained no evidence indicating that he might have spoken at any point of putting an end to his life. There was no written note. The victim did not wait to be alone at home. Instead, he committed his act in a routine situation: his wife was watching television late at night and he was upstairs, presumably going to sleep. Thus, he had one to two hours at his disposal, and he ingested a very fast-acting drug which would make any attempt at reanimation impossible, even after a brief period of time. This may have induced the physician in charge to believe that the cause of death was cardiac origin, a likely hypothesis given the age of the victim.”
What to do when a terminally ill patient talks suicide
When a terminally ill patient expresses the desire to end his or her life, it’s important to understand that desire is often a result of existential suffering, a sense of hopelessness, and lack of social support, said Lynn A. Jansen, PhD, a bioethicist at the University of Arizona in Tucson.
“The duty of beneficence requires that physicians attempt to provide the support and care that is needed,” said Dr. Jansen. “Here, interdisciplinary teamwork is important and should be utilized. Physicians should refer patients to professionals, such as social workers, pastoral care, psychologists, etc., who are better able to address these issues.”
The rate of desire for a hastened death among terminally ill patients ranges from 17% to 45%, depending on the population studied and how the desire is evaluated, according to an analysis in the Primary Care Companion to the Journal of Clinical Psychiatry. In one study, 14% of about 130 palliative care patients with cancer had a strong desire to quicken the dying process.
In addition, patients with neurologic disorders have a significantly higher suicide rate than that of those without neurologic disorders, a recent JAMA study found. About 1 in 150 patients diagnosed with a neurological disorder dies by suicide, the analysis determined.
A tricky point to remember is that a desire by a terminally ill patient to hasten his or her death by suicide should not be taken by itself to indicate depression, Dr. Jansen noted.
“In principle, such patients can make an autonomous decision to end their lives,” she said. “However, the expression of such a desire is very often associated with depression and forms of suffering that can be effectively addressed by the health care team.”
Physicians can also explore other avenues with the patient such as palliative care or making sure adequate pain relief is available, added Robert Klitzman, MD, professor of psychiatry and academic director of the master of science in bioethics program at Columbia University, New York.
“If they are saying it’s because they are distressed, ethically, a doctor can and should find ways to decrease their distress,” he said.
Of course, those who practice in the U.S. jurisdictions that have physician-assisted-dying laws have different legal and ethical elements to consider. Physicians in these areas have no ethical duty to participate in the process, Dr. Jansen said, but they have a duty to refer patients who express a desire to pursue physician aid-in-dying to another provider who can assist them.
Physician aid-in-dying laws vary somewhat so it’s important that physicians in these areas be aware of their specific statute, Dr. Klitzman said. California, Colorado, Hawaii, Maine, New Jersey, New Mexico, Oregon, Vermont, Washington, and the District of Columbia have these laws.
“In these states, if a terminally ill patient says they don’t want to live anymore, a physician would first decide if this is a result of depression or if it’s a request for physician aid-in-dying,” he said. “Even then, in most cases, the patient would be evaluated by not one, but two different health professionals at two different points. We want to see if it is a consistent decision that the person has made that they want physician aid-in-dying, and not just that they’ve had a bad day or a setback in their treatment.”
In the case of the internist who told no one of his patient’s suicide plan, Dr. Klitzman said he would have dug deeper into the patient’s mindset.
“Not knowing anything about the patient or the doctor, I would have responded differently,” he said. “I think a physician should address why a patient feels that way. They may feel their pain is unbearable, and we potentially offer more pain relief. Maybe the patient shows evidence of having depression, which may be treatable [with medication]. The patient would then feel better and be able to spend quality time with family and loved ones, make sure their affairs are in order, and have a chance to say goodbye.”
A version of this article first appeared on Medscape.com.
An internist will never forget the dark secret his patient revealed during a routine visit – or the grim aftermath.
The patient, who had a progressive, incurable neurological condition, confided that he planned to kill himself. The patient intended to conceal the true manner and make the death look natural.
“[He planned to do it] very carefully at home so no one would know,” said the internist, who remains anonymous. “[He shared] the methods he would use.”
Perhaps more shocking than the patient’s confession was the physician’s response.
“He did not require my help to do what he planned, and I did not try to stop him,” said the internist. “I reported his death as ‘natural causes’ and never told anyone.”
An ob.gyn., for instance, wrote about struggling with whether to tell a father that his newborn baby was not his genetic child. The newborn had a blood type that made it impossible for the father to be biologically related to the infant, the anonymous doctor wrote.
“I told the wife who then informed me she had a lover,” the ob.gyn. said. “I never told the husband.”
It’s uncertain whether carrying the burden of such hidden knowledge affected the physicians involved in these cases. However, in general, secrets can weigh heavily on the minds of those who keep them and can contribute to stress, said Malia Mason, PhD, a psychologist and dean of research at Columbia Business School in New York. Holding onto secrets can cause depression and anxiety, research shows. The more often people think about the secret, the greater the impact, according to a recent study coauthored by Dr. Mason.
“Keeping a secret diminishes well-being,” Dr. Mason said. “It makes people feel socially distant. It lowers relationship satisfaction, and it leads people to feel inauthentic. The reason that secrets do this is because people think about them all the time. The more you think about it, the more you see these consequences.”
Feelings that stem from a secret depend on the content. The more immoral a secret is thought to be, the more people feel ashamed, according to a 2021 analysis of thousands of secrets, reported by Michael L. Slepian, PhD, and Alex Koch, PhD. However, secrets more related to a person’s profession are often internalized differently, the study found. The more a secret fell higher on the profession/goal-oriented dimension, the more people felt they had insight into the secret, according to the analysis. For example, having clear thinking about the secret and/or knowing how to handle it.
“The more shame participants felt from their secret, the more they indicated the secret hurt their well-being,” Dr. Slepian and Dr. Koch wrote in the study. “The more insight participants felt they had into their secret, the less they indicated the secret hurt their well-being.”
Suspicious deaths exposed after investigations
The internist’s account of keeping his patient’s suicide a secret raises many questions, such as how the patient masked his manner of death. The internist did not share any more details about the incident.
Suicides are among the most challenging manners of deaths to certify, according to James Gill, MD, a pathologist and president of the National Association of Medical Examiners. Death investigators must demonstrate intent, meaning the individuals caused the injury to intentionally harm themselves. Fewer than half of people who die by suicide leave a note, Dr. Gill said, so investigators can’t rely on the absence or the presence of a note in making their determination.
A decedent who had cancer or a severe neurological disorder presents further challenges, said Dr. Gill, who serves as chief medical examiner for the state of Connecticut.
“These [deaths] may not be unexpected and may not be reported to the medical examiner/coroner,” Dr. Gill said. “If there is no suspicion and the treating doctor is willing to sign the death certificate, the death will not come under the jurisdiction of the medical examiner.”
Dr. Gill recalled a death his colleague once investigated that appeared to be natural but emerged as something else after a deeper look.
A woman with metastatic breast cancer was about to be discharged from a hospital into hospice the next morning. The night before, she had a “going away” party with friends who came to visit her in the hospital. Shortly after the friends left, the woman was found dead. Because of her condition, she could have died at any time, Dr. Gill said, but she also had a history of depression and hospital staff were suspicious. The death was reported to the medical examiner’s office.
Toxicology testing found markedly elevated concentrations of phenytoin and pentobarbital, neither of which were prescribed during her hospital stay. Dr. Gill said it turned out that the woman and her friends worked at a veterinarian’s office, and the medication they used to euthanize dogs was a combination of phenytoin and pentobarbital.
“The death was certified as a homicide because of the direct actions of another, but a reasonable argument could be made for suicide,” Dr. Gill said.
In a similar case reported in the journal Science & Justice, a 64-year-old cardiologist was found lifeless by his wife after he collapsed near the stairs of his home. Next to his body was a bottle of whiskey and two cups, one that appeared to be used for the alcohol and one with a yellowish liquid smelling of honey. The wife reported that her husband always drank whiskey with honey before bed. The death was initially classified as natural, but after vehement protest by the family, a forensic autopsy was performed.
Prior to the autopsy, death investigators learned the decedent, who was a well-known and successful practitioner in his community, had Parkinson’s disease. At times, he could not sign his prescriptions because of the increasing tremor in his hands, according to the case study. Investigators learned the patient’s mother had also suffered from Parkinson’s, and that her son had witnessed her decline.
The autopsy revealed only nonspecific lesions such as acute stasis of the viscera, moderate pulmonary and cerebral edema, and moderate generalized atheromatosis. Histological examinations did not yield any unusual findings.
An analysis of the beverage containers detected pentobarbital in the yellowish syrup residue of the second cup. Testing of the doctor’s peripheral blood revealed the presence of a metabolite of pentobarbital, ethanol, and traces of phenobarbital. In addition, a urine analysis showed the presence of venlafaxine, an antidepressant, as well as the benzophenone of lorazepam, a sedating benzodiazepine, and metoclopramide, an antiemetic.
Lead author C. Brandt-Casadevall, MD, and colleagues wrote that the levels were clearly compatible with a scenario of a pentobarbital overdose with a lethal outcome.
“... It is obvious that the victim attempted to hide his suicide from his family circle,” Dr. Brandt-Casadevall and colleagues wrote. “Thus, we obtained no evidence indicating that he might have spoken at any point of putting an end to his life. There was no written note. The victim did not wait to be alone at home. Instead, he committed his act in a routine situation: his wife was watching television late at night and he was upstairs, presumably going to sleep. Thus, he had one to two hours at his disposal, and he ingested a very fast-acting drug which would make any attempt at reanimation impossible, even after a brief period of time. This may have induced the physician in charge to believe that the cause of death was cardiac origin, a likely hypothesis given the age of the victim.”
What to do when a terminally ill patient talks suicide
When a terminally ill patient expresses the desire to end his or her life, it’s important to understand that desire is often a result of existential suffering, a sense of hopelessness, and lack of social support, said Lynn A. Jansen, PhD, a bioethicist at the University of Arizona in Tucson.
“The duty of beneficence requires that physicians attempt to provide the support and care that is needed,” said Dr. Jansen. “Here, interdisciplinary teamwork is important and should be utilized. Physicians should refer patients to professionals, such as social workers, pastoral care, psychologists, etc., who are better able to address these issues.”
The rate of desire for a hastened death among terminally ill patients ranges from 17% to 45%, depending on the population studied and how the desire is evaluated, according to an analysis in the Primary Care Companion to the Journal of Clinical Psychiatry. In one study, 14% of about 130 palliative care patients with cancer had a strong desire to quicken the dying process.
In addition, patients with neurologic disorders have a significantly higher suicide rate than that of those without neurologic disorders, a recent JAMA study found. About 1 in 150 patients diagnosed with a neurological disorder dies by suicide, the analysis determined.
A tricky point to remember is that a desire by a terminally ill patient to hasten his or her death by suicide should not be taken by itself to indicate depression, Dr. Jansen noted.
“In principle, such patients can make an autonomous decision to end their lives,” she said. “However, the expression of such a desire is very often associated with depression and forms of suffering that can be effectively addressed by the health care team.”
Physicians can also explore other avenues with the patient such as palliative care or making sure adequate pain relief is available, added Robert Klitzman, MD, professor of psychiatry and academic director of the master of science in bioethics program at Columbia University, New York.
“If they are saying it’s because they are distressed, ethically, a doctor can and should find ways to decrease their distress,” he said.
Of course, those who practice in the U.S. jurisdictions that have physician-assisted-dying laws have different legal and ethical elements to consider. Physicians in these areas have no ethical duty to participate in the process, Dr. Jansen said, but they have a duty to refer patients who express a desire to pursue physician aid-in-dying to another provider who can assist them.
Physician aid-in-dying laws vary somewhat so it’s important that physicians in these areas be aware of their specific statute, Dr. Klitzman said. California, Colorado, Hawaii, Maine, New Jersey, New Mexico, Oregon, Vermont, Washington, and the District of Columbia have these laws.
“In these states, if a terminally ill patient says they don’t want to live anymore, a physician would first decide if this is a result of depression or if it’s a request for physician aid-in-dying,” he said. “Even then, in most cases, the patient would be evaluated by not one, but two different health professionals at two different points. We want to see if it is a consistent decision that the person has made that they want physician aid-in-dying, and not just that they’ve had a bad day or a setback in their treatment.”
In the case of the internist who told no one of his patient’s suicide plan, Dr. Klitzman said he would have dug deeper into the patient’s mindset.
“Not knowing anything about the patient or the doctor, I would have responded differently,” he said. “I think a physician should address why a patient feels that way. They may feel their pain is unbearable, and we potentially offer more pain relief. Maybe the patient shows evidence of having depression, which may be treatable [with medication]. The patient would then feel better and be able to spend quality time with family and loved ones, make sure their affairs are in order, and have a chance to say goodbye.”
A version of this article first appeared on Medscape.com.
Human brain patterns may help build a better AI system
new research suggests. “This work opens new opportunities to discover how the network organization of the brain optimizes cognitive capacity,” wrote researchers from The Neuro (Montreal Neurological Institute–Hospital) and the Quebec Artificial Intelligence Institute.
Senior investigator Bratislav Misic, PhD, said the research has potential clinical application for studying diseases of the brain, which is something his team is actively working on. “For example, using MRI techniques, we can measure different patterns of atrophy in neurodegenerative diseases such as Alzheimer’s disease,” he said.
“We can use these disease patterns from real patients to artificially lesion these connectomes and to ask how a particular disease causes a particular pattern of symptoms and cognitive deficits,” he added.
The findings were published online in Nature Machine Intelligence.
Unique approach
Using brain imaging data, the investigators reconstructed a human brain connectivity pattern and applied it to an artificial neural network. After training, the artificial neural network successfully performed a working memory task more flexibly and efficiently than other “benchmark” AI systems.
The researchers noted that their approach is unique because previous work on brain connectivity, also known as connectomics, has focused on describing brain organization without regard to how it actually functions.
Traditional artificial neural network have arbitrary structures that do not reflect how real brain networks are organized. Integrating brain connectomics into the construction of artificial neural network can reveal how the wiring of the brain supports specific cognitive skills, the investigators wrote.
“Up until now, if you look at how neural networks are constructed, the architectures that are used are very ad hoc and very problem specific,” Dr. Misic said. “But the connectomics revolution that’s happened in neuroscience over the past 20 years or so has given us the ability to really measure and trace out connection patterns in a variety of organisms, including the human brain.”
He noted that the researchers took wiring patterns of the real human brain and implemented it as an artificial neural network. They then “trained that network to perform a very simple cognitive task, and when you compare it to other benchmark architectures, it actually does better.”
This shows that there is “something fundamentally different about how the human brain is wired up and that the design principles that we can see in the human brain could be used to potentially build better artificial networks,” Dr. Misic concluded.
Funding for the research was provided by the Canada First Research Excellence Fund, awarded to McGill University for the Healthy Brains, Healthy Lives initiative, and by the Natural Sciences and Engineering Research Council of Canada, Fonds de Recherche du Quebec – Santé, the Canadian Institute for Advanced Research, Canada Research Chairs, Fonds de Recherche du Quebec – Nature et Technologies, and the Centre UNIQUE (Union of Neuroscience and Artificial Intelligence). The investigators have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests. “This work opens new opportunities to discover how the network organization of the brain optimizes cognitive capacity,” wrote researchers from The Neuro (Montreal Neurological Institute–Hospital) and the Quebec Artificial Intelligence Institute.
Senior investigator Bratislav Misic, PhD, said the research has potential clinical application for studying diseases of the brain, which is something his team is actively working on. “For example, using MRI techniques, we can measure different patterns of atrophy in neurodegenerative diseases such as Alzheimer’s disease,” he said.
“We can use these disease patterns from real patients to artificially lesion these connectomes and to ask how a particular disease causes a particular pattern of symptoms and cognitive deficits,” he added.
The findings were published online in Nature Machine Intelligence.
Unique approach
Using brain imaging data, the investigators reconstructed a human brain connectivity pattern and applied it to an artificial neural network. After training, the artificial neural network successfully performed a working memory task more flexibly and efficiently than other “benchmark” AI systems.
The researchers noted that their approach is unique because previous work on brain connectivity, also known as connectomics, has focused on describing brain organization without regard to how it actually functions.
Traditional artificial neural network have arbitrary structures that do not reflect how real brain networks are organized. Integrating brain connectomics into the construction of artificial neural network can reveal how the wiring of the brain supports specific cognitive skills, the investigators wrote.
“Up until now, if you look at how neural networks are constructed, the architectures that are used are very ad hoc and very problem specific,” Dr. Misic said. “But the connectomics revolution that’s happened in neuroscience over the past 20 years or so has given us the ability to really measure and trace out connection patterns in a variety of organisms, including the human brain.”
He noted that the researchers took wiring patterns of the real human brain and implemented it as an artificial neural network. They then “trained that network to perform a very simple cognitive task, and when you compare it to other benchmark architectures, it actually does better.”
This shows that there is “something fundamentally different about how the human brain is wired up and that the design principles that we can see in the human brain could be used to potentially build better artificial networks,” Dr. Misic concluded.
Funding for the research was provided by the Canada First Research Excellence Fund, awarded to McGill University for the Healthy Brains, Healthy Lives initiative, and by the Natural Sciences and Engineering Research Council of Canada, Fonds de Recherche du Quebec – Santé, the Canadian Institute for Advanced Research, Canada Research Chairs, Fonds de Recherche du Quebec – Nature et Technologies, and the Centre UNIQUE (Union of Neuroscience and Artificial Intelligence). The investigators have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests. “This work opens new opportunities to discover how the network organization of the brain optimizes cognitive capacity,” wrote researchers from The Neuro (Montreal Neurological Institute–Hospital) and the Quebec Artificial Intelligence Institute.
Senior investigator Bratislav Misic, PhD, said the research has potential clinical application for studying diseases of the brain, which is something his team is actively working on. “For example, using MRI techniques, we can measure different patterns of atrophy in neurodegenerative diseases such as Alzheimer’s disease,” he said.
“We can use these disease patterns from real patients to artificially lesion these connectomes and to ask how a particular disease causes a particular pattern of symptoms and cognitive deficits,” he added.
The findings were published online in Nature Machine Intelligence.
Unique approach
Using brain imaging data, the investigators reconstructed a human brain connectivity pattern and applied it to an artificial neural network. After training, the artificial neural network successfully performed a working memory task more flexibly and efficiently than other “benchmark” AI systems.
The researchers noted that their approach is unique because previous work on brain connectivity, also known as connectomics, has focused on describing brain organization without regard to how it actually functions.
Traditional artificial neural network have arbitrary structures that do not reflect how real brain networks are organized. Integrating brain connectomics into the construction of artificial neural network can reveal how the wiring of the brain supports specific cognitive skills, the investigators wrote.
“Up until now, if you look at how neural networks are constructed, the architectures that are used are very ad hoc and very problem specific,” Dr. Misic said. “But the connectomics revolution that’s happened in neuroscience over the past 20 years or so has given us the ability to really measure and trace out connection patterns in a variety of organisms, including the human brain.”
He noted that the researchers took wiring patterns of the real human brain and implemented it as an artificial neural network. They then “trained that network to perform a very simple cognitive task, and when you compare it to other benchmark architectures, it actually does better.”
This shows that there is “something fundamentally different about how the human brain is wired up and that the design principles that we can see in the human brain could be used to potentially build better artificial networks,” Dr. Misic concluded.
Funding for the research was provided by the Canada First Research Excellence Fund, awarded to McGill University for the Healthy Brains, Healthy Lives initiative, and by the Natural Sciences and Engineering Research Council of Canada, Fonds de Recherche du Quebec – Santé, the Canadian Institute for Advanced Research, Canada Research Chairs, Fonds de Recherche du Quebec – Nature et Technologies, and the Centre UNIQUE (Union of Neuroscience and Artificial Intelligence). The investigators have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM NATURE MACHINE INTELLIGENCE




