User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
‘Emerging Threat’ Xylazine Use Continues to Spread Across the United States
Illicit use of the veterinary tranquilizer xylazine continues to spread across the United States. The drug, which is increasingly mixed with fentanyl, often fails to respond to the opioid overdose reversal medication naloxone and can cause severe necrotic lesions.
A report released by Millennium Health, a specialty lab that provides medication monitoring for pain management, drug treatment, and behavioral and substance use disorder treatment centers across the country, showed the number of urine specimens collected and tested at the US drug treatment centers were positive for xylazine in the most recent 6 months.
As previously reported by this news organization, in late 2022, the US Food and Drug Administration (FDA) issued a communication alerting clinicians about the special management required for opioid overdoses tainted with xylazine, which is also known as “tranq” or “tranq dope.”
Subsequently, in early 2023, The White House Office of National Drug Control Policy designated xylazine combined with fentanyl as an emerging threat to the United States.
Both the FDA and the Drug Enforcement Administration have taken steps to try to stop trafficking of the combination. However, despite these efforts, xylazine use has continued to spread.
The Millennium Health Signals report showed that the greatest increase in xylazine use was largely in the western United States. In the first 6 months of 2023, 3% of urine drug tests (UDTs) in Washington, Oregon, California, Hawaii, and Alaska were positive for xylazine. From November 2023 to April 2024, this rose to 8%, a 147% increase. In the Mountain West, xylazine-positive UDTs increased from 2% in 2023 to 4% in 2024, an increase of 94%. In addition to growth in the West, the report showed that xylazine use increased by more than 100% in New England — from 14% in 2023 to 28% in 2024.
Nationally, 16% of all urine specimens were positive for xylazine from late 2023 to April 2024, up slightly from 14% from April to October 2023.
Xylazine use was highest in the East and in the mid-Atlantic United States. Still, positivity rates in the mid-Atlantic dropped from 44% to 33%. The states included in that group were New York, Pennsylvania, Delaware, and New Jersey. East North Central states (Ohio, Michigan, Wisconsin, Indiana, and Illinois) also experienced a decline in positive tests from 32% to 30%.
The South Atlantic states, which include Maryland, Virginia, West Virginia, North and South Carolina, Georgia, and Florida, had a 17% increase in positivity — from 22% to 26%.
From April 2023 to April 2024 state-level UDT positivity rates were 40% in Pennsylvania, 37% in New York, and 35% in Ohio. But rates vary by locality. In Clermont and Hamilton counties in Ohio — both in the Cincinnati area — about 70% of specimens were positive for xylazine.
About one third of specimens in Maryland and South Carolina contained xylazine.
“Because xylazine exposure remains a significant challenge in the East and is a growing concern in the West, clinicians across the US need to be prepared to recognize and address the consequences of xylazine use — like diminished responses to naloxone and severe skin wounds that may lead to amputation — among people who use fentanyl,” Millennium Health Chief Clinical Officer Angela Huskey, PharmD, said in a press release.
The Health Signals Alert analyzed more than 50,000 fentanyl-positive UDT specimens collected between April 12, 2023, and April 11, 2024. Millennium Health researchers analyzed xylazine positivity rates in fentanyl-positive UDT specimens by the US Census Division and state.
A version of this article first appeared on Medscape.com.
Illicit use of the veterinary tranquilizer xylazine continues to spread across the United States. The drug, which is increasingly mixed with fentanyl, often fails to respond to the opioid overdose reversal medication naloxone and can cause severe necrotic lesions.
A report released by Millennium Health, a specialty lab that provides medication monitoring for pain management, drug treatment, and behavioral and substance use disorder treatment centers across the country, showed the number of urine specimens collected and tested at the US drug treatment centers were positive for xylazine in the most recent 6 months.
As previously reported by this news organization, in late 2022, the US Food and Drug Administration (FDA) issued a communication alerting clinicians about the special management required for opioid overdoses tainted with xylazine, which is also known as “tranq” or “tranq dope.”
Subsequently, in early 2023, The White House Office of National Drug Control Policy designated xylazine combined with fentanyl as an emerging threat to the United States.
Both the FDA and the Drug Enforcement Administration have taken steps to try to stop trafficking of the combination. However, despite these efforts, xylazine use has continued to spread.
The Millennium Health Signals report showed that the greatest increase in xylazine use was largely in the western United States. In the first 6 months of 2023, 3% of urine drug tests (UDTs) in Washington, Oregon, California, Hawaii, and Alaska were positive for xylazine. From November 2023 to April 2024, this rose to 8%, a 147% increase. In the Mountain West, xylazine-positive UDTs increased from 2% in 2023 to 4% in 2024, an increase of 94%. In addition to growth in the West, the report showed that xylazine use increased by more than 100% in New England — from 14% in 2023 to 28% in 2024.
Nationally, 16% of all urine specimens were positive for xylazine from late 2023 to April 2024, up slightly from 14% from April to October 2023.
Xylazine use was highest in the East and in the mid-Atlantic United States. Still, positivity rates in the mid-Atlantic dropped from 44% to 33%. The states included in that group were New York, Pennsylvania, Delaware, and New Jersey. East North Central states (Ohio, Michigan, Wisconsin, Indiana, and Illinois) also experienced a decline in positive tests from 32% to 30%.
The South Atlantic states, which include Maryland, Virginia, West Virginia, North and South Carolina, Georgia, and Florida, had a 17% increase in positivity — from 22% to 26%.
From April 2023 to April 2024 state-level UDT positivity rates were 40% in Pennsylvania, 37% in New York, and 35% in Ohio. But rates vary by locality. In Clermont and Hamilton counties in Ohio — both in the Cincinnati area — about 70% of specimens were positive for xylazine.
About one third of specimens in Maryland and South Carolina contained xylazine.
“Because xylazine exposure remains a significant challenge in the East and is a growing concern in the West, clinicians across the US need to be prepared to recognize and address the consequences of xylazine use — like diminished responses to naloxone and severe skin wounds that may lead to amputation — among people who use fentanyl,” Millennium Health Chief Clinical Officer Angela Huskey, PharmD, said in a press release.
The Health Signals Alert analyzed more than 50,000 fentanyl-positive UDT specimens collected between April 12, 2023, and April 11, 2024. Millennium Health researchers analyzed xylazine positivity rates in fentanyl-positive UDT specimens by the US Census Division and state.
A version of this article first appeared on Medscape.com.
Illicit use of the veterinary tranquilizer xylazine continues to spread across the United States. The drug, which is increasingly mixed with fentanyl, often fails to respond to the opioid overdose reversal medication naloxone and can cause severe necrotic lesions.
A report released by Millennium Health, a specialty lab that provides medication monitoring for pain management, drug treatment, and behavioral and substance use disorder treatment centers across the country, showed the number of urine specimens collected and tested at the US drug treatment centers were positive for xylazine in the most recent 6 months.
As previously reported by this news organization, in late 2022, the US Food and Drug Administration (FDA) issued a communication alerting clinicians about the special management required for opioid overdoses tainted with xylazine, which is also known as “tranq” or “tranq dope.”
Subsequently, in early 2023, The White House Office of National Drug Control Policy designated xylazine combined with fentanyl as an emerging threat to the United States.
Both the FDA and the Drug Enforcement Administration have taken steps to try to stop trafficking of the combination. However, despite these efforts, xylazine use has continued to spread.
The Millennium Health Signals report showed that the greatest increase in xylazine use was largely in the western United States. In the first 6 months of 2023, 3% of urine drug tests (UDTs) in Washington, Oregon, California, Hawaii, and Alaska were positive for xylazine. From November 2023 to April 2024, this rose to 8%, a 147% increase. In the Mountain West, xylazine-positive UDTs increased from 2% in 2023 to 4% in 2024, an increase of 94%. In addition to growth in the West, the report showed that xylazine use increased by more than 100% in New England — from 14% in 2023 to 28% in 2024.
Nationally, 16% of all urine specimens were positive for xylazine from late 2023 to April 2024, up slightly from 14% from April to October 2023.
Xylazine use was highest in the East and in the mid-Atlantic United States. Still, positivity rates in the mid-Atlantic dropped from 44% to 33%. The states included in that group were New York, Pennsylvania, Delaware, and New Jersey. East North Central states (Ohio, Michigan, Wisconsin, Indiana, and Illinois) also experienced a decline in positive tests from 32% to 30%.
The South Atlantic states, which include Maryland, Virginia, West Virginia, North and South Carolina, Georgia, and Florida, had a 17% increase in positivity — from 22% to 26%.
From April 2023 to April 2024 state-level UDT positivity rates were 40% in Pennsylvania, 37% in New York, and 35% in Ohio. But rates vary by locality. In Clermont and Hamilton counties in Ohio — both in the Cincinnati area — about 70% of specimens were positive for xylazine.
About one third of specimens in Maryland and South Carolina contained xylazine.
“Because xylazine exposure remains a significant challenge in the East and is a growing concern in the West, clinicians across the US need to be prepared to recognize and address the consequences of xylazine use — like diminished responses to naloxone and severe skin wounds that may lead to amputation — among people who use fentanyl,” Millennium Health Chief Clinical Officer Angela Huskey, PharmD, said in a press release.
The Health Signals Alert analyzed more than 50,000 fentanyl-positive UDT specimens collected between April 12, 2023, and April 11, 2024. Millennium Health researchers analyzed xylazine positivity rates in fentanyl-positive UDT specimens by the US Census Division and state.
A version of this article first appeared on Medscape.com.
Revamping Resident Schedules to Reduce Burnout
It’s the difference between running a marathon and taking a leisurely stroll. That’s how recent pediatrics resident Joey Whelihan, MD, compared an 11-hour inpatient hospital day with an 8-hour outpatient shift where residents see patients in a clinic.
With inpatient training, “you are lucky if you have time to cook dinner, go to bed, and get ready for the next day,” said Dr. Whelihan, who recently started his adolescent medicine fellowship at Children’s Hospital of Philadelphia after 3 years of residency there. Some residents have call every fourth day during inpatient rotations, working 24-28 hours at a time. They come in one morning and go home the next, he told this news organization.
“Outpatient blocks give you more time to catch your breath and feel somewhat refreshed and ready to take care of patients.”
Longer stretches of inpatient rotations are not sustainable, Dr. Whelihan added, and residents are likely to become exhausted. Fatigue is a leading cause of burnout, a mental, physical, and emotional challenge that residency programs and national medical organizations have been struggling to address.
In recent years, there has been a movement to reduce the maximum consecutive duration of resident duty hours in residency programs across the country. Fueled by resident health and patient safety concerns, the movement is a shift from the previous 24- to 36-hour call duty schedules.
Improved Call Systems = Better Residents
The connection between burnout, well-being, and work schedules appears regularly in national program standards. “Residents and faculty members are at risk for burnout and depression,” according to the current Accreditation Council for Graduate Medical Education’s standard residency program requirements.
“Programs, in partnership with their sponsoring institutions, have the same responsibility to address well-being as other aspects of resident competence,” the guidelines state. That charge includes “attention to scheduling, work intensity, and work compression that impacts resident well-being.”
In Medscape’s Residents Lifestyle & Happiness Report 2023, a third of residents surveyed rarely or never paid attention to their well-being, which closely mirrors the 31% who rarely or never had time for a social life. Slightly more residents (37%) said their work-life balance was “somewhat worse” or “much worse” than they expected.
“I think everyone has burnout as a resident, regardless of the type of program they are in,” Dr. Whelihan said. He described the experience as when you lack fulfillment and empathy and feel exhausted, callous, and removed from interactions with colleagues and patients.
The American Medical Association’s recently released report on the state of residency well-being in 2023 also found that about 43% of residents and fellows had at least one symptom of burnout, about a 2% increase from 2022.
Efforts to Combat Burnout
One residency program found a way to reduce burnout by changing its block scheduling from 4 inpatient weeks followed by 1 outpatient week (4 + 1) to 4 inpatient call-based weeks and 4 outpatient ambulatory, non-call weeks (4 + 4), according to a survey study published recently in JAMA Network Open. The initiative drew praise from some residents and a med school professor who studies wellness issues.
In the survey of postgraduate year (PGY) 1 and PGY-2 hospitalist and primary care residents from the University of Colorado’s Internal Medicine Residency Program, Aurora, between June 2019 and June 2021, the schedule change resulted in improved burnout scores and self-reported professional, educational, and health benefits.
As part of the survey, residents rated symptoms on a 7-point scale on the basis of how frequently they experienced emotional exhaustion, depersonalization, and personal accomplishment.
Investigators also used a questionnaire to evaluate how participants perceived the rotation structure with various outcomes, including the ability to acquire clinical skills, access educational and scholarly opportunities, job satisfaction, and health.
The study concluded that the schedule change improved burnout, health, wellness, and professional development without weakening residents perceived clinical skills or standardized exam scores.
Still, the study authors acknowledged that several factors, including the pandemic, may have limited the findings. During that time, the study transitioned from in-person to electronic submissions, resulting in reduced response rates because of changes in staffing needs and fewer research and scholarly activities.
“One of the things we worried about was that the pandemic would make [burnout findings] look worse,” said lead author Dan Heppe, MD, a hospitalist and associate director of the CU Internal Medicine Residency Program. “Anecdotally, residents may have had more support in our program than perhaps some other programs. Though they had long hours with very sick patients, we tried to keep going in a positive direction.”
Dr. Heppe said in an interview that the purpose of the schedule change was to space out more intense rotations and build in more time for research, leadership, teaching, and professional development. He suggested the new schedule could help with other aspects of residents’ careers, exposing them to alternate avenues earlier in their training and in a more structured way.
Like most of the study authors, Dr. Heppe is a graduate of the residency program. He recalled how the program changed from multiple inpatient months in a row with clinic half days during those rotations to a 4 + 1 schedule. But the 1 week between inpatient rotations wasn’t enough time to recover or catch up on clinical work, said Dr. Heppe, who is also an associate professor of medicine at CU.
“It was too erratic,” he said of his former residency schedule. “There was a month of research here or there and clinic and then right back to the ICU for a couple of months without a break, and it was less predictable.”
Dr. Heppe said other residency programs have expressed interest in duplicating CU’s schedule change. He admits it may be difficult because of intensive schedule coordination, and some hospitals may not want to reduce clinical services.
The Yale Internal Medicine Traditional Residency Program also recently ended its 28-hour call, during which residents worked 24 hours with an additional 4 hours to transfer the patient to the incoming team. The move was made in response to residents’ requests, saying that the grueling call rotation’s time had come. The reaction has been overwhelmingly positive.
Proponents of alternate scheduling blocks [4 + 4 or 6 + 2] say that they improve residents’ educational experience, patient care, and continuity of care, reduce burnout, and guarantee residents time off.
Advancing Resident Well-Being
“The premise of looking at scheduling in a more intentional way is a sound one in the process of trying to support and advance resident well-being,” said Mark Greenawald, MD, vice chair of academic affairs, well-being, and professional development for the Virginia Tech Carilion School of Medicine’s Department of Family and Community Medicine in Roanoke.
He said it’s up to residency program directors or graduate medical education departments within a specialty to determine whether such scheduling changes fit their requirements for inpatient and outpatient care and training electives. Requirements may limit some scheduling changes, but within the specialty, there’s some flexibility to be creative with rotations. The CU study considered how to create a residency rhythm without stacking inpatient rotations so there’s recovery time.
“Human beings need a break. If residents work 80 hours continually, they will start to experience greater distress, which for many leads to burnout,” he said
Still, the study includes design flaws because it doesn’t explain how call times and hours differ between inpatient and outpatient rotations. “My own [family medicine] program also does outpatient clinics when we have inpatient service. We have half days in the clinic, which ensures better continuity care with the patient.”
Dr. Greenawald has yet to see much research published about the impact of resident schedule changes. By taking an experimental approach, the CU study showed that their particular change positively affected burnout. If the study leads to improvements in rotation schedules or encourages other programs to experiment with their schedules, it will be a step in the right direction.
How Residents Respond
Haidn Foster, MD, a third-year internal medicine resident at Penn State Health Milton S. Hershey Medical Center, Hershey, remembered experiencing burnout as an intern. At that time, he occasionally dealt with poor patient outcomes and sick patients while working long hours with only 1 day off each week. During a particularly challenging rotation, he felt overwhelmed and numb, which was exacerbated if a patient’s condition worsened or they passed away, he said.
His program follows a schedule of 6 weeks of inpatient training and 2 weeks of outpatient rotations (6 + 2). He said that restructuring residents’ schedules may be more effective than commonly used individual wellness modules, referring to the CU study. “The authors tried out a novel systematic way to tackle the epidemic of physician burnout overwhelming people in the medical community.”
Although the study found that schedule changes don’t affect standardized exam scores, Dr. Foster wondered about preceptor ratings, another marker for clinical competency.
He said future studies should attempt to change the structure of medical training delivery by evaluating models that best reduce burnout, are consistent with residents’ career goals, and produce competent physicians. “Burnout plagues our medical system and leads to too many physicians and physicians-in-training leaving the field or taking their lives. I’m not sure this particular mechanism gets us there, but it’s a step, and so that’s very important.”
Like Dr. Foster, Dr. Whelihan follows a 6 + 2 schedule. He said he would have welcomed a schedule that included more outpatient and less inpatient training and can see how changes in scheduling could reduce burnout. “More outpatient time gives you an opportunity to breathe. You get a little more time off working in clinic with less sick people at a slower pace.”
Ally Fuher, MD, said she chose CU’s Internal Medicine Residency Program 4 years ago largely because of its innovative schedule. Now the program’s chief medical resident, she knew the structure would give her more time to pursue other nonclinical interests including research and medical education, meet regularly with mentors, visit family in another state, and attend important life events.
She acknowledged that the alternative would have meant a more irregular schedule with the possibility of working as many as 80 hours a week on back-to-back inpatient rotations with only 1 day off a week, leaving minimal time to plan other activities, let alone rest and recover.
Dr. Fuher said a balanced schedule made her a more well-rounded person excited to engage in her profession. While she hasn’t personally experienced burnout, she realizes a schedule change may not completely solve the issue for others. However, it shows what progress programs can make when they create systemic structural change.
A version of this article first appeared on Medscape.com.
It’s the difference between running a marathon and taking a leisurely stroll. That’s how recent pediatrics resident Joey Whelihan, MD, compared an 11-hour inpatient hospital day with an 8-hour outpatient shift where residents see patients in a clinic.
With inpatient training, “you are lucky if you have time to cook dinner, go to bed, and get ready for the next day,” said Dr. Whelihan, who recently started his adolescent medicine fellowship at Children’s Hospital of Philadelphia after 3 years of residency there. Some residents have call every fourth day during inpatient rotations, working 24-28 hours at a time. They come in one morning and go home the next, he told this news organization.
“Outpatient blocks give you more time to catch your breath and feel somewhat refreshed and ready to take care of patients.”
Longer stretches of inpatient rotations are not sustainable, Dr. Whelihan added, and residents are likely to become exhausted. Fatigue is a leading cause of burnout, a mental, physical, and emotional challenge that residency programs and national medical organizations have been struggling to address.
In recent years, there has been a movement to reduce the maximum consecutive duration of resident duty hours in residency programs across the country. Fueled by resident health and patient safety concerns, the movement is a shift from the previous 24- to 36-hour call duty schedules.
Improved Call Systems = Better Residents
The connection between burnout, well-being, and work schedules appears regularly in national program standards. “Residents and faculty members are at risk for burnout and depression,” according to the current Accreditation Council for Graduate Medical Education’s standard residency program requirements.
“Programs, in partnership with their sponsoring institutions, have the same responsibility to address well-being as other aspects of resident competence,” the guidelines state. That charge includes “attention to scheduling, work intensity, and work compression that impacts resident well-being.”
In Medscape’s Residents Lifestyle & Happiness Report 2023, a third of residents surveyed rarely or never paid attention to their well-being, which closely mirrors the 31% who rarely or never had time for a social life. Slightly more residents (37%) said their work-life balance was “somewhat worse” or “much worse” than they expected.
“I think everyone has burnout as a resident, regardless of the type of program they are in,” Dr. Whelihan said. He described the experience as when you lack fulfillment and empathy and feel exhausted, callous, and removed from interactions with colleagues and patients.
The American Medical Association’s recently released report on the state of residency well-being in 2023 also found that about 43% of residents and fellows had at least one symptom of burnout, about a 2% increase from 2022.
Efforts to Combat Burnout
One residency program found a way to reduce burnout by changing its block scheduling from 4 inpatient weeks followed by 1 outpatient week (4 + 1) to 4 inpatient call-based weeks and 4 outpatient ambulatory, non-call weeks (4 + 4), according to a survey study published recently in JAMA Network Open. The initiative drew praise from some residents and a med school professor who studies wellness issues.
In the survey of postgraduate year (PGY) 1 and PGY-2 hospitalist and primary care residents from the University of Colorado’s Internal Medicine Residency Program, Aurora, between June 2019 and June 2021, the schedule change resulted in improved burnout scores and self-reported professional, educational, and health benefits.
As part of the survey, residents rated symptoms on a 7-point scale on the basis of how frequently they experienced emotional exhaustion, depersonalization, and personal accomplishment.
Investigators also used a questionnaire to evaluate how participants perceived the rotation structure with various outcomes, including the ability to acquire clinical skills, access educational and scholarly opportunities, job satisfaction, and health.
The study concluded that the schedule change improved burnout, health, wellness, and professional development without weakening residents perceived clinical skills or standardized exam scores.
Still, the study authors acknowledged that several factors, including the pandemic, may have limited the findings. During that time, the study transitioned from in-person to electronic submissions, resulting in reduced response rates because of changes in staffing needs and fewer research and scholarly activities.
“One of the things we worried about was that the pandemic would make [burnout findings] look worse,” said lead author Dan Heppe, MD, a hospitalist and associate director of the CU Internal Medicine Residency Program. “Anecdotally, residents may have had more support in our program than perhaps some other programs. Though they had long hours with very sick patients, we tried to keep going in a positive direction.”
Dr. Heppe said in an interview that the purpose of the schedule change was to space out more intense rotations and build in more time for research, leadership, teaching, and professional development. He suggested the new schedule could help with other aspects of residents’ careers, exposing them to alternate avenues earlier in their training and in a more structured way.
Like most of the study authors, Dr. Heppe is a graduate of the residency program. He recalled how the program changed from multiple inpatient months in a row with clinic half days during those rotations to a 4 + 1 schedule. But the 1 week between inpatient rotations wasn’t enough time to recover or catch up on clinical work, said Dr. Heppe, who is also an associate professor of medicine at CU.
“It was too erratic,” he said of his former residency schedule. “There was a month of research here or there and clinic and then right back to the ICU for a couple of months without a break, and it was less predictable.”
Dr. Heppe said other residency programs have expressed interest in duplicating CU’s schedule change. He admits it may be difficult because of intensive schedule coordination, and some hospitals may not want to reduce clinical services.
The Yale Internal Medicine Traditional Residency Program also recently ended its 28-hour call, during which residents worked 24 hours with an additional 4 hours to transfer the patient to the incoming team. The move was made in response to residents’ requests, saying that the grueling call rotation’s time had come. The reaction has been overwhelmingly positive.
Proponents of alternate scheduling blocks [4 + 4 or 6 + 2] say that they improve residents’ educational experience, patient care, and continuity of care, reduce burnout, and guarantee residents time off.
Advancing Resident Well-Being
“The premise of looking at scheduling in a more intentional way is a sound one in the process of trying to support and advance resident well-being,” said Mark Greenawald, MD, vice chair of academic affairs, well-being, and professional development for the Virginia Tech Carilion School of Medicine’s Department of Family and Community Medicine in Roanoke.
He said it’s up to residency program directors or graduate medical education departments within a specialty to determine whether such scheduling changes fit their requirements for inpatient and outpatient care and training electives. Requirements may limit some scheduling changes, but within the specialty, there’s some flexibility to be creative with rotations. The CU study considered how to create a residency rhythm without stacking inpatient rotations so there’s recovery time.
“Human beings need a break. If residents work 80 hours continually, they will start to experience greater distress, which for many leads to burnout,” he said
Still, the study includes design flaws because it doesn’t explain how call times and hours differ between inpatient and outpatient rotations. “My own [family medicine] program also does outpatient clinics when we have inpatient service. We have half days in the clinic, which ensures better continuity care with the patient.”
Dr. Greenawald has yet to see much research published about the impact of resident schedule changes. By taking an experimental approach, the CU study showed that their particular change positively affected burnout. If the study leads to improvements in rotation schedules or encourages other programs to experiment with their schedules, it will be a step in the right direction.
How Residents Respond
Haidn Foster, MD, a third-year internal medicine resident at Penn State Health Milton S. Hershey Medical Center, Hershey, remembered experiencing burnout as an intern. At that time, he occasionally dealt with poor patient outcomes and sick patients while working long hours with only 1 day off each week. During a particularly challenging rotation, he felt overwhelmed and numb, which was exacerbated if a patient’s condition worsened or they passed away, he said.
His program follows a schedule of 6 weeks of inpatient training and 2 weeks of outpatient rotations (6 + 2). He said that restructuring residents’ schedules may be more effective than commonly used individual wellness modules, referring to the CU study. “The authors tried out a novel systematic way to tackle the epidemic of physician burnout overwhelming people in the medical community.”
Although the study found that schedule changes don’t affect standardized exam scores, Dr. Foster wondered about preceptor ratings, another marker for clinical competency.
He said future studies should attempt to change the structure of medical training delivery by evaluating models that best reduce burnout, are consistent with residents’ career goals, and produce competent physicians. “Burnout plagues our medical system and leads to too many physicians and physicians-in-training leaving the field or taking their lives. I’m not sure this particular mechanism gets us there, but it’s a step, and so that’s very important.”
Like Dr. Foster, Dr. Whelihan follows a 6 + 2 schedule. He said he would have welcomed a schedule that included more outpatient and less inpatient training and can see how changes in scheduling could reduce burnout. “More outpatient time gives you an opportunity to breathe. You get a little more time off working in clinic with less sick people at a slower pace.”
Ally Fuher, MD, said she chose CU’s Internal Medicine Residency Program 4 years ago largely because of its innovative schedule. Now the program’s chief medical resident, she knew the structure would give her more time to pursue other nonclinical interests including research and medical education, meet regularly with mentors, visit family in another state, and attend important life events.
She acknowledged that the alternative would have meant a more irregular schedule with the possibility of working as many as 80 hours a week on back-to-back inpatient rotations with only 1 day off a week, leaving minimal time to plan other activities, let alone rest and recover.
Dr. Fuher said a balanced schedule made her a more well-rounded person excited to engage in her profession. While she hasn’t personally experienced burnout, she realizes a schedule change may not completely solve the issue for others. However, it shows what progress programs can make when they create systemic structural change.
A version of this article first appeared on Medscape.com.
It’s the difference between running a marathon and taking a leisurely stroll. That’s how recent pediatrics resident Joey Whelihan, MD, compared an 11-hour inpatient hospital day with an 8-hour outpatient shift where residents see patients in a clinic.
With inpatient training, “you are lucky if you have time to cook dinner, go to bed, and get ready for the next day,” said Dr. Whelihan, who recently started his adolescent medicine fellowship at Children’s Hospital of Philadelphia after 3 years of residency there. Some residents have call every fourth day during inpatient rotations, working 24-28 hours at a time. They come in one morning and go home the next, he told this news organization.
“Outpatient blocks give you more time to catch your breath and feel somewhat refreshed and ready to take care of patients.”
Longer stretches of inpatient rotations are not sustainable, Dr. Whelihan added, and residents are likely to become exhausted. Fatigue is a leading cause of burnout, a mental, physical, and emotional challenge that residency programs and national medical organizations have been struggling to address.
In recent years, there has been a movement to reduce the maximum consecutive duration of resident duty hours in residency programs across the country. Fueled by resident health and patient safety concerns, the movement is a shift from the previous 24- to 36-hour call duty schedules.
Improved Call Systems = Better Residents
The connection between burnout, well-being, and work schedules appears regularly in national program standards. “Residents and faculty members are at risk for burnout and depression,” according to the current Accreditation Council for Graduate Medical Education’s standard residency program requirements.
“Programs, in partnership with their sponsoring institutions, have the same responsibility to address well-being as other aspects of resident competence,” the guidelines state. That charge includes “attention to scheduling, work intensity, and work compression that impacts resident well-being.”
In Medscape’s Residents Lifestyle & Happiness Report 2023, a third of residents surveyed rarely or never paid attention to their well-being, which closely mirrors the 31% who rarely or never had time for a social life. Slightly more residents (37%) said their work-life balance was “somewhat worse” or “much worse” than they expected.
“I think everyone has burnout as a resident, regardless of the type of program they are in,” Dr. Whelihan said. He described the experience as when you lack fulfillment and empathy and feel exhausted, callous, and removed from interactions with colleagues and patients.
The American Medical Association’s recently released report on the state of residency well-being in 2023 also found that about 43% of residents and fellows had at least one symptom of burnout, about a 2% increase from 2022.
Efforts to Combat Burnout
One residency program found a way to reduce burnout by changing its block scheduling from 4 inpatient weeks followed by 1 outpatient week (4 + 1) to 4 inpatient call-based weeks and 4 outpatient ambulatory, non-call weeks (4 + 4), according to a survey study published recently in JAMA Network Open. The initiative drew praise from some residents and a med school professor who studies wellness issues.
In the survey of postgraduate year (PGY) 1 and PGY-2 hospitalist and primary care residents from the University of Colorado’s Internal Medicine Residency Program, Aurora, between June 2019 and June 2021, the schedule change resulted in improved burnout scores and self-reported professional, educational, and health benefits.
As part of the survey, residents rated symptoms on a 7-point scale on the basis of how frequently they experienced emotional exhaustion, depersonalization, and personal accomplishment.
Investigators also used a questionnaire to evaluate how participants perceived the rotation structure with various outcomes, including the ability to acquire clinical skills, access educational and scholarly opportunities, job satisfaction, and health.
The study concluded that the schedule change improved burnout, health, wellness, and professional development without weakening residents perceived clinical skills or standardized exam scores.
Still, the study authors acknowledged that several factors, including the pandemic, may have limited the findings. During that time, the study transitioned from in-person to electronic submissions, resulting in reduced response rates because of changes in staffing needs and fewer research and scholarly activities.
“One of the things we worried about was that the pandemic would make [burnout findings] look worse,” said lead author Dan Heppe, MD, a hospitalist and associate director of the CU Internal Medicine Residency Program. “Anecdotally, residents may have had more support in our program than perhaps some other programs. Though they had long hours with very sick patients, we tried to keep going in a positive direction.”
Dr. Heppe said in an interview that the purpose of the schedule change was to space out more intense rotations and build in more time for research, leadership, teaching, and professional development. He suggested the new schedule could help with other aspects of residents’ careers, exposing them to alternate avenues earlier in their training and in a more structured way.
Like most of the study authors, Dr. Heppe is a graduate of the residency program. He recalled how the program changed from multiple inpatient months in a row with clinic half days during those rotations to a 4 + 1 schedule. But the 1 week between inpatient rotations wasn’t enough time to recover or catch up on clinical work, said Dr. Heppe, who is also an associate professor of medicine at CU.
“It was too erratic,” he said of his former residency schedule. “There was a month of research here or there and clinic and then right back to the ICU for a couple of months without a break, and it was less predictable.”
Dr. Heppe said other residency programs have expressed interest in duplicating CU’s schedule change. He admits it may be difficult because of intensive schedule coordination, and some hospitals may not want to reduce clinical services.
The Yale Internal Medicine Traditional Residency Program also recently ended its 28-hour call, during which residents worked 24 hours with an additional 4 hours to transfer the patient to the incoming team. The move was made in response to residents’ requests, saying that the grueling call rotation’s time had come. The reaction has been overwhelmingly positive.
Proponents of alternate scheduling blocks [4 + 4 or 6 + 2] say that they improve residents’ educational experience, patient care, and continuity of care, reduce burnout, and guarantee residents time off.
Advancing Resident Well-Being
“The premise of looking at scheduling in a more intentional way is a sound one in the process of trying to support and advance resident well-being,” said Mark Greenawald, MD, vice chair of academic affairs, well-being, and professional development for the Virginia Tech Carilion School of Medicine’s Department of Family and Community Medicine in Roanoke.
He said it’s up to residency program directors or graduate medical education departments within a specialty to determine whether such scheduling changes fit their requirements for inpatient and outpatient care and training electives. Requirements may limit some scheduling changes, but within the specialty, there’s some flexibility to be creative with rotations. The CU study considered how to create a residency rhythm without stacking inpatient rotations so there’s recovery time.
“Human beings need a break. If residents work 80 hours continually, they will start to experience greater distress, which for many leads to burnout,” he said
Still, the study includes design flaws because it doesn’t explain how call times and hours differ between inpatient and outpatient rotations. “My own [family medicine] program also does outpatient clinics when we have inpatient service. We have half days in the clinic, which ensures better continuity care with the patient.”
Dr. Greenawald has yet to see much research published about the impact of resident schedule changes. By taking an experimental approach, the CU study showed that their particular change positively affected burnout. If the study leads to improvements in rotation schedules or encourages other programs to experiment with their schedules, it will be a step in the right direction.
How Residents Respond
Haidn Foster, MD, a third-year internal medicine resident at Penn State Health Milton S. Hershey Medical Center, Hershey, remembered experiencing burnout as an intern. At that time, he occasionally dealt with poor patient outcomes and sick patients while working long hours with only 1 day off each week. During a particularly challenging rotation, he felt overwhelmed and numb, which was exacerbated if a patient’s condition worsened or they passed away, he said.
His program follows a schedule of 6 weeks of inpatient training and 2 weeks of outpatient rotations (6 + 2). He said that restructuring residents’ schedules may be more effective than commonly used individual wellness modules, referring to the CU study. “The authors tried out a novel systematic way to tackle the epidemic of physician burnout overwhelming people in the medical community.”
Although the study found that schedule changes don’t affect standardized exam scores, Dr. Foster wondered about preceptor ratings, another marker for clinical competency.
He said future studies should attempt to change the structure of medical training delivery by evaluating models that best reduce burnout, are consistent with residents’ career goals, and produce competent physicians. “Burnout plagues our medical system and leads to too many physicians and physicians-in-training leaving the field or taking their lives. I’m not sure this particular mechanism gets us there, but it’s a step, and so that’s very important.”
Like Dr. Foster, Dr. Whelihan follows a 6 + 2 schedule. He said he would have welcomed a schedule that included more outpatient and less inpatient training and can see how changes in scheduling could reduce burnout. “More outpatient time gives you an opportunity to breathe. You get a little more time off working in clinic with less sick people at a slower pace.”
Ally Fuher, MD, said she chose CU’s Internal Medicine Residency Program 4 years ago largely because of its innovative schedule. Now the program’s chief medical resident, she knew the structure would give her more time to pursue other nonclinical interests including research and medical education, meet regularly with mentors, visit family in another state, and attend important life events.
She acknowledged that the alternative would have meant a more irregular schedule with the possibility of working as many as 80 hours a week on back-to-back inpatient rotations with only 1 day off a week, leaving minimal time to plan other activities, let alone rest and recover.
Dr. Fuher said a balanced schedule made her a more well-rounded person excited to engage in her profession. While she hasn’t personally experienced burnout, she realizes a schedule change may not completely solve the issue for others. However, it shows what progress programs can make when they create systemic structural change.
A version of this article first appeared on Medscape.com.
Study Finds Potential benefits of Spironolactone for Women with HS
TOPLINE:
according to the results of a single-center retrospective study.
METHODOLOGY:
- This retrospective study included 157 women (median age, 36.5 years) with HS who received spironolactone for at least 3 months between 2000 and 2021 at Michigan Medicine outpatient dermatology clinics. The majority of patients were White (59%) or Black (37%) individuals.
- The median prescribed dose was 100 mg/d, the most common dose was 50-100 mg/d, and the median time spironolactone was initiated was 8.8 years after HS was diagnosed.
- Improvement status was classified on the basis of objective clinician assessments, including documented reductions in the lesion count, pain, and symptoms.
TAKEAWAY:
- Overall, 31 patients (20%) showed improvements with spironolactone treatment.
- A shorter duration between the diagnosis of HS and the initiation of spironolactone was associated with improvement (P = .047).
- Axillary involvement (P = .003), the use of intralesional steroids (P = .015), previous treatments (P = .023), and previous treatment failures (P = .030) were linked to a lack of improvement with spironolactone.
- Patients with Hurley stage III were 85% less likely to experience improvement with spironolactone (P = .036).
IN PRACTICE:
Spironolactone, which has antiandrogenic properties, “may be beneficial for patients with mild HS, notably those at Hurley stage I if implemented early as a primary or ancillary treatment,” the authors concluded, adding that prospective, multicenter studies are needed to “elucidate further the safety and efficacy of spironolactone for treating HS.”
SOURCE:
The study was led by Suma V. Gangidi, BS, Carle Illinois College of Medicine, University of Illinois Urbana-Champaign, and was published online in the International Journal of Women’s Dermatology.
LIMITATIONS:
Retrospective design can introduce inherent biases, including the potential for missing or misclassified data. Additionally, the study was conducted at a single center, which may limit the generalizability, and findings were also limited by lack of standardized objective measures for assessing treatment improvement, presence of confounding variables from concomitant treatments, small sample size, and potential multicollinearity.
DISCLOSURES:
This study did not receive any funding. One author declared ties with various pharmaceutical companies. The other authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
according to the results of a single-center retrospective study.
METHODOLOGY:
- This retrospective study included 157 women (median age, 36.5 years) with HS who received spironolactone for at least 3 months between 2000 and 2021 at Michigan Medicine outpatient dermatology clinics. The majority of patients were White (59%) or Black (37%) individuals.
- The median prescribed dose was 100 mg/d, the most common dose was 50-100 mg/d, and the median time spironolactone was initiated was 8.8 years after HS was diagnosed.
- Improvement status was classified on the basis of objective clinician assessments, including documented reductions in the lesion count, pain, and symptoms.
TAKEAWAY:
- Overall, 31 patients (20%) showed improvements with spironolactone treatment.
- A shorter duration between the diagnosis of HS and the initiation of spironolactone was associated with improvement (P = .047).
- Axillary involvement (P = .003), the use of intralesional steroids (P = .015), previous treatments (P = .023), and previous treatment failures (P = .030) were linked to a lack of improvement with spironolactone.
- Patients with Hurley stage III were 85% less likely to experience improvement with spironolactone (P = .036).
IN PRACTICE:
Spironolactone, which has antiandrogenic properties, “may be beneficial for patients with mild HS, notably those at Hurley stage I if implemented early as a primary or ancillary treatment,” the authors concluded, adding that prospective, multicenter studies are needed to “elucidate further the safety and efficacy of spironolactone for treating HS.”
SOURCE:
The study was led by Suma V. Gangidi, BS, Carle Illinois College of Medicine, University of Illinois Urbana-Champaign, and was published online in the International Journal of Women’s Dermatology.
LIMITATIONS:
Retrospective design can introduce inherent biases, including the potential for missing or misclassified data. Additionally, the study was conducted at a single center, which may limit the generalizability, and findings were also limited by lack of standardized objective measures for assessing treatment improvement, presence of confounding variables from concomitant treatments, small sample size, and potential multicollinearity.
DISCLOSURES:
This study did not receive any funding. One author declared ties with various pharmaceutical companies. The other authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
according to the results of a single-center retrospective study.
METHODOLOGY:
- This retrospective study included 157 women (median age, 36.5 years) with HS who received spironolactone for at least 3 months between 2000 and 2021 at Michigan Medicine outpatient dermatology clinics. The majority of patients were White (59%) or Black (37%) individuals.
- The median prescribed dose was 100 mg/d, the most common dose was 50-100 mg/d, and the median time spironolactone was initiated was 8.8 years after HS was diagnosed.
- Improvement status was classified on the basis of objective clinician assessments, including documented reductions in the lesion count, pain, and symptoms.
TAKEAWAY:
- Overall, 31 patients (20%) showed improvements with spironolactone treatment.
- A shorter duration between the diagnosis of HS and the initiation of spironolactone was associated with improvement (P = .047).
- Axillary involvement (P = .003), the use of intralesional steroids (P = .015), previous treatments (P = .023), and previous treatment failures (P = .030) were linked to a lack of improvement with spironolactone.
- Patients with Hurley stage III were 85% less likely to experience improvement with spironolactone (P = .036).
IN PRACTICE:
Spironolactone, which has antiandrogenic properties, “may be beneficial for patients with mild HS, notably those at Hurley stage I if implemented early as a primary or ancillary treatment,” the authors concluded, adding that prospective, multicenter studies are needed to “elucidate further the safety and efficacy of spironolactone for treating HS.”
SOURCE:
The study was led by Suma V. Gangidi, BS, Carle Illinois College of Medicine, University of Illinois Urbana-Champaign, and was published online in the International Journal of Women’s Dermatology.
LIMITATIONS:
Retrospective design can introduce inherent biases, including the potential for missing or misclassified data. Additionally, the study was conducted at a single center, which may limit the generalizability, and findings were also limited by lack of standardized objective measures for assessing treatment improvement, presence of confounding variables from concomitant treatments, small sample size, and potential multicollinearity.
DISCLOSURES:
This study did not receive any funding. One author declared ties with various pharmaceutical companies. The other authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Studies Show Dupilumab Effects In Children with Both Atopic Dermatitis and Alopecia
TOPLINE:
(AA) in a review.
METHODOLOGY:
- Researchers conducted a scoping review of seven studies, a result of a MEDLINE and Embase search on March 1, 2024, which included 31 patients aged 4-17 years with both AD and AA (average age, 11.4 years; 64.5% women).
- The review included four case reports, two case series, and one retrospective chart review.
- Patients had an average duration of AA and AD of 3.31 years and 5.33 years, respectively, before starting dupilumab.
- The type of AA was listed in 22 patients; among these patients, alopecia universalis was the most common (50%), followed by alopecia ophiasis (22.7%), patchy alopecia (18.2%), and alopecia totalis (9.09%).
TAKEAWAY:
- Overall, 77.4% of patients in the trials achieved hair regrowth with dupilumab treatment with a mean 42.6 reduction in SALT score (measuring scalp hair loss on a scale of 0-100) over an average of 3.21 months (P < .01).
- Severity of AD was reduced by an average of 2.14 units to an average of 0.857 (clear or almost clear AD; P < .01) on the AD Investigator Global Assessment dropping from an average of 3 (severe disease) before treatment.
- There were no characteristics that significantly distinguished patients with AA who responded to treatment from those who did not.
- Four patients reported worsening of preexisting AA after starting dupilumab; two of these continued dupilumab and showed improvement at subsequent follow-ups.
IN PRACTICE:
“Our review highlights the efficacy of dupilumab in pediatric AA with concurrent AD,” wrote the authors, noting that “the exact mechanism for this efficacy remains speculative.” Although there have been reports of new or worsening AA with dupilumab, they added, its “favorable safety profile in pediatrics enhances its appeal for AA treatment, as monotherapy or in combination with other AA medications.”
SOURCE:
The study was led by Dea Metko, Michael G. DeGroote School of Medicine in Hamilton, Ontario, Canada. It was published online on July 4, 2024, in Pediatric Dermatology.
LIMITATIONS:
Potential publication bias, inconsistent data reporting, the small number of patients, and short follow-up duration were the main limitations of this study.
DISCLOSURES:
The study funding source was not disclosed. One author received honoraria outside this work. Other authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
(AA) in a review.
METHODOLOGY:
- Researchers conducted a scoping review of seven studies, a result of a MEDLINE and Embase search on March 1, 2024, which included 31 patients aged 4-17 years with both AD and AA (average age, 11.4 years; 64.5% women).
- The review included four case reports, two case series, and one retrospective chart review.
- Patients had an average duration of AA and AD of 3.31 years and 5.33 years, respectively, before starting dupilumab.
- The type of AA was listed in 22 patients; among these patients, alopecia universalis was the most common (50%), followed by alopecia ophiasis (22.7%), patchy alopecia (18.2%), and alopecia totalis (9.09%).
TAKEAWAY:
- Overall, 77.4% of patients in the trials achieved hair regrowth with dupilumab treatment with a mean 42.6 reduction in SALT score (measuring scalp hair loss on a scale of 0-100) over an average of 3.21 months (P < .01).
- Severity of AD was reduced by an average of 2.14 units to an average of 0.857 (clear or almost clear AD; P < .01) on the AD Investigator Global Assessment dropping from an average of 3 (severe disease) before treatment.
- There were no characteristics that significantly distinguished patients with AA who responded to treatment from those who did not.
- Four patients reported worsening of preexisting AA after starting dupilumab; two of these continued dupilumab and showed improvement at subsequent follow-ups.
IN PRACTICE:
“Our review highlights the efficacy of dupilumab in pediatric AA with concurrent AD,” wrote the authors, noting that “the exact mechanism for this efficacy remains speculative.” Although there have been reports of new or worsening AA with dupilumab, they added, its “favorable safety profile in pediatrics enhances its appeal for AA treatment, as monotherapy or in combination with other AA medications.”
SOURCE:
The study was led by Dea Metko, Michael G. DeGroote School of Medicine in Hamilton, Ontario, Canada. It was published online on July 4, 2024, in Pediatric Dermatology.
LIMITATIONS:
Potential publication bias, inconsistent data reporting, the small number of patients, and short follow-up duration were the main limitations of this study.
DISCLOSURES:
The study funding source was not disclosed. One author received honoraria outside this work. Other authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
(AA) in a review.
METHODOLOGY:
- Researchers conducted a scoping review of seven studies, a result of a MEDLINE and Embase search on March 1, 2024, which included 31 patients aged 4-17 years with both AD and AA (average age, 11.4 years; 64.5% women).
- The review included four case reports, two case series, and one retrospective chart review.
- Patients had an average duration of AA and AD of 3.31 years and 5.33 years, respectively, before starting dupilumab.
- The type of AA was listed in 22 patients; among these patients, alopecia universalis was the most common (50%), followed by alopecia ophiasis (22.7%), patchy alopecia (18.2%), and alopecia totalis (9.09%).
TAKEAWAY:
- Overall, 77.4% of patients in the trials achieved hair regrowth with dupilumab treatment with a mean 42.6 reduction in SALT score (measuring scalp hair loss on a scale of 0-100) over an average of 3.21 months (P < .01).
- Severity of AD was reduced by an average of 2.14 units to an average of 0.857 (clear or almost clear AD; P < .01) on the AD Investigator Global Assessment dropping from an average of 3 (severe disease) before treatment.
- There were no characteristics that significantly distinguished patients with AA who responded to treatment from those who did not.
- Four patients reported worsening of preexisting AA after starting dupilumab; two of these continued dupilumab and showed improvement at subsequent follow-ups.
IN PRACTICE:
“Our review highlights the efficacy of dupilumab in pediatric AA with concurrent AD,” wrote the authors, noting that “the exact mechanism for this efficacy remains speculative.” Although there have been reports of new or worsening AA with dupilumab, they added, its “favorable safety profile in pediatrics enhances its appeal for AA treatment, as monotherapy or in combination with other AA medications.”
SOURCE:
The study was led by Dea Metko, Michael G. DeGroote School of Medicine in Hamilton, Ontario, Canada. It was published online on July 4, 2024, in Pediatric Dermatology.
LIMITATIONS:
Potential publication bias, inconsistent data reporting, the small number of patients, and short follow-up duration were the main limitations of this study.
DISCLOSURES:
The study funding source was not disclosed. One author received honoraria outside this work. Other authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Study Estimates Global Prevalence of Seborrheic Dermatitis
TOPLINE:
, according to a meta-analysis that also found a higher prevalence in adults than in children.
METHODOLOGY:
- Researchers conducted a meta-analysis of 121 studies, which included 1,260,163 people with clinician-diagnosed seborrheic dermatitis.
- The included studies represented nine countries; most were from India (n = 18), Turkey (n = 13), and the United States (n = 8).
- The primary outcome was the pooled prevalence of seborrheic dermatitis.
TAKEAWAY:
- The overall pooled prevalence of seborrheic dermatitis was 4.38%, 4.08% in clinical settings, and 4.71% in the studies conducted in the general population.
- The prevalence of seborrheic dermatitis was higher among adults (5.64%) than in children (3.7%) and neonates (0.23%).
- A significant variation was observed across countries, with South Africa having the highest prevalence at 8.82%, followed by the United States at 5.86% and Turkey at 3.74%, while India had the lowest prevalence at 2.62%.
IN PRACTICE:
The global prevalence in this meta-analysis was “higher than previous large-scale global estimates, with notable geographic and sociodemographic variability, highlighting the potential impact of environmental factors and cultural practices,” the authors wrote.
SOURCE:
The study was led by Meredith Tyree Polaskey, MS, Chicago Medical School, Rosalind Franklin University of Medicine and Science, North Chicago, Illinois, and was published online on July 3, 2024, in the JAMA Dermatology.
LIMITATIONS:
Interpretation of the findings is limited by research gaps in Central Asia, much of Sub-Saharan Africa, Eastern Europe, Southeast Asia, Latin America (excluding Brazil), and the Caribbean, along with potential underreporting in regions with restricted healthcare access and significant heterogeneity across studies.
DISCLOSURES:
Funding information was not available. One author reported serving as an advisor, consultant, speaker, and/or investigator for multiple pharmaceutical companies, including AbbVie, Amgen, and Pfizer.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
, according to a meta-analysis that also found a higher prevalence in adults than in children.
METHODOLOGY:
- Researchers conducted a meta-analysis of 121 studies, which included 1,260,163 people with clinician-diagnosed seborrheic dermatitis.
- The included studies represented nine countries; most were from India (n = 18), Turkey (n = 13), and the United States (n = 8).
- The primary outcome was the pooled prevalence of seborrheic dermatitis.
TAKEAWAY:
- The overall pooled prevalence of seborrheic dermatitis was 4.38%, 4.08% in clinical settings, and 4.71% in the studies conducted in the general population.
- The prevalence of seborrheic dermatitis was higher among adults (5.64%) than in children (3.7%) and neonates (0.23%).
- A significant variation was observed across countries, with South Africa having the highest prevalence at 8.82%, followed by the United States at 5.86% and Turkey at 3.74%, while India had the lowest prevalence at 2.62%.
IN PRACTICE:
The global prevalence in this meta-analysis was “higher than previous large-scale global estimates, with notable geographic and sociodemographic variability, highlighting the potential impact of environmental factors and cultural practices,” the authors wrote.
SOURCE:
The study was led by Meredith Tyree Polaskey, MS, Chicago Medical School, Rosalind Franklin University of Medicine and Science, North Chicago, Illinois, and was published online on July 3, 2024, in the JAMA Dermatology.
LIMITATIONS:
Interpretation of the findings is limited by research gaps in Central Asia, much of Sub-Saharan Africa, Eastern Europe, Southeast Asia, Latin America (excluding Brazil), and the Caribbean, along with potential underreporting in regions with restricted healthcare access and significant heterogeneity across studies.
DISCLOSURES:
Funding information was not available. One author reported serving as an advisor, consultant, speaker, and/or investigator for multiple pharmaceutical companies, including AbbVie, Amgen, and Pfizer.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
, according to a meta-analysis that also found a higher prevalence in adults than in children.
METHODOLOGY:
- Researchers conducted a meta-analysis of 121 studies, which included 1,260,163 people with clinician-diagnosed seborrheic dermatitis.
- The included studies represented nine countries; most were from India (n = 18), Turkey (n = 13), and the United States (n = 8).
- The primary outcome was the pooled prevalence of seborrheic dermatitis.
TAKEAWAY:
- The overall pooled prevalence of seborrheic dermatitis was 4.38%, 4.08% in clinical settings, and 4.71% in the studies conducted in the general population.
- The prevalence of seborrheic dermatitis was higher among adults (5.64%) than in children (3.7%) and neonates (0.23%).
- A significant variation was observed across countries, with South Africa having the highest prevalence at 8.82%, followed by the United States at 5.86% and Turkey at 3.74%, while India had the lowest prevalence at 2.62%.
IN PRACTICE:
The global prevalence in this meta-analysis was “higher than previous large-scale global estimates, with notable geographic and sociodemographic variability, highlighting the potential impact of environmental factors and cultural practices,” the authors wrote.
SOURCE:
The study was led by Meredith Tyree Polaskey, MS, Chicago Medical School, Rosalind Franklin University of Medicine and Science, North Chicago, Illinois, and was published online on July 3, 2024, in the JAMA Dermatology.
LIMITATIONS:
Interpretation of the findings is limited by research gaps in Central Asia, much of Sub-Saharan Africa, Eastern Europe, Southeast Asia, Latin America (excluding Brazil), and the Caribbean, along with potential underreporting in regions with restricted healthcare access and significant heterogeneity across studies.
DISCLOSURES:
Funding information was not available. One author reported serving as an advisor, consultant, speaker, and/or investigator for multiple pharmaceutical companies, including AbbVie, Amgen, and Pfizer.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
How Common Are Life-Threatening Infections In Infants with Pustules, Vesicles?
TOPLINE:
, according to the findings from a retrospective study.
METHODOLOGY:
- Researchers reviewed the electronic medical records of infants aged ≤ 60 days who received a pediatric dermatology consultation at six US academic institutions between September 2013 and August 2019.
- Among 879 consults, 183 afebrile infants were identified as having presented with pustules, vesicles, and/or bullae.
- Infectious disease workups included blood cultures, urine cultures, lumbar punctures, and HSV testing using viral skin culture, direct immunofluorescence assay, and/or polymerase chain reaction.
- Patients were categorized by gestational age as preterm (< 37 weeks), full-term (37-42 weeks), and post-term (≥ 42 weeks).
- Overall, 67.8% of infants had pustules, 31.1% had vesicles, and 10.4% had bullae.
TAKEAWAY:
- None of the cases showed positive cerebrospinal fluid or pathogenic blood cultures. In 122 of the cases (66.6%), a noninfectious cause was diagnosed, and an infectious cause was diagnosed in 71 cases (38.8%; some patients had more than one diagnosis).
- Of the 127 newborns evaluated for HSV infection, nine (7.1%) tested positive, of whom seven (5.5%) had disease affecting the skin, eye, and mouth and were full- term infants, and two (1.6%) had disseminated HSV and were preterm infants.
- Angioinvasive fungal infection was diagnosed in five infants (2.7%), all of whom were preterm infants (< 28 weeks gestational age).
- The risk for life-threatening disease was higher in preterm infants born before 32 weeks of gestational age (P < .01) compared with those born after 32 weeks.
IN PRACTICE:
“Full-term, well-appearing, afebrile infants ≤ 60 days of age presenting with pustules or vesicles may not require full SBI [serious bacterial infection] work-up, although larger studies are needed,” the authors concluded. Testing for HSV, they added, “is recommended in all infants with vesicles, grouped pustules, or pustules accompanied by punched out or grouped erosions,” and preterm infants “should be assessed for disseminated fungal infection and HSV in the setting of fluid-filled skin lesions.”
SOURCE:
The study was led by Sonora Yun, BA, Columbia University, New York City, and was published online in Pediatrics.
LIMITATIONS:
The data were limited by the sample size and very low incidence of serious infections. Infants probably had atypical or severe presentations that warranted pediatric dermatology consultation, which may have led to overrepresentation of infectious disease rates. The study inclusion was restricted to those who received a dermatology consult; therefore, the findings may not be generalizable to outpatient primary care.
DISCLOSURES:
This study did not receive any external funding. The authors declared that they had no relevant conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
, according to the findings from a retrospective study.
METHODOLOGY:
- Researchers reviewed the electronic medical records of infants aged ≤ 60 days who received a pediatric dermatology consultation at six US academic institutions between September 2013 and August 2019.
- Among 879 consults, 183 afebrile infants were identified as having presented with pustules, vesicles, and/or bullae.
- Infectious disease workups included blood cultures, urine cultures, lumbar punctures, and HSV testing using viral skin culture, direct immunofluorescence assay, and/or polymerase chain reaction.
- Patients were categorized by gestational age as preterm (< 37 weeks), full-term (37-42 weeks), and post-term (≥ 42 weeks).
- Overall, 67.8% of infants had pustules, 31.1% had vesicles, and 10.4% had bullae.
TAKEAWAY:
- None of the cases showed positive cerebrospinal fluid or pathogenic blood cultures. In 122 of the cases (66.6%), a noninfectious cause was diagnosed, and an infectious cause was diagnosed in 71 cases (38.8%; some patients had more than one diagnosis).
- Of the 127 newborns evaluated for HSV infection, nine (7.1%) tested positive, of whom seven (5.5%) had disease affecting the skin, eye, and mouth and were full- term infants, and two (1.6%) had disseminated HSV and were preterm infants.
- Angioinvasive fungal infection was diagnosed in five infants (2.7%), all of whom were preterm infants (< 28 weeks gestational age).
- The risk for life-threatening disease was higher in preterm infants born before 32 weeks of gestational age (P < .01) compared with those born after 32 weeks.
IN PRACTICE:
“Full-term, well-appearing, afebrile infants ≤ 60 days of age presenting with pustules or vesicles may not require full SBI [serious bacterial infection] work-up, although larger studies are needed,” the authors concluded. Testing for HSV, they added, “is recommended in all infants with vesicles, grouped pustules, or pustules accompanied by punched out or grouped erosions,” and preterm infants “should be assessed for disseminated fungal infection and HSV in the setting of fluid-filled skin lesions.”
SOURCE:
The study was led by Sonora Yun, BA, Columbia University, New York City, and was published online in Pediatrics.
LIMITATIONS:
The data were limited by the sample size and very low incidence of serious infections. Infants probably had atypical or severe presentations that warranted pediatric dermatology consultation, which may have led to overrepresentation of infectious disease rates. The study inclusion was restricted to those who received a dermatology consult; therefore, the findings may not be generalizable to outpatient primary care.
DISCLOSURES:
This study did not receive any external funding. The authors declared that they had no relevant conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
, according to the findings from a retrospective study.
METHODOLOGY:
- Researchers reviewed the electronic medical records of infants aged ≤ 60 days who received a pediatric dermatology consultation at six US academic institutions between September 2013 and August 2019.
- Among 879 consults, 183 afebrile infants were identified as having presented with pustules, vesicles, and/or bullae.
- Infectious disease workups included blood cultures, urine cultures, lumbar punctures, and HSV testing using viral skin culture, direct immunofluorescence assay, and/or polymerase chain reaction.
- Patients were categorized by gestational age as preterm (< 37 weeks), full-term (37-42 weeks), and post-term (≥ 42 weeks).
- Overall, 67.8% of infants had pustules, 31.1% had vesicles, and 10.4% had bullae.
TAKEAWAY:
- None of the cases showed positive cerebrospinal fluid or pathogenic blood cultures. In 122 of the cases (66.6%), a noninfectious cause was diagnosed, and an infectious cause was diagnosed in 71 cases (38.8%; some patients had more than one diagnosis).
- Of the 127 newborns evaluated for HSV infection, nine (7.1%) tested positive, of whom seven (5.5%) had disease affecting the skin, eye, and mouth and were full- term infants, and two (1.6%) had disseminated HSV and were preterm infants.
- Angioinvasive fungal infection was diagnosed in five infants (2.7%), all of whom were preterm infants (< 28 weeks gestational age).
- The risk for life-threatening disease was higher in preterm infants born before 32 weeks of gestational age (P < .01) compared with those born after 32 weeks.
IN PRACTICE:
“Full-term, well-appearing, afebrile infants ≤ 60 days of age presenting with pustules or vesicles may not require full SBI [serious bacterial infection] work-up, although larger studies are needed,” the authors concluded. Testing for HSV, they added, “is recommended in all infants with vesicles, grouped pustules, or pustules accompanied by punched out or grouped erosions,” and preterm infants “should be assessed for disseminated fungal infection and HSV in the setting of fluid-filled skin lesions.”
SOURCE:
The study was led by Sonora Yun, BA, Columbia University, New York City, and was published online in Pediatrics.
LIMITATIONS:
The data were limited by the sample size and very low incidence of serious infections. Infants probably had atypical or severe presentations that warranted pediatric dermatology consultation, which may have led to overrepresentation of infectious disease rates. The study inclusion was restricted to those who received a dermatology consult; therefore, the findings may not be generalizable to outpatient primary care.
DISCLOSURES:
This study did not receive any external funding. The authors declared that they had no relevant conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Topical PDE4 Inhibitor Now Approved for Atopic Dermatitis in Children, Adults
On July 9, the aged 6 years or older.
Roflumilast cream 0.15%, which has been developed by Arcutis Biotherapeutics and is marketed under the brand name Zoryve, is a steroid-free topical phosphodiesterase-4 inhibitor that was previously approved in a higher concentration to treat seborrheic dermatitis and plaque psoriasis.
According to a press release from Arcutis, approval for AD was supported by positive results from three phase 3 studies, a phase 2 dose-ranging study, and two phase 1 pharmacokinetic trials. In two identical phase 3 studies known as INTEGUMENT-1 and INTEGUMENT-2, about 40% of children and adults treated with roflumilast cream 0.15% achieved a Validated Investigator Global Assessment for Atopic Dermatitis score of clear (0) or almost clear (1) at week 4 (INTEGUMENT-1: 41.5% vs 25.2%; P < .0001; INTEGUMENT-2: 39% vs 16.9%; P < .0001), with significant improvement as early as week 1 (P < .0001).
Among children and adults who participated in the INTEGUMENT studies for 28 and 56 weeks, 61.3% and 65.7% achieved a 75% reduction in their Eczema Area and Severity Index scores, respectively. According to the company, there were no adverse reactions in the combined phase 3 pivotal trials that occurred in more than 2.9% of participants in either arm. The most common adverse reactions included headache (2.9%), nausea (1.9%), application-site pain (1.5%), diarrhea (1.5%), and vomiting (1.5%).
The product is expected to be available commercially at the end of July 2024, according to Arcutis. Roflumilast cream 0.3% is indicated for topical treatment of plaque psoriasis, including intertriginous areas, in adult and pediatric patients aged 6 years or older; roflumilast foam 0.3% is indicated for the treatment of seborrheic dermatitis in adult and pediatric patients aged 9 years or older.
A version of this article first appeared on Medscape.com.
On July 9, the aged 6 years or older.
Roflumilast cream 0.15%, which has been developed by Arcutis Biotherapeutics and is marketed under the brand name Zoryve, is a steroid-free topical phosphodiesterase-4 inhibitor that was previously approved in a higher concentration to treat seborrheic dermatitis and plaque psoriasis.
According to a press release from Arcutis, approval for AD was supported by positive results from three phase 3 studies, a phase 2 dose-ranging study, and two phase 1 pharmacokinetic trials. In two identical phase 3 studies known as INTEGUMENT-1 and INTEGUMENT-2, about 40% of children and adults treated with roflumilast cream 0.15% achieved a Validated Investigator Global Assessment for Atopic Dermatitis score of clear (0) or almost clear (1) at week 4 (INTEGUMENT-1: 41.5% vs 25.2%; P < .0001; INTEGUMENT-2: 39% vs 16.9%; P < .0001), with significant improvement as early as week 1 (P < .0001).
Among children and adults who participated in the INTEGUMENT studies for 28 and 56 weeks, 61.3% and 65.7% achieved a 75% reduction in their Eczema Area and Severity Index scores, respectively. According to the company, there were no adverse reactions in the combined phase 3 pivotal trials that occurred in more than 2.9% of participants in either arm. The most common adverse reactions included headache (2.9%), nausea (1.9%), application-site pain (1.5%), diarrhea (1.5%), and vomiting (1.5%).
The product is expected to be available commercially at the end of July 2024, according to Arcutis. Roflumilast cream 0.3% is indicated for topical treatment of plaque psoriasis, including intertriginous areas, in adult and pediatric patients aged 6 years or older; roflumilast foam 0.3% is indicated for the treatment of seborrheic dermatitis in adult and pediatric patients aged 9 years or older.
A version of this article first appeared on Medscape.com.
On July 9, the aged 6 years or older.
Roflumilast cream 0.15%, which has been developed by Arcutis Biotherapeutics and is marketed under the brand name Zoryve, is a steroid-free topical phosphodiesterase-4 inhibitor that was previously approved in a higher concentration to treat seborrheic dermatitis and plaque psoriasis.
According to a press release from Arcutis, approval for AD was supported by positive results from three phase 3 studies, a phase 2 dose-ranging study, and two phase 1 pharmacokinetic trials. In two identical phase 3 studies known as INTEGUMENT-1 and INTEGUMENT-2, about 40% of children and adults treated with roflumilast cream 0.15% achieved a Validated Investigator Global Assessment for Atopic Dermatitis score of clear (0) or almost clear (1) at week 4 (INTEGUMENT-1: 41.5% vs 25.2%; P < .0001; INTEGUMENT-2: 39% vs 16.9%; P < .0001), with significant improvement as early as week 1 (P < .0001).
Among children and adults who participated in the INTEGUMENT studies for 28 and 56 weeks, 61.3% and 65.7% achieved a 75% reduction in their Eczema Area and Severity Index scores, respectively. According to the company, there were no adverse reactions in the combined phase 3 pivotal trials that occurred in more than 2.9% of participants in either arm. The most common adverse reactions included headache (2.9%), nausea (1.9%), application-site pain (1.5%), diarrhea (1.5%), and vomiting (1.5%).
The product is expected to be available commercially at the end of July 2024, according to Arcutis. Roflumilast cream 0.3% is indicated for topical treatment of plaque psoriasis, including intertriginous areas, in adult and pediatric patients aged 6 years or older; roflumilast foam 0.3% is indicated for the treatment of seborrheic dermatitis in adult and pediatric patients aged 9 years or older.
A version of this article first appeared on Medscape.com.
Brazilian Peppertree: Watch Out for This Lesser-Known Relative of Poison Ivy
Brazilian peppertree (Schinus terebinthifolia), a member of the Anacardiaceae family, is an internationally invasive plant that causes allergic contact dermatitis (ACD) in susceptible individuals. This noxious weed has settled into the landscape of the southern United States and continues to expand. Its key identifying features include its year-round white flowers as well as a peppery and turpentinelike aroma created by cracking its bright red berries. The ACD associated with contact—primarily with the plant’s sap—stems from known alkenyl phenols, cardol and cardanol. Treatment of Brazilian peppertree–associated ACD parallels that for poison ivy. As this pest increases its range, dermatologists living in endemic areas should familiarize themselves with Brazilian peppertree and its potential for harm.
Brazilian Peppertree Morphology and Geography
Plants in the Anacardiaceae family contribute to more ACD than any other family, and its 80 genera include most of the urushiol-containing plants, such as Toxicodendron (poison ivy, poison oak, poison sumac, Japanese lacquer tree), Anacardium (cashew tree), Mangifera (mango fruit), Semecarpus (India marking nut tree), and Schinus (Brazilian peppertree). Deciduous and evergreen tree members of the Anacardiaceae family grow primarily in tropical and subtropical locations and produce thick resins, 5-petalled flowers, and small fruit known as drupes. The genus name for Brazilian peppertree, Schinus, derives from Latin and Greek words meaning “mastic tree,” a relative of the pistachio tree that the Brazilian peppertree resembles.1 Brazilian peppertree leaves look and smell similar to Pistacia terebinthus (turpentine tree or terebinth), from which the species name terebinthifolia derives.2
Brazilian peppertree originated in South America, particularly Brazil, Paraguay, and Argentina.3 Since the 1840s,4 it has been an invasive weed in the United States, notably in Florida, California, Hawaii, Alabama, Georgia,5 Arizona,6 Nevada,3 and Texas.5,7 The plant also grows throughout the world, including parts of Africa, Asia, Central America, Europe,6 New Zealand,8 Australia, and various islands.9 The plant expertly outcompetes neighboring plants and has prompted control and eradication efforts in many locations.3
Identifying Features and Allergenic Plant Parts
Brazilian peppertree can be either a shrub or tree up to 30 feet tall.4 As an evergreen, it retains its leaves year-round. During fruiting seasons (primarily December through March7), bright red or pink (depending on the variety3) berries appear (Figure 1A) and contribute to its nickname “Florida holly.” Although generally considered an unwelcome guest in Florida, it does display white flowers (Figure 1B) year-round, especially from September to November.9 It characteristically exhibits 3 to 13 leaflets per leaf.10 The leaflets’ ovoid and ridged edges, netlike vasculature, shiny hue, and aroma can help identify the plant (Figure 2A). For decades, the sap of the Brazilian peppertree has been associated with skin irritation (Figure 2B).6 Although the sap of the plant serves as the main culprit of Brazilian peppertree–associated ACD, it appears that other parts of the plant, including the fruit, can cause irritating effects to skin on contact.11,12 The leaves, trunk, and fruit can be harmful to both humans and animals.6 Chemicals from flowers and crushed fruit also can lead to irritating effects in the respiratory tract if aspirated.13


Urushiol, an oily resin present in most plants of the Anacardiaceae family,14 contains many chemicals, including allergenic phenols, catechols, and resorcinols.15 Urushiol-allergic individuals develop dermatitis upon exposure to Brazilian peppertree sap.6 Alkenyl phenols found in Brazilian peppertree lead to the cutaneous manifestations in sensitized patients.11,12 In 1983, Stahl et al11 identified a phenol, cardanol (chemical name 3-pentadecylphenol16) C15:1, in Brazilian peppertree fruit. The group further tested this compound’s effect on skin via patch testing, which showed an allergic response.11 Cashew nut shells (Anacardium occidentale) contain cardanol, anacardic acid (a phenolic acid), and cardol (a phenol with the chemical name 5-pentadecylresorcinol),15,16 though Stahl et al11 were unable to extract these 2 substances (if present) from Brazilian peppertree fruit. When exposed to cardol and anacardic acid, those allergic to poison ivy often develop ACD,15 and these 2 substances are more irritating than cardanol.11 A later study did identify cardol in addition to cardanol in Brazilian peppertree.12
Cutaneous Manifestations
Brazilian peppertree–induced ACD appears similar to other plant-induced ACD with linear streaks of erythema, juicy papules, vesicles, coalescing erythematous plaques, and/or occasional edema and bullae accompanied by intense pruritus.
Treatment
Avoiding contact with Brazilian peppertree is the first line of defense, and treatment for a reaction associated with exposure is similar to that of poison ivy.17 Application of cool compresses, calamine lotion, and topical astringents offer symptom alleviation, and topical steroids (eg, clobetasol propionate 0.05% twice daily) can improve mild localized ACD when given prior to formation of blisters. For more severe and diffuse ACD, oral steroids (eg, prednisone 1 mg/kg/d tapered over 2–3 weeks) likely are necessary, though intramuscular options greatly alleviate discomfort in more severe cases (eg, intramuscular triamcinolone acetonide 1 mg/kg combined with betamethasone 0.1 mg/kg). Physicians should monitor sites for any signs of superimposed bacterial infection and initiate antibiotics as necessary.17
- Zona S. The correct gender of Schinus (Anacardiaceae). Phytotaxa. 2015;222:075-077.
- Terebinth. Encyclopedia.com website. Updated May 17, 2018. Accessed July 9, 2024. https://www.encyclopedia.com/plants-and-animals/plants/plants/terebinth
- Brazilian pepper tree. iNaturalist website. Accessed July 1, 2024. https://www.inaturalist.org/guide_taxa/841531#:~:text=Throughout% 20South%20and%20Central%20America,and%20as%20a%20topical%20antiseptic
- Center for Aquatic and Invasive Plants. Schinus terebinthifolia. Brazilian peppertree. Accessed July 1, 2024. https://plants.ifas.ufl.edu/plant-directory/schinus-terebinthifolia/#:~:text=Species%20Overview&text=People%20sensitive%20to%20poison%20ivy,associated%20with%20its%20bloom%20period
- Brazilian peppertree (Schinus terebinthifolia). Early Detection & Distribution Mapping System. Accessed July 4, 2024. https://www.eddmaps.org/distribution/usstate.cfm?sub=78819
- Morton F. Brazilian pepper: its impact on people, animals, and the environment. Econ Bot. 1978;32:353-359.
- Fire Effects Information System. Schinus terebinthifolius. US Department of Agriculture website. Accessed July 4, 2024. https://www.fs.usda.gov/database/feis/plants/shrub/schter/all.html
- New Zealand Plant Conservation Network. Schinus terebinthifolius. Accessed July 1, 2024. https://www.nzpcn.org.nz/flora/species/schinus-terebinthifolius
- Rojas-Sandoval J, Acevedo-Rodriguez P. Schinus terebinthifolius (Brazilian pepper tree). CABI Compendium. July 23, 2014. Accessed July 1, 2024. https://www.cabidigitallibrary.org/doi/10.1079/cabicompendium.49031
- Patocka J, Diz de Almeida J. Brazilian peppertree: review of pharmacology. Mil Med Sci Lett. 2017;86:32-41.
- Stahl E, Keller K, Blinn C. Cardanol, a skin irritant in pink pepper. Plant Medica. 1983;48:5-9.
- Skopp G, Opferkuch H-J, Schqenker G. n-Alkylphenols from Schinus terebinthifolius Raddi (Anacardiaceae). In German. Zeitschrift für Naturforschung C. 1987;42:1-16. https://doi.org/10.1515/znc-1987-1-203.
- Lloyd HA, Jaouni TM, Evans SL, et al. Terpenes of Schinus terebinthifolius. Phytochemistry. 1977;16:1301-1302.
- Goon ATJ, Goh CL. Plant dermatitis: Asian perspective. Indian J Dermatol. 2011;56:707-710.
- Rozas-Muñoz E, Lepoittevin JP, Pujol RM, et al. Allergic contact dermatitis to plants: understanding the chemistry will help our diagnostic approach. Actas Dermosifiliogr. 2012;103:456-477.
- Caillol S. Cardanol: a promising building block for biobased polymers and additives. Curr Opin Green Sustain Chem. 2018;14: 26-32.
- Prok L, McGovern T. Poison ivy (Toxicodendron) dermatitis. UpToDate. Updated June 21, 2024. Accessed July 7, 2024. https://www.uptodate.com/contents/poison-ivy-toxicodendron-dermatitis#
Brazilian peppertree (Schinus terebinthifolia), a member of the Anacardiaceae family, is an internationally invasive plant that causes allergic contact dermatitis (ACD) in susceptible individuals. This noxious weed has settled into the landscape of the southern United States and continues to expand. Its key identifying features include its year-round white flowers as well as a peppery and turpentinelike aroma created by cracking its bright red berries. The ACD associated with contact—primarily with the plant’s sap—stems from known alkenyl phenols, cardol and cardanol. Treatment of Brazilian peppertree–associated ACD parallels that for poison ivy. As this pest increases its range, dermatologists living in endemic areas should familiarize themselves with Brazilian peppertree and its potential for harm.
Brazilian Peppertree Morphology and Geography
Plants in the Anacardiaceae family contribute to more ACD than any other family, and its 80 genera include most of the urushiol-containing plants, such as Toxicodendron (poison ivy, poison oak, poison sumac, Japanese lacquer tree), Anacardium (cashew tree), Mangifera (mango fruit), Semecarpus (India marking nut tree), and Schinus (Brazilian peppertree). Deciduous and evergreen tree members of the Anacardiaceae family grow primarily in tropical and subtropical locations and produce thick resins, 5-petalled flowers, and small fruit known as drupes. The genus name for Brazilian peppertree, Schinus, derives from Latin and Greek words meaning “mastic tree,” a relative of the pistachio tree that the Brazilian peppertree resembles.1 Brazilian peppertree leaves look and smell similar to Pistacia terebinthus (turpentine tree or terebinth), from which the species name terebinthifolia derives.2
Brazilian peppertree originated in South America, particularly Brazil, Paraguay, and Argentina.3 Since the 1840s,4 it has been an invasive weed in the United States, notably in Florida, California, Hawaii, Alabama, Georgia,5 Arizona,6 Nevada,3 and Texas.5,7 The plant also grows throughout the world, including parts of Africa, Asia, Central America, Europe,6 New Zealand,8 Australia, and various islands.9 The plant expertly outcompetes neighboring plants and has prompted control and eradication efforts in many locations.3
Identifying Features and Allergenic Plant Parts
Brazilian peppertree can be either a shrub or tree up to 30 feet tall.4 As an evergreen, it retains its leaves year-round. During fruiting seasons (primarily December through March7), bright red or pink (depending on the variety3) berries appear (Figure 1A) and contribute to its nickname “Florida holly.” Although generally considered an unwelcome guest in Florida, it does display white flowers (Figure 1B) year-round, especially from September to November.9 It characteristically exhibits 3 to 13 leaflets per leaf.10 The leaflets’ ovoid and ridged edges, netlike vasculature, shiny hue, and aroma can help identify the plant (Figure 2A). For decades, the sap of the Brazilian peppertree has been associated with skin irritation (Figure 2B).6 Although the sap of the plant serves as the main culprit of Brazilian peppertree–associated ACD, it appears that other parts of the plant, including the fruit, can cause irritating effects to skin on contact.11,12 The leaves, trunk, and fruit can be harmful to both humans and animals.6 Chemicals from flowers and crushed fruit also can lead to irritating effects in the respiratory tract if aspirated.13


Urushiol, an oily resin present in most plants of the Anacardiaceae family,14 contains many chemicals, including allergenic phenols, catechols, and resorcinols.15 Urushiol-allergic individuals develop dermatitis upon exposure to Brazilian peppertree sap.6 Alkenyl phenols found in Brazilian peppertree lead to the cutaneous manifestations in sensitized patients.11,12 In 1983, Stahl et al11 identified a phenol, cardanol (chemical name 3-pentadecylphenol16) C15:1, in Brazilian peppertree fruit. The group further tested this compound’s effect on skin via patch testing, which showed an allergic response.11 Cashew nut shells (Anacardium occidentale) contain cardanol, anacardic acid (a phenolic acid), and cardol (a phenol with the chemical name 5-pentadecylresorcinol),15,16 though Stahl et al11 were unable to extract these 2 substances (if present) from Brazilian peppertree fruit. When exposed to cardol and anacardic acid, those allergic to poison ivy often develop ACD,15 and these 2 substances are more irritating than cardanol.11 A later study did identify cardol in addition to cardanol in Brazilian peppertree.12
Cutaneous Manifestations
Brazilian peppertree–induced ACD appears similar to other plant-induced ACD with linear streaks of erythema, juicy papules, vesicles, coalescing erythematous plaques, and/or occasional edema and bullae accompanied by intense pruritus.
Treatment
Avoiding contact with Brazilian peppertree is the first line of defense, and treatment for a reaction associated with exposure is similar to that of poison ivy.17 Application of cool compresses, calamine lotion, and topical astringents offer symptom alleviation, and topical steroids (eg, clobetasol propionate 0.05% twice daily) can improve mild localized ACD when given prior to formation of blisters. For more severe and diffuse ACD, oral steroids (eg, prednisone 1 mg/kg/d tapered over 2–3 weeks) likely are necessary, though intramuscular options greatly alleviate discomfort in more severe cases (eg, intramuscular triamcinolone acetonide 1 mg/kg combined with betamethasone 0.1 mg/kg). Physicians should monitor sites for any signs of superimposed bacterial infection and initiate antibiotics as necessary.17
Brazilian peppertree (Schinus terebinthifolia), a member of the Anacardiaceae family, is an internationally invasive plant that causes allergic contact dermatitis (ACD) in susceptible individuals. This noxious weed has settled into the landscape of the southern United States and continues to expand. Its key identifying features include its year-round white flowers as well as a peppery and turpentinelike aroma created by cracking its bright red berries. The ACD associated with contact—primarily with the plant’s sap—stems from known alkenyl phenols, cardol and cardanol. Treatment of Brazilian peppertree–associated ACD parallels that for poison ivy. As this pest increases its range, dermatologists living in endemic areas should familiarize themselves with Brazilian peppertree and its potential for harm.
Brazilian Peppertree Morphology and Geography
Plants in the Anacardiaceae family contribute to more ACD than any other family, and its 80 genera include most of the urushiol-containing plants, such as Toxicodendron (poison ivy, poison oak, poison sumac, Japanese lacquer tree), Anacardium (cashew tree), Mangifera (mango fruit), Semecarpus (India marking nut tree), and Schinus (Brazilian peppertree). Deciduous and evergreen tree members of the Anacardiaceae family grow primarily in tropical and subtropical locations and produce thick resins, 5-petalled flowers, and small fruit known as drupes. The genus name for Brazilian peppertree, Schinus, derives from Latin and Greek words meaning “mastic tree,” a relative of the pistachio tree that the Brazilian peppertree resembles.1 Brazilian peppertree leaves look and smell similar to Pistacia terebinthus (turpentine tree or terebinth), from which the species name terebinthifolia derives.2
Brazilian peppertree originated in South America, particularly Brazil, Paraguay, and Argentina.3 Since the 1840s,4 it has been an invasive weed in the United States, notably in Florida, California, Hawaii, Alabama, Georgia,5 Arizona,6 Nevada,3 and Texas.5,7 The plant also grows throughout the world, including parts of Africa, Asia, Central America, Europe,6 New Zealand,8 Australia, and various islands.9 The plant expertly outcompetes neighboring plants and has prompted control and eradication efforts in many locations.3
Identifying Features and Allergenic Plant Parts
Brazilian peppertree can be either a shrub or tree up to 30 feet tall.4 As an evergreen, it retains its leaves year-round. During fruiting seasons (primarily December through March7), bright red or pink (depending on the variety3) berries appear (Figure 1A) and contribute to its nickname “Florida holly.” Although generally considered an unwelcome guest in Florida, it does display white flowers (Figure 1B) year-round, especially from September to November.9 It characteristically exhibits 3 to 13 leaflets per leaf.10 The leaflets’ ovoid and ridged edges, netlike vasculature, shiny hue, and aroma can help identify the plant (Figure 2A). For decades, the sap of the Brazilian peppertree has been associated with skin irritation (Figure 2B).6 Although the sap of the plant serves as the main culprit of Brazilian peppertree–associated ACD, it appears that other parts of the plant, including the fruit, can cause irritating effects to skin on contact.11,12 The leaves, trunk, and fruit can be harmful to both humans and animals.6 Chemicals from flowers and crushed fruit also can lead to irritating effects in the respiratory tract if aspirated.13


Urushiol, an oily resin present in most plants of the Anacardiaceae family,14 contains many chemicals, including allergenic phenols, catechols, and resorcinols.15 Urushiol-allergic individuals develop dermatitis upon exposure to Brazilian peppertree sap.6 Alkenyl phenols found in Brazilian peppertree lead to the cutaneous manifestations in sensitized patients.11,12 In 1983, Stahl et al11 identified a phenol, cardanol (chemical name 3-pentadecylphenol16) C15:1, in Brazilian peppertree fruit. The group further tested this compound’s effect on skin via patch testing, which showed an allergic response.11 Cashew nut shells (Anacardium occidentale) contain cardanol, anacardic acid (a phenolic acid), and cardol (a phenol with the chemical name 5-pentadecylresorcinol),15,16 though Stahl et al11 were unable to extract these 2 substances (if present) from Brazilian peppertree fruit. When exposed to cardol and anacardic acid, those allergic to poison ivy often develop ACD,15 and these 2 substances are more irritating than cardanol.11 A later study did identify cardol in addition to cardanol in Brazilian peppertree.12
Cutaneous Manifestations
Brazilian peppertree–induced ACD appears similar to other plant-induced ACD with linear streaks of erythema, juicy papules, vesicles, coalescing erythematous plaques, and/or occasional edema and bullae accompanied by intense pruritus.
Treatment
Avoiding contact with Brazilian peppertree is the first line of defense, and treatment for a reaction associated with exposure is similar to that of poison ivy.17 Application of cool compresses, calamine lotion, and topical astringents offer symptom alleviation, and topical steroids (eg, clobetasol propionate 0.05% twice daily) can improve mild localized ACD when given prior to formation of blisters. For more severe and diffuse ACD, oral steroids (eg, prednisone 1 mg/kg/d tapered over 2–3 weeks) likely are necessary, though intramuscular options greatly alleviate discomfort in more severe cases (eg, intramuscular triamcinolone acetonide 1 mg/kg combined with betamethasone 0.1 mg/kg). Physicians should monitor sites for any signs of superimposed bacterial infection and initiate antibiotics as necessary.17
- Zona S. The correct gender of Schinus (Anacardiaceae). Phytotaxa. 2015;222:075-077.
- Terebinth. Encyclopedia.com website. Updated May 17, 2018. Accessed July 9, 2024. https://www.encyclopedia.com/plants-and-animals/plants/plants/terebinth
- Brazilian pepper tree. iNaturalist website. Accessed July 1, 2024. https://www.inaturalist.org/guide_taxa/841531#:~:text=Throughout% 20South%20and%20Central%20America,and%20as%20a%20topical%20antiseptic
- Center for Aquatic and Invasive Plants. Schinus terebinthifolia. Brazilian peppertree. Accessed July 1, 2024. https://plants.ifas.ufl.edu/plant-directory/schinus-terebinthifolia/#:~:text=Species%20Overview&text=People%20sensitive%20to%20poison%20ivy,associated%20with%20its%20bloom%20period
- Brazilian peppertree (Schinus terebinthifolia). Early Detection & Distribution Mapping System. Accessed July 4, 2024. https://www.eddmaps.org/distribution/usstate.cfm?sub=78819
- Morton F. Brazilian pepper: its impact on people, animals, and the environment. Econ Bot. 1978;32:353-359.
- Fire Effects Information System. Schinus terebinthifolius. US Department of Agriculture website. Accessed July 4, 2024. https://www.fs.usda.gov/database/feis/plants/shrub/schter/all.html
- New Zealand Plant Conservation Network. Schinus terebinthifolius. Accessed July 1, 2024. https://www.nzpcn.org.nz/flora/species/schinus-terebinthifolius
- Rojas-Sandoval J, Acevedo-Rodriguez P. Schinus terebinthifolius (Brazilian pepper tree). CABI Compendium. July 23, 2014. Accessed July 1, 2024. https://www.cabidigitallibrary.org/doi/10.1079/cabicompendium.49031
- Patocka J, Diz de Almeida J. Brazilian peppertree: review of pharmacology. Mil Med Sci Lett. 2017;86:32-41.
- Stahl E, Keller K, Blinn C. Cardanol, a skin irritant in pink pepper. Plant Medica. 1983;48:5-9.
- Skopp G, Opferkuch H-J, Schqenker G. n-Alkylphenols from Schinus terebinthifolius Raddi (Anacardiaceae). In German. Zeitschrift für Naturforschung C. 1987;42:1-16. https://doi.org/10.1515/znc-1987-1-203.
- Lloyd HA, Jaouni TM, Evans SL, et al. Terpenes of Schinus terebinthifolius. Phytochemistry. 1977;16:1301-1302.
- Goon ATJ, Goh CL. Plant dermatitis: Asian perspective. Indian J Dermatol. 2011;56:707-710.
- Rozas-Muñoz E, Lepoittevin JP, Pujol RM, et al. Allergic contact dermatitis to plants: understanding the chemistry will help our diagnostic approach. Actas Dermosifiliogr. 2012;103:456-477.
- Caillol S. Cardanol: a promising building block for biobased polymers and additives. Curr Opin Green Sustain Chem. 2018;14: 26-32.
- Prok L, McGovern T. Poison ivy (Toxicodendron) dermatitis. UpToDate. Updated June 21, 2024. Accessed July 7, 2024. https://www.uptodate.com/contents/poison-ivy-toxicodendron-dermatitis#
- Zona S. The correct gender of Schinus (Anacardiaceae). Phytotaxa. 2015;222:075-077.
- Terebinth. Encyclopedia.com website. Updated May 17, 2018. Accessed July 9, 2024. https://www.encyclopedia.com/plants-and-animals/plants/plants/terebinth
- Brazilian pepper tree. iNaturalist website. Accessed July 1, 2024. https://www.inaturalist.org/guide_taxa/841531#:~:text=Throughout% 20South%20and%20Central%20America,and%20as%20a%20topical%20antiseptic
- Center for Aquatic and Invasive Plants. Schinus terebinthifolia. Brazilian peppertree. Accessed July 1, 2024. https://plants.ifas.ufl.edu/plant-directory/schinus-terebinthifolia/#:~:text=Species%20Overview&text=People%20sensitive%20to%20poison%20ivy,associated%20with%20its%20bloom%20period
- Brazilian peppertree (Schinus terebinthifolia). Early Detection & Distribution Mapping System. Accessed July 4, 2024. https://www.eddmaps.org/distribution/usstate.cfm?sub=78819
- Morton F. Brazilian pepper: its impact on people, animals, and the environment. Econ Bot. 1978;32:353-359.
- Fire Effects Information System. Schinus terebinthifolius. US Department of Agriculture website. Accessed July 4, 2024. https://www.fs.usda.gov/database/feis/plants/shrub/schter/all.html
- New Zealand Plant Conservation Network. Schinus terebinthifolius. Accessed July 1, 2024. https://www.nzpcn.org.nz/flora/species/schinus-terebinthifolius
- Rojas-Sandoval J, Acevedo-Rodriguez P. Schinus terebinthifolius (Brazilian pepper tree). CABI Compendium. July 23, 2014. Accessed July 1, 2024. https://www.cabidigitallibrary.org/doi/10.1079/cabicompendium.49031
- Patocka J, Diz de Almeida J. Brazilian peppertree: review of pharmacology. Mil Med Sci Lett. 2017;86:32-41.
- Stahl E, Keller K, Blinn C. Cardanol, a skin irritant in pink pepper. Plant Medica. 1983;48:5-9.
- Skopp G, Opferkuch H-J, Schqenker G. n-Alkylphenols from Schinus terebinthifolius Raddi (Anacardiaceae). In German. Zeitschrift für Naturforschung C. 1987;42:1-16. https://doi.org/10.1515/znc-1987-1-203.
- Lloyd HA, Jaouni TM, Evans SL, et al. Terpenes of Schinus terebinthifolius. Phytochemistry. 1977;16:1301-1302.
- Goon ATJ, Goh CL. Plant dermatitis: Asian perspective. Indian J Dermatol. 2011;56:707-710.
- Rozas-Muñoz E, Lepoittevin JP, Pujol RM, et al. Allergic contact dermatitis to plants: understanding the chemistry will help our diagnostic approach. Actas Dermosifiliogr. 2012;103:456-477.
- Caillol S. Cardanol: a promising building block for biobased polymers and additives. Curr Opin Green Sustain Chem. 2018;14: 26-32.
- Prok L, McGovern T. Poison ivy (Toxicodendron) dermatitis. UpToDate. Updated June 21, 2024. Accessed July 7, 2024. https://www.uptodate.com/contents/poison-ivy-toxicodendron-dermatitis#
Practice Points
- The Anacardiaceae family contains several plants, including Brazilian peppertree and poison ivy, that have the potential to cause allergic contact dermatitis (ACD).
- Hot spots for Brazilian peppertree include Florida and California, though it also has been reported in Texas, Hawaii, Georgia, Alabama, Arkansas, Nevada, and Arizona.
- Alkenyl phenols (eg, cardol, cardanol) are the key sensitizers found in Brazilian peppertree.
- Treatment consists of supportive care and either topical, oral, or intramuscular steroids depending on the extent and severity of the ACD.
Barriers to Mohs Micrographic Surgery in Japanese Patients With Basal Cell Carcinoma
Margin-controlled surgery for squamous cell carcinoma (SCC) on the lower lip was first performed by Dr. Frederic Mohs on June 30, 1936. Since then, thousands of skin cancer surgeons have refined and adopted the technique. Due to the high cure rate and sparing of normal tissue, Mohs micrographic surgery (MMS) has become the gold standard treatment for facial and special-site nonmelanoma skin cancer worldwide. Mohs micrographic surgery is performed on more than 876,000 tumors annually in the United States.1 Among 3.5 million Americans diagnosed with nonmelanoma skin cancer in 2006, one-quarter were treated with MMS.2 In Japan, basal cell carcinoma (BCC) is the most common skin malignancy, with an incidence of 3.34 cases per 100,000 individuals; SCC is the second most common, with an incidence of 2.5 cases per 100,000 individuals.3
The essential element that makes MMS unique is the careful microscopic examination of the entire margin of the removed specimen. Tissue processing is done with careful en face orientation to ensure that circumferential and deep margins are entirely visible. The surgeon interprets the slides and proceeds to remove the additional tumor as necessary. Because the same physician performs both the surgery and the pathologic assessment throughout the procedure, a precise correlation between the microscopic and surgical findings can be made. The surgeon can begin with smaller margins, removing minimal healthy tissue while removing all the cancer cells, which results in the smallest-possible skin defect and the best prognosis for the malignancy (Figure 1).
At the only facility in Japan offering MMS, the lead author (S.S.) has treated 52 lesions with MMS in 46 patients (2020-2022). Of these patients, 40 were White, 5 were Japanese, and 1 was of African descent. In this case series, we present 5 Japanese patients who had BCC treated with MMS.
Case Series
Patient 1—A 50-year-old Japanese woman presented to dermatology with a brown papule on the nasal tip of 1.25 year’s duration (Figure 2). A biopsy revealed infiltrative BCC (Figure 3), and the patient was referred to the dermatology department at a nearby university hospital. Because the BCC was an aggressive variant, wide local excision (WLE) with subsequent flap reconstruction was recommended as well as radiation therapy. The patient learned about MMS through an internet search and refused both options, seeking MMS treatment at our clinic. Although Japanese health insurance does not cover MMS, the patient had supplemental private insurance that did cover the cost. She provided consent to undergo the procedure. Physical examination revealed a 7.5×6-mm, brown-red macule with ill-defined borders on the tip of the nose. We used a 1.5-mm margin for the first stage of MMS (Figure 4A). The frozen section revealed that the tumor had been entirely excised in the first stage, leaving only a 10.5×9-mm skin defect that was reconstructed with a Dufourmentel flap (Figure 4B). No signs of recurrence were noted at 3.5-year follow-up, and the cosmetic outcome was favorable (Figure 4C). National Comprehensive Cancer Network guidelines recommend a margin greater than 4 mm for infiltrative BCCs4; therefore, our technique reduced the total defect by at least 4 mm in a cosmetically sensitive area. The patient also did not need radiation therapy, which reduced morbidity. She continues to be recurrence free at 3.5-year follow-up.
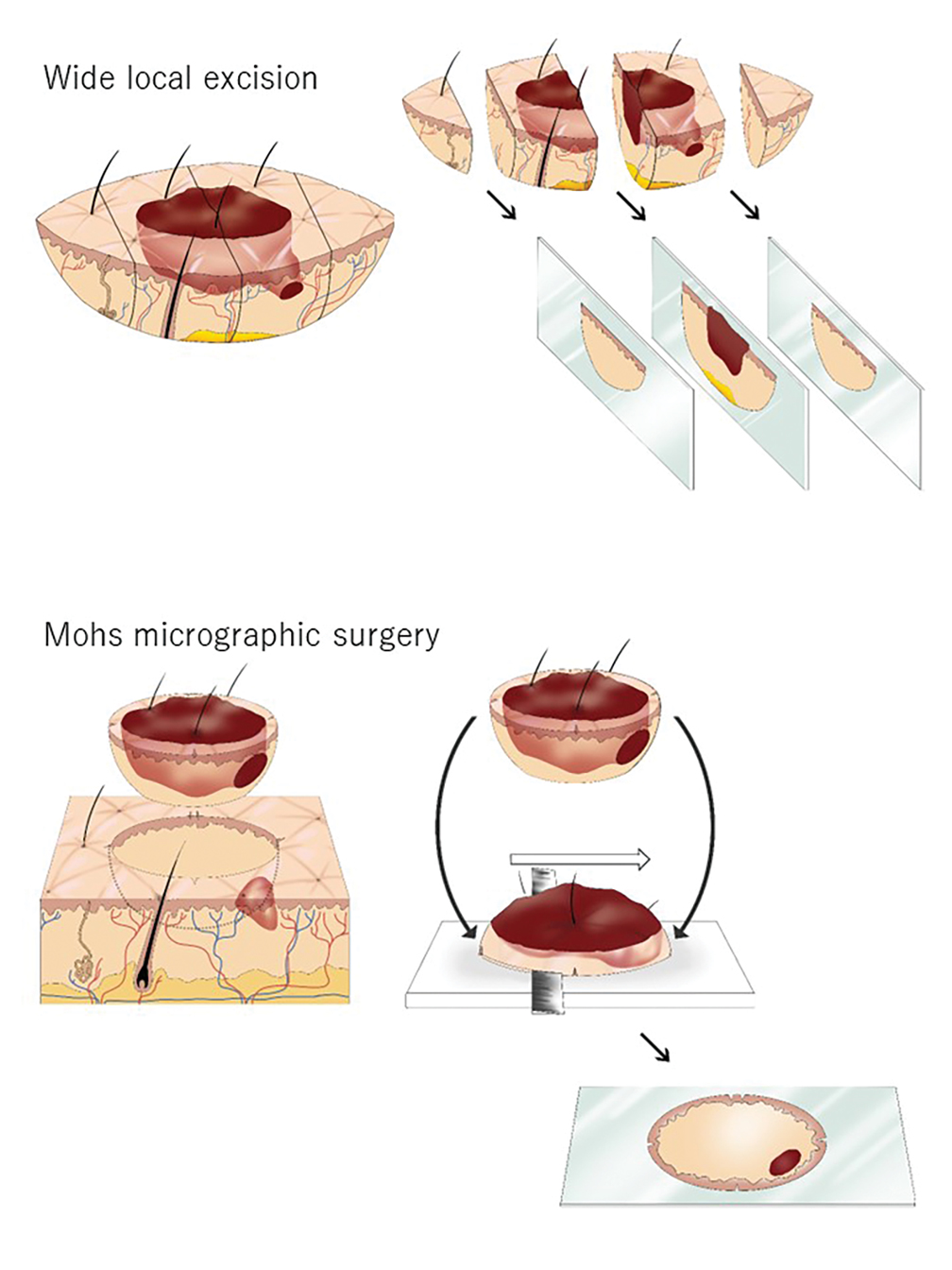

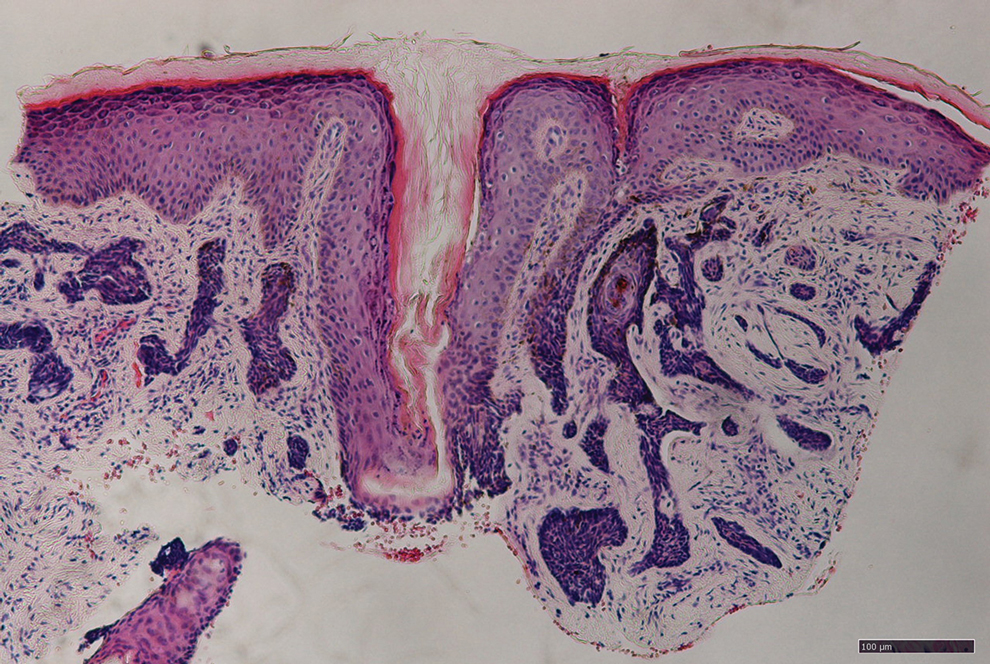
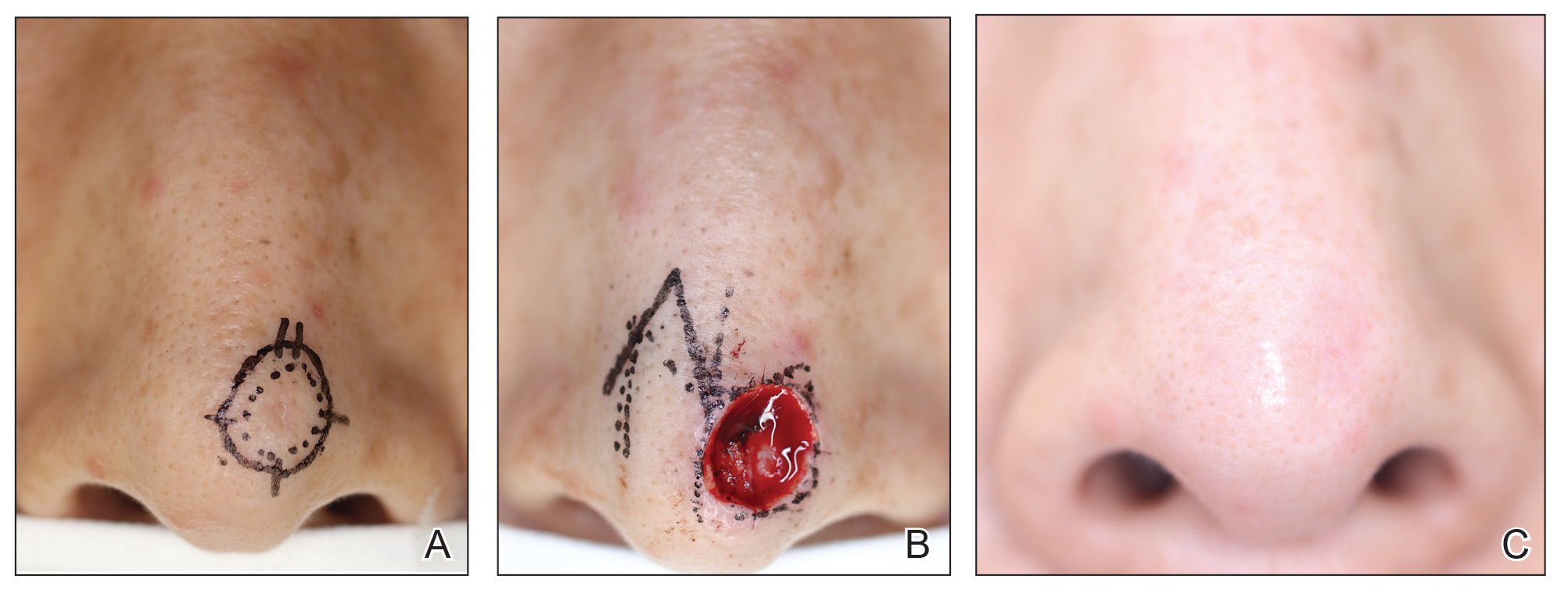
Patient 2—A 63-year-old Japanese man presented to dermatology with a brown macule on the right lower eyelid of 2 years’ duration. A biopsy of the lesion was positive for nodular BCC. After being advised to undergo WLE and extensive reconstruction with plastic surgery, the patient learned of MMS through an internet search and found our clinic. Physical examination revealed a 7×5-mm brown macule on the right lower eyelid. The patient had supplemental private insurance that covered the cost of MMS, and he provided consent for the procedure. A 1.5-mm margin was taken for the first stage, resulting in a 10×8-mm defect superficial to the orbicularis oculi muscle. The frozen section revealed residual tumor exposure in the dermis at the 9- to 10-o’clock position. A second-stage excision was performed to remove an additional 1.5 mm of skin at the 9- to 12-o’clock position with a thin layer of the orbicularis oculi muscle. The subsequent histologic examination revealed no residual BCC, and the final 13×9-mm skin defect was reconstructed with a rotation flap. There were no signs of recurrence at 2.5-year follow-up with an excellent cosmetic outcome.
Patient 3—A 73-year-old Japanese man presented to a local university dermatology clinic with a new papule on the nose. The dermatologist suggested WLE with 4-mm margins and reconstruction of the skin defect 2 weeks later by a plastic surgeon. The patient was not satisfied with the proposed surgical plan, which led him to learn about MMS on the internet; he subsequently found our clinic. Physical examination revealed a 4×3.5-mm brown papule on the tip of the nose. He understood the nature of MMS and chose to pay out-of-pocket because Japanese health insurance did not cover the procedure. We used a 2-mm margin for the first stage, which created a 7.5×7-mm skin defect. The frozen section pathology revealed no residual BCC at the cut surface. The skin defect was reconstructed with a Limberg rhombic flap. There were no signs of recurrence at 1.5-year follow-up with a favorable cosmetic outcome.
Patient 4—A 45-year-old man presented to a dermatology clinic with a papule on the right side of the nose of 1 year’s duration. A biopsy revealed the lesion was a nodular BCC. The dermatologist recommended WLE at a general hospital, but the patient refused after learning about MMS. He subsequently made an appointment with our clinic. Physical examination revealed a 7×4-mm white papule on the right side of the nose. The patient had private insurance that covered the cost of MMS. The first stage was performed with 1.5-mm margins and was clear of residual tumor. A Limberg rhombic flap from the adjacent cheek was used to repair the final 10×7-mm skin defect. There were no signs of recurrence at 1 year and 9 months’ follow-up with a favorable cosmetic outcome.
Patient 5—A 76-year-old Japanese woman presented to a university hospital near Tokyo with a black papule on the left cutaneous lip of 5 years’ duration. A biopsy revealed nodular BCC, and WLE with flap reconstruction was recommended. The patient’s son learned about MMS through internet research and referred her to our clinic. Physical examination revealed a 7×5-mm black papule on the left upper lip. The patient’s private insurance covered the cost of MMS, and she consented to the procedure. We used a 2-mm initial margin, and the immediate frozen section revealed no signs of BCC at the cut surface. The 11×9-mm skin defect was reconstructed with a Limberg rhombic flap. There were no signs of recurrence at 1.5-year follow-up with a favorable cosmetic outcome.
Comment
We presented 5 cases of MMS in Japanese patients with BCC. More than 7000 new cases of nonmelanoma skin cancer occur every year in Japan.3 Only 0.04% of these cases—the 5 cases presented here—were treated with MMS in Japan in 2020 and 2021, in contrast to 25% in the United States in 2006.2
MMS vs Other BCC Treatments—Mohs micrographic surgery offers 2 distinct advantages over conventional excision: an improved cure rate while achieving a smaller final defect size, generally leading to better cosmetic outcomes. Overall 5-year recurrence rates of BCC are 10% for conventional surgical excision vs 1% for MMS, while the recurrence rates for SCC are 8% and 3%, respectively.5 A study of well-demarcated BCCs smaller than 2 cm that were treated with MMS with 2-mm increments revealed that 95% of the cases were free of malignancy within a 4-mm margin of the normal-appearing skin surrounding the tumor.6 Several articles have reported a 95% cure rate or higher with conventional excision of localized BCC,7 but 4- to 5-mm excision margins are required, resulting in a greater skin defect and a lower cure rate compared to MMS.
Aggressive subtypes of BCC have a higher recurrence rate. Rowe et al8 reported the following 5-year recurrence rates: 5.6% for MMS, 17.4% for conventional surgical excision, 40.0% for curettage and electrodesiccation, and 9.8% for radiation therapy. Primary BCCs with high-risk histologic subtypes has a 10-year recurrence rate of 4.4% with MMS vs 12.2% with conventional excision.9 These findings reveal that MMS yields a better prognosis compared to traditional treatment methods for recurrent BCCs and BCCs of high-risk histologic subtypes.
The primary reason for the excellent cure rate seen in MMS is the ability to perform complete margin assessment. Peripheral and deep en face margin assessment (PDEMA) is crucial in achieving high cure rates with narrow margins. In WLE (Figure 1), vertical sectioning (also known as bread-loafing) does not achieve direct visualization of the entire surgical margin, as this technique only evaluates random sections and does not achieve PDEMA.10 The bread-loafing method is used almost exclusively in Japan and visualizes only 0.1% of the entire margin compared to 100% with MMS.11 Beyond the superior cure rate, the MMS technique often yields smaller final defects compared to WLE. All 5 of our patients achieved complete tumor removal while sparing more normal tissue compared to conventional WLE, which takes at least a 4-mm margin in all directions.
Barriers to Adopting MMS in Japan—There are many barriers to the broader adoption of MMS in Japan. A guideline of the Japanese Dermatological Association says, MMS “is complicated, requires special training for acquisition, and requires time and labor for implementation of a series of processes, and it has not gained wide acceptance in Japan because of these disadvantages.”3 There currently are no MMS training programs in Japan. We refute this statement from the Japanese Dermatological Association because, in our experience, only 1 surgeon plus a single histotechnician familiar with MMS is sufficient for a facility to offer the procedure (the lead author of this study [S.S.] acts as both the surgeon and the histotechnician). Another misconception among some physicians in Japan is that cancer on ethnically Japanese skin is uniquely suited to excision without microscopic verification of tumor clearance because the borders of the tumors are easily identified, which was based on good cure rates for the excision of well-demarcated pigmented BCCs in a Japanese cohort. This study of a Japanese cohort investigated the specimens with the conventional bread-loafing technique but not with the PDEMA.12
Eighty percent (4/5) of our patients presented with nodular BCC, and only 1 required a second stage. In comparison, we also treated 16 White patients with nodular BCC with MMS during the same period, and 31% (5/16) required more than 1 stage, with 1 patient requiring 3 stages. This cohort, however, is too small to demonstrate a statistically significant difference (S.S., unpublished data, 2020-2022).
A study in Singapore reported the postsurgical complication rate and 5-year recurrence rate for 481 tumors (92% BCC and 7.5% SCC). The median follow-up duration after MMS was 36 months, and the recurrence rate was 0.6%. The postsurgical complications included 11 (2.3%) cases with superficial tip necrosis of surgical flaps/grafts, 2 (0.4%) with mild wound dehiscence, 1 (0.2%) with minor surgical site bleeding, and 1 (0.2%) with minor wound infection.13 This study supports the notion that MMS is equally effective for Asian patients.
Awareness of MMS in Japan is lacking, and most Japanese dermatologists do not know about the technique. All 5 patients in our case series asked their dermatologists about alternative treatment options and were not offered MMS. In each case, the patients learned of the technique through internet research.
The lack of insurance reimbursement for MMS in Japan is another barrier. Because the national health insurance does not reimburse for MMS, the procedure is relatively unavailable to most Japanese citizens who cannot pay out-of-pocket for the treatment and do not have supplemental insurance. Mohs micrographic surgery may seem expensive compared to WLE followed by repair; however, in the authors’ experience, in Japan, excision without MMS may require general sedation and multiple surgeries to reconstruct larger skin defects, leading to greater morbidity and risk for the patient.
Conclusion
Mohs micrographic surgery in Japan is in its infancy, and further studies showing recurrence rates and long-term prognosis are needed. Such data should help increase awareness of MMS among Japanese physicians as an excellent treatment option for their patients. Furthermore, as Japan becomes more heterogenous as a society and the US Military increases its presence in the region, the need for MMS is likely to increase.
Acknowledgments—We appreciate the proofreading support by Mark Bivens, MBA, MSc (Tokyo, Japan), as well as the technical support from Ben Tallon, MBChB, and Robyn Mason (both in Tauranga, New Zealand) to start MMS at our clinic.
- Asgari MM, Olson J, Alam M. Needs assessment for Mohs micrographic surgery. Dermatol Clin. 2012;30:167-175. doi:10.1016/j.det.2011.08.010
- Connolly SM, Baker DR, Baker DR, et al. AAD/ACMS/ASDSA/ASMS 2012 appropriate use criteria for Mohs micrographic surgery: a report of the American Academy of Dermatology, American College of Mohs Surgery, American Society for Dermatologic Surgery Association, and the American Society for Mohs Surgery. J Am Acad Dermatol. 2012;67:531-550.
- Ansai SI, Umebayashi Y, Katsumata N, et al. Japanese Dermatological Association Guidelines: outlines of guidelines for cutaneous squamous cell carcinoma 2020. J Dermatol. 2021;48:E288-E311.
- Schmults CD, Blitzblau R, Aasi SZ, et at. Basal cell skin cancer, version 2.2024, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2023;21:1181-1203. doi:10.6004/jncn.2023.0056
- Snow SN, Gunkel J. Mohs surgery. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Elsevier; 2017:2445-2455. doi:10.1016/b978-0-070-94171-3.00041-7
- Wolf DJ, Zitelli JA. Surgical margins for basal cell carcinoma. Arch Dermatol. 1987;123:340-344.
- Quazi SJ, Aslam N, Saleem H, et al. Surgical margin of excision in basal cell carcinoma: a systematic review of literature. Cureus. 2020;12:E9211.
- Rowe DE, Carroll RJ, Day Jus CL. Mohs surgery is the treatment of choice for recurrent (previously treated) basal cell carcinoma. J Dermatol Surg Oncol. 1989;15:424-431.
- Van Loo, Mosterd K, Krekels GA. Surgical excision versus Mohs’ micrographic surgery for basal cell carcinoma of the face. Eur J Cancer. 2014;50:3011-3020.
- Schmults CD, Blitzblau R, Aasi SZ, et al. NCCN Guidelines Insights: Squamous Cell Skin Cancer, Version 1.2022. J Natl Compr Canc Netw. 2021;19:1382-1394.
- Hui AM, Jacobson M, Markowitz O, et al. Mohs micrographic surgery for the treatment of melanoma. Dermatol Clin. 2012;30:503-515.
- Ito T, Inatomi Y, Nagae K, et al. Narrow-margin excision is a safe, reliable treatment for well-defined, primary pigmented basal cell carcinoma: an analysis of 288 lesions in Japan. J Eur Acad Dermatol Venereol. 2015;29:1828-1831.
- Ho WYB, Zhao X, Tan WPM. Mohs micrographic surgery in Singapore: a long-term follow-up review. Ann Acad Med Singap. 2021;50:922-923.
Margin-controlled surgery for squamous cell carcinoma (SCC) on the lower lip was first performed by Dr. Frederic Mohs on June 30, 1936. Since then, thousands of skin cancer surgeons have refined and adopted the technique. Due to the high cure rate and sparing of normal tissue, Mohs micrographic surgery (MMS) has become the gold standard treatment for facial and special-site nonmelanoma skin cancer worldwide. Mohs micrographic surgery is performed on more than 876,000 tumors annually in the United States.1 Among 3.5 million Americans diagnosed with nonmelanoma skin cancer in 2006, one-quarter were treated with MMS.2 In Japan, basal cell carcinoma (BCC) is the most common skin malignancy, with an incidence of 3.34 cases per 100,000 individuals; SCC is the second most common, with an incidence of 2.5 cases per 100,000 individuals.3
The essential element that makes MMS unique is the careful microscopic examination of the entire margin of the removed specimen. Tissue processing is done with careful en face orientation to ensure that circumferential and deep margins are entirely visible. The surgeon interprets the slides and proceeds to remove the additional tumor as necessary. Because the same physician performs both the surgery and the pathologic assessment throughout the procedure, a precise correlation between the microscopic and surgical findings can be made. The surgeon can begin with smaller margins, removing minimal healthy tissue while removing all the cancer cells, which results in the smallest-possible skin defect and the best prognosis for the malignancy (Figure 1).
At the only facility in Japan offering MMS, the lead author (S.S.) has treated 52 lesions with MMS in 46 patients (2020-2022). Of these patients, 40 were White, 5 were Japanese, and 1 was of African descent. In this case series, we present 5 Japanese patients who had BCC treated with MMS.
Case Series
Patient 1—A 50-year-old Japanese woman presented to dermatology with a brown papule on the nasal tip of 1.25 year’s duration (Figure 2). A biopsy revealed infiltrative BCC (Figure 3), and the patient was referred to the dermatology department at a nearby university hospital. Because the BCC was an aggressive variant, wide local excision (WLE) with subsequent flap reconstruction was recommended as well as radiation therapy. The patient learned about MMS through an internet search and refused both options, seeking MMS treatment at our clinic. Although Japanese health insurance does not cover MMS, the patient had supplemental private insurance that did cover the cost. She provided consent to undergo the procedure. Physical examination revealed a 7.5×6-mm, brown-red macule with ill-defined borders on the tip of the nose. We used a 1.5-mm margin for the first stage of MMS (Figure 4A). The frozen section revealed that the tumor had been entirely excised in the first stage, leaving only a 10.5×9-mm skin defect that was reconstructed with a Dufourmentel flap (Figure 4B). No signs of recurrence were noted at 3.5-year follow-up, and the cosmetic outcome was favorable (Figure 4C). National Comprehensive Cancer Network guidelines recommend a margin greater than 4 mm for infiltrative BCCs4; therefore, our technique reduced the total defect by at least 4 mm in a cosmetically sensitive area. The patient also did not need radiation therapy, which reduced morbidity. She continues to be recurrence free at 3.5-year follow-up.
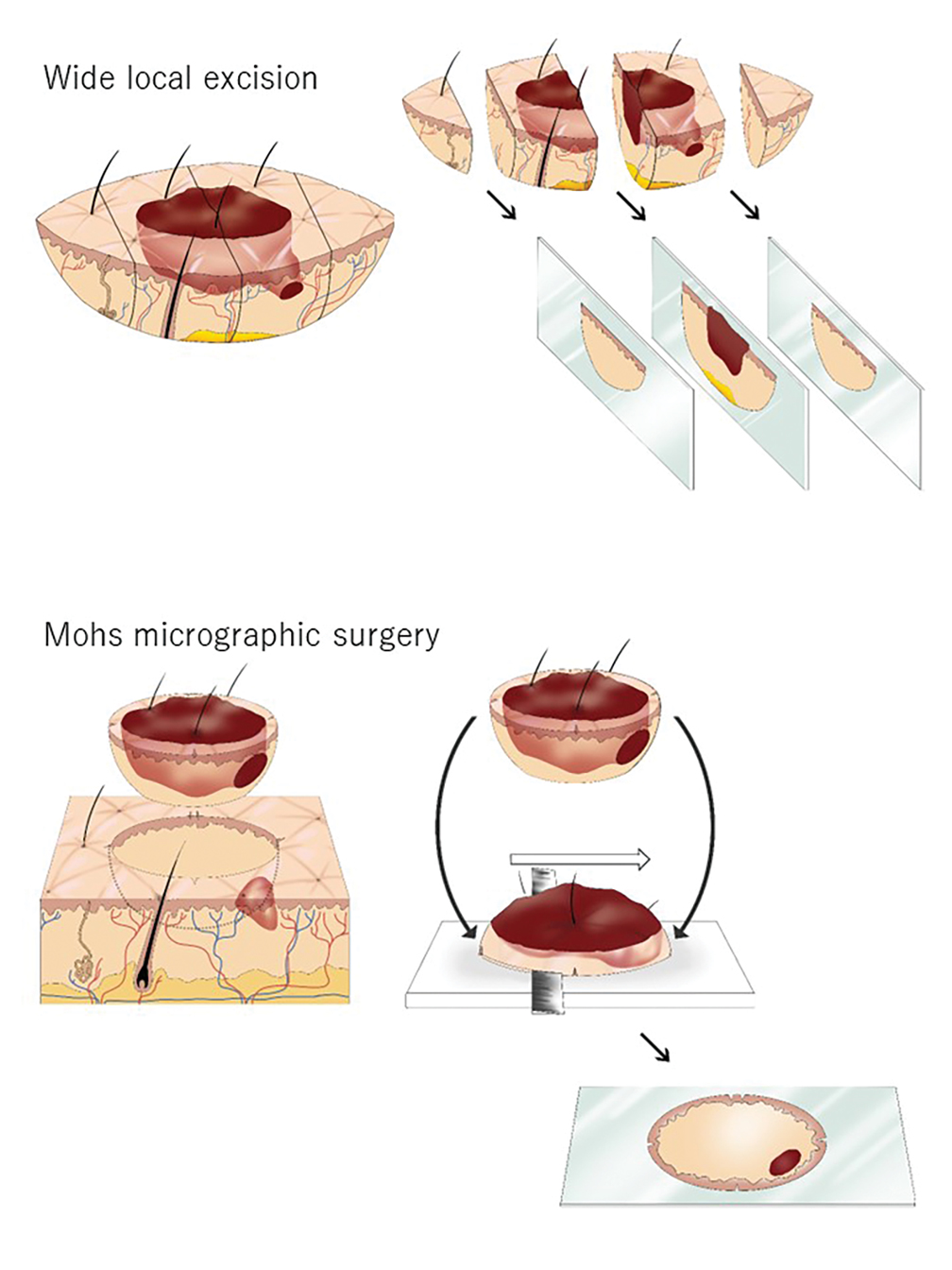

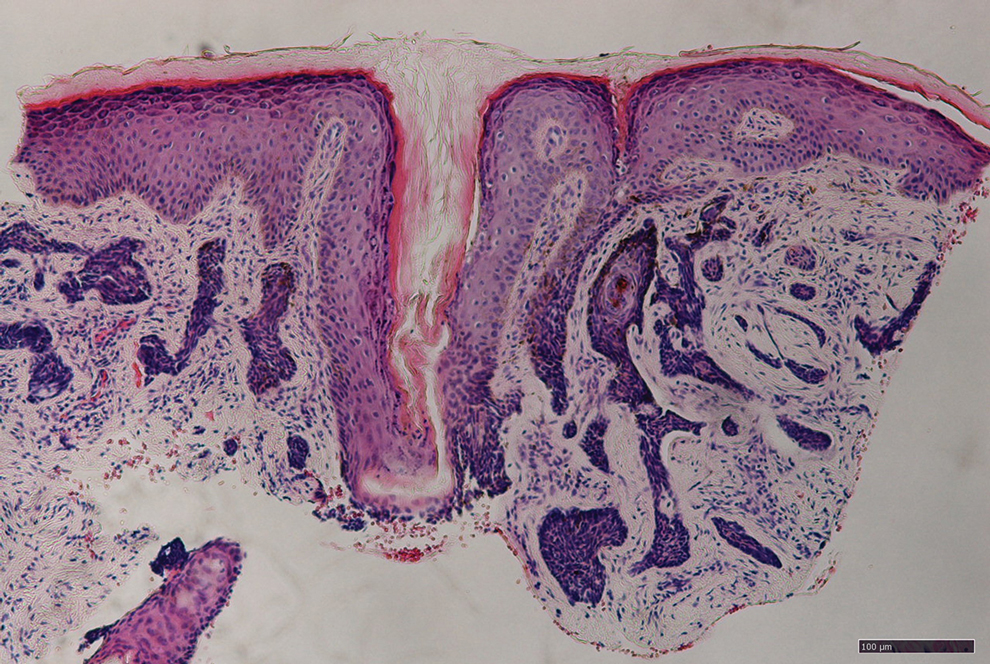
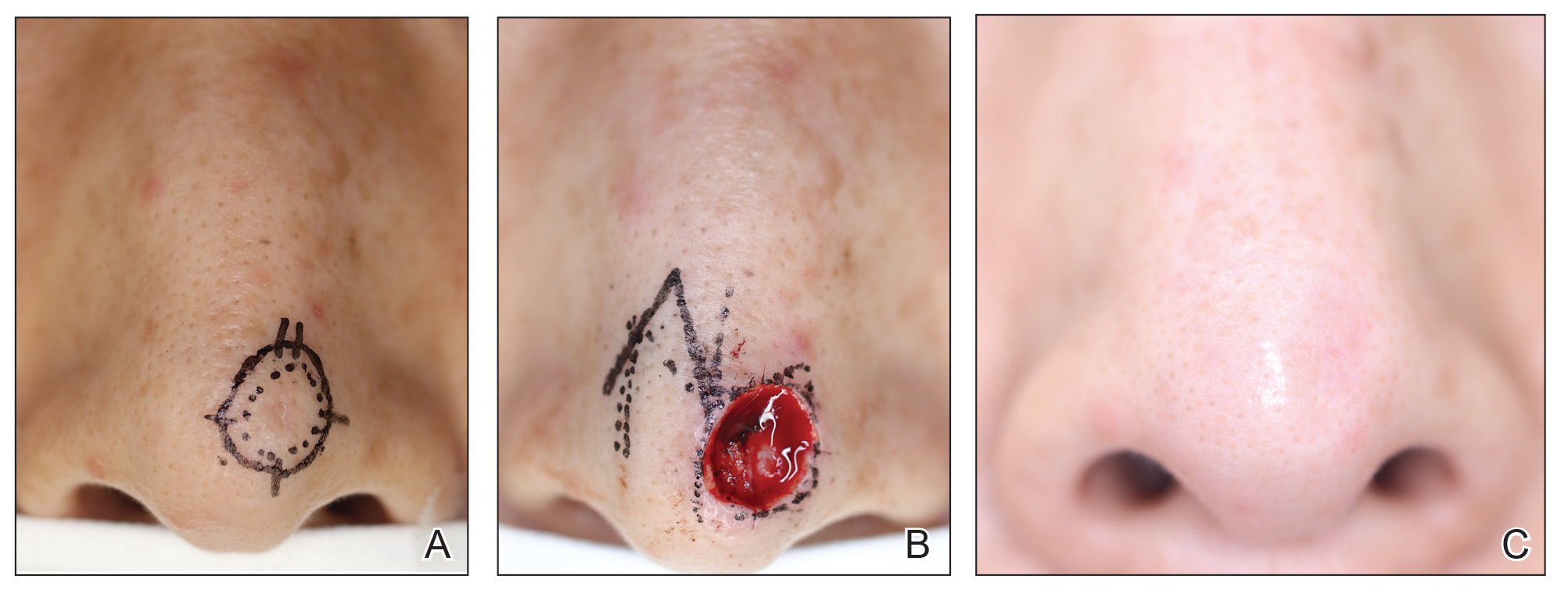
Patient 2—A 63-year-old Japanese man presented to dermatology with a brown macule on the right lower eyelid of 2 years’ duration. A biopsy of the lesion was positive for nodular BCC. After being advised to undergo WLE and extensive reconstruction with plastic surgery, the patient learned of MMS through an internet search and found our clinic. Physical examination revealed a 7×5-mm brown macule on the right lower eyelid. The patient had supplemental private insurance that covered the cost of MMS, and he provided consent for the procedure. A 1.5-mm margin was taken for the first stage, resulting in a 10×8-mm defect superficial to the orbicularis oculi muscle. The frozen section revealed residual tumor exposure in the dermis at the 9- to 10-o’clock position. A second-stage excision was performed to remove an additional 1.5 mm of skin at the 9- to 12-o’clock position with a thin layer of the orbicularis oculi muscle. The subsequent histologic examination revealed no residual BCC, and the final 13×9-mm skin defect was reconstructed with a rotation flap. There were no signs of recurrence at 2.5-year follow-up with an excellent cosmetic outcome.
Patient 3—A 73-year-old Japanese man presented to a local university dermatology clinic with a new papule on the nose. The dermatologist suggested WLE with 4-mm margins and reconstruction of the skin defect 2 weeks later by a plastic surgeon. The patient was not satisfied with the proposed surgical plan, which led him to learn about MMS on the internet; he subsequently found our clinic. Physical examination revealed a 4×3.5-mm brown papule on the tip of the nose. He understood the nature of MMS and chose to pay out-of-pocket because Japanese health insurance did not cover the procedure. We used a 2-mm margin for the first stage, which created a 7.5×7-mm skin defect. The frozen section pathology revealed no residual BCC at the cut surface. The skin defect was reconstructed with a Limberg rhombic flap. There were no signs of recurrence at 1.5-year follow-up with a favorable cosmetic outcome.
Patient 4—A 45-year-old man presented to a dermatology clinic with a papule on the right side of the nose of 1 year’s duration. A biopsy revealed the lesion was a nodular BCC. The dermatologist recommended WLE at a general hospital, but the patient refused after learning about MMS. He subsequently made an appointment with our clinic. Physical examination revealed a 7×4-mm white papule on the right side of the nose. The patient had private insurance that covered the cost of MMS. The first stage was performed with 1.5-mm margins and was clear of residual tumor. A Limberg rhombic flap from the adjacent cheek was used to repair the final 10×7-mm skin defect. There were no signs of recurrence at 1 year and 9 months’ follow-up with a favorable cosmetic outcome.
Patient 5—A 76-year-old Japanese woman presented to a university hospital near Tokyo with a black papule on the left cutaneous lip of 5 years’ duration. A biopsy revealed nodular BCC, and WLE with flap reconstruction was recommended. The patient’s son learned about MMS through internet research and referred her to our clinic. Physical examination revealed a 7×5-mm black papule on the left upper lip. The patient’s private insurance covered the cost of MMS, and she consented to the procedure. We used a 2-mm initial margin, and the immediate frozen section revealed no signs of BCC at the cut surface. The 11×9-mm skin defect was reconstructed with a Limberg rhombic flap. There were no signs of recurrence at 1.5-year follow-up with a favorable cosmetic outcome.
Comment
We presented 5 cases of MMS in Japanese patients with BCC. More than 7000 new cases of nonmelanoma skin cancer occur every year in Japan.3 Only 0.04% of these cases—the 5 cases presented here—were treated with MMS in Japan in 2020 and 2021, in contrast to 25% in the United States in 2006.2
MMS vs Other BCC Treatments—Mohs micrographic surgery offers 2 distinct advantages over conventional excision: an improved cure rate while achieving a smaller final defect size, generally leading to better cosmetic outcomes. Overall 5-year recurrence rates of BCC are 10% for conventional surgical excision vs 1% for MMS, while the recurrence rates for SCC are 8% and 3%, respectively.5 A study of well-demarcated BCCs smaller than 2 cm that were treated with MMS with 2-mm increments revealed that 95% of the cases were free of malignancy within a 4-mm margin of the normal-appearing skin surrounding the tumor.6 Several articles have reported a 95% cure rate or higher with conventional excision of localized BCC,7 but 4- to 5-mm excision margins are required, resulting in a greater skin defect and a lower cure rate compared to MMS.
Aggressive subtypes of BCC have a higher recurrence rate. Rowe et al8 reported the following 5-year recurrence rates: 5.6% for MMS, 17.4% for conventional surgical excision, 40.0% for curettage and electrodesiccation, and 9.8% for radiation therapy. Primary BCCs with high-risk histologic subtypes has a 10-year recurrence rate of 4.4% with MMS vs 12.2% with conventional excision.9 These findings reveal that MMS yields a better prognosis compared to traditional treatment methods for recurrent BCCs and BCCs of high-risk histologic subtypes.
The primary reason for the excellent cure rate seen in MMS is the ability to perform complete margin assessment. Peripheral and deep en face margin assessment (PDEMA) is crucial in achieving high cure rates with narrow margins. In WLE (Figure 1), vertical sectioning (also known as bread-loafing) does not achieve direct visualization of the entire surgical margin, as this technique only evaluates random sections and does not achieve PDEMA.10 The bread-loafing method is used almost exclusively in Japan and visualizes only 0.1% of the entire margin compared to 100% with MMS.11 Beyond the superior cure rate, the MMS technique often yields smaller final defects compared to WLE. All 5 of our patients achieved complete tumor removal while sparing more normal tissue compared to conventional WLE, which takes at least a 4-mm margin in all directions.
Barriers to Adopting MMS in Japan—There are many barriers to the broader adoption of MMS in Japan. A guideline of the Japanese Dermatological Association says, MMS “is complicated, requires special training for acquisition, and requires time and labor for implementation of a series of processes, and it has not gained wide acceptance in Japan because of these disadvantages.”3 There currently are no MMS training programs in Japan. We refute this statement from the Japanese Dermatological Association because, in our experience, only 1 surgeon plus a single histotechnician familiar with MMS is sufficient for a facility to offer the procedure (the lead author of this study [S.S.] acts as both the surgeon and the histotechnician). Another misconception among some physicians in Japan is that cancer on ethnically Japanese skin is uniquely suited to excision without microscopic verification of tumor clearance because the borders of the tumors are easily identified, which was based on good cure rates for the excision of well-demarcated pigmented BCCs in a Japanese cohort. This study of a Japanese cohort investigated the specimens with the conventional bread-loafing technique but not with the PDEMA.12
Eighty percent (4/5) of our patients presented with nodular BCC, and only 1 required a second stage. In comparison, we also treated 16 White patients with nodular BCC with MMS during the same period, and 31% (5/16) required more than 1 stage, with 1 patient requiring 3 stages. This cohort, however, is too small to demonstrate a statistically significant difference (S.S., unpublished data, 2020-2022).
A study in Singapore reported the postsurgical complication rate and 5-year recurrence rate for 481 tumors (92% BCC and 7.5% SCC). The median follow-up duration after MMS was 36 months, and the recurrence rate was 0.6%. The postsurgical complications included 11 (2.3%) cases with superficial tip necrosis of surgical flaps/grafts, 2 (0.4%) with mild wound dehiscence, 1 (0.2%) with minor surgical site bleeding, and 1 (0.2%) with minor wound infection.13 This study supports the notion that MMS is equally effective for Asian patients.
Awareness of MMS in Japan is lacking, and most Japanese dermatologists do not know about the technique. All 5 patients in our case series asked their dermatologists about alternative treatment options and were not offered MMS. In each case, the patients learned of the technique through internet research.
The lack of insurance reimbursement for MMS in Japan is another barrier. Because the national health insurance does not reimburse for MMS, the procedure is relatively unavailable to most Japanese citizens who cannot pay out-of-pocket for the treatment and do not have supplemental insurance. Mohs micrographic surgery may seem expensive compared to WLE followed by repair; however, in the authors’ experience, in Japan, excision without MMS may require general sedation and multiple surgeries to reconstruct larger skin defects, leading to greater morbidity and risk for the patient.
Conclusion
Mohs micrographic surgery in Japan is in its infancy, and further studies showing recurrence rates and long-term prognosis are needed. Such data should help increase awareness of MMS among Japanese physicians as an excellent treatment option for their patients. Furthermore, as Japan becomes more heterogenous as a society and the US Military increases its presence in the region, the need for MMS is likely to increase.
Acknowledgments—We appreciate the proofreading support by Mark Bivens, MBA, MSc (Tokyo, Japan), as well as the technical support from Ben Tallon, MBChB, and Robyn Mason (both in Tauranga, New Zealand) to start MMS at our clinic.
Margin-controlled surgery for squamous cell carcinoma (SCC) on the lower lip was first performed by Dr. Frederic Mohs on June 30, 1936. Since then, thousands of skin cancer surgeons have refined and adopted the technique. Due to the high cure rate and sparing of normal tissue, Mohs micrographic surgery (MMS) has become the gold standard treatment for facial and special-site nonmelanoma skin cancer worldwide. Mohs micrographic surgery is performed on more than 876,000 tumors annually in the United States.1 Among 3.5 million Americans diagnosed with nonmelanoma skin cancer in 2006, one-quarter were treated with MMS.2 In Japan, basal cell carcinoma (BCC) is the most common skin malignancy, with an incidence of 3.34 cases per 100,000 individuals; SCC is the second most common, with an incidence of 2.5 cases per 100,000 individuals.3
The essential element that makes MMS unique is the careful microscopic examination of the entire margin of the removed specimen. Tissue processing is done with careful en face orientation to ensure that circumferential and deep margins are entirely visible. The surgeon interprets the slides and proceeds to remove the additional tumor as necessary. Because the same physician performs both the surgery and the pathologic assessment throughout the procedure, a precise correlation between the microscopic and surgical findings can be made. The surgeon can begin with smaller margins, removing minimal healthy tissue while removing all the cancer cells, which results in the smallest-possible skin defect and the best prognosis for the malignancy (Figure 1).
At the only facility in Japan offering MMS, the lead author (S.S.) has treated 52 lesions with MMS in 46 patients (2020-2022). Of these patients, 40 were White, 5 were Japanese, and 1 was of African descent. In this case series, we present 5 Japanese patients who had BCC treated with MMS.
Case Series
Patient 1—A 50-year-old Japanese woman presented to dermatology with a brown papule on the nasal tip of 1.25 year’s duration (Figure 2). A biopsy revealed infiltrative BCC (Figure 3), and the patient was referred to the dermatology department at a nearby university hospital. Because the BCC was an aggressive variant, wide local excision (WLE) with subsequent flap reconstruction was recommended as well as radiation therapy. The patient learned about MMS through an internet search and refused both options, seeking MMS treatment at our clinic. Although Japanese health insurance does not cover MMS, the patient had supplemental private insurance that did cover the cost. She provided consent to undergo the procedure. Physical examination revealed a 7.5×6-mm, brown-red macule with ill-defined borders on the tip of the nose. We used a 1.5-mm margin for the first stage of MMS (Figure 4A). The frozen section revealed that the tumor had been entirely excised in the first stage, leaving only a 10.5×9-mm skin defect that was reconstructed with a Dufourmentel flap (Figure 4B). No signs of recurrence were noted at 3.5-year follow-up, and the cosmetic outcome was favorable (Figure 4C). National Comprehensive Cancer Network guidelines recommend a margin greater than 4 mm for infiltrative BCCs4; therefore, our technique reduced the total defect by at least 4 mm in a cosmetically sensitive area. The patient also did not need radiation therapy, which reduced morbidity. She continues to be recurrence free at 3.5-year follow-up.
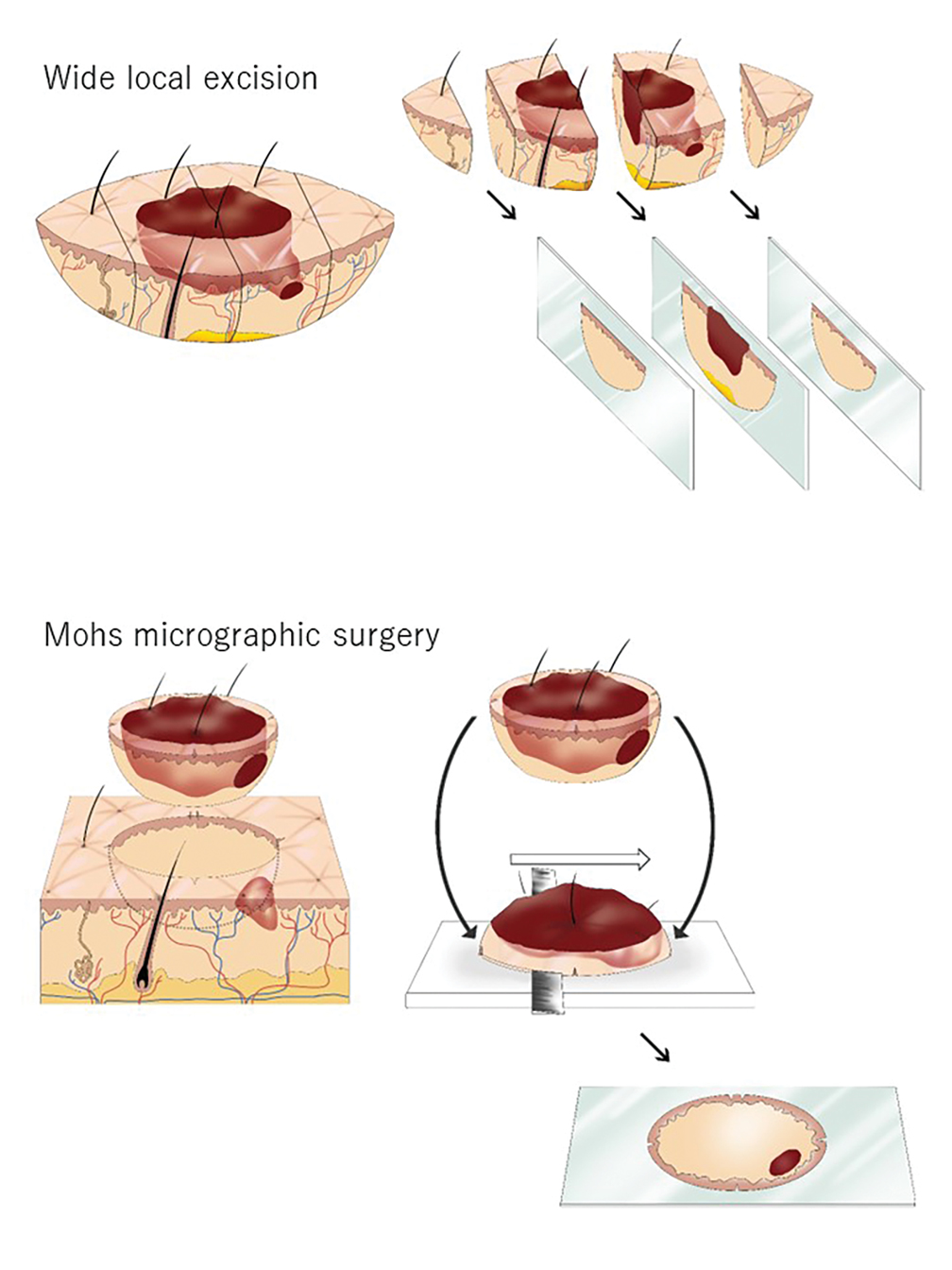

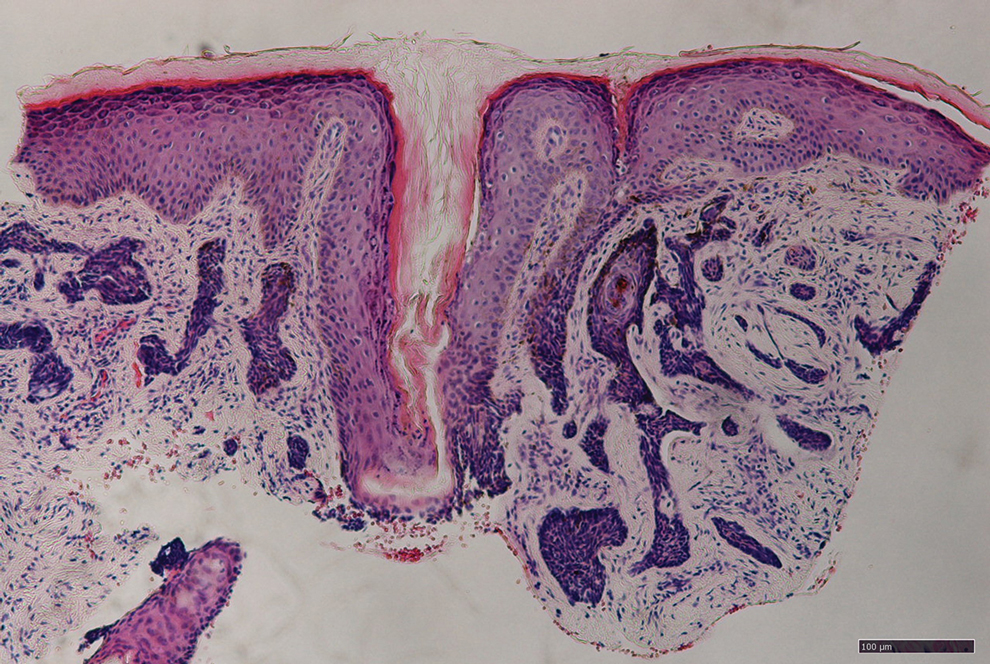
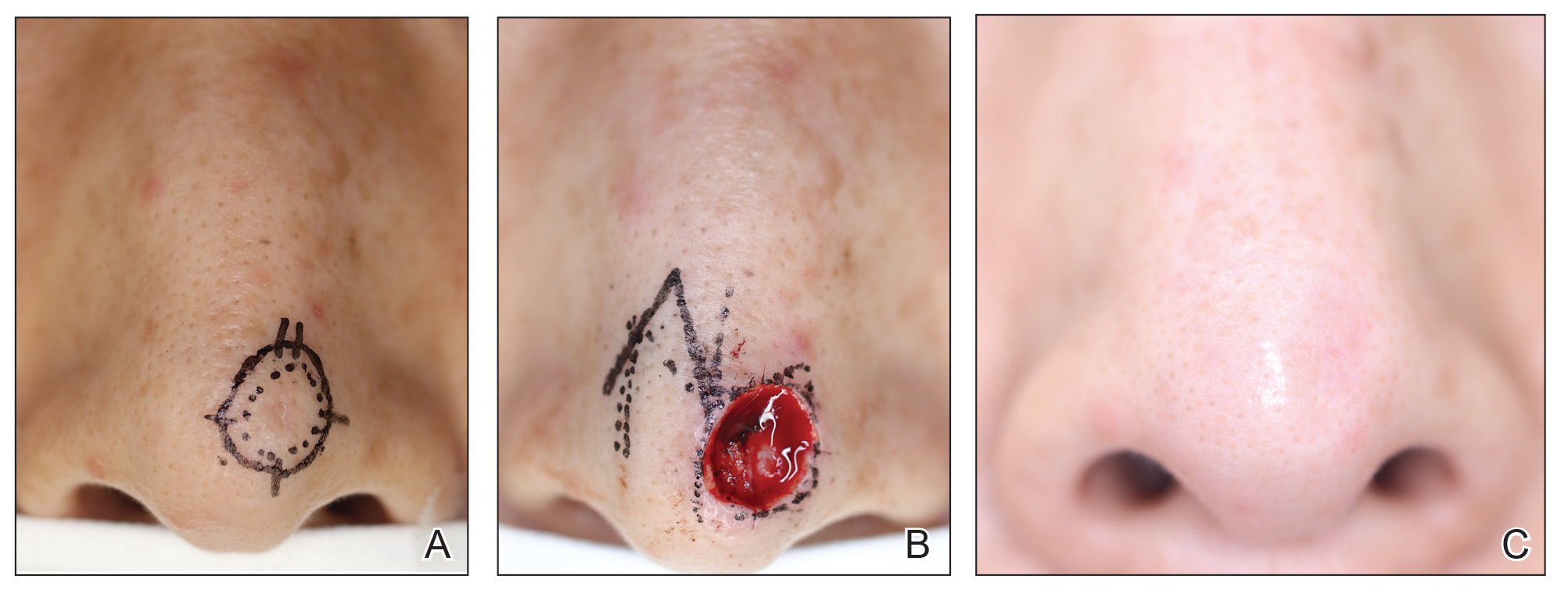
Patient 2—A 63-year-old Japanese man presented to dermatology with a brown macule on the right lower eyelid of 2 years’ duration. A biopsy of the lesion was positive for nodular BCC. After being advised to undergo WLE and extensive reconstruction with plastic surgery, the patient learned of MMS through an internet search and found our clinic. Physical examination revealed a 7×5-mm brown macule on the right lower eyelid. The patient had supplemental private insurance that covered the cost of MMS, and he provided consent for the procedure. A 1.5-mm margin was taken for the first stage, resulting in a 10×8-mm defect superficial to the orbicularis oculi muscle. The frozen section revealed residual tumor exposure in the dermis at the 9- to 10-o’clock position. A second-stage excision was performed to remove an additional 1.5 mm of skin at the 9- to 12-o’clock position with a thin layer of the orbicularis oculi muscle. The subsequent histologic examination revealed no residual BCC, and the final 13×9-mm skin defect was reconstructed with a rotation flap. There were no signs of recurrence at 2.5-year follow-up with an excellent cosmetic outcome.
Patient 3—A 73-year-old Japanese man presented to a local university dermatology clinic with a new papule on the nose. The dermatologist suggested WLE with 4-mm margins and reconstruction of the skin defect 2 weeks later by a plastic surgeon. The patient was not satisfied with the proposed surgical plan, which led him to learn about MMS on the internet; he subsequently found our clinic. Physical examination revealed a 4×3.5-mm brown papule on the tip of the nose. He understood the nature of MMS and chose to pay out-of-pocket because Japanese health insurance did not cover the procedure. We used a 2-mm margin for the first stage, which created a 7.5×7-mm skin defect. The frozen section pathology revealed no residual BCC at the cut surface. The skin defect was reconstructed with a Limberg rhombic flap. There were no signs of recurrence at 1.5-year follow-up with a favorable cosmetic outcome.
Patient 4—A 45-year-old man presented to a dermatology clinic with a papule on the right side of the nose of 1 year’s duration. A biopsy revealed the lesion was a nodular BCC. The dermatologist recommended WLE at a general hospital, but the patient refused after learning about MMS. He subsequently made an appointment with our clinic. Physical examination revealed a 7×4-mm white papule on the right side of the nose. The patient had private insurance that covered the cost of MMS. The first stage was performed with 1.5-mm margins and was clear of residual tumor. A Limberg rhombic flap from the adjacent cheek was used to repair the final 10×7-mm skin defect. There were no signs of recurrence at 1 year and 9 months’ follow-up with a favorable cosmetic outcome.
Patient 5—A 76-year-old Japanese woman presented to a university hospital near Tokyo with a black papule on the left cutaneous lip of 5 years’ duration. A biopsy revealed nodular BCC, and WLE with flap reconstruction was recommended. The patient’s son learned about MMS through internet research and referred her to our clinic. Physical examination revealed a 7×5-mm black papule on the left upper lip. The patient’s private insurance covered the cost of MMS, and she consented to the procedure. We used a 2-mm initial margin, and the immediate frozen section revealed no signs of BCC at the cut surface. The 11×9-mm skin defect was reconstructed with a Limberg rhombic flap. There were no signs of recurrence at 1.5-year follow-up with a favorable cosmetic outcome.
Comment
We presented 5 cases of MMS in Japanese patients with BCC. More than 7000 new cases of nonmelanoma skin cancer occur every year in Japan.3 Only 0.04% of these cases—the 5 cases presented here—were treated with MMS in Japan in 2020 and 2021, in contrast to 25% in the United States in 2006.2
MMS vs Other BCC Treatments—Mohs micrographic surgery offers 2 distinct advantages over conventional excision: an improved cure rate while achieving a smaller final defect size, generally leading to better cosmetic outcomes. Overall 5-year recurrence rates of BCC are 10% for conventional surgical excision vs 1% for MMS, while the recurrence rates for SCC are 8% and 3%, respectively.5 A study of well-demarcated BCCs smaller than 2 cm that were treated with MMS with 2-mm increments revealed that 95% of the cases were free of malignancy within a 4-mm margin of the normal-appearing skin surrounding the tumor.6 Several articles have reported a 95% cure rate or higher with conventional excision of localized BCC,7 but 4- to 5-mm excision margins are required, resulting in a greater skin defect and a lower cure rate compared to MMS.
Aggressive subtypes of BCC have a higher recurrence rate. Rowe et al8 reported the following 5-year recurrence rates: 5.6% for MMS, 17.4% for conventional surgical excision, 40.0% for curettage and electrodesiccation, and 9.8% for radiation therapy. Primary BCCs with high-risk histologic subtypes has a 10-year recurrence rate of 4.4% with MMS vs 12.2% with conventional excision.9 These findings reveal that MMS yields a better prognosis compared to traditional treatment methods for recurrent BCCs and BCCs of high-risk histologic subtypes.
The primary reason for the excellent cure rate seen in MMS is the ability to perform complete margin assessment. Peripheral and deep en face margin assessment (PDEMA) is crucial in achieving high cure rates with narrow margins. In WLE (Figure 1), vertical sectioning (also known as bread-loafing) does not achieve direct visualization of the entire surgical margin, as this technique only evaluates random sections and does not achieve PDEMA.10 The bread-loafing method is used almost exclusively in Japan and visualizes only 0.1% of the entire margin compared to 100% with MMS.11 Beyond the superior cure rate, the MMS technique often yields smaller final defects compared to WLE. All 5 of our patients achieved complete tumor removal while sparing more normal tissue compared to conventional WLE, which takes at least a 4-mm margin in all directions.
Barriers to Adopting MMS in Japan—There are many barriers to the broader adoption of MMS in Japan. A guideline of the Japanese Dermatological Association says, MMS “is complicated, requires special training for acquisition, and requires time and labor for implementation of a series of processes, and it has not gained wide acceptance in Japan because of these disadvantages.”3 There currently are no MMS training programs in Japan. We refute this statement from the Japanese Dermatological Association because, in our experience, only 1 surgeon plus a single histotechnician familiar with MMS is sufficient for a facility to offer the procedure (the lead author of this study [S.S.] acts as both the surgeon and the histotechnician). Another misconception among some physicians in Japan is that cancer on ethnically Japanese skin is uniquely suited to excision without microscopic verification of tumor clearance because the borders of the tumors are easily identified, which was based on good cure rates for the excision of well-demarcated pigmented BCCs in a Japanese cohort. This study of a Japanese cohort investigated the specimens with the conventional bread-loafing technique but not with the PDEMA.12
Eighty percent (4/5) of our patients presented with nodular BCC, and only 1 required a second stage. In comparison, we also treated 16 White patients with nodular BCC with MMS during the same period, and 31% (5/16) required more than 1 stage, with 1 patient requiring 3 stages. This cohort, however, is too small to demonstrate a statistically significant difference (S.S., unpublished data, 2020-2022).
A study in Singapore reported the postsurgical complication rate and 5-year recurrence rate for 481 tumors (92% BCC and 7.5% SCC). The median follow-up duration after MMS was 36 months, and the recurrence rate was 0.6%. The postsurgical complications included 11 (2.3%) cases with superficial tip necrosis of surgical flaps/grafts, 2 (0.4%) with mild wound dehiscence, 1 (0.2%) with minor surgical site bleeding, and 1 (0.2%) with minor wound infection.13 This study supports the notion that MMS is equally effective for Asian patients.
Awareness of MMS in Japan is lacking, and most Japanese dermatologists do not know about the technique. All 5 patients in our case series asked their dermatologists about alternative treatment options and were not offered MMS. In each case, the patients learned of the technique through internet research.
The lack of insurance reimbursement for MMS in Japan is another barrier. Because the national health insurance does not reimburse for MMS, the procedure is relatively unavailable to most Japanese citizens who cannot pay out-of-pocket for the treatment and do not have supplemental insurance. Mohs micrographic surgery may seem expensive compared to WLE followed by repair; however, in the authors’ experience, in Japan, excision without MMS may require general sedation and multiple surgeries to reconstruct larger skin defects, leading to greater morbidity and risk for the patient.
Conclusion
Mohs micrographic surgery in Japan is in its infancy, and further studies showing recurrence rates and long-term prognosis are needed. Such data should help increase awareness of MMS among Japanese physicians as an excellent treatment option for their patients. Furthermore, as Japan becomes more heterogenous as a society and the US Military increases its presence in the region, the need for MMS is likely to increase.
Acknowledgments—We appreciate the proofreading support by Mark Bivens, MBA, MSc (Tokyo, Japan), as well as the technical support from Ben Tallon, MBChB, and Robyn Mason (both in Tauranga, New Zealand) to start MMS at our clinic.
- Asgari MM, Olson J, Alam M. Needs assessment for Mohs micrographic surgery. Dermatol Clin. 2012;30:167-175. doi:10.1016/j.det.2011.08.010
- Connolly SM, Baker DR, Baker DR, et al. AAD/ACMS/ASDSA/ASMS 2012 appropriate use criteria for Mohs micrographic surgery: a report of the American Academy of Dermatology, American College of Mohs Surgery, American Society for Dermatologic Surgery Association, and the American Society for Mohs Surgery. J Am Acad Dermatol. 2012;67:531-550.
- Ansai SI, Umebayashi Y, Katsumata N, et al. Japanese Dermatological Association Guidelines: outlines of guidelines for cutaneous squamous cell carcinoma 2020. J Dermatol. 2021;48:E288-E311.
- Schmults CD, Blitzblau R, Aasi SZ, et at. Basal cell skin cancer, version 2.2024, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2023;21:1181-1203. doi:10.6004/jncn.2023.0056
- Snow SN, Gunkel J. Mohs surgery. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Elsevier; 2017:2445-2455. doi:10.1016/b978-0-070-94171-3.00041-7
- Wolf DJ, Zitelli JA. Surgical margins for basal cell carcinoma. Arch Dermatol. 1987;123:340-344.
- Quazi SJ, Aslam N, Saleem H, et al. Surgical margin of excision in basal cell carcinoma: a systematic review of literature. Cureus. 2020;12:E9211.
- Rowe DE, Carroll RJ, Day Jus CL. Mohs surgery is the treatment of choice for recurrent (previously treated) basal cell carcinoma. J Dermatol Surg Oncol. 1989;15:424-431.
- Van Loo, Mosterd K, Krekels GA. Surgical excision versus Mohs’ micrographic surgery for basal cell carcinoma of the face. Eur J Cancer. 2014;50:3011-3020.
- Schmults CD, Blitzblau R, Aasi SZ, et al. NCCN Guidelines Insights: Squamous Cell Skin Cancer, Version 1.2022. J Natl Compr Canc Netw. 2021;19:1382-1394.
- Hui AM, Jacobson M, Markowitz O, et al. Mohs micrographic surgery for the treatment of melanoma. Dermatol Clin. 2012;30:503-515.
- Ito T, Inatomi Y, Nagae K, et al. Narrow-margin excision is a safe, reliable treatment for well-defined, primary pigmented basal cell carcinoma: an analysis of 288 lesions in Japan. J Eur Acad Dermatol Venereol. 2015;29:1828-1831.
- Ho WYB, Zhao X, Tan WPM. Mohs micrographic surgery in Singapore: a long-term follow-up review. Ann Acad Med Singap. 2021;50:922-923.
- Asgari MM, Olson J, Alam M. Needs assessment for Mohs micrographic surgery. Dermatol Clin. 2012;30:167-175. doi:10.1016/j.det.2011.08.010
- Connolly SM, Baker DR, Baker DR, et al. AAD/ACMS/ASDSA/ASMS 2012 appropriate use criteria for Mohs micrographic surgery: a report of the American Academy of Dermatology, American College of Mohs Surgery, American Society for Dermatologic Surgery Association, and the American Society for Mohs Surgery. J Am Acad Dermatol. 2012;67:531-550.
- Ansai SI, Umebayashi Y, Katsumata N, et al. Japanese Dermatological Association Guidelines: outlines of guidelines for cutaneous squamous cell carcinoma 2020. J Dermatol. 2021;48:E288-E311.
- Schmults CD, Blitzblau R, Aasi SZ, et at. Basal cell skin cancer, version 2.2024, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2023;21:1181-1203. doi:10.6004/jncn.2023.0056
- Snow SN, Gunkel J. Mohs surgery. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Elsevier; 2017:2445-2455. doi:10.1016/b978-0-070-94171-3.00041-7
- Wolf DJ, Zitelli JA. Surgical margins for basal cell carcinoma. Arch Dermatol. 1987;123:340-344.
- Quazi SJ, Aslam N, Saleem H, et al. Surgical margin of excision in basal cell carcinoma: a systematic review of literature. Cureus. 2020;12:E9211.
- Rowe DE, Carroll RJ, Day Jus CL. Mohs surgery is the treatment of choice for recurrent (previously treated) basal cell carcinoma. J Dermatol Surg Oncol. 1989;15:424-431.
- Van Loo, Mosterd K, Krekels GA. Surgical excision versus Mohs’ micrographic surgery for basal cell carcinoma of the face. Eur J Cancer. 2014;50:3011-3020.
- Schmults CD, Blitzblau R, Aasi SZ, et al. NCCN Guidelines Insights: Squamous Cell Skin Cancer, Version 1.2022. J Natl Compr Canc Netw. 2021;19:1382-1394.
- Hui AM, Jacobson M, Markowitz O, et al. Mohs micrographic surgery for the treatment of melanoma. Dermatol Clin. 2012;30:503-515.
- Ito T, Inatomi Y, Nagae K, et al. Narrow-margin excision is a safe, reliable treatment for well-defined, primary pigmented basal cell carcinoma: an analysis of 288 lesions in Japan. J Eur Acad Dermatol Venereol. 2015;29:1828-1831.
- Ho WYB, Zhao X, Tan WPM. Mohs micrographic surgery in Singapore: a long-term follow-up review. Ann Acad Med Singap. 2021;50:922-923.
Practice Points
- Mohs micrographic surgery (MMS) is a safe and effective treatment method for nonmelanoma skin cancer. In some cases, this procedure is superior to standard wide local excision and repair.
- For the broader adaptation of this vital technique in Japan—where MMS is not well established—increased awareness of treatment outcomes among Japanese physicians is needed.
Uproar Over Vitamin D Disease-Prevention Guideline
A recent report by this news organization of a vitamin D clinical practice guideline released by the Endocrine Society in June triggered an outpouring of objections in the comments section from doctors and other readers.
A society press release listed the key new recommendations on the use of vitamin D supplementation and screening to reduce disease risks in individuals without established indications for such treatment or testing:
- For healthy adults younger than 75, no supplementation at doses above the recommended dietary intakes.
- Populations that may benefit from higher doses include: children and adolescents 18 and younger to prevent rickets and to reduce risk for respiratory infection, individuals 75 and older to possibly lower mortality risk, “pregnant people” to potentially reduce various risks, and people with prediabetes to potentially reduce risk of progression.
- No routine testing for 25-hydroxyvitamin D levels because outcome-specific benefits based on those levels have not been identified (including screening in people with dark complexion or obesity).
- Based on insufficient evidence, the panel could not determine specific blood-level thresholds for 25-hydroxyvitamin D for adequacy or for target levels for disease prevention.
This news organization covered the guideline release and simultaneous presentation at the Endocrine Society annual meeting. In response to the coverage, more than 200 doctors and other readers expressed concerns about the guideline, and some said outright that they would not follow it (readers quoted below are identified by the usernames they registered with on the website).
One reader who posted as Dr. Joseph Destefano went so far as to call the guideline “dangerous” and “almost ... evil.” Ironically, some readers attacked this news organization, thinking that the coverage implied an endorsement, rather than a news report.
Ignores Potential Benefits
“They address issues dealing only with endocrinology and bone health for the most part,” Dr. Emilio Gonzalez wrote. “However, vitamin D insufficiency and deficiency are not rare, and they impact the treatment of autoimmune disorders, chronic pain control, immunosuppression, cancer prevention, cardiovascular health, etc. There is plenty of literature in this regard.”
“They make these claims as if quality studies contradicting their guidelines have not been out there for years,” Dr. Brian Batcheldor said. “What about the huge demographic with diseases that impact intestinal absorption, eg, Crohn’s and celiac disease, cystic fibrosis, and ulcerative colitis? What about the one in nine that now have autoimmune diseases still awaiting diagnosis? What about night workers or anyone with more restricted access to sun exposure? How about those whose cultural or religious dress code limit skin exposure?”
The latter group was also mentioned in a post from Dr. Eve Finkelstein who said, “They don’t take into account women who are totally covered for religious reasons. They have no skin other than part of their face exposed. It does not make sense not to supplement them. Ignoring women’s health needs seems to be the norm.”
“I don’t think they considered the oral health effects of vitamin D deficiency,” pointed out commenter Corie Lewis. “Excess dental calculus (tartar) from excess calcium/phosphate in saliva significantly increases an individual’s periodontal disease risks (gum disease), and low saliva calcium/phosphate increases dental caries (cavities) risks, which generally indicates an imbalance of the oral microbiome. Vitamin D can help create balance and reduce those oral health risks.”
Noted Kimberley Morris-Windisch, “Having worked in rheumatology and pain for most of my career, I have seen too many people benefit from correcting deficiency of vitamin D. To ignore this is to miss opportunities to improve patient health.” Furthermore, “I find it unlikely that it would only improve mortality after age 75. That makes no sense.”
“Also,” she added, “what is the number [needed] to harm? In my 25 years, I have seen vitamin D toxicity once and an excessively high level without symptoms one other time.”
“WHY? Just WHY?” lamented Anne Kinchen. “Low levels in pregnant women have long-term effects on the developing fetus — higher and earlier rates of osteopenia in female children, weaker immune systems overall. There are just SO many reasons to test. These guidelines for no testing are absurd!”
No Screening, No Need for Decision-Making?
Several readers questioned the society’s rationale for not screening, as expressed by session moderator Clifford J. Rosen, MD, director of Clinical and Translational Research and senior scientist at Maine Medical Center Research Institute, Scarborough, Maine.
“When clinicians measure vitamin D, then they’re forced to make a decision what to do about it,” Dr. Rosen said. “That’s where questions about the levels come in. And that’s a big problem. So what the panel’s saying is, don’t screen. ... This really gets to the heart of the issue, because we have no data that there’s anything about screening that allows us to improve quality of life. ... Screening is probably not worthwhile in any age group.”
Among the reader comments in this regard:
“So misguided. Don’t look because we don’t know what do to with data. That’s the message this article exposes. The recommendation is do nothing. But, doing nothing IS an action — not a default.” (Lisa Tracy)
“So now, you will not screen for vitamin D because you do not know what to do next? See a naturopathic doctor — we know what to do next!” (Dr. Joyce Roberson)
“Gee, how do we treat it? ... What to do? Sounds incompetent at minimum. I suspect it’s vital, easy, and inexpensive ... so hide it.” (Holly Kohley)
“Just because we do not know is not a rationale for not testing. The opposite should be done.” (Dr. JJ Gold)
Caters to Industry?
Many commentators intimated that pharma and/or insurance company considerations played a role in the recommendations. Their comments included the following:
“I have been under the impression people do routine checkups to verify there are no hidden problems. If only some testing is done, the probability of not finding a problem is huge. ... Preventive healthcare should be looking for something to prevent instead of waiting until they can cure it. Of course, it might come back to ‘follow the money.’ It is much more profitable to diagnose and treat than it is to prevent.” (Grace Kyser)
“The current irrational ‘recommendation’ gives insurance companies an excuse to deny ALL tests of vitamin D — even if the proper code is supplied. The result is — people suffer. This recommendation does harm!” (Dr JJ Gold)
“Essentially, they are saying let’s not screen ‘healthy’ individuals and ignore it altogether. Better to wait till they’re old, pregnant, or already sick and diagnosed with a disease. This is the problem with the healthcare in this country.” (Brittney Lesher)
“Until allopathic medicine stops waiting for severe symptoms to develop before even screening for potential health problems, the most expensive healthcare (aka, sick care) system in the world will continue to be content to focus on medical emergencies and ignore prevention. ...” (Dean Raffelock)
“Don’t test? Are you kidding me? Especially when people are supplementing? That is akin to taking a blood pressure medication without measuring blood pressures! ... Don’t test? Don’t supplement? ... I have only one explanation for such nonsense: Pharma lives off sick people, not healthy ones.” (Georg Schlomka)
On a somewhat conciliatory and pointed note, Dr Francesca Luna-Rudin commented, “I would like to remind all of my fellow physicians that recommendations should be regarded as just that, a ‘recommendation.’ As doctors, we can use guidelines and recommendations in our practice, but if a new one is presented that does not make sense or would lead to harm based on our education and training, then we are not bound to follow it!”
A version of this article first appeared on Medscape.com.
A recent report by this news organization of a vitamin D clinical practice guideline released by the Endocrine Society in June triggered an outpouring of objections in the comments section from doctors and other readers.
A society press release listed the key new recommendations on the use of vitamin D supplementation and screening to reduce disease risks in individuals without established indications for such treatment or testing:
- For healthy adults younger than 75, no supplementation at doses above the recommended dietary intakes.
- Populations that may benefit from higher doses include: children and adolescents 18 and younger to prevent rickets and to reduce risk for respiratory infection, individuals 75 and older to possibly lower mortality risk, “pregnant people” to potentially reduce various risks, and people with prediabetes to potentially reduce risk of progression.
- No routine testing for 25-hydroxyvitamin D levels because outcome-specific benefits based on those levels have not been identified (including screening in people with dark complexion or obesity).
- Based on insufficient evidence, the panel could not determine specific blood-level thresholds for 25-hydroxyvitamin D for adequacy or for target levels for disease prevention.
This news organization covered the guideline release and simultaneous presentation at the Endocrine Society annual meeting. In response to the coverage, more than 200 doctors and other readers expressed concerns about the guideline, and some said outright that they would not follow it (readers quoted below are identified by the usernames they registered with on the website).
One reader who posted as Dr. Joseph Destefano went so far as to call the guideline “dangerous” and “almost ... evil.” Ironically, some readers attacked this news organization, thinking that the coverage implied an endorsement, rather than a news report.
Ignores Potential Benefits
“They address issues dealing only with endocrinology and bone health for the most part,” Dr. Emilio Gonzalez wrote. “However, vitamin D insufficiency and deficiency are not rare, and they impact the treatment of autoimmune disorders, chronic pain control, immunosuppression, cancer prevention, cardiovascular health, etc. There is plenty of literature in this regard.”
“They make these claims as if quality studies contradicting their guidelines have not been out there for years,” Dr. Brian Batcheldor said. “What about the huge demographic with diseases that impact intestinal absorption, eg, Crohn’s and celiac disease, cystic fibrosis, and ulcerative colitis? What about the one in nine that now have autoimmune diseases still awaiting diagnosis? What about night workers or anyone with more restricted access to sun exposure? How about those whose cultural or religious dress code limit skin exposure?”
The latter group was also mentioned in a post from Dr. Eve Finkelstein who said, “They don’t take into account women who are totally covered for religious reasons. They have no skin other than part of their face exposed. It does not make sense not to supplement them. Ignoring women’s health needs seems to be the norm.”
“I don’t think they considered the oral health effects of vitamin D deficiency,” pointed out commenter Corie Lewis. “Excess dental calculus (tartar) from excess calcium/phosphate in saliva significantly increases an individual’s periodontal disease risks (gum disease), and low saliva calcium/phosphate increases dental caries (cavities) risks, which generally indicates an imbalance of the oral microbiome. Vitamin D can help create balance and reduce those oral health risks.”
Noted Kimberley Morris-Windisch, “Having worked in rheumatology and pain for most of my career, I have seen too many people benefit from correcting deficiency of vitamin D. To ignore this is to miss opportunities to improve patient health.” Furthermore, “I find it unlikely that it would only improve mortality after age 75. That makes no sense.”
“Also,” she added, “what is the number [needed] to harm? In my 25 years, I have seen vitamin D toxicity once and an excessively high level without symptoms one other time.”
“WHY? Just WHY?” lamented Anne Kinchen. “Low levels in pregnant women have long-term effects on the developing fetus — higher and earlier rates of osteopenia in female children, weaker immune systems overall. There are just SO many reasons to test. These guidelines for no testing are absurd!”
No Screening, No Need for Decision-Making?
Several readers questioned the society’s rationale for not screening, as expressed by session moderator Clifford J. Rosen, MD, director of Clinical and Translational Research and senior scientist at Maine Medical Center Research Institute, Scarborough, Maine.
“When clinicians measure vitamin D, then they’re forced to make a decision what to do about it,” Dr. Rosen said. “That’s where questions about the levels come in. And that’s a big problem. So what the panel’s saying is, don’t screen. ... This really gets to the heart of the issue, because we have no data that there’s anything about screening that allows us to improve quality of life. ... Screening is probably not worthwhile in any age group.”
Among the reader comments in this regard:
“So misguided. Don’t look because we don’t know what do to with data. That’s the message this article exposes. The recommendation is do nothing. But, doing nothing IS an action — not a default.” (Lisa Tracy)
“So now, you will not screen for vitamin D because you do not know what to do next? See a naturopathic doctor — we know what to do next!” (Dr. Joyce Roberson)
“Gee, how do we treat it? ... What to do? Sounds incompetent at minimum. I suspect it’s vital, easy, and inexpensive ... so hide it.” (Holly Kohley)
“Just because we do not know is not a rationale for not testing. The opposite should be done.” (Dr. JJ Gold)
Caters to Industry?
Many commentators intimated that pharma and/or insurance company considerations played a role in the recommendations. Their comments included the following:
“I have been under the impression people do routine checkups to verify there are no hidden problems. If only some testing is done, the probability of not finding a problem is huge. ... Preventive healthcare should be looking for something to prevent instead of waiting until they can cure it. Of course, it might come back to ‘follow the money.’ It is much more profitable to diagnose and treat than it is to prevent.” (Grace Kyser)
“The current irrational ‘recommendation’ gives insurance companies an excuse to deny ALL tests of vitamin D — even if the proper code is supplied. The result is — people suffer. This recommendation does harm!” (Dr JJ Gold)
“Essentially, they are saying let’s not screen ‘healthy’ individuals and ignore it altogether. Better to wait till they’re old, pregnant, or already sick and diagnosed with a disease. This is the problem with the healthcare in this country.” (Brittney Lesher)
“Until allopathic medicine stops waiting for severe symptoms to develop before even screening for potential health problems, the most expensive healthcare (aka, sick care) system in the world will continue to be content to focus on medical emergencies and ignore prevention. ...” (Dean Raffelock)
“Don’t test? Are you kidding me? Especially when people are supplementing? That is akin to taking a blood pressure medication without measuring blood pressures! ... Don’t test? Don’t supplement? ... I have only one explanation for such nonsense: Pharma lives off sick people, not healthy ones.” (Georg Schlomka)
On a somewhat conciliatory and pointed note, Dr Francesca Luna-Rudin commented, “I would like to remind all of my fellow physicians that recommendations should be regarded as just that, a ‘recommendation.’ As doctors, we can use guidelines and recommendations in our practice, but if a new one is presented that does not make sense or would lead to harm based on our education and training, then we are not bound to follow it!”
A version of this article first appeared on Medscape.com.
A recent report by this news organization of a vitamin D clinical practice guideline released by the Endocrine Society in June triggered an outpouring of objections in the comments section from doctors and other readers.
A society press release listed the key new recommendations on the use of vitamin D supplementation and screening to reduce disease risks in individuals without established indications for such treatment or testing:
- For healthy adults younger than 75, no supplementation at doses above the recommended dietary intakes.
- Populations that may benefit from higher doses include: children and adolescents 18 and younger to prevent rickets and to reduce risk for respiratory infection, individuals 75 and older to possibly lower mortality risk, “pregnant people” to potentially reduce various risks, and people with prediabetes to potentially reduce risk of progression.
- No routine testing for 25-hydroxyvitamin D levels because outcome-specific benefits based on those levels have not been identified (including screening in people with dark complexion or obesity).
- Based on insufficient evidence, the panel could not determine specific blood-level thresholds for 25-hydroxyvitamin D for adequacy or for target levels for disease prevention.
This news organization covered the guideline release and simultaneous presentation at the Endocrine Society annual meeting. In response to the coverage, more than 200 doctors and other readers expressed concerns about the guideline, and some said outright that they would not follow it (readers quoted below are identified by the usernames they registered with on the website).
One reader who posted as Dr. Joseph Destefano went so far as to call the guideline “dangerous” and “almost ... evil.” Ironically, some readers attacked this news organization, thinking that the coverage implied an endorsement, rather than a news report.
Ignores Potential Benefits
“They address issues dealing only with endocrinology and bone health for the most part,” Dr. Emilio Gonzalez wrote. “However, vitamin D insufficiency and deficiency are not rare, and they impact the treatment of autoimmune disorders, chronic pain control, immunosuppression, cancer prevention, cardiovascular health, etc. There is plenty of literature in this regard.”
“They make these claims as if quality studies contradicting their guidelines have not been out there for years,” Dr. Brian Batcheldor said. “What about the huge demographic with diseases that impact intestinal absorption, eg, Crohn’s and celiac disease, cystic fibrosis, and ulcerative colitis? What about the one in nine that now have autoimmune diseases still awaiting diagnosis? What about night workers or anyone with more restricted access to sun exposure? How about those whose cultural or religious dress code limit skin exposure?”
The latter group was also mentioned in a post from Dr. Eve Finkelstein who said, “They don’t take into account women who are totally covered for religious reasons. They have no skin other than part of their face exposed. It does not make sense not to supplement them. Ignoring women’s health needs seems to be the norm.”
“I don’t think they considered the oral health effects of vitamin D deficiency,” pointed out commenter Corie Lewis. “Excess dental calculus (tartar) from excess calcium/phosphate in saliva significantly increases an individual’s periodontal disease risks (gum disease), and low saliva calcium/phosphate increases dental caries (cavities) risks, which generally indicates an imbalance of the oral microbiome. Vitamin D can help create balance and reduce those oral health risks.”
Noted Kimberley Morris-Windisch, “Having worked in rheumatology and pain for most of my career, I have seen too many people benefit from correcting deficiency of vitamin D. To ignore this is to miss opportunities to improve patient health.” Furthermore, “I find it unlikely that it would only improve mortality after age 75. That makes no sense.”
“Also,” she added, “what is the number [needed] to harm? In my 25 years, I have seen vitamin D toxicity once and an excessively high level without symptoms one other time.”
“WHY? Just WHY?” lamented Anne Kinchen. “Low levels in pregnant women have long-term effects on the developing fetus — higher and earlier rates of osteopenia in female children, weaker immune systems overall. There are just SO many reasons to test. These guidelines for no testing are absurd!”
No Screening, No Need for Decision-Making?
Several readers questioned the society’s rationale for not screening, as expressed by session moderator Clifford J. Rosen, MD, director of Clinical and Translational Research and senior scientist at Maine Medical Center Research Institute, Scarborough, Maine.
“When clinicians measure vitamin D, then they’re forced to make a decision what to do about it,” Dr. Rosen said. “That’s where questions about the levels come in. And that’s a big problem. So what the panel’s saying is, don’t screen. ... This really gets to the heart of the issue, because we have no data that there’s anything about screening that allows us to improve quality of life. ... Screening is probably not worthwhile in any age group.”
Among the reader comments in this regard:
“So misguided. Don’t look because we don’t know what do to with data. That’s the message this article exposes. The recommendation is do nothing. But, doing nothing IS an action — not a default.” (Lisa Tracy)
“So now, you will not screen for vitamin D because you do not know what to do next? See a naturopathic doctor — we know what to do next!” (Dr. Joyce Roberson)
“Gee, how do we treat it? ... What to do? Sounds incompetent at minimum. I suspect it’s vital, easy, and inexpensive ... so hide it.” (Holly Kohley)
“Just because we do not know is not a rationale for not testing. The opposite should be done.” (Dr. JJ Gold)
Caters to Industry?
Many commentators intimated that pharma and/or insurance company considerations played a role in the recommendations. Their comments included the following:
“I have been under the impression people do routine checkups to verify there are no hidden problems. If only some testing is done, the probability of not finding a problem is huge. ... Preventive healthcare should be looking for something to prevent instead of waiting until they can cure it. Of course, it might come back to ‘follow the money.’ It is much more profitable to diagnose and treat than it is to prevent.” (Grace Kyser)
“The current irrational ‘recommendation’ gives insurance companies an excuse to deny ALL tests of vitamin D — even if the proper code is supplied. The result is — people suffer. This recommendation does harm!” (Dr JJ Gold)
“Essentially, they are saying let’s not screen ‘healthy’ individuals and ignore it altogether. Better to wait till they’re old, pregnant, or already sick and diagnosed with a disease. This is the problem with the healthcare in this country.” (Brittney Lesher)
“Until allopathic medicine stops waiting for severe symptoms to develop before even screening for potential health problems, the most expensive healthcare (aka, sick care) system in the world will continue to be content to focus on medical emergencies and ignore prevention. ...” (Dean Raffelock)
“Don’t test? Are you kidding me? Especially when people are supplementing? That is akin to taking a blood pressure medication without measuring blood pressures! ... Don’t test? Don’t supplement? ... I have only one explanation for such nonsense: Pharma lives off sick people, not healthy ones.” (Georg Schlomka)
On a somewhat conciliatory and pointed note, Dr Francesca Luna-Rudin commented, “I would like to remind all of my fellow physicians that recommendations should be regarded as just that, a ‘recommendation.’ As doctors, we can use guidelines and recommendations in our practice, but if a new one is presented that does not make sense or would lead to harm based on our education and training, then we are not bound to follow it!”
A version of this article first appeared on Medscape.com.

