User login
Diabetes Hub contains news and clinical review articles for physicians seeking the most up-to-date information on the rapidly evolving options for treating and preventing Type 2 Diabetes in at-risk patients. The Diabetes Hub is powered by Frontline Medical Communications.
Gastric bypass T2D benefit can fade over time
but the effect diminished over time, according to findings published Jan. 16 in JAMA.
In a randomized study of 113 obese patients with diabetes, about 50% of those who received gastric bypass in addition to lifestyle and medical management achieved the composite endpoint of a hemoglobin A1c (HbA1c) value of less than 7%, an LDL cholesterol level of less than 100 mg/dL, and a systolic blood pressure of less than 130 mm Hg after 1 year, reported Sayeed Ikramuddin, MD, FACS, of the department of surgery at the University of Minnesota, Minneapolis, and his coauthors. For comparison, just 16% in the lifestyle/medical management group achieved the endpoint (difference, 34%; 95% confidence interval, 14%-54%; P = .003) .
At 5 years’ follow-up, about 23% of patients in the gastric bypass group and 4% in the lifestyle/medical management group achieved the composite triple endpoint (difference, 19%; 95% CI, 4%-34%; P = .01), the authors reported.
The study included 120 patients at four sites in the United States and Taiwan, 7 of whom either died or were lost to follow-up before completion of the study. Participants had an HbA1c level of 8% or higher and a body mass index between 30 and 39.9 kg/m2.
Patients were randomized to receive either 2 years of lifestyle and medical management alone or in conjunction with standardized Roux-en-Y gastric bypass. During the first 2 years of intervention, patients were told to record weight, exercise, and food intake and were prescribed 325 minutes of physical activity per week. Participants also met regularly with a trained interventionist and an endocrinologist and were given pharmacologic therapy for hyperglycemia, cholesterol, and hypertension, the authors said. Aside from usual visits with a primary physician, all study interventions ceased after the initial 2-year period.
At baseline, the group that received only lifestyle/medical management had a mean BMI of 34.4 and HbA1c level of 9.6%, compared with a mean BMI of 34.9 and HbA1c level of 9.6% in the gastric bypass group.
Primary endpoint success rates decreased in both groups between years 1 and 3, going from 50% to 23% in the gastric bypass group and from 16% to 4% in the lifestyle/medical management group, but it remained stable from year 3 through year 5, Dr. Ikramuddin and his coauthors said in the report.
Overall, 26% of patients who had gastric bypass surgery during the first year achieved the triple endpoint at 5 years, compared with 8% of those who did not have surgery (difference, 18%; 95% CI, 6%-32%; P = .04).
The mean weight loss for participants in the gastric bypass group was 21.8% at 5 years, compared with 9.6% in the lifestyle/medical management group (difference, 12.2%; 95% CI, 8.9%-15.5%).
The results suggest that “gastric bypass provides significant benefit but with a smaller and less durable effect size than what is seen in the evaluation of glycemic control alone,” the authors wrote.
“Because the effect size diminished over 5 years, further follow-up is needed to understand the durability of the improvement,” Dr. Ikramuddin and his colleagues concluded.
Dr. Ikramuddin disclosed relationships with Novo Nordisk, USGI Medical, Medica, Metamodix, Medtronic, ReShape Medical, and EnteroMedics.
acssurgerynews@frontlinemedcom.com
SOURCE: Ikramuddin S. JAMA. 2018;319(3):266-278.
but the effect diminished over time, according to findings published Jan. 16 in JAMA.
In a randomized study of 113 obese patients with diabetes, about 50% of those who received gastric bypass in addition to lifestyle and medical management achieved the composite endpoint of a hemoglobin A1c (HbA1c) value of less than 7%, an LDL cholesterol level of less than 100 mg/dL, and a systolic blood pressure of less than 130 mm Hg after 1 year, reported Sayeed Ikramuddin, MD, FACS, of the department of surgery at the University of Minnesota, Minneapolis, and his coauthors. For comparison, just 16% in the lifestyle/medical management group achieved the endpoint (difference, 34%; 95% confidence interval, 14%-54%; P = .003) .
At 5 years’ follow-up, about 23% of patients in the gastric bypass group and 4% in the lifestyle/medical management group achieved the composite triple endpoint (difference, 19%; 95% CI, 4%-34%; P = .01), the authors reported.
The study included 120 patients at four sites in the United States and Taiwan, 7 of whom either died or were lost to follow-up before completion of the study. Participants had an HbA1c level of 8% or higher and a body mass index between 30 and 39.9 kg/m2.
Patients were randomized to receive either 2 years of lifestyle and medical management alone or in conjunction with standardized Roux-en-Y gastric bypass. During the first 2 years of intervention, patients were told to record weight, exercise, and food intake and were prescribed 325 minutes of physical activity per week. Participants also met regularly with a trained interventionist and an endocrinologist and were given pharmacologic therapy for hyperglycemia, cholesterol, and hypertension, the authors said. Aside from usual visits with a primary physician, all study interventions ceased after the initial 2-year period.
At baseline, the group that received only lifestyle/medical management had a mean BMI of 34.4 and HbA1c level of 9.6%, compared with a mean BMI of 34.9 and HbA1c level of 9.6% in the gastric bypass group.
Primary endpoint success rates decreased in both groups between years 1 and 3, going from 50% to 23% in the gastric bypass group and from 16% to 4% in the lifestyle/medical management group, but it remained stable from year 3 through year 5, Dr. Ikramuddin and his coauthors said in the report.
Overall, 26% of patients who had gastric bypass surgery during the first year achieved the triple endpoint at 5 years, compared with 8% of those who did not have surgery (difference, 18%; 95% CI, 6%-32%; P = .04).
The mean weight loss for participants in the gastric bypass group was 21.8% at 5 years, compared with 9.6% in the lifestyle/medical management group (difference, 12.2%; 95% CI, 8.9%-15.5%).
The results suggest that “gastric bypass provides significant benefit but with a smaller and less durable effect size than what is seen in the evaluation of glycemic control alone,” the authors wrote.
“Because the effect size diminished over 5 years, further follow-up is needed to understand the durability of the improvement,” Dr. Ikramuddin and his colleagues concluded.
Dr. Ikramuddin disclosed relationships with Novo Nordisk, USGI Medical, Medica, Metamodix, Medtronic, ReShape Medical, and EnteroMedics.
acssurgerynews@frontlinemedcom.com
SOURCE: Ikramuddin S. JAMA. 2018;319(3):266-278.
but the effect diminished over time, according to findings published Jan. 16 in JAMA.
In a randomized study of 113 obese patients with diabetes, about 50% of those who received gastric bypass in addition to lifestyle and medical management achieved the composite endpoint of a hemoglobin A1c (HbA1c) value of less than 7%, an LDL cholesterol level of less than 100 mg/dL, and a systolic blood pressure of less than 130 mm Hg after 1 year, reported Sayeed Ikramuddin, MD, FACS, of the department of surgery at the University of Minnesota, Minneapolis, and his coauthors. For comparison, just 16% in the lifestyle/medical management group achieved the endpoint (difference, 34%; 95% confidence interval, 14%-54%; P = .003) .
At 5 years’ follow-up, about 23% of patients in the gastric bypass group and 4% in the lifestyle/medical management group achieved the composite triple endpoint (difference, 19%; 95% CI, 4%-34%; P = .01), the authors reported.
The study included 120 patients at four sites in the United States and Taiwan, 7 of whom either died or were lost to follow-up before completion of the study. Participants had an HbA1c level of 8% or higher and a body mass index between 30 and 39.9 kg/m2.
Patients were randomized to receive either 2 years of lifestyle and medical management alone or in conjunction with standardized Roux-en-Y gastric bypass. During the first 2 years of intervention, patients were told to record weight, exercise, and food intake and were prescribed 325 minutes of physical activity per week. Participants also met regularly with a trained interventionist and an endocrinologist and were given pharmacologic therapy for hyperglycemia, cholesterol, and hypertension, the authors said. Aside from usual visits with a primary physician, all study interventions ceased after the initial 2-year period.
At baseline, the group that received only lifestyle/medical management had a mean BMI of 34.4 and HbA1c level of 9.6%, compared with a mean BMI of 34.9 and HbA1c level of 9.6% in the gastric bypass group.
Primary endpoint success rates decreased in both groups between years 1 and 3, going from 50% to 23% in the gastric bypass group and from 16% to 4% in the lifestyle/medical management group, but it remained stable from year 3 through year 5, Dr. Ikramuddin and his coauthors said in the report.
Overall, 26% of patients who had gastric bypass surgery during the first year achieved the triple endpoint at 5 years, compared with 8% of those who did not have surgery (difference, 18%; 95% CI, 6%-32%; P = .04).
The mean weight loss for participants in the gastric bypass group was 21.8% at 5 years, compared with 9.6% in the lifestyle/medical management group (difference, 12.2%; 95% CI, 8.9%-15.5%).
The results suggest that “gastric bypass provides significant benefit but with a smaller and less durable effect size than what is seen in the evaluation of glycemic control alone,” the authors wrote.
“Because the effect size diminished over 5 years, further follow-up is needed to understand the durability of the improvement,” Dr. Ikramuddin and his colleagues concluded.
Dr. Ikramuddin disclosed relationships with Novo Nordisk, USGI Medical, Medica, Metamodix, Medtronic, ReShape Medical, and EnteroMedics.
acssurgerynews@frontlinemedcom.com
SOURCE: Ikramuddin S. JAMA. 2018;319(3):266-278.
FROM JAMA
Key clinical point: Adding gastric bypass surgery to lifestyle and medical management improves diabetes outcomes – but with diminished effect over time.
Major finding: Primary endpoint success rates decreased in both groups between years 1 and 3, going from 50% to 23% in the gastric bypass group and from 16% to 4% in the lifestyle/medical management group.
Data source: A randomized study of 113 patients at four sites in the United States and Taiwan with a HbA1c level of 8% or higher and a BMI of 30-39.9 kg/m2.
Disclosures: Dr. Ikramuddin disclosed relationships with Novo Nordisk, USGI Medical, Medica, Metamodix, Medtronic, ReShape Medical, and EnteroMedics
SOURCE: Ikramuddin S et al. JAMA. 2018;319(3):266-278.
Insulin delivery devices now covered under Part D
Older Americans will now have access to insulin delivery devices under Part D of Medicare coverage, according to guidance issued by the Centers for Medicare & Medicaid Services (CMS). The CMS guidance clarified that devices not previously covered under Medicare Part B will be covered under Part D of the prescription drug program. As a result, older Americans will now have access to a wider range of insulin delivery devices.
Insulin delivery devices help patients manage blood sugar levels effectively. The devices prevent dangerous blood sugar fluctuations that can lead to complications like hypoglycemia.
In the guidance, the CMS wrote: “With the introduction of new insulin delivery devices to the market, questions have arisen about Part D coverage for these products. Specifically, we have been asked whether newer insulin delivery devices that are not covered under Medicare Part B meet the Part D definition of ‘medical supplies associated with the injection of insulin. … The examples that were previously provided were never intended to be an exhaustive list of products that could be covered under Part D. Instead, they represented our understanding of the types of medical supplies associated with the injection of insulin that were available at the time.”
Since then, new delivery devices have been introduced to market “in the form of both mechanical and electronic insulin pumps” that are not covered under the Medicare Part B durable medical equipment (DME) benefit.
“We expect that technology will continue to advance and that ‘medical supplies associated with the injection of insulin’ will become significantly more sophisticated,” wrote the CMS. “As new products become available, Part D sponsors may evaluate these products for formulary placement and medical necessity and, subject to Part D coverage determination and appeals requirements, allow access and restrict use accordingly.”
According to the guidance, Part D will cover supplies “that are alternatives to insulin syringes,” and the CMS will not require insurers who offer Part D plan coverage to include these on their formularies. If these alternatives are included on formularies, sponsors may use utilization management criteria for the products.
In a statement praising the CMS’s decision, the Endocrine Society wrote: “This opens the door for older Americans to gain coverage for devices such as the Omnipod insulin management system, a popular insulin pump system. Until the new guidance was issued, Omnipod was the only FDA [Food and Drug Administration]–approved insulin pump system not covered by Medicare. Previously, people with diabetes who qualified for Medicare at age 65 had to pay out of pocket to continue using the Omnipod, and many lost access to the device.”
Robert Lash, MD, chief professional and clinical affairs officer for the Endocrine Society, said in an interview that the new CMS guidance "gives physicians and people with diabetes access to a wider range of technology options, since some people with type 1 diabetes prefer the Omnipod’s tubing-free design because it makes it easier to participate in sports and safer to work in certain environments.
“Before this guidance was issued, those patients had to switch pumps or revert to insulin injections when they turned 65 years old. We are pleased this guidance will open the door to greater choice” for patients, said Dr. Lash.
The CMS’s decision on insulin delivery devices follows a decision last year to cover continuous glucose monitors (CGMs) through Medicare. Last week, the CMS also announced it will provide coverage for the Abbott Freestyle Libre CGM, a welcome move for patients seeking additional choices.
This article was revised 1/18/18.
Older Americans will now have access to insulin delivery devices under Part D of Medicare coverage, according to guidance issued by the Centers for Medicare & Medicaid Services (CMS). The CMS guidance clarified that devices not previously covered under Medicare Part B will be covered under Part D of the prescription drug program. As a result, older Americans will now have access to a wider range of insulin delivery devices.
Insulin delivery devices help patients manage blood sugar levels effectively. The devices prevent dangerous blood sugar fluctuations that can lead to complications like hypoglycemia.
In the guidance, the CMS wrote: “With the introduction of new insulin delivery devices to the market, questions have arisen about Part D coverage for these products. Specifically, we have been asked whether newer insulin delivery devices that are not covered under Medicare Part B meet the Part D definition of ‘medical supplies associated with the injection of insulin. … The examples that were previously provided were never intended to be an exhaustive list of products that could be covered under Part D. Instead, they represented our understanding of the types of medical supplies associated with the injection of insulin that were available at the time.”
Since then, new delivery devices have been introduced to market “in the form of both mechanical and electronic insulin pumps” that are not covered under the Medicare Part B durable medical equipment (DME) benefit.
“We expect that technology will continue to advance and that ‘medical supplies associated with the injection of insulin’ will become significantly more sophisticated,” wrote the CMS. “As new products become available, Part D sponsors may evaluate these products for formulary placement and medical necessity and, subject to Part D coverage determination and appeals requirements, allow access and restrict use accordingly.”
According to the guidance, Part D will cover supplies “that are alternatives to insulin syringes,” and the CMS will not require insurers who offer Part D plan coverage to include these on their formularies. If these alternatives are included on formularies, sponsors may use utilization management criteria for the products.
In a statement praising the CMS’s decision, the Endocrine Society wrote: “This opens the door for older Americans to gain coverage for devices such as the Omnipod insulin management system, a popular insulin pump system. Until the new guidance was issued, Omnipod was the only FDA [Food and Drug Administration]–approved insulin pump system not covered by Medicare. Previously, people with diabetes who qualified for Medicare at age 65 had to pay out of pocket to continue using the Omnipod, and many lost access to the device.”
Robert Lash, MD, chief professional and clinical affairs officer for the Endocrine Society, said in an interview that the new CMS guidance "gives physicians and people with diabetes access to a wider range of technology options, since some people with type 1 diabetes prefer the Omnipod’s tubing-free design because it makes it easier to participate in sports and safer to work in certain environments.
“Before this guidance was issued, those patients had to switch pumps or revert to insulin injections when they turned 65 years old. We are pleased this guidance will open the door to greater choice” for patients, said Dr. Lash.
The CMS’s decision on insulin delivery devices follows a decision last year to cover continuous glucose monitors (CGMs) through Medicare. Last week, the CMS also announced it will provide coverage for the Abbott Freestyle Libre CGM, a welcome move for patients seeking additional choices.
This article was revised 1/18/18.
Older Americans will now have access to insulin delivery devices under Part D of Medicare coverage, according to guidance issued by the Centers for Medicare & Medicaid Services (CMS). The CMS guidance clarified that devices not previously covered under Medicare Part B will be covered under Part D of the prescription drug program. As a result, older Americans will now have access to a wider range of insulin delivery devices.
Insulin delivery devices help patients manage blood sugar levels effectively. The devices prevent dangerous blood sugar fluctuations that can lead to complications like hypoglycemia.
In the guidance, the CMS wrote: “With the introduction of new insulin delivery devices to the market, questions have arisen about Part D coverage for these products. Specifically, we have been asked whether newer insulin delivery devices that are not covered under Medicare Part B meet the Part D definition of ‘medical supplies associated with the injection of insulin. … The examples that were previously provided were never intended to be an exhaustive list of products that could be covered under Part D. Instead, they represented our understanding of the types of medical supplies associated with the injection of insulin that were available at the time.”
Since then, new delivery devices have been introduced to market “in the form of both mechanical and electronic insulin pumps” that are not covered under the Medicare Part B durable medical equipment (DME) benefit.
“We expect that technology will continue to advance and that ‘medical supplies associated with the injection of insulin’ will become significantly more sophisticated,” wrote the CMS. “As new products become available, Part D sponsors may evaluate these products for formulary placement and medical necessity and, subject to Part D coverage determination and appeals requirements, allow access and restrict use accordingly.”
According to the guidance, Part D will cover supplies “that are alternatives to insulin syringes,” and the CMS will not require insurers who offer Part D plan coverage to include these on their formularies. If these alternatives are included on formularies, sponsors may use utilization management criteria for the products.
In a statement praising the CMS’s decision, the Endocrine Society wrote: “This opens the door for older Americans to gain coverage for devices such as the Omnipod insulin management system, a popular insulin pump system. Until the new guidance was issued, Omnipod was the only FDA [Food and Drug Administration]–approved insulin pump system not covered by Medicare. Previously, people with diabetes who qualified for Medicare at age 65 had to pay out of pocket to continue using the Omnipod, and many lost access to the device.”
Robert Lash, MD, chief professional and clinical affairs officer for the Endocrine Society, said in an interview that the new CMS guidance "gives physicians and people with diabetes access to a wider range of technology options, since some people with type 1 diabetes prefer the Omnipod’s tubing-free design because it makes it easier to participate in sports and safer to work in certain environments.
“Before this guidance was issued, those patients had to switch pumps or revert to insulin injections when they turned 65 years old. We are pleased this guidance will open the door to greater choice” for patients, said Dr. Lash.
The CMS’s decision on insulin delivery devices follows a decision last year to cover continuous glucose monitors (CGMs) through Medicare. Last week, the CMS also announced it will provide coverage for the Abbott Freestyle Libre CGM, a welcome move for patients seeking additional choices.
This article was revised 1/18/18.
Breastfeeding lowers later diabetes risk in women
Breastfeeding may reduce a woman’s risk of developing diabetes, with a prospective cohort study showing a strong, inverse association between lactation duration and risk of diabetes.
In a report published in the Jan. 16 online edition of JAMA Internal Medicine, researchers analyzed data from the Coronary Artery Risk Development Study in Young Adults (CARDIA), which followed 1,238 women aged 18-30 for 30 years, with multiple assessments of glucose tolerance over the course of the study.
Women who breastfed for 6-12 months had a 48% reduction in the risk of diabetes (95% CI, 0.31-0.87), and those who breastfed for up to 6 months had a 25% lower risk (95% CI, 0.51-1.09), with the trend being significant.
In women with a history of gestational diabetes, those who did not breastfeed at all had a 2.08% higher excess risk of incident diabetes per year, compared with women who breastfed for at least 12 months. The increase in excess risk for the same comparison in women without a history of gestational diabetes was 0.48% per year.
Erica P. Gunderson, PhD, of Kaiser Permanente Northern California, Oakland, and her coauthors noted that previous meta-analyses of the effect of lactation on diabetes incidence or prevalence pointed to protective summary estimates of 9%-11% per year of lactation.
“Lactating women have lower circulating glucose in both fasting and post absorptive states, as well as lower insulin secretion, despite increased glucose production rates,” the authors wrote. “About 50 g of glucose per 24 hours is diverted into the mammary gland for milk synthesis via non–insulin mediated pathways.”
Studies in mice have also suggested that lactating animals have greater pancreatic beta-cell proliferation.
While the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists recommend breastfeeding for 1 year, only 55% of women in the United States are still breastfeeding at 6 months and 33% are still breastfeeding at 1 year after birth. Black women are also less likely to breastfeed, regardless of socioeconomic status or body size.
“Lactation is a natural biological process with the enormous potential to provide long-term benefits to maternal health, but has been underappreciated as a potential key strategy for early primary prevention of metabolic diseases in women across the childbearing years and beyond.”
The study and analyses were supported by the National Institute of Diabetes and Digestive and Kidney Diseases, and two authors declared funding from pharmaceutical companies.
SOURCE: JAMA Intern Med. 2016 Jan 16. doi: 10.1001/jamainternmed.2017.7978.
Breastfeeding may reduce a woman’s risk of developing diabetes, with a prospective cohort study showing a strong, inverse association between lactation duration and risk of diabetes.
In a report published in the Jan. 16 online edition of JAMA Internal Medicine, researchers analyzed data from the Coronary Artery Risk Development Study in Young Adults (CARDIA), which followed 1,238 women aged 18-30 for 30 years, with multiple assessments of glucose tolerance over the course of the study.
Women who breastfed for 6-12 months had a 48% reduction in the risk of diabetes (95% CI, 0.31-0.87), and those who breastfed for up to 6 months had a 25% lower risk (95% CI, 0.51-1.09), with the trend being significant.
In women with a history of gestational diabetes, those who did not breastfeed at all had a 2.08% higher excess risk of incident diabetes per year, compared with women who breastfed for at least 12 months. The increase in excess risk for the same comparison in women without a history of gestational diabetes was 0.48% per year.
Erica P. Gunderson, PhD, of Kaiser Permanente Northern California, Oakland, and her coauthors noted that previous meta-analyses of the effect of lactation on diabetes incidence or prevalence pointed to protective summary estimates of 9%-11% per year of lactation.
“Lactating women have lower circulating glucose in both fasting and post absorptive states, as well as lower insulin secretion, despite increased glucose production rates,” the authors wrote. “About 50 g of glucose per 24 hours is diverted into the mammary gland for milk synthesis via non–insulin mediated pathways.”
Studies in mice have also suggested that lactating animals have greater pancreatic beta-cell proliferation.
While the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists recommend breastfeeding for 1 year, only 55% of women in the United States are still breastfeeding at 6 months and 33% are still breastfeeding at 1 year after birth. Black women are also less likely to breastfeed, regardless of socioeconomic status or body size.
“Lactation is a natural biological process with the enormous potential to provide long-term benefits to maternal health, but has been underappreciated as a potential key strategy for early primary prevention of metabolic diseases in women across the childbearing years and beyond.”
The study and analyses were supported by the National Institute of Diabetes and Digestive and Kidney Diseases, and two authors declared funding from pharmaceutical companies.
SOURCE: JAMA Intern Med. 2016 Jan 16. doi: 10.1001/jamainternmed.2017.7978.
Breastfeeding may reduce a woman’s risk of developing diabetes, with a prospective cohort study showing a strong, inverse association between lactation duration and risk of diabetes.
In a report published in the Jan. 16 online edition of JAMA Internal Medicine, researchers analyzed data from the Coronary Artery Risk Development Study in Young Adults (CARDIA), which followed 1,238 women aged 18-30 for 30 years, with multiple assessments of glucose tolerance over the course of the study.
Women who breastfed for 6-12 months had a 48% reduction in the risk of diabetes (95% CI, 0.31-0.87), and those who breastfed for up to 6 months had a 25% lower risk (95% CI, 0.51-1.09), with the trend being significant.
In women with a history of gestational diabetes, those who did not breastfeed at all had a 2.08% higher excess risk of incident diabetes per year, compared with women who breastfed for at least 12 months. The increase in excess risk for the same comparison in women without a history of gestational diabetes was 0.48% per year.
Erica P. Gunderson, PhD, of Kaiser Permanente Northern California, Oakland, and her coauthors noted that previous meta-analyses of the effect of lactation on diabetes incidence or prevalence pointed to protective summary estimates of 9%-11% per year of lactation.
“Lactating women have lower circulating glucose in both fasting and post absorptive states, as well as lower insulin secretion, despite increased glucose production rates,” the authors wrote. “About 50 g of glucose per 24 hours is diverted into the mammary gland for milk synthesis via non–insulin mediated pathways.”
Studies in mice have also suggested that lactating animals have greater pancreatic beta-cell proliferation.
While the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists recommend breastfeeding for 1 year, only 55% of women in the United States are still breastfeeding at 6 months and 33% are still breastfeeding at 1 year after birth. Black women are also less likely to breastfeed, regardless of socioeconomic status or body size.
“Lactation is a natural biological process with the enormous potential to provide long-term benefits to maternal health, but has been underappreciated as a potential key strategy for early primary prevention of metabolic diseases in women across the childbearing years and beyond.”
The study and analyses were supported by the National Institute of Diabetes and Digestive and Kidney Diseases, and two authors declared funding from pharmaceutical companies.
SOURCE: JAMA Intern Med. 2016 Jan 16. doi: 10.1001/jamainternmed.2017.7978.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Duration of breastfeeding is inversely associated with risk of developing diabetes.
Major finding: Women who breastfeed for 12 months or more have a 47% lower risk of developing diabetes compared with women who do not breastfeed at all.
Data source: Analysis of data from the CARDIA population-based prospective cohort study in 1,238 women.
Disclosures: The study and analyses were supported by the National Institute of Diabetes and Digestive and Kidney Diseases, and two authors declared funding from pharmaceutical companies.
Source: JAMA Intern Med. 2016 Jan 16. doi: 10.1001/jamainternmed.2017.7978.
Bariatric surgery comes with some risk of complications
that should acknowledged by clinicians and understood by patients, a large cohort study has shown.
Gunn Signe Jakobsen, MD, of Vestfold Hospital Trust, Tønsberg, Norway, and her colleagues wrote in an article published in JAMA, “Few studies report long-term complication rates. ... No large-scale clinical practice–based study has compared the long-term association of bariatric surgery and specialized medical obesity treatment with obesity-related somatic and mental comorbidities, nor the irrespective complication rates.”
The investigators compared outcomes from 932 patients who underwent bariatric surgery and 956 who underwent specialized medical treatment that involved either individual or group lifestyle intervention programs. The study population included 1,249 women and 639 men with an average age of 44 years and an average baseline body mass index of 44 kg/m2.
The surgery patients were more likely than the medical treatment patients to have hypertension remission (absolute risk 32% vs. 12%, respectively), and less likely to develop new-onset hypertension (absolute risk 4% vs. 12%, respectively). Diabetes remission was significantly higher among surgery patients, compared with medical treatment patients (58% vs. 13%) as was the likelihood of dyslipidemia remission (43% vs. 13%). Surgery patients also were less likely to develop new-onset diabetes or dyslipidemia than the medical treatment patients.
However, more patients who underwent bariatric surgery had low ferritin levels, compared with the medical treatment patients (26% vs. 12%). The surgery patients were significantly more likely than the medical treatment patients to develop new-onset depression (adjusted relative risk, 1.5; 95% confidence interval, 1.4-1.7), anxiety and sleep disorders (aRR, 1.3; 95% CI, 1.2-1.5), and treatment with opioids (aRR, 1.3; 95% CI, 1.2-1.4). In addition, bariatric patients were more likely to have at least one additional gastrointestinal surgical procedure (aRR, 2.0; 95% CI, 1.7-2.4), an operation for intestinal obstruction (aRR, 10.5; 95% CI, 5.1-21.5), abdominal pain (aRR, 1.9; 95% CI, 1.6-2.3), and gastroduodenal ulcers (aRR, 3.4; 95% CI 2.0-5.6).
The study was limited by several factors, including selection bias of younger, heavier patients in the bariatric surgery group, the lack of data on actual weight loss, incomplete laboratory data, and a relatively homogeneous white population, the researchers noted. However, the nearly 100% follow-up over approximately 6 years adds to the strength of the findings, which suggest that “the risk for complications should be considered in the decision-making process,” for obese patients considering bariatric surgery, they said.
Dr. Jakobsen was supported by the Vestfold Hospital Trust, with no financial conflicts to disclose.
SOURCE: Jakobsen G et al. JAMA. 2018 Jan 16;319(3):291-301.
that should acknowledged by clinicians and understood by patients, a large cohort study has shown.
Gunn Signe Jakobsen, MD, of Vestfold Hospital Trust, Tønsberg, Norway, and her colleagues wrote in an article published in JAMA, “Few studies report long-term complication rates. ... No large-scale clinical practice–based study has compared the long-term association of bariatric surgery and specialized medical obesity treatment with obesity-related somatic and mental comorbidities, nor the irrespective complication rates.”
The investigators compared outcomes from 932 patients who underwent bariatric surgery and 956 who underwent specialized medical treatment that involved either individual or group lifestyle intervention programs. The study population included 1,249 women and 639 men with an average age of 44 years and an average baseline body mass index of 44 kg/m2.
The surgery patients were more likely than the medical treatment patients to have hypertension remission (absolute risk 32% vs. 12%, respectively), and less likely to develop new-onset hypertension (absolute risk 4% vs. 12%, respectively). Diabetes remission was significantly higher among surgery patients, compared with medical treatment patients (58% vs. 13%) as was the likelihood of dyslipidemia remission (43% vs. 13%). Surgery patients also were less likely to develop new-onset diabetes or dyslipidemia than the medical treatment patients.
However, more patients who underwent bariatric surgery had low ferritin levels, compared with the medical treatment patients (26% vs. 12%). The surgery patients were significantly more likely than the medical treatment patients to develop new-onset depression (adjusted relative risk, 1.5; 95% confidence interval, 1.4-1.7), anxiety and sleep disorders (aRR, 1.3; 95% CI, 1.2-1.5), and treatment with opioids (aRR, 1.3; 95% CI, 1.2-1.4). In addition, bariatric patients were more likely to have at least one additional gastrointestinal surgical procedure (aRR, 2.0; 95% CI, 1.7-2.4), an operation for intestinal obstruction (aRR, 10.5; 95% CI, 5.1-21.5), abdominal pain (aRR, 1.9; 95% CI, 1.6-2.3), and gastroduodenal ulcers (aRR, 3.4; 95% CI 2.0-5.6).
The study was limited by several factors, including selection bias of younger, heavier patients in the bariatric surgery group, the lack of data on actual weight loss, incomplete laboratory data, and a relatively homogeneous white population, the researchers noted. However, the nearly 100% follow-up over approximately 6 years adds to the strength of the findings, which suggest that “the risk for complications should be considered in the decision-making process,” for obese patients considering bariatric surgery, they said.
Dr. Jakobsen was supported by the Vestfold Hospital Trust, with no financial conflicts to disclose.
SOURCE: Jakobsen G et al. JAMA. 2018 Jan 16;319(3):291-301.
that should acknowledged by clinicians and understood by patients, a large cohort study has shown.
Gunn Signe Jakobsen, MD, of Vestfold Hospital Trust, Tønsberg, Norway, and her colleagues wrote in an article published in JAMA, “Few studies report long-term complication rates. ... No large-scale clinical practice–based study has compared the long-term association of bariatric surgery and specialized medical obesity treatment with obesity-related somatic and mental comorbidities, nor the irrespective complication rates.”
The investigators compared outcomes from 932 patients who underwent bariatric surgery and 956 who underwent specialized medical treatment that involved either individual or group lifestyle intervention programs. The study population included 1,249 women and 639 men with an average age of 44 years and an average baseline body mass index of 44 kg/m2.
The surgery patients were more likely than the medical treatment patients to have hypertension remission (absolute risk 32% vs. 12%, respectively), and less likely to develop new-onset hypertension (absolute risk 4% vs. 12%, respectively). Diabetes remission was significantly higher among surgery patients, compared with medical treatment patients (58% vs. 13%) as was the likelihood of dyslipidemia remission (43% vs. 13%). Surgery patients also were less likely to develop new-onset diabetes or dyslipidemia than the medical treatment patients.
However, more patients who underwent bariatric surgery had low ferritin levels, compared with the medical treatment patients (26% vs. 12%). The surgery patients were significantly more likely than the medical treatment patients to develop new-onset depression (adjusted relative risk, 1.5; 95% confidence interval, 1.4-1.7), anxiety and sleep disorders (aRR, 1.3; 95% CI, 1.2-1.5), and treatment with opioids (aRR, 1.3; 95% CI, 1.2-1.4). In addition, bariatric patients were more likely to have at least one additional gastrointestinal surgical procedure (aRR, 2.0; 95% CI, 1.7-2.4), an operation for intestinal obstruction (aRR, 10.5; 95% CI, 5.1-21.5), abdominal pain (aRR, 1.9; 95% CI, 1.6-2.3), and gastroduodenal ulcers (aRR, 3.4; 95% CI 2.0-5.6).
The study was limited by several factors, including selection bias of younger, heavier patients in the bariatric surgery group, the lack of data on actual weight loss, incomplete laboratory data, and a relatively homogeneous white population, the researchers noted. However, the nearly 100% follow-up over approximately 6 years adds to the strength of the findings, which suggest that “the risk for complications should be considered in the decision-making process,” for obese patients considering bariatric surgery, they said.
Dr. Jakobsen was supported by the Vestfold Hospital Trust, with no financial conflicts to disclose.
SOURCE: Jakobsen G et al. JAMA. 2018 Jan 16;319(3):291-301.
FROM JAMA
Key clinical point: Bariatric surgery was associated with reduced hypertension but more complications, including iron deficiency and ulcers.
Major finding: Obese adults who had bariatric surgery were at greater risk for new-onset depression (aRR, 1.5), anxiety and sleep disorders (aRR, 1.3), and ulcers (aRR 3.4).
Study details: A cohort study of 1,888 adults treated with bariatric surgery or medical therapy.
Disclosures: Dr. Jakobsen was supported by the Vestfold Hospital Trust, with no financial conflicts to disclose.
Source: Jakobsen G et al. JAMA. 2018 Jan 16;319(3):291-301.
Shedding light on shift work’s influence on cardiometabolic risk
LOS ANGELES – Current and previous night workers had significantly increased levels of hemoglobin A1c, compared with diurnal workers, preliminary results from an ongoing study showed. The finding sheds further insight into the link between environmental light, circadian rhythms, and metabolic disorders.
“To date, observational studies on bright light have revealed that evening bright light is associated with increased appetite and that bedroom light intensity is correlated with obesity,” Massimo Federici, MD, said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “It’s also been reported that artificial light is correlated with type 2 diabetes in the home setting and that daytime light exposure is positively correlated with body mass index. However, no studies have directly investigated the effect of acute light on human glucose metabolism.”
Although few metabolic intervention studies using light have been done, Dr. Federici mentioned three of note. One, in patients with seasonal affective disorder and type 2 diabetes, showed reduced insulin requirements after light therapy (Lancet. 1992;339[8800]:1065-6). Another, a short-term study of 25 obese subjects treated with 5,000 lux bright light therapy in addition to exercise, showed reduced body fat after 6 weeks (Obesity 2007; 15[7]:1749-57). A third, in 34 obese subjects who were exposed to 1,300 lux bright light every morning for 3 weeks, showed a small but significant reduction in fat mass (Obes Facts 2013;6:28-38).
As part of an ongoing project known as EuRhythDia, researchers including Dr. Federici set out to identify metabolic and molecular variables associated with shift work, and to test the effect of a lifestyle intervention that comprised light exposure, exercise, and melatonin. He presented unpublished results from one aspect of the trial: a cross-sectional analysis of 273 nurses divided into one of three groups: 64 diurnal workers (DW), 111 active night shift workers (aNW), and 98 prior night shift workers (pNW). Those with diabetes or taking oral antidiabetic drugs were excluded from the study.
The analysis showed that nurses in the pNW group were significantly older, at a mean of 39.7 years, than those in the DW group, whose mean age was 37 years, and the aNW group, who averaged 36.1 years. Those in the pNW group also had a significantly greater body mass index, compared with their counterparts in the aNW and DW groups (a mean of 25.7 kg/m2, vs. 24.8 and 23.7, respectively) as well has a higher mean waist circumference (a mean of 87.2 cm, vs. 84.6 cm and 82 cm).
The mean HbA1c was higher in the nurses with prior and active night shift work, at 5.3% each, than in the diurnal workers (5.1%, P less than .001).
When Pittsburgh Sleep Quality Index scores were used to evaluate sleep quality independent of work status, more than half of the study subjects (163) were classified as being “good sleepers,” while 110 were considered to be “bad sleepers.” Bad sleepers had a significantly higher mean HbA1c level compared with good sleepers (5.3% vs. 5.2%). Bad sleepers also had higher levels of HDL cholesterol (a mean of 60.8 mg/dL vs. 56.3 mg/dL).
Dr. Federici highlighted preliminary findings from a study of 32 aNW subjects who were assigned to treatment with warm light therapy at 1,000 lux for 30 minutes at 30 cm every morning for 3 months. They observed a mild improvement in the area under the curve of the oral glucose tolerance test at 24 weeks (12 weeks’ washout after 12 weeks of light therapy). “However, the effect was obtained not at the end of the intervention but at the end of the washout period,” he said.
He called for more studies going forward that take into account the effect of seasons as well as the effects of diet and exercise.
Dr. Federici disclosed that he receives editorial fees from Springer Nature group.
LOS ANGELES – Current and previous night workers had significantly increased levels of hemoglobin A1c, compared with diurnal workers, preliminary results from an ongoing study showed. The finding sheds further insight into the link between environmental light, circadian rhythms, and metabolic disorders.
“To date, observational studies on bright light have revealed that evening bright light is associated with increased appetite and that bedroom light intensity is correlated with obesity,” Massimo Federici, MD, said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “It’s also been reported that artificial light is correlated with type 2 diabetes in the home setting and that daytime light exposure is positively correlated with body mass index. However, no studies have directly investigated the effect of acute light on human glucose metabolism.”
Although few metabolic intervention studies using light have been done, Dr. Federici mentioned three of note. One, in patients with seasonal affective disorder and type 2 diabetes, showed reduced insulin requirements after light therapy (Lancet. 1992;339[8800]:1065-6). Another, a short-term study of 25 obese subjects treated with 5,000 lux bright light therapy in addition to exercise, showed reduced body fat after 6 weeks (Obesity 2007; 15[7]:1749-57). A third, in 34 obese subjects who were exposed to 1,300 lux bright light every morning for 3 weeks, showed a small but significant reduction in fat mass (Obes Facts 2013;6:28-38).
As part of an ongoing project known as EuRhythDia, researchers including Dr. Federici set out to identify metabolic and molecular variables associated with shift work, and to test the effect of a lifestyle intervention that comprised light exposure, exercise, and melatonin. He presented unpublished results from one aspect of the trial: a cross-sectional analysis of 273 nurses divided into one of three groups: 64 diurnal workers (DW), 111 active night shift workers (aNW), and 98 prior night shift workers (pNW). Those with diabetes or taking oral antidiabetic drugs were excluded from the study.
The analysis showed that nurses in the pNW group were significantly older, at a mean of 39.7 years, than those in the DW group, whose mean age was 37 years, and the aNW group, who averaged 36.1 years. Those in the pNW group also had a significantly greater body mass index, compared with their counterparts in the aNW and DW groups (a mean of 25.7 kg/m2, vs. 24.8 and 23.7, respectively) as well has a higher mean waist circumference (a mean of 87.2 cm, vs. 84.6 cm and 82 cm).
The mean HbA1c was higher in the nurses with prior and active night shift work, at 5.3% each, than in the diurnal workers (5.1%, P less than .001).
When Pittsburgh Sleep Quality Index scores were used to evaluate sleep quality independent of work status, more than half of the study subjects (163) were classified as being “good sleepers,” while 110 were considered to be “bad sleepers.” Bad sleepers had a significantly higher mean HbA1c level compared with good sleepers (5.3% vs. 5.2%). Bad sleepers also had higher levels of HDL cholesterol (a mean of 60.8 mg/dL vs. 56.3 mg/dL).
Dr. Federici highlighted preliminary findings from a study of 32 aNW subjects who were assigned to treatment with warm light therapy at 1,000 lux for 30 minutes at 30 cm every morning for 3 months. They observed a mild improvement in the area under the curve of the oral glucose tolerance test at 24 weeks (12 weeks’ washout after 12 weeks of light therapy). “However, the effect was obtained not at the end of the intervention but at the end of the washout period,” he said.
He called for more studies going forward that take into account the effect of seasons as well as the effects of diet and exercise.
Dr. Federici disclosed that he receives editorial fees from Springer Nature group.
LOS ANGELES – Current and previous night workers had significantly increased levels of hemoglobin A1c, compared with diurnal workers, preliminary results from an ongoing study showed. The finding sheds further insight into the link between environmental light, circadian rhythms, and metabolic disorders.
“To date, observational studies on bright light have revealed that evening bright light is associated with increased appetite and that bedroom light intensity is correlated with obesity,” Massimo Federici, MD, said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “It’s also been reported that artificial light is correlated with type 2 diabetes in the home setting and that daytime light exposure is positively correlated with body mass index. However, no studies have directly investigated the effect of acute light on human glucose metabolism.”
Although few metabolic intervention studies using light have been done, Dr. Federici mentioned three of note. One, in patients with seasonal affective disorder and type 2 diabetes, showed reduced insulin requirements after light therapy (Lancet. 1992;339[8800]:1065-6). Another, a short-term study of 25 obese subjects treated with 5,000 lux bright light therapy in addition to exercise, showed reduced body fat after 6 weeks (Obesity 2007; 15[7]:1749-57). A third, in 34 obese subjects who were exposed to 1,300 lux bright light every morning for 3 weeks, showed a small but significant reduction in fat mass (Obes Facts 2013;6:28-38).
As part of an ongoing project known as EuRhythDia, researchers including Dr. Federici set out to identify metabolic and molecular variables associated with shift work, and to test the effect of a lifestyle intervention that comprised light exposure, exercise, and melatonin. He presented unpublished results from one aspect of the trial: a cross-sectional analysis of 273 nurses divided into one of three groups: 64 diurnal workers (DW), 111 active night shift workers (aNW), and 98 prior night shift workers (pNW). Those with diabetes or taking oral antidiabetic drugs were excluded from the study.
The analysis showed that nurses in the pNW group were significantly older, at a mean of 39.7 years, than those in the DW group, whose mean age was 37 years, and the aNW group, who averaged 36.1 years. Those in the pNW group also had a significantly greater body mass index, compared with their counterparts in the aNW and DW groups (a mean of 25.7 kg/m2, vs. 24.8 and 23.7, respectively) as well has a higher mean waist circumference (a mean of 87.2 cm, vs. 84.6 cm and 82 cm).
The mean HbA1c was higher in the nurses with prior and active night shift work, at 5.3% each, than in the diurnal workers (5.1%, P less than .001).
When Pittsburgh Sleep Quality Index scores were used to evaluate sleep quality independent of work status, more than half of the study subjects (163) were classified as being “good sleepers,” while 110 were considered to be “bad sleepers.” Bad sleepers had a significantly higher mean HbA1c level compared with good sleepers (5.3% vs. 5.2%). Bad sleepers also had higher levels of HDL cholesterol (a mean of 60.8 mg/dL vs. 56.3 mg/dL).
Dr. Federici highlighted preliminary findings from a study of 32 aNW subjects who were assigned to treatment with warm light therapy at 1,000 lux for 30 minutes at 30 cm every morning for 3 months. They observed a mild improvement in the area under the curve of the oral glucose tolerance test at 24 weeks (12 weeks’ washout after 12 weeks of light therapy). “However, the effect was obtained not at the end of the intervention but at the end of the washout period,” he said.
He called for more studies going forward that take into account the effect of seasons as well as the effects of diet and exercise.
Dr. Federici disclosed that he receives editorial fees from Springer Nature group.
EXPERT ANALYSIS FROM WCIRDC 2017
Cars that recognize hypoglycemia? Maybe soon
SAN DIEGO – When researchers at the University of Nebraska placed sensors in the cars of patients with type 1 diabetes, they found something interesting: About 3.4% of the time, the patients were driving with a blood glucose below 70 mg/dL.
Almost 10% of the time, it was above 300 mg/dL, and both hyper and hypoglycemia, but especially hypoglycemia, corresponded with erratic driving, especially at highway speeds.
The finding explains why patients taking insulin for type 1 diabetes have a 12%-19% higher risk of crashing their cars, compared with the general population. But in a larger sense, the study speaks to a new possibility as cars become smarter: monitoring drivers’ mental states and pulling over to the side of the road or otherwise taking control if there’s a problem.
The “results show that vehicle sensor and physiologic data can be successfully linked to quantify individual driver performance and behavior in drivers with metabolic disorders that affect brain function. The work we are doing could be used to tune the algorithm that drive these automated vehicles. I think this is a very important area of study,” said senior investigator Matthew Rizzo, MD, chair of the university’s department of neurological sciences in Omaha.
Participants had the devices in their cars for a month, during which time the diabetes patients were also on continuous, 24-hour blood glucose monitoring. The investigators then synched the car data with the glucose readings, and compared it with the data from the controls’ cars. In all, the system recorded more than 1,000 hours of road time across 3,687 drives and 21,232 miles.
“What we found was that the drivers with diabetes had trouble,” Dr. Rizzo said at the American Neurological Association annual meeting.
Glucose was dangerously high or low about 13% of the time when people with diabetes were behind the wheel. Their accelerometer profiles revealed more risky maneuvering and variability in pedal control even during periods of euglycemia and moderate hyperglycemia, but particularly when hypoglycemia occurred at highway speeds.
One driver almost blacked out behind the wheel when his blood glucose fell below 40 mg/dL. “He might have been driving because he was not aware he had a problem,” Dr. Rizzo said. He is now; he was shown the video.
The team reviewed their subjects’ department of motor vehicles records for the 2 years before the study. All three car crashes in the study population were among drivers with diabetes, and they received 11 of the 13 citations (85%).
The technology has many implications. In the short term, it’s a feedback tool to help people with diabetes stay safer on the road. But the work is also “a model for us to be able to approach all kinds of medical disorders in the real world. We want generalizable models that go beyond type 1 diabetes to type 2 diabetes and other forms of encephalopathy, of which there are many in neurology.” Those models could one day lead to “automated in-vehicle technology responsive to driver’s momentary neurocognitive state. You could have [systems] that alert the car that the driver is in no state to drive; the car could even take over. We are very excited about” the possibilities, Dr. Rizzo said.
Meanwhile, “just the diagnosis of diabetes itself is not enough to restrict a person from driving. But if you record their sugars over long periods of time, and you see the kind of changes we saw in some of the drivers, it means the license might need to be adjusted slightly,” he said.
Dr. Rizzo had no relevant disclosures. One of the investigators was an employee of the Toyota Collaborative Safety Research Center.
SAN DIEGO – When researchers at the University of Nebraska placed sensors in the cars of patients with type 1 diabetes, they found something interesting: About 3.4% of the time, the patients were driving with a blood glucose below 70 mg/dL.
Almost 10% of the time, it was above 300 mg/dL, and both hyper and hypoglycemia, but especially hypoglycemia, corresponded with erratic driving, especially at highway speeds.
The finding explains why patients taking insulin for type 1 diabetes have a 12%-19% higher risk of crashing their cars, compared with the general population. But in a larger sense, the study speaks to a new possibility as cars become smarter: monitoring drivers’ mental states and pulling over to the side of the road or otherwise taking control if there’s a problem.
The “results show that vehicle sensor and physiologic data can be successfully linked to quantify individual driver performance and behavior in drivers with metabolic disorders that affect brain function. The work we are doing could be used to tune the algorithm that drive these automated vehicles. I think this is a very important area of study,” said senior investigator Matthew Rizzo, MD, chair of the university’s department of neurological sciences in Omaha.
Participants had the devices in their cars for a month, during which time the diabetes patients were also on continuous, 24-hour blood glucose monitoring. The investigators then synched the car data with the glucose readings, and compared it with the data from the controls’ cars. In all, the system recorded more than 1,000 hours of road time across 3,687 drives and 21,232 miles.
“What we found was that the drivers with diabetes had trouble,” Dr. Rizzo said at the American Neurological Association annual meeting.
Glucose was dangerously high or low about 13% of the time when people with diabetes were behind the wheel. Their accelerometer profiles revealed more risky maneuvering and variability in pedal control even during periods of euglycemia and moderate hyperglycemia, but particularly when hypoglycemia occurred at highway speeds.
One driver almost blacked out behind the wheel when his blood glucose fell below 40 mg/dL. “He might have been driving because he was not aware he had a problem,” Dr. Rizzo said. He is now; he was shown the video.
The team reviewed their subjects’ department of motor vehicles records for the 2 years before the study. All three car crashes in the study population were among drivers with diabetes, and they received 11 of the 13 citations (85%).
The technology has many implications. In the short term, it’s a feedback tool to help people with diabetes stay safer on the road. But the work is also “a model for us to be able to approach all kinds of medical disorders in the real world. We want generalizable models that go beyond type 1 diabetes to type 2 diabetes and other forms of encephalopathy, of which there are many in neurology.” Those models could one day lead to “automated in-vehicle technology responsive to driver’s momentary neurocognitive state. You could have [systems] that alert the car that the driver is in no state to drive; the car could even take over. We are very excited about” the possibilities, Dr. Rizzo said.
Meanwhile, “just the diagnosis of diabetes itself is not enough to restrict a person from driving. But if you record their sugars over long periods of time, and you see the kind of changes we saw in some of the drivers, it means the license might need to be adjusted slightly,” he said.
Dr. Rizzo had no relevant disclosures. One of the investigators was an employee of the Toyota Collaborative Safety Research Center.
SAN DIEGO – When researchers at the University of Nebraska placed sensors in the cars of patients with type 1 diabetes, they found something interesting: About 3.4% of the time, the patients were driving with a blood glucose below 70 mg/dL.
Almost 10% of the time, it was above 300 mg/dL, and both hyper and hypoglycemia, but especially hypoglycemia, corresponded with erratic driving, especially at highway speeds.
The finding explains why patients taking insulin for type 1 diabetes have a 12%-19% higher risk of crashing their cars, compared with the general population. But in a larger sense, the study speaks to a new possibility as cars become smarter: monitoring drivers’ mental states and pulling over to the side of the road or otherwise taking control if there’s a problem.
The “results show that vehicle sensor and physiologic data can be successfully linked to quantify individual driver performance and behavior in drivers with metabolic disorders that affect brain function. The work we are doing could be used to tune the algorithm that drive these automated vehicles. I think this is a very important area of study,” said senior investigator Matthew Rizzo, MD, chair of the university’s department of neurological sciences in Omaha.
Participants had the devices in their cars for a month, during which time the diabetes patients were also on continuous, 24-hour blood glucose monitoring. The investigators then synched the car data with the glucose readings, and compared it with the data from the controls’ cars. In all, the system recorded more than 1,000 hours of road time across 3,687 drives and 21,232 miles.
“What we found was that the drivers with diabetes had trouble,” Dr. Rizzo said at the American Neurological Association annual meeting.
Glucose was dangerously high or low about 13% of the time when people with diabetes were behind the wheel. Their accelerometer profiles revealed more risky maneuvering and variability in pedal control even during periods of euglycemia and moderate hyperglycemia, but particularly when hypoglycemia occurred at highway speeds.
One driver almost blacked out behind the wheel when his blood glucose fell below 40 mg/dL. “He might have been driving because he was not aware he had a problem,” Dr. Rizzo said. He is now; he was shown the video.
The team reviewed their subjects’ department of motor vehicles records for the 2 years before the study. All three car crashes in the study population were among drivers with diabetes, and they received 11 of the 13 citations (85%).
The technology has many implications. In the short term, it’s a feedback tool to help people with diabetes stay safer on the road. But the work is also “a model for us to be able to approach all kinds of medical disorders in the real world. We want generalizable models that go beyond type 1 diabetes to type 2 diabetes and other forms of encephalopathy, of which there are many in neurology.” Those models could one day lead to “automated in-vehicle technology responsive to driver’s momentary neurocognitive state. You could have [systems] that alert the car that the driver is in no state to drive; the car could even take over. We are very excited about” the possibilities, Dr. Rizzo said.
Meanwhile, “just the diagnosis of diabetes itself is not enough to restrict a person from driving. But if you record their sugars over long periods of time, and you see the kind of changes we saw in some of the drivers, it means the license might need to be adjusted slightly,” he said.
Dr. Rizzo had no relevant disclosures. One of the investigators was an employee of the Toyota Collaborative Safety Research Center.
REPORTING FROM ANA 2017
Key clinical point:
Major finding: Glucose was dangerously high or low about 13% of the time when people with diabetes were behind the wheel.
Study details: Investigators paired real-time driving data with continuous glucose monitoring in patients with type 1 diabetes to asses how blood sugar levels affected driving.
Disclosures: Toyota funded the work. The senior investigator had no relevant disclosures.
Source: Rizzo M, et al. ANA 2017 abstract number S131.
FDA approves first follow-on short-acting insulin product using abbreviated approval pathway
aged 3 years and older with type 1 and type 2 diabetes mellitus, according to a news release from the FDA.
Insulin lispro injections are to be administered subcutaneously by injection, infusion via an insulin pump, or intravenously. Doses should be individualized based on route of administration and patients’ individual metabolic needs. All diabetes patients should regularly monitor their blood sugar levels and insulin regimens should be exclusively modified under medical supervision.
“With today’s approval, we are providing an important short-acting insulin option for patients that meets our standards for safety and effectiveness,” Mary T. Thanh Hai, MD, deputy director of the Office of New Drug Evaluation II in the FDA’s Center for Drug Evaluation and Research, said in a statement.
Admelog, a biosimilar to Eli Lilly’s Humalog, was approved as a follow-on product based on the prior approval of Humalog. This allowed insulin lispro injections to be passed through the abbreviated approval pathway under the Federal Food, Drug, and Cosmetic Act, formally known as the 505(b)(2) pathway. The makers of insulin lispro found it was scientifically justified to use the previous safety and effectiveness data from the approval of Humalog to support the approval of insulin lispro injections. In addition to the Humalog data, the insulin lispro injection data included findings from two phase 3 clinical trials, each of which comprised about 500 diabetes patients. Using this abbreviated pathway can reduce the costs of drug development significantly, allowing new products to be offered to patients at lower prices.
“One of my key policy efforts is increasing competition in the market for prescription drugs and helping facilitate the entry of lower-cost alternatives. This is particularly important for drugs like insulin that are taken by millions of Americans every day for a patient’s lifetime to manage a chronic disease,” FDA Commissioner Scott Gottlieb, MD, said in a statement “In the coming months, we’ll be taking additional policy steps to help to make sure patients continue to benefit from improved access to lower cost, safe and effective alternatives to brand name drugs approved through the agency’s abbreviated pathways.”
Insulin lispro injections are short-acting insulin products that can help improve blood sugar levels in diabetes patients. This can be useful in controlling blood sugar levels after eating. This contrasts with long-acting insulin products, which are intended to control background insulin levels between meals. The blood sugar control needs of type 1 and type 2 diabetes patients are unique. Type 1 patients require both short- and long-term controls, while some type 2 patients may never need a short-acting insulin product. Because of these differences, providing insulin lispro injections as a blood sugar control method may be particularly useful to type 1 diabetes patients who need to control mealtime blood sugar levels.
aged 3 years and older with type 1 and type 2 diabetes mellitus, according to a news release from the FDA.
Insulin lispro injections are to be administered subcutaneously by injection, infusion via an insulin pump, or intravenously. Doses should be individualized based on route of administration and patients’ individual metabolic needs. All diabetes patients should regularly monitor their blood sugar levels and insulin regimens should be exclusively modified under medical supervision.
“With today’s approval, we are providing an important short-acting insulin option for patients that meets our standards for safety and effectiveness,” Mary T. Thanh Hai, MD, deputy director of the Office of New Drug Evaluation II in the FDA’s Center for Drug Evaluation and Research, said in a statement.
Admelog, a biosimilar to Eli Lilly’s Humalog, was approved as a follow-on product based on the prior approval of Humalog. This allowed insulin lispro injections to be passed through the abbreviated approval pathway under the Federal Food, Drug, and Cosmetic Act, formally known as the 505(b)(2) pathway. The makers of insulin lispro found it was scientifically justified to use the previous safety and effectiveness data from the approval of Humalog to support the approval of insulin lispro injections. In addition to the Humalog data, the insulin lispro injection data included findings from two phase 3 clinical trials, each of which comprised about 500 diabetes patients. Using this abbreviated pathway can reduce the costs of drug development significantly, allowing new products to be offered to patients at lower prices.
“One of my key policy efforts is increasing competition in the market for prescription drugs and helping facilitate the entry of lower-cost alternatives. This is particularly important for drugs like insulin that are taken by millions of Americans every day for a patient’s lifetime to manage a chronic disease,” FDA Commissioner Scott Gottlieb, MD, said in a statement “In the coming months, we’ll be taking additional policy steps to help to make sure patients continue to benefit from improved access to lower cost, safe and effective alternatives to brand name drugs approved through the agency’s abbreviated pathways.”
Insulin lispro injections are short-acting insulin products that can help improve blood sugar levels in diabetes patients. This can be useful in controlling blood sugar levels after eating. This contrasts with long-acting insulin products, which are intended to control background insulin levels between meals. The blood sugar control needs of type 1 and type 2 diabetes patients are unique. Type 1 patients require both short- and long-term controls, while some type 2 patients may never need a short-acting insulin product. Because of these differences, providing insulin lispro injections as a blood sugar control method may be particularly useful to type 1 diabetes patients who need to control mealtime blood sugar levels.
aged 3 years and older with type 1 and type 2 diabetes mellitus, according to a news release from the FDA.
Insulin lispro injections are to be administered subcutaneously by injection, infusion via an insulin pump, or intravenously. Doses should be individualized based on route of administration and patients’ individual metabolic needs. All diabetes patients should regularly monitor their blood sugar levels and insulin regimens should be exclusively modified under medical supervision.
“With today’s approval, we are providing an important short-acting insulin option for patients that meets our standards for safety and effectiveness,” Mary T. Thanh Hai, MD, deputy director of the Office of New Drug Evaluation II in the FDA’s Center for Drug Evaluation and Research, said in a statement.
Admelog, a biosimilar to Eli Lilly’s Humalog, was approved as a follow-on product based on the prior approval of Humalog. This allowed insulin lispro injections to be passed through the abbreviated approval pathway under the Federal Food, Drug, and Cosmetic Act, formally known as the 505(b)(2) pathway. The makers of insulin lispro found it was scientifically justified to use the previous safety and effectiveness data from the approval of Humalog to support the approval of insulin lispro injections. In addition to the Humalog data, the insulin lispro injection data included findings from two phase 3 clinical trials, each of which comprised about 500 diabetes patients. Using this abbreviated pathway can reduce the costs of drug development significantly, allowing new products to be offered to patients at lower prices.
“One of my key policy efforts is increasing competition in the market for prescription drugs and helping facilitate the entry of lower-cost alternatives. This is particularly important for drugs like insulin that are taken by millions of Americans every day for a patient’s lifetime to manage a chronic disease,” FDA Commissioner Scott Gottlieb, MD, said in a statement “In the coming months, we’ll be taking additional policy steps to help to make sure patients continue to benefit from improved access to lower cost, safe and effective alternatives to brand name drugs approved through the agency’s abbreviated pathways.”
Insulin lispro injections are short-acting insulin products that can help improve blood sugar levels in diabetes patients. This can be useful in controlling blood sugar levels after eating. This contrasts with long-acting insulin products, which are intended to control background insulin levels between meals. The blood sugar control needs of type 1 and type 2 diabetes patients are unique. Type 1 patients require both short- and long-term controls, while some type 2 patients may never need a short-acting insulin product. Because of these differences, providing insulin lispro injections as a blood sugar control method may be particularly useful to type 1 diabetes patients who need to control mealtime blood sugar levels.
Type 2 diabetes remitted with low-calorie diet
Type 2 diabetes mellitus remitted without medication in 46% of subjects who followed a strict, calorie-controlled diet for 1 year, judging from the findings of an open-label, cluster-randomized trial.
Remission rates closely tracked weight loss, Michael E.J. Lean, MD, reported in the Dec. 5 online issue of the Lancet. Among those who lost 15 kg or more, 86% also normalized their hemoglobin A1c levels. Lesser weight losses were successful too, with diabetes remitting in 57% of those who lost 10-15 kg and 34% of those who lost 5-10 kg, reported Dr. Lean, who is chair of human nutrition at the University of Glasgow.
Weight loss conferred other benefits as well. Quality of life improved significantly, triglycerides declined, and about half of the subjects were able to discontinue both their antidiabetic and antihypertension prescriptions.
DiRECT (the Diabetes Remission Clinical Trial) didn’t include a strict exercise component – something that sets it apart from most dietary interventions, Dr. Lean noted in a press statement. Instead, the study’s “Counterweight-plus” diet intervention focused on very strict calorie control. Counterweight is a proprietary, subscription-based weight-loss program that costs about $570 for 1 year.
The paper offered few details about the intervention, which was supervised by a nurse and/or dietitian. For the first 3-5 months, patients consumed only Counterweight-branded soups and shakes, amounting to about 850 calories per day. After that, solid foods were reintroduced over 2-8 weeks. There was ongoing support for weight-loss maintenance, including cognitive-behavioral therapy, combined with strategies to increase physical activity. Activity strategies were confined to encouraging subjects to walk up to 15,000 steps per day in the second and third phase, but the investigators had little hope that this would actually occur.
“It was recognized that this target was unlikely to be achieved by many, and objectively measured physical activity showed no increase in physical activity in either group between baseline and 12 months, which underlines the difficulty this population has in maintaining increased activity,” they noted.
DiRECT enrolled 298 adults with type 2 diabetes recruited from 49 primary care practices across Scotland and England. They were about 54 years old, with a mean diabetes duration of about 3 years. Subjects were assigned to either the Counterweight-plus weight management program or best practice care under current guidelines. At baseline, subjects’ mean body mass index was 35 mg/m2. Their mean HbA1c was about 7.6%; about 75% were taking at least one antidiabetic medication, and 30% taking two or more. Hypertension was present in more than half.
In the active group, investigators withdrew all antidiabetic and antihypertensive medications when the diet commenced. Antihypertensives were restarted only if subjects experienced an increase in systolic blood pressure. Patients in the control group stayed on their medications.
At 12 months, the mean weight loss was significantly greater in the intervention group than the control group (10 kg vs. 1 kg). Weight loss of at least 15 kg occurred in 24% of the intervention group and none of the control group. It was most pronounced in the total diet replacement phase, falling by a mean of 14.5 kg; participants regained weigh during the food reintroduction phase (mean, 1 kg) and again during the maintenance phase (mean, 1.9 kg). Four subjects in the intervention group who experienced diabetes remission needed a “short rescue plan” on the total diet replacement phase because of weight regain within 60 days of the study’s end. The authors didn’t say how much weight these patients regained.
By the end of the study period, diabetes had remitted in 46% of the intervention group and 4% of the control group (odds ratio, 19.7) and was positively associated with the amount of weight loss.
At 12 months, 74% of the intervention group and 18% of the control group were off antidiabetic medications. HbA1c was significantly better in the intervention group (mean 6.4% vs. 7.2%). Antihypertensive drugs also were less common among the intervention group (32% vs. 61%) at 12 months. Despite the reduction in medication, there were no significant changes in blood pressure from baseline.
Nine serious adverse events occurred among seven intervention subjects. Two (biliary colic and abdominal pain) occurred in the same subject and were considered related to the diet, but they did not withdraw promptly.
Counterweight sponsored the trial, and several of the coinvestigators are stockholders and were company employees during the study. Dr. Lean reported financial remuneration from Counterweight.
SOURCE: Lean M et al. Lancet 2017 Dec 5; doi: 10.1016/ S0140-6736(17)33102-1.
The results of the DiRECT are “impressive and strongly support the view that type 2 diabetes is tightly associated with excessive fat mass in the body,” Matti Uusitupa, MD, wrote in an accompanying editorial.
Emerging data point at weight loss as the most effective treatment for type 2 diabetes, Dr. Uusitupa wrote. It confers a variety of benefits: improved insulin sensitivity in muscles and liver, decreased organ fat, and improved insulin secretion. Some studies suggest that fat loss also helps preserve beta cells in the pancreas.
Nevertheless, the study raises some questions. Without long-term data, it’s tough to know whether DiRECT should be a watershed moment in type 2 diabetes treatment, shifting efforts more toward weight loss and less toward medications.
“In view of the results of the DiRECT trial, a nonpharmacologic approach should be revived. In clinical practice, antidiabetic drugs seldom result in normalization of glucose metabolism if patients’ lifestyles remain unchanged. Mechanisms of action of some drugs for type 2 diabetes might not be in line with current knowledge of pathophysiology of disease, whereas intensive weight management along with physical activity and healthy diet is targeted therapy for type 2 diabetes.”
The best time to start a weight-loss war on type 2 diabetes is probably at the time of diagnosis, Dr. Uusitupa suggested, because patients are most highly motivated at that point.
“However, disease prevention should be maintained as the primary goal that requires both individual-level and population-based strategies.”
Dr. Uusitupa is an emeritus professor at the University of Eastern Finland, Kuopio.
The results of the DiRECT are “impressive and strongly support the view that type 2 diabetes is tightly associated with excessive fat mass in the body,” Matti Uusitupa, MD, wrote in an accompanying editorial.
Emerging data point at weight loss as the most effective treatment for type 2 diabetes, Dr. Uusitupa wrote. It confers a variety of benefits: improved insulin sensitivity in muscles and liver, decreased organ fat, and improved insulin secretion. Some studies suggest that fat loss also helps preserve beta cells in the pancreas.
Nevertheless, the study raises some questions. Without long-term data, it’s tough to know whether DiRECT should be a watershed moment in type 2 diabetes treatment, shifting efforts more toward weight loss and less toward medications.
“In view of the results of the DiRECT trial, a nonpharmacologic approach should be revived. In clinical practice, antidiabetic drugs seldom result in normalization of glucose metabolism if patients’ lifestyles remain unchanged. Mechanisms of action of some drugs for type 2 diabetes might not be in line with current knowledge of pathophysiology of disease, whereas intensive weight management along with physical activity and healthy diet is targeted therapy for type 2 diabetes.”
The best time to start a weight-loss war on type 2 diabetes is probably at the time of diagnosis, Dr. Uusitupa suggested, because patients are most highly motivated at that point.
“However, disease prevention should be maintained as the primary goal that requires both individual-level and population-based strategies.”
Dr. Uusitupa is an emeritus professor at the University of Eastern Finland, Kuopio.
The results of the DiRECT are “impressive and strongly support the view that type 2 diabetes is tightly associated with excessive fat mass in the body,” Matti Uusitupa, MD, wrote in an accompanying editorial.
Emerging data point at weight loss as the most effective treatment for type 2 diabetes, Dr. Uusitupa wrote. It confers a variety of benefits: improved insulin sensitivity in muscles and liver, decreased organ fat, and improved insulin secretion. Some studies suggest that fat loss also helps preserve beta cells in the pancreas.
Nevertheless, the study raises some questions. Without long-term data, it’s tough to know whether DiRECT should be a watershed moment in type 2 diabetes treatment, shifting efforts more toward weight loss and less toward medications.
“In view of the results of the DiRECT trial, a nonpharmacologic approach should be revived. In clinical practice, antidiabetic drugs seldom result in normalization of glucose metabolism if patients’ lifestyles remain unchanged. Mechanisms of action of some drugs for type 2 diabetes might not be in line with current knowledge of pathophysiology of disease, whereas intensive weight management along with physical activity and healthy diet is targeted therapy for type 2 diabetes.”
The best time to start a weight-loss war on type 2 diabetes is probably at the time of diagnosis, Dr. Uusitupa suggested, because patients are most highly motivated at that point.
“However, disease prevention should be maintained as the primary goal that requires both individual-level and population-based strategies.”
Dr. Uusitupa is an emeritus professor at the University of Eastern Finland, Kuopio.
Type 2 diabetes mellitus remitted without medication in 46% of subjects who followed a strict, calorie-controlled diet for 1 year, judging from the findings of an open-label, cluster-randomized trial.
Remission rates closely tracked weight loss, Michael E.J. Lean, MD, reported in the Dec. 5 online issue of the Lancet. Among those who lost 15 kg or more, 86% also normalized their hemoglobin A1c levels. Lesser weight losses were successful too, with diabetes remitting in 57% of those who lost 10-15 kg and 34% of those who lost 5-10 kg, reported Dr. Lean, who is chair of human nutrition at the University of Glasgow.
Weight loss conferred other benefits as well. Quality of life improved significantly, triglycerides declined, and about half of the subjects were able to discontinue both their antidiabetic and antihypertension prescriptions.
DiRECT (the Diabetes Remission Clinical Trial) didn’t include a strict exercise component – something that sets it apart from most dietary interventions, Dr. Lean noted in a press statement. Instead, the study’s “Counterweight-plus” diet intervention focused on very strict calorie control. Counterweight is a proprietary, subscription-based weight-loss program that costs about $570 for 1 year.
The paper offered few details about the intervention, which was supervised by a nurse and/or dietitian. For the first 3-5 months, patients consumed only Counterweight-branded soups and shakes, amounting to about 850 calories per day. After that, solid foods were reintroduced over 2-8 weeks. There was ongoing support for weight-loss maintenance, including cognitive-behavioral therapy, combined with strategies to increase physical activity. Activity strategies were confined to encouraging subjects to walk up to 15,000 steps per day in the second and third phase, but the investigators had little hope that this would actually occur.
“It was recognized that this target was unlikely to be achieved by many, and objectively measured physical activity showed no increase in physical activity in either group between baseline and 12 months, which underlines the difficulty this population has in maintaining increased activity,” they noted.
DiRECT enrolled 298 adults with type 2 diabetes recruited from 49 primary care practices across Scotland and England. They were about 54 years old, with a mean diabetes duration of about 3 years. Subjects were assigned to either the Counterweight-plus weight management program or best practice care under current guidelines. At baseline, subjects’ mean body mass index was 35 mg/m2. Their mean HbA1c was about 7.6%; about 75% were taking at least one antidiabetic medication, and 30% taking two or more. Hypertension was present in more than half.
In the active group, investigators withdrew all antidiabetic and antihypertensive medications when the diet commenced. Antihypertensives were restarted only if subjects experienced an increase in systolic blood pressure. Patients in the control group stayed on their medications.
At 12 months, the mean weight loss was significantly greater in the intervention group than the control group (10 kg vs. 1 kg). Weight loss of at least 15 kg occurred in 24% of the intervention group and none of the control group. It was most pronounced in the total diet replacement phase, falling by a mean of 14.5 kg; participants regained weigh during the food reintroduction phase (mean, 1 kg) and again during the maintenance phase (mean, 1.9 kg). Four subjects in the intervention group who experienced diabetes remission needed a “short rescue plan” on the total diet replacement phase because of weight regain within 60 days of the study’s end. The authors didn’t say how much weight these patients regained.
By the end of the study period, diabetes had remitted in 46% of the intervention group and 4% of the control group (odds ratio, 19.7) and was positively associated with the amount of weight loss.
At 12 months, 74% of the intervention group and 18% of the control group were off antidiabetic medications. HbA1c was significantly better in the intervention group (mean 6.4% vs. 7.2%). Antihypertensive drugs also were less common among the intervention group (32% vs. 61%) at 12 months. Despite the reduction in medication, there were no significant changes in blood pressure from baseline.
Nine serious adverse events occurred among seven intervention subjects. Two (biliary colic and abdominal pain) occurred in the same subject and were considered related to the diet, but they did not withdraw promptly.
Counterweight sponsored the trial, and several of the coinvestigators are stockholders and were company employees during the study. Dr. Lean reported financial remuneration from Counterweight.
SOURCE: Lean M et al. Lancet 2017 Dec 5; doi: 10.1016/ S0140-6736(17)33102-1.
Type 2 diabetes mellitus remitted without medication in 46% of subjects who followed a strict, calorie-controlled diet for 1 year, judging from the findings of an open-label, cluster-randomized trial.
Remission rates closely tracked weight loss, Michael E.J. Lean, MD, reported in the Dec. 5 online issue of the Lancet. Among those who lost 15 kg or more, 86% also normalized their hemoglobin A1c levels. Lesser weight losses were successful too, with diabetes remitting in 57% of those who lost 10-15 kg and 34% of those who lost 5-10 kg, reported Dr. Lean, who is chair of human nutrition at the University of Glasgow.
Weight loss conferred other benefits as well. Quality of life improved significantly, triglycerides declined, and about half of the subjects were able to discontinue both their antidiabetic and antihypertension prescriptions.
DiRECT (the Diabetes Remission Clinical Trial) didn’t include a strict exercise component – something that sets it apart from most dietary interventions, Dr. Lean noted in a press statement. Instead, the study’s “Counterweight-plus” diet intervention focused on very strict calorie control. Counterweight is a proprietary, subscription-based weight-loss program that costs about $570 for 1 year.
The paper offered few details about the intervention, which was supervised by a nurse and/or dietitian. For the first 3-5 months, patients consumed only Counterweight-branded soups and shakes, amounting to about 850 calories per day. After that, solid foods were reintroduced over 2-8 weeks. There was ongoing support for weight-loss maintenance, including cognitive-behavioral therapy, combined with strategies to increase physical activity. Activity strategies were confined to encouraging subjects to walk up to 15,000 steps per day in the second and third phase, but the investigators had little hope that this would actually occur.
“It was recognized that this target was unlikely to be achieved by many, and objectively measured physical activity showed no increase in physical activity in either group between baseline and 12 months, which underlines the difficulty this population has in maintaining increased activity,” they noted.
DiRECT enrolled 298 adults with type 2 diabetes recruited from 49 primary care practices across Scotland and England. They were about 54 years old, with a mean diabetes duration of about 3 years. Subjects were assigned to either the Counterweight-plus weight management program or best practice care under current guidelines. At baseline, subjects’ mean body mass index was 35 mg/m2. Their mean HbA1c was about 7.6%; about 75% were taking at least one antidiabetic medication, and 30% taking two or more. Hypertension was present in more than half.
In the active group, investigators withdrew all antidiabetic and antihypertensive medications when the diet commenced. Antihypertensives were restarted only if subjects experienced an increase in systolic blood pressure. Patients in the control group stayed on their medications.
At 12 months, the mean weight loss was significantly greater in the intervention group than the control group (10 kg vs. 1 kg). Weight loss of at least 15 kg occurred in 24% of the intervention group and none of the control group. It was most pronounced in the total diet replacement phase, falling by a mean of 14.5 kg; participants regained weigh during the food reintroduction phase (mean, 1 kg) and again during the maintenance phase (mean, 1.9 kg). Four subjects in the intervention group who experienced diabetes remission needed a “short rescue plan” on the total diet replacement phase because of weight regain within 60 days of the study’s end. The authors didn’t say how much weight these patients regained.
By the end of the study period, diabetes had remitted in 46% of the intervention group and 4% of the control group (odds ratio, 19.7) and was positively associated with the amount of weight loss.
At 12 months, 74% of the intervention group and 18% of the control group were off antidiabetic medications. HbA1c was significantly better in the intervention group (mean 6.4% vs. 7.2%). Antihypertensive drugs also were less common among the intervention group (32% vs. 61%) at 12 months. Despite the reduction in medication, there were no significant changes in blood pressure from baseline.
Nine serious adverse events occurred among seven intervention subjects. Two (biliary colic and abdominal pain) occurred in the same subject and were considered related to the diet, but they did not withdraw promptly.
Counterweight sponsored the trial, and several of the coinvestigators are stockholders and were company employees during the study. Dr. Lean reported financial remuneration from Counterweight.
SOURCE: Lean M et al. Lancet 2017 Dec 5; doi: 10.1016/ S0140-6736(17)33102-1.
FROM LANCET
Key clinical point: Diet alone may be enough to cause remission of type 2 diabetes.
Major finding: Type 2 diabetes remitted without medication in 46% of subjects who followed a strict, calorie-controlled diet for 1 year, according to results from a randomized, controlled trial.
Study details: The randomized study comprised 298 subjects.
Disclosures: Counterweight sponsored the trial, and several of the coinvestigators are stockholders and were company employees during the study. Dr. Lean reported financial remuneration from Counterweight.
Source: Lean M et al. Lancet. 2017. doi: 10.1016/ S0140-6736(17)33102-1.
Health disparities in rural America: Chronic conditions
Among rural adults, multiple chronic health conditions are most common in non-Hispanic blacks and American Indians/Alaska Natives (AI/ANs) and least common among Asians and Native Hawaiians/other Pacific Islanders (NHOPIs), according to the Centers for Disease Control and Prevention.
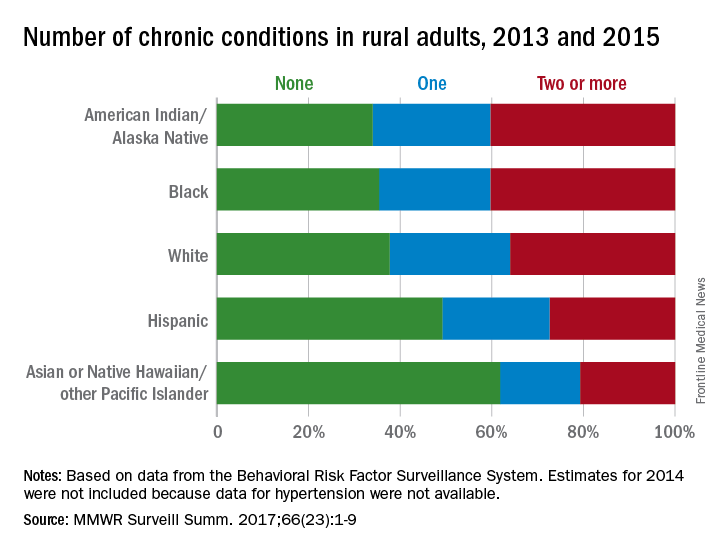
The order was reversed for adults reporting no chronic conditions: Asians and NHOPIs at 61.8%, Hispanics at 49.2%, whites at 37.8%, blacks at 35.4%, and AI/ANs at 34.0%, the researchers said.
For the chronic health conditions included separately in the report, blacks had the highest rate (45.9%) and Asians and NHOPIs had the lowest rate (15.5%) of obesity; AI/ANs were most likely (23.2%) and Asians and NHOPIs were least likely (5.8%) to report depressive disorder. Other conditions considered in the estimates were myocardial infarction; coronary heart disease; stroke; hypertension; asthma; skin cancer; other types of cancer; chronic obstructive pulmonary disease; kidney disease; some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia; and diabetes. Estimates for 2014 were not included because data for hypertension were not available, the investigators noted.
Of the 3,143 counties categorized by the National Center for Health Statistics’ Urban-Rural Classification Scheme for Counties, a total of 1,325 were considered rural and included 6.1% of the U.S. population, they said.
Among rural adults, multiple chronic health conditions are most common in non-Hispanic blacks and American Indians/Alaska Natives (AI/ANs) and least common among Asians and Native Hawaiians/other Pacific Islanders (NHOPIs), according to the Centers for Disease Control and Prevention.
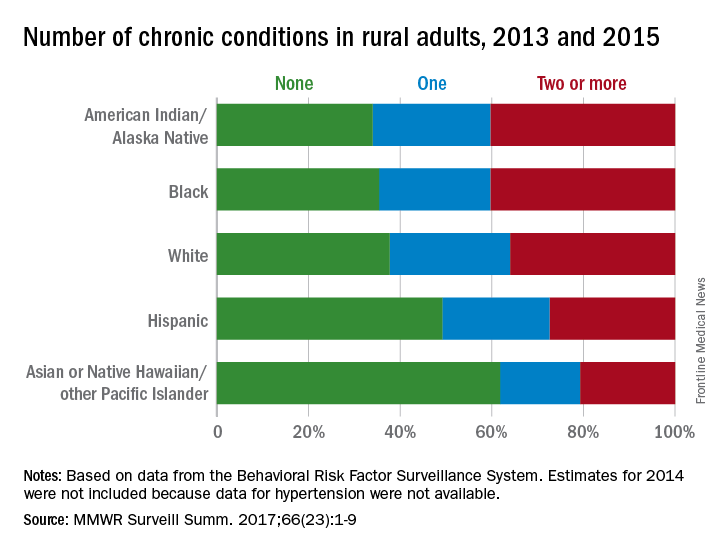
The order was reversed for adults reporting no chronic conditions: Asians and NHOPIs at 61.8%, Hispanics at 49.2%, whites at 37.8%, blacks at 35.4%, and AI/ANs at 34.0%, the researchers said.
For the chronic health conditions included separately in the report, blacks had the highest rate (45.9%) and Asians and NHOPIs had the lowest rate (15.5%) of obesity; AI/ANs were most likely (23.2%) and Asians and NHOPIs were least likely (5.8%) to report depressive disorder. Other conditions considered in the estimates were myocardial infarction; coronary heart disease; stroke; hypertension; asthma; skin cancer; other types of cancer; chronic obstructive pulmonary disease; kidney disease; some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia; and diabetes. Estimates for 2014 were not included because data for hypertension were not available, the investigators noted.
Of the 3,143 counties categorized by the National Center for Health Statistics’ Urban-Rural Classification Scheme for Counties, a total of 1,325 were considered rural and included 6.1% of the U.S. population, they said.
Among rural adults, multiple chronic health conditions are most common in non-Hispanic blacks and American Indians/Alaska Natives (AI/ANs) and least common among Asians and Native Hawaiians/other Pacific Islanders (NHOPIs), according to the Centers for Disease Control and Prevention.
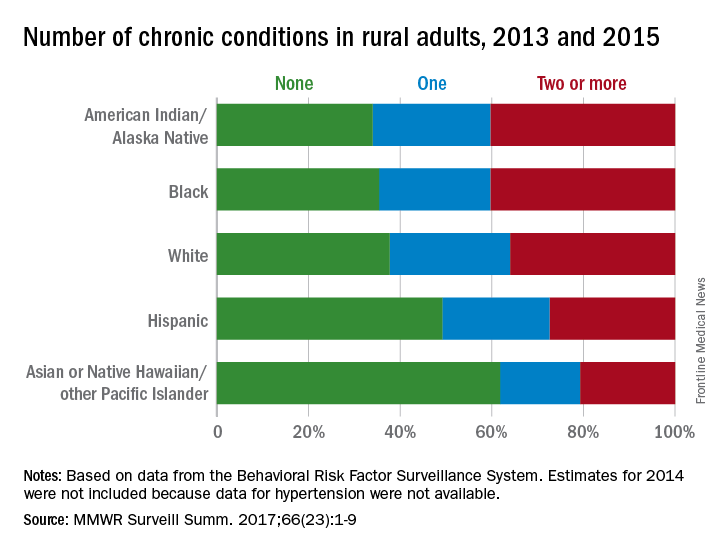
The order was reversed for adults reporting no chronic conditions: Asians and NHOPIs at 61.8%, Hispanics at 49.2%, whites at 37.8%, blacks at 35.4%, and AI/ANs at 34.0%, the researchers said.
For the chronic health conditions included separately in the report, blacks had the highest rate (45.9%) and Asians and NHOPIs had the lowest rate (15.5%) of obesity; AI/ANs were most likely (23.2%) and Asians and NHOPIs were least likely (5.8%) to report depressive disorder. Other conditions considered in the estimates were myocardial infarction; coronary heart disease; stroke; hypertension; asthma; skin cancer; other types of cancer; chronic obstructive pulmonary disease; kidney disease; some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia; and diabetes. Estimates for 2014 were not included because data for hypertension were not available, the investigators noted.
Of the 3,143 counties categorized by the National Center for Health Statistics’ Urban-Rural Classification Scheme for Counties, a total of 1,325 were considered rural and included 6.1% of the U.S. population, they said.
FROM MMWR SURVEILLANCE SUMMARIES
Alcohol use, abuse rise after bariatric surgery
ORLANDO –
Following any of several methods of bariatric surgery, patients showed a statistically significant 8% higher rate of new onset alcohol abuse, and a relative 50% increased rate of significant alcohol use, compared with rates before surgery, Prandeet Wander, MD, said at the World Congress of Gastroenterology at ACG 2017.
Her meta-analysis identified prospective, retrospective, and cross-sectional studies of alcohol use that included more than 100 bariatric surgery patients and that had follow-up beyond 1 year. Patients could have undergone Roux-en-Y gastric bypass, sleeve gastrectomy, or laparoscopic adjustable gastric banding. Comparator populations had to be either the surgery patients prior to the procedure or the controls matched by age and body mass index.
The 28 included studies enrolled 15,714 patients who averaged 43 years old, with more than three quarters women. Follow-up averaged 2.6 years. The most common surgery was Roux-en-Y, used in 23 studies, followed by banding in 12 studies, and sleeves in 8 studies (some studies used more than one type of surgery).
Nineteen of the studies examined the prevalence of “significant alcohol abuse” following surgery in a total of 4,552 patients, with 23% of patients overall showing this behavior. Five studies, involving 2,698 patients, documented the rate of new-onset alcohol abuse after surgery, with an overall rate of 8% that was statistically significant. All five studies individually showed increased incidence of alcohol abuse, with rates that ranged from 4% to 8%.
The analysis that showed a relative 50% higher rate of “significant” alcohol use after surgery, compared with the same patients before their surgery used data from 11 studies with 3,370 patients. Five of these 11 studies individually showed a statistically significant increase in alcohol use, 1 showed a significant, 34% relative decrease, and the remaining 5 studies did not show statistically significant changes, with 3 studies trending toward an increased rate and two trending toward a decreased rate after surgery.
None of the 28 included studies had a randomized control arm, and the studies collectively ran in six countries, including the United States, and hence involved different societal norms of alcohol use. Changes in alcohol absorption and metabolism following bariatric surgery may play roles in the observed effects, as might undiagnosed depression or substance use by patients who undergo this surgery, Dr. Wander suggested.
SOURCE: Wander P et al. World Congress of Gastroenterology, abstract 10.
ORLANDO –
Following any of several methods of bariatric surgery, patients showed a statistically significant 8% higher rate of new onset alcohol abuse, and a relative 50% increased rate of significant alcohol use, compared with rates before surgery, Prandeet Wander, MD, said at the World Congress of Gastroenterology at ACG 2017.
Her meta-analysis identified prospective, retrospective, and cross-sectional studies of alcohol use that included more than 100 bariatric surgery patients and that had follow-up beyond 1 year. Patients could have undergone Roux-en-Y gastric bypass, sleeve gastrectomy, or laparoscopic adjustable gastric banding. Comparator populations had to be either the surgery patients prior to the procedure or the controls matched by age and body mass index.
The 28 included studies enrolled 15,714 patients who averaged 43 years old, with more than three quarters women. Follow-up averaged 2.6 years. The most common surgery was Roux-en-Y, used in 23 studies, followed by banding in 12 studies, and sleeves in 8 studies (some studies used more than one type of surgery).
Nineteen of the studies examined the prevalence of “significant alcohol abuse” following surgery in a total of 4,552 patients, with 23% of patients overall showing this behavior. Five studies, involving 2,698 patients, documented the rate of new-onset alcohol abuse after surgery, with an overall rate of 8% that was statistically significant. All five studies individually showed increased incidence of alcohol abuse, with rates that ranged from 4% to 8%.
The analysis that showed a relative 50% higher rate of “significant” alcohol use after surgery, compared with the same patients before their surgery used data from 11 studies with 3,370 patients. Five of these 11 studies individually showed a statistically significant increase in alcohol use, 1 showed a significant, 34% relative decrease, and the remaining 5 studies did not show statistically significant changes, with 3 studies trending toward an increased rate and two trending toward a decreased rate after surgery.
None of the 28 included studies had a randomized control arm, and the studies collectively ran in six countries, including the United States, and hence involved different societal norms of alcohol use. Changes in alcohol absorption and metabolism following bariatric surgery may play roles in the observed effects, as might undiagnosed depression or substance use by patients who undergo this surgery, Dr. Wander suggested.
SOURCE: Wander P et al. World Congress of Gastroenterology, abstract 10.
ORLANDO –
Following any of several methods of bariatric surgery, patients showed a statistically significant 8% higher rate of new onset alcohol abuse, and a relative 50% increased rate of significant alcohol use, compared with rates before surgery, Prandeet Wander, MD, said at the World Congress of Gastroenterology at ACG 2017.
Her meta-analysis identified prospective, retrospective, and cross-sectional studies of alcohol use that included more than 100 bariatric surgery patients and that had follow-up beyond 1 year. Patients could have undergone Roux-en-Y gastric bypass, sleeve gastrectomy, or laparoscopic adjustable gastric banding. Comparator populations had to be either the surgery patients prior to the procedure or the controls matched by age and body mass index.
The 28 included studies enrolled 15,714 patients who averaged 43 years old, with more than three quarters women. Follow-up averaged 2.6 years. The most common surgery was Roux-en-Y, used in 23 studies, followed by banding in 12 studies, and sleeves in 8 studies (some studies used more than one type of surgery).
Nineteen of the studies examined the prevalence of “significant alcohol abuse” following surgery in a total of 4,552 patients, with 23% of patients overall showing this behavior. Five studies, involving 2,698 patients, documented the rate of new-onset alcohol abuse after surgery, with an overall rate of 8% that was statistically significant. All five studies individually showed increased incidence of alcohol abuse, with rates that ranged from 4% to 8%.
The analysis that showed a relative 50% higher rate of “significant” alcohol use after surgery, compared with the same patients before their surgery used data from 11 studies with 3,370 patients. Five of these 11 studies individually showed a statistically significant increase in alcohol use, 1 showed a significant, 34% relative decrease, and the remaining 5 studies did not show statistically significant changes, with 3 studies trending toward an increased rate and two trending toward a decreased rate after surgery.
None of the 28 included studies had a randomized control arm, and the studies collectively ran in six countries, including the United States, and hence involved different societal norms of alcohol use. Changes in alcohol absorption and metabolism following bariatric surgery may play roles in the observed effects, as might undiagnosed depression or substance use by patients who undergo this surgery, Dr. Wander suggested.
SOURCE: Wander P et al. World Congress of Gastroenterology, abstract 10.
REPORTING FROM WORLD CONGRESS OF GASTROENTEROLOGY
Key clinical point: Following bariatric surgery patients have increased alcohol use and abuse.
Major finding: Alcohol abuse rose by 8%; significant alcohol use rose by a relative 50%.
Study details: Meta-analysis of 28 reports with 15,714 patients
Disclosures: Dr. Wander had no disclosures.
Source: Wander P et al. World Congress of Gastroenterology, abstract 10.