User login
Cardiology News is an independent news source that provides cardiologists with timely and relevant news and commentary about clinical developments and the impact of health care policy on cardiology and the cardiologist's practice. Cardiology News Digital Network is the online destination and multimedia properties of Cardiology News, the independent news publication for cardiologists. Cardiology news is the leading source of news and commentary about clinical developments in cardiology as well as health care policy and regulations that affect the cardiologist's practice. Cardiology News Digital Network is owned by Frontline Medical Communications.
FDA Clears Medical Grade Over-the-Counter Pulse Oximeter
The MightySat Medical, an over-the-counter medical fingertip pulse oximeter, has received clearance from the US Food and Drug Administration (FDA) for use without a prescription, according to a press release from manufacturer Masimo.
The device is the first medical fingertip pulse oximeter available directly to consumers without a prescription that includes the same technology used by many hospitals, according to the company.
According to the FDA, home pulse oximeters are currently generally of two classes: hospital-grade prescription devices which have been vetted for accuracy through clinical trials, and over-the-counter devices which are sold direct to consumers but often estimate oxygen saturation. FDA communication on pulse oximeter accuracy states "OTC oximeters that are sold as either general wellness or sporting/aviation products are not intended for medical purposes, so they do not undergo FDA review."
Pulse oximeter use is important for patients diagnosed with breathing problems or lung diseases such as asthma, chronic obstructive pulmonary disease, pulmonary fibrosis, lung cancer, flu, pneumonia, or COVID-19 to collect accurate data on arterial blood oxygen saturation that they can share with their healthcare providers, according to the company. Patients with cardiac conditions, including pulmonary hypertension and heart failure may also benefit from pulse oximeter monitoring.
However, challenges of pulse oximeter use include measuring accuracy when patients are moving, measuring patients with poor circulation, and measuring patients with cool, thick, or darker skin. The MightySat Medical is designed to provide reliable measures of oxygen saturation and pulse rate across all patient groups, the manufacturers wrote in the press release.
Asked for additional comment, Diego J. Maselli, MD, FCCP, Professor and Chief in the division of Pulmonary Diseases and Critical Care at UT Health at San Antonio, noted, "Over the past decades, there has been an increased interest in home monitoring of medical conditions, particulrly with the development of more portable and accessible technology."
"This was heightended by the COVID-19 pandemic where telemedicine was frequently required as a means of delivering care," Dr. Maselli continued. "One of the important characteristics to monitor was the oxgen saturation in patients that had an active COVID-19 infection as it would dictate management and was part of the protocol for monitoring the clinical course of infection. Because of this need, many companies developed portable pulse oximeters for home use. This resulted in widespread use of pulse oximeters at home and other places outside clinic or hospital."
Other over-the-counter pulse oximeters that are not cleared by the FDA may create confusion among patients about the accuracy of their measurements, according to the company.
Dr. Maselli also commented that pulse oximeters' value can vary. "Unfortunately, these devices vary in quality and reliability and patients may not be fully aware of this. Most recently, the FDA approved a hospital-grade pulse oximeter that requires no prescription. This device may provide a more accurate reading in a wide range of clinical situations outside the healthcare setting. Patients should be aware that there are different grades of pulse oximeter before selecting one for home use. In addition, patients should work closely with their providers to better select the monitoring modaility that best fits their clinical situation," he said.
MightySat Medical is indicated for individuals aged 18 years and older who are well or poorly perfused under no motion conditions and is not intended as a diagnostic or screening tool for lung disease, according to the release. Treatment decisions based on data from the device should be made only in consultation with a healthcare provider, the company said. Dr. Maselli serves as a member of the CHEST Physician editorial board.
The FDA’s website offers further guidance related to at-home pulse oximeter use, with recommendations and limitations, as well as information on initiatives to ensure accurate and equitable pulse oximetry for all patients.
A version of this article appeared on Medscape.com.
The MightySat Medical, an over-the-counter medical fingertip pulse oximeter, has received clearance from the US Food and Drug Administration (FDA) for use without a prescription, according to a press release from manufacturer Masimo.
The device is the first medical fingertip pulse oximeter available directly to consumers without a prescription that includes the same technology used by many hospitals, according to the company.
According to the FDA, home pulse oximeters are currently generally of two classes: hospital-grade prescription devices which have been vetted for accuracy through clinical trials, and over-the-counter devices which are sold direct to consumers but often estimate oxygen saturation. FDA communication on pulse oximeter accuracy states "OTC oximeters that are sold as either general wellness or sporting/aviation products are not intended for medical purposes, so they do not undergo FDA review."
Pulse oximeter use is important for patients diagnosed with breathing problems or lung diseases such as asthma, chronic obstructive pulmonary disease, pulmonary fibrosis, lung cancer, flu, pneumonia, or COVID-19 to collect accurate data on arterial blood oxygen saturation that they can share with their healthcare providers, according to the company. Patients with cardiac conditions, including pulmonary hypertension and heart failure may also benefit from pulse oximeter monitoring.
However, challenges of pulse oximeter use include measuring accuracy when patients are moving, measuring patients with poor circulation, and measuring patients with cool, thick, or darker skin. The MightySat Medical is designed to provide reliable measures of oxygen saturation and pulse rate across all patient groups, the manufacturers wrote in the press release.
Asked for additional comment, Diego J. Maselli, MD, FCCP, Professor and Chief in the division of Pulmonary Diseases and Critical Care at UT Health at San Antonio, noted, "Over the past decades, there has been an increased interest in home monitoring of medical conditions, particulrly with the development of more portable and accessible technology."
"This was heightended by the COVID-19 pandemic where telemedicine was frequently required as a means of delivering care," Dr. Maselli continued. "One of the important characteristics to monitor was the oxgen saturation in patients that had an active COVID-19 infection as it would dictate management and was part of the protocol for monitoring the clinical course of infection. Because of this need, many companies developed portable pulse oximeters for home use. This resulted in widespread use of pulse oximeters at home and other places outside clinic or hospital."
Other over-the-counter pulse oximeters that are not cleared by the FDA may create confusion among patients about the accuracy of their measurements, according to the company.
Dr. Maselli also commented that pulse oximeters' value can vary. "Unfortunately, these devices vary in quality and reliability and patients may not be fully aware of this. Most recently, the FDA approved a hospital-grade pulse oximeter that requires no prescription. This device may provide a more accurate reading in a wide range of clinical situations outside the healthcare setting. Patients should be aware that there are different grades of pulse oximeter before selecting one for home use. In addition, patients should work closely with their providers to better select the monitoring modaility that best fits their clinical situation," he said.
MightySat Medical is indicated for individuals aged 18 years and older who are well or poorly perfused under no motion conditions and is not intended as a diagnostic or screening tool for lung disease, according to the release. Treatment decisions based on data from the device should be made only in consultation with a healthcare provider, the company said. Dr. Maselli serves as a member of the CHEST Physician editorial board.
The FDA’s website offers further guidance related to at-home pulse oximeter use, with recommendations and limitations, as well as information on initiatives to ensure accurate and equitable pulse oximetry for all patients.
A version of this article appeared on Medscape.com.
The MightySat Medical, an over-the-counter medical fingertip pulse oximeter, has received clearance from the US Food and Drug Administration (FDA) for use without a prescription, according to a press release from manufacturer Masimo.
The device is the first medical fingertip pulse oximeter available directly to consumers without a prescription that includes the same technology used by many hospitals, according to the company.
According to the FDA, home pulse oximeters are currently generally of two classes: hospital-grade prescription devices which have been vetted for accuracy through clinical trials, and over-the-counter devices which are sold direct to consumers but often estimate oxygen saturation. FDA communication on pulse oximeter accuracy states "OTC oximeters that are sold as either general wellness or sporting/aviation products are not intended for medical purposes, so they do not undergo FDA review."
Pulse oximeter use is important for patients diagnosed with breathing problems or lung diseases such as asthma, chronic obstructive pulmonary disease, pulmonary fibrosis, lung cancer, flu, pneumonia, or COVID-19 to collect accurate data on arterial blood oxygen saturation that they can share with their healthcare providers, according to the company. Patients with cardiac conditions, including pulmonary hypertension and heart failure may also benefit from pulse oximeter monitoring.
However, challenges of pulse oximeter use include measuring accuracy when patients are moving, measuring patients with poor circulation, and measuring patients with cool, thick, or darker skin. The MightySat Medical is designed to provide reliable measures of oxygen saturation and pulse rate across all patient groups, the manufacturers wrote in the press release.
Asked for additional comment, Diego J. Maselli, MD, FCCP, Professor and Chief in the division of Pulmonary Diseases and Critical Care at UT Health at San Antonio, noted, "Over the past decades, there has been an increased interest in home monitoring of medical conditions, particulrly with the development of more portable and accessible technology."
"This was heightended by the COVID-19 pandemic where telemedicine was frequently required as a means of delivering care," Dr. Maselli continued. "One of the important characteristics to monitor was the oxgen saturation in patients that had an active COVID-19 infection as it would dictate management and was part of the protocol for monitoring the clinical course of infection. Because of this need, many companies developed portable pulse oximeters for home use. This resulted in widespread use of pulse oximeters at home and other places outside clinic or hospital."
Other over-the-counter pulse oximeters that are not cleared by the FDA may create confusion among patients about the accuracy of their measurements, according to the company.
Dr. Maselli also commented that pulse oximeters' value can vary. "Unfortunately, these devices vary in quality and reliability and patients may not be fully aware of this. Most recently, the FDA approved a hospital-grade pulse oximeter that requires no prescription. This device may provide a more accurate reading in a wide range of clinical situations outside the healthcare setting. Patients should be aware that there are different grades of pulse oximeter before selecting one for home use. In addition, patients should work closely with their providers to better select the monitoring modaility that best fits their clinical situation," he said.
MightySat Medical is indicated for individuals aged 18 years and older who are well or poorly perfused under no motion conditions and is not intended as a diagnostic or screening tool for lung disease, according to the release. Treatment decisions based on data from the device should be made only in consultation with a healthcare provider, the company said. Dr. Maselli serves as a member of the CHEST Physician editorial board.
The FDA’s website offers further guidance related to at-home pulse oximeter use, with recommendations and limitations, as well as information on initiatives to ensure accurate and equitable pulse oximetry for all patients.
A version of this article appeared on Medscape.com.
It Sure Looks Like Cannabis Is Bad for the Heart, Doesn’t It?
This transcript has been edited for clarity.
If you’re an epidemiologist trying to explore whether some exposure is a risk factor for a disease, you can run into a tough problem when your exposure of interest is highly correlated with another risk factor for the disease. For decades, this stymied investigations into the link, if any, between marijuana use and cardiovascular disease because, for decades, most people who used marijuana in some way also smoked cigarettes — which is a very clear risk factor for heart disease.
But the times they are a-changing.
Thanks to the legalization of marijuana for recreational use in many states, and even broader social trends, there is now a large population of people who use marijuana but do not use cigarettes. That means we can start to determine whether marijuana use is an independent risk factor for heart disease.
And this week, we have the largest study yet to attempt to answer that question, though, as I’ll explain momentarily, the smoke hasn’t entirely cleared yet.
The centerpiece of the study we are discussing this week, “Association of Cannabis Use With Cardiovascular Outcomes Among US Adults,” which appeared in the Journal of the American Heart Association, is the Behavioral Risk Factor Surveillance System, an annual telephone survey conducted by the Centers for Disease Control and Prevention since 1984 that gathers data on all sorts of stuff that we do to ourselves: our drinking habits, our smoking habits, and, more recently, our marijuana habits.
The paper combines annual data from 2016 to 2020 representing 27 states and two US territories for a total sample size of more than 430,000 individuals. The key exposure? Marijuana use, which was coded as the number of days of marijuana use in the past 30 days. The key outcome? Coronary heart disease, collected through questions such as “Has a doctor, nurse, or other health professional ever told you that you had a heart attack?”
Right away you might detect a couple of problems here. But let me show you the results before we worry about what they mean.
You can see the rates of the major cardiovascular outcomes here, stratified by daily use of marijuana, nondaily use, and no use. Broadly speaking, the risk was highest for daily users, lowest for occasional users, and in the middle for non-users.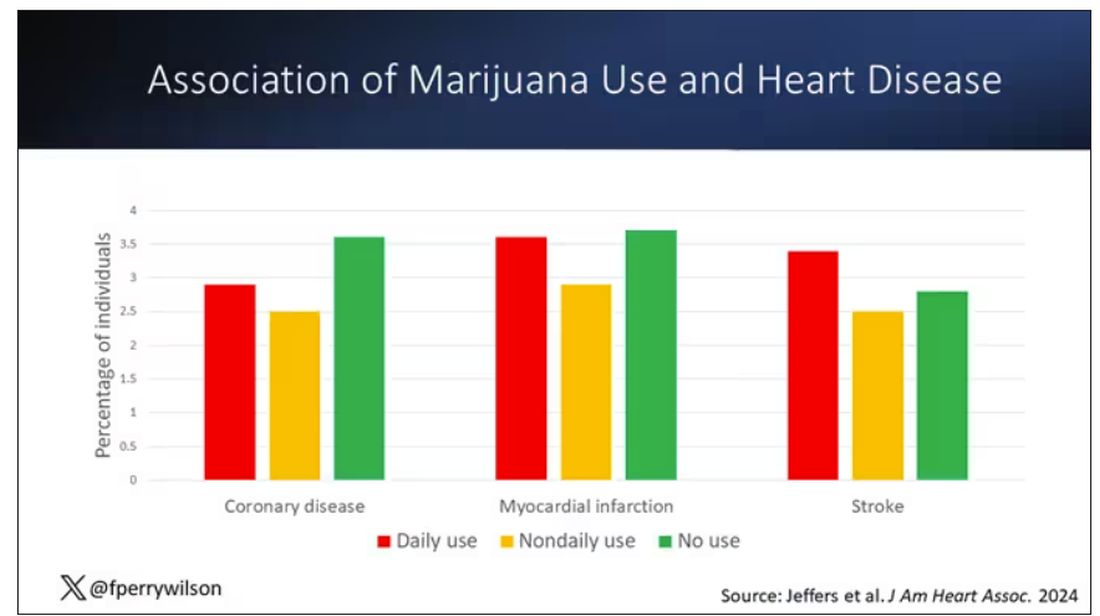
Of course, non-users and users are different in lots of other ways; non-users were quite a bit older, for example. Adjusting for all those factors showed that, independent of age, smoking status, the presence of diabetes, and so on, there was an independently increased risk for cardiovascular outcomes in people who used marijuana.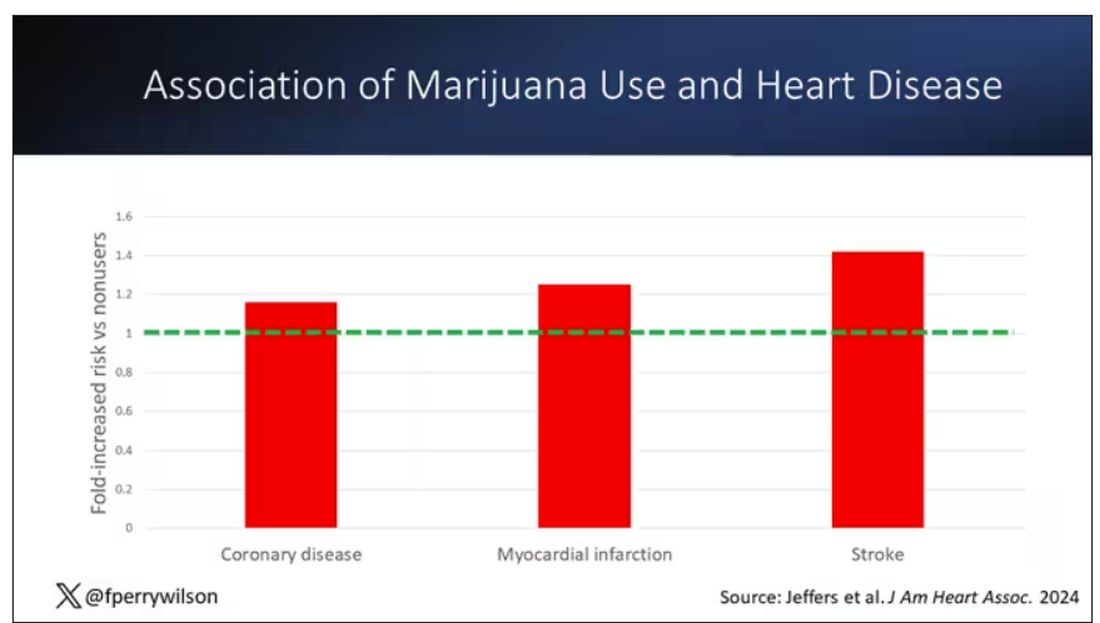
Importantly, 60% of people in this study were never smokers, and the results in that group looked pretty similar to the results overall.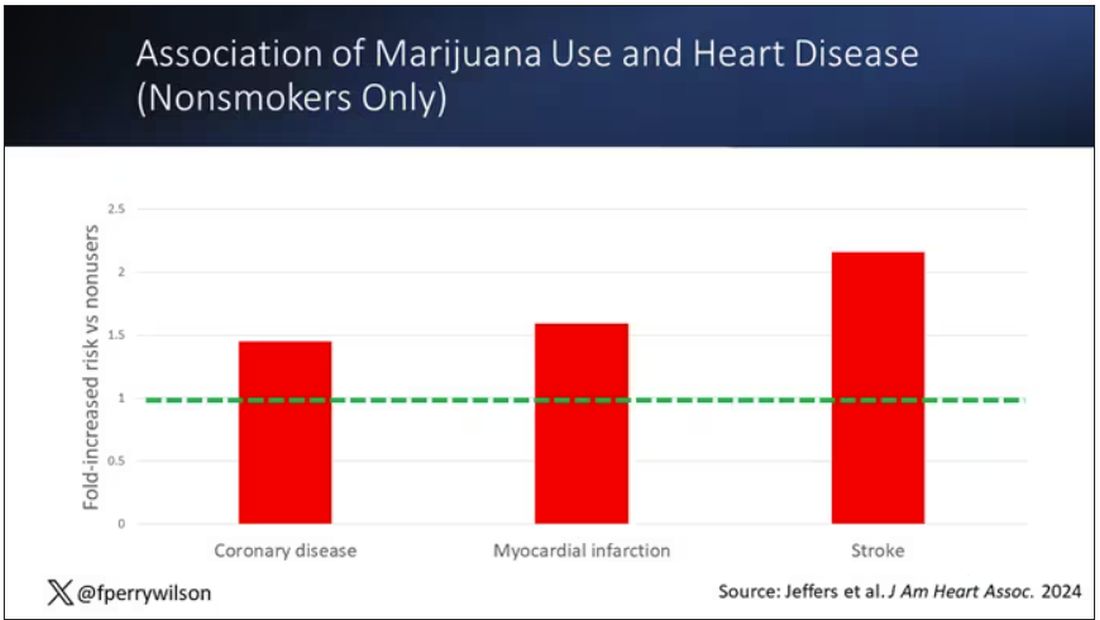
But I said there were a couple of problems, so let’s dig into those a bit.
First, like most survey studies, this one requires honest and accurate reporting from its subjects. There was no verification of heart disease using electronic health records or of marijuana usage based on biosamples. Broadly, miscategorization of exposure and outcomes in surveys tends to bias the results toward the null hypothesis, toward concluding that there is no link between exposure and outcome, so perhaps this is okay.
The bigger problem is the fact that this is a cross-sectional design. If you really wanted to know whether marijuana led to heart disease, you’d do a longitudinal study following users and non-users for some number of decades and see who developed heart disease and who didn’t. (For the pedants out there, I suppose you’d actually want to randomize people to use marijuana or not and then see who had a heart attack, but the IRB keeps rejecting my protocol when I submit it.)
Here, though, we literally can’t tell whether people who use marijuana have more heart attacks or whether people who have heart attacks use more marijuana. The authors argue that there are no data that show that people are more likely to use marijuana after a heart attack or stroke, but at the time the survey was conducted, they had already had their heart attack or stroke.
The authors also imply that they found a dose-response relationship between marijuana use and these cardiovascular outcomes. This is an important statement because dose response is one factor that we use to determine whether a risk factor may actually be causative as opposed to just correlative.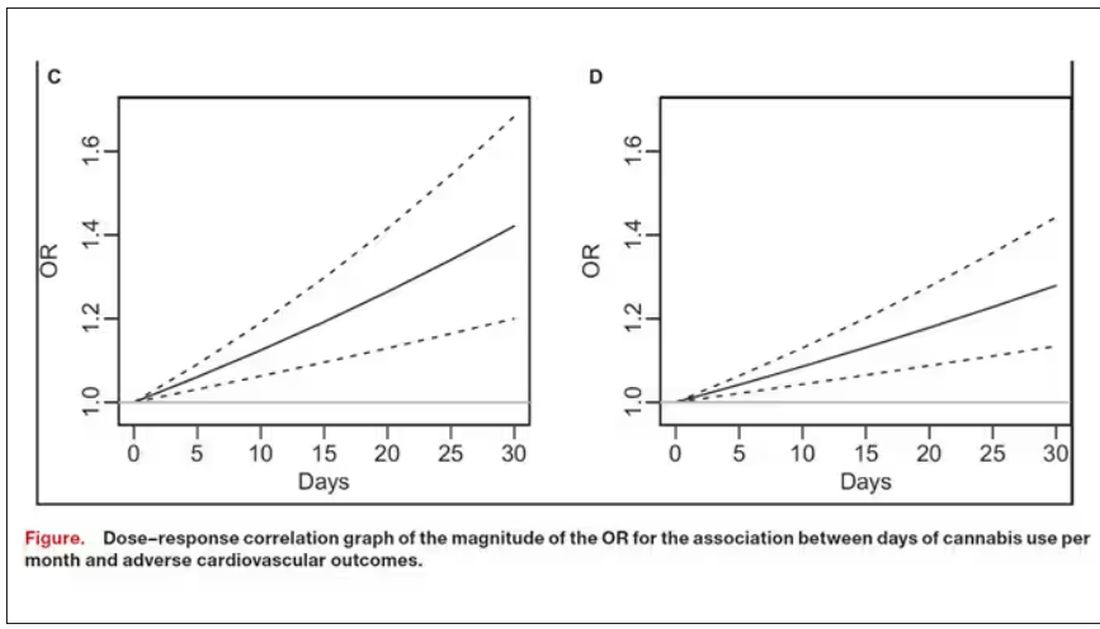
But I take issue with the dose-response language here. The model used to make these graphs classifies marijuana use as a single continuous variable ranging from 0 (no days of use in the past 30 days) to 1 (30 days of use in the past 30 days). The model is thus constrained to monotonically increase or decrease with respect to the outcome. To prove a dose response, you have to give the model the option to find something that isn’t a dose response — for example, by classifying marijuana use into discrete, independent categories rather than a single continuous number.
Am I arguing here that marijuana use is good for you? Of course not. Nor am I even arguing that it has no effect on the cardiovascular system. There are endocannabinoid receptors all over your vasculature. But a cross-sectional survey study, while a good start, is not quite the right way to answer the question. So, while the jury is still out, it’s high time for more research.
Dr. F. Perry Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
If you’re an epidemiologist trying to explore whether some exposure is a risk factor for a disease, you can run into a tough problem when your exposure of interest is highly correlated with another risk factor for the disease. For decades, this stymied investigations into the link, if any, between marijuana use and cardiovascular disease because, for decades, most people who used marijuana in some way also smoked cigarettes — which is a very clear risk factor for heart disease.
But the times they are a-changing.
Thanks to the legalization of marijuana for recreational use in many states, and even broader social trends, there is now a large population of people who use marijuana but do not use cigarettes. That means we can start to determine whether marijuana use is an independent risk factor for heart disease.
And this week, we have the largest study yet to attempt to answer that question, though, as I’ll explain momentarily, the smoke hasn’t entirely cleared yet.
The centerpiece of the study we are discussing this week, “Association of Cannabis Use With Cardiovascular Outcomes Among US Adults,” which appeared in the Journal of the American Heart Association, is the Behavioral Risk Factor Surveillance System, an annual telephone survey conducted by the Centers for Disease Control and Prevention since 1984 that gathers data on all sorts of stuff that we do to ourselves: our drinking habits, our smoking habits, and, more recently, our marijuana habits.
The paper combines annual data from 2016 to 2020 representing 27 states and two US territories for a total sample size of more than 430,000 individuals. The key exposure? Marijuana use, which was coded as the number of days of marijuana use in the past 30 days. The key outcome? Coronary heart disease, collected through questions such as “Has a doctor, nurse, or other health professional ever told you that you had a heart attack?”
Right away you might detect a couple of problems here. But let me show you the results before we worry about what they mean.
You can see the rates of the major cardiovascular outcomes here, stratified by daily use of marijuana, nondaily use, and no use. Broadly speaking, the risk was highest for daily users, lowest for occasional users, and in the middle for non-users.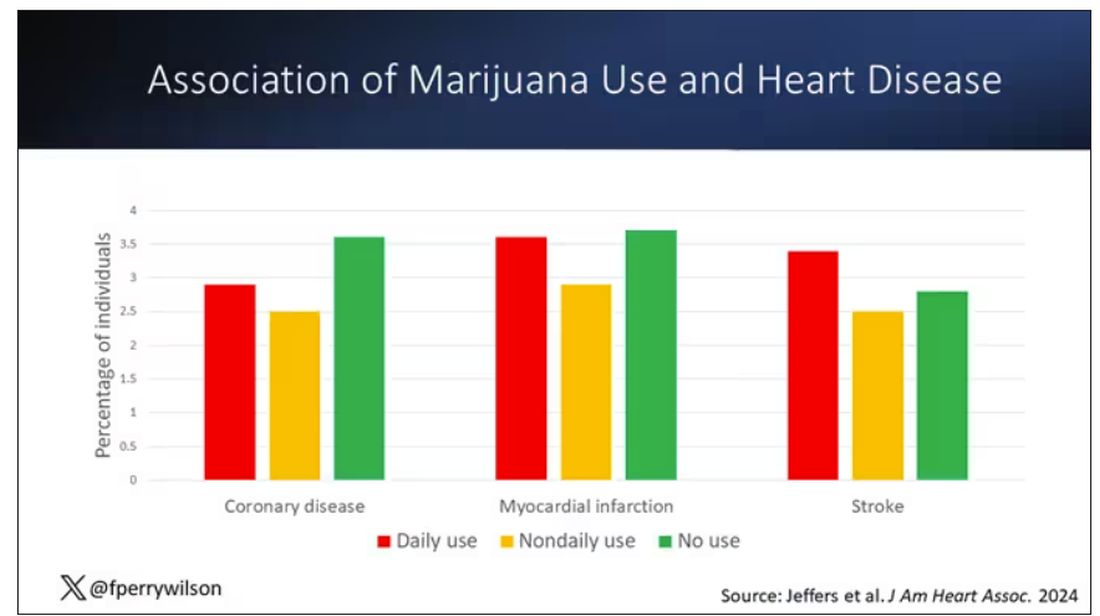
Of course, non-users and users are different in lots of other ways; non-users were quite a bit older, for example. Adjusting for all those factors showed that, independent of age, smoking status, the presence of diabetes, and so on, there was an independently increased risk for cardiovascular outcomes in people who used marijuana.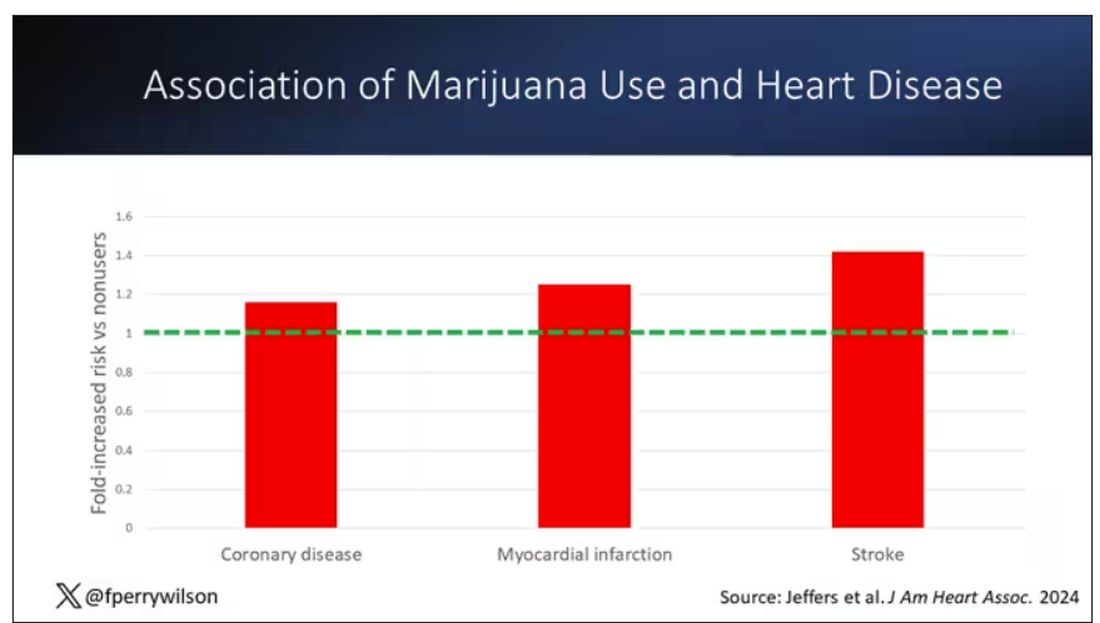
Importantly, 60% of people in this study were never smokers, and the results in that group looked pretty similar to the results overall.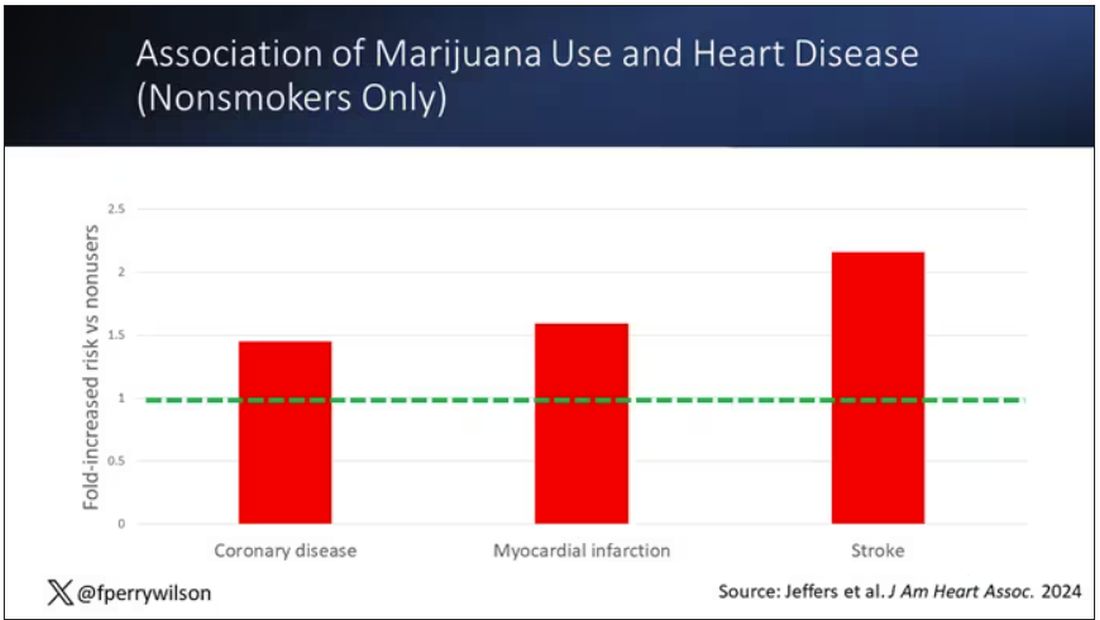
But I said there were a couple of problems, so let’s dig into those a bit.
First, like most survey studies, this one requires honest and accurate reporting from its subjects. There was no verification of heart disease using electronic health records or of marijuana usage based on biosamples. Broadly, miscategorization of exposure and outcomes in surveys tends to bias the results toward the null hypothesis, toward concluding that there is no link between exposure and outcome, so perhaps this is okay.
The bigger problem is the fact that this is a cross-sectional design. If you really wanted to know whether marijuana led to heart disease, you’d do a longitudinal study following users and non-users for some number of decades and see who developed heart disease and who didn’t. (For the pedants out there, I suppose you’d actually want to randomize people to use marijuana or not and then see who had a heart attack, but the IRB keeps rejecting my protocol when I submit it.)
Here, though, we literally can’t tell whether people who use marijuana have more heart attacks or whether people who have heart attacks use more marijuana. The authors argue that there are no data that show that people are more likely to use marijuana after a heart attack or stroke, but at the time the survey was conducted, they had already had their heart attack or stroke.
The authors also imply that they found a dose-response relationship between marijuana use and these cardiovascular outcomes. This is an important statement because dose response is one factor that we use to determine whether a risk factor may actually be causative as opposed to just correlative.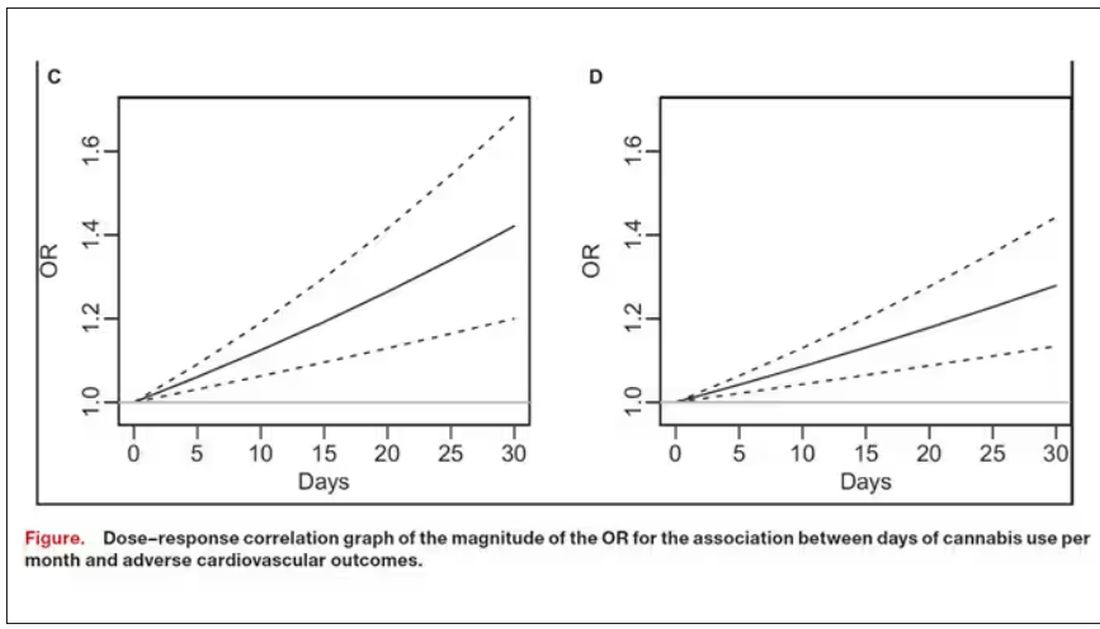
But I take issue with the dose-response language here. The model used to make these graphs classifies marijuana use as a single continuous variable ranging from 0 (no days of use in the past 30 days) to 1 (30 days of use in the past 30 days). The model is thus constrained to monotonically increase or decrease with respect to the outcome. To prove a dose response, you have to give the model the option to find something that isn’t a dose response — for example, by classifying marijuana use into discrete, independent categories rather than a single continuous number.
Am I arguing here that marijuana use is good for you? Of course not. Nor am I even arguing that it has no effect on the cardiovascular system. There are endocannabinoid receptors all over your vasculature. But a cross-sectional survey study, while a good start, is not quite the right way to answer the question. So, while the jury is still out, it’s high time for more research.
Dr. F. Perry Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
If you’re an epidemiologist trying to explore whether some exposure is a risk factor for a disease, you can run into a tough problem when your exposure of interest is highly correlated with another risk factor for the disease. For decades, this stymied investigations into the link, if any, between marijuana use and cardiovascular disease because, for decades, most people who used marijuana in some way also smoked cigarettes — which is a very clear risk factor for heart disease.
But the times they are a-changing.
Thanks to the legalization of marijuana for recreational use in many states, and even broader social trends, there is now a large population of people who use marijuana but do not use cigarettes. That means we can start to determine whether marijuana use is an independent risk factor for heart disease.
And this week, we have the largest study yet to attempt to answer that question, though, as I’ll explain momentarily, the smoke hasn’t entirely cleared yet.
The centerpiece of the study we are discussing this week, “Association of Cannabis Use With Cardiovascular Outcomes Among US Adults,” which appeared in the Journal of the American Heart Association, is the Behavioral Risk Factor Surveillance System, an annual telephone survey conducted by the Centers for Disease Control and Prevention since 1984 that gathers data on all sorts of stuff that we do to ourselves: our drinking habits, our smoking habits, and, more recently, our marijuana habits.
The paper combines annual data from 2016 to 2020 representing 27 states and two US territories for a total sample size of more than 430,000 individuals. The key exposure? Marijuana use, which was coded as the number of days of marijuana use in the past 30 days. The key outcome? Coronary heart disease, collected through questions such as “Has a doctor, nurse, or other health professional ever told you that you had a heart attack?”
Right away you might detect a couple of problems here. But let me show you the results before we worry about what they mean.
You can see the rates of the major cardiovascular outcomes here, stratified by daily use of marijuana, nondaily use, and no use. Broadly speaking, the risk was highest for daily users, lowest for occasional users, and in the middle for non-users.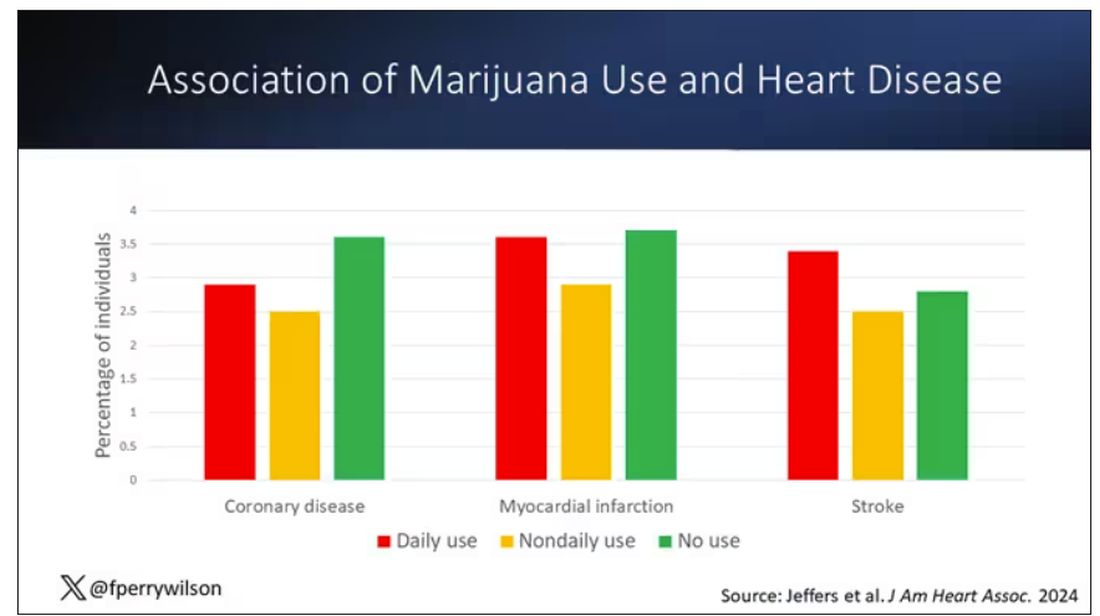
Of course, non-users and users are different in lots of other ways; non-users were quite a bit older, for example. Adjusting for all those factors showed that, independent of age, smoking status, the presence of diabetes, and so on, there was an independently increased risk for cardiovascular outcomes in people who used marijuana.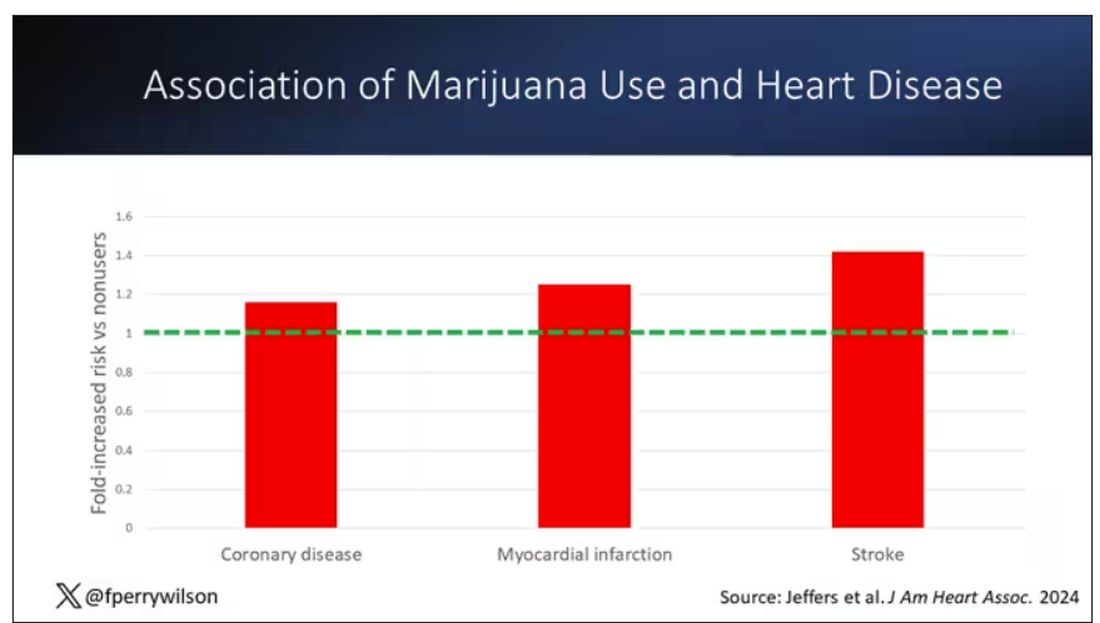
Importantly, 60% of people in this study were never smokers, and the results in that group looked pretty similar to the results overall.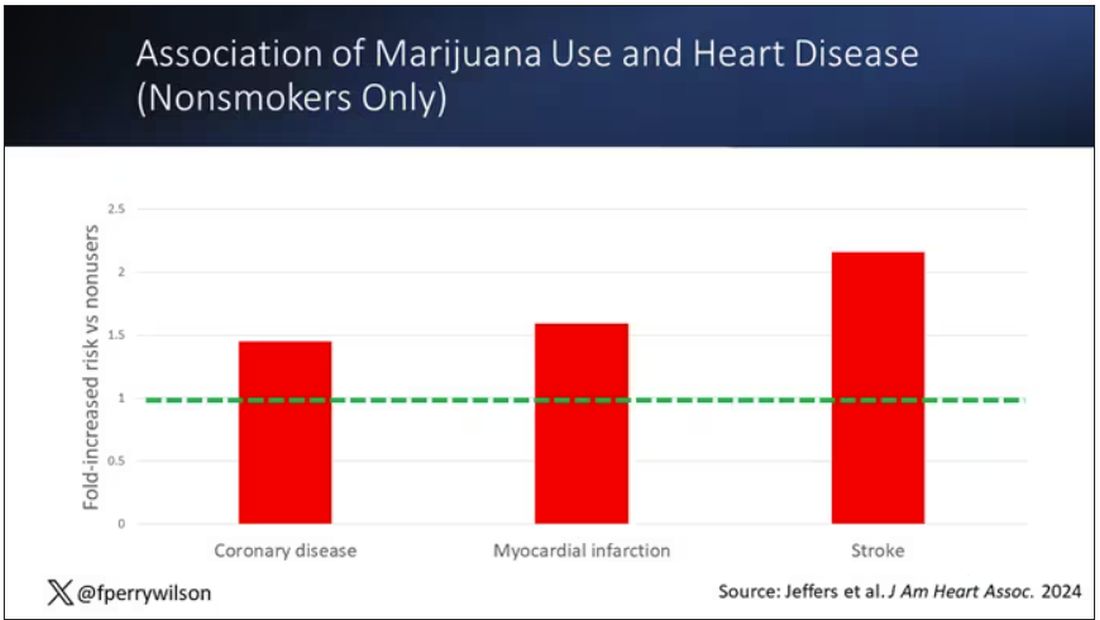
But I said there were a couple of problems, so let’s dig into those a bit.
First, like most survey studies, this one requires honest and accurate reporting from its subjects. There was no verification of heart disease using electronic health records or of marijuana usage based on biosamples. Broadly, miscategorization of exposure and outcomes in surveys tends to bias the results toward the null hypothesis, toward concluding that there is no link between exposure and outcome, so perhaps this is okay.
The bigger problem is the fact that this is a cross-sectional design. If you really wanted to know whether marijuana led to heart disease, you’d do a longitudinal study following users and non-users for some number of decades and see who developed heart disease and who didn’t. (For the pedants out there, I suppose you’d actually want to randomize people to use marijuana or not and then see who had a heart attack, but the IRB keeps rejecting my protocol when I submit it.)
Here, though, we literally can’t tell whether people who use marijuana have more heart attacks or whether people who have heart attacks use more marijuana. The authors argue that there are no data that show that people are more likely to use marijuana after a heart attack or stroke, but at the time the survey was conducted, they had already had their heart attack or stroke.
The authors also imply that they found a dose-response relationship between marijuana use and these cardiovascular outcomes. This is an important statement because dose response is one factor that we use to determine whether a risk factor may actually be causative as opposed to just correlative.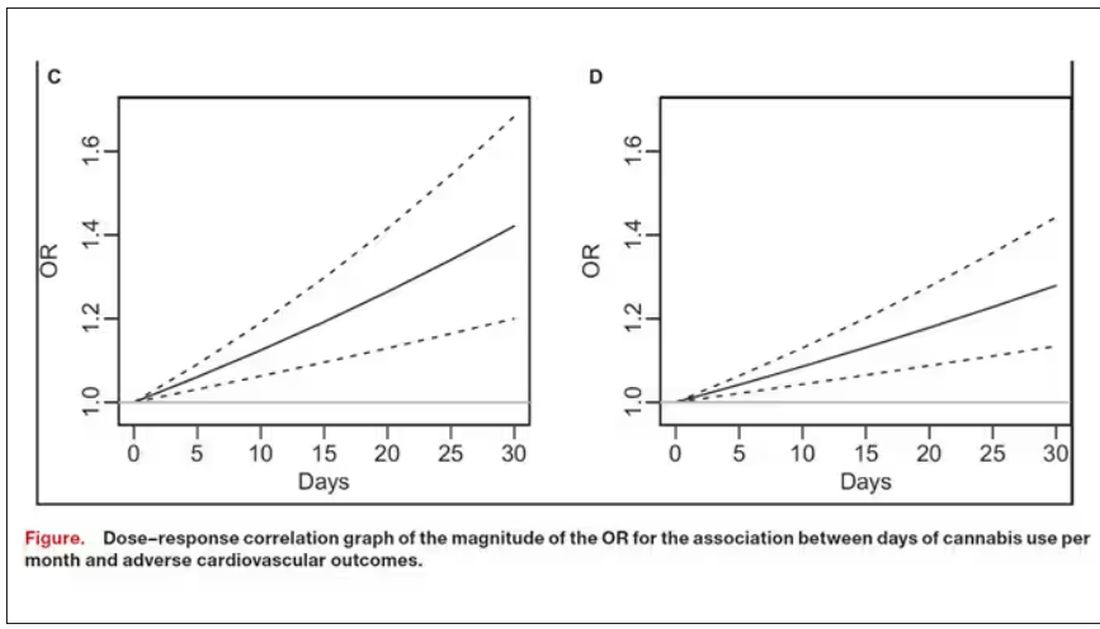
But I take issue with the dose-response language here. The model used to make these graphs classifies marijuana use as a single continuous variable ranging from 0 (no days of use in the past 30 days) to 1 (30 days of use in the past 30 days). The model is thus constrained to monotonically increase or decrease with respect to the outcome. To prove a dose response, you have to give the model the option to find something that isn’t a dose response — for example, by classifying marijuana use into discrete, independent categories rather than a single continuous number.
Am I arguing here that marijuana use is good for you? Of course not. Nor am I even arguing that it has no effect on the cardiovascular system. There are endocannabinoid receptors all over your vasculature. But a cross-sectional survey study, while a good start, is not quite the right way to answer the question. So, while the jury is still out, it’s high time for more research.
Dr. F. Perry Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Gout Increases the Risk for a Wide Range of Cardiovascular Diseases
People with gout are 58% more likely to develop cardiovascular disease (CVD), according to a new analysis. This increased risk was observed across 12 different cardiovascular conditions, including heart failure, arrhythmias, and valve diseases.
“These findings suggest that the organ damage associated with gout is likely to be much broader than originally thought,” Nathalie Conrad, PhD, senior author of the research and cardiovascular epidemiologist at KU Leuven, Leuven, Belgium, said in an email. This could be useful for future research on underlying biological mechanisms driving CVD risk in gout, she added.
While previous research has tied gout to increased cardiovascular risk, these studies “largely focused on coronary heart disease, stroke, and thromboembolic outcomes,” she explained, and have been smaller in size.
This new study included more than 862,000 individuals, which permitted researchers to investigate rarer CVD outcomes such as myocarditis and pericarditis.
For the study, researchers used electronic health records from the UK Clinical Practice Research Datalink, a primary care database that contains anonymized health data for about 22 million individuals. Using these data, they identified more than 152,600 individuals with gout. Patients included in the analysis were diagnosed between 2000 and 2017, younger than 80 years at diagnosis, and free of CVD for at least 12 months after their gout diagnosis.
Patients with gout were compared with nearly 710,000 controls, matched on demographic factors such as age, sex, and geographic region.
Researchers then investigated the incidence of 12 CVDs, including atherosclerotic diseases, degenerative and thromboembolic diseases, and arrythmias, between the two groups from January 1, 2000, to June 30, 2019.
The findings were published in the March 2024 issue of The Lancet Rheumatology. Overall, patients with gout were 58% more likely to develop any CVD than their matched comparators without gout. There was a higher disease incidence among patients with gout for each of the 12 conditions. This association was more pronounced in women (hazard ratio [HR], 1.88) than in men (HR, 1.49), and gout amplified the risk for CVD in younger individuals to a greater extent.
Individuals younger than 45 years with gout were more than twice as likely to develop CVD compared with similarly aged individuals without gout. For comparison, individuals aged 45-54 years with gout were 84% more likely to develop CVD, and individuals aged 55-64 years were 57% more likely to develop CVD than matched controls.
Conduction system disease had the highest incident risk (HR, 1.88), followed by heart failure and valve disease (HR, 1.85 for both).
Individuals with gout had higher rates of comorbidities than the controls, including hypertension, obesity, and dyslipidemia. Overall, CVD risk was slightly attenuated after adjustment for traditional CVD risk factors such as smoking, blood pressure, and body mass index but still significant: Patients with gout had a 31% higher risk for CVD than comparators.
This shows “that known CVD risk factors only explain part of the CVD risks seen in patients with gout,” Dr. Conrad said. Other factors such as inflammation and other disease activity factors could be at play, she explained, which would need to be explored in future research.
The study “shows the whole landscape” of CVD and gout, Michael H. Pillinger, MD, rheumatologist and professor of medicine, biochemistry, and molecular pharmacology at NYU Grossman School of Medicine in New York City, said in an interview. He was not involved with the research.
“Every possible cardiovascular disease that they could think of was something that gout patients had more of than the non-gout patients,” he added. “I think this is going to be a paper that gets cited a lot, at minimum when describing the background of risk when we look at gout patients.”
The study had some limitations, including that researchers were unable to account for how medications such as nonsteroidal anti-inflammatory drugs, corticosteroids, colchicine, or allopurinol may have affected the association between gout and CVD.
“This is because analyses of nonrandomized treatment can be confounded by indication, wherein it is difficult to differentiate the effects of the treatment from underlying disease severity,” the authors wrote.
There was also a large amount of missing data on blood pressure, body mass index, smoking status, and other health information relevant to cardiovascular risk, so sensitivity analyses adjusting for these factors “should be interpreted with caution,” they added.
Dr. Pillinger also noted that the rates of comorbidities in the gout study population were lower than what have been found in US study populations. For example, about 40% of patients with gout in the analysis had hypertension, while other studies have suggested higher rates of 60%-70%, he said. However, it’s not clear if these differences could have affected outcomes. He added that these limitations do not “in any way weaken [the authors’] conclusion.”
The findings call for better strategies to reduce CVD risk in patients with gout, Dr. Conrad noted.
“Further improvements could come from better recognition and intervention on CVD risk factors (eg, through lifestyle changes or drug therapies where they are indicated), as well as proactive screening for heart disease in patients with gout, which could allow early diagnosis and interventions to delay more severe outcomes,” she added.
This study was funded by Research Foundation Flanders. Dr. Conrad was funded by a personal fellowship from the Research Foundation Flanders and a European Society of Cardiology research grant. She received royalties from Oxford University Innovation. Four of Dr. Conrad’s eight coauthors also reported financial relationships with pharmaceutical companies. Dr. Pillinger served as a consultant to Amgen, Federation Bio, Fortress Biotech, and Scilex, and he holds an investigator-initiated grant from Hikma.
A version of this article appeared on Medscape.com.
People with gout are 58% more likely to develop cardiovascular disease (CVD), according to a new analysis. This increased risk was observed across 12 different cardiovascular conditions, including heart failure, arrhythmias, and valve diseases.
“These findings suggest that the organ damage associated with gout is likely to be much broader than originally thought,” Nathalie Conrad, PhD, senior author of the research and cardiovascular epidemiologist at KU Leuven, Leuven, Belgium, said in an email. This could be useful for future research on underlying biological mechanisms driving CVD risk in gout, she added.
While previous research has tied gout to increased cardiovascular risk, these studies “largely focused on coronary heart disease, stroke, and thromboembolic outcomes,” she explained, and have been smaller in size.
This new study included more than 862,000 individuals, which permitted researchers to investigate rarer CVD outcomes such as myocarditis and pericarditis.
For the study, researchers used electronic health records from the UK Clinical Practice Research Datalink, a primary care database that contains anonymized health data for about 22 million individuals. Using these data, they identified more than 152,600 individuals with gout. Patients included in the analysis were diagnosed between 2000 and 2017, younger than 80 years at diagnosis, and free of CVD for at least 12 months after their gout diagnosis.
Patients with gout were compared with nearly 710,000 controls, matched on demographic factors such as age, sex, and geographic region.
Researchers then investigated the incidence of 12 CVDs, including atherosclerotic diseases, degenerative and thromboembolic diseases, and arrythmias, between the two groups from January 1, 2000, to June 30, 2019.
The findings were published in the March 2024 issue of The Lancet Rheumatology. Overall, patients with gout were 58% more likely to develop any CVD than their matched comparators without gout. There was a higher disease incidence among patients with gout for each of the 12 conditions. This association was more pronounced in women (hazard ratio [HR], 1.88) than in men (HR, 1.49), and gout amplified the risk for CVD in younger individuals to a greater extent.
Individuals younger than 45 years with gout were more than twice as likely to develop CVD compared with similarly aged individuals without gout. For comparison, individuals aged 45-54 years with gout were 84% more likely to develop CVD, and individuals aged 55-64 years were 57% more likely to develop CVD than matched controls.
Conduction system disease had the highest incident risk (HR, 1.88), followed by heart failure and valve disease (HR, 1.85 for both).
Individuals with gout had higher rates of comorbidities than the controls, including hypertension, obesity, and dyslipidemia. Overall, CVD risk was slightly attenuated after adjustment for traditional CVD risk factors such as smoking, blood pressure, and body mass index but still significant: Patients with gout had a 31% higher risk for CVD than comparators.
This shows “that known CVD risk factors only explain part of the CVD risks seen in patients with gout,” Dr. Conrad said. Other factors such as inflammation and other disease activity factors could be at play, she explained, which would need to be explored in future research.
The study “shows the whole landscape” of CVD and gout, Michael H. Pillinger, MD, rheumatologist and professor of medicine, biochemistry, and molecular pharmacology at NYU Grossman School of Medicine in New York City, said in an interview. He was not involved with the research.
“Every possible cardiovascular disease that they could think of was something that gout patients had more of than the non-gout patients,” he added. “I think this is going to be a paper that gets cited a lot, at minimum when describing the background of risk when we look at gout patients.”
The study had some limitations, including that researchers were unable to account for how medications such as nonsteroidal anti-inflammatory drugs, corticosteroids, colchicine, or allopurinol may have affected the association between gout and CVD.
“This is because analyses of nonrandomized treatment can be confounded by indication, wherein it is difficult to differentiate the effects of the treatment from underlying disease severity,” the authors wrote.
There was also a large amount of missing data on blood pressure, body mass index, smoking status, and other health information relevant to cardiovascular risk, so sensitivity analyses adjusting for these factors “should be interpreted with caution,” they added.
Dr. Pillinger also noted that the rates of comorbidities in the gout study population were lower than what have been found in US study populations. For example, about 40% of patients with gout in the analysis had hypertension, while other studies have suggested higher rates of 60%-70%, he said. However, it’s not clear if these differences could have affected outcomes. He added that these limitations do not “in any way weaken [the authors’] conclusion.”
The findings call for better strategies to reduce CVD risk in patients with gout, Dr. Conrad noted.
“Further improvements could come from better recognition and intervention on CVD risk factors (eg, through lifestyle changes or drug therapies where they are indicated), as well as proactive screening for heart disease in patients with gout, which could allow early diagnosis and interventions to delay more severe outcomes,” she added.
This study was funded by Research Foundation Flanders. Dr. Conrad was funded by a personal fellowship from the Research Foundation Flanders and a European Society of Cardiology research grant. She received royalties from Oxford University Innovation. Four of Dr. Conrad’s eight coauthors also reported financial relationships with pharmaceutical companies. Dr. Pillinger served as a consultant to Amgen, Federation Bio, Fortress Biotech, and Scilex, and he holds an investigator-initiated grant from Hikma.
A version of this article appeared on Medscape.com.
People with gout are 58% more likely to develop cardiovascular disease (CVD), according to a new analysis. This increased risk was observed across 12 different cardiovascular conditions, including heart failure, arrhythmias, and valve diseases.
“These findings suggest that the organ damage associated with gout is likely to be much broader than originally thought,” Nathalie Conrad, PhD, senior author of the research and cardiovascular epidemiologist at KU Leuven, Leuven, Belgium, said in an email. This could be useful for future research on underlying biological mechanisms driving CVD risk in gout, she added.
While previous research has tied gout to increased cardiovascular risk, these studies “largely focused on coronary heart disease, stroke, and thromboembolic outcomes,” she explained, and have been smaller in size.
This new study included more than 862,000 individuals, which permitted researchers to investigate rarer CVD outcomes such as myocarditis and pericarditis.
For the study, researchers used electronic health records from the UK Clinical Practice Research Datalink, a primary care database that contains anonymized health data for about 22 million individuals. Using these data, they identified more than 152,600 individuals with gout. Patients included in the analysis were diagnosed between 2000 and 2017, younger than 80 years at diagnosis, and free of CVD for at least 12 months after their gout diagnosis.
Patients with gout were compared with nearly 710,000 controls, matched on demographic factors such as age, sex, and geographic region.
Researchers then investigated the incidence of 12 CVDs, including atherosclerotic diseases, degenerative and thromboembolic diseases, and arrythmias, between the two groups from January 1, 2000, to June 30, 2019.
The findings were published in the March 2024 issue of The Lancet Rheumatology. Overall, patients with gout were 58% more likely to develop any CVD than their matched comparators without gout. There was a higher disease incidence among patients with gout for each of the 12 conditions. This association was more pronounced in women (hazard ratio [HR], 1.88) than in men (HR, 1.49), and gout amplified the risk for CVD in younger individuals to a greater extent.
Individuals younger than 45 years with gout were more than twice as likely to develop CVD compared with similarly aged individuals without gout. For comparison, individuals aged 45-54 years with gout were 84% more likely to develop CVD, and individuals aged 55-64 years were 57% more likely to develop CVD than matched controls.
Conduction system disease had the highest incident risk (HR, 1.88), followed by heart failure and valve disease (HR, 1.85 for both).
Individuals with gout had higher rates of comorbidities than the controls, including hypertension, obesity, and dyslipidemia. Overall, CVD risk was slightly attenuated after adjustment for traditional CVD risk factors such as smoking, blood pressure, and body mass index but still significant: Patients with gout had a 31% higher risk for CVD than comparators.
This shows “that known CVD risk factors only explain part of the CVD risks seen in patients with gout,” Dr. Conrad said. Other factors such as inflammation and other disease activity factors could be at play, she explained, which would need to be explored in future research.
The study “shows the whole landscape” of CVD and gout, Michael H. Pillinger, MD, rheumatologist and professor of medicine, biochemistry, and molecular pharmacology at NYU Grossman School of Medicine in New York City, said in an interview. He was not involved with the research.
“Every possible cardiovascular disease that they could think of was something that gout patients had more of than the non-gout patients,” he added. “I think this is going to be a paper that gets cited a lot, at minimum when describing the background of risk when we look at gout patients.”
The study had some limitations, including that researchers were unable to account for how medications such as nonsteroidal anti-inflammatory drugs, corticosteroids, colchicine, or allopurinol may have affected the association between gout and CVD.
“This is because analyses of nonrandomized treatment can be confounded by indication, wherein it is difficult to differentiate the effects of the treatment from underlying disease severity,” the authors wrote.
There was also a large amount of missing data on blood pressure, body mass index, smoking status, and other health information relevant to cardiovascular risk, so sensitivity analyses adjusting for these factors “should be interpreted with caution,” they added.
Dr. Pillinger also noted that the rates of comorbidities in the gout study population were lower than what have been found in US study populations. For example, about 40% of patients with gout in the analysis had hypertension, while other studies have suggested higher rates of 60%-70%, he said. However, it’s not clear if these differences could have affected outcomes. He added that these limitations do not “in any way weaken [the authors’] conclusion.”
The findings call for better strategies to reduce CVD risk in patients with gout, Dr. Conrad noted.
“Further improvements could come from better recognition and intervention on CVD risk factors (eg, through lifestyle changes or drug therapies where they are indicated), as well as proactive screening for heart disease in patients with gout, which could allow early diagnosis and interventions to delay more severe outcomes,” she added.
This study was funded by Research Foundation Flanders. Dr. Conrad was funded by a personal fellowship from the Research Foundation Flanders and a European Society of Cardiology research grant. She received royalties from Oxford University Innovation. Four of Dr. Conrad’s eight coauthors also reported financial relationships with pharmaceutical companies. Dr. Pillinger served as a consultant to Amgen, Federation Bio, Fortress Biotech, and Scilex, and he holds an investigator-initiated grant from Hikma.
A version of this article appeared on Medscape.com.
Is Stretching Now Underrated? Accumulating Research Says Yes
For many, stretching is the fitness equivalent of awkward small talk. It’s the opening act, the thing you tolerate because you know it will be over soon.
Others have challenged the practice, suggesting that stretching isn’t necessary at all. Some research has found that a preworkout stretch may even be disadvantageous, weakening muscles and hindering performance.
To put it plainly, no one seems terribly enthusiastic about touching their toes.
That’s why a 2020 study on exercise and mortality was such a head-scratcher. The study found that stretching was uniquely associated with a lower risk for all-cause mortality among American adults. That’s after controlling for participation in other types of exercise.
The finding seemed like a fluke, until a 2023 study found essentially the same thing.
That was slightly better than the risk reduction associated with high volumes of aerobic exercise and resistance training.
How can that be ? It turns out, stretching is linked to several health benefits that you might not expect.
The Surprising Benefits of Stretching
When we talk about stretching, we usually mean static stretching — getting into and holding a position that challenges a muscle, with the goal of improving range of motion around a joint.
It doesn’t need to be a big challenge. “Research shows you can get increases in flexibility by stretching to the initial point of discomfort,” said David Behm, PhD, an exercise scientist at Memorial University of Newfoundland in Canada who’s published dozens of studies on stretching over the past quarter-century.
That brings us to the first benefit.
Stretching Benefit #1: More Strength
At first glance, flexibility training and strength training have little in common. You lengthen muscles in the former and contract them in the latter.
But in both cases, Dr. Behm said, you’re applying tension to muscles and connective tissues. Tension activates proteins called integrins, which send and receive signals across cellular membranes. Those signals are the start of a cascade that leads to protein synthesis. That’s how muscles get bigger and stronger when you lift weights.
That mechanism could explain the small gains in muscle strength and size associated with static stretching, Dr. Behm said.
But can you really stretch your way to muscle growth? Theoretically, yes. But strength training is far more time-efficient, Dr. Behm says. Studies showing increases in muscle mass have typically stretched a single muscle (usually the calves, using a specialized device) for > 30 min/session, 6 d/wk for 6 weeks. And that’s for just one leg.
Still, stretching may be more accessible for some patients — research suggested that older and more sedentary people are most likely to benefit from stretching-induced gains in strength.
Stretching Benefit #2: Reduced Arterial Stiffness
“Most people don’t think about the cardiovascular benefits of stretching,” Dr. Behm said. There are some big ones.
If your body doesn’t move well, it’s not unreasonable to assume your blood doesn’t flow well. That is indeed the case: Poor flexibility is associated with arterial stiffness.
Stretching is associated not only with improved arterial function but also with reductions in resting heart rate and blood pressure and increased vasodilation.
Mobility improvements may have an indirect benefit on cardiovascular health as well.
“Studies show runners are more economical when they’re more flexible,” Dr. Behm said. If your movement is more efficient, you’ll probably do more of it. Doing more, in turn, would lead to improved fitness.
Stretching Benefit #3: Improved Performance
Research is equivocal on whether stretching improves athletic performance, said Joe Yoon, a sports massage therapist in Orlando, Florida, and author of Better Stretching.
“But I’ve always taken the approach that if you can improve your range of motion and get into positions” required for your sport, you’ll probably perform better, with less risk for injury, Mr. Yoon said.
It’s worth noting that some research over the past 30 years has linked pre-exercise static stretching with a loss of strength, power, and/or speed.
But consider this: In a 2016 review, Dr. Behm and his coauthors showed that performance reductions were most likely to occur in two situations:
When participants did extremely long stretches (duration, ≥ 60 sec per muscle).
When researchers tested the participants’ strength, power, or speed immediately after they stretched.
Avoiding those problems is easy, Dr. Behm said: Stretch each muscle for < 60 sec, and combine static stretches with more active warm-up exercises.
“Stretching can impair your performance but only if you do it wrong,” he said.
Stretching Benefit #4: Fewer Injuries
When you stretch, the point where you feel tension is where the muscle is most vulnerable. “That’s where injuries usually happen,” Dr. Behm said.
More flexibility in those areas allows your muscles to safely generate force at longer lengths. For an athlete, that means fewer injuries when they’re doing explosive movements or changing direction.
For nonathletes, flexibility reduces injuries by improving balance. Better balance reduces the risk of falling and helps mitigate the damage if you do take a tumble.
Help Your Patients Get the Benefits of Stretching
Stretching, like training for endurance or strength, can be as complex as you want to make it. But Mr. Yoon advocates a simpler approach.
“You see this flashy stuff online,” he said. “But if you see those trainers in real life or you book a session with them, they go right back to the basics.”
Ideally, Mr. Yoon said, a flexibility routine will work the entire body. But if that’s too big a stretch for your patient, he recommends starting with one or two stretches for the most problematic area.
For example, for a stiff back, try doing the puppy pose at least once a day, although twice is better. Hold the position for 30 seconds to 2 minutes, said Mr. Yoon. Even if you combine it with a dynamic movement like the cat-cow, the two exercises would take just a few minutes a day.
“There’s this misconception that you have to do a lot of it to be successful,” Mr. Yoon said.
Consistency is far more important than volume. Mr. Yoon recommends “a little bit every day — the minimum viable dose.”
As a bonus, stretching an area like your upper back will probably improve your shoulder mobility, Mr. Yoon said. Same with your lower body: Stretches for your hips, over time, should also benefit your knees and lower back.
And thanks to a phenomenon called nonlocal flexibility transfer, lower-body stretches should improve upper-body flexibility, at least temporarily. Shoulder stretches can also have an immediate effect on hip mobility.
“It’s all connected,” Mr. Yoon said, which brings us back to where we started.
If stretching can indeed reduce mortality risk, it’s probably because of interconnected pathways, rather than any single mechanism.
Most obviously, stretching improves flexibility, which makes movement easier, improves balance, and reduces the risk for falls and other types of injuries. It can also lead to small improvements in strength. Less obviously, stretching improves several aspects of cardiovascular function, including circulation.
“There seems to be a global effect in everything we do,” Dr. Behm said. “Whether you’re stretching or weight training, the message is sent throughout your body."
A version of this article appeared on Medscape.com.
For many, stretching is the fitness equivalent of awkward small talk. It’s the opening act, the thing you tolerate because you know it will be over soon.
Others have challenged the practice, suggesting that stretching isn’t necessary at all. Some research has found that a preworkout stretch may even be disadvantageous, weakening muscles and hindering performance.
To put it plainly, no one seems terribly enthusiastic about touching their toes.
That’s why a 2020 study on exercise and mortality was such a head-scratcher. The study found that stretching was uniquely associated with a lower risk for all-cause mortality among American adults. That’s after controlling for participation in other types of exercise.
The finding seemed like a fluke, until a 2023 study found essentially the same thing.
That was slightly better than the risk reduction associated with high volumes of aerobic exercise and resistance training.
How can that be ? It turns out, stretching is linked to several health benefits that you might not expect.
The Surprising Benefits of Stretching
When we talk about stretching, we usually mean static stretching — getting into and holding a position that challenges a muscle, with the goal of improving range of motion around a joint.
It doesn’t need to be a big challenge. “Research shows you can get increases in flexibility by stretching to the initial point of discomfort,” said David Behm, PhD, an exercise scientist at Memorial University of Newfoundland in Canada who’s published dozens of studies on stretching over the past quarter-century.
That brings us to the first benefit.
Stretching Benefit #1: More Strength
At first glance, flexibility training and strength training have little in common. You lengthen muscles in the former and contract them in the latter.
But in both cases, Dr. Behm said, you’re applying tension to muscles and connective tissues. Tension activates proteins called integrins, which send and receive signals across cellular membranes. Those signals are the start of a cascade that leads to protein synthesis. That’s how muscles get bigger and stronger when you lift weights.
That mechanism could explain the small gains in muscle strength and size associated with static stretching, Dr. Behm said.
But can you really stretch your way to muscle growth? Theoretically, yes. But strength training is far more time-efficient, Dr. Behm says. Studies showing increases in muscle mass have typically stretched a single muscle (usually the calves, using a specialized device) for > 30 min/session, 6 d/wk for 6 weeks. And that’s for just one leg.
Still, stretching may be more accessible for some patients — research suggested that older and more sedentary people are most likely to benefit from stretching-induced gains in strength.
Stretching Benefit #2: Reduced Arterial Stiffness
“Most people don’t think about the cardiovascular benefits of stretching,” Dr. Behm said. There are some big ones.
If your body doesn’t move well, it’s not unreasonable to assume your blood doesn’t flow well. That is indeed the case: Poor flexibility is associated with arterial stiffness.
Stretching is associated not only with improved arterial function but also with reductions in resting heart rate and blood pressure and increased vasodilation.
Mobility improvements may have an indirect benefit on cardiovascular health as well.
“Studies show runners are more economical when they’re more flexible,” Dr. Behm said. If your movement is more efficient, you’ll probably do more of it. Doing more, in turn, would lead to improved fitness.
Stretching Benefit #3: Improved Performance
Research is equivocal on whether stretching improves athletic performance, said Joe Yoon, a sports massage therapist in Orlando, Florida, and author of Better Stretching.
“But I’ve always taken the approach that if you can improve your range of motion and get into positions” required for your sport, you’ll probably perform better, with less risk for injury, Mr. Yoon said.
It’s worth noting that some research over the past 30 years has linked pre-exercise static stretching with a loss of strength, power, and/or speed.
But consider this: In a 2016 review, Dr. Behm and his coauthors showed that performance reductions were most likely to occur in two situations:
When participants did extremely long stretches (duration, ≥ 60 sec per muscle).
When researchers tested the participants’ strength, power, or speed immediately after they stretched.
Avoiding those problems is easy, Dr. Behm said: Stretch each muscle for < 60 sec, and combine static stretches with more active warm-up exercises.
“Stretching can impair your performance but only if you do it wrong,” he said.
Stretching Benefit #4: Fewer Injuries
When you stretch, the point where you feel tension is where the muscle is most vulnerable. “That’s where injuries usually happen,” Dr. Behm said.
More flexibility in those areas allows your muscles to safely generate force at longer lengths. For an athlete, that means fewer injuries when they’re doing explosive movements or changing direction.
For nonathletes, flexibility reduces injuries by improving balance. Better balance reduces the risk of falling and helps mitigate the damage if you do take a tumble.
Help Your Patients Get the Benefits of Stretching
Stretching, like training for endurance or strength, can be as complex as you want to make it. But Mr. Yoon advocates a simpler approach.
“You see this flashy stuff online,” he said. “But if you see those trainers in real life or you book a session with them, they go right back to the basics.”
Ideally, Mr. Yoon said, a flexibility routine will work the entire body. But if that’s too big a stretch for your patient, he recommends starting with one or two stretches for the most problematic area.
For example, for a stiff back, try doing the puppy pose at least once a day, although twice is better. Hold the position for 30 seconds to 2 minutes, said Mr. Yoon. Even if you combine it with a dynamic movement like the cat-cow, the two exercises would take just a few minutes a day.
“There’s this misconception that you have to do a lot of it to be successful,” Mr. Yoon said.
Consistency is far more important than volume. Mr. Yoon recommends “a little bit every day — the minimum viable dose.”
As a bonus, stretching an area like your upper back will probably improve your shoulder mobility, Mr. Yoon said. Same with your lower body: Stretches for your hips, over time, should also benefit your knees and lower back.
And thanks to a phenomenon called nonlocal flexibility transfer, lower-body stretches should improve upper-body flexibility, at least temporarily. Shoulder stretches can also have an immediate effect on hip mobility.
“It’s all connected,” Mr. Yoon said, which brings us back to where we started.
If stretching can indeed reduce mortality risk, it’s probably because of interconnected pathways, rather than any single mechanism.
Most obviously, stretching improves flexibility, which makes movement easier, improves balance, and reduces the risk for falls and other types of injuries. It can also lead to small improvements in strength. Less obviously, stretching improves several aspects of cardiovascular function, including circulation.
“There seems to be a global effect in everything we do,” Dr. Behm said. “Whether you’re stretching or weight training, the message is sent throughout your body."
A version of this article appeared on Medscape.com.
For many, stretching is the fitness equivalent of awkward small talk. It’s the opening act, the thing you tolerate because you know it will be over soon.
Others have challenged the practice, suggesting that stretching isn’t necessary at all. Some research has found that a preworkout stretch may even be disadvantageous, weakening muscles and hindering performance.
To put it plainly, no one seems terribly enthusiastic about touching their toes.
That’s why a 2020 study on exercise and mortality was such a head-scratcher. The study found that stretching was uniquely associated with a lower risk for all-cause mortality among American adults. That’s after controlling for participation in other types of exercise.
The finding seemed like a fluke, until a 2023 study found essentially the same thing.
That was slightly better than the risk reduction associated with high volumes of aerobic exercise and resistance training.
How can that be ? It turns out, stretching is linked to several health benefits that you might not expect.
The Surprising Benefits of Stretching
When we talk about stretching, we usually mean static stretching — getting into and holding a position that challenges a muscle, with the goal of improving range of motion around a joint.
It doesn’t need to be a big challenge. “Research shows you can get increases in flexibility by stretching to the initial point of discomfort,” said David Behm, PhD, an exercise scientist at Memorial University of Newfoundland in Canada who’s published dozens of studies on stretching over the past quarter-century.
That brings us to the first benefit.
Stretching Benefit #1: More Strength
At first glance, flexibility training and strength training have little in common. You lengthen muscles in the former and contract them in the latter.
But in both cases, Dr. Behm said, you’re applying tension to muscles and connective tissues. Tension activates proteins called integrins, which send and receive signals across cellular membranes. Those signals are the start of a cascade that leads to protein synthesis. That’s how muscles get bigger and stronger when you lift weights.
That mechanism could explain the small gains in muscle strength and size associated with static stretching, Dr. Behm said.
But can you really stretch your way to muscle growth? Theoretically, yes. But strength training is far more time-efficient, Dr. Behm says. Studies showing increases in muscle mass have typically stretched a single muscle (usually the calves, using a specialized device) for > 30 min/session, 6 d/wk for 6 weeks. And that’s for just one leg.
Still, stretching may be more accessible for some patients — research suggested that older and more sedentary people are most likely to benefit from stretching-induced gains in strength.
Stretching Benefit #2: Reduced Arterial Stiffness
“Most people don’t think about the cardiovascular benefits of stretching,” Dr. Behm said. There are some big ones.
If your body doesn’t move well, it’s not unreasonable to assume your blood doesn’t flow well. That is indeed the case: Poor flexibility is associated with arterial stiffness.
Stretching is associated not only with improved arterial function but also with reductions in resting heart rate and blood pressure and increased vasodilation.
Mobility improvements may have an indirect benefit on cardiovascular health as well.
“Studies show runners are more economical when they’re more flexible,” Dr. Behm said. If your movement is more efficient, you’ll probably do more of it. Doing more, in turn, would lead to improved fitness.
Stretching Benefit #3: Improved Performance
Research is equivocal on whether stretching improves athletic performance, said Joe Yoon, a sports massage therapist in Orlando, Florida, and author of Better Stretching.
“But I’ve always taken the approach that if you can improve your range of motion and get into positions” required for your sport, you’ll probably perform better, with less risk for injury, Mr. Yoon said.
It’s worth noting that some research over the past 30 years has linked pre-exercise static stretching with a loss of strength, power, and/or speed.
But consider this: In a 2016 review, Dr. Behm and his coauthors showed that performance reductions were most likely to occur in two situations:
When participants did extremely long stretches (duration, ≥ 60 sec per muscle).
When researchers tested the participants’ strength, power, or speed immediately after they stretched.
Avoiding those problems is easy, Dr. Behm said: Stretch each muscle for < 60 sec, and combine static stretches with more active warm-up exercises.
“Stretching can impair your performance but only if you do it wrong,” he said.
Stretching Benefit #4: Fewer Injuries
When you stretch, the point where you feel tension is where the muscle is most vulnerable. “That’s where injuries usually happen,” Dr. Behm said.
More flexibility in those areas allows your muscles to safely generate force at longer lengths. For an athlete, that means fewer injuries when they’re doing explosive movements or changing direction.
For nonathletes, flexibility reduces injuries by improving balance. Better balance reduces the risk of falling and helps mitigate the damage if you do take a tumble.
Help Your Patients Get the Benefits of Stretching
Stretching, like training for endurance or strength, can be as complex as you want to make it. But Mr. Yoon advocates a simpler approach.
“You see this flashy stuff online,” he said. “But if you see those trainers in real life or you book a session with them, they go right back to the basics.”
Ideally, Mr. Yoon said, a flexibility routine will work the entire body. But if that’s too big a stretch for your patient, he recommends starting with one or two stretches for the most problematic area.
For example, for a stiff back, try doing the puppy pose at least once a day, although twice is better. Hold the position for 30 seconds to 2 minutes, said Mr. Yoon. Even if you combine it with a dynamic movement like the cat-cow, the two exercises would take just a few minutes a day.
“There’s this misconception that you have to do a lot of it to be successful,” Mr. Yoon said.
Consistency is far more important than volume. Mr. Yoon recommends “a little bit every day — the minimum viable dose.”
As a bonus, stretching an area like your upper back will probably improve your shoulder mobility, Mr. Yoon said. Same with your lower body: Stretches for your hips, over time, should also benefit your knees and lower back.
And thanks to a phenomenon called nonlocal flexibility transfer, lower-body stretches should improve upper-body flexibility, at least temporarily. Shoulder stretches can also have an immediate effect on hip mobility.
“It’s all connected,” Mr. Yoon said, which brings us back to where we started.
If stretching can indeed reduce mortality risk, it’s probably because of interconnected pathways, rather than any single mechanism.
Most obviously, stretching improves flexibility, which makes movement easier, improves balance, and reduces the risk for falls and other types of injuries. It can also lead to small improvements in strength. Less obviously, stretching improves several aspects of cardiovascular function, including circulation.
“There seems to be a global effect in everything we do,” Dr. Behm said. “Whether you’re stretching or weight training, the message is sent throughout your body."
A version of this article appeared on Medscape.com.
Judge Won’t Overturn Invalidated USMLE Scores
(USMLE).
In a February 23 order, Judge Christopher R. Cooper, of the US District Court for the District of Columbia, denied Latika Giri’s emergency motion to block the National Board of Medical Examiners (NBME) from invalidating the scores, ruling the public interest plainly weighs against granting the request.
“First and foremost, is the overriding interest in public safety,” Cooper wrote in his 32-page order. “This is a case about the credentials of doctors applying to medical residency programs…Granting the preliminary injunction would create an unacceptable risk that individuals who lack the requisite knowledge and skills they purport to possess because they achieved their exam scores fraudulently will be administering medical care to unsuspecting patients across the nation.”
Attorneys for Giri did not return messages seeking comment about the order.
The NBME also did not return messages seeking comment. The board previously said it does not comment on pending litigation.
The decision is the latest development in a widespread cheating scandal. Giri, an international medical graduate (IMG) from Kathmandu, sued NBME earlier this month claiming the board discriminated against Nepali medical graduates when it invalidated hundreds of exam scores linked to the country.
Giri also accused NBME of violating its own procedures when it voided the scores before giving examinees a chance to argue and appeal. She asked the district court to block NBME from invalidating her exam scores while the lawsuit continues and restore her original results.
In court documents, NBME argued that it did not invalidate the scores because the examinees were Nepali but because staff concluded that there was “a good faith basis for questioning the validity of the scores.”
The invalidations were based on concerns that the results reflected prior access to secure exam content rather than knowledge and understanding of the medical principles and skills the exams are intended to assess, according to the NBME’s legal response.
“The USMLE program took reasonable and appropriate actions to prevent the significant harm and disruption that would result from allowing potentially unqualified individuals to participate in the 2024 residency Match,” the NBME stated in court documents. “If granted, the requested injunction would cause enormous harm not only to NBME… but also to state licensing authorities, which rely upon USMLE results to help ensure that physicians have the minimum competencies needed to provide safe and effective health care.”
In his order, Cooper wrote that Giri has not proven the board’s actions were discriminatory against Nepali doctors.
“Nothing in the present record suggests that NBME went looking for a problem in Nepal out of ethnicity-or national-origin based [sic] suspicion,” Cooper wrote. “[It] followed the trail of evidence, including tips about organized cheating taking place in medical schools and at a testing center located in Nepal, and on an online forum for which a ‘nexus to Nepal’ was a ticket to admission.”
NBME: Nepal Outperformed All Other Countries on USMLE
Court documents shed more light on NBME’s investigation into the suspected cheating and on the anomalous patterns the board allegedly discovered from Nepal medical graduates.
In response to anonymous tips, the USMLE program in early 2023 asked the NBME Psychometrics and Data Analysis (PADA) unit to analyze examinee performance data for test centers in Jordan, Nepal, and Pakistan, according to court records. Within the initial data analysis, the data involving the single test center in Nepal was “the most extreme,” the unit found.
Out of more than 400 test centers across the world, including those in the United States, the test center in Nepal produced the highest test scores in the world for Step 1 in 2021 and 2022 and the highest test scores in the world for Step 2 CK in 2022, according to court documents. For the 2022 Step 1 exam for example, the average score of examinees testing in the Nepal test center was 240. No other test center in the world had an average examinee score above 227, according to the NBME’s legal response.
The median item response time for examinees who tested at the Nepal test center in 2022 was also among the fastest of all international test centers for Step 1 and Step 2 CK, investigators found.
In addition, the volume of examinees taking the USMLE Step 1 and Step 2 CK at the Nepal test center in Nepal had sharply increased. Step 1 volume more than doubled in the Nepal test center from 281 examinees in 2019 to 662 examinees in 2022, according to court documents.
The rapid increase continued in 2023, when examinee volume was nearly three-and-a-half times higher than the 2019 volume. The data were consistent with anonymous tips received by the USMLE program office, suggesting there may be wide-scale collection and sharing of live USMLE exam content within Nepal.
Investigation Finds Similar Correct and Incorrect Answers
Agreement similarity among the exams analyzed also raised red flags. Investigators ran an “agreement analysis” for all examinees who tested at centers in Jordan, Nepal, and Pakistan as well as two centers in India, according to court documents.
For the 2022 Step 1 exam and the 2021 and 2022 Step 2 CK exam, the analysis showed a substantially higher percentage of examinees with a statistically significant level of agreement matches in the examine group that tested at centers in Jordan, Nepal, Pakistan, and India compared with the baseline group, according to legal records.
The vast majority of examinees with a statistically significant number of matching incorrect answers tested at the Nepal test center, data showed.
Further analysis found that examinee volumes increased considerably at the Nepal test center in the months prior to the USMLE program releasing new test items, “suggesting that candidates who had prior access to disclosed exam questions wanted to test before new questions came into the item pool.”
Investigators also identified posts on social medial and in online chat rooms suggesting groups were collecting and sharing large amounts of secure exam material in private groups. Some posts advised examinees to use the full examination time when taking the USMLE “to avoid raising suspicion about having had prior access to secure exam materials,” according to court documents.
From its investigation and analysis, the USMLE program identified 832 examinees who had passing level exam results whose validity the USMLE program had a significant and good faith basis for questioning, according to court records.
Of the total, 618 examinees had one Step score flagged as being of questioned validity, 202 examinees had two Step exam scores flagged, and 12 examinees had scores flagged on all three Step exams.
NBME Defends Departure From Traditional Procedures
In court documents, NBME disputed claims that it violated its own procedures by invalidating the exam scores. Giri’s report contends that examinees suspected of cheating are typically first advised of the matter, given an opportunity to share relevant information, and provided the right to appeal — during which time, their scores are treated as valid.
But the NBME said the USMLE program is authorized to take any actions it deems appropriate in response to concerns regarding score validity if the USMLE Committee for Individualized Review or the USMLE Composite Committee concludes that alternative or supplemental procedures are warranted in response to a given set of facts or circumstances.
“Following the month-long investigation and analysis…the USMLE program concluded that alternative procedures were warranted to address the score invalidity concerns identified in the interest of providing a process that is timely, efficient, effective, and fair, and given the large number of examinees involved in the investigation,” the board stated in its legal response.
In his order, Cooper wrote the current scenario, which implicates that more than 800 test-takers, is “clearly a situation calling for a procedure geared toward efficiency.” No evidence shows the board would not have taken similarly swift action if confronted with evidence of cheating on a comparable scale elsewhere, he wrote.
The judge also denied Giri’s motion to certify the lawsuit as a class action. The motion was denied without prejudice, meaning the plaintiff has the option to renew the motion should the case proceed.
A version of this article appeared on Medscape.com.
(USMLE).
In a February 23 order, Judge Christopher R. Cooper, of the US District Court for the District of Columbia, denied Latika Giri’s emergency motion to block the National Board of Medical Examiners (NBME) from invalidating the scores, ruling the public interest plainly weighs against granting the request.
“First and foremost, is the overriding interest in public safety,” Cooper wrote in his 32-page order. “This is a case about the credentials of doctors applying to medical residency programs…Granting the preliminary injunction would create an unacceptable risk that individuals who lack the requisite knowledge and skills they purport to possess because they achieved their exam scores fraudulently will be administering medical care to unsuspecting patients across the nation.”
Attorneys for Giri did not return messages seeking comment about the order.
The NBME also did not return messages seeking comment. The board previously said it does not comment on pending litigation.
The decision is the latest development in a widespread cheating scandal. Giri, an international medical graduate (IMG) from Kathmandu, sued NBME earlier this month claiming the board discriminated against Nepali medical graduates when it invalidated hundreds of exam scores linked to the country.
Giri also accused NBME of violating its own procedures when it voided the scores before giving examinees a chance to argue and appeal. She asked the district court to block NBME from invalidating her exam scores while the lawsuit continues and restore her original results.
In court documents, NBME argued that it did not invalidate the scores because the examinees were Nepali but because staff concluded that there was “a good faith basis for questioning the validity of the scores.”
The invalidations were based on concerns that the results reflected prior access to secure exam content rather than knowledge and understanding of the medical principles and skills the exams are intended to assess, according to the NBME’s legal response.
“The USMLE program took reasonable and appropriate actions to prevent the significant harm and disruption that would result from allowing potentially unqualified individuals to participate in the 2024 residency Match,” the NBME stated in court documents. “If granted, the requested injunction would cause enormous harm not only to NBME… but also to state licensing authorities, which rely upon USMLE results to help ensure that physicians have the minimum competencies needed to provide safe and effective health care.”
In his order, Cooper wrote that Giri has not proven the board’s actions were discriminatory against Nepali doctors.
“Nothing in the present record suggests that NBME went looking for a problem in Nepal out of ethnicity-or national-origin based [sic] suspicion,” Cooper wrote. “[It] followed the trail of evidence, including tips about organized cheating taking place in medical schools and at a testing center located in Nepal, and on an online forum for which a ‘nexus to Nepal’ was a ticket to admission.”
NBME: Nepal Outperformed All Other Countries on USMLE
Court documents shed more light on NBME’s investigation into the suspected cheating and on the anomalous patterns the board allegedly discovered from Nepal medical graduates.
In response to anonymous tips, the USMLE program in early 2023 asked the NBME Psychometrics and Data Analysis (PADA) unit to analyze examinee performance data for test centers in Jordan, Nepal, and Pakistan, according to court records. Within the initial data analysis, the data involving the single test center in Nepal was “the most extreme,” the unit found.
Out of more than 400 test centers across the world, including those in the United States, the test center in Nepal produced the highest test scores in the world for Step 1 in 2021 and 2022 and the highest test scores in the world for Step 2 CK in 2022, according to court documents. For the 2022 Step 1 exam for example, the average score of examinees testing in the Nepal test center was 240. No other test center in the world had an average examinee score above 227, according to the NBME’s legal response.
The median item response time for examinees who tested at the Nepal test center in 2022 was also among the fastest of all international test centers for Step 1 and Step 2 CK, investigators found.
In addition, the volume of examinees taking the USMLE Step 1 and Step 2 CK at the Nepal test center in Nepal had sharply increased. Step 1 volume more than doubled in the Nepal test center from 281 examinees in 2019 to 662 examinees in 2022, according to court documents.
The rapid increase continued in 2023, when examinee volume was nearly three-and-a-half times higher than the 2019 volume. The data were consistent with anonymous tips received by the USMLE program office, suggesting there may be wide-scale collection and sharing of live USMLE exam content within Nepal.
Investigation Finds Similar Correct and Incorrect Answers
Agreement similarity among the exams analyzed also raised red flags. Investigators ran an “agreement analysis” for all examinees who tested at centers in Jordan, Nepal, and Pakistan as well as two centers in India, according to court documents.
For the 2022 Step 1 exam and the 2021 and 2022 Step 2 CK exam, the analysis showed a substantially higher percentage of examinees with a statistically significant level of agreement matches in the examine group that tested at centers in Jordan, Nepal, Pakistan, and India compared with the baseline group, according to legal records.
The vast majority of examinees with a statistically significant number of matching incorrect answers tested at the Nepal test center, data showed.
Further analysis found that examinee volumes increased considerably at the Nepal test center in the months prior to the USMLE program releasing new test items, “suggesting that candidates who had prior access to disclosed exam questions wanted to test before new questions came into the item pool.”
Investigators also identified posts on social medial and in online chat rooms suggesting groups were collecting and sharing large amounts of secure exam material in private groups. Some posts advised examinees to use the full examination time when taking the USMLE “to avoid raising suspicion about having had prior access to secure exam materials,” according to court documents.
From its investigation and analysis, the USMLE program identified 832 examinees who had passing level exam results whose validity the USMLE program had a significant and good faith basis for questioning, according to court records.
Of the total, 618 examinees had one Step score flagged as being of questioned validity, 202 examinees had two Step exam scores flagged, and 12 examinees had scores flagged on all three Step exams.
NBME Defends Departure From Traditional Procedures
In court documents, NBME disputed claims that it violated its own procedures by invalidating the exam scores. Giri’s report contends that examinees suspected of cheating are typically first advised of the matter, given an opportunity to share relevant information, and provided the right to appeal — during which time, their scores are treated as valid.
But the NBME said the USMLE program is authorized to take any actions it deems appropriate in response to concerns regarding score validity if the USMLE Committee for Individualized Review or the USMLE Composite Committee concludes that alternative or supplemental procedures are warranted in response to a given set of facts or circumstances.
“Following the month-long investigation and analysis…the USMLE program concluded that alternative procedures were warranted to address the score invalidity concerns identified in the interest of providing a process that is timely, efficient, effective, and fair, and given the large number of examinees involved in the investigation,” the board stated in its legal response.
In his order, Cooper wrote the current scenario, which implicates that more than 800 test-takers, is “clearly a situation calling for a procedure geared toward efficiency.” No evidence shows the board would not have taken similarly swift action if confronted with evidence of cheating on a comparable scale elsewhere, he wrote.
The judge also denied Giri’s motion to certify the lawsuit as a class action. The motion was denied without prejudice, meaning the plaintiff has the option to renew the motion should the case proceed.
A version of this article appeared on Medscape.com.
(USMLE).
In a February 23 order, Judge Christopher R. Cooper, of the US District Court for the District of Columbia, denied Latika Giri’s emergency motion to block the National Board of Medical Examiners (NBME) from invalidating the scores, ruling the public interest plainly weighs against granting the request.
“First and foremost, is the overriding interest in public safety,” Cooper wrote in his 32-page order. “This is a case about the credentials of doctors applying to medical residency programs…Granting the preliminary injunction would create an unacceptable risk that individuals who lack the requisite knowledge and skills they purport to possess because they achieved their exam scores fraudulently will be administering medical care to unsuspecting patients across the nation.”
Attorneys for Giri did not return messages seeking comment about the order.
The NBME also did not return messages seeking comment. The board previously said it does not comment on pending litigation.
The decision is the latest development in a widespread cheating scandal. Giri, an international medical graduate (IMG) from Kathmandu, sued NBME earlier this month claiming the board discriminated against Nepali medical graduates when it invalidated hundreds of exam scores linked to the country.
Giri also accused NBME of violating its own procedures when it voided the scores before giving examinees a chance to argue and appeal. She asked the district court to block NBME from invalidating her exam scores while the lawsuit continues and restore her original results.
In court documents, NBME argued that it did not invalidate the scores because the examinees were Nepali but because staff concluded that there was “a good faith basis for questioning the validity of the scores.”
The invalidations were based on concerns that the results reflected prior access to secure exam content rather than knowledge and understanding of the medical principles and skills the exams are intended to assess, according to the NBME’s legal response.
“The USMLE program took reasonable and appropriate actions to prevent the significant harm and disruption that would result from allowing potentially unqualified individuals to participate in the 2024 residency Match,” the NBME stated in court documents. “If granted, the requested injunction would cause enormous harm not only to NBME… but also to state licensing authorities, which rely upon USMLE results to help ensure that physicians have the minimum competencies needed to provide safe and effective health care.”
In his order, Cooper wrote that Giri has not proven the board’s actions were discriminatory against Nepali doctors.
“Nothing in the present record suggests that NBME went looking for a problem in Nepal out of ethnicity-or national-origin based [sic] suspicion,” Cooper wrote. “[It] followed the trail of evidence, including tips about organized cheating taking place in medical schools and at a testing center located in Nepal, and on an online forum for which a ‘nexus to Nepal’ was a ticket to admission.”
NBME: Nepal Outperformed All Other Countries on USMLE
Court documents shed more light on NBME’s investigation into the suspected cheating and on the anomalous patterns the board allegedly discovered from Nepal medical graduates.
In response to anonymous tips, the USMLE program in early 2023 asked the NBME Psychometrics and Data Analysis (PADA) unit to analyze examinee performance data for test centers in Jordan, Nepal, and Pakistan, according to court records. Within the initial data analysis, the data involving the single test center in Nepal was “the most extreme,” the unit found.
Out of more than 400 test centers across the world, including those in the United States, the test center in Nepal produced the highest test scores in the world for Step 1 in 2021 and 2022 and the highest test scores in the world for Step 2 CK in 2022, according to court documents. For the 2022 Step 1 exam for example, the average score of examinees testing in the Nepal test center was 240. No other test center in the world had an average examinee score above 227, according to the NBME’s legal response.
The median item response time for examinees who tested at the Nepal test center in 2022 was also among the fastest of all international test centers for Step 1 and Step 2 CK, investigators found.
In addition, the volume of examinees taking the USMLE Step 1 and Step 2 CK at the Nepal test center in Nepal had sharply increased. Step 1 volume more than doubled in the Nepal test center from 281 examinees in 2019 to 662 examinees in 2022, according to court documents.
The rapid increase continued in 2023, when examinee volume was nearly three-and-a-half times higher than the 2019 volume. The data were consistent with anonymous tips received by the USMLE program office, suggesting there may be wide-scale collection and sharing of live USMLE exam content within Nepal.
Investigation Finds Similar Correct and Incorrect Answers
Agreement similarity among the exams analyzed also raised red flags. Investigators ran an “agreement analysis” for all examinees who tested at centers in Jordan, Nepal, and Pakistan as well as two centers in India, according to court documents.
For the 2022 Step 1 exam and the 2021 and 2022 Step 2 CK exam, the analysis showed a substantially higher percentage of examinees with a statistically significant level of agreement matches in the examine group that tested at centers in Jordan, Nepal, Pakistan, and India compared with the baseline group, according to legal records.
The vast majority of examinees with a statistically significant number of matching incorrect answers tested at the Nepal test center, data showed.
Further analysis found that examinee volumes increased considerably at the Nepal test center in the months prior to the USMLE program releasing new test items, “suggesting that candidates who had prior access to disclosed exam questions wanted to test before new questions came into the item pool.”
Investigators also identified posts on social medial and in online chat rooms suggesting groups were collecting and sharing large amounts of secure exam material in private groups. Some posts advised examinees to use the full examination time when taking the USMLE “to avoid raising suspicion about having had prior access to secure exam materials,” according to court documents.
From its investigation and analysis, the USMLE program identified 832 examinees who had passing level exam results whose validity the USMLE program had a significant and good faith basis for questioning, according to court records.
Of the total, 618 examinees had one Step score flagged as being of questioned validity, 202 examinees had two Step exam scores flagged, and 12 examinees had scores flagged on all three Step exams.
NBME Defends Departure From Traditional Procedures
In court documents, NBME disputed claims that it violated its own procedures by invalidating the exam scores. Giri’s report contends that examinees suspected of cheating are typically first advised of the matter, given an opportunity to share relevant information, and provided the right to appeal — during which time, their scores are treated as valid.
But the NBME said the USMLE program is authorized to take any actions it deems appropriate in response to concerns regarding score validity if the USMLE Committee for Individualized Review or the USMLE Composite Committee concludes that alternative or supplemental procedures are warranted in response to a given set of facts or circumstances.
“Following the month-long investigation and analysis…the USMLE program concluded that alternative procedures were warranted to address the score invalidity concerns identified in the interest of providing a process that is timely, efficient, effective, and fair, and given the large number of examinees involved in the investigation,” the board stated in its legal response.
In his order, Cooper wrote the current scenario, which implicates that more than 800 test-takers, is “clearly a situation calling for a procedure geared toward efficiency.” No evidence shows the board would not have taken similarly swift action if confronted with evidence of cheating on a comparable scale elsewhere, he wrote.
The judge also denied Giri’s motion to certify the lawsuit as a class action. The motion was denied without prejudice, meaning the plaintiff has the option to renew the motion should the case proceed.
A version of this article appeared on Medscape.com.
Is Metformin a ‘Drug for All Diseases’?
In 2021 alone, clinicians wrote more than 91 million orders for the medication — up from 40 million 2004.
But is metformin just getting started? Emerging evidence suggests the drug may be effective for a much broader range of conditions beyond managing high blood glucose, including various cancers, obesity, liver disease, cardiovascular, neurodegenerative, and renal diseases. As the evidence for diverse uses accumulates, many trials have launched, with researchers looking to expand metformin’s indications and validate or explore new directions.
Metformin’s long history as a pharmaceutical includes an herbal ancestry, recognition in 1918 for its ability to lower blood glucose, being cast aside because of toxicity fears in the 1930s, rediscovery and synthesis in Europe in the 1940s, the first reported use for diabetes in 1957, and approval in the United States in 1994.
The drug has maintained its place as the preferred first-line treatment for type 2 diabetes since 2011, when it was first included in the World Health Organization’s essential medicines list.
“The focus hitherto has been primarily on its insulin sensitization effects,” Akshay Jain, MD, a clinical and research endocrinologist at TLC Diabetes and Endocrinology, in Surrey, British Columbia, Canada, told this news organization.
“The recent surge of renewed interest is in part related to its postulated effects on multiple other receptors,” he said. “In my mind, the metformin data on coronary artery disease reduction and cancer-protective effects have come farther along than other disease states.”
Cardiovascular Outcomes
Gregory G. Schwartz, MD, PhD, chief of the cardiology section at Rocky Mountain Regional VA Medical Center and professor of medicine at the University of Colorado School of Medicine in Aurora, is leading the VA-IMPACT trial. Despite metformin’s long history and widespread use, he said his study is the first placebo-controlled cardiovascular outcomes trial of the drug.
Launched in 2023, the study tests the hypothesis that metformin reduces the risk for death or nonfatal ischemic cardiovascular events in patients with prediabetes and established coronary, cerebrovascular, or peripheral artery disease, Dr. Schwartz said. The trial is being conducted at roughly 40 VA medical centers, with a planned enrollment of 7410 patients. The estimated completion date is March 2029.
“The principal mechanism of action of metformin is through activation of AMP [adenosine monophosphate]–activated protein kinase, a central pathway in metabolic regulation, cell protection, and survival,” Dr. Schwartz explained. “Experimental data have demonstrated attenuated development of atherosclerosis, reduced myocardial infarct size, improved endothelial function, and antiarrhythmic actions — none of those dependent on the presence of diabetes.”
Dr. Schwartz and his colleagues decided to test their hypothesis in people with prediabetes, rather than diabetes, to create a “true placebo-controlled comparison,” he said.
“If patients with type 2 diabetes had been chosen, there would be potential for confounding because a placebo group would require more treatment with other active antihyperglycemic medications to achieve the same degree of glycemic control as a metformin group,” Dr. Schwartz said.
“If proven efficacious in the VA-IMPACT trial, metformin could provide an inexpensive, generally safe, and well-tolerated approach to reduce cardiovascular morbidity and mortality in a large segment of the population,” Dr. Schwartz added. “Perhaps the old dog can learn some new tricks.”
Other recruiting trials looking at cardiovascular-related outcomes include Met-PEF, LIMIT, and Metformin as an Adjunctive Therapy to Catheter Ablation in Atrial Fibrillation.
Reducing Cancer Risks
Sai Yendamuri, MD, chair of the Department of Thoracic Surgery and director of the Thoracic Surgery Laboratory at Roswell Park Comprehensive Cancer Center in Buffalo, New York, is leading a phase 2 trial exploring whether metformin can prevent lung cancer in people with overweight or obesity who are at a high risk for the malignancy.
The study, which has accrued about 60% of its estimated enrollment, also will assess whether metformin can reprogram participants’ immune systems, with a view toward reducing the activity of regulatory T cells that are linked to development of tumors.
“In our preclinical and retrospective clinical data, we found that metformin had anticancer effects but only if the patients were overweight,” Dr. Yendamuri said. “In mice, we find that obesity increases regulatory T-cell function, which suppresses the immune system of the lungs. This effect is reversed by metformin.” The team is conducting the current study to examine if this happens in patients, as well. Results are expected next year.
Research is underway in other tumor types, including oral and endometrial, and brain cancers.
Preventing Alzheimer’s Disease
Cognitive function — or at least delaying its erosion — represents another front for metformin. José A. Luchsinger, MD, MPH, vice-chair for clinical and epidemiological research and director of the section on geriatrics, gerontology, and aging at Columbia University Irving Medical Center in New York City, is heading a phase 2/3 randomized controlled trial assessing the ability of the drug to prevent Alzheimer›s disease.
The study investigators hope to enroll 326 men and women aged 55-90 years with early and late mild cognitive impairment, overweight or obesity, and no diabetes.
“The hypothesis is that improving insulin and glucose levels can lead to lowering the risk of Alzheimer’s disease,” Dr. Luchsinger said. Recruitment should be complete by the end of 2024 and results are expected in late 2026.
Similar studies are underway in Europe and Asia.
Other areas of investigation, while tantalizing, are mostly in early stages, although bolstered by preclinical and mechanistic studies. The authors of a recent review on the potential mechanisms of action of metformin and existing evidence of the drug›s effectiveness — or lack thereof — in treating diseases other than diabetes, wrote: “Collectively, these data raise the question: Is metformin a drug for all diseases? It remains unclear as to whether all of these putative beneficial effects are secondary to its actions as an antihyperglycemic and insulin-sensitizing drug, or result from other cellular actions, including inhibition of mTOR (mammalian target for rapamycin), or direct antiviral actions.”
Off-Label Uses
Metformin currently is approved by the US Food and Drug Administration only for the treatment of type 2 diabetes, although it is also the only antidiabetic medication for prediabetes currently recommended by the American Diabetes Association.
Some studies currently are looking at its use in a variety of off-label indications, including obesity, gestational diabetes, weight gain from antipsychotics, and polycystic ovary syndrome.
For the most part, metformin is considered a safe drug, but it is not risk-free, Dr. Jain cautioned.
“Although it would certainly be helpful to see if this inexpensive medication that’s universally available can help in disease states, one shouldn’t overlook the potential risk of adverse effects, such as gastrointestinal, potential vitamin B12 deficiency, blunting of skeletal muscle development and the rare risk of lactic acidosis in those with kidney impairment,” he said.
“Similarly, with recent reports of the carcinogenic potential of certain formulations of long-acting metformin that contained NDMA [N-nitrosodimethylamine], it would be imperative that these kinks are removed before we incorporate metformin as the gift that keeps giving.”
Dr. Jain reported financial relationships with Abbott, Amgen, Boehringer Ingelheim, Dexcom, Eli Lilly, Janssen, Medtronic, Merck, and Novo Nordisk. Dr. Yendamuri disclosed serving on the scientific advisory board member of Karkinos Healthcare and research funding from Lumeda for the metformin study. Dr. Luchsinger reported receiving donated metformin and matching placebo from EMD Serono, a subsidiary of Merck, for the MAP study. Dr. Schwartz received research support from the US Department of Veterans Affairs as National Chair of the VA-IMPACT trial.
A version of this article appeared on Medscape.com.
In 2021 alone, clinicians wrote more than 91 million orders for the medication — up from 40 million 2004.
But is metformin just getting started? Emerging evidence suggests the drug may be effective for a much broader range of conditions beyond managing high blood glucose, including various cancers, obesity, liver disease, cardiovascular, neurodegenerative, and renal diseases. As the evidence for diverse uses accumulates, many trials have launched, with researchers looking to expand metformin’s indications and validate or explore new directions.
Metformin’s long history as a pharmaceutical includes an herbal ancestry, recognition in 1918 for its ability to lower blood glucose, being cast aside because of toxicity fears in the 1930s, rediscovery and synthesis in Europe in the 1940s, the first reported use for diabetes in 1957, and approval in the United States in 1994.
The drug has maintained its place as the preferred first-line treatment for type 2 diabetes since 2011, when it was first included in the World Health Organization’s essential medicines list.
“The focus hitherto has been primarily on its insulin sensitization effects,” Akshay Jain, MD, a clinical and research endocrinologist at TLC Diabetes and Endocrinology, in Surrey, British Columbia, Canada, told this news organization.
“The recent surge of renewed interest is in part related to its postulated effects on multiple other receptors,” he said. “In my mind, the metformin data on coronary artery disease reduction and cancer-protective effects have come farther along than other disease states.”
Cardiovascular Outcomes
Gregory G. Schwartz, MD, PhD, chief of the cardiology section at Rocky Mountain Regional VA Medical Center and professor of medicine at the University of Colorado School of Medicine in Aurora, is leading the VA-IMPACT trial. Despite metformin’s long history and widespread use, he said his study is the first placebo-controlled cardiovascular outcomes trial of the drug.
Launched in 2023, the study tests the hypothesis that metformin reduces the risk for death or nonfatal ischemic cardiovascular events in patients with prediabetes and established coronary, cerebrovascular, or peripheral artery disease, Dr. Schwartz said. The trial is being conducted at roughly 40 VA medical centers, with a planned enrollment of 7410 patients. The estimated completion date is March 2029.
“The principal mechanism of action of metformin is through activation of AMP [adenosine monophosphate]–activated protein kinase, a central pathway in metabolic regulation, cell protection, and survival,” Dr. Schwartz explained. “Experimental data have demonstrated attenuated development of atherosclerosis, reduced myocardial infarct size, improved endothelial function, and antiarrhythmic actions — none of those dependent on the presence of diabetes.”
Dr. Schwartz and his colleagues decided to test their hypothesis in people with prediabetes, rather than diabetes, to create a “true placebo-controlled comparison,” he said.
“If patients with type 2 diabetes had been chosen, there would be potential for confounding because a placebo group would require more treatment with other active antihyperglycemic medications to achieve the same degree of glycemic control as a metformin group,” Dr. Schwartz said.
“If proven efficacious in the VA-IMPACT trial, metformin could provide an inexpensive, generally safe, and well-tolerated approach to reduce cardiovascular morbidity and mortality in a large segment of the population,” Dr. Schwartz added. “Perhaps the old dog can learn some new tricks.”
Other recruiting trials looking at cardiovascular-related outcomes include Met-PEF, LIMIT, and Metformin as an Adjunctive Therapy to Catheter Ablation in Atrial Fibrillation.
Reducing Cancer Risks
Sai Yendamuri, MD, chair of the Department of Thoracic Surgery and director of the Thoracic Surgery Laboratory at Roswell Park Comprehensive Cancer Center in Buffalo, New York, is leading a phase 2 trial exploring whether metformin can prevent lung cancer in people with overweight or obesity who are at a high risk for the malignancy.
The study, which has accrued about 60% of its estimated enrollment, also will assess whether metformin can reprogram participants’ immune systems, with a view toward reducing the activity of regulatory T cells that are linked to development of tumors.
“In our preclinical and retrospective clinical data, we found that metformin had anticancer effects but only if the patients were overweight,” Dr. Yendamuri said. “In mice, we find that obesity increases regulatory T-cell function, which suppresses the immune system of the lungs. This effect is reversed by metformin.” The team is conducting the current study to examine if this happens in patients, as well. Results are expected next year.
Research is underway in other tumor types, including oral and endometrial, and brain cancers.
Preventing Alzheimer’s Disease
Cognitive function — or at least delaying its erosion — represents another front for metformin. José A. Luchsinger, MD, MPH, vice-chair for clinical and epidemiological research and director of the section on geriatrics, gerontology, and aging at Columbia University Irving Medical Center in New York City, is heading a phase 2/3 randomized controlled trial assessing the ability of the drug to prevent Alzheimer›s disease.
The study investigators hope to enroll 326 men and women aged 55-90 years with early and late mild cognitive impairment, overweight or obesity, and no diabetes.
“The hypothesis is that improving insulin and glucose levels can lead to lowering the risk of Alzheimer’s disease,” Dr. Luchsinger said. Recruitment should be complete by the end of 2024 and results are expected in late 2026.
Similar studies are underway in Europe and Asia.
Other areas of investigation, while tantalizing, are mostly in early stages, although bolstered by preclinical and mechanistic studies. The authors of a recent review on the potential mechanisms of action of metformin and existing evidence of the drug›s effectiveness — or lack thereof — in treating diseases other than diabetes, wrote: “Collectively, these data raise the question: Is metformin a drug for all diseases? It remains unclear as to whether all of these putative beneficial effects are secondary to its actions as an antihyperglycemic and insulin-sensitizing drug, or result from other cellular actions, including inhibition of mTOR (mammalian target for rapamycin), or direct antiviral actions.”
Off-Label Uses
Metformin currently is approved by the US Food and Drug Administration only for the treatment of type 2 diabetes, although it is also the only antidiabetic medication for prediabetes currently recommended by the American Diabetes Association.
Some studies currently are looking at its use in a variety of off-label indications, including obesity, gestational diabetes, weight gain from antipsychotics, and polycystic ovary syndrome.
For the most part, metformin is considered a safe drug, but it is not risk-free, Dr. Jain cautioned.
“Although it would certainly be helpful to see if this inexpensive medication that’s universally available can help in disease states, one shouldn’t overlook the potential risk of adverse effects, such as gastrointestinal, potential vitamin B12 deficiency, blunting of skeletal muscle development and the rare risk of lactic acidosis in those with kidney impairment,” he said.
“Similarly, with recent reports of the carcinogenic potential of certain formulations of long-acting metformin that contained NDMA [N-nitrosodimethylamine], it would be imperative that these kinks are removed before we incorporate metformin as the gift that keeps giving.”
Dr. Jain reported financial relationships with Abbott, Amgen, Boehringer Ingelheim, Dexcom, Eli Lilly, Janssen, Medtronic, Merck, and Novo Nordisk. Dr. Yendamuri disclosed serving on the scientific advisory board member of Karkinos Healthcare and research funding from Lumeda for the metformin study. Dr. Luchsinger reported receiving donated metformin and matching placebo from EMD Serono, a subsidiary of Merck, for the MAP study. Dr. Schwartz received research support from the US Department of Veterans Affairs as National Chair of the VA-IMPACT trial.
A version of this article appeared on Medscape.com.
In 2021 alone, clinicians wrote more than 91 million orders for the medication — up from 40 million 2004.
But is metformin just getting started? Emerging evidence suggests the drug may be effective for a much broader range of conditions beyond managing high blood glucose, including various cancers, obesity, liver disease, cardiovascular, neurodegenerative, and renal diseases. As the evidence for diverse uses accumulates, many trials have launched, with researchers looking to expand metformin’s indications and validate or explore new directions.
Metformin’s long history as a pharmaceutical includes an herbal ancestry, recognition in 1918 for its ability to lower blood glucose, being cast aside because of toxicity fears in the 1930s, rediscovery and synthesis in Europe in the 1940s, the first reported use for diabetes in 1957, and approval in the United States in 1994.
The drug has maintained its place as the preferred first-line treatment for type 2 diabetes since 2011, when it was first included in the World Health Organization’s essential medicines list.
“The focus hitherto has been primarily on its insulin sensitization effects,” Akshay Jain, MD, a clinical and research endocrinologist at TLC Diabetes and Endocrinology, in Surrey, British Columbia, Canada, told this news organization.
“The recent surge of renewed interest is in part related to its postulated effects on multiple other receptors,” he said. “In my mind, the metformin data on coronary artery disease reduction and cancer-protective effects have come farther along than other disease states.”
Cardiovascular Outcomes
Gregory G. Schwartz, MD, PhD, chief of the cardiology section at Rocky Mountain Regional VA Medical Center and professor of medicine at the University of Colorado School of Medicine in Aurora, is leading the VA-IMPACT trial. Despite metformin’s long history and widespread use, he said his study is the first placebo-controlled cardiovascular outcomes trial of the drug.
Launched in 2023, the study tests the hypothesis that metformin reduces the risk for death or nonfatal ischemic cardiovascular events in patients with prediabetes and established coronary, cerebrovascular, or peripheral artery disease, Dr. Schwartz said. The trial is being conducted at roughly 40 VA medical centers, with a planned enrollment of 7410 patients. The estimated completion date is March 2029.
“The principal mechanism of action of metformin is through activation of AMP [adenosine monophosphate]–activated protein kinase, a central pathway in metabolic regulation, cell protection, and survival,” Dr. Schwartz explained. “Experimental data have demonstrated attenuated development of atherosclerosis, reduced myocardial infarct size, improved endothelial function, and antiarrhythmic actions — none of those dependent on the presence of diabetes.”
Dr. Schwartz and his colleagues decided to test their hypothesis in people with prediabetes, rather than diabetes, to create a “true placebo-controlled comparison,” he said.
“If patients with type 2 diabetes had been chosen, there would be potential for confounding because a placebo group would require more treatment with other active antihyperglycemic medications to achieve the same degree of glycemic control as a metformin group,” Dr. Schwartz said.
“If proven efficacious in the VA-IMPACT trial, metformin could provide an inexpensive, generally safe, and well-tolerated approach to reduce cardiovascular morbidity and mortality in a large segment of the population,” Dr. Schwartz added. “Perhaps the old dog can learn some new tricks.”
Other recruiting trials looking at cardiovascular-related outcomes include Met-PEF, LIMIT, and Metformin as an Adjunctive Therapy to Catheter Ablation in Atrial Fibrillation.
Reducing Cancer Risks
Sai Yendamuri, MD, chair of the Department of Thoracic Surgery and director of the Thoracic Surgery Laboratory at Roswell Park Comprehensive Cancer Center in Buffalo, New York, is leading a phase 2 trial exploring whether metformin can prevent lung cancer in people with overweight or obesity who are at a high risk for the malignancy.
The study, which has accrued about 60% of its estimated enrollment, also will assess whether metformin can reprogram participants’ immune systems, with a view toward reducing the activity of regulatory T cells that are linked to development of tumors.
“In our preclinical and retrospective clinical data, we found that metformin had anticancer effects but only if the patients were overweight,” Dr. Yendamuri said. “In mice, we find that obesity increases regulatory T-cell function, which suppresses the immune system of the lungs. This effect is reversed by metformin.” The team is conducting the current study to examine if this happens in patients, as well. Results are expected next year.
Research is underway in other tumor types, including oral and endometrial, and brain cancers.
Preventing Alzheimer’s Disease
Cognitive function — or at least delaying its erosion — represents another front for metformin. José A. Luchsinger, MD, MPH, vice-chair for clinical and epidemiological research and director of the section on geriatrics, gerontology, and aging at Columbia University Irving Medical Center in New York City, is heading a phase 2/3 randomized controlled trial assessing the ability of the drug to prevent Alzheimer›s disease.
The study investigators hope to enroll 326 men and women aged 55-90 years with early and late mild cognitive impairment, overweight or obesity, and no diabetes.
“The hypothesis is that improving insulin and glucose levels can lead to lowering the risk of Alzheimer’s disease,” Dr. Luchsinger said. Recruitment should be complete by the end of 2024 and results are expected in late 2026.
Similar studies are underway in Europe and Asia.
Other areas of investigation, while tantalizing, are mostly in early stages, although bolstered by preclinical and mechanistic studies. The authors of a recent review on the potential mechanisms of action of metformin and existing evidence of the drug›s effectiveness — or lack thereof — in treating diseases other than diabetes, wrote: “Collectively, these data raise the question: Is metformin a drug for all diseases? It remains unclear as to whether all of these putative beneficial effects are secondary to its actions as an antihyperglycemic and insulin-sensitizing drug, or result from other cellular actions, including inhibition of mTOR (mammalian target for rapamycin), or direct antiviral actions.”
Off-Label Uses
Metformin currently is approved by the US Food and Drug Administration only for the treatment of type 2 diabetes, although it is also the only antidiabetic medication for prediabetes currently recommended by the American Diabetes Association.
Some studies currently are looking at its use in a variety of off-label indications, including obesity, gestational diabetes, weight gain from antipsychotics, and polycystic ovary syndrome.
For the most part, metformin is considered a safe drug, but it is not risk-free, Dr. Jain cautioned.
“Although it would certainly be helpful to see if this inexpensive medication that’s universally available can help in disease states, one shouldn’t overlook the potential risk of adverse effects, such as gastrointestinal, potential vitamin B12 deficiency, blunting of skeletal muscle development and the rare risk of lactic acidosis in those with kidney impairment,” he said.
“Similarly, with recent reports of the carcinogenic potential of certain formulations of long-acting metformin that contained NDMA [N-nitrosodimethylamine], it would be imperative that these kinks are removed before we incorporate metformin as the gift that keeps giving.”
Dr. Jain reported financial relationships with Abbott, Amgen, Boehringer Ingelheim, Dexcom, Eli Lilly, Janssen, Medtronic, Merck, and Novo Nordisk. Dr. Yendamuri disclosed serving on the scientific advisory board member of Karkinos Healthcare and research funding from Lumeda for the metformin study. Dr. Luchsinger reported receiving donated metformin and matching placebo from EMD Serono, a subsidiary of Merck, for the MAP study. Dr. Schwartz received research support from the US Department of Veterans Affairs as National Chair of the VA-IMPACT trial.
A version of this article appeared on Medscape.com.
Just 2000 Steps a Day Linked to Reduced Heart Failure Risk
TOPLINE:
Accelerometer-measured physical activity (PA), whether light, moderate, or vigorous, is associated with lower risk for heart failure (HF) in older women while more sedentary time is associated with higher HF risk in these women, results of a new study suggest.
METHODOLOGY:
- The analysis included 5951 women aged 63-99 years (mean age, 78.6 years), including 33.7% Black, 17.2% Hispanic, and 49.2% White individuals without HF from the Objective Physical Activity and Cardiovascular Health (OPACH) study, an ancillary to the Women’s Health Initiative Long-Life Study.
- Participants wore an accelerometer on their hip 24 hours a day for up to 7 consecutive days except when in water, kept nightly sleep logs, completed questionnaires to provide information on medical history and sociodemographic and lifestyle factors, and self-rated their general health status.
- Researchers recorded their use of assistive walking devices; determined body mass index as well as blood pressure; obtained fasting serum glucose, total and high-density lipoprotein cholesterol, triglyceride, and high-sensitivity C-reactive protein concentrations; and scored participants’ multimorbidity.
- They determined intensity-specific PA using vector magnitude acceleration cut points (light PA, 19-518 counts/15 s; moderate to vigorous PA [MVPA], > 518) and steps per day using dedicated software, and they quantified sedentary time (total and mean bout duration).
- The primary outcome was overall self-reported HF later adjudicated by physicians using medical record reviews; secondary endpoints were heart failure with reduced ejection fraction (HFrEF) and preserved EF (HFpEF), classified by an EF of < 45% or 45% or > 45%, respectively, after cardiac imaging.
TAKEAWAY:
- A total of 407 HF cases (including 257 HFpEF and 110 HFrEF) were identified during a mean of 7.5 years of follow-up.
- HFrEF was not associated with PA measures in the fully adjusted model (which controlled extensively for health and physical functioning status), but overall HF and HFpEF were inversely associated with total PA (per 1-standard deviation [SD] increment: hazard ratio [HR] 0.85; 95% CI, 0.75-0.95 and HR, 0.78; 95% CI, 0.67-0.91, respectively), light PA (HR, 0.88; 95% CI, 0.78-0.98 and HR, 0.80; 95% CI, 0.70-0.93, respectively) and MVPA (HR, 0.84; 95% CI, 0.73-0.97 and HR, 0.85; 95% CI, 0.72-1.01, respectively).
- With regard to daily steps, each 1-SD increment was associated with a significant 26% lower risk for overall HF (HR 0.74; 95% CI, 0.63-0.88) and 29% lower risk for HFpEF (HR, 0.71; 95% CI, 0.57-0.88), with these inverse risks becoming significant at about 2000 steps/d, “far less than the often touted 10,000 steps/d for promoting health benefits,” noted the authors.
- but not HFrEF; mean sedentary bout duration was significantly inversely associated with HFrEF (per 1 SD: HR, 0.76; 95% CI, 0.61-0.97), although the relatively small number of cases at the extremes of bout duration may contribute to this unexpected inverse association, said the authors.
IN PRACTICE:
The implications of promoting PA, regardless of intensity, for primary HFpEF prevention in later life, “has profound public health and clinical relevance,” the authors concluded. They noted that HFpEF is a “burgeoning epidemic” that disproportionately affects women and minorities with limited available therapies.
STUDY DETAILS:
The study, led by Michael J. LaMonte, PhD, MPH, University at Buffalo-SUNY, Buffalo, New York, was published online on February 21, 2024, in JAMA Cardiology.
LIMITATIONS:
There was only a single accelerometer assessment of PA and sedentary exposures and relatively small numbers of HFrEF cases, which restricted analytic precision. Although researchers controlled for several established vascular biomarkers, they did not have HF-specific measures such as cardiac troponin or N-terminal pro–brain natriuretic peptide. It’s unknown if the findings can be generalized to men and populations dissimilar to women in OPACH.
DISCLOSURES:
The study was funded in part by the National Heart, Lung, and Blood Institute, National Institutes of Health, and US Department of Health and Human Services. LaMonte reported receiving grants from the National Institutes of Health during the conduct of the study; see paper for disclosures of the other authors.
A version of this article appeared on Medscape.com.
TOPLINE:
Accelerometer-measured physical activity (PA), whether light, moderate, or vigorous, is associated with lower risk for heart failure (HF) in older women while more sedentary time is associated with higher HF risk in these women, results of a new study suggest.
METHODOLOGY:
- The analysis included 5951 women aged 63-99 years (mean age, 78.6 years), including 33.7% Black, 17.2% Hispanic, and 49.2% White individuals without HF from the Objective Physical Activity and Cardiovascular Health (OPACH) study, an ancillary to the Women’s Health Initiative Long-Life Study.
- Participants wore an accelerometer on their hip 24 hours a day for up to 7 consecutive days except when in water, kept nightly sleep logs, completed questionnaires to provide information on medical history and sociodemographic and lifestyle factors, and self-rated their general health status.
- Researchers recorded their use of assistive walking devices; determined body mass index as well as blood pressure; obtained fasting serum glucose, total and high-density lipoprotein cholesterol, triglyceride, and high-sensitivity C-reactive protein concentrations; and scored participants’ multimorbidity.
- They determined intensity-specific PA using vector magnitude acceleration cut points (light PA, 19-518 counts/15 s; moderate to vigorous PA [MVPA], > 518) and steps per day using dedicated software, and they quantified sedentary time (total and mean bout duration).
- The primary outcome was overall self-reported HF later adjudicated by physicians using medical record reviews; secondary endpoints were heart failure with reduced ejection fraction (HFrEF) and preserved EF (HFpEF), classified by an EF of < 45% or 45% or > 45%, respectively, after cardiac imaging.
TAKEAWAY:
- A total of 407 HF cases (including 257 HFpEF and 110 HFrEF) were identified during a mean of 7.5 years of follow-up.
- HFrEF was not associated with PA measures in the fully adjusted model (which controlled extensively for health and physical functioning status), but overall HF and HFpEF were inversely associated with total PA (per 1-standard deviation [SD] increment: hazard ratio [HR] 0.85; 95% CI, 0.75-0.95 and HR, 0.78; 95% CI, 0.67-0.91, respectively), light PA (HR, 0.88; 95% CI, 0.78-0.98 and HR, 0.80; 95% CI, 0.70-0.93, respectively) and MVPA (HR, 0.84; 95% CI, 0.73-0.97 and HR, 0.85; 95% CI, 0.72-1.01, respectively).
- With regard to daily steps, each 1-SD increment was associated with a significant 26% lower risk for overall HF (HR 0.74; 95% CI, 0.63-0.88) and 29% lower risk for HFpEF (HR, 0.71; 95% CI, 0.57-0.88), with these inverse risks becoming significant at about 2000 steps/d, “far less than the often touted 10,000 steps/d for promoting health benefits,” noted the authors.
- but not HFrEF; mean sedentary bout duration was significantly inversely associated with HFrEF (per 1 SD: HR, 0.76; 95% CI, 0.61-0.97), although the relatively small number of cases at the extremes of bout duration may contribute to this unexpected inverse association, said the authors.
IN PRACTICE:
The implications of promoting PA, regardless of intensity, for primary HFpEF prevention in later life, “has profound public health and clinical relevance,” the authors concluded. They noted that HFpEF is a “burgeoning epidemic” that disproportionately affects women and minorities with limited available therapies.
STUDY DETAILS:
The study, led by Michael J. LaMonte, PhD, MPH, University at Buffalo-SUNY, Buffalo, New York, was published online on February 21, 2024, in JAMA Cardiology.
LIMITATIONS:
There was only a single accelerometer assessment of PA and sedentary exposures and relatively small numbers of HFrEF cases, which restricted analytic precision. Although researchers controlled for several established vascular biomarkers, they did not have HF-specific measures such as cardiac troponin or N-terminal pro–brain natriuretic peptide. It’s unknown if the findings can be generalized to men and populations dissimilar to women in OPACH.
DISCLOSURES:
The study was funded in part by the National Heart, Lung, and Blood Institute, National Institutes of Health, and US Department of Health and Human Services. LaMonte reported receiving grants from the National Institutes of Health during the conduct of the study; see paper for disclosures of the other authors.
A version of this article appeared on Medscape.com.
TOPLINE:
Accelerometer-measured physical activity (PA), whether light, moderate, or vigorous, is associated with lower risk for heart failure (HF) in older women while more sedentary time is associated with higher HF risk in these women, results of a new study suggest.
METHODOLOGY:
- The analysis included 5951 women aged 63-99 years (mean age, 78.6 years), including 33.7% Black, 17.2% Hispanic, and 49.2% White individuals without HF from the Objective Physical Activity and Cardiovascular Health (OPACH) study, an ancillary to the Women’s Health Initiative Long-Life Study.
- Participants wore an accelerometer on their hip 24 hours a day for up to 7 consecutive days except when in water, kept nightly sleep logs, completed questionnaires to provide information on medical history and sociodemographic and lifestyle factors, and self-rated their general health status.
- Researchers recorded their use of assistive walking devices; determined body mass index as well as blood pressure; obtained fasting serum glucose, total and high-density lipoprotein cholesterol, triglyceride, and high-sensitivity C-reactive protein concentrations; and scored participants’ multimorbidity.
- They determined intensity-specific PA using vector magnitude acceleration cut points (light PA, 19-518 counts/15 s; moderate to vigorous PA [MVPA], > 518) and steps per day using dedicated software, and they quantified sedentary time (total and mean bout duration).
- The primary outcome was overall self-reported HF later adjudicated by physicians using medical record reviews; secondary endpoints were heart failure with reduced ejection fraction (HFrEF) and preserved EF (HFpEF), classified by an EF of < 45% or 45% or > 45%, respectively, after cardiac imaging.
TAKEAWAY:
- A total of 407 HF cases (including 257 HFpEF and 110 HFrEF) were identified during a mean of 7.5 years of follow-up.
- HFrEF was not associated with PA measures in the fully adjusted model (which controlled extensively for health and physical functioning status), but overall HF and HFpEF were inversely associated with total PA (per 1-standard deviation [SD] increment: hazard ratio [HR] 0.85; 95% CI, 0.75-0.95 and HR, 0.78; 95% CI, 0.67-0.91, respectively), light PA (HR, 0.88; 95% CI, 0.78-0.98 and HR, 0.80; 95% CI, 0.70-0.93, respectively) and MVPA (HR, 0.84; 95% CI, 0.73-0.97 and HR, 0.85; 95% CI, 0.72-1.01, respectively).
- With regard to daily steps, each 1-SD increment was associated with a significant 26% lower risk for overall HF (HR 0.74; 95% CI, 0.63-0.88) and 29% lower risk for HFpEF (HR, 0.71; 95% CI, 0.57-0.88), with these inverse risks becoming significant at about 2000 steps/d, “far less than the often touted 10,000 steps/d for promoting health benefits,” noted the authors.
- but not HFrEF; mean sedentary bout duration was significantly inversely associated with HFrEF (per 1 SD: HR, 0.76; 95% CI, 0.61-0.97), although the relatively small number of cases at the extremes of bout duration may contribute to this unexpected inverse association, said the authors.
IN PRACTICE:
The implications of promoting PA, regardless of intensity, for primary HFpEF prevention in later life, “has profound public health and clinical relevance,” the authors concluded. They noted that HFpEF is a “burgeoning epidemic” that disproportionately affects women and minorities with limited available therapies.
STUDY DETAILS:
The study, led by Michael J. LaMonte, PhD, MPH, University at Buffalo-SUNY, Buffalo, New York, was published online on February 21, 2024, in JAMA Cardiology.
LIMITATIONS:
There was only a single accelerometer assessment of PA and sedentary exposures and relatively small numbers of HFrEF cases, which restricted analytic precision. Although researchers controlled for several established vascular biomarkers, they did not have HF-specific measures such as cardiac troponin or N-terminal pro–brain natriuretic peptide. It’s unknown if the findings can be generalized to men and populations dissimilar to women in OPACH.
DISCLOSURES:
The study was funded in part by the National Heart, Lung, and Blood Institute, National Institutes of Health, and US Department of Health and Human Services. LaMonte reported receiving grants from the National Institutes of Health during the conduct of the study; see paper for disclosures of the other authors.
A version of this article appeared on Medscape.com.
Sex Matters in Postprandial Response to Hypoxemia
TOPLINE:
METHODOLOGY:
- Potential gender differences in the impact of intermittent hypoxemia on triglycerides have not been well studied, despite the increased risk for metabolic comorbidities in obstructive sleep apnea (OSA).
- The researchers recruited 24 healthy young adults with a mean age of 23.3 years for the 12 men and 21.3 years for the 12 women.
- Participants consumed a high-fat meal followed by 6 hours of exposure to intermittent hypoxemia or ambient air; the primary outcome was changes in postprandial plasma triglyceride levels.
TAKEAWAY:
- Intermittent hypoxemia was associated with significantly higher postprandial triglycerides in men but not in women.
- Women had lower levels of total triglycerides as well as denser triglyceride-rich lipoprotein triglycerides (TRL-TG) and buoyant TRL-TG in both normoxia and hypoxemia conditions compared with men.
- Glucose levels were significantly higher in men and significantly lower in women during intermittent hypoxemia compared with normoxia (P < .001 for both sexes).
IN PRACTICE:
“Although there is a need for larger confirmatory studies in individuals living with obstructive sleep apnea, this study demonstrates that intermittent hypoxemia alters triglyceride metabolism differently between men and women,” the researchers wrote.
SOURCE:
The lead author of the study was Nicholas Goulet, MD, of the University of Ottawa, Ottawa, Ontario, Canada. The study was published online in The Journal of Physiology on January 29, 2024.
LIMITATIONS:
Limitations of the study included the experimental design with simulated OSA, the small and homogeneous study population, the use of a specific profile for intermittent hypoxemia, and the use of a specific high-fat meal.
DISCLOSURES:
The study was supported by the Natural Sciences and Engineering Research Council of Canada and the Association Médicale Universitaire de l’Hôpital Montfort. The researchers had no financial conflicts to disclose.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Potential gender differences in the impact of intermittent hypoxemia on triglycerides have not been well studied, despite the increased risk for metabolic comorbidities in obstructive sleep apnea (OSA).
- The researchers recruited 24 healthy young adults with a mean age of 23.3 years for the 12 men and 21.3 years for the 12 women.
- Participants consumed a high-fat meal followed by 6 hours of exposure to intermittent hypoxemia or ambient air; the primary outcome was changes in postprandial plasma triglyceride levels.
TAKEAWAY:
- Intermittent hypoxemia was associated with significantly higher postprandial triglycerides in men but not in women.
- Women had lower levels of total triglycerides as well as denser triglyceride-rich lipoprotein triglycerides (TRL-TG) and buoyant TRL-TG in both normoxia and hypoxemia conditions compared with men.
- Glucose levels were significantly higher in men and significantly lower in women during intermittent hypoxemia compared with normoxia (P < .001 for both sexes).
IN PRACTICE:
“Although there is a need for larger confirmatory studies in individuals living with obstructive sleep apnea, this study demonstrates that intermittent hypoxemia alters triglyceride metabolism differently between men and women,” the researchers wrote.
SOURCE:
The lead author of the study was Nicholas Goulet, MD, of the University of Ottawa, Ottawa, Ontario, Canada. The study was published online in The Journal of Physiology on January 29, 2024.
LIMITATIONS:
Limitations of the study included the experimental design with simulated OSA, the small and homogeneous study population, the use of a specific profile for intermittent hypoxemia, and the use of a specific high-fat meal.
DISCLOSURES:
The study was supported by the Natural Sciences and Engineering Research Council of Canada and the Association Médicale Universitaire de l’Hôpital Montfort. The researchers had no financial conflicts to disclose.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Potential gender differences in the impact of intermittent hypoxemia on triglycerides have not been well studied, despite the increased risk for metabolic comorbidities in obstructive sleep apnea (OSA).
- The researchers recruited 24 healthy young adults with a mean age of 23.3 years for the 12 men and 21.3 years for the 12 women.
- Participants consumed a high-fat meal followed by 6 hours of exposure to intermittent hypoxemia or ambient air; the primary outcome was changes in postprandial plasma triglyceride levels.
TAKEAWAY:
- Intermittent hypoxemia was associated with significantly higher postprandial triglycerides in men but not in women.
- Women had lower levels of total triglycerides as well as denser triglyceride-rich lipoprotein triglycerides (TRL-TG) and buoyant TRL-TG in both normoxia and hypoxemia conditions compared with men.
- Glucose levels were significantly higher in men and significantly lower in women during intermittent hypoxemia compared with normoxia (P < .001 for both sexes).
IN PRACTICE:
“Although there is a need for larger confirmatory studies in individuals living with obstructive sleep apnea, this study demonstrates that intermittent hypoxemia alters triglyceride metabolism differently between men and women,” the researchers wrote.
SOURCE:
The lead author of the study was Nicholas Goulet, MD, of the University of Ottawa, Ottawa, Ontario, Canada. The study was published online in The Journal of Physiology on January 29, 2024.
LIMITATIONS:
Limitations of the study included the experimental design with simulated OSA, the small and homogeneous study population, the use of a specific profile for intermittent hypoxemia, and the use of a specific high-fat meal.
DISCLOSURES:
The study was supported by the Natural Sciences and Engineering Research Council of Canada and the Association Médicale Universitaire de l’Hôpital Montfort. The researchers had no financial conflicts to disclose.
A version of this article appeared on Medscape.com.
Lung Cancer Radiation May Up AF Risk
TOPLINE:
METHODOLOGY:
- Arrhythmia — with AF being the most common type — affects roughly 11% of patients following lung cancer RT.
- Given RT’s recognized impact on cardiac tissues over time, researchers hypothesized that the dosage affecting pulmonary veins might contribute to the observed increased rates of AF after RT.
- To investigate, researchers looked back at 420 patients with NSCLC (52% women, median age 70) undergoing definitive RT (± chemo) with modern planning techniques at 55 Gy in 20 once-daily fractions over 4 weeks.
- Most patients underwent treatment planning using volumetric modulated arc therapy (50%) or static gantry intensity-modulated RT (20%). Chemotherapy was administered in a minority of cases (33%).
- Pulmonary veins were contoured on planning CT scans, and dose metrics were calculated. The association between pulmonary veins dose and incidence of new AF was evaluated, with AF verified by a cardiologist.
TAKEAWAY:
- Out of the entire cohort, 26 patients (6%) developed AF a median of 13 months after treatment. All cases of AF were grade 3 except for two grade 4 events.
- Radiation dose to the left and right pulmonary veins was significantly associated with incident AF. Dose volumes most strongly associated with AF were ≥ 55 Gy (V55) on the left and ≥ 10 Gy (V10) on the right.
- The risk for AF increased by 2% per percentage point increase in the left pulmonary veins V55 and 1% in the right pulmonary veins V10. The associations were statistically significant after accounting for cardiovascular factors and risk for death risk.
- The area under the curve for prediction of AF events was 0.64 (P = .02) for the left pulmonary veins V55 and 0.61 (P = .03) for the right pulmonary veins V10. The optimal thresholds for predicting AF were 2% and 54%, respectively.
IN PRACTICE:
“The implications of these data are that actively sparing these structures could reduce the incidence of [AF], and where this is not possible, patients identified as being at high risk of AF could undergo active screening during follow-up,” the researchers said, adding that further validation of these findings should take place before implementation.
SOURCE:
The study, with first author Gerard M. Walls, MB, MRCP, Patrick G Johnston Centre for Cancer Research, Queen’s University Belfast, Belfast, Northern Ireland, was published online on January 4 in Radiotherapy and Oncology .
LIMITATIONS:
This was a single-center, retrospective study with a small number of AF events. The study may have underestimated the relationship between pulmonary vein irradiation and new AF events. The findings needed validation in larger datasets.
DISCLOSURES:
The study had no commercial funding. The authors declared no conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Arrhythmia — with AF being the most common type — affects roughly 11% of patients following lung cancer RT.
- Given RT’s recognized impact on cardiac tissues over time, researchers hypothesized that the dosage affecting pulmonary veins might contribute to the observed increased rates of AF after RT.
- To investigate, researchers looked back at 420 patients with NSCLC (52% women, median age 70) undergoing definitive RT (± chemo) with modern planning techniques at 55 Gy in 20 once-daily fractions over 4 weeks.
- Most patients underwent treatment planning using volumetric modulated arc therapy (50%) or static gantry intensity-modulated RT (20%). Chemotherapy was administered in a minority of cases (33%).
- Pulmonary veins were contoured on planning CT scans, and dose metrics were calculated. The association between pulmonary veins dose and incidence of new AF was evaluated, with AF verified by a cardiologist.
TAKEAWAY:
- Out of the entire cohort, 26 patients (6%) developed AF a median of 13 months after treatment. All cases of AF were grade 3 except for two grade 4 events.
- Radiation dose to the left and right pulmonary veins was significantly associated with incident AF. Dose volumes most strongly associated with AF were ≥ 55 Gy (V55) on the left and ≥ 10 Gy (V10) on the right.
- The risk for AF increased by 2% per percentage point increase in the left pulmonary veins V55 and 1% in the right pulmonary veins V10. The associations were statistically significant after accounting for cardiovascular factors and risk for death risk.
- The area under the curve for prediction of AF events was 0.64 (P = .02) for the left pulmonary veins V55 and 0.61 (P = .03) for the right pulmonary veins V10. The optimal thresholds for predicting AF were 2% and 54%, respectively.
IN PRACTICE:
“The implications of these data are that actively sparing these structures could reduce the incidence of [AF], and where this is not possible, patients identified as being at high risk of AF could undergo active screening during follow-up,” the researchers said, adding that further validation of these findings should take place before implementation.
SOURCE:
The study, with first author Gerard M. Walls, MB, MRCP, Patrick G Johnston Centre for Cancer Research, Queen’s University Belfast, Belfast, Northern Ireland, was published online on January 4 in Radiotherapy and Oncology .
LIMITATIONS:
This was a single-center, retrospective study with a small number of AF events. The study may have underestimated the relationship between pulmonary vein irradiation and new AF events. The findings needed validation in larger datasets.
DISCLOSURES:
The study had no commercial funding. The authors declared no conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Arrhythmia — with AF being the most common type — affects roughly 11% of patients following lung cancer RT.
- Given RT’s recognized impact on cardiac tissues over time, researchers hypothesized that the dosage affecting pulmonary veins might contribute to the observed increased rates of AF after RT.
- To investigate, researchers looked back at 420 patients with NSCLC (52% women, median age 70) undergoing definitive RT (± chemo) with modern planning techniques at 55 Gy in 20 once-daily fractions over 4 weeks.
- Most patients underwent treatment planning using volumetric modulated arc therapy (50%) or static gantry intensity-modulated RT (20%). Chemotherapy was administered in a minority of cases (33%).
- Pulmonary veins were contoured on planning CT scans, and dose metrics were calculated. The association between pulmonary veins dose and incidence of new AF was evaluated, with AF verified by a cardiologist.
TAKEAWAY:
- Out of the entire cohort, 26 patients (6%) developed AF a median of 13 months after treatment. All cases of AF were grade 3 except for two grade 4 events.
- Radiation dose to the left and right pulmonary veins was significantly associated with incident AF. Dose volumes most strongly associated with AF were ≥ 55 Gy (V55) on the left and ≥ 10 Gy (V10) on the right.
- The risk for AF increased by 2% per percentage point increase in the left pulmonary veins V55 and 1% in the right pulmonary veins V10. The associations were statistically significant after accounting for cardiovascular factors and risk for death risk.
- The area under the curve for prediction of AF events was 0.64 (P = .02) for the left pulmonary veins V55 and 0.61 (P = .03) for the right pulmonary veins V10. The optimal thresholds for predicting AF were 2% and 54%, respectively.
IN PRACTICE:
“The implications of these data are that actively sparing these structures could reduce the incidence of [AF], and where this is not possible, patients identified as being at high risk of AF could undergo active screening during follow-up,” the researchers said, adding that further validation of these findings should take place before implementation.
SOURCE:
The study, with first author Gerard M. Walls, MB, MRCP, Patrick G Johnston Centre for Cancer Research, Queen’s University Belfast, Belfast, Northern Ireland, was published online on January 4 in Radiotherapy and Oncology .
LIMITATIONS:
This was a single-center, retrospective study with a small number of AF events. The study may have underestimated the relationship between pulmonary vein irradiation and new AF events. The findings needed validation in larger datasets.
DISCLOSURES:
The study had no commercial funding. The authors declared no conflicts of interest.
A version of this article appeared on Medscape.com.
Communicating Bad News to Patients
Communicating bad news to patients is one of the most stressful and challenging clinical tasks for any physician, regardless of his or her specialty. This task is more frequent for physicians caring for oncology patients and can also affect the physician’s emotional state.
The manner in which bad news is communicated plays a significant role in the psychological burden on the patient, and various communication techniques and guidelines have been developed to enable physicians to perform this difficult task effectively.
Revealing bad news in person whenever possible, to address the emotional responses of patients or relatives, is part of the prevailing expert recommendations. However, it has been acknowledged that in certain situations, communicating bad news over the phone is more feasible.
Since the beginning of the COVID-19 pandemic, the disclosure of bad news over the phone has become a necessary substitute for in-person visits and an integral part of clinical practice worldwide. It remains to be clarified what the real psychological impact on patients and their closest relatives is when delivering bad news over the phone compared with delivering it in person.
Right and Wrong Ways
The most popular guideline for communicating bad news is SPIKES, a six-phase protocol with a special application for cancer patients. It is used in various countries (eg, the United States, France, and Germany) as a guide for this sensitive practice and for training in communication skills in this context. The SPIKES acronym refers to the following six recommended steps for delivering bad news:
- Setting: Set up the conversation.
- Perception: Assess the patient’s perception.
- Invitation: Ask the patient what he or she would like to know.
- Knowledge: Provide the patient with knowledge and information, breaking it down into small parts.
- Emotions: Acknowledge and empathetically address the patient’s emotions.
- Strategy and Summary: Summarize and define a medical action plan.
The lesson from SPIKES is that when a person experiences strong emotions, it is difficult to continue discussing anything, and they will struggle to hear anything. Allowing for silence is fundamental. In addition, empathy allows the patient to express his or her feelings and concerns, as well as provide support. The aim is not to argue but to allow the expression of emotions without criticism. However, these recommendations are primarily based on expert opinion and less on empirical evidence, due to the difficulty of studies in assessing patient outcomes in various phases of these protocols.
A recent study analyzed the differences in psychological distress between patients who received bad news over the phone vs those who received it in person. The study was a systematic review and meta-analysis.
The investigators examined 5944 studies, including 11 qualitative analysis studies, nine meta-analyses, and four randomized controlled trials.
In a set of studies ranging from moderate to good quality, no difference in psychological distress was found when bad news was disclosed over the phone compared with in person, regarding anxiety, depression, and posttraumatic stress disorder.
There was no average difference in patient satisfaction levels when bad news was delivered over the phone compared with in person. The risk for dissatisfaction was similar between groups.
Clinical Practice Guidelines
The demand for telemedicine, including the disclosure of bad news, is growing despite the limited knowledge of potential adverse effects. The results of existing studies suggest that the mode of disclosure may play a secondary role, and the manner in which bad news is communicated may be more important.
Therefore, it is paramount to prepare patients or their families for the possibility of receiving bad news well in advance and, during the conversation, to ensure first and foremost that they are in an appropriate environment. The structure and content of the conversation may be relevant, and adhering to dedicated communication strategies can be a wise choice for the physician and the interlocutor.
This story was translated from Univadis Italy, which is part of the Medscape professional network, using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Communicating bad news to patients is one of the most stressful and challenging clinical tasks for any physician, regardless of his or her specialty. This task is more frequent for physicians caring for oncology patients and can also affect the physician’s emotional state.
The manner in which bad news is communicated plays a significant role in the psychological burden on the patient, and various communication techniques and guidelines have been developed to enable physicians to perform this difficult task effectively.
Revealing bad news in person whenever possible, to address the emotional responses of patients or relatives, is part of the prevailing expert recommendations. However, it has been acknowledged that in certain situations, communicating bad news over the phone is more feasible.
Since the beginning of the COVID-19 pandemic, the disclosure of bad news over the phone has become a necessary substitute for in-person visits and an integral part of clinical practice worldwide. It remains to be clarified what the real psychological impact on patients and their closest relatives is when delivering bad news over the phone compared with delivering it in person.
Right and Wrong Ways
The most popular guideline for communicating bad news is SPIKES, a six-phase protocol with a special application for cancer patients. It is used in various countries (eg, the United States, France, and Germany) as a guide for this sensitive practice and for training in communication skills in this context. The SPIKES acronym refers to the following six recommended steps for delivering bad news:
- Setting: Set up the conversation.
- Perception: Assess the patient’s perception.
- Invitation: Ask the patient what he or she would like to know.
- Knowledge: Provide the patient with knowledge and information, breaking it down into small parts.
- Emotions: Acknowledge and empathetically address the patient’s emotions.
- Strategy and Summary: Summarize and define a medical action plan.
The lesson from SPIKES is that when a person experiences strong emotions, it is difficult to continue discussing anything, and they will struggle to hear anything. Allowing for silence is fundamental. In addition, empathy allows the patient to express his or her feelings and concerns, as well as provide support. The aim is not to argue but to allow the expression of emotions without criticism. However, these recommendations are primarily based on expert opinion and less on empirical evidence, due to the difficulty of studies in assessing patient outcomes in various phases of these protocols.
A recent study analyzed the differences in psychological distress between patients who received bad news over the phone vs those who received it in person. The study was a systematic review and meta-analysis.
The investigators examined 5944 studies, including 11 qualitative analysis studies, nine meta-analyses, and four randomized controlled trials.
In a set of studies ranging from moderate to good quality, no difference in psychological distress was found when bad news was disclosed over the phone compared with in person, regarding anxiety, depression, and posttraumatic stress disorder.
There was no average difference in patient satisfaction levels when bad news was delivered over the phone compared with in person. The risk for dissatisfaction was similar between groups.
Clinical Practice Guidelines
The demand for telemedicine, including the disclosure of bad news, is growing despite the limited knowledge of potential adverse effects. The results of existing studies suggest that the mode of disclosure may play a secondary role, and the manner in which bad news is communicated may be more important.
Therefore, it is paramount to prepare patients or their families for the possibility of receiving bad news well in advance and, during the conversation, to ensure first and foremost that they are in an appropriate environment. The structure and content of the conversation may be relevant, and adhering to dedicated communication strategies can be a wise choice for the physician and the interlocutor.
This story was translated from Univadis Italy, which is part of the Medscape professional network, using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Communicating bad news to patients is one of the most stressful and challenging clinical tasks for any physician, regardless of his or her specialty. This task is more frequent for physicians caring for oncology patients and can also affect the physician’s emotional state.
The manner in which bad news is communicated plays a significant role in the psychological burden on the patient, and various communication techniques and guidelines have been developed to enable physicians to perform this difficult task effectively.
Revealing bad news in person whenever possible, to address the emotional responses of patients or relatives, is part of the prevailing expert recommendations. However, it has been acknowledged that in certain situations, communicating bad news over the phone is more feasible.
Since the beginning of the COVID-19 pandemic, the disclosure of bad news over the phone has become a necessary substitute for in-person visits and an integral part of clinical practice worldwide. It remains to be clarified what the real psychological impact on patients and their closest relatives is when delivering bad news over the phone compared with delivering it in person.
Right and Wrong Ways
The most popular guideline for communicating bad news is SPIKES, a six-phase protocol with a special application for cancer patients. It is used in various countries (eg, the United States, France, and Germany) as a guide for this sensitive practice and for training in communication skills in this context. The SPIKES acronym refers to the following six recommended steps for delivering bad news:
- Setting: Set up the conversation.
- Perception: Assess the patient’s perception.
- Invitation: Ask the patient what he or she would like to know.
- Knowledge: Provide the patient with knowledge and information, breaking it down into small parts.
- Emotions: Acknowledge and empathetically address the patient’s emotions.
- Strategy and Summary: Summarize and define a medical action plan.
The lesson from SPIKES is that when a person experiences strong emotions, it is difficult to continue discussing anything, and they will struggle to hear anything. Allowing for silence is fundamental. In addition, empathy allows the patient to express his or her feelings and concerns, as well as provide support. The aim is not to argue but to allow the expression of emotions without criticism. However, these recommendations are primarily based on expert opinion and less on empirical evidence, due to the difficulty of studies in assessing patient outcomes in various phases of these protocols.
A recent study analyzed the differences in psychological distress between patients who received bad news over the phone vs those who received it in person. The study was a systematic review and meta-analysis.
The investigators examined 5944 studies, including 11 qualitative analysis studies, nine meta-analyses, and four randomized controlled trials.
In a set of studies ranging from moderate to good quality, no difference in psychological distress was found when bad news was disclosed over the phone compared with in person, regarding anxiety, depression, and posttraumatic stress disorder.
There was no average difference in patient satisfaction levels when bad news was delivered over the phone compared with in person. The risk for dissatisfaction was similar between groups.
Clinical Practice Guidelines
The demand for telemedicine, including the disclosure of bad news, is growing despite the limited knowledge of potential adverse effects. The results of existing studies suggest that the mode of disclosure may play a secondary role, and the manner in which bad news is communicated may be more important.
Therefore, it is paramount to prepare patients or their families for the possibility of receiving bad news well in advance and, during the conversation, to ensure first and foremost that they are in an appropriate environment. The structure and content of the conversation may be relevant, and adhering to dedicated communication strategies can be a wise choice for the physician and the interlocutor.
This story was translated from Univadis Italy, which is part of the Medscape professional network, using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.