User login
ID Practitioner is an independent news source that provides infectious disease specialists with timely and relevant news and commentary about clinical developments and the impact of health care policy on the infectious disease specialist’s practice. Specialty focus topics include antimicrobial resistance, emerging infections, global ID, hepatitis, HIV, hospital-acquired infections, immunizations and vaccines, influenza, mycoses, pediatric infections, and STIs. Infectious Diseases News is owned by Frontline Medical Communications.
sofosbuvir
ritonavir with dasabuvir
discount
support path
program
ritonavir
greedy
ledipasvir
assistance
viekira pak
vpak
advocacy
needy
protest
abbvie
paritaprevir
ombitasvir
direct-acting antivirals
dasabuvir
gilead
fake-ovir
support
v pak
oasis
harvoni
section[contains(@class, 'footer-nav-section-wrapper')]
div[contains(@class, 'pane-pub-article-idp')]
div[contains(@class, 'pane-medstat-latest-articles-articles-section')]
div[contains(@class, 'pane-pub-home-idp')]
div[contains(@class, 'pane-pub-topic-idp')]
70% of Doctors Would Discharge Noncompliant Patients, Medscape Survey Finds
Physicians shared their views on frequently discussed (and sometimes controversial) topics ranging from romances with patients to age-related competency tests in the latest report from Medscape Medical News.
The report captured data from over 1000 full- or part-time US physicians across more than 29 specialties who were surveyed over a 3-month period in 2024.
Responsibility toward their patients was a clear priority among the doctors surveyed.
While around 6 in 10 physicians said they would immediately discharge a patient who refused to follow their treatment recommendations, 8% said they would wait, and 31% indicated they would keep the patient.
Most doctors (91%) said they would not accept a gift of substantial monetary or sentimental value from a patient, adhering to the AMA Code of Medical Ethics.
Big gifts “may signal psychological issues, and it is not fair to patients who can’t afford big gifts, since they may encourage better care,” said Jason Doctor, PhD, a senior scholar at the USC Leonard D. Schaeffer Center for Health Policy & Economics in Los Angeles, California. “It also taints the doctor-patient relationship, which should not involve large gifts of expectations of reciprocity.”
The vast majority of doctors said a romantic relationship with a patient still in their care was unacceptable, although 1% felt it would be OK, and 9% said, “it depends.”
When asked if they might withhold information about a patient’s condition if disclosure could do more harm than good, the majority of doctors said no. But 38% said it depended on the situation.
“This is how the profession and public expectations are evolving from the old paternalistic approach,” said Peter Angood, MD, president and CEO of the American Association for Physician Leadership.
Meanwhile, most doctors (62%) said that an annual flu shot should be mandatory for physicians who see patients. And a substantial majority of doctors surveyed agreed that taking care of their physical and mental health amounts to an ethical duty.
Around three in four physicians surveyed said felt periodic bias training was necessary for doctors.
“We all need refreshers about our own bias and how to manage it,” one respondent said. But another physician said, “I think we all know what appropriate behavior is and don’t need to add yet another CME course, ugh.”
Roughly equal shares of doctors surveyed felt some obligation to take at least some Medicaid patients or felt no societal obligation. The remaining 18% were willing to treat Medicaid patients once states streamlined the rules and improved reimbursements.
And finally, nearly all the survey respondents said physicians should advise patients on the risks of marijuana, notwithstanding the number of states and localities that recently have legalized pot or cannabis products.
A version of this article first appeared on Medscape.com.
Physicians shared their views on frequently discussed (and sometimes controversial) topics ranging from romances with patients to age-related competency tests in the latest report from Medscape Medical News.
The report captured data from over 1000 full- or part-time US physicians across more than 29 specialties who were surveyed over a 3-month period in 2024.
Responsibility toward their patients was a clear priority among the doctors surveyed.
While around 6 in 10 physicians said they would immediately discharge a patient who refused to follow their treatment recommendations, 8% said they would wait, and 31% indicated they would keep the patient.
Most doctors (91%) said they would not accept a gift of substantial monetary or sentimental value from a patient, adhering to the AMA Code of Medical Ethics.
Big gifts “may signal psychological issues, and it is not fair to patients who can’t afford big gifts, since they may encourage better care,” said Jason Doctor, PhD, a senior scholar at the USC Leonard D. Schaeffer Center for Health Policy & Economics in Los Angeles, California. “It also taints the doctor-patient relationship, which should not involve large gifts of expectations of reciprocity.”
The vast majority of doctors said a romantic relationship with a patient still in their care was unacceptable, although 1% felt it would be OK, and 9% said, “it depends.”
When asked if they might withhold information about a patient’s condition if disclosure could do more harm than good, the majority of doctors said no. But 38% said it depended on the situation.
“This is how the profession and public expectations are evolving from the old paternalistic approach,” said Peter Angood, MD, president and CEO of the American Association for Physician Leadership.
Meanwhile, most doctors (62%) said that an annual flu shot should be mandatory for physicians who see patients. And a substantial majority of doctors surveyed agreed that taking care of their physical and mental health amounts to an ethical duty.
Around three in four physicians surveyed said felt periodic bias training was necessary for doctors.
“We all need refreshers about our own bias and how to manage it,” one respondent said. But another physician said, “I think we all know what appropriate behavior is and don’t need to add yet another CME course, ugh.”
Roughly equal shares of doctors surveyed felt some obligation to take at least some Medicaid patients or felt no societal obligation. The remaining 18% were willing to treat Medicaid patients once states streamlined the rules and improved reimbursements.
And finally, nearly all the survey respondents said physicians should advise patients on the risks of marijuana, notwithstanding the number of states and localities that recently have legalized pot or cannabis products.
A version of this article first appeared on Medscape.com.
Physicians shared their views on frequently discussed (and sometimes controversial) topics ranging from romances with patients to age-related competency tests in the latest report from Medscape Medical News.
The report captured data from over 1000 full- or part-time US physicians across more than 29 specialties who were surveyed over a 3-month period in 2024.
Responsibility toward their patients was a clear priority among the doctors surveyed.
While around 6 in 10 physicians said they would immediately discharge a patient who refused to follow their treatment recommendations, 8% said they would wait, and 31% indicated they would keep the patient.
Most doctors (91%) said they would not accept a gift of substantial monetary or sentimental value from a patient, adhering to the AMA Code of Medical Ethics.
Big gifts “may signal psychological issues, and it is not fair to patients who can’t afford big gifts, since they may encourage better care,” said Jason Doctor, PhD, a senior scholar at the USC Leonard D. Schaeffer Center for Health Policy & Economics in Los Angeles, California. “It also taints the doctor-patient relationship, which should not involve large gifts of expectations of reciprocity.”
The vast majority of doctors said a romantic relationship with a patient still in their care was unacceptable, although 1% felt it would be OK, and 9% said, “it depends.”
When asked if they might withhold information about a patient’s condition if disclosure could do more harm than good, the majority of doctors said no. But 38% said it depended on the situation.
“This is how the profession and public expectations are evolving from the old paternalistic approach,” said Peter Angood, MD, president and CEO of the American Association for Physician Leadership.
Meanwhile, most doctors (62%) said that an annual flu shot should be mandatory for physicians who see patients. And a substantial majority of doctors surveyed agreed that taking care of their physical and mental health amounts to an ethical duty.
Around three in four physicians surveyed said felt periodic bias training was necessary for doctors.
“We all need refreshers about our own bias and how to manage it,” one respondent said. But another physician said, “I think we all know what appropriate behavior is and don’t need to add yet another CME course, ugh.”
Roughly equal shares of doctors surveyed felt some obligation to take at least some Medicaid patients or felt no societal obligation. The remaining 18% were willing to treat Medicaid patients once states streamlined the rules and improved reimbursements.
And finally, nearly all the survey respondents said physicians should advise patients on the risks of marijuana, notwithstanding the number of states and localities that recently have legalized pot or cannabis products.
A version of this article first appeared on Medscape.com.
Heart Attack, Stroke Survivors at High Risk for Long COVID
Primary care doctors and specialists should advise patients who have already experienced a heart attack or stroke that they are at a higher risk for long COVID and need to take steps to avoid contracting the virus, according to new research.
The study, led by researchers at Columbia University, New York City, suggests that anyone with cardiovascular disease (CVD) — defined as having experienced a heart attack or stroke — should consider getting the updated COVID vaccine boosters. They also suggest patients with CVD take other steps to avoid an acute infection, such as avoiding crowded indoor spaces.
There is no specific test or treatment for long COVID, which can become disabling and chronic. Long COVID is defined by the failure to recover from acute COVID-19 in 90 days.
The scientists used data from nearly 5000 people enrolled in 14 established, ongoing research programs, including the 76-year-old Framingham Heart Study. The results of the analysis of the “mega-cohort” were published in JAMA Network Open.
Most of the 14 studies already had 10-20 years of data on the cardiac health of thousands of enrollees, said Norrina B. Allen, one of the authors and a cardiac epidemiologist at Northwestern University Feinberg School of Medicine in Chicago, Illinois.
“This is a particularly strong study that looked at risk factors — or individual health — prior to developing COVID and their impact on the likely of recovering from COVID,” she said.
In addition to those with CVD, women and adults with preexisting chronic illnesses took longer to recover.
More than 20% of those in the large, racially and ethnically diverse US population–based study did not recover from COVID in 90 days. The researchers found that the median self-reported time to recovery from acute infection was 20 days.
While women and those with chronic illness had a higher risk for long COVID, vaccination and infection with the Omicron variant wave were associated with shorter recovery times.
These findings make sense, said Ziyad Al-Aly, MD, chief of research at Veterans Affairs St. Louis Health Care System and clinical epidemiologist at Washington University in St. Louis, Missouri.
“We also see that COVID-19 can lead to new-onset cardiovascular disease,” said Al-Aly, who was not involved in the study. “There is clearly a (link) between COVID and cardiovascular disease. These two seem to be intimately intertwined. In my view, this emphasizes the importance of targeting these individuals for vaccination and potentially antivirals (when they get infected) to help reduce their risk of adverse events and ameliorate their chance of full and fast recovery.”
The study used data from the Collaborative Cohort of Cohorts for COVID-19 Research. The long list of researchers contributing to this study includes epidemiologists, biostatisticians, neurologists, pulmonologists, and cardiologists. The data come from a list of cohorts like the Framingham Heart Study, which identified key risk factors for CVD, including cholesterol levels. Other studies include the Atherosclerosis Risk in Communities study, which began in the mid-1980s. Researchers there recruited a cohort of 15,792 men and women in rural North Carolina and Mississippi and suburban Minneapolis. They enrolled a high number of African American participants, who have been underrepresented in past studies. Other cohorts focused on young adults with CVD and Hispanics, while another focused on people with chronic obstructive pulmonary disease.
Lead author Elizabeth C. Oelsner, MD, of Columbia University Irving Medical Center in New York City, said she was not surprised by the CVD-long COVID link.
“We were aware that individuals with CVD were at higher risk of a more severe acute infection,” she said. “We were also seeing evidence that long and severe infection led to persistent symptoms.”
Oelsner noted that many patients still take more than 3 months to recover, even during the Omicron wave.
“While that has improved over the course of the pandemic, many individuals are taking a very long time to recover, and that can have a huge burden on the patient,” she said.
She encourages healthcare providers to tell patients at higher risk to take steps to avoid the virus, including vaccination and boosters.
A version of this article first appeared on Medscape.com.
Primary care doctors and specialists should advise patients who have already experienced a heart attack or stroke that they are at a higher risk for long COVID and need to take steps to avoid contracting the virus, according to new research.
The study, led by researchers at Columbia University, New York City, suggests that anyone with cardiovascular disease (CVD) — defined as having experienced a heart attack or stroke — should consider getting the updated COVID vaccine boosters. They also suggest patients with CVD take other steps to avoid an acute infection, such as avoiding crowded indoor spaces.
There is no specific test or treatment for long COVID, which can become disabling and chronic. Long COVID is defined by the failure to recover from acute COVID-19 in 90 days.
The scientists used data from nearly 5000 people enrolled in 14 established, ongoing research programs, including the 76-year-old Framingham Heart Study. The results of the analysis of the “mega-cohort” were published in JAMA Network Open.
Most of the 14 studies already had 10-20 years of data on the cardiac health of thousands of enrollees, said Norrina B. Allen, one of the authors and a cardiac epidemiologist at Northwestern University Feinberg School of Medicine in Chicago, Illinois.
“This is a particularly strong study that looked at risk factors — or individual health — prior to developing COVID and their impact on the likely of recovering from COVID,” she said.
In addition to those with CVD, women and adults with preexisting chronic illnesses took longer to recover.
More than 20% of those in the large, racially and ethnically diverse US population–based study did not recover from COVID in 90 days. The researchers found that the median self-reported time to recovery from acute infection was 20 days.
While women and those with chronic illness had a higher risk for long COVID, vaccination and infection with the Omicron variant wave were associated with shorter recovery times.
These findings make sense, said Ziyad Al-Aly, MD, chief of research at Veterans Affairs St. Louis Health Care System and clinical epidemiologist at Washington University in St. Louis, Missouri.
“We also see that COVID-19 can lead to new-onset cardiovascular disease,” said Al-Aly, who was not involved in the study. “There is clearly a (link) between COVID and cardiovascular disease. These two seem to be intimately intertwined. In my view, this emphasizes the importance of targeting these individuals for vaccination and potentially antivirals (when they get infected) to help reduce their risk of adverse events and ameliorate their chance of full and fast recovery.”
The study used data from the Collaborative Cohort of Cohorts for COVID-19 Research. The long list of researchers contributing to this study includes epidemiologists, biostatisticians, neurologists, pulmonologists, and cardiologists. The data come from a list of cohorts like the Framingham Heart Study, which identified key risk factors for CVD, including cholesterol levels. Other studies include the Atherosclerosis Risk in Communities study, which began in the mid-1980s. Researchers there recruited a cohort of 15,792 men and women in rural North Carolina and Mississippi and suburban Minneapolis. They enrolled a high number of African American participants, who have been underrepresented in past studies. Other cohorts focused on young adults with CVD and Hispanics, while another focused on people with chronic obstructive pulmonary disease.
Lead author Elizabeth C. Oelsner, MD, of Columbia University Irving Medical Center in New York City, said she was not surprised by the CVD-long COVID link.
“We were aware that individuals with CVD were at higher risk of a more severe acute infection,” she said. “We were also seeing evidence that long and severe infection led to persistent symptoms.”
Oelsner noted that many patients still take more than 3 months to recover, even during the Omicron wave.
“While that has improved over the course of the pandemic, many individuals are taking a very long time to recover, and that can have a huge burden on the patient,” she said.
She encourages healthcare providers to tell patients at higher risk to take steps to avoid the virus, including vaccination and boosters.
A version of this article first appeared on Medscape.com.
Primary care doctors and specialists should advise patients who have already experienced a heart attack or stroke that they are at a higher risk for long COVID and need to take steps to avoid contracting the virus, according to new research.
The study, led by researchers at Columbia University, New York City, suggests that anyone with cardiovascular disease (CVD) — defined as having experienced a heart attack or stroke — should consider getting the updated COVID vaccine boosters. They also suggest patients with CVD take other steps to avoid an acute infection, such as avoiding crowded indoor spaces.
There is no specific test or treatment for long COVID, which can become disabling and chronic. Long COVID is defined by the failure to recover from acute COVID-19 in 90 days.
The scientists used data from nearly 5000 people enrolled in 14 established, ongoing research programs, including the 76-year-old Framingham Heart Study. The results of the analysis of the “mega-cohort” were published in JAMA Network Open.
Most of the 14 studies already had 10-20 years of data on the cardiac health of thousands of enrollees, said Norrina B. Allen, one of the authors and a cardiac epidemiologist at Northwestern University Feinberg School of Medicine in Chicago, Illinois.
“This is a particularly strong study that looked at risk factors — or individual health — prior to developing COVID and their impact on the likely of recovering from COVID,” she said.
In addition to those with CVD, women and adults with preexisting chronic illnesses took longer to recover.
More than 20% of those in the large, racially and ethnically diverse US population–based study did not recover from COVID in 90 days. The researchers found that the median self-reported time to recovery from acute infection was 20 days.
While women and those with chronic illness had a higher risk for long COVID, vaccination and infection with the Omicron variant wave were associated with shorter recovery times.
These findings make sense, said Ziyad Al-Aly, MD, chief of research at Veterans Affairs St. Louis Health Care System and clinical epidemiologist at Washington University in St. Louis, Missouri.
“We also see that COVID-19 can lead to new-onset cardiovascular disease,” said Al-Aly, who was not involved in the study. “There is clearly a (link) between COVID and cardiovascular disease. These two seem to be intimately intertwined. In my view, this emphasizes the importance of targeting these individuals for vaccination and potentially antivirals (when they get infected) to help reduce their risk of adverse events and ameliorate their chance of full and fast recovery.”
The study used data from the Collaborative Cohort of Cohorts for COVID-19 Research. The long list of researchers contributing to this study includes epidemiologists, biostatisticians, neurologists, pulmonologists, and cardiologists. The data come from a list of cohorts like the Framingham Heart Study, which identified key risk factors for CVD, including cholesterol levels. Other studies include the Atherosclerosis Risk in Communities study, which began in the mid-1980s. Researchers there recruited a cohort of 15,792 men and women in rural North Carolina and Mississippi and suburban Minneapolis. They enrolled a high number of African American participants, who have been underrepresented in past studies. Other cohorts focused on young adults with CVD and Hispanics, while another focused on people with chronic obstructive pulmonary disease.
Lead author Elizabeth C. Oelsner, MD, of Columbia University Irving Medical Center in New York City, said she was not surprised by the CVD-long COVID link.
“We were aware that individuals with CVD were at higher risk of a more severe acute infection,” she said. “We were also seeing evidence that long and severe infection led to persistent symptoms.”
Oelsner noted that many patients still take more than 3 months to recover, even during the Omicron wave.
“While that has improved over the course of the pandemic, many individuals are taking a very long time to recover, and that can have a huge burden on the patient,” she said.
She encourages healthcare providers to tell patients at higher risk to take steps to avoid the virus, including vaccination and boosters.
A version of this article first appeared on Medscape.com.
Sperm Appear to Have a Nonreproductive Function
Brazilian researchers have identified a previously unrecognized function of sperm that is unrelated to reproduction. A study of 13 patients admitted to the Hospital das Clínicas da Universidade de São Paulo with moderate to severe COVID-19 showed that male gametes released extracellular traps (in a process called ETosis) in response to the infection. This immune response, which is common to macrophages and neutrophils, had never been observed in mammalian reproductive cells.
“It opens up a new line of research,” said Jorge Hallak, a professor at the University of São Paulo School of Medicine, São Paulo, Brazil, and first author of the article published in Andrology. “This may be an innovative mechanism, or it may have always existed, and no one knew.”
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was identified in cells more than 3 months after infection in 11 participants, although polymerase chain reaction tests were negative. These findings suggest the potential for drafting a protocol or guidance on when to attempt a pregnancy. “My concern is with assisted reproduction, in which, in general, only one basic spermogram is done, without diagnostic investigation or serology for coronavirus,” said Hallak.
Symptomatic infections hinder the reproductive process because symptoms such as high fever impair cell function by triggering increased DNA fragmentation, reduced mitochondrial activity, decreased acrosome reaction, and cell death, thus affecting sperm count and gamete mobility.
The new findings indicate that the impact of SARS-CoV-2 infection can continue for as long as 90 days after symptoms and signs disappear and affect sperm count and gamete quality for even longer. “With the sperm selection technique, you are at risk of taking a cell with viruses and injecting it into the egg. It is not known what changes this may cause to the embryo,” said Hallak.
The expert emphasized that the finding contributes to the understanding of reproductive difficulties that previously had no plausible explanation. It serves as a warning against negligence in the evaluation of men in assisted reproductive treatments.
Daniel Zylberstein, urologist and member of the Brazilian Association of Assisted Reproduction, who did not participate in the research, noted that the result comes from a small study that should be expanded to try to develop guidance for doctors.
“There is still no protocol for these cases. The ideal approach would be to wait for complete spermatogenesis, which takes about 3 months, before putting patients on treatment. This often does not happen, and treatment begins shortly after clinical recovery. In the case of moderate to severe COVID-19, this period should be longer than 90 days,” he said.
The study suggests establishing a quarantine period for reproduction until the sperm are free of the virus, said Zylberstein. “With infected sperm, it makes no sense to start reproductive treatment. This sperm is spending energy to fight the pathogen. Assisted reproduction is expensive and exhaustive and may not have the expected outcome because of SARS-CoV-2 infectivity.”
This story was translated from the Medscape Portuguese edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Brazilian researchers have identified a previously unrecognized function of sperm that is unrelated to reproduction. A study of 13 patients admitted to the Hospital das Clínicas da Universidade de São Paulo with moderate to severe COVID-19 showed that male gametes released extracellular traps (in a process called ETosis) in response to the infection. This immune response, which is common to macrophages and neutrophils, had never been observed in mammalian reproductive cells.
“It opens up a new line of research,” said Jorge Hallak, a professor at the University of São Paulo School of Medicine, São Paulo, Brazil, and first author of the article published in Andrology. “This may be an innovative mechanism, or it may have always existed, and no one knew.”
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was identified in cells more than 3 months after infection in 11 participants, although polymerase chain reaction tests were negative. These findings suggest the potential for drafting a protocol or guidance on when to attempt a pregnancy. “My concern is with assisted reproduction, in which, in general, only one basic spermogram is done, without diagnostic investigation or serology for coronavirus,” said Hallak.
Symptomatic infections hinder the reproductive process because symptoms such as high fever impair cell function by triggering increased DNA fragmentation, reduced mitochondrial activity, decreased acrosome reaction, and cell death, thus affecting sperm count and gamete mobility.
The new findings indicate that the impact of SARS-CoV-2 infection can continue for as long as 90 days after symptoms and signs disappear and affect sperm count and gamete quality for even longer. “With the sperm selection technique, you are at risk of taking a cell with viruses and injecting it into the egg. It is not known what changes this may cause to the embryo,” said Hallak.
The expert emphasized that the finding contributes to the understanding of reproductive difficulties that previously had no plausible explanation. It serves as a warning against negligence in the evaluation of men in assisted reproductive treatments.
Daniel Zylberstein, urologist and member of the Brazilian Association of Assisted Reproduction, who did not participate in the research, noted that the result comes from a small study that should be expanded to try to develop guidance for doctors.
“There is still no protocol for these cases. The ideal approach would be to wait for complete spermatogenesis, which takes about 3 months, before putting patients on treatment. This often does not happen, and treatment begins shortly after clinical recovery. In the case of moderate to severe COVID-19, this period should be longer than 90 days,” he said.
The study suggests establishing a quarantine period for reproduction until the sperm are free of the virus, said Zylberstein. “With infected sperm, it makes no sense to start reproductive treatment. This sperm is spending energy to fight the pathogen. Assisted reproduction is expensive and exhaustive and may not have the expected outcome because of SARS-CoV-2 infectivity.”
This story was translated from the Medscape Portuguese edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Brazilian researchers have identified a previously unrecognized function of sperm that is unrelated to reproduction. A study of 13 patients admitted to the Hospital das Clínicas da Universidade de São Paulo with moderate to severe COVID-19 showed that male gametes released extracellular traps (in a process called ETosis) in response to the infection. This immune response, which is common to macrophages and neutrophils, had never been observed in mammalian reproductive cells.
“It opens up a new line of research,” said Jorge Hallak, a professor at the University of São Paulo School of Medicine, São Paulo, Brazil, and first author of the article published in Andrology. “This may be an innovative mechanism, or it may have always existed, and no one knew.”
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was identified in cells more than 3 months after infection in 11 participants, although polymerase chain reaction tests were negative. These findings suggest the potential for drafting a protocol or guidance on when to attempt a pregnancy. “My concern is with assisted reproduction, in which, in general, only one basic spermogram is done, without diagnostic investigation or serology for coronavirus,” said Hallak.
Symptomatic infections hinder the reproductive process because symptoms such as high fever impair cell function by triggering increased DNA fragmentation, reduced mitochondrial activity, decreased acrosome reaction, and cell death, thus affecting sperm count and gamete mobility.
The new findings indicate that the impact of SARS-CoV-2 infection can continue for as long as 90 days after symptoms and signs disappear and affect sperm count and gamete quality for even longer. “With the sperm selection technique, you are at risk of taking a cell with viruses and injecting it into the egg. It is not known what changes this may cause to the embryo,” said Hallak.
The expert emphasized that the finding contributes to the understanding of reproductive difficulties that previously had no plausible explanation. It serves as a warning against negligence in the evaluation of men in assisted reproductive treatments.
Daniel Zylberstein, urologist and member of the Brazilian Association of Assisted Reproduction, who did not participate in the research, noted that the result comes from a small study that should be expanded to try to develop guidance for doctors.
“There is still no protocol for these cases. The ideal approach would be to wait for complete spermatogenesis, which takes about 3 months, before putting patients on treatment. This often does not happen, and treatment begins shortly after clinical recovery. In the case of moderate to severe COVID-19, this period should be longer than 90 days,” he said.
The study suggests establishing a quarantine period for reproduction until the sperm are free of the virus, said Zylberstein. “With infected sperm, it makes no sense to start reproductive treatment. This sperm is spending energy to fight the pathogen. Assisted reproduction is expensive and exhaustive and may not have the expected outcome because of SARS-CoV-2 infectivity.”
This story was translated from the Medscape Portuguese edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
FROM ANDROLOGY
Too Few Immunocompromised Veterans Are Getting Zoster Vaccinations
TOPLINE:
the low rate of herpes zoster vaccination in this immunocompromised group, especially among younger individuals, is concerning.
METHODOLOGY:
- In 2021, the Food and Drug Administration authorized the use of RZV for adults aged 18 years or older on chronic immunosuppressive medications because of their high risk for herpes zoster and its related complications, followed by updated guidance from the Centers for Disease Control and Prevention and American College of Rheumatology in 2021 and 2022, respectively.
- This study aimed to assess the receipt of RZV among veterans receiving immunosuppressive medications within the Veterans Health Administration (VHA) healthcare system before and after the expanded indications in February 2022.
- It included 190,162 veterans who were prescribed one or more immunosuppressive medications for at least 90 days at 130 medical facilities between January 1, 2018, and June 30, 2023.
- A total of 23,295 veterans (12.3%) were younger than 50 years by the end of the study period.
- The outcome measured was the percentage of veterans with one or more doses of RZV documented during the study period.
TAKEAWAY:
- Among veterans aged 50 years or older, 36.2% and 49.8% received an RZV before the expanded indication and by mid-2023, respectively. Even though the rate of vaccination is higher than that observed in the 2021 National Health Interview Survey, significant room for improvement remains.
- Among veterans younger than 50 years, very few (2.8%) received an RZV before the expanded indication, and only 13.4% received it by mid-2023.
- Demographic factors associated with lower odds of vaccination included male sex, African American or unknown race, and nonurban residence (P ≤ .004 for all).
- Those who received targeted synthetic disease-modifying antirheumatic drugs (DMARDs) alone or in combination with other drugs or those who received other vaccines were more likely to receive RZV than those who received conventional synthetic DMARD monotherapy (P < .001 for both).
IN PRACTICE:
“Future work to improve RZV vaccination in patients at high risk should focus on creating informatics tools to identify individuals at high risk and standardizing vaccination guidelines across subspecialties,” the authors wrote.
SOURCE:
This study was led by Sharon Abada, MD, University of California, San Francisco. It was published online on October 11, 2024, in JAMA Network Open.
LIMITATIONS:
This study may not be generalizable to nonveteran populations or countries outside the United States. Limitations also included difficulty with capturing vaccinations not administered within the VHA system, which may have resulted in an underestimation of the percentage of patients vaccinated.
DISCLOSURES:
This work was funded by grants from the VA Quality Enhancement Research Initiative and the Agency for Healthcare Research and Quality. Some authors reported receiving grants from institutions and pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
the low rate of herpes zoster vaccination in this immunocompromised group, especially among younger individuals, is concerning.
METHODOLOGY:
- In 2021, the Food and Drug Administration authorized the use of RZV for adults aged 18 years or older on chronic immunosuppressive medications because of their high risk for herpes zoster and its related complications, followed by updated guidance from the Centers for Disease Control and Prevention and American College of Rheumatology in 2021 and 2022, respectively.
- This study aimed to assess the receipt of RZV among veterans receiving immunosuppressive medications within the Veterans Health Administration (VHA) healthcare system before and after the expanded indications in February 2022.
- It included 190,162 veterans who were prescribed one or more immunosuppressive medications for at least 90 days at 130 medical facilities between January 1, 2018, and June 30, 2023.
- A total of 23,295 veterans (12.3%) were younger than 50 years by the end of the study period.
- The outcome measured was the percentage of veterans with one or more doses of RZV documented during the study period.
TAKEAWAY:
- Among veterans aged 50 years or older, 36.2% and 49.8% received an RZV before the expanded indication and by mid-2023, respectively. Even though the rate of vaccination is higher than that observed in the 2021 National Health Interview Survey, significant room for improvement remains.
- Among veterans younger than 50 years, very few (2.8%) received an RZV before the expanded indication, and only 13.4% received it by mid-2023.
- Demographic factors associated with lower odds of vaccination included male sex, African American or unknown race, and nonurban residence (P ≤ .004 for all).
- Those who received targeted synthetic disease-modifying antirheumatic drugs (DMARDs) alone or in combination with other drugs or those who received other vaccines were more likely to receive RZV than those who received conventional synthetic DMARD monotherapy (P < .001 for both).
IN PRACTICE:
“Future work to improve RZV vaccination in patients at high risk should focus on creating informatics tools to identify individuals at high risk and standardizing vaccination guidelines across subspecialties,” the authors wrote.
SOURCE:
This study was led by Sharon Abada, MD, University of California, San Francisco. It was published online on October 11, 2024, in JAMA Network Open.
LIMITATIONS:
This study may not be generalizable to nonveteran populations or countries outside the United States. Limitations also included difficulty with capturing vaccinations not administered within the VHA system, which may have resulted in an underestimation of the percentage of patients vaccinated.
DISCLOSURES:
This work was funded by grants from the VA Quality Enhancement Research Initiative and the Agency for Healthcare Research and Quality. Some authors reported receiving grants from institutions and pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
the low rate of herpes zoster vaccination in this immunocompromised group, especially among younger individuals, is concerning.
METHODOLOGY:
- In 2021, the Food and Drug Administration authorized the use of RZV for adults aged 18 years or older on chronic immunosuppressive medications because of their high risk for herpes zoster and its related complications, followed by updated guidance from the Centers for Disease Control and Prevention and American College of Rheumatology in 2021 and 2022, respectively.
- This study aimed to assess the receipt of RZV among veterans receiving immunosuppressive medications within the Veterans Health Administration (VHA) healthcare system before and after the expanded indications in February 2022.
- It included 190,162 veterans who were prescribed one or more immunosuppressive medications for at least 90 days at 130 medical facilities between January 1, 2018, and June 30, 2023.
- A total of 23,295 veterans (12.3%) were younger than 50 years by the end of the study period.
- The outcome measured was the percentage of veterans with one or more doses of RZV documented during the study period.
TAKEAWAY:
- Among veterans aged 50 years or older, 36.2% and 49.8% received an RZV before the expanded indication and by mid-2023, respectively. Even though the rate of vaccination is higher than that observed in the 2021 National Health Interview Survey, significant room for improvement remains.
- Among veterans younger than 50 years, very few (2.8%) received an RZV before the expanded indication, and only 13.4% received it by mid-2023.
- Demographic factors associated with lower odds of vaccination included male sex, African American or unknown race, and nonurban residence (P ≤ .004 for all).
- Those who received targeted synthetic disease-modifying antirheumatic drugs (DMARDs) alone or in combination with other drugs or those who received other vaccines were more likely to receive RZV than those who received conventional synthetic DMARD monotherapy (P < .001 for both).
IN PRACTICE:
“Future work to improve RZV vaccination in patients at high risk should focus on creating informatics tools to identify individuals at high risk and standardizing vaccination guidelines across subspecialties,” the authors wrote.
SOURCE:
This study was led by Sharon Abada, MD, University of California, San Francisco. It was published online on October 11, 2024, in JAMA Network Open.
LIMITATIONS:
This study may not be generalizable to nonveteran populations or countries outside the United States. Limitations also included difficulty with capturing vaccinations not administered within the VHA system, which may have resulted in an underestimation of the percentage of patients vaccinated.
DISCLOSURES:
This work was funded by grants from the VA Quality Enhancement Research Initiative and the Agency for Healthcare Research and Quality. Some authors reported receiving grants from institutions and pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
A Hard Look at Toxic Workplace Culture in Medicine
While Kellie Lease Stecher, MD, was working as an ob.gyn. in Minneapolis, Minnesota, a patient confided in her a sexual assault allegation about one of Stecher’s male colleagues. Stecher shared the allegation with her supervisor, who told Stecher not to file a report and chose not to address the issue with the patient. Stecher weighed how to do the right thing: Should she speak up? What were the ethical and legal implications of speaking up vs staying silent?
After seeking advice from her mentors, Stecher felt it was her moral and legal duty to report the allegation to the Minnesota Medical Board. Once she did, her supervisor chastised her repeatedly for reporting the allegation. Stecher soon found herself in a hostile work environment where she was regularly singled out and silenced by her supervisor and colleagues.
“I got to a point where I felt like I couldn’t say anything at any meetings without somehow being targeted after the meeting. There was an individual who was even allowed to fat-shame me with no consequences,” Stecher said. “[Being bullied at work is] a struggle because you have no voice, you have no opportunities, and there’s someone who is intentionally making your life uncomfortable.”
Stecher’s experience is not unusual. Mistreatment is a common issue among healthcare workers, ranging from rudeness to bullying and harassment and permeating every level and specialty of the medical profession. A 2019 research review estimated that 26.3% of healthcare workers had experienced bullying and found bullying in healthcare to be associated with mental health problems such as burnout and depression, physical health problems such as insomnia and headaches, and physicians taking more sick leave.
The Medscape Physician Workplace Culture Report 2024 found similarly bleak results:
- 38% said workplace culture is declining.
- 70% don’t see a big commitment from employers for positive culture.
- 48% said staff isn’t committed to positive culture.
The irony, of course, is that most physicians enter the field to care for people. As individuals go from medical school to residency and on with the rest of their careers, they often experience a rude awakening.
It’s Everywhere
Noticing the prevalence of workplace bullying in the medical field, endocrinologist Farah Khan, MD, at UW Medicine in Seattle, Washington, decided to conduct a survey on the issue.
Khan collected 122 responses from colleagues, friends, and acquaintances in the field. When asked if they had ever been bullied in medicine, 68% of respondents said yes. But here’s the fascinating part: She tried to pinpoint one particular area or source of toxicity in the progression of a physician’s career — and couldn’t because it existed at all levels.
More than one third of respondents said their worst bullying experiences occurred in residency, while 30% said mistreatment was worst in medical school, and 24% indicated their worst experience had occurred once they became an attending.
The litany of experiences included being belittled, excluded, yelled at, criticized, shamed, unfairly blamed, threatened, sexually harassed, subjected to bigotry and slurs, and humiliated.
“What surprised me the most was how widespread this problem is and the many different layers of healthcare it permeates through, from operating room staff to medical students to hospital HR to residents and attendings,” Khan said of her findings.
Who Cares for the Caregivers?
When hematologist Mikkael Sekeres, MD, was in medical school, he seriously considered a career as a surgeon. Following success in his surgical rotations, he scrubbed in with a cardiothoracic surgeon who was well known for both his status as a surgeon and his fiery temper. Sekeres witnessed the surgeon yelling at whoever was nearby: Medical students, fellows, residents, operating room nurses.
“At the end of that experience, any passing thoughts I had of going into cardiothoracic surgery were gone,” Sekeres said. “Some of the people I met in surgery were truly wonderful. Some were unhappy people.”
He has clear ideas why. Mental health struggles that are all too common among physicians can be caused or exacerbated by mistreatment and can also lead a physician to mistreat others.
“People bully when they themselves are hurting,” Sekeres said. “It begs the question, why are people hurting? What’s driving them to be bullies? I think part of the reason is that they’re working really hard and they’re tired, and nobody’s caring for them. It’s hard to care for others when you feel as if you’re hurting more than they are.”
Gail Gazelle, MD, experienced something like this. In her case, the pressure to please and to be a perfect professional and mother affected how she interacted with those around her. While working as a hospice medical director and an academician and clinician at Harvard Medical School, Boston, Massachusetts, she found herself feeling exhausted and burnt out but simultaneously guilty for not doing enough at work or at home.
Guess what happened? She became irritable, lashing out at her son and not putting her best foot forward with coworkers or patients.
After trying traditional therapy and self-help through books and podcasts, Gazelle found her solution in life coaching. “I realized just how harsh I was being on myself and found ways to reverse that pattern,” she said. “I learned ways of regulating myself emotionally that I definitely didn’t learn in my training.”
Today, Gazelle works as a life coach herself, guiding physicians through common challenges of the profession — particularly bullying, which she sees often. She remembers one client, an oncologist, who was being targeted by a nurse practitioner she was training. The nurse practitioner began talking back to the oncologist, as well as gossiping and bad-mouthing her to the nurses in the practice. The nurses then began excluding the oncologist from their cafeteria table at lunchtime, which felt blatant in such a small practice.
A core component of Gazelle’s coaching strategy was helping the client reclaim her self-esteem by focusing on her strengths. She instructed the client to write down what went well that day each night rather than lying in bed ruminating. Such self-care strategies can not only help bullied physicians but also prevent some of the challenges that might cause a physician to bully or lash out at another in the first place.
Such strategies, along with the recent influx of wellness programs available in healthcare facilities, can help physicians cope with the mental health impacts of bullying and the job in general. But even life coaches like Gazelle acknowledge that they are often band-aids on the system’s deeper wounds. Bullying in healthcare is not an individual issue; at its core, it’s an institutional one.
Negative Hierarchies in Healthcare
When Stecher’s contract expired, she was fired by the supervisor who had been bullying her. Stecher has since filed a lawsuit, claiming sexual discrimination, defamation, and wrongful termination.
The medical field has a long history of hierarchy, and while this rigidity has softened over time, negative hierarchical dynamics are often perpetuated by leaders. Phenomena like cronyism and cliques and behaviors like petty gossip, lunchroom exclusion (which in the worst cases can mimic high school dynamics), and targeting can be at play in the healthcare workplace.
The classic examples, Stecher said, can usually be spotted: “If you threaten the status quo or offer different ideas, you are seen as a threat. Cronyism ... strict hierarchies ... people who elevate individuals in their social arena into leadership positions. Physicians don’t get the leadership training that they really need; they are often just dumped into roles with no previous experience because they’re someone’s golfing buddy.”
The question is how to get workplace culture momentum moving in a positive direction. When Gazelle’s clients are hesitant to voice concerns, she emphasizes doing so can and should benefit leadership, as well as patients and the wider healthcare system.
“The win-win is that you have a healthy culture of respect and dignity and civility rather than the opposite,” she said. “The leader will actually have more staff retention, which everybody’s concerned about, given the shortage of healthcare workers.”
And that’s a key incentive that may not be discussed as much: Talent drain from toxicity. The Medscape Workplace Culture Report asked about culture as it applies to physicians looking to join up. Notably, 93% of doctors say culture is important when mulling a job offer, 70% said culture is equal to money, and 18% ranked it as more important than money, and 46% say a positive atmosphere is the top priority.
Ultimately, it comes down to who is willing to step in and stand up. Respondents to Khan’s survey counted anonymous reporting systems, more supportive administration teams, and zero-tolerance policies as potential remedies. Gazelle, Sekeres, and Stecher all emphasize the need for zero-tolerance policies for bullying and mistreatment.
“We can’t afford to have things going on like this that just destroy the fabric of the healthcare endeavor,” Gazelle said. “They come out sideways eventually. They come out in terms of poor patient care because there are greater errors. There’s a lack of respect for patients. There’s anger and irritability and so much spillover. We have to have zero-tolerance policies from the top down.”
A version of this article appeared on Medscape.com.
While Kellie Lease Stecher, MD, was working as an ob.gyn. in Minneapolis, Minnesota, a patient confided in her a sexual assault allegation about one of Stecher’s male colleagues. Stecher shared the allegation with her supervisor, who told Stecher not to file a report and chose not to address the issue with the patient. Stecher weighed how to do the right thing: Should she speak up? What were the ethical and legal implications of speaking up vs staying silent?
After seeking advice from her mentors, Stecher felt it was her moral and legal duty to report the allegation to the Minnesota Medical Board. Once she did, her supervisor chastised her repeatedly for reporting the allegation. Stecher soon found herself in a hostile work environment where she was regularly singled out and silenced by her supervisor and colleagues.
“I got to a point where I felt like I couldn’t say anything at any meetings without somehow being targeted after the meeting. There was an individual who was even allowed to fat-shame me with no consequences,” Stecher said. “[Being bullied at work is] a struggle because you have no voice, you have no opportunities, and there’s someone who is intentionally making your life uncomfortable.”
Stecher’s experience is not unusual. Mistreatment is a common issue among healthcare workers, ranging from rudeness to bullying and harassment and permeating every level and specialty of the medical profession. A 2019 research review estimated that 26.3% of healthcare workers had experienced bullying and found bullying in healthcare to be associated with mental health problems such as burnout and depression, physical health problems such as insomnia and headaches, and physicians taking more sick leave.
The Medscape Physician Workplace Culture Report 2024 found similarly bleak results:
- 38% said workplace culture is declining.
- 70% don’t see a big commitment from employers for positive culture.
- 48% said staff isn’t committed to positive culture.
The irony, of course, is that most physicians enter the field to care for people. As individuals go from medical school to residency and on with the rest of their careers, they often experience a rude awakening.
It’s Everywhere
Noticing the prevalence of workplace bullying in the medical field, endocrinologist Farah Khan, MD, at UW Medicine in Seattle, Washington, decided to conduct a survey on the issue.
Khan collected 122 responses from colleagues, friends, and acquaintances in the field. When asked if they had ever been bullied in medicine, 68% of respondents said yes. But here’s the fascinating part: She tried to pinpoint one particular area or source of toxicity in the progression of a physician’s career — and couldn’t because it existed at all levels.
More than one third of respondents said their worst bullying experiences occurred in residency, while 30% said mistreatment was worst in medical school, and 24% indicated their worst experience had occurred once they became an attending.
The litany of experiences included being belittled, excluded, yelled at, criticized, shamed, unfairly blamed, threatened, sexually harassed, subjected to bigotry and slurs, and humiliated.
“What surprised me the most was how widespread this problem is and the many different layers of healthcare it permeates through, from operating room staff to medical students to hospital HR to residents and attendings,” Khan said of her findings.
Who Cares for the Caregivers?
When hematologist Mikkael Sekeres, MD, was in medical school, he seriously considered a career as a surgeon. Following success in his surgical rotations, he scrubbed in with a cardiothoracic surgeon who was well known for both his status as a surgeon and his fiery temper. Sekeres witnessed the surgeon yelling at whoever was nearby: Medical students, fellows, residents, operating room nurses.
“At the end of that experience, any passing thoughts I had of going into cardiothoracic surgery were gone,” Sekeres said. “Some of the people I met in surgery were truly wonderful. Some were unhappy people.”
He has clear ideas why. Mental health struggles that are all too common among physicians can be caused or exacerbated by mistreatment and can also lead a physician to mistreat others.
“People bully when they themselves are hurting,” Sekeres said. “It begs the question, why are people hurting? What’s driving them to be bullies? I think part of the reason is that they’re working really hard and they’re tired, and nobody’s caring for them. It’s hard to care for others when you feel as if you’re hurting more than they are.”
Gail Gazelle, MD, experienced something like this. In her case, the pressure to please and to be a perfect professional and mother affected how she interacted with those around her. While working as a hospice medical director and an academician and clinician at Harvard Medical School, Boston, Massachusetts, she found herself feeling exhausted and burnt out but simultaneously guilty for not doing enough at work or at home.
Guess what happened? She became irritable, lashing out at her son and not putting her best foot forward with coworkers or patients.
After trying traditional therapy and self-help through books and podcasts, Gazelle found her solution in life coaching. “I realized just how harsh I was being on myself and found ways to reverse that pattern,” she said. “I learned ways of regulating myself emotionally that I definitely didn’t learn in my training.”
Today, Gazelle works as a life coach herself, guiding physicians through common challenges of the profession — particularly bullying, which she sees often. She remembers one client, an oncologist, who was being targeted by a nurse practitioner she was training. The nurse practitioner began talking back to the oncologist, as well as gossiping and bad-mouthing her to the nurses in the practice. The nurses then began excluding the oncologist from their cafeteria table at lunchtime, which felt blatant in such a small practice.
A core component of Gazelle’s coaching strategy was helping the client reclaim her self-esteem by focusing on her strengths. She instructed the client to write down what went well that day each night rather than lying in bed ruminating. Such self-care strategies can not only help bullied physicians but also prevent some of the challenges that might cause a physician to bully or lash out at another in the first place.
Such strategies, along with the recent influx of wellness programs available in healthcare facilities, can help physicians cope with the mental health impacts of bullying and the job in general. But even life coaches like Gazelle acknowledge that they are often band-aids on the system’s deeper wounds. Bullying in healthcare is not an individual issue; at its core, it’s an institutional one.
Negative Hierarchies in Healthcare
When Stecher’s contract expired, she was fired by the supervisor who had been bullying her. Stecher has since filed a lawsuit, claiming sexual discrimination, defamation, and wrongful termination.
The medical field has a long history of hierarchy, and while this rigidity has softened over time, negative hierarchical dynamics are often perpetuated by leaders. Phenomena like cronyism and cliques and behaviors like petty gossip, lunchroom exclusion (which in the worst cases can mimic high school dynamics), and targeting can be at play in the healthcare workplace.
The classic examples, Stecher said, can usually be spotted: “If you threaten the status quo or offer different ideas, you are seen as a threat. Cronyism ... strict hierarchies ... people who elevate individuals in their social arena into leadership positions. Physicians don’t get the leadership training that they really need; they are often just dumped into roles with no previous experience because they’re someone’s golfing buddy.”
The question is how to get workplace culture momentum moving in a positive direction. When Gazelle’s clients are hesitant to voice concerns, she emphasizes doing so can and should benefit leadership, as well as patients and the wider healthcare system.
“The win-win is that you have a healthy culture of respect and dignity and civility rather than the opposite,” she said. “The leader will actually have more staff retention, which everybody’s concerned about, given the shortage of healthcare workers.”
And that’s a key incentive that may not be discussed as much: Talent drain from toxicity. The Medscape Workplace Culture Report asked about culture as it applies to physicians looking to join up. Notably, 93% of doctors say culture is important when mulling a job offer, 70% said culture is equal to money, and 18% ranked it as more important than money, and 46% say a positive atmosphere is the top priority.
Ultimately, it comes down to who is willing to step in and stand up. Respondents to Khan’s survey counted anonymous reporting systems, more supportive administration teams, and zero-tolerance policies as potential remedies. Gazelle, Sekeres, and Stecher all emphasize the need for zero-tolerance policies for bullying and mistreatment.
“We can’t afford to have things going on like this that just destroy the fabric of the healthcare endeavor,” Gazelle said. “They come out sideways eventually. They come out in terms of poor patient care because there are greater errors. There’s a lack of respect for patients. There’s anger and irritability and so much spillover. We have to have zero-tolerance policies from the top down.”
A version of this article appeared on Medscape.com.
While Kellie Lease Stecher, MD, was working as an ob.gyn. in Minneapolis, Minnesota, a patient confided in her a sexual assault allegation about one of Stecher’s male colleagues. Stecher shared the allegation with her supervisor, who told Stecher not to file a report and chose not to address the issue with the patient. Stecher weighed how to do the right thing: Should she speak up? What were the ethical and legal implications of speaking up vs staying silent?
After seeking advice from her mentors, Stecher felt it was her moral and legal duty to report the allegation to the Minnesota Medical Board. Once she did, her supervisor chastised her repeatedly for reporting the allegation. Stecher soon found herself in a hostile work environment where she was regularly singled out and silenced by her supervisor and colleagues.
“I got to a point where I felt like I couldn’t say anything at any meetings without somehow being targeted after the meeting. There was an individual who was even allowed to fat-shame me with no consequences,” Stecher said. “[Being bullied at work is] a struggle because you have no voice, you have no opportunities, and there’s someone who is intentionally making your life uncomfortable.”
Stecher’s experience is not unusual. Mistreatment is a common issue among healthcare workers, ranging from rudeness to bullying and harassment and permeating every level and specialty of the medical profession. A 2019 research review estimated that 26.3% of healthcare workers had experienced bullying and found bullying in healthcare to be associated with mental health problems such as burnout and depression, physical health problems such as insomnia and headaches, and physicians taking more sick leave.
The Medscape Physician Workplace Culture Report 2024 found similarly bleak results:
- 38% said workplace culture is declining.
- 70% don’t see a big commitment from employers for positive culture.
- 48% said staff isn’t committed to positive culture.
The irony, of course, is that most physicians enter the field to care for people. As individuals go from medical school to residency and on with the rest of their careers, they often experience a rude awakening.
It’s Everywhere
Noticing the prevalence of workplace bullying in the medical field, endocrinologist Farah Khan, MD, at UW Medicine in Seattle, Washington, decided to conduct a survey on the issue.
Khan collected 122 responses from colleagues, friends, and acquaintances in the field. When asked if they had ever been bullied in medicine, 68% of respondents said yes. But here’s the fascinating part: She tried to pinpoint one particular area or source of toxicity in the progression of a physician’s career — and couldn’t because it existed at all levels.
More than one third of respondents said their worst bullying experiences occurred in residency, while 30% said mistreatment was worst in medical school, and 24% indicated their worst experience had occurred once they became an attending.
The litany of experiences included being belittled, excluded, yelled at, criticized, shamed, unfairly blamed, threatened, sexually harassed, subjected to bigotry and slurs, and humiliated.
“What surprised me the most was how widespread this problem is and the many different layers of healthcare it permeates through, from operating room staff to medical students to hospital HR to residents and attendings,” Khan said of her findings.
Who Cares for the Caregivers?
When hematologist Mikkael Sekeres, MD, was in medical school, he seriously considered a career as a surgeon. Following success in his surgical rotations, he scrubbed in with a cardiothoracic surgeon who was well known for both his status as a surgeon and his fiery temper. Sekeres witnessed the surgeon yelling at whoever was nearby: Medical students, fellows, residents, operating room nurses.
“At the end of that experience, any passing thoughts I had of going into cardiothoracic surgery were gone,” Sekeres said. “Some of the people I met in surgery were truly wonderful. Some were unhappy people.”
He has clear ideas why. Mental health struggles that are all too common among physicians can be caused or exacerbated by mistreatment and can also lead a physician to mistreat others.
“People bully when they themselves are hurting,” Sekeres said. “It begs the question, why are people hurting? What’s driving them to be bullies? I think part of the reason is that they’re working really hard and they’re tired, and nobody’s caring for them. It’s hard to care for others when you feel as if you’re hurting more than they are.”
Gail Gazelle, MD, experienced something like this. In her case, the pressure to please and to be a perfect professional and mother affected how she interacted with those around her. While working as a hospice medical director and an academician and clinician at Harvard Medical School, Boston, Massachusetts, she found herself feeling exhausted and burnt out but simultaneously guilty for not doing enough at work or at home.
Guess what happened? She became irritable, lashing out at her son and not putting her best foot forward with coworkers or patients.
After trying traditional therapy and self-help through books and podcasts, Gazelle found her solution in life coaching. “I realized just how harsh I was being on myself and found ways to reverse that pattern,” she said. “I learned ways of regulating myself emotionally that I definitely didn’t learn in my training.”
Today, Gazelle works as a life coach herself, guiding physicians through common challenges of the profession — particularly bullying, which she sees often. She remembers one client, an oncologist, who was being targeted by a nurse practitioner she was training. The nurse practitioner began talking back to the oncologist, as well as gossiping and bad-mouthing her to the nurses in the practice. The nurses then began excluding the oncologist from their cafeteria table at lunchtime, which felt blatant in such a small practice.
A core component of Gazelle’s coaching strategy was helping the client reclaim her self-esteem by focusing on her strengths. She instructed the client to write down what went well that day each night rather than lying in bed ruminating. Such self-care strategies can not only help bullied physicians but also prevent some of the challenges that might cause a physician to bully or lash out at another in the first place.
Such strategies, along with the recent influx of wellness programs available in healthcare facilities, can help physicians cope with the mental health impacts of bullying and the job in general. But even life coaches like Gazelle acknowledge that they are often band-aids on the system’s deeper wounds. Bullying in healthcare is not an individual issue; at its core, it’s an institutional one.
Negative Hierarchies in Healthcare
When Stecher’s contract expired, she was fired by the supervisor who had been bullying her. Stecher has since filed a lawsuit, claiming sexual discrimination, defamation, and wrongful termination.
The medical field has a long history of hierarchy, and while this rigidity has softened over time, negative hierarchical dynamics are often perpetuated by leaders. Phenomena like cronyism and cliques and behaviors like petty gossip, lunchroom exclusion (which in the worst cases can mimic high school dynamics), and targeting can be at play in the healthcare workplace.
The classic examples, Stecher said, can usually be spotted: “If you threaten the status quo or offer different ideas, you are seen as a threat. Cronyism ... strict hierarchies ... people who elevate individuals in their social arena into leadership positions. Physicians don’t get the leadership training that they really need; they are often just dumped into roles with no previous experience because they’re someone’s golfing buddy.”
The question is how to get workplace culture momentum moving in a positive direction. When Gazelle’s clients are hesitant to voice concerns, she emphasizes doing so can and should benefit leadership, as well as patients and the wider healthcare system.
“The win-win is that you have a healthy culture of respect and dignity and civility rather than the opposite,” she said. “The leader will actually have more staff retention, which everybody’s concerned about, given the shortage of healthcare workers.”
And that’s a key incentive that may not be discussed as much: Talent drain from toxicity. The Medscape Workplace Culture Report asked about culture as it applies to physicians looking to join up. Notably, 93% of doctors say culture is important when mulling a job offer, 70% said culture is equal to money, and 18% ranked it as more important than money, and 46% say a positive atmosphere is the top priority.
Ultimately, it comes down to who is willing to step in and stand up. Respondents to Khan’s survey counted anonymous reporting systems, more supportive administration teams, and zero-tolerance policies as potential remedies. Gazelle, Sekeres, and Stecher all emphasize the need for zero-tolerance policies for bullying and mistreatment.
“We can’t afford to have things going on like this that just destroy the fabric of the healthcare endeavor,” Gazelle said. “They come out sideways eventually. They come out in terms of poor patient care because there are greater errors. There’s a lack of respect for patients. There’s anger and irritability and so much spillover. We have to have zero-tolerance policies from the top down.”
A version of this article appeared on Medscape.com.
NY Nurse Practitioners Sue State Over Pay Equity, Alleged Gender Inequality
A
The New York State Civil Service Commission understates the job function of NPs, overstates their dependence on physicians, and inadequately pays them for their work, according to the complaint filed in the US District Court for the Northern District of New York.
The nurses claim the mistreatment is a consequence of the fact that “at least 80% of the state’s employed NPs are women.”
Michael H. Sussman, a Goshen, New York–based attorney for the nurses, said in an interview that New York NPs are increasingly being used essentially as doctors at state-run facilities, including prisons, yet the state has failed to adequately pay them.
The lawsuit comes after a decade-long attempt by NPs to attain equitable pay and the ability to advance their civil service careers, he said.
“New York state has not addressed the heart of the issue, which is that the classification of this position is much lower than other positions in the state which are not so female-dominated and which engage in very similar activities,” Sussman said.
The lawsuit claims that “the work of NPs is complex, equaling that of a medical specialist, psychiatrist, or clinical physician.”
A spokesman for the New York State Civil Service Commission declined comment, saying the department does not comment on pending litigation.
Novel Gender Discrimination Argument
Gender discrimination is a relatively new argument avenue in the larger equal work, equal pay debate, said Joanne Spetz, PhD, director of the Institute for Health Policy Studies at the University of California, San Francisco.
“This is the first time I’ve heard of [such] a case being really gender discrimination focused,” she said in an interview. “On one level, I think it’s groundbreaking as a legal approach, but it’s also limited because it’s focused on public, state employees.”
Spetz noted that New York has significantly expanded NPs’ scope of practice, enacting in 2022 legislation that granted NPs full practice authority. The law means NPs can evaluate, order, diagnose, manage treatments, and prescribe medications for patients without physician supervision.
“They are in a role where they are stepping back and saying, ‘Wait, why are [we] not receiving equal pay for equal work?’ ” Spetz said. “It’s a totally fair area for debate, especially because they are now authorized to do essentially equal work with a high degree of autonomy.”
Debate Over Pay Grade
The nurses’ complaint centers on the New York State Civil Service Commission’s classification for NPs, which hasn’t changed since 2006. NPs are classified at grade 24, and they have no possibility of internal advancement associated with their title, according to the legal complaint filed on September 17.
To comply with a state legislative directive, the commission in 2018 conducted a study of the NP classification but recommended against reclassification or implementing a career ladder. The study noted the subordinate role of NPs to physicians and the substantial difference between physician classification (entry at grade 34) and that of NPs, psychologists (grade 25), and pharmacists (grade 25).
The study concluded that higher classified positions have higher levels of educational attainment and licensure requirements and no supervision or collaboration requirements, according to the complaint.
At the time, groups such as the Nurse Practitioner Association and the Public Employees Federation (PEF) criticized the findings, but the commission stuck to its classification.
Following the NP Modernization Act that allowed NPs to practice independently, PEF sought an increase for NPs to grade 28 with a progression to grade 34 depending on experience.
“But to this date, despite altering the starting salaries of NPs, defendants have failed and refused to alter the compensation offered to the substantial majority of NPs, and each plaintiff remains cabined in a grade 24 with a discriminatorily low salary when compared with males in other job classifications doing highly similar functions,” the lawsuit contended.
Six plaintiffs are named in the lawsuit, all of whom are women and work for state agencies. Plaintiff Rachel Burns, for instance, works as a psychiatric mental health NP in West Seneca and is responsible for performing psychiatric evaluations for patients, diagnosis, prescribing medication, ordering labs, and determining risks. The evaluations are identical for a psychiatrist and require her to complete the same forms, according to the suit.
Another plaintiff, Amber Hawthorne Lashway, works at a correctional facility in Altona, where for many years she was the sole medical provider, according to the lawsuit. Lashway’s duties, which include diagnoses and treatment of inmates’ medical conditions, mirror those performed by clinical physicians, the suit stated.
The plaintiffs are requesting the court accept jurisdiction of the matter and certify the class they seek to represent. They are also demanding prospective pay equity and compensatory damages for the distress caused by “the long-standing discriminatory” treatment by the state.
The Civil Service Commission and state of New York have not yet responded to the complaint. Their responses are due on November 12.
Attorney: Case Impact Limited
Benjamin McMichael, PhD, JD, said the New York case is not surprising as more states across the country are granting nurses more practice autonomy. The current landscape tends to favor the nurses, he said, with about half of states now allowing NPs full practice authority.
“I think the [New York] NPs are correct that they are underpaid,” said McMichael, an associate professor of law and director of the Interdisciplinary Legal Studies Initiative at The University of Alabama in Tuscaloosa. “With that said, the nature of the case does not clearly lend itself to national change.”
The fact that the NP plaintiffs are employed by the state means they are using a specific set of laws to advance their cause, he said. Other NPs in other employment situations may not have access to the same laws.
A version of this article first appeared on Medscape.com.
A
The New York State Civil Service Commission understates the job function of NPs, overstates their dependence on physicians, and inadequately pays them for their work, according to the complaint filed in the US District Court for the Northern District of New York.
The nurses claim the mistreatment is a consequence of the fact that “at least 80% of the state’s employed NPs are women.”
Michael H. Sussman, a Goshen, New York–based attorney for the nurses, said in an interview that New York NPs are increasingly being used essentially as doctors at state-run facilities, including prisons, yet the state has failed to adequately pay them.
The lawsuit comes after a decade-long attempt by NPs to attain equitable pay and the ability to advance their civil service careers, he said.
“New York state has not addressed the heart of the issue, which is that the classification of this position is much lower than other positions in the state which are not so female-dominated and which engage in very similar activities,” Sussman said.
The lawsuit claims that “the work of NPs is complex, equaling that of a medical specialist, psychiatrist, or clinical physician.”
A spokesman for the New York State Civil Service Commission declined comment, saying the department does not comment on pending litigation.
Novel Gender Discrimination Argument
Gender discrimination is a relatively new argument avenue in the larger equal work, equal pay debate, said Joanne Spetz, PhD, director of the Institute for Health Policy Studies at the University of California, San Francisco.
“This is the first time I’ve heard of [such] a case being really gender discrimination focused,” she said in an interview. “On one level, I think it’s groundbreaking as a legal approach, but it’s also limited because it’s focused on public, state employees.”
Spetz noted that New York has significantly expanded NPs’ scope of practice, enacting in 2022 legislation that granted NPs full practice authority. The law means NPs can evaluate, order, diagnose, manage treatments, and prescribe medications for patients without physician supervision.
“They are in a role where they are stepping back and saying, ‘Wait, why are [we] not receiving equal pay for equal work?’ ” Spetz said. “It’s a totally fair area for debate, especially because they are now authorized to do essentially equal work with a high degree of autonomy.”
Debate Over Pay Grade
The nurses’ complaint centers on the New York State Civil Service Commission’s classification for NPs, which hasn’t changed since 2006. NPs are classified at grade 24, and they have no possibility of internal advancement associated with their title, according to the legal complaint filed on September 17.
To comply with a state legislative directive, the commission in 2018 conducted a study of the NP classification but recommended against reclassification or implementing a career ladder. The study noted the subordinate role of NPs to physicians and the substantial difference between physician classification (entry at grade 34) and that of NPs, psychologists (grade 25), and pharmacists (grade 25).
The study concluded that higher classified positions have higher levels of educational attainment and licensure requirements and no supervision or collaboration requirements, according to the complaint.
At the time, groups such as the Nurse Practitioner Association and the Public Employees Federation (PEF) criticized the findings, but the commission stuck to its classification.
Following the NP Modernization Act that allowed NPs to practice independently, PEF sought an increase for NPs to grade 28 with a progression to grade 34 depending on experience.
“But to this date, despite altering the starting salaries of NPs, defendants have failed and refused to alter the compensation offered to the substantial majority of NPs, and each plaintiff remains cabined in a grade 24 with a discriminatorily low salary when compared with males in other job classifications doing highly similar functions,” the lawsuit contended.
Six plaintiffs are named in the lawsuit, all of whom are women and work for state agencies. Plaintiff Rachel Burns, for instance, works as a psychiatric mental health NP in West Seneca and is responsible for performing psychiatric evaluations for patients, diagnosis, prescribing medication, ordering labs, and determining risks. The evaluations are identical for a psychiatrist and require her to complete the same forms, according to the suit.
Another plaintiff, Amber Hawthorne Lashway, works at a correctional facility in Altona, where for many years she was the sole medical provider, according to the lawsuit. Lashway’s duties, which include diagnoses and treatment of inmates’ medical conditions, mirror those performed by clinical physicians, the suit stated.
The plaintiffs are requesting the court accept jurisdiction of the matter and certify the class they seek to represent. They are also demanding prospective pay equity and compensatory damages for the distress caused by “the long-standing discriminatory” treatment by the state.
The Civil Service Commission and state of New York have not yet responded to the complaint. Their responses are due on November 12.
Attorney: Case Impact Limited
Benjamin McMichael, PhD, JD, said the New York case is not surprising as more states across the country are granting nurses more practice autonomy. The current landscape tends to favor the nurses, he said, with about half of states now allowing NPs full practice authority.
“I think the [New York] NPs are correct that they are underpaid,” said McMichael, an associate professor of law and director of the Interdisciplinary Legal Studies Initiative at The University of Alabama in Tuscaloosa. “With that said, the nature of the case does not clearly lend itself to national change.”
The fact that the NP plaintiffs are employed by the state means they are using a specific set of laws to advance their cause, he said. Other NPs in other employment situations may not have access to the same laws.
A version of this article first appeared on Medscape.com.
A
The New York State Civil Service Commission understates the job function of NPs, overstates their dependence on physicians, and inadequately pays them for their work, according to the complaint filed in the US District Court for the Northern District of New York.
The nurses claim the mistreatment is a consequence of the fact that “at least 80% of the state’s employed NPs are women.”
Michael H. Sussman, a Goshen, New York–based attorney for the nurses, said in an interview that New York NPs are increasingly being used essentially as doctors at state-run facilities, including prisons, yet the state has failed to adequately pay them.
The lawsuit comes after a decade-long attempt by NPs to attain equitable pay and the ability to advance their civil service careers, he said.
“New York state has not addressed the heart of the issue, which is that the classification of this position is much lower than other positions in the state which are not so female-dominated and which engage in very similar activities,” Sussman said.
The lawsuit claims that “the work of NPs is complex, equaling that of a medical specialist, psychiatrist, or clinical physician.”
A spokesman for the New York State Civil Service Commission declined comment, saying the department does not comment on pending litigation.
Novel Gender Discrimination Argument
Gender discrimination is a relatively new argument avenue in the larger equal work, equal pay debate, said Joanne Spetz, PhD, director of the Institute for Health Policy Studies at the University of California, San Francisco.
“This is the first time I’ve heard of [such] a case being really gender discrimination focused,” she said in an interview. “On one level, I think it’s groundbreaking as a legal approach, but it’s also limited because it’s focused on public, state employees.”
Spetz noted that New York has significantly expanded NPs’ scope of practice, enacting in 2022 legislation that granted NPs full practice authority. The law means NPs can evaluate, order, diagnose, manage treatments, and prescribe medications for patients without physician supervision.
“They are in a role where they are stepping back and saying, ‘Wait, why are [we] not receiving equal pay for equal work?’ ” Spetz said. “It’s a totally fair area for debate, especially because they are now authorized to do essentially equal work with a high degree of autonomy.”
Debate Over Pay Grade
The nurses’ complaint centers on the New York State Civil Service Commission’s classification for NPs, which hasn’t changed since 2006. NPs are classified at grade 24, and they have no possibility of internal advancement associated with their title, according to the legal complaint filed on September 17.
To comply with a state legislative directive, the commission in 2018 conducted a study of the NP classification but recommended against reclassification or implementing a career ladder. The study noted the subordinate role of NPs to physicians and the substantial difference between physician classification (entry at grade 34) and that of NPs, psychologists (grade 25), and pharmacists (grade 25).
The study concluded that higher classified positions have higher levels of educational attainment and licensure requirements and no supervision or collaboration requirements, according to the complaint.
At the time, groups such as the Nurse Practitioner Association and the Public Employees Federation (PEF) criticized the findings, but the commission stuck to its classification.
Following the NP Modernization Act that allowed NPs to practice independently, PEF sought an increase for NPs to grade 28 with a progression to grade 34 depending on experience.
“But to this date, despite altering the starting salaries of NPs, defendants have failed and refused to alter the compensation offered to the substantial majority of NPs, and each plaintiff remains cabined in a grade 24 with a discriminatorily low salary when compared with males in other job classifications doing highly similar functions,” the lawsuit contended.
Six plaintiffs are named in the lawsuit, all of whom are women and work for state agencies. Plaintiff Rachel Burns, for instance, works as a psychiatric mental health NP in West Seneca and is responsible for performing psychiatric evaluations for patients, diagnosis, prescribing medication, ordering labs, and determining risks. The evaluations are identical for a psychiatrist and require her to complete the same forms, according to the suit.
Another plaintiff, Amber Hawthorne Lashway, works at a correctional facility in Altona, where for many years she was the sole medical provider, according to the lawsuit. Lashway’s duties, which include diagnoses and treatment of inmates’ medical conditions, mirror those performed by clinical physicians, the suit stated.
The plaintiffs are requesting the court accept jurisdiction of the matter and certify the class they seek to represent. They are also demanding prospective pay equity and compensatory damages for the distress caused by “the long-standing discriminatory” treatment by the state.
The Civil Service Commission and state of New York have not yet responded to the complaint. Their responses are due on November 12.
Attorney: Case Impact Limited
Benjamin McMichael, PhD, JD, said the New York case is not surprising as more states across the country are granting nurses more practice autonomy. The current landscape tends to favor the nurses, he said, with about half of states now allowing NPs full practice authority.
“I think the [New York] NPs are correct that they are underpaid,” said McMichael, an associate professor of law and director of the Interdisciplinary Legal Studies Initiative at The University of Alabama in Tuscaloosa. “With that said, the nature of the case does not clearly lend itself to national change.”
The fact that the NP plaintiffs are employed by the state means they are using a specific set of laws to advance their cause, he said. Other NPs in other employment situations may not have access to the same laws.
A version of this article first appeared on Medscape.com.
Beyond Scope Creep: Why Physicians and PAs Should Come Together for Patients
Over the past few years, many states have attempted to address the ongoing shortage of healthcare workers by introducing new bills to increase the scope of practice for nurse practitioners (NPs) and physician assistants (PAs). The goal of each bill was to improve access to care, particularly for patients who may live in areas where it’s difficult to find a doctor.
In response, the American Medical Association (AMA) launched a targeted campaign to fight “scope creep.” Their goal was to gain the momentum necessary to block proposed legislation to modify or expand the practice authority of nonphysicians, including PAs. A spokesperson for the organization told this news organization that the AMA “greatly values and respects the contributions of PAs as important members of the healthcare team” but emphasized that they do not have the same “skill set or breadth of experience of physicians.”
As such, the AMA argued that expanded practice authority would not only dismantle physician-led care teams but also ultimately lead to higher costs and lower-quality patient care.
The AMA has since launched a large-scale advocacy effort to fight practice expansion legislation — and has a specific page on its website to highlight those efforts. In addition, they have authored model legislation, talking points for AMA members, and a widely read article in AMA News to help them in what they call a “fight for physicians.”
These resources have also been disseminated to the greater healthcare stakeholder community.
Marilyn Suri, PA-C, chief operating officer and senior executive for Advanced Practice Professional Affairs at Vincenzo Novara MDPA and Associates, a critical care pulmonary medicine practice in Miami, Florida, said she found the AMA’s campaign to be “very misleading.”
“PAs are created in the image of physicians to help manage the physician shortage. We are trained very rigorously — to diagnose illness, develop treatment plans, and prescribe medications,” she said. “We’re not trying to expand our scope. We are trying to eliminate or lessen barriers that prevent patients from getting access to care.”
Suri is not alone. Last summer, the American Academy of Physician Associates (AAPA) requested a meeting with the AMA to find ways for the two organizations to collaborate to improve care delivery — as well as find common ground to address issues regarding patient access to care. When the AMA did not respond, the AAPA sent a second letter in September 2024, reiterating their request for a meeting.
That correspondence also included a letter, signed by more than 8000 PAs from across the country, calling for an end to what the AAPA refers to as “damaging rhetoric,” as well as data from a recent survey of PAs regarding the fallout of AMA’s scope creep messaging.
Those survey results highlighted that the vast majority of PAs surveyed feel that the AMA is doing more than just attacking proposed legislation: They believe the association is negatively influencing patients’ understanding of PA qualifications, ultimately affecting their ability to provide care.
“The campaign is unintentionally harming patients by suggesting we are doing more than what we are trained to do,” said Elisa Hock, PA-C, a behavioral health PA in Texas. “And when you work in a place with limited resources, medically speaking — including limited access to providers — this kind of campaign is really detrimental to helping patients.”
Lisa M. Gables, CEO of the AAPA, said the organization is “deeply disappointed” in the AMA’s lack of response to their letters thus far — but remains committed to working with the organization to bring forward new solutions to address healthcare’s most pressing challenges.
“AAPA remains committed to pushing for modernization of practice laws to ensure all providers can practice medicine to the fullest extent of their training, education, and experience,” she said. “That is what patients deserve and want.”
Hock agreed. She told this news organization that the public is not always aware of what PAs can offer in terms of patient care. That said, she believes newer generations of physicians understand the value of PAs and the many skills they bring to the table.
“I’ve been doing this for 17 years, and it’s been an uphill battle, at times, to educate the public about what PAs can and can’t do,” she explained. “To throw more mud in the mix that will confuse patients more about what we do doesn’t help. Healthcare works best with a team-based approach. And that team has been and always will be led by the physician. We are aware of our role and our limitations. But we also know what we can offer patients, especially in areas like El Paso, where there is a real shortage of providers.”
With a growing aging population — and the physician shortage expected to increase in the coming decade — Suri hopes that the AMA will accept AAPA’s invitation to meet — because no one wins with this kind of healthcare infighting. In fact, she said patients will suffer because of it. She hopes that future discussions and collaborations can show providers and patients what team-based healthcare can offer.
“I think it’s important for those in healthcare to be aware that none of us work alone. Even physicians collaborate with other subspecialties, as well as nurses and other healthcare professionals,” said Suri.
A version of this article appeared on Medscape.com.
Over the past few years, many states have attempted to address the ongoing shortage of healthcare workers by introducing new bills to increase the scope of practice for nurse practitioners (NPs) and physician assistants (PAs). The goal of each bill was to improve access to care, particularly for patients who may live in areas where it’s difficult to find a doctor.
In response, the American Medical Association (AMA) launched a targeted campaign to fight “scope creep.” Their goal was to gain the momentum necessary to block proposed legislation to modify or expand the practice authority of nonphysicians, including PAs. A spokesperson for the organization told this news organization that the AMA “greatly values and respects the contributions of PAs as important members of the healthcare team” but emphasized that they do not have the same “skill set or breadth of experience of physicians.”
As such, the AMA argued that expanded practice authority would not only dismantle physician-led care teams but also ultimately lead to higher costs and lower-quality patient care.
The AMA has since launched a large-scale advocacy effort to fight practice expansion legislation — and has a specific page on its website to highlight those efforts. In addition, they have authored model legislation, talking points for AMA members, and a widely read article in AMA News to help them in what they call a “fight for physicians.”
These resources have also been disseminated to the greater healthcare stakeholder community.
Marilyn Suri, PA-C, chief operating officer and senior executive for Advanced Practice Professional Affairs at Vincenzo Novara MDPA and Associates, a critical care pulmonary medicine practice in Miami, Florida, said she found the AMA’s campaign to be “very misleading.”
“PAs are created in the image of physicians to help manage the physician shortage. We are trained very rigorously — to diagnose illness, develop treatment plans, and prescribe medications,” she said. “We’re not trying to expand our scope. We are trying to eliminate or lessen barriers that prevent patients from getting access to care.”
Suri is not alone. Last summer, the American Academy of Physician Associates (AAPA) requested a meeting with the AMA to find ways for the two organizations to collaborate to improve care delivery — as well as find common ground to address issues regarding patient access to care. When the AMA did not respond, the AAPA sent a second letter in September 2024, reiterating their request for a meeting.
That correspondence also included a letter, signed by more than 8000 PAs from across the country, calling for an end to what the AAPA refers to as “damaging rhetoric,” as well as data from a recent survey of PAs regarding the fallout of AMA’s scope creep messaging.
Those survey results highlighted that the vast majority of PAs surveyed feel that the AMA is doing more than just attacking proposed legislation: They believe the association is negatively influencing patients’ understanding of PA qualifications, ultimately affecting their ability to provide care.
“The campaign is unintentionally harming patients by suggesting we are doing more than what we are trained to do,” said Elisa Hock, PA-C, a behavioral health PA in Texas. “And when you work in a place with limited resources, medically speaking — including limited access to providers — this kind of campaign is really detrimental to helping patients.”
Lisa M. Gables, CEO of the AAPA, said the organization is “deeply disappointed” in the AMA’s lack of response to their letters thus far — but remains committed to working with the organization to bring forward new solutions to address healthcare’s most pressing challenges.
“AAPA remains committed to pushing for modernization of practice laws to ensure all providers can practice medicine to the fullest extent of their training, education, and experience,” she said. “That is what patients deserve and want.”
Hock agreed. She told this news organization that the public is not always aware of what PAs can offer in terms of patient care. That said, she believes newer generations of physicians understand the value of PAs and the many skills they bring to the table.
“I’ve been doing this for 17 years, and it’s been an uphill battle, at times, to educate the public about what PAs can and can’t do,” she explained. “To throw more mud in the mix that will confuse patients more about what we do doesn’t help. Healthcare works best with a team-based approach. And that team has been and always will be led by the physician. We are aware of our role and our limitations. But we also know what we can offer patients, especially in areas like El Paso, where there is a real shortage of providers.”
With a growing aging population — and the physician shortage expected to increase in the coming decade — Suri hopes that the AMA will accept AAPA’s invitation to meet — because no one wins with this kind of healthcare infighting. In fact, she said patients will suffer because of it. She hopes that future discussions and collaborations can show providers and patients what team-based healthcare can offer.
“I think it’s important for those in healthcare to be aware that none of us work alone. Even physicians collaborate with other subspecialties, as well as nurses and other healthcare professionals,” said Suri.
A version of this article appeared on Medscape.com.
Over the past few years, many states have attempted to address the ongoing shortage of healthcare workers by introducing new bills to increase the scope of practice for nurse practitioners (NPs) and physician assistants (PAs). The goal of each bill was to improve access to care, particularly for patients who may live in areas where it’s difficult to find a doctor.
In response, the American Medical Association (AMA) launched a targeted campaign to fight “scope creep.” Their goal was to gain the momentum necessary to block proposed legislation to modify or expand the practice authority of nonphysicians, including PAs. A spokesperson for the organization told this news organization that the AMA “greatly values and respects the contributions of PAs as important members of the healthcare team” but emphasized that they do not have the same “skill set or breadth of experience of physicians.”
As such, the AMA argued that expanded practice authority would not only dismantle physician-led care teams but also ultimately lead to higher costs and lower-quality patient care.
The AMA has since launched a large-scale advocacy effort to fight practice expansion legislation — and has a specific page on its website to highlight those efforts. In addition, they have authored model legislation, talking points for AMA members, and a widely read article in AMA News to help them in what they call a “fight for physicians.”
These resources have also been disseminated to the greater healthcare stakeholder community.
Marilyn Suri, PA-C, chief operating officer and senior executive for Advanced Practice Professional Affairs at Vincenzo Novara MDPA and Associates, a critical care pulmonary medicine practice in Miami, Florida, said she found the AMA’s campaign to be “very misleading.”
“PAs are created in the image of physicians to help manage the physician shortage. We are trained very rigorously — to diagnose illness, develop treatment plans, and prescribe medications,” she said. “We’re not trying to expand our scope. We are trying to eliminate or lessen barriers that prevent patients from getting access to care.”
Suri is not alone. Last summer, the American Academy of Physician Associates (AAPA) requested a meeting with the AMA to find ways for the two organizations to collaborate to improve care delivery — as well as find common ground to address issues regarding patient access to care. When the AMA did not respond, the AAPA sent a second letter in September 2024, reiterating their request for a meeting.
That correspondence also included a letter, signed by more than 8000 PAs from across the country, calling for an end to what the AAPA refers to as “damaging rhetoric,” as well as data from a recent survey of PAs regarding the fallout of AMA’s scope creep messaging.
Those survey results highlighted that the vast majority of PAs surveyed feel that the AMA is doing more than just attacking proposed legislation: They believe the association is negatively influencing patients’ understanding of PA qualifications, ultimately affecting their ability to provide care.
“The campaign is unintentionally harming patients by suggesting we are doing more than what we are trained to do,” said Elisa Hock, PA-C, a behavioral health PA in Texas. “And when you work in a place with limited resources, medically speaking — including limited access to providers — this kind of campaign is really detrimental to helping patients.”
Lisa M. Gables, CEO of the AAPA, said the organization is “deeply disappointed” in the AMA’s lack of response to their letters thus far — but remains committed to working with the organization to bring forward new solutions to address healthcare’s most pressing challenges.
“AAPA remains committed to pushing for modernization of practice laws to ensure all providers can practice medicine to the fullest extent of their training, education, and experience,” she said. “That is what patients deserve and want.”
Hock agreed. She told this news organization that the public is not always aware of what PAs can offer in terms of patient care. That said, she believes newer generations of physicians understand the value of PAs and the many skills they bring to the table.
“I’ve been doing this for 17 years, and it’s been an uphill battle, at times, to educate the public about what PAs can and can’t do,” she explained. “To throw more mud in the mix that will confuse patients more about what we do doesn’t help. Healthcare works best with a team-based approach. And that team has been and always will be led by the physician. We are aware of our role and our limitations. But we also know what we can offer patients, especially in areas like El Paso, where there is a real shortage of providers.”
With a growing aging population — and the physician shortage expected to increase in the coming decade — Suri hopes that the AMA will accept AAPA’s invitation to meet — because no one wins with this kind of healthcare infighting. In fact, she said patients will suffer because of it. She hopes that future discussions and collaborations can show providers and patients what team-based healthcare can offer.
“I think it’s important for those in healthcare to be aware that none of us work alone. Even physicians collaborate with other subspecialties, as well as nurses and other healthcare professionals,” said Suri.
A version of this article appeared on Medscape.com.
Maternal Immunization to Prevent Serious Respiratory Illness
Editor’s Note: Sadly, this is the last column in the Master Class Obstetrics series. This award-winning column has been part of Ob.Gyn. News for 20 years. The deep discussion of cutting-edge topics in obstetrics by specialists and researchers will be missed as will the leadership and curation of topics by Dr. E. Albert Reece.
Introduction: The Need for Increased Vigilance About Maternal Immunization
Viruses are becoming increasingly prevalent in our world and the consequences of viral infections are implicated in a growing number of disease states. It is well established that certain cancers are caused by viruses and it is increasingly evident that viral infections can trigger the development of chronic illness. In pregnant women, viruses such as cytomegalovirus can cause infection in utero and lead to long-term impairments for the baby.
Likewise, it appears that the virulence of viruses is increasing, whether it be the respiratory syncytial virus (RSV) in children or the severe acute respiratory syndrome (SARS) coronaviruses in adults. Clearly, our environment is changing, with increases in population growth and urbanization, for instance, and an intensification of climate change and its effects. Viruses are part of this changing background.
Vaccines are our most powerful tool to protect people of all ages against viral threats, and fortunately, we benefit from increasing expertise in vaccinology. Since 1974, the University of Maryland School of Medicine has a Center for Vaccine Development and Global Health that has conducted research on vaccines to defend against the Zika virus, H1N1, Ebola, and SARS-CoV-2.
We’re not alone. Other vaccinology centers across the country — as well as the National Institutes of Health at the national level, through its National Institute of Allergy and Infectious Diseases — are doing research and developing vaccines to combat viral diseases.
In this column, we are focused on viral diseases in pregnancy and the role that vaccines can play in preventing serious respiratory illness in mothers and their newborns. I have invited Laura E. Riley, MD, the Given Foundation Professor and Chair of Obstetrics and Gynecology at Weill Cornell Medicine, to address the importance of maternal immunization and how we can best counsel our patients and improve immunization rates.
As Dr. Riley explains, we are in a new era, and it behooves us all to be more vigilant about recommending vaccines, combating misperceptions, addressing patients’ knowledge gaps, and administering vaccines whenever possible.
Dr. Reece is the former Dean of Medicine & University Executive VP, and The Distinguished University and Endowed Professor & Director of the Center for Advanced Research Training and Innovation (CARTI) at the University of Maryland School of Medicine, as well as senior scientist at the Center for Birth Defects Research.
The alarming decline in maternal immunization rates that occurred in the wake of the COVID-19 pandemic means that, now more than ever, we must fully embrace our responsibility to recommend immunizations in pregnancy and to communicate what is known about their efficacy and safety. Data show that vaccination rates drop when we do not offer vaccines in our offices, so whenever possible, we should administer them as well.
The ob.gyn. is the patient’s most trusted person in pregnancy. When patients decline or express hesitancy about vaccines, it is incumbent upon us to ask why. Oftentimes, we can identify areas in which patients lack knowledge or have misperceptions and we can successfully educate the patient or change their perspective or misunderstanding concerning the importance of vaccination for themselves and their babies. (See Table 1.) We can also successfully address concerns about safety.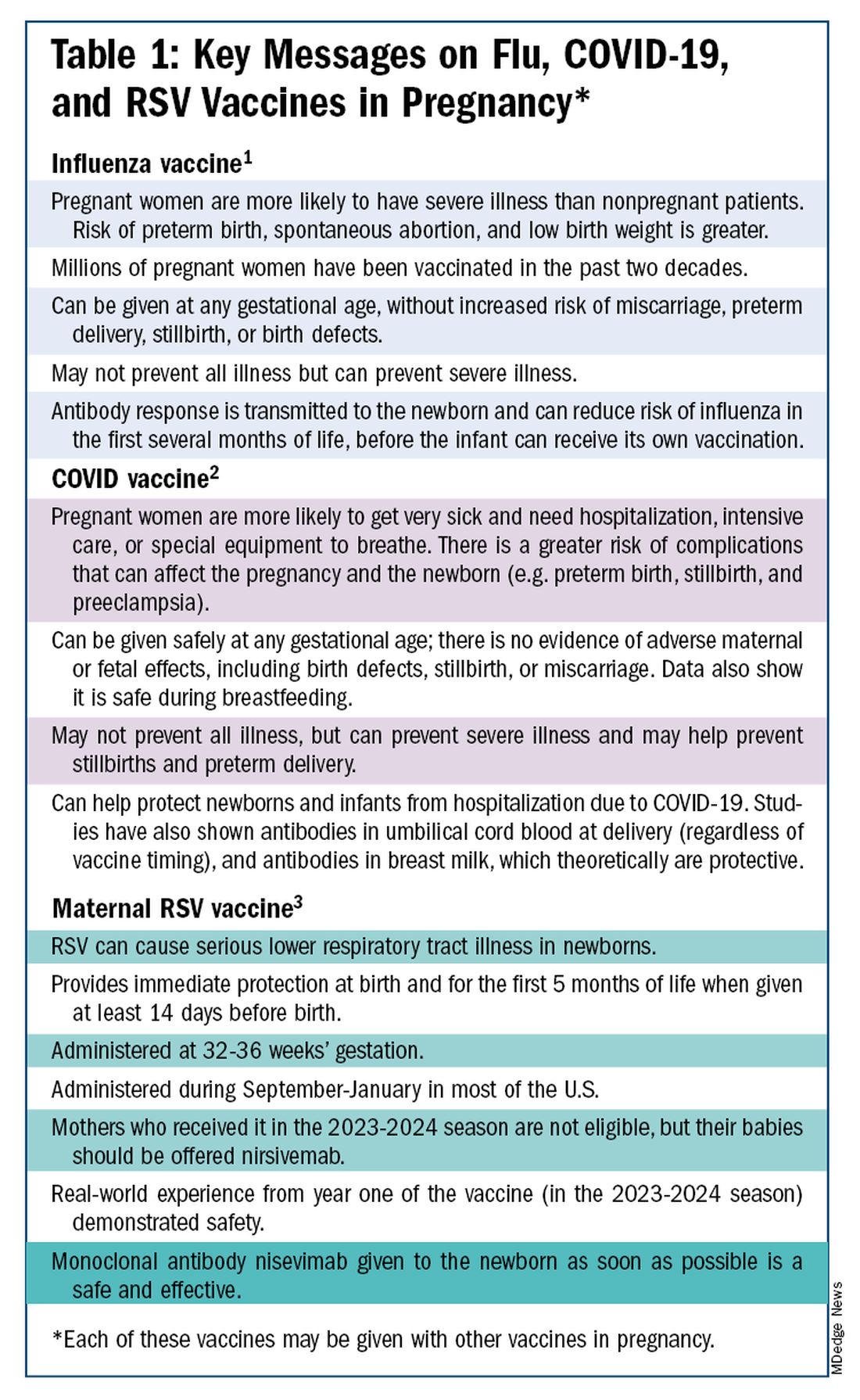
The safety of COVID-19 vaccinations in pregnancy is now backed by several years of data from multiple studies showing no increase in birth defects, preterm delivery, miscarriage, or stillbirth.
Data also show that pregnant patients are more likely than patients who are not pregnant to need hospitalization and intensive care when infected with SARS-CoV-2 and are at risk of having complications that can affect pregnancy and the newborn, including preterm birth and stillbirth. Vaccination has been shown to reduce the risk of severe illness and the risk of such adverse obstetrical outcomes, in addition to providing protection for the infant early on.
Similarly, influenza has long been more likely to be severe in pregnant patients, with an increased risk of poor obstetrical outcomes. Vaccines similarly provide “two for one protection,” protecting both mother and baby, and are, of course, backed by many years of safety and efficacy data.
With the new maternal respiratory syncytial virus (RSV) vaccine, now in its second year of availability, the goal is to protect the baby from RSV-caused serious lower respiratory tract illness. The illness has contributed to tens of thousands of annual hospitalizations and up to several hundred deaths every year in children younger than 5 years — particularly in those under age 6 months.
The RSV monoclonal antibody nirsevimab is available for the newborn as an alternative to maternal immunization but the maternal vaccine is optimal in that it will provide immediate rather than delayed protection for the newborn. The maternal vaccine is recommended during weeks 32-36 of pregnancy in mothers who were not vaccinated during last year’s RSV season. With real-world experience from year one, the available safety data are reassuring.
Counseling About Influenza and COVID-19 Vaccination
The COVID-19 pandemic took a toll on vaccination interest/receptivity broadly in pregnant and nonpregnant people. Among pregnant individuals, influenza vaccination coverage declined from 71% in the 2019-2020 influenza season to 56% in the 2021-2022 season, according to data from the Centers for Disease Control and Prevention’s Vaccine Safety Datalink.4 Coverage for the 2022-2023 and 2023-2024 influenza seasons was even worse: well under 50%.5
Fewer pregnant women have received updated COVID-19 vaccines. Only 13% of pregnant persons overall received the updated 2023-2024 COVID-19 booster vaccine (through March 30, 2024), according to the CDC.6
Maternal immunization for influenza has been recommended in the United States since 2004 (part of the recommendation that everyone over the age of 6 months receive an annual flu vaccine), and flu vaccines have been given to millions of pregnant women, but the H1N1 pandemic of 2009 reinforced its value as a priority for prenatal care. Most of the women who became severely ill from the H1N1 virus were young and healthy, without co-existing conditions known to increase risk.7
It became clearer during the H1N1 pandemic that pregnancy itself — which is associated with physiologic changes such as decreased lung capacity, increased nasal congestion and changes in the immune system – is its own significant risk factor for severe illness from the influenza virus. This increased risk applies to COVID-19 as well.
As COVID-19 has become endemic, with hospitalizations and deaths not reaching the levels of previous surges — and with mask-wearing and other preventive measures having declined — patients understandably have become more complacent. Some patients are vaccine deniers, but in my practice, these patients are a much smaller group than those who believe COVID-19 “is no big deal,” especially if they have had infections recently.
This is why it’s important to actively listen to concerns and to ask patients who decline a vaccination why they are hesitant. Blanket messages about vaccine efficacy and safety are the first step, but individualized, more pointed conversations based on the patient’s personal experiences and beliefs have become increasingly important.
I routinely tell pregnant patients about the risks of COVID-19 and I explain that it has been difficult to predict who will develop severe illness. Sometimes more conversation is needed. For those who are still hesitant or who tell me they feel protected by a recent infection, for instance, I provide more detail on the unique risks of pregnancy — the fact that “pregnancy is different” — and that natural immunity wanes while the protection afforded by immunization is believed to last longer. Many women are also concerned about the safety of the COVID-19 vaccine, so having safety data at your fingertips is helpful. (See Table 2.)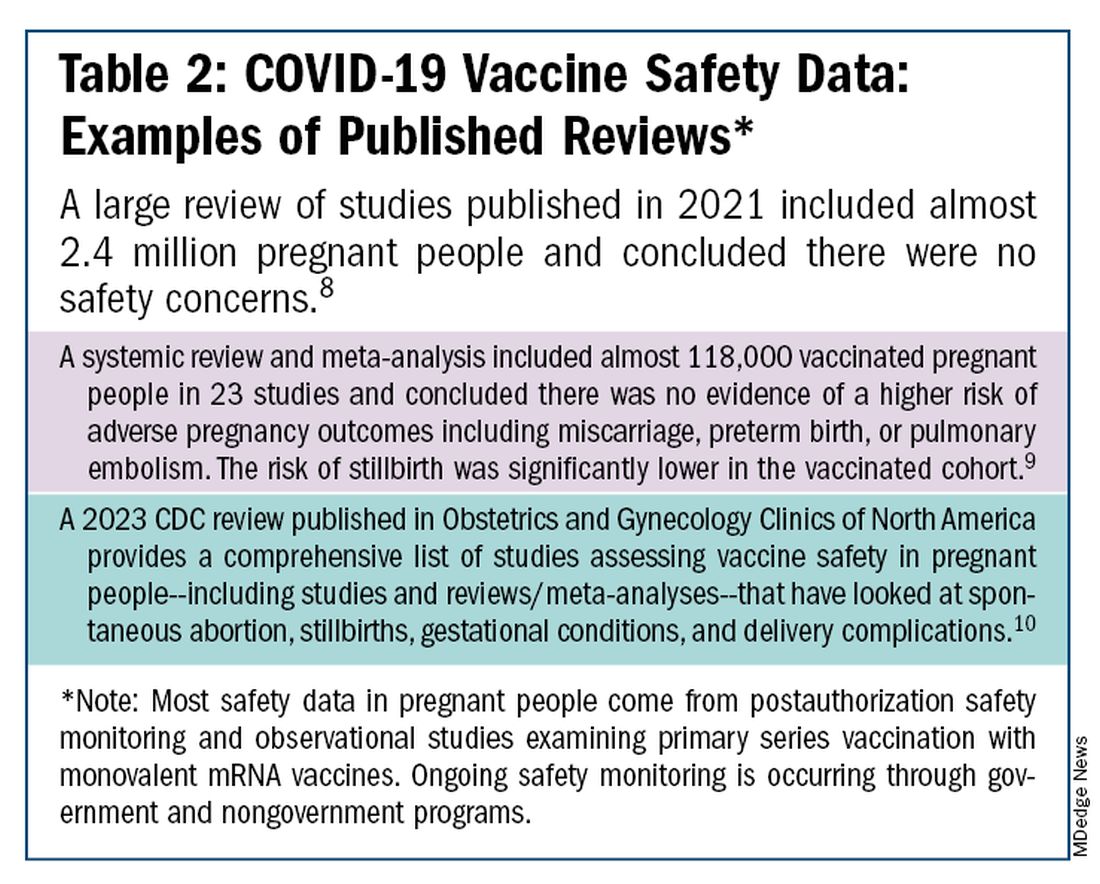
The fact that influenza and COVID-19 vaccination protect the newborn as well as the mother is something that I find is underappreciated by many patients. Explaining that infants likely benefit from the passage of antibodies across the placenta should be part of patient counseling.
Counseling About RSV Vaccination
Importantly, for the 2024-2025 RSV season, the maternal RSV vaccine (Abrysvo, Pfizer) is recommended only for pregnant women who did not receive the vaccine during the 2023-2024 season. When more research is done and more data are obtained showing how long the immune response persists post vaccination, it may be that the US Food and Drug Administration (FDA) will approve the maternal RSV vaccine for use in every pregnancy.
The later timing of the vaccination recommendation — 32-36 weeks’ gestation — reflects a conservative approach taken by the FDA in response to data from one of the pivotal trials showing a numerical trend toward more preterm deliveries among vaccinated compared with unvaccinated patients. This imbalance in the original trial, which administered the vaccine during 24-36 weeks of gestation, was seen only in low-income countries with no temporal association, however.
In our experience at two Weill Cornell Medical College–associated hospitals we did not see this trend. Our cohort study of almost 3000 pregnant patients who delivered at 32 weeks’ gestation or later found no increased risk of preterm birth among the 35% of patients who received the RSV vaccine during the 2023-2024 RSV season. We also did not see any difference in preeclampsia, in contrast with original trial data that showed a signal for increased risk.11
When fewer than 2 weeks have elapsed between maternal vaccination and delivery, the monoclonal antibody nirsevimab is recommended for the newborn — ideally before the newborn leaves the hospital. Nirsevimab is also recommended for newborns of mothers who decline vaccination or were not candidates (e.g. vaccinated in a previous pregnancy), or when there is concern about the adequacy of the maternal immune response to the vaccine (e.g. in cases of immunosuppression).
While there was a limited supply of the monoclonal antibody last year, limitations are not expected this year, especially after October.
The ultimate goal is that patients choose the vaccine or the immunoglobulin, given the severity of RSV disease. Patient preferences should be considered. However, given that it takes 2 weeks after vaccination for protection to build up, I stress to patients that if they’ve vaccinated themselves, their newborn will leave the hospital with protection. If nirsevimab is relied upon, I explain, their newborn may not be protected for some period of time.
Take-home Messages
- When patients decline or are hesitant about vaccines, ask why. Listen actively, and work to correct misperceptions and knowledge gaps.
- Whenever possible, offer vaccines in your practice. Vaccination rates drop when this does not occur.
- COVID-vaccine safety is backed by many studies showing no increase in birth defects, preterm delivery, miscarriage, or stillbirth.
- Pregnant women are more likely to have severe illness from the influenza and SARS-CoV-2 viruses. Vaccines can prevent severe illness and can protect the newborn as well as the mother.
- Recommend/administer the maternal RSV vaccine at 32-36 weeks’ gestation in women who did not receive the vaccine in the 2023-2024 season. If mothers aren’t eligible their babies should be offered nirsevimab.
Dr. Riley is the Given Foundation Professor and Chair of Obstetrics and Gynecology at Weill Cornell Medicine and the obstetrician and gynecologist-in-chief at New York Presbyterian Hospital. She disclosed that she has provided one-time consultations to Pfizer (Abrysvo RSV vaccine) and GSK (cytomegalovirus vaccine), and is providing consultant education on CMV for Moderna. She is chair of ACOG’s task force on immunization and emerging infectious diseases, serves on the medical advisory board for MAVEN, and serves as an editor or editorial board member for several medical publications.
References
1. ACOG Committee Opinion No. 741: Maternal Immunization. Obstet Gynecol. 2018;131(6):e214-e217.
2. Centers for Disease Control and Prevention. COVID-19 Vaccination for People Who are Pregnant or Breastfeeding. https://www.cdc.gov/covid/vaccines/pregnant-or-breastfeeding.html.
3. ACOG Practice Advisory on Maternal Respiratory Syncytial Virus Vaccination, September 2023. (Updated August 2024).4. Irving S et al. Open Forum Infect Dis. 2023;10(Suppl 2):ofad500.1002.
5. Flu Vaccination Dashboard, CDC, National Center for Immunization and Respiratory Diseases.
6. Weekly COVID-19 Vaccination Dashboard, CDC. https://www.cdc.gov/covidvaxview/weekly-dashboard/index.html
7. Louie JK et al. N Engl J Med. 2010;362:27-35. 8. Ciapponi A et al. Vaccine. 2021;39(40):5891-908.
9. Prasad S et al. Nature Communications. 2022;13:2414. 10. Fleming-Dutra KE et al. Obstet Gynecol Clin North Am 2023;50(2):279-97. 11. Mouen S et al. JAMA Network Open 2024;7(7):e2419268.
Editor’s Note: Sadly, this is the last column in the Master Class Obstetrics series. This award-winning column has been part of Ob.Gyn. News for 20 years. The deep discussion of cutting-edge topics in obstetrics by specialists and researchers will be missed as will the leadership and curation of topics by Dr. E. Albert Reece.
Introduction: The Need for Increased Vigilance About Maternal Immunization
Viruses are becoming increasingly prevalent in our world and the consequences of viral infections are implicated in a growing number of disease states. It is well established that certain cancers are caused by viruses and it is increasingly evident that viral infections can trigger the development of chronic illness. In pregnant women, viruses such as cytomegalovirus can cause infection in utero and lead to long-term impairments for the baby.
Likewise, it appears that the virulence of viruses is increasing, whether it be the respiratory syncytial virus (RSV) in children or the severe acute respiratory syndrome (SARS) coronaviruses in adults. Clearly, our environment is changing, with increases in population growth and urbanization, for instance, and an intensification of climate change and its effects. Viruses are part of this changing background.
Vaccines are our most powerful tool to protect people of all ages against viral threats, and fortunately, we benefit from increasing expertise in vaccinology. Since 1974, the University of Maryland School of Medicine has a Center for Vaccine Development and Global Health that has conducted research on vaccines to defend against the Zika virus, H1N1, Ebola, and SARS-CoV-2.
We’re not alone. Other vaccinology centers across the country — as well as the National Institutes of Health at the national level, through its National Institute of Allergy and Infectious Diseases — are doing research and developing vaccines to combat viral diseases.
In this column, we are focused on viral diseases in pregnancy and the role that vaccines can play in preventing serious respiratory illness in mothers and their newborns. I have invited Laura E. Riley, MD, the Given Foundation Professor and Chair of Obstetrics and Gynecology at Weill Cornell Medicine, to address the importance of maternal immunization and how we can best counsel our patients and improve immunization rates.
As Dr. Riley explains, we are in a new era, and it behooves us all to be more vigilant about recommending vaccines, combating misperceptions, addressing patients’ knowledge gaps, and administering vaccines whenever possible.
Dr. Reece is the former Dean of Medicine & University Executive VP, and The Distinguished University and Endowed Professor & Director of the Center for Advanced Research Training and Innovation (CARTI) at the University of Maryland School of Medicine, as well as senior scientist at the Center for Birth Defects Research.
The alarming decline in maternal immunization rates that occurred in the wake of the COVID-19 pandemic means that, now more than ever, we must fully embrace our responsibility to recommend immunizations in pregnancy and to communicate what is known about their efficacy and safety. Data show that vaccination rates drop when we do not offer vaccines in our offices, so whenever possible, we should administer them as well.
The ob.gyn. is the patient’s most trusted person in pregnancy. When patients decline or express hesitancy about vaccines, it is incumbent upon us to ask why. Oftentimes, we can identify areas in which patients lack knowledge or have misperceptions and we can successfully educate the patient or change their perspective or misunderstanding concerning the importance of vaccination for themselves and their babies. (See Table 1.) We can also successfully address concerns about safety.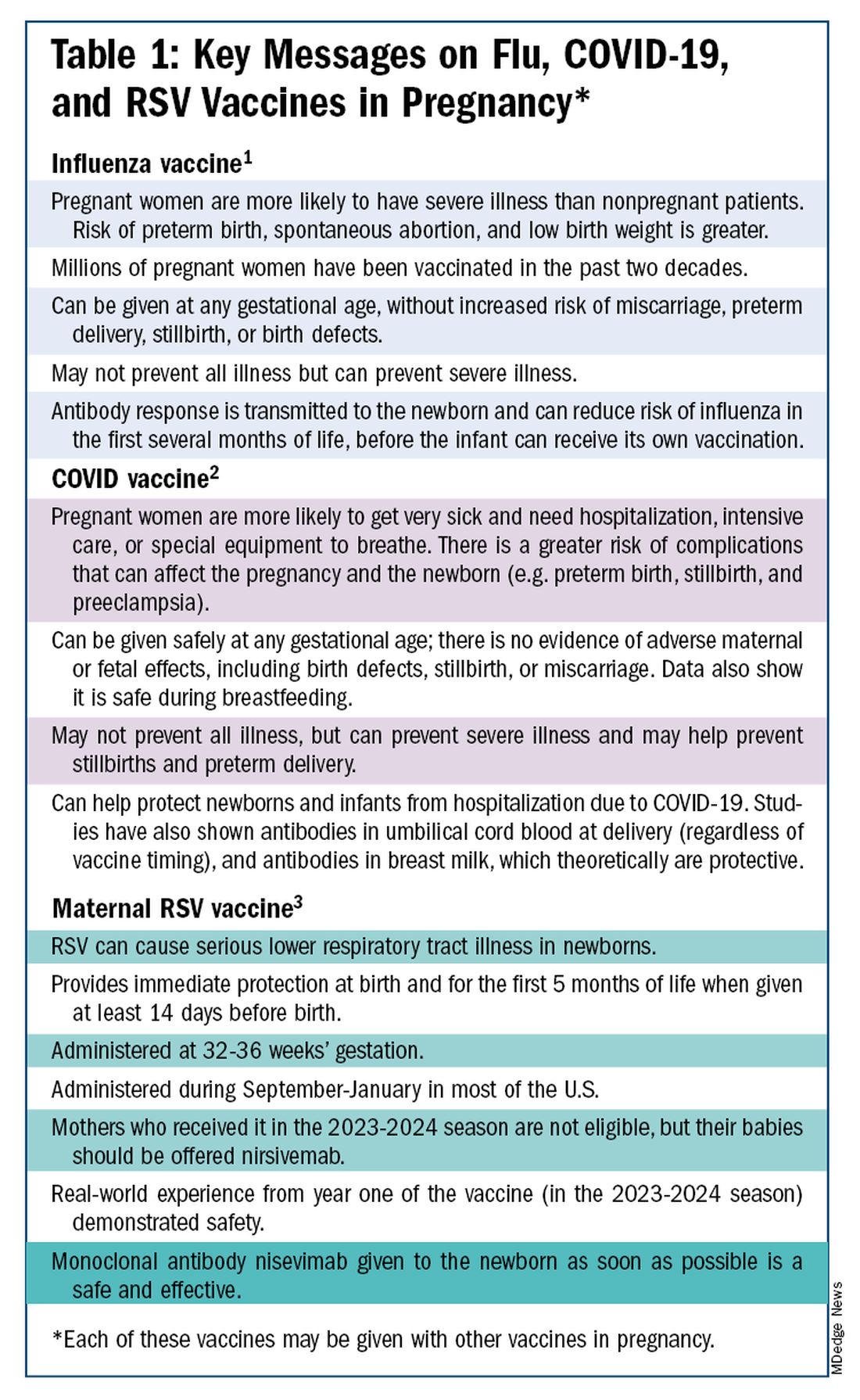
The safety of COVID-19 vaccinations in pregnancy is now backed by several years of data from multiple studies showing no increase in birth defects, preterm delivery, miscarriage, or stillbirth.
Data also show that pregnant patients are more likely than patients who are not pregnant to need hospitalization and intensive care when infected with SARS-CoV-2 and are at risk of having complications that can affect pregnancy and the newborn, including preterm birth and stillbirth. Vaccination has been shown to reduce the risk of severe illness and the risk of such adverse obstetrical outcomes, in addition to providing protection for the infant early on.
Similarly, influenza has long been more likely to be severe in pregnant patients, with an increased risk of poor obstetrical outcomes. Vaccines similarly provide “two for one protection,” protecting both mother and baby, and are, of course, backed by many years of safety and efficacy data.
With the new maternal respiratory syncytial virus (RSV) vaccine, now in its second year of availability, the goal is to protect the baby from RSV-caused serious lower respiratory tract illness. The illness has contributed to tens of thousands of annual hospitalizations and up to several hundred deaths every year in children younger than 5 years — particularly in those under age 6 months.
The RSV monoclonal antibody nirsevimab is available for the newborn as an alternative to maternal immunization but the maternal vaccine is optimal in that it will provide immediate rather than delayed protection for the newborn. The maternal vaccine is recommended during weeks 32-36 of pregnancy in mothers who were not vaccinated during last year’s RSV season. With real-world experience from year one, the available safety data are reassuring.
Counseling About Influenza and COVID-19 Vaccination
The COVID-19 pandemic took a toll on vaccination interest/receptivity broadly in pregnant and nonpregnant people. Among pregnant individuals, influenza vaccination coverage declined from 71% in the 2019-2020 influenza season to 56% in the 2021-2022 season, according to data from the Centers for Disease Control and Prevention’s Vaccine Safety Datalink.4 Coverage for the 2022-2023 and 2023-2024 influenza seasons was even worse: well under 50%.5
Fewer pregnant women have received updated COVID-19 vaccines. Only 13% of pregnant persons overall received the updated 2023-2024 COVID-19 booster vaccine (through March 30, 2024), according to the CDC.6
Maternal immunization for influenza has been recommended in the United States since 2004 (part of the recommendation that everyone over the age of 6 months receive an annual flu vaccine), and flu vaccines have been given to millions of pregnant women, but the H1N1 pandemic of 2009 reinforced its value as a priority for prenatal care. Most of the women who became severely ill from the H1N1 virus were young and healthy, without co-existing conditions known to increase risk.7
It became clearer during the H1N1 pandemic that pregnancy itself — which is associated with physiologic changes such as decreased lung capacity, increased nasal congestion and changes in the immune system – is its own significant risk factor for severe illness from the influenza virus. This increased risk applies to COVID-19 as well.
As COVID-19 has become endemic, with hospitalizations and deaths not reaching the levels of previous surges — and with mask-wearing and other preventive measures having declined — patients understandably have become more complacent. Some patients are vaccine deniers, but in my practice, these patients are a much smaller group than those who believe COVID-19 “is no big deal,” especially if they have had infections recently.
This is why it’s important to actively listen to concerns and to ask patients who decline a vaccination why they are hesitant. Blanket messages about vaccine efficacy and safety are the first step, but individualized, more pointed conversations based on the patient’s personal experiences and beliefs have become increasingly important.
I routinely tell pregnant patients about the risks of COVID-19 and I explain that it has been difficult to predict who will develop severe illness. Sometimes more conversation is needed. For those who are still hesitant or who tell me they feel protected by a recent infection, for instance, I provide more detail on the unique risks of pregnancy — the fact that “pregnancy is different” — and that natural immunity wanes while the protection afforded by immunization is believed to last longer. Many women are also concerned about the safety of the COVID-19 vaccine, so having safety data at your fingertips is helpful. (See Table 2.)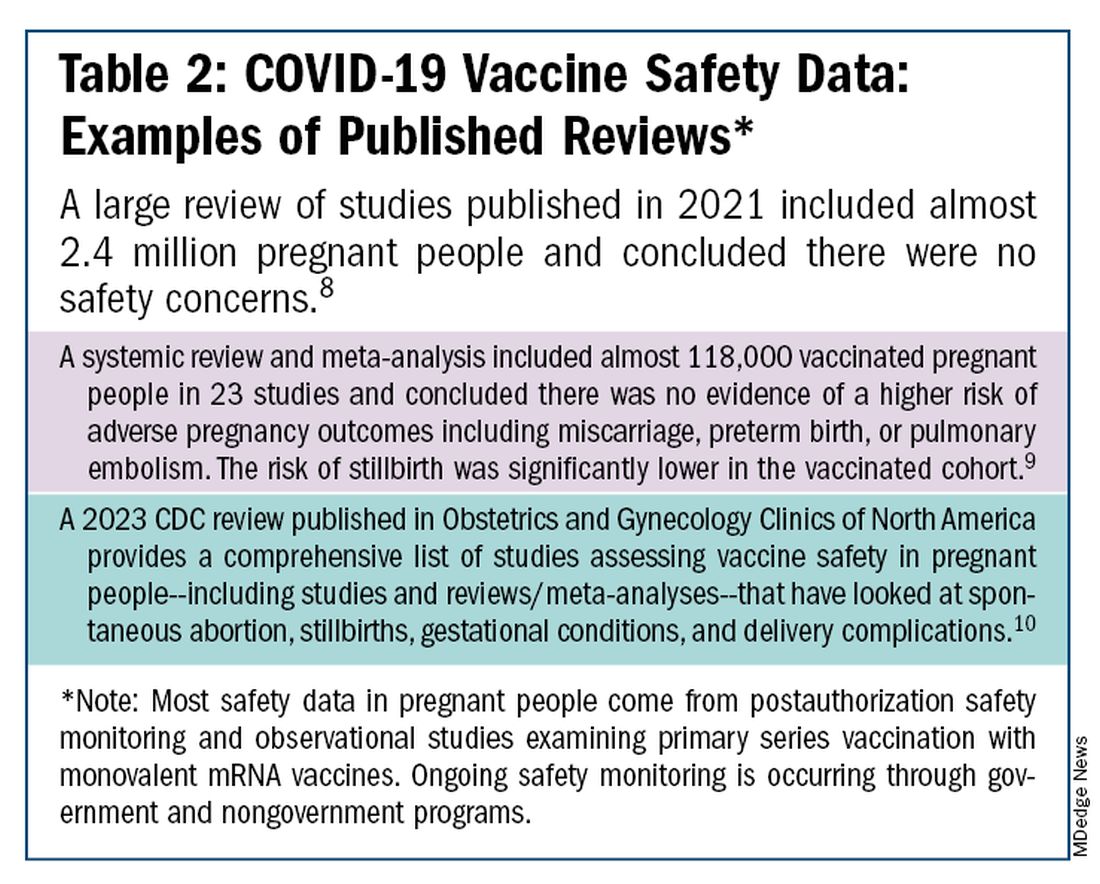
The fact that influenza and COVID-19 vaccination protect the newborn as well as the mother is something that I find is underappreciated by many patients. Explaining that infants likely benefit from the passage of antibodies across the placenta should be part of patient counseling.
Counseling About RSV Vaccination
Importantly, for the 2024-2025 RSV season, the maternal RSV vaccine (Abrysvo, Pfizer) is recommended only for pregnant women who did not receive the vaccine during the 2023-2024 season. When more research is done and more data are obtained showing how long the immune response persists post vaccination, it may be that the US Food and Drug Administration (FDA) will approve the maternal RSV vaccine for use in every pregnancy.
The later timing of the vaccination recommendation — 32-36 weeks’ gestation — reflects a conservative approach taken by the FDA in response to data from one of the pivotal trials showing a numerical trend toward more preterm deliveries among vaccinated compared with unvaccinated patients. This imbalance in the original trial, which administered the vaccine during 24-36 weeks of gestation, was seen only in low-income countries with no temporal association, however.
In our experience at two Weill Cornell Medical College–associated hospitals we did not see this trend. Our cohort study of almost 3000 pregnant patients who delivered at 32 weeks’ gestation or later found no increased risk of preterm birth among the 35% of patients who received the RSV vaccine during the 2023-2024 RSV season. We also did not see any difference in preeclampsia, in contrast with original trial data that showed a signal for increased risk.11
When fewer than 2 weeks have elapsed between maternal vaccination and delivery, the monoclonal antibody nirsevimab is recommended for the newborn — ideally before the newborn leaves the hospital. Nirsevimab is also recommended for newborns of mothers who decline vaccination or were not candidates (e.g. vaccinated in a previous pregnancy), or when there is concern about the adequacy of the maternal immune response to the vaccine (e.g. in cases of immunosuppression).
While there was a limited supply of the monoclonal antibody last year, limitations are not expected this year, especially after October.
The ultimate goal is that patients choose the vaccine or the immunoglobulin, given the severity of RSV disease. Patient preferences should be considered. However, given that it takes 2 weeks after vaccination for protection to build up, I stress to patients that if they’ve vaccinated themselves, their newborn will leave the hospital with protection. If nirsevimab is relied upon, I explain, their newborn may not be protected for some period of time.
Take-home Messages
- When patients decline or are hesitant about vaccines, ask why. Listen actively, and work to correct misperceptions and knowledge gaps.
- Whenever possible, offer vaccines in your practice. Vaccination rates drop when this does not occur.
- COVID-vaccine safety is backed by many studies showing no increase in birth defects, preterm delivery, miscarriage, or stillbirth.
- Pregnant women are more likely to have severe illness from the influenza and SARS-CoV-2 viruses. Vaccines can prevent severe illness and can protect the newborn as well as the mother.
- Recommend/administer the maternal RSV vaccine at 32-36 weeks’ gestation in women who did not receive the vaccine in the 2023-2024 season. If mothers aren’t eligible their babies should be offered nirsevimab.
Dr. Riley is the Given Foundation Professor and Chair of Obstetrics and Gynecology at Weill Cornell Medicine and the obstetrician and gynecologist-in-chief at New York Presbyterian Hospital. She disclosed that she has provided one-time consultations to Pfizer (Abrysvo RSV vaccine) and GSK (cytomegalovirus vaccine), and is providing consultant education on CMV for Moderna. She is chair of ACOG’s task force on immunization and emerging infectious diseases, serves on the medical advisory board for MAVEN, and serves as an editor or editorial board member for several medical publications.
References
1. ACOG Committee Opinion No. 741: Maternal Immunization. Obstet Gynecol. 2018;131(6):e214-e217.
2. Centers for Disease Control and Prevention. COVID-19 Vaccination for People Who are Pregnant or Breastfeeding. https://www.cdc.gov/covid/vaccines/pregnant-or-breastfeeding.html.
3. ACOG Practice Advisory on Maternal Respiratory Syncytial Virus Vaccination, September 2023. (Updated August 2024).4. Irving S et al. Open Forum Infect Dis. 2023;10(Suppl 2):ofad500.1002.
5. Flu Vaccination Dashboard, CDC, National Center for Immunization and Respiratory Diseases.
6. Weekly COVID-19 Vaccination Dashboard, CDC. https://www.cdc.gov/covidvaxview/weekly-dashboard/index.html
7. Louie JK et al. N Engl J Med. 2010;362:27-35. 8. Ciapponi A et al. Vaccine. 2021;39(40):5891-908.
9. Prasad S et al. Nature Communications. 2022;13:2414. 10. Fleming-Dutra KE et al. Obstet Gynecol Clin North Am 2023;50(2):279-97. 11. Mouen S et al. JAMA Network Open 2024;7(7):e2419268.
Editor’s Note: Sadly, this is the last column in the Master Class Obstetrics series. This award-winning column has been part of Ob.Gyn. News for 20 years. The deep discussion of cutting-edge topics in obstetrics by specialists and researchers will be missed as will the leadership and curation of topics by Dr. E. Albert Reece.
Introduction: The Need for Increased Vigilance About Maternal Immunization
Viruses are becoming increasingly prevalent in our world and the consequences of viral infections are implicated in a growing number of disease states. It is well established that certain cancers are caused by viruses and it is increasingly evident that viral infections can trigger the development of chronic illness. In pregnant women, viruses such as cytomegalovirus can cause infection in utero and lead to long-term impairments for the baby.
Likewise, it appears that the virulence of viruses is increasing, whether it be the respiratory syncytial virus (RSV) in children or the severe acute respiratory syndrome (SARS) coronaviruses in adults. Clearly, our environment is changing, with increases in population growth and urbanization, for instance, and an intensification of climate change and its effects. Viruses are part of this changing background.
Vaccines are our most powerful tool to protect people of all ages against viral threats, and fortunately, we benefit from increasing expertise in vaccinology. Since 1974, the University of Maryland School of Medicine has a Center for Vaccine Development and Global Health that has conducted research on vaccines to defend against the Zika virus, H1N1, Ebola, and SARS-CoV-2.
We’re not alone. Other vaccinology centers across the country — as well as the National Institutes of Health at the national level, through its National Institute of Allergy and Infectious Diseases — are doing research and developing vaccines to combat viral diseases.
In this column, we are focused on viral diseases in pregnancy and the role that vaccines can play in preventing serious respiratory illness in mothers and their newborns. I have invited Laura E. Riley, MD, the Given Foundation Professor and Chair of Obstetrics and Gynecology at Weill Cornell Medicine, to address the importance of maternal immunization and how we can best counsel our patients and improve immunization rates.
As Dr. Riley explains, we are in a new era, and it behooves us all to be more vigilant about recommending vaccines, combating misperceptions, addressing patients’ knowledge gaps, and administering vaccines whenever possible.
Dr. Reece is the former Dean of Medicine & University Executive VP, and The Distinguished University and Endowed Professor & Director of the Center for Advanced Research Training and Innovation (CARTI) at the University of Maryland School of Medicine, as well as senior scientist at the Center for Birth Defects Research.
The alarming decline in maternal immunization rates that occurred in the wake of the COVID-19 pandemic means that, now more than ever, we must fully embrace our responsibility to recommend immunizations in pregnancy and to communicate what is known about their efficacy and safety. Data show that vaccination rates drop when we do not offer vaccines in our offices, so whenever possible, we should administer them as well.
The ob.gyn. is the patient’s most trusted person in pregnancy. When patients decline or express hesitancy about vaccines, it is incumbent upon us to ask why. Oftentimes, we can identify areas in which patients lack knowledge or have misperceptions and we can successfully educate the patient or change their perspective or misunderstanding concerning the importance of vaccination for themselves and their babies. (See Table 1.) We can also successfully address concerns about safety.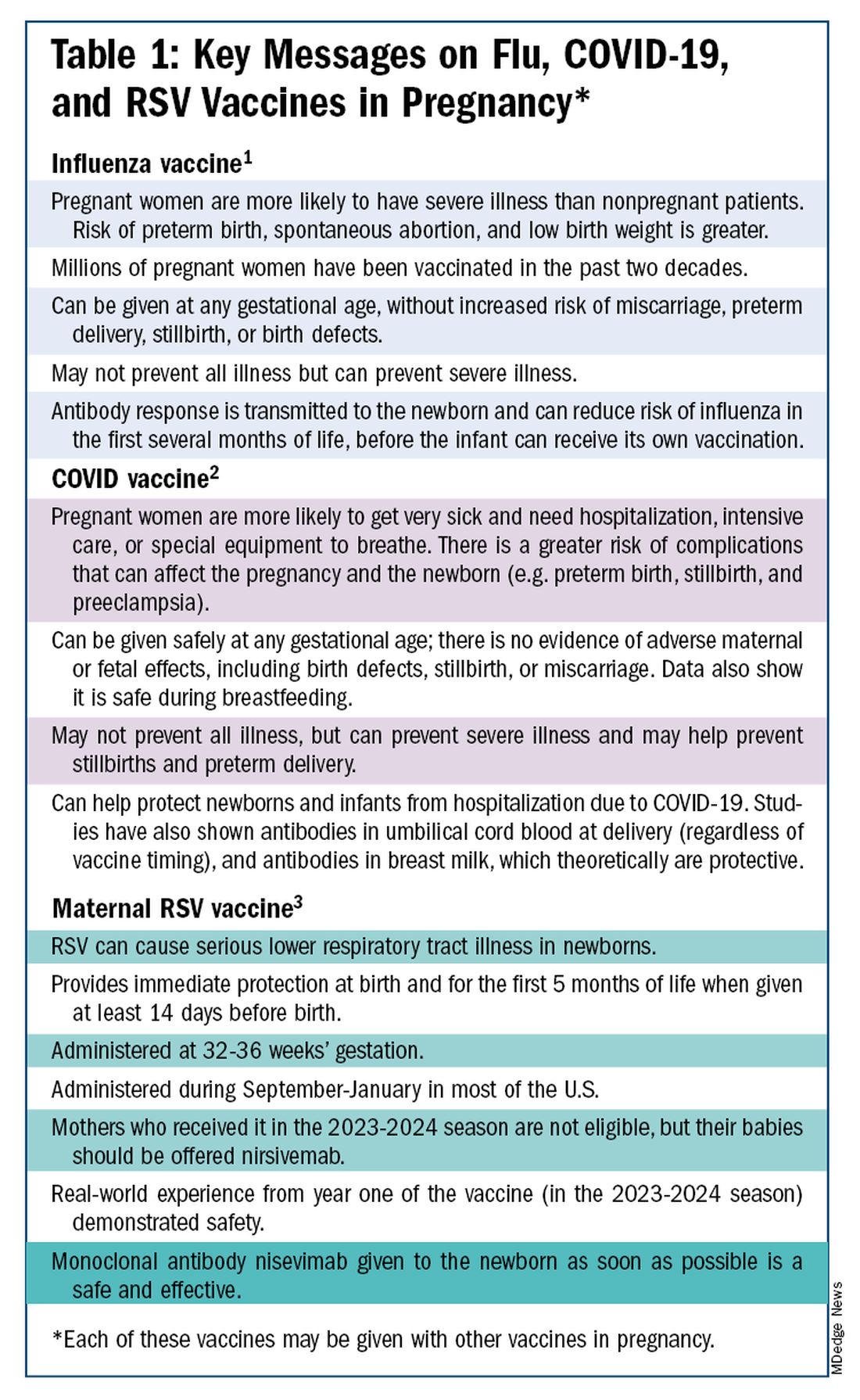
The safety of COVID-19 vaccinations in pregnancy is now backed by several years of data from multiple studies showing no increase in birth defects, preterm delivery, miscarriage, or stillbirth.
Data also show that pregnant patients are more likely than patients who are not pregnant to need hospitalization and intensive care when infected with SARS-CoV-2 and are at risk of having complications that can affect pregnancy and the newborn, including preterm birth and stillbirth. Vaccination has been shown to reduce the risk of severe illness and the risk of such adverse obstetrical outcomes, in addition to providing protection for the infant early on.
Similarly, influenza has long been more likely to be severe in pregnant patients, with an increased risk of poor obstetrical outcomes. Vaccines similarly provide “two for one protection,” protecting both mother and baby, and are, of course, backed by many years of safety and efficacy data.
With the new maternal respiratory syncytial virus (RSV) vaccine, now in its second year of availability, the goal is to protect the baby from RSV-caused serious lower respiratory tract illness. The illness has contributed to tens of thousands of annual hospitalizations and up to several hundred deaths every year in children younger than 5 years — particularly in those under age 6 months.
The RSV monoclonal antibody nirsevimab is available for the newborn as an alternative to maternal immunization but the maternal vaccine is optimal in that it will provide immediate rather than delayed protection for the newborn. The maternal vaccine is recommended during weeks 32-36 of pregnancy in mothers who were not vaccinated during last year’s RSV season. With real-world experience from year one, the available safety data are reassuring.
Counseling About Influenza and COVID-19 Vaccination
The COVID-19 pandemic took a toll on vaccination interest/receptivity broadly in pregnant and nonpregnant people. Among pregnant individuals, influenza vaccination coverage declined from 71% in the 2019-2020 influenza season to 56% in the 2021-2022 season, according to data from the Centers for Disease Control and Prevention’s Vaccine Safety Datalink.4 Coverage for the 2022-2023 and 2023-2024 influenza seasons was even worse: well under 50%.5
Fewer pregnant women have received updated COVID-19 vaccines. Only 13% of pregnant persons overall received the updated 2023-2024 COVID-19 booster vaccine (through March 30, 2024), according to the CDC.6
Maternal immunization for influenza has been recommended in the United States since 2004 (part of the recommendation that everyone over the age of 6 months receive an annual flu vaccine), and flu vaccines have been given to millions of pregnant women, but the H1N1 pandemic of 2009 reinforced its value as a priority for prenatal care. Most of the women who became severely ill from the H1N1 virus were young and healthy, without co-existing conditions known to increase risk.7
It became clearer during the H1N1 pandemic that pregnancy itself — which is associated with physiologic changes such as decreased lung capacity, increased nasal congestion and changes in the immune system – is its own significant risk factor for severe illness from the influenza virus. This increased risk applies to COVID-19 as well.
As COVID-19 has become endemic, with hospitalizations and deaths not reaching the levels of previous surges — and with mask-wearing and other preventive measures having declined — patients understandably have become more complacent. Some patients are vaccine deniers, but in my practice, these patients are a much smaller group than those who believe COVID-19 “is no big deal,” especially if they have had infections recently.
This is why it’s important to actively listen to concerns and to ask patients who decline a vaccination why they are hesitant. Blanket messages about vaccine efficacy and safety are the first step, but individualized, more pointed conversations based on the patient’s personal experiences and beliefs have become increasingly important.
I routinely tell pregnant patients about the risks of COVID-19 and I explain that it has been difficult to predict who will develop severe illness. Sometimes more conversation is needed. For those who are still hesitant or who tell me they feel protected by a recent infection, for instance, I provide more detail on the unique risks of pregnancy — the fact that “pregnancy is different” — and that natural immunity wanes while the protection afforded by immunization is believed to last longer. Many women are also concerned about the safety of the COVID-19 vaccine, so having safety data at your fingertips is helpful. (See Table 2.)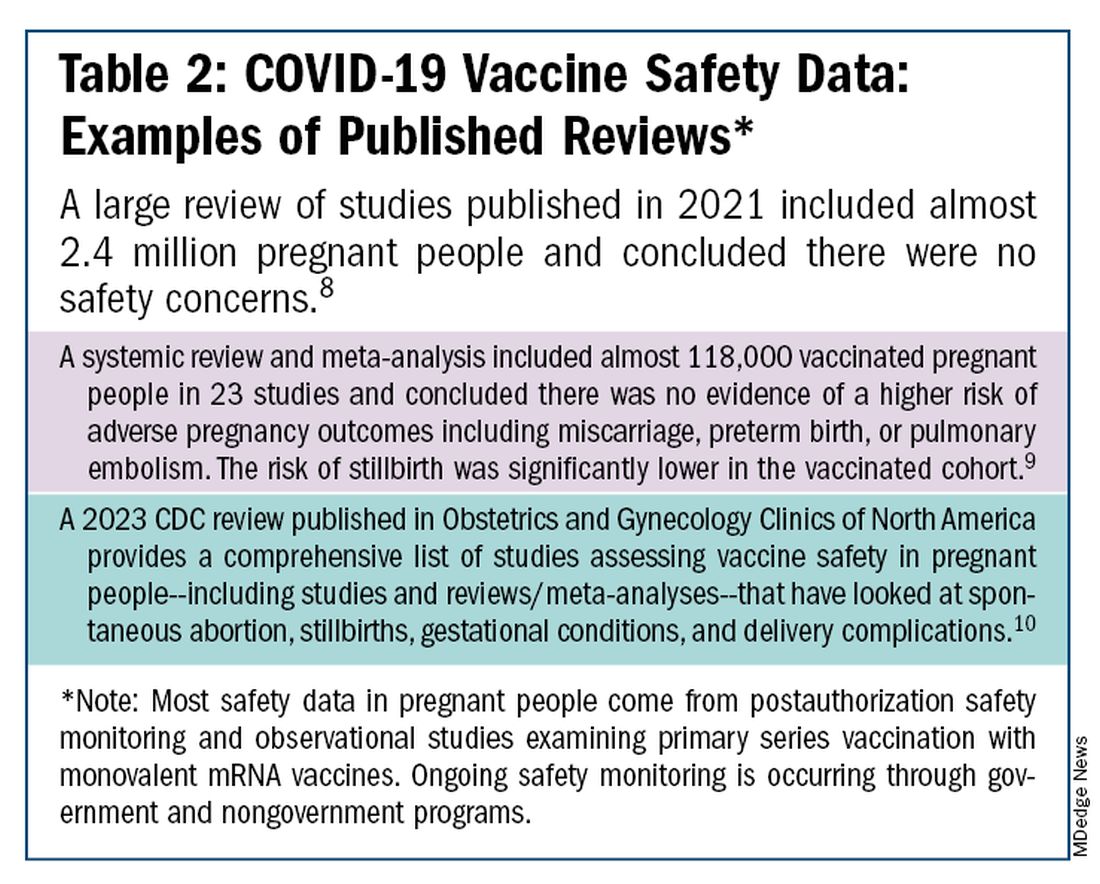
The fact that influenza and COVID-19 vaccination protect the newborn as well as the mother is something that I find is underappreciated by many patients. Explaining that infants likely benefit from the passage of antibodies across the placenta should be part of patient counseling.
Counseling About RSV Vaccination
Importantly, for the 2024-2025 RSV season, the maternal RSV vaccine (Abrysvo, Pfizer) is recommended only for pregnant women who did not receive the vaccine during the 2023-2024 season. When more research is done and more data are obtained showing how long the immune response persists post vaccination, it may be that the US Food and Drug Administration (FDA) will approve the maternal RSV vaccine for use in every pregnancy.
The later timing of the vaccination recommendation — 32-36 weeks’ gestation — reflects a conservative approach taken by the FDA in response to data from one of the pivotal trials showing a numerical trend toward more preterm deliveries among vaccinated compared with unvaccinated patients. This imbalance in the original trial, which administered the vaccine during 24-36 weeks of gestation, was seen only in low-income countries with no temporal association, however.
In our experience at two Weill Cornell Medical College–associated hospitals we did not see this trend. Our cohort study of almost 3000 pregnant patients who delivered at 32 weeks’ gestation or later found no increased risk of preterm birth among the 35% of patients who received the RSV vaccine during the 2023-2024 RSV season. We also did not see any difference in preeclampsia, in contrast with original trial data that showed a signal for increased risk.11
When fewer than 2 weeks have elapsed between maternal vaccination and delivery, the monoclonal antibody nirsevimab is recommended for the newborn — ideally before the newborn leaves the hospital. Nirsevimab is also recommended for newborns of mothers who decline vaccination or were not candidates (e.g. vaccinated in a previous pregnancy), or when there is concern about the adequacy of the maternal immune response to the vaccine (e.g. in cases of immunosuppression).
While there was a limited supply of the monoclonal antibody last year, limitations are not expected this year, especially after October.
The ultimate goal is that patients choose the vaccine or the immunoglobulin, given the severity of RSV disease. Patient preferences should be considered. However, given that it takes 2 weeks after vaccination for protection to build up, I stress to patients that if they’ve vaccinated themselves, their newborn will leave the hospital with protection. If nirsevimab is relied upon, I explain, their newborn may not be protected for some period of time.
Take-home Messages
- When patients decline or are hesitant about vaccines, ask why. Listen actively, and work to correct misperceptions and knowledge gaps.
- Whenever possible, offer vaccines in your practice. Vaccination rates drop when this does not occur.
- COVID-vaccine safety is backed by many studies showing no increase in birth defects, preterm delivery, miscarriage, or stillbirth.
- Pregnant women are more likely to have severe illness from the influenza and SARS-CoV-2 viruses. Vaccines can prevent severe illness and can protect the newborn as well as the mother.
- Recommend/administer the maternal RSV vaccine at 32-36 weeks’ gestation in women who did not receive the vaccine in the 2023-2024 season. If mothers aren’t eligible their babies should be offered nirsevimab.
Dr. Riley is the Given Foundation Professor and Chair of Obstetrics and Gynecology at Weill Cornell Medicine and the obstetrician and gynecologist-in-chief at New York Presbyterian Hospital. She disclosed that she has provided one-time consultations to Pfizer (Abrysvo RSV vaccine) and GSK (cytomegalovirus vaccine), and is providing consultant education on CMV for Moderna. She is chair of ACOG’s task force on immunization and emerging infectious diseases, serves on the medical advisory board for MAVEN, and serves as an editor or editorial board member for several medical publications.
References
1. ACOG Committee Opinion No. 741: Maternal Immunization. Obstet Gynecol. 2018;131(6):e214-e217.
2. Centers for Disease Control and Prevention. COVID-19 Vaccination for People Who are Pregnant or Breastfeeding. https://www.cdc.gov/covid/vaccines/pregnant-or-breastfeeding.html.
3. ACOG Practice Advisory on Maternal Respiratory Syncytial Virus Vaccination, September 2023. (Updated August 2024).4. Irving S et al. Open Forum Infect Dis. 2023;10(Suppl 2):ofad500.1002.
5. Flu Vaccination Dashboard, CDC, National Center for Immunization and Respiratory Diseases.
6. Weekly COVID-19 Vaccination Dashboard, CDC. https://www.cdc.gov/covidvaxview/weekly-dashboard/index.html
7. Louie JK et al. N Engl J Med. 2010;362:27-35. 8. Ciapponi A et al. Vaccine. 2021;39(40):5891-908.
9. Prasad S et al. Nature Communications. 2022;13:2414. 10. Fleming-Dutra KE et al. Obstet Gynecol Clin North Am 2023;50(2):279-97. 11. Mouen S et al. JAMA Network Open 2024;7(7):e2419268.
Lawsuit Targets Publishers: Is Peer Review Flawed?
The peer-review process, which is used by scientific journals to validate legitimate research, is now under legal scrutiny. The US District Court for the Southern District of New York will soon rule on whether scientific publishers have compromised this system for profit. In mid-September, University of California, Los Angeles neuroscientist Lucina Uddin filed a class action lawsuit against six leading academic publishers — Elsevier, Wolters Kluwer, Wiley, Sage Publications, Taylor & Francis, and Springer Nature — accusing them of violating antitrust laws and obstructing academic research.
The lawsuit targets several long-standing practices in scientific publishing, including the lack of compensation for peer reviewers, restrictions that require submitting to only one journal at a time, and bans on sharing manuscripts under review. Uddin’s complaint argues that these practices contribute to inefficiencies in the review process, thus delaying the publication of critical discoveries, which could hinder research, clinical advancements, and the development of new medical treatments.
The suit also noted that these publishers generated $10 billion in revenue in 2023 in peer-reviewed journals. However, the complaint seemingly overlooks the widespread practice of preprint repositories, where many manuscripts are shared while awaiting peer review.
Flawed Reviews
A growing number of studies have highlighted subpar or unethical behaviors among reviewers, who are supposed to adhere to the highest standards of methodological rigor, both in conducting research and reviewing work for journals. One recent study published in Scientometrics in August examined 263 reviews from 37 journals across various disciplines and found alarming patterns of duplication. Many of the reviews contained identical or highly similar language. Some reviewers were found to be suggesting that the authors expand their bibliographies to include the reviewers’ own work, thus inflating their citation counts.
As María Ángeles Oviedo-García from the University of Seville in Spain, pointed out: “The analysis of 263 review reports shows a pattern of vague, repetitive statements — often identical or very similar — along with coercive citations, ultimately resulting in misleading reviews.”
Experts in research integrity and ethics argue that while issues persist, the integrity of scientific research is improving. Increasing research and public disclosure reflect a heightened awareness of problems long overlooked.
Speaking to this news organization, Fanelli, who has been studying scientific misconduct for about 20 years, noted that while his early work left him disillusioned, further research has replaced his cynicism with what he describes as healthy skepticism and a more optimistic outlook. Fanelli also collaborates with the Luxembourg Agency for Research Integrity and the Advisory Committee on Research Ethics and Bioethics at the Italian National Research Council (CNR), where he helped develop the first research integrity guidelines.
Lack of Awareness
A recurring challenge is the difficulty in distinguishing between honest mistakes and intentional misconduct. “This is why greater investment in education is essential,” said Daniel Pizzolato, European Network of Research Ethics Committees, Bonn, Germany, and the Centre for Biomedical Ethics and Law, KU Leuven in Belgium.
While Pizzolato acknowledged that institutions such as the CNR in Italy provide a positive example, awareness of research integrity is generally still lacking across much of Europe, and there are few offices dedicated to promoting research integrity. However, he pointed to promising developments in other countries. “In France and Denmark, researchers are required to be familiar with integrity norms because codes of conduct have legal standing. Some major international funding bodies like the European Molecular Biology Organization are making participation in research integrity courses a condition for receiving grants.”
Pizzolato remains optimistic. “There is a growing willingness to move past this impasse,” he said.
A recent study published in The Journal of Clinical Epidemiology reveals troubling gaps in how retracted biomedical articles are flagged and cited. Led by Caitlin Bakkera, Department of Epidemiology, Maastricht University, Maastricht, the Netherlands, the research sought to determine whether articles retracted because of errors or fraud were properly flagged across various databases.
The results were concerning: Less than 5% of retracted articles had consistent retraction notices across all databases that hosted them, and less than 50% of citations referenced the retraction. None of the 414 retraction notices analyzed met best-practice guidelines for completeness. Bakkera and colleagues warned that these shortcomings threaten the integrity of public health research.
Fanelli’s Perspective
Despite the concerns, Fanelli remains calm. “Science is based on debate and a perspective called organized skepticism, which helps reveal the truth,” he explained. “While there is often excessive skepticism today, the overall quality of clinical trials is improving.
“It’s important to remember that reliable results take time and shouldn’t depend on the outcome of a single study. It’s essential to consider the broader context, the history of the research field, and potential conflicts of interest, both financial and otherwise. Biomedical research requires constant updates,” he concluded.
This story was translated from Univadis Italy using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
The peer-review process, which is used by scientific journals to validate legitimate research, is now under legal scrutiny. The US District Court for the Southern District of New York will soon rule on whether scientific publishers have compromised this system for profit. In mid-September, University of California, Los Angeles neuroscientist Lucina Uddin filed a class action lawsuit against six leading academic publishers — Elsevier, Wolters Kluwer, Wiley, Sage Publications, Taylor & Francis, and Springer Nature — accusing them of violating antitrust laws and obstructing academic research.
The lawsuit targets several long-standing practices in scientific publishing, including the lack of compensation for peer reviewers, restrictions that require submitting to only one journal at a time, and bans on sharing manuscripts under review. Uddin’s complaint argues that these practices contribute to inefficiencies in the review process, thus delaying the publication of critical discoveries, which could hinder research, clinical advancements, and the development of new medical treatments.
The suit also noted that these publishers generated $10 billion in revenue in 2023 in peer-reviewed journals. However, the complaint seemingly overlooks the widespread practice of preprint repositories, where many manuscripts are shared while awaiting peer review.
Flawed Reviews
A growing number of studies have highlighted subpar or unethical behaviors among reviewers, who are supposed to adhere to the highest standards of methodological rigor, both in conducting research and reviewing work for journals. One recent study published in Scientometrics in August examined 263 reviews from 37 journals across various disciplines and found alarming patterns of duplication. Many of the reviews contained identical or highly similar language. Some reviewers were found to be suggesting that the authors expand their bibliographies to include the reviewers’ own work, thus inflating their citation counts.
As María Ángeles Oviedo-García from the University of Seville in Spain, pointed out: “The analysis of 263 review reports shows a pattern of vague, repetitive statements — often identical or very similar — along with coercive citations, ultimately resulting in misleading reviews.”
Experts in research integrity and ethics argue that while issues persist, the integrity of scientific research is improving. Increasing research and public disclosure reflect a heightened awareness of problems long overlooked.
Speaking to this news organization, Fanelli, who has been studying scientific misconduct for about 20 years, noted that while his early work left him disillusioned, further research has replaced his cynicism with what he describes as healthy skepticism and a more optimistic outlook. Fanelli also collaborates with the Luxembourg Agency for Research Integrity and the Advisory Committee on Research Ethics and Bioethics at the Italian National Research Council (CNR), where he helped develop the first research integrity guidelines.
Lack of Awareness
A recurring challenge is the difficulty in distinguishing between honest mistakes and intentional misconduct. “This is why greater investment in education is essential,” said Daniel Pizzolato, European Network of Research Ethics Committees, Bonn, Germany, and the Centre for Biomedical Ethics and Law, KU Leuven in Belgium.
While Pizzolato acknowledged that institutions such as the CNR in Italy provide a positive example, awareness of research integrity is generally still lacking across much of Europe, and there are few offices dedicated to promoting research integrity. However, he pointed to promising developments in other countries. “In France and Denmark, researchers are required to be familiar with integrity norms because codes of conduct have legal standing. Some major international funding bodies like the European Molecular Biology Organization are making participation in research integrity courses a condition for receiving grants.”
Pizzolato remains optimistic. “There is a growing willingness to move past this impasse,” he said.
A recent study published in The Journal of Clinical Epidemiology reveals troubling gaps in how retracted biomedical articles are flagged and cited. Led by Caitlin Bakkera, Department of Epidemiology, Maastricht University, Maastricht, the Netherlands, the research sought to determine whether articles retracted because of errors or fraud were properly flagged across various databases.
The results were concerning: Less than 5% of retracted articles had consistent retraction notices across all databases that hosted them, and less than 50% of citations referenced the retraction. None of the 414 retraction notices analyzed met best-practice guidelines for completeness. Bakkera and colleagues warned that these shortcomings threaten the integrity of public health research.
Fanelli’s Perspective
Despite the concerns, Fanelli remains calm. “Science is based on debate and a perspective called organized skepticism, which helps reveal the truth,” he explained. “While there is often excessive skepticism today, the overall quality of clinical trials is improving.
“It’s important to remember that reliable results take time and shouldn’t depend on the outcome of a single study. It’s essential to consider the broader context, the history of the research field, and potential conflicts of interest, both financial and otherwise. Biomedical research requires constant updates,” he concluded.
This story was translated from Univadis Italy using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
The peer-review process, which is used by scientific journals to validate legitimate research, is now under legal scrutiny. The US District Court for the Southern District of New York will soon rule on whether scientific publishers have compromised this system for profit. In mid-September, University of California, Los Angeles neuroscientist Lucina Uddin filed a class action lawsuit against six leading academic publishers — Elsevier, Wolters Kluwer, Wiley, Sage Publications, Taylor & Francis, and Springer Nature — accusing them of violating antitrust laws and obstructing academic research.
The lawsuit targets several long-standing practices in scientific publishing, including the lack of compensation for peer reviewers, restrictions that require submitting to only one journal at a time, and bans on sharing manuscripts under review. Uddin’s complaint argues that these practices contribute to inefficiencies in the review process, thus delaying the publication of critical discoveries, which could hinder research, clinical advancements, and the development of new medical treatments.
The suit also noted that these publishers generated $10 billion in revenue in 2023 in peer-reviewed journals. However, the complaint seemingly overlooks the widespread practice of preprint repositories, where many manuscripts are shared while awaiting peer review.
Flawed Reviews
A growing number of studies have highlighted subpar or unethical behaviors among reviewers, who are supposed to adhere to the highest standards of methodological rigor, both in conducting research and reviewing work for journals. One recent study published in Scientometrics in August examined 263 reviews from 37 journals across various disciplines and found alarming patterns of duplication. Many of the reviews contained identical or highly similar language. Some reviewers were found to be suggesting that the authors expand their bibliographies to include the reviewers’ own work, thus inflating their citation counts.
As María Ángeles Oviedo-García from the University of Seville in Spain, pointed out: “The analysis of 263 review reports shows a pattern of vague, repetitive statements — often identical or very similar — along with coercive citations, ultimately resulting in misleading reviews.”
Experts in research integrity and ethics argue that while issues persist, the integrity of scientific research is improving. Increasing research and public disclosure reflect a heightened awareness of problems long overlooked.
Speaking to this news organization, Fanelli, who has been studying scientific misconduct for about 20 years, noted that while his early work left him disillusioned, further research has replaced his cynicism with what he describes as healthy skepticism and a more optimistic outlook. Fanelli also collaborates with the Luxembourg Agency for Research Integrity and the Advisory Committee on Research Ethics and Bioethics at the Italian National Research Council (CNR), where he helped develop the first research integrity guidelines.
Lack of Awareness
A recurring challenge is the difficulty in distinguishing between honest mistakes and intentional misconduct. “This is why greater investment in education is essential,” said Daniel Pizzolato, European Network of Research Ethics Committees, Bonn, Germany, and the Centre for Biomedical Ethics and Law, KU Leuven in Belgium.
While Pizzolato acknowledged that institutions such as the CNR in Italy provide a positive example, awareness of research integrity is generally still lacking across much of Europe, and there are few offices dedicated to promoting research integrity. However, he pointed to promising developments in other countries. “In France and Denmark, researchers are required to be familiar with integrity norms because codes of conduct have legal standing. Some major international funding bodies like the European Molecular Biology Organization are making participation in research integrity courses a condition for receiving grants.”
Pizzolato remains optimistic. “There is a growing willingness to move past this impasse,” he said.
A recent study published in The Journal of Clinical Epidemiology reveals troubling gaps in how retracted biomedical articles are flagged and cited. Led by Caitlin Bakkera, Department of Epidemiology, Maastricht University, Maastricht, the Netherlands, the research sought to determine whether articles retracted because of errors or fraud were properly flagged across various databases.
The results were concerning: Less than 5% of retracted articles had consistent retraction notices across all databases that hosted them, and less than 50% of citations referenced the retraction. None of the 414 retraction notices analyzed met best-practice guidelines for completeness. Bakkera and colleagues warned that these shortcomings threaten the integrity of public health research.
Fanelli’s Perspective
Despite the concerns, Fanelli remains calm. “Science is based on debate and a perspective called organized skepticism, which helps reveal the truth,” he explained. “While there is often excessive skepticism today, the overall quality of clinical trials is improving.
“It’s important to remember that reliable results take time and shouldn’t depend on the outcome of a single study. It’s essential to consider the broader context, the history of the research field, and potential conflicts of interest, both financial and otherwise. Biomedical research requires constant updates,” he concluded.
This story was translated from Univadis Italy using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Is Metformin An Unexpected Ally Against Long COVID?
TOPLINE:
METHODOLOGY:
- Previous studies have shown that metformin use before and during SARS-CoV-2 infection reduces severe COVID-19 and postacute sequelae of SARS-CoV-2 (PASC), also referred to as long COVID, in adults.
- A retrospective cohort analysis was conducted to evaluate the association between metformin use before and during SARS-CoV-2 infection and the subsequent incidence of PASC.
- Researchers used data from the National COVID Cohort Collaborative (N3C) and National Patient-Centered Clinical Research Network (PCORnet) electronic health record (EHR) databases to identify adults (age, ≥ 21 years) with T2D prescribed a diabetes medication within the past 12 months.
- Participants were categorized into those using metformin (metformin group) and those using other noninsulin diabetes medications such as sulfonylureas, dipeptidyl peptidase-4 inhibitors, or thiazolidinediones (the comparator group); those who used glucagon-like peptide 1 receptor agonists or sodium-glucose cotransporter-2 inhibitors were excluded.
- The primary outcome was the incidence of PASC or death within 180 days after SARS-CoV-2 infection, defined using International Classification of Diseases U09.9 diagnosis code and/or computable phenotype defined by a predicted probability of > 75% for PASC using a machine learning model trained on patients diagnosed using U09.9 (PASC computable phenotype).
TAKEAWAY:
- Researchers identified 51,385 and 37,947 participants from the N3C and PCORnet datasets, respectively.
- Metformin use was associated with a 21% lower risk for death or PASC using the U09.9 diagnosis code (P < .001) and a 15% lower risk using the PASC computable phenotype (P < .001) in the N3C dataset than non-metformin use.
- In the PCORnet dataset, the risk for death or PASC was 13% lower using the U09.9 diagnosis code (P = .08) with metformin use vs non-metformin use, whereas the risk did not differ significantly between the groups when using the PASC computable phenotype (P = .58).
- The incidence of PASC using the U09.9 diagnosis code for the metformin and comparator groups was similar between the two datasets (1.6% and 2.0% in N3C and 2.2 and 2.6% in PCORnet, respectively).
- However, when using the computable phenotype, the incidence rates of PASC for the metformin and comparator groups were 4.8% and 5.2% in N3C and 25.2% and 24.2% in PCORnet, respectively.
IN PRACTICE:
“The incidence of PASC was lower when defined by [International Classification of Diseases] code, compared with a computable phenotype in both databases,” the authors wrote. “This may reflect the challenges of clinical care for adults needing chronic medication management and the likelihood of those adults receiving a formal PASC diagnosis.”
SOURCE:
The study was led by Steven G. Johnson, PhD, Institute for Health Informatics, University of Minnesota, Minneapolis. It was published online in Diabetes Care.
LIMITATIONS:
The use of EHR data had several limitations, including the inability to examine a dose-dependent relationship and the lack of information on whether medications were taken before, during, or after the acute infection. The outcome definition involved the need for a medical encounter and, thus, may not capture data on all patients experiencing symptoms of PASC. The analysis focused on the prevalent use of chronic medications, limiting the assessment of initiating metformin in those diagnosed with COVID-19.
DISCLOSURES:
The study was supported by the National Institutes of Health Agreement as part of the RECOVER research program. One author reported receiving salary support from the Center for Pharmacoepidemiology and owning stock options in various pharmaceutical and biopharmaceutical companies. Another author reported receiving grant support and consulting contracts, being involved in expert witness engagement, and owning stock options in various pharmaceutical, biopharmaceutical, diabetes management, and medical device companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Previous studies have shown that metformin use before and during SARS-CoV-2 infection reduces severe COVID-19 and postacute sequelae of SARS-CoV-2 (PASC), also referred to as long COVID, in adults.
- A retrospective cohort analysis was conducted to evaluate the association between metformin use before and during SARS-CoV-2 infection and the subsequent incidence of PASC.
- Researchers used data from the National COVID Cohort Collaborative (N3C) and National Patient-Centered Clinical Research Network (PCORnet) electronic health record (EHR) databases to identify adults (age, ≥ 21 years) with T2D prescribed a diabetes medication within the past 12 months.
- Participants were categorized into those using metformin (metformin group) and those using other noninsulin diabetes medications such as sulfonylureas, dipeptidyl peptidase-4 inhibitors, or thiazolidinediones (the comparator group); those who used glucagon-like peptide 1 receptor agonists or sodium-glucose cotransporter-2 inhibitors were excluded.
- The primary outcome was the incidence of PASC or death within 180 days after SARS-CoV-2 infection, defined using International Classification of Diseases U09.9 diagnosis code and/or computable phenotype defined by a predicted probability of > 75% for PASC using a machine learning model trained on patients diagnosed using U09.9 (PASC computable phenotype).
TAKEAWAY:
- Researchers identified 51,385 and 37,947 participants from the N3C and PCORnet datasets, respectively.
- Metformin use was associated with a 21% lower risk for death or PASC using the U09.9 diagnosis code (P < .001) and a 15% lower risk using the PASC computable phenotype (P < .001) in the N3C dataset than non-metformin use.
- In the PCORnet dataset, the risk for death or PASC was 13% lower using the U09.9 diagnosis code (P = .08) with metformin use vs non-metformin use, whereas the risk did not differ significantly between the groups when using the PASC computable phenotype (P = .58).
- The incidence of PASC using the U09.9 diagnosis code for the metformin and comparator groups was similar between the two datasets (1.6% and 2.0% in N3C and 2.2 and 2.6% in PCORnet, respectively).
- However, when using the computable phenotype, the incidence rates of PASC for the metformin and comparator groups were 4.8% and 5.2% in N3C and 25.2% and 24.2% in PCORnet, respectively.
IN PRACTICE:
“The incidence of PASC was lower when defined by [International Classification of Diseases] code, compared with a computable phenotype in both databases,” the authors wrote. “This may reflect the challenges of clinical care for adults needing chronic medication management and the likelihood of those adults receiving a formal PASC diagnosis.”
SOURCE:
The study was led by Steven G. Johnson, PhD, Institute for Health Informatics, University of Minnesota, Minneapolis. It was published online in Diabetes Care.
LIMITATIONS:
The use of EHR data had several limitations, including the inability to examine a dose-dependent relationship and the lack of information on whether medications were taken before, during, or after the acute infection. The outcome definition involved the need for a medical encounter and, thus, may not capture data on all patients experiencing symptoms of PASC. The analysis focused on the prevalent use of chronic medications, limiting the assessment of initiating metformin in those diagnosed with COVID-19.
DISCLOSURES:
The study was supported by the National Institutes of Health Agreement as part of the RECOVER research program. One author reported receiving salary support from the Center for Pharmacoepidemiology and owning stock options in various pharmaceutical and biopharmaceutical companies. Another author reported receiving grant support and consulting contracts, being involved in expert witness engagement, and owning stock options in various pharmaceutical, biopharmaceutical, diabetes management, and medical device companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Previous studies have shown that metformin use before and during SARS-CoV-2 infection reduces severe COVID-19 and postacute sequelae of SARS-CoV-2 (PASC), also referred to as long COVID, in adults.
- A retrospective cohort analysis was conducted to evaluate the association between metformin use before and during SARS-CoV-2 infection and the subsequent incidence of PASC.
- Researchers used data from the National COVID Cohort Collaborative (N3C) and National Patient-Centered Clinical Research Network (PCORnet) electronic health record (EHR) databases to identify adults (age, ≥ 21 years) with T2D prescribed a diabetes medication within the past 12 months.
- Participants were categorized into those using metformin (metformin group) and those using other noninsulin diabetes medications such as sulfonylureas, dipeptidyl peptidase-4 inhibitors, or thiazolidinediones (the comparator group); those who used glucagon-like peptide 1 receptor agonists or sodium-glucose cotransporter-2 inhibitors were excluded.
- The primary outcome was the incidence of PASC or death within 180 days after SARS-CoV-2 infection, defined using International Classification of Diseases U09.9 diagnosis code and/or computable phenotype defined by a predicted probability of > 75% for PASC using a machine learning model trained on patients diagnosed using U09.9 (PASC computable phenotype).
TAKEAWAY:
- Researchers identified 51,385 and 37,947 participants from the N3C and PCORnet datasets, respectively.
- Metformin use was associated with a 21% lower risk for death or PASC using the U09.9 diagnosis code (P < .001) and a 15% lower risk using the PASC computable phenotype (P < .001) in the N3C dataset than non-metformin use.
- In the PCORnet dataset, the risk for death or PASC was 13% lower using the U09.9 diagnosis code (P = .08) with metformin use vs non-metformin use, whereas the risk did not differ significantly between the groups when using the PASC computable phenotype (P = .58).
- The incidence of PASC using the U09.9 diagnosis code for the metformin and comparator groups was similar between the two datasets (1.6% and 2.0% in N3C and 2.2 and 2.6% in PCORnet, respectively).
- However, when using the computable phenotype, the incidence rates of PASC for the metformin and comparator groups were 4.8% and 5.2% in N3C and 25.2% and 24.2% in PCORnet, respectively.
IN PRACTICE:
“The incidence of PASC was lower when defined by [International Classification of Diseases] code, compared with a computable phenotype in both databases,” the authors wrote. “This may reflect the challenges of clinical care for adults needing chronic medication management and the likelihood of those adults receiving a formal PASC diagnosis.”
SOURCE:
The study was led by Steven G. Johnson, PhD, Institute for Health Informatics, University of Minnesota, Minneapolis. It was published online in Diabetes Care.
LIMITATIONS:
The use of EHR data had several limitations, including the inability to examine a dose-dependent relationship and the lack of information on whether medications were taken before, during, or after the acute infection. The outcome definition involved the need for a medical encounter and, thus, may not capture data on all patients experiencing symptoms of PASC. The analysis focused on the prevalent use of chronic medications, limiting the assessment of initiating metformin in those diagnosed with COVID-19.
DISCLOSURES:
The study was supported by the National Institutes of Health Agreement as part of the RECOVER research program. One author reported receiving salary support from the Center for Pharmacoepidemiology and owning stock options in various pharmaceutical and biopharmaceutical companies. Another author reported receiving grant support and consulting contracts, being involved in expert witness engagement, and owning stock options in various pharmaceutical, biopharmaceutical, diabetes management, and medical device companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.


