User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Novel neural cell therapy: A cure for focal epilepsy?
BOSTON – (MTLE) in the first-in-human test of the novel therapy.
“It is notable that the early significant seizure reduction observed in this study appears to be durable in these first two patients treated with a single administration of NRTX-1001,” principal investigator Robert Beach, MD, PhD, said in a news release.
“It is also encouraging that the first patient has been free from disabling seizures from the second month on and has shown improved memory performance on multiple cognitive tests, as memory problems can be an issue for individuals with drug-resistant MTLE,” said Dr. Beach, chief of epilepsy and professor of neurology at State University of New York, Syracuse.
The findings were presented at the annual meeting of the American Academy of Neurology.
Restorative not destructive
NRTX-1001 therapy (Neurona Therapeutics) is a one-time dose of an injectable suspension of high-purity inhibitory interneurons that secrete the inhibitory neurotransmitter gamma-aminobutyric acid (GABA). The interneurons are intended to integrate and innervate on-target, providing long-term GABAergic inhibition to repair hyperexcitable neural networks.
Preclinical work in animal models of epilepsy has provided strong support for both the safety and the efficacy of boosting inhibition in the seizure focus using implanted human inhibitory interneurons.
This therapy is “potentially restorative instead of just destructive, like epilepsy surgery,” study investigator David Spencer, MD, professor of neurology and director of the Comprehensive Epilepsy Center, Oregon Health & Science University in Portland, said during a press briefing.
In the first two patients, the cells were implanted in the seizure focus using MRI guidance through a tiny opening in the back of the skull. The patients recovered overnight and went home the next day.
The first patient had a 9-year history of drug-resistant epilepsy and was averaging 30 seizures per month at baseline. Testing confirmed that the seizures were coming from a single focus on the right temporal lobe. The implant was uncomplicated, and the cells were delivered to the seizure focus on target.
To date, there have been no serious or unexpected adverse events from the implant. At 9 months of follow-up the patient has had a 93% reduction in seizures overall and is free of all seizures causing impairment of awareness, “which was the most debilitating seizure type for this patient,” Dr. Spencer noted.
Studies of brain metabolism in the area of the implant have shown favorable markers of increased inhibition and decreased inflammation. Cognitive testing at 6 months showed no worsening of memory function or cognition. And, in fact, there were some mild improvements, he said.
The second patient had an 8-year history of drug-resistant epilepsy, averaging 14 focal seizures per month at baseline. Testing also confirmed seizure onset in a single focus in the right temporal lobe and the cells were again implanted without complication on target. Five months after treatment, the patient has had a 94% reduction in seizures and no serious adverse events.
‘Hot off the press’
Epilepsy affects about 3.5 million people in the United States. About two-thirds of people with epilepsy get good control of their seizures using antiseizure medication.
For seizures that are uncontrolled with medication, identifying the seizure focus and removing it surgically can often result in seizure freedom in a high proportion of patients. But not all patients are candidates for epilepsy surgery, and for those who can have it the surgery itself carries some risks, including diminished cognition and memory.
“While these are still early days, we’re encouraged by the positive safety findings so far, and the early seizure responses” with neural cell therapy, Dr. Spencer told reporters.
Given the positive results in the first two patients, additional patients will be treated “with careful safety review all along the way. This is going to be rolling out over the next several years,” Dr. Spencer said. Patient recruitment is underway at epilepsy centers across the United States.
Briefing moderator Natalia Rost, MD, MPH, chair of the AAN science committee, said, “This is a true example of emerging science. It’s literally hot off the press,” and the preliminary results are “very promising.”
Dr. Rost, chief of the stroke division at Massachusetts General Hospital in Boston, noted that this type of cell therapy implant is “very novel and representative of where the field is moving, when no traditional solutions exist for common neurological problems.”
The study was sponsored by Neurona Therapeutics and funded in part by the California Institute for Regenerative Medicine. Dr. Beach and Dr. Spencer report no relevant financial relationships. Several investigators are employees of Neurona Therapeutics. Dr. Rost reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
BOSTON – (MTLE) in the first-in-human test of the novel therapy.
“It is notable that the early significant seizure reduction observed in this study appears to be durable in these first two patients treated with a single administration of NRTX-1001,” principal investigator Robert Beach, MD, PhD, said in a news release.
“It is also encouraging that the first patient has been free from disabling seizures from the second month on and has shown improved memory performance on multiple cognitive tests, as memory problems can be an issue for individuals with drug-resistant MTLE,” said Dr. Beach, chief of epilepsy and professor of neurology at State University of New York, Syracuse.
The findings were presented at the annual meeting of the American Academy of Neurology.
Restorative not destructive
NRTX-1001 therapy (Neurona Therapeutics) is a one-time dose of an injectable suspension of high-purity inhibitory interneurons that secrete the inhibitory neurotransmitter gamma-aminobutyric acid (GABA). The interneurons are intended to integrate and innervate on-target, providing long-term GABAergic inhibition to repair hyperexcitable neural networks.
Preclinical work in animal models of epilepsy has provided strong support for both the safety and the efficacy of boosting inhibition in the seizure focus using implanted human inhibitory interneurons.
This therapy is “potentially restorative instead of just destructive, like epilepsy surgery,” study investigator David Spencer, MD, professor of neurology and director of the Comprehensive Epilepsy Center, Oregon Health & Science University in Portland, said during a press briefing.
In the first two patients, the cells were implanted in the seizure focus using MRI guidance through a tiny opening in the back of the skull. The patients recovered overnight and went home the next day.
The first patient had a 9-year history of drug-resistant epilepsy and was averaging 30 seizures per month at baseline. Testing confirmed that the seizures were coming from a single focus on the right temporal lobe. The implant was uncomplicated, and the cells were delivered to the seizure focus on target.
To date, there have been no serious or unexpected adverse events from the implant. At 9 months of follow-up the patient has had a 93% reduction in seizures overall and is free of all seizures causing impairment of awareness, “which was the most debilitating seizure type for this patient,” Dr. Spencer noted.
Studies of brain metabolism in the area of the implant have shown favorable markers of increased inhibition and decreased inflammation. Cognitive testing at 6 months showed no worsening of memory function or cognition. And, in fact, there were some mild improvements, he said.
The second patient had an 8-year history of drug-resistant epilepsy, averaging 14 focal seizures per month at baseline. Testing also confirmed seizure onset in a single focus in the right temporal lobe and the cells were again implanted without complication on target. Five months after treatment, the patient has had a 94% reduction in seizures and no serious adverse events.
‘Hot off the press’
Epilepsy affects about 3.5 million people in the United States. About two-thirds of people with epilepsy get good control of their seizures using antiseizure medication.
For seizures that are uncontrolled with medication, identifying the seizure focus and removing it surgically can often result in seizure freedom in a high proportion of patients. But not all patients are candidates for epilepsy surgery, and for those who can have it the surgery itself carries some risks, including diminished cognition and memory.
“While these are still early days, we’re encouraged by the positive safety findings so far, and the early seizure responses” with neural cell therapy, Dr. Spencer told reporters.
Given the positive results in the first two patients, additional patients will be treated “with careful safety review all along the way. This is going to be rolling out over the next several years,” Dr. Spencer said. Patient recruitment is underway at epilepsy centers across the United States.
Briefing moderator Natalia Rost, MD, MPH, chair of the AAN science committee, said, “This is a true example of emerging science. It’s literally hot off the press,” and the preliminary results are “very promising.”
Dr. Rost, chief of the stroke division at Massachusetts General Hospital in Boston, noted that this type of cell therapy implant is “very novel and representative of where the field is moving, when no traditional solutions exist for common neurological problems.”
The study was sponsored by Neurona Therapeutics and funded in part by the California Institute for Regenerative Medicine. Dr. Beach and Dr. Spencer report no relevant financial relationships. Several investigators are employees of Neurona Therapeutics. Dr. Rost reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
BOSTON – (MTLE) in the first-in-human test of the novel therapy.
“It is notable that the early significant seizure reduction observed in this study appears to be durable in these first two patients treated with a single administration of NRTX-1001,” principal investigator Robert Beach, MD, PhD, said in a news release.
“It is also encouraging that the first patient has been free from disabling seizures from the second month on and has shown improved memory performance on multiple cognitive tests, as memory problems can be an issue for individuals with drug-resistant MTLE,” said Dr. Beach, chief of epilepsy and professor of neurology at State University of New York, Syracuse.
The findings were presented at the annual meeting of the American Academy of Neurology.
Restorative not destructive
NRTX-1001 therapy (Neurona Therapeutics) is a one-time dose of an injectable suspension of high-purity inhibitory interneurons that secrete the inhibitory neurotransmitter gamma-aminobutyric acid (GABA). The interneurons are intended to integrate and innervate on-target, providing long-term GABAergic inhibition to repair hyperexcitable neural networks.
Preclinical work in animal models of epilepsy has provided strong support for both the safety and the efficacy of boosting inhibition in the seizure focus using implanted human inhibitory interneurons.
This therapy is “potentially restorative instead of just destructive, like epilepsy surgery,” study investigator David Spencer, MD, professor of neurology and director of the Comprehensive Epilepsy Center, Oregon Health & Science University in Portland, said during a press briefing.
In the first two patients, the cells were implanted in the seizure focus using MRI guidance through a tiny opening in the back of the skull. The patients recovered overnight and went home the next day.
The first patient had a 9-year history of drug-resistant epilepsy and was averaging 30 seizures per month at baseline. Testing confirmed that the seizures were coming from a single focus on the right temporal lobe. The implant was uncomplicated, and the cells were delivered to the seizure focus on target.
To date, there have been no serious or unexpected adverse events from the implant. At 9 months of follow-up the patient has had a 93% reduction in seizures overall and is free of all seizures causing impairment of awareness, “which was the most debilitating seizure type for this patient,” Dr. Spencer noted.
Studies of brain metabolism in the area of the implant have shown favorable markers of increased inhibition and decreased inflammation. Cognitive testing at 6 months showed no worsening of memory function or cognition. And, in fact, there were some mild improvements, he said.
The second patient had an 8-year history of drug-resistant epilepsy, averaging 14 focal seizures per month at baseline. Testing also confirmed seizure onset in a single focus in the right temporal lobe and the cells were again implanted without complication on target. Five months after treatment, the patient has had a 94% reduction in seizures and no serious adverse events.
‘Hot off the press’
Epilepsy affects about 3.5 million people in the United States. About two-thirds of people with epilepsy get good control of their seizures using antiseizure medication.
For seizures that are uncontrolled with medication, identifying the seizure focus and removing it surgically can often result in seizure freedom in a high proportion of patients. But not all patients are candidates for epilepsy surgery, and for those who can have it the surgery itself carries some risks, including diminished cognition and memory.
“While these are still early days, we’re encouraged by the positive safety findings so far, and the early seizure responses” with neural cell therapy, Dr. Spencer told reporters.
Given the positive results in the first two patients, additional patients will be treated “with careful safety review all along the way. This is going to be rolling out over the next several years,” Dr. Spencer said. Patient recruitment is underway at epilepsy centers across the United States.
Briefing moderator Natalia Rost, MD, MPH, chair of the AAN science committee, said, “This is a true example of emerging science. It’s literally hot off the press,” and the preliminary results are “very promising.”
Dr. Rost, chief of the stroke division at Massachusetts General Hospital in Boston, noted that this type of cell therapy implant is “very novel and representative of where the field is moving, when no traditional solutions exist for common neurological problems.”
The study was sponsored by Neurona Therapeutics and funded in part by the California Institute for Regenerative Medicine. Dr. Beach and Dr. Spencer report no relevant financial relationships. Several investigators are employees of Neurona Therapeutics. Dr. Rost reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AAN 2023
Explanation proposed for long-COVID symptoms in the CNS
BOSTON – , according to a collaborative study presented at the 2023 annual meeting of the American Academy of Neurology.
Already documented in several other viral infections, such as influenza and human immunodeficiency virus, antigenic imprinting results in production of antibodies to previously encountered viral infections rather than to the immediate threat, according to Marianna Spatola, MD, PhD, a research fellow at the Ragon Institute, Harvard University, Cambridge, Mass.
Original antigenic sin
In the case of persistent neurologic symptoms after COVID, a condition known as neuroPASC (neurological postacute sequelae of SARS-CoV2 infection), antibodies produced for previously encountered coronaviruses rather than for SARS-CoV2 might explain most or all cases, according to the data Dr. Spatola presented.
The evidence for this explanation was drawn from a study of 112 patients evaluated months after an acute episode of COVID-19. Of these, 18 patients had persistent neurologic dysfunction. When compared with the 94 whose infection resolved without sequelae, the patients with prolonged neurologic impairments had relatively low systemic antibody response to SARS-CoV2. However, they showed relatively high antibody responses against other coronaviruses.
This is a pattern consistent with antigenic imprinting, a concept first described more than 60 years ago as original antigenic sin. When the immune system becomes imprinted with an antigen from the first encountered virus from a family of pathogens, it governs all subsequent antibody responses, according to several published studies that have described and evaluated this concept.
Additional evidence
In Dr. Spatola’s study, other differences, particularly in regard to the cerebrospinal fluid (CSF), further supported the role of antigenic imprinting as a cause of neuroPASC. For one, those with elevated immune responses to other common coronaviruses rather than SARS-CoV2 in the CSF relative to the periphery were more likely to have a bad outcome in regard to neurologic symptoms.
Moreover, the CSF in neuroPASC patients “was characterized by increased IgG1 and absence of IgM, suggesting compartmentalized humoral responses within the CSF through selective transfer of antibodies from the serum to the CSF across the blood-brain barrier rather than through intrathecal synthesis,” Dr. Spatola reported.
In the case of COVID-19, the propensity for antigenic imprinting is not difficult to understand.
“The common cold coronaviruses are pretty similar to SARS-CoV2, but they are not exactly the same,” Dr. Spatola said. Her work and studies by others suggest that when antigenic imprinting occurs, “it prevents full maturation of the antibody response.”
NeuroPASC is one of many manifestations of long COVID, but Dr. Spatola pointed out that the immune response in the CSF is unique and the causes of prolonged neurologic impairment after COVID-19 are likely to involve different mechanisms than other long-COVID symptoms.
“Antibodies in the brain are functionally different,” said Dr. Spatola, noting for example that antibody-directed defenses against viral threats show a greater relative reliance on phagocytosis. This might become important in the development of therapeutics for neurologic symptoms of long COVID.
A different phenomenon
The manifestations of neuroPASC are heterogeneous and can include confusion, cognitive dysfunction, headache, encephalitis, and other impairments. Neurologic symptoms occur during acute SARS-CoV2 infections, but neuroPASC appears to be a different phenomenon. These symptoms, which develop after the initial respiratory disease has resolved, were attributed by Dr. Spatola to persistent inflammation that is not necessarily directly related to ongoing infection.
“The reason why some patients develop neuroPASC is unknown, but I think the evidence has pointed to a role for the immune system rather than the virus itself,” Dr. Spatola said.
Currently, neuroPASC is a clinical diagnosis but Dr. Spatola and her coinvestigators are conducting research to identify biomarkers. A viable diagnostic test is not expected imminently. They have identified 150 different features with potential relevance to neuroPASC.
In their comparison of those who did relative to those who did not develop neuroPASC, the initial studies were undertaken 2-4 months after the acute COVID-19 symptoms had resolved. The patients with neuroPASC and those without neurologic sequelae have now been followed for 6-8 months, which Dr. Spatola said was too short to draw firm conclusions about outcomes.
An evolving concept
Despite the small sample size of this study, these are “very interesting data” for considering the pathogenesis of neuroPASC, which is “a concept that is still evolving,” according to Natalia S. Rost, MD, chief of the stroke division, department of neurology, Massachusetts General Hospital, Boston.
Applied to SARS-CoV2, the concept of original antigenic sin “is new” but Dr. Rost said that it might help differentiate neuroPASC from acute neurologic symptoms of COVID-19, which include stroke. She indicated that the work performed by Dr. Spatola and others might eventually explain the pathology while leading to treatment strategies. She cautioned that the concepts explored in this study “need to be further developed” through larger sample sizes and the exploration of other variables that support the hypothesis.
Dr. Spatola and Dr. Rost report no potential conflicts of interest.
BOSTON – , according to a collaborative study presented at the 2023 annual meeting of the American Academy of Neurology.
Already documented in several other viral infections, such as influenza and human immunodeficiency virus, antigenic imprinting results in production of antibodies to previously encountered viral infections rather than to the immediate threat, according to Marianna Spatola, MD, PhD, a research fellow at the Ragon Institute, Harvard University, Cambridge, Mass.
Original antigenic sin
In the case of persistent neurologic symptoms after COVID, a condition known as neuroPASC (neurological postacute sequelae of SARS-CoV2 infection), antibodies produced for previously encountered coronaviruses rather than for SARS-CoV2 might explain most or all cases, according to the data Dr. Spatola presented.
The evidence for this explanation was drawn from a study of 112 patients evaluated months after an acute episode of COVID-19. Of these, 18 patients had persistent neurologic dysfunction. When compared with the 94 whose infection resolved without sequelae, the patients with prolonged neurologic impairments had relatively low systemic antibody response to SARS-CoV2. However, they showed relatively high antibody responses against other coronaviruses.
This is a pattern consistent with antigenic imprinting, a concept first described more than 60 years ago as original antigenic sin. When the immune system becomes imprinted with an antigen from the first encountered virus from a family of pathogens, it governs all subsequent antibody responses, according to several published studies that have described and evaluated this concept.
Additional evidence
In Dr. Spatola’s study, other differences, particularly in regard to the cerebrospinal fluid (CSF), further supported the role of antigenic imprinting as a cause of neuroPASC. For one, those with elevated immune responses to other common coronaviruses rather than SARS-CoV2 in the CSF relative to the periphery were more likely to have a bad outcome in regard to neurologic symptoms.
Moreover, the CSF in neuroPASC patients “was characterized by increased IgG1 and absence of IgM, suggesting compartmentalized humoral responses within the CSF through selective transfer of antibodies from the serum to the CSF across the blood-brain barrier rather than through intrathecal synthesis,” Dr. Spatola reported.
In the case of COVID-19, the propensity for antigenic imprinting is not difficult to understand.
“The common cold coronaviruses are pretty similar to SARS-CoV2, but they are not exactly the same,” Dr. Spatola said. Her work and studies by others suggest that when antigenic imprinting occurs, “it prevents full maturation of the antibody response.”
NeuroPASC is one of many manifestations of long COVID, but Dr. Spatola pointed out that the immune response in the CSF is unique and the causes of prolonged neurologic impairment after COVID-19 are likely to involve different mechanisms than other long-COVID symptoms.
“Antibodies in the brain are functionally different,” said Dr. Spatola, noting for example that antibody-directed defenses against viral threats show a greater relative reliance on phagocytosis. This might become important in the development of therapeutics for neurologic symptoms of long COVID.
A different phenomenon
The manifestations of neuroPASC are heterogeneous and can include confusion, cognitive dysfunction, headache, encephalitis, and other impairments. Neurologic symptoms occur during acute SARS-CoV2 infections, but neuroPASC appears to be a different phenomenon. These symptoms, which develop after the initial respiratory disease has resolved, were attributed by Dr. Spatola to persistent inflammation that is not necessarily directly related to ongoing infection.
“The reason why some patients develop neuroPASC is unknown, but I think the evidence has pointed to a role for the immune system rather than the virus itself,” Dr. Spatola said.
Currently, neuroPASC is a clinical diagnosis but Dr. Spatola and her coinvestigators are conducting research to identify biomarkers. A viable diagnostic test is not expected imminently. They have identified 150 different features with potential relevance to neuroPASC.
In their comparison of those who did relative to those who did not develop neuroPASC, the initial studies were undertaken 2-4 months after the acute COVID-19 symptoms had resolved. The patients with neuroPASC and those without neurologic sequelae have now been followed for 6-8 months, which Dr. Spatola said was too short to draw firm conclusions about outcomes.
An evolving concept
Despite the small sample size of this study, these are “very interesting data” for considering the pathogenesis of neuroPASC, which is “a concept that is still evolving,” according to Natalia S. Rost, MD, chief of the stroke division, department of neurology, Massachusetts General Hospital, Boston.
Applied to SARS-CoV2, the concept of original antigenic sin “is new” but Dr. Rost said that it might help differentiate neuroPASC from acute neurologic symptoms of COVID-19, which include stroke. She indicated that the work performed by Dr. Spatola and others might eventually explain the pathology while leading to treatment strategies. She cautioned that the concepts explored in this study “need to be further developed” through larger sample sizes and the exploration of other variables that support the hypothesis.
Dr. Spatola and Dr. Rost report no potential conflicts of interest.
BOSTON – , according to a collaborative study presented at the 2023 annual meeting of the American Academy of Neurology.
Already documented in several other viral infections, such as influenza and human immunodeficiency virus, antigenic imprinting results in production of antibodies to previously encountered viral infections rather than to the immediate threat, according to Marianna Spatola, MD, PhD, a research fellow at the Ragon Institute, Harvard University, Cambridge, Mass.
Original antigenic sin
In the case of persistent neurologic symptoms after COVID, a condition known as neuroPASC (neurological postacute sequelae of SARS-CoV2 infection), antibodies produced for previously encountered coronaviruses rather than for SARS-CoV2 might explain most or all cases, according to the data Dr. Spatola presented.
The evidence for this explanation was drawn from a study of 112 patients evaluated months after an acute episode of COVID-19. Of these, 18 patients had persistent neurologic dysfunction. When compared with the 94 whose infection resolved without sequelae, the patients with prolonged neurologic impairments had relatively low systemic antibody response to SARS-CoV2. However, they showed relatively high antibody responses against other coronaviruses.
This is a pattern consistent with antigenic imprinting, a concept first described more than 60 years ago as original antigenic sin. When the immune system becomes imprinted with an antigen from the first encountered virus from a family of pathogens, it governs all subsequent antibody responses, according to several published studies that have described and evaluated this concept.
Additional evidence
In Dr. Spatola’s study, other differences, particularly in regard to the cerebrospinal fluid (CSF), further supported the role of antigenic imprinting as a cause of neuroPASC. For one, those with elevated immune responses to other common coronaviruses rather than SARS-CoV2 in the CSF relative to the periphery were more likely to have a bad outcome in regard to neurologic symptoms.
Moreover, the CSF in neuroPASC patients “was characterized by increased IgG1 and absence of IgM, suggesting compartmentalized humoral responses within the CSF through selective transfer of antibodies from the serum to the CSF across the blood-brain barrier rather than through intrathecal synthesis,” Dr. Spatola reported.
In the case of COVID-19, the propensity for antigenic imprinting is not difficult to understand.
“The common cold coronaviruses are pretty similar to SARS-CoV2, but they are not exactly the same,” Dr. Spatola said. Her work and studies by others suggest that when antigenic imprinting occurs, “it prevents full maturation of the antibody response.”
NeuroPASC is one of many manifestations of long COVID, but Dr. Spatola pointed out that the immune response in the CSF is unique and the causes of prolonged neurologic impairment after COVID-19 are likely to involve different mechanisms than other long-COVID symptoms.
“Antibodies in the brain are functionally different,” said Dr. Spatola, noting for example that antibody-directed defenses against viral threats show a greater relative reliance on phagocytosis. This might become important in the development of therapeutics for neurologic symptoms of long COVID.
A different phenomenon
The manifestations of neuroPASC are heterogeneous and can include confusion, cognitive dysfunction, headache, encephalitis, and other impairments. Neurologic symptoms occur during acute SARS-CoV2 infections, but neuroPASC appears to be a different phenomenon. These symptoms, which develop after the initial respiratory disease has resolved, were attributed by Dr. Spatola to persistent inflammation that is not necessarily directly related to ongoing infection.
“The reason why some patients develop neuroPASC is unknown, but I think the evidence has pointed to a role for the immune system rather than the virus itself,” Dr. Spatola said.
Currently, neuroPASC is a clinical diagnosis but Dr. Spatola and her coinvestigators are conducting research to identify biomarkers. A viable diagnostic test is not expected imminently. They have identified 150 different features with potential relevance to neuroPASC.
In their comparison of those who did relative to those who did not develop neuroPASC, the initial studies were undertaken 2-4 months after the acute COVID-19 symptoms had resolved. The patients with neuroPASC and those without neurologic sequelae have now been followed for 6-8 months, which Dr. Spatola said was too short to draw firm conclusions about outcomes.
An evolving concept
Despite the small sample size of this study, these are “very interesting data” for considering the pathogenesis of neuroPASC, which is “a concept that is still evolving,” according to Natalia S. Rost, MD, chief of the stroke division, department of neurology, Massachusetts General Hospital, Boston.
Applied to SARS-CoV2, the concept of original antigenic sin “is new” but Dr. Rost said that it might help differentiate neuroPASC from acute neurologic symptoms of COVID-19, which include stroke. She indicated that the work performed by Dr. Spatola and others might eventually explain the pathology while leading to treatment strategies. She cautioned that the concepts explored in this study “need to be further developed” through larger sample sizes and the exploration of other variables that support the hypothesis.
Dr. Spatola and Dr. Rost report no potential conflicts of interest.
FROM AAN 2023
The amazing brain
Last week, unbeknownst to most people, Dayton, Ohio, hosted the world championships of Winter Drumline. It’s a combination of percussion instruments, dance, and music, with a storyline. Think of it as a very fast-paced half-time show, with only percussion, in 6 minutes or less.
My daughter fell in love with it her second year of high school, and has participated in it through college. Her specialty is the pit – marimba, vibraphone, xylophone. This gives our house a cruise ship atmosphere when she comes home to practice on weekends.
Over the years my wife and I have gone to many of her shows and competitions, streamed others online, and always been amazed by the variety of costumes, choreography, music numbers, and overall themes different teams come up with. We’ve seen shows based on 1930s detective fiction, ocean life, westerns, science fiction, toxic waste, emotions, relationships, flamenco, pirate ships, and many others.
And, as always, I marvel at the human brain.
Only 2-3 pounds but still an amazing thing. The capacity for imagination is endless, and one of the things that got us where we are today. The ability to see things that don’t exist yet, and work out the details on how to get there. The pyramids, Petra, the Great Wall, flight, the steam engine, landing on the moon, the ISS. And, of course, Winter Drumline.
It’s a uniquely (as far as we know) human capacity. To look at a rock and envision what it might be carved into. To look at Jupiter and think of a way to get a probe there. To sit in an empty gym and imagine the floor covered with dozens of percussion instruments and their players, imagining what each will be playing and doing at a given moment.
It’s really a remarkable capacity when you think about it. I’m sure it originally began as a way to figure out where you might find shelter or food, or simply to outwit the other tribe. But it’s become so much more than that. Someone envisioned every movie you see, book you read, and the computer I’m writing this on.
In his 1968 novelization of “2001: A Space Odyssey” Arthur C. Clarke described the thoughts of the unknown civilization that had left the Monolith behind for us as “in all the galaxy they had found nothing more precious than Mind.”
I’d agree with that. Even after 30 years of learning about the 2-3 pounds of semi-solid tissue we all carry upstairs, and doing my best to treat its malfunctions, I’ve never ceased to be amazed by it.
I hope I always will be.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Last week, unbeknownst to most people, Dayton, Ohio, hosted the world championships of Winter Drumline. It’s a combination of percussion instruments, dance, and music, with a storyline. Think of it as a very fast-paced half-time show, with only percussion, in 6 minutes or less.
My daughter fell in love with it her second year of high school, and has participated in it through college. Her specialty is the pit – marimba, vibraphone, xylophone. This gives our house a cruise ship atmosphere when she comes home to practice on weekends.
Over the years my wife and I have gone to many of her shows and competitions, streamed others online, and always been amazed by the variety of costumes, choreography, music numbers, and overall themes different teams come up with. We’ve seen shows based on 1930s detective fiction, ocean life, westerns, science fiction, toxic waste, emotions, relationships, flamenco, pirate ships, and many others.
And, as always, I marvel at the human brain.
Only 2-3 pounds but still an amazing thing. The capacity for imagination is endless, and one of the things that got us where we are today. The ability to see things that don’t exist yet, and work out the details on how to get there. The pyramids, Petra, the Great Wall, flight, the steam engine, landing on the moon, the ISS. And, of course, Winter Drumline.
It’s a uniquely (as far as we know) human capacity. To look at a rock and envision what it might be carved into. To look at Jupiter and think of a way to get a probe there. To sit in an empty gym and imagine the floor covered with dozens of percussion instruments and their players, imagining what each will be playing and doing at a given moment.
It’s really a remarkable capacity when you think about it. I’m sure it originally began as a way to figure out where you might find shelter or food, or simply to outwit the other tribe. But it’s become so much more than that. Someone envisioned every movie you see, book you read, and the computer I’m writing this on.
In his 1968 novelization of “2001: A Space Odyssey” Arthur C. Clarke described the thoughts of the unknown civilization that had left the Monolith behind for us as “in all the galaxy they had found nothing more precious than Mind.”
I’d agree with that. Even after 30 years of learning about the 2-3 pounds of semi-solid tissue we all carry upstairs, and doing my best to treat its malfunctions, I’ve never ceased to be amazed by it.
I hope I always will be.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Last week, unbeknownst to most people, Dayton, Ohio, hosted the world championships of Winter Drumline. It’s a combination of percussion instruments, dance, and music, with a storyline. Think of it as a very fast-paced half-time show, with only percussion, in 6 minutes or less.
My daughter fell in love with it her second year of high school, and has participated in it through college. Her specialty is the pit – marimba, vibraphone, xylophone. This gives our house a cruise ship atmosphere when she comes home to practice on weekends.
Over the years my wife and I have gone to many of her shows and competitions, streamed others online, and always been amazed by the variety of costumes, choreography, music numbers, and overall themes different teams come up with. We’ve seen shows based on 1930s detective fiction, ocean life, westerns, science fiction, toxic waste, emotions, relationships, flamenco, pirate ships, and many others.
And, as always, I marvel at the human brain.
Only 2-3 pounds but still an amazing thing. The capacity for imagination is endless, and one of the things that got us where we are today. The ability to see things that don’t exist yet, and work out the details on how to get there. The pyramids, Petra, the Great Wall, flight, the steam engine, landing on the moon, the ISS. And, of course, Winter Drumline.
It’s a uniquely (as far as we know) human capacity. To look at a rock and envision what it might be carved into. To look at Jupiter and think of a way to get a probe there. To sit in an empty gym and imagine the floor covered with dozens of percussion instruments and their players, imagining what each will be playing and doing at a given moment.
It’s really a remarkable capacity when you think about it. I’m sure it originally began as a way to figure out where you might find shelter or food, or simply to outwit the other tribe. But it’s become so much more than that. Someone envisioned every movie you see, book you read, and the computer I’m writing this on.
In his 1968 novelization of “2001: A Space Odyssey” Arthur C. Clarke described the thoughts of the unknown civilization that had left the Monolith behind for us as “in all the galaxy they had found nothing more precious than Mind.”
I’d agree with that. Even after 30 years of learning about the 2-3 pounds of semi-solid tissue we all carry upstairs, and doing my best to treat its malfunctions, I’ve never ceased to be amazed by it.
I hope I always will be.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Proposed Medicare bill would raise docs’ pay with inflation
Introduced by four physician U.S. House representatives, HR 2474 would link Medicare fee schedule updates to the Medicare Economic Index, a measure of inflation related to physicians’ practice costs and wages.
That’s a long-sought goal of the American Medical Association, which is leading 120 state medical societies and medical specialty groups in championing the bill.
The legislation is essential to enabling physician practices to better absorb payment distributions triggered by budget neutrality rules, performance adjustments, and periods of high inflation, the groups wrote in a joint letter sent to the bill’s sponsors. The sponsors say they hope the legislation will improve access to care, as low reimbursements cause some physicians to limit their number of Medicare patients.
Physicians groups for years have urged federal lawmakers to scrap short-term fixes staving off Medicare pay cuts in favor of permanent reforms. Unlike nearly all other Medicare clinicians including hospitals, physicians’ Medicare payment updates aren’t currently tied to inflation.
Adjusted for inflation, Medicare payments to physicians have declined 26% between 2001 and 2023, including a 2% payment reduction in 2023, according to the AMA. Small and rural physician practices have been disproportionately affected by these reductions, as have doctors treating low-income or uninsured patients, the AMA said.
Last month, an influential federal advisory panel recommended permanently tying Medicare physician pay increases to inflation. Clinicians’ cost of providing services, measured by the Medicare Economic Index, rose by 2.6% in 2021 and are estimated to have risen 4.7% in 2022, significantly more than in recent years, the Medicare Payment Advisory Commission said.
A version of this article originally appeared on Medscape.com.
Introduced by four physician U.S. House representatives, HR 2474 would link Medicare fee schedule updates to the Medicare Economic Index, a measure of inflation related to physicians’ practice costs and wages.
That’s a long-sought goal of the American Medical Association, which is leading 120 state medical societies and medical specialty groups in championing the bill.
The legislation is essential to enabling physician practices to better absorb payment distributions triggered by budget neutrality rules, performance adjustments, and periods of high inflation, the groups wrote in a joint letter sent to the bill’s sponsors. The sponsors say they hope the legislation will improve access to care, as low reimbursements cause some physicians to limit their number of Medicare patients.
Physicians groups for years have urged federal lawmakers to scrap short-term fixes staving off Medicare pay cuts in favor of permanent reforms. Unlike nearly all other Medicare clinicians including hospitals, physicians’ Medicare payment updates aren’t currently tied to inflation.
Adjusted for inflation, Medicare payments to physicians have declined 26% between 2001 and 2023, including a 2% payment reduction in 2023, according to the AMA. Small and rural physician practices have been disproportionately affected by these reductions, as have doctors treating low-income or uninsured patients, the AMA said.
Last month, an influential federal advisory panel recommended permanently tying Medicare physician pay increases to inflation. Clinicians’ cost of providing services, measured by the Medicare Economic Index, rose by 2.6% in 2021 and are estimated to have risen 4.7% in 2022, significantly more than in recent years, the Medicare Payment Advisory Commission said.
A version of this article originally appeared on Medscape.com.
Introduced by four physician U.S. House representatives, HR 2474 would link Medicare fee schedule updates to the Medicare Economic Index, a measure of inflation related to physicians’ practice costs and wages.
That’s a long-sought goal of the American Medical Association, which is leading 120 state medical societies and medical specialty groups in championing the bill.
The legislation is essential to enabling physician practices to better absorb payment distributions triggered by budget neutrality rules, performance adjustments, and periods of high inflation, the groups wrote in a joint letter sent to the bill’s sponsors. The sponsors say they hope the legislation will improve access to care, as low reimbursements cause some physicians to limit their number of Medicare patients.
Physicians groups for years have urged federal lawmakers to scrap short-term fixes staving off Medicare pay cuts in favor of permanent reforms. Unlike nearly all other Medicare clinicians including hospitals, physicians’ Medicare payment updates aren’t currently tied to inflation.
Adjusted for inflation, Medicare payments to physicians have declined 26% between 2001 and 2023, including a 2% payment reduction in 2023, according to the AMA. Small and rural physician practices have been disproportionately affected by these reductions, as have doctors treating low-income or uninsured patients, the AMA said.
Last month, an influential federal advisory panel recommended permanently tying Medicare physician pay increases to inflation. Clinicians’ cost of providing services, measured by the Medicare Economic Index, rose by 2.6% in 2021 and are estimated to have risen 4.7% in 2022, significantly more than in recent years, the Medicare Payment Advisory Commission said.
A version of this article originally appeared on Medscape.com.
Surgeons, intensivists earn more than do colleagues from private insurance
General and orthopedic surgeons and intensivists earn the highest net reimbursements from private U.S. insurers, a new report estimates.
On average in 2021, they were paid $5.8 million, $4.9 million, and $3.3 million, respectively, according to figures compiled by AMN Healthcare, a Dallas-based health staffing company.
None of 15 other physician specialties topped $3 million in net reimbursement on average, and three – dermatology, pediatrics, and family medicine – didn’t reach $1 million.
The report doesn’t include data about reimbursement from Medicare and Medicaid, and its numbers assume that 50% of insurance claims are denied. Denial rates differ from practice to practice.
Still, the findings offer a “benchmark tool” to help clinicians understand how they rank against their peers, Linda Murphy, president of AMN Healthcare’s Revenue Cycle Solutions division, said in an interview.
This is the first year that the company has calculated physician reimbursement levels by using claim and clearinghouse data, Ms. Murphy said. Previously, a division of the firm compiled data by surveying chief financial officers from hospitals.
The report’s estimate that insurers deny 50% of claims is “conservative,” Ms. Murphy said. Miscoding is a significant factor behind that number.
The estimated 2021 net private insurance reimbursements by specialty for direct services, assuming a 50% denial rate:
- Anesthesiology: $1,665,510
- Cardiology: $1,703,013
- Critical Care (intensivist): $3,338,656
- Dermatology: $729,107
- Family medicine: $697,094
- Gastroenterology: $2,765,110
- Internal medicine: $1,297,200
- Neurology: $1,390,181
- Obstetrician/gynecology: $1,880,888
- Otolaryngology: $2,095,277
- Pediatrics: $661,552
- Psychiatry: $1,348,730
- Pulmonology: $1,561,617
- Radiology: $1,015,750
- Rheumatology: $1,705,140
- General surgery: $5,834,508
- Orthopedic surgery: $4,904,757
- Urology: $2,943,381
Among 18 physician specialties overall, the report estimated that the average net reimbursement in 2021 was $1.9 million.
The report also estimated that the net reimbursement amounts at $875,140 for certified registered nurse anesthetists and $388,696 for nurse practitioners.
Surprisingly, Ms. Murphy said, there’s “a really large swing” among reimbursement levels for individual specialties. The quartile of cardiologists with the lowest level of reimbursement, for example, submitted $2.1 million in claims in 2021, netting about $1 million at a 50% denial rate versus the $7.3 million made by those in the highest quartile, netting about $3.6 million.
The gap seems to be due to regional variations, she said, adding that a rural cardiologist will have different billing practices than does one practicing in New York City.
The quartile of general surgeons with the highest reimbursement levels billed for $21.1 million on average in 2021, making about $10.5 million at a 50% denial rate. The lowest quartile billed for $5.5 million, making about $2.7 million at a 50% denial rate.
The report noted that primary care physicians – that is, family medicine, internal medicine, and pediatrics specialists – have much lower levels of reimbursement, compared with most other specialties. But the work of primary care physicians “may lead to considerable ‘downstream revenue’ through the hospital admissions, tests and treatment they order.”
A previous analysis by a division of AMN Healthcare found that primary care physicians, on average, generate $2,113,273 a year in net annual revenue for their affiliated hospitals, nearing the $2,446,429 in net annual hospital revenue generated by specialists.
AMN Healthcare is preparing another report that will examine Medicare reimbursements, Ms. Murphy said. According to the new report, payments by nonprivate insurers amount to about one-third of the total amount of reimbursement by commercial insurers.
A version of this article originally appeared on Medscape.com.
General and orthopedic surgeons and intensivists earn the highest net reimbursements from private U.S. insurers, a new report estimates.
On average in 2021, they were paid $5.8 million, $4.9 million, and $3.3 million, respectively, according to figures compiled by AMN Healthcare, a Dallas-based health staffing company.
None of 15 other physician specialties topped $3 million in net reimbursement on average, and three – dermatology, pediatrics, and family medicine – didn’t reach $1 million.
The report doesn’t include data about reimbursement from Medicare and Medicaid, and its numbers assume that 50% of insurance claims are denied. Denial rates differ from practice to practice.
Still, the findings offer a “benchmark tool” to help clinicians understand how they rank against their peers, Linda Murphy, president of AMN Healthcare’s Revenue Cycle Solutions division, said in an interview.
This is the first year that the company has calculated physician reimbursement levels by using claim and clearinghouse data, Ms. Murphy said. Previously, a division of the firm compiled data by surveying chief financial officers from hospitals.
The report’s estimate that insurers deny 50% of claims is “conservative,” Ms. Murphy said. Miscoding is a significant factor behind that number.
The estimated 2021 net private insurance reimbursements by specialty for direct services, assuming a 50% denial rate:
- Anesthesiology: $1,665,510
- Cardiology: $1,703,013
- Critical Care (intensivist): $3,338,656
- Dermatology: $729,107
- Family medicine: $697,094
- Gastroenterology: $2,765,110
- Internal medicine: $1,297,200
- Neurology: $1,390,181
- Obstetrician/gynecology: $1,880,888
- Otolaryngology: $2,095,277
- Pediatrics: $661,552
- Psychiatry: $1,348,730
- Pulmonology: $1,561,617
- Radiology: $1,015,750
- Rheumatology: $1,705,140
- General surgery: $5,834,508
- Orthopedic surgery: $4,904,757
- Urology: $2,943,381
Among 18 physician specialties overall, the report estimated that the average net reimbursement in 2021 was $1.9 million.
The report also estimated that the net reimbursement amounts at $875,140 for certified registered nurse anesthetists and $388,696 for nurse practitioners.
Surprisingly, Ms. Murphy said, there’s “a really large swing” among reimbursement levels for individual specialties. The quartile of cardiologists with the lowest level of reimbursement, for example, submitted $2.1 million in claims in 2021, netting about $1 million at a 50% denial rate versus the $7.3 million made by those in the highest quartile, netting about $3.6 million.
The gap seems to be due to regional variations, she said, adding that a rural cardiologist will have different billing practices than does one practicing in New York City.
The quartile of general surgeons with the highest reimbursement levels billed for $21.1 million on average in 2021, making about $10.5 million at a 50% denial rate. The lowest quartile billed for $5.5 million, making about $2.7 million at a 50% denial rate.
The report noted that primary care physicians – that is, family medicine, internal medicine, and pediatrics specialists – have much lower levels of reimbursement, compared with most other specialties. But the work of primary care physicians “may lead to considerable ‘downstream revenue’ through the hospital admissions, tests and treatment they order.”
A previous analysis by a division of AMN Healthcare found that primary care physicians, on average, generate $2,113,273 a year in net annual revenue for their affiliated hospitals, nearing the $2,446,429 in net annual hospital revenue generated by specialists.
AMN Healthcare is preparing another report that will examine Medicare reimbursements, Ms. Murphy said. According to the new report, payments by nonprivate insurers amount to about one-third of the total amount of reimbursement by commercial insurers.
A version of this article originally appeared on Medscape.com.
General and orthopedic surgeons and intensivists earn the highest net reimbursements from private U.S. insurers, a new report estimates.
On average in 2021, they were paid $5.8 million, $4.9 million, and $3.3 million, respectively, according to figures compiled by AMN Healthcare, a Dallas-based health staffing company.
None of 15 other physician specialties topped $3 million in net reimbursement on average, and three – dermatology, pediatrics, and family medicine – didn’t reach $1 million.
The report doesn’t include data about reimbursement from Medicare and Medicaid, and its numbers assume that 50% of insurance claims are denied. Denial rates differ from practice to practice.
Still, the findings offer a “benchmark tool” to help clinicians understand how they rank against their peers, Linda Murphy, president of AMN Healthcare’s Revenue Cycle Solutions division, said in an interview.
This is the first year that the company has calculated physician reimbursement levels by using claim and clearinghouse data, Ms. Murphy said. Previously, a division of the firm compiled data by surveying chief financial officers from hospitals.
The report’s estimate that insurers deny 50% of claims is “conservative,” Ms. Murphy said. Miscoding is a significant factor behind that number.
The estimated 2021 net private insurance reimbursements by specialty for direct services, assuming a 50% denial rate:
- Anesthesiology: $1,665,510
- Cardiology: $1,703,013
- Critical Care (intensivist): $3,338,656
- Dermatology: $729,107
- Family medicine: $697,094
- Gastroenterology: $2,765,110
- Internal medicine: $1,297,200
- Neurology: $1,390,181
- Obstetrician/gynecology: $1,880,888
- Otolaryngology: $2,095,277
- Pediatrics: $661,552
- Psychiatry: $1,348,730
- Pulmonology: $1,561,617
- Radiology: $1,015,750
- Rheumatology: $1,705,140
- General surgery: $5,834,508
- Orthopedic surgery: $4,904,757
- Urology: $2,943,381
Among 18 physician specialties overall, the report estimated that the average net reimbursement in 2021 was $1.9 million.
The report also estimated that the net reimbursement amounts at $875,140 for certified registered nurse anesthetists and $388,696 for nurse practitioners.
Surprisingly, Ms. Murphy said, there’s “a really large swing” among reimbursement levels for individual specialties. The quartile of cardiologists with the lowest level of reimbursement, for example, submitted $2.1 million in claims in 2021, netting about $1 million at a 50% denial rate versus the $7.3 million made by those in the highest quartile, netting about $3.6 million.
The gap seems to be due to regional variations, she said, adding that a rural cardiologist will have different billing practices than does one practicing in New York City.
The quartile of general surgeons with the highest reimbursement levels billed for $21.1 million on average in 2021, making about $10.5 million at a 50% denial rate. The lowest quartile billed for $5.5 million, making about $2.7 million at a 50% denial rate.
The report noted that primary care physicians – that is, family medicine, internal medicine, and pediatrics specialists – have much lower levels of reimbursement, compared with most other specialties. But the work of primary care physicians “may lead to considerable ‘downstream revenue’ through the hospital admissions, tests and treatment they order.”
A previous analysis by a division of AMN Healthcare found that primary care physicians, on average, generate $2,113,273 a year in net annual revenue for their affiliated hospitals, nearing the $2,446,429 in net annual hospital revenue generated by specialists.
AMN Healthcare is preparing another report that will examine Medicare reimbursements, Ms. Murphy said. According to the new report, payments by nonprivate insurers amount to about one-third of the total amount of reimbursement by commercial insurers.
A version of this article originally appeared on Medscape.com.
Early menopause, delayed HT tied to Alzheimer’s pathology
Investigators found elevated levels of tau protein in the brains of women who initiated HT more than 5 years after menopause onset, while those who started the therapy earlier had normal levels.
Tau levels were also higher in women who started menopause before age 45, either naturally or following surgery, but only in those who already had high levels of beta-amyloid.
The findings were published online in JAMA Neurology.
Hotly debated
Previous research has suggested the timing of menopause and HT initiation may be associated with AD. However, the current research is the first to suggest tau deposition may explain that link.
“There have been a lot of conflicting findings around whether HT induces risk for Alzheimer’s disease dementia or not, and – at least in our hands – our observational evidence suggests that any risk is fairly limited to those rarer cases when women might delay their initiation of HT considerably,” senior investigator Rachel Buckley, PhD, assistant investigator in neurology at Massachusetts General Hospital and assistant professor of neurology at Harvard Medical School, Boston, told this news organization.
The link between HT, dementia, and cognitive decline has been hotly debated since the initial release of findings from the Women’s Health Initiative Memory Study, reported 20 years ago.
Since then, dozens of studies have yielded conflicting evidence about HT and AD risk, with some showing a protective effect and others showing the treatment may increase AD risk.
For this study, researchers analyzed data from 292 cognitively unimpaired participants (66.1% female) in the Wisconsin Registry for Alzheimer Prevention. About half of the women had received HT.
Women had higher levels of tau measured on PET imaging than age-matched males, even after adjustment for APOE status and other potential confounders.
Higher tau levels were found in those with an earlier age at menopause (P < .001) and HT use (P = .008) compared with male sex; later menopause onset; or HT nonuse – but only in patients who also had a higher beta-amyloid burden.
Late initiation of HT (> 5 years following age at menopause) was associated with higher tau compared with early initiation (P = .001), regardless of amyloid levels.
Surprising finding
Although researchers expected to find that surgical history (specifically oophorectomy) might have a greater impact on risk, that wasn’t the case.
“Given that bilateral oophorectomy involves the removal of both ovaries, and the immediate ceasing of estrogen production, I had expected this to be the primary driver of higher tau levels,” Dr. Buckley said. “But early age at menopause – regardless of whether the genesis was natural or surgical – seemed to have similar impacts.”
These findings are the latest from Dr. Buckley’s group that indicate that women tend to have higher levels of tau than men, regardless of preexisting amyloid burden in the brain.
“We see this in healthy older women, women with dementia, and even in postmortem cases,” Dr. Buckley said. “It really remains to be seen whether women tend to accumulate tau faster in the brain than men, or whether this is simply a one-shot phenomenon that we see in observational studies at the baseline.”
“One could really flip this finding on its head and suggest that women are truly resilient to the disease,” she continued. “That is, they can hold much more tau in their brain and remain well enough to be studied, unlike men.”
Among the study’s limitations is that the data were collected at a single time point and did not include information on subsequent Alzheimer’s diagnosis or cognitive decline.
“It is important to remember that the participants in this study were not as representative of the general population in the United States, so we cannot extrapolate our findings to women from a range of socioeconomic, racial and ethnic backgrounds or education levels,” she said.
The study’s observational design left researchers unable to demonstrate causation. What’s more, the findings don’t support the assertion that hormone therapy may protect against AD, Dr. Buckley added.
“I would more confidently say that evidence from our work, and that of many others, seems to suggest that HT initiated around the time of menopause may be benign – not providing benefit or risk, at least in the context of Alzheimer’s disease risk,” she said.
Another important takeaway from the study, Dr. Buckley said, is that not all women are at high risk for AD.
“Often the headlines might make you think that most women are destined to progress to dementia, but this simply is not the case,” Dr. Buckley said. “We are now starting to really drill down on what might elevate risk for AD in women and use this information to better inform clinical trials and doctors on how best to think about treating these higher-risk groups.”
New mechanism?
Commenting on the findings, Pauline Maki, PhD, professor of psychiatry, psychology and obstetrics & gynecology at the University of Illinois at Chicago, called the study “interesting.”
“It identifies a new mechanism in humans that could underlie a possible link between sex hormones and dementia,” Dr. Maki said.
However, Dr. Maki noted that the study wasn’t randomized and information about menopause onset was self-reported.
“We must remember that many of the hypotheses about hormone therapy and brain health that came from observational studies were not validated in randomized trials, including the hypothesis that hormone therapy prevents dementia,” she said.
The findings don’t resolve the debate over hormone therapy and AD risk and point to the need for randomized, prospective studies on the topic, Dr. Maki added. Still, she said, they underscore the gender disparity in AD risk.
“It’s a good reminder to clinicians that women have a higher lifetime risk of Alzheimer’s disease and should be advised on factors that might lower their risk,” she said.
The study was funded by the National Institutes of Health. Dr. Buckley reports no relevant financial conflicts. Dr. Maki serves on the advisory boards for Astellas, Bayer, Johnson & Johnson, consults for Pfizer and Mithra, and has equity in Estrigenix, Midi-Health, and Alloy.
A version of this article originally appeared on Medscape.com.
Investigators found elevated levels of tau protein in the brains of women who initiated HT more than 5 years after menopause onset, while those who started the therapy earlier had normal levels.
Tau levels were also higher in women who started menopause before age 45, either naturally or following surgery, but only in those who already had high levels of beta-amyloid.
The findings were published online in JAMA Neurology.
Hotly debated
Previous research has suggested the timing of menopause and HT initiation may be associated with AD. However, the current research is the first to suggest tau deposition may explain that link.
“There have been a lot of conflicting findings around whether HT induces risk for Alzheimer’s disease dementia or not, and – at least in our hands – our observational evidence suggests that any risk is fairly limited to those rarer cases when women might delay their initiation of HT considerably,” senior investigator Rachel Buckley, PhD, assistant investigator in neurology at Massachusetts General Hospital and assistant professor of neurology at Harvard Medical School, Boston, told this news organization.
The link between HT, dementia, and cognitive decline has been hotly debated since the initial release of findings from the Women’s Health Initiative Memory Study, reported 20 years ago.
Since then, dozens of studies have yielded conflicting evidence about HT and AD risk, with some showing a protective effect and others showing the treatment may increase AD risk.
For this study, researchers analyzed data from 292 cognitively unimpaired participants (66.1% female) in the Wisconsin Registry for Alzheimer Prevention. About half of the women had received HT.
Women had higher levels of tau measured on PET imaging than age-matched males, even after adjustment for APOE status and other potential confounders.
Higher tau levels were found in those with an earlier age at menopause (P < .001) and HT use (P = .008) compared with male sex; later menopause onset; or HT nonuse – but only in patients who also had a higher beta-amyloid burden.
Late initiation of HT (> 5 years following age at menopause) was associated with higher tau compared with early initiation (P = .001), regardless of amyloid levels.
Surprising finding
Although researchers expected to find that surgical history (specifically oophorectomy) might have a greater impact on risk, that wasn’t the case.
“Given that bilateral oophorectomy involves the removal of both ovaries, and the immediate ceasing of estrogen production, I had expected this to be the primary driver of higher tau levels,” Dr. Buckley said. “But early age at menopause – regardless of whether the genesis was natural or surgical – seemed to have similar impacts.”
These findings are the latest from Dr. Buckley’s group that indicate that women tend to have higher levels of tau than men, regardless of preexisting amyloid burden in the brain.
“We see this in healthy older women, women with dementia, and even in postmortem cases,” Dr. Buckley said. “It really remains to be seen whether women tend to accumulate tau faster in the brain than men, or whether this is simply a one-shot phenomenon that we see in observational studies at the baseline.”
“One could really flip this finding on its head and suggest that women are truly resilient to the disease,” she continued. “That is, they can hold much more tau in their brain and remain well enough to be studied, unlike men.”
Among the study’s limitations is that the data were collected at a single time point and did not include information on subsequent Alzheimer’s diagnosis or cognitive decline.
“It is important to remember that the participants in this study were not as representative of the general population in the United States, so we cannot extrapolate our findings to women from a range of socioeconomic, racial and ethnic backgrounds or education levels,” she said.
The study’s observational design left researchers unable to demonstrate causation. What’s more, the findings don’t support the assertion that hormone therapy may protect against AD, Dr. Buckley added.
“I would more confidently say that evidence from our work, and that of many others, seems to suggest that HT initiated around the time of menopause may be benign – not providing benefit or risk, at least in the context of Alzheimer’s disease risk,” she said.
Another important takeaway from the study, Dr. Buckley said, is that not all women are at high risk for AD.
“Often the headlines might make you think that most women are destined to progress to dementia, but this simply is not the case,” Dr. Buckley said. “We are now starting to really drill down on what might elevate risk for AD in women and use this information to better inform clinical trials and doctors on how best to think about treating these higher-risk groups.”
New mechanism?
Commenting on the findings, Pauline Maki, PhD, professor of psychiatry, psychology and obstetrics & gynecology at the University of Illinois at Chicago, called the study “interesting.”
“It identifies a new mechanism in humans that could underlie a possible link between sex hormones and dementia,” Dr. Maki said.
However, Dr. Maki noted that the study wasn’t randomized and information about menopause onset was self-reported.
“We must remember that many of the hypotheses about hormone therapy and brain health that came from observational studies were not validated in randomized trials, including the hypothesis that hormone therapy prevents dementia,” she said.
The findings don’t resolve the debate over hormone therapy and AD risk and point to the need for randomized, prospective studies on the topic, Dr. Maki added. Still, she said, they underscore the gender disparity in AD risk.
“It’s a good reminder to clinicians that women have a higher lifetime risk of Alzheimer’s disease and should be advised on factors that might lower their risk,” she said.
The study was funded by the National Institutes of Health. Dr. Buckley reports no relevant financial conflicts. Dr. Maki serves on the advisory boards for Astellas, Bayer, Johnson & Johnson, consults for Pfizer and Mithra, and has equity in Estrigenix, Midi-Health, and Alloy.
A version of this article originally appeared on Medscape.com.
Investigators found elevated levels of tau protein in the brains of women who initiated HT more than 5 years after menopause onset, while those who started the therapy earlier had normal levels.
Tau levels were also higher in women who started menopause before age 45, either naturally or following surgery, but only in those who already had high levels of beta-amyloid.
The findings were published online in JAMA Neurology.
Hotly debated
Previous research has suggested the timing of menopause and HT initiation may be associated with AD. However, the current research is the first to suggest tau deposition may explain that link.
“There have been a lot of conflicting findings around whether HT induces risk for Alzheimer’s disease dementia or not, and – at least in our hands – our observational evidence suggests that any risk is fairly limited to those rarer cases when women might delay their initiation of HT considerably,” senior investigator Rachel Buckley, PhD, assistant investigator in neurology at Massachusetts General Hospital and assistant professor of neurology at Harvard Medical School, Boston, told this news organization.
The link between HT, dementia, and cognitive decline has been hotly debated since the initial release of findings from the Women’s Health Initiative Memory Study, reported 20 years ago.
Since then, dozens of studies have yielded conflicting evidence about HT and AD risk, with some showing a protective effect and others showing the treatment may increase AD risk.
For this study, researchers analyzed data from 292 cognitively unimpaired participants (66.1% female) in the Wisconsin Registry for Alzheimer Prevention. About half of the women had received HT.
Women had higher levels of tau measured on PET imaging than age-matched males, even after adjustment for APOE status and other potential confounders.
Higher tau levels were found in those with an earlier age at menopause (P < .001) and HT use (P = .008) compared with male sex; later menopause onset; or HT nonuse – but only in patients who also had a higher beta-amyloid burden.
Late initiation of HT (> 5 years following age at menopause) was associated with higher tau compared with early initiation (P = .001), regardless of amyloid levels.
Surprising finding
Although researchers expected to find that surgical history (specifically oophorectomy) might have a greater impact on risk, that wasn’t the case.
“Given that bilateral oophorectomy involves the removal of both ovaries, and the immediate ceasing of estrogen production, I had expected this to be the primary driver of higher tau levels,” Dr. Buckley said. “But early age at menopause – regardless of whether the genesis was natural or surgical – seemed to have similar impacts.”
These findings are the latest from Dr. Buckley’s group that indicate that women tend to have higher levels of tau than men, regardless of preexisting amyloid burden in the brain.
“We see this in healthy older women, women with dementia, and even in postmortem cases,” Dr. Buckley said. “It really remains to be seen whether women tend to accumulate tau faster in the brain than men, or whether this is simply a one-shot phenomenon that we see in observational studies at the baseline.”
“One could really flip this finding on its head and suggest that women are truly resilient to the disease,” she continued. “That is, they can hold much more tau in their brain and remain well enough to be studied, unlike men.”
Among the study’s limitations is that the data were collected at a single time point and did not include information on subsequent Alzheimer’s diagnosis or cognitive decline.
“It is important to remember that the participants in this study were not as representative of the general population in the United States, so we cannot extrapolate our findings to women from a range of socioeconomic, racial and ethnic backgrounds or education levels,” she said.
The study’s observational design left researchers unable to demonstrate causation. What’s more, the findings don’t support the assertion that hormone therapy may protect against AD, Dr. Buckley added.
“I would more confidently say that evidence from our work, and that of many others, seems to suggest that HT initiated around the time of menopause may be benign – not providing benefit or risk, at least in the context of Alzheimer’s disease risk,” she said.
Another important takeaway from the study, Dr. Buckley said, is that not all women are at high risk for AD.
“Often the headlines might make you think that most women are destined to progress to dementia, but this simply is not the case,” Dr. Buckley said. “We are now starting to really drill down on what might elevate risk for AD in women and use this information to better inform clinical trials and doctors on how best to think about treating these higher-risk groups.”
New mechanism?
Commenting on the findings, Pauline Maki, PhD, professor of psychiatry, psychology and obstetrics & gynecology at the University of Illinois at Chicago, called the study “interesting.”
“It identifies a new mechanism in humans that could underlie a possible link between sex hormones and dementia,” Dr. Maki said.
However, Dr. Maki noted that the study wasn’t randomized and information about menopause onset was self-reported.
“We must remember that many of the hypotheses about hormone therapy and brain health that came from observational studies were not validated in randomized trials, including the hypothesis that hormone therapy prevents dementia,” she said.
The findings don’t resolve the debate over hormone therapy and AD risk and point to the need for randomized, prospective studies on the topic, Dr. Maki added. Still, she said, they underscore the gender disparity in AD risk.
“It’s a good reminder to clinicians that women have a higher lifetime risk of Alzheimer’s disease and should be advised on factors that might lower their risk,” she said.
The study was funded by the National Institutes of Health. Dr. Buckley reports no relevant financial conflicts. Dr. Maki serves on the advisory boards for Astellas, Bayer, Johnson & Johnson, consults for Pfizer and Mithra, and has equity in Estrigenix, Midi-Health, and Alloy.
A version of this article originally appeared on Medscape.com.
FROM JAMA NEUROLOGY
‘Bony’ stroke: Bone defects can cause recurrent stroke
These so-called “bony” strokes constitute a possible cause of recurrent ischemia in the same vascular territory as previous episodes, note the authors, led by Johanna Haertl, MD, Technical University of Munich.
“In patients with recurrent strokes in one vascular territory the presence of a symptomatic anatomic bone or cartilage anomaly may be considered as a differential diagnosis after sufficient exclusion of competing etiologies of an ischemic stroke,” they conclude.
“Due to the possibly high risk of stroke recurrence and potentially causative treatment options, bony strokes seem to be highly relevant for clinical practice,” they add.
The study was published online in the journal Stroke.
In their report, investigators explain that diagnosis of a bony stroke is based on a combination of imaging devices including CT, MRI, angiography, and sonography of brain-supplying vessels.
In addition to conventional static imaging, dynamic imaging modalities with the patients’ head in a fixed rotation or reclination has been shown to be useful as this enables the detection of a compressive effect on brain-supplying arteries caused by head movement.
They note that these bony strokes have been described previously – mainly as single case reports or small case series – but a systematic evaluation of each anatomical type of bony stroke is currently lacking.
For the current paper, the authors describe the identification and therapeutic workup of six patients with a bony stroke among 4,200 patients with ischemic stroke treated from January 2017 to March 2022 at their comprehensive stroke care center, constituting an incidence of 0.14%.
But they caution, “Given our retrospective study design, the method of patient acquisition, and the lack of systematic evaluation of bony strokes during acute stroke treatment, epidemiologic conclusions can be drawn only very carefully.”
In each of these six cases, the recurrent stroke was found to be caused by large-artery embolism from mechanical stress by bone or cartilage anomalies on arteries supplying the brain.
“Our case series aims to raise awareness for the rare entity of bony strokes, emphasizing the necessity to evaluate structural bone or cartilage lesions as a possible cause of ischemic stroke in patients with stroke recurrence of unknown cause in one vascular territory. We further aim on highlighting individual diagnostic and therapeutic options,” they state.
They note that it has previously been suggested that ischemic strokes based on bone or cartilage anomalies are more common in the relatively young patients with stroke, which is in line with their current patient data (mean age, 55 years), but this may reflect a selection bias.
A medical history with an association between changes in the head position and the occurrence of ischemic stroke may also raise awareness of the possibility of a bony stroke.
The authors outline treatment options for bony stroke, which they describe as diverse: They include conservative treatment, endovascular stenting, occlusion of the affected vessel, surgical bypass, and bone/cartilage removal.
From a pathophysiologic point of view, it seems reasonable to eliminate a causative lesion by surgical removal of the mechanical stressor, they note.
In cases of vascular stenting, they caution that the remainder of the mechanical stressor may provoke stent fracture and recurrent stroke, which occurred in two of their patients, a situation that may be observed more often in the future with the increasing use of vascular stenting.
The authors report that, compared with annual stroke rates in atrial fibrillation patients, stroke recurrence in this patient cohort ahead of definite treatment was high (cumulative 2.14 strokes per year). And as no patient had further ischemia after treatment, they argue that diagnosis and appropriate treatment of bony stroke may reduce or even eliminate the risk for future stroke recurrence.
They propose that for the diagnosis an exact medical history, with emphasis on a possible change of head position at the onset of stroke symptoms, is useful.
Furthermore, previously acquired diagnostic scans including CT or MRI may be evaluated for a symptomatic vessel-bone or cartilage contact. Then, the additional application of dynamic imaging modalities, including dynamic ultrasound of brain-supplying vessels and CT-angiography, may be discussed.
“An appropriate diagnosis and the evaluation of individual and interdisciplinary treatment options seem crucial to prevent recurrent ischemic strokes. Future prospective trials seem mandatory to optimize patient care,” they conclude.
The study had no specific funding. Coauthor Jan S. Kirschke, MD, received research support from the German Research Foundation, Bonescreen, H2020 European Research Council, and Philips. The other authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
These so-called “bony” strokes constitute a possible cause of recurrent ischemia in the same vascular territory as previous episodes, note the authors, led by Johanna Haertl, MD, Technical University of Munich.
“In patients with recurrent strokes in one vascular territory the presence of a symptomatic anatomic bone or cartilage anomaly may be considered as a differential diagnosis after sufficient exclusion of competing etiologies of an ischemic stroke,” they conclude.
“Due to the possibly high risk of stroke recurrence and potentially causative treatment options, bony strokes seem to be highly relevant for clinical practice,” they add.
The study was published online in the journal Stroke.
In their report, investigators explain that diagnosis of a bony stroke is based on a combination of imaging devices including CT, MRI, angiography, and sonography of brain-supplying vessels.
In addition to conventional static imaging, dynamic imaging modalities with the patients’ head in a fixed rotation or reclination has been shown to be useful as this enables the detection of a compressive effect on brain-supplying arteries caused by head movement.
They note that these bony strokes have been described previously – mainly as single case reports or small case series – but a systematic evaluation of each anatomical type of bony stroke is currently lacking.
For the current paper, the authors describe the identification and therapeutic workup of six patients with a bony stroke among 4,200 patients with ischemic stroke treated from January 2017 to March 2022 at their comprehensive stroke care center, constituting an incidence of 0.14%.
But they caution, “Given our retrospective study design, the method of patient acquisition, and the lack of systematic evaluation of bony strokes during acute stroke treatment, epidemiologic conclusions can be drawn only very carefully.”
In each of these six cases, the recurrent stroke was found to be caused by large-artery embolism from mechanical stress by bone or cartilage anomalies on arteries supplying the brain.
“Our case series aims to raise awareness for the rare entity of bony strokes, emphasizing the necessity to evaluate structural bone or cartilage lesions as a possible cause of ischemic stroke in patients with stroke recurrence of unknown cause in one vascular territory. We further aim on highlighting individual diagnostic and therapeutic options,” they state.
They note that it has previously been suggested that ischemic strokes based on bone or cartilage anomalies are more common in the relatively young patients with stroke, which is in line with their current patient data (mean age, 55 years), but this may reflect a selection bias.
A medical history with an association between changes in the head position and the occurrence of ischemic stroke may also raise awareness of the possibility of a bony stroke.
The authors outline treatment options for bony stroke, which they describe as diverse: They include conservative treatment, endovascular stenting, occlusion of the affected vessel, surgical bypass, and bone/cartilage removal.
From a pathophysiologic point of view, it seems reasonable to eliminate a causative lesion by surgical removal of the mechanical stressor, they note.
In cases of vascular stenting, they caution that the remainder of the mechanical stressor may provoke stent fracture and recurrent stroke, which occurred in two of their patients, a situation that may be observed more often in the future with the increasing use of vascular stenting.
The authors report that, compared with annual stroke rates in atrial fibrillation patients, stroke recurrence in this patient cohort ahead of definite treatment was high (cumulative 2.14 strokes per year). And as no patient had further ischemia after treatment, they argue that diagnosis and appropriate treatment of bony stroke may reduce or even eliminate the risk for future stroke recurrence.
They propose that for the diagnosis an exact medical history, with emphasis on a possible change of head position at the onset of stroke symptoms, is useful.
Furthermore, previously acquired diagnostic scans including CT or MRI may be evaluated for a symptomatic vessel-bone or cartilage contact. Then, the additional application of dynamic imaging modalities, including dynamic ultrasound of brain-supplying vessels and CT-angiography, may be discussed.
“An appropriate diagnosis and the evaluation of individual and interdisciplinary treatment options seem crucial to prevent recurrent ischemic strokes. Future prospective trials seem mandatory to optimize patient care,” they conclude.
The study had no specific funding. Coauthor Jan S. Kirschke, MD, received research support from the German Research Foundation, Bonescreen, H2020 European Research Council, and Philips. The other authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
These so-called “bony” strokes constitute a possible cause of recurrent ischemia in the same vascular territory as previous episodes, note the authors, led by Johanna Haertl, MD, Technical University of Munich.
“In patients with recurrent strokes in one vascular territory the presence of a symptomatic anatomic bone or cartilage anomaly may be considered as a differential diagnosis after sufficient exclusion of competing etiologies of an ischemic stroke,” they conclude.
“Due to the possibly high risk of stroke recurrence and potentially causative treatment options, bony strokes seem to be highly relevant for clinical practice,” they add.
The study was published online in the journal Stroke.
In their report, investigators explain that diagnosis of a bony stroke is based on a combination of imaging devices including CT, MRI, angiography, and sonography of brain-supplying vessels.
In addition to conventional static imaging, dynamic imaging modalities with the patients’ head in a fixed rotation or reclination has been shown to be useful as this enables the detection of a compressive effect on brain-supplying arteries caused by head movement.
They note that these bony strokes have been described previously – mainly as single case reports or small case series – but a systematic evaluation of each anatomical type of bony stroke is currently lacking.
For the current paper, the authors describe the identification and therapeutic workup of six patients with a bony stroke among 4,200 patients with ischemic stroke treated from January 2017 to March 2022 at their comprehensive stroke care center, constituting an incidence of 0.14%.
But they caution, “Given our retrospective study design, the method of patient acquisition, and the lack of systematic evaluation of bony strokes during acute stroke treatment, epidemiologic conclusions can be drawn only very carefully.”
In each of these six cases, the recurrent stroke was found to be caused by large-artery embolism from mechanical stress by bone or cartilage anomalies on arteries supplying the brain.
“Our case series aims to raise awareness for the rare entity of bony strokes, emphasizing the necessity to evaluate structural bone or cartilage lesions as a possible cause of ischemic stroke in patients with stroke recurrence of unknown cause in one vascular territory. We further aim on highlighting individual diagnostic and therapeutic options,” they state.
They note that it has previously been suggested that ischemic strokes based on bone or cartilage anomalies are more common in the relatively young patients with stroke, which is in line with their current patient data (mean age, 55 years), but this may reflect a selection bias.
A medical history with an association between changes in the head position and the occurrence of ischemic stroke may also raise awareness of the possibility of a bony stroke.
The authors outline treatment options for bony stroke, which they describe as diverse: They include conservative treatment, endovascular stenting, occlusion of the affected vessel, surgical bypass, and bone/cartilage removal.
From a pathophysiologic point of view, it seems reasonable to eliminate a causative lesion by surgical removal of the mechanical stressor, they note.
In cases of vascular stenting, they caution that the remainder of the mechanical stressor may provoke stent fracture and recurrent stroke, which occurred in two of their patients, a situation that may be observed more often in the future with the increasing use of vascular stenting.
The authors report that, compared with annual stroke rates in atrial fibrillation patients, stroke recurrence in this patient cohort ahead of definite treatment was high (cumulative 2.14 strokes per year). And as no patient had further ischemia after treatment, they argue that diagnosis and appropriate treatment of bony stroke may reduce or even eliminate the risk for future stroke recurrence.
They propose that for the diagnosis an exact medical history, with emphasis on a possible change of head position at the onset of stroke symptoms, is useful.
Furthermore, previously acquired diagnostic scans including CT or MRI may be evaluated for a symptomatic vessel-bone or cartilage contact. Then, the additional application of dynamic imaging modalities, including dynamic ultrasound of brain-supplying vessels and CT-angiography, may be discussed.
“An appropriate diagnosis and the evaluation of individual and interdisciplinary treatment options seem crucial to prevent recurrent ischemic strokes. Future prospective trials seem mandatory to optimize patient care,” they conclude.
The study had no specific funding. Coauthor Jan S. Kirschke, MD, received research support from the German Research Foundation, Bonescreen, H2020 European Research Council, and Philips. The other authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM STROKE
CMS inpatient payment rule for 2024: Key takeaways
The Centers for Medicare & Medicaid Services (CMS) released its annual update to the inpatient prospective payment system (IPPS) and long-term care hospital (LTCH) PPS on April 10, with many changes centered around improving health equity and quality as well as alleviating rural clinician shortages.
“This proposed rule reflects our person-centric approach to better measure health care quality and safety in hospitals to reduce preventable harm and our commitment to ensure that people with Medicare in rural and underserved areas have improved access to high-quality health care,” said CMS Administrator Chiquita Brooks-LaSure said in a statement.
Here are 14 things to know about the fiscal year (FY) 2024 proposal:
1. New payment rate: Acute-care hospitals that report inpatient quality data and participate in the EHR Meaningful Use program will receive a 2.8% net increase in payment rates. The rate adjustment will send approximately $3.3 billion more funding to hospitals compared with 2023.
2. LTCH payments: CMS projects that the LTCH standard payment rate will increase by 2.9%, whereas discharge payments will decrease by 2.5% or $59 million.
3. Disproportionate share hospital payments: Medicare disproportionate share hospital payments and Medicare uncompensated care payments will decrease by about $115 million for FY 2024.
4. Health equity categories: CMS proposes adding 15 new health equity hospital categorizations for IPPS payments to advance the goals of its Framework for Health Equity initiative.
5. Social determinants of health codes: To reflect increased resource utilization, the severity designation for the three International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) diagnosis codes describing homelessness will change from noncomplication or comorbidity to complication or comorbidity.
6. Rural emergency hospitals: The proposed rule will allow designated rural emergency hospitals to serve as training sites and receive Medicare graduate medical education payments to address concerns over rural hospital closures.
7. COVID treatment add-on payments: If the public health emergency ends in May, add-on payments for discharges involving eligible products like convalescent plasma and nirmatrelvir-ritonavir will expire on Sept. 30.
8. Technology add-on payments: Requests for new technology add-on payments must include a complete, active Food and Drug Administration market authorization application. Beginning with FY 2025 applications, the FDA approval deadline will move from July 1 to May 1.
9. Physician-owned hospitals: To receive Medicare payment for services referred by a physician owner or investor, the hospital must satisfy all requirements of the whole hospital exception or the rural provider exception to the Stark Law. In either case, a hospital may not increase the aggregate number of operating rooms, procedure rooms, or beds above the level it was licensed for on March 23, 2010, unless CMS grants an exception.
10. Electronic clinical quality measures: The new rule will remove and modify several existing electronic clinical quality measures and add three new ones: hospital harm, pressure injury; hospital harm, acute kidney injury; and excessive radiation dose or inadequate image quality for diagnostic CT in adult inpatients.
11. HCAHPS survey: Beginning Jan. 1, 2025, modifications to the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey will extend the data collection period from 42 to 49 days, limit supplemental survey items to 12, and require an official Spanish translation for patients.
12. Safety-net hospitals request for information: CMS seeks public input about the unique challenges faced by safety-net hospitals and potential solutions to ensure that uninsured, underinsured, and other vulnerable populations have access to essential services.
13. LTCH quality reporting: CMS proposes several quality-measure updates, including a functional discharge score measure beginning in FY 2025 and reporting the percentage of patients current with Centers for Disease Control and Prevention–recommended COVID vaccinations starting in FY 2026.
14. Commenting period: CMS will accept comments on the proposed rule through June 9.
A version of this article originally appeared on Medscape.com.
The Centers for Medicare & Medicaid Services (CMS) released its annual update to the inpatient prospective payment system (IPPS) and long-term care hospital (LTCH) PPS on April 10, with many changes centered around improving health equity and quality as well as alleviating rural clinician shortages.
“This proposed rule reflects our person-centric approach to better measure health care quality and safety in hospitals to reduce preventable harm and our commitment to ensure that people with Medicare in rural and underserved areas have improved access to high-quality health care,” said CMS Administrator Chiquita Brooks-LaSure said in a statement.
Here are 14 things to know about the fiscal year (FY) 2024 proposal:
1. New payment rate: Acute-care hospitals that report inpatient quality data and participate in the EHR Meaningful Use program will receive a 2.8% net increase in payment rates. The rate adjustment will send approximately $3.3 billion more funding to hospitals compared with 2023.
2. LTCH payments: CMS projects that the LTCH standard payment rate will increase by 2.9%, whereas discharge payments will decrease by 2.5% or $59 million.
3. Disproportionate share hospital payments: Medicare disproportionate share hospital payments and Medicare uncompensated care payments will decrease by about $115 million for FY 2024.
4. Health equity categories: CMS proposes adding 15 new health equity hospital categorizations for IPPS payments to advance the goals of its Framework for Health Equity initiative.
5. Social determinants of health codes: To reflect increased resource utilization, the severity designation for the three International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) diagnosis codes describing homelessness will change from noncomplication or comorbidity to complication or comorbidity.
6. Rural emergency hospitals: The proposed rule will allow designated rural emergency hospitals to serve as training sites and receive Medicare graduate medical education payments to address concerns over rural hospital closures.
7. COVID treatment add-on payments: If the public health emergency ends in May, add-on payments for discharges involving eligible products like convalescent plasma and nirmatrelvir-ritonavir will expire on Sept. 30.
8. Technology add-on payments: Requests for new technology add-on payments must include a complete, active Food and Drug Administration market authorization application. Beginning with FY 2025 applications, the FDA approval deadline will move from July 1 to May 1.
9. Physician-owned hospitals: To receive Medicare payment for services referred by a physician owner or investor, the hospital must satisfy all requirements of the whole hospital exception or the rural provider exception to the Stark Law. In either case, a hospital may not increase the aggregate number of operating rooms, procedure rooms, or beds above the level it was licensed for on March 23, 2010, unless CMS grants an exception.
10. Electronic clinical quality measures: The new rule will remove and modify several existing electronic clinical quality measures and add three new ones: hospital harm, pressure injury; hospital harm, acute kidney injury; and excessive radiation dose or inadequate image quality for diagnostic CT in adult inpatients.
11. HCAHPS survey: Beginning Jan. 1, 2025, modifications to the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey will extend the data collection period from 42 to 49 days, limit supplemental survey items to 12, and require an official Spanish translation for patients.
12. Safety-net hospitals request for information: CMS seeks public input about the unique challenges faced by safety-net hospitals and potential solutions to ensure that uninsured, underinsured, and other vulnerable populations have access to essential services.
13. LTCH quality reporting: CMS proposes several quality-measure updates, including a functional discharge score measure beginning in FY 2025 and reporting the percentage of patients current with Centers for Disease Control and Prevention–recommended COVID vaccinations starting in FY 2026.
14. Commenting period: CMS will accept comments on the proposed rule through June 9.
A version of this article originally appeared on Medscape.com.
The Centers for Medicare & Medicaid Services (CMS) released its annual update to the inpatient prospective payment system (IPPS) and long-term care hospital (LTCH) PPS on April 10, with many changes centered around improving health equity and quality as well as alleviating rural clinician shortages.
“This proposed rule reflects our person-centric approach to better measure health care quality and safety in hospitals to reduce preventable harm and our commitment to ensure that people with Medicare in rural and underserved areas have improved access to high-quality health care,” said CMS Administrator Chiquita Brooks-LaSure said in a statement.
Here are 14 things to know about the fiscal year (FY) 2024 proposal:
1. New payment rate: Acute-care hospitals that report inpatient quality data and participate in the EHR Meaningful Use program will receive a 2.8% net increase in payment rates. The rate adjustment will send approximately $3.3 billion more funding to hospitals compared with 2023.
2. LTCH payments: CMS projects that the LTCH standard payment rate will increase by 2.9%, whereas discharge payments will decrease by 2.5% or $59 million.
3. Disproportionate share hospital payments: Medicare disproportionate share hospital payments and Medicare uncompensated care payments will decrease by about $115 million for FY 2024.
4. Health equity categories: CMS proposes adding 15 new health equity hospital categorizations for IPPS payments to advance the goals of its Framework for Health Equity initiative.
5. Social determinants of health codes: To reflect increased resource utilization, the severity designation for the three International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) diagnosis codes describing homelessness will change from noncomplication or comorbidity to complication or comorbidity.
6. Rural emergency hospitals: The proposed rule will allow designated rural emergency hospitals to serve as training sites and receive Medicare graduate medical education payments to address concerns over rural hospital closures.
7. COVID treatment add-on payments: If the public health emergency ends in May, add-on payments for discharges involving eligible products like convalescent plasma and nirmatrelvir-ritonavir will expire on Sept. 30.
8. Technology add-on payments: Requests for new technology add-on payments must include a complete, active Food and Drug Administration market authorization application. Beginning with FY 2025 applications, the FDA approval deadline will move from July 1 to May 1.
9. Physician-owned hospitals: To receive Medicare payment for services referred by a physician owner or investor, the hospital must satisfy all requirements of the whole hospital exception or the rural provider exception to the Stark Law. In either case, a hospital may not increase the aggregate number of operating rooms, procedure rooms, or beds above the level it was licensed for on March 23, 2010, unless CMS grants an exception.
10. Electronic clinical quality measures: The new rule will remove and modify several existing electronic clinical quality measures and add three new ones: hospital harm, pressure injury; hospital harm, acute kidney injury; and excessive radiation dose or inadequate image quality for diagnostic CT in adult inpatients.
11. HCAHPS survey: Beginning Jan. 1, 2025, modifications to the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey will extend the data collection period from 42 to 49 days, limit supplemental survey items to 12, and require an official Spanish translation for patients.
12. Safety-net hospitals request for information: CMS seeks public input about the unique challenges faced by safety-net hospitals and potential solutions to ensure that uninsured, underinsured, and other vulnerable populations have access to essential services.
13. LTCH quality reporting: CMS proposes several quality-measure updates, including a functional discharge score measure beginning in FY 2025 and reporting the percentage of patients current with Centers for Disease Control and Prevention–recommended COVID vaccinations starting in FY 2026.
14. Commenting period: CMS will accept comments on the proposed rule through June 9.
A version of this article originally appeared on Medscape.com.
Infographic: Is your compensation rising as fast as your peers?
Did doctors’ salaries continue their zesty postpandemic rise in 2022? Are female physicians making pay gains versus their male counterparts that spark optimism for the future?
reveals which medical specialties pay better than others, and evaluates the current gender pay gap in medicine. If you’re interested in delving deeper into the data, check out Your Income vs. Your Peers’: Physician Compensation Report 2023.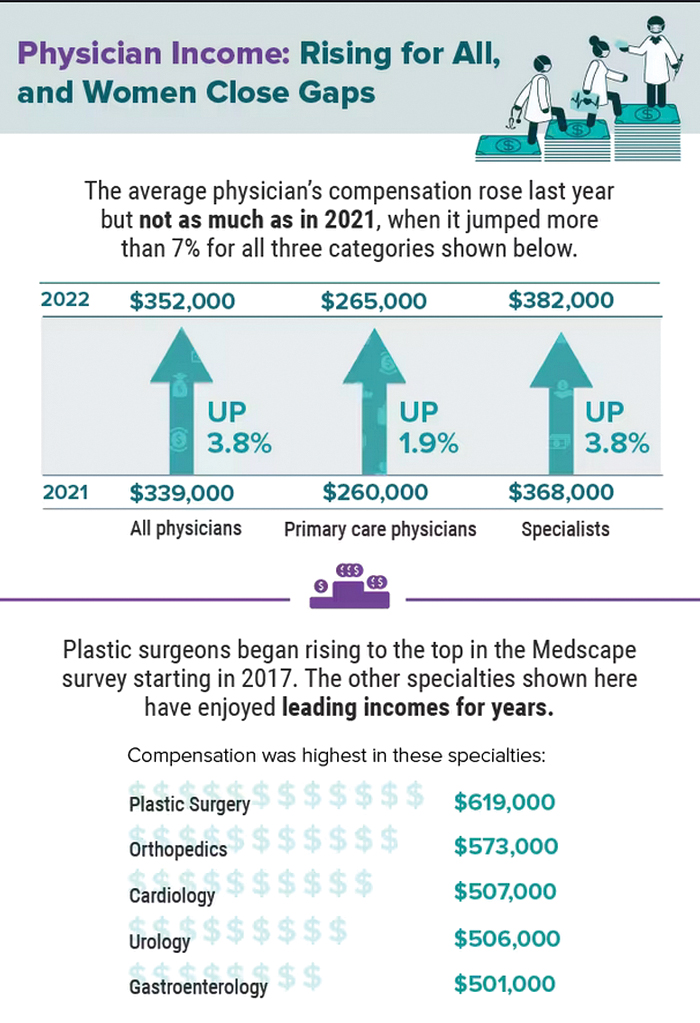
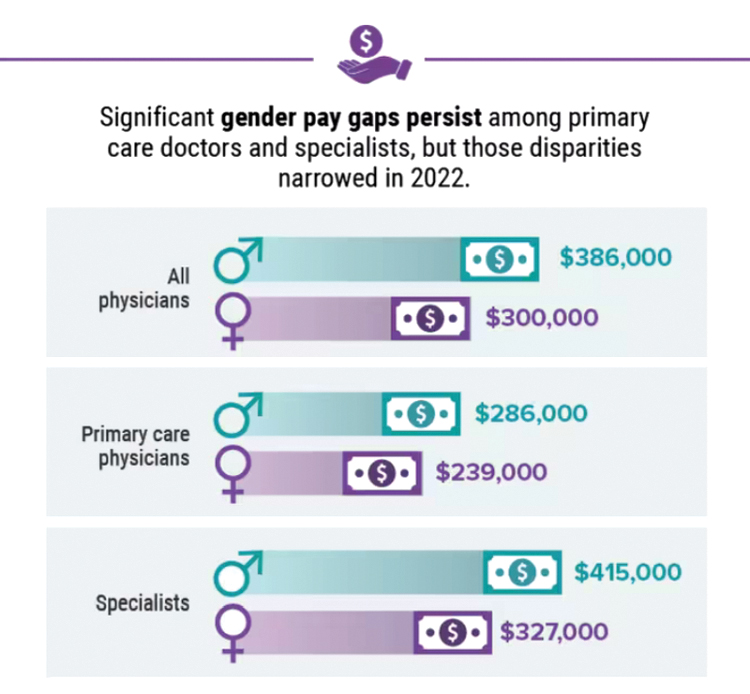
A version of this article first appeared on Medscape.com.
Did doctors’ salaries continue their zesty postpandemic rise in 2022? Are female physicians making pay gains versus their male counterparts that spark optimism for the future?
reveals which medical specialties pay better than others, and evaluates the current gender pay gap in medicine. If you’re interested in delving deeper into the data, check out Your Income vs. Your Peers’: Physician Compensation Report 2023.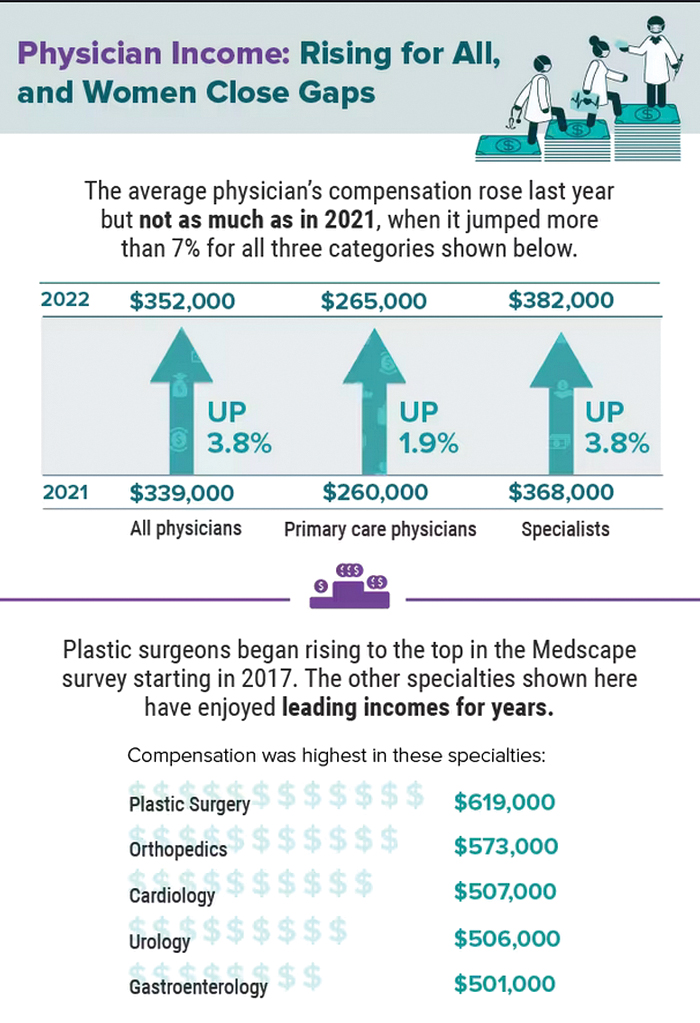
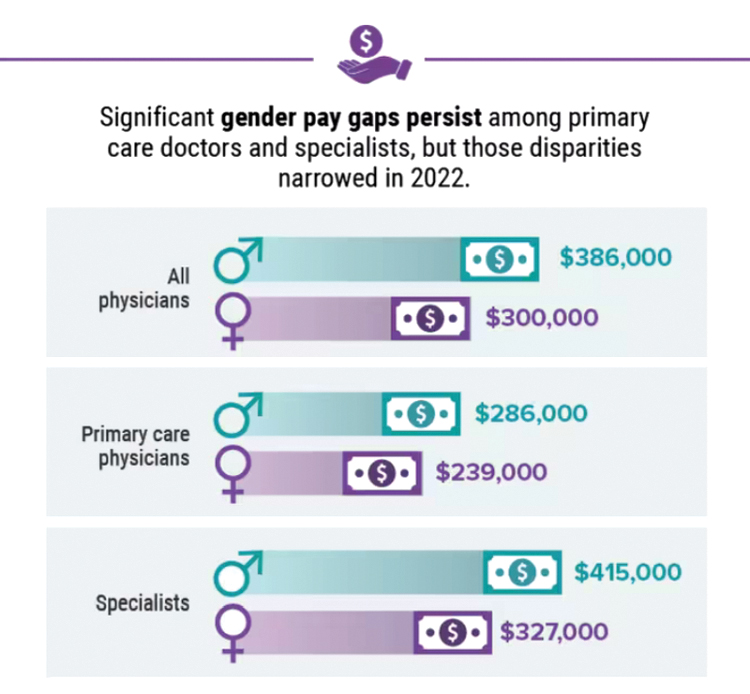
A version of this article first appeared on Medscape.com.
Did doctors’ salaries continue their zesty postpandemic rise in 2022? Are female physicians making pay gains versus their male counterparts that spark optimism for the future?
reveals which medical specialties pay better than others, and evaluates the current gender pay gap in medicine. If you’re interested in delving deeper into the data, check out Your Income vs. Your Peers’: Physician Compensation Report 2023.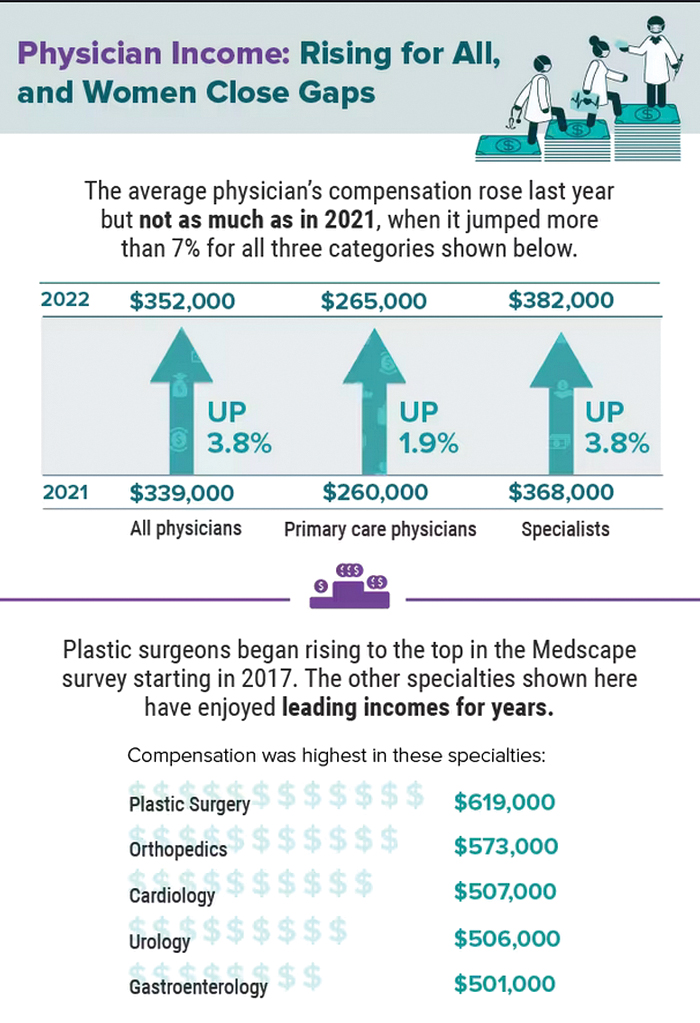
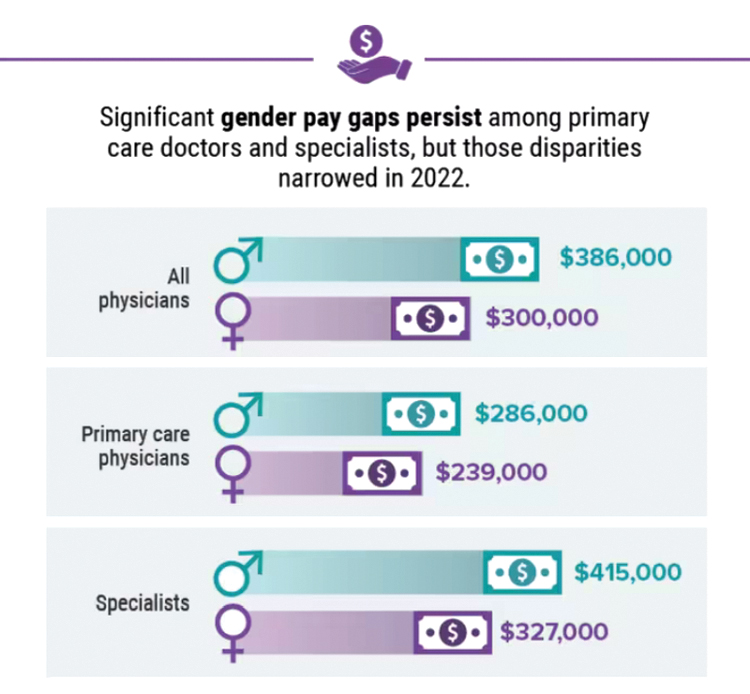
A version of this article first appeared on Medscape.com.
Five chronic mistakes that can sabotage your medical practice
A physician who in the past has led medical groups as both chief medical officer and president, Gerda Maissel, MD, president of My MD Advisor, a private patient advocacy group, has seen the good, bad, and ugly of practice administration. There’s a spectrum of infractions: Anything from doctors making inappropriate jokes with staff or patients, to failing to establish key relationships with other critical entities, says Dr. Maissel.
“Being a good physician who provides value is important in building a practice,” explained Dr. Maissel. “But it is not the be-all and end-all.”
While the number of physician-owned practices is declining, just under 50% are still in private practice, according to the American Medical Association’s 2020 survey. There’s also a continuing trend toward larger practices. Whatever the size, the physicians are responsible for strategy, marketing, building the practice, and maintaining profitability.
Catherine Lightfoot, CPA, CHBC, president of the National Society of Certified Healthcare Business Consultants (NSCHBC), has her finger on the pulse of what’s right and what’s wrong when it comes to running a medical practice. Although she says there are no hard and fast rules on how to run a thriving medical group, there are common mistakes that physicians often don’t recognize.
Here are the five key mistakes that commonly crop up, and the experts’ thoughts on how to prevent or fix them.
1. Failing to engage in outreach activities and community efforts to build your practice.
Yes, physicians earn good reputations through dedicated work, and that often precedes them when it comes to building a practice. But assuming that hanging a shingle backed by strong credentials is all it takes for success is akin to building a website and assuming people will find it organically. Maybe there was a time, in a small community, where this was good enough. But no longer.
It’s important to plan to get your practice and your name known to potential patients. “Most physicians think that means advertising, but that’s not the complete case,” Dr. Maissel said.
Much of the equation involves ensuring availability. This means setting office hours that work for your target audience of patients, and then ensuring you stick to those hours. This extends beyond scheduling your current patients and into referral patients, too. And it’s particularly true while in the building phase of a new practice.
“If one of your colleagues calls with a referral patient, and they consider the matter urgent, you need to heed that,” explained Dr. Maissel. “So have a breadth of availability for these referral cases.” Through word of mouth, you’ll get a good reputation for patient care and availability, and that will go a long way toward helping to grow your practice.
Establishing a culture that doesn’t involve canceling and rescheduling patients is part of the scheduling equation, too. “I’ve seen the full gamut of cancellation policies, ranging from a month’s notice on changes to 3 months’ notice,” said Dr. Maissel. “It all gets at the same issue, which is failing to set up a culture where doctors don’t change their schedules and leave patients hanging.”
In the end, wonky scheduling, cancellations, and a lack of respect for the urgency of referrals can cost a practice. Forge a reputation in reliability and word will get around, in all the right ways.
2. Not having enough oversight of your outsourced billing service
Billing is one of the biggest pieces of running a successful and profitable practice, yet too many practices ignore it once they’ve handed it off to a billing company. That can cost you in more ways than one, said Ms. Lightfoot. “Billing changes all the time, and if you’re not monitoring your billing partner, you don’t know what you’re getting,” she said.
Ms. Lightfoot said that a decade ago, billing was much more straightforward – essentially, you did the work and received payment. Today’s complex insurance, Medicare, and Medicaid environment have changed the landscape. “Now you have to fight for every dollar you’re billing,” said Ms. Lightfoot. “Rates get cut all the time, you might miss out on a claim, and the rules are constantly changing.”
The solution for many practices is to outsource billing, which Ms. Lightfoot supports. “They specialize in this, and that’s a great start,” she said. “But it’s not as simple as handing it off and forgetting it.”
Instead, ensure your internal staff is up to date on all things coding and billing so that they can catch what your outsourced billing partner doesn’t. Your internal staff should be prepared to carry out coding, check coding, and stay on top of the billing company if they aren’t processing claims quickly enough. For instance: If there’s a denial, how many times will the billing company go after that money?
Other questions to ask when entering a billing relationship: What does the billing company expect from your practice? Do they communicate what needs to be worked on or fixed? Are they providing you with monthly reports? “You want to make sure you’re getting those reports every month and reading them over carefully,” said Ms. Lightfoot.
This means that if you have a large practice, you should have a point person within your billing department to handle the relationship with your billing partner. If it’s a smaller practice, the task will likely fall to the office manager. The ‘who’ isn’t important, but having someone on the case is.
Another important aspect of this billing relationship is understanding what you’re receiving for your payment. “Sometimes going with the cheapest offer amounts to a billing partner who isn’t working on those claims and denials as much as they should,” said Ms. Lightfoot. “I’ve seen fees anywhere from 4% to 9%, and the lower end can mean you’ll need to chase down every penny.”
3. Neglecting to forge the right relationships in the community.
Another common mistake physicians make is failing to develop the professional relationships that will help you thrive. Successful practices need to establish relationships with the right people and organizations. While the occasional afternoon of golf used to serve this purpose, today outreach must go beyond that, said Dr. Maissel. “You need to create relationships with hospitals and hospital-based practices because you may have value to them,” she said. “You should also get into some sort of relationship with your local ACO (Accountable Care Organization) or PHO (Physician Hospital Organization). Identify the leaders there and let them know you exist.”
Establishing these relationships goes beyond that first step of introducing yourself, or you risk losing their benefits. You must also nurture and “fertilize” these relationships in an ongoing fashion. “For years, as the head of employee practice, I had a competitor who would go out of his way to invite me to lunch regularly,” said Dr. Maissel. “When there were opportunities for his group, I would connect him. I wouldn’t have done that had he not worked on our relationship over time.”
The adage of “it’s not what you know but who you know” holds up here. If you don’t do the reach out to the right people and organizations in your community, you will have a harder time succeeding as a practice.
4. Hiring the wrong person/a family member for the job.
When starting a new practice, or if you’re running a small practice, it can be tempting to look for affordable or reliable staffing from among family members or friends. That’s fine if your family member or friend is also qualified for the job. If they aren’t, however, you might be setting up for failure.
“When you hire someone without the right qualifications, you need to be willing to train them for the job,” said Ms. Lightfoot. “Doctors don’t have that kind of time.”
Too often, Ms. Lightfoot said, a doctor will have a position like officer manager open and fill it with an in-law, whether he or she is experienced or not. “Now you have someone in the role who is unqualified, and the rest of the office can’t speak up about that because it’s a relative to the lead physician,” she said. “That doesn’t create a good environment for anyone.”
Also, a setup for failure is hiring someone who might be qualified, but not possessing the right personality for the role. A front desk position, for instance, should be held by someone who’s a bit upbeat and able to multitask. “You can’t put a shy, quiet person in that job,” said Ms. Lightfoot. “So, if you see a person with 10 years’ experience in a medical practice, but they’re reserved, what will happen? You must think about this when hiring.”
One PA recalled a small family practice in which the lead physician’s wife was the office manager. To save money, the wife removed lights from the staff restroom and staff lunchroom and declined staff requests for earned vacation. The staff felt unable to speak up, and they – and all new office staff members – ultimately left the practice.
5. Overlooking the importance of acting like a professional and respecting your staff.
This one might seem obvious, but many physicians get a bit too comfortable in the office environment, said Dr. Maissel. This can encompass a whole host of bad behaviors, from making inappropriate jokes to staff and patients, to trash-talking colleagues. None of this behavior is acceptable and can set you up for things to go wrong, especially when good labor is hard to come by. “Your staff is made up of people for whom 50 cents an hour is meaningful,” she said. “If they don’t have a warm, supportive office, they will look elsewhere.”
This is especially true of younger people now entering the workforce – they are less tolerant than generations past of egregious behavior. Try to establish a professional, yet nurturing environment for your staff. “Inquire about things that matter to them,” said Dr. Maissel. “Small talk can go a long way. See them as human beings, not cogs in the wheel.”
Inappropriate and uncaring behaviors will give physician leaders a reputation, one that sticks. “The medical community is pretty connected, and if you behave inappropriately enough times, it will circle back to you,” said Dr. Maissel.
Launching, and sustaining, a successful medical practice is never a given, but mistakes are. With the right approach, however, you can avoid these common – and impactful – errors and set your practice up for success.
A version of this article first appeared on Medscape.com.
A physician who in the past has led medical groups as both chief medical officer and president, Gerda Maissel, MD, president of My MD Advisor, a private patient advocacy group, has seen the good, bad, and ugly of practice administration. There’s a spectrum of infractions: Anything from doctors making inappropriate jokes with staff or patients, to failing to establish key relationships with other critical entities, says Dr. Maissel.
“Being a good physician who provides value is important in building a practice,” explained Dr. Maissel. “But it is not the be-all and end-all.”
While the number of physician-owned practices is declining, just under 50% are still in private practice, according to the American Medical Association’s 2020 survey. There’s also a continuing trend toward larger practices. Whatever the size, the physicians are responsible for strategy, marketing, building the practice, and maintaining profitability.
Catherine Lightfoot, CPA, CHBC, president of the National Society of Certified Healthcare Business Consultants (NSCHBC), has her finger on the pulse of what’s right and what’s wrong when it comes to running a medical practice. Although she says there are no hard and fast rules on how to run a thriving medical group, there are common mistakes that physicians often don’t recognize.
Here are the five key mistakes that commonly crop up, and the experts’ thoughts on how to prevent or fix them.
1. Failing to engage in outreach activities and community efforts to build your practice.
Yes, physicians earn good reputations through dedicated work, and that often precedes them when it comes to building a practice. But assuming that hanging a shingle backed by strong credentials is all it takes for success is akin to building a website and assuming people will find it organically. Maybe there was a time, in a small community, where this was good enough. But no longer.
It’s important to plan to get your practice and your name known to potential patients. “Most physicians think that means advertising, but that’s not the complete case,” Dr. Maissel said.
Much of the equation involves ensuring availability. This means setting office hours that work for your target audience of patients, and then ensuring you stick to those hours. This extends beyond scheduling your current patients and into referral patients, too. And it’s particularly true while in the building phase of a new practice.
“If one of your colleagues calls with a referral patient, and they consider the matter urgent, you need to heed that,” explained Dr. Maissel. “So have a breadth of availability for these referral cases.” Through word of mouth, you’ll get a good reputation for patient care and availability, and that will go a long way toward helping to grow your practice.
Establishing a culture that doesn’t involve canceling and rescheduling patients is part of the scheduling equation, too. “I’ve seen the full gamut of cancellation policies, ranging from a month’s notice on changes to 3 months’ notice,” said Dr. Maissel. “It all gets at the same issue, which is failing to set up a culture where doctors don’t change their schedules and leave patients hanging.”
In the end, wonky scheduling, cancellations, and a lack of respect for the urgency of referrals can cost a practice. Forge a reputation in reliability and word will get around, in all the right ways.
2. Not having enough oversight of your outsourced billing service
Billing is one of the biggest pieces of running a successful and profitable practice, yet too many practices ignore it once they’ve handed it off to a billing company. That can cost you in more ways than one, said Ms. Lightfoot. “Billing changes all the time, and if you’re not monitoring your billing partner, you don’t know what you’re getting,” she said.
Ms. Lightfoot said that a decade ago, billing was much more straightforward – essentially, you did the work and received payment. Today’s complex insurance, Medicare, and Medicaid environment have changed the landscape. “Now you have to fight for every dollar you’re billing,” said Ms. Lightfoot. “Rates get cut all the time, you might miss out on a claim, and the rules are constantly changing.”
The solution for many practices is to outsource billing, which Ms. Lightfoot supports. “They specialize in this, and that’s a great start,” she said. “But it’s not as simple as handing it off and forgetting it.”
Instead, ensure your internal staff is up to date on all things coding and billing so that they can catch what your outsourced billing partner doesn’t. Your internal staff should be prepared to carry out coding, check coding, and stay on top of the billing company if they aren’t processing claims quickly enough. For instance: If there’s a denial, how many times will the billing company go after that money?
Other questions to ask when entering a billing relationship: What does the billing company expect from your practice? Do they communicate what needs to be worked on or fixed? Are they providing you with monthly reports? “You want to make sure you’re getting those reports every month and reading them over carefully,” said Ms. Lightfoot.
This means that if you have a large practice, you should have a point person within your billing department to handle the relationship with your billing partner. If it’s a smaller practice, the task will likely fall to the office manager. The ‘who’ isn’t important, but having someone on the case is.
Another important aspect of this billing relationship is understanding what you’re receiving for your payment. “Sometimes going with the cheapest offer amounts to a billing partner who isn’t working on those claims and denials as much as they should,” said Ms. Lightfoot. “I’ve seen fees anywhere from 4% to 9%, and the lower end can mean you’ll need to chase down every penny.”
3. Neglecting to forge the right relationships in the community.
Another common mistake physicians make is failing to develop the professional relationships that will help you thrive. Successful practices need to establish relationships with the right people and organizations. While the occasional afternoon of golf used to serve this purpose, today outreach must go beyond that, said Dr. Maissel. “You need to create relationships with hospitals and hospital-based practices because you may have value to them,” she said. “You should also get into some sort of relationship with your local ACO (Accountable Care Organization) or PHO (Physician Hospital Organization). Identify the leaders there and let them know you exist.”
Establishing these relationships goes beyond that first step of introducing yourself, or you risk losing their benefits. You must also nurture and “fertilize” these relationships in an ongoing fashion. “For years, as the head of employee practice, I had a competitor who would go out of his way to invite me to lunch regularly,” said Dr. Maissel. “When there were opportunities for his group, I would connect him. I wouldn’t have done that had he not worked on our relationship over time.”
The adage of “it’s not what you know but who you know” holds up here. If you don’t do the reach out to the right people and organizations in your community, you will have a harder time succeeding as a practice.
4. Hiring the wrong person/a family member for the job.
When starting a new practice, or if you’re running a small practice, it can be tempting to look for affordable or reliable staffing from among family members or friends. That’s fine if your family member or friend is also qualified for the job. If they aren’t, however, you might be setting up for failure.
“When you hire someone without the right qualifications, you need to be willing to train them for the job,” said Ms. Lightfoot. “Doctors don’t have that kind of time.”
Too often, Ms. Lightfoot said, a doctor will have a position like officer manager open and fill it with an in-law, whether he or she is experienced or not. “Now you have someone in the role who is unqualified, and the rest of the office can’t speak up about that because it’s a relative to the lead physician,” she said. “That doesn’t create a good environment for anyone.”
Also, a setup for failure is hiring someone who might be qualified, but not possessing the right personality for the role. A front desk position, for instance, should be held by someone who’s a bit upbeat and able to multitask. “You can’t put a shy, quiet person in that job,” said Ms. Lightfoot. “So, if you see a person with 10 years’ experience in a medical practice, but they’re reserved, what will happen? You must think about this when hiring.”
One PA recalled a small family practice in which the lead physician’s wife was the office manager. To save money, the wife removed lights from the staff restroom and staff lunchroom and declined staff requests for earned vacation. The staff felt unable to speak up, and they – and all new office staff members – ultimately left the practice.
5. Overlooking the importance of acting like a professional and respecting your staff.
This one might seem obvious, but many physicians get a bit too comfortable in the office environment, said Dr. Maissel. This can encompass a whole host of bad behaviors, from making inappropriate jokes to staff and patients, to trash-talking colleagues. None of this behavior is acceptable and can set you up for things to go wrong, especially when good labor is hard to come by. “Your staff is made up of people for whom 50 cents an hour is meaningful,” she said. “If they don’t have a warm, supportive office, they will look elsewhere.”
This is especially true of younger people now entering the workforce – they are less tolerant than generations past of egregious behavior. Try to establish a professional, yet nurturing environment for your staff. “Inquire about things that matter to them,” said Dr. Maissel. “Small talk can go a long way. See them as human beings, not cogs in the wheel.”
Inappropriate and uncaring behaviors will give physician leaders a reputation, one that sticks. “The medical community is pretty connected, and if you behave inappropriately enough times, it will circle back to you,” said Dr. Maissel.
Launching, and sustaining, a successful medical practice is never a given, but mistakes are. With the right approach, however, you can avoid these common – and impactful – errors and set your practice up for success.
A version of this article first appeared on Medscape.com.
A physician who in the past has led medical groups as both chief medical officer and president, Gerda Maissel, MD, president of My MD Advisor, a private patient advocacy group, has seen the good, bad, and ugly of practice administration. There’s a spectrum of infractions: Anything from doctors making inappropriate jokes with staff or patients, to failing to establish key relationships with other critical entities, says Dr. Maissel.
“Being a good physician who provides value is important in building a practice,” explained Dr. Maissel. “But it is not the be-all and end-all.”
While the number of physician-owned practices is declining, just under 50% are still in private practice, according to the American Medical Association’s 2020 survey. There’s also a continuing trend toward larger practices. Whatever the size, the physicians are responsible for strategy, marketing, building the practice, and maintaining profitability.
Catherine Lightfoot, CPA, CHBC, president of the National Society of Certified Healthcare Business Consultants (NSCHBC), has her finger on the pulse of what’s right and what’s wrong when it comes to running a medical practice. Although she says there are no hard and fast rules on how to run a thriving medical group, there are common mistakes that physicians often don’t recognize.
Here are the five key mistakes that commonly crop up, and the experts’ thoughts on how to prevent or fix them.
1. Failing to engage in outreach activities and community efforts to build your practice.
Yes, physicians earn good reputations through dedicated work, and that often precedes them when it comes to building a practice. But assuming that hanging a shingle backed by strong credentials is all it takes for success is akin to building a website and assuming people will find it organically. Maybe there was a time, in a small community, where this was good enough. But no longer.
It’s important to plan to get your practice and your name known to potential patients. “Most physicians think that means advertising, but that’s not the complete case,” Dr. Maissel said.
Much of the equation involves ensuring availability. This means setting office hours that work for your target audience of patients, and then ensuring you stick to those hours. This extends beyond scheduling your current patients and into referral patients, too. And it’s particularly true while in the building phase of a new practice.
“If one of your colleagues calls with a referral patient, and they consider the matter urgent, you need to heed that,” explained Dr. Maissel. “So have a breadth of availability for these referral cases.” Through word of mouth, you’ll get a good reputation for patient care and availability, and that will go a long way toward helping to grow your practice.
Establishing a culture that doesn’t involve canceling and rescheduling patients is part of the scheduling equation, too. “I’ve seen the full gamut of cancellation policies, ranging from a month’s notice on changes to 3 months’ notice,” said Dr. Maissel. “It all gets at the same issue, which is failing to set up a culture where doctors don’t change their schedules and leave patients hanging.”
In the end, wonky scheduling, cancellations, and a lack of respect for the urgency of referrals can cost a practice. Forge a reputation in reliability and word will get around, in all the right ways.
2. Not having enough oversight of your outsourced billing service
Billing is one of the biggest pieces of running a successful and profitable practice, yet too many practices ignore it once they’ve handed it off to a billing company. That can cost you in more ways than one, said Ms. Lightfoot. “Billing changes all the time, and if you’re not monitoring your billing partner, you don’t know what you’re getting,” she said.
Ms. Lightfoot said that a decade ago, billing was much more straightforward – essentially, you did the work and received payment. Today’s complex insurance, Medicare, and Medicaid environment have changed the landscape. “Now you have to fight for every dollar you’re billing,” said Ms. Lightfoot. “Rates get cut all the time, you might miss out on a claim, and the rules are constantly changing.”
The solution for many practices is to outsource billing, which Ms. Lightfoot supports. “They specialize in this, and that’s a great start,” she said. “But it’s not as simple as handing it off and forgetting it.”
Instead, ensure your internal staff is up to date on all things coding and billing so that they can catch what your outsourced billing partner doesn’t. Your internal staff should be prepared to carry out coding, check coding, and stay on top of the billing company if they aren’t processing claims quickly enough. For instance: If there’s a denial, how many times will the billing company go after that money?
Other questions to ask when entering a billing relationship: What does the billing company expect from your practice? Do they communicate what needs to be worked on or fixed? Are they providing you with monthly reports? “You want to make sure you’re getting those reports every month and reading them over carefully,” said Ms. Lightfoot.
This means that if you have a large practice, you should have a point person within your billing department to handle the relationship with your billing partner. If it’s a smaller practice, the task will likely fall to the office manager. The ‘who’ isn’t important, but having someone on the case is.
Another important aspect of this billing relationship is understanding what you’re receiving for your payment. “Sometimes going with the cheapest offer amounts to a billing partner who isn’t working on those claims and denials as much as they should,” said Ms. Lightfoot. “I’ve seen fees anywhere from 4% to 9%, and the lower end can mean you’ll need to chase down every penny.”
3. Neglecting to forge the right relationships in the community.
Another common mistake physicians make is failing to develop the professional relationships that will help you thrive. Successful practices need to establish relationships with the right people and organizations. While the occasional afternoon of golf used to serve this purpose, today outreach must go beyond that, said Dr. Maissel. “You need to create relationships with hospitals and hospital-based practices because you may have value to them,” she said. “You should also get into some sort of relationship with your local ACO (Accountable Care Organization) or PHO (Physician Hospital Organization). Identify the leaders there and let them know you exist.”
Establishing these relationships goes beyond that first step of introducing yourself, or you risk losing their benefits. You must also nurture and “fertilize” these relationships in an ongoing fashion. “For years, as the head of employee practice, I had a competitor who would go out of his way to invite me to lunch regularly,” said Dr. Maissel. “When there were opportunities for his group, I would connect him. I wouldn’t have done that had he not worked on our relationship over time.”
The adage of “it’s not what you know but who you know” holds up here. If you don’t do the reach out to the right people and organizations in your community, you will have a harder time succeeding as a practice.
4. Hiring the wrong person/a family member for the job.
When starting a new practice, or if you’re running a small practice, it can be tempting to look for affordable or reliable staffing from among family members or friends. That’s fine if your family member or friend is also qualified for the job. If they aren’t, however, you might be setting up for failure.
“When you hire someone without the right qualifications, you need to be willing to train them for the job,” said Ms. Lightfoot. “Doctors don’t have that kind of time.”
Too often, Ms. Lightfoot said, a doctor will have a position like officer manager open and fill it with an in-law, whether he or she is experienced or not. “Now you have someone in the role who is unqualified, and the rest of the office can’t speak up about that because it’s a relative to the lead physician,” she said. “That doesn’t create a good environment for anyone.”
Also, a setup for failure is hiring someone who might be qualified, but not possessing the right personality for the role. A front desk position, for instance, should be held by someone who’s a bit upbeat and able to multitask. “You can’t put a shy, quiet person in that job,” said Ms. Lightfoot. “So, if you see a person with 10 years’ experience in a medical practice, but they’re reserved, what will happen? You must think about this when hiring.”
One PA recalled a small family practice in which the lead physician’s wife was the office manager. To save money, the wife removed lights from the staff restroom and staff lunchroom and declined staff requests for earned vacation. The staff felt unable to speak up, and they – and all new office staff members – ultimately left the practice.
5. Overlooking the importance of acting like a professional and respecting your staff.
This one might seem obvious, but many physicians get a bit too comfortable in the office environment, said Dr. Maissel. This can encompass a whole host of bad behaviors, from making inappropriate jokes to staff and patients, to trash-talking colleagues. None of this behavior is acceptable and can set you up for things to go wrong, especially when good labor is hard to come by. “Your staff is made up of people for whom 50 cents an hour is meaningful,” she said. “If they don’t have a warm, supportive office, they will look elsewhere.”
This is especially true of younger people now entering the workforce – they are less tolerant than generations past of egregious behavior. Try to establish a professional, yet nurturing environment for your staff. “Inquire about things that matter to them,” said Dr. Maissel. “Small talk can go a long way. See them as human beings, not cogs in the wheel.”
Inappropriate and uncaring behaviors will give physician leaders a reputation, one that sticks. “The medical community is pretty connected, and if you behave inappropriately enough times, it will circle back to you,” said Dr. Maissel.
Launching, and sustaining, a successful medical practice is never a given, but mistakes are. With the right approach, however, you can avoid these common – and impactful – errors and set your practice up for success.
A version of this article first appeared on Medscape.com.

