User login
Administration of ketamine for depression should be limited to psychiatrists
In the modern-day practice of medicine, turf wars are more common than one may realize. Presently, an ongoing battle over who should be prescribing and administering ketamine for novel treatment uses is being waged among psychiatrists, anesthesiologists, family physicians, and emergency physicians. Whoever emerges victorious will determine whether psychiatric care is administered in a safe and cost-effective manner, or if it will merely benefit the bottom line of the prescriber. In this article, we discuss how ketamine may have a role for treatment-resistant depression (TRD), and why psychiatrists are uniquely qualified to prescribe and administer this medication for this purpose.
New approaches to treatment-resistant depression
Antidepressant medications, long the mainstay of depression treatment, have been shown to be safe and relatively equally effective, with varying tolerability. However, 33% percent of patients do not achieve remission after 4 trials of antidepressant therapy.1 Most antidepressant efficacy studies report remission rates of 35% to 40%,2 which means many patients require subsequent switching and/or augmentation of their treatment.3 The STAR*D trial demonstrated that after 2 adequate antidepressant trials, the likelihood of remission diminishes.4
After a patient’s depression is found to be treatment-resistant, the onus of guiding treatment shifts away from the patient’s primary care physician to the more specialized psychiatrist. Few would question the suitability of a psychiatrist’s expertise in handling complicated and nuanced mental illness. In order to manage TRD, psychiatrists enter a terrain of emerging novel therapies with rapid onset, different mechanisms of action, and parenteral routes of administration.
One such therapy is esketamine, the S-enantiomer of ketamine. The FDA approved the intranasal (IN) formulation of esketamine in March 2019 after the medication had been designated as a breakthrough therapy for TRD in 2013 and studied in 6 Phase III clinical trials.5 The S-enantiomer of ketamine is known to bind to the N-methyl-
Ketamine may be administered intranasally, intravenously, or orally. A meta-analysis aimed at assessing differences in ketamine efficacy for depression based on route of administration have shown that both IV and IN ketamine are effective, though it is not possible to draw conclusions regarding a direct comparison based on available data.9 Despite several landmark published studies, such as those by Zarate et al,10 IV ketamine is not FDA-approved for TRD.
Continue to: Why psychiatrists?
Why psychiatrists?
Psychiatrists have been prescribing IN esketamine, which is covered by most commercial insurances and administered in certified healthcare settings under a Risk Evaluation and Mitigation Strategy program.5 However, anesthesiologists and emergency physicians have opened a crop of boutique and concierge health clinics offering various “packages” of IV ketamine infusions for a slew of mental ailments, including depression, anxiety, bipolar disorder, and posttraumatic stress disorder.11 Minimal investigation reveals that these services are being prescribed mainly by practitioners in fields other than psychiatry. Intravenous ketamine has long been used off-label as a treatment for depression not by psychiatrists but by practitioners of anesthesiology or emergency medicine. Although these clinicians are likely familiar with ketamine as an anesthetic, they have no foundation or expertise in the diagnosis and treatment of complex mood disorders. The FDA-approved indication for esketamine falls firmly in the realm of psychiatric treatment. Physicians who have not completed a psychiatry residency have neither the training nor experience necessary to determine whether a patient is a candidate for this treatment.
One potential adverse effect of ketamine is an emergence phenomenon, colloquially named a “K-hole,” that can induce symptoms of psychosis such as disturbing hallucinations. Patients who have a history of psychosis need to be carefully evaluated for appropriateness to receive this treatment.
Furthermore, ketamine treatments administered by physicians who are not psychiatrists are billed not through insurance but mostly via private pay. A patient may therefore be charged $350 to $1,000 per infusion, to be paid out of pocket.11 Tally that up over the standard 6 to 12 initial treatment infusions, followed by maintenance infusions, and these patients with profound depression are potentially building up significant debt. Does this practice align with the ethical principles of autonomy, justice, beneficence, and nonmaleficence that all physicians swore to uphold? Will psychiatrists take a stand against the financial exploitation of a vulnerable group that is desperate to find any potential relief from their depression?
1. Hillhouse TM, Porter JH. A brief history of the development of antidepressant drugs: from monoamines to glutamate. Exp Clin Psychopharmacol. 2015;23(1):1-21.
2. Fava M, Rush A, Trivedi M, et al. Background and rationale for the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study. Psychiatr Clin North Am. 2003;26(2):457-494.
3. Gaynes BN, Rush AJ, Trivedi MH, et al. Primary versus specialty care outcomes for depressed outpatients managed with measurement-based care: results from STAR*D. J Gen Intern Med. 2008;23(5):551-560.
4. Gaynes BN, Warden D, Trivedi MH, et al. What did STAR*D teach us? Results from a large-scale, practical, clinical trial for patients with depression. Psychiatr Serv. 2009;60(11):1439-1445.
5. US Food and Drug Administration. Center for Drug Evaluation and Research. Esketamine clinical review. Published March 5, 2019. Accessed August 9, 2021. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2019/211243Orig1s000MedR.pdf
6. Zanos P, Moaddel R, Morris PJ, et al. Ketamine and ketamine metabolite pharmacology: insights into therapeutic mechanisms. Pharmacol Rev. 2018;70(3):621-660.
7. Zanos P, Gould TD. Mechanisms of ketamine action as an antidepressant. Mol Psychiatry. 2018;23(4):801-811.
8. Kaur U, Pathak BK, Singh A, et al. Esketamine: a glimmer of hope in treatment-resistant depression. Eur Arch Psychiatry Clin Neurosci. 2021;271(3):417-429.
9. McIntyre RS, Carvalho IP, Lui LMW, et al. The effect of intravenous, intranasal, and oral ketamine/esketamine in mood disorders: a meta-analysis. J Affect Disord. 2020;276:576-584.
10. Zarate CA Jr, Singh JB, Carlson PJ, et al. A randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression. Arch Gen Psychiatry. 2006;63(8):856-864.
11. Thielking M. Ketamine gives hope to patients with severe depression. But some clinics stray from the science and hype its benefits. STAT+. Published September 18, 2018. Accessed August 5, 2021. www.statnews.com/2018/09/24/ketamine-clinics-severe-depression-treatment/
In the modern-day practice of medicine, turf wars are more common than one may realize. Presently, an ongoing battle over who should be prescribing and administering ketamine for novel treatment uses is being waged among psychiatrists, anesthesiologists, family physicians, and emergency physicians. Whoever emerges victorious will determine whether psychiatric care is administered in a safe and cost-effective manner, or if it will merely benefit the bottom line of the prescriber. In this article, we discuss how ketamine may have a role for treatment-resistant depression (TRD), and why psychiatrists are uniquely qualified to prescribe and administer this medication for this purpose.
New approaches to treatment-resistant depression
Antidepressant medications, long the mainstay of depression treatment, have been shown to be safe and relatively equally effective, with varying tolerability. However, 33% percent of patients do not achieve remission after 4 trials of antidepressant therapy.1 Most antidepressant efficacy studies report remission rates of 35% to 40%,2 which means many patients require subsequent switching and/or augmentation of their treatment.3 The STAR*D trial demonstrated that after 2 adequate antidepressant trials, the likelihood of remission diminishes.4
After a patient’s depression is found to be treatment-resistant, the onus of guiding treatment shifts away from the patient’s primary care physician to the more specialized psychiatrist. Few would question the suitability of a psychiatrist’s expertise in handling complicated and nuanced mental illness. In order to manage TRD, psychiatrists enter a terrain of emerging novel therapies with rapid onset, different mechanisms of action, and parenteral routes of administration.
One such therapy is esketamine, the S-enantiomer of ketamine. The FDA approved the intranasal (IN) formulation of esketamine in March 2019 after the medication had been designated as a breakthrough therapy for TRD in 2013 and studied in 6 Phase III clinical trials.5 The S-enantiomer of ketamine is known to bind to the N-methyl-
Ketamine may be administered intranasally, intravenously, or orally. A meta-analysis aimed at assessing differences in ketamine efficacy for depression based on route of administration have shown that both IV and IN ketamine are effective, though it is not possible to draw conclusions regarding a direct comparison based on available data.9 Despite several landmark published studies, such as those by Zarate et al,10 IV ketamine is not FDA-approved for TRD.
Continue to: Why psychiatrists?
Why psychiatrists?
Psychiatrists have been prescribing IN esketamine, which is covered by most commercial insurances and administered in certified healthcare settings under a Risk Evaluation and Mitigation Strategy program.5 However, anesthesiologists and emergency physicians have opened a crop of boutique and concierge health clinics offering various “packages” of IV ketamine infusions for a slew of mental ailments, including depression, anxiety, bipolar disorder, and posttraumatic stress disorder.11 Minimal investigation reveals that these services are being prescribed mainly by practitioners in fields other than psychiatry. Intravenous ketamine has long been used off-label as a treatment for depression not by psychiatrists but by practitioners of anesthesiology or emergency medicine. Although these clinicians are likely familiar with ketamine as an anesthetic, they have no foundation or expertise in the diagnosis and treatment of complex mood disorders. The FDA-approved indication for esketamine falls firmly in the realm of psychiatric treatment. Physicians who have not completed a psychiatry residency have neither the training nor experience necessary to determine whether a patient is a candidate for this treatment.
One potential adverse effect of ketamine is an emergence phenomenon, colloquially named a “K-hole,” that can induce symptoms of psychosis such as disturbing hallucinations. Patients who have a history of psychosis need to be carefully evaluated for appropriateness to receive this treatment.
Furthermore, ketamine treatments administered by physicians who are not psychiatrists are billed not through insurance but mostly via private pay. A patient may therefore be charged $350 to $1,000 per infusion, to be paid out of pocket.11 Tally that up over the standard 6 to 12 initial treatment infusions, followed by maintenance infusions, and these patients with profound depression are potentially building up significant debt. Does this practice align with the ethical principles of autonomy, justice, beneficence, and nonmaleficence that all physicians swore to uphold? Will psychiatrists take a stand against the financial exploitation of a vulnerable group that is desperate to find any potential relief from their depression?
In the modern-day practice of medicine, turf wars are more common than one may realize. Presently, an ongoing battle over who should be prescribing and administering ketamine for novel treatment uses is being waged among psychiatrists, anesthesiologists, family physicians, and emergency physicians. Whoever emerges victorious will determine whether psychiatric care is administered in a safe and cost-effective manner, or if it will merely benefit the bottom line of the prescriber. In this article, we discuss how ketamine may have a role for treatment-resistant depression (TRD), and why psychiatrists are uniquely qualified to prescribe and administer this medication for this purpose.
New approaches to treatment-resistant depression
Antidepressant medications, long the mainstay of depression treatment, have been shown to be safe and relatively equally effective, with varying tolerability. However, 33% percent of patients do not achieve remission after 4 trials of antidepressant therapy.1 Most antidepressant efficacy studies report remission rates of 35% to 40%,2 which means many patients require subsequent switching and/or augmentation of their treatment.3 The STAR*D trial demonstrated that after 2 adequate antidepressant trials, the likelihood of remission diminishes.4
After a patient’s depression is found to be treatment-resistant, the onus of guiding treatment shifts away from the patient’s primary care physician to the more specialized psychiatrist. Few would question the suitability of a psychiatrist’s expertise in handling complicated and nuanced mental illness. In order to manage TRD, psychiatrists enter a terrain of emerging novel therapies with rapid onset, different mechanisms of action, and parenteral routes of administration.
One such therapy is esketamine, the S-enantiomer of ketamine. The FDA approved the intranasal (IN) formulation of esketamine in March 2019 after the medication had been designated as a breakthrough therapy for TRD in 2013 and studied in 6 Phase III clinical trials.5 The S-enantiomer of ketamine is known to bind to the N-methyl-
Ketamine may be administered intranasally, intravenously, or orally. A meta-analysis aimed at assessing differences in ketamine efficacy for depression based on route of administration have shown that both IV and IN ketamine are effective, though it is not possible to draw conclusions regarding a direct comparison based on available data.9 Despite several landmark published studies, such as those by Zarate et al,10 IV ketamine is not FDA-approved for TRD.
Continue to: Why psychiatrists?
Why psychiatrists?
Psychiatrists have been prescribing IN esketamine, which is covered by most commercial insurances and administered in certified healthcare settings under a Risk Evaluation and Mitigation Strategy program.5 However, anesthesiologists and emergency physicians have opened a crop of boutique and concierge health clinics offering various “packages” of IV ketamine infusions for a slew of mental ailments, including depression, anxiety, bipolar disorder, and posttraumatic stress disorder.11 Minimal investigation reveals that these services are being prescribed mainly by practitioners in fields other than psychiatry. Intravenous ketamine has long been used off-label as a treatment for depression not by psychiatrists but by practitioners of anesthesiology or emergency medicine. Although these clinicians are likely familiar with ketamine as an anesthetic, they have no foundation or expertise in the diagnosis and treatment of complex mood disorders. The FDA-approved indication for esketamine falls firmly in the realm of psychiatric treatment. Physicians who have not completed a psychiatry residency have neither the training nor experience necessary to determine whether a patient is a candidate for this treatment.
One potential adverse effect of ketamine is an emergence phenomenon, colloquially named a “K-hole,” that can induce symptoms of psychosis such as disturbing hallucinations. Patients who have a history of psychosis need to be carefully evaluated for appropriateness to receive this treatment.
Furthermore, ketamine treatments administered by physicians who are not psychiatrists are billed not through insurance but mostly via private pay. A patient may therefore be charged $350 to $1,000 per infusion, to be paid out of pocket.11 Tally that up over the standard 6 to 12 initial treatment infusions, followed by maintenance infusions, and these patients with profound depression are potentially building up significant debt. Does this practice align with the ethical principles of autonomy, justice, beneficence, and nonmaleficence that all physicians swore to uphold? Will psychiatrists take a stand against the financial exploitation of a vulnerable group that is desperate to find any potential relief from their depression?
1. Hillhouse TM, Porter JH. A brief history of the development of antidepressant drugs: from monoamines to glutamate. Exp Clin Psychopharmacol. 2015;23(1):1-21.
2. Fava M, Rush A, Trivedi M, et al. Background and rationale for the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study. Psychiatr Clin North Am. 2003;26(2):457-494.
3. Gaynes BN, Rush AJ, Trivedi MH, et al. Primary versus specialty care outcomes for depressed outpatients managed with measurement-based care: results from STAR*D. J Gen Intern Med. 2008;23(5):551-560.
4. Gaynes BN, Warden D, Trivedi MH, et al. What did STAR*D teach us? Results from a large-scale, practical, clinical trial for patients with depression. Psychiatr Serv. 2009;60(11):1439-1445.
5. US Food and Drug Administration. Center for Drug Evaluation and Research. Esketamine clinical review. Published March 5, 2019. Accessed August 9, 2021. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2019/211243Orig1s000MedR.pdf
6. Zanos P, Moaddel R, Morris PJ, et al. Ketamine and ketamine metabolite pharmacology: insights into therapeutic mechanisms. Pharmacol Rev. 2018;70(3):621-660.
7. Zanos P, Gould TD. Mechanisms of ketamine action as an antidepressant. Mol Psychiatry. 2018;23(4):801-811.
8. Kaur U, Pathak BK, Singh A, et al. Esketamine: a glimmer of hope in treatment-resistant depression. Eur Arch Psychiatry Clin Neurosci. 2021;271(3):417-429.
9. McIntyre RS, Carvalho IP, Lui LMW, et al. The effect of intravenous, intranasal, and oral ketamine/esketamine in mood disorders: a meta-analysis. J Affect Disord. 2020;276:576-584.
10. Zarate CA Jr, Singh JB, Carlson PJ, et al. A randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression. Arch Gen Psychiatry. 2006;63(8):856-864.
11. Thielking M. Ketamine gives hope to patients with severe depression. But some clinics stray from the science and hype its benefits. STAT+. Published September 18, 2018. Accessed August 5, 2021. www.statnews.com/2018/09/24/ketamine-clinics-severe-depression-treatment/
1. Hillhouse TM, Porter JH. A brief history of the development of antidepressant drugs: from monoamines to glutamate. Exp Clin Psychopharmacol. 2015;23(1):1-21.
2. Fava M, Rush A, Trivedi M, et al. Background and rationale for the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study. Psychiatr Clin North Am. 2003;26(2):457-494.
3. Gaynes BN, Rush AJ, Trivedi MH, et al. Primary versus specialty care outcomes for depressed outpatients managed with measurement-based care: results from STAR*D. J Gen Intern Med. 2008;23(5):551-560.
4. Gaynes BN, Warden D, Trivedi MH, et al. What did STAR*D teach us? Results from a large-scale, practical, clinical trial for patients with depression. Psychiatr Serv. 2009;60(11):1439-1445.
5. US Food and Drug Administration. Center for Drug Evaluation and Research. Esketamine clinical review. Published March 5, 2019. Accessed August 9, 2021. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2019/211243Orig1s000MedR.pdf
6. Zanos P, Moaddel R, Morris PJ, et al. Ketamine and ketamine metabolite pharmacology: insights into therapeutic mechanisms. Pharmacol Rev. 2018;70(3):621-660.
7. Zanos P, Gould TD. Mechanisms of ketamine action as an antidepressant. Mol Psychiatry. 2018;23(4):801-811.
8. Kaur U, Pathak BK, Singh A, et al. Esketamine: a glimmer of hope in treatment-resistant depression. Eur Arch Psychiatry Clin Neurosci. 2021;271(3):417-429.
9. McIntyre RS, Carvalho IP, Lui LMW, et al. The effect of intravenous, intranasal, and oral ketamine/esketamine in mood disorders: a meta-analysis. J Affect Disord. 2020;276:576-584.
10. Zarate CA Jr, Singh JB, Carlson PJ, et al. A randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression. Arch Gen Psychiatry. 2006;63(8):856-864.
11. Thielking M. Ketamine gives hope to patients with severe depression. But some clinics stray from the science and hype its benefits. STAT+. Published September 18, 2018. Accessed August 5, 2021. www.statnews.com/2018/09/24/ketamine-clinics-severe-depression-treatment/
APA, ABPN, and Maintenance of Certification: Stop this MOCkery
Editor’s note: Readers’ Forum is a department for correspondence from readers that is not in response to articles published in
The Accreditation Council for Graduate Medical Education (ACGME) is entrusted with assuring that upon graduation every resident is a competent doctor, a trained professional, and prepared to practice in their own field at a level that assures patient safety and meets the standard of care. The American Board of Psychiatry and Neurology (ABPN) is a private company that sells certificates claiming to attest the capacity or competence of the doctor but does not make public the test questions or algorithms used to win its qualifications or approval. The certifying business and the newer Maintenance of Certification (MOC) process developed by ABPN have unfortunately been embraced by ACGME and many hospitals, despite the lack of any good scientific support that board certification or MOC are meaningful for quality of patient care or outcomes. By that I mean there is no evidence that the voluntary board certification process or MOC have been shown to produce better outcomes for patients, save money for the country drowning in an ocean of health care costs, or allow doctors to get paid at a higher level by insurers for the same billing codes compared with those who bill without possessing these qualifications. The only entity that “profits” from the board certification/MOC process is ABPN, a private corporation that is supposed to be a nonprofit, but was sitting on a treasury of more than $140M in assets in 2019,1 with revenues growing annually. Including the interest earned on the investment and added revenues every year, the estimated total assets of ABPN will be in the range of $150M at the end of 2021!
Collaboration between ACGME and ABPN
The collaboration between ACGME and ABPN for graduate education for designing training programs for residents and fellows, with progressively increasing competencies and their assessments to dovetail with the board examinations offered by ABPN, sounds very legitimate. This arrangement is designed to enhance the quality of training and establish a minimum level of competence in each trainee who completes the training program. However, ACGME is catering to a monopoly recognized by the US Department of Justice (DOJ) Antitrust Division.2 ACGME has not entertained other evaluators of competence to discourage competition to the monopolistic ABPN. ACGME is only involved with the accredited training programs and has no business in assessing the continued competence of graduated trainees after they leave the program, although most will voluntarily opt to become board-certified by ABPN. Maintenance of Certification definitely does not come within the purview of “graduate medical education” for ACGME to be getting drawn into this collaboration.
ACGME and ABPN are unregulated and are not member-driven. As such, they operate outside of any real oversight. Their power derives from the status given to them by hospitals, some insurers, and many of our colleagues, who fail to see the reality that they are nothing more than diploma shops.
I am board-certified in psychiatry and child and adolescent psychiatry, and I have participated in obtaining board certification by ABPN in 3 other subspecialties (geriatric, addiction, and forensic). I decided to not participate in MOC for the latter 3 subspecialty certifications beyond 10 and 20 years for my own practical reasons. Obviously, then, I am not at all against initial certifications in any specialty, nor am I opposed to practitioners keeping up with progress in their fields and maintaining their competence. I am opposed to the continued efforts to engage professionals to pay a high price for the repeated MOC, riding on the hard work and earnings of the graduated specialists and continuously suctioning their income over their careers, with no evidence that MOC measures clinical competence or patient outcomes of their subscribers, who pay a chunk of money to the American Board of Medical Specialties (ABMS)/ABPN annually and every 10 years.
MOC and the APA
Many American Psychiatric Association (APA) members are opposed to the APA giving ABPN a piggyback ride to accomplish this profit seeking. This is becoming obvious to many APA members, who see this as a great exploitation.
Over the last 6 years, physicians have begun to question the validity of board certification and MOC by ABPN, mostly as a response to ever-increasing costs to them and ever-increasing revenues to ABPN. While APA members have long pressed the APA to push back against ABPN, the APA Board of Trustees has done the opposite by accepting yearly “unrestricted educational grants” from ABPN. In this manner, ABPN has essentially silenced the APA and has made it ineffective as our member organization in what has become a fight against ABPN’s unchecked power, influence, and intrusion. Every poll conducted by every APA District Branch or subspecialty organization has shown widespread discontent and anger at the ABPN/MOC process and APA’s deliberate inaction. Even when the APA commissioned its own member survey on the topic, wrote the questions, picked who would get the survey, decided which responses to count, and determined what statistics to apply, the results were damning. Despite its obviously transparent machinations, the APA failed to glorify the MOC process.
Continue to: The APA's membership...
The APA’s membership is declining, and the Board of Trustee’s position on MOC is partly to blame. The APA is once again not listening to its members! As a membership-driven organization, the APA must not exclusively support and promote this commercial educational product termed MOC when other, less expensive alternatives are now available. The APA can easily endorse these alternatives, in addition to offering its own less expensive products for attesting maintenance of competence. The latter effort will help eliminate the monopoly held by ABMS/ABPN in this domain and please all members as well as the DOJ.
The APA’s failure to provide less expensive alternatives or at least endorse existing ones despite repeated requests from a large number of APA members has led to frustration and a surge of strong feelings that are expressed on the APA email listservs, and especially that of the MOC caucus. These expressions are legitimate and need to be publicized to the general membership. I have collected the opinions of various loyal, long-standing APA members and put together a separate, yet-unpublished article to drive home the point that APA has resisted breaking the monopoly of ABPN, which the DOJ would encourage organizations such as the APA to do. Instead, APA is acting as an enabler to ABPN to create a multi-million dollar (and eventually a billion dollar) monopolistic industry at their members’ expense, literally endangering the careers of members if they fail to participate when employed by institutions that overvalue the MOC offered by ABPN.
I believe the recent exhibition of “collaboration” between the APA and ABPN is not similar to that between ACGME and ABPN, but is a most blatant effort on the part of the APA to help ABPN build a billion-dollar educational industry over the next 10 to 15 years. One can easily lose sight of this and get lost in the intricacies of how candidates can maintain their competency by obtaining free CME credits. The APA is distracting its members by citing this. They will continue to pay a high price for certification and recertification, with no real discount.
Most of the APA’s 38,000 members are in the dark about the above-mentioned process. They need to do their own research, especially when there are alternatives to the ABPN’s MOC program. They need to insist that the APA stop exclusively promoting ABPN products, and publicize other, much cheaper, alternatives. It will please all APA members to see the ABPN’s monopoly vanish. This is especially the case for younger psychiatrists, who average nearly $250,000 in educational loans. They need to prevent the APA/ABPN collaboration from having a far-reaching effect on their careers and finances, with potentially destructive consequences for their families, employers and—most importantly—their patients. Even some state licensing boards are being tempted to buy into the illusion.
Stop this MOCkery.
1. ProPublica. American Board of Psychiatry and Neurology. Accessed July 16, 2021. https://projects.propublica.org/nonprofits/organizations/410654864
2. US Department of Justice, Antitrust Division. Comments on Maryland House Bill 857. Published September 10, 2018. Accessed July 16, 2021. https://www.justice.gov/atr/page/file/1092791/download
Editor’s note: Readers’ Forum is a department for correspondence from readers that is not in response to articles published in
The Accreditation Council for Graduate Medical Education (ACGME) is entrusted with assuring that upon graduation every resident is a competent doctor, a trained professional, and prepared to practice in their own field at a level that assures patient safety and meets the standard of care. The American Board of Psychiatry and Neurology (ABPN) is a private company that sells certificates claiming to attest the capacity or competence of the doctor but does not make public the test questions or algorithms used to win its qualifications or approval. The certifying business and the newer Maintenance of Certification (MOC) process developed by ABPN have unfortunately been embraced by ACGME and many hospitals, despite the lack of any good scientific support that board certification or MOC are meaningful for quality of patient care or outcomes. By that I mean there is no evidence that the voluntary board certification process or MOC have been shown to produce better outcomes for patients, save money for the country drowning in an ocean of health care costs, or allow doctors to get paid at a higher level by insurers for the same billing codes compared with those who bill without possessing these qualifications. The only entity that “profits” from the board certification/MOC process is ABPN, a private corporation that is supposed to be a nonprofit, but was sitting on a treasury of more than $140M in assets in 2019,1 with revenues growing annually. Including the interest earned on the investment and added revenues every year, the estimated total assets of ABPN will be in the range of $150M at the end of 2021!
Collaboration between ACGME and ABPN
The collaboration between ACGME and ABPN for graduate education for designing training programs for residents and fellows, with progressively increasing competencies and their assessments to dovetail with the board examinations offered by ABPN, sounds very legitimate. This arrangement is designed to enhance the quality of training and establish a minimum level of competence in each trainee who completes the training program. However, ACGME is catering to a monopoly recognized by the US Department of Justice (DOJ) Antitrust Division.2 ACGME has not entertained other evaluators of competence to discourage competition to the monopolistic ABPN. ACGME is only involved with the accredited training programs and has no business in assessing the continued competence of graduated trainees after they leave the program, although most will voluntarily opt to become board-certified by ABPN. Maintenance of Certification definitely does not come within the purview of “graduate medical education” for ACGME to be getting drawn into this collaboration.
ACGME and ABPN are unregulated and are not member-driven. As such, they operate outside of any real oversight. Their power derives from the status given to them by hospitals, some insurers, and many of our colleagues, who fail to see the reality that they are nothing more than diploma shops.
I am board-certified in psychiatry and child and adolescent psychiatry, and I have participated in obtaining board certification by ABPN in 3 other subspecialties (geriatric, addiction, and forensic). I decided to not participate in MOC for the latter 3 subspecialty certifications beyond 10 and 20 years for my own practical reasons. Obviously, then, I am not at all against initial certifications in any specialty, nor am I opposed to practitioners keeping up with progress in their fields and maintaining their competence. I am opposed to the continued efforts to engage professionals to pay a high price for the repeated MOC, riding on the hard work and earnings of the graduated specialists and continuously suctioning their income over their careers, with no evidence that MOC measures clinical competence or patient outcomes of their subscribers, who pay a chunk of money to the American Board of Medical Specialties (ABMS)/ABPN annually and every 10 years.
MOC and the APA
Many American Psychiatric Association (APA) members are opposed to the APA giving ABPN a piggyback ride to accomplish this profit seeking. This is becoming obvious to many APA members, who see this as a great exploitation.
Over the last 6 years, physicians have begun to question the validity of board certification and MOC by ABPN, mostly as a response to ever-increasing costs to them and ever-increasing revenues to ABPN. While APA members have long pressed the APA to push back against ABPN, the APA Board of Trustees has done the opposite by accepting yearly “unrestricted educational grants” from ABPN. In this manner, ABPN has essentially silenced the APA and has made it ineffective as our member organization in what has become a fight against ABPN’s unchecked power, influence, and intrusion. Every poll conducted by every APA District Branch or subspecialty organization has shown widespread discontent and anger at the ABPN/MOC process and APA’s deliberate inaction. Even when the APA commissioned its own member survey on the topic, wrote the questions, picked who would get the survey, decided which responses to count, and determined what statistics to apply, the results were damning. Despite its obviously transparent machinations, the APA failed to glorify the MOC process.
Continue to: The APA's membership...
The APA’s membership is declining, and the Board of Trustee’s position on MOC is partly to blame. The APA is once again not listening to its members! As a membership-driven organization, the APA must not exclusively support and promote this commercial educational product termed MOC when other, less expensive alternatives are now available. The APA can easily endorse these alternatives, in addition to offering its own less expensive products for attesting maintenance of competence. The latter effort will help eliminate the monopoly held by ABMS/ABPN in this domain and please all members as well as the DOJ.
The APA’s failure to provide less expensive alternatives or at least endorse existing ones despite repeated requests from a large number of APA members has led to frustration and a surge of strong feelings that are expressed on the APA email listservs, and especially that of the MOC caucus. These expressions are legitimate and need to be publicized to the general membership. I have collected the opinions of various loyal, long-standing APA members and put together a separate, yet-unpublished article to drive home the point that APA has resisted breaking the monopoly of ABPN, which the DOJ would encourage organizations such as the APA to do. Instead, APA is acting as an enabler to ABPN to create a multi-million dollar (and eventually a billion dollar) monopolistic industry at their members’ expense, literally endangering the careers of members if they fail to participate when employed by institutions that overvalue the MOC offered by ABPN.
I believe the recent exhibition of “collaboration” between the APA and ABPN is not similar to that between ACGME and ABPN, but is a most blatant effort on the part of the APA to help ABPN build a billion-dollar educational industry over the next 10 to 15 years. One can easily lose sight of this and get lost in the intricacies of how candidates can maintain their competency by obtaining free CME credits. The APA is distracting its members by citing this. They will continue to pay a high price for certification and recertification, with no real discount.
Most of the APA’s 38,000 members are in the dark about the above-mentioned process. They need to do their own research, especially when there are alternatives to the ABPN’s MOC program. They need to insist that the APA stop exclusively promoting ABPN products, and publicize other, much cheaper, alternatives. It will please all APA members to see the ABPN’s monopoly vanish. This is especially the case for younger psychiatrists, who average nearly $250,000 in educational loans. They need to prevent the APA/ABPN collaboration from having a far-reaching effect on their careers and finances, with potentially destructive consequences for their families, employers and—most importantly—their patients. Even some state licensing boards are being tempted to buy into the illusion.
Stop this MOCkery.
Editor’s note: Readers’ Forum is a department for correspondence from readers that is not in response to articles published in
The Accreditation Council for Graduate Medical Education (ACGME) is entrusted with assuring that upon graduation every resident is a competent doctor, a trained professional, and prepared to practice in their own field at a level that assures patient safety and meets the standard of care. The American Board of Psychiatry and Neurology (ABPN) is a private company that sells certificates claiming to attest the capacity or competence of the doctor but does not make public the test questions or algorithms used to win its qualifications or approval. The certifying business and the newer Maintenance of Certification (MOC) process developed by ABPN have unfortunately been embraced by ACGME and many hospitals, despite the lack of any good scientific support that board certification or MOC are meaningful for quality of patient care or outcomes. By that I mean there is no evidence that the voluntary board certification process or MOC have been shown to produce better outcomes for patients, save money for the country drowning in an ocean of health care costs, or allow doctors to get paid at a higher level by insurers for the same billing codes compared with those who bill without possessing these qualifications. The only entity that “profits” from the board certification/MOC process is ABPN, a private corporation that is supposed to be a nonprofit, but was sitting on a treasury of more than $140M in assets in 2019,1 with revenues growing annually. Including the interest earned on the investment and added revenues every year, the estimated total assets of ABPN will be in the range of $150M at the end of 2021!
Collaboration between ACGME and ABPN
The collaboration between ACGME and ABPN for graduate education for designing training programs for residents and fellows, with progressively increasing competencies and their assessments to dovetail with the board examinations offered by ABPN, sounds very legitimate. This arrangement is designed to enhance the quality of training and establish a minimum level of competence in each trainee who completes the training program. However, ACGME is catering to a monopoly recognized by the US Department of Justice (DOJ) Antitrust Division.2 ACGME has not entertained other evaluators of competence to discourage competition to the monopolistic ABPN. ACGME is only involved with the accredited training programs and has no business in assessing the continued competence of graduated trainees after they leave the program, although most will voluntarily opt to become board-certified by ABPN. Maintenance of Certification definitely does not come within the purview of “graduate medical education” for ACGME to be getting drawn into this collaboration.
ACGME and ABPN are unregulated and are not member-driven. As such, they operate outside of any real oversight. Their power derives from the status given to them by hospitals, some insurers, and many of our colleagues, who fail to see the reality that they are nothing more than diploma shops.
I am board-certified in psychiatry and child and adolescent psychiatry, and I have participated in obtaining board certification by ABPN in 3 other subspecialties (geriatric, addiction, and forensic). I decided to not participate in MOC for the latter 3 subspecialty certifications beyond 10 and 20 years for my own practical reasons. Obviously, then, I am not at all against initial certifications in any specialty, nor am I opposed to practitioners keeping up with progress in their fields and maintaining their competence. I am opposed to the continued efforts to engage professionals to pay a high price for the repeated MOC, riding on the hard work and earnings of the graduated specialists and continuously suctioning their income over their careers, with no evidence that MOC measures clinical competence or patient outcomes of their subscribers, who pay a chunk of money to the American Board of Medical Specialties (ABMS)/ABPN annually and every 10 years.
MOC and the APA
Many American Psychiatric Association (APA) members are opposed to the APA giving ABPN a piggyback ride to accomplish this profit seeking. This is becoming obvious to many APA members, who see this as a great exploitation.
Over the last 6 years, physicians have begun to question the validity of board certification and MOC by ABPN, mostly as a response to ever-increasing costs to them and ever-increasing revenues to ABPN. While APA members have long pressed the APA to push back against ABPN, the APA Board of Trustees has done the opposite by accepting yearly “unrestricted educational grants” from ABPN. In this manner, ABPN has essentially silenced the APA and has made it ineffective as our member organization in what has become a fight against ABPN’s unchecked power, influence, and intrusion. Every poll conducted by every APA District Branch or subspecialty organization has shown widespread discontent and anger at the ABPN/MOC process and APA’s deliberate inaction. Even when the APA commissioned its own member survey on the topic, wrote the questions, picked who would get the survey, decided which responses to count, and determined what statistics to apply, the results were damning. Despite its obviously transparent machinations, the APA failed to glorify the MOC process.
Continue to: The APA's membership...
The APA’s membership is declining, and the Board of Trustee’s position on MOC is partly to blame. The APA is once again not listening to its members! As a membership-driven organization, the APA must not exclusively support and promote this commercial educational product termed MOC when other, less expensive alternatives are now available. The APA can easily endorse these alternatives, in addition to offering its own less expensive products for attesting maintenance of competence. The latter effort will help eliminate the monopoly held by ABMS/ABPN in this domain and please all members as well as the DOJ.
The APA’s failure to provide less expensive alternatives or at least endorse existing ones despite repeated requests from a large number of APA members has led to frustration and a surge of strong feelings that are expressed on the APA email listservs, and especially that of the MOC caucus. These expressions are legitimate and need to be publicized to the general membership. I have collected the opinions of various loyal, long-standing APA members and put together a separate, yet-unpublished article to drive home the point that APA has resisted breaking the monopoly of ABPN, which the DOJ would encourage organizations such as the APA to do. Instead, APA is acting as an enabler to ABPN to create a multi-million dollar (and eventually a billion dollar) monopolistic industry at their members’ expense, literally endangering the careers of members if they fail to participate when employed by institutions that overvalue the MOC offered by ABPN.
I believe the recent exhibition of “collaboration” between the APA and ABPN is not similar to that between ACGME and ABPN, but is a most blatant effort on the part of the APA to help ABPN build a billion-dollar educational industry over the next 10 to 15 years. One can easily lose sight of this and get lost in the intricacies of how candidates can maintain their competency by obtaining free CME credits. The APA is distracting its members by citing this. They will continue to pay a high price for certification and recertification, with no real discount.
Most of the APA’s 38,000 members are in the dark about the above-mentioned process. They need to do their own research, especially when there are alternatives to the ABPN’s MOC program. They need to insist that the APA stop exclusively promoting ABPN products, and publicize other, much cheaper, alternatives. It will please all APA members to see the ABPN’s monopoly vanish. This is especially the case for younger psychiatrists, who average nearly $250,000 in educational loans. They need to prevent the APA/ABPN collaboration from having a far-reaching effect on their careers and finances, with potentially destructive consequences for their families, employers and—most importantly—their patients. Even some state licensing boards are being tempted to buy into the illusion.
Stop this MOCkery.
1. ProPublica. American Board of Psychiatry and Neurology. Accessed July 16, 2021. https://projects.propublica.org/nonprofits/organizations/410654864
2. US Department of Justice, Antitrust Division. Comments on Maryland House Bill 857. Published September 10, 2018. Accessed July 16, 2021. https://www.justice.gov/atr/page/file/1092791/download
1. ProPublica. American Board of Psychiatry and Neurology. Accessed July 16, 2021. https://projects.propublica.org/nonprofits/organizations/410654864
2. US Department of Justice, Antitrust Division. Comments on Maryland House Bill 857. Published September 10, 2018. Accessed July 16, 2021. https://www.justice.gov/atr/page/file/1092791/download
From past to future
This month, the current Editor-in-Chief and his Editorial Board will conclude our 5-year term. Megan Adams MD, JD, MSc, from the University of Michigan School of Medicine will assume my position. She has a stellar academic, research, and teaching record and is one of the best writers I know. She and her Board of Editors will carry on the tradition of GIHN.
The idea of an official newspaper of the AGA came from AGA staff in 2006. The goals of the newspaper were twofold: to communicate the latest news and information to practitioners to help them stay at the forefront of patient care and to develop another revenue stream for our society. The newspaper was launched in January 2007 with Charles Lightdale MD, AGAF, as the first editor and Colin W. Howden MD, AGAF, as the second (each with 5-year terms). While they wrote occasional editorials, I began writing 300-word essays for each issue. I have tried diligently to maintain a balanced viewpoint for all my editorials, although this has been difficult in the recent past and current national environment.
The paper evolved from a simple print publication to a multimedia communications vehicle that includes online-only content, videos, supplements, quizzes, and more. Last year, we published our first “Data Trends,” a supplement containing 10 or so brief articles written by content experts, covering current topics of high interest. As the paper evolved, we broadened our target audience to include research scientists, international practitioners and others interested in digestive diseases.
As I did last month, I would like to thank the AGA and Frontline Medical Communications staff for their dedication and constant work to bring you this newspaper.
Finally, I would like to pay tribute to Tadataka “Tachi” Yamada, who died this last month at the age of 76 years. He was one of the premier advocates for global health. His contributions to our field thru research, philanthropy, and leadership were enormous. We will miss him greatly.
John I Allen, MD, MBA, AGAF
Editor in Chief
This month, the current Editor-in-Chief and his Editorial Board will conclude our 5-year term. Megan Adams MD, JD, MSc, from the University of Michigan School of Medicine will assume my position. She has a stellar academic, research, and teaching record and is one of the best writers I know. She and her Board of Editors will carry on the tradition of GIHN.
The idea of an official newspaper of the AGA came from AGA staff in 2006. The goals of the newspaper were twofold: to communicate the latest news and information to practitioners to help them stay at the forefront of patient care and to develop another revenue stream for our society. The newspaper was launched in January 2007 with Charles Lightdale MD, AGAF, as the first editor and Colin W. Howden MD, AGAF, as the second (each with 5-year terms). While they wrote occasional editorials, I began writing 300-word essays for each issue. I have tried diligently to maintain a balanced viewpoint for all my editorials, although this has been difficult in the recent past and current national environment.
The paper evolved from a simple print publication to a multimedia communications vehicle that includes online-only content, videos, supplements, quizzes, and more. Last year, we published our first “Data Trends,” a supplement containing 10 or so brief articles written by content experts, covering current topics of high interest. As the paper evolved, we broadened our target audience to include research scientists, international practitioners and others interested in digestive diseases.
As I did last month, I would like to thank the AGA and Frontline Medical Communications staff for their dedication and constant work to bring you this newspaper.
Finally, I would like to pay tribute to Tadataka “Tachi” Yamada, who died this last month at the age of 76 years. He was one of the premier advocates for global health. His contributions to our field thru research, philanthropy, and leadership were enormous. We will miss him greatly.
John I Allen, MD, MBA, AGAF
Editor in Chief
This month, the current Editor-in-Chief and his Editorial Board will conclude our 5-year term. Megan Adams MD, JD, MSc, from the University of Michigan School of Medicine will assume my position. She has a stellar academic, research, and teaching record and is one of the best writers I know. She and her Board of Editors will carry on the tradition of GIHN.
The idea of an official newspaper of the AGA came from AGA staff in 2006. The goals of the newspaper were twofold: to communicate the latest news and information to practitioners to help them stay at the forefront of patient care and to develop another revenue stream for our society. The newspaper was launched in January 2007 with Charles Lightdale MD, AGAF, as the first editor and Colin W. Howden MD, AGAF, as the second (each with 5-year terms). While they wrote occasional editorials, I began writing 300-word essays for each issue. I have tried diligently to maintain a balanced viewpoint for all my editorials, although this has been difficult in the recent past and current national environment.
The paper evolved from a simple print publication to a multimedia communications vehicle that includes online-only content, videos, supplements, quizzes, and more. Last year, we published our first “Data Trends,” a supplement containing 10 or so brief articles written by content experts, covering current topics of high interest. As the paper evolved, we broadened our target audience to include research scientists, international practitioners and others interested in digestive diseases.
As I did last month, I would like to thank the AGA and Frontline Medical Communications staff for their dedication and constant work to bring you this newspaper.
Finally, I would like to pay tribute to Tadataka “Tachi” Yamada, who died this last month at the age of 76 years. He was one of the premier advocates for global health. His contributions to our field thru research, philanthropy, and leadership were enormous. We will miss him greatly.
John I Allen, MD, MBA, AGAF
Editor in Chief
Clinical Edge Journal Scan Commentary: EPI September 2021
Our first study comes out of Sheffield, UK, and Halle, Germany, and looks at the correlation between sarcopenia and EPI (Jalal et al). Notably sarcopenia, or reduction in muscle mass, is a known complication of malnutrition and conditions like EPI. It has traditionally been difficult to diagnose because traditional methods have suffered from low accuracy (i.e., mid-arm circumference). In recent years, commercially available software has been developed to digitally assess skeletal muscle mass on axial CT imaging. Digital imaging allows for granular assessments of metrics such as myosteatosis and sacropenic obesity, both of which remained relatively elusive metrics in prior ways of assessing sarcopenia.
In this study, researchers postulate that, since CT scans are recently performed in the evaluation of those patients with suspected pancreatic pathology, it would be natural to assess for sarcopenia on said CT imaging. Identifying sarcopenia might allow clinicians to identify those patients with or at risk for EPI.
Patients referred to EUS for suspected pancreatic pathology were included in the study (except those found to have pancreatic cancer). This prospective study included 102 patients with suspected or proven benign pancreatic pathology, chronic pancreatitis, or recurrent pancreatic type pain. Fecal elastase testing was used to determine those with EPI, and digital CT analysis was used to recognize patients with sarcopenia.
Overall, EPI was present in 45.1% of patients. The prevalence of sarcopenia (67.4% vs. 37.55%; P < .003), myosteatosis (52.2% vs. 10.7%; P = .046), and sarcopenic obesity (66.7% vs. 24.3%; P = .002) was significantly higher in patients with vs without EPI. Sarcopenia (odds ratio [OR], 4.8; P = .02) was strongly associated with EPI. The authors conclude that digital skeletal mass analysis can be performed on patients already undergoing CT scans for suspected pancreatic pathology for possible further diagnosis, risk assessment and to better inform clinical management.
Another notable study came out of Baylor College of Medicine that looked at the clinical significance of fatty pancreas (FP) (Krill et al). Diffuse echogenicity of the pancreas is a common finding on endoscopic ultrasound (EUS), but of unknown clinical significance. Krill’s group aimed to determine if diffuse fatty infiltration of the pancreas had any clinical implication on pancreatic function. They conducted a retrospective case-control study comparing adult patients with diffuse echogenicity of the pancreas to those without known pancreatic disease with chronic diarrhea. Notably, the incidence of EPI (47% vs. 6%) and chronic pancreatitis (18% vs. 0%) was significantly higher (both P < .001) in the fatty pancreas group vs. the control group.
The authors conclude “Our findings suggest that FP may not merely be a benign sonographic finding, but rather imply underlying parenchymal dysfunction, such as that seen when fat deposition occurs in the liver (i.e., nonalcoholic fatty liver disease).” Additionally the paper states that recent literature has found an association between fatty pancreas and increasing body mass index (BMI), hyperlipidemia, insulin resistance, and metabolic syndrome. Perhaps we will further appreciate the likely prominent and under-appreciated role of metabolic syndrome in the development of acute and chronic pancreatitis.
References:
Jalal M, Rosendahl J, Campbell JA, Vinayagam R, Al-Mukhtar A, Hopper AD. Identification of “digital sarcopenia” can aid the detection of pancreatic exocrine insufficiency and malnutrition assessment in patients with suspected pancreatic pathology. Dig Dis 2021 (Jun 8), (in press).
Krill JT, Szafron D, Elhanafi S, et al. Endoscopic ultrasound finding of diffuse echogenicity in the pancreas, is it relevant? Dig Dis Sci 2021 (Aug 4), (in press).
Our first study comes out of Sheffield, UK, and Halle, Germany, and looks at the correlation between sarcopenia and EPI (Jalal et al). Notably sarcopenia, or reduction in muscle mass, is a known complication of malnutrition and conditions like EPI. It has traditionally been difficult to diagnose because traditional methods have suffered from low accuracy (i.e., mid-arm circumference). In recent years, commercially available software has been developed to digitally assess skeletal muscle mass on axial CT imaging. Digital imaging allows for granular assessments of metrics such as myosteatosis and sacropenic obesity, both of which remained relatively elusive metrics in prior ways of assessing sarcopenia.
In this study, researchers postulate that, since CT scans are recently performed in the evaluation of those patients with suspected pancreatic pathology, it would be natural to assess for sarcopenia on said CT imaging. Identifying sarcopenia might allow clinicians to identify those patients with or at risk for EPI.
Patients referred to EUS for suspected pancreatic pathology were included in the study (except those found to have pancreatic cancer). This prospective study included 102 patients with suspected or proven benign pancreatic pathology, chronic pancreatitis, or recurrent pancreatic type pain. Fecal elastase testing was used to determine those with EPI, and digital CT analysis was used to recognize patients with sarcopenia.
Overall, EPI was present in 45.1% of patients. The prevalence of sarcopenia (67.4% vs. 37.55%; P < .003), myosteatosis (52.2% vs. 10.7%; P = .046), and sarcopenic obesity (66.7% vs. 24.3%; P = .002) was significantly higher in patients with vs without EPI. Sarcopenia (odds ratio [OR], 4.8; P = .02) was strongly associated with EPI. The authors conclude that digital skeletal mass analysis can be performed on patients already undergoing CT scans for suspected pancreatic pathology for possible further diagnosis, risk assessment and to better inform clinical management.
Another notable study came out of Baylor College of Medicine that looked at the clinical significance of fatty pancreas (FP) (Krill et al). Diffuse echogenicity of the pancreas is a common finding on endoscopic ultrasound (EUS), but of unknown clinical significance. Krill’s group aimed to determine if diffuse fatty infiltration of the pancreas had any clinical implication on pancreatic function. They conducted a retrospective case-control study comparing adult patients with diffuse echogenicity of the pancreas to those without known pancreatic disease with chronic diarrhea. Notably, the incidence of EPI (47% vs. 6%) and chronic pancreatitis (18% vs. 0%) was significantly higher (both P < .001) in the fatty pancreas group vs. the control group.
The authors conclude “Our findings suggest that FP may not merely be a benign sonographic finding, but rather imply underlying parenchymal dysfunction, such as that seen when fat deposition occurs in the liver (i.e., nonalcoholic fatty liver disease).” Additionally the paper states that recent literature has found an association between fatty pancreas and increasing body mass index (BMI), hyperlipidemia, insulin resistance, and metabolic syndrome. Perhaps we will further appreciate the likely prominent and under-appreciated role of metabolic syndrome in the development of acute and chronic pancreatitis.
References:
Jalal M, Rosendahl J, Campbell JA, Vinayagam R, Al-Mukhtar A, Hopper AD. Identification of “digital sarcopenia” can aid the detection of pancreatic exocrine insufficiency and malnutrition assessment in patients with suspected pancreatic pathology. Dig Dis 2021 (Jun 8), (in press).
Krill JT, Szafron D, Elhanafi S, et al. Endoscopic ultrasound finding of diffuse echogenicity in the pancreas, is it relevant? Dig Dis Sci 2021 (Aug 4), (in press).
Our first study comes out of Sheffield, UK, and Halle, Germany, and looks at the correlation between sarcopenia and EPI (Jalal et al). Notably sarcopenia, or reduction in muscle mass, is a known complication of malnutrition and conditions like EPI. It has traditionally been difficult to diagnose because traditional methods have suffered from low accuracy (i.e., mid-arm circumference). In recent years, commercially available software has been developed to digitally assess skeletal muscle mass on axial CT imaging. Digital imaging allows for granular assessments of metrics such as myosteatosis and sacropenic obesity, both of which remained relatively elusive metrics in prior ways of assessing sarcopenia.
In this study, researchers postulate that, since CT scans are recently performed in the evaluation of those patients with suspected pancreatic pathology, it would be natural to assess for sarcopenia on said CT imaging. Identifying sarcopenia might allow clinicians to identify those patients with or at risk for EPI.
Patients referred to EUS for suspected pancreatic pathology were included in the study (except those found to have pancreatic cancer). This prospective study included 102 patients with suspected or proven benign pancreatic pathology, chronic pancreatitis, or recurrent pancreatic type pain. Fecal elastase testing was used to determine those with EPI, and digital CT analysis was used to recognize patients with sarcopenia.
Overall, EPI was present in 45.1% of patients. The prevalence of sarcopenia (67.4% vs. 37.55%; P < .003), myosteatosis (52.2% vs. 10.7%; P = .046), and sarcopenic obesity (66.7% vs. 24.3%; P = .002) was significantly higher in patients with vs without EPI. Sarcopenia (odds ratio [OR], 4.8; P = .02) was strongly associated with EPI. The authors conclude that digital skeletal mass analysis can be performed on patients already undergoing CT scans for suspected pancreatic pathology for possible further diagnosis, risk assessment and to better inform clinical management.
Another notable study came out of Baylor College of Medicine that looked at the clinical significance of fatty pancreas (FP) (Krill et al). Diffuse echogenicity of the pancreas is a common finding on endoscopic ultrasound (EUS), but of unknown clinical significance. Krill’s group aimed to determine if diffuse fatty infiltration of the pancreas had any clinical implication on pancreatic function. They conducted a retrospective case-control study comparing adult patients with diffuse echogenicity of the pancreas to those without known pancreatic disease with chronic diarrhea. Notably, the incidence of EPI (47% vs. 6%) and chronic pancreatitis (18% vs. 0%) was significantly higher (both P < .001) in the fatty pancreas group vs. the control group.
The authors conclude “Our findings suggest that FP may not merely be a benign sonographic finding, but rather imply underlying parenchymal dysfunction, such as that seen when fat deposition occurs in the liver (i.e., nonalcoholic fatty liver disease).” Additionally the paper states that recent literature has found an association between fatty pancreas and increasing body mass index (BMI), hyperlipidemia, insulin resistance, and metabolic syndrome. Perhaps we will further appreciate the likely prominent and under-appreciated role of metabolic syndrome in the development of acute and chronic pancreatitis.
References:
Jalal M, Rosendahl J, Campbell JA, Vinayagam R, Al-Mukhtar A, Hopper AD. Identification of “digital sarcopenia” can aid the detection of pancreatic exocrine insufficiency and malnutrition assessment in patients with suspected pancreatic pathology. Dig Dis 2021 (Jun 8), (in press).
Krill JT, Szafron D, Elhanafi S, et al. Endoscopic ultrasound finding of diffuse echogenicity in the pancreas, is it relevant? Dig Dis Sci 2021 (Aug 4), (in press).
Clinical Edge Journal Scan Commentary: PsA September 2021
Identifying risk factors for onset of Psoriatic Arthritis (PsA) is a major unmet need. Comparing potential risk factors for the diagnosis of PsA, rheumatoid arthritis (RA), and ankylosing spondylitis (AS) is of interest. Such studies may help us identify shared and unique risk factors of onset of chronic inflammatory arthritis. Meer E et al compared potential risk factors for the diagnosis of PsA, psoriasis, RA, and AS. They conducted four parallel case-control studies using data collected between 1994 and 2015 in The Health Improvement Network, an anonymized longitudinal patient dataset collected at primary care clinics throughout the United Kingdom. PsA was associated with obesity, pharyngitis, skin infections, moderate alcohol intake, gout, and uveitis. As expected, PsA and AS were associated with uveitis. Interestingly, PsA and RA were associated with preceding gout. Smoking was a risk factor for all disease and statin use was inversely associated with all 4 diseases. This study has identified potential risk factors for inflammatory diseases including PsA and may help in early identification as well as risk mitigation.
Most patients develop psoriatic arthritis (PsA) after or simultaneously with cutaneous psoriasis. The mechanisms underlying progression from cutaneous psoriasis to arthritis psoriasis are currently unclear. An important question is whether modern targeted treatment of cutaneous psoriasis reduces the risk of developing PsA. To address this, Acosta Felquer ML et al conducted a retrospective cohort study to compare the incidence of PsA in 1719 patients with psoriasis (14,721 patient/years of follow up) grouped according to different treatments for their skin psoriasis: topicals, phototherapy or no treatment (n= 1387), conventional disease-modifying antirheumatic drugs (cDMARDs) or biological DMARDs (bDMARDs). During follow-up, 239 patients (14%) developed PsA. The risk of developing PsA in patients treated with bDMARDs was significantly lower (incidence rate ratio (IRR)=0.26; 95% CI 0.03 to 0.94), compared with topicals, but not compared with cDMARDs (IRR=0.35; 95% CI 0.035 to 1.96). Male sex, nail involvement and higher body mass index were associated with increased risk of developing PsA, while bDMARD use was protective. Thus, this study provides some evidence that systemic treatment might ‘protect’ against development if PsA. Appropriately designed prospective studies are required.
One important clinical question is whether patients with oligoarthritis (involvement of <5 joints) progress to polyarthritis. In an observational study Gladman DD et al reported that in 407 patients evaluated within 12 months of diagnosis, 192 (47%) presented with oligoarthritis. More patients with polyarthritis presented with dactylitis, enthesitis, higher HAQ and lower SF-36 scores. Of the 192 patients with oligoarthritis, 75 (39%) progressed to polyarthritis. Lower SF-36 mental component summary score was the predictor for progressing to polyarthritis. Thus, except for the burden of musculoskeletal involvement, oligoarticular PsA resembles polyarticular PsA and therefore the two PsA subclasses should simply be classified together as peripheral arthritis.
Identifying risk factors for onset of Psoriatic Arthritis (PsA) is a major unmet need. Comparing potential risk factors for the diagnosis of PsA, rheumatoid arthritis (RA), and ankylosing spondylitis (AS) is of interest. Such studies may help us identify shared and unique risk factors of onset of chronic inflammatory arthritis. Meer E et al compared potential risk factors for the diagnosis of PsA, psoriasis, RA, and AS. They conducted four parallel case-control studies using data collected between 1994 and 2015 in The Health Improvement Network, an anonymized longitudinal patient dataset collected at primary care clinics throughout the United Kingdom. PsA was associated with obesity, pharyngitis, skin infections, moderate alcohol intake, gout, and uveitis. As expected, PsA and AS were associated with uveitis. Interestingly, PsA and RA were associated with preceding gout. Smoking was a risk factor for all disease and statin use was inversely associated with all 4 diseases. This study has identified potential risk factors for inflammatory diseases including PsA and may help in early identification as well as risk mitigation.
Most patients develop psoriatic arthritis (PsA) after or simultaneously with cutaneous psoriasis. The mechanisms underlying progression from cutaneous psoriasis to arthritis psoriasis are currently unclear. An important question is whether modern targeted treatment of cutaneous psoriasis reduces the risk of developing PsA. To address this, Acosta Felquer ML et al conducted a retrospective cohort study to compare the incidence of PsA in 1719 patients with psoriasis (14,721 patient/years of follow up) grouped according to different treatments for their skin psoriasis: topicals, phototherapy or no treatment (n= 1387), conventional disease-modifying antirheumatic drugs (cDMARDs) or biological DMARDs (bDMARDs). During follow-up, 239 patients (14%) developed PsA. The risk of developing PsA in patients treated with bDMARDs was significantly lower (incidence rate ratio (IRR)=0.26; 95% CI 0.03 to 0.94), compared with topicals, but not compared with cDMARDs (IRR=0.35; 95% CI 0.035 to 1.96). Male sex, nail involvement and higher body mass index were associated with increased risk of developing PsA, while bDMARD use was protective. Thus, this study provides some evidence that systemic treatment might ‘protect’ against development if PsA. Appropriately designed prospective studies are required.
One important clinical question is whether patients with oligoarthritis (involvement of <5 joints) progress to polyarthritis. In an observational study Gladman DD et al reported that in 407 patients evaluated within 12 months of diagnosis, 192 (47%) presented with oligoarthritis. More patients with polyarthritis presented with dactylitis, enthesitis, higher HAQ and lower SF-36 scores. Of the 192 patients with oligoarthritis, 75 (39%) progressed to polyarthritis. Lower SF-36 mental component summary score was the predictor for progressing to polyarthritis. Thus, except for the burden of musculoskeletal involvement, oligoarticular PsA resembles polyarticular PsA and therefore the two PsA subclasses should simply be classified together as peripheral arthritis.
Identifying risk factors for onset of Psoriatic Arthritis (PsA) is a major unmet need. Comparing potential risk factors for the diagnosis of PsA, rheumatoid arthritis (RA), and ankylosing spondylitis (AS) is of interest. Such studies may help us identify shared and unique risk factors of onset of chronic inflammatory arthritis. Meer E et al compared potential risk factors for the diagnosis of PsA, psoriasis, RA, and AS. They conducted four parallel case-control studies using data collected between 1994 and 2015 in The Health Improvement Network, an anonymized longitudinal patient dataset collected at primary care clinics throughout the United Kingdom. PsA was associated with obesity, pharyngitis, skin infections, moderate alcohol intake, gout, and uveitis. As expected, PsA and AS were associated with uveitis. Interestingly, PsA and RA were associated with preceding gout. Smoking was a risk factor for all disease and statin use was inversely associated with all 4 diseases. This study has identified potential risk factors for inflammatory diseases including PsA and may help in early identification as well as risk mitigation.
Most patients develop psoriatic arthritis (PsA) after or simultaneously with cutaneous psoriasis. The mechanisms underlying progression from cutaneous psoriasis to arthritis psoriasis are currently unclear. An important question is whether modern targeted treatment of cutaneous psoriasis reduces the risk of developing PsA. To address this, Acosta Felquer ML et al conducted a retrospective cohort study to compare the incidence of PsA in 1719 patients with psoriasis (14,721 patient/years of follow up) grouped according to different treatments for their skin psoriasis: topicals, phototherapy or no treatment (n= 1387), conventional disease-modifying antirheumatic drugs (cDMARDs) or biological DMARDs (bDMARDs). During follow-up, 239 patients (14%) developed PsA. The risk of developing PsA in patients treated with bDMARDs was significantly lower (incidence rate ratio (IRR)=0.26; 95% CI 0.03 to 0.94), compared with topicals, but not compared with cDMARDs (IRR=0.35; 95% CI 0.035 to 1.96). Male sex, nail involvement and higher body mass index were associated with increased risk of developing PsA, while bDMARD use was protective. Thus, this study provides some evidence that systemic treatment might ‘protect’ against development if PsA. Appropriately designed prospective studies are required.
One important clinical question is whether patients with oligoarthritis (involvement of <5 joints) progress to polyarthritis. In an observational study Gladman DD et al reported that in 407 patients evaluated within 12 months of diagnosis, 192 (47%) presented with oligoarthritis. More patients with polyarthritis presented with dactylitis, enthesitis, higher HAQ and lower SF-36 scores. Of the 192 patients with oligoarthritis, 75 (39%) progressed to polyarthritis. Lower SF-36 mental component summary score was the predictor for progressing to polyarthritis. Thus, except for the burden of musculoskeletal involvement, oligoarticular PsA resembles polyarticular PsA and therefore the two PsA subclasses should simply be classified together as peripheral arthritis.
Clinical Edge Journal Scan Commentary: Uterine Fibroid September 2021
Chiuve et al published a large cohort study in the Journal of Epidemiology and Community Health that evaluated the association between uterine fibroids and diagnosed depression, anxiety and self-directed violence. Women aged 18-50 years with diagnosed uterine fibroids (n=313,754) were identified in the Optum Clinformatics commercial insurance claims database and matched 1:2 on age and calendar time to women without (n=627,539). After adjusting for confounders, women with uterine fibroids had a higher rate of depression, anxiety and self-directed violence then women not diagnosed with fibroids. Among women with pain symptoms and heavy menstrual bleeding, the hazard ratio comparing women with fibroids to women without was 1.21 for depression, 1.18 for anxiety and 1.68 for self-directed violence. Among women with fibroids, those who underwent hysterectomy had higher rates of depression, anxiety and self-directed violence.
A third study by Wesselink et al in Human Reproduction examined ambient air pollution exposure and the risk of developing uterine fibroids. This was a prospective cohort study of 21,998 premenopausal Black women in 56 US metropolitan areas from 1997 to 2011. During the follow up, 28.4% of participants (n=6238) reported uterine fibroid diagnosis by ultrasound or surgery. Increased ozone concentrations were associated with an increased risk of being diagnosed with uterine fibroids, with a stronger association among women less than 35 years of age and parous women. Other pollutants, specifically particulate matter <2.5 microns and nitrogen dioxide, were not associated with an increased risk of uterine fibroids.
Chiuve et al published a large cohort study in the Journal of Epidemiology and Community Health that evaluated the association between uterine fibroids and diagnosed depression, anxiety and self-directed violence. Women aged 18-50 years with diagnosed uterine fibroids (n=313,754) were identified in the Optum Clinformatics commercial insurance claims database and matched 1:2 on age and calendar time to women without (n=627,539). After adjusting for confounders, women with uterine fibroids had a higher rate of depression, anxiety and self-directed violence then women not diagnosed with fibroids. Among women with pain symptoms and heavy menstrual bleeding, the hazard ratio comparing women with fibroids to women without was 1.21 for depression, 1.18 for anxiety and 1.68 for self-directed violence. Among women with fibroids, those who underwent hysterectomy had higher rates of depression, anxiety and self-directed violence.
A third study by Wesselink et al in Human Reproduction examined ambient air pollution exposure and the risk of developing uterine fibroids. This was a prospective cohort study of 21,998 premenopausal Black women in 56 US metropolitan areas from 1997 to 2011. During the follow up, 28.4% of participants (n=6238) reported uterine fibroid diagnosis by ultrasound or surgery. Increased ozone concentrations were associated with an increased risk of being diagnosed with uterine fibroids, with a stronger association among women less than 35 years of age and parous women. Other pollutants, specifically particulate matter <2.5 microns and nitrogen dioxide, were not associated with an increased risk of uterine fibroids.
Chiuve et al published a large cohort study in the Journal of Epidemiology and Community Health that evaluated the association between uterine fibroids and diagnosed depression, anxiety and self-directed violence. Women aged 18-50 years with diagnosed uterine fibroids (n=313,754) were identified in the Optum Clinformatics commercial insurance claims database and matched 1:2 on age and calendar time to women without (n=627,539). After adjusting for confounders, women with uterine fibroids had a higher rate of depression, anxiety and self-directed violence then women not diagnosed with fibroids. Among women with pain symptoms and heavy menstrual bleeding, the hazard ratio comparing women with fibroids to women without was 1.21 for depression, 1.18 for anxiety and 1.68 for self-directed violence. Among women with fibroids, those who underwent hysterectomy had higher rates of depression, anxiety and self-directed violence.
A third study by Wesselink et al in Human Reproduction examined ambient air pollution exposure and the risk of developing uterine fibroids. This was a prospective cohort study of 21,998 premenopausal Black women in 56 US metropolitan areas from 1997 to 2011. During the follow up, 28.4% of participants (n=6238) reported uterine fibroid diagnosis by ultrasound or surgery. Increased ozone concentrations were associated with an increased risk of being diagnosed with uterine fibroids, with a stronger association among women less than 35 years of age and parous women. Other pollutants, specifically particulate matter <2.5 microns and nitrogen dioxide, were not associated with an increased risk of uterine fibroids.
Clinical Edge Journal Scan Commentary: HCC September 2021
Patients with hepatocellular carcinoma (HCC) that has not spread outside the liver have several treatment options available. This month we will review articles that analyze outcomes after liver transplantation, liver resection, as well as radiofrequency ablation.
In HCC patients within the Milan criteria, the 5-year overall survival rate after transplant is about 70%, and the 5-year HCC recurrence rate is about 10%. Patients with tumors beyond the Milan criteria are frequently down staged with locoregional therapies to fall within the Milan criteria. The incidence of HCC recurrence in these patients is around 15.5% at 5 years. In this study, Lee et al demonstrated that statin use substantially reduced the risk of HCC recurrence. In this retrospective analysis of a longitudinal cohort of 430 patients transplanted between September 1995 and December 2019, 323 patients (75.1%) were statin non-users and 107 (24.9%) were statin users. Statin use was defined as at least 90 days of statin therapy, prescribed according to the treatment guidelines for dyslipidemia for primary or secondary prevention of CVD. At a median follow-up of 64.9 months, HCC recurred in 79 patients (18.4%), including 72 (22.3%) in the statin non-user group and 7 (6.5%) in the statin user group. Of those, 61 (77.2%) patients had HCC recurrence that initially presented at extrahepatic site regardless of the presence of intrahepatic tumors. Sixty-three patients (79.7%) had recurrence within 2 years of liver transplantation. The cumulative incidence of HCC recurrence at 2 and 5 years was 18.9% and 22.3% in the statin non-user group, and 3.8% and 5.7% in the statin user group, respectively (P < 0.001).
Liang et al evaluated the importance of tumor size in predicting the likelihood of HCC recurrence following surgical resection. In this retrospective study, a total of 813 cirrhotic patients who underwent curative-intent hepatectomy for solitary HCC without macrovascular invasion between 2001 and 2014 were evaluated. Overall, 464 patients had tumor size ≤ 5 cm, and 349 had tumor size > 5 cm. The 5-year RFS and OS rates were 38.3% and 61.5% in the ≤ 5 cm group, compared with 25.1% and 59.9% in the > 5 cm group. Long-term survival outcomes were significantly worse as tumor size increased. Multivariate analysis indicated that tumor size > 5 cm was an independent risk factor for tumor recurrence and long-term survival.
Finally, Sulaiman et al reported the survival rate of the early and intermediate stage HCC patients who underwent radiofrequency ablation (RFA). In this retrospective analysis, patients with BCLC A and B HCC who underwent RFA treatments between January 2015 to December 2017 were evaluated. Out of 62 patients 46 (74.2%) were reported to have RFA as their only first line of treatment, while 12 (25.8%) were reported to have a combination of RFA and other therapeutic modalities. At a mean follow up of 27 months, the survival rate at 12 and 36 months in patients who received RFA was 82.3% and 57.8%, respectively. A relatively high 36-month survival rate was seen in patients who had a response to RFA compared to the non-response group (100% vs 44.8%, P = 0.021). In terms of prognosis, BCLC staging of liver cancer and response after RFA were significantly associated with survival.
Patients with hepatocellular carcinoma (HCC) that has not spread outside the liver have several treatment options available. This month we will review articles that analyze outcomes after liver transplantation, liver resection, as well as radiofrequency ablation.
In HCC patients within the Milan criteria, the 5-year overall survival rate after transplant is about 70%, and the 5-year HCC recurrence rate is about 10%. Patients with tumors beyond the Milan criteria are frequently down staged with locoregional therapies to fall within the Milan criteria. The incidence of HCC recurrence in these patients is around 15.5% at 5 years. In this study, Lee et al demonstrated that statin use substantially reduced the risk of HCC recurrence. In this retrospective analysis of a longitudinal cohort of 430 patients transplanted between September 1995 and December 2019, 323 patients (75.1%) were statin non-users and 107 (24.9%) were statin users. Statin use was defined as at least 90 days of statin therapy, prescribed according to the treatment guidelines for dyslipidemia for primary or secondary prevention of CVD. At a median follow-up of 64.9 months, HCC recurred in 79 patients (18.4%), including 72 (22.3%) in the statin non-user group and 7 (6.5%) in the statin user group. Of those, 61 (77.2%) patients had HCC recurrence that initially presented at extrahepatic site regardless of the presence of intrahepatic tumors. Sixty-three patients (79.7%) had recurrence within 2 years of liver transplantation. The cumulative incidence of HCC recurrence at 2 and 5 years was 18.9% and 22.3% in the statin non-user group, and 3.8% and 5.7% in the statin user group, respectively (P < 0.001).
Liang et al evaluated the importance of tumor size in predicting the likelihood of HCC recurrence following surgical resection. In this retrospective study, a total of 813 cirrhotic patients who underwent curative-intent hepatectomy for solitary HCC without macrovascular invasion between 2001 and 2014 were evaluated. Overall, 464 patients had tumor size ≤ 5 cm, and 349 had tumor size > 5 cm. The 5-year RFS and OS rates were 38.3% and 61.5% in the ≤ 5 cm group, compared with 25.1% and 59.9% in the > 5 cm group. Long-term survival outcomes were significantly worse as tumor size increased. Multivariate analysis indicated that tumor size > 5 cm was an independent risk factor for tumor recurrence and long-term survival.
Finally, Sulaiman et al reported the survival rate of the early and intermediate stage HCC patients who underwent radiofrequency ablation (RFA). In this retrospective analysis, patients with BCLC A and B HCC who underwent RFA treatments between January 2015 to December 2017 were evaluated. Out of 62 patients 46 (74.2%) were reported to have RFA as their only first line of treatment, while 12 (25.8%) were reported to have a combination of RFA and other therapeutic modalities. At a mean follow up of 27 months, the survival rate at 12 and 36 months in patients who received RFA was 82.3% and 57.8%, respectively. A relatively high 36-month survival rate was seen in patients who had a response to RFA compared to the non-response group (100% vs 44.8%, P = 0.021). In terms of prognosis, BCLC staging of liver cancer and response after RFA were significantly associated with survival.
Patients with hepatocellular carcinoma (HCC) that has not spread outside the liver have several treatment options available. This month we will review articles that analyze outcomes after liver transplantation, liver resection, as well as radiofrequency ablation.
In HCC patients within the Milan criteria, the 5-year overall survival rate after transplant is about 70%, and the 5-year HCC recurrence rate is about 10%. Patients with tumors beyond the Milan criteria are frequently down staged with locoregional therapies to fall within the Milan criteria. The incidence of HCC recurrence in these patients is around 15.5% at 5 years. In this study, Lee et al demonstrated that statin use substantially reduced the risk of HCC recurrence. In this retrospective analysis of a longitudinal cohort of 430 patients transplanted between September 1995 and December 2019, 323 patients (75.1%) were statin non-users and 107 (24.9%) were statin users. Statin use was defined as at least 90 days of statin therapy, prescribed according to the treatment guidelines for dyslipidemia for primary or secondary prevention of CVD. At a median follow-up of 64.9 months, HCC recurred in 79 patients (18.4%), including 72 (22.3%) in the statin non-user group and 7 (6.5%) in the statin user group. Of those, 61 (77.2%) patients had HCC recurrence that initially presented at extrahepatic site regardless of the presence of intrahepatic tumors. Sixty-three patients (79.7%) had recurrence within 2 years of liver transplantation. The cumulative incidence of HCC recurrence at 2 and 5 years was 18.9% and 22.3% in the statin non-user group, and 3.8% and 5.7% in the statin user group, respectively (P < 0.001).
Liang et al evaluated the importance of tumor size in predicting the likelihood of HCC recurrence following surgical resection. In this retrospective study, a total of 813 cirrhotic patients who underwent curative-intent hepatectomy for solitary HCC without macrovascular invasion between 2001 and 2014 were evaluated. Overall, 464 patients had tumor size ≤ 5 cm, and 349 had tumor size > 5 cm. The 5-year RFS and OS rates were 38.3% and 61.5% in the ≤ 5 cm group, compared with 25.1% and 59.9% in the > 5 cm group. Long-term survival outcomes were significantly worse as tumor size increased. Multivariate analysis indicated that tumor size > 5 cm was an independent risk factor for tumor recurrence and long-term survival.
Finally, Sulaiman et al reported the survival rate of the early and intermediate stage HCC patients who underwent radiofrequency ablation (RFA). In this retrospective analysis, patients with BCLC A and B HCC who underwent RFA treatments between January 2015 to December 2017 were evaluated. Out of 62 patients 46 (74.2%) were reported to have RFA as their only first line of treatment, while 12 (25.8%) were reported to have a combination of RFA and other therapeutic modalities. At a mean follow up of 27 months, the survival rate at 12 and 36 months in patients who received RFA was 82.3% and 57.8%, respectively. A relatively high 36-month survival rate was seen in patients who had a response to RFA compared to the non-response group (100% vs 44.8%, P = 0.021). In terms of prognosis, BCLC staging of liver cancer and response after RFA were significantly associated with survival.
Children and COVID: Weekly cases top 200,000, vaccinations down
Weekly pediatric cases of COVID-19 exceeded 200,000 for just the second time during the pandemic, while new vaccinations in children continued to decline.
The weekly count has now increased for 9 consecutive weeks, during which time it has risen by over 2,300%, the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID-19 report. Total cases in children number almost 4.8 million since the pandemic started.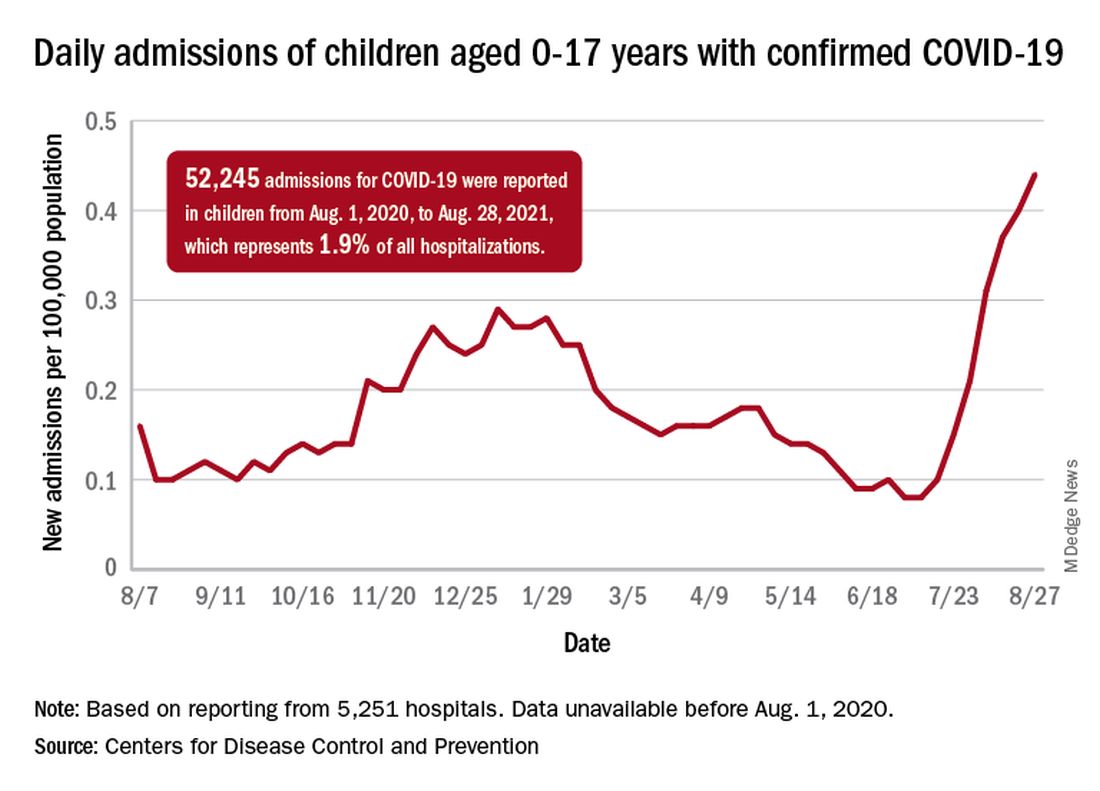
Vaccinations in children are following a different trend. Vaccine initiation has dropped 3 weeks in a row for both of the eligible age groups: First doses administered were down by 29% among 12- to 15-year-olds over that span and by 32% in 16- to 17-year-olds, according to data from the Centers for Disease Control and Prevention.
Since vaccination for children aged 12-15 years started in May, 49% had received at least one dose, and just over 36% were fully vaccinated as of Aug. 30. Among children aged 16-17 years, who have been eligible since December, 57.5% had gotten at least one dose of the vaccine and 46% have completed the two-dose regimen. The total number of children with at least one dose, including those under age 12 who are involved in clinical trials, was about 12 million, the CDC said on its COVID Data Tracker.
Hospitalizations are higher than ever
The recent rise in new child cases has been accompanied by an unprecedented increase in hospitalizations. The daily rate in children aged 0-17 years, which did not surpass 0.30 new admissions per 100,000 population during the worst of the winter surge, had risen to 0.45 per 100,000 by Aug. 26. Since July 4, when the new-admission rate was at its low point of 0.07 per 100,000, hospitalizations in children have jumped by 543%, based on data reported to the CDC by 5,251 hospitals.
A total of 52,245 children were admitted with confirmed COVID-19 from Aug. 1, 2020, when the CDC dataset begins, to Aug. 28, 2021. Those children represent 1.9% of all COVID admissions (2.7 million) in the United States over that period, the CDC said.
Total COVID-related deaths in children are up to 425 in the 48 jurisdictions (45 states, New York City, Puerto Rico, and Guam) that provide mortality data by age, the AAP and the CHA said.
Record-high numbers for the previous 2 reporting weeks – 23 deaths during Aug. 20-26 and 24 deaths during Aug. 13-19, when the previous weekly high was 16 – at least partially reflect the recent addition of South Carolina and New Mexico to the AAP/CHA database, as the two states just started reporting age-related data.
Weekly pediatric cases of COVID-19 exceeded 200,000 for just the second time during the pandemic, while new vaccinations in children continued to decline.
The weekly count has now increased for 9 consecutive weeks, during which time it has risen by over 2,300%, the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID-19 report. Total cases in children number almost 4.8 million since the pandemic started.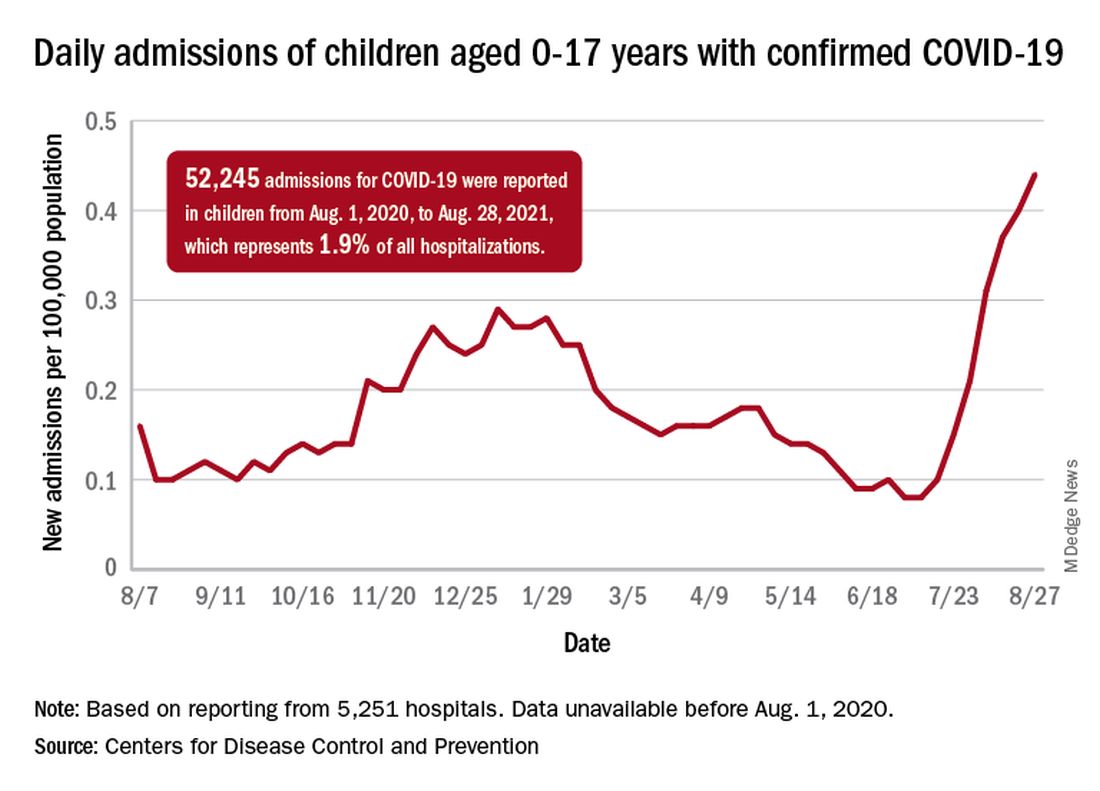
Vaccinations in children are following a different trend. Vaccine initiation has dropped 3 weeks in a row for both of the eligible age groups: First doses administered were down by 29% among 12- to 15-year-olds over that span and by 32% in 16- to 17-year-olds, according to data from the Centers for Disease Control and Prevention.
Since vaccination for children aged 12-15 years started in May, 49% had received at least one dose, and just over 36% were fully vaccinated as of Aug. 30. Among children aged 16-17 years, who have been eligible since December, 57.5% had gotten at least one dose of the vaccine and 46% have completed the two-dose regimen. The total number of children with at least one dose, including those under age 12 who are involved in clinical trials, was about 12 million, the CDC said on its COVID Data Tracker.
Hospitalizations are higher than ever
The recent rise in new child cases has been accompanied by an unprecedented increase in hospitalizations. The daily rate in children aged 0-17 years, which did not surpass 0.30 new admissions per 100,000 population during the worst of the winter surge, had risen to 0.45 per 100,000 by Aug. 26. Since July 4, when the new-admission rate was at its low point of 0.07 per 100,000, hospitalizations in children have jumped by 543%, based on data reported to the CDC by 5,251 hospitals.
A total of 52,245 children were admitted with confirmed COVID-19 from Aug. 1, 2020, when the CDC dataset begins, to Aug. 28, 2021. Those children represent 1.9% of all COVID admissions (2.7 million) in the United States over that period, the CDC said.
Total COVID-related deaths in children are up to 425 in the 48 jurisdictions (45 states, New York City, Puerto Rico, and Guam) that provide mortality data by age, the AAP and the CHA said.
Record-high numbers for the previous 2 reporting weeks – 23 deaths during Aug. 20-26 and 24 deaths during Aug. 13-19, when the previous weekly high was 16 – at least partially reflect the recent addition of South Carolina and New Mexico to the AAP/CHA database, as the two states just started reporting age-related data.
Weekly pediatric cases of COVID-19 exceeded 200,000 for just the second time during the pandemic, while new vaccinations in children continued to decline.
The weekly count has now increased for 9 consecutive weeks, during which time it has risen by over 2,300%, the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID-19 report. Total cases in children number almost 4.8 million since the pandemic started.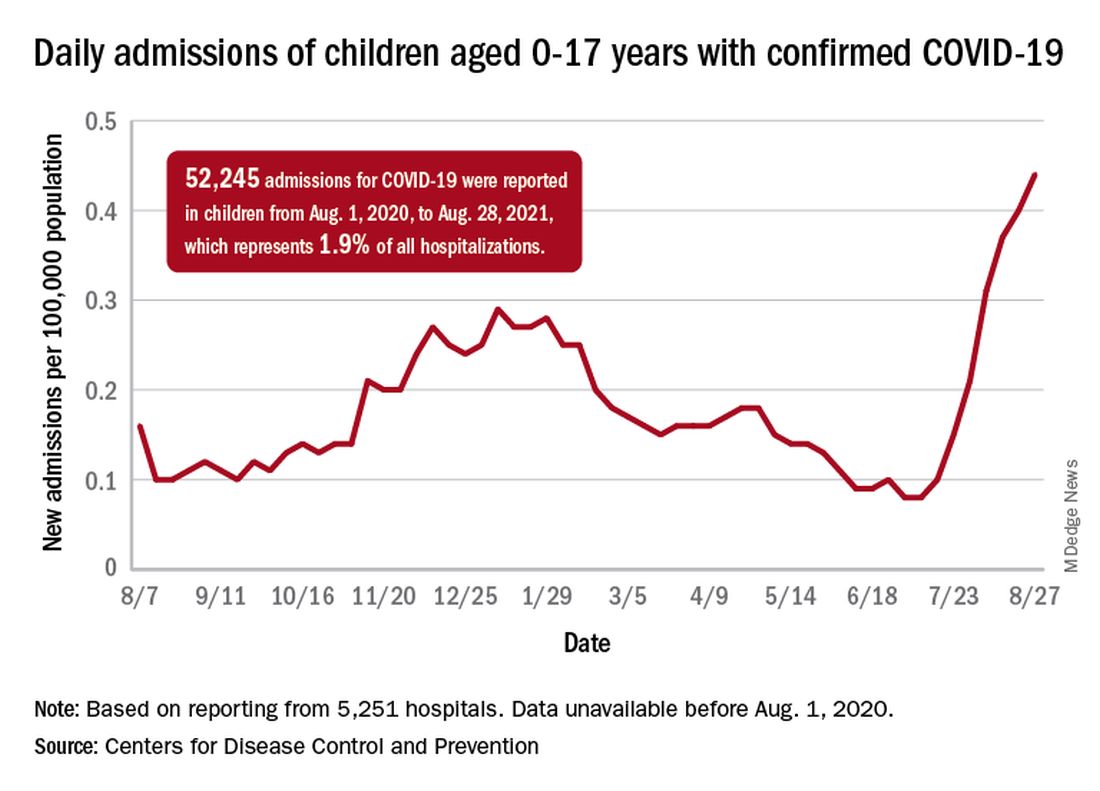
Vaccinations in children are following a different trend. Vaccine initiation has dropped 3 weeks in a row for both of the eligible age groups: First doses administered were down by 29% among 12- to 15-year-olds over that span and by 32% in 16- to 17-year-olds, according to data from the Centers for Disease Control and Prevention.
Since vaccination for children aged 12-15 years started in May, 49% had received at least one dose, and just over 36% were fully vaccinated as of Aug. 30. Among children aged 16-17 years, who have been eligible since December, 57.5% had gotten at least one dose of the vaccine and 46% have completed the two-dose regimen. The total number of children with at least one dose, including those under age 12 who are involved in clinical trials, was about 12 million, the CDC said on its COVID Data Tracker.
Hospitalizations are higher than ever
The recent rise in new child cases has been accompanied by an unprecedented increase in hospitalizations. The daily rate in children aged 0-17 years, which did not surpass 0.30 new admissions per 100,000 population during the worst of the winter surge, had risen to 0.45 per 100,000 by Aug. 26. Since July 4, when the new-admission rate was at its low point of 0.07 per 100,000, hospitalizations in children have jumped by 543%, based on data reported to the CDC by 5,251 hospitals.
A total of 52,245 children were admitted with confirmed COVID-19 from Aug. 1, 2020, when the CDC dataset begins, to Aug. 28, 2021. Those children represent 1.9% of all COVID admissions (2.7 million) in the United States over that period, the CDC said.
Total COVID-related deaths in children are up to 425 in the 48 jurisdictions (45 states, New York City, Puerto Rico, and Guam) that provide mortality data by age, the AAP and the CHA said.
Record-high numbers for the previous 2 reporting weeks – 23 deaths during Aug. 20-26 and 24 deaths during Aug. 13-19, when the previous weekly high was 16 – at least partially reflect the recent addition of South Carolina and New Mexico to the AAP/CHA database, as the two states just started reporting age-related data.
Clinical Edge Journal Scan Commentary: Breast Cancer September 2021
Metastatic triple-negative breast cancer (TNBC) is a heterogeneous, biologically complex subtype, with continuing efforts to identify therapeutic targets. The PI3K/AKT signaling pathway plays a key role in cell proliferation, survival, invasion, and metabolism. In the phase II LOTUS trial (Dent et al) including 124 patients with advanced TNBC (no prior therapy for advanced disease), addition of the oral AKT inhibitor, ipatasertib, to paclitaxel led to a numerical improvement in OS that was not statistically significant. The median OS was 25.8 vs 16.9 months for the ipatasertib-paclitaxel vs placebo-paclitaxel, respectively (HR 0.80, 95% CI 0.50-1.28). Findings from cohort A of the phase III IPATunity130 trial showed that ipatasertib-paclitaxel did not lead to a statistically significant improvement in PFS vs placebo-paclitaxel in patients with PIK3CA/AKT1/PTEN-altered advanced TNBC in the first-line metastatic setting (mPFS 7.4 vs 6.1 months, respectively; HR 1.02, p=0.9237). These findings support further investigation into predictors of response and other molecular markers that may play a role in the diversity of mTNBC.
Endocrine therapy resistance remains a significant challenge in advanced HR+/HER2- breast cancer, and initial studies with the oral histone deacetylase inhibitor, etinostat, showed promise in this space. Unfortunately, these findings were not upheld in the phase III E2112 trial (Connolly et al), which failed to show an improvement in PFS or OS with exemestane-etinostat (EE) compared to exemestane-placebo (EP) among patients who had progressed on prior non-steroidal AI. Median PFS was 3.3 vs 3.1 months (HR 0.87; p=0.30) and median OS was 23.4 vs 21.7 months (HR 0.99; p=0.94) for the EE vs EP arms, respectively. The combination of an alternative HDAC inhibitor, tucidinostat, has been approved in China in combination with exemestane based on PFS benefit (3.6 months) in the phase III ACE trial. There are notable difference between E2112 and ACE trials, including patient population and design, and importantly OS has not been reported for the latter. The relatively short mPFS and low response rate (5-6%) in E2112 argues for more efficacious therapeutics. There is also value in correlative studies to help further elucidate if there is a role for HDAC inhibitors in this space.
Although adjuvant endocrine therapy has had a significantly beneficial effect on outcomes in early-stage HR+ breast cancer, late recurrences are characteristic of the luminal subtype, and have led to trials investigating extended adjuvant endocrine therapy. The phase III SALSA trial included 3484 women with early HR+ breast cancer who had received 5 years of adjuvant endocrine therapy with randomization to anastrozole for an additional 2 vs 5 years (comparing total of 7 vs 10 years). There was no significant difference in disease-free survival (DFS) at 8 years (73.6% vs 73.9% in the 2 vs 5-year groups, respectively; HR 0.99, p=0.90). Additionally, there was a lower risk of bone fracture in the 2 vs 5-year group (4.7% vs 6.3%; HR 1.35). It is essential to balance modest benefits with toxicities of prolonged AI use, and valuable to identify high-risk patients who may benefit from extended adjuvant endocrine therapy.
References:
Chan A, Moy B, Mansi J, et al; ExteNET Study Group. Final efficacy results of neratinib in HER2-positive hormone receptor-positive early-stage breast cancer from the phase III ExteNET trial. Clin Breast Cancer. 2021;21(1):80-91.e7.
von Minckwitz G, Huang CS, Mano MS, et al; KATHERINE Investigators. Trastuzumab emtansine for residual invasive HER2-positive breast cancer. N Engl J Med. 2019;380(7):617-628.
Dent R, Kim SB, Oliveira M, et al. Double-blind placebo-controlled randomized phase III trial evaluating first-line ipatasertib combined with paclitaxel for PIK3CA/AKT1/PTEN-altered locally advanced unresectable or metastatic triple-negative breast cancer: primary results from IPATunity130 cohort A. Presented at: 2020 San Antonio Breast Cancer Symposium; December 8-11, 2020; Virtual. Oral GS3-04.
Jiang Z, Li W, Hu X, et al. Tucidinostat plus exemestane for postmenopausal patients with advanced, hormone receptor-positive breast cancer (ACE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2019;20(6):806-815.
Mamounas EP, Bandos H, Lembersky BC, et al. Use of letrozole after aromatase inhibitor-based therapy in postmenopausal breast cancer (NRG Oncology/NSABP B-42): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2019;20(1):88-99.
Metastatic triple-negative breast cancer (TNBC) is a heterogeneous, biologically complex subtype, with continuing efforts to identify therapeutic targets. The PI3K/AKT signaling pathway plays a key role in cell proliferation, survival, invasion, and metabolism. In the phase II LOTUS trial (Dent et al) including 124 patients with advanced TNBC (no prior therapy for advanced disease), addition of the oral AKT inhibitor, ipatasertib, to paclitaxel led to a numerical improvement in OS that was not statistically significant. The median OS was 25.8 vs 16.9 months for the ipatasertib-paclitaxel vs placebo-paclitaxel, respectively (HR 0.80, 95% CI 0.50-1.28). Findings from cohort A of the phase III IPATunity130 trial showed that ipatasertib-paclitaxel did not lead to a statistically significant improvement in PFS vs placebo-paclitaxel in patients with PIK3CA/AKT1/PTEN-altered advanced TNBC in the first-line metastatic setting (mPFS 7.4 vs 6.1 months, respectively; HR 1.02, p=0.9237). These findings support further investigation into predictors of response and other molecular markers that may play a role in the diversity of mTNBC.
Endocrine therapy resistance remains a significant challenge in advanced HR+/HER2- breast cancer, and initial studies with the oral histone deacetylase inhibitor, etinostat, showed promise in this space. Unfortunately, these findings were not upheld in the phase III E2112 trial (Connolly et al), which failed to show an improvement in PFS or OS with exemestane-etinostat (EE) compared to exemestane-placebo (EP) among patients who had progressed on prior non-steroidal AI. Median PFS was 3.3 vs 3.1 months (HR 0.87; p=0.30) and median OS was 23.4 vs 21.7 months (HR 0.99; p=0.94) for the EE vs EP arms, respectively. The combination of an alternative HDAC inhibitor, tucidinostat, has been approved in China in combination with exemestane based on PFS benefit (3.6 months) in the phase III ACE trial. There are notable difference between E2112 and ACE trials, including patient population and design, and importantly OS has not been reported for the latter. The relatively short mPFS and low response rate (5-6%) in E2112 argues for more efficacious therapeutics. There is also value in correlative studies to help further elucidate if there is a role for HDAC inhibitors in this space.
Although adjuvant endocrine therapy has had a significantly beneficial effect on outcomes in early-stage HR+ breast cancer, late recurrences are characteristic of the luminal subtype, and have led to trials investigating extended adjuvant endocrine therapy. The phase III SALSA trial included 3484 women with early HR+ breast cancer who had received 5 years of adjuvant endocrine therapy with randomization to anastrozole for an additional 2 vs 5 years (comparing total of 7 vs 10 years). There was no significant difference in disease-free survival (DFS) at 8 years (73.6% vs 73.9% in the 2 vs 5-year groups, respectively; HR 0.99, p=0.90). Additionally, there was a lower risk of bone fracture in the 2 vs 5-year group (4.7% vs 6.3%; HR 1.35). It is essential to balance modest benefits with toxicities of prolonged AI use, and valuable to identify high-risk patients who may benefit from extended adjuvant endocrine therapy.
References:
Chan A, Moy B, Mansi J, et al; ExteNET Study Group. Final efficacy results of neratinib in HER2-positive hormone receptor-positive early-stage breast cancer from the phase III ExteNET trial. Clin Breast Cancer. 2021;21(1):80-91.e7.
von Minckwitz G, Huang CS, Mano MS, et al; KATHERINE Investigators. Trastuzumab emtansine for residual invasive HER2-positive breast cancer. N Engl J Med. 2019;380(7):617-628.
Dent R, Kim SB, Oliveira M, et al. Double-blind placebo-controlled randomized phase III trial evaluating first-line ipatasertib combined with paclitaxel for PIK3CA/AKT1/PTEN-altered locally advanced unresectable or metastatic triple-negative breast cancer: primary results from IPATunity130 cohort A. Presented at: 2020 San Antonio Breast Cancer Symposium; December 8-11, 2020; Virtual. Oral GS3-04.
Jiang Z, Li W, Hu X, et al. Tucidinostat plus exemestane for postmenopausal patients with advanced, hormone receptor-positive breast cancer (ACE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2019;20(6):806-815.
Mamounas EP, Bandos H, Lembersky BC, et al. Use of letrozole after aromatase inhibitor-based therapy in postmenopausal breast cancer (NRG Oncology/NSABP B-42): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2019;20(1):88-99.
Metastatic triple-negative breast cancer (TNBC) is a heterogeneous, biologically complex subtype, with continuing efforts to identify therapeutic targets. The PI3K/AKT signaling pathway plays a key role in cell proliferation, survival, invasion, and metabolism. In the phase II LOTUS trial (Dent et al) including 124 patients with advanced TNBC (no prior therapy for advanced disease), addition of the oral AKT inhibitor, ipatasertib, to paclitaxel led to a numerical improvement in OS that was not statistically significant. The median OS was 25.8 vs 16.9 months for the ipatasertib-paclitaxel vs placebo-paclitaxel, respectively (HR 0.80, 95% CI 0.50-1.28). Findings from cohort A of the phase III IPATunity130 trial showed that ipatasertib-paclitaxel did not lead to a statistically significant improvement in PFS vs placebo-paclitaxel in patients with PIK3CA/AKT1/PTEN-altered advanced TNBC in the first-line metastatic setting (mPFS 7.4 vs 6.1 months, respectively; HR 1.02, p=0.9237). These findings support further investigation into predictors of response and other molecular markers that may play a role in the diversity of mTNBC.
Endocrine therapy resistance remains a significant challenge in advanced HR+/HER2- breast cancer, and initial studies with the oral histone deacetylase inhibitor, etinostat, showed promise in this space. Unfortunately, these findings were not upheld in the phase III E2112 trial (Connolly et al), which failed to show an improvement in PFS or OS with exemestane-etinostat (EE) compared to exemestane-placebo (EP) among patients who had progressed on prior non-steroidal AI. Median PFS was 3.3 vs 3.1 months (HR 0.87; p=0.30) and median OS was 23.4 vs 21.7 months (HR 0.99; p=0.94) for the EE vs EP arms, respectively. The combination of an alternative HDAC inhibitor, tucidinostat, has been approved in China in combination with exemestane based on PFS benefit (3.6 months) in the phase III ACE trial. There are notable difference between E2112 and ACE trials, including patient population and design, and importantly OS has not been reported for the latter. The relatively short mPFS and low response rate (5-6%) in E2112 argues for more efficacious therapeutics. There is also value in correlative studies to help further elucidate if there is a role for HDAC inhibitors in this space.
Although adjuvant endocrine therapy has had a significantly beneficial effect on outcomes in early-stage HR+ breast cancer, late recurrences are characteristic of the luminal subtype, and have led to trials investigating extended adjuvant endocrine therapy. The phase III SALSA trial included 3484 women with early HR+ breast cancer who had received 5 years of adjuvant endocrine therapy with randomization to anastrozole for an additional 2 vs 5 years (comparing total of 7 vs 10 years). There was no significant difference in disease-free survival (DFS) at 8 years (73.6% vs 73.9% in the 2 vs 5-year groups, respectively; HR 0.99, p=0.90). Additionally, there was a lower risk of bone fracture in the 2 vs 5-year group (4.7% vs 6.3%; HR 1.35). It is essential to balance modest benefits with toxicities of prolonged AI use, and valuable to identify high-risk patients who may benefit from extended adjuvant endocrine therapy.
References:
Chan A, Moy B, Mansi J, et al; ExteNET Study Group. Final efficacy results of neratinib in HER2-positive hormone receptor-positive early-stage breast cancer from the phase III ExteNET trial. Clin Breast Cancer. 2021;21(1):80-91.e7.
von Minckwitz G, Huang CS, Mano MS, et al; KATHERINE Investigators. Trastuzumab emtansine for residual invasive HER2-positive breast cancer. N Engl J Med. 2019;380(7):617-628.
Dent R, Kim SB, Oliveira M, et al. Double-blind placebo-controlled randomized phase III trial evaluating first-line ipatasertib combined with paclitaxel for PIK3CA/AKT1/PTEN-altered locally advanced unresectable or metastatic triple-negative breast cancer: primary results from IPATunity130 cohort A. Presented at: 2020 San Antonio Breast Cancer Symposium; December 8-11, 2020; Virtual. Oral GS3-04.
Jiang Z, Li W, Hu X, et al. Tucidinostat plus exemestane for postmenopausal patients with advanced, hormone receptor-positive breast cancer (ACE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2019;20(6):806-815.
Mamounas EP, Bandos H, Lembersky BC, et al. Use of letrozole after aromatase inhibitor-based therapy in postmenopausal breast cancer (NRG Oncology/NSABP B-42): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2019;20(1):88-99.
TNBC: Statin use is linked to survival benefit
Key clinical point: Initiation of statin treatment within 12 months of diagnosis improves survival in women with stage I-III triple-negative breast cancer (TNBC).
Major finding: Statin treatment was initiated in 2,281 patients within 12 months of diagnosis. In 1,534 patients with TNBC, statin use was associated with a significant improvement in breast cancer-specific survival (standardized hazard ratio [HR], 0.42; P = 0.022) and overall survival (HR, 0.70; P = 0.046). No significant association was observed between statin use and survival in patients without TNBC.
Study details: retrospective study of 23,192 patients with stage I-III breast cancer from the Surveillance, Epidemiology, and End Results-Medicare and Texas Cancer Registry-Medicare database between 2008 and 2015.
Disclosures: The study was supported by National Institutes of Health and Cancer Prevention Research Institute of Texas. The authors received grants, research funding, and personal fees outside this work.
Source: Nowakowska MK et al. Cancer. 2021 Aug 3. doi: 10.1002/cncr.33797.
Key clinical point: Initiation of statin treatment within 12 months of diagnosis improves survival in women with stage I-III triple-negative breast cancer (TNBC).
Major finding: Statin treatment was initiated in 2,281 patients within 12 months of diagnosis. In 1,534 patients with TNBC, statin use was associated with a significant improvement in breast cancer-specific survival (standardized hazard ratio [HR], 0.42; P = 0.022) and overall survival (HR, 0.70; P = 0.046). No significant association was observed between statin use and survival in patients without TNBC.
Study details: retrospective study of 23,192 patients with stage I-III breast cancer from the Surveillance, Epidemiology, and End Results-Medicare and Texas Cancer Registry-Medicare database between 2008 and 2015.
Disclosures: The study was supported by National Institutes of Health and Cancer Prevention Research Institute of Texas. The authors received grants, research funding, and personal fees outside this work.
Source: Nowakowska MK et al. Cancer. 2021 Aug 3. doi: 10.1002/cncr.33797.
Key clinical point: Initiation of statin treatment within 12 months of diagnosis improves survival in women with stage I-III triple-negative breast cancer (TNBC).
Major finding: Statin treatment was initiated in 2,281 patients within 12 months of diagnosis. In 1,534 patients with TNBC, statin use was associated with a significant improvement in breast cancer-specific survival (standardized hazard ratio [HR], 0.42; P = 0.022) and overall survival (HR, 0.70; P = 0.046). No significant association was observed between statin use and survival in patients without TNBC.
Study details: retrospective study of 23,192 patients with stage I-III breast cancer from the Surveillance, Epidemiology, and End Results-Medicare and Texas Cancer Registry-Medicare database between 2008 and 2015.
Disclosures: The study was supported by National Institutes of Health and Cancer Prevention Research Institute of Texas. The authors received grants, research funding, and personal fees outside this work.
Source: Nowakowska MK et al. Cancer. 2021 Aug 3. doi: 10.1002/cncr.33797.