User login
Many ED visits may be preventable for NSCLC patients
The leading cause of ED visits in the study was the cancer itself, although many visits were unrelated to non–small cell lung cancer (NSCLC) or cancer therapy.
Less than 10% of ED visits were related to cancer therapy, but visits were much more common among patients receiving chemotherapy than among those receiving immunotherapy or tyrosine kinase inhibitors (TKIs).
Manan P. Shah, MD, and Joel W. Neal, MD, PhD, both of Stanford (Calif. ) University, reported these results in JCO Oncology Practice.
The authors noted that, in the United States, care of patients with cancer, among all diseases, leads to the highest per-person cost. Unplanned hospital visits are among the largest drivers of increased spending in advanced cancer care, accounting for 48% of spending. However, that spending may not be indicative of better quality care, but rather of inefficiency, according to the authors.
One registry spanning 2009-2012 and including more than 400,000 newly diagnosed cancer patients found lung cancer to have the third-highest rate of unplanned hospitalizations (after hepatobiliary and pancreatic cancer). Those findings were published in JCO Oncology Practice in 2018.
While the reason for presentation to the ED is often the cancer or its therapy in this population, there is a paucity of research on the relative contribution of factors leading to unplanned hospital visits.
Common precipitants of medical emergencies in advanced stages of lung cancer include pulmonary embolism, obstructive pneumonia, spinal cord compression caused by metastasis, and tumor progression or pleural effusion leading to respiratory failure.
Lung cancer therapies, such as TKIs, immunotherapy, and cytotoxic chemotherapy, can also cause various medical emergencies arising out of skin reactions, gastrointestinal dysfunction, organ inflammatory processes, and bone marrow suppression.
Identifying drivers of unplanned ED visits
The primary goals of Dr. Shah and Dr. Neal’s study were to understand the drivers of unplanned ED visits and identify potential strategies to prevent them.
Drawing from the Stanford Medicine Research Data Repository, the authors identified 97 NSCLC patients with 173 ED visits at Stanford.
Patients were sorted according to which of the three therapies they had been receiving in the 3 months prior to the unplanned visit – TKIs (n = 47), immunotherapy (n = 24), or chemotherapy (n = 26). Patients receiving a combination of chemotherapy and immunotherapy were classified under the immunotherapy category.
ED visits were divided into four categories: cancer related, therapy related, unrelated to cancer or therapy, and rule-out (when an outpatient provider sent the patient to rule out medico-oncologic emergencies such as pulmonary embolism or cord compression).
If the patient’s main complaint(s) began 2 or more days before presentation, the diagnostics or therapeutics could have been provided in an outpatient setting (e.g., in clinic or urgent care), and the patient was discharged directly from the ED, the encounter was classified as potentially preventable. Among these preventable encounters, those made during business hours were also labeled unnecessary because they could have been managed through the Stanford sick call system for same-day urgent visits.
Leading cause is cancer
Overall, the leading cause of ED visits was NSCLC itself (54%). The patient’s cancer contributed to 61% of ED visits in the TKI group, 49% in the immunotherapy group, and 42% in the chemotherapy group.
Many ED visits were deemed unrelated to cancer or its therapies – 30% in the TKI group, 26% in the immunotherapy group, and 32% in the chemotherapy group.
Rule-out cases contributed to 7% of ED visits in the TKI group, 14% in the immunotherapy group, and 5% in the chemotherapy group.
Overall, 9% of ED visits were therapy related. The smallest proportion of these was observed in the TKI group (2%), which was significantly smaller than in the immunotherapy group (12%), a rate also significantly smaller than in the chemotherapy group (21%, P < .001).
Most unplanned ED visits did not lead to admissions (55%), were for complaints that began 2 or more days prior to presentation (53%), led to diagnostics or therapeutics that could have been administered in an outpatient setting (48%), and were during business hours (52%).
As a result, 24% of visits were classified as preventable, and 10% were deemed unnecessary.
Preventive strategies
“Our study suggests that TKIs lead to fewer emergency room visits than immunotherapy and chemotherapy,” Dr. Shah said in an interview.
“Overall, this may not necessarily change which therapy we prescribe,” he added, “as TKI therapy is often first line for patients with targeted mutations. However, recognizing that those on chemotherapy or immunotherapy are at higher risk for emergency room visits, we may target preventative strategies, for example, nursing phone calls, telemonitoring of symptoms, and frequent video visits toward this high-risk population.”
Dr. Shah and Dr. Neal said it’s “reassuring” that TKIs and immunotherapy are small drivers of unplanned hospital care. However, they also said efforts aimed at reducing chemotherapy-related ED visits are warranted.
The authors speculated that early intervention, extension of ambulatory care, and patient education about outpatient avenues of care could eliminate a significant proportion (at least 20%) of unplanned ED visits by NSCLC patients.
There was no specific funding for this study. Dr. Shah disclosed no conflicts of interest. Dr. Neal disclosed relationships with many companies, including this news organization.
The leading cause of ED visits in the study was the cancer itself, although many visits were unrelated to non–small cell lung cancer (NSCLC) or cancer therapy.
Less than 10% of ED visits were related to cancer therapy, but visits were much more common among patients receiving chemotherapy than among those receiving immunotherapy or tyrosine kinase inhibitors (TKIs).
Manan P. Shah, MD, and Joel W. Neal, MD, PhD, both of Stanford (Calif. ) University, reported these results in JCO Oncology Practice.
The authors noted that, in the United States, care of patients with cancer, among all diseases, leads to the highest per-person cost. Unplanned hospital visits are among the largest drivers of increased spending in advanced cancer care, accounting for 48% of spending. However, that spending may not be indicative of better quality care, but rather of inefficiency, according to the authors.
One registry spanning 2009-2012 and including more than 400,000 newly diagnosed cancer patients found lung cancer to have the third-highest rate of unplanned hospitalizations (after hepatobiliary and pancreatic cancer). Those findings were published in JCO Oncology Practice in 2018.
While the reason for presentation to the ED is often the cancer or its therapy in this population, there is a paucity of research on the relative contribution of factors leading to unplanned hospital visits.
Common precipitants of medical emergencies in advanced stages of lung cancer include pulmonary embolism, obstructive pneumonia, spinal cord compression caused by metastasis, and tumor progression or pleural effusion leading to respiratory failure.
Lung cancer therapies, such as TKIs, immunotherapy, and cytotoxic chemotherapy, can also cause various medical emergencies arising out of skin reactions, gastrointestinal dysfunction, organ inflammatory processes, and bone marrow suppression.
Identifying drivers of unplanned ED visits
The primary goals of Dr. Shah and Dr. Neal’s study were to understand the drivers of unplanned ED visits and identify potential strategies to prevent them.
Drawing from the Stanford Medicine Research Data Repository, the authors identified 97 NSCLC patients with 173 ED visits at Stanford.
Patients were sorted according to which of the three therapies they had been receiving in the 3 months prior to the unplanned visit – TKIs (n = 47), immunotherapy (n = 24), or chemotherapy (n = 26). Patients receiving a combination of chemotherapy and immunotherapy were classified under the immunotherapy category.
ED visits were divided into four categories: cancer related, therapy related, unrelated to cancer or therapy, and rule-out (when an outpatient provider sent the patient to rule out medico-oncologic emergencies such as pulmonary embolism or cord compression).
If the patient’s main complaint(s) began 2 or more days before presentation, the diagnostics or therapeutics could have been provided in an outpatient setting (e.g., in clinic or urgent care), and the patient was discharged directly from the ED, the encounter was classified as potentially preventable. Among these preventable encounters, those made during business hours were also labeled unnecessary because they could have been managed through the Stanford sick call system for same-day urgent visits.
Leading cause is cancer
Overall, the leading cause of ED visits was NSCLC itself (54%). The patient’s cancer contributed to 61% of ED visits in the TKI group, 49% in the immunotherapy group, and 42% in the chemotherapy group.
Many ED visits were deemed unrelated to cancer or its therapies – 30% in the TKI group, 26% in the immunotherapy group, and 32% in the chemotherapy group.
Rule-out cases contributed to 7% of ED visits in the TKI group, 14% in the immunotherapy group, and 5% in the chemotherapy group.
Overall, 9% of ED visits were therapy related. The smallest proportion of these was observed in the TKI group (2%), which was significantly smaller than in the immunotherapy group (12%), a rate also significantly smaller than in the chemotherapy group (21%, P < .001).
Most unplanned ED visits did not lead to admissions (55%), were for complaints that began 2 or more days prior to presentation (53%), led to diagnostics or therapeutics that could have been administered in an outpatient setting (48%), and were during business hours (52%).
As a result, 24% of visits were classified as preventable, and 10% were deemed unnecessary.
Preventive strategies
“Our study suggests that TKIs lead to fewer emergency room visits than immunotherapy and chemotherapy,” Dr. Shah said in an interview.
“Overall, this may not necessarily change which therapy we prescribe,” he added, “as TKI therapy is often first line for patients with targeted mutations. However, recognizing that those on chemotherapy or immunotherapy are at higher risk for emergency room visits, we may target preventative strategies, for example, nursing phone calls, telemonitoring of symptoms, and frequent video visits toward this high-risk population.”
Dr. Shah and Dr. Neal said it’s “reassuring” that TKIs and immunotherapy are small drivers of unplanned hospital care. However, they also said efforts aimed at reducing chemotherapy-related ED visits are warranted.
The authors speculated that early intervention, extension of ambulatory care, and patient education about outpatient avenues of care could eliminate a significant proportion (at least 20%) of unplanned ED visits by NSCLC patients.
There was no specific funding for this study. Dr. Shah disclosed no conflicts of interest. Dr. Neal disclosed relationships with many companies, including this news organization.
The leading cause of ED visits in the study was the cancer itself, although many visits were unrelated to non–small cell lung cancer (NSCLC) or cancer therapy.
Less than 10% of ED visits were related to cancer therapy, but visits were much more common among patients receiving chemotherapy than among those receiving immunotherapy or tyrosine kinase inhibitors (TKIs).
Manan P. Shah, MD, and Joel W. Neal, MD, PhD, both of Stanford (Calif. ) University, reported these results in JCO Oncology Practice.
The authors noted that, in the United States, care of patients with cancer, among all diseases, leads to the highest per-person cost. Unplanned hospital visits are among the largest drivers of increased spending in advanced cancer care, accounting for 48% of spending. However, that spending may not be indicative of better quality care, but rather of inefficiency, according to the authors.
One registry spanning 2009-2012 and including more than 400,000 newly diagnosed cancer patients found lung cancer to have the third-highest rate of unplanned hospitalizations (after hepatobiliary and pancreatic cancer). Those findings were published in JCO Oncology Practice in 2018.
While the reason for presentation to the ED is often the cancer or its therapy in this population, there is a paucity of research on the relative contribution of factors leading to unplanned hospital visits.
Common precipitants of medical emergencies in advanced stages of lung cancer include pulmonary embolism, obstructive pneumonia, spinal cord compression caused by metastasis, and tumor progression or pleural effusion leading to respiratory failure.
Lung cancer therapies, such as TKIs, immunotherapy, and cytotoxic chemotherapy, can also cause various medical emergencies arising out of skin reactions, gastrointestinal dysfunction, organ inflammatory processes, and bone marrow suppression.
Identifying drivers of unplanned ED visits
The primary goals of Dr. Shah and Dr. Neal’s study were to understand the drivers of unplanned ED visits and identify potential strategies to prevent them.
Drawing from the Stanford Medicine Research Data Repository, the authors identified 97 NSCLC patients with 173 ED visits at Stanford.
Patients were sorted according to which of the three therapies they had been receiving in the 3 months prior to the unplanned visit – TKIs (n = 47), immunotherapy (n = 24), or chemotherapy (n = 26). Patients receiving a combination of chemotherapy and immunotherapy were classified under the immunotherapy category.
ED visits were divided into four categories: cancer related, therapy related, unrelated to cancer or therapy, and rule-out (when an outpatient provider sent the patient to rule out medico-oncologic emergencies such as pulmonary embolism or cord compression).
If the patient’s main complaint(s) began 2 or more days before presentation, the diagnostics or therapeutics could have been provided in an outpatient setting (e.g., in clinic or urgent care), and the patient was discharged directly from the ED, the encounter was classified as potentially preventable. Among these preventable encounters, those made during business hours were also labeled unnecessary because they could have been managed through the Stanford sick call system for same-day urgent visits.
Leading cause is cancer
Overall, the leading cause of ED visits was NSCLC itself (54%). The patient’s cancer contributed to 61% of ED visits in the TKI group, 49% in the immunotherapy group, and 42% in the chemotherapy group.
Many ED visits were deemed unrelated to cancer or its therapies – 30% in the TKI group, 26% in the immunotherapy group, and 32% in the chemotherapy group.
Rule-out cases contributed to 7% of ED visits in the TKI group, 14% in the immunotherapy group, and 5% in the chemotherapy group.
Overall, 9% of ED visits were therapy related. The smallest proportion of these was observed in the TKI group (2%), which was significantly smaller than in the immunotherapy group (12%), a rate also significantly smaller than in the chemotherapy group (21%, P < .001).
Most unplanned ED visits did not lead to admissions (55%), were for complaints that began 2 or more days prior to presentation (53%), led to diagnostics or therapeutics that could have been administered in an outpatient setting (48%), and were during business hours (52%).
As a result, 24% of visits were classified as preventable, and 10% were deemed unnecessary.
Preventive strategies
“Our study suggests that TKIs lead to fewer emergency room visits than immunotherapy and chemotherapy,” Dr. Shah said in an interview.
“Overall, this may not necessarily change which therapy we prescribe,” he added, “as TKI therapy is often first line for patients with targeted mutations. However, recognizing that those on chemotherapy or immunotherapy are at higher risk for emergency room visits, we may target preventative strategies, for example, nursing phone calls, telemonitoring of symptoms, and frequent video visits toward this high-risk population.”
Dr. Shah and Dr. Neal said it’s “reassuring” that TKIs and immunotherapy are small drivers of unplanned hospital care. However, they also said efforts aimed at reducing chemotherapy-related ED visits are warranted.
The authors speculated that early intervention, extension of ambulatory care, and patient education about outpatient avenues of care could eliminate a significant proportion (at least 20%) of unplanned ED visits by NSCLC patients.
There was no specific funding for this study. Dr. Shah disclosed no conflicts of interest. Dr. Neal disclosed relationships with many companies, including this news organization.
FROM JCO ONCOLOGY PRACTICE
Moderna needs more kids for COVID vaccine trials
according to the company CEO and a federal official.
The Moderna vaccine was authorized for use in December and is now being given to people 18 and over. But children would receive lower doses, so new clinical trials must be done, Moderna CEO Stephane Bancel said at the JPMorgan virtual Health Care Conference on Monday.
Clinical trials on children 11 and younger “will take much longer, because we have to age deescalate and start at a lower dose. So we should not anticipate clinical data in 2021, but more in 2022,” Ms. Bancel said, according to Business Insider.
Moderna’s clinical trials for 12- to 17-year-olds started 4 weeks ago, but the company is having trouble getting enough participants, said Moncef Slaoui, PhD, the scientific head of Operation Warp Speed, the U.S. government’s vaccine effort. That could delay Food and Drug Administration approval, he said.
“It’s really very important for all of us, for all the population in America, to realize that we can’t have that indication unless adolescents aged 12-18 decide to participate,” Dr. Slaoui said, according to USA Today.
He said the adolescent trials are getting only about 800 volunteers a month, but need at least 3,000 volunteers to complete the study, USA Today reported. Parents interested in having their child participate can check eligibility and sign at this website.
The Pfizer/BioNTech vaccine won authorization for use in 16- to 17-year-olds as well as adults.
The coronavirus doesn’t appear to have as serious complications for children as for adults.
“At this time, it appears that severe illness due to COVID-19 is rare among children,” the American Association of Pediatrics says. “However, there is an urgent need to collect more data on longer-term impacts of the pandemic on children, including ways the virus may harm the long-term physical health of infected children, as well as its emotional and mental health effects.”
The association says 179 children had died of COVID-related reasons in 43 states and New York City as of Dec. 31, 2020. That’s about 0.06% of total COVID deaths, it says.
But children do get sick. As of Jan. 7, 2021, nearly 2.3 million children had tested positive for COVID-19 since the start of the pandemic, the association says.
A version of this article first appeared on WebMD.com.
according to the company CEO and a federal official.
The Moderna vaccine was authorized for use in December and is now being given to people 18 and over. But children would receive lower doses, so new clinical trials must be done, Moderna CEO Stephane Bancel said at the JPMorgan virtual Health Care Conference on Monday.
Clinical trials on children 11 and younger “will take much longer, because we have to age deescalate and start at a lower dose. So we should not anticipate clinical data in 2021, but more in 2022,” Ms. Bancel said, according to Business Insider.
Moderna’s clinical trials for 12- to 17-year-olds started 4 weeks ago, but the company is having trouble getting enough participants, said Moncef Slaoui, PhD, the scientific head of Operation Warp Speed, the U.S. government’s vaccine effort. That could delay Food and Drug Administration approval, he said.
“It’s really very important for all of us, for all the population in America, to realize that we can’t have that indication unless adolescents aged 12-18 decide to participate,” Dr. Slaoui said, according to USA Today.
He said the adolescent trials are getting only about 800 volunteers a month, but need at least 3,000 volunteers to complete the study, USA Today reported. Parents interested in having their child participate can check eligibility and sign at this website.
The Pfizer/BioNTech vaccine won authorization for use in 16- to 17-year-olds as well as adults.
The coronavirus doesn’t appear to have as serious complications for children as for adults.
“At this time, it appears that severe illness due to COVID-19 is rare among children,” the American Association of Pediatrics says. “However, there is an urgent need to collect more data on longer-term impacts of the pandemic on children, including ways the virus may harm the long-term physical health of infected children, as well as its emotional and mental health effects.”
The association says 179 children had died of COVID-related reasons in 43 states and New York City as of Dec. 31, 2020. That’s about 0.06% of total COVID deaths, it says.
But children do get sick. As of Jan. 7, 2021, nearly 2.3 million children had tested positive for COVID-19 since the start of the pandemic, the association says.
A version of this article first appeared on WebMD.com.
according to the company CEO and a federal official.
The Moderna vaccine was authorized for use in December and is now being given to people 18 and over. But children would receive lower doses, so new clinical trials must be done, Moderna CEO Stephane Bancel said at the JPMorgan virtual Health Care Conference on Monday.
Clinical trials on children 11 and younger “will take much longer, because we have to age deescalate and start at a lower dose. So we should not anticipate clinical data in 2021, but more in 2022,” Ms. Bancel said, according to Business Insider.
Moderna’s clinical trials for 12- to 17-year-olds started 4 weeks ago, but the company is having trouble getting enough participants, said Moncef Slaoui, PhD, the scientific head of Operation Warp Speed, the U.S. government’s vaccine effort. That could delay Food and Drug Administration approval, he said.
“It’s really very important for all of us, for all the population in America, to realize that we can’t have that indication unless adolescents aged 12-18 decide to participate,” Dr. Slaoui said, according to USA Today.
He said the adolescent trials are getting only about 800 volunteers a month, but need at least 3,000 volunteers to complete the study, USA Today reported. Parents interested in having their child participate can check eligibility and sign at this website.
The Pfizer/BioNTech vaccine won authorization for use in 16- to 17-year-olds as well as adults.
The coronavirus doesn’t appear to have as serious complications for children as for adults.
“At this time, it appears that severe illness due to COVID-19 is rare among children,” the American Association of Pediatrics says. “However, there is an urgent need to collect more data on longer-term impacts of the pandemic on children, including ways the virus may harm the long-term physical health of infected children, as well as its emotional and mental health effects.”
The association says 179 children had died of COVID-related reasons in 43 states and New York City as of Dec. 31, 2020. That’s about 0.06% of total COVID deaths, it says.
But children do get sick. As of Jan. 7, 2021, nearly 2.3 million children had tested positive for COVID-19 since the start of the pandemic, the association says.
A version of this article first appeared on WebMD.com.
Nulliparity, not ART, likely raises risk of ovarian cancer
Women who receive ovarian stimulation for assisted reproductive technology (ART) procedures don’t have an increased risk of developing ovarian cancer when compared to subfertile women who don’t undergo ART, according to a new study.
The results suggest that nulliparity is likely responsible for the increased risk of ovarian cancer observed in patients treated with ART, the researchers said.
Earlier, shorter studies had only compared ART-treated women with women from the general population.
“Subfertile women differ from women in the general population according to several ovarian cancer risk factors. Therefore, to estimate the risk of ovarian cancer associated with ART, it was important to include a comparison group of women who were subfertile and not treated with ART,” said senior study author Flora E. van Leeuwen, PhD, of Netherlands Cancer Institute in Amsterdam.
She and her colleagues conducted a nationwide cohort study of 30,625 women who received ovarian stimulation for ART during 1983-2000 and 9,988 women who received fertility treatments other than ART.
Incident invasive and borderline ovarian tumors were ascertained through linkage with the Netherlands Cancer Registry and the Dutch Pathology Registry. Ovarian tumor risk in ART-treated women was compared with risks in the general population and the subfertile non-ART group.
The researchers reported the results in the Journal of the National Cancer Institute.
Risk of ovarian cancer
Women treated with ART were no more likely to develop ovarian cancer than subfertile women not treated with ART (adjusted hazard ratio, 1.02), but the ART group did have an increased risk of ovarian cancer when compared to the general population (standardized incidence ratio, 1.43).
“This, however, turned out to be due to the fact that the women who had received ART were less likely to have children. Not having children is a known risk factor for ovarian cancer,” Dr. van Leeuwen said.
Women with more ART procedures that resulted in the birth of a child were at lower risk of developing ovarian cancer, compared with women without any successful cycle (Ptrend = .001). However, women who had only cycles not resulting in a birth were not at higher risk of ovarian cancer when they had a greater number of cycles.
“These results indicate that parity decreases the risk of ovarian cancer, also in ART-treated women. But more unsuccessful ART cycles do not increase the risk of ovarian cancer,” Dr. van Leeuwen said.
Risk of borderline ovarian tumors
The risk of developing borderline ovarian tumors was roughly twice as high in women who had received ART, both compared with women who had received other fertility treatments (hazard ratio, 1.84) and women from the general population (standardized incidence ratio, 2.20).
However, the risk of developing borderline ovarian tumors did not increase in women who had received multiple ART procedures.
“If there was a causal association between ART and increased risk of borderline ovarian tumors, we would expect to see this risk increase with a greater number of ART procedures from more hormones and more stimulation of the ovaries. This makes the direct link between ART and increased risk of borderline tumors a bit uncertain. It might be caused by other factors, such as the severity of infertility,” Dr. van Leeuwen said.
Borderline ovarian tumors are rare in the general population in the Netherlands, and women who develop these tumors generally have a good prognosis, she said.
The risk of developing a borderline tumor before the age of 55 for women in the Netherlands is approximately 0.2%. After ART, the study found a risk of approximately 0.3%.
Causal associations with ART 'unlikely'
“Women who develop cancer and have undergone ART procedures in the past may wonder whether their cancer may be caused by ART. Based on the results from our study, that seems unlikely, and that is a very reassuring message from practicing oncologists to women diagnosed with ovarian cancer. Another important message is that, in ART-treated women, increasing parity reduces the risk of ovarian cancer,” Dr. van Leeuwen said.
She added that the risk of borderline ovarian tumors did not increase in women who received multiple ART procedures, “which makes it somewhat less likely that ART would have caused their borderline ovarian tumor.”
The study does not exclude the possibility that ART might increase the risk of ovarian tumors after age 60.
“Despite our long follow-up, the age of the women at the end of our study was still relatively young [average 56 years]. Because the incidence of ovarian cancer increases with older age, it is vital to continue to follow these women. Only then can we be sure that ART does not increase the risk of ovarian tumors in the very long run,” Dr. van Leeuwen said.
“This study offers confirmation of several previous studies and provides reassurance about the risk of ovarian cancer after ART procedures,” said Daniel Kenigsberg, MD, of RMA Long Island IVF in New York. Dr. Kenigsberg was not involved in this study but has performed more than 30,000 ART procedures over the past 32 years.
“Researchers have looked at whether fertility drugs cause ovarian cancer in different ways and in different countries, and there is no cause-and-effect relationship. There was no dose-response relationship between ART and ovarian tumors in this study. It’s more likely there is something wrong with the women’s ovaries that lead to borderline tumors and infertility more than any treatment,” Dr. Kenigsberg added.
“Perhaps both fertility and cancer relate to an underlying ovarian issue, but this would not explain the increased cancer incidence in those who never attempted pregnancy, that is, women who are voluntarily childless. Pregnancy is statistically protective: more pregnancies lead to less ovarian cancer, but this is far from absolute,” he explained.
Dr. Kenigsberg suggested that oncologists should be aware of a patient’s obstetrical history and fertility history as well as any related medical interventions.
“Borderline tumors look like cancer and have histologic features of cancer but do not meet the criteria for a cancer diagnosis,” he said. “They require close surveillance because their relationship to the development of full-fledged cancer is uncertain.”
This research was supported by grants from the Dutch Cancer Society. The authors and Dr. Kenigsberg have no conflicts of interest.
Women who receive ovarian stimulation for assisted reproductive technology (ART) procedures don’t have an increased risk of developing ovarian cancer when compared to subfertile women who don’t undergo ART, according to a new study.
The results suggest that nulliparity is likely responsible for the increased risk of ovarian cancer observed in patients treated with ART, the researchers said.
Earlier, shorter studies had only compared ART-treated women with women from the general population.
“Subfertile women differ from women in the general population according to several ovarian cancer risk factors. Therefore, to estimate the risk of ovarian cancer associated with ART, it was important to include a comparison group of women who were subfertile and not treated with ART,” said senior study author Flora E. van Leeuwen, PhD, of Netherlands Cancer Institute in Amsterdam.
She and her colleagues conducted a nationwide cohort study of 30,625 women who received ovarian stimulation for ART during 1983-2000 and 9,988 women who received fertility treatments other than ART.
Incident invasive and borderline ovarian tumors were ascertained through linkage with the Netherlands Cancer Registry and the Dutch Pathology Registry. Ovarian tumor risk in ART-treated women was compared with risks in the general population and the subfertile non-ART group.
The researchers reported the results in the Journal of the National Cancer Institute.
Risk of ovarian cancer
Women treated with ART were no more likely to develop ovarian cancer than subfertile women not treated with ART (adjusted hazard ratio, 1.02), but the ART group did have an increased risk of ovarian cancer when compared to the general population (standardized incidence ratio, 1.43).
“This, however, turned out to be due to the fact that the women who had received ART were less likely to have children. Not having children is a known risk factor for ovarian cancer,” Dr. van Leeuwen said.
Women with more ART procedures that resulted in the birth of a child were at lower risk of developing ovarian cancer, compared with women without any successful cycle (Ptrend = .001). However, women who had only cycles not resulting in a birth were not at higher risk of ovarian cancer when they had a greater number of cycles.
“These results indicate that parity decreases the risk of ovarian cancer, also in ART-treated women. But more unsuccessful ART cycles do not increase the risk of ovarian cancer,” Dr. van Leeuwen said.
Risk of borderline ovarian tumors
The risk of developing borderline ovarian tumors was roughly twice as high in women who had received ART, both compared with women who had received other fertility treatments (hazard ratio, 1.84) and women from the general population (standardized incidence ratio, 2.20).
However, the risk of developing borderline ovarian tumors did not increase in women who had received multiple ART procedures.
“If there was a causal association between ART and increased risk of borderline ovarian tumors, we would expect to see this risk increase with a greater number of ART procedures from more hormones and more stimulation of the ovaries. This makes the direct link between ART and increased risk of borderline tumors a bit uncertain. It might be caused by other factors, such as the severity of infertility,” Dr. van Leeuwen said.
Borderline ovarian tumors are rare in the general population in the Netherlands, and women who develop these tumors generally have a good prognosis, she said.
The risk of developing a borderline tumor before the age of 55 for women in the Netherlands is approximately 0.2%. After ART, the study found a risk of approximately 0.3%.
Causal associations with ART 'unlikely'
“Women who develop cancer and have undergone ART procedures in the past may wonder whether their cancer may be caused by ART. Based on the results from our study, that seems unlikely, and that is a very reassuring message from practicing oncologists to women diagnosed with ovarian cancer. Another important message is that, in ART-treated women, increasing parity reduces the risk of ovarian cancer,” Dr. van Leeuwen said.
She added that the risk of borderline ovarian tumors did not increase in women who received multiple ART procedures, “which makes it somewhat less likely that ART would have caused their borderline ovarian tumor.”
The study does not exclude the possibility that ART might increase the risk of ovarian tumors after age 60.
“Despite our long follow-up, the age of the women at the end of our study was still relatively young [average 56 years]. Because the incidence of ovarian cancer increases with older age, it is vital to continue to follow these women. Only then can we be sure that ART does not increase the risk of ovarian tumors in the very long run,” Dr. van Leeuwen said.
“This study offers confirmation of several previous studies and provides reassurance about the risk of ovarian cancer after ART procedures,” said Daniel Kenigsberg, MD, of RMA Long Island IVF in New York. Dr. Kenigsberg was not involved in this study but has performed more than 30,000 ART procedures over the past 32 years.
“Researchers have looked at whether fertility drugs cause ovarian cancer in different ways and in different countries, and there is no cause-and-effect relationship. There was no dose-response relationship between ART and ovarian tumors in this study. It’s more likely there is something wrong with the women’s ovaries that lead to borderline tumors and infertility more than any treatment,” Dr. Kenigsberg added.
“Perhaps both fertility and cancer relate to an underlying ovarian issue, but this would not explain the increased cancer incidence in those who never attempted pregnancy, that is, women who are voluntarily childless. Pregnancy is statistically protective: more pregnancies lead to less ovarian cancer, but this is far from absolute,” he explained.
Dr. Kenigsberg suggested that oncologists should be aware of a patient’s obstetrical history and fertility history as well as any related medical interventions.
“Borderline tumors look like cancer and have histologic features of cancer but do not meet the criteria for a cancer diagnosis,” he said. “They require close surveillance because their relationship to the development of full-fledged cancer is uncertain.”
This research was supported by grants from the Dutch Cancer Society. The authors and Dr. Kenigsberg have no conflicts of interest.
Women who receive ovarian stimulation for assisted reproductive technology (ART) procedures don’t have an increased risk of developing ovarian cancer when compared to subfertile women who don’t undergo ART, according to a new study.
The results suggest that nulliparity is likely responsible for the increased risk of ovarian cancer observed in patients treated with ART, the researchers said.
Earlier, shorter studies had only compared ART-treated women with women from the general population.
“Subfertile women differ from women in the general population according to several ovarian cancer risk factors. Therefore, to estimate the risk of ovarian cancer associated with ART, it was important to include a comparison group of women who were subfertile and not treated with ART,” said senior study author Flora E. van Leeuwen, PhD, of Netherlands Cancer Institute in Amsterdam.
She and her colleagues conducted a nationwide cohort study of 30,625 women who received ovarian stimulation for ART during 1983-2000 and 9,988 women who received fertility treatments other than ART.
Incident invasive and borderline ovarian tumors were ascertained through linkage with the Netherlands Cancer Registry and the Dutch Pathology Registry. Ovarian tumor risk in ART-treated women was compared with risks in the general population and the subfertile non-ART group.
The researchers reported the results in the Journal of the National Cancer Institute.
Risk of ovarian cancer
Women treated with ART were no more likely to develop ovarian cancer than subfertile women not treated with ART (adjusted hazard ratio, 1.02), but the ART group did have an increased risk of ovarian cancer when compared to the general population (standardized incidence ratio, 1.43).
“This, however, turned out to be due to the fact that the women who had received ART were less likely to have children. Not having children is a known risk factor for ovarian cancer,” Dr. van Leeuwen said.
Women with more ART procedures that resulted in the birth of a child were at lower risk of developing ovarian cancer, compared with women without any successful cycle (Ptrend = .001). However, women who had only cycles not resulting in a birth were not at higher risk of ovarian cancer when they had a greater number of cycles.
“These results indicate that parity decreases the risk of ovarian cancer, also in ART-treated women. But more unsuccessful ART cycles do not increase the risk of ovarian cancer,” Dr. van Leeuwen said.
Risk of borderline ovarian tumors
The risk of developing borderline ovarian tumors was roughly twice as high in women who had received ART, both compared with women who had received other fertility treatments (hazard ratio, 1.84) and women from the general population (standardized incidence ratio, 2.20).
However, the risk of developing borderline ovarian tumors did not increase in women who had received multiple ART procedures.
“If there was a causal association between ART and increased risk of borderline ovarian tumors, we would expect to see this risk increase with a greater number of ART procedures from more hormones and more stimulation of the ovaries. This makes the direct link between ART and increased risk of borderline tumors a bit uncertain. It might be caused by other factors, such as the severity of infertility,” Dr. van Leeuwen said.
Borderline ovarian tumors are rare in the general population in the Netherlands, and women who develop these tumors generally have a good prognosis, she said.
The risk of developing a borderline tumor before the age of 55 for women in the Netherlands is approximately 0.2%. After ART, the study found a risk of approximately 0.3%.
Causal associations with ART 'unlikely'
“Women who develop cancer and have undergone ART procedures in the past may wonder whether their cancer may be caused by ART. Based on the results from our study, that seems unlikely, and that is a very reassuring message from practicing oncologists to women diagnosed with ovarian cancer. Another important message is that, in ART-treated women, increasing parity reduces the risk of ovarian cancer,” Dr. van Leeuwen said.
She added that the risk of borderline ovarian tumors did not increase in women who received multiple ART procedures, “which makes it somewhat less likely that ART would have caused their borderline ovarian tumor.”
The study does not exclude the possibility that ART might increase the risk of ovarian tumors after age 60.
“Despite our long follow-up, the age of the women at the end of our study was still relatively young [average 56 years]. Because the incidence of ovarian cancer increases with older age, it is vital to continue to follow these women. Only then can we be sure that ART does not increase the risk of ovarian tumors in the very long run,” Dr. van Leeuwen said.
“This study offers confirmation of several previous studies and provides reassurance about the risk of ovarian cancer after ART procedures,” said Daniel Kenigsberg, MD, of RMA Long Island IVF in New York. Dr. Kenigsberg was not involved in this study but has performed more than 30,000 ART procedures over the past 32 years.
“Researchers have looked at whether fertility drugs cause ovarian cancer in different ways and in different countries, and there is no cause-and-effect relationship. There was no dose-response relationship between ART and ovarian tumors in this study. It’s more likely there is something wrong with the women’s ovaries that lead to borderline tumors and infertility more than any treatment,” Dr. Kenigsberg added.
“Perhaps both fertility and cancer relate to an underlying ovarian issue, but this would not explain the increased cancer incidence in those who never attempted pregnancy, that is, women who are voluntarily childless. Pregnancy is statistically protective: more pregnancies lead to less ovarian cancer, but this is far from absolute,” he explained.
Dr. Kenigsberg suggested that oncologists should be aware of a patient’s obstetrical history and fertility history as well as any related medical interventions.
“Borderline tumors look like cancer and have histologic features of cancer but do not meet the criteria for a cancer diagnosis,” he said. “They require close surveillance because their relationship to the development of full-fledged cancer is uncertain.”
This research was supported by grants from the Dutch Cancer Society. The authors and Dr. Kenigsberg have no conflicts of interest.
FROM JOURNAL OF THE NATIONAL CANCER INSTITUTE
American Academy of Sleep Medicine (AASM) advocates for year-round standard time
Although the United States has observed daylight saving time (DST) continuously, in some form, for the last 5 decades (Table), the twice a year switches have never been less popular. In 2019, an American Academy of Sleep Medicine (AASM) survey of more than 2,000 US adults found that 63% support the elimination of seasonal time changes in favor of a national, fixed, year-round time, and only 11% oppose it. Indeed, multiple states have pending legislations to adopt year-round daylight saving time or year-round standard time (Updated September 30, 2020, Congressional Research Service. https://crsreports.congress.gov. R45208 Daylight Saving Time. Accessed Dec 14, 2020). Adjacent states, to limit confusion to interstate travel and commerce, tend to lobby for similar changes together. Most importantly, because of the scientific evidence of detrimental health effects to the public and safety concerns, the American Academy of Sleep Medicine has issued a position statement for year-round standard time (Rishi MA, et al. Daylight saving time: an American Academy of Sleep Medicine position statement. J Clin Sleep Med. 2020;16(10):1781).
Railroad industry successfully lobbied the US government for consistent time in the United States to keep transportation schedules uniform in 1883; standard time was implemented. When war efforts were over, DST was dropped. Some regions, such as New York and Chicago, maintained DST, but no national standard was applied. Retailers and the recreational activity industry advocated for DST to increase business after work in the afternoon and evenings. In 1966, Congress passed the Uniform Time Act of 1966 to implement 6 months of DST and 6 months of standard time (Waxman OB. The real reason why daylight saving time is a thing. https://time.com/4549397/daylight-saving-time-history-politics/; November 1, 2017. Accessed Dec 14, 2020). Local jurisdictions can opt out of DST, but it requires an act of congress to enforce perennial DST.
When the OPEC embargo occurred, the Emergency Daylight Saving Time Energy Conservation Act was enacted in 1973, but it was quickly ended in October 1974 due to its unpopularity. The dairy industry was opposed to earlier rise time that disrupted the animals’ feeding schedules and their farm operations (Feldman R. Five myths about daylight saving time. https://www.washingtonpost.com/opinions/five-myths-about-daylight-saving-time/2015/03/06/970092d4-c2c1-11e4-9271-610273846239_story.html. Accessed Dec 14, 2020.). Public safety was raised as a concern as early as 1975. The Department of Transportation found increased fatalities of school-aged children in the mornings from January to April of 1974 as compared with 1973. However, the National Bureau of Standards, that performed a review subsequently, stated that other factors might also be at play. Further extension of DST from 6 months of the year to the subsequent 7, and then 8 months per year were enacted in 1986 and 2005, respectively (The reasoning behind changing daylight saving. https://www.npr.org/templates/story/story.php?storyId=7779869. NPR. Accessed Nov 1, 2020.)
An exemption of a state from DST is allowable under existing law, but to establish permanent DST will require an act of Congress. Since then, Arizona and Hawaii, as well as US territories, such as Puerto Rico, Guam, American Samoa and Northern Mariana Islands, and US Virgin Islands, have all opted out of DST by state exemption. Because of Hawaii’s proximity to the equator, the timing of sunrise and sunset were fairly constant throughout the year that made DST unnecessary. The Navajo Nation in Arizona, because of its extension into adjacent New Mexico and Utah, participates in DST. Most of the countries along the tropics, parts of Australia, China, Japan, South Korea, India, and majority of African countries do not observe DST. The European Union has voted to abolish twice yearly change in time in 2021; and individual member states will be able to decide whether they wish to remain on permanent standard time or DST. Since 2015, more than 45 states have proposed legislation to change their observance of DST.
The human biological rhythm is most consistent with standard time (Antle M. Circadian rhythm expert argues against permanent daylight saving time. https://www.ucalgary.ca/news/circadian-rhythm-expert-argues-against-permanent-daylight-saving-time. Accessed Dec 14, 2020.). Since the biological clock for most individuals is not exactly 24 hours long, zeitgebers such as sunlight, exercise, and feeding behaviors are important time cues to foster a regular rhythm. Acutely, the adjustment to 1 hour’s sleep loss at the spring switch from standard time to DST generally requires several days to adapt (Kalidindi A. Daylight saving time is bad for your health. https://massivesci.com/articles/daylight-saving-savings-time-dst-november-standard-time. Accessed Dec 14, 2020.). During this adjustment period, the internal bodily functions are disrupted. The sense of sleepiness and fatigue are increased with earlier morning awakenings, and the inability to fall asleep earlier leads to symptoms of insomnia and poor sleep quality.
The health and economic costs due to accidents, injuries, and medical errors are now well known. Individual biological rhythm disruptions at the spring switch from standard time to DST with the loss of sleep likely contributes to higher risks of myocardial infarctions (Janszky I, et al. Shifts to and from daylight saving time and incidence of myocardial infarction. N Engl J Med. 2008; 359(18):1966) that are not mostly seen during the fall switch from DST to standard time. An estimated 40 minutes of sleep loss occurs within the Sunday to Monday transition of DST in the spring. Medical errors, car crashes, suicide risks, and fatigue are all reportedly higher on the Monday after the spring switch. Some of these effects have been cited as remaining elevated through the first week and possibly chronically during the entire duration of DST. Some people have difficulty adapting to sleep loss from DST, creating social jetlag, and complaints of fatigue and increased prevalence of metabolic syndromes are more common in this population (Koopman ADM, et al. The association between social jetlag, the metabolic syndrome, and type 2 diabetes mellitus in the general population: The New Hoorn study. J Biol Rhythms. 2017 Aug:32(4):359; Roenneberg T, et al. Social jetlag and obesity. Curr Biol. 2012 May 22; 22(10):939). “Cyber-loafing,” describing those at work but who chose to peruse entertaining websites, reportedly occurred more during DST compared with the fall.
Delaying school start time has been associated with improved school attendance and performance. The American Academy of Pediatrics and AASM support delaying school start time; this measure has been adopted by California, and legislation is pending in other states (https://www.startschoollater.net/legislation.html). In spring, the loss of 1 hour’s sleep would negate any benefit of beginning the school day later. Students would suffer inattention, decrease ability to focus, and be less effective learners. Obesity and metabolic syndromes that have been found in adults, are also observed in children whose biological rhythms are delayed compared with their peers who have morning lark tendencies. Risks of mood disorder may be elevated at onset of DST due to earlier arise time or standard time when less sunlight is available in the evenings.
During the current pandemic with SARS-CoV-2, there are new reports of teens and college students able to obtain more sleep because of online education (How children’s sleep habits have changed in the pandemic. https://www.nytimes.com/2020/08/17/well/family/children-sleep-pandemic.html. Accessed Dec 14, 2020.) and they had more restful sleep and improved mood. This positive trend will be monitored closely with some schools returning to in-person instruction.
Societal costs of decreased productivity, on the job accidents and injuries, and increased risk of motor vehicle crashes (Robb D, et al. Accident rates and the impact of daylight saving transitions. Accid Anal Prev. 2018 Feb; 111:193), in addition to individual well-being, have also been reported. Energy savings that propelled arguments for DST did not translate into significant savings after all. Although less electricity was used with more abundance of sunlight in the afternoon, people drove more and used more gasoline to attend their after work activities.
Adaptation of a year-round time schedule will need to balance the impact and disruption to the health and well-being of its citizens, as well as the interests of its commercial sector. The argument for maintaining year-round standard time states that to prevent the loss of the 1 hour’s sleep that DST creates in the spring. Therefore, it preserves a more aligned biological rhythm, lowers the risks of preventable myocardial infarction, improves attention and focus, lessens daytime fatigue, and improves sense of well-being year round. Certainly, it will ensure that the teens who are likely to have later sleep schedules, will not lose more sleep and negate the benefit of starting school later.
Timeline for DST
1784 Benjamin Franklin advocated to rise earlier so as to burn fewer candles in the evenings.
1883 Railroads need standard time for operations.
1890 Merchants and retailers (clothing, cigars) advocated for longer shopping hours.
1916 Germany conserves energy.
1918 DST: fuel conservation during World War I.
1942 DST during World War II.
1963 “Chaos of clocks” needs uniform time for commerce.
1966 Uniform Time Act: DST 6 months per year.
1973 Emergency DST Energy Conservation Act: Arab oil embargo to extend DST to 8 months; ended prematurely in October 1974.
1986 Extended start date from last Sunday of April to first Sunday of November.
2005 Energy Act of 2005: 2nd week of March.
Dr. Yuen is Assistant Professor, UCSF Department of Internal Medicine-Pulmonary Department, and Adjunct Clinical Assistant Professor at Department of Psychiatry & Behavioral Sciences at Stanford (Calif.) University. Dr. Rishi is Consultant – Pulmonary, Critical Care and Sleep Medicine, Mayo Clinic Health System, Eau Claire, WI; and Assistant Professor of Medicine, Alix School of Medicine, Mayo Clinic, Rochester, MN.
Correction 3/16/21: A photo caption in an earlier version of this article misstated Dr. Kin Yuen's name.
Although the United States has observed daylight saving time (DST) continuously, in some form, for the last 5 decades (Table), the twice a year switches have never been less popular. In 2019, an American Academy of Sleep Medicine (AASM) survey of more than 2,000 US adults found that 63% support the elimination of seasonal time changes in favor of a national, fixed, year-round time, and only 11% oppose it. Indeed, multiple states have pending legislations to adopt year-round daylight saving time or year-round standard time (Updated September 30, 2020, Congressional Research Service. https://crsreports.congress.gov. R45208 Daylight Saving Time. Accessed Dec 14, 2020). Adjacent states, to limit confusion to interstate travel and commerce, tend to lobby for similar changes together. Most importantly, because of the scientific evidence of detrimental health effects to the public and safety concerns, the American Academy of Sleep Medicine has issued a position statement for year-round standard time (Rishi MA, et al. Daylight saving time: an American Academy of Sleep Medicine position statement. J Clin Sleep Med. 2020;16(10):1781).
Railroad industry successfully lobbied the US government for consistent time in the United States to keep transportation schedules uniform in 1883; standard time was implemented. When war efforts were over, DST was dropped. Some regions, such as New York and Chicago, maintained DST, but no national standard was applied. Retailers and the recreational activity industry advocated for DST to increase business after work in the afternoon and evenings. In 1966, Congress passed the Uniform Time Act of 1966 to implement 6 months of DST and 6 months of standard time (Waxman OB. The real reason why daylight saving time is a thing. https://time.com/4549397/daylight-saving-time-history-politics/; November 1, 2017. Accessed Dec 14, 2020). Local jurisdictions can opt out of DST, but it requires an act of congress to enforce perennial DST.
When the OPEC embargo occurred, the Emergency Daylight Saving Time Energy Conservation Act was enacted in 1973, but it was quickly ended in October 1974 due to its unpopularity. The dairy industry was opposed to earlier rise time that disrupted the animals’ feeding schedules and their farm operations (Feldman R. Five myths about daylight saving time. https://www.washingtonpost.com/opinions/five-myths-about-daylight-saving-time/2015/03/06/970092d4-c2c1-11e4-9271-610273846239_story.html. Accessed Dec 14, 2020.). Public safety was raised as a concern as early as 1975. The Department of Transportation found increased fatalities of school-aged children in the mornings from January to April of 1974 as compared with 1973. However, the National Bureau of Standards, that performed a review subsequently, stated that other factors might also be at play. Further extension of DST from 6 months of the year to the subsequent 7, and then 8 months per year were enacted in 1986 and 2005, respectively (The reasoning behind changing daylight saving. https://www.npr.org/templates/story/story.php?storyId=7779869. NPR. Accessed Nov 1, 2020.)
An exemption of a state from DST is allowable under existing law, but to establish permanent DST will require an act of Congress. Since then, Arizona and Hawaii, as well as US territories, such as Puerto Rico, Guam, American Samoa and Northern Mariana Islands, and US Virgin Islands, have all opted out of DST by state exemption. Because of Hawaii’s proximity to the equator, the timing of sunrise and sunset were fairly constant throughout the year that made DST unnecessary. The Navajo Nation in Arizona, because of its extension into adjacent New Mexico and Utah, participates in DST. Most of the countries along the tropics, parts of Australia, China, Japan, South Korea, India, and majority of African countries do not observe DST. The European Union has voted to abolish twice yearly change in time in 2021; and individual member states will be able to decide whether they wish to remain on permanent standard time or DST. Since 2015, more than 45 states have proposed legislation to change their observance of DST.
The human biological rhythm is most consistent with standard time (Antle M. Circadian rhythm expert argues against permanent daylight saving time. https://www.ucalgary.ca/news/circadian-rhythm-expert-argues-against-permanent-daylight-saving-time. Accessed Dec 14, 2020.). Since the biological clock for most individuals is not exactly 24 hours long, zeitgebers such as sunlight, exercise, and feeding behaviors are important time cues to foster a regular rhythm. Acutely, the adjustment to 1 hour’s sleep loss at the spring switch from standard time to DST generally requires several days to adapt (Kalidindi A. Daylight saving time is bad for your health. https://massivesci.com/articles/daylight-saving-savings-time-dst-november-standard-time. Accessed Dec 14, 2020.). During this adjustment period, the internal bodily functions are disrupted. The sense of sleepiness and fatigue are increased with earlier morning awakenings, and the inability to fall asleep earlier leads to symptoms of insomnia and poor sleep quality.
The health and economic costs due to accidents, injuries, and medical errors are now well known. Individual biological rhythm disruptions at the spring switch from standard time to DST with the loss of sleep likely contributes to higher risks of myocardial infarctions (Janszky I, et al. Shifts to and from daylight saving time and incidence of myocardial infarction. N Engl J Med. 2008; 359(18):1966) that are not mostly seen during the fall switch from DST to standard time. An estimated 40 minutes of sleep loss occurs within the Sunday to Monday transition of DST in the spring. Medical errors, car crashes, suicide risks, and fatigue are all reportedly higher on the Monday after the spring switch. Some of these effects have been cited as remaining elevated through the first week and possibly chronically during the entire duration of DST. Some people have difficulty adapting to sleep loss from DST, creating social jetlag, and complaints of fatigue and increased prevalence of metabolic syndromes are more common in this population (Koopman ADM, et al. The association between social jetlag, the metabolic syndrome, and type 2 diabetes mellitus in the general population: The New Hoorn study. J Biol Rhythms. 2017 Aug:32(4):359; Roenneberg T, et al. Social jetlag and obesity. Curr Biol. 2012 May 22; 22(10):939). “Cyber-loafing,” describing those at work but who chose to peruse entertaining websites, reportedly occurred more during DST compared with the fall.
Delaying school start time has been associated with improved school attendance and performance. The American Academy of Pediatrics and AASM support delaying school start time; this measure has been adopted by California, and legislation is pending in other states (https://www.startschoollater.net/legislation.html). In spring, the loss of 1 hour’s sleep would negate any benefit of beginning the school day later. Students would suffer inattention, decrease ability to focus, and be less effective learners. Obesity and metabolic syndromes that have been found in adults, are also observed in children whose biological rhythms are delayed compared with their peers who have morning lark tendencies. Risks of mood disorder may be elevated at onset of DST due to earlier arise time or standard time when less sunlight is available in the evenings.
During the current pandemic with SARS-CoV-2, there are new reports of teens and college students able to obtain more sleep because of online education (How children’s sleep habits have changed in the pandemic. https://www.nytimes.com/2020/08/17/well/family/children-sleep-pandemic.html. Accessed Dec 14, 2020.) and they had more restful sleep and improved mood. This positive trend will be monitored closely with some schools returning to in-person instruction.
Societal costs of decreased productivity, on the job accidents and injuries, and increased risk of motor vehicle crashes (Robb D, et al. Accident rates and the impact of daylight saving transitions. Accid Anal Prev. 2018 Feb; 111:193), in addition to individual well-being, have also been reported. Energy savings that propelled arguments for DST did not translate into significant savings after all. Although less electricity was used with more abundance of sunlight in the afternoon, people drove more and used more gasoline to attend their after work activities.
Adaptation of a year-round time schedule will need to balance the impact and disruption to the health and well-being of its citizens, as well as the interests of its commercial sector. The argument for maintaining year-round standard time states that to prevent the loss of the 1 hour’s sleep that DST creates in the spring. Therefore, it preserves a more aligned biological rhythm, lowers the risks of preventable myocardial infarction, improves attention and focus, lessens daytime fatigue, and improves sense of well-being year round. Certainly, it will ensure that the teens who are likely to have later sleep schedules, will not lose more sleep and negate the benefit of starting school later.
Timeline for DST
1784 Benjamin Franklin advocated to rise earlier so as to burn fewer candles in the evenings.
1883 Railroads need standard time for operations.
1890 Merchants and retailers (clothing, cigars) advocated for longer shopping hours.
1916 Germany conserves energy.
1918 DST: fuel conservation during World War I.
1942 DST during World War II.
1963 “Chaos of clocks” needs uniform time for commerce.
1966 Uniform Time Act: DST 6 months per year.
1973 Emergency DST Energy Conservation Act: Arab oil embargo to extend DST to 8 months; ended prematurely in October 1974.
1986 Extended start date from last Sunday of April to first Sunday of November.
2005 Energy Act of 2005: 2nd week of March.
Dr. Yuen is Assistant Professor, UCSF Department of Internal Medicine-Pulmonary Department, and Adjunct Clinical Assistant Professor at Department of Psychiatry & Behavioral Sciences at Stanford (Calif.) University. Dr. Rishi is Consultant – Pulmonary, Critical Care and Sleep Medicine, Mayo Clinic Health System, Eau Claire, WI; and Assistant Professor of Medicine, Alix School of Medicine, Mayo Clinic, Rochester, MN.
Correction 3/16/21: A photo caption in an earlier version of this article misstated Dr. Kin Yuen's name.
Although the United States has observed daylight saving time (DST) continuously, in some form, for the last 5 decades (Table), the twice a year switches have never been less popular. In 2019, an American Academy of Sleep Medicine (AASM) survey of more than 2,000 US adults found that 63% support the elimination of seasonal time changes in favor of a national, fixed, year-round time, and only 11% oppose it. Indeed, multiple states have pending legislations to adopt year-round daylight saving time or year-round standard time (Updated September 30, 2020, Congressional Research Service. https://crsreports.congress.gov. R45208 Daylight Saving Time. Accessed Dec 14, 2020). Adjacent states, to limit confusion to interstate travel and commerce, tend to lobby for similar changes together. Most importantly, because of the scientific evidence of detrimental health effects to the public and safety concerns, the American Academy of Sleep Medicine has issued a position statement for year-round standard time (Rishi MA, et al. Daylight saving time: an American Academy of Sleep Medicine position statement. J Clin Sleep Med. 2020;16(10):1781).
Railroad industry successfully lobbied the US government for consistent time in the United States to keep transportation schedules uniform in 1883; standard time was implemented. When war efforts were over, DST was dropped. Some regions, such as New York and Chicago, maintained DST, but no national standard was applied. Retailers and the recreational activity industry advocated for DST to increase business after work in the afternoon and evenings. In 1966, Congress passed the Uniform Time Act of 1966 to implement 6 months of DST and 6 months of standard time (Waxman OB. The real reason why daylight saving time is a thing. https://time.com/4549397/daylight-saving-time-history-politics/; November 1, 2017. Accessed Dec 14, 2020). Local jurisdictions can opt out of DST, but it requires an act of congress to enforce perennial DST.
When the OPEC embargo occurred, the Emergency Daylight Saving Time Energy Conservation Act was enacted in 1973, but it was quickly ended in October 1974 due to its unpopularity. The dairy industry was opposed to earlier rise time that disrupted the animals’ feeding schedules and their farm operations (Feldman R. Five myths about daylight saving time. https://www.washingtonpost.com/opinions/five-myths-about-daylight-saving-time/2015/03/06/970092d4-c2c1-11e4-9271-610273846239_story.html. Accessed Dec 14, 2020.). Public safety was raised as a concern as early as 1975. The Department of Transportation found increased fatalities of school-aged children in the mornings from January to April of 1974 as compared with 1973. However, the National Bureau of Standards, that performed a review subsequently, stated that other factors might also be at play. Further extension of DST from 6 months of the year to the subsequent 7, and then 8 months per year were enacted in 1986 and 2005, respectively (The reasoning behind changing daylight saving. https://www.npr.org/templates/story/story.php?storyId=7779869. NPR. Accessed Nov 1, 2020.)
An exemption of a state from DST is allowable under existing law, but to establish permanent DST will require an act of Congress. Since then, Arizona and Hawaii, as well as US territories, such as Puerto Rico, Guam, American Samoa and Northern Mariana Islands, and US Virgin Islands, have all opted out of DST by state exemption. Because of Hawaii’s proximity to the equator, the timing of sunrise and sunset were fairly constant throughout the year that made DST unnecessary. The Navajo Nation in Arizona, because of its extension into adjacent New Mexico and Utah, participates in DST. Most of the countries along the tropics, parts of Australia, China, Japan, South Korea, India, and majority of African countries do not observe DST. The European Union has voted to abolish twice yearly change in time in 2021; and individual member states will be able to decide whether they wish to remain on permanent standard time or DST. Since 2015, more than 45 states have proposed legislation to change their observance of DST.
The human biological rhythm is most consistent with standard time (Antle M. Circadian rhythm expert argues against permanent daylight saving time. https://www.ucalgary.ca/news/circadian-rhythm-expert-argues-against-permanent-daylight-saving-time. Accessed Dec 14, 2020.). Since the biological clock for most individuals is not exactly 24 hours long, zeitgebers such as sunlight, exercise, and feeding behaviors are important time cues to foster a regular rhythm. Acutely, the adjustment to 1 hour’s sleep loss at the spring switch from standard time to DST generally requires several days to adapt (Kalidindi A. Daylight saving time is bad for your health. https://massivesci.com/articles/daylight-saving-savings-time-dst-november-standard-time. Accessed Dec 14, 2020.). During this adjustment period, the internal bodily functions are disrupted. The sense of sleepiness and fatigue are increased with earlier morning awakenings, and the inability to fall asleep earlier leads to symptoms of insomnia and poor sleep quality.
The health and economic costs due to accidents, injuries, and medical errors are now well known. Individual biological rhythm disruptions at the spring switch from standard time to DST with the loss of sleep likely contributes to higher risks of myocardial infarctions (Janszky I, et al. Shifts to and from daylight saving time and incidence of myocardial infarction. N Engl J Med. 2008; 359(18):1966) that are not mostly seen during the fall switch from DST to standard time. An estimated 40 minutes of sleep loss occurs within the Sunday to Monday transition of DST in the spring. Medical errors, car crashes, suicide risks, and fatigue are all reportedly higher on the Monday after the spring switch. Some of these effects have been cited as remaining elevated through the first week and possibly chronically during the entire duration of DST. Some people have difficulty adapting to sleep loss from DST, creating social jetlag, and complaints of fatigue and increased prevalence of metabolic syndromes are more common in this population (Koopman ADM, et al. The association between social jetlag, the metabolic syndrome, and type 2 diabetes mellitus in the general population: The New Hoorn study. J Biol Rhythms. 2017 Aug:32(4):359; Roenneberg T, et al. Social jetlag and obesity. Curr Biol. 2012 May 22; 22(10):939). “Cyber-loafing,” describing those at work but who chose to peruse entertaining websites, reportedly occurred more during DST compared with the fall.
Delaying school start time has been associated with improved school attendance and performance. The American Academy of Pediatrics and AASM support delaying school start time; this measure has been adopted by California, and legislation is pending in other states (https://www.startschoollater.net/legislation.html). In spring, the loss of 1 hour’s sleep would negate any benefit of beginning the school day later. Students would suffer inattention, decrease ability to focus, and be less effective learners. Obesity and metabolic syndromes that have been found in adults, are also observed in children whose biological rhythms are delayed compared with their peers who have morning lark tendencies. Risks of mood disorder may be elevated at onset of DST due to earlier arise time or standard time when less sunlight is available in the evenings.
During the current pandemic with SARS-CoV-2, there are new reports of teens and college students able to obtain more sleep because of online education (How children’s sleep habits have changed in the pandemic. https://www.nytimes.com/2020/08/17/well/family/children-sleep-pandemic.html. Accessed Dec 14, 2020.) and they had more restful sleep and improved mood. This positive trend will be monitored closely with some schools returning to in-person instruction.
Societal costs of decreased productivity, on the job accidents and injuries, and increased risk of motor vehicle crashes (Robb D, et al. Accident rates and the impact of daylight saving transitions. Accid Anal Prev. 2018 Feb; 111:193), in addition to individual well-being, have also been reported. Energy savings that propelled arguments for DST did not translate into significant savings after all. Although less electricity was used with more abundance of sunlight in the afternoon, people drove more and used more gasoline to attend their after work activities.
Adaptation of a year-round time schedule will need to balance the impact and disruption to the health and well-being of its citizens, as well as the interests of its commercial sector. The argument for maintaining year-round standard time states that to prevent the loss of the 1 hour’s sleep that DST creates in the spring. Therefore, it preserves a more aligned biological rhythm, lowers the risks of preventable myocardial infarction, improves attention and focus, lessens daytime fatigue, and improves sense of well-being year round. Certainly, it will ensure that the teens who are likely to have later sleep schedules, will not lose more sleep and negate the benefit of starting school later.
Timeline for DST
1784 Benjamin Franklin advocated to rise earlier so as to burn fewer candles in the evenings.
1883 Railroads need standard time for operations.
1890 Merchants and retailers (clothing, cigars) advocated for longer shopping hours.
1916 Germany conserves energy.
1918 DST: fuel conservation during World War I.
1942 DST during World War II.
1963 “Chaos of clocks” needs uniform time for commerce.
1966 Uniform Time Act: DST 6 months per year.
1973 Emergency DST Energy Conservation Act: Arab oil embargo to extend DST to 8 months; ended prematurely in October 1974.
1986 Extended start date from last Sunday of April to first Sunday of November.
2005 Energy Act of 2005: 2nd week of March.
Dr. Yuen is Assistant Professor, UCSF Department of Internal Medicine-Pulmonary Department, and Adjunct Clinical Assistant Professor at Department of Psychiatry & Behavioral Sciences at Stanford (Calif.) University. Dr. Rishi is Consultant – Pulmonary, Critical Care and Sleep Medicine, Mayo Clinic Health System, Eau Claire, WI; and Assistant Professor of Medicine, Alix School of Medicine, Mayo Clinic, Rochester, MN.
Correction 3/16/21: A photo caption in an earlier version of this article misstated Dr. Kin Yuen's name.
Updates from the AMA House of Delegates: November 2020 special meeting
The American Medical Association (AMA) had its November 2020 AMA Special Meeting of the AMA House of Delegates (HOD) from November 13-17.
Delegates from over 170 societies (state societies, specialties, subspecialties, and uniformed services), including physicians, residents, and students, gathered virtually for the meeting(https://tinyurl.com/y7494mwa) to consider a wide array of proposals to help fulfill the AMA’s core mission of promoting medicine and improving public health. The AMA House of Delegates, also known as the “House” or the “HOD,” is the principal policy-making body of the AMA. This democratic forum represents the views and interests of a diverse group of member physicians from more than 170 societies. These delegates meet twice per year to establish policies on health; medical, professional, and governance matters; and the principles within which the AMA’s business activities are conducted.
During the COVID-19 pandemic, the AMA has been the leading physician and patient ally—voicing recommendations to key Congressional leaders and agency staff, state policymakers, and private sector stakeholders. Acting on both federal and state levels, examples of AMA’s recent efforts include actions in financial relief, telehealth, testing and vaccine development, health equity, and more.
CHEST is an active member, and through the HOD and Specialty and Service Society (SSS), CHEST can partner with AMA other societies to support each other on important regulatory issues. CHEST/Allergy Section Council (participants at this meeting were from the AAAAI, AAOA, AASM, ACAAI, ATS, CHEST, and SCCM) met before voting in the House to discuss pending business. The meeting was hosted by the current CHEST/Allergy council chair Dr. Wesley Vander Ark (AMA Delegate AAOA) and Jami Lucas, CEO AAOA.
Policy and resolutions
Overview of the process
Policies originate via resolutions submitted by individuals or societies. These resolutions then go to one of several Reference Committees for open discussion. These committees then report their recommendations back to the HOD, which then discusses and votes on the recommendations. In some instances, the question is referred for further studies by one of several Councils, which reports go to the Board of Trustees or back to the House. Details can be found in the April 2018 CHEST Physician® article on the process. (https://tinyurl.com/yacysxar).
This year, due to the virtual nature, prioritization matrix was utilized and based on urgency. Resolutions were divided into top priority, priority, medium priority, low priority, and not a priority.
The following reference committees convened at this Special Meeting Constitution & Bylaws, Medical Service, Legislation Medical Education, Public Health, Science and Technology, Finance and Medical Practice.
Some of the issues discussed at the House of Delegates are as follows:
Medical education
Continuing board certification (Adapted as a new policy)
The policy states that American Medical Association (AMA), through its Council on Medical Education, continue to work with the American Board of Medical Specialties (ABMS) and ABMS member boards to implement key recommendations outlined by the Continuing Board Certification: Vision for the Future Commission in its final report, including the development of new, integrated standards for continuing certification programs by 2020 that will address the Commission’s recommendations for flexibility in knowledge assessment and advancing practice, feedback to diplomates, and consistency.
Graduate medical education and the corporate practice of medicine (modified existing policy)
The existing policy was amended to urge AMA to continue to monitor issues, including waiver of due process requirements, created by corporate-owned graduate medical education sites.
Public health
Bullying in the Practice of Medicine
Health-care organizations, including academic medical centers, should establish policies to prevent and address bullying in their workplaces. An effective workplace policy should:
• Describe the management’s commitment to providing a safe and healthy workplace.
• Show the staff that their leaders are concerned about bullying and unprofessional behavior and that they take it seriously.
• Clearly define workplace violence, harassment, and bullying, specifically including intimidation, threats, and other forms of aggressive behavior.
• Specify to whom the policy applies (ie, medical staff, students, administration, patients, employees, contractors, vendors, etc).
• Define both expected and prohibited behaviors.
• Outline steps for individuals to take when they feel they are a victim of workplace bullying.
• Provide contact information for a confidential means for documenting and reporting incidents.
• Prohibit retaliation and ensure privacy and confidentiality.
• Document training requirements and establish clear expectations about the training objectives.
Availability of personal protective equipment (PPE)
That our American Medical Association actively support that physicians and health-care professionals are empowered to use workplace modifications to continue professional patient care when they determine such action to be appropriate and in the best interest of patient and physician wellbeing. Physicians and health-care professionals must be permitted to use their professional judgment and augment institution-provided PPE with additional, appropriately decontaminated, personally provided personal protective equipment (PPE) without penalty (Directive to Take Action); and be it further that AMA affirm that the medical staff of each healt-care institution should integrally be involved in disaster planning, strategy, and tactical management of ongoing crises (New HOD Policy).
AMA governance and finance
The establishment of private practice physicians’ section was approved.
Medical practice
Merit-based incentive payment system (MIPS)
That our American Medical Association (AMA) support legislation that ensures Medicare physician payment is sufficient to safeguard beneficiary access to care, replaces or supplements budget neutrality in MIPS with incentive payments, or implements positive annual physician payment updates. (Directive to Take Action).
Establishing professional services claims-based payment enhancement for activities associated with the COVID-19 pandemic
American Medical Association work with other interested parties to advocate for regulatory action on the part of the Centers for Medicare & Medicaid Services to implement a professional services claims-based payment enhancement to help recognize the enhanced, nonseparately reimbursable work performed by physicians during the COVID-19 Public Health Emergency. (Directive to Take Action).
This is just a small sampling of the activities and more information, including reports from the various Councils, are available on the AMA website, http://ama-assn.org.
CHEST members interested in the AMA policy-making process may observe any AMA-HOD meeting or participate in the AMA’s democratic processes. Attendees will also be able to increase their knowledge and skills at no cost. They will also be able to connect with more than 1,500 peers and other meeting attendees from across the country. CHEST members with the time (there are two 5-day meetings each year) and interest are invited to apply to be an official CHEST delegate to the AMA. Contact Jennifer Nemkovich at jnemkovich@chestnet.org for details.
Dr. Desai is with the Chicago Chest Center and AMITA Health Suburban Lung Associates; and the Division of Pulmonary, Critical Care, Sleep and Allergy, University of Illinois at Chicago. He is also the CHEST Delegate to the AMA House of Delegates.
The American Medical Association (AMA) had its November 2020 AMA Special Meeting of the AMA House of Delegates (HOD) from November 13-17.
Delegates from over 170 societies (state societies, specialties, subspecialties, and uniformed services), including physicians, residents, and students, gathered virtually for the meeting(https://tinyurl.com/y7494mwa) to consider a wide array of proposals to help fulfill the AMA’s core mission of promoting medicine and improving public health. The AMA House of Delegates, also known as the “House” or the “HOD,” is the principal policy-making body of the AMA. This democratic forum represents the views and interests of a diverse group of member physicians from more than 170 societies. These delegates meet twice per year to establish policies on health; medical, professional, and governance matters; and the principles within which the AMA’s business activities are conducted.
During the COVID-19 pandemic, the AMA has been the leading physician and patient ally—voicing recommendations to key Congressional leaders and agency staff, state policymakers, and private sector stakeholders. Acting on both federal and state levels, examples of AMA’s recent efforts include actions in financial relief, telehealth, testing and vaccine development, health equity, and more.
CHEST is an active member, and through the HOD and Specialty and Service Society (SSS), CHEST can partner with AMA other societies to support each other on important regulatory issues. CHEST/Allergy Section Council (participants at this meeting were from the AAAAI, AAOA, AASM, ACAAI, ATS, CHEST, and SCCM) met before voting in the House to discuss pending business. The meeting was hosted by the current CHEST/Allergy council chair Dr. Wesley Vander Ark (AMA Delegate AAOA) and Jami Lucas, CEO AAOA.
Policy and resolutions
Overview of the process
Policies originate via resolutions submitted by individuals or societies. These resolutions then go to one of several Reference Committees for open discussion. These committees then report their recommendations back to the HOD, which then discusses and votes on the recommendations. In some instances, the question is referred for further studies by one of several Councils, which reports go to the Board of Trustees or back to the House. Details can be found in the April 2018 CHEST Physician® article on the process. (https://tinyurl.com/yacysxar).
This year, due to the virtual nature, prioritization matrix was utilized and based on urgency. Resolutions were divided into top priority, priority, medium priority, low priority, and not a priority.
The following reference committees convened at this Special Meeting Constitution & Bylaws, Medical Service, Legislation Medical Education, Public Health, Science and Technology, Finance and Medical Practice.
Some of the issues discussed at the House of Delegates are as follows:
Medical education
Continuing board certification (Adapted as a new policy)
The policy states that American Medical Association (AMA), through its Council on Medical Education, continue to work with the American Board of Medical Specialties (ABMS) and ABMS member boards to implement key recommendations outlined by the Continuing Board Certification: Vision for the Future Commission in its final report, including the development of new, integrated standards for continuing certification programs by 2020 that will address the Commission’s recommendations for flexibility in knowledge assessment and advancing practice, feedback to diplomates, and consistency.
Graduate medical education and the corporate practice of medicine (modified existing policy)
The existing policy was amended to urge AMA to continue to monitor issues, including waiver of due process requirements, created by corporate-owned graduate medical education sites.
Public health
Bullying in the Practice of Medicine
Health-care organizations, including academic medical centers, should establish policies to prevent and address bullying in their workplaces. An effective workplace policy should:
• Describe the management’s commitment to providing a safe and healthy workplace.
• Show the staff that their leaders are concerned about bullying and unprofessional behavior and that they take it seriously.
• Clearly define workplace violence, harassment, and bullying, specifically including intimidation, threats, and other forms of aggressive behavior.
• Specify to whom the policy applies (ie, medical staff, students, administration, patients, employees, contractors, vendors, etc).
• Define both expected and prohibited behaviors.
• Outline steps for individuals to take when they feel they are a victim of workplace bullying.
• Provide contact information for a confidential means for documenting and reporting incidents.
• Prohibit retaliation and ensure privacy and confidentiality.
• Document training requirements and establish clear expectations about the training objectives.
Availability of personal protective equipment (PPE)
That our American Medical Association actively support that physicians and health-care professionals are empowered to use workplace modifications to continue professional patient care when they determine such action to be appropriate and in the best interest of patient and physician wellbeing. Physicians and health-care professionals must be permitted to use their professional judgment and augment institution-provided PPE with additional, appropriately decontaminated, personally provided personal protective equipment (PPE) without penalty (Directive to Take Action); and be it further that AMA affirm that the medical staff of each healt-care institution should integrally be involved in disaster planning, strategy, and tactical management of ongoing crises (New HOD Policy).
AMA governance and finance
The establishment of private practice physicians’ section was approved.
Medical practice
Merit-based incentive payment system (MIPS)
That our American Medical Association (AMA) support legislation that ensures Medicare physician payment is sufficient to safeguard beneficiary access to care, replaces or supplements budget neutrality in MIPS with incentive payments, or implements positive annual physician payment updates. (Directive to Take Action).
Establishing professional services claims-based payment enhancement for activities associated with the COVID-19 pandemic
American Medical Association work with other interested parties to advocate for regulatory action on the part of the Centers for Medicare & Medicaid Services to implement a professional services claims-based payment enhancement to help recognize the enhanced, nonseparately reimbursable work performed by physicians during the COVID-19 Public Health Emergency. (Directive to Take Action).
This is just a small sampling of the activities and more information, including reports from the various Councils, are available on the AMA website, http://ama-assn.org.
CHEST members interested in the AMA policy-making process may observe any AMA-HOD meeting or participate in the AMA’s democratic processes. Attendees will also be able to increase their knowledge and skills at no cost. They will also be able to connect with more than 1,500 peers and other meeting attendees from across the country. CHEST members with the time (there are two 5-day meetings each year) and interest are invited to apply to be an official CHEST delegate to the AMA. Contact Jennifer Nemkovich at jnemkovich@chestnet.org for details.
Dr. Desai is with the Chicago Chest Center and AMITA Health Suburban Lung Associates; and the Division of Pulmonary, Critical Care, Sleep and Allergy, University of Illinois at Chicago. He is also the CHEST Delegate to the AMA House of Delegates.
The American Medical Association (AMA) had its November 2020 AMA Special Meeting of the AMA House of Delegates (HOD) from November 13-17.
Delegates from over 170 societies (state societies, specialties, subspecialties, and uniformed services), including physicians, residents, and students, gathered virtually for the meeting(https://tinyurl.com/y7494mwa) to consider a wide array of proposals to help fulfill the AMA’s core mission of promoting medicine and improving public health. The AMA House of Delegates, also known as the “House” or the “HOD,” is the principal policy-making body of the AMA. This democratic forum represents the views and interests of a diverse group of member physicians from more than 170 societies. These delegates meet twice per year to establish policies on health; medical, professional, and governance matters; and the principles within which the AMA’s business activities are conducted.
During the COVID-19 pandemic, the AMA has been the leading physician and patient ally—voicing recommendations to key Congressional leaders and agency staff, state policymakers, and private sector stakeholders. Acting on both federal and state levels, examples of AMA’s recent efforts include actions in financial relief, telehealth, testing and vaccine development, health equity, and more.
CHEST is an active member, and through the HOD and Specialty and Service Society (SSS), CHEST can partner with AMA other societies to support each other on important regulatory issues. CHEST/Allergy Section Council (participants at this meeting were from the AAAAI, AAOA, AASM, ACAAI, ATS, CHEST, and SCCM) met before voting in the House to discuss pending business. The meeting was hosted by the current CHEST/Allergy council chair Dr. Wesley Vander Ark (AMA Delegate AAOA) and Jami Lucas, CEO AAOA.
Policy and resolutions
Overview of the process
Policies originate via resolutions submitted by individuals or societies. These resolutions then go to one of several Reference Committees for open discussion. These committees then report their recommendations back to the HOD, which then discusses and votes on the recommendations. In some instances, the question is referred for further studies by one of several Councils, which reports go to the Board of Trustees or back to the House. Details can be found in the April 2018 CHEST Physician® article on the process. (https://tinyurl.com/yacysxar).
This year, due to the virtual nature, prioritization matrix was utilized and based on urgency. Resolutions were divided into top priority, priority, medium priority, low priority, and not a priority.
The following reference committees convened at this Special Meeting Constitution & Bylaws, Medical Service, Legislation Medical Education, Public Health, Science and Technology, Finance and Medical Practice.
Some of the issues discussed at the House of Delegates are as follows:
Medical education
Continuing board certification (Adapted as a new policy)
The policy states that American Medical Association (AMA), through its Council on Medical Education, continue to work with the American Board of Medical Specialties (ABMS) and ABMS member boards to implement key recommendations outlined by the Continuing Board Certification: Vision for the Future Commission in its final report, including the development of new, integrated standards for continuing certification programs by 2020 that will address the Commission’s recommendations for flexibility in knowledge assessment and advancing practice, feedback to diplomates, and consistency.
Graduate medical education and the corporate practice of medicine (modified existing policy)
The existing policy was amended to urge AMA to continue to monitor issues, including waiver of due process requirements, created by corporate-owned graduate medical education sites.
Public health
Bullying in the Practice of Medicine
Health-care organizations, including academic medical centers, should establish policies to prevent and address bullying in their workplaces. An effective workplace policy should:
• Describe the management’s commitment to providing a safe and healthy workplace.
• Show the staff that their leaders are concerned about bullying and unprofessional behavior and that they take it seriously.
• Clearly define workplace violence, harassment, and bullying, specifically including intimidation, threats, and other forms of aggressive behavior.
• Specify to whom the policy applies (ie, medical staff, students, administration, patients, employees, contractors, vendors, etc).
• Define both expected and prohibited behaviors.
• Outline steps for individuals to take when they feel they are a victim of workplace bullying.
• Provide contact information for a confidential means for documenting and reporting incidents.
• Prohibit retaliation and ensure privacy and confidentiality.
• Document training requirements and establish clear expectations about the training objectives.
Availability of personal protective equipment (PPE)
That our American Medical Association actively support that physicians and health-care professionals are empowered to use workplace modifications to continue professional patient care when they determine such action to be appropriate and in the best interest of patient and physician wellbeing. Physicians and health-care professionals must be permitted to use their professional judgment and augment institution-provided PPE with additional, appropriately decontaminated, personally provided personal protective equipment (PPE) without penalty (Directive to Take Action); and be it further that AMA affirm that the medical staff of each healt-care institution should integrally be involved in disaster planning, strategy, and tactical management of ongoing crises (New HOD Policy).
AMA governance and finance
The establishment of private practice physicians’ section was approved.
Medical practice
Merit-based incentive payment system (MIPS)
That our American Medical Association (AMA) support legislation that ensures Medicare physician payment is sufficient to safeguard beneficiary access to care, replaces or supplements budget neutrality in MIPS with incentive payments, or implements positive annual physician payment updates. (Directive to Take Action).
Establishing professional services claims-based payment enhancement for activities associated with the COVID-19 pandemic
American Medical Association work with other interested parties to advocate for regulatory action on the part of the Centers for Medicare & Medicaid Services to implement a professional services claims-based payment enhancement to help recognize the enhanced, nonseparately reimbursable work performed by physicians during the COVID-19 Public Health Emergency. (Directive to Take Action).
This is just a small sampling of the activities and more information, including reports from the various Councils, are available on the AMA website, http://ama-assn.org.
CHEST members interested in the AMA policy-making process may observe any AMA-HOD meeting or participate in the AMA’s democratic processes. Attendees will also be able to increase their knowledge and skills at no cost. They will also be able to connect with more than 1,500 peers and other meeting attendees from across the country. CHEST members with the time (there are two 5-day meetings each year) and interest are invited to apply to be an official CHEST delegate to the AMA. Contact Jennifer Nemkovich at jnemkovich@chestnet.org for details.
Dr. Desai is with the Chicago Chest Center and AMITA Health Suburban Lung Associates; and the Division of Pulmonary, Critical Care, Sleep and Allergy, University of Illinois at Chicago. He is also the CHEST Delegate to the AMA House of Delegates.
Meet the new members of the CHEST Physician® Editorial Board
We’re happy to introduce these new board members whose primary responsibility is the active review each month of potential articles for publication that could have an impact on or be of interest to our health-care professional readership.
Carolyn M. D’Ambrosio, MD, FCCP, is the Program Director for the Harvard-Brigham and Women’s Hospital Fellowship in Pulmonary and Critical Care Medicine and is Associate Professor of Medicine at Harvard Medical School. Most recently, she was awarded the Pillar Award for Educational Program Leadership, the top award for program directors throughout the Mass General Brigham institutions. In addition to teaching and clinical work, Dr. D’Ambrosio has conducted research on sleep and menopause, sleep and breathing in infants, and participated as the sleep medicine expert in two systemic reviews on home sleep apnea testing and fixed vs auto-titrating CPAP. She continues her work in Medical Ethics as a Senior Ethics Consultant at Brigham and Women’s Hospital.
Jonathan (Jona) Ludmir, MD, FCCP
After completing internal medicine/pediatrics, cardiology, and critical care training, Dr. Ludmir joined the Massachusetts General Hospital staff as a cardiac intensivist and noninvasive cardiologist. His clinical focus is in the heart center ICU, the echocardiography lab, as well as in outpatient cardiology. Additionally, he is the lead physician for the Family-Centered Care Initiative, where he focuses on incorporating evidence-based guidelines and leads in the science of family-centered cardiovascular care delivery. Dr. Ludmir’s research focuses on identifying and addressing psychological symptoms in the ICU, optimizing ICU communication, and enhancing delivery of family-centered care.
Abbie Begnaud, MD, FCCP
Dr. Begnaud hails from south Louisiana and reveals that she attended her first CHEST Annual Meeting in 2011 in Hawaii, and she was “instantly hooked.” Clinically, she practices general pulmonology, critical care, and interventional pulmonology and focuses her research on lung cancer screening and health disparities. She has been on faculty at the University of Minnesota since 2013 and is passionate about lung cancer, health equity, and mentoring.
Shyam Subramanian, MD , FCCP
Dr. Subramanian is currently the Section Chief for Specialty Clinics and the Division Chief for Pulmonary/Critical Care and Sleep Medicine at Sutter Gould Medical Foundation, Tracy, California.
He previously was Systems Director at Baylor College of Medicine in Houston and Section Chief at Case Western Reserve University in Cleveland. Dr. Subramanian currently serves as Chair for the CHEST Clinical Pulmonary NetWork and has previously served as Chair of the Practice Operations NetWork. He is a member of the Executive Committee of the Council of NetWorks and the Scientific Program Committee for the CHEST Annual Meeting.
Mary Jo S. Farmer, MD, PhD, FCCP
Dr. Farmer is a pulmonary, critical care, and sleep medicine physician at Baystate Medical Center (Springfield, MA); Assistant Professor of Medicine University at Massachusetts Medical School – Baystate; and adjunct faculty Tufts University School of Medicine. Dr. Farmer serves as director of pulmonary hypertension services for the Pulmonary & Critical Care Division. Pulmonary vascular disease, interprofessional education, clinical trials research, endobronchial ultrasound, and medical student, resident, and fellow education are her major interests. She is a member of the CHEST Interprofessional NetWork and Clinical Pulmonary NetWork.
We’re happy to introduce these new board members whose primary responsibility is the active review each month of potential articles for publication that could have an impact on or be of interest to our health-care professional readership.
Carolyn M. D’Ambrosio, MD, FCCP, is the Program Director for the Harvard-Brigham and Women’s Hospital Fellowship in Pulmonary and Critical Care Medicine and is Associate Professor of Medicine at Harvard Medical School. Most recently, she was awarded the Pillar Award for Educational Program Leadership, the top award for program directors throughout the Mass General Brigham institutions. In addition to teaching and clinical work, Dr. D’Ambrosio has conducted research on sleep and menopause, sleep and breathing in infants, and participated as the sleep medicine expert in two systemic reviews on home sleep apnea testing and fixed vs auto-titrating CPAP. She continues her work in Medical Ethics as a Senior Ethics Consultant at Brigham and Women’s Hospital.
Jonathan (Jona) Ludmir, MD, FCCP
After completing internal medicine/pediatrics, cardiology, and critical care training, Dr. Ludmir joined the Massachusetts General Hospital staff as a cardiac intensivist and noninvasive cardiologist. His clinical focus is in the heart center ICU, the echocardiography lab, as well as in outpatient cardiology. Additionally, he is the lead physician for the Family-Centered Care Initiative, where he focuses on incorporating evidence-based guidelines and leads in the science of family-centered cardiovascular care delivery. Dr. Ludmir’s research focuses on identifying and addressing psychological symptoms in the ICU, optimizing ICU communication, and enhancing delivery of family-centered care.
Abbie Begnaud, MD, FCCP
Dr. Begnaud hails from south Louisiana and reveals that she attended her first CHEST Annual Meeting in 2011 in Hawaii, and she was “instantly hooked.” Clinically, she practices general pulmonology, critical care, and interventional pulmonology and focuses her research on lung cancer screening and health disparities. She has been on faculty at the University of Minnesota since 2013 and is passionate about lung cancer, health equity, and mentoring.
Shyam Subramanian, MD , FCCP
Dr. Subramanian is currently the Section Chief for Specialty Clinics and the Division Chief for Pulmonary/Critical Care and Sleep Medicine at Sutter Gould Medical Foundation, Tracy, California.
He previously was Systems Director at Baylor College of Medicine in Houston and Section Chief at Case Western Reserve University in Cleveland. Dr. Subramanian currently serves as Chair for the CHEST Clinical Pulmonary NetWork and has previously served as Chair of the Practice Operations NetWork. He is a member of the Executive Committee of the Council of NetWorks and the Scientific Program Committee for the CHEST Annual Meeting.
Mary Jo S. Farmer, MD, PhD, FCCP
Dr. Farmer is a pulmonary, critical care, and sleep medicine physician at Baystate Medical Center (Springfield, MA); Assistant Professor of Medicine University at Massachusetts Medical School – Baystate; and adjunct faculty Tufts University School of Medicine. Dr. Farmer serves as director of pulmonary hypertension services for the Pulmonary & Critical Care Division. Pulmonary vascular disease, interprofessional education, clinical trials research, endobronchial ultrasound, and medical student, resident, and fellow education are her major interests. She is a member of the CHEST Interprofessional NetWork and Clinical Pulmonary NetWork.
We’re happy to introduce these new board members whose primary responsibility is the active review each month of potential articles for publication that could have an impact on or be of interest to our health-care professional readership.
Carolyn M. D’Ambrosio, MD, FCCP, is the Program Director for the Harvard-Brigham and Women’s Hospital Fellowship in Pulmonary and Critical Care Medicine and is Associate Professor of Medicine at Harvard Medical School. Most recently, she was awarded the Pillar Award for Educational Program Leadership, the top award for program directors throughout the Mass General Brigham institutions. In addition to teaching and clinical work, Dr. D’Ambrosio has conducted research on sleep and menopause, sleep and breathing in infants, and participated as the sleep medicine expert in two systemic reviews on home sleep apnea testing and fixed vs auto-titrating CPAP. She continues her work in Medical Ethics as a Senior Ethics Consultant at Brigham and Women’s Hospital.
Jonathan (Jona) Ludmir, MD, FCCP
After completing internal medicine/pediatrics, cardiology, and critical care training, Dr. Ludmir joined the Massachusetts General Hospital staff as a cardiac intensivist and noninvasive cardiologist. His clinical focus is in the heart center ICU, the echocardiography lab, as well as in outpatient cardiology. Additionally, he is the lead physician for the Family-Centered Care Initiative, where he focuses on incorporating evidence-based guidelines and leads in the science of family-centered cardiovascular care delivery. Dr. Ludmir’s research focuses on identifying and addressing psychological symptoms in the ICU, optimizing ICU communication, and enhancing delivery of family-centered care.
Abbie Begnaud, MD, FCCP
Dr. Begnaud hails from south Louisiana and reveals that she attended her first CHEST Annual Meeting in 2011 in Hawaii, and she was “instantly hooked.” Clinically, she practices general pulmonology, critical care, and interventional pulmonology and focuses her research on lung cancer screening and health disparities. She has been on faculty at the University of Minnesota since 2013 and is passionate about lung cancer, health equity, and mentoring.
Shyam Subramanian, MD , FCCP
Dr. Subramanian is currently the Section Chief for Specialty Clinics and the Division Chief for Pulmonary/Critical Care and Sleep Medicine at Sutter Gould Medical Foundation, Tracy, California.
He previously was Systems Director at Baylor College of Medicine in Houston and Section Chief at Case Western Reserve University in Cleveland. Dr. Subramanian currently serves as Chair for the CHEST Clinical Pulmonary NetWork and has previously served as Chair of the Practice Operations NetWork. He is a member of the Executive Committee of the Council of NetWorks and the Scientific Program Committee for the CHEST Annual Meeting.
Mary Jo S. Farmer, MD, PhD, FCCP
Dr. Farmer is a pulmonary, critical care, and sleep medicine physician at Baystate Medical Center (Springfield, MA); Assistant Professor of Medicine University at Massachusetts Medical School – Baystate; and adjunct faculty Tufts University School of Medicine. Dr. Farmer serves as director of pulmonary hypertension services for the Pulmonary & Critical Care Division. Pulmonary vascular disease, interprofessional education, clinical trials research, endobronchial ultrasound, and medical student, resident, and fellow education are her major interests. She is a member of the CHEST Interprofessional NetWork and Clinical Pulmonary NetWork.
How the Foundation’s virtual listening tour aims to help patients like James
Constance Baker was juggling the dual stresses of mothering a newborn and raising a teenager when she noticed a skin patch on her father looked discolored. His breathing soon became labored, and the skin on his hands turned calloused. Then he passed out. Initially, doctors thought his problems were cardiovascular.
Since James didn’t have a primary doctor, Constance repeatedly took him to the emergency room to receive care. His frequent visits attracted the attention of a medical intern who ordered tests and asked James to see a specialist. More than half a year later, Constance and James met pulmonologist Dr. Demondes Haynes and learned the cause of James’ troubled breathing. James has a rare disease called scleroderma, which hardens patches of skin and created scarring of his lung tissue. He also had pulmonary hypertension. James needed rapid intervention with a complicated regimen of medication.
At first, James didn’t want to go along with the program, but Dr. Haynes’ attentive and gentle nature changed his mind. “Dr. Haynes always made us comfortable, taking the time to listen and show us his concern. He even explained that we wouldn’t have to worry about paying for anything, which was a huge relief.”
Before Dr. Haynes, James and Constance had never met a doctor who didn’t treat them like a case file. “He actually acknowledged our circumstances, which meant he acknowledged us.”
As a native Mississippian, Dr. Haynes knows the plight of many of his patients. “Not everyone with lung disease can access a pulmonologist, like me, and not everyone can afford appropriate treatment. You have to recognize these disparities in order to build a relationship of trust with your patients.”
James was ready to start treatment with Dr. Haynes’ guidance, but since he couldn’t read, he couldn’t understand how to put the medication together. That’s when Constance had to step up. They worked together to change and clean the tubing to the port by his heart and make his medication. “We leaned on each other a lot during that time, and you know what? We made it through.”
Even though James’ disease can be debilitating at times, and his care can seem completely overwhelming, Constance wouldn’t have it any other way. “It’s always been my father and I, just us two. He’s always taken care of me, and now it’s my turn to take care of him.”
Unfortunately, Constance and James’ story is not unique. So many patients don’t have access to doctors, specialists, and caregivers, and many aren’t empowered enough to take
their medications. These stories don’t get posted on Instagram and they don’t make the evening news. Underprivileged and underserved patients have been left behind – left without a voice.
That’s why the foundation launched its virtual listening tours across America in September. Our tours give patients, caregivers, and physicians the opportunity to raise issues that they believe are impacting health care in their communities.
How can physicians work to understand their patients better? How can patients learn to trust their providers? These are all the questions we aim to answer.
James is doing as well as he is because of his relationship with Dr. Haynes. What can we do with that information? We can listen, we can learn, and we can spread the word.
Read more about the work of the CHEST Foundation in its 2020 Impact Report at chestfoundation.org.
Constance Baker was juggling the dual stresses of mothering a newborn and raising a teenager when she noticed a skin patch on her father looked discolored. His breathing soon became labored, and the skin on his hands turned calloused. Then he passed out. Initially, doctors thought his problems were cardiovascular.
Since James didn’t have a primary doctor, Constance repeatedly took him to the emergency room to receive care. His frequent visits attracted the attention of a medical intern who ordered tests and asked James to see a specialist. More than half a year later, Constance and James met pulmonologist Dr. Demondes Haynes and learned the cause of James’ troubled breathing. James has a rare disease called scleroderma, which hardens patches of skin and created scarring of his lung tissue. He also had pulmonary hypertension. James needed rapid intervention with a complicated regimen of medication.
At first, James didn’t want to go along with the program, but Dr. Haynes’ attentive and gentle nature changed his mind. “Dr. Haynes always made us comfortable, taking the time to listen and show us his concern. He even explained that we wouldn’t have to worry about paying for anything, which was a huge relief.”
Before Dr. Haynes, James and Constance had never met a doctor who didn’t treat them like a case file. “He actually acknowledged our circumstances, which meant he acknowledged us.”
As a native Mississippian, Dr. Haynes knows the plight of many of his patients. “Not everyone with lung disease can access a pulmonologist, like me, and not everyone can afford appropriate treatment. You have to recognize these disparities in order to build a relationship of trust with your patients.”
James was ready to start treatment with Dr. Haynes’ guidance, but since he couldn’t read, he couldn’t understand how to put the medication together. That’s when Constance had to step up. They worked together to change and clean the tubing to the port by his heart and make his medication. “We leaned on each other a lot during that time, and you know what? We made it through.”
Even though James’ disease can be debilitating at times, and his care can seem completely overwhelming, Constance wouldn’t have it any other way. “It’s always been my father and I, just us two. He’s always taken care of me, and now it’s my turn to take care of him.”
Unfortunately, Constance and James’ story is not unique. So many patients don’t have access to doctors, specialists, and caregivers, and many aren’t empowered enough to take
their medications. These stories don’t get posted on Instagram and they don’t make the evening news. Underprivileged and underserved patients have been left behind – left without a voice.
That’s why the foundation launched its virtual listening tours across America in September. Our tours give patients, caregivers, and physicians the opportunity to raise issues that they believe are impacting health care in their communities.
How can physicians work to understand their patients better? How can patients learn to trust their providers? These are all the questions we aim to answer.
James is doing as well as he is because of his relationship with Dr. Haynes. What can we do with that information? We can listen, we can learn, and we can spread the word.
Read more about the work of the CHEST Foundation in its 2020 Impact Report at chestfoundation.org.
Constance Baker was juggling the dual stresses of mothering a newborn and raising a teenager when she noticed a skin patch on her father looked discolored. His breathing soon became labored, and the skin on his hands turned calloused. Then he passed out. Initially, doctors thought his problems were cardiovascular.
Since James didn’t have a primary doctor, Constance repeatedly took him to the emergency room to receive care. His frequent visits attracted the attention of a medical intern who ordered tests and asked James to see a specialist. More than half a year later, Constance and James met pulmonologist Dr. Demondes Haynes and learned the cause of James’ troubled breathing. James has a rare disease called scleroderma, which hardens patches of skin and created scarring of his lung tissue. He also had pulmonary hypertension. James needed rapid intervention with a complicated regimen of medication.
At first, James didn’t want to go along with the program, but Dr. Haynes’ attentive and gentle nature changed his mind. “Dr. Haynes always made us comfortable, taking the time to listen and show us his concern. He even explained that we wouldn’t have to worry about paying for anything, which was a huge relief.”
Before Dr. Haynes, James and Constance had never met a doctor who didn’t treat them like a case file. “He actually acknowledged our circumstances, which meant he acknowledged us.”
As a native Mississippian, Dr. Haynes knows the plight of many of his patients. “Not everyone with lung disease can access a pulmonologist, like me, and not everyone can afford appropriate treatment. You have to recognize these disparities in order to build a relationship of trust with your patients.”
James was ready to start treatment with Dr. Haynes’ guidance, but since he couldn’t read, he couldn’t understand how to put the medication together. That’s when Constance had to step up. They worked together to change and clean the tubing to the port by his heart and make his medication. “We leaned on each other a lot during that time, and you know what? We made it through.”
Even though James’ disease can be debilitating at times, and his care can seem completely overwhelming, Constance wouldn’t have it any other way. “It’s always been my father and I, just us two. He’s always taken care of me, and now it’s my turn to take care of him.”
Unfortunately, Constance and James’ story is not unique. So many patients don’t have access to doctors, specialists, and caregivers, and many aren’t empowered enough to take
their medications. These stories don’t get posted on Instagram and they don’t make the evening news. Underprivileged and underserved patients have been left behind – left without a voice.
That’s why the foundation launched its virtual listening tours across America in September. Our tours give patients, caregivers, and physicians the opportunity to raise issues that they believe are impacting health care in their communities.
How can physicians work to understand their patients better? How can patients learn to trust their providers? These are all the questions we aim to answer.
James is doing as well as he is because of his relationship with Dr. Haynes. What can we do with that information? We can listen, we can learn, and we can spread the word.
Read more about the work of the CHEST Foundation in its 2020 Impact Report at chestfoundation.org.
This month in CHEST
Editor’s picks
Original Research
A behaviour change intervention aimed at increasing physical activity improves clinical control in adults with asthma: a randomised controlled trial. By Dr. C. Carvalho, et al.
Critically ill adults with COVID-19 in New Orleans and care with an evidence-based protocol. By Dr. D. Janz, et al.
Mortality trends of idiopathic pulmonary fibrosis in the United States from 2004 to 2017.By Dr. N. Jeganathan, et al.
United States Pulmonary Hypertension Scientific Registry (USPHSR): Baseline characteristics. By Dr. J. Badlam, et al.
CHEST Review
Pulmonary exacerbations in adults with cystic fibrosis: A grown-up issue in a changing CF landscape. By Dr. G. Stanford, et al.
Computed tomography imaging and comorbidities in chronic obstructive pulmonary disease: Beyond lung cancer screening. By Dr. J. Bon, et al.
How I Do It
The PERT concept: A step-by-step approach to managing PE. By Dr. B. Rivera-Lebron, et al.
Special Feature
A brief overview of the national outbreak of e-cigarette, or vaping, product use-associated lung injury (EVALI) and the primary causes. By Dr. E. Kiernan, et al.
Editor’s picks
Editor’s picks
Original Research
A behaviour change intervention aimed at increasing physical activity improves clinical control in adults with asthma: a randomised controlled trial. By Dr. C. Carvalho, et al.
Critically ill adults with COVID-19 in New Orleans and care with an evidence-based protocol. By Dr. D. Janz, et al.
Mortality trends of idiopathic pulmonary fibrosis in the United States from 2004 to 2017.By Dr. N. Jeganathan, et al.
United States Pulmonary Hypertension Scientific Registry (USPHSR): Baseline characteristics. By Dr. J. Badlam, et al.
CHEST Review
Pulmonary exacerbations in adults with cystic fibrosis: A grown-up issue in a changing CF landscape. By Dr. G. Stanford, et al.
Computed tomography imaging and comorbidities in chronic obstructive pulmonary disease: Beyond lung cancer screening. By Dr. J. Bon, et al.
How I Do It
The PERT concept: A step-by-step approach to managing PE. By Dr. B. Rivera-Lebron, et al.
Special Feature
A brief overview of the national outbreak of e-cigarette, or vaping, product use-associated lung injury (EVALI) and the primary causes. By Dr. E. Kiernan, et al.
Original Research
A behaviour change intervention aimed at increasing physical activity improves clinical control in adults with asthma: a randomised controlled trial. By Dr. C. Carvalho, et al.
Critically ill adults with COVID-19 in New Orleans and care with an evidence-based protocol. By Dr. D. Janz, et al.
Mortality trends of idiopathic pulmonary fibrosis in the United States from 2004 to 2017.By Dr. N. Jeganathan, et al.
United States Pulmonary Hypertension Scientific Registry (USPHSR): Baseline characteristics. By Dr. J. Badlam, et al.
CHEST Review
Pulmonary exacerbations in adults with cystic fibrosis: A grown-up issue in a changing CF landscape. By Dr. G. Stanford, et al.
Computed tomography imaging and comorbidities in chronic obstructive pulmonary disease: Beyond lung cancer screening. By Dr. J. Bon, et al.
How I Do It
The PERT concept: A step-by-step approach to managing PE. By Dr. B. Rivera-Lebron, et al.
Special Feature
A brief overview of the national outbreak of e-cigarette, or vaping, product use-associated lung injury (EVALI) and the primary causes. By Dr. E. Kiernan, et al.
Cardiovascular Medicine and Surgery
Cardiovascular Medicine and Surgery
Use of hepatitis C donors in thoracic organ transplantation: Reportedly associated with increased risk of rejection
Mark Jay Zucker, MD, JD, FCCP
Vice-Chair
Transplanting organs from hepatitis C (HCV) antibody and/or antigen-positive donors is associated with a greater than 8%-90% likelihood that the recipient will acquire the infection. Several studies reported that if HCV conversion happened, the outcomes in both heart and lung recipients were worse, even if treated with interferon/ribavirin (Haji SA, et al J Heart Lung Transplant. 2004;23:277; Wang BY, et al. Ann Thorac Surg. 2010 May;89[5]:1645; Carreno MC, et al. J Heart Lung Transplant. 2001;20(2):224). Thus, despite the shortage of thoracic organ donors and high wait-list mortality, the practice was strongly discouraged.
In 2016, the successful use of a direct-acting antiviral (DAA) for 12 weeks to eliminate HCV in a lung transplant recipient of a seropositive organ was published (Khan B, et al. Am J Transplant. 2017;17:1129). Two years later, the outcomes of seronegative heart (n=8) or lung (n=36) transplant recipients receiving organs from seropositive donors were presented (Woolley AE, et al. N Engl J Med. 2019;380:1606). Forty-two of the patients had viremia within days of the operation. All patients were treated with 4 weeks of a DAA and, of the 35 patients available for 6-month analysis, viral load was undetectable in all. Of concern, however—more cellular rejection requiring treatment was seen in the lung recipients of HCV+ donors compared with recipients of HCV- donors. The difference was not statistically significant.
The largest analysis of the safety of HCV+ donors in HCV- thoracic organ transplant recipients involved 343 heart transplant recipients (Kilic A, et al. J Am Heart Assoc. 2020;9(2):e014495). No differences were noted in outcomes, strokes, need for dialysis, or incidence of treated rejection during the first year. However, the observation regarding rejection was not subsequently confirmed by the NYU team (Gidea CG, et al. J Heart Lung Transplant. 2020;39:1199). Of 22 HCV- recipients of an HCV donor with viremia, the rate of rejection was 64% vs 18% in 28 patients receiving a donor without viremia (through day 180 (P=.001)).
In summary, the ability of DAAs to render 97%-99% of immunosuppressed transplant recipients HCV seronegative has transformed the landscape and HCV viremia in the donor (or recipient) and is no longer an absolute contraindication to transplantation. However, more information is needed as to whether there is an increased incidence of rejection.
Cardiovascular Medicine and Surgery
Use of hepatitis C donors in thoracic organ transplantation: Reportedly associated with increased risk of rejection
Mark Jay Zucker, MD, JD, FCCP
Vice-Chair
Transplanting organs from hepatitis C (HCV) antibody and/or antigen-positive donors is associated with a greater than 8%-90% likelihood that the recipient will acquire the infection. Several studies reported that if HCV conversion happened, the outcomes in both heart and lung recipients were worse, even if treated with interferon/ribavirin (Haji SA, et al J Heart Lung Transplant. 2004;23:277; Wang BY, et al. Ann Thorac Surg. 2010 May;89[5]:1645; Carreno MC, et al. J Heart Lung Transplant. 2001;20(2):224). Thus, despite the shortage of thoracic organ donors and high wait-list mortality, the practice was strongly discouraged.
In 2016, the successful use of a direct-acting antiviral (DAA) for 12 weeks to eliminate HCV in a lung transplant recipient of a seropositive organ was published (Khan B, et al. Am J Transplant. 2017;17:1129). Two years later, the outcomes of seronegative heart (n=8) or lung (n=36) transplant recipients receiving organs from seropositive donors were presented (Woolley AE, et al. N Engl J Med. 2019;380:1606). Forty-two of the patients had viremia within days of the operation. All patients were treated with 4 weeks of a DAA and, of the 35 patients available for 6-month analysis, viral load was undetectable in all. Of concern, however—more cellular rejection requiring treatment was seen in the lung recipients of HCV+ donors compared with recipients of HCV- donors. The difference was not statistically significant.
The largest analysis of the safety of HCV+ donors in HCV- thoracic organ transplant recipients involved 343 heart transplant recipients (Kilic A, et al. J Am Heart Assoc. 2020;9(2):e014495). No differences were noted in outcomes, strokes, need for dialysis, or incidence of treated rejection during the first year. However, the observation regarding rejection was not subsequently confirmed by the NYU team (Gidea CG, et al. J Heart Lung Transplant. 2020;39:1199). Of 22 HCV- recipients of an HCV donor with viremia, the rate of rejection was 64% vs 18% in 28 patients receiving a donor without viremia (through day 180 (P=.001)).
In summary, the ability of DAAs to render 97%-99% of immunosuppressed transplant recipients HCV seronegative has transformed the landscape and HCV viremia in the donor (or recipient) and is no longer an absolute contraindication to transplantation. However, more information is needed as to whether there is an increased incidence of rejection.
Cardiovascular Medicine and Surgery
Use of hepatitis C donors in thoracic organ transplantation: Reportedly associated with increased risk of rejection
Mark Jay Zucker, MD, JD, FCCP
Vice-Chair
Transplanting organs from hepatitis C (HCV) antibody and/or antigen-positive donors is associated with a greater than 8%-90% likelihood that the recipient will acquire the infection. Several studies reported that if HCV conversion happened, the outcomes in both heart and lung recipients were worse, even if treated with interferon/ribavirin (Haji SA, et al J Heart Lung Transplant. 2004;23:277; Wang BY, et al. Ann Thorac Surg. 2010 May;89[5]:1645; Carreno MC, et al. J Heart Lung Transplant. 2001;20(2):224). Thus, despite the shortage of thoracic organ donors and high wait-list mortality, the practice was strongly discouraged.
In 2016, the successful use of a direct-acting antiviral (DAA) for 12 weeks to eliminate HCV in a lung transplant recipient of a seropositive organ was published (Khan B, et al. Am J Transplant. 2017;17:1129). Two years later, the outcomes of seronegative heart (n=8) or lung (n=36) transplant recipients receiving organs from seropositive donors were presented (Woolley AE, et al. N Engl J Med. 2019;380:1606). Forty-two of the patients had viremia within days of the operation. All patients were treated with 4 weeks of a DAA and, of the 35 patients available for 6-month analysis, viral load was undetectable in all. Of concern, however—more cellular rejection requiring treatment was seen in the lung recipients of HCV+ donors compared with recipients of HCV- donors. The difference was not statistically significant.
The largest analysis of the safety of HCV+ donors in HCV- thoracic organ transplant recipients involved 343 heart transplant recipients (Kilic A, et al. J Am Heart Assoc. 2020;9(2):e014495). No differences were noted in outcomes, strokes, need for dialysis, or incidence of treated rejection during the first year. However, the observation regarding rejection was not subsequently confirmed by the NYU team (Gidea CG, et al. J Heart Lung Transplant. 2020;39:1199). Of 22 HCV- recipients of an HCV donor with viremia, the rate of rejection was 64% vs 18% in 28 patients receiving a donor without viremia (through day 180 (P=.001)).
In summary, the ability of DAAs to render 97%-99% of immunosuppressed transplant recipients HCV seronegative has transformed the landscape and HCV viremia in the donor (or recipient) and is no longer an absolute contraindication to transplantation. However, more information is needed as to whether there is an increased incidence of rejection.
Finding meaning in ‘Lean’?
Using systems improvement strategies to support the Quadruple Aim
General background on well-being and burnout
With burnout increasingly recognized as a shared responsibility that requires addressing organizational drivers while supporting individuals to be well,1-4 practical strategies and examples of successful implementation of systems interventions to address burnout will be helpful for service directors to support their staff. The Charter on Physician Well-being, recently developed through collaborative input from multiple organizations, defines guiding principles and key commitments at the societal, organizational, interpersonal, and individual levels and may be a useful framework for organizations that are developing well-being initiatives.5
The charter advocates including physician well-being as a quality improvement metric for health systems, aligned with the concept of the Quadruple Aim of optimizing patient care by enhancing provider experience, promoting high-value care, and improving population health.6 Identifying areas of alignment between the charter’s recommendations and systems improvement strategies that seek to optimize efficiency and reduce waste, such as Lean Management, may help physician leaders to contextualize well-being initiatives more easily within ongoing systems improvement efforts. In this perspective, we provide one division’s experience using the Charter to assess successes and identify additional areas of improvement for well-being initiatives developed using Lean Management methodology.
Past and current state of affairs
In 2011, the division of hospital medicine at Zuckerberg San Francisco General Hospital was established and has seen continual expansion in terms of direct patient care, medical education, and hospital leadership.
In 2015, the division of hospital medicine experienced leadership transitions, faculty attrition, and insufficient recruitment resulting in staffing shortages, service line closure, schedule instability, and ultimately, low morale. A baseline survey conducted using the 2-Item Maslach Burnout Inventory. This survey, which uses one item in the domain of emotional exhaustion and one item in the domain of depersonalization, has shown good correlation with the full Maslach Burnout Inventory.7 At baseline, approximately one-third of the division’s physicians experienced burnout.
In response, a subsequent retreat focused on the three greatest areas of concern identified by the survey: scheduling, faculty development, and well-being.
Like many health systems, the hospital has adopted Lean as its preferred systems-improvement framework. The retreat was structured around the principles of Lean philosophy, and was designed to emulate that of a consolidated Kaizen workshop.
“Kaizen” in Japanese means “change for the better.” A typical Kaizen workshop revolves around rapid problem-solving over the course of 3-5 days, in which a team of people come together to identify and implement significant improvements for a selected process. To this end, the retreat was divided into subgroups for each area of concern. In turn, each subgroup mapped out existing workflows (“value stream”), identified areas of waste and non–value added time, and generated ideas of what an idealized process would be. Next, a root-cause analysis was performed and subsequent interventions (“countermeasures”) developed to address each problem. At the conclusion of the retreat, each subgroup shared a summary of their findings with the larger group.
Moving forward, this information served as a guiding framework for service and division leadership to run small tests of change. We enacted a series of countermeasures over the course of several years, and multiple cycles of improvement work addressed the three areas of concern. We developed an A3 report (a Lean project management tool that incorporates the plan-do-study-act cycle, organizes strategic efforts, and tracks progress on a single page) to summarize and present these initiatives to the Performance Improvement and Patient Safety Committee of the hospital executive leadership team. This structure illustrated alignment with the hospital’s core values (“true north”) of “developing people” and “care experience.”
In 2018, interval surveys demonstrated a gradual reduction of burnout to approximately one-fifth of division physicians as measured by the 2-item Maslach Burnout Inventory.
Initiatives in faculty well-being
The Charter of Physician Well-being outlines a framework to promote well-being among doctors by maximizing a sense of fulfillment and minimizing the harms of burnout. It shares this responsibility among societal, organizational, and interpersonal and individual commitments.5
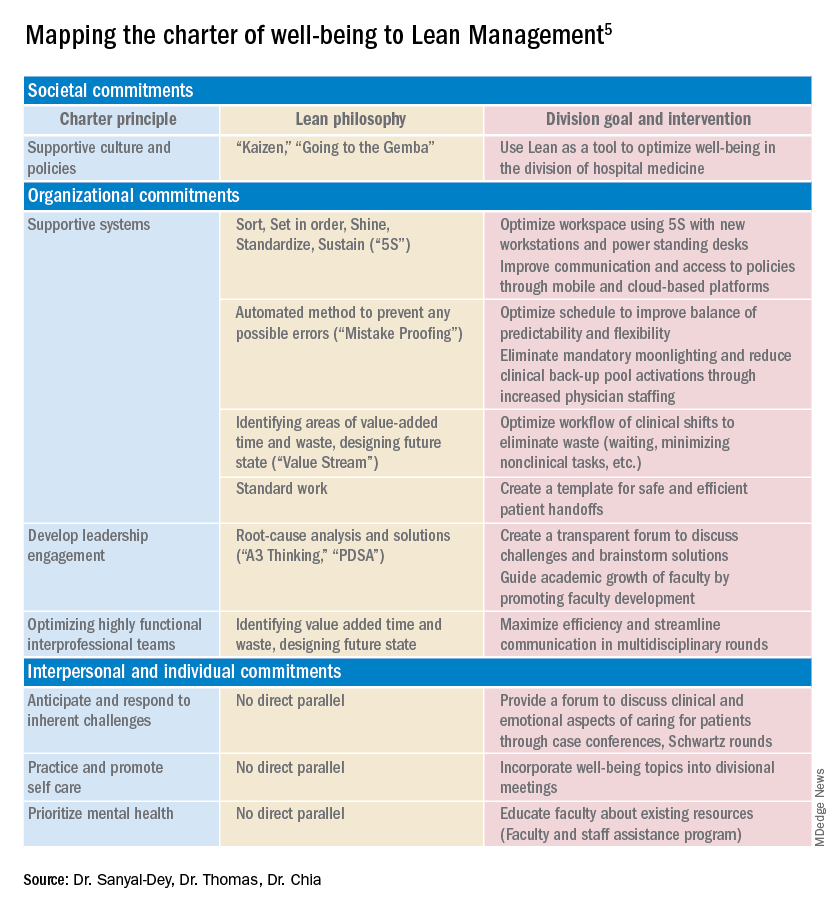
As illustrated above, we used principles of Lean Management to prospectively create initiatives to improve well-being in our division. Lean in health care is designed to optimize primarily the patient experience; its implementation has subsequently demonstrated mixed provider and staff experiences,8,9 and many providers are skeptical of Lean’s potential to improve their own well-being. If, however, Lean is aligned with best practice frameworks for well-being such as those outline in the charter, it may also help to meet the Quadruple Aim of optimizing both provider well-being and patient experience. To further test this hypothesis, we retrospectively categorized our Lean-based interventions into the commitments described by the charter to identify areas of alignment and gaps that were not initially addressed using Lean Management (Table).
Organizational commitments5Supportive systems
We optimized scheduling and enhanced physician staffing by budgeting for a physician staffing buffer each academic year in order to minimize mandatory moonlighting and jeopardy pool activations that result from operating on a thin staffing margin when expected personal leave and reductions in clinical effort occur. Furthermore, we revised scheduling principles to balance patient continuity and individual time off requests while setting limits on the maximum duration of clinical stretches and instituting mandatory minimum time off between them.
Leadership engagement
We initiated monthly operations meetings as a forum to discuss challenges, brainstorm solutions, and message new initiatives with group input. For example, as a result of these meetings, we designed and implemented an additional service line to address the high census, revised the distribution of new patient admissions to level-load clinical shifts, and established a maximum number of weekends worked per month and year. This approach aligns with recommendations to use participatory leadership strategies to enhance physician well-being.10 Engaging both executive level and service level management to focus on burnout and other related well-being metrics is necessary for sustaining such work.
Interprofessional teamwork
We revised multidisciplinary rounds with social work, utilization management, and physical therapy to maximize efficiency and streamline communication by developing standard approaches for each patient presentation.
Interpersonal and individual commitments5Address emotional challenges of physician work
Although these commitments did not have a direct corollary with Lean philosophy, some of these needs were identified by our physician group at our annual retreats. As a result, we initiated a monthly faculty-led noon conference series focused on the clinical challenges of caring for vulnerable populations, a particular source of distress in our practice setting, and revised the division schedule to encourage attendance at the hospital’s Schwartz rounds.
Mental health and self-care
We organized focus groups and faculty development sessions on provider well-being and burnout and dealing with challenging patients and invited the Faculty and Staff Assistance Program, our institution’s mental health service provider, to our weekly division meeting.
Future directions
After using Lean Management as an approach to prospectively improve physician well-being, we were able to use the Charter on Physician Well-being retrospectively as a “checklist” to identify additional gaps for targeted intervention to ensure all commitments are sufficiently addressed.
Overall, we found that, not surprisingly, Lean Management aligned best with the organizational commitments in the charter. Reviewing the organizational commitments, we found our biggest remaining challenges are in building supportive systems, namely ensuring sustainable workloads, offloading and delegating nonphysician tasks, and minimizing the burden of documentation and administration.
Reviewing the societal commitments helped us to identify opportunities for future directions that we may not have otherwise considered. As a safety-net institution, we benefit from a strong sense of mission and shared values within our hospital and division. However, we recognize the need to continue to be vigilant to ensure that our physicians perceive that their own values are aligned with the division’s stated mission. Devoting a Kaizen-style retreat to well-being likely helped, and allocating divisional resources to a well-being committee indirectly helped, to foster a culture of well-being; however, we could more deliberately identify local policies that may benefit from advocacy or revision. Although our faculty identified interventions to improve interpersonal and individual drivers of well-being, these charter commitments did not have direct parallels in Lean philosophy, and organizations may need to deliberately seek to address these commitments outside of a Lean approach. Specifically, by reviewing the charter, we identified opportunities to provide additional resources for peer support and protected time for mental health care and self-care.
Conclusion
Lean Management can be an effective strategy to address many of the organizational commitments outlined in the Charter on Physician Well-being. This approach may be particularly effective for solving local challenges with systems and workflows. Those who use Lean as a primary method to approach systems improvement in support of the Quadruple Aim may need to use additional strategies to address societal and interpersonal and individual commitments outlined in the charter.
Dr. Sanyal-Dey is visiting associate clinical professor of medicine at Zuckerberg San Francisco General Hospital and director of client services, LeanTaaS. Dr. Thomas is associate clinical professor of medicine at Zuckerberg San Francisco General Hospital. Dr. Chia is associate professor of clinical medicine at Zuckerberg San Francisco General Hospital.
References
1. West CP et al. Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. Lancet. 2016;388(10057):2272-81.
2. Shanafelt TD, Noseworthy JH. Executive leadership and physician: Nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92(1):129-46.
3. Shanafelt T et al. The business case for investing in physician well-being. JAMA Intern Med. 2017;177(12):1826-32.
4. Shanafelt T et al. Building a program on well-being: Key design considerations to meet the unique needs of each organization. Acad Med. 2019 Feb;94(2):156-161.
5. Thomas LR et al. Charter on physician well-being. JAMA. 2018;319(15):1541-42.
6. Bodenheimer T, Sinsky C. From triple to quadruple aim: Care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573-6.
7. West CP et al. Concurrent Validity of Single-Item Measures of Emotional Exhaustion and Depersonalization in Burnout Assessment. J Gen Intern Med. 2012;27(11):1445-52.
8. Hung DY et al. Experiences of primary care physicians and staff following lean workflow redesign. BMC Health Serv Res. 2018 Apr 10;18(1):274.
9. Zibrowski E et al. Easier and faster is not always better: Grounded theory of the impact of large-scale system transformation on the clinical work of emergency medicine nurses and physicians. JMIR Hum Factors. 2018. doi: 10.2196/11013.
10. Shanafelt TD et al. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clin Proc. 2015;90(4):432-40.
Using systems improvement strategies to support the Quadruple Aim
Using systems improvement strategies to support the Quadruple Aim
General background on well-being and burnout
With burnout increasingly recognized as a shared responsibility that requires addressing organizational drivers while supporting individuals to be well,1-4 practical strategies and examples of successful implementation of systems interventions to address burnout will be helpful for service directors to support their staff. The Charter on Physician Well-being, recently developed through collaborative input from multiple organizations, defines guiding principles and key commitments at the societal, organizational, interpersonal, and individual levels and may be a useful framework for organizations that are developing well-being initiatives.5
The charter advocates including physician well-being as a quality improvement metric for health systems, aligned with the concept of the Quadruple Aim of optimizing patient care by enhancing provider experience, promoting high-value care, and improving population health.6 Identifying areas of alignment between the charter’s recommendations and systems improvement strategies that seek to optimize efficiency and reduce waste, such as Lean Management, may help physician leaders to contextualize well-being initiatives more easily within ongoing systems improvement efforts. In this perspective, we provide one division’s experience using the Charter to assess successes and identify additional areas of improvement for well-being initiatives developed using Lean Management methodology.
Past and current state of affairs
In 2011, the division of hospital medicine at Zuckerberg San Francisco General Hospital was established and has seen continual expansion in terms of direct patient care, medical education, and hospital leadership.
In 2015, the division of hospital medicine experienced leadership transitions, faculty attrition, and insufficient recruitment resulting in staffing shortages, service line closure, schedule instability, and ultimately, low morale. A baseline survey conducted using the 2-Item Maslach Burnout Inventory. This survey, which uses one item in the domain of emotional exhaustion and one item in the domain of depersonalization, has shown good correlation with the full Maslach Burnout Inventory.7 At baseline, approximately one-third of the division’s physicians experienced burnout.
In response, a subsequent retreat focused on the three greatest areas of concern identified by the survey: scheduling, faculty development, and well-being.
Like many health systems, the hospital has adopted Lean as its preferred systems-improvement framework. The retreat was structured around the principles of Lean philosophy, and was designed to emulate that of a consolidated Kaizen workshop.
“Kaizen” in Japanese means “change for the better.” A typical Kaizen workshop revolves around rapid problem-solving over the course of 3-5 days, in which a team of people come together to identify and implement significant improvements for a selected process. To this end, the retreat was divided into subgroups for each area of concern. In turn, each subgroup mapped out existing workflows (“value stream”), identified areas of waste and non–value added time, and generated ideas of what an idealized process would be. Next, a root-cause analysis was performed and subsequent interventions (“countermeasures”) developed to address each problem. At the conclusion of the retreat, each subgroup shared a summary of their findings with the larger group.
Moving forward, this information served as a guiding framework for service and division leadership to run small tests of change. We enacted a series of countermeasures over the course of several years, and multiple cycles of improvement work addressed the three areas of concern. We developed an A3 report (a Lean project management tool that incorporates the plan-do-study-act cycle, organizes strategic efforts, and tracks progress on a single page) to summarize and present these initiatives to the Performance Improvement and Patient Safety Committee of the hospital executive leadership team. This structure illustrated alignment with the hospital’s core values (“true north”) of “developing people” and “care experience.”
In 2018, interval surveys demonstrated a gradual reduction of burnout to approximately one-fifth of division physicians as measured by the 2-item Maslach Burnout Inventory.
Initiatives in faculty well-being
The Charter of Physician Well-being outlines a framework to promote well-being among doctors by maximizing a sense of fulfillment and minimizing the harms of burnout. It shares this responsibility among societal, organizational, and interpersonal and individual commitments.5
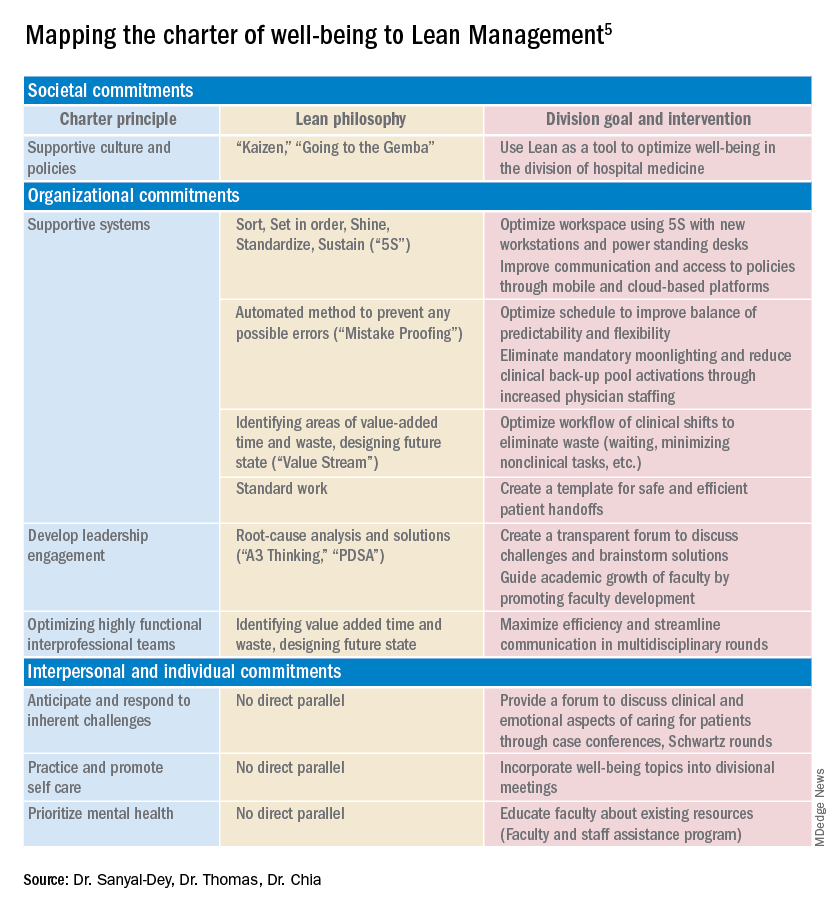
As illustrated above, we used principles of Lean Management to prospectively create initiatives to improve well-being in our division. Lean in health care is designed to optimize primarily the patient experience; its implementation has subsequently demonstrated mixed provider and staff experiences,8,9 and many providers are skeptical of Lean’s potential to improve their own well-being. If, however, Lean is aligned with best practice frameworks for well-being such as those outline in the charter, it may also help to meet the Quadruple Aim of optimizing both provider well-being and patient experience. To further test this hypothesis, we retrospectively categorized our Lean-based interventions into the commitments described by the charter to identify areas of alignment and gaps that were not initially addressed using Lean Management (Table).
Organizational commitments5Supportive systems
We optimized scheduling and enhanced physician staffing by budgeting for a physician staffing buffer each academic year in order to minimize mandatory moonlighting and jeopardy pool activations that result from operating on a thin staffing margin when expected personal leave and reductions in clinical effort occur. Furthermore, we revised scheduling principles to balance patient continuity and individual time off requests while setting limits on the maximum duration of clinical stretches and instituting mandatory minimum time off between them.
Leadership engagement
We initiated monthly operations meetings as a forum to discuss challenges, brainstorm solutions, and message new initiatives with group input. For example, as a result of these meetings, we designed and implemented an additional service line to address the high census, revised the distribution of new patient admissions to level-load clinical shifts, and established a maximum number of weekends worked per month and year. This approach aligns with recommendations to use participatory leadership strategies to enhance physician well-being.10 Engaging both executive level and service level management to focus on burnout and other related well-being metrics is necessary for sustaining such work.
Interprofessional teamwork
We revised multidisciplinary rounds with social work, utilization management, and physical therapy to maximize efficiency and streamline communication by developing standard approaches for each patient presentation.
Interpersonal and individual commitments5Address emotional challenges of physician work
Although these commitments did not have a direct corollary with Lean philosophy, some of these needs were identified by our physician group at our annual retreats. As a result, we initiated a monthly faculty-led noon conference series focused on the clinical challenges of caring for vulnerable populations, a particular source of distress in our practice setting, and revised the division schedule to encourage attendance at the hospital’s Schwartz rounds.
Mental health and self-care
We organized focus groups and faculty development sessions on provider well-being and burnout and dealing with challenging patients and invited the Faculty and Staff Assistance Program, our institution’s mental health service provider, to our weekly division meeting.
Future directions
After using Lean Management as an approach to prospectively improve physician well-being, we were able to use the Charter on Physician Well-being retrospectively as a “checklist” to identify additional gaps for targeted intervention to ensure all commitments are sufficiently addressed.
Overall, we found that, not surprisingly, Lean Management aligned best with the organizational commitments in the charter. Reviewing the organizational commitments, we found our biggest remaining challenges are in building supportive systems, namely ensuring sustainable workloads, offloading and delegating nonphysician tasks, and minimizing the burden of documentation and administration.
Reviewing the societal commitments helped us to identify opportunities for future directions that we may not have otherwise considered. As a safety-net institution, we benefit from a strong sense of mission and shared values within our hospital and division. However, we recognize the need to continue to be vigilant to ensure that our physicians perceive that their own values are aligned with the division’s stated mission. Devoting a Kaizen-style retreat to well-being likely helped, and allocating divisional resources to a well-being committee indirectly helped, to foster a culture of well-being; however, we could more deliberately identify local policies that may benefit from advocacy or revision. Although our faculty identified interventions to improve interpersonal and individual drivers of well-being, these charter commitments did not have direct parallels in Lean philosophy, and organizations may need to deliberately seek to address these commitments outside of a Lean approach. Specifically, by reviewing the charter, we identified opportunities to provide additional resources for peer support and protected time for mental health care and self-care.
Conclusion
Lean Management can be an effective strategy to address many of the organizational commitments outlined in the Charter on Physician Well-being. This approach may be particularly effective for solving local challenges with systems and workflows. Those who use Lean as a primary method to approach systems improvement in support of the Quadruple Aim may need to use additional strategies to address societal and interpersonal and individual commitments outlined in the charter.
Dr. Sanyal-Dey is visiting associate clinical professor of medicine at Zuckerberg San Francisco General Hospital and director of client services, LeanTaaS. Dr. Thomas is associate clinical professor of medicine at Zuckerberg San Francisco General Hospital. Dr. Chia is associate professor of clinical medicine at Zuckerberg San Francisco General Hospital.
References
1. West CP et al. Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. Lancet. 2016;388(10057):2272-81.
2. Shanafelt TD, Noseworthy JH. Executive leadership and physician: Nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92(1):129-46.
3. Shanafelt T et al. The business case for investing in physician well-being. JAMA Intern Med. 2017;177(12):1826-32.
4. Shanafelt T et al. Building a program on well-being: Key design considerations to meet the unique needs of each organization. Acad Med. 2019 Feb;94(2):156-161.
5. Thomas LR et al. Charter on physician well-being. JAMA. 2018;319(15):1541-42.
6. Bodenheimer T, Sinsky C. From triple to quadruple aim: Care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573-6.
7. West CP et al. Concurrent Validity of Single-Item Measures of Emotional Exhaustion and Depersonalization in Burnout Assessment. J Gen Intern Med. 2012;27(11):1445-52.
8. Hung DY et al. Experiences of primary care physicians and staff following lean workflow redesign. BMC Health Serv Res. 2018 Apr 10;18(1):274.
9. Zibrowski E et al. Easier and faster is not always better: Grounded theory of the impact of large-scale system transformation on the clinical work of emergency medicine nurses and physicians. JMIR Hum Factors. 2018. doi: 10.2196/11013.
10. Shanafelt TD et al. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clin Proc. 2015;90(4):432-40.
General background on well-being and burnout
With burnout increasingly recognized as a shared responsibility that requires addressing organizational drivers while supporting individuals to be well,1-4 practical strategies and examples of successful implementation of systems interventions to address burnout will be helpful for service directors to support their staff. The Charter on Physician Well-being, recently developed through collaborative input from multiple organizations, defines guiding principles and key commitments at the societal, organizational, interpersonal, and individual levels and may be a useful framework for organizations that are developing well-being initiatives.5
The charter advocates including physician well-being as a quality improvement metric for health systems, aligned with the concept of the Quadruple Aim of optimizing patient care by enhancing provider experience, promoting high-value care, and improving population health.6 Identifying areas of alignment between the charter’s recommendations and systems improvement strategies that seek to optimize efficiency and reduce waste, such as Lean Management, may help physician leaders to contextualize well-being initiatives more easily within ongoing systems improvement efforts. In this perspective, we provide one division’s experience using the Charter to assess successes and identify additional areas of improvement for well-being initiatives developed using Lean Management methodology.
Past and current state of affairs
In 2011, the division of hospital medicine at Zuckerberg San Francisco General Hospital was established and has seen continual expansion in terms of direct patient care, medical education, and hospital leadership.
In 2015, the division of hospital medicine experienced leadership transitions, faculty attrition, and insufficient recruitment resulting in staffing shortages, service line closure, schedule instability, and ultimately, low morale. A baseline survey conducted using the 2-Item Maslach Burnout Inventory. This survey, which uses one item in the domain of emotional exhaustion and one item in the domain of depersonalization, has shown good correlation with the full Maslach Burnout Inventory.7 At baseline, approximately one-third of the division’s physicians experienced burnout.
In response, a subsequent retreat focused on the three greatest areas of concern identified by the survey: scheduling, faculty development, and well-being.
Like many health systems, the hospital has adopted Lean as its preferred systems-improvement framework. The retreat was structured around the principles of Lean philosophy, and was designed to emulate that of a consolidated Kaizen workshop.
“Kaizen” in Japanese means “change for the better.” A typical Kaizen workshop revolves around rapid problem-solving over the course of 3-5 days, in which a team of people come together to identify and implement significant improvements for a selected process. To this end, the retreat was divided into subgroups for each area of concern. In turn, each subgroup mapped out existing workflows (“value stream”), identified areas of waste and non–value added time, and generated ideas of what an idealized process would be. Next, a root-cause analysis was performed and subsequent interventions (“countermeasures”) developed to address each problem. At the conclusion of the retreat, each subgroup shared a summary of their findings with the larger group.
Moving forward, this information served as a guiding framework for service and division leadership to run small tests of change. We enacted a series of countermeasures over the course of several years, and multiple cycles of improvement work addressed the three areas of concern. We developed an A3 report (a Lean project management tool that incorporates the plan-do-study-act cycle, organizes strategic efforts, and tracks progress on a single page) to summarize and present these initiatives to the Performance Improvement and Patient Safety Committee of the hospital executive leadership team. This structure illustrated alignment with the hospital’s core values (“true north”) of “developing people” and “care experience.”
In 2018, interval surveys demonstrated a gradual reduction of burnout to approximately one-fifth of division physicians as measured by the 2-item Maslach Burnout Inventory.
Initiatives in faculty well-being
The Charter of Physician Well-being outlines a framework to promote well-being among doctors by maximizing a sense of fulfillment and minimizing the harms of burnout. It shares this responsibility among societal, organizational, and interpersonal and individual commitments.5
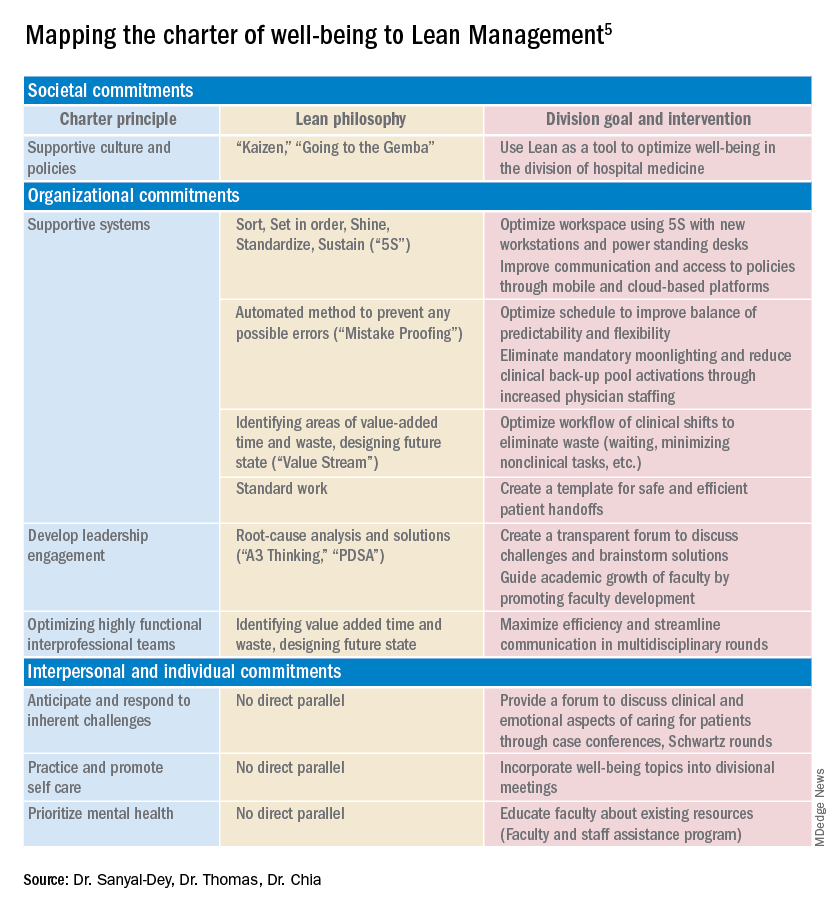
As illustrated above, we used principles of Lean Management to prospectively create initiatives to improve well-being in our division. Lean in health care is designed to optimize primarily the patient experience; its implementation has subsequently demonstrated mixed provider and staff experiences,8,9 and many providers are skeptical of Lean’s potential to improve their own well-being. If, however, Lean is aligned with best practice frameworks for well-being such as those outline in the charter, it may also help to meet the Quadruple Aim of optimizing both provider well-being and patient experience. To further test this hypothesis, we retrospectively categorized our Lean-based interventions into the commitments described by the charter to identify areas of alignment and gaps that were not initially addressed using Lean Management (Table).
Organizational commitments5Supportive systems
We optimized scheduling and enhanced physician staffing by budgeting for a physician staffing buffer each academic year in order to minimize mandatory moonlighting and jeopardy pool activations that result from operating on a thin staffing margin when expected personal leave and reductions in clinical effort occur. Furthermore, we revised scheduling principles to balance patient continuity and individual time off requests while setting limits on the maximum duration of clinical stretches and instituting mandatory minimum time off between them.
Leadership engagement
We initiated monthly operations meetings as a forum to discuss challenges, brainstorm solutions, and message new initiatives with group input. For example, as a result of these meetings, we designed and implemented an additional service line to address the high census, revised the distribution of new patient admissions to level-load clinical shifts, and established a maximum number of weekends worked per month and year. This approach aligns with recommendations to use participatory leadership strategies to enhance physician well-being.10 Engaging both executive level and service level management to focus on burnout and other related well-being metrics is necessary for sustaining such work.
Interprofessional teamwork
We revised multidisciplinary rounds with social work, utilization management, and physical therapy to maximize efficiency and streamline communication by developing standard approaches for each patient presentation.
Interpersonal and individual commitments5Address emotional challenges of physician work
Although these commitments did not have a direct corollary with Lean philosophy, some of these needs were identified by our physician group at our annual retreats. As a result, we initiated a monthly faculty-led noon conference series focused on the clinical challenges of caring for vulnerable populations, a particular source of distress in our practice setting, and revised the division schedule to encourage attendance at the hospital’s Schwartz rounds.
Mental health and self-care
We organized focus groups and faculty development sessions on provider well-being and burnout and dealing with challenging patients and invited the Faculty and Staff Assistance Program, our institution’s mental health service provider, to our weekly division meeting.
Future directions
After using Lean Management as an approach to prospectively improve physician well-being, we were able to use the Charter on Physician Well-being retrospectively as a “checklist” to identify additional gaps for targeted intervention to ensure all commitments are sufficiently addressed.
Overall, we found that, not surprisingly, Lean Management aligned best with the organizational commitments in the charter. Reviewing the organizational commitments, we found our biggest remaining challenges are in building supportive systems, namely ensuring sustainable workloads, offloading and delegating nonphysician tasks, and minimizing the burden of documentation and administration.
Reviewing the societal commitments helped us to identify opportunities for future directions that we may not have otherwise considered. As a safety-net institution, we benefit from a strong sense of mission and shared values within our hospital and division. However, we recognize the need to continue to be vigilant to ensure that our physicians perceive that their own values are aligned with the division’s stated mission. Devoting a Kaizen-style retreat to well-being likely helped, and allocating divisional resources to a well-being committee indirectly helped, to foster a culture of well-being; however, we could more deliberately identify local policies that may benefit from advocacy or revision. Although our faculty identified interventions to improve interpersonal and individual drivers of well-being, these charter commitments did not have direct parallels in Lean philosophy, and organizations may need to deliberately seek to address these commitments outside of a Lean approach. Specifically, by reviewing the charter, we identified opportunities to provide additional resources for peer support and protected time for mental health care and self-care.
Conclusion
Lean Management can be an effective strategy to address many of the organizational commitments outlined in the Charter on Physician Well-being. This approach may be particularly effective for solving local challenges with systems and workflows. Those who use Lean as a primary method to approach systems improvement in support of the Quadruple Aim may need to use additional strategies to address societal and interpersonal and individual commitments outlined in the charter.
Dr. Sanyal-Dey is visiting associate clinical professor of medicine at Zuckerberg San Francisco General Hospital and director of client services, LeanTaaS. Dr. Thomas is associate clinical professor of medicine at Zuckerberg San Francisco General Hospital. Dr. Chia is associate professor of clinical medicine at Zuckerberg San Francisco General Hospital.
References
1. West CP et al. Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. Lancet. 2016;388(10057):2272-81.
2. Shanafelt TD, Noseworthy JH. Executive leadership and physician: Nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92(1):129-46.
3. Shanafelt T et al. The business case for investing in physician well-being. JAMA Intern Med. 2017;177(12):1826-32.
4. Shanafelt T et al. Building a program on well-being: Key design considerations to meet the unique needs of each organization. Acad Med. 2019 Feb;94(2):156-161.
5. Thomas LR et al. Charter on physician well-being. JAMA. 2018;319(15):1541-42.
6. Bodenheimer T, Sinsky C. From triple to quadruple aim: Care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573-6.
7. West CP et al. Concurrent Validity of Single-Item Measures of Emotional Exhaustion and Depersonalization in Burnout Assessment. J Gen Intern Med. 2012;27(11):1445-52.
8. Hung DY et al. Experiences of primary care physicians and staff following lean workflow redesign. BMC Health Serv Res. 2018 Apr 10;18(1):274.
9. Zibrowski E et al. Easier and faster is not always better: Grounded theory of the impact of large-scale system transformation on the clinical work of emergency medicine nurses and physicians. JMIR Hum Factors. 2018. doi: 10.2196/11013.
10. Shanafelt TD et al. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clin Proc. 2015;90(4):432-40.