User login
Biden’s COVID-19 challenge: 100 million vaccinations in the first 100 days. It won’t be easy.
It’s in the nature of presidential candidates and new presidents to promise big things. Just months after his 1961 inauguration, President John F. Kennedy vowed to send a man to the moon by the end of the decade. That pledge was kept, but many others haven’t been, such as candidate Bill Clinton’s promise to provide universal health care and presidential hopeful George H.W. Bush’s guarantee of no new taxes.
Now, during a once-in-a-century pandemic, incoming President Joe Biden has promised to provide 100 million COVID-19 vaccinations in his first 100 days in office.
“This team will help get … at least 100 million covid vaccine shots into the arms of the American people in the first 100 days,” Biden said during a Dec. 8 news conference introducing key members of his health team.
When first asked about his pledge, the Biden team said the president-elect meant 50 million people would get their two-dose regimen. The incoming administration has since updated this plan, saying it will release vaccine doses as soon as they’re available instead of holding back some of that supply for second doses.
Either way, Biden may run into difficulty meeting that 100 million mark.
“I think it’s an attainable goal. I think it’s going to be extremely challenging,” said Claire Hannan, executive director of the Association of Immunization Managers.
While a pace of 1 million doses a day is “somewhat of an increase over what we’re already doing,” a much higher rate of vaccinations will be necessary to stem the pandemic, said Larry Levitt, executive vice president for health policy at Kaiser Family Foundation. (KHN is an editorially independent program of KFF.) “The Biden administration has plans to rationalize vaccine distribution, but increasing the supply quickly” could be a difficult task.
Under the Trump administration, vaccine deployment has been much slower than Biden’s plan. The rollout began on Dec. 14. Since then, 12 million shots have been given and 31 million doses have been shipped out, according to the Centers for Disease Control and Prevention’s vaccine tracker.
This sluggishness has been attributed to a lack of communication between the federal government and state and local health departments, not enough funding for large-scale vaccination efforts, and confusing federal guidance on distribution of the vaccines.
The same problems could plague the Biden administration, said experts.
States still aren’t sure how much vaccine they’ll get and whether there will be a sufficient supply, said Dr. Marcus Plescia, chief medical officer for the Association of State and Territorial Health Officials, which represents state public health agencies.
“We have been given little information about the amount of vaccine the states will receive in the near future and are of the impression that there may not be 1 million doses available per day in the first 100 days of the Biden administration,” said Dr. Plescia. “Or at least not in the early stages of the 100 days.”
Another challenge has been a lack of funding. Public health departments have had to start vaccination campaigns while also operating testing centers and conducting contact tracing efforts with budgets that have been critically underfunded for years.
“States have to pay for creating the systems, identifying the personnel, training, staffing, tracking people, information campaigns – all the things that go into getting a shot in someone’s arm,” said Jennifer Kates, director of global health & HIV policy at KFF. “They’re having to create an unprecedented mass vaccination program on a shaky foundation.”
The latest covid stimulus bill, signed into law in December, allocates almost $9 billion in funding to the CDC for vaccination efforts. About $4.5 billion is supposed to go to states, territories and tribal organizations, and $3 billion of that is slated to arrive soon.
But it’s not clear that level of funding can sustain mass vaccination campaigns as more groups become eligible for the vaccine.
Biden released a $1.9 trillion plan last week to address covid and the struggling economy. It includes $160 billion to create national vaccination and testing programs, but also earmarks funds for $1,400 stimulus payments to individuals, state and local government aid, extension of unemployment insurance, and financial assistance for schools to reopen safely.
Though it took Congress almost eight months to pass the last covid relief bill after Republican objections to the cost, Biden seems optimistic he’ll get some Republicans on board for his plan. But it’s not yet clear that will work.
There’s also the question of whether outgoing President Donald Trump’s impeachment trial will get in the way of Biden’s legislative priorities.
In addition, states have complained about a lack of guidance and confusing instructions on which groups should be given priority status for vaccination, an issue the Biden administration will need to address.
On Dec. 3, the CDC recommended health care personnel, residents of long-term care facilities, those 75 and older, and front-line essential workers should be immunized first. But on Jan. 12, the CDC shifted course and recommended that everyone over age 65 should be immunized. In a speech Biden gave on Jan. 15 detailing his vaccination plan, he said he would stick to the CDC’s recommendation to prioritize those over 65.
Outgoing Health and Human Services Secretary Alex Azar also said on Jan. 12 that states that moved their vaccine supply fastest would be prioritized in getting more shipments. It’s not known yet whether the Biden administration’s CDC will stick to this guidance. Critics have said it could make vaccine distribution less equitable.
In general, taking over with a strong vision and clear communication will be key to ramping up vaccine distribution, said Ms. Hannan.
“Everyone needs to understand what the goal is and how it’s going to work,” she said.
A challenge for Biden will be tamping expectations that the vaccine is all that is needed to end the pandemic. Across the country, covid cases are higher than ever, and in many locations officials cannot control the spread.
Public health experts said Biden must amp up efforts to increase testing across the country, as he has suggested he will do by promising to establish a national pandemic testing board.
With so much focus on vaccine distribution, it’s important that this part of the equation not be lost. Right now, “it’s completely all over the map,” said KFF’s Ms. Kates, adding that the federal government will need a “good sense” of who is and is not being tested in different areas in order to “fix” public health capacity.
Jan. 20, 2021, marks the launch of The Biden Promise Tracker, which monitors the 100 most important campaign promises of President Joseph R. Biden. Biden listed the coronavirus and a variety of other health-related issues among his top priorities. You can see the entire list – including improving the economy, responding to calls for racial justice and combating climate change – here. As part of KHN’s partnership with PolitiFact, we will follow the health-related issues and then rate them on whether the promise was achieved: Promise Kept, Promise Broken, Compromise, Stalled, In the Works or Not Yet Rated. We rate the promise not on the president’s intentions or effort, but on verifiable outcomes. PolitiFact previously tracked the promises of President Donald Trump and President Barack Obama.
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF, which is not affiliated with Kaiser Permanente.
It’s in the nature of presidential candidates and new presidents to promise big things. Just months after his 1961 inauguration, President John F. Kennedy vowed to send a man to the moon by the end of the decade. That pledge was kept, but many others haven’t been, such as candidate Bill Clinton’s promise to provide universal health care and presidential hopeful George H.W. Bush’s guarantee of no new taxes.
Now, during a once-in-a-century pandemic, incoming President Joe Biden has promised to provide 100 million COVID-19 vaccinations in his first 100 days in office.
“This team will help get … at least 100 million covid vaccine shots into the arms of the American people in the first 100 days,” Biden said during a Dec. 8 news conference introducing key members of his health team.
When first asked about his pledge, the Biden team said the president-elect meant 50 million people would get their two-dose regimen. The incoming administration has since updated this plan, saying it will release vaccine doses as soon as they’re available instead of holding back some of that supply for second doses.
Either way, Biden may run into difficulty meeting that 100 million mark.
“I think it’s an attainable goal. I think it’s going to be extremely challenging,” said Claire Hannan, executive director of the Association of Immunization Managers.
While a pace of 1 million doses a day is “somewhat of an increase over what we’re already doing,” a much higher rate of vaccinations will be necessary to stem the pandemic, said Larry Levitt, executive vice president for health policy at Kaiser Family Foundation. (KHN is an editorially independent program of KFF.) “The Biden administration has plans to rationalize vaccine distribution, but increasing the supply quickly” could be a difficult task.
Under the Trump administration, vaccine deployment has been much slower than Biden’s plan. The rollout began on Dec. 14. Since then, 12 million shots have been given and 31 million doses have been shipped out, according to the Centers for Disease Control and Prevention’s vaccine tracker.
This sluggishness has been attributed to a lack of communication between the federal government and state and local health departments, not enough funding for large-scale vaccination efforts, and confusing federal guidance on distribution of the vaccines.
The same problems could plague the Biden administration, said experts.
States still aren’t sure how much vaccine they’ll get and whether there will be a sufficient supply, said Dr. Marcus Plescia, chief medical officer for the Association of State and Territorial Health Officials, which represents state public health agencies.
“We have been given little information about the amount of vaccine the states will receive in the near future and are of the impression that there may not be 1 million doses available per day in the first 100 days of the Biden administration,” said Dr. Plescia. “Or at least not in the early stages of the 100 days.”
Another challenge has been a lack of funding. Public health departments have had to start vaccination campaigns while also operating testing centers and conducting contact tracing efforts with budgets that have been critically underfunded for years.
“States have to pay for creating the systems, identifying the personnel, training, staffing, tracking people, information campaigns – all the things that go into getting a shot in someone’s arm,” said Jennifer Kates, director of global health & HIV policy at KFF. “They’re having to create an unprecedented mass vaccination program on a shaky foundation.”
The latest covid stimulus bill, signed into law in December, allocates almost $9 billion in funding to the CDC for vaccination efforts. About $4.5 billion is supposed to go to states, territories and tribal organizations, and $3 billion of that is slated to arrive soon.
But it’s not clear that level of funding can sustain mass vaccination campaigns as more groups become eligible for the vaccine.
Biden released a $1.9 trillion plan last week to address covid and the struggling economy. It includes $160 billion to create national vaccination and testing programs, but also earmarks funds for $1,400 stimulus payments to individuals, state and local government aid, extension of unemployment insurance, and financial assistance for schools to reopen safely.
Though it took Congress almost eight months to pass the last covid relief bill after Republican objections to the cost, Biden seems optimistic he’ll get some Republicans on board for his plan. But it’s not yet clear that will work.
There’s also the question of whether outgoing President Donald Trump’s impeachment trial will get in the way of Biden’s legislative priorities.
In addition, states have complained about a lack of guidance and confusing instructions on which groups should be given priority status for vaccination, an issue the Biden administration will need to address.
On Dec. 3, the CDC recommended health care personnel, residents of long-term care facilities, those 75 and older, and front-line essential workers should be immunized first. But on Jan. 12, the CDC shifted course and recommended that everyone over age 65 should be immunized. In a speech Biden gave on Jan. 15 detailing his vaccination plan, he said he would stick to the CDC’s recommendation to prioritize those over 65.
Outgoing Health and Human Services Secretary Alex Azar also said on Jan. 12 that states that moved their vaccine supply fastest would be prioritized in getting more shipments. It’s not known yet whether the Biden administration’s CDC will stick to this guidance. Critics have said it could make vaccine distribution less equitable.
In general, taking over with a strong vision and clear communication will be key to ramping up vaccine distribution, said Ms. Hannan.
“Everyone needs to understand what the goal is and how it’s going to work,” she said.
A challenge for Biden will be tamping expectations that the vaccine is all that is needed to end the pandemic. Across the country, covid cases are higher than ever, and in many locations officials cannot control the spread.
Public health experts said Biden must amp up efforts to increase testing across the country, as he has suggested he will do by promising to establish a national pandemic testing board.
With so much focus on vaccine distribution, it’s important that this part of the equation not be lost. Right now, “it’s completely all over the map,” said KFF’s Ms. Kates, adding that the federal government will need a “good sense” of who is and is not being tested in different areas in order to “fix” public health capacity.
Jan. 20, 2021, marks the launch of The Biden Promise Tracker, which monitors the 100 most important campaign promises of President Joseph R. Biden. Biden listed the coronavirus and a variety of other health-related issues among his top priorities. You can see the entire list – including improving the economy, responding to calls for racial justice and combating climate change – here. As part of KHN’s partnership with PolitiFact, we will follow the health-related issues and then rate them on whether the promise was achieved: Promise Kept, Promise Broken, Compromise, Stalled, In the Works or Not Yet Rated. We rate the promise not on the president’s intentions or effort, but on verifiable outcomes. PolitiFact previously tracked the promises of President Donald Trump and President Barack Obama.
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF, which is not affiliated with Kaiser Permanente.
It’s in the nature of presidential candidates and new presidents to promise big things. Just months after his 1961 inauguration, President John F. Kennedy vowed to send a man to the moon by the end of the decade. That pledge was kept, but many others haven’t been, such as candidate Bill Clinton’s promise to provide universal health care and presidential hopeful George H.W. Bush’s guarantee of no new taxes.
Now, during a once-in-a-century pandemic, incoming President Joe Biden has promised to provide 100 million COVID-19 vaccinations in his first 100 days in office.
“This team will help get … at least 100 million covid vaccine shots into the arms of the American people in the first 100 days,” Biden said during a Dec. 8 news conference introducing key members of his health team.
When first asked about his pledge, the Biden team said the president-elect meant 50 million people would get their two-dose regimen. The incoming administration has since updated this plan, saying it will release vaccine doses as soon as they’re available instead of holding back some of that supply for second doses.
Either way, Biden may run into difficulty meeting that 100 million mark.
“I think it’s an attainable goal. I think it’s going to be extremely challenging,” said Claire Hannan, executive director of the Association of Immunization Managers.
While a pace of 1 million doses a day is “somewhat of an increase over what we’re already doing,” a much higher rate of vaccinations will be necessary to stem the pandemic, said Larry Levitt, executive vice president for health policy at Kaiser Family Foundation. (KHN is an editorially independent program of KFF.) “The Biden administration has plans to rationalize vaccine distribution, but increasing the supply quickly” could be a difficult task.
Under the Trump administration, vaccine deployment has been much slower than Biden’s plan. The rollout began on Dec. 14. Since then, 12 million shots have been given and 31 million doses have been shipped out, according to the Centers for Disease Control and Prevention’s vaccine tracker.
This sluggishness has been attributed to a lack of communication between the federal government and state and local health departments, not enough funding for large-scale vaccination efforts, and confusing federal guidance on distribution of the vaccines.
The same problems could plague the Biden administration, said experts.
States still aren’t sure how much vaccine they’ll get and whether there will be a sufficient supply, said Dr. Marcus Plescia, chief medical officer for the Association of State and Territorial Health Officials, which represents state public health agencies.
“We have been given little information about the amount of vaccine the states will receive in the near future and are of the impression that there may not be 1 million doses available per day in the first 100 days of the Biden administration,” said Dr. Plescia. “Or at least not in the early stages of the 100 days.”
Another challenge has been a lack of funding. Public health departments have had to start vaccination campaigns while also operating testing centers and conducting contact tracing efforts with budgets that have been critically underfunded for years.
“States have to pay for creating the systems, identifying the personnel, training, staffing, tracking people, information campaigns – all the things that go into getting a shot in someone’s arm,” said Jennifer Kates, director of global health & HIV policy at KFF. “They’re having to create an unprecedented mass vaccination program on a shaky foundation.”
The latest covid stimulus bill, signed into law in December, allocates almost $9 billion in funding to the CDC for vaccination efforts. About $4.5 billion is supposed to go to states, territories and tribal organizations, and $3 billion of that is slated to arrive soon.
But it’s not clear that level of funding can sustain mass vaccination campaigns as more groups become eligible for the vaccine.
Biden released a $1.9 trillion plan last week to address covid and the struggling economy. It includes $160 billion to create national vaccination and testing programs, but also earmarks funds for $1,400 stimulus payments to individuals, state and local government aid, extension of unemployment insurance, and financial assistance for schools to reopen safely.
Though it took Congress almost eight months to pass the last covid relief bill after Republican objections to the cost, Biden seems optimistic he’ll get some Republicans on board for his plan. But it’s not yet clear that will work.
There’s also the question of whether outgoing President Donald Trump’s impeachment trial will get in the way of Biden’s legislative priorities.
In addition, states have complained about a lack of guidance and confusing instructions on which groups should be given priority status for vaccination, an issue the Biden administration will need to address.
On Dec. 3, the CDC recommended health care personnel, residents of long-term care facilities, those 75 and older, and front-line essential workers should be immunized first. But on Jan. 12, the CDC shifted course and recommended that everyone over age 65 should be immunized. In a speech Biden gave on Jan. 15 detailing his vaccination plan, he said he would stick to the CDC’s recommendation to prioritize those over 65.
Outgoing Health and Human Services Secretary Alex Azar also said on Jan. 12 that states that moved their vaccine supply fastest would be prioritized in getting more shipments. It’s not known yet whether the Biden administration’s CDC will stick to this guidance. Critics have said it could make vaccine distribution less equitable.
In general, taking over with a strong vision and clear communication will be key to ramping up vaccine distribution, said Ms. Hannan.
“Everyone needs to understand what the goal is and how it’s going to work,” she said.
A challenge for Biden will be tamping expectations that the vaccine is all that is needed to end the pandemic. Across the country, covid cases are higher than ever, and in many locations officials cannot control the spread.
Public health experts said Biden must amp up efforts to increase testing across the country, as he has suggested he will do by promising to establish a national pandemic testing board.
With so much focus on vaccine distribution, it’s important that this part of the equation not be lost. Right now, “it’s completely all over the map,” said KFF’s Ms. Kates, adding that the federal government will need a “good sense” of who is and is not being tested in different areas in order to “fix” public health capacity.
Jan. 20, 2021, marks the launch of The Biden Promise Tracker, which monitors the 100 most important campaign promises of President Joseph R. Biden. Biden listed the coronavirus and a variety of other health-related issues among his top priorities. You can see the entire list – including improving the economy, responding to calls for racial justice and combating climate change – here. As part of KHN’s partnership with PolitiFact, we will follow the health-related issues and then rate them on whether the promise was achieved: Promise Kept, Promise Broken, Compromise, Stalled, In the Works or Not Yet Rated. We rate the promise not on the president’s intentions or effort, but on verifiable outcomes. PolitiFact previously tracked the promises of President Donald Trump and President Barack Obama.
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF, which is not affiliated with Kaiser Permanente.
Many EM docs have treated COVID-19 patients without proper PPE: Survey
Many emergency medicine (EM) physicians who responded to a Medscape survey said they have treated COVID-19 patients without appropriate personal protective equipment (PPE).
In the Medscape Emergency Medicine Physicians’ COVID-19 Experience Report, 21% of respondents said that that was sometimes the case; 7% said that it was often the case; and 1% said they always treat patients without appropriate PPE.
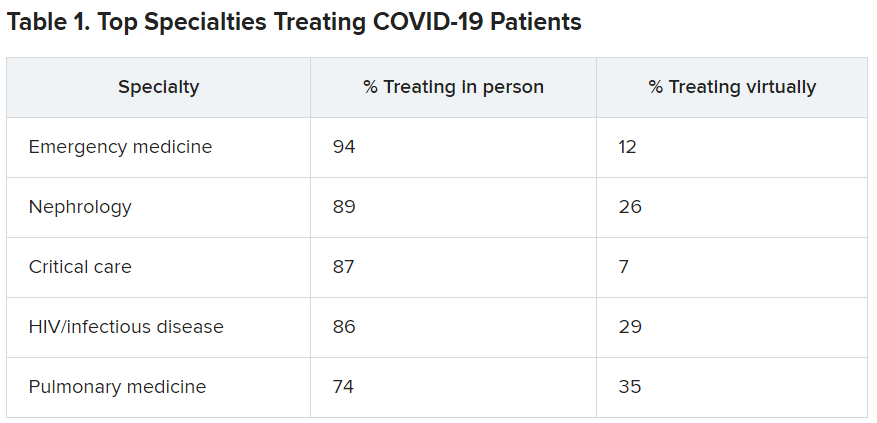
EM physicians were the physicians most likely to treat COVID-19 patients in person.
For comparison, among family medicine physicians, 58% said that they have treated COVID-19 patients in person, and 45% said they were treating them via telemedicine.
Data for the report were gathered from June 9 to July 20 as part of Medscape’s COVID-19 experience survey for all physicians. That survey drew more than 5,000 responses.
Nearly all (98%) of EM physicians who have treated COVID-19 patients said that they have done so since the beginning, when the World Health Organization declared a pandemic on March 11, 2020. For all U.S. physicians, the percentage was much higher than that – 73% said they had treated COVID-19 patients from the start.
EM physicians have often found themselves sacrificing their own safety for the sake of patients. More than half of EM physicians (54%) said that they had knowingly taken personal safety risks to treat a COVID-19 emergency, a percentage far higher than the 30% of all physicians who said they had done so.
Four percent of EM physicians have received a positive diagnosis of COVID-19 via testing. An additional 2% have been confirmed as having COVID on the basis of symptoms.
Steep income drops
Survey authors wrote that two-thirds of EM physicians have experienced income loss during the pandemic. Most (71%) saw their income drop by between 11% and 50%; 11% saw a decrease of more than 50%. Among other specialties, the percentages of those who have experienced a drop of more than 50% are far higher. Among ophthalmologists, 51% said they had experienced such a drop; among allergists, 46%; plastic surgeons, 46%; and otolaryngologists, 45%.
Asked whether their burnout levels have increased in the wake of COVID-19, 74% of EM physicians said burnout had intensified; 23% reported no change; and 3% said burnout had lessened.
Reports of loneliness have been widespread during the pandemic, owing to stay-at-home orders and social distancing. More EM physicians than physicians in general said feelings of loneliness had increased for them in the past year.
More than half of EM doctors (55%) said they are experiencing more loneliness in the pandemic, compared with 46% of all physicians who felt that way; 42% said those feelings have not changed; and 3% said they have been less lonely.
Grief and stress relief
Fewer than half (42%) of the respondents reported that their workplace offers clinician activities to help with grief and stress; 39% said their workplace didn’t offer such help; and 19% said they were unsure.
The percentages were nearly identical to the percentages of physicians overall who answered whether their workplace offered help for grief and stress.
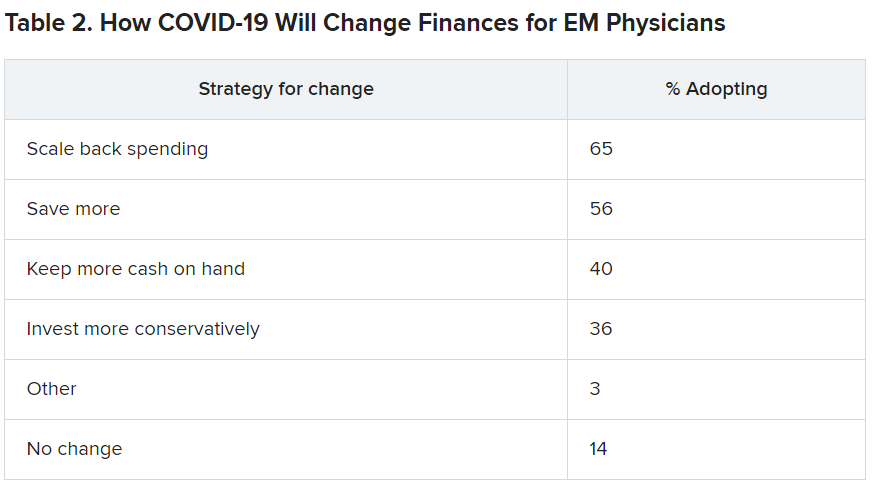
Along with insecurity regarding physical and mental health, COVID-19 has introduced more questions about financial health. Here’s a look at how emergency physicians said they would change the way they save and spend.
Challenges to daily practice
By the time this survey was taken, a large percentage of patients had delayed or avoided urgent or routine medical care for reasons related to COVID-19, so survey authors asked whether EM physicians’ patient population had changed.
Survey authors wrote that “most EM physicians (82%) are seeing patients with non-COVID diseases, such as cardiovascular problems or diabetes, who otherwise probably would have sought treatment earlier.”
COVID-19 has also thrown a major obstacle into most EM physicians’ careers by preventing them from doing the job to the best of their ability. That loss is one of the three primary components of burnout.
More than two-thirds (67%) said COVID-19 has hampered their ability to be as good a doctor as they would like.
A version of this article first appeared on Medscape.com.
Many emergency medicine (EM) physicians who responded to a Medscape survey said they have treated COVID-19 patients without appropriate personal protective equipment (PPE).
In the Medscape Emergency Medicine Physicians’ COVID-19 Experience Report, 21% of respondents said that that was sometimes the case; 7% said that it was often the case; and 1% said they always treat patients without appropriate PPE.
EM physicians were the physicians most likely to treat COVID-19 patients in person.
For comparison, among family medicine physicians, 58% said that they have treated COVID-19 patients in person, and 45% said they were treating them via telemedicine.
Data for the report were gathered from June 9 to July 20 as part of Medscape’s COVID-19 experience survey for all physicians. That survey drew more than 5,000 responses.
Nearly all (98%) of EM physicians who have treated COVID-19 patients said that they have done so since the beginning, when the World Health Organization declared a pandemic on March 11, 2020. For all U.S. physicians, the percentage was much higher than that – 73% said they had treated COVID-19 patients from the start.
EM physicians have often found themselves sacrificing their own safety for the sake of patients. More than half of EM physicians (54%) said that they had knowingly taken personal safety risks to treat a COVID-19 emergency, a percentage far higher than the 30% of all physicians who said they had done so.
Four percent of EM physicians have received a positive diagnosis of COVID-19 via testing. An additional 2% have been confirmed as having COVID on the basis of symptoms.
Steep income drops
Survey authors wrote that two-thirds of EM physicians have experienced income loss during the pandemic. Most (71%) saw their income drop by between 11% and 50%; 11% saw a decrease of more than 50%. Among other specialties, the percentages of those who have experienced a drop of more than 50% are far higher. Among ophthalmologists, 51% said they had experienced such a drop; among allergists, 46%; plastic surgeons, 46%; and otolaryngologists, 45%.
Asked whether their burnout levels have increased in the wake of COVID-19, 74% of EM physicians said burnout had intensified; 23% reported no change; and 3% said burnout had lessened.
Reports of loneliness have been widespread during the pandemic, owing to stay-at-home orders and social distancing. More EM physicians than physicians in general said feelings of loneliness had increased for them in the past year.
More than half of EM doctors (55%) said they are experiencing more loneliness in the pandemic, compared with 46% of all physicians who felt that way; 42% said those feelings have not changed; and 3% said they have been less lonely.
Grief and stress relief
Fewer than half (42%) of the respondents reported that their workplace offers clinician activities to help with grief and stress; 39% said their workplace didn’t offer such help; and 19% said they were unsure.
The percentages were nearly identical to the percentages of physicians overall who answered whether their workplace offered help for grief and stress.
Along with insecurity regarding physical and mental health, COVID-19 has introduced more questions about financial health. Here’s a look at how emergency physicians said they would change the way they save and spend.
Challenges to daily practice
By the time this survey was taken, a large percentage of patients had delayed or avoided urgent or routine medical care for reasons related to COVID-19, so survey authors asked whether EM physicians’ patient population had changed.
Survey authors wrote that “most EM physicians (82%) are seeing patients with non-COVID diseases, such as cardiovascular problems or diabetes, who otherwise probably would have sought treatment earlier.”
COVID-19 has also thrown a major obstacle into most EM physicians’ careers by preventing them from doing the job to the best of their ability. That loss is one of the three primary components of burnout.
More than two-thirds (67%) said COVID-19 has hampered their ability to be as good a doctor as they would like.
A version of this article first appeared on Medscape.com.
Many emergency medicine (EM) physicians who responded to a Medscape survey said they have treated COVID-19 patients without appropriate personal protective equipment (PPE).
In the Medscape Emergency Medicine Physicians’ COVID-19 Experience Report, 21% of respondents said that that was sometimes the case; 7% said that it was often the case; and 1% said they always treat patients without appropriate PPE.
EM physicians were the physicians most likely to treat COVID-19 patients in person.
For comparison, among family medicine physicians, 58% said that they have treated COVID-19 patients in person, and 45% said they were treating them via telemedicine.
Data for the report were gathered from June 9 to July 20 as part of Medscape’s COVID-19 experience survey for all physicians. That survey drew more than 5,000 responses.
Nearly all (98%) of EM physicians who have treated COVID-19 patients said that they have done so since the beginning, when the World Health Organization declared a pandemic on March 11, 2020. For all U.S. physicians, the percentage was much higher than that – 73% said they had treated COVID-19 patients from the start.
EM physicians have often found themselves sacrificing their own safety for the sake of patients. More than half of EM physicians (54%) said that they had knowingly taken personal safety risks to treat a COVID-19 emergency, a percentage far higher than the 30% of all physicians who said they had done so.
Four percent of EM physicians have received a positive diagnosis of COVID-19 via testing. An additional 2% have been confirmed as having COVID on the basis of symptoms.
Steep income drops
Survey authors wrote that two-thirds of EM physicians have experienced income loss during the pandemic. Most (71%) saw their income drop by between 11% and 50%; 11% saw a decrease of more than 50%. Among other specialties, the percentages of those who have experienced a drop of more than 50% are far higher. Among ophthalmologists, 51% said they had experienced such a drop; among allergists, 46%; plastic surgeons, 46%; and otolaryngologists, 45%.
Asked whether their burnout levels have increased in the wake of COVID-19, 74% of EM physicians said burnout had intensified; 23% reported no change; and 3% said burnout had lessened.
Reports of loneliness have been widespread during the pandemic, owing to stay-at-home orders and social distancing. More EM physicians than physicians in general said feelings of loneliness had increased for them in the past year.
More than half of EM doctors (55%) said they are experiencing more loneliness in the pandemic, compared with 46% of all physicians who felt that way; 42% said those feelings have not changed; and 3% said they have been less lonely.
Grief and stress relief
Fewer than half (42%) of the respondents reported that their workplace offers clinician activities to help with grief and stress; 39% said their workplace didn’t offer such help; and 19% said they were unsure.
The percentages were nearly identical to the percentages of physicians overall who answered whether their workplace offered help for grief and stress.
Along with insecurity regarding physical and mental health, COVID-19 has introduced more questions about financial health. Here’s a look at how emergency physicians said they would change the way they save and spend.
Challenges to daily practice
By the time this survey was taken, a large percentage of patients had delayed or avoided urgent or routine medical care for reasons related to COVID-19, so survey authors asked whether EM physicians’ patient population had changed.
Survey authors wrote that “most EM physicians (82%) are seeing patients with non-COVID diseases, such as cardiovascular problems or diabetes, who otherwise probably would have sought treatment earlier.”
COVID-19 has also thrown a major obstacle into most EM physicians’ careers by preventing them from doing the job to the best of their ability. That loss is one of the three primary components of burnout.
More than two-thirds (67%) said COVID-19 has hampered their ability to be as good a doctor as they would like.
A version of this article first appeared on Medscape.com.
Cardiometabolic Center Alliance promotes multiorgan, integrated T2D treatment
A one-stop shop approach to managing the spectrum of complications in patients with type 2 diabetes with a coordinated, multidisciplinary team of clinicians has taken root in at least two U.S. medical centers, and their efforts have now joined to take this concept national through the Cardiometabolic Center Alliance, which hopes to have at least 20 such centers running by the end of 2022.
In patients with type 2 diabetes (T2D), “multiple organs are affected by the same disease process,” notably the heart, kidneys, vasculature, and liver, but the care these patients often receive today is “fragmented, and typically without good coordination,” explained Mikhail N. Kosiborod, MD, a cardiologist and codirector of the Saint Luke’s Michael & Marlys Haverty Cardiometabolic Center of Excellence in Kansas City, Mo.
“We need to depart from the outdated idea that each medical specialty focuses on an organ system. It’s one patient with one disease that affects multiple organs and needs comprehensive, multidisciplinary care,” he said.
Historically, “we’ve looked to primary care physicians to ‘conduct the orchestra’ for complex, multispecialty care” for patients with T2D, but a recent “avalanche” of new treatments with new data and recommendations has made coordination by a single, generalist physician essentially impossible. “It isn’t realistic” to expect a single primary care physician to coordinate all the care a patient with T2D now needs to receive, said Dr. Kosiborod, who is also a professor of medicine at the University of Missouri–Kansas City. Plus, “patients can get lost” when they try to navigate on their own among several physicians, possibly in disparate locations, and without fully understanding what each physician is responsible for managing.
Application of recommended treatments ‘lagging’
“The data are there, and the recommendations are there for T2D and cardiovascular disease, heart failure, and diabetic kidney disease, but the problem has been implementation,” said Dr. Kosiborod. “Application in practice is lagging way behind the recommendations.” That led him and his associates to devise a “new model of care for patients with T2D,” the cardiometabolic center (CMC), as a status quo alternative.
The CMC paradigm is that patients with T2D, especially those with existing cardiovascular or chronic kidney disease or at high risk for these complications, undergo assessment and treatment at one site from a multidisciplinary staff of physicians and allied caregivers including nurse practitioners, nurse coordinators, pharmacists, dieticians, and diabetes educators who are cross-trained for managing both T2D and cardiovascular diseases.
The Cardiometabolic Center Alliance builds on the idea that this care model is defined by a set of detailed treatment protocols and processes of care that other sites can adopt to boost the number of patients aided by this approach, to gather data from a larger patient pool in a dedicated registry to better document the program’s impact, and to form a quality-improvement network that can collectively improve performance.
“It’s absolutely replicable,” maintained Dr. Kosiborod, who is also executive director of the Cardiometabolic Center Alliance. “We’ve codified all of the care and medications into an impressive package. We now have something that works, and many other centers are interested in building programs like this. By establishing a base of well-defined protocols and operating procedures we can train a cadre of allied professionals who can effectively implement the program across wider populations of patients, while using the brick and mortar center to manage more complex patients,” he added.
“We’re not taking patients” from primary care physicians, Dr. Kosiborod stressed. “We’re helping generalists give better care. They already have their hands full. We’re here to help physicians do better.”
He cited a recent study of 1,735 patients with atherosclerotic cardiovascular disease and diabetes (96% with T2D) enrolled in a registry at 119 U.S. sites during 2016-2018 that found less than 7% were on the full range of guideline-directed medical therapy that they qualified for based on existing treatment guidelines. “This is not acceptable,” Dr. Kosiborod declared.
“It’s so obvious that this needs to be a combined approach. It’s very difficult to have one provider take care of all of the T2D complications. There needs to be a new approach, and [the Cardiometabolic Center program at Saint Luke’s] has done a great job getting their initiative underway to take a more global approach,” commented Ralph A. DeFronzo, MD, chief of the diabetes division and professor of medicine at the University of Texas Health Science Center, San Antonio.
Early results show improved metrics
The Saint Luke’s Haverty CMC launched in 2019, and data from its first 129 patients with at least one follow-up visit documented early efficacy for the program, as reported at the American Heart Association’s Quality of Care and Outcome’s Research meeting, held virtually on May 15 and 16, 2020.
That analysis from Dr. Kosiborod and associates compared various short-term metrics among their CMC patients against a control cohort of 387 similar patients with T2D who also received care in the Saint Luke’s Health System during 2019 but outside of the CMC. This observational study involved no patient randomization, but the researchers used propensity scoring to match the control patients with those managed in the CMC by several demographic and clinical parameters.
During follow-up that was generally less than 6 months, patients managed in the CMC averaged 12 pounds of weight loss, a 0.5% reduction in their average hemoglobin A1c, a mean 4.6–mm Hg cut in their systolic blood pressure, an average drop in their LDL cholesterol of 11.4 mg/dL, and among those receiving insulin the daily, average insulin dose fell by a relative 43%, compared with baseline. Among the controls, averages for these five parameters were weight loss of 2 pounds, a cut in A1c of 0.2%, a systolic blood pressure reduction of 0.6 mm Hg, a drop in LDL cholesterol of 4.9 mg/dL, and a relative rise in insulin dose of 6%. All of these between group differences were statistically significant except for LDL cholesterol.
Additional analysis of the medications that patients in the CMC and control group received also showed striking differences. Combined prescriptions for all components of guideline-directed medical therapy went to 41% of the CMC patients, compared with 2% of the controls, a statistically significant difference. Contributing to this difference were significantly increased rates of prescriptions for ACE inhibitors and statins.
The CMC staff also started 57% of their patients on a SGLT2 inhibitor and 90% on a GLP-1 receptor agonist (GLP-1 RA), compared with rates of 18% and 13%, respectively, among controls. Both of these between-group differences were also significant, and they highlighted the willingness and success of the CMC clinicians to put a large number of their patients on agents from both of these beneficial drug classes. This is a notable change from usual recent practice that limits most patients who actually receive these medications to a drug from just one of these two classes, often because of real or perceived limits on insurance coverage.
The data from these initial patients in the Saint Luke’s CMC show that the program was “very successful; it looks very promising,” said Dr. Kosiborod. The results show “transformational improvement in the quality of care.” Subsequent to this initial cohort from 2019, the Saint Luke’s CMC has seen “hundreds” of additional patients with T2D.
The Cardiometabolic Center Alliance gets started
The second member of the Cardiometabolic Center Alliance is a program run by the University Hospitals system based in Cleveland that had begun earlier in 2020. The University Hospitals’ Center for Integrated and Novel Approaches in Vascular-Metabolic Disease (CINEMA) uses a comprehensive, multidisciplinary-care model developed independently of but very similar to the Saint Luke’s CMC. By the end of 2020, the CINEMA program had managed about 150 patients, said Sanjay Rajagopalan, MD, director of CINEMA and a professor of medicine at Case Western Reserve University, Cleveland.
“Our outcomes have been quite similar” to what the Saint Luke’s program reported, he said. “We had better use of guideline-directed therapies, more weight loss, and better control of metabolic parameters.” The CINEMA program entered the Cardiometabolic Center Alliance as a “key strategic partner,” which means it will have a role in shaping the alliance going forward. One issue the alliance faces is how to leverage its growth to improve management of patients with T2D who do not have access to a CMC.
The CMCs “are not meant for every patient with T2D, but for those with high risk for cardiovascular complications who require extra attention,” Dr. Rajagopalan said in an interview. Both he and Dr. Kosiborod acknowledged that, even if 200 CMCs were to eventually open, and even if each center averaged 5,000 managed patients, those 1 million patients would be a small fraction of the total number of U.S. patients with T2D.
“Having these centers will produce a ripple effect. The protocols will percolate to primary care physicians,” Dr. Rajagopalan predicted. Once that happens, “not all patients will need to go to a cardiometabolic center.” In addition, leveraging established protocols via nurse coordinators and virtual care could bring this model to many more patients, Dr. Kosiborod noted.
By the end of 2020, a total of three additional U.S. centers had joined Saint Luke’s and University Hospitals in the alliance, but Dr. Kosiborod said that none of the three had yet been officially announced. The alliance has also started a national cardiometabolic registry, which will be “instrumental for its mission to track, benchmark, and improve quality of care and outcomes; enable mechanisms for “learning health care systems”; and can be used to answer important research questions,” Dr. Kosiborod said.
Combined SGLT2 inhibitor and GLP-1 RA treatment takes off
A key element of the more aggressive, risk-driven management emphasized in the CMC approach is frequent use of combined treatment with an SGLT2 inhibitor and a GLP-1 RA. Both classes of glucose-lowering drugs have well-documented, risk-reducing benefits, notably reduced atherosclerotic cardiovascular events and weight loss produced by the GLP1-RAs, and cuts in heart failure onset and hospitalizations and slowing of chronic kidney disease progression by the SGLT2 inhibitors.
Until now, medical society recommendations as well as opinion leaders have approached these two drug classes with a presumption that physicians would usually prescribe patients an agent from only one of these two classes, largely because the high cost of agents in both classes, all still under patent, often means coverage limits by insurers. Physicians at both the Saint Luke’s and University Hospitals programs have been more proactive, and successful, in prescribing agents from both classes to their high-risk patients with T2D.
“We use combination treatment quite a bit,” said Dr. Kosiborod. “It’s very sensible to use both. Their mechanisms of action are different and likely don’t overlap, so it’s reasonable to presume their activity is complimentary.” But he acknowledged that this has not yet been formally studied for cardiovascular or renal outcomes. Study results have documented complimentary effects between the two classes for weight loss, blood pressure reduction, and to some extent A1c reduction. A key reason for more frequent combined treatment with an SGLT2 inhibitor and GLP-1 RA is increased focus on the ability of both drug classes to lower risk in patients with T2D and high cardiovascular-disease risk, rather than prescribing decisions driven largely by trying to further reduce a patient’s A1c.
Although insurance coverage is not a given, the Saint Luke’s CMC has had good results using patient-assistance programs run by various drug companies. Some patients have received their medications free of charge or with modest copays, depending on their income and insurance coverage. At Saint Luke’s, “many” patients with T2D have been able to get free medications through assistance programs, he said. And for patients with health insurance, getting coverage for an agent from each class “is easier now than it was 3-4 years ago.”
Dr. Kosiborod has been a consultant to several companies, and has received research grants from AstraZeneca and Boehringer Ingelheim. Dr. DeFronzo received research grants from Astra Zeneca, Janssen, and Merck; he has been an adviser to AstraZeneca, Boehringer Ingelheim, Intarcia, Janssen, and Novo Nordisk; and he has been a speaker on behalf of AstraZeneca and Novo Nordisk. Dr. Rajagopalan has been a consultant to Novo Nordisk and Takeda.
A one-stop shop approach to managing the spectrum of complications in patients with type 2 diabetes with a coordinated, multidisciplinary team of clinicians has taken root in at least two U.S. medical centers, and their efforts have now joined to take this concept national through the Cardiometabolic Center Alliance, which hopes to have at least 20 such centers running by the end of 2022.
In patients with type 2 diabetes (T2D), “multiple organs are affected by the same disease process,” notably the heart, kidneys, vasculature, and liver, but the care these patients often receive today is “fragmented, and typically without good coordination,” explained Mikhail N. Kosiborod, MD, a cardiologist and codirector of the Saint Luke’s Michael & Marlys Haverty Cardiometabolic Center of Excellence in Kansas City, Mo.
“We need to depart from the outdated idea that each medical specialty focuses on an organ system. It’s one patient with one disease that affects multiple organs and needs comprehensive, multidisciplinary care,” he said.
Historically, “we’ve looked to primary care physicians to ‘conduct the orchestra’ for complex, multispecialty care” for patients with T2D, but a recent “avalanche” of new treatments with new data and recommendations has made coordination by a single, generalist physician essentially impossible. “It isn’t realistic” to expect a single primary care physician to coordinate all the care a patient with T2D now needs to receive, said Dr. Kosiborod, who is also a professor of medicine at the University of Missouri–Kansas City. Plus, “patients can get lost” when they try to navigate on their own among several physicians, possibly in disparate locations, and without fully understanding what each physician is responsible for managing.
Application of recommended treatments ‘lagging’
“The data are there, and the recommendations are there for T2D and cardiovascular disease, heart failure, and diabetic kidney disease, but the problem has been implementation,” said Dr. Kosiborod. “Application in practice is lagging way behind the recommendations.” That led him and his associates to devise a “new model of care for patients with T2D,” the cardiometabolic center (CMC), as a status quo alternative.
The CMC paradigm is that patients with T2D, especially those with existing cardiovascular or chronic kidney disease or at high risk for these complications, undergo assessment and treatment at one site from a multidisciplinary staff of physicians and allied caregivers including nurse practitioners, nurse coordinators, pharmacists, dieticians, and diabetes educators who are cross-trained for managing both T2D and cardiovascular diseases.
The Cardiometabolic Center Alliance builds on the idea that this care model is defined by a set of detailed treatment protocols and processes of care that other sites can adopt to boost the number of patients aided by this approach, to gather data from a larger patient pool in a dedicated registry to better document the program’s impact, and to form a quality-improvement network that can collectively improve performance.
“It’s absolutely replicable,” maintained Dr. Kosiborod, who is also executive director of the Cardiometabolic Center Alliance. “We’ve codified all of the care and medications into an impressive package. We now have something that works, and many other centers are interested in building programs like this. By establishing a base of well-defined protocols and operating procedures we can train a cadre of allied professionals who can effectively implement the program across wider populations of patients, while using the brick and mortar center to manage more complex patients,” he added.
“We’re not taking patients” from primary care physicians, Dr. Kosiborod stressed. “We’re helping generalists give better care. They already have their hands full. We’re here to help physicians do better.”
He cited a recent study of 1,735 patients with atherosclerotic cardiovascular disease and diabetes (96% with T2D) enrolled in a registry at 119 U.S. sites during 2016-2018 that found less than 7% were on the full range of guideline-directed medical therapy that they qualified for based on existing treatment guidelines. “This is not acceptable,” Dr. Kosiborod declared.
“It’s so obvious that this needs to be a combined approach. It’s very difficult to have one provider take care of all of the T2D complications. There needs to be a new approach, and [the Cardiometabolic Center program at Saint Luke’s] has done a great job getting their initiative underway to take a more global approach,” commented Ralph A. DeFronzo, MD, chief of the diabetes division and professor of medicine at the University of Texas Health Science Center, San Antonio.
Early results show improved metrics
The Saint Luke’s Haverty CMC launched in 2019, and data from its first 129 patients with at least one follow-up visit documented early efficacy for the program, as reported at the American Heart Association’s Quality of Care and Outcome’s Research meeting, held virtually on May 15 and 16, 2020.
That analysis from Dr. Kosiborod and associates compared various short-term metrics among their CMC patients against a control cohort of 387 similar patients with T2D who also received care in the Saint Luke’s Health System during 2019 but outside of the CMC. This observational study involved no patient randomization, but the researchers used propensity scoring to match the control patients with those managed in the CMC by several demographic and clinical parameters.
During follow-up that was generally less than 6 months, patients managed in the CMC averaged 12 pounds of weight loss, a 0.5% reduction in their average hemoglobin A1c, a mean 4.6–mm Hg cut in their systolic blood pressure, an average drop in their LDL cholesterol of 11.4 mg/dL, and among those receiving insulin the daily, average insulin dose fell by a relative 43%, compared with baseline. Among the controls, averages for these five parameters were weight loss of 2 pounds, a cut in A1c of 0.2%, a systolic blood pressure reduction of 0.6 mm Hg, a drop in LDL cholesterol of 4.9 mg/dL, and a relative rise in insulin dose of 6%. All of these between group differences were statistically significant except for LDL cholesterol.
Additional analysis of the medications that patients in the CMC and control group received also showed striking differences. Combined prescriptions for all components of guideline-directed medical therapy went to 41% of the CMC patients, compared with 2% of the controls, a statistically significant difference. Contributing to this difference were significantly increased rates of prescriptions for ACE inhibitors and statins.
The CMC staff also started 57% of their patients on a SGLT2 inhibitor and 90% on a GLP-1 receptor agonist (GLP-1 RA), compared with rates of 18% and 13%, respectively, among controls. Both of these between-group differences were also significant, and they highlighted the willingness and success of the CMC clinicians to put a large number of their patients on agents from both of these beneficial drug classes. This is a notable change from usual recent practice that limits most patients who actually receive these medications to a drug from just one of these two classes, often because of real or perceived limits on insurance coverage.
The data from these initial patients in the Saint Luke’s CMC show that the program was “very successful; it looks very promising,” said Dr. Kosiborod. The results show “transformational improvement in the quality of care.” Subsequent to this initial cohort from 2019, the Saint Luke’s CMC has seen “hundreds” of additional patients with T2D.
The Cardiometabolic Center Alliance gets started
The second member of the Cardiometabolic Center Alliance is a program run by the University Hospitals system based in Cleveland that had begun earlier in 2020. The University Hospitals’ Center for Integrated and Novel Approaches in Vascular-Metabolic Disease (CINEMA) uses a comprehensive, multidisciplinary-care model developed independently of but very similar to the Saint Luke’s CMC. By the end of 2020, the CINEMA program had managed about 150 patients, said Sanjay Rajagopalan, MD, director of CINEMA and a professor of medicine at Case Western Reserve University, Cleveland.
“Our outcomes have been quite similar” to what the Saint Luke’s program reported, he said. “We had better use of guideline-directed therapies, more weight loss, and better control of metabolic parameters.” The CINEMA program entered the Cardiometabolic Center Alliance as a “key strategic partner,” which means it will have a role in shaping the alliance going forward. One issue the alliance faces is how to leverage its growth to improve management of patients with T2D who do not have access to a CMC.
The CMCs “are not meant for every patient with T2D, but for those with high risk for cardiovascular complications who require extra attention,” Dr. Rajagopalan said in an interview. Both he and Dr. Kosiborod acknowledged that, even if 200 CMCs were to eventually open, and even if each center averaged 5,000 managed patients, those 1 million patients would be a small fraction of the total number of U.S. patients with T2D.
“Having these centers will produce a ripple effect. The protocols will percolate to primary care physicians,” Dr. Rajagopalan predicted. Once that happens, “not all patients will need to go to a cardiometabolic center.” In addition, leveraging established protocols via nurse coordinators and virtual care could bring this model to many more patients, Dr. Kosiborod noted.
By the end of 2020, a total of three additional U.S. centers had joined Saint Luke’s and University Hospitals in the alliance, but Dr. Kosiborod said that none of the three had yet been officially announced. The alliance has also started a national cardiometabolic registry, which will be “instrumental for its mission to track, benchmark, and improve quality of care and outcomes; enable mechanisms for “learning health care systems”; and can be used to answer important research questions,” Dr. Kosiborod said.
Combined SGLT2 inhibitor and GLP-1 RA treatment takes off
A key element of the more aggressive, risk-driven management emphasized in the CMC approach is frequent use of combined treatment with an SGLT2 inhibitor and a GLP-1 RA. Both classes of glucose-lowering drugs have well-documented, risk-reducing benefits, notably reduced atherosclerotic cardiovascular events and weight loss produced by the GLP1-RAs, and cuts in heart failure onset and hospitalizations and slowing of chronic kidney disease progression by the SGLT2 inhibitors.
Until now, medical society recommendations as well as opinion leaders have approached these two drug classes with a presumption that physicians would usually prescribe patients an agent from only one of these two classes, largely because the high cost of agents in both classes, all still under patent, often means coverage limits by insurers. Physicians at both the Saint Luke’s and University Hospitals programs have been more proactive, and successful, in prescribing agents from both classes to their high-risk patients with T2D.
“We use combination treatment quite a bit,” said Dr. Kosiborod. “It’s very sensible to use both. Their mechanisms of action are different and likely don’t overlap, so it’s reasonable to presume their activity is complimentary.” But he acknowledged that this has not yet been formally studied for cardiovascular or renal outcomes. Study results have documented complimentary effects between the two classes for weight loss, blood pressure reduction, and to some extent A1c reduction. A key reason for more frequent combined treatment with an SGLT2 inhibitor and GLP-1 RA is increased focus on the ability of both drug classes to lower risk in patients with T2D and high cardiovascular-disease risk, rather than prescribing decisions driven largely by trying to further reduce a patient’s A1c.
Although insurance coverage is not a given, the Saint Luke’s CMC has had good results using patient-assistance programs run by various drug companies. Some patients have received their medications free of charge or with modest copays, depending on their income and insurance coverage. At Saint Luke’s, “many” patients with T2D have been able to get free medications through assistance programs, he said. And for patients with health insurance, getting coverage for an agent from each class “is easier now than it was 3-4 years ago.”
Dr. Kosiborod has been a consultant to several companies, and has received research grants from AstraZeneca and Boehringer Ingelheim. Dr. DeFronzo received research grants from Astra Zeneca, Janssen, and Merck; he has been an adviser to AstraZeneca, Boehringer Ingelheim, Intarcia, Janssen, and Novo Nordisk; and he has been a speaker on behalf of AstraZeneca and Novo Nordisk. Dr. Rajagopalan has been a consultant to Novo Nordisk and Takeda.
A one-stop shop approach to managing the spectrum of complications in patients with type 2 diabetes with a coordinated, multidisciplinary team of clinicians has taken root in at least two U.S. medical centers, and their efforts have now joined to take this concept national through the Cardiometabolic Center Alliance, which hopes to have at least 20 such centers running by the end of 2022.
In patients with type 2 diabetes (T2D), “multiple organs are affected by the same disease process,” notably the heart, kidneys, vasculature, and liver, but the care these patients often receive today is “fragmented, and typically without good coordination,” explained Mikhail N. Kosiborod, MD, a cardiologist and codirector of the Saint Luke’s Michael & Marlys Haverty Cardiometabolic Center of Excellence in Kansas City, Mo.
“We need to depart from the outdated idea that each medical specialty focuses on an organ system. It’s one patient with one disease that affects multiple organs and needs comprehensive, multidisciplinary care,” he said.
Historically, “we’ve looked to primary care physicians to ‘conduct the orchestra’ for complex, multispecialty care” for patients with T2D, but a recent “avalanche” of new treatments with new data and recommendations has made coordination by a single, generalist physician essentially impossible. “It isn’t realistic” to expect a single primary care physician to coordinate all the care a patient with T2D now needs to receive, said Dr. Kosiborod, who is also a professor of medicine at the University of Missouri–Kansas City. Plus, “patients can get lost” when they try to navigate on their own among several physicians, possibly in disparate locations, and without fully understanding what each physician is responsible for managing.
Application of recommended treatments ‘lagging’
“The data are there, and the recommendations are there for T2D and cardiovascular disease, heart failure, and diabetic kidney disease, but the problem has been implementation,” said Dr. Kosiborod. “Application in practice is lagging way behind the recommendations.” That led him and his associates to devise a “new model of care for patients with T2D,” the cardiometabolic center (CMC), as a status quo alternative.
The CMC paradigm is that patients with T2D, especially those with existing cardiovascular or chronic kidney disease or at high risk for these complications, undergo assessment and treatment at one site from a multidisciplinary staff of physicians and allied caregivers including nurse practitioners, nurse coordinators, pharmacists, dieticians, and diabetes educators who are cross-trained for managing both T2D and cardiovascular diseases.
The Cardiometabolic Center Alliance builds on the idea that this care model is defined by a set of detailed treatment protocols and processes of care that other sites can adopt to boost the number of patients aided by this approach, to gather data from a larger patient pool in a dedicated registry to better document the program’s impact, and to form a quality-improvement network that can collectively improve performance.
“It’s absolutely replicable,” maintained Dr. Kosiborod, who is also executive director of the Cardiometabolic Center Alliance. “We’ve codified all of the care and medications into an impressive package. We now have something that works, and many other centers are interested in building programs like this. By establishing a base of well-defined protocols and operating procedures we can train a cadre of allied professionals who can effectively implement the program across wider populations of patients, while using the brick and mortar center to manage more complex patients,” he added.
“We’re not taking patients” from primary care physicians, Dr. Kosiborod stressed. “We’re helping generalists give better care. They already have their hands full. We’re here to help physicians do better.”
He cited a recent study of 1,735 patients with atherosclerotic cardiovascular disease and diabetes (96% with T2D) enrolled in a registry at 119 U.S. sites during 2016-2018 that found less than 7% were on the full range of guideline-directed medical therapy that they qualified for based on existing treatment guidelines. “This is not acceptable,” Dr. Kosiborod declared.
“It’s so obvious that this needs to be a combined approach. It’s very difficult to have one provider take care of all of the T2D complications. There needs to be a new approach, and [the Cardiometabolic Center program at Saint Luke’s] has done a great job getting their initiative underway to take a more global approach,” commented Ralph A. DeFronzo, MD, chief of the diabetes division and professor of medicine at the University of Texas Health Science Center, San Antonio.
Early results show improved metrics
The Saint Luke’s Haverty CMC launched in 2019, and data from its first 129 patients with at least one follow-up visit documented early efficacy for the program, as reported at the American Heart Association’s Quality of Care and Outcome’s Research meeting, held virtually on May 15 and 16, 2020.
That analysis from Dr. Kosiborod and associates compared various short-term metrics among their CMC patients against a control cohort of 387 similar patients with T2D who also received care in the Saint Luke’s Health System during 2019 but outside of the CMC. This observational study involved no patient randomization, but the researchers used propensity scoring to match the control patients with those managed in the CMC by several demographic and clinical parameters.
During follow-up that was generally less than 6 months, patients managed in the CMC averaged 12 pounds of weight loss, a 0.5% reduction in their average hemoglobin A1c, a mean 4.6–mm Hg cut in their systolic blood pressure, an average drop in their LDL cholesterol of 11.4 mg/dL, and among those receiving insulin the daily, average insulin dose fell by a relative 43%, compared with baseline. Among the controls, averages for these five parameters were weight loss of 2 pounds, a cut in A1c of 0.2%, a systolic blood pressure reduction of 0.6 mm Hg, a drop in LDL cholesterol of 4.9 mg/dL, and a relative rise in insulin dose of 6%. All of these between group differences were statistically significant except for LDL cholesterol.
Additional analysis of the medications that patients in the CMC and control group received also showed striking differences. Combined prescriptions for all components of guideline-directed medical therapy went to 41% of the CMC patients, compared with 2% of the controls, a statistically significant difference. Contributing to this difference were significantly increased rates of prescriptions for ACE inhibitors and statins.
The CMC staff also started 57% of their patients on a SGLT2 inhibitor and 90% on a GLP-1 receptor agonist (GLP-1 RA), compared with rates of 18% and 13%, respectively, among controls. Both of these between-group differences were also significant, and they highlighted the willingness and success of the CMC clinicians to put a large number of their patients on agents from both of these beneficial drug classes. This is a notable change from usual recent practice that limits most patients who actually receive these medications to a drug from just one of these two classes, often because of real or perceived limits on insurance coverage.
The data from these initial patients in the Saint Luke’s CMC show that the program was “very successful; it looks very promising,” said Dr. Kosiborod. The results show “transformational improvement in the quality of care.” Subsequent to this initial cohort from 2019, the Saint Luke’s CMC has seen “hundreds” of additional patients with T2D.
The Cardiometabolic Center Alliance gets started
The second member of the Cardiometabolic Center Alliance is a program run by the University Hospitals system based in Cleveland that had begun earlier in 2020. The University Hospitals’ Center for Integrated and Novel Approaches in Vascular-Metabolic Disease (CINEMA) uses a comprehensive, multidisciplinary-care model developed independently of but very similar to the Saint Luke’s CMC. By the end of 2020, the CINEMA program had managed about 150 patients, said Sanjay Rajagopalan, MD, director of CINEMA and a professor of medicine at Case Western Reserve University, Cleveland.
“Our outcomes have been quite similar” to what the Saint Luke’s program reported, he said. “We had better use of guideline-directed therapies, more weight loss, and better control of metabolic parameters.” The CINEMA program entered the Cardiometabolic Center Alliance as a “key strategic partner,” which means it will have a role in shaping the alliance going forward. One issue the alliance faces is how to leverage its growth to improve management of patients with T2D who do not have access to a CMC.
The CMCs “are not meant for every patient with T2D, but for those with high risk for cardiovascular complications who require extra attention,” Dr. Rajagopalan said in an interview. Both he and Dr. Kosiborod acknowledged that, even if 200 CMCs were to eventually open, and even if each center averaged 5,000 managed patients, those 1 million patients would be a small fraction of the total number of U.S. patients with T2D.
“Having these centers will produce a ripple effect. The protocols will percolate to primary care physicians,” Dr. Rajagopalan predicted. Once that happens, “not all patients will need to go to a cardiometabolic center.” In addition, leveraging established protocols via nurse coordinators and virtual care could bring this model to many more patients, Dr. Kosiborod noted.
By the end of 2020, a total of three additional U.S. centers had joined Saint Luke’s and University Hospitals in the alliance, but Dr. Kosiborod said that none of the three had yet been officially announced. The alliance has also started a national cardiometabolic registry, which will be “instrumental for its mission to track, benchmark, and improve quality of care and outcomes; enable mechanisms for “learning health care systems”; and can be used to answer important research questions,” Dr. Kosiborod said.
Combined SGLT2 inhibitor and GLP-1 RA treatment takes off
A key element of the more aggressive, risk-driven management emphasized in the CMC approach is frequent use of combined treatment with an SGLT2 inhibitor and a GLP-1 RA. Both classes of glucose-lowering drugs have well-documented, risk-reducing benefits, notably reduced atherosclerotic cardiovascular events and weight loss produced by the GLP1-RAs, and cuts in heart failure onset and hospitalizations and slowing of chronic kidney disease progression by the SGLT2 inhibitors.
Until now, medical society recommendations as well as opinion leaders have approached these two drug classes with a presumption that physicians would usually prescribe patients an agent from only one of these two classes, largely because the high cost of agents in both classes, all still under patent, often means coverage limits by insurers. Physicians at both the Saint Luke’s and University Hospitals programs have been more proactive, and successful, in prescribing agents from both classes to their high-risk patients with T2D.
“We use combination treatment quite a bit,” said Dr. Kosiborod. “It’s very sensible to use both. Their mechanisms of action are different and likely don’t overlap, so it’s reasonable to presume their activity is complimentary.” But he acknowledged that this has not yet been formally studied for cardiovascular or renal outcomes. Study results have documented complimentary effects between the two classes for weight loss, blood pressure reduction, and to some extent A1c reduction. A key reason for more frequent combined treatment with an SGLT2 inhibitor and GLP-1 RA is increased focus on the ability of both drug classes to lower risk in patients with T2D and high cardiovascular-disease risk, rather than prescribing decisions driven largely by trying to further reduce a patient’s A1c.
Although insurance coverage is not a given, the Saint Luke’s CMC has had good results using patient-assistance programs run by various drug companies. Some patients have received their medications free of charge or with modest copays, depending on their income and insurance coverage. At Saint Luke’s, “many” patients with T2D have been able to get free medications through assistance programs, he said. And for patients with health insurance, getting coverage for an agent from each class “is easier now than it was 3-4 years ago.”
Dr. Kosiborod has been a consultant to several companies, and has received research grants from AstraZeneca and Boehringer Ingelheim. Dr. DeFronzo received research grants from Astra Zeneca, Janssen, and Merck; he has been an adviser to AstraZeneca, Boehringer Ingelheim, Intarcia, Janssen, and Novo Nordisk; and he has been a speaker on behalf of AstraZeneca and Novo Nordisk. Dr. Rajagopalan has been a consultant to Novo Nordisk and Takeda.
How COVID-19 will continue to alter patient visits
Finding the current domestic and global situations too disheartening to write about, I have decided for the moment to take the long view in hopes of finding something to stimulate your imaginations. It appears that we have several vaccines effective against SARS-CoV-2 if not in your hands at the moment at least in someone’s freezer or at the very least somewhere near beginning of their journey in the production pipeline. It may be a year of more but thanks to the vaccines and herd immunity there will be a time when parents may feel more comfortable about bringing their children into your office. How are you going to dial back your office routine to something even vaguely familiar?
To keep your office afloat financially you have probably been forced to adopt and adapt telemedicine strategies to your practice style. Prior to the pandemic you may have been among the few who were actively experimenting with practicing remotely. But, it is more likely that you had given little serious thought to how you would manage your patients without them being physically present.
You probably carried in your mind a list of symptoms and complaints which you had promised yourself that you would never treat without first laying eyes and hands on the patient. You may have even codified this list into a set of guidelines that you included in the office manual for your nurses, assistants, and receptionists. You may have looked askance at some of your colleagues whom you felt too often treated their patients (and yours when they were covering) based on what seemed to be scanty information gleaned from a phone call. The impropriety of this kind of clinical behavior may have even come up at staff meetings or at least been the topic of hallway discussions.
How did your list of complaints that demanded an in-person visit evolve? I suspect that in large part it was formed as you modeled the behavior of your mentors and teachers. In some cases you may have heard of tragic cases in which a child had died or suffered serious consequences of being treated without an in-person evaluation. In many cases you were following a tradition or ethic that said treating in certain circumstances without an exam just wasn’t done.
Have the realities of the pandemic forced you to alter your list of must-see-before-I’ll-treat complaints? Have you found yourself calling in antibiotic prescriptions for children with ear pain who 1 year ago you would have told to come in for an office visit? Are you treating “strep throats” without a rapid strep test or culture? How many stimulant prescriptions have you refilled for children who haven’t been reevaluated in the office in over a year? How are you going to manage the tsunami of requests for sports physicals once the junior high and high school teams are allowed to return to action? You probably won’t have the time to examine all of the sports candidates who show up in your office with crumpled forms recently retrieved from crumb-filled backpacks.
Where are you going to reset the bar as the pandemic lifts and the barriers that have prevented patients from coming to your office over the last year or year and a half recede? Have you realized that many of your office visits in prepandemic times were unnecessary? How many children with otitis really needed to be followed up with an ear recheck visit? Which children with sore throats and a fever needed to be examined? Was a yearly exam really necessary for a high school sophomore who wanted to play basketball? Has your comfort zone widened to include more patient complaints that can be managed without a face to face encounter? Where will telemedicine fit into the mix?
At some time in the next 12 months you will have to recalibrate and reset the bar. It will probably be a gradual process that in large part can be molded by the responses of the families who may have also come to realize that seeing you in the office isn’t quite as necessary as you both may have thought it was.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com
Finding the current domestic and global situations too disheartening to write about, I have decided for the moment to take the long view in hopes of finding something to stimulate your imaginations. It appears that we have several vaccines effective against SARS-CoV-2 if not in your hands at the moment at least in someone’s freezer or at the very least somewhere near beginning of their journey in the production pipeline. It may be a year of more but thanks to the vaccines and herd immunity there will be a time when parents may feel more comfortable about bringing their children into your office. How are you going to dial back your office routine to something even vaguely familiar?
To keep your office afloat financially you have probably been forced to adopt and adapt telemedicine strategies to your practice style. Prior to the pandemic you may have been among the few who were actively experimenting with practicing remotely. But, it is more likely that you had given little serious thought to how you would manage your patients without them being physically present.
You probably carried in your mind a list of symptoms and complaints which you had promised yourself that you would never treat without first laying eyes and hands on the patient. You may have even codified this list into a set of guidelines that you included in the office manual for your nurses, assistants, and receptionists. You may have looked askance at some of your colleagues whom you felt too often treated their patients (and yours when they were covering) based on what seemed to be scanty information gleaned from a phone call. The impropriety of this kind of clinical behavior may have even come up at staff meetings or at least been the topic of hallway discussions.
How did your list of complaints that demanded an in-person visit evolve? I suspect that in large part it was formed as you modeled the behavior of your mentors and teachers. In some cases you may have heard of tragic cases in which a child had died or suffered serious consequences of being treated without an in-person evaluation. In many cases you were following a tradition or ethic that said treating in certain circumstances without an exam just wasn’t done.
Have the realities of the pandemic forced you to alter your list of must-see-before-I’ll-treat complaints? Have you found yourself calling in antibiotic prescriptions for children with ear pain who 1 year ago you would have told to come in for an office visit? Are you treating “strep throats” without a rapid strep test or culture? How many stimulant prescriptions have you refilled for children who haven’t been reevaluated in the office in over a year? How are you going to manage the tsunami of requests for sports physicals once the junior high and high school teams are allowed to return to action? You probably won’t have the time to examine all of the sports candidates who show up in your office with crumpled forms recently retrieved from crumb-filled backpacks.
Where are you going to reset the bar as the pandemic lifts and the barriers that have prevented patients from coming to your office over the last year or year and a half recede? Have you realized that many of your office visits in prepandemic times were unnecessary? How many children with otitis really needed to be followed up with an ear recheck visit? Which children with sore throats and a fever needed to be examined? Was a yearly exam really necessary for a high school sophomore who wanted to play basketball? Has your comfort zone widened to include more patient complaints that can be managed without a face to face encounter? Where will telemedicine fit into the mix?
At some time in the next 12 months you will have to recalibrate and reset the bar. It will probably be a gradual process that in large part can be molded by the responses of the families who may have also come to realize that seeing you in the office isn’t quite as necessary as you both may have thought it was.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com
Finding the current domestic and global situations too disheartening to write about, I have decided for the moment to take the long view in hopes of finding something to stimulate your imaginations. It appears that we have several vaccines effective against SARS-CoV-2 if not in your hands at the moment at least in someone’s freezer or at the very least somewhere near beginning of their journey in the production pipeline. It may be a year of more but thanks to the vaccines and herd immunity there will be a time when parents may feel more comfortable about bringing their children into your office. How are you going to dial back your office routine to something even vaguely familiar?
To keep your office afloat financially you have probably been forced to adopt and adapt telemedicine strategies to your practice style. Prior to the pandemic you may have been among the few who were actively experimenting with practicing remotely. But, it is more likely that you had given little serious thought to how you would manage your patients without them being physically present.
You probably carried in your mind a list of symptoms and complaints which you had promised yourself that you would never treat without first laying eyes and hands on the patient. You may have even codified this list into a set of guidelines that you included in the office manual for your nurses, assistants, and receptionists. You may have looked askance at some of your colleagues whom you felt too often treated their patients (and yours when they were covering) based on what seemed to be scanty information gleaned from a phone call. The impropriety of this kind of clinical behavior may have even come up at staff meetings or at least been the topic of hallway discussions.
How did your list of complaints that demanded an in-person visit evolve? I suspect that in large part it was formed as you modeled the behavior of your mentors and teachers. In some cases you may have heard of tragic cases in which a child had died or suffered serious consequences of being treated without an in-person evaluation. In many cases you were following a tradition or ethic that said treating in certain circumstances without an exam just wasn’t done.
Have the realities of the pandemic forced you to alter your list of must-see-before-I’ll-treat complaints? Have you found yourself calling in antibiotic prescriptions for children with ear pain who 1 year ago you would have told to come in for an office visit? Are you treating “strep throats” without a rapid strep test or culture? How many stimulant prescriptions have you refilled for children who haven’t been reevaluated in the office in over a year? How are you going to manage the tsunami of requests for sports physicals once the junior high and high school teams are allowed to return to action? You probably won’t have the time to examine all of the sports candidates who show up in your office with crumpled forms recently retrieved from crumb-filled backpacks.
Where are you going to reset the bar as the pandemic lifts and the barriers that have prevented patients from coming to your office over the last year or year and a half recede? Have you realized that many of your office visits in prepandemic times were unnecessary? How many children with otitis really needed to be followed up with an ear recheck visit? Which children with sore throats and a fever needed to be examined? Was a yearly exam really necessary for a high school sophomore who wanted to play basketball? Has your comfort zone widened to include more patient complaints that can be managed without a face to face encounter? Where will telemedicine fit into the mix?
At some time in the next 12 months you will have to recalibrate and reset the bar. It will probably be a gradual process that in large part can be molded by the responses of the families who may have also come to realize that seeing you in the office isn’t quite as necessary as you both may have thought it was.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com
How much is enough?
How much do I make compared with other doctors?
I see questions like that on surveys I get, asking me to fill something out on the Internet, then I’ll get back a list of how well other docs in my field/city/state/blood type are doing.
Nah. I’ll pass.
Realistically, why? So I can feel I’m superior or inferior to others? Isn’t keeping up with the Joneses the purpose of the doctors’ parking lot at the hospital? (Actually, the number of pricey cars there has dropped off over time).
I really don’t want to know how much others make. It’s probably more than what I make, but that’s the trade-off I accepted when I went with a small solo practice instead of a large group 20 years ago.
We become so obsessed with the question of “how much money should I be making?” and comparing it with the salaries of others that we lose track of the real question: “How much money do I need?”
That should be the real number to look at. How much money do I really need to pay for a comfortable home, support my family, pay for my kids’ education, fund my retirement?
Enough should be as good as a feast.
Yet, even when content we get caught in the trap of comparing ourselves with others. This is human nature. We’re programmed to be competitive to survive. Whether that means anything when we don’t have to be hunters and gatherers is irrelevant. It is who we are.
But we’re also intelligent enough to realize that. I for one, don’t want to know, or care, how much money the neurologist down the street is earning.
To quote Sheryl Crow, “it’s not having what you want, it’s wanting what you’ve got.”
So I’ll skip the comparisons and focus on the only people that really matter to me.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
How much do I make compared with other doctors?
I see questions like that on surveys I get, asking me to fill something out on the Internet, then I’ll get back a list of how well other docs in my field/city/state/blood type are doing.
Nah. I’ll pass.
Realistically, why? So I can feel I’m superior or inferior to others? Isn’t keeping up with the Joneses the purpose of the doctors’ parking lot at the hospital? (Actually, the number of pricey cars there has dropped off over time).
I really don’t want to know how much others make. It’s probably more than what I make, but that’s the trade-off I accepted when I went with a small solo practice instead of a large group 20 years ago.
We become so obsessed with the question of “how much money should I be making?” and comparing it with the salaries of others that we lose track of the real question: “How much money do I need?”
That should be the real number to look at. How much money do I really need to pay for a comfortable home, support my family, pay for my kids’ education, fund my retirement?
Enough should be as good as a feast.
Yet, even when content we get caught in the trap of comparing ourselves with others. This is human nature. We’re programmed to be competitive to survive. Whether that means anything when we don’t have to be hunters and gatherers is irrelevant. It is who we are.
But we’re also intelligent enough to realize that. I for one, don’t want to know, or care, how much money the neurologist down the street is earning.
To quote Sheryl Crow, “it’s not having what you want, it’s wanting what you’ve got.”
So I’ll skip the comparisons and focus on the only people that really matter to me.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
How much do I make compared with other doctors?
I see questions like that on surveys I get, asking me to fill something out on the Internet, then I’ll get back a list of how well other docs in my field/city/state/blood type are doing.
Nah. I’ll pass.
Realistically, why? So I can feel I’m superior or inferior to others? Isn’t keeping up with the Joneses the purpose of the doctors’ parking lot at the hospital? (Actually, the number of pricey cars there has dropped off over time).
I really don’t want to know how much others make. It’s probably more than what I make, but that’s the trade-off I accepted when I went with a small solo practice instead of a large group 20 years ago.
We become so obsessed with the question of “how much money should I be making?” and comparing it with the salaries of others that we lose track of the real question: “How much money do I need?”
That should be the real number to look at. How much money do I really need to pay for a comfortable home, support my family, pay for my kids’ education, fund my retirement?
Enough should be as good as a feast.
Yet, even when content we get caught in the trap of comparing ourselves with others. This is human nature. We’re programmed to be competitive to survive. Whether that means anything when we don’t have to be hunters and gatherers is irrelevant. It is who we are.
But we’re also intelligent enough to realize that. I for one, don’t want to know, or care, how much money the neurologist down the street is earning.
To quote Sheryl Crow, “it’s not having what you want, it’s wanting what you’ve got.”
So I’ll skip the comparisons and focus on the only people that really matter to me.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Cutaneous Insulin-Derived Amyloidosis Presenting as Hyperkeratotic Nodules
Amyloidosis consists of approximately 30 protein-folding disorders sharing the common feature of abnormal extracellular amyloid deposition. In each condition, a specific soluble precursor protein aggregates to form the insoluble fibrils of amyloid, characterized by the beta-pleated sheet structure.1 Amyloidosis occurs as either a systemic or localized process. Insulin-derived (AIns) amyloidosis, a localized process occurring at insulin injection sites, was first reported in 1983.2 There were fewer than 20 reported cases until 2014, when 57 additional cases were reported by just 2 institutions,3,4 indicating that AIns amyloidosis may be more common than previously thought.3,5
Despite the increasing prevalence of diabetes mellitus and insulin use, there is a paucity of published cases of AIns amyloidosis. The lack of awareness of this condition among both dermatologists and general practitioners may be in part due to its variable clinical manifestations. We describe 2 patients with unique presentations of localized amyloidosis at repeated insulin injection sites.
Case Reports
Patient 1
A 39-year-old man with a history of type 1 diabetes mellitus presented with 4 asymptomatic nodules on the lateral thighs in areas of previous insulin injection. He first noticed the lesions 9 months prior to presentation and subsequently switched the injection site to the abdomen without development of new nodules. Despite being compliant with his insulin regimen, he had a long history of irregular glucose control, including frequent hypoglycemic episodes. The patient was using regular and neutral protamine hagedorn insulin.
On physical examination, 2 soft, nontender, exophytic nodules were noted on each upper thigh with surrounding hyperpigmented and hyperkeratotic collarettes (Figure 1). The nodules ranged in size from 2 to 3.5 cm in diameter.

Remarkable laboratory data included a fasting glucose level of 207 mg/dL (reference range, 70–110 mg/dL) and a glycohemoglobin of 8.8% (reference range, <5.7%). Serum protein electrophoresis and immunofixation were normal. Histopathology of the lesions demonstrated diffuse deposition of pink amorphous material associated with prominent papillomatosis, hyperkeratosis, and acanthosis (Figure 2). Congo red staining was positive with green birefringence under polarized light, indicative of amyloid deposits (Figure 3). Liquid chromatography–tandem mass spectrometry of the specimens was consistent with deposition of AIns amyloidosis.
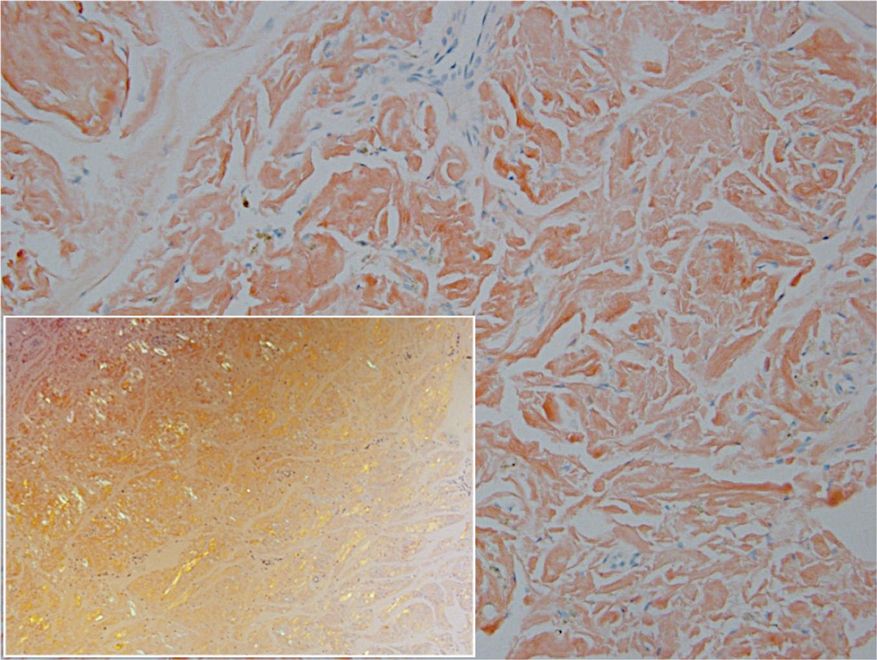
Due to the size and persistent nature of the lesions, the nodules were removed by tangential excision. In addition, the patient was advised to continue rotating injection sites frequently. His blood glucose levels are now well controlled, and he has not developed any new nodules.
Patient 2
A 53-year-old woman with a history of type 2 diabetes mellitus presented with painful subcutaneous nodules on the lower abdomen at sites of previous insulin injections. The nodules developed approximately 1 month after she started treatment with neutral protamine hagedorn insulin and had been slowly enlarging over the past year. She tried switching injection sites after noticing the lesions, but the nodules persisted. The patient had a long history of poor glucose control with chronically elevated glycohemoglobin and blood glucose levels.
On physical examination, 2 hyperpigmented, exophytic, smooth nodules were noted on the right and left lower abdomen, ranging in size from 2.5 to 5.5 cm in diameter (Figure 4).

Relevant laboratory data included a fasting glucose level of 197 mg/dL and a glycohemoglobin of 9.3%. A biopsy of the lesion on the left lower abdomen revealed eosinophilic amorphous deposits with fissuring in the dermis (Figure 5). Congo red stain was positive with green birefringence under polarized light. Liquid chromatography–tandem mass spectrometry of the specimen showed deposition of AIns amyloid. The patient began injecting away from the amyloid nodules without development of any new lesions. The original nodules have persisted, and surgical excision is planned.
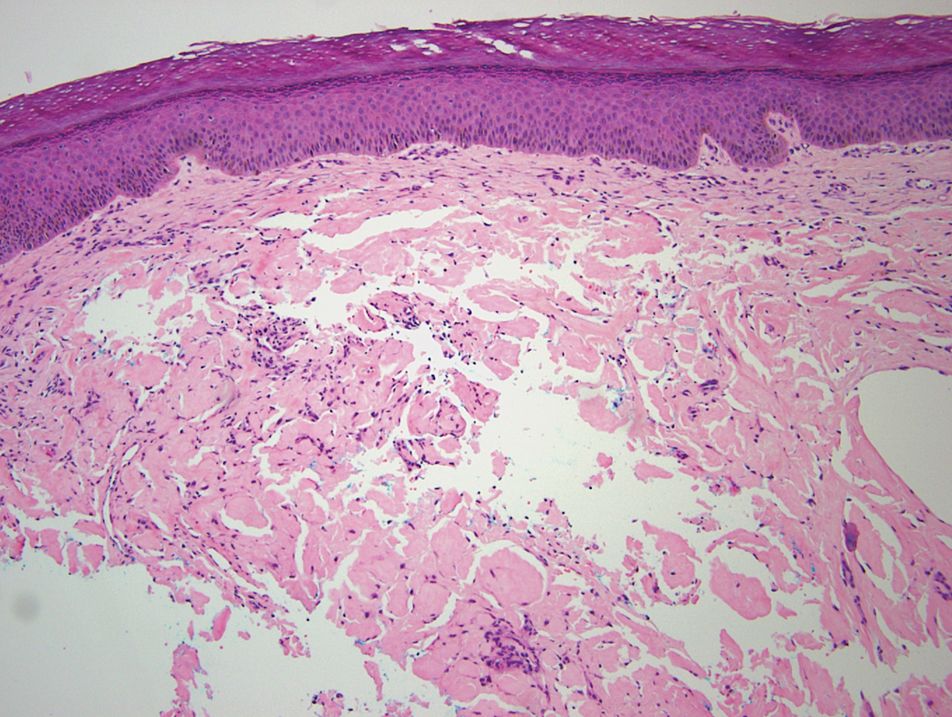
Comment
Insulin is the suspected precursor protein in AIns amyloidosis, but the exact pathogenesis is unknown. The protein that is derived from insulin in these tumors is now identified as AIns amyloidosis.5,6 It is hypothesized that insulin accumulates locally and is converted to amyloid by an unknown mechanism.7 Other potential contributory factors include chronic inflammation and foreign body reactions developing around amyloid deposits, as well as repeated trauma from injections into a single site.4,5 It appears that lesions may derive from a wide range of insulin types and occur after variable time periods.
A majority of cases of iatrogenic amyloid have been described as single, firm, subcutaneous masses at an injection site that commonly are misdiagnosed as lipomas or lipohypertrophy.7-11 To our knowledge, none of the reported cases resembled the multiple, discrete, exophytic nodules seen in our patients.3,4 The surrounding hyperkeratosis noted in patient 1 is another uncommon feature of AIns amyloidosis (Figures 1 and 2). Only 3 AIns amyloidosis cases described lesions with acanthosis nigricans–like changes, only 1 of which provided a clinical image.6,7,12The mechanism for the acanthosis nigricans–like changes may have been due to the high levels of insulin at the injection site. It has been suggested that the activation of insulinlike growth factor receptor by insulin leads to the proliferation of keratinocytes and fibroblasts.6 Histologic examination of AIns amyloidosis lesions generally demonstrates deposition of homogenous eosinophilic material consistent with amyloid, as well as positive Congo red staining with green birefringence by polarization. Immunohistologic staining with insulin antibody with or without proteomic analysis of the amyloid deposits can confirm the diagnosis. In both of our patients’ specimens, liquid chromatography–tandem mass spectrometry was performed for proteomic analysis, and results were consistent with AIns amyloidosis.
Reports in the literature have suggested that the deposition of amyloid at insulin injection sites has the potential to interfere with insulin absorption, leading to poor glucose control.4,11,13 Hence, injection site rotation is a crucial aspect of treatment and prevention of AIns amyloidosis. In their study of 4 patients, Nagase et al4 compared serum insulin levels after insulin injection into amyloid nodules vs insulin levels after injection into normal skin. Insulin absorption at the amyloid sites was 34% of that at normal sites. Given these results, patients should be instructed to inject away from the amyloid deposit once it is identified.6 Glucose levels should be monitored closely when patients first inject away from the amyloid mass, as injection of the same dosage to an area of normal skin can lead to increased insulin absorption and hypoglycemia.4,6 It is possible that the frequent hypoglycemic episodes noted in patient 1 were due to increased insulin sensitivity after switching to injection sites away from amyloid lesions.
Conclusion
Our patients demonstrate unique presentations of localized cutaneous amyloidosis at repeated insulin injection sites. We report these cases to complement the current data of iatrogenic amyloidosis and provide insight into this likely underreported phenomenon.
- Hazenberg BPC. Amyloidosis: a clinical overview. Rheum Dis Clin North Am. 2013;39:323-345.
- Storkel S, Schneider HM, Muntefering H, et al. Iatrogenic, insulin-dependent, local amyloidosis. Lab Invest. 1983;48:108-111.
- D’souza A, Theis JD, Vrana JA, et al. Pharmaceutical amyloidosis associated with subcutaneous insulin and enfuvirtide administration. Amyloid. 2014;21:71-75.
- Nagase T, Iwaya K, Iwaki Y, et al. Insulin-derived amyloidosis and poor glycemic control: a case series. Am J Med. 2014;127:450-454.
- Gupta Y, Singla G, Singla R. Insulin-derived amyloidosis. Indian J Endocrinol Metab. 2015;19:174-177.
- Kudo-Watanuki S, Kurihara E, Yamamoto K, et al. Coexistence of insulin-derived amyloidosis and an overlying acanthosis nigricans-like lesion at the site of insulin injection. Clin Exp Dermatol. 2013;38:25-29.
- Yumlu S, Barany R, Eriksson M, et al. Localized insulin-derived amyloidosis in patients with diabetes mellitus: a case report. Hum Pathol. 2009;40:1655-1660.
- Okamura S, Hayashino Y, Kore-Eda S, et al. Localized amyloidosis at the site of repeated insulin injection in a patient with type 2 diabetes. Diabetes Care. 2013;36:E200.
- Dische FE, Wernstedt C, Westermark GT, et al. Insulin as an amyloid-fibril protein at sites of repeated insulin injections in a diabetic patient. Diabetologia. 1988;31:158-161.
- Swift B, Hawkins PN, Richards C, et al. Examination of insulin injection sites: an unexpected finding of localized amyloidosis. Diabetic Med. 2002;19:881-882.
- Albert SG, Obadiah J, Parseghian SA, et al. Severe insulin resistance associated with subcutaneous amyloid deposition. Diabetes Res Clin Pract. 2007;75:374-376.
- Nandeesh BN, Rajalakshmi T, Shubha B. Cutaneous amyloidosis and insulin with coexistence of acanthosis nigricans. Indian J Pathol Microbiol. 2014;57:127-129.
- Endo JO, Rocken C, Lamb S, et al. Nodular amyloidosis in a diabetic patient with frequent hypoglycemia: sequelae of repeatedly injecting insulin without site rotation. J Am Acad Dermatol. 2010;63:E113-E114.
Amyloidosis consists of approximately 30 protein-folding disorders sharing the common feature of abnormal extracellular amyloid deposition. In each condition, a specific soluble precursor protein aggregates to form the insoluble fibrils of amyloid, characterized by the beta-pleated sheet structure.1 Amyloidosis occurs as either a systemic or localized process. Insulin-derived (AIns) amyloidosis, a localized process occurring at insulin injection sites, was first reported in 1983.2 There were fewer than 20 reported cases until 2014, when 57 additional cases were reported by just 2 institutions,3,4 indicating that AIns amyloidosis may be more common than previously thought.3,5
Despite the increasing prevalence of diabetes mellitus and insulin use, there is a paucity of published cases of AIns amyloidosis. The lack of awareness of this condition among both dermatologists and general practitioners may be in part due to its variable clinical manifestations. We describe 2 patients with unique presentations of localized amyloidosis at repeated insulin injection sites.
Case Reports
Patient 1
A 39-year-old man with a history of type 1 diabetes mellitus presented with 4 asymptomatic nodules on the lateral thighs in areas of previous insulin injection. He first noticed the lesions 9 months prior to presentation and subsequently switched the injection site to the abdomen without development of new nodules. Despite being compliant with his insulin regimen, he had a long history of irregular glucose control, including frequent hypoglycemic episodes. The patient was using regular and neutral protamine hagedorn insulin.
On physical examination, 2 soft, nontender, exophytic nodules were noted on each upper thigh with surrounding hyperpigmented and hyperkeratotic collarettes (Figure 1). The nodules ranged in size from 2 to 3.5 cm in diameter.

Remarkable laboratory data included a fasting glucose level of 207 mg/dL (reference range, 70–110 mg/dL) and a glycohemoglobin of 8.8% (reference range, <5.7%). Serum protein electrophoresis and immunofixation were normal. Histopathology of the lesions demonstrated diffuse deposition of pink amorphous material associated with prominent papillomatosis, hyperkeratosis, and acanthosis (Figure 2). Congo red staining was positive with green birefringence under polarized light, indicative of amyloid deposits (Figure 3). Liquid chromatography–tandem mass spectrometry of the specimens was consistent with deposition of AIns amyloidosis.
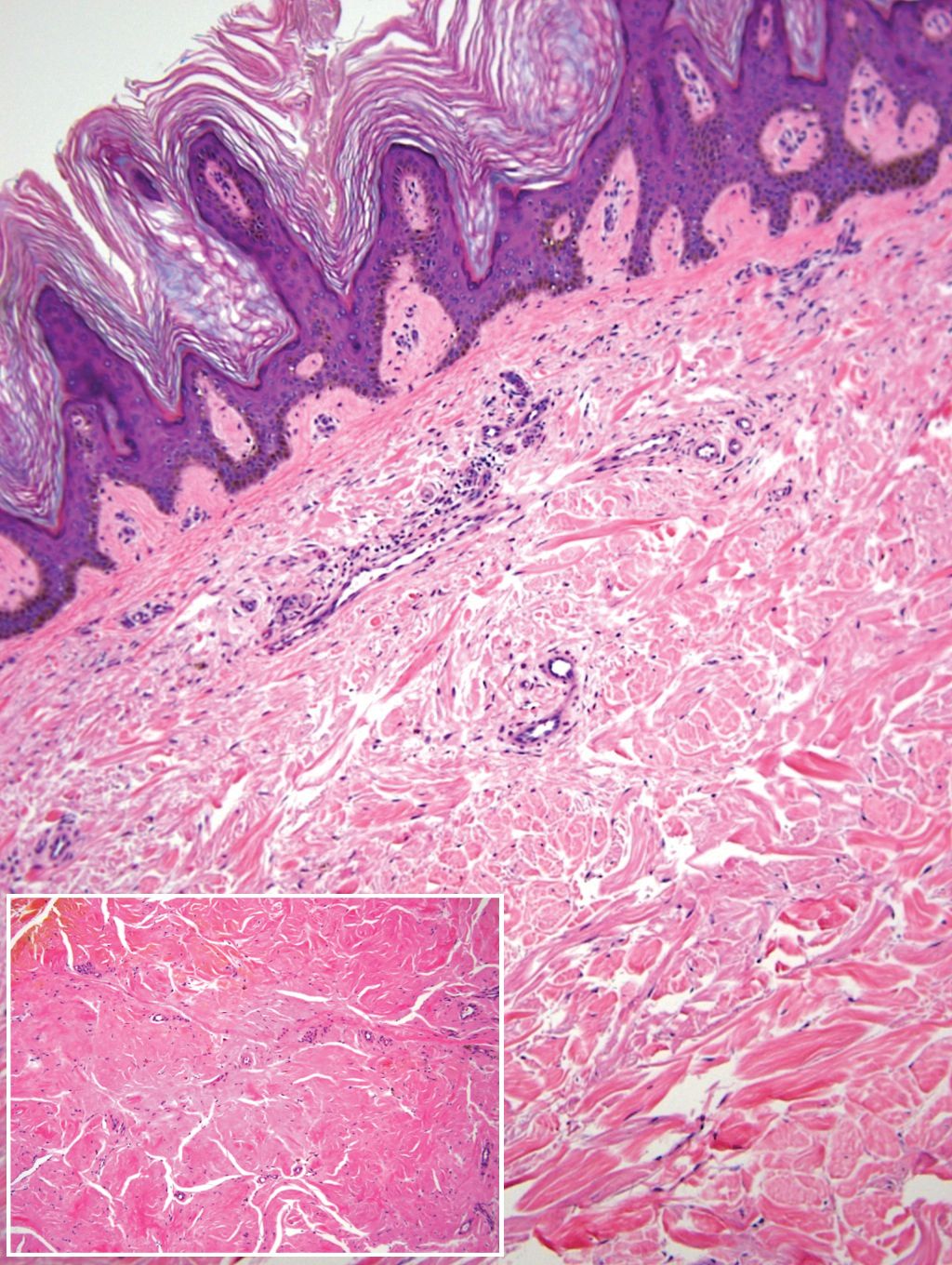
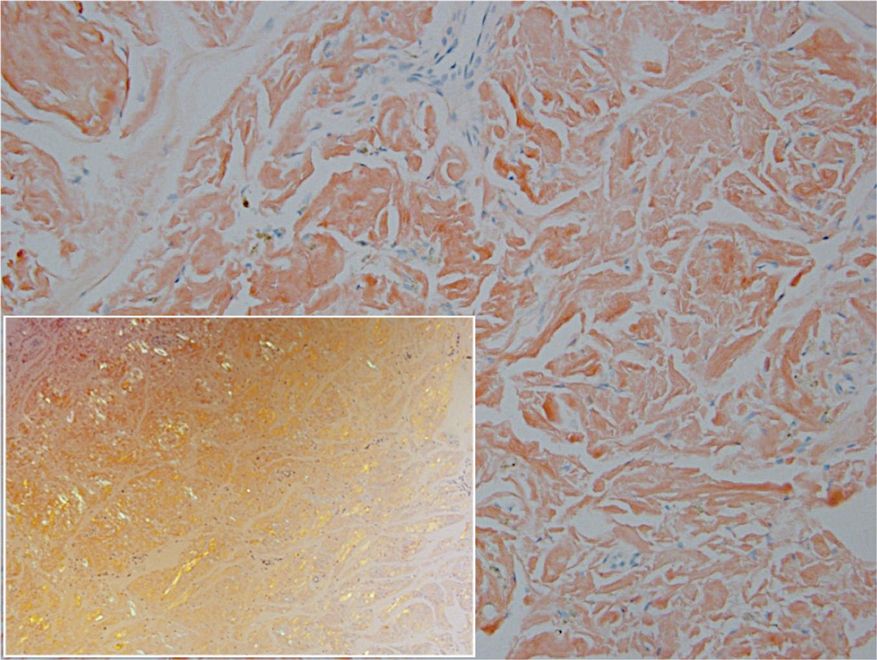
Due to the size and persistent nature of the lesions, the nodules were removed by tangential excision. In addition, the patient was advised to continue rotating injection sites frequently. His blood glucose levels are now well controlled, and he has not developed any new nodules.
Patient 2
A 53-year-old woman with a history of type 2 diabetes mellitus presented with painful subcutaneous nodules on the lower abdomen at sites of previous insulin injections. The nodules developed approximately 1 month after she started treatment with neutral protamine hagedorn insulin and had been slowly enlarging over the past year. She tried switching injection sites after noticing the lesions, but the nodules persisted. The patient had a long history of poor glucose control with chronically elevated glycohemoglobin and blood glucose levels.
On physical examination, 2 hyperpigmented, exophytic, smooth nodules were noted on the right and left lower abdomen, ranging in size from 2.5 to 5.5 cm in diameter (Figure 4).

Relevant laboratory data included a fasting glucose level of 197 mg/dL and a glycohemoglobin of 9.3%. A biopsy of the lesion on the left lower abdomen revealed eosinophilic amorphous deposits with fissuring in the dermis (Figure 5). Congo red stain was positive with green birefringence under polarized light. Liquid chromatography–tandem mass spectrometry of the specimen showed deposition of AIns amyloid. The patient began injecting away from the amyloid nodules without development of any new lesions. The original nodules have persisted, and surgical excision is planned.
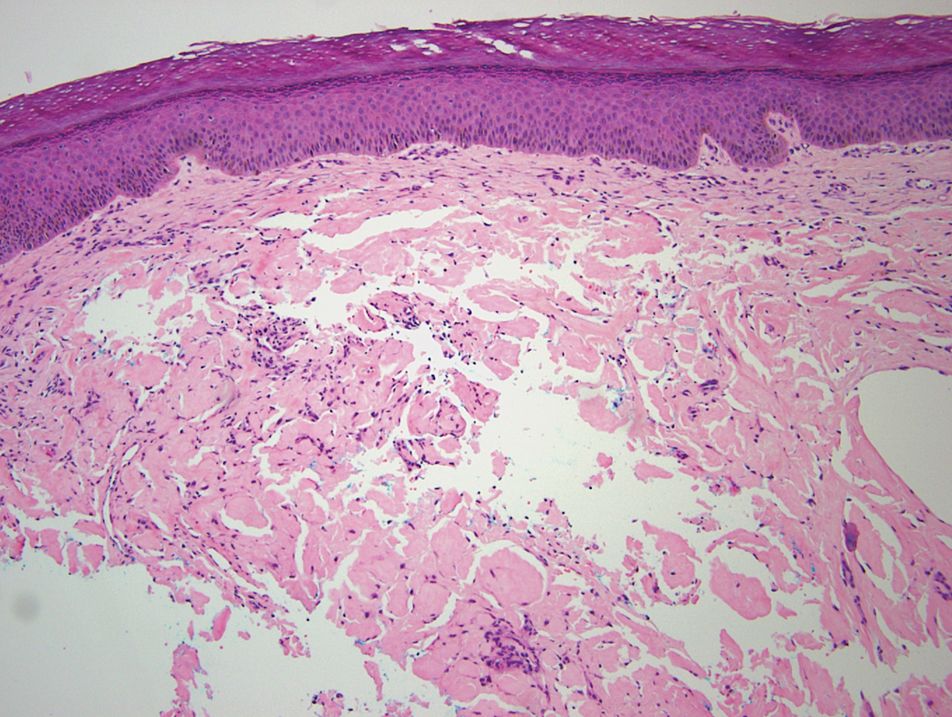
Comment
Insulin is the suspected precursor protein in AIns amyloidosis, but the exact pathogenesis is unknown. The protein that is derived from insulin in these tumors is now identified as AIns amyloidosis.5,6 It is hypothesized that insulin accumulates locally and is converted to amyloid by an unknown mechanism.7 Other potential contributory factors include chronic inflammation and foreign body reactions developing around amyloid deposits, as well as repeated trauma from injections into a single site.4,5 It appears that lesions may derive from a wide range of insulin types and occur after variable time periods.
A majority of cases of iatrogenic amyloid have been described as single, firm, subcutaneous masses at an injection site that commonly are misdiagnosed as lipomas or lipohypertrophy.7-11 To our knowledge, none of the reported cases resembled the multiple, discrete, exophytic nodules seen in our patients.3,4 The surrounding hyperkeratosis noted in patient 1 is another uncommon feature of AIns amyloidosis (Figures 1 and 2). Only 3 AIns amyloidosis cases described lesions with acanthosis nigricans–like changes, only 1 of which provided a clinical image.6,7,12The mechanism for the acanthosis nigricans–like changes may have been due to the high levels of insulin at the injection site. It has been suggested that the activation of insulinlike growth factor receptor by insulin leads to the proliferation of keratinocytes and fibroblasts.6 Histologic examination of AIns amyloidosis lesions generally demonstrates deposition of homogenous eosinophilic material consistent with amyloid, as well as positive Congo red staining with green birefringence by polarization. Immunohistologic staining with insulin antibody with or without proteomic analysis of the amyloid deposits can confirm the diagnosis. In both of our patients’ specimens, liquid chromatography–tandem mass spectrometry was performed for proteomic analysis, and results were consistent with AIns amyloidosis.
Reports in the literature have suggested that the deposition of amyloid at insulin injection sites has the potential to interfere with insulin absorption, leading to poor glucose control.4,11,13 Hence, injection site rotation is a crucial aspect of treatment and prevention of AIns amyloidosis. In their study of 4 patients, Nagase et al4 compared serum insulin levels after insulin injection into amyloid nodules vs insulin levels after injection into normal skin. Insulin absorption at the amyloid sites was 34% of that at normal sites. Given these results, patients should be instructed to inject away from the amyloid deposit once it is identified.6 Glucose levels should be monitored closely when patients first inject away from the amyloid mass, as injection of the same dosage to an area of normal skin can lead to increased insulin absorption and hypoglycemia.4,6 It is possible that the frequent hypoglycemic episodes noted in patient 1 were due to increased insulin sensitivity after switching to injection sites away from amyloid lesions.
Conclusion
Our patients demonstrate unique presentations of localized cutaneous amyloidosis at repeated insulin injection sites. We report these cases to complement the current data of iatrogenic amyloidosis and provide insight into this likely underreported phenomenon.
Amyloidosis consists of approximately 30 protein-folding disorders sharing the common feature of abnormal extracellular amyloid deposition. In each condition, a specific soluble precursor protein aggregates to form the insoluble fibrils of amyloid, characterized by the beta-pleated sheet structure.1 Amyloidosis occurs as either a systemic or localized process. Insulin-derived (AIns) amyloidosis, a localized process occurring at insulin injection sites, was first reported in 1983.2 There were fewer than 20 reported cases until 2014, when 57 additional cases were reported by just 2 institutions,3,4 indicating that AIns amyloidosis may be more common than previously thought.3,5
Despite the increasing prevalence of diabetes mellitus and insulin use, there is a paucity of published cases of AIns amyloidosis. The lack of awareness of this condition among both dermatologists and general practitioners may be in part due to its variable clinical manifestations. We describe 2 patients with unique presentations of localized amyloidosis at repeated insulin injection sites.
Case Reports
Patient 1
A 39-year-old man with a history of type 1 diabetes mellitus presented with 4 asymptomatic nodules on the lateral thighs in areas of previous insulin injection. He first noticed the lesions 9 months prior to presentation and subsequently switched the injection site to the abdomen without development of new nodules. Despite being compliant with his insulin regimen, he had a long history of irregular glucose control, including frequent hypoglycemic episodes. The patient was using regular and neutral protamine hagedorn insulin.
On physical examination, 2 soft, nontender, exophytic nodules were noted on each upper thigh with surrounding hyperpigmented and hyperkeratotic collarettes (Figure 1). The nodules ranged in size from 2 to 3.5 cm in diameter.

Remarkable laboratory data included a fasting glucose level of 207 mg/dL (reference range, 70–110 mg/dL) and a glycohemoglobin of 8.8% (reference range, <5.7%). Serum protein electrophoresis and immunofixation were normal. Histopathology of the lesions demonstrated diffuse deposition of pink amorphous material associated with prominent papillomatosis, hyperkeratosis, and acanthosis (Figure 2). Congo red staining was positive with green birefringence under polarized light, indicative of amyloid deposits (Figure 3). Liquid chromatography–tandem mass spectrometry of the specimens was consistent with deposition of AIns amyloidosis.
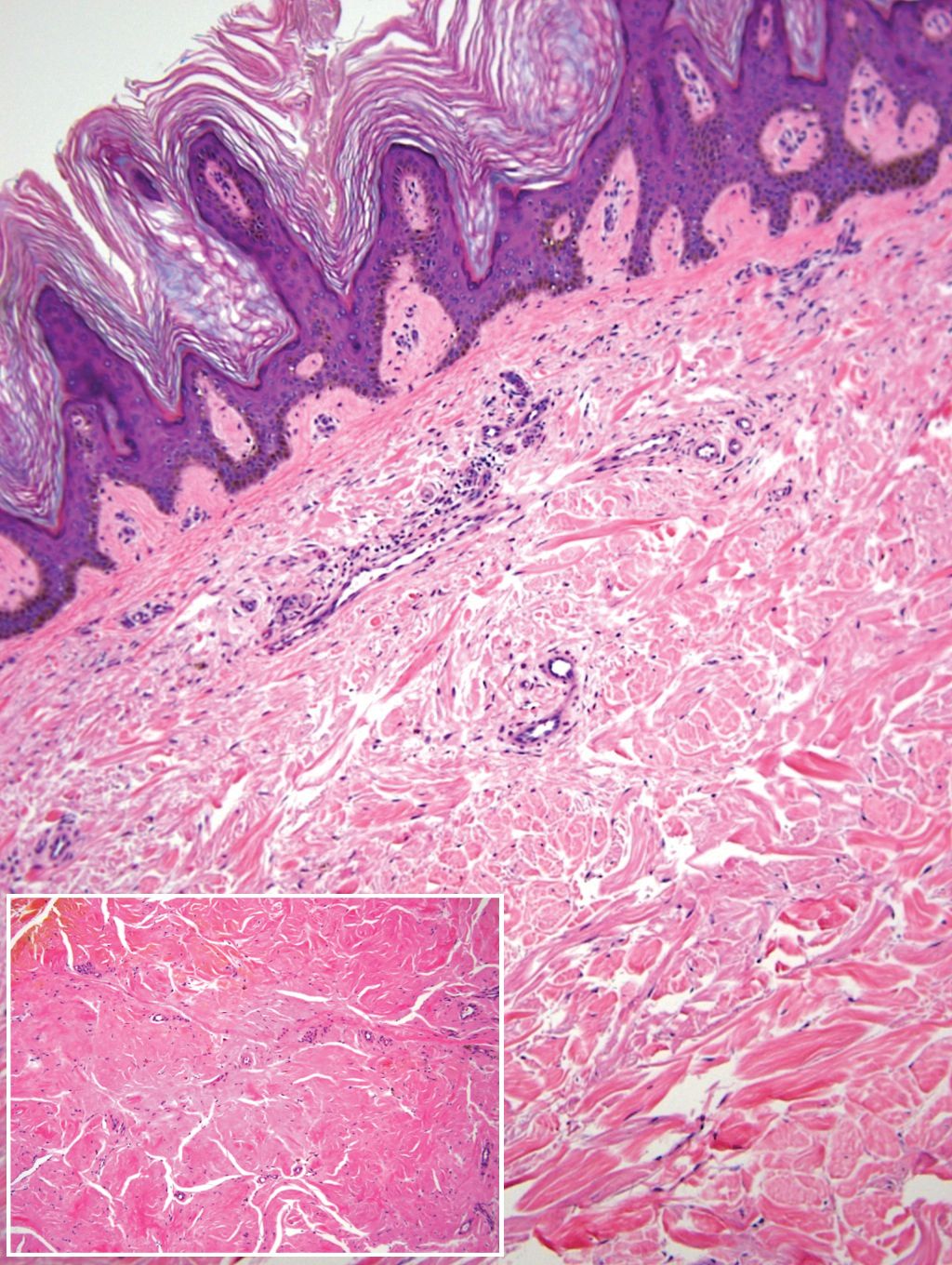
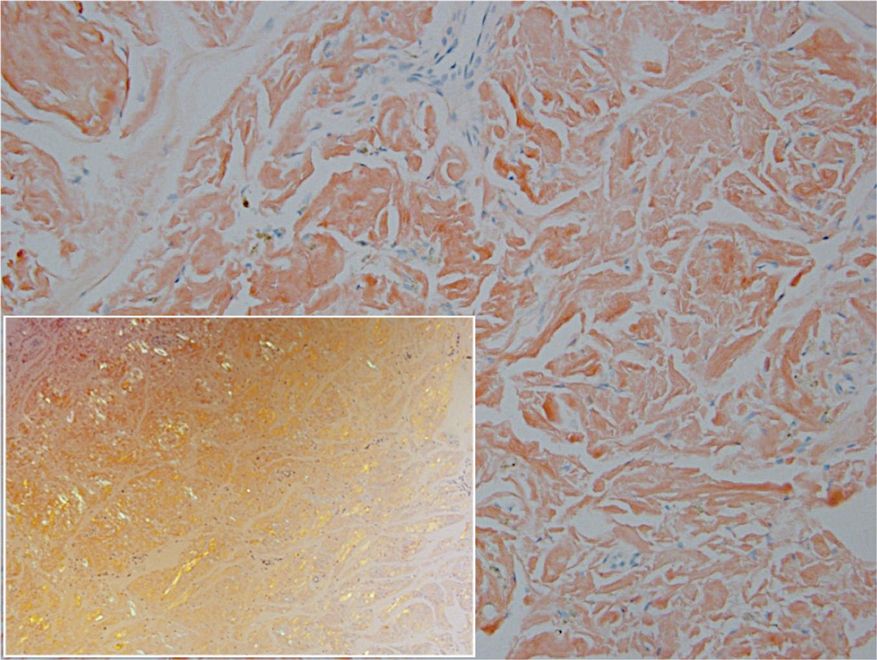
Due to the size and persistent nature of the lesions, the nodules were removed by tangential excision. In addition, the patient was advised to continue rotating injection sites frequently. His blood glucose levels are now well controlled, and he has not developed any new nodules.
Patient 2
A 53-year-old woman with a history of type 2 diabetes mellitus presented with painful subcutaneous nodules on the lower abdomen at sites of previous insulin injections. The nodules developed approximately 1 month after she started treatment with neutral protamine hagedorn insulin and had been slowly enlarging over the past year. She tried switching injection sites after noticing the lesions, but the nodules persisted. The patient had a long history of poor glucose control with chronically elevated glycohemoglobin and blood glucose levels.
On physical examination, 2 hyperpigmented, exophytic, smooth nodules were noted on the right and left lower abdomen, ranging in size from 2.5 to 5.5 cm in diameter (Figure 4).

Relevant laboratory data included a fasting glucose level of 197 mg/dL and a glycohemoglobin of 9.3%. A biopsy of the lesion on the left lower abdomen revealed eosinophilic amorphous deposits with fissuring in the dermis (Figure 5). Congo red stain was positive with green birefringence under polarized light. Liquid chromatography–tandem mass spectrometry of the specimen showed deposition of AIns amyloid. The patient began injecting away from the amyloid nodules without development of any new lesions. The original nodules have persisted, and surgical excision is planned.
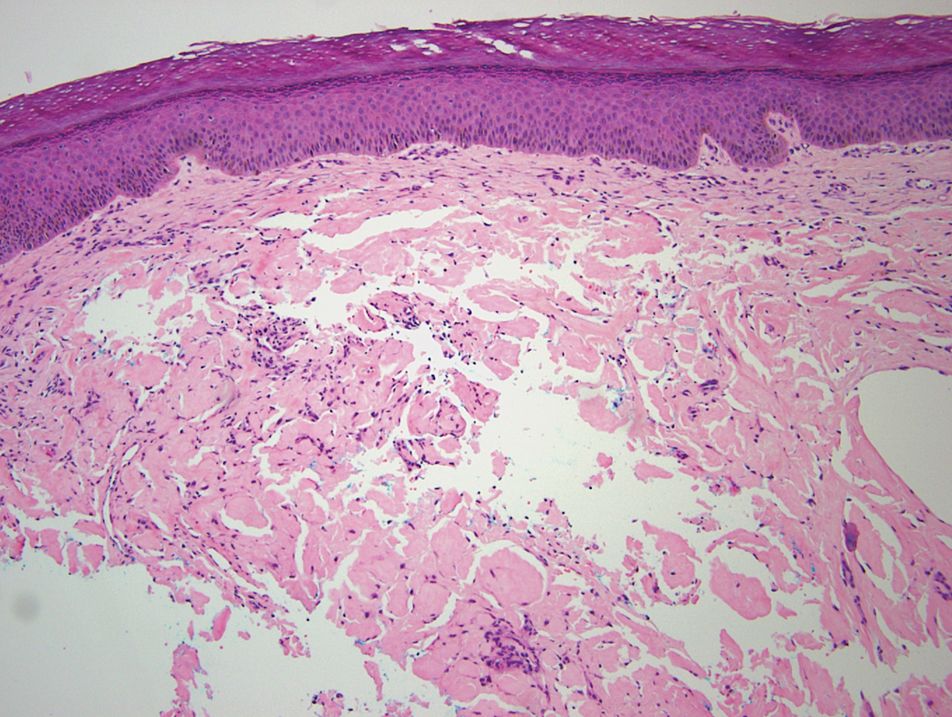
Comment
Insulin is the suspected precursor protein in AIns amyloidosis, but the exact pathogenesis is unknown. The protein that is derived from insulin in these tumors is now identified as AIns amyloidosis.5,6 It is hypothesized that insulin accumulates locally and is converted to amyloid by an unknown mechanism.7 Other potential contributory factors include chronic inflammation and foreign body reactions developing around amyloid deposits, as well as repeated trauma from injections into a single site.4,5 It appears that lesions may derive from a wide range of insulin types and occur after variable time periods.
A majority of cases of iatrogenic amyloid have been described as single, firm, subcutaneous masses at an injection site that commonly are misdiagnosed as lipomas or lipohypertrophy.7-11 To our knowledge, none of the reported cases resembled the multiple, discrete, exophytic nodules seen in our patients.3,4 The surrounding hyperkeratosis noted in patient 1 is another uncommon feature of AIns amyloidosis (Figures 1 and 2). Only 3 AIns amyloidosis cases described lesions with acanthosis nigricans–like changes, only 1 of which provided a clinical image.6,7,12The mechanism for the acanthosis nigricans–like changes may have been due to the high levels of insulin at the injection site. It has been suggested that the activation of insulinlike growth factor receptor by insulin leads to the proliferation of keratinocytes and fibroblasts.6 Histologic examination of AIns amyloidosis lesions generally demonstrates deposition of homogenous eosinophilic material consistent with amyloid, as well as positive Congo red staining with green birefringence by polarization. Immunohistologic staining with insulin antibody with or without proteomic analysis of the amyloid deposits can confirm the diagnosis. In both of our patients’ specimens, liquid chromatography–tandem mass spectrometry was performed for proteomic analysis, and results were consistent with AIns amyloidosis.
Reports in the literature have suggested that the deposition of amyloid at insulin injection sites has the potential to interfere with insulin absorption, leading to poor glucose control.4,11,13 Hence, injection site rotation is a crucial aspect of treatment and prevention of AIns amyloidosis. In their study of 4 patients, Nagase et al4 compared serum insulin levels after insulin injection into amyloid nodules vs insulin levels after injection into normal skin. Insulin absorption at the amyloid sites was 34% of that at normal sites. Given these results, patients should be instructed to inject away from the amyloid deposit once it is identified.6 Glucose levels should be monitored closely when patients first inject away from the amyloid mass, as injection of the same dosage to an area of normal skin can lead to increased insulin absorption and hypoglycemia.4,6 It is possible that the frequent hypoglycemic episodes noted in patient 1 were due to increased insulin sensitivity after switching to injection sites away from amyloid lesions.
Conclusion
Our patients demonstrate unique presentations of localized cutaneous amyloidosis at repeated insulin injection sites. We report these cases to complement the current data of iatrogenic amyloidosis and provide insight into this likely underreported phenomenon.
- Hazenberg BPC. Amyloidosis: a clinical overview. Rheum Dis Clin North Am. 2013;39:323-345.
- Storkel S, Schneider HM, Muntefering H, et al. Iatrogenic, insulin-dependent, local amyloidosis. Lab Invest. 1983;48:108-111.
- D’souza A, Theis JD, Vrana JA, et al. Pharmaceutical amyloidosis associated with subcutaneous insulin and enfuvirtide administration. Amyloid. 2014;21:71-75.
- Nagase T, Iwaya K, Iwaki Y, et al. Insulin-derived amyloidosis and poor glycemic control: a case series. Am J Med. 2014;127:450-454.
- Gupta Y, Singla G, Singla R. Insulin-derived amyloidosis. Indian J Endocrinol Metab. 2015;19:174-177.
- Kudo-Watanuki S, Kurihara E, Yamamoto K, et al. Coexistence of insulin-derived amyloidosis and an overlying acanthosis nigricans-like lesion at the site of insulin injection. Clin Exp Dermatol. 2013;38:25-29.
- Yumlu S, Barany R, Eriksson M, et al. Localized insulin-derived amyloidosis in patients with diabetes mellitus: a case report. Hum Pathol. 2009;40:1655-1660.
- Okamura S, Hayashino Y, Kore-Eda S, et al. Localized amyloidosis at the site of repeated insulin injection in a patient with type 2 diabetes. Diabetes Care. 2013;36:E200.
- Dische FE, Wernstedt C, Westermark GT, et al. Insulin as an amyloid-fibril protein at sites of repeated insulin injections in a diabetic patient. Diabetologia. 1988;31:158-161.
- Swift B, Hawkins PN, Richards C, et al. Examination of insulin injection sites: an unexpected finding of localized amyloidosis. Diabetic Med. 2002;19:881-882.
- Albert SG, Obadiah J, Parseghian SA, et al. Severe insulin resistance associated with subcutaneous amyloid deposition. Diabetes Res Clin Pract. 2007;75:374-376.
- Nandeesh BN, Rajalakshmi T, Shubha B. Cutaneous amyloidosis and insulin with coexistence of acanthosis nigricans. Indian J Pathol Microbiol. 2014;57:127-129.
- Endo JO, Rocken C, Lamb S, et al. Nodular amyloidosis in a diabetic patient with frequent hypoglycemia: sequelae of repeatedly injecting insulin without site rotation. J Am Acad Dermatol. 2010;63:E113-E114.
- Hazenberg BPC. Amyloidosis: a clinical overview. Rheum Dis Clin North Am. 2013;39:323-345.
- Storkel S, Schneider HM, Muntefering H, et al. Iatrogenic, insulin-dependent, local amyloidosis. Lab Invest. 1983;48:108-111.
- D’souza A, Theis JD, Vrana JA, et al. Pharmaceutical amyloidosis associated with subcutaneous insulin and enfuvirtide administration. Amyloid. 2014;21:71-75.
- Nagase T, Iwaya K, Iwaki Y, et al. Insulin-derived amyloidosis and poor glycemic control: a case series. Am J Med. 2014;127:450-454.
- Gupta Y, Singla G, Singla R. Insulin-derived amyloidosis. Indian J Endocrinol Metab. 2015;19:174-177.
- Kudo-Watanuki S, Kurihara E, Yamamoto K, et al. Coexistence of insulin-derived amyloidosis and an overlying acanthosis nigricans-like lesion at the site of insulin injection. Clin Exp Dermatol. 2013;38:25-29.
- Yumlu S, Barany R, Eriksson M, et al. Localized insulin-derived amyloidosis in patients with diabetes mellitus: a case report. Hum Pathol. 2009;40:1655-1660.
- Okamura S, Hayashino Y, Kore-Eda S, et al. Localized amyloidosis at the site of repeated insulin injection in a patient with type 2 diabetes. Diabetes Care. 2013;36:E200.
- Dische FE, Wernstedt C, Westermark GT, et al. Insulin as an amyloid-fibril protein at sites of repeated insulin injections in a diabetic patient. Diabetologia. 1988;31:158-161.
- Swift B, Hawkins PN, Richards C, et al. Examination of insulin injection sites: an unexpected finding of localized amyloidosis. Diabetic Med. 2002;19:881-882.
- Albert SG, Obadiah J, Parseghian SA, et al. Severe insulin resistance associated with subcutaneous amyloid deposition. Diabetes Res Clin Pract. 2007;75:374-376.
- Nandeesh BN, Rajalakshmi T, Shubha B. Cutaneous amyloidosis and insulin with coexistence of acanthosis nigricans. Indian J Pathol Microbiol. 2014;57:127-129.
- Endo JO, Rocken C, Lamb S, et al. Nodular amyloidosis in a diabetic patient with frequent hypoglycemia: sequelae of repeatedly injecting insulin without site rotation. J Am Acad Dermatol. 2010;63:E113-E114.
Practice Points
- Deposition of amyloid at insulin injection sites has the potential to interfere with insulin absorption, leading to poor glucose control.
- Patients with insulin-derived (AIns) amyloidosis may initially present after noticing nodular deposits.
- Insulin injection site rotation is a crucial aspect of treatment and prevention of AIns amyloidosis.
Boost dose reduces recurrence in high-risk DCIS
Giving a tumor bed boost (TBB) reduced the risk of local recurrence and overall disease recurrence, but there were no significant differences in recurrence rates between conventional WBI and hypofractionated WBI.
Boon Hui Chua, MD, of the University of New South Wales, Sydney, presented these results at the 2020 San Antonio Breast Cancer Symposium.
Dr. Chua and colleagues studied 1,608 women with DCIS resected by conservative surgery. Patients were either younger than 50 years or age 50 and older with at least one of the following risk factors: symptomatic presentation, palpable tumor, multifocal disease, tumor size 1.5 cm or larger, intermediate or high nuclear grade, central necrosis, comedo histology, and/or surgical margins less than 10 mm.
The patients were randomized to treatment in three categories. In randomization A (n = 503), patients were randomized to one of the following treatments:
- WBI at 50 Gy in 25 fractions
- WBI at 42.5 Gy in 16 fractions
- WBI at 50 Gy in 25 fractions plus TBB at 16 Gy in 8 fractions
- WBI at 42.5 Gy in 16 fractions plus TBB at 16 Gy in 8 fractions.
In randomization B (n = 581), patients received WBI at 50 Gy in 25 fractions, with or without TBB at 16 Gy in 8 fractions. In randomization C (n = 524), patients received WBI at 42.5 Gy in 16 fractions, with or without TBB at 16 Gy in 8 fractions.
All patients underwent CT-based radiation planning. WBI was delivered with tangential MV photon beams, and TBB was performed with CT contouring of protocol-defined tumor bed target volumes, with electron or photon energy. The median follow-up was 6.6 years.
Giving a boost to better outcomes
The 5-year rate of freedom from local recurrence was 97% for patients who received TBB and 93% for patients who did not (hazard ratio, 0.47; P < .001). The benefit of TBB was consistent across subgroups.
There were no significant differences in 5-year rates of freedom from local recurrence by WBI fractionation, either in randomization A (P = .837) or among all randomized patients (P = .887).
The tests for interactions between TBB and WBI fractionation on local recurrence were not significant in randomization A (P = .89) or in all randomized patients (P = .89).
The risk of overall disease recurrence was lower among patients who had received TBB, with an HR of 0.63 (P = .004). The 5-year rate of freedom from disease recurrence was 97% with TBB and 91% with no boost (P = .002).
There were no significant differences in freedom from disease recurrence rates by WBI fractionation either in randomization A (P = .443) or among all randomized patients (P = .605).
Acute radiation dermatitis occurred in significantly more patients who received TBB (P = .006), as did late breast pain (P = .003), induration or fibrosis (P < .0001), and telangiectasia (P = .02). There were no significant differences by boost status for acute or late fatigue, pneumonitis, cardiac complications, or second malignancies.
Reduce the boost dose?
A radiation oncologist who was not involved in this study said that, while the results confirm a benefit of boost dose for patients with non–low-risk DCIS, the doses used in the BIG-3-07 study may be higher than needed to achieve a protective effect.
“Here in America, we usually give 10 Gy in five fractions, and, in many countries, actually, it’s 10 Gy in five fractions, although a few European centers give 16 Gy in eight fractions,” said Alphose Taghian, MD, of Massachusetts General Hospital in Boston.
“I personally only give 10 Gy in five fractions. I am not under the impression that 16 Gy in eight fractions will give better results. The local failure rate is so low, it’s likely that 10 Gy will do the job,” Dr. Taghian said in an interview.
Dr. Taghian noted that raising the dose to 16 Gy increases the risk of fibrosis, as seen in the BIG-3-07 trial.
Nonetheless, the trial demonstrates the benefit of radiation boost dose in patients with high-risk DCIS, he said, adding that the local recurrence-free benefit curves may separate further with longer follow-up.
The study was sponsored by the Trans Tasman Radiation Oncology Group. Dr. Chua and Dr. Taghian reported no conflicts of interest.
Giving a tumor bed boost (TBB) reduced the risk of local recurrence and overall disease recurrence, but there were no significant differences in recurrence rates between conventional WBI and hypofractionated WBI.
Boon Hui Chua, MD, of the University of New South Wales, Sydney, presented these results at the 2020 San Antonio Breast Cancer Symposium.
Dr. Chua and colleagues studied 1,608 women with DCIS resected by conservative surgery. Patients were either younger than 50 years or age 50 and older with at least one of the following risk factors: symptomatic presentation, palpable tumor, multifocal disease, tumor size 1.5 cm or larger, intermediate or high nuclear grade, central necrosis, comedo histology, and/or surgical margins less than 10 mm.
The patients were randomized to treatment in three categories. In randomization A (n = 503), patients were randomized to one of the following treatments:
- WBI at 50 Gy in 25 fractions
- WBI at 42.5 Gy in 16 fractions
- WBI at 50 Gy in 25 fractions plus TBB at 16 Gy in 8 fractions
- WBI at 42.5 Gy in 16 fractions plus TBB at 16 Gy in 8 fractions.
In randomization B (n = 581), patients received WBI at 50 Gy in 25 fractions, with or without TBB at 16 Gy in 8 fractions. In randomization C (n = 524), patients received WBI at 42.5 Gy in 16 fractions, with or without TBB at 16 Gy in 8 fractions.
All patients underwent CT-based radiation planning. WBI was delivered with tangential MV photon beams, and TBB was performed with CT contouring of protocol-defined tumor bed target volumes, with electron or photon energy. The median follow-up was 6.6 years.
Giving a boost to better outcomes
The 5-year rate of freedom from local recurrence was 97% for patients who received TBB and 93% for patients who did not (hazard ratio, 0.47; P < .001). The benefit of TBB was consistent across subgroups.
There were no significant differences in 5-year rates of freedom from local recurrence by WBI fractionation, either in randomization A (P = .837) or among all randomized patients (P = .887).
The tests for interactions between TBB and WBI fractionation on local recurrence were not significant in randomization A (P = .89) or in all randomized patients (P = .89).
The risk of overall disease recurrence was lower among patients who had received TBB, with an HR of 0.63 (P = .004). The 5-year rate of freedom from disease recurrence was 97% with TBB and 91% with no boost (P = .002).
There were no significant differences in freedom from disease recurrence rates by WBI fractionation either in randomization A (P = .443) or among all randomized patients (P = .605).
Acute radiation dermatitis occurred in significantly more patients who received TBB (P = .006), as did late breast pain (P = .003), induration or fibrosis (P < .0001), and telangiectasia (P = .02). There were no significant differences by boost status for acute or late fatigue, pneumonitis, cardiac complications, or second malignancies.
Reduce the boost dose?
A radiation oncologist who was not involved in this study said that, while the results confirm a benefit of boost dose for patients with non–low-risk DCIS, the doses used in the BIG-3-07 study may be higher than needed to achieve a protective effect.
“Here in America, we usually give 10 Gy in five fractions, and, in many countries, actually, it’s 10 Gy in five fractions, although a few European centers give 16 Gy in eight fractions,” said Alphose Taghian, MD, of Massachusetts General Hospital in Boston.
“I personally only give 10 Gy in five fractions. I am not under the impression that 16 Gy in eight fractions will give better results. The local failure rate is so low, it’s likely that 10 Gy will do the job,” Dr. Taghian said in an interview.
Dr. Taghian noted that raising the dose to 16 Gy increases the risk of fibrosis, as seen in the BIG-3-07 trial.
Nonetheless, the trial demonstrates the benefit of radiation boost dose in patients with high-risk DCIS, he said, adding that the local recurrence-free benefit curves may separate further with longer follow-up.
The study was sponsored by the Trans Tasman Radiation Oncology Group. Dr. Chua and Dr. Taghian reported no conflicts of interest.
Giving a tumor bed boost (TBB) reduced the risk of local recurrence and overall disease recurrence, but there were no significant differences in recurrence rates between conventional WBI and hypofractionated WBI.
Boon Hui Chua, MD, of the University of New South Wales, Sydney, presented these results at the 2020 San Antonio Breast Cancer Symposium.
Dr. Chua and colleagues studied 1,608 women with DCIS resected by conservative surgery. Patients were either younger than 50 years or age 50 and older with at least one of the following risk factors: symptomatic presentation, palpable tumor, multifocal disease, tumor size 1.5 cm or larger, intermediate or high nuclear grade, central necrosis, comedo histology, and/or surgical margins less than 10 mm.
The patients were randomized to treatment in three categories. In randomization A (n = 503), patients were randomized to one of the following treatments:
- WBI at 50 Gy in 25 fractions
- WBI at 42.5 Gy in 16 fractions
- WBI at 50 Gy in 25 fractions plus TBB at 16 Gy in 8 fractions
- WBI at 42.5 Gy in 16 fractions plus TBB at 16 Gy in 8 fractions.
In randomization B (n = 581), patients received WBI at 50 Gy in 25 fractions, with or without TBB at 16 Gy in 8 fractions. In randomization C (n = 524), patients received WBI at 42.5 Gy in 16 fractions, with or without TBB at 16 Gy in 8 fractions.
All patients underwent CT-based radiation planning. WBI was delivered with tangential MV photon beams, and TBB was performed with CT contouring of protocol-defined tumor bed target volumes, with electron or photon energy. The median follow-up was 6.6 years.
Giving a boost to better outcomes
The 5-year rate of freedom from local recurrence was 97% for patients who received TBB and 93% for patients who did not (hazard ratio, 0.47; P < .001). The benefit of TBB was consistent across subgroups.
There were no significant differences in 5-year rates of freedom from local recurrence by WBI fractionation, either in randomization A (P = .837) or among all randomized patients (P = .887).
The tests for interactions between TBB and WBI fractionation on local recurrence were not significant in randomization A (P = .89) or in all randomized patients (P = .89).
The risk of overall disease recurrence was lower among patients who had received TBB, with an HR of 0.63 (P = .004). The 5-year rate of freedom from disease recurrence was 97% with TBB and 91% with no boost (P = .002).
There were no significant differences in freedom from disease recurrence rates by WBI fractionation either in randomization A (P = .443) or among all randomized patients (P = .605).
Acute radiation dermatitis occurred in significantly more patients who received TBB (P = .006), as did late breast pain (P = .003), induration or fibrosis (P < .0001), and telangiectasia (P = .02). There were no significant differences by boost status for acute or late fatigue, pneumonitis, cardiac complications, or second malignancies.
Reduce the boost dose?
A radiation oncologist who was not involved in this study said that, while the results confirm a benefit of boost dose for patients with non–low-risk DCIS, the doses used in the BIG-3-07 study may be higher than needed to achieve a protective effect.
“Here in America, we usually give 10 Gy in five fractions, and, in many countries, actually, it’s 10 Gy in five fractions, although a few European centers give 16 Gy in eight fractions,” said Alphose Taghian, MD, of Massachusetts General Hospital in Boston.
“I personally only give 10 Gy in five fractions. I am not under the impression that 16 Gy in eight fractions will give better results. The local failure rate is so low, it’s likely that 10 Gy will do the job,” Dr. Taghian said in an interview.
Dr. Taghian noted that raising the dose to 16 Gy increases the risk of fibrosis, as seen in the BIG-3-07 trial.
Nonetheless, the trial demonstrates the benefit of radiation boost dose in patients with high-risk DCIS, he said, adding that the local recurrence-free benefit curves may separate further with longer follow-up.
The study was sponsored by the Trans Tasman Radiation Oncology Group. Dr. Chua and Dr. Taghian reported no conflicts of interest.
FROM SABCS 2020
Immunotherapy response linked to low TMB in recurrent glioblastoma
In contrast to what has been seen in other tumor types, recurrent glioblastoma (rGBM) may respond better to immunotherapy when tumor mutational burden (TMB) is low, new research suggests.
There’s an “unexpected correlation between TMB, tumor-intrinsic inflammation, and survival after immunotherapy” in this patient population, researchers noted in a Nature Communications report.
Cases of rGBM in which TMB is low are more likely to respond to immunotherapy than cases in which TMB is higher, the investigators concluded from an analysis of tumor tissue from more than 100 patients.
“We need to do a prospective study and establish a threshold in a particular assay format,” senior author David Ashley, MBBS, PhD, a neurosurgery professor at Duke University, Durham, N.C., said in an interview.
Andrew Sloan, MD, a neurosurgery professor at the Seidman Cancer Center, Cleveland, said in a comment that “many have given up on immunotherapy for GBM because these tumors tend to have lower TMB than tumors that typically respond to immunotherapy, including checkpoint inhibitors.” (Examples include melanoma and lung cancer.)
“If the findings are confirmed, it would be very useful clinically to select” patients for immunotherapy, Dr. Sloan commented.
Correlation seen with rGBM, not primary tumor
Recurrence of GBM is almost inevitable, even when aggressive standard-of-care therapy is given initially, according to Dr. Ashley and colleagues. Studies have indicated that, in 10%-20% of patients with rGBM, disease responds to subsequent immunotherapy, and patients live beyond the predicted median survival of about 12 months. It’s been unclear, however, what distinguishes these survivors from the other patients.
Dr. Ashley and colleagues looked for common genetic factors that distinguish survivors.
The tumor tissue the team analyzed came from three studies. The first was a trial of an intratumoral infusion of a recombinant nonpathogenic poliorhinovirus chimera (PVSRIPO), developed at Duke University, that induces innate inflammation and T-cell attack. Among 61 patients, 21% were alive at 3 years versus 4% of historical control patients.
The second study was a review of 66 patients with GBM who underwent treatment with pembrolizumab or nivolumab. The median survival was 14.3 months among those who experienced a response versus10.1 months for those who did not.
The third study involved more than 1,000 patients with advanced cancer who underwent treatment with checkpoint inhibitors. There was no survival benefit among the 117 patients with glioma who were treated with checkpoint inhibitors.
In the PVSRIPO trial, rGBM tumors from patients who survived longer than 20 months harbored very low TMB, less than 0.6 mutations/Mb. In the two checkpoint inhibitor trials, among 110 patients with rGBM, survival was longer for those whose TMB was at or below the median level.
The differences in survival were not driven by differences in steroid dosing, unfavorable responses among patients with hypermutations, or the presence or absence of IDH1 or PTEN mutations or MGMT promoter methylation, according to Dr. Ashley and colleagues.
“Increased survival of immunotherapy-treated rGBM patients with very low TMB is due to immunotherapy response,” the investigators concluded.
As for the explanation, the team found that rGBM tumors with lower TMB levels had enriched inflammatory gene signatures, compared with tumors with higher TMB levels.
The correlation – and longer survival with low TMB – was not observed in primary GBM tumors, “indicating that a relationship between tumor-intrinsic inflammation and TMB develops upon recurrence. ... We postulate that the baseline inflammatory status of rGBM tumors determines their susceptibility to immunotherapy,” the authors wrote.
Because the correlation between tumor inflammation and TMB was robust in rGBM but not in primary tumors, it might well have been caused by standard-of-care therapy, which affects mutation levels.
“Chemotherapy, which is the standard of care for newly diagnosed glioblastoma, might be altering the inflammatory response in these tumors” and priming an inflammatory process that increases vulnerability to immunotherapy in recurrent tumors, Dr. Ashley said in a press release.
Shorter time to recurrence also correlated with lower TMB and favorable response to PVSRIPO, so shorter duration of standard therapy or shorter time from initial surgery might improve immunotherapy response, he speculated.
The study was funded by the National Institutes of Health and other organizations. Dr. Ashley and other investigators own intellectual property related to PVSRIPO, which has been licensed to Istari Oncology. Several investigators hold equity in and/or are paid consultants for Istari. Dr. Sloan is the Ohio principal investigator for an rGBM PVSRIPO and pembrolizumab study funded by the company.
A version of this article first appeared on Medscape.com.
In contrast to what has been seen in other tumor types, recurrent glioblastoma (rGBM) may respond better to immunotherapy when tumor mutational burden (TMB) is low, new research suggests.
There’s an “unexpected correlation between TMB, tumor-intrinsic inflammation, and survival after immunotherapy” in this patient population, researchers noted in a Nature Communications report.
Cases of rGBM in which TMB is low are more likely to respond to immunotherapy than cases in which TMB is higher, the investigators concluded from an analysis of tumor tissue from more than 100 patients.
“We need to do a prospective study and establish a threshold in a particular assay format,” senior author David Ashley, MBBS, PhD, a neurosurgery professor at Duke University, Durham, N.C., said in an interview.
Andrew Sloan, MD, a neurosurgery professor at the Seidman Cancer Center, Cleveland, said in a comment that “many have given up on immunotherapy for GBM because these tumors tend to have lower TMB than tumors that typically respond to immunotherapy, including checkpoint inhibitors.” (Examples include melanoma and lung cancer.)
“If the findings are confirmed, it would be very useful clinically to select” patients for immunotherapy, Dr. Sloan commented.
Correlation seen with rGBM, not primary tumor
Recurrence of GBM is almost inevitable, even when aggressive standard-of-care therapy is given initially, according to Dr. Ashley and colleagues. Studies have indicated that, in 10%-20% of patients with rGBM, disease responds to subsequent immunotherapy, and patients live beyond the predicted median survival of about 12 months. It’s been unclear, however, what distinguishes these survivors from the other patients.
Dr. Ashley and colleagues looked for common genetic factors that distinguish survivors.
The tumor tissue the team analyzed came from three studies. The first was a trial of an intratumoral infusion of a recombinant nonpathogenic poliorhinovirus chimera (PVSRIPO), developed at Duke University, that induces innate inflammation and T-cell attack. Among 61 patients, 21% were alive at 3 years versus 4% of historical control patients.
The second study was a review of 66 patients with GBM who underwent treatment with pembrolizumab or nivolumab. The median survival was 14.3 months among those who experienced a response versus10.1 months for those who did not.
The third study involved more than 1,000 patients with advanced cancer who underwent treatment with checkpoint inhibitors. There was no survival benefit among the 117 patients with glioma who were treated with checkpoint inhibitors.
In the PVSRIPO trial, rGBM tumors from patients who survived longer than 20 months harbored very low TMB, less than 0.6 mutations/Mb. In the two checkpoint inhibitor trials, among 110 patients with rGBM, survival was longer for those whose TMB was at or below the median level.
The differences in survival were not driven by differences in steroid dosing, unfavorable responses among patients with hypermutations, or the presence or absence of IDH1 or PTEN mutations or MGMT promoter methylation, according to Dr. Ashley and colleagues.
“Increased survival of immunotherapy-treated rGBM patients with very low TMB is due to immunotherapy response,” the investigators concluded.
As for the explanation, the team found that rGBM tumors with lower TMB levels had enriched inflammatory gene signatures, compared with tumors with higher TMB levels.
The correlation – and longer survival with low TMB – was not observed in primary GBM tumors, “indicating that a relationship between tumor-intrinsic inflammation and TMB develops upon recurrence. ... We postulate that the baseline inflammatory status of rGBM tumors determines their susceptibility to immunotherapy,” the authors wrote.
Because the correlation between tumor inflammation and TMB was robust in rGBM but not in primary tumors, it might well have been caused by standard-of-care therapy, which affects mutation levels.
“Chemotherapy, which is the standard of care for newly diagnosed glioblastoma, might be altering the inflammatory response in these tumors” and priming an inflammatory process that increases vulnerability to immunotherapy in recurrent tumors, Dr. Ashley said in a press release.
Shorter time to recurrence also correlated with lower TMB and favorable response to PVSRIPO, so shorter duration of standard therapy or shorter time from initial surgery might improve immunotherapy response, he speculated.
The study was funded by the National Institutes of Health and other organizations. Dr. Ashley and other investigators own intellectual property related to PVSRIPO, which has been licensed to Istari Oncology. Several investigators hold equity in and/or are paid consultants for Istari. Dr. Sloan is the Ohio principal investigator for an rGBM PVSRIPO and pembrolizumab study funded by the company.
A version of this article first appeared on Medscape.com.
In contrast to what has been seen in other tumor types, recurrent glioblastoma (rGBM) may respond better to immunotherapy when tumor mutational burden (TMB) is low, new research suggests.
There’s an “unexpected correlation between TMB, tumor-intrinsic inflammation, and survival after immunotherapy” in this patient population, researchers noted in a Nature Communications report.
Cases of rGBM in which TMB is low are more likely to respond to immunotherapy than cases in which TMB is higher, the investigators concluded from an analysis of tumor tissue from more than 100 patients.
“We need to do a prospective study and establish a threshold in a particular assay format,” senior author David Ashley, MBBS, PhD, a neurosurgery professor at Duke University, Durham, N.C., said in an interview.
Andrew Sloan, MD, a neurosurgery professor at the Seidman Cancer Center, Cleveland, said in a comment that “many have given up on immunotherapy for GBM because these tumors tend to have lower TMB than tumors that typically respond to immunotherapy, including checkpoint inhibitors.” (Examples include melanoma and lung cancer.)
“If the findings are confirmed, it would be very useful clinically to select” patients for immunotherapy, Dr. Sloan commented.
Correlation seen with rGBM, not primary tumor
Recurrence of GBM is almost inevitable, even when aggressive standard-of-care therapy is given initially, according to Dr. Ashley and colleagues. Studies have indicated that, in 10%-20% of patients with rGBM, disease responds to subsequent immunotherapy, and patients live beyond the predicted median survival of about 12 months. It’s been unclear, however, what distinguishes these survivors from the other patients.
Dr. Ashley and colleagues looked for common genetic factors that distinguish survivors.
The tumor tissue the team analyzed came from three studies. The first was a trial of an intratumoral infusion of a recombinant nonpathogenic poliorhinovirus chimera (PVSRIPO), developed at Duke University, that induces innate inflammation and T-cell attack. Among 61 patients, 21% were alive at 3 years versus 4% of historical control patients.
The second study was a review of 66 patients with GBM who underwent treatment with pembrolizumab or nivolumab. The median survival was 14.3 months among those who experienced a response versus10.1 months for those who did not.
The third study involved more than 1,000 patients with advanced cancer who underwent treatment with checkpoint inhibitors. There was no survival benefit among the 117 patients with glioma who were treated with checkpoint inhibitors.
In the PVSRIPO trial, rGBM tumors from patients who survived longer than 20 months harbored very low TMB, less than 0.6 mutations/Mb. In the two checkpoint inhibitor trials, among 110 patients with rGBM, survival was longer for those whose TMB was at or below the median level.
The differences in survival were not driven by differences in steroid dosing, unfavorable responses among patients with hypermutations, or the presence or absence of IDH1 or PTEN mutations or MGMT promoter methylation, according to Dr. Ashley and colleagues.
“Increased survival of immunotherapy-treated rGBM patients with very low TMB is due to immunotherapy response,” the investigators concluded.
As for the explanation, the team found that rGBM tumors with lower TMB levels had enriched inflammatory gene signatures, compared with tumors with higher TMB levels.
The correlation – and longer survival with low TMB – was not observed in primary GBM tumors, “indicating that a relationship between tumor-intrinsic inflammation and TMB develops upon recurrence. ... We postulate that the baseline inflammatory status of rGBM tumors determines their susceptibility to immunotherapy,” the authors wrote.
Because the correlation between tumor inflammation and TMB was robust in rGBM but not in primary tumors, it might well have been caused by standard-of-care therapy, which affects mutation levels.
“Chemotherapy, which is the standard of care for newly diagnosed glioblastoma, might be altering the inflammatory response in these tumors” and priming an inflammatory process that increases vulnerability to immunotherapy in recurrent tumors, Dr. Ashley said in a press release.
Shorter time to recurrence also correlated with lower TMB and favorable response to PVSRIPO, so shorter duration of standard therapy or shorter time from initial surgery might improve immunotherapy response, he speculated.
The study was funded by the National Institutes of Health and other organizations. Dr. Ashley and other investigators own intellectual property related to PVSRIPO, which has been licensed to Istari Oncology. Several investigators hold equity in and/or are paid consultants for Istari. Dr. Sloan is the Ohio principal investigator for an rGBM PVSRIPO and pembrolizumab study funded by the company.
A version of this article first appeared on Medscape.com.
Surprise medical billing may eliminate restrictive networks
Certainly, this has been a tumultuous year for health care, as well as the nation in general. There is so much to cover it is hard to know where to begin.
Against a background of a swelling pandemic, I remain confused about the new evaluation and management coding system, and suspect there will be much more training to be rolled out. It is excellent news that the Paycheck Protection Program has been renewed for a second pass, if you can demonstrate that you suffered at least a 25% drop in income for at least one quarter last year, and have fewer than 300 employees – which covers most dermatology practices. I plan to discuss the impact of price transparency in a future column, but today will discuss one area, where we have had the passage of major health care legislation, that may have been overlooked.
Starting in January 2022, patients are protected from surprise medical bills. For nonemergency services and services outside hospitals and other facilities, a patient can only be billed for the coinsurance/copay that they would have had if the patient had been in network unless you go through a consent process by which you inform the patient that you are out-of-network, inform them of the costs, and inform them of other in-network providers. It also requires that patients’ in-network cost-sharing payments for out-of-network surprise bills are attributed to a patient’s in-network deductible.
In section 103, it further states that, where out-of-network rates are determined, there will be a 30-day open negotiation period for providers and payers to settle out-of-network claims. It also states that if the parties are unable to reach a negotiated agreement, they may access a binding arbitration process – referred to as an independent dispute resolution (IDR) – in which one offer prevails. Providers may batch similar services in one proceeding when claims are from the same payer. The IDR process will be administered by independent, unbiased entities with no affiliation to providers or payers.
The IDR entity is required to consider the market-based median in-network rate, alongside relevant information brought by either party, information requested by the reviewer, as well as factors such as the provider’s training and experience patient acuity, and the complexity of furnishing the item or service, in the case of a provider that is a facility. Other factors include the teaching status, case mix and scope of services of such facility, demonstrations of good faith efforts (or lack of good faith efforts) to enter into a network agreement, prior contracted rates during the previous 4 plan-years, and other items. Billed charges and public payer (Medicare and Medicaid) rates are excluded from consideration. This should result in a payment closer to private insurance rates.
As many of you know, another one of the long-term outrages by insurers has been the closure of their networks and delisting of dermatologists. I have written about this situation before in this column. Insurers have also refused to update their provider lists, effectively denying care by the magical process of not having to pay for medical care, because there aren’t any medical providers.
Inaccurate physician rosters
Obviously, one source of surprise medical bills that is easily correctable are inaccurate insurance company physician rosters. The Centers for Medicare & Medicaid Services implemented new rules with stiff fines instructing Medicare advantage plans to improve the accuracy of physician rosters, after a scathing General Accounting Office report 5 years ago. This process, however, was effectively neutered by the last administration by referring all enforcement action to the states, which did not have the manpower or political will to enforce them. This new surprise billing law directly addresses this issue, requiring insurers to update their provider directories every 90 days and keeping them available to patients on line.
This law also eliminates gag clauses between physicians and patients regarding insurer policies.
In short, this bill solves many problems for dermatologists in their constant struggle with insurers. In particular, accurate provider directories will allow patients and companies buying insurance for their employees, to see what they are getting. I suspect the revelation of the paucity of dermatologists in many of these networks will result in increased demand for your services and perhaps provide you a little negotiating leverage.
Also, if I read this law correctly, and I inform patients of our out-of-network status and give them a reasonable estimate of the cost of their care, network participation will no longer restrict patients who want to see me. I acknowledge that we will have to make good-faith efforts to join their networks (which most of us have repeatedly) and learn how to navigate the arbitration process, but this could be a boon for small-practice dermatologists who have been shut out of participating. In fact, it may be less trouble for insurers to simply invite us in, than going through repeated arbitration.
In the bigger picture, I would remind you of the importance of your legislative participation at the past American Academy of Dermatology Association Washington fly-ins, your support of the American Medical Association, and your support of SkinPac. These issues were always in our top three asks in Washington. All this favorable language was suggested, supported, and aided by your efforts and support of organized medicine.
There is a sign on my desk my wife gave me that reads “Never, Never, Never, Give Up.” I am proud of all of you for never giving up, and think you all deserve a “way to go” and a pat on the back. This law, which is a far walk from abusive air ambulance bills and unexpected anesthesia charges, amply and happily demonstrates that things can be changed for the better, and that access to care for our patients can be improved.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at dermnews@mdedge.com.
Certainly, this has been a tumultuous year for health care, as well as the nation in general. There is so much to cover it is hard to know where to begin.
Against a background of a swelling pandemic, I remain confused about the new evaluation and management coding system, and suspect there will be much more training to be rolled out. It is excellent news that the Paycheck Protection Program has been renewed for a second pass, if you can demonstrate that you suffered at least a 25% drop in income for at least one quarter last year, and have fewer than 300 employees – which covers most dermatology practices. I plan to discuss the impact of price transparency in a future column, but today will discuss one area, where we have had the passage of major health care legislation, that may have been overlooked.
Starting in January 2022, patients are protected from surprise medical bills. For nonemergency services and services outside hospitals and other facilities, a patient can only be billed for the coinsurance/copay that they would have had if the patient had been in network unless you go through a consent process by which you inform the patient that you are out-of-network, inform them of the costs, and inform them of other in-network providers. It also requires that patients’ in-network cost-sharing payments for out-of-network surprise bills are attributed to a patient’s in-network deductible.
In section 103, it further states that, where out-of-network rates are determined, there will be a 30-day open negotiation period for providers and payers to settle out-of-network claims. It also states that if the parties are unable to reach a negotiated agreement, they may access a binding arbitration process – referred to as an independent dispute resolution (IDR) – in which one offer prevails. Providers may batch similar services in one proceeding when claims are from the same payer. The IDR process will be administered by independent, unbiased entities with no affiliation to providers or payers.
The IDR entity is required to consider the market-based median in-network rate, alongside relevant information brought by either party, information requested by the reviewer, as well as factors such as the provider’s training and experience patient acuity, and the complexity of furnishing the item or service, in the case of a provider that is a facility. Other factors include the teaching status, case mix and scope of services of such facility, demonstrations of good faith efforts (or lack of good faith efforts) to enter into a network agreement, prior contracted rates during the previous 4 plan-years, and other items. Billed charges and public payer (Medicare and Medicaid) rates are excluded from consideration. This should result in a payment closer to private insurance rates.
As many of you know, another one of the long-term outrages by insurers has been the closure of their networks and delisting of dermatologists. I have written about this situation before in this column. Insurers have also refused to update their provider lists, effectively denying care by the magical process of not having to pay for medical care, because there aren’t any medical providers.
Inaccurate physician rosters
Obviously, one source of surprise medical bills that is easily correctable are inaccurate insurance company physician rosters. The Centers for Medicare & Medicaid Services implemented new rules with stiff fines instructing Medicare advantage plans to improve the accuracy of physician rosters, after a scathing General Accounting Office report 5 years ago. This process, however, was effectively neutered by the last administration by referring all enforcement action to the states, which did not have the manpower or political will to enforce them. This new surprise billing law directly addresses this issue, requiring insurers to update their provider directories every 90 days and keeping them available to patients on line.
This law also eliminates gag clauses between physicians and patients regarding insurer policies.
In short, this bill solves many problems for dermatologists in their constant struggle with insurers. In particular, accurate provider directories will allow patients and companies buying insurance for their employees, to see what they are getting. I suspect the revelation of the paucity of dermatologists in many of these networks will result in increased demand for your services and perhaps provide you a little negotiating leverage.
Also, if I read this law correctly, and I inform patients of our out-of-network status and give them a reasonable estimate of the cost of their care, network participation will no longer restrict patients who want to see me. I acknowledge that we will have to make good-faith efforts to join their networks (which most of us have repeatedly) and learn how to navigate the arbitration process, but this could be a boon for small-practice dermatologists who have been shut out of participating. In fact, it may be less trouble for insurers to simply invite us in, than going through repeated arbitration.
In the bigger picture, I would remind you of the importance of your legislative participation at the past American Academy of Dermatology Association Washington fly-ins, your support of the American Medical Association, and your support of SkinPac. These issues were always in our top three asks in Washington. All this favorable language was suggested, supported, and aided by your efforts and support of organized medicine.
There is a sign on my desk my wife gave me that reads “Never, Never, Never, Give Up.” I am proud of all of you for never giving up, and think you all deserve a “way to go” and a pat on the back. This law, which is a far walk from abusive air ambulance bills and unexpected anesthesia charges, amply and happily demonstrates that things can be changed for the better, and that access to care for our patients can be improved.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at dermnews@mdedge.com.
Certainly, this has been a tumultuous year for health care, as well as the nation in general. There is so much to cover it is hard to know where to begin.
Against a background of a swelling pandemic, I remain confused about the new evaluation and management coding system, and suspect there will be much more training to be rolled out. It is excellent news that the Paycheck Protection Program has been renewed for a second pass, if you can demonstrate that you suffered at least a 25% drop in income for at least one quarter last year, and have fewer than 300 employees – which covers most dermatology practices. I plan to discuss the impact of price transparency in a future column, but today will discuss one area, where we have had the passage of major health care legislation, that may have been overlooked.
Starting in January 2022, patients are protected from surprise medical bills. For nonemergency services and services outside hospitals and other facilities, a patient can only be billed for the coinsurance/copay that they would have had if the patient had been in network unless you go through a consent process by which you inform the patient that you are out-of-network, inform them of the costs, and inform them of other in-network providers. It also requires that patients’ in-network cost-sharing payments for out-of-network surprise bills are attributed to a patient’s in-network deductible.
In section 103, it further states that, where out-of-network rates are determined, there will be a 30-day open negotiation period for providers and payers to settle out-of-network claims. It also states that if the parties are unable to reach a negotiated agreement, they may access a binding arbitration process – referred to as an independent dispute resolution (IDR) – in which one offer prevails. Providers may batch similar services in one proceeding when claims are from the same payer. The IDR process will be administered by independent, unbiased entities with no affiliation to providers or payers.
The IDR entity is required to consider the market-based median in-network rate, alongside relevant information brought by either party, information requested by the reviewer, as well as factors such as the provider’s training and experience patient acuity, and the complexity of furnishing the item or service, in the case of a provider that is a facility. Other factors include the teaching status, case mix and scope of services of such facility, demonstrations of good faith efforts (or lack of good faith efforts) to enter into a network agreement, prior contracted rates during the previous 4 plan-years, and other items. Billed charges and public payer (Medicare and Medicaid) rates are excluded from consideration. This should result in a payment closer to private insurance rates.
As many of you know, another one of the long-term outrages by insurers has been the closure of their networks and delisting of dermatologists. I have written about this situation before in this column. Insurers have also refused to update their provider lists, effectively denying care by the magical process of not having to pay for medical care, because there aren’t any medical providers.
Inaccurate physician rosters
Obviously, one source of surprise medical bills that is easily correctable are inaccurate insurance company physician rosters. The Centers for Medicare & Medicaid Services implemented new rules with stiff fines instructing Medicare advantage plans to improve the accuracy of physician rosters, after a scathing General Accounting Office report 5 years ago. This process, however, was effectively neutered by the last administration by referring all enforcement action to the states, which did not have the manpower or political will to enforce them. This new surprise billing law directly addresses this issue, requiring insurers to update their provider directories every 90 days and keeping them available to patients on line.
This law also eliminates gag clauses between physicians and patients regarding insurer policies.
In short, this bill solves many problems for dermatologists in their constant struggle with insurers. In particular, accurate provider directories will allow patients and companies buying insurance for their employees, to see what they are getting. I suspect the revelation of the paucity of dermatologists in many of these networks will result in increased demand for your services and perhaps provide you a little negotiating leverage.
Also, if I read this law correctly, and I inform patients of our out-of-network status and give them a reasonable estimate of the cost of their care, network participation will no longer restrict patients who want to see me. I acknowledge that we will have to make good-faith efforts to join their networks (which most of us have repeatedly) and learn how to navigate the arbitration process, but this could be a boon for small-practice dermatologists who have been shut out of participating. In fact, it may be less trouble for insurers to simply invite us in, than going through repeated arbitration.
In the bigger picture, I would remind you of the importance of your legislative participation at the past American Academy of Dermatology Association Washington fly-ins, your support of the American Medical Association, and your support of SkinPac. These issues were always in our top three asks in Washington. All this favorable language was suggested, supported, and aided by your efforts and support of organized medicine.
There is a sign on my desk my wife gave me that reads “Never, Never, Never, Give Up.” I am proud of all of you for never giving up, and think you all deserve a “way to go” and a pat on the back. This law, which is a far walk from abusive air ambulance bills and unexpected anesthesia charges, amply and happily demonstrates that things can be changed for the better, and that access to care for our patients can be improved.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at dermnews@mdedge.com.
Early Head Start program boosts healthy eating, self-regulation
Home-based preventive interventions not only improve healthy eating habits and self-regulation in toddlers but also guide their parents toward better food presentation and response to picky behaviors, reported Robert L. Nix, PhD, of the University of Wisconsin, Madison, and his associates.
In a small, randomized controlled trial of 73 families with toddlers aged 18-36 months enrolled in home-based Early Head Start (EHS), the researchers evaluated four protective factors, including toddlers’ healthy eating habits, toddlers’ self-regulation, parents’ responsive feeding practices, and parents’ sensitive scaffolding. The study, conducted from April to October 2013, is the first clinical trial of Recipe 4 Success, a preschool-focused intervention created by administrators and home visitors of EHS that promotes healthy eating and self-regulation in toddlers living in poverty who may otherwise face weight challenges and obesity later in life. Integrating the intervention into EHS allowed the researchers to take full advantage of its national infrastructure and to make dissemination more efficient.
Of the families selected to participate, all of whom were living below the Federal poverty threshold, 66 were retained through post treatment. Most participating parents were biological mothers; 61% were single; 29% were not high school graduates; just 11% were employed full time. The toddlers averaged 30.72 months; 44% were female. Roughly 48% of families were non-Hispanic White; 29% were Black; and 23% were Hispanic or Latinx, the investigators reported in Pediatrics. More than three-quarters of participants were enrolled in the Special Supplemental Nutrition Program for Women, Infants, and Children or the Supplemental Nutrition Assistance Program.
The program allowed parents to transform toddler eating habits quickly
The study, which was designed to evaluate for posttreatment differences in the primary outcomes, involved 10 consecutive weekly lessons implemented by regularly assigned EHS home visitors. Parents were required to adhere to feeding practices carefully targeted with sensitive, structured scaffolding designed to keep toddlers from becoming overwhelmed. Parents were guided to understand, for instance, that toddlers frequently need to be exposed to a new food 10-20 times before eating it, and that poor sleep can have a detrimental influence on emotional and behavioral controls that can progress to weight gain.
Parent recall of what food and drinks their toddlers consumed in the previous 24-hour period was collected by interviewers. The percentage of all meals that included a fruit and/or vegetable, a protein source, and the absence of sweets and junk food were noted. Toddler self-regulation was assessed in accordance with delay of gratification, task orientation, and emotional/behavioral control. Parents were asked to rate toddler ability to cease desired activities to comply with parental requests. Parental responsive feeding practices were also recorded to observe how they introduce unique healthy foods and how they responded to their toddlers’ reactions. Parental sensitive scaffolding was similarly observed for their ability to structure activities in a developmentally appropriate manner promoting self-regulation.
The researchers noted no statistically significant differences between families in the treatment and control groups, nor were there differences in outcome measures or covariates. Study findings showed that, compared with toddlers who continued to receive just EHS support, the toddlers randomly assigned to Recipe 4 Success were more likely to consume snacks and meals that contained fruits, vegetables, protein, and no sweets or junk food.
As the results of this study and others have shown, early food preferences offer the strongest indication of later diet and healthy eating habits throughout life. The program targeted in this study is significant in its ability to accelerate the adoption of better toddler eating habits in just a 10-week period.
Recipe 4 Success along with other successful preventive interventions for young children are most effective when parents drive the change. “In the present trial, the quality of parenting was most highly related to healthy eating habits and self-regulation at baseline,” the researchers noted.
Specifically, the authors attributed the success of the program to “targeting specific interrelated outcomes with an integrated, theoretically driven intervention model,” which allowed Recipe 4 Success to boost the effectiveness of EHS substantially “in just 10 weeks with a minimal increase in funding,” the authors added.
The authors noted several weaknesses as well as strengths of the study. Its primary weakness was a baseline-posttreatment design, which made it impossible to assert that intervention effects can be sustained. The study was also limited to English-speaking families. Given that most home visitors attended to families in both Recipe 4 Success and EHS, the researchers noted the possibility for contamination across conditions, but they added that this would have actually reduced the intervention effects. The study’s primary strength was the evidenced-based nature of the randomized control. That Recipe 4 Success was operated as an intervention only strengthen the benefits of normal EHS visits.
Patient parents who promote self-regulation have the best chance of success
“This small study emphasizes the importance of parent education and support in setting the toddlers’ palate for lifelong eating habits and self-regulation,” observed Silver Spring, MD, private practice pediatrician and associate clinical professor of pediatrics at George Washington University, Washington, Lillian M. Beard, MD, in a separate interview.
“With the goal of promoting eating habits and self-regulation, I try to guide parents’ choices of what they offer to their toddler. I applaud parents’ patience as I encourage them not to give in and quickly resort to offering salty or sweet snacks. I suggest that if during the course of a day, a palette of colorful healthy choices is offered, most toddlers will graze independently as they go about their play. The challenge is to really support the parent through this quirky stage of their child’s development,” she explained.
“The ultimate challenge today with so much food insecurity, COVID-19 related job losses, and shrinking dollars to feed families is that too many families are feeling a food crisis! A program such as Recipe 4 Success can provide invaluable education for families on how to best stretch their few dollars, with knowledge of which items to seek from their community food pantries, how to best utilize items from the State WIC programs and still seek nutrition tips from their pediatricians while avoiding expensive fast foods that only offer immediate satiety and gratification. The Recipe 4 Success educator, pediatrician, or any community educator can give recommendations about which fresh produce may be inexpensive, but nutritional,” Dr. Beard suggested.
Dr. Nix and colleagues as well as Dr. Beard had no conflicts of interest and no relevant financial disclosures.
Home-based preventive interventions not only improve healthy eating habits and self-regulation in toddlers but also guide their parents toward better food presentation and response to picky behaviors, reported Robert L. Nix, PhD, of the University of Wisconsin, Madison, and his associates.
In a small, randomized controlled trial of 73 families with toddlers aged 18-36 months enrolled in home-based Early Head Start (EHS), the researchers evaluated four protective factors, including toddlers’ healthy eating habits, toddlers’ self-regulation, parents’ responsive feeding practices, and parents’ sensitive scaffolding. The study, conducted from April to October 2013, is the first clinical trial of Recipe 4 Success, a preschool-focused intervention created by administrators and home visitors of EHS that promotes healthy eating and self-regulation in toddlers living in poverty who may otherwise face weight challenges and obesity later in life. Integrating the intervention into EHS allowed the researchers to take full advantage of its national infrastructure and to make dissemination more efficient.
Of the families selected to participate, all of whom were living below the Federal poverty threshold, 66 were retained through post treatment. Most participating parents were biological mothers; 61% were single; 29% were not high school graduates; just 11% were employed full time. The toddlers averaged 30.72 months; 44% were female. Roughly 48% of families were non-Hispanic White; 29% were Black; and 23% were Hispanic or Latinx, the investigators reported in Pediatrics. More than three-quarters of participants were enrolled in the Special Supplemental Nutrition Program for Women, Infants, and Children or the Supplemental Nutrition Assistance Program.
The program allowed parents to transform toddler eating habits quickly
The study, which was designed to evaluate for posttreatment differences in the primary outcomes, involved 10 consecutive weekly lessons implemented by regularly assigned EHS home visitors. Parents were required to adhere to feeding practices carefully targeted with sensitive, structured scaffolding designed to keep toddlers from becoming overwhelmed. Parents were guided to understand, for instance, that toddlers frequently need to be exposed to a new food 10-20 times before eating it, and that poor sleep can have a detrimental influence on emotional and behavioral controls that can progress to weight gain.
Parent recall of what food and drinks their toddlers consumed in the previous 24-hour period was collected by interviewers. The percentage of all meals that included a fruit and/or vegetable, a protein source, and the absence of sweets and junk food were noted. Toddler self-regulation was assessed in accordance with delay of gratification, task orientation, and emotional/behavioral control. Parents were asked to rate toddler ability to cease desired activities to comply with parental requests. Parental responsive feeding practices were also recorded to observe how they introduce unique healthy foods and how they responded to their toddlers’ reactions. Parental sensitive scaffolding was similarly observed for their ability to structure activities in a developmentally appropriate manner promoting self-regulation.
The researchers noted no statistically significant differences between families in the treatment and control groups, nor were there differences in outcome measures or covariates. Study findings showed that, compared with toddlers who continued to receive just EHS support, the toddlers randomly assigned to Recipe 4 Success were more likely to consume snacks and meals that contained fruits, vegetables, protein, and no sweets or junk food.
As the results of this study and others have shown, early food preferences offer the strongest indication of later diet and healthy eating habits throughout life. The program targeted in this study is significant in its ability to accelerate the adoption of better toddler eating habits in just a 10-week period.
Recipe 4 Success along with other successful preventive interventions for young children are most effective when parents drive the change. “In the present trial, the quality of parenting was most highly related to healthy eating habits and self-regulation at baseline,” the researchers noted.
Specifically, the authors attributed the success of the program to “targeting specific interrelated outcomes with an integrated, theoretically driven intervention model,” which allowed Recipe 4 Success to boost the effectiveness of EHS substantially “in just 10 weeks with a minimal increase in funding,” the authors added.
The authors noted several weaknesses as well as strengths of the study. Its primary weakness was a baseline-posttreatment design, which made it impossible to assert that intervention effects can be sustained. The study was also limited to English-speaking families. Given that most home visitors attended to families in both Recipe 4 Success and EHS, the researchers noted the possibility for contamination across conditions, but they added that this would have actually reduced the intervention effects. The study’s primary strength was the evidenced-based nature of the randomized control. That Recipe 4 Success was operated as an intervention only strengthen the benefits of normal EHS visits.
Patient parents who promote self-regulation have the best chance of success
“This small study emphasizes the importance of parent education and support in setting the toddlers’ palate for lifelong eating habits and self-regulation,” observed Silver Spring, MD, private practice pediatrician and associate clinical professor of pediatrics at George Washington University, Washington, Lillian M. Beard, MD, in a separate interview.
“With the goal of promoting eating habits and self-regulation, I try to guide parents’ choices of what they offer to their toddler. I applaud parents’ patience as I encourage them not to give in and quickly resort to offering salty or sweet snacks. I suggest that if during the course of a day, a palette of colorful healthy choices is offered, most toddlers will graze independently as they go about their play. The challenge is to really support the parent through this quirky stage of their child’s development,” she explained.
“The ultimate challenge today with so much food insecurity, COVID-19 related job losses, and shrinking dollars to feed families is that too many families are feeling a food crisis! A program such as Recipe 4 Success can provide invaluable education for families on how to best stretch their few dollars, with knowledge of which items to seek from their community food pantries, how to best utilize items from the State WIC programs and still seek nutrition tips from their pediatricians while avoiding expensive fast foods that only offer immediate satiety and gratification. The Recipe 4 Success educator, pediatrician, or any community educator can give recommendations about which fresh produce may be inexpensive, but nutritional,” Dr. Beard suggested.
Dr. Nix and colleagues as well as Dr. Beard had no conflicts of interest and no relevant financial disclosures.
Home-based preventive interventions not only improve healthy eating habits and self-regulation in toddlers but also guide their parents toward better food presentation and response to picky behaviors, reported Robert L. Nix, PhD, of the University of Wisconsin, Madison, and his associates.
In a small, randomized controlled trial of 73 families with toddlers aged 18-36 months enrolled in home-based Early Head Start (EHS), the researchers evaluated four protective factors, including toddlers’ healthy eating habits, toddlers’ self-regulation, parents’ responsive feeding practices, and parents’ sensitive scaffolding. The study, conducted from April to October 2013, is the first clinical trial of Recipe 4 Success, a preschool-focused intervention created by administrators and home visitors of EHS that promotes healthy eating and self-regulation in toddlers living in poverty who may otherwise face weight challenges and obesity later in life. Integrating the intervention into EHS allowed the researchers to take full advantage of its national infrastructure and to make dissemination more efficient.
Of the families selected to participate, all of whom were living below the Federal poverty threshold, 66 were retained through post treatment. Most participating parents were biological mothers; 61% were single; 29% were not high school graduates; just 11% were employed full time. The toddlers averaged 30.72 months; 44% were female. Roughly 48% of families were non-Hispanic White; 29% were Black; and 23% were Hispanic or Latinx, the investigators reported in Pediatrics. More than three-quarters of participants were enrolled in the Special Supplemental Nutrition Program for Women, Infants, and Children or the Supplemental Nutrition Assistance Program.
The program allowed parents to transform toddler eating habits quickly
The study, which was designed to evaluate for posttreatment differences in the primary outcomes, involved 10 consecutive weekly lessons implemented by regularly assigned EHS home visitors. Parents were required to adhere to feeding practices carefully targeted with sensitive, structured scaffolding designed to keep toddlers from becoming overwhelmed. Parents were guided to understand, for instance, that toddlers frequently need to be exposed to a new food 10-20 times before eating it, and that poor sleep can have a detrimental influence on emotional and behavioral controls that can progress to weight gain.
Parent recall of what food and drinks their toddlers consumed in the previous 24-hour period was collected by interviewers. The percentage of all meals that included a fruit and/or vegetable, a protein source, and the absence of sweets and junk food were noted. Toddler self-regulation was assessed in accordance with delay of gratification, task orientation, and emotional/behavioral control. Parents were asked to rate toddler ability to cease desired activities to comply with parental requests. Parental responsive feeding practices were also recorded to observe how they introduce unique healthy foods and how they responded to their toddlers’ reactions. Parental sensitive scaffolding was similarly observed for their ability to structure activities in a developmentally appropriate manner promoting self-regulation.
The researchers noted no statistically significant differences between families in the treatment and control groups, nor were there differences in outcome measures or covariates. Study findings showed that, compared with toddlers who continued to receive just EHS support, the toddlers randomly assigned to Recipe 4 Success were more likely to consume snacks and meals that contained fruits, vegetables, protein, and no sweets or junk food.
As the results of this study and others have shown, early food preferences offer the strongest indication of later diet and healthy eating habits throughout life. The program targeted in this study is significant in its ability to accelerate the adoption of better toddler eating habits in just a 10-week period.
Recipe 4 Success along with other successful preventive interventions for young children are most effective when parents drive the change. “In the present trial, the quality of parenting was most highly related to healthy eating habits and self-regulation at baseline,” the researchers noted.
Specifically, the authors attributed the success of the program to “targeting specific interrelated outcomes with an integrated, theoretically driven intervention model,” which allowed Recipe 4 Success to boost the effectiveness of EHS substantially “in just 10 weeks with a minimal increase in funding,” the authors added.
The authors noted several weaknesses as well as strengths of the study. Its primary weakness was a baseline-posttreatment design, which made it impossible to assert that intervention effects can be sustained. The study was also limited to English-speaking families. Given that most home visitors attended to families in both Recipe 4 Success and EHS, the researchers noted the possibility for contamination across conditions, but they added that this would have actually reduced the intervention effects. The study’s primary strength was the evidenced-based nature of the randomized control. That Recipe 4 Success was operated as an intervention only strengthen the benefits of normal EHS visits.
Patient parents who promote self-regulation have the best chance of success
“This small study emphasizes the importance of parent education and support in setting the toddlers’ palate for lifelong eating habits and self-regulation,” observed Silver Spring, MD, private practice pediatrician and associate clinical professor of pediatrics at George Washington University, Washington, Lillian M. Beard, MD, in a separate interview.
“With the goal of promoting eating habits and self-regulation, I try to guide parents’ choices of what they offer to their toddler. I applaud parents’ patience as I encourage them not to give in and quickly resort to offering salty or sweet snacks. I suggest that if during the course of a day, a palette of colorful healthy choices is offered, most toddlers will graze independently as they go about their play. The challenge is to really support the parent through this quirky stage of their child’s development,” she explained.
“The ultimate challenge today with so much food insecurity, COVID-19 related job losses, and shrinking dollars to feed families is that too many families are feeling a food crisis! A program such as Recipe 4 Success can provide invaluable education for families on how to best stretch their few dollars, with knowledge of which items to seek from their community food pantries, how to best utilize items from the State WIC programs and still seek nutrition tips from their pediatricians while avoiding expensive fast foods that only offer immediate satiety and gratification. The Recipe 4 Success educator, pediatrician, or any community educator can give recommendations about which fresh produce may be inexpensive, but nutritional,” Dr. Beard suggested.
Dr. Nix and colleagues as well as Dr. Beard had no conflicts of interest and no relevant financial disclosures.
FROM PEDIATRICS