User login
Blood donated after mass shootings may go to waste
Public calls for blood donations in response to mass shootings may be unnecessary and result in waste, according to researchers.
Mass shootings often trigger a sharp increase in blood donations for affected communities.
In response to the recent mass shooting at the Tree Of Life Synagogue in Pittsburgh, Pennsylvania, multiple news outlets called for blood donations, and local blood centers extended their hours to compensate for the increase in donations.
However, a new study suggests that blood products donated in response to mass shootings may go unused and have to be discarded.
This study was published in The Journal of Trauma and Acute Care Surgery.
The study authors focused on blood donated in response to the mass shooting that took place in Las Vegas on October 1, 2017. This shooting resulted in 58 deaths, 869 injuries, 220 hospital admissions, and at least 68 critical care admissions.
Three healthcare systems provided data for the study. In all, 519 shooting victims were treated within these systems, and 185 were admitted to the hospitals. During the first 24 hours, these patients received 499 blood components, or 2.7 units per admission.
“From our data, it is likely that the total 1-day blood component transfusions needed in Las Vegas were more than in any mass shooting on record,” said study author M. James Lozada, DO, of Vanderbilt University Medical Center in Nashville, Tennessee.
However, the blood donations made in response to the shooting surpassed the need.
A public call for blood donations was issued during a press conference in the early hours of October 2, and that call was amplified in news stories. Stories about blood donation in Las Vegas increased from a daily average of 10 to more than 100 on October 2.
From October 2 to 4, the American Red Cross saw a 53% increase in blood donations nationwide.
The Las Vegas blood bank, United Blood Services, reported receiving 791 donations right after the shooting.
Unfortunately, 137 of these donations (17%) went unused and were subsequently discarded, compared to an average of 26 wasted donations per month at the blood bank.
Therefore, Dr. Lozada and his colleagues concluded that a call for immediate blood donation was unnecessary.
“There is an emotional desire after these events on the part of the public to immediately donate blood, but that’s not always necessary, and it’s not always the best immediate response,” Dr. Lozada said. “The best thing you can do is donate blood year-round.”
“One of the things that we propose in the paper is for cities to develop some protocols for these kind of scenarios, where instead of issuing a blanket call for blood donation, you would do it in a systematic way. As one suggestion, you might do it by ZIP code.”
“Our findings are important to help us prepare for the next mass shooting in the United States. It shows us the amount of blood components we likely will need. It will also help first responders adequately prepare to save lives.”
There was no funding for this research, and the study authors declared no conflicts of interest.
Public calls for blood donations in response to mass shootings may be unnecessary and result in waste, according to researchers.
Mass shootings often trigger a sharp increase in blood donations for affected communities.
In response to the recent mass shooting at the Tree Of Life Synagogue in Pittsburgh, Pennsylvania, multiple news outlets called for blood donations, and local blood centers extended their hours to compensate for the increase in donations.
However, a new study suggests that blood products donated in response to mass shootings may go unused and have to be discarded.
This study was published in The Journal of Trauma and Acute Care Surgery.
The study authors focused on blood donated in response to the mass shooting that took place in Las Vegas on October 1, 2017. This shooting resulted in 58 deaths, 869 injuries, 220 hospital admissions, and at least 68 critical care admissions.
Three healthcare systems provided data for the study. In all, 519 shooting victims were treated within these systems, and 185 were admitted to the hospitals. During the first 24 hours, these patients received 499 blood components, or 2.7 units per admission.
“From our data, it is likely that the total 1-day blood component transfusions needed in Las Vegas were more than in any mass shooting on record,” said study author M. James Lozada, DO, of Vanderbilt University Medical Center in Nashville, Tennessee.
However, the blood donations made in response to the shooting surpassed the need.
A public call for blood donations was issued during a press conference in the early hours of October 2, and that call was amplified in news stories. Stories about blood donation in Las Vegas increased from a daily average of 10 to more than 100 on October 2.
From October 2 to 4, the American Red Cross saw a 53% increase in blood donations nationwide.
The Las Vegas blood bank, United Blood Services, reported receiving 791 donations right after the shooting.
Unfortunately, 137 of these donations (17%) went unused and were subsequently discarded, compared to an average of 26 wasted donations per month at the blood bank.
Therefore, Dr. Lozada and his colleagues concluded that a call for immediate blood donation was unnecessary.
“There is an emotional desire after these events on the part of the public to immediately donate blood, but that’s not always necessary, and it’s not always the best immediate response,” Dr. Lozada said. “The best thing you can do is donate blood year-round.”
“One of the things that we propose in the paper is for cities to develop some protocols for these kind of scenarios, where instead of issuing a blanket call for blood donation, you would do it in a systematic way. As one suggestion, you might do it by ZIP code.”
“Our findings are important to help us prepare for the next mass shooting in the United States. It shows us the amount of blood components we likely will need. It will also help first responders adequately prepare to save lives.”
There was no funding for this research, and the study authors declared no conflicts of interest.
Public calls for blood donations in response to mass shootings may be unnecessary and result in waste, according to researchers.
Mass shootings often trigger a sharp increase in blood donations for affected communities.
In response to the recent mass shooting at the Tree Of Life Synagogue in Pittsburgh, Pennsylvania, multiple news outlets called for blood donations, and local blood centers extended their hours to compensate for the increase in donations.
However, a new study suggests that blood products donated in response to mass shootings may go unused and have to be discarded.
This study was published in The Journal of Trauma and Acute Care Surgery.
The study authors focused on blood donated in response to the mass shooting that took place in Las Vegas on October 1, 2017. This shooting resulted in 58 deaths, 869 injuries, 220 hospital admissions, and at least 68 critical care admissions.
Three healthcare systems provided data for the study. In all, 519 shooting victims were treated within these systems, and 185 were admitted to the hospitals. During the first 24 hours, these patients received 499 blood components, or 2.7 units per admission.
“From our data, it is likely that the total 1-day blood component transfusions needed in Las Vegas were more than in any mass shooting on record,” said study author M. James Lozada, DO, of Vanderbilt University Medical Center in Nashville, Tennessee.
However, the blood donations made in response to the shooting surpassed the need.
A public call for blood donations was issued during a press conference in the early hours of October 2, and that call was amplified in news stories. Stories about blood donation in Las Vegas increased from a daily average of 10 to more than 100 on October 2.
From October 2 to 4, the American Red Cross saw a 53% increase in blood donations nationwide.
The Las Vegas blood bank, United Blood Services, reported receiving 791 donations right after the shooting.
Unfortunately, 137 of these donations (17%) went unused and were subsequently discarded, compared to an average of 26 wasted donations per month at the blood bank.
Therefore, Dr. Lozada and his colleagues concluded that a call for immediate blood donation was unnecessary.
“There is an emotional desire after these events on the part of the public to immediately donate blood, but that’s not always necessary, and it’s not always the best immediate response,” Dr. Lozada said. “The best thing you can do is donate blood year-round.”
“One of the things that we propose in the paper is for cities to develop some protocols for these kind of scenarios, where instead of issuing a blanket call for blood donation, you would do it in a systematic way. As one suggestion, you might do it by ZIP code.”
“Our findings are important to help us prepare for the next mass shooting in the United States. It shows us the amount of blood components we likely will need. It will also help first responders adequately prepare to save lives.”
There was no funding for this research, and the study authors declared no conflicts of interest.
Dogs can sniff out malaria, team says
NEW ORLEANS—Dogs can be trained to sniff out malaria in humans, according to research presented at the American Society of Tropical Medicine and Hygiene Annual Meeting.
Researchers found that dogs could detect malaria by sniffing socks worn by children from a malaria-endemic area of West Africa.
“While our findings are at an early stage, in principle, we have shown that dogs could be trained to detect malaria-infected people by their odor with a credible degree of accuracy,” said study investigator Steve Lindsay, PhD, of Durham University in Durham City, U.K.
Dr. Lindsay presented these findings at the meeting as abstract 32.
The research began in The Gambia, where 600 school children were recruited to join the study. They were checked for overall general health, sampled for malaria parasites, and fitted with a pair of socks they were asked to wear overnight.
The next day, the socks were collected. The socks were sorted according to the malaria infection status of the children. The researchers only selected socks from uninfected children and children with malaria who did not have fever.
The socks were shipped to the United Kingdom, where they were stored in a freezer for several months while dogs were trained to sniff out malaria.
The dogs had to distinguish between socks from children with malaria parasites and socks from uninfected children. The animals were trained to sniff each sample, freeze if they thought they detected malaria, and move on if they did not.
In total, 175 sock samples were tested, including those from 30 malaria-positive children and those from 145 uninfected children.
The dogs correctly identified 70% of the infected children and 90% of the uninfected children.
Dr. Lindsay and his colleagues believe that, with more training and more samples, the dogs could provide a level of accuracy approaching that of a clinical test.
Now, the researchers are considering a follow-up study that would take samples from people in different parts of Africa to test whether parasites from one part of the continent present odors that are different from another part of the continent.
As for putting malaria-detecting dogs to work in the field, Dr. Lindsay said they could be helpful assistants in malaria elimination campaigns.
Currently, the only way to address the problem of asymptomatic malaria carriers is to test or treat an entire community. Dr. Lindsay said detection dogs could be useful for significantly narrowing the focus of clinical testing and treatment efforts.
Dr. Lindsay also believes detection dogs could be used at ports of entry into countries that have eliminated malaria or are close to elimination.
“This could provide a non-invasive way of screening for the disease at ports of entry in a similar way to how sniffer dogs are routinely used to detect fruit and vegetables or drugs at airports,” he said.
“This could help prevent the spread of malaria to countries that have been declared malaria-free and also ensure that people, many of whom might be unaware that they are infected with the malaria parasite, receive antimalarial drug treatment for the disease.”
Dr. Lindsay and his colleagues’ research was funded by the Bill & Melinda Gates Foundation. Dr. Lindsay reported no conflicts of interest.
NEW ORLEANS—Dogs can be trained to sniff out malaria in humans, according to research presented at the American Society of Tropical Medicine and Hygiene Annual Meeting.
Researchers found that dogs could detect malaria by sniffing socks worn by children from a malaria-endemic area of West Africa.
“While our findings are at an early stage, in principle, we have shown that dogs could be trained to detect malaria-infected people by their odor with a credible degree of accuracy,” said study investigator Steve Lindsay, PhD, of Durham University in Durham City, U.K.
Dr. Lindsay presented these findings at the meeting as abstract 32.
The research began in The Gambia, where 600 school children were recruited to join the study. They were checked for overall general health, sampled for malaria parasites, and fitted with a pair of socks they were asked to wear overnight.
The next day, the socks were collected. The socks were sorted according to the malaria infection status of the children. The researchers only selected socks from uninfected children and children with malaria who did not have fever.
The socks were shipped to the United Kingdom, where they were stored in a freezer for several months while dogs were trained to sniff out malaria.
The dogs had to distinguish between socks from children with malaria parasites and socks from uninfected children. The animals were trained to sniff each sample, freeze if they thought they detected malaria, and move on if they did not.
In total, 175 sock samples were tested, including those from 30 malaria-positive children and those from 145 uninfected children.
The dogs correctly identified 70% of the infected children and 90% of the uninfected children.
Dr. Lindsay and his colleagues believe that, with more training and more samples, the dogs could provide a level of accuracy approaching that of a clinical test.
Now, the researchers are considering a follow-up study that would take samples from people in different parts of Africa to test whether parasites from one part of the continent present odors that are different from another part of the continent.
As for putting malaria-detecting dogs to work in the field, Dr. Lindsay said they could be helpful assistants in malaria elimination campaigns.
Currently, the only way to address the problem of asymptomatic malaria carriers is to test or treat an entire community. Dr. Lindsay said detection dogs could be useful for significantly narrowing the focus of clinical testing and treatment efforts.
Dr. Lindsay also believes detection dogs could be used at ports of entry into countries that have eliminated malaria or are close to elimination.
“This could provide a non-invasive way of screening for the disease at ports of entry in a similar way to how sniffer dogs are routinely used to detect fruit and vegetables or drugs at airports,” he said.
“This could help prevent the spread of malaria to countries that have been declared malaria-free and also ensure that people, many of whom might be unaware that they are infected with the malaria parasite, receive antimalarial drug treatment for the disease.”
Dr. Lindsay and his colleagues’ research was funded by the Bill & Melinda Gates Foundation. Dr. Lindsay reported no conflicts of interest.
NEW ORLEANS—Dogs can be trained to sniff out malaria in humans, according to research presented at the American Society of Tropical Medicine and Hygiene Annual Meeting.
Researchers found that dogs could detect malaria by sniffing socks worn by children from a malaria-endemic area of West Africa.
“While our findings are at an early stage, in principle, we have shown that dogs could be trained to detect malaria-infected people by their odor with a credible degree of accuracy,” said study investigator Steve Lindsay, PhD, of Durham University in Durham City, U.K.
Dr. Lindsay presented these findings at the meeting as abstract 32.
The research began in The Gambia, where 600 school children were recruited to join the study. They were checked for overall general health, sampled for malaria parasites, and fitted with a pair of socks they were asked to wear overnight.
The next day, the socks were collected. The socks were sorted according to the malaria infection status of the children. The researchers only selected socks from uninfected children and children with malaria who did not have fever.
The socks were shipped to the United Kingdom, where they were stored in a freezer for several months while dogs were trained to sniff out malaria.
The dogs had to distinguish between socks from children with malaria parasites and socks from uninfected children. The animals were trained to sniff each sample, freeze if they thought they detected malaria, and move on if they did not.
In total, 175 sock samples were tested, including those from 30 malaria-positive children and those from 145 uninfected children.
The dogs correctly identified 70% of the infected children and 90% of the uninfected children.
Dr. Lindsay and his colleagues believe that, with more training and more samples, the dogs could provide a level of accuracy approaching that of a clinical test.
Now, the researchers are considering a follow-up study that would take samples from people in different parts of Africa to test whether parasites from one part of the continent present odors that are different from another part of the continent.
As for putting malaria-detecting dogs to work in the field, Dr. Lindsay said they could be helpful assistants in malaria elimination campaigns.
Currently, the only way to address the problem of asymptomatic malaria carriers is to test or treat an entire community. Dr. Lindsay said detection dogs could be useful for significantly narrowing the focus of clinical testing and treatment efforts.
Dr. Lindsay also believes detection dogs could be used at ports of entry into countries that have eliminated malaria or are close to elimination.
“This could provide a non-invasive way of screening for the disease at ports of entry in a similar way to how sniffer dogs are routinely used to detect fruit and vegetables or drugs at airports,” he said.
“This could help prevent the spread of malaria to countries that have been declared malaria-free and also ensure that people, many of whom might be unaware that they are infected with the malaria parasite, receive antimalarial drug treatment for the disease.”
Dr. Lindsay and his colleagues’ research was funded by the Bill & Melinda Gates Foundation. Dr. Lindsay reported no conflicts of interest.
Healthy, ethical environments can alleviate ‘moral distress’ in clinicians
SAN ANTONIO – Understanding the experience of “moral distress” in critical care is essential because of its potential negative effects on health care providers and the need to prevent or address those effects, according to Marian Altman, PhD, RN, a clinical practice specialist from the American Association of Critical Care Nurses.
Dr. Altman spoke about moral distress as part of a panel discussion at the annual meeting of the American College of Chest Physicians on how to handle nonbeneficial treatment requests from families, including the legal and ethical obligations of care providers when a patient is receiving life-sustaining treatment.
“The key point about moral distress is that these are personal constraints, and so the choices of what is best for a patient often conflicts with what is best for the organization,” Dr. Altman told CHEST 2018 attendees. “It could conflict with what’s best for the care providers, the family, or even other patients, and so it’s that personal experience of moral compromise that often originates in this broader practice of our routine.”
While it does not necessarily occur frequently, moral distress is intense when it does occur.
“It really threatens the identity and the integrity of those who experience it because they truly believe they are seriously compromised with this deep personal effect,” Dr. Altman said.
Dr. Altman credited Andrew Jameton, a bioethicist who authored a seminal book on ethical issues in nursing in 1984, with defining exactly what moral distress is: “painful feelings and/or the psychological disequilibrium that occurs when a person is conscious of the morally appropriate action a situation requires but cannot carry out that action because of the institutionalized obstacles, such as lack of time, lack of supervisory support, exercise of medical power, and institutional policy or legal limits.” Or, in plainer terms, “Moral distress occurs when one knows the ethically correct action to take but feels powerless to take that action,” as Elizabeth G. Epstein, PhD, RN, and Sarah Delgado, MSN, RN, wrote in the Online Journal of Issues in Nursing.
To understand moral distress, it’s important to know what it’s not, too, Dr. Altman said. It’s not the daily stress of work or compassion fatigue or even burnout, though it can lead to burnout.
“Burnout is the state of physical, emotional, and mental fatigue and exhaustion caused by long-term involvement in situations that are emotionally demanding,” Dr. Altman said. “Burnout has been linked with moral distress, but they are two very different things.”
It’s also not a disagreement among colleagues or “an excuse to avoid a challenging situation.” In fact, the No. 1 cause of moral distress, in study after study, Dr. Altman said, is providing medical care, particularly medically futile care.
“Providing really unnecessary treatments and providing end-of-life care can lead to it as well as complex patients and challenging situations,” Dr. Altman said. Other causes include inadequate staffing, incompetent providers, poor communication, and advanced technology used to sustain life.
Though people often associate moral distress with intensive care, it can occur “wherever care is provided” and can “affect all members of the health care team,” Dr. Altman said. Though the early research into moral distress focused on critical care nurses, the field has since exploded, across all medical disciplines and in countries around the world.
That research has revealed how intensely moral distress can impact the psychological, biological, and social health of people. Physical symptoms that can result from moral distress include diarrhea, headache, heart palpitations, neck pain, muscle aches, and vomiting. The emotions it rouses include frustration, fear, anger, anxiety, and, especially, powerlessness and guilt.
Moral distress can lead to burnout and dissatisfaction in individuals and, subsequently, reduced retention and productivity within institutions. Health care providers who experience moral distress may leave their position, their unit, or the profession altogether.
“That can have a huge impact in a time when we need many more health care providers to care for this exploding population,” Dr. Altman said. It can also negatively influence the patient-provider relationship, potentially affecting the quantity and safety of care delivered, she explained.
But there are ways to address moral distress, she said.
“We’re not going to eradicate it because we will never eradicate critical care or end-of-life care, and those are the causes that lead to moral distress,” Dr. Altman said. “But what we can do, and what the research is now focusing on, is concentrate on improving our work environment, and help people recognize that they’re experiencing moral distress before it gets to burnout … or mitigating moral distress when it occurs.”
Those improvements include fostering both a positive ethical environment, with ethics education, an ethics committee, and on-site ethics experts, and a healthy work environment with collaboration and skillful communication.
Research has shown that “a higher ethical work environment is correlated with a decrease in moral distress frequency,” Dr. Altman said. And structured communication processes should focus on the goals of care, she said. More formal programs may include moral distress workshops, a moral distress consult service, an ethics consult service, and distress debriefings, during which a facilitator leads providers in a structured, collaborative discussion about a distressing event that has occurred.
SAN ANTONIO – Understanding the experience of “moral distress” in critical care is essential because of its potential negative effects on health care providers and the need to prevent or address those effects, according to Marian Altman, PhD, RN, a clinical practice specialist from the American Association of Critical Care Nurses.
Dr. Altman spoke about moral distress as part of a panel discussion at the annual meeting of the American College of Chest Physicians on how to handle nonbeneficial treatment requests from families, including the legal and ethical obligations of care providers when a patient is receiving life-sustaining treatment.
“The key point about moral distress is that these are personal constraints, and so the choices of what is best for a patient often conflicts with what is best for the organization,” Dr. Altman told CHEST 2018 attendees. “It could conflict with what’s best for the care providers, the family, or even other patients, and so it’s that personal experience of moral compromise that often originates in this broader practice of our routine.”
While it does not necessarily occur frequently, moral distress is intense when it does occur.
“It really threatens the identity and the integrity of those who experience it because they truly believe they are seriously compromised with this deep personal effect,” Dr. Altman said.
Dr. Altman credited Andrew Jameton, a bioethicist who authored a seminal book on ethical issues in nursing in 1984, with defining exactly what moral distress is: “painful feelings and/or the psychological disequilibrium that occurs when a person is conscious of the morally appropriate action a situation requires but cannot carry out that action because of the institutionalized obstacles, such as lack of time, lack of supervisory support, exercise of medical power, and institutional policy or legal limits.” Or, in plainer terms, “Moral distress occurs when one knows the ethically correct action to take but feels powerless to take that action,” as Elizabeth G. Epstein, PhD, RN, and Sarah Delgado, MSN, RN, wrote in the Online Journal of Issues in Nursing.
To understand moral distress, it’s important to know what it’s not, too, Dr. Altman said. It’s not the daily stress of work or compassion fatigue or even burnout, though it can lead to burnout.
“Burnout is the state of physical, emotional, and mental fatigue and exhaustion caused by long-term involvement in situations that are emotionally demanding,” Dr. Altman said. “Burnout has been linked with moral distress, but they are two very different things.”
It’s also not a disagreement among colleagues or “an excuse to avoid a challenging situation.” In fact, the No. 1 cause of moral distress, in study after study, Dr. Altman said, is providing medical care, particularly medically futile care.
“Providing really unnecessary treatments and providing end-of-life care can lead to it as well as complex patients and challenging situations,” Dr. Altman said. Other causes include inadequate staffing, incompetent providers, poor communication, and advanced technology used to sustain life.
Though people often associate moral distress with intensive care, it can occur “wherever care is provided” and can “affect all members of the health care team,” Dr. Altman said. Though the early research into moral distress focused on critical care nurses, the field has since exploded, across all medical disciplines and in countries around the world.
That research has revealed how intensely moral distress can impact the psychological, biological, and social health of people. Physical symptoms that can result from moral distress include diarrhea, headache, heart palpitations, neck pain, muscle aches, and vomiting. The emotions it rouses include frustration, fear, anger, anxiety, and, especially, powerlessness and guilt.
Moral distress can lead to burnout and dissatisfaction in individuals and, subsequently, reduced retention and productivity within institutions. Health care providers who experience moral distress may leave their position, their unit, or the profession altogether.
“That can have a huge impact in a time when we need many more health care providers to care for this exploding population,” Dr. Altman said. It can also negatively influence the patient-provider relationship, potentially affecting the quantity and safety of care delivered, she explained.
But there are ways to address moral distress, she said.
“We’re not going to eradicate it because we will never eradicate critical care or end-of-life care, and those are the causes that lead to moral distress,” Dr. Altman said. “But what we can do, and what the research is now focusing on, is concentrate on improving our work environment, and help people recognize that they’re experiencing moral distress before it gets to burnout … or mitigating moral distress when it occurs.”
Those improvements include fostering both a positive ethical environment, with ethics education, an ethics committee, and on-site ethics experts, and a healthy work environment with collaboration and skillful communication.
Research has shown that “a higher ethical work environment is correlated with a decrease in moral distress frequency,” Dr. Altman said. And structured communication processes should focus on the goals of care, she said. More formal programs may include moral distress workshops, a moral distress consult service, an ethics consult service, and distress debriefings, during which a facilitator leads providers in a structured, collaborative discussion about a distressing event that has occurred.
SAN ANTONIO – Understanding the experience of “moral distress” in critical care is essential because of its potential negative effects on health care providers and the need to prevent or address those effects, according to Marian Altman, PhD, RN, a clinical practice specialist from the American Association of Critical Care Nurses.
Dr. Altman spoke about moral distress as part of a panel discussion at the annual meeting of the American College of Chest Physicians on how to handle nonbeneficial treatment requests from families, including the legal and ethical obligations of care providers when a patient is receiving life-sustaining treatment.
“The key point about moral distress is that these are personal constraints, and so the choices of what is best for a patient often conflicts with what is best for the organization,” Dr. Altman told CHEST 2018 attendees. “It could conflict with what’s best for the care providers, the family, or even other patients, and so it’s that personal experience of moral compromise that often originates in this broader practice of our routine.”
While it does not necessarily occur frequently, moral distress is intense when it does occur.
“It really threatens the identity and the integrity of those who experience it because they truly believe they are seriously compromised with this deep personal effect,” Dr. Altman said.
Dr. Altman credited Andrew Jameton, a bioethicist who authored a seminal book on ethical issues in nursing in 1984, with defining exactly what moral distress is: “painful feelings and/or the psychological disequilibrium that occurs when a person is conscious of the morally appropriate action a situation requires but cannot carry out that action because of the institutionalized obstacles, such as lack of time, lack of supervisory support, exercise of medical power, and institutional policy or legal limits.” Or, in plainer terms, “Moral distress occurs when one knows the ethically correct action to take but feels powerless to take that action,” as Elizabeth G. Epstein, PhD, RN, and Sarah Delgado, MSN, RN, wrote in the Online Journal of Issues in Nursing.
To understand moral distress, it’s important to know what it’s not, too, Dr. Altman said. It’s not the daily stress of work or compassion fatigue or even burnout, though it can lead to burnout.
“Burnout is the state of physical, emotional, and mental fatigue and exhaustion caused by long-term involvement in situations that are emotionally demanding,” Dr. Altman said. “Burnout has been linked with moral distress, but they are two very different things.”
It’s also not a disagreement among colleagues or “an excuse to avoid a challenging situation.” In fact, the No. 1 cause of moral distress, in study after study, Dr. Altman said, is providing medical care, particularly medically futile care.
“Providing really unnecessary treatments and providing end-of-life care can lead to it as well as complex patients and challenging situations,” Dr. Altman said. Other causes include inadequate staffing, incompetent providers, poor communication, and advanced technology used to sustain life.
Though people often associate moral distress with intensive care, it can occur “wherever care is provided” and can “affect all members of the health care team,” Dr. Altman said. Though the early research into moral distress focused on critical care nurses, the field has since exploded, across all medical disciplines and in countries around the world.
That research has revealed how intensely moral distress can impact the psychological, biological, and social health of people. Physical symptoms that can result from moral distress include diarrhea, headache, heart palpitations, neck pain, muscle aches, and vomiting. The emotions it rouses include frustration, fear, anger, anxiety, and, especially, powerlessness and guilt.
Moral distress can lead to burnout and dissatisfaction in individuals and, subsequently, reduced retention and productivity within institutions. Health care providers who experience moral distress may leave their position, their unit, or the profession altogether.
“That can have a huge impact in a time when we need many more health care providers to care for this exploding population,” Dr. Altman said. It can also negatively influence the patient-provider relationship, potentially affecting the quantity and safety of care delivered, she explained.
But there are ways to address moral distress, she said.
“We’re not going to eradicate it because we will never eradicate critical care or end-of-life care, and those are the causes that lead to moral distress,” Dr. Altman said. “But what we can do, and what the research is now focusing on, is concentrate on improving our work environment, and help people recognize that they’re experiencing moral distress before it gets to burnout … or mitigating moral distress when it occurs.”
Those improvements include fostering both a positive ethical environment, with ethics education, an ethics committee, and on-site ethics experts, and a healthy work environment with collaboration and skillful communication.
Research has shown that “a higher ethical work environment is correlated with a decrease in moral distress frequency,” Dr. Altman said. And structured communication processes should focus on the goals of care, she said. More formal programs may include moral distress workshops, a moral distress consult service, an ethics consult service, and distress debriefings, during which a facilitator leads providers in a structured, collaborative discussion about a distressing event that has occurred.
REPORTING FROM CHEST 2018
Surgical checklist benefits depend on culture change
BOSTON – The success of surgical safety checklists to reduce postoperative mortality appears to depend not only on implementation but also on the degree to which a hospital embraces a culture of teamwork, Atul Gawande, MD, MPH, FACS, said at the annual clinical congress of the American College of Surgeons.
The session “Checking in on the Checklist – Ten Years of the WHO Surgical Safety Checklist” moderated by Thomas Geoghegan Weiser, MD, FACS, and Alex B. Haynes, MD, FACS,considered the progress of the past decade in implementing the World Health Organization initiative in medical institutions around the world.
Team-based approaches to the checklist accompanied by other institutional support have demonstrated double-digit reductions in mortality, while in contrast, a mandate-only approach resulted in a 0% change, said Dr. Gawande, a general and endocrine surgeon at Brigham and Women’s Hospital and professor in the department of health policy and management at the Harvard T.H. Chan School of Public Health and the Samuel O. Thier Professor of Surgery at Harvard Medical School, all in Boston.
Variables including respect among team members, clinical leadership, and assertiveness on behalf of patient safety appeared to be predictive of postoperative death rates in one recent implementation of the WHO Surgical Safety Checklist, he added.
Dr. Gawande said the 29-item surgical safety checklist has earned support but also skepticism and “some outright opposition” in the nearly 10 years since landmark study published in the New England Journal of Medicine, coauthored by Dr. Haynes, reported that the approach cut mortality by 47% and postoperative complication rates by 36%, on average, in a diverse group of eight hospitals throughout the world.
“It’s a challenge in a fundamental way, to our values,” Dr. Gawande told attendees. “What we have valued in our life as surgeons is our autonomy as clinicians, and here was an approach which required you to work with different values: humility, discipline, teamwork.”
That 47% mortality reduction was achieved in a clinical trial setting with “very carefully selected sites” that were enthusiastic about giving the checklist a try, and toward that end, received weekly support, Dr. Gawande said.
Subsequent implementations of the checklist have had varying success rates, he said.
Implementations that have included a mandate plus regular feedback have yielded mortality reductions upward of 26%he said, while a mandate plus team training reduced mortality by 18% in a Veterans Health Administration hospital setting, according to Dr. Gawande. By contrast, a mandate-alone approach in Ontario yielded a 0% reduction in mortality.
“What we came to realize is a kind of formula that underlies how you create change in organizations generally, where you’re trying to create systems that make it easier for people to get the right kinds of things done,” Dr. Gawande said.
“You have a systems tool that has been carefully crafted around the ‘killer items’ – the failure points that even experts fail at – you have an implementation pathway, and then you bring it into a ready environment where people are capable and they’re motivated,” he explained.
A South Carolina initiative that was voluntary and included light-touch support yielded a 22% reduction in hospitals that completed the adoption program, Dr. Gawande said. Of note, investigators in the Safe Surgery 2015: South Carolina Initiative found that perceptions of safety among operating room personnel were associated with the all-cause 30-day postoperative death rate.
“The team found in South Carolina that the predictor of how much change you get is how effective your implementation was in changing the culture to be more team oriented,” Dr. Gawande said.
“You could recognize it by how much change you saw in what the frontline people reported about how much they are respected, how much clinical leadership was actually involved in the way the team works, and the ultimate test; how assertive could people be in raising issues,” he continued. “Did they feel safe to raise issues, and not get their head bitten off, but in fact, find that what they offered had value.”
Dr. Gawande is the founder and executive director of Ariadne Labs, a center for health systems innovation, and the chairman of Lifebox, a not-for-profit organization.
SOURCE: Gawande AA et al. ACS Clinical Congress 2018, Session PS232.
BOSTON – The success of surgical safety checklists to reduce postoperative mortality appears to depend not only on implementation but also on the degree to which a hospital embraces a culture of teamwork, Atul Gawande, MD, MPH, FACS, said at the annual clinical congress of the American College of Surgeons.
The session “Checking in on the Checklist – Ten Years of the WHO Surgical Safety Checklist” moderated by Thomas Geoghegan Weiser, MD, FACS, and Alex B. Haynes, MD, FACS,considered the progress of the past decade in implementing the World Health Organization initiative in medical institutions around the world.
Team-based approaches to the checklist accompanied by other institutional support have demonstrated double-digit reductions in mortality, while in contrast, a mandate-only approach resulted in a 0% change, said Dr. Gawande, a general and endocrine surgeon at Brigham and Women’s Hospital and professor in the department of health policy and management at the Harvard T.H. Chan School of Public Health and the Samuel O. Thier Professor of Surgery at Harvard Medical School, all in Boston.
Variables including respect among team members, clinical leadership, and assertiveness on behalf of patient safety appeared to be predictive of postoperative death rates in one recent implementation of the WHO Surgical Safety Checklist, he added.
Dr. Gawande said the 29-item surgical safety checklist has earned support but also skepticism and “some outright opposition” in the nearly 10 years since landmark study published in the New England Journal of Medicine, coauthored by Dr. Haynes, reported that the approach cut mortality by 47% and postoperative complication rates by 36%, on average, in a diverse group of eight hospitals throughout the world.
“It’s a challenge in a fundamental way, to our values,” Dr. Gawande told attendees. “What we have valued in our life as surgeons is our autonomy as clinicians, and here was an approach which required you to work with different values: humility, discipline, teamwork.”
That 47% mortality reduction was achieved in a clinical trial setting with “very carefully selected sites” that were enthusiastic about giving the checklist a try, and toward that end, received weekly support, Dr. Gawande said.
Subsequent implementations of the checklist have had varying success rates, he said.
Implementations that have included a mandate plus regular feedback have yielded mortality reductions upward of 26%he said, while a mandate plus team training reduced mortality by 18% in a Veterans Health Administration hospital setting, according to Dr. Gawande. By contrast, a mandate-alone approach in Ontario yielded a 0% reduction in mortality.
“What we came to realize is a kind of formula that underlies how you create change in organizations generally, where you’re trying to create systems that make it easier for people to get the right kinds of things done,” Dr. Gawande said.
“You have a systems tool that has been carefully crafted around the ‘killer items’ – the failure points that even experts fail at – you have an implementation pathway, and then you bring it into a ready environment where people are capable and they’re motivated,” he explained.
A South Carolina initiative that was voluntary and included light-touch support yielded a 22% reduction in hospitals that completed the adoption program, Dr. Gawande said. Of note, investigators in the Safe Surgery 2015: South Carolina Initiative found that perceptions of safety among operating room personnel were associated with the all-cause 30-day postoperative death rate.
“The team found in South Carolina that the predictor of how much change you get is how effective your implementation was in changing the culture to be more team oriented,” Dr. Gawande said.
“You could recognize it by how much change you saw in what the frontline people reported about how much they are respected, how much clinical leadership was actually involved in the way the team works, and the ultimate test; how assertive could people be in raising issues,” he continued. “Did they feel safe to raise issues, and not get their head bitten off, but in fact, find that what they offered had value.”
Dr. Gawande is the founder and executive director of Ariadne Labs, a center for health systems innovation, and the chairman of Lifebox, a not-for-profit organization.
SOURCE: Gawande AA et al. ACS Clinical Congress 2018, Session PS232.
BOSTON – The success of surgical safety checklists to reduce postoperative mortality appears to depend not only on implementation but also on the degree to which a hospital embraces a culture of teamwork, Atul Gawande, MD, MPH, FACS, said at the annual clinical congress of the American College of Surgeons.
The session “Checking in on the Checklist – Ten Years of the WHO Surgical Safety Checklist” moderated by Thomas Geoghegan Weiser, MD, FACS, and Alex B. Haynes, MD, FACS,considered the progress of the past decade in implementing the World Health Organization initiative in medical institutions around the world.
Team-based approaches to the checklist accompanied by other institutional support have demonstrated double-digit reductions in mortality, while in contrast, a mandate-only approach resulted in a 0% change, said Dr. Gawande, a general and endocrine surgeon at Brigham and Women’s Hospital and professor in the department of health policy and management at the Harvard T.H. Chan School of Public Health and the Samuel O. Thier Professor of Surgery at Harvard Medical School, all in Boston.
Variables including respect among team members, clinical leadership, and assertiveness on behalf of patient safety appeared to be predictive of postoperative death rates in one recent implementation of the WHO Surgical Safety Checklist, he added.
Dr. Gawande said the 29-item surgical safety checklist has earned support but also skepticism and “some outright opposition” in the nearly 10 years since landmark study published in the New England Journal of Medicine, coauthored by Dr. Haynes, reported that the approach cut mortality by 47% and postoperative complication rates by 36%, on average, in a diverse group of eight hospitals throughout the world.
“It’s a challenge in a fundamental way, to our values,” Dr. Gawande told attendees. “What we have valued in our life as surgeons is our autonomy as clinicians, and here was an approach which required you to work with different values: humility, discipline, teamwork.”
That 47% mortality reduction was achieved in a clinical trial setting with “very carefully selected sites” that were enthusiastic about giving the checklist a try, and toward that end, received weekly support, Dr. Gawande said.
Subsequent implementations of the checklist have had varying success rates, he said.
Implementations that have included a mandate plus regular feedback have yielded mortality reductions upward of 26%he said, while a mandate plus team training reduced mortality by 18% in a Veterans Health Administration hospital setting, according to Dr. Gawande. By contrast, a mandate-alone approach in Ontario yielded a 0% reduction in mortality.
“What we came to realize is a kind of formula that underlies how you create change in organizations generally, where you’re trying to create systems that make it easier for people to get the right kinds of things done,” Dr. Gawande said.
“You have a systems tool that has been carefully crafted around the ‘killer items’ – the failure points that even experts fail at – you have an implementation pathway, and then you bring it into a ready environment where people are capable and they’re motivated,” he explained.
A South Carolina initiative that was voluntary and included light-touch support yielded a 22% reduction in hospitals that completed the adoption program, Dr. Gawande said. Of note, investigators in the Safe Surgery 2015: South Carolina Initiative found that perceptions of safety among operating room personnel were associated with the all-cause 30-day postoperative death rate.
“The team found in South Carolina that the predictor of how much change you get is how effective your implementation was in changing the culture to be more team oriented,” Dr. Gawande said.
“You could recognize it by how much change you saw in what the frontline people reported about how much they are respected, how much clinical leadership was actually involved in the way the team works, and the ultimate test; how assertive could people be in raising issues,” he continued. “Did they feel safe to raise issues, and not get their head bitten off, but in fact, find that what they offered had value.”
Dr. Gawande is the founder and executive director of Ariadne Labs, a center for health systems innovation, and the chairman of Lifebox, a not-for-profit organization.
SOURCE: Gawande AA et al. ACS Clinical Congress 2018, Session PS232.
REPORTING FROM THE ACS CLINICAL CONGRESS
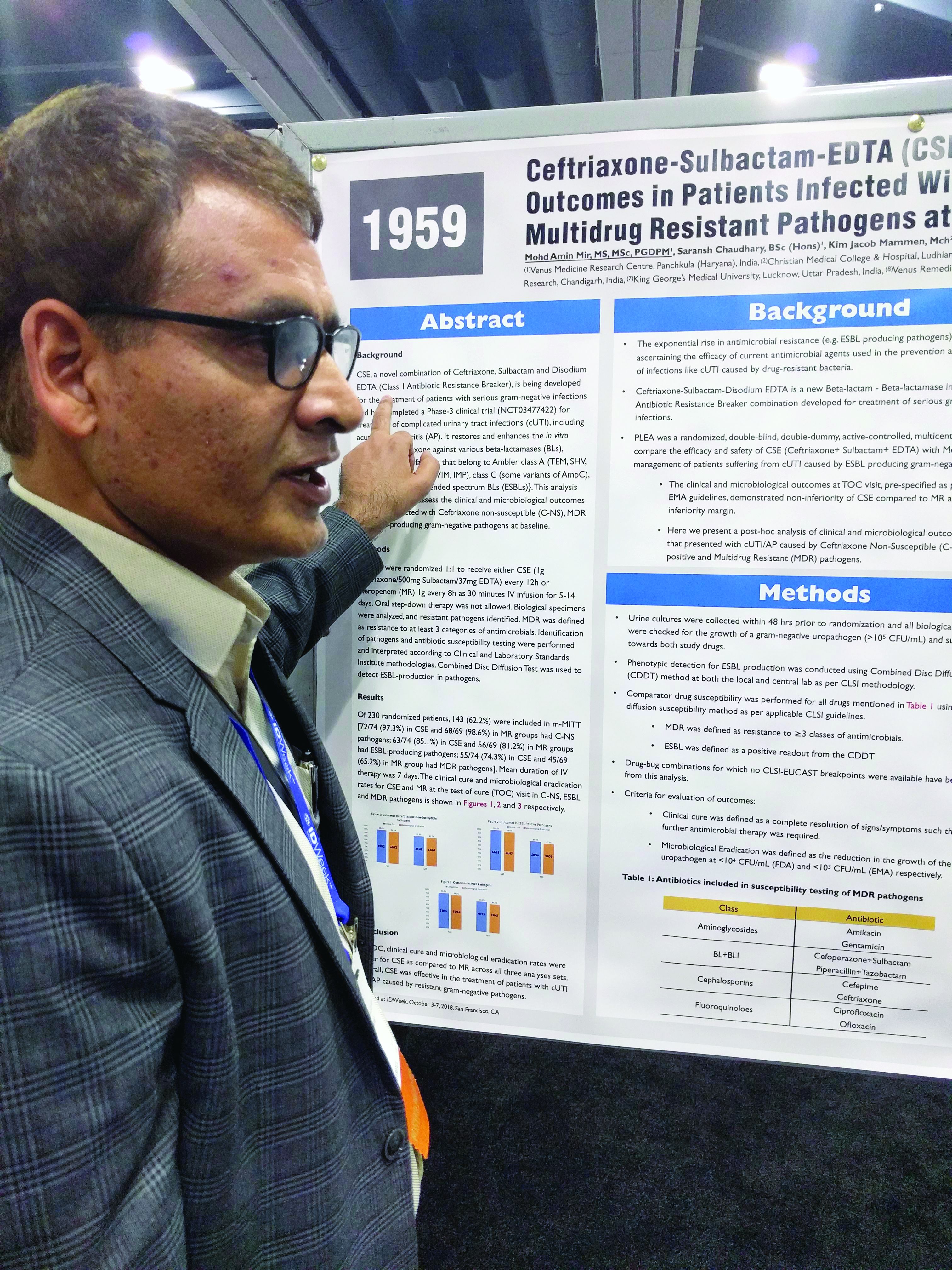
Three-drug combo proves effective against multidrug-resistant UTIs
SAN FRANCISCO – A combination of ceftriaxone, a beta-lactamase inhibitor, and disodium ethylenediaminetetraacetic acid (EDTA) is superior to meropenem in the treatment of complicated urinary tract infections caused by extended-spectrum beta-lactamase (ESBL) gram-negative bacteria, according to a new study.
The post-hoc analysis also found that the three-drug combination – known as CSE – is noninferior to meropenem in multidrug-resistant (MDR) and ceftriaxone-nonsusceptible (C-NS) pathogens.
CSE is aimed at the growing problem of antibiotic resistance, particularly the mechanisms used by bacteria to counter beta-lactamase inhibitors. EDTA chelates zinc and calcium, and many of the resistance mechanisms rely on one or the other of these ions to function. In in vitro models, the combination of sulbactam and EDTA restores activity of ceftriaxone against various beta-lactamases.
Mohd Amin Mir, MD, head of clinical research at the Venus Medicine Research Center, Panchkula, India, and presenter of the study, said that, in the case of efflux pumps, “when there is EDTA present, it chelates the calcium, and that means there is no energy for the efflux pump to throw out the drug.”
The penems, which include meropenem, are a class of synthetic antibiotics with an unsaturated beta-lactam ring. Like other antibiotics, they are under assault from antibiotic resistance, especially beta-lactamase enzymes. “Penems are very precious drugs. The objective of developing [EDTA combinations] is to save the penems,” Dr. Mir said at an annual scientific meeting on infectious diseases.
The PLEA trial randomized 143 patients with complicated urinary tract infections or acute pyelonephritis to CSE (1 g ceftriaxone/500 mg sulbactam/37 mg EDTA) every 12 hours or 1 g meropenem (MR) as a 30-minute intravenous infusion over 30 minutes. Patients received treatment for 5-14 days.
The original study demonstrated that CSE is noninferior to meropenem at a 10% noninferiority margin. The researchers conducted a post-hoc analysis of patients who presented with complicated UTIs or acute pyelonephritis cases that were C-NS, ESBL-positive, or multidrug-resistant (MDR) pathogens. The researchers defined MDR as resistance to three or more categories of antimicrobial agents.
Of patients who received CSE, 97.3% had pathogens that were nonsusceptible to ceftriaxone, as did 98.6% of those who received MR; 85.1% of CSE and 81.2% of MR patients had an ESBL-producing pathogen; and 74.3% of infections in the CSE group were MDR, as were 65.2% of the MR group.
In all three resistant phenotypes, CSE at least trended to more favorable outcomes. In the MDR group, 96.4% of CSE patients achieved a clinical cure, compared with 88.9% in the MR group, and 94.5% achieved microbial eradication, compared with 86.75% in the MR group.
In the ESBL subgroup, 100% of patients in the CSE group achieved a clinical cure, compared with 89.3%, while 98.4% had complete eradication in the CSE group, compared with 87.5%. In the C-NS subgroup, 95.8% in the CSE group achieved a clinical cure, compared with 91.2%, and 94.4% achieved eradication, compared with 89.7% in the MR group.
In the ESBL subgroup, the lower bound of the 95% confidence interval of the between-group difference was greater than 0, indicating superiority of CSE over MR for both clinical cure and eradication. In the MDR and C-NS subgroups, CSE achieved noninferiority at a –10% margin.
CSE is currently commercially available in India, and the manufacturer is now seeking approval in Europe and the United States.
SOURCE: Mir MA et al. IDWeek 2018, Abstract 1959.
SAN FRANCISCO – A combination of ceftriaxone, a beta-lactamase inhibitor, and disodium ethylenediaminetetraacetic acid (EDTA) is superior to meropenem in the treatment of complicated urinary tract infections caused by extended-spectrum beta-lactamase (ESBL) gram-negative bacteria, according to a new study.
The post-hoc analysis also found that the three-drug combination – known as CSE – is noninferior to meropenem in multidrug-resistant (MDR) and ceftriaxone-nonsusceptible (C-NS) pathogens.
CSE is aimed at the growing problem of antibiotic resistance, particularly the mechanisms used by bacteria to counter beta-lactamase inhibitors. EDTA chelates zinc and calcium, and many of the resistance mechanisms rely on one or the other of these ions to function. In in vitro models, the combination of sulbactam and EDTA restores activity of ceftriaxone against various beta-lactamases.
Mohd Amin Mir, MD, head of clinical research at the Venus Medicine Research Center, Panchkula, India, and presenter of the study, said that, in the case of efflux pumps, “when there is EDTA present, it chelates the calcium, and that means there is no energy for the efflux pump to throw out the drug.”
The penems, which include meropenem, are a class of synthetic antibiotics with an unsaturated beta-lactam ring. Like other antibiotics, they are under assault from antibiotic resistance, especially beta-lactamase enzymes. “Penems are very precious drugs. The objective of developing [EDTA combinations] is to save the penems,” Dr. Mir said at an annual scientific meeting on infectious diseases.
The PLEA trial randomized 143 patients with complicated urinary tract infections or acute pyelonephritis to CSE (1 g ceftriaxone/500 mg sulbactam/37 mg EDTA) every 12 hours or 1 g meropenem (MR) as a 30-minute intravenous infusion over 30 minutes. Patients received treatment for 5-14 days.
The original study demonstrated that CSE is noninferior to meropenem at a 10% noninferiority margin. The researchers conducted a post-hoc analysis of patients who presented with complicated UTIs or acute pyelonephritis cases that were C-NS, ESBL-positive, or multidrug-resistant (MDR) pathogens. The researchers defined MDR as resistance to three or more categories of antimicrobial agents.
Of patients who received CSE, 97.3% had pathogens that were nonsusceptible to ceftriaxone, as did 98.6% of those who received MR; 85.1% of CSE and 81.2% of MR patients had an ESBL-producing pathogen; and 74.3% of infections in the CSE group were MDR, as were 65.2% of the MR group.
In all three resistant phenotypes, CSE at least trended to more favorable outcomes. In the MDR group, 96.4% of CSE patients achieved a clinical cure, compared with 88.9% in the MR group, and 94.5% achieved microbial eradication, compared with 86.75% in the MR group.
In the ESBL subgroup, 100% of patients in the CSE group achieved a clinical cure, compared with 89.3%, while 98.4% had complete eradication in the CSE group, compared with 87.5%. In the C-NS subgroup, 95.8% in the CSE group achieved a clinical cure, compared with 91.2%, and 94.4% achieved eradication, compared with 89.7% in the MR group.
In the ESBL subgroup, the lower bound of the 95% confidence interval of the between-group difference was greater than 0, indicating superiority of CSE over MR for both clinical cure and eradication. In the MDR and C-NS subgroups, CSE achieved noninferiority at a –10% margin.
CSE is currently commercially available in India, and the manufacturer is now seeking approval in Europe and the United States.
SOURCE: Mir MA et al. IDWeek 2018, Abstract 1959.
SAN FRANCISCO – A combination of ceftriaxone, a beta-lactamase inhibitor, and disodium ethylenediaminetetraacetic acid (EDTA) is superior to meropenem in the treatment of complicated urinary tract infections caused by extended-spectrum beta-lactamase (ESBL) gram-negative bacteria, according to a new study.
The post-hoc analysis also found that the three-drug combination – known as CSE – is noninferior to meropenem in multidrug-resistant (MDR) and ceftriaxone-nonsusceptible (C-NS) pathogens.
CSE is aimed at the growing problem of antibiotic resistance, particularly the mechanisms used by bacteria to counter beta-lactamase inhibitors. EDTA chelates zinc and calcium, and many of the resistance mechanisms rely on one or the other of these ions to function. In in vitro models, the combination of sulbactam and EDTA restores activity of ceftriaxone against various beta-lactamases.
Mohd Amin Mir, MD, head of clinical research at the Venus Medicine Research Center, Panchkula, India, and presenter of the study, said that, in the case of efflux pumps, “when there is EDTA present, it chelates the calcium, and that means there is no energy for the efflux pump to throw out the drug.”
The penems, which include meropenem, are a class of synthetic antibiotics with an unsaturated beta-lactam ring. Like other antibiotics, they are under assault from antibiotic resistance, especially beta-lactamase enzymes. “Penems are very precious drugs. The objective of developing [EDTA combinations] is to save the penems,” Dr. Mir said at an annual scientific meeting on infectious diseases.
The PLEA trial randomized 143 patients with complicated urinary tract infections or acute pyelonephritis to CSE (1 g ceftriaxone/500 mg sulbactam/37 mg EDTA) every 12 hours or 1 g meropenem (MR) as a 30-minute intravenous infusion over 30 minutes. Patients received treatment for 5-14 days.
The original study demonstrated that CSE is noninferior to meropenem at a 10% noninferiority margin. The researchers conducted a post-hoc analysis of patients who presented with complicated UTIs or acute pyelonephritis cases that were C-NS, ESBL-positive, or multidrug-resistant (MDR) pathogens. The researchers defined MDR as resistance to three or more categories of antimicrobial agents.
Of patients who received CSE, 97.3% had pathogens that were nonsusceptible to ceftriaxone, as did 98.6% of those who received MR; 85.1% of CSE and 81.2% of MR patients had an ESBL-producing pathogen; and 74.3% of infections in the CSE group were MDR, as were 65.2% of the MR group.
In all three resistant phenotypes, CSE at least trended to more favorable outcomes. In the MDR group, 96.4% of CSE patients achieved a clinical cure, compared with 88.9% in the MR group, and 94.5% achieved microbial eradication, compared with 86.75% in the MR group.
In the ESBL subgroup, 100% of patients in the CSE group achieved a clinical cure, compared with 89.3%, while 98.4% had complete eradication in the CSE group, compared with 87.5%. In the C-NS subgroup, 95.8% in the CSE group achieved a clinical cure, compared with 91.2%, and 94.4% achieved eradication, compared with 89.7% in the MR group.
In the ESBL subgroup, the lower bound of the 95% confidence interval of the between-group difference was greater than 0, indicating superiority of CSE over MR for both clinical cure and eradication. In the MDR and C-NS subgroups, CSE achieved noninferiority at a –10% margin.
CSE is currently commercially available in India, and the manufacturer is now seeking approval in Europe and the United States.
SOURCE: Mir MA et al. IDWeek 2018, Abstract 1959.
REPORTING FROM IDWEEK 2018
Key clinical point:
Major finding: The combination was noninferior in the context of different resistant subtypes.
Study details: Posthoc analysis of a randomized, controlled trial (n = 143).
Disclosures: The study was funded by Venus Medicine Research Center, which employs Dr. Mir.
Source: Mir MA et al. IDWeek 2018, Abstract 1959.
ACP beefs up firearms policy
The American College of Physicians supports appropriate regulations surrounding the purchase of firearms; best practices ownership, storage, and safe use to minimize the risk of accidental or intentional death or injury; and a ban on civilian use of semiautomatic weapons and large capacity magazines, according to an expanded and updated policy statement issued Oct. 29.
The updated policy statement was issued at the end of a week that saw a mass shooting at a Pittsburgh synagogue where 11 people were killed as well as an incident in which two others were shot to death in a Kentucky grocery store.
“Physicians regularly come face to face with the tragedy that gun violence brings, whether maliciously or unintentionally,” ACP President Ana María López, MD, said in a statement after the synagogue shooting. “The rate of injuries and deaths related to firearms and the growing incidence of mass shootings brings to light, once again, the glaring lack of firearm policy in the United States – a country with one of the highest rates of gun violence in the world. This most recent event makes it more important than ever that Congress and states implement common-sense policies that could prevent injuries and deaths from firearms.”
The policy statement reaffirms all policies included in the college’s 2014 policy.
New to the ACP policy is the college’s support for “appropriate regulation of the purchase of legal firearms to reduce firearms-related injuries and deaths.” ACP specifies that any policy “must be consistent with the Supreme Court ruling establishing that individual ownership of firearms is a constitutional right under the Second Amendment of the Bill of Rights.”
The expanded policy calls for universal criminal background checks for firearms purchase and completion of an educational program on firearm safety; strengthening and enforcing laws on prohibiting convicted domestic violence offenders from purchasing firearms; banning firearms that cannot be detected by metal detectors and standard security screening devices; and a reexamining of concealed carry laws. ACP also favors strong penalties and criminal prosecution for those who sell firearms illegally and for those who legally purchase firearms for the sole purpose of acting as the purchaser for someone who is not legally able to possess the firearm.
The policy also “favors enactment of legislation to ban the manufacture, sale, transfer, and subsequent ownership for civilian use of semiautomatic firearms that are designed to increase their rapid killing capacity (often called ‘assault weapons’) and large-capacity magazines, and retaining the current ban on automatic weapons for civilian use.”
As part of this, ACP is calling for a comprehensive definition of semiautomatic firearms that would be subject to the ban as well as a definition of sporting and hunting purposes that should be narrowly defined.
The policy also calls for raising of the minimum age to purchase a semiautomatic weapon to 21 years, prior to the full ban being put in place.
Finally, ACP is calling on firearm owners to “adhere to best practices to reduce the risk of accidental or intentional injuries or deaths from firearms,” including ensuring that firearms “cannot be accessed by children, adolescents, people with dementia, people with substance use disorder, and the subset of people with serious mental illness that are associated with greater risk of harming themselves and others.”
Finally, the expanded policy calls for enactment of extreme risk protection order laws, under which a family member or law enforcement officer can seek a court order to temporarily remove firearms from an individual who is at imminent risk of self-harm or to others, while preserving the individual’s due process protections.
gtwachtman@mdedge.com
SOURCE: Butkus R et al. Ann Intern Med. 2018 Oct 29. doi: 10.7326/M18-1530.
“Do you have guns in the home?”
This simple question should be asked as if it were any other question about health status and potentially unsafe behavior that doctors routinely ask.
It opens the door to further discuss firearms-related issues, especially if there is a concern regarding the patient’s mental state that could impact the health and safety of the patient or others around the individual.
James Kahn, MD, of Stanford (Calif.) University, makes this suggestion in an editorial accompanying the ACP policy statement (Ann Intern Med. 2018 Oct 29. doi: 10.7326/M18-2756).
“Do you have guns in the home?”
This simple question should be asked as if it were any other question about health status and potentially unsafe behavior that doctors routinely ask.
It opens the door to further discuss firearms-related issues, especially if there is a concern regarding the patient’s mental state that could impact the health and safety of the patient or others around the individual.
James Kahn, MD, of Stanford (Calif.) University, makes this suggestion in an editorial accompanying the ACP policy statement (Ann Intern Med. 2018 Oct 29. doi: 10.7326/M18-2756).
“Do you have guns in the home?”
This simple question should be asked as if it were any other question about health status and potentially unsafe behavior that doctors routinely ask.
It opens the door to further discuss firearms-related issues, especially if there is a concern regarding the patient’s mental state that could impact the health and safety of the patient or others around the individual.
James Kahn, MD, of Stanford (Calif.) University, makes this suggestion in an editorial accompanying the ACP policy statement (Ann Intern Med. 2018 Oct 29. doi: 10.7326/M18-2756).
The American College of Physicians supports appropriate regulations surrounding the purchase of firearms; best practices ownership, storage, and safe use to minimize the risk of accidental or intentional death or injury; and a ban on civilian use of semiautomatic weapons and large capacity magazines, according to an expanded and updated policy statement issued Oct. 29.
The updated policy statement was issued at the end of a week that saw a mass shooting at a Pittsburgh synagogue where 11 people were killed as well as an incident in which two others were shot to death in a Kentucky grocery store.
“Physicians regularly come face to face with the tragedy that gun violence brings, whether maliciously or unintentionally,” ACP President Ana María López, MD, said in a statement after the synagogue shooting. “The rate of injuries and deaths related to firearms and the growing incidence of mass shootings brings to light, once again, the glaring lack of firearm policy in the United States – a country with one of the highest rates of gun violence in the world. This most recent event makes it more important than ever that Congress and states implement common-sense policies that could prevent injuries and deaths from firearms.”
The policy statement reaffirms all policies included in the college’s 2014 policy.
New to the ACP policy is the college’s support for “appropriate regulation of the purchase of legal firearms to reduce firearms-related injuries and deaths.” ACP specifies that any policy “must be consistent with the Supreme Court ruling establishing that individual ownership of firearms is a constitutional right under the Second Amendment of the Bill of Rights.”
The expanded policy calls for universal criminal background checks for firearms purchase and completion of an educational program on firearm safety; strengthening and enforcing laws on prohibiting convicted domestic violence offenders from purchasing firearms; banning firearms that cannot be detected by metal detectors and standard security screening devices; and a reexamining of concealed carry laws. ACP also favors strong penalties and criminal prosecution for those who sell firearms illegally and for those who legally purchase firearms for the sole purpose of acting as the purchaser for someone who is not legally able to possess the firearm.
The policy also “favors enactment of legislation to ban the manufacture, sale, transfer, and subsequent ownership for civilian use of semiautomatic firearms that are designed to increase their rapid killing capacity (often called ‘assault weapons’) and large-capacity magazines, and retaining the current ban on automatic weapons for civilian use.”
As part of this, ACP is calling for a comprehensive definition of semiautomatic firearms that would be subject to the ban as well as a definition of sporting and hunting purposes that should be narrowly defined.
The policy also calls for raising of the minimum age to purchase a semiautomatic weapon to 21 years, prior to the full ban being put in place.
Finally, ACP is calling on firearm owners to “adhere to best practices to reduce the risk of accidental or intentional injuries or deaths from firearms,” including ensuring that firearms “cannot be accessed by children, adolescents, people with dementia, people with substance use disorder, and the subset of people with serious mental illness that are associated with greater risk of harming themselves and others.”
Finally, the expanded policy calls for enactment of extreme risk protection order laws, under which a family member or law enforcement officer can seek a court order to temporarily remove firearms from an individual who is at imminent risk of self-harm or to others, while preserving the individual’s due process protections.
gtwachtman@mdedge.com
SOURCE: Butkus R et al. Ann Intern Med. 2018 Oct 29. doi: 10.7326/M18-1530.
The American College of Physicians supports appropriate regulations surrounding the purchase of firearms; best practices ownership, storage, and safe use to minimize the risk of accidental or intentional death or injury; and a ban on civilian use of semiautomatic weapons and large capacity magazines, according to an expanded and updated policy statement issued Oct. 29.
The updated policy statement was issued at the end of a week that saw a mass shooting at a Pittsburgh synagogue where 11 people were killed as well as an incident in which two others were shot to death in a Kentucky grocery store.
“Physicians regularly come face to face with the tragedy that gun violence brings, whether maliciously or unintentionally,” ACP President Ana María López, MD, said in a statement after the synagogue shooting. “The rate of injuries and deaths related to firearms and the growing incidence of mass shootings brings to light, once again, the glaring lack of firearm policy in the United States – a country with one of the highest rates of gun violence in the world. This most recent event makes it more important than ever that Congress and states implement common-sense policies that could prevent injuries and deaths from firearms.”
The policy statement reaffirms all policies included in the college’s 2014 policy.
New to the ACP policy is the college’s support for “appropriate regulation of the purchase of legal firearms to reduce firearms-related injuries and deaths.” ACP specifies that any policy “must be consistent with the Supreme Court ruling establishing that individual ownership of firearms is a constitutional right under the Second Amendment of the Bill of Rights.”
The expanded policy calls for universal criminal background checks for firearms purchase and completion of an educational program on firearm safety; strengthening and enforcing laws on prohibiting convicted domestic violence offenders from purchasing firearms; banning firearms that cannot be detected by metal detectors and standard security screening devices; and a reexamining of concealed carry laws. ACP also favors strong penalties and criminal prosecution for those who sell firearms illegally and for those who legally purchase firearms for the sole purpose of acting as the purchaser for someone who is not legally able to possess the firearm.
The policy also “favors enactment of legislation to ban the manufacture, sale, transfer, and subsequent ownership for civilian use of semiautomatic firearms that are designed to increase their rapid killing capacity (often called ‘assault weapons’) and large-capacity magazines, and retaining the current ban on automatic weapons for civilian use.”
As part of this, ACP is calling for a comprehensive definition of semiautomatic firearms that would be subject to the ban as well as a definition of sporting and hunting purposes that should be narrowly defined.
The policy also calls for raising of the minimum age to purchase a semiautomatic weapon to 21 years, prior to the full ban being put in place.
Finally, ACP is calling on firearm owners to “adhere to best practices to reduce the risk of accidental or intentional injuries or deaths from firearms,” including ensuring that firearms “cannot be accessed by children, adolescents, people with dementia, people with substance use disorder, and the subset of people with serious mental illness that are associated with greater risk of harming themselves and others.”
Finally, the expanded policy calls for enactment of extreme risk protection order laws, under which a family member or law enforcement officer can seek a court order to temporarily remove firearms from an individual who is at imminent risk of self-harm or to others, while preserving the individual’s due process protections.
gtwachtman@mdedge.com
SOURCE: Butkus R et al. Ann Intern Med. 2018 Oct 29. doi: 10.7326/M18-1530.
FROM ANNALS OF INTERNAL MEDICINE
Few clinical outcomes convincingly linked to sickle cell trait
Although sickle cell trait (SCT) has been linked to numerous adverse clinical outcomes in multiple studies, only a handful of those associations have strong supporting evidence, results of a systematic review suggest.
Venous and renal complications had the strongest evidence supporting an association with SCT, while exertion-related sudden death – perhaps the highest-profile potential complication of SCT – had moderate-strength evidence supporting a link, according to the review.
By contrast, most other associations between SCT and clinical outcomes had either low-strength evidence or insufficient data to support a link, according to Rakhi P. Naik, MD, of Johns Hopkins University, Baltimore, and coauthors of the review.
“Future rigorous studies are needed to address potential complications of SCT and to determine modifiers of risk,” they wrote. The report in the Annals of Internal Medicine.
The systematic review by Dr. Naik and colleagues focused on 41 studies, most of which were population-based cohort or case-control studies. They rated the evidence quality of each study and grouped 24 clinical outcomes of interest into six categories: exertion-related injury, renal, vascular, pediatric, surgery- and trauma-related outcomes, and mortality.
Exercise-related injury has received considerable attention, particularly in relation to the military and athletics.
The strength of evidence for a link between SCT and exertion-related death was low in their analysis, which included two studies evaluating the outcome. However, Dr. Naik and coauthors did note that SCT may be associated with a small absolute risk of exertion-related death in extreme conditions such a highly strenuous athletic training or the military.
“We do concur with the American Society of Hematology statement recommending against routine SCT screening in athletics and supporting the consistent use of universal precautions to mitigate exertion-related risk in all persons, regardless of SCT status,” they wrote.
Similarly, the absolute risk of exertional rhabdomyolysis in SCT is small and probably occurs only in high-intensity settings, with risk modified by other genetic and environmental factors, Dr. Naik and coauthors said, based on their analysis of two studies looking at this outcome.
Venous complications had a stronger body of evidence, including several studies showing high levels of procoagulants, which makes elevated venous thromboembolism risk plausible in individuals with SCT.
High-strength evidence linked pulmonary embolism, with or without deep-vein thrombosis, to SCT. In contrast, there was no increased risk of isolated deep-vein thrombosis in these individuals.
“The cause of this paradoxical observation is unknown but may be an increased risk for clot embolization in SCT,” Dr. Naik and colleagues wrote in a discussion of the results.
Renal outcomes were often attributed to SCT, and in this review, the authors said there was evidence to support SCT as a risk factor for both proteinuria and chronic kidney disease.
Out of six studies looking at proteinuria, the one high-quality study found a 1.86-fold increased risk for baseline albuminuria in African Americans with SCT versus those without, according to the review.
Out of four studies looking at chronic kidney disease, the two high-quality studies found 1.57- to 1.89-fold increased risk of those outcomes in African Americans with SCT.
Support for the study came in part from the National Human Genome Research Institute and the National Heart, Lung, and Blood Institute. The authors reported disclosures related to Novartis, Addmedica, and Global Blood Therapeutics, among others.
SOURCE: Naik RP et al. Ann Intern Med. 2018 Oct 30. doi:10.7326/M18-1161.
Although sickle cell trait (SCT) has been linked to numerous adverse clinical outcomes in multiple studies, only a handful of those associations have strong supporting evidence, results of a systematic review suggest.
Venous and renal complications had the strongest evidence supporting an association with SCT, while exertion-related sudden death – perhaps the highest-profile potential complication of SCT – had moderate-strength evidence supporting a link, according to the review.
By contrast, most other associations between SCT and clinical outcomes had either low-strength evidence or insufficient data to support a link, according to Rakhi P. Naik, MD, of Johns Hopkins University, Baltimore, and coauthors of the review.
“Future rigorous studies are needed to address potential complications of SCT and to determine modifiers of risk,” they wrote. The report in the Annals of Internal Medicine.
The systematic review by Dr. Naik and colleagues focused on 41 studies, most of which were population-based cohort or case-control studies. They rated the evidence quality of each study and grouped 24 clinical outcomes of interest into six categories: exertion-related injury, renal, vascular, pediatric, surgery- and trauma-related outcomes, and mortality.
Exercise-related injury has received considerable attention, particularly in relation to the military and athletics.
The strength of evidence for a link between SCT and exertion-related death was low in their analysis, which included two studies evaluating the outcome. However, Dr. Naik and coauthors did note that SCT may be associated with a small absolute risk of exertion-related death in extreme conditions such a highly strenuous athletic training or the military.
“We do concur with the American Society of Hematology statement recommending against routine SCT screening in athletics and supporting the consistent use of universal precautions to mitigate exertion-related risk in all persons, regardless of SCT status,” they wrote.
Similarly, the absolute risk of exertional rhabdomyolysis in SCT is small and probably occurs only in high-intensity settings, with risk modified by other genetic and environmental factors, Dr. Naik and coauthors said, based on their analysis of two studies looking at this outcome.
Venous complications had a stronger body of evidence, including several studies showing high levels of procoagulants, which makes elevated venous thromboembolism risk plausible in individuals with SCT.
High-strength evidence linked pulmonary embolism, with or without deep-vein thrombosis, to SCT. In contrast, there was no increased risk of isolated deep-vein thrombosis in these individuals.
“The cause of this paradoxical observation is unknown but may be an increased risk for clot embolization in SCT,” Dr. Naik and colleagues wrote in a discussion of the results.
Renal outcomes were often attributed to SCT, and in this review, the authors said there was evidence to support SCT as a risk factor for both proteinuria and chronic kidney disease.
Out of six studies looking at proteinuria, the one high-quality study found a 1.86-fold increased risk for baseline albuminuria in African Americans with SCT versus those without, according to the review.
Out of four studies looking at chronic kidney disease, the two high-quality studies found 1.57- to 1.89-fold increased risk of those outcomes in African Americans with SCT.
Support for the study came in part from the National Human Genome Research Institute and the National Heart, Lung, and Blood Institute. The authors reported disclosures related to Novartis, Addmedica, and Global Blood Therapeutics, among others.
SOURCE: Naik RP et al. Ann Intern Med. 2018 Oct 30. doi:10.7326/M18-1161.
Although sickle cell trait (SCT) has been linked to numerous adverse clinical outcomes in multiple studies, only a handful of those associations have strong supporting evidence, results of a systematic review suggest.
Venous and renal complications had the strongest evidence supporting an association with SCT, while exertion-related sudden death – perhaps the highest-profile potential complication of SCT – had moderate-strength evidence supporting a link, according to the review.
By contrast, most other associations between SCT and clinical outcomes had either low-strength evidence or insufficient data to support a link, according to Rakhi P. Naik, MD, of Johns Hopkins University, Baltimore, and coauthors of the review.
“Future rigorous studies are needed to address potential complications of SCT and to determine modifiers of risk,” they wrote. The report in the Annals of Internal Medicine.
The systematic review by Dr. Naik and colleagues focused on 41 studies, most of which were population-based cohort or case-control studies. They rated the evidence quality of each study and grouped 24 clinical outcomes of interest into six categories: exertion-related injury, renal, vascular, pediatric, surgery- and trauma-related outcomes, and mortality.
Exercise-related injury has received considerable attention, particularly in relation to the military and athletics.
The strength of evidence for a link between SCT and exertion-related death was low in their analysis, which included two studies evaluating the outcome. However, Dr. Naik and coauthors did note that SCT may be associated with a small absolute risk of exertion-related death in extreme conditions such a highly strenuous athletic training or the military.
“We do concur with the American Society of Hematology statement recommending against routine SCT screening in athletics and supporting the consistent use of universal precautions to mitigate exertion-related risk in all persons, regardless of SCT status,” they wrote.
Similarly, the absolute risk of exertional rhabdomyolysis in SCT is small and probably occurs only in high-intensity settings, with risk modified by other genetic and environmental factors, Dr. Naik and coauthors said, based on their analysis of two studies looking at this outcome.
Venous complications had a stronger body of evidence, including several studies showing high levels of procoagulants, which makes elevated venous thromboembolism risk plausible in individuals with SCT.
High-strength evidence linked pulmonary embolism, with or without deep-vein thrombosis, to SCT. In contrast, there was no increased risk of isolated deep-vein thrombosis in these individuals.
“The cause of this paradoxical observation is unknown but may be an increased risk for clot embolization in SCT,” Dr. Naik and colleagues wrote in a discussion of the results.
Renal outcomes were often attributed to SCT, and in this review, the authors said there was evidence to support SCT as a risk factor for both proteinuria and chronic kidney disease.
Out of six studies looking at proteinuria, the one high-quality study found a 1.86-fold increased risk for baseline albuminuria in African Americans with SCT versus those without, according to the review.
Out of four studies looking at chronic kidney disease, the two high-quality studies found 1.57- to 1.89-fold increased risk of those outcomes in African Americans with SCT.
Support for the study came in part from the National Human Genome Research Institute and the National Heart, Lung, and Blood Institute. The authors reported disclosures related to Novartis, Addmedica, and Global Blood Therapeutics, among others.
SOURCE: Naik RP et al. Ann Intern Med. 2018 Oct 30. doi:10.7326/M18-1161.
FROM ANNALS OF INTERNAL MEDICINE
Key clinical point:
Major finding: Risks of 1.57-fold and higher were seen in high-quality studies linking SCT to venous and renal complications, while studies of moderate quality suggested small absolute risks of exertion-related mortality or rhabdomyolysis.
Study details: A systematic review including 41 mostly population-based cohort or case-control studies looking at 24 clinical outcomes of interest.
Disclosures: Support for the study came in part from the National Human Genome Research Institute and the National Heart, Lung, and Blood Institute. The authors reported disclosures related to Novartis, Addmedica, and Global Blood Therapeutics, among others.
Source: Naik RP et al. Ann Intern Med. 2018 Oct 30. doi:10.7326/M18-1161.
Most Americans incorrectly identify homicide as more common than suicide
Most adults do not realize that suicide is a more frequent cause of death than homicide, according to the first nationally representative study of public perceptions of firearm and non-firearm-related violent death in the United States.
“These findings are consistent with the well-established relationship between risk perception and the ease with which a pertinent categorical example can be summoned from memory, which in most persons is probably affected by the salience of homicides in media coverage,” lead author Erin R. Morgan, MS, and her coauthors wrote in the Annals of Internal Medicine.
The coauthors reviewed 3,811 responses to a question in the National Firearms Survey on the intent and means of violent death; participants were given 4 options – homicide with a gun, homicide with a weapon other than a gun, suicide with a gun, and suicide by a method other than a gun – and asked to rank them by frequency. A study of those responses found that only 13.5% of U.S. adults could correctly identify their state’s most frequent cause of violent death. Of the 1,880 respondents who shared their occupations, only 20% of health care professionals answered the question correctly.
The survey was conducted in April 2015; between 2014 and 2015, suicide was more common than homicide in all 50 states. Suicide by firearm was also more common than homicide by firearm in every state but Illinois, Maryland, and New Jersey. When reviewing firearm options only, the percentage of respondents who identified suicide as most frequent increased to 25.9%, according to Ms. Morgan of the School of Public Health and of Harborview Injury Prevention & Research Center at the University of Washington in Seattle, and her colleagues.
The coauthors noted that accurate identification was not impacted by the respondents’ firearm ownership status, but also that future research should evaluate if promoting awareness of suicide frequency and risk might “motivate behavioral change regarding firearm storage.”
“Our findings suggest that correcting misperceptions about the relative frequency of firearm-related violent deaths may make persons more cognizant of the actuarial risks to themselves and their family, thus creating new opportunities for prevention,” they wrote.
The study was funded by the Fund for a Safer Future and the Joyce Foundation. No conflicts of interest were reported.
SOURCE: Morgan E et al. Ann Intern Med. 2018 Oct 30. doi:10.7326/M18-1533.
Most adults do not realize that suicide is a more frequent cause of death than homicide, according to the first nationally representative study of public perceptions of firearm and non-firearm-related violent death in the United States.
“These findings are consistent with the well-established relationship between risk perception and the ease with which a pertinent categorical example can be summoned from memory, which in most persons is probably affected by the salience of homicides in media coverage,” lead author Erin R. Morgan, MS, and her coauthors wrote in the Annals of Internal Medicine.
The coauthors reviewed 3,811 responses to a question in the National Firearms Survey on the intent and means of violent death; participants were given 4 options – homicide with a gun, homicide with a weapon other than a gun, suicide with a gun, and suicide by a method other than a gun – and asked to rank them by frequency. A study of those responses found that only 13.5% of U.S. adults could correctly identify their state’s most frequent cause of violent death. Of the 1,880 respondents who shared their occupations, only 20% of health care professionals answered the question correctly.
The survey was conducted in April 2015; between 2014 and 2015, suicide was more common than homicide in all 50 states. Suicide by firearm was also more common than homicide by firearm in every state but Illinois, Maryland, and New Jersey. When reviewing firearm options only, the percentage of respondents who identified suicide as most frequent increased to 25.9%, according to Ms. Morgan of the School of Public Health and of Harborview Injury Prevention & Research Center at the University of Washington in Seattle, and her colleagues.
The coauthors noted that accurate identification was not impacted by the respondents’ firearm ownership status, but also that future research should evaluate if promoting awareness of suicide frequency and risk might “motivate behavioral change regarding firearm storage.”
“Our findings suggest that correcting misperceptions about the relative frequency of firearm-related violent deaths may make persons more cognizant of the actuarial risks to themselves and their family, thus creating new opportunities for prevention,” they wrote.
The study was funded by the Fund for a Safer Future and the Joyce Foundation. No conflicts of interest were reported.
SOURCE: Morgan E et al. Ann Intern Med. 2018 Oct 30. doi:10.7326/M18-1533.
Most adults do not realize that suicide is a more frequent cause of death than homicide, according to the first nationally representative study of public perceptions of firearm and non-firearm-related violent death in the United States.
“These findings are consistent with the well-established relationship between risk perception and the ease with which a pertinent categorical example can be summoned from memory, which in most persons is probably affected by the salience of homicides in media coverage,” lead author Erin R. Morgan, MS, and her coauthors wrote in the Annals of Internal Medicine.
The coauthors reviewed 3,811 responses to a question in the National Firearms Survey on the intent and means of violent death; participants were given 4 options – homicide with a gun, homicide with a weapon other than a gun, suicide with a gun, and suicide by a method other than a gun – and asked to rank them by frequency. A study of those responses found that only 13.5% of U.S. adults could correctly identify their state’s most frequent cause of violent death. Of the 1,880 respondents who shared their occupations, only 20% of health care professionals answered the question correctly.
The survey was conducted in April 2015; between 2014 and 2015, suicide was more common than homicide in all 50 states. Suicide by firearm was also more common than homicide by firearm in every state but Illinois, Maryland, and New Jersey. When reviewing firearm options only, the percentage of respondents who identified suicide as most frequent increased to 25.9%, according to Ms. Morgan of the School of Public Health and of Harborview Injury Prevention & Research Center at the University of Washington in Seattle, and her colleagues.
The coauthors noted that accurate identification was not impacted by the respondents’ firearm ownership status, but also that future research should evaluate if promoting awareness of suicide frequency and risk might “motivate behavioral change regarding firearm storage.”
“Our findings suggest that correcting misperceptions about the relative frequency of firearm-related violent deaths may make persons more cognizant of the actuarial risks to themselves and their family, thus creating new opportunities for prevention,” they wrote.
The study was funded by the Fund for a Safer Future and the Joyce Foundation. No conflicts of interest were reported.
SOURCE: Morgan E et al. Ann Intern Med. 2018 Oct 30. doi:10.7326/M18-1533.
FROM ANNALS OF INTERNAL MEDICINE
Key clinical point: Only 13.5% of U.S. adults – and 20% of health care professionals – could identify the most frequent cause of violent death in their state.
Major finding:
Study details: A study of 3,811 responses to the National Firearms Survey.
Disclosures: The study was funded by the Fund for a Safer Future and the Joyce Foundation. No conflicts of interest were reported.
Source: Morgan E et al. Ann Intern Med. 2018 Oct 30. doi:10.7326/M18-1533.
Investigational gene therapy for medically refractory Parkinson’s shows promise
ATLANTA – VY-AADC01, an investigational gene therapy for individuals with medically refractory Parkinson’s disease being developed by Voyager Therapeutics, was well tolerated and decreased the need for antiparkinsonian medications, results from an ongoing phase 1b study showed.
“Prior phase 1 trials also introduced the aromatic l-amino acid decarboxylase (AADC) gene using an adeno-associated virus serotype-2 (AAV2) vector into the putamen of people with Parkinson’s disease (PD),” lead study author Chad Christine, MD, said in an interview in advance of the annual meeting of the American Neurological Association. “Unlike the previous trials, here we increased both vector genome concentration and volume of the AAV2-AADC vector (VY-AADC01) across cohorts and used intraoperative MRI guidance to administer the gene product.”
According to Dr. Christine, a neurologist at the University of California, San Francisco, Parkinson’s Disease Clinic and Research Center, prior trials showed that AAV2-AADC was safe, but there was limited clinical efficacy. This may have been because of the limited volume of putamen treated with the gene therapy. “In our current trial, we admixed VY-AADC01 with gadoteridol (ProHance), an MR imaging agent, which allowed both near real-time MRI monitoring of the location and volume of product infused and postsurgical assessment of the area of the putamen covered by VY-AADC01,” he said. “In addition, we used 18F-Dopa PET, which allowed us to assess the activity of the AADC enzyme in the putamen.”
The researchers enrolled three cohorts of patients who received bilateral infusions of VY-AADC01, admixed with gadoteridol to facilitate intraoperative MRI monitoring of the infusions. In cohort 1, five patients received up to 450 μL/putamen at a concentration of 8.3 × 1011 vg (viral genomes)/mL and were followed for 36 months. In cohort 2, five patients received up to 900 μL/putamen at 8.3 × 1011 vg/mL and were followed for 18 months. In cohort 3, five patients received up to 900 μL/putamen at 2.6 × 1012 vg/mL and were followed for 12 months.
At 12 months, Dr. Christine and his associates observed mean levodopa-equivalent dose (LED) reductions of –10.2%, –32.8%, and –39.3% in cohort 1, cohort 2, and cohort 3, respectively; LED reductions were sustained to 18 months in cohorts 1 and 2. “We were impressed by how well the decrease in need for antiparkinsonian medications paralleled the AADC activity we measured in the putamen of our subjects, which is consistent with the proposed mechanism of action of VY-AADC01,” he said.
In addition, subjects in cohort 1 showed a mean 2.3-hour improvement in Parkinson’s diary-“on” time without troublesome dyskinesia at 24 months, which was maintained at 36 months, while subjects in cohort 2 showed a clinically meaningful 3.5-hour improvement at 18 months. Subjects in cohort 3 showed somewhat less improvement than the other cohorts (1.5 hours at 12 months), but they also had more severe baseline dyskinesia on the Unified Dyskinesia Rating Scale (a mean of 30.2 vs. 19.2 and 17.4 in cohorts 1 and 2, respectively). One patient in the trial experienced two surgery-related serious adverse events (pulmonary embolism and related heart arrhythmia) which resolved completely.
“I think we were somewhat surprised by some of the challenges of the surgical administration,” Dr. Christine said. “Our surgeons improved the administration technique throughout the trial and made a major transition from administering VY-AADC01 using a frontal approach to the putamen to using a posterior approach in our second phase 1 trial.”
He concluded that findings of the current trial suggest that AAV2-AADC gene therapy, administered using intraoperative MRI guidance, appears to be safe and well tolerated. “A number of outcomes suggest that it may offer clinical benefit to patients with advancing Parkinson’s disease, but this will have to be tested in a randomized trial which has recently started,” he said.
Dr. Christine acknowledged that the small sample size and the open-label design of the study limits the generalizability of the findings. The trial received support from Voyager Therapeutics and the Michael J. Fox Foundation. Dr. Christine reported having no disclosures.
Source: Christine et al. ANA 2018, Abstract M300.
ATLANTA – VY-AADC01, an investigational gene therapy for individuals with medically refractory Parkinson’s disease being developed by Voyager Therapeutics, was well tolerated and decreased the need for antiparkinsonian medications, results from an ongoing phase 1b study showed.
“Prior phase 1 trials also introduced the aromatic l-amino acid decarboxylase (AADC) gene using an adeno-associated virus serotype-2 (AAV2) vector into the putamen of people with Parkinson’s disease (PD),” lead study author Chad Christine, MD, said in an interview in advance of the annual meeting of the American Neurological Association. “Unlike the previous trials, here we increased both vector genome concentration and volume of the AAV2-AADC vector (VY-AADC01) across cohorts and used intraoperative MRI guidance to administer the gene product.”
According to Dr. Christine, a neurologist at the University of California, San Francisco, Parkinson’s Disease Clinic and Research Center, prior trials showed that AAV2-AADC was safe, but there was limited clinical efficacy. This may have been because of the limited volume of putamen treated with the gene therapy. “In our current trial, we admixed VY-AADC01 with gadoteridol (ProHance), an MR imaging agent, which allowed both near real-time MRI monitoring of the location and volume of product infused and postsurgical assessment of the area of the putamen covered by VY-AADC01,” he said. “In addition, we used 18F-Dopa PET, which allowed us to assess the activity of the AADC enzyme in the putamen.”
The researchers enrolled three cohorts of patients who received bilateral infusions of VY-AADC01, admixed with gadoteridol to facilitate intraoperative MRI monitoring of the infusions. In cohort 1, five patients received up to 450 μL/putamen at a concentration of 8.3 × 1011 vg (viral genomes)/mL and were followed for 36 months. In cohort 2, five patients received up to 900 μL/putamen at 8.3 × 1011 vg/mL and were followed for 18 months. In cohort 3, five patients received up to 900 μL/putamen at 2.6 × 1012 vg/mL and were followed for 12 months.
At 12 months, Dr. Christine and his associates observed mean levodopa-equivalent dose (LED) reductions of –10.2%, –32.8%, and –39.3% in cohort 1, cohort 2, and cohort 3, respectively; LED reductions were sustained to 18 months in cohorts 1 and 2. “We were impressed by how well the decrease in need for antiparkinsonian medications paralleled the AADC activity we measured in the putamen of our subjects, which is consistent with the proposed mechanism of action of VY-AADC01,” he said.
In addition, subjects in cohort 1 showed a mean 2.3-hour improvement in Parkinson’s diary-“on” time without troublesome dyskinesia at 24 months, which was maintained at 36 months, while subjects in cohort 2 showed a clinically meaningful 3.5-hour improvement at 18 months. Subjects in cohort 3 showed somewhat less improvement than the other cohorts (1.5 hours at 12 months), but they also had more severe baseline dyskinesia on the Unified Dyskinesia Rating Scale (a mean of 30.2 vs. 19.2 and 17.4 in cohorts 1 and 2, respectively). One patient in the trial experienced two surgery-related serious adverse events (pulmonary embolism and related heart arrhythmia) which resolved completely.
“I think we were somewhat surprised by some of the challenges of the surgical administration,” Dr. Christine said. “Our surgeons improved the administration technique throughout the trial and made a major transition from administering VY-AADC01 using a frontal approach to the putamen to using a posterior approach in our second phase 1 trial.”
He concluded that findings of the current trial suggest that AAV2-AADC gene therapy, administered using intraoperative MRI guidance, appears to be safe and well tolerated. “A number of outcomes suggest that it may offer clinical benefit to patients with advancing Parkinson’s disease, but this will have to be tested in a randomized trial which has recently started,” he said.
Dr. Christine acknowledged that the small sample size and the open-label design of the study limits the generalizability of the findings. The trial received support from Voyager Therapeutics and the Michael J. Fox Foundation. Dr. Christine reported having no disclosures.
Source: Christine et al. ANA 2018, Abstract M300.
ATLANTA – VY-AADC01, an investigational gene therapy for individuals with medically refractory Parkinson’s disease being developed by Voyager Therapeutics, was well tolerated and decreased the need for antiparkinsonian medications, results from an ongoing phase 1b study showed.
“Prior phase 1 trials also introduced the aromatic l-amino acid decarboxylase (AADC) gene using an adeno-associated virus serotype-2 (AAV2) vector into the putamen of people with Parkinson’s disease (PD),” lead study author Chad Christine, MD, said in an interview in advance of the annual meeting of the American Neurological Association. “Unlike the previous trials, here we increased both vector genome concentration and volume of the AAV2-AADC vector (VY-AADC01) across cohorts and used intraoperative MRI guidance to administer the gene product.”
According to Dr. Christine, a neurologist at the University of California, San Francisco, Parkinson’s Disease Clinic and Research Center, prior trials showed that AAV2-AADC was safe, but there was limited clinical efficacy. This may have been because of the limited volume of putamen treated with the gene therapy. “In our current trial, we admixed VY-AADC01 with gadoteridol (ProHance), an MR imaging agent, which allowed both near real-time MRI monitoring of the location and volume of product infused and postsurgical assessment of the area of the putamen covered by VY-AADC01,” he said. “In addition, we used 18F-Dopa PET, which allowed us to assess the activity of the AADC enzyme in the putamen.”
The researchers enrolled three cohorts of patients who received bilateral infusions of VY-AADC01, admixed with gadoteridol to facilitate intraoperative MRI monitoring of the infusions. In cohort 1, five patients received up to 450 μL/putamen at a concentration of 8.3 × 1011 vg (viral genomes)/mL and were followed for 36 months. In cohort 2, five patients received up to 900 μL/putamen at 8.3 × 1011 vg/mL and were followed for 18 months. In cohort 3, five patients received up to 900 μL/putamen at 2.6 × 1012 vg/mL and were followed for 12 months.
At 12 months, Dr. Christine and his associates observed mean levodopa-equivalent dose (LED) reductions of –10.2%, –32.8%, and –39.3% in cohort 1, cohort 2, and cohort 3, respectively; LED reductions were sustained to 18 months in cohorts 1 and 2. “We were impressed by how well the decrease in need for antiparkinsonian medications paralleled the AADC activity we measured in the putamen of our subjects, which is consistent with the proposed mechanism of action of VY-AADC01,” he said.
In addition, subjects in cohort 1 showed a mean 2.3-hour improvement in Parkinson’s diary-“on” time without troublesome dyskinesia at 24 months, which was maintained at 36 months, while subjects in cohort 2 showed a clinically meaningful 3.5-hour improvement at 18 months. Subjects in cohort 3 showed somewhat less improvement than the other cohorts (1.5 hours at 12 months), but they also had more severe baseline dyskinesia on the Unified Dyskinesia Rating Scale (a mean of 30.2 vs. 19.2 and 17.4 in cohorts 1 and 2, respectively). One patient in the trial experienced two surgery-related serious adverse events (pulmonary embolism and related heart arrhythmia) which resolved completely.
“I think we were somewhat surprised by some of the challenges of the surgical administration,” Dr. Christine said. “Our surgeons improved the administration technique throughout the trial and made a major transition from administering VY-AADC01 using a frontal approach to the putamen to using a posterior approach in our second phase 1 trial.”
He concluded that findings of the current trial suggest that AAV2-AADC gene therapy, administered using intraoperative MRI guidance, appears to be safe and well tolerated. “A number of outcomes suggest that it may offer clinical benefit to patients with advancing Parkinson’s disease, but this will have to be tested in a randomized trial which has recently started,” he said.
Dr. Christine acknowledged that the small sample size and the open-label design of the study limits the generalizability of the findings. The trial received support from Voyager Therapeutics and the Michael J. Fox Foundation. Dr. Christine reported having no disclosures.
Source: Christine et al. ANA 2018, Abstract M300.
REPORTING FROM ANA 2018
Key clinical point: AAV2-AADC gene therapy, administered using intraoperative MRI guidance, appears to be safe and well tolerated.
Major finding: At 12 months, the researchers observed mean levodopa-equivalent dose (LED) reductions of –10.2%, –32.8%, and –39.3% in cohort 1, cohort 2, and cohort 3, respectively.
Study details: A study of 15 patients in three cohorts who received bilateral infusions of VY-AADC01, admixed with gadoteridol to facilitate intraoperative MRI monitoring of the infusions.
Disclosures: The trial received support from Voyager Therapeutics and the Michael J. Fox Foundation. Dr. Christine reported having no disclosures.
Source: Christine et al. ANA 2018, Abstract M300.
Many oromandibular dystonia patients report improvement after botulinum toxin injections
ATLANTA – A majority of oromandibular dystonia patients treated with botulinum toxin injections reported improvement in symptoms in the largest cohort of patients to date.
Improvements in the range of 50%-100% occurred in 78% of oromandibular dystonia (OMD) patients who received botulinum toxin injections in the retrospective, multicenter analysis, which was presented by Laura Scorr, MD, at the annual meeting of the American Neurological Association.
In an effort to better describe the clinical characteristics of patients with OMD, Dr. Scorr, a movement disorders specialist at Emory University, Atlanta, and her colleagues analyzed data collected from 164 OMD patients enrolled at 26 international sites in the Dystonia Coalition and 37 additional patients who were evaluated at the Emory University within the last year. Subjects enrolled at Dystonia Coalition centers underwent evaluation by a movement disorders specialist to determine distribution of dystonia, areas affected, and severity as measured by the Global Dystonia Rating Scale. A subgroup of patients also completed the SF 36-item Health Survey, the Beck Depression Scale, and the Liebowitz social anxiety scale. Meanwhile, the charts of patients seen at Emory underwent review for data on clinical characteristics, treatment type, botulinum toxin doses, and response.
Among all 201 patients, the average age of onset was 54 years and 65% were female. About 45% were determined to have focal dystonia, 36% had segmental dystonia, and 19% had generalized dystonia. Among a cohort of 47 patients evaluated in the Dystonia Coalition biorepository, the researchers observed significantly increased social anxiety and impaired quality of life on the Liebowitz social anxiety scale and the SF-36 Health Survey.
Of the 37 Emory patients, 31 (84%) received botulinum toxin injections. Of these, 39% reported symptom improvement that ranged from 75%-100% while 39% reported symptom improvement that ranged from 50%-74%. Only 13% had a minimal response, defined as improvement that ranged from 1%-24%.
“Oromandibular dystonia is particularly disabling,” Dr. Scorr said. “There have been a few reports in the literature that say it does not respond to botulinum toxin injections. But in our retrospective review, the majority of patients not only have a response, but a response that’s greater than 50% improvement, which is significant.” She acknowledged that the study’s retrospective design is a limitation. “I think we need more prospective studies, specifically on response to treatment with botulinum toxin,” she said.
The study was funded in part by the Dystonia Medical Research Foundation. Dr. Scorr reported having no financial disclosures.
SOURCE: Scorr L et al. Ann Neurol. 2018;84[S22]:S90, Abstract S216.
ATLANTA – A majority of oromandibular dystonia patients treated with botulinum toxin injections reported improvement in symptoms in the largest cohort of patients to date.
Improvements in the range of 50%-100% occurred in 78% of oromandibular dystonia (OMD) patients who received botulinum toxin injections in the retrospective, multicenter analysis, which was presented by Laura Scorr, MD, at the annual meeting of the American Neurological Association.
In an effort to better describe the clinical characteristics of patients with OMD, Dr. Scorr, a movement disorders specialist at Emory University, Atlanta, and her colleagues analyzed data collected from 164 OMD patients enrolled at 26 international sites in the Dystonia Coalition and 37 additional patients who were evaluated at the Emory University within the last year. Subjects enrolled at Dystonia Coalition centers underwent evaluation by a movement disorders specialist to determine distribution of dystonia, areas affected, and severity as measured by the Global Dystonia Rating Scale. A subgroup of patients also completed the SF 36-item Health Survey, the Beck Depression Scale, and the Liebowitz social anxiety scale. Meanwhile, the charts of patients seen at Emory underwent review for data on clinical characteristics, treatment type, botulinum toxin doses, and response.
Among all 201 patients, the average age of onset was 54 years and 65% were female. About 45% were determined to have focal dystonia, 36% had segmental dystonia, and 19% had generalized dystonia. Among a cohort of 47 patients evaluated in the Dystonia Coalition biorepository, the researchers observed significantly increased social anxiety and impaired quality of life on the Liebowitz social anxiety scale and the SF-36 Health Survey.
Of the 37 Emory patients, 31 (84%) received botulinum toxin injections. Of these, 39% reported symptom improvement that ranged from 75%-100% while 39% reported symptom improvement that ranged from 50%-74%. Only 13% had a minimal response, defined as improvement that ranged from 1%-24%.
“Oromandibular dystonia is particularly disabling,” Dr. Scorr said. “There have been a few reports in the literature that say it does not respond to botulinum toxin injections. But in our retrospective review, the majority of patients not only have a response, but a response that’s greater than 50% improvement, which is significant.” She acknowledged that the study’s retrospective design is a limitation. “I think we need more prospective studies, specifically on response to treatment with botulinum toxin,” she said.
The study was funded in part by the Dystonia Medical Research Foundation. Dr. Scorr reported having no financial disclosures.
SOURCE: Scorr L et al. Ann Neurol. 2018;84[S22]:S90, Abstract S216.
ATLANTA – A majority of oromandibular dystonia patients treated with botulinum toxin injections reported improvement in symptoms in the largest cohort of patients to date.
Improvements in the range of 50%-100% occurred in 78% of oromandibular dystonia (OMD) patients who received botulinum toxin injections in the retrospective, multicenter analysis, which was presented by Laura Scorr, MD, at the annual meeting of the American Neurological Association.
In an effort to better describe the clinical characteristics of patients with OMD, Dr. Scorr, a movement disorders specialist at Emory University, Atlanta, and her colleagues analyzed data collected from 164 OMD patients enrolled at 26 international sites in the Dystonia Coalition and 37 additional patients who were evaluated at the Emory University within the last year. Subjects enrolled at Dystonia Coalition centers underwent evaluation by a movement disorders specialist to determine distribution of dystonia, areas affected, and severity as measured by the Global Dystonia Rating Scale. A subgroup of patients also completed the SF 36-item Health Survey, the Beck Depression Scale, and the Liebowitz social anxiety scale. Meanwhile, the charts of patients seen at Emory underwent review for data on clinical characteristics, treatment type, botulinum toxin doses, and response.
Among all 201 patients, the average age of onset was 54 years and 65% were female. About 45% were determined to have focal dystonia, 36% had segmental dystonia, and 19% had generalized dystonia. Among a cohort of 47 patients evaluated in the Dystonia Coalition biorepository, the researchers observed significantly increased social anxiety and impaired quality of life on the Liebowitz social anxiety scale and the SF-36 Health Survey.
Of the 37 Emory patients, 31 (84%) received botulinum toxin injections. Of these, 39% reported symptom improvement that ranged from 75%-100% while 39% reported symptom improvement that ranged from 50%-74%. Only 13% had a minimal response, defined as improvement that ranged from 1%-24%.
“Oromandibular dystonia is particularly disabling,” Dr. Scorr said. “There have been a few reports in the literature that say it does not respond to botulinum toxin injections. But in our retrospective review, the majority of patients not only have a response, but a response that’s greater than 50% improvement, which is significant.” She acknowledged that the study’s retrospective design is a limitation. “I think we need more prospective studies, specifically on response to treatment with botulinum toxin,” she said.
The study was funded in part by the Dystonia Medical Research Foundation. Dr. Scorr reported having no financial disclosures.
SOURCE: Scorr L et al. Ann Neurol. 2018;84[S22]:S90, Abstract S216.
AT ANA 2018
Key clinical point: Oromandibular dystonia is associated with increased social anxiety and impaired quality of life.
Major finding: After receiving botulinum toxin injections, 78% of patients with oromandibular dystonia reported improvements in the range of 50%-100%.
Study details: A retrospective review of 201 patients with oromandibular dystonia.
Disclosures: The study was funded in part by the Dystonia Medical Research Foundation. Dr. Scorr researchers reported having no financial disclosures.
Source: Scorr L et al. Ann Neurol. 2018;84[S22]:S90, Abstract S216.