User login
Aspirin May Be an Effective Pretreatment for Exercise in Patients With MS
Time to exhaustion was significantly greater after pretreatment with aspirin versus placebo.
LOS ANGELES—Aspirin may be an effective pretreatment for exercise in patients with multiple sclerosis (MS), according to a study described at the 70th Annual Meeting of the American Academy of Neurology.
“Exercise in MS we know to be beneficial on multiple levels,” said Victoria M. Leavitt, PhD, Assistant Professor of Neuropsychology at Columbia University Medical Center in New York. “In addition to physical benefits like gait, balance, and improved cardiovascular fitness, exercise is also associated with improved mood, reduced fatigue, and improved memory performance. The challenge, of course, is that exercise is only beneficial if people actually do it.”
Exercise-induced overheating, exhaustion, and symptom worsening (Uhtoff’s phenomenon) deter many patients with MS from exercise, and patients may have elevated resting body temperatures that are associated with worse fatigue.
To test whether aspirin pretreatment improves exercise performance in people with MS, Dr. Leavitt and colleagues conducted a randomized, placebo-controlled, crossover pilot study. The researchers studied aspirin because of its antipyretic effects and its efficacy in reducing fatigue in nonexercising patients with MS. The primary outcome was total time spent exercising. Change in exercise-induced body temperature was a secondary outcome.
In all, 12 patients participated in the study (nine females; mean age, 39.8; mean disease duration, 7.7 years; Expanded Disability Status Scale scores of 6.5 or less). Eight patients reported heat sensitivity during exercise.
Participants completed two maximal progressive ramped lower body cycle ergometer exercise tests one week apart after taking 650 mg of aspirin or placebo one hour before each test.
Patients exercised an average of 16.4 seconds longer after taking aspirin (9 minutes 28.6 seconds), versus placebo (9 minutes 12.2 seconds). In heat-sensitive patients, average body temperature increase after exercise with aspirin (0.41°F) was lower than the increase with placebo (0.88°F). This difference was not statistically significant.
Larger studies are needed, but the results are encouraging, Dr. Leavitt said. “The next thing we want to look at is how this translates to everyday exercise,” she said. “Does aspirin use in people with MS result in increased physical activity levels or increased adherence to exercise regimens?”
—Jake Remaly
Suggested Reading
Leavitt VM, Blanchard AR, Guo CY, et al. Aspirin is an effective pretreatment for exercise in multiple sclerosis: a double-blin
Wingerchuk DM, Benarroch EE, O’Brien PC, et al. A randomized controlled crossover trial of aspirin for fatigue in multiple sclerosis. Neurology. 2005;64(7):1267-1269.
Time to exhaustion was significantly greater after pretreatment with aspirin versus placebo.
Time to exhaustion was significantly greater after pretreatment with aspirin versus placebo.
LOS ANGELES—Aspirin may be an effective pretreatment for exercise in patients with multiple sclerosis (MS), according to a study described at the 70th Annual Meeting of the American Academy of Neurology.
“Exercise in MS we know to be beneficial on multiple levels,” said Victoria M. Leavitt, PhD, Assistant Professor of Neuropsychology at Columbia University Medical Center in New York. “In addition to physical benefits like gait, balance, and improved cardiovascular fitness, exercise is also associated with improved mood, reduced fatigue, and improved memory performance. The challenge, of course, is that exercise is only beneficial if people actually do it.”
Exercise-induced overheating, exhaustion, and symptom worsening (Uhtoff’s phenomenon) deter many patients with MS from exercise, and patients may have elevated resting body temperatures that are associated with worse fatigue.
To test whether aspirin pretreatment improves exercise performance in people with MS, Dr. Leavitt and colleagues conducted a randomized, placebo-controlled, crossover pilot study. The researchers studied aspirin because of its antipyretic effects and its efficacy in reducing fatigue in nonexercising patients with MS. The primary outcome was total time spent exercising. Change in exercise-induced body temperature was a secondary outcome.
In all, 12 patients participated in the study (nine females; mean age, 39.8; mean disease duration, 7.7 years; Expanded Disability Status Scale scores of 6.5 or less). Eight patients reported heat sensitivity during exercise.
Participants completed two maximal progressive ramped lower body cycle ergometer exercise tests one week apart after taking 650 mg of aspirin or placebo one hour before each test.
Patients exercised an average of 16.4 seconds longer after taking aspirin (9 minutes 28.6 seconds), versus placebo (9 minutes 12.2 seconds). In heat-sensitive patients, average body temperature increase after exercise with aspirin (0.41°F) was lower than the increase with placebo (0.88°F). This difference was not statistically significant.
Larger studies are needed, but the results are encouraging, Dr. Leavitt said. “The next thing we want to look at is how this translates to everyday exercise,” she said. “Does aspirin use in people with MS result in increased physical activity levels or increased adherence to exercise regimens?”
—Jake Remaly
Suggested Reading
Leavitt VM, Blanchard AR, Guo CY, et al. Aspirin is an effective pretreatment for exercise in multiple sclerosis: a double-blin
Wingerchuk DM, Benarroch EE, O’Brien PC, et al. A randomized controlled crossover trial of aspirin for fatigue in multiple sclerosis. Neurology. 2005;64(7):1267-1269.
LOS ANGELES—Aspirin may be an effective pretreatment for exercise in patients with multiple sclerosis (MS), according to a study described at the 70th Annual Meeting of the American Academy of Neurology.
“Exercise in MS we know to be beneficial on multiple levels,” said Victoria M. Leavitt, PhD, Assistant Professor of Neuropsychology at Columbia University Medical Center in New York. “In addition to physical benefits like gait, balance, and improved cardiovascular fitness, exercise is also associated with improved mood, reduced fatigue, and improved memory performance. The challenge, of course, is that exercise is only beneficial if people actually do it.”
Exercise-induced overheating, exhaustion, and symptom worsening (Uhtoff’s phenomenon) deter many patients with MS from exercise, and patients may have elevated resting body temperatures that are associated with worse fatigue.
To test whether aspirin pretreatment improves exercise performance in people with MS, Dr. Leavitt and colleagues conducted a randomized, placebo-controlled, crossover pilot study. The researchers studied aspirin because of its antipyretic effects and its efficacy in reducing fatigue in nonexercising patients with MS. The primary outcome was total time spent exercising. Change in exercise-induced body temperature was a secondary outcome.
In all, 12 patients participated in the study (nine females; mean age, 39.8; mean disease duration, 7.7 years; Expanded Disability Status Scale scores of 6.5 or less). Eight patients reported heat sensitivity during exercise.
Participants completed two maximal progressive ramped lower body cycle ergometer exercise tests one week apart after taking 650 mg of aspirin or placebo one hour before each test.
Patients exercised an average of 16.4 seconds longer after taking aspirin (9 minutes 28.6 seconds), versus placebo (9 minutes 12.2 seconds). In heat-sensitive patients, average body temperature increase after exercise with aspirin (0.41°F) was lower than the increase with placebo (0.88°F). This difference was not statistically significant.
Larger studies are needed, but the results are encouraging, Dr. Leavitt said. “The next thing we want to look at is how this translates to everyday exercise,” she said. “Does aspirin use in people with MS result in increased physical activity levels or increased adherence to exercise regimens?”
—Jake Remaly
Suggested Reading
Leavitt VM, Blanchard AR, Guo CY, et al. Aspirin is an effective pretreatment for exercise in multiple sclerosis: a double-blin
Wingerchuk DM, Benarroch EE, O’Brien PC, et al. A randomized controlled crossover trial of aspirin for fatigue in multiple sclerosis. Neurology. 2005;64(7):1267-1269.
Rare clear cell papillary RCC has indolent course
Clear cell papillary renal cell carcinoma (CCPRCC), a recently identified, rare type of renal tumor, appears to have an indolent course with low risk of either local invasion or distant metastasis, results of a small retrospective study suggest.
Among 25 patients with CCPRCC followed for as long as 119 months, there were no cases of local recurrence or distant metastasis, reported Wei-Jen Chen, MD, of Tapei (Taiwan) Veterans General Hospital, and colleagues.
“Based on our findings, CCPRCC has an indolent behavior even if the patients are immunosuppressed or if they receive less invasive therapy. Microscopically, CCPRCC is considered to be a tumor of low malignant potential, as all tumors in our series were of low nuclear grade,” they wrote in a study published online in the Journal of the Chinese Medical Association.
“Whenever the diagnosis is made in a high grade renal tumor, it should be carefully re-confirmed by either cytogenetic or molecular genetic methods,” the authors reported.
CCPRCC was newly recognized as a distinct renal malignancy in the 2016 World Health Organization Classification of Tumors of the Urinary System and Male Genital Organs. The classification describes CCPRCC as “a renal epithelial neoplasm composed of low-grade clear epithelial cells arranged in tubules and papillae with a predominantly linear nuclear alignment away from the basement membrane.”
Although rare, these tumors account for up to 5% of all resected renal tumors, and arise sporadically in patients with end-stage renal disease (ESRD) and von Hippel-Lindau syndrome, the classification states, adding that “according to current knowledge, these tumors have indolent behavior.”
To see if they could verify that last statement, Dr. Chen and associates collected data on all patients diagnosed at their institution with CCPRCC from January 2008 through September 2016.
They identified a total of 25 patients (11 men and 14 women) with a mean age at diagnosis of 62.8 years. Of this group, three patients with poor general condition underwent cryotherapy after a biopsy-confirmed diagnosis of CCPRCC.
All of the remaining 22 patients underwent surgical resection. Of this group, four had ESRD; three of these patients had received a kidney transplant prior to diagnosis of CCPRCC in the native kidneys, and one had three tumors over both kidneys.
“Three patients had other types of synchronous RCC; one with acquired cystic kidney disease-associated RCC, and the others with ccRCC. All CCPRCCs were localized and low grade (pT1a- pT1b, Fuhrman grade 2), and all of the patients are currently alive with no evidence of disease,” the investigators wrote.
Mean follow-up was 49.7 months (range 12 to 119 months).
One additional patient who was not included in the series was initially diagnosed with CCPRCC with lung metastasis. This patient, who died 3 years and 8 months after cytoreductive nephrectomy, had a clinical course distinct from that of all the other patients, leading the investigators to reexamine his kidney specimen with whole-exome sequencing. The sequencing led to a revision of the diagnosis to clear cell RCC.
The investigators noted that clear cell RCC, papillary RCC, and translocation RCC are three RCC subtypes that should be considered in the differential diagnosis of CCPRCC.
The investigators did not report a study funding source. They reported having no conflicts of interest relevant to the subject matter or materials discussed in the article.
SOURCE: Chen W-J et al. J Chinese Med Assoc. 2018 July 20. doi: 10.1016/j.jcma.2018.04.005.
Clear cell papillary renal cell carcinoma (CCPRCC), a recently identified, rare type of renal tumor, appears to have an indolent course with low risk of either local invasion or distant metastasis, results of a small retrospective study suggest.
Among 25 patients with CCPRCC followed for as long as 119 months, there were no cases of local recurrence or distant metastasis, reported Wei-Jen Chen, MD, of Tapei (Taiwan) Veterans General Hospital, and colleagues.
“Based on our findings, CCPRCC has an indolent behavior even if the patients are immunosuppressed or if they receive less invasive therapy. Microscopically, CCPRCC is considered to be a tumor of low malignant potential, as all tumors in our series were of low nuclear grade,” they wrote in a study published online in the Journal of the Chinese Medical Association.
“Whenever the diagnosis is made in a high grade renal tumor, it should be carefully re-confirmed by either cytogenetic or molecular genetic methods,” the authors reported.
CCPRCC was newly recognized as a distinct renal malignancy in the 2016 World Health Organization Classification of Tumors of the Urinary System and Male Genital Organs. The classification describes CCPRCC as “a renal epithelial neoplasm composed of low-grade clear epithelial cells arranged in tubules and papillae with a predominantly linear nuclear alignment away from the basement membrane.”
Although rare, these tumors account for up to 5% of all resected renal tumors, and arise sporadically in patients with end-stage renal disease (ESRD) and von Hippel-Lindau syndrome, the classification states, adding that “according to current knowledge, these tumors have indolent behavior.”
To see if they could verify that last statement, Dr. Chen and associates collected data on all patients diagnosed at their institution with CCPRCC from January 2008 through September 2016.
They identified a total of 25 patients (11 men and 14 women) with a mean age at diagnosis of 62.8 years. Of this group, three patients with poor general condition underwent cryotherapy after a biopsy-confirmed diagnosis of CCPRCC.
All of the remaining 22 patients underwent surgical resection. Of this group, four had ESRD; three of these patients had received a kidney transplant prior to diagnosis of CCPRCC in the native kidneys, and one had three tumors over both kidneys.
“Three patients had other types of synchronous RCC; one with acquired cystic kidney disease-associated RCC, and the others with ccRCC. All CCPRCCs were localized and low grade (pT1a- pT1b, Fuhrman grade 2), and all of the patients are currently alive with no evidence of disease,” the investigators wrote.
Mean follow-up was 49.7 months (range 12 to 119 months).
One additional patient who was not included in the series was initially diagnosed with CCPRCC with lung metastasis. This patient, who died 3 years and 8 months after cytoreductive nephrectomy, had a clinical course distinct from that of all the other patients, leading the investigators to reexamine his kidney specimen with whole-exome sequencing. The sequencing led to a revision of the diagnosis to clear cell RCC.
The investigators noted that clear cell RCC, papillary RCC, and translocation RCC are three RCC subtypes that should be considered in the differential diagnosis of CCPRCC.
The investigators did not report a study funding source. They reported having no conflicts of interest relevant to the subject matter or materials discussed in the article.
SOURCE: Chen W-J et al. J Chinese Med Assoc. 2018 July 20. doi: 10.1016/j.jcma.2018.04.005.
Clear cell papillary renal cell carcinoma (CCPRCC), a recently identified, rare type of renal tumor, appears to have an indolent course with low risk of either local invasion or distant metastasis, results of a small retrospective study suggest.
Among 25 patients with CCPRCC followed for as long as 119 months, there were no cases of local recurrence or distant metastasis, reported Wei-Jen Chen, MD, of Tapei (Taiwan) Veterans General Hospital, and colleagues.
“Based on our findings, CCPRCC has an indolent behavior even if the patients are immunosuppressed or if they receive less invasive therapy. Microscopically, CCPRCC is considered to be a tumor of low malignant potential, as all tumors in our series were of low nuclear grade,” they wrote in a study published online in the Journal of the Chinese Medical Association.
“Whenever the diagnosis is made in a high grade renal tumor, it should be carefully re-confirmed by either cytogenetic or molecular genetic methods,” the authors reported.
CCPRCC was newly recognized as a distinct renal malignancy in the 2016 World Health Organization Classification of Tumors of the Urinary System and Male Genital Organs. The classification describes CCPRCC as “a renal epithelial neoplasm composed of low-grade clear epithelial cells arranged in tubules and papillae with a predominantly linear nuclear alignment away from the basement membrane.”
Although rare, these tumors account for up to 5% of all resected renal tumors, and arise sporadically in patients with end-stage renal disease (ESRD) and von Hippel-Lindau syndrome, the classification states, adding that “according to current knowledge, these tumors have indolent behavior.”
To see if they could verify that last statement, Dr. Chen and associates collected data on all patients diagnosed at their institution with CCPRCC from January 2008 through September 2016.
They identified a total of 25 patients (11 men and 14 women) with a mean age at diagnosis of 62.8 years. Of this group, three patients with poor general condition underwent cryotherapy after a biopsy-confirmed diagnosis of CCPRCC.
All of the remaining 22 patients underwent surgical resection. Of this group, four had ESRD; three of these patients had received a kidney transplant prior to diagnosis of CCPRCC in the native kidneys, and one had three tumors over both kidneys.
“Three patients had other types of synchronous RCC; one with acquired cystic kidney disease-associated RCC, and the others with ccRCC. All CCPRCCs were localized and low grade (pT1a- pT1b, Fuhrman grade 2), and all of the patients are currently alive with no evidence of disease,” the investigators wrote.
Mean follow-up was 49.7 months (range 12 to 119 months).
One additional patient who was not included in the series was initially diagnosed with CCPRCC with lung metastasis. This patient, who died 3 years and 8 months after cytoreductive nephrectomy, had a clinical course distinct from that of all the other patients, leading the investigators to reexamine his kidney specimen with whole-exome sequencing. The sequencing led to a revision of the diagnosis to clear cell RCC.
The investigators noted that clear cell RCC, papillary RCC, and translocation RCC are three RCC subtypes that should be considered in the differential diagnosis of CCPRCC.
The investigators did not report a study funding source. They reported having no conflicts of interest relevant to the subject matter or materials discussed in the article.
SOURCE: Chen W-J et al. J Chinese Med Assoc. 2018 July 20. doi: 10.1016/j.jcma.2018.04.005.
FROM JOURNAL OF THE CHINESE MEDICAL SOCIETY
Key clinical point: Clear cell papillary renal cell carcinoma (CCPRCC) is a distinct renal tumor type with an apparently indolent clinical course.
Major finding: There were no cases of local recurrence or distant metastasis of CCPRCC after a mean of 49.7 months of follow-up (range 12-119 months).
Study details: Retrospective case study of 25 patients diagnosed and treated at a single center.
Disclosures: The investigators did not report a study funding source. They reported having no conflicts of interest relevant to the subject matter or materials discussed in the article.
Source: Chen W-J et al. J Chinese Med Assoc. 2018 July 20 doi: 10.1016/j.jcma.2018.04.005.
Treatment of relapsing progressive MS may reduce disability progression
Superimposed relapses were associated with a significantly reduced risk of disability progression in a longitudinal, prospective cohort study of 1,419 multiple sclerosis patients (MS) of the progressive-onset type.
To determine the role of inflammatory relapses on disability in the progressive-relapsing phenotype of progressive-onset MS, the researchers collected data from MSBase, an international, observational cohort of MS patients, from January 1995 to February 2017. The study population included 1,419 adults with MS (553 in the relapse subgroup, 866 in a nonrelapse subgroup) from 83 centers in 28 countries; the median prospective follow-up period was 5 years. The patients included in the analysis had adult-onset disease, at least three clinic visits with Expanded Disability Status Scale (EDSS) score recorded, and a time frame of more than 3 months between the second and last visit.
Overall, patients with relapses had significantly less risk of disability progression after adjusting for confounding variables (adjusted hazard ratio, 0.83; 95% confidence interval, 0.74-0.94; P = .003). Disease progression was defined as worsening of the EDSS score.
In addition, the researchers examined the data in a stratified model and found a 4% relative decrease in the hazard of confirmed disability progression events for each 10% increment of follow-up time for receiving disease-modifying therapy (DMT). However, DMT did not reduce disease progression risk in progressive-onset MS patients without relapse.
“This suggests that relapses in progressive-onset MS, as a clinical correlate of episodic inflammatory activity, represent a positive prognostic marker and provide an opportunity to improve disease outcomes through prevention of relapse-related disability accrual,” the researchers wrote.
Interferon-beta was the most common DMT, given to 73% of the relapse patients and 56% of the nonrelapse patients, followed by glatiramer acetate (20% and 13%, respectively), and fingolimod (12% and 16%, respectively).
The study’s main limitation was the use of the EDSS as a measure of disability, as well as the absence of quantifiable disability change to confirm relapse, the researchers noted. However, “these findings provide further evidence for a progressive-onset MS phenotype with acute episodic inflammatory changes, thereby identifying patients who may respond to existing immunotherapies.”
The study was supported by grants from the National Health and Medical Research Council of Australia and the MSBase Foundation, a nonprofit organization that itself receives support from multiple companies, including Merck, Novartis, and Sanofi. Dr. Hughes had no financial conflicts to disclose, but most coauthors disclosed relationships with multiple companies including Merck, Novartis, Sanofi. Genzyme, and Biogen.
SOURCE: Hughes J et al. JAMA Neurol. 2018 Aug 6. doi: 10.1001/jamaneurol.2018.2109.
This study is important because it addresses an area of controversy in management of patients with a progressive multiple sclerosis (MS) phenotype. The role of superimposed relapses in patients with progressive MS has long been debated, with some studies reporting no impact on long-term disability accrual and other reporting a negative impact of relapses. Treatment of progressive MS remains controversial as well, with only one therapy approved by the Food and Drug Administration for any form of progressive MS. There is considerable ongoing debate about whether MS disease-modifying therapies (MSDMT) are effective in progressive forms of MS, and whether clinical or MRI evidence of active inflammation predicts a better chance of response.
This study has several important strengths and limitations. The large sample size allowed statistical power to detect relatively small differences in disability progression risk between progressive MS subtypes. The better prognosis in progressive patients with superimposed relapses contradicts some earlier studies that suggested a worse prognosis or no difference in prognosis between progressive patients with and without relapses. This study also supports a role for MSDMT in progressive MS patients, at least those with clinical evidence of relapses, and possibly MRI evidence of inflammatory disease activity (although this was not specifically addressed in the current study). Limitations of the study include the observational nature of the database, variable periods of follow-up, lack of objective verification of recorded relapses either with EDSS scores or MRI confirmation, and lack of an untreated control group. Therefore, no conclusions can be drawn as to whether MSDMT exposure had a favorable impact on the whole cohort of progressive patients versus no treatment.
Jonathan L. Carter, MD , is an MS specialist at the Mayo Clinic in Scottsdale, Ariz. He had no relevant disclosures to report.
This study is important because it addresses an area of controversy in management of patients with a progressive multiple sclerosis (MS) phenotype. The role of superimposed relapses in patients with progressive MS has long been debated, with some studies reporting no impact on long-term disability accrual and other reporting a negative impact of relapses. Treatment of progressive MS remains controversial as well, with only one therapy approved by the Food and Drug Administration for any form of progressive MS. There is considerable ongoing debate about whether MS disease-modifying therapies (MSDMT) are effective in progressive forms of MS, and whether clinical or MRI evidence of active inflammation predicts a better chance of response.
This study has several important strengths and limitations. The large sample size allowed statistical power to detect relatively small differences in disability progression risk between progressive MS subtypes. The better prognosis in progressive patients with superimposed relapses contradicts some earlier studies that suggested a worse prognosis or no difference in prognosis between progressive patients with and without relapses. This study also supports a role for MSDMT in progressive MS patients, at least those with clinical evidence of relapses, and possibly MRI evidence of inflammatory disease activity (although this was not specifically addressed in the current study). Limitations of the study include the observational nature of the database, variable periods of follow-up, lack of objective verification of recorded relapses either with EDSS scores or MRI confirmation, and lack of an untreated control group. Therefore, no conclusions can be drawn as to whether MSDMT exposure had a favorable impact on the whole cohort of progressive patients versus no treatment.
Jonathan L. Carter, MD , is an MS specialist at the Mayo Clinic in Scottsdale, Ariz. He had no relevant disclosures to report.
This study is important because it addresses an area of controversy in management of patients with a progressive multiple sclerosis (MS) phenotype. The role of superimposed relapses in patients with progressive MS has long been debated, with some studies reporting no impact on long-term disability accrual and other reporting a negative impact of relapses. Treatment of progressive MS remains controversial as well, with only one therapy approved by the Food and Drug Administration for any form of progressive MS. There is considerable ongoing debate about whether MS disease-modifying therapies (MSDMT) are effective in progressive forms of MS, and whether clinical or MRI evidence of active inflammation predicts a better chance of response.
This study has several important strengths and limitations. The large sample size allowed statistical power to detect relatively small differences in disability progression risk between progressive MS subtypes. The better prognosis in progressive patients with superimposed relapses contradicts some earlier studies that suggested a worse prognosis or no difference in prognosis between progressive patients with and without relapses. This study also supports a role for MSDMT in progressive MS patients, at least those with clinical evidence of relapses, and possibly MRI evidence of inflammatory disease activity (although this was not specifically addressed in the current study). Limitations of the study include the observational nature of the database, variable periods of follow-up, lack of objective verification of recorded relapses either with EDSS scores or MRI confirmation, and lack of an untreated control group. Therefore, no conclusions can be drawn as to whether MSDMT exposure had a favorable impact on the whole cohort of progressive patients versus no treatment.
Jonathan L. Carter, MD , is an MS specialist at the Mayo Clinic in Scottsdale, Ariz. He had no relevant disclosures to report.
Superimposed relapses were associated with a significantly reduced risk of disability progression in a longitudinal, prospective cohort study of 1,419 multiple sclerosis patients (MS) of the progressive-onset type.
To determine the role of inflammatory relapses on disability in the progressive-relapsing phenotype of progressive-onset MS, the researchers collected data from MSBase, an international, observational cohort of MS patients, from January 1995 to February 2017. The study population included 1,419 adults with MS (553 in the relapse subgroup, 866 in a nonrelapse subgroup) from 83 centers in 28 countries; the median prospective follow-up period was 5 years. The patients included in the analysis had adult-onset disease, at least three clinic visits with Expanded Disability Status Scale (EDSS) score recorded, and a time frame of more than 3 months between the second and last visit.
Overall, patients with relapses had significantly less risk of disability progression after adjusting for confounding variables (adjusted hazard ratio, 0.83; 95% confidence interval, 0.74-0.94; P = .003). Disease progression was defined as worsening of the EDSS score.
In addition, the researchers examined the data in a stratified model and found a 4% relative decrease in the hazard of confirmed disability progression events for each 10% increment of follow-up time for receiving disease-modifying therapy (DMT). However, DMT did not reduce disease progression risk in progressive-onset MS patients without relapse.
“This suggests that relapses in progressive-onset MS, as a clinical correlate of episodic inflammatory activity, represent a positive prognostic marker and provide an opportunity to improve disease outcomes through prevention of relapse-related disability accrual,” the researchers wrote.
Interferon-beta was the most common DMT, given to 73% of the relapse patients and 56% of the nonrelapse patients, followed by glatiramer acetate (20% and 13%, respectively), and fingolimod (12% and 16%, respectively).
The study’s main limitation was the use of the EDSS as a measure of disability, as well as the absence of quantifiable disability change to confirm relapse, the researchers noted. However, “these findings provide further evidence for a progressive-onset MS phenotype with acute episodic inflammatory changes, thereby identifying patients who may respond to existing immunotherapies.”
The study was supported by grants from the National Health and Medical Research Council of Australia and the MSBase Foundation, a nonprofit organization that itself receives support from multiple companies, including Merck, Novartis, and Sanofi. Dr. Hughes had no financial conflicts to disclose, but most coauthors disclosed relationships with multiple companies including Merck, Novartis, Sanofi. Genzyme, and Biogen.
SOURCE: Hughes J et al. JAMA Neurol. 2018 Aug 6. doi: 10.1001/jamaneurol.2018.2109.
Superimposed relapses were associated with a significantly reduced risk of disability progression in a longitudinal, prospective cohort study of 1,419 multiple sclerosis patients (MS) of the progressive-onset type.
To determine the role of inflammatory relapses on disability in the progressive-relapsing phenotype of progressive-onset MS, the researchers collected data from MSBase, an international, observational cohort of MS patients, from January 1995 to February 2017. The study population included 1,419 adults with MS (553 in the relapse subgroup, 866 in a nonrelapse subgroup) from 83 centers in 28 countries; the median prospective follow-up period was 5 years. The patients included in the analysis had adult-onset disease, at least three clinic visits with Expanded Disability Status Scale (EDSS) score recorded, and a time frame of more than 3 months between the second and last visit.
Overall, patients with relapses had significantly less risk of disability progression after adjusting for confounding variables (adjusted hazard ratio, 0.83; 95% confidence interval, 0.74-0.94; P = .003). Disease progression was defined as worsening of the EDSS score.
In addition, the researchers examined the data in a stratified model and found a 4% relative decrease in the hazard of confirmed disability progression events for each 10% increment of follow-up time for receiving disease-modifying therapy (DMT). However, DMT did not reduce disease progression risk in progressive-onset MS patients without relapse.
“This suggests that relapses in progressive-onset MS, as a clinical correlate of episodic inflammatory activity, represent a positive prognostic marker and provide an opportunity to improve disease outcomes through prevention of relapse-related disability accrual,” the researchers wrote.
Interferon-beta was the most common DMT, given to 73% of the relapse patients and 56% of the nonrelapse patients, followed by glatiramer acetate (20% and 13%, respectively), and fingolimod (12% and 16%, respectively).
The study’s main limitation was the use of the EDSS as a measure of disability, as well as the absence of quantifiable disability change to confirm relapse, the researchers noted. However, “these findings provide further evidence for a progressive-onset MS phenotype with acute episodic inflammatory changes, thereby identifying patients who may respond to existing immunotherapies.”
The study was supported by grants from the National Health and Medical Research Council of Australia and the MSBase Foundation, a nonprofit organization that itself receives support from multiple companies, including Merck, Novartis, and Sanofi. Dr. Hughes had no financial conflicts to disclose, but most coauthors disclosed relationships with multiple companies including Merck, Novartis, Sanofi. Genzyme, and Biogen.
SOURCE: Hughes J et al. JAMA Neurol. 2018 Aug 6. doi: 10.1001/jamaneurol.2018.2109.
FROM JAMA NEUROLOGY
Key clinical point: Disease-modifying therapy was significantly associated with less disability progression in multiple sclerosis patients with superimposed relapses, compared with those without relapses.
Major finding: Progressive-onset multiple sclerosis patients with superimposed relapses were significantly less likely to have confirmed disability progression (adjusted hazard ratio, 0.83).
Study details: The data came from a longitudinal, prospective cohort study of 1,419 adults with progressive-onset multiple sclerosis.
Disclosures: The study was supported by grants from the National Health and Medical Research Council of Australia and the MSBase Foundation, a nonprofit organization that itself receives support from multiple companies, including Merck, Novartis, and Sanofi. Dr. Hughes had no financial conflicts to disclose, but most coauthors disclosed relationships with multiple companies, including Merck, Novartis, Sanofi, Genzyme, and Biogen.
Source: Hughes J et al. JAMA Neurol. 2018 Aug 6. doi: 10.1001/jamaneurol.2018.2109.
Help Develop 3 SVS Guidelines
The Society for Vascular Surgery needs members to participate in guideline writing groups on three topics: Enhanced Recovery After Surgery, Trauma and Genetic Aneurysms/Dissections. SVS welcomes applicants with expertise and experience in diverse practice settings. Visit here for more information and the survey/application forms for each guideline. Completed forms are due Aug. 15.
The Society for Vascular Surgery needs members to participate in guideline writing groups on three topics: Enhanced Recovery After Surgery, Trauma and Genetic Aneurysms/Dissections. SVS welcomes applicants with expertise and experience in diverse practice settings. Visit here for more information and the survey/application forms for each guideline. Completed forms are due Aug. 15.
The Society for Vascular Surgery needs members to participate in guideline writing groups on three topics: Enhanced Recovery After Surgery, Trauma and Genetic Aneurysms/Dissections. SVS welcomes applicants with expertise and experience in diverse practice settings. Visit here for more information and the survey/application forms for each guideline. Completed forms are due Aug. 15.
Submit Ideas for VAM 2019
Do you have an idea for an informative session at the 2019 Vascular Annual Meeting? The Society for Vascular Surgery is seeking proposals for invited sessions — postgraduate courses; breakfast, concurrent or small-group sessions; and/or Tips and Tricks and Ask the Experts sessions — for next year’s meeting. Suggestions are due by Aug. 27. See more information and find the submission form here. The 2019 VAM will be June 12-15 at the Gaylord National Resort and Convention Center in National Harbor, Md., just outside Washington, D.C.
Do you have an idea for an informative session at the 2019 Vascular Annual Meeting? The Society for Vascular Surgery is seeking proposals for invited sessions — postgraduate courses; breakfast, concurrent or small-group sessions; and/or Tips and Tricks and Ask the Experts sessions — for next year’s meeting. Suggestions are due by Aug. 27. See more information and find the submission form here. The 2019 VAM will be June 12-15 at the Gaylord National Resort and Convention Center in National Harbor, Md., just outside Washington, D.C.
Do you have an idea for an informative session at the 2019 Vascular Annual Meeting? The Society for Vascular Surgery is seeking proposals for invited sessions — postgraduate courses; breakfast, concurrent or small-group sessions; and/or Tips and Tricks and Ask the Experts sessions — for next year’s meeting. Suggestions are due by Aug. 27. See more information and find the submission form here. The 2019 VAM will be June 12-15 at the Gaylord National Resort and Convention Center in National Harbor, Md., just outside Washington, D.C.
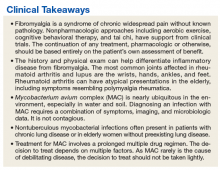
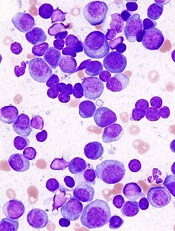
Insurance is a matter of life or death for lymphoma patients
Having health insurance can mean the difference between life and death for patients with follicular lymphoma, suggest results of a study showing that patients with private health insurance had nearly twofold better survival outcomes than patients without insurance or those who were covered by Medicare or Medicaid.
A review of records on more than 43,000 patients with follicular lymphoma (FL) in a national cancer registry showed that, compared with patients under age 65 with private insurance, the hazard ratios (HR) for death among patients in the same age bracket with either no insurance, Medicaid, or Medicare were, respectively, 1.96, 1.83, and 1.96 (P less than .0001 for each comparison).
“Our study finds that insurance status contributes to survival disparities in FL. Future studies on outcomes in FL should include insurance status as an important predictor,” Christopher R. Flowers, MD, of Emory University in Atlanta and his colleagues wrote in Blood.
“Further research on prognosis for FL should examine the impact of public policy, such as the passage of the [Affordable Care Act], on FL outcomes, as well as examine other factors that influence access to care, such as individual-level socioeconomic status, regular primary care visits, access to prescription medications, and care affordability,” they added.
The investigators noted that earlier research found that patients with Medicaid or no insurance were more likely than privately-insured patients to be diagnosed with cancers at advanced stages, and that some patients with aggressive non-Hodgkin lymphomas have been shown to have insurance-related disparities in treatments and outcomes.
To see whether the same could be true for patients with indolent-histology lymphomas such as FL, they extracted data from the National Cancer Database, a nationwide hospital-based cancer registry sponsored jointly by the American College of Surgeons and the American Cancer Society.
They identified a total of 43,648 patients aged 18 years or older who were diagnosed with FL from 2004 through 2014. They looked at both patients 18-64 years and those 65 years and older to account for changes in insurance with Medicare eligibility.
Overall survival among patients younger than age 65 was significantly worse for patients with public insurance (Medicaid or Medicare) or no insurance in Cox proportional hazard models controlling for available data on sociodemographic factors and prognostic indicators.
However, compared with patients aged 65 and older with private insurance, only patients with Medicare as their sole source of insurance had significantly worse overall survival (HR, 1.28; P less than .0001).
Patients who were uninsured or had Medicaid were more likely than others to have lower socioeconomic status, present with advanced-stage disease, have systemic symptoms, and have multiple comorbidities that persisted after controlling for known sociodemographic and prognostic factors.
The investigators found that, among patients under age 65, those with a comorbidity score of 1 had an HR for death of 1.71, compared with patients with no comorbidities, and that patients with a score of 2 or greater had a HR of 3.1 (P less than .0001 for each comparison).
“The findings of the study indicate that improving access to affordable, quality health care may reduce disparities in survival for those currently lacking coverage,” the investigators wrote.
The study was supported by Emory University, the National Institutes of Health, and the National Center for Advancing Translational Sciences. Dr. Flowers reported financial relationships with AbbVie, Spectrum, Celgene, and several other companies. The other authors reported having nothing to disclose.
SOURCE: Goldstein JS et al. Blood. 2018 Jul 24. doi: 10.1182/blood-2018-03-839035.
Having health insurance can mean the difference between life and death for patients with follicular lymphoma, suggest results of a study showing that patients with private health insurance had nearly twofold better survival outcomes than patients without insurance or those who were covered by Medicare or Medicaid.
A review of records on more than 43,000 patients with follicular lymphoma (FL) in a national cancer registry showed that, compared with patients under age 65 with private insurance, the hazard ratios (HR) for death among patients in the same age bracket with either no insurance, Medicaid, or Medicare were, respectively, 1.96, 1.83, and 1.96 (P less than .0001 for each comparison).
“Our study finds that insurance status contributes to survival disparities in FL. Future studies on outcomes in FL should include insurance status as an important predictor,” Christopher R. Flowers, MD, of Emory University in Atlanta and his colleagues wrote in Blood.
“Further research on prognosis for FL should examine the impact of public policy, such as the passage of the [Affordable Care Act], on FL outcomes, as well as examine other factors that influence access to care, such as individual-level socioeconomic status, regular primary care visits, access to prescription medications, and care affordability,” they added.
The investigators noted that earlier research found that patients with Medicaid or no insurance were more likely than privately-insured patients to be diagnosed with cancers at advanced stages, and that some patients with aggressive non-Hodgkin lymphomas have been shown to have insurance-related disparities in treatments and outcomes.
To see whether the same could be true for patients with indolent-histology lymphomas such as FL, they extracted data from the National Cancer Database, a nationwide hospital-based cancer registry sponsored jointly by the American College of Surgeons and the American Cancer Society.
They identified a total of 43,648 patients aged 18 years or older who were diagnosed with FL from 2004 through 2014. They looked at both patients 18-64 years and those 65 years and older to account for changes in insurance with Medicare eligibility.
Overall survival among patients younger than age 65 was significantly worse for patients with public insurance (Medicaid or Medicare) or no insurance in Cox proportional hazard models controlling for available data on sociodemographic factors and prognostic indicators.
However, compared with patients aged 65 and older with private insurance, only patients with Medicare as their sole source of insurance had significantly worse overall survival (HR, 1.28; P less than .0001).
Patients who were uninsured or had Medicaid were more likely than others to have lower socioeconomic status, present with advanced-stage disease, have systemic symptoms, and have multiple comorbidities that persisted after controlling for known sociodemographic and prognostic factors.
The investigators found that, among patients under age 65, those with a comorbidity score of 1 had an HR for death of 1.71, compared with patients with no comorbidities, and that patients with a score of 2 or greater had a HR of 3.1 (P less than .0001 for each comparison).
“The findings of the study indicate that improving access to affordable, quality health care may reduce disparities in survival for those currently lacking coverage,” the investigators wrote.
The study was supported by Emory University, the National Institutes of Health, and the National Center for Advancing Translational Sciences. Dr. Flowers reported financial relationships with AbbVie, Spectrum, Celgene, and several other companies. The other authors reported having nothing to disclose.
SOURCE: Goldstein JS et al. Blood. 2018 Jul 24. doi: 10.1182/blood-2018-03-839035.
Having health insurance can mean the difference between life and death for patients with follicular lymphoma, suggest results of a study showing that patients with private health insurance had nearly twofold better survival outcomes than patients without insurance or those who were covered by Medicare or Medicaid.
A review of records on more than 43,000 patients with follicular lymphoma (FL) in a national cancer registry showed that, compared with patients under age 65 with private insurance, the hazard ratios (HR) for death among patients in the same age bracket with either no insurance, Medicaid, or Medicare were, respectively, 1.96, 1.83, and 1.96 (P less than .0001 for each comparison).
“Our study finds that insurance status contributes to survival disparities in FL. Future studies on outcomes in FL should include insurance status as an important predictor,” Christopher R. Flowers, MD, of Emory University in Atlanta and his colleagues wrote in Blood.
“Further research on prognosis for FL should examine the impact of public policy, such as the passage of the [Affordable Care Act], on FL outcomes, as well as examine other factors that influence access to care, such as individual-level socioeconomic status, regular primary care visits, access to prescription medications, and care affordability,” they added.
The investigators noted that earlier research found that patients with Medicaid or no insurance were more likely than privately-insured patients to be diagnosed with cancers at advanced stages, and that some patients with aggressive non-Hodgkin lymphomas have been shown to have insurance-related disparities in treatments and outcomes.
To see whether the same could be true for patients with indolent-histology lymphomas such as FL, they extracted data from the National Cancer Database, a nationwide hospital-based cancer registry sponsored jointly by the American College of Surgeons and the American Cancer Society.
They identified a total of 43,648 patients aged 18 years or older who were diagnosed with FL from 2004 through 2014. They looked at both patients 18-64 years and those 65 years and older to account for changes in insurance with Medicare eligibility.
Overall survival among patients younger than age 65 was significantly worse for patients with public insurance (Medicaid or Medicare) or no insurance in Cox proportional hazard models controlling for available data on sociodemographic factors and prognostic indicators.
However, compared with patients aged 65 and older with private insurance, only patients with Medicare as their sole source of insurance had significantly worse overall survival (HR, 1.28; P less than .0001).
Patients who were uninsured or had Medicaid were more likely than others to have lower socioeconomic status, present with advanced-stage disease, have systemic symptoms, and have multiple comorbidities that persisted after controlling for known sociodemographic and prognostic factors.
The investigators found that, among patients under age 65, those with a comorbidity score of 1 had an HR for death of 1.71, compared with patients with no comorbidities, and that patients with a score of 2 or greater had a HR of 3.1 (P less than .0001 for each comparison).
“The findings of the study indicate that improving access to affordable, quality health care may reduce disparities in survival for those currently lacking coverage,” the investigators wrote.
The study was supported by Emory University, the National Institutes of Health, and the National Center for Advancing Translational Sciences. Dr. Flowers reported financial relationships with AbbVie, Spectrum, Celgene, and several other companies. The other authors reported having nothing to disclose.
SOURCE: Goldstein JS et al. Blood. 2018 Jul 24. doi: 10.1182/blood-2018-03-839035.
FROM BLOOD
Key clinical point:
Major finding: The risk for death among patients under age 65 with no insurance, Medicaid, or Medicare was nearly twice that of similar patients with private health insurance.
Study details: Review of data on 43,648 patients with follicular lymphoma in the National Cancer Database.
Disclosures: The study was supported by Emory University, the National Institutes of Health, and the National Center for Advancing Translational Sciences. Dr. Flowers reported financial relationships with AbbVie, Spectrum, Celgene, and several other companies. The other authors reported having nothing to disclose.
Source: Goldstein JS et al. Blood. 2018 Jul 24. doi: 10.1182/blood-2018-03-839035.
A Veteran With Fibromyalgia Presenting With Dyspnea
Case Presentation. A 64-year-old US Army veteran with a history of colorectal cancer, melanoma, and fibrinolytic presented with dyspnea to VA Boston Healthcare System (VABHS). Seven years prior to the current presentation, at the time of her diagnosis of colorectal cancer, the patient was found to be HIV negative but to have a positive purified protein derivative (PPD) test. She was treated with isoniazid (INH) therapy for 9 months. Sputum cultures collected prior to initiation of therapy grew Mycobacterium avium complex (MAC) in 1 of 3 samples, with these results reported several months after initiation of therapy. She was a never smoker with no known travel or exposure. At the time of the current presentation, her medications included bupropion, levothyroxine, capsaicin, cyclobenzaprine, ibuprofen, and acetaminophen.
►Lakshmana Swamy, MD, Chief Medical Resident, VABHS and Boston Medical Center. Dr. Monach, this patient is on a variety of pain medications and has a diagnosis of fibromyalgia. This diagnosis often frustrates doctors and patients alike. Can you tell us about fibromyalgia from the rheumatologist’s perspective and what you think of her current treatment regimen?
►Paul A. Monach, MD, PhD, Chief, Section of Rheumatology, VABHS and Associate Professor of Medicine, Boston University School of Medicine. Fibromyalgia is a syndrome of chronic widespread pain without known pathology in the musculoskeletal system. It is thought to be caused by chronic dysfunction of pain-processing pathways in the central nervous system (CNS). It is often accompanied by other somatic symptoms such as chronic fatigue, irritable bowel syndrome, and bladder pain. It is a common condition, affecting up to 5% of otherwise healthy women. It is particularly common in persons with chronic nonrestorative sleep or posttraumatic stress disorder from a wide range of causes. However, it also is more common in persons with autoimmune inflammatory diseases, such as lupus, Sjögren syndrome, or rheumatoid arthritis. Concern for one of these diseases is the main reason to consider referring a patient for evaluation by a rheumatologist. Often rheumatologists participate in the management of fibromyalgia. A patient should be given appropriate expectations by the referring physician.
Effectiveness of treatment varies widely among patients. Nonpharmacologic approaches such as aerobic exercise, cognitive behavioral therapy, and tai chi have support from clinical trials, and yoga and aquatherapy also are widely used.1,2 The classes of drugs used are the same as for neuropathic pain: tricyclics, including cyclobenzaprine; serotonin and norepinephrine reuptake inhibitors (SNRIs); and gabapentinoids. In contrast, nonsteroidal anti-inflammatory drugs and opioids are ineffective unless there is a superimposed mechanical or inflammatory cause in the periphery. The key point is that continuation of any treatment should be based entirely on the patient’s own assessment of benefit.
►Dr. Swamy. Seven years later, the patient returned to her primary care provider, reporting increased dyspnea on exertion as well as significant fatigue. She was referred to the pulmonary department and had repeat computed tomography (CT) scans of the chest, which indicated persistent right middle lobe (RML) bronchiectasis. She then underwent bronchoscopy with a subsequent bronchoalveolar lavage (BAL) culture growing MAC. Dr. Fine, please interpret the baseline and follow-up CT scans and help us understand the significance of the MAC on sputum and BAL cultures.
►Alan Fine, MD, Section of Pulmonary and Critical Care, VABHS and Professor of Medicine, Boston University School of Medicine. Prior to this presentation, the patient had a pleural-based area of fibrosis with possible associated RML bronchiectasis. This appears to be a postinflammatory process without classic features of malignant or metastatic disease. She then had a sputum, which grew MAC in only 1 of 3 samples and in liquid media only. Importantly, the sputum was not smear positive. All of this suggests a low organism burden. One possibility is that this could reflect colonization with MAC; it is not uncommon for patients with underlying chronic changes in their lung to grow MAC, and it is often difficult to tell whether it is indicative of active disease. Structural lung disease, such as bronchiectasis, predisposes a patient to MAC, but chronic MAC also may cause bronchiectasis. This chicken-and-egg scenario comes up frequently. She may have a MAC infection, but as she is HIV negative and asymptomatic, there is no urgent indication to treat, especially as the burden of therapy is not insignificant.
►Dr. Swamy. Do we need to worry about Mycobacterium tuberculosis (MTB)?
►Dr. Fine. Although she was previously PPD positive, she had already completed 1 year of isoniazid (INH) therapy, making active MTB less likely. From an infection control standpoint, it is important to distinguish MAC from MTB. The former is not contagious, and there is no need for airborne isolation.
►Dr. Swamy. Dr. Fine, where does MAC come from? Does it commonly cause disease?
►Dr. Fine. In the environment, MAC is nearly ubiquitous , especially in water and soil. In one study, 20% of showerheads were positive for MAC; when patients are infected, we may suggest changing/bleaching the showerhead, but there are no definitive recommendations.3 Because MAC is so common in the environment, it is unlikely that measures to target MAC colonization will be clinically meaningful. On the other hand, the incidence of nontuberculous mycobacterial infections is increasing across the US, and it may be a common and frequently underdiagnosed cause of chronic cough, especially in postmenopausal women.
►Dr. Swamy. Four years prior to the current presentation, the patient developed a cough after an upper respiratory tract infection that persisted for more than 2 weeks. Given her history, she underwent a repeat chest CT, which noted a slight increase in nodularity and ground-glass opacity restricted to the RML. She also reported dyspnea on exertion and was referred to the pulmonary medicine department. By the time she arrived, her dyspnea had largely resolved, but she reported persistent fatigue without other systemic symptoms, such as fevers or chills. Dr. Fine, does MAC explain this patient’s dyspnea?
►Dr. Fine. As her pulmonary symptoms resolved in a short period of time with only azithromycin, it is very unlikely that her symptoms were related to her prior disease. The MAC infection is not likely to cause dyspnea on exertion and fatigue and should be worked up more broadly before attributing it to MAC. In view of this, it would not be unreasonable to follow her clinically and see her again in 6 to 8 weeks. In this context, we also should consider the untoward impact of repeated radiation exposure derived from multiple CT scans. When a patient has an abnormality on CT scan, it often leads to further scans even if the symptoms do not match the previous findings, as in this case.
►Dr. Swamy. Given her ongoing fatigue and systemic symptoms (morning stiffness of the shoulders, legs, and thighs, and leg cramps), she was referred to the rheumatology department where the physical examination revealed muscle tenderness in her proximal arms and legs with normal strength, tender points at the elbows and medial side of the bilateral knees, significant tenderness of lower legs, and no synovitis.
Dr. Monach, can you walk us through your approach to this patient? Are we seeing manifestations of fibromyalgia? What diagnoses concerns you and how would you proceed?
►Dr. Monach. The history and exam are most helpful in raising or reducing suspicion for an underlying inflammatory disease. Areas of tenderness described in her case are typical of fibromyalgia, although it can be difficult to interpret symptoms in the hip girdle and shoulder girdle because objective findings are often absent on exam in patients with inflammatory arthritis or bursitis. Similarly, tenderness at sites of tendon insertion (enthuses) without objective abnormalities is common in different forms of spondyloarthritis, so tenderness at the elbow, knee, lateral hip, and low back can be difficult to interpret. What this patient is lacking is prominent subjective or objective findings in the joints most commonly affected in rheumatoid arthritis and lupus: wrists, hands, ankles, and feet.
►Dr. Swamy. Initial laboratory data include an erythrocyte sedimentation rate of 79 with a normal C-reactive protein. A tentative diagnosis of polymyalgia rheumatic is made with consideration of a trial treatment of prednisone.
Dr. Monach, this patient has an indolent infection and is about to be given glucocorticoids. Could you describe the situations in which you feel that glucocorticoids cause a relative immunosuppression?
►Dr. Monach. Glucocorticoids are considered safe in a patient whose infection is not intrinsically dangerous or who has started appropriate antibiotics for that infection. Although all toxicities of glucocorticoids are dose dependent, the long-standing assertion that doses below 10 mg to 15 mg do not increase risk of infection is contradicted by data published in the past 10 to 15 years, with the caveat that these patients were on long-term treatment.
►Dr. Swamy. The patient was started on prednisone 15 mg per day for 15 days. She returned to the clinic after 1 week of prednisone troutment and noted “significant improvement in fatigue, morning stiffness of shoulders, thighs, leg, back is better, leg cramps resolved, shooting pain in many joints resolved.” Further laboratory results were notable for a negative rheumatoid factor, negative antinuclear antibody, and a cyclic citrullinated peptide of 60. A presumptive diagnosis of rheumatoid arthritis (RA) was made and plaquenil 200 mg twice daily was started.
Dr. Monach, can you explain why RA comes up now on serology but was not considered initially? Why does this presentation fit RA, and was her response to treatment typical? How does this fit in with her previous diagnosis of fibromyalgia? Was that just an atypical, indolent presentation of RA?
►Dr. Monach. Though her presentation is atypical for RA, in elderly patients, RA can present with symptoms resembling polymyalgia rheumatica. The question is whether she had RA all along (in which case “elderly onset” would not apply) or had fibromyalgia and developed RA more recently. The response to empiric glucocorticoid therapy is helpful, since fibromyalgia should not improve with prednisone even in a patient with RA unless treatment of RA would allow better sleep and ability to exercise. Rheumatoid arthritis typically responds very well to prednisone in the 5-mg to 15-mg range.
►Dr. Swamy. Given the new diagnosis of an inflammatory arthritis requiring immunosuppression, bronchoscopy with BAL is performed to evaluate for the presence of MAC. These cultures were positive for MAC.
Dr. Fine, does the positive BAL culture indicate an active MAC infection?
►Dr. Fine. Yes, based on these updated data, the patient has an active MAC infection. Active infection is defined as symptoms or imaging consistent with the diagnosis, supporting microbiology data (either 2 sputum or 1 BAL sample growing MAC) and the exclusion of other causes. Previously, this patient grew MAC in just one expectorated sputum; this did not meet the microbiologic criteria. Now sputum has grown in the BAL sample; along with the CT imaging, this is enough to diagnosis active MAC infection.
Treatment for MAC must consider the details of each case. First, this is not an emergency; treatment decisions should be made with the rheumatologist to consider the planned immunosuppression. For example, we must consider potential drug interactions. A specific point should be made of the use of tumor necrosis factor (TNF)-α inhibition, which data indicate can reactivate TB and may inhibit mechanisms that restrain mycobacterial disease. Serious cases of MAC infection have been reported in the literature in the setting of TNF-α inhibition.5,6 Despite these concerns, there is not a contraindication to using these therapies from the perspective of the active MAC disease. All of these decisions will impact the need to commit the patient to MAC therapy.
►Dr. Swamy. Dr. Fine, what do you consider prior to initiating MAC therapy?
► Dr. Fine. The decision to pursue MAC therapy should not be taken lightly. Therapy often entails prolonged multidrug regimens, usually spanning more than a year, with frequent adverse effects. Outside of very specific cases, such as TNF-β inhibition, MAC is rarely a life-threatening disease, so the benefit may be limited. Treatment for MAC is certainly unlikely to be fruitful without a diligent and motivated patient able to handle the high and prolonged pill burden. Of note, it is also important to keep this patient up-to-date with influenza and pneumonia vaccination given her structural lung disease.
►Dr. Swamy. The decision is made to treat MAC with azithromycin, rifampin, and ethambutol. The disease is noted to be nonfibrocavitary. The patient underwent monthly liver function test monitoring and visual acuity testing, which were unremarkable. Dr. Fine, can you describe the phenotypes of nontuberculous mycobacterial (NTM) disease?
►Dr. Fine. There are 3 main phenotypes of NTM.3 First, we see the elderly man with preexisting lung disease—usually chronic obstructive pulmonary disease—with fibrocavitary and/or reticulonodular appearance. Second, we see the slim, elderly woman often without any preexisting lung disease presenting with focal bronchiectasis and nodular lesions in right middle lobe and lingula—the Lady Windermere syndrome. This eponym is derived from Oscar Wilde’s play “Lady Windermere’s Fan, a Play About a Good Woman,” and was first associated with this disease in 1992.7 At the time, it was thought that the voluntary suppression of cough led to poorly draining lung regions, vulnerable to engraftment by atypical mycobacteria. Infection with atypical mycobacteria are associated with this population; however, it is no longer thought to be due to the voluntary suppression of cough.7,8 Third, we do occasionally see atypical presentations, such as focal masses and solitary nodules.
►Dr. Swamy. At 1-year follow-up she successfully completed MAC therapy and noted ongoing control of rheumatoid symptoms.
1. Bernardy K, Klose P, Welsch P, Häuser W. Efficacy, acceptability and safety of cognitive behavioural therapies in fibromyalgia syndrome—a systematic review and meta-analysis of randomized controlled trials. Eur J Pain. 2018;22(2):242-260.
2. Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA, Smith BH. Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2017;4:CD011279.
3. Aksamit TR, Philley JV, Griffith DE. Nontuberculous mycobacterial (NTM) lung disease: the top ten essentials. Respir Med. 2014;108(3):417-425.
4. Aucott JN. Glucocorticoids and infection. Endocrinol Metab Clin North Am. 1994;23(3):655-670.
5. Curtis JR, Yang S, Patkar NM, et al. Risk of hospitalized bacterial infections associated with biologic treatment among US veterans with rheumatoid arthritis. Arthritis Care Res (Hoboken). 2014;66(7):990-997.
6. Lane MA, McDonald JR, Zeringue AL, et al. TNF-α antagonist use and risk of hospitalization for infection in a national cohort of veterans with rheumatoid arthritis. Medicine (Baltimore). 2011;90(2):139-145.
7. Reich JM, Johnson RE. Mycobacterium avium complex pulmonary disease presenting as an isolated lingular or middle lobe pattern. The Lady Windermere syndrome. Chest. 1992;101(6):1605-1609.
8. Kasthoori JJ, Liam CK, Wastie ML. Lady Windermere syndrome: an inappropriate eponym for an increasingly important condition. Singapore Med J. 2008;49(2):e47-e49.
Case Presentation. A 64-year-old US Army veteran with a history of colorectal cancer, melanoma, and fibrinolytic presented with dyspnea to VA Boston Healthcare System (VABHS). Seven years prior to the current presentation, at the time of her diagnosis of colorectal cancer, the patient was found to be HIV negative but to have a positive purified protein derivative (PPD) test. She was treated with isoniazid (INH) therapy for 9 months. Sputum cultures collected prior to initiation of therapy grew Mycobacterium avium complex (MAC) in 1 of 3 samples, with these results reported several months after initiation of therapy. She was a never smoker with no known travel or exposure. At the time of the current presentation, her medications included bupropion, levothyroxine, capsaicin, cyclobenzaprine, ibuprofen, and acetaminophen.
►Lakshmana Swamy, MD, Chief Medical Resident, VABHS and Boston Medical Center. Dr. Monach, this patient is on a variety of pain medications and has a diagnosis of fibromyalgia. This diagnosis often frustrates doctors and patients alike. Can you tell us about fibromyalgia from the rheumatologist’s perspective and what you think of her current treatment regimen?
►Paul A. Monach, MD, PhD, Chief, Section of Rheumatology, VABHS and Associate Professor of Medicine, Boston University School of Medicine. Fibromyalgia is a syndrome of chronic widespread pain without known pathology in the musculoskeletal system. It is thought to be caused by chronic dysfunction of pain-processing pathways in the central nervous system (CNS). It is often accompanied by other somatic symptoms such as chronic fatigue, irritable bowel syndrome, and bladder pain. It is a common condition, affecting up to 5% of otherwise healthy women. It is particularly common in persons with chronic nonrestorative sleep or posttraumatic stress disorder from a wide range of causes. However, it also is more common in persons with autoimmune inflammatory diseases, such as lupus, Sjögren syndrome, or rheumatoid arthritis. Concern for one of these diseases is the main reason to consider referring a patient for evaluation by a rheumatologist. Often rheumatologists participate in the management of fibromyalgia. A patient should be given appropriate expectations by the referring physician.
Effectiveness of treatment varies widely among patients. Nonpharmacologic approaches such as aerobic exercise, cognitive behavioral therapy, and tai chi have support from clinical trials, and yoga and aquatherapy also are widely used.1,2 The classes of drugs used are the same as for neuropathic pain: tricyclics, including cyclobenzaprine; serotonin and norepinephrine reuptake inhibitors (SNRIs); and gabapentinoids. In contrast, nonsteroidal anti-inflammatory drugs and opioids are ineffective unless there is a superimposed mechanical or inflammatory cause in the periphery. The key point is that continuation of any treatment should be based entirely on the patient’s own assessment of benefit.
►Dr. Swamy. Seven years later, the patient returned to her primary care provider, reporting increased dyspnea on exertion as well as significant fatigue. She was referred to the pulmonary department and had repeat computed tomography (CT) scans of the chest, which indicated persistent right middle lobe (RML) bronchiectasis. She then underwent bronchoscopy with a subsequent bronchoalveolar lavage (BAL) culture growing MAC. Dr. Fine, please interpret the baseline and follow-up CT scans and help us understand the significance of the MAC on sputum and BAL cultures.
►Alan Fine, MD, Section of Pulmonary and Critical Care, VABHS and Professor of Medicine, Boston University School of Medicine. Prior to this presentation, the patient had a pleural-based area of fibrosis with possible associated RML bronchiectasis. This appears to be a postinflammatory process without classic features of malignant or metastatic disease. She then had a sputum, which grew MAC in only 1 of 3 samples and in liquid media only. Importantly, the sputum was not smear positive. All of this suggests a low organism burden. One possibility is that this could reflect colonization with MAC; it is not uncommon for patients with underlying chronic changes in their lung to grow MAC, and it is often difficult to tell whether it is indicative of active disease. Structural lung disease, such as bronchiectasis, predisposes a patient to MAC, but chronic MAC also may cause bronchiectasis. This chicken-and-egg scenario comes up frequently. She may have a MAC infection, but as she is HIV negative and asymptomatic, there is no urgent indication to treat, especially as the burden of therapy is not insignificant.
►Dr. Swamy. Do we need to worry about Mycobacterium tuberculosis (MTB)?
►Dr. Fine. Although she was previously PPD positive, she had already completed 1 year of isoniazid (INH) therapy, making active MTB less likely. From an infection control standpoint, it is important to distinguish MAC from MTB. The former is not contagious, and there is no need for airborne isolation.
►Dr. Swamy. Dr. Fine, where does MAC come from? Does it commonly cause disease?
►Dr. Fine. In the environment, MAC is nearly ubiquitous , especially in water and soil. In one study, 20% of showerheads were positive for MAC; when patients are infected, we may suggest changing/bleaching the showerhead, but there are no definitive recommendations.3 Because MAC is so common in the environment, it is unlikely that measures to target MAC colonization will be clinically meaningful. On the other hand, the incidence of nontuberculous mycobacterial infections is increasing across the US, and it may be a common and frequently underdiagnosed cause of chronic cough, especially in postmenopausal women.
►Dr. Swamy. Four years prior to the current presentation, the patient developed a cough after an upper respiratory tract infection that persisted for more than 2 weeks. Given her history, she underwent a repeat chest CT, which noted a slight increase in nodularity and ground-glass opacity restricted to the RML. She also reported dyspnea on exertion and was referred to the pulmonary medicine department. By the time she arrived, her dyspnea had largely resolved, but she reported persistent fatigue without other systemic symptoms, such as fevers or chills. Dr. Fine, does MAC explain this patient’s dyspnea?
►Dr. Fine. As her pulmonary symptoms resolved in a short period of time with only azithromycin, it is very unlikely that her symptoms were related to her prior disease. The MAC infection is not likely to cause dyspnea on exertion and fatigue and should be worked up more broadly before attributing it to MAC. In view of this, it would not be unreasonable to follow her clinically and see her again in 6 to 8 weeks. In this context, we also should consider the untoward impact of repeated radiation exposure derived from multiple CT scans. When a patient has an abnormality on CT scan, it often leads to further scans even if the symptoms do not match the previous findings, as in this case.
►Dr. Swamy. Given her ongoing fatigue and systemic symptoms (morning stiffness of the shoulders, legs, and thighs, and leg cramps), she was referred to the rheumatology department where the physical examination revealed muscle tenderness in her proximal arms and legs with normal strength, tender points at the elbows and medial side of the bilateral knees, significant tenderness of lower legs, and no synovitis.
Dr. Monach, can you walk us through your approach to this patient? Are we seeing manifestations of fibromyalgia? What diagnoses concerns you and how would you proceed?
►Dr. Monach. The history and exam are most helpful in raising or reducing suspicion for an underlying inflammatory disease. Areas of tenderness described in her case are typical of fibromyalgia, although it can be difficult to interpret symptoms in the hip girdle and shoulder girdle because objective findings are often absent on exam in patients with inflammatory arthritis or bursitis. Similarly, tenderness at sites of tendon insertion (enthuses) without objective abnormalities is common in different forms of spondyloarthritis, so tenderness at the elbow, knee, lateral hip, and low back can be difficult to interpret. What this patient is lacking is prominent subjective or objective findings in the joints most commonly affected in rheumatoid arthritis and lupus: wrists, hands, ankles, and feet.
►Dr. Swamy. Initial laboratory data include an erythrocyte sedimentation rate of 79 with a normal C-reactive protein. A tentative diagnosis of polymyalgia rheumatic is made with consideration of a trial treatment of prednisone.
Dr. Monach, this patient has an indolent infection and is about to be given glucocorticoids. Could you describe the situations in which you feel that glucocorticoids cause a relative immunosuppression?
►Dr. Monach. Glucocorticoids are considered safe in a patient whose infection is not intrinsically dangerous or who has started appropriate antibiotics for that infection. Although all toxicities of glucocorticoids are dose dependent, the long-standing assertion that doses below 10 mg to 15 mg do not increase risk of infection is contradicted by data published in the past 10 to 15 years, with the caveat that these patients were on long-term treatment.
►Dr. Swamy. The patient was started on prednisone 15 mg per day for 15 days. She returned to the clinic after 1 week of prednisone troutment and noted “significant improvement in fatigue, morning stiffness of shoulders, thighs, leg, back is better, leg cramps resolved, shooting pain in many joints resolved.” Further laboratory results were notable for a negative rheumatoid factor, negative antinuclear antibody, and a cyclic citrullinated peptide of 60. A presumptive diagnosis of rheumatoid arthritis (RA) was made and plaquenil 200 mg twice daily was started.
Dr. Monach, can you explain why RA comes up now on serology but was not considered initially? Why does this presentation fit RA, and was her response to treatment typical? How does this fit in with her previous diagnosis of fibromyalgia? Was that just an atypical, indolent presentation of RA?
►Dr. Monach. Though her presentation is atypical for RA, in elderly patients, RA can present with symptoms resembling polymyalgia rheumatica. The question is whether she had RA all along (in which case “elderly onset” would not apply) or had fibromyalgia and developed RA more recently. The response to empiric glucocorticoid therapy is helpful, since fibromyalgia should not improve with prednisone even in a patient with RA unless treatment of RA would allow better sleep and ability to exercise. Rheumatoid arthritis typically responds very well to prednisone in the 5-mg to 15-mg range.
►Dr. Swamy. Given the new diagnosis of an inflammatory arthritis requiring immunosuppression, bronchoscopy with BAL is performed to evaluate for the presence of MAC. These cultures were positive for MAC.
Dr. Fine, does the positive BAL culture indicate an active MAC infection?
►Dr. Fine. Yes, based on these updated data, the patient has an active MAC infection. Active infection is defined as symptoms or imaging consistent with the diagnosis, supporting microbiology data (either 2 sputum or 1 BAL sample growing MAC) and the exclusion of other causes. Previously, this patient grew MAC in just one expectorated sputum; this did not meet the microbiologic criteria. Now sputum has grown in the BAL sample; along with the CT imaging, this is enough to diagnosis active MAC infection.
Treatment for MAC must consider the details of each case. First, this is not an emergency; treatment decisions should be made with the rheumatologist to consider the planned immunosuppression. For example, we must consider potential drug interactions. A specific point should be made of the use of tumor necrosis factor (TNF)-α inhibition, which data indicate can reactivate TB and may inhibit mechanisms that restrain mycobacterial disease. Serious cases of MAC infection have been reported in the literature in the setting of TNF-α inhibition.5,6 Despite these concerns, there is not a contraindication to using these therapies from the perspective of the active MAC disease. All of these decisions will impact the need to commit the patient to MAC therapy.
►Dr. Swamy. Dr. Fine, what do you consider prior to initiating MAC therapy?
► Dr. Fine. The decision to pursue MAC therapy should not be taken lightly. Therapy often entails prolonged multidrug regimens, usually spanning more than a year, with frequent adverse effects. Outside of very specific cases, such as TNF-β inhibition, MAC is rarely a life-threatening disease, so the benefit may be limited. Treatment for MAC is certainly unlikely to be fruitful without a diligent and motivated patient able to handle the high and prolonged pill burden. Of note, it is also important to keep this patient up-to-date with influenza and pneumonia vaccination given her structural lung disease.
►Dr. Swamy. The decision is made to treat MAC with azithromycin, rifampin, and ethambutol. The disease is noted to be nonfibrocavitary. The patient underwent monthly liver function test monitoring and visual acuity testing, which were unremarkable. Dr. Fine, can you describe the phenotypes of nontuberculous mycobacterial (NTM) disease?
►Dr. Fine. There are 3 main phenotypes of NTM.3 First, we see the elderly man with preexisting lung disease—usually chronic obstructive pulmonary disease—with fibrocavitary and/or reticulonodular appearance. Second, we see the slim, elderly woman often without any preexisting lung disease presenting with focal bronchiectasis and nodular lesions in right middle lobe and lingula—the Lady Windermere syndrome. This eponym is derived from Oscar Wilde’s play “Lady Windermere’s Fan, a Play About a Good Woman,” and was first associated with this disease in 1992.7 At the time, it was thought that the voluntary suppression of cough led to poorly draining lung regions, vulnerable to engraftment by atypical mycobacteria. Infection with atypical mycobacteria are associated with this population; however, it is no longer thought to be due to the voluntary suppression of cough.7,8 Third, we do occasionally see atypical presentations, such as focal masses and solitary nodules.
►Dr. Swamy. At 1-year follow-up she successfully completed MAC therapy and noted ongoing control of rheumatoid symptoms.
Case Presentation. A 64-year-old US Army veteran with a history of colorectal cancer, melanoma, and fibrinolytic presented with dyspnea to VA Boston Healthcare System (VABHS). Seven years prior to the current presentation, at the time of her diagnosis of colorectal cancer, the patient was found to be HIV negative but to have a positive purified protein derivative (PPD) test. She was treated with isoniazid (INH) therapy for 9 months. Sputum cultures collected prior to initiation of therapy grew Mycobacterium avium complex (MAC) in 1 of 3 samples, with these results reported several months after initiation of therapy. She was a never smoker with no known travel or exposure. At the time of the current presentation, her medications included bupropion, levothyroxine, capsaicin, cyclobenzaprine, ibuprofen, and acetaminophen.
►Lakshmana Swamy, MD, Chief Medical Resident, VABHS and Boston Medical Center. Dr. Monach, this patient is on a variety of pain medications and has a diagnosis of fibromyalgia. This diagnosis often frustrates doctors and patients alike. Can you tell us about fibromyalgia from the rheumatologist’s perspective and what you think of her current treatment regimen?
►Paul A. Monach, MD, PhD, Chief, Section of Rheumatology, VABHS and Associate Professor of Medicine, Boston University School of Medicine. Fibromyalgia is a syndrome of chronic widespread pain without known pathology in the musculoskeletal system. It is thought to be caused by chronic dysfunction of pain-processing pathways in the central nervous system (CNS). It is often accompanied by other somatic symptoms such as chronic fatigue, irritable bowel syndrome, and bladder pain. It is a common condition, affecting up to 5% of otherwise healthy women. It is particularly common in persons with chronic nonrestorative sleep or posttraumatic stress disorder from a wide range of causes. However, it also is more common in persons with autoimmune inflammatory diseases, such as lupus, Sjögren syndrome, or rheumatoid arthritis. Concern for one of these diseases is the main reason to consider referring a patient for evaluation by a rheumatologist. Often rheumatologists participate in the management of fibromyalgia. A patient should be given appropriate expectations by the referring physician.
Effectiveness of treatment varies widely among patients. Nonpharmacologic approaches such as aerobic exercise, cognitive behavioral therapy, and tai chi have support from clinical trials, and yoga and aquatherapy also are widely used.1,2 The classes of drugs used are the same as for neuropathic pain: tricyclics, including cyclobenzaprine; serotonin and norepinephrine reuptake inhibitors (SNRIs); and gabapentinoids. In contrast, nonsteroidal anti-inflammatory drugs and opioids are ineffective unless there is a superimposed mechanical or inflammatory cause in the periphery. The key point is that continuation of any treatment should be based entirely on the patient’s own assessment of benefit.
►Dr. Swamy. Seven years later, the patient returned to her primary care provider, reporting increased dyspnea on exertion as well as significant fatigue. She was referred to the pulmonary department and had repeat computed tomography (CT) scans of the chest, which indicated persistent right middle lobe (RML) bronchiectasis. She then underwent bronchoscopy with a subsequent bronchoalveolar lavage (BAL) culture growing MAC. Dr. Fine, please interpret the baseline and follow-up CT scans and help us understand the significance of the MAC on sputum and BAL cultures.
►Alan Fine, MD, Section of Pulmonary and Critical Care, VABHS and Professor of Medicine, Boston University School of Medicine. Prior to this presentation, the patient had a pleural-based area of fibrosis with possible associated RML bronchiectasis. This appears to be a postinflammatory process without classic features of malignant or metastatic disease. She then had a sputum, which grew MAC in only 1 of 3 samples and in liquid media only. Importantly, the sputum was not smear positive. All of this suggests a low organism burden. One possibility is that this could reflect colonization with MAC; it is not uncommon for patients with underlying chronic changes in their lung to grow MAC, and it is often difficult to tell whether it is indicative of active disease. Structural lung disease, such as bronchiectasis, predisposes a patient to MAC, but chronic MAC also may cause bronchiectasis. This chicken-and-egg scenario comes up frequently. She may have a MAC infection, but as she is HIV negative and asymptomatic, there is no urgent indication to treat, especially as the burden of therapy is not insignificant.
►Dr. Swamy. Do we need to worry about Mycobacterium tuberculosis (MTB)?
►Dr. Fine. Although she was previously PPD positive, she had already completed 1 year of isoniazid (INH) therapy, making active MTB less likely. From an infection control standpoint, it is important to distinguish MAC from MTB. The former is not contagious, and there is no need for airborne isolation.
►Dr. Swamy. Dr. Fine, where does MAC come from? Does it commonly cause disease?
►Dr. Fine. In the environment, MAC is nearly ubiquitous , especially in water and soil. In one study, 20% of showerheads were positive for MAC; when patients are infected, we may suggest changing/bleaching the showerhead, but there are no definitive recommendations.3 Because MAC is so common in the environment, it is unlikely that measures to target MAC colonization will be clinically meaningful. On the other hand, the incidence of nontuberculous mycobacterial infections is increasing across the US, and it may be a common and frequently underdiagnosed cause of chronic cough, especially in postmenopausal women.
►Dr. Swamy. Four years prior to the current presentation, the patient developed a cough after an upper respiratory tract infection that persisted for more than 2 weeks. Given her history, she underwent a repeat chest CT, which noted a slight increase in nodularity and ground-glass opacity restricted to the RML. She also reported dyspnea on exertion and was referred to the pulmonary medicine department. By the time she arrived, her dyspnea had largely resolved, but she reported persistent fatigue without other systemic symptoms, such as fevers or chills. Dr. Fine, does MAC explain this patient’s dyspnea?
►Dr. Fine. As her pulmonary symptoms resolved in a short period of time with only azithromycin, it is very unlikely that her symptoms were related to her prior disease. The MAC infection is not likely to cause dyspnea on exertion and fatigue and should be worked up more broadly before attributing it to MAC. In view of this, it would not be unreasonable to follow her clinically and see her again in 6 to 8 weeks. In this context, we also should consider the untoward impact of repeated radiation exposure derived from multiple CT scans. When a patient has an abnormality on CT scan, it often leads to further scans even if the symptoms do not match the previous findings, as in this case.
►Dr. Swamy. Given her ongoing fatigue and systemic symptoms (morning stiffness of the shoulders, legs, and thighs, and leg cramps), she was referred to the rheumatology department where the physical examination revealed muscle tenderness in her proximal arms and legs with normal strength, tender points at the elbows and medial side of the bilateral knees, significant tenderness of lower legs, and no synovitis.
Dr. Monach, can you walk us through your approach to this patient? Are we seeing manifestations of fibromyalgia? What diagnoses concerns you and how would you proceed?
►Dr. Monach. The history and exam are most helpful in raising or reducing suspicion for an underlying inflammatory disease. Areas of tenderness described in her case are typical of fibromyalgia, although it can be difficult to interpret symptoms in the hip girdle and shoulder girdle because objective findings are often absent on exam in patients with inflammatory arthritis or bursitis. Similarly, tenderness at sites of tendon insertion (enthuses) without objective abnormalities is common in different forms of spondyloarthritis, so tenderness at the elbow, knee, lateral hip, and low back can be difficult to interpret. What this patient is lacking is prominent subjective or objective findings in the joints most commonly affected in rheumatoid arthritis and lupus: wrists, hands, ankles, and feet.
►Dr. Swamy. Initial laboratory data include an erythrocyte sedimentation rate of 79 with a normal C-reactive protein. A tentative diagnosis of polymyalgia rheumatic is made with consideration of a trial treatment of prednisone.
Dr. Monach, this patient has an indolent infection and is about to be given glucocorticoids. Could you describe the situations in which you feel that glucocorticoids cause a relative immunosuppression?
►Dr. Monach. Glucocorticoids are considered safe in a patient whose infection is not intrinsically dangerous or who has started appropriate antibiotics for that infection. Although all toxicities of glucocorticoids are dose dependent, the long-standing assertion that doses below 10 mg to 15 mg do not increase risk of infection is contradicted by data published in the past 10 to 15 years, with the caveat that these patients were on long-term treatment.
►Dr. Swamy. The patient was started on prednisone 15 mg per day for 15 days. She returned to the clinic after 1 week of prednisone troutment and noted “significant improvement in fatigue, morning stiffness of shoulders, thighs, leg, back is better, leg cramps resolved, shooting pain in many joints resolved.” Further laboratory results were notable for a negative rheumatoid factor, negative antinuclear antibody, and a cyclic citrullinated peptide of 60. A presumptive diagnosis of rheumatoid arthritis (RA) was made and plaquenil 200 mg twice daily was started.
Dr. Monach, can you explain why RA comes up now on serology but was not considered initially? Why does this presentation fit RA, and was her response to treatment typical? How does this fit in with her previous diagnosis of fibromyalgia? Was that just an atypical, indolent presentation of RA?
►Dr. Monach. Though her presentation is atypical for RA, in elderly patients, RA can present with symptoms resembling polymyalgia rheumatica. The question is whether she had RA all along (in which case “elderly onset” would not apply) or had fibromyalgia and developed RA more recently. The response to empiric glucocorticoid therapy is helpful, since fibromyalgia should not improve with prednisone even in a patient with RA unless treatment of RA would allow better sleep and ability to exercise. Rheumatoid arthritis typically responds very well to prednisone in the 5-mg to 15-mg range.
►Dr. Swamy. Given the new diagnosis of an inflammatory arthritis requiring immunosuppression, bronchoscopy with BAL is performed to evaluate for the presence of MAC. These cultures were positive for MAC.
Dr. Fine, does the positive BAL culture indicate an active MAC infection?
►Dr. Fine. Yes, based on these updated data, the patient has an active MAC infection. Active infection is defined as symptoms or imaging consistent with the diagnosis, supporting microbiology data (either 2 sputum or 1 BAL sample growing MAC) and the exclusion of other causes. Previously, this patient grew MAC in just one expectorated sputum; this did not meet the microbiologic criteria. Now sputum has grown in the BAL sample; along with the CT imaging, this is enough to diagnosis active MAC infection.
Treatment for MAC must consider the details of each case. First, this is not an emergency; treatment decisions should be made with the rheumatologist to consider the planned immunosuppression. For example, we must consider potential drug interactions. A specific point should be made of the use of tumor necrosis factor (TNF)-α inhibition, which data indicate can reactivate TB and may inhibit mechanisms that restrain mycobacterial disease. Serious cases of MAC infection have been reported in the literature in the setting of TNF-α inhibition.5,6 Despite these concerns, there is not a contraindication to using these therapies from the perspective of the active MAC disease. All of these decisions will impact the need to commit the patient to MAC therapy.
►Dr. Swamy. Dr. Fine, what do you consider prior to initiating MAC therapy?
► Dr. Fine. The decision to pursue MAC therapy should not be taken lightly. Therapy often entails prolonged multidrug regimens, usually spanning more than a year, with frequent adverse effects. Outside of very specific cases, such as TNF-β inhibition, MAC is rarely a life-threatening disease, so the benefit may be limited. Treatment for MAC is certainly unlikely to be fruitful without a diligent and motivated patient able to handle the high and prolonged pill burden. Of note, it is also important to keep this patient up-to-date with influenza and pneumonia vaccination given her structural lung disease.
►Dr. Swamy. The decision is made to treat MAC with azithromycin, rifampin, and ethambutol. The disease is noted to be nonfibrocavitary. The patient underwent monthly liver function test monitoring and visual acuity testing, which were unremarkable. Dr. Fine, can you describe the phenotypes of nontuberculous mycobacterial (NTM) disease?
►Dr. Fine. There are 3 main phenotypes of NTM.3 First, we see the elderly man with preexisting lung disease—usually chronic obstructive pulmonary disease—with fibrocavitary and/or reticulonodular appearance. Second, we see the slim, elderly woman often without any preexisting lung disease presenting with focal bronchiectasis and nodular lesions in right middle lobe and lingula—the Lady Windermere syndrome. This eponym is derived from Oscar Wilde’s play “Lady Windermere’s Fan, a Play About a Good Woman,” and was first associated with this disease in 1992.7 At the time, it was thought that the voluntary suppression of cough led to poorly draining lung regions, vulnerable to engraftment by atypical mycobacteria. Infection with atypical mycobacteria are associated with this population; however, it is no longer thought to be due to the voluntary suppression of cough.7,8 Third, we do occasionally see atypical presentations, such as focal masses and solitary nodules.
►Dr. Swamy. At 1-year follow-up she successfully completed MAC therapy and noted ongoing control of rheumatoid symptoms.
1. Bernardy K, Klose P, Welsch P, Häuser W. Efficacy, acceptability and safety of cognitive behavioural therapies in fibromyalgia syndrome—a systematic review and meta-analysis of randomized controlled trials. Eur J Pain. 2018;22(2):242-260.
2. Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA, Smith BH. Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2017;4:CD011279.
3. Aksamit TR, Philley JV, Griffith DE. Nontuberculous mycobacterial (NTM) lung disease: the top ten essentials. Respir Med. 2014;108(3):417-425.
4. Aucott JN. Glucocorticoids and infection. Endocrinol Metab Clin North Am. 1994;23(3):655-670.
5. Curtis JR, Yang S, Patkar NM, et al. Risk of hospitalized bacterial infections associated with biologic treatment among US veterans with rheumatoid arthritis. Arthritis Care Res (Hoboken). 2014;66(7):990-997.
6. Lane MA, McDonald JR, Zeringue AL, et al. TNF-α antagonist use and risk of hospitalization for infection in a national cohort of veterans with rheumatoid arthritis. Medicine (Baltimore). 2011;90(2):139-145.
7. Reich JM, Johnson RE. Mycobacterium avium complex pulmonary disease presenting as an isolated lingular or middle lobe pattern. The Lady Windermere syndrome. Chest. 1992;101(6):1605-1609.
8. Kasthoori JJ, Liam CK, Wastie ML. Lady Windermere syndrome: an inappropriate eponym for an increasingly important condition. Singapore Med J. 2008;49(2):e47-e49.
1. Bernardy K, Klose P, Welsch P, Häuser W. Efficacy, acceptability and safety of cognitive behavioural therapies in fibromyalgia syndrome—a systematic review and meta-analysis of randomized controlled trials. Eur J Pain. 2018;22(2):242-260.
2. Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA, Smith BH. Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2017;4:CD011279.
3. Aksamit TR, Philley JV, Griffith DE. Nontuberculous mycobacterial (NTM) lung disease: the top ten essentials. Respir Med. 2014;108(3):417-425.
4. Aucott JN. Glucocorticoids and infection. Endocrinol Metab Clin North Am. 1994;23(3):655-670.
5. Curtis JR, Yang S, Patkar NM, et al. Risk of hospitalized bacterial infections associated with biologic treatment among US veterans with rheumatoid arthritis. Arthritis Care Res (Hoboken). 2014;66(7):990-997.
6. Lane MA, McDonald JR, Zeringue AL, et al. TNF-α antagonist use and risk of hospitalization for infection in a national cohort of veterans with rheumatoid arthritis. Medicine (Baltimore). 2011;90(2):139-145.
7. Reich JM, Johnson RE. Mycobacterium avium complex pulmonary disease presenting as an isolated lingular or middle lobe pattern. The Lady Windermere syndrome. Chest. 1992;101(6):1605-1609.
8. Kasthoori JJ, Liam CK, Wastie ML. Lady Windermere syndrome: an inappropriate eponym for an increasingly important condition. Singapore Med J. 2008;49(2):e47-e49.
Company stops development of drug for MM
MorphoSys AG has decided to stop developing MOR202 as a treatment for multiple myeloma (MM).
However, MorphoSys said it will complete the ongoing phase 1/2a trial of MOR202, and I-Mab Biopharma will continue developing MOR202 as an MM therapy for the Greater China region.
MOR202 is a human monoclonal HuCAL antibody directed against CD38, a validated target in MM.
MorphoSys is testing MOR202 in combination with other drugs in a phase 1/2a trial of patients with relapsed/refractory MM (NCT01421186).
The patients were assigned to receive MOR202 plus dexamethasone (Dex), MOR202 plus lenalidomide (Len) and Dex, or MOR202 plus pomalidomide (Pom) and Dex.
Results from this study were presented at the 2016 Annual Meeting of the German, Austrian and Swiss Societies for Hematology and Medical Oncology.
Data were reported for 38 patients—18 who had received MOR202 plus Dex, 7 who had received MOR202 plus Pom and Dex, and 13 who had received MOR202 plus Len and Dex.
The researchers said the maximum-tolerated dose of MOR202, alone or in combination, had not yet been reached. However, the data suggested MOR202 can be safely administered as a 2-hour intravenous infusion at doses up to 16 mg/kg.
The most frequent grade 3 or higher adverse events observed were hematologic in nature (leukopenia, lymphopenia, neutropenia, thrombocytopenia, and anemia).
One patient discontinued treatment due to an adverse event (decrease in platelet count) that may have been caused by MOR202 or Dex. One patient developed a transient anti-MOR202 antibody response.
There were no treatment-related deaths.
Efficacy data were available for 31 of the 38 patients. Fifteen patients responded (2 with complete responses). There were 7 responses in the Len/Dex arm, 5 in the Dex arm, and 3 in the Pom/Dex arm. Twelve responses were ongoing for up to 56 weeks.
MorphoSys said it expects to present final results from this study at an upcoming medical conference.
MorphoSys also said it will continue to support I-Mab Biopharma’s development of MOR202 in Greater China (China, Taiwan, Hong Kong, and Macao).
In November 2017, MorphoSys and I-Mab entered into an exclusive regional licensing agreement to develop and commercialize MOR202 in Greater China. I-Mab assumed exclusive responsibility for all subsequent development and commercialization of MOR202 in the agreed territory.
MorphoSys AG has decided to stop developing MOR202 as a treatment for multiple myeloma (MM).
However, MorphoSys said it will complete the ongoing phase 1/2a trial of MOR202, and I-Mab Biopharma will continue developing MOR202 as an MM therapy for the Greater China region.
MOR202 is a human monoclonal HuCAL antibody directed against CD38, a validated target in MM.
MorphoSys is testing MOR202 in combination with other drugs in a phase 1/2a trial of patients with relapsed/refractory MM (NCT01421186).
The patients were assigned to receive MOR202 plus dexamethasone (Dex), MOR202 plus lenalidomide (Len) and Dex, or MOR202 plus pomalidomide (Pom) and Dex.
Results from this study were presented at the 2016 Annual Meeting of the German, Austrian and Swiss Societies for Hematology and Medical Oncology.
Data were reported for 38 patients—18 who had received MOR202 plus Dex, 7 who had received MOR202 plus Pom and Dex, and 13 who had received MOR202 plus Len and Dex.
The researchers said the maximum-tolerated dose of MOR202, alone or in combination, had not yet been reached. However, the data suggested MOR202 can be safely administered as a 2-hour intravenous infusion at doses up to 16 mg/kg.
The most frequent grade 3 or higher adverse events observed were hematologic in nature (leukopenia, lymphopenia, neutropenia, thrombocytopenia, and anemia).
One patient discontinued treatment due to an adverse event (decrease in platelet count) that may have been caused by MOR202 or Dex. One patient developed a transient anti-MOR202 antibody response.
There were no treatment-related deaths.
Efficacy data were available for 31 of the 38 patients. Fifteen patients responded (2 with complete responses). There were 7 responses in the Len/Dex arm, 5 in the Dex arm, and 3 in the Pom/Dex arm. Twelve responses were ongoing for up to 56 weeks.
MorphoSys said it expects to present final results from this study at an upcoming medical conference.
MorphoSys also said it will continue to support I-Mab Biopharma’s development of MOR202 in Greater China (China, Taiwan, Hong Kong, and Macao).
In November 2017, MorphoSys and I-Mab entered into an exclusive regional licensing agreement to develop and commercialize MOR202 in Greater China. I-Mab assumed exclusive responsibility for all subsequent development and commercialization of MOR202 in the agreed territory.
MorphoSys AG has decided to stop developing MOR202 as a treatment for multiple myeloma (MM).
However, MorphoSys said it will complete the ongoing phase 1/2a trial of MOR202, and I-Mab Biopharma will continue developing MOR202 as an MM therapy for the Greater China region.
MOR202 is a human monoclonal HuCAL antibody directed against CD38, a validated target in MM.
MorphoSys is testing MOR202 in combination with other drugs in a phase 1/2a trial of patients with relapsed/refractory MM (NCT01421186).
The patients were assigned to receive MOR202 plus dexamethasone (Dex), MOR202 plus lenalidomide (Len) and Dex, or MOR202 plus pomalidomide (Pom) and Dex.
Results from this study were presented at the 2016 Annual Meeting of the German, Austrian and Swiss Societies for Hematology and Medical Oncology.
Data were reported for 38 patients—18 who had received MOR202 plus Dex, 7 who had received MOR202 plus Pom and Dex, and 13 who had received MOR202 plus Len and Dex.
The researchers said the maximum-tolerated dose of MOR202, alone or in combination, had not yet been reached. However, the data suggested MOR202 can be safely administered as a 2-hour intravenous infusion at doses up to 16 mg/kg.
The most frequent grade 3 or higher adverse events observed were hematologic in nature (leukopenia, lymphopenia, neutropenia, thrombocytopenia, and anemia).
One patient discontinued treatment due to an adverse event (decrease in platelet count) that may have been caused by MOR202 or Dex. One patient developed a transient anti-MOR202 antibody response.
There were no treatment-related deaths.
Efficacy data were available for 31 of the 38 patients. Fifteen patients responded (2 with complete responses). There were 7 responses in the Len/Dex arm, 5 in the Dex arm, and 3 in the Pom/Dex arm. Twelve responses were ongoing for up to 56 weeks.
MorphoSys said it expects to present final results from this study at an upcoming medical conference.
MorphoSys also said it will continue to support I-Mab Biopharma’s development of MOR202 in Greater China (China, Taiwan, Hong Kong, and Macao).
In November 2017, MorphoSys and I-Mab entered into an exclusive regional licensing agreement to develop and commercialize MOR202 in Greater China. I-Mab assumed exclusive responsibility for all subsequent development and commercialization of MOR202 in the agreed territory.
Xenomelia: Profile of a man with intense desire to amputate a healthy limb
Xenomelia, literally meaning “foreign limb,” is a neuropsychiatric condition in which nonpsychotic individuals have an intense, persistent belief that one or more of their limbs does not belong to their body; instead they regard it as an alien appendage that should be discarded.1 This unwavering, fixed belief resembles a delusion and is often debilitating to the point where the affected person strongly desires amputation of the unwanted limb. Traditionally, such requests often are denied by the medical community, which may cause an individual who has xenomelia to attempt risky self-amputation, or to injure the limb in a manner that makes subsequent amputation medically necessary.1
The name for this condition has evolved over the years, depending on the emphasis given to specific characteristics. It was once called apotemnophilia, meaning “love of amputation,” when the condition was believed to be a fetish involving sexual gratification derived from being an amputee.2,3 The term “body integrity identity disorder” (BIID) was introduced several decades later to incorporate the condition into a broader spectrum of accepted psychiatric pathologies, reasoning that it was the cause of a mismatch between objective and subjective body schema, similar to anorexia nervosa or body dysmorphic disorder.4,5 This name also served to draw parallels between this condition and gender identity disorder. However, unlike these other disorders, individuals with this condition have sufficient factual insight to know they appear “normal” to others. The newest term, xenomelia, was established to acknowledge the neurologic component of the condition after neuroimaging studies showed structural changes to the right parietal lobe in individuals who desired amputation of their left lower limb, thus linking the part of the brain that processes sensory input from the affected limb.6
While particular nuances in symptomatology were modified in formulating these older names, certain hallmark features of xenomelia have remained the same.7 The condition starts in early childhood, prior to puberty. Those who have it feel intense distress, and are resigned to the notion that nothing but amputation can alleviate their distress. Xenomelia is overwhelmingly more common in males than females. It is accompanied by nontraditional attitudes about disability, including admiration of amputees and complete apathy and disregard toward the impairment that amputation would cause.
While the data are insufficient to draw a definitive conclusion, the trend in the published literature suggests in xenomelia, the lower left leg is predominantly the limb implicated in the condition, in right-handed individuals.1
Here, we describe the case of a young man, Mr. H, with xenomelia who contacted us after reading about this condition in a review we recently published.1 He agreed to allow us to anonymously describe his history and symptoms so that clinicians can recognize and help other individuals with xenomelia. His history may also help stimulate exploration of etiological factors and novel treatment strategies for xenomelia, other than amputation of a healthy limb.
CASE
‘I have this limb that should not be’
Mr. H, age 31, is a white male of Eastern European descent who was born, raised, and resides in a major metropolitan area in the western United States. He is married, college-educated, and currently works as a computer programmer for a prominent technology company. During our conversation via telephone, he exhibits above-average intelligence, appears to be in euthymic mood, and speaks with broad affect. Mr. H displays no psychotic symptoms such as overt delusions, hallucinations, reality distortion, or response to internal stimuli. His past psychiatric history includes attention-deficit/hyperactivity disorder (ADHD), which was diagnosed at age 6 and treated with appropriate medication under the care of a psychiatrist until age 18, when Mr. H decided to discontinue treatment. He no longer endorses symptoms of ADHD. He has no chronic medical conditions other than season allergies, for which he sometimes takes antihistamines, and occasional exacerbation of sciatica, for which he takes an over-the-counter nonsteroidal anti-inflammatory medication. Mr. H also has episodic insomnia, which he attributes to job-related stress and working odd hours. He was treated for meningitis as an infant, and underwent a bilateral myringotomy as a young child to treat recurrent ear infections. He has no other surgical history. He was raised in a middle-class Christian household that included both parents, who are still alive, still together, and have no significant psychiatric or medical history. He has no siblings.
Although he lives an ostensibly normal life, Mr. H suffers in silence and secrecy with xenomelia. According to him, there was never a time in his life when he didn’t feel that his left leg was “too long” and he was “walking on a stilt.” He says, “It takes a daily toll on my health and well-being.” He can clearly recall being 4 years old and playing games in which he would pretend to injure his left leg. He says, “When we played ‘make believe,’ the game would always end with something ‘happening’ to [my left leg].” He enjoys outdoor sports like snowboarding and mountain biking, and although he denies self-injurious behavior, he says in the event of an accident, he would prefer to land on his left leg, because it is the part of his body that he considers most “expendable.” One of his most vivid memories of childhood was going shopping with his parents and seeing an older man with only one leg standing on crutches in the parking lot outside the entrance. He remembers feeling “jealous” of this man.
Continue to: Although his parents were not particularly wealthy...
Although his parents were not particularly wealthy, they sent him to a private Christian school for most of his childhood. Mr. H admits that while there he didn’t fit in and felt like an outcast, in part because he didn’t come from the level of wealth of his classmates, and because having ADHD left him isolative and avoidant. “I was always the one going away to take medication,” he explains, and he also developed a hostile attitude. He was suspended from school multiple times for fighting. These years left him tremendously anxious and depressed, and he would often find it therapeutic to sit with his left leg bent underneath him, so as to hide its undesired portion. It was common for him to tie his leg up and stare at himself in the mirror for minutes to hours as a form of stress reduction.
Most of Mr. H’s social circle is composed of friends he has known since childhood, none of whom are aware of his condition. He acknowledges that his feelings are “bizarre in nature” and so he has kept this secret on a “need-to-know” basis out of “fear of rejection, mockery, and damage to my reputation.” Through the years, he has sought out and encountered others with this condition, first anonymously on the internet, then in-person once he gets to know and trust them. He claims to know and be friendly with several people with xenomelia in his own city, some of whom have undergone amputation and are extremely happy with the results. According to Mr. H, there is a community aspect to xenomelia in his city, and people with the condition often meet each other socially. He has revealed his secret to 2 women he dated, including his present wife, who he told 3 years into their relationship. “I was prepared for her to leave me,” he recalls. Although he has never connected the desire for amputation with sexuality, he certainly believes that amputating his left leg would enhance his sex life. “Do I find amputees sexy?” he asks, “I would say yes.” On a 10-point scale, he considers his sex life to be a “7 or 8,” and it would reach 10 if he underwent amputation.
Mr. H has a calendar on which he keeps track of the days when he feels “impaired” by his xenomelia. He marks each day as either “red” or “green.” So far, he does not recognize a pattern of exacerbation. “I have my good days, then I have my bad days,” he laments. “On good days, I think about amputation and where my leg should actually end, but it is something I can quickly push off. On my bad days, I am constantly reminded in one way or another that, yes, I have this limb that should not be.” While he has never sought treatment for this condition from a health care professional, he developed his own therapeutic regimen that includes yoga, hiking, and daily use of cannabis, which “helps take the edge off.” He used alcohol in the past as self-medication, but stopped drinking to excess when it started to disrupt other aspects of his life. According to Mr. H, the goal is to distract himself from the condition, which provides temporary relief. “I find if my mind is more engaged, the amputation thoughts are fewer and less in intensity.” He reports that the months leading up to his wedding were particularly therapeutic because wedding planning provided an excellent distraction.
Overall, his current desire for amputation is steadily increasing. “Lately it has become more of a roller coaster,” he says. “If there’s a safe way to do it, I’ll do it.” An amputation would allow him to “feel good, complete, grounded, and content.” If he were to undergo amputation, he would use a prosthetic in order to retain mobility and keep his physique as discreet as possible. He has made initial inquiries into getting an amputation, saying, “I have heard of rumors of surgeons willing to perform the surgery, for a price. However, I have not completed the ‘vetting process’ to actually come into contact with the surgeons themselves.” Similar to others with xenomelia, he is easily able to draw a line on his leg, exactly where the desired amputation should occur.8 For most of his life, that line would have been 2 inches above his knee, but in recent years, the line has drifted lower, to 2 inches below the knee. However, he “wouldn’t mind either” line of amputation. He indicates the area below the desired line is less sensitive to pain than the corresponding part of his right leg, particularly his toes.
Mr. H’s wife is extremely supportive and understanding of her husband’s condition, but is opposed to the possibility of amputation (Box).
Box
Xenomelia: A spouse's perspective
Mr. H's wife is extremely compassionate, empathetic, and supportive of her husband's struggle with xenomelia. She denies noticing any hint of his condition until he informed her. "He expected me to freak out more than I did," she recalls. In her experience, Mr. H can go days at a time without having a "flare-up" of his condition. She believes that the intermittent worsening of her husband's condition might be associated with increased work-related stress and anxiety. She encouraged him to maintain a calendar for tracking the days with exacerbations. On days when Mr. H's xenomelia is worse, she attempts to distract him with hobbies and activities. She has accompanied Mr. H when he meets others with xenomelia, although she finds these meetings quite unremarkable. "They all seem like normal people," she says. "It's usually just an average conversation." While she is committed to helping her husband cope with xenomelia, she is averse to the possibility of amputation. "I'm willing to help in any way I can, but I'm hesitant for him to amputate a healthy limb," she admits. "I'm worried about his mobility."
Continue to: Much left to be learned about xenomelia
Much left to be learned about xenomelia
What remains to be discovered about xenomelia falls into 2 areas:
- the possible usefulness of various neuroimaging modalities (morphological MRI, functional MRI, magnetic resonance spectroscopy, and diffusion tensor imaging) to identify and localize anomalous neural pathways or neuroanatomical foci associated with this condition, such as an aberrantly developed or poorly myelinated right parietal lobe, which houses the limb’s physical proprioception
- a biopsychosocial inquiry into whether there exists a specific combination of a given individual’s organic brain, mind, and environmental interactions that may give rise to this condition, and whether we might detect a prodrome that arises in early childhood. The objective of any research into this condition would be to minimize its effects, if not prevent them altogether.1
As this case illustrates, xenomelia begins in early childhood, with symptoms being reported in children as young as age 3.7 However, no published literature has investigated these early stages. We’ve learned that individuals with xenomelia often can point to key childhood experiences or memories related to seeing people with amputated limbs. They remember feeling a sense of wonder, fascination, or other strong emotion. It may be in this memory that xenomelia is permanently imprinted. This was definitely true for Mr. H, who never knew a time when he didn’t endure some level of debilitation from xenomelia, and distinctly remembers feeling jealous upon seeing a man with the amputated leg standing on crutches in a store parking lot. Although he has come across many amputees in his life, Mr. H says he vividly remembers everything about that particular man in that particular moment, adding “I can still see the clothes he was wearing. I can still see the cars in the parking lot.” That was likely his moment of vivid and powerful imprinting.
Particularly influential changes occur in adolescence, not just in the course of physical development, but in the formulation of self-identity, which involves the inevitable comparison of one’s own appearance to that of others, with heightened awareness of what others might perceive. This phenomenon is known as “the imaginary audience,” and it is often overemphasized in the minds of individuals with xenomelia.7 Mr. H is a textbook example of someone acutely aware of his “audience,” suffering from the embarrassment that came from being less wealthy than others at his school, and having to manage his ADHD in plain sight of his classmates, who knew that he required medication. It is no surprise that he felt like an outcast and got suspended for fighting. He would relieve anxiety by tying his leg up and staring at himself in the mirror, finding refuge in front of an audience of one that understood and sympathized with his suffering.
Among the most notorious aspects of this condition is investigation into the possibility of there being a sexual component to the desire for amputation. The notion that the desire is a fetish employed for the purpose of sexual arousal was first propagated by Penthouse magazine in the 1970s.9 Learning that xenomelia exists in a child long before sexual maturation—and in an older adult long after sexual drive peaks—suggests the condition is independent of sexuality. However, this aspect of xenomelia continues to be investigated. A recent study found that >70% of individuals with xenomelia are at least partially motivated by the perceived enhancement in sexual gratification.10 Individuals with this motivation are predominantly male, homosexual, come from a religious background, and are far more likely to self-amputate.10 Mr. H admitted that he is sexually attracted to amputees, and while he had no complaints about his sex life, he felt it could only reach the highest levels of gratification if he were an amputee.
It is reasonable to posit that there is a genetic mechanism that creates a cortical template of one’s body, and this template connects with the limbic system, encoding a visual preference for and attraction to one’s own idealized and preferred body morphology that includes an amputated limb.11 Therefore, if Mr. H sees himself as an amputee, it would be reasonable for him to identify with and be attracted to other amputees. However, Mr. H is clearly not preoccupied with sexuality, and believes that heightened sexual gratification would be an ancillary bonus, and not the main objective, of amputation.
Continue to: Most individuals who have particpated in research studies about xenomelia tend to...
Most individuals who have participated in research studies about xenomelia tend to be older, mainly in their 60s. This is particularly true of individuals who go through with amputation. At some point, the need for a person to invoke their autonomy, alleviate their debilitation, and fulfill their desire may supersede their aversion to physical disability and social ridicule. At this stage in his life, Mr. H can’t commit to going forward with the amputation. However, he regards the likelihood of undergoing amputation to be quite high. He made initial inquiries to find a surgeon who would be willing to perform the procedure. Given that he has found people with xenomelia who have undergone amputation, he will likely will be able find a surgeon to perform the procedure. Mr. H reports that just about everyone he has ever known with xenomelia who underwent amputation is completely satisfied with their decision, even years later. He has come across only one person who regretted the amputation, and he believes that person was likely suffering from other psychiatric issues, and did not have true xenomelia.
In the mind of an individual with xenomelia, the desire for amputation is separate from a desire to be disabled. Mr. H is mindful of the assumed irrationality of removing a healthy but “alien” limb to replace it with a prosthetic limb that is equally alien. The perceived irony is not lost on him. He values his mobility, and has no desire to use crutches, a wheelchair, or any other ambulatory tool. This is consistent with most individuals with xenomelia, who are neither motived by the desire to flaunt their amputated limb, nor by the sympathy they might receive from others by endorsing impaired mobility. They don’t consider themselves disabled. On the contrary, for them, amputation is a much-desired enhancement to their health and well-being.
Increased opportunities for research
The internet, social media, and even peer-reviewed medical journals offer ever-increasing opportunities for individuals with xenomelia, such as Mr. H, to have their story told, regardless of whether they choose to identify themselves or remain anonymous. There are no published data about the prevalence of xenomelia, but it is almost certainly rare. However, if Mr. H was able to meet multiple people with xenomelia in his own city and form a supportive community with them, then perhaps it isn’t exactly as rare as one might initially assume. People with xenomelia may tend to look for each other, hoping those with the same condition might show them the greatest empathy.
From Mr. H’s experience, it appears that it would be possible to locate a sufficient number of individuals with xenomelia for the purposes of conducting research, which might allow for results with acceptable statistical power. There are plenty of individual patient stories, and by documenting these stories in published literature, it is likely that patterns would emerge and causality might be determined. Such data might be bolstered by a possible strong neurologic corroboration based on what is found via neuroimaging.
Informed research into xenomelia is still in the early stages, and it is clear that there is much left to discover. It is vital that, moving forward, investigation into this condition be thorough and objective, with the goal of alleviating this secretive and debilitating neuropsychiatric condition.
Continue to: Bottom Line
Bottom Line
Individuals with xenomelia have the persistent belief that one or more of their limbs does not belong to their body but is an alien appendage that should be removed. Patients with this condition may resort to self-amputation or self-mutilation that requires subsequent surgical amputation. Xenomelia may be related to anomalous brain development, with a lack of neural representation of a limb in the right parietal lobe.
Related Resources
- Hilti LM, Hänggi J, Vitacco DA, et al. The desire for healthy limb amputation: structural brain correlates and clinical features of xenomelia. Brain. 2013;136(pt 1):318-329.
- Brugger P, Lenggenhager B, Giummarra MJ. Xenomelia: a social neuroscience view of altered bodily self-consciousness. Front Psychol. 2013;4:204. doi:10.3389/fpsyg.2013.00204.
1. Upadhyaya MA, Nasrallah HA. The intense desire for healthy limb amputation: a dis-proprioceptive neuropsychiatric disorder. Ann Clin Psychiatry. 2017;29(2):125-132.
2. Sedda A, Bottini G. Apotemnophilia, body integrity identity disorder or xenomelia? Psychiatric and neurologic etiologies face each other. Neuropsychiatr Dis Treat. 2014;10:1255-1265.
3. Money J, Jobaris R, Furth G. Apotemnophilia: two cases of self-demand amputation as a paraphilia. J Sex Res. 1977;13(2):115-125.
4. Blom RM, Hennekam RC, Denys D. Body integrity identity disorder. PLoS One. 2012;7(4):e34702. doi: 10.1371/journal.pone.0034702.
5. First MB. Desire for amputation of a limb: paraphilia, psychosis, or a new type of identity disorder. Psychol Med. 2005;35(6):919-928.
6. McGeoch PD, Brang D, Song T, et al. Xenomelia: a new right parietal lobe syndrome. J Neurol Neurosurg Psychiatry. 2011;82(12):1314-1319.
7. Nowakowski P, Karczmarczyk A. The rest is not me… An attempt to explain xenomelia--neurodevelopmental hypothesis. Postepy Psychiatrii i Neurologii. 2016;25(3):196-208.
8. Brang D, McGeoch PD, Ramachandran VS. Apotemnophilia: a neurological disorder. Neuroreport. 2008;19(13):1305-1306.
9. Forum. Penthouse. September 1972:128.
10. Blom RM, van der Wal SJ, Vulink NC, et al. Role of sexuality in body integrity identity disorder (BIID): a cross-sectional internet-based survey study. J Sex Med. 2017;14(8):1028-1035.
11. Ramachandran VS, Brang D, McGeoch PD, et al. Sexual and food preference in apotemnophilia and anorexia: interactions between ‘beliefs’ and ‘needs’ regulated by two-way connections between body image and limbic structures. Perception. 2009;38(5):775-777.
Xenomelia, literally meaning “foreign limb,” is a neuropsychiatric condition in which nonpsychotic individuals have an intense, persistent belief that one or more of their limbs does not belong to their body; instead they regard it as an alien appendage that should be discarded.1 This unwavering, fixed belief resembles a delusion and is often debilitating to the point where the affected person strongly desires amputation of the unwanted limb. Traditionally, such requests often are denied by the medical community, which may cause an individual who has xenomelia to attempt risky self-amputation, or to injure the limb in a manner that makes subsequent amputation medically necessary.1
The name for this condition has evolved over the years, depending on the emphasis given to specific characteristics. It was once called apotemnophilia, meaning “love of amputation,” when the condition was believed to be a fetish involving sexual gratification derived from being an amputee.2,3 The term “body integrity identity disorder” (BIID) was introduced several decades later to incorporate the condition into a broader spectrum of accepted psychiatric pathologies, reasoning that it was the cause of a mismatch between objective and subjective body schema, similar to anorexia nervosa or body dysmorphic disorder.4,5 This name also served to draw parallels between this condition and gender identity disorder. However, unlike these other disorders, individuals with this condition have sufficient factual insight to know they appear “normal” to others. The newest term, xenomelia, was established to acknowledge the neurologic component of the condition after neuroimaging studies showed structural changes to the right parietal lobe in individuals who desired amputation of their left lower limb, thus linking the part of the brain that processes sensory input from the affected limb.6
While particular nuances in symptomatology were modified in formulating these older names, certain hallmark features of xenomelia have remained the same.7 The condition starts in early childhood, prior to puberty. Those who have it feel intense distress, and are resigned to the notion that nothing but amputation can alleviate their distress. Xenomelia is overwhelmingly more common in males than females. It is accompanied by nontraditional attitudes about disability, including admiration of amputees and complete apathy and disregard toward the impairment that amputation would cause.
While the data are insufficient to draw a definitive conclusion, the trend in the published literature suggests in xenomelia, the lower left leg is predominantly the limb implicated in the condition, in right-handed individuals.1
Here, we describe the case of a young man, Mr. H, with xenomelia who contacted us after reading about this condition in a review we recently published.1 He agreed to allow us to anonymously describe his history and symptoms so that clinicians can recognize and help other individuals with xenomelia. His history may also help stimulate exploration of etiological factors and novel treatment strategies for xenomelia, other than amputation of a healthy limb.
CASE
‘I have this limb that should not be’
Mr. H, age 31, is a white male of Eastern European descent who was born, raised, and resides in a major metropolitan area in the western United States. He is married, college-educated, and currently works as a computer programmer for a prominent technology company. During our conversation via telephone, he exhibits above-average intelligence, appears to be in euthymic mood, and speaks with broad affect. Mr. H displays no psychotic symptoms such as overt delusions, hallucinations, reality distortion, or response to internal stimuli. His past psychiatric history includes attention-deficit/hyperactivity disorder (ADHD), which was diagnosed at age 6 and treated with appropriate medication under the care of a psychiatrist until age 18, when Mr. H decided to discontinue treatment. He no longer endorses symptoms of ADHD. He has no chronic medical conditions other than season allergies, for which he sometimes takes antihistamines, and occasional exacerbation of sciatica, for which he takes an over-the-counter nonsteroidal anti-inflammatory medication. Mr. H also has episodic insomnia, which he attributes to job-related stress and working odd hours. He was treated for meningitis as an infant, and underwent a bilateral myringotomy as a young child to treat recurrent ear infections. He has no other surgical history. He was raised in a middle-class Christian household that included both parents, who are still alive, still together, and have no significant psychiatric or medical history. He has no siblings.
Although he lives an ostensibly normal life, Mr. H suffers in silence and secrecy with xenomelia. According to him, there was never a time in his life when he didn’t feel that his left leg was “too long” and he was “walking on a stilt.” He says, “It takes a daily toll on my health and well-being.” He can clearly recall being 4 years old and playing games in which he would pretend to injure his left leg. He says, “When we played ‘make believe,’ the game would always end with something ‘happening’ to [my left leg].” He enjoys outdoor sports like snowboarding and mountain biking, and although he denies self-injurious behavior, he says in the event of an accident, he would prefer to land on his left leg, because it is the part of his body that he considers most “expendable.” One of his most vivid memories of childhood was going shopping with his parents and seeing an older man with only one leg standing on crutches in the parking lot outside the entrance. He remembers feeling “jealous” of this man.
Continue to: Although his parents were not particularly wealthy...
Although his parents were not particularly wealthy, they sent him to a private Christian school for most of his childhood. Mr. H admits that while there he didn’t fit in and felt like an outcast, in part because he didn’t come from the level of wealth of his classmates, and because having ADHD left him isolative and avoidant. “I was always the one going away to take medication,” he explains, and he also developed a hostile attitude. He was suspended from school multiple times for fighting. These years left him tremendously anxious and depressed, and he would often find it therapeutic to sit with his left leg bent underneath him, so as to hide its undesired portion. It was common for him to tie his leg up and stare at himself in the mirror for minutes to hours as a form of stress reduction.
Most of Mr. H’s social circle is composed of friends he has known since childhood, none of whom are aware of his condition. He acknowledges that his feelings are “bizarre in nature” and so he has kept this secret on a “need-to-know” basis out of “fear of rejection, mockery, and damage to my reputation.” Through the years, he has sought out and encountered others with this condition, first anonymously on the internet, then in-person once he gets to know and trust them. He claims to know and be friendly with several people with xenomelia in his own city, some of whom have undergone amputation and are extremely happy with the results. According to Mr. H, there is a community aspect to xenomelia in his city, and people with the condition often meet each other socially. He has revealed his secret to 2 women he dated, including his present wife, who he told 3 years into their relationship. “I was prepared for her to leave me,” he recalls. Although he has never connected the desire for amputation with sexuality, he certainly believes that amputating his left leg would enhance his sex life. “Do I find amputees sexy?” he asks, “I would say yes.” On a 10-point scale, he considers his sex life to be a “7 or 8,” and it would reach 10 if he underwent amputation.
Mr. H has a calendar on which he keeps track of the days when he feels “impaired” by his xenomelia. He marks each day as either “red” or “green.” So far, he does not recognize a pattern of exacerbation. “I have my good days, then I have my bad days,” he laments. “On good days, I think about amputation and where my leg should actually end, but it is something I can quickly push off. On my bad days, I am constantly reminded in one way or another that, yes, I have this limb that should not be.” While he has never sought treatment for this condition from a health care professional, he developed his own therapeutic regimen that includes yoga, hiking, and daily use of cannabis, which “helps take the edge off.” He used alcohol in the past as self-medication, but stopped drinking to excess when it started to disrupt other aspects of his life. According to Mr. H, the goal is to distract himself from the condition, which provides temporary relief. “I find if my mind is more engaged, the amputation thoughts are fewer and less in intensity.” He reports that the months leading up to his wedding were particularly therapeutic because wedding planning provided an excellent distraction.
Overall, his current desire for amputation is steadily increasing. “Lately it has become more of a roller coaster,” he says. “If there’s a safe way to do it, I’ll do it.” An amputation would allow him to “feel good, complete, grounded, and content.” If he were to undergo amputation, he would use a prosthetic in order to retain mobility and keep his physique as discreet as possible. He has made initial inquiries into getting an amputation, saying, “I have heard of rumors of surgeons willing to perform the surgery, for a price. However, I have not completed the ‘vetting process’ to actually come into contact with the surgeons themselves.” Similar to others with xenomelia, he is easily able to draw a line on his leg, exactly where the desired amputation should occur.8 For most of his life, that line would have been 2 inches above his knee, but in recent years, the line has drifted lower, to 2 inches below the knee. However, he “wouldn’t mind either” line of amputation. He indicates the area below the desired line is less sensitive to pain than the corresponding part of his right leg, particularly his toes.
Mr. H’s wife is extremely supportive and understanding of her husband’s condition, but is opposed to the possibility of amputation (Box).
Box
Xenomelia: A spouse's perspective
Mr. H's wife is extremely compassionate, empathetic, and supportive of her husband's struggle with xenomelia. She denies noticing any hint of his condition until he informed her. "He expected me to freak out more than I did," she recalls. In her experience, Mr. H can go days at a time without having a "flare-up" of his condition. She believes that the intermittent worsening of her husband's condition might be associated with increased work-related stress and anxiety. She encouraged him to maintain a calendar for tracking the days with exacerbations. On days when Mr. H's xenomelia is worse, she attempts to distract him with hobbies and activities. She has accompanied Mr. H when he meets others with xenomelia, although she finds these meetings quite unremarkable. "They all seem like normal people," she says. "It's usually just an average conversation." While she is committed to helping her husband cope with xenomelia, she is averse to the possibility of amputation. "I'm willing to help in any way I can, but I'm hesitant for him to amputate a healthy limb," she admits. "I'm worried about his mobility."
Continue to: Much left to be learned about xenomelia
Much left to be learned about xenomelia
What remains to be discovered about xenomelia falls into 2 areas:
- the possible usefulness of various neuroimaging modalities (morphological MRI, functional MRI, magnetic resonance spectroscopy, and diffusion tensor imaging) to identify and localize anomalous neural pathways or neuroanatomical foci associated with this condition, such as an aberrantly developed or poorly myelinated right parietal lobe, which houses the limb’s physical proprioception
- a biopsychosocial inquiry into whether there exists a specific combination of a given individual’s organic brain, mind, and environmental interactions that may give rise to this condition, and whether we might detect a prodrome that arises in early childhood. The objective of any research into this condition would be to minimize its effects, if not prevent them altogether.1
As this case illustrates, xenomelia begins in early childhood, with symptoms being reported in children as young as age 3.7 However, no published literature has investigated these early stages. We’ve learned that individuals with xenomelia often can point to key childhood experiences or memories related to seeing people with amputated limbs. They remember feeling a sense of wonder, fascination, or other strong emotion. It may be in this memory that xenomelia is permanently imprinted. This was definitely true for Mr. H, who never knew a time when he didn’t endure some level of debilitation from xenomelia, and distinctly remembers feeling jealous upon seeing a man with the amputated leg standing on crutches in a store parking lot. Although he has come across many amputees in his life, Mr. H says he vividly remembers everything about that particular man in that particular moment, adding “I can still see the clothes he was wearing. I can still see the cars in the parking lot.” That was likely his moment of vivid and powerful imprinting.
Particularly influential changes occur in adolescence, not just in the course of physical development, but in the formulation of self-identity, which involves the inevitable comparison of one’s own appearance to that of others, with heightened awareness of what others might perceive. This phenomenon is known as “the imaginary audience,” and it is often overemphasized in the minds of individuals with xenomelia.7 Mr. H is a textbook example of someone acutely aware of his “audience,” suffering from the embarrassment that came from being less wealthy than others at his school, and having to manage his ADHD in plain sight of his classmates, who knew that he required medication. It is no surprise that he felt like an outcast and got suspended for fighting. He would relieve anxiety by tying his leg up and staring at himself in the mirror, finding refuge in front of an audience of one that understood and sympathized with his suffering.
Among the most notorious aspects of this condition is investigation into the possibility of there being a sexual component to the desire for amputation. The notion that the desire is a fetish employed for the purpose of sexual arousal was first propagated by Penthouse magazine in the 1970s.9 Learning that xenomelia exists in a child long before sexual maturation—and in an older adult long after sexual drive peaks—suggests the condition is independent of sexuality. However, this aspect of xenomelia continues to be investigated. A recent study found that >70% of individuals with xenomelia are at least partially motivated by the perceived enhancement in sexual gratification.10 Individuals with this motivation are predominantly male, homosexual, come from a religious background, and are far more likely to self-amputate.10 Mr. H admitted that he is sexually attracted to amputees, and while he had no complaints about his sex life, he felt it could only reach the highest levels of gratification if he were an amputee.
It is reasonable to posit that there is a genetic mechanism that creates a cortical template of one’s body, and this template connects with the limbic system, encoding a visual preference for and attraction to one’s own idealized and preferred body morphology that includes an amputated limb.11 Therefore, if Mr. H sees himself as an amputee, it would be reasonable for him to identify with and be attracted to other amputees. However, Mr. H is clearly not preoccupied with sexuality, and believes that heightened sexual gratification would be an ancillary bonus, and not the main objective, of amputation.
Continue to: Most individuals who have particpated in research studies about xenomelia tend to...
Most individuals who have participated in research studies about xenomelia tend to be older, mainly in their 60s. This is particularly true of individuals who go through with amputation. At some point, the need for a person to invoke their autonomy, alleviate their debilitation, and fulfill their desire may supersede their aversion to physical disability and social ridicule. At this stage in his life, Mr. H can’t commit to going forward with the amputation. However, he regards the likelihood of undergoing amputation to be quite high. He made initial inquiries to find a surgeon who would be willing to perform the procedure. Given that he has found people with xenomelia who have undergone amputation, he will likely will be able find a surgeon to perform the procedure. Mr. H reports that just about everyone he has ever known with xenomelia who underwent amputation is completely satisfied with their decision, even years later. He has come across only one person who regretted the amputation, and he believes that person was likely suffering from other psychiatric issues, and did not have true xenomelia.
In the mind of an individual with xenomelia, the desire for amputation is separate from a desire to be disabled. Mr. H is mindful of the assumed irrationality of removing a healthy but “alien” limb to replace it with a prosthetic limb that is equally alien. The perceived irony is not lost on him. He values his mobility, and has no desire to use crutches, a wheelchair, or any other ambulatory tool. This is consistent with most individuals with xenomelia, who are neither motived by the desire to flaunt their amputated limb, nor by the sympathy they might receive from others by endorsing impaired mobility. They don’t consider themselves disabled. On the contrary, for them, amputation is a much-desired enhancement to their health and well-being.
Increased opportunities for research
The internet, social media, and even peer-reviewed medical journals offer ever-increasing opportunities for individuals with xenomelia, such as Mr. H, to have their story told, regardless of whether they choose to identify themselves or remain anonymous. There are no published data about the prevalence of xenomelia, but it is almost certainly rare. However, if Mr. H was able to meet multiple people with xenomelia in his own city and form a supportive community with them, then perhaps it isn’t exactly as rare as one might initially assume. People with xenomelia may tend to look for each other, hoping those with the same condition might show them the greatest empathy.
From Mr. H’s experience, it appears that it would be possible to locate a sufficient number of individuals with xenomelia for the purposes of conducting research, which might allow for results with acceptable statistical power. There are plenty of individual patient stories, and by documenting these stories in published literature, it is likely that patterns would emerge and causality might be determined. Such data might be bolstered by a possible strong neurologic corroboration based on what is found via neuroimaging.
Informed research into xenomelia is still in the early stages, and it is clear that there is much left to discover. It is vital that, moving forward, investigation into this condition be thorough and objective, with the goal of alleviating this secretive and debilitating neuropsychiatric condition.
Continue to: Bottom Line
Bottom Line
Individuals with xenomelia have the persistent belief that one or more of their limbs does not belong to their body but is an alien appendage that should be removed. Patients with this condition may resort to self-amputation or self-mutilation that requires subsequent surgical amputation. Xenomelia may be related to anomalous brain development, with a lack of neural representation of a limb in the right parietal lobe.
Related Resources
- Hilti LM, Hänggi J, Vitacco DA, et al. The desire for healthy limb amputation: structural brain correlates and clinical features of xenomelia. Brain. 2013;136(pt 1):318-329.
- Brugger P, Lenggenhager B, Giummarra MJ. Xenomelia: a social neuroscience view of altered bodily self-consciousness. Front Psychol. 2013;4:204. doi:10.3389/fpsyg.2013.00204.
Xenomelia, literally meaning “foreign limb,” is a neuropsychiatric condition in which nonpsychotic individuals have an intense, persistent belief that one or more of their limbs does not belong to their body; instead they regard it as an alien appendage that should be discarded.1 This unwavering, fixed belief resembles a delusion and is often debilitating to the point where the affected person strongly desires amputation of the unwanted limb. Traditionally, such requests often are denied by the medical community, which may cause an individual who has xenomelia to attempt risky self-amputation, or to injure the limb in a manner that makes subsequent amputation medically necessary.1
The name for this condition has evolved over the years, depending on the emphasis given to specific characteristics. It was once called apotemnophilia, meaning “love of amputation,” when the condition was believed to be a fetish involving sexual gratification derived from being an amputee.2,3 The term “body integrity identity disorder” (BIID) was introduced several decades later to incorporate the condition into a broader spectrum of accepted psychiatric pathologies, reasoning that it was the cause of a mismatch between objective and subjective body schema, similar to anorexia nervosa or body dysmorphic disorder.4,5 This name also served to draw parallels between this condition and gender identity disorder. However, unlike these other disorders, individuals with this condition have sufficient factual insight to know they appear “normal” to others. The newest term, xenomelia, was established to acknowledge the neurologic component of the condition after neuroimaging studies showed structural changes to the right parietal lobe in individuals who desired amputation of their left lower limb, thus linking the part of the brain that processes sensory input from the affected limb.6
While particular nuances in symptomatology were modified in formulating these older names, certain hallmark features of xenomelia have remained the same.7 The condition starts in early childhood, prior to puberty. Those who have it feel intense distress, and are resigned to the notion that nothing but amputation can alleviate their distress. Xenomelia is overwhelmingly more common in males than females. It is accompanied by nontraditional attitudes about disability, including admiration of amputees and complete apathy and disregard toward the impairment that amputation would cause.
While the data are insufficient to draw a definitive conclusion, the trend in the published literature suggests in xenomelia, the lower left leg is predominantly the limb implicated in the condition, in right-handed individuals.1
Here, we describe the case of a young man, Mr. H, with xenomelia who contacted us after reading about this condition in a review we recently published.1 He agreed to allow us to anonymously describe his history and symptoms so that clinicians can recognize and help other individuals with xenomelia. His history may also help stimulate exploration of etiological factors and novel treatment strategies for xenomelia, other than amputation of a healthy limb.
CASE
‘I have this limb that should not be’
Mr. H, age 31, is a white male of Eastern European descent who was born, raised, and resides in a major metropolitan area in the western United States. He is married, college-educated, and currently works as a computer programmer for a prominent technology company. During our conversation via telephone, he exhibits above-average intelligence, appears to be in euthymic mood, and speaks with broad affect. Mr. H displays no psychotic symptoms such as overt delusions, hallucinations, reality distortion, or response to internal stimuli. His past psychiatric history includes attention-deficit/hyperactivity disorder (ADHD), which was diagnosed at age 6 and treated with appropriate medication under the care of a psychiatrist until age 18, when Mr. H decided to discontinue treatment. He no longer endorses symptoms of ADHD. He has no chronic medical conditions other than season allergies, for which he sometimes takes antihistamines, and occasional exacerbation of sciatica, for which he takes an over-the-counter nonsteroidal anti-inflammatory medication. Mr. H also has episodic insomnia, which he attributes to job-related stress and working odd hours. He was treated for meningitis as an infant, and underwent a bilateral myringotomy as a young child to treat recurrent ear infections. He has no other surgical history. He was raised in a middle-class Christian household that included both parents, who are still alive, still together, and have no significant psychiatric or medical history. He has no siblings.
Although he lives an ostensibly normal life, Mr. H suffers in silence and secrecy with xenomelia. According to him, there was never a time in his life when he didn’t feel that his left leg was “too long” and he was “walking on a stilt.” He says, “It takes a daily toll on my health and well-being.” He can clearly recall being 4 years old and playing games in which he would pretend to injure his left leg. He says, “When we played ‘make believe,’ the game would always end with something ‘happening’ to [my left leg].” He enjoys outdoor sports like snowboarding and mountain biking, and although he denies self-injurious behavior, he says in the event of an accident, he would prefer to land on his left leg, because it is the part of his body that he considers most “expendable.” One of his most vivid memories of childhood was going shopping with his parents and seeing an older man with only one leg standing on crutches in the parking lot outside the entrance. He remembers feeling “jealous” of this man.
Continue to: Although his parents were not particularly wealthy...
Although his parents were not particularly wealthy, they sent him to a private Christian school for most of his childhood. Mr. H admits that while there he didn’t fit in and felt like an outcast, in part because he didn’t come from the level of wealth of his classmates, and because having ADHD left him isolative and avoidant. “I was always the one going away to take medication,” he explains, and he also developed a hostile attitude. He was suspended from school multiple times for fighting. These years left him tremendously anxious and depressed, and he would often find it therapeutic to sit with his left leg bent underneath him, so as to hide its undesired portion. It was common for him to tie his leg up and stare at himself in the mirror for minutes to hours as a form of stress reduction.
Most of Mr. H’s social circle is composed of friends he has known since childhood, none of whom are aware of his condition. He acknowledges that his feelings are “bizarre in nature” and so he has kept this secret on a “need-to-know” basis out of “fear of rejection, mockery, and damage to my reputation.” Through the years, he has sought out and encountered others with this condition, first anonymously on the internet, then in-person once he gets to know and trust them. He claims to know and be friendly with several people with xenomelia in his own city, some of whom have undergone amputation and are extremely happy with the results. According to Mr. H, there is a community aspect to xenomelia in his city, and people with the condition often meet each other socially. He has revealed his secret to 2 women he dated, including his present wife, who he told 3 years into their relationship. “I was prepared for her to leave me,” he recalls. Although he has never connected the desire for amputation with sexuality, he certainly believes that amputating his left leg would enhance his sex life. “Do I find amputees sexy?” he asks, “I would say yes.” On a 10-point scale, he considers his sex life to be a “7 or 8,” and it would reach 10 if he underwent amputation.
Mr. H has a calendar on which he keeps track of the days when he feels “impaired” by his xenomelia. He marks each day as either “red” or “green.” So far, he does not recognize a pattern of exacerbation. “I have my good days, then I have my bad days,” he laments. “On good days, I think about amputation and where my leg should actually end, but it is something I can quickly push off. On my bad days, I am constantly reminded in one way or another that, yes, I have this limb that should not be.” While he has never sought treatment for this condition from a health care professional, he developed his own therapeutic regimen that includes yoga, hiking, and daily use of cannabis, which “helps take the edge off.” He used alcohol in the past as self-medication, but stopped drinking to excess when it started to disrupt other aspects of his life. According to Mr. H, the goal is to distract himself from the condition, which provides temporary relief. “I find if my mind is more engaged, the amputation thoughts are fewer and less in intensity.” He reports that the months leading up to his wedding were particularly therapeutic because wedding planning provided an excellent distraction.
Overall, his current desire for amputation is steadily increasing. “Lately it has become more of a roller coaster,” he says. “If there’s a safe way to do it, I’ll do it.” An amputation would allow him to “feel good, complete, grounded, and content.” If he were to undergo amputation, he would use a prosthetic in order to retain mobility and keep his physique as discreet as possible. He has made initial inquiries into getting an amputation, saying, “I have heard of rumors of surgeons willing to perform the surgery, for a price. However, I have not completed the ‘vetting process’ to actually come into contact with the surgeons themselves.” Similar to others with xenomelia, he is easily able to draw a line on his leg, exactly where the desired amputation should occur.8 For most of his life, that line would have been 2 inches above his knee, but in recent years, the line has drifted lower, to 2 inches below the knee. However, he “wouldn’t mind either” line of amputation. He indicates the area below the desired line is less sensitive to pain than the corresponding part of his right leg, particularly his toes.
Mr. H’s wife is extremely supportive and understanding of her husband’s condition, but is opposed to the possibility of amputation (Box).
Box
Xenomelia: A spouse's perspective
Mr. H's wife is extremely compassionate, empathetic, and supportive of her husband's struggle with xenomelia. She denies noticing any hint of his condition until he informed her. "He expected me to freak out more than I did," she recalls. In her experience, Mr. H can go days at a time without having a "flare-up" of his condition. She believes that the intermittent worsening of her husband's condition might be associated with increased work-related stress and anxiety. She encouraged him to maintain a calendar for tracking the days with exacerbations. On days when Mr. H's xenomelia is worse, she attempts to distract him with hobbies and activities. She has accompanied Mr. H when he meets others with xenomelia, although she finds these meetings quite unremarkable. "They all seem like normal people," she says. "It's usually just an average conversation." While she is committed to helping her husband cope with xenomelia, she is averse to the possibility of amputation. "I'm willing to help in any way I can, but I'm hesitant for him to amputate a healthy limb," she admits. "I'm worried about his mobility."
Continue to: Much left to be learned about xenomelia
Much left to be learned about xenomelia
What remains to be discovered about xenomelia falls into 2 areas:
- the possible usefulness of various neuroimaging modalities (morphological MRI, functional MRI, magnetic resonance spectroscopy, and diffusion tensor imaging) to identify and localize anomalous neural pathways or neuroanatomical foci associated with this condition, such as an aberrantly developed or poorly myelinated right parietal lobe, which houses the limb’s physical proprioception
- a biopsychosocial inquiry into whether there exists a specific combination of a given individual’s organic brain, mind, and environmental interactions that may give rise to this condition, and whether we might detect a prodrome that arises in early childhood. The objective of any research into this condition would be to minimize its effects, if not prevent them altogether.1
As this case illustrates, xenomelia begins in early childhood, with symptoms being reported in children as young as age 3.7 However, no published literature has investigated these early stages. We’ve learned that individuals with xenomelia often can point to key childhood experiences or memories related to seeing people with amputated limbs. They remember feeling a sense of wonder, fascination, or other strong emotion. It may be in this memory that xenomelia is permanently imprinted. This was definitely true for Mr. H, who never knew a time when he didn’t endure some level of debilitation from xenomelia, and distinctly remembers feeling jealous upon seeing a man with the amputated leg standing on crutches in a store parking lot. Although he has come across many amputees in his life, Mr. H says he vividly remembers everything about that particular man in that particular moment, adding “I can still see the clothes he was wearing. I can still see the cars in the parking lot.” That was likely his moment of vivid and powerful imprinting.
Particularly influential changes occur in adolescence, not just in the course of physical development, but in the formulation of self-identity, which involves the inevitable comparison of one’s own appearance to that of others, with heightened awareness of what others might perceive. This phenomenon is known as “the imaginary audience,” and it is often overemphasized in the minds of individuals with xenomelia.7 Mr. H is a textbook example of someone acutely aware of his “audience,” suffering from the embarrassment that came from being less wealthy than others at his school, and having to manage his ADHD in plain sight of his classmates, who knew that he required medication. It is no surprise that he felt like an outcast and got suspended for fighting. He would relieve anxiety by tying his leg up and staring at himself in the mirror, finding refuge in front of an audience of one that understood and sympathized with his suffering.
Among the most notorious aspects of this condition is investigation into the possibility of there being a sexual component to the desire for amputation. The notion that the desire is a fetish employed for the purpose of sexual arousal was first propagated by Penthouse magazine in the 1970s.9 Learning that xenomelia exists in a child long before sexual maturation—and in an older adult long after sexual drive peaks—suggests the condition is independent of sexuality. However, this aspect of xenomelia continues to be investigated. A recent study found that >70% of individuals with xenomelia are at least partially motivated by the perceived enhancement in sexual gratification.10 Individuals with this motivation are predominantly male, homosexual, come from a religious background, and are far more likely to self-amputate.10 Mr. H admitted that he is sexually attracted to amputees, and while he had no complaints about his sex life, he felt it could only reach the highest levels of gratification if he were an amputee.
It is reasonable to posit that there is a genetic mechanism that creates a cortical template of one’s body, and this template connects with the limbic system, encoding a visual preference for and attraction to one’s own idealized and preferred body morphology that includes an amputated limb.11 Therefore, if Mr. H sees himself as an amputee, it would be reasonable for him to identify with and be attracted to other amputees. However, Mr. H is clearly not preoccupied with sexuality, and believes that heightened sexual gratification would be an ancillary bonus, and not the main objective, of amputation.
Continue to: Most individuals who have particpated in research studies about xenomelia tend to...
Most individuals who have participated in research studies about xenomelia tend to be older, mainly in their 60s. This is particularly true of individuals who go through with amputation. At some point, the need for a person to invoke their autonomy, alleviate their debilitation, and fulfill their desire may supersede their aversion to physical disability and social ridicule. At this stage in his life, Mr. H can’t commit to going forward with the amputation. However, he regards the likelihood of undergoing amputation to be quite high. He made initial inquiries to find a surgeon who would be willing to perform the procedure. Given that he has found people with xenomelia who have undergone amputation, he will likely will be able find a surgeon to perform the procedure. Mr. H reports that just about everyone he has ever known with xenomelia who underwent amputation is completely satisfied with their decision, even years later. He has come across only one person who regretted the amputation, and he believes that person was likely suffering from other psychiatric issues, and did not have true xenomelia.
In the mind of an individual with xenomelia, the desire for amputation is separate from a desire to be disabled. Mr. H is mindful of the assumed irrationality of removing a healthy but “alien” limb to replace it with a prosthetic limb that is equally alien. The perceived irony is not lost on him. He values his mobility, and has no desire to use crutches, a wheelchair, or any other ambulatory tool. This is consistent with most individuals with xenomelia, who are neither motived by the desire to flaunt their amputated limb, nor by the sympathy they might receive from others by endorsing impaired mobility. They don’t consider themselves disabled. On the contrary, for them, amputation is a much-desired enhancement to their health and well-being.
Increased opportunities for research
The internet, social media, and even peer-reviewed medical journals offer ever-increasing opportunities for individuals with xenomelia, such as Mr. H, to have their story told, regardless of whether they choose to identify themselves or remain anonymous. There are no published data about the prevalence of xenomelia, but it is almost certainly rare. However, if Mr. H was able to meet multiple people with xenomelia in his own city and form a supportive community with them, then perhaps it isn’t exactly as rare as one might initially assume. People with xenomelia may tend to look for each other, hoping those with the same condition might show them the greatest empathy.
From Mr. H’s experience, it appears that it would be possible to locate a sufficient number of individuals with xenomelia for the purposes of conducting research, which might allow for results with acceptable statistical power. There are plenty of individual patient stories, and by documenting these stories in published literature, it is likely that patterns would emerge and causality might be determined. Such data might be bolstered by a possible strong neurologic corroboration based on what is found via neuroimaging.
Informed research into xenomelia is still in the early stages, and it is clear that there is much left to discover. It is vital that, moving forward, investigation into this condition be thorough and objective, with the goal of alleviating this secretive and debilitating neuropsychiatric condition.
Continue to: Bottom Line
Bottom Line
Individuals with xenomelia have the persistent belief that one or more of their limbs does not belong to their body but is an alien appendage that should be removed. Patients with this condition may resort to self-amputation or self-mutilation that requires subsequent surgical amputation. Xenomelia may be related to anomalous brain development, with a lack of neural representation of a limb in the right parietal lobe.
Related Resources
- Hilti LM, Hänggi J, Vitacco DA, et al. The desire for healthy limb amputation: structural brain correlates and clinical features of xenomelia. Brain. 2013;136(pt 1):318-329.
- Brugger P, Lenggenhager B, Giummarra MJ. Xenomelia: a social neuroscience view of altered bodily self-consciousness. Front Psychol. 2013;4:204. doi:10.3389/fpsyg.2013.00204.
1. Upadhyaya MA, Nasrallah HA. The intense desire for healthy limb amputation: a dis-proprioceptive neuropsychiatric disorder. Ann Clin Psychiatry. 2017;29(2):125-132.
2. Sedda A, Bottini G. Apotemnophilia, body integrity identity disorder or xenomelia? Psychiatric and neurologic etiologies face each other. Neuropsychiatr Dis Treat. 2014;10:1255-1265.
3. Money J, Jobaris R, Furth G. Apotemnophilia: two cases of self-demand amputation as a paraphilia. J Sex Res. 1977;13(2):115-125.
4. Blom RM, Hennekam RC, Denys D. Body integrity identity disorder. PLoS One. 2012;7(4):e34702. doi: 10.1371/journal.pone.0034702.
5. First MB. Desire for amputation of a limb: paraphilia, psychosis, or a new type of identity disorder. Psychol Med. 2005;35(6):919-928.
6. McGeoch PD, Brang D, Song T, et al. Xenomelia: a new right parietal lobe syndrome. J Neurol Neurosurg Psychiatry. 2011;82(12):1314-1319.
7. Nowakowski P, Karczmarczyk A. The rest is not me… An attempt to explain xenomelia--neurodevelopmental hypothesis. Postepy Psychiatrii i Neurologii. 2016;25(3):196-208.
8. Brang D, McGeoch PD, Ramachandran VS. Apotemnophilia: a neurological disorder. Neuroreport. 2008;19(13):1305-1306.
9. Forum. Penthouse. September 1972:128.
10. Blom RM, van der Wal SJ, Vulink NC, et al. Role of sexuality in body integrity identity disorder (BIID): a cross-sectional internet-based survey study. J Sex Med. 2017;14(8):1028-1035.
11. Ramachandran VS, Brang D, McGeoch PD, et al. Sexual and food preference in apotemnophilia and anorexia: interactions between ‘beliefs’ and ‘needs’ regulated by two-way connections between body image and limbic structures. Perception. 2009;38(5):775-777.
1. Upadhyaya MA, Nasrallah HA. The intense desire for healthy limb amputation: a dis-proprioceptive neuropsychiatric disorder. Ann Clin Psychiatry. 2017;29(2):125-132.
2. Sedda A, Bottini G. Apotemnophilia, body integrity identity disorder or xenomelia? Psychiatric and neurologic etiologies face each other. Neuropsychiatr Dis Treat. 2014;10:1255-1265.
3. Money J, Jobaris R, Furth G. Apotemnophilia: two cases of self-demand amputation as a paraphilia. J Sex Res. 1977;13(2):115-125.
4. Blom RM, Hennekam RC, Denys D. Body integrity identity disorder. PLoS One. 2012;7(4):e34702. doi: 10.1371/journal.pone.0034702.
5. First MB. Desire for amputation of a limb: paraphilia, psychosis, or a new type of identity disorder. Psychol Med. 2005;35(6):919-928.
6. McGeoch PD, Brang D, Song T, et al. Xenomelia: a new right parietal lobe syndrome. J Neurol Neurosurg Psychiatry. 2011;82(12):1314-1319.
7. Nowakowski P, Karczmarczyk A. The rest is not me… An attempt to explain xenomelia--neurodevelopmental hypothesis. Postepy Psychiatrii i Neurologii. 2016;25(3):196-208.
8. Brang D, McGeoch PD, Ramachandran VS. Apotemnophilia: a neurological disorder. Neuroreport. 2008;19(13):1305-1306.
9. Forum. Penthouse. September 1972:128.
10. Blom RM, van der Wal SJ, Vulink NC, et al. Role of sexuality in body integrity identity disorder (BIID): a cross-sectional internet-based survey study. J Sex Med. 2017;14(8):1028-1035.
11. Ramachandran VS, Brang D, McGeoch PD, et al. Sexual and food preference in apotemnophilia and anorexia: interactions between ‘beliefs’ and ‘needs’ regulated by two-way connections between body image and limbic structures. Perception. 2009;38(5):775-777.
OTP: Pipe Dream, Smoke Screen, or the Right Thing?
We live in a world of acronyms. OMG, GOAT, and the like are ubiquitous on social media and increasingly sprinkled into more traditional journalistic formats. But if you’re a PA, the most important acronym for at least the past two years has been OTP—optimal team practice.
In my February 2017 editorial, I opined on the related concept of full practice authority (FPA), discussing the hurdles the NP and PA professions face to achieve this goal (Clinician Reviews. 2017;27[2]:12-14). Both professions, now more than a half-century old, assert that they have demonstrated, through practice and research, a commitment to competent, quality health care. In recent years, these assertions have been increasingly centered around acquiring more autonomy and responsibility—what NPs refer to as the ability to practice to the fullest extent of their education and training. As a profession, the NPs have done an excellent job of breaking down unnecessary barriers to their practice.
PAs, however, continue to have challenges with this concept. To address this, a mere three months after my FPA editorial, the House of Delegates of the American Academy of PAs (AAPA) adopted OTP as a policy. The Academy says OTP is designed to increase access to care and help align the PA profession with modern societal health care needs.1
- Allow PAs to practice without a formal agreement with a particular physician
- Create separate majority-PA regulatory boards (or give authority to boards comprised of PAs and physicians who practice with PAs), and
- Allow PAs to be directly reimbursed by all public and private insurers. (PAs continue to be the only health care professionals who bill Medicare but are not entitled to direct reimbursement.)
These changes encourage PAs to practice to the full extent of their training and remove restrictions that currently obstruct delivery of care.1,2 Yet there are unintended consequences as the profession pursues this path.
The Physician Assistant Education Association (PAEA), while supporting most of the OTP policy, has raised concerns about changing curricula to reflect increased autonomy, which would require longer educational programs and incur higher costs for students.3 A significant part of PA education for the past half-century has been the social integration into the health care realm with physicians. There is also concern that changes to accommodate OTP might ultimately lead to a requirement for PAs to have a doctorate degree in order to practice—although not everyone sees that as a drawback!
Proponents of OTP, on the other hand, insist that times have changed and the profession must change with them—or at least, the rules governing the profession must be amended to reflect practical realities. AAPA leaders believe that physician oversight provisions are no longer necessary, and that PAs must acclimate to the changing health care marketplace to solidify the future of the profession and meet the needs of patients.
Continue to: Barriers to PA recruitment continue to...
Barriers to PA recruitment continue to exist as a result of statutory requirements. In today’s health care system, physicians are more likely to be employed by a large institution. Because of this, they may no longer see a financial benefit to entering into a formal agreement with a PA, which is currently required by statute for PAs to practice. Furthermore, as PAs and physicians increasingly practice in groups, the requirement for PAs to have an agreement with a specific physician is challenging to manage and places all providers involved at risk for disciplinary action for administrative infractions unrelated to patient care or outcomes.
Advocates for OTP also emphasize the perception that our NP colleagues are preferentially hired over PAs. In 22 states and the District of Columbia, NPs are allowed to practice without a collaborative agreement with a specific physician, anecdotally making them easier to hire.4 Even in states where NPs do not have FPA, the perception that hiring an NP is less burdensome than hiring a PA often exists. If accurate, these reports suggest PAs are at a disadvantage relative to NPs, resulting in lost opportunities for employment and advancement. (At least one study—based on a survey of members of the American College of Emergency Physicians council, who have direct experience in hiring NPs and PAs—demonstrated no differences in hiring preferences between the two professions. The same survey also revealed wide variability in supervisory requirements, however.5)
By recommending the elimination of the requirement for PAs to have an agreement with a specific physician in order to practice, AAPA is in effect broadening an evolution already occurring at the state level. In 2016, Michigan removed the supervisory requirement and repealed the stipulation of physician responsibility for PA-provided care; PAs in Michigan now practice with a “participating physician.” In 2017, New Mexico amended its Medical Practice Act to allow PAs who practice primary care to collaborate with a physician, while PAs who practice specialty care must be supervised by a physician.6 Illinois recently signed a 10-year extension of the state’s PA Practice Act that also better reflects the relationship between PAs and physicians, substituting “collaborating physician” for “supervising physician.”7 West Virginia has also adopted legislation referring to the physician/PA relationship as a “collaboration” (terminology Alaska has used since the 1980s).
In supporting the recent changes in Illinois, Dr. Nestor Ramirez, President of the Illinois State Medical Society, noted that “Patients are best served by physician-led teams of professionals practicing within the scope of their licensure, and physicians work collaboratively with PAs and other allied healthcare professionals to ensure that the care provided is of the highest quality.” Changing the terminology to collaboration, he added, simply “brings the language of the Physician Assistant Practice Act in line with that of other licensure acts.”7
Perhaps the larger challenge in implementing OTP will be achieving this level of support from all our physician colleagues. In a small survey on this topic conducted by researchers at the Hofstra Northwell School of Graduate Nursing and Physician Assistant Studies, nearly 80% of physician respondents had no previous knowledge of OTP. The majority (62.8%) agreed with the notion that PAs are committed to team practice (first component of OTP); however, less than half of the respondents (47.3%) said they would support OTP policy. The authors concluded that OTP advocacy efforts should target physician awareness and support.8
Continue to: One thing is clear...
One thing is clear: the OTP train has left the proverbial station. My concern is: Are we on the right track, with the right strategic plan, and with the right people on board? In my opinion, we need to turn to our professional organizational leaders and ask them to carefully evaluate all the unintended consequences of OTP and outline a carefully thought-out plan for the next decade of PA practice. While state efforts are thus far focused on amending supervisory requirements, I think we would be best served focusing on the development of PA-specific regulatory boards (currently, only five states have one). In the long term, this would make the profession responsible for its own practice regulations.
There is no doubt that we must find appropriate responses to the changing practice environment. As we work toward professional solutions, we must take into consideration the needs of all stakeholders, including our physician colleagues, PA educators, PA regulators, current and future students, and patients. How do we best partner with them—and with our NP colleagues—for the sake of continuity of patient care? Send your ideas to me at PAeditor@mdedge.com.
1. AAPA. Frequently asked questions: optimal team practice. www.aapa.org/wp-content/uploads/2018/01/Core-FAQ.pdf. Accessed July 12, 2018.
2. AAPA. Guidelines for state regulation of PAs. www.aapa.org/download/35030/. Accessed July 12, 2018.
3. Physician Assistant Education Association. Optimal team practice: the right prescription for all PAs? http://paeaonline.org/wp-content/uploads/2017/05/PAEA-OTP-Task-Force-Report_2017_2.pdf. Accessed July 12, 2018.
4. Japsen B. Nurse practitioners boost presence by 43% in rural America. www.forbes.com/sites/brucejapsen/2018/06/05/nurse-practitioners-boost-presence-by-43-in-rural-america/#39542d52648b. Accessed July 12, 2018.
5. Phillips AW, Klauer KM, Kessler CS. Emergency physician evaluation of PA and NP practice patterns. JAAPA. 2018;31(5):38-43.
6. AAPA. New Mexico PAs celebrate the enactment of collaboration bill. April 18, 2017. www.aapa.org/news-central/2017/04/new-mexico-pas-celebrate-enactment-collaboration-bill/. Accessed July 12, 2018.
7. Japsen B. States lift more hurdles to physician assistants. September 8, 2017. Forbes. www.forbes.com/sites/brucejapsen/2017/09/08/states-lift-more-hurdles-to-physician-assistants/#57ec3e822eff. Accessed July 12, 2018.
8. DeForte L, Doerler A, Oliphant A, et al. Assessing physicians’ opinions regarding optimal team practice. Presented at: AAPA 2018 annual conference; May 19-23, 2018; New Orleans, LA. Poster 115.
We live in a world of acronyms. OMG, GOAT, and the like are ubiquitous on social media and increasingly sprinkled into more traditional journalistic formats. But if you’re a PA, the most important acronym for at least the past two years has been OTP—optimal team practice.
In my February 2017 editorial, I opined on the related concept of full practice authority (FPA), discussing the hurdles the NP and PA professions face to achieve this goal (Clinician Reviews. 2017;27[2]:12-14). Both professions, now more than a half-century old, assert that they have demonstrated, through practice and research, a commitment to competent, quality health care. In recent years, these assertions have been increasingly centered around acquiring more autonomy and responsibility—what NPs refer to as the ability to practice to the fullest extent of their education and training. As a profession, the NPs have done an excellent job of breaking down unnecessary barriers to their practice.
PAs, however, continue to have challenges with this concept. To address this, a mere three months after my FPA editorial, the House of Delegates of the American Academy of PAs (AAPA) adopted OTP as a policy. The Academy says OTP is designed to increase access to care and help align the PA profession with modern societal health care needs.1
- Allow PAs to practice without a formal agreement with a particular physician
- Create separate majority-PA regulatory boards (or give authority to boards comprised of PAs and physicians who practice with PAs), and
- Allow PAs to be directly reimbursed by all public and private insurers. (PAs continue to be the only health care professionals who bill Medicare but are not entitled to direct reimbursement.)
These changes encourage PAs to practice to the full extent of their training and remove restrictions that currently obstruct delivery of care.1,2 Yet there are unintended consequences as the profession pursues this path.
The Physician Assistant Education Association (PAEA), while supporting most of the OTP policy, has raised concerns about changing curricula to reflect increased autonomy, which would require longer educational programs and incur higher costs for students.3 A significant part of PA education for the past half-century has been the social integration into the health care realm with physicians. There is also concern that changes to accommodate OTP might ultimately lead to a requirement for PAs to have a doctorate degree in order to practice—although not everyone sees that as a drawback!
Proponents of OTP, on the other hand, insist that times have changed and the profession must change with them—or at least, the rules governing the profession must be amended to reflect practical realities. AAPA leaders believe that physician oversight provisions are no longer necessary, and that PAs must acclimate to the changing health care marketplace to solidify the future of the profession and meet the needs of patients.
Continue to: Barriers to PA recruitment continue to...
Barriers to PA recruitment continue to exist as a result of statutory requirements. In today’s health care system, physicians are more likely to be employed by a large institution. Because of this, they may no longer see a financial benefit to entering into a formal agreement with a PA, which is currently required by statute for PAs to practice. Furthermore, as PAs and physicians increasingly practice in groups, the requirement for PAs to have an agreement with a specific physician is challenging to manage and places all providers involved at risk for disciplinary action for administrative infractions unrelated to patient care or outcomes.
Advocates for OTP also emphasize the perception that our NP colleagues are preferentially hired over PAs. In 22 states and the District of Columbia, NPs are allowed to practice without a collaborative agreement with a specific physician, anecdotally making them easier to hire.4 Even in states where NPs do not have FPA, the perception that hiring an NP is less burdensome than hiring a PA often exists. If accurate, these reports suggest PAs are at a disadvantage relative to NPs, resulting in lost opportunities for employment and advancement. (At least one study—based on a survey of members of the American College of Emergency Physicians council, who have direct experience in hiring NPs and PAs—demonstrated no differences in hiring preferences between the two professions. The same survey also revealed wide variability in supervisory requirements, however.5)
By recommending the elimination of the requirement for PAs to have an agreement with a specific physician in order to practice, AAPA is in effect broadening an evolution already occurring at the state level. In 2016, Michigan removed the supervisory requirement and repealed the stipulation of physician responsibility for PA-provided care; PAs in Michigan now practice with a “participating physician.” In 2017, New Mexico amended its Medical Practice Act to allow PAs who practice primary care to collaborate with a physician, while PAs who practice specialty care must be supervised by a physician.6 Illinois recently signed a 10-year extension of the state’s PA Practice Act that also better reflects the relationship between PAs and physicians, substituting “collaborating physician” for “supervising physician.”7 West Virginia has also adopted legislation referring to the physician/PA relationship as a “collaboration” (terminology Alaska has used since the 1980s).
In supporting the recent changes in Illinois, Dr. Nestor Ramirez, President of the Illinois State Medical Society, noted that “Patients are best served by physician-led teams of professionals practicing within the scope of their licensure, and physicians work collaboratively with PAs and other allied healthcare professionals to ensure that the care provided is of the highest quality.” Changing the terminology to collaboration, he added, simply “brings the language of the Physician Assistant Practice Act in line with that of other licensure acts.”7
Perhaps the larger challenge in implementing OTP will be achieving this level of support from all our physician colleagues. In a small survey on this topic conducted by researchers at the Hofstra Northwell School of Graduate Nursing and Physician Assistant Studies, nearly 80% of physician respondents had no previous knowledge of OTP. The majority (62.8%) agreed with the notion that PAs are committed to team practice (first component of OTP); however, less than half of the respondents (47.3%) said they would support OTP policy. The authors concluded that OTP advocacy efforts should target physician awareness and support.8
Continue to: One thing is clear...
One thing is clear: the OTP train has left the proverbial station. My concern is: Are we on the right track, with the right strategic plan, and with the right people on board? In my opinion, we need to turn to our professional organizational leaders and ask them to carefully evaluate all the unintended consequences of OTP and outline a carefully thought-out plan for the next decade of PA practice. While state efforts are thus far focused on amending supervisory requirements, I think we would be best served focusing on the development of PA-specific regulatory boards (currently, only five states have one). In the long term, this would make the profession responsible for its own practice regulations.
There is no doubt that we must find appropriate responses to the changing practice environment. As we work toward professional solutions, we must take into consideration the needs of all stakeholders, including our physician colleagues, PA educators, PA regulators, current and future students, and patients. How do we best partner with them—and with our NP colleagues—for the sake of continuity of patient care? Send your ideas to me at PAeditor@mdedge.com.
We live in a world of acronyms. OMG, GOAT, and the like are ubiquitous on social media and increasingly sprinkled into more traditional journalistic formats. But if you’re a PA, the most important acronym for at least the past two years has been OTP—optimal team practice.
In my February 2017 editorial, I opined on the related concept of full practice authority (FPA), discussing the hurdles the NP and PA professions face to achieve this goal (Clinician Reviews. 2017;27[2]:12-14). Both professions, now more than a half-century old, assert that they have demonstrated, through practice and research, a commitment to competent, quality health care. In recent years, these assertions have been increasingly centered around acquiring more autonomy and responsibility—what NPs refer to as the ability to practice to the fullest extent of their education and training. As a profession, the NPs have done an excellent job of breaking down unnecessary barriers to their practice.
PAs, however, continue to have challenges with this concept. To address this, a mere three months after my FPA editorial, the House of Delegates of the American Academy of PAs (AAPA) adopted OTP as a policy. The Academy says OTP is designed to increase access to care and help align the PA profession with modern societal health care needs.1
- Allow PAs to practice without a formal agreement with a particular physician
- Create separate majority-PA regulatory boards (or give authority to boards comprised of PAs and physicians who practice with PAs), and
- Allow PAs to be directly reimbursed by all public and private insurers. (PAs continue to be the only health care professionals who bill Medicare but are not entitled to direct reimbursement.)
These changes encourage PAs to practice to the full extent of their training and remove restrictions that currently obstruct delivery of care.1,2 Yet there are unintended consequences as the profession pursues this path.
The Physician Assistant Education Association (PAEA), while supporting most of the OTP policy, has raised concerns about changing curricula to reflect increased autonomy, which would require longer educational programs and incur higher costs for students.3 A significant part of PA education for the past half-century has been the social integration into the health care realm with physicians. There is also concern that changes to accommodate OTP might ultimately lead to a requirement for PAs to have a doctorate degree in order to practice—although not everyone sees that as a drawback!
Proponents of OTP, on the other hand, insist that times have changed and the profession must change with them—or at least, the rules governing the profession must be amended to reflect practical realities. AAPA leaders believe that physician oversight provisions are no longer necessary, and that PAs must acclimate to the changing health care marketplace to solidify the future of the profession and meet the needs of patients.
Continue to: Barriers to PA recruitment continue to...
Barriers to PA recruitment continue to exist as a result of statutory requirements. In today’s health care system, physicians are more likely to be employed by a large institution. Because of this, they may no longer see a financial benefit to entering into a formal agreement with a PA, which is currently required by statute for PAs to practice. Furthermore, as PAs and physicians increasingly practice in groups, the requirement for PAs to have an agreement with a specific physician is challenging to manage and places all providers involved at risk for disciplinary action for administrative infractions unrelated to patient care or outcomes.
Advocates for OTP also emphasize the perception that our NP colleagues are preferentially hired over PAs. In 22 states and the District of Columbia, NPs are allowed to practice without a collaborative agreement with a specific physician, anecdotally making them easier to hire.4 Even in states where NPs do not have FPA, the perception that hiring an NP is less burdensome than hiring a PA often exists. If accurate, these reports suggest PAs are at a disadvantage relative to NPs, resulting in lost opportunities for employment and advancement. (At least one study—based on a survey of members of the American College of Emergency Physicians council, who have direct experience in hiring NPs and PAs—demonstrated no differences in hiring preferences between the two professions. The same survey also revealed wide variability in supervisory requirements, however.5)
By recommending the elimination of the requirement for PAs to have an agreement with a specific physician in order to practice, AAPA is in effect broadening an evolution already occurring at the state level. In 2016, Michigan removed the supervisory requirement and repealed the stipulation of physician responsibility for PA-provided care; PAs in Michigan now practice with a “participating physician.” In 2017, New Mexico amended its Medical Practice Act to allow PAs who practice primary care to collaborate with a physician, while PAs who practice specialty care must be supervised by a physician.6 Illinois recently signed a 10-year extension of the state’s PA Practice Act that also better reflects the relationship between PAs and physicians, substituting “collaborating physician” for “supervising physician.”7 West Virginia has also adopted legislation referring to the physician/PA relationship as a “collaboration” (terminology Alaska has used since the 1980s).
In supporting the recent changes in Illinois, Dr. Nestor Ramirez, President of the Illinois State Medical Society, noted that “Patients are best served by physician-led teams of professionals practicing within the scope of their licensure, and physicians work collaboratively with PAs and other allied healthcare professionals to ensure that the care provided is of the highest quality.” Changing the terminology to collaboration, he added, simply “brings the language of the Physician Assistant Practice Act in line with that of other licensure acts.”7
Perhaps the larger challenge in implementing OTP will be achieving this level of support from all our physician colleagues. In a small survey on this topic conducted by researchers at the Hofstra Northwell School of Graduate Nursing and Physician Assistant Studies, nearly 80% of physician respondents had no previous knowledge of OTP. The majority (62.8%) agreed with the notion that PAs are committed to team practice (first component of OTP); however, less than half of the respondents (47.3%) said they would support OTP policy. The authors concluded that OTP advocacy efforts should target physician awareness and support.8
Continue to: One thing is clear...
One thing is clear: the OTP train has left the proverbial station. My concern is: Are we on the right track, with the right strategic plan, and with the right people on board? In my opinion, we need to turn to our professional organizational leaders and ask them to carefully evaluate all the unintended consequences of OTP and outline a carefully thought-out plan for the next decade of PA practice. While state efforts are thus far focused on amending supervisory requirements, I think we would be best served focusing on the development of PA-specific regulatory boards (currently, only five states have one). In the long term, this would make the profession responsible for its own practice regulations.
There is no doubt that we must find appropriate responses to the changing practice environment. As we work toward professional solutions, we must take into consideration the needs of all stakeholders, including our physician colleagues, PA educators, PA regulators, current and future students, and patients. How do we best partner with them—and with our NP colleagues—for the sake of continuity of patient care? Send your ideas to me at PAeditor@mdedge.com.
1. AAPA. Frequently asked questions: optimal team practice. www.aapa.org/wp-content/uploads/2018/01/Core-FAQ.pdf. Accessed July 12, 2018.
2. AAPA. Guidelines for state regulation of PAs. www.aapa.org/download/35030/. Accessed July 12, 2018.
3. Physician Assistant Education Association. Optimal team practice: the right prescription for all PAs? http://paeaonline.org/wp-content/uploads/2017/05/PAEA-OTP-Task-Force-Report_2017_2.pdf. Accessed July 12, 2018.
4. Japsen B. Nurse practitioners boost presence by 43% in rural America. www.forbes.com/sites/brucejapsen/2018/06/05/nurse-practitioners-boost-presence-by-43-in-rural-america/#39542d52648b. Accessed July 12, 2018.
5. Phillips AW, Klauer KM, Kessler CS. Emergency physician evaluation of PA and NP practice patterns. JAAPA. 2018;31(5):38-43.
6. AAPA. New Mexico PAs celebrate the enactment of collaboration bill. April 18, 2017. www.aapa.org/news-central/2017/04/new-mexico-pas-celebrate-enactment-collaboration-bill/. Accessed July 12, 2018.
7. Japsen B. States lift more hurdles to physician assistants. September 8, 2017. Forbes. www.forbes.com/sites/brucejapsen/2017/09/08/states-lift-more-hurdles-to-physician-assistants/#57ec3e822eff. Accessed July 12, 2018.
8. DeForte L, Doerler A, Oliphant A, et al. Assessing physicians’ opinions regarding optimal team practice. Presented at: AAPA 2018 annual conference; May 19-23, 2018; New Orleans, LA. Poster 115.
1. AAPA. Frequently asked questions: optimal team practice. www.aapa.org/wp-content/uploads/2018/01/Core-FAQ.pdf. Accessed July 12, 2018.
2. AAPA. Guidelines for state regulation of PAs. www.aapa.org/download/35030/. Accessed July 12, 2018.
3. Physician Assistant Education Association. Optimal team practice: the right prescription for all PAs? http://paeaonline.org/wp-content/uploads/2017/05/PAEA-OTP-Task-Force-Report_2017_2.pdf. Accessed July 12, 2018.
4. Japsen B. Nurse practitioners boost presence by 43% in rural America. www.forbes.com/sites/brucejapsen/2018/06/05/nurse-practitioners-boost-presence-by-43-in-rural-america/#39542d52648b. Accessed July 12, 2018.
5. Phillips AW, Klauer KM, Kessler CS. Emergency physician evaluation of PA and NP practice patterns. JAAPA. 2018;31(5):38-43.
6. AAPA. New Mexico PAs celebrate the enactment of collaboration bill. April 18, 2017. www.aapa.org/news-central/2017/04/new-mexico-pas-celebrate-enactment-collaboration-bill/. Accessed July 12, 2018.
7. Japsen B. States lift more hurdles to physician assistants. September 8, 2017. Forbes. www.forbes.com/sites/brucejapsen/2017/09/08/states-lift-more-hurdles-to-physician-assistants/#57ec3e822eff. Accessed July 12, 2018.
8. DeForte L, Doerler A, Oliphant A, et al. Assessing physicians’ opinions regarding optimal team practice. Presented at: AAPA 2018 annual conference; May 19-23, 2018; New Orleans, LA. Poster 115.