User login
Can Antihypertensive Medication Reduce Dementia Risk in Older Adults?
LONDON—Calcium channel blockers and angiotensin receptor blockers are independently associated with a decreased risk of dementia in older patients, according to a study presented at the 2017 Alzheimer’s Association International Conference and published in the October issue of Journal of Hypertension.
“Calcium channel blockers regulate calcium influx, which may prevent neuronal cell death, inhibit the production of amyloid beta and neurofibrillary tangles, and improve cerebrovascular perfusion. Angiotensin receptor blockers may improve the cerebral blood flow, decrease levels of amyloid beta, and have an anti-inflammatory effect,” said Tessa van Middelaar, MD, a PhD student in the Department of Neurology at the Academic Medical Center in Amsterdam and the Radboud University Medical Center in Nijmegen.
Epidemiologic evidence has suggested that hypertension is an important risk factor for dementia. Trials studying the effect of antihypertensive medication on the incidence of dementia have had inconclusive results, however.
Post Hoc Analysis of Data
Dr. van Middelaar and colleagues conducted a post hoc analysis of data from the Prevention of Dementia by Intensive Vascular Care (preDIVA) trial. In this randomized controlled trial, 3,526 community-dwelling adults ranging in age from 70 to 78 received either intensive vascular care or standard care.
At baseline and during follow-up, data on medication use and medical history were collected every two years. Researchers identified five classes of antihypertensive medication used by participants (ie, beta-blockers, diuretics, ACE inhibitors, calcium channel blockers, and angiotensin receptor blockers).
The investigators used the Mini-Mental State Examination to measure cognition and defined dementia using the Diagnostic and Statistical Manual of Mental Disorders IV criteria. Analyses were restricted to participants who were using antihypertensive medications at baseline. Dr. van Middelaar and colleagues compared incident dementia rates associated with the use of different antihypertensive medication classes, including monotherapy and combination therapy, with those associ
Two Classes Reduced Dementia Risk
At baseline, 1,951 patients used antihypertensive medication. The study population’s mean age was 74.4, and 46.2% of participants were men. In all, 986 patients used beta-blockers, 798 used diuretics, 623 used ACE inhibitors, 522 used calcium channel blockers, and 402 used angiotensin receptor blockers. After a median of 6.7 years of follow-up, 136 participants developed dementia.
The use of calcium channel blockers and the use of angiotensin receptor blockers were associated with a lower incidence of dementia, compared with the use of other antihypertensive medications (hazard ratios, 0.56 and 0.60, respectively). The reduced risk of dementia associated with calcium channel blockers was the most evident in participants without a history of cardiovascular disease and those with uncontrolled hypertension. “A possible explanation for this increased benefit in older people without a history of cardiovascular disease could be related to less pronounced vascular lesions and, therefore, more brain reserve and capacity for functional resilience to cognitive decline,” said Dr. van Middelaar and colleagues. Researchers also found that systolic blood pressure was not significantly lower in participants using calcium channel blockers or angiotensin receptor blockers.
—Erica Tricarico
Suggested Reading
van Middelaar T, van Vught LA, Moll van Charante EP, et al. Lower dementia risk with different classes of antihypertensive medication in older patients. J Hypertens. 2017;35(10):2095-2101.
LONDON—Calcium channel blockers and angiotensin receptor blockers are independently associated with a decreased risk of dementia in older patients, according to a study presented at the 2017 Alzheimer’s Association International Conference and published in the October issue of Journal of Hypertension.
“Calcium channel blockers regulate calcium influx, which may prevent neuronal cell death, inhibit the production of amyloid beta and neurofibrillary tangles, and improve cerebrovascular perfusion. Angiotensin receptor blockers may improve the cerebral blood flow, decrease levels of amyloid beta, and have an anti-inflammatory effect,” said Tessa van Middelaar, MD, a PhD student in the Department of Neurology at the Academic Medical Center in Amsterdam and the Radboud University Medical Center in Nijmegen.
Epidemiologic evidence has suggested that hypertension is an important risk factor for dementia. Trials studying the effect of antihypertensive medication on the incidence of dementia have had inconclusive results, however.
Post Hoc Analysis of Data
Dr. van Middelaar and colleagues conducted a post hoc analysis of data from the Prevention of Dementia by Intensive Vascular Care (preDIVA) trial. In this randomized controlled trial, 3,526 community-dwelling adults ranging in age from 70 to 78 received either intensive vascular care or standard care.
At baseline and during follow-up, data on medication use and medical history were collected every two years. Researchers identified five classes of antihypertensive medication used by participants (ie, beta-blockers, diuretics, ACE inhibitors, calcium channel blockers, and angiotensin receptor blockers).
The investigators used the Mini-Mental State Examination to measure cognition and defined dementia using the Diagnostic and Statistical Manual of Mental Disorders IV criteria. Analyses were restricted to participants who were using antihypertensive medications at baseline. Dr. van Middelaar and colleagues compared incident dementia rates associated with the use of different antihypertensive medication classes, including monotherapy and combination therapy, with those associ
Two Classes Reduced Dementia Risk
At baseline, 1,951 patients used antihypertensive medication. The study population’s mean age was 74.4, and 46.2% of participants were men. In all, 986 patients used beta-blockers, 798 used diuretics, 623 used ACE inhibitors, 522 used calcium channel blockers, and 402 used angiotensin receptor blockers. After a median of 6.7 years of follow-up, 136 participants developed dementia.
The use of calcium channel blockers and the use of angiotensin receptor blockers were associated with a lower incidence of dementia, compared with the use of other antihypertensive medications (hazard ratios, 0.56 and 0.60, respectively). The reduced risk of dementia associated with calcium channel blockers was the most evident in participants without a history of cardiovascular disease and those with uncontrolled hypertension. “A possible explanation for this increased benefit in older people without a history of cardiovascular disease could be related to less pronounced vascular lesions and, therefore, more brain reserve and capacity for functional resilience to cognitive decline,” said Dr. van Middelaar and colleagues. Researchers also found that systolic blood pressure was not significantly lower in participants using calcium channel blockers or angiotensin receptor blockers.
—Erica Tricarico
Suggested Reading
van Middelaar T, van Vught LA, Moll van Charante EP, et al. Lower dementia risk with different classes of antihypertensive medication in older patients. J Hypertens. 2017;35(10):2095-2101.
LONDON—Calcium channel blockers and angiotensin receptor blockers are independently associated with a decreased risk of dementia in older patients, according to a study presented at the 2017 Alzheimer’s Association International Conference and published in the October issue of Journal of Hypertension.
“Calcium channel blockers regulate calcium influx, which may prevent neuronal cell death, inhibit the production of amyloid beta and neurofibrillary tangles, and improve cerebrovascular perfusion. Angiotensin receptor blockers may improve the cerebral blood flow, decrease levels of amyloid beta, and have an anti-inflammatory effect,” said Tessa van Middelaar, MD, a PhD student in the Department of Neurology at the Academic Medical Center in Amsterdam and the Radboud University Medical Center in Nijmegen.
Epidemiologic evidence has suggested that hypertension is an important risk factor for dementia. Trials studying the effect of antihypertensive medication on the incidence of dementia have had inconclusive results, however.
Post Hoc Analysis of Data
Dr. van Middelaar and colleagues conducted a post hoc analysis of data from the Prevention of Dementia by Intensive Vascular Care (preDIVA) trial. In this randomized controlled trial, 3,526 community-dwelling adults ranging in age from 70 to 78 received either intensive vascular care or standard care.
At baseline and during follow-up, data on medication use and medical history were collected every two years. Researchers identified five classes of antihypertensive medication used by participants (ie, beta-blockers, diuretics, ACE inhibitors, calcium channel blockers, and angiotensin receptor blockers).
The investigators used the Mini-Mental State Examination to measure cognition and defined dementia using the Diagnostic and Statistical Manual of Mental Disorders IV criteria. Analyses were restricted to participants who were using antihypertensive medications at baseline. Dr. van Middelaar and colleagues compared incident dementia rates associated with the use of different antihypertensive medication classes, including monotherapy and combination therapy, with those associ
Two Classes Reduced Dementia Risk
At baseline, 1,951 patients used antihypertensive medication. The study population’s mean age was 74.4, and 46.2% of participants were men. In all, 986 patients used beta-blockers, 798 used diuretics, 623 used ACE inhibitors, 522 used calcium channel blockers, and 402 used angiotensin receptor blockers. After a median of 6.7 years of follow-up, 136 participants developed dementia.
The use of calcium channel blockers and the use of angiotensin receptor blockers were associated with a lower incidence of dementia, compared with the use of other antihypertensive medications (hazard ratios, 0.56 and 0.60, respectively). The reduced risk of dementia associated with calcium channel blockers was the most evident in participants without a history of cardiovascular disease and those with uncontrolled hypertension. “A possible explanation for this increased benefit in older people without a history of cardiovascular disease could be related to less pronounced vascular lesions and, therefore, more brain reserve and capacity for functional resilience to cognitive decline,” said Dr. van Middelaar and colleagues. Researchers also found that systolic blood pressure was not significantly lower in participants using calcium channel blockers or angiotensin receptor blockers.
—Erica Tricarico
Suggested Reading
van Middelaar T, van Vught LA, Moll van Charante EP, et al. Lower dementia risk with different classes of antihypertensive medication in older patients. J Hypertens. 2017;35(10):2095-2101.
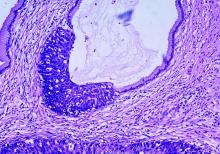
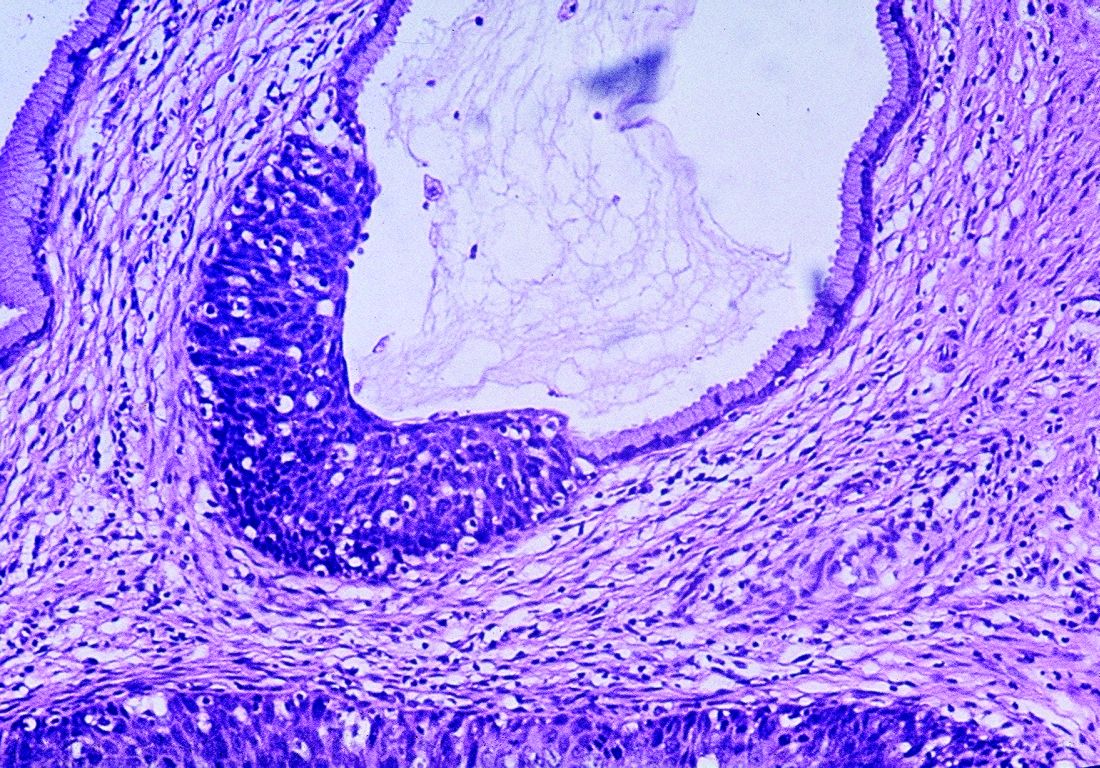
Real-world data support extended cervical cancer screening interval
A cervical cancer screening interval of 5 years or longer may be safe for women with one or more negative cotests using the high-risk human papillomavirus (HPV) test and cervical cytology, according to the results of a large observational study.
The findings also suggest that one or two negative HPV tests, regardless of cytology, may be enough to extend the screening interval, the researchers noted.
The 5-year risk decreased with each successive HPV-negative and cytology-negative result, falling from 0.098% in the first cotesting round, to 0.052% in the second round, and 0.035% in the third round. The 5-year risks were similar with an HPV-negative cotest result, regardless of the outcome of cytology: 0.114%, 0.061%, and 0.041%.
The results are based on data from more than 990,000 women in the Kaiser Permanente Northern California health care system who had one or more cotests from 2003 to 2014.
These findings come as the U.S. Preventive Services Task Force (USPSTF) has issued draft recommendations that would call for either HPV testing alone every 5 years starting at age 30 years or cytology every 3 years, but no cotesting. The American College of Obstetricians and Gynecologists currently recommends cotesting with cytology and HPV testing every 5 years or cytology alone every 3 years in women aged 30-65 years (Obstet Gynecol. 2016;128[4]:e111-30).
The study was partially funded by the National Cancer Institute. Some of the researchers are employees of the National Cancer Institute. The researchers reported receiving cervical screening tests and diagnostics at reduced or no cost from Roche, BD Biosciences, Cepheid, Arbor Vita, and Hologic.
The study by Castle et al provides important insight into the effects of repeated testing of HPV, cervical cytology, and testing both together. The authors are to be commended for performing their analysis, which involved almost 1 million women.
There are several important observations that can be made. One is that the risk of detecting cancer is decreased after cotesting HPV and cervical cytology both show a negative result, and that this risk is further reduced after the second and third negative HPV/cytology test. This could mean less frequent screening could be safely adopted in women who are HPV and cytology negative, which would lead to fewer women referred for unnecessary colposcopy and treatment, reducing their stress and discomfort.
These data could alter how women are triaged on the basis of the HPV test. In HPV-positive women, for example, current practices are appropriate for the first and perhaps second round of HPV testing, but perhaps subsequent rounds could become less stringent. Conversely, when there is an HPV-negative result, even in the presence of a positive or equivocal cytology, screening intervals may still be safe to lengthen as there is only a small increase in risk versus being both HPV and cytology negative.
Guglielmo Ronco, MD, PhD, is formerly of the City of Health and Science University Hospital of Turin (Italy). Silvia Franceschi, MD, PhD, is with the International Agency for Research on Cancer in Lyon, France. They reported having no relevant financial disclosures. Their comments were adapted from an accompanying editorial (Ann Intern Med. 2017. doi: 10.7326/M17-2872).
The study by Castle et al provides important insight into the effects of repeated testing of HPV, cervical cytology, and testing both together. The authors are to be commended for performing their analysis, which involved almost 1 million women.
There are several important observations that can be made. One is that the risk of detecting cancer is decreased after cotesting HPV and cervical cytology both show a negative result, and that this risk is further reduced after the second and third negative HPV/cytology test. This could mean less frequent screening could be safely adopted in women who are HPV and cytology negative, which would lead to fewer women referred for unnecessary colposcopy and treatment, reducing their stress and discomfort.
These data could alter how women are triaged on the basis of the HPV test. In HPV-positive women, for example, current practices are appropriate for the first and perhaps second round of HPV testing, but perhaps subsequent rounds could become less stringent. Conversely, when there is an HPV-negative result, even in the presence of a positive or equivocal cytology, screening intervals may still be safe to lengthen as there is only a small increase in risk versus being both HPV and cytology negative.
Guglielmo Ronco, MD, PhD, is formerly of the City of Health and Science University Hospital of Turin (Italy). Silvia Franceschi, MD, PhD, is with the International Agency for Research on Cancer in Lyon, France. They reported having no relevant financial disclosures. Their comments were adapted from an accompanying editorial (Ann Intern Med. 2017. doi: 10.7326/M17-2872).
The study by Castle et al provides important insight into the effects of repeated testing of HPV, cervical cytology, and testing both together. The authors are to be commended for performing their analysis, which involved almost 1 million women.
There are several important observations that can be made. One is that the risk of detecting cancer is decreased after cotesting HPV and cervical cytology both show a negative result, and that this risk is further reduced after the second and third negative HPV/cytology test. This could mean less frequent screening could be safely adopted in women who are HPV and cytology negative, which would lead to fewer women referred for unnecessary colposcopy and treatment, reducing their stress and discomfort.
These data could alter how women are triaged on the basis of the HPV test. In HPV-positive women, for example, current practices are appropriate for the first and perhaps second round of HPV testing, but perhaps subsequent rounds could become less stringent. Conversely, when there is an HPV-negative result, even in the presence of a positive or equivocal cytology, screening intervals may still be safe to lengthen as there is only a small increase in risk versus being both HPV and cytology negative.
Guglielmo Ronco, MD, PhD, is formerly of the City of Health and Science University Hospital of Turin (Italy). Silvia Franceschi, MD, PhD, is with the International Agency for Research on Cancer in Lyon, France. They reported having no relevant financial disclosures. Their comments were adapted from an accompanying editorial (Ann Intern Med. 2017. doi: 10.7326/M17-2872).
A cervical cancer screening interval of 5 years or longer may be safe for women with one or more negative cotests using the high-risk human papillomavirus (HPV) test and cervical cytology, according to the results of a large observational study.
The findings also suggest that one or two negative HPV tests, regardless of cytology, may be enough to extend the screening interval, the researchers noted.
The 5-year risk decreased with each successive HPV-negative and cytology-negative result, falling from 0.098% in the first cotesting round, to 0.052% in the second round, and 0.035% in the third round. The 5-year risks were similar with an HPV-negative cotest result, regardless of the outcome of cytology: 0.114%, 0.061%, and 0.041%.
The results are based on data from more than 990,000 women in the Kaiser Permanente Northern California health care system who had one or more cotests from 2003 to 2014.
These findings come as the U.S. Preventive Services Task Force (USPSTF) has issued draft recommendations that would call for either HPV testing alone every 5 years starting at age 30 years or cytology every 3 years, but no cotesting. The American College of Obstetricians and Gynecologists currently recommends cotesting with cytology and HPV testing every 5 years or cytology alone every 3 years in women aged 30-65 years (Obstet Gynecol. 2016;128[4]:e111-30).
The study was partially funded by the National Cancer Institute. Some of the researchers are employees of the National Cancer Institute. The researchers reported receiving cervical screening tests and diagnostics at reduced or no cost from Roche, BD Biosciences, Cepheid, Arbor Vita, and Hologic.
A cervical cancer screening interval of 5 years or longer may be safe for women with one or more negative cotests using the high-risk human papillomavirus (HPV) test and cervical cytology, according to the results of a large observational study.
The findings also suggest that one or two negative HPV tests, regardless of cytology, may be enough to extend the screening interval, the researchers noted.
The 5-year risk decreased with each successive HPV-negative and cytology-negative result, falling from 0.098% in the first cotesting round, to 0.052% in the second round, and 0.035% in the third round. The 5-year risks were similar with an HPV-negative cotest result, regardless of the outcome of cytology: 0.114%, 0.061%, and 0.041%.
The results are based on data from more than 990,000 women in the Kaiser Permanente Northern California health care system who had one or more cotests from 2003 to 2014.
These findings come as the U.S. Preventive Services Task Force (USPSTF) has issued draft recommendations that would call for either HPV testing alone every 5 years starting at age 30 years or cytology every 3 years, but no cotesting. The American College of Obstetricians and Gynecologists currently recommends cotesting with cytology and HPV testing every 5 years or cytology alone every 3 years in women aged 30-65 years (Obstet Gynecol. 2016;128[4]:e111-30).
The study was partially funded by the National Cancer Institute. Some of the researchers are employees of the National Cancer Institute. The researchers reported receiving cervical screening tests and diagnostics at reduced or no cost from Roche, BD Biosciences, Cepheid, Arbor Vita, and Hologic.
FROM ANNALS OF INTERNAL MEDICINE
Key clinical point:
Major finding: The 5-year cumulative detection of invasive cervical cancer, CIN3, and adenocarcinoma in situ decreased with each successive HPV-negative and cytology-negative result (0.098%, 0.052%, and 0.035%).
Data source: Data on more than 990,000 women who received cotesting between 2003 and 2014.
Disclosures: The research was partially supported by the National Cancer Institute. Some of the researchers are employees of the National Cancer Institute. The researchers reported receiving cervical screening tests and diagnostics at reduced or no cost from Roche, BD Biosciences, Cepheid, Arbor Vita, and Hologic.
From the Washington Office: Year Two of MIPS …The song remains the same (largely)
The interim final rule for the second year of Centers for Medicare and Medicaid Services (CMS) Quality Payment Program (QPP) was released on November 2, 2017. This rule will apply to performance and reporting for calendar year 2018 and impact payment in 2020. Below, I have highlighted a few of the key components of the 1,653-page rule with special attention to the Merit-based Incentive Payment System (MIPS).
To briefly review, there are two pathways for participation in the QPP, namely MIPS and the Advanced Alternative Payment Models (A-APMs). For 2018, we still expect that the majority of surgeons eligible to participate in the QPP will do so via the MIPS pathway. That said, and for reasons discussed below, CMS estimates that approximately half of the 1.2 million MIPS-eligible clinicians will be required to submit MIPS data in 2018. In addition, CMS estimates that approximately 200,000 eligible clinicians will participate in the QPP in 2018 via the A-APMs.
1) Quality – For 2018, CMS continues to require reporting on six measures, one of which must be an outcome measure or other high-priority measure. Should surgeons choose to report on more than six measures, CMS will use the six with the highest score for purposes of calculating their score for the Quality component. However, CMS did increase the percentage of patients on which reporting is required, aka the completeness threshold, in 2018 to 60%. Measures submitted that fall below the completeness threshold will receive one point. Small practices will receive three points for measures that fail to meet the completeness threshold. Multiple options remain available for submission of data, i.e., electronic health record (EHR), Medicare claims, a qualified registry or a qualified clinical data registry (QCDR). For 2018, the Quality component will make up 50% of the MIPS final score.
Cost
Those familiar with the 2017 version of MIPS will remember that the Cost component was weighted at zero for the first year of the program. CMS discussed, and indeed, initially proposed, to continue weighing cost at zero for 2018. However, because current law requires CMS to weigh cost at 30% beginning with the 2019 performance period, CMS finalized a 10% weight for cost in 2018 with the goal of making the impact of the transition in 2019 less dramatic. CMS will base its calculation of the cost component on the total per capita costs for all beneficiaries attributed to a provider and the Medicare Spending per Beneficiary measure for the entirety of the 2018 performance period. CMS intends to provide performance feedback on both measures by July 1, 2018. Surgeons are not required to submit data for purposes of cost component.
Advancing Care Information (ACI)
There are no major changes to the scoring policy for 2018 and all the applicable Base Score measures must still be reported in order to receive a score for the ACI component. The performance period requirement remains a minimum of 90 continuous days. For 2018, both 2014 Edition and 2015 Edition certified electronic health record technology (CEHRT) remain acceptable. However, those using only a 2015 Edition will be eligible for a 10% bonus. Regardless of edition used , bonus points are also available for reporting to a public health agency or clinical data registry and for the completion of an Improvement Activity (IA) using CEHRT. A significant hardship exemption remains available for those in small practices. As was the case in 2017, the ACI component represents 25% of the final score. However, as was also the case in 2017, one is not required to have an electronic health record to avoid a penalty in 2018.
Improvement Activities
The weight assigned to the IA component remains at 15%. CMS added 21 new IAs in the final rule, bringing the number of IA available from which to choose up to well over 110. CMS also made changes to 27 activities previously adopted. Reporting remains a simple attestation of participation in the activity for 90 continuous days. To receive full credit for the IA component, most surgeons will be required to attest to having participated in two, three, or four activities depending on whether the activities chosen are of medium value or high value. This is not a change. However, those in small or rural practices must only participate in one or two activities to receive full credit. It should be noted that for 2018, one will be able to avoid a penalty in 2020 solely by fulfillment of the requirements imposed by the Improvement Activities component.
As mentioned above, CMS estimates that only approximately 622,000 providers out of the 1.2 million eligible will be required to submit data under MIPS. Many providers are excluded from MIPS based on the low-volume threshold. For 2018, CMS set this threshold at less than or equal to $90,000 in Medicare Part B charges OR less than or equal to 200 Medicare Part B beneficiaries. The effect of this change, compared to the values set for 2017 low-volume threshold, is to exclude more providers from MIPS reporting.
Lastly, many will remember that for 2017, the performance threshold was set at three points, and thus, required only minimal reporting in either quality, ACI, or IA to avoid a penalty. It was expected that the threshold necessary to avoid a penalty for 2018 performance would be increased and indeed, CMS has set that value at 15. Those scoring above 15 will be eligible for a positive update in their Medicare payments in 2020, while those scoring below 15 will receive a penalty. Those who choose to not participate in 2018 will receive a 5% penalty in 2020. However, two points made above warrant reiteration:
a) By fully participating in the IA component, one can accrue the 15 points necessary to avoid a penalty.
b) An EHR is not required to avoid a penalty.
In the coming weeks, we will be updating the QPP website (www.facs.org/qpp) to reflect the changes in the program for 2018. New videos will be available as will be new electronic and print materials to assist Fellows to participate in the program.
Dr. Bailey is a pediatric surgeon and Medical Director, Advocacy, for the Division of Advocacy and Health Policy in the ACS offices in Washington, DC.
The interim final rule for the second year of Centers for Medicare and Medicaid Services (CMS) Quality Payment Program (QPP) was released on November 2, 2017. This rule will apply to performance and reporting for calendar year 2018 and impact payment in 2020. Below, I have highlighted a few of the key components of the 1,653-page rule with special attention to the Merit-based Incentive Payment System (MIPS).
To briefly review, there are two pathways for participation in the QPP, namely MIPS and the Advanced Alternative Payment Models (A-APMs). For 2018, we still expect that the majority of surgeons eligible to participate in the QPP will do so via the MIPS pathway. That said, and for reasons discussed below, CMS estimates that approximately half of the 1.2 million MIPS-eligible clinicians will be required to submit MIPS data in 2018. In addition, CMS estimates that approximately 200,000 eligible clinicians will participate in the QPP in 2018 via the A-APMs.
1) Quality – For 2018, CMS continues to require reporting on six measures, one of which must be an outcome measure or other high-priority measure. Should surgeons choose to report on more than six measures, CMS will use the six with the highest score for purposes of calculating their score for the Quality component. However, CMS did increase the percentage of patients on which reporting is required, aka the completeness threshold, in 2018 to 60%. Measures submitted that fall below the completeness threshold will receive one point. Small practices will receive three points for measures that fail to meet the completeness threshold. Multiple options remain available for submission of data, i.e., electronic health record (EHR), Medicare claims, a qualified registry or a qualified clinical data registry (QCDR). For 2018, the Quality component will make up 50% of the MIPS final score.
Cost
Those familiar with the 2017 version of MIPS will remember that the Cost component was weighted at zero for the first year of the program. CMS discussed, and indeed, initially proposed, to continue weighing cost at zero for 2018. However, because current law requires CMS to weigh cost at 30% beginning with the 2019 performance period, CMS finalized a 10% weight for cost in 2018 with the goal of making the impact of the transition in 2019 less dramatic. CMS will base its calculation of the cost component on the total per capita costs for all beneficiaries attributed to a provider and the Medicare Spending per Beneficiary measure for the entirety of the 2018 performance period. CMS intends to provide performance feedback on both measures by July 1, 2018. Surgeons are not required to submit data for purposes of cost component.
Advancing Care Information (ACI)
There are no major changes to the scoring policy for 2018 and all the applicable Base Score measures must still be reported in order to receive a score for the ACI component. The performance period requirement remains a minimum of 90 continuous days. For 2018, both 2014 Edition and 2015 Edition certified electronic health record technology (CEHRT) remain acceptable. However, those using only a 2015 Edition will be eligible for a 10% bonus. Regardless of edition used , bonus points are also available for reporting to a public health agency or clinical data registry and for the completion of an Improvement Activity (IA) using CEHRT. A significant hardship exemption remains available for those in small practices. As was the case in 2017, the ACI component represents 25% of the final score. However, as was also the case in 2017, one is not required to have an electronic health record to avoid a penalty in 2018.
Improvement Activities
The weight assigned to the IA component remains at 15%. CMS added 21 new IAs in the final rule, bringing the number of IA available from which to choose up to well over 110. CMS also made changes to 27 activities previously adopted. Reporting remains a simple attestation of participation in the activity for 90 continuous days. To receive full credit for the IA component, most surgeons will be required to attest to having participated in two, three, or four activities depending on whether the activities chosen are of medium value or high value. This is not a change. However, those in small or rural practices must only participate in one or two activities to receive full credit. It should be noted that for 2018, one will be able to avoid a penalty in 2020 solely by fulfillment of the requirements imposed by the Improvement Activities component.
As mentioned above, CMS estimates that only approximately 622,000 providers out of the 1.2 million eligible will be required to submit data under MIPS. Many providers are excluded from MIPS based on the low-volume threshold. For 2018, CMS set this threshold at less than or equal to $90,000 in Medicare Part B charges OR less than or equal to 200 Medicare Part B beneficiaries. The effect of this change, compared to the values set for 2017 low-volume threshold, is to exclude more providers from MIPS reporting.
Lastly, many will remember that for 2017, the performance threshold was set at three points, and thus, required only minimal reporting in either quality, ACI, or IA to avoid a penalty. It was expected that the threshold necessary to avoid a penalty for 2018 performance would be increased and indeed, CMS has set that value at 15. Those scoring above 15 will be eligible for a positive update in their Medicare payments in 2020, while those scoring below 15 will receive a penalty. Those who choose to not participate in 2018 will receive a 5% penalty in 2020. However, two points made above warrant reiteration:
a) By fully participating in the IA component, one can accrue the 15 points necessary to avoid a penalty.
b) An EHR is not required to avoid a penalty.
In the coming weeks, we will be updating the QPP website (www.facs.org/qpp) to reflect the changes in the program for 2018. New videos will be available as will be new electronic and print materials to assist Fellows to participate in the program.
Dr. Bailey is a pediatric surgeon and Medical Director, Advocacy, for the Division of Advocacy and Health Policy in the ACS offices in Washington, DC.
The interim final rule for the second year of Centers for Medicare and Medicaid Services (CMS) Quality Payment Program (QPP) was released on November 2, 2017. This rule will apply to performance and reporting for calendar year 2018 and impact payment in 2020. Below, I have highlighted a few of the key components of the 1,653-page rule with special attention to the Merit-based Incentive Payment System (MIPS).
To briefly review, there are two pathways for participation in the QPP, namely MIPS and the Advanced Alternative Payment Models (A-APMs). For 2018, we still expect that the majority of surgeons eligible to participate in the QPP will do so via the MIPS pathway. That said, and for reasons discussed below, CMS estimates that approximately half of the 1.2 million MIPS-eligible clinicians will be required to submit MIPS data in 2018. In addition, CMS estimates that approximately 200,000 eligible clinicians will participate in the QPP in 2018 via the A-APMs.
1) Quality – For 2018, CMS continues to require reporting on six measures, one of which must be an outcome measure or other high-priority measure. Should surgeons choose to report on more than six measures, CMS will use the six with the highest score for purposes of calculating their score for the Quality component. However, CMS did increase the percentage of patients on which reporting is required, aka the completeness threshold, in 2018 to 60%. Measures submitted that fall below the completeness threshold will receive one point. Small practices will receive three points for measures that fail to meet the completeness threshold. Multiple options remain available for submission of data, i.e., electronic health record (EHR), Medicare claims, a qualified registry or a qualified clinical data registry (QCDR). For 2018, the Quality component will make up 50% of the MIPS final score.
Cost
Those familiar with the 2017 version of MIPS will remember that the Cost component was weighted at zero for the first year of the program. CMS discussed, and indeed, initially proposed, to continue weighing cost at zero for 2018. However, because current law requires CMS to weigh cost at 30% beginning with the 2019 performance period, CMS finalized a 10% weight for cost in 2018 with the goal of making the impact of the transition in 2019 less dramatic. CMS will base its calculation of the cost component on the total per capita costs for all beneficiaries attributed to a provider and the Medicare Spending per Beneficiary measure for the entirety of the 2018 performance period. CMS intends to provide performance feedback on both measures by July 1, 2018. Surgeons are not required to submit data for purposes of cost component.
Advancing Care Information (ACI)
There are no major changes to the scoring policy for 2018 and all the applicable Base Score measures must still be reported in order to receive a score for the ACI component. The performance period requirement remains a minimum of 90 continuous days. For 2018, both 2014 Edition and 2015 Edition certified electronic health record technology (CEHRT) remain acceptable. However, those using only a 2015 Edition will be eligible for a 10% bonus. Regardless of edition used , bonus points are also available for reporting to a public health agency or clinical data registry and for the completion of an Improvement Activity (IA) using CEHRT. A significant hardship exemption remains available for those in small practices. As was the case in 2017, the ACI component represents 25% of the final score. However, as was also the case in 2017, one is not required to have an electronic health record to avoid a penalty in 2018.
Improvement Activities
The weight assigned to the IA component remains at 15%. CMS added 21 new IAs in the final rule, bringing the number of IA available from which to choose up to well over 110. CMS also made changes to 27 activities previously adopted. Reporting remains a simple attestation of participation in the activity for 90 continuous days. To receive full credit for the IA component, most surgeons will be required to attest to having participated in two, three, or four activities depending on whether the activities chosen are of medium value or high value. This is not a change. However, those in small or rural practices must only participate in one or two activities to receive full credit. It should be noted that for 2018, one will be able to avoid a penalty in 2020 solely by fulfillment of the requirements imposed by the Improvement Activities component.
As mentioned above, CMS estimates that only approximately 622,000 providers out of the 1.2 million eligible will be required to submit data under MIPS. Many providers are excluded from MIPS based on the low-volume threshold. For 2018, CMS set this threshold at less than or equal to $90,000 in Medicare Part B charges OR less than or equal to 200 Medicare Part B beneficiaries. The effect of this change, compared to the values set for 2017 low-volume threshold, is to exclude more providers from MIPS reporting.
Lastly, many will remember that for 2017, the performance threshold was set at three points, and thus, required only minimal reporting in either quality, ACI, or IA to avoid a penalty. It was expected that the threshold necessary to avoid a penalty for 2018 performance would be increased and indeed, CMS has set that value at 15. Those scoring above 15 will be eligible for a positive update in their Medicare payments in 2020, while those scoring below 15 will receive a penalty. Those who choose to not participate in 2018 will receive a 5% penalty in 2020. However, two points made above warrant reiteration:
a) By fully participating in the IA component, one can accrue the 15 points necessary to avoid a penalty.
b) An EHR is not required to avoid a penalty.
In the coming weeks, we will be updating the QPP website (www.facs.org/qpp) to reflect the changes in the program for 2018. New videos will be available as will be new electronic and print materials to assist Fellows to participate in the program.
Dr. Bailey is a pediatric surgeon and Medical Director, Advocacy, for the Division of Advocacy and Health Policy in the ACS offices in Washington, DC.
Two Antiamyloid Antibodies Will Undergo Further Study
BOSTON—Solanezumab and gantenerumab, both of which failed in phase III studies, will be examined in further trials at much higher doses, according to lectures presented at the 10th Edition of Clinical Trials on Alzheimer’s Disease.
Gantenerumab will be tested in two new phase III studies at a much higher dose than was used in the Scarlet Road and Marguerite Road studies, according to Gregory Klein, PhD, Principal Scientist and Biomarker Experimental Medicine Leader at Roche in Basel, Switzerland.
The Challenges of Antiamyloid Therapies
Solanezumab and gantenerumab are antiamyloid antibodies. In their prior trials, both effectively cleared amyloid plaques, but neither significantly improved cognition in patients with mild to moderate disease. Other studies of antiamyloid therapies have had similar results. Although these drugs stimulate several mechanisms of plaque removal, none has significantly improved thinking or memory.
Some investigators have questioned whether the drugs’ doses were high enough. Doses had been chosen with caution, partly because antiamyloid antibodies can cause amyloid-related imaging abnormalities (ARIA), an inflammatory response of brain edema or microhemorrhages. Concern over this side effect has decreased with the accumulation of more adverse-event data. Most cases of ARIA have been asymptomatic and resolved spontaneously. New open-label extension data from the Scarlet Road and Marguerite Road trials of gantenerumab, plus a new titration model, have increased confidence that patients will tolerate the antibody at subcutaneous doses as high as 1,200 mg.
Researchers also have examined the question of therapeutic timing. It is increasingly apparent that plaque eradication does not rescue cognition. It is possible that Alzheimer’s disease must be treated before amyloid and tau damage the hippocampus and neocortex.
After evaluating the failures of solanezumab and gantenerumab, researchers hypothesized that higher doses delivered earlier in the disease process might be effective, not at restoring lost cognition, but at preventing cognitive decline.
“One of the greatest advances in this field over the past 10 years is the recognition that Alzheimer’s disease is a continuum that likely begins well before the stage we recognize as dementia, and even before the stages of mild cognitive impairment [MCI] and prodromal Alzheimer’s [disease],” said Dr. Sperling. “Treating in the presymptomatic phase may be the best opportunity to bend this curve back toward the trajectory of normal aging.”
Other investigators hold that tau is the prime concern and the main cause of declines in memory and cognition. Tau is present in the brains of most people experiencing cognitively normal aging, but amyloid deposition may spur tau to spread into the neocortex. Preventing amyloid accumulation may prevent dementia not only by controlling amyloid levels, but also by removing a stimulus for the spread of tau.
Dr. Sperling cited unpublished data showing subtle cognitive decline in cognitively normal patients who have amyloid and tau in the brain. Although the cognitive scores were within the normal range, subjects with both proteins declined over two years on specific measures of memory and were more likely to progress to MCI.
“This [result] is striking to me and made me a little worried about the critical window of intervention,” she said. “What is also striking is that even though we restricted the eligibility criteria of A4 to those with normal memory and normal cognition, we do see that tau positivity at baseline is associated with lower baseline performance. Again, we have this suggestion that amyloid is associated with tau, and tau is associated with poor memory, even in normal people.”
A New Study of Solanezumab
Solanezumab’s failure in the series of EXPEDITION studies has prompted the modification of the A4 protocol. “We think solanezumab has an increased chance of success here [compared with the EXPEDITION trial] because we are employing it 10 to 15 years earlier in the disease. But we also want to maximize its chances.”
Thus, she said, investigators have decided to quadruple the dose administered in A4. Subjects will undergo titration from 600 mg to 800 mg for two months and then to 1,600 mg every four weeks. A safety cohort of 200 patients will be monitored for adverse events, especially hemorrhagic or edematous ARIA. “We are also extending the double-blind phase to 240 weeks, which allows everyone to dose-escalate and increases our power to detect small effect sizes,” said Dr. Sperling.
So far, 1,151 patients have been recruited into the study. Dr. Sperling expects the full 1,200-subject cohort to be randomized by the end of 2017.
Gantenerumab May Reduce Amyloid Burden
Gantenerumab will be examined in further trials, following investigators’ analyses of open-label extension data from the Scarlet Road and Marguerite Road studies, said Dr. Klein. Patients in these studies were randomized to either 105 mg or 225 mg of the antibody. Researchers observed no significant cognitive benefits of therapy, but noted trends toward improvement with the higher dose, as well as dose-dependent plaque clearance. These results encouraged researchers to examine higher doses in 52-week open-label extensions of each study.
Dr. Klein presented new imaging data for these studies. In both studies combined, 40 patients were maintained for six to nine months on the highest doses (ie, from 900 mg to 1,200 mg). Of these participants, 17 had almost total clearance of their amyloid burden. Their scans, Dr. Klein said, appear to show traces of amyloid or to be amyloid-negative. The effect was consistent, regardless of the amount of amyloid at baseline. “These are encouraging biomarker data,” he said. “We are going into our new phase III studies, Graduate I and II, optimistic.”
According to a Roche press release, these studies will target patients with prodromal to mild disease at the higher doses. Emails to Roche and its German partner, MorphoSys, were not returned by press time. Dr. Klein’s comments suggest that studies of gantenerumab will continue.
—Michele G. Sullivan
BOSTON—Solanezumab and gantenerumab, both of which failed in phase III studies, will be examined in further trials at much higher doses, according to lectures presented at the 10th Edition of Clinical Trials on Alzheimer’s Disease.
Gantenerumab will be tested in two new phase III studies at a much higher dose than was used in the Scarlet Road and Marguerite Road studies, according to Gregory Klein, PhD, Principal Scientist and Biomarker Experimental Medicine Leader at Roche in Basel, Switzerland.
The Challenges of Antiamyloid Therapies
Solanezumab and gantenerumab are antiamyloid antibodies. In their prior trials, both effectively cleared amyloid plaques, but neither significantly improved cognition in patients with mild to moderate disease. Other studies of antiamyloid therapies have had similar results. Although these drugs stimulate several mechanisms of plaque removal, none has significantly improved thinking or memory.
Some investigators have questioned whether the drugs’ doses were high enough. Doses had been chosen with caution, partly because antiamyloid antibodies can cause amyloid-related imaging abnormalities (ARIA), an inflammatory response of brain edema or microhemorrhages. Concern over this side effect has decreased with the accumulation of more adverse-event data. Most cases of ARIA have been asymptomatic and resolved spontaneously. New open-label extension data from the Scarlet Road and Marguerite Road trials of gantenerumab, plus a new titration model, have increased confidence that patients will tolerate the antibody at subcutaneous doses as high as 1,200 mg.
Researchers also have examined the question of therapeutic timing. It is increasingly apparent that plaque eradication does not rescue cognition. It is possible that Alzheimer’s disease must be treated before amyloid and tau damage the hippocampus and neocortex.
After evaluating the failures of solanezumab and gantenerumab, researchers hypothesized that higher doses delivered earlier in the disease process might be effective, not at restoring lost cognition, but at preventing cognitive decline.
“One of the greatest advances in this field over the past 10 years is the recognition that Alzheimer’s disease is a continuum that likely begins well before the stage we recognize as dementia, and even before the stages of mild cognitive impairment [MCI] and prodromal Alzheimer’s [disease],” said Dr. Sperling. “Treating in the presymptomatic phase may be the best opportunity to bend this curve back toward the trajectory of normal aging.”
Other investigators hold that tau is the prime concern and the main cause of declines in memory and cognition. Tau is present in the brains of most people experiencing cognitively normal aging, but amyloid deposition may spur tau to spread into the neocortex. Preventing amyloid accumulation may prevent dementia not only by controlling amyloid levels, but also by removing a stimulus for the spread of tau.
Dr. Sperling cited unpublished data showing subtle cognitive decline in cognitively normal patients who have amyloid and tau in the brain. Although the cognitive scores were within the normal range, subjects with both proteins declined over two years on specific measures of memory and were more likely to progress to MCI.
“This [result] is striking to me and made me a little worried about the critical window of intervention,” she said. “What is also striking is that even though we restricted the eligibility criteria of A4 to those with normal memory and normal cognition, we do see that tau positivity at baseline is associated with lower baseline performance. Again, we have this suggestion that amyloid is associated with tau, and tau is associated with poor memory, even in normal people.”
A New Study of Solanezumab
Solanezumab’s failure in the series of EXPEDITION studies has prompted the modification of the A4 protocol. “We think solanezumab has an increased chance of success here [compared with the EXPEDITION trial] because we are employing it 10 to 15 years earlier in the disease. But we also want to maximize its chances.”
Thus, she said, investigators have decided to quadruple the dose administered in A4. Subjects will undergo titration from 600 mg to 800 mg for two months and then to 1,600 mg every four weeks. A safety cohort of 200 patients will be monitored for adverse events, especially hemorrhagic or edematous ARIA. “We are also extending the double-blind phase to 240 weeks, which allows everyone to dose-escalate and increases our power to detect small effect sizes,” said Dr. Sperling.
So far, 1,151 patients have been recruited into the study. Dr. Sperling expects the full 1,200-subject cohort to be randomized by the end of 2017.
Gantenerumab May Reduce Amyloid Burden
Gantenerumab will be examined in further trials, following investigators’ analyses of open-label extension data from the Scarlet Road and Marguerite Road studies, said Dr. Klein. Patients in these studies were randomized to either 105 mg or 225 mg of the antibody. Researchers observed no significant cognitive benefits of therapy, but noted trends toward improvement with the higher dose, as well as dose-dependent plaque clearance. These results encouraged researchers to examine higher doses in 52-week open-label extensions of each study.
Dr. Klein presented new imaging data for these studies. In both studies combined, 40 patients were maintained for six to nine months on the highest doses (ie, from 900 mg to 1,200 mg). Of these participants, 17 had almost total clearance of their amyloid burden. Their scans, Dr. Klein said, appear to show traces of amyloid or to be amyloid-negative. The effect was consistent, regardless of the amount of amyloid at baseline. “These are encouraging biomarker data,” he said. “We are going into our new phase III studies, Graduate I and II, optimistic.”
According to a Roche press release, these studies will target patients with prodromal to mild disease at the higher doses. Emails to Roche and its German partner, MorphoSys, were not returned by press time. Dr. Klein’s comments suggest that studies of gantenerumab will continue.
—Michele G. Sullivan
BOSTON—Solanezumab and gantenerumab, both of which failed in phase III studies, will be examined in further trials at much higher doses, according to lectures presented at the 10th Edition of Clinical Trials on Alzheimer’s Disease.
Gantenerumab will be tested in two new phase III studies at a much higher dose than was used in the Scarlet Road and Marguerite Road studies, according to Gregory Klein, PhD, Principal Scientist and Biomarker Experimental Medicine Leader at Roche in Basel, Switzerland.
The Challenges of Antiamyloid Therapies
Solanezumab and gantenerumab are antiamyloid antibodies. In their prior trials, both effectively cleared amyloid plaques, but neither significantly improved cognition in patients with mild to moderate disease. Other studies of antiamyloid therapies have had similar results. Although these drugs stimulate several mechanisms of plaque removal, none has significantly improved thinking or memory.
Some investigators have questioned whether the drugs’ doses were high enough. Doses had been chosen with caution, partly because antiamyloid antibodies can cause amyloid-related imaging abnormalities (ARIA), an inflammatory response of brain edema or microhemorrhages. Concern over this side effect has decreased with the accumulation of more adverse-event data. Most cases of ARIA have been asymptomatic and resolved spontaneously. New open-label extension data from the Scarlet Road and Marguerite Road trials of gantenerumab, plus a new titration model, have increased confidence that patients will tolerate the antibody at subcutaneous doses as high as 1,200 mg.
Researchers also have examined the question of therapeutic timing. It is increasingly apparent that plaque eradication does not rescue cognition. It is possible that Alzheimer’s disease must be treated before amyloid and tau damage the hippocampus and neocortex.
After evaluating the failures of solanezumab and gantenerumab, researchers hypothesized that higher doses delivered earlier in the disease process might be effective, not at restoring lost cognition, but at preventing cognitive decline.
“One of the greatest advances in this field over the past 10 years is the recognition that Alzheimer’s disease is a continuum that likely begins well before the stage we recognize as dementia, and even before the stages of mild cognitive impairment [MCI] and prodromal Alzheimer’s [disease],” said Dr. Sperling. “Treating in the presymptomatic phase may be the best opportunity to bend this curve back toward the trajectory of normal aging.”
Other investigators hold that tau is the prime concern and the main cause of declines in memory and cognition. Tau is present in the brains of most people experiencing cognitively normal aging, but amyloid deposition may spur tau to spread into the neocortex. Preventing amyloid accumulation may prevent dementia not only by controlling amyloid levels, but also by removing a stimulus for the spread of tau.
Dr. Sperling cited unpublished data showing subtle cognitive decline in cognitively normal patients who have amyloid and tau in the brain. Although the cognitive scores were within the normal range, subjects with both proteins declined over two years on specific measures of memory and were more likely to progress to MCI.
“This [result] is striking to me and made me a little worried about the critical window of intervention,” she said. “What is also striking is that even though we restricted the eligibility criteria of A4 to those with normal memory and normal cognition, we do see that tau positivity at baseline is associated with lower baseline performance. Again, we have this suggestion that amyloid is associated with tau, and tau is associated with poor memory, even in normal people.”
A New Study of Solanezumab
Solanezumab’s failure in the series of EXPEDITION studies has prompted the modification of the A4 protocol. “We think solanezumab has an increased chance of success here [compared with the EXPEDITION trial] because we are employing it 10 to 15 years earlier in the disease. But we also want to maximize its chances.”
Thus, she said, investigators have decided to quadruple the dose administered in A4. Subjects will undergo titration from 600 mg to 800 mg for two months and then to 1,600 mg every four weeks. A safety cohort of 200 patients will be monitored for adverse events, especially hemorrhagic or edematous ARIA. “We are also extending the double-blind phase to 240 weeks, which allows everyone to dose-escalate and increases our power to detect small effect sizes,” said Dr. Sperling.
So far, 1,151 patients have been recruited into the study. Dr. Sperling expects the full 1,200-subject cohort to be randomized by the end of 2017.
Gantenerumab May Reduce Amyloid Burden
Gantenerumab will be examined in further trials, following investigators’ analyses of open-label extension data from the Scarlet Road and Marguerite Road studies, said Dr. Klein. Patients in these studies were randomized to either 105 mg or 225 mg of the antibody. Researchers observed no significant cognitive benefits of therapy, but noted trends toward improvement with the higher dose, as well as dose-dependent plaque clearance. These results encouraged researchers to examine higher doses in 52-week open-label extensions of each study.
Dr. Klein presented new imaging data for these studies. In both studies combined, 40 patients were maintained for six to nine months on the highest doses (ie, from 900 mg to 1,200 mg). Of these participants, 17 had almost total clearance of their amyloid burden. Their scans, Dr. Klein said, appear to show traces of amyloid or to be amyloid-negative. The effect was consistent, regardless of the amount of amyloid at baseline. “These are encouraging biomarker data,” he said. “We are going into our new phase III studies, Graduate I and II, optimistic.”
According to a Roche press release, these studies will target patients with prodromal to mild disease at the higher doses. Emails to Roche and its German partner, MorphoSys, were not returned by press time. Dr. Klein’s comments suggest that studies of gantenerumab will continue.
—Michele G. Sullivan
Bilateral ACP shown similar to unilateral in arch replacement study
What may be the largest study comparing unilateral and bilateral antegrade cerebral perfusion during total arch replacement for type A aortic dissection has reported that outcomes between the two approaches are comparable, although the bilateral approach showed some advantages during the operation itself, investigators from China reported in the Journal of Thoracic and Cardiovascular Surgery (2017;154:767-75).
The effectiveness of bilateral antegrade cerebral perfusion (b-ACP) vs. unilateral antegrade cerebral perfusion (u-ACP) has been the focus of extensive debate, lead study author Guang Tong, MD, of the Guangzhou (China) General Hospital, and coauthors said. They compared outcomes in six different metrics, ranging from cardiopulmonary bypass time to length of stay (LOS) in the ICU and hospital, in 203 patients with type A aortic dissection who had total aortic arch replacement with hypothermic circulatory arrest over an 8-year period ending in August 2014; 121 had b-ACP and 82 had u-ACP. “The issue of u-ACP vs. b-ACP has been examined in aortic arch surgery, but few reports have focused on type A aortic dissection,” Dr. Tong and coauthors wrote.
They acknowledged that some surgeons are reluctant to use b-ACP because of its complexity, but their study found no increase in cross-clamp time, cardiopulmonary bypass time, or surgery time in the b-ACP group. They cited another reason surgeons give for avoiding b-ACP: the risk of embolic injury caused by canulating the left common carotid artery in an atheromatous aorta. “In the present study, this risk was avoided by attaching the left common carotid artery to the four-branched prosthetic graft for left hemisphere perfusion,” Dr. Tong and coauthors wrote.
Key outcomes that the researchers found not statistically significant were:
- Overall 30-day mortality (11.6% for b-ACP vs. 20.7% for u-ACP; P = .075).
- Prevalence of postoperative permanent neurologic dysfunction (8.4% vs. 16.9%; P = .091).
- Average ICU LOS (16 ± 17.75 days vs. 17 ± 11.5 days, P =.454).
- Average hospital LOS (26.5 ± 20.6 days vs. 24.8 ± 10.3 days, P = .434).
However, average ventilation time was lower in the b-ACP group (95.5 hours vs. 147 hours; P less than or equal to.001).
Dr. Tong and coauthors used an aggressive approach, as advocated by Dhaval Trivedi, MD, and colleagues (Ann Thorac Surg. 2016;101:896-903), and had a total arch replacement rate of 57.8%. This rate is higher than most published series in the west but comparable to other studies from China, perhaps because of the relatively young age of this study cohort – an average age of 51 years – compared to data sets other studies have used. Dr. Tong and coauthors used a b-ACP strategy that established both cerebral perfusion routes before circulatory arrest.
Rates of the following complications were also not significantly different across the study population: paraplegia (2.8% for b-ACP vs. 3.1% for u-ACP), temporary neurologic dysfunction (4.7% vs. 9.2%), permanent neurologic dysfunction (8.4% vs. 16.9%), renal failure (18% vs. 23.1%), reoperation for bleeding (2.8% vs. 4.6%), and mediastinal infection (3.7% vs. 6.2%).
While b-ACP patients did not have a statistically significant lower incidence of TND, Dr. Tong and coauthors noted the shorter time on ventilation and significantly lower tracheostomy rates for the b-ACP patients, 3.7% vs. 16.9% for the u-ACP group (P = .003). “In our institute, protocols to wean patients from ventilation were normally initiated as soon as consciousness was regained,” Dr. Tong and coauthors wrote.
Among the study limits Dr. Tong and coauthors acknowledged were its retrospective, nonrandomized, single-center nature, and the fact that the surgeries were performed over an 8-year period representing different eras.
The investigators reported having no relevant financial disclosures.
The study by Dr. Tong and coauthors adds to the discussion between the “bilateralists” and “unilateralists,” as Jean Bachet, MD, called the two prevailing camps on cerebral perfusion strategies in his invited commentary (J Thorac Cardiovasc Surg. 2017;154:765-6). And while most clinical reports find outcomes similar between the two approaches, the evidence favors the bilateral approach for total arch replacement.
Citing how the study implied mortality and neurologic morbidity rates almost half those for unilateral perfusion, but not reaching statistical significance, Dr. Bachet said, “The statisticians would say that this is only a trend and no proof, but some trends might be indicative, and significance might only be a matter of number in each arm of the comparison.”
Dr. Bachet raised a question about the unilateral approach – that once the arch is opened it takes a minute or so to insert the small balloon canula into the origin of the left carotid artery or divided vessel and start bilateral perfusion. “A major question arises,” said Dr. Bachet: “Why should we expose our patients to any undue risk just to avoid a simple maneuver, to spare a little time, or for any other fancy and questionable reason?”
Cardiologists have raised that question for more than 20 years. Said Dr. Bachet, “We still wait for the answer.”
Dr. Bachet is a cardiac surgeon in Surgenes, France. He reported having no financial relationships to disclose.
The study by Dr. Tong and coauthors adds to the discussion between the “bilateralists” and “unilateralists,” as Jean Bachet, MD, called the two prevailing camps on cerebral perfusion strategies in his invited commentary (J Thorac Cardiovasc Surg. 2017;154:765-6). And while most clinical reports find outcomes similar between the two approaches, the evidence favors the bilateral approach for total arch replacement.
Citing how the study implied mortality and neurologic morbidity rates almost half those for unilateral perfusion, but not reaching statistical significance, Dr. Bachet said, “The statisticians would say that this is only a trend and no proof, but some trends might be indicative, and significance might only be a matter of number in each arm of the comparison.”
Dr. Bachet raised a question about the unilateral approach – that once the arch is opened it takes a minute or so to insert the small balloon canula into the origin of the left carotid artery or divided vessel and start bilateral perfusion. “A major question arises,” said Dr. Bachet: “Why should we expose our patients to any undue risk just to avoid a simple maneuver, to spare a little time, or for any other fancy and questionable reason?”
Cardiologists have raised that question for more than 20 years. Said Dr. Bachet, “We still wait for the answer.”
Dr. Bachet is a cardiac surgeon in Surgenes, France. He reported having no financial relationships to disclose.
The study by Dr. Tong and coauthors adds to the discussion between the “bilateralists” and “unilateralists,” as Jean Bachet, MD, called the two prevailing camps on cerebral perfusion strategies in his invited commentary (J Thorac Cardiovasc Surg. 2017;154:765-6). And while most clinical reports find outcomes similar between the two approaches, the evidence favors the bilateral approach for total arch replacement.
Citing how the study implied mortality and neurologic morbidity rates almost half those for unilateral perfusion, but not reaching statistical significance, Dr. Bachet said, “The statisticians would say that this is only a trend and no proof, but some trends might be indicative, and significance might only be a matter of number in each arm of the comparison.”
Dr. Bachet raised a question about the unilateral approach – that once the arch is opened it takes a minute or so to insert the small balloon canula into the origin of the left carotid artery or divided vessel and start bilateral perfusion. “A major question arises,” said Dr. Bachet: “Why should we expose our patients to any undue risk just to avoid a simple maneuver, to spare a little time, or for any other fancy and questionable reason?”
Cardiologists have raised that question for more than 20 years. Said Dr. Bachet, “We still wait for the answer.”
Dr. Bachet is a cardiac surgeon in Surgenes, France. He reported having no financial relationships to disclose.
What may be the largest study comparing unilateral and bilateral antegrade cerebral perfusion during total arch replacement for type A aortic dissection has reported that outcomes between the two approaches are comparable, although the bilateral approach showed some advantages during the operation itself, investigators from China reported in the Journal of Thoracic and Cardiovascular Surgery (2017;154:767-75).
The effectiveness of bilateral antegrade cerebral perfusion (b-ACP) vs. unilateral antegrade cerebral perfusion (u-ACP) has been the focus of extensive debate, lead study author Guang Tong, MD, of the Guangzhou (China) General Hospital, and coauthors said. They compared outcomes in six different metrics, ranging from cardiopulmonary bypass time to length of stay (LOS) in the ICU and hospital, in 203 patients with type A aortic dissection who had total aortic arch replacement with hypothermic circulatory arrest over an 8-year period ending in August 2014; 121 had b-ACP and 82 had u-ACP. “The issue of u-ACP vs. b-ACP has been examined in aortic arch surgery, but few reports have focused on type A aortic dissection,” Dr. Tong and coauthors wrote.
They acknowledged that some surgeons are reluctant to use b-ACP because of its complexity, but their study found no increase in cross-clamp time, cardiopulmonary bypass time, or surgery time in the b-ACP group. They cited another reason surgeons give for avoiding b-ACP: the risk of embolic injury caused by canulating the left common carotid artery in an atheromatous aorta. “In the present study, this risk was avoided by attaching the left common carotid artery to the four-branched prosthetic graft for left hemisphere perfusion,” Dr. Tong and coauthors wrote.
Key outcomes that the researchers found not statistically significant were:
- Overall 30-day mortality (11.6% for b-ACP vs. 20.7% for u-ACP; P = .075).
- Prevalence of postoperative permanent neurologic dysfunction (8.4% vs. 16.9%; P = .091).
- Average ICU LOS (16 ± 17.75 days vs. 17 ± 11.5 days, P =.454).
- Average hospital LOS (26.5 ± 20.6 days vs. 24.8 ± 10.3 days, P = .434).
However, average ventilation time was lower in the b-ACP group (95.5 hours vs. 147 hours; P less than or equal to.001).
Dr. Tong and coauthors used an aggressive approach, as advocated by Dhaval Trivedi, MD, and colleagues (Ann Thorac Surg. 2016;101:896-903), and had a total arch replacement rate of 57.8%. This rate is higher than most published series in the west but comparable to other studies from China, perhaps because of the relatively young age of this study cohort – an average age of 51 years – compared to data sets other studies have used. Dr. Tong and coauthors used a b-ACP strategy that established both cerebral perfusion routes before circulatory arrest.
Rates of the following complications were also not significantly different across the study population: paraplegia (2.8% for b-ACP vs. 3.1% for u-ACP), temporary neurologic dysfunction (4.7% vs. 9.2%), permanent neurologic dysfunction (8.4% vs. 16.9%), renal failure (18% vs. 23.1%), reoperation for bleeding (2.8% vs. 4.6%), and mediastinal infection (3.7% vs. 6.2%).
While b-ACP patients did not have a statistically significant lower incidence of TND, Dr. Tong and coauthors noted the shorter time on ventilation and significantly lower tracheostomy rates for the b-ACP patients, 3.7% vs. 16.9% for the u-ACP group (P = .003). “In our institute, protocols to wean patients from ventilation were normally initiated as soon as consciousness was regained,” Dr. Tong and coauthors wrote.
Among the study limits Dr. Tong and coauthors acknowledged were its retrospective, nonrandomized, single-center nature, and the fact that the surgeries were performed over an 8-year period representing different eras.
The investigators reported having no relevant financial disclosures.
What may be the largest study comparing unilateral and bilateral antegrade cerebral perfusion during total arch replacement for type A aortic dissection has reported that outcomes between the two approaches are comparable, although the bilateral approach showed some advantages during the operation itself, investigators from China reported in the Journal of Thoracic and Cardiovascular Surgery (2017;154:767-75).
The effectiveness of bilateral antegrade cerebral perfusion (b-ACP) vs. unilateral antegrade cerebral perfusion (u-ACP) has been the focus of extensive debate, lead study author Guang Tong, MD, of the Guangzhou (China) General Hospital, and coauthors said. They compared outcomes in six different metrics, ranging from cardiopulmonary bypass time to length of stay (LOS) in the ICU and hospital, in 203 patients with type A aortic dissection who had total aortic arch replacement with hypothermic circulatory arrest over an 8-year period ending in August 2014; 121 had b-ACP and 82 had u-ACP. “The issue of u-ACP vs. b-ACP has been examined in aortic arch surgery, but few reports have focused on type A aortic dissection,” Dr. Tong and coauthors wrote.
They acknowledged that some surgeons are reluctant to use b-ACP because of its complexity, but their study found no increase in cross-clamp time, cardiopulmonary bypass time, or surgery time in the b-ACP group. They cited another reason surgeons give for avoiding b-ACP: the risk of embolic injury caused by canulating the left common carotid artery in an atheromatous aorta. “In the present study, this risk was avoided by attaching the left common carotid artery to the four-branched prosthetic graft for left hemisphere perfusion,” Dr. Tong and coauthors wrote.
Key outcomes that the researchers found not statistically significant were:
- Overall 30-day mortality (11.6% for b-ACP vs. 20.7% for u-ACP; P = .075).
- Prevalence of postoperative permanent neurologic dysfunction (8.4% vs. 16.9%; P = .091).
- Average ICU LOS (16 ± 17.75 days vs. 17 ± 11.5 days, P =.454).
- Average hospital LOS (26.5 ± 20.6 days vs. 24.8 ± 10.3 days, P = .434).
However, average ventilation time was lower in the b-ACP group (95.5 hours vs. 147 hours; P less than or equal to.001).
Dr. Tong and coauthors used an aggressive approach, as advocated by Dhaval Trivedi, MD, and colleagues (Ann Thorac Surg. 2016;101:896-903), and had a total arch replacement rate of 57.8%. This rate is higher than most published series in the west but comparable to other studies from China, perhaps because of the relatively young age of this study cohort – an average age of 51 years – compared to data sets other studies have used. Dr. Tong and coauthors used a b-ACP strategy that established both cerebral perfusion routes before circulatory arrest.
Rates of the following complications were also not significantly different across the study population: paraplegia (2.8% for b-ACP vs. 3.1% for u-ACP), temporary neurologic dysfunction (4.7% vs. 9.2%), permanent neurologic dysfunction (8.4% vs. 16.9%), renal failure (18% vs. 23.1%), reoperation for bleeding (2.8% vs. 4.6%), and mediastinal infection (3.7% vs. 6.2%).
While b-ACP patients did not have a statistically significant lower incidence of TND, Dr. Tong and coauthors noted the shorter time on ventilation and significantly lower tracheostomy rates for the b-ACP patients, 3.7% vs. 16.9% for the u-ACP group (P = .003). “In our institute, protocols to wean patients from ventilation were normally initiated as soon as consciousness was regained,” Dr. Tong and coauthors wrote.
Among the study limits Dr. Tong and coauthors acknowledged were its retrospective, nonrandomized, single-center nature, and the fact that the surgeries were performed over an 8-year period representing different eras.
The investigators reported having no relevant financial disclosures.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Clinical outcomes were comparable between groups who underwent unilateral or bilateral antegrade cerebral perfusion in total arch replacement for type A aortic dissection.
Major finding: Overall 30-day mortality was 11.6% in the bilateral ACP group vs. 20.7% for unilateral ACP (P =.075).
Data source: Population of 203 patients who had aortic arch replacement surgery for type A aortic dissection between September 2006 and August 2014.
Disclosures: Dr. Tong and coauthors reported having no relevant financial disclosures.
Kidney transplant for GPA boosts survival
SAN DIEGO – Receiving a kidney transplant increased the likelihood of survival in patients with end-stage renal disease (ESRD) due to granulomatosis with polyangiitis, a study showed.
“We found that there was a huge survival advantage of having a renal transplant,” lead author Zachary S. Wallace, MD, MS, of Harvard Medical School, Boston, said in an interview. “In addition, this improvement in survival seems to be due to a dramatic reduction in death due to cardiovascular disease.”
An estimated 25% of patients with GPA develop ESRD, according to Dr. Wallace, who also works at the vasculitis and glomerulonephritis center at Massachusetts General Hospital, Boston. “GPA and ANCA [antineutrophil cytoplasmic autoantibody]–associated vasculitis in general have a propensity to affect the kidneys, and the reason for that is not entirely known,” he said during the interview. “In the kidney, it most commonly causes a rapidly progressive glomerulonephritis which can cause irreversible renal failure if not aggressively treated.”
Dr. Wallace and his colleagues launched their study to better understand the impact of kidney transplants. “We know that patients with ESRD from more common causes – such as diabetes and hypertension – benefit in terms of survival and quality of life from transplantation,” he said in the interview. “It was unknown if GPA patients similarly benefit. Often, GPA patients have fewer comorbidities than patients with ESRD due to diabetes or hypertension. Since they may be relatively healthier, one might wonder if the survival benefit would be as great in ESRD patients with GPA.”
Dr. Wallace and his colleagues tracked 2,471 cases of ESRD due to GPA from the U.S. Renal Data System. All were wait-listed for a kidney transplant from 1995 to 2014, and the researchers tracked them as late as Jan. 1, 2016. Of the patients studied, 946 received a transplant. The study’s participants tended to be male (59%) and white (86-87%), and they rarely had comorbidities outside of diabetes (64-67%).
There were 438 deaths in the entire group. Those who received transplants were much less likely to die than those who didn’t (adjusted hazard ratio, 0.30; 95% confidence interval, 0.25-0.37; P less than .001), he reported at the annual meeting of the American College of Rheumatology.
Also, those who received transplants were much less likely than those who didn’t to die of cardiovascular disease (adjusted HR, 0.13; 95% CI, 0.08-0.22; P less than .001) and infection (adjusted HR, 0.61; 95% CI, 0.34-1.08; P = .09). There was no statistically significant difference between the groups in terms of deaths from cancer.
“The improvement in survival seems to be due to a dramatic reduction in death due to cardiovascular disease,” Dr. Wallace said in the interview. “While cardiovascular disease is a common cause of death in GPA and ESRD due to other causes, this was not known specifically in patients with ESRD due to GPA.”
The findings provide the following messages to rheumatologists: Renal transplantation in patients with ESRD due to GPA offers a significant survival benefit, and it is important to refer patients early to a renal transplant center, he noted.
“[Rheumatologists] should work closely with primary care physicians and nephrologists to make sure that the patient’s cardiovascular disease risk is being assessed – checking lipids, A1c, etc. – and addressed as necessary,” Dr. Wallace added.
The study authors reported no relevant financial disclosures. Funding included support from the Rheumatology Research Foundation, the Executive Committee on Research at Massachusetts General, and the National Institutes of Health Loan Repayment Program.
SAN DIEGO – Receiving a kidney transplant increased the likelihood of survival in patients with end-stage renal disease (ESRD) due to granulomatosis with polyangiitis, a study showed.
“We found that there was a huge survival advantage of having a renal transplant,” lead author Zachary S. Wallace, MD, MS, of Harvard Medical School, Boston, said in an interview. “In addition, this improvement in survival seems to be due to a dramatic reduction in death due to cardiovascular disease.”
An estimated 25% of patients with GPA develop ESRD, according to Dr. Wallace, who also works at the vasculitis and glomerulonephritis center at Massachusetts General Hospital, Boston. “GPA and ANCA [antineutrophil cytoplasmic autoantibody]–associated vasculitis in general have a propensity to affect the kidneys, and the reason for that is not entirely known,” he said during the interview. “In the kidney, it most commonly causes a rapidly progressive glomerulonephritis which can cause irreversible renal failure if not aggressively treated.”
Dr. Wallace and his colleagues launched their study to better understand the impact of kidney transplants. “We know that patients with ESRD from more common causes – such as diabetes and hypertension – benefit in terms of survival and quality of life from transplantation,” he said in the interview. “It was unknown if GPA patients similarly benefit. Often, GPA patients have fewer comorbidities than patients with ESRD due to diabetes or hypertension. Since they may be relatively healthier, one might wonder if the survival benefit would be as great in ESRD patients with GPA.”
Dr. Wallace and his colleagues tracked 2,471 cases of ESRD due to GPA from the U.S. Renal Data System. All were wait-listed for a kidney transplant from 1995 to 2014, and the researchers tracked them as late as Jan. 1, 2016. Of the patients studied, 946 received a transplant. The study’s participants tended to be male (59%) and white (86-87%), and they rarely had comorbidities outside of diabetes (64-67%).
There were 438 deaths in the entire group. Those who received transplants were much less likely to die than those who didn’t (adjusted hazard ratio, 0.30; 95% confidence interval, 0.25-0.37; P less than .001), he reported at the annual meeting of the American College of Rheumatology.
Also, those who received transplants were much less likely than those who didn’t to die of cardiovascular disease (adjusted HR, 0.13; 95% CI, 0.08-0.22; P less than .001) and infection (adjusted HR, 0.61; 95% CI, 0.34-1.08; P = .09). There was no statistically significant difference between the groups in terms of deaths from cancer.
“The improvement in survival seems to be due to a dramatic reduction in death due to cardiovascular disease,” Dr. Wallace said in the interview. “While cardiovascular disease is a common cause of death in GPA and ESRD due to other causes, this was not known specifically in patients with ESRD due to GPA.”
The findings provide the following messages to rheumatologists: Renal transplantation in patients with ESRD due to GPA offers a significant survival benefit, and it is important to refer patients early to a renal transplant center, he noted.
“[Rheumatologists] should work closely with primary care physicians and nephrologists to make sure that the patient’s cardiovascular disease risk is being assessed – checking lipids, A1c, etc. – and addressed as necessary,” Dr. Wallace added.
The study authors reported no relevant financial disclosures. Funding included support from the Rheumatology Research Foundation, the Executive Committee on Research at Massachusetts General, and the National Institutes of Health Loan Repayment Program.
SAN DIEGO – Receiving a kidney transplant increased the likelihood of survival in patients with end-stage renal disease (ESRD) due to granulomatosis with polyangiitis, a study showed.
“We found that there was a huge survival advantage of having a renal transplant,” lead author Zachary S. Wallace, MD, MS, of Harvard Medical School, Boston, said in an interview. “In addition, this improvement in survival seems to be due to a dramatic reduction in death due to cardiovascular disease.”
An estimated 25% of patients with GPA develop ESRD, according to Dr. Wallace, who also works at the vasculitis and glomerulonephritis center at Massachusetts General Hospital, Boston. “GPA and ANCA [antineutrophil cytoplasmic autoantibody]–associated vasculitis in general have a propensity to affect the kidneys, and the reason for that is not entirely known,” he said during the interview. “In the kidney, it most commonly causes a rapidly progressive glomerulonephritis which can cause irreversible renal failure if not aggressively treated.”
Dr. Wallace and his colleagues launched their study to better understand the impact of kidney transplants. “We know that patients with ESRD from more common causes – such as diabetes and hypertension – benefit in terms of survival and quality of life from transplantation,” he said in the interview. “It was unknown if GPA patients similarly benefit. Often, GPA patients have fewer comorbidities than patients with ESRD due to diabetes or hypertension. Since they may be relatively healthier, one might wonder if the survival benefit would be as great in ESRD patients with GPA.”
Dr. Wallace and his colleagues tracked 2,471 cases of ESRD due to GPA from the U.S. Renal Data System. All were wait-listed for a kidney transplant from 1995 to 2014, and the researchers tracked them as late as Jan. 1, 2016. Of the patients studied, 946 received a transplant. The study’s participants tended to be male (59%) and white (86-87%), and they rarely had comorbidities outside of diabetes (64-67%).
There were 438 deaths in the entire group. Those who received transplants were much less likely to die than those who didn’t (adjusted hazard ratio, 0.30; 95% confidence interval, 0.25-0.37; P less than .001), he reported at the annual meeting of the American College of Rheumatology.
Also, those who received transplants were much less likely than those who didn’t to die of cardiovascular disease (adjusted HR, 0.13; 95% CI, 0.08-0.22; P less than .001) and infection (adjusted HR, 0.61; 95% CI, 0.34-1.08; P = .09). There was no statistically significant difference between the groups in terms of deaths from cancer.
“The improvement in survival seems to be due to a dramatic reduction in death due to cardiovascular disease,” Dr. Wallace said in the interview. “While cardiovascular disease is a common cause of death in GPA and ESRD due to other causes, this was not known specifically in patients with ESRD due to GPA.”
The findings provide the following messages to rheumatologists: Renal transplantation in patients with ESRD due to GPA offers a significant survival benefit, and it is important to refer patients early to a renal transplant center, he noted.
“[Rheumatologists] should work closely with primary care physicians and nephrologists to make sure that the patient’s cardiovascular disease risk is being assessed – checking lipids, A1c, etc. – and addressed as necessary,” Dr. Wallace added.
The study authors reported no relevant financial disclosures. Funding included support from the Rheumatology Research Foundation, the Executive Committee on Research at Massachusetts General, and the National Institutes of Health Loan Repayment Program.
AT ACR 2017
Key clinical point:
Major finding: Compared with patients who were wait-listed for a transplant but didn’t receive one, those who got transplants were much less likely to die during the study period (adjusted HR, 0.30; 95% CI, 0.25-0.37; P less than .001).
Data source: 2,471 patients with ESRD due to GPA who were wait-listed for a kidney transplant from 1995 to 2014 and tracked as late as 2016; 946 received a transplant.
Disclosures: The study authors reported no relevant financial disclosures. Funding included support from the Rheumatology Research Foundation, the Executive Committee on Research at Massachusetts General, and the National Institutes of Health Loan Repayment Program.
CSF May Reveal Dementia Risk in Lewy Body Disease
SAN DIEGO—In patients with Lewy body disease, CSF biomarkers may predict the extent of Alzheimer’s disease pathology, according to a new postmortem analysis presented at the 142nd Annual Meeting of the American Neurological Association.
In the small, prospective study, David Irwin, MD, Assistant Professor of Neurology at the University of Pennsylvania in Philadelphia, and colleagues found that higher antemortem CSF levels of total tau protein and lower amyloid beta1–42 levels were associated with postmortem evidence of cerebral Alzheimer’s disease and synuclein pathology. The connection between CSF amyloid beta1–42 and tau protein had been shown in Alzheimer’s disease, but not in Lewy body disease.
The findings could have prognostic implications, because about 40% of patients with Lewy body disease have enough amyloid beta1–42 and tau tangle pathology to have a secondary diagnosis of Alzheimer’s disease, and greater Alzheimer’s disease pathology has been linked to shorter survival. The results also could help individualize therapy, because patients with Lewy body disease and Alzheimer’s disease characteristics might respond better to antisynuclein and Alzheimer’s disease therapies, according to Dr. Irwin.
The CSF ratio of total tau to amyloid beta1–42 predicted the presence or absence of Alzheimer’s disease pathology with 90% sensitivity and 100% specificity.
If the results are confirmed, “we can identify who has Alzheimer’s copathology and who has a more aggressive form of Lewy body disease where it is reaching the cortex rather than being in the brainstem, and that correlates with memory loss, dementia, and other things that impair the patient’s functioning,” said Dr. Irwin.
The Udall Center for Parkinson’s Research at the University of Pennsylvania has an active autopsy program, and a significant number of patients with Parkinson’s disease donated their brains for research. “It is rare to have autopsy-confirmed samples where we can validate what we are measuring in the spinal fluid to what is actually accumulating in the brain,” Dr. Irwin said.
The study included 24 patients with autopsy-confirmed Lewy body disease who had undergone CSF testing during life. The researchers calculated ordinal pathology scores of tau tangles, amyloid beta1–42 plaques, and alpha-synuclein pathology in seven regions of the brain, producing a global pathology score for each variable. The subjects were then categorized into a group of participants with Lewy body synuclein stages and medium to high Alzheimer’s copathology (SYN+AD, n = 10) and a group with little or no Alzheimer’s copathology (SYN−AD, n = 14).
The researchers analyzed potential associations involving total tau, phosphorylated tau, and amyloid beta1–42. They found that amyloid beta1–42 levels were significantly different between SYN+AD and SYN−AD patients (147.2 pg/mL vs 231.1 pg/mL, respectively), as were CSF total tau levels (63.9 pg/mL vs 36.9 pg/mL). Phosphorylated tau was not significantly different between groups (20.2 pg/mL vs 15.5 pg/mL), which surprised the researchers, since it “is usually the strongest correlate of tangles in the brain,” said Dr. Irwin.
A ratio of CSF total tau to amyloid beta1–42 higher than 0.30 distinguished between SYN+AD and SYN−AD (area under the curve [AUC], 0.92; 90% sensitivity; 100% specificity), while CSF amyloid beta1–42 less than 185 pg/mL identified the neocortical synuclein stage (AUC, 0.92; 77% sensitivity; 82% specificity).
—Jim Kling
SAN DIEGO—In patients with Lewy body disease, CSF biomarkers may predict the extent of Alzheimer’s disease pathology, according to a new postmortem analysis presented at the 142nd Annual Meeting of the American Neurological Association.
In the small, prospective study, David Irwin, MD, Assistant Professor of Neurology at the University of Pennsylvania in Philadelphia, and colleagues found that higher antemortem CSF levels of total tau protein and lower amyloid beta1–42 levels were associated with postmortem evidence of cerebral Alzheimer’s disease and synuclein pathology. The connection between CSF amyloid beta1–42 and tau protein had been shown in Alzheimer’s disease, but not in Lewy body disease.
The findings could have prognostic implications, because about 40% of patients with Lewy body disease have enough amyloid beta1–42 and tau tangle pathology to have a secondary diagnosis of Alzheimer’s disease, and greater Alzheimer’s disease pathology has been linked to shorter survival. The results also could help individualize therapy, because patients with Lewy body disease and Alzheimer’s disease characteristics might respond better to antisynuclein and Alzheimer’s disease therapies, according to Dr. Irwin.
The CSF ratio of total tau to amyloid beta1–42 predicted the presence or absence of Alzheimer’s disease pathology with 90% sensitivity and 100% specificity.
If the results are confirmed, “we can identify who has Alzheimer’s copathology and who has a more aggressive form of Lewy body disease where it is reaching the cortex rather than being in the brainstem, and that correlates with memory loss, dementia, and other things that impair the patient’s functioning,” said Dr. Irwin.
The Udall Center for Parkinson’s Research at the University of Pennsylvania has an active autopsy program, and a significant number of patients with Parkinson’s disease donated their brains for research. “It is rare to have autopsy-confirmed samples where we can validate what we are measuring in the spinal fluid to what is actually accumulating in the brain,” Dr. Irwin said.
The study included 24 patients with autopsy-confirmed Lewy body disease who had undergone CSF testing during life. The researchers calculated ordinal pathology scores of tau tangles, amyloid beta1–42 plaques, and alpha-synuclein pathology in seven regions of the brain, producing a global pathology score for each variable. The subjects were then categorized into a group of participants with Lewy body synuclein stages and medium to high Alzheimer’s copathology (SYN+AD, n = 10) and a group with little or no Alzheimer’s copathology (SYN−AD, n = 14).
The researchers analyzed potential associations involving total tau, phosphorylated tau, and amyloid beta1–42. They found that amyloid beta1–42 levels were significantly different between SYN+AD and SYN−AD patients (147.2 pg/mL vs 231.1 pg/mL, respectively), as were CSF total tau levels (63.9 pg/mL vs 36.9 pg/mL). Phosphorylated tau was not significantly different between groups (20.2 pg/mL vs 15.5 pg/mL), which surprised the researchers, since it “is usually the strongest correlate of tangles in the brain,” said Dr. Irwin.
A ratio of CSF total tau to amyloid beta1–42 higher than 0.30 distinguished between SYN+AD and SYN−AD (area under the curve [AUC], 0.92; 90% sensitivity; 100% specificity), while CSF amyloid beta1–42 less than 185 pg/mL identified the neocortical synuclein stage (AUC, 0.92; 77% sensitivity; 82% specificity).
—Jim Kling
SAN DIEGO—In patients with Lewy body disease, CSF biomarkers may predict the extent of Alzheimer’s disease pathology, according to a new postmortem analysis presented at the 142nd Annual Meeting of the American Neurological Association.
In the small, prospective study, David Irwin, MD, Assistant Professor of Neurology at the University of Pennsylvania in Philadelphia, and colleagues found that higher antemortem CSF levels of total tau protein and lower amyloid beta1–42 levels were associated with postmortem evidence of cerebral Alzheimer’s disease and synuclein pathology. The connection between CSF amyloid beta1–42 and tau protein had been shown in Alzheimer’s disease, but not in Lewy body disease.
The findings could have prognostic implications, because about 40% of patients with Lewy body disease have enough amyloid beta1–42 and tau tangle pathology to have a secondary diagnosis of Alzheimer’s disease, and greater Alzheimer’s disease pathology has been linked to shorter survival. The results also could help individualize therapy, because patients with Lewy body disease and Alzheimer’s disease characteristics might respond better to antisynuclein and Alzheimer’s disease therapies, according to Dr. Irwin.
The CSF ratio of total tau to amyloid beta1–42 predicted the presence or absence of Alzheimer’s disease pathology with 90% sensitivity and 100% specificity.
If the results are confirmed, “we can identify who has Alzheimer’s copathology and who has a more aggressive form of Lewy body disease where it is reaching the cortex rather than being in the brainstem, and that correlates with memory loss, dementia, and other things that impair the patient’s functioning,” said Dr. Irwin.
The Udall Center for Parkinson’s Research at the University of Pennsylvania has an active autopsy program, and a significant number of patients with Parkinson’s disease donated their brains for research. “It is rare to have autopsy-confirmed samples where we can validate what we are measuring in the spinal fluid to what is actually accumulating in the brain,” Dr. Irwin said.
The study included 24 patients with autopsy-confirmed Lewy body disease who had undergone CSF testing during life. The researchers calculated ordinal pathology scores of tau tangles, amyloid beta1–42 plaques, and alpha-synuclein pathology in seven regions of the brain, producing a global pathology score for each variable. The subjects were then categorized into a group of participants with Lewy body synuclein stages and medium to high Alzheimer’s copathology (SYN+AD, n = 10) and a group with little or no Alzheimer’s copathology (SYN−AD, n = 14).
The researchers analyzed potential associations involving total tau, phosphorylated tau, and amyloid beta1–42. They found that amyloid beta1–42 levels were significantly different between SYN+AD and SYN−AD patients (147.2 pg/mL vs 231.1 pg/mL, respectively), as were CSF total tau levels (63.9 pg/mL vs 36.9 pg/mL). Phosphorylated tau was not significantly different between groups (20.2 pg/mL vs 15.5 pg/mL), which surprised the researchers, since it “is usually the strongest correlate of tangles in the brain,” said Dr. Irwin.
A ratio of CSF total tau to amyloid beta1–42 higher than 0.30 distinguished between SYN+AD and SYN−AD (area under the curve [AUC], 0.92; 90% sensitivity; 100% specificity), while CSF amyloid beta1–42 less than 185 pg/mL identified the neocortical synuclein stage (AUC, 0.92; 77% sensitivity; 82% specificity).
—Jim Kling
Does Midlife Physical Activity Affect Cognitive Health in Later Life?
In contrast with previous research, a study published in the Journal of Alzheimer’s Disease indicates that exercise in midlife is not associated with cognitive fitness in late life. The data suggest that physical activity may not help maintain cognitive function or prevent the onset of Alzheimer’s disease. Physical activity in late life, however, is associated with high cognitive function two years later, according to the researchers.
The literature contains few prospective data on the relationship between midlife and late-life physical activity and late-life cognitive performance. Cross-sectional study designs and short durations of follow-up have made several studies of this relationship unsatisfactory, according to Alden L. Gross, PhD, Assistant Professor of Epidemiology at Johns Hopkins Bloomberg School of Public Health in Baltimore, and colleagues.
A Prospective Study of Medical Graduates
To conduct a prospective analysis of the possible association between exercise in midlife and cognitive performance in later life, Dr. Gross and colleagues examined 30 years of longitudinal data from the Johns Hopkins Precursors study. This study enrolled medical graduates from 1948 to 1964 and followed them annually with health questionnaires. Surveys of physical activity were mailed in 1978, 1986, 1989, 1993, 1995, 1997, 2003, and 2006. Participants underwent cognitive testing in 2005 and 2008.
An adjudication committee consisting of physicians assigned diagnoses of dementia and dates of onset based on participants’ medical records. The investigators assigned a metabolic equivalent value (MET) to each category of activity (ie, vigorous, moderate, light, and sleep). They used linear regression for cognitive tests and Cox proportional hazards models for dementia onset to characterize associations with midlife physical activity. Models were adjusted for age, sex, smoking, diabetes, and hypertension.
Exercise Had No Long-Term Cognitive Effects
The study sample included 646 participants (48 women). In 1978, participants’ mean age was 47, mean BMI was 23.7 kg/m2, the prevalence of hypertension was 8.8%, and the prevalence of diabetes was 0.8%. Approximately 74% of participants reported regular exercise. In 2006, 54% of participants had hypertension, and 12% had diabetes. The incidence of dementia was 4.3%, and mean age at onset was 77.
No measure of activity in 1978, including MET h/day, decile of physical activity, and engagement in regular exercise, was associated with cognitive performance in demographic-adjusted or fully adjusted models. Regular exercise in 2006 and MET h/day expended in 2006, however, were associated with better cognitive performance. In addition, no physical activity exposure in 1978 was associated with onset of dementia. Greater physical activity in 2006, however, had a modest inverse association with risk of dementia.
The strength of the association between cognitive outcomes and physical activity in 1978 did not vary by gender. In 2006, however, greater MET h/day in a typical week and regular exercise were significantly associated with better cognitive performance in women, but not in men.
Homogeneous Sample Reduced Confounders
Previous studies included diverse cross sections of people and thus may have been susceptible to residual confounding by factors such as years of education, said the investigators. The Precursors study represents a highly homogeneous sample, however, which reduces the likelihood of such confounding. Nevertheless, the homogenous sample may limit the results’ generalizability, particularly to women.
“The prevailing notion that higher levels of physical activity protect against cognitive impairment in later life may result from the artifact of reverse causation,” said the authors. “While physical activity is strongly recommended for many reasons, our data suggest cognitive health may not be one of those reasons.”
“These findings have implications for intervention work moving forward,” said Dr. Gross. “We still need to focus on causes and mechanisms of Alzheimer’s [disease] and dementia, since we do not yet know which preventive measures may or may not work. For now, when I speak in the community about Alzheimer’s [disease], I find that people take some relief in understanding that there was not anything that anyone might have done to avoid a loved one developing Alzheimer’s [disease]. Of course, the goal for researchers is to identify factors that may help older people maintain their cognitive function into their later years. More long-term studies like the Precursors study are needed.”
—Erik Greb
Suggested Reading
Gross AL, Lu H, Meoni L, et al. Physical activity in midlife is not associated with cognitive health in later life among cognitively normal older adults. J Alzheimers Dis. 2017;59(4):1349-1358.
In contrast with previous research, a study published in the Journal of Alzheimer’s Disease indicates that exercise in midlife is not associated with cognitive fitness in late life. The data suggest that physical activity may not help maintain cognitive function or prevent the onset of Alzheimer’s disease. Physical activity in late life, however, is associated with high cognitive function two years later, according to the researchers.
The literature contains few prospective data on the relationship between midlife and late-life physical activity and late-life cognitive performance. Cross-sectional study designs and short durations of follow-up have made several studies of this relationship unsatisfactory, according to Alden L. Gross, PhD, Assistant Professor of Epidemiology at Johns Hopkins Bloomberg School of Public Health in Baltimore, and colleagues.
A Prospective Study of Medical Graduates
To conduct a prospective analysis of the possible association between exercise in midlife and cognitive performance in later life, Dr. Gross and colleagues examined 30 years of longitudinal data from the Johns Hopkins Precursors study. This study enrolled medical graduates from 1948 to 1964 and followed them annually with health questionnaires. Surveys of physical activity were mailed in 1978, 1986, 1989, 1993, 1995, 1997, 2003, and 2006. Participants underwent cognitive testing in 2005 and 2008.
An adjudication committee consisting of physicians assigned diagnoses of dementia and dates of onset based on participants’ medical records. The investigators assigned a metabolic equivalent value (MET) to each category of activity (ie, vigorous, moderate, light, and sleep). They used linear regression for cognitive tests and Cox proportional hazards models for dementia onset to characterize associations with midlife physical activity. Models were adjusted for age, sex, smoking, diabetes, and hypertension.
Exercise Had No Long-Term Cognitive Effects
The study sample included 646 participants (48 women). In 1978, participants’ mean age was 47, mean BMI was 23.7 kg/m2, the prevalence of hypertension was 8.8%, and the prevalence of diabetes was 0.8%. Approximately 74% of participants reported regular exercise. In 2006, 54% of participants had hypertension, and 12% had diabetes. The incidence of dementia was 4.3%, and mean age at onset was 77.
No measure of activity in 1978, including MET h/day, decile of physical activity, and engagement in regular exercise, was associated with cognitive performance in demographic-adjusted or fully adjusted models. Regular exercise in 2006 and MET h/day expended in 2006, however, were associated with better cognitive performance. In addition, no physical activity exposure in 1978 was associated with onset of dementia. Greater physical activity in 2006, however, had a modest inverse association with risk of dementia.
The strength of the association between cognitive outcomes and physical activity in 1978 did not vary by gender. In 2006, however, greater MET h/day in a typical week and regular exercise were significantly associated with better cognitive performance in women, but not in men.
Homogeneous Sample Reduced Confounders
Previous studies included diverse cross sections of people and thus may have been susceptible to residual confounding by factors such as years of education, said the investigators. The Precursors study represents a highly homogeneous sample, however, which reduces the likelihood of such confounding. Nevertheless, the homogenous sample may limit the results’ generalizability, particularly to women.
“The prevailing notion that higher levels of physical activity protect against cognitive impairment in later life may result from the artifact of reverse causation,” said the authors. “While physical activity is strongly recommended for many reasons, our data suggest cognitive health may not be one of those reasons.”
“These findings have implications for intervention work moving forward,” said Dr. Gross. “We still need to focus on causes and mechanisms of Alzheimer’s [disease] and dementia, since we do not yet know which preventive measures may or may not work. For now, when I speak in the community about Alzheimer’s [disease], I find that people take some relief in understanding that there was not anything that anyone might have done to avoid a loved one developing Alzheimer’s [disease]. Of course, the goal for researchers is to identify factors that may help older people maintain their cognitive function into their later years. More long-term studies like the Precursors study are needed.”
—Erik Greb
Suggested Reading
Gross AL, Lu H, Meoni L, et al. Physical activity in midlife is not associated with cognitive health in later life among cognitively normal older adults. J Alzheimers Dis. 2017;59(4):1349-1358.
In contrast with previous research, a study published in the Journal of Alzheimer’s Disease indicates that exercise in midlife is not associated with cognitive fitness in late life. The data suggest that physical activity may not help maintain cognitive function or prevent the onset of Alzheimer’s disease. Physical activity in late life, however, is associated with high cognitive function two years later, according to the researchers.
The literature contains few prospective data on the relationship between midlife and late-life physical activity and late-life cognitive performance. Cross-sectional study designs and short durations of follow-up have made several studies of this relationship unsatisfactory, according to Alden L. Gross, PhD, Assistant Professor of Epidemiology at Johns Hopkins Bloomberg School of Public Health in Baltimore, and colleagues.
A Prospective Study of Medical Graduates
To conduct a prospective analysis of the possible association between exercise in midlife and cognitive performance in later life, Dr. Gross and colleagues examined 30 years of longitudinal data from the Johns Hopkins Precursors study. This study enrolled medical graduates from 1948 to 1964 and followed them annually with health questionnaires. Surveys of physical activity were mailed in 1978, 1986, 1989, 1993, 1995, 1997, 2003, and 2006. Participants underwent cognitive testing in 2005 and 2008.
An adjudication committee consisting of physicians assigned diagnoses of dementia and dates of onset based on participants’ medical records. The investigators assigned a metabolic equivalent value (MET) to each category of activity (ie, vigorous, moderate, light, and sleep). They used linear regression for cognitive tests and Cox proportional hazards models for dementia onset to characterize associations with midlife physical activity. Models were adjusted for age, sex, smoking, diabetes, and hypertension.
Exercise Had No Long-Term Cognitive Effects
The study sample included 646 participants (48 women). In 1978, participants’ mean age was 47, mean BMI was 23.7 kg/m2, the prevalence of hypertension was 8.8%, and the prevalence of diabetes was 0.8%. Approximately 74% of participants reported regular exercise. In 2006, 54% of participants had hypertension, and 12% had diabetes. The incidence of dementia was 4.3%, and mean age at onset was 77.
No measure of activity in 1978, including MET h/day, decile of physical activity, and engagement in regular exercise, was associated with cognitive performance in demographic-adjusted or fully adjusted models. Regular exercise in 2006 and MET h/day expended in 2006, however, were associated with better cognitive performance. In addition, no physical activity exposure in 1978 was associated with onset of dementia. Greater physical activity in 2006, however, had a modest inverse association with risk of dementia.
The strength of the association between cognitive outcomes and physical activity in 1978 did not vary by gender. In 2006, however, greater MET h/day in a typical week and regular exercise were significantly associated with better cognitive performance in women, but not in men.
Homogeneous Sample Reduced Confounders
Previous studies included diverse cross sections of people and thus may have been susceptible to residual confounding by factors such as years of education, said the investigators. The Precursors study represents a highly homogeneous sample, however, which reduces the likelihood of such confounding. Nevertheless, the homogenous sample may limit the results’ generalizability, particularly to women.
“The prevailing notion that higher levels of physical activity protect against cognitive impairment in later life may result from the artifact of reverse causation,” said the authors. “While physical activity is strongly recommended for many reasons, our data suggest cognitive health may not be one of those reasons.”
“These findings have implications for intervention work moving forward,” said Dr. Gross. “We still need to focus on causes and mechanisms of Alzheimer’s [disease] and dementia, since we do not yet know which preventive measures may or may not work. For now, when I speak in the community about Alzheimer’s [disease], I find that people take some relief in understanding that there was not anything that anyone might have done to avoid a loved one developing Alzheimer’s [disease]. Of course, the goal for researchers is to identify factors that may help older people maintain their cognitive function into their later years. More long-term studies like the Precursors study are needed.”
—Erik Greb
Suggested Reading
Gross AL, Lu H, Meoni L, et al. Physical activity in midlife is not associated with cognitive health in later life among cognitively normal older adults. J Alzheimers Dis. 2017;59(4):1349-1358.
Two-thirds of abortions occur by 8 weeks’ gestation
, although there was variation by maternal age and race/ethnicity, according to the Centers for Disease Control and Prevention.
That year, 65.3% of abortions were performed at a gestational age of 8 weeks or earlier, with 25.6% occurring at 9-13 weeks. Gestational distribution of the remaining abortions was fairly even: 3.4% at 14-15 weeks, 2.2% at 16-17 weeks, 2.0% at 18-20 weeks, and 1.4% at 21 weeks or later, the CDC investigators reported (MMWR Surveill Summ. 2017 Nov 25;66[24]:1-48).
The percentage of abortions occurring at 8 weeks or earlier was lowest for the youngest age group and increased along with maternal age: 43% for those under 15 years of age and progressing up to 72.5% for women over age 40. That scenario was basically reversed for all of the other gestational periods, as the under-15 group had the highest percentage for 9-13 weeks (34.4%), 14-15 (6.7%), 16-17 (3.6%), 18-20 (5.0%), and 21 weeks and later (7.3%). Those over age 40 had the lowest or almost the lowest percentage in each period, reported Tara C. Jatlaoui, MD, and her associates.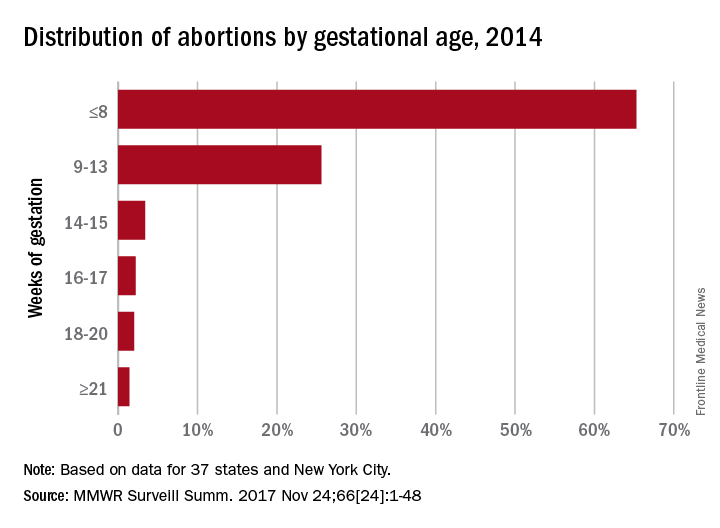
The data for gestational period analysis came from 37 states and New York City. New York State, along with 12 other states, did not report, did not report by gestational age, or did not meet reporting standards.
, although there was variation by maternal age and race/ethnicity, according to the Centers for Disease Control and Prevention.
That year, 65.3% of abortions were performed at a gestational age of 8 weeks or earlier, with 25.6% occurring at 9-13 weeks. Gestational distribution of the remaining abortions was fairly even: 3.4% at 14-15 weeks, 2.2% at 16-17 weeks, 2.0% at 18-20 weeks, and 1.4% at 21 weeks or later, the CDC investigators reported (MMWR Surveill Summ. 2017 Nov 25;66[24]:1-48).
The percentage of abortions occurring at 8 weeks or earlier was lowest for the youngest age group and increased along with maternal age: 43% for those under 15 years of age and progressing up to 72.5% for women over age 40. That scenario was basically reversed for all of the other gestational periods, as the under-15 group had the highest percentage for 9-13 weeks (34.4%), 14-15 (6.7%), 16-17 (3.6%), 18-20 (5.0%), and 21 weeks and later (7.3%). Those over age 40 had the lowest or almost the lowest percentage in each period, reported Tara C. Jatlaoui, MD, and her associates.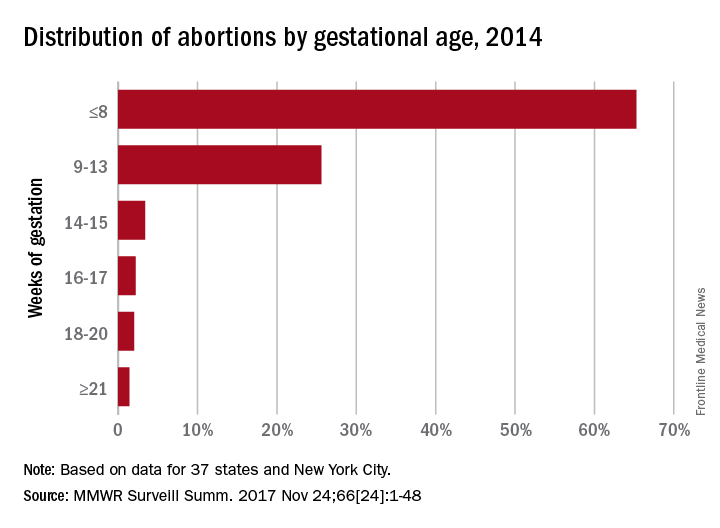
The data for gestational period analysis came from 37 states and New York City. New York State, along with 12 other states, did not report, did not report by gestational age, or did not meet reporting standards.
, although there was variation by maternal age and race/ethnicity, according to the Centers for Disease Control and Prevention.
That year, 65.3% of abortions were performed at a gestational age of 8 weeks or earlier, with 25.6% occurring at 9-13 weeks. Gestational distribution of the remaining abortions was fairly even: 3.4% at 14-15 weeks, 2.2% at 16-17 weeks, 2.0% at 18-20 weeks, and 1.4% at 21 weeks or later, the CDC investigators reported (MMWR Surveill Summ. 2017 Nov 25;66[24]:1-48).
The percentage of abortions occurring at 8 weeks or earlier was lowest for the youngest age group and increased along with maternal age: 43% for those under 15 years of age and progressing up to 72.5% for women over age 40. That scenario was basically reversed for all of the other gestational periods, as the under-15 group had the highest percentage for 9-13 weeks (34.4%), 14-15 (6.7%), 16-17 (3.6%), 18-20 (5.0%), and 21 weeks and later (7.3%). Those over age 40 had the lowest or almost the lowest percentage in each period, reported Tara C. Jatlaoui, MD, and her associates.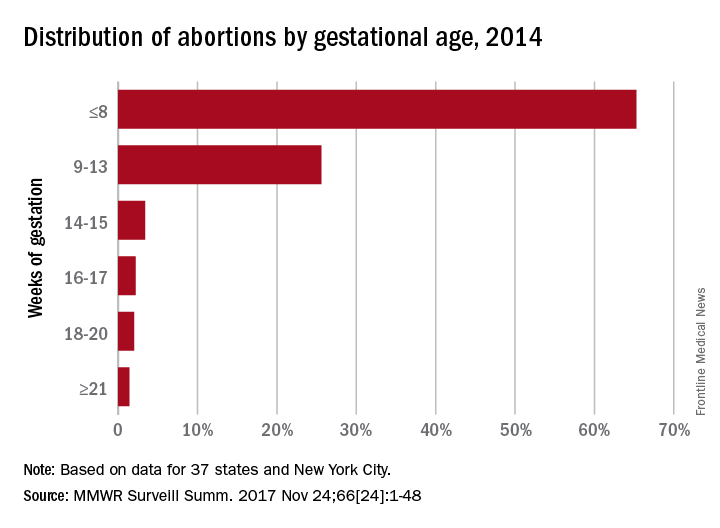
The data for gestational period analysis came from 37 states and New York City. New York State, along with 12 other states, did not report, did not report by gestational age, or did not meet reporting standards.
FROM MMWR SURVEILLANCE SUMMARIES
The clear and present future: Telehealth and telemedicine in obstetrics and gynecology
I recently spoke with 2 outstanding leaders in our field, members of the American College of Obstetricians and Gynecologists (ACOG) task force on telehealth and telemedicine, about the future of providing health care to women in remote locations.
Haywood Brown, MD, is President of ACOG for 2017–2018 and is F. Bayard Carter Professor of Obstetrics and Gynecology at Duke University Medical Center in Durham, North Carolina, and Peter Nielsen, MD, is Professor and Vice Chair of the Department of Obstetrics and Gynecology at Baylor College of Medicine in Houston, Texas, and Obstetrician-in-Chief at Children’s Hospital of San Antonio. Dr. Nielsen is a retired US Army colonel.
Why an ACOG telehealth task force?
Haywood Brown, MD: Our overall goals in telehealth and telemedicine are to coordinate and better facilitate the health care of women in remote locations and to improve maternal morbidity and mortality. Telehealth can be used on both an outpatient and an inpatient basis.
Outpatient telehealth is used for consultations. In maternal-fetal medicine, for instance, we use it for ultrasonography consultations. I also have used telehealth technology to “see” a pregnant patient with type 1diabetes. During our sessions, I managed her blood sugar levels and did all the other things I would have done if we had been together at my clinic. Without telehealth technology, however, this patient would have needed to drive 4 hours round-trip for each appointment.
Our colleagues in rural communities and at lower-level hospitals can use telehealth and telemedicine as aids in treating their high-risk patients, such as those with preeclampsia, prematurity risk, or other conditions. Physicians can consult with specialists through a face-to-face conversation that takes place through telecommunications. The result is that the quality of care for women in our communities is improved.
Genetic counseling, infertility consultation, and fetal anomaly management are some of the other applications. Our task force is discussing different ways to improve patient care and ways to collaborate with our colleagues around the country. Ultimately, we are developing best practices—a model for the best uses of technology to improve women’s health care in the United States.
Task force focus: Telehealth technology, billing, services
Dr. Brown: Our task force, a diverse group of members from all over the country, represents the spectrum of ObGyns. Although task force members have various levels of telehealth experience, all are very interested in these new channels of communication. The task force also includes billers, who understand billing ramifications, and payers, who know firsthand what will and will not be paid.
Technology and its availability is the most important topic for the task force. While some communities have Internet service, not all do. We need to determine which areas need service, how much it would cost, and who pays for it. Can a hospital afford it? A practice? Their partners? Identifying partners in tertiary care settings is a task force goal.
We are engaging a broad range of experts to study all the components and associated costs of technology, licensing, and cross-state credentialing. Gathering this information will help in developing a best practices model that general ObGyns can use.
Telehealth is redefining aspects of care: prenatal care (how many visits are required?), postpartum care, and other types of services that can be done remotely. Genetic counseling—who can provide it, what education is required—is another topic of discussion. Once we surmount the billing obstacles, we can do much with teleconferencing, such as provide genetic consultation with ObGyns in various settings.
The terms "telehealth" and "telemedicine" are often used interchangeably. Telemedicine is the older phrase, while telehealth entered the vernacular more recently and encompasses a broader definition.
The HealthIT.gov website explains the differences in terminology this way1:
- The Health Resources Services Administration defines telehealth as the use of electronic information and telecommunications technologies to support long-distance clinical health care, patient and professional health-related education, public health and health administration. Technologies include videoconferencing, the Internet, store-and-forward imaging, streaming media, and terrestrial and wireless communications.
- Telehealth is different from telemedicine because it refers to a broader scope of remote health care services than telemedicine. While telemedicine refers specifically to remote clinical services, telehealth can refer to remote nonclinical services, such as provider training, administrative meetings, and continuing medical education, in addition to clinical services.
A World Health Organization report, however, uses the 2 terms synonymously and interchangeably, defining telemedicine as2:
- The delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interests of advancing the health of individuals and their communities.
The American Telemedicine Association (ATA) describes their use of the terms this way3:
- ATA largely views telemedicine and telehealth to be interchangeable terms, encompassing a wide definition of remote healthcare, although telehealth may not always involve clinical care.
References
- HealthIT.gov website. Frequently asked questions. https://www.healthit.gov/providers-professionals/frequently-asked-questions/485. Accessed November 15, 2017.
- World Health Organization. Telemedicine: opportunities and developments in member states. 2010. http://www.who.int/goe/publications/goe_telemedicine_2010.pdf. Accessed November 15, 2017.
- American Telemedicine Association. About telemedicine: the ultimate frontier for superior healthcare delivery. http://www.americantelemed.org/about/about-telemedicine. Accessed November 15, 2017.
Learn about ways clinicians can use telemedicine.
Making progress in rural and underserved communities
Peter Nielsen, MD: When we saw that some high-risk obstetrics patients were having a difficult time getting to our downtown San Antonio office—the trip from surrounding communities was taking too long, or city driving and parking were stressful or too costly—we looked to improve access to care. Collaborating with a health care network that has a hospital in a town north of San Antonio, we set up a pilot program to provide telemedicine perinatal consultation services.
In this kind of service, which occurs entirely in real time, ultrasound images taken at the hospital are streamed by high-speed fiberoptic cable to our office, where a maternal-fetal medicine physician views them. If a repeat image or a different image is needed, the physician requests another scan. Linked to the physician and listening through an earpiece, the ultrasonographer performs the new scan with little delay and without disturbing the patient. The conversation between physician and ultrasonographer is private.
After ultrasound scanning is complete, the patient goes to a private room at the hospital for a video conference with our physician in San Antonio, who has reviewed the images in the PACS (picture archiving and communication system) or ultrasound recording system. They discuss the images, the findings, and the follow-up.
We tested the technology during a 6-month pilot program to make sure it worked at the highest quality and safety levels. Then the program went live and we started seeing patients remotely. Now we have a robust telemedicine training capability at that hospital outside San Antonio, and we are looking to expand to other south and west Texas areas, some even farther from our office.
I have done some of these remote consultations. In response to my informal queries about the experience, patients said that no one else was offering it, and they were participating for the first time. Naturally they had questions and concerns. Nevertheless, patients, family members, and the ultrasonographer and physicians in the communities seem to think this is a high-quality, safe program that makes it easier for patients to access health care.
Patients uniformly describe these consultations in positive terms. They do not have to drive far, into the city, and deal with traffic; parking is easy and free; and less travel means much less time off from work. Given these very practical advantages, patients are interested in having more appointments done remotely. In addition, they say the appointment itself is easy, being there is effortless, and they feel their physician is sitting in the same room. It is like video chatting with family members—they are comfortable with the technology.
Related article:
Landmark women’s health care remains law of the land
The patients’ perspective
Dr. Brown: Patient satisfaction is an important issue. In psychiatry, dermatology, and other disciplines, patients have indicated that they are very satisfied with telehealth sessions. Telehealth in obstetrics and gynecology, I think, will receive similar positive feedback.
The issue of driving distance led us to reconsider the number of face-to-face prenatal visits a normal, healthy patient needs. These days, a patient can use a prenatal care app to track her weight and blood pressure and send the data to her physician. Besides being convenient, these monitoring apps can give a patient an important sense of control. Our pilot programs found that a patient who self-monitors understands her weight gain better and is more in tune with it. Apps and other technologies can thus improve quality of care and, in reducing the number of trips to an office, increase patient satisfaction.
Many people use or are familiar with the programs Skype and FaceTime (audiovideo chat software), and I envision that our postpartum task force will recommend using such programs for follow-up appointments. For each visit, the question to ask is whether the patient really needs to meet with her physician in person, or can she stay with her new baby and receive postpartum counseling at home. I am excited about the potential of telehealth in obstetrics and gynecology. Our task force is exploring that potential.
Telehealth for both routine and specialized care
Dr. Brown: Specialized care applications are here. In a pilot program in Wisconsin, a colleague has been providing remote psychiatric care. Perhaps such a program can be used to follow up on patients with postpartum depression. In addition, other psychiatry colleagues have long been using telehealth for adolescent behavior follow-ups, and we can do this too.
Another colleague has been performing remote perinatal follow-up for children with congenital anomalies. The physician interacts with the parent or parents as well as the patient. This seems to represent only the tip of the iceberg of what can be done in terms of follow-up.
We can also use telehealth in infertility settings. High-risk patients can benefit, too. Our guidelines say patients with preeclampsia should be seen within 3 days to 1 week. Many are transferred from low-access hospitals to our office. This follow-up, however, also can be done remotely, with patients at health department clinics or even at home. Reporting blood pressure readings and health-related feelings to a physician during a teleconsultation removes driving as a potential inconvenience or obstacle.
Telemedicine can be advantageous in gynecology. Physicians are doing important work with telecolposcopy as a follow-up to abnormal Pap test findings in patients in sub-Saharan Africa.
Routine wound care, which is commonly needed, can be performed in the home by a home health nurse telecommunicating with a physician. I can see broad telehealth use, and indeed our dermatology colleagues have been practicing telemedicine for quite some time.
Read about solving financial barriers and physician shortages.
An affordable solution to financial barriers and physician shortages
Dr. Nielsen: Telehealth can reduce barriers to care. For example, knowing that our teleconsultation services are covered by insurance, referring physicians and patients are more likely to try them and continue to use them. Payers are on board as well. Other barriers can be harder to overcome, particularly for patients at risk for complex diagnoses and medical decisions. Our pilot program, however, has demonstrated success in this area. It has provided safe, high-quality imaging, accurate diagnoses, productive discussions, and helpful management recommendations.
Telehealth also helps address relative and absolute physician shortages. In some areas, a relative shortage may indicate misdistribution. In other areas, specialists simply are too few in number. This absolute shortage of specialists likely will increase, as many communities are too small to sustain and support having them in person.
Outpatients can obtain care 5 days a week with telemedicine, as opposed to only 1 to 3 times a month in person. Physicians travel to remote clinics that are staffed only 1 or 2 days a month. Where the window for care is so small, patients and physicians are likely to turn to telemedicine. In addition, that utility results in better use of resources. For example, studies that were performed earlier would not need to be repeated, since you could access centrally located archives.
Related article:
ICD-10-CM code changes: What's new for 2018
Dr. Brown: For teleconsultations and televisits, all that payers need do is modify the billing codes they use for our usual services. Once that is done, payers can develop a payment model that works for both themselves and the teleconsultants.
The US health care system is fragmented. Health care is provided in various facilities, including federally qualified health centers and health department clinics. As Dr. Nielsen said, physicians travel to remote facilities once or twice a week or even a month, whereas telehealth can be offered 5 days a week. Many residents go to remote clinics, where an attending physician is required. Instead of an attending driving there, he or she could be teleconsulting—interacting with residents and patients from afar. So, telehealth is a win-win situation. It increases access to physicians and facilitates appropriate interactions with them, wherever they are. Telehealth can be an important contribution to developing a more effective health care delivery system than the fragmented one we have now.
Effective health care delivery is so important for obstetrics and gynecology, and the reported workforce challenges are real. A maternal-fetal medicine physician is unlikely to travel to remote communities once a week or even every 2 weeks, but that same physician can teleconsult multiple days each week.
How telehealth can close service gaps
Dr. Brown: Having established relationships with physicians in other clinics and communities paves the way for teleconsultation and remote supervision. Technology can help Planned Parenthood and other clinics continue to provide contraceptive counseling and other health care services. Even medical abortions can be supervised through teleconsultation.
With funds to Medicaid being cut, with the potential for Planned Parenthood to be defunded, physicians must think of ways they can continue to provide care to all patients and communities. By addressing these issues now, we will be ready to take charge of patient care, wherever it is needed.
But, we need partners, no question. We need hospital partners in all communities, and especially in rural communities. Rural hospitals and maternity care are at risk. Health care in rural communities faces many challenges. Telehealth, teleconferencing, and teleconsultation not only can improve access to services, but also can curb travel costs as well as costs to the communities and hospitals.
Who pays the operating costs, and who benefits
Dr. Brown: Payers are already discovering that teleconsultations are as billable as in-person visits. In addition, physicians are realizing that remote consultation can work as well as in-person consultation, with its own merits and advantages. Education is key—education about billing and about what is doable in telehealth. We can learn from colleagues in other specialties.
Dr. Nielsen: Several entities and groups must start covering the technology costs. Federal and state entities need to determine how the country’s information infrastructure can be improved to give rural areas access to high-quality, high-speed, wide-bandwidth communications, which will help expand telehealth and increase other industries’ opportunities to grow and sustain these communities. Improving the infrastructure also can help keep rural areas sustainable.
Health care systems themselves can join federal, state, and local governments in building this infrastructure. They can also start identifying opportunities to support and sustain physicians and hospitals in smaller towns and start combating the perception that the infrastructure is being developed only to migrate patients over to accessing their care through telehealth provided by physicians in the larger cities.
Many payers see telehealth as improving access and outcomes and already support it, but more payers need to become involved. All need to understand how routine and complex consultations, even inpatient consultations, can be performed remotely and can be properly reimbursed, and incentivized with payments for improved outcomes and value.
As barriers fall and telehealth improves, acceptance by patients and physicians will increase. In addition, telehealth will enter medical education in a significant way. The instruction that students, residents, and Fellows receive will be enhanced by new telehealth approaches in various specialties, and residents will come out of these programs with telehealth experience and a sense of both financial benefits and payment structures. This early exposure will pique their interest in using telehealth and advocating its use where it may never before have been considered, owing to real and perceived barriers.
Read about telehealth solutions for ObGyns.
Learning from other specialties and agencies
Dr. Brown: The physician shortage negatively affects access to health care in rural areas. Many city and suburban physicians, including ObGyns, want to stay where they are. Education is needed to show them that a rural practice can be successful. They would have a good patient base and be able to use telehealth to improve care and maintain contact with tertiary care centers.
Several task force members have described their experience within their health systems, and we hope to borrow from that. A health system in South Dakota received a Health Resources and Services Administration grant to use telehealth and teleconsultation in the Indian Health Service (IHS). To women who access their health care through the IHS, being able to remain in the community is culturally important. Telehealth and teleconsultation bring care to these women where they live.
To develop the best telehealth and teleconsultation model, we are borrowing from these health systems and from the experience of our colleagues in dermatology, behavioral health, psychiatry, and other disciplines. These physicians already have overcome many hurdles and discovered the importance of patient satisfaction in providing remote health care.
Patients will benefit in various ways, and here is another example: A clinic refers a patient to an ObGyn to discuss whether it is possible to have a vaginal birth after a cesarean delivery. The drive to the ObGyn’s office takes an hour, but the patient just as easily could have had all her questions answered during a teleconsultation.
Related articles:
Telehealth and you (4-part audiocast)
Telehealth recommendations for ObGyns
Dr. Brown: Our task force will develop recommended best practices for telehealth. We will outline how a practice can engage with telehealth and will address licensing requirements, as a practice must be licensed in each state where it uses telehealth. Our goal is to help our specialty get started in telehealth and telemedicine.
In practices with telehealth, it will be incumbent on ObGyns to identify any barriers to care. For example, we are concerned about early discontinuation of breastfeeding, particularly among African American communities. Fortunately, we have learned that video chat follow-ups can help improve breastfeeding continuation rates.
It also will be incumbent on ObGyns to think differently about how best to follow up. For a patient who calls to say she thinks she has mastitis, much of the consultation can be handled by telephone or video conference with the physician and a nurse practi‑tioner, and then medication can be prescribed without the need for in-person follow-up. We must then determine how to ensure these follow-up methods are compensated.
Direct-to-patient virtual visits
- Virtual home visits
- Low-risk pregnancy
- Postpartum visits
- Lactation support
- Routine gynecologic care
- Postoperative follow-up
Remote patient monitoring
- Chronic disease management
- Antenatal testing
- Fetal heart rate monitoring
- Transfer of care
Final thoughts
Dr. Nielsen: It is time for all US health care players to more seriously and aggressively consider how telehealth can improve health care access, quality, and safety. Even more important, patients and physicians in small communities need to feel that they can access specialists and care that is as good as those available in larger communities without having to pull up stakes and move.
Telehealth can help small communities become sustainable over the long term. As the majority of the people in this country are born in and receive health care in community hospitals, not large tertiary care centers, the state of US health care should be measured by the ability to provide as much care as is technically possible in the small communities where patients live and work and raise their kids.
Dr. Brown: More than 50% of all babies are born in hospitals where fewer than 1,000 deliveries are performed, and almost 40% are born in hospitals where fewer than 500 are performed. To provide high-level care and have patients feel comfortable, to improve morbidity and mortality, we need telehealth and telemedicine.
If I can help a physician in East Africa place a Bakri balloon for postpartum hemorrhaging, surely I can help a physician in rural areas of Wyoming, South Dakota, or North Carolina deal with this obstetric emergency. In obstetrics and gynecology, telehealth and telemedicine have great potential in terms of morbidity and mortality, but we are also doing genetic counseling and a great deal of patient follow-up, and so much more can be done.
That is the key, and the reason for the training, the task force, the deliberations, and the best practices model that we will be sharing with our colleagues.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
I recently spoke with 2 outstanding leaders in our field, members of the American College of Obstetricians and Gynecologists (ACOG) task force on telehealth and telemedicine, about the future of providing health care to women in remote locations.
Haywood Brown, MD, is President of ACOG for 2017–2018 and is F. Bayard Carter Professor of Obstetrics and Gynecology at Duke University Medical Center in Durham, North Carolina, and Peter Nielsen, MD, is Professor and Vice Chair of the Department of Obstetrics and Gynecology at Baylor College of Medicine in Houston, Texas, and Obstetrician-in-Chief at Children’s Hospital of San Antonio. Dr. Nielsen is a retired US Army colonel.
Why an ACOG telehealth task force?
Haywood Brown, MD: Our overall goals in telehealth and telemedicine are to coordinate and better facilitate the health care of women in remote locations and to improve maternal morbidity and mortality. Telehealth can be used on both an outpatient and an inpatient basis.
Outpatient telehealth is used for consultations. In maternal-fetal medicine, for instance, we use it for ultrasonography consultations. I also have used telehealth technology to “see” a pregnant patient with type 1diabetes. During our sessions, I managed her blood sugar levels and did all the other things I would have done if we had been together at my clinic. Without telehealth technology, however, this patient would have needed to drive 4 hours round-trip for each appointment.
Our colleagues in rural communities and at lower-level hospitals can use telehealth and telemedicine as aids in treating their high-risk patients, such as those with preeclampsia, prematurity risk, or other conditions. Physicians can consult with specialists through a face-to-face conversation that takes place through telecommunications. The result is that the quality of care for women in our communities is improved.
Genetic counseling, infertility consultation, and fetal anomaly management are some of the other applications. Our task force is discussing different ways to improve patient care and ways to collaborate with our colleagues around the country. Ultimately, we are developing best practices—a model for the best uses of technology to improve women’s health care in the United States.
Task force focus: Telehealth technology, billing, services
Dr. Brown: Our task force, a diverse group of members from all over the country, represents the spectrum of ObGyns. Although task force members have various levels of telehealth experience, all are very interested in these new channels of communication. The task force also includes billers, who understand billing ramifications, and payers, who know firsthand what will and will not be paid.
Technology and its availability is the most important topic for the task force. While some communities have Internet service, not all do. We need to determine which areas need service, how much it would cost, and who pays for it. Can a hospital afford it? A practice? Their partners? Identifying partners in tertiary care settings is a task force goal.
We are engaging a broad range of experts to study all the components and associated costs of technology, licensing, and cross-state credentialing. Gathering this information will help in developing a best practices model that general ObGyns can use.
Telehealth is redefining aspects of care: prenatal care (how many visits are required?), postpartum care, and other types of services that can be done remotely. Genetic counseling—who can provide it, what education is required—is another topic of discussion. Once we surmount the billing obstacles, we can do much with teleconferencing, such as provide genetic consultation with ObGyns in various settings.
The terms "telehealth" and "telemedicine" are often used interchangeably. Telemedicine is the older phrase, while telehealth entered the vernacular more recently and encompasses a broader definition.
The HealthIT.gov website explains the differences in terminology this way1:
- The Health Resources Services Administration defines telehealth as the use of electronic information and telecommunications technologies to support long-distance clinical health care, patient and professional health-related education, public health and health administration. Technologies include videoconferencing, the Internet, store-and-forward imaging, streaming media, and terrestrial and wireless communications.
- Telehealth is different from telemedicine because it refers to a broader scope of remote health care services than telemedicine. While telemedicine refers specifically to remote clinical services, telehealth can refer to remote nonclinical services, such as provider training, administrative meetings, and continuing medical education, in addition to clinical services.
A World Health Organization report, however, uses the 2 terms synonymously and interchangeably, defining telemedicine as2:
- The delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interests of advancing the health of individuals and their communities.
The American Telemedicine Association (ATA) describes their use of the terms this way3:
- ATA largely views telemedicine and telehealth to be interchangeable terms, encompassing a wide definition of remote healthcare, although telehealth may not always involve clinical care.
References
- HealthIT.gov website. Frequently asked questions. https://www.healthit.gov/providers-professionals/frequently-asked-questions/485. Accessed November 15, 2017.
- World Health Organization. Telemedicine: opportunities and developments in member states. 2010. http://www.who.int/goe/publications/goe_telemedicine_2010.pdf. Accessed November 15, 2017.
- American Telemedicine Association. About telemedicine: the ultimate frontier for superior healthcare delivery. http://www.americantelemed.org/about/about-telemedicine. Accessed November 15, 2017.
Learn about ways clinicians can use telemedicine.
Making progress in rural and underserved communities
Peter Nielsen, MD: When we saw that some high-risk obstetrics patients were having a difficult time getting to our downtown San Antonio office—the trip from surrounding communities was taking too long, or city driving and parking were stressful or too costly—we looked to improve access to care. Collaborating with a health care network that has a hospital in a town north of San Antonio, we set up a pilot program to provide telemedicine perinatal consultation services.
In this kind of service, which occurs entirely in real time, ultrasound images taken at the hospital are streamed by high-speed fiberoptic cable to our office, where a maternal-fetal medicine physician views them. If a repeat image or a different image is needed, the physician requests another scan. Linked to the physician and listening through an earpiece, the ultrasonographer performs the new scan with little delay and without disturbing the patient. The conversation between physician and ultrasonographer is private.
After ultrasound scanning is complete, the patient goes to a private room at the hospital for a video conference with our physician in San Antonio, who has reviewed the images in the PACS (picture archiving and communication system) or ultrasound recording system. They discuss the images, the findings, and the follow-up.
We tested the technology during a 6-month pilot program to make sure it worked at the highest quality and safety levels. Then the program went live and we started seeing patients remotely. Now we have a robust telemedicine training capability at that hospital outside San Antonio, and we are looking to expand to other south and west Texas areas, some even farther from our office.
I have done some of these remote consultations. In response to my informal queries about the experience, patients said that no one else was offering it, and they were participating for the first time. Naturally they had questions and concerns. Nevertheless, patients, family members, and the ultrasonographer and physicians in the communities seem to think this is a high-quality, safe program that makes it easier for patients to access health care.
Patients uniformly describe these consultations in positive terms. They do not have to drive far, into the city, and deal with traffic; parking is easy and free; and less travel means much less time off from work. Given these very practical advantages, patients are interested in having more appointments done remotely. In addition, they say the appointment itself is easy, being there is effortless, and they feel their physician is sitting in the same room. It is like video chatting with family members—they are comfortable with the technology.
Related article:
Landmark women’s health care remains law of the land
The patients’ perspective
Dr. Brown: Patient satisfaction is an important issue. In psychiatry, dermatology, and other disciplines, patients have indicated that they are very satisfied with telehealth sessions. Telehealth in obstetrics and gynecology, I think, will receive similar positive feedback.
The issue of driving distance led us to reconsider the number of face-to-face prenatal visits a normal, healthy patient needs. These days, a patient can use a prenatal care app to track her weight and blood pressure and send the data to her physician. Besides being convenient, these monitoring apps can give a patient an important sense of control. Our pilot programs found that a patient who self-monitors understands her weight gain better and is more in tune with it. Apps and other technologies can thus improve quality of care and, in reducing the number of trips to an office, increase patient satisfaction.
Many people use or are familiar with the programs Skype and FaceTime (audiovideo chat software), and I envision that our postpartum task force will recommend using such programs for follow-up appointments. For each visit, the question to ask is whether the patient really needs to meet with her physician in person, or can she stay with her new baby and receive postpartum counseling at home. I am excited about the potential of telehealth in obstetrics and gynecology. Our task force is exploring that potential.
Telehealth for both routine and specialized care
Dr. Brown: Specialized care applications are here. In a pilot program in Wisconsin, a colleague has been providing remote psychiatric care. Perhaps such a program can be used to follow up on patients with postpartum depression. In addition, other psychiatry colleagues have long been using telehealth for adolescent behavior follow-ups, and we can do this too.
Another colleague has been performing remote perinatal follow-up for children with congenital anomalies. The physician interacts with the parent or parents as well as the patient. This seems to represent only the tip of the iceberg of what can be done in terms of follow-up.
We can also use telehealth in infertility settings. High-risk patients can benefit, too. Our guidelines say patients with preeclampsia should be seen within 3 days to 1 week. Many are transferred from low-access hospitals to our office. This follow-up, however, also can be done remotely, with patients at health department clinics or even at home. Reporting blood pressure readings and health-related feelings to a physician during a teleconsultation removes driving as a potential inconvenience or obstacle.
Telemedicine can be advantageous in gynecology. Physicians are doing important work with telecolposcopy as a follow-up to abnormal Pap test findings in patients in sub-Saharan Africa.
Routine wound care, which is commonly needed, can be performed in the home by a home health nurse telecommunicating with a physician. I can see broad telehealth use, and indeed our dermatology colleagues have been practicing telemedicine for quite some time.
Read about solving financial barriers and physician shortages.
An affordable solution to financial barriers and physician shortages
Dr. Nielsen: Telehealth can reduce barriers to care. For example, knowing that our teleconsultation services are covered by insurance, referring physicians and patients are more likely to try them and continue to use them. Payers are on board as well. Other barriers can be harder to overcome, particularly for patients at risk for complex diagnoses and medical decisions. Our pilot program, however, has demonstrated success in this area. It has provided safe, high-quality imaging, accurate diagnoses, productive discussions, and helpful management recommendations.
Telehealth also helps address relative and absolute physician shortages. In some areas, a relative shortage may indicate misdistribution. In other areas, specialists simply are too few in number. This absolute shortage of specialists likely will increase, as many communities are too small to sustain and support having them in person.
Outpatients can obtain care 5 days a week with telemedicine, as opposed to only 1 to 3 times a month in person. Physicians travel to remote clinics that are staffed only 1 or 2 days a month. Where the window for care is so small, patients and physicians are likely to turn to telemedicine. In addition, that utility results in better use of resources. For example, studies that were performed earlier would not need to be repeated, since you could access centrally located archives.
Related article:
ICD-10-CM code changes: What's new for 2018
Dr. Brown: For teleconsultations and televisits, all that payers need do is modify the billing codes they use for our usual services. Once that is done, payers can develop a payment model that works for both themselves and the teleconsultants.
The US health care system is fragmented. Health care is provided in various facilities, including federally qualified health centers and health department clinics. As Dr. Nielsen said, physicians travel to remote facilities once or twice a week or even a month, whereas telehealth can be offered 5 days a week. Many residents go to remote clinics, where an attending physician is required. Instead of an attending driving there, he or she could be teleconsulting—interacting with residents and patients from afar. So, telehealth is a win-win situation. It increases access to physicians and facilitates appropriate interactions with them, wherever they are. Telehealth can be an important contribution to developing a more effective health care delivery system than the fragmented one we have now.
Effective health care delivery is so important for obstetrics and gynecology, and the reported workforce challenges are real. A maternal-fetal medicine physician is unlikely to travel to remote communities once a week or even every 2 weeks, but that same physician can teleconsult multiple days each week.
How telehealth can close service gaps
Dr. Brown: Having established relationships with physicians in other clinics and communities paves the way for teleconsultation and remote supervision. Technology can help Planned Parenthood and other clinics continue to provide contraceptive counseling and other health care services. Even medical abortions can be supervised through teleconsultation.
With funds to Medicaid being cut, with the potential for Planned Parenthood to be defunded, physicians must think of ways they can continue to provide care to all patients and communities. By addressing these issues now, we will be ready to take charge of patient care, wherever it is needed.
But, we need partners, no question. We need hospital partners in all communities, and especially in rural communities. Rural hospitals and maternity care are at risk. Health care in rural communities faces many challenges. Telehealth, teleconferencing, and teleconsultation not only can improve access to services, but also can curb travel costs as well as costs to the communities and hospitals.
Who pays the operating costs, and who benefits
Dr. Brown: Payers are already discovering that teleconsultations are as billable as in-person visits. In addition, physicians are realizing that remote consultation can work as well as in-person consultation, with its own merits and advantages. Education is key—education about billing and about what is doable in telehealth. We can learn from colleagues in other specialties.
Dr. Nielsen: Several entities and groups must start covering the technology costs. Federal and state entities need to determine how the country’s information infrastructure can be improved to give rural areas access to high-quality, high-speed, wide-bandwidth communications, which will help expand telehealth and increase other industries’ opportunities to grow and sustain these communities. Improving the infrastructure also can help keep rural areas sustainable.
Health care systems themselves can join federal, state, and local governments in building this infrastructure. They can also start identifying opportunities to support and sustain physicians and hospitals in smaller towns and start combating the perception that the infrastructure is being developed only to migrate patients over to accessing their care through telehealth provided by physicians in the larger cities.
Many payers see telehealth as improving access and outcomes and already support it, but more payers need to become involved. All need to understand how routine and complex consultations, even inpatient consultations, can be performed remotely and can be properly reimbursed, and incentivized with payments for improved outcomes and value.
As barriers fall and telehealth improves, acceptance by patients and physicians will increase. In addition, telehealth will enter medical education in a significant way. The instruction that students, residents, and Fellows receive will be enhanced by new telehealth approaches in various specialties, and residents will come out of these programs with telehealth experience and a sense of both financial benefits and payment structures. This early exposure will pique their interest in using telehealth and advocating its use where it may never before have been considered, owing to real and perceived barriers.
Read about telehealth solutions for ObGyns.
Learning from other specialties and agencies
Dr. Brown: The physician shortage negatively affects access to health care in rural areas. Many city and suburban physicians, including ObGyns, want to stay where they are. Education is needed to show them that a rural practice can be successful. They would have a good patient base and be able to use telehealth to improve care and maintain contact with tertiary care centers.
Several task force members have described their experience within their health systems, and we hope to borrow from that. A health system in South Dakota received a Health Resources and Services Administration grant to use telehealth and teleconsultation in the Indian Health Service (IHS). To women who access their health care through the IHS, being able to remain in the community is culturally important. Telehealth and teleconsultation bring care to these women where they live.
To develop the best telehealth and teleconsultation model, we are borrowing from these health systems and from the experience of our colleagues in dermatology, behavioral health, psychiatry, and other disciplines. These physicians already have overcome many hurdles and discovered the importance of patient satisfaction in providing remote health care.
Patients will benefit in various ways, and here is another example: A clinic refers a patient to an ObGyn to discuss whether it is possible to have a vaginal birth after a cesarean delivery. The drive to the ObGyn’s office takes an hour, but the patient just as easily could have had all her questions answered during a teleconsultation.
Related articles:
Telehealth and you (4-part audiocast)
Telehealth recommendations for ObGyns
Dr. Brown: Our task force will develop recommended best practices for telehealth. We will outline how a practice can engage with telehealth and will address licensing requirements, as a practice must be licensed in each state where it uses telehealth. Our goal is to help our specialty get started in telehealth and telemedicine.
In practices with telehealth, it will be incumbent on ObGyns to identify any barriers to care. For example, we are concerned about early discontinuation of breastfeeding, particularly among African American communities. Fortunately, we have learned that video chat follow-ups can help improve breastfeeding continuation rates.
It also will be incumbent on ObGyns to think differently about how best to follow up. For a patient who calls to say she thinks she has mastitis, much of the consultation can be handled by telephone or video conference with the physician and a nurse practi‑tioner, and then medication can be prescribed without the need for in-person follow-up. We must then determine how to ensure these follow-up methods are compensated.
Direct-to-patient virtual visits
- Virtual home visits
- Low-risk pregnancy
- Postpartum visits
- Lactation support
- Routine gynecologic care
- Postoperative follow-up
Remote patient monitoring
- Chronic disease management
- Antenatal testing
- Fetal heart rate monitoring
- Transfer of care
Final thoughts
Dr. Nielsen: It is time for all US health care players to more seriously and aggressively consider how telehealth can improve health care access, quality, and safety. Even more important, patients and physicians in small communities need to feel that they can access specialists and care that is as good as those available in larger communities without having to pull up stakes and move.
Telehealth can help small communities become sustainable over the long term. As the majority of the people in this country are born in and receive health care in community hospitals, not large tertiary care centers, the state of US health care should be measured by the ability to provide as much care as is technically possible in the small communities where patients live and work and raise their kids.
Dr. Brown: More than 50% of all babies are born in hospitals where fewer than 1,000 deliveries are performed, and almost 40% are born in hospitals where fewer than 500 are performed. To provide high-level care and have patients feel comfortable, to improve morbidity and mortality, we need telehealth and telemedicine.
If I can help a physician in East Africa place a Bakri balloon for postpartum hemorrhaging, surely I can help a physician in rural areas of Wyoming, South Dakota, or North Carolina deal with this obstetric emergency. In obstetrics and gynecology, telehealth and telemedicine have great potential in terms of morbidity and mortality, but we are also doing genetic counseling and a great deal of patient follow-up, and so much more can be done.
That is the key, and the reason for the training, the task force, the deliberations, and the best practices model that we will be sharing with our colleagues.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
I recently spoke with 2 outstanding leaders in our field, members of the American College of Obstetricians and Gynecologists (ACOG) task force on telehealth and telemedicine, about the future of providing health care to women in remote locations.
Haywood Brown, MD, is President of ACOG for 2017–2018 and is F. Bayard Carter Professor of Obstetrics and Gynecology at Duke University Medical Center in Durham, North Carolina, and Peter Nielsen, MD, is Professor and Vice Chair of the Department of Obstetrics and Gynecology at Baylor College of Medicine in Houston, Texas, and Obstetrician-in-Chief at Children’s Hospital of San Antonio. Dr. Nielsen is a retired US Army colonel.
Why an ACOG telehealth task force?
Haywood Brown, MD: Our overall goals in telehealth and telemedicine are to coordinate and better facilitate the health care of women in remote locations and to improve maternal morbidity and mortality. Telehealth can be used on both an outpatient and an inpatient basis.
Outpatient telehealth is used for consultations. In maternal-fetal medicine, for instance, we use it for ultrasonography consultations. I also have used telehealth technology to “see” a pregnant patient with type 1diabetes. During our sessions, I managed her blood sugar levels and did all the other things I would have done if we had been together at my clinic. Without telehealth technology, however, this patient would have needed to drive 4 hours round-trip for each appointment.
Our colleagues in rural communities and at lower-level hospitals can use telehealth and telemedicine as aids in treating their high-risk patients, such as those with preeclampsia, prematurity risk, or other conditions. Physicians can consult with specialists through a face-to-face conversation that takes place through telecommunications. The result is that the quality of care for women in our communities is improved.
Genetic counseling, infertility consultation, and fetal anomaly management are some of the other applications. Our task force is discussing different ways to improve patient care and ways to collaborate with our colleagues around the country. Ultimately, we are developing best practices—a model for the best uses of technology to improve women’s health care in the United States.
Task force focus: Telehealth technology, billing, services
Dr. Brown: Our task force, a diverse group of members from all over the country, represents the spectrum of ObGyns. Although task force members have various levels of telehealth experience, all are very interested in these new channels of communication. The task force also includes billers, who understand billing ramifications, and payers, who know firsthand what will and will not be paid.
Technology and its availability is the most important topic for the task force. While some communities have Internet service, not all do. We need to determine which areas need service, how much it would cost, and who pays for it. Can a hospital afford it? A practice? Their partners? Identifying partners in tertiary care settings is a task force goal.
We are engaging a broad range of experts to study all the components and associated costs of technology, licensing, and cross-state credentialing. Gathering this information will help in developing a best practices model that general ObGyns can use.
Telehealth is redefining aspects of care: prenatal care (how many visits are required?), postpartum care, and other types of services that can be done remotely. Genetic counseling—who can provide it, what education is required—is another topic of discussion. Once we surmount the billing obstacles, we can do much with teleconferencing, such as provide genetic consultation with ObGyns in various settings.
The terms "telehealth" and "telemedicine" are often used interchangeably. Telemedicine is the older phrase, while telehealth entered the vernacular more recently and encompasses a broader definition.
The HealthIT.gov website explains the differences in terminology this way1:
- The Health Resources Services Administration defines telehealth as the use of electronic information and telecommunications technologies to support long-distance clinical health care, patient and professional health-related education, public health and health administration. Technologies include videoconferencing, the Internet, store-and-forward imaging, streaming media, and terrestrial and wireless communications.
- Telehealth is different from telemedicine because it refers to a broader scope of remote health care services than telemedicine. While telemedicine refers specifically to remote clinical services, telehealth can refer to remote nonclinical services, such as provider training, administrative meetings, and continuing medical education, in addition to clinical services.
A World Health Organization report, however, uses the 2 terms synonymously and interchangeably, defining telemedicine as2:
- The delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interests of advancing the health of individuals and their communities.
The American Telemedicine Association (ATA) describes their use of the terms this way3:
- ATA largely views telemedicine and telehealth to be interchangeable terms, encompassing a wide definition of remote healthcare, although telehealth may not always involve clinical care.
References
- HealthIT.gov website. Frequently asked questions. https://www.healthit.gov/providers-professionals/frequently-asked-questions/485. Accessed November 15, 2017.
- World Health Organization. Telemedicine: opportunities and developments in member states. 2010. http://www.who.int/goe/publications/goe_telemedicine_2010.pdf. Accessed November 15, 2017.
- American Telemedicine Association. About telemedicine: the ultimate frontier for superior healthcare delivery. http://www.americantelemed.org/about/about-telemedicine. Accessed November 15, 2017.
Learn about ways clinicians can use telemedicine.
Making progress in rural and underserved communities
Peter Nielsen, MD: When we saw that some high-risk obstetrics patients were having a difficult time getting to our downtown San Antonio office—the trip from surrounding communities was taking too long, or city driving and parking were stressful or too costly—we looked to improve access to care. Collaborating with a health care network that has a hospital in a town north of San Antonio, we set up a pilot program to provide telemedicine perinatal consultation services.
In this kind of service, which occurs entirely in real time, ultrasound images taken at the hospital are streamed by high-speed fiberoptic cable to our office, where a maternal-fetal medicine physician views them. If a repeat image or a different image is needed, the physician requests another scan. Linked to the physician and listening through an earpiece, the ultrasonographer performs the new scan with little delay and without disturbing the patient. The conversation between physician and ultrasonographer is private.
After ultrasound scanning is complete, the patient goes to a private room at the hospital for a video conference with our physician in San Antonio, who has reviewed the images in the PACS (picture archiving and communication system) or ultrasound recording system. They discuss the images, the findings, and the follow-up.
We tested the technology during a 6-month pilot program to make sure it worked at the highest quality and safety levels. Then the program went live and we started seeing patients remotely. Now we have a robust telemedicine training capability at that hospital outside San Antonio, and we are looking to expand to other south and west Texas areas, some even farther from our office.
I have done some of these remote consultations. In response to my informal queries about the experience, patients said that no one else was offering it, and they were participating for the first time. Naturally they had questions and concerns. Nevertheless, patients, family members, and the ultrasonographer and physicians in the communities seem to think this is a high-quality, safe program that makes it easier for patients to access health care.
Patients uniformly describe these consultations in positive terms. They do not have to drive far, into the city, and deal with traffic; parking is easy and free; and less travel means much less time off from work. Given these very practical advantages, patients are interested in having more appointments done remotely. In addition, they say the appointment itself is easy, being there is effortless, and they feel their physician is sitting in the same room. It is like video chatting with family members—they are comfortable with the technology.
Related article:
Landmark women’s health care remains law of the land
The patients’ perspective
Dr. Brown: Patient satisfaction is an important issue. In psychiatry, dermatology, and other disciplines, patients have indicated that they are very satisfied with telehealth sessions. Telehealth in obstetrics and gynecology, I think, will receive similar positive feedback.
The issue of driving distance led us to reconsider the number of face-to-face prenatal visits a normal, healthy patient needs. These days, a patient can use a prenatal care app to track her weight and blood pressure and send the data to her physician. Besides being convenient, these monitoring apps can give a patient an important sense of control. Our pilot programs found that a patient who self-monitors understands her weight gain better and is more in tune with it. Apps and other technologies can thus improve quality of care and, in reducing the number of trips to an office, increase patient satisfaction.
Many people use or are familiar with the programs Skype and FaceTime (audiovideo chat software), and I envision that our postpartum task force will recommend using such programs for follow-up appointments. For each visit, the question to ask is whether the patient really needs to meet with her physician in person, or can she stay with her new baby and receive postpartum counseling at home. I am excited about the potential of telehealth in obstetrics and gynecology. Our task force is exploring that potential.
Telehealth for both routine and specialized care
Dr. Brown: Specialized care applications are here. In a pilot program in Wisconsin, a colleague has been providing remote psychiatric care. Perhaps such a program can be used to follow up on patients with postpartum depression. In addition, other psychiatry colleagues have long been using telehealth for adolescent behavior follow-ups, and we can do this too.
Another colleague has been performing remote perinatal follow-up for children with congenital anomalies. The physician interacts with the parent or parents as well as the patient. This seems to represent only the tip of the iceberg of what can be done in terms of follow-up.
We can also use telehealth in infertility settings. High-risk patients can benefit, too. Our guidelines say patients with preeclampsia should be seen within 3 days to 1 week. Many are transferred from low-access hospitals to our office. This follow-up, however, also can be done remotely, with patients at health department clinics or even at home. Reporting blood pressure readings and health-related feelings to a physician during a teleconsultation removes driving as a potential inconvenience or obstacle.
Telemedicine can be advantageous in gynecology. Physicians are doing important work with telecolposcopy as a follow-up to abnormal Pap test findings in patients in sub-Saharan Africa.
Routine wound care, which is commonly needed, can be performed in the home by a home health nurse telecommunicating with a physician. I can see broad telehealth use, and indeed our dermatology colleagues have been practicing telemedicine for quite some time.
Read about solving financial barriers and physician shortages.
An affordable solution to financial barriers and physician shortages
Dr. Nielsen: Telehealth can reduce barriers to care. For example, knowing that our teleconsultation services are covered by insurance, referring physicians and patients are more likely to try them and continue to use them. Payers are on board as well. Other barriers can be harder to overcome, particularly for patients at risk for complex diagnoses and medical decisions. Our pilot program, however, has demonstrated success in this area. It has provided safe, high-quality imaging, accurate diagnoses, productive discussions, and helpful management recommendations.
Telehealth also helps address relative and absolute physician shortages. In some areas, a relative shortage may indicate misdistribution. In other areas, specialists simply are too few in number. This absolute shortage of specialists likely will increase, as many communities are too small to sustain and support having them in person.
Outpatients can obtain care 5 days a week with telemedicine, as opposed to only 1 to 3 times a month in person. Physicians travel to remote clinics that are staffed only 1 or 2 days a month. Where the window for care is so small, patients and physicians are likely to turn to telemedicine. In addition, that utility results in better use of resources. For example, studies that were performed earlier would not need to be repeated, since you could access centrally located archives.
Related article:
ICD-10-CM code changes: What's new for 2018
Dr. Brown: For teleconsultations and televisits, all that payers need do is modify the billing codes they use for our usual services. Once that is done, payers can develop a payment model that works for both themselves and the teleconsultants.
The US health care system is fragmented. Health care is provided in various facilities, including federally qualified health centers and health department clinics. As Dr. Nielsen said, physicians travel to remote facilities once or twice a week or even a month, whereas telehealth can be offered 5 days a week. Many residents go to remote clinics, where an attending physician is required. Instead of an attending driving there, he or she could be teleconsulting—interacting with residents and patients from afar. So, telehealth is a win-win situation. It increases access to physicians and facilitates appropriate interactions with them, wherever they are. Telehealth can be an important contribution to developing a more effective health care delivery system than the fragmented one we have now.
Effective health care delivery is so important for obstetrics and gynecology, and the reported workforce challenges are real. A maternal-fetal medicine physician is unlikely to travel to remote communities once a week or even every 2 weeks, but that same physician can teleconsult multiple days each week.
How telehealth can close service gaps
Dr. Brown: Having established relationships with physicians in other clinics and communities paves the way for teleconsultation and remote supervision. Technology can help Planned Parenthood and other clinics continue to provide contraceptive counseling and other health care services. Even medical abortions can be supervised through teleconsultation.
With funds to Medicaid being cut, with the potential for Planned Parenthood to be defunded, physicians must think of ways they can continue to provide care to all patients and communities. By addressing these issues now, we will be ready to take charge of patient care, wherever it is needed.
But, we need partners, no question. We need hospital partners in all communities, and especially in rural communities. Rural hospitals and maternity care are at risk. Health care in rural communities faces many challenges. Telehealth, teleconferencing, and teleconsultation not only can improve access to services, but also can curb travel costs as well as costs to the communities and hospitals.
Who pays the operating costs, and who benefits
Dr. Brown: Payers are already discovering that teleconsultations are as billable as in-person visits. In addition, physicians are realizing that remote consultation can work as well as in-person consultation, with its own merits and advantages. Education is key—education about billing and about what is doable in telehealth. We can learn from colleagues in other specialties.
Dr. Nielsen: Several entities and groups must start covering the technology costs. Federal and state entities need to determine how the country’s information infrastructure can be improved to give rural areas access to high-quality, high-speed, wide-bandwidth communications, which will help expand telehealth and increase other industries’ opportunities to grow and sustain these communities. Improving the infrastructure also can help keep rural areas sustainable.
Health care systems themselves can join federal, state, and local governments in building this infrastructure. They can also start identifying opportunities to support and sustain physicians and hospitals in smaller towns and start combating the perception that the infrastructure is being developed only to migrate patients over to accessing their care through telehealth provided by physicians in the larger cities.
Many payers see telehealth as improving access and outcomes and already support it, but more payers need to become involved. All need to understand how routine and complex consultations, even inpatient consultations, can be performed remotely and can be properly reimbursed, and incentivized with payments for improved outcomes and value.
As barriers fall and telehealth improves, acceptance by patients and physicians will increase. In addition, telehealth will enter medical education in a significant way. The instruction that students, residents, and Fellows receive will be enhanced by new telehealth approaches in various specialties, and residents will come out of these programs with telehealth experience and a sense of both financial benefits and payment structures. This early exposure will pique their interest in using telehealth and advocating its use where it may never before have been considered, owing to real and perceived barriers.
Read about telehealth solutions for ObGyns.
Learning from other specialties and agencies
Dr. Brown: The physician shortage negatively affects access to health care in rural areas. Many city and suburban physicians, including ObGyns, want to stay where they are. Education is needed to show them that a rural practice can be successful. They would have a good patient base and be able to use telehealth to improve care and maintain contact with tertiary care centers.
Several task force members have described their experience within their health systems, and we hope to borrow from that. A health system in South Dakota received a Health Resources and Services Administration grant to use telehealth and teleconsultation in the Indian Health Service (IHS). To women who access their health care through the IHS, being able to remain in the community is culturally important. Telehealth and teleconsultation bring care to these women where they live.
To develop the best telehealth and teleconsultation model, we are borrowing from these health systems and from the experience of our colleagues in dermatology, behavioral health, psychiatry, and other disciplines. These physicians already have overcome many hurdles and discovered the importance of patient satisfaction in providing remote health care.
Patients will benefit in various ways, and here is another example: A clinic refers a patient to an ObGyn to discuss whether it is possible to have a vaginal birth after a cesarean delivery. The drive to the ObGyn’s office takes an hour, but the patient just as easily could have had all her questions answered during a teleconsultation.
Related articles:
Telehealth and you (4-part audiocast)
Telehealth recommendations for ObGyns
Dr. Brown: Our task force will develop recommended best practices for telehealth. We will outline how a practice can engage with telehealth and will address licensing requirements, as a practice must be licensed in each state where it uses telehealth. Our goal is to help our specialty get started in telehealth and telemedicine.
In practices with telehealth, it will be incumbent on ObGyns to identify any barriers to care. For example, we are concerned about early discontinuation of breastfeeding, particularly among African American communities. Fortunately, we have learned that video chat follow-ups can help improve breastfeeding continuation rates.
It also will be incumbent on ObGyns to think differently about how best to follow up. For a patient who calls to say she thinks she has mastitis, much of the consultation can be handled by telephone or video conference with the physician and a nurse practi‑tioner, and then medication can be prescribed without the need for in-person follow-up. We must then determine how to ensure these follow-up methods are compensated.
Direct-to-patient virtual visits
- Virtual home visits
- Low-risk pregnancy
- Postpartum visits
- Lactation support
- Routine gynecologic care
- Postoperative follow-up
Remote patient monitoring
- Chronic disease management
- Antenatal testing
- Fetal heart rate monitoring
- Transfer of care
Final thoughts
Dr. Nielsen: It is time for all US health care players to more seriously and aggressively consider how telehealth can improve health care access, quality, and safety. Even more important, patients and physicians in small communities need to feel that they can access specialists and care that is as good as those available in larger communities without having to pull up stakes and move.
Telehealth can help small communities become sustainable over the long term. As the majority of the people in this country are born in and receive health care in community hospitals, not large tertiary care centers, the state of US health care should be measured by the ability to provide as much care as is technically possible in the small communities where patients live and work and raise their kids.
Dr. Brown: More than 50% of all babies are born in hospitals where fewer than 1,000 deliveries are performed, and almost 40% are born in hospitals where fewer than 500 are performed. To provide high-level care and have patients feel comfortable, to improve morbidity and mortality, we need telehealth and telemedicine.
If I can help a physician in East Africa place a Bakri balloon for postpartum hemorrhaging, surely I can help a physician in rural areas of Wyoming, South Dakota, or North Carolina deal with this obstetric emergency. In obstetrics and gynecology, telehealth and telemedicine have great potential in terms of morbidity and mortality, but we are also doing genetic counseling and a great deal of patient follow-up, and so much more can be done.
That is the key, and the reason for the training, the task force, the deliberations, and the best practices model that we will be sharing with our colleagues.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.