User login
Study supports wider use of dried blood samples
Researchers have found evidence to suggest that dried blood samples may sometimes be a suitable alternative to conventional blood sampling.
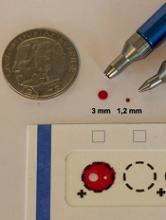
The team measured levels of 92 proteins in millimeter-sized circles punched out of dried blood samples.
They found that, in many cases, little happens to these proteins when they are allowed to dry.
Most of the proteins remain unaltered after 30 years, or they change only minimally.
However, the proteins can be affected by storage temperatures.
Still, the researchers believe these results suggest dried blood samples could be used more widely—for routine health checks and to set up large-scale biobanks, with patients collecting the blood samples themselves.
“[Y]ou can prick your own finger and send in a dried blood spot by post,” study author Ulf Landegren, MD, PhD, of Uppsala University in Sweden.
“[A]t a minimal cost, it will be possible to build gigantic biobanks of samples obtained on a routine clinical basis. This means that samples can be taken before the clinical debut of a disease to identify markers of value for early diagnosis, improving the scope for curative treatment.”
Dr Landegren and his colleagues discussed these possibilities in a paper published in Molecular and Cellular Proteomics.
The researchers analyzed dried blood samples, measuring levels of 92 proteins that are relevant in oncology. To determine the effects of long-term storage, the team examined what happens to protein detection as an effect of the drying process.
Some of the dried blood samples analyzed had been collected recently, while others had been preserved for up to 30 years in biobanks in Sweden and Denmark. These 2 biobanks keep their dried blood samples at different temperatures: the Swedish one at +4°C and the Danish one at -24°C.
The researchers also looked at wet plasma samples kept at -70°C for corresponding periods of time.
“Our conclusion is that we can measure levels of 92 proteins with very high precision and sensitivity using PEA [proximity extension assay] technology in the tiny, punched-out discs from a dried blood spot,” said study author Johan Björkesten, a doctoral student at Uppsala University.
“The actual drying process has a negligible effect on the various proteins, and the effect is reproducible, which means that it can be included in the calculation.”
The researchers did find that long-term storage affects the detectability of certain proteins more than others.
Most proteins remain completely intact after 30 years or exhibit minimal changes. However, levels of some proteins decrease so that half the quantity remains after a period of between 10 and 50 years.
The researchers also found that a relatively low storage temperature is preferable for proteins that are affected by storage.
Protein detection was less affected when dried blood samples were stored at -24°C than when they were stored at +4°C. Over the 30-year period, detectability was not affected for 34% of proteins stored at +4°C and 76% of proteins stored at -24°C.
However, storing wet plasma at -70°C preserved proteins better than dried blood sample storage at -24°C. Detectability decreased for 5% of the proteins stored wet at -70°C for 45 years, compared to 24% for proteins in dried samples stored at -24°C for 30 years.
The researchers did note, though, that this part of their analysis was complicated by some confounding factors, so this was not a clear, direct comparison between wet and dry samples. ![]()
Researchers have found evidence to suggest that dried blood samples may sometimes be a suitable alternative to conventional blood sampling.
The team measured levels of 92 proteins in millimeter-sized circles punched out of dried blood samples.
They found that, in many cases, little happens to these proteins when they are allowed to dry.
Most of the proteins remain unaltered after 30 years, or they change only minimally.
However, the proteins can be affected by storage temperatures.
Still, the researchers believe these results suggest dried blood samples could be used more widely—for routine health checks and to set up large-scale biobanks, with patients collecting the blood samples themselves.
“[Y]ou can prick your own finger and send in a dried blood spot by post,” study author Ulf Landegren, MD, PhD, of Uppsala University in Sweden.
“[A]t a minimal cost, it will be possible to build gigantic biobanks of samples obtained on a routine clinical basis. This means that samples can be taken before the clinical debut of a disease to identify markers of value for early diagnosis, improving the scope for curative treatment.”
Dr Landegren and his colleagues discussed these possibilities in a paper published in Molecular and Cellular Proteomics.
The researchers analyzed dried blood samples, measuring levels of 92 proteins that are relevant in oncology. To determine the effects of long-term storage, the team examined what happens to protein detection as an effect of the drying process.
Some of the dried blood samples analyzed had been collected recently, while others had been preserved for up to 30 years in biobanks in Sweden and Denmark. These 2 biobanks keep their dried blood samples at different temperatures: the Swedish one at +4°C and the Danish one at -24°C.
The researchers also looked at wet plasma samples kept at -70°C for corresponding periods of time.
“Our conclusion is that we can measure levels of 92 proteins with very high precision and sensitivity using PEA [proximity extension assay] technology in the tiny, punched-out discs from a dried blood spot,” said study author Johan Björkesten, a doctoral student at Uppsala University.
“The actual drying process has a negligible effect on the various proteins, and the effect is reproducible, which means that it can be included in the calculation.”
The researchers did find that long-term storage affects the detectability of certain proteins more than others.
Most proteins remain completely intact after 30 years or exhibit minimal changes. However, levels of some proteins decrease so that half the quantity remains after a period of between 10 and 50 years.
The researchers also found that a relatively low storage temperature is preferable for proteins that are affected by storage.
Protein detection was less affected when dried blood samples were stored at -24°C than when they were stored at +4°C. Over the 30-year period, detectability was not affected for 34% of proteins stored at +4°C and 76% of proteins stored at -24°C.
However, storing wet plasma at -70°C preserved proteins better than dried blood sample storage at -24°C. Detectability decreased for 5% of the proteins stored wet at -70°C for 45 years, compared to 24% for proteins in dried samples stored at -24°C for 30 years.
The researchers did note, though, that this part of their analysis was complicated by some confounding factors, so this was not a clear, direct comparison between wet and dry samples. ![]()
Researchers have found evidence to suggest that dried blood samples may sometimes be a suitable alternative to conventional blood sampling.
The team measured levels of 92 proteins in millimeter-sized circles punched out of dried blood samples.
They found that, in many cases, little happens to these proteins when they are allowed to dry.
Most of the proteins remain unaltered after 30 years, or they change only minimally.
However, the proteins can be affected by storage temperatures.
Still, the researchers believe these results suggest dried blood samples could be used more widely—for routine health checks and to set up large-scale biobanks, with patients collecting the blood samples themselves.
“[Y]ou can prick your own finger and send in a dried blood spot by post,” study author Ulf Landegren, MD, PhD, of Uppsala University in Sweden.
“[A]t a minimal cost, it will be possible to build gigantic biobanks of samples obtained on a routine clinical basis. This means that samples can be taken before the clinical debut of a disease to identify markers of value for early diagnosis, improving the scope for curative treatment.”
Dr Landegren and his colleagues discussed these possibilities in a paper published in Molecular and Cellular Proteomics.
The researchers analyzed dried blood samples, measuring levels of 92 proteins that are relevant in oncology. To determine the effects of long-term storage, the team examined what happens to protein detection as an effect of the drying process.
Some of the dried blood samples analyzed had been collected recently, while others had been preserved for up to 30 years in biobanks in Sweden and Denmark. These 2 biobanks keep their dried blood samples at different temperatures: the Swedish one at +4°C and the Danish one at -24°C.
The researchers also looked at wet plasma samples kept at -70°C for corresponding periods of time.
“Our conclusion is that we can measure levels of 92 proteins with very high precision and sensitivity using PEA [proximity extension assay] technology in the tiny, punched-out discs from a dried blood spot,” said study author Johan Björkesten, a doctoral student at Uppsala University.
“The actual drying process has a negligible effect on the various proteins, and the effect is reproducible, which means that it can be included in the calculation.”
The researchers did find that long-term storage affects the detectability of certain proteins more than others.
Most proteins remain completely intact after 30 years or exhibit minimal changes. However, levels of some proteins decrease so that half the quantity remains after a period of between 10 and 50 years.
The researchers also found that a relatively low storage temperature is preferable for proteins that are affected by storage.
Protein detection was less affected when dried blood samples were stored at -24°C than when they were stored at +4°C. Over the 30-year period, detectability was not affected for 34% of proteins stored at +4°C and 76% of proteins stored at -24°C.
However, storing wet plasma at -70°C preserved proteins better than dried blood sample storage at -24°C. Detectability decreased for 5% of the proteins stored wet at -70°C for 45 years, compared to 24% for proteins in dried samples stored at -24°C for 30 years.
The researchers did note, though, that this part of their analysis was complicated by some confounding factors, so this was not a clear, direct comparison between wet and dry samples. ![]()
EC grants drug orphan designation for AML
The European Commission (EC) has granted orphan designation to GMI-1271 for the treatment of acute myeloid leukemia (AML).
GMI-1271 is an E-selectin antagonist being developed by GlycoMimetics, Inc.
The product also has orphan designation, fast track designation, and breakthrough therapy designation in the US.
GMI-1271 is currently being evaluated in a phase 1/2 trial of patients with relapsed or refractory AML and patients age 60 and older with newly diagnosed AML.
The patients are receiving GM-1271 in combination with chemotherapy. The relapsed/refractory group is receiving mitoxantrone, etoposide, and cytarabine. The newly diagnosed patients are receiving cytarabine and idarubicin (7+3).
GlycoMimetics plans to present data from this trial at the 2017 American Society of Clinical Oncology (ASCO) Annual Meeting as abstracts 2520 and 2560.
The company also plans to present the research at the 22nd Congress of the European Hematology Association (EHA) as abstracts P547 and P203.
About orphan designation
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure.
The European Medicines Agency adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the EC for a final decision. The EC typically makes a decision within 30 days of that submission. ![]()
The European Commission (EC) has granted orphan designation to GMI-1271 for the treatment of acute myeloid leukemia (AML).
GMI-1271 is an E-selectin antagonist being developed by GlycoMimetics, Inc.
The product also has orphan designation, fast track designation, and breakthrough therapy designation in the US.
GMI-1271 is currently being evaluated in a phase 1/2 trial of patients with relapsed or refractory AML and patients age 60 and older with newly diagnosed AML.
The patients are receiving GM-1271 in combination with chemotherapy. The relapsed/refractory group is receiving mitoxantrone, etoposide, and cytarabine. The newly diagnosed patients are receiving cytarabine and idarubicin (7+3).
GlycoMimetics plans to present data from this trial at the 2017 American Society of Clinical Oncology (ASCO) Annual Meeting as abstracts 2520 and 2560.
The company also plans to present the research at the 22nd Congress of the European Hematology Association (EHA) as abstracts P547 and P203.
About orphan designation
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure.
The European Medicines Agency adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the EC for a final decision. The EC typically makes a decision within 30 days of that submission. ![]()
The European Commission (EC) has granted orphan designation to GMI-1271 for the treatment of acute myeloid leukemia (AML).
GMI-1271 is an E-selectin antagonist being developed by GlycoMimetics, Inc.
The product also has orphan designation, fast track designation, and breakthrough therapy designation in the US.
GMI-1271 is currently being evaluated in a phase 1/2 trial of patients with relapsed or refractory AML and patients age 60 and older with newly diagnosed AML.
The patients are receiving GM-1271 in combination with chemotherapy. The relapsed/refractory group is receiving mitoxantrone, etoposide, and cytarabine. The newly diagnosed patients are receiving cytarabine and idarubicin (7+3).
GlycoMimetics plans to present data from this trial at the 2017 American Society of Clinical Oncology (ASCO) Annual Meeting as abstracts 2520 and 2560.
The company also plans to present the research at the 22nd Congress of the European Hematology Association (EHA) as abstracts P547 and P203.
About orphan designation
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure.
The European Medicines Agency adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the EC for a final decision. The EC typically makes a decision within 30 days of that submission. ![]()
President’s budget: Malpractice reform but deep health care cuts
President Trump’s proposed budget for fiscal 2018 could mean crushing blows for some of the nation’s largest health care programs, if it makes it through Congress.
The proposed budget “clearly reflects the priorities of the Trump administration, which is to cut taxes, to increase defense spending and spending on boarder security, and also to cut domestic spending,” Timothy S. Jost, a health law professor at Washington and Lee University in Lexington, Va., said in an interview*.
The proposed CHIP reduction would eliminate the increased federal match provided by the Affordable Care Act and cap eligibility for federal CHIP funding at 250% of the federal poverty level, according to a summary of the proposal by the Kaiser Family Foundation. States would be able to transfer children in families with incomes below 133% of the poverty line who were moved from CHIP to Medicaid under the ACA back to CHIP.
If the cuts are approved, physicians face the challenge of caring for more uninsured and underinsured patients, said John D. Abramson, MD, a family physician and health policy lecturer at Harvard Medical School in Boston. He notes that the budget’s proposed Medicaid cuts come on top of Medicaid reductions included in the AHCA.
Meanwhile, the Food and Drug Administration stands to lose $850 million for 2018 through the budget, although medical product user fees would increase, resulting in a program increase of about $450 million. The President proposes to cut CDC funds by $1.3 billion and withdraw $252 million in funding from the Substance Abuse and Mental Health Services Administration. The cuts and savings are further outlined in a U.S. Department of Health & Human Services budget summary.
The cuts to mental health care funding would no doubt affect mental health care providers and the patients they seek to treat, Mr. Jost said. “Given the seriousness of the opioid crisis, it doesn’t seem like a great time to be cutting funding for substance abuse treatment.”
Medical research may also suffer under the proposed budget. The President intends to cut funding for the National Institutes of Health by $5.8 billion, while eliminating the Agency for Health Care Research and Quality as a stand alone agency and folding it into the NIH with less funding.
The American Association for the Advancement of Science expressed concern that the research cuts could devastate the country’s science and technology enterprise and weaken the nation’s economic growth.
“Slashing funding of critically important federal agencies threatens our nation’s ability to advance cures for disease, develop new energy technologies, improve public health, train the next generation of scientists and engineers and grow the American economy,” Rush Holt, association CEO said in a statement.
Other proposals in the budget could be positive for health care, experts say.
IPAB “really hasn’t had any impact on health care over the past 7 years,” Dr. Ayanian said. ““That’s potentially one area of compromise as senators and representatives discuss ways in which the Affordable Care Act can be reformed.”
Medical malpractice reforms are also included in the proposed budget. The proposal includes a $250,000 cap on noneconomic damages, a 3-year statute of limitations, and an established safe harbor for clinicians following evidence-based clinical practice guidelines. The changes are estimated to save the federal government $55 billion over 10 years.
“That’s an area of frequent concern for practicing physicians,” Dr. Ayanian said. “To the extent that reforms can be developed that are acceptable to patients and physicians that create the right incentives for improving health care quality and avoiding medical errors, that could be a positive. It’ll depend very much on the reform proposals that are developed. I think there is potential for bipartisan agreement in this area.”
Ms. Carpenter stressed that the President’s budget is only the first step in a lengthy budget process that will include congressional hearings and debate before legislators draft budget resolutions. “I expect Congress to debate some of the cuts to domestic spending, including things like NIH. There seems to be a good bit of alignment in terms of repeal and replace of the [ACA] and potentially some of the Medicaid reforms.”
“Trump’s budget breaks his promise not to touch Social Security, which at its core is lifeline insurance for Americans who can no longer work, not just in retirement, but also due to a disability,” Sen. Wyden said in a statement. “It also slashes Medicaid by over $600 billion beyond the damage done by Trumpcare, further threatening pediatric care, the nursing home benefit, special education programs in schools, and other health care like substance misuse treatment.”
House Energy and Commerce Committee Chairman Greg Walden (R-Ore.) commended the budget proposal as one that demonstrates President Trump’s commitment to balancing the budget and responsibly prioritizing taxpayer dollars.
“The initiatives modernizing our energy infrastructure and promoting our nation’s energy abundance would undoubtedly make positive impacts on our constituents’ lives,” he said in a statement. “The president’s proposals show the difficult choices facing the country as we work to reduce the deficit, protect our security, and grow jobs.”
Additional proposals in the President’s budget include:
• Nearly $70 billion in cuts for Social Security disability benefits over the next 10 years.
• A funding increase for the Veterans Administration, including $29 billion over the next decade for a program that enables veterans to seek outside health services from private doctors.
• A ban on funds for clinics and medical centers that provide abortions, such as Planned Parenthood.
• A $70 million increase for Medicare and Medicaid fraud prevention efforts in 2018.
• A $114 million funding increase for the Center for Medicare and Medicaid Innovation.
agallegos@frontlinemedcom.com
On Twitter @legal_med
*This story was updated May 26, 2017
President Trump’s proposed budget for fiscal 2018 could mean crushing blows for some of the nation’s largest health care programs, if it makes it through Congress.
The proposed budget “clearly reflects the priorities of the Trump administration, which is to cut taxes, to increase defense spending and spending on boarder security, and also to cut domestic spending,” Timothy S. Jost, a health law professor at Washington and Lee University in Lexington, Va., said in an interview*.
The proposed CHIP reduction would eliminate the increased federal match provided by the Affordable Care Act and cap eligibility for federal CHIP funding at 250% of the federal poverty level, according to a summary of the proposal by the Kaiser Family Foundation. States would be able to transfer children in families with incomes below 133% of the poverty line who were moved from CHIP to Medicaid under the ACA back to CHIP.
If the cuts are approved, physicians face the challenge of caring for more uninsured and underinsured patients, said John D. Abramson, MD, a family physician and health policy lecturer at Harvard Medical School in Boston. He notes that the budget’s proposed Medicaid cuts come on top of Medicaid reductions included in the AHCA.
Meanwhile, the Food and Drug Administration stands to lose $850 million for 2018 through the budget, although medical product user fees would increase, resulting in a program increase of about $450 million. The President proposes to cut CDC funds by $1.3 billion and withdraw $252 million in funding from the Substance Abuse and Mental Health Services Administration. The cuts and savings are further outlined in a U.S. Department of Health & Human Services budget summary.
The cuts to mental health care funding would no doubt affect mental health care providers and the patients they seek to treat, Mr. Jost said. “Given the seriousness of the opioid crisis, it doesn’t seem like a great time to be cutting funding for substance abuse treatment.”
Medical research may also suffer under the proposed budget. The President intends to cut funding for the National Institutes of Health by $5.8 billion, while eliminating the Agency for Health Care Research and Quality as a stand alone agency and folding it into the NIH with less funding.
The American Association for the Advancement of Science expressed concern that the research cuts could devastate the country’s science and technology enterprise and weaken the nation’s economic growth.
“Slashing funding of critically important federal agencies threatens our nation’s ability to advance cures for disease, develop new energy technologies, improve public health, train the next generation of scientists and engineers and grow the American economy,” Rush Holt, association CEO said in a statement.
Other proposals in the budget could be positive for health care, experts say.
IPAB “really hasn’t had any impact on health care over the past 7 years,” Dr. Ayanian said. ““That’s potentially one area of compromise as senators and representatives discuss ways in which the Affordable Care Act can be reformed.”
Medical malpractice reforms are also included in the proposed budget. The proposal includes a $250,000 cap on noneconomic damages, a 3-year statute of limitations, and an established safe harbor for clinicians following evidence-based clinical practice guidelines. The changes are estimated to save the federal government $55 billion over 10 years.
“That’s an area of frequent concern for practicing physicians,” Dr. Ayanian said. “To the extent that reforms can be developed that are acceptable to patients and physicians that create the right incentives for improving health care quality and avoiding medical errors, that could be a positive. It’ll depend very much on the reform proposals that are developed. I think there is potential for bipartisan agreement in this area.”
Ms. Carpenter stressed that the President’s budget is only the first step in a lengthy budget process that will include congressional hearings and debate before legislators draft budget resolutions. “I expect Congress to debate some of the cuts to domestic spending, including things like NIH. There seems to be a good bit of alignment in terms of repeal and replace of the [ACA] and potentially some of the Medicaid reforms.”
“Trump’s budget breaks his promise not to touch Social Security, which at its core is lifeline insurance for Americans who can no longer work, not just in retirement, but also due to a disability,” Sen. Wyden said in a statement. “It also slashes Medicaid by over $600 billion beyond the damage done by Trumpcare, further threatening pediatric care, the nursing home benefit, special education programs in schools, and other health care like substance misuse treatment.”
House Energy and Commerce Committee Chairman Greg Walden (R-Ore.) commended the budget proposal as one that demonstrates President Trump’s commitment to balancing the budget and responsibly prioritizing taxpayer dollars.
“The initiatives modernizing our energy infrastructure and promoting our nation’s energy abundance would undoubtedly make positive impacts on our constituents’ lives,” he said in a statement. “The president’s proposals show the difficult choices facing the country as we work to reduce the deficit, protect our security, and grow jobs.”
Additional proposals in the President’s budget include:
• Nearly $70 billion in cuts for Social Security disability benefits over the next 10 years.
• A funding increase for the Veterans Administration, including $29 billion over the next decade for a program that enables veterans to seek outside health services from private doctors.
• A ban on funds for clinics and medical centers that provide abortions, such as Planned Parenthood.
• A $70 million increase for Medicare and Medicaid fraud prevention efforts in 2018.
• A $114 million funding increase for the Center for Medicare and Medicaid Innovation.
agallegos@frontlinemedcom.com
On Twitter @legal_med
*This story was updated May 26, 2017
President Trump’s proposed budget for fiscal 2018 could mean crushing blows for some of the nation’s largest health care programs, if it makes it through Congress.
The proposed budget “clearly reflects the priorities of the Trump administration, which is to cut taxes, to increase defense spending and spending on boarder security, and also to cut domestic spending,” Timothy S. Jost, a health law professor at Washington and Lee University in Lexington, Va., said in an interview*.
The proposed CHIP reduction would eliminate the increased federal match provided by the Affordable Care Act and cap eligibility for federal CHIP funding at 250% of the federal poverty level, according to a summary of the proposal by the Kaiser Family Foundation. States would be able to transfer children in families with incomes below 133% of the poverty line who were moved from CHIP to Medicaid under the ACA back to CHIP.
If the cuts are approved, physicians face the challenge of caring for more uninsured and underinsured patients, said John D. Abramson, MD, a family physician and health policy lecturer at Harvard Medical School in Boston. He notes that the budget’s proposed Medicaid cuts come on top of Medicaid reductions included in the AHCA.
Meanwhile, the Food and Drug Administration stands to lose $850 million for 2018 through the budget, although medical product user fees would increase, resulting in a program increase of about $450 million. The President proposes to cut CDC funds by $1.3 billion and withdraw $252 million in funding from the Substance Abuse and Mental Health Services Administration. The cuts and savings are further outlined in a U.S. Department of Health & Human Services budget summary.
The cuts to mental health care funding would no doubt affect mental health care providers and the patients they seek to treat, Mr. Jost said. “Given the seriousness of the opioid crisis, it doesn’t seem like a great time to be cutting funding for substance abuse treatment.”
Medical research may also suffer under the proposed budget. The President intends to cut funding for the National Institutes of Health by $5.8 billion, while eliminating the Agency for Health Care Research and Quality as a stand alone agency and folding it into the NIH with less funding.
The American Association for the Advancement of Science expressed concern that the research cuts could devastate the country’s science and technology enterprise and weaken the nation’s economic growth.
“Slashing funding of critically important federal agencies threatens our nation’s ability to advance cures for disease, develop new energy technologies, improve public health, train the next generation of scientists and engineers and grow the American economy,” Rush Holt, association CEO said in a statement.
Other proposals in the budget could be positive for health care, experts say.
IPAB “really hasn’t had any impact on health care over the past 7 years,” Dr. Ayanian said. ““That’s potentially one area of compromise as senators and representatives discuss ways in which the Affordable Care Act can be reformed.”
Medical malpractice reforms are also included in the proposed budget. The proposal includes a $250,000 cap on noneconomic damages, a 3-year statute of limitations, and an established safe harbor for clinicians following evidence-based clinical practice guidelines. The changes are estimated to save the federal government $55 billion over 10 years.
“That’s an area of frequent concern for practicing physicians,” Dr. Ayanian said. “To the extent that reforms can be developed that are acceptable to patients and physicians that create the right incentives for improving health care quality and avoiding medical errors, that could be a positive. It’ll depend very much on the reform proposals that are developed. I think there is potential for bipartisan agreement in this area.”
Ms. Carpenter stressed that the President’s budget is only the first step in a lengthy budget process that will include congressional hearings and debate before legislators draft budget resolutions. “I expect Congress to debate some of the cuts to domestic spending, including things like NIH. There seems to be a good bit of alignment in terms of repeal and replace of the [ACA] and potentially some of the Medicaid reforms.”
“Trump’s budget breaks his promise not to touch Social Security, which at its core is lifeline insurance for Americans who can no longer work, not just in retirement, but also due to a disability,” Sen. Wyden said in a statement. “It also slashes Medicaid by over $600 billion beyond the damage done by Trumpcare, further threatening pediatric care, the nursing home benefit, special education programs in schools, and other health care like substance misuse treatment.”
House Energy and Commerce Committee Chairman Greg Walden (R-Ore.) commended the budget proposal as one that demonstrates President Trump’s commitment to balancing the budget and responsibly prioritizing taxpayer dollars.
“The initiatives modernizing our energy infrastructure and promoting our nation’s energy abundance would undoubtedly make positive impacts on our constituents’ lives,” he said in a statement. “The president’s proposals show the difficult choices facing the country as we work to reduce the deficit, protect our security, and grow jobs.”
Additional proposals in the President’s budget include:
• Nearly $70 billion in cuts for Social Security disability benefits over the next 10 years.
• A funding increase for the Veterans Administration, including $29 billion over the next decade for a program that enables veterans to seek outside health services from private doctors.
• A ban on funds for clinics and medical centers that provide abortions, such as Planned Parenthood.
• A $70 million increase for Medicare and Medicaid fraud prevention efforts in 2018.
• A $114 million funding increase for the Center for Medicare and Medicaid Innovation.
agallegos@frontlinemedcom.com
On Twitter @legal_med
*This story was updated May 26, 2017
App Identifies Stress and Missed Sleep as Seizure Triggers
BOSTON—Research using an Apple Watch app to track seizures in people with epilepsy finds that common triggers include stress and missed sleep, according to a preliminary study presented at the 69th Annual Meeting of the American Academy of Neurology.
Gregory Krauss, MD, Professor of Neurology at Johns Hopkins University in Baltimore, and colleagues conducted the study to identify common seizure triggers and estimate their relative frequency in a US population of people with epilepsy. For the 10-month study, 598 people signed up to track their seizures with an app called EpiWatch that had been created using ResearchKit, a software framework designed by Apple to make it easy for researchers to gather data more frequently and more accurately from participants using an iPhone or Apple Watch.
When a participant felt a seizure aura starting, he or she opened the app. Using the Apple Watch's biosensors, EpiWatch recorded the participant's heart rate and movements for 10 minutes. The app asked him or her to perform tasks to test responsiveness. After the seizure ended, the participant was given a brief survey about seizure type, aura, loss of awareness, and possible seizure triggers.
"The data collected will help researchers better understand epilepsy, while helping people with epilepsy keep a more complete history of their seizures," said Dr. Krauss. "The app also provides helpful tracking of seizures, prescription medication use, and drug side effects--activities that are important in helping people manage their condition."
In all, 40% of the group tracked a total of 1,485 seizures, and 177 participants reported what triggered their seizures. Stress was the most common trigger and was linked to 37% of seizures. Participants also identified lack of sleep as a trigger for 18% of the seizures, menstruation for 12%, and overexertion for 11%. Other reported triggers included diet (9%), missed medications (7%), and fever or infection (6%). Demographics and seizure types were generally similar between participants who reported seizure triggers and those who did not. Seizure triggers did not vary by the type of seizure people had.
The investigators found that stress was more commonly reported as a trigger for participants who worked full-time (35%), compared with those who worked part-time (21%), were unemployed (27%), or were disabled (29%). Nonadherence to medication was reported slightly more frequently among younger participants (ie, ages 16 to 25), among whom 40% reported a missed medication as a trigger, compared with older participants (ie, ages 26 to 66), among whom 34% reported a missed medication.
"Seizures are very unpredictable," said Dr. Krauss. "Our eventual goal is to be able to use wearable technology to predict an oncoming seizure. This could potentially save lives, as well as give people with epilepsy more freedom. The data collected in this study help us take a step in that direction."
BOSTON—Research using an Apple Watch app to track seizures in people with epilepsy finds that common triggers include stress and missed sleep, according to a preliminary study presented at the 69th Annual Meeting of the American Academy of Neurology.
Gregory Krauss, MD, Professor of Neurology at Johns Hopkins University in Baltimore, and colleagues conducted the study to identify common seizure triggers and estimate their relative frequency in a US population of people with epilepsy. For the 10-month study, 598 people signed up to track their seizures with an app called EpiWatch that had been created using ResearchKit, a software framework designed by Apple to make it easy for researchers to gather data more frequently and more accurately from participants using an iPhone or Apple Watch.
When a participant felt a seizure aura starting, he or she opened the app. Using the Apple Watch's biosensors, EpiWatch recorded the participant's heart rate and movements for 10 minutes. The app asked him or her to perform tasks to test responsiveness. After the seizure ended, the participant was given a brief survey about seizure type, aura, loss of awareness, and possible seizure triggers.
"The data collected will help researchers better understand epilepsy, while helping people with epilepsy keep a more complete history of their seizures," said Dr. Krauss. "The app also provides helpful tracking of seizures, prescription medication use, and drug side effects--activities that are important in helping people manage their condition."
In all, 40% of the group tracked a total of 1,485 seizures, and 177 participants reported what triggered their seizures. Stress was the most common trigger and was linked to 37% of seizures. Participants also identified lack of sleep as a trigger for 18% of the seizures, menstruation for 12%, and overexertion for 11%. Other reported triggers included diet (9%), missed medications (7%), and fever or infection (6%). Demographics and seizure types were generally similar between participants who reported seizure triggers and those who did not. Seizure triggers did not vary by the type of seizure people had.
The investigators found that stress was more commonly reported as a trigger for participants who worked full-time (35%), compared with those who worked part-time (21%), were unemployed (27%), or were disabled (29%). Nonadherence to medication was reported slightly more frequently among younger participants (ie, ages 16 to 25), among whom 40% reported a missed medication as a trigger, compared with older participants (ie, ages 26 to 66), among whom 34% reported a missed medication.
"Seizures are very unpredictable," said Dr. Krauss. "Our eventual goal is to be able to use wearable technology to predict an oncoming seizure. This could potentially save lives, as well as give people with epilepsy more freedom. The data collected in this study help us take a step in that direction."
BOSTON—Research using an Apple Watch app to track seizures in people with epilepsy finds that common triggers include stress and missed sleep, according to a preliminary study presented at the 69th Annual Meeting of the American Academy of Neurology.
Gregory Krauss, MD, Professor of Neurology at Johns Hopkins University in Baltimore, and colleagues conducted the study to identify common seizure triggers and estimate their relative frequency in a US population of people with epilepsy. For the 10-month study, 598 people signed up to track their seizures with an app called EpiWatch that had been created using ResearchKit, a software framework designed by Apple to make it easy for researchers to gather data more frequently and more accurately from participants using an iPhone or Apple Watch.
When a participant felt a seizure aura starting, he or she opened the app. Using the Apple Watch's biosensors, EpiWatch recorded the participant's heart rate and movements for 10 minutes. The app asked him or her to perform tasks to test responsiveness. After the seizure ended, the participant was given a brief survey about seizure type, aura, loss of awareness, and possible seizure triggers.
"The data collected will help researchers better understand epilepsy, while helping people with epilepsy keep a more complete history of their seizures," said Dr. Krauss. "The app also provides helpful tracking of seizures, prescription medication use, and drug side effects--activities that are important in helping people manage their condition."
In all, 40% of the group tracked a total of 1,485 seizures, and 177 participants reported what triggered their seizures. Stress was the most common trigger and was linked to 37% of seizures. Participants also identified lack of sleep as a trigger for 18% of the seizures, menstruation for 12%, and overexertion for 11%. Other reported triggers included diet (9%), missed medications (7%), and fever or infection (6%). Demographics and seizure types were generally similar between participants who reported seizure triggers and those who did not. Seizure triggers did not vary by the type of seizure people had.
The investigators found that stress was more commonly reported as a trigger for participants who worked full-time (35%), compared with those who worked part-time (21%), were unemployed (27%), or were disabled (29%). Nonadherence to medication was reported slightly more frequently among younger participants (ie, ages 16 to 25), among whom 40% reported a missed medication as a trigger, compared with older participants (ie, ages 26 to 66), among whom 34% reported a missed medication.
"Seizures are very unpredictable," said Dr. Krauss. "Our eventual goal is to be able to use wearable technology to predict an oncoming seizure. This could potentially save lives, as well as give people with epilepsy more freedom. The data collected in this study help us take a step in that direction."
Extrapolation of AED Efficacy Data From Adults to Pediatric Patients
BOSTON—Across a likely spectrum of syndromes with generalized seizures, the effect of adjunctive antiepileptic drug (AED) treatment on primary generalized tonic-clonic seizures appears similar between adults and children, according to a report presented at the 69th Annual Meeting of the American Academy of Neurology.
The availability of new AEDs for pediatric patients has been delayed due to the challenges of conducting clinical trials in children. In response to this challenge, the feasibility of extrapolation of adjunctive efficacy results for partial-onset seizures has been previously shown by Pellock et al from adult to pediatric populations when the disease course and pharmacokinetics of drug effects are comparable between populations. In response to a request from the Pediatric Committee of the European Medicines Agency, Douglas Nordli Jr, MD, and colleagues explored the feasibility of extrapolating AED efficacy data from adults to pediatric patients with primary generalized tonic-clonic seizures. Dr. Nordli is the Chief of the Division of Pediatric Neurology and Codirector of the Neurosciences Institute at Children's Hospital Los Angeles.
Dr. Nordli and colleagues conducted literature searches in EMBASE, Medline, and the Cochrane Central Register of Controlled Trials for randomized, placebo-controlled clinical trials of adjunctive AED treatment for primary generalized tonic-clonic seizures in adults and children published from 1970 to 2015. Outcome data, expressed as median percent reduction in seizure frequency and greater than or equal to 50% responder rate, were extracted from eligible trials for adult and pediatric patients receiving adjunctive AEDs or placebo and used to determine the relative strength of baseline-subtracted efficacy measures.
Seven published trials of AED adjunctive therapy for primary generalized tonic-clonic seizures were eligible for quantitative analysis. Dr. Nordli and colleagues found that changes in efficacy measures were similar in adults and children with primary generalized tonic-clonic seizures and were not age-dependent. The 95% confidence intervals for the standardized mean difference in median percent reduction of seizure frequency and estimated risk ratios in greater than or equal to 50% responder rate were consistently in favor of the AED treatment and comparable between adult and pediatric groups.
Dr. Nordli's study was supported by Eisai.
Suggested Reading
Pellock JM, Carman WJ, Thyagarajan V, et al. Efficacy of antiepileptic drugs in adults predicts efficacy in children: a systematic review. Neurology. 2012;79(14):1482-1489.
BOSTON—Across a likely spectrum of syndromes with generalized seizures, the effect of adjunctive antiepileptic drug (AED) treatment on primary generalized tonic-clonic seizures appears similar between adults and children, according to a report presented at the 69th Annual Meeting of the American Academy of Neurology.
The availability of new AEDs for pediatric patients has been delayed due to the challenges of conducting clinical trials in children. In response to this challenge, the feasibility of extrapolation of adjunctive efficacy results for partial-onset seizures has been previously shown by Pellock et al from adult to pediatric populations when the disease course and pharmacokinetics of drug effects are comparable between populations. In response to a request from the Pediatric Committee of the European Medicines Agency, Douglas Nordli Jr, MD, and colleagues explored the feasibility of extrapolating AED efficacy data from adults to pediatric patients with primary generalized tonic-clonic seizures. Dr. Nordli is the Chief of the Division of Pediatric Neurology and Codirector of the Neurosciences Institute at Children's Hospital Los Angeles.
Dr. Nordli and colleagues conducted literature searches in EMBASE, Medline, and the Cochrane Central Register of Controlled Trials for randomized, placebo-controlled clinical trials of adjunctive AED treatment for primary generalized tonic-clonic seizures in adults and children published from 1970 to 2015. Outcome data, expressed as median percent reduction in seizure frequency and greater than or equal to 50% responder rate, were extracted from eligible trials for adult and pediatric patients receiving adjunctive AEDs or placebo and used to determine the relative strength of baseline-subtracted efficacy measures.
Seven published trials of AED adjunctive therapy for primary generalized tonic-clonic seizures were eligible for quantitative analysis. Dr. Nordli and colleagues found that changes in efficacy measures were similar in adults and children with primary generalized tonic-clonic seizures and were not age-dependent. The 95% confidence intervals for the standardized mean difference in median percent reduction of seizure frequency and estimated risk ratios in greater than or equal to 50% responder rate were consistently in favor of the AED treatment and comparable between adult and pediatric groups.
Dr. Nordli's study was supported by Eisai.
Suggested Reading
Pellock JM, Carman WJ, Thyagarajan V, et al. Efficacy of antiepileptic drugs in adults predicts efficacy in children: a systematic review. Neurology. 2012;79(14):1482-1489.
BOSTON—Across a likely spectrum of syndromes with generalized seizures, the effect of adjunctive antiepileptic drug (AED) treatment on primary generalized tonic-clonic seizures appears similar between adults and children, according to a report presented at the 69th Annual Meeting of the American Academy of Neurology.
The availability of new AEDs for pediatric patients has been delayed due to the challenges of conducting clinical trials in children. In response to this challenge, the feasibility of extrapolation of adjunctive efficacy results for partial-onset seizures has been previously shown by Pellock et al from adult to pediatric populations when the disease course and pharmacokinetics of drug effects are comparable between populations. In response to a request from the Pediatric Committee of the European Medicines Agency, Douglas Nordli Jr, MD, and colleagues explored the feasibility of extrapolating AED efficacy data from adults to pediatric patients with primary generalized tonic-clonic seizures. Dr. Nordli is the Chief of the Division of Pediatric Neurology and Codirector of the Neurosciences Institute at Children's Hospital Los Angeles.
Dr. Nordli and colleagues conducted literature searches in EMBASE, Medline, and the Cochrane Central Register of Controlled Trials for randomized, placebo-controlled clinical trials of adjunctive AED treatment for primary generalized tonic-clonic seizures in adults and children published from 1970 to 2015. Outcome data, expressed as median percent reduction in seizure frequency and greater than or equal to 50% responder rate, were extracted from eligible trials for adult and pediatric patients receiving adjunctive AEDs or placebo and used to determine the relative strength of baseline-subtracted efficacy measures.
Seven published trials of AED adjunctive therapy for primary generalized tonic-clonic seizures were eligible for quantitative analysis. Dr. Nordli and colleagues found that changes in efficacy measures were similar in adults and children with primary generalized tonic-clonic seizures and were not age-dependent. The 95% confidence intervals for the standardized mean difference in median percent reduction of seizure frequency and estimated risk ratios in greater than or equal to 50% responder rate were consistently in favor of the AED treatment and comparable between adult and pediatric groups.
Dr. Nordli's study was supported by Eisai.
Suggested Reading
Pellock JM, Carman WJ, Thyagarajan V, et al. Efficacy of antiepileptic drugs in adults predicts efficacy in children: a systematic review. Neurology. 2012;79(14):1482-1489.
Oral GnRH antagonist offers endometriosis pain relief in trials
VANCOUVER – An oral agent reduced dysmenorrhea and nonmenstrual pelvic pain in endometriosis patients, with more fine control over estrogen levels than historically seen with injectable gonadotropin-releasing hormone (GnRH) agonists, according to findings from two randomized controlled trials.
Elagolix is an oral, nonpeptide, gonadotropin-releasing hormone (GnRH) antagonist being developed by Neurocrine Biosciences and AbbVie. Its dose can be adjusted in an attempt to achieve estrogen levels in the optimal “therapeutic window” that controls endometriosis pain while reducing menopausal symptoms, according to Hugh S. Taylor, MD, professor of obstetrics, gynecology and reproductive services at Yale University, New Haven, Conn., and chief of obstetrics and gynecology at Yale–New Haven Hospital, who presented the research at the World Congress on Endometriosis.
Results from two phase III clinical trials, simultaneously published in the New England Journal of Medicine, show that two different doses of elagolix – 150 mg once daily or 200 mg twice daily – improved moderate or severe endometriosis-associated pain. However, patients taking the drug experienced heightened frequencies of hot flushes and increased serum lipid levels, and decreases from baseline in bone mineral density (N Engl J Med. 2017 May 19. doi: 10.1056/NEJMoa1700089).
Still, the two doses give physicians options in tailoring the drug for their patients, Dr. Taylor said. The key is to keep the levels within the therapeutic window. “That’s always been the goal, and now we have a drug that does that. You can customize it for your patient, using the stronger dose for those who need it,” he said.
He described the results from two parallel clinical trials, one conducted in the United States and Canada (Elaris Endometriosis I, n = 872) and one conducted at 187 sites on five continents (Elaris Endometriosis II, n = 817).
Patients were allowed to use NSAIDs (500 mg of naproxen) or an opioid, or both, as needed. Dr. Taylor reported the results after 6 months of treatment.
Both doses of the drug outperformed placebo in reducing dysmenorrhea at 3 months. In Elaris EM-I, 75.8% in the high-dose group and 46.4% in the low-dose group had a clinically significant reduction in dysmenorrhea and decreased or stable use of analgesics at 3 months, compared with 19.6% in the placebo group. In Elaris EM-II, 72.4% in the high-dose group and 43.4% in the low-dose group achieved a clinically significant reduction, compared with 22.7% in the placebo group (P less than .001 for all comparisons).
For nonmenstrual pelvic pain, the two doses of elagolix again bested placebo. In Elaris EM-I, 54.5% in the high-dose group and 50.4% in the low-dose group achieved a clinically significant reduction and a decreased or stable use of analgesics, compared with 36.5% on placebo (P less than .001 for all). In Elaris EM-II, 57.8% in the high-dose group and 49.8% in the low-dose group achieved a clinically significant response, compared with 36.5% in the placebo group (P less than .001 and P = .003, respectively).
The responses were sustained at 6 months for both outcomes.
In Elaris EM-I, hot flushes were reported by 7.0% of the placebo group, 23.7% of the low-dose group, and 42.3% of the high-dose group (P less than .001). In Elaris EM-II, they were reported in 10.3% of the placebo group, 22.6% of the low-dose group, and 47.6% of the high-dose group (P less than .001).
Patients in the elagolix groups experienced increases in total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides, though the researchers noted that less than 20% of participants in each group had LDL levels higher than 160 mg/dL or triglycerides levels higher than 200 mg/dL at any point during treatment.
There were also decreases in bone mineral density in the elagolix groups, but after 6 months of treatment, a z score of –1.5 or less at the lumbar spine occurred in fewer than 5% of women in the elagolix groups.
The drug should provide a more palatable option to GnRH agonists, according to Dr. Taylor. “This is a big step forward, very effective and much more tolerable. I think having an oral, rapidly acting, reversible drug, with a couple of doses available, will make this much more widely accepted and just as effective.”
The study was sponsored by AbbVie. Dr. Taylor and other researchers on the study reported financial ties to AbbVie and other pharmaceutical companies.
VANCOUVER – An oral agent reduced dysmenorrhea and nonmenstrual pelvic pain in endometriosis patients, with more fine control over estrogen levels than historically seen with injectable gonadotropin-releasing hormone (GnRH) agonists, according to findings from two randomized controlled trials.
Elagolix is an oral, nonpeptide, gonadotropin-releasing hormone (GnRH) antagonist being developed by Neurocrine Biosciences and AbbVie. Its dose can be adjusted in an attempt to achieve estrogen levels in the optimal “therapeutic window” that controls endometriosis pain while reducing menopausal symptoms, according to Hugh S. Taylor, MD, professor of obstetrics, gynecology and reproductive services at Yale University, New Haven, Conn., and chief of obstetrics and gynecology at Yale–New Haven Hospital, who presented the research at the World Congress on Endometriosis.
Results from two phase III clinical trials, simultaneously published in the New England Journal of Medicine, show that two different doses of elagolix – 150 mg once daily or 200 mg twice daily – improved moderate or severe endometriosis-associated pain. However, patients taking the drug experienced heightened frequencies of hot flushes and increased serum lipid levels, and decreases from baseline in bone mineral density (N Engl J Med. 2017 May 19. doi: 10.1056/NEJMoa1700089).
Still, the two doses give physicians options in tailoring the drug for their patients, Dr. Taylor said. The key is to keep the levels within the therapeutic window. “That’s always been the goal, and now we have a drug that does that. You can customize it for your patient, using the stronger dose for those who need it,” he said.
He described the results from two parallel clinical trials, one conducted in the United States and Canada (Elaris Endometriosis I, n = 872) and one conducted at 187 sites on five continents (Elaris Endometriosis II, n = 817).
Patients were allowed to use NSAIDs (500 mg of naproxen) or an opioid, or both, as needed. Dr. Taylor reported the results after 6 months of treatment.
Both doses of the drug outperformed placebo in reducing dysmenorrhea at 3 months. In Elaris EM-I, 75.8% in the high-dose group and 46.4% in the low-dose group had a clinically significant reduction in dysmenorrhea and decreased or stable use of analgesics at 3 months, compared with 19.6% in the placebo group. In Elaris EM-II, 72.4% in the high-dose group and 43.4% in the low-dose group achieved a clinically significant reduction, compared with 22.7% in the placebo group (P less than .001 for all comparisons).
For nonmenstrual pelvic pain, the two doses of elagolix again bested placebo. In Elaris EM-I, 54.5% in the high-dose group and 50.4% in the low-dose group achieved a clinically significant reduction and a decreased or stable use of analgesics, compared with 36.5% on placebo (P less than .001 for all). In Elaris EM-II, 57.8% in the high-dose group and 49.8% in the low-dose group achieved a clinically significant response, compared with 36.5% in the placebo group (P less than .001 and P = .003, respectively).
The responses were sustained at 6 months for both outcomes.
In Elaris EM-I, hot flushes were reported by 7.0% of the placebo group, 23.7% of the low-dose group, and 42.3% of the high-dose group (P less than .001). In Elaris EM-II, they were reported in 10.3% of the placebo group, 22.6% of the low-dose group, and 47.6% of the high-dose group (P less than .001).
Patients in the elagolix groups experienced increases in total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides, though the researchers noted that less than 20% of participants in each group had LDL levels higher than 160 mg/dL or triglycerides levels higher than 200 mg/dL at any point during treatment.
There were also decreases in bone mineral density in the elagolix groups, but after 6 months of treatment, a z score of –1.5 or less at the lumbar spine occurred in fewer than 5% of women in the elagolix groups.
The drug should provide a more palatable option to GnRH agonists, according to Dr. Taylor. “This is a big step forward, very effective and much more tolerable. I think having an oral, rapidly acting, reversible drug, with a couple of doses available, will make this much more widely accepted and just as effective.”
The study was sponsored by AbbVie. Dr. Taylor and other researchers on the study reported financial ties to AbbVie and other pharmaceutical companies.
VANCOUVER – An oral agent reduced dysmenorrhea and nonmenstrual pelvic pain in endometriosis patients, with more fine control over estrogen levels than historically seen with injectable gonadotropin-releasing hormone (GnRH) agonists, according to findings from two randomized controlled trials.
Elagolix is an oral, nonpeptide, gonadotropin-releasing hormone (GnRH) antagonist being developed by Neurocrine Biosciences and AbbVie. Its dose can be adjusted in an attempt to achieve estrogen levels in the optimal “therapeutic window” that controls endometriosis pain while reducing menopausal symptoms, according to Hugh S. Taylor, MD, professor of obstetrics, gynecology and reproductive services at Yale University, New Haven, Conn., and chief of obstetrics and gynecology at Yale–New Haven Hospital, who presented the research at the World Congress on Endometriosis.
Results from two phase III clinical trials, simultaneously published in the New England Journal of Medicine, show that two different doses of elagolix – 150 mg once daily or 200 mg twice daily – improved moderate or severe endometriosis-associated pain. However, patients taking the drug experienced heightened frequencies of hot flushes and increased serum lipid levels, and decreases from baseline in bone mineral density (N Engl J Med. 2017 May 19. doi: 10.1056/NEJMoa1700089).
Still, the two doses give physicians options in tailoring the drug for their patients, Dr. Taylor said. The key is to keep the levels within the therapeutic window. “That’s always been the goal, and now we have a drug that does that. You can customize it for your patient, using the stronger dose for those who need it,” he said.
He described the results from two parallel clinical trials, one conducted in the United States and Canada (Elaris Endometriosis I, n = 872) and one conducted at 187 sites on five continents (Elaris Endometriosis II, n = 817).
Patients were allowed to use NSAIDs (500 mg of naproxen) or an opioid, or both, as needed. Dr. Taylor reported the results after 6 months of treatment.
Both doses of the drug outperformed placebo in reducing dysmenorrhea at 3 months. In Elaris EM-I, 75.8% in the high-dose group and 46.4% in the low-dose group had a clinically significant reduction in dysmenorrhea and decreased or stable use of analgesics at 3 months, compared with 19.6% in the placebo group. In Elaris EM-II, 72.4% in the high-dose group and 43.4% in the low-dose group achieved a clinically significant reduction, compared with 22.7% in the placebo group (P less than .001 for all comparisons).
For nonmenstrual pelvic pain, the two doses of elagolix again bested placebo. In Elaris EM-I, 54.5% in the high-dose group and 50.4% in the low-dose group achieved a clinically significant reduction and a decreased or stable use of analgesics, compared with 36.5% on placebo (P less than .001 for all). In Elaris EM-II, 57.8% in the high-dose group and 49.8% in the low-dose group achieved a clinically significant response, compared with 36.5% in the placebo group (P less than .001 and P = .003, respectively).
The responses were sustained at 6 months for both outcomes.
In Elaris EM-I, hot flushes were reported by 7.0% of the placebo group, 23.7% of the low-dose group, and 42.3% of the high-dose group (P less than .001). In Elaris EM-II, they were reported in 10.3% of the placebo group, 22.6% of the low-dose group, and 47.6% of the high-dose group (P less than .001).
Patients in the elagolix groups experienced increases in total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides, though the researchers noted that less than 20% of participants in each group had LDL levels higher than 160 mg/dL or triglycerides levels higher than 200 mg/dL at any point during treatment.
There were also decreases in bone mineral density in the elagolix groups, but after 6 months of treatment, a z score of –1.5 or less at the lumbar spine occurred in fewer than 5% of women in the elagolix groups.
The drug should provide a more palatable option to GnRH agonists, according to Dr. Taylor. “This is a big step forward, very effective and much more tolerable. I think having an oral, rapidly acting, reversible drug, with a couple of doses available, will make this much more widely accepted and just as effective.”
The study was sponsored by AbbVie. Dr. Taylor and other researchers on the study reported financial ties to AbbVie and other pharmaceutical companies.
Key clinical point:
Major finding: At 3 and 6 months, the drug achieved a clinically significant reduction in dysmenorrhea for between 43% and 77% of women, compared with placebo (P less than .001).
Data source: Two phase III controlled trials randomizing nearly 1,700 with surgically confirmed endometriosis.
Disclosures: The study was sponsored by AbbVie. Dr. Taylor and other researchers on the study reported financial ties to AbbVie and other pharmaceutical companies.
Infections up the risk for pregnancy-associated stroke in preeclampsia
A host of factors, some of them preventable or treatable, increase the risk of pregnancy-related stroke among women hospitalized for preeclampsia, according to findings from a case-control study of nearly 800 preeclamptic women in New York.
Women who experienced a stroke were roughly seven times more likely to have severe preeclampsia or eclampsia, and about three to four times more likely to have an infection, a prothrombotic state, a coagulopathy, or chronic hypertension, according to the findings (Stroke. 2017 May 25. doi: 10.1161/STROKEAHA.117.017374).
“Prospective studies are needed to confirm these findings and develop interventions aimed at preventing strokes in this uniquely vulnerable group,” they added.
For the study, the investigators used billing data from the 2003-2012 New York State Department of Health inpatient database to identify women aged 12-55 years admitted with preeclampsia.
They matched each woman who experienced pregnancy-associated stroke with three randomly selected controls of the same age, race/ethnicity, and insurance status. They then compared the groups on a set of predefined risk factors.
Results showed that of 88,857 women admitted for preeclampsia during the study period, 0.2% experienced pregnancy-associated stroke, translating to a cumulative incidence of 222 per 100,000 preeclamptic women, a value more than six times that seen in the general pregnant population, the investigators noted.
The majority of strokes occurred post partum (66.5%), but more than a quarter occurred before delivery (27.9%). The single most common type of stroke was hemorrhagic (46.7%).
The 197 women with preeclampsia who experienced pregnancy-associated stroke had a sharply higher rate of in-hospital mortality (13.2%), compared with the 591 controls (0.2%).
In multivariate analysis, women with preeclampsia experiencing stroke were more likely to have severe preeclampsia or eclampsia (odds ratio, 7.2; 95% confidence interval, 4.6-11.3), or infections at the time of admission (OR, 3.0; 95% CI, 1.6-5.8), predominantly genitourinary infections.
Other risk factors for pregnancy-associated stroke included prothrombotic states (OR, 3.5; 95% CI, 1.3-9.2), coagulopathies (OR, 3.1; 95% CI, 1.3-7.1), or chronic hypertension (OR, 3.2; 95% CI, 1.8-5.5).
The findings were similar when women were matched by the severity of preeclampsia, when women with eclampsia were excluded, or when women with only postpartum stroke were included.
Heart disease, multiple gestation, and previous pregnancies were not significantly independently associated with the risk of pregnancy-associated stroke.
“The ethnic and regional diversity of New York State increases the generalizability of our findings,” the investigators wrote. “Matching of cases and controls allowed for nuanced analysis of other risk factors.”
But the study may have missed some cases of preeclampsia not formally diagnosed, and the timing of infections relative to stroke was unknown, they acknowledged. Additionally, they noted that causality cannot be inferred from the observational study, and therefore the results should be interpreted cautiously.
The investigators reported research support from the National Institutes of Health. They had no other financial disclosures.
A host of factors, some of them preventable or treatable, increase the risk of pregnancy-related stroke among women hospitalized for preeclampsia, according to findings from a case-control study of nearly 800 preeclamptic women in New York.
Women who experienced a stroke were roughly seven times more likely to have severe preeclampsia or eclampsia, and about three to four times more likely to have an infection, a prothrombotic state, a coagulopathy, or chronic hypertension, according to the findings (Stroke. 2017 May 25. doi: 10.1161/STROKEAHA.117.017374).
“Prospective studies are needed to confirm these findings and develop interventions aimed at preventing strokes in this uniquely vulnerable group,” they added.
For the study, the investigators used billing data from the 2003-2012 New York State Department of Health inpatient database to identify women aged 12-55 years admitted with preeclampsia.
They matched each woman who experienced pregnancy-associated stroke with three randomly selected controls of the same age, race/ethnicity, and insurance status. They then compared the groups on a set of predefined risk factors.
Results showed that of 88,857 women admitted for preeclampsia during the study period, 0.2% experienced pregnancy-associated stroke, translating to a cumulative incidence of 222 per 100,000 preeclamptic women, a value more than six times that seen in the general pregnant population, the investigators noted.
The majority of strokes occurred post partum (66.5%), but more than a quarter occurred before delivery (27.9%). The single most common type of stroke was hemorrhagic (46.7%).
The 197 women with preeclampsia who experienced pregnancy-associated stroke had a sharply higher rate of in-hospital mortality (13.2%), compared with the 591 controls (0.2%).
In multivariate analysis, women with preeclampsia experiencing stroke were more likely to have severe preeclampsia or eclampsia (odds ratio, 7.2; 95% confidence interval, 4.6-11.3), or infections at the time of admission (OR, 3.0; 95% CI, 1.6-5.8), predominantly genitourinary infections.
Other risk factors for pregnancy-associated stroke included prothrombotic states (OR, 3.5; 95% CI, 1.3-9.2), coagulopathies (OR, 3.1; 95% CI, 1.3-7.1), or chronic hypertension (OR, 3.2; 95% CI, 1.8-5.5).
The findings were similar when women were matched by the severity of preeclampsia, when women with eclampsia were excluded, or when women with only postpartum stroke were included.
Heart disease, multiple gestation, and previous pregnancies were not significantly independently associated with the risk of pregnancy-associated stroke.
“The ethnic and regional diversity of New York State increases the generalizability of our findings,” the investigators wrote. “Matching of cases and controls allowed for nuanced analysis of other risk factors.”
But the study may have missed some cases of preeclampsia not formally diagnosed, and the timing of infections relative to stroke was unknown, they acknowledged. Additionally, they noted that causality cannot be inferred from the observational study, and therefore the results should be interpreted cautiously.
The investigators reported research support from the National Institutes of Health. They had no other financial disclosures.
A host of factors, some of them preventable or treatable, increase the risk of pregnancy-related stroke among women hospitalized for preeclampsia, according to findings from a case-control study of nearly 800 preeclamptic women in New York.
Women who experienced a stroke were roughly seven times more likely to have severe preeclampsia or eclampsia, and about three to four times more likely to have an infection, a prothrombotic state, a coagulopathy, or chronic hypertension, according to the findings (Stroke. 2017 May 25. doi: 10.1161/STROKEAHA.117.017374).
“Prospective studies are needed to confirm these findings and develop interventions aimed at preventing strokes in this uniquely vulnerable group,” they added.
For the study, the investigators used billing data from the 2003-2012 New York State Department of Health inpatient database to identify women aged 12-55 years admitted with preeclampsia.
They matched each woman who experienced pregnancy-associated stroke with three randomly selected controls of the same age, race/ethnicity, and insurance status. They then compared the groups on a set of predefined risk factors.
Results showed that of 88,857 women admitted for preeclampsia during the study period, 0.2% experienced pregnancy-associated stroke, translating to a cumulative incidence of 222 per 100,000 preeclamptic women, a value more than six times that seen in the general pregnant population, the investigators noted.
The majority of strokes occurred post partum (66.5%), but more than a quarter occurred before delivery (27.9%). The single most common type of stroke was hemorrhagic (46.7%).
The 197 women with preeclampsia who experienced pregnancy-associated stroke had a sharply higher rate of in-hospital mortality (13.2%), compared with the 591 controls (0.2%).
In multivariate analysis, women with preeclampsia experiencing stroke were more likely to have severe preeclampsia or eclampsia (odds ratio, 7.2; 95% confidence interval, 4.6-11.3), or infections at the time of admission (OR, 3.0; 95% CI, 1.6-5.8), predominantly genitourinary infections.
Other risk factors for pregnancy-associated stroke included prothrombotic states (OR, 3.5; 95% CI, 1.3-9.2), coagulopathies (OR, 3.1; 95% CI, 1.3-7.1), or chronic hypertension (OR, 3.2; 95% CI, 1.8-5.5).
The findings were similar when women were matched by the severity of preeclampsia, when women with eclampsia were excluded, or when women with only postpartum stroke were included.
Heart disease, multiple gestation, and previous pregnancies were not significantly independently associated with the risk of pregnancy-associated stroke.
“The ethnic and regional diversity of New York State increases the generalizability of our findings,” the investigators wrote. “Matching of cases and controls allowed for nuanced analysis of other risk factors.”
But the study may have missed some cases of preeclampsia not formally diagnosed, and the timing of infections relative to stroke was unknown, they acknowledged. Additionally, they noted that causality cannot be inferred from the observational study, and therefore the results should be interpreted cautiously.
The investigators reported research support from the National Institutes of Health. They had no other financial disclosures.
FROM STROKE
Key clinical point:
Major finding: Independent risk factors for pregnancy-associated stroke were severe preeclampsia or eclampsia (OR, 7.2), infections (OR, 3.0), prothrombotic states (OR, 3.5), coagulopathies (OR, 3.1), or chronic hypertension (OR, 3.2).
Data source: A matched, case-control study of 788 women from a New York inpatient database who were hospitalized for preeclampsia.
Disclosures: The investigators reported research support from the National Institutes of Health. They had no other financial disclosures.
MS May Have a Measurable Prodrome
A Large Case–Control Analysis
Previous studies have provided evidence for an MS prodrome that occurs years before a demyelinating event or the onset of clinical symptoms. Many of these studies, however, have been limited by a retrospective design or by the absence of a control group.
To analyze the question further, Dr. Tremlett and colleagues examined data from linked health administrative and clinical databases in the Canadian provinces of British Columbia, Saskatchewan, Manitoba, and Nova Scotia, which were chosen for their geographic diversity and comprehensive data. The researchers created a health administrative cohort, which was based on administrative data, and an MS clinic-derived cohort, which used administrative and clinical data. The study’s primary outcome was all-cause use of health care during each of the five years before the health administrative index date (ie, the first demyelinating disease-related claim) or clinical index date (ie, the date of MS symptom onset).
Health Care Use Increased in Prodromal MS
The health administrative cohort included 14,428 people with MS and 72,059 matched controls. In all, 10,525 (73%) of the patients with MS were women, and their mean age at the health administrative index date was 43. Compared with controls, annual health care use increased steadily between five years and one year before the first demyelinating disease claim in these patients.
The mean number of hospital admissions was 26% higher in people with MS than in controls in the fifth year before the index date, and 78% higher in the year before the index date. The mean number of physician claims was 24% higher in people with MS than in controls in the fifth year before the index date, and 88% higher in people with MS than in controls in the year before the index date. Also, the mean number of prescribed drug classes was 23% higher in people with MS than in matched controls in the fifth year before the index date, and 49% higher in people with MS than in controls in the year before the index date.
The MS clinic cohort included 3,202 people with MS and 16,006 matched controls. In all, 2,368 (74%) of people with MS were women, and the mean age at the clinical index date was approximately 37. Compared with the health administrative cohort, this cohort had similar patterns for physician claims and prescriptions, although the differences in use in each of the five years mostly did not reach statistical significance.
“To gain a better insight into the MS prodrome, the complex reasons for increased health care use will need to be established, for example, through access of additional administrative data such as the specific diagnostic codes related to a hospital admission or physician visit, or the therapeutic drug class for a prescription,” Dr. Tremlett concluded.
—Erik Greb
Suggested Reading
Wijnands JMA, Kingwell E, Zhu F, et al. Health-care use before a first demyelinating event suggestive of a multiple sclerosis prodrome: a matched cohort study. Lancet Neurol. 2017 Apr 20 [Epub ahead of print].
A Large Case–Control Analysis
Previous studies have provided evidence for an MS prodrome that occurs years before a demyelinating event or the onset of clinical symptoms. Many of these studies, however, have been limited by a retrospective design or by the absence of a control group.
To analyze the question further, Dr. Tremlett and colleagues examined data from linked health administrative and clinical databases in the Canadian provinces of British Columbia, Saskatchewan, Manitoba, and Nova Scotia, which were chosen for their geographic diversity and comprehensive data. The researchers created a health administrative cohort, which was based on administrative data, and an MS clinic-derived cohort, which used administrative and clinical data. The study’s primary outcome was all-cause use of health care during each of the five years before the health administrative index date (ie, the first demyelinating disease-related claim) or clinical index date (ie, the date of MS symptom onset).
Health Care Use Increased in Prodromal MS
The health administrative cohort included 14,428 people with MS and 72,059 matched controls. In all, 10,525 (73%) of the patients with MS were women, and their mean age at the health administrative index date was 43. Compared with controls, annual health care use increased steadily between five years and one year before the first demyelinating disease claim in these patients.
The mean number of hospital admissions was 26% higher in people with MS than in controls in the fifth year before the index date, and 78% higher in the year before the index date. The mean number of physician claims was 24% higher in people with MS than in controls in the fifth year before the index date, and 88% higher in people with MS than in controls in the year before the index date. Also, the mean number of prescribed drug classes was 23% higher in people with MS than in matched controls in the fifth year before the index date, and 49% higher in people with MS than in controls in the year before the index date.
The MS clinic cohort included 3,202 people with MS and 16,006 matched controls. In all, 2,368 (74%) of people with MS were women, and the mean age at the clinical index date was approximately 37. Compared with the health administrative cohort, this cohort had similar patterns for physician claims and prescriptions, although the differences in use in each of the five years mostly did not reach statistical significance.
“To gain a better insight into the MS prodrome, the complex reasons for increased health care use will need to be established, for example, through access of additional administrative data such as the specific diagnostic codes related to a hospital admission or physician visit, or the therapeutic drug class for a prescription,” Dr. Tremlett concluded.
—Erik Greb
Suggested Reading
Wijnands JMA, Kingwell E, Zhu F, et al. Health-care use before a first demyelinating event suggestive of a multiple sclerosis prodrome: a matched cohort study. Lancet Neurol. 2017 Apr 20 [Epub ahead of print].
A Large Case–Control Analysis
Previous studies have provided evidence for an MS prodrome that occurs years before a demyelinating event or the onset of clinical symptoms. Many of these studies, however, have been limited by a retrospective design or by the absence of a control group.
To analyze the question further, Dr. Tremlett and colleagues examined data from linked health administrative and clinical databases in the Canadian provinces of British Columbia, Saskatchewan, Manitoba, and Nova Scotia, which were chosen for their geographic diversity and comprehensive data. The researchers created a health administrative cohort, which was based on administrative data, and an MS clinic-derived cohort, which used administrative and clinical data. The study’s primary outcome was all-cause use of health care during each of the five years before the health administrative index date (ie, the first demyelinating disease-related claim) or clinical index date (ie, the date of MS symptom onset).
Health Care Use Increased in Prodromal MS
The health administrative cohort included 14,428 people with MS and 72,059 matched controls. In all, 10,525 (73%) of the patients with MS were women, and their mean age at the health administrative index date was 43. Compared with controls, annual health care use increased steadily between five years and one year before the first demyelinating disease claim in these patients.
The mean number of hospital admissions was 26% higher in people with MS than in controls in the fifth year before the index date, and 78% higher in the year before the index date. The mean number of physician claims was 24% higher in people with MS than in controls in the fifth year before the index date, and 88% higher in people with MS than in controls in the year before the index date. Also, the mean number of prescribed drug classes was 23% higher in people with MS than in matched controls in the fifth year before the index date, and 49% higher in people with MS than in controls in the year before the index date.
The MS clinic cohort included 3,202 people with MS and 16,006 matched controls. In all, 2,368 (74%) of people with MS were women, and the mean age at the clinical index date was approximately 37. Compared with the health administrative cohort, this cohort had similar patterns for physician claims and prescriptions, although the differences in use in each of the five years mostly did not reach statistical significance.
“To gain a better insight into the MS prodrome, the complex reasons for increased health care use will need to be established, for example, through access of additional administrative data such as the specific diagnostic codes related to a hospital admission or physician visit, or the therapeutic drug class for a prescription,” Dr. Tremlett concluded.
—Erik Greb
Suggested Reading
Wijnands JMA, Kingwell E, Zhu F, et al. Health-care use before a first demyelinating event suggestive of a multiple sclerosis prodrome: a matched cohort study. Lancet Neurol. 2017 Apr 20 [Epub ahead of print].
How Can Neurologists Diagnose Traumatic Encephalopathy Syndrome?
BOSTON—Proposed diagnostic criteria for probable or possible chronic traumatic encephalopathy (CTE), a progressive neurodegenerative disease associated with repetitive brain trauma, include a history of head impacts and various core clinical and supportive features.
The preliminary criteria, which were presented by Andrew Budson, MD, Professor of Neurology at Boston University School of Medicine, at the 69th Annual Meeting of the American Academy of Neurology, primarily were designed for research purposes, but can serve as a guide for neurologists for the diagnosis of traumatic encephalopathy syndrome. CTE is a neuropathologic diagnosis, whereas traumatic encephalopathy syndrome is a clinical diagnosis. In addition to presenting the general criteria, Dr. Budson shared diagnostic subtypes, potential biomarkers, and treatment options.
General Criteria
There are five general criteria that patients must meet to receive a diagnosis of traumatic encephalopathy syndrome, said Dr. Budson. First, there must be a history of impacts to the head based on types of injuries (eg, mild or severe traumatic brain injury, concussions, or subconcussive trauma) and sources of exposure, such as military service or involvement in contact sports for a minimum of six years, including at least two years at the college level or higher.
Second, patients must not have another neurologic disorder that likely accounts for the clinical features. Third, clinical features must be present for at least 12 months. The fourth requirement is that at least one core clinical feature (ie, cognitive, behavioral, or mood features) must be present and considered a change from baseline. Finally, at least two of nine supportive features must be present.
Core Clinical and Supportive Features
Of the core clinical features, difficulties in cognition must be reported by the patient, an informant, or a clinician and substantiated by standardized tests. Core behavioral clinical features include emotionally explosive behavior or physical and verbal abuse. Core mood clinical features include feeling overly sad, depressed, or hopeless.
In addition to core clinical features, two of the following supportive features must be present: impulsivity, anxiety, apathy, paranoia, suicidality, headache, motor signs (eg, dysarthria, dysgraphia, or other features of parkinsonism), documented decline for at least a year, or delayed onset of clinical features after a significant head impact exposure (usually at least two years).
Syndrome Subtypes
Patients may have one of four possible traumatic encephalopathy syndrome diagnostic subtypes. A behavioral/mood variant is more common among younger patients, whereas a cognitive variant is more common in older populations, said Dr. Budson. Patients also may have a mixed variant or dementia. Patients with the dementia subtype must have a progressive course of cognitive core clinical features, with or without behavior or mood features. In addition, patients with dementia must have cognitive impairment that interferes with their ability to function independently during normal daily activities.
Biomarkers and Treatment
Cavum septum pellucidum, cavum vergae, or fenestrations on neuroimaging are potential CTE biomarkers, said Dr. Budson. Normal beta amyloid CSF levels, elevated CSF p-tau/tau ratio, negative amyloid imaging, as well as cortical atrophy beyond that expected for age could also be signs of CTE. Potential experimental biomarkers include positive tau imaging and cortical thinning based on MRI.
Once physicians have made a diagnosis of probable or possible CTE, there are several treatments that may benefit patients, although no medications are approved for the treatment of CTE. Cholinesterase inhibitors may help to treat memory impairment, said Dr. Budson. For patients with depression and anxiety, selective serotonin reuptake inhibitors may be helpful. For patients with violent or explosive behavior, atypical neuroleptics may be efficacious. Memantine may benefit patients with moderate or severe dementia. Finally, to manage agitation, a combination of dextromethorphan and quinidine may be a treatment option.
—Erica Tricarico
Suggested Reading
Montenigro PH, Baugh CM, Daneshvar DH, et al. Clinical subtypes of chronic traumatic encephalopathy: literature review and proposed research diagnostic criteria for traumatic encephalopathy syndrome. Alzheimers Res Ther. 2014;6(5):68.
BOSTON—Proposed diagnostic criteria for probable or possible chronic traumatic encephalopathy (CTE), a progressive neurodegenerative disease associated with repetitive brain trauma, include a history of head impacts and various core clinical and supportive features.
The preliminary criteria, which were presented by Andrew Budson, MD, Professor of Neurology at Boston University School of Medicine, at the 69th Annual Meeting of the American Academy of Neurology, primarily were designed for research purposes, but can serve as a guide for neurologists for the diagnosis of traumatic encephalopathy syndrome. CTE is a neuropathologic diagnosis, whereas traumatic encephalopathy syndrome is a clinical diagnosis. In addition to presenting the general criteria, Dr. Budson shared diagnostic subtypes, potential biomarkers, and treatment options.
General Criteria
There are five general criteria that patients must meet to receive a diagnosis of traumatic encephalopathy syndrome, said Dr. Budson. First, there must be a history of impacts to the head based on types of injuries (eg, mild or severe traumatic brain injury, concussions, or subconcussive trauma) and sources of exposure, such as military service or involvement in contact sports for a minimum of six years, including at least two years at the college level or higher.
Second, patients must not have another neurologic disorder that likely accounts for the clinical features. Third, clinical features must be present for at least 12 months. The fourth requirement is that at least one core clinical feature (ie, cognitive, behavioral, or mood features) must be present and considered a change from baseline. Finally, at least two of nine supportive features must be present.
Core Clinical and Supportive Features
Of the core clinical features, difficulties in cognition must be reported by the patient, an informant, or a clinician and substantiated by standardized tests. Core behavioral clinical features include emotionally explosive behavior or physical and verbal abuse. Core mood clinical features include feeling overly sad, depressed, or hopeless.
In addition to core clinical features, two of the following supportive features must be present: impulsivity, anxiety, apathy, paranoia, suicidality, headache, motor signs (eg, dysarthria, dysgraphia, or other features of parkinsonism), documented decline for at least a year, or delayed onset of clinical features after a significant head impact exposure (usually at least two years).
Syndrome Subtypes
Patients may have one of four possible traumatic encephalopathy syndrome diagnostic subtypes. A behavioral/mood variant is more common among younger patients, whereas a cognitive variant is more common in older populations, said Dr. Budson. Patients also may have a mixed variant or dementia. Patients with the dementia subtype must have a progressive course of cognitive core clinical features, with or without behavior or mood features. In addition, patients with dementia must have cognitive impairment that interferes with their ability to function independently during normal daily activities.
Biomarkers and Treatment
Cavum septum pellucidum, cavum vergae, or fenestrations on neuroimaging are potential CTE biomarkers, said Dr. Budson. Normal beta amyloid CSF levels, elevated CSF p-tau/tau ratio, negative amyloid imaging, as well as cortical atrophy beyond that expected for age could also be signs of CTE. Potential experimental biomarkers include positive tau imaging and cortical thinning based on MRI.
Once physicians have made a diagnosis of probable or possible CTE, there are several treatments that may benefit patients, although no medications are approved for the treatment of CTE. Cholinesterase inhibitors may help to treat memory impairment, said Dr. Budson. For patients with depression and anxiety, selective serotonin reuptake inhibitors may be helpful. For patients with violent or explosive behavior, atypical neuroleptics may be efficacious. Memantine may benefit patients with moderate or severe dementia. Finally, to manage agitation, a combination of dextromethorphan and quinidine may be a treatment option.
—Erica Tricarico
Suggested Reading
Montenigro PH, Baugh CM, Daneshvar DH, et al. Clinical subtypes of chronic traumatic encephalopathy: literature review and proposed research diagnostic criteria for traumatic encephalopathy syndrome. Alzheimers Res Ther. 2014;6(5):68.
BOSTON—Proposed diagnostic criteria for probable or possible chronic traumatic encephalopathy (CTE), a progressive neurodegenerative disease associated with repetitive brain trauma, include a history of head impacts and various core clinical and supportive features.
The preliminary criteria, which were presented by Andrew Budson, MD, Professor of Neurology at Boston University School of Medicine, at the 69th Annual Meeting of the American Academy of Neurology, primarily were designed for research purposes, but can serve as a guide for neurologists for the diagnosis of traumatic encephalopathy syndrome. CTE is a neuropathologic diagnosis, whereas traumatic encephalopathy syndrome is a clinical diagnosis. In addition to presenting the general criteria, Dr. Budson shared diagnostic subtypes, potential biomarkers, and treatment options.
General Criteria
There are five general criteria that patients must meet to receive a diagnosis of traumatic encephalopathy syndrome, said Dr. Budson. First, there must be a history of impacts to the head based on types of injuries (eg, mild or severe traumatic brain injury, concussions, or subconcussive trauma) and sources of exposure, such as military service or involvement in contact sports for a minimum of six years, including at least two years at the college level or higher.
Second, patients must not have another neurologic disorder that likely accounts for the clinical features. Third, clinical features must be present for at least 12 months. The fourth requirement is that at least one core clinical feature (ie, cognitive, behavioral, or mood features) must be present and considered a change from baseline. Finally, at least two of nine supportive features must be present.
Core Clinical and Supportive Features
Of the core clinical features, difficulties in cognition must be reported by the patient, an informant, or a clinician and substantiated by standardized tests. Core behavioral clinical features include emotionally explosive behavior or physical and verbal abuse. Core mood clinical features include feeling overly sad, depressed, or hopeless.
In addition to core clinical features, two of the following supportive features must be present: impulsivity, anxiety, apathy, paranoia, suicidality, headache, motor signs (eg, dysarthria, dysgraphia, or other features of parkinsonism), documented decline for at least a year, or delayed onset of clinical features after a significant head impact exposure (usually at least two years).
Syndrome Subtypes
Patients may have one of four possible traumatic encephalopathy syndrome diagnostic subtypes. A behavioral/mood variant is more common among younger patients, whereas a cognitive variant is more common in older populations, said Dr. Budson. Patients also may have a mixed variant or dementia. Patients with the dementia subtype must have a progressive course of cognitive core clinical features, with or without behavior or mood features. In addition, patients with dementia must have cognitive impairment that interferes with their ability to function independently during normal daily activities.
Biomarkers and Treatment
Cavum septum pellucidum, cavum vergae, or fenestrations on neuroimaging are potential CTE biomarkers, said Dr. Budson. Normal beta amyloid CSF levels, elevated CSF p-tau/tau ratio, negative amyloid imaging, as well as cortical atrophy beyond that expected for age could also be signs of CTE. Potential experimental biomarkers include positive tau imaging and cortical thinning based on MRI.
Once physicians have made a diagnosis of probable or possible CTE, there are several treatments that may benefit patients, although no medications are approved for the treatment of CTE. Cholinesterase inhibitors may help to treat memory impairment, said Dr. Budson. For patients with depression and anxiety, selective serotonin reuptake inhibitors may be helpful. For patients with violent or explosive behavior, atypical neuroleptics may be efficacious. Memantine may benefit patients with moderate or severe dementia. Finally, to manage agitation, a combination of dextromethorphan and quinidine may be a treatment option.
—Erica Tricarico
Suggested Reading
Montenigro PH, Baugh CM, Daneshvar DH, et al. Clinical subtypes of chronic traumatic encephalopathy: literature review and proposed research diagnostic criteria for traumatic encephalopathy syndrome. Alzheimers Res Ther. 2014;6(5):68.
Breast cancer liquid biopsies don’t change outcomes....yet
LAS VEGAS – Although circulating tumor cells are prognostic in breast cancer, they aren’t likely to become a part of routine practice until they’ve been shown to improve outcomes, and that hasn’t happened yet, according to Anthony Lucci, MD, professor of breast surgical oncology at MD Anderson Cancer Center, Houston.
MD Anderson and other institutions have established that in breast cancer, from baseline through treatment follow-up, the presence of circulating tumor cells (CTCs) in the blood predicts worse outcomes in both metastatic and local disease, even among women who have a pathologic complete response to treatment.
That knowledge has not yet translated into better outcomes. In a pivotal trial, survival was no better in metastatic breast cancer when women were switched to an alternative chemotherapy regimen after their CTC levels did not fall in response to first-line treatment, compared with women who remained on their initial agent despite persistently high CTCs (J Clin Oncol. 2014 Nov 1;32[31]:3483-9).
“When we tried to switch chemotherapy” based on CTCs, “it really didn’t make a difference, so no one is really quite sure yet what to do with this information. We can’t tell a patient that they are likely to have a much worse outcome, but there’s nothing we can do about it,” and “I don’t think payers will pay” for CTC testing in breast cancer until “we establish a predictive benefit, and show what agents will reduce CTCs and improve outcomes,” Dr. Lucci said at the American Society of Breast Surgeons annual meeting.
Even so, the promise of CTCs as a clinical tool is too great to abandon research, and work continues at MD Anderson and elsewhere. It’s thought that tumor cells in the blood aren’t simply a marker of disease, but rather microscopic disease in themselves that contributes to recurrence and progression. It’s possible that cells shed by tumors lie dormant in the bone marrow, then reactivate and reseed the original tumor site or give rise to distant metastases.
CTCs are similar to tumor cells that have been found in the bone marrow of women with apparently quiescent breast cancer, but finding them in the blood means “you don’t have to poke a needle in someone’s bone. You can just take a sample of their blood, and it tells you the same information,” Dr. Lucci said.
CTCs have been shown in breast cancer to rise and fall depending on tumor response. “In the future, I do think we will [use them] as a serial monitoring tool and a guide to therapy.” There might even be a role for breast cancer screening, he said.
Analyzing the blood for evidence of solid tumors – popularly called “liquid biopsy” – has shown benefits in a variety of cancers, particularly for identifying disease, and in some cases mutations, sooner than with conventional methods. Science is catching up to the old-school notion that cancer spreads through the blood.
Another approach is to look for circulating tumor DNA, which has been shown to be useful for early detection in gynecologic cancers. The idea is that a few tumor cells shatter and spill their genetic material into the blood early on. “In the majority of breast cancer patients,” however, “you don’t find actionable mutations” with circulating tumor DNA, especially in earlier-stage, nonmetastatic disease. “There’s not enough DNA released into the blood,” Dr. Lucci said.
But “we need to be monitoring the blood on a routine basis” for breast cancer clues. “That, I think, is the wave of the future. Just looking at x-rays and waiting for something to happen is too late,” he said.
Dr. Lucci had no disclosures related to his talk.
LAS VEGAS – Although circulating tumor cells are prognostic in breast cancer, they aren’t likely to become a part of routine practice until they’ve been shown to improve outcomes, and that hasn’t happened yet, according to Anthony Lucci, MD, professor of breast surgical oncology at MD Anderson Cancer Center, Houston.
MD Anderson and other institutions have established that in breast cancer, from baseline through treatment follow-up, the presence of circulating tumor cells (CTCs) in the blood predicts worse outcomes in both metastatic and local disease, even among women who have a pathologic complete response to treatment.
That knowledge has not yet translated into better outcomes. In a pivotal trial, survival was no better in metastatic breast cancer when women were switched to an alternative chemotherapy regimen after their CTC levels did not fall in response to first-line treatment, compared with women who remained on their initial agent despite persistently high CTCs (J Clin Oncol. 2014 Nov 1;32[31]:3483-9).
“When we tried to switch chemotherapy” based on CTCs, “it really didn’t make a difference, so no one is really quite sure yet what to do with this information. We can’t tell a patient that they are likely to have a much worse outcome, but there’s nothing we can do about it,” and “I don’t think payers will pay” for CTC testing in breast cancer until “we establish a predictive benefit, and show what agents will reduce CTCs and improve outcomes,” Dr. Lucci said at the American Society of Breast Surgeons annual meeting.
Even so, the promise of CTCs as a clinical tool is too great to abandon research, and work continues at MD Anderson and elsewhere. It’s thought that tumor cells in the blood aren’t simply a marker of disease, but rather microscopic disease in themselves that contributes to recurrence and progression. It’s possible that cells shed by tumors lie dormant in the bone marrow, then reactivate and reseed the original tumor site or give rise to distant metastases.
CTCs are similar to tumor cells that have been found in the bone marrow of women with apparently quiescent breast cancer, but finding them in the blood means “you don’t have to poke a needle in someone’s bone. You can just take a sample of their blood, and it tells you the same information,” Dr. Lucci said.
CTCs have been shown in breast cancer to rise and fall depending on tumor response. “In the future, I do think we will [use them] as a serial monitoring tool and a guide to therapy.” There might even be a role for breast cancer screening, he said.
Analyzing the blood for evidence of solid tumors – popularly called “liquid biopsy” – has shown benefits in a variety of cancers, particularly for identifying disease, and in some cases mutations, sooner than with conventional methods. Science is catching up to the old-school notion that cancer spreads through the blood.
Another approach is to look for circulating tumor DNA, which has been shown to be useful for early detection in gynecologic cancers. The idea is that a few tumor cells shatter and spill their genetic material into the blood early on. “In the majority of breast cancer patients,” however, “you don’t find actionable mutations” with circulating tumor DNA, especially in earlier-stage, nonmetastatic disease. “There’s not enough DNA released into the blood,” Dr. Lucci said.
But “we need to be monitoring the blood on a routine basis” for breast cancer clues. “That, I think, is the wave of the future. Just looking at x-rays and waiting for something to happen is too late,” he said.
Dr. Lucci had no disclosures related to his talk.
LAS VEGAS – Although circulating tumor cells are prognostic in breast cancer, they aren’t likely to become a part of routine practice until they’ve been shown to improve outcomes, and that hasn’t happened yet, according to Anthony Lucci, MD, professor of breast surgical oncology at MD Anderson Cancer Center, Houston.
MD Anderson and other institutions have established that in breast cancer, from baseline through treatment follow-up, the presence of circulating tumor cells (CTCs) in the blood predicts worse outcomes in both metastatic and local disease, even among women who have a pathologic complete response to treatment.
That knowledge has not yet translated into better outcomes. In a pivotal trial, survival was no better in metastatic breast cancer when women were switched to an alternative chemotherapy regimen after their CTC levels did not fall in response to first-line treatment, compared with women who remained on their initial agent despite persistently high CTCs (J Clin Oncol. 2014 Nov 1;32[31]:3483-9).
“When we tried to switch chemotherapy” based on CTCs, “it really didn’t make a difference, so no one is really quite sure yet what to do with this information. We can’t tell a patient that they are likely to have a much worse outcome, but there’s nothing we can do about it,” and “I don’t think payers will pay” for CTC testing in breast cancer until “we establish a predictive benefit, and show what agents will reduce CTCs and improve outcomes,” Dr. Lucci said at the American Society of Breast Surgeons annual meeting.
Even so, the promise of CTCs as a clinical tool is too great to abandon research, and work continues at MD Anderson and elsewhere. It’s thought that tumor cells in the blood aren’t simply a marker of disease, but rather microscopic disease in themselves that contributes to recurrence and progression. It’s possible that cells shed by tumors lie dormant in the bone marrow, then reactivate and reseed the original tumor site or give rise to distant metastases.
CTCs are similar to tumor cells that have been found in the bone marrow of women with apparently quiescent breast cancer, but finding them in the blood means “you don’t have to poke a needle in someone’s bone. You can just take a sample of their blood, and it tells you the same information,” Dr. Lucci said.
CTCs have been shown in breast cancer to rise and fall depending on tumor response. “In the future, I do think we will [use them] as a serial monitoring tool and a guide to therapy.” There might even be a role for breast cancer screening, he said.
Analyzing the blood for evidence of solid tumors – popularly called “liquid biopsy” – has shown benefits in a variety of cancers, particularly for identifying disease, and in some cases mutations, sooner than with conventional methods. Science is catching up to the old-school notion that cancer spreads through the blood.
Another approach is to look for circulating tumor DNA, which has been shown to be useful for early detection in gynecologic cancers. The idea is that a few tumor cells shatter and spill their genetic material into the blood early on. “In the majority of breast cancer patients,” however, “you don’t find actionable mutations” with circulating tumor DNA, especially in earlier-stage, nonmetastatic disease. “There’s not enough DNA released into the blood,” Dr. Lucci said.
But “we need to be monitoring the blood on a routine basis” for breast cancer clues. “That, I think, is the wave of the future. Just looking at x-rays and waiting for something to happen is too late,” he said.
Dr. Lucci had no disclosures related to his talk.
AT ASBS 2017