User login
Weight fluctuations linked to higher mortality, CV events
Weight fluctuations – like the typical pattern of weight loss followed by partial or total regain that affects most people attempting to lose weight – are strongly associated with higher mortality, more cardiovascular events, and new-onset diabetes, according to an analysis of the Treating to New Targets trial published online April 6 in the New England Journal of Medicine.
Weight loss is commonly prescribed as a lifestyle intervention to improve health, especially cardiovascular health. However, “the usual pattern for most patients ... is weight loss followed by weight gain” (also termed weight cycling), which has been linked to poor cardiovascular outcomes, especially when the pattern is repeated over time, said Sripal Bangalore, MD, of New York University, and his coinvestigators.
The primary outcome measure – the composite rate of death from coronary heart disease, nonfatal MI, resuscitated cardiac arrest, revascularization, or angina – was significantly associated with weight fluctuations in a dose-dependent fashion so that greater degrees of variability in body weight were linked to higher event rates (N Engl J Med. 2017 April 6. doi: 10.1056/NEJMoa1606148).
“When compared with the lowest quintile, patients with the highest quintile of variability had an increase in the risk of any coronary event of 64%, an increase in the risk of any cardiovascular event of 85%, an increase in the risk of death of 124%, an increase in the risk of MI of 117%, an increase in the risk of stroke of 136%, and an increase in the risk of new-onset diabetes of 78%, independent of traditional risk factors,” Dr. Bangalore and his associates reported.
This association remained strong regardless of the patients’ weight at baseline, consistent among those of normal body weight and those who were overweight or obese. And the association also persisted across multiple sensitivity analyses.
This study was supported by Pfizer. Dr. Bangalore reported serving as a consultant to Pfizer, Daiichi-Sankyo, Boehringer Ingelheim, Merck, Menarini, Gilead, and Abbott Vascular; his associates reported ties to numerous industry sources.
Weight fluctuations – like the typical pattern of weight loss followed by partial or total regain that affects most people attempting to lose weight – are strongly associated with higher mortality, more cardiovascular events, and new-onset diabetes, according to an analysis of the Treating to New Targets trial published online April 6 in the New England Journal of Medicine.
Weight loss is commonly prescribed as a lifestyle intervention to improve health, especially cardiovascular health. However, “the usual pattern for most patients ... is weight loss followed by weight gain” (also termed weight cycling), which has been linked to poor cardiovascular outcomes, especially when the pattern is repeated over time, said Sripal Bangalore, MD, of New York University, and his coinvestigators.
The primary outcome measure – the composite rate of death from coronary heart disease, nonfatal MI, resuscitated cardiac arrest, revascularization, or angina – was significantly associated with weight fluctuations in a dose-dependent fashion so that greater degrees of variability in body weight were linked to higher event rates (N Engl J Med. 2017 April 6. doi: 10.1056/NEJMoa1606148).
“When compared with the lowest quintile, patients with the highest quintile of variability had an increase in the risk of any coronary event of 64%, an increase in the risk of any cardiovascular event of 85%, an increase in the risk of death of 124%, an increase in the risk of MI of 117%, an increase in the risk of stroke of 136%, and an increase in the risk of new-onset diabetes of 78%, independent of traditional risk factors,” Dr. Bangalore and his associates reported.
This association remained strong regardless of the patients’ weight at baseline, consistent among those of normal body weight and those who were overweight or obese. And the association also persisted across multiple sensitivity analyses.
This study was supported by Pfizer. Dr. Bangalore reported serving as a consultant to Pfizer, Daiichi-Sankyo, Boehringer Ingelheim, Merck, Menarini, Gilead, and Abbott Vascular; his associates reported ties to numerous industry sources.
Weight fluctuations – like the typical pattern of weight loss followed by partial or total regain that affects most people attempting to lose weight – are strongly associated with higher mortality, more cardiovascular events, and new-onset diabetes, according to an analysis of the Treating to New Targets trial published online April 6 in the New England Journal of Medicine.
Weight loss is commonly prescribed as a lifestyle intervention to improve health, especially cardiovascular health. However, “the usual pattern for most patients ... is weight loss followed by weight gain” (also termed weight cycling), which has been linked to poor cardiovascular outcomes, especially when the pattern is repeated over time, said Sripal Bangalore, MD, of New York University, and his coinvestigators.
The primary outcome measure – the composite rate of death from coronary heart disease, nonfatal MI, resuscitated cardiac arrest, revascularization, or angina – was significantly associated with weight fluctuations in a dose-dependent fashion so that greater degrees of variability in body weight were linked to higher event rates (N Engl J Med. 2017 April 6. doi: 10.1056/NEJMoa1606148).
“When compared with the lowest quintile, patients with the highest quintile of variability had an increase in the risk of any coronary event of 64%, an increase in the risk of any cardiovascular event of 85%, an increase in the risk of death of 124%, an increase in the risk of MI of 117%, an increase in the risk of stroke of 136%, and an increase in the risk of new-onset diabetes of 78%, independent of traditional risk factors,” Dr. Bangalore and his associates reported.
This association remained strong regardless of the patients’ weight at baseline, consistent among those of normal body weight and those who were overweight or obese. And the association also persisted across multiple sensitivity analyses.
This study was supported by Pfizer. Dr. Bangalore reported serving as a consultant to Pfizer, Daiichi-Sankyo, Boehringer Ingelheim, Merck, Menarini, Gilead, and Abbott Vascular; his associates reported ties to numerous industry sources.
Key clinical point: Weight fluctuations are strongly associated with higher mortality, more cardiovascular events, and new-onset diabetes.
Major finding: Patients with the highest quintile of weight variability had increased risks of coronary events (64%), cardiovascular events (85%), death (124%), MI (117%), stroke (136%), and new-onset diabetes (78%).
Data source: A secondary analysis of data for 9,509 adults with coronary artery disease participating in the Treating to New Targets trial of cholesterol therapy.
Disclosures: This study was supported by Pfizer. Dr. Bangalore reported serving as a consultant to Pfizer, Daiichi-Sankyo, Boehringer Ingelheim, Merck, Menarini, Gilead, and Abbott Vascular; his associates reported ties to numerous industry sources.
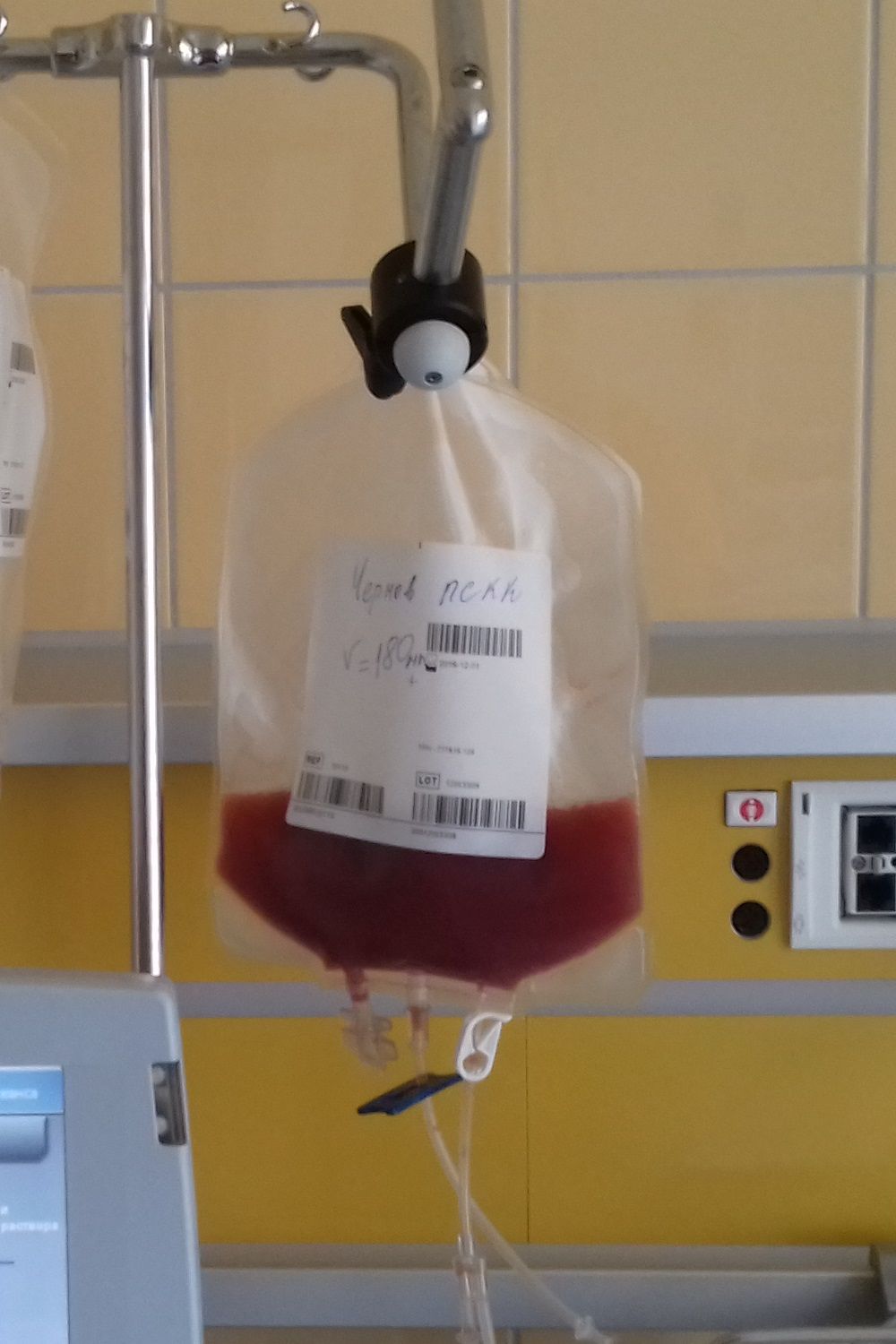
Transplantation plus VRD tops VRD alone in myeloma
Adding high-dose chemotherapy and autologous stem cell transplantation to two cycles of bortezomib, lenalidomide, and dexamethasone (VRD) significantly improved progression-free survival in adults with newly diagnosed multiple myeloma, according to new analyses from the multicenter, randomized, phase III IFM 2009 Study.
Median PFS was 50 months in the transplantation group, versus 36 months when patients only received five cycles of VRD for consolidation (adjusted hazard ratio for disease progression or death, 0.65; 95% confidence interval, 0.53 to 0.80; P less than .001), reported Michel Attal, MD, of Institut Universitaire du Cancer de Toulouse-Oncopole in Toulouse, France, and his associates. “Transplantation was also associated with a higher rate of complete response, a lower rate of minimal residual disease detection, and a longer median time to progression,” they wrote (N Engl J Med. 2017 April 6. doi: 10.1056/NEJMoa1611750).
Transplantation did not improve 4-year overall survival (81% with transplantation plus VRD and 82% with VRD only), perhaps because VRD-only patients had the option of salvage transplantation if their disease progressed, the investigators said. In addition, grade 3 or 4 neutropenias were significantly more common with transplantation than otherwise (92% versus 47%), as were grade 3 or 4 gastrointestinal disorders (28% versus 7%) and infections (20% versus 9%). However, the groups did not significantly differ in terms of treatment-related deaths, second primary cancers, thromboembolic events, or peripheral neuropathy.
Before the advent of immunomodulatory drugs and proteasome inhibitors, several randomized trials showed that the benefits of high-dose chemotherapy with autologous stem cell transplantation outperformed conventional chemotherapy in multiple myeloma. For IFM 2009, 700 newly diagnosed patients aged up to 65 years received three 21-day cycles of VRD induction: bortezomib 1.3 mg/m2 on days 1, 4, 8, and 11; lenalidomide 25 mg on days 1-14; and dexamethasone 20 mg on days 1, 2, 4, 5, 8, 9, 11, and 12. Consolidation consisted of either five more VRD cycles with dexamethasone reduced to 10 mg/day, or high-dose (200 mg/m2) melphalan plus transplantation followed by two VRD cycles with the reduced dexamethasone dose. Both arms received 1 year of lenalidomide maintenance (10 mg/day for 3 months, followed by 15/mg day, depending on side effects).
Transplantation was associated with a significantly higher likelihood of complete response (59% versus 48%; P = .03) and undetectable minimal residual disease (79% versus 65%; P less than .001). Undetectable minimal residual disease, in turn, predicted longer PFS (adjusted hazard ratio, 0.30; P = .001). In contrast, age, sex, isotype of the monoclonal component, International Staging System disease stage, and cytogenetic risk profile did not significantly affect PFS among transplant patients.
The PFS benefit of transplantation “must be weighed against the increased risk of toxic effects associated with high-dose chemotherapy plus transplantation, especially since we found that later transplantation might be as effective as early transplantation in securing long- term survival,” the researchers said. “Our results suggest that the use of a combination therapy that incorporates newer proteasome inhibitors, next-generation immunomodulatory drugs, and potent monoclonal antibodies along with transplantation tailored according to minimal residual disease detection could further improve outcomes among adults up to 65 years of age who have multiple myeloma.”
Celgene, Janssen, the French Ministry of Health Programme Hospitalier de Recherche Clinique, and the French National Research Agency funded the study. Dr. Attal had no conflicts. Nine coinvestigators disclosed ties to Celgene, Janssen, and several other pharmaceutical companies. Two coinvestigators disclosed ownership or founder roles in OncoPep, one of whom disclosed patent licensure to OncoPep for a multipeptide vaccine. The other investigators had no conflicts.
In the IFM 2009 trial, the planned treatments were realistic. The combination of immunomodulatory drugs and proteasome inhibitors is associated with high response rates similar to those achieved with transplantation, whereas previous trials had used less effective chemotherapy regimens as comparators.
[Transplantation] resulted in a deeper and longer initial treatment response than did nontransplantation. However, the benefits of transplantation were more modest than some might have hoped, and it did not appear to be curative.
A question remains as to whether all patients with multiple myeloma should undergo immediate autologous stem-cell transplantation, since the use of delayed transplantation resulted in similar overall survival, with some patients not needing transplantation to date. The observed lack of a survival benefit for early transplantation was consistent with previous results that suggested salvage transplantation is an equalizer in this regard.
Charles A. Schiffer, MD, and Jeffrey A. Zonder, MD, are with Karmanos Cancer Institute, Wayne State University, Detroit, Mich. Dr. Zonder is a member of the editorial advisory board of Hematology News. Their comments were taken from an editorial (N Engl J Med. 2017 April 6. doi: 10.1056/NEJMe1700453).
In the IFM 2009 trial, the planned treatments were realistic. The combination of immunomodulatory drugs and proteasome inhibitors is associated with high response rates similar to those achieved with transplantation, whereas previous trials had used less effective chemotherapy regimens as comparators.
[Transplantation] resulted in a deeper and longer initial treatment response than did nontransplantation. However, the benefits of transplantation were more modest than some might have hoped, and it did not appear to be curative.
A question remains as to whether all patients with multiple myeloma should undergo immediate autologous stem-cell transplantation, since the use of delayed transplantation resulted in similar overall survival, with some patients not needing transplantation to date. The observed lack of a survival benefit for early transplantation was consistent with previous results that suggested salvage transplantation is an equalizer in this regard.
Charles A. Schiffer, MD, and Jeffrey A. Zonder, MD, are with Karmanos Cancer Institute, Wayne State University, Detroit, Mich. Dr. Zonder is a member of the editorial advisory board of Hematology News. Their comments were taken from an editorial (N Engl J Med. 2017 April 6. doi: 10.1056/NEJMe1700453).
In the IFM 2009 trial, the planned treatments were realistic. The combination of immunomodulatory drugs and proteasome inhibitors is associated with high response rates similar to those achieved with transplantation, whereas previous trials had used less effective chemotherapy regimens as comparators.
[Transplantation] resulted in a deeper and longer initial treatment response than did nontransplantation. However, the benefits of transplantation were more modest than some might have hoped, and it did not appear to be curative.
A question remains as to whether all patients with multiple myeloma should undergo immediate autologous stem-cell transplantation, since the use of delayed transplantation resulted in similar overall survival, with some patients not needing transplantation to date. The observed lack of a survival benefit for early transplantation was consistent with previous results that suggested salvage transplantation is an equalizer in this regard.
Charles A. Schiffer, MD, and Jeffrey A. Zonder, MD, are with Karmanos Cancer Institute, Wayne State University, Detroit, Mich. Dr. Zonder is a member of the editorial advisory board of Hematology News. Their comments were taken from an editorial (N Engl J Med. 2017 April 6. doi: 10.1056/NEJMe1700453).
Adding high-dose chemotherapy and autologous stem cell transplantation to two cycles of bortezomib, lenalidomide, and dexamethasone (VRD) significantly improved progression-free survival in adults with newly diagnosed multiple myeloma, according to new analyses from the multicenter, randomized, phase III IFM 2009 Study.
Median PFS was 50 months in the transplantation group, versus 36 months when patients only received five cycles of VRD for consolidation (adjusted hazard ratio for disease progression or death, 0.65; 95% confidence interval, 0.53 to 0.80; P less than .001), reported Michel Attal, MD, of Institut Universitaire du Cancer de Toulouse-Oncopole in Toulouse, France, and his associates. “Transplantation was also associated with a higher rate of complete response, a lower rate of minimal residual disease detection, and a longer median time to progression,” they wrote (N Engl J Med. 2017 April 6. doi: 10.1056/NEJMoa1611750).
Transplantation did not improve 4-year overall survival (81% with transplantation plus VRD and 82% with VRD only), perhaps because VRD-only patients had the option of salvage transplantation if their disease progressed, the investigators said. In addition, grade 3 or 4 neutropenias were significantly more common with transplantation than otherwise (92% versus 47%), as were grade 3 or 4 gastrointestinal disorders (28% versus 7%) and infections (20% versus 9%). However, the groups did not significantly differ in terms of treatment-related deaths, second primary cancers, thromboembolic events, or peripheral neuropathy.
Before the advent of immunomodulatory drugs and proteasome inhibitors, several randomized trials showed that the benefits of high-dose chemotherapy with autologous stem cell transplantation outperformed conventional chemotherapy in multiple myeloma. For IFM 2009, 700 newly diagnosed patients aged up to 65 years received three 21-day cycles of VRD induction: bortezomib 1.3 mg/m2 on days 1, 4, 8, and 11; lenalidomide 25 mg on days 1-14; and dexamethasone 20 mg on days 1, 2, 4, 5, 8, 9, 11, and 12. Consolidation consisted of either five more VRD cycles with dexamethasone reduced to 10 mg/day, or high-dose (200 mg/m2) melphalan plus transplantation followed by two VRD cycles with the reduced dexamethasone dose. Both arms received 1 year of lenalidomide maintenance (10 mg/day for 3 months, followed by 15/mg day, depending on side effects).
Transplantation was associated with a significantly higher likelihood of complete response (59% versus 48%; P = .03) and undetectable minimal residual disease (79% versus 65%; P less than .001). Undetectable minimal residual disease, in turn, predicted longer PFS (adjusted hazard ratio, 0.30; P = .001). In contrast, age, sex, isotype of the monoclonal component, International Staging System disease stage, and cytogenetic risk profile did not significantly affect PFS among transplant patients.
The PFS benefit of transplantation “must be weighed against the increased risk of toxic effects associated with high-dose chemotherapy plus transplantation, especially since we found that later transplantation might be as effective as early transplantation in securing long- term survival,” the researchers said. “Our results suggest that the use of a combination therapy that incorporates newer proteasome inhibitors, next-generation immunomodulatory drugs, and potent monoclonal antibodies along with transplantation tailored according to minimal residual disease detection could further improve outcomes among adults up to 65 years of age who have multiple myeloma.”
Celgene, Janssen, the French Ministry of Health Programme Hospitalier de Recherche Clinique, and the French National Research Agency funded the study. Dr. Attal had no conflicts. Nine coinvestigators disclosed ties to Celgene, Janssen, and several other pharmaceutical companies. Two coinvestigators disclosed ownership or founder roles in OncoPep, one of whom disclosed patent licensure to OncoPep for a multipeptide vaccine. The other investigators had no conflicts.
Adding high-dose chemotherapy and autologous stem cell transplantation to two cycles of bortezomib, lenalidomide, and dexamethasone (VRD) significantly improved progression-free survival in adults with newly diagnosed multiple myeloma, according to new analyses from the multicenter, randomized, phase III IFM 2009 Study.
Median PFS was 50 months in the transplantation group, versus 36 months when patients only received five cycles of VRD for consolidation (adjusted hazard ratio for disease progression or death, 0.65; 95% confidence interval, 0.53 to 0.80; P less than .001), reported Michel Attal, MD, of Institut Universitaire du Cancer de Toulouse-Oncopole in Toulouse, France, and his associates. “Transplantation was also associated with a higher rate of complete response, a lower rate of minimal residual disease detection, and a longer median time to progression,” they wrote (N Engl J Med. 2017 April 6. doi: 10.1056/NEJMoa1611750).
Transplantation did not improve 4-year overall survival (81% with transplantation plus VRD and 82% with VRD only), perhaps because VRD-only patients had the option of salvage transplantation if their disease progressed, the investigators said. In addition, grade 3 or 4 neutropenias were significantly more common with transplantation than otherwise (92% versus 47%), as were grade 3 or 4 gastrointestinal disorders (28% versus 7%) and infections (20% versus 9%). However, the groups did not significantly differ in terms of treatment-related deaths, second primary cancers, thromboembolic events, or peripheral neuropathy.
Before the advent of immunomodulatory drugs and proteasome inhibitors, several randomized trials showed that the benefits of high-dose chemotherapy with autologous stem cell transplantation outperformed conventional chemotherapy in multiple myeloma. For IFM 2009, 700 newly diagnosed patients aged up to 65 years received three 21-day cycles of VRD induction: bortezomib 1.3 mg/m2 on days 1, 4, 8, and 11; lenalidomide 25 mg on days 1-14; and dexamethasone 20 mg on days 1, 2, 4, 5, 8, 9, 11, and 12. Consolidation consisted of either five more VRD cycles with dexamethasone reduced to 10 mg/day, or high-dose (200 mg/m2) melphalan plus transplantation followed by two VRD cycles with the reduced dexamethasone dose. Both arms received 1 year of lenalidomide maintenance (10 mg/day for 3 months, followed by 15/mg day, depending on side effects).
Transplantation was associated with a significantly higher likelihood of complete response (59% versus 48%; P = .03) and undetectable minimal residual disease (79% versus 65%; P less than .001). Undetectable minimal residual disease, in turn, predicted longer PFS (adjusted hazard ratio, 0.30; P = .001). In contrast, age, sex, isotype of the monoclonal component, International Staging System disease stage, and cytogenetic risk profile did not significantly affect PFS among transplant patients.
The PFS benefit of transplantation “must be weighed against the increased risk of toxic effects associated with high-dose chemotherapy plus transplantation, especially since we found that later transplantation might be as effective as early transplantation in securing long- term survival,” the researchers said. “Our results suggest that the use of a combination therapy that incorporates newer proteasome inhibitors, next-generation immunomodulatory drugs, and potent monoclonal antibodies along with transplantation tailored according to minimal residual disease detection could further improve outcomes among adults up to 65 years of age who have multiple myeloma.”
Celgene, Janssen, the French Ministry of Health Programme Hospitalier de Recherche Clinique, and the French National Research Agency funded the study. Dr. Attal had no conflicts. Nine coinvestigators disclosed ties to Celgene, Janssen, and several other pharmaceutical companies. Two coinvestigators disclosed ownership or founder roles in OncoPep, one of whom disclosed patent licensure to OncoPep for a multipeptide vaccine. The other investigators had no conflicts.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: High-dose chemotherapy and autologous stem cell transplantation plus bortezomib, lenalidomide, and dexamethasone (VRD) outperformed consolidation with VRD only in adults with newly diagnosed multiple myeloma.
Major finding: Median progression-free survival was 50 months with transplantation plus VRD and 36 months with VRD only (adjusted hazard ratio for disease progression or death, 0.65; P less than .001).
Data source: A randomized, multicenter, open-label, phase III trial of 700 patients with multiple myeloma.
Disclosures: Celgene, Janssen, the French Ministry of Health Programme Hospitalier de Recherche Clinique, and the French National Research Agency funded the study. Dr. Attal had no conflicts. Nine coinvestigators disclosed ties to Celgene, Janssen, and several other pharmaceutical companies. Two coinvestigators disclosed ownership or founder roles in OncoPep, one of whom disclosed patent licensure to OncoPep for a multipeptide vaccine. The other investigators had no conflicts.
Fatigue in rheumatoid arthritis declines with pedometer use
Rheumatoid arthritis patients given pedometers reported a decrease in fatigue over a 21-week period, coupled with a small but significant increase in steps walked, according to a study from investigators at the University of California, San Francisco.
“Our results provide evidence that pedometers are effective at increasing physical activity among people with RA and provide support for the hypothesis that increasing physical activity by walking has important effects on fatigue and other RA symptoms,” wrote the researchers, led by Patricia Katz, PhD.
Patients who were given only pedometers increased their walking from baseline to week 21 by an average of 1,441 steps, while those given pedometers plus a step goal walked a mean of 1,656 steps additionally. The control group had a mean decrease of 747 steps.
Scores on the Patient-Reported Outcome Measurement Information System fatigue short form at 21 weeks declined by –3.2 for those who received pedometers only (P = .02) and by –4.8 for those who received pedometers plus a step goal (P = .0002), compared with the control group, which reported a decrease of –1.6 (P = .26).
While both intervention groups saw increased activity when compared with controls, patients given a step goal saw constant improvement, averaging an increase of 22 steps per week, while those without a step goal reported a decrease of 37 steps per week, which the researchers suspected could be from a larger initial increase in activity that could have discouraged a continued increase over time.
Dr. Katz and her associates said that the positive change that a rise in physical activity had on all other aspects of patients’ self-reported assessment shows promising results for the efficacy of exercise in patients, which some physicians had questioned.
“In the past, there was concern that physical activity or exercise might exacerbate rheumatoid arthritis symptoms, [however], our findings are similar to previous reports that exercise did not lead to worsened rheumatoid arthritis,” they wrote.
This study was limited by the small number of participants in the study, as well as the self-reported method of data collection. Researchers were also unable to gather activity intensity, as well as the amount of time patients wore the pedometer, causing the measure of adherence to “only be considered an estimate.”
The researchers reported technical difficulties with the devices, creating missing data.
The study was supported by the Rheumatology Research Foundation. The researchers reported no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
On Twitter @EAZTweets
Rheumatoid arthritis patients given pedometers reported a decrease in fatigue over a 21-week period, coupled with a small but significant increase in steps walked, according to a study from investigators at the University of California, San Francisco.
“Our results provide evidence that pedometers are effective at increasing physical activity among people with RA and provide support for the hypothesis that increasing physical activity by walking has important effects on fatigue and other RA symptoms,” wrote the researchers, led by Patricia Katz, PhD.
Patients who were given only pedometers increased their walking from baseline to week 21 by an average of 1,441 steps, while those given pedometers plus a step goal walked a mean of 1,656 steps additionally. The control group had a mean decrease of 747 steps.
Scores on the Patient-Reported Outcome Measurement Information System fatigue short form at 21 weeks declined by –3.2 for those who received pedometers only (P = .02) and by –4.8 for those who received pedometers plus a step goal (P = .0002), compared with the control group, which reported a decrease of –1.6 (P = .26).
While both intervention groups saw increased activity when compared with controls, patients given a step goal saw constant improvement, averaging an increase of 22 steps per week, while those without a step goal reported a decrease of 37 steps per week, which the researchers suspected could be from a larger initial increase in activity that could have discouraged a continued increase over time.
Dr. Katz and her associates said that the positive change that a rise in physical activity had on all other aspects of patients’ self-reported assessment shows promising results for the efficacy of exercise in patients, which some physicians had questioned.
“In the past, there was concern that physical activity or exercise might exacerbate rheumatoid arthritis symptoms, [however], our findings are similar to previous reports that exercise did not lead to worsened rheumatoid arthritis,” they wrote.
This study was limited by the small number of participants in the study, as well as the self-reported method of data collection. Researchers were also unable to gather activity intensity, as well as the amount of time patients wore the pedometer, causing the measure of adherence to “only be considered an estimate.”
The researchers reported technical difficulties with the devices, creating missing data.
The study was supported by the Rheumatology Research Foundation. The researchers reported no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
On Twitter @EAZTweets
Rheumatoid arthritis patients given pedometers reported a decrease in fatigue over a 21-week period, coupled with a small but significant increase in steps walked, according to a study from investigators at the University of California, San Francisco.
“Our results provide evidence that pedometers are effective at increasing physical activity among people with RA and provide support for the hypothesis that increasing physical activity by walking has important effects on fatigue and other RA symptoms,” wrote the researchers, led by Patricia Katz, PhD.
Patients who were given only pedometers increased their walking from baseline to week 21 by an average of 1,441 steps, while those given pedometers plus a step goal walked a mean of 1,656 steps additionally. The control group had a mean decrease of 747 steps.
Scores on the Patient-Reported Outcome Measurement Information System fatigue short form at 21 weeks declined by –3.2 for those who received pedometers only (P = .02) and by –4.8 for those who received pedometers plus a step goal (P = .0002), compared with the control group, which reported a decrease of –1.6 (P = .26).
While both intervention groups saw increased activity when compared with controls, patients given a step goal saw constant improvement, averaging an increase of 22 steps per week, while those without a step goal reported a decrease of 37 steps per week, which the researchers suspected could be from a larger initial increase in activity that could have discouraged a continued increase over time.
Dr. Katz and her associates said that the positive change that a rise in physical activity had on all other aspects of patients’ self-reported assessment shows promising results for the efficacy of exercise in patients, which some physicians had questioned.
“In the past, there was concern that physical activity or exercise might exacerbate rheumatoid arthritis symptoms, [however], our findings are similar to previous reports that exercise did not lead to worsened rheumatoid arthritis,” they wrote.
This study was limited by the small number of participants in the study, as well as the self-reported method of data collection. Researchers were also unable to gather activity intensity, as well as the amount of time patients wore the pedometer, causing the measure of adherence to “only be considered an estimate.”
The researchers reported technical difficulties with the devices, creating missing data.
The study was supported by the Rheumatology Research Foundation. The researchers reported no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
On Twitter @EAZTweets
FROM ARTHRITIS CARE & RESEARCH
Key clinical point:
Major finding: Mean fatigue scores dropped –3.2 (P = .02) and –4.8 (P = .0002) for patients given only pedometers and pedometers with step goals, respectively.
Data source: Controlled study of 96 rheumatoid arthritis patients observed over a 21-week period.
Disclosures: The study was supported by the Rheumatology Research Foundation. The researchers reported no relevant financial disclosures.
Inpatient cost of atopic dermatitis called ‘substantial’
Inpatient care for atopic dermatitis in the U.S. totaled almost $128 million between 2002 and 2012, indicating a rising financial burden, according to a study funded by the Agency for Healthcare Research and Quality (AHRQ).
Cost of care averaged $8.3 million per year for adults and $3.3 million per year for children, with per-day costs for adult care increasing from $3,200 in 2002 to $3,783 in 2012 and per-day costs for pediatric care increasing from $2,430 to $2,914 in the same period, according to Shanthi Narla, a doctoral research fellow at Northwestern University, Chicago, and her colleagues (J Invest Dermatol. 2017 Mar 1. doi: 10.1016/j.jid.2017.02.975)
Growth in hospitalizations was seen especially in adult AD patients, which rose from 58 million to 76 million over the decade.
Despite such high comparative rates of hospitalization, most adult (80%) and child (97%) AD patients had a shorter average length of stay than those without AD (adults: 2.7 vs. 3.5 days; children: 2.4 vs. 2.7 days; P = .0004),
Growing prevalence of AD hospitalization contributed to the larger financial burden for AD patients, compared with psoriasis and pemphigus, the researchers noted, considering length of stay per AD hospitalization averaged 62.5% and 50% shorter than those for pemphigus or psoriasis.
“The acute signs and symptoms of [AD or eczema]... erythema, oozing/weeping, scaling and pruritus, may resolve faster with optimized treatment than vesicobullae and erosions in pemphigus or ‘lakes of pus’ and skin sloughing in generalized pustular psoriasis,” they wrote.
Additionally, hospitalization costs for AD were 60% and 33% of the cost per psoriasis and pemphigus hospitalizations, respectively, according to Ms. Narla and her colleagues.
The researchers said they were concerned that the prevalence of AD, and subsequently the inpatient financial burden, will continue to increase if left unchecked.
“Prevalences and costs of hospitalization for AD significantly increased during the study period without plateauing, indicating that the total cost of inpatient care for AD may continue to increase,” the researchers asserted.
This study was limited by a lack of information on the severity of patients’ symptoms, as well as whether a dermatologist or other physician diagnosed the patients and by which criteria.
ezimmerman@frontlinemedcom.com
On Twitter @EAZTweets
Inpatient care for atopic dermatitis in the U.S. totaled almost $128 million between 2002 and 2012, indicating a rising financial burden, according to a study funded by the Agency for Healthcare Research and Quality (AHRQ).
Cost of care averaged $8.3 million per year for adults and $3.3 million per year for children, with per-day costs for adult care increasing from $3,200 in 2002 to $3,783 in 2012 and per-day costs for pediatric care increasing from $2,430 to $2,914 in the same period, according to Shanthi Narla, a doctoral research fellow at Northwestern University, Chicago, and her colleagues (J Invest Dermatol. 2017 Mar 1. doi: 10.1016/j.jid.2017.02.975)
Growth in hospitalizations was seen especially in adult AD patients, which rose from 58 million to 76 million over the decade.
Despite such high comparative rates of hospitalization, most adult (80%) and child (97%) AD patients had a shorter average length of stay than those without AD (adults: 2.7 vs. 3.5 days; children: 2.4 vs. 2.7 days; P = .0004),
Growing prevalence of AD hospitalization contributed to the larger financial burden for AD patients, compared with psoriasis and pemphigus, the researchers noted, considering length of stay per AD hospitalization averaged 62.5% and 50% shorter than those for pemphigus or psoriasis.
“The acute signs and symptoms of [AD or eczema]... erythema, oozing/weeping, scaling and pruritus, may resolve faster with optimized treatment than vesicobullae and erosions in pemphigus or ‘lakes of pus’ and skin sloughing in generalized pustular psoriasis,” they wrote.
Additionally, hospitalization costs for AD were 60% and 33% of the cost per psoriasis and pemphigus hospitalizations, respectively, according to Ms. Narla and her colleagues.
The researchers said they were concerned that the prevalence of AD, and subsequently the inpatient financial burden, will continue to increase if left unchecked.
“Prevalences and costs of hospitalization for AD significantly increased during the study period without plateauing, indicating that the total cost of inpatient care for AD may continue to increase,” the researchers asserted.
This study was limited by a lack of information on the severity of patients’ symptoms, as well as whether a dermatologist or other physician diagnosed the patients and by which criteria.
ezimmerman@frontlinemedcom.com
On Twitter @EAZTweets
Inpatient care for atopic dermatitis in the U.S. totaled almost $128 million between 2002 and 2012, indicating a rising financial burden, according to a study funded by the Agency for Healthcare Research and Quality (AHRQ).
Cost of care averaged $8.3 million per year for adults and $3.3 million per year for children, with per-day costs for adult care increasing from $3,200 in 2002 to $3,783 in 2012 and per-day costs for pediatric care increasing from $2,430 to $2,914 in the same period, according to Shanthi Narla, a doctoral research fellow at Northwestern University, Chicago, and her colleagues (J Invest Dermatol. 2017 Mar 1. doi: 10.1016/j.jid.2017.02.975)
Growth in hospitalizations was seen especially in adult AD patients, which rose from 58 million to 76 million over the decade.
Despite such high comparative rates of hospitalization, most adult (80%) and child (97%) AD patients had a shorter average length of stay than those without AD (adults: 2.7 vs. 3.5 days; children: 2.4 vs. 2.7 days; P = .0004),
Growing prevalence of AD hospitalization contributed to the larger financial burden for AD patients, compared with psoriasis and pemphigus, the researchers noted, considering length of stay per AD hospitalization averaged 62.5% and 50% shorter than those for pemphigus or psoriasis.
“The acute signs and symptoms of [AD or eczema]... erythema, oozing/weeping, scaling and pruritus, may resolve faster with optimized treatment than vesicobullae and erosions in pemphigus or ‘lakes of pus’ and skin sloughing in generalized pustular psoriasis,” they wrote.
Additionally, hospitalization costs for AD were 60% and 33% of the cost per psoriasis and pemphigus hospitalizations, respectively, according to Ms. Narla and her colleagues.
The researchers said they were concerned that the prevalence of AD, and subsequently the inpatient financial burden, will continue to increase if left unchecked.
“Prevalences and costs of hospitalization for AD significantly increased during the study period without plateauing, indicating that the total cost of inpatient care for AD may continue to increase,” the researchers asserted.
This study was limited by a lack of information on the severity of patients’ symptoms, as well as whether a dermatologist or other physician diagnosed the patients and by which criteria.
ezimmerman@frontlinemedcom.com
On Twitter @EAZTweets
FROM THE JOURNAL OF INVESTIGATIVE DERMATOLOGY
Key clinical point:
Major finding: Hospitalization costs for atopic dermatitis or eczema in adults and children in the U.S. totaled $127.8 million between 2002 and 2012.
Data source: Retrospective analysis of 87 million patient records from the 2002-2012 National Inpatient Sample, with cost of care adjusted for inflation.
Disclosures: Study was sponsored by the Agency for Healthcare Research and Quality (AHRQ), the Dermatology Foundation, and American Medical Association Foundation. The investigators report no relevant financial disclosures.
Cell sheet transplantation improves ischemic cardiomyopathy at 1 year
For patients with ischemic cardiomyopathy (ICM), transplanting sheets of autologous myoblasts onto the epicardial surface was safe and led to “marked” improvements in functional and laboratory measures, investigators reported.
However, cell sheet transplantation was much less effective for patients with dilated cardiomyopathy in this phase I trial, wrote Shigeru Miyagawa, MD, PhD, of Osaka (Japan) University, and his associates in the Journal of the American Heart Association. The findings merit additional follow-up in larger clinical studies, the investigators asserted.
Heart failure remains life threatening even with the best approved treatments. Previously, the researchers transplanted scaffold-free sheets of autologous myoblasts derived from skeletal muscle into small and large animals with heart failure and found that this approach healed severely damaged myocardium. Transplantation caused secreted cytokines to induce native regeneration through paracrine effects, Dr. Miyagawa noted in a prior review article (BioMed Research International. 2013. doi: 10.1155/2013/583912).
To evaluate this approach in humans, the researchers transplanted 15 patients with ischemic cardiomyopathy and 12 patients with dilated cardiomyopathy (DCM). Patients were 20-75 years old, had ejection fractions under 35% and New York Heart Association (NYHA) classifications of II or more, and were responding inadequately to standard treatment with a beta-blocker or ACE inhibitor and an angiotensin receptor blocker. The sole intervention was transplantation of the cell sheet over the left ventricular-free wall during left thoracotomy (J Am Heart Assoc. 2017 Apr 5. doi: 10.1161/JAHA.116.003918). There were no major procedure-related complications during follow-up, the researchers said. For patients with ICM, NYHA classifications dropped significantly at 6 months, from 2.9 at baseline to 2.1 at 6 months and 1.9 at 1 year. Six-Minute Walk Test scores improved significantly, from 416 m at baseline to 475 m at 6 months to 484 m at 1 year. Transplantation also led to significant drops in serum brain natriuretic peptide levels (baseline average, 308 pg/mL; 6 months, 191 pg/mL; 1 year, 182 pg/mL). Additionally, ICM patients improved significantly on measures of pulmonary artery pressure, pulmonary capillary wedge pressure, pulmonary vein resistance, and left ventricular wall stress.
In contrast, DCM patients did not significantly improve based on the 6-Minute Walk Test, NYHA classification, or brain natriuretic peptide serum levels. Of 12, 3 progressed to NYHA functional class IV by 1-year follow-up and there were five cardiac deaths. There were no cardiac deaths in the ICM group. “It has been reported that regeneration mechanisms in cell sheet mainly depend on angiogenesis induced by secreted cytokines, so cell-sheet implantation may be more suitable for ICM patients, compared with DCM patients, considering pathophysiological aspects,” the researchers wrote.
The study was funded by grants from Regenerative Medicine for Clinical Application, Health and Labor Sciences Research, and the Japan Agency for Medical Research and Development. The investigators disclosed laboratory funding from Terumo for cooperative research in cell sheet.
For patients with ischemic cardiomyopathy (ICM), transplanting sheets of autologous myoblasts onto the epicardial surface was safe and led to “marked” improvements in functional and laboratory measures, investigators reported.
However, cell sheet transplantation was much less effective for patients with dilated cardiomyopathy in this phase I trial, wrote Shigeru Miyagawa, MD, PhD, of Osaka (Japan) University, and his associates in the Journal of the American Heart Association. The findings merit additional follow-up in larger clinical studies, the investigators asserted.
Heart failure remains life threatening even with the best approved treatments. Previously, the researchers transplanted scaffold-free sheets of autologous myoblasts derived from skeletal muscle into small and large animals with heart failure and found that this approach healed severely damaged myocardium. Transplantation caused secreted cytokines to induce native regeneration through paracrine effects, Dr. Miyagawa noted in a prior review article (BioMed Research International. 2013. doi: 10.1155/2013/583912).
To evaluate this approach in humans, the researchers transplanted 15 patients with ischemic cardiomyopathy and 12 patients with dilated cardiomyopathy (DCM). Patients were 20-75 years old, had ejection fractions under 35% and New York Heart Association (NYHA) classifications of II or more, and were responding inadequately to standard treatment with a beta-blocker or ACE inhibitor and an angiotensin receptor blocker. The sole intervention was transplantation of the cell sheet over the left ventricular-free wall during left thoracotomy (J Am Heart Assoc. 2017 Apr 5. doi: 10.1161/JAHA.116.003918). There were no major procedure-related complications during follow-up, the researchers said. For patients with ICM, NYHA classifications dropped significantly at 6 months, from 2.9 at baseline to 2.1 at 6 months and 1.9 at 1 year. Six-Minute Walk Test scores improved significantly, from 416 m at baseline to 475 m at 6 months to 484 m at 1 year. Transplantation also led to significant drops in serum brain natriuretic peptide levels (baseline average, 308 pg/mL; 6 months, 191 pg/mL; 1 year, 182 pg/mL). Additionally, ICM patients improved significantly on measures of pulmonary artery pressure, pulmonary capillary wedge pressure, pulmonary vein resistance, and left ventricular wall stress.
In contrast, DCM patients did not significantly improve based on the 6-Minute Walk Test, NYHA classification, or brain natriuretic peptide serum levels. Of 12, 3 progressed to NYHA functional class IV by 1-year follow-up and there were five cardiac deaths. There were no cardiac deaths in the ICM group. “It has been reported that regeneration mechanisms in cell sheet mainly depend on angiogenesis induced by secreted cytokines, so cell-sheet implantation may be more suitable for ICM patients, compared with DCM patients, considering pathophysiological aspects,” the researchers wrote.
The study was funded by grants from Regenerative Medicine for Clinical Application, Health and Labor Sciences Research, and the Japan Agency for Medical Research and Development. The investigators disclosed laboratory funding from Terumo for cooperative research in cell sheet.
For patients with ischemic cardiomyopathy (ICM), transplanting sheets of autologous myoblasts onto the epicardial surface was safe and led to “marked” improvements in functional and laboratory measures, investigators reported.
However, cell sheet transplantation was much less effective for patients with dilated cardiomyopathy in this phase I trial, wrote Shigeru Miyagawa, MD, PhD, of Osaka (Japan) University, and his associates in the Journal of the American Heart Association. The findings merit additional follow-up in larger clinical studies, the investigators asserted.
Heart failure remains life threatening even with the best approved treatments. Previously, the researchers transplanted scaffold-free sheets of autologous myoblasts derived from skeletal muscle into small and large animals with heart failure and found that this approach healed severely damaged myocardium. Transplantation caused secreted cytokines to induce native regeneration through paracrine effects, Dr. Miyagawa noted in a prior review article (BioMed Research International. 2013. doi: 10.1155/2013/583912).
To evaluate this approach in humans, the researchers transplanted 15 patients with ischemic cardiomyopathy and 12 patients with dilated cardiomyopathy (DCM). Patients were 20-75 years old, had ejection fractions under 35% and New York Heart Association (NYHA) classifications of II or more, and were responding inadequately to standard treatment with a beta-blocker or ACE inhibitor and an angiotensin receptor blocker. The sole intervention was transplantation of the cell sheet over the left ventricular-free wall during left thoracotomy (J Am Heart Assoc. 2017 Apr 5. doi: 10.1161/JAHA.116.003918). There were no major procedure-related complications during follow-up, the researchers said. For patients with ICM, NYHA classifications dropped significantly at 6 months, from 2.9 at baseline to 2.1 at 6 months and 1.9 at 1 year. Six-Minute Walk Test scores improved significantly, from 416 m at baseline to 475 m at 6 months to 484 m at 1 year. Transplantation also led to significant drops in serum brain natriuretic peptide levels (baseline average, 308 pg/mL; 6 months, 191 pg/mL; 1 year, 182 pg/mL). Additionally, ICM patients improved significantly on measures of pulmonary artery pressure, pulmonary capillary wedge pressure, pulmonary vein resistance, and left ventricular wall stress.
In contrast, DCM patients did not significantly improve based on the 6-Minute Walk Test, NYHA classification, or brain natriuretic peptide serum levels. Of 12, 3 progressed to NYHA functional class IV by 1-year follow-up and there were five cardiac deaths. There were no cardiac deaths in the ICM group. “It has been reported that regeneration mechanisms in cell sheet mainly depend on angiogenesis induced by secreted cytokines, so cell-sheet implantation may be more suitable for ICM patients, compared with DCM patients, considering pathophysiological aspects,” the researchers wrote.
The study was funded by grants from Regenerative Medicine for Clinical Application, Health and Labor Sciences Research, and the Japan Agency for Medical Research and Development. The investigators disclosed laboratory funding from Terumo for cooperative research in cell sheet.
Key clinical point: Transplanting a sheet of autologous myoblasts onto the epicardial surface was safe and was associated with functional and symptomatic improvements in patients with ischemic cardiomyopathy.
Major finding: Patients improved significantly on the 6-Minute Walk Test, New York Heart Classification, and on measures of brain natriuretic peptide, pulmonary artery pressure, pulmonary capillary wedge pressure, pulmonary vein resistance, and left ventricular wall stress. These effects did not extend to patients with dilated cardiomyopathy.
Data source: A phase I trial of 27 patients with ischemic or dilated cardiomyopathy.
Disclosures: The study was funded by grants from Regenerative Medicine for Clinical Application, Health and Labor Sciences Research, and the Japan Agency for Medical Research and Development. The investigators disclosed laboratory funding from Terumo for cooperative research in cell sheet.
Pushing the Boundaries of Conventional Surgery
With the myriad procedures and complications that thoracic surgeons are required to be familiar with, the Adult Cardiac Skills course, “100 Years of Training – More Skills Still Needed!” aims to shed some light on the more unconventional procedures that thoracic surgeons see less frequently.
The course will consist of sessions that will each highlight a specific topic: mitral valve repairs. imaging, coronary surgery, and “complex case presentations,” which will feature demonstrations of groundbreaking techniques for challenging presentations a surgeon could encounter.
The mitral valve repair session will focus on bileaflet and endoscopic mitral valve repair, along with talks on right perfusion management, transapical artificial chordae implantation, and using aortic valve repair on a bicuspid aortic valve. These talks – given by Patrick Perier, MD, of the Herz und Gefaess Klinik, Andrea Colli, MD, of the University of Padova, and David Fitzgerald, MD, of the Medical Center of South Carolina, among others – will each last about 15 minutes and will culminate in a panel discussion.
The following hour will be spent discussing imaging in cardiac surgery, where speakers such as Eric E. Roselli, MD, of the Cleveland Clinic, will discuss using imaging in TEVAR to facilitate aortic stenting. Wilson Y. Szeto, MD, of the University of Pennsylvania, will give a talk on transfemoral TAVR, and Mary Beth Brady, MD, of Johns Hopkins University, will discuss the use of transesophageal echocardiogram in thoracic surgery.
After lunch, the coronary surgery session will feature presentations on internal thoracic artery grafts – presented by course chair Dr. Zehr – along with discussions on hybrid revascularization and minimal access off-pump coronary artery bypass. And finally, the last session will highlight the most unusual and rare cases surgeons are likely to come across, such as redoing a mitral valve repair and operating on an infected aortic root. Dr. Zehr hopes the session will address some needs and questions for attendees to improve their practice. “What extra skill sets are necessary to do a few more mitral repairs than you’re already doing and to be a little bit more successful in aortic dissections? Or to know some of the subtleties between doing an open aortic valve versus a minimally invasive transapical or transcathetic aortic valve.”
With the myriad procedures and complications that thoracic surgeons are required to be familiar with, the Adult Cardiac Skills course, “100 Years of Training – More Skills Still Needed!” aims to shed some light on the more unconventional procedures that thoracic surgeons see less frequently.
The course will consist of sessions that will each highlight a specific topic: mitral valve repairs. imaging, coronary surgery, and “complex case presentations,” which will feature demonstrations of groundbreaking techniques for challenging presentations a surgeon could encounter.
The mitral valve repair session will focus on bileaflet and endoscopic mitral valve repair, along with talks on right perfusion management, transapical artificial chordae implantation, and using aortic valve repair on a bicuspid aortic valve. These talks – given by Patrick Perier, MD, of the Herz und Gefaess Klinik, Andrea Colli, MD, of the University of Padova, and David Fitzgerald, MD, of the Medical Center of South Carolina, among others – will each last about 15 minutes and will culminate in a panel discussion.
The following hour will be spent discussing imaging in cardiac surgery, where speakers such as Eric E. Roselli, MD, of the Cleveland Clinic, will discuss using imaging in TEVAR to facilitate aortic stenting. Wilson Y. Szeto, MD, of the University of Pennsylvania, will give a talk on transfemoral TAVR, and Mary Beth Brady, MD, of Johns Hopkins University, will discuss the use of transesophageal echocardiogram in thoracic surgery.
After lunch, the coronary surgery session will feature presentations on internal thoracic artery grafts – presented by course chair Dr. Zehr – along with discussions on hybrid revascularization and minimal access off-pump coronary artery bypass. And finally, the last session will highlight the most unusual and rare cases surgeons are likely to come across, such as redoing a mitral valve repair and operating on an infected aortic root. Dr. Zehr hopes the session will address some needs and questions for attendees to improve their practice. “What extra skill sets are necessary to do a few more mitral repairs than you’re already doing and to be a little bit more successful in aortic dissections? Or to know some of the subtleties between doing an open aortic valve versus a minimally invasive transapical or transcathetic aortic valve.”
With the myriad procedures and complications that thoracic surgeons are required to be familiar with, the Adult Cardiac Skills course, “100 Years of Training – More Skills Still Needed!” aims to shed some light on the more unconventional procedures that thoracic surgeons see less frequently.
The course will consist of sessions that will each highlight a specific topic: mitral valve repairs. imaging, coronary surgery, and “complex case presentations,” which will feature demonstrations of groundbreaking techniques for challenging presentations a surgeon could encounter.
The mitral valve repair session will focus on bileaflet and endoscopic mitral valve repair, along with talks on right perfusion management, transapical artificial chordae implantation, and using aortic valve repair on a bicuspid aortic valve. These talks – given by Patrick Perier, MD, of the Herz und Gefaess Klinik, Andrea Colli, MD, of the University of Padova, and David Fitzgerald, MD, of the Medical Center of South Carolina, among others – will each last about 15 minutes and will culminate in a panel discussion.
The following hour will be spent discussing imaging in cardiac surgery, where speakers such as Eric E. Roselli, MD, of the Cleveland Clinic, will discuss using imaging in TEVAR to facilitate aortic stenting. Wilson Y. Szeto, MD, of the University of Pennsylvania, will give a talk on transfemoral TAVR, and Mary Beth Brady, MD, of Johns Hopkins University, will discuss the use of transesophageal echocardiogram in thoracic surgery.
After lunch, the coronary surgery session will feature presentations on internal thoracic artery grafts – presented by course chair Dr. Zehr – along with discussions on hybrid revascularization and minimal access off-pump coronary artery bypass. And finally, the last session will highlight the most unusual and rare cases surgeons are likely to come across, such as redoing a mitral valve repair and operating on an infected aortic root. Dr. Zehr hopes the session will address some needs and questions for attendees to improve their practice. “What extra skill sets are necessary to do a few more mitral repairs than you’re already doing and to be a little bit more successful in aortic dissections? Or to know some of the subtleties between doing an open aortic valve versus a minimally invasive transapical or transcathetic aortic valve.”
Does laparoscopy have an advantage for emergency VHR?
HOUSTON – The benefits of elective laparoscopic ventral hernia repair over the open approach have been well documented, but, when presented with emergency cases, surgeons still are about 10 times more likely to employ open surgery, possibly exposing patients to greater risk of complications, as well as longer hospital stays, according to an analysis of a national database.
“Despite the benefits of laparoscopic surgery, its utilization in ventral hernia repair (VHR) remains low,” said David Pechman, MD, MBA, of Mount Sinai Beth Israel Medical Center, New York, at the annual meeting of the American Society of Gastrointestinal and Endoscopic Surgeons. “This study suggests that utilization is further decreased in emergency cases. Relative to elective cases, emergency VHR is associated with markedly increased rates of morbidity, giving us more room to improve patient outcomes with the use of laparoscopy in these cases.”
The study analyzed 330 emergency VHR operations in the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database for 2012 and 2013. Thirty-two (9.3%) of those operations were performed laparoscopically, and the remainder were open. Because the sample size of laparoscopic operations was so small, drawing statistically significant conclusions from the findings is difficult without a larger, higher-powered study, Dr. Pechman said. “We do think that further research is warranted and believe that analysis of a larger sample would display that increased utilization of laparoscopy in emergency VHR could significantly improve outcomes.”
The analysis found significant differences in outcomes between the laparoscopic and the open operations for emergency VHR. Average hospital stay after laparoscopic emergency VHR was 2.8 days vs. 5.9 days for open VHR (P = .02). Surgical site infection rates were 0% vs. 7.7% (P = .15). Demographics between both laparoscopic and open groups were similar, Dr. Pechman said.
Session moderator E. Matthew Ritter, MD, of Walter Reed National Military Medical Center, Bethesda, Md., noted that the study conclusion is in line with the goals of SAGES’s minimally invasive surgery initiative to increase utilization of laparoscopy. When referring to the findings Dr. Pechman reported, Dr. Ritter said, “This is a remarkably low complication rate for a procedure that could seemingly have some benefit.”
Dr. Pechman’s response acknowledged the concerns of the surgeons doing the procedures: “A lot of this has to do with surgeon comfort and the preoperative decision-making, especially in an emergency setting.”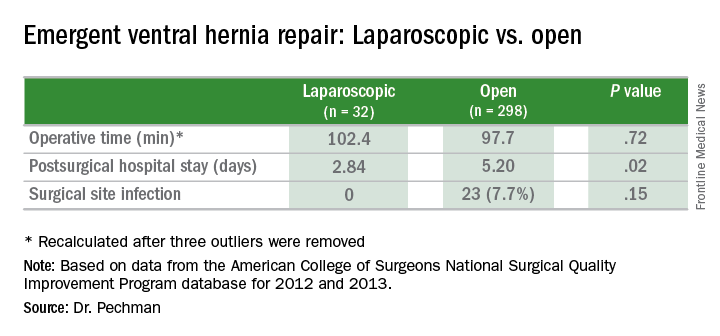
HOUSTON – The benefits of elective laparoscopic ventral hernia repair over the open approach have been well documented, but, when presented with emergency cases, surgeons still are about 10 times more likely to employ open surgery, possibly exposing patients to greater risk of complications, as well as longer hospital stays, according to an analysis of a national database.
“Despite the benefits of laparoscopic surgery, its utilization in ventral hernia repair (VHR) remains low,” said David Pechman, MD, MBA, of Mount Sinai Beth Israel Medical Center, New York, at the annual meeting of the American Society of Gastrointestinal and Endoscopic Surgeons. “This study suggests that utilization is further decreased in emergency cases. Relative to elective cases, emergency VHR is associated with markedly increased rates of morbidity, giving us more room to improve patient outcomes with the use of laparoscopy in these cases.”
The study analyzed 330 emergency VHR operations in the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database for 2012 and 2013. Thirty-two (9.3%) of those operations were performed laparoscopically, and the remainder were open. Because the sample size of laparoscopic operations was so small, drawing statistically significant conclusions from the findings is difficult without a larger, higher-powered study, Dr. Pechman said. “We do think that further research is warranted and believe that analysis of a larger sample would display that increased utilization of laparoscopy in emergency VHR could significantly improve outcomes.”
The analysis found significant differences in outcomes between the laparoscopic and the open operations for emergency VHR. Average hospital stay after laparoscopic emergency VHR was 2.8 days vs. 5.9 days for open VHR (P = .02). Surgical site infection rates were 0% vs. 7.7% (P = .15). Demographics between both laparoscopic and open groups were similar, Dr. Pechman said.
Session moderator E. Matthew Ritter, MD, of Walter Reed National Military Medical Center, Bethesda, Md., noted that the study conclusion is in line with the goals of SAGES’s minimally invasive surgery initiative to increase utilization of laparoscopy. When referring to the findings Dr. Pechman reported, Dr. Ritter said, “This is a remarkably low complication rate for a procedure that could seemingly have some benefit.”
Dr. Pechman’s response acknowledged the concerns of the surgeons doing the procedures: “A lot of this has to do with surgeon comfort and the preoperative decision-making, especially in an emergency setting.”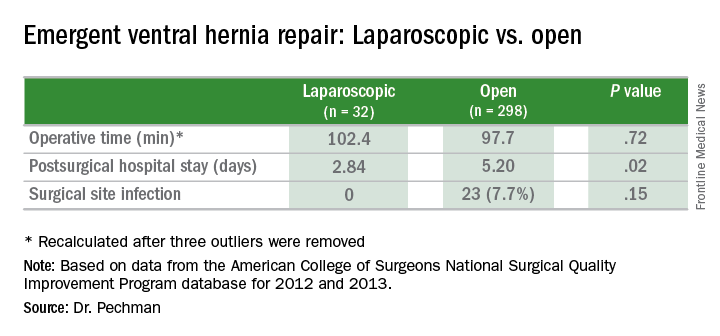
HOUSTON – The benefits of elective laparoscopic ventral hernia repair over the open approach have been well documented, but, when presented with emergency cases, surgeons still are about 10 times more likely to employ open surgery, possibly exposing patients to greater risk of complications, as well as longer hospital stays, according to an analysis of a national database.
“Despite the benefits of laparoscopic surgery, its utilization in ventral hernia repair (VHR) remains low,” said David Pechman, MD, MBA, of Mount Sinai Beth Israel Medical Center, New York, at the annual meeting of the American Society of Gastrointestinal and Endoscopic Surgeons. “This study suggests that utilization is further decreased in emergency cases. Relative to elective cases, emergency VHR is associated with markedly increased rates of morbidity, giving us more room to improve patient outcomes with the use of laparoscopy in these cases.”
The study analyzed 330 emergency VHR operations in the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database for 2012 and 2013. Thirty-two (9.3%) of those operations were performed laparoscopically, and the remainder were open. Because the sample size of laparoscopic operations was so small, drawing statistically significant conclusions from the findings is difficult without a larger, higher-powered study, Dr. Pechman said. “We do think that further research is warranted and believe that analysis of a larger sample would display that increased utilization of laparoscopy in emergency VHR could significantly improve outcomes.”
The analysis found significant differences in outcomes between the laparoscopic and the open operations for emergency VHR. Average hospital stay after laparoscopic emergency VHR was 2.8 days vs. 5.9 days for open VHR (P = .02). Surgical site infection rates were 0% vs. 7.7% (P = .15). Demographics between both laparoscopic and open groups were similar, Dr. Pechman said.
Session moderator E. Matthew Ritter, MD, of Walter Reed National Military Medical Center, Bethesda, Md., noted that the study conclusion is in line with the goals of SAGES’s minimally invasive surgery initiative to increase utilization of laparoscopy. When referring to the findings Dr. Pechman reported, Dr. Ritter said, “This is a remarkably low complication rate for a procedure that could seemingly have some benefit.”
Dr. Pechman’s response acknowledged the concerns of the surgeons doing the procedures: “A lot of this has to do with surgeon comfort and the preoperative decision-making, especially in an emergency setting.”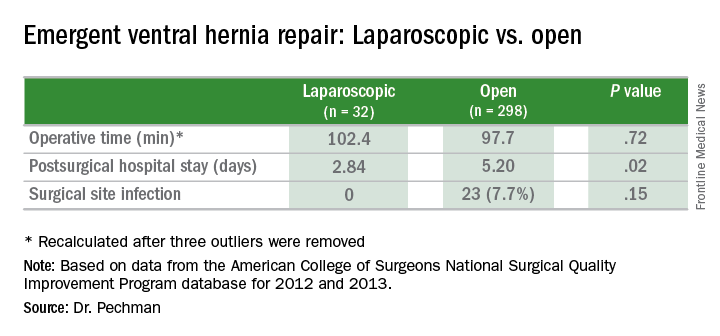
Key clinical point: Outcomes of laparoscopic ventral hernia repair (VHR) may be superior to those for open surgery in the emergency setting.
Major finding: Average hospital stay after laparoscopic emergency VHR was 2.8 days vs. 5.9 days for open surgery, and surgical site infection rates were 0% vs. 7.7%.
Data source: Analysis of 329 cases of emergency VHR enrolled in the American College of Surgeons National Surgical Quality Improvement Program in 2012 and 2013.
Disclosures: Dr. Pechman reported no financial disclosures.
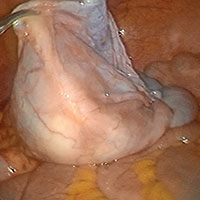
Advanced techniques in cystectomy for mature cystic teratomas

Visit the Society of Gynecologic Surgeons online: sgsonline.org
More videos from SGS:
- Novel classification of labial anatomy and evaluation in the treatment of labial agglutination
- Strategies for prophylactic oophoropexy
- Tips and tricks for open laparoscopy
- Complete colpectomy & colpocleisis: Model for simulation
- Natural orifice sacral colpopexy
- Alternative options for visualizing ureteral patency during intraoperative cystoscopy
- Use of suprapubic Carter-Thomason needle to assist in cystoscopic excision of an intravesical foreign object
- Uterine artery ligation: Advanced techniques and considerations for the difficult laparoscopic hysterectomy
- Cervical injection of methylene blue for identification of sentinel lymph nodes in cervical cancer
- Misplaced hysteroscopic sterilization micro-insert in the peritoneal cavity: A corpus alienum
- Laparoscopic cystectomy for large, bilateral ovarian dermoids
- Small bowel surgery for the benign gynecologist

Visit the Society of Gynecologic Surgeons online: sgsonline.org
More videos from SGS:
- Novel classification of labial anatomy and evaluation in the treatment of labial agglutination
- Strategies for prophylactic oophoropexy
- Tips and tricks for open laparoscopy
- Complete colpectomy & colpocleisis: Model for simulation
- Natural orifice sacral colpopexy
- Alternative options for visualizing ureteral patency during intraoperative cystoscopy
- Use of suprapubic Carter-Thomason needle to assist in cystoscopic excision of an intravesical foreign object
- Uterine artery ligation: Advanced techniques and considerations for the difficult laparoscopic hysterectomy
- Cervical injection of methylene blue for identification of sentinel lymph nodes in cervical cancer
- Misplaced hysteroscopic sterilization micro-insert in the peritoneal cavity: A corpus alienum
- Laparoscopic cystectomy for large, bilateral ovarian dermoids
- Small bowel surgery for the benign gynecologist

Visit the Society of Gynecologic Surgeons online: sgsonline.org
More videos from SGS:
- Novel classification of labial anatomy and evaluation in the treatment of labial agglutination
- Strategies for prophylactic oophoropexy
- Tips and tricks for open laparoscopy
- Complete colpectomy & colpocleisis: Model for simulation
- Natural orifice sacral colpopexy
- Alternative options for visualizing ureteral patency during intraoperative cystoscopy
- Use of suprapubic Carter-Thomason needle to assist in cystoscopic excision of an intravesical foreign object
- Uterine artery ligation: Advanced techniques and considerations for the difficult laparoscopic hysterectomy
- Cervical injection of methylene blue for identification of sentinel lymph nodes in cervical cancer
- Misplaced hysteroscopic sterilization micro-insert in the peritoneal cavity: A corpus alienum
- Laparoscopic cystectomy for large, bilateral ovarian dermoids
- Small bowel surgery for the benign gynecologist
This video is brought to you by
Course Takes Aim at Innovative Approaches to Rare Congenital Heart Disease
One of the noteworthy courses to be held on Saturday will focus exclusively on congenital heart disease and the skills necessary to treat some of its most unusual and difficult complications.
“We looked at previous years to see what are some good areas that are either complicated or controversial, that have not been covered in recent years, and that will bring something new to practitioners or to present various views of controversies,” explained session chair David P. Bichell, MD, of Vanderbilt University. “And it’s really centered on techniques.”
Repairing and replacing atrioventricular valves will also be discussed at length. Special attention will be paid to Ebstein’s tricuspid valve – something that comes up very rarely for most surgeons, which will be presented by Joseph A. Dearani, MD, of the Mayo Clinic – along with a way to reconstruct a tricuspid valve called the Cone Technique. Dr. Bichell noted that too many surgeons are unaware of the Cone Technique.
“Replacing valves in infants is a really special problem because the infants grow, because prosthetic knobs are too small, [and] because anticoagulation is a headache,” explained Dr. Bichell. “There are various options for replacing a valve, creating a valve out of a cylinder of material, and putting in a valve that is balloon deployed. We depend on those colleagues who see these rare things to share their experiences.
“There will be some profusion talks on miniaturizing the circuit, bloodless surgery, and other topics that are of interest to everyone, but few have good answers for,” said Dr. Bichell. “But those who have put more thought and experience into it are going to share what they know.”
The sessions will run about 15 minutes each and will feature a video of the technique being demonstrated while the speaker discusses the procedure. The overarching goal of the session is to give attendees the confidence to go into their practice the next day and, should they see a patient with a presentation they’ve never seen before, have the confidence to perform the necessary procedure. “We want to focus on the rare but relevant end of what people would be interested in,” said Dr. Bichell.
One of the noteworthy courses to be held on Saturday will focus exclusively on congenital heart disease and the skills necessary to treat some of its most unusual and difficult complications.
“We looked at previous years to see what are some good areas that are either complicated or controversial, that have not been covered in recent years, and that will bring something new to practitioners or to present various views of controversies,” explained session chair David P. Bichell, MD, of Vanderbilt University. “And it’s really centered on techniques.”
Repairing and replacing atrioventricular valves will also be discussed at length. Special attention will be paid to Ebstein’s tricuspid valve – something that comes up very rarely for most surgeons, which will be presented by Joseph A. Dearani, MD, of the Mayo Clinic – along with a way to reconstruct a tricuspid valve called the Cone Technique. Dr. Bichell noted that too many surgeons are unaware of the Cone Technique.
“Replacing valves in infants is a really special problem because the infants grow, because prosthetic knobs are too small, [and] because anticoagulation is a headache,” explained Dr. Bichell. “There are various options for replacing a valve, creating a valve out of a cylinder of material, and putting in a valve that is balloon deployed. We depend on those colleagues who see these rare things to share their experiences.
“There will be some profusion talks on miniaturizing the circuit, bloodless surgery, and other topics that are of interest to everyone, but few have good answers for,” said Dr. Bichell. “But those who have put more thought and experience into it are going to share what they know.”
The sessions will run about 15 minutes each and will feature a video of the technique being demonstrated while the speaker discusses the procedure. The overarching goal of the session is to give attendees the confidence to go into their practice the next day and, should they see a patient with a presentation they’ve never seen before, have the confidence to perform the necessary procedure. “We want to focus on the rare but relevant end of what people would be interested in,” said Dr. Bichell.
One of the noteworthy courses to be held on Saturday will focus exclusively on congenital heart disease and the skills necessary to treat some of its most unusual and difficult complications.
“We looked at previous years to see what are some good areas that are either complicated or controversial, that have not been covered in recent years, and that will bring something new to practitioners or to present various views of controversies,” explained session chair David P. Bichell, MD, of Vanderbilt University. “And it’s really centered on techniques.”
Repairing and replacing atrioventricular valves will also be discussed at length. Special attention will be paid to Ebstein’s tricuspid valve – something that comes up very rarely for most surgeons, which will be presented by Joseph A. Dearani, MD, of the Mayo Clinic – along with a way to reconstruct a tricuspid valve called the Cone Technique. Dr. Bichell noted that too many surgeons are unaware of the Cone Technique.
“Replacing valves in infants is a really special problem because the infants grow, because prosthetic knobs are too small, [and] because anticoagulation is a headache,” explained Dr. Bichell. “There are various options for replacing a valve, creating a valve out of a cylinder of material, and putting in a valve that is balloon deployed. We depend on those colleagues who see these rare things to share their experiences.
“There will be some profusion talks on miniaturizing the circuit, bloodless surgery, and other topics that are of interest to everyone, but few have good answers for,” said Dr. Bichell. “But those who have put more thought and experience into it are going to share what they know.”
The sessions will run about 15 minutes each and will feature a video of the technique being demonstrated while the speaker discusses the procedure. The overarching goal of the session is to give attendees the confidence to go into their practice the next day and, should they see a patient with a presentation they’ve never seen before, have the confidence to perform the necessary procedure. “We want to focus on the rare but relevant end of what people would be interested in,” said Dr. Bichell.
NCCN myelofibrosis guideline: Patient voice is key
ORLANDO – Referral to a specialized center with expertise in the management of myeloproliferative neoplasms is strongly recommended for all patients diagnosed with myelofibrosis, according to a new treatment guideline from the National Comprehensive Cancer Network.
The guideline is the first in a series addressing myeloproliferative neoplasms (MPNs), and it focuses on the diagnostic work-up of MPNs, as well as the treatment of myelofibrosis. The guideline panel, led by panel chair Ruben A. Mesa, MD, is working next on guidelines for the other two “core classic” Philadelphia chromosome–negative MPNs: polycythemia vera, and essential thrombocythemia.
Nearly two-thirds of myelofibrosis patients have intermediate-risk 2 or high-risk disease, and treatment decisions in these patients are complex and require patient input – particularly in candidates for allogeneic hematopoietic stem cell transplantation, he said.
“These diseases can be a little different than other malignant diseases,” Dr. Mesa said, explaining that while there is a clear risk of progression to acute myeloid leukemia, and from polycythemia vera and essential thrombocythemia to myelofibrosis, and while the diseases can be fatal, the burden patients face is not solely related to mortality.
There are implications in terms of health that are independent of that, such as the risk of thrombosis and bleeding, the potential for cytopenia, and severe splenomegaly that results in significant symptoms, he said.
Further, while molecular mutations and their implications for prognosis are a “rapidly moving part of the discussion,” the care of patients with MPNs involves far more than a molecular understanding of the disease.
In fact, the role of molecular changes in these patients is speculative, he said.
While such changes can be assessed and used for patient stratification, their role in myelofibrosis – unlike in other diseases such as chronic myeloid leukemia where the level of change in a target gene is highly relevant and prognostic, is not yet clear.
Thus, a core aspect of the guideline is inclusion of the voice of the patient in individualizing care, he said, noting that many factors should be considered, including how well the patient metabolizes drugs, and the symptom profile, psychosocial circumstances, support structure, and personal beliefs.
“It’s not solely about the tumor,” he stressed.
In fact, the answer to the question of whether a patient can be symptomatic enough to require a specific treatment is “no,” because of the potential for side effects, risk, expense, and other considerations.
“So the voice of the patient is always a key part [of the decision],” he said, noting also that as with all NCCN guidelines, this guideline is a partnership with the treating physician; deciding who is a transplant candidate is a nuanced issue for which the panel provides “discussion and guidance.”
“But clearly, these guidelines are the most useful and helpful in the setting of experienced providers bringing all of their experiences to bear,” he said.
In general, however, the guidelines call for allogeneic hematopoietic stem cell transplantation (HCT) in those with intermediate-risk 2 or high-risk disease who are transplant candidates, and treatment based on assessment of symptom burden (using the MPN–Symptom Assessment Form Total Symptom Score–10 Items) in those who are not HCT candidates. Those with platelets at 50,000 or below should be considered for clinical trial enrollment, and those with platelets above 50,000 should be considered for a clinical trial or treatment with the oral JAK1 and JAK2 inhibitor ruxolitinib, which has been shown to have beneficial effects on both symptoms and survival and which is approved for patients with platelets above 50,000. .
Treated patients should be monitored for response and for signs and symptoms of disease progression every 3-6 months. Treatment should continue in those who respond, as well as in those who do not – as long as there is no disease progression.
Those with progressive disease include patients who are moving toward acute leukemia, and those with overt acute leukemia.
“Here is where the key decision occurs. Are they or are they not a transplant candidate? If they are a candidate, we have a potentially curative track which would include cytoreduction followed by transplant,” Dr. Mesa said.
Cytoreduction can involve hypomethylating agents if the patient doesn’t have excess blast cells or too high a burden of disease.
Acute myeloid leukemia–like induction chemotherapy followed by allogeneic HCT is also an option in these patients.
As for treatment of low-risk myelofibrosis, the guideline states that asymptomatic patients can be observed or enrolled in a clinical trial and monitored for progression every 3-6 months, and that symptomatic patients should receive ruxolitinib or interferons (which are used off label), or be enrolled in a clinical trial. Treatment is important for patients with particularly difficult symptoms, he said, noting that some patients have had pruritus so severe that they have committed suicide. Treatment should continue unless monitoring shows signs of progression to intermediate risk 1, intermediate risk 2/high-risk, or advanced stage disease.
For those with intermediate risk 1 disease, the guideline calls for observation or ruxolitinib in those who are symptomatic, or clinical trial enrollment or allogeneic HCT. Treatment should continue unless monitoring shows disease progression, in which case the appropriate algorithm should be considered.
The guideline also addresses several special circumstances, including the management of anemia in myelofibrosis patients, which can be a difficult issue, he said.
Since the guideline was first published in December, two updates have been incorporated, and Dr. Mesa said that he anticipates regular updates given the rapidly evolving understanding of MPNs and new findings with respect to potential treatment strategies.
He noted that a number of drugs are currently in clinical trials involving patients with myelofibrosis, including the JAK2/FLT3 inhibitor pacritinib, the JAK1/JAK2 inhibitor momelotinib, the active antifibrosing agent PRM-151, and the telomerase inhibitor imetelstat, as well as numerous drug combinations.
Going forward, the guideline panel will be focusing on four different areas of assessment, including new therapies and new genetic therapies, improving transplant outcomes, MPN symptom and quality of life assessment, and nonpharmacologic interventions such as yoga.
“We certainly hope to complement things over time, to look not only at pharmacologic interventions, but others that patients may be able to utilize from a toolkit of resources,” he said.
COMFORT-1 update: ruxolitinib responses durable in myelofibrosis
To date, ruxolitinib is the only Food and Drug Administration–approved drug for the treatment of myelofibrosis.
The randomized controlled phase III COMFORT I and II trials conducted in the United States and Europe, respectively, demonstrated that the oral JAK1/JAK2 inhibitor has a rapid, beneficial impact on both survival and disease-associated enlargement of the spleen and improvement in related symptoms, Dr. Mesa said.
A 5-year update on data from 309 patients in the COMFORT-1 trial, as reported at the annual meeting of the American Society of Clinical Oncology in 2016, confirmed the durability of treatment responses to ruxolitinib in patients initially randomized to receive the drug, he said.
“We were able to demonstrate a continued survival advantage for those individuals receiving ruxolitinib,” he added.
At weeks 24 and 264, the mean spleen volume reduction was 31.6% and 37.6%, respectively, in those originally randomized to ruxolitinib. The median duration of at least 35% spleen volume reduction was 168.3 weeks.
Overall survival favored ruxolitinib (hazard ratio, 0.69). Median overall survival in the ruxolitinib group had not yet been reached.
“But we realize our work is not done. The survival curve does not plateau; we are not curing these patients. We’re having meaningful impact, but we have room to continue to improve,” he said.
Also, there is an initial drop in platelet counts that tends to stabilize, but not improve, and there is worsening of anemia (new onset grade 3 or 4 anemia was 25.2% with ruxolitinib, and 26.1% in 111 of 154 patients who crossed over from the placebo group), and although this tends to improve, these are among areas of unmet need, he added.
Further, long-term risks of treatment include cutaneous malignancies (basal cell carcinoma occurred in 7.7% and 9.0% of treatment and crossover patients, respectively), which are difficult to separate from baseline hydroxyurea use, and increased risk of herpes zoster (which occurred in 10.3% and 13.5% of treated and crossover patients).
However, there appears to be no increased risk – and there may be a slight decreased risk – of progression to acute leukemia, Dr. Mesa said.
Dr. Mesa disclosed that he has received consulting fees, honoraria, and/or grant/research support from ARIAD Pharmaceuticals, Celgene, CTI BioPharma, Galena Biopharma, Gilead Sciences, Incyte, Novartis Pharmaceuticals, and Promedior.
A step toward harmonizing treatment
Myelofibrosis is a rare chronic leukemia with a complex biology. Disease heterogeneity poses several challenges in the appropriate selection and timing of treatments in this disorder. The NCCN Practice Guidelines in Myelofibrosis is an important step towards harmonizing clinical practice for treating this disease and improving the care of patients.
Vikas Gupta, MD, FRCP, FRCPath, is Director of The Elizabeth and Tony Comper MPN Program at Princess Margaret Cancer Centre in Toronto and a member of the editorial advisory board of Hematology News.
A step toward harmonizing treatment
Myelofibrosis is a rare chronic leukemia with a complex biology. Disease heterogeneity poses several challenges in the appropriate selection and timing of treatments in this disorder. The NCCN Practice Guidelines in Myelofibrosis is an important step towards harmonizing clinical practice for treating this disease and improving the care of patients.
Vikas Gupta, MD, FRCP, FRCPath, is Director of The Elizabeth and Tony Comper MPN Program at Princess Margaret Cancer Centre in Toronto and a member of the editorial advisory board of Hematology News.
A step toward harmonizing treatment
Myelofibrosis is a rare chronic leukemia with a complex biology. Disease heterogeneity poses several challenges in the appropriate selection and timing of treatments in this disorder. The NCCN Practice Guidelines in Myelofibrosis is an important step towards harmonizing clinical practice for treating this disease and improving the care of patients.
Vikas Gupta, MD, FRCP, FRCPath, is Director of The Elizabeth and Tony Comper MPN Program at Princess Margaret Cancer Centre in Toronto and a member of the editorial advisory board of Hematology News.
ORLANDO – Referral to a specialized center with expertise in the management of myeloproliferative neoplasms is strongly recommended for all patients diagnosed with myelofibrosis, according to a new treatment guideline from the National Comprehensive Cancer Network.
The guideline is the first in a series addressing myeloproliferative neoplasms (MPNs), and it focuses on the diagnostic work-up of MPNs, as well as the treatment of myelofibrosis. The guideline panel, led by panel chair Ruben A. Mesa, MD, is working next on guidelines for the other two “core classic” Philadelphia chromosome–negative MPNs: polycythemia vera, and essential thrombocythemia.
Nearly two-thirds of myelofibrosis patients have intermediate-risk 2 or high-risk disease, and treatment decisions in these patients are complex and require patient input – particularly in candidates for allogeneic hematopoietic stem cell transplantation, he said.
“These diseases can be a little different than other malignant diseases,” Dr. Mesa said, explaining that while there is a clear risk of progression to acute myeloid leukemia, and from polycythemia vera and essential thrombocythemia to myelofibrosis, and while the diseases can be fatal, the burden patients face is not solely related to mortality.
There are implications in terms of health that are independent of that, such as the risk of thrombosis and bleeding, the potential for cytopenia, and severe splenomegaly that results in significant symptoms, he said.
Further, while molecular mutations and their implications for prognosis are a “rapidly moving part of the discussion,” the care of patients with MPNs involves far more than a molecular understanding of the disease.
In fact, the role of molecular changes in these patients is speculative, he said.
While such changes can be assessed and used for patient stratification, their role in myelofibrosis – unlike in other diseases such as chronic myeloid leukemia where the level of change in a target gene is highly relevant and prognostic, is not yet clear.
Thus, a core aspect of the guideline is inclusion of the voice of the patient in individualizing care, he said, noting that many factors should be considered, including how well the patient metabolizes drugs, and the symptom profile, psychosocial circumstances, support structure, and personal beliefs.
“It’s not solely about the tumor,” he stressed.
In fact, the answer to the question of whether a patient can be symptomatic enough to require a specific treatment is “no,” because of the potential for side effects, risk, expense, and other considerations.
“So the voice of the patient is always a key part [of the decision],” he said, noting also that as with all NCCN guidelines, this guideline is a partnership with the treating physician; deciding who is a transplant candidate is a nuanced issue for which the panel provides “discussion and guidance.”
“But clearly, these guidelines are the most useful and helpful in the setting of experienced providers bringing all of their experiences to bear,” he said.
In general, however, the guidelines call for allogeneic hematopoietic stem cell transplantation (HCT) in those with intermediate-risk 2 or high-risk disease who are transplant candidates, and treatment based on assessment of symptom burden (using the MPN–Symptom Assessment Form Total Symptom Score–10 Items) in those who are not HCT candidates. Those with platelets at 50,000 or below should be considered for clinical trial enrollment, and those with platelets above 50,000 should be considered for a clinical trial or treatment with the oral JAK1 and JAK2 inhibitor ruxolitinib, which has been shown to have beneficial effects on both symptoms and survival and which is approved for patients with platelets above 50,000. .
Treated patients should be monitored for response and for signs and symptoms of disease progression every 3-6 months. Treatment should continue in those who respond, as well as in those who do not – as long as there is no disease progression.
Those with progressive disease include patients who are moving toward acute leukemia, and those with overt acute leukemia.
“Here is where the key decision occurs. Are they or are they not a transplant candidate? If they are a candidate, we have a potentially curative track which would include cytoreduction followed by transplant,” Dr. Mesa said.
Cytoreduction can involve hypomethylating agents if the patient doesn’t have excess blast cells or too high a burden of disease.
Acute myeloid leukemia–like induction chemotherapy followed by allogeneic HCT is also an option in these patients.
As for treatment of low-risk myelofibrosis, the guideline states that asymptomatic patients can be observed or enrolled in a clinical trial and monitored for progression every 3-6 months, and that symptomatic patients should receive ruxolitinib or interferons (which are used off label), or be enrolled in a clinical trial. Treatment is important for patients with particularly difficult symptoms, he said, noting that some patients have had pruritus so severe that they have committed suicide. Treatment should continue unless monitoring shows signs of progression to intermediate risk 1, intermediate risk 2/high-risk, or advanced stage disease.
For those with intermediate risk 1 disease, the guideline calls for observation or ruxolitinib in those who are symptomatic, or clinical trial enrollment or allogeneic HCT. Treatment should continue unless monitoring shows disease progression, in which case the appropriate algorithm should be considered.
The guideline also addresses several special circumstances, including the management of anemia in myelofibrosis patients, which can be a difficult issue, he said.
Since the guideline was first published in December, two updates have been incorporated, and Dr. Mesa said that he anticipates regular updates given the rapidly evolving understanding of MPNs and new findings with respect to potential treatment strategies.
He noted that a number of drugs are currently in clinical trials involving patients with myelofibrosis, including the JAK2/FLT3 inhibitor pacritinib, the JAK1/JAK2 inhibitor momelotinib, the active antifibrosing agent PRM-151, and the telomerase inhibitor imetelstat, as well as numerous drug combinations.
Going forward, the guideline panel will be focusing on four different areas of assessment, including new therapies and new genetic therapies, improving transplant outcomes, MPN symptom and quality of life assessment, and nonpharmacologic interventions such as yoga.
“We certainly hope to complement things over time, to look not only at pharmacologic interventions, but others that patients may be able to utilize from a toolkit of resources,” he said.
COMFORT-1 update: ruxolitinib responses durable in myelofibrosis
To date, ruxolitinib is the only Food and Drug Administration–approved drug for the treatment of myelofibrosis.
The randomized controlled phase III COMFORT I and II trials conducted in the United States and Europe, respectively, demonstrated that the oral JAK1/JAK2 inhibitor has a rapid, beneficial impact on both survival and disease-associated enlargement of the spleen and improvement in related symptoms, Dr. Mesa said.
A 5-year update on data from 309 patients in the COMFORT-1 trial, as reported at the annual meeting of the American Society of Clinical Oncology in 2016, confirmed the durability of treatment responses to ruxolitinib in patients initially randomized to receive the drug, he said.
“We were able to demonstrate a continued survival advantage for those individuals receiving ruxolitinib,” he added.
At weeks 24 and 264, the mean spleen volume reduction was 31.6% and 37.6%, respectively, in those originally randomized to ruxolitinib. The median duration of at least 35% spleen volume reduction was 168.3 weeks.
Overall survival favored ruxolitinib (hazard ratio, 0.69). Median overall survival in the ruxolitinib group had not yet been reached.
“But we realize our work is not done. The survival curve does not plateau; we are not curing these patients. We’re having meaningful impact, but we have room to continue to improve,” he said.
Also, there is an initial drop in platelet counts that tends to stabilize, but not improve, and there is worsening of anemia (new onset grade 3 or 4 anemia was 25.2% with ruxolitinib, and 26.1% in 111 of 154 patients who crossed over from the placebo group), and although this tends to improve, these are among areas of unmet need, he added.
Further, long-term risks of treatment include cutaneous malignancies (basal cell carcinoma occurred in 7.7% and 9.0% of treatment and crossover patients, respectively), which are difficult to separate from baseline hydroxyurea use, and increased risk of herpes zoster (which occurred in 10.3% and 13.5% of treated and crossover patients).
However, there appears to be no increased risk – and there may be a slight decreased risk – of progression to acute leukemia, Dr. Mesa said.
Dr. Mesa disclosed that he has received consulting fees, honoraria, and/or grant/research support from ARIAD Pharmaceuticals, Celgene, CTI BioPharma, Galena Biopharma, Gilead Sciences, Incyte, Novartis Pharmaceuticals, and Promedior.
ORLANDO – Referral to a specialized center with expertise in the management of myeloproliferative neoplasms is strongly recommended for all patients diagnosed with myelofibrosis, according to a new treatment guideline from the National Comprehensive Cancer Network.
The guideline is the first in a series addressing myeloproliferative neoplasms (MPNs), and it focuses on the diagnostic work-up of MPNs, as well as the treatment of myelofibrosis. The guideline panel, led by panel chair Ruben A. Mesa, MD, is working next on guidelines for the other two “core classic” Philadelphia chromosome–negative MPNs: polycythemia vera, and essential thrombocythemia.
Nearly two-thirds of myelofibrosis patients have intermediate-risk 2 or high-risk disease, and treatment decisions in these patients are complex and require patient input – particularly in candidates for allogeneic hematopoietic stem cell transplantation, he said.
“These diseases can be a little different than other malignant diseases,” Dr. Mesa said, explaining that while there is a clear risk of progression to acute myeloid leukemia, and from polycythemia vera and essential thrombocythemia to myelofibrosis, and while the diseases can be fatal, the burden patients face is not solely related to mortality.
There are implications in terms of health that are independent of that, such as the risk of thrombosis and bleeding, the potential for cytopenia, and severe splenomegaly that results in significant symptoms, he said.
Further, while molecular mutations and their implications for prognosis are a “rapidly moving part of the discussion,” the care of patients with MPNs involves far more than a molecular understanding of the disease.
In fact, the role of molecular changes in these patients is speculative, he said.
While such changes can be assessed and used for patient stratification, their role in myelofibrosis – unlike in other diseases such as chronic myeloid leukemia where the level of change in a target gene is highly relevant and prognostic, is not yet clear.
Thus, a core aspect of the guideline is inclusion of the voice of the patient in individualizing care, he said, noting that many factors should be considered, including how well the patient metabolizes drugs, and the symptom profile, psychosocial circumstances, support structure, and personal beliefs.
“It’s not solely about the tumor,” he stressed.
In fact, the answer to the question of whether a patient can be symptomatic enough to require a specific treatment is “no,” because of the potential for side effects, risk, expense, and other considerations.
“So the voice of the patient is always a key part [of the decision],” he said, noting also that as with all NCCN guidelines, this guideline is a partnership with the treating physician; deciding who is a transplant candidate is a nuanced issue for which the panel provides “discussion and guidance.”
“But clearly, these guidelines are the most useful and helpful in the setting of experienced providers bringing all of their experiences to bear,” he said.
In general, however, the guidelines call for allogeneic hematopoietic stem cell transplantation (HCT) in those with intermediate-risk 2 or high-risk disease who are transplant candidates, and treatment based on assessment of symptom burden (using the MPN–Symptom Assessment Form Total Symptom Score–10 Items) in those who are not HCT candidates. Those with platelets at 50,000 or below should be considered for clinical trial enrollment, and those with platelets above 50,000 should be considered for a clinical trial or treatment with the oral JAK1 and JAK2 inhibitor ruxolitinib, which has been shown to have beneficial effects on both symptoms and survival and which is approved for patients with platelets above 50,000. .
Treated patients should be monitored for response and for signs and symptoms of disease progression every 3-6 months. Treatment should continue in those who respond, as well as in those who do not – as long as there is no disease progression.
Those with progressive disease include patients who are moving toward acute leukemia, and those with overt acute leukemia.
“Here is where the key decision occurs. Are they or are they not a transplant candidate? If they are a candidate, we have a potentially curative track which would include cytoreduction followed by transplant,” Dr. Mesa said.
Cytoreduction can involve hypomethylating agents if the patient doesn’t have excess blast cells or too high a burden of disease.
Acute myeloid leukemia–like induction chemotherapy followed by allogeneic HCT is also an option in these patients.
As for treatment of low-risk myelofibrosis, the guideline states that asymptomatic patients can be observed or enrolled in a clinical trial and monitored for progression every 3-6 months, and that symptomatic patients should receive ruxolitinib or interferons (which are used off label), or be enrolled in a clinical trial. Treatment is important for patients with particularly difficult symptoms, he said, noting that some patients have had pruritus so severe that they have committed suicide. Treatment should continue unless monitoring shows signs of progression to intermediate risk 1, intermediate risk 2/high-risk, or advanced stage disease.
For those with intermediate risk 1 disease, the guideline calls for observation or ruxolitinib in those who are symptomatic, or clinical trial enrollment or allogeneic HCT. Treatment should continue unless monitoring shows disease progression, in which case the appropriate algorithm should be considered.
The guideline also addresses several special circumstances, including the management of anemia in myelofibrosis patients, which can be a difficult issue, he said.
Since the guideline was first published in December, two updates have been incorporated, and Dr. Mesa said that he anticipates regular updates given the rapidly evolving understanding of MPNs and new findings with respect to potential treatment strategies.
He noted that a number of drugs are currently in clinical trials involving patients with myelofibrosis, including the JAK2/FLT3 inhibitor pacritinib, the JAK1/JAK2 inhibitor momelotinib, the active antifibrosing agent PRM-151, and the telomerase inhibitor imetelstat, as well as numerous drug combinations.
Going forward, the guideline panel will be focusing on four different areas of assessment, including new therapies and new genetic therapies, improving transplant outcomes, MPN symptom and quality of life assessment, and nonpharmacologic interventions such as yoga.
“We certainly hope to complement things over time, to look not only at pharmacologic interventions, but others that patients may be able to utilize from a toolkit of resources,” he said.
COMFORT-1 update: ruxolitinib responses durable in myelofibrosis
To date, ruxolitinib is the only Food and Drug Administration–approved drug for the treatment of myelofibrosis.
The randomized controlled phase III COMFORT I and II trials conducted in the United States and Europe, respectively, demonstrated that the oral JAK1/JAK2 inhibitor has a rapid, beneficial impact on both survival and disease-associated enlargement of the spleen and improvement in related symptoms, Dr. Mesa said.
A 5-year update on data from 309 patients in the COMFORT-1 trial, as reported at the annual meeting of the American Society of Clinical Oncology in 2016, confirmed the durability of treatment responses to ruxolitinib in patients initially randomized to receive the drug, he said.
“We were able to demonstrate a continued survival advantage for those individuals receiving ruxolitinib,” he added.
At weeks 24 and 264, the mean spleen volume reduction was 31.6% and 37.6%, respectively, in those originally randomized to ruxolitinib. The median duration of at least 35% spleen volume reduction was 168.3 weeks.
Overall survival favored ruxolitinib (hazard ratio, 0.69). Median overall survival in the ruxolitinib group had not yet been reached.
“But we realize our work is not done. The survival curve does not plateau; we are not curing these patients. We’re having meaningful impact, but we have room to continue to improve,” he said.
Also, there is an initial drop in platelet counts that tends to stabilize, but not improve, and there is worsening of anemia (new onset grade 3 or 4 anemia was 25.2% with ruxolitinib, and 26.1% in 111 of 154 patients who crossed over from the placebo group), and although this tends to improve, these are among areas of unmet need, he added.
Further, long-term risks of treatment include cutaneous malignancies (basal cell carcinoma occurred in 7.7% and 9.0% of treatment and crossover patients, respectively), which are difficult to separate from baseline hydroxyurea use, and increased risk of herpes zoster (which occurred in 10.3% and 13.5% of treated and crossover patients).
However, there appears to be no increased risk – and there may be a slight decreased risk – of progression to acute leukemia, Dr. Mesa said.
Dr. Mesa disclosed that he has received consulting fees, honoraria, and/or grant/research support from ARIAD Pharmaceuticals, Celgene, CTI BioPharma, Galena Biopharma, Gilead Sciences, Incyte, Novartis Pharmaceuticals, and Promedior.
EXPERT ANALYSIS AT THE NCCN ANNUAL CONFERENCE