User login
Terminalia chebula
Terminalia chebula, a member of the Combretaceae family, is an evergreen plant found abundantly in India, Pakistan, China, Thailand, Sri Lanka, and Malaysia.1,2 It has long been used in traditional medicine, particularly Ayurveda, as well as in Thai traditional medicine.3 It also has also been used for many years in the traditional medicine of the Samahni valley of Pakistan to treat chronic ulcers as well as dental caries and heart ailments.4 Other traditional indications include asthma and urinary disorders.5 In Thailand, it has been used to treat skin diseases and to promote wound healing and rejuvenation.1 It is particularly known for its potent antioxidant and antimicrobial properties.6 The wide array of health benefits associated with T. chebula is attributed to its high content of phenolic compounds, flavonol glycosides, and other phytonutrients.7
Antioxidant, anti-aging, and depigmenting effects
In 2004, Na et al. observed that T. chebula fruit extract exerted an inhibitory effect on the age-dependent shortening of telomeres and UVB-induced oxidative damage in vitro.8
Kim et al. screened 50 Korean plants to identify natural sources of elastase and hyaluronidase inhibitors in 2010. The strong efficacy of T. chebula led the investigators to choose it for additional study in which the fruits of the methanol crude extract at 1 mg/mL demonstrated 80% elastase and 87% hyaluronidase inhibitory activities. In addition, the investigators isolated 1,2,3,4,6-penta-O-galloyl-beta-D-glucose (PGG), which also exhibited significant inhibition of elastase and hyaluronidase and induction of type II collagen expression. The authors concluded that PGG has the potential as a cutaneous anti-aging agent posing no cytotoxicity concerns and warrants further in vivo study.9
A 2010 in vitro study of the anti-aging properties of the extracts of 15 plant species, including T. chebula galls, outgrowths that result from insect bites, was conducted by Manosroi et al. The cold aqueous extract of T. chebula manifested the highest 2,2-diphenyl-1-picrylhydrazyl (DPPH) radical-scavenging activity and highest stimulation index for proliferation of normal human skin fibroblasts. T. chebula, which also inhibited matrix metalloproteinase (MMP)-2 activity, was compared against compounds such as ascorbic acid, alpha-tocopherol, and butylated hydroxytoluene. The investigators concluded that their findings supported the traditional uses of T. chebula gall in Thai medicine and suggest that T. chebula would be beneficial for inclusion in new anti-aging formulations.3
Later that year, Manosroi et al. characterized the biological activities of the phenolic compounds isolated from T. chebula galls, finding that these compounds (gallic acid, punicalagin, isoterchebulin, 1,3,6-tri-O-galloyl-beta-D-glucopyranose, chebulagic acid, and chebulinic acid) exhibited greater radical-scavenging and melanin-inhibitory activity than the reference compounds ascorbic acid, butylated hydroxytoluene, alpha-tocopherol, arbutin, and kojic acid. Although the T. chebula constituents were less effective than the reference compounds in mushroom tyrosinase inhibition and human tumor cytotoxicity assays, the investigators concluded that the antioxidant and depigmenting activity of the constituents of T. chebula accounted for the beneficial profile of the plant that has emerged over time.10
The next year, Manosroi et al. assessed the cutaneous anti-aging effects of a gel containing niosomes incorporating a semi-purified fraction including gallic acid derived from T. chebula galls or outgrowths. Human volunteers were enlisted to test skin elasticity and roughness and rabbit skin was used to evaluate skin irritation. The gel containing the semi-purified fractions loaded in niosomes was compared with an unloaded fraction, revealing that the loaded niosomes yielded greater gallic acid chemical stability as well as in vivo anti-aging effects.11 Earlier that year, the team had shown the viability of niosomes, particularly elastic ones, to promote chemical stability for the transdermal absorption of gallic acid in semipurified T. chebula gall fractions in rats. Their findings, they concluded, point to the potential for achieving topical anti-aging benefits from such formulations.12
In 2012, Akhtar et al. developed a water-in-oil T. chebula formulation and assessed its effects on various parameters. The investigators prepared a base with no active ingredients and a 5% T. chebula formulation, which remained stable at various storage conditions. For 8 weeks, they applied the base as well as the formulation to the cheeks of human volunteers, with weekly evaluations indicating that the formulation as opposed to the base yielded significant improvement, irrespective of time elapsed, in skin moisture content and erythema. The authors concluded that their T. chebula topical cream was effective in rejuvenating human skin.13
Wound healing
In 2002, Suguna et al. investigated in vivo the effects of a topically administered alcohol extract of the leaves of T. chebula on the healing of rat dermal wounds. The researchers found that treatment with T. chebula accelerated wound healing, with improved contraction rates and shorter epithelialization periods. T. chebula treatment yielded a 40% increase in the tensile strength of tissues from treated wounds. The authors concluded that T. chebula is beneficial in speeding the wound healing process.2
Immature T. chebula fruit extracts high in tannins are thought to be effective in enhancing the wound healing process, according to Li et al., who found in 2011 that the extracts promoted wound healing in rats, likely due to the antibacterial and angiogenic potency of its tannins.1
In a 2014 study on wound healing, Singh et al. observed in vitro that T. chebula extracts effectively scavenged free radicals in a DPPH assay and enhanced proliferation of keratinocytes and fibroblasts. They concluded that T. chebula can be considered for use as a bioactive approach to wound healing for its effects in promoting cellular proliferation and inhibiting production of free radicals.7
Other biologic activities
A 1995 study by Kurokawa et al. showed that T. chebula was one of four herbal extracts among 10 tested to exhibit a discrete anti–herpes simplex virus type 1 (HSV-1) activity in vitro when combined with acyclovir. Oral administration of the herbs with acyclovir in mice in doses corresponding to human use significantly limited skin lesion development and/or extended mean survival time of infected mice in comparison to any of the herbs or acyclovir used alone.14
Nam et al. used a 2,4-dinitrofluorobenzene (DNFB)-induced mouse model of atopic symptoms in 2011 and found that a T. chebula seed extract attenuated atopic dermatitis symptoms, resulting in a 52% decrease in the immune response and lower eosinophil levels in nearby skin tissue.6
In 2013, Manosroi et al. found that various tannins and one oleanane-type triterpene acid isolated from T. chebula galls displayed strong inhibitory capacity against melanogenesis in mice, with one of the tannins (isoterchebulin) shown to decrease protein levels of tyrosinase, microphthalmia-associated transcription factor, and tyrosine-related protein 1 in mainly a concentration-dependent fashion. Another tannin and several triterpenoids were noted for suppressing 12-O-tetradecanoylphorbol 13-acetate (TPA)-induced inflammation. In addition, constituent phenols manifested strong radical-scavenging activity. In a two-stage carcinogenesis mouse model, the investigators observed that the triterpene acid arjungenin hindered skin tumor promotion after initiation with 7,12-dimethylbenz[a]anthracene (DMBA) and promotion by TPA. Their findings indicate a wide range of biologic activity and potential health benefits associated with T. chebula.15
In a mouse study in 2014, Singh et al. determined that a new antifungal agent, an apigenin ointment containing extract of T. chebula stem, was effective in significantly reducing the fungal burden from the experimentally-induced dermatophyte Trichopython mentagrophytes. They suggested that this agent warrants consideration in clinically treating dermatophytosis in humans.16
Triphala, a traditional combination formulation
Long used in Ayurveda, triphala (the word is derived from the Sanskrit tri, three, and phala, fruits) is an antioxidant-rich herbal formulation that combines the dried fruits of T. chebula, Terminalia bellirica, and Emblica officinalis. Naik et al. observed, in a 2005 in vitro study of the aqueous extract of the fruits of T. chebula, T. bellirica, and E. officinalis, as well as their equiproportional mixture triphala, that T. chebula was the most effective at scavenging free radicals. They noted that triphala appears to synergistically combine the strengths of each of its primary components.17 Subsequent studies have demonstrated that triphala is a strong source of natural antioxidants and exhibits a wide range of beneficial activities, including free radical scavenging, antioxidant, anti-inflammatory, analgesic, antibacterial, antimutagenic, wound healing, antistress, adaptogenic, hypoglycemic, anticancer, chemoprotective, radioprotective, chemopreventive, and wound healing.5,18-21
Extracts of T. chebula also have been combined with those of E. officinalis, T. bellirica, Albizia lebbeck, Piper nigrum, Zingiber officinale, and Piper longum in a polyherbal formulation (Aller-7/NR-A2) that has been found safe for the treatment of allergic rhinitis.22
Conclusion
The use of T. chebula in various traditional medical practices around the world is well established. There is ample evidence supporting multiple biologic properties of this Ayurvedic staple. While it is not a standard ingredient in dermatologic health care in the West, the data support continued research as to how best to incorporate this agent.
References
1. BMC Complement Altern Med. 2011 Oct 7;11:86.
2. Phytother Res. 2002 May;16(3):227-31.
3. Pharm Biol. 2010 Apr;48(4):469-81.
4. Pak J Biol Sci. 2007 Jul 1;10(13):2241-56.
5. BMC Complement Altern Med. 2010 May 13;10:20.
6. Int J Mol Med. 2011 Dec;28(6):1013-8.
7. Evid Based Complement Alternat Med. 2014;2014:701656.
8. Phytother Res. 2004 Sep;18:737-41.
9. Acta Pol Pharm. 2010 Mar-Apr;67(2):145-50.
10. Nat Prod Res. 2010 Dec;24(20):1915-26.
11. Pharm Biol. 2011 Nov;49(11):1190-203.
12. Pharm Biol. 2011 Jun;49(6):553-62.
13. Forsch Komplementmed. 2012;19(1):20-5.
14. Antiviral Res. 1995 May;27(1-2):19-37.
15. Chem Biodivers. 2013 Aug;10(8):1448-63.
16. Mycoses. 2014 Aug;57(8):497-506.
17. Phytother Res. 2005 Jul;19(7):582-6.
18. Chin J Integr Med. 2012 Dec;18(12):946-54.
19. J Surg Res. 2008 Jan;144(1):94-101.
20. J Surg Res. 2010 Jan;158(1):162-70.
21. J Altern Complement Med. 2010 Dec;16(12):1301-8.
22. Toxicol Mech Methods. 2005;15(3):193-204.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in the Design District in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote the textbook, “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and a book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). She has contributed to the Cosmeceutical Critique column in Dermatology News since January 2001. Her latest book, “Cosmeceuticals and Cosmetic Ingredients,” was published in November 2014. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Evolus, Galderma, GlaxoSmithKline, Kythera Biopharmaceuticals, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Topix Pharmaceuticals, and Unilever.
Terminalia chebula, a member of the Combretaceae family, is an evergreen plant found abundantly in India, Pakistan, China, Thailand, Sri Lanka, and Malaysia.1,2 It has long been used in traditional medicine, particularly Ayurveda, as well as in Thai traditional medicine.3 It also has also been used for many years in the traditional medicine of the Samahni valley of Pakistan to treat chronic ulcers as well as dental caries and heart ailments.4 Other traditional indications include asthma and urinary disorders.5 In Thailand, it has been used to treat skin diseases and to promote wound healing and rejuvenation.1 It is particularly known for its potent antioxidant and antimicrobial properties.6 The wide array of health benefits associated with T. chebula is attributed to its high content of phenolic compounds, flavonol glycosides, and other phytonutrients.7
Antioxidant, anti-aging, and depigmenting effects
In 2004, Na et al. observed that T. chebula fruit extract exerted an inhibitory effect on the age-dependent shortening of telomeres and UVB-induced oxidative damage in vitro.8
Kim et al. screened 50 Korean plants to identify natural sources of elastase and hyaluronidase inhibitors in 2010. The strong efficacy of T. chebula led the investigators to choose it for additional study in which the fruits of the methanol crude extract at 1 mg/mL demonstrated 80% elastase and 87% hyaluronidase inhibitory activities. In addition, the investigators isolated 1,2,3,4,6-penta-O-galloyl-beta-D-glucose (PGG), which also exhibited significant inhibition of elastase and hyaluronidase and induction of type II collagen expression. The authors concluded that PGG has the potential as a cutaneous anti-aging agent posing no cytotoxicity concerns and warrants further in vivo study.9
A 2010 in vitro study of the anti-aging properties of the extracts of 15 plant species, including T. chebula galls, outgrowths that result from insect bites, was conducted by Manosroi et al. The cold aqueous extract of T. chebula manifested the highest 2,2-diphenyl-1-picrylhydrazyl (DPPH) radical-scavenging activity and highest stimulation index for proliferation of normal human skin fibroblasts. T. chebula, which also inhibited matrix metalloproteinase (MMP)-2 activity, was compared against compounds such as ascorbic acid, alpha-tocopherol, and butylated hydroxytoluene. The investigators concluded that their findings supported the traditional uses of T. chebula gall in Thai medicine and suggest that T. chebula would be beneficial for inclusion in new anti-aging formulations.3
Later that year, Manosroi et al. characterized the biological activities of the phenolic compounds isolated from T. chebula galls, finding that these compounds (gallic acid, punicalagin, isoterchebulin, 1,3,6-tri-O-galloyl-beta-D-glucopyranose, chebulagic acid, and chebulinic acid) exhibited greater radical-scavenging and melanin-inhibitory activity than the reference compounds ascorbic acid, butylated hydroxytoluene, alpha-tocopherol, arbutin, and kojic acid. Although the T. chebula constituents were less effective than the reference compounds in mushroom tyrosinase inhibition and human tumor cytotoxicity assays, the investigators concluded that the antioxidant and depigmenting activity of the constituents of T. chebula accounted for the beneficial profile of the plant that has emerged over time.10
The next year, Manosroi et al. assessed the cutaneous anti-aging effects of a gel containing niosomes incorporating a semi-purified fraction including gallic acid derived from T. chebula galls or outgrowths. Human volunteers were enlisted to test skin elasticity and roughness and rabbit skin was used to evaluate skin irritation. The gel containing the semi-purified fractions loaded in niosomes was compared with an unloaded fraction, revealing that the loaded niosomes yielded greater gallic acid chemical stability as well as in vivo anti-aging effects.11 Earlier that year, the team had shown the viability of niosomes, particularly elastic ones, to promote chemical stability for the transdermal absorption of gallic acid in semipurified T. chebula gall fractions in rats. Their findings, they concluded, point to the potential for achieving topical anti-aging benefits from such formulations.12
In 2012, Akhtar et al. developed a water-in-oil T. chebula formulation and assessed its effects on various parameters. The investigators prepared a base with no active ingredients and a 5% T. chebula formulation, which remained stable at various storage conditions. For 8 weeks, they applied the base as well as the formulation to the cheeks of human volunteers, with weekly evaluations indicating that the formulation as opposed to the base yielded significant improvement, irrespective of time elapsed, in skin moisture content and erythema. The authors concluded that their T. chebula topical cream was effective in rejuvenating human skin.13
Wound healing
In 2002, Suguna et al. investigated in vivo the effects of a topically administered alcohol extract of the leaves of T. chebula on the healing of rat dermal wounds. The researchers found that treatment with T. chebula accelerated wound healing, with improved contraction rates and shorter epithelialization periods. T. chebula treatment yielded a 40% increase in the tensile strength of tissues from treated wounds. The authors concluded that T. chebula is beneficial in speeding the wound healing process.2
Immature T. chebula fruit extracts high in tannins are thought to be effective in enhancing the wound healing process, according to Li et al., who found in 2011 that the extracts promoted wound healing in rats, likely due to the antibacterial and angiogenic potency of its tannins.1
In a 2014 study on wound healing, Singh et al. observed in vitro that T. chebula extracts effectively scavenged free radicals in a DPPH assay and enhanced proliferation of keratinocytes and fibroblasts. They concluded that T. chebula can be considered for use as a bioactive approach to wound healing for its effects in promoting cellular proliferation and inhibiting production of free radicals.7
Other biologic activities
A 1995 study by Kurokawa et al. showed that T. chebula was one of four herbal extracts among 10 tested to exhibit a discrete anti–herpes simplex virus type 1 (HSV-1) activity in vitro when combined with acyclovir. Oral administration of the herbs with acyclovir in mice in doses corresponding to human use significantly limited skin lesion development and/or extended mean survival time of infected mice in comparison to any of the herbs or acyclovir used alone.14
Nam et al. used a 2,4-dinitrofluorobenzene (DNFB)-induced mouse model of atopic symptoms in 2011 and found that a T. chebula seed extract attenuated atopic dermatitis symptoms, resulting in a 52% decrease in the immune response and lower eosinophil levels in nearby skin tissue.6
In 2013, Manosroi et al. found that various tannins and one oleanane-type triterpene acid isolated from T. chebula galls displayed strong inhibitory capacity against melanogenesis in mice, with one of the tannins (isoterchebulin) shown to decrease protein levels of tyrosinase, microphthalmia-associated transcription factor, and tyrosine-related protein 1 in mainly a concentration-dependent fashion. Another tannin and several triterpenoids were noted for suppressing 12-O-tetradecanoylphorbol 13-acetate (TPA)-induced inflammation. In addition, constituent phenols manifested strong radical-scavenging activity. In a two-stage carcinogenesis mouse model, the investigators observed that the triterpene acid arjungenin hindered skin tumor promotion after initiation with 7,12-dimethylbenz[a]anthracene (DMBA) and promotion by TPA. Their findings indicate a wide range of biologic activity and potential health benefits associated with T. chebula.15
In a mouse study in 2014, Singh et al. determined that a new antifungal agent, an apigenin ointment containing extract of T. chebula stem, was effective in significantly reducing the fungal burden from the experimentally-induced dermatophyte Trichopython mentagrophytes. They suggested that this agent warrants consideration in clinically treating dermatophytosis in humans.16
Triphala, a traditional combination formulation
Long used in Ayurveda, triphala (the word is derived from the Sanskrit tri, three, and phala, fruits) is an antioxidant-rich herbal formulation that combines the dried fruits of T. chebula, Terminalia bellirica, and Emblica officinalis. Naik et al. observed, in a 2005 in vitro study of the aqueous extract of the fruits of T. chebula, T. bellirica, and E. officinalis, as well as their equiproportional mixture triphala, that T. chebula was the most effective at scavenging free radicals. They noted that triphala appears to synergistically combine the strengths of each of its primary components.17 Subsequent studies have demonstrated that triphala is a strong source of natural antioxidants and exhibits a wide range of beneficial activities, including free radical scavenging, antioxidant, anti-inflammatory, analgesic, antibacterial, antimutagenic, wound healing, antistress, adaptogenic, hypoglycemic, anticancer, chemoprotective, radioprotective, chemopreventive, and wound healing.5,18-21
Extracts of T. chebula also have been combined with those of E. officinalis, T. bellirica, Albizia lebbeck, Piper nigrum, Zingiber officinale, and Piper longum in a polyherbal formulation (Aller-7/NR-A2) that has been found safe for the treatment of allergic rhinitis.22
Conclusion
The use of T. chebula in various traditional medical practices around the world is well established. There is ample evidence supporting multiple biologic properties of this Ayurvedic staple. While it is not a standard ingredient in dermatologic health care in the West, the data support continued research as to how best to incorporate this agent.
References
1. BMC Complement Altern Med. 2011 Oct 7;11:86.
2. Phytother Res. 2002 May;16(3):227-31.
3. Pharm Biol. 2010 Apr;48(4):469-81.
4. Pak J Biol Sci. 2007 Jul 1;10(13):2241-56.
5. BMC Complement Altern Med. 2010 May 13;10:20.
6. Int J Mol Med. 2011 Dec;28(6):1013-8.
7. Evid Based Complement Alternat Med. 2014;2014:701656.
8. Phytother Res. 2004 Sep;18:737-41.
9. Acta Pol Pharm. 2010 Mar-Apr;67(2):145-50.
10. Nat Prod Res. 2010 Dec;24(20):1915-26.
11. Pharm Biol. 2011 Nov;49(11):1190-203.
12. Pharm Biol. 2011 Jun;49(6):553-62.
13. Forsch Komplementmed. 2012;19(1):20-5.
14. Antiviral Res. 1995 May;27(1-2):19-37.
15. Chem Biodivers. 2013 Aug;10(8):1448-63.
16. Mycoses. 2014 Aug;57(8):497-506.
17. Phytother Res. 2005 Jul;19(7):582-6.
18. Chin J Integr Med. 2012 Dec;18(12):946-54.
19. J Surg Res. 2008 Jan;144(1):94-101.
20. J Surg Res. 2010 Jan;158(1):162-70.
21. J Altern Complement Med. 2010 Dec;16(12):1301-8.
22. Toxicol Mech Methods. 2005;15(3):193-204.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in the Design District in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote the textbook, “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and a book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). She has contributed to the Cosmeceutical Critique column in Dermatology News since January 2001. Her latest book, “Cosmeceuticals and Cosmetic Ingredients,” was published in November 2014. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Evolus, Galderma, GlaxoSmithKline, Kythera Biopharmaceuticals, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Topix Pharmaceuticals, and Unilever.
Terminalia chebula, a member of the Combretaceae family, is an evergreen plant found abundantly in India, Pakistan, China, Thailand, Sri Lanka, and Malaysia.1,2 It has long been used in traditional medicine, particularly Ayurveda, as well as in Thai traditional medicine.3 It also has also been used for many years in the traditional medicine of the Samahni valley of Pakistan to treat chronic ulcers as well as dental caries and heart ailments.4 Other traditional indications include asthma and urinary disorders.5 In Thailand, it has been used to treat skin diseases and to promote wound healing and rejuvenation.1 It is particularly known for its potent antioxidant and antimicrobial properties.6 The wide array of health benefits associated with T. chebula is attributed to its high content of phenolic compounds, flavonol glycosides, and other phytonutrients.7
Antioxidant, anti-aging, and depigmenting effects
In 2004, Na et al. observed that T. chebula fruit extract exerted an inhibitory effect on the age-dependent shortening of telomeres and UVB-induced oxidative damage in vitro.8
Kim et al. screened 50 Korean plants to identify natural sources of elastase and hyaluronidase inhibitors in 2010. The strong efficacy of T. chebula led the investigators to choose it for additional study in which the fruits of the methanol crude extract at 1 mg/mL demonstrated 80% elastase and 87% hyaluronidase inhibitory activities. In addition, the investigators isolated 1,2,3,4,6-penta-O-galloyl-beta-D-glucose (PGG), which also exhibited significant inhibition of elastase and hyaluronidase and induction of type II collagen expression. The authors concluded that PGG has the potential as a cutaneous anti-aging agent posing no cytotoxicity concerns and warrants further in vivo study.9
A 2010 in vitro study of the anti-aging properties of the extracts of 15 plant species, including T. chebula galls, outgrowths that result from insect bites, was conducted by Manosroi et al. The cold aqueous extract of T. chebula manifested the highest 2,2-diphenyl-1-picrylhydrazyl (DPPH) radical-scavenging activity and highest stimulation index for proliferation of normal human skin fibroblasts. T. chebula, which also inhibited matrix metalloproteinase (MMP)-2 activity, was compared against compounds such as ascorbic acid, alpha-tocopherol, and butylated hydroxytoluene. The investigators concluded that their findings supported the traditional uses of T. chebula gall in Thai medicine and suggest that T. chebula would be beneficial for inclusion in new anti-aging formulations.3
Later that year, Manosroi et al. characterized the biological activities of the phenolic compounds isolated from T. chebula galls, finding that these compounds (gallic acid, punicalagin, isoterchebulin, 1,3,6-tri-O-galloyl-beta-D-glucopyranose, chebulagic acid, and chebulinic acid) exhibited greater radical-scavenging and melanin-inhibitory activity than the reference compounds ascorbic acid, butylated hydroxytoluene, alpha-tocopherol, arbutin, and kojic acid. Although the T. chebula constituents were less effective than the reference compounds in mushroom tyrosinase inhibition and human tumor cytotoxicity assays, the investigators concluded that the antioxidant and depigmenting activity of the constituents of T. chebula accounted for the beneficial profile of the plant that has emerged over time.10
The next year, Manosroi et al. assessed the cutaneous anti-aging effects of a gel containing niosomes incorporating a semi-purified fraction including gallic acid derived from T. chebula galls or outgrowths. Human volunteers were enlisted to test skin elasticity and roughness and rabbit skin was used to evaluate skin irritation. The gel containing the semi-purified fractions loaded in niosomes was compared with an unloaded fraction, revealing that the loaded niosomes yielded greater gallic acid chemical stability as well as in vivo anti-aging effects.11 Earlier that year, the team had shown the viability of niosomes, particularly elastic ones, to promote chemical stability for the transdermal absorption of gallic acid in semipurified T. chebula gall fractions in rats. Their findings, they concluded, point to the potential for achieving topical anti-aging benefits from such formulations.12
In 2012, Akhtar et al. developed a water-in-oil T. chebula formulation and assessed its effects on various parameters. The investigators prepared a base with no active ingredients and a 5% T. chebula formulation, which remained stable at various storage conditions. For 8 weeks, they applied the base as well as the formulation to the cheeks of human volunteers, with weekly evaluations indicating that the formulation as opposed to the base yielded significant improvement, irrespective of time elapsed, in skin moisture content and erythema. The authors concluded that their T. chebula topical cream was effective in rejuvenating human skin.13
Wound healing
In 2002, Suguna et al. investigated in vivo the effects of a topically administered alcohol extract of the leaves of T. chebula on the healing of rat dermal wounds. The researchers found that treatment with T. chebula accelerated wound healing, with improved contraction rates and shorter epithelialization periods. T. chebula treatment yielded a 40% increase in the tensile strength of tissues from treated wounds. The authors concluded that T. chebula is beneficial in speeding the wound healing process.2
Immature T. chebula fruit extracts high in tannins are thought to be effective in enhancing the wound healing process, according to Li et al., who found in 2011 that the extracts promoted wound healing in rats, likely due to the antibacterial and angiogenic potency of its tannins.1
In a 2014 study on wound healing, Singh et al. observed in vitro that T. chebula extracts effectively scavenged free radicals in a DPPH assay and enhanced proliferation of keratinocytes and fibroblasts. They concluded that T. chebula can be considered for use as a bioactive approach to wound healing for its effects in promoting cellular proliferation and inhibiting production of free radicals.7
Other biologic activities
A 1995 study by Kurokawa et al. showed that T. chebula was one of four herbal extracts among 10 tested to exhibit a discrete anti–herpes simplex virus type 1 (HSV-1) activity in vitro when combined with acyclovir. Oral administration of the herbs with acyclovir in mice in doses corresponding to human use significantly limited skin lesion development and/or extended mean survival time of infected mice in comparison to any of the herbs or acyclovir used alone.14
Nam et al. used a 2,4-dinitrofluorobenzene (DNFB)-induced mouse model of atopic symptoms in 2011 and found that a T. chebula seed extract attenuated atopic dermatitis symptoms, resulting in a 52% decrease in the immune response and lower eosinophil levels in nearby skin tissue.6
In 2013, Manosroi et al. found that various tannins and one oleanane-type triterpene acid isolated from T. chebula galls displayed strong inhibitory capacity against melanogenesis in mice, with one of the tannins (isoterchebulin) shown to decrease protein levels of tyrosinase, microphthalmia-associated transcription factor, and tyrosine-related protein 1 in mainly a concentration-dependent fashion. Another tannin and several triterpenoids were noted for suppressing 12-O-tetradecanoylphorbol 13-acetate (TPA)-induced inflammation. In addition, constituent phenols manifested strong radical-scavenging activity. In a two-stage carcinogenesis mouse model, the investigators observed that the triterpene acid arjungenin hindered skin tumor promotion after initiation with 7,12-dimethylbenz[a]anthracene (DMBA) and promotion by TPA. Their findings indicate a wide range of biologic activity and potential health benefits associated with T. chebula.15
In a mouse study in 2014, Singh et al. determined that a new antifungal agent, an apigenin ointment containing extract of T. chebula stem, was effective in significantly reducing the fungal burden from the experimentally-induced dermatophyte Trichopython mentagrophytes. They suggested that this agent warrants consideration in clinically treating dermatophytosis in humans.16
Triphala, a traditional combination formulation
Long used in Ayurveda, triphala (the word is derived from the Sanskrit tri, three, and phala, fruits) is an antioxidant-rich herbal formulation that combines the dried fruits of T. chebula, Terminalia bellirica, and Emblica officinalis. Naik et al. observed, in a 2005 in vitro study of the aqueous extract of the fruits of T. chebula, T. bellirica, and E. officinalis, as well as their equiproportional mixture triphala, that T. chebula was the most effective at scavenging free radicals. They noted that triphala appears to synergistically combine the strengths of each of its primary components.17 Subsequent studies have demonstrated that triphala is a strong source of natural antioxidants and exhibits a wide range of beneficial activities, including free radical scavenging, antioxidant, anti-inflammatory, analgesic, antibacterial, antimutagenic, wound healing, antistress, adaptogenic, hypoglycemic, anticancer, chemoprotective, radioprotective, chemopreventive, and wound healing.5,18-21
Extracts of T. chebula also have been combined with those of E. officinalis, T. bellirica, Albizia lebbeck, Piper nigrum, Zingiber officinale, and Piper longum in a polyherbal formulation (Aller-7/NR-A2) that has been found safe for the treatment of allergic rhinitis.22
Conclusion
The use of T. chebula in various traditional medical practices around the world is well established. There is ample evidence supporting multiple biologic properties of this Ayurvedic staple. While it is not a standard ingredient in dermatologic health care in the West, the data support continued research as to how best to incorporate this agent.
References
1. BMC Complement Altern Med. 2011 Oct 7;11:86.
2. Phytother Res. 2002 May;16(3):227-31.
3. Pharm Biol. 2010 Apr;48(4):469-81.
4. Pak J Biol Sci. 2007 Jul 1;10(13):2241-56.
5. BMC Complement Altern Med. 2010 May 13;10:20.
6. Int J Mol Med. 2011 Dec;28(6):1013-8.
7. Evid Based Complement Alternat Med. 2014;2014:701656.
8. Phytother Res. 2004 Sep;18:737-41.
9. Acta Pol Pharm. 2010 Mar-Apr;67(2):145-50.
10. Nat Prod Res. 2010 Dec;24(20):1915-26.
11. Pharm Biol. 2011 Nov;49(11):1190-203.
12. Pharm Biol. 2011 Jun;49(6):553-62.
13. Forsch Komplementmed. 2012;19(1):20-5.
14. Antiviral Res. 1995 May;27(1-2):19-37.
15. Chem Biodivers. 2013 Aug;10(8):1448-63.
16. Mycoses. 2014 Aug;57(8):497-506.
17. Phytother Res. 2005 Jul;19(7):582-6.
18. Chin J Integr Med. 2012 Dec;18(12):946-54.
19. J Surg Res. 2008 Jan;144(1):94-101.
20. J Surg Res. 2010 Jan;158(1):162-70.
21. J Altern Complement Med. 2010 Dec;16(12):1301-8.
22. Toxicol Mech Methods. 2005;15(3):193-204.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in the Design District in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote the textbook, “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and a book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). She has contributed to the Cosmeceutical Critique column in Dermatology News since January 2001. Her latest book, “Cosmeceuticals and Cosmetic Ingredients,” was published in November 2014. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Evolus, Galderma, GlaxoSmithKline, Kythera Biopharmaceuticals, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Topix Pharmaceuticals, and Unilever.
Hospitalist Cynthia Cheung, MD, Joins Hospital Committee, Promotes Antibiotic Stewardship
Each year in the United States, at least 2 million people become infected with bacteria that are resistant to antibiotics, and at least 23,000 people die as a result of these infections. To promote improved antibiotic-prescribing behaviors among the nation’s hospitalists, SHM launched its “Fight the Resistance” campaign in November 2015. Cynthia Cheung, MD, a hospitalist in the Triton Hospitalists group at Houston Methodist Willowbrook Hospital and assistant professor of clinical medicine at Houston Methodist, recently shared efforts by a team at her hospital that are closely aligned with SHM’s campaign.
Question: What led you to a career in hospital medicine?
Answer: I was very fortunate to train in a program that had excellent hospitalists at the University of California at Los Angeles. Our general wards were staffed by very talented attending physicians, many of whom were hospitalists, and I quickly fell in love with the fast pace of hospital medicine. My UCLA experience confirmed that hospital medicine was the path for me. I finished my residency in 2010 and began my current role at Houston Methodist early in 2014. Almost two years later, I still love what I do.
Q: How did you get involved in antibiotic stewardship at your hospital?
A: One of my colleagues, an infectious disease specialist and chair of our antimicrobial stewardship committee, invited me to join her team. In retrospect, I had never really thought very much about antibiotic stewardship aside from trying to prescribe the proper antibiotics and the appropriate dosages to my patients. I had not fully considered the quality perspective under such a focused lens; being a part of this committee really opened my eyes, especially since the committee’s goals are completely focused on optimizing clinical outcomes and minimizing unintended consequences of antibiotic use.
Q: What most excites you about SHM’s “Fight the Resistance” campaign?
A: I joined SHM a year ago, and I think it’s really exciting that SHM is drawing attention to hospitalists’ roles in promoting antibiotic stewardship in addition to its other quality improvement initiatives. Previously, antibiotic stewardship appeared to be mostly the province of infectious disease physicians, but that isn’t the case anymore. As frontline providers, we are poised to make a difference in appropriate antibiotic use if armed with the proper knowledge and tools.
Q: As part of “Fight the Resistance,” SHM developed recommendations for promoting antibiotic stewardship in hospitals. How do your team efforts align with SHM’s campaign?
A: One of SHM’s recommendations is to engage with a team of hospital-based clinicians to improve stewardship, and our committee oversees a pharmacist-driven real-time audit and feedback intervention to optimize antibiotic use. Often, after a provider places an antibiotic order, additional culture results and clinical information become available. Our pharmacists evaluate this information and contact the provider if they feel the antibiotic dose prescribed is not the most effective or if there is a culture-antibiotic mismatch.
Or the pharmacist might notice that a patient has been taking an antibiotic for an extended duration and may discuss with the provider whether an appropriate duration can be defined. They will call and consult with providers to help them consider discontinuation or de-escalation if necessary. This is in line with SHM’s recommendation to rethink antibiotic treatment time course. Our clinician acceptance rate has been 90 percent in favor of interventions proposed by the pharmacists.
Any time a provider declines pharmacist intervention, our committee reviews these cases to determine whether or not the decision was in the best interest of the patient given the information available. The reviewers include an interdisciplinary team of hospitalists, infectious disease physicians, critical care physicians, and emergency physicians. If one particular clinician has a record of prescribing suboptimally, the team would review that particular provider’s prescribing habits with more detail.
Our committee is also aligned with SHM’s recommendation to identify mechanisms to educate providers on appropriate prescribing by creating guidelines for different classes of bacterial infections and communicating them to our clinical staff. For gram-negative infections, we recommend avoiding the use of carbapenems and antipseudomonal agents in known pathogens that are not pseudonomous. For gram-positive infections, we advise against use of MRSA/VRE-active antibiotics in known pathogens that are not resistant and the use of double coverage in non-synergistic settings. In the case of anaerobic infections, our guidelines suggest clinicians not use double coverage when susceptibilities are known. These guidelines form the backbone of our reviews and assist the pharmacists in their feedback and audit.
Moving forward, one of our committee’s primary action items is to develop a method of communicating our resistance patterns effectively to our clinical staff to make them more widely known. The information is currently sitting in a silo and is not as easily accessible to assist clinicians in their decision-making process when prescribing antibiotics. We also hope to address appropriate usage of daptomycin and ceftaroline, reduce rates of inappropriate treatment of asymptomatic bacteriuria, and seek additional ways to reduce rates of Clostridium difficile infection.
Q: What do you think is most important for hospitalists to know about their roles in antibiotic stewardship?
A: It is extremely important to remember that antibiotics are one of the few classes of drugs that can harm a patient through promotion of resistance—even if the medication was not given to the patient directly. A lot of clinicians may have been taught a certain way to prescribe antibiotics in training or have become rooted in habit. Hospitalists need to proactively stay abreast of antibiotic stewardship developments, share with fellow providers, and not be afraid to alter the way they prescribe.
While this personal education process might seem daunting at first, medicine is a lifelong learning experience. As physicians, we see new things and learn new things every day. I encourage all hospitalists—and all hospital-based staff—to try to take a greater role in stewardship. You do not have to be a specialist to make a difference, and it doesn’t matter at which point in your career you are. Antibiotic resistance affects everyone. Now is the time to step up and fight it. TH
Brett Radler is SHM’s communications coordinator.
Each year in the United States, at least 2 million people become infected with bacteria that are resistant to antibiotics, and at least 23,000 people die as a result of these infections. To promote improved antibiotic-prescribing behaviors among the nation’s hospitalists, SHM launched its “Fight the Resistance” campaign in November 2015. Cynthia Cheung, MD, a hospitalist in the Triton Hospitalists group at Houston Methodist Willowbrook Hospital and assistant professor of clinical medicine at Houston Methodist, recently shared efforts by a team at her hospital that are closely aligned with SHM’s campaign.
Question: What led you to a career in hospital medicine?
Answer: I was very fortunate to train in a program that had excellent hospitalists at the University of California at Los Angeles. Our general wards were staffed by very talented attending physicians, many of whom were hospitalists, and I quickly fell in love with the fast pace of hospital medicine. My UCLA experience confirmed that hospital medicine was the path for me. I finished my residency in 2010 and began my current role at Houston Methodist early in 2014. Almost two years later, I still love what I do.
Q: How did you get involved in antibiotic stewardship at your hospital?
A: One of my colleagues, an infectious disease specialist and chair of our antimicrobial stewardship committee, invited me to join her team. In retrospect, I had never really thought very much about antibiotic stewardship aside from trying to prescribe the proper antibiotics and the appropriate dosages to my patients. I had not fully considered the quality perspective under such a focused lens; being a part of this committee really opened my eyes, especially since the committee’s goals are completely focused on optimizing clinical outcomes and minimizing unintended consequences of antibiotic use.
Q: What most excites you about SHM’s “Fight the Resistance” campaign?
A: I joined SHM a year ago, and I think it’s really exciting that SHM is drawing attention to hospitalists’ roles in promoting antibiotic stewardship in addition to its other quality improvement initiatives. Previously, antibiotic stewardship appeared to be mostly the province of infectious disease physicians, but that isn’t the case anymore. As frontline providers, we are poised to make a difference in appropriate antibiotic use if armed with the proper knowledge and tools.
Q: As part of “Fight the Resistance,” SHM developed recommendations for promoting antibiotic stewardship in hospitals. How do your team efforts align with SHM’s campaign?
A: One of SHM’s recommendations is to engage with a team of hospital-based clinicians to improve stewardship, and our committee oversees a pharmacist-driven real-time audit and feedback intervention to optimize antibiotic use. Often, after a provider places an antibiotic order, additional culture results and clinical information become available. Our pharmacists evaluate this information and contact the provider if they feel the antibiotic dose prescribed is not the most effective or if there is a culture-antibiotic mismatch.
Or the pharmacist might notice that a patient has been taking an antibiotic for an extended duration and may discuss with the provider whether an appropriate duration can be defined. They will call and consult with providers to help them consider discontinuation or de-escalation if necessary. This is in line with SHM’s recommendation to rethink antibiotic treatment time course. Our clinician acceptance rate has been 90 percent in favor of interventions proposed by the pharmacists.
Any time a provider declines pharmacist intervention, our committee reviews these cases to determine whether or not the decision was in the best interest of the patient given the information available. The reviewers include an interdisciplinary team of hospitalists, infectious disease physicians, critical care physicians, and emergency physicians. If one particular clinician has a record of prescribing suboptimally, the team would review that particular provider’s prescribing habits with more detail.
Our committee is also aligned with SHM’s recommendation to identify mechanisms to educate providers on appropriate prescribing by creating guidelines for different classes of bacterial infections and communicating them to our clinical staff. For gram-negative infections, we recommend avoiding the use of carbapenems and antipseudomonal agents in known pathogens that are not pseudonomous. For gram-positive infections, we advise against use of MRSA/VRE-active antibiotics in known pathogens that are not resistant and the use of double coverage in non-synergistic settings. In the case of anaerobic infections, our guidelines suggest clinicians not use double coverage when susceptibilities are known. These guidelines form the backbone of our reviews and assist the pharmacists in their feedback and audit.
Moving forward, one of our committee’s primary action items is to develop a method of communicating our resistance patterns effectively to our clinical staff to make them more widely known. The information is currently sitting in a silo and is not as easily accessible to assist clinicians in their decision-making process when prescribing antibiotics. We also hope to address appropriate usage of daptomycin and ceftaroline, reduce rates of inappropriate treatment of asymptomatic bacteriuria, and seek additional ways to reduce rates of Clostridium difficile infection.
Q: What do you think is most important for hospitalists to know about their roles in antibiotic stewardship?
A: It is extremely important to remember that antibiotics are one of the few classes of drugs that can harm a patient through promotion of resistance—even if the medication was not given to the patient directly. A lot of clinicians may have been taught a certain way to prescribe antibiotics in training or have become rooted in habit. Hospitalists need to proactively stay abreast of antibiotic stewardship developments, share with fellow providers, and not be afraid to alter the way they prescribe.
While this personal education process might seem daunting at first, medicine is a lifelong learning experience. As physicians, we see new things and learn new things every day. I encourage all hospitalists—and all hospital-based staff—to try to take a greater role in stewardship. You do not have to be a specialist to make a difference, and it doesn’t matter at which point in your career you are. Antibiotic resistance affects everyone. Now is the time to step up and fight it. TH
Brett Radler is SHM’s communications coordinator.
Each year in the United States, at least 2 million people become infected with bacteria that are resistant to antibiotics, and at least 23,000 people die as a result of these infections. To promote improved antibiotic-prescribing behaviors among the nation’s hospitalists, SHM launched its “Fight the Resistance” campaign in November 2015. Cynthia Cheung, MD, a hospitalist in the Triton Hospitalists group at Houston Methodist Willowbrook Hospital and assistant professor of clinical medicine at Houston Methodist, recently shared efforts by a team at her hospital that are closely aligned with SHM’s campaign.
Question: What led you to a career in hospital medicine?
Answer: I was very fortunate to train in a program that had excellent hospitalists at the University of California at Los Angeles. Our general wards were staffed by very talented attending physicians, many of whom were hospitalists, and I quickly fell in love with the fast pace of hospital medicine. My UCLA experience confirmed that hospital medicine was the path for me. I finished my residency in 2010 and began my current role at Houston Methodist early in 2014. Almost two years later, I still love what I do.
Q: How did you get involved in antibiotic stewardship at your hospital?
A: One of my colleagues, an infectious disease specialist and chair of our antimicrobial stewardship committee, invited me to join her team. In retrospect, I had never really thought very much about antibiotic stewardship aside from trying to prescribe the proper antibiotics and the appropriate dosages to my patients. I had not fully considered the quality perspective under such a focused lens; being a part of this committee really opened my eyes, especially since the committee’s goals are completely focused on optimizing clinical outcomes and minimizing unintended consequences of antibiotic use.
Q: What most excites you about SHM’s “Fight the Resistance” campaign?
A: I joined SHM a year ago, and I think it’s really exciting that SHM is drawing attention to hospitalists’ roles in promoting antibiotic stewardship in addition to its other quality improvement initiatives. Previously, antibiotic stewardship appeared to be mostly the province of infectious disease physicians, but that isn’t the case anymore. As frontline providers, we are poised to make a difference in appropriate antibiotic use if armed with the proper knowledge and tools.
Q: As part of “Fight the Resistance,” SHM developed recommendations for promoting antibiotic stewardship in hospitals. How do your team efforts align with SHM’s campaign?
A: One of SHM’s recommendations is to engage with a team of hospital-based clinicians to improve stewardship, and our committee oversees a pharmacist-driven real-time audit and feedback intervention to optimize antibiotic use. Often, after a provider places an antibiotic order, additional culture results and clinical information become available. Our pharmacists evaluate this information and contact the provider if they feel the antibiotic dose prescribed is not the most effective or if there is a culture-antibiotic mismatch.
Or the pharmacist might notice that a patient has been taking an antibiotic for an extended duration and may discuss with the provider whether an appropriate duration can be defined. They will call and consult with providers to help them consider discontinuation or de-escalation if necessary. This is in line with SHM’s recommendation to rethink antibiotic treatment time course. Our clinician acceptance rate has been 90 percent in favor of interventions proposed by the pharmacists.
Any time a provider declines pharmacist intervention, our committee reviews these cases to determine whether or not the decision was in the best interest of the patient given the information available. The reviewers include an interdisciplinary team of hospitalists, infectious disease physicians, critical care physicians, and emergency physicians. If one particular clinician has a record of prescribing suboptimally, the team would review that particular provider’s prescribing habits with more detail.
Our committee is also aligned with SHM’s recommendation to identify mechanisms to educate providers on appropriate prescribing by creating guidelines for different classes of bacterial infections and communicating them to our clinical staff. For gram-negative infections, we recommend avoiding the use of carbapenems and antipseudomonal agents in known pathogens that are not pseudonomous. For gram-positive infections, we advise against use of MRSA/VRE-active antibiotics in known pathogens that are not resistant and the use of double coverage in non-synergistic settings. In the case of anaerobic infections, our guidelines suggest clinicians not use double coverage when susceptibilities are known. These guidelines form the backbone of our reviews and assist the pharmacists in their feedback and audit.
Moving forward, one of our committee’s primary action items is to develop a method of communicating our resistance patterns effectively to our clinical staff to make them more widely known. The information is currently sitting in a silo and is not as easily accessible to assist clinicians in their decision-making process when prescribing antibiotics. We also hope to address appropriate usage of daptomycin and ceftaroline, reduce rates of inappropriate treatment of asymptomatic bacteriuria, and seek additional ways to reduce rates of Clostridium difficile infection.
Q: What do you think is most important for hospitalists to know about their roles in antibiotic stewardship?
A: It is extremely important to remember that antibiotics are one of the few classes of drugs that can harm a patient through promotion of resistance—even if the medication was not given to the patient directly. A lot of clinicians may have been taught a certain way to prescribe antibiotics in training or have become rooted in habit. Hospitalists need to proactively stay abreast of antibiotic stewardship developments, share with fellow providers, and not be afraid to alter the way they prescribe.
While this personal education process might seem daunting at first, medicine is a lifelong learning experience. As physicians, we see new things and learn new things every day. I encourage all hospitalists—and all hospital-based staff—to try to take a greater role in stewardship. You do not have to be a specialist to make a difference, and it doesn’t matter at which point in your career you are. Antibiotic resistance affects everyone. Now is the time to step up and fight it. TH
Brett Radler is SHM’s communications coordinator.
2016 Update on fertility
Patients seeking fertility care commonly ask the physician for advice regarding ways to optimize their conception attempts. While evidence from randomized controlled trials is not available, data from observational studies provide parameters that can inform patient decision making. Knowledge about the fertility window, the decline in fecundability with age, and lifestyle practices that promote conception may be helpful to clinicians and aid in their ability to guide patients.
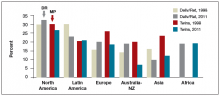
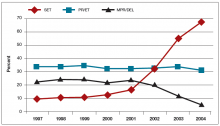
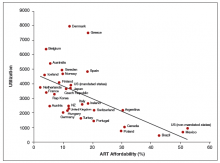
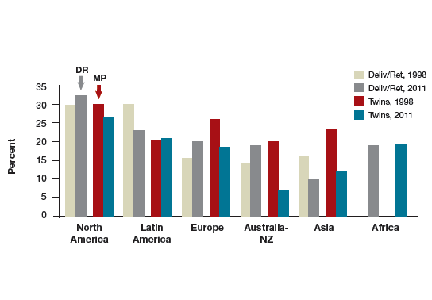
For those patients who will not achieve conception naturally, assisted reproductive technologies (ART) offer a promising alternative. ART options have improved greatly in effectiveness and safety since Louise Brown was born in 1978. More than 5 million babies have been born globally.1 However, even though the United States is wealthy, access to in vitro fertilization (IVF) is poor relative to many other countries, with not more than 1 in 3 people needing IVF actually receiving the treatment. Understanding the international experience enables physicians to take actions that help increase access for their patients who need IVF.
In this article we not only address ways in which your patients can optimize their natural fertility but also examine this country’s ability to offer ART options when they are needed. Without such examination, fundamental changes in societal attitudes toward infertility and payor attitudes toward reproductive care will not occur, and it is these changes, among others, that can move this country to more equitable ART access.
- Adamson GD, Tabangin M, Macaluso M, de Mouzon J. The number of babies born globally after treatment with the Assisted Reproductive Technologies (ART). Paper presented at International Federation of Fertility Societies/American Society for Reproductive Medicine Conjoint Meeting; October 12–17, 2013; Boston, Massachusetts.
- Dunson DB, Baird DD, Wilcox AJ, Weinberg CR. Day-specific probabilities of clinical pregnancy based on two studies with imperfect measures of ovulation. Hum Reprod. 1999;14(7):1835–1839.
- Keulers MJ, Hamilton CJ, Franx A, et al. The length of the fertile window is associated with the chance of spontaneously conceiving an ongoing pregnancy in subfertile couples. Hum Reprod. 2007;22(6):1652–1656.
- Wilcox AJ, Weinberg CR, Baird DD. Timing of sexual intercourse in relation to ovulation. Effects on the probability of conception, survival of the pregnancy, and sex of the baby. N Engl J Med. 1995;333(23):1517–1521.
- Levitas E, Lunenfeld E, Weiss N, et al. Relationship between the duration of sexual abstinence and semen quality: analysis of 9,489 semen samples. Fertil Steril. 2005;83(6):1680–1686.
- Elzanaty S, Malm J, Giwercman A. Duration of sexual abstinence: epididymal and accessory sex gland secretions and their relationship to sperm motility. Hum Reprod. 2005;20(1):221–225.
- Check JH, Epstein R, Long R. Effect of time interval between ejaculations on semen parameters. Arch Androl. 1991;27(2):93–95.
- Practice Committee of American Society for Reproductive Medicine in collaboration with Society for Reproductive Endocrinology and Infertility. Optimizing natural fertility: a committee opinion. Fertil Steril. 2013;100(3):631–637.
- Gnoth C, Godehardt E, Frank-Herrmann P, Friol K, Tigges J, Freundi G. Definition and prevalence of subfertility and infertility. Hum Reprod. 2005;20(5):1144–1447.
- Howe G, Westhoff C, Vessey M, Yeates D. Effects of age, cigarette smoking, and other factors on fertility: findings in a large prospective study. BMJ (Clin Res Ed). 1985;290(6483):1697–700.
- Dunson DB, Baird DD, Colombo B. Increased infertility with age in men and women. Obstet Gynecol. 2004;103(1):51–56.
- Dunson DB, Colombo B, Baird DD. Changes with age in the level and duration of fertility in the menstrual cycle. Hum Reprod. 2002;17(5):1399–1403.
- Lumley J, Watson L, Watson M, Bower C. Periconceptional supplementation with folate and/or multivitamins for preventing neural tube defects. Cochrane Database Syst Rev. 2001;(3):CD001056.
- Augood C, Duckitt K, Templeton AA. Smoking and female infertility: a systematic review and meta-analysis. Hum Reprod. 1998;13(6):1532–1539.
- Winter E, Wang J, Davies MJ, Norman R. Early pregnancy loss following assisted reproductive technology treatment. Hum Reprod. 2002;17(12):3220–3223.
- Ness RB, Grisso JA, Hirschinger N, et al. Cocaine and tobacco use and the risk of spontaneous abortion. New Engl J Med. 1999;340(5):333–339.
- Mattison DR, Plowchalk DR, Meadows MJ, Miller MM, Malek A, London S. The effect of smoking on oogenesis, fertilization and implantation. Semin Reprod Med. 1989;7(4):291–304.
- Adena MA, Gallagher HG. Cigarette smoking and the age at menopause. Ann Hum Biol. 1982;9(2):121–130.
- Bolumar F, Olsen J, Rebagliato M, Bisanti L. Caffeine intake and delayed conception: a European multicenter study on infertility and subfecundity. European Study Group on Infertility Subfecundity. Am J Epidemiol. 1997;145(4):324–334.
- Wilcox A, Weinberg C, Baird D. Caffeinated beverages and decreased fertility. Lancet. 1988;2(8626–8627):1453–1456.
- Signorello LB, McLaughlin JK. Maternal caffeine consumption and spontaneous abortion: a review of the epidemiologic evidence. Epidemiology. 2004;15(2):229–239.
- Kesmodel U, Wisborg K, Olsen SF, Henriksen TB, Secher NJ. Moderate alcohol intake in pregnancy and the risk of spontaneous abortion. Alcohol. 2002;37(1):87–92.
- Adamson GD; International Council of Medical Acupuncture and Related Techniques (ICMART). ICMART World Report 2011. Webcast presented at: Annual Meeting European Society of Human Reproduction and Embryology (ESHRE); June 16, 2015; Lisbon, Portugal.
- Chambers G, Phuong Hoang V, et al. The impact of consumer affordability on access to assisted reproductive technologies and embryo transfer practices: an international analysis. Fertil Steril. 2014;101(1):191–198.
- Stovall DW, Allen BD, Sparks AE, Syrop CH, Saunders RG, VanVoorhis BJ. The cost of infertility evaluation and therapy: findings of a self-insured university healthcare plan. Fertil Steril. 1999;72(5):778–784.
- Chambers GM, Sullivan E, Ishihara O, Chapman MG, Adamson GD. The economic impact of assisted reproductive technology: a review of selected developed countries. Fertil Steril. 2009;91(6):2281–2294.
- Hamilton BH, McManus B. The effects of insurance mandates on choices and outcomes in infertility treatment markets. Health Econ. 2012;21(8):994–1016.
- Chambers GM, Adamson GD, Eijkemans MJC. Acceptable cost for the patient and society. Fertil Steril. 2013;100(2):319–327.
- Zegers-Hochschild F, Adamson GD, de Mouzon J, et al; ICMART, WHO. International Committee for Monitoring Assisted Reproductive Technology (ICMART); World Health Organization (WHO) revised glossary of ART terminology, 2009. Fertil Steril. 2009;92(5):1520–1524.
Patients seeking fertility care commonly ask the physician for advice regarding ways to optimize their conception attempts. While evidence from randomized controlled trials is not available, data from observational studies provide parameters that can inform patient decision making. Knowledge about the fertility window, the decline in fecundability with age, and lifestyle practices that promote conception may be helpful to clinicians and aid in their ability to guide patients.
For those patients who will not achieve conception naturally, assisted reproductive technologies (ART) offer a promising alternative. ART options have improved greatly in effectiveness and safety since Louise Brown was born in 1978. More than 5 million babies have been born globally.1 However, even though the United States is wealthy, access to in vitro fertilization (IVF) is poor relative to many other countries, with not more than 1 in 3 people needing IVF actually receiving the treatment. Understanding the international experience enables physicians to take actions that help increase access for their patients who need IVF.
In this article we not only address ways in which your patients can optimize their natural fertility but also examine this country’s ability to offer ART options when they are needed. Without such examination, fundamental changes in societal attitudes toward infertility and payor attitudes toward reproductive care will not occur, and it is these changes, among others, that can move this country to more equitable ART access.
Patients seeking fertility care commonly ask the physician for advice regarding ways to optimize their conception attempts. While evidence from randomized controlled trials is not available, data from observational studies provide parameters that can inform patient decision making. Knowledge about the fertility window, the decline in fecundability with age, and lifestyle practices that promote conception may be helpful to clinicians and aid in their ability to guide patients.
For those patients who will not achieve conception naturally, assisted reproductive technologies (ART) offer a promising alternative. ART options have improved greatly in effectiveness and safety since Louise Brown was born in 1978. More than 5 million babies have been born globally.1 However, even though the United States is wealthy, access to in vitro fertilization (IVF) is poor relative to many other countries, with not more than 1 in 3 people needing IVF actually receiving the treatment. Understanding the international experience enables physicians to take actions that help increase access for their patients who need IVF.
In this article we not only address ways in which your patients can optimize their natural fertility but also examine this country’s ability to offer ART options when they are needed. Without such examination, fundamental changes in societal attitudes toward infertility and payor attitudes toward reproductive care will not occur, and it is these changes, among others, that can move this country to more equitable ART access.
- Adamson GD, Tabangin M, Macaluso M, de Mouzon J. The number of babies born globally after treatment with the Assisted Reproductive Technologies (ART). Paper presented at International Federation of Fertility Societies/American Society for Reproductive Medicine Conjoint Meeting; October 12–17, 2013; Boston, Massachusetts.
- Dunson DB, Baird DD, Wilcox AJ, Weinberg CR. Day-specific probabilities of clinical pregnancy based on two studies with imperfect measures of ovulation. Hum Reprod. 1999;14(7):1835–1839.
- Keulers MJ, Hamilton CJ, Franx A, et al. The length of the fertile window is associated with the chance of spontaneously conceiving an ongoing pregnancy in subfertile couples. Hum Reprod. 2007;22(6):1652–1656.
- Wilcox AJ, Weinberg CR, Baird DD. Timing of sexual intercourse in relation to ovulation. Effects on the probability of conception, survival of the pregnancy, and sex of the baby. N Engl J Med. 1995;333(23):1517–1521.
- Levitas E, Lunenfeld E, Weiss N, et al. Relationship between the duration of sexual abstinence and semen quality: analysis of 9,489 semen samples. Fertil Steril. 2005;83(6):1680–1686.
- Elzanaty S, Malm J, Giwercman A. Duration of sexual abstinence: epididymal and accessory sex gland secretions and their relationship to sperm motility. Hum Reprod. 2005;20(1):221–225.
- Check JH, Epstein R, Long R. Effect of time interval between ejaculations on semen parameters. Arch Androl. 1991;27(2):93–95.
- Practice Committee of American Society for Reproductive Medicine in collaboration with Society for Reproductive Endocrinology and Infertility. Optimizing natural fertility: a committee opinion. Fertil Steril. 2013;100(3):631–637.
- Gnoth C, Godehardt E, Frank-Herrmann P, Friol K, Tigges J, Freundi G. Definition and prevalence of subfertility and infertility. Hum Reprod. 2005;20(5):1144–1447.
- Howe G, Westhoff C, Vessey M, Yeates D. Effects of age, cigarette smoking, and other factors on fertility: findings in a large prospective study. BMJ (Clin Res Ed). 1985;290(6483):1697–700.
- Dunson DB, Baird DD, Colombo B. Increased infertility with age in men and women. Obstet Gynecol. 2004;103(1):51–56.
- Dunson DB, Colombo B, Baird DD. Changes with age in the level and duration of fertility in the menstrual cycle. Hum Reprod. 2002;17(5):1399–1403.
- Lumley J, Watson L, Watson M, Bower C. Periconceptional supplementation with folate and/or multivitamins for preventing neural tube defects. Cochrane Database Syst Rev. 2001;(3):CD001056.
- Augood C, Duckitt K, Templeton AA. Smoking and female infertility: a systematic review and meta-analysis. Hum Reprod. 1998;13(6):1532–1539.
- Winter E, Wang J, Davies MJ, Norman R. Early pregnancy loss following assisted reproductive technology treatment. Hum Reprod. 2002;17(12):3220–3223.
- Ness RB, Grisso JA, Hirschinger N, et al. Cocaine and tobacco use and the risk of spontaneous abortion. New Engl J Med. 1999;340(5):333–339.
- Mattison DR, Plowchalk DR, Meadows MJ, Miller MM, Malek A, London S. The effect of smoking on oogenesis, fertilization and implantation. Semin Reprod Med. 1989;7(4):291–304.
- Adena MA, Gallagher HG. Cigarette smoking and the age at menopause. Ann Hum Biol. 1982;9(2):121–130.
- Bolumar F, Olsen J, Rebagliato M, Bisanti L. Caffeine intake and delayed conception: a European multicenter study on infertility and subfecundity. European Study Group on Infertility Subfecundity. Am J Epidemiol. 1997;145(4):324–334.
- Wilcox A, Weinberg C, Baird D. Caffeinated beverages and decreased fertility. Lancet. 1988;2(8626–8627):1453–1456.
- Signorello LB, McLaughlin JK. Maternal caffeine consumption and spontaneous abortion: a review of the epidemiologic evidence. Epidemiology. 2004;15(2):229–239.
- Kesmodel U, Wisborg K, Olsen SF, Henriksen TB, Secher NJ. Moderate alcohol intake in pregnancy and the risk of spontaneous abortion. Alcohol. 2002;37(1):87–92.
- Adamson GD; International Council of Medical Acupuncture and Related Techniques (ICMART). ICMART World Report 2011. Webcast presented at: Annual Meeting European Society of Human Reproduction and Embryology (ESHRE); June 16, 2015; Lisbon, Portugal.
- Chambers G, Phuong Hoang V, et al. The impact of consumer affordability on access to assisted reproductive technologies and embryo transfer practices: an international analysis. Fertil Steril. 2014;101(1):191–198.
- Stovall DW, Allen BD, Sparks AE, Syrop CH, Saunders RG, VanVoorhis BJ. The cost of infertility evaluation and therapy: findings of a self-insured university healthcare plan. Fertil Steril. 1999;72(5):778–784.
- Chambers GM, Sullivan E, Ishihara O, Chapman MG, Adamson GD. The economic impact of assisted reproductive technology: a review of selected developed countries. Fertil Steril. 2009;91(6):2281–2294.
- Hamilton BH, McManus B. The effects of insurance mandates on choices and outcomes in infertility treatment markets. Health Econ. 2012;21(8):994–1016.
- Chambers GM, Adamson GD, Eijkemans MJC. Acceptable cost for the patient and society. Fertil Steril. 2013;100(2):319–327.
- Zegers-Hochschild F, Adamson GD, de Mouzon J, et al; ICMART, WHO. International Committee for Monitoring Assisted Reproductive Technology (ICMART); World Health Organization (WHO) revised glossary of ART terminology, 2009. Fertil Steril. 2009;92(5):1520–1524.
- Adamson GD, Tabangin M, Macaluso M, de Mouzon J. The number of babies born globally after treatment with the Assisted Reproductive Technologies (ART). Paper presented at International Federation of Fertility Societies/American Society for Reproductive Medicine Conjoint Meeting; October 12–17, 2013; Boston, Massachusetts.
- Dunson DB, Baird DD, Wilcox AJ, Weinberg CR. Day-specific probabilities of clinical pregnancy based on two studies with imperfect measures of ovulation. Hum Reprod. 1999;14(7):1835–1839.
- Keulers MJ, Hamilton CJ, Franx A, et al. The length of the fertile window is associated with the chance of spontaneously conceiving an ongoing pregnancy in subfertile couples. Hum Reprod. 2007;22(6):1652–1656.
- Wilcox AJ, Weinberg CR, Baird DD. Timing of sexual intercourse in relation to ovulation. Effects on the probability of conception, survival of the pregnancy, and sex of the baby. N Engl J Med. 1995;333(23):1517–1521.
- Levitas E, Lunenfeld E, Weiss N, et al. Relationship between the duration of sexual abstinence and semen quality: analysis of 9,489 semen samples. Fertil Steril. 2005;83(6):1680–1686.
- Elzanaty S, Malm J, Giwercman A. Duration of sexual abstinence: epididymal and accessory sex gland secretions and their relationship to sperm motility. Hum Reprod. 2005;20(1):221–225.
- Check JH, Epstein R, Long R. Effect of time interval between ejaculations on semen parameters. Arch Androl. 1991;27(2):93–95.
- Practice Committee of American Society for Reproductive Medicine in collaboration with Society for Reproductive Endocrinology and Infertility. Optimizing natural fertility: a committee opinion. Fertil Steril. 2013;100(3):631–637.
- Gnoth C, Godehardt E, Frank-Herrmann P, Friol K, Tigges J, Freundi G. Definition and prevalence of subfertility and infertility. Hum Reprod. 2005;20(5):1144–1447.
- Howe G, Westhoff C, Vessey M, Yeates D. Effects of age, cigarette smoking, and other factors on fertility: findings in a large prospective study. BMJ (Clin Res Ed). 1985;290(6483):1697–700.
- Dunson DB, Baird DD, Colombo B. Increased infertility with age in men and women. Obstet Gynecol. 2004;103(1):51–56.
- Dunson DB, Colombo B, Baird DD. Changes with age in the level and duration of fertility in the menstrual cycle. Hum Reprod. 2002;17(5):1399–1403.
- Lumley J, Watson L, Watson M, Bower C. Periconceptional supplementation with folate and/or multivitamins for preventing neural tube defects. Cochrane Database Syst Rev. 2001;(3):CD001056.
- Augood C, Duckitt K, Templeton AA. Smoking and female infertility: a systematic review and meta-analysis. Hum Reprod. 1998;13(6):1532–1539.
- Winter E, Wang J, Davies MJ, Norman R. Early pregnancy loss following assisted reproductive technology treatment. Hum Reprod. 2002;17(12):3220–3223.
- Ness RB, Grisso JA, Hirschinger N, et al. Cocaine and tobacco use and the risk of spontaneous abortion. New Engl J Med. 1999;340(5):333–339.
- Mattison DR, Plowchalk DR, Meadows MJ, Miller MM, Malek A, London S. The effect of smoking on oogenesis, fertilization and implantation. Semin Reprod Med. 1989;7(4):291–304.
- Adena MA, Gallagher HG. Cigarette smoking and the age at menopause. Ann Hum Biol. 1982;9(2):121–130.
- Bolumar F, Olsen J, Rebagliato M, Bisanti L. Caffeine intake and delayed conception: a European multicenter study on infertility and subfecundity. European Study Group on Infertility Subfecundity. Am J Epidemiol. 1997;145(4):324–334.
- Wilcox A, Weinberg C, Baird D. Caffeinated beverages and decreased fertility. Lancet. 1988;2(8626–8627):1453–1456.
- Signorello LB, McLaughlin JK. Maternal caffeine consumption and spontaneous abortion: a review of the epidemiologic evidence. Epidemiology. 2004;15(2):229–239.
- Kesmodel U, Wisborg K, Olsen SF, Henriksen TB, Secher NJ. Moderate alcohol intake in pregnancy and the risk of spontaneous abortion. Alcohol. 2002;37(1):87–92.
- Adamson GD; International Council of Medical Acupuncture and Related Techniques (ICMART). ICMART World Report 2011. Webcast presented at: Annual Meeting European Society of Human Reproduction and Embryology (ESHRE); June 16, 2015; Lisbon, Portugal.
- Chambers G, Phuong Hoang V, et al. The impact of consumer affordability on access to assisted reproductive technologies and embryo transfer practices: an international analysis. Fertil Steril. 2014;101(1):191–198.
- Stovall DW, Allen BD, Sparks AE, Syrop CH, Saunders RG, VanVoorhis BJ. The cost of infertility evaluation and therapy: findings of a self-insured university healthcare plan. Fertil Steril. 1999;72(5):778–784.
- Chambers GM, Sullivan E, Ishihara O, Chapman MG, Adamson GD. The economic impact of assisted reproductive technology: a review of selected developed countries. Fertil Steril. 2009;91(6):2281–2294.
- Hamilton BH, McManus B. The effects of insurance mandates on choices and outcomes in infertility treatment markets. Health Econ. 2012;21(8):994–1016.
- Chambers GM, Adamson GD, Eijkemans MJC. Acceptable cost for the patient and society. Fertil Steril. 2013;100(2):319–327.
- Zegers-Hochschild F, Adamson GD, de Mouzon J, et al; ICMART, WHO. International Committee for Monitoring Assisted Reproductive Technology (ICMART); World Health Organization (WHO) revised glossary of ART terminology, 2009. Fertil Steril. 2009;92(5):1520–1524.
In this Article
- Factors affecting the probability of conception
- Barriers to ART access
- Ways to increase ART funding
Psychotropics low on list of therapies for autism
NEW YORK – Some of the behavioral and psychiatric problems observed in children with autism spectrum disorder (ASD) may improve on atypical antipsychotics, but these drugs do not improve core symptoms and should be used sparingly in this population, according to an expert’s analysis at a psychopharmacology update held by the American Academy of Child and Adolescent Psychiatry.
“Most children with ASD either do not need or will not benefit from available psychotropic medications,” reported Dr. Jeremy M. Veenstra-VanderWeele of the Center for Autism and the Developing Brain, Columbia University, New York.
In a review of the evidence, he suggested that psychopharmacologic treatments for children with ASD, when indicated at all, are only relevant to behavioral issues and psychiatric comorbidities. On an evidence basis, behavioral modification and psychosocial support for the patient and family should come first or at least accompany psychotropic agents.
“These families are desperate and, oftentimes, they cannot get the services that would actually make things better for their child on a behavioral level,” Dr. Veenstra-VanderWeele said. He said that the “pressure to prescribe,” along with a desire to help, drive many clinicians to offer medications, “but we just should be honest and recognize that our evidence does not suggest that we are able to help the majority.”
Most children with ASD do receive one or more prescriptions for psychotropic agents, according to Dr. Veenstra-VanderWeele’s experience. In fact, he reported that he often is asked to consult on a child who has been prescribed two or three medications when it is unclear which, if any, are offering benefit. While he also finds that these agents often are prescribed at low doses, a better approach would be to use an evidence-based therapy at an adequate dose after carefully evaluating the risk-to-benefit ratio.
“I find that a lot of the kids I see in consultation have had, in desperation, more than one medicine started within the time window of response, and that’s really problematic. That is how kids end up on three or four medicines without a clear sense of what led to improvement,” Dr. Veenstra-VanderWeele noted. He suggested that the more appropriate strategy is to attempt to maximize benefit on one therapy, including behavioral therapies, before initiating another.
In his review of psychotropic medicines for ASD comorbidities, he suggested the evidence is “high” that the atypical antipsychotics risperidone and aripiprazole are effective in at least some children for irritability and agitation. He also reported that the evidence of lack of benefit from secretin also should now be labeled as high.
The evidence for benefit from long-acting stimulants for behavioral improvement was labeled as “moderate,” particularly when considered in the context of adverse events. Atomoxetine, a selective norepinephrine reuptake inhibitor also used for attention-deficit/hyperactivity disorder, is another drug placed by Dr. Veenstra-VanderWeele in the category for “moderate” evidence. Two controlled studies have demonstrated activity, but the overall response in each was relatively modest.
In a third group, labeled “insufficient evidence,” he placed both guanfacine, particularly for irritability, and selective serotonin reuptake inhibitors.
Although the strongest evidence for pharmacotherapy to control comorbidities in ASD is related to atypical antipsychotics, he emphasized that these are accompanied with adverse events. Some, such as weight gain, can be difficult to reverse after long-term therapy.
“Particularly in this population, I talk about stopping the medicine at the time that I start the medicine,” Dr. Veenstra-VanderWeele reported. Citing the frequency of rapid weight gain in patients on some atypical antipsychotics, he said that it is important to warn patients that a switch in therapy may be necessary.
“It is often hard to say we are going to switch when everyone feels that the patient is much better. You have to lay it out in advance and write it down, so the family knows what to expect,” Dr. Veenstra-VanderWeele said.
Management of pediatric ASD typically involves multiple coexisting clinical issues. Because “there is always something else going on” in the ASD patient, he emphasized the need for a systematic approach in which medical and behavioral issues and psychiatric comorbidities are addressed in the context of clear goals for each targeted symptom.
Dr. Veenstra-VanderWeele reported financial relationships with Forest Laboratories, Hoffmann-La Roche, Novartis, Seaside Therapeutics, Sunovion Pharmaceuticals, and SynapDx.
NEW YORK – Some of the behavioral and psychiatric problems observed in children with autism spectrum disorder (ASD) may improve on atypical antipsychotics, but these drugs do not improve core symptoms and should be used sparingly in this population, according to an expert’s analysis at a psychopharmacology update held by the American Academy of Child and Adolescent Psychiatry.
“Most children with ASD either do not need or will not benefit from available psychotropic medications,” reported Dr. Jeremy M. Veenstra-VanderWeele of the Center for Autism and the Developing Brain, Columbia University, New York.
In a review of the evidence, he suggested that psychopharmacologic treatments for children with ASD, when indicated at all, are only relevant to behavioral issues and psychiatric comorbidities. On an evidence basis, behavioral modification and psychosocial support for the patient and family should come first or at least accompany psychotropic agents.
“These families are desperate and, oftentimes, they cannot get the services that would actually make things better for their child on a behavioral level,” Dr. Veenstra-VanderWeele said. He said that the “pressure to prescribe,” along with a desire to help, drive many clinicians to offer medications, “but we just should be honest and recognize that our evidence does not suggest that we are able to help the majority.”
Most children with ASD do receive one or more prescriptions for psychotropic agents, according to Dr. Veenstra-VanderWeele’s experience. In fact, he reported that he often is asked to consult on a child who has been prescribed two or three medications when it is unclear which, if any, are offering benefit. While he also finds that these agents often are prescribed at low doses, a better approach would be to use an evidence-based therapy at an adequate dose after carefully evaluating the risk-to-benefit ratio.
“I find that a lot of the kids I see in consultation have had, in desperation, more than one medicine started within the time window of response, and that’s really problematic. That is how kids end up on three or four medicines without a clear sense of what led to improvement,” Dr. Veenstra-VanderWeele noted. He suggested that the more appropriate strategy is to attempt to maximize benefit on one therapy, including behavioral therapies, before initiating another.
In his review of psychotropic medicines for ASD comorbidities, he suggested the evidence is “high” that the atypical antipsychotics risperidone and aripiprazole are effective in at least some children for irritability and agitation. He also reported that the evidence of lack of benefit from secretin also should now be labeled as high.
The evidence for benefit from long-acting stimulants for behavioral improvement was labeled as “moderate,” particularly when considered in the context of adverse events. Atomoxetine, a selective norepinephrine reuptake inhibitor also used for attention-deficit/hyperactivity disorder, is another drug placed by Dr. Veenstra-VanderWeele in the category for “moderate” evidence. Two controlled studies have demonstrated activity, but the overall response in each was relatively modest.
In a third group, labeled “insufficient evidence,” he placed both guanfacine, particularly for irritability, and selective serotonin reuptake inhibitors.
Although the strongest evidence for pharmacotherapy to control comorbidities in ASD is related to atypical antipsychotics, he emphasized that these are accompanied with adverse events. Some, such as weight gain, can be difficult to reverse after long-term therapy.
“Particularly in this population, I talk about stopping the medicine at the time that I start the medicine,” Dr. Veenstra-VanderWeele reported. Citing the frequency of rapid weight gain in patients on some atypical antipsychotics, he said that it is important to warn patients that a switch in therapy may be necessary.
“It is often hard to say we are going to switch when everyone feels that the patient is much better. You have to lay it out in advance and write it down, so the family knows what to expect,” Dr. Veenstra-VanderWeele said.
Management of pediatric ASD typically involves multiple coexisting clinical issues. Because “there is always something else going on” in the ASD patient, he emphasized the need for a systematic approach in which medical and behavioral issues and psychiatric comorbidities are addressed in the context of clear goals for each targeted symptom.
Dr. Veenstra-VanderWeele reported financial relationships with Forest Laboratories, Hoffmann-La Roche, Novartis, Seaside Therapeutics, Sunovion Pharmaceuticals, and SynapDx.
NEW YORK – Some of the behavioral and psychiatric problems observed in children with autism spectrum disorder (ASD) may improve on atypical antipsychotics, but these drugs do not improve core symptoms and should be used sparingly in this population, according to an expert’s analysis at a psychopharmacology update held by the American Academy of Child and Adolescent Psychiatry.
“Most children with ASD either do not need or will not benefit from available psychotropic medications,” reported Dr. Jeremy M. Veenstra-VanderWeele of the Center for Autism and the Developing Brain, Columbia University, New York.
In a review of the evidence, he suggested that psychopharmacologic treatments for children with ASD, when indicated at all, are only relevant to behavioral issues and psychiatric comorbidities. On an evidence basis, behavioral modification and psychosocial support for the patient and family should come first or at least accompany psychotropic agents.
“These families are desperate and, oftentimes, they cannot get the services that would actually make things better for their child on a behavioral level,” Dr. Veenstra-VanderWeele said. He said that the “pressure to prescribe,” along with a desire to help, drive many clinicians to offer medications, “but we just should be honest and recognize that our evidence does not suggest that we are able to help the majority.”
Most children with ASD do receive one or more prescriptions for psychotropic agents, according to Dr. Veenstra-VanderWeele’s experience. In fact, he reported that he often is asked to consult on a child who has been prescribed two or three medications when it is unclear which, if any, are offering benefit. While he also finds that these agents often are prescribed at low doses, a better approach would be to use an evidence-based therapy at an adequate dose after carefully evaluating the risk-to-benefit ratio.
“I find that a lot of the kids I see in consultation have had, in desperation, more than one medicine started within the time window of response, and that’s really problematic. That is how kids end up on three or four medicines without a clear sense of what led to improvement,” Dr. Veenstra-VanderWeele noted. He suggested that the more appropriate strategy is to attempt to maximize benefit on one therapy, including behavioral therapies, before initiating another.
In his review of psychotropic medicines for ASD comorbidities, he suggested the evidence is “high” that the atypical antipsychotics risperidone and aripiprazole are effective in at least some children for irritability and agitation. He also reported that the evidence of lack of benefit from secretin also should now be labeled as high.
The evidence for benefit from long-acting stimulants for behavioral improvement was labeled as “moderate,” particularly when considered in the context of adverse events. Atomoxetine, a selective norepinephrine reuptake inhibitor also used for attention-deficit/hyperactivity disorder, is another drug placed by Dr. Veenstra-VanderWeele in the category for “moderate” evidence. Two controlled studies have demonstrated activity, but the overall response in each was relatively modest.
In a third group, labeled “insufficient evidence,” he placed both guanfacine, particularly for irritability, and selective serotonin reuptake inhibitors.
Although the strongest evidence for pharmacotherapy to control comorbidities in ASD is related to atypical antipsychotics, he emphasized that these are accompanied with adverse events. Some, such as weight gain, can be difficult to reverse after long-term therapy.
“Particularly in this population, I talk about stopping the medicine at the time that I start the medicine,” Dr. Veenstra-VanderWeele reported. Citing the frequency of rapid weight gain in patients on some atypical antipsychotics, he said that it is important to warn patients that a switch in therapy may be necessary.
“It is often hard to say we are going to switch when everyone feels that the patient is much better. You have to lay it out in advance and write it down, so the family knows what to expect,” Dr. Veenstra-VanderWeele said.
Management of pediatric ASD typically involves multiple coexisting clinical issues. Because “there is always something else going on” in the ASD patient, he emphasized the need for a systematic approach in which medical and behavioral issues and psychiatric comorbidities are addressed in the context of clear goals for each targeted symptom.
Dr. Veenstra-VanderWeele reported financial relationships with Forest Laboratories, Hoffmann-La Roche, Novartis, Seaside Therapeutics, Sunovion Pharmaceuticals, and SynapDx.
EXPERT ANALYSIS FROM THE PSYCHOPHARMACOLOGY UPDATE INSTITUTE
Can we solve the problem of inadequate contraception for women at high risk for adverse pregnancy outcomes?
In the United States contraception practices are slowly improving, with robust evidence for the increased use of long-acting reversible contraceptives and preliminary data that the unintended pregnancy rate may be decreasing for the first time in many years.1 There remains a major gap in contraception practice, however: US women with chronic disease who are at high risk for adverse pregnancy outcomes are not receiving adequate contraceptive counseling or adequate contraception.2,3 In one study, the majority of women with hypertension, diabetes, epilepsy, stroke, heart disease, lupus, or thrombophilia were not using a prescription contraceptive.3
Recently, I have seen women with major medical problems, who have had many visits with specialists and primary care clinicians, but who have not had their contraceptive needs prioritized. Here are but a few examples:
- We recently cared for a patient with heart disease and severe pulmonary hypertension, who had many procedures performed by cardiologists and cardiac surgeons, but contraception had not been prioritized as one of her foremost medical needs.
- A young woman who had a pulmonary embolism 1-month postpartum reported that her primary care clinician said that she could never use any hormonal contraceptive, including the progestin-only pill, progestin-implant, and the progestin-releasing intrauterine device (IUD). She was not taking a contraceptive and had an unplanned pregnancy.
- A middle-aged woman with diabetes and a glycosylated hemoglo‑ bin A1c (HbA1c) value greater than 10% was regularly seeing her primary care clinician, but was not using an effective contraceptive. She became pregnant with a fetus that had a major congenital anomaly.
Clearly, there is a major gap between current and optimal contraceptive services for women with chronic medical problems. Women with diabetes and heart disease are affected substantially, as the evidence I present in this editorial indicates. Studies also show that women taking teratogenic medications do not receive the vital counseling that they should regarding contraception. Given the potential detrimental adverse events to both mother and fetus, obstetrician-gynecologists are poised to offer solutions to this concerning inadequacy of care.
DiabetesWomen with diabetes and an abnormally elevated HbA1c level are at high risk for many adverse pregnancy outcomes, including major congenital malformations and intrauterine fetal demise.4 Unfortunately, results of many studies indicate that women with diabetes are not receiving adequate contraceptive services.5–7 In one review of records at Kaiser Permanente Northern California, investigators reported that 62% of 122,921 healthy women, but only 48% of 8,182 women with diabetes, received contraceptive counseling, a contraceptive prescription, or contraceptive services.5
Why is it that so many women with diabetes do not receive contraceptive services? One possibility is that clinicians are reluctant to prescribe oral hormonal contraceptives that contain estrogen to their patients with diabetes because of a perceived increased risk of cardiovascular events.8 In the Kaiser study, 31% of the healthy women, and only 13% of the women with diabetes, were using a pill, patch, or ring (most of which contain estrogen).5 In this same study, the rate of utilization of an IUD was similar in the healthy (6.5%) and diabetic (5.6%) women. The IUD is known to be safe for use in women with diabetes.9
The low rate of utilization of intrauterine contraception by women with diabetes is a gap that gynecologists are well positioned to help solve.
Heart diseaseIn developed countries, a major cause of maternal mortality is pregnancy among women with congenital or acquired heart disease.10 Misinformation is a common problem in contraceptive counseling. In a recent study of 83 sexually active women with congenital heart disease, 6 women were told that they could not use an IUD or progestin-implant because they were unsafe for those with repaired congenital heart disease.11 In this cohort of women, who were at high risk for adverse pregnancy outcomes, 45% of pregnancies were unplanned, similar to the rate among healthy women.
On a positive note, authors of a small study from Maryland found that, among women with heart disease, the self-reported use of a contraceptive increased from 60% prepregnancy to 93% following delivery.12
Clearly, patient interaction with qualified women’s health clinicians can increase contraceptive use in those with high-risk medical issues.
Teratogenic medicationsShould reproductive-age women taking long-term methotrexate for treatment of rheumatoid conditions receive contraceptive counseling? The answer is clearly, “yes.” Methotrexate can cause fetal death or major congenital malformations, such as absence of digits and oxycephaly (premature closure of the skull sutures). All women of reproductive age prescribed known teratogens should receive effective contraception. Unfortunately, data do not indicate this is occurring.
In one study of 1,694 adolescents and young women aged 14 to 25 years who were prescribed a teratogen, only 29% received documented contraception counseling, and only 11% received a contraceptive prescription or were documented to be actively using a contraceptive.13 The most commonly prescribed teratogens in this study were topiramate, methotrexate, and isoretinoin. Among the specialists who prescribed the medications, dermatologists documented contraceptive counseling in 47% of visits—likely because of the federally mandated risk mitigation system for prescribing isoretinoin. Neurologists and hematologists were least likely to document contraceptive counseling, at 16% and 28%, respectively.13
In a study of 488,175 women aged 15 to 44 years receiving care from clinicians at Kaiser Permanente Northern California, contraceptive counseling documentation was compared among women prescribed US Food and Drug Administration (FDA) category A or B medications (nonteratogenic) versus FDA category D or X medications (teratogenic).14 The rate at which women had no contraceptive counseling recorded was similar whether a teratogenic (47.6%) or nonteratogenic (46%) medication was prescribed. Clearly, there is a gap between current and optimal practice when teratogens are prescribed to women of reproductive age.
What could improve contraceptive services for women with serious medical problems?One promising approach is to include contraception status as a vital sign for all women and men of reproductive age. Most electronic medical records prioritize assessment of such health vital signs as allergies, smoking status, depression screening, falls prevention, blood pressure, temperature, heart rate, weight, and height. Contraception status is of equal importance to these vital signs in women and men of reproductive age and should be routinely documented.
Another intervention is to create a standard of care in which reproductive-age women with major medical problems are routinely referred to a clinician who has the time and skill to provide a comprehensive contraception visit. Health systems could take greater responsibility for managing the contraception practices of their members. For example, within a given accountable care organization the electronic health record could be used to identify adult women of reproductive age with diabetes and an HbA1c level greater than 7%. These women could be contacted to ascertain their contraception status and their need for a contraception health visit. Electronic health records could be utilized to identify all reproductive-age women taking a teratogenic medication. A computer-generated alert could be sent to the responsible clinician recommending referral to an obstetrician-gynecologist for a contraceptive services visit.15
Pharmacists could be more proactive in highlighting the importance of contraception for women prescribed teratogens and in recommending a contraceptive visit. In some states pharmacists can offer an oral hormonal contraceptive to women who are prescribed a teratogen and at risk for becoming pregnant.
How do you propose to address lack of counseling?As an experienced clinician, you likely have ideas about how to improve contraceptive counseling for women with significant medical problems. Please let me know what interventions you think would best improve the use of contraception in this group of high-risk women by emailing me at OBG Management: rbarbieri@frontlinemedcom.com.
Tell us…What are your ideas to improve contraception counseling for women with significant medical problems that put them at high risk for adverse pregnancy outcomes?
Send your letter to the editor to rbarbieri@frontlinemedcom.com. Please include the city and state in which you practice
- Kavanaugh ML, Jerman J, Finer LB. Changes in use of long-acting reversible contraceptive methods among US women, 2009-2012. Obstet Gynecol. 2015;126(5):917–927.
- DeNoble AE, Hall KS, Xu X, Zochowski MK, Piehl K, Dalton VK. Receipt of prescription contraception by commercially insured women with chronic medical conditions. Obstet Gynecol. 2014;123(6):1213–1220.
- Champaloux SW, Tepper NK, Curtis KM, et al. Contraceptive use among women with medical conditions in a nationwide privately insured population. Obstet Gynecol. 2015;126(6):1151–1159.
- Klingensmith GJ, Pyle L, Nadeau KJ, et al; TODAY Study Group. Pregnancy outcomes in youth with type 2 diabetes: the TODAY study experience. Diabetes Care. 2016;39(1):122–129.
- Schwarz EB, Postlethwaite D, Hung YY, Lantzman E, Armstrong MA, Horberg MA. Provision of contraceptive services to women with diabetes mellitus. J Gen Int Med. 2011;27(2):196–201.
- Schwarz EB, Maselli J, Gonzales R. Contraceptive counseling of diabetic women of reproductive age. Obstet Gynecol. 2006;107(5):1070–1074.
- Chuang CH, Chase GA, Bensyl DM, Weisman CS. Contraceptive use by diabetic and obese women. Womens Health Issues. 2005;15(4):167–173.
- Lidegaard O. Hormonal contraception, thrombosis and age. Expert Opin Drug Safe. 2014;13(10):1353–1360.
- Goldstuck ND, Steyn PS. The intrauterine device in women with diabetes mellitus type I and II: a systematic review. ISRN Obstet Gynecol. 2013:814062. doi.10.1155/2013/814062.
- Thompson JL, Kuklina EV, Bateman BT, Callaghan WM, James AH, Grotegut CA. Medical and obstetric outcomes among pregnant women with congenital heart disease. Obstet Gynecol. 2015;126(2):346–354.
- Lindley KJ, Madden T, Cahill AG, Ludbrook PA, Billadello JJ. Contraceptive use and unintended pregnancy in women with congenital heart disease. Obstet Gynecol. 2015;126(2):363–369.
- Perritt JB, Burke A, Jasmshidli R, Wang J, Fox M. Contraception counseling, pregnancy intention and contraception use in women with medical problems: an analysis of data from the Maryland Pregnancy Risk Assessment Monitoring System (PRAMS). Contraception. 2013;88(2):263–268.
- Stancil SL, Miller M, Briggs H, Lynch D, Goggin K, Kearns G. Contraceptive provision to adolescent females prescribed teratogenic medications. Pediatrics. 2016;137(1):1–8.
- Schwarz EB, Postlewaite DA, Hung YY, Armstrong MA. Documentation of contraception and pregnancy when prescribing potentially teratogenic medications for reproductive-age women. Ann Int Med. 2007;147(6):370–376.
- Mody SK, Wu J, Ornelas M, et al. Using the electronic medical record to refer women taking category D or X medications for teratogen and contraceptive counseling. Birth Defects Res A Clin Mol Teratol. 2015;103(7):644–647.
In the United States contraception practices are slowly improving, with robust evidence for the increased use of long-acting reversible contraceptives and preliminary data that the unintended pregnancy rate may be decreasing for the first time in many years.1 There remains a major gap in contraception practice, however: US women with chronic disease who are at high risk for adverse pregnancy outcomes are not receiving adequate contraceptive counseling or adequate contraception.2,3 In one study, the majority of women with hypertension, diabetes, epilepsy, stroke, heart disease, lupus, or thrombophilia were not using a prescription contraceptive.3
Recently, I have seen women with major medical problems, who have had many visits with specialists and primary care clinicians, but who have not had their contraceptive needs prioritized. Here are but a few examples:
- We recently cared for a patient with heart disease and severe pulmonary hypertension, who had many procedures performed by cardiologists and cardiac surgeons, but contraception had not been prioritized as one of her foremost medical needs.
- A young woman who had a pulmonary embolism 1-month postpartum reported that her primary care clinician said that she could never use any hormonal contraceptive, including the progestin-only pill, progestin-implant, and the progestin-releasing intrauterine device (IUD). She was not taking a contraceptive and had an unplanned pregnancy.
- A middle-aged woman with diabetes and a glycosylated hemoglo‑ bin A1c (HbA1c) value greater than 10% was regularly seeing her primary care clinician, but was not using an effective contraceptive. She became pregnant with a fetus that had a major congenital anomaly.
Clearly, there is a major gap between current and optimal contraceptive services for women with chronic medical problems. Women with diabetes and heart disease are affected substantially, as the evidence I present in this editorial indicates. Studies also show that women taking teratogenic medications do not receive the vital counseling that they should regarding contraception. Given the potential detrimental adverse events to both mother and fetus, obstetrician-gynecologists are poised to offer solutions to this concerning inadequacy of care.
DiabetesWomen with diabetes and an abnormally elevated HbA1c level are at high risk for many adverse pregnancy outcomes, including major congenital malformations and intrauterine fetal demise.4 Unfortunately, results of many studies indicate that women with diabetes are not receiving adequate contraceptive services.5–7 In one review of records at Kaiser Permanente Northern California, investigators reported that 62% of 122,921 healthy women, but only 48% of 8,182 women with diabetes, received contraceptive counseling, a contraceptive prescription, or contraceptive services.5
Why is it that so many women with diabetes do not receive contraceptive services? One possibility is that clinicians are reluctant to prescribe oral hormonal contraceptives that contain estrogen to their patients with diabetes because of a perceived increased risk of cardiovascular events.8 In the Kaiser study, 31% of the healthy women, and only 13% of the women with diabetes, were using a pill, patch, or ring (most of which contain estrogen).5 In this same study, the rate of utilization of an IUD was similar in the healthy (6.5%) and diabetic (5.6%) women. The IUD is known to be safe for use in women with diabetes.9
The low rate of utilization of intrauterine contraception by women with diabetes is a gap that gynecologists are well positioned to help solve.
Heart diseaseIn developed countries, a major cause of maternal mortality is pregnancy among women with congenital or acquired heart disease.10 Misinformation is a common problem in contraceptive counseling. In a recent study of 83 sexually active women with congenital heart disease, 6 women were told that they could not use an IUD or progestin-implant because they were unsafe for those with repaired congenital heart disease.11 In this cohort of women, who were at high risk for adverse pregnancy outcomes, 45% of pregnancies were unplanned, similar to the rate among healthy women.
On a positive note, authors of a small study from Maryland found that, among women with heart disease, the self-reported use of a contraceptive increased from 60% prepregnancy to 93% following delivery.12
Clearly, patient interaction with qualified women’s health clinicians can increase contraceptive use in those with high-risk medical issues.
Teratogenic medicationsShould reproductive-age women taking long-term methotrexate for treatment of rheumatoid conditions receive contraceptive counseling? The answer is clearly, “yes.” Methotrexate can cause fetal death or major congenital malformations, such as absence of digits and oxycephaly (premature closure of the skull sutures). All women of reproductive age prescribed known teratogens should receive effective contraception. Unfortunately, data do not indicate this is occurring.
In one study of 1,694 adolescents and young women aged 14 to 25 years who were prescribed a teratogen, only 29% received documented contraception counseling, and only 11% received a contraceptive prescription or were documented to be actively using a contraceptive.13 The most commonly prescribed teratogens in this study were topiramate, methotrexate, and isoretinoin. Among the specialists who prescribed the medications, dermatologists documented contraceptive counseling in 47% of visits—likely because of the federally mandated risk mitigation system for prescribing isoretinoin. Neurologists and hematologists were least likely to document contraceptive counseling, at 16% and 28%, respectively.13
In a study of 488,175 women aged 15 to 44 years receiving care from clinicians at Kaiser Permanente Northern California, contraceptive counseling documentation was compared among women prescribed US Food and Drug Administration (FDA) category A or B medications (nonteratogenic) versus FDA category D or X medications (teratogenic).14 The rate at which women had no contraceptive counseling recorded was similar whether a teratogenic (47.6%) or nonteratogenic (46%) medication was prescribed. Clearly, there is a gap between current and optimal practice when teratogens are prescribed to women of reproductive age.
What could improve contraceptive services for women with serious medical problems?One promising approach is to include contraception status as a vital sign for all women and men of reproductive age. Most electronic medical records prioritize assessment of such health vital signs as allergies, smoking status, depression screening, falls prevention, blood pressure, temperature, heart rate, weight, and height. Contraception status is of equal importance to these vital signs in women and men of reproductive age and should be routinely documented.
Another intervention is to create a standard of care in which reproductive-age women with major medical problems are routinely referred to a clinician who has the time and skill to provide a comprehensive contraception visit. Health systems could take greater responsibility for managing the contraception practices of their members. For example, within a given accountable care organization the electronic health record could be used to identify adult women of reproductive age with diabetes and an HbA1c level greater than 7%. These women could be contacted to ascertain their contraception status and their need for a contraception health visit. Electronic health records could be utilized to identify all reproductive-age women taking a teratogenic medication. A computer-generated alert could be sent to the responsible clinician recommending referral to an obstetrician-gynecologist for a contraceptive services visit.15
Pharmacists could be more proactive in highlighting the importance of contraception for women prescribed teratogens and in recommending a contraceptive visit. In some states pharmacists can offer an oral hormonal contraceptive to women who are prescribed a teratogen and at risk for becoming pregnant.
How do you propose to address lack of counseling?As an experienced clinician, you likely have ideas about how to improve contraceptive counseling for women with significant medical problems. Please let me know what interventions you think would best improve the use of contraception in this group of high-risk women by emailing me at OBG Management: rbarbieri@frontlinemedcom.com.
Tell us…What are your ideas to improve contraception counseling for women with significant medical problems that put them at high risk for adverse pregnancy outcomes?
Send your letter to the editor to rbarbieri@frontlinemedcom.com. Please include the city and state in which you practice
In the United States contraception practices are slowly improving, with robust evidence for the increased use of long-acting reversible contraceptives and preliminary data that the unintended pregnancy rate may be decreasing for the first time in many years.1 There remains a major gap in contraception practice, however: US women with chronic disease who are at high risk for adverse pregnancy outcomes are not receiving adequate contraceptive counseling or adequate contraception.2,3 In one study, the majority of women with hypertension, diabetes, epilepsy, stroke, heart disease, lupus, or thrombophilia were not using a prescription contraceptive.3
Recently, I have seen women with major medical problems, who have had many visits with specialists and primary care clinicians, but who have not had their contraceptive needs prioritized. Here are but a few examples:
- We recently cared for a patient with heart disease and severe pulmonary hypertension, who had many procedures performed by cardiologists and cardiac surgeons, but contraception had not been prioritized as one of her foremost medical needs.
- A young woman who had a pulmonary embolism 1-month postpartum reported that her primary care clinician said that she could never use any hormonal contraceptive, including the progestin-only pill, progestin-implant, and the progestin-releasing intrauterine device (IUD). She was not taking a contraceptive and had an unplanned pregnancy.
- A middle-aged woman with diabetes and a glycosylated hemoglo‑ bin A1c (HbA1c) value greater than 10% was regularly seeing her primary care clinician, but was not using an effective contraceptive. She became pregnant with a fetus that had a major congenital anomaly.
Clearly, there is a major gap between current and optimal contraceptive services for women with chronic medical problems. Women with diabetes and heart disease are affected substantially, as the evidence I present in this editorial indicates. Studies also show that women taking teratogenic medications do not receive the vital counseling that they should regarding contraception. Given the potential detrimental adverse events to both mother and fetus, obstetrician-gynecologists are poised to offer solutions to this concerning inadequacy of care.
DiabetesWomen with diabetes and an abnormally elevated HbA1c level are at high risk for many adverse pregnancy outcomes, including major congenital malformations and intrauterine fetal demise.4 Unfortunately, results of many studies indicate that women with diabetes are not receiving adequate contraceptive services.5–7 In one review of records at Kaiser Permanente Northern California, investigators reported that 62% of 122,921 healthy women, but only 48% of 8,182 women with diabetes, received contraceptive counseling, a contraceptive prescription, or contraceptive services.5
Why is it that so many women with diabetes do not receive contraceptive services? One possibility is that clinicians are reluctant to prescribe oral hormonal contraceptives that contain estrogen to their patients with diabetes because of a perceived increased risk of cardiovascular events.8 In the Kaiser study, 31% of the healthy women, and only 13% of the women with diabetes, were using a pill, patch, or ring (most of which contain estrogen).5 In this same study, the rate of utilization of an IUD was similar in the healthy (6.5%) and diabetic (5.6%) women. The IUD is known to be safe for use in women with diabetes.9
The low rate of utilization of intrauterine contraception by women with diabetes is a gap that gynecologists are well positioned to help solve.
Heart diseaseIn developed countries, a major cause of maternal mortality is pregnancy among women with congenital or acquired heart disease.10 Misinformation is a common problem in contraceptive counseling. In a recent study of 83 sexually active women with congenital heart disease, 6 women were told that they could not use an IUD or progestin-implant because they were unsafe for those with repaired congenital heart disease.11 In this cohort of women, who were at high risk for adverse pregnancy outcomes, 45% of pregnancies were unplanned, similar to the rate among healthy women.
On a positive note, authors of a small study from Maryland found that, among women with heart disease, the self-reported use of a contraceptive increased from 60% prepregnancy to 93% following delivery.12
Clearly, patient interaction with qualified women’s health clinicians can increase contraceptive use in those with high-risk medical issues.
Teratogenic medicationsShould reproductive-age women taking long-term methotrexate for treatment of rheumatoid conditions receive contraceptive counseling? The answer is clearly, “yes.” Methotrexate can cause fetal death or major congenital malformations, such as absence of digits and oxycephaly (premature closure of the skull sutures). All women of reproductive age prescribed known teratogens should receive effective contraception. Unfortunately, data do not indicate this is occurring.
In one study of 1,694 adolescents and young women aged 14 to 25 years who were prescribed a teratogen, only 29% received documented contraception counseling, and only 11% received a contraceptive prescription or were documented to be actively using a contraceptive.13 The most commonly prescribed teratogens in this study were topiramate, methotrexate, and isoretinoin. Among the specialists who prescribed the medications, dermatologists documented contraceptive counseling in 47% of visits—likely because of the federally mandated risk mitigation system for prescribing isoretinoin. Neurologists and hematologists were least likely to document contraceptive counseling, at 16% and 28%, respectively.13
In a study of 488,175 women aged 15 to 44 years receiving care from clinicians at Kaiser Permanente Northern California, contraceptive counseling documentation was compared among women prescribed US Food and Drug Administration (FDA) category A or B medications (nonteratogenic) versus FDA category D or X medications (teratogenic).14 The rate at which women had no contraceptive counseling recorded was similar whether a teratogenic (47.6%) or nonteratogenic (46%) medication was prescribed. Clearly, there is a gap between current and optimal practice when teratogens are prescribed to women of reproductive age.
What could improve contraceptive services for women with serious medical problems?One promising approach is to include contraception status as a vital sign for all women and men of reproductive age. Most electronic medical records prioritize assessment of such health vital signs as allergies, smoking status, depression screening, falls prevention, blood pressure, temperature, heart rate, weight, and height. Contraception status is of equal importance to these vital signs in women and men of reproductive age and should be routinely documented.
Another intervention is to create a standard of care in which reproductive-age women with major medical problems are routinely referred to a clinician who has the time and skill to provide a comprehensive contraception visit. Health systems could take greater responsibility for managing the contraception practices of their members. For example, within a given accountable care organization the electronic health record could be used to identify adult women of reproductive age with diabetes and an HbA1c level greater than 7%. These women could be contacted to ascertain their contraception status and their need for a contraception health visit. Electronic health records could be utilized to identify all reproductive-age women taking a teratogenic medication. A computer-generated alert could be sent to the responsible clinician recommending referral to an obstetrician-gynecologist for a contraceptive services visit.15
Pharmacists could be more proactive in highlighting the importance of contraception for women prescribed teratogens and in recommending a contraceptive visit. In some states pharmacists can offer an oral hormonal contraceptive to women who are prescribed a teratogen and at risk for becoming pregnant.
How do you propose to address lack of counseling?As an experienced clinician, you likely have ideas about how to improve contraceptive counseling for women with significant medical problems. Please let me know what interventions you think would best improve the use of contraception in this group of high-risk women by emailing me at OBG Management: rbarbieri@frontlinemedcom.com.
Tell us…What are your ideas to improve contraception counseling for women with significant medical problems that put them at high risk for adverse pregnancy outcomes?
Send your letter to the editor to rbarbieri@frontlinemedcom.com. Please include the city and state in which you practice
- Kavanaugh ML, Jerman J, Finer LB. Changes in use of long-acting reversible contraceptive methods among US women, 2009-2012. Obstet Gynecol. 2015;126(5):917–927.
- DeNoble AE, Hall KS, Xu X, Zochowski MK, Piehl K, Dalton VK. Receipt of prescription contraception by commercially insured women with chronic medical conditions. Obstet Gynecol. 2014;123(6):1213–1220.
- Champaloux SW, Tepper NK, Curtis KM, et al. Contraceptive use among women with medical conditions in a nationwide privately insured population. Obstet Gynecol. 2015;126(6):1151–1159.
- Klingensmith GJ, Pyle L, Nadeau KJ, et al; TODAY Study Group. Pregnancy outcomes in youth with type 2 diabetes: the TODAY study experience. Diabetes Care. 2016;39(1):122–129.
- Schwarz EB, Postlethwaite D, Hung YY, Lantzman E, Armstrong MA, Horberg MA. Provision of contraceptive services to women with diabetes mellitus. J Gen Int Med. 2011;27(2):196–201.
- Schwarz EB, Maselli J, Gonzales R. Contraceptive counseling of diabetic women of reproductive age. Obstet Gynecol. 2006;107(5):1070–1074.
- Chuang CH, Chase GA, Bensyl DM, Weisman CS. Contraceptive use by diabetic and obese women. Womens Health Issues. 2005;15(4):167–173.
- Lidegaard O. Hormonal contraception, thrombosis and age. Expert Opin Drug Safe. 2014;13(10):1353–1360.
- Goldstuck ND, Steyn PS. The intrauterine device in women with diabetes mellitus type I and II: a systematic review. ISRN Obstet Gynecol. 2013:814062. doi.10.1155/2013/814062.
- Thompson JL, Kuklina EV, Bateman BT, Callaghan WM, James AH, Grotegut CA. Medical and obstetric outcomes among pregnant women with congenital heart disease. Obstet Gynecol. 2015;126(2):346–354.
- Lindley KJ, Madden T, Cahill AG, Ludbrook PA, Billadello JJ. Contraceptive use and unintended pregnancy in women with congenital heart disease. Obstet Gynecol. 2015;126(2):363–369.
- Perritt JB, Burke A, Jasmshidli R, Wang J, Fox M. Contraception counseling, pregnancy intention and contraception use in women with medical problems: an analysis of data from the Maryland Pregnancy Risk Assessment Monitoring System (PRAMS). Contraception. 2013;88(2):263–268.
- Stancil SL, Miller M, Briggs H, Lynch D, Goggin K, Kearns G. Contraceptive provision to adolescent females prescribed teratogenic medications. Pediatrics. 2016;137(1):1–8.
- Schwarz EB, Postlewaite DA, Hung YY, Armstrong MA. Documentation of contraception and pregnancy when prescribing potentially teratogenic medications for reproductive-age women. Ann Int Med. 2007;147(6):370–376.
- Mody SK, Wu J, Ornelas M, et al. Using the electronic medical record to refer women taking category D or X medications for teratogen and contraceptive counseling. Birth Defects Res A Clin Mol Teratol. 2015;103(7):644–647.
- Kavanaugh ML, Jerman J, Finer LB. Changes in use of long-acting reversible contraceptive methods among US women, 2009-2012. Obstet Gynecol. 2015;126(5):917–927.
- DeNoble AE, Hall KS, Xu X, Zochowski MK, Piehl K, Dalton VK. Receipt of prescription contraception by commercially insured women with chronic medical conditions. Obstet Gynecol. 2014;123(6):1213–1220.
- Champaloux SW, Tepper NK, Curtis KM, et al. Contraceptive use among women with medical conditions in a nationwide privately insured population. Obstet Gynecol. 2015;126(6):1151–1159.
- Klingensmith GJ, Pyle L, Nadeau KJ, et al; TODAY Study Group. Pregnancy outcomes in youth with type 2 diabetes: the TODAY study experience. Diabetes Care. 2016;39(1):122–129.
- Schwarz EB, Postlethwaite D, Hung YY, Lantzman E, Armstrong MA, Horberg MA. Provision of contraceptive services to women with diabetes mellitus. J Gen Int Med. 2011;27(2):196–201.
- Schwarz EB, Maselli J, Gonzales R. Contraceptive counseling of diabetic women of reproductive age. Obstet Gynecol. 2006;107(5):1070–1074.
- Chuang CH, Chase GA, Bensyl DM, Weisman CS. Contraceptive use by diabetic and obese women. Womens Health Issues. 2005;15(4):167–173.
- Lidegaard O. Hormonal contraception, thrombosis and age. Expert Opin Drug Safe. 2014;13(10):1353–1360.
- Goldstuck ND, Steyn PS. The intrauterine device in women with diabetes mellitus type I and II: a systematic review. ISRN Obstet Gynecol. 2013:814062. doi.10.1155/2013/814062.
- Thompson JL, Kuklina EV, Bateman BT, Callaghan WM, James AH, Grotegut CA. Medical and obstetric outcomes among pregnant women with congenital heart disease. Obstet Gynecol. 2015;126(2):346–354.
- Lindley KJ, Madden T, Cahill AG, Ludbrook PA, Billadello JJ. Contraceptive use and unintended pregnancy in women with congenital heart disease. Obstet Gynecol. 2015;126(2):363–369.
- Perritt JB, Burke A, Jasmshidli R, Wang J, Fox M. Contraception counseling, pregnancy intention and contraception use in women with medical problems: an analysis of data from the Maryland Pregnancy Risk Assessment Monitoring System (PRAMS). Contraception. 2013;88(2):263–268.
- Stancil SL, Miller M, Briggs H, Lynch D, Goggin K, Kearns G. Contraceptive provision to adolescent females prescribed teratogenic medications. Pediatrics. 2016;137(1):1–8.
- Schwarz EB, Postlewaite DA, Hung YY, Armstrong MA. Documentation of contraception and pregnancy when prescribing potentially teratogenic medications for reproductive-age women. Ann Int Med. 2007;147(6):370–376.
- Mody SK, Wu J, Ornelas M, et al. Using the electronic medical record to refer women taking category D or X medications for teratogen and contraceptive counseling. Birth Defects Res A Clin Mol Teratol. 2015;103(7):644–647.
Uterus transplantation comes to the United States
After previous attempts in Turkey and Saudi Arabia, the first successful uterine transplantation occurred in 2013. The team of successful surgeons was located in Gothenburg, Sweden, led by Mats Brännström, MD. The team performed 9 transplants in all, and the first birth of a healthy baby boy in October 2014 marked a medical breakthrough.1 The woman who received the transplanted uterus was born without one, a condition known as Mayer-Rokitanksy-Küster-Hauser syndrome, a cause of uterine factor infertility (UFI).
The previous options for having a child for women with UFI (which is the absence of a functional uterus, either congenital or acquired) were adoption or a gestational carrier/surrogacy.2 Surrogacy is not an option for many women, however, as in many countries, including Sweden, the use of gestational carriers and its associated contracts is illegal. All Muslim countries prohibit gestational carriers. Surrogacy also is prohibited in 3 US states, including New York, Michigan, and Arizona. Laws in other US states vary widely.3
Tommaso Falcone, MD, professor and chair, Department of Obstetrics and Gynecology, at the Cleveland Clinic in Cleveland, Ohio, is now co–Principal Investigator on a clinical trial assessing uterine transplantation at his institution, the first such surgeries to be performed in the United States. There will be 7 phases involved in the study: primary and secondary screening, medical evaluation, in vitro fertilization (IVF) with cryopreservation of sufficient number of embryos, transplantation and use of antirejection drugs, embryo transfer, pregnancy/delivery, and ultimately removal of the transplanted uterus. The study team is approved to enroll 10 women.4
OBG Management recently caught up with Dr. Falcone on his groundbreaking, and controversial, endeavor.
OBG Management: When did the thought of performing uterus transplantation enter your mind?
Tommaso Falcone, MD: The idea for uterus transplants was brought to my attention for the first time in Boston in 2007, at an annual meeting of the International Society for Fertility Preservation (ISFP). It was the inaugural meeting for ISFP, a society focused on helping women with cancer to protect their fertility. In 2007, we talked about the standard topics regarding fertility preservation: IVF and ovarian tissue cryopreservation. Then, right at the end of the meeting, was a presentation on uterus transplantation. Upon hearing the presenter, my thought was, “This will never happen in America, for many reasons.”
As time went on, I concentrated my energy more on ovarian tissue transplants for fertility preservation. Then a couple of years ago Andreas G. Tzakis, MD, a transplant surgeon from the University of Miami joined the Cleveland Clinic Florida. Dr. Tzakis was involved with the Swedish Group, including Mats Brännström’s transplant work in humans.
Of course, Dr. Tzakis had had a completely different journey to lead him to uterus transplantation. But as the director of solid organ transplant surgery at the Cleveland Clinic hospital in Florida, he said to me, “I think we should do this. There are many women who have asked for this procedure.” I was not sure at first, but I was interested in going to Sweden to see Dr. Brännström perform his last of 9 uterus transplants.
In Sweden, I asked Dr. Brännström if I could meet the women he already had performed the transplants on. I had certain preconceived notions on which types of women would accept this kind of major surgery to treat their infertility due to absence of a uterus. I expected perhaps that these women could have been coerced into accepting this surgery as a plausible option since surrogacy was not possible for them. I found out, as people usually do, that my preconceived notions were wrong. The women that I met said, “No, we’ve done this because we wanted to.” The women had independently come to a decision that experiencing pregnancy was important in their lives. There was no coercion. They understood the risks. However, I did not meet the uterus donors.
When I got on the plane to return home, I said to myself, we have to offer this service because it is part of the choices that women have to treat their reproductive infertility.
OBG Management: What are the hurdles you have had to overcome to bring this groundbreaking surgery to the Cleveland Clinic?
Dr. Falcone, MD: As soon as I returned from Sweden, we began the internal review board (IRB) approval process, which was extremely long. The first decision was: Do we use a live donor, as they do in Sweden, in America?
We analyzed the data from the Swedes and found that the surgery is very long for the donor and it put some of the donors, especially those who were older and placed on hormones, at risk for venous thromboembolism. (No blood clots had occurred in the Swedish trial.) In addition, there were some complications for patients. Although not major complications, we felt that these could be limited.
To remove the variable of risks for the donor, we decided that we would go in another direction and use the typical approach to donor transplants that is taken in this country, which is to use cadaveric, or brain dead, donors. The use of deceased donors allows us to isolate larger vascular pedicles for transplantation. Although we do not have IRB approval for live donors we are working in animal models to come up with an alternative technique to obtain vessels appropriate for anastomosis.
To address complications for the recipient, including the necessity to continually take antirejection, or immunosuppressive, medications, our recommendation to patients who undergo uterus transplantation surgery is to remove the uterus after delivery of 2 babies. Our plan at that time will be to perform a cesarean delivery and remove the uterus.
Right now in the process we are going through the screening phase and beginning IVF. We are approved for 10 women, and all potential recipients went through the necessary criteria, including psychological counseling. During IVF, each woman needs to have between 6 and 10 embryos (blastocysts).
OBG Management: Do you think that organ transplant pioneers foresaw successful transplantation of a uterus?
Dr. Falcone, MD: I do not think Dr. Tzakis, who is a transplant pioneer and has been doing this his entire career of 25 years or so, even foresaw this. This is something that has evolved over time. The first transplants (of kidney, heart, and liver) were to save lives. Subsequently, quality-of- life transplants have occurred, such as the face transplant and the larynx transplant. Uterus transplants are not to save lives, but they do improve quality of life, and I think that is what is important.
There is a lot of controversy surrounding this procedure—just like many aspects of reproductive medicine. A lot of what we do is full of controversy: IVF, gestational carriers, and genetic screening in utero. But we are in the quality-of-life era with transplantation medicine. If women have a strong desire to carry their own child, and surrogacy is not an option, then this may be one.
Tommasso Falcone, MD, was co-director of the Pelvic Anatomy and Gynecologic Surgery (PAGS) Symposium held in Las Vegas, Nevada, December 10–12, 2015. He offered workshops and seminars during the Scientific Program on diverse topics, including: hysteroscopy; ultrasonography; pelvic and abdominal anatomy; myometomy; hysterectomy; endometriosis; avoiding laparoscopic complications; medicolegal considerations; and surgical tips and techniques.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Brännström M, Johannesson L, Bokström H. Livebirth after uterus transplantation. Lancet. 2015;385(9968):607−616.
- Barbieri RL. Uterus transplantation: Medical breakthrough or surgical folly? OBG Manag. 2015;27(4):8, 10, 12.
- Surrogacy laws in the United States. Milwaukee Wisconsin Journal Sentinel Web site. http://www.jsonline.com/news/health/163772546.html. Published August 4, 2012. Accessed January 19, 2016.
- Uterine transplantation for the treatment of uterine factor infertility. ClinicalTrials.gov Web site. https://clinicaltrials.gov/ct2/show/NCT02573415. Updated October 28, 2015. Accessed January 19, 2016.
After previous attempts in Turkey and Saudi Arabia, the first successful uterine transplantation occurred in 2013. The team of successful surgeons was located in Gothenburg, Sweden, led by Mats Brännström, MD. The team performed 9 transplants in all, and the first birth of a healthy baby boy in October 2014 marked a medical breakthrough.1 The woman who received the transplanted uterus was born without one, a condition known as Mayer-Rokitanksy-Küster-Hauser syndrome, a cause of uterine factor infertility (UFI).
The previous options for having a child for women with UFI (which is the absence of a functional uterus, either congenital or acquired) were adoption or a gestational carrier/surrogacy.2 Surrogacy is not an option for many women, however, as in many countries, including Sweden, the use of gestational carriers and its associated contracts is illegal. All Muslim countries prohibit gestational carriers. Surrogacy also is prohibited in 3 US states, including New York, Michigan, and Arizona. Laws in other US states vary widely.3
Tommaso Falcone, MD, professor and chair, Department of Obstetrics and Gynecology, at the Cleveland Clinic in Cleveland, Ohio, is now co–Principal Investigator on a clinical trial assessing uterine transplantation at his institution, the first such surgeries to be performed in the United States. There will be 7 phases involved in the study: primary and secondary screening, medical evaluation, in vitro fertilization (IVF) with cryopreservation of sufficient number of embryos, transplantation and use of antirejection drugs, embryo transfer, pregnancy/delivery, and ultimately removal of the transplanted uterus. The study team is approved to enroll 10 women.4
OBG Management recently caught up with Dr. Falcone on his groundbreaking, and controversial, endeavor.
OBG Management: When did the thought of performing uterus transplantation enter your mind?
Tommaso Falcone, MD: The idea for uterus transplants was brought to my attention for the first time in Boston in 2007, at an annual meeting of the International Society for Fertility Preservation (ISFP). It was the inaugural meeting for ISFP, a society focused on helping women with cancer to protect their fertility. In 2007, we talked about the standard topics regarding fertility preservation: IVF and ovarian tissue cryopreservation. Then, right at the end of the meeting, was a presentation on uterus transplantation. Upon hearing the presenter, my thought was, “This will never happen in America, for many reasons.”
As time went on, I concentrated my energy more on ovarian tissue transplants for fertility preservation. Then a couple of years ago Andreas G. Tzakis, MD, a transplant surgeon from the University of Miami joined the Cleveland Clinic Florida. Dr. Tzakis was involved with the Swedish Group, including Mats Brännström’s transplant work in humans.
Of course, Dr. Tzakis had had a completely different journey to lead him to uterus transplantation. But as the director of solid organ transplant surgery at the Cleveland Clinic hospital in Florida, he said to me, “I think we should do this. There are many women who have asked for this procedure.” I was not sure at first, but I was interested in going to Sweden to see Dr. Brännström perform his last of 9 uterus transplants.
In Sweden, I asked Dr. Brännström if I could meet the women he already had performed the transplants on. I had certain preconceived notions on which types of women would accept this kind of major surgery to treat their infertility due to absence of a uterus. I expected perhaps that these women could have been coerced into accepting this surgery as a plausible option since surrogacy was not possible for them. I found out, as people usually do, that my preconceived notions were wrong. The women that I met said, “No, we’ve done this because we wanted to.” The women had independently come to a decision that experiencing pregnancy was important in their lives. There was no coercion. They understood the risks. However, I did not meet the uterus donors.
When I got on the plane to return home, I said to myself, we have to offer this service because it is part of the choices that women have to treat their reproductive infertility.
OBG Management: What are the hurdles you have had to overcome to bring this groundbreaking surgery to the Cleveland Clinic?
Dr. Falcone, MD: As soon as I returned from Sweden, we began the internal review board (IRB) approval process, which was extremely long. The first decision was: Do we use a live donor, as they do in Sweden, in America?
We analyzed the data from the Swedes and found that the surgery is very long for the donor and it put some of the donors, especially those who were older and placed on hormones, at risk for venous thromboembolism. (No blood clots had occurred in the Swedish trial.) In addition, there were some complications for patients. Although not major complications, we felt that these could be limited.
To remove the variable of risks for the donor, we decided that we would go in another direction and use the typical approach to donor transplants that is taken in this country, which is to use cadaveric, or brain dead, donors. The use of deceased donors allows us to isolate larger vascular pedicles for transplantation. Although we do not have IRB approval for live donors we are working in animal models to come up with an alternative technique to obtain vessels appropriate for anastomosis.
To address complications for the recipient, including the necessity to continually take antirejection, or immunosuppressive, medications, our recommendation to patients who undergo uterus transplantation surgery is to remove the uterus after delivery of 2 babies. Our plan at that time will be to perform a cesarean delivery and remove the uterus.
Right now in the process we are going through the screening phase and beginning IVF. We are approved for 10 women, and all potential recipients went through the necessary criteria, including psychological counseling. During IVF, each woman needs to have between 6 and 10 embryos (blastocysts).
OBG Management: Do you think that organ transplant pioneers foresaw successful transplantation of a uterus?
Dr. Falcone, MD: I do not think Dr. Tzakis, who is a transplant pioneer and has been doing this his entire career of 25 years or so, even foresaw this. This is something that has evolved over time. The first transplants (of kidney, heart, and liver) were to save lives. Subsequently, quality-of- life transplants have occurred, such as the face transplant and the larynx transplant. Uterus transplants are not to save lives, but they do improve quality of life, and I think that is what is important.
There is a lot of controversy surrounding this procedure—just like many aspects of reproductive medicine. A lot of what we do is full of controversy: IVF, gestational carriers, and genetic screening in utero. But we are in the quality-of-life era with transplantation medicine. If women have a strong desire to carry their own child, and surrogacy is not an option, then this may be one.
Tommasso Falcone, MD, was co-director of the Pelvic Anatomy and Gynecologic Surgery (PAGS) Symposium held in Las Vegas, Nevada, December 10–12, 2015. He offered workshops and seminars during the Scientific Program on diverse topics, including: hysteroscopy; ultrasonography; pelvic and abdominal anatomy; myometomy; hysterectomy; endometriosis; avoiding laparoscopic complications; medicolegal considerations; and surgical tips and techniques.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
After previous attempts in Turkey and Saudi Arabia, the first successful uterine transplantation occurred in 2013. The team of successful surgeons was located in Gothenburg, Sweden, led by Mats Brännström, MD. The team performed 9 transplants in all, and the first birth of a healthy baby boy in October 2014 marked a medical breakthrough.1 The woman who received the transplanted uterus was born without one, a condition known as Mayer-Rokitanksy-Küster-Hauser syndrome, a cause of uterine factor infertility (UFI).
The previous options for having a child for women with UFI (which is the absence of a functional uterus, either congenital or acquired) were adoption or a gestational carrier/surrogacy.2 Surrogacy is not an option for many women, however, as in many countries, including Sweden, the use of gestational carriers and its associated contracts is illegal. All Muslim countries prohibit gestational carriers. Surrogacy also is prohibited in 3 US states, including New York, Michigan, and Arizona. Laws in other US states vary widely.3
Tommaso Falcone, MD, professor and chair, Department of Obstetrics and Gynecology, at the Cleveland Clinic in Cleveland, Ohio, is now co–Principal Investigator on a clinical trial assessing uterine transplantation at his institution, the first such surgeries to be performed in the United States. There will be 7 phases involved in the study: primary and secondary screening, medical evaluation, in vitro fertilization (IVF) with cryopreservation of sufficient number of embryos, transplantation and use of antirejection drugs, embryo transfer, pregnancy/delivery, and ultimately removal of the transplanted uterus. The study team is approved to enroll 10 women.4
OBG Management recently caught up with Dr. Falcone on his groundbreaking, and controversial, endeavor.
OBG Management: When did the thought of performing uterus transplantation enter your mind?
Tommaso Falcone, MD: The idea for uterus transplants was brought to my attention for the first time in Boston in 2007, at an annual meeting of the International Society for Fertility Preservation (ISFP). It was the inaugural meeting for ISFP, a society focused on helping women with cancer to protect their fertility. In 2007, we talked about the standard topics regarding fertility preservation: IVF and ovarian tissue cryopreservation. Then, right at the end of the meeting, was a presentation on uterus transplantation. Upon hearing the presenter, my thought was, “This will never happen in America, for many reasons.”
As time went on, I concentrated my energy more on ovarian tissue transplants for fertility preservation. Then a couple of years ago Andreas G. Tzakis, MD, a transplant surgeon from the University of Miami joined the Cleveland Clinic Florida. Dr. Tzakis was involved with the Swedish Group, including Mats Brännström’s transplant work in humans.
Of course, Dr. Tzakis had had a completely different journey to lead him to uterus transplantation. But as the director of solid organ transplant surgery at the Cleveland Clinic hospital in Florida, he said to me, “I think we should do this. There are many women who have asked for this procedure.” I was not sure at first, but I was interested in going to Sweden to see Dr. Brännström perform his last of 9 uterus transplants.
In Sweden, I asked Dr. Brännström if I could meet the women he already had performed the transplants on. I had certain preconceived notions on which types of women would accept this kind of major surgery to treat their infertility due to absence of a uterus. I expected perhaps that these women could have been coerced into accepting this surgery as a plausible option since surrogacy was not possible for them. I found out, as people usually do, that my preconceived notions were wrong. The women that I met said, “No, we’ve done this because we wanted to.” The women had independently come to a decision that experiencing pregnancy was important in their lives. There was no coercion. They understood the risks. However, I did not meet the uterus donors.
When I got on the plane to return home, I said to myself, we have to offer this service because it is part of the choices that women have to treat their reproductive infertility.
OBG Management: What are the hurdles you have had to overcome to bring this groundbreaking surgery to the Cleveland Clinic?
Dr. Falcone, MD: As soon as I returned from Sweden, we began the internal review board (IRB) approval process, which was extremely long. The first decision was: Do we use a live donor, as they do in Sweden, in America?
We analyzed the data from the Swedes and found that the surgery is very long for the donor and it put some of the donors, especially those who were older and placed on hormones, at risk for venous thromboembolism. (No blood clots had occurred in the Swedish trial.) In addition, there were some complications for patients. Although not major complications, we felt that these could be limited.
To remove the variable of risks for the donor, we decided that we would go in another direction and use the typical approach to donor transplants that is taken in this country, which is to use cadaveric, or brain dead, donors. The use of deceased donors allows us to isolate larger vascular pedicles for transplantation. Although we do not have IRB approval for live donors we are working in animal models to come up with an alternative technique to obtain vessels appropriate for anastomosis.
To address complications for the recipient, including the necessity to continually take antirejection, or immunosuppressive, medications, our recommendation to patients who undergo uterus transplantation surgery is to remove the uterus after delivery of 2 babies. Our plan at that time will be to perform a cesarean delivery and remove the uterus.
Right now in the process we are going through the screening phase and beginning IVF. We are approved for 10 women, and all potential recipients went through the necessary criteria, including psychological counseling. During IVF, each woman needs to have between 6 and 10 embryos (blastocysts).
OBG Management: Do you think that organ transplant pioneers foresaw successful transplantation of a uterus?
Dr. Falcone, MD: I do not think Dr. Tzakis, who is a transplant pioneer and has been doing this his entire career of 25 years or so, even foresaw this. This is something that has evolved over time. The first transplants (of kidney, heart, and liver) were to save lives. Subsequently, quality-of- life transplants have occurred, such as the face transplant and the larynx transplant. Uterus transplants are not to save lives, but they do improve quality of life, and I think that is what is important.
There is a lot of controversy surrounding this procedure—just like many aspects of reproductive medicine. A lot of what we do is full of controversy: IVF, gestational carriers, and genetic screening in utero. But we are in the quality-of-life era with transplantation medicine. If women have a strong desire to carry their own child, and surrogacy is not an option, then this may be one.
Tommasso Falcone, MD, was co-director of the Pelvic Anatomy and Gynecologic Surgery (PAGS) Symposium held in Las Vegas, Nevada, December 10–12, 2015. He offered workshops and seminars during the Scientific Program on diverse topics, including: hysteroscopy; ultrasonography; pelvic and abdominal anatomy; myometomy; hysterectomy; endometriosis; avoiding laparoscopic complications; medicolegal considerations; and surgical tips and techniques.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Brännström M, Johannesson L, Bokström H. Livebirth after uterus transplantation. Lancet. 2015;385(9968):607−616.
- Barbieri RL. Uterus transplantation: Medical breakthrough or surgical folly? OBG Manag. 2015;27(4):8, 10, 12.
- Surrogacy laws in the United States. Milwaukee Wisconsin Journal Sentinel Web site. http://www.jsonline.com/news/health/163772546.html. Published August 4, 2012. Accessed January 19, 2016.
- Uterine transplantation for the treatment of uterine factor infertility. ClinicalTrials.gov Web site. https://clinicaltrials.gov/ct2/show/NCT02573415. Updated October 28, 2015. Accessed January 19, 2016.
- Brännström M, Johannesson L, Bokström H. Livebirth after uterus transplantation. Lancet. 2015;385(9968):607−616.
- Barbieri RL. Uterus transplantation: Medical breakthrough or surgical folly? OBG Manag. 2015;27(4):8, 10, 12.
- Surrogacy laws in the United States. Milwaukee Wisconsin Journal Sentinel Web site. http://www.jsonline.com/news/health/163772546.html. Published August 4, 2012. Accessed January 19, 2016.
- Uterine transplantation for the treatment of uterine factor infertility. ClinicalTrials.gov Web site. https://clinicaltrials.gov/ct2/show/NCT02573415. Updated October 28, 2015. Accessed January 19, 2016.
In this Article
- Hurdles to IRB approval
- The quality-of-life era in transplant medicine
Product Update: FemTouch, Lunette Menstrual Cups, ROCA Test, NextGen Home Sperm Banking Kit

CO2 Laser To Treat Vaginal Conditions FemTouch™ FemTouch™ is a fractional CO2 laser that addresses vaginal health-related conditions such as stress urinary incontinence, vaginal laxity, and vaginal atrophy. Lumenis® says that FemTouch promotes the restoration of the vaginal mucous epithelium layer. The laser is applied along the vaginal wall, resulting in gentle, controlled ablation and coagulation of the vaginal lining. Lumenis states that the FemTouch in-office procedure takes only a few minutes, is efficient (with 2 to 4 treatments needed), and requires no anesthesia or special postprocedural care. The treatment is associated with minimal discomfort for patients, according to Lumenis, and some women being treated with FemTouch report improvement in their condition after 1 or 2 procedures.
FemTouch is designed for use with the Lumenis AcuPulse™ MultiMode™ SuperPulse™ CO2 Laser System, offering 10 built-in treatment modes.
FOR MORE INFORMATION, VISIT: www.lumenis.com
According to the manufacturer’s instructions, a woman folds and inserts the cup in the lower vagina above the pelvic bone. She empties the cup 2 to 4 times per day and can use it overnight. Between uses, she rinses the cup with water and washes it with warm soapy water before reinsertion. When water is not available, toilet paper can be used for cleaning. For thorough cleaning, a woman can place the cup in boiling water then disinfect it with alcohol. Lunette should be cleaned after menses and stored in its own bag. The FDA recommends replacing the cup every 2 to 3 years.
Lunette is designed for all women, including those who have not had sexual intercourse and those who use an IUD or contraceptive ring (consult a physician). Lunette is available in 2 sizes: Model 1 is generally for those with light to moderate flow; Model 2 is recommended for normal or heavier flow. A detailed sizing guide is found on the website.
FOR MORE INFORMATION, VISIT: www.lunette.com/us

Detect Ovarian Cancer EarlyThe ROCA® Test from Abcodia offers early detection of ovarian cancer. Data reported from a large prospective randomized controlled study recently published in The Lancet demonstrate that a screening strategy using ROCA (Risk of Ovarian Cancer Algorithm) may reduce ovarian cancer mortality by an estimated 20%.
The ROCA Test uses a woman’s age, menopausal status, risk status, and serial blood measurements of CA 125 to produce a score that indicates current likelihood of having ovarian cancer. The initial risk assessment is then modified based on how closely a patient’s CA 125 profile matches the profiles seen in healthy women and women with ovarian cancer.
The test is intended for postmenopausal women between the ages of 50 and 85 years with no known risk factors other than age and for women between the ages of 35 and 85 years who are considered high risk due to family history of ovarian or breast cancer, have BRCA1 or BRCA2 gene mutations, or have Lynch Syndrome. The ROCA Test is now available in 15 states and the District of Columbia, and will be offered to additional areas of the United States in 2016.
After purchasing a ROCA Test online, the patient will receive an instructional kit, which she will take to her physician to review her medical history and sign a consent form. A blood sample will be drawn and sent to the ROCA Test laboratory. The physician will receive and share the test results with the patient. High-risk patients are encouraged to complete 3 tests per year.
FOR MORE INFORMATION, VISIT: www.rocatest.com

A semen sample can be collected at home and then shipped to the sperm banking facilities at Cleveland Clinic’s Andrology Center in Cleveland,Ohio. There, the sperm will be cryopreserved for as long as desired; an annual storage fee will be charged.
FOR MORE INFORMATION, VISIT: www.fairhavenhealth.com/nextgen-home-sperm-banking-kit.html

CO2 Laser To Treat Vaginal Conditions FemTouch™ FemTouch™ is a fractional CO2 laser that addresses vaginal health-related conditions such as stress urinary incontinence, vaginal laxity, and vaginal atrophy. Lumenis® says that FemTouch promotes the restoration of the vaginal mucous epithelium layer. The laser is applied along the vaginal wall, resulting in gentle, controlled ablation and coagulation of the vaginal lining. Lumenis states that the FemTouch in-office procedure takes only a few minutes, is efficient (with 2 to 4 treatments needed), and requires no anesthesia or special postprocedural care. The treatment is associated with minimal discomfort for patients, according to Lumenis, and some women being treated with FemTouch report improvement in their condition after 1 or 2 procedures.
FemTouch is designed for use with the Lumenis AcuPulse™ MultiMode™ SuperPulse™ CO2 Laser System, offering 10 built-in treatment modes.
FOR MORE INFORMATION, VISIT: www.lumenis.com
According to the manufacturer’s instructions, a woman folds and inserts the cup in the lower vagina above the pelvic bone. She empties the cup 2 to 4 times per day and can use it overnight. Between uses, she rinses the cup with water and washes it with warm soapy water before reinsertion. When water is not available, toilet paper can be used for cleaning. For thorough cleaning, a woman can place the cup in boiling water then disinfect it with alcohol. Lunette should be cleaned after menses and stored in its own bag. The FDA recommends replacing the cup every 2 to 3 years.
Lunette is designed for all women, including those who have not had sexual intercourse and those who use an IUD or contraceptive ring (consult a physician). Lunette is available in 2 sizes: Model 1 is generally for those with light to moderate flow; Model 2 is recommended for normal or heavier flow. A detailed sizing guide is found on the website.
FOR MORE INFORMATION, VISIT: www.lunette.com/us

Detect Ovarian Cancer EarlyThe ROCA® Test from Abcodia offers early detection of ovarian cancer. Data reported from a large prospective randomized controlled study recently published in The Lancet demonstrate that a screening strategy using ROCA (Risk of Ovarian Cancer Algorithm) may reduce ovarian cancer mortality by an estimated 20%.
The ROCA Test uses a woman’s age, menopausal status, risk status, and serial blood measurements of CA 125 to produce a score that indicates current likelihood of having ovarian cancer. The initial risk assessment is then modified based on how closely a patient’s CA 125 profile matches the profiles seen in healthy women and women with ovarian cancer.
The test is intended for postmenopausal women between the ages of 50 and 85 years with no known risk factors other than age and for women between the ages of 35 and 85 years who are considered high risk due to family history of ovarian or breast cancer, have BRCA1 or BRCA2 gene mutations, or have Lynch Syndrome. The ROCA Test is now available in 15 states and the District of Columbia, and will be offered to additional areas of the United States in 2016.
After purchasing a ROCA Test online, the patient will receive an instructional kit, which she will take to her physician to review her medical history and sign a consent form. A blood sample will be drawn and sent to the ROCA Test laboratory. The physician will receive and share the test results with the patient. High-risk patients are encouraged to complete 3 tests per year.
FOR MORE INFORMATION, VISIT: www.rocatest.com

A semen sample can be collected at home and then shipped to the sperm banking facilities at Cleveland Clinic’s Andrology Center in Cleveland,Ohio. There, the sperm will be cryopreserved for as long as desired; an annual storage fee will be charged.
FOR MORE INFORMATION, VISIT: www.fairhavenhealth.com/nextgen-home-sperm-banking-kit.html

CO2 Laser To Treat Vaginal Conditions FemTouch™ FemTouch™ is a fractional CO2 laser that addresses vaginal health-related conditions such as stress urinary incontinence, vaginal laxity, and vaginal atrophy. Lumenis® says that FemTouch promotes the restoration of the vaginal mucous epithelium layer. The laser is applied along the vaginal wall, resulting in gentle, controlled ablation and coagulation of the vaginal lining. Lumenis states that the FemTouch in-office procedure takes only a few minutes, is efficient (with 2 to 4 treatments needed), and requires no anesthesia or special postprocedural care. The treatment is associated with minimal discomfort for patients, according to Lumenis, and some women being treated with FemTouch report improvement in their condition after 1 or 2 procedures.
FemTouch is designed for use with the Lumenis AcuPulse™ MultiMode™ SuperPulse™ CO2 Laser System, offering 10 built-in treatment modes.
FOR MORE INFORMATION, VISIT: www.lumenis.com
According to the manufacturer’s instructions, a woman folds and inserts the cup in the lower vagina above the pelvic bone. She empties the cup 2 to 4 times per day and can use it overnight. Between uses, she rinses the cup with water and washes it with warm soapy water before reinsertion. When water is not available, toilet paper can be used for cleaning. For thorough cleaning, a woman can place the cup in boiling water then disinfect it with alcohol. Lunette should be cleaned after menses and stored in its own bag. The FDA recommends replacing the cup every 2 to 3 years.
Lunette is designed for all women, including those who have not had sexual intercourse and those who use an IUD or contraceptive ring (consult a physician). Lunette is available in 2 sizes: Model 1 is generally for those with light to moderate flow; Model 2 is recommended for normal or heavier flow. A detailed sizing guide is found on the website.
FOR MORE INFORMATION, VISIT: www.lunette.com/us

Detect Ovarian Cancer EarlyThe ROCA® Test from Abcodia offers early detection of ovarian cancer. Data reported from a large prospective randomized controlled study recently published in The Lancet demonstrate that a screening strategy using ROCA (Risk of Ovarian Cancer Algorithm) may reduce ovarian cancer mortality by an estimated 20%.
The ROCA Test uses a woman’s age, menopausal status, risk status, and serial blood measurements of CA 125 to produce a score that indicates current likelihood of having ovarian cancer. The initial risk assessment is then modified based on how closely a patient’s CA 125 profile matches the profiles seen in healthy women and women with ovarian cancer.
The test is intended for postmenopausal women between the ages of 50 and 85 years with no known risk factors other than age and for women between the ages of 35 and 85 years who are considered high risk due to family history of ovarian or breast cancer, have BRCA1 or BRCA2 gene mutations, or have Lynch Syndrome. The ROCA Test is now available in 15 states and the District of Columbia, and will be offered to additional areas of the United States in 2016.
After purchasing a ROCA Test online, the patient will receive an instructional kit, which she will take to her physician to review her medical history and sign a consent form. A blood sample will be drawn and sent to the ROCA Test laboratory. The physician will receive and share the test results with the patient. High-risk patients are encouraged to complete 3 tests per year.
FOR MORE INFORMATION, VISIT: www.rocatest.com

A semen sample can be collected at home and then shipped to the sperm banking facilities at Cleveland Clinic’s Andrology Center in Cleveland,Ohio. There, the sperm will be cryopreserved for as long as desired; an annual storage fee will be charged.
FOR MORE INFORMATION, VISIT: www.fairhavenhealth.com/nextgen-home-sperm-banking-kit.html
Is double-layer closure with unlocked first-layer associated with better uterine scar healing than locked single-layer closure?
Cesarean delivery (CD), the most common surgery performed worldwide, is associated with increased morbidity and mortality compared with vaginal delivery. More than 230 randomized controlled trials (RCTs) have been published on varying technical aspects of CD, yet uncertainty remains regarding the optimal approach(es) to minimize perinatal morbidity.
Previous trials of one such technique, uterine closure, have not demonstrated short-term outcome differences among those randomized to single- versus double-layer closure. Results of long-term outcomes such as uterine rupture remain unclear. Emerging evidence also has associated cesarean scar defects with gynecologic problems like dysmenorrhea, pelvic pain, and postmenstrual spotting, further highlighting the importance of identifying surgical techniques that optimize uterine scar healing after CD.
Details of the study
In their recent RCT, Roberge and colleagues randomly assigned 81 women with singleton pregnancies undergoing elective primary CD (at ≥38 0/7 weeks) and compared the following uterine closure types on residual myometrial thickness during postpartum transvaginal ultrasound at 6 months:
- single-layer locked closure (control)
- double-layer locked closure
- double-layer unlocked closure.
In addition to addressing the single- versus double-layer debate, this study highlights another important aspect of closure technique: locked versus unlocked first-layer suture closure. The residual myometrial thickness, a surrogate measure of uterine scar healing, was significantly greater in those women randomly assigned to double-layer (locked or unlocked) closure compared with controls. Additionally, total myometrial thickness significantly increased in the double- layer unlocked closure group. There were no differences in the short-term outcomes of operative time or estimated blood loss among any of the groups.
Based on these findings, the authors advocate for double-layer unlocked uterine closure during CD to maximize uterine scar healing.
Bottom line
Double-layer uterine closure with unlocked first-layer at CD appears to maximize postpartum uterine scar thickness compared with other techniques; it remains unclear, however, if this improves short- or long-term outcomes. What this evidence means for practice
While residual and total myometrial thickness presents a feasible, albeit indirect, assessment of uterine scar healing, it remains unclear if double-layer unlocked first-layer closure decreases long-term adverse outcomes, such as subsequent uterine rupture, cesarean scar defects, or gynecologic morbidity compared with other techniques. Nevertheless, this study highlights the importance of future research specifying both single- or double-layer and locked or unlocked uterine closure techniques.
— Joshua D. Dahlke, MD
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Cesarean delivery (CD), the most common surgery performed worldwide, is associated with increased morbidity and mortality compared with vaginal delivery. More than 230 randomized controlled trials (RCTs) have been published on varying technical aspects of CD, yet uncertainty remains regarding the optimal approach(es) to minimize perinatal morbidity.
Previous trials of one such technique, uterine closure, have not demonstrated short-term outcome differences among those randomized to single- versus double-layer closure. Results of long-term outcomes such as uterine rupture remain unclear. Emerging evidence also has associated cesarean scar defects with gynecologic problems like dysmenorrhea, pelvic pain, and postmenstrual spotting, further highlighting the importance of identifying surgical techniques that optimize uterine scar healing after CD.
Details of the study
In their recent RCT, Roberge and colleagues randomly assigned 81 women with singleton pregnancies undergoing elective primary CD (at ≥38 0/7 weeks) and compared the following uterine closure types on residual myometrial thickness during postpartum transvaginal ultrasound at 6 months:
- single-layer locked closure (control)
- double-layer locked closure
- double-layer unlocked closure.
In addition to addressing the single- versus double-layer debate, this study highlights another important aspect of closure technique: locked versus unlocked first-layer suture closure. The residual myometrial thickness, a surrogate measure of uterine scar healing, was significantly greater in those women randomly assigned to double-layer (locked or unlocked) closure compared with controls. Additionally, total myometrial thickness significantly increased in the double- layer unlocked closure group. There were no differences in the short-term outcomes of operative time or estimated blood loss among any of the groups.
Based on these findings, the authors advocate for double-layer unlocked uterine closure during CD to maximize uterine scar healing.
Bottom line
Double-layer uterine closure with unlocked first-layer at CD appears to maximize postpartum uterine scar thickness compared with other techniques; it remains unclear, however, if this improves short- or long-term outcomes. What this evidence means for practice
While residual and total myometrial thickness presents a feasible, albeit indirect, assessment of uterine scar healing, it remains unclear if double-layer unlocked first-layer closure decreases long-term adverse outcomes, such as subsequent uterine rupture, cesarean scar defects, or gynecologic morbidity compared with other techniques. Nevertheless, this study highlights the importance of future research specifying both single- or double-layer and locked or unlocked uterine closure techniques.
— Joshua D. Dahlke, MD
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Cesarean delivery (CD), the most common surgery performed worldwide, is associated with increased morbidity and mortality compared with vaginal delivery. More than 230 randomized controlled trials (RCTs) have been published on varying technical aspects of CD, yet uncertainty remains regarding the optimal approach(es) to minimize perinatal morbidity.
Previous trials of one such technique, uterine closure, have not demonstrated short-term outcome differences among those randomized to single- versus double-layer closure. Results of long-term outcomes such as uterine rupture remain unclear. Emerging evidence also has associated cesarean scar defects with gynecologic problems like dysmenorrhea, pelvic pain, and postmenstrual spotting, further highlighting the importance of identifying surgical techniques that optimize uterine scar healing after CD.
Details of the study
In their recent RCT, Roberge and colleagues randomly assigned 81 women with singleton pregnancies undergoing elective primary CD (at ≥38 0/7 weeks) and compared the following uterine closure types on residual myometrial thickness during postpartum transvaginal ultrasound at 6 months:
- single-layer locked closure (control)
- double-layer locked closure
- double-layer unlocked closure.
In addition to addressing the single- versus double-layer debate, this study highlights another important aspect of closure technique: locked versus unlocked first-layer suture closure. The residual myometrial thickness, a surrogate measure of uterine scar healing, was significantly greater in those women randomly assigned to double-layer (locked or unlocked) closure compared with controls. Additionally, total myometrial thickness significantly increased in the double- layer unlocked closure group. There were no differences in the short-term outcomes of operative time or estimated blood loss among any of the groups.
Based on these findings, the authors advocate for double-layer unlocked uterine closure during CD to maximize uterine scar healing.
Bottom line
Double-layer uterine closure with unlocked first-layer at CD appears to maximize postpartum uterine scar thickness compared with other techniques; it remains unclear, however, if this improves short- or long-term outcomes. What this evidence means for practice
While residual and total myometrial thickness presents a feasible, albeit indirect, assessment of uterine scar healing, it remains unclear if double-layer unlocked first-layer closure decreases long-term adverse outcomes, such as subsequent uterine rupture, cesarean scar defects, or gynecologic morbidity compared with other techniques. Nevertheless, this study highlights the importance of future research specifying both single- or double-layer and locked or unlocked uterine closure techniques.
— Joshua D. Dahlke, MD
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Failure to find breast cancer; later diagnosed at Stage 3
Stroke during delivery: $35.4M verdict
Stroke during delivery: $35.4M verdict
During delivery, a 25-year-old woman had a hemorrhagic stroke that left her unable to care for herself or her child.
Patient’s claim The patient’s neurologist failed to advise the ObGyn that the patient had a history of brain aneurysm and a venous varix, which increased the risk for stroke during labor and delivery. The patient had shared her history with the ObGyn, and she requested that her neurologist contact the ObGyn.
Neurologist’s defense There was no negligence. The entire medical file had been delivered to the ObGyn. Any negligence was on the part of the ObGyn for failure to educate herself as to the patient’s condition.
Verdict A $35.4 million Massachusetts verdict was returned against the neurologist, including $12.9 million for past and future pain and suffering, $4 million for past medical care, $11 million for future medical care, $4.5 million for the husband’s loss of consortium, $1.5 million for lost wages, and $1.5 million for the child’s loss of consortium.
IUGR detected but not immediately treated: $15.5M settlement
During a prenatal visit at 38 weeks’ gestation, a mother’s ObGyn saw signs of intrauterine growth restriction (IUGR) but did not order ultrasono- graphy to confirm the diagnosis or induce labor. When born 15 days later, the baby had a low birth weight and low Apgar scores. The child has permanent brain injury due to hypoxia.
Parents’ claim The ObGyn should have confirmed the presence of IUGR and appropriately managed the mother’s prenatal care. The child’s injuries could have been prevented if an earlier delivery had occurred.
Physician’s defense The case was settled during the trial.
Verdict A $15.5 million Illinois settlement was reached.
Ureter injured during total abdominal hysterectomy
A 40-year-old woman with uterine fibroids, excessive bleeding, and pelvic pain underwent total abdominal hysterectomy performed by her ObGyn.
Postoperatively, the patient reported abdominal pain, but she was discharged from the hospital. Two days later, she returned to the emergency department reporting continued and increasing abdominal pain and urine leakage. The ObGyn referred her to a urologist who diagnosed stricture of the left ureter with a ureterovaginal fistula. A nephrostomy procedure was performed. Three months later, left ureter reimplantation surgery was completed.
Patient’s claim The ObGyn was negligent in injuring the ureter during hysterectomy, in not identifying the injury during surgery, and in not diagnosing and treating the injury in a timely manner, despite the patient’s reports of increasing pain.
Physician’s defense The case was settled during the trial.
Verdict A $350,000 Virginia settlement was reached.
Breech presentation but cesarean not performed
When her water broke, a mother was admitted to the hospital. The ObGyn ordered induction of labor but deferred vaginal examination to avoid infection. After labor was induced, a nurse noticed the presence of meconium. She performed a vaginal examination and found that the baby was in breech position; she did not immediately contact the ObGyn. After several hours of labor, the baby was born limp and not breathing with a heart rate of 50 bpm. The baby was resuscitated but sustained severe brain damage.
Parents’ claim The mother should have been examined before induction of labor. When it was determined that the baby was in breech position, a cesarean delivery should have been ordered. Communication between the nurse and ObGyn was poor.
Defendants' defense There was no negligence; labor was managed according to the standard of care.
Verdict A New Jersey defense verdict was returned.
Stroke during delivery: $35.4M verdict
During delivery, a 25-year-old woman had a hemorrhagic stroke that left her unable to care for herself or her child.
Patient’s claim The patient’s neurologist failed to advise the ObGyn that the patient had a history of brain aneurysm and a venous varix, which increased the risk for stroke during labor and delivery. The patient had shared her history with the ObGyn, and she requested that her neurologist contact the ObGyn.
Neurologist’s defense There was no negligence. The entire medical file had been delivered to the ObGyn. Any negligence was on the part of the ObGyn for failure to educate herself as to the patient’s condition.
Verdict A $35.4 million Massachusetts verdict was returned against the neurologist, including $12.9 million for past and future pain and suffering, $4 million for past medical care, $11 million for future medical care, $4.5 million for the husband’s loss of consortium, $1.5 million for lost wages, and $1.5 million for the child’s loss of consortium.
IUGR detected but not immediately treated: $15.5M settlement
During a prenatal visit at 38 weeks’ gestation, a mother’s ObGyn saw signs of intrauterine growth restriction (IUGR) but did not order ultrasono- graphy to confirm the diagnosis or induce labor. When born 15 days later, the baby had a low birth weight and low Apgar scores. The child has permanent brain injury due to hypoxia.
Parents’ claim The ObGyn should have confirmed the presence of IUGR and appropriately managed the mother’s prenatal care. The child’s injuries could have been prevented if an earlier delivery had occurred.
Physician’s defense The case was settled during the trial.
Verdict A $15.5 million Illinois settlement was reached.
Ureter injured during total abdominal hysterectomy
A 40-year-old woman with uterine fibroids, excessive bleeding, and pelvic pain underwent total abdominal hysterectomy performed by her ObGyn.
Postoperatively, the patient reported abdominal pain, but she was discharged from the hospital. Two days later, she returned to the emergency department reporting continued and increasing abdominal pain and urine leakage. The ObGyn referred her to a urologist who diagnosed stricture of the left ureter with a ureterovaginal fistula. A nephrostomy procedure was performed. Three months later, left ureter reimplantation surgery was completed.
Patient’s claim The ObGyn was negligent in injuring the ureter during hysterectomy, in not identifying the injury during surgery, and in not diagnosing and treating the injury in a timely manner, despite the patient’s reports of increasing pain.
Physician’s defense The case was settled during the trial.
Verdict A $350,000 Virginia settlement was reached.
Breech presentation but cesarean not performed
When her water broke, a mother was admitted to the hospital. The ObGyn ordered induction of labor but deferred vaginal examination to avoid infection. After labor was induced, a nurse noticed the presence of meconium. She performed a vaginal examination and found that the baby was in breech position; she did not immediately contact the ObGyn. After several hours of labor, the baby was born limp and not breathing with a heart rate of 50 bpm. The baby was resuscitated but sustained severe brain damage.
Parents’ claim The mother should have been examined before induction of labor. When it was determined that the baby was in breech position, a cesarean delivery should have been ordered. Communication between the nurse and ObGyn was poor.
Defendants' defense There was no negligence; labor was managed according to the standard of care.
Verdict A New Jersey defense verdict was returned.
Stroke during delivery: $35.4M verdict
During delivery, a 25-year-old woman had a hemorrhagic stroke that left her unable to care for herself or her child.
Patient’s claim The patient’s neurologist failed to advise the ObGyn that the patient had a history of brain aneurysm and a venous varix, which increased the risk for stroke during labor and delivery. The patient had shared her history with the ObGyn, and she requested that her neurologist contact the ObGyn.
Neurologist’s defense There was no negligence. The entire medical file had been delivered to the ObGyn. Any negligence was on the part of the ObGyn for failure to educate herself as to the patient’s condition.
Verdict A $35.4 million Massachusetts verdict was returned against the neurologist, including $12.9 million for past and future pain and suffering, $4 million for past medical care, $11 million for future medical care, $4.5 million for the husband’s loss of consortium, $1.5 million for lost wages, and $1.5 million for the child’s loss of consortium.
IUGR detected but not immediately treated: $15.5M settlement
During a prenatal visit at 38 weeks’ gestation, a mother’s ObGyn saw signs of intrauterine growth restriction (IUGR) but did not order ultrasono- graphy to confirm the diagnosis or induce labor. When born 15 days later, the baby had a low birth weight and low Apgar scores. The child has permanent brain injury due to hypoxia.
Parents’ claim The ObGyn should have confirmed the presence of IUGR and appropriately managed the mother’s prenatal care. The child’s injuries could have been prevented if an earlier delivery had occurred.
Physician’s defense The case was settled during the trial.
Verdict A $15.5 million Illinois settlement was reached.
Ureter injured during total abdominal hysterectomy
A 40-year-old woman with uterine fibroids, excessive bleeding, and pelvic pain underwent total abdominal hysterectomy performed by her ObGyn.
Postoperatively, the patient reported abdominal pain, but she was discharged from the hospital. Two days later, she returned to the emergency department reporting continued and increasing abdominal pain and urine leakage. The ObGyn referred her to a urologist who diagnosed stricture of the left ureter with a ureterovaginal fistula. A nephrostomy procedure was performed. Three months later, left ureter reimplantation surgery was completed.
Patient’s claim The ObGyn was negligent in injuring the ureter during hysterectomy, in not identifying the injury during surgery, and in not diagnosing and treating the injury in a timely manner, despite the patient’s reports of increasing pain.
Physician’s defense The case was settled during the trial.
Verdict A $350,000 Virginia settlement was reached.
Breech presentation but cesarean not performed
When her water broke, a mother was admitted to the hospital. The ObGyn ordered induction of labor but deferred vaginal examination to avoid infection. After labor was induced, a nurse noticed the presence of meconium. She performed a vaginal examination and found that the baby was in breech position; she did not immediately contact the ObGyn. After several hours of labor, the baby was born limp and not breathing with a heart rate of 50 bpm. The baby was resuscitated but sustained severe brain damage.
Parents’ claim The mother should have been examined before induction of labor. When it was determined that the baby was in breech position, a cesarean delivery should have been ordered. Communication between the nurse and ObGyn was poor.
Defendants' defense There was no negligence; labor was managed according to the standard of care.
Verdict A New Jersey defense verdict was returned.
Additional Medical Verdicts cases
Failure to find breast cancer; later diagnosed at Stage 3
Endometrial cancer after unopposed estrogen: $7.5M