User login
STS: BMI impacts risk for complications after lung resection
PHOENIX – Being underweight is associated with a substantially increased risk of complications following lung resection for cancer, results from a large database study found.
“This is not generally known among surgeons or their patients,” Dr. Trevor Williams said in an interview before the annual meeting of the Society of Thoracic Surgeons. “Studies are conflicting about the relationship of BMI [body mass index] to surgical outcomes. Most of the previous studies simply categorize BMI as overweight or not. We’ve stratified based on World Health Organization categories to get a more precise look at BMI.”
Dr. Williams, a surgeon at the University of Chicago Medical Center, and his associates evaluated 41,446 patients in the STS General Thoracic Surgery Database who underwent elective anatomic lung resection for cancer between 2009 and 2014. Their mean age was 68 years, and 53% were female. The researchers performed multivariable analysis after adjusting for validated STS risk model covariates, including gender and spirometry.
According to WHO criteria for BMI, 3% were underweight (less than 18.5 kg/m2); 33.5% were normal weight (18.5-24.9 kg/m2); 35.4% were overweight (25-29.9 kg/m2); 18.1% were obese I (30-34.9 kg/m2); 6.4% were obese II (35-39.9 kg/m2), and 3.6% were obese III (40 kg/m2 or greater). Dr. Williams and his associates observed that women were more often underweight, compared with men (4.1% vs. 1.8%, respectively; P less than .001), and underweight patients more often had chronic obstructive pulmonary disease (51.7% vs. 35.2%; P less than .001). Pulmonary complication rates were higher among underweight and obese III patients (P less than .001), while being underweight was also associated with higher rates of infections and any surgical complications.
Multivariable analysis revealed that pulmonary and any postoperative complications were more common among underweight patients (odds ratio, 1.44 and OR, 1.41, respectively), while any major complication was more common among obese III patients (OR, 1.18). Overweight and obese I-II patients were less likely to have any postoperative and pulmonary complications, compared with patients who had a normal BMI. “The finding of underweight patients being such a high-risk patient population is suggested in the literature but not demonstrated as clearly as in this study,” Dr. Williams said. “A truly surprising finding was that obese patients actually have a lower risk of pulmonary and overall complications than ‘normal’-BMI patients.”
He concluded that according to the current analysis, “careful risk assessment is appropriate when considering operating on underweight patients. Whether there are interventions that could be instituted to improve an individual’s risk profile has not been determined. Any preconceived notions about not operating on obese patients due to elevated risk appear to be unfounded.”
Dr. Williams reported having no financial disclosures.
PHOENIX – Being underweight is associated with a substantially increased risk of complications following lung resection for cancer, results from a large database study found.
“This is not generally known among surgeons or their patients,” Dr. Trevor Williams said in an interview before the annual meeting of the Society of Thoracic Surgeons. “Studies are conflicting about the relationship of BMI [body mass index] to surgical outcomes. Most of the previous studies simply categorize BMI as overweight or not. We’ve stratified based on World Health Organization categories to get a more precise look at BMI.”
Dr. Williams, a surgeon at the University of Chicago Medical Center, and his associates evaluated 41,446 patients in the STS General Thoracic Surgery Database who underwent elective anatomic lung resection for cancer between 2009 and 2014. Their mean age was 68 years, and 53% were female. The researchers performed multivariable analysis after adjusting for validated STS risk model covariates, including gender and spirometry.
According to WHO criteria for BMI, 3% were underweight (less than 18.5 kg/m2); 33.5% were normal weight (18.5-24.9 kg/m2); 35.4% were overweight (25-29.9 kg/m2); 18.1% were obese I (30-34.9 kg/m2); 6.4% were obese II (35-39.9 kg/m2), and 3.6% were obese III (40 kg/m2 or greater). Dr. Williams and his associates observed that women were more often underweight, compared with men (4.1% vs. 1.8%, respectively; P less than .001), and underweight patients more often had chronic obstructive pulmonary disease (51.7% vs. 35.2%; P less than .001). Pulmonary complication rates were higher among underweight and obese III patients (P less than .001), while being underweight was also associated with higher rates of infections and any surgical complications.
Multivariable analysis revealed that pulmonary and any postoperative complications were more common among underweight patients (odds ratio, 1.44 and OR, 1.41, respectively), while any major complication was more common among obese III patients (OR, 1.18). Overweight and obese I-II patients were less likely to have any postoperative and pulmonary complications, compared with patients who had a normal BMI. “The finding of underweight patients being such a high-risk patient population is suggested in the literature but not demonstrated as clearly as in this study,” Dr. Williams said. “A truly surprising finding was that obese patients actually have a lower risk of pulmonary and overall complications than ‘normal’-BMI patients.”
He concluded that according to the current analysis, “careful risk assessment is appropriate when considering operating on underweight patients. Whether there are interventions that could be instituted to improve an individual’s risk profile has not been determined. Any preconceived notions about not operating on obese patients due to elevated risk appear to be unfounded.”
Dr. Williams reported having no financial disclosures.
PHOENIX – Being underweight is associated with a substantially increased risk of complications following lung resection for cancer, results from a large database study found.
“This is not generally known among surgeons or their patients,” Dr. Trevor Williams said in an interview before the annual meeting of the Society of Thoracic Surgeons. “Studies are conflicting about the relationship of BMI [body mass index] to surgical outcomes. Most of the previous studies simply categorize BMI as overweight or not. We’ve stratified based on World Health Organization categories to get a more precise look at BMI.”
Dr. Williams, a surgeon at the University of Chicago Medical Center, and his associates evaluated 41,446 patients in the STS General Thoracic Surgery Database who underwent elective anatomic lung resection for cancer between 2009 and 2014. Their mean age was 68 years, and 53% were female. The researchers performed multivariable analysis after adjusting for validated STS risk model covariates, including gender and spirometry.
According to WHO criteria for BMI, 3% were underweight (less than 18.5 kg/m2); 33.5% were normal weight (18.5-24.9 kg/m2); 35.4% were overweight (25-29.9 kg/m2); 18.1% were obese I (30-34.9 kg/m2); 6.4% were obese II (35-39.9 kg/m2), and 3.6% were obese III (40 kg/m2 or greater). Dr. Williams and his associates observed that women were more often underweight, compared with men (4.1% vs. 1.8%, respectively; P less than .001), and underweight patients more often had chronic obstructive pulmonary disease (51.7% vs. 35.2%; P less than .001). Pulmonary complication rates were higher among underweight and obese III patients (P less than .001), while being underweight was also associated with higher rates of infections and any surgical complications.
Multivariable analysis revealed that pulmonary and any postoperative complications were more common among underweight patients (odds ratio, 1.44 and OR, 1.41, respectively), while any major complication was more common among obese III patients (OR, 1.18). Overweight and obese I-II patients were less likely to have any postoperative and pulmonary complications, compared with patients who had a normal BMI. “The finding of underweight patients being such a high-risk patient population is suggested in the literature but not demonstrated as clearly as in this study,” Dr. Williams said. “A truly surprising finding was that obese patients actually have a lower risk of pulmonary and overall complications than ‘normal’-BMI patients.”
He concluded that according to the current analysis, “careful risk assessment is appropriate when considering operating on underweight patients. Whether there are interventions that could be instituted to improve an individual’s risk profile has not been determined. Any preconceived notions about not operating on obese patients due to elevated risk appear to be unfounded.”
Dr. Williams reported having no financial disclosures.
AT THE STS ANNUAL MEETING
Key clinical point: Careful risk assessment is appropriate when considering performing lung resection on underweight patients.
Major finding: Multivariable analysis revealed that pulmonary and any postoperative complications were more common among underweight patients (OR, 1.44 and OR, 1.41, respectively), while any major complication was more common among obese III patients (OR, 1.18).
Data source: An analysis of 41,446 patients in the STS General Thoracic Surgery Database who underwent elective lung resection for cancer between 2009 and 2014.
Disclosures: Dr. Williams reported having no financial disclosures.
VIDEO: Novel imaging technique helps hunt for pulmonary lesions
PHOENIX – Each year more than 250,000 patients present with ground-glass opacities and other solitary pulmonary nodules, and they are difficult to locate.
“There’s been a need for our field to develop new technologies to find these nodules in the OR,” Dr. Sunil Singhal said in a video interview at the annual meeting of the Society of Thoracic Surgeons. “The fallback plan has always been that we can make a thoracotomy. Some studies have shown that in about one out of every two cases you end up opening a patient just to find a tiny little nodule.”
Dr. Singhal of the division of cardiothoracic surgery at the University of Pennsylvania School of Medicine, Philadelphia, discussed preoperative and intraoperative localization methods, including an investigational technology in which patients receive an intravascular dye that localizes the pulmonary tumor. “When we put our video-assisted thoracoscopic surgery camera in, the tumors are glowing,” he said. “We can then do a localized wedge excision and confirm margins of the staple line. We’ve done this [in] about 80 patients, and it’s been non-toxic, very safe, and very effective. Our biggest limitation has been our depth of penetration.”
Dr. Singhal reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
PHOENIX – Each year more than 250,000 patients present with ground-glass opacities and other solitary pulmonary nodules, and they are difficult to locate.
“There’s been a need for our field to develop new technologies to find these nodules in the OR,” Dr. Sunil Singhal said in a video interview at the annual meeting of the Society of Thoracic Surgeons. “The fallback plan has always been that we can make a thoracotomy. Some studies have shown that in about one out of every two cases you end up opening a patient just to find a tiny little nodule.”
Dr. Singhal of the division of cardiothoracic surgery at the University of Pennsylvania School of Medicine, Philadelphia, discussed preoperative and intraoperative localization methods, including an investigational technology in which patients receive an intravascular dye that localizes the pulmonary tumor. “When we put our video-assisted thoracoscopic surgery camera in, the tumors are glowing,” he said. “We can then do a localized wedge excision and confirm margins of the staple line. We’ve done this [in] about 80 patients, and it’s been non-toxic, very safe, and very effective. Our biggest limitation has been our depth of penetration.”
Dr. Singhal reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
PHOENIX – Each year more than 250,000 patients present with ground-glass opacities and other solitary pulmonary nodules, and they are difficult to locate.
“There’s been a need for our field to develop new technologies to find these nodules in the OR,” Dr. Sunil Singhal said in a video interview at the annual meeting of the Society of Thoracic Surgeons. “The fallback plan has always been that we can make a thoracotomy. Some studies have shown that in about one out of every two cases you end up opening a patient just to find a tiny little nodule.”
Dr. Singhal of the division of cardiothoracic surgery at the University of Pennsylvania School of Medicine, Philadelphia, discussed preoperative and intraoperative localization methods, including an investigational technology in which patients receive an intravascular dye that localizes the pulmonary tumor. “When we put our video-assisted thoracoscopic surgery camera in, the tumors are glowing,” he said. “We can then do a localized wedge excision and confirm margins of the staple line. We’ve done this [in] about 80 patients, and it’s been non-toxic, very safe, and very effective. Our biggest limitation has been our depth of penetration.”
Dr. Singhal reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
EXPERT ANALYSIS FROM THE STS ANNUAL MEETING
Viruses, Part 2: RNA Viruses
Review the PDF of the fact sheet on RNA viruses with board-relevant, easy-to-review material. This fact sheet will review the spectrum of RNA viruses that cause or are associated with cutaneous manifestations. RNA virus classification, clinical findings, potential treatments, and other board-relevant facts will be discussed.
Practice Questions
1. Which virus is transmitted by Culex mosquitos?
a. chikungunya virus
b. coxsackievirus A16
c. dengue virus
d. human T-lymphotropic virus
e. West Nile virus
2. Which virus causes an illness associated with an enanthem of grey papules on the buccal mucosa?
a. Paramyxoviridae
b. Parvoviridae
c. Picornaviridae
d. Retroviridae
e. Togaviridae
3. Illness associated with which viral infection may be prevented via vaccination?
a. coxsackievirus
b. dengue virus
c. enterovirus
d. hepatitis C virus
e. togavirus
4. Which virus is classically associated with retro-orbital pain and a morbilliform eruption with areas of sparing?
a. chikungunya virus
b. dengue virus
c. human immunodeficiency virus
d. West Nile virus
e. yellow fever virus
5. Which of the following may be included in the treatment of hepatitis C virus (HCV) infection?
a. doxorubicin
b. HCV vaccine
c. ribavirin
d. tenofovir
e. vitamin A
1. Which virus is transmitted by Culex mosquitos?
a. chikungunya virus
b. coxsackievirus A16
c. dengue virus
d. human T-lymphotropic virus
e. West Nile virus
2. Which virus causes an illness associated with an enanthem of grey papules on the buccal mucosa?
a. Paramyxoviridae
b. Parvoviridae
c. Picornaviridae
d. Retroviridae
e. Togaviridae
3. Illness associated with which viral infection may be prevented via vaccination?
a. coxsackievirus
b. dengue virus c. enterovirus
d. hepatitis C virus
e. togavirus
4. Which virus is classically associated with retro-orbital pain and a morbilliform eruption with areas of sparing?
a. chikungunya virus
b. dengue virus
c. human immunodeficiency virus
d. West Nile virus
e. yellow fever virus
5. Which of the following may be included in the treatment of hepatitis C virus (HCV) infection?
a. doxorubicin
b. HCV vaccine
c. ribavirin
d. tenofovir
e. vitamin A
Review the PDF of the fact sheet on RNA viruses with board-relevant, easy-to-review material. This fact sheet will review the spectrum of RNA viruses that cause or are associated with cutaneous manifestations. RNA virus classification, clinical findings, potential treatments, and other board-relevant facts will be discussed.
Practice Questions
1. Which virus is transmitted by Culex mosquitos?
a. chikungunya virus
b. coxsackievirus A16
c. dengue virus
d. human T-lymphotropic virus
e. West Nile virus
2. Which virus causes an illness associated with an enanthem of grey papules on the buccal mucosa?
a. Paramyxoviridae
b. Parvoviridae
c. Picornaviridae
d. Retroviridae
e. Togaviridae
3. Illness associated with which viral infection may be prevented via vaccination?
a. coxsackievirus
b. dengue virus
c. enterovirus
d. hepatitis C virus
e. togavirus
4. Which virus is classically associated with retro-orbital pain and a morbilliform eruption with areas of sparing?
a. chikungunya virus
b. dengue virus
c. human immunodeficiency virus
d. West Nile virus
e. yellow fever virus
5. Which of the following may be included in the treatment of hepatitis C virus (HCV) infection?
a. doxorubicin
b. HCV vaccine
c. ribavirin
d. tenofovir
e. vitamin A
1. Which virus is transmitted by Culex mosquitos?
a. chikungunya virus
b. coxsackievirus A16
c. dengue virus
d. human T-lymphotropic virus
e. West Nile virus
2. Which virus causes an illness associated with an enanthem of grey papules on the buccal mucosa?
a. Paramyxoviridae
b. Parvoviridae
c. Picornaviridae
d. Retroviridae
e. Togaviridae
3. Illness associated with which viral infection may be prevented via vaccination?
a. coxsackievirus
b. dengue virus c. enterovirus
d. hepatitis C virus
e. togavirus
4. Which virus is classically associated with retro-orbital pain and a morbilliform eruption with areas of sparing?
a. chikungunya virus
b. dengue virus
c. human immunodeficiency virus
d. West Nile virus
e. yellow fever virus
5. Which of the following may be included in the treatment of hepatitis C virus (HCV) infection?
a. doxorubicin
b. HCV vaccine
c. ribavirin
d. tenofovir
e. vitamin A
Review the PDF of the fact sheet on RNA viruses with board-relevant, easy-to-review material. This fact sheet will review the spectrum of RNA viruses that cause or are associated with cutaneous manifestations. RNA virus classification, clinical findings, potential treatments, and other board-relevant facts will be discussed.
Practice Questions
1. Which virus is transmitted by Culex mosquitos?
a. chikungunya virus
b. coxsackievirus A16
c. dengue virus
d. human T-lymphotropic virus
e. West Nile virus
2. Which virus causes an illness associated with an enanthem of grey papules on the buccal mucosa?
a. Paramyxoviridae
b. Parvoviridae
c. Picornaviridae
d. Retroviridae
e. Togaviridae
3. Illness associated with which viral infection may be prevented via vaccination?
a. coxsackievirus
b. dengue virus
c. enterovirus
d. hepatitis C virus
e. togavirus
4. Which virus is classically associated with retro-orbital pain and a morbilliform eruption with areas of sparing?
a. chikungunya virus
b. dengue virus
c. human immunodeficiency virus
d. West Nile virus
e. yellow fever virus
5. Which of the following may be included in the treatment of hepatitis C virus (HCV) infection?
a. doxorubicin
b. HCV vaccine
c. ribavirin
d. tenofovir
e. vitamin A
1. Which virus is transmitted by Culex mosquitos?
a. chikungunya virus
b. coxsackievirus A16
c. dengue virus
d. human T-lymphotropic virus
e. West Nile virus
2. Which virus causes an illness associated with an enanthem of grey papules on the buccal mucosa?
a. Paramyxoviridae
b. Parvoviridae
c. Picornaviridae
d. Retroviridae
e. Togaviridae
3. Illness associated with which viral infection may be prevented via vaccination?
a. coxsackievirus
b. dengue virus c. enterovirus
d. hepatitis C virus
e. togavirus
4. Which virus is classically associated with retro-orbital pain and a morbilliform eruption with areas of sparing?
a. chikungunya virus
b. dengue virus
c. human immunodeficiency virus
d. West Nile virus
e. yellow fever virus
5. Which of the following may be included in the treatment of hepatitis C virus (HCV) infection?
a. doxorubicin
b. HCV vaccine
c. ribavirin
d. tenofovir
e. vitamin A
STS: Score stratifies risks for isolated tricuspid valve surgery patients
PHOENIX – A team of cardiac surgeons has developed the first clinical risk score for predicting the risk that patients face for operative mortality and postsurgical major morbidity when undergoing isolated tricuspid valve repair or replacement.
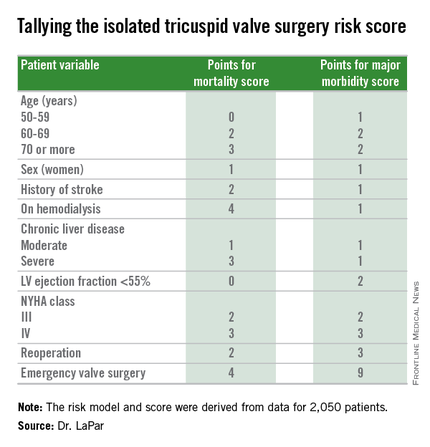
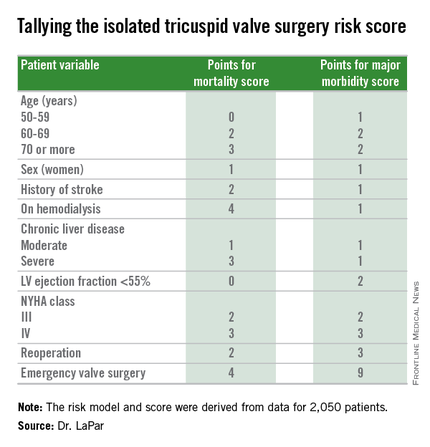
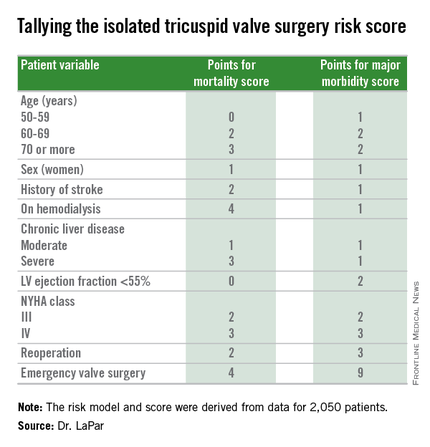
The risk score uses nine easily collected variables, and the derived model discriminates outcomes based on patients who score from 0-10 or more points on both a mortality and a morbidity risk scale, Dr. Damien J. LaPar said at the annual meeting of the Society of Thoracic Surgeons.
The risk scores allow surgeons to better describe and quantify to patients considering isolated tricuspid valve surgery the risks they face from the operation, and they have already been incorporated into practice at the University of Virginia, in Charlottesville, where Dr. LaPar practices.
“Patients love to better understand their risks. We can provide them with empirical data from a large, heterogeneous population that are better than a surgeon’s gut feeling” about the risks they face, said Dr. LaPar, a cardiothoracic surgeon at the University.
Another consequence of having the new risk model and score is that it identified certain key risk factors that are controllable, and thereby, “makes the case for early referrals” for isolated tricuspid valve surgery, Dr. LaPar said in an interview. For example, the risk score shows that patients who are older, on hemodialysis, have a reduced left ventricular ejection fraction, or require emergency intervention all contribute to worse outcomes, compared with patients who are younger, have better renal function, better cardiac output, or can be treated on a more routine basis.
Many physicians have viewed isolated tricuspid valve surgery as posing similar risks to all patients, with an overall average operative mortality rate of about 10%, he noted. The new risk score model shows that some patients who are younger and healthier have operative mortality rates below 5%, while older and sicker patients have rates that can surpass 20%.
“Our data show a spectrum of risk, and that it is better to operate sooner than later. That is the huge clinical message of these data,” Dr. LaPar said.
Designated discussant Dr. Michael A. Acker noted that the risk score for tricuspid-valve surgery “is a first of its kind and a major contribution.” Dr. Acker is professor of surgery and chief of cardiovascular surgery at the University of Pennsylvania in Philadelphia. He is a consultant to Thoratec and HeartWare.
Dr. LaPar and his associates derived the risk model and score from data collected on 2,050 patients who underwent isolated tricuspid valve repair or replacement at 49 hospitals in Virginia or Michigan during 2002-2014. The data came from databases maintained by the Virginia Cardiac Surgery Quality Initiative and by the Michigan Society of Thoracic & Cardiovascular Surgeons, and reported to the Adult Cardiac Surgery Database of the Society of Thoracic Surgeons. The model they developed showed operative mortality rates that ranged from 2%, for patients with a mortality score of zero, to 34% for patients with a score of 10 or more. It further showed major morbidity rates of 13%, for patients with a morbidity score of zero, to 71% for those with a score of 10 or more. Scoring for mortality uses a slightly different system than the scoring for morbidity, so the scores must be calculated individually, and the score totals for a patient can differ for each endpoint. The maximum score is 22 for mortality and 23 for morbidity.
Only 5%-15% of patients undergoing tricuspid valve surgery have an isolated procedure, so a relatively limited number of patients fall into this category, a fact that has in the past limited collection of data from large numbers of patients. The dataset used for this analysis, with 2,050 patients “is one of the largest series collected,” and made possible derivation of a robust risk model and scoring system. Future analysis of even more patients should further improve the model and scoring system.
“These data set the stage for looking at national-level data to further refine the model and make it even more generalizable,” Dr. LaPar said.
On Twitter @mitchelzoler
PHOENIX – A team of cardiac surgeons has developed the first clinical risk score for predicting the risk that patients face for operative mortality and postsurgical major morbidity when undergoing isolated tricuspid valve repair or replacement.
The risk score uses nine easily collected variables, and the derived model discriminates outcomes based on patients who score from 0-10 or more points on both a mortality and a morbidity risk scale, Dr. Damien J. LaPar said at the annual meeting of the Society of Thoracic Surgeons.
The risk scores allow surgeons to better describe and quantify to patients considering isolated tricuspid valve surgery the risks they face from the operation, and they have already been incorporated into practice at the University of Virginia, in Charlottesville, where Dr. LaPar practices.
“Patients love to better understand their risks. We can provide them with empirical data from a large, heterogeneous population that are better than a surgeon’s gut feeling” about the risks they face, said Dr. LaPar, a cardiothoracic surgeon at the University.
Another consequence of having the new risk model and score is that it identified certain key risk factors that are controllable, and thereby, “makes the case for early referrals” for isolated tricuspid valve surgery, Dr. LaPar said in an interview. For example, the risk score shows that patients who are older, on hemodialysis, have a reduced left ventricular ejection fraction, or require emergency intervention all contribute to worse outcomes, compared with patients who are younger, have better renal function, better cardiac output, or can be treated on a more routine basis.
Many physicians have viewed isolated tricuspid valve surgery as posing similar risks to all patients, with an overall average operative mortality rate of about 10%, he noted. The new risk score model shows that some patients who are younger and healthier have operative mortality rates below 5%, while older and sicker patients have rates that can surpass 20%.
“Our data show a spectrum of risk, and that it is better to operate sooner than later. That is the huge clinical message of these data,” Dr. LaPar said.
Designated discussant Dr. Michael A. Acker noted that the risk score for tricuspid-valve surgery “is a first of its kind and a major contribution.” Dr. Acker is professor of surgery and chief of cardiovascular surgery at the University of Pennsylvania in Philadelphia. He is a consultant to Thoratec and HeartWare.
Dr. LaPar and his associates derived the risk model and score from data collected on 2,050 patients who underwent isolated tricuspid valve repair or replacement at 49 hospitals in Virginia or Michigan during 2002-2014. The data came from databases maintained by the Virginia Cardiac Surgery Quality Initiative and by the Michigan Society of Thoracic & Cardiovascular Surgeons, and reported to the Adult Cardiac Surgery Database of the Society of Thoracic Surgeons. The model they developed showed operative mortality rates that ranged from 2%, for patients with a mortality score of zero, to 34% for patients with a score of 10 or more. It further showed major morbidity rates of 13%, for patients with a morbidity score of zero, to 71% for those with a score of 10 or more. Scoring for mortality uses a slightly different system than the scoring for morbidity, so the scores must be calculated individually, and the score totals for a patient can differ for each endpoint. The maximum score is 22 for mortality and 23 for morbidity.
Only 5%-15% of patients undergoing tricuspid valve surgery have an isolated procedure, so a relatively limited number of patients fall into this category, a fact that has in the past limited collection of data from large numbers of patients. The dataset used for this analysis, with 2,050 patients “is one of the largest series collected,” and made possible derivation of a robust risk model and scoring system. Future analysis of even more patients should further improve the model and scoring system.
“These data set the stage for looking at national-level data to further refine the model and make it even more generalizable,” Dr. LaPar said.
On Twitter @mitchelzoler
PHOENIX – A team of cardiac surgeons has developed the first clinical risk score for predicting the risk that patients face for operative mortality and postsurgical major morbidity when undergoing isolated tricuspid valve repair or replacement.
The risk score uses nine easily collected variables, and the derived model discriminates outcomes based on patients who score from 0-10 or more points on both a mortality and a morbidity risk scale, Dr. Damien J. LaPar said at the annual meeting of the Society of Thoracic Surgeons.
The risk scores allow surgeons to better describe and quantify to patients considering isolated tricuspid valve surgery the risks they face from the operation, and they have already been incorporated into practice at the University of Virginia, in Charlottesville, where Dr. LaPar practices.
“Patients love to better understand their risks. We can provide them with empirical data from a large, heterogeneous population that are better than a surgeon’s gut feeling” about the risks they face, said Dr. LaPar, a cardiothoracic surgeon at the University.
Another consequence of having the new risk model and score is that it identified certain key risk factors that are controllable, and thereby, “makes the case for early referrals” for isolated tricuspid valve surgery, Dr. LaPar said in an interview. For example, the risk score shows that patients who are older, on hemodialysis, have a reduced left ventricular ejection fraction, or require emergency intervention all contribute to worse outcomes, compared with patients who are younger, have better renal function, better cardiac output, or can be treated on a more routine basis.
Many physicians have viewed isolated tricuspid valve surgery as posing similar risks to all patients, with an overall average operative mortality rate of about 10%, he noted. The new risk score model shows that some patients who are younger and healthier have operative mortality rates below 5%, while older and sicker patients have rates that can surpass 20%.
“Our data show a spectrum of risk, and that it is better to operate sooner than later. That is the huge clinical message of these data,” Dr. LaPar said.
Designated discussant Dr. Michael A. Acker noted that the risk score for tricuspid-valve surgery “is a first of its kind and a major contribution.” Dr. Acker is professor of surgery and chief of cardiovascular surgery at the University of Pennsylvania in Philadelphia. He is a consultant to Thoratec and HeartWare.
Dr. LaPar and his associates derived the risk model and score from data collected on 2,050 patients who underwent isolated tricuspid valve repair or replacement at 49 hospitals in Virginia or Michigan during 2002-2014. The data came from databases maintained by the Virginia Cardiac Surgery Quality Initiative and by the Michigan Society of Thoracic & Cardiovascular Surgeons, and reported to the Adult Cardiac Surgery Database of the Society of Thoracic Surgeons. The model they developed showed operative mortality rates that ranged from 2%, for patients with a mortality score of zero, to 34% for patients with a score of 10 or more. It further showed major morbidity rates of 13%, for patients with a morbidity score of zero, to 71% for those with a score of 10 or more. Scoring for mortality uses a slightly different system than the scoring for morbidity, so the scores must be calculated individually, and the score totals for a patient can differ for each endpoint. The maximum score is 22 for mortality and 23 for morbidity.
Only 5%-15% of patients undergoing tricuspid valve surgery have an isolated procedure, so a relatively limited number of patients fall into this category, a fact that has in the past limited collection of data from large numbers of patients. The dataset used for this analysis, with 2,050 patients “is one of the largest series collected,” and made possible derivation of a robust risk model and scoring system. Future analysis of even more patients should further improve the model and scoring system.
“These data set the stage for looking at national-level data to further refine the model and make it even more generalizable,” Dr. LaPar said.
On Twitter @mitchelzoler
AT THE STS ANNUAL MEETING
Key clinical point: A risk-scoring system estimates a patient’s mortality and morbidity risk when undergoing isolated tricuspid valve surgery.
Major finding: The scoring system discriminated mortality risk from 2% to 34%, and major morbidity risk from 13% to 71%.
Data source: Analysis of 2,050 patients who underwent isolated tricuspid valve surgery in the STS Adult Cardiac Surgery Database.
Disclosures: Dr. LaPar had no disclosures.
Workplace Interactions for Rosacea Patients
A new survey from the National Rosacea Society of 794 rosacea patients revealed that the majority of respondents indicated the disease had affected interactions with others in the workplace. More than 82% of respondents said they would notice people staring when they were experiencing a flare-up, and nearly 54% reported hearing rude or inappropriate comments about their facial appearance. More than 66% of the survey respondents said rosacea had negatively impacted interactions with customers or coworkers. Twenty-nine percent of patients with mild symptoms and 43% of those with severe symptoms reported they had missed work because of the condition.
Although rosacea may impact workplace interactions, 76.5% of respondents did not feel their appearance had cost them a promotion or new responsibilities, and 77.5% indicated that it had not kept them from landing a new job. Most respondents indicated that workplace problems were resolved when medical therapy was started, with nearly 67% reporting that effective treatment had improved their interactions with others at work.
In a January 2015 Cutis article, “The Rosacea Patient Journey: A Novel Approach to Conceptualizing Patient Experiences,” Kuo and colleagues discussed how patients can be educated to prepare for the rosacea patient experience. “Rosacea patients are faced with confusing and aggravating symptoms that can cause anxiety and may lead them to seek treatment from a physician,” the authors said. Rosacea can be a socially stigmatizing disease because the facial flushing and phymatous changes may be mistaken for alcohol abuse. It can also disrupt social and professional interactions, leading to quality-of-life effects such as difficulty functioning on a day-to-day basis.
Because there is no cure for rosacea, the patient and dermatologist must work together to devise a treatment plan that will help control the symptoms of rosacea. “Ultimately, with the alleviation of visible symptoms, the patient’s quality of life also can improve,” Kuo and colleagues reported. “Better understanding of the rosacea patient perspective can lead to a more efficient health care system, improved patient care, and better patient satisfaction.”
Share a copy of the Cutis rosacea patient journey guide with your patients today.
A new survey from the National Rosacea Society of 794 rosacea patients revealed that the majority of respondents indicated the disease had affected interactions with others in the workplace. More than 82% of respondents said they would notice people staring when they were experiencing a flare-up, and nearly 54% reported hearing rude or inappropriate comments about their facial appearance. More than 66% of the survey respondents said rosacea had negatively impacted interactions with customers or coworkers. Twenty-nine percent of patients with mild symptoms and 43% of those with severe symptoms reported they had missed work because of the condition.
Although rosacea may impact workplace interactions, 76.5% of respondents did not feel their appearance had cost them a promotion or new responsibilities, and 77.5% indicated that it had not kept them from landing a new job. Most respondents indicated that workplace problems were resolved when medical therapy was started, with nearly 67% reporting that effective treatment had improved their interactions with others at work.
In a January 2015 Cutis article, “The Rosacea Patient Journey: A Novel Approach to Conceptualizing Patient Experiences,” Kuo and colleagues discussed how patients can be educated to prepare for the rosacea patient experience. “Rosacea patients are faced with confusing and aggravating symptoms that can cause anxiety and may lead them to seek treatment from a physician,” the authors said. Rosacea can be a socially stigmatizing disease because the facial flushing and phymatous changes may be mistaken for alcohol abuse. It can also disrupt social and professional interactions, leading to quality-of-life effects such as difficulty functioning on a day-to-day basis.
Because there is no cure for rosacea, the patient and dermatologist must work together to devise a treatment plan that will help control the symptoms of rosacea. “Ultimately, with the alleviation of visible symptoms, the patient’s quality of life also can improve,” Kuo and colleagues reported. “Better understanding of the rosacea patient perspective can lead to a more efficient health care system, improved patient care, and better patient satisfaction.”
Share a copy of the Cutis rosacea patient journey guide with your patients today.
A new survey from the National Rosacea Society of 794 rosacea patients revealed that the majority of respondents indicated the disease had affected interactions with others in the workplace. More than 82% of respondents said they would notice people staring when they were experiencing a flare-up, and nearly 54% reported hearing rude or inappropriate comments about their facial appearance. More than 66% of the survey respondents said rosacea had negatively impacted interactions with customers or coworkers. Twenty-nine percent of patients with mild symptoms and 43% of those with severe symptoms reported they had missed work because of the condition.
Although rosacea may impact workplace interactions, 76.5% of respondents did not feel their appearance had cost them a promotion or new responsibilities, and 77.5% indicated that it had not kept them from landing a new job. Most respondents indicated that workplace problems were resolved when medical therapy was started, with nearly 67% reporting that effective treatment had improved their interactions with others at work.
In a January 2015 Cutis article, “The Rosacea Patient Journey: A Novel Approach to Conceptualizing Patient Experiences,” Kuo and colleagues discussed how patients can be educated to prepare for the rosacea patient experience. “Rosacea patients are faced with confusing and aggravating symptoms that can cause anxiety and may lead them to seek treatment from a physician,” the authors said. Rosacea can be a socially stigmatizing disease because the facial flushing and phymatous changes may be mistaken for alcohol abuse. It can also disrupt social and professional interactions, leading to quality-of-life effects such as difficulty functioning on a day-to-day basis.
Because there is no cure for rosacea, the patient and dermatologist must work together to devise a treatment plan that will help control the symptoms of rosacea. “Ultimately, with the alleviation of visible symptoms, the patient’s quality of life also can improve,” Kuo and colleagues reported. “Better understanding of the rosacea patient perspective can lead to a more efficient health care system, improved patient care, and better patient satisfaction.”
Share a copy of the Cutis rosacea patient journey guide with your patients today.
Dealing with adversity in vascular surgery
Adversity is part of life and everyone must deal with it. How one manages adversity matters, separates the winners from the losers, and is a major determinant of success.
Adverse challenges may be minor, intermediate or major. Although everyone is faced with such challenges, they are particularly relevant in a vascular surgery career. This is because of the serious nature and consequences of vascular diseases which can threaten loss of life, limb, and neurological function, and because of the complicated administrative world in which vascular surgery functions.
Minor frustrations are almost daily occurrences in a busy vascular surgeon’s life. They occur in and out of the operating room or angio suite, and many of them relate to other coworkers and associates making errors that interfere with smooth work flow or even good patient care. An angry response to these minor frustrations can exacerbate the problem and lead to strained, unpleasant working relationships and further errors. In contrast, a calm, measured response to these minor frustrations can minimize the damage caused and lead to a tranquil and effective work place.
Moreover, the individuals who control their responses are destined to be more effective and well liked. Equanimity when things go wrong during a stressful procedure in the operating room or angio suite is an even more valuable asset. Such composed responses will usually yield a better outcome than will loud and angry expressions of blame. The more serious the situation, the greater will be the value of composure.
Intermediate adversity in a work environment can take the form of rejection of a paper, denial of a grant request, or failure to get a sought promotion or assignment to a particular area of one’s interest. The latter two failures can best be managed by quietly continuing to work and strive. Success should only be regarded as delayed not denied. Rejection of grants and articles is almost routine despite the amount of time and hard work required to prepare them. Calm persistence can overcome many of these adverse events. Rewriting the paper or grant to correct the deficiencies detected by the reviewers followed by resubmission, even re-resubmission or submission to another journal, will ultimately result in publication of the work. To paraphrase Winston Churchill’s credo: Never, never, never, never, never, never give up.
A particularly challenging case can also be stressful and disheartening. It can appear at first to be an adverse event to the person faced with it. By staying calm and thinking clearly, it is sometimes possible to devise a new solution to the problem – one never described before. Thus, by meeting the challenge of this adversity, the vascular surgeon serendipitously turns adversity to his or her advantage and becomes an innovator. The seeming adversity becomes a creative opportunity. Many new developments and progress in vascular surgery have begun this way. No problem should be viewed as unsolvable despite so-called current wisdom.
More major adversity in a job setting can take the form of firing or termination. Such termination may be warranted or not. Often it is totally unjustified and based on personality differences or ego issues. Jealousy or negative bias are often involved. Such firings may take the form of a witch hunt based on a clinical or administrative superior highlighting selective and unrepresentative bad outcomes in a few difficult cases – something every good vascular surgeon has because of the difficult nature of the diseases we treat.
How should one deal with such a termination – unfair or not? Do not seek revenge. Get over it. Get another job and move on. Fortunately other jobs are abundant in the United States. Moreover, the new job often turns out to be better than the one left behind. The termination actually becomes a blessing in disguise, although it may take time for this to become apparent. Interestingly, many first-line leaders or biggest names in vascular surgery have profited in this way from the apparent major adversity of a termination. As one door closes, another may open if one is alert to the possibilities that may arise from change. Furthermore, the best revenge for an unfair termination is gained by achieving great success in one’s next position.
Although the discussion about dealing with adversity has thus far dealt largely with professional issues, the same principles can be applied to dealing with other aspects of life in general. Vigorous and excessive responses to adversity often result in greater pain and enhancing the wealth of lawyers. Equanimity, minimizing reactivity, and succeeding in the new venture one is forced into – even if unfairly – usually produce the best long-term outcome. It is an imperfect world, and how one deals with the many adversities that are part of it can make it less imperfect.
Adversity is part of life and everyone must deal with it. How one manages adversity matters, separates the winners from the losers, and is a major determinant of success.
Adverse challenges may be minor, intermediate or major. Although everyone is faced with such challenges, they are particularly relevant in a vascular surgery career. This is because of the serious nature and consequences of vascular diseases which can threaten loss of life, limb, and neurological function, and because of the complicated administrative world in which vascular surgery functions.
Minor frustrations are almost daily occurrences in a busy vascular surgeon’s life. They occur in and out of the operating room or angio suite, and many of them relate to other coworkers and associates making errors that interfere with smooth work flow or even good patient care. An angry response to these minor frustrations can exacerbate the problem and lead to strained, unpleasant working relationships and further errors. In contrast, a calm, measured response to these minor frustrations can minimize the damage caused and lead to a tranquil and effective work place.
Moreover, the individuals who control their responses are destined to be more effective and well liked. Equanimity when things go wrong during a stressful procedure in the operating room or angio suite is an even more valuable asset. Such composed responses will usually yield a better outcome than will loud and angry expressions of blame. The more serious the situation, the greater will be the value of composure.
Intermediate adversity in a work environment can take the form of rejection of a paper, denial of a grant request, or failure to get a sought promotion or assignment to a particular area of one’s interest. The latter two failures can best be managed by quietly continuing to work and strive. Success should only be regarded as delayed not denied. Rejection of grants and articles is almost routine despite the amount of time and hard work required to prepare them. Calm persistence can overcome many of these adverse events. Rewriting the paper or grant to correct the deficiencies detected by the reviewers followed by resubmission, even re-resubmission or submission to another journal, will ultimately result in publication of the work. To paraphrase Winston Churchill’s credo: Never, never, never, never, never, never give up.
A particularly challenging case can also be stressful and disheartening. It can appear at first to be an adverse event to the person faced with it. By staying calm and thinking clearly, it is sometimes possible to devise a new solution to the problem – one never described before. Thus, by meeting the challenge of this adversity, the vascular surgeon serendipitously turns adversity to his or her advantage and becomes an innovator. The seeming adversity becomes a creative opportunity. Many new developments and progress in vascular surgery have begun this way. No problem should be viewed as unsolvable despite so-called current wisdom.
More major adversity in a job setting can take the form of firing or termination. Such termination may be warranted or not. Often it is totally unjustified and based on personality differences or ego issues. Jealousy or negative bias are often involved. Such firings may take the form of a witch hunt based on a clinical or administrative superior highlighting selective and unrepresentative bad outcomes in a few difficult cases – something every good vascular surgeon has because of the difficult nature of the diseases we treat.
How should one deal with such a termination – unfair or not? Do not seek revenge. Get over it. Get another job and move on. Fortunately other jobs are abundant in the United States. Moreover, the new job often turns out to be better than the one left behind. The termination actually becomes a blessing in disguise, although it may take time for this to become apparent. Interestingly, many first-line leaders or biggest names in vascular surgery have profited in this way from the apparent major adversity of a termination. As one door closes, another may open if one is alert to the possibilities that may arise from change. Furthermore, the best revenge for an unfair termination is gained by achieving great success in one’s next position.
Although the discussion about dealing with adversity has thus far dealt largely with professional issues, the same principles can be applied to dealing with other aspects of life in general. Vigorous and excessive responses to adversity often result in greater pain and enhancing the wealth of lawyers. Equanimity, minimizing reactivity, and succeeding in the new venture one is forced into – even if unfairly – usually produce the best long-term outcome. It is an imperfect world, and how one deals with the many adversities that are part of it can make it less imperfect.
Adversity is part of life and everyone must deal with it. How one manages adversity matters, separates the winners from the losers, and is a major determinant of success.
Adverse challenges may be minor, intermediate or major. Although everyone is faced with such challenges, they are particularly relevant in a vascular surgery career. This is because of the serious nature and consequences of vascular diseases which can threaten loss of life, limb, and neurological function, and because of the complicated administrative world in which vascular surgery functions.
Minor frustrations are almost daily occurrences in a busy vascular surgeon’s life. They occur in and out of the operating room or angio suite, and many of them relate to other coworkers and associates making errors that interfere with smooth work flow or even good patient care. An angry response to these minor frustrations can exacerbate the problem and lead to strained, unpleasant working relationships and further errors. In contrast, a calm, measured response to these minor frustrations can minimize the damage caused and lead to a tranquil and effective work place.
Moreover, the individuals who control their responses are destined to be more effective and well liked. Equanimity when things go wrong during a stressful procedure in the operating room or angio suite is an even more valuable asset. Such composed responses will usually yield a better outcome than will loud and angry expressions of blame. The more serious the situation, the greater will be the value of composure.
Intermediate adversity in a work environment can take the form of rejection of a paper, denial of a grant request, or failure to get a sought promotion or assignment to a particular area of one’s interest. The latter two failures can best be managed by quietly continuing to work and strive. Success should only be regarded as delayed not denied. Rejection of grants and articles is almost routine despite the amount of time and hard work required to prepare them. Calm persistence can overcome many of these adverse events. Rewriting the paper or grant to correct the deficiencies detected by the reviewers followed by resubmission, even re-resubmission or submission to another journal, will ultimately result in publication of the work. To paraphrase Winston Churchill’s credo: Never, never, never, never, never, never give up.
A particularly challenging case can also be stressful and disheartening. It can appear at first to be an adverse event to the person faced with it. By staying calm and thinking clearly, it is sometimes possible to devise a new solution to the problem – one never described before. Thus, by meeting the challenge of this adversity, the vascular surgeon serendipitously turns adversity to his or her advantage and becomes an innovator. The seeming adversity becomes a creative opportunity. Many new developments and progress in vascular surgery have begun this way. No problem should be viewed as unsolvable despite so-called current wisdom.
More major adversity in a job setting can take the form of firing or termination. Such termination may be warranted or not. Often it is totally unjustified and based on personality differences or ego issues. Jealousy or negative bias are often involved. Such firings may take the form of a witch hunt based on a clinical or administrative superior highlighting selective and unrepresentative bad outcomes in a few difficult cases – something every good vascular surgeon has because of the difficult nature of the diseases we treat.
How should one deal with such a termination – unfair or not? Do not seek revenge. Get over it. Get another job and move on. Fortunately other jobs are abundant in the United States. Moreover, the new job often turns out to be better than the one left behind. The termination actually becomes a blessing in disguise, although it may take time for this to become apparent. Interestingly, many first-line leaders or biggest names in vascular surgery have profited in this way from the apparent major adversity of a termination. As one door closes, another may open if one is alert to the possibilities that may arise from change. Furthermore, the best revenge for an unfair termination is gained by achieving great success in one’s next position.
Although the discussion about dealing with adversity has thus far dealt largely with professional issues, the same principles can be applied to dealing with other aspects of life in general. Vigorous and excessive responses to adversity often result in greater pain and enhancing the wealth of lawyers. Equanimity, minimizing reactivity, and succeeding in the new venture one is forced into – even if unfairly – usually produce the best long-term outcome. It is an imperfect world, and how one deals with the many adversities that are part of it can make it less imperfect.
Overall Patient Satisfaction Better on Hospitalist Teams Compared with Teaching Teams
Clinical question: Is there a difference in patient experience on hospitalist teams compared with teaching teams?
Background: Hospitalist-intensive hospitals tend to perform better on patient-satisfaction measures on HCAHPS survey; however, little is known about the difference in patient experience between patients cared for by hospitalist and trainee teams.
Study design: Retrospective cohort analysis.
Setting: University of Chicago Medical Center.
Synopsis: A 30-day post-discharge survey was sent to 14,855 patients cared for by hospitalist and teaching teams, with 57% of teaching and 31% of hospitalist team patients returning fully completed surveys. A higher percentage of hospitalist team patients reported satisfaction with their overall care (73% vs. 67%; P<0.001; regression model odds ratio = 1.33; 95% CI, 1.15–1.47). There was no statistically significant difference in patient satisfaction with the teamwork of their providers, confidence in identifying their provider, or ability to understand the role of their provider.
Other than the inability to mitigate response-selection bias, the main limitation of this study is the single-center setting, which impacts the generalizability of the findings. Hospital-specific factors like different services and structures (hospitalists at their institution care for renal and lung transplant and oncology patients) could influence patients’ perception of their care. More research needs to be done to determine the specific factors that lead to a better patient experience.
Bottom line: At a single academic center, overall patient satisfaction was higher on a hospitalist service compared with teaching teams.
Citation: Wray CM, Flores A, Padula WV, Prochaska MT, Meltzer DO, Arora VM. Measuring patient experiences on hospitalist and teaching services: patient responses to a 30-day postdischarge questionnaire [published online ahead of print September 18, 2015]. J Hosp Med. doi:10.1002/jhm.2485.
Clinical question: Is there a difference in patient experience on hospitalist teams compared with teaching teams?
Background: Hospitalist-intensive hospitals tend to perform better on patient-satisfaction measures on HCAHPS survey; however, little is known about the difference in patient experience between patients cared for by hospitalist and trainee teams.
Study design: Retrospective cohort analysis.
Setting: University of Chicago Medical Center.
Synopsis: A 30-day post-discharge survey was sent to 14,855 patients cared for by hospitalist and teaching teams, with 57% of teaching and 31% of hospitalist team patients returning fully completed surveys. A higher percentage of hospitalist team patients reported satisfaction with their overall care (73% vs. 67%; P<0.001; regression model odds ratio = 1.33; 95% CI, 1.15–1.47). There was no statistically significant difference in patient satisfaction with the teamwork of their providers, confidence in identifying their provider, or ability to understand the role of their provider.
Other than the inability to mitigate response-selection bias, the main limitation of this study is the single-center setting, which impacts the generalizability of the findings. Hospital-specific factors like different services and structures (hospitalists at their institution care for renal and lung transplant and oncology patients) could influence patients’ perception of their care. More research needs to be done to determine the specific factors that lead to a better patient experience.
Bottom line: At a single academic center, overall patient satisfaction was higher on a hospitalist service compared with teaching teams.
Citation: Wray CM, Flores A, Padula WV, Prochaska MT, Meltzer DO, Arora VM. Measuring patient experiences on hospitalist and teaching services: patient responses to a 30-day postdischarge questionnaire [published online ahead of print September 18, 2015]. J Hosp Med. doi:10.1002/jhm.2485.
Clinical question: Is there a difference in patient experience on hospitalist teams compared with teaching teams?
Background: Hospitalist-intensive hospitals tend to perform better on patient-satisfaction measures on HCAHPS survey; however, little is known about the difference in patient experience between patients cared for by hospitalist and trainee teams.
Study design: Retrospective cohort analysis.
Setting: University of Chicago Medical Center.
Synopsis: A 30-day post-discharge survey was sent to 14,855 patients cared for by hospitalist and teaching teams, with 57% of teaching and 31% of hospitalist team patients returning fully completed surveys. A higher percentage of hospitalist team patients reported satisfaction with their overall care (73% vs. 67%; P<0.001; regression model odds ratio = 1.33; 95% CI, 1.15–1.47). There was no statistically significant difference in patient satisfaction with the teamwork of their providers, confidence in identifying their provider, or ability to understand the role of their provider.
Other than the inability to mitigate response-selection bias, the main limitation of this study is the single-center setting, which impacts the generalizability of the findings. Hospital-specific factors like different services and structures (hospitalists at their institution care for renal and lung transplant and oncology patients) could influence patients’ perception of their care. More research needs to be done to determine the specific factors that lead to a better patient experience.
Bottom line: At a single academic center, overall patient satisfaction was higher on a hospitalist service compared with teaching teams.
Citation: Wray CM, Flores A, Padula WV, Prochaska MT, Meltzer DO, Arora VM. Measuring patient experiences on hospitalist and teaching services: patient responses to a 30-day postdischarge questionnaire [published online ahead of print September 18, 2015]. J Hosp Med. doi:10.1002/jhm.2485.
Antiplatelet drug appears effective for women

while another doctor looks on
Photo courtesy of NCI
An analysis of data from the CHAMPION PHOENIX trial suggests cangrelor is more effective than clopidogrel for preventing complications in women undergoing percutaneous coronary intervention (PCI).
Rates of severe bleeding did not differ significantly between the treatment arms, but women who received cangrelor had a higher rate of moderate bleeding than those who received clopidogrel.
Researchers relayed these results in Circulation.
The CHAMPION PHOENIX trial was funded by The Medicines Company, which manufactures cangrelor.
For this phase 3 trial, researchers compared the safety and efficacy of clopidogrel and cangrelor in 11,145 patients who were undergoing elective or urgent PCI.
In the initial analysis of trial data, cangrelor reduced the overall odds of complications from PCI, which included death, myocardial infarction, ischemia-driven revascularization, and stent thrombosis.
But cangrelor also resulted in significantly higher rates of major and minor bleeding when compared to clopidogrel. The rates of severe bleeding were similar between the treatment arms.
With the current analysis, researchers wanted to determine if the effects of cangrelor and clopidogrel differed between men and women.
“In the past, questions have been raised about the safety and efficacy of blood thinners in women,” said study author Michelle O’Donoghue, MD, of Brigham and Women’s Hospital in Boston, Massachusetts.
“This study provides important reassurance, overall, that [cangrelor] appears to offer as much benefit for women as it does for men.”
The primary efficacy endpoint was the composite of death, myocardial infarction, ischemia-driven revascularization, and stent thrombosis at 48 hours. The primary safety endpoint was GUSTO severe bleeding at 48 hours.
Sex differences
Of the 11,451 patients in this trial, 3051 (28%) were female. These patients were more likely than males to be older and to have a history of diabetes mellitus, hypertension, hyperlipidemia, prior stroke, or transient ischemic attack.
Women were more likely than men to be enrolled with stable angina or non ST-segment elevation myocardial infarction, and ST-segment elevation myocardial infarction was more common in men.
The women were less likely to have a prior history of myocardial infarction or coronary revascularization, and they had lower baseline hemoglobin and hematocrit levels than men.
Men were more likely than women to receive aspirin, but there was no difference between the sexes when it came to the choice of clopidogrel loading dose and the use of unfractionated heparin and bivalirudin. The median duration of PCI was longer in men than women, but the choice of access site was similar.
When the researchers adjusted for potentially confounding factors, they found that being female was independently associated with higher odds of the primary efficacy outcome (adjusted odds ratio [aOR]=1.30) and GUSTO moderate or severe bleeding (aOR=2.70).
Efficacy and safety
For women, cangrelor was associated with a significant decrease in the odds of achieving the primary efficacy endpoint. Men were less likely to achieve the endpoint when on cangrelor as well, but the difference between the cangrelor and clopidogrel arms was not statistically significant for men.
The percentage of women who met criteria for the primary efficacy endpoint was 4.8% in the cangrelor arm and 6.9% in the clopidogrel arm (aOR=0.65, P=0.01). The percentage of men who did so was 4.7% in the cangrelor arm and 5.5% in the clopidogrel arm (aOR=0.86, P=0.14, P interaction=0.23).
Cangrelor was associated with a significantly lower risk of stent thrombosis at 48 hours for women but not men.
For women, the incidence of stent thrombosis was 0.8% in the cangrelor arm and 1.9% in the clopidogrel arm (aOR=0.39, P=0.01). For men, the rates were 0.9% and 1.1%, respectively (aOR=0.84, P=0.44, P interaction=0.11).
There was no significant difference in severe bleeding between the treatment arms for men or women, but women had a significantly higher risk of moderate bleeding if they received cangrelor.
For women, the rate of severe bleeding was 0.3% in the cangrelor arm and 0.2% in the clopidogrel arm (aOR=2.37, P=0.30). For men, the rates were 0.1% in both arms (aOR=2.04, P=0.41, P interaction=0.88 ).
For women, the rate of moderate bleeding was 0.9% in the cangrelor arm and 0.3% in the clopidogrel arm (aOR=3.63, P=0.02). For men, the rates were 0.2% in both arms (aOR=0.81, P=0.68, P interaction=0.04). ![]()

while another doctor looks on
Photo courtesy of NCI
An analysis of data from the CHAMPION PHOENIX trial suggests cangrelor is more effective than clopidogrel for preventing complications in women undergoing percutaneous coronary intervention (PCI).
Rates of severe bleeding did not differ significantly between the treatment arms, but women who received cangrelor had a higher rate of moderate bleeding than those who received clopidogrel.
Researchers relayed these results in Circulation.
The CHAMPION PHOENIX trial was funded by The Medicines Company, which manufactures cangrelor.
For this phase 3 trial, researchers compared the safety and efficacy of clopidogrel and cangrelor in 11,145 patients who were undergoing elective or urgent PCI.
In the initial analysis of trial data, cangrelor reduced the overall odds of complications from PCI, which included death, myocardial infarction, ischemia-driven revascularization, and stent thrombosis.
But cangrelor also resulted in significantly higher rates of major and minor bleeding when compared to clopidogrel. The rates of severe bleeding were similar between the treatment arms.
With the current analysis, researchers wanted to determine if the effects of cangrelor and clopidogrel differed between men and women.
“In the past, questions have been raised about the safety and efficacy of blood thinners in women,” said study author Michelle O’Donoghue, MD, of Brigham and Women’s Hospital in Boston, Massachusetts.
“This study provides important reassurance, overall, that [cangrelor] appears to offer as much benefit for women as it does for men.”
The primary efficacy endpoint was the composite of death, myocardial infarction, ischemia-driven revascularization, and stent thrombosis at 48 hours. The primary safety endpoint was GUSTO severe bleeding at 48 hours.
Sex differences
Of the 11,451 patients in this trial, 3051 (28%) were female. These patients were more likely than males to be older and to have a history of diabetes mellitus, hypertension, hyperlipidemia, prior stroke, or transient ischemic attack.
Women were more likely than men to be enrolled with stable angina or non ST-segment elevation myocardial infarction, and ST-segment elevation myocardial infarction was more common in men.
The women were less likely to have a prior history of myocardial infarction or coronary revascularization, and they had lower baseline hemoglobin and hematocrit levels than men.
Men were more likely than women to receive aspirin, but there was no difference between the sexes when it came to the choice of clopidogrel loading dose and the use of unfractionated heparin and bivalirudin. The median duration of PCI was longer in men than women, but the choice of access site was similar.
When the researchers adjusted for potentially confounding factors, they found that being female was independently associated with higher odds of the primary efficacy outcome (adjusted odds ratio [aOR]=1.30) and GUSTO moderate or severe bleeding (aOR=2.70).
Efficacy and safety
For women, cangrelor was associated with a significant decrease in the odds of achieving the primary efficacy endpoint. Men were less likely to achieve the endpoint when on cangrelor as well, but the difference between the cangrelor and clopidogrel arms was not statistically significant for men.
The percentage of women who met criteria for the primary efficacy endpoint was 4.8% in the cangrelor arm and 6.9% in the clopidogrel arm (aOR=0.65, P=0.01). The percentage of men who did so was 4.7% in the cangrelor arm and 5.5% in the clopidogrel arm (aOR=0.86, P=0.14, P interaction=0.23).
Cangrelor was associated with a significantly lower risk of stent thrombosis at 48 hours for women but not men.
For women, the incidence of stent thrombosis was 0.8% in the cangrelor arm and 1.9% in the clopidogrel arm (aOR=0.39, P=0.01). For men, the rates were 0.9% and 1.1%, respectively (aOR=0.84, P=0.44, P interaction=0.11).
There was no significant difference in severe bleeding between the treatment arms for men or women, but women had a significantly higher risk of moderate bleeding if they received cangrelor.
For women, the rate of severe bleeding was 0.3% in the cangrelor arm and 0.2% in the clopidogrel arm (aOR=2.37, P=0.30). For men, the rates were 0.1% in both arms (aOR=2.04, P=0.41, P interaction=0.88 ).
For women, the rate of moderate bleeding was 0.9% in the cangrelor arm and 0.3% in the clopidogrel arm (aOR=3.63, P=0.02). For men, the rates were 0.2% in both arms (aOR=0.81, P=0.68, P interaction=0.04). ![]()

while another doctor looks on
Photo courtesy of NCI
An analysis of data from the CHAMPION PHOENIX trial suggests cangrelor is more effective than clopidogrel for preventing complications in women undergoing percutaneous coronary intervention (PCI).
Rates of severe bleeding did not differ significantly between the treatment arms, but women who received cangrelor had a higher rate of moderate bleeding than those who received clopidogrel.
Researchers relayed these results in Circulation.
The CHAMPION PHOENIX trial was funded by The Medicines Company, which manufactures cangrelor.
For this phase 3 trial, researchers compared the safety and efficacy of clopidogrel and cangrelor in 11,145 patients who were undergoing elective or urgent PCI.
In the initial analysis of trial data, cangrelor reduced the overall odds of complications from PCI, which included death, myocardial infarction, ischemia-driven revascularization, and stent thrombosis.
But cangrelor also resulted in significantly higher rates of major and minor bleeding when compared to clopidogrel. The rates of severe bleeding were similar between the treatment arms.
With the current analysis, researchers wanted to determine if the effects of cangrelor and clopidogrel differed between men and women.
“In the past, questions have been raised about the safety and efficacy of blood thinners in women,” said study author Michelle O’Donoghue, MD, of Brigham and Women’s Hospital in Boston, Massachusetts.
“This study provides important reassurance, overall, that [cangrelor] appears to offer as much benefit for women as it does for men.”
The primary efficacy endpoint was the composite of death, myocardial infarction, ischemia-driven revascularization, and stent thrombosis at 48 hours. The primary safety endpoint was GUSTO severe bleeding at 48 hours.
Sex differences
Of the 11,451 patients in this trial, 3051 (28%) were female. These patients were more likely than males to be older and to have a history of diabetes mellitus, hypertension, hyperlipidemia, prior stroke, or transient ischemic attack.
Women were more likely than men to be enrolled with stable angina or non ST-segment elevation myocardial infarction, and ST-segment elevation myocardial infarction was more common in men.
The women were less likely to have a prior history of myocardial infarction or coronary revascularization, and they had lower baseline hemoglobin and hematocrit levels than men.
Men were more likely than women to receive aspirin, but there was no difference between the sexes when it came to the choice of clopidogrel loading dose and the use of unfractionated heparin and bivalirudin. The median duration of PCI was longer in men than women, but the choice of access site was similar.
When the researchers adjusted for potentially confounding factors, they found that being female was independently associated with higher odds of the primary efficacy outcome (adjusted odds ratio [aOR]=1.30) and GUSTO moderate or severe bleeding (aOR=2.70).
Efficacy and safety
For women, cangrelor was associated with a significant decrease in the odds of achieving the primary efficacy endpoint. Men were less likely to achieve the endpoint when on cangrelor as well, but the difference between the cangrelor and clopidogrel arms was not statistically significant for men.
The percentage of women who met criteria for the primary efficacy endpoint was 4.8% in the cangrelor arm and 6.9% in the clopidogrel arm (aOR=0.65, P=0.01). The percentage of men who did so was 4.7% in the cangrelor arm and 5.5% in the clopidogrel arm (aOR=0.86, P=0.14, P interaction=0.23).
Cangrelor was associated with a significantly lower risk of stent thrombosis at 48 hours for women but not men.
For women, the incidence of stent thrombosis was 0.8% in the cangrelor arm and 1.9% in the clopidogrel arm (aOR=0.39, P=0.01). For men, the rates were 0.9% and 1.1%, respectively (aOR=0.84, P=0.44, P interaction=0.11).
There was no significant difference in severe bleeding between the treatment arms for men or women, but women had a significantly higher risk of moderate bleeding if they received cangrelor.
For women, the rate of severe bleeding was 0.3% in the cangrelor arm and 0.2% in the clopidogrel arm (aOR=2.37, P=0.30). For men, the rates were 0.1% in both arms (aOR=2.04, P=0.41, P interaction=0.88 ).
For women, the rate of moderate bleeding was 0.9% in the cangrelor arm and 0.3% in the clopidogrel arm (aOR=3.63, P=0.02). For men, the rates were 0.2% in both arms (aOR=0.81, P=0.68, P interaction=0.04). ![]()
New insight into CLL development

Photo by Graham Colm
New research indicates that chronic lymphocytic leukemia (CLL) can develop during nearly any stage of B-cell maturation.
However, CLL that arises from more progressive maturation stages responds better to therapy.
The study also suggests that most methylation events that were previously thought to be tumor-specific are normally present in non-malignant B cells.
These findings were published in Nature Genetics.
Christoph Plass, PhD, of the German Cancer Research Center (DKFZ) in Heidelberg, and his colleagues conducted this study to determine which development stage of B cells marks the origin of B-cell CLL.
The team took blood samples from 268 CLL patients, separated the blood cells using specific B-cell maturation markers and analyzed the methylation patterns of each individual maturation stage.
The investigators were surprised to find that CLL can develop from almost all maturation stages. They also found that maturation was associated with “increasingly favorable clinical outcomes.”
In addition, methylation patterns that were previously regarded as cancer-specific actually reflect the characteristic patterns of the development stages at the moment of cancerous transformation.
The investigators found that the cell “freezes” this methylation pattern, and this is followed by only a few changes that are truly cancer-specific.
The team said they used advanced bioinformatic methods to calculate the small percentage of cancer-specific methylation patterns from the wealth of maturation-related variations.
“Up until recently, it was technically impossible to study the various maturation stages in such detail as we have done,” Dr Plass said. “It took the advanced sequencing technology and the powerful bioinformatic methods that we have available now to make such a detailed comparison possible.”
The investigators said their findings differ from those of prior studies because, with the current study, they compared CLL cells with the whole pool of B-cell maturation stages.
“All differences found were attributed to cancer,” Dr Plass said, adding that some previous works on the cancer epigenome will need to be re-interpreted in the light of the current results.
Next, Dr Plass and his colleagues want to examine other cancer types to determine whether methylation patterns that are thought to be cancer-specific also arise from the normal cellular maturation program. In particular, they plan to study other hematologic malignancies and prostate cancer. ![]()

Photo by Graham Colm
New research indicates that chronic lymphocytic leukemia (CLL) can develop during nearly any stage of B-cell maturation.
However, CLL that arises from more progressive maturation stages responds better to therapy.
The study also suggests that most methylation events that were previously thought to be tumor-specific are normally present in non-malignant B cells.
These findings were published in Nature Genetics.
Christoph Plass, PhD, of the German Cancer Research Center (DKFZ) in Heidelberg, and his colleagues conducted this study to determine which development stage of B cells marks the origin of B-cell CLL.
The team took blood samples from 268 CLL patients, separated the blood cells using specific B-cell maturation markers and analyzed the methylation patterns of each individual maturation stage.
The investigators were surprised to find that CLL can develop from almost all maturation stages. They also found that maturation was associated with “increasingly favorable clinical outcomes.”
In addition, methylation patterns that were previously regarded as cancer-specific actually reflect the characteristic patterns of the development stages at the moment of cancerous transformation.
The investigators found that the cell “freezes” this methylation pattern, and this is followed by only a few changes that are truly cancer-specific.
The team said they used advanced bioinformatic methods to calculate the small percentage of cancer-specific methylation patterns from the wealth of maturation-related variations.
“Up until recently, it was technically impossible to study the various maturation stages in such detail as we have done,” Dr Plass said. “It took the advanced sequencing technology and the powerful bioinformatic methods that we have available now to make such a detailed comparison possible.”
The investigators said their findings differ from those of prior studies because, with the current study, they compared CLL cells with the whole pool of B-cell maturation stages.
“All differences found were attributed to cancer,” Dr Plass said, adding that some previous works on the cancer epigenome will need to be re-interpreted in the light of the current results.
Next, Dr Plass and his colleagues want to examine other cancer types to determine whether methylation patterns that are thought to be cancer-specific also arise from the normal cellular maturation program. In particular, they plan to study other hematologic malignancies and prostate cancer. ![]()

Photo by Graham Colm
New research indicates that chronic lymphocytic leukemia (CLL) can develop during nearly any stage of B-cell maturation.
However, CLL that arises from more progressive maturation stages responds better to therapy.
The study also suggests that most methylation events that were previously thought to be tumor-specific are normally present in non-malignant B cells.
These findings were published in Nature Genetics.
Christoph Plass, PhD, of the German Cancer Research Center (DKFZ) in Heidelberg, and his colleagues conducted this study to determine which development stage of B cells marks the origin of B-cell CLL.
The team took blood samples from 268 CLL patients, separated the blood cells using specific B-cell maturation markers and analyzed the methylation patterns of each individual maturation stage.
The investigators were surprised to find that CLL can develop from almost all maturation stages. They also found that maturation was associated with “increasingly favorable clinical outcomes.”
In addition, methylation patterns that were previously regarded as cancer-specific actually reflect the characteristic patterns of the development stages at the moment of cancerous transformation.
The investigators found that the cell “freezes” this methylation pattern, and this is followed by only a few changes that are truly cancer-specific.
The team said they used advanced bioinformatic methods to calculate the small percentage of cancer-specific methylation patterns from the wealth of maturation-related variations.
“Up until recently, it was technically impossible to study the various maturation stages in such detail as we have done,” Dr Plass said. “It took the advanced sequencing technology and the powerful bioinformatic methods that we have available now to make such a detailed comparison possible.”
The investigators said their findings differ from those of prior studies because, with the current study, they compared CLL cells with the whole pool of B-cell maturation stages.
“All differences found were attributed to cancer,” Dr Plass said, adding that some previous works on the cancer epigenome will need to be re-interpreted in the light of the current results.
Next, Dr Plass and his colleagues want to examine other cancer types to determine whether methylation patterns that are thought to be cancer-specific also arise from the normal cellular maturation program. In particular, they plan to study other hematologic malignancies and prostate cancer. ![]()
VIDEO: Preventing healthcare acquired infections after CT surgery
PHOENIX – More and more attention is being paid to preventing healthcare acquired infections (HAIs) in the hospital setting, and the role of HAIs in cardiothoracic surgery is a particlularly important area of focus.
“The good news is that cardiothoracic surgeons are really good at preventing infections. There’s been a lot of pressure over the past many years to report infections after cardiothoracic surgery, and so they’ve gotten a lot of things right,” Dr. Emily Landon said in a video interview at the annual meeting of the Society of Thoracic Surgeons.
“However, patients that undergo cardiothoracic surgery are still at risk of the infections that plague everyone in hospitals ... all of these are a problem based on whatever the hospital’s current situation is.”
Dr. Landon, who is the medical director of antimicrobial stewardship and infection control at University of Chicago Medicine, Chicago, discussed how cardiothroacic surgeons can maintain their own good outcomes and how they can have a postive impact outside the OR on protecting their patients after surgery.
Dr. Landon reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
PHOENIX – More and more attention is being paid to preventing healthcare acquired infections (HAIs) in the hospital setting, and the role of HAIs in cardiothoracic surgery is a particlularly important area of focus.
“The good news is that cardiothoracic surgeons are really good at preventing infections. There’s been a lot of pressure over the past many years to report infections after cardiothoracic surgery, and so they’ve gotten a lot of things right,” Dr. Emily Landon said in a video interview at the annual meeting of the Society of Thoracic Surgeons.
“However, patients that undergo cardiothoracic surgery are still at risk of the infections that plague everyone in hospitals ... all of these are a problem based on whatever the hospital’s current situation is.”
Dr. Landon, who is the medical director of antimicrobial stewardship and infection control at University of Chicago Medicine, Chicago, discussed how cardiothroacic surgeons can maintain their own good outcomes and how they can have a postive impact outside the OR on protecting their patients after surgery.
Dr. Landon reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
PHOENIX – More and more attention is being paid to preventing healthcare acquired infections (HAIs) in the hospital setting, and the role of HAIs in cardiothoracic surgery is a particlularly important area of focus.
“The good news is that cardiothoracic surgeons are really good at preventing infections. There’s been a lot of pressure over the past many years to report infections after cardiothoracic surgery, and so they’ve gotten a lot of things right,” Dr. Emily Landon said in a video interview at the annual meeting of the Society of Thoracic Surgeons.
“However, patients that undergo cardiothoracic surgery are still at risk of the infections that plague everyone in hospitals ... all of these are a problem based on whatever the hospital’s current situation is.”
Dr. Landon, who is the medical director of antimicrobial stewardship and infection control at University of Chicago Medicine, Chicago, discussed how cardiothroacic surgeons can maintain their own good outcomes and how they can have a postive impact outside the OR on protecting their patients after surgery.
Dr. Landon reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
EXPERT ANALYSIS FROM THE STS ANNUAL MEETING










