User login
Finding more transplant hearts but not more donors
Heart transplant volumes in the United States have remained static since the start of the century because of improved trauma prevention and treatment, but that has challenged cardiologists to find enough donor hearts for the growing ranks of advanced heart failure patients. So a multidisciplinary team at the University of Washington in Seattle initiated a quality improvement program that doubled transplant volume without any change in transplant-related deaths by accepting hearts they would have otherwise discarded.
The study came about after the researchers determined that a large number of donor hearts from their own organ procurement program were being sent to other transplant centers. So they gathered a multidisciplinary team of transplant surgeons, cardiologists, and members of the organ procurement program to study ways to improve its center-specific organ utilization rate. The endeavor resulted in an increase in utilization rates from 28% to 49% in a year, a rate that has been sustained through a second year, according to study findings published in the January issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:238-43).
“The simple process of systematically reviewing donor turn down events as a group tended to reduce variability [and] increase confidence in expanded criteria donors and resulted in improved donor organ utilization and transplant volumes,” lead author Dr. Jason Smith and colleagues said.
The 30-day and 1-year death rates were similar before and after the quality improvement program started, but the death rates of those on the heart wait list declined from 17.2% to 12%, “which was not statistically significant,” Dr. Smith and coauthors said, “but does show that increasing use of organs that may be outside of the usual pattern has a trend toward improved wait list survival and needs to be considered when assessing donor hearts.”
Because of excellent results of heart transplants in patients with advanced heart failure, a number of investigators have proposed expanding the population of heart donors to include older people, those with higher risk of infectious disease, or with heart disease such as coronary artery disease and left ventricular hypertrophy, Dr. Smith and coauthors said. Their own review found a higher-than-expected rate of donor hearts sent to other centers from the University of Washington organ procurement program.
The multidisciplinary team analyzed the organs the University of Washington surgeons refused and sent to other institutions from July 2012 to June 2013.
For a year after that, the multidisciplinary group did real-time analysis of organ refusal along with quarterly reviews “in a non-confrontational, proactive” setting, as Dr. Smith and his colleagues described it. The group held open discussions on refused organs that were ultimately transplanted elsewhere. “The review process was facilitated to provide a constructive environment to encourage development of best practices and consistency,” the researchers noted. The quality improvement program led to an increase in the unit’s transplant volume despite fewer donor offers.
The researchers acknowledged that donor assessment has been the focus of much controversy. They pointed out that average donor age has increased over the last 20 years from 29 years to 33 years and has since retreated to 31 years, and some programs utilize donors up to their mid-60s. Also, previous studies have advocated for the use of donors who meet the criteria of the Centers for Disease Control and Prevention high risk behavior of infection as well as some drug abusers because of the low-risk of transmission and emerging evidence affirming the safety of hearts of drug users.
“The individual decision to utilize or discard a donor organ is one of the most challenging aspects of transplant medicine,” Dr. Smith and colleagues said. “It requires balancing donor risks against the exigencies of the recipient.”
Today, the multidisciplinary team evaluates each heart offered for donation and is exploring ways to accept even more donor hearts, even discarded hearts. “This represents a large, untapped pool of potential donor hearts that might add to the net number of transplants performed nationally and not merely redistribute organ usage,” Dr. Smith and colleagues said.
Dr. Smith is a consultant for Thoratec and is a primary site investigator for the EXPAND Trial sponsored by TransMedics. Dr. Todd Dardas is supported by the American College of Cardiology/Daiichi Sankyo Career Development Award. Dr. Jay Pal receives grant support from Tenax. Dr. Wayne Levy is a consultant for HeartWare, Novartis, GE Healthcare, Pharmin, and Biotronik. Dr. Claudius Mahr is a consultant for Thoratec, HeartWare and Abiomed. Dr. Nahush Mokadam is a consultant for Thoratec, HeartWare, Syncardia and St. Jude Medical, and has research grants from Thoratec, HeartWare and Syncardia. The other coauthors had no relationships to disclose.
How the University of Washington researchers brought about such a dramatic increase in donor heart utilization raises a number of questions, Dr. Nicholas Smedira of Cleveland Clinic said in his invited commentary (J Thorac Cardiovasc Surg 2016;151:243-4).
“They refer euphemistically to ‘behavioral adaptation’ and ‘frank discussions’ regarding ‘individual and group bias’ as explanations, but understanding exactly how this is accomplished is not easy,” Dr. Smedira said.
Noteworthy is that the researchers used more donors who meet Center for Disease Control and Prevention high risk criteria for infectious disease. However, cardiologists tend to weigh their decision for accepting donor hearts “by the last memorable or distressful experience,” Dr. Smedira said. Hence, many of these donor hearts go unused. At the same time, assessing risk without complete information is challenging, he said.
Besides their thought processes, other factors that influence cardiologists’ decisions on accepting donor hearts include fatigue, scheduling conflicts, reimbursement issues, and outcome metrics. He credited the University of Washington for its “courage” to examine their decision-making process, including exploring biases as well as working “collectively and blamelessly” to support their decisions. “I would encourage more transplant centers to follow a program similar to the University of Washington’s and maybe we will be hearing more yeses and fewer nos,” Dr. Smedira said.
He had no relationships to disclose.
How the University of Washington researchers brought about such a dramatic increase in donor heart utilization raises a number of questions, Dr. Nicholas Smedira of Cleveland Clinic said in his invited commentary (J Thorac Cardiovasc Surg 2016;151:243-4).
“They refer euphemistically to ‘behavioral adaptation’ and ‘frank discussions’ regarding ‘individual and group bias’ as explanations, but understanding exactly how this is accomplished is not easy,” Dr. Smedira said.
Noteworthy is that the researchers used more donors who meet Center for Disease Control and Prevention high risk criteria for infectious disease. However, cardiologists tend to weigh their decision for accepting donor hearts “by the last memorable or distressful experience,” Dr. Smedira said. Hence, many of these donor hearts go unused. At the same time, assessing risk without complete information is challenging, he said.
Besides their thought processes, other factors that influence cardiologists’ decisions on accepting donor hearts include fatigue, scheduling conflicts, reimbursement issues, and outcome metrics. He credited the University of Washington for its “courage” to examine their decision-making process, including exploring biases as well as working “collectively and blamelessly” to support their decisions. “I would encourage more transplant centers to follow a program similar to the University of Washington’s and maybe we will be hearing more yeses and fewer nos,” Dr. Smedira said.
He had no relationships to disclose.
How the University of Washington researchers brought about such a dramatic increase in donor heart utilization raises a number of questions, Dr. Nicholas Smedira of Cleveland Clinic said in his invited commentary (J Thorac Cardiovasc Surg 2016;151:243-4).
“They refer euphemistically to ‘behavioral adaptation’ and ‘frank discussions’ regarding ‘individual and group bias’ as explanations, but understanding exactly how this is accomplished is not easy,” Dr. Smedira said.
Noteworthy is that the researchers used more donors who meet Center for Disease Control and Prevention high risk criteria for infectious disease. However, cardiologists tend to weigh their decision for accepting donor hearts “by the last memorable or distressful experience,” Dr. Smedira said. Hence, many of these donor hearts go unused. At the same time, assessing risk without complete information is challenging, he said.
Besides their thought processes, other factors that influence cardiologists’ decisions on accepting donor hearts include fatigue, scheduling conflicts, reimbursement issues, and outcome metrics. He credited the University of Washington for its “courage” to examine their decision-making process, including exploring biases as well as working “collectively and blamelessly” to support their decisions. “I would encourage more transplant centers to follow a program similar to the University of Washington’s and maybe we will be hearing more yeses and fewer nos,” Dr. Smedira said.
He had no relationships to disclose.
Heart transplant volumes in the United States have remained static since the start of the century because of improved trauma prevention and treatment, but that has challenged cardiologists to find enough donor hearts for the growing ranks of advanced heart failure patients. So a multidisciplinary team at the University of Washington in Seattle initiated a quality improvement program that doubled transplant volume without any change in transplant-related deaths by accepting hearts they would have otherwise discarded.
The study came about after the researchers determined that a large number of donor hearts from their own organ procurement program were being sent to other transplant centers. So they gathered a multidisciplinary team of transplant surgeons, cardiologists, and members of the organ procurement program to study ways to improve its center-specific organ utilization rate. The endeavor resulted in an increase in utilization rates from 28% to 49% in a year, a rate that has been sustained through a second year, according to study findings published in the January issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:238-43).
“The simple process of systematically reviewing donor turn down events as a group tended to reduce variability [and] increase confidence in expanded criteria donors and resulted in improved donor organ utilization and transplant volumes,” lead author Dr. Jason Smith and colleagues said.
The 30-day and 1-year death rates were similar before and after the quality improvement program started, but the death rates of those on the heart wait list declined from 17.2% to 12%, “which was not statistically significant,” Dr. Smith and coauthors said, “but does show that increasing use of organs that may be outside of the usual pattern has a trend toward improved wait list survival and needs to be considered when assessing donor hearts.”
Because of excellent results of heart transplants in patients with advanced heart failure, a number of investigators have proposed expanding the population of heart donors to include older people, those with higher risk of infectious disease, or with heart disease such as coronary artery disease and left ventricular hypertrophy, Dr. Smith and coauthors said. Their own review found a higher-than-expected rate of donor hearts sent to other centers from the University of Washington organ procurement program.
The multidisciplinary team analyzed the organs the University of Washington surgeons refused and sent to other institutions from July 2012 to June 2013.
For a year after that, the multidisciplinary group did real-time analysis of organ refusal along with quarterly reviews “in a non-confrontational, proactive” setting, as Dr. Smith and his colleagues described it. The group held open discussions on refused organs that were ultimately transplanted elsewhere. “The review process was facilitated to provide a constructive environment to encourage development of best practices and consistency,” the researchers noted. The quality improvement program led to an increase in the unit’s transplant volume despite fewer donor offers.
The researchers acknowledged that donor assessment has been the focus of much controversy. They pointed out that average donor age has increased over the last 20 years from 29 years to 33 years and has since retreated to 31 years, and some programs utilize donors up to their mid-60s. Also, previous studies have advocated for the use of donors who meet the criteria of the Centers for Disease Control and Prevention high risk behavior of infection as well as some drug abusers because of the low-risk of transmission and emerging evidence affirming the safety of hearts of drug users.
“The individual decision to utilize or discard a donor organ is one of the most challenging aspects of transplant medicine,” Dr. Smith and colleagues said. “It requires balancing donor risks against the exigencies of the recipient.”
Today, the multidisciplinary team evaluates each heart offered for donation and is exploring ways to accept even more donor hearts, even discarded hearts. “This represents a large, untapped pool of potential donor hearts that might add to the net number of transplants performed nationally and not merely redistribute organ usage,” Dr. Smith and colleagues said.
Dr. Smith is a consultant for Thoratec and is a primary site investigator for the EXPAND Trial sponsored by TransMedics. Dr. Todd Dardas is supported by the American College of Cardiology/Daiichi Sankyo Career Development Award. Dr. Jay Pal receives grant support from Tenax. Dr. Wayne Levy is a consultant for HeartWare, Novartis, GE Healthcare, Pharmin, and Biotronik. Dr. Claudius Mahr is a consultant for Thoratec, HeartWare and Abiomed. Dr. Nahush Mokadam is a consultant for Thoratec, HeartWare, Syncardia and St. Jude Medical, and has research grants from Thoratec, HeartWare and Syncardia. The other coauthors had no relationships to disclose.
Heart transplant volumes in the United States have remained static since the start of the century because of improved trauma prevention and treatment, but that has challenged cardiologists to find enough donor hearts for the growing ranks of advanced heart failure patients. So a multidisciplinary team at the University of Washington in Seattle initiated a quality improvement program that doubled transplant volume without any change in transplant-related deaths by accepting hearts they would have otherwise discarded.
The study came about after the researchers determined that a large number of donor hearts from their own organ procurement program were being sent to other transplant centers. So they gathered a multidisciplinary team of transplant surgeons, cardiologists, and members of the organ procurement program to study ways to improve its center-specific organ utilization rate. The endeavor resulted in an increase in utilization rates from 28% to 49% in a year, a rate that has been sustained through a second year, according to study findings published in the January issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:238-43).
“The simple process of systematically reviewing donor turn down events as a group tended to reduce variability [and] increase confidence in expanded criteria donors and resulted in improved donor organ utilization and transplant volumes,” lead author Dr. Jason Smith and colleagues said.
The 30-day and 1-year death rates were similar before and after the quality improvement program started, but the death rates of those on the heart wait list declined from 17.2% to 12%, “which was not statistically significant,” Dr. Smith and coauthors said, “but does show that increasing use of organs that may be outside of the usual pattern has a trend toward improved wait list survival and needs to be considered when assessing donor hearts.”
Because of excellent results of heart transplants in patients with advanced heart failure, a number of investigators have proposed expanding the population of heart donors to include older people, those with higher risk of infectious disease, or with heart disease such as coronary artery disease and left ventricular hypertrophy, Dr. Smith and coauthors said. Their own review found a higher-than-expected rate of donor hearts sent to other centers from the University of Washington organ procurement program.
The multidisciplinary team analyzed the organs the University of Washington surgeons refused and sent to other institutions from July 2012 to June 2013.
For a year after that, the multidisciplinary group did real-time analysis of organ refusal along with quarterly reviews “in a non-confrontational, proactive” setting, as Dr. Smith and his colleagues described it. The group held open discussions on refused organs that were ultimately transplanted elsewhere. “The review process was facilitated to provide a constructive environment to encourage development of best practices and consistency,” the researchers noted. The quality improvement program led to an increase in the unit’s transplant volume despite fewer donor offers.
The researchers acknowledged that donor assessment has been the focus of much controversy. They pointed out that average donor age has increased over the last 20 years from 29 years to 33 years and has since retreated to 31 years, and some programs utilize donors up to their mid-60s. Also, previous studies have advocated for the use of donors who meet the criteria of the Centers for Disease Control and Prevention high risk behavior of infection as well as some drug abusers because of the low-risk of transmission and emerging evidence affirming the safety of hearts of drug users.
“The individual decision to utilize or discard a donor organ is one of the most challenging aspects of transplant medicine,” Dr. Smith and colleagues said. “It requires balancing donor risks against the exigencies of the recipient.”
Today, the multidisciplinary team evaluates each heart offered for donation and is exploring ways to accept even more donor hearts, even discarded hearts. “This represents a large, untapped pool of potential donor hearts that might add to the net number of transplants performed nationally and not merely redistribute organ usage,” Dr. Smith and colleagues said.
Dr. Smith is a consultant for Thoratec and is a primary site investigator for the EXPAND Trial sponsored by TransMedics. Dr. Todd Dardas is supported by the American College of Cardiology/Daiichi Sankyo Career Development Award. Dr. Jay Pal receives grant support from Tenax. Dr. Wayne Levy is a consultant for HeartWare, Novartis, GE Healthcare, Pharmin, and Biotronik. Dr. Claudius Mahr is a consultant for Thoratec, HeartWare and Abiomed. Dr. Nahush Mokadam is a consultant for Thoratec, HeartWare, Syncardia and St. Jude Medical, and has research grants from Thoratec, HeartWare and Syncardia. The other coauthors had no relationships to disclose.
Key clinical point: A group approach to systematically review rejected donor organs has led to expanded donor criteria and resulted in improved donor organ utilization and transplant volume.
Major finding: Transplant utilization rate increased from 28% to 49% with no significant change in 30-day survival after implementation of a donor review protocol.
Data source: Retrospective review of 293 total donor heart offers at a single center from July 2012 to June 2013 compared with review of 279 heart offers from July 2013 to June 2014.
Disclosures: Lead author Dr. Jason Smith is a consultant for Thoratec and is a primary site investigator for the EXPAND Trial sponsored by TransMedics. Dr. Todd Dardas is supported by the American College of Cardiology/Daiichi Sankyo Career Development Award. Dr. Jay Pal receives grant support from Tenax. Dr. Wayne Levy is a consultant for HeartWare, Novartis, GE Healthcare, Pharmin, and Biotronik. Dr. Claudius Mahr is a consultant for Thoratec, HeartWare and Abiomed. Dr. Nahush Mokadam is a consultant for Thoratec, HeartWare, Syncardia, and St. Jude Medical, and has research grants from Thoratec, HeartWare and Syncardia. The other coauthors had no relationships to disclose.
False Estradiol Results From Interaction With Fulvestrant
Estradiol testing may guide treatment for patients with estrogen receptor-positive breast cancer, but researchers from Rush University Medical Center in Chicago, Illinois, have a cautionary report about relying on that when fulvestrant, an estrogen receptor antagonist, is used with standard steroid immunoassays. They report on a patient who had a falsely elevated estradiol reading that led to unnecessary procedures.
Related: Delayed Adjuvant Chemotherapy Significantly Affects Breast Cancer Recovery
Their patient underwent a bilateral oophorectomy and was then started on anti-estrogen therapy with letrozole and fulvestrant, as well as zoledronic acid. At the patient’s request, her primary oncologist obtained a serum estradiol level, which was “unexpectedly” high. The finding was puzzling, the authors say, because she had reported menopausal symptoms, such as hot flashes, which were not consistent with the estradiol level obtained. She also had a complete clinical response to treatment, according to symptoms, radiologic findings, and decreasing levels of carcinoma antigen 125.
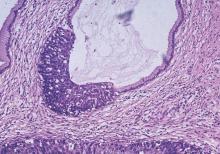
A pelvic ultrasound revealed a possible small soft tissue density in the left adnexal region—a “concerning” finding suggesting ovarian remnant syndrome, a rare condition in which ovarian tissue remains after oophorectomy.
Related: Extending Therapy for Breast Cancer
After additional imaging and laparoscopy, pathology revealed fibrovascular and adipose tissue, but no ovarian tissue, ruling out ovarian remnant syndrome as the cause of the elevated estradiol.
Endocrinologists suspected that fulvestrant, which has a molecular structure similar to that of estradiol, was reacting with the standard estradiol immunoassay. That theory was confirmed by testing the serum estradiol levels with the more sensitive, specific liquid chromatography-tandem mass spectrometry, which showed that the levels were actually undetectable.
Related: USPSTF Supports Mammography Starting at Age 50
Fulvestrant has no known agonist effects; it has not previously been reported to elevate estradiol levels or cross-react with estradiol immunoassays, the authors say. Neither the package insert for fulvestrant nor the product insert for the immunoassay warn about the interaction. The authors, therefore, advise clinicians to be aware of the “high likelihood” of this potential drug-assay interaction.
Source:
Berger D, Waheed S, Fattout Y, Kazlauskaite LU. Clin Breast Cancer. 2016;16(1)e11-e16.
doi: 10.1016/j.clbc.2015.07.004.
Estradiol testing may guide treatment for patients with estrogen receptor-positive breast cancer, but researchers from Rush University Medical Center in Chicago, Illinois, have a cautionary report about relying on that when fulvestrant, an estrogen receptor antagonist, is used with standard steroid immunoassays. They report on a patient who had a falsely elevated estradiol reading that led to unnecessary procedures.
Related: Delayed Adjuvant Chemotherapy Significantly Affects Breast Cancer Recovery
Their patient underwent a bilateral oophorectomy and was then started on anti-estrogen therapy with letrozole and fulvestrant, as well as zoledronic acid. At the patient’s request, her primary oncologist obtained a serum estradiol level, which was “unexpectedly” high. The finding was puzzling, the authors say, because she had reported menopausal symptoms, such as hot flashes, which were not consistent with the estradiol level obtained. She also had a complete clinical response to treatment, according to symptoms, radiologic findings, and decreasing levels of carcinoma antigen 125.
A pelvic ultrasound revealed a possible small soft tissue density in the left adnexal region—a “concerning” finding suggesting ovarian remnant syndrome, a rare condition in which ovarian tissue remains after oophorectomy.
Related: Extending Therapy for Breast Cancer
After additional imaging and laparoscopy, pathology revealed fibrovascular and adipose tissue, but no ovarian tissue, ruling out ovarian remnant syndrome as the cause of the elevated estradiol.
Endocrinologists suspected that fulvestrant, which has a molecular structure similar to that of estradiol, was reacting with the standard estradiol immunoassay. That theory was confirmed by testing the serum estradiol levels with the more sensitive, specific liquid chromatography-tandem mass spectrometry, which showed that the levels were actually undetectable.
Related: USPSTF Supports Mammography Starting at Age 50
Fulvestrant has no known agonist effects; it has not previously been reported to elevate estradiol levels or cross-react with estradiol immunoassays, the authors say. Neither the package insert for fulvestrant nor the product insert for the immunoassay warn about the interaction. The authors, therefore, advise clinicians to be aware of the “high likelihood” of this potential drug-assay interaction.
Source:
Berger D, Waheed S, Fattout Y, Kazlauskaite LU. Clin Breast Cancer. 2016;16(1)e11-e16.
doi: 10.1016/j.clbc.2015.07.004.
Estradiol testing may guide treatment for patients with estrogen receptor-positive breast cancer, but researchers from Rush University Medical Center in Chicago, Illinois, have a cautionary report about relying on that when fulvestrant, an estrogen receptor antagonist, is used with standard steroid immunoassays. They report on a patient who had a falsely elevated estradiol reading that led to unnecessary procedures.
Related: Delayed Adjuvant Chemotherapy Significantly Affects Breast Cancer Recovery
Their patient underwent a bilateral oophorectomy and was then started on anti-estrogen therapy with letrozole and fulvestrant, as well as zoledronic acid. At the patient’s request, her primary oncologist obtained a serum estradiol level, which was “unexpectedly” high. The finding was puzzling, the authors say, because she had reported menopausal symptoms, such as hot flashes, which were not consistent with the estradiol level obtained. She also had a complete clinical response to treatment, according to symptoms, radiologic findings, and decreasing levels of carcinoma antigen 125.
A pelvic ultrasound revealed a possible small soft tissue density in the left adnexal region—a “concerning” finding suggesting ovarian remnant syndrome, a rare condition in which ovarian tissue remains after oophorectomy.
Related: Extending Therapy for Breast Cancer
After additional imaging and laparoscopy, pathology revealed fibrovascular and adipose tissue, but no ovarian tissue, ruling out ovarian remnant syndrome as the cause of the elevated estradiol.
Endocrinologists suspected that fulvestrant, which has a molecular structure similar to that of estradiol, was reacting with the standard estradiol immunoassay. That theory was confirmed by testing the serum estradiol levels with the more sensitive, specific liquid chromatography-tandem mass spectrometry, which showed that the levels were actually undetectable.
Related: USPSTF Supports Mammography Starting at Age 50
Fulvestrant has no known agonist effects; it has not previously been reported to elevate estradiol levels or cross-react with estradiol immunoassays, the authors say. Neither the package insert for fulvestrant nor the product insert for the immunoassay warn about the interaction. The authors, therefore, advise clinicians to be aware of the “high likelihood” of this potential drug-assay interaction.
Source:
Berger D, Waheed S, Fattout Y, Kazlauskaite LU. Clin Breast Cancer. 2016;16(1)e11-e16.
doi: 10.1016/j.clbc.2015.07.004.
Investigating Isotretinoin Inconsistencies
In a JAMA Dermatology article published online on December 2, Lee et al challenged the commonly held belief that laboratory studies should be monitored frequently for patients on isotretinoin. In this systematic review and meta-analysis, abnormalities in liver function tests (LFTs), complete blood cell count (CBC), and lipid panel were compared in a set of 22 randomized clinical trials and 4 retrospective studies (1574 patients). Results revealed changes in the mean laboratory values from baseline (99% CI) of the following: aspartate aminotransferase, 22.67 U/L (19.94–25.41 U/L); alanine aminotransferase, 21.77 U/L (18.96–24.59 U/L); alkaline phosphatase, 88.35 U/L (58.94–117.76 U/L); white blood cell count portion of CBC, 6890/µL (5700–8030/µL); lipid panel (triglycerides, 119.98 mg/dL [98.58–141.39 mg/dL]; total cholesterol, 184.74 mg/dL [178.17–191.31 mg/dL]; low-density lipoprotein cholesterol, 109.23 mg/dL [103.68–114.79 mg/dL]; high-density lipoprotein cholesterol, 42.80 mg/dL [39.84–45.76 mg/dL]).
Although these laboratory values were altered as noted above, only 0.5% of patients exhibited test results statistically above or below the mean laboratory values. Additionally, of these laboratory abnormalities, mean changes were not considered to be high risk based on National Institutes of Health clinical center reference ranges.
What’s the issue?
Last year the residents in-training in our department noted variations in what each faculty member was recommending for isotretinoin laboratory monitoring. Practices ranged from initial then monthly full CBC, LFTs, and lipid panel, to those who only checked these laboratory results initially and at 1 month, to those who only performed review of systems-germane parameters. After reviewing the literature, individual preferences, and cost comparisons, a consensus was reached: tests for aspartate aminotransferase, alanine aminotransferase (in lieu of LFT panel), total cholesterol, triglycerides (in lieu of lipid panel), and relevant pregnancy screens would be performed initially, at month 1, and at month 2.
Lee et al also determined that monthly laboratory testing may not be necessary, especially for this low-risk category of patients, but further study is required to determine if there is a standardized way to approach laboratory testing from a safety and economic standpoint, as each dermatologist who prescribes isotretinoin can identify individual cases in which laboratory monitoring was helpful or uncovered individual comorbidities or toxicities in addition to instances where blood work was prohibitively redundant and expensive.
What is your approach to blood work in isotretinoin patients, and can you identify individual patient populations that require more or less stringent laboratory monitoring?
In a JAMA Dermatology article published online on December 2, Lee et al challenged the commonly held belief that laboratory studies should be monitored frequently for patients on isotretinoin. In this systematic review and meta-analysis, abnormalities in liver function tests (LFTs), complete blood cell count (CBC), and lipid panel were compared in a set of 22 randomized clinical trials and 4 retrospective studies (1574 patients). Results revealed changes in the mean laboratory values from baseline (99% CI) of the following: aspartate aminotransferase, 22.67 U/L (19.94–25.41 U/L); alanine aminotransferase, 21.77 U/L (18.96–24.59 U/L); alkaline phosphatase, 88.35 U/L (58.94–117.76 U/L); white blood cell count portion of CBC, 6890/µL (5700–8030/µL); lipid panel (triglycerides, 119.98 mg/dL [98.58–141.39 mg/dL]; total cholesterol, 184.74 mg/dL [178.17–191.31 mg/dL]; low-density lipoprotein cholesterol, 109.23 mg/dL [103.68–114.79 mg/dL]; high-density lipoprotein cholesterol, 42.80 mg/dL [39.84–45.76 mg/dL]).
Although these laboratory values were altered as noted above, only 0.5% of patients exhibited test results statistically above or below the mean laboratory values. Additionally, of these laboratory abnormalities, mean changes were not considered to be high risk based on National Institutes of Health clinical center reference ranges.
What’s the issue?
Last year the residents in-training in our department noted variations in what each faculty member was recommending for isotretinoin laboratory monitoring. Practices ranged from initial then monthly full CBC, LFTs, and lipid panel, to those who only checked these laboratory results initially and at 1 month, to those who only performed review of systems-germane parameters. After reviewing the literature, individual preferences, and cost comparisons, a consensus was reached: tests for aspartate aminotransferase, alanine aminotransferase (in lieu of LFT panel), total cholesterol, triglycerides (in lieu of lipid panel), and relevant pregnancy screens would be performed initially, at month 1, and at month 2.
Lee et al also determined that monthly laboratory testing may not be necessary, especially for this low-risk category of patients, but further study is required to determine if there is a standardized way to approach laboratory testing from a safety and economic standpoint, as each dermatologist who prescribes isotretinoin can identify individual cases in which laboratory monitoring was helpful or uncovered individual comorbidities or toxicities in addition to instances where blood work was prohibitively redundant and expensive.
What is your approach to blood work in isotretinoin patients, and can you identify individual patient populations that require more or less stringent laboratory monitoring?
In a JAMA Dermatology article published online on December 2, Lee et al challenged the commonly held belief that laboratory studies should be monitored frequently for patients on isotretinoin. In this systematic review and meta-analysis, abnormalities in liver function tests (LFTs), complete blood cell count (CBC), and lipid panel were compared in a set of 22 randomized clinical trials and 4 retrospective studies (1574 patients). Results revealed changes in the mean laboratory values from baseline (99% CI) of the following: aspartate aminotransferase, 22.67 U/L (19.94–25.41 U/L); alanine aminotransferase, 21.77 U/L (18.96–24.59 U/L); alkaline phosphatase, 88.35 U/L (58.94–117.76 U/L); white blood cell count portion of CBC, 6890/µL (5700–8030/µL); lipid panel (triglycerides, 119.98 mg/dL [98.58–141.39 mg/dL]; total cholesterol, 184.74 mg/dL [178.17–191.31 mg/dL]; low-density lipoprotein cholesterol, 109.23 mg/dL [103.68–114.79 mg/dL]; high-density lipoprotein cholesterol, 42.80 mg/dL [39.84–45.76 mg/dL]).
Although these laboratory values were altered as noted above, only 0.5% of patients exhibited test results statistically above or below the mean laboratory values. Additionally, of these laboratory abnormalities, mean changes were not considered to be high risk based on National Institutes of Health clinical center reference ranges.
What’s the issue?
Last year the residents in-training in our department noted variations in what each faculty member was recommending for isotretinoin laboratory monitoring. Practices ranged from initial then monthly full CBC, LFTs, and lipid panel, to those who only checked these laboratory results initially and at 1 month, to those who only performed review of systems-germane parameters. After reviewing the literature, individual preferences, and cost comparisons, a consensus was reached: tests for aspartate aminotransferase, alanine aminotransferase (in lieu of LFT panel), total cholesterol, triglycerides (in lieu of lipid panel), and relevant pregnancy screens would be performed initially, at month 1, and at month 2.
Lee et al also determined that monthly laboratory testing may not be necessary, especially for this low-risk category of patients, but further study is required to determine if there is a standardized way to approach laboratory testing from a safety and economic standpoint, as each dermatologist who prescribes isotretinoin can identify individual cases in which laboratory monitoring was helpful or uncovered individual comorbidities or toxicities in addition to instances where blood work was prohibitively redundant and expensive.
What is your approach to blood work in isotretinoin patients, and can you identify individual patient populations that require more or less stringent laboratory monitoring?
Fertility preservation in early cervical cancer
Historically, the standard of care for women diagnosed with early cervical cancer has been radical hysterectomy. Thus, young women are not only being confronted with a cancer diagnosis, but may also be forced to cope with the loss of their fertility.
As many young women with cervical cancer were not accepting of this treatment, Dr. Daniel Dargent pioneered the vaginal radical trachelectomy as a fertility-preserving treatment option for early cervical cancer in 1994. There have now been more than 900 vaginal radical trachelectomies performed and they have been shown to have oncologic outcomes similar to those of traditional radical hysterectomy, while sparing a woman’s fertility (Int J Gynecol Cancer. 2013 Jul;23[6]:982-9).
Obstetric outcomes following vaginal radical trachelectomy are acceptable with 17% miscarriage rate in the first trimester (compared to 10%-20% in the general population) and 8% in the second trimester (compared to 1%-5% in the general population) (Am Fam Physician. 2007 Nov 1;76[9]:1341-6). Following vaginal radical trachelectomy, 64% of pregnancies deliver at term.
The usual criteria required to undergo radical trachelectomy include:
1) Reproductive age with desire for fertility.
2) Stage IA1 with LVSI (lymphovascular space invasion), IA2, or IB1 with tumor less than 2 cm.
3) Limited endocervical involvement via preoperative MRI.
4) Negative pelvic lymph nodes.
Preoperative PET scan can be used to evaluate nodal status, but suspicious lymph nodes should be evaluated on frozen section at the time of surgery. The presence of LVSI alone is not a contraindication to trachelectomy.
A key limitation of vaginal radical trachelectomy is the specialized training required to perform this technically challenging procedure. Few surgeons in the United States are trained to perform vaginal radical trachelectomy. In response to this limitation, surgeons began to attempt radical trachelectomy via laparotomy (Gynecol Oncol. 2006 Dec;103[3]:807-13). Oncologic outcomes following fertility-sparing abdominal radical trachelectomy have been reported to be equivalent to radical hysterectomy. Concerns regarding the abdominal approach to radical trachelectomy include higher rates of second trimester loss (19%) when compared to the vaginal approach (8%), higher rate of loss of fertility (30%), and risk of postoperative adhesions.
The advent of minimally invasive surgery, particularly robotic surgery, now offers surgeons the ability to perform a procedure technically similar to radical hysterectomy using a minimally invasive approach. Given the similarity of procedural steps of radical trachelectomy to radical hysterectomy using the robotic platform, this procedure is gaining acceptance in the United States with an associated improved surgeon learning curve (Gynecol Oncol. 2008 Nov;111[2]:255-60). In addition, the use of minimally invasive surgery should result in less adhesion formation facilitating natural fertility options postoperatively.
Obstetric and fertility outcomes are limited following minimally invasive radical trachelectomy via laparoscopy or robotic surgery given the novelty of this procedure. Emerging obstetric outcomes appear reassuring, but further data are needed to fully understand the effects of this procedure on pregnancy outcomes and the need for assisted reproductive techniques to achieve pregnancy.
The management of pregnancies following radical trachelectomy is also an area with limited data, which presents a clinical challenge to obstetricians. Many gynecologic oncologists perform a permanent cerclage at the time of trachelectomy and recommend delivery via scheduled cesarean at term for all subsequent pregnancies prior to labor (usually 37-38 weeks).
At our institution, we recommend the use of progesterone from 16 to 36 weeks despite no clear evidence on the role of progesterone in this setting. Maternal-fetal medicine consultation should be considered to either follow these patients during their pregnancies or to perform a single consultative visit to guide antepartum care.
Some have advocated for less radical surgery, such as simple trachelectomy or large cold knife conization, as the risk of parametrial extension in these patients is low (Gynecol Oncol. 2011 Dec;123[3]:557-60). More data are needed to determine if this is a safe approach. Further, the use of neoadjuvant chemotherapy followed by cold knife conization for fertility preservation in women with larger tumors has been proposed. This may be a feasible option in women with chemo-sensitive tumors, but progression on chemotherapy and increased recurrences have been reported with this approach (Gynecol Oncol. 2008 Dec;111[3]:438-43).
Women of reproductive age diagnosed with early cervical cancer now have multiple options for fertility preservation. Ongoing research regarding obstetric and fertility outcomes is needed; however, oncologic outcomes appear to be equivalent.
Dr. Clark is a fellow in the division of gynecologic oncology, department of obstetrics and gynecology, at the University of North Carolina, Chapel Hill. Dr. Boggess is an expert in robotic surgery in gynecologic oncology and is a professor in the division of gynecologic oncology at UNC–Chapel Hill. They reported having no financial disclosures relevant to this column. Email them at obnews@frontlinemedcom.com.
Historically, the standard of care for women diagnosed with early cervical cancer has been radical hysterectomy. Thus, young women are not only being confronted with a cancer diagnosis, but may also be forced to cope with the loss of their fertility.
As many young women with cervical cancer were not accepting of this treatment, Dr. Daniel Dargent pioneered the vaginal radical trachelectomy as a fertility-preserving treatment option for early cervical cancer in 1994. There have now been more than 900 vaginal radical trachelectomies performed and they have been shown to have oncologic outcomes similar to those of traditional radical hysterectomy, while sparing a woman’s fertility (Int J Gynecol Cancer. 2013 Jul;23[6]:982-9).
Obstetric outcomes following vaginal radical trachelectomy are acceptable with 17% miscarriage rate in the first trimester (compared to 10%-20% in the general population) and 8% in the second trimester (compared to 1%-5% in the general population) (Am Fam Physician. 2007 Nov 1;76[9]:1341-6). Following vaginal radical trachelectomy, 64% of pregnancies deliver at term.
The usual criteria required to undergo radical trachelectomy include:
1) Reproductive age with desire for fertility.
2) Stage IA1 with LVSI (lymphovascular space invasion), IA2, or IB1 with tumor less than 2 cm.
3) Limited endocervical involvement via preoperative MRI.
4) Negative pelvic lymph nodes.
Preoperative PET scan can be used to evaluate nodal status, but suspicious lymph nodes should be evaluated on frozen section at the time of surgery. The presence of LVSI alone is not a contraindication to trachelectomy.
A key limitation of vaginal radical trachelectomy is the specialized training required to perform this technically challenging procedure. Few surgeons in the United States are trained to perform vaginal radical trachelectomy. In response to this limitation, surgeons began to attempt radical trachelectomy via laparotomy (Gynecol Oncol. 2006 Dec;103[3]:807-13). Oncologic outcomes following fertility-sparing abdominal radical trachelectomy have been reported to be equivalent to radical hysterectomy. Concerns regarding the abdominal approach to radical trachelectomy include higher rates of second trimester loss (19%) when compared to the vaginal approach (8%), higher rate of loss of fertility (30%), and risk of postoperative adhesions.
The advent of minimally invasive surgery, particularly robotic surgery, now offers surgeons the ability to perform a procedure technically similar to radical hysterectomy using a minimally invasive approach. Given the similarity of procedural steps of radical trachelectomy to radical hysterectomy using the robotic platform, this procedure is gaining acceptance in the United States with an associated improved surgeon learning curve (Gynecol Oncol. 2008 Nov;111[2]:255-60). In addition, the use of minimally invasive surgery should result in less adhesion formation facilitating natural fertility options postoperatively.
Obstetric and fertility outcomes are limited following minimally invasive radical trachelectomy via laparoscopy or robotic surgery given the novelty of this procedure. Emerging obstetric outcomes appear reassuring, but further data are needed to fully understand the effects of this procedure on pregnancy outcomes and the need for assisted reproductive techniques to achieve pregnancy.
The management of pregnancies following radical trachelectomy is also an area with limited data, which presents a clinical challenge to obstetricians. Many gynecologic oncologists perform a permanent cerclage at the time of trachelectomy and recommend delivery via scheduled cesarean at term for all subsequent pregnancies prior to labor (usually 37-38 weeks).
At our institution, we recommend the use of progesterone from 16 to 36 weeks despite no clear evidence on the role of progesterone in this setting. Maternal-fetal medicine consultation should be considered to either follow these patients during their pregnancies or to perform a single consultative visit to guide antepartum care.
Some have advocated for less radical surgery, such as simple trachelectomy or large cold knife conization, as the risk of parametrial extension in these patients is low (Gynecol Oncol. 2011 Dec;123[3]:557-60). More data are needed to determine if this is a safe approach. Further, the use of neoadjuvant chemotherapy followed by cold knife conization for fertility preservation in women with larger tumors has been proposed. This may be a feasible option in women with chemo-sensitive tumors, but progression on chemotherapy and increased recurrences have been reported with this approach (Gynecol Oncol. 2008 Dec;111[3]:438-43).
Women of reproductive age diagnosed with early cervical cancer now have multiple options for fertility preservation. Ongoing research regarding obstetric and fertility outcomes is needed; however, oncologic outcomes appear to be equivalent.
Dr. Clark is a fellow in the division of gynecologic oncology, department of obstetrics and gynecology, at the University of North Carolina, Chapel Hill. Dr. Boggess is an expert in robotic surgery in gynecologic oncology and is a professor in the division of gynecologic oncology at UNC–Chapel Hill. They reported having no financial disclosures relevant to this column. Email them at obnews@frontlinemedcom.com.
Historically, the standard of care for women diagnosed with early cervical cancer has been radical hysterectomy. Thus, young women are not only being confronted with a cancer diagnosis, but may also be forced to cope with the loss of their fertility.
As many young women with cervical cancer were not accepting of this treatment, Dr. Daniel Dargent pioneered the vaginal radical trachelectomy as a fertility-preserving treatment option for early cervical cancer in 1994. There have now been more than 900 vaginal radical trachelectomies performed and they have been shown to have oncologic outcomes similar to those of traditional radical hysterectomy, while sparing a woman’s fertility (Int J Gynecol Cancer. 2013 Jul;23[6]:982-9).
Obstetric outcomes following vaginal radical trachelectomy are acceptable with 17% miscarriage rate in the first trimester (compared to 10%-20% in the general population) and 8% in the second trimester (compared to 1%-5% in the general population) (Am Fam Physician. 2007 Nov 1;76[9]:1341-6). Following vaginal radical trachelectomy, 64% of pregnancies deliver at term.
The usual criteria required to undergo radical trachelectomy include:
1) Reproductive age with desire for fertility.
2) Stage IA1 with LVSI (lymphovascular space invasion), IA2, or IB1 with tumor less than 2 cm.
3) Limited endocervical involvement via preoperative MRI.
4) Negative pelvic lymph nodes.
Preoperative PET scan can be used to evaluate nodal status, but suspicious lymph nodes should be evaluated on frozen section at the time of surgery. The presence of LVSI alone is not a contraindication to trachelectomy.
A key limitation of vaginal radical trachelectomy is the specialized training required to perform this technically challenging procedure. Few surgeons in the United States are trained to perform vaginal radical trachelectomy. In response to this limitation, surgeons began to attempt radical trachelectomy via laparotomy (Gynecol Oncol. 2006 Dec;103[3]:807-13). Oncologic outcomes following fertility-sparing abdominal radical trachelectomy have been reported to be equivalent to radical hysterectomy. Concerns regarding the abdominal approach to radical trachelectomy include higher rates of second trimester loss (19%) when compared to the vaginal approach (8%), higher rate of loss of fertility (30%), and risk of postoperative adhesions.
The advent of minimally invasive surgery, particularly robotic surgery, now offers surgeons the ability to perform a procedure technically similar to radical hysterectomy using a minimally invasive approach. Given the similarity of procedural steps of radical trachelectomy to radical hysterectomy using the robotic platform, this procedure is gaining acceptance in the United States with an associated improved surgeon learning curve (Gynecol Oncol. 2008 Nov;111[2]:255-60). In addition, the use of minimally invasive surgery should result in less adhesion formation facilitating natural fertility options postoperatively.
Obstetric and fertility outcomes are limited following minimally invasive radical trachelectomy via laparoscopy or robotic surgery given the novelty of this procedure. Emerging obstetric outcomes appear reassuring, but further data are needed to fully understand the effects of this procedure on pregnancy outcomes and the need for assisted reproductive techniques to achieve pregnancy.
The management of pregnancies following radical trachelectomy is also an area with limited data, which presents a clinical challenge to obstetricians. Many gynecologic oncologists perform a permanent cerclage at the time of trachelectomy and recommend delivery via scheduled cesarean at term for all subsequent pregnancies prior to labor (usually 37-38 weeks).
At our institution, we recommend the use of progesterone from 16 to 36 weeks despite no clear evidence on the role of progesterone in this setting. Maternal-fetal medicine consultation should be considered to either follow these patients during their pregnancies or to perform a single consultative visit to guide antepartum care.
Some have advocated for less radical surgery, such as simple trachelectomy or large cold knife conization, as the risk of parametrial extension in these patients is low (Gynecol Oncol. 2011 Dec;123[3]:557-60). More data are needed to determine if this is a safe approach. Further, the use of neoadjuvant chemotherapy followed by cold knife conization for fertility preservation in women with larger tumors has been proposed. This may be a feasible option in women with chemo-sensitive tumors, but progression on chemotherapy and increased recurrences have been reported with this approach (Gynecol Oncol. 2008 Dec;111[3]:438-43).
Women of reproductive age diagnosed with early cervical cancer now have multiple options for fertility preservation. Ongoing research regarding obstetric and fertility outcomes is needed; however, oncologic outcomes appear to be equivalent.
Dr. Clark is a fellow in the division of gynecologic oncology, department of obstetrics and gynecology, at the University of North Carolina, Chapel Hill. Dr. Boggess is an expert in robotic surgery in gynecologic oncology and is a professor in the division of gynecologic oncology at UNC–Chapel Hill. They reported having no financial disclosures relevant to this column. Email them at obnews@frontlinemedcom.com.
Families Perceive Few Benefits From Aggressive End-of-Life Care
Bereaved families were substantially more satisfied with end-of-life cancer care when patients did not die in hospital, received more than 3 days of hospice care, and did not enter the ICU within 30 days of dying, according to a multicenter, prospective study published online Jan. 19 in JAMA.
The analysis is one of the first of its type to assess these end-of-life care indicators, said Dr. Alexi Wright of Harvard Medical School, Boston, and her associates. The findings could affect health policy as electronic health records expand under the Health Information Technology for Economic and Clinical Health Act, they said.
End-of-life cancer care has become increasingly aggressive, belying evidence that this approach does not improve patient outcomes, quality of life, or caregiver bereavement. To explore alternatives, the researchers analyzed 1,146 interviews of family members of Medicare patients who died of lung or colorectal cancer by 2011. Their data source was the multiregional, prospective, observational Cancer Care Outcomes Research and Surveillance (CanCORS) study (JAMA 2016;315:284-92).
Family members described end-of-life care as “excellent” 59% of the time when hospice care lasted more 3 days, but 43% of the time otherwise (95% confidence interval for adjusted difference, 11% to 22%). Notably, 73% of patients who received more than 3 days of hospice care died in their preferred location, compared with 40% of patients who received less or no hospice care. Care was rated as excellent 52% of the time when ICU admission was avoided within 30 days of death, and 57% of the time when patients died outside the hospital, compared with 45% and 42% of the time otherwise.
The results support “advance care planning consistent with the preferences of patients,” said the investigators. They recommended more extensive counseling of cancer patients and families, earlier palliative care referrals, and an audit and feedback system to monitor the use of aggressive end-of-life care.
The National Cancer Institute and the Cancer Care Outcomes Research and Surveillance Consortium funded the study. One coinvestigator reported financial relationships with the American Academy of Hospice and Palliative Medicine, National Institute of Nursing Research, National Institute on Aging, Retirement Research Retirement Foundation, California Healthcare Foundation, Commonwealth Fund, West Health Institute, University of Wisconsin, and UpToDate.com. Senior author Dr. Mary Landrum, also of Harvard Medical School, reported grant funding from Pfizer and personal fees from McKinsey and Company and Greylock McKinnon Associates. The other authors had no disclosures.
Bereaved families were substantially more satisfied with end-of-life cancer care when patients did not die in hospital, received more than 3 days of hospice care, and did not enter the ICU within 30 days of dying, according to a multicenter, prospective study published online Jan. 19 in JAMA.
The analysis is one of the first of its type to assess these end-of-life care indicators, said Dr. Alexi Wright of Harvard Medical School, Boston, and her associates. The findings could affect health policy as electronic health records expand under the Health Information Technology for Economic and Clinical Health Act, they said.
End-of-life cancer care has become increasingly aggressive, belying evidence that this approach does not improve patient outcomes, quality of life, or caregiver bereavement. To explore alternatives, the researchers analyzed 1,146 interviews of family members of Medicare patients who died of lung or colorectal cancer by 2011. Their data source was the multiregional, prospective, observational Cancer Care Outcomes Research and Surveillance (CanCORS) study (JAMA 2016;315:284-92).
Family members described end-of-life care as “excellent” 59% of the time when hospice care lasted more 3 days, but 43% of the time otherwise (95% confidence interval for adjusted difference, 11% to 22%). Notably, 73% of patients who received more than 3 days of hospice care died in their preferred location, compared with 40% of patients who received less or no hospice care. Care was rated as excellent 52% of the time when ICU admission was avoided within 30 days of death, and 57% of the time when patients died outside the hospital, compared with 45% and 42% of the time otherwise.
The results support “advance care planning consistent with the preferences of patients,” said the investigators. They recommended more extensive counseling of cancer patients and families, earlier palliative care referrals, and an audit and feedback system to monitor the use of aggressive end-of-life care.
The National Cancer Institute and the Cancer Care Outcomes Research and Surveillance Consortium funded the study. One coinvestigator reported financial relationships with the American Academy of Hospice and Palliative Medicine, National Institute of Nursing Research, National Institute on Aging, Retirement Research Retirement Foundation, California Healthcare Foundation, Commonwealth Fund, West Health Institute, University of Wisconsin, and UpToDate.com. Senior author Dr. Mary Landrum, also of Harvard Medical School, reported grant funding from Pfizer and personal fees from McKinsey and Company and Greylock McKinnon Associates. The other authors had no disclosures.
Bereaved families were substantially more satisfied with end-of-life cancer care when patients did not die in hospital, received more than 3 days of hospice care, and did not enter the ICU within 30 days of dying, according to a multicenter, prospective study published online Jan. 19 in JAMA.
The analysis is one of the first of its type to assess these end-of-life care indicators, said Dr. Alexi Wright of Harvard Medical School, Boston, and her associates. The findings could affect health policy as electronic health records expand under the Health Information Technology for Economic and Clinical Health Act, they said.
End-of-life cancer care has become increasingly aggressive, belying evidence that this approach does not improve patient outcomes, quality of life, or caregiver bereavement. To explore alternatives, the researchers analyzed 1,146 interviews of family members of Medicare patients who died of lung or colorectal cancer by 2011. Their data source was the multiregional, prospective, observational Cancer Care Outcomes Research and Surveillance (CanCORS) study (JAMA 2016;315:284-92).
Family members described end-of-life care as “excellent” 59% of the time when hospice care lasted more 3 days, but 43% of the time otherwise (95% confidence interval for adjusted difference, 11% to 22%). Notably, 73% of patients who received more than 3 days of hospice care died in their preferred location, compared with 40% of patients who received less or no hospice care. Care was rated as excellent 52% of the time when ICU admission was avoided within 30 days of death, and 57% of the time when patients died outside the hospital, compared with 45% and 42% of the time otherwise.
The results support “advance care planning consistent with the preferences of patients,” said the investigators. They recommended more extensive counseling of cancer patients and families, earlier palliative care referrals, and an audit and feedback system to monitor the use of aggressive end-of-life care.
The National Cancer Institute and the Cancer Care Outcomes Research and Surveillance Consortium funded the study. One coinvestigator reported financial relationships with the American Academy of Hospice and Palliative Medicine, National Institute of Nursing Research, National Institute on Aging, Retirement Research Retirement Foundation, California Healthcare Foundation, Commonwealth Fund, West Health Institute, University of Wisconsin, and UpToDate.com. Senior author Dr. Mary Landrum, also of Harvard Medical School, reported grant funding from Pfizer and personal fees from McKinsey and Company and Greylock McKinnon Associates. The other authors had no disclosures.
FROM JAMA
HM Groups Invited to Participate in 2016 State of Hospital Medicine Survey
Every other year, SHM’s practice analysis subcommittee invites all U.S. hospital medicine groups to participate in the State of Hospital Medicine (SOHM) survey. Your responses generate the authoritative report on how today’s hospital medicine groups are organized, scheduled, funded, compensated, staffed, and much more. After months of refining and updating, the survey opened on Jan. 11. The time has arrived for you to respond to this critical survey!
Empower Your Hospitalist Program
Hospital medicine has seen the most dramatic growth and evolution of any specialty in the last two decades. Although all practices innovate in response to shifting demands, leaders and hospitalists alike need to understand how the frontrunners in this dynamic field have adapted. The SoHM report summarizes thousands of data points about the latest trends in hospital medicine practice design and productivity.
Hospitalist group leaders depend on this information to draw comparisons against national benchmarks, both for improvement and as a frame of reference for demonstrating the value your group provides to your hospital. However, the report is only as good as the number and quality of the responses to the survey.
How To Get Engaged
Responding to the survey is straightforward through the web-based questionnaire, and only one response is needed from each group. The survey does require some modest preparation to look up such practice characteristics as CPT code distribution, total RVU generation, and average number of shifts per FTE. For many groups, a hospitalist and a practice manager can collaborate to answer all of the questions accurately. If you haven’t already, take some basic steps to prepare:
- Discuss the survey at your next group meeting and advocate for responding.
- Determine who will complete the survey on behalf of your group.
- Visit www.hospitalmedicine.org/survey and download the survey instrument and instructions, share them with the lead respondent for your group.
- Submit your responses by March 11.
Of note, you’ll also want to participate in the Medical Group Management Association (MGMA) survey, as well. SHM licenses key portions of the SoHM report from MGMA, such as provider compensation, so the complete report depends on having great responses to both instruments.
Why Participate?
First, hospitalist groups that respond to the Survey will get a FREE copy of the report. Have you wondered things like:
- “How many groups are using a scheduling model other than 7-on, 7-off?”
- “What percentage of groups staff an observation unit?”
- “Are hospitalists groups taking on new roles in Accountable Care Organizations (ACOs)?”
- “How does compensation differ for providers who see children or are in academics?”
If so, you’ll have those answers at your fingertips and a whole lot more.
Second, you’ll have the satisfaction of knowing that you helped to make the SoHM report the indispensable tool upon which group leaders everywhere depend. The survey is anonymous, but respondents will know that the report presents data on the most relevant HM group of all—your own! Don’t wait.
Participate today at www.hospitalmedicine.org/survey. TH
Dr. White is assistant professor of medicine at the University of Washington and group director at the University of Washington Medical Center in Seattle, Wash.
Every other year, SHM’s practice analysis subcommittee invites all U.S. hospital medicine groups to participate in the State of Hospital Medicine (SOHM) survey. Your responses generate the authoritative report on how today’s hospital medicine groups are organized, scheduled, funded, compensated, staffed, and much more. After months of refining and updating, the survey opened on Jan. 11. The time has arrived for you to respond to this critical survey!
Empower Your Hospitalist Program
Hospital medicine has seen the most dramatic growth and evolution of any specialty in the last two decades. Although all practices innovate in response to shifting demands, leaders and hospitalists alike need to understand how the frontrunners in this dynamic field have adapted. The SoHM report summarizes thousands of data points about the latest trends in hospital medicine practice design and productivity.
Hospitalist group leaders depend on this information to draw comparisons against national benchmarks, both for improvement and as a frame of reference for demonstrating the value your group provides to your hospital. However, the report is only as good as the number and quality of the responses to the survey.
How To Get Engaged
Responding to the survey is straightforward through the web-based questionnaire, and only one response is needed from each group. The survey does require some modest preparation to look up such practice characteristics as CPT code distribution, total RVU generation, and average number of shifts per FTE. For many groups, a hospitalist and a practice manager can collaborate to answer all of the questions accurately. If you haven’t already, take some basic steps to prepare:
- Discuss the survey at your next group meeting and advocate for responding.
- Determine who will complete the survey on behalf of your group.
- Visit www.hospitalmedicine.org/survey and download the survey instrument and instructions, share them with the lead respondent for your group.
- Submit your responses by March 11.
Of note, you’ll also want to participate in the Medical Group Management Association (MGMA) survey, as well. SHM licenses key portions of the SoHM report from MGMA, such as provider compensation, so the complete report depends on having great responses to both instruments.
Why Participate?
First, hospitalist groups that respond to the Survey will get a FREE copy of the report. Have you wondered things like:
- “How many groups are using a scheduling model other than 7-on, 7-off?”
- “What percentage of groups staff an observation unit?”
- “Are hospitalists groups taking on new roles in Accountable Care Organizations (ACOs)?”
- “How does compensation differ for providers who see children or are in academics?”
If so, you’ll have those answers at your fingertips and a whole lot more.
Second, you’ll have the satisfaction of knowing that you helped to make the SoHM report the indispensable tool upon which group leaders everywhere depend. The survey is anonymous, but respondents will know that the report presents data on the most relevant HM group of all—your own! Don’t wait.
Participate today at www.hospitalmedicine.org/survey. TH
Dr. White is assistant professor of medicine at the University of Washington and group director at the University of Washington Medical Center in Seattle, Wash.
Every other year, SHM’s practice analysis subcommittee invites all U.S. hospital medicine groups to participate in the State of Hospital Medicine (SOHM) survey. Your responses generate the authoritative report on how today’s hospital medicine groups are organized, scheduled, funded, compensated, staffed, and much more. After months of refining and updating, the survey opened on Jan. 11. The time has arrived for you to respond to this critical survey!
Empower Your Hospitalist Program
Hospital medicine has seen the most dramatic growth and evolution of any specialty in the last two decades. Although all practices innovate in response to shifting demands, leaders and hospitalists alike need to understand how the frontrunners in this dynamic field have adapted. The SoHM report summarizes thousands of data points about the latest trends in hospital medicine practice design and productivity.
Hospitalist group leaders depend on this information to draw comparisons against national benchmarks, both for improvement and as a frame of reference for demonstrating the value your group provides to your hospital. However, the report is only as good as the number and quality of the responses to the survey.
How To Get Engaged
Responding to the survey is straightforward through the web-based questionnaire, and only one response is needed from each group. The survey does require some modest preparation to look up such practice characteristics as CPT code distribution, total RVU generation, and average number of shifts per FTE. For many groups, a hospitalist and a practice manager can collaborate to answer all of the questions accurately. If you haven’t already, take some basic steps to prepare:
- Discuss the survey at your next group meeting and advocate for responding.
- Determine who will complete the survey on behalf of your group.
- Visit www.hospitalmedicine.org/survey and download the survey instrument and instructions, share them with the lead respondent for your group.
- Submit your responses by March 11.
Of note, you’ll also want to participate in the Medical Group Management Association (MGMA) survey, as well. SHM licenses key portions of the SoHM report from MGMA, such as provider compensation, so the complete report depends on having great responses to both instruments.
Why Participate?
First, hospitalist groups that respond to the Survey will get a FREE copy of the report. Have you wondered things like:
- “How many groups are using a scheduling model other than 7-on, 7-off?”
- “What percentage of groups staff an observation unit?”
- “Are hospitalists groups taking on new roles in Accountable Care Organizations (ACOs)?”
- “How does compensation differ for providers who see children or are in academics?”
If so, you’ll have those answers at your fingertips and a whole lot more.
Second, you’ll have the satisfaction of knowing that you helped to make the SoHM report the indispensable tool upon which group leaders everywhere depend. The survey is anonymous, but respondents will know that the report presents data on the most relevant HM group of all—your own! Don’t wait.
Participate today at www.hospitalmedicine.org/survey. TH
Dr. White is assistant professor of medicine at the University of Washington and group director at the University of Washington Medical Center in Seattle, Wash.
End-of-life cancer care by country

in the intensive care unit
A study of end-of-life cancer care practices in 7 countries suggests the US has the lowest proportion of deaths in the hospital and the lowest number of days in the hospital for patients in their last 6 months of life.
However, the US performed poorly in other aspects of care, particularly intensive care unit admissions and hospital expenditures.
The other countries included in the study were Belgium, Canada, England, Germany, the Netherlands, and Norway.
The research was published in JAMA.
Ezekiel J. Emanuel, MD, PhD, of the University of Pennsylvania in Philadelphia, and his colleagues examined patterns of care, healthcare utilization, and expenditures for dying cancer patients in the 7 aforementioned countries.
The researchers first analyzed data from 2010 that included subjects older than 65 years of age who died with cancer.
The proportion of patients who died in the hospital was 22.2% in the US, 29.4% in the Netherlands, 38.3% in Germany, 41.7% in England, 44.7% in Norway, 51.2% in Belgium, and 52.1% in Canada.
In the last 180 days of life, the mean number of days in the hospital per capita was 27.7 in Belgium, 24.8 in Norway, 21.7 in Germany, 19 in Canada, 18.3 in England, 17.8 in the Netherlands, and 10.7 in the US.
The proportion of patients admitted to the intensive care unit in their last 180 days of life was 40.3% in the US, 18.5% in Belgium, 15.2% in Canada, 10.2% in the Netherlands, and 8.2% in Germany. Data were not available for England and Norway.
In the last 180 days of life, average per capita hospital expenditures (in USD) were higher in Canada ($21,840), Norway ($19,783), and the US ($18,500), intermediate in Germany ($16,221) and Belgium ($15,699), and lowest in the Netherlands ($10,936) and England ($9342).
Analyses that included decedents of any age, decedents older than 65 years of age with lung cancer, and decedents older than 65 years in the US and Germany from 2012 showed similar results.
The researchers said this suggests the differences observed were driven more by end-of-life care practices and organization rather than differences in cohort identification. ![]()

in the intensive care unit
A study of end-of-life cancer care practices in 7 countries suggests the US has the lowest proportion of deaths in the hospital and the lowest number of days in the hospital for patients in their last 6 months of life.
However, the US performed poorly in other aspects of care, particularly intensive care unit admissions and hospital expenditures.
The other countries included in the study were Belgium, Canada, England, Germany, the Netherlands, and Norway.
The research was published in JAMA.
Ezekiel J. Emanuel, MD, PhD, of the University of Pennsylvania in Philadelphia, and his colleagues examined patterns of care, healthcare utilization, and expenditures for dying cancer patients in the 7 aforementioned countries.
The researchers first analyzed data from 2010 that included subjects older than 65 years of age who died with cancer.
The proportion of patients who died in the hospital was 22.2% in the US, 29.4% in the Netherlands, 38.3% in Germany, 41.7% in England, 44.7% in Norway, 51.2% in Belgium, and 52.1% in Canada.
In the last 180 days of life, the mean number of days in the hospital per capita was 27.7 in Belgium, 24.8 in Norway, 21.7 in Germany, 19 in Canada, 18.3 in England, 17.8 in the Netherlands, and 10.7 in the US.
The proportion of patients admitted to the intensive care unit in their last 180 days of life was 40.3% in the US, 18.5% in Belgium, 15.2% in Canada, 10.2% in the Netherlands, and 8.2% in Germany. Data were not available for England and Norway.
In the last 180 days of life, average per capita hospital expenditures (in USD) were higher in Canada ($21,840), Norway ($19,783), and the US ($18,500), intermediate in Germany ($16,221) and Belgium ($15,699), and lowest in the Netherlands ($10,936) and England ($9342).
Analyses that included decedents of any age, decedents older than 65 years of age with lung cancer, and decedents older than 65 years in the US and Germany from 2012 showed similar results.
The researchers said this suggests the differences observed were driven more by end-of-life care practices and organization rather than differences in cohort identification. ![]()

in the intensive care unit
A study of end-of-life cancer care practices in 7 countries suggests the US has the lowest proportion of deaths in the hospital and the lowest number of days in the hospital for patients in their last 6 months of life.
However, the US performed poorly in other aspects of care, particularly intensive care unit admissions and hospital expenditures.
The other countries included in the study were Belgium, Canada, England, Germany, the Netherlands, and Norway.
The research was published in JAMA.
Ezekiel J. Emanuel, MD, PhD, of the University of Pennsylvania in Philadelphia, and his colleagues examined patterns of care, healthcare utilization, and expenditures for dying cancer patients in the 7 aforementioned countries.
The researchers first analyzed data from 2010 that included subjects older than 65 years of age who died with cancer.
The proportion of patients who died in the hospital was 22.2% in the US, 29.4% in the Netherlands, 38.3% in Germany, 41.7% in England, 44.7% in Norway, 51.2% in Belgium, and 52.1% in Canada.
In the last 180 days of life, the mean number of days in the hospital per capita was 27.7 in Belgium, 24.8 in Norway, 21.7 in Germany, 19 in Canada, 18.3 in England, 17.8 in the Netherlands, and 10.7 in the US.
The proportion of patients admitted to the intensive care unit in their last 180 days of life was 40.3% in the US, 18.5% in Belgium, 15.2% in Canada, 10.2% in the Netherlands, and 8.2% in Germany. Data were not available for England and Norway.
In the last 180 days of life, average per capita hospital expenditures (in USD) were higher in Canada ($21,840), Norway ($19,783), and the US ($18,500), intermediate in Germany ($16,221) and Belgium ($15,699), and lowest in the Netherlands ($10,936) and England ($9342).
Analyses that included decedents of any age, decedents older than 65 years of age with lung cancer, and decedents older than 65 years in the US and Germany from 2012 showed similar results.
The researchers said this suggests the differences observed were driven more by end-of-life care practices and organization rather than differences in cohort identification. ![]()
Drug granted another breakthrough designation for CLL

The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to the BCL-2 inhibitor venetoclax when given with rituximab to treat patients with relapsed or refractory chronic lymphocytic leukemia (CLL).
Venetoclax already had breakthrough designation from the FDA as single-agent treatment for patients with relapsed or refractory CLL and 17p deletion.
The drug was granted priority review for this indication as well.
Breakthrough therapy designation is designed to accelerate the development and review of medicines that demonstrate early clinical evidence of a substantial improvement over current treatment options for serious diseases.
The latest breakthrough designation for venetoclax is supported by a phase 2 study of the drug in combination with rituximab in patients with relapsed/refractory CLL. Results from this trial were presented at the 2015 ASH Annual Meeting (abstract 325).
Another phase 2 trial presented at that meeting (abstract LBA-6) showed that single-agent venetoclax is effective against CLL as well.
The drug has also proven active against other hematologic malignancies, including acute myeloid lekemia and multiple myeloma.
However, venetoclax has been shown to pose a risk of tumor lysis syndrome (TLS). In fact, TLS-related deaths temporarily halted enrollment in trials of venetoclax. But researchers discovered ways to reduce the risk of TLS, and the trials continued.
Venetoclax is being developed by AbbVie in partnership with Genentech and Roche. ![]()

The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to the BCL-2 inhibitor venetoclax when given with rituximab to treat patients with relapsed or refractory chronic lymphocytic leukemia (CLL).
Venetoclax already had breakthrough designation from the FDA as single-agent treatment for patients with relapsed or refractory CLL and 17p deletion.
The drug was granted priority review for this indication as well.
Breakthrough therapy designation is designed to accelerate the development and review of medicines that demonstrate early clinical evidence of a substantial improvement over current treatment options for serious diseases.
The latest breakthrough designation for venetoclax is supported by a phase 2 study of the drug in combination with rituximab in patients with relapsed/refractory CLL. Results from this trial were presented at the 2015 ASH Annual Meeting (abstract 325).
Another phase 2 trial presented at that meeting (abstract LBA-6) showed that single-agent venetoclax is effective against CLL as well.
The drug has also proven active against other hematologic malignancies, including acute myeloid lekemia and multiple myeloma.
However, venetoclax has been shown to pose a risk of tumor lysis syndrome (TLS). In fact, TLS-related deaths temporarily halted enrollment in trials of venetoclax. But researchers discovered ways to reduce the risk of TLS, and the trials continued.
Venetoclax is being developed by AbbVie in partnership with Genentech and Roche. ![]()

The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to the BCL-2 inhibitor venetoclax when given with rituximab to treat patients with relapsed or refractory chronic lymphocytic leukemia (CLL).
Venetoclax already had breakthrough designation from the FDA as single-agent treatment for patients with relapsed or refractory CLL and 17p deletion.
The drug was granted priority review for this indication as well.
Breakthrough therapy designation is designed to accelerate the development and review of medicines that demonstrate early clinical evidence of a substantial improvement over current treatment options for serious diseases.
The latest breakthrough designation for venetoclax is supported by a phase 2 study of the drug in combination with rituximab in patients with relapsed/refractory CLL. Results from this trial were presented at the 2015 ASH Annual Meeting (abstract 325).
Another phase 2 trial presented at that meeting (abstract LBA-6) showed that single-agent venetoclax is effective against CLL as well.
The drug has also proven active against other hematologic malignancies, including acute myeloid lekemia and multiple myeloma.
However, venetoclax has been shown to pose a risk of tumor lysis syndrome (TLS). In fact, TLS-related deaths temporarily halted enrollment in trials of venetoclax. But researchers discovered ways to reduce the risk of TLS, and the trials continued.
Venetoclax is being developed by AbbVie in partnership with Genentech and Roche. ![]()
Obesity linked to VTE in kids

Photo by Matthew Lester
A single-center, retrospective study has revealed an association between obesity and venous thromboembolism (VTE) in children and adolescents.
While obesity is a well-established risk factor for VTE in adults, previous studies in pediatric populations have yielded mixed results.
The new study, however, showed that obesity, as determined by body mass index (BMI), was a statistically significant predictor of VTE in juveniles.
The research was published in Hospital Pediatrics.
“This is important because the incidence of pediatric VTE has increased dramatically over the last 20 years, and childhood obesity remains highly prevalent in the United States,” said study author Elizabeth Halvorson, MD, of Wake Forest Baptist Medical Center in Winston-Salem, North Carolina.
For this study, she and her colleagues conducted a retrospective chart review of inpatients at Wake Forest Baptist’s Brenner Children’s Hospital between January 2000 and September 2012.
The researchers identified 88 patients, ages 2 to 18, who had confirmed cases of VTE. The team compared these patients to control subjects (2 controls per case) matched by age, gender, and the presence of a central venous catheter.
Of the 88 patients with VTE, 33 (37.5%) were obese, although most of them had known risk factors for VTE in addition to obesity.
In univariate analysis, the researchers found a statistically significant association between VTE and obesity, or increased BMI z score (P=0.002).
In a multivariate analysis, obesity remained a significant predictor of VTE. The odds ratio (OR) was 3.1 (P=0.007).
Other factors were significant predictors of VTE as well, including bacteremia (OR: 4.9; P=0.02), a stay in the intensive care unit (OR: 2.5; P=0.02), and the use of oral contraceptives (OR: 17.4; P<0.001).
“Our study presents data from a single institution with a relatively small sample size,” Dr Halvorson noted. “But it does demonstrate an association between obesity and VTE in children, which should be explored further in larger future studies.” ![]()

Photo by Matthew Lester
A single-center, retrospective study has revealed an association between obesity and venous thromboembolism (VTE) in children and adolescents.
While obesity is a well-established risk factor for VTE in adults, previous studies in pediatric populations have yielded mixed results.
The new study, however, showed that obesity, as determined by body mass index (BMI), was a statistically significant predictor of VTE in juveniles.
The research was published in Hospital Pediatrics.
“This is important because the incidence of pediatric VTE has increased dramatically over the last 20 years, and childhood obesity remains highly prevalent in the United States,” said study author Elizabeth Halvorson, MD, of Wake Forest Baptist Medical Center in Winston-Salem, North Carolina.
For this study, she and her colleagues conducted a retrospective chart review of inpatients at Wake Forest Baptist’s Brenner Children’s Hospital between January 2000 and September 2012.
The researchers identified 88 patients, ages 2 to 18, who had confirmed cases of VTE. The team compared these patients to control subjects (2 controls per case) matched by age, gender, and the presence of a central venous catheter.
Of the 88 patients with VTE, 33 (37.5%) were obese, although most of them had known risk factors for VTE in addition to obesity.
In univariate analysis, the researchers found a statistically significant association between VTE and obesity, or increased BMI z score (P=0.002).
In a multivariate analysis, obesity remained a significant predictor of VTE. The odds ratio (OR) was 3.1 (P=0.007).
Other factors were significant predictors of VTE as well, including bacteremia (OR: 4.9; P=0.02), a stay in the intensive care unit (OR: 2.5; P=0.02), and the use of oral contraceptives (OR: 17.4; P<0.001).
“Our study presents data from a single institution with a relatively small sample size,” Dr Halvorson noted. “But it does demonstrate an association between obesity and VTE in children, which should be explored further in larger future studies.” ![]()

Photo by Matthew Lester
A single-center, retrospective study has revealed an association between obesity and venous thromboembolism (VTE) in children and adolescents.
While obesity is a well-established risk factor for VTE in adults, previous studies in pediatric populations have yielded mixed results.
The new study, however, showed that obesity, as determined by body mass index (BMI), was a statistically significant predictor of VTE in juveniles.
The research was published in Hospital Pediatrics.
“This is important because the incidence of pediatric VTE has increased dramatically over the last 20 years, and childhood obesity remains highly prevalent in the United States,” said study author Elizabeth Halvorson, MD, of Wake Forest Baptist Medical Center in Winston-Salem, North Carolina.
For this study, she and her colleagues conducted a retrospective chart review of inpatients at Wake Forest Baptist’s Brenner Children’s Hospital between January 2000 and September 2012.
The researchers identified 88 patients, ages 2 to 18, who had confirmed cases of VTE. The team compared these patients to control subjects (2 controls per case) matched by age, gender, and the presence of a central venous catheter.
Of the 88 patients with VTE, 33 (37.5%) were obese, although most of them had known risk factors for VTE in addition to obesity.
In univariate analysis, the researchers found a statistically significant association between VTE and obesity, or increased BMI z score (P=0.002).
In a multivariate analysis, obesity remained a significant predictor of VTE. The odds ratio (OR) was 3.1 (P=0.007).
Other factors were significant predictors of VTE as well, including bacteremia (OR: 4.9; P=0.02), a stay in the intensive care unit (OR: 2.5; P=0.02), and the use of oral contraceptives (OR: 17.4; P<0.001).
“Our study presents data from a single institution with a relatively small sample size,” Dr Halvorson noted. “But it does demonstrate an association between obesity and VTE in children, which should be explored further in larger future studies.” ![]()
Protein may be therapeutic target for AML

and Matt McCormack, PhD
Photo courtesy of the
Walter and Eliza Hall
Institute of Medical Research
Preclinical research suggests the Hhex protein could be a cancer-specific therapeutic target for acute myeloid leukemia (AML).
Investigators discovered that loss of the Hhex protein halted leukemia cell growth and division in vitro and in vivo, but normal cells were unaffected by the loss of Hhex.
Matt McCormack, PhD, of the Walter and Eliza Hall Institute of Medical Research in Parkville, Victoria, Australia, and his colleagues relayed these findings in Genes and Development.
“There is an urgent need for new therapies to treat AML,” Dr McCormack said. “We showed blocking the Hhex protein could put the brakes on leukemia growth and completely eliminate AML in preclinical models. This could be targeted by new drugs to treat AML in humans.”
Specifically, the investigators found that Hhex was overexpressed in human AML, and the protein was essential for the maintenance of AML driven by the oncogenic fusion protein MLL-ENL and its downstream effectors, HoxA9 and Meis1.
However, Hhex was not required for normal myelopoiesis.
“Hhex is only essential for the leukemic cells, meaning we could target and treat leukemia without toxic effects on normal cells, avoiding many of the serious side effects that come with standard cancer treatments,” Dr McCormack said.
“We also know that most people with AML have increased levels of Hhex, often associated with adverse outcomes, further indicating it is an important target for new AML drugs.”
Dr McCormack and his colleagues also attempted to determine the mechanism by which Hhex promotes AML.
They found the protein represses the tumor suppressors p16INK4a and p19ARF in leukemic stem cells by regulating the Polycomb-repressive complex 2 (PRC2). They said that Hhex binds to the Cdkn2a locus and directly interacts with PRC2 to enable H3K27me3-mediated epigenetic repression.
“Hhex works by recruiting epigenetic factors to growth-control genes, effectively silencing them,” said author Ben Shields, PhD, also of the Walter and Eliza Hall Institute.
“This allows the leukemia cells to reproduce and accumulate more damage, contributing to the speed of AML progression.”
Dr McCormack said that although drugs inhibiting epigenetic modification have been tested against AML in the past, they have caused significant toxicity because their targets are also required for normal blood cell function.
“Unlike the epigenetic factors targeted previously, Hhex only regulates a small number of genes and is dispensable for normal blood cells,” Dr McCormack reiterated.
“This gives us a rare opportunity to kill AML cells without causing many side effects. We now hope to identify the critical regions of the Hhex protein that enable it to function, which will allow us to design much-needed new drugs to treat AML.” ![]()

and Matt McCormack, PhD
Photo courtesy of the
Walter and Eliza Hall
Institute of Medical Research
Preclinical research suggests the Hhex protein could be a cancer-specific therapeutic target for acute myeloid leukemia (AML).
Investigators discovered that loss of the Hhex protein halted leukemia cell growth and division in vitro and in vivo, but normal cells were unaffected by the loss of Hhex.
Matt McCormack, PhD, of the Walter and Eliza Hall Institute of Medical Research in Parkville, Victoria, Australia, and his colleagues relayed these findings in Genes and Development.
“There is an urgent need for new therapies to treat AML,” Dr McCormack said. “We showed blocking the Hhex protein could put the brakes on leukemia growth and completely eliminate AML in preclinical models. This could be targeted by new drugs to treat AML in humans.”
Specifically, the investigators found that Hhex was overexpressed in human AML, and the protein was essential for the maintenance of AML driven by the oncogenic fusion protein MLL-ENL and its downstream effectors, HoxA9 and Meis1.
However, Hhex was not required for normal myelopoiesis.
“Hhex is only essential for the leukemic cells, meaning we could target and treat leukemia without toxic effects on normal cells, avoiding many of the serious side effects that come with standard cancer treatments,” Dr McCormack said.
“We also know that most people with AML have increased levels of Hhex, often associated with adverse outcomes, further indicating it is an important target for new AML drugs.”
Dr McCormack and his colleagues also attempted to determine the mechanism by which Hhex promotes AML.
They found the protein represses the tumor suppressors p16INK4a and p19ARF in leukemic stem cells by regulating the Polycomb-repressive complex 2 (PRC2). They said that Hhex binds to the Cdkn2a locus and directly interacts with PRC2 to enable H3K27me3-mediated epigenetic repression.
“Hhex works by recruiting epigenetic factors to growth-control genes, effectively silencing them,” said author Ben Shields, PhD, also of the Walter and Eliza Hall Institute.
“This allows the leukemia cells to reproduce and accumulate more damage, contributing to the speed of AML progression.”
Dr McCormack said that although drugs inhibiting epigenetic modification have been tested against AML in the past, they have caused significant toxicity because their targets are also required for normal blood cell function.
“Unlike the epigenetic factors targeted previously, Hhex only regulates a small number of genes and is dispensable for normal blood cells,” Dr McCormack reiterated.
“This gives us a rare opportunity to kill AML cells without causing many side effects. We now hope to identify the critical regions of the Hhex protein that enable it to function, which will allow us to design much-needed new drugs to treat AML.” ![]()

and Matt McCormack, PhD
Photo courtesy of the
Walter and Eliza Hall
Institute of Medical Research
Preclinical research suggests the Hhex protein could be a cancer-specific therapeutic target for acute myeloid leukemia (AML).
Investigators discovered that loss of the Hhex protein halted leukemia cell growth and division in vitro and in vivo, but normal cells were unaffected by the loss of Hhex.
Matt McCormack, PhD, of the Walter and Eliza Hall Institute of Medical Research in Parkville, Victoria, Australia, and his colleagues relayed these findings in Genes and Development.
“There is an urgent need for new therapies to treat AML,” Dr McCormack said. “We showed blocking the Hhex protein could put the brakes on leukemia growth and completely eliminate AML in preclinical models. This could be targeted by new drugs to treat AML in humans.”
Specifically, the investigators found that Hhex was overexpressed in human AML, and the protein was essential for the maintenance of AML driven by the oncogenic fusion protein MLL-ENL and its downstream effectors, HoxA9 and Meis1.
However, Hhex was not required for normal myelopoiesis.
“Hhex is only essential for the leukemic cells, meaning we could target and treat leukemia without toxic effects on normal cells, avoiding many of the serious side effects that come with standard cancer treatments,” Dr McCormack said.
“We also know that most people with AML have increased levels of Hhex, often associated with adverse outcomes, further indicating it is an important target for new AML drugs.”
Dr McCormack and his colleagues also attempted to determine the mechanism by which Hhex promotes AML.
They found the protein represses the tumor suppressors p16INK4a and p19ARF in leukemic stem cells by regulating the Polycomb-repressive complex 2 (PRC2). They said that Hhex binds to the Cdkn2a locus and directly interacts with PRC2 to enable H3K27me3-mediated epigenetic repression.
“Hhex works by recruiting epigenetic factors to growth-control genes, effectively silencing them,” said author Ben Shields, PhD, also of the Walter and Eliza Hall Institute.
“This allows the leukemia cells to reproduce and accumulate more damage, contributing to the speed of AML progression.”
Dr McCormack said that although drugs inhibiting epigenetic modification have been tested against AML in the past, they have caused significant toxicity because their targets are also required for normal blood cell function.
“Unlike the epigenetic factors targeted previously, Hhex only regulates a small number of genes and is dispensable for normal blood cells,” Dr McCormack reiterated.
“This gives us a rare opportunity to kill AML cells without causing many side effects. We now hope to identify the critical regions of the Hhex protein that enable it to function, which will allow us to design much-needed new drugs to treat AML.” ![]()