User login
Lifelong Problem Has Caused Embarrassment
ANSWER
The correct answer is discoid lupus (choice “d”); see discussion for further details.
Sarcoidosis (choice “a”) is a worthy item in this differential, since it can be chronic, often affects the face (especially in African-Americans), and frequently defies ready diagnosis. But the biopsy was totally inconsistent with this diagnosis; in a case of sarcoidosis, it instead would have shown noncaseating granulomas, which are characteristic of the condition.
Lichen planus (choice “b”) is likewise worth consideration, since it can present in a similar fashion (although the chronicity of this patient’s lesions would have been atypical). Moreover, lichen planus is almost invariably symptomatic (itch). Biopsy would have shown obliteration of the dermoepidermal junction by an intense lymphocytic infiltrate—findings totally at odds with what was seen.
Polymorphous light eruption (PMLE; choice “c”) is the name given to a variety of photosensitivities that, true to the term polymorphous (or polymorphic), can present in numerous ways—although the lesions on any given patient tend to be monomorphic. These can take the form of vesicles, papules, and even erythema multiforme–like targetoid lesions, most commonly (as expected) on sun-exposed skin. Curiously, though, PMLE seldom affects the face or hands. It can manifest early in a patient’s life, but it would have been “seasonal,” disappearing in winter, and would have revealed a totally different picture on biopsy.
DISCUSSION
This patient suffered needlessly for more than half his life for lack of one simple thing: a correct diagnosis. Truth be known, the patient and his family probably bear some responsibility—but at some point, one of his many providers should have either obtained a punch biopsy or sent him to someone who would do so.
Instead, as is often the case, the emphasis was on treatment: trying one thing after another. The lack of success with these endeavors speaks loudly for the need for a definitive diagnosis. This could only be established one way: with a biopsy.
All the items mentioned in the above differential were legitimately considered. So was the possibility of infection, especially atypical types such as mycobacterial, deep fungal, or those involving other unusual organisms (eg, Nocardia, Actinomycetes). As in this case, tissue can be collected and submitted for culture, but the usual formalin preservative will kill any organism, necessitating prompt processing in saline.
Discoid lupus erythematosus (DLE) can be purely cutaneous (as seen here) or can be a manifestation of more serious systemic lupus. In any case, it is an autoimmune process, made worse by the sun, and can be chronic (though this case is exceptional in that regard).
This patient’s chance of developing systemic lupus erythematosus is slight, at most, since his antinuclear antibody test was negative. But his lifetime risk for another autoimmune disease is high.
TREATMENT
DLE is usually treated successfully with a combination of sun avoidance and a course of oral hydroxychloroquine (200 mg QD to bid, depending on the patient’s body habitus and the severity of the disease). Given the advanced state of this patient’s condition, he received the more frequent dosage, which should yield positive results. However, he will likely be on this regimen for some time.
ANSWER
The correct answer is discoid lupus (choice “d”); see discussion for further details.
Sarcoidosis (choice “a”) is a worthy item in this differential, since it can be chronic, often affects the face (especially in African-Americans), and frequently defies ready diagnosis. But the biopsy was totally inconsistent with this diagnosis; in a case of sarcoidosis, it instead would have shown noncaseating granulomas, which are characteristic of the condition.
Lichen planus (choice “b”) is likewise worth consideration, since it can present in a similar fashion (although the chronicity of this patient’s lesions would have been atypical). Moreover, lichen planus is almost invariably symptomatic (itch). Biopsy would have shown obliteration of the dermoepidermal junction by an intense lymphocytic infiltrate—findings totally at odds with what was seen.
Polymorphous light eruption (PMLE; choice “c”) is the name given to a variety of photosensitivities that, true to the term polymorphous (or polymorphic), can present in numerous ways—although the lesions on any given patient tend to be monomorphic. These can take the form of vesicles, papules, and even erythema multiforme–like targetoid lesions, most commonly (as expected) on sun-exposed skin. Curiously, though, PMLE seldom affects the face or hands. It can manifest early in a patient’s life, but it would have been “seasonal,” disappearing in winter, and would have revealed a totally different picture on biopsy.
DISCUSSION
This patient suffered needlessly for more than half his life for lack of one simple thing: a correct diagnosis. Truth be known, the patient and his family probably bear some responsibility—but at some point, one of his many providers should have either obtained a punch biopsy or sent him to someone who would do so.
Instead, as is often the case, the emphasis was on treatment: trying one thing after another. The lack of success with these endeavors speaks loudly for the need for a definitive diagnosis. This could only be established one way: with a biopsy.
All the items mentioned in the above differential were legitimately considered. So was the possibility of infection, especially atypical types such as mycobacterial, deep fungal, or those involving other unusual organisms (eg, Nocardia, Actinomycetes). As in this case, tissue can be collected and submitted for culture, but the usual formalin preservative will kill any organism, necessitating prompt processing in saline.
Discoid lupus erythematosus (DLE) can be purely cutaneous (as seen here) or can be a manifestation of more serious systemic lupus. In any case, it is an autoimmune process, made worse by the sun, and can be chronic (though this case is exceptional in that regard).
This patient’s chance of developing systemic lupus erythematosus is slight, at most, since his antinuclear antibody test was negative. But his lifetime risk for another autoimmune disease is high.
TREATMENT
DLE is usually treated successfully with a combination of sun avoidance and a course of oral hydroxychloroquine (200 mg QD to bid, depending on the patient’s body habitus and the severity of the disease). Given the advanced state of this patient’s condition, he received the more frequent dosage, which should yield positive results. However, he will likely be on this regimen for some time.
ANSWER
The correct answer is discoid lupus (choice “d”); see discussion for further details.
Sarcoidosis (choice “a”) is a worthy item in this differential, since it can be chronic, often affects the face (especially in African-Americans), and frequently defies ready diagnosis. But the biopsy was totally inconsistent with this diagnosis; in a case of sarcoidosis, it instead would have shown noncaseating granulomas, which are characteristic of the condition.
Lichen planus (choice “b”) is likewise worth consideration, since it can present in a similar fashion (although the chronicity of this patient’s lesions would have been atypical). Moreover, lichen planus is almost invariably symptomatic (itch). Biopsy would have shown obliteration of the dermoepidermal junction by an intense lymphocytic infiltrate—findings totally at odds with what was seen.
Polymorphous light eruption (PMLE; choice “c”) is the name given to a variety of photosensitivities that, true to the term polymorphous (or polymorphic), can present in numerous ways—although the lesions on any given patient tend to be monomorphic. These can take the form of vesicles, papules, and even erythema multiforme–like targetoid lesions, most commonly (as expected) on sun-exposed skin. Curiously, though, PMLE seldom affects the face or hands. It can manifest early in a patient’s life, but it would have been “seasonal,” disappearing in winter, and would have revealed a totally different picture on biopsy.
DISCUSSION
This patient suffered needlessly for more than half his life for lack of one simple thing: a correct diagnosis. Truth be known, the patient and his family probably bear some responsibility—but at some point, one of his many providers should have either obtained a punch biopsy or sent him to someone who would do so.
Instead, as is often the case, the emphasis was on treatment: trying one thing after another. The lack of success with these endeavors speaks loudly for the need for a definitive diagnosis. This could only be established one way: with a biopsy.
All the items mentioned in the above differential were legitimately considered. So was the possibility of infection, especially atypical types such as mycobacterial, deep fungal, or those involving other unusual organisms (eg, Nocardia, Actinomycetes). As in this case, tissue can be collected and submitted for culture, but the usual formalin preservative will kill any organism, necessitating prompt processing in saline.
Discoid lupus erythematosus (DLE) can be purely cutaneous (as seen here) or can be a manifestation of more serious systemic lupus. In any case, it is an autoimmune process, made worse by the sun, and can be chronic (though this case is exceptional in that regard).
This patient’s chance of developing systemic lupus erythematosus is slight, at most, since his antinuclear antibody test was negative. But his lifetime risk for another autoimmune disease is high.
TREATMENT
DLE is usually treated successfully with a combination of sun avoidance and a course of oral hydroxychloroquine (200 mg QD to bid, depending on the patient’s body habitus and the severity of the disease). Given the advanced state of this patient’s condition, he received the more frequent dosage, which should yield positive results. However, he will likely be on this regimen for some time.

Since the fourth grade, this 22-year-old African-American man has had facial lesions that, although constantly present, worsen in the summer. The problem is so severe that it has greatly affected his quality of life: In school and in his neighborhood, he has been subjected to rumors that his condition might be contagious. Despite numerous treatment attempts—including topical and oral anti-acne medications, topical and oral antifungal medications, and oral antibiotics—the condition has persisted. Once, at his mother’s urging, the patient even sought the assistance of a faith healer at a religious revival. Initially seen by a primary care provider at a free clinic, he was then referred to a dermatology clinician at the same facility. History taking reveals that the lesions are asymptomatic and appear in additional locations (eg, arms, ears, and neck). The patient denies any family history of similar problems, as well as persistent fever, cough, or shortness of breath. Lab studies obtained by his primary care provider, including a complete blood count and chem screen, were within normal limits. Most of the lesions on the patient’s face are round areas of slightly erythematous erosion covered by eschar. They range in size from 3 mm to more than 1 cm. Focal postinflammatory hyperpigmentation is noted (a common finding in those with type V/VI skin). Focal hyperpigmentation is also seen on both ears, in some cases with scaling and faint erosion on the surface. A KOH prep is performed with scale collected from perilesional skin; results are negative for fungal elements. There are no palpable nodes in the adjacent nodal locations. Two punch biopsies are done, with samples taken from the active margins of the lesions. One is submitted for routine H&E (hematoxylin and eosin) handling and the other in saline for bacterial, acid-fast bacilli (AFB), and fungal cultures. The biopsy shows hyperkeratosis, follicular plugging, and epidermal atrophy. Marked vacuolar degeneration of the dermoepidermal junction is also noted, along with mucin deposition. Stains for bacteria, AFB, and fungi yield negative results.
Woman Assaulted on Street
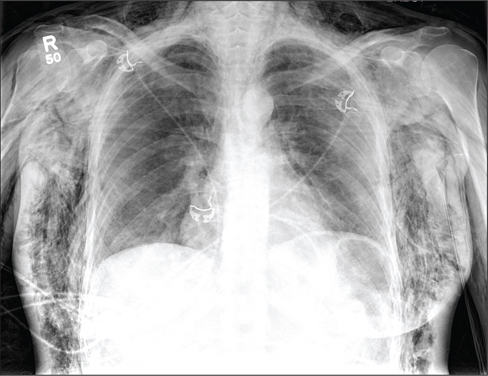
The chest radiograph demonstrates a massive amount of soft tissue and subcutaneous emphysema extending from the neck down through the chest and into the lower chest/upper abdomen. In addition, there are several fractured posterior ribs bilaterally. No large pneumothorax or pneumomediastinum is noted.
Because of the extent and mechanism of injury, CT of the chest, abdomen, and pelvis had already been ordered. Arrangements were also made for the patient to be admitted to the ICU for closer observation.
The chest radiograph demonstrates a massive amount of soft tissue and subcutaneous emphysema extending from the neck down through the chest and into the lower chest/upper abdomen. In addition, there are several fractured posterior ribs bilaterally. No large pneumothorax or pneumomediastinum is noted.
Because of the extent and mechanism of injury, CT of the chest, abdomen, and pelvis had already been ordered. Arrangements were also made for the patient to be admitted to the ICU for closer observation.
The chest radiograph demonstrates a massive amount of soft tissue and subcutaneous emphysema extending from the neck down through the chest and into the lower chest/upper abdomen. In addition, there are several fractured posterior ribs bilaterally. No large pneumothorax or pneumomediastinum is noted.
Because of the extent and mechanism of injury, CT of the chest, abdomen, and pelvis had already been ordered. Arrangements were also made for the patient to be admitted to the ICU for closer observation.
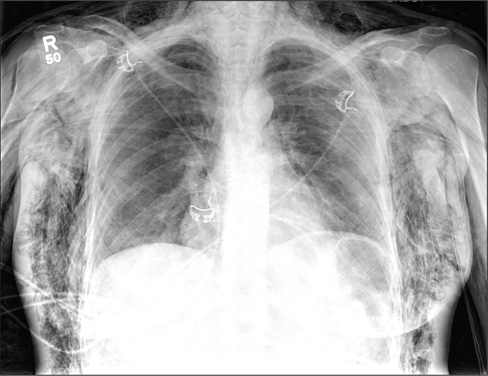
A 40-year-old woman is brought in by EMS for evaluation of injuries secondary to being assaulted. She was out walking late last night when she was approached by two men who pushed her to the ground and began punching and kicking her repeatedly on her face, chest, and back. She is primarily complaining of chest wall and back pain. Her medical history is significant for hypertension, diet-controlled diabetes, and “some sort of heart problem” for which she takes medication. Surgical history is significant for hysterectomy, cholecystectomy, and appendectomy. She smokes more than a pack of cigarettes per day and consumes at least a six-pack of beer daily. Initial exam shows an anxious female who appears somewhat uncomfortable but is in no obvious distress. Her vital signs are as follows: blood pressure, 130/88 mm Hg; pulse, 120 beats/min; respiratory rate, 22 breaths/min; and O2 saturation, 100% on room air. Physical exam reveals extensive facial/periorbital swelling, as well as swelling in the neck. Some splinting is noted. There is extensive crepitus noted within the soft tissue of the face, neck, and chest wall. Also, there is moderate tenderness bilaterally over the ribs. Chest radiograph is obtained (shown). What is your impression?
Observation Status Not So Well-Defined in Hospitals
New research suggests use of the designation "observation status" for admitted hospital patients varies in clinical practice, despite rigid criteria the Centers for Medicare & Medicaid Services (CMS) uses to define the term.
CMS defines observation status as "well-defined sets of specific, clinically appropriate services." In most cases, the status applies to inpatient stays of less than 24 hours. Longer than 48 hours is dubbed "rare and exceptional" by the federal agency.
But in the report, “Hospitalized But Not Admitted: Characteristics of Patients With ‘Observation Status’ at an Academic Medical Center," lead author and hospitalist Ann Sheehy, MD, MS, of Wisconsin School of Medicine and Public Health in Madison found that patients' mean length of stay (LOS) in observation was 33.3 hours, but it was longer than 48 hours in 16.5% of cases. Dr. Sheehy adds that 1,141 distinct observation diagnosis codes were used for observation stays during the study period, which ran from July 1, 2010, to Dec. 31, 2011.
"What CMS has as a definition for observation status is clearly not what's happening in clinical practice, based on the length of stay and the wide variety of diagnosis codes," Dr. Sheehy says. "We had over 1,000 diagnosis codes for something CMS says is well-defined."
The issue is of particular note to hospital medicine groups as observation status disproportionately affects the general-medicine population, Dr. Sheehy says. Just over 52% of all observation stays in the study were adult general-medicine patients.
The paper adds that while the cost per encounter for observation care was less than that for inpatient care, the average reimbursement for observation care failed to cover it. The net loss per encounter for an observation stay was $331, compared with a net gain of $2,163 for an inpatient stay.
"We don't want to have hospitals operating on a huge profit margin," Dr. Sheehy says, but "you can't have hospitals delivering care at a loss consistently and have them stay solvent. It's just not going to work."
Visit our website for more information on observation status rules.
New research suggests use of the designation "observation status" for admitted hospital patients varies in clinical practice, despite rigid criteria the Centers for Medicare & Medicaid Services (CMS) uses to define the term.
CMS defines observation status as "well-defined sets of specific, clinically appropriate services." In most cases, the status applies to inpatient stays of less than 24 hours. Longer than 48 hours is dubbed "rare and exceptional" by the federal agency.
But in the report, “Hospitalized But Not Admitted: Characteristics of Patients With ‘Observation Status’ at an Academic Medical Center," lead author and hospitalist Ann Sheehy, MD, MS, of Wisconsin School of Medicine and Public Health in Madison found that patients' mean length of stay (LOS) in observation was 33.3 hours, but it was longer than 48 hours in 16.5% of cases. Dr. Sheehy adds that 1,141 distinct observation diagnosis codes were used for observation stays during the study period, which ran from July 1, 2010, to Dec. 31, 2011.
"What CMS has as a definition for observation status is clearly not what's happening in clinical practice, based on the length of stay and the wide variety of diagnosis codes," Dr. Sheehy says. "We had over 1,000 diagnosis codes for something CMS says is well-defined."
The issue is of particular note to hospital medicine groups as observation status disproportionately affects the general-medicine population, Dr. Sheehy says. Just over 52% of all observation stays in the study were adult general-medicine patients.
The paper adds that while the cost per encounter for observation care was less than that for inpatient care, the average reimbursement for observation care failed to cover it. The net loss per encounter for an observation stay was $331, compared with a net gain of $2,163 for an inpatient stay.
"We don't want to have hospitals operating on a huge profit margin," Dr. Sheehy says, but "you can't have hospitals delivering care at a loss consistently and have them stay solvent. It's just not going to work."
Visit our website for more information on observation status rules.
New research suggests use of the designation "observation status" for admitted hospital patients varies in clinical practice, despite rigid criteria the Centers for Medicare & Medicaid Services (CMS) uses to define the term.
CMS defines observation status as "well-defined sets of specific, clinically appropriate services." In most cases, the status applies to inpatient stays of less than 24 hours. Longer than 48 hours is dubbed "rare and exceptional" by the federal agency.
But in the report, “Hospitalized But Not Admitted: Characteristics of Patients With ‘Observation Status’ at an Academic Medical Center," lead author and hospitalist Ann Sheehy, MD, MS, of Wisconsin School of Medicine and Public Health in Madison found that patients' mean length of stay (LOS) in observation was 33.3 hours, but it was longer than 48 hours in 16.5% of cases. Dr. Sheehy adds that 1,141 distinct observation diagnosis codes were used for observation stays during the study period, which ran from July 1, 2010, to Dec. 31, 2011.
"What CMS has as a definition for observation status is clearly not what's happening in clinical practice, based on the length of stay and the wide variety of diagnosis codes," Dr. Sheehy says. "We had over 1,000 diagnosis codes for something CMS says is well-defined."
The issue is of particular note to hospital medicine groups as observation status disproportionately affects the general-medicine population, Dr. Sheehy says. Just over 52% of all observation stays in the study were adult general-medicine patients.
The paper adds that while the cost per encounter for observation care was less than that for inpatient care, the average reimbursement for observation care failed to cover it. The net loss per encounter for an observation stay was $331, compared with a net gain of $2,163 for an inpatient stay.
"We don't want to have hospitals operating on a huge profit margin," Dr. Sheehy says, but "you can't have hospitals delivering care at a loss consistently and have them stay solvent. It's just not going to work."
Visit our website for more information on observation status rules.
CMS Allows Residents, Advanced Practitioners to Admit Inpatients
A federal rule that some hospitalists feared would bar nonstaff physicians from writing admission orders for hospital inpatients has been clarified to extend those privileges to resident physicians and advanced practitioners.
On Aug. 19, the Centers for Medicare & Medicaid Services (CMS) published its fiscal 2014 hospital Inpatient Prospective Payment System (IPPS) Final Rule, which is effective Oct. 1. Although this document impacts a number of important areas for hospitals, including the use of inpatient admission and observation status, hospitalists also were left with the impression that resident physicians and advanced practitioners (NPs and PAs) were being barred from writing admission orders.
Medical residents, NPs, and PAs do not have admitting privileges in most hospitals, and their inability to write admission orders would pose significant logistical and financial hurdles for many hospitals and physician groups, including hospitalists.
In most academic centers, residents have the opportunity and responsibility to evaluate patients at the time of hospitalization, write initial hospitalization orders, and then discuss patients with the attending physician. The "staffing" of patients typically occurs either later the same day or the following morning. The provision requiring an attending physician knowledgeable of the case to furnish the admission order, and not allowing delegation of this order to their residents, could fundamentally change the way our physicians are trained.
Many hospitals rely on NPs and PAs for the care of hospitalized patients under the supervision of a staff physician. These nonphysician providers often care for hospitalized patients, admit patients, and provide overnight coverage. Requiring admission orders to be placed by physicians with admitting privileges would require a greater presence of staff physicians, which would increase costs.
Some of these concerns were voiced Aug. 15 on CMS' Special Open Door Forum on CMS Rule 1599-F. While clarification was not offered, it was indicated that CMS did not intend to place such limitations on residents, NPs, and PAs. On Sept. 5, CMS released clarifications to some of these provisions in the IPPS Final Rule, and noted that admission orders may come from a physician or other practitioner.
This clarification suggests that when a resident, NP, or PA writes admission orders, they are doing so at the direction of a physician with admitting privileges. This may occur in the form of a verbal order, which requires documentation of the name of the admitting physician, as well as the date and time of the verbal order. This verbal order must then be countersigned by a qualified physician prior to patient discharge.
Failures to obtain appropriate orders co-signed by an appropriate physician are likely at high risk for Medicare payment denial. This clarification appears to address previously held concerns about this new rule.
A federal rule that some hospitalists feared would bar nonstaff physicians from writing admission orders for hospital inpatients has been clarified to extend those privileges to resident physicians and advanced practitioners.
On Aug. 19, the Centers for Medicare & Medicaid Services (CMS) published its fiscal 2014 hospital Inpatient Prospective Payment System (IPPS) Final Rule, which is effective Oct. 1. Although this document impacts a number of important areas for hospitals, including the use of inpatient admission and observation status, hospitalists also were left with the impression that resident physicians and advanced practitioners (NPs and PAs) were being barred from writing admission orders.
Medical residents, NPs, and PAs do not have admitting privileges in most hospitals, and their inability to write admission orders would pose significant logistical and financial hurdles for many hospitals and physician groups, including hospitalists.
In most academic centers, residents have the opportunity and responsibility to evaluate patients at the time of hospitalization, write initial hospitalization orders, and then discuss patients with the attending physician. The "staffing" of patients typically occurs either later the same day or the following morning. The provision requiring an attending physician knowledgeable of the case to furnish the admission order, and not allowing delegation of this order to their residents, could fundamentally change the way our physicians are trained.
Many hospitals rely on NPs and PAs for the care of hospitalized patients under the supervision of a staff physician. These nonphysician providers often care for hospitalized patients, admit patients, and provide overnight coverage. Requiring admission orders to be placed by physicians with admitting privileges would require a greater presence of staff physicians, which would increase costs.
Some of these concerns were voiced Aug. 15 on CMS' Special Open Door Forum on CMS Rule 1599-F. While clarification was not offered, it was indicated that CMS did not intend to place such limitations on residents, NPs, and PAs. On Sept. 5, CMS released clarifications to some of these provisions in the IPPS Final Rule, and noted that admission orders may come from a physician or other practitioner.
This clarification suggests that when a resident, NP, or PA writes admission orders, they are doing so at the direction of a physician with admitting privileges. This may occur in the form of a verbal order, which requires documentation of the name of the admitting physician, as well as the date and time of the verbal order. This verbal order must then be countersigned by a qualified physician prior to patient discharge.
Failures to obtain appropriate orders co-signed by an appropriate physician are likely at high risk for Medicare payment denial. This clarification appears to address previously held concerns about this new rule.
A federal rule that some hospitalists feared would bar nonstaff physicians from writing admission orders for hospital inpatients has been clarified to extend those privileges to resident physicians and advanced practitioners.
On Aug. 19, the Centers for Medicare & Medicaid Services (CMS) published its fiscal 2014 hospital Inpatient Prospective Payment System (IPPS) Final Rule, which is effective Oct. 1. Although this document impacts a number of important areas for hospitals, including the use of inpatient admission and observation status, hospitalists also were left with the impression that resident physicians and advanced practitioners (NPs and PAs) were being barred from writing admission orders.
Medical residents, NPs, and PAs do not have admitting privileges in most hospitals, and their inability to write admission orders would pose significant logistical and financial hurdles for many hospitals and physician groups, including hospitalists.
In most academic centers, residents have the opportunity and responsibility to evaluate patients at the time of hospitalization, write initial hospitalization orders, and then discuss patients with the attending physician. The "staffing" of patients typically occurs either later the same day or the following morning. The provision requiring an attending physician knowledgeable of the case to furnish the admission order, and not allowing delegation of this order to their residents, could fundamentally change the way our physicians are trained.
Many hospitals rely on NPs and PAs for the care of hospitalized patients under the supervision of a staff physician. These nonphysician providers often care for hospitalized patients, admit patients, and provide overnight coverage. Requiring admission orders to be placed by physicians with admitting privileges would require a greater presence of staff physicians, which would increase costs.
Some of these concerns were voiced Aug. 15 on CMS' Special Open Door Forum on CMS Rule 1599-F. While clarification was not offered, it was indicated that CMS did not intend to place such limitations on residents, NPs, and PAs. On Sept. 5, CMS released clarifications to some of these provisions in the IPPS Final Rule, and noted that admission orders may come from a physician or other practitioner.
This clarification suggests that when a resident, NP, or PA writes admission orders, they are doing so at the direction of a physician with admitting privileges. This may occur in the form of a verbal order, which requires documentation of the name of the admitting physician, as well as the date and time of the verbal order. This verbal order must then be countersigned by a qualified physician prior to patient discharge.
Failures to obtain appropriate orders co-signed by an appropriate physician are likely at high risk for Medicare payment denial. This clarification appears to address previously held concerns about this new rule.
Cranial radiotherapy for acute lymphoblastic leukemia linked to impaired neurocognition
Reduced white matter and impaired neuropsychological function were seen 20-30 years later in childhood acute lymphoblastic leukemia and lymphoma survivors who received cranial radiotherapy.
Survivors treated with chemotherapy alone appeared to have milder impairments, with measures that were within one standard deviation of the measures seen in healthy controls, reported Ilse Schuitema of the University of Leiden and her associates.
They also found that a young age at the time of cranial radiotherapy and the radiation dosage were associated with poorer results on the MRI measure used to evaluate the white matter's microstructure. Decreases in this measure were associated with neuropsychological dysfunction. The study was published in the Sept. 20 issue of the Journal of Clinical Oncology (2013;31:3378-88).
The finding "warrants a recommendation to use CRT [cranial radiotherapy] only as a last resort," since chemotherapy is just as effective, based on survival and recurrence rates in patients with acute lymphoblastic leukemia (ALL). Further, indications of accelerated aging seen in survivors given cranial radiotherapy may support screening for early-onset dementia as well as recommending lifestyle modifications such as not smoking and getting regular physical exercise to slow the progress of dementia.
Ms. Schuitema of the department of clinical child and adolescent studies, faculty of social sciences at Leiden (the Netherlands) University, and her co-investigators, followed up with 93 survivors of ALL or lymphoma who had been treated between 1978 and 1990 with cranial radiotherapy or CNS-directed chemotherapy, and compared them with 49 healthy controls. The mean age of patients given chemotherapy only was 27 years and the mean age of those treated with radiotherapy was 31 years.
Testing included magnetic resonance diffusion tensor imaging and neuropsychological tests. Differences in fractional anisotropy on the MRI test were used to analyze white matter microstructure, and whole-brain, voxel-based analysis was performed.
Survivors treated with chemotherapy only had reductions in the MRI measure and neuropsychological performance, but the measures were no more than one standard deviation below the mean values of controls.
When compared with controls, survivors who had cranial radiotherapy had significant reductions in white matter integrity and lower neurocognitive function, with effects that included lower IQ, poorer visuomotor accuracy, and poorer work flow during sustained attention.
Further, there was a "steep decline," in the MRI measure within the frontal and parietal white matter, which "is a strong indication of accelerated aging" the researchers wrote. Some of the anatomical findings among those treated with CRT were similar to those found in people with Alzheimer's disease, suggesting that "the irradiated survivors could be at increased risk of developing early-onset dementia."
The study results highlight the importance of long-term follow-up of children who receive neurotoxic treatments and increase support "for the concept of accelerated aging after CRT implicates screening for early-onset dementia,"the researchers said.
The tests used in the study included the computerized Amsterdam Neuropsychological Tasks (ANT) program, used to assess executive functions, and the four subtest short-form of the Wechsler Adult Intelligence Scale Revised (WAIS-R III).
Ms. Schuitema's coauthors are from the University of Leiden; University Hospitals Leuven, Belgium; and Academic Medical Center, Amsterdam. The authors had no disclosures. The study was funded by grants, including one from the Dutch Cancer Society.
This is one of the first studies to look at the long-term effects of treatment in childhood ALL survivors. These findings raise a significant concern about the long-term CNS and neurocognitive integrity of children who have been treated and are currently being treated with cranial radiotherapy. A significant number of children continue to receive radiation doses that are similar to or higher than the doses that were used to treat the patients in this study. Additional confirmatory studies are needed as is research that may bring about changes in treatment and long-term outcomes for the children we are treating today.
F. Daniel Armstrong, Ph.D., is director of the Mailman Center for Child Development, and professor of pediatrics & psychology at the University of Miami. He made his remarks in an editorial that accompanied the study (J. Clin. Oncol 2013;31:3309-11). He had no relevant disclosures.
This is one of the first studies to look at the long-term effects of treatment in childhood ALL survivors. These findings raise a significant concern about the long-term CNS and neurocognitive integrity of children who have been treated and are currently being treated with cranial radiotherapy. A significant number of children continue to receive radiation doses that are similar to or higher than the doses that were used to treat the patients in this study. Additional confirmatory studies are needed as is research that may bring about changes in treatment and long-term outcomes for the children we are treating today.
F. Daniel Armstrong, Ph.D., is director of the Mailman Center for Child Development, and professor of pediatrics & psychology at the University of Miami. He made his remarks in an editorial that accompanied the study (J. Clin. Oncol 2013;31:3309-11). He had no relevant disclosures.
This is one of the first studies to look at the long-term effects of treatment in childhood ALL survivors. These findings raise a significant concern about the long-term CNS and neurocognitive integrity of children who have been treated and are currently being treated with cranial radiotherapy. A significant number of children continue to receive radiation doses that are similar to or higher than the doses that were used to treat the patients in this study. Additional confirmatory studies are needed as is research that may bring about changes in treatment and long-term outcomes for the children we are treating today.
F. Daniel Armstrong, Ph.D., is director of the Mailman Center for Child Development, and professor of pediatrics & psychology at the University of Miami. He made his remarks in an editorial that accompanied the study (J. Clin. Oncol 2013;31:3309-11). He had no relevant disclosures.
Reduced white matter and impaired neuropsychological function were seen 20-30 years later in childhood acute lymphoblastic leukemia and lymphoma survivors who received cranial radiotherapy.
Survivors treated with chemotherapy alone appeared to have milder impairments, with measures that were within one standard deviation of the measures seen in healthy controls, reported Ilse Schuitema of the University of Leiden and her associates.
They also found that a young age at the time of cranial radiotherapy and the radiation dosage were associated with poorer results on the MRI measure used to evaluate the white matter's microstructure. Decreases in this measure were associated with neuropsychological dysfunction. The study was published in the Sept. 20 issue of the Journal of Clinical Oncology (2013;31:3378-88).
The finding "warrants a recommendation to use CRT [cranial radiotherapy] only as a last resort," since chemotherapy is just as effective, based on survival and recurrence rates in patients with acute lymphoblastic leukemia (ALL). Further, indications of accelerated aging seen in survivors given cranial radiotherapy may support screening for early-onset dementia as well as recommending lifestyle modifications such as not smoking and getting regular physical exercise to slow the progress of dementia.
Ms. Schuitema of the department of clinical child and adolescent studies, faculty of social sciences at Leiden (the Netherlands) University, and her co-investigators, followed up with 93 survivors of ALL or lymphoma who had been treated between 1978 and 1990 with cranial radiotherapy or CNS-directed chemotherapy, and compared them with 49 healthy controls. The mean age of patients given chemotherapy only was 27 years and the mean age of those treated with radiotherapy was 31 years.
Testing included magnetic resonance diffusion tensor imaging and neuropsychological tests. Differences in fractional anisotropy on the MRI test were used to analyze white matter microstructure, and whole-brain, voxel-based analysis was performed.
Survivors treated with chemotherapy only had reductions in the MRI measure and neuropsychological performance, but the measures were no more than one standard deviation below the mean values of controls.
When compared with controls, survivors who had cranial radiotherapy had significant reductions in white matter integrity and lower neurocognitive function, with effects that included lower IQ, poorer visuomotor accuracy, and poorer work flow during sustained attention.
Further, there was a "steep decline," in the MRI measure within the frontal and parietal white matter, which "is a strong indication of accelerated aging" the researchers wrote. Some of the anatomical findings among those treated with CRT were similar to those found in people with Alzheimer's disease, suggesting that "the irradiated survivors could be at increased risk of developing early-onset dementia."
The study results highlight the importance of long-term follow-up of children who receive neurotoxic treatments and increase support "for the concept of accelerated aging after CRT implicates screening for early-onset dementia,"the researchers said.
The tests used in the study included the computerized Amsterdam Neuropsychological Tasks (ANT) program, used to assess executive functions, and the four subtest short-form of the Wechsler Adult Intelligence Scale Revised (WAIS-R III).
Ms. Schuitema's coauthors are from the University of Leiden; University Hospitals Leuven, Belgium; and Academic Medical Center, Amsterdam. The authors had no disclosures. The study was funded by grants, including one from the Dutch Cancer Society.
Reduced white matter and impaired neuropsychological function were seen 20-30 years later in childhood acute lymphoblastic leukemia and lymphoma survivors who received cranial radiotherapy.
Survivors treated with chemotherapy alone appeared to have milder impairments, with measures that were within one standard deviation of the measures seen in healthy controls, reported Ilse Schuitema of the University of Leiden and her associates.
They also found that a young age at the time of cranial radiotherapy and the radiation dosage were associated with poorer results on the MRI measure used to evaluate the white matter's microstructure. Decreases in this measure were associated with neuropsychological dysfunction. The study was published in the Sept. 20 issue of the Journal of Clinical Oncology (2013;31:3378-88).
The finding "warrants a recommendation to use CRT [cranial radiotherapy] only as a last resort," since chemotherapy is just as effective, based on survival and recurrence rates in patients with acute lymphoblastic leukemia (ALL). Further, indications of accelerated aging seen in survivors given cranial radiotherapy may support screening for early-onset dementia as well as recommending lifestyle modifications such as not smoking and getting regular physical exercise to slow the progress of dementia.
Ms. Schuitema of the department of clinical child and adolescent studies, faculty of social sciences at Leiden (the Netherlands) University, and her co-investigators, followed up with 93 survivors of ALL or lymphoma who had been treated between 1978 and 1990 with cranial radiotherapy or CNS-directed chemotherapy, and compared them with 49 healthy controls. The mean age of patients given chemotherapy only was 27 years and the mean age of those treated with radiotherapy was 31 years.
Testing included magnetic resonance diffusion tensor imaging and neuropsychological tests. Differences in fractional anisotropy on the MRI test were used to analyze white matter microstructure, and whole-brain, voxel-based analysis was performed.
Survivors treated with chemotherapy only had reductions in the MRI measure and neuropsychological performance, but the measures were no more than one standard deviation below the mean values of controls.
When compared with controls, survivors who had cranial radiotherapy had significant reductions in white matter integrity and lower neurocognitive function, with effects that included lower IQ, poorer visuomotor accuracy, and poorer work flow during sustained attention.
Further, there was a "steep decline," in the MRI measure within the frontal and parietal white matter, which "is a strong indication of accelerated aging" the researchers wrote. Some of the anatomical findings among those treated with CRT were similar to those found in people with Alzheimer's disease, suggesting that "the irradiated survivors could be at increased risk of developing early-onset dementia."
The study results highlight the importance of long-term follow-up of children who receive neurotoxic treatments and increase support "for the concept of accelerated aging after CRT implicates screening for early-onset dementia,"the researchers said.
The tests used in the study included the computerized Amsterdam Neuropsychological Tasks (ANT) program, used to assess executive functions, and the four subtest short-form of the Wechsler Adult Intelligence Scale Revised (WAIS-R III).
Ms. Schuitema's coauthors are from the University of Leiden; University Hospitals Leuven, Belgium; and Academic Medical Center, Amsterdam. The authors had no disclosures. The study was funded by grants, including one from the Dutch Cancer Society.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Major finding: Compared with controls, survivors who had cranial radiotherapy had significant reductions in white matter integrity and lower neurocognitive function, with effects that included lower IQ, poorer visuomotor accuracy, and poorer work flow during sustained attention.
Data source: Magnetic resonance imaging and neuropsychological test results in 93 survivors of childhood ALL or lymphoma and 49 healthy controls.
Disclosures: The study was supported with grants, including one from the Dutch Cancer Society. The authors had no disclosures.
Ten tips for chronic venous ulcers
The underlying pathophysiology of chronic venous insufficiency is complex and involves many factors. Studies have shown that average venous ulcers may need 6-12 months for complete healing with an anticipated recurrence rate exceeding 2/3 cases in 5 years. These numbers reflect the magnitude of the problem and mandate deploying all efforts to stop progression of the disease. Our group has found the following 10 tips have significantly improved our healing rates.
1. First, rule out any associated arterial, immunologic, endocrine, or other systemic causes for leg/foot ulceration.
2. Be aggressive to stop progression of the disease (fight CEAP 6): any local tenderness at the site of discolored skin at the gaiter area for venous ulcers should initiate a prompt reflux study to evaluate for incompetent perforators.
3. Venous ulcers are associated with an incompetent perforator within 2 cm of the ulcer area.
4. Recurrent venous ulcers at the same location may be associated with venous outflow obstruction, (May-Thurner syndrome is an underestimated pathology) which affects mainly the left leg.
5. When performing iliac vein venograms, make liberal use of intravascular ultrasound.
6. Exudative venous ulcers need multilayer compression dressings and appropriate antibiotics if infection exists.
7. Pentoxifylline (Trental) 800 mg, 3 times daily.
8. Frequent debridement and frequent objective evaluation for ulcer area with each office visit.
9. Bi-layered living cell treatment (Apligraf?) to promote healing.
10. Office/clinic visit every 3 months after complete healing (CEAP 5) and further testing as needed.
Dr. Mousa is an associate professor at the Department of Surgery, West Virginia University, Morgantown.
The underlying pathophysiology of chronic venous insufficiency is complex and involves many factors. Studies have shown that average venous ulcers may need 6-12 months for complete healing with an anticipated recurrence rate exceeding 2/3 cases in 5 years. These numbers reflect the magnitude of the problem and mandate deploying all efforts to stop progression of the disease. Our group has found the following 10 tips have significantly improved our healing rates.
1. First, rule out any associated arterial, immunologic, endocrine, or other systemic causes for leg/foot ulceration.
2. Be aggressive to stop progression of the disease (fight CEAP 6): any local tenderness at the site of discolored skin at the gaiter area for venous ulcers should initiate a prompt reflux study to evaluate for incompetent perforators.
3. Venous ulcers are associated with an incompetent perforator within 2 cm of the ulcer area.
4. Recurrent venous ulcers at the same location may be associated with venous outflow obstruction, (May-Thurner syndrome is an underestimated pathology) which affects mainly the left leg.
5. When performing iliac vein venograms, make liberal use of intravascular ultrasound.
6. Exudative venous ulcers need multilayer compression dressings and appropriate antibiotics if infection exists.
7. Pentoxifylline (Trental) 800 mg, 3 times daily.
8. Frequent debridement and frequent objective evaluation for ulcer area with each office visit.
9. Bi-layered living cell treatment (Apligraf?) to promote healing.
10. Office/clinic visit every 3 months after complete healing (CEAP 5) and further testing as needed.
Dr. Mousa is an associate professor at the Department of Surgery, West Virginia University, Morgantown.
The underlying pathophysiology of chronic venous insufficiency is complex and involves many factors. Studies have shown that average venous ulcers may need 6-12 months for complete healing with an anticipated recurrence rate exceeding 2/3 cases in 5 years. These numbers reflect the magnitude of the problem and mandate deploying all efforts to stop progression of the disease. Our group has found the following 10 tips have significantly improved our healing rates.
1. First, rule out any associated arterial, immunologic, endocrine, or other systemic causes for leg/foot ulceration.
2. Be aggressive to stop progression of the disease (fight CEAP 6): any local tenderness at the site of discolored skin at the gaiter area for venous ulcers should initiate a prompt reflux study to evaluate for incompetent perforators.
3. Venous ulcers are associated with an incompetent perforator within 2 cm of the ulcer area.
4. Recurrent venous ulcers at the same location may be associated with venous outflow obstruction, (May-Thurner syndrome is an underestimated pathology) which affects mainly the left leg.
5. When performing iliac vein venograms, make liberal use of intravascular ultrasound.
6. Exudative venous ulcers need multilayer compression dressings and appropriate antibiotics if infection exists.
7. Pentoxifylline (Trental) 800 mg, 3 times daily.
8. Frequent debridement and frequent objective evaluation for ulcer area with each office visit.
9. Bi-layered living cell treatment (Apligraf?) to promote healing.
10. Office/clinic visit every 3 months after complete healing (CEAP 5) and further testing as needed.
Dr. Mousa is an associate professor at the Department of Surgery, West Virginia University, Morgantown.
Peripheral neuropathy linked to obstructive sleep apnea?
CASE A 57-year-old white woman presented with symptoms of bilateral “stocking-like numbness” and the sensation of “wearing socks for a few weeks” but denied any injury, previous chemotherapy, or diabetes. Her medical history was positive for untreated obstructive sleep apnea (OSA), obesity (body mass index, 36 kg/m2), osteoarthritis in various joints, impaired fasting glucose with normal glycosylated hemoglobin (HbA1c), hypertension, gastroesophageal reflux disease, hypothyroidism, hypercholesterolemia, and osteoporosis.
Our initial examination revealed decreased sensation to light palpation and pin prick over the distal portion of her lower extremities in a stocking-like fashion. Proprioception was decreased at the distal joint of the big toe. Her deep tendon reflex pattern was symmetric with 2+ at the knees, ankles, and toes. The rest of her lower extremity exam was within normal limits and there were no obvious vascular abnormalities.
Given the suspicion of peripheral neuropathy, the patient underwent laboratory tests and a nerve conduction study. Vitamin B12, vitamin B1, methylmalonic acid (MMA), thyroid function, thyroid peroxidase (TPO), serum protein electrophoresis (SPEP), rapid plasma reagin (RPR), sedimentation rate, vitamin D, complete blood count, and chemistry profile 24 were all negative. The antinuclear antibody test revealed a homogenous 1:80 titer with a negative nuclear deoxyribonucleic acid. Her fasting glucose had been elevated between 107 to 117 mg/dL in the last 5 years but HbA1c was normal (5.8%). The patient had not been diagnosed with diabetes and her latest glucose values had been stable.
However, electromyography and a nerve conduction study were abnormal, with electrophysiological evidence of mild axonal polyneuropathy. During the month prior to her presentation, she had developed burning pain in addition to the numbness/stocking sensation. Pregabalin, gabapentin, duloxetine, celecoxib, hydrocodone, methadone, and other medications were ineffective. Eventually the foot pain became so severe—she described it as “walking on tacks”—that she was unable to walk.
Our team decided to do a nerve block to relieve the pain. Initially she underwent right and later left peroneal and posterior tibial nerve blocks, which gave her immediate relief that lasted about 2 months.
Relief from the pain, but what about the OSA symptoms?
In the meantime, our patient developed increasing OSA symptoms, including snoring, nonrestorative sleep, daytime somnolence, and fatigue. (To learn more about OSA, see “Obstructive sleep apnea: A diagnostic and treatment guide” on page 565.)
Her history of mild-to-moderate OSA dated back 2 years, and included an apnea-hypopnea index (AHI) of 20 events per hour and 133 episodes of oxygen desaturation with a low O2 desaturation of 83%. The patient had never been treated, however, because she felt that she couldn’t tolerate the continuous positive airway pressure (CPAP) mask.
The patient finally agreed to a CPAP titration study. Her AHI improved from 20 to <2 events per hour; the oxygen desaturation dropped from 133 to 104 episodes; and the lowest O2 desaturation went from 83% to 85%.
When we initially started CPAP, our patient did not tolerate it very well. However, after consulting with our sleep clinic, she was placed on bilevel positive airway pressure, which she did tolerate. Surprisingly, she also noticed immediate improvement of the neuropathic foot pain; after a few weeks it resolved completely.
Still no foot pain…We continue to follow the patient’s progress and, after 3 years, she remains free of foot pain. Her initial numbness remains, however. She has not developed diabetes, with similar fasting sugar levels and an HbA1c of 5.4%. She is not taking any medication for neuropathic pain, but remains on methadone for unrelated severe intractable osteoarthritic pain of the lumbar spine, bilateral knee joints, and left hip.
The link between sleep apnea and neuropathy
Our case report suggests that clinicians should consider OSA as a cause of neuropathic pain. A recent review of the literature supports the relationship between the 2 conditions.
The prevalence of neuropathy in the general population is 2.4%, rising to 8% with advancing age.1 Many different types of peripheral neuropathy have been described; they have different symptoms and characteristics, depending on the specific part of the nervous system that is affected.2
The literature reveals a strong association between OSA and peripheral neuropathy and sight-threatening retinopathy.3 One study found that nearly 60% of patients with diabetes and OSA also have peripheral neuropathy.4 Another report found that OSA is an independent risk factor for axonal damage of peripheral nerves.5 Furthermore, a case-control study revealed that the impaired neural function is at least partly reversible with treatment for sleep apnea.4 Finally, Tahrani et al6 have found that “neuropathy prevalence was higher in patients with OSA than those without” (60% vs 27%; P<.001), which supports our case finding.
The specific mechanism linking OSA and neuropathy remains elusive, but the evidence suggests that peripheral nervous tissue is affected by chronic endoneural hypoxia in this patient population.7 In patients with OSA, 2 types of nerve dysfunction are apparent: ischemia-related axonal degeneration and resistance to ischemic nerve failure.8
An approach worth considering. While nerve blocks did provide some relief for our patient, they are not a long-term solution. To our knowledge, this case report is the first one published in the United States describing resolution of neuropathic pain by treatment of OSA. This approach is certainly worth considering in patients who have not responded to more traditional therapy.
Correspondence
Fong Wong, DDS, MS, Associate Professor, Department of Restorative Dental Sciences, College of Dentistry, University of Florida, 1395 Center Drive, PO Box 100435, Gainesville, FL 32610; Fwong@dental.ufl.edu
1. Martyn C, Hughes R. Epidemiology of peripheral neuropathy. J Neurol Neurosurg Psychiatry. 1997;62:310-318.
2. NINDS peripheral neuropathy information page. Available at: http://www.ninds.nih.gov/disorders/peripheralneuropathy/peripheralneuropathy.htm. Last updated September 19, 2012. Accessed September 16, 2013.
3. Waller E, Bendel R, Kaplan J. Sleep disorders and the eye. Mayo Clin Proc. 2008;83:1251-1261.
4. Dziewas R, Schilling M, Engel P, et al. Treatment for obstructive sleep apnoea: effect on peripheral nerve function. J Neurol Neurosurg Psychiatry. 2007;78:295-297.
5. Ludemann P, Dziewas R, Soros P, et al. Axonal polyneuropathy in obstructive sleep apnoea. J Neurol Neurosurg Psychiatry. 2001;70:685-687.
6. Tahrani AA, Ali A, Raymond NT, et al. Obstructive sleep apnea and diabetic neuropathy: a novel association in patients with type 2 diabetes. Am J Respir Crit Care Med. 2012;186:434-441.
7. Pfeiffer G, Kunze K, Bruch M, et al. Polyneuropathy associated with chronic hypoxaemia: prevalence in patients with chronic obstructive pulmonary disease. J Neurol. 1990;237:230-233.
8. Mayer P, Dematteis M, Pepin J, et al. Peripheral neuropathy in sleep apnea. A tissue marker of the severity of nocturnal desaturation. Am J Respir Crit Care Med. 1999;159:213-219.
CASE A 57-year-old white woman presented with symptoms of bilateral “stocking-like numbness” and the sensation of “wearing socks for a few weeks” but denied any injury, previous chemotherapy, or diabetes. Her medical history was positive for untreated obstructive sleep apnea (OSA), obesity (body mass index, 36 kg/m2), osteoarthritis in various joints, impaired fasting glucose with normal glycosylated hemoglobin (HbA1c), hypertension, gastroesophageal reflux disease, hypothyroidism, hypercholesterolemia, and osteoporosis.
Our initial examination revealed decreased sensation to light palpation and pin prick over the distal portion of her lower extremities in a stocking-like fashion. Proprioception was decreased at the distal joint of the big toe. Her deep tendon reflex pattern was symmetric with 2+ at the knees, ankles, and toes. The rest of her lower extremity exam was within normal limits and there were no obvious vascular abnormalities.
Given the suspicion of peripheral neuropathy, the patient underwent laboratory tests and a nerve conduction study. Vitamin B12, vitamin B1, methylmalonic acid (MMA), thyroid function, thyroid peroxidase (TPO), serum protein electrophoresis (SPEP), rapid plasma reagin (RPR), sedimentation rate, vitamin D, complete blood count, and chemistry profile 24 were all negative. The antinuclear antibody test revealed a homogenous 1:80 titer with a negative nuclear deoxyribonucleic acid. Her fasting glucose had been elevated between 107 to 117 mg/dL in the last 5 years but HbA1c was normal (5.8%). The patient had not been diagnosed with diabetes and her latest glucose values had been stable.
However, electromyography and a nerve conduction study were abnormal, with electrophysiological evidence of mild axonal polyneuropathy. During the month prior to her presentation, she had developed burning pain in addition to the numbness/stocking sensation. Pregabalin, gabapentin, duloxetine, celecoxib, hydrocodone, methadone, and other medications were ineffective. Eventually the foot pain became so severe—she described it as “walking on tacks”—that she was unable to walk.
Our team decided to do a nerve block to relieve the pain. Initially she underwent right and later left peroneal and posterior tibial nerve blocks, which gave her immediate relief that lasted about 2 months.
Relief from the pain, but what about the OSA symptoms?
In the meantime, our patient developed increasing OSA symptoms, including snoring, nonrestorative sleep, daytime somnolence, and fatigue. (To learn more about OSA, see “Obstructive sleep apnea: A diagnostic and treatment guide” on page 565.)
Her history of mild-to-moderate OSA dated back 2 years, and included an apnea-hypopnea index (AHI) of 20 events per hour and 133 episodes of oxygen desaturation with a low O2 desaturation of 83%. The patient had never been treated, however, because she felt that she couldn’t tolerate the continuous positive airway pressure (CPAP) mask.
The patient finally agreed to a CPAP titration study. Her AHI improved from 20 to <2 events per hour; the oxygen desaturation dropped from 133 to 104 episodes; and the lowest O2 desaturation went from 83% to 85%.
When we initially started CPAP, our patient did not tolerate it very well. However, after consulting with our sleep clinic, she was placed on bilevel positive airway pressure, which she did tolerate. Surprisingly, she also noticed immediate improvement of the neuropathic foot pain; after a few weeks it resolved completely.
Still no foot pain…We continue to follow the patient’s progress and, after 3 years, she remains free of foot pain. Her initial numbness remains, however. She has not developed diabetes, with similar fasting sugar levels and an HbA1c of 5.4%. She is not taking any medication for neuropathic pain, but remains on methadone for unrelated severe intractable osteoarthritic pain of the lumbar spine, bilateral knee joints, and left hip.
The link between sleep apnea and neuropathy
Our case report suggests that clinicians should consider OSA as a cause of neuropathic pain. A recent review of the literature supports the relationship between the 2 conditions.
The prevalence of neuropathy in the general population is 2.4%, rising to 8% with advancing age.1 Many different types of peripheral neuropathy have been described; they have different symptoms and characteristics, depending on the specific part of the nervous system that is affected.2
The literature reveals a strong association between OSA and peripheral neuropathy and sight-threatening retinopathy.3 One study found that nearly 60% of patients with diabetes and OSA also have peripheral neuropathy.4 Another report found that OSA is an independent risk factor for axonal damage of peripheral nerves.5 Furthermore, a case-control study revealed that the impaired neural function is at least partly reversible with treatment for sleep apnea.4 Finally, Tahrani et al6 have found that “neuropathy prevalence was higher in patients with OSA than those without” (60% vs 27%; P<.001), which supports our case finding.
The specific mechanism linking OSA and neuropathy remains elusive, but the evidence suggests that peripheral nervous tissue is affected by chronic endoneural hypoxia in this patient population.7 In patients with OSA, 2 types of nerve dysfunction are apparent: ischemia-related axonal degeneration and resistance to ischemic nerve failure.8
An approach worth considering. While nerve blocks did provide some relief for our patient, they are not a long-term solution. To our knowledge, this case report is the first one published in the United States describing resolution of neuropathic pain by treatment of OSA. This approach is certainly worth considering in patients who have not responded to more traditional therapy.
Correspondence
Fong Wong, DDS, MS, Associate Professor, Department of Restorative Dental Sciences, College of Dentistry, University of Florida, 1395 Center Drive, PO Box 100435, Gainesville, FL 32610; Fwong@dental.ufl.edu
CASE A 57-year-old white woman presented with symptoms of bilateral “stocking-like numbness” and the sensation of “wearing socks for a few weeks” but denied any injury, previous chemotherapy, or diabetes. Her medical history was positive for untreated obstructive sleep apnea (OSA), obesity (body mass index, 36 kg/m2), osteoarthritis in various joints, impaired fasting glucose with normal glycosylated hemoglobin (HbA1c), hypertension, gastroesophageal reflux disease, hypothyroidism, hypercholesterolemia, and osteoporosis.
Our initial examination revealed decreased sensation to light palpation and pin prick over the distal portion of her lower extremities in a stocking-like fashion. Proprioception was decreased at the distal joint of the big toe. Her deep tendon reflex pattern was symmetric with 2+ at the knees, ankles, and toes. The rest of her lower extremity exam was within normal limits and there were no obvious vascular abnormalities.
Given the suspicion of peripheral neuropathy, the patient underwent laboratory tests and a nerve conduction study. Vitamin B12, vitamin B1, methylmalonic acid (MMA), thyroid function, thyroid peroxidase (TPO), serum protein electrophoresis (SPEP), rapid plasma reagin (RPR), sedimentation rate, vitamin D, complete blood count, and chemistry profile 24 were all negative. The antinuclear antibody test revealed a homogenous 1:80 titer with a negative nuclear deoxyribonucleic acid. Her fasting glucose had been elevated between 107 to 117 mg/dL in the last 5 years but HbA1c was normal (5.8%). The patient had not been diagnosed with diabetes and her latest glucose values had been stable.
However, electromyography and a nerve conduction study were abnormal, with electrophysiological evidence of mild axonal polyneuropathy. During the month prior to her presentation, she had developed burning pain in addition to the numbness/stocking sensation. Pregabalin, gabapentin, duloxetine, celecoxib, hydrocodone, methadone, and other medications were ineffective. Eventually the foot pain became so severe—she described it as “walking on tacks”—that she was unable to walk.
Our team decided to do a nerve block to relieve the pain. Initially she underwent right and later left peroneal and posterior tibial nerve blocks, which gave her immediate relief that lasted about 2 months.
Relief from the pain, but what about the OSA symptoms?
In the meantime, our patient developed increasing OSA symptoms, including snoring, nonrestorative sleep, daytime somnolence, and fatigue. (To learn more about OSA, see “Obstructive sleep apnea: A diagnostic and treatment guide” on page 565.)
Her history of mild-to-moderate OSA dated back 2 years, and included an apnea-hypopnea index (AHI) of 20 events per hour and 133 episodes of oxygen desaturation with a low O2 desaturation of 83%. The patient had never been treated, however, because she felt that she couldn’t tolerate the continuous positive airway pressure (CPAP) mask.
The patient finally agreed to a CPAP titration study. Her AHI improved from 20 to <2 events per hour; the oxygen desaturation dropped from 133 to 104 episodes; and the lowest O2 desaturation went from 83% to 85%.
When we initially started CPAP, our patient did not tolerate it very well. However, after consulting with our sleep clinic, she was placed on bilevel positive airway pressure, which she did tolerate. Surprisingly, she also noticed immediate improvement of the neuropathic foot pain; after a few weeks it resolved completely.
Still no foot pain…We continue to follow the patient’s progress and, after 3 years, she remains free of foot pain. Her initial numbness remains, however. She has not developed diabetes, with similar fasting sugar levels and an HbA1c of 5.4%. She is not taking any medication for neuropathic pain, but remains on methadone for unrelated severe intractable osteoarthritic pain of the lumbar spine, bilateral knee joints, and left hip.
The link between sleep apnea and neuropathy
Our case report suggests that clinicians should consider OSA as a cause of neuropathic pain. A recent review of the literature supports the relationship between the 2 conditions.
The prevalence of neuropathy in the general population is 2.4%, rising to 8% with advancing age.1 Many different types of peripheral neuropathy have been described; they have different symptoms and characteristics, depending on the specific part of the nervous system that is affected.2
The literature reveals a strong association between OSA and peripheral neuropathy and sight-threatening retinopathy.3 One study found that nearly 60% of patients with diabetes and OSA also have peripheral neuropathy.4 Another report found that OSA is an independent risk factor for axonal damage of peripheral nerves.5 Furthermore, a case-control study revealed that the impaired neural function is at least partly reversible with treatment for sleep apnea.4 Finally, Tahrani et al6 have found that “neuropathy prevalence was higher in patients with OSA than those without” (60% vs 27%; P<.001), which supports our case finding.
The specific mechanism linking OSA and neuropathy remains elusive, but the evidence suggests that peripheral nervous tissue is affected by chronic endoneural hypoxia in this patient population.7 In patients with OSA, 2 types of nerve dysfunction are apparent: ischemia-related axonal degeneration and resistance to ischemic nerve failure.8
An approach worth considering. While nerve blocks did provide some relief for our patient, they are not a long-term solution. To our knowledge, this case report is the first one published in the United States describing resolution of neuropathic pain by treatment of OSA. This approach is certainly worth considering in patients who have not responded to more traditional therapy.
Correspondence
Fong Wong, DDS, MS, Associate Professor, Department of Restorative Dental Sciences, College of Dentistry, University of Florida, 1395 Center Drive, PO Box 100435, Gainesville, FL 32610; Fwong@dental.ufl.edu
1. Martyn C, Hughes R. Epidemiology of peripheral neuropathy. J Neurol Neurosurg Psychiatry. 1997;62:310-318.
2. NINDS peripheral neuropathy information page. Available at: http://www.ninds.nih.gov/disorders/peripheralneuropathy/peripheralneuropathy.htm. Last updated September 19, 2012. Accessed September 16, 2013.
3. Waller E, Bendel R, Kaplan J. Sleep disorders and the eye. Mayo Clin Proc. 2008;83:1251-1261.
4. Dziewas R, Schilling M, Engel P, et al. Treatment for obstructive sleep apnoea: effect on peripheral nerve function. J Neurol Neurosurg Psychiatry. 2007;78:295-297.
5. Ludemann P, Dziewas R, Soros P, et al. Axonal polyneuropathy in obstructive sleep apnoea. J Neurol Neurosurg Psychiatry. 2001;70:685-687.
6. Tahrani AA, Ali A, Raymond NT, et al. Obstructive sleep apnea and diabetic neuropathy: a novel association in patients with type 2 diabetes. Am J Respir Crit Care Med. 2012;186:434-441.
7. Pfeiffer G, Kunze K, Bruch M, et al. Polyneuropathy associated with chronic hypoxaemia: prevalence in patients with chronic obstructive pulmonary disease. J Neurol. 1990;237:230-233.
8. Mayer P, Dematteis M, Pepin J, et al. Peripheral neuropathy in sleep apnea. A tissue marker of the severity of nocturnal desaturation. Am J Respir Crit Care Med. 1999;159:213-219.
1. Martyn C, Hughes R. Epidemiology of peripheral neuropathy. J Neurol Neurosurg Psychiatry. 1997;62:310-318.
2. NINDS peripheral neuropathy information page. Available at: http://www.ninds.nih.gov/disorders/peripheralneuropathy/peripheralneuropathy.htm. Last updated September 19, 2012. Accessed September 16, 2013.
3. Waller E, Bendel R, Kaplan J. Sleep disorders and the eye. Mayo Clin Proc. 2008;83:1251-1261.
4. Dziewas R, Schilling M, Engel P, et al. Treatment for obstructive sleep apnoea: effect on peripheral nerve function. J Neurol Neurosurg Psychiatry. 2007;78:295-297.
5. Ludemann P, Dziewas R, Soros P, et al. Axonal polyneuropathy in obstructive sleep apnoea. J Neurol Neurosurg Psychiatry. 2001;70:685-687.
6. Tahrani AA, Ali A, Raymond NT, et al. Obstructive sleep apnea and diabetic neuropathy: a novel association in patients with type 2 diabetes. Am J Respir Crit Care Med. 2012;186:434-441.
7. Pfeiffer G, Kunze K, Bruch M, et al. Polyneuropathy associated with chronic hypoxaemia: prevalence in patients with chronic obstructive pulmonary disease. J Neurol. 1990;237:230-233.
8. Mayer P, Dematteis M, Pepin J, et al. Peripheral neuropathy in sleep apnea. A tissue marker of the severity of nocturnal desaturation. Am J Respir Crit Care Med. 1999;159:213-219.
Democracy - best, but only if....
A stated goal of the United States is to support and promote democracy throughout the world. This seems reasonable, because democracy has often worked well in our own and other Western countries, and because no other form of government has consistently been better. So is democracy the best form of government? I submit that it is the best only if certain conditions are met.
For democracy to work, the public must be well informed and willing to consider, at least to some extent, the country’s interests in addition to their own self-interests. If a major fraction of the public does not care about or know what is good for the country or is totally motivated by self-interest, the government and the country will fail. Sadly this appears to be the case in the U.S. today as evidenced by Jay Leno’s "JayWalking Segments" in which most young people interviewed – even college graduates – have no idea about issues important to our country. They appear to be more interested in sports and their social life and more knowledgeable about TV sitcoms and reality shows.
How can such individuals be relied upon to pick government leaders who will take care of our country’s interests in the trying times it faces politically and economically? An ill-informed and non-caring public is more likely to pick leaders who are the slickest talkers and who promise the most despite the impossibility or negative effects of keeping these promises. This know-nothing or self-interested nature of our electorate contributes importantly to the ever expanding entitlement culture in the U.S. and the resulting dangerous expansion of our national debt.
Another related requirement for democracy to be an effective form of government is the need for an honest and objective media and press. A controlled or biased source of information contributes hugely to an ill-informed public. Whoever controls the media and the press controls the minds of the voters. For democracy to work effectively, the public must not only want to be informed, they must also be given the necessary objective facts to make valid judgments. The press has a vital responsibility to provide such facts with minimal bias. There is considerable doubt about whether or not this is occurring today in the U.S.
Of even greater importance to a successful democracy is the ethical stature of its leaders and their motivation – once elected – to act in the best interests of the country. Many forces act upon our leaders and are counter to these interests. These include obligations to those who helped elect them, ideology, personal gain, a desire to be re-elected, and most importantly the corrupting requirement to solicit campaign financing. In the U.S. currently, the need to finance expensive campaigns is a major flaw in our democracy, and is really a veiled form of bribery.
For a democratic leader to be successful in terms of doing a good job of leading the country, all these forces must be overridden by the desire to do what is right and best for the whole country. This means the leader must not serve solely special or self-interests, and must have the courage and inner strength to do what may at the moment be unpopular with his or her electoral base. He or she must unite the country rather than divide it for short-term political or parochial gain. Unfortunately many of our recently elected U.S. leaders have not met any of these requirements. If this trend continues, our democracy will serve the country’s interests poorly, and the U.S. will decline rather than gain in stature and strength.
Efforts at democracy in the Middle East and elsewhere have failed because some or all of the requirements discussed here have not been met. A similar decline awaits our U.S. democracy if the current flaws in the underlying system cannot be corrected.
So far this discussion has largely been related to the U.S. federal government. However, the same considerations apply to effective governments at the county, state, and city levels, and to governing bodies of other entities which purport to be managed in a democratic fashion. This even applies to our vascular societies. The ethics and character of the leaders and those choosing them are important to effective governance and the success of the organization. If special interests, financial conflicts, and self-interest prevail over the needs of the organization, the latter will fail and decline.
Dr. Veith is Professor of Surgery at New York University Medical Center and the Cleveland Clinic. He is an associate medical editor for Vascular Specialist.
The ideas and opinions expressed in Vascular Specialist do not necessarily reflect those of the Society or Publisher.
A stated goal of the United States is to support and promote democracy throughout the world. This seems reasonable, because democracy has often worked well in our own and other Western countries, and because no other form of government has consistently been better. So is democracy the best form of government? I submit that it is the best only if certain conditions are met.
For democracy to work, the public must be well informed and willing to consider, at least to some extent, the country’s interests in addition to their own self-interests. If a major fraction of the public does not care about or know what is good for the country or is totally motivated by self-interest, the government and the country will fail. Sadly this appears to be the case in the U.S. today as evidenced by Jay Leno’s "JayWalking Segments" in which most young people interviewed – even college graduates – have no idea about issues important to our country. They appear to be more interested in sports and their social life and more knowledgeable about TV sitcoms and reality shows.
How can such individuals be relied upon to pick government leaders who will take care of our country’s interests in the trying times it faces politically and economically? An ill-informed and non-caring public is more likely to pick leaders who are the slickest talkers and who promise the most despite the impossibility or negative effects of keeping these promises. This know-nothing or self-interested nature of our electorate contributes importantly to the ever expanding entitlement culture in the U.S. and the resulting dangerous expansion of our national debt.
Another related requirement for democracy to be an effective form of government is the need for an honest and objective media and press. A controlled or biased source of information contributes hugely to an ill-informed public. Whoever controls the media and the press controls the minds of the voters. For democracy to work effectively, the public must not only want to be informed, they must also be given the necessary objective facts to make valid judgments. The press has a vital responsibility to provide such facts with minimal bias. There is considerable doubt about whether or not this is occurring today in the U.S.
Of even greater importance to a successful democracy is the ethical stature of its leaders and their motivation – once elected – to act in the best interests of the country. Many forces act upon our leaders and are counter to these interests. These include obligations to those who helped elect them, ideology, personal gain, a desire to be re-elected, and most importantly the corrupting requirement to solicit campaign financing. In the U.S. currently, the need to finance expensive campaigns is a major flaw in our democracy, and is really a veiled form of bribery.
For a democratic leader to be successful in terms of doing a good job of leading the country, all these forces must be overridden by the desire to do what is right and best for the whole country. This means the leader must not serve solely special or self-interests, and must have the courage and inner strength to do what may at the moment be unpopular with his or her electoral base. He or she must unite the country rather than divide it for short-term political or parochial gain. Unfortunately many of our recently elected U.S. leaders have not met any of these requirements. If this trend continues, our democracy will serve the country’s interests poorly, and the U.S. will decline rather than gain in stature and strength.
Efforts at democracy in the Middle East and elsewhere have failed because some or all of the requirements discussed here have not been met. A similar decline awaits our U.S. democracy if the current flaws in the underlying system cannot be corrected.
So far this discussion has largely been related to the U.S. federal government. However, the same considerations apply to effective governments at the county, state, and city levels, and to governing bodies of other entities which purport to be managed in a democratic fashion. This even applies to our vascular societies. The ethics and character of the leaders and those choosing them are important to effective governance and the success of the organization. If special interests, financial conflicts, and self-interest prevail over the needs of the organization, the latter will fail and decline.
Dr. Veith is Professor of Surgery at New York University Medical Center and the Cleveland Clinic. He is an associate medical editor for Vascular Specialist.
The ideas and opinions expressed in Vascular Specialist do not necessarily reflect those of the Society or Publisher.
A stated goal of the United States is to support and promote democracy throughout the world. This seems reasonable, because democracy has often worked well in our own and other Western countries, and because no other form of government has consistently been better. So is democracy the best form of government? I submit that it is the best only if certain conditions are met.
For democracy to work, the public must be well informed and willing to consider, at least to some extent, the country’s interests in addition to their own self-interests. If a major fraction of the public does not care about or know what is good for the country or is totally motivated by self-interest, the government and the country will fail. Sadly this appears to be the case in the U.S. today as evidenced by Jay Leno’s "JayWalking Segments" in which most young people interviewed – even college graduates – have no idea about issues important to our country. They appear to be more interested in sports and their social life and more knowledgeable about TV sitcoms and reality shows.
How can such individuals be relied upon to pick government leaders who will take care of our country’s interests in the trying times it faces politically and economically? An ill-informed and non-caring public is more likely to pick leaders who are the slickest talkers and who promise the most despite the impossibility or negative effects of keeping these promises. This know-nothing or self-interested nature of our electorate contributes importantly to the ever expanding entitlement culture in the U.S. and the resulting dangerous expansion of our national debt.
Another related requirement for democracy to be an effective form of government is the need for an honest and objective media and press. A controlled or biased source of information contributes hugely to an ill-informed public. Whoever controls the media and the press controls the minds of the voters. For democracy to work effectively, the public must not only want to be informed, they must also be given the necessary objective facts to make valid judgments. The press has a vital responsibility to provide such facts with minimal bias. There is considerable doubt about whether or not this is occurring today in the U.S.
Of even greater importance to a successful democracy is the ethical stature of its leaders and their motivation – once elected – to act in the best interests of the country. Many forces act upon our leaders and are counter to these interests. These include obligations to those who helped elect them, ideology, personal gain, a desire to be re-elected, and most importantly the corrupting requirement to solicit campaign financing. In the U.S. currently, the need to finance expensive campaigns is a major flaw in our democracy, and is really a veiled form of bribery.
For a democratic leader to be successful in terms of doing a good job of leading the country, all these forces must be overridden by the desire to do what is right and best for the whole country. This means the leader must not serve solely special or self-interests, and must have the courage and inner strength to do what may at the moment be unpopular with his or her electoral base. He or she must unite the country rather than divide it for short-term political or parochial gain. Unfortunately many of our recently elected U.S. leaders have not met any of these requirements. If this trend continues, our democracy will serve the country’s interests poorly, and the U.S. will decline rather than gain in stature and strength.
Efforts at democracy in the Middle East and elsewhere have failed because some or all of the requirements discussed here have not been met. A similar decline awaits our U.S. democracy if the current flaws in the underlying system cannot be corrected.
So far this discussion has largely been related to the U.S. federal government. However, the same considerations apply to effective governments at the county, state, and city levels, and to governing bodies of other entities which purport to be managed in a democratic fashion. This even applies to our vascular societies. The ethics and character of the leaders and those choosing them are important to effective governance and the success of the organization. If special interests, financial conflicts, and self-interest prevail over the needs of the organization, the latter will fail and decline.
Dr. Veith is Professor of Surgery at New York University Medical Center and the Cleveland Clinic. He is an associate medical editor for Vascular Specialist.
The ideas and opinions expressed in Vascular Specialist do not necessarily reflect those of the Society or Publisher.
Online tool calculates Medicare incentives, penalties
Not sure if you’re going to be getting a bonus or paying a penalty to Medicare this year? You’re not alone.
Between the Medicare e-prescribing program, the "meaningful use" incentives for implementing electronic health records (EHRs), and the Physician Quality Reporting System (PQRS) – all with different incentive and penalty schedules – it’s hard to keep track of whether payments are going up or down and by how much.
Apparently, officials at the Centers for Medicare and Medicaid Services (CMS) agree. They have launched an online tool that allows physicians to click through a few questions and figure out what their payment adjustments will look like based on 2013 participation in the eRx Incentive Program, the Medicare EHR Incentive Program, and the PQRS.
For instance, if a physician attested to meaningful use of certified EHR technology in 2013 and plans on demonstrating that use, then he will avoid the 2015 payment adjustment and be eligible for incentive payments of between $8,000 and $12,000, depending on the year that he first demonstrated meaningful use.
The tool can also help physicians figure out how the three programs interact. If a physician reported the eRx measure’s numerator code at least 25 times in 2012, he will avoid the 2014 eRx penalty. But if he also successfully attested to meaningful use in 2012, then he can’t "double dip" and pick up the 1% eRx bonus, according to the CMS.
–By Mary Ellen Schneider
Dr. Stuart M. Garay, FCCP, comments:
Meeting CMS requirements for Medicare reimbursement is becoming increasingly complicated. During the past few years e-prescribing, EHR meaningful use, and PQRS have been rolled out to physicians with different incentive and penalty schedules. Physicians have been presented a confusing mess! Finally CMS has provided an online tool to sort this out. Take advantage; don't miss out!
Dr. Stuart M. Garay, FCCP, comments:
Meeting CMS requirements for Medicare reimbursement is becoming increasingly complicated. During the past few years e-prescribing, EHR meaningful use, and PQRS have been rolled out to physicians with different incentive and penalty schedules. Physicians have been presented a confusing mess! Finally CMS has provided an online tool to sort this out. Take advantage; don't miss out!
Dr. Stuart M. Garay, FCCP, comments:
Meeting CMS requirements for Medicare reimbursement is becoming increasingly complicated. During the past few years e-prescribing, EHR meaningful use, and PQRS have been rolled out to physicians with different incentive and penalty schedules. Physicians have been presented a confusing mess! Finally CMS has provided an online tool to sort this out. Take advantage; don't miss out!
Not sure if you’re going to be getting a bonus or paying a penalty to Medicare this year? You’re not alone.
Between the Medicare e-prescribing program, the "meaningful use" incentives for implementing electronic health records (EHRs), and the Physician Quality Reporting System (PQRS) – all with different incentive and penalty schedules – it’s hard to keep track of whether payments are going up or down and by how much.
Apparently, officials at the Centers for Medicare and Medicaid Services (CMS) agree. They have launched an online tool that allows physicians to click through a few questions and figure out what their payment adjustments will look like based on 2013 participation in the eRx Incentive Program, the Medicare EHR Incentive Program, and the PQRS.
For instance, if a physician attested to meaningful use of certified EHR technology in 2013 and plans on demonstrating that use, then he will avoid the 2015 payment adjustment and be eligible for incentive payments of between $8,000 and $12,000, depending on the year that he first demonstrated meaningful use.
The tool can also help physicians figure out how the three programs interact. If a physician reported the eRx measure’s numerator code at least 25 times in 2012, he will avoid the 2014 eRx penalty. But if he also successfully attested to meaningful use in 2012, then he can’t "double dip" and pick up the 1% eRx bonus, according to the CMS.
–By Mary Ellen Schneider
Not sure if you’re going to be getting a bonus or paying a penalty to Medicare this year? You’re not alone.
Between the Medicare e-prescribing program, the "meaningful use" incentives for implementing electronic health records (EHRs), and the Physician Quality Reporting System (PQRS) – all with different incentive and penalty schedules – it’s hard to keep track of whether payments are going up or down and by how much.
Apparently, officials at the Centers for Medicare and Medicaid Services (CMS) agree. They have launched an online tool that allows physicians to click through a few questions and figure out what their payment adjustments will look like based on 2013 participation in the eRx Incentive Program, the Medicare EHR Incentive Program, and the PQRS.
For instance, if a physician attested to meaningful use of certified EHR technology in 2013 and plans on demonstrating that use, then he will avoid the 2015 payment adjustment and be eligible for incentive payments of between $8,000 and $12,000, depending on the year that he first demonstrated meaningful use.
The tool can also help physicians figure out how the three programs interact. If a physician reported the eRx measure’s numerator code at least 25 times in 2012, he will avoid the 2014 eRx penalty. But if he also successfully attested to meaningful use in 2012, then he can’t "double dip" and pick up the 1% eRx bonus, according to the CMS.
–By Mary Ellen Schneider
Elevated troponin but no CVD: What’s the prognosis?
Patients with elevated troponin levels and chronic renal disease, pulmonary hypertension, pulmonary embolism, chronic obstructive pulmonary disease, sepsis, or acute ischemic stroke have a 2- to 5-fold increased risk of death, even in the absence of known cardiovascular disease (TABLE)1-6 (strength of recommendation: B, meta-analysis, multiple prospective and retrospective observational studies.)
EVIDENCE SUMMARY
To investigate the prognostic value of troponin on overall mortality, a multicenter prospective study followed 847 patients 18 years and older (mean age 59 years) with end-stage renal disease whose troponin T levels were measured 3 months from the start of peritoneal dialysis or hemodialysis until transplantation or death.1 At enrollment, 566 patients had a troponin level of ≤0.04 ng/dL, 188 had a value between 0.05 and 0.10 ng/dL, and 93 had a level of more than 0.10 ng/dL.
Using Cox regression, patients whose troponin levels were more than 0.10 ng/dL had an increased hazard ratio (HR) for all-cause mortality of 2.2 (95% confidence interval [CI], 1.7-2.8) compared with patients who had levels ≤0.04 ng/dL. Cardiovascular mortality also was higher (HR=1.9; 95% CI, 0.9-3.7) with troponin elevations, but didn’t reach statistical significance. Investigators found no significant differences in mortality risk between patients on peritoneal or hemodialysis, patients with or without a history of acute myocardial infarction, or patients who suffered cerebrovascular accidents.
Elevated troponin raises risk of death 5-fold in pulmonary embolism patients
A meta-analysis of 20 trials with a total of 1985 patients assessed the prognostic value of troponin for short-term mortality in patients admitted with acute pulmonary embolism.2 Sixteen studies (1527 patients) were prospective trials and the remainder (458 patients) were retrospective trials. Investigators obtained troponin levels for all patients at admission. They used several different troponin assays (both I and T), but most of the studies used the assay manufacturers’ cutoff points (exceeding the 99th percentile).
High troponin levels were associated with a 5-fold increased risk of short-term death, defined as in-hospital death up to 30 days after discharge (19.7% with elevated troponin vs 3.7% with normal troponin; odds ratio [OR]=5.24; 95% CI, 3.3-8.4).
Increased risk of death among those with pulmonary hypertension, COPD A prospective single-center study of 56 patients with chronic pulmonary hypertension found that the 14% of those whose troponin T was elevated (≥0.01 ng/mL) had a lower survival rate than the other patients. Patients who either had a positive troponin on initial assessment or developed troponin elevation within the 2-year follow-up period had a cumulative 24-month survival rate of 29%, compared with 81% for their troponin T-negative counterparts (P=.001).3
Patients with elevated troponin levels and certain conditions have a 2- to 5-fold increased risk of death, even without known cardiovascular disease.
Elevated troponin I is an independent predictor of mortality in severe sepsis
A double-blind, placebo-controlled, phase 3 trial evaluated the effect of drotrecogin alfa (activated)—withdrawn from the market in 2011—on survival of patients with severe sepsis.5 Investigators used positive troponin I levels (≥0.06 ng/mL) as a prognostic indicator of mortality. Patients who were troponin-positive had a 28-day mortality rate of 32%, compared with 14% in the troponin-negative group (P<.0001).
A bias of this study is that the patients with positive troponin levels tended to be older and more critically ill. However, in a multivariate model, troponin I still remained an independent predictor of mortality.
Elevated troponin predicts increased death risk in up to 20% of stroke patients
A systematic review of 15 trials with a total of 2901 patients evaluated the relationship between troponin levels and stroke.6 Investigators assessed the prevalence of elevated troponin in acute stroke patients, the association of elevated troponin levels with electrocardiographic changes, and the overall morbidity and mortality associated with troponin levels. Thirteen of the 15 studies used a troponin T or I level obtained within 72 hours of admission and a cut-off level of 0.1 ng/mL. The remaining 2 studies used troponin I cut-off levels >0.2 and 0.4 ng/mL.
Overall, 18% of acute stroke patients had elevated troponin levels. Studies that excluded patients with known cardiac disease had a lower prevalence of elevated levels (10% vs 22%). Patients with elevated troponin levels had an associated overall increased risk of death (OR=2.9; 95% CI, 1.7-4.8) and were 3 times more likely to have ischemic changes on electrocardiogram (OR=3.0; 95% CI, 1.5-6.2). Investigators concluded that elevated troponin levels occur in as many as one in 5 patients and are associated with an increased risk of death.
Troponin elevations may be observed in congestive heart failure, chest wall trauma, cardioversion/defibrillator shocks, rhabdomyolysis, and ultra-endurance activities.7 However, this analysis didn’t address prognostic implications of elevated troponins.
RECOMMENDATIONS
No recommendation exists for biochemical testing of troponins in various medical conditions except in the presence of signs and symptoms consistent with acute coronary syndrome. The American College of Cardiology and American Heart Association recommend routine testing of cardiac troponins in patients hospitalized for worsening congestive heart failure symptoms.8
The European Society of Cardiology recommends measuring troponin levels to further stratify risk in non-high-risk patients with confirmed pulmonary embolus.9
The National Academy of Clinical Biochemistry recommends using cardiac troponins to help define mortality risk in end-stage renal disease and critically ill patients.10
1. Havekes B, van Manen J, Krediet R, et al. Serum troponin T concentration as a predictor of mortality in hemodialysis and peritoneal dialysis patients. Am J Kidney Dis. 2006;47:823-829.
2. Becattini C, Vedovati MC, Agnelli G. Prognostic value of tropo- nins in acute pulmonary embolism. Circulation. 2007;116:427- 433.
3. Torbicki A, Kurzyna M, Kuca P, et al. Detectable serum cardiac troponin T as a marker of poor prognosis among patients with chronic precapillary pulmonary hypertension. Circulation. 2003;108:844-848.
4. Brekke PH, Omland T, Holmedal SH, et al. Troponin T eleva- tion and long-term mortality after chronic obstructive pulmo- nary disease exacerbation. Eur Respir J. 2008;31:563-570.
5. John J, Woodward DB, Wang Y, et al. Troponin I as a prog- nosticator of mortality in severe sepsis patients. J Crit Care. 2010;25:270-275.
6. Kerr G, Ray G, Wu O, et al. Elevated troponin after stroke: a sys- tematic review. Cerebrovasc Dis. 2009;28:220-226.
7. Korff S, Katus HA, Giannitsis E. Differential diagnosis of el- evated troponins. Heart. 2006;92:987-993.
8. Hunt SA, Abraham WT, Chin MH, et al. 2009 Focused update incorporated into the ACC/AHA 2005 guidelines for the diag- nosis and management of heart failure in adults. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines devel- oped in collaboration with the International Society for Heart and Lung Transplantation. J Am Coll Cardiol. 2009;53:e1-e90.
9. Torbicki A, Perrier A, Konstantinides S, et al. Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology. Eur Heart J. 2008;29:2276-2315.
10. Wu AH, Jaffe AS, Apple FS, et al. National Academy of Clinical Biochemistry laboratory medicine practice guidelines: use of cardiac troponin and B-type natriuretic peptide or N-terminal proB-type natriuretic peptide for etiologies other than acute coronary syndromes and heart failure. Clin Chem. 2007;53:2086-2096.
Patients with elevated troponin levels and chronic renal disease, pulmonary hypertension, pulmonary embolism, chronic obstructive pulmonary disease, sepsis, or acute ischemic stroke have a 2- to 5-fold increased risk of death, even in the absence of known cardiovascular disease (TABLE)1-6 (strength of recommendation: B, meta-analysis, multiple prospective and retrospective observational studies.)
EVIDENCE SUMMARY
To investigate the prognostic value of troponin on overall mortality, a multicenter prospective study followed 847 patients 18 years and older (mean age 59 years) with end-stage renal disease whose troponin T levels were measured 3 months from the start of peritoneal dialysis or hemodialysis until transplantation or death.1 At enrollment, 566 patients had a troponin level of ≤0.04 ng/dL, 188 had a value between 0.05 and 0.10 ng/dL, and 93 had a level of more than 0.10 ng/dL.
Using Cox regression, patients whose troponin levels were more than 0.10 ng/dL had an increased hazard ratio (HR) for all-cause mortality of 2.2 (95% confidence interval [CI], 1.7-2.8) compared with patients who had levels ≤0.04 ng/dL. Cardiovascular mortality also was higher (HR=1.9; 95% CI, 0.9-3.7) with troponin elevations, but didn’t reach statistical significance. Investigators found no significant differences in mortality risk between patients on peritoneal or hemodialysis, patients with or without a history of acute myocardial infarction, or patients who suffered cerebrovascular accidents.
Elevated troponin raises risk of death 5-fold in pulmonary embolism patients
A meta-analysis of 20 trials with a total of 1985 patients assessed the prognostic value of troponin for short-term mortality in patients admitted with acute pulmonary embolism.2 Sixteen studies (1527 patients) were prospective trials and the remainder (458 patients) were retrospective trials. Investigators obtained troponin levels for all patients at admission. They used several different troponin assays (both I and T), but most of the studies used the assay manufacturers’ cutoff points (exceeding the 99th percentile).
High troponin levels were associated with a 5-fold increased risk of short-term death, defined as in-hospital death up to 30 days after discharge (19.7% with elevated troponin vs 3.7% with normal troponin; odds ratio [OR]=5.24; 95% CI, 3.3-8.4).
Increased risk of death among those with pulmonary hypertension, COPD A prospective single-center study of 56 patients with chronic pulmonary hypertension found that the 14% of those whose troponin T was elevated (≥0.01 ng/mL) had a lower survival rate than the other patients. Patients who either had a positive troponin on initial assessment or developed troponin elevation within the 2-year follow-up period had a cumulative 24-month survival rate of 29%, compared with 81% for their troponin T-negative counterparts (P=.001).3
Patients with elevated troponin levels and certain conditions have a 2- to 5-fold increased risk of death, even without known cardiovascular disease.
Elevated troponin I is an independent predictor of mortality in severe sepsis
A double-blind, placebo-controlled, phase 3 trial evaluated the effect of drotrecogin alfa (activated)—withdrawn from the market in 2011—on survival of patients with severe sepsis.5 Investigators used positive troponin I levels (≥0.06 ng/mL) as a prognostic indicator of mortality. Patients who were troponin-positive had a 28-day mortality rate of 32%, compared with 14% in the troponin-negative group (P<.0001).
A bias of this study is that the patients with positive troponin levels tended to be older and more critically ill. However, in a multivariate model, troponin I still remained an independent predictor of mortality.
Elevated troponin predicts increased death risk in up to 20% of stroke patients
A systematic review of 15 trials with a total of 2901 patients evaluated the relationship between troponin levels and stroke.6 Investigators assessed the prevalence of elevated troponin in acute stroke patients, the association of elevated troponin levels with electrocardiographic changes, and the overall morbidity and mortality associated with troponin levels. Thirteen of the 15 studies used a troponin T or I level obtained within 72 hours of admission and a cut-off level of 0.1 ng/mL. The remaining 2 studies used troponin I cut-off levels >0.2 and 0.4 ng/mL.
Overall, 18% of acute stroke patients had elevated troponin levels. Studies that excluded patients with known cardiac disease had a lower prevalence of elevated levels (10% vs 22%). Patients with elevated troponin levels had an associated overall increased risk of death (OR=2.9; 95% CI, 1.7-4.8) and were 3 times more likely to have ischemic changes on electrocardiogram (OR=3.0; 95% CI, 1.5-6.2). Investigators concluded that elevated troponin levels occur in as many as one in 5 patients and are associated with an increased risk of death.
Troponin elevations may be observed in congestive heart failure, chest wall trauma, cardioversion/defibrillator shocks, rhabdomyolysis, and ultra-endurance activities.7 However, this analysis didn’t address prognostic implications of elevated troponins.
RECOMMENDATIONS
No recommendation exists for biochemical testing of troponins in various medical conditions except in the presence of signs and symptoms consistent with acute coronary syndrome. The American College of Cardiology and American Heart Association recommend routine testing of cardiac troponins in patients hospitalized for worsening congestive heart failure symptoms.8
The European Society of Cardiology recommends measuring troponin levels to further stratify risk in non-high-risk patients with confirmed pulmonary embolus.9
The National Academy of Clinical Biochemistry recommends using cardiac troponins to help define mortality risk in end-stage renal disease and critically ill patients.10
Patients with elevated troponin levels and chronic renal disease, pulmonary hypertension, pulmonary embolism, chronic obstructive pulmonary disease, sepsis, or acute ischemic stroke have a 2- to 5-fold increased risk of death, even in the absence of known cardiovascular disease (TABLE)1-6 (strength of recommendation: B, meta-analysis, multiple prospective and retrospective observational studies.)
EVIDENCE SUMMARY
To investigate the prognostic value of troponin on overall mortality, a multicenter prospective study followed 847 patients 18 years and older (mean age 59 years) with end-stage renal disease whose troponin T levels were measured 3 months from the start of peritoneal dialysis or hemodialysis until transplantation or death.1 At enrollment, 566 patients had a troponin level of ≤0.04 ng/dL, 188 had a value between 0.05 and 0.10 ng/dL, and 93 had a level of more than 0.10 ng/dL.
Using Cox regression, patients whose troponin levels were more than 0.10 ng/dL had an increased hazard ratio (HR) for all-cause mortality of 2.2 (95% confidence interval [CI], 1.7-2.8) compared with patients who had levels ≤0.04 ng/dL. Cardiovascular mortality also was higher (HR=1.9; 95% CI, 0.9-3.7) with troponin elevations, but didn’t reach statistical significance. Investigators found no significant differences in mortality risk between patients on peritoneal or hemodialysis, patients with or without a history of acute myocardial infarction, or patients who suffered cerebrovascular accidents.
Elevated troponin raises risk of death 5-fold in pulmonary embolism patients
A meta-analysis of 20 trials with a total of 1985 patients assessed the prognostic value of troponin for short-term mortality in patients admitted with acute pulmonary embolism.2 Sixteen studies (1527 patients) were prospective trials and the remainder (458 patients) were retrospective trials. Investigators obtained troponin levels for all patients at admission. They used several different troponin assays (both I and T), but most of the studies used the assay manufacturers’ cutoff points (exceeding the 99th percentile).
High troponin levels were associated with a 5-fold increased risk of short-term death, defined as in-hospital death up to 30 days after discharge (19.7% with elevated troponin vs 3.7% with normal troponin; odds ratio [OR]=5.24; 95% CI, 3.3-8.4).
Increased risk of death among those with pulmonary hypertension, COPD A prospective single-center study of 56 patients with chronic pulmonary hypertension found that the 14% of those whose troponin T was elevated (≥0.01 ng/mL) had a lower survival rate than the other patients. Patients who either had a positive troponin on initial assessment or developed troponin elevation within the 2-year follow-up period had a cumulative 24-month survival rate of 29%, compared with 81% for their troponin T-negative counterparts (P=.001).3
Patients with elevated troponin levels and certain conditions have a 2- to 5-fold increased risk of death, even without known cardiovascular disease.
Elevated troponin I is an independent predictor of mortality in severe sepsis
A double-blind, placebo-controlled, phase 3 trial evaluated the effect of drotrecogin alfa (activated)—withdrawn from the market in 2011—on survival of patients with severe sepsis.5 Investigators used positive troponin I levels (≥0.06 ng/mL) as a prognostic indicator of mortality. Patients who were troponin-positive had a 28-day mortality rate of 32%, compared with 14% in the troponin-negative group (P<.0001).
A bias of this study is that the patients with positive troponin levels tended to be older and more critically ill. However, in a multivariate model, troponin I still remained an independent predictor of mortality.
Elevated troponin predicts increased death risk in up to 20% of stroke patients
A systematic review of 15 trials with a total of 2901 patients evaluated the relationship between troponin levels and stroke.6 Investigators assessed the prevalence of elevated troponin in acute stroke patients, the association of elevated troponin levels with electrocardiographic changes, and the overall morbidity and mortality associated with troponin levels. Thirteen of the 15 studies used a troponin T or I level obtained within 72 hours of admission and a cut-off level of 0.1 ng/mL. The remaining 2 studies used troponin I cut-off levels >0.2 and 0.4 ng/mL.
Overall, 18% of acute stroke patients had elevated troponin levels. Studies that excluded patients with known cardiac disease had a lower prevalence of elevated levels (10% vs 22%). Patients with elevated troponin levels had an associated overall increased risk of death (OR=2.9; 95% CI, 1.7-4.8) and were 3 times more likely to have ischemic changes on electrocardiogram (OR=3.0; 95% CI, 1.5-6.2). Investigators concluded that elevated troponin levels occur in as many as one in 5 patients and are associated with an increased risk of death.
Troponin elevations may be observed in congestive heart failure, chest wall trauma, cardioversion/defibrillator shocks, rhabdomyolysis, and ultra-endurance activities.7 However, this analysis didn’t address prognostic implications of elevated troponins.
RECOMMENDATIONS
No recommendation exists for biochemical testing of troponins in various medical conditions except in the presence of signs and symptoms consistent with acute coronary syndrome. The American College of Cardiology and American Heart Association recommend routine testing of cardiac troponins in patients hospitalized for worsening congestive heart failure symptoms.8
The European Society of Cardiology recommends measuring troponin levels to further stratify risk in non-high-risk patients with confirmed pulmonary embolus.9
The National Academy of Clinical Biochemistry recommends using cardiac troponins to help define mortality risk in end-stage renal disease and critically ill patients.10
1. Havekes B, van Manen J, Krediet R, et al. Serum troponin T concentration as a predictor of mortality in hemodialysis and peritoneal dialysis patients. Am J Kidney Dis. 2006;47:823-829.
2. Becattini C, Vedovati MC, Agnelli G. Prognostic value of tropo- nins in acute pulmonary embolism. Circulation. 2007;116:427- 433.
3. Torbicki A, Kurzyna M, Kuca P, et al. Detectable serum cardiac troponin T as a marker of poor prognosis among patients with chronic precapillary pulmonary hypertension. Circulation. 2003;108:844-848.
4. Brekke PH, Omland T, Holmedal SH, et al. Troponin T eleva- tion and long-term mortality after chronic obstructive pulmo- nary disease exacerbation. Eur Respir J. 2008;31:563-570.
5. John J, Woodward DB, Wang Y, et al. Troponin I as a prog- nosticator of mortality in severe sepsis patients. J Crit Care. 2010;25:270-275.
6. Kerr G, Ray G, Wu O, et al. Elevated troponin after stroke: a sys- tematic review. Cerebrovasc Dis. 2009;28:220-226.
7. Korff S, Katus HA, Giannitsis E. Differential diagnosis of el- evated troponins. Heart. 2006;92:987-993.
8. Hunt SA, Abraham WT, Chin MH, et al. 2009 Focused update incorporated into the ACC/AHA 2005 guidelines for the diag- nosis and management of heart failure in adults. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines devel- oped in collaboration with the International Society for Heart and Lung Transplantation. J Am Coll Cardiol. 2009;53:e1-e90.
9. Torbicki A, Perrier A, Konstantinides S, et al. Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology. Eur Heart J. 2008;29:2276-2315.
10. Wu AH, Jaffe AS, Apple FS, et al. National Academy of Clinical Biochemistry laboratory medicine practice guidelines: use of cardiac troponin and B-type natriuretic peptide or N-terminal proB-type natriuretic peptide for etiologies other than acute coronary syndromes and heart failure. Clin Chem. 2007;53:2086-2096.
1. Havekes B, van Manen J, Krediet R, et al. Serum troponin T concentration as a predictor of mortality in hemodialysis and peritoneal dialysis patients. Am J Kidney Dis. 2006;47:823-829.
2. Becattini C, Vedovati MC, Agnelli G. Prognostic value of tropo- nins in acute pulmonary embolism. Circulation. 2007;116:427- 433.
3. Torbicki A, Kurzyna M, Kuca P, et al. Detectable serum cardiac troponin T as a marker of poor prognosis among patients with chronic precapillary pulmonary hypertension. Circulation. 2003;108:844-848.
4. Brekke PH, Omland T, Holmedal SH, et al. Troponin T eleva- tion and long-term mortality after chronic obstructive pulmo- nary disease exacerbation. Eur Respir J. 2008;31:563-570.
5. John J, Woodward DB, Wang Y, et al. Troponin I as a prog- nosticator of mortality in severe sepsis patients. J Crit Care. 2010;25:270-275.
6. Kerr G, Ray G, Wu O, et al. Elevated troponin after stroke: a sys- tematic review. Cerebrovasc Dis. 2009;28:220-226.
7. Korff S, Katus HA, Giannitsis E. Differential diagnosis of el- evated troponins. Heart. 2006;92:987-993.
8. Hunt SA, Abraham WT, Chin MH, et al. 2009 Focused update incorporated into the ACC/AHA 2005 guidelines for the diag- nosis and management of heart failure in adults. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines devel- oped in collaboration with the International Society for Heart and Lung Transplantation. J Am Coll Cardiol. 2009;53:e1-e90.
9. Torbicki A, Perrier A, Konstantinides S, et al. Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology. Eur Heart J. 2008;29:2276-2315.
10. Wu AH, Jaffe AS, Apple FS, et al. National Academy of Clinical Biochemistry laboratory medicine practice guidelines: use of cardiac troponin and B-type natriuretic peptide or N-terminal proB-type natriuretic peptide for etiologies other than acute coronary syndromes and heart failure. Clin Chem. 2007;53:2086-2096.
Evidence-based answers from the Family Physicians Inquiries Network