User login
Possible Simeprevir/Sofosbuvir-Induced Hepatic Decompensation With Acute Kidney Failure
The emergence of hepatitis C (HCV) treatment regimens in the past 5 years has resulted in a major paradigm shift in the management of those infected with this virus. The 2011 approval of boceprevir and telaprevir was associated with a higher virologic response (50%-75%) and a shorter length of therapy depending on the patient population. Despite these gains, first generation direct-acting antivirals (DAAs) required multiple doses, had a higher pill burden with numerous drug interactions, and adverse effects (AEs). In addition, viral resistance limited the full use of the first generation DAAs for all genotypes.
Sofosbuvir, simeprevir, and ledipasvir-sofosbuvir (second generation DAAs) boast even higher (> 90%) sustained virologic response rates (SVR) and more tolerable AE profiles especially anemia, depression, and gastrointestinal symptoms compared with the first generation DAAs. At the time of treatment for this case study, sofosbuvir/ledipasvir was not commercially available. Sofosbuvir in combination with simeprevir with or without ribavirin was one of the preferred treatment options for chronic HCV.1
Unlike the first generation DAAs, which have been associated with a decline in renal function compared with conventional pegylated interferon and ribavirin, sofosbuvir is extensively renally eliminated by glomerular filtration and active tubular secretion as the metabolite GS-331007. On the other hand, simeprevir is hepatically metabolized.
A PubMed literature search for reports of “simeprevir-induced” or “sofosbuvir-induced with hepatic, renal failure, acute kidney injury” yielded only 1 published case of hepatic decompensation likely related to simeprevir, but no case report of simeprevir and sofosbuvir associated with hepatic decompensation and acute kidney injury.4 In this article, the authors describe a case of hepatic decompensation and acute kidney injury caused by simeprevir/sofosbuvir initiation for chronic HCV that required intensive care and dialysis.
Case Report
The patient was a 62-year-old African American man with chronic HCV, genotype 1b, TT IL28B, and 4,980,000 IU baseline viral load. He was treatment naïve with biopsy proven compensated cirrhosis, and Child-Turcotte-Pugh class A with a pretreatment model for end-stage liver disease score of 12. His past medical history included hypertension, chronic kidney disease (CKD) (baseline serum creatinine [SCr] 1.4-1.8 mg/dL), benign prostatic hypertrophy, depression, obesity (30.6 body mass index, 246 lb), and psoriasis. In addition, the patient was on the following maintenance medications: allopurinol, bupropion, diltiazem, sustained-release and immediate-release morphine, sennosides, and terazosin.
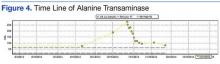
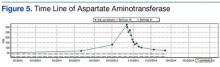
In September 2014, the patient was diagnosed with biopsy-confirmed hepatocellular carcinoma (HCC) Barcelona clinic liver cancer stage B T3aN0M0 stage III. He was considered for transarterial chemoembolization (TACE), but treatment was withheld due to subsequent increase in liver function tests (LFTs) with total bilirubin (TB) 2.9 mg/dL, direct bilirubin (DB) 1.8 mg/dL, aspartate aminotransferase test (AST) 130 U/L, and alanine aminotransferase test (ALT) 188 U/L (baseline: TB 1.1 mg/dL, AST 69 U/L, and ALT 76 U/L). These results were thought to be the result of worsening hepatic function from untreated HCV, therefore, treatment was initiated.
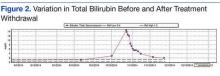
The patient was started on simeprevir 150 mg orally daily and sofosbuvir 400 mg orally daily with an estimated baseline creatinine clearance of 67 mL/min per Cockcroft-Gault equation.5 Two days after therapy initiation, the patient presented to the emergency department with the following symptoms: hiccups, nausea, vomiting, and abdominal pain. Laboratory results showed 10.85 mg/dL SCr and 91 mg/dL blood urea nitrogen (BUN), TB increased to 14.6 mg/dL with AST of 325 U/L and ALT 277 U/L. The patient reported no use of acetaminophen, alcohol, nonsteroidal anti-inflammatory drugs, or other nephrotoxic agents.
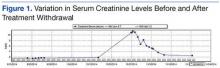
Upon admission, the patient was diagnosed with drug-induced hepatitis and acute kidney injury (AKI). Simeprevir/sofosbuvir was discontinued along with allopurinol, bupropion, lisinopril, and morphine. An abdominal ultrasound was negative for obstructive uropathy. The patient did not respond to fluid boluses. A nephrologist was consulted, and dialysis was initiated. The patient underwent dialysis for 3 days and his LFTs and SCr levels started trending downward (Figures 1 to 5).
The patient was discharged after 8 days. After 3 weeks, the SCr decreased to 2.29 mg/dL, BUN was 26 mg/dL, TB was 2 mg/dL, DB was 0.9 mg/dL, AST was 73 U/L, and ALT was 81 U/L. Weekly laboratory values continued to improve following discharge but did not return to baseline levels. The patient remained off HCV treatment.
Discussion
The patient had baseline CKD with SCr > 1.5 mg/dL; however, the significant decline in renal function and worsening hepatic function were thought to be the result of external factors. Although hepatorenal syndrome was considered, the authors suspected that the AKI and hepatic decompensation were related to simeprevir/sofosbuvir regimens due to their presumed relationship and probability analysis. Osinusi and colleagues noted a decline in renal function in a patient who received ledipasvir/sofosbuvir for 6 weeks in an open-label pilot study.6 Stine and colleagues also reported on cases of simeprevir-related hepatic decompensation.4
In this case, the authors employed the Naranjo algorithm adverse drug reaction probability scale to assess whether there was a causal relationship between this event and initiation of simeprevir/sofosbuvir regimen.7 The Naranjo score was 4, indicating a possible link between simeprevir/sofosbuvir initiation and hepatic decompensation and AKI. This case may be the first postmarketing report of significant hepatic decompensation and AKI related to simeprevir/sofosbuvir.
Unlike simeprevir, which undergoes extensive oxidative metabolism by CYP3A in the liver and has negligible renal clearance with < 1% of the dose recovered in the urine, sofosbuvir is extensively metabolized by the kidneys with an active metabolite, GS-331007, and about 80% of the dose is recovered in urine (78% as GS-331007; 3.5% as sofosbuvir).8,9 The potential for drug-drug interaction also was assessed because simeprevir is extensively metabolized by the hepatic cytochrome CYP34 system and possibly CYP2C8 and CYP2C19. Clinically significant interactions could have occurred with diltiazem and morphine, because the coadministration of these medications along with simeprevir, an inhibitor of P-glycoprotein (P-gp), and intestinal CYP3A4, may result in increased diltiazem and morphine plasma concentrations.
Of note, because sofosbuvir is a substrate of P-gp, it may have its serum concentration increased by simeprevir. Inducers and inhibitors of P-gp may alter the plasma concentration of sofosbuvir. The major metabolite, GS-331007, is not a substrate of P-gp. Drugs that induce P-gp may reduce the therapeutic effect of sofosbuvir; however, the FDA-labeling suggests that inhibitors of P-gp may be coadministered with sofosbuvir.
According to simeprevir prescribing information, drug interaction studies have demonstrated that moderate CYP3A4 inhibitors, such as diltiazem (although coadministration have not been studied), increased the maximum serum concentration (Cmax), minumum serum concentration (Cmin), and AUC of simeprevir.7 As a result, concurrent use of simeprevir with a moderate CYP3A4 inhibitors is not recommended. Morphine and simeprevir interaction also is possible via the P-gp inhibition of simeprevir. Morphine concentration may have increased and metabolites may have accumulated, leading to urinary retention and elevated creatinine. In addition, decreased oral intake and subsequent nausea/vomiting may have compounded the renal insult.
Conclusion
Given that updated HCV treatment guidelines include simeprevir/sofosbuvir as an alternative treatment option, clinicians should be aware of hepatic decompensation with markedly elevated bilirubin and AKI during simeprevir and sofosbuvir treatment. Careful consideration is needed prior to the initiation of simeprevir/sofosbuvir, particularly in patients with advanced liver disease or known HCC and baseline renal impairment.
1. American Association for the Study of Liver Diseases and the Infectious Diseases Society of America. Recommendations for testing, managing, and treating hepatitis C: Initial Treatment of HCV. American Association for the Study of Liver Diseases and the Infectious Diseases Society of America Website. http://www.hcvguidelines.org. Accessed February 8, 2016.
2. Mauss S, Hueppe D, Alshuth U. Renal impairment is frequent in chronic hepatitis C patient under triple therapy with telaprevir or boceprevir. Hepatology. 2014;59(1):46-48.
3. Virlogeux V, Pradat P, Bailly F, et al. Boceprevir and telaprevir-based triple therapy for chronic hepatitis C: virolgical efficacy and impact on kidney function and model for end-stage liver disease score. J Viral Hepat. 2014;21(9):e98-e107.
4. Stine JG, Intagliata N, Shah L, et al. Hepatic decompensation likely attributable to simeprevir in patients with advanced cirrhosis. Dig Dis Sci. 2015;60(4):1031-1035.
5. Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16(1):31-41.
6. Osinusi A, Kohli A, Marti MM, et al. Re-treamtent of chronic hepatitis C virus genotype 1 infection after relapse: an open-label pilot study. Ann Intern Med. 2014;161(9):634-638.
7. Naranjo CA, Busto U, Sellers EM, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30(2):239-245.
8. Olysio (simeprevir) [package insert]. Titusville, NJ: Janssen Therapeutics; 2014.
9. Sovaldi (sofosbuvir) [package insert]. Foster City, CA: Gilead Sciences, Inc; 2014.
The emergence of hepatitis C (HCV) treatment regimens in the past 5 years has resulted in a major paradigm shift in the management of those infected with this virus. The 2011 approval of boceprevir and telaprevir was associated with a higher virologic response (50%-75%) and a shorter length of therapy depending on the patient population. Despite these gains, first generation direct-acting antivirals (DAAs) required multiple doses, had a higher pill burden with numerous drug interactions, and adverse effects (AEs). In addition, viral resistance limited the full use of the first generation DAAs for all genotypes.
Sofosbuvir, simeprevir, and ledipasvir-sofosbuvir (second generation DAAs) boast even higher (> 90%) sustained virologic response rates (SVR) and more tolerable AE profiles especially anemia, depression, and gastrointestinal symptoms compared with the first generation DAAs. At the time of treatment for this case study, sofosbuvir/ledipasvir was not commercially available. Sofosbuvir in combination with simeprevir with or without ribavirin was one of the preferred treatment options for chronic HCV.1
Unlike the first generation DAAs, which have been associated with a decline in renal function compared with conventional pegylated interferon and ribavirin, sofosbuvir is extensively renally eliminated by glomerular filtration and active tubular secretion as the metabolite GS-331007. On the other hand, simeprevir is hepatically metabolized.
A PubMed literature search for reports of “simeprevir-induced” or “sofosbuvir-induced with hepatic, renal failure, acute kidney injury” yielded only 1 published case of hepatic decompensation likely related to simeprevir, but no case report of simeprevir and sofosbuvir associated with hepatic decompensation and acute kidney injury.4 In this article, the authors describe a case of hepatic decompensation and acute kidney injury caused by simeprevir/sofosbuvir initiation for chronic HCV that required intensive care and dialysis.
Case Report
The patient was a 62-year-old African American man with chronic HCV, genotype 1b, TT IL28B, and 4,980,000 IU baseline viral load. He was treatment naïve with biopsy proven compensated cirrhosis, and Child-Turcotte-Pugh class A with a pretreatment model for end-stage liver disease score of 12. His past medical history included hypertension, chronic kidney disease (CKD) (baseline serum creatinine [SCr] 1.4-1.8 mg/dL), benign prostatic hypertrophy, depression, obesity (30.6 body mass index, 246 lb), and psoriasis. In addition, the patient was on the following maintenance medications: allopurinol, bupropion, diltiazem, sustained-release and immediate-release morphine, sennosides, and terazosin.
In September 2014, the patient was diagnosed with biopsy-confirmed hepatocellular carcinoma (HCC) Barcelona clinic liver cancer stage B T3aN0M0 stage III. He was considered for transarterial chemoembolization (TACE), but treatment was withheld due to subsequent increase in liver function tests (LFTs) with total bilirubin (TB) 2.9 mg/dL, direct bilirubin (DB) 1.8 mg/dL, aspartate aminotransferase test (AST) 130 U/L, and alanine aminotransferase test (ALT) 188 U/L (baseline: TB 1.1 mg/dL, AST 69 U/L, and ALT 76 U/L). These results were thought to be the result of worsening hepatic function from untreated HCV, therefore, treatment was initiated.
The patient was started on simeprevir 150 mg orally daily and sofosbuvir 400 mg orally daily with an estimated baseline creatinine clearance of 67 mL/min per Cockcroft-Gault equation.5 Two days after therapy initiation, the patient presented to the emergency department with the following symptoms: hiccups, nausea, vomiting, and abdominal pain. Laboratory results showed 10.85 mg/dL SCr and 91 mg/dL blood urea nitrogen (BUN), TB increased to 14.6 mg/dL with AST of 325 U/L and ALT 277 U/L. The patient reported no use of acetaminophen, alcohol, nonsteroidal anti-inflammatory drugs, or other nephrotoxic agents.
Upon admission, the patient was diagnosed with drug-induced hepatitis and acute kidney injury (AKI). Simeprevir/sofosbuvir was discontinued along with allopurinol, bupropion, lisinopril, and morphine. An abdominal ultrasound was negative for obstructive uropathy. The patient did not respond to fluid boluses. A nephrologist was consulted, and dialysis was initiated. The patient underwent dialysis for 3 days and his LFTs and SCr levels started trending downward (Figures 1 to 5).
The patient was discharged after 8 days. After 3 weeks, the SCr decreased to 2.29 mg/dL, BUN was 26 mg/dL, TB was 2 mg/dL, DB was 0.9 mg/dL, AST was 73 U/L, and ALT was 81 U/L. Weekly laboratory values continued to improve following discharge but did not return to baseline levels. The patient remained off HCV treatment.
Discussion
The patient had baseline CKD with SCr > 1.5 mg/dL; however, the significant decline in renal function and worsening hepatic function were thought to be the result of external factors. Although hepatorenal syndrome was considered, the authors suspected that the AKI and hepatic decompensation were related to simeprevir/sofosbuvir regimens due to their presumed relationship and probability analysis. Osinusi and colleagues noted a decline in renal function in a patient who received ledipasvir/sofosbuvir for 6 weeks in an open-label pilot study.6 Stine and colleagues also reported on cases of simeprevir-related hepatic decompensation.4
In this case, the authors employed the Naranjo algorithm adverse drug reaction probability scale to assess whether there was a causal relationship between this event and initiation of simeprevir/sofosbuvir regimen.7 The Naranjo score was 4, indicating a possible link between simeprevir/sofosbuvir initiation and hepatic decompensation and AKI. This case may be the first postmarketing report of significant hepatic decompensation and AKI related to simeprevir/sofosbuvir.
Unlike simeprevir, which undergoes extensive oxidative metabolism by CYP3A in the liver and has negligible renal clearance with < 1% of the dose recovered in the urine, sofosbuvir is extensively metabolized by the kidneys with an active metabolite, GS-331007, and about 80% of the dose is recovered in urine (78% as GS-331007; 3.5% as sofosbuvir).8,9 The potential for drug-drug interaction also was assessed because simeprevir is extensively metabolized by the hepatic cytochrome CYP34 system and possibly CYP2C8 and CYP2C19. Clinically significant interactions could have occurred with diltiazem and morphine, because the coadministration of these medications along with simeprevir, an inhibitor of P-glycoprotein (P-gp), and intestinal CYP3A4, may result in increased diltiazem and morphine plasma concentrations.
Of note, because sofosbuvir is a substrate of P-gp, it may have its serum concentration increased by simeprevir. Inducers and inhibitors of P-gp may alter the plasma concentration of sofosbuvir. The major metabolite, GS-331007, is not a substrate of P-gp. Drugs that induce P-gp may reduce the therapeutic effect of sofosbuvir; however, the FDA-labeling suggests that inhibitors of P-gp may be coadministered with sofosbuvir.
According to simeprevir prescribing information, drug interaction studies have demonstrated that moderate CYP3A4 inhibitors, such as diltiazem (although coadministration have not been studied), increased the maximum serum concentration (Cmax), minumum serum concentration (Cmin), and AUC of simeprevir.7 As a result, concurrent use of simeprevir with a moderate CYP3A4 inhibitors is not recommended. Morphine and simeprevir interaction also is possible via the P-gp inhibition of simeprevir. Morphine concentration may have increased and metabolites may have accumulated, leading to urinary retention and elevated creatinine. In addition, decreased oral intake and subsequent nausea/vomiting may have compounded the renal insult.
Conclusion
Given that updated HCV treatment guidelines include simeprevir/sofosbuvir as an alternative treatment option, clinicians should be aware of hepatic decompensation with markedly elevated bilirubin and AKI during simeprevir and sofosbuvir treatment. Careful consideration is needed prior to the initiation of simeprevir/sofosbuvir, particularly in patients with advanced liver disease or known HCC and baseline renal impairment.
The emergence of hepatitis C (HCV) treatment regimens in the past 5 years has resulted in a major paradigm shift in the management of those infected with this virus. The 2011 approval of boceprevir and telaprevir was associated with a higher virologic response (50%-75%) and a shorter length of therapy depending on the patient population. Despite these gains, first generation direct-acting antivirals (DAAs) required multiple doses, had a higher pill burden with numerous drug interactions, and adverse effects (AEs). In addition, viral resistance limited the full use of the first generation DAAs for all genotypes.
Sofosbuvir, simeprevir, and ledipasvir-sofosbuvir (second generation DAAs) boast even higher (> 90%) sustained virologic response rates (SVR) and more tolerable AE profiles especially anemia, depression, and gastrointestinal symptoms compared with the first generation DAAs. At the time of treatment for this case study, sofosbuvir/ledipasvir was not commercially available. Sofosbuvir in combination with simeprevir with or without ribavirin was one of the preferred treatment options for chronic HCV.1
Unlike the first generation DAAs, which have been associated with a decline in renal function compared with conventional pegylated interferon and ribavirin, sofosbuvir is extensively renally eliminated by glomerular filtration and active tubular secretion as the metabolite GS-331007. On the other hand, simeprevir is hepatically metabolized.
A PubMed literature search for reports of “simeprevir-induced” or “sofosbuvir-induced with hepatic, renal failure, acute kidney injury” yielded only 1 published case of hepatic decompensation likely related to simeprevir, but no case report of simeprevir and sofosbuvir associated with hepatic decompensation and acute kidney injury.4 In this article, the authors describe a case of hepatic decompensation and acute kidney injury caused by simeprevir/sofosbuvir initiation for chronic HCV that required intensive care and dialysis.
Case Report
The patient was a 62-year-old African American man with chronic HCV, genotype 1b, TT IL28B, and 4,980,000 IU baseline viral load. He was treatment naïve with biopsy proven compensated cirrhosis, and Child-Turcotte-Pugh class A with a pretreatment model for end-stage liver disease score of 12. His past medical history included hypertension, chronic kidney disease (CKD) (baseline serum creatinine [SCr] 1.4-1.8 mg/dL), benign prostatic hypertrophy, depression, obesity (30.6 body mass index, 246 lb), and psoriasis. In addition, the patient was on the following maintenance medications: allopurinol, bupropion, diltiazem, sustained-release and immediate-release morphine, sennosides, and terazosin.
In September 2014, the patient was diagnosed with biopsy-confirmed hepatocellular carcinoma (HCC) Barcelona clinic liver cancer stage B T3aN0M0 stage III. He was considered for transarterial chemoembolization (TACE), but treatment was withheld due to subsequent increase in liver function tests (LFTs) with total bilirubin (TB) 2.9 mg/dL, direct bilirubin (DB) 1.8 mg/dL, aspartate aminotransferase test (AST) 130 U/L, and alanine aminotransferase test (ALT) 188 U/L (baseline: TB 1.1 mg/dL, AST 69 U/L, and ALT 76 U/L). These results were thought to be the result of worsening hepatic function from untreated HCV, therefore, treatment was initiated.
The patient was started on simeprevir 150 mg orally daily and sofosbuvir 400 mg orally daily with an estimated baseline creatinine clearance of 67 mL/min per Cockcroft-Gault equation.5 Two days after therapy initiation, the patient presented to the emergency department with the following symptoms: hiccups, nausea, vomiting, and abdominal pain. Laboratory results showed 10.85 mg/dL SCr and 91 mg/dL blood urea nitrogen (BUN), TB increased to 14.6 mg/dL with AST of 325 U/L and ALT 277 U/L. The patient reported no use of acetaminophen, alcohol, nonsteroidal anti-inflammatory drugs, or other nephrotoxic agents.
Upon admission, the patient was diagnosed with drug-induced hepatitis and acute kidney injury (AKI). Simeprevir/sofosbuvir was discontinued along with allopurinol, bupropion, lisinopril, and morphine. An abdominal ultrasound was negative for obstructive uropathy. The patient did not respond to fluid boluses. A nephrologist was consulted, and dialysis was initiated. The patient underwent dialysis for 3 days and his LFTs and SCr levels started trending downward (Figures 1 to 5).
The patient was discharged after 8 days. After 3 weeks, the SCr decreased to 2.29 mg/dL, BUN was 26 mg/dL, TB was 2 mg/dL, DB was 0.9 mg/dL, AST was 73 U/L, and ALT was 81 U/L. Weekly laboratory values continued to improve following discharge but did not return to baseline levels. The patient remained off HCV treatment.
Discussion
The patient had baseline CKD with SCr > 1.5 mg/dL; however, the significant decline in renal function and worsening hepatic function were thought to be the result of external factors. Although hepatorenal syndrome was considered, the authors suspected that the AKI and hepatic decompensation were related to simeprevir/sofosbuvir regimens due to their presumed relationship and probability analysis. Osinusi and colleagues noted a decline in renal function in a patient who received ledipasvir/sofosbuvir for 6 weeks in an open-label pilot study.6 Stine and colleagues also reported on cases of simeprevir-related hepatic decompensation.4
In this case, the authors employed the Naranjo algorithm adverse drug reaction probability scale to assess whether there was a causal relationship between this event and initiation of simeprevir/sofosbuvir regimen.7 The Naranjo score was 4, indicating a possible link between simeprevir/sofosbuvir initiation and hepatic decompensation and AKI. This case may be the first postmarketing report of significant hepatic decompensation and AKI related to simeprevir/sofosbuvir.
Unlike simeprevir, which undergoes extensive oxidative metabolism by CYP3A in the liver and has negligible renal clearance with < 1% of the dose recovered in the urine, sofosbuvir is extensively metabolized by the kidneys with an active metabolite, GS-331007, and about 80% of the dose is recovered in urine (78% as GS-331007; 3.5% as sofosbuvir).8,9 The potential for drug-drug interaction also was assessed because simeprevir is extensively metabolized by the hepatic cytochrome CYP34 system and possibly CYP2C8 and CYP2C19. Clinically significant interactions could have occurred with diltiazem and morphine, because the coadministration of these medications along with simeprevir, an inhibitor of P-glycoprotein (P-gp), and intestinal CYP3A4, may result in increased diltiazem and morphine plasma concentrations.
Of note, because sofosbuvir is a substrate of P-gp, it may have its serum concentration increased by simeprevir. Inducers and inhibitors of P-gp may alter the plasma concentration of sofosbuvir. The major metabolite, GS-331007, is not a substrate of P-gp. Drugs that induce P-gp may reduce the therapeutic effect of sofosbuvir; however, the FDA-labeling suggests that inhibitors of P-gp may be coadministered with sofosbuvir.
According to simeprevir prescribing information, drug interaction studies have demonstrated that moderate CYP3A4 inhibitors, such as diltiazem (although coadministration have not been studied), increased the maximum serum concentration (Cmax), minumum serum concentration (Cmin), and AUC of simeprevir.7 As a result, concurrent use of simeprevir with a moderate CYP3A4 inhibitors is not recommended. Morphine and simeprevir interaction also is possible via the P-gp inhibition of simeprevir. Morphine concentration may have increased and metabolites may have accumulated, leading to urinary retention and elevated creatinine. In addition, decreased oral intake and subsequent nausea/vomiting may have compounded the renal insult.
Conclusion
Given that updated HCV treatment guidelines include simeprevir/sofosbuvir as an alternative treatment option, clinicians should be aware of hepatic decompensation with markedly elevated bilirubin and AKI during simeprevir and sofosbuvir treatment. Careful consideration is needed prior to the initiation of simeprevir/sofosbuvir, particularly in patients with advanced liver disease or known HCC and baseline renal impairment.
1. American Association for the Study of Liver Diseases and the Infectious Diseases Society of America. Recommendations for testing, managing, and treating hepatitis C: Initial Treatment of HCV. American Association for the Study of Liver Diseases and the Infectious Diseases Society of America Website. http://www.hcvguidelines.org. Accessed February 8, 2016.
2. Mauss S, Hueppe D, Alshuth U. Renal impairment is frequent in chronic hepatitis C patient under triple therapy with telaprevir or boceprevir. Hepatology. 2014;59(1):46-48.
3. Virlogeux V, Pradat P, Bailly F, et al. Boceprevir and telaprevir-based triple therapy for chronic hepatitis C: virolgical efficacy and impact on kidney function and model for end-stage liver disease score. J Viral Hepat. 2014;21(9):e98-e107.
4. Stine JG, Intagliata N, Shah L, et al. Hepatic decompensation likely attributable to simeprevir in patients with advanced cirrhosis. Dig Dis Sci. 2015;60(4):1031-1035.
5. Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16(1):31-41.
6. Osinusi A, Kohli A, Marti MM, et al. Re-treamtent of chronic hepatitis C virus genotype 1 infection after relapse: an open-label pilot study. Ann Intern Med. 2014;161(9):634-638.
7. Naranjo CA, Busto U, Sellers EM, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30(2):239-245.
8. Olysio (simeprevir) [package insert]. Titusville, NJ: Janssen Therapeutics; 2014.
9. Sovaldi (sofosbuvir) [package insert]. Foster City, CA: Gilead Sciences, Inc; 2014.
1. American Association for the Study of Liver Diseases and the Infectious Diseases Society of America. Recommendations for testing, managing, and treating hepatitis C: Initial Treatment of HCV. American Association for the Study of Liver Diseases and the Infectious Diseases Society of America Website. http://www.hcvguidelines.org. Accessed February 8, 2016.
2. Mauss S, Hueppe D, Alshuth U. Renal impairment is frequent in chronic hepatitis C patient under triple therapy with telaprevir or boceprevir. Hepatology. 2014;59(1):46-48.
3. Virlogeux V, Pradat P, Bailly F, et al. Boceprevir and telaprevir-based triple therapy for chronic hepatitis C: virolgical efficacy and impact on kidney function and model for end-stage liver disease score. J Viral Hepat. 2014;21(9):e98-e107.
4. Stine JG, Intagliata N, Shah L, et al. Hepatic decompensation likely attributable to simeprevir in patients with advanced cirrhosis. Dig Dis Sci. 2015;60(4):1031-1035.
5. Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16(1):31-41.
6. Osinusi A, Kohli A, Marti MM, et al. Re-treamtent of chronic hepatitis C virus genotype 1 infection after relapse: an open-label pilot study. Ann Intern Med. 2014;161(9):634-638.
7. Naranjo CA, Busto U, Sellers EM, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30(2):239-245.
8. Olysio (simeprevir) [package insert]. Titusville, NJ: Janssen Therapeutics; 2014.
9. Sovaldi (sofosbuvir) [package insert]. Foster City, CA: Gilead Sciences, Inc; 2014.
Onychomatricoma: A Rare Case of Unguioblastic Fibroma of the Fingernail Associated With Trauma
Onychomatricoma (OM) is a rare benign neoplasm of the nail matrix. Even less common is its possible association with both trauma to the nail apparatus and onychomycosis. This case illustrates both of these findings.
Case Report
A 72-year-old white man presented to the dermatology clinic with a 26-year history of a thickened nail plate on the right third finger that had developed soon after a baseball injury. The patient reported that the nail was completely normal prior to the trauma. According to the patient, the distal aspect of the finger was directly hit by a baseball and subsequently was wrapped by the patient for a few weeks. The nail then turned black and eventually fell off. When the nail grew back, it appeared abnormal and in its current state. The patient stated the lesion was asymptomatic at the time of presentation.
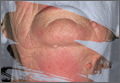
Physical examination revealed thickening, yellow discoloration, and transverse overcurvature of the nail plate on the right third finger with longitudinal ridging (Figure 1). A culture of the nail plate grew Chaetomium species. Application of topical clotrimazole for 3 months followed by a 6-week course of oral terbinafine produced no improvement. The patient then consented to a nail matrix incisional biopsy 6 months after initial presentation. After a digital nerve block was administered and a tourniquet of the proximal digit was applied, a nail avulsion was performed. Subsequently, a 3-mm punch biopsy was taken of the clinically apparent tumor in the nail matrix.
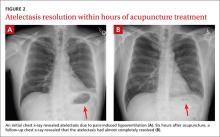
On microscopic examination of the removed tissue, a benign mixed epithelial and stromal proliferative lesion was noted. The basaloid epithelium, lacking a granular layer, arose from the surface epithelial layer and formed a reticulated pattern extending into the stromal component, which was moderately cellular with spindle to fusiform nuclei dissecting between collagen bundles arranged in parallel arrays (Figure 2). The stromal component predominated over the epithelial component in this neoplasm. The nail was preserved in formalin and underwent hematoxylin and eosin staining. It was thickened and grossly showed filiform fibrous projections extending into the nail plate. Histologically, the nail displayed prominent oval clear channels. Periodic acid–Schiff staining was negative for fungal organisms.
A diagnosis of unguioblastic fibroma–type OM was made. After receiving the diagnosis, expected course, and treatment options, the patient was offered conservative surgical excision but preferred clinical monitoring. At his last visit (6 months after the biopsy), the nail plate distal to the biopsy site had thinning and improvement, while the nail plate distal to the matrix that was not removed continued to show thickening, yellow discoloration, overcurvature, and longitudinal ridging (Figure 3).
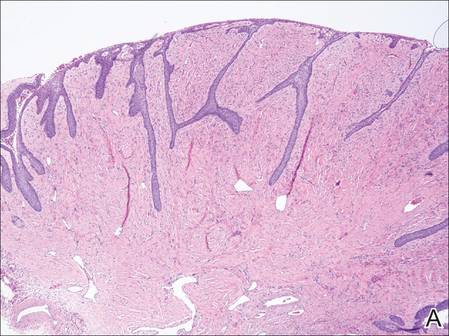 | 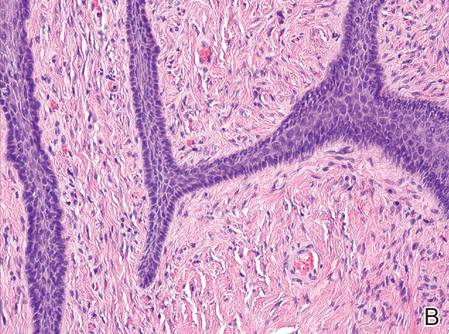 | |
Figure 2. The basaloid epithelium arose from the surface epithelial layer and formed a reticulated pattern extending into the stromal component (A)(H&E, original magnification ×2). At higher magnification, the stromal component was moderately cellular with spindle to fusiform nuclei dissecting between collagen bundles arranged in parallel arrays (B)(H&E, original magnification ×10). | ||
|
|
Comment
Onychomatricoma is a rare tumor originating from the nail matrix. The tumor was first described by Baran and Kint1 in 1992 using the term onychomatrixoma, but later the term onychomatricoma became more widely used.2 Onychomatricomas are more common in adults (mean age, 48 years) and white individuals with no gender predilection.3,4 Fingernail involvement is twice as common as toenail involvement.3 Onychomatricoma is the only tumor that actively produces a nail plate.4
Clinically, OM presents with yellow discoloration along the entire nail plate and proximal splinter hemorrhages. It has a tendency toward transverse overcurvature of the nail plate with prominent longitudinal ridging.4 Trauma has been associated in at least 3 cases reported in the literature, though the association was sometimes weak.3,4 Xanthonychia and onychodystrophy of the nail are common.3 Pterygium, melanonychia, nail bleeding, and cutaneous horns have been reported but are rare.3-5 The tumor typically is painless with no radiographic bone involvement.3 Onychomycosis can be present,3 which may either be a predisposing factor for the tumor or secondary due to the deformed nail plate.4
When the nail plate is avulsed and the proximal nail fold is turned back, the matrix tumor is exposed. This polypoid and filiform tumor has characteristic fingerlike fibrokeratogenous projections extending from the nail matrix into the nail plate.3
Histologically, the tumor is fibroepithelial or biphasic with stromal and epithelial components. It has a lobulated and papillary growth pattern with 2 distinct areas that correspond to 2 anatomic zones.3 The base of the tumor corresponds to the proximal anatomic zone, which begins at the root of the nail and extends to the cuticle. This area is composed of V-shaped keratinous zones similar to the normal matrix. If the nail is removed prior to excision, these areas can be avulsed, leaving clear clefts. The superficial aspect of the tumor corresponds to the distal anatomic zone, which is located in the region of the lunula. This area is composed of multiple digitate or fingerlike projections with a fibrous core and a thick matrical epithelial covering.3 These digitations extend into small cavities in the nail plate, which can be visualized as clear channels or woodwormlike holes in hematoxylin and eosin–stained specimens. A biphasic fibrous stroma also can be observed with the superficial dermis being cellular with fibrillary collagen and the deep dermis more hypocellular with thicker collagen bundles.3,4
An analysis of keratins in the nail matrix, bed, and isthmus showed that OM has the capacity to recapitulate the entire nail unit with differentiation toward the nail bed and isthmus.6 It appears that the mesenchymal component has an inductive effect that can lead to complete epithelial onychogenic differentiation.6
Due to the histological differences among the described cases of OM in the literature, a new classification based on the spectrum of epithelial to stromal ratio of stromal cellularity and the extent of nuclear pleomorphism was proposed in 2004.7 The prominent feature of the unguioblastoma type of OM is epithelial, while the cellular stroma is the prominent feature in the unguioblastic fibroma type. Atypical unguioblastic fibroma refers to a tumor with increased mitotic activity and nuclear pleomorphism among the stroma.7
Most OM tumors follow a benign clinical course; however, complete excision is advised to include the normal nail matrix proximal to the lesion, which may prevent recurrence and serves as a primary treatment.
Conclusion
Onychomatricoma is a benign neoplasm of the nail matrix that may be triggered by trauma; however, due to the weak association, further observations and studies should be conducted to substantiate this possibility. Patients with the classic clinical presentation possibly may be spared a nail avulsion and biopsy. Onychomycosis occurs in the setting of OM, and culture and treatment are unlikely to change the appearance or course of this nail condition.
1. Baran R, Kint A. Onychomatrixoma. filamentous tufted tumour in the matrix of a funnel-shaped nail: a new entity (report of three cases). Br J Dermatol. 1992;126:510-515.
2. Haneke E, Franken J. Onychomatricoma. Dermatol Surg. 1995;21:984-987.
3. Gaertner EM, Gordon M, Reed T. Onychomatricoma: case report of an unusual subungual tumor with literature review. J Cutan Pathol. 2009;36(suppl 1):66-69.
4. Cañueto J, Santos-Briz Á, García JL, et al. Onychomatricoma: genome-wide analyses of a rare nail matrix tumor. J Am Acad Dermatol. 2011;64:573-578.
5. Perrin C, Baran R. Onychomatricoma with dorsalpterygium: pathogenic mechanisms in 3 cases. J Am Acad Dermatol. 2008;59:990-994.
6. Perrin C, Langbein L, Schweizer J, et al. Onychomatricoma in the light of the microanatomy of the normal nail unit. Am J Dermatopathol. 2011;33:131-139.
7. Ko CJ, Shi L, Barr RJ, et al. Unguioblastoma and unguioblastic fibroma—an expanded spectrum of onychomatricoma. J Cutan Pathol. 2004;31:307-311.
Onychomatricoma (OM) is a rare benign neoplasm of the nail matrix. Even less common is its possible association with both trauma to the nail apparatus and onychomycosis. This case illustrates both of these findings.
Case Report
A 72-year-old white man presented to the dermatology clinic with a 26-year history of a thickened nail plate on the right third finger that had developed soon after a baseball injury. The patient reported that the nail was completely normal prior to the trauma. According to the patient, the distal aspect of the finger was directly hit by a baseball and subsequently was wrapped by the patient for a few weeks. The nail then turned black and eventually fell off. When the nail grew back, it appeared abnormal and in its current state. The patient stated the lesion was asymptomatic at the time of presentation.
Physical examination revealed thickening, yellow discoloration, and transverse overcurvature of the nail plate on the right third finger with longitudinal ridging (Figure 1). A culture of the nail plate grew Chaetomium species. Application of topical clotrimazole for 3 months followed by a 6-week course of oral terbinafine produced no improvement. The patient then consented to a nail matrix incisional biopsy 6 months after initial presentation. After a digital nerve block was administered and a tourniquet of the proximal digit was applied, a nail avulsion was performed. Subsequently, a 3-mm punch biopsy was taken of the clinically apparent tumor in the nail matrix.
On microscopic examination of the removed tissue, a benign mixed epithelial and stromal proliferative lesion was noted. The basaloid epithelium, lacking a granular layer, arose from the surface epithelial layer and formed a reticulated pattern extending into the stromal component, which was moderately cellular with spindle to fusiform nuclei dissecting between collagen bundles arranged in parallel arrays (Figure 2). The stromal component predominated over the epithelial component in this neoplasm. The nail was preserved in formalin and underwent hematoxylin and eosin staining. It was thickened and grossly showed filiform fibrous projections extending into the nail plate. Histologically, the nail displayed prominent oval clear channels. Periodic acid–Schiff staining was negative for fungal organisms.
A diagnosis of unguioblastic fibroma–type OM was made. After receiving the diagnosis, expected course, and treatment options, the patient was offered conservative surgical excision but preferred clinical monitoring. At his last visit (6 months after the biopsy), the nail plate distal to the biopsy site had thinning and improvement, while the nail plate distal to the matrix that was not removed continued to show thickening, yellow discoloration, overcurvature, and longitudinal ridging (Figure 3).
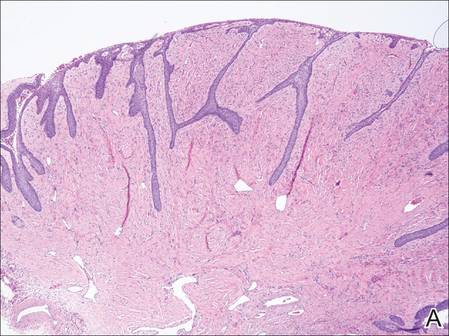 | 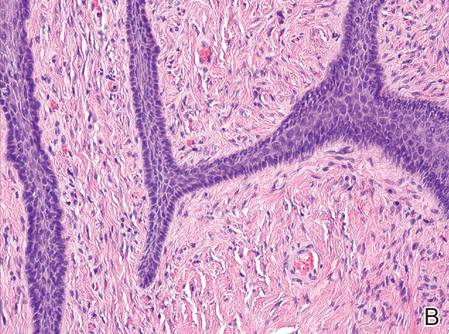 | |
Figure 2. The basaloid epithelium arose from the surface epithelial layer and formed a reticulated pattern extending into the stromal component (A)(H&E, original magnification ×2). At higher magnification, the stromal component was moderately cellular with spindle to fusiform nuclei dissecting between collagen bundles arranged in parallel arrays (B)(H&E, original magnification ×10). | ||
|
|
Comment
Onychomatricoma is a rare tumor originating from the nail matrix. The tumor was first described by Baran and Kint1 in 1992 using the term onychomatrixoma, but later the term onychomatricoma became more widely used.2 Onychomatricomas are more common in adults (mean age, 48 years) and white individuals with no gender predilection.3,4 Fingernail involvement is twice as common as toenail involvement.3 Onychomatricoma is the only tumor that actively produces a nail plate.4
Clinically, OM presents with yellow discoloration along the entire nail plate and proximal splinter hemorrhages. It has a tendency toward transverse overcurvature of the nail plate with prominent longitudinal ridging.4 Trauma has been associated in at least 3 cases reported in the literature, though the association was sometimes weak.3,4 Xanthonychia and onychodystrophy of the nail are common.3 Pterygium, melanonychia, nail bleeding, and cutaneous horns have been reported but are rare.3-5 The tumor typically is painless with no radiographic bone involvement.3 Onychomycosis can be present,3 which may either be a predisposing factor for the tumor or secondary due to the deformed nail plate.4
When the nail plate is avulsed and the proximal nail fold is turned back, the matrix tumor is exposed. This polypoid and filiform tumor has characteristic fingerlike fibrokeratogenous projections extending from the nail matrix into the nail plate.3
Histologically, the tumor is fibroepithelial or biphasic with stromal and epithelial components. It has a lobulated and papillary growth pattern with 2 distinct areas that correspond to 2 anatomic zones.3 The base of the tumor corresponds to the proximal anatomic zone, which begins at the root of the nail and extends to the cuticle. This area is composed of V-shaped keratinous zones similar to the normal matrix. If the nail is removed prior to excision, these areas can be avulsed, leaving clear clefts. The superficial aspect of the tumor corresponds to the distal anatomic zone, which is located in the region of the lunula. This area is composed of multiple digitate or fingerlike projections with a fibrous core and a thick matrical epithelial covering.3 These digitations extend into small cavities in the nail plate, which can be visualized as clear channels or woodwormlike holes in hematoxylin and eosin–stained specimens. A biphasic fibrous stroma also can be observed with the superficial dermis being cellular with fibrillary collagen and the deep dermis more hypocellular with thicker collagen bundles.3,4
An analysis of keratins in the nail matrix, bed, and isthmus showed that OM has the capacity to recapitulate the entire nail unit with differentiation toward the nail bed and isthmus.6 It appears that the mesenchymal component has an inductive effect that can lead to complete epithelial onychogenic differentiation.6
Due to the histological differences among the described cases of OM in the literature, a new classification based on the spectrum of epithelial to stromal ratio of stromal cellularity and the extent of nuclear pleomorphism was proposed in 2004.7 The prominent feature of the unguioblastoma type of OM is epithelial, while the cellular stroma is the prominent feature in the unguioblastic fibroma type. Atypical unguioblastic fibroma refers to a tumor with increased mitotic activity and nuclear pleomorphism among the stroma.7
Most OM tumors follow a benign clinical course; however, complete excision is advised to include the normal nail matrix proximal to the lesion, which may prevent recurrence and serves as a primary treatment.
Conclusion
Onychomatricoma is a benign neoplasm of the nail matrix that may be triggered by trauma; however, due to the weak association, further observations and studies should be conducted to substantiate this possibility. Patients with the classic clinical presentation possibly may be spared a nail avulsion and biopsy. Onychomycosis occurs in the setting of OM, and culture and treatment are unlikely to change the appearance or course of this nail condition.
Onychomatricoma (OM) is a rare benign neoplasm of the nail matrix. Even less common is its possible association with both trauma to the nail apparatus and onychomycosis. This case illustrates both of these findings.
Case Report
A 72-year-old white man presented to the dermatology clinic with a 26-year history of a thickened nail plate on the right third finger that had developed soon after a baseball injury. The patient reported that the nail was completely normal prior to the trauma. According to the patient, the distal aspect of the finger was directly hit by a baseball and subsequently was wrapped by the patient for a few weeks. The nail then turned black and eventually fell off. When the nail grew back, it appeared abnormal and in its current state. The patient stated the lesion was asymptomatic at the time of presentation.
Physical examination revealed thickening, yellow discoloration, and transverse overcurvature of the nail plate on the right third finger with longitudinal ridging (Figure 1). A culture of the nail plate grew Chaetomium species. Application of topical clotrimazole for 3 months followed by a 6-week course of oral terbinafine produced no improvement. The patient then consented to a nail matrix incisional biopsy 6 months after initial presentation. After a digital nerve block was administered and a tourniquet of the proximal digit was applied, a nail avulsion was performed. Subsequently, a 3-mm punch biopsy was taken of the clinically apparent tumor in the nail matrix.
On microscopic examination of the removed tissue, a benign mixed epithelial and stromal proliferative lesion was noted. The basaloid epithelium, lacking a granular layer, arose from the surface epithelial layer and formed a reticulated pattern extending into the stromal component, which was moderately cellular with spindle to fusiform nuclei dissecting between collagen bundles arranged in parallel arrays (Figure 2). The stromal component predominated over the epithelial component in this neoplasm. The nail was preserved in formalin and underwent hematoxylin and eosin staining. It was thickened and grossly showed filiform fibrous projections extending into the nail plate. Histologically, the nail displayed prominent oval clear channels. Periodic acid–Schiff staining was negative for fungal organisms.
A diagnosis of unguioblastic fibroma–type OM was made. After receiving the diagnosis, expected course, and treatment options, the patient was offered conservative surgical excision but preferred clinical monitoring. At his last visit (6 months after the biopsy), the nail plate distal to the biopsy site had thinning and improvement, while the nail plate distal to the matrix that was not removed continued to show thickening, yellow discoloration, overcurvature, and longitudinal ridging (Figure 3).
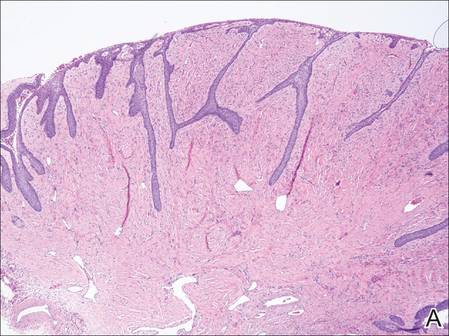 | 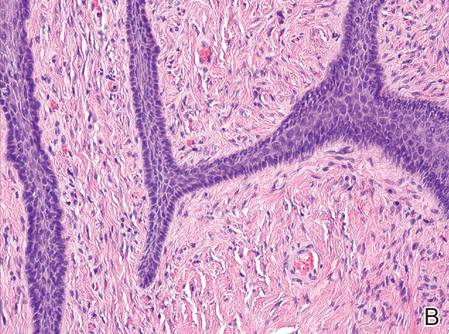 | |
Figure 2. The basaloid epithelium arose from the surface epithelial layer and formed a reticulated pattern extending into the stromal component (A)(H&E, original magnification ×2). At higher magnification, the stromal component was moderately cellular with spindle to fusiform nuclei dissecting between collagen bundles arranged in parallel arrays (B)(H&E, original magnification ×10). | ||
|
|
Comment
Onychomatricoma is a rare tumor originating from the nail matrix. The tumor was first described by Baran and Kint1 in 1992 using the term onychomatrixoma, but later the term onychomatricoma became more widely used.2 Onychomatricomas are more common in adults (mean age, 48 years) and white individuals with no gender predilection.3,4 Fingernail involvement is twice as common as toenail involvement.3 Onychomatricoma is the only tumor that actively produces a nail plate.4
Clinically, OM presents with yellow discoloration along the entire nail plate and proximal splinter hemorrhages. It has a tendency toward transverse overcurvature of the nail plate with prominent longitudinal ridging.4 Trauma has been associated in at least 3 cases reported in the literature, though the association was sometimes weak.3,4 Xanthonychia and onychodystrophy of the nail are common.3 Pterygium, melanonychia, nail bleeding, and cutaneous horns have been reported but are rare.3-5 The tumor typically is painless with no radiographic bone involvement.3 Onychomycosis can be present,3 which may either be a predisposing factor for the tumor or secondary due to the deformed nail plate.4
When the nail plate is avulsed and the proximal nail fold is turned back, the matrix tumor is exposed. This polypoid and filiform tumor has characteristic fingerlike fibrokeratogenous projections extending from the nail matrix into the nail plate.3
Histologically, the tumor is fibroepithelial or biphasic with stromal and epithelial components. It has a lobulated and papillary growth pattern with 2 distinct areas that correspond to 2 anatomic zones.3 The base of the tumor corresponds to the proximal anatomic zone, which begins at the root of the nail and extends to the cuticle. This area is composed of V-shaped keratinous zones similar to the normal matrix. If the nail is removed prior to excision, these areas can be avulsed, leaving clear clefts. The superficial aspect of the tumor corresponds to the distal anatomic zone, which is located in the region of the lunula. This area is composed of multiple digitate or fingerlike projections with a fibrous core and a thick matrical epithelial covering.3 These digitations extend into small cavities in the nail plate, which can be visualized as clear channels or woodwormlike holes in hematoxylin and eosin–stained specimens. A biphasic fibrous stroma also can be observed with the superficial dermis being cellular with fibrillary collagen and the deep dermis more hypocellular with thicker collagen bundles.3,4
An analysis of keratins in the nail matrix, bed, and isthmus showed that OM has the capacity to recapitulate the entire nail unit with differentiation toward the nail bed and isthmus.6 It appears that the mesenchymal component has an inductive effect that can lead to complete epithelial onychogenic differentiation.6
Due to the histological differences among the described cases of OM in the literature, a new classification based on the spectrum of epithelial to stromal ratio of stromal cellularity and the extent of nuclear pleomorphism was proposed in 2004.7 The prominent feature of the unguioblastoma type of OM is epithelial, while the cellular stroma is the prominent feature in the unguioblastic fibroma type. Atypical unguioblastic fibroma refers to a tumor with increased mitotic activity and nuclear pleomorphism among the stroma.7
Most OM tumors follow a benign clinical course; however, complete excision is advised to include the normal nail matrix proximal to the lesion, which may prevent recurrence and serves as a primary treatment.
Conclusion
Onychomatricoma is a benign neoplasm of the nail matrix that may be triggered by trauma; however, due to the weak association, further observations and studies should be conducted to substantiate this possibility. Patients with the classic clinical presentation possibly may be spared a nail avulsion and biopsy. Onychomycosis occurs in the setting of OM, and culture and treatment are unlikely to change the appearance or course of this nail condition.
1. Baran R, Kint A. Onychomatrixoma. filamentous tufted tumour in the matrix of a funnel-shaped nail: a new entity (report of three cases). Br J Dermatol. 1992;126:510-515.
2. Haneke E, Franken J. Onychomatricoma. Dermatol Surg. 1995;21:984-987.
3. Gaertner EM, Gordon M, Reed T. Onychomatricoma: case report of an unusual subungual tumor with literature review. J Cutan Pathol. 2009;36(suppl 1):66-69.
4. Cañueto J, Santos-Briz Á, García JL, et al. Onychomatricoma: genome-wide analyses of a rare nail matrix tumor. J Am Acad Dermatol. 2011;64:573-578.
5. Perrin C, Baran R. Onychomatricoma with dorsalpterygium: pathogenic mechanisms in 3 cases. J Am Acad Dermatol. 2008;59:990-994.
6. Perrin C, Langbein L, Schweizer J, et al. Onychomatricoma in the light of the microanatomy of the normal nail unit. Am J Dermatopathol. 2011;33:131-139.
7. Ko CJ, Shi L, Barr RJ, et al. Unguioblastoma and unguioblastic fibroma—an expanded spectrum of onychomatricoma. J Cutan Pathol. 2004;31:307-311.
1. Baran R, Kint A. Onychomatrixoma. filamentous tufted tumour in the matrix of a funnel-shaped nail: a new entity (report of three cases). Br J Dermatol. 1992;126:510-515.
2. Haneke E, Franken J. Onychomatricoma. Dermatol Surg. 1995;21:984-987.
3. Gaertner EM, Gordon M, Reed T. Onychomatricoma: case report of an unusual subungual tumor with literature review. J Cutan Pathol. 2009;36(suppl 1):66-69.
4. Cañueto J, Santos-Briz Á, García JL, et al. Onychomatricoma: genome-wide analyses of a rare nail matrix tumor. J Am Acad Dermatol. 2011;64:573-578.
5. Perrin C, Baran R. Onychomatricoma with dorsalpterygium: pathogenic mechanisms in 3 cases. J Am Acad Dermatol. 2008;59:990-994.
6. Perrin C, Langbein L, Schweizer J, et al. Onychomatricoma in the light of the microanatomy of the normal nail unit. Am J Dermatopathol. 2011;33:131-139.
7. Ko CJ, Shi L, Barr RJ, et al. Unguioblastoma and unguioblastic fibroma—an expanded spectrum of onychomatricoma. J Cutan Pathol. 2004;31:307-311.
Practice Points
- Onychomatricoma is a rare benign neoplasm of the nail matrix that actively produces a nail plate.
- Onychomatricoma should be in the differential diagnosis of a thickened discolored nail plate with transverse overcurvature.
- Onychomatricoma has been associated with onychomycosis and trauma to the nail apparatus.
Angioedema Following tPA Administration for Acute Cerebrovascular Accident
The use of thrombolytic medications for the treatment of acute ischemic cerebral infarctions has dynamically altered stroke care. However, there are both major and minor side effects associated with its use—most notably major bleeding, which led to strict inclusion and exclusion criteria governing the administration of this medication class. One less recognized but potentially serious complication is angioedema secondary to tissue plasminogen activator (tPA). Our case emphasizes the importance of early recognition of this clinical syndrome as it relates to airway compromise and potential respiratory failure in patients who are treated with tPA.
Case
A 70-year-old woman with a history of diabetes and hypertension and a remote history of breast cancer, nonhemiplegic migraines, and hypothyroidism presented to the ED with complaints of aphasia and right-sided paralysis, with onset 2 hours prior. Regarding the patient’s medication history, she had been taking lisinopril for hypertension.
Upon assessment, the patient was awake and alert and her vital signs were normal and stable, but she was aphasic, unable to accurately phonate, and was not able to move her right arm or leg against gravity. Her sensation appeared intact, and she had mild facial asymmetry with inability to raise the right corner of her mouth; her tongue had midline protrusion.
An emergent computed tomography (CT) scan of the head demonstrated mild brain atrophy and minimal low attenuation within the cerebral hemispheric white matter—most noticeably within the subcortical region of the left frontal lobe, consistent with small vessel ischemia. There was no evidence of acute intracranial hemorrhage, midline shift, or focal mass effect, and no convincing CT evidence for acute large vessel, cortical-based infarction.
The patient was determined to be an appropriate candidate for tPA, and was consented in the usual fashion. Within 15 minutes of administration of intravenous (IV) tPA, her symptoms improved, the aphasia resolved, and she was able to lift her right arm and leg against gravity and verbally communicate. Approximately 30 minutes following the resolution of her neurological symptoms, however, the patient was noted to have bleeding around a tooth socket, which was controlled with gauze and pressure. She subsequently began to complain of swelling on her right inferior lip without acute airway compromise. Over the next 10 to 15 minutes, she began to develop tongue swelling and feelings of dyspnea without wheezing.
The patient’s airway was reassessed and was classified as a Mallampati class IV. Anesthesia services were consulted for an emergent, awake intubation for airway protection. She was medicated with midazolam IV, as well as atomized lidocaine and lidocaine gargle for local anesthesia. The patient was successfully intubated awake using a flexible fiber optic technique. She was admitted to the medical intensive care unit for further monitoring, where she was treated with IV methylprednisolone, famotidine, and diphenhydramine. She was extubated the following day, had a relatively uncomplicated hospital course, and was discharged on hospital day 5 with improvement in her speech and right-sided weakness.
Discussion
The risk of angioedema associated with tPA administration has been previously described, with an estimated rate of 1.3 to 5.1%.1-3 Studies have shown the risk of developing angioedema is significantly increased in the setting of concomitant use of an angiotensin converting enzyme inhibitor (ACE-I); CT studies have also shown evidence of frontal and insular ischemia, with an odds radio of 13.6 and 9.1, respectively.2 Our patient was on lisinopril and had early signs of ischemia in the frontal lobe on initial CT scan, which likely increased her risk for angioedema.
How tPA Can Trigger Angioedema
The development of angioedema after administration of tPA has a well-described biochemical basis. Angioedema has been linked to the local vasodilatory effects of bradykinin, mast cell degranulation, and histamine release from activation of the complement pathway.4 Tissue plasminogen activator may trigger both of these pathways. It is a serine protease that cleaves plasminogen to plasmin; the plasmin in turn cleaves fibrin, resulting in the desired thrombolytic effects.5 Plasmin can cause mast cell degranulation through conversion of C3 to C3a and through activation of the complement pathway through conversion of C1 to C1a.6
Studies have shown tPA to have low antigenicity, and activation of this pathway is most likely secondary to direct proteolytic effects as opposed to antibody complexes.7 In a study by Bennett et al,6 tPA was shown to significantly increase C3a, C4a, and C5a serum levels when given in the setting of myocardial infarction (MI). It has also been shown to activate and increase serum kallikrein, which cleaves high-molecular weight kininogen to bradykinin, a potent vasodilator.8,9
Since bradykinin is broken down by several enzymes, including ACE, degradation is therefore delayed in patients on ACE-I.10 The alternate pathway for bradykinin degradation in the absence of ACE may also result in formation of des-Arg bradykinin, another similar active metabolite that mimics the effects of bradykinins.9 The formation of bradykinin through the proteolytic effects of tPA, in combination with the delayed breakdown in patient’s taking an ACE-I, likely plays a significant role in the development of angioedema.
In addition to the direct proteolytic effect of tPA resulting in angioedema, the underlying ischemic insult may also predispose patients to angioedema. As was the case with our patient, angioedema preferentially affects the ipsilateral side of the patient’s deficit.2,11,12 Theories suggest this is due to the lack of autonomic compensatory responses in the setting of ischemic insult.2 Interestingly, the development of angioedema in relation to the use of recombinant-tPA (eg, alteplase) in the setting of MI has not been as well described and may be related to the effect of central nervous system insult.3
Treatment
Although hemorrhagic complications of tPA therapy for cerebrovascular accident are well known, the risk for angioedema as a complication is less recognized. In most cases, angioedema is transient, and very few patients require aggressive support.3,12 Treatments that have previously been described include antihistamines and steroids.1,11,13 Epinephrine has been reported in one case study as an adjunct treatment of tPA-induced angioedema; however, it was given in combination with steroids and antihistimines.14 Therefore, caution should be taken regarding the use of epinephrine in this setting as there may be a theoretical precipitation of intracranial hypertension or hemorrhage.2
Given the likely significant role of the bradykinin-mediated pathway in tPA-induced angioedema, the true efficacy of these agents is unknown. Our patient had significant labial and lingual involvement, and given the concern for impending airway compromise, fiber optic intubation was performed. The decision to intubate and the technique employed must be carefully considered as a failed airway and need for a surgical airway is a concerning prospect in the setting of fibrinolytics. Successful cricothyroidotomy without significant complications has been described in the setting of streptokinase-induced angioedema when given for MI.15
Conclusion
The use of tPA for the treatment of ischemic stroke has been increasing over the last decade.16,17 Given the high prevalence of ACE-I use in patients who are also at risk for ischemic stroke, physicians administering tPA must be aware of the risk of tPA-associated angioedema. Patients with a known history of angioedema or anaphylaxis to tPA should be counseled on these risks and should not be given this medication, but rather considered for potential endovascular or mechanical clot retrieval therapy if they meet inclusion criteria for its use.
1. Hill MD, Barber PA, Takahashi J, Demchuk AM, Feasby TE, Buchan AM. Anaphylactoid reactions and angioedema during alteplase treatment of acute ischemic stroke. CMAJ. 2000;162(9):1281-1284.
2. Hill MD, Lye T, Moss H, et al. Hemi-orolingual angioedema and ACE inhibition after alteplase treatment of stroke. Neurology. 2003;60(9):1525-1527.
3. Hill MD, Buchan AM; Canadian Alteplase for Stroke Effectiveness Study (CASES) Investigators. Thrombolysis for acute ischemic stroke: results of the Canadian Alteplase for Stroke Effectiveness Study. CMAJ. 2005;172(10):1307-1312.
4. Lewis LM. Angioedema: etiology, pathophysiology, current and emerging therapies. J Emerg Med. 2013;45(5):789-796.
5. Loscalzo J, Braunwald E. Tissue plasminogen activator. N Engl J Med. 1988;319(14):935-931.
6. Bennett WR, Yawn DH, Migliore PJ, et al. Activation of the complement system by recombinant tissue plasminogen activator. J Am Coll Cardiol. 1987;10(3):627-632.
7. Reed BR, Chen AB, Tanswell P, et al. Low incidence of antibodies to recombinant human tissue-type plasminogen activator in treated patients. Thromb Haemost. 1990;64(2):276-280.
8. Hoffmeister HM, Szabo S, Kastner C, et al. Thrombolytic therapy in acute myocardial infarction: comparison of procoagulant effects of streptokinase and alteplase regimens with focus on the kallikrein system and plasmin. Circulation. 1998;98(23):2527-2533.
9. Molinaro G, Gervais N, Adam A. Biochemical basis of angioedema associated with recombinant tissue plasminogen activator treatment: an in vitro experimental approach. Stroke. 2002;33(6):1712-1716.
10. Bezalel S, Mahlab-Guri K, Asher I, Werner B, Sthoeger ZM. Angiotensin-converting enzyme inhibitor-induced angioedema. Am J Med. 2015;128(2):120-125.
11. Pancioli A, Brott T, Donaldson V, Miller R. Asymmetric angioneurotic edema associated with thrombolysis for acute stroke. Ann Emerg Med. 1997;30(2):227-229.
12. Correia AS, Matias G, Calado S, Lourenço A, Viana-Baptista M. Orolingual angiodema associated with alteplase treatment of acute stroke: a reappraisal. J Stroke Cerebrovasc Dis. 2015;24(1):31-40.
13. Maertins M, Wol R, Swider M. Angioedema after administration of tPA for ischemic stroke: case report. Air Med J. 2011;30(5):276-278.
14. Fugate JE, Kalimullah EA, Wijdicks EF. Angioedema after tPA: what neurointensivists should know. Neurocrit Care. 2012;16(3):440-443.
15. Walls RM, Pollack CV Jr. Successful cricothyrotomy after thrombolytic therapy for acute myocardial infarction: a report of two cases. Ann Emerg Med. 2000;35(2):188-191.
16. Lichtman JH, Watanabe E, Allen NB, Jones SB, Dostal J, Goldstein LB. Hospital arrival time and intravenous t-PA use in US Academic Medical Centers, 2001-2004. Stroke. 2009;40(12):3845-3850.
17. Schwamm LH, Ali SF, Reeves MJ, et al. Temporal trends in patient characteristics and treatment with intravenous thrombolysis among acute ischemic stroke patients at Get With the Guidelines-Stroke hospitals. Circ Cardiovasc Qual Outcomes. 2013;6(5):543-549.
The use of thrombolytic medications for the treatment of acute ischemic cerebral infarctions has dynamically altered stroke care. However, there are both major and minor side effects associated with its use—most notably major bleeding, which led to strict inclusion and exclusion criteria governing the administration of this medication class. One less recognized but potentially serious complication is angioedema secondary to tissue plasminogen activator (tPA). Our case emphasizes the importance of early recognition of this clinical syndrome as it relates to airway compromise and potential respiratory failure in patients who are treated with tPA.
Case
A 70-year-old woman with a history of diabetes and hypertension and a remote history of breast cancer, nonhemiplegic migraines, and hypothyroidism presented to the ED with complaints of aphasia and right-sided paralysis, with onset 2 hours prior. Regarding the patient’s medication history, she had been taking lisinopril for hypertension.
Upon assessment, the patient was awake and alert and her vital signs were normal and stable, but she was aphasic, unable to accurately phonate, and was not able to move her right arm or leg against gravity. Her sensation appeared intact, and she had mild facial asymmetry with inability to raise the right corner of her mouth; her tongue had midline protrusion.
An emergent computed tomography (CT) scan of the head demonstrated mild brain atrophy and minimal low attenuation within the cerebral hemispheric white matter—most noticeably within the subcortical region of the left frontal lobe, consistent with small vessel ischemia. There was no evidence of acute intracranial hemorrhage, midline shift, or focal mass effect, and no convincing CT evidence for acute large vessel, cortical-based infarction.
The patient was determined to be an appropriate candidate for tPA, and was consented in the usual fashion. Within 15 minutes of administration of intravenous (IV) tPA, her symptoms improved, the aphasia resolved, and she was able to lift her right arm and leg against gravity and verbally communicate. Approximately 30 minutes following the resolution of her neurological symptoms, however, the patient was noted to have bleeding around a tooth socket, which was controlled with gauze and pressure. She subsequently began to complain of swelling on her right inferior lip without acute airway compromise. Over the next 10 to 15 minutes, she began to develop tongue swelling and feelings of dyspnea without wheezing.
The patient’s airway was reassessed and was classified as a Mallampati class IV. Anesthesia services were consulted for an emergent, awake intubation for airway protection. She was medicated with midazolam IV, as well as atomized lidocaine and lidocaine gargle for local anesthesia. The patient was successfully intubated awake using a flexible fiber optic technique. She was admitted to the medical intensive care unit for further monitoring, where she was treated with IV methylprednisolone, famotidine, and diphenhydramine. She was extubated the following day, had a relatively uncomplicated hospital course, and was discharged on hospital day 5 with improvement in her speech and right-sided weakness.
Discussion
The risk of angioedema associated with tPA administration has been previously described, with an estimated rate of 1.3 to 5.1%.1-3 Studies have shown the risk of developing angioedema is significantly increased in the setting of concomitant use of an angiotensin converting enzyme inhibitor (ACE-I); CT studies have also shown evidence of frontal and insular ischemia, with an odds radio of 13.6 and 9.1, respectively.2 Our patient was on lisinopril and had early signs of ischemia in the frontal lobe on initial CT scan, which likely increased her risk for angioedema.
How tPA Can Trigger Angioedema
The development of angioedema after administration of tPA has a well-described biochemical basis. Angioedema has been linked to the local vasodilatory effects of bradykinin, mast cell degranulation, and histamine release from activation of the complement pathway.4 Tissue plasminogen activator may trigger both of these pathways. It is a serine protease that cleaves plasminogen to plasmin; the plasmin in turn cleaves fibrin, resulting in the desired thrombolytic effects.5 Plasmin can cause mast cell degranulation through conversion of C3 to C3a and through activation of the complement pathway through conversion of C1 to C1a.6
Studies have shown tPA to have low antigenicity, and activation of this pathway is most likely secondary to direct proteolytic effects as opposed to antibody complexes.7 In a study by Bennett et al,6 tPA was shown to significantly increase C3a, C4a, and C5a serum levels when given in the setting of myocardial infarction (MI). It has also been shown to activate and increase serum kallikrein, which cleaves high-molecular weight kininogen to bradykinin, a potent vasodilator.8,9
Since bradykinin is broken down by several enzymes, including ACE, degradation is therefore delayed in patients on ACE-I.10 The alternate pathway for bradykinin degradation in the absence of ACE may also result in formation of des-Arg bradykinin, another similar active metabolite that mimics the effects of bradykinins.9 The formation of bradykinin through the proteolytic effects of tPA, in combination with the delayed breakdown in patient’s taking an ACE-I, likely plays a significant role in the development of angioedema.
In addition to the direct proteolytic effect of tPA resulting in angioedema, the underlying ischemic insult may also predispose patients to angioedema. As was the case with our patient, angioedema preferentially affects the ipsilateral side of the patient’s deficit.2,11,12 Theories suggest this is due to the lack of autonomic compensatory responses in the setting of ischemic insult.2 Interestingly, the development of angioedema in relation to the use of recombinant-tPA (eg, alteplase) in the setting of MI has not been as well described and may be related to the effect of central nervous system insult.3
Treatment
Although hemorrhagic complications of tPA therapy for cerebrovascular accident are well known, the risk for angioedema as a complication is less recognized. In most cases, angioedema is transient, and very few patients require aggressive support.3,12 Treatments that have previously been described include antihistamines and steroids.1,11,13 Epinephrine has been reported in one case study as an adjunct treatment of tPA-induced angioedema; however, it was given in combination with steroids and antihistimines.14 Therefore, caution should be taken regarding the use of epinephrine in this setting as there may be a theoretical precipitation of intracranial hypertension or hemorrhage.2
Given the likely significant role of the bradykinin-mediated pathway in tPA-induced angioedema, the true efficacy of these agents is unknown. Our patient had significant labial and lingual involvement, and given the concern for impending airway compromise, fiber optic intubation was performed. The decision to intubate and the technique employed must be carefully considered as a failed airway and need for a surgical airway is a concerning prospect in the setting of fibrinolytics. Successful cricothyroidotomy without significant complications has been described in the setting of streptokinase-induced angioedema when given for MI.15
Conclusion
The use of tPA for the treatment of ischemic stroke has been increasing over the last decade.16,17 Given the high prevalence of ACE-I use in patients who are also at risk for ischemic stroke, physicians administering tPA must be aware of the risk of tPA-associated angioedema. Patients with a known history of angioedema or anaphylaxis to tPA should be counseled on these risks and should not be given this medication, but rather considered for potential endovascular or mechanical clot retrieval therapy if they meet inclusion criteria for its use.
The use of thrombolytic medications for the treatment of acute ischemic cerebral infarctions has dynamically altered stroke care. However, there are both major and minor side effects associated with its use—most notably major bleeding, which led to strict inclusion and exclusion criteria governing the administration of this medication class. One less recognized but potentially serious complication is angioedema secondary to tissue plasminogen activator (tPA). Our case emphasizes the importance of early recognition of this clinical syndrome as it relates to airway compromise and potential respiratory failure in patients who are treated with tPA.
Case
A 70-year-old woman with a history of diabetes and hypertension and a remote history of breast cancer, nonhemiplegic migraines, and hypothyroidism presented to the ED with complaints of aphasia and right-sided paralysis, with onset 2 hours prior. Regarding the patient’s medication history, she had been taking lisinopril for hypertension.
Upon assessment, the patient was awake and alert and her vital signs were normal and stable, but she was aphasic, unable to accurately phonate, and was not able to move her right arm or leg against gravity. Her sensation appeared intact, and she had mild facial asymmetry with inability to raise the right corner of her mouth; her tongue had midline protrusion.
An emergent computed tomography (CT) scan of the head demonstrated mild brain atrophy and minimal low attenuation within the cerebral hemispheric white matter—most noticeably within the subcortical region of the left frontal lobe, consistent with small vessel ischemia. There was no evidence of acute intracranial hemorrhage, midline shift, or focal mass effect, and no convincing CT evidence for acute large vessel, cortical-based infarction.
The patient was determined to be an appropriate candidate for tPA, and was consented in the usual fashion. Within 15 minutes of administration of intravenous (IV) tPA, her symptoms improved, the aphasia resolved, and she was able to lift her right arm and leg against gravity and verbally communicate. Approximately 30 minutes following the resolution of her neurological symptoms, however, the patient was noted to have bleeding around a tooth socket, which was controlled with gauze and pressure. She subsequently began to complain of swelling on her right inferior lip without acute airway compromise. Over the next 10 to 15 minutes, she began to develop tongue swelling and feelings of dyspnea without wheezing.
The patient’s airway was reassessed and was classified as a Mallampati class IV. Anesthesia services were consulted for an emergent, awake intubation for airway protection. She was medicated with midazolam IV, as well as atomized lidocaine and lidocaine gargle for local anesthesia. The patient was successfully intubated awake using a flexible fiber optic technique. She was admitted to the medical intensive care unit for further monitoring, where she was treated with IV methylprednisolone, famotidine, and diphenhydramine. She was extubated the following day, had a relatively uncomplicated hospital course, and was discharged on hospital day 5 with improvement in her speech and right-sided weakness.
Discussion
The risk of angioedema associated with tPA administration has been previously described, with an estimated rate of 1.3 to 5.1%.1-3 Studies have shown the risk of developing angioedema is significantly increased in the setting of concomitant use of an angiotensin converting enzyme inhibitor (ACE-I); CT studies have also shown evidence of frontal and insular ischemia, with an odds radio of 13.6 and 9.1, respectively.2 Our patient was on lisinopril and had early signs of ischemia in the frontal lobe on initial CT scan, which likely increased her risk for angioedema.
How tPA Can Trigger Angioedema
The development of angioedema after administration of tPA has a well-described biochemical basis. Angioedema has been linked to the local vasodilatory effects of bradykinin, mast cell degranulation, and histamine release from activation of the complement pathway.4 Tissue plasminogen activator may trigger both of these pathways. It is a serine protease that cleaves plasminogen to plasmin; the plasmin in turn cleaves fibrin, resulting in the desired thrombolytic effects.5 Plasmin can cause mast cell degranulation through conversion of C3 to C3a and through activation of the complement pathway through conversion of C1 to C1a.6
Studies have shown tPA to have low antigenicity, and activation of this pathway is most likely secondary to direct proteolytic effects as opposed to antibody complexes.7 In a study by Bennett et al,6 tPA was shown to significantly increase C3a, C4a, and C5a serum levels when given in the setting of myocardial infarction (MI). It has also been shown to activate and increase serum kallikrein, which cleaves high-molecular weight kininogen to bradykinin, a potent vasodilator.8,9
Since bradykinin is broken down by several enzymes, including ACE, degradation is therefore delayed in patients on ACE-I.10 The alternate pathway for bradykinin degradation in the absence of ACE may also result in formation of des-Arg bradykinin, another similar active metabolite that mimics the effects of bradykinins.9 The formation of bradykinin through the proteolytic effects of tPA, in combination with the delayed breakdown in patient’s taking an ACE-I, likely plays a significant role in the development of angioedema.
In addition to the direct proteolytic effect of tPA resulting in angioedema, the underlying ischemic insult may also predispose patients to angioedema. As was the case with our patient, angioedema preferentially affects the ipsilateral side of the patient’s deficit.2,11,12 Theories suggest this is due to the lack of autonomic compensatory responses in the setting of ischemic insult.2 Interestingly, the development of angioedema in relation to the use of recombinant-tPA (eg, alteplase) in the setting of MI has not been as well described and may be related to the effect of central nervous system insult.3
Treatment
Although hemorrhagic complications of tPA therapy for cerebrovascular accident are well known, the risk for angioedema as a complication is less recognized. In most cases, angioedema is transient, and very few patients require aggressive support.3,12 Treatments that have previously been described include antihistamines and steroids.1,11,13 Epinephrine has been reported in one case study as an adjunct treatment of tPA-induced angioedema; however, it was given in combination with steroids and antihistimines.14 Therefore, caution should be taken regarding the use of epinephrine in this setting as there may be a theoretical precipitation of intracranial hypertension or hemorrhage.2
Given the likely significant role of the bradykinin-mediated pathway in tPA-induced angioedema, the true efficacy of these agents is unknown. Our patient had significant labial and lingual involvement, and given the concern for impending airway compromise, fiber optic intubation was performed. The decision to intubate and the technique employed must be carefully considered as a failed airway and need for a surgical airway is a concerning prospect in the setting of fibrinolytics. Successful cricothyroidotomy without significant complications has been described in the setting of streptokinase-induced angioedema when given for MI.15
Conclusion
The use of tPA for the treatment of ischemic stroke has been increasing over the last decade.16,17 Given the high prevalence of ACE-I use in patients who are also at risk for ischemic stroke, physicians administering tPA must be aware of the risk of tPA-associated angioedema. Patients with a known history of angioedema or anaphylaxis to tPA should be counseled on these risks and should not be given this medication, but rather considered for potential endovascular or mechanical clot retrieval therapy if they meet inclusion criteria for its use.
1. Hill MD, Barber PA, Takahashi J, Demchuk AM, Feasby TE, Buchan AM. Anaphylactoid reactions and angioedema during alteplase treatment of acute ischemic stroke. CMAJ. 2000;162(9):1281-1284.
2. Hill MD, Lye T, Moss H, et al. Hemi-orolingual angioedema and ACE inhibition after alteplase treatment of stroke. Neurology. 2003;60(9):1525-1527.
3. Hill MD, Buchan AM; Canadian Alteplase for Stroke Effectiveness Study (CASES) Investigators. Thrombolysis for acute ischemic stroke: results of the Canadian Alteplase for Stroke Effectiveness Study. CMAJ. 2005;172(10):1307-1312.
4. Lewis LM. Angioedema: etiology, pathophysiology, current and emerging therapies. J Emerg Med. 2013;45(5):789-796.
5. Loscalzo J, Braunwald E. Tissue plasminogen activator. N Engl J Med. 1988;319(14):935-931.
6. Bennett WR, Yawn DH, Migliore PJ, et al. Activation of the complement system by recombinant tissue plasminogen activator. J Am Coll Cardiol. 1987;10(3):627-632.
7. Reed BR, Chen AB, Tanswell P, et al. Low incidence of antibodies to recombinant human tissue-type plasminogen activator in treated patients. Thromb Haemost. 1990;64(2):276-280.
8. Hoffmeister HM, Szabo S, Kastner C, et al. Thrombolytic therapy in acute myocardial infarction: comparison of procoagulant effects of streptokinase and alteplase regimens with focus on the kallikrein system and plasmin. Circulation. 1998;98(23):2527-2533.
9. Molinaro G, Gervais N, Adam A. Biochemical basis of angioedema associated with recombinant tissue plasminogen activator treatment: an in vitro experimental approach. Stroke. 2002;33(6):1712-1716.
10. Bezalel S, Mahlab-Guri K, Asher I, Werner B, Sthoeger ZM. Angiotensin-converting enzyme inhibitor-induced angioedema. Am J Med. 2015;128(2):120-125.
11. Pancioli A, Brott T, Donaldson V, Miller R. Asymmetric angioneurotic edema associated with thrombolysis for acute stroke. Ann Emerg Med. 1997;30(2):227-229.
12. Correia AS, Matias G, Calado S, Lourenço A, Viana-Baptista M. Orolingual angiodema associated with alteplase treatment of acute stroke: a reappraisal. J Stroke Cerebrovasc Dis. 2015;24(1):31-40.
13. Maertins M, Wol R, Swider M. Angioedema after administration of tPA for ischemic stroke: case report. Air Med J. 2011;30(5):276-278.
14. Fugate JE, Kalimullah EA, Wijdicks EF. Angioedema after tPA: what neurointensivists should know. Neurocrit Care. 2012;16(3):440-443.
15. Walls RM, Pollack CV Jr. Successful cricothyrotomy after thrombolytic therapy for acute myocardial infarction: a report of two cases. Ann Emerg Med. 2000;35(2):188-191.
16. Lichtman JH, Watanabe E, Allen NB, Jones SB, Dostal J, Goldstein LB. Hospital arrival time and intravenous t-PA use in US Academic Medical Centers, 2001-2004. Stroke. 2009;40(12):3845-3850.
17. Schwamm LH, Ali SF, Reeves MJ, et al. Temporal trends in patient characteristics and treatment with intravenous thrombolysis among acute ischemic stroke patients at Get With the Guidelines-Stroke hospitals. Circ Cardiovasc Qual Outcomes. 2013;6(5):543-549.
1. Hill MD, Barber PA, Takahashi J, Demchuk AM, Feasby TE, Buchan AM. Anaphylactoid reactions and angioedema during alteplase treatment of acute ischemic stroke. CMAJ. 2000;162(9):1281-1284.
2. Hill MD, Lye T, Moss H, et al. Hemi-orolingual angioedema and ACE inhibition after alteplase treatment of stroke. Neurology. 2003;60(9):1525-1527.
3. Hill MD, Buchan AM; Canadian Alteplase for Stroke Effectiveness Study (CASES) Investigators. Thrombolysis for acute ischemic stroke: results of the Canadian Alteplase for Stroke Effectiveness Study. CMAJ. 2005;172(10):1307-1312.
4. Lewis LM. Angioedema: etiology, pathophysiology, current and emerging therapies. J Emerg Med. 2013;45(5):789-796.
5. Loscalzo J, Braunwald E. Tissue plasminogen activator. N Engl J Med. 1988;319(14):935-931.
6. Bennett WR, Yawn DH, Migliore PJ, et al. Activation of the complement system by recombinant tissue plasminogen activator. J Am Coll Cardiol. 1987;10(3):627-632.
7. Reed BR, Chen AB, Tanswell P, et al. Low incidence of antibodies to recombinant human tissue-type plasminogen activator in treated patients. Thromb Haemost. 1990;64(2):276-280.
8. Hoffmeister HM, Szabo S, Kastner C, et al. Thrombolytic therapy in acute myocardial infarction: comparison of procoagulant effects of streptokinase and alteplase regimens with focus on the kallikrein system and plasmin. Circulation. 1998;98(23):2527-2533.
9. Molinaro G, Gervais N, Adam A. Biochemical basis of angioedema associated with recombinant tissue plasminogen activator treatment: an in vitro experimental approach. Stroke. 2002;33(6):1712-1716.
10. Bezalel S, Mahlab-Guri K, Asher I, Werner B, Sthoeger ZM. Angiotensin-converting enzyme inhibitor-induced angioedema. Am J Med. 2015;128(2):120-125.
11. Pancioli A, Brott T, Donaldson V, Miller R. Asymmetric angioneurotic edema associated with thrombolysis for acute stroke. Ann Emerg Med. 1997;30(2):227-229.
12. Correia AS, Matias G, Calado S, Lourenço A, Viana-Baptista M. Orolingual angiodema associated with alteplase treatment of acute stroke: a reappraisal. J Stroke Cerebrovasc Dis. 2015;24(1):31-40.
13. Maertins M, Wol R, Swider M. Angioedema after administration of tPA for ischemic stroke: case report. Air Med J. 2011;30(5):276-278.
14. Fugate JE, Kalimullah EA, Wijdicks EF. Angioedema after tPA: what neurointensivists should know. Neurocrit Care. 2012;16(3):440-443.
15. Walls RM, Pollack CV Jr. Successful cricothyrotomy after thrombolytic therapy for acute myocardial infarction: a report of two cases. Ann Emerg Med. 2000;35(2):188-191.
16. Lichtman JH, Watanabe E, Allen NB, Jones SB, Dostal J, Goldstein LB. Hospital arrival time and intravenous t-PA use in US Academic Medical Centers, 2001-2004. Stroke. 2009;40(12):3845-3850.
17. Schwamm LH, Ali SF, Reeves MJ, et al. Temporal trends in patient characteristics and treatment with intravenous thrombolysis among acute ischemic stroke patients at Get With the Guidelines-Stroke hospitals. Circ Cardiovasc Qual Outcomes. 2013;6(5):543-549.
An unconventional approach to chest wall pain
THE CASE
A 45-year-old airman presented to our medical group with acute onset of sharp, positional left lateral chest wall pain that he’d had for 2 days. The pain began after an extreme core body workout. Treatment with ibuprofen 800 mg and local electrical stimulation one day prior provided no benefit. The patient reported the pain to be a 6 out of 10 when still and a 9 to 10 when sitting for more than a few minutes, turning, or taking a medium to deep breath. The patient felt “dangerously distracted by the pain” while driving in for his appointment.
We noted focal left lower lateral intercostal muscle tenderness without trigger point-like thickness or spasm. The patient also had restricted inspiration, secondary to the severe pain, and decreased left lower field breath sounds. His vital signs were normal, as was his cardiac exam.
THE DIAGNOSIS
While awaiting a chest x-ray, the patient was offered and opted to try acupuncture for pain relief. (We have medical acupuncturists on staff.) Analgesics had already been used, but had provided little relief.
We identified 4 acupuncture sites in the ear: 2 were battlefield acupuncture (BFA) points (more on this in a bit) and 2 points were deemed active by a skin conductance point finder (a handheld device that assesses changes in electrical skin resistance at auricular acupuncture points). The left ear points that were treated included the cingulate gyrus (intertragic notch), Shen Men (triangular fossa), and chest and abdomen regional points (antihelix) (FIGURE 1).
Within 15 minutes, the patient reported significant pain relief and was able to inspire deeply without pain. The patient also underwent a chest x-ray, which revealed atelectasis of the left lower lobe (FIGURE 2A) caused by pain-induced hypoventilation.
Because the patient’s pain was so well controlled, he returned to work immediately after the appointment. At the end of his shift 6 hours later he returned, unscheduled, to report pain at a level of one out of 10 and said he was able to breathe normally. In addition, lung auscultation was normal and a repeat chest x-ray revealed that the atelectasis had almost completely resolved (FIGURE 2B). This occurred without medication or other therapy. The pain did not return.
DISCUSSION
Although acupuncture is over 2000 years old, it has been largely disregarded in the United States due to a lack of mainstream evidence supporting its efficacy. Research is hindered by significant variation in approach between providers, the difficulties inherent to blinding patients and providers to treatment vs placebo, and poor insurance coverage and reimbursement.
Acupuncture research is burgeoning. A 2012 meta-analysis concluded that patients receiving acupuncture had less pain than those receiving sham or no acupuncture for several pain conditions. Specifically, scores for back and neck pain, osteoarthritis, and chronic headache were 0.23, 0.16, and 0.15 standard deviations (SDs), respectively, lower for patients receiving acupuncture than for those who got sham acupuncture. The effect sizes for acupuncture patients compared to no acupuncture controls were 0.55, 0.57, and 0.42 respectively (all P<.001).1
Several theories explain how auricular acupuncture may work. Paul Nogier, MD, noted that the ear is composed of ectodermal, mesodermal, and endodermal tissues, and mapped the “inverted fetus” homunculus in the ear, which corresponds to specific body points.2 Functional magnetic resonance imaging has demonstrated increased brain activity in the cingulate gyrus and thalamic regions in response to a painful stimulus, as well as attenuation of this activity after the placement of needles in corresponding auricular cingulate gyrus and thalamus points.3 In addition, research has confirmed that acupuncture raises serum and cerebrospinal levels of endorphins and enkephalins.4
Battlefield acupuncture (BFA) was developed by Richard Niemtzow, MD, and has been used for acute injuries in the front lines of battle as well as for many health conditions. BFA treats pain using a sequence of 5 predetermined auricular acupuncture points.5 Onset and duration of pain relief vary depending on the location and nature of the pathology. We’ve noted that BFA for chronic pain has a shorter duration of benefit and is more likely to need to be repeated.
One randomized pilot study involving 87 patients presenting to the emergency room blinded emergency health care providers to the inclusion of the first 2 BFA points in their otherwise usual care of acute pain patients. Participants in the acupuncture group experienced a 23% reduction in pain before discharge compared to no change in the standard care group (P<.0005).6
Our patient. We inserted semi-permanent needles with a needle length of 2 mm into 4 locations on the ear. (These needles can remain in the ear for several days and fall out on their own or they may be removed by pulling the stud ends.) As noted earlier, our patient reported pain relief within 15 minutes and was pain free by the next day.
THE TAKEAWAY
Auricular acupuncture can treat acute and chronic pain. As proof, the BFA technique is widely used by health care providers throughout the US military and Department of Veterans Affairs. In this case, the immediate pain relief and x-ray documentation of atelectasis resolution within 6 hours of treatment provide support that auricular acupuncture was beneficial in reversing the cause of this atelectasis, which was pain-induced hypoventilation.
While the acute pain control observed with this patient is not unusual in our experience, what is unusual is the rare visual confirmation of the striking degree of pain reduction possible with auricular acupuncture.
1. Vickers AJ, Cronin AM, Maschino AC, et al. Acupuncture Trialists’ Collaboration. Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med. 2012;172:1444-1453.
2. Oleson T. Auriculotherapy Manual: Chinese and Western Systems of Ear Acupuncture. 4th ed. Los Angeles: Churchill Livingstone; 2014.
3. Sjölund B, Eriksson M. Electro-acupunture and endogenous morphines. Lancet. 1976;2:1085.
4. Cho ZH, Chung SC, Jones JP, et al. New findings of the correlation between acupoints and corresponding brain cortices using functional MRI. Proc Natl Acad Sci U S A. 1998;95:2670-2673.
5. Niemtzow RC. Battlefield acupuncture: Update. Medical Acupuncture. 2007;19:225-228.
6.Goertz CM, Niemtzow R, Burns SM, et al. Auricular acupuncture in the treatment of acute pain syndromes: A pilot study. Mil Med. 2006;171:1010-1014.
THE CASE
A 45-year-old airman presented to our medical group with acute onset of sharp, positional left lateral chest wall pain that he’d had for 2 days. The pain began after an extreme core body workout. Treatment with ibuprofen 800 mg and local electrical stimulation one day prior provided no benefit. The patient reported the pain to be a 6 out of 10 when still and a 9 to 10 when sitting for more than a few minutes, turning, or taking a medium to deep breath. The patient felt “dangerously distracted by the pain” while driving in for his appointment.
We noted focal left lower lateral intercostal muscle tenderness without trigger point-like thickness or spasm. The patient also had restricted inspiration, secondary to the severe pain, and decreased left lower field breath sounds. His vital signs were normal, as was his cardiac exam.
THE DIAGNOSIS
While awaiting a chest x-ray, the patient was offered and opted to try acupuncture for pain relief. (We have medical acupuncturists on staff.) Analgesics had already been used, but had provided little relief.
We identified 4 acupuncture sites in the ear: 2 were battlefield acupuncture (BFA) points (more on this in a bit) and 2 points were deemed active by a skin conductance point finder (a handheld device that assesses changes in electrical skin resistance at auricular acupuncture points). The left ear points that were treated included the cingulate gyrus (intertragic notch), Shen Men (triangular fossa), and chest and abdomen regional points (antihelix) (FIGURE 1).
Within 15 minutes, the patient reported significant pain relief and was able to inspire deeply without pain. The patient also underwent a chest x-ray, which revealed atelectasis of the left lower lobe (FIGURE 2A) caused by pain-induced hypoventilation.
Because the patient’s pain was so well controlled, he returned to work immediately after the appointment. At the end of his shift 6 hours later he returned, unscheduled, to report pain at a level of one out of 10 and said he was able to breathe normally. In addition, lung auscultation was normal and a repeat chest x-ray revealed that the atelectasis had almost completely resolved (FIGURE 2B). This occurred without medication or other therapy. The pain did not return.
DISCUSSION
Although acupuncture is over 2000 years old, it has been largely disregarded in the United States due to a lack of mainstream evidence supporting its efficacy. Research is hindered by significant variation in approach between providers, the difficulties inherent to blinding patients and providers to treatment vs placebo, and poor insurance coverage and reimbursement.
Acupuncture research is burgeoning. A 2012 meta-analysis concluded that patients receiving acupuncture had less pain than those receiving sham or no acupuncture for several pain conditions. Specifically, scores for back and neck pain, osteoarthritis, and chronic headache were 0.23, 0.16, and 0.15 standard deviations (SDs), respectively, lower for patients receiving acupuncture than for those who got sham acupuncture. The effect sizes for acupuncture patients compared to no acupuncture controls were 0.55, 0.57, and 0.42 respectively (all P<.001).1
Several theories explain how auricular acupuncture may work. Paul Nogier, MD, noted that the ear is composed of ectodermal, mesodermal, and endodermal tissues, and mapped the “inverted fetus” homunculus in the ear, which corresponds to specific body points.2 Functional magnetic resonance imaging has demonstrated increased brain activity in the cingulate gyrus and thalamic regions in response to a painful stimulus, as well as attenuation of this activity after the placement of needles in corresponding auricular cingulate gyrus and thalamus points.3 In addition, research has confirmed that acupuncture raises serum and cerebrospinal levels of endorphins and enkephalins.4
Battlefield acupuncture (BFA) was developed by Richard Niemtzow, MD, and has been used for acute injuries in the front lines of battle as well as for many health conditions. BFA treats pain using a sequence of 5 predetermined auricular acupuncture points.5 Onset and duration of pain relief vary depending on the location and nature of the pathology. We’ve noted that BFA for chronic pain has a shorter duration of benefit and is more likely to need to be repeated.
One randomized pilot study involving 87 patients presenting to the emergency room blinded emergency health care providers to the inclusion of the first 2 BFA points in their otherwise usual care of acute pain patients. Participants in the acupuncture group experienced a 23% reduction in pain before discharge compared to no change in the standard care group (P<.0005).6
Our patient. We inserted semi-permanent needles with a needle length of 2 mm into 4 locations on the ear. (These needles can remain in the ear for several days and fall out on their own or they may be removed by pulling the stud ends.) As noted earlier, our patient reported pain relief within 15 minutes and was pain free by the next day.
THE TAKEAWAY
Auricular acupuncture can treat acute and chronic pain. As proof, the BFA technique is widely used by health care providers throughout the US military and Department of Veterans Affairs. In this case, the immediate pain relief and x-ray documentation of atelectasis resolution within 6 hours of treatment provide support that auricular acupuncture was beneficial in reversing the cause of this atelectasis, which was pain-induced hypoventilation.
While the acute pain control observed with this patient is not unusual in our experience, what is unusual is the rare visual confirmation of the striking degree of pain reduction possible with auricular acupuncture.
THE CASE
A 45-year-old airman presented to our medical group with acute onset of sharp, positional left lateral chest wall pain that he’d had for 2 days. The pain began after an extreme core body workout. Treatment with ibuprofen 800 mg and local electrical stimulation one day prior provided no benefit. The patient reported the pain to be a 6 out of 10 when still and a 9 to 10 when sitting for more than a few minutes, turning, or taking a medium to deep breath. The patient felt “dangerously distracted by the pain” while driving in for his appointment.
We noted focal left lower lateral intercostal muscle tenderness without trigger point-like thickness or spasm. The patient also had restricted inspiration, secondary to the severe pain, and decreased left lower field breath sounds. His vital signs were normal, as was his cardiac exam.
THE DIAGNOSIS
While awaiting a chest x-ray, the patient was offered and opted to try acupuncture for pain relief. (We have medical acupuncturists on staff.) Analgesics had already been used, but had provided little relief.
We identified 4 acupuncture sites in the ear: 2 were battlefield acupuncture (BFA) points (more on this in a bit) and 2 points were deemed active by a skin conductance point finder (a handheld device that assesses changes in electrical skin resistance at auricular acupuncture points). The left ear points that were treated included the cingulate gyrus (intertragic notch), Shen Men (triangular fossa), and chest and abdomen regional points (antihelix) (FIGURE 1).
Within 15 minutes, the patient reported significant pain relief and was able to inspire deeply without pain. The patient also underwent a chest x-ray, which revealed atelectasis of the left lower lobe (FIGURE 2A) caused by pain-induced hypoventilation.
Because the patient’s pain was so well controlled, he returned to work immediately after the appointment. At the end of his shift 6 hours later he returned, unscheduled, to report pain at a level of one out of 10 and said he was able to breathe normally. In addition, lung auscultation was normal and a repeat chest x-ray revealed that the atelectasis had almost completely resolved (FIGURE 2B). This occurred without medication or other therapy. The pain did not return.
DISCUSSION
Although acupuncture is over 2000 years old, it has been largely disregarded in the United States due to a lack of mainstream evidence supporting its efficacy. Research is hindered by significant variation in approach between providers, the difficulties inherent to blinding patients and providers to treatment vs placebo, and poor insurance coverage and reimbursement.
Acupuncture research is burgeoning. A 2012 meta-analysis concluded that patients receiving acupuncture had less pain than those receiving sham or no acupuncture for several pain conditions. Specifically, scores for back and neck pain, osteoarthritis, and chronic headache were 0.23, 0.16, and 0.15 standard deviations (SDs), respectively, lower for patients receiving acupuncture than for those who got sham acupuncture. The effect sizes for acupuncture patients compared to no acupuncture controls were 0.55, 0.57, and 0.42 respectively (all P<.001).1
Several theories explain how auricular acupuncture may work. Paul Nogier, MD, noted that the ear is composed of ectodermal, mesodermal, and endodermal tissues, and mapped the “inverted fetus” homunculus in the ear, which corresponds to specific body points.2 Functional magnetic resonance imaging has demonstrated increased brain activity in the cingulate gyrus and thalamic regions in response to a painful stimulus, as well as attenuation of this activity after the placement of needles in corresponding auricular cingulate gyrus and thalamus points.3 In addition, research has confirmed that acupuncture raises serum and cerebrospinal levels of endorphins and enkephalins.4
Battlefield acupuncture (BFA) was developed by Richard Niemtzow, MD, and has been used for acute injuries in the front lines of battle as well as for many health conditions. BFA treats pain using a sequence of 5 predetermined auricular acupuncture points.5 Onset and duration of pain relief vary depending on the location and nature of the pathology. We’ve noted that BFA for chronic pain has a shorter duration of benefit and is more likely to need to be repeated.
One randomized pilot study involving 87 patients presenting to the emergency room blinded emergency health care providers to the inclusion of the first 2 BFA points in their otherwise usual care of acute pain patients. Participants in the acupuncture group experienced a 23% reduction in pain before discharge compared to no change in the standard care group (P<.0005).6
Our patient. We inserted semi-permanent needles with a needle length of 2 mm into 4 locations on the ear. (These needles can remain in the ear for several days and fall out on their own or they may be removed by pulling the stud ends.) As noted earlier, our patient reported pain relief within 15 minutes and was pain free by the next day.
THE TAKEAWAY
Auricular acupuncture can treat acute and chronic pain. As proof, the BFA technique is widely used by health care providers throughout the US military and Department of Veterans Affairs. In this case, the immediate pain relief and x-ray documentation of atelectasis resolution within 6 hours of treatment provide support that auricular acupuncture was beneficial in reversing the cause of this atelectasis, which was pain-induced hypoventilation.
While the acute pain control observed with this patient is not unusual in our experience, what is unusual is the rare visual confirmation of the striking degree of pain reduction possible with auricular acupuncture.
1. Vickers AJ, Cronin AM, Maschino AC, et al. Acupuncture Trialists’ Collaboration. Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med. 2012;172:1444-1453.
2. Oleson T. Auriculotherapy Manual: Chinese and Western Systems of Ear Acupuncture. 4th ed. Los Angeles: Churchill Livingstone; 2014.
3. Sjölund B, Eriksson M. Electro-acupunture and endogenous morphines. Lancet. 1976;2:1085.
4. Cho ZH, Chung SC, Jones JP, et al. New findings of the correlation between acupoints and corresponding brain cortices using functional MRI. Proc Natl Acad Sci U S A. 1998;95:2670-2673.
5. Niemtzow RC. Battlefield acupuncture: Update. Medical Acupuncture. 2007;19:225-228.
6.Goertz CM, Niemtzow R, Burns SM, et al. Auricular acupuncture in the treatment of acute pain syndromes: A pilot study. Mil Med. 2006;171:1010-1014.
1. Vickers AJ, Cronin AM, Maschino AC, et al. Acupuncture Trialists’ Collaboration. Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med. 2012;172:1444-1453.
2. Oleson T. Auriculotherapy Manual: Chinese and Western Systems of Ear Acupuncture. 4th ed. Los Angeles: Churchill Livingstone; 2014.
3. Sjölund B, Eriksson M. Electro-acupunture and endogenous morphines. Lancet. 1976;2:1085.
4. Cho ZH, Chung SC, Jones JP, et al. New findings of the correlation between acupoints and corresponding brain cortices using functional MRI. Proc Natl Acad Sci U S A. 1998;95:2670-2673.
5. Niemtzow RC. Battlefield acupuncture: Update. Medical Acupuncture. 2007;19:225-228.
6.Goertz CM, Niemtzow R, Burns SM, et al. Auricular acupuncture in the treatment of acute pain syndromes: A pilot study. Mil Med. 2006;171:1010-1014.
Uninjured athlete with edematous arm • Dx?
THE CASE
A 16-year-old boy presented to the emergency room (ER) with pain, redness, and swelling of his right upper arm that had been bothering him for 2 days. He was the quarterback of his high school football team, a sport that he’d been playing since he was 8 years old. He indicated that his football training—which involved repetitive throwing with his right arm—had intensified over the previous 2 months.
Prior to the ER visit, the patient was healthy and active with no significant medical history. He’d had no shoulder trauma and there was no family history of any coagulopathies, venous thrombosis, or pulmonary embolism. He denied chest pain, shortness of breath, palpitations, and fever, and said that he did not smoke cigarettes or drink alcohol.
On physical examination, his blood pressure was 118/70 mm Hg and his heart rate was 74 beats per minute. He had nonpitting edema and erythema of his right upper arm. His radial and brachial pulses were strong and equal in both arms. Assessment of neurologic and vascular integrity produced positive Wright’s and Adson’s tests, but a negative Halstead’s test. (For more on these tests, see: Wright’s test, Adson’s test, and Halstead’s test.) The circumference of the patient’s right upper arm was 2.5 cm greater than the left upper arm. The remainder of the physical exam was normal.
THE DIAGNOSIS
A duplex ultrasound of the right upper arm revealed an acute occlusive thrombus in the axillary vein. We started the patient on intravenous heparin. A venogram confirmed thrombosis of the axillary-subclavian vein (FIGURE 1A). Based on the patient’s clinical presentation and the results of the venogram, we diagnosed Paget-Schroetter syndrome. The venogram was followed by thrombolysis with alteplase (FIGURE 1B) and a balloon angioplasty (FIGURE 1C). One week later, a repeat venogram demonstrated partial removal of the thrombus and an area of compression on the inferior aspect of the subclavian vein due to a cervical band (FIGURE 1D).
DISCUSSION
Paget-Schroetter syndrome (PSS), or effort thrombosis of the upper extremities, is defined as spontaneous thrombus in the axillary and subclavian veins that occurs as a consequence of strenuous upper-extremity activity. It is a rare condition with an incidence of one to 2 cases per 100,000 people per year, and represents 1% to 4% of all cases of deep vein thrombosis (DVT).1
Spontaneous thrombosis of the upper extremities typically presents in young, otherwise healthy individuals. It has been described in athletes who are involved in ball games, games with rackets or clubs, aquatic sports, combatant sports, and in violin players.2 The repetitive movements used in these activities can lead to compression of the axillary and subclavian veins by hypertrophied muscles. Repetitive trauma causes intimal damage and thrombogenesis.3
PSS is characterized by the abrupt, spontaneous swelling of the entire arm, cyanosis, and pain that occurs with use or overhead positioning. Enlarged subcutaneous veins are present in the upper arm, around the shoulder, or in the upper anterior chest wall (Urschel’s sign). The classic presentation is acute onset of upper extremity pain and swelling in the dominant arm following a particularly strenuous activity.4 A low-grade fever, superficial thrombophlebitis, or neurologic symptoms may coexist. Certain provocative maneuvers can help reproduce the symptoms (TABLE 15,6). Complications of PSS include pulmonary embolism, postthrombotic syndrome (pain, heaviness, and swelling), and recurrent thrombosis.7
Contrast venography best shows the extent of thrombosis
Duplex ultrasound, with its high sensitivity and specificity, is the initial, noninvasive test of choice (TABLE 24,8-11). However, duplex ultrasound has a false-negative rate of 30% because it is highly technician-dependent and can be complicated by acoustic shadows from the clavicle or sternum.8
The most direct and definitive means to confirm the diagnosis of PSS is catheter-directed contrast venography.9 This method provides complete anatomic information regarding the site and extent of thrombosis, allows definitive evaluation of the collateral venous pathways, and is a necessary step toward the use of thrombolytic therapy. Contrast load, however, contraindicates the procedure in patients with renal failure and in those who are pregnant.
Contrast-enhanced computed tomography (CT) and magnetic resonance angiography (MRA) are also highly sensitive for detecting focal stenosis at the level of the first rib, the presence or absence of enlarged collateral veins, and the chronicity of any thrombus present. However, the usefulness of CT and magnetic resonance venography in initial screening is unclear, due to a lack of randomized controlled trials.
Treatment involves anticoagulants, thrombolytics, and possibly surgery
Prompt use of anticoagulation is indicated in PSS. Initial anticoagulation with low molecular weight unfractionated heparin or a direct thrombin inhibitor followed by warfarin for a minimum of 3 to 6 months is recommended.12
Patients treated with anticoagulation alone have a higher incidence of long-term residual symptoms, disability, and recurrent thrombosis.7 As a result, a more aggressive approach with the use of thrombolytic therapy is indicated, especially in young, active patients, to minimize long-term consequences. Alteplase or reteplase are used for this purpose. Thrombolysis is less likely to be beneficial if the thrombus is more than 2 weeks old or if there are inflammatory changes in the vein. The use of catheter-directed thrombolysis minimizes the risk of systemic adverse effects and achieves higher clot resolution rates.13
Because PSS is caused by compression of the vein, rather than a disorder of blood clotting, there is still a 50% to 70% risk of recurrent thrombosis despite thrombolysis and anticoagulation.14 Therefore, the most definitive management approach remains surgical treatment. Patients with recent thrombosis who are within the first several weeks of undergoing successful thrombolytic therapy are excellent candidates for surgery. Operative treatment for PSS includes first rib resection, scalene muscle removal, or subclavius muscle removal, along with removal of constricting scar tissue from around the vein.7
THE TAKEAWAY
PSS is characterized by upper-extremity DVT resulting from repetitive trauma to the subclavian-axillary vein. Early diagnosis of PSS with contrast venography and prompt use of anticoagulation can effectively restore venous patency, reduce the risk of rethrombosis, and return the patient to normal function. Primary care physicians should be aware of this condition, because delayed recognition in a high-functioning person can be potentially disabling.
Our patient had a first rib resection, partial division of the scalenus anterior and medius muscles, and lysis of the cervical band. Follow-up venography confirmed resolution of thrombosis without any complications. The patient was continued on anticoagulation with warfarin for 3 months.
1. Isma N, Svensson PJ, Gottsäter A, et al. Upper extremity deep venous thrombosis in the population-based Malmö thrombophilia study (MATS). Epidemiology, risk factors, recurrence risk, and mortality. Thromb Res. 2010;125:e335-e338.
2. DiFelice GS, Paletta GA Jr, Phillips BB, et al. Effort thrombosis in the elite throwing athlete. Am J Sports Med. 2002;30:708-712.
3. Thompson JF, Winterborn RJ, Bays S, et al. Venous thoracic outlet compression and the Paget-Schroetter syndrome: a review and recommendations for management. Cardiovasc Intervent Radiol. 2011;34:903-910.
4. Joffe HV, Kucher N, Tapson VF, et al; Deep vein thrombosis (DVT) FREE steering committee. Upper-extremity deep vein thrombosis: a prospective registry of 592 patients. Circulation. 2004;110:1605-1611.
5. Osterman AL, Lincoski C. Thoracic outlet syndrome. In: Skirven TM, Osterman AL, Fedorczyk JM, et al, eds. Rehabilitation of the Hand and Upper Extremity. 6th ed. Philadelphia, Pa: Mosby, Inc; 2011:723-732.
6. Laker S, Sullivan WJ, Whitehill TA. Thoracic outlet syndrome. In: Akuthota V, Herring SA, eds. Nerve and vascular injuries in sports medicine. New York, NY: Springer; 2009:117.
7. Urschel HC Jr, Patel AN. Surgery remains the most effective treatment for Paget-Schroetter syndrome: 50 years’ experience. Ann Thorac Surg. 2008;86:254-260; discussion 260.
8. Melby SJ, Vedantham S, Narra VR, et al. Comprehensive surgical management of the competitive athlete with effort thrombosis of the subclavian vein (Paget-Schroetter syndrome). J Vasc Surg. 2008;47:809-820; discussion 821.
9. Di Nisio M, Van Sluis GL, Bossuyt PM, et al. Accuracy of diagnostic tests for clinically suspected upper extremity deep vein thrombosis: a systematic review. J Thromb Haemost. 2010;8:684-692.
10. Thompson RW. Comprehensive management of subclavian vein effort thrombosis. Semin Intervent Radiol. 2012;29:44-51.
11. Desjardins B, Rybicki FJ, Kim HS, et al. ACR Appropriateness Criteria® Suspected upper extremity deep vein thrombosis. J Am Coll Radiol. 2012;9:613-619.
12. Savage KJ, Wells PS, Schulz V, et al. Outpatient use of low molecular weight heparin (Dalteparin) for the treatment of deep vein thrombosis of the upper extremity. Thromb Haemost. 1999;82:1008-1010.
13. Machleder HI. Evaluation of a new treatment strategy for Paget-Schroetter syndrome: spontaneous thrombosis of the axillary-subclavian vein. J Vasc Surg. 1993;17:305-315; discussion 316-317.
14. Thomas IH, Zierler BK. An integrative review of outcomes in patients with acute primary upper extremity deep venous thrombosis following no treatment or treatment with anticoagulation, thrombolysis, or surgical algorithms. Vasc Endovascular Surg. 2005;39:163-174.
THE CASE
A 16-year-old boy presented to the emergency room (ER) with pain, redness, and swelling of his right upper arm that had been bothering him for 2 days. He was the quarterback of his high school football team, a sport that he’d been playing since he was 8 years old. He indicated that his football training—which involved repetitive throwing with his right arm—had intensified over the previous 2 months.
Prior to the ER visit, the patient was healthy and active with no significant medical history. He’d had no shoulder trauma and there was no family history of any coagulopathies, venous thrombosis, or pulmonary embolism. He denied chest pain, shortness of breath, palpitations, and fever, and said that he did not smoke cigarettes or drink alcohol.
On physical examination, his blood pressure was 118/70 mm Hg and his heart rate was 74 beats per minute. He had nonpitting edema and erythema of his right upper arm. His radial and brachial pulses were strong and equal in both arms. Assessment of neurologic and vascular integrity produced positive Wright’s and Adson’s tests, but a negative Halstead’s test. (For more on these tests, see: Wright’s test, Adson’s test, and Halstead’s test.) The circumference of the patient’s right upper arm was 2.5 cm greater than the left upper arm. The remainder of the physical exam was normal.
THE DIAGNOSIS
A duplex ultrasound of the right upper arm revealed an acute occlusive thrombus in the axillary vein. We started the patient on intravenous heparin. A venogram confirmed thrombosis of the axillary-subclavian vein (FIGURE 1A). Based on the patient’s clinical presentation and the results of the venogram, we diagnosed Paget-Schroetter syndrome. The venogram was followed by thrombolysis with alteplase (FIGURE 1B) and a balloon angioplasty (FIGURE 1C). One week later, a repeat venogram demonstrated partial removal of the thrombus and an area of compression on the inferior aspect of the subclavian vein due to a cervical band (FIGURE 1D).
DISCUSSION
Paget-Schroetter syndrome (PSS), or effort thrombosis of the upper extremities, is defined as spontaneous thrombus in the axillary and subclavian veins that occurs as a consequence of strenuous upper-extremity activity. It is a rare condition with an incidence of one to 2 cases per 100,000 people per year, and represents 1% to 4% of all cases of deep vein thrombosis (DVT).1
Spontaneous thrombosis of the upper extremities typically presents in young, otherwise healthy individuals. It has been described in athletes who are involved in ball games, games with rackets or clubs, aquatic sports, combatant sports, and in violin players.2 The repetitive movements used in these activities can lead to compression of the axillary and subclavian veins by hypertrophied muscles. Repetitive trauma causes intimal damage and thrombogenesis.3
PSS is characterized by the abrupt, spontaneous swelling of the entire arm, cyanosis, and pain that occurs with use or overhead positioning. Enlarged subcutaneous veins are present in the upper arm, around the shoulder, or in the upper anterior chest wall (Urschel’s sign). The classic presentation is acute onset of upper extremity pain and swelling in the dominant arm following a particularly strenuous activity.4 A low-grade fever, superficial thrombophlebitis, or neurologic symptoms may coexist. Certain provocative maneuvers can help reproduce the symptoms (TABLE 15,6). Complications of PSS include pulmonary embolism, postthrombotic syndrome (pain, heaviness, and swelling), and recurrent thrombosis.7
Contrast venography best shows the extent of thrombosis
Duplex ultrasound, with its high sensitivity and specificity, is the initial, noninvasive test of choice (TABLE 24,8-11). However, duplex ultrasound has a false-negative rate of 30% because it is highly technician-dependent and can be complicated by acoustic shadows from the clavicle or sternum.8
The most direct and definitive means to confirm the diagnosis of PSS is catheter-directed contrast venography.9 This method provides complete anatomic information regarding the site and extent of thrombosis, allows definitive evaluation of the collateral venous pathways, and is a necessary step toward the use of thrombolytic therapy. Contrast load, however, contraindicates the procedure in patients with renal failure and in those who are pregnant.
Contrast-enhanced computed tomography (CT) and magnetic resonance angiography (MRA) are also highly sensitive for detecting focal stenosis at the level of the first rib, the presence or absence of enlarged collateral veins, and the chronicity of any thrombus present. However, the usefulness of CT and magnetic resonance venography in initial screening is unclear, due to a lack of randomized controlled trials.
Treatment involves anticoagulants, thrombolytics, and possibly surgery
Prompt use of anticoagulation is indicated in PSS. Initial anticoagulation with low molecular weight unfractionated heparin or a direct thrombin inhibitor followed by warfarin for a minimum of 3 to 6 months is recommended.12
Patients treated with anticoagulation alone have a higher incidence of long-term residual symptoms, disability, and recurrent thrombosis.7 As a result, a more aggressive approach with the use of thrombolytic therapy is indicated, especially in young, active patients, to minimize long-term consequences. Alteplase or reteplase are used for this purpose. Thrombolysis is less likely to be beneficial if the thrombus is more than 2 weeks old or if there are inflammatory changes in the vein. The use of catheter-directed thrombolysis minimizes the risk of systemic adverse effects and achieves higher clot resolution rates.13
Because PSS is caused by compression of the vein, rather than a disorder of blood clotting, there is still a 50% to 70% risk of recurrent thrombosis despite thrombolysis and anticoagulation.14 Therefore, the most definitive management approach remains surgical treatment. Patients with recent thrombosis who are within the first several weeks of undergoing successful thrombolytic therapy are excellent candidates for surgery. Operative treatment for PSS includes first rib resection, scalene muscle removal, or subclavius muscle removal, along with removal of constricting scar tissue from around the vein.7
THE TAKEAWAY
PSS is characterized by upper-extremity DVT resulting from repetitive trauma to the subclavian-axillary vein. Early diagnosis of PSS with contrast venography and prompt use of anticoagulation can effectively restore venous patency, reduce the risk of rethrombosis, and return the patient to normal function. Primary care physicians should be aware of this condition, because delayed recognition in a high-functioning person can be potentially disabling.
Our patient had a first rib resection, partial division of the scalenus anterior and medius muscles, and lysis of the cervical band. Follow-up venography confirmed resolution of thrombosis without any complications. The patient was continued on anticoagulation with warfarin for 3 months.
THE CASE
A 16-year-old boy presented to the emergency room (ER) with pain, redness, and swelling of his right upper arm that had been bothering him for 2 days. He was the quarterback of his high school football team, a sport that he’d been playing since he was 8 years old. He indicated that his football training—which involved repetitive throwing with his right arm—had intensified over the previous 2 months.
Prior to the ER visit, the patient was healthy and active with no significant medical history. He’d had no shoulder trauma and there was no family history of any coagulopathies, venous thrombosis, or pulmonary embolism. He denied chest pain, shortness of breath, palpitations, and fever, and said that he did not smoke cigarettes or drink alcohol.
On physical examination, his blood pressure was 118/70 mm Hg and his heart rate was 74 beats per minute. He had nonpitting edema and erythema of his right upper arm. His radial and brachial pulses were strong and equal in both arms. Assessment of neurologic and vascular integrity produced positive Wright’s and Adson’s tests, but a negative Halstead’s test. (For more on these tests, see: Wright’s test, Adson’s test, and Halstead’s test.) The circumference of the patient’s right upper arm was 2.5 cm greater than the left upper arm. The remainder of the physical exam was normal.
THE DIAGNOSIS
A duplex ultrasound of the right upper arm revealed an acute occlusive thrombus in the axillary vein. We started the patient on intravenous heparin. A venogram confirmed thrombosis of the axillary-subclavian vein (FIGURE 1A). Based on the patient’s clinical presentation and the results of the venogram, we diagnosed Paget-Schroetter syndrome. The venogram was followed by thrombolysis with alteplase (FIGURE 1B) and a balloon angioplasty (FIGURE 1C). One week later, a repeat venogram demonstrated partial removal of the thrombus and an area of compression on the inferior aspect of the subclavian vein due to a cervical band (FIGURE 1D).
DISCUSSION
Paget-Schroetter syndrome (PSS), or effort thrombosis of the upper extremities, is defined as spontaneous thrombus in the axillary and subclavian veins that occurs as a consequence of strenuous upper-extremity activity. It is a rare condition with an incidence of one to 2 cases per 100,000 people per year, and represents 1% to 4% of all cases of deep vein thrombosis (DVT).1
Spontaneous thrombosis of the upper extremities typically presents in young, otherwise healthy individuals. It has been described in athletes who are involved in ball games, games with rackets or clubs, aquatic sports, combatant sports, and in violin players.2 The repetitive movements used in these activities can lead to compression of the axillary and subclavian veins by hypertrophied muscles. Repetitive trauma causes intimal damage and thrombogenesis.3
PSS is characterized by the abrupt, spontaneous swelling of the entire arm, cyanosis, and pain that occurs with use or overhead positioning. Enlarged subcutaneous veins are present in the upper arm, around the shoulder, or in the upper anterior chest wall (Urschel’s sign). The classic presentation is acute onset of upper extremity pain and swelling in the dominant arm following a particularly strenuous activity.4 A low-grade fever, superficial thrombophlebitis, or neurologic symptoms may coexist. Certain provocative maneuvers can help reproduce the symptoms (TABLE 15,6). Complications of PSS include pulmonary embolism, postthrombotic syndrome (pain, heaviness, and swelling), and recurrent thrombosis.7
Contrast venography best shows the extent of thrombosis
Duplex ultrasound, with its high sensitivity and specificity, is the initial, noninvasive test of choice (TABLE 24,8-11). However, duplex ultrasound has a false-negative rate of 30% because it is highly technician-dependent and can be complicated by acoustic shadows from the clavicle or sternum.8
The most direct and definitive means to confirm the diagnosis of PSS is catheter-directed contrast venography.9 This method provides complete anatomic information regarding the site and extent of thrombosis, allows definitive evaluation of the collateral venous pathways, and is a necessary step toward the use of thrombolytic therapy. Contrast load, however, contraindicates the procedure in patients with renal failure and in those who are pregnant.
Contrast-enhanced computed tomography (CT) and magnetic resonance angiography (MRA) are also highly sensitive for detecting focal stenosis at the level of the first rib, the presence or absence of enlarged collateral veins, and the chronicity of any thrombus present. However, the usefulness of CT and magnetic resonance venography in initial screening is unclear, due to a lack of randomized controlled trials.
Treatment involves anticoagulants, thrombolytics, and possibly surgery
Prompt use of anticoagulation is indicated in PSS. Initial anticoagulation with low molecular weight unfractionated heparin or a direct thrombin inhibitor followed by warfarin for a minimum of 3 to 6 months is recommended.12
Patients treated with anticoagulation alone have a higher incidence of long-term residual symptoms, disability, and recurrent thrombosis.7 As a result, a more aggressive approach with the use of thrombolytic therapy is indicated, especially in young, active patients, to minimize long-term consequences. Alteplase or reteplase are used for this purpose. Thrombolysis is less likely to be beneficial if the thrombus is more than 2 weeks old or if there are inflammatory changes in the vein. The use of catheter-directed thrombolysis minimizes the risk of systemic adverse effects and achieves higher clot resolution rates.13
Because PSS is caused by compression of the vein, rather than a disorder of blood clotting, there is still a 50% to 70% risk of recurrent thrombosis despite thrombolysis and anticoagulation.14 Therefore, the most definitive management approach remains surgical treatment. Patients with recent thrombosis who are within the first several weeks of undergoing successful thrombolytic therapy are excellent candidates for surgery. Operative treatment for PSS includes first rib resection, scalene muscle removal, or subclavius muscle removal, along with removal of constricting scar tissue from around the vein.7
THE TAKEAWAY
PSS is characterized by upper-extremity DVT resulting from repetitive trauma to the subclavian-axillary vein. Early diagnosis of PSS with contrast venography and prompt use of anticoagulation can effectively restore venous patency, reduce the risk of rethrombosis, and return the patient to normal function. Primary care physicians should be aware of this condition, because delayed recognition in a high-functioning person can be potentially disabling.
Our patient had a first rib resection, partial division of the scalenus anterior and medius muscles, and lysis of the cervical band. Follow-up venography confirmed resolution of thrombosis without any complications. The patient was continued on anticoagulation with warfarin for 3 months.
1. Isma N, Svensson PJ, Gottsäter A, et al. Upper extremity deep venous thrombosis in the population-based Malmö thrombophilia study (MATS). Epidemiology, risk factors, recurrence risk, and mortality. Thromb Res. 2010;125:e335-e338.
2. DiFelice GS, Paletta GA Jr, Phillips BB, et al. Effort thrombosis in the elite throwing athlete. Am J Sports Med. 2002;30:708-712.
3. Thompson JF, Winterborn RJ, Bays S, et al. Venous thoracic outlet compression and the Paget-Schroetter syndrome: a review and recommendations for management. Cardiovasc Intervent Radiol. 2011;34:903-910.
4. Joffe HV, Kucher N, Tapson VF, et al; Deep vein thrombosis (DVT) FREE steering committee. Upper-extremity deep vein thrombosis: a prospective registry of 592 patients. Circulation. 2004;110:1605-1611.
5. Osterman AL, Lincoski C. Thoracic outlet syndrome. In: Skirven TM, Osterman AL, Fedorczyk JM, et al, eds. Rehabilitation of the Hand and Upper Extremity. 6th ed. Philadelphia, Pa: Mosby, Inc; 2011:723-732.
6. Laker S, Sullivan WJ, Whitehill TA. Thoracic outlet syndrome. In: Akuthota V, Herring SA, eds. Nerve and vascular injuries in sports medicine. New York, NY: Springer; 2009:117.
7. Urschel HC Jr, Patel AN. Surgery remains the most effective treatment for Paget-Schroetter syndrome: 50 years’ experience. Ann Thorac Surg. 2008;86:254-260; discussion 260.
8. Melby SJ, Vedantham S, Narra VR, et al. Comprehensive surgical management of the competitive athlete with effort thrombosis of the subclavian vein (Paget-Schroetter syndrome). J Vasc Surg. 2008;47:809-820; discussion 821.
9. Di Nisio M, Van Sluis GL, Bossuyt PM, et al. Accuracy of diagnostic tests for clinically suspected upper extremity deep vein thrombosis: a systematic review. J Thromb Haemost. 2010;8:684-692.
10. Thompson RW. Comprehensive management of subclavian vein effort thrombosis. Semin Intervent Radiol. 2012;29:44-51.
11. Desjardins B, Rybicki FJ, Kim HS, et al. ACR Appropriateness Criteria® Suspected upper extremity deep vein thrombosis. J Am Coll Radiol. 2012;9:613-619.
12. Savage KJ, Wells PS, Schulz V, et al. Outpatient use of low molecular weight heparin (Dalteparin) for the treatment of deep vein thrombosis of the upper extremity. Thromb Haemost. 1999;82:1008-1010.
13. Machleder HI. Evaluation of a new treatment strategy for Paget-Schroetter syndrome: spontaneous thrombosis of the axillary-subclavian vein. J Vasc Surg. 1993;17:305-315; discussion 316-317.
14. Thomas IH, Zierler BK. An integrative review of outcomes in patients with acute primary upper extremity deep venous thrombosis following no treatment or treatment with anticoagulation, thrombolysis, or surgical algorithms. Vasc Endovascular Surg. 2005;39:163-174.
1. Isma N, Svensson PJ, Gottsäter A, et al. Upper extremity deep venous thrombosis in the population-based Malmö thrombophilia study (MATS). Epidemiology, risk factors, recurrence risk, and mortality. Thromb Res. 2010;125:e335-e338.
2. DiFelice GS, Paletta GA Jr, Phillips BB, et al. Effort thrombosis in the elite throwing athlete. Am J Sports Med. 2002;30:708-712.
3. Thompson JF, Winterborn RJ, Bays S, et al. Venous thoracic outlet compression and the Paget-Schroetter syndrome: a review and recommendations for management. Cardiovasc Intervent Radiol. 2011;34:903-910.
4. Joffe HV, Kucher N, Tapson VF, et al; Deep vein thrombosis (DVT) FREE steering committee. Upper-extremity deep vein thrombosis: a prospective registry of 592 patients. Circulation. 2004;110:1605-1611.
5. Osterman AL, Lincoski C. Thoracic outlet syndrome. In: Skirven TM, Osterman AL, Fedorczyk JM, et al, eds. Rehabilitation of the Hand and Upper Extremity. 6th ed. Philadelphia, Pa: Mosby, Inc; 2011:723-732.
6. Laker S, Sullivan WJ, Whitehill TA. Thoracic outlet syndrome. In: Akuthota V, Herring SA, eds. Nerve and vascular injuries in sports medicine. New York, NY: Springer; 2009:117.
7. Urschel HC Jr, Patel AN. Surgery remains the most effective treatment for Paget-Schroetter syndrome: 50 years’ experience. Ann Thorac Surg. 2008;86:254-260; discussion 260.
8. Melby SJ, Vedantham S, Narra VR, et al. Comprehensive surgical management of the competitive athlete with effort thrombosis of the subclavian vein (Paget-Schroetter syndrome). J Vasc Surg. 2008;47:809-820; discussion 821.
9. Di Nisio M, Van Sluis GL, Bossuyt PM, et al. Accuracy of diagnostic tests for clinically suspected upper extremity deep vein thrombosis: a systematic review. J Thromb Haemost. 2010;8:684-692.
10. Thompson RW. Comprehensive management of subclavian vein effort thrombosis. Semin Intervent Radiol. 2012;29:44-51.
11. Desjardins B, Rybicki FJ, Kim HS, et al. ACR Appropriateness Criteria® Suspected upper extremity deep vein thrombosis. J Am Coll Radiol. 2012;9:613-619.
12. Savage KJ, Wells PS, Schulz V, et al. Outpatient use of low molecular weight heparin (Dalteparin) for the treatment of deep vein thrombosis of the upper extremity. Thromb Haemost. 1999;82:1008-1010.
13. Machleder HI. Evaluation of a new treatment strategy for Paget-Schroetter syndrome: spontaneous thrombosis of the axillary-subclavian vein. J Vasc Surg. 1993;17:305-315; discussion 316-317.
14. Thomas IH, Zierler BK. An integrative review of outcomes in patients with acute primary upper extremity deep venous thrombosis following no treatment or treatment with anticoagulation, thrombolysis, or surgical algorithms. Vasc Endovascular Surg. 2005;39:163-174.
Acute promyelocytic leukemia presenting as a paraspinal mass
Acute promyelocytic leukemia (APL) is a distinct subtype of acute myeloid leukemia (AML) that is characterized by a balanced translocation between chromosomes 15 and 17 [t(15;17)], which results in the fusion of the promyelocytic leukemia (PML) and retinoic acid receptor α (RARA) genes.1,2 Historically, APL was a fatal disease because of the high relapse rates with cytotoxic chemotherapy alone and a significant bleeding risk secondary to disseminated intravascular coagulation (DIC).
Click on the PDF icon at the top of this introduction to read the full article.
Acute promyelocytic leukemia (APL) is a distinct subtype of acute myeloid leukemia (AML) that is characterized by a balanced translocation between chromosomes 15 and 17 [t(15;17)], which results in the fusion of the promyelocytic leukemia (PML) and retinoic acid receptor α (RARA) genes.1,2 Historically, APL was a fatal disease because of the high relapse rates with cytotoxic chemotherapy alone and a significant bleeding risk secondary to disseminated intravascular coagulation (DIC).
Click on the PDF icon at the top of this introduction to read the full article.
Acute promyelocytic leukemia (APL) is a distinct subtype of acute myeloid leukemia (AML) that is characterized by a balanced translocation between chromosomes 15 and 17 [t(15;17)], which results in the fusion of the promyelocytic leukemia (PML) and retinoic acid receptor α (RARA) genes.1,2 Historically, APL was a fatal disease because of the high relapse rates with cytotoxic chemotherapy alone and a significant bleeding risk secondary to disseminated intravascular coagulation (DIC).
Click on the PDF icon at the top of this introduction to read the full article.
An uncommon presentation of non-small-cell lung cancer with acrometastases to the great toe and index finger
Case presentation and summary
A 71-year-old white woman was referred to the emergency department by her primary care physician for necrosis and swelling of the left great toe for work-up of possible osteomyelitis (Figure 1). Before she presented to her physician, she had been complaining of severe pain, swelling, and erythema of the left great toe that had lasted for 1-2 months. Infection was initially suspected. She completed 2 courses of oral antibiotics with no improvement. She was also complaining of similar symptoms on the left index finger and attributed her symptoms to an injury a month earlier (Figure 2). The pain was so severe that she was not able to bear weight on her left foot. An outpatient X-ray of her left great toe raised her physician’s concerns that it might be osteomyelitis so she was referred to the emergency department.
Click on the PDF icon at the top of this introduction to read the full article.
Case presentation and summary
A 71-year-old white woman was referred to the emergency department by her primary care physician for necrosis and swelling of the left great toe for work-up of possible osteomyelitis (Figure 1). Before she presented to her physician, she had been complaining of severe pain, swelling, and erythema of the left great toe that had lasted for 1-2 months. Infection was initially suspected. She completed 2 courses of oral antibiotics with no improvement. She was also complaining of similar symptoms on the left index finger and attributed her symptoms to an injury a month earlier (Figure 2). The pain was so severe that she was not able to bear weight on her left foot. An outpatient X-ray of her left great toe raised her physician’s concerns that it might be osteomyelitis so she was referred to the emergency department.
Click on the PDF icon at the top of this introduction to read the full article.
Case presentation and summary
A 71-year-old white woman was referred to the emergency department by her primary care physician for necrosis and swelling of the left great toe for work-up of possible osteomyelitis (Figure 1). Before she presented to her physician, she had been complaining of severe pain, swelling, and erythema of the left great toe that had lasted for 1-2 months. Infection was initially suspected. She completed 2 courses of oral antibiotics with no improvement. She was also complaining of similar symptoms on the left index finger and attributed her symptoms to an injury a month earlier (Figure 2). The pain was so severe that she was not able to bear weight on her left foot. An outpatient X-ray of her left great toe raised her physician’s concerns that it might be osteomyelitis so she was referred to the emergency department.
Click on the PDF icon at the top of this introduction to read the full article.
Night of the Living Thrips: An Unusual Outbreak of Thysanoptera Dermatitis
Case Reports
A platoon of 24 US Marines participated in a 1-week outdoor training exercise (February 4–8) at the Marine Corps Training Area Bellows in Oahu, Hawaii. During the last 3 days of training, 15 (62.5%) marines presented to the same primary care provider with what appeared to be diffuse scattered lesions on the face, neck, and dorsal aspect of the hands. All 15 patients reported that they noticed the lesions upon waking up the morning after their second night at the training area. The patients were unable to recollect specific direct arthropod interactions, but they reported the presence of “bugs” in the training area and denied use of any insect repellents, insect nets, or sunscreen. Sleeping arrangements varied from covered vehicles and cots to sleeping bags on the ground, which were laundered independently by each marine and thereby were ruled out as a commonality. The patients denied working with any chemicals or cleansers while in the field. Further questioning of all 15 patients revealed a history of extended contact with live foliage as branches were broken off to build camouflaged sites.
The following week, a second platoon of 20 marines occupied a separate undisturbed portion of the same training area for a similar 1-week training evolution. Manifestation of similar symptoms among members of the second group, who had no contact with the initial 15 patients, supported the likely environmental etiology of the eruptions.
 |
| Figure 1. Numerous well-circumscribed, discrete, pink-red papules diffusely scattered across the face. |
 |
| Figure 2. Papules with classic anemic halos. |
Referral
Two patients from the first group were evaluated at the dermatology clinic at Tripler Army Medical Center (Honolulu, Hawaii) on day 10 of the initial outbreak. Cutaneous examination revealed numerous discrete, pink-red, well-circumscribed, 2- to 4-mm, dome-shaped papules exclusive to exposed areas on the face, neck, and dorsal aspect of the hands (Figures 1 and 2). Anemic halos surrounding the hand papules were noted (Figure 2). A punch biopsy in both patients revealed spongiotic dermatitis with superficial perivascular and interstitial lymphohistiocytic inflammation with eosinophils, suggestive of an arthropod bite (Figure 3). No retained arthropod parts wereidentified. Both patients were treated with triamcinolone ointment twice daily for 7 days with total resolution of the lesions.
Site Survey Results
Five days following the initial presentation of the first outbreak, a daytime site survey of the training area was conducted by a medical entomologist, an environmental health scientist, and a wildlife biologist. Records indicated that prior to the current utilization, the training area had not been used for 9 months. Approximately half of the training area was covered with mixed scrub vegetation and the remainder was clear pavement or sand (clear of vegetation). Feral hogs (Sus scrofa), cats (Felis domesticus), and mongooses (Herpestes javanicus) were observed at the site. Patient interviews and site survey ruled out a number of potential environmental irritants, including contact with fresh or salt water and chemical contaminants in the air or soil.
Because biting insects were suspected as the cause of the eruptions, an overnight entomological survey was conducted 3 weeks after the first outbreak under similar weather conditions and was centered in the area of an Australian pine (Casuarina equisetifolia) forest where most of the marines had slept during training. Mosquitoes (Aedes albopictus and Culex quinquefasciatus) were observed in the area, with an estimated biting rate of 1 to 2 bites per hour. Centipedes (Scolopendra subspinipes) were commonly observed after dark. There was no sign of heavy bird roosting or nesting, which would be a possible source of biting ectoparasites. Other than the Australian pine, notable vegetation present included Christmasberry (Schinus terebinthifolius), koa haole (Leucaena leucocephala), and Chinese banyan (Ficus microcarpa). A survey of the vegetation uncovered no notable insects, and no damage to the leaves of the Chinese banyans, which is typical of thrip infestation, was noted.
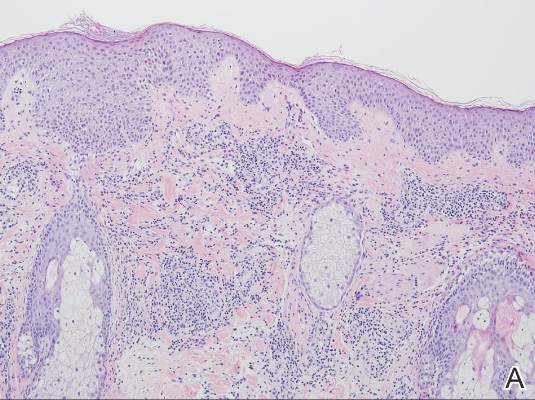 |  |
| Figure 3. Superficial and deep perivascular and interstitial dermatitis (A)(H&E, original magnification ×10) with lymphocytic predominance (B)(H&E, original magnification ×40). | |
After completion of a resource-intensive investigation that included site survey, literature review, detailed patient history including thrips-associated skin manifestations, and thorough consultation with local dermatologists and entomologists, the findings seemingly pointed to thrips as the most likely etiology of the eruption seen in our patients and a diagnosis of Thysanoptera dermatitis was made.
Comment
Thrips are small winged insects in the order Thysanoptera, which comprises more than 5000 identified species ranging in size from 0.5 to 15 mm, though most are approximately 1 mm.1 The insects typically are phytophagous (feeding on plants) and are attracted to humidity and seemingly the sweat of animals and humans.2 Although largely a phytophagous organism, a few published cases of thrips exposure reported papular skin eruptions known as Thysanoptera dermatitis.3-8 Several species of thrips across the globe have been associated with incidental attacks on humans to include “Heliothrips indicus Bagnall, a cotton pest of the Sudan; Thrips imagines Bagnall, reported in Australia; Limothrips cerealium (Haliday), in Germany; Gynaitkothrips uzeli Zimmerman, in Algeria; and other species.”7 In Hawaii, Gynaikothrips ficorum (Cuban laurel thrips) is a common pest of the Chinese banyan tree (F microcarpa) tree.9
A case series reported by Goldstein and Skipworth5 in the late 1960s of military personnel stationed in Oahu described exposure to similar environmental conditions with resultant lesions that were nearly identical to those seen in our patients. The final conclusion of the investigation was that Cuban laurel thrips were the likely etiology, though mites also were considered.5 In a subsequent commentary in 1968, Waisman10 reported similar eruptions in hospitalized patients with further comment regarding the nocturnal occurrence of the bites. Additionally, the eruptions were reported to be short lasting and devoid of discomfort, similar to our patient population.10
Following suit, Aeling6 published a case series in 1974 depicting several service members who presented with symptoms that were nearly identical to the symptoms experienced by our patients as well as those of Goldstein and Skipworth.5 The investigator coined the term hypoanesthetic halos in Hawaii to describe the findings and further reported that Hawaiian dermatologists were familiar with the symptoms and clinical presentation of the disease. Patients in this outbreak had observed small flying insects, similar to the reports from our patients, and postulated that the symptoms occurred secondary to insect bites.6
Since the report by Goldstein and Skipworth5 in 1968, the majority of the literature regarding Thysanoptera dermatitis has largely been in case reports. In 1987, Fishman7 reported the case of a 43-year-old woman who presented with a palm-sized area of grouped red puncta on the lateral neck with the subsequent entrapment and identification of a flower thrips from the patient’s clothing. In 2005, Leigheb et al2 reported the case of a 30-year-old man with an erythematous papular cutaneous eruption on the anterior chest. In this case, the causative etiology was unequivocally confirmed upon identification of the presence of thrips on biopsy.2 In 2006, Guarneri et al1 reported the case of a 59-year-old farmer who had tentatively been diagnosed with delusional parasitosis until persistent presentation to a dermatologist for evaluation enabled the capture and identification of grain thrips. More recently, another case of likely Thysanoptera dermatitis was published in 2012 after a man presented with a slide-mounted thrip from his skin for evaluation as to a potential cause of a recurrent rash he had been experiencing.11 In all of these cases, it was fortunate that a specific organism could be identified for 2 reasons: (1) members of the order Thysanoptera have a biological cycle of only 11 to 36 days, and (2) thrips may go virtually unnoticed by humans, as they are often difficult to see due to their small size.2,12 Perhaps the most extensive report, however, comes from Childers et al8 in a descriptive case series published in 2005. In this report, the investigators provided a thorough detailing of multiple encounters dating back to 1883 through which patients were inadvertently exposed to various species of thrips and subsequently presented with arthropod bites.
Conclusion
The rapid and clustered manner of patient presentation in this case series makes it unique and highlights the need for further consideration of Thysanoptera dermatitis as a potential etiology for an outbreak of a papular eruption. Further reporting may help to better contextualize the true epidemiology of the condition and subsequently may trigger its greater inclusion in the differential diagnosis for a pruritic papular eruption.
Acknowledgments
We would like to extend our appreciation to Amy Spizuoco, DO (New York, New York), for her assistance with the initial diagnosis; Steve Montgomery, PhD (Honolulu, Hawaii), for his assistance with further entomological discussion of potential etiologies; and John R. Gilstad, MD (Honolulu, Hawaii), for contributing his thoughts on the differential diagnosis of the presenting symptoms.
1. Guarneri F, Guarneri C, Mento G, et al. Pseudo‐delusory syndrome caused by Limothrips cerealium. Int J Dermatol. 2006;45:197-199.
2. Leigheb G, Tiberio R, Filosa G, et al. Thysanoptera dermatitis. J Eur Acad Dermatol Venereol. 2005;19:722-724.
3. Williams CB. A blood sucking thrips. The Entomologist. 1921;54:164.
4. Bailey SF. Thrips attacking man. Can Entomol. 1936;68:95-98.
5. Goldstein N, Skipworth GB. Papular eruption secondary to thrips bites. JAMA. 1968;203:53-55.
6. Aeling JL. Hypoanesthetic halos in Hawaii. Cutis. 1974;14:541-544.
7. Fishman HC. Thrips. Arch Dermatol. 1987;123:993.
8. Childers CC, Beshear RJ, Frantz G, et al. A review of thrips species biting man including records in Florida and Georgia between 1986-1997. Florida Entomologist. 2005;88:447-451.
9. Funasaki GY. Studies on the life cycle and propagation technique of Montandoniola moraguesi (Puton)(Heteroptera: Anthocoridae). Proc Hawaii Entomol Soc. 1966;XIX.2:209-211.
10. Waisman M. Thrips bites dermatitis. JAMA. 1968;204:82.
11. Martin J, Richmond A, Davis BM, et al. Thysanoptera dermatitis presenting as folie à deux. Arch Dermatol. 2012;148:864-865.
12. Cooper RG. Dermatitis & conjunctivitis in workers on an ostrich farm following thrips infestation. Indian J Med Res. 2007;125:588-589.
Case Reports
A platoon of 24 US Marines participated in a 1-week outdoor training exercise (February 4–8) at the Marine Corps Training Area Bellows in Oahu, Hawaii. During the last 3 days of training, 15 (62.5%) marines presented to the same primary care provider with what appeared to be diffuse scattered lesions on the face, neck, and dorsal aspect of the hands. All 15 patients reported that they noticed the lesions upon waking up the morning after their second night at the training area. The patients were unable to recollect specific direct arthropod interactions, but they reported the presence of “bugs” in the training area and denied use of any insect repellents, insect nets, or sunscreen. Sleeping arrangements varied from covered vehicles and cots to sleeping bags on the ground, which were laundered independently by each marine and thereby were ruled out as a commonality. The patients denied working with any chemicals or cleansers while in the field. Further questioning of all 15 patients revealed a history of extended contact with live foliage as branches were broken off to build camouflaged sites.
The following week, a second platoon of 20 marines occupied a separate undisturbed portion of the same training area for a similar 1-week training evolution. Manifestation of similar symptoms among members of the second group, who had no contact with the initial 15 patients, supported the likely environmental etiology of the eruptions.
 |
| Figure 1. Numerous well-circumscribed, discrete, pink-red papules diffusely scattered across the face. |
 |
| Figure 2. Papules with classic anemic halos. |
Referral
Two patients from the first group were evaluated at the dermatology clinic at Tripler Army Medical Center (Honolulu, Hawaii) on day 10 of the initial outbreak. Cutaneous examination revealed numerous discrete, pink-red, well-circumscribed, 2- to 4-mm, dome-shaped papules exclusive to exposed areas on the face, neck, and dorsal aspect of the hands (Figures 1 and 2). Anemic halos surrounding the hand papules were noted (Figure 2). A punch biopsy in both patients revealed spongiotic dermatitis with superficial perivascular and interstitial lymphohistiocytic inflammation with eosinophils, suggestive of an arthropod bite (Figure 3). No retained arthropod parts wereidentified. Both patients were treated with triamcinolone ointment twice daily for 7 days with total resolution of the lesions.
Site Survey Results
Five days following the initial presentation of the first outbreak, a daytime site survey of the training area was conducted by a medical entomologist, an environmental health scientist, and a wildlife biologist. Records indicated that prior to the current utilization, the training area had not been used for 9 months. Approximately half of the training area was covered with mixed scrub vegetation and the remainder was clear pavement or sand (clear of vegetation). Feral hogs (Sus scrofa), cats (Felis domesticus), and mongooses (Herpestes javanicus) were observed at the site. Patient interviews and site survey ruled out a number of potential environmental irritants, including contact with fresh or salt water and chemical contaminants in the air or soil.
Because biting insects were suspected as the cause of the eruptions, an overnight entomological survey was conducted 3 weeks after the first outbreak under similar weather conditions and was centered in the area of an Australian pine (Casuarina equisetifolia) forest where most of the marines had slept during training. Mosquitoes (Aedes albopictus and Culex quinquefasciatus) were observed in the area, with an estimated biting rate of 1 to 2 bites per hour. Centipedes (Scolopendra subspinipes) were commonly observed after dark. There was no sign of heavy bird roosting or nesting, which would be a possible source of biting ectoparasites. Other than the Australian pine, notable vegetation present included Christmasberry (Schinus terebinthifolius), koa haole (Leucaena leucocephala), and Chinese banyan (Ficus microcarpa). A survey of the vegetation uncovered no notable insects, and no damage to the leaves of the Chinese banyans, which is typical of thrip infestation, was noted.
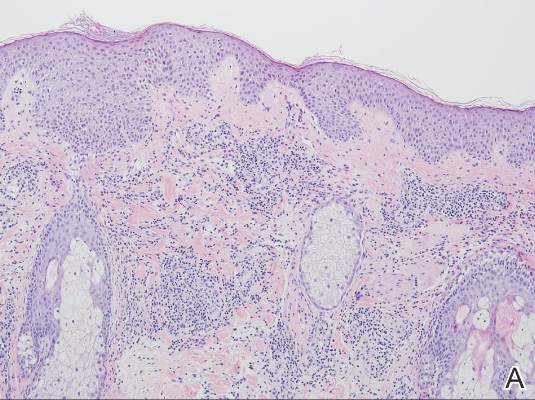 |  |
| Figure 3. Superficial and deep perivascular and interstitial dermatitis (A)(H&E, original magnification ×10) with lymphocytic predominance (B)(H&E, original magnification ×40). | |
After completion of a resource-intensive investigation that included site survey, literature review, detailed patient history including thrips-associated skin manifestations, and thorough consultation with local dermatologists and entomologists, the findings seemingly pointed to thrips as the most likely etiology of the eruption seen in our patients and a diagnosis of Thysanoptera dermatitis was made.
Comment
Thrips are small winged insects in the order Thysanoptera, which comprises more than 5000 identified species ranging in size from 0.5 to 15 mm, though most are approximately 1 mm.1 The insects typically are phytophagous (feeding on plants) and are attracted to humidity and seemingly the sweat of animals and humans.2 Although largely a phytophagous organism, a few published cases of thrips exposure reported papular skin eruptions known as Thysanoptera dermatitis.3-8 Several species of thrips across the globe have been associated with incidental attacks on humans to include “Heliothrips indicus Bagnall, a cotton pest of the Sudan; Thrips imagines Bagnall, reported in Australia; Limothrips cerealium (Haliday), in Germany; Gynaitkothrips uzeli Zimmerman, in Algeria; and other species.”7 In Hawaii, Gynaikothrips ficorum (Cuban laurel thrips) is a common pest of the Chinese banyan tree (F microcarpa) tree.9
A case series reported by Goldstein and Skipworth5 in the late 1960s of military personnel stationed in Oahu described exposure to similar environmental conditions with resultant lesions that were nearly identical to those seen in our patients. The final conclusion of the investigation was that Cuban laurel thrips were the likely etiology, though mites also were considered.5 In a subsequent commentary in 1968, Waisman10 reported similar eruptions in hospitalized patients with further comment regarding the nocturnal occurrence of the bites. Additionally, the eruptions were reported to be short lasting and devoid of discomfort, similar to our patient population.10
Following suit, Aeling6 published a case series in 1974 depicting several service members who presented with symptoms that were nearly identical to the symptoms experienced by our patients as well as those of Goldstein and Skipworth.5 The investigator coined the term hypoanesthetic halos in Hawaii to describe the findings and further reported that Hawaiian dermatologists were familiar with the symptoms and clinical presentation of the disease. Patients in this outbreak had observed small flying insects, similar to the reports from our patients, and postulated that the symptoms occurred secondary to insect bites.6
Since the report by Goldstein and Skipworth5 in 1968, the majority of the literature regarding Thysanoptera dermatitis has largely been in case reports. In 1987, Fishman7 reported the case of a 43-year-old woman who presented with a palm-sized area of grouped red puncta on the lateral neck with the subsequent entrapment and identification of a flower thrips from the patient’s clothing. In 2005, Leigheb et al2 reported the case of a 30-year-old man with an erythematous papular cutaneous eruption on the anterior chest. In this case, the causative etiology was unequivocally confirmed upon identification of the presence of thrips on biopsy.2 In 2006, Guarneri et al1 reported the case of a 59-year-old farmer who had tentatively been diagnosed with delusional parasitosis until persistent presentation to a dermatologist for evaluation enabled the capture and identification of grain thrips. More recently, another case of likely Thysanoptera dermatitis was published in 2012 after a man presented with a slide-mounted thrip from his skin for evaluation as to a potential cause of a recurrent rash he had been experiencing.11 In all of these cases, it was fortunate that a specific organism could be identified for 2 reasons: (1) members of the order Thysanoptera have a biological cycle of only 11 to 36 days, and (2) thrips may go virtually unnoticed by humans, as they are often difficult to see due to their small size.2,12 Perhaps the most extensive report, however, comes from Childers et al8 in a descriptive case series published in 2005. In this report, the investigators provided a thorough detailing of multiple encounters dating back to 1883 through which patients were inadvertently exposed to various species of thrips and subsequently presented with arthropod bites.
Conclusion
The rapid and clustered manner of patient presentation in this case series makes it unique and highlights the need for further consideration of Thysanoptera dermatitis as a potential etiology for an outbreak of a papular eruption. Further reporting may help to better contextualize the true epidemiology of the condition and subsequently may trigger its greater inclusion in the differential diagnosis for a pruritic papular eruption.
Acknowledgments
We would like to extend our appreciation to Amy Spizuoco, DO (New York, New York), for her assistance with the initial diagnosis; Steve Montgomery, PhD (Honolulu, Hawaii), for his assistance with further entomological discussion of potential etiologies; and John R. Gilstad, MD (Honolulu, Hawaii), for contributing his thoughts on the differential diagnosis of the presenting symptoms.
Case Reports
A platoon of 24 US Marines participated in a 1-week outdoor training exercise (February 4–8) at the Marine Corps Training Area Bellows in Oahu, Hawaii. During the last 3 days of training, 15 (62.5%) marines presented to the same primary care provider with what appeared to be diffuse scattered lesions on the face, neck, and dorsal aspect of the hands. All 15 patients reported that they noticed the lesions upon waking up the morning after their second night at the training area. The patients were unable to recollect specific direct arthropod interactions, but they reported the presence of “bugs” in the training area and denied use of any insect repellents, insect nets, or sunscreen. Sleeping arrangements varied from covered vehicles and cots to sleeping bags on the ground, which were laundered independently by each marine and thereby were ruled out as a commonality. The patients denied working with any chemicals or cleansers while in the field. Further questioning of all 15 patients revealed a history of extended contact with live foliage as branches were broken off to build camouflaged sites.
The following week, a second platoon of 20 marines occupied a separate undisturbed portion of the same training area for a similar 1-week training evolution. Manifestation of similar symptoms among members of the second group, who had no contact with the initial 15 patients, supported the likely environmental etiology of the eruptions.
 |
| Figure 1. Numerous well-circumscribed, discrete, pink-red papules diffusely scattered across the face. |
 |
| Figure 2. Papules with classic anemic halos. |
Referral
Two patients from the first group were evaluated at the dermatology clinic at Tripler Army Medical Center (Honolulu, Hawaii) on day 10 of the initial outbreak. Cutaneous examination revealed numerous discrete, pink-red, well-circumscribed, 2- to 4-mm, dome-shaped papules exclusive to exposed areas on the face, neck, and dorsal aspect of the hands (Figures 1 and 2). Anemic halos surrounding the hand papules were noted (Figure 2). A punch biopsy in both patients revealed spongiotic dermatitis with superficial perivascular and interstitial lymphohistiocytic inflammation with eosinophils, suggestive of an arthropod bite (Figure 3). No retained arthropod parts wereidentified. Both patients were treated with triamcinolone ointment twice daily for 7 days with total resolution of the lesions.
Site Survey Results
Five days following the initial presentation of the first outbreak, a daytime site survey of the training area was conducted by a medical entomologist, an environmental health scientist, and a wildlife biologist. Records indicated that prior to the current utilization, the training area had not been used for 9 months. Approximately half of the training area was covered with mixed scrub vegetation and the remainder was clear pavement or sand (clear of vegetation). Feral hogs (Sus scrofa), cats (Felis domesticus), and mongooses (Herpestes javanicus) were observed at the site. Patient interviews and site survey ruled out a number of potential environmental irritants, including contact with fresh or salt water and chemical contaminants in the air or soil.
Because biting insects were suspected as the cause of the eruptions, an overnight entomological survey was conducted 3 weeks after the first outbreak under similar weather conditions and was centered in the area of an Australian pine (Casuarina equisetifolia) forest where most of the marines had slept during training. Mosquitoes (Aedes albopictus and Culex quinquefasciatus) were observed in the area, with an estimated biting rate of 1 to 2 bites per hour. Centipedes (Scolopendra subspinipes) were commonly observed after dark. There was no sign of heavy bird roosting or nesting, which would be a possible source of biting ectoparasites. Other than the Australian pine, notable vegetation present included Christmasberry (Schinus terebinthifolius), koa haole (Leucaena leucocephala), and Chinese banyan (Ficus microcarpa). A survey of the vegetation uncovered no notable insects, and no damage to the leaves of the Chinese banyans, which is typical of thrip infestation, was noted.
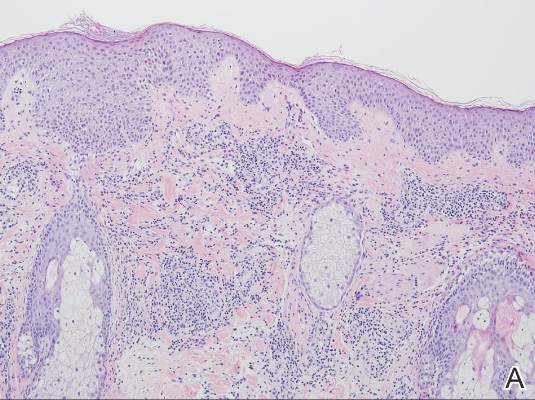 |  |
| Figure 3. Superficial and deep perivascular and interstitial dermatitis (A)(H&E, original magnification ×10) with lymphocytic predominance (B)(H&E, original magnification ×40). | |
After completion of a resource-intensive investigation that included site survey, literature review, detailed patient history including thrips-associated skin manifestations, and thorough consultation with local dermatologists and entomologists, the findings seemingly pointed to thrips as the most likely etiology of the eruption seen in our patients and a diagnosis of Thysanoptera dermatitis was made.
Comment
Thrips are small winged insects in the order Thysanoptera, which comprises more than 5000 identified species ranging in size from 0.5 to 15 mm, though most are approximately 1 mm.1 The insects typically are phytophagous (feeding on plants) and are attracted to humidity and seemingly the sweat of animals and humans.2 Although largely a phytophagous organism, a few published cases of thrips exposure reported papular skin eruptions known as Thysanoptera dermatitis.3-8 Several species of thrips across the globe have been associated with incidental attacks on humans to include “Heliothrips indicus Bagnall, a cotton pest of the Sudan; Thrips imagines Bagnall, reported in Australia; Limothrips cerealium (Haliday), in Germany; Gynaitkothrips uzeli Zimmerman, in Algeria; and other species.”7 In Hawaii, Gynaikothrips ficorum (Cuban laurel thrips) is a common pest of the Chinese banyan tree (F microcarpa) tree.9
A case series reported by Goldstein and Skipworth5 in the late 1960s of military personnel stationed in Oahu described exposure to similar environmental conditions with resultant lesions that were nearly identical to those seen in our patients. The final conclusion of the investigation was that Cuban laurel thrips were the likely etiology, though mites also were considered.5 In a subsequent commentary in 1968, Waisman10 reported similar eruptions in hospitalized patients with further comment regarding the nocturnal occurrence of the bites. Additionally, the eruptions were reported to be short lasting and devoid of discomfort, similar to our patient population.10
Following suit, Aeling6 published a case series in 1974 depicting several service members who presented with symptoms that were nearly identical to the symptoms experienced by our patients as well as those of Goldstein and Skipworth.5 The investigator coined the term hypoanesthetic halos in Hawaii to describe the findings and further reported that Hawaiian dermatologists were familiar with the symptoms and clinical presentation of the disease. Patients in this outbreak had observed small flying insects, similar to the reports from our patients, and postulated that the symptoms occurred secondary to insect bites.6
Since the report by Goldstein and Skipworth5 in 1968, the majority of the literature regarding Thysanoptera dermatitis has largely been in case reports. In 1987, Fishman7 reported the case of a 43-year-old woman who presented with a palm-sized area of grouped red puncta on the lateral neck with the subsequent entrapment and identification of a flower thrips from the patient’s clothing. In 2005, Leigheb et al2 reported the case of a 30-year-old man with an erythematous papular cutaneous eruption on the anterior chest. In this case, the causative etiology was unequivocally confirmed upon identification of the presence of thrips on biopsy.2 In 2006, Guarneri et al1 reported the case of a 59-year-old farmer who had tentatively been diagnosed with delusional parasitosis until persistent presentation to a dermatologist for evaluation enabled the capture and identification of grain thrips. More recently, another case of likely Thysanoptera dermatitis was published in 2012 after a man presented with a slide-mounted thrip from his skin for evaluation as to a potential cause of a recurrent rash he had been experiencing.11 In all of these cases, it was fortunate that a specific organism could be identified for 2 reasons: (1) members of the order Thysanoptera have a biological cycle of only 11 to 36 days, and (2) thrips may go virtually unnoticed by humans, as they are often difficult to see due to their small size.2,12 Perhaps the most extensive report, however, comes from Childers et al8 in a descriptive case series published in 2005. In this report, the investigators provided a thorough detailing of multiple encounters dating back to 1883 through which patients were inadvertently exposed to various species of thrips and subsequently presented with arthropod bites.
Conclusion
The rapid and clustered manner of patient presentation in this case series makes it unique and highlights the need for further consideration of Thysanoptera dermatitis as a potential etiology for an outbreak of a papular eruption. Further reporting may help to better contextualize the true epidemiology of the condition and subsequently may trigger its greater inclusion in the differential diagnosis for a pruritic papular eruption.
Acknowledgments
We would like to extend our appreciation to Amy Spizuoco, DO (New York, New York), for her assistance with the initial diagnosis; Steve Montgomery, PhD (Honolulu, Hawaii), for his assistance with further entomological discussion of potential etiologies; and John R. Gilstad, MD (Honolulu, Hawaii), for contributing his thoughts on the differential diagnosis of the presenting symptoms.
1. Guarneri F, Guarneri C, Mento G, et al. Pseudo‐delusory syndrome caused by Limothrips cerealium. Int J Dermatol. 2006;45:197-199.
2. Leigheb G, Tiberio R, Filosa G, et al. Thysanoptera dermatitis. J Eur Acad Dermatol Venereol. 2005;19:722-724.
3. Williams CB. A blood sucking thrips. The Entomologist. 1921;54:164.
4. Bailey SF. Thrips attacking man. Can Entomol. 1936;68:95-98.
5. Goldstein N, Skipworth GB. Papular eruption secondary to thrips bites. JAMA. 1968;203:53-55.
6. Aeling JL. Hypoanesthetic halos in Hawaii. Cutis. 1974;14:541-544.
7. Fishman HC. Thrips. Arch Dermatol. 1987;123:993.
8. Childers CC, Beshear RJ, Frantz G, et al. A review of thrips species biting man including records in Florida and Georgia between 1986-1997. Florida Entomologist. 2005;88:447-451.
9. Funasaki GY. Studies on the life cycle and propagation technique of Montandoniola moraguesi (Puton)(Heteroptera: Anthocoridae). Proc Hawaii Entomol Soc. 1966;XIX.2:209-211.
10. Waisman M. Thrips bites dermatitis. JAMA. 1968;204:82.
11. Martin J, Richmond A, Davis BM, et al. Thysanoptera dermatitis presenting as folie à deux. Arch Dermatol. 2012;148:864-865.
12. Cooper RG. Dermatitis & conjunctivitis in workers on an ostrich farm following thrips infestation. Indian J Med Res. 2007;125:588-589.
1. Guarneri F, Guarneri C, Mento G, et al. Pseudo‐delusory syndrome caused by Limothrips cerealium. Int J Dermatol. 2006;45:197-199.
2. Leigheb G, Tiberio R, Filosa G, et al. Thysanoptera dermatitis. J Eur Acad Dermatol Venereol. 2005;19:722-724.
3. Williams CB. A blood sucking thrips. The Entomologist. 1921;54:164.
4. Bailey SF. Thrips attacking man. Can Entomol. 1936;68:95-98.
5. Goldstein N, Skipworth GB. Papular eruption secondary to thrips bites. JAMA. 1968;203:53-55.
6. Aeling JL. Hypoanesthetic halos in Hawaii. Cutis. 1974;14:541-544.
7. Fishman HC. Thrips. Arch Dermatol. 1987;123:993.
8. Childers CC, Beshear RJ, Frantz G, et al. A review of thrips species biting man including records in Florida and Georgia between 1986-1997. Florida Entomologist. 2005;88:447-451.
9. Funasaki GY. Studies on the life cycle and propagation technique of Montandoniola moraguesi (Puton)(Heteroptera: Anthocoridae). Proc Hawaii Entomol Soc. 1966;XIX.2:209-211.
10. Waisman M. Thrips bites dermatitis. JAMA. 1968;204:82.
11. Martin J, Richmond A, Davis BM, et al. Thysanoptera dermatitis presenting as folie à deux. Arch Dermatol. 2012;148:864-865.
12. Cooper RG. Dermatitis & conjunctivitis in workers on an ostrich farm following thrips infestation. Indian J Med Res. 2007;125:588-589.
Practice Points
- Thysanoptera dermatitis presents as a diffuse cutaneous eruption consisting of scattered pruritic papules to exposed skin surfaces.
- The importance of considering the environmental component of a cutaneous eruption via a thorough understanding of local flora and fauna cannot be underestimated.
- The role of a dermatologist in the rapid identification of a cutaneous eruption in the setting of an acute cluster outbreak is of utmost importance to assist with eliminating infectious and environmental public health threats from the differential diagnosis.
Complete Atrioventricular Nodal Block Due to Malignancy-Related Hypercalcemia
Complete atrioventricular (AV) block can occur due to structural or functional causes. Common structural etiologies include sclerodegenerative disease of the conduction system, ischemic heart disease in the acute or chronic setting, infiltrative myocardial disease, congenital heart disease, and cardiac surgery. Reversible etiologies of complete AV block include drug overdose and electrolyte abnormalities. In the following case study, the authors present a rare case of complete AV block caused by severe hypercalcemia related to malignancy that completely normalized after treatment of the hypercalcemia.
Case Report
A 63-year-old African-American man with metastatic carcinoma of the lungs (Figure 1) with unknown primary cancer was found to have a serum calcium level of 17.5 mg/dL (reference range:8.4-10.2 mg/dL) on routine preoperative laboratory testing prior to placement of a surgical port for chemotherapy. The patient also was noted to have a slow heart rate, and his electrocardiogram revealed a third-degree AV block with an escape rhythm at 29 bpm with a prolonged corrected QT (QTc) of 556 ms (Figure 2).
Although the patient reported nonspecific symptoms of fatigue, anorexia, dysphagia, and weight loss for 3 months, there were no new symptoms of dizziness, chest discomfort, or syncope. His past medical history included hypertension, hyperlipidemia, chronic kidney disease, obstructive sleep apnea, and the recently discovered bilateral lung metastasis. The patient reported no prior history of cardiac arrhythmias, coronary artery disease, or structural heart defects. His outpatient medications included aspirin, amlodipine, bupropion, hydralazine, and simvastatin.
At the physical examination the patient was cachectic but in no apparent distress. His heart rate escape rhythm was 29 bpm, with no murmurs and mildly reduced breath sounds. The patient’s blood pressure was 110/70. After correction for albumin, the serum calcium level was 17.8 mg/dL; ionized calcium level was 8.6 mg/dL; parathyroid hormone was 7.6 pg/mL (normal range, 12-88 pg/mL); parathyroid hormone-related protein was 6.4 pmol/L (normal range, < 2.0 pmol/L); potassium was 3.4 mmol/L (normal range, 3.5 – 5.1 mmol/L); and magnesium was 2.01 mg/dL. The patient’s thyroid stimulating hormone level was normal, and serial cardiac enzymes stayed within the reference range.
The patient was admitted to a cardiac care unit. A temporary transvenous pacemaker was placed, and the hypercalcemia was treated with aggressive fluid hydration, calcitonin, and zoledronic acid. Serum calcium gradually decreased to 14.6 mg/dL the following day and 9.6 mg/dL the subsequent day. The normalization of calcium resulted in resolution of complete heart block (Figure 3). The patient did not experience recurrence of AV nodal dysfunction and eventually died 3 months later due to his advanced metastatic disease.
Discussion
The reported cardiovascular effects of hypercalcemia include hypertension, arrhythmias, increased myocardial contractility at serum calcium level below 15 mg/dL, and myocardial depression above that level. Electrocardiographic manifestations of hypercalcemia include a shortened ST segment leading to a short corrected QT interval (QTc), slight increase in T wave duration, and rarely, Osborn waves or J waves.1-3 However, its influence on the AV node is less clear.
One small study assessed the prevalence of cardiac arrhythmias and conduction disturbances in 20 patients with hyperparathyroidism and moderate hypercalcemia and found no increase in the frequency of arrhythmias or high grade AV block.4
There are reports of conduction abnormality secondary to experimentally induced hypercalcemia in the literature. Hoff and colleagues described findings of AV block generated by the injection of IV calcium in dogs.5 In 2 human subjects, sinus bradycardia was precipitated after they received IV infusion of calcium gluconate.6 Shah and colleagues described 2 patients with sinus node dysfunction attributed to hypercalcemia secondary to hyperparathyroidism.7
Case reports of AV nodal dysfunction provoked by hypercalcemia have primarily occurred in the setting of primary hyperparathyroidism.8,9 Milk-alkali syndrome and vitamin D related hypercalcemia also have been reported to cause complete heart block.10,11 Reports of malignancy-related hypercalcemia causing conduction abnormalities are rare. The authors also found one case report of marked sinus bradycardia due to hypercalcemia related to breast cancer.12The case study presented in this report is rare because the patient developed complete AV block due to malignancy-related hypercalcemia that resolved completely with resolution of hypercalcemia. The prolongation of the QTc interval was another unique electrocardiographic change observed in this case. Calcium levels are inversely proportional to the QTc interval, and hypercalcemia is typically associated with a shortened QTc interval. However, this patient had a prolonged QTc without any other clear-cut cause. His hypokalemia was of a mild degree and not severe enough to produce such a long QTc interval. A possible explanation of QTc prolongation may be an increase in the T wave width associated with a serum calcium level above 16 mg/dL.
The pathophysiology of hypercalcemia-induced AV nodal conduction system disease is unknown. Calcium deposition in AV nodes of elderly patients has been associated with paroxysmal 2:1 AV block.8 It could be postulated that elevated serum calcium levels predispose to calcium deposition in cardiac conduction tissue, leading to progressive dysfunction. Although this theory may be applicable in a chronic setting, the mechanism in an acute setting likely relates to elevated serum levels of calcium that causes an alteration in electrochemical gradients. These elevated serum levels also increase intracellular calcium. This rise may result in increased calmodulin activation on the intracellular portion of the myocyte cell membrane and consequent enhanced sodium channel activation, which may then inhibit AV nodal conduction.13
Conclusion
Physicians should be aware that severe hypercalcemia can cause significant conduction system alterations, including complete AV block. A short QTc interval is typical, but a prolonged QTc interval also may be seen. While temporary support with a transvenous pacemaker may be needed, the conduction system abnormality is expected to resolve by treatment of the underlying hypercalcemia.
1. Nierenberg DW, Ransil BJ. Q-aTc interval as a clinical indicator of hypercalcemia. Am J Cardiol. 1979;44(2):243-248.
2. Bronsky D, Dubin A, Waldstein SS, Kushner DS. Calcium and the electrocardiogram II. The electrocardiographic manifestations of hyperparathyroidism and of marked hypercalcemia from various other etiologies. Am J Cardiol. 1961;7(6):833-839.
3. Otero J, Lenihan DJ. The "normothermic" Osborn wave induced by severe hypercalcemia. Tex Heart Inst J. 2000;27(3):316-317.
4. Rosenqvist M, Nordenström J, Andersson M, Edhag OK. Cardiac conduction inpatients with hypercalcaemia due to primary hyperparathyroidism. Clin Endocrinol (Oxf). 1992;37(1):29-33.
5. Hoff H, Smith P, Winkler A. Electrocardiographic changes and concentration of calcium in serum following injection of calcium chloride. Am J Physiol. 1939;125:162-171.
6. Howard JE, Hopkins TR, Connor TB. The use of intravenous calcium as a measure of activity of the parathyroid glands. Trans Assoc Am Physicians. 1952;65:351-358.
7. Shah AP, Lopez A, Wachsner RY, Meymandi SK, El-Bialy AK, Ichiuji AM. Sinus node dysfunction secondary to hyperparathyroidism. J Cardiovasc Pharmacol Ther. 2004;9(2):145-147.
8. Vosnakidis A, Polymeropoulos K, Zaragoulidis P, Zarifis I. Atrioventricular nodal dysfunction secondary to hyperparathyroidism. J Thoracic Dis. 2013;5(3):E90-E92.
9. Crum WB, Till HJ. Hyperparathyroidism with Wenckebach's phenomenon. Am J Cardiol. 1960;6:838-840.
10. Ginsberg H, Schwarz KV. Letter: hypercalcemia and complete heart block. Ann Intern Med. 1973;79(6):903.
11. Garg G, Khadgwat R, Khandelwal D, Gupta N. Vitamin D toxicity presenting as hypercalcemia and complete heart block: an interesting case report. Indian J Endocrinol Metab. 2012;16 (suppl 2):S423-S425.
12. Badertscher E, Warnica JW, Ernst DS. Acute hypercalcemia and severe bradycardia in a patient with breast cancer. CMAJ. 1993;148(9):1506-1508.
13. Potet F, Chagot B, Anghelescu M, et al. Functional interactions between distinct sodium channel cytoplasmic domains through the action of calmodulin. J Biol Chem. 2009;284(13):8846-8854.
Complete atrioventricular (AV) block can occur due to structural or functional causes. Common structural etiologies include sclerodegenerative disease of the conduction system, ischemic heart disease in the acute or chronic setting, infiltrative myocardial disease, congenital heart disease, and cardiac surgery. Reversible etiologies of complete AV block include drug overdose and electrolyte abnormalities. In the following case study, the authors present a rare case of complete AV block caused by severe hypercalcemia related to malignancy that completely normalized after treatment of the hypercalcemia.
Case Report
A 63-year-old African-American man with metastatic carcinoma of the lungs (Figure 1) with unknown primary cancer was found to have a serum calcium level of 17.5 mg/dL (reference range:8.4-10.2 mg/dL) on routine preoperative laboratory testing prior to placement of a surgical port for chemotherapy. The patient also was noted to have a slow heart rate, and his electrocardiogram revealed a third-degree AV block with an escape rhythm at 29 bpm with a prolonged corrected QT (QTc) of 556 ms (Figure 2).
Although the patient reported nonspecific symptoms of fatigue, anorexia, dysphagia, and weight loss for 3 months, there were no new symptoms of dizziness, chest discomfort, or syncope. His past medical history included hypertension, hyperlipidemia, chronic kidney disease, obstructive sleep apnea, and the recently discovered bilateral lung metastasis. The patient reported no prior history of cardiac arrhythmias, coronary artery disease, or structural heart defects. His outpatient medications included aspirin, amlodipine, bupropion, hydralazine, and simvastatin.
At the physical examination the patient was cachectic but in no apparent distress. His heart rate escape rhythm was 29 bpm, with no murmurs and mildly reduced breath sounds. The patient’s blood pressure was 110/70. After correction for albumin, the serum calcium level was 17.8 mg/dL; ionized calcium level was 8.6 mg/dL; parathyroid hormone was 7.6 pg/mL (normal range, 12-88 pg/mL); parathyroid hormone-related protein was 6.4 pmol/L (normal range, < 2.0 pmol/L); potassium was 3.4 mmol/L (normal range, 3.5 – 5.1 mmol/L); and magnesium was 2.01 mg/dL. The patient’s thyroid stimulating hormone level was normal, and serial cardiac enzymes stayed within the reference range.
The patient was admitted to a cardiac care unit. A temporary transvenous pacemaker was placed, and the hypercalcemia was treated with aggressive fluid hydration, calcitonin, and zoledronic acid. Serum calcium gradually decreased to 14.6 mg/dL the following day and 9.6 mg/dL the subsequent day. The normalization of calcium resulted in resolution of complete heart block (Figure 3). The patient did not experience recurrence of AV nodal dysfunction and eventually died 3 months later due to his advanced metastatic disease.
Discussion
The reported cardiovascular effects of hypercalcemia include hypertension, arrhythmias, increased myocardial contractility at serum calcium level below 15 mg/dL, and myocardial depression above that level. Electrocardiographic manifestations of hypercalcemia include a shortened ST segment leading to a short corrected QT interval (QTc), slight increase in T wave duration, and rarely, Osborn waves or J waves.1-3 However, its influence on the AV node is less clear.
One small study assessed the prevalence of cardiac arrhythmias and conduction disturbances in 20 patients with hyperparathyroidism and moderate hypercalcemia and found no increase in the frequency of arrhythmias or high grade AV block.4
There are reports of conduction abnormality secondary to experimentally induced hypercalcemia in the literature. Hoff and colleagues described findings of AV block generated by the injection of IV calcium in dogs.5 In 2 human subjects, sinus bradycardia was precipitated after they received IV infusion of calcium gluconate.6 Shah and colleagues described 2 patients with sinus node dysfunction attributed to hypercalcemia secondary to hyperparathyroidism.7
Case reports of AV nodal dysfunction provoked by hypercalcemia have primarily occurred in the setting of primary hyperparathyroidism.8,9 Milk-alkali syndrome and vitamin D related hypercalcemia also have been reported to cause complete heart block.10,11 Reports of malignancy-related hypercalcemia causing conduction abnormalities are rare. The authors also found one case report of marked sinus bradycardia due to hypercalcemia related to breast cancer.12The case study presented in this report is rare because the patient developed complete AV block due to malignancy-related hypercalcemia that resolved completely with resolution of hypercalcemia. The prolongation of the QTc interval was another unique electrocardiographic change observed in this case. Calcium levels are inversely proportional to the QTc interval, and hypercalcemia is typically associated with a shortened QTc interval. However, this patient had a prolonged QTc without any other clear-cut cause. His hypokalemia was of a mild degree and not severe enough to produce such a long QTc interval. A possible explanation of QTc prolongation may be an increase in the T wave width associated with a serum calcium level above 16 mg/dL.
The pathophysiology of hypercalcemia-induced AV nodal conduction system disease is unknown. Calcium deposition in AV nodes of elderly patients has been associated with paroxysmal 2:1 AV block.8 It could be postulated that elevated serum calcium levels predispose to calcium deposition in cardiac conduction tissue, leading to progressive dysfunction. Although this theory may be applicable in a chronic setting, the mechanism in an acute setting likely relates to elevated serum levels of calcium that causes an alteration in electrochemical gradients. These elevated serum levels also increase intracellular calcium. This rise may result in increased calmodulin activation on the intracellular portion of the myocyte cell membrane and consequent enhanced sodium channel activation, which may then inhibit AV nodal conduction.13
Conclusion
Physicians should be aware that severe hypercalcemia can cause significant conduction system alterations, including complete AV block. A short QTc interval is typical, but a prolonged QTc interval also may be seen. While temporary support with a transvenous pacemaker may be needed, the conduction system abnormality is expected to resolve by treatment of the underlying hypercalcemia.
Complete atrioventricular (AV) block can occur due to structural or functional causes. Common structural etiologies include sclerodegenerative disease of the conduction system, ischemic heart disease in the acute or chronic setting, infiltrative myocardial disease, congenital heart disease, and cardiac surgery. Reversible etiologies of complete AV block include drug overdose and electrolyte abnormalities. In the following case study, the authors present a rare case of complete AV block caused by severe hypercalcemia related to malignancy that completely normalized after treatment of the hypercalcemia.
Case Report
A 63-year-old African-American man with metastatic carcinoma of the lungs (Figure 1) with unknown primary cancer was found to have a serum calcium level of 17.5 mg/dL (reference range:8.4-10.2 mg/dL) on routine preoperative laboratory testing prior to placement of a surgical port for chemotherapy. The patient also was noted to have a slow heart rate, and his electrocardiogram revealed a third-degree AV block with an escape rhythm at 29 bpm with a prolonged corrected QT (QTc) of 556 ms (Figure 2).
Although the patient reported nonspecific symptoms of fatigue, anorexia, dysphagia, and weight loss for 3 months, there were no new symptoms of dizziness, chest discomfort, or syncope. His past medical history included hypertension, hyperlipidemia, chronic kidney disease, obstructive sleep apnea, and the recently discovered bilateral lung metastasis. The patient reported no prior history of cardiac arrhythmias, coronary artery disease, or structural heart defects. His outpatient medications included aspirin, amlodipine, bupropion, hydralazine, and simvastatin.
At the physical examination the patient was cachectic but in no apparent distress. His heart rate escape rhythm was 29 bpm, with no murmurs and mildly reduced breath sounds. The patient’s blood pressure was 110/70. After correction for albumin, the serum calcium level was 17.8 mg/dL; ionized calcium level was 8.6 mg/dL; parathyroid hormone was 7.6 pg/mL (normal range, 12-88 pg/mL); parathyroid hormone-related protein was 6.4 pmol/L (normal range, < 2.0 pmol/L); potassium was 3.4 mmol/L (normal range, 3.5 – 5.1 mmol/L); and magnesium was 2.01 mg/dL. The patient’s thyroid stimulating hormone level was normal, and serial cardiac enzymes stayed within the reference range.
The patient was admitted to a cardiac care unit. A temporary transvenous pacemaker was placed, and the hypercalcemia was treated with aggressive fluid hydration, calcitonin, and zoledronic acid. Serum calcium gradually decreased to 14.6 mg/dL the following day and 9.6 mg/dL the subsequent day. The normalization of calcium resulted in resolution of complete heart block (Figure 3). The patient did not experience recurrence of AV nodal dysfunction and eventually died 3 months later due to his advanced metastatic disease.
Discussion
The reported cardiovascular effects of hypercalcemia include hypertension, arrhythmias, increased myocardial contractility at serum calcium level below 15 mg/dL, and myocardial depression above that level. Electrocardiographic manifestations of hypercalcemia include a shortened ST segment leading to a short corrected QT interval (QTc), slight increase in T wave duration, and rarely, Osborn waves or J waves.1-3 However, its influence on the AV node is less clear.
One small study assessed the prevalence of cardiac arrhythmias and conduction disturbances in 20 patients with hyperparathyroidism and moderate hypercalcemia and found no increase in the frequency of arrhythmias or high grade AV block.4
There are reports of conduction abnormality secondary to experimentally induced hypercalcemia in the literature. Hoff and colleagues described findings of AV block generated by the injection of IV calcium in dogs.5 In 2 human subjects, sinus bradycardia was precipitated after they received IV infusion of calcium gluconate.6 Shah and colleagues described 2 patients with sinus node dysfunction attributed to hypercalcemia secondary to hyperparathyroidism.7
Case reports of AV nodal dysfunction provoked by hypercalcemia have primarily occurred in the setting of primary hyperparathyroidism.8,9 Milk-alkali syndrome and vitamin D related hypercalcemia also have been reported to cause complete heart block.10,11 Reports of malignancy-related hypercalcemia causing conduction abnormalities are rare. The authors also found one case report of marked sinus bradycardia due to hypercalcemia related to breast cancer.12The case study presented in this report is rare because the patient developed complete AV block due to malignancy-related hypercalcemia that resolved completely with resolution of hypercalcemia. The prolongation of the QTc interval was another unique electrocardiographic change observed in this case. Calcium levels are inversely proportional to the QTc interval, and hypercalcemia is typically associated with a shortened QTc interval. However, this patient had a prolonged QTc without any other clear-cut cause. His hypokalemia was of a mild degree and not severe enough to produce such a long QTc interval. A possible explanation of QTc prolongation may be an increase in the T wave width associated with a serum calcium level above 16 mg/dL.
The pathophysiology of hypercalcemia-induced AV nodal conduction system disease is unknown. Calcium deposition in AV nodes of elderly patients has been associated with paroxysmal 2:1 AV block.8 It could be postulated that elevated serum calcium levels predispose to calcium deposition in cardiac conduction tissue, leading to progressive dysfunction. Although this theory may be applicable in a chronic setting, the mechanism in an acute setting likely relates to elevated serum levels of calcium that causes an alteration in electrochemical gradients. These elevated serum levels also increase intracellular calcium. This rise may result in increased calmodulin activation on the intracellular portion of the myocyte cell membrane and consequent enhanced sodium channel activation, which may then inhibit AV nodal conduction.13
Conclusion
Physicians should be aware that severe hypercalcemia can cause significant conduction system alterations, including complete AV block. A short QTc interval is typical, but a prolonged QTc interval also may be seen. While temporary support with a transvenous pacemaker may be needed, the conduction system abnormality is expected to resolve by treatment of the underlying hypercalcemia.
1. Nierenberg DW, Ransil BJ. Q-aTc interval as a clinical indicator of hypercalcemia. Am J Cardiol. 1979;44(2):243-248.
2. Bronsky D, Dubin A, Waldstein SS, Kushner DS. Calcium and the electrocardiogram II. The electrocardiographic manifestations of hyperparathyroidism and of marked hypercalcemia from various other etiologies. Am J Cardiol. 1961;7(6):833-839.
3. Otero J, Lenihan DJ. The "normothermic" Osborn wave induced by severe hypercalcemia. Tex Heart Inst J. 2000;27(3):316-317.
4. Rosenqvist M, Nordenström J, Andersson M, Edhag OK. Cardiac conduction inpatients with hypercalcaemia due to primary hyperparathyroidism. Clin Endocrinol (Oxf). 1992;37(1):29-33.
5. Hoff H, Smith P, Winkler A. Electrocardiographic changes and concentration of calcium in serum following injection of calcium chloride. Am J Physiol. 1939;125:162-171.
6. Howard JE, Hopkins TR, Connor TB. The use of intravenous calcium as a measure of activity of the parathyroid glands. Trans Assoc Am Physicians. 1952;65:351-358.
7. Shah AP, Lopez A, Wachsner RY, Meymandi SK, El-Bialy AK, Ichiuji AM. Sinus node dysfunction secondary to hyperparathyroidism. J Cardiovasc Pharmacol Ther. 2004;9(2):145-147.
8. Vosnakidis A, Polymeropoulos K, Zaragoulidis P, Zarifis I. Atrioventricular nodal dysfunction secondary to hyperparathyroidism. J Thoracic Dis. 2013;5(3):E90-E92.
9. Crum WB, Till HJ. Hyperparathyroidism with Wenckebach's phenomenon. Am J Cardiol. 1960;6:838-840.
10. Ginsberg H, Schwarz KV. Letter: hypercalcemia and complete heart block. Ann Intern Med. 1973;79(6):903.
11. Garg G, Khadgwat R, Khandelwal D, Gupta N. Vitamin D toxicity presenting as hypercalcemia and complete heart block: an interesting case report. Indian J Endocrinol Metab. 2012;16 (suppl 2):S423-S425.
12. Badertscher E, Warnica JW, Ernst DS. Acute hypercalcemia and severe bradycardia in a patient with breast cancer. CMAJ. 1993;148(9):1506-1508.
13. Potet F, Chagot B, Anghelescu M, et al. Functional interactions between distinct sodium channel cytoplasmic domains through the action of calmodulin. J Biol Chem. 2009;284(13):8846-8854.
1. Nierenberg DW, Ransil BJ. Q-aTc interval as a clinical indicator of hypercalcemia. Am J Cardiol. 1979;44(2):243-248.
2. Bronsky D, Dubin A, Waldstein SS, Kushner DS. Calcium and the electrocardiogram II. The electrocardiographic manifestations of hyperparathyroidism and of marked hypercalcemia from various other etiologies. Am J Cardiol. 1961;7(6):833-839.
3. Otero J, Lenihan DJ. The "normothermic" Osborn wave induced by severe hypercalcemia. Tex Heart Inst J. 2000;27(3):316-317.
4. Rosenqvist M, Nordenström J, Andersson M, Edhag OK. Cardiac conduction inpatients with hypercalcaemia due to primary hyperparathyroidism. Clin Endocrinol (Oxf). 1992;37(1):29-33.
5. Hoff H, Smith P, Winkler A. Electrocardiographic changes and concentration of calcium in serum following injection of calcium chloride. Am J Physiol. 1939;125:162-171.
6. Howard JE, Hopkins TR, Connor TB. The use of intravenous calcium as a measure of activity of the parathyroid glands. Trans Assoc Am Physicians. 1952;65:351-358.
7. Shah AP, Lopez A, Wachsner RY, Meymandi SK, El-Bialy AK, Ichiuji AM. Sinus node dysfunction secondary to hyperparathyroidism. J Cardiovasc Pharmacol Ther. 2004;9(2):145-147.
8. Vosnakidis A, Polymeropoulos K, Zaragoulidis P, Zarifis I. Atrioventricular nodal dysfunction secondary to hyperparathyroidism. J Thoracic Dis. 2013;5(3):E90-E92.
9. Crum WB, Till HJ. Hyperparathyroidism with Wenckebach's phenomenon. Am J Cardiol. 1960;6:838-840.
10. Ginsberg H, Schwarz KV. Letter: hypercalcemia and complete heart block. Ann Intern Med. 1973;79(6):903.
11. Garg G, Khadgwat R, Khandelwal D, Gupta N. Vitamin D toxicity presenting as hypercalcemia and complete heart block: an interesting case report. Indian J Endocrinol Metab. 2012;16 (suppl 2):S423-S425.
12. Badertscher E, Warnica JW, Ernst DS. Acute hypercalcemia and severe bradycardia in a patient with breast cancer. CMAJ. 1993;148(9):1506-1508.
13. Potet F, Chagot B, Anghelescu M, et al. Functional interactions between distinct sodium channel cytoplasmic domains through the action of calmodulin. J Biol Chem. 2009;284(13):8846-8854.
Progressive Cardiomyopathy in a Patient With Elevated Cobalt Ion Levels and Bilateral Metal-on-Metal Hip Arthroplasties
Systemic cobalt toxicity has been reported in the literature after hip arthroplasty revisions for failed ceramic components secondary to third-body abrasive wear of cobalt-chrome (CoCr) components, as well as with metal-on-metal (MOM) hip arthroplasty designs. There have been several cases of systemic cobalt toxicity after revision for fractured ceramic components.1,2 Of these 7 reported cases, all patients had neurologic complaints and 4 patients developed cardiomyopathy secondary to toxic cobalt levels, with 1 case being fatal.1 MOM hip prostheses have also been associated with local and systemic problems secondary to metal debris. Adverse local tissue reactions have been reported to occur in up to 59% of patients, and, in some registries, the failure rate of MOM arthroplasty caused by these soft-tissue reactions is 2 to 3 times that of conventional metal-on-polyethylene design failures.3,4 The occurrence of systemic complications from MOM total hip arthroplasty (THA) wear debris is much less common. There have been 6 cases of systemic cobalt toxicity reported in the literature resulting from MOM total hip prosthesis design.1,2
We present a case of biopsy-confirmed cardiomyopathy secondary to cobalt toxicity from a MOM THA design with subsequent requirement for left ventricular assist device (LVAD) implantation despite prosthesis removal. To our knowledge, this is the first report in the literature of this specific implant design causing systemic cobalt toxicity. The patient provided written informed consent for print and electronic publication of this case report.
Case Report
The patient was a healthy nondiabetic man age 54 years who presented to our clinic 6 years after undergoing left THA and 5 years after undergoing right THA with the Biomet M2a-Magnum MOM prosthesis at an outside facility. The left-side components placed at the index procedure were a size 50 cup, 44 magnum head, 10 Taperloc stem (Biomet), and +9 neck. The right-side components were a size 52 cup, 46 magnum head, 10 Taperloc stem, and +3 neck. The patient emphasized that he was very happy with his hip prostheses and denied groin or thigh pain. His medical history was significant for exogenous obesity, and he denied any history of alcohol, tobacco, steroid, or recreational drug use.
The patient’s review of systems suggested that, approximately 11 months prior to presentation at our facility, he began having difficulty with his activities of daily living secondary to chest pressure with exertion, fatigue, and associated diaphoresis. He complained of decreased sensation in his feet bilaterally but denied any hearing loss, tinnitus, or vision changes. He underwent evaluation of the new-onset chest discomfort with a cardiac stress test that suggested no active cardiac ischemia. An echocardiogram revealed mitral regurgitation, stage II diastolic dysfunction with a left ventricular ejection fraction of 55%. Additionally, during this time period, the patient was being followed by his local orthopedic surgeon for an elevated cobalt level of 120 ppb and a chromium level of 109 ppb. The patient was referred to our clinic for recommendations regarding the elevated metal-ion levels. Upon initial evaluation, the patient denied any hip or groin pain. His physical examination revealed a nonantalgic gait with full range of motion and no signs of instability, tenderness, or masses. The patient was also noted to have no vibratory sensation in his feet bilaterally. The plain radiographs indicated bilateral MOM THA with acetabular inclination levels of 55º on the right and left sides. No cystic changes or other worrisome signs that would suggest implant loosening or failure were present (Figure 1). The serum metal levels were repeated and showed a cobalt level of 189 ppb and a chromium level of 71 ppb. Whole venous blood samples were drawn at our request using trace element tubes and were sent to Medtox Laboratories Inc. for analysis. Other pertinent laboratory values, including hematocrit and thyroid levels, were within normal limits. Because of concerns of systemic toxicity from significantly elevated cobalt and chromium levels, the patient elected to proceed with revision of the MOM components.
During the preoperative medical evaluation, the patient’s cardiac status was a concern, and the etiology of the cardiac dysfunction was unclear. Cardiac magnetic resonance imaging (MRI), which was performed to evaluate the extent and etiology of cardiac dysfunction, showed biventricular dysfunction. To evaluate the underlying myocardial tissue characteristics, delayed contrast imaging was performed and showed diffuse myocardial hyperenhancement of the anterior, lateral, and apical walls, with sparing of the base and midseptum. This type of extensive hyperenhancement is commonly seen with cardiac amyloidosis; however, the blood-pool kinetics during contrast administration is unusual for amyloidosis, as well as the diffuse edema noted on T2-weighted MRI. Importantly, cardiac MRI is very specific in excluding alternative diagnoses, such as postinfarct, infiltrative, acquired, viral, or alcoholic/drugs of abuse etiologies. In the absence of amyloidosis, the only other pattern that would be consistent with symptoms was diffuse, fulminant myocarditis of toxic origin lacking clinical evidence for an infectious origin. The patient’s prior exposure to cobalt was noted. Thus, the hyperenhancement and edema could be strong supportive evidence of cobalt infiltration, despite no reported cases in the literature of cobalt cardiomyopathy found on cardiac MRI.
Additional workup was initiated, and cardiac catheterization showed that the patient continued to decompensate, with worsening global left ventricular dysfunction with an ejection fraction of 30% without evidence of coronary artery disease. Also, he was noted to have mild renal impairment with a blood urea nitrogen level of 31 mg/dL and a creatinine level of 1.7 mg/dL. The etiology of the renal impairment was unknown and had not been established, according to the patient and his wife. The renal impairment was not thought to be caused by the elevated metal ions levels but likely resulted from prerenal azotemia secondary to decreased cardiac output. During catheterization, an endomyocardial biopsy was performed and the tissue sent to the Mayo Clinic pathology department for analysis. The sample showed myocyte hypertrophy and interstitial fibrosis with scattered myofibers containing large cytoplasmic vacuoles. Also present was karyomegaly consistent with myocyte hypertrophy (Figures 2A, 2B). Trichrome stain confirmed replacement of myofibers by collagen (Figure 2C). Electron microscopy performed on a paraffin block showed reduced contractile elements, vacuolar spaces, and increased lipofuscin. The findings were very consistent with, but not specific for, cardiomyopathy from cobalt toxicity. No evidence of an inflammatory infiltrate was identified. The diagnosis was cobalt cardiomyopathy based on biopsy, presentation, cobalt levels, and intraoperative findings.
The patient was admitted to the cardiac intensive care unit preoperatively and optimized with inotropic agents. A multidisciplinary consultation with the cardiology and anesthesia departments was obtained. Both recommended cardiac anesthesia with intraoperative Swan-Ganz catheter and transesophageal echo monitoring. Assuming that the patient remained hemodynamically stable with limited blood loss and the first hip was timely performed, the cardiology department recommended a single surgery, because fewer risks and complications could be expected than from a staged procedure. Subsequently, surgery was performed on the left hip via a conservative anterior approach on the fracture table. The patient remained stable with limited blood loss. During the same operating room time, revision of the right hip was performed using an anterior approach. The intraoperative findings showed evidence of pseudotumors in the adjacent soft tissues and abundant brown, creamy fluid upon entering the joint capsule, consistent with a metallic appearance. Both hips showed similar prosthetic findings. There was no significant visible wear of the large diameter metal heads or gross abnormality of the acetabular components. The trunnion area on both femoral implants was abnormal, revealing a black coating suggestive of marked corrosion. The components were all well fixed, without visible damage, and, because of his fragile cardiac status, the patient’s acetabular components were not revised. The trunnions were cleaned and the femoral heads were revised to active articulation dual-mobility metal-on-polyethylene constructs using 28-mm Biolox Option ceramic (CeramTec). The tissue specimens from the operation showed chronic inflammation with areas of fibroconnective tissue and bland fibrinoid necrosis with extensive brown pigment-laden macrophage reaction. The intraoperative cultures were negative.
The patient tolerated the surgery without complication, and his postoperative period was without incident. Nine months after surgery, the patient’s cobalt and chromium levels had declined to 16 ppb and 32 ppb, respectively (normal, <1 ppb). However, his cardiac status continued to worsen with significant shortness of breath and bilateral lower extremity edema despite diuresis. Follow-up cardiac MRI indicated progressive left and right dysfunction with ejection fractions of 23% and 25%, respectively. After progressive heart-failure symptoms, the patient was admitted to the hospital for severe congestive heart failure and underwent implantation of a HeartWare LVAD with tricuspid valve repair using an Edwards annuloplasty ring. He has since had a cardiac transplant and is doing well.
Discussion
To our knowledge, this is the first reported case of cardiomyopathy in a patient with elevated cobalt ion levels and a Biomet M2a-Magnum hip prosthesis. This is also the first reported case of cardiac MRI–defined cobalt cardiomyopathy. The cobalt levels seen in this patient were similar to those of other cases with systemic cobalt toxicity from a MOM hip construct. Mao and colleagues5 reported 2 cases of systemic cobalt toxicity in 2 patients with articular surface replacement hip prostheses.One patient presented with mild groin pain, neurologic symptoms, and a cobalt level of 410 ppb 5 years after her index procedure. The other patient presented with cardiac and neurologic symptoms but no hip complaints. The patient’s cobalt levels ranged from 185 ppb to 210 ppb. Both patients improved after their revision surgery, and their cobalt levels decreased. The 2 patients in Tower’s report6 were 49-year-old men who had articular surface replacement implants (DePuy). One patient who presented with progressive hip pain 11 months postoperatively developed neurologic symptoms and cardiomyopathy, with cobalt levels of 83 ppb before revision surgery 43 months after his index procedure. The other patient presented with hip pain and vertigo, headaches, fatigue, and dyspnea. He underwent hip revision 40 months postoperatively and required closed reduction under sedation for dislocation. Finally, and most recently, Allen and colleagues2 reported a 59-year-old woman with a cobalt level of 287 ppb whose symptoms did not resolve after implantation of an LVAD or cardiac transplantation but only after removal of her bilateral hip prosthesis. Our case is most similar to this report but significantly adds to the literature in 2 distinct manners: (1) Biomet M2a-Magnum has not been implicated in cobalt toxicity; and (2) this is the first reported use of dedicated cardiac MRI to noninvasively define underlying cardiac pathology.
The cardiac manifestations secondary to systemic cobalt toxicity in this patient represent a frightening consequence of MOM prosthetic wear. The effects of cobalt toxicity on cardiac tissues were first described in a series of alcoholic patients from Manchester in 1900;7 however, it was not until 1967, in a series of patients in Quebec, that cobalt was found to be the inciting factor. In the modern era, hip arthroplasty techniques resulting in excessive cobalt and chromium wear have demonstrated the same findings of myocyte hypertrophy, interstitial fibrosis, and scattered myofibers containing large cytoplasmic inclusions.8,9 The patient presented here has pathologic findings consistent with previous cases of cobalt cardiomyopathy; however, in the other cases of cardiomyopathy due to MOM total hip components, the patients’ cardiac conditions improved after the prostheses were revised and the cobalt levels began to diminish.5,6In our case, the patient has sustained permanent damage to his myocardium and a progressive decline in his cardiac status, which is a deviation from reported cases as of 2014.
While there is no guideline to unequivocally diagnose cobalt cardiomyopathy, the constellation of findings, including pathologic, biologic, blood levels, imaging, and surgical, all uniformly indicate a unifying diagnosis. The lack of improvement after prosthetic device removal supports a diagnosis of permanent myocardial damage, which is consistent with cardiomyopathy of advanced toxic etiology.
Conclusion
This case presents a patient with bilateral MOM THAs, acetabular cup inclinations of greater than 55º, renal impairment, and cobalt levels greater than 60 ppb, with occult cardiac failure leading to LVAD implantation as a prelude to cardiac transplantation in order to avoid certain death. These factors have been shown, in prior case reports, to be associated with cardiac damage that may be reversible.6 However; it is important for orthopedic surgeons to recognize that certain hip prostheses can be associated or lead to irreversible cardiac damage.
1. Zywiel MG, Brandt JM, Overgaard CB, Cheung AC, Turgeon TR, Syed KA. Fatal cardiomyopathy after revision total hip replacement for fracture of a ceramic liner. Bone Joint J. 2013;95(1):31-37.
2. Allen LA, Ambardekar AV, Devaraj KM, Maleszewski JJ, Wolfel EE. Clinical problem-solving. Missing elements of the history. N Engl J Med. 2014;370(6):559-566.
3. Hart AJ, Satchihananda K, Liddle AD, et al. Pseudotumors in association with well-functioning metal-on-metal hip prostheses: a case-control study using three-dimensional tomography and magnetic resonance imaging. J Bone Joint Surg Am. 2012;94(4);317-325.
4. Kwon MK, Jacobs JJ, MacDonald SJ, Potter HG, Fehring TK, Lombardi AV. Evidence-based understanding of management perils for metal-on-metal hip arthroplasty patients. J Arthroplasty. 2012;27(8 suppl):20-25.
5. Mao X, Wong AA, Crawford RW. Cobalt toxicity- -an emerging clinical problem in patients with metal-on-metal hip prostheses? Med J Aust. 2011;194(12):649-651.
6. Tower SS. Arthroprosthetic cobaltism: neurological and cardiac manifestations in two patients with metal-on-metal arthroplasty: a case report. J Bone Joint Surg Am. 2010;92(17):2847-2851.
7. Morin Y, Daniel P. Quebec beer-drinkers’ cardiomyopathy: etiological considerations. Can Med Assoc J. 1967;97(15):926-928.
8. Gilbert C, Cheung A, Butany J, et al. Hip pain and heart failure: the missing link. Can J Cardiol. 2013;29(5):639.e1-e2.
9. Seghizzi P, D’Adda F, Borleri D, Barbic F, Mosconi G. Cobalt myocardiopathy. A critical review of literature. Sci Total Environ. 1994;150(1-3):105-109.
Systemic cobalt toxicity has been reported in the literature after hip arthroplasty revisions for failed ceramic components secondary to third-body abrasive wear of cobalt-chrome (CoCr) components, as well as with metal-on-metal (MOM) hip arthroplasty designs. There have been several cases of systemic cobalt toxicity after revision for fractured ceramic components.1,2 Of these 7 reported cases, all patients had neurologic complaints and 4 patients developed cardiomyopathy secondary to toxic cobalt levels, with 1 case being fatal.1 MOM hip prostheses have also been associated with local and systemic problems secondary to metal debris. Adverse local tissue reactions have been reported to occur in up to 59% of patients, and, in some registries, the failure rate of MOM arthroplasty caused by these soft-tissue reactions is 2 to 3 times that of conventional metal-on-polyethylene design failures.3,4 The occurrence of systemic complications from MOM total hip arthroplasty (THA) wear debris is much less common. There have been 6 cases of systemic cobalt toxicity reported in the literature resulting from MOM total hip prosthesis design.1,2
We present a case of biopsy-confirmed cardiomyopathy secondary to cobalt toxicity from a MOM THA design with subsequent requirement for left ventricular assist device (LVAD) implantation despite prosthesis removal. To our knowledge, this is the first report in the literature of this specific implant design causing systemic cobalt toxicity. The patient provided written informed consent for print and electronic publication of this case report.
Case Report
The patient was a healthy nondiabetic man age 54 years who presented to our clinic 6 years after undergoing left THA and 5 years after undergoing right THA with the Biomet M2a-Magnum MOM prosthesis at an outside facility. The left-side components placed at the index procedure were a size 50 cup, 44 magnum head, 10 Taperloc stem (Biomet), and +9 neck. The right-side components were a size 52 cup, 46 magnum head, 10 Taperloc stem, and +3 neck. The patient emphasized that he was very happy with his hip prostheses and denied groin or thigh pain. His medical history was significant for exogenous obesity, and he denied any history of alcohol, tobacco, steroid, or recreational drug use.
The patient’s review of systems suggested that, approximately 11 months prior to presentation at our facility, he began having difficulty with his activities of daily living secondary to chest pressure with exertion, fatigue, and associated diaphoresis. He complained of decreased sensation in his feet bilaterally but denied any hearing loss, tinnitus, or vision changes. He underwent evaluation of the new-onset chest discomfort with a cardiac stress test that suggested no active cardiac ischemia. An echocardiogram revealed mitral regurgitation, stage II diastolic dysfunction with a left ventricular ejection fraction of 55%. Additionally, during this time period, the patient was being followed by his local orthopedic surgeon for an elevated cobalt level of 120 ppb and a chromium level of 109 ppb. The patient was referred to our clinic for recommendations regarding the elevated metal-ion levels. Upon initial evaluation, the patient denied any hip or groin pain. His physical examination revealed a nonantalgic gait with full range of motion and no signs of instability, tenderness, or masses. The patient was also noted to have no vibratory sensation in his feet bilaterally. The plain radiographs indicated bilateral MOM THA with acetabular inclination levels of 55º on the right and left sides. No cystic changes or other worrisome signs that would suggest implant loosening or failure were present (Figure 1). The serum metal levels were repeated and showed a cobalt level of 189 ppb and a chromium level of 71 ppb. Whole venous blood samples were drawn at our request using trace element tubes and were sent to Medtox Laboratories Inc. for analysis. Other pertinent laboratory values, including hematocrit and thyroid levels, were within normal limits. Because of concerns of systemic toxicity from significantly elevated cobalt and chromium levels, the patient elected to proceed with revision of the MOM components.
During the preoperative medical evaluation, the patient’s cardiac status was a concern, and the etiology of the cardiac dysfunction was unclear. Cardiac magnetic resonance imaging (MRI), which was performed to evaluate the extent and etiology of cardiac dysfunction, showed biventricular dysfunction. To evaluate the underlying myocardial tissue characteristics, delayed contrast imaging was performed and showed diffuse myocardial hyperenhancement of the anterior, lateral, and apical walls, with sparing of the base and midseptum. This type of extensive hyperenhancement is commonly seen with cardiac amyloidosis; however, the blood-pool kinetics during contrast administration is unusual for amyloidosis, as well as the diffuse edema noted on T2-weighted MRI. Importantly, cardiac MRI is very specific in excluding alternative diagnoses, such as postinfarct, infiltrative, acquired, viral, or alcoholic/drugs of abuse etiologies. In the absence of amyloidosis, the only other pattern that would be consistent with symptoms was diffuse, fulminant myocarditis of toxic origin lacking clinical evidence for an infectious origin. The patient’s prior exposure to cobalt was noted. Thus, the hyperenhancement and edema could be strong supportive evidence of cobalt infiltration, despite no reported cases in the literature of cobalt cardiomyopathy found on cardiac MRI.
Additional workup was initiated, and cardiac catheterization showed that the patient continued to decompensate, with worsening global left ventricular dysfunction with an ejection fraction of 30% without evidence of coronary artery disease. Also, he was noted to have mild renal impairment with a blood urea nitrogen level of 31 mg/dL and a creatinine level of 1.7 mg/dL. The etiology of the renal impairment was unknown and had not been established, according to the patient and his wife. The renal impairment was not thought to be caused by the elevated metal ions levels but likely resulted from prerenal azotemia secondary to decreased cardiac output. During catheterization, an endomyocardial biopsy was performed and the tissue sent to the Mayo Clinic pathology department for analysis. The sample showed myocyte hypertrophy and interstitial fibrosis with scattered myofibers containing large cytoplasmic vacuoles. Also present was karyomegaly consistent with myocyte hypertrophy (Figures 2A, 2B). Trichrome stain confirmed replacement of myofibers by collagen (Figure 2C). Electron microscopy performed on a paraffin block showed reduced contractile elements, vacuolar spaces, and increased lipofuscin. The findings were very consistent with, but not specific for, cardiomyopathy from cobalt toxicity. No evidence of an inflammatory infiltrate was identified. The diagnosis was cobalt cardiomyopathy based on biopsy, presentation, cobalt levels, and intraoperative findings.
The patient was admitted to the cardiac intensive care unit preoperatively and optimized with inotropic agents. A multidisciplinary consultation with the cardiology and anesthesia departments was obtained. Both recommended cardiac anesthesia with intraoperative Swan-Ganz catheter and transesophageal echo monitoring. Assuming that the patient remained hemodynamically stable with limited blood loss and the first hip was timely performed, the cardiology department recommended a single surgery, because fewer risks and complications could be expected than from a staged procedure. Subsequently, surgery was performed on the left hip via a conservative anterior approach on the fracture table. The patient remained stable with limited blood loss. During the same operating room time, revision of the right hip was performed using an anterior approach. The intraoperative findings showed evidence of pseudotumors in the adjacent soft tissues and abundant brown, creamy fluid upon entering the joint capsule, consistent with a metallic appearance. Both hips showed similar prosthetic findings. There was no significant visible wear of the large diameter metal heads or gross abnormality of the acetabular components. The trunnion area on both femoral implants was abnormal, revealing a black coating suggestive of marked corrosion. The components were all well fixed, without visible damage, and, because of his fragile cardiac status, the patient’s acetabular components were not revised. The trunnions were cleaned and the femoral heads were revised to active articulation dual-mobility metal-on-polyethylene constructs using 28-mm Biolox Option ceramic (CeramTec). The tissue specimens from the operation showed chronic inflammation with areas of fibroconnective tissue and bland fibrinoid necrosis with extensive brown pigment-laden macrophage reaction. The intraoperative cultures were negative.
The patient tolerated the surgery without complication, and his postoperative period was without incident. Nine months after surgery, the patient’s cobalt and chromium levels had declined to 16 ppb and 32 ppb, respectively (normal, <1 ppb). However, his cardiac status continued to worsen with significant shortness of breath and bilateral lower extremity edema despite diuresis. Follow-up cardiac MRI indicated progressive left and right dysfunction with ejection fractions of 23% and 25%, respectively. After progressive heart-failure symptoms, the patient was admitted to the hospital for severe congestive heart failure and underwent implantation of a HeartWare LVAD with tricuspid valve repair using an Edwards annuloplasty ring. He has since had a cardiac transplant and is doing well.
Discussion
To our knowledge, this is the first reported case of cardiomyopathy in a patient with elevated cobalt ion levels and a Biomet M2a-Magnum hip prosthesis. This is also the first reported case of cardiac MRI–defined cobalt cardiomyopathy. The cobalt levels seen in this patient were similar to those of other cases with systemic cobalt toxicity from a MOM hip construct. Mao and colleagues5 reported 2 cases of systemic cobalt toxicity in 2 patients with articular surface replacement hip prostheses.One patient presented with mild groin pain, neurologic symptoms, and a cobalt level of 410 ppb 5 years after her index procedure. The other patient presented with cardiac and neurologic symptoms but no hip complaints. The patient’s cobalt levels ranged from 185 ppb to 210 ppb. Both patients improved after their revision surgery, and their cobalt levels decreased. The 2 patients in Tower’s report6 were 49-year-old men who had articular surface replacement implants (DePuy). One patient who presented with progressive hip pain 11 months postoperatively developed neurologic symptoms and cardiomyopathy, with cobalt levels of 83 ppb before revision surgery 43 months after his index procedure. The other patient presented with hip pain and vertigo, headaches, fatigue, and dyspnea. He underwent hip revision 40 months postoperatively and required closed reduction under sedation for dislocation. Finally, and most recently, Allen and colleagues2 reported a 59-year-old woman with a cobalt level of 287 ppb whose symptoms did not resolve after implantation of an LVAD or cardiac transplantation but only after removal of her bilateral hip prosthesis. Our case is most similar to this report but significantly adds to the literature in 2 distinct manners: (1) Biomet M2a-Magnum has not been implicated in cobalt toxicity; and (2) this is the first reported use of dedicated cardiac MRI to noninvasively define underlying cardiac pathology.
The cardiac manifestations secondary to systemic cobalt toxicity in this patient represent a frightening consequence of MOM prosthetic wear. The effects of cobalt toxicity on cardiac tissues were first described in a series of alcoholic patients from Manchester in 1900;7 however, it was not until 1967, in a series of patients in Quebec, that cobalt was found to be the inciting factor. In the modern era, hip arthroplasty techniques resulting in excessive cobalt and chromium wear have demonstrated the same findings of myocyte hypertrophy, interstitial fibrosis, and scattered myofibers containing large cytoplasmic inclusions.8,9 The patient presented here has pathologic findings consistent with previous cases of cobalt cardiomyopathy; however, in the other cases of cardiomyopathy due to MOM total hip components, the patients’ cardiac conditions improved after the prostheses were revised and the cobalt levels began to diminish.5,6In our case, the patient has sustained permanent damage to his myocardium and a progressive decline in his cardiac status, which is a deviation from reported cases as of 2014.
While there is no guideline to unequivocally diagnose cobalt cardiomyopathy, the constellation of findings, including pathologic, biologic, blood levels, imaging, and surgical, all uniformly indicate a unifying diagnosis. The lack of improvement after prosthetic device removal supports a diagnosis of permanent myocardial damage, which is consistent with cardiomyopathy of advanced toxic etiology.
Conclusion
This case presents a patient with bilateral MOM THAs, acetabular cup inclinations of greater than 55º, renal impairment, and cobalt levels greater than 60 ppb, with occult cardiac failure leading to LVAD implantation as a prelude to cardiac transplantation in order to avoid certain death. These factors have been shown, in prior case reports, to be associated with cardiac damage that may be reversible.6 However; it is important for orthopedic surgeons to recognize that certain hip prostheses can be associated or lead to irreversible cardiac damage.
Systemic cobalt toxicity has been reported in the literature after hip arthroplasty revisions for failed ceramic components secondary to third-body abrasive wear of cobalt-chrome (CoCr) components, as well as with metal-on-metal (MOM) hip arthroplasty designs. There have been several cases of systemic cobalt toxicity after revision for fractured ceramic components.1,2 Of these 7 reported cases, all patients had neurologic complaints and 4 patients developed cardiomyopathy secondary to toxic cobalt levels, with 1 case being fatal.1 MOM hip prostheses have also been associated with local and systemic problems secondary to metal debris. Adverse local tissue reactions have been reported to occur in up to 59% of patients, and, in some registries, the failure rate of MOM arthroplasty caused by these soft-tissue reactions is 2 to 3 times that of conventional metal-on-polyethylene design failures.3,4 The occurrence of systemic complications from MOM total hip arthroplasty (THA) wear debris is much less common. There have been 6 cases of systemic cobalt toxicity reported in the literature resulting from MOM total hip prosthesis design.1,2
We present a case of biopsy-confirmed cardiomyopathy secondary to cobalt toxicity from a MOM THA design with subsequent requirement for left ventricular assist device (LVAD) implantation despite prosthesis removal. To our knowledge, this is the first report in the literature of this specific implant design causing systemic cobalt toxicity. The patient provided written informed consent for print and electronic publication of this case report.
Case Report
The patient was a healthy nondiabetic man age 54 years who presented to our clinic 6 years after undergoing left THA and 5 years after undergoing right THA with the Biomet M2a-Magnum MOM prosthesis at an outside facility. The left-side components placed at the index procedure were a size 50 cup, 44 magnum head, 10 Taperloc stem (Biomet), and +9 neck. The right-side components were a size 52 cup, 46 magnum head, 10 Taperloc stem, and +3 neck. The patient emphasized that he was very happy with his hip prostheses and denied groin or thigh pain. His medical history was significant for exogenous obesity, and he denied any history of alcohol, tobacco, steroid, or recreational drug use.
The patient’s review of systems suggested that, approximately 11 months prior to presentation at our facility, he began having difficulty with his activities of daily living secondary to chest pressure with exertion, fatigue, and associated diaphoresis. He complained of decreased sensation in his feet bilaterally but denied any hearing loss, tinnitus, or vision changes. He underwent evaluation of the new-onset chest discomfort with a cardiac stress test that suggested no active cardiac ischemia. An echocardiogram revealed mitral regurgitation, stage II diastolic dysfunction with a left ventricular ejection fraction of 55%. Additionally, during this time period, the patient was being followed by his local orthopedic surgeon for an elevated cobalt level of 120 ppb and a chromium level of 109 ppb. The patient was referred to our clinic for recommendations regarding the elevated metal-ion levels. Upon initial evaluation, the patient denied any hip or groin pain. His physical examination revealed a nonantalgic gait with full range of motion and no signs of instability, tenderness, or masses. The patient was also noted to have no vibratory sensation in his feet bilaterally. The plain radiographs indicated bilateral MOM THA with acetabular inclination levels of 55º on the right and left sides. No cystic changes or other worrisome signs that would suggest implant loosening or failure were present (Figure 1). The serum metal levels were repeated and showed a cobalt level of 189 ppb and a chromium level of 71 ppb. Whole venous blood samples were drawn at our request using trace element tubes and were sent to Medtox Laboratories Inc. for analysis. Other pertinent laboratory values, including hematocrit and thyroid levels, were within normal limits. Because of concerns of systemic toxicity from significantly elevated cobalt and chromium levels, the patient elected to proceed with revision of the MOM components.
During the preoperative medical evaluation, the patient’s cardiac status was a concern, and the etiology of the cardiac dysfunction was unclear. Cardiac magnetic resonance imaging (MRI), which was performed to evaluate the extent and etiology of cardiac dysfunction, showed biventricular dysfunction. To evaluate the underlying myocardial tissue characteristics, delayed contrast imaging was performed and showed diffuse myocardial hyperenhancement of the anterior, lateral, and apical walls, with sparing of the base and midseptum. This type of extensive hyperenhancement is commonly seen with cardiac amyloidosis; however, the blood-pool kinetics during contrast administration is unusual for amyloidosis, as well as the diffuse edema noted on T2-weighted MRI. Importantly, cardiac MRI is very specific in excluding alternative diagnoses, such as postinfarct, infiltrative, acquired, viral, or alcoholic/drugs of abuse etiologies. In the absence of amyloidosis, the only other pattern that would be consistent with symptoms was diffuse, fulminant myocarditis of toxic origin lacking clinical evidence for an infectious origin. The patient’s prior exposure to cobalt was noted. Thus, the hyperenhancement and edema could be strong supportive evidence of cobalt infiltration, despite no reported cases in the literature of cobalt cardiomyopathy found on cardiac MRI.
Additional workup was initiated, and cardiac catheterization showed that the patient continued to decompensate, with worsening global left ventricular dysfunction with an ejection fraction of 30% without evidence of coronary artery disease. Also, he was noted to have mild renal impairment with a blood urea nitrogen level of 31 mg/dL and a creatinine level of 1.7 mg/dL. The etiology of the renal impairment was unknown and had not been established, according to the patient and his wife. The renal impairment was not thought to be caused by the elevated metal ions levels but likely resulted from prerenal azotemia secondary to decreased cardiac output. During catheterization, an endomyocardial biopsy was performed and the tissue sent to the Mayo Clinic pathology department for analysis. The sample showed myocyte hypertrophy and interstitial fibrosis with scattered myofibers containing large cytoplasmic vacuoles. Also present was karyomegaly consistent with myocyte hypertrophy (Figures 2A, 2B). Trichrome stain confirmed replacement of myofibers by collagen (Figure 2C). Electron microscopy performed on a paraffin block showed reduced contractile elements, vacuolar spaces, and increased lipofuscin. The findings were very consistent with, but not specific for, cardiomyopathy from cobalt toxicity. No evidence of an inflammatory infiltrate was identified. The diagnosis was cobalt cardiomyopathy based on biopsy, presentation, cobalt levels, and intraoperative findings.
The patient was admitted to the cardiac intensive care unit preoperatively and optimized with inotropic agents. A multidisciplinary consultation with the cardiology and anesthesia departments was obtained. Both recommended cardiac anesthesia with intraoperative Swan-Ganz catheter and transesophageal echo monitoring. Assuming that the patient remained hemodynamically stable with limited blood loss and the first hip was timely performed, the cardiology department recommended a single surgery, because fewer risks and complications could be expected than from a staged procedure. Subsequently, surgery was performed on the left hip via a conservative anterior approach on the fracture table. The patient remained stable with limited blood loss. During the same operating room time, revision of the right hip was performed using an anterior approach. The intraoperative findings showed evidence of pseudotumors in the adjacent soft tissues and abundant brown, creamy fluid upon entering the joint capsule, consistent with a metallic appearance. Both hips showed similar prosthetic findings. There was no significant visible wear of the large diameter metal heads or gross abnormality of the acetabular components. The trunnion area on both femoral implants was abnormal, revealing a black coating suggestive of marked corrosion. The components were all well fixed, without visible damage, and, because of his fragile cardiac status, the patient’s acetabular components were not revised. The trunnions were cleaned and the femoral heads were revised to active articulation dual-mobility metal-on-polyethylene constructs using 28-mm Biolox Option ceramic (CeramTec). The tissue specimens from the operation showed chronic inflammation with areas of fibroconnective tissue and bland fibrinoid necrosis with extensive brown pigment-laden macrophage reaction. The intraoperative cultures were negative.
The patient tolerated the surgery without complication, and his postoperative period was without incident. Nine months after surgery, the patient’s cobalt and chromium levels had declined to 16 ppb and 32 ppb, respectively (normal, <1 ppb). However, his cardiac status continued to worsen with significant shortness of breath and bilateral lower extremity edema despite diuresis. Follow-up cardiac MRI indicated progressive left and right dysfunction with ejection fractions of 23% and 25%, respectively. After progressive heart-failure symptoms, the patient was admitted to the hospital for severe congestive heart failure and underwent implantation of a HeartWare LVAD with tricuspid valve repair using an Edwards annuloplasty ring. He has since had a cardiac transplant and is doing well.
Discussion
To our knowledge, this is the first reported case of cardiomyopathy in a patient with elevated cobalt ion levels and a Biomet M2a-Magnum hip prosthesis. This is also the first reported case of cardiac MRI–defined cobalt cardiomyopathy. The cobalt levels seen in this patient were similar to those of other cases with systemic cobalt toxicity from a MOM hip construct. Mao and colleagues5 reported 2 cases of systemic cobalt toxicity in 2 patients with articular surface replacement hip prostheses.One patient presented with mild groin pain, neurologic symptoms, and a cobalt level of 410 ppb 5 years after her index procedure. The other patient presented with cardiac and neurologic symptoms but no hip complaints. The patient’s cobalt levels ranged from 185 ppb to 210 ppb. Both patients improved after their revision surgery, and their cobalt levels decreased. The 2 patients in Tower’s report6 were 49-year-old men who had articular surface replacement implants (DePuy). One patient who presented with progressive hip pain 11 months postoperatively developed neurologic symptoms and cardiomyopathy, with cobalt levels of 83 ppb before revision surgery 43 months after his index procedure. The other patient presented with hip pain and vertigo, headaches, fatigue, and dyspnea. He underwent hip revision 40 months postoperatively and required closed reduction under sedation for dislocation. Finally, and most recently, Allen and colleagues2 reported a 59-year-old woman with a cobalt level of 287 ppb whose symptoms did not resolve after implantation of an LVAD or cardiac transplantation but only after removal of her bilateral hip prosthesis. Our case is most similar to this report but significantly adds to the literature in 2 distinct manners: (1) Biomet M2a-Magnum has not been implicated in cobalt toxicity; and (2) this is the first reported use of dedicated cardiac MRI to noninvasively define underlying cardiac pathology.
The cardiac manifestations secondary to systemic cobalt toxicity in this patient represent a frightening consequence of MOM prosthetic wear. The effects of cobalt toxicity on cardiac tissues were first described in a series of alcoholic patients from Manchester in 1900;7 however, it was not until 1967, in a series of patients in Quebec, that cobalt was found to be the inciting factor. In the modern era, hip arthroplasty techniques resulting in excessive cobalt and chromium wear have demonstrated the same findings of myocyte hypertrophy, interstitial fibrosis, and scattered myofibers containing large cytoplasmic inclusions.8,9 The patient presented here has pathologic findings consistent with previous cases of cobalt cardiomyopathy; however, in the other cases of cardiomyopathy due to MOM total hip components, the patients’ cardiac conditions improved after the prostheses were revised and the cobalt levels began to diminish.5,6In our case, the patient has sustained permanent damage to his myocardium and a progressive decline in his cardiac status, which is a deviation from reported cases as of 2014.
While there is no guideline to unequivocally diagnose cobalt cardiomyopathy, the constellation of findings, including pathologic, biologic, blood levels, imaging, and surgical, all uniformly indicate a unifying diagnosis. The lack of improvement after prosthetic device removal supports a diagnosis of permanent myocardial damage, which is consistent with cardiomyopathy of advanced toxic etiology.
Conclusion
This case presents a patient with bilateral MOM THAs, acetabular cup inclinations of greater than 55º, renal impairment, and cobalt levels greater than 60 ppb, with occult cardiac failure leading to LVAD implantation as a prelude to cardiac transplantation in order to avoid certain death. These factors have been shown, in prior case reports, to be associated with cardiac damage that may be reversible.6 However; it is important for orthopedic surgeons to recognize that certain hip prostheses can be associated or lead to irreversible cardiac damage.
1. Zywiel MG, Brandt JM, Overgaard CB, Cheung AC, Turgeon TR, Syed KA. Fatal cardiomyopathy after revision total hip replacement for fracture of a ceramic liner. Bone Joint J. 2013;95(1):31-37.
2. Allen LA, Ambardekar AV, Devaraj KM, Maleszewski JJ, Wolfel EE. Clinical problem-solving. Missing elements of the history. N Engl J Med. 2014;370(6):559-566.
3. Hart AJ, Satchihananda K, Liddle AD, et al. Pseudotumors in association with well-functioning metal-on-metal hip prostheses: a case-control study using three-dimensional tomography and magnetic resonance imaging. J Bone Joint Surg Am. 2012;94(4);317-325.
4. Kwon MK, Jacobs JJ, MacDonald SJ, Potter HG, Fehring TK, Lombardi AV. Evidence-based understanding of management perils for metal-on-metal hip arthroplasty patients. J Arthroplasty. 2012;27(8 suppl):20-25.
5. Mao X, Wong AA, Crawford RW. Cobalt toxicity- -an emerging clinical problem in patients with metal-on-metal hip prostheses? Med J Aust. 2011;194(12):649-651.
6. Tower SS. Arthroprosthetic cobaltism: neurological and cardiac manifestations in two patients with metal-on-metal arthroplasty: a case report. J Bone Joint Surg Am. 2010;92(17):2847-2851.
7. Morin Y, Daniel P. Quebec beer-drinkers’ cardiomyopathy: etiological considerations. Can Med Assoc J. 1967;97(15):926-928.
8. Gilbert C, Cheung A, Butany J, et al. Hip pain and heart failure: the missing link. Can J Cardiol. 2013;29(5):639.e1-e2.
9. Seghizzi P, D’Adda F, Borleri D, Barbic F, Mosconi G. Cobalt myocardiopathy. A critical review of literature. Sci Total Environ. 1994;150(1-3):105-109.
1. Zywiel MG, Brandt JM, Overgaard CB, Cheung AC, Turgeon TR, Syed KA. Fatal cardiomyopathy after revision total hip replacement for fracture of a ceramic liner. Bone Joint J. 2013;95(1):31-37.
2. Allen LA, Ambardekar AV, Devaraj KM, Maleszewski JJ, Wolfel EE. Clinical problem-solving. Missing elements of the history. N Engl J Med. 2014;370(6):559-566.
3. Hart AJ, Satchihananda K, Liddle AD, et al. Pseudotumors in association with well-functioning metal-on-metal hip prostheses: a case-control study using three-dimensional tomography and magnetic resonance imaging. J Bone Joint Surg Am. 2012;94(4);317-325.
4. Kwon MK, Jacobs JJ, MacDonald SJ, Potter HG, Fehring TK, Lombardi AV. Evidence-based understanding of management perils for metal-on-metal hip arthroplasty patients. J Arthroplasty. 2012;27(8 suppl):20-25.
5. Mao X, Wong AA, Crawford RW. Cobalt toxicity- -an emerging clinical problem in patients with metal-on-metal hip prostheses? Med J Aust. 2011;194(12):649-651.
6. Tower SS. Arthroprosthetic cobaltism: neurological and cardiac manifestations in two patients with metal-on-metal arthroplasty: a case report. J Bone Joint Surg Am. 2010;92(17):2847-2851.
7. Morin Y, Daniel P. Quebec beer-drinkers’ cardiomyopathy: etiological considerations. Can Med Assoc J. 1967;97(15):926-928.
8. Gilbert C, Cheung A, Butany J, et al. Hip pain and heart failure: the missing link. Can J Cardiol. 2013;29(5):639.e1-e2.
9. Seghizzi P, D’Adda F, Borleri D, Barbic F, Mosconi G. Cobalt myocardiopathy. A critical review of literature. Sci Total Environ. 1994;150(1-3):105-109.