User login
MDedge latest news is breaking news from medical conferences, journals, guidelines, the FDA and CDC.
Most US Adults Plan to Skip Annual COVID Vaccines
Most US adults continue to plan on skipping an annual COVID vaccine.
according to results of a new survey from the Pew Research Center.
When asked why people wouldn’t get an updated COVID vaccine, 61% said a major reason was that they don’t think they need it, and 60% said a major reason is that they are concerned about side effects. Cost was a factor for 14% of people, and 46% of people said they don’t get vaccines in general.
There were some differences in intention to get vaccinated based on a person’s age. Among people ages 65 and older, 27% said they had already gotten the vaccine, and another 27% said they probably will get the shot, leaving 45% who said they probably won’t roll up their sleeves. People ages 30-49 years old were the least likely to plan on getting a COVID shot – 66% said they probably won’t get one.
Public health officials say everyone should get an annual COVID vaccine, just as they should get a flu shot, because the vaccines are formulated each year to target virus strains predicted to be in wide circulation. Also, immunity – either from past vaccination or past infection – wanes over time.
Research shows that the vaccines reduce the likelihood of hospitalization or death caused by severe illness, particularly among people who have risk factors, like being over age 65 or having health issues that are becoming increasingly common in the United States, like diabetes, heart problems, and lung conditions.
The survey included 9,593 adults who were asked about their COVID vaccine intentions with this question: “Public health officials recently recommended an updated vaccine for COVID-19. Do you think you will probably get an updated vaccine, probably not get an updated vaccine, or have you already received an updated vaccine?” The survey was done online and by telephone from October 21 to October 27.
So far in 2024, the CDC’s ongoing immunization survey shows that 17% of adults say that, as of November 2, they have gotten vaccinated for COVID-19 this season, and 14% said they will definitely get vaccinated. The Pew Research Center survey found that 15% of people said they’ve already gotten the shot this season.
Reports of positive COVID tests, emergency room visits, and hospitalizations remain very low. About 3.6% of test results shared with the CDC were positive for COVID the week ending November 9. Less than 1% of ER visits involve a COVID diagnosis, and hospitalizations are well below the rate seen at this time last year. Last year, COVID activity in the United States began rising around Thanksgiving and continued upward, peaking in early January.
The protection from a COVID-19 vaccination usually fully kicks in about 2 weeks after you get the shot, and the vaccines are most effective for the following 3 months.
A version of this article first appeared on WebMD.com.
Most US adults continue to plan on skipping an annual COVID vaccine.
according to results of a new survey from the Pew Research Center.
When asked why people wouldn’t get an updated COVID vaccine, 61% said a major reason was that they don’t think they need it, and 60% said a major reason is that they are concerned about side effects. Cost was a factor for 14% of people, and 46% of people said they don’t get vaccines in general.
There were some differences in intention to get vaccinated based on a person’s age. Among people ages 65 and older, 27% said they had already gotten the vaccine, and another 27% said they probably will get the shot, leaving 45% who said they probably won’t roll up their sleeves. People ages 30-49 years old were the least likely to plan on getting a COVID shot – 66% said they probably won’t get one.
Public health officials say everyone should get an annual COVID vaccine, just as they should get a flu shot, because the vaccines are formulated each year to target virus strains predicted to be in wide circulation. Also, immunity – either from past vaccination or past infection – wanes over time.
Research shows that the vaccines reduce the likelihood of hospitalization or death caused by severe illness, particularly among people who have risk factors, like being over age 65 or having health issues that are becoming increasingly common in the United States, like diabetes, heart problems, and lung conditions.
The survey included 9,593 adults who were asked about their COVID vaccine intentions with this question: “Public health officials recently recommended an updated vaccine for COVID-19. Do you think you will probably get an updated vaccine, probably not get an updated vaccine, or have you already received an updated vaccine?” The survey was done online and by telephone from October 21 to October 27.
So far in 2024, the CDC’s ongoing immunization survey shows that 17% of adults say that, as of November 2, they have gotten vaccinated for COVID-19 this season, and 14% said they will definitely get vaccinated. The Pew Research Center survey found that 15% of people said they’ve already gotten the shot this season.
Reports of positive COVID tests, emergency room visits, and hospitalizations remain very low. About 3.6% of test results shared with the CDC were positive for COVID the week ending November 9. Less than 1% of ER visits involve a COVID diagnosis, and hospitalizations are well below the rate seen at this time last year. Last year, COVID activity in the United States began rising around Thanksgiving and continued upward, peaking in early January.
The protection from a COVID-19 vaccination usually fully kicks in about 2 weeks after you get the shot, and the vaccines are most effective for the following 3 months.
A version of this article first appeared on WebMD.com.
Most US adults continue to plan on skipping an annual COVID vaccine.
according to results of a new survey from the Pew Research Center.
When asked why people wouldn’t get an updated COVID vaccine, 61% said a major reason was that they don’t think they need it, and 60% said a major reason is that they are concerned about side effects. Cost was a factor for 14% of people, and 46% of people said they don’t get vaccines in general.
There were some differences in intention to get vaccinated based on a person’s age. Among people ages 65 and older, 27% said they had already gotten the vaccine, and another 27% said they probably will get the shot, leaving 45% who said they probably won’t roll up their sleeves. People ages 30-49 years old were the least likely to plan on getting a COVID shot – 66% said they probably won’t get one.
Public health officials say everyone should get an annual COVID vaccine, just as they should get a flu shot, because the vaccines are formulated each year to target virus strains predicted to be in wide circulation. Also, immunity – either from past vaccination or past infection – wanes over time.
Research shows that the vaccines reduce the likelihood of hospitalization or death caused by severe illness, particularly among people who have risk factors, like being over age 65 or having health issues that are becoming increasingly common in the United States, like diabetes, heart problems, and lung conditions.
The survey included 9,593 adults who were asked about their COVID vaccine intentions with this question: “Public health officials recently recommended an updated vaccine for COVID-19. Do you think you will probably get an updated vaccine, probably not get an updated vaccine, or have you already received an updated vaccine?” The survey was done online and by telephone from October 21 to October 27.
So far in 2024, the CDC’s ongoing immunization survey shows that 17% of adults say that, as of November 2, they have gotten vaccinated for COVID-19 this season, and 14% said they will definitely get vaccinated. The Pew Research Center survey found that 15% of people said they’ve already gotten the shot this season.
Reports of positive COVID tests, emergency room visits, and hospitalizations remain very low. About 3.6% of test results shared with the CDC were positive for COVID the week ending November 9. Less than 1% of ER visits involve a COVID diagnosis, and hospitalizations are well below the rate seen at this time last year. Last year, COVID activity in the United States began rising around Thanksgiving and continued upward, peaking in early January.
The protection from a COVID-19 vaccination usually fully kicks in about 2 weeks after you get the shot, and the vaccines are most effective for the following 3 months.
A version of this article first appeared on WebMD.com.
Pertussis Cases Spike in November
Six times as many cases of pertussis were reported in the United States for the week ending November 16, 2024, as the same week in 2023, according to new data from the Centers for Disease Control and Prevention (CDC).
Of the 434 cases reported for the week ending November 16, 2024, a majority (109) occurred in the East North Central region, mostly in Ohio (93). Another 70 cases occurred in the West North Central region, with 32 cases and 37 cases in Missouri and Nebraska, respectively.
None of the 75 cases in the Middle Atlantic region occurred in New Jersey or New York City; 38 were reported elsewhere in New York, and 37 in Pennsylvania. The South Atlantic region reported 55 cases, including 29 in Florida. The East South Central and West South Central regions reported 11 and 20 cases, respectively. The Mountain and Pacific regions reported 31 (20 in Arizona) and 47 (20 in Washington State) cases, respectively.
The CDC tracks pertussis cases through a national surveillance system, but many cases are likely unrecognized and unreported, according to the CDC.
Although vaccines for pertussis (whooping cough) provide protection, their effectiveness decreases over time, and the CDC expects rates to increase in vaccinated and unvaccinated populations as case levels rebound with the lifting of pandemic mitigation strategies such as masking and remote learning.
Recent CDC data reported by Medscape Medical News showed an association between lower vaccination rates and 2024’s uptick in pertussis cases.
A version of this article first appeared on Medscape.com.
Six times as many cases of pertussis were reported in the United States for the week ending November 16, 2024, as the same week in 2023, according to new data from the Centers for Disease Control and Prevention (CDC).
Of the 434 cases reported for the week ending November 16, 2024, a majority (109) occurred in the East North Central region, mostly in Ohio (93). Another 70 cases occurred in the West North Central region, with 32 cases and 37 cases in Missouri and Nebraska, respectively.
None of the 75 cases in the Middle Atlantic region occurred in New Jersey or New York City; 38 were reported elsewhere in New York, and 37 in Pennsylvania. The South Atlantic region reported 55 cases, including 29 in Florida. The East South Central and West South Central regions reported 11 and 20 cases, respectively. The Mountain and Pacific regions reported 31 (20 in Arizona) and 47 (20 in Washington State) cases, respectively.
The CDC tracks pertussis cases through a national surveillance system, but many cases are likely unrecognized and unreported, according to the CDC.
Although vaccines for pertussis (whooping cough) provide protection, their effectiveness decreases over time, and the CDC expects rates to increase in vaccinated and unvaccinated populations as case levels rebound with the lifting of pandemic mitigation strategies such as masking and remote learning.
Recent CDC data reported by Medscape Medical News showed an association between lower vaccination rates and 2024’s uptick in pertussis cases.
A version of this article first appeared on Medscape.com.
Six times as many cases of pertussis were reported in the United States for the week ending November 16, 2024, as the same week in 2023, according to new data from the Centers for Disease Control and Prevention (CDC).
Of the 434 cases reported for the week ending November 16, 2024, a majority (109) occurred in the East North Central region, mostly in Ohio (93). Another 70 cases occurred in the West North Central region, with 32 cases and 37 cases in Missouri and Nebraska, respectively.
None of the 75 cases in the Middle Atlantic region occurred in New Jersey or New York City; 38 were reported elsewhere in New York, and 37 in Pennsylvania. The South Atlantic region reported 55 cases, including 29 in Florida. The East South Central and West South Central regions reported 11 and 20 cases, respectively. The Mountain and Pacific regions reported 31 (20 in Arizona) and 47 (20 in Washington State) cases, respectively.
The CDC tracks pertussis cases through a national surveillance system, but many cases are likely unrecognized and unreported, according to the CDC.
Although vaccines for pertussis (whooping cough) provide protection, their effectiveness decreases over time, and the CDC expects rates to increase in vaccinated and unvaccinated populations as case levels rebound with the lifting of pandemic mitigation strategies such as masking and remote learning.
Recent CDC data reported by Medscape Medical News showed an association between lower vaccination rates and 2024’s uptick in pertussis cases.
A version of this article first appeared on Medscape.com.
BCG Vaccine May Protect Against Long COVID Symptoms
TOPLINE:
METHODOLOGY:
- A phase 3 clinical trial initiated in early 2020 investigated the effect of the BCG vaccine injected during active infection on COVID-19 progression in adults with mild or moderate COVID-19. The current study summarizes the 6- and 12-month follow-up data with a focus on long-COVID symptoms.
- Patients who tested positive for severe acute respiratory syndrome coronavirus 2 were randomly assigned to receive either 0.1 mL of intradermal BCG (n = 191) or 0.9% saline placebo (n = 202) within 14 days of symptom onset and were followed up at 7, 14, 21, and 45 days and at 6 and 12 months postinjection.
- Overall, 157 BCG (median age, 40 years; 54.1% women) and 142 placebo (median age, 41 years; 65.5% women) recipients completed the 6-month follow-up, and 97 BCG (median age, 37 years; 49.5% women) and 95 placebo (median age, 40 years; 67.4% women) recipients completed the 12-month follow-up.
- The researchers primarily assessed the effect of the BCG vaccine on the development of the symptoms of long COVID at 6 and 12 months.
TAKEAWAY:
- Hearing problems were less frequent among BCG recipients at 6 months compared with those who received placebo (odds ratio [OR], 0.26; 95% CI, 0.045-1.0; P = .044).
- At 12 months, participants who received the BCG vaccine exhibited fewer issues with sleeping (P = .027), concentration (P = .009), memory (P = .009), and vision (P = .022) along with a lower long-COVID score (one-sided Wilcoxon test, P = .002) than those who received placebo.
- At 6 months, BCG demonstrated a sex-specific paradoxical effect on hair loss, decreasing it in men (P = .031), while causing a slight, though statistically nonsignificant, increase in women.
- Male sex was the strongest predictive factor for long COVID, cognitive dysfunction, and cardiopulmonary scores at both follow-up assessments.
IN PRACTICE:
“[The study] findings suggest that BCG immunotherapy for an existing ailment may be superior to prophylaxis in healthy individuals,” the authors wrote.
SOURCE:
The study was led by Mehrsa Jalalizadeh and Keini Buosi, UroScience, State University of Campinas, Unicamp, São Paulo, Brazil. It was published online on November 19, 2024, in the Journal of Internal Medicine.
LIMITATIONS:
Previous mycobacterial exposure was not tested among the study participants. A notable loss to follow-up, particularly at 12 months, may have introduced bias into the results.
DISCLOSURES:
The study was supported by the Coordination for the Improvement of Higher Education Personnel, Federal Government of Brazil, the General Coordination of the National Immunization Program, Ministry of Health (Brazil), and the National Council for Scientific and Technological Development-Research Productivity. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- A phase 3 clinical trial initiated in early 2020 investigated the effect of the BCG vaccine injected during active infection on COVID-19 progression in adults with mild or moderate COVID-19. The current study summarizes the 6- and 12-month follow-up data with a focus on long-COVID symptoms.
- Patients who tested positive for severe acute respiratory syndrome coronavirus 2 were randomly assigned to receive either 0.1 mL of intradermal BCG (n = 191) or 0.9% saline placebo (n = 202) within 14 days of symptom onset and were followed up at 7, 14, 21, and 45 days and at 6 and 12 months postinjection.
- Overall, 157 BCG (median age, 40 years; 54.1% women) and 142 placebo (median age, 41 years; 65.5% women) recipients completed the 6-month follow-up, and 97 BCG (median age, 37 years; 49.5% women) and 95 placebo (median age, 40 years; 67.4% women) recipients completed the 12-month follow-up.
- The researchers primarily assessed the effect of the BCG vaccine on the development of the symptoms of long COVID at 6 and 12 months.
TAKEAWAY:
- Hearing problems were less frequent among BCG recipients at 6 months compared with those who received placebo (odds ratio [OR], 0.26; 95% CI, 0.045-1.0; P = .044).
- At 12 months, participants who received the BCG vaccine exhibited fewer issues with sleeping (P = .027), concentration (P = .009), memory (P = .009), and vision (P = .022) along with a lower long-COVID score (one-sided Wilcoxon test, P = .002) than those who received placebo.
- At 6 months, BCG demonstrated a sex-specific paradoxical effect on hair loss, decreasing it in men (P = .031), while causing a slight, though statistically nonsignificant, increase in women.
- Male sex was the strongest predictive factor for long COVID, cognitive dysfunction, and cardiopulmonary scores at both follow-up assessments.
IN PRACTICE:
“[The study] findings suggest that BCG immunotherapy for an existing ailment may be superior to prophylaxis in healthy individuals,” the authors wrote.
SOURCE:
The study was led by Mehrsa Jalalizadeh and Keini Buosi, UroScience, State University of Campinas, Unicamp, São Paulo, Brazil. It was published online on November 19, 2024, in the Journal of Internal Medicine.
LIMITATIONS:
Previous mycobacterial exposure was not tested among the study participants. A notable loss to follow-up, particularly at 12 months, may have introduced bias into the results.
DISCLOSURES:
The study was supported by the Coordination for the Improvement of Higher Education Personnel, Federal Government of Brazil, the General Coordination of the National Immunization Program, Ministry of Health (Brazil), and the National Council for Scientific and Technological Development-Research Productivity. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- A phase 3 clinical trial initiated in early 2020 investigated the effect of the BCG vaccine injected during active infection on COVID-19 progression in adults with mild or moderate COVID-19. The current study summarizes the 6- and 12-month follow-up data with a focus on long-COVID symptoms.
- Patients who tested positive for severe acute respiratory syndrome coronavirus 2 were randomly assigned to receive either 0.1 mL of intradermal BCG (n = 191) or 0.9% saline placebo (n = 202) within 14 days of symptom onset and were followed up at 7, 14, 21, and 45 days and at 6 and 12 months postinjection.
- Overall, 157 BCG (median age, 40 years; 54.1% women) and 142 placebo (median age, 41 years; 65.5% women) recipients completed the 6-month follow-up, and 97 BCG (median age, 37 years; 49.5% women) and 95 placebo (median age, 40 years; 67.4% women) recipients completed the 12-month follow-up.
- The researchers primarily assessed the effect of the BCG vaccine on the development of the symptoms of long COVID at 6 and 12 months.
TAKEAWAY:
- Hearing problems were less frequent among BCG recipients at 6 months compared with those who received placebo (odds ratio [OR], 0.26; 95% CI, 0.045-1.0; P = .044).
- At 12 months, participants who received the BCG vaccine exhibited fewer issues with sleeping (P = .027), concentration (P = .009), memory (P = .009), and vision (P = .022) along with a lower long-COVID score (one-sided Wilcoxon test, P = .002) than those who received placebo.
- At 6 months, BCG demonstrated a sex-specific paradoxical effect on hair loss, decreasing it in men (P = .031), while causing a slight, though statistically nonsignificant, increase in women.
- Male sex was the strongest predictive factor for long COVID, cognitive dysfunction, and cardiopulmonary scores at both follow-up assessments.
IN PRACTICE:
“[The study] findings suggest that BCG immunotherapy for an existing ailment may be superior to prophylaxis in healthy individuals,” the authors wrote.
SOURCE:
The study was led by Mehrsa Jalalizadeh and Keini Buosi, UroScience, State University of Campinas, Unicamp, São Paulo, Brazil. It was published online on November 19, 2024, in the Journal of Internal Medicine.
LIMITATIONS:
Previous mycobacterial exposure was not tested among the study participants. A notable loss to follow-up, particularly at 12 months, may have introduced bias into the results.
DISCLOSURES:
The study was supported by the Coordination for the Improvement of Higher Education Personnel, Federal Government of Brazil, the General Coordination of the National Immunization Program, Ministry of Health (Brazil), and the National Council for Scientific and Technological Development-Research Productivity. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
How Metals Affect the Brain
This transcript has been edited for clarity.
It has always amazed me that our bodies require these tiny amounts of incredibly rare substances to function. Sure, we need oxygen. We need water. But we also need molybdenum, which makes up just 1.2 parts per million of the Earth’s crust.
Without adequate molybdenum intake, we develop seizures, developmental delays, death. Fortunately, we need so little molybdenum that true molybdenum deficiency is incredibly rare — seen only in people on total parenteral nutrition without supplementation or those with certain rare genetic conditions. But still, molybdenum is necessary for life.
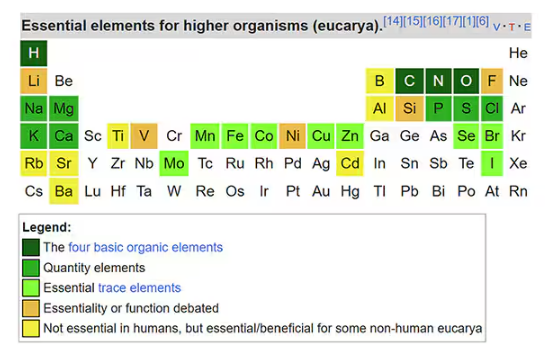
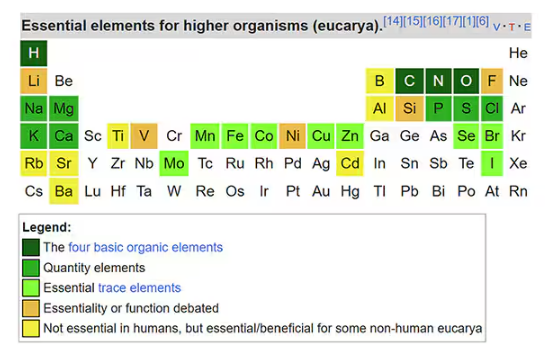
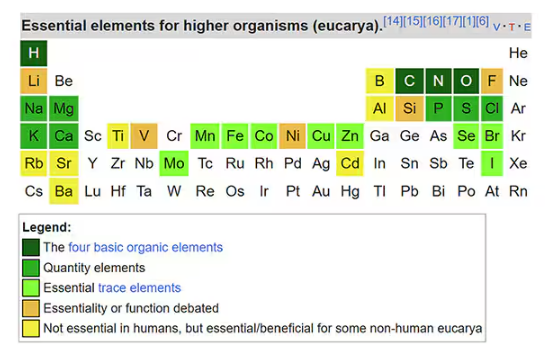
Many metals are. Figure 1 colors the essential minerals on the periodic table. You can see that to stay alive, we humans need not only things like sodium, but selenium, bromine, zinc, copper, and cobalt.
Some metals are very clearly not essential; we can all do without lead and mercury, and probably should.
But just because something is essential for life does not mean that more is better. The dose is the poison, as they say. And this week, we explore whether metals — even essential metals — might be adversely affecting our brains.
It’s not a stretch to think that metal intake could have weird effects on our nervous system. Lead exposure, primarily due to leaded gasoline, has been blamed for an average reduction of about 3 points in our national IQ, for example . But not all metals are created equal. Researchers set out to find out which might be more strongly associated with performance on cognitive tests and dementia, and reported their results in this study in JAMA Network Open.
To do this, they leveraged the MESA cohort study. This is a longitudinal study of a relatively diverse group of 6300 adults who were enrolled from 2000 to 2002 around the United States. At enrollment, they gave a urine sample and took a variety of cognitive tests. Important for this study was the digit symbol substitution test, where participants are provided a code and need to replace a list of numbers with symbols as per that code. Performance on this test worsens with age, depression, and cognitive impairment.
Participants were followed for more than a decade, and over that time, 559 (about 9%) were diagnosed with dementia.
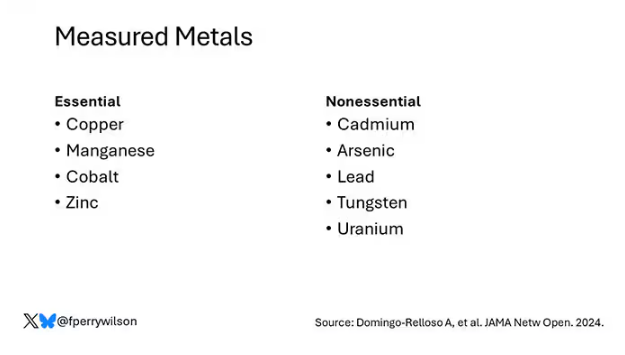
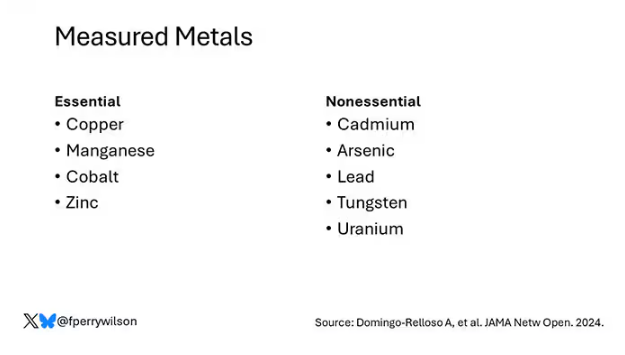
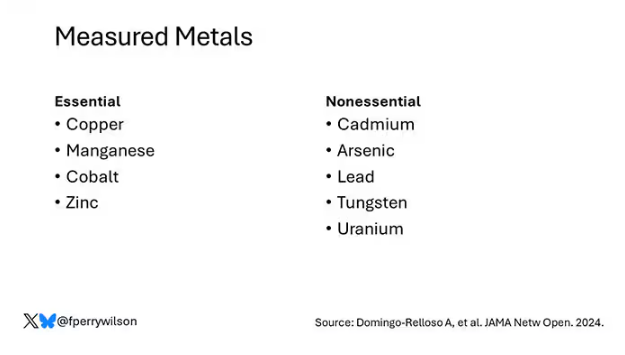
Those baseline urine samples were assayed for a variety of metals — some essential, some very much not, as you can see in Figure 2.
Now, I have to put my kidney doctor hat on for a second and talk about urine measurement ... of anything. The problem with urine is that the concentration can change a lot — by more than 10-fold, in fact — based on how much water you drank recently. Researchers correct for this, and in the case of this study, they do what a lot of researchers do: divide the measured concentration by the urine creatinine level.
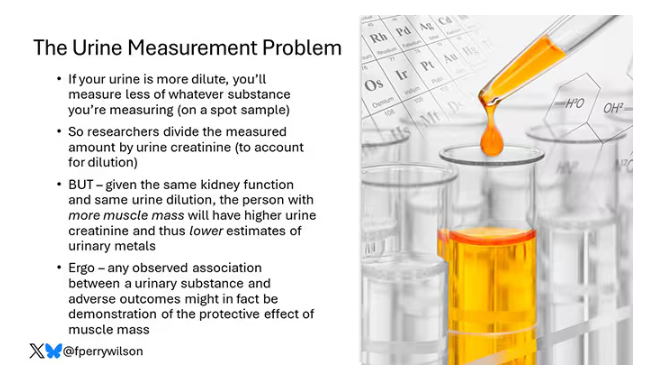
This introduces a bit of a problem. Take two people with exactly the same kidney function, who drank exactly the same water, whose urine is exactly the same concentration. The person with more muscle mass will have more creatinine in that urine sample, since creatinine is a byproduct of muscle metabolism. Because people with more muscle mass are generally healthier, when you divide your metal concentration by urine creatinine, you get a lower number, which might lead you to believe that lower levels of the metal in the urine are protective. But in fact, what you’re seeing is that higher levels of creatinine are protective. I see this issue all the time and it will always color results of studies like this.
Okay, I am doffing my kidney doctor hat now to show you the results.
The researchers first looked at the relationship between metal concentrations in the urine and performance on cognitive tests. The results were fairly equivocal, save for that digit substitution test which is shown in Figure 4.
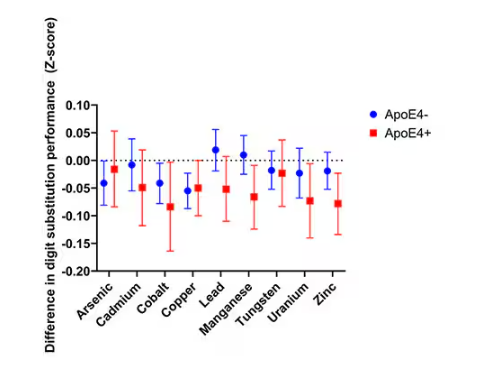
Even these results don’t ring major alarm bells for me. What you’re seeing here is the change in scores on the digit substitution test for each 25-percentile increase in urinary metal level — a pretty big change. And yet, you see really minor changes in the performance on the test. The digit substitution test is not an IQ test; but to give you a feeling for the magnitude of this change, if we looked at copper level, moving from the 25th to the 50th percentile would be associated with a loss of nine tenths of an IQ point.
You see two colors on the Figure 4 graph, by the way. That’s because the researchers stratified their findings based on whether the individual carried the ApoE4 gene allele, which is a risk factor for the development of dementia. There are reasons to believe that neurotoxic metals might be worse in this population, and I suppose you do see generally more adverse effects on scores in the red lines compared with the blue lines. But still, we’re not talking about a huge effect size here.
Let’s look at the relationship between these metals and the development of dementia itself, a clearly more important outcome than how well you can replace numeric digits with symbols. I’ll highlight a few of the results that are particularly telling.
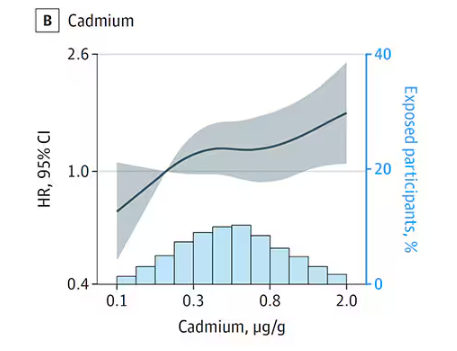
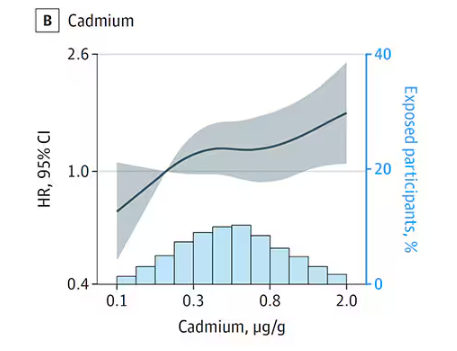
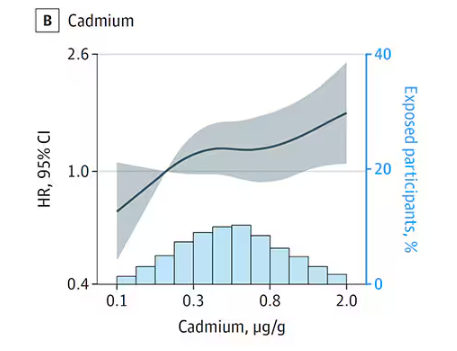
First, the nonessential mineral cadmium, which displays the type of relationship we would expect if the metal were neurotoxic: a clear, roughly linear increase in risk for dementia as urinary concentration increases.
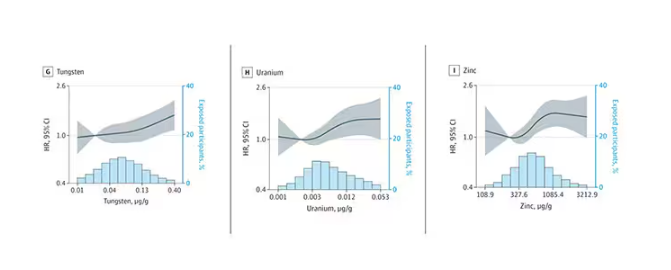
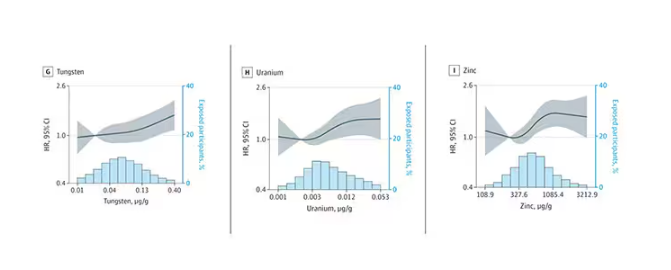
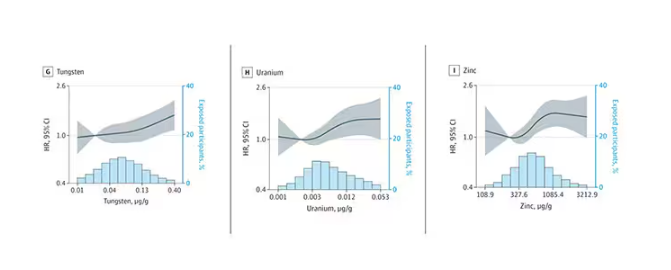
We see roughly similar patterns with the nonessential minerals tungsten and uranium, and the essential mineral zinc (beloved of respiratory-virus avoiders everywhere).
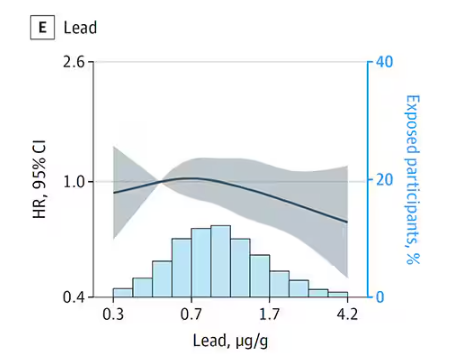
But it is very much not what we see for all metals. Strangest of all, look at lead, which shows basically no relationship with dementia.
This concerns me a bit. Earlier, I discussed the issue of measuring stuff in urine and how standardizing levels to the urine creatinine level introduces a bias due to muscle mass. One way around this is to standardize urine levels to some other marker of urine dilution, like osmolality. But more fundamental than that, I like to see positive and negative controls in studies like this. For example, lead strikes me as a good positive control here. If the experimental framework were valid, I would think we’d see a relationship between lead level and dementia.
For a negative control? Well, something we are quite sure is not neurotoxic — something like sulfur, which is relatively ubiquitous, used in a variety of biological processes, and efficiently eliminated. We don’t have that in this study.
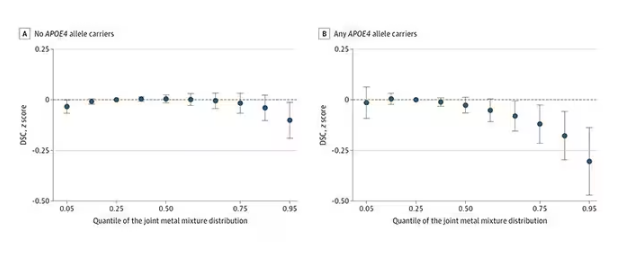
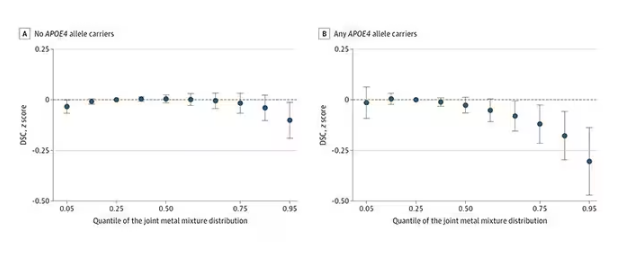
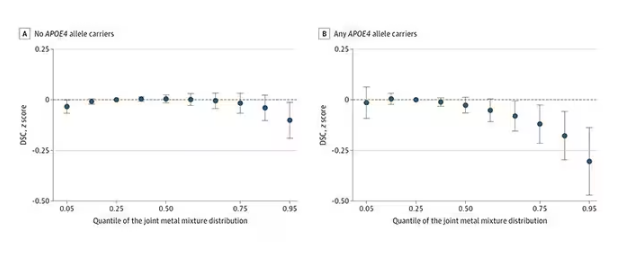
The authors close their case by creating a model that combines all the metal levels, asking the question of whether higher levels of metals in the urine in general worsen cognitive scores. And they find that the relationship exists, as you can see in Figure 8, both in carriers and noncarriers of ApoE4. But, to me, this is even more argument for the creatinine problem. If it’s not a specific metal but just the sort of general concentration of all metals, the risk for confounding by muscle mass is even higher.
So should we worry about ingesting metals? I suppose the answer is ... kind of.
I am sure we should be avoiding lead, despite the results of this study. It’s probably best to stay away from uranium too.
As for the essential metals, I’m sure there is some toxic dose; there’s a toxic dose for everything at some point. But I don’t see evidence in this study to make me worry that a significant chunk of the population is anywhere close to that.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
It has always amazed me that our bodies require these tiny amounts of incredibly rare substances to function. Sure, we need oxygen. We need water. But we also need molybdenum, which makes up just 1.2 parts per million of the Earth’s crust.
Without adequate molybdenum intake, we develop seizures, developmental delays, death. Fortunately, we need so little molybdenum that true molybdenum deficiency is incredibly rare — seen only in people on total parenteral nutrition without supplementation or those with certain rare genetic conditions. But still, molybdenum is necessary for life.
Many metals are. Figure 1 colors the essential minerals on the periodic table. You can see that to stay alive, we humans need not only things like sodium, but selenium, bromine, zinc, copper, and cobalt.
Some metals are very clearly not essential; we can all do without lead and mercury, and probably should.
But just because something is essential for life does not mean that more is better. The dose is the poison, as they say. And this week, we explore whether metals — even essential metals — might be adversely affecting our brains.
It’s not a stretch to think that metal intake could have weird effects on our nervous system. Lead exposure, primarily due to leaded gasoline, has been blamed for an average reduction of about 3 points in our national IQ, for example . But not all metals are created equal. Researchers set out to find out which might be more strongly associated with performance on cognitive tests and dementia, and reported their results in this study in JAMA Network Open.
To do this, they leveraged the MESA cohort study. This is a longitudinal study of a relatively diverse group of 6300 adults who were enrolled from 2000 to 2002 around the United States. At enrollment, they gave a urine sample and took a variety of cognitive tests. Important for this study was the digit symbol substitution test, where participants are provided a code and need to replace a list of numbers with symbols as per that code. Performance on this test worsens with age, depression, and cognitive impairment.
Participants were followed for more than a decade, and over that time, 559 (about 9%) were diagnosed with dementia.
Those baseline urine samples were assayed for a variety of metals — some essential, some very much not, as you can see in Figure 2.
Now, I have to put my kidney doctor hat on for a second and talk about urine measurement ... of anything. The problem with urine is that the concentration can change a lot — by more than 10-fold, in fact — based on how much water you drank recently. Researchers correct for this, and in the case of this study, they do what a lot of researchers do: divide the measured concentration by the urine creatinine level.
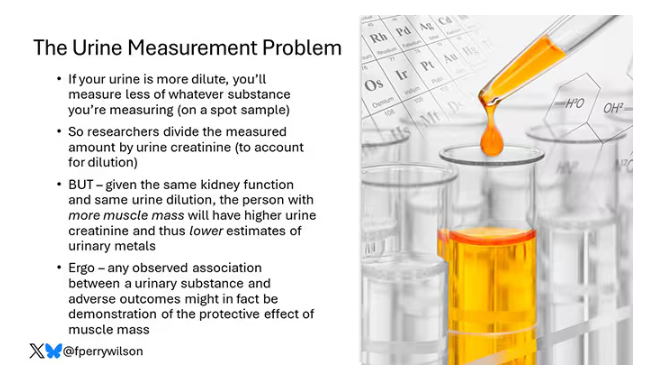
This introduces a bit of a problem. Take two people with exactly the same kidney function, who drank exactly the same water, whose urine is exactly the same concentration. The person with more muscle mass will have more creatinine in that urine sample, since creatinine is a byproduct of muscle metabolism. Because people with more muscle mass are generally healthier, when you divide your metal concentration by urine creatinine, you get a lower number, which might lead you to believe that lower levels of the metal in the urine are protective. But in fact, what you’re seeing is that higher levels of creatinine are protective. I see this issue all the time and it will always color results of studies like this.
Okay, I am doffing my kidney doctor hat now to show you the results.
The researchers first looked at the relationship between metal concentrations in the urine and performance on cognitive tests. The results were fairly equivocal, save for that digit substitution test which is shown in Figure 4.
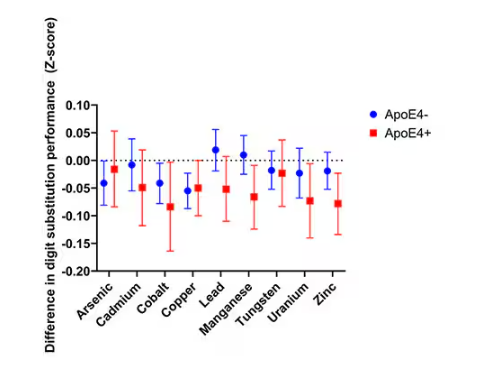
Even these results don’t ring major alarm bells for me. What you’re seeing here is the change in scores on the digit substitution test for each 25-percentile increase in urinary metal level — a pretty big change. And yet, you see really minor changes in the performance on the test. The digit substitution test is not an IQ test; but to give you a feeling for the magnitude of this change, if we looked at copper level, moving from the 25th to the 50th percentile would be associated with a loss of nine tenths of an IQ point.
You see two colors on the Figure 4 graph, by the way. That’s because the researchers stratified their findings based on whether the individual carried the ApoE4 gene allele, which is a risk factor for the development of dementia. There are reasons to believe that neurotoxic metals might be worse in this population, and I suppose you do see generally more adverse effects on scores in the red lines compared with the blue lines. But still, we’re not talking about a huge effect size here.
Let’s look at the relationship between these metals and the development of dementia itself, a clearly more important outcome than how well you can replace numeric digits with symbols. I’ll highlight a few of the results that are particularly telling.
First, the nonessential mineral cadmium, which displays the type of relationship we would expect if the metal were neurotoxic: a clear, roughly linear increase in risk for dementia as urinary concentration increases.
We see roughly similar patterns with the nonessential minerals tungsten and uranium, and the essential mineral zinc (beloved of respiratory-virus avoiders everywhere).
But it is very much not what we see for all metals. Strangest of all, look at lead, which shows basically no relationship with dementia.
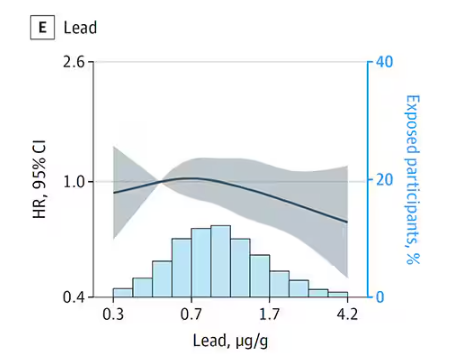
This concerns me a bit. Earlier, I discussed the issue of measuring stuff in urine and how standardizing levels to the urine creatinine level introduces a bias due to muscle mass. One way around this is to standardize urine levels to some other marker of urine dilution, like osmolality. But more fundamental than that, I like to see positive and negative controls in studies like this. For example, lead strikes me as a good positive control here. If the experimental framework were valid, I would think we’d see a relationship between lead level and dementia.
For a negative control? Well, something we are quite sure is not neurotoxic — something like sulfur, which is relatively ubiquitous, used in a variety of biological processes, and efficiently eliminated. We don’t have that in this study.
The authors close their case by creating a model that combines all the metal levels, asking the question of whether higher levels of metals in the urine in general worsen cognitive scores. And they find that the relationship exists, as you can see in Figure 8, both in carriers and noncarriers of ApoE4. But, to me, this is even more argument for the creatinine problem. If it’s not a specific metal but just the sort of general concentration of all metals, the risk for confounding by muscle mass is even higher.
So should we worry about ingesting metals? I suppose the answer is ... kind of.
I am sure we should be avoiding lead, despite the results of this study. It’s probably best to stay away from uranium too.
As for the essential metals, I’m sure there is some toxic dose; there’s a toxic dose for everything at some point. But I don’t see evidence in this study to make me worry that a significant chunk of the population is anywhere close to that.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
It has always amazed me that our bodies require these tiny amounts of incredibly rare substances to function. Sure, we need oxygen. We need water. But we also need molybdenum, which makes up just 1.2 parts per million of the Earth’s crust.
Without adequate molybdenum intake, we develop seizures, developmental delays, death. Fortunately, we need so little molybdenum that true molybdenum deficiency is incredibly rare — seen only in people on total parenteral nutrition without supplementation or those with certain rare genetic conditions. But still, molybdenum is necessary for life.
Many metals are. Figure 1 colors the essential minerals on the periodic table. You can see that to stay alive, we humans need not only things like sodium, but selenium, bromine, zinc, copper, and cobalt.
Some metals are very clearly not essential; we can all do without lead and mercury, and probably should.
But just because something is essential for life does not mean that more is better. The dose is the poison, as they say. And this week, we explore whether metals — even essential metals — might be adversely affecting our brains.
It’s not a stretch to think that metal intake could have weird effects on our nervous system. Lead exposure, primarily due to leaded gasoline, has been blamed for an average reduction of about 3 points in our national IQ, for example . But not all metals are created equal. Researchers set out to find out which might be more strongly associated with performance on cognitive tests and dementia, and reported their results in this study in JAMA Network Open.
To do this, they leveraged the MESA cohort study. This is a longitudinal study of a relatively diverse group of 6300 adults who were enrolled from 2000 to 2002 around the United States. At enrollment, they gave a urine sample and took a variety of cognitive tests. Important for this study was the digit symbol substitution test, where participants are provided a code and need to replace a list of numbers with symbols as per that code. Performance on this test worsens with age, depression, and cognitive impairment.
Participants were followed for more than a decade, and over that time, 559 (about 9%) were diagnosed with dementia.
Those baseline urine samples were assayed for a variety of metals — some essential, some very much not, as you can see in Figure 2.
Now, I have to put my kidney doctor hat on for a second and talk about urine measurement ... of anything. The problem with urine is that the concentration can change a lot — by more than 10-fold, in fact — based on how much water you drank recently. Researchers correct for this, and in the case of this study, they do what a lot of researchers do: divide the measured concentration by the urine creatinine level.
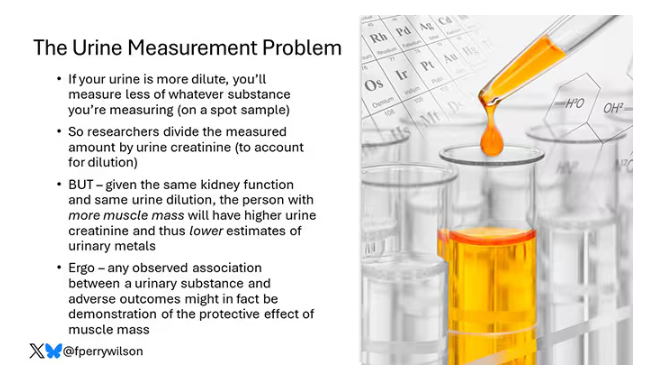
This introduces a bit of a problem. Take two people with exactly the same kidney function, who drank exactly the same water, whose urine is exactly the same concentration. The person with more muscle mass will have more creatinine in that urine sample, since creatinine is a byproduct of muscle metabolism. Because people with more muscle mass are generally healthier, when you divide your metal concentration by urine creatinine, you get a lower number, which might lead you to believe that lower levels of the metal in the urine are protective. But in fact, what you’re seeing is that higher levels of creatinine are protective. I see this issue all the time and it will always color results of studies like this.
Okay, I am doffing my kidney doctor hat now to show you the results.
The researchers first looked at the relationship between metal concentrations in the urine and performance on cognitive tests. The results were fairly equivocal, save for that digit substitution test which is shown in Figure 4.
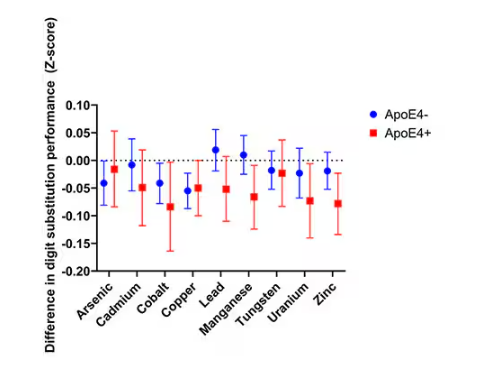
Even these results don’t ring major alarm bells for me. What you’re seeing here is the change in scores on the digit substitution test for each 25-percentile increase in urinary metal level — a pretty big change. And yet, you see really minor changes in the performance on the test. The digit substitution test is not an IQ test; but to give you a feeling for the magnitude of this change, if we looked at copper level, moving from the 25th to the 50th percentile would be associated with a loss of nine tenths of an IQ point.
You see two colors on the Figure 4 graph, by the way. That’s because the researchers stratified their findings based on whether the individual carried the ApoE4 gene allele, which is a risk factor for the development of dementia. There are reasons to believe that neurotoxic metals might be worse in this population, and I suppose you do see generally more adverse effects on scores in the red lines compared with the blue lines. But still, we’re not talking about a huge effect size here.
Let’s look at the relationship between these metals and the development of dementia itself, a clearly more important outcome than how well you can replace numeric digits with symbols. I’ll highlight a few of the results that are particularly telling.
First, the nonessential mineral cadmium, which displays the type of relationship we would expect if the metal were neurotoxic: a clear, roughly linear increase in risk for dementia as urinary concentration increases.
We see roughly similar patterns with the nonessential minerals tungsten and uranium, and the essential mineral zinc (beloved of respiratory-virus avoiders everywhere).
But it is very much not what we see for all metals. Strangest of all, look at lead, which shows basically no relationship with dementia.
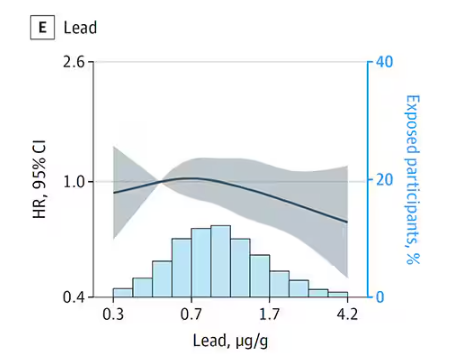
This concerns me a bit. Earlier, I discussed the issue of measuring stuff in urine and how standardizing levels to the urine creatinine level introduces a bias due to muscle mass. One way around this is to standardize urine levels to some other marker of urine dilution, like osmolality. But more fundamental than that, I like to see positive and negative controls in studies like this. For example, lead strikes me as a good positive control here. If the experimental framework were valid, I would think we’d see a relationship between lead level and dementia.
For a negative control? Well, something we are quite sure is not neurotoxic — something like sulfur, which is relatively ubiquitous, used in a variety of biological processes, and efficiently eliminated. We don’t have that in this study.
The authors close their case by creating a model that combines all the metal levels, asking the question of whether higher levels of metals in the urine in general worsen cognitive scores. And they find that the relationship exists, as you can see in Figure 8, both in carriers and noncarriers of ApoE4. But, to me, this is even more argument for the creatinine problem. If it’s not a specific metal but just the sort of general concentration of all metals, the risk for confounding by muscle mass is even higher.
So should we worry about ingesting metals? I suppose the answer is ... kind of.
I am sure we should be avoiding lead, despite the results of this study. It’s probably best to stay away from uranium too.
As for the essential metals, I’m sure there is some toxic dose; there’s a toxic dose for everything at some point. But I don’t see evidence in this study to make me worry that a significant chunk of the population is anywhere close to that.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
There Are ‘Four Pillars of Acne Pathogenesis’: Make Sure Treatment Hits as Many as Possible
LAS VEGAS — For clinicians who rely on generic tretinoin 0.5% as their go-to treatment for patients with acne, Shanna Miranti, MPAS, PA-C, offers some straightforward advice: You can do better.
“Friends don’t let friends write generic tretinoin only because there are so many better options out there,” Miranti, who practices dermatology in Naples, Florida, said at the Society of Dermatology Physician Associates (SDPA) 22nd Annual Fall Dermatology Conference. “Don’t get lazy; your patients deserve better.”
In her wide-ranging presentation, Miranti described the four pillars of acne pathogenesis as increased sebum production caused by androgens, follicular hyperkeratinization in the pilosebaceous unit, colonization by Cutibacterium acnes (formerly Proprionibacterium acnes), and inflammation. Acne “starts with androgens, but this is a cascade, so you have to find treatment options that hit as many of these four pillars as possible,” Miranti explained. “If you’re only using generic tretinoin, you’re only hitting maybe two of the four pillars at best.”
She then discussed the best treatment options for each pillar:
Follicular plugging and hyperkeratinization. Topical retinoids, including tretinoin, adapalene, tazarotene, and trifarotene, are highly effective for this issue. Systemic isotretinoin is also a strong option. For patients who are pregnant or trying to conceive, azelaic acid is a helpful alternative.
Excessive sebum production and androgens. “This may be the genesis of when acne begins — during puberty,” Miranti said. “With rising androgens comes rising amounts of sebum.” The only topical treatment that specifically targets this is clascoterone (Winlevi), which should be applied twice daily. For systemic management of excessive sebum, isotretinoin is highly effective. In women, spironolactone (50 mg daily, or split into two doses) and oral contraceptives are also options.
Inflammation. Topical options include retinoids, antibiotics, benzoyl peroxide (BPO), topical dapsone, azelaic acid, and clascoterone. Systemic options include isotretinoin; the antibiotics doxycycline, minocycline, and sarecycline; spironolactone; and oral contraceptives. “So, when you see patients with intense inflammation, and they’re starting to get post-inflammatory erythema or post-inflammatory hyperpigmentation, you need something to address this inflammatory problem,” she noted.
C acnes. Topical treatment options include BPO and antibiotics. However, topical antibiotics should never be used alone, Miranti said; they must always be combined with BPO to prevent bacterial resistance. Oral options include sarecycline, “which has a low propensity for antibiotic resistance and spares the gut microbiome to some degree,” and the “old-school” antibiotics doxycycline, minocycline, and tetracycline. “But all oral antibiotics should be used concomitantly with BPO,” she added.
Regardless of which treatment is chosen for any pillar, Miranti emphasized that monotherapy with a single agent is often insufficient. “Historically, we have combined therapies to treat the multiple causes of acne,” she said. “The average number of acne products used per patient is 2.53, but that’s also the average number of copays. We have to be conscious of that. If you are a mom with four kids who are on acne medication, you want to minimize your copay burden. So, if you can find a topical medication that hits three out of the four pillars of acne pathogenesis, that would be fantastic.” The only topical that targets excess sebum is clascoterone, she noted, and the only medication that hits all four pillars is isotretinoin.
In October 2023, the Food and Drug Administration approved a once-daily topical gel for patients aged 12 years or older that contains clindamycin 1.2%, adapalene 0.15%, and BPO 3.1%. The first-ever triple combination therapy, known as Cabtreo, was released to pharmacies in March 2024. In a phase 2 trial, researchers randomized 394 patients aged 9 years or older with moderate to severe acne to once-daily IDP-126, one of three dyad combination gels, or vehicle gel for 12 weeks. Patients in the Cabtreo arm achieved significantly greater lesion reductions than those in the vehicle arm (inflammatory: 78.3% vs 45.1%; noninflammatory: 70.0% vs 37.6%; P < .001 for both). They also experienced lesion reductions that were 9.2%-16.6% greater than those observed with any of the dyad combination gels. Miranti characterized the study results as “pretty phenomenal,” noting that the ease of use makes Cabtreo stand out as a treatment option. “Simplicity drives compliance, and compliance drives results,” she said. “This is one product to apply once a day. Any of you who have a teenage son like me, you know it is hard to get them to brush their teeth twice a day, let alone take medicine before they leave the house in the morning. This can be a home run for a lot of patients, and not just our teenagers. Adult females have done very well with this medication.”
In a network meta-analysis, researchers reviewed 221 randomized controlled trials to compare the efficacy of pharmacologic treatment for acne. The most effective treatment in reducing inflammatory and noninflammatory lesions was oral isotretinoin, followed by Cabtreo.
Miranti disclosed being a speaker, consultant, and/or an advisory board member for Arcutis Biotherapeutics, Bausch Health, Dermavant Sciences, Galderma, Incyte, LEO Pharma, Eli Lilly, Sun Pharma, Swift USA, and Verrica Pharmaceuticals.
A version of this article first appeared on Medscape.com.
LAS VEGAS — For clinicians who rely on generic tretinoin 0.5% as their go-to treatment for patients with acne, Shanna Miranti, MPAS, PA-C, offers some straightforward advice: You can do better.
“Friends don’t let friends write generic tretinoin only because there are so many better options out there,” Miranti, who practices dermatology in Naples, Florida, said at the Society of Dermatology Physician Associates (SDPA) 22nd Annual Fall Dermatology Conference. “Don’t get lazy; your patients deserve better.”
In her wide-ranging presentation, Miranti described the four pillars of acne pathogenesis as increased sebum production caused by androgens, follicular hyperkeratinization in the pilosebaceous unit, colonization by Cutibacterium acnes (formerly Proprionibacterium acnes), and inflammation. Acne “starts with androgens, but this is a cascade, so you have to find treatment options that hit as many of these four pillars as possible,” Miranti explained. “If you’re only using generic tretinoin, you’re only hitting maybe two of the four pillars at best.”
She then discussed the best treatment options for each pillar:
Follicular plugging and hyperkeratinization. Topical retinoids, including tretinoin, adapalene, tazarotene, and trifarotene, are highly effective for this issue. Systemic isotretinoin is also a strong option. For patients who are pregnant or trying to conceive, azelaic acid is a helpful alternative.
Excessive sebum production and androgens. “This may be the genesis of when acne begins — during puberty,” Miranti said. “With rising androgens comes rising amounts of sebum.” The only topical treatment that specifically targets this is clascoterone (Winlevi), which should be applied twice daily. For systemic management of excessive sebum, isotretinoin is highly effective. In women, spironolactone (50 mg daily, or split into two doses) and oral contraceptives are also options.
Inflammation. Topical options include retinoids, antibiotics, benzoyl peroxide (BPO), topical dapsone, azelaic acid, and clascoterone. Systemic options include isotretinoin; the antibiotics doxycycline, minocycline, and sarecycline; spironolactone; and oral contraceptives. “So, when you see patients with intense inflammation, and they’re starting to get post-inflammatory erythema or post-inflammatory hyperpigmentation, you need something to address this inflammatory problem,” she noted.
C acnes. Topical treatment options include BPO and antibiotics. However, topical antibiotics should never be used alone, Miranti said; they must always be combined with BPO to prevent bacterial resistance. Oral options include sarecycline, “which has a low propensity for antibiotic resistance and spares the gut microbiome to some degree,” and the “old-school” antibiotics doxycycline, minocycline, and tetracycline. “But all oral antibiotics should be used concomitantly with BPO,” she added.
Regardless of which treatment is chosen for any pillar, Miranti emphasized that monotherapy with a single agent is often insufficient. “Historically, we have combined therapies to treat the multiple causes of acne,” she said. “The average number of acne products used per patient is 2.53, but that’s also the average number of copays. We have to be conscious of that. If you are a mom with four kids who are on acne medication, you want to minimize your copay burden. So, if you can find a topical medication that hits three out of the four pillars of acne pathogenesis, that would be fantastic.” The only topical that targets excess sebum is clascoterone, she noted, and the only medication that hits all four pillars is isotretinoin.
In October 2023, the Food and Drug Administration approved a once-daily topical gel for patients aged 12 years or older that contains clindamycin 1.2%, adapalene 0.15%, and BPO 3.1%. The first-ever triple combination therapy, known as Cabtreo, was released to pharmacies in March 2024. In a phase 2 trial, researchers randomized 394 patients aged 9 years or older with moderate to severe acne to once-daily IDP-126, one of three dyad combination gels, or vehicle gel for 12 weeks. Patients in the Cabtreo arm achieved significantly greater lesion reductions than those in the vehicle arm (inflammatory: 78.3% vs 45.1%; noninflammatory: 70.0% vs 37.6%; P < .001 for both). They also experienced lesion reductions that were 9.2%-16.6% greater than those observed with any of the dyad combination gels. Miranti characterized the study results as “pretty phenomenal,” noting that the ease of use makes Cabtreo stand out as a treatment option. “Simplicity drives compliance, and compliance drives results,” she said. “This is one product to apply once a day. Any of you who have a teenage son like me, you know it is hard to get them to brush their teeth twice a day, let alone take medicine before they leave the house in the morning. This can be a home run for a lot of patients, and not just our teenagers. Adult females have done very well with this medication.”
In a network meta-analysis, researchers reviewed 221 randomized controlled trials to compare the efficacy of pharmacologic treatment for acne. The most effective treatment in reducing inflammatory and noninflammatory lesions was oral isotretinoin, followed by Cabtreo.
Miranti disclosed being a speaker, consultant, and/or an advisory board member for Arcutis Biotherapeutics, Bausch Health, Dermavant Sciences, Galderma, Incyte, LEO Pharma, Eli Lilly, Sun Pharma, Swift USA, and Verrica Pharmaceuticals.
A version of this article first appeared on Medscape.com.
LAS VEGAS — For clinicians who rely on generic tretinoin 0.5% as their go-to treatment for patients with acne, Shanna Miranti, MPAS, PA-C, offers some straightforward advice: You can do better.
“Friends don’t let friends write generic tretinoin only because there are so many better options out there,” Miranti, who practices dermatology in Naples, Florida, said at the Society of Dermatology Physician Associates (SDPA) 22nd Annual Fall Dermatology Conference. “Don’t get lazy; your patients deserve better.”
In her wide-ranging presentation, Miranti described the four pillars of acne pathogenesis as increased sebum production caused by androgens, follicular hyperkeratinization in the pilosebaceous unit, colonization by Cutibacterium acnes (formerly Proprionibacterium acnes), and inflammation. Acne “starts with androgens, but this is a cascade, so you have to find treatment options that hit as many of these four pillars as possible,” Miranti explained. “If you’re only using generic tretinoin, you’re only hitting maybe two of the four pillars at best.”
She then discussed the best treatment options for each pillar:
Follicular plugging and hyperkeratinization. Topical retinoids, including tretinoin, adapalene, tazarotene, and trifarotene, are highly effective for this issue. Systemic isotretinoin is also a strong option. For patients who are pregnant or trying to conceive, azelaic acid is a helpful alternative.
Excessive sebum production and androgens. “This may be the genesis of when acne begins — during puberty,” Miranti said. “With rising androgens comes rising amounts of sebum.” The only topical treatment that specifically targets this is clascoterone (Winlevi), which should be applied twice daily. For systemic management of excessive sebum, isotretinoin is highly effective. In women, spironolactone (50 mg daily, or split into two doses) and oral contraceptives are also options.
Inflammation. Topical options include retinoids, antibiotics, benzoyl peroxide (BPO), topical dapsone, azelaic acid, and clascoterone. Systemic options include isotretinoin; the antibiotics doxycycline, minocycline, and sarecycline; spironolactone; and oral contraceptives. “So, when you see patients with intense inflammation, and they’re starting to get post-inflammatory erythema or post-inflammatory hyperpigmentation, you need something to address this inflammatory problem,” she noted.
C acnes. Topical treatment options include BPO and antibiotics. However, topical antibiotics should never be used alone, Miranti said; they must always be combined with BPO to prevent bacterial resistance. Oral options include sarecycline, “which has a low propensity for antibiotic resistance and spares the gut microbiome to some degree,” and the “old-school” antibiotics doxycycline, minocycline, and tetracycline. “But all oral antibiotics should be used concomitantly with BPO,” she added.
Regardless of which treatment is chosen for any pillar, Miranti emphasized that monotherapy with a single agent is often insufficient. “Historically, we have combined therapies to treat the multiple causes of acne,” she said. “The average number of acne products used per patient is 2.53, but that’s also the average number of copays. We have to be conscious of that. If you are a mom with four kids who are on acne medication, you want to minimize your copay burden. So, if you can find a topical medication that hits three out of the four pillars of acne pathogenesis, that would be fantastic.” The only topical that targets excess sebum is clascoterone, she noted, and the only medication that hits all four pillars is isotretinoin.
In October 2023, the Food and Drug Administration approved a once-daily topical gel for patients aged 12 years or older that contains clindamycin 1.2%, adapalene 0.15%, and BPO 3.1%. The first-ever triple combination therapy, known as Cabtreo, was released to pharmacies in March 2024. In a phase 2 trial, researchers randomized 394 patients aged 9 years or older with moderate to severe acne to once-daily IDP-126, one of three dyad combination gels, or vehicle gel for 12 weeks. Patients in the Cabtreo arm achieved significantly greater lesion reductions than those in the vehicle arm (inflammatory: 78.3% vs 45.1%; noninflammatory: 70.0% vs 37.6%; P < .001 for both). They also experienced lesion reductions that were 9.2%-16.6% greater than those observed with any of the dyad combination gels. Miranti characterized the study results as “pretty phenomenal,” noting that the ease of use makes Cabtreo stand out as a treatment option. “Simplicity drives compliance, and compliance drives results,” she said. “This is one product to apply once a day. Any of you who have a teenage son like me, you know it is hard to get them to brush their teeth twice a day, let alone take medicine before they leave the house in the morning. This can be a home run for a lot of patients, and not just our teenagers. Adult females have done very well with this medication.”
In a network meta-analysis, researchers reviewed 221 randomized controlled trials to compare the efficacy of pharmacologic treatment for acne. The most effective treatment in reducing inflammatory and noninflammatory lesions was oral isotretinoin, followed by Cabtreo.
Miranti disclosed being a speaker, consultant, and/or an advisory board member for Arcutis Biotherapeutics, Bausch Health, Dermavant Sciences, Galderma, Incyte, LEO Pharma, Eli Lilly, Sun Pharma, Swift USA, and Verrica Pharmaceuticals.
A version of this article first appeared on Medscape.com.
FROM SDPA 2024
Flu Vaccine Guards Household Contacts of Infected People
TOPLINE:
Vaccination lowers the risk of contracting the infection among household contacts.
METHODOLOGY:
- Researchers conducted a prospective cohort study of data between 2017 and 2020 to determine the estimated effectiveness of influenza vaccines in preventing secondary infections in household contacts.
- Overall, 699 people were primary contacts, or the first in a household to get infected (median age, 13 years; 54.5% women); there were 1581 household contacts (median age, 31 years; 52.7% women), and both groups were followed for 7 days.
- Participants collected daily symptom diaries and nasal swabs during the follow-up period.
- Participants also submitted their history of influenza vaccination; 50.1% of household contacts had received a shot at least 14 days before the first case of disease onset in the household.
- The risk for secondary infection and vaccine effectiveness in preventing infection among household contacts was estimated overall and by virus type, subtype, and lineage.
TAKEAWAY:
- Nearly half (48.2%) of primary cases were from children and teens between ages 5 and 17 years.
- Overall, 22% household contacts had laboratory-confirmed influenza during follow-up, of which 7% were asymptomatic.
- The overall risk for secondary infection among unvaccinated household contacts was 18.8%, with the highest risk observed among children younger than age 5 years (29.9%).
- The overall effectiveness of influenza vaccines in preventing laboratory-confirmed infections among household contacts was 21% (95% CI, 1.4%-36.7%).
- The vaccine demonstrated specific protection against influenza B infection (56.4%; 95% CI, 30.1%-72.8%), particularly among those between ages 5 and 17 years.
IN PRACTICE:
“Although complementary preventive strategies to prevent influenza in household settings may be considered, seasonal influenza vaccination is the primary strategy recommended for prevention of influenza illness and its complications,” the authors wrote.
SOURCE:
The study was led by Carlos G. Grijalva, MD, MPH, of Vanderbilt University Medical Center in Nashville, Tennessee, and was published online in JAMA Network Open.
LIMITATIONS:
The recruitment of infected individuals from clinical testing pools may have limited the generalizability of the risk for secondary infection in households in which the primary case had a milder or asymptomatic infection. The study was unable to assess the effectiveness of specific vaccine formulations, such as those receiving high doses. The stratification of estimates by influenza subtypes and lineages was challenging because of small cell sizes.
DISCLOSURES:
This study was supported by grants from the Centers for Disease Control and Prevention (CDC) and authors reported support from grants from the National Institute Of Allergy And Infectious Diseases. Some authors reported contracts, receiving personal fees and grants from the CDC and various pharmaceutical companies such as Merck and Sanofi.
This article was created using several editorial tools, including artificial intelligence, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Vaccination lowers the risk of contracting the infection among household contacts.
METHODOLOGY:
- Researchers conducted a prospective cohort study of data between 2017 and 2020 to determine the estimated effectiveness of influenza vaccines in preventing secondary infections in household contacts.
- Overall, 699 people were primary contacts, or the first in a household to get infected (median age, 13 years; 54.5% women); there were 1581 household contacts (median age, 31 years; 52.7% women), and both groups were followed for 7 days.
- Participants collected daily symptom diaries and nasal swabs during the follow-up period.
- Participants also submitted their history of influenza vaccination; 50.1% of household contacts had received a shot at least 14 days before the first case of disease onset in the household.
- The risk for secondary infection and vaccine effectiveness in preventing infection among household contacts was estimated overall and by virus type, subtype, and lineage.
TAKEAWAY:
- Nearly half (48.2%) of primary cases were from children and teens between ages 5 and 17 years.
- Overall, 22% household contacts had laboratory-confirmed influenza during follow-up, of which 7% were asymptomatic.
- The overall risk for secondary infection among unvaccinated household contacts was 18.8%, with the highest risk observed among children younger than age 5 years (29.9%).
- The overall effectiveness of influenza vaccines in preventing laboratory-confirmed infections among household contacts was 21% (95% CI, 1.4%-36.7%).
- The vaccine demonstrated specific protection against influenza B infection (56.4%; 95% CI, 30.1%-72.8%), particularly among those between ages 5 and 17 years.
IN PRACTICE:
“Although complementary preventive strategies to prevent influenza in household settings may be considered, seasonal influenza vaccination is the primary strategy recommended for prevention of influenza illness and its complications,” the authors wrote.
SOURCE:
The study was led by Carlos G. Grijalva, MD, MPH, of Vanderbilt University Medical Center in Nashville, Tennessee, and was published online in JAMA Network Open.
LIMITATIONS:
The recruitment of infected individuals from clinical testing pools may have limited the generalizability of the risk for secondary infection in households in which the primary case had a milder or asymptomatic infection. The study was unable to assess the effectiveness of specific vaccine formulations, such as those receiving high doses. The stratification of estimates by influenza subtypes and lineages was challenging because of small cell sizes.
DISCLOSURES:
This study was supported by grants from the Centers for Disease Control and Prevention (CDC) and authors reported support from grants from the National Institute Of Allergy And Infectious Diseases. Some authors reported contracts, receiving personal fees and grants from the CDC and various pharmaceutical companies such as Merck and Sanofi.
This article was created using several editorial tools, including artificial intelligence, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Vaccination lowers the risk of contracting the infection among household contacts.
METHODOLOGY:
- Researchers conducted a prospective cohort study of data between 2017 and 2020 to determine the estimated effectiveness of influenza vaccines in preventing secondary infections in household contacts.
- Overall, 699 people were primary contacts, or the first in a household to get infected (median age, 13 years; 54.5% women); there were 1581 household contacts (median age, 31 years; 52.7% women), and both groups were followed for 7 days.
- Participants collected daily symptom diaries and nasal swabs during the follow-up period.
- Participants also submitted their history of influenza vaccination; 50.1% of household contacts had received a shot at least 14 days before the first case of disease onset in the household.
- The risk for secondary infection and vaccine effectiveness in preventing infection among household contacts was estimated overall and by virus type, subtype, and lineage.
TAKEAWAY:
- Nearly half (48.2%) of primary cases were from children and teens between ages 5 and 17 years.
- Overall, 22% household contacts had laboratory-confirmed influenza during follow-up, of which 7% were asymptomatic.
- The overall risk for secondary infection among unvaccinated household contacts was 18.8%, with the highest risk observed among children younger than age 5 years (29.9%).
- The overall effectiveness of influenza vaccines in preventing laboratory-confirmed infections among household contacts was 21% (95% CI, 1.4%-36.7%).
- The vaccine demonstrated specific protection against influenza B infection (56.4%; 95% CI, 30.1%-72.8%), particularly among those between ages 5 and 17 years.
IN PRACTICE:
“Although complementary preventive strategies to prevent influenza in household settings may be considered, seasonal influenza vaccination is the primary strategy recommended for prevention of influenza illness and its complications,” the authors wrote.
SOURCE:
The study was led by Carlos G. Grijalva, MD, MPH, of Vanderbilt University Medical Center in Nashville, Tennessee, and was published online in JAMA Network Open.
LIMITATIONS:
The recruitment of infected individuals from clinical testing pools may have limited the generalizability of the risk for secondary infection in households in which the primary case had a milder or asymptomatic infection. The study was unable to assess the effectiveness of specific vaccine formulations, such as those receiving high doses. The stratification of estimates by influenza subtypes and lineages was challenging because of small cell sizes.
DISCLOSURES:
This study was supported by grants from the Centers for Disease Control and Prevention (CDC) and authors reported support from grants from the National Institute Of Allergy And Infectious Diseases. Some authors reported contracts, receiving personal fees and grants from the CDC and various pharmaceutical companies such as Merck and Sanofi.
This article was created using several editorial tools, including artificial intelligence, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
US Study Pinpoints Merkel Cell Risk Factors
TOPLINE:
in the United States.
METHODOLOGY:
- Researchers evaluated 38,020 MCC cases (38% women; 93% non-Hispanic White, 4% Hispanic, 1% non-Hispanic Black) diagnosed in the United States from 2001 to 2019 to estimate the contribution of potentially modifiable risk factors to the burden of MCC.
- Population-based cancer registries and linkages with HIV and transplant registries were utilized to identify MCC cases in patients with HIV, solid organ transplant recipients, and patients with chronic lymphocytic leukemia (CLL).
- Data on cloud-adjusted daily ambient UVR irradiance were merged with cancer registry information on the county of residence at diagnosis to assess UVR exposure. Studies reporting the prevalence of MCPyV in MCC specimens collected in the United States were combined via a meta-analysis.
- The study assessed population attributable fractions of MCC cases that were attributable to major immunosuppressive conditions (HIV, solid organ transplant, and chronic CLL), ambient UVR exposure, and MCPyV.
TAKEAWAY:
- The incidence of MCC was higher in people with HIV (standardized incidence ratio [SIR], 2.78), organ transplant recipients (SIR, 13.1), and patients with CLL (SIR, 5.75) than in the general US population. However, only 2.5% of MCC cases were attributable to these immunosuppressive conditions.
- Non-Hispanic White individuals showed elevated MCC incidence at both lower and higher ambient UVR exposure levels, with incidence rate ratios of 4.05 and 4.91, respectively, for MCC on the head and neck.
- A meta-analysis of 19 case series revealed that 63.8% of MCC cases were attributable to MCPyV, with a similar prevalence observed between immunocompromised and immunocompetent patients.
- Overall, 65.1% of MCC cases were attributable to ambient UVR exposure, with higher attribution for cases diagnosed on the head and neck than those diagnosed on other sites (72.1% vs 60.2%).
IN PRACTICE:
“The results of this study suggest that most MCC cases in the US are attributable to MCPyV and/or ambient UVR [UV radiation] exposure, with a smaller fraction attributable to three major immunosuppressive conditions,” the authors wrote. “Future studies should investigate UVR mutational signature, TMB [tumor mutational burden], and MCPyV prevalence according to race and ethnicity and patient immune status to help clarify the overlap between MCC risk factors.”
SOURCE:
The study was led by Jacob T. Tribble, BA, Division of Cancer Epidemiology and Genetics, National Cancer Institute (NCI), Rockville, Maryland. It was published online on November 27, 2024, in JAMA Dermatology.
LIMITATIONS:
Incidences of MCC may have been inflated because of increased medical surveillance in immunosuppressed populations. The analysis assumed that only cases among non-Hispanic White individuals were associated with UVR. Additionally, the meta-analysis of MCPyV prevalence primarily included studies from large academic institutions, which may not be representative of the entire US population.
DISCLOSURES:
This study was supported in part by the Intramural Research Program of the NCI and the National Institutes of Health Medical Research Scholars Program. Additional funding was provided through a public-private partnership with contributions from the American Association for Dental Research and the Colgate-Palmolive Company to the Foundation for the National Institutes of Health. The authors reported no relevant conflicts of interest.
This article was created using several editorial tools, including artificial intelligence, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
in the United States.
METHODOLOGY:
- Researchers evaluated 38,020 MCC cases (38% women; 93% non-Hispanic White, 4% Hispanic, 1% non-Hispanic Black) diagnosed in the United States from 2001 to 2019 to estimate the contribution of potentially modifiable risk factors to the burden of MCC.
- Population-based cancer registries and linkages with HIV and transplant registries were utilized to identify MCC cases in patients with HIV, solid organ transplant recipients, and patients with chronic lymphocytic leukemia (CLL).
- Data on cloud-adjusted daily ambient UVR irradiance were merged with cancer registry information on the county of residence at diagnosis to assess UVR exposure. Studies reporting the prevalence of MCPyV in MCC specimens collected in the United States were combined via a meta-analysis.
- The study assessed population attributable fractions of MCC cases that were attributable to major immunosuppressive conditions (HIV, solid organ transplant, and chronic CLL), ambient UVR exposure, and MCPyV.
TAKEAWAY:
- The incidence of MCC was higher in people with HIV (standardized incidence ratio [SIR], 2.78), organ transplant recipients (SIR, 13.1), and patients with CLL (SIR, 5.75) than in the general US population. However, only 2.5% of MCC cases were attributable to these immunosuppressive conditions.
- Non-Hispanic White individuals showed elevated MCC incidence at both lower and higher ambient UVR exposure levels, with incidence rate ratios of 4.05 and 4.91, respectively, for MCC on the head and neck.
- A meta-analysis of 19 case series revealed that 63.8% of MCC cases were attributable to MCPyV, with a similar prevalence observed between immunocompromised and immunocompetent patients.
- Overall, 65.1% of MCC cases were attributable to ambient UVR exposure, with higher attribution for cases diagnosed on the head and neck than those diagnosed on other sites (72.1% vs 60.2%).
IN PRACTICE:
“The results of this study suggest that most MCC cases in the US are attributable to MCPyV and/or ambient UVR [UV radiation] exposure, with a smaller fraction attributable to three major immunosuppressive conditions,” the authors wrote. “Future studies should investigate UVR mutational signature, TMB [tumor mutational burden], and MCPyV prevalence according to race and ethnicity and patient immune status to help clarify the overlap between MCC risk factors.”
SOURCE:
The study was led by Jacob T. Tribble, BA, Division of Cancer Epidemiology and Genetics, National Cancer Institute (NCI), Rockville, Maryland. It was published online on November 27, 2024, in JAMA Dermatology.
LIMITATIONS:
Incidences of MCC may have been inflated because of increased medical surveillance in immunosuppressed populations. The analysis assumed that only cases among non-Hispanic White individuals were associated with UVR. Additionally, the meta-analysis of MCPyV prevalence primarily included studies from large academic institutions, which may not be representative of the entire US population.
DISCLOSURES:
This study was supported in part by the Intramural Research Program of the NCI and the National Institutes of Health Medical Research Scholars Program. Additional funding was provided through a public-private partnership with contributions from the American Association for Dental Research and the Colgate-Palmolive Company to the Foundation for the National Institutes of Health. The authors reported no relevant conflicts of interest.
This article was created using several editorial tools, including artificial intelligence, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
in the United States.
METHODOLOGY:
- Researchers evaluated 38,020 MCC cases (38% women; 93% non-Hispanic White, 4% Hispanic, 1% non-Hispanic Black) diagnosed in the United States from 2001 to 2019 to estimate the contribution of potentially modifiable risk factors to the burden of MCC.
- Population-based cancer registries and linkages with HIV and transplant registries were utilized to identify MCC cases in patients with HIV, solid organ transplant recipients, and patients with chronic lymphocytic leukemia (CLL).
- Data on cloud-adjusted daily ambient UVR irradiance were merged with cancer registry information on the county of residence at diagnosis to assess UVR exposure. Studies reporting the prevalence of MCPyV in MCC specimens collected in the United States were combined via a meta-analysis.
- The study assessed population attributable fractions of MCC cases that were attributable to major immunosuppressive conditions (HIV, solid organ transplant, and chronic CLL), ambient UVR exposure, and MCPyV.
TAKEAWAY:
- The incidence of MCC was higher in people with HIV (standardized incidence ratio [SIR], 2.78), organ transplant recipients (SIR, 13.1), and patients with CLL (SIR, 5.75) than in the general US population. However, only 2.5% of MCC cases were attributable to these immunosuppressive conditions.
- Non-Hispanic White individuals showed elevated MCC incidence at both lower and higher ambient UVR exposure levels, with incidence rate ratios of 4.05 and 4.91, respectively, for MCC on the head and neck.
- A meta-analysis of 19 case series revealed that 63.8% of MCC cases were attributable to MCPyV, with a similar prevalence observed between immunocompromised and immunocompetent patients.
- Overall, 65.1% of MCC cases were attributable to ambient UVR exposure, with higher attribution for cases diagnosed on the head and neck than those diagnosed on other sites (72.1% vs 60.2%).
IN PRACTICE:
“The results of this study suggest that most MCC cases in the US are attributable to MCPyV and/or ambient UVR [UV radiation] exposure, with a smaller fraction attributable to three major immunosuppressive conditions,” the authors wrote. “Future studies should investigate UVR mutational signature, TMB [tumor mutational burden], and MCPyV prevalence according to race and ethnicity and patient immune status to help clarify the overlap between MCC risk factors.”
SOURCE:
The study was led by Jacob T. Tribble, BA, Division of Cancer Epidemiology and Genetics, National Cancer Institute (NCI), Rockville, Maryland. It was published online on November 27, 2024, in JAMA Dermatology.
LIMITATIONS:
Incidences of MCC may have been inflated because of increased medical surveillance in immunosuppressed populations. The analysis assumed that only cases among non-Hispanic White individuals were associated with UVR. Additionally, the meta-analysis of MCPyV prevalence primarily included studies from large academic institutions, which may not be representative of the entire US population.
DISCLOSURES:
This study was supported in part by the Intramural Research Program of the NCI and the National Institutes of Health Medical Research Scholars Program. Additional funding was provided through a public-private partnership with contributions from the American Association for Dental Research and the Colgate-Palmolive Company to the Foundation for the National Institutes of Health. The authors reported no relevant conflicts of interest.
This article was created using several editorial tools, including artificial intelligence, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
AMR Could Surpass Cancer as Leading Cause of Death by 2050
Antimicrobial resistance (AMR) is globally recognized as one of the greatest health threats of the 21st century, responsible for 1.27 million deaths annually. “According to the WHO, if no measures are taken promptly, AMR could lead to more deaths than cancer by 2050,” Arnaud Marchant, MD, PhD, director of the European Plotkin Institute for Vaccinology at Université libre de Bruxelles (EPIV-ULB), Anderlecht, Belgium, said in an interview with MediQuality, part of the Medscape Professional Network. “This is a huge problem, and vaccination could be part of the solution.”
EPIV-ULB marked the start of the World AMR Awareness Week (November 18-24) with an event highlighting the critical role of vaccination to counter the rise for resistant pathogens. During the event, MediQuality interviewed Marchant, along with several other experts in the field.
Antibiotics Losing Effectiveness
Marc Van Ranst, PhD, virologist at Rega Institute KU Leuven in Leuven, Belgium, echoed Marchant’s concerns. He noted that “an increasing number of bacteria are becoming resistant to more antibiotics.” “While antibiotics were once miracle drugs, they have now stopped — or almost stopped — working against certain bacteria. Although we are discovering more effective therapies, bacterial infections are increasingly likely to worsen due to AMR.”
Van Ranst issued a stark warning: “If this trend continues, it is entirely reasonable to predict that in 25 years, some antibiotics will become useless, certain bacterial infections will be much harder to treat, and deaths will outnumber those caused by cancer. It’s worth noting, however, that as cancer treatments improve, cancer-related deaths are expected to decline, further highlighting the growing burden of AMR-related fatalities.”
Viruses, Vaccines, and Resistance
Van Ranst emphasized that while AMR primarily involves bacteria, viral infections and vaccination against them also play a role in addressing the issue. “When vaccines prevent illness, they reduce the need for unnecessary antibiotic use. In the past, antibiotics were frequently prescribed for respiratory infections — typically caused by viruses — leading to misuse and heightened resistance. By preventing viral infections through vaccines, we reduce inappropriate antibiotic prescriptions and, subsequently, AMR.”
Strategic Areas of Focus
To maximize the impact of vaccination in combating AMR, Belgium must prioritize several strategic areas, according to EPIV-ULB. “Expanding vaccination coverage for recommended vaccines is crucial to effectively preventing the spread of resistant pathogens,” said Marchant.
“Innovation and development of new vaccines are also essential, including targeted research into vaccines for infections that are currently unavoidable through other means. Enhancing epidemiological surveillance through national data collection and analysis will further clarify the impact of vaccines on AMR and inform policy decisions.”
EPIV-ULB underscored the importance of educating the public and healthcare professionals. “Public awareness is essential to addressing vaccine hesitancy by providing clear information on the importance of prevention,” Marchant explained. “Healthcare professional training must also improve, encouraging preventive practices and judicious antibiotic use. Furthermore, additional research is necessary to fill data gaps and develop predictive models that can guide vaccine development in the future.”
Role of Vaccination
According to EPIV-ULB, Belgium needs a strengthened national strategy to address AMR effectively. “Complementary solutions are increasingly important as antimicrobials lose efficacy and treatments become more complex,” Marchant said. “Vaccination offers a proactive and effective preventive solution, directly and indirectly reducing the spread of resistant pathogens.”
Vaccines combat AMR through various mechanisms. “They prevent diseases such as pneumococcal pneumonia and meningitis, reducing the need for antibiotics to treat these infections,” Marchant explained. “Additionally, vaccination lowers inappropriate antibiotic use by preventing viral infections, reducing the risk of overprescribing antibiotics in cases where they are unnecessary. Lastly, herd immunity from vaccination slows the circulation of resistant pathogens, limiting their spread.”
Van Ranst urged healthcare professionals to prioritize vaccinating at-risk populations as identified by Belgium’s Superior Health Council. These include the elderly with underlying conditions and pregnant women, especially for influenza vaccines. University Hospitals Leuven in Belgium, also conducts annual vaccination campaigns for its staff, combining flu and COVID vaccines to increase uptake.
A Global Challenge
Marc Noppen, MD, PhD, director of University Hospital Brussels, Belgium, emphasized the complexity of AMR as a global issue. “The problem isn’t solely due to human antibiotic use; it also stems from veterinary medicine, plant breeding, and animal husbandry. This is a multifactorial, worldwide issue that requires public awareness. Improved vaccination strategies are one way to address AMR, particularly in this post-COVID era of heightened skepticism toward vaccines,” he explained.
Marie-Lise Verschelden from Pfizer highlighted the need for cooperation across the healthcare sector. “Belgium is fortunate to have a fantastic ecosystem of academics, clinicians, and industry experts. Collaboration, including government involvement, is critical to advancing our efforts. At Pfizer, we continue to develop new vaccines and technologies, and the COVID crisis has reinforced the critical role of vaccination in combating AMR. Through our vaccine portfolio and ongoing developments, we are well-positioned to contribute significantly to this global challenge.”
Elisabeth Van Damme from GSK reiterated that AMR is a global issue requiring joint efforts. “Existing vaccines are underutilized. Vaccination protects against certain infectious diseases, reducing the need for antibiotics. Antibiotics, in turn, are sometimes prescribed incorrectly, especially for viral infections they cannot treat. At GSK, we are already developing new vaccines to meet future needs.”
Vaccination remains a cornerstone in the fight against AMR. As pathogens grow increasingly resistant to antibiotics, coordinated efforts and innovative vaccine development are essential to mitigating this global health crisis.
This story was translated and adapted from MediQuality using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Antimicrobial resistance (AMR) is globally recognized as one of the greatest health threats of the 21st century, responsible for 1.27 million deaths annually. “According to the WHO, if no measures are taken promptly, AMR could lead to more deaths than cancer by 2050,” Arnaud Marchant, MD, PhD, director of the European Plotkin Institute for Vaccinology at Université libre de Bruxelles (EPIV-ULB), Anderlecht, Belgium, said in an interview with MediQuality, part of the Medscape Professional Network. “This is a huge problem, and vaccination could be part of the solution.”
EPIV-ULB marked the start of the World AMR Awareness Week (November 18-24) with an event highlighting the critical role of vaccination to counter the rise for resistant pathogens. During the event, MediQuality interviewed Marchant, along with several other experts in the field.
Antibiotics Losing Effectiveness
Marc Van Ranst, PhD, virologist at Rega Institute KU Leuven in Leuven, Belgium, echoed Marchant’s concerns. He noted that “an increasing number of bacteria are becoming resistant to more antibiotics.” “While antibiotics were once miracle drugs, they have now stopped — or almost stopped — working against certain bacteria. Although we are discovering more effective therapies, bacterial infections are increasingly likely to worsen due to AMR.”
Van Ranst issued a stark warning: “If this trend continues, it is entirely reasonable to predict that in 25 years, some antibiotics will become useless, certain bacterial infections will be much harder to treat, and deaths will outnumber those caused by cancer. It’s worth noting, however, that as cancer treatments improve, cancer-related deaths are expected to decline, further highlighting the growing burden of AMR-related fatalities.”
Viruses, Vaccines, and Resistance
Van Ranst emphasized that while AMR primarily involves bacteria, viral infections and vaccination against them also play a role in addressing the issue. “When vaccines prevent illness, they reduce the need for unnecessary antibiotic use. In the past, antibiotics were frequently prescribed for respiratory infections — typically caused by viruses — leading to misuse and heightened resistance. By preventing viral infections through vaccines, we reduce inappropriate antibiotic prescriptions and, subsequently, AMR.”
Strategic Areas of Focus
To maximize the impact of vaccination in combating AMR, Belgium must prioritize several strategic areas, according to EPIV-ULB. “Expanding vaccination coverage for recommended vaccines is crucial to effectively preventing the spread of resistant pathogens,” said Marchant.
“Innovation and development of new vaccines are also essential, including targeted research into vaccines for infections that are currently unavoidable through other means. Enhancing epidemiological surveillance through national data collection and analysis will further clarify the impact of vaccines on AMR and inform policy decisions.”
EPIV-ULB underscored the importance of educating the public and healthcare professionals. “Public awareness is essential to addressing vaccine hesitancy by providing clear information on the importance of prevention,” Marchant explained. “Healthcare professional training must also improve, encouraging preventive practices and judicious antibiotic use. Furthermore, additional research is necessary to fill data gaps and develop predictive models that can guide vaccine development in the future.”
Role of Vaccination
According to EPIV-ULB, Belgium needs a strengthened national strategy to address AMR effectively. “Complementary solutions are increasingly important as antimicrobials lose efficacy and treatments become more complex,” Marchant said. “Vaccination offers a proactive and effective preventive solution, directly and indirectly reducing the spread of resistant pathogens.”
Vaccines combat AMR through various mechanisms. “They prevent diseases such as pneumococcal pneumonia and meningitis, reducing the need for antibiotics to treat these infections,” Marchant explained. “Additionally, vaccination lowers inappropriate antibiotic use by preventing viral infections, reducing the risk of overprescribing antibiotics in cases where they are unnecessary. Lastly, herd immunity from vaccination slows the circulation of resistant pathogens, limiting their spread.”
Van Ranst urged healthcare professionals to prioritize vaccinating at-risk populations as identified by Belgium’s Superior Health Council. These include the elderly with underlying conditions and pregnant women, especially for influenza vaccines. University Hospitals Leuven in Belgium, also conducts annual vaccination campaigns for its staff, combining flu and COVID vaccines to increase uptake.
A Global Challenge
Marc Noppen, MD, PhD, director of University Hospital Brussels, Belgium, emphasized the complexity of AMR as a global issue. “The problem isn’t solely due to human antibiotic use; it also stems from veterinary medicine, plant breeding, and animal husbandry. This is a multifactorial, worldwide issue that requires public awareness. Improved vaccination strategies are one way to address AMR, particularly in this post-COVID era of heightened skepticism toward vaccines,” he explained.
Marie-Lise Verschelden from Pfizer highlighted the need for cooperation across the healthcare sector. “Belgium is fortunate to have a fantastic ecosystem of academics, clinicians, and industry experts. Collaboration, including government involvement, is critical to advancing our efforts. At Pfizer, we continue to develop new vaccines and technologies, and the COVID crisis has reinforced the critical role of vaccination in combating AMR. Through our vaccine portfolio and ongoing developments, we are well-positioned to contribute significantly to this global challenge.”
Elisabeth Van Damme from GSK reiterated that AMR is a global issue requiring joint efforts. “Existing vaccines are underutilized. Vaccination protects against certain infectious diseases, reducing the need for antibiotics. Antibiotics, in turn, are sometimes prescribed incorrectly, especially for viral infections they cannot treat. At GSK, we are already developing new vaccines to meet future needs.”
Vaccination remains a cornerstone in the fight against AMR. As pathogens grow increasingly resistant to antibiotics, coordinated efforts and innovative vaccine development are essential to mitigating this global health crisis.
This story was translated and adapted from MediQuality using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Antimicrobial resistance (AMR) is globally recognized as one of the greatest health threats of the 21st century, responsible for 1.27 million deaths annually. “According to the WHO, if no measures are taken promptly, AMR could lead to more deaths than cancer by 2050,” Arnaud Marchant, MD, PhD, director of the European Plotkin Institute for Vaccinology at Université libre de Bruxelles (EPIV-ULB), Anderlecht, Belgium, said in an interview with MediQuality, part of the Medscape Professional Network. “This is a huge problem, and vaccination could be part of the solution.”
EPIV-ULB marked the start of the World AMR Awareness Week (November 18-24) with an event highlighting the critical role of vaccination to counter the rise for resistant pathogens. During the event, MediQuality interviewed Marchant, along with several other experts in the field.
Antibiotics Losing Effectiveness
Marc Van Ranst, PhD, virologist at Rega Institute KU Leuven in Leuven, Belgium, echoed Marchant’s concerns. He noted that “an increasing number of bacteria are becoming resistant to more antibiotics.” “While antibiotics were once miracle drugs, they have now stopped — or almost stopped — working against certain bacteria. Although we are discovering more effective therapies, bacterial infections are increasingly likely to worsen due to AMR.”
Van Ranst issued a stark warning: “If this trend continues, it is entirely reasonable to predict that in 25 years, some antibiotics will become useless, certain bacterial infections will be much harder to treat, and deaths will outnumber those caused by cancer. It’s worth noting, however, that as cancer treatments improve, cancer-related deaths are expected to decline, further highlighting the growing burden of AMR-related fatalities.”
Viruses, Vaccines, and Resistance
Van Ranst emphasized that while AMR primarily involves bacteria, viral infections and vaccination against them also play a role in addressing the issue. “When vaccines prevent illness, they reduce the need for unnecessary antibiotic use. In the past, antibiotics were frequently prescribed for respiratory infections — typically caused by viruses — leading to misuse and heightened resistance. By preventing viral infections through vaccines, we reduce inappropriate antibiotic prescriptions and, subsequently, AMR.”
Strategic Areas of Focus
To maximize the impact of vaccination in combating AMR, Belgium must prioritize several strategic areas, according to EPIV-ULB. “Expanding vaccination coverage for recommended vaccines is crucial to effectively preventing the spread of resistant pathogens,” said Marchant.
“Innovation and development of new vaccines are also essential, including targeted research into vaccines for infections that are currently unavoidable through other means. Enhancing epidemiological surveillance through national data collection and analysis will further clarify the impact of vaccines on AMR and inform policy decisions.”
EPIV-ULB underscored the importance of educating the public and healthcare professionals. “Public awareness is essential to addressing vaccine hesitancy by providing clear information on the importance of prevention,” Marchant explained. “Healthcare professional training must also improve, encouraging preventive practices and judicious antibiotic use. Furthermore, additional research is necessary to fill data gaps and develop predictive models that can guide vaccine development in the future.”
Role of Vaccination
According to EPIV-ULB, Belgium needs a strengthened national strategy to address AMR effectively. “Complementary solutions are increasingly important as antimicrobials lose efficacy and treatments become more complex,” Marchant said. “Vaccination offers a proactive and effective preventive solution, directly and indirectly reducing the spread of resistant pathogens.”
Vaccines combat AMR through various mechanisms. “They prevent diseases such as pneumococcal pneumonia and meningitis, reducing the need for antibiotics to treat these infections,” Marchant explained. “Additionally, vaccination lowers inappropriate antibiotic use by preventing viral infections, reducing the risk of overprescribing antibiotics in cases where they are unnecessary. Lastly, herd immunity from vaccination slows the circulation of resistant pathogens, limiting their spread.”
Van Ranst urged healthcare professionals to prioritize vaccinating at-risk populations as identified by Belgium’s Superior Health Council. These include the elderly with underlying conditions and pregnant women, especially for influenza vaccines. University Hospitals Leuven in Belgium, also conducts annual vaccination campaigns for its staff, combining flu and COVID vaccines to increase uptake.
A Global Challenge
Marc Noppen, MD, PhD, director of University Hospital Brussels, Belgium, emphasized the complexity of AMR as a global issue. “The problem isn’t solely due to human antibiotic use; it also stems from veterinary medicine, plant breeding, and animal husbandry. This is a multifactorial, worldwide issue that requires public awareness. Improved vaccination strategies are one way to address AMR, particularly in this post-COVID era of heightened skepticism toward vaccines,” he explained.
Marie-Lise Verschelden from Pfizer highlighted the need for cooperation across the healthcare sector. “Belgium is fortunate to have a fantastic ecosystem of academics, clinicians, and industry experts. Collaboration, including government involvement, is critical to advancing our efforts. At Pfizer, we continue to develop new vaccines and technologies, and the COVID crisis has reinforced the critical role of vaccination in combating AMR. Through our vaccine portfolio and ongoing developments, we are well-positioned to contribute significantly to this global challenge.”
Elisabeth Van Damme from GSK reiterated that AMR is a global issue requiring joint efforts. “Existing vaccines are underutilized. Vaccination protects against certain infectious diseases, reducing the need for antibiotics. Antibiotics, in turn, are sometimes prescribed incorrectly, especially for viral infections they cannot treat. At GSK, we are already developing new vaccines to meet future needs.”
Vaccination remains a cornerstone in the fight against AMR. As pathogens grow increasingly resistant to antibiotics, coordinated efforts and innovative vaccine development are essential to mitigating this global health crisis.
This story was translated and adapted from MediQuality using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Watch That Attitude: Is There Ageism in Healthcare?
People are living longer in Europe. Life expectancy increased on the continent by around 12 years between 1960 and 2022. And despite slower progress during the COVID-19 pandemic, the trend appears to be continuing.
Not only are Europeans living longer, their fertility rates are declining. This means that the number of people aged 75-84 years is projected to grow in Europe a full 56.1% by 2050, while the population younger than 55 years is expected to fall by 13.5%.
This means that attitudes toward age need to change, and fast — even among healthcare professionals.
Healthcare Is Not Exempt From Ageist Attitudes
A systematic review published in the journal PLOS ONE in 2020 found that age was a determinant factor in dictating who received certain medical procedures or treatments. For example, a study of 9105 hospitalized patients found that healthcare providers were significantly more likely to withhold life-sustaining treatments from older patients. Another study found evidence that older people are excluded from clinical trials, even when the trials are for diseases that appear later in life, like Parkinson’s.
“In healthcare, there are different levels of ageism,” explained Hannah Swift, PhD, reader in social and organizational psychology at the University of Kent in the United Kingdom.
Ageism is embedded in the laws, rules, and practices of institutions, she explained. This became especially obvious during the pandemic, when health professionals had to decide who to treat, possibly using age as a proxy for making some of these decisions, she said.
“When you categorize people, you might be using stereotypes, assumptions, and expectations about age and that age group to make those decisions, and that’s where errors can occur.”
She added that ageist attitudes also become apparent at the interpersonal level by using patronizing language or offering unnecessary help to older people based on assumptions about their cognitive and physical abilities.
“Older age is often wrongly associated with declining levels of health and activity,” said Ittay Mannheim, PhD, guest postdoctoral researcher on aging and ageism at the Open University of the Netherlands. “However, older adults are a very diverse group, varying widely in many aspects, including health conditions. This stereotype can influence how healthcare professionals interact with them, assuming frailty or memory issues simply based on age. It’s important to recognize that being older doesn’t necessarily mean being ill.”
Mannheim’s research found that healthcare professionals often stand in the way of older people using technology-based treatments due to negative attitudes towards age. “So, actually, a barrier to using these technologies could be that healthcare professionals don’t think that someone can use it or won’t even offer it because someone looks old or is old,” he said.
The Impacts
Discrimination impacts the physical, mental, and social well-being of its victims. This includes attitudes towards age.
The PLOS ONE review of research on the global reach of ageism found that experienced or self-determined ageism was associated with significantly worse health outcomes across all countries examined. The same research team calculated that an estimated 6.3 million cases of depression worldwide are linked to ageism.
Other research has found that exposure to negative age stereotyping impacts willingness to adopt a healthy lifestyle in addition to increasing the risk for cardiovascular events.
What Can Be Done?
“Healthcare professionals frequently interact with older adults at their most vulnerable, which can reinforce negative stereotypes of older people being vulnerable or ill,” said Swift. “However, not all older adults fit these stereotypes. Many can live well and independently. Perhaps healthcare education should include reminders of the diverse experiences of older individuals rather than solely focusing on the moments when they require help.”
Research indicates that although progress has been made in geriatric training and the care of older individuals by healthcare education institutions, improved education and training are still needed at all levels of geriatric healthcare, including hospital administrators, physicians, nurses, personal caregivers, and associated health professions.
“Generally speaking, what healthcare professionals learn about aging tends to focus more on the biological aspects,” said Mannheim. “However, they may not fully understand what it means to be old or how to interact with older individuals, especially regarding technology. It is important to raise awareness about ageism because, in my experience working with healthcare professionals, even a single workshop on ageism can have a profound impact. Participants often respond with surprise, saying something like, ‘Wow, I never thought about this before.’”
Mannheim said that training healthcare providers to understand the aging process better could help to reduce any biases they might have and better prepare them to respond more adequately to the needs of older patients.
“We cannot devalue the lives of older people simply because they are older. It is crucial for all of us, especially governments, to acknowledge our responsibility to protect and promote human rights for individuals of all ages. If we fail to do this, the strategies we’ve witnessed during this pandemic will be repeated in the future,” said Nena Georgantzi, PhD, Barcelona-based human rights manager at AGE Platform Europe, an EU network of organizations of and for older people.
A version of this article appeared on Medscape.com.
People are living longer in Europe. Life expectancy increased on the continent by around 12 years between 1960 and 2022. And despite slower progress during the COVID-19 pandemic, the trend appears to be continuing.
Not only are Europeans living longer, their fertility rates are declining. This means that the number of people aged 75-84 years is projected to grow in Europe a full 56.1% by 2050, while the population younger than 55 years is expected to fall by 13.5%.
This means that attitudes toward age need to change, and fast — even among healthcare professionals.
Healthcare Is Not Exempt From Ageist Attitudes
A systematic review published in the journal PLOS ONE in 2020 found that age was a determinant factor in dictating who received certain medical procedures or treatments. For example, a study of 9105 hospitalized patients found that healthcare providers were significantly more likely to withhold life-sustaining treatments from older patients. Another study found evidence that older people are excluded from clinical trials, even when the trials are for diseases that appear later in life, like Parkinson’s.
“In healthcare, there are different levels of ageism,” explained Hannah Swift, PhD, reader in social and organizational psychology at the University of Kent in the United Kingdom.
Ageism is embedded in the laws, rules, and practices of institutions, she explained. This became especially obvious during the pandemic, when health professionals had to decide who to treat, possibly using age as a proxy for making some of these decisions, she said.
“When you categorize people, you might be using stereotypes, assumptions, and expectations about age and that age group to make those decisions, and that’s where errors can occur.”
She added that ageist attitudes also become apparent at the interpersonal level by using patronizing language or offering unnecessary help to older people based on assumptions about their cognitive and physical abilities.
“Older age is often wrongly associated with declining levels of health and activity,” said Ittay Mannheim, PhD, guest postdoctoral researcher on aging and ageism at the Open University of the Netherlands. “However, older adults are a very diverse group, varying widely in many aspects, including health conditions. This stereotype can influence how healthcare professionals interact with them, assuming frailty or memory issues simply based on age. It’s important to recognize that being older doesn’t necessarily mean being ill.”
Mannheim’s research found that healthcare professionals often stand in the way of older people using technology-based treatments due to negative attitudes towards age. “So, actually, a barrier to using these technologies could be that healthcare professionals don’t think that someone can use it or won’t even offer it because someone looks old or is old,” he said.
The Impacts
Discrimination impacts the physical, mental, and social well-being of its victims. This includes attitudes towards age.
The PLOS ONE review of research on the global reach of ageism found that experienced or self-determined ageism was associated with significantly worse health outcomes across all countries examined. The same research team calculated that an estimated 6.3 million cases of depression worldwide are linked to ageism.
Other research has found that exposure to negative age stereotyping impacts willingness to adopt a healthy lifestyle in addition to increasing the risk for cardiovascular events.
What Can Be Done?
“Healthcare professionals frequently interact with older adults at their most vulnerable, which can reinforce negative stereotypes of older people being vulnerable or ill,” said Swift. “However, not all older adults fit these stereotypes. Many can live well and independently. Perhaps healthcare education should include reminders of the diverse experiences of older individuals rather than solely focusing on the moments when they require help.”
Research indicates that although progress has been made in geriatric training and the care of older individuals by healthcare education institutions, improved education and training are still needed at all levels of geriatric healthcare, including hospital administrators, physicians, nurses, personal caregivers, and associated health professions.
“Generally speaking, what healthcare professionals learn about aging tends to focus more on the biological aspects,” said Mannheim. “However, they may not fully understand what it means to be old or how to interact with older individuals, especially regarding technology. It is important to raise awareness about ageism because, in my experience working with healthcare professionals, even a single workshop on ageism can have a profound impact. Participants often respond with surprise, saying something like, ‘Wow, I never thought about this before.’”
Mannheim said that training healthcare providers to understand the aging process better could help to reduce any biases they might have and better prepare them to respond more adequately to the needs of older patients.
“We cannot devalue the lives of older people simply because they are older. It is crucial for all of us, especially governments, to acknowledge our responsibility to protect and promote human rights for individuals of all ages. If we fail to do this, the strategies we’ve witnessed during this pandemic will be repeated in the future,” said Nena Georgantzi, PhD, Barcelona-based human rights manager at AGE Platform Europe, an EU network of organizations of and for older people.
A version of this article appeared on Medscape.com.
People are living longer in Europe. Life expectancy increased on the continent by around 12 years between 1960 and 2022. And despite slower progress during the COVID-19 pandemic, the trend appears to be continuing.
Not only are Europeans living longer, their fertility rates are declining. This means that the number of people aged 75-84 years is projected to grow in Europe a full 56.1% by 2050, while the population younger than 55 years is expected to fall by 13.5%.
This means that attitudes toward age need to change, and fast — even among healthcare professionals.
Healthcare Is Not Exempt From Ageist Attitudes
A systematic review published in the journal PLOS ONE in 2020 found that age was a determinant factor in dictating who received certain medical procedures or treatments. For example, a study of 9105 hospitalized patients found that healthcare providers were significantly more likely to withhold life-sustaining treatments from older patients. Another study found evidence that older people are excluded from clinical trials, even when the trials are for diseases that appear later in life, like Parkinson’s.
“In healthcare, there are different levels of ageism,” explained Hannah Swift, PhD, reader in social and organizational psychology at the University of Kent in the United Kingdom.
Ageism is embedded in the laws, rules, and practices of institutions, she explained. This became especially obvious during the pandemic, when health professionals had to decide who to treat, possibly using age as a proxy for making some of these decisions, she said.
“When you categorize people, you might be using stereotypes, assumptions, and expectations about age and that age group to make those decisions, and that’s where errors can occur.”
She added that ageist attitudes also become apparent at the interpersonal level by using patronizing language or offering unnecessary help to older people based on assumptions about their cognitive and physical abilities.
“Older age is often wrongly associated with declining levels of health and activity,” said Ittay Mannheim, PhD, guest postdoctoral researcher on aging and ageism at the Open University of the Netherlands. “However, older adults are a very diverse group, varying widely in many aspects, including health conditions. This stereotype can influence how healthcare professionals interact with them, assuming frailty or memory issues simply based on age. It’s important to recognize that being older doesn’t necessarily mean being ill.”
Mannheim’s research found that healthcare professionals often stand in the way of older people using technology-based treatments due to negative attitudes towards age. “So, actually, a barrier to using these technologies could be that healthcare professionals don’t think that someone can use it or won’t even offer it because someone looks old or is old,” he said.
The Impacts
Discrimination impacts the physical, mental, and social well-being of its victims. This includes attitudes towards age.
The PLOS ONE review of research on the global reach of ageism found that experienced or self-determined ageism was associated with significantly worse health outcomes across all countries examined. The same research team calculated that an estimated 6.3 million cases of depression worldwide are linked to ageism.
Other research has found that exposure to negative age stereotyping impacts willingness to adopt a healthy lifestyle in addition to increasing the risk for cardiovascular events.
What Can Be Done?
“Healthcare professionals frequently interact with older adults at their most vulnerable, which can reinforce negative stereotypes of older people being vulnerable or ill,” said Swift. “However, not all older adults fit these stereotypes. Many can live well and independently. Perhaps healthcare education should include reminders of the diverse experiences of older individuals rather than solely focusing on the moments when they require help.”
Research indicates that although progress has been made in geriatric training and the care of older individuals by healthcare education institutions, improved education and training are still needed at all levels of geriatric healthcare, including hospital administrators, physicians, nurses, personal caregivers, and associated health professions.
“Generally speaking, what healthcare professionals learn about aging tends to focus more on the biological aspects,” said Mannheim. “However, they may not fully understand what it means to be old or how to interact with older individuals, especially regarding technology. It is important to raise awareness about ageism because, in my experience working with healthcare professionals, even a single workshop on ageism can have a profound impact. Participants often respond with surprise, saying something like, ‘Wow, I never thought about this before.’”
Mannheim said that training healthcare providers to understand the aging process better could help to reduce any biases they might have and better prepare them to respond more adequately to the needs of older patients.
“We cannot devalue the lives of older people simply because they are older. It is crucial for all of us, especially governments, to acknowledge our responsibility to protect and promote human rights for individuals of all ages. If we fail to do this, the strategies we’ve witnessed during this pandemic will be repeated in the future,” said Nena Georgantzi, PhD, Barcelona-based human rights manager at AGE Platform Europe, an EU network of organizations of and for older people.
A version of this article appeared on Medscape.com.
Does Screening at 40-49 Years Boost Breast Cancer Survival?
The data call into question draft guidelines from the Canadian Task Force on Preventive Health Care, which suggest not systematically screening women in this age group with mammography.
Overdiagnosis Challenged
Given that some jurisdictions in Canada have organized screening programs and some do not, there was an opportunity to compare breast cancer 10-year net survival of women who lived in jurisdictions with and without such programs, explained family physician Anna N. Wilkinson, MD, Ottawa regional cancer primary care lead and associate professor at the University of Ottawa in Ontario, Canada.
“The question was [whether] we could use big cancer data to figure out what’s going on,” she told this news organization.
To investigate, Wilkinson and co-investigators reviewed data from the Canadian Cancer Registry linked to mortality information and assessed outcomes for women aged 40-49 and 50-59 years diagnosed with breast cancer from 2002 to 2007. They compared 10-year net survival estimates in jurisdictions with organized screening programs for those aged 40-49 years with the jurisdictions without them.
“Net survival is important because it’s a survival measure that looks at only the cancer in question,” Wilkinson explained.
Investigators determined breast cancer to be the primary cause of 10-year mortality in women aged 40-49 years diagnosed with the disease (90.7% of deaths).
Furthermore, the 10-year net survival in jurisdictions that screened these women (84.8%) was 1.9 percentage points higher than for jurisdictions that did not (82.9%).
The difference in 10-year net survival favoring jurisdictions that offered screening was significant for women aged 45-49 years (2.6 percentage points) but not for those aged 40-44 years (0.9 percentage points).
Given that 90% of the deaths in women in their 40s who had a breast cancer diagnosis were due to breast cancer, Wilkinson challenged the concept of women in their 40s being overdiagnosed with breast cancer, meaning that the cancers detected were indolent and did not require treatment nor result in death.
Earlier detection would generally mean finding disease at an earlier stage and the need for less invasive treatment, she noted. “And one of the biggest benefits [of screening women in their 40s] is that you have diagnosis at earlier stage disease, which means fewer intensive therapies, less time off work, less long-term morbidity, and less cost to our healthcare system.”
Modeling Shows Little Screening Benefit
The task force’s draft guidelines, released earlier this year, were based on evidence from 165 studies including randomized, controlled trials, observational studies, time-trend studies and modeling. They suggest not systematically screening women 40-49 with mammography who are not high risk.
Family physician Guylène Thériault, MD, chair of the task force and its breast cancer working group, and director of the Pedagogy Center at the Outaouais Campus, McGill University, Montreal, Quebec, Canada, explained that to come to that conclusion, the task force had assessed the impact of organized screening for women in Canada aged 40-49 years and calculated the impact of mammography for every 1000 women over 10 years.
The model suggested that screening would yield 368 false positives, leading to 55 biopsies, and then to a breast cancer diagnosis in 19 women. Of those 19, the task force estimated 17 or 18 would not die of breast cancer over 10 years, two would be treated for breast cancer that would not have caused problems, ie, overdiagnosis, and one to two would die of breast cancer.
Without screening, on the other hand, the model suggested that 983 of 1000 women aged 40-49 years would not be diagnosed with breast cancer, and 17 would be, 15 of whom would not die from breast cancer over 10 years (no overdiagnosis, no deaths prevented) and two would die.
It is important that family physicians provide their patients with this information to assist in shared decision making about screening, Thériault said.
Wilkinson concluded that screening programs that included women in their 40s were associated with a significantly higher breast cancer 10-year survival, without an increased rate of diagnosis. She suggested that the study findings can inform the screening guidelines for women aged 40-49 years.
The study was supported by the University of Ottawa’s department of family medicine.
Wilkinson, MD, is a consultant for Thrive Health. Thériault, MD, disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
The data call into question draft guidelines from the Canadian Task Force on Preventive Health Care, which suggest not systematically screening women in this age group with mammography.
Overdiagnosis Challenged
Given that some jurisdictions in Canada have organized screening programs and some do not, there was an opportunity to compare breast cancer 10-year net survival of women who lived in jurisdictions with and without such programs, explained family physician Anna N. Wilkinson, MD, Ottawa regional cancer primary care lead and associate professor at the University of Ottawa in Ontario, Canada.
“The question was [whether] we could use big cancer data to figure out what’s going on,” she told this news organization.
To investigate, Wilkinson and co-investigators reviewed data from the Canadian Cancer Registry linked to mortality information and assessed outcomes for women aged 40-49 and 50-59 years diagnosed with breast cancer from 2002 to 2007. They compared 10-year net survival estimates in jurisdictions with organized screening programs for those aged 40-49 years with the jurisdictions without them.
“Net survival is important because it’s a survival measure that looks at only the cancer in question,” Wilkinson explained.
Investigators determined breast cancer to be the primary cause of 10-year mortality in women aged 40-49 years diagnosed with the disease (90.7% of deaths).
Furthermore, the 10-year net survival in jurisdictions that screened these women (84.8%) was 1.9 percentage points higher than for jurisdictions that did not (82.9%).
The difference in 10-year net survival favoring jurisdictions that offered screening was significant for women aged 45-49 years (2.6 percentage points) but not for those aged 40-44 years (0.9 percentage points).
Given that 90% of the deaths in women in their 40s who had a breast cancer diagnosis were due to breast cancer, Wilkinson challenged the concept of women in their 40s being overdiagnosed with breast cancer, meaning that the cancers detected were indolent and did not require treatment nor result in death.
Earlier detection would generally mean finding disease at an earlier stage and the need for less invasive treatment, she noted. “And one of the biggest benefits [of screening women in their 40s] is that you have diagnosis at earlier stage disease, which means fewer intensive therapies, less time off work, less long-term morbidity, and less cost to our healthcare system.”
Modeling Shows Little Screening Benefit
The task force’s draft guidelines, released earlier this year, were based on evidence from 165 studies including randomized, controlled trials, observational studies, time-trend studies and modeling. They suggest not systematically screening women 40-49 with mammography who are not high risk.
Family physician Guylène Thériault, MD, chair of the task force and its breast cancer working group, and director of the Pedagogy Center at the Outaouais Campus, McGill University, Montreal, Quebec, Canada, explained that to come to that conclusion, the task force had assessed the impact of organized screening for women in Canada aged 40-49 years and calculated the impact of mammography for every 1000 women over 10 years.
The model suggested that screening would yield 368 false positives, leading to 55 biopsies, and then to a breast cancer diagnosis in 19 women. Of those 19, the task force estimated 17 or 18 would not die of breast cancer over 10 years, two would be treated for breast cancer that would not have caused problems, ie, overdiagnosis, and one to two would die of breast cancer.
Without screening, on the other hand, the model suggested that 983 of 1000 women aged 40-49 years would not be diagnosed with breast cancer, and 17 would be, 15 of whom would not die from breast cancer over 10 years (no overdiagnosis, no deaths prevented) and two would die.
It is important that family physicians provide their patients with this information to assist in shared decision making about screening, Thériault said.
Wilkinson concluded that screening programs that included women in their 40s were associated with a significantly higher breast cancer 10-year survival, without an increased rate of diagnosis. She suggested that the study findings can inform the screening guidelines for women aged 40-49 years.
The study was supported by the University of Ottawa’s department of family medicine.
Wilkinson, MD, is a consultant for Thrive Health. Thériault, MD, disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
The data call into question draft guidelines from the Canadian Task Force on Preventive Health Care, which suggest not systematically screening women in this age group with mammography.
Overdiagnosis Challenged
Given that some jurisdictions in Canada have organized screening programs and some do not, there was an opportunity to compare breast cancer 10-year net survival of women who lived in jurisdictions with and without such programs, explained family physician Anna N. Wilkinson, MD, Ottawa regional cancer primary care lead and associate professor at the University of Ottawa in Ontario, Canada.
“The question was [whether] we could use big cancer data to figure out what’s going on,” she told this news organization.
To investigate, Wilkinson and co-investigators reviewed data from the Canadian Cancer Registry linked to mortality information and assessed outcomes for women aged 40-49 and 50-59 years diagnosed with breast cancer from 2002 to 2007. They compared 10-year net survival estimates in jurisdictions with organized screening programs for those aged 40-49 years with the jurisdictions without them.
“Net survival is important because it’s a survival measure that looks at only the cancer in question,” Wilkinson explained.
Investigators determined breast cancer to be the primary cause of 10-year mortality in women aged 40-49 years diagnosed with the disease (90.7% of deaths).
Furthermore, the 10-year net survival in jurisdictions that screened these women (84.8%) was 1.9 percentage points higher than for jurisdictions that did not (82.9%).
The difference in 10-year net survival favoring jurisdictions that offered screening was significant for women aged 45-49 years (2.6 percentage points) but not for those aged 40-44 years (0.9 percentage points).
Given that 90% of the deaths in women in their 40s who had a breast cancer diagnosis were due to breast cancer, Wilkinson challenged the concept of women in their 40s being overdiagnosed with breast cancer, meaning that the cancers detected were indolent and did not require treatment nor result in death.
Earlier detection would generally mean finding disease at an earlier stage and the need for less invasive treatment, she noted. “And one of the biggest benefits [of screening women in their 40s] is that you have diagnosis at earlier stage disease, which means fewer intensive therapies, less time off work, less long-term morbidity, and less cost to our healthcare system.”
Modeling Shows Little Screening Benefit
The task force’s draft guidelines, released earlier this year, were based on evidence from 165 studies including randomized, controlled trials, observational studies, time-trend studies and modeling. They suggest not systematically screening women 40-49 with mammography who are not high risk.
Family physician Guylène Thériault, MD, chair of the task force and its breast cancer working group, and director of the Pedagogy Center at the Outaouais Campus, McGill University, Montreal, Quebec, Canada, explained that to come to that conclusion, the task force had assessed the impact of organized screening for women in Canada aged 40-49 years and calculated the impact of mammography for every 1000 women over 10 years.
The model suggested that screening would yield 368 false positives, leading to 55 biopsies, and then to a breast cancer diagnosis in 19 women. Of those 19, the task force estimated 17 or 18 would not die of breast cancer over 10 years, two would be treated for breast cancer that would not have caused problems, ie, overdiagnosis, and one to two would die of breast cancer.
Without screening, on the other hand, the model suggested that 983 of 1000 women aged 40-49 years would not be diagnosed with breast cancer, and 17 would be, 15 of whom would not die from breast cancer over 10 years (no overdiagnosis, no deaths prevented) and two would die.
It is important that family physicians provide their patients with this information to assist in shared decision making about screening, Thériault said.
Wilkinson concluded that screening programs that included women in their 40s were associated with a significantly higher breast cancer 10-year survival, without an increased rate of diagnosis. She suggested that the study findings can inform the screening guidelines for women aged 40-49 years.
The study was supported by the University of Ottawa’s department of family medicine.
Wilkinson, MD, is a consultant for Thrive Health. Thériault, MD, disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
FROM FMF 2024
