User login
An appeal for equitable access to care for early pregnancy loss
Remarkable advances in care for early pregnancy loss (EPL) have occurred over the past several years. Misoprostol with mifepristone pretreatment is now the gold standard for medical management after recent research showed that this regimen improves both the efficacy and cost-effectiveness of medical management.1 Manual vacuum aspiration (MVA)’s portability, effectiveness, and safety ensure that providers can offer procedural EPL management in almost any clinical setting. Medication management and in-office uterine aspiration are two evidence-based options for EPL management that may increase access for the 25% of pregnant women who experience EPL. Unfortunately, many women do not have access to either option. Equitable access to early pregnancy loss management can be achieved by expanding access to mifepristone and office-based MVA.
However, access to mifepristone and initiating office-based MVA is challenging. Mifepristone is one of several medications regulated under the Food and Drug Administration’s Risk Evaluation and Management Strategies (REMS) program.2
The REMS guidelines restrict clinicians in prescribing and dispensing mifepristone, including the key provision that mifepristone may be dispensed only in clinics, medical offices, and hospitals. Clinicians cannot write a prescription for mifepristone for a patient to pick up at the pharmacy. Efforts are underway to roll back the REMS. Barriers to office-based MVA include time, culture shift among staff, gathering equipment, and creating protocols. Clinicians can improve access to EPL management in a variety of ways:
- MVA training: Ob.gyns. who lack training in MVA use can take advantage of several programs designed to teach the skill to clinicians, including programs such as Training, Education, and Advocacy in Miscarriage Management (TEAMM).3,4 MVA is easy to learn for ob.gyns. and procedural complications are uncommon. In the office setting, complications requiring transfer to a higher level of care are rare.5 With adequate training, whether during residency or afterward, ob.gyns. can learn to safely and effectively use MVA for procedural EPL management in the office and in the emergency department.
- Partnerships with pharmacists to reduce barriers to mifepristone: Ob.gyns. working in a variety of clinical settings, including independent clinics, critical access hospitals, community hospitals, and academic medical centers, have worked closely with on-site pharmacists to place mifepristone on their practice sites’ formularies.6 These ob.gyn.–pharmacist collaborations often require explanations to institutional Pharmacy and Therapeutics (P&T) committees of the benefits of mifepristone to patients, detailed indications for mifepristone’s use, and methods to secure mifepristone on site.
- Partnerships with emergency department and outpatient nursing and administration to promote MVA: Provision of MVA is ideal for safe, effective, and cost-efficient procedural EPL management in both the emergency department and outpatient setting. However, access to MVA in emergency rooms and outpatient clinical settings is suboptimal. Some clinicians push back against MVA use in the emergency department, citing fears that performing the procedure in the emergency department unnecessarily uses staff and resources reserved for patients with more critical illnesses. Ob.gyns. should also work with emergency medicine physicians and emergency department nursing staff and hospital administrators in explaining that MVA in the emergency room is patient centered and cost effective.
Interdisciplinary collaboration and training are two strategies that can increase access to mifepristone and MVA for EPL management. Use of mifepristone/misoprostol and office/emergency department MVA for treatment of EPL is patient centered, evidence based, feasible, highly effective, and timely. These two health care interventions are practical in almost any setting, including rural and other low-resource settings. By using these strategies to overcome the logistical and institutional challenges, ob.gyns. can help countless women with EPL gain access to the best EPL care.
Dr. Espey is chair of the department of obstetrics and gynecology at the University of New Mexico, Albuquerque. Dr. Jackson is an obstetrician/gynecologist at Michigan State University in Flint. They have no disclosures to report.
References
1. Schreiber CA et al. N Engl J Med. 2018 Jun 7;378(23):2161-70.
2. Food and Drug Administration. Mifeprex (mifepristone) information.
3. The TEAMM (Training, Education, and Advocacy in Miscarriage Management) Project. Training interprofessional teams to manage miscarriage. Accessed March 15, 2021.
4. Quinley KE et al. Ann Emerg Med. 2019 Jul;72(1):86-92.
5. Milingos DS et al. BJOG. 2009 Aug;116(9):1268-71.
6. Calloway D et al. Contraception. 2021 Jul;104(1):24-8.
Remarkable advances in care for early pregnancy loss (EPL) have occurred over the past several years. Misoprostol with mifepristone pretreatment is now the gold standard for medical management after recent research showed that this regimen improves both the efficacy and cost-effectiveness of medical management.1 Manual vacuum aspiration (MVA)’s portability, effectiveness, and safety ensure that providers can offer procedural EPL management in almost any clinical setting. Medication management and in-office uterine aspiration are two evidence-based options for EPL management that may increase access for the 25% of pregnant women who experience EPL. Unfortunately, many women do not have access to either option. Equitable access to early pregnancy loss management can be achieved by expanding access to mifepristone and office-based MVA.
However, access to mifepristone and initiating office-based MVA is challenging. Mifepristone is one of several medications regulated under the Food and Drug Administration’s Risk Evaluation and Management Strategies (REMS) program.2
The REMS guidelines restrict clinicians in prescribing and dispensing mifepristone, including the key provision that mifepristone may be dispensed only in clinics, medical offices, and hospitals. Clinicians cannot write a prescription for mifepristone for a patient to pick up at the pharmacy. Efforts are underway to roll back the REMS. Barriers to office-based MVA include time, culture shift among staff, gathering equipment, and creating protocols. Clinicians can improve access to EPL management in a variety of ways:
- MVA training: Ob.gyns. who lack training in MVA use can take advantage of several programs designed to teach the skill to clinicians, including programs such as Training, Education, and Advocacy in Miscarriage Management (TEAMM).3,4 MVA is easy to learn for ob.gyns. and procedural complications are uncommon. In the office setting, complications requiring transfer to a higher level of care are rare.5 With adequate training, whether during residency or afterward, ob.gyns. can learn to safely and effectively use MVA for procedural EPL management in the office and in the emergency department.
- Partnerships with pharmacists to reduce barriers to mifepristone: Ob.gyns. working in a variety of clinical settings, including independent clinics, critical access hospitals, community hospitals, and academic medical centers, have worked closely with on-site pharmacists to place mifepristone on their practice sites’ formularies.6 These ob.gyn.–pharmacist collaborations often require explanations to institutional Pharmacy and Therapeutics (P&T) committees of the benefits of mifepristone to patients, detailed indications for mifepristone’s use, and methods to secure mifepristone on site.
- Partnerships with emergency department and outpatient nursing and administration to promote MVA: Provision of MVA is ideal for safe, effective, and cost-efficient procedural EPL management in both the emergency department and outpatient setting. However, access to MVA in emergency rooms and outpatient clinical settings is suboptimal. Some clinicians push back against MVA use in the emergency department, citing fears that performing the procedure in the emergency department unnecessarily uses staff and resources reserved for patients with more critical illnesses. Ob.gyns. should also work with emergency medicine physicians and emergency department nursing staff and hospital administrators in explaining that MVA in the emergency room is patient centered and cost effective.
Interdisciplinary collaboration and training are two strategies that can increase access to mifepristone and MVA for EPL management. Use of mifepristone/misoprostol and office/emergency department MVA for treatment of EPL is patient centered, evidence based, feasible, highly effective, and timely. These two health care interventions are practical in almost any setting, including rural and other low-resource settings. By using these strategies to overcome the logistical and institutional challenges, ob.gyns. can help countless women with EPL gain access to the best EPL care.
Dr. Espey is chair of the department of obstetrics and gynecology at the University of New Mexico, Albuquerque. Dr. Jackson is an obstetrician/gynecologist at Michigan State University in Flint. They have no disclosures to report.
References
1. Schreiber CA et al. N Engl J Med. 2018 Jun 7;378(23):2161-70.
2. Food and Drug Administration. Mifeprex (mifepristone) information.
3. The TEAMM (Training, Education, and Advocacy in Miscarriage Management) Project. Training interprofessional teams to manage miscarriage. Accessed March 15, 2021.
4. Quinley KE et al. Ann Emerg Med. 2019 Jul;72(1):86-92.
5. Milingos DS et al. BJOG. 2009 Aug;116(9):1268-71.
6. Calloway D et al. Contraception. 2021 Jul;104(1):24-8.
Remarkable advances in care for early pregnancy loss (EPL) have occurred over the past several years. Misoprostol with mifepristone pretreatment is now the gold standard for medical management after recent research showed that this regimen improves both the efficacy and cost-effectiveness of medical management.1 Manual vacuum aspiration (MVA)’s portability, effectiveness, and safety ensure that providers can offer procedural EPL management in almost any clinical setting. Medication management and in-office uterine aspiration are two evidence-based options for EPL management that may increase access for the 25% of pregnant women who experience EPL. Unfortunately, many women do not have access to either option. Equitable access to early pregnancy loss management can be achieved by expanding access to mifepristone and office-based MVA.
However, access to mifepristone and initiating office-based MVA is challenging. Mifepristone is one of several medications regulated under the Food and Drug Administration’s Risk Evaluation and Management Strategies (REMS) program.2
The REMS guidelines restrict clinicians in prescribing and dispensing mifepristone, including the key provision that mifepristone may be dispensed only in clinics, medical offices, and hospitals. Clinicians cannot write a prescription for mifepristone for a patient to pick up at the pharmacy. Efforts are underway to roll back the REMS. Barriers to office-based MVA include time, culture shift among staff, gathering equipment, and creating protocols. Clinicians can improve access to EPL management in a variety of ways:
- MVA training: Ob.gyns. who lack training in MVA use can take advantage of several programs designed to teach the skill to clinicians, including programs such as Training, Education, and Advocacy in Miscarriage Management (TEAMM).3,4 MVA is easy to learn for ob.gyns. and procedural complications are uncommon. In the office setting, complications requiring transfer to a higher level of care are rare.5 With adequate training, whether during residency or afterward, ob.gyns. can learn to safely and effectively use MVA for procedural EPL management in the office and in the emergency department.
- Partnerships with pharmacists to reduce barriers to mifepristone: Ob.gyns. working in a variety of clinical settings, including independent clinics, critical access hospitals, community hospitals, and academic medical centers, have worked closely with on-site pharmacists to place mifepristone on their practice sites’ formularies.6 These ob.gyn.–pharmacist collaborations often require explanations to institutional Pharmacy and Therapeutics (P&T) committees of the benefits of mifepristone to patients, detailed indications for mifepristone’s use, and methods to secure mifepristone on site.
- Partnerships with emergency department and outpatient nursing and administration to promote MVA: Provision of MVA is ideal for safe, effective, and cost-efficient procedural EPL management in both the emergency department and outpatient setting. However, access to MVA in emergency rooms and outpatient clinical settings is suboptimal. Some clinicians push back against MVA use in the emergency department, citing fears that performing the procedure in the emergency department unnecessarily uses staff and resources reserved for patients with more critical illnesses. Ob.gyns. should also work with emergency medicine physicians and emergency department nursing staff and hospital administrators in explaining that MVA in the emergency room is patient centered and cost effective.
Interdisciplinary collaboration and training are two strategies that can increase access to mifepristone and MVA for EPL management. Use of mifepristone/misoprostol and office/emergency department MVA for treatment of EPL is patient centered, evidence based, feasible, highly effective, and timely. These two health care interventions are practical in almost any setting, including rural and other low-resource settings. By using these strategies to overcome the logistical and institutional challenges, ob.gyns. can help countless women with EPL gain access to the best EPL care.
Dr. Espey is chair of the department of obstetrics and gynecology at the University of New Mexico, Albuquerque. Dr. Jackson is an obstetrician/gynecologist at Michigan State University in Flint. They have no disclosures to report.
References
1. Schreiber CA et al. N Engl J Med. 2018 Jun 7;378(23):2161-70.
2. Food and Drug Administration. Mifeprex (mifepristone) information.
3. The TEAMM (Training, Education, and Advocacy in Miscarriage Management) Project. Training interprofessional teams to manage miscarriage. Accessed March 15, 2021.
4. Quinley KE et al. Ann Emerg Med. 2019 Jul;72(1):86-92.
5. Milingos DS et al. BJOG. 2009 Aug;116(9):1268-71.
6. Calloway D et al. Contraception. 2021 Jul;104(1):24-8.
Authors’ response
My co-authors and I appreciate the excellent comments regarding our Photo Rounds column, “Foot rash and joint pain,” and would like to provide some additional detail.
After our patient’s 27-day hospital stay, he was admitted to a rehabilitation center for continued inpatient physical therapy for 14 days due to weakness and deconditioning. Following his discharge from the rehabilitation center, the patient was still confined to a wheelchair. He was prescribed an oral prednisone taper (as mentioned in our article) and celecoxib 200 mg bid and referred for outpatient physical therapy. At a follow-up appointment with the rheumatologist, he received adalimumab 80 mg followed by 40 mg every other week, which led to improvement in his range of motion and pain. Two months after outpatient physical therapy, the patient was lost to follow-up.
We agree with Dr. Hahn et al that many of these patients with chlamydia-associated ReA become “long-haulers.” In medicine—especially when rare diseases are considered—we must often make decisions without perfect science. The studies referenced by Dr. Hahn et al suggest that combinations of doxycycline and rifampin or azithromycin and rifampin may treat not only chlamydial infection, but ReA and associated cutaneous disease, as well.1,2 While these studies are small in size, larger studies may never be funded. We agree that combination therapy should be considered in this population of patients.
Hannah R. Badon, MD
Ross L. Pearlman, MD
Robert T. Brodell, MD
Jackson, MS
1. Carter JD, Valeriano J, Vasey FB. Doxycycline versus doxycycline and rifampin in undifferentiated spondyloarthropathy, with special reference to chlamydia-induced arthritis. A prospective, randomized 9-month comparison. J Rheumatol. 2004;31:1973-1980.
2. Carter JD, Espinoza LR, Inman RD, et al. Combination antibiotics as a treatment for chronic Chlamydia-induced reactive arthritis: a double-blind, placebo-controlled, prospective trial. Arthritis Rheum. 2010;62:1298-1307. doi: 10.1002/art.27394
My co-authors and I appreciate the excellent comments regarding our Photo Rounds column, “Foot rash and joint pain,” and would like to provide some additional detail.
After our patient’s 27-day hospital stay, he was admitted to a rehabilitation center for continued inpatient physical therapy for 14 days due to weakness and deconditioning. Following his discharge from the rehabilitation center, the patient was still confined to a wheelchair. He was prescribed an oral prednisone taper (as mentioned in our article) and celecoxib 200 mg bid and referred for outpatient physical therapy. At a follow-up appointment with the rheumatologist, he received adalimumab 80 mg followed by 40 mg every other week, which led to improvement in his range of motion and pain. Two months after outpatient physical therapy, the patient was lost to follow-up.
We agree with Dr. Hahn et al that many of these patients with chlamydia-associated ReA become “long-haulers.” In medicine—especially when rare diseases are considered—we must often make decisions without perfect science. The studies referenced by Dr. Hahn et al suggest that combinations of doxycycline and rifampin or azithromycin and rifampin may treat not only chlamydial infection, but ReA and associated cutaneous disease, as well.1,2 While these studies are small in size, larger studies may never be funded. We agree that combination therapy should be considered in this population of patients.
Hannah R. Badon, MD
Ross L. Pearlman, MD
Robert T. Brodell, MD
Jackson, MS
My co-authors and I appreciate the excellent comments regarding our Photo Rounds column, “Foot rash and joint pain,” and would like to provide some additional detail.
After our patient’s 27-day hospital stay, he was admitted to a rehabilitation center for continued inpatient physical therapy for 14 days due to weakness and deconditioning. Following his discharge from the rehabilitation center, the patient was still confined to a wheelchair. He was prescribed an oral prednisone taper (as mentioned in our article) and celecoxib 200 mg bid and referred for outpatient physical therapy. At a follow-up appointment with the rheumatologist, he received adalimumab 80 mg followed by 40 mg every other week, which led to improvement in his range of motion and pain. Two months after outpatient physical therapy, the patient was lost to follow-up.
We agree with Dr. Hahn et al that many of these patients with chlamydia-associated ReA become “long-haulers.” In medicine—especially when rare diseases are considered—we must often make decisions without perfect science. The studies referenced by Dr. Hahn et al suggest that combinations of doxycycline and rifampin or azithromycin and rifampin may treat not only chlamydial infection, but ReA and associated cutaneous disease, as well.1,2 While these studies are small in size, larger studies may never be funded. We agree that combination therapy should be considered in this population of patients.
Hannah R. Badon, MD
Ross L. Pearlman, MD
Robert T. Brodell, MD
Jackson, MS
1. Carter JD, Valeriano J, Vasey FB. Doxycycline versus doxycycline and rifampin in undifferentiated spondyloarthropathy, with special reference to chlamydia-induced arthritis. A prospective, randomized 9-month comparison. J Rheumatol. 2004;31:1973-1980.
2. Carter JD, Espinoza LR, Inman RD, et al. Combination antibiotics as a treatment for chronic Chlamydia-induced reactive arthritis: a double-blind, placebo-controlled, prospective trial. Arthritis Rheum. 2010;62:1298-1307. doi: 10.1002/art.27394
1. Carter JD, Valeriano J, Vasey FB. Doxycycline versus doxycycline and rifampin in undifferentiated spondyloarthropathy, with special reference to chlamydia-induced arthritis. A prospective, randomized 9-month comparison. J Rheumatol. 2004;31:1973-1980.
2. Carter JD, Espinoza LR, Inman RD, et al. Combination antibiotics as a treatment for chronic Chlamydia-induced reactive arthritis: a double-blind, placebo-controlled, prospective trial. Arthritis Rheum. 2010;62:1298-1307. doi: 10.1002/art.27394
How best to treat “long-haulers” with reactive arthritis?
In the June Photo Rounds column, “Foot rash and joint pain” (J Fam Pract. 2021;70:249-251), Badon et al presented a case of chlamydia-associated reactive arthritis (ReA), formerly called Reiter syndrome, in a 21-year-old man following Chlamydia trachomatis urethritis. We would like to point out that, contrary to the conventional definition of ReA, in which the causative pathogen can’t be cultured from the affected joints,1 chlamydia-associated ReA is associated with evidence of chronic joint infection that, while not cultivable, can be confirmed by real-time polymerase chain reaction testing of metabolically active pathogens in synovial tissue and/or fluid.2
C trachomatis and C pneumoniae are the most frequent causative pathogens to elicit ReA.3 Short-course antibiotics and anti-inflammatory treatments can palliate ReA, but these treatments often do not provide a cure.3 Two controlled clinical trials demonstrated that chlamydia-associated ReA can be treated successfully with longer-term combination antibiotic therapy.4,5 ReA is usually diagnosed in the acute stage (first 6 months) and can become chronic in 30% of cases.6 It would be interesting to know the long-term treatment and outcome data for the case patient.
David L. Hahn, MD, MS
Alan P. Hudson, PhD
Charles Stratton, MD
Wilmore Webley, PhD
Judith Whittum-Hudson, PhD
1. Yu D, van Tubergenm A. Reactive arthritis. UpToDate. Updated 2021. Accessed August 10, 2021. www.uptodate.com/contents/reactive-arthritis
2. Gérard HC, Carter JD, Hudson AP. Chlamydia trachomatis is present and metabolically active during the remitting phase in synovial tissues from patients with chronic chlamydia-induced reactive arthritis. Am J Med Sci. 2013;346:22-25. doi: 10.1097/MAJ.0b013e3182648740
3. Zeidler H, Hudson AP. New insights into chlamydia and arthritis. Promise of a cure? Ann Rheum Dis. 2014;73:637-644. doi: 10.1136/annrheumdis-2013-204110
4. Carter JD, Valeriano J, Vasey FB. Doxycycline versus doxycycline and rifampin in undifferentiated spondyloarthropathy, with special reference to chlamydia-induced arthritis. A prospective, randomized 9-month comparison. J Rheumatol. 2004;31:1973-1980.
5. Carter JD, Espinoza LR, Inman RD, et al. Combination antibiotics as a treatment for chronic Chlamydia-induced reactive arthritis: a double-blind, placebo-controlled, prospective trial. Arthritis Rheum. 2010;62:1298-1307. doi: 10.1002/art.27394
6. Carter JD, Inman RD, Whittum-Hudson J, et al. Chlamydia and chronic arthritis. Ann Med. 2012;44:784-792. doi: 10.3109/07853890.2011.606830
In the June Photo Rounds column, “Foot rash and joint pain” (J Fam Pract. 2021;70:249-251), Badon et al presented a case of chlamydia-associated reactive arthritis (ReA), formerly called Reiter syndrome, in a 21-year-old man following Chlamydia trachomatis urethritis. We would like to point out that, contrary to the conventional definition of ReA, in which the causative pathogen can’t be cultured from the affected joints,1 chlamydia-associated ReA is associated with evidence of chronic joint infection that, while not cultivable, can be confirmed by real-time polymerase chain reaction testing of metabolically active pathogens in synovial tissue and/or fluid.2
C trachomatis and C pneumoniae are the most frequent causative pathogens to elicit ReA.3 Short-course antibiotics and anti-inflammatory treatments can palliate ReA, but these treatments often do not provide a cure.3 Two controlled clinical trials demonstrated that chlamydia-associated ReA can be treated successfully with longer-term combination antibiotic therapy.4,5 ReA is usually diagnosed in the acute stage (first 6 months) and can become chronic in 30% of cases.6 It would be interesting to know the long-term treatment and outcome data for the case patient.
David L. Hahn, MD, MS
Alan P. Hudson, PhD
Charles Stratton, MD
Wilmore Webley, PhD
Judith Whittum-Hudson, PhD
In the June Photo Rounds column, “Foot rash and joint pain” (J Fam Pract. 2021;70:249-251), Badon et al presented a case of chlamydia-associated reactive arthritis (ReA), formerly called Reiter syndrome, in a 21-year-old man following Chlamydia trachomatis urethritis. We would like to point out that, contrary to the conventional definition of ReA, in which the causative pathogen can’t be cultured from the affected joints,1 chlamydia-associated ReA is associated with evidence of chronic joint infection that, while not cultivable, can be confirmed by real-time polymerase chain reaction testing of metabolically active pathogens in synovial tissue and/or fluid.2
C trachomatis and C pneumoniae are the most frequent causative pathogens to elicit ReA.3 Short-course antibiotics and anti-inflammatory treatments can palliate ReA, but these treatments often do not provide a cure.3 Two controlled clinical trials demonstrated that chlamydia-associated ReA can be treated successfully with longer-term combination antibiotic therapy.4,5 ReA is usually diagnosed in the acute stage (first 6 months) and can become chronic in 30% of cases.6 It would be interesting to know the long-term treatment and outcome data for the case patient.
David L. Hahn, MD, MS
Alan P. Hudson, PhD
Charles Stratton, MD
Wilmore Webley, PhD
Judith Whittum-Hudson, PhD
1. Yu D, van Tubergenm A. Reactive arthritis. UpToDate. Updated 2021. Accessed August 10, 2021. www.uptodate.com/contents/reactive-arthritis
2. Gérard HC, Carter JD, Hudson AP. Chlamydia trachomatis is present and metabolically active during the remitting phase in synovial tissues from patients with chronic chlamydia-induced reactive arthritis. Am J Med Sci. 2013;346:22-25. doi: 10.1097/MAJ.0b013e3182648740
3. Zeidler H, Hudson AP. New insights into chlamydia and arthritis. Promise of a cure? Ann Rheum Dis. 2014;73:637-644. doi: 10.1136/annrheumdis-2013-204110
4. Carter JD, Valeriano J, Vasey FB. Doxycycline versus doxycycline and rifampin in undifferentiated spondyloarthropathy, with special reference to chlamydia-induced arthritis. A prospective, randomized 9-month comparison. J Rheumatol. 2004;31:1973-1980.
5. Carter JD, Espinoza LR, Inman RD, et al. Combination antibiotics as a treatment for chronic Chlamydia-induced reactive arthritis: a double-blind, placebo-controlled, prospective trial. Arthritis Rheum. 2010;62:1298-1307. doi: 10.1002/art.27394
6. Carter JD, Inman RD, Whittum-Hudson J, et al. Chlamydia and chronic arthritis. Ann Med. 2012;44:784-792. doi: 10.3109/07853890.2011.606830
1. Yu D, van Tubergenm A. Reactive arthritis. UpToDate. Updated 2021. Accessed August 10, 2021. www.uptodate.com/contents/reactive-arthritis
2. Gérard HC, Carter JD, Hudson AP. Chlamydia trachomatis is present and metabolically active during the remitting phase in synovial tissues from patients with chronic chlamydia-induced reactive arthritis. Am J Med Sci. 2013;346:22-25. doi: 10.1097/MAJ.0b013e3182648740
3. Zeidler H, Hudson AP. New insights into chlamydia and arthritis. Promise of a cure? Ann Rheum Dis. 2014;73:637-644. doi: 10.1136/annrheumdis-2013-204110
4. Carter JD, Valeriano J, Vasey FB. Doxycycline versus doxycycline and rifampin in undifferentiated spondyloarthropathy, with special reference to chlamydia-induced arthritis. A prospective, randomized 9-month comparison. J Rheumatol. 2004;31:1973-1980.
5. Carter JD, Espinoza LR, Inman RD, et al. Combination antibiotics as a treatment for chronic Chlamydia-induced reactive arthritis: a double-blind, placebo-controlled, prospective trial. Arthritis Rheum. 2010;62:1298-1307. doi: 10.1002/art.27394
6. Carter JD, Inman RD, Whittum-Hudson J, et al. Chlamydia and chronic arthritis. Ann Med. 2012;44:784-792. doi: 10.3109/07853890.2011.606830
Buprenorphine offers a way to rise from the ashes of addiction
One of the most rewarding aspects of being a physician is having a direct impact on alleviating patient suffering. On the other hand, one of the more difficult elements is a confrontational patient with unreasonable expectations or inappropriate demands. I have experienced both ends of the spectrum while engaging with patients who have opioid use disorder (OUD).
An untreated patient with OUD might provide an untruthful history, attempt to falsify exam findings, or even become threatening or abusive in an attempt to secure opiate pain medication. Managing a patient with OUD by providing buprenorphine treatment, however, is a completely different experience.
There is no controversy about the effectiveness of buprenorphine treatment for OUD. Patients seeking it are not looking for inappropriate care but rather a treatment that is established as an unequivocal standard with proven results for better treatment outcomes1-3 and reduced mortality.4 Personally, I’ve found offering buprenorphine treatment to be one of the most rewarding aspects of practicing medicine. It is a real joy to witness people turn their lives around with meaningful outcomes such as gainful employment, eradication of hepatitis C, reconciliation of broken relationships, resolution of legal troubles, and long-term sobriety. Being a part of lives that are practically resurrected from the ashes of addiction by prescribing medicine is indeed an exceptional experience.
On April 28, 2021, the Department of Health and Human Services provided notice for immediate action allowing for any DEA-licensed provider to obtain an X-waiver to treat 30 active patients without educational prerequisite or certification of behavioral health referral capacity.5 The X-waiver requirements were reduced, as outlined by SAMSHA,6 to a simple online notice of intent7 that can be completed in less than 5 minutes.
I encourage my colleagues to obtain the X-waiver by the simplified process, start prescribing buprenorphine, and be a part of the solution to the opioid epidemic. Of course, there will be struggles and lessons learned, but these can most certainly be eclipsed by a focus on the rewarding experience of restoring wholeness to the lives of many patients.
Aaron Newcomb, DO
Carbondale, IL
1. Norton BL, Beitin A, Glenn M, et al. Retention in buprenorphine treatment is associated with improved HCV care outcomes. J Subst Abuse Treat. 2017;75:38-42. doi: 10.1016/j.jsat.2017.01.015
2. Evans EA, Zhu Y, Yoo C, et al. Criminal justice outcomes over 5 years after randomization to buprenorphine-naloxone or methadone treatment for opioid use disorder. Addiction. 2019;114:1396-1404. doi: 10.1111/add.14620
3. Mattick RP, Breen C, Kimber J, et al. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane. Published February 6, 2014. Accessed August 10, 2021. www.cochrane.org/CD002207/ADDICTN_buprenorphine-maintenance-versus-placebo-or-methadone-maintenance-for-opioid-dependence
4. Methadone and buprenorphine reduce risk of death after opioid overdose. National Institutes of Health. Published June 19, 2018. Accessed August 10, 2021. www.nih.gov/news-events/news-releases/methadone-buprenorphine-reduce-risk-death-after-opioid-overdose
5. Practice Guidelines for the Administration of Buprenorphine for Treating Opioid Use Disorder. Department of Health and Human Services; 2021. Accessed August 10, 2021. www.federalregister.gov/documents/2021/04/28/2021-08961/practice-guidelines-for-the-administration-of-buprenorphine-for-treating-opioid-use-disorder
6. US Department of Health & Human Services. Become a buprenorphine waivered practitioner. SAMHSA. Updated May 14, 2021. Accessed August 10, 2021. www.samhsa.gov/medication-assisted-treatment/become-buprenorphine-waivered-practitioner
7. Buprenorphine waiver notification. SAMHSA. Accessed August 10, 2021. https://buprenorphine.samhsa.gov/forms/select-practitioner-type.php
One of the most rewarding aspects of being a physician is having a direct impact on alleviating patient suffering. On the other hand, one of the more difficult elements is a confrontational patient with unreasonable expectations or inappropriate demands. I have experienced both ends of the spectrum while engaging with patients who have opioid use disorder (OUD).
An untreated patient with OUD might provide an untruthful history, attempt to falsify exam findings, or even become threatening or abusive in an attempt to secure opiate pain medication. Managing a patient with OUD by providing buprenorphine treatment, however, is a completely different experience.
There is no controversy about the effectiveness of buprenorphine treatment for OUD. Patients seeking it are not looking for inappropriate care but rather a treatment that is established as an unequivocal standard with proven results for better treatment outcomes1-3 and reduced mortality.4 Personally, I’ve found offering buprenorphine treatment to be one of the most rewarding aspects of practicing medicine. It is a real joy to witness people turn their lives around with meaningful outcomes such as gainful employment, eradication of hepatitis C, reconciliation of broken relationships, resolution of legal troubles, and long-term sobriety. Being a part of lives that are practically resurrected from the ashes of addiction by prescribing medicine is indeed an exceptional experience.
On April 28, 2021, the Department of Health and Human Services provided notice for immediate action allowing for any DEA-licensed provider to obtain an X-waiver to treat 30 active patients without educational prerequisite or certification of behavioral health referral capacity.5 The X-waiver requirements were reduced, as outlined by SAMSHA,6 to a simple online notice of intent7 that can be completed in less than 5 minutes.
I encourage my colleagues to obtain the X-waiver by the simplified process, start prescribing buprenorphine, and be a part of the solution to the opioid epidemic. Of course, there will be struggles and lessons learned, but these can most certainly be eclipsed by a focus on the rewarding experience of restoring wholeness to the lives of many patients.
Aaron Newcomb, DO
Carbondale, IL
One of the most rewarding aspects of being a physician is having a direct impact on alleviating patient suffering. On the other hand, one of the more difficult elements is a confrontational patient with unreasonable expectations or inappropriate demands. I have experienced both ends of the spectrum while engaging with patients who have opioid use disorder (OUD).
An untreated patient with OUD might provide an untruthful history, attempt to falsify exam findings, or even become threatening or abusive in an attempt to secure opiate pain medication. Managing a patient with OUD by providing buprenorphine treatment, however, is a completely different experience.
There is no controversy about the effectiveness of buprenorphine treatment for OUD. Patients seeking it are not looking for inappropriate care but rather a treatment that is established as an unequivocal standard with proven results for better treatment outcomes1-3 and reduced mortality.4 Personally, I’ve found offering buprenorphine treatment to be one of the most rewarding aspects of practicing medicine. It is a real joy to witness people turn their lives around with meaningful outcomes such as gainful employment, eradication of hepatitis C, reconciliation of broken relationships, resolution of legal troubles, and long-term sobriety. Being a part of lives that are practically resurrected from the ashes of addiction by prescribing medicine is indeed an exceptional experience.
On April 28, 2021, the Department of Health and Human Services provided notice for immediate action allowing for any DEA-licensed provider to obtain an X-waiver to treat 30 active patients without educational prerequisite or certification of behavioral health referral capacity.5 The X-waiver requirements were reduced, as outlined by SAMSHA,6 to a simple online notice of intent7 that can be completed in less than 5 minutes.
I encourage my colleagues to obtain the X-waiver by the simplified process, start prescribing buprenorphine, and be a part of the solution to the opioid epidemic. Of course, there will be struggles and lessons learned, but these can most certainly be eclipsed by a focus on the rewarding experience of restoring wholeness to the lives of many patients.
Aaron Newcomb, DO
Carbondale, IL
1. Norton BL, Beitin A, Glenn M, et al. Retention in buprenorphine treatment is associated with improved HCV care outcomes. J Subst Abuse Treat. 2017;75:38-42. doi: 10.1016/j.jsat.2017.01.015
2. Evans EA, Zhu Y, Yoo C, et al. Criminal justice outcomes over 5 years after randomization to buprenorphine-naloxone or methadone treatment for opioid use disorder. Addiction. 2019;114:1396-1404. doi: 10.1111/add.14620
3. Mattick RP, Breen C, Kimber J, et al. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane. Published February 6, 2014. Accessed August 10, 2021. www.cochrane.org/CD002207/ADDICTN_buprenorphine-maintenance-versus-placebo-or-methadone-maintenance-for-opioid-dependence
4. Methadone and buprenorphine reduce risk of death after opioid overdose. National Institutes of Health. Published June 19, 2018. Accessed August 10, 2021. www.nih.gov/news-events/news-releases/methadone-buprenorphine-reduce-risk-death-after-opioid-overdose
5. Practice Guidelines for the Administration of Buprenorphine for Treating Opioid Use Disorder. Department of Health and Human Services; 2021. Accessed August 10, 2021. www.federalregister.gov/documents/2021/04/28/2021-08961/practice-guidelines-for-the-administration-of-buprenorphine-for-treating-opioid-use-disorder
6. US Department of Health & Human Services. Become a buprenorphine waivered practitioner. SAMHSA. Updated May 14, 2021. Accessed August 10, 2021. www.samhsa.gov/medication-assisted-treatment/become-buprenorphine-waivered-practitioner
7. Buprenorphine waiver notification. SAMHSA. Accessed August 10, 2021. https://buprenorphine.samhsa.gov/forms/select-practitioner-type.php
1. Norton BL, Beitin A, Glenn M, et al. Retention in buprenorphine treatment is associated with improved HCV care outcomes. J Subst Abuse Treat. 2017;75:38-42. doi: 10.1016/j.jsat.2017.01.015
2. Evans EA, Zhu Y, Yoo C, et al. Criminal justice outcomes over 5 years after randomization to buprenorphine-naloxone or methadone treatment for opioid use disorder. Addiction. 2019;114:1396-1404. doi: 10.1111/add.14620
3. Mattick RP, Breen C, Kimber J, et al. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane. Published February 6, 2014. Accessed August 10, 2021. www.cochrane.org/CD002207/ADDICTN_buprenorphine-maintenance-versus-placebo-or-methadone-maintenance-for-opioid-dependence
4. Methadone and buprenorphine reduce risk of death after opioid overdose. National Institutes of Health. Published June 19, 2018. Accessed August 10, 2021. www.nih.gov/news-events/news-releases/methadone-buprenorphine-reduce-risk-death-after-opioid-overdose
5. Practice Guidelines for the Administration of Buprenorphine for Treating Opioid Use Disorder. Department of Health and Human Services; 2021. Accessed August 10, 2021. www.federalregister.gov/documents/2021/04/28/2021-08961/practice-guidelines-for-the-administration-of-buprenorphine-for-treating-opioid-use-disorder
6. US Department of Health & Human Services. Become a buprenorphine waivered practitioner. SAMHSA. Updated May 14, 2021. Accessed August 10, 2021. www.samhsa.gov/medication-assisted-treatment/become-buprenorphine-waivered-practitioner
7. Buprenorphine waiver notification. SAMHSA. Accessed August 10, 2021. https://buprenorphine.samhsa.gov/forms/select-practitioner-type.php
Smart watch glucose monitoring on the horizon
Earlier this year, technology news sites reported that the Apple Watch Series 7 and the Samsung Galaxy Watch 4 were going to have integrated optical sensors for checking interstitial fluid glucose levels with no blood sampling needed. By the summer, new articles indicated that the glucose sensing watches would not be released this year for either Apple or Samsung.
For now, the newest technology available for monitoring glucose is continuous glucose monitoring (CGM), which involves a tiny sensor being inserted under the skin. The sensor tests glucose every few minutes, and a transmitter wirelessly sends the information to a monitor, which may be part of an insulin pump or a separate device. Some CGMs send information directly to a smartphone or tablet, according to the National Institutes of Health.
In 1999 the Food and Drug Administration approved the first CGM, which was only approved for downloading 3 days of data at a doctor’s office. Interestingly, the first real-time CGM device for patients to use on their own was a watch, the Glucowatch Biographer. Because of irritation and other issues, that watch never caught on. In 2006 and 2008, Dexcom and then Abbott released the first real-time CGMs that allowed patients to frequently check their own blood sugars.1,2
How CGM has advanced diabetes management
The advent of CGM has advanced the field of diabetes management in many ways.
It has allowed patients to get real time feedback on how their behavior affects their blood sugar. The use of CGM along with the ensuing behavioral changes actually leads to a decrease in hemoglobin A1c, along with a lower risk of hypoglycemia. CGM has also resulted in patients having a better understanding of several aspects of glucose control, including glucose variability and nocturnal hypoglycemia.
Affordable, readily accessible CGM monitors that allow patients to intermittently use CGM have become available over the last 3 years.
In the United States alone, 34.2 million people have diabetes – nearly 1 in every 10 people. Many do not do self-monitoring of blood glucose and most do not use CGM. The current alternative to CGM – self monitoring of blood glucose – is cumbersome, and, since it requires regular finger sticks, is painful. Also, there is significant cost to each test strip that is used to self-monitor, and most insurance limits the number of times a day a patient can check their blood sugar. CGM used to be reserved only for patients who use multiple doses of insulin daily, and only began being approved for use for patients on basal insulin alone in June 2021.3
Most primary care doctors are just beginning to learn how to interpret CGM data.
Smart watch glucose monitoring predictions
When smart watch glucose monitoring arrives, it will suddenly change the playing field for patients with diabetes and their doctors alike.
We expect it to bring down the price of CGM and make it readily available to any patient who owns a smart watch with that function.
For doctors, the new technology will result in them suddenly being asked to advise their patients on how to use the data generated by watch-based CGM.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. They have no conflicts related to the content of this piece. Dr. Persampiere is a second-year resident in the family medicine residency program at Abington Jefferson Health. You can contact them at fpnews@mdedge.com.
References
1. Hirsh I. Introduction: History of Glucose Monitoring, in “Role of Continuous Glucose Monitoring in Diabetes Treatment.” American Diabetes Association. 2018.
2. Peters A. The Evidence Base for Continuous Glucose Monitoring, in “Role of Continuous Glucose Monitoring in Diabetes Treatment.” American Diabetes Association 2018.
3. “Medicare Loosening Restrictions for Continuous Glucose Monitor (CGM) Coverage,” Healthline. 2021 Jul 13.
Earlier this year, technology news sites reported that the Apple Watch Series 7 and the Samsung Galaxy Watch 4 were going to have integrated optical sensors for checking interstitial fluid glucose levels with no blood sampling needed. By the summer, new articles indicated that the glucose sensing watches would not be released this year for either Apple or Samsung.
For now, the newest technology available for monitoring glucose is continuous glucose monitoring (CGM), which involves a tiny sensor being inserted under the skin. The sensor tests glucose every few minutes, and a transmitter wirelessly sends the information to a monitor, which may be part of an insulin pump or a separate device. Some CGMs send information directly to a smartphone or tablet, according to the National Institutes of Health.
In 1999 the Food and Drug Administration approved the first CGM, which was only approved for downloading 3 days of data at a doctor’s office. Interestingly, the first real-time CGM device for patients to use on their own was a watch, the Glucowatch Biographer. Because of irritation and other issues, that watch never caught on. In 2006 and 2008, Dexcom and then Abbott released the first real-time CGMs that allowed patients to frequently check their own blood sugars.1,2
How CGM has advanced diabetes management
The advent of CGM has advanced the field of diabetes management in many ways.
It has allowed patients to get real time feedback on how their behavior affects their blood sugar. The use of CGM along with the ensuing behavioral changes actually leads to a decrease in hemoglobin A1c, along with a lower risk of hypoglycemia. CGM has also resulted in patients having a better understanding of several aspects of glucose control, including glucose variability and nocturnal hypoglycemia.
Affordable, readily accessible CGM monitors that allow patients to intermittently use CGM have become available over the last 3 years.
In the United States alone, 34.2 million people have diabetes – nearly 1 in every 10 people. Many do not do self-monitoring of blood glucose and most do not use CGM. The current alternative to CGM – self monitoring of blood glucose – is cumbersome, and, since it requires regular finger sticks, is painful. Also, there is significant cost to each test strip that is used to self-monitor, and most insurance limits the number of times a day a patient can check their blood sugar. CGM used to be reserved only for patients who use multiple doses of insulin daily, and only began being approved for use for patients on basal insulin alone in June 2021.3
Most primary care doctors are just beginning to learn how to interpret CGM data.
Smart watch glucose monitoring predictions
When smart watch glucose monitoring arrives, it will suddenly change the playing field for patients with diabetes and their doctors alike.
We expect it to bring down the price of CGM and make it readily available to any patient who owns a smart watch with that function.
For doctors, the new technology will result in them suddenly being asked to advise their patients on how to use the data generated by watch-based CGM.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. They have no conflicts related to the content of this piece. Dr. Persampiere is a second-year resident in the family medicine residency program at Abington Jefferson Health. You can contact them at fpnews@mdedge.com.
References
1. Hirsh I. Introduction: History of Glucose Monitoring, in “Role of Continuous Glucose Monitoring in Diabetes Treatment.” American Diabetes Association. 2018.
2. Peters A. The Evidence Base for Continuous Glucose Monitoring, in “Role of Continuous Glucose Monitoring in Diabetes Treatment.” American Diabetes Association 2018.
3. “Medicare Loosening Restrictions for Continuous Glucose Monitor (CGM) Coverage,” Healthline. 2021 Jul 13.
Earlier this year, technology news sites reported that the Apple Watch Series 7 and the Samsung Galaxy Watch 4 were going to have integrated optical sensors for checking interstitial fluid glucose levels with no blood sampling needed. By the summer, new articles indicated that the glucose sensing watches would not be released this year for either Apple or Samsung.
For now, the newest technology available for monitoring glucose is continuous glucose monitoring (CGM), which involves a tiny sensor being inserted under the skin. The sensor tests glucose every few minutes, and a transmitter wirelessly sends the information to a monitor, which may be part of an insulin pump or a separate device. Some CGMs send information directly to a smartphone or tablet, according to the National Institutes of Health.
In 1999 the Food and Drug Administration approved the first CGM, which was only approved for downloading 3 days of data at a doctor’s office. Interestingly, the first real-time CGM device for patients to use on their own was a watch, the Glucowatch Biographer. Because of irritation and other issues, that watch never caught on. In 2006 and 2008, Dexcom and then Abbott released the first real-time CGMs that allowed patients to frequently check their own blood sugars.1,2
How CGM has advanced diabetes management
The advent of CGM has advanced the field of diabetes management in many ways.
It has allowed patients to get real time feedback on how their behavior affects their blood sugar. The use of CGM along with the ensuing behavioral changes actually leads to a decrease in hemoglobin A1c, along with a lower risk of hypoglycemia. CGM has also resulted in patients having a better understanding of several aspects of glucose control, including glucose variability and nocturnal hypoglycemia.
Affordable, readily accessible CGM monitors that allow patients to intermittently use CGM have become available over the last 3 years.
In the United States alone, 34.2 million people have diabetes – nearly 1 in every 10 people. Many do not do self-monitoring of blood glucose and most do not use CGM. The current alternative to CGM – self monitoring of blood glucose – is cumbersome, and, since it requires regular finger sticks, is painful. Also, there is significant cost to each test strip that is used to self-monitor, and most insurance limits the number of times a day a patient can check their blood sugar. CGM used to be reserved only for patients who use multiple doses of insulin daily, and only began being approved for use for patients on basal insulin alone in June 2021.3
Most primary care doctors are just beginning to learn how to interpret CGM data.
Smart watch glucose monitoring predictions
When smart watch glucose monitoring arrives, it will suddenly change the playing field for patients with diabetes and their doctors alike.
We expect it to bring down the price of CGM and make it readily available to any patient who owns a smart watch with that function.
For doctors, the new technology will result in them suddenly being asked to advise their patients on how to use the data generated by watch-based CGM.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. They have no conflicts related to the content of this piece. Dr. Persampiere is a second-year resident in the family medicine residency program at Abington Jefferson Health. You can contact them at fpnews@mdedge.com.
References
1. Hirsh I. Introduction: History of Glucose Monitoring, in “Role of Continuous Glucose Monitoring in Diabetes Treatment.” American Diabetes Association. 2018.
2. Peters A. The Evidence Base for Continuous Glucose Monitoring, in “Role of Continuous Glucose Monitoring in Diabetes Treatment.” American Diabetes Association 2018.
3. “Medicare Loosening Restrictions for Continuous Glucose Monitor (CGM) Coverage,” Healthline. 2021 Jul 13.
Embedding diversity, equity, inclusion, and justice in hospital medicine
A road map for success
The language of equality in America’s founding was never truly embraced, resulting in a painful legacy of slavery, racial injustice, and gender inequality inherited by all generations. However, for as long as America has fallen short of this unfulfilled promise, individuals have dedicated their lives to the tireless work of correcting injustice. Although the process has been painstakingly slow, our nation has incrementally inched toward the promised vision of equality, and these efforts continue today. With increased attention to social justice movements such as #MeToo and Black Lives Matter, our collective social consciousness may be finally waking up to the systemic injustices embedded into our fundamental institutions.
Medicine is not immune to these injustices. Persistent underrepresentation of women and minorities remains in medical school faculty and the broader physician workforce, and the same inequities exist in hospital medicine.1-6 The report by the Association of American Medical Colleges (AAMC) on diversity in medicine highlights the impact widespread implicit and explicit bias has on creating exclusionary environments, exemplified by research demonstrating lower promotion rates in non-White faculty.7-8 The report calls us, as physicians, to a broader mission: “Focusing solely on increasing compositional diversity along the academic continuum is insufficient. To effectively enact institutional change at academic medical centers ... leaders must focus their efforts on developing inclusive, equity-minded environments.”7
We have a clear moral imperative to correct these shortcomings for our profession and our patients. It is incumbent on our institutions and hospital medicine groups (HMGs) to embark on the necessary process of systemic institutional change to address inequality and justice within our field.
A road map for DEI and justice in hospital medicine
The policies and biases allowing these inequities to persist have existed for decades, and superficial efforts will not bring sufficient change. Our institutions require new building blocks from which the foundation of a wholly inclusive and equal system of practice can be constructed. Encouragingly, some institutions and HMGs have taken steps to modernize their practices. We offer examples and suggestions of concrete practices to begin this journey, organizing these efforts into three broad categories:
1. Recruitment and retention
2. Scholarship, mentorship, and sponsorship
3. Community engagement and partnership.
Recruitment and retention
Improving equity and inclusion begins with recruitment. Search and hiring committees should be assembled intentionally, with gender balance, and ideally with diversity or equity experts invited to join. All members should receive unconscious bias training. For example, the University of Colorado utilizes a toolkit to ensure appropriate steps are followed in the recruitment process, including predetermined candidate selection criteria that are ranked in advance.
Job descriptions should be reviewed by a diversity expert, ensuring unbiased and ungendered language within written text. Advertisements should be wide-reaching, and the committee should consider asking applicants for a diversity statement. Interviews should include a variety of interviewers and interview types (e.g., 1:1, group, etc.). Letters of recommendation deserve special scrutiny; letters for women and minorities may be at risk of being shorter and less record focused, and may be subject to less professional respect, such as use of first names over honorifics or titles.
Once candidates are hired, institutions and HMGs should prioritize developing strategies to improve retention of a diverse workforce. This includes special attention to workplace culture, and thoughtfully striving for cultural intelligence within the group. Some examples may include developing affinity groups, such as underrepresented in medicine (UIM), women in medicine (WIM), or LGBTQ+ groups. Affinity groups provide a safe space for members and allies to support and uplift each other. Institutional and HMG leaders must educate themselves and their members on the importance of language (see table), and the more insidious forms of bias and discrimination that adversely affect workplace culture. Microinsults and microinvalidations, for example, can hurt and result in failure to recruit or turnover. 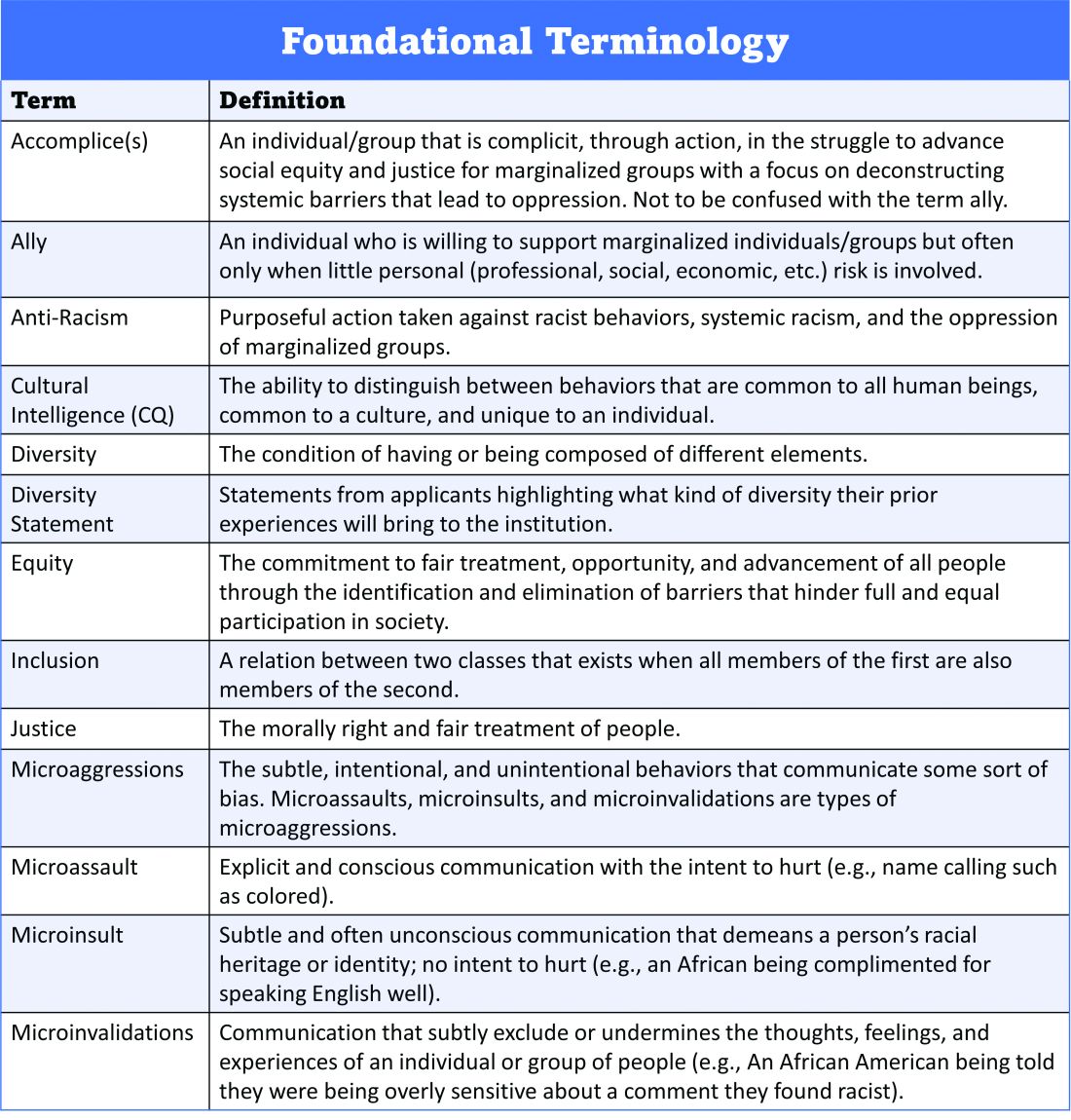
Conducting exit interviews when any hospitalist leaves is important to learn how to improve, but holding ‘stay’ interviews is mission critical. Stay interviews are an opportunity for HMG leaders to proactively understand why hospitalists stay, and what can be done to create more inclusive and equitable environments to retain them. This process creates psychological safety that brings challenges to the fore to be addressed, and spotlights best practices to be maintained and scaled.
Scholarship, mentorship, and sponsorship
Women and minorities are known to be over-mentored and under-sponsored. Sponsorship is defined by Ayyala et al. as “active support by someone appropriately placed in the organization who has significant influence on decision making processes or structures and who is advocating for the career advancement of an individual and recommends them for leadership roles, awards, or high-profile speaking opportunities.”9 While the goal of mentorship is professional development, sponsorship emphasizes professional advancement. Deliberate steps to both mentor and then sponsor diverse hospitalists and future hospitalists (including trainees) are important to ensure equity.
More inclusive HMGs can be bolstered by prioritizing peer education on the professional imperative that we have a diverse workforce and equitable, just workplaces. Academic institutions may use existing structures such as grand rounds to provide education on these crucial topics, and all HMGs can host journal clubs and professional development sessions on leadership competencies that foster inclusion and equity. Sessions coordinated by women and minorities are also a form of justice, by helping overcome barriers to career advancement. Diverse faculty presenting in educational venues will result in content that is relevant to more audience members and will exemplify that leaders and experts are of all races, ethnicities, genders, ages, and abilities.
Groups should prioritize mentoring trainees and early-career hospitalists on scholarly projects that examine equity in opportunities of care, which signals that this science is valued as much as basic research. When used to demonstrate areas needing improvement, these projects can drive meaningful change. Even projects as straightforward as studying diversity in conference presenters, disparities in adherence to guidelines, or QI projects on how race is portrayed in the medical record can be powerful tools in advancing equity.
A key part of mentoring is training hospitalists and future hospitalists in how to be an upstander, as in how to intervene when a peer or patient is affected by bias, harassment, or discrimination. Receiving such training can prepare hospitalists for these nearly inevitable experiences and receiving training during usual work hours communicates that this is a valuable and necessary professional competency.
Community engagement and partnership
Institutions and HMGs should deliberately work to promote community engagement and partnership within their groups. Beyond promoting health equity, community engagement also fosters inclusivity by allowing community members to share their ideas and give recommendations to the institutions that serve them.
There is a growing body of literature that demonstrates how disadvantages by individual and neighborhood-level socioeconomic status (SES) contribute to disparities in specific disease conditions.10-11 Strategies to narrow the gap in SES disadvantages may help reduce race-related health disparities. Institutions that engage the community and develop programs to promote health equity can do so through bidirectional exchange of knowledge and mutual benefit.
An institution-specific example is Medicine for the Greater Good at Johns Hopkins. The founders of this program wrote, “health is not synonymous with medicine. To truly care for our patients and their communities, health care professionals must understand how to deliver equitable health care that meets the needs of the diverse populations we care for. The mission of Medicine for the Greater Good is to promote health and wellness beyond the confines of the hospital through an interactive and engaging partnership with the community ...” Community engagement also provides an opportunity for growing the cultural intelligence of institutions and HMGs.
Tools for advancing comprehensive change – Repurposing PDSA cycles
Whether institutions and HMGs are at the beginning of their journey or further along in the work of reducing disparities, having a systematic approach for implementing and refining policies and procedures can cultivate more inclusive and equitable environments. Thankfully, hospitalists are already equipped with the fundamental tools needed to advance change across their institutions – QI processes in the form of Plan-Do-Study-Act (PDSA) cycles.
They allow a continuous cycle of successful incremental change based on direct evidence and experience. Any efforts to deconstruct systematic bias within our organizations must also be a continual process. Our female colleagues and colleagues of color need our institutions to engage unceasingly to bring about the equality they deserve. To that end, PDSA cycles are an apt tool to utilize in this work as they can naturally function in a never-ending process of improvement.
With PDSA as a model, we envision a cycle with steps that are intentionally purposed to fit the needs of equitable institutional change: Target-Engage-Assess-Modify. As highlighted (see graphic), these modifications ensure that stakeholders (i.e., those that unequal practices and policies affect the most) are engaged early and remain involved throughout the cycle. 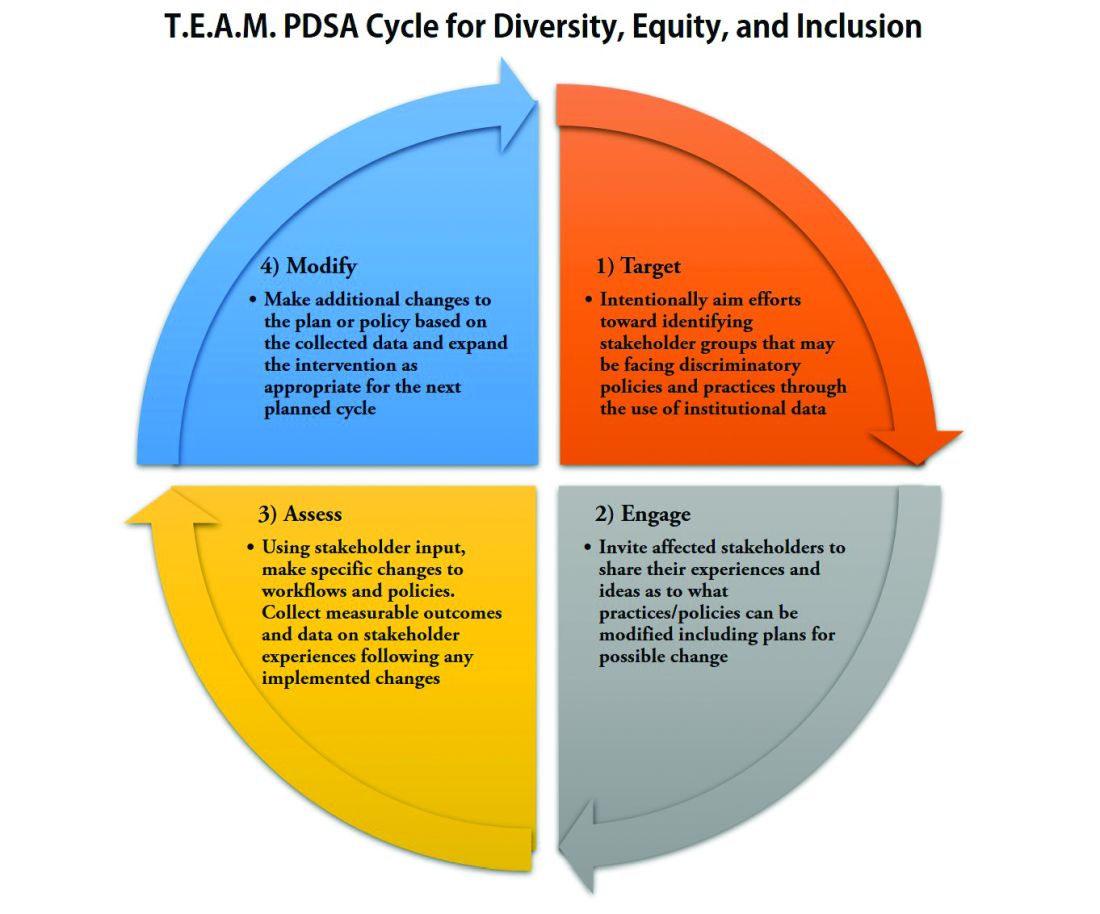
As hospitalists, we have significant work ahead to ensure that we develop and maintain a diverse, equitable and inclusive workforce. This work to bring change will not be easy and will require a considerable investment of time and resources. However, with the strategies and tools that we have outlined, our institutions and HMGs can start the change needed in our profession for our patients and the workforce. In doing so, we can all be accomplices in the fight to achieve racial and gender equity, and social justice.
Dr. Delapenha and Dr. Kisuule are based in the department of internal medicine, division of hospital medicine, at the Johns Hopkins University, Baltimore. Dr. Martin is based in the department of medicine, section of hospital medicine at the University of Chicago. Dr. Barrett is a hospitalist in the department of internal medicine, University of New Mexico, Albuquerque.
References
1. Diversity in Medicine: Facts and Figures 2019: Figure 19. Percentage of physicians by sex, 2018. AAMC website.
2. Diversity in Medicine: Facts and Figures 2019. Figure 16. Percentage of full-time U.S. medical school faculty by sex and race/ethnicity, 2018. AAMC website.
3. Diversity in Medicine: Facts and Figures 2019. Figure 15. Percentage of full-time U.S. medical school faculty by race/ethnicity, 2018. AAMC website.
4. Diversity in Medicine: Facts and Figures 2019. Figure 6. Percentage of acceptees to U.S. medical schools by race/ethnicity (alone), academic year 2018-2019. AAMC website.
5. Diversity in Medicine: Facts and Figures 2019 Figure 18. Percentage of all active physicians by race/ethnicity, 2018. AAMC website.
6. Herzke C et al. Gender issues in academic hospital medicine: A national survey of hospitalist leaders. J Gen Intern Med. 2020;35(6):1641-6.
7. Diversity in Medicine: Facts and Figures 2019. Fostering diversity and inclusion. AAMC website.
8. Diversity in Medicine: Facts and Figures 2019. Executive summary. AAMC website.
9. Ayyala MS et al. Mentorship is not enough: Exploring sponsorship and its role in career advancement in academic medicine. Acad Med. 2019;94(1):94-100.
10. Ejike OC et al. Contribution of individual and neighborhood factors to racial disparities in respiratory outcomes. Am J Respir Crit Care Med. 2021 Apr 15;203(8):987-97.
11. Galiatsatos P et al. The effect of community socioeconomic status on sepsis-attributable mortality. J Crit Care. 2018 Aug;46:129-33.
A road map for success
A road map for success
The language of equality in America’s founding was never truly embraced, resulting in a painful legacy of slavery, racial injustice, and gender inequality inherited by all generations. However, for as long as America has fallen short of this unfulfilled promise, individuals have dedicated their lives to the tireless work of correcting injustice. Although the process has been painstakingly slow, our nation has incrementally inched toward the promised vision of equality, and these efforts continue today. With increased attention to social justice movements such as #MeToo and Black Lives Matter, our collective social consciousness may be finally waking up to the systemic injustices embedded into our fundamental institutions.
Medicine is not immune to these injustices. Persistent underrepresentation of women and minorities remains in medical school faculty and the broader physician workforce, and the same inequities exist in hospital medicine.1-6 The report by the Association of American Medical Colleges (AAMC) on diversity in medicine highlights the impact widespread implicit and explicit bias has on creating exclusionary environments, exemplified by research demonstrating lower promotion rates in non-White faculty.7-8 The report calls us, as physicians, to a broader mission: “Focusing solely on increasing compositional diversity along the academic continuum is insufficient. To effectively enact institutional change at academic medical centers ... leaders must focus their efforts on developing inclusive, equity-minded environments.”7
We have a clear moral imperative to correct these shortcomings for our profession and our patients. It is incumbent on our institutions and hospital medicine groups (HMGs) to embark on the necessary process of systemic institutional change to address inequality and justice within our field.
A road map for DEI and justice in hospital medicine
The policies and biases allowing these inequities to persist have existed for decades, and superficial efforts will not bring sufficient change. Our institutions require new building blocks from which the foundation of a wholly inclusive and equal system of practice can be constructed. Encouragingly, some institutions and HMGs have taken steps to modernize their practices. We offer examples and suggestions of concrete practices to begin this journey, organizing these efforts into three broad categories:
1. Recruitment and retention
2. Scholarship, mentorship, and sponsorship
3. Community engagement and partnership.
Recruitment and retention
Improving equity and inclusion begins with recruitment. Search and hiring committees should be assembled intentionally, with gender balance, and ideally with diversity or equity experts invited to join. All members should receive unconscious bias training. For example, the University of Colorado utilizes a toolkit to ensure appropriate steps are followed in the recruitment process, including predetermined candidate selection criteria that are ranked in advance.
Job descriptions should be reviewed by a diversity expert, ensuring unbiased and ungendered language within written text. Advertisements should be wide-reaching, and the committee should consider asking applicants for a diversity statement. Interviews should include a variety of interviewers and interview types (e.g., 1:1, group, etc.). Letters of recommendation deserve special scrutiny; letters for women and minorities may be at risk of being shorter and less record focused, and may be subject to less professional respect, such as use of first names over honorifics or titles.
Once candidates are hired, institutions and HMGs should prioritize developing strategies to improve retention of a diverse workforce. This includes special attention to workplace culture, and thoughtfully striving for cultural intelligence within the group. Some examples may include developing affinity groups, such as underrepresented in medicine (UIM), women in medicine (WIM), or LGBTQ+ groups. Affinity groups provide a safe space for members and allies to support and uplift each other. Institutional and HMG leaders must educate themselves and their members on the importance of language (see table), and the more insidious forms of bias and discrimination that adversely affect workplace culture. Microinsults and microinvalidations, for example, can hurt and result in failure to recruit or turnover. 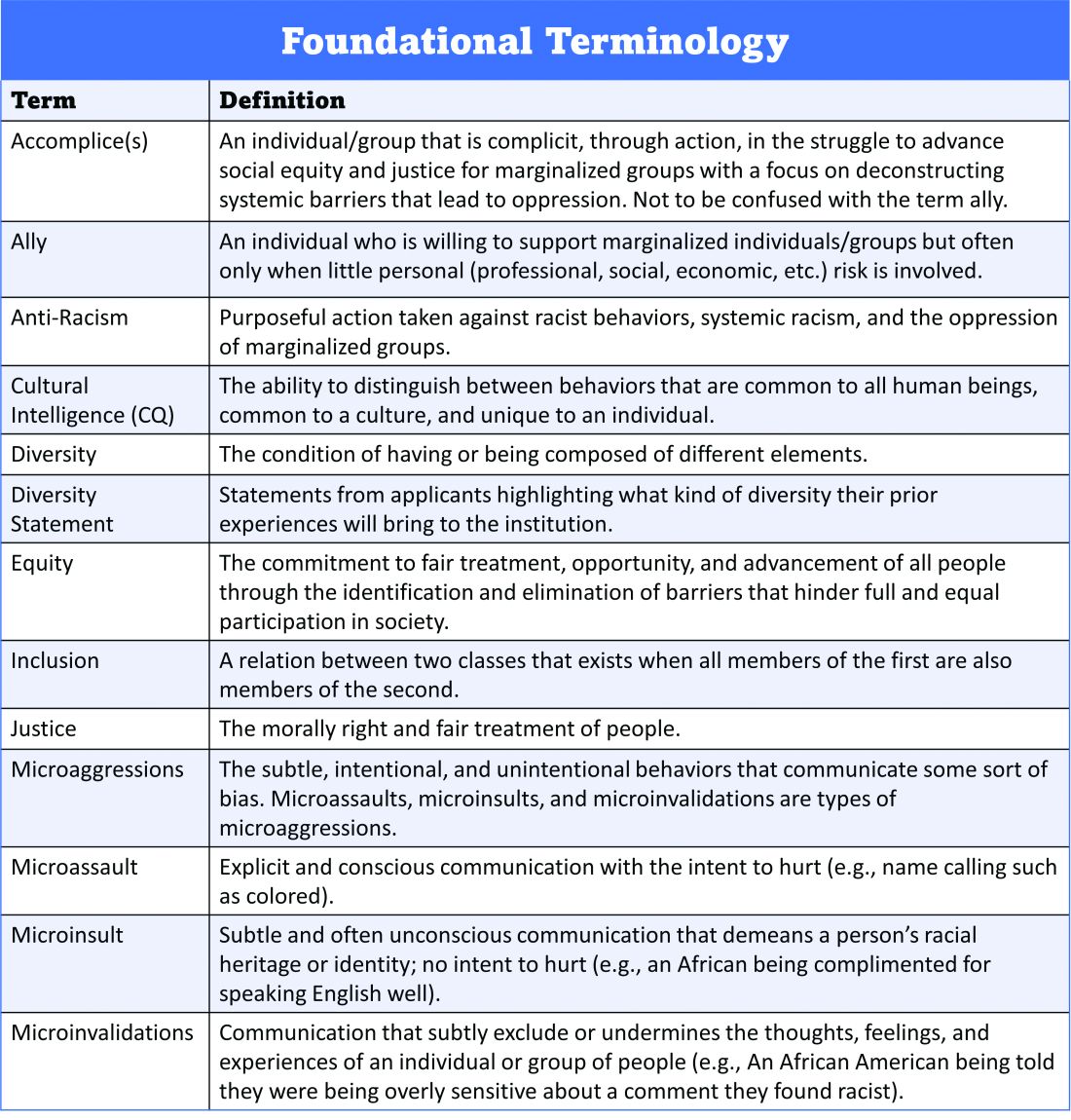
Conducting exit interviews when any hospitalist leaves is important to learn how to improve, but holding ‘stay’ interviews is mission critical. Stay interviews are an opportunity for HMG leaders to proactively understand why hospitalists stay, and what can be done to create more inclusive and equitable environments to retain them. This process creates psychological safety that brings challenges to the fore to be addressed, and spotlights best practices to be maintained and scaled.
Scholarship, mentorship, and sponsorship
Women and minorities are known to be over-mentored and under-sponsored. Sponsorship is defined by Ayyala et al. as “active support by someone appropriately placed in the organization who has significant influence on decision making processes or structures and who is advocating for the career advancement of an individual and recommends them for leadership roles, awards, or high-profile speaking opportunities.”9 While the goal of mentorship is professional development, sponsorship emphasizes professional advancement. Deliberate steps to both mentor and then sponsor diverse hospitalists and future hospitalists (including trainees) are important to ensure equity.
More inclusive HMGs can be bolstered by prioritizing peer education on the professional imperative that we have a diverse workforce and equitable, just workplaces. Academic institutions may use existing structures such as grand rounds to provide education on these crucial topics, and all HMGs can host journal clubs and professional development sessions on leadership competencies that foster inclusion and equity. Sessions coordinated by women and minorities are also a form of justice, by helping overcome barriers to career advancement. Diverse faculty presenting in educational venues will result in content that is relevant to more audience members and will exemplify that leaders and experts are of all races, ethnicities, genders, ages, and abilities.
Groups should prioritize mentoring trainees and early-career hospitalists on scholarly projects that examine equity in opportunities of care, which signals that this science is valued as much as basic research. When used to demonstrate areas needing improvement, these projects can drive meaningful change. Even projects as straightforward as studying diversity in conference presenters, disparities in adherence to guidelines, or QI projects on how race is portrayed in the medical record can be powerful tools in advancing equity.
A key part of mentoring is training hospitalists and future hospitalists in how to be an upstander, as in how to intervene when a peer or patient is affected by bias, harassment, or discrimination. Receiving such training can prepare hospitalists for these nearly inevitable experiences and receiving training during usual work hours communicates that this is a valuable and necessary professional competency.
Community engagement and partnership
Institutions and HMGs should deliberately work to promote community engagement and partnership within their groups. Beyond promoting health equity, community engagement also fosters inclusivity by allowing community members to share their ideas and give recommendations to the institutions that serve them.
There is a growing body of literature that demonstrates how disadvantages by individual and neighborhood-level socioeconomic status (SES) contribute to disparities in specific disease conditions.10-11 Strategies to narrow the gap in SES disadvantages may help reduce race-related health disparities. Institutions that engage the community and develop programs to promote health equity can do so through bidirectional exchange of knowledge and mutual benefit.
An institution-specific example is Medicine for the Greater Good at Johns Hopkins. The founders of this program wrote, “health is not synonymous with medicine. To truly care for our patients and their communities, health care professionals must understand how to deliver equitable health care that meets the needs of the diverse populations we care for. The mission of Medicine for the Greater Good is to promote health and wellness beyond the confines of the hospital through an interactive and engaging partnership with the community ...” Community engagement also provides an opportunity for growing the cultural intelligence of institutions and HMGs.
Tools for advancing comprehensive change – Repurposing PDSA cycles
Whether institutions and HMGs are at the beginning of their journey or further along in the work of reducing disparities, having a systematic approach for implementing and refining policies and procedures can cultivate more inclusive and equitable environments. Thankfully, hospitalists are already equipped with the fundamental tools needed to advance change across their institutions – QI processes in the form of Plan-Do-Study-Act (PDSA) cycles.
They allow a continuous cycle of successful incremental change based on direct evidence and experience. Any efforts to deconstruct systematic bias within our organizations must also be a continual process. Our female colleagues and colleagues of color need our institutions to engage unceasingly to bring about the equality they deserve. To that end, PDSA cycles are an apt tool to utilize in this work as they can naturally function in a never-ending process of improvement.
With PDSA as a model, we envision a cycle with steps that are intentionally purposed to fit the needs of equitable institutional change: Target-Engage-Assess-Modify. As highlighted (see graphic), these modifications ensure that stakeholders (i.e., those that unequal practices and policies affect the most) are engaged early and remain involved throughout the cycle. 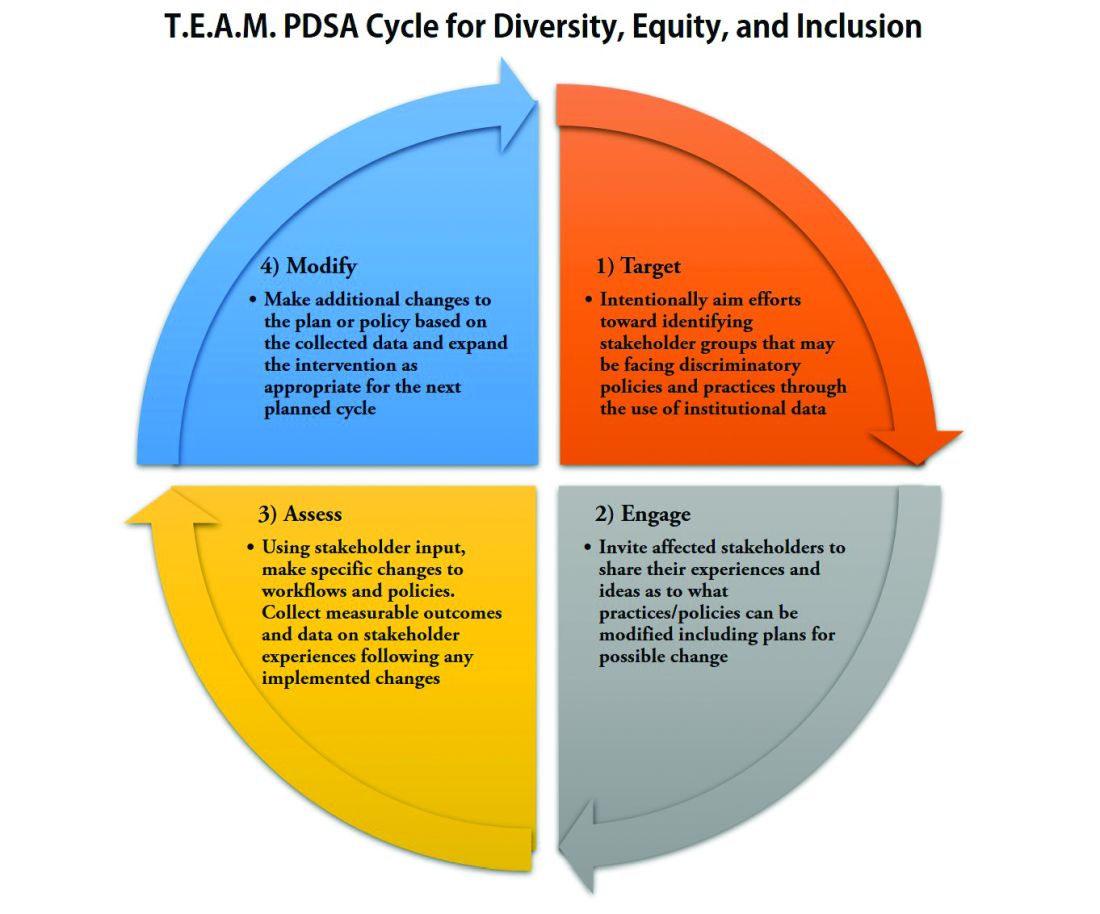
As hospitalists, we have significant work ahead to ensure that we develop and maintain a diverse, equitable and inclusive workforce. This work to bring change will not be easy and will require a considerable investment of time and resources. However, with the strategies and tools that we have outlined, our institutions and HMGs can start the change needed in our profession for our patients and the workforce. In doing so, we can all be accomplices in the fight to achieve racial and gender equity, and social justice.
Dr. Delapenha and Dr. Kisuule are based in the department of internal medicine, division of hospital medicine, at the Johns Hopkins University, Baltimore. Dr. Martin is based in the department of medicine, section of hospital medicine at the University of Chicago. Dr. Barrett is a hospitalist in the department of internal medicine, University of New Mexico, Albuquerque.
References
1. Diversity in Medicine: Facts and Figures 2019: Figure 19. Percentage of physicians by sex, 2018. AAMC website.
2. Diversity in Medicine: Facts and Figures 2019. Figure 16. Percentage of full-time U.S. medical school faculty by sex and race/ethnicity, 2018. AAMC website.
3. Diversity in Medicine: Facts and Figures 2019. Figure 15. Percentage of full-time U.S. medical school faculty by race/ethnicity, 2018. AAMC website.
4. Diversity in Medicine: Facts and Figures 2019. Figure 6. Percentage of acceptees to U.S. medical schools by race/ethnicity (alone), academic year 2018-2019. AAMC website.
5. Diversity in Medicine: Facts and Figures 2019 Figure 18. Percentage of all active physicians by race/ethnicity, 2018. AAMC website.
6. Herzke C et al. Gender issues in academic hospital medicine: A national survey of hospitalist leaders. J Gen Intern Med. 2020;35(6):1641-6.
7. Diversity in Medicine: Facts and Figures 2019. Fostering diversity and inclusion. AAMC website.
8. Diversity in Medicine: Facts and Figures 2019. Executive summary. AAMC website.
9. Ayyala MS et al. Mentorship is not enough: Exploring sponsorship and its role in career advancement in academic medicine. Acad Med. 2019;94(1):94-100.
10. Ejike OC et al. Contribution of individual and neighborhood factors to racial disparities in respiratory outcomes. Am J Respir Crit Care Med. 2021 Apr 15;203(8):987-97.
11. Galiatsatos P et al. The effect of community socioeconomic status on sepsis-attributable mortality. J Crit Care. 2018 Aug;46:129-33.
The language of equality in America’s founding was never truly embraced, resulting in a painful legacy of slavery, racial injustice, and gender inequality inherited by all generations. However, for as long as America has fallen short of this unfulfilled promise, individuals have dedicated their lives to the tireless work of correcting injustice. Although the process has been painstakingly slow, our nation has incrementally inched toward the promised vision of equality, and these efforts continue today. With increased attention to social justice movements such as #MeToo and Black Lives Matter, our collective social consciousness may be finally waking up to the systemic injustices embedded into our fundamental institutions.
Medicine is not immune to these injustices. Persistent underrepresentation of women and minorities remains in medical school faculty and the broader physician workforce, and the same inequities exist in hospital medicine.1-6 The report by the Association of American Medical Colleges (AAMC) on diversity in medicine highlights the impact widespread implicit and explicit bias has on creating exclusionary environments, exemplified by research demonstrating lower promotion rates in non-White faculty.7-8 The report calls us, as physicians, to a broader mission: “Focusing solely on increasing compositional diversity along the academic continuum is insufficient. To effectively enact institutional change at academic medical centers ... leaders must focus their efforts on developing inclusive, equity-minded environments.”7
We have a clear moral imperative to correct these shortcomings for our profession and our patients. It is incumbent on our institutions and hospital medicine groups (HMGs) to embark on the necessary process of systemic institutional change to address inequality and justice within our field.
A road map for DEI and justice in hospital medicine
The policies and biases allowing these inequities to persist have existed for decades, and superficial efforts will not bring sufficient change. Our institutions require new building blocks from which the foundation of a wholly inclusive and equal system of practice can be constructed. Encouragingly, some institutions and HMGs have taken steps to modernize their practices. We offer examples and suggestions of concrete practices to begin this journey, organizing these efforts into three broad categories:
1. Recruitment and retention
2. Scholarship, mentorship, and sponsorship
3. Community engagement and partnership.
Recruitment and retention
Improving equity and inclusion begins with recruitment. Search and hiring committees should be assembled intentionally, with gender balance, and ideally with diversity or equity experts invited to join. All members should receive unconscious bias training. For example, the University of Colorado utilizes a toolkit to ensure appropriate steps are followed in the recruitment process, including predetermined candidate selection criteria that are ranked in advance.
Job descriptions should be reviewed by a diversity expert, ensuring unbiased and ungendered language within written text. Advertisements should be wide-reaching, and the committee should consider asking applicants for a diversity statement. Interviews should include a variety of interviewers and interview types (e.g., 1:1, group, etc.). Letters of recommendation deserve special scrutiny; letters for women and minorities may be at risk of being shorter and less record focused, and may be subject to less professional respect, such as use of first names over honorifics or titles.
Once candidates are hired, institutions and HMGs should prioritize developing strategies to improve retention of a diverse workforce. This includes special attention to workplace culture, and thoughtfully striving for cultural intelligence within the group. Some examples may include developing affinity groups, such as underrepresented in medicine (UIM), women in medicine (WIM), or LGBTQ+ groups. Affinity groups provide a safe space for members and allies to support and uplift each other. Institutional and HMG leaders must educate themselves and their members on the importance of language (see table), and the more insidious forms of bias and discrimination that adversely affect workplace culture. Microinsults and microinvalidations, for example, can hurt and result in failure to recruit or turnover. 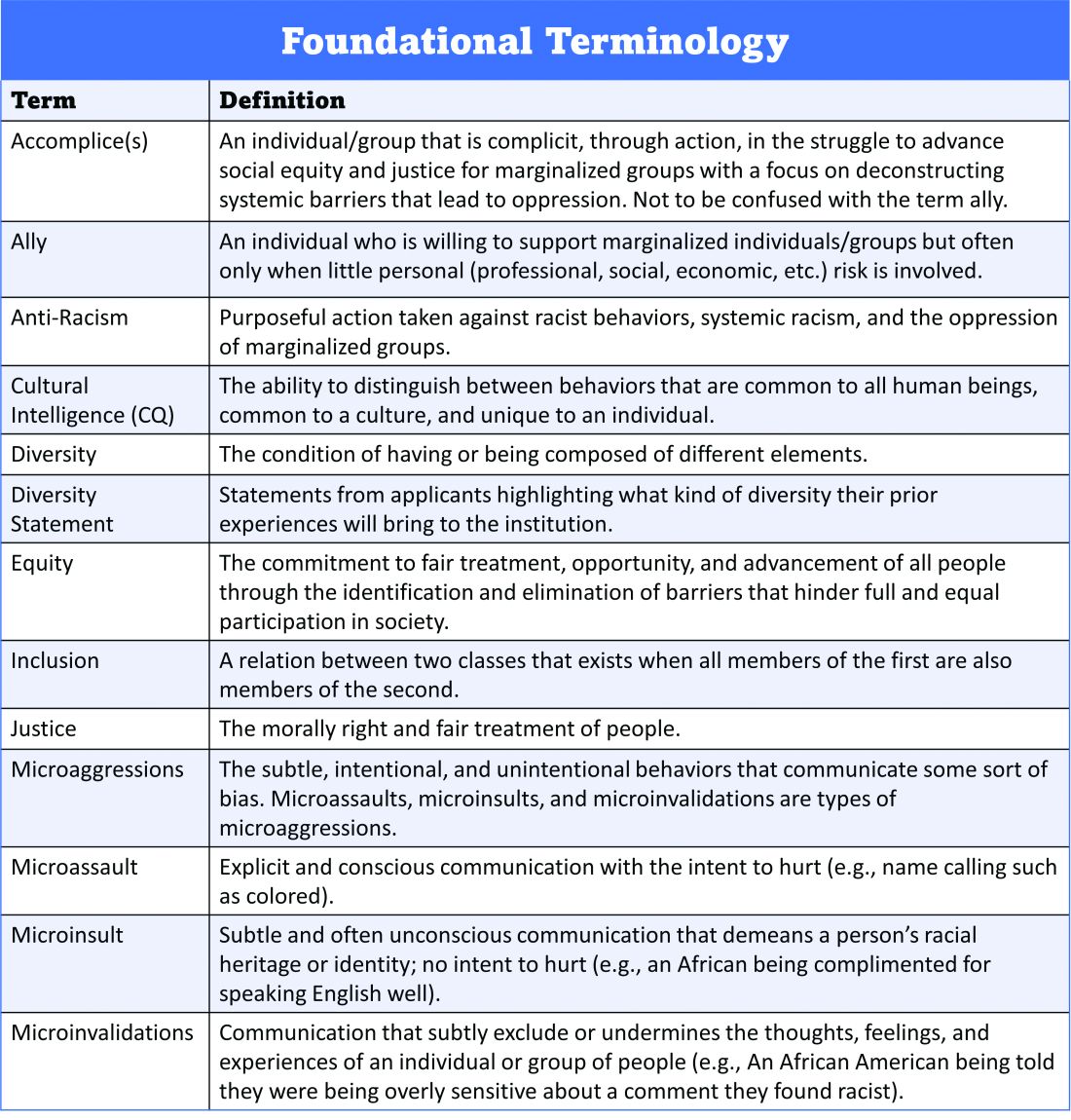
Conducting exit interviews when any hospitalist leaves is important to learn how to improve, but holding ‘stay’ interviews is mission critical. Stay interviews are an opportunity for HMG leaders to proactively understand why hospitalists stay, and what can be done to create more inclusive and equitable environments to retain them. This process creates psychological safety that brings challenges to the fore to be addressed, and spotlights best practices to be maintained and scaled.
Scholarship, mentorship, and sponsorship
Women and minorities are known to be over-mentored and under-sponsored. Sponsorship is defined by Ayyala et al. as “active support by someone appropriately placed in the organization who has significant influence on decision making processes or structures and who is advocating for the career advancement of an individual and recommends them for leadership roles, awards, or high-profile speaking opportunities.”9 While the goal of mentorship is professional development, sponsorship emphasizes professional advancement. Deliberate steps to both mentor and then sponsor diverse hospitalists and future hospitalists (including trainees) are important to ensure equity.
More inclusive HMGs can be bolstered by prioritizing peer education on the professional imperative that we have a diverse workforce and equitable, just workplaces. Academic institutions may use existing structures such as grand rounds to provide education on these crucial topics, and all HMGs can host journal clubs and professional development sessions on leadership competencies that foster inclusion and equity. Sessions coordinated by women and minorities are also a form of justice, by helping overcome barriers to career advancement. Diverse faculty presenting in educational venues will result in content that is relevant to more audience members and will exemplify that leaders and experts are of all races, ethnicities, genders, ages, and abilities.
Groups should prioritize mentoring trainees and early-career hospitalists on scholarly projects that examine equity in opportunities of care, which signals that this science is valued as much as basic research. When used to demonstrate areas needing improvement, these projects can drive meaningful change. Even projects as straightforward as studying diversity in conference presenters, disparities in adherence to guidelines, or QI projects on how race is portrayed in the medical record can be powerful tools in advancing equity.
A key part of mentoring is training hospitalists and future hospitalists in how to be an upstander, as in how to intervene when a peer or patient is affected by bias, harassment, or discrimination. Receiving such training can prepare hospitalists for these nearly inevitable experiences and receiving training during usual work hours communicates that this is a valuable and necessary professional competency.
Community engagement and partnership
Institutions and HMGs should deliberately work to promote community engagement and partnership within their groups. Beyond promoting health equity, community engagement also fosters inclusivity by allowing community members to share their ideas and give recommendations to the institutions that serve them.
There is a growing body of literature that demonstrates how disadvantages by individual and neighborhood-level socioeconomic status (SES) contribute to disparities in specific disease conditions.10-11 Strategies to narrow the gap in SES disadvantages may help reduce race-related health disparities. Institutions that engage the community and develop programs to promote health equity can do so through bidirectional exchange of knowledge and mutual benefit.
An institution-specific example is Medicine for the Greater Good at Johns Hopkins. The founders of this program wrote, “health is not synonymous with medicine. To truly care for our patients and their communities, health care professionals must understand how to deliver equitable health care that meets the needs of the diverse populations we care for. The mission of Medicine for the Greater Good is to promote health and wellness beyond the confines of the hospital through an interactive and engaging partnership with the community ...” Community engagement also provides an opportunity for growing the cultural intelligence of institutions and HMGs.
Tools for advancing comprehensive change – Repurposing PDSA cycles
Whether institutions and HMGs are at the beginning of their journey or further along in the work of reducing disparities, having a systematic approach for implementing and refining policies and procedures can cultivate more inclusive and equitable environments. Thankfully, hospitalists are already equipped with the fundamental tools needed to advance change across their institutions – QI processes in the form of Plan-Do-Study-Act (PDSA) cycles.
They allow a continuous cycle of successful incremental change based on direct evidence and experience. Any efforts to deconstruct systematic bias within our organizations must also be a continual process. Our female colleagues and colleagues of color need our institutions to engage unceasingly to bring about the equality they deserve. To that end, PDSA cycles are an apt tool to utilize in this work as they can naturally function in a never-ending process of improvement.
With PDSA as a model, we envision a cycle with steps that are intentionally purposed to fit the needs of equitable institutional change: Target-Engage-Assess-Modify. As highlighted (see graphic), these modifications ensure that stakeholders (i.e., those that unequal practices and policies affect the most) are engaged early and remain involved throughout the cycle. 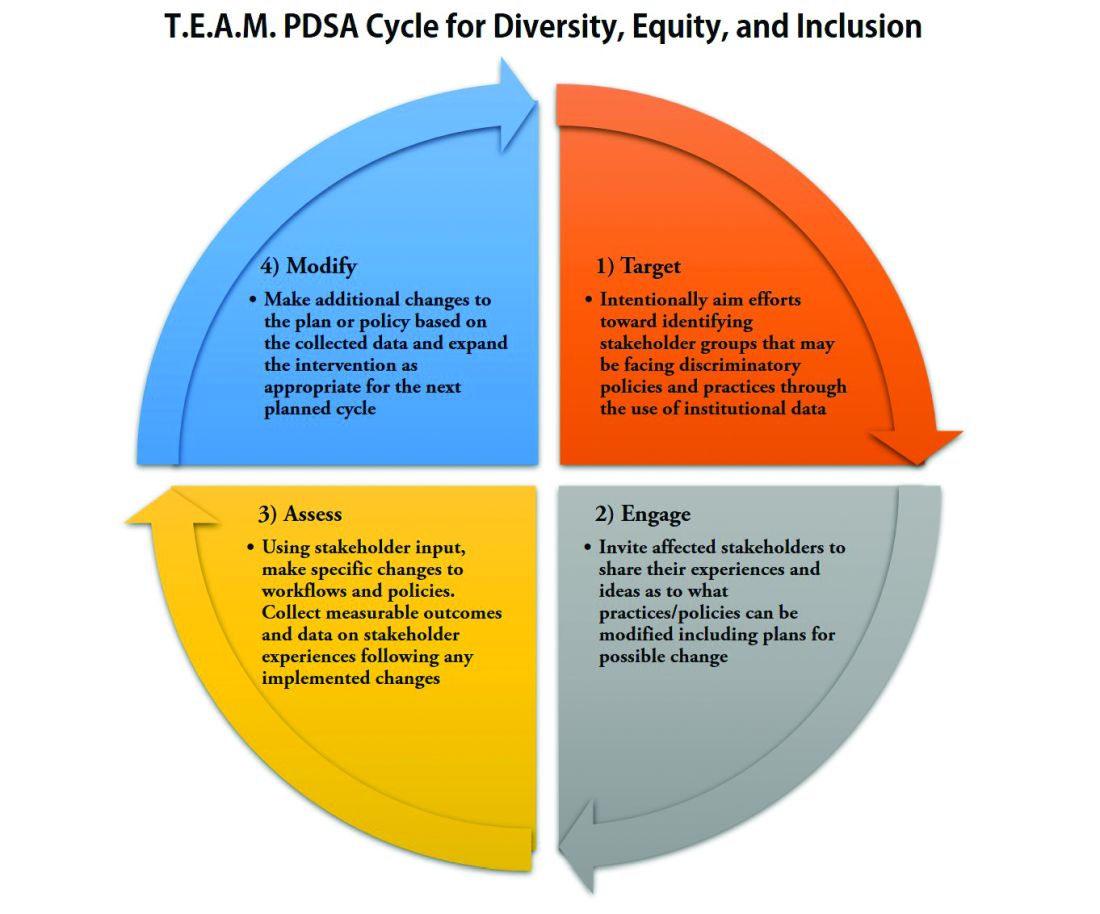
As hospitalists, we have significant work ahead to ensure that we develop and maintain a diverse, equitable and inclusive workforce. This work to bring change will not be easy and will require a considerable investment of time and resources. However, with the strategies and tools that we have outlined, our institutions and HMGs can start the change needed in our profession for our patients and the workforce. In doing so, we can all be accomplices in the fight to achieve racial and gender equity, and social justice.
Dr. Delapenha and Dr. Kisuule are based in the department of internal medicine, division of hospital medicine, at the Johns Hopkins University, Baltimore. Dr. Martin is based in the department of medicine, section of hospital medicine at the University of Chicago. Dr. Barrett is a hospitalist in the department of internal medicine, University of New Mexico, Albuquerque.
References
1. Diversity in Medicine: Facts and Figures 2019: Figure 19. Percentage of physicians by sex, 2018. AAMC website.
2. Diversity in Medicine: Facts and Figures 2019. Figure 16. Percentage of full-time U.S. medical school faculty by sex and race/ethnicity, 2018. AAMC website.
3. Diversity in Medicine: Facts and Figures 2019. Figure 15. Percentage of full-time U.S. medical school faculty by race/ethnicity, 2018. AAMC website.
4. Diversity in Medicine: Facts and Figures 2019. Figure 6. Percentage of acceptees to U.S. medical schools by race/ethnicity (alone), academic year 2018-2019. AAMC website.
5. Diversity in Medicine: Facts and Figures 2019 Figure 18. Percentage of all active physicians by race/ethnicity, 2018. AAMC website.
6. Herzke C et al. Gender issues in academic hospital medicine: A national survey of hospitalist leaders. J Gen Intern Med. 2020;35(6):1641-6.
7. Diversity in Medicine: Facts and Figures 2019. Fostering diversity and inclusion. AAMC website.
8. Diversity in Medicine: Facts and Figures 2019. Executive summary. AAMC website.
9. Ayyala MS et al. Mentorship is not enough: Exploring sponsorship and its role in career advancement in academic medicine. Acad Med. 2019;94(1):94-100.
10. Ejike OC et al. Contribution of individual and neighborhood factors to racial disparities in respiratory outcomes. Am J Respir Crit Care Med. 2021 Apr 15;203(8):987-97.
11. Galiatsatos P et al. The effect of community socioeconomic status on sepsis-attributable mortality. J Crit Care. 2018 Aug;46:129-33.
Adolescent immunizations and protecting our children from COVID-19
I began thinking of a topic for this column weeks ago determined to discuss anything except COVID-19. Yet, news reports from all sources blasted daily reminders of rising COVID-19 cases overall and specifically in children.
In August, school resumed for many of our patients and the battle over mandating masks for school attendance was in full swing. The fact that it is a Centers for Disease Control and Prevention recommendation supported by both the American Academy of Pediatrics and the Pediatric Infectious Disease Society fell on deaf ears. One day, I heard a report that over 25,000 students attending Texas public schools were diagnosed with COVID-19 between Aug. 23 and Aug. 29. This peak in activity occurred just 2 weeks after the start of school and led to the closure of 45 school districts. Texas does not have a monopoly on these rising cases. Delta, a more contagious variant, began circulating in June 2021 and by July it was the most predominant. Emergency department visits and hospitalizations have increased nationwide. During the latter 2 weeks of August 2021, COVID-19–related ED visits and hospitalizations for persons aged 0-17 years were 3.4 and 3.7 times higher in states with the lowest vaccination coverage, compared with states with high vaccination coverage (MMWR Morb Mortal Wkly Rep. 2021;70:1249-54). Specifically, the rates of hospitalization the week ending Aug. 14, 2021, were nearly 5 times the rates for the week ending June 26, 2021, for 0- to 17-year-olds and nearly 10 times the rates for children 0-4 years of age. Hospitalization rates were 10.1 times higher for unimmunized adolescents than for fully vaccinated ones (MMWR Morb Mortal Wkly Rep. 2021;70:1255-60).
Multiple elected state leaders have opposed interventions such as mandating masks in school, and our children are paying for it. These leaders have relinquished their responsibility to local school boards. Several have reinforced the no-mask mandate while others have had the courage and insight to ignore state government leaders and have established mask mandates.
How is this lack of enforcement of national recommendations affecting our patients? Let’s look at two neighboring school districts in Texas. School districts have COVID-19 dashboards that are updated daily and accessible to the general public. School District A requires masks for school entry. It serves 196,171 students and has 27,195 teachers and staff. Since school opened in August, 1,606 cumulative cases of COVID-19 in students (0.8%) and 282 in staff (1%) have been reported. Fifty-five percent of the student cases occurred in elementary schools. In contrast, School District B located in the adjacent county serves 64,517 students and has 3,906 teachers and staff with no mask mandate. Since August, there have been 4,506 cumulative COVID-19 cases in students (6.9%) and 578 (14.7%) in staff. Information regarding the specific school type was not provided; however, the dashboard indicates that 2,924 cases (64.8%) occurred in children younger than 11 years of age. County data indicate 62% of those older than 12 years of age were fully vaccinated in District A, compared with 54% of persons older than 12 years in District B. The county COVID-19 positivity rate in District A is 17.6% and in District B it is 20%. Both counties are experiencing increased COVID-19 activity yet have had strikingly different outcomes in the student/staff population. While supporting the case for wearing masks to prevent disease transmission, one can’t ignore the adolescents who were infected and vaccine eligible (District A: 706; District B: 1,582). Their vaccination status could not be determined.
As pediatricians we have played an integral part in the elimination of diseases through educating and administering vaccinations. Adolescents are relatively healthy, thus limiting the number of encounters with them. The majority complete the 11-year visit; however, many fail to return for the 16- to 18-year visit.
So how are we doing? CDC data from 10 U.S. jurisdictions demonstrated a substantial decrease in vaccine administration between March and May of 2020, compared with the same period in 2018 and 2019. A decline was anticipated because of the nationwide lockdown. Doses of HPV administered declined almost 64% and 71% for 9- to 12-year-olds and 13- to 17-year-olds, respectively. Tdap administration declined 66% and 61% for the same respective age groups. Although administered doses increased between June and September of 2020, it was not sufficient to achieve catch-up coverage. Compared to the same period in 2018-2019, administration of the HPV vaccine declined 12.8% and 28% (ages 9-12 and ages 13-17) and for Tdap it was 21% and 30% lower (ages 9-12 and ages 13-17) (MMWR Morb Mortal Wkly Rep. 2021;70:840-5).
Now, we have another adolescent vaccine to discuss and encourage our patients to receive. We also need to address their concerns and/or to at least direct them to a reliable source to obtain accurate information. For the first time, a recommended vaccine may not be available at their medical home. Many don’t know where to go to receive it (http://www.vaccines.gov). Results of a Kaiser Family Foundation COVID-19 survey (August 2021) indicated that parents trusted their pediatricians most often (78%) for vaccine advice. The respondents voiced concern about trusting the location where the child would be immunized and long-term effects especially related to fertility. Parents who received communications regarding the benefits of vaccination were twice as likely to have their adolescents immunized. Finally, remember: Like parent, like child. An immunized parent is more likely to immunize the adolescent. (See Fig. 1.)

It is beyond the scope of this column to discuss the psychosocial aspects of this disease: children experiencing the death of teachers, classmates, family members, and those viewing the vitriol between pro- and antimask proponents often exhibited on school premises. And let’s not forget the child who wants to wear a mask but may be ostracized or bullied for doing so.
Our job is to do our very best to advocate for and to protect our patients by promoting mandatory masks at schools and encouraging vaccination of adolescents as we patiently wait for vaccines to become available for all of our children.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
I began thinking of a topic for this column weeks ago determined to discuss anything except COVID-19. Yet, news reports from all sources blasted daily reminders of rising COVID-19 cases overall and specifically in children.
In August, school resumed for many of our patients and the battle over mandating masks for school attendance was in full swing. The fact that it is a Centers for Disease Control and Prevention recommendation supported by both the American Academy of Pediatrics and the Pediatric Infectious Disease Society fell on deaf ears. One day, I heard a report that over 25,000 students attending Texas public schools were diagnosed with COVID-19 between Aug. 23 and Aug. 29. This peak in activity occurred just 2 weeks after the start of school and led to the closure of 45 school districts. Texas does not have a monopoly on these rising cases. Delta, a more contagious variant, began circulating in June 2021 and by July it was the most predominant. Emergency department visits and hospitalizations have increased nationwide. During the latter 2 weeks of August 2021, COVID-19–related ED visits and hospitalizations for persons aged 0-17 years were 3.4 and 3.7 times higher in states with the lowest vaccination coverage, compared with states with high vaccination coverage (MMWR Morb Mortal Wkly Rep. 2021;70:1249-54). Specifically, the rates of hospitalization the week ending Aug. 14, 2021, were nearly 5 times the rates for the week ending June 26, 2021, for 0- to 17-year-olds and nearly 10 times the rates for children 0-4 years of age. Hospitalization rates were 10.1 times higher for unimmunized adolescents than for fully vaccinated ones (MMWR Morb Mortal Wkly Rep. 2021;70:1255-60).
Multiple elected state leaders have opposed interventions such as mandating masks in school, and our children are paying for it. These leaders have relinquished their responsibility to local school boards. Several have reinforced the no-mask mandate while others have had the courage and insight to ignore state government leaders and have established mask mandates.
How is this lack of enforcement of national recommendations affecting our patients? Let’s look at two neighboring school districts in Texas. School districts have COVID-19 dashboards that are updated daily and accessible to the general public. School District A requires masks for school entry. It serves 196,171 students and has 27,195 teachers and staff. Since school opened in August, 1,606 cumulative cases of COVID-19 in students (0.8%) and 282 in staff (1%) have been reported. Fifty-five percent of the student cases occurred in elementary schools. In contrast, School District B located in the adjacent county serves 64,517 students and has 3,906 teachers and staff with no mask mandate. Since August, there have been 4,506 cumulative COVID-19 cases in students (6.9%) and 578 (14.7%) in staff. Information regarding the specific school type was not provided; however, the dashboard indicates that 2,924 cases (64.8%) occurred in children younger than 11 years of age. County data indicate 62% of those older than 12 years of age were fully vaccinated in District A, compared with 54% of persons older than 12 years in District B. The county COVID-19 positivity rate in District A is 17.6% and in District B it is 20%. Both counties are experiencing increased COVID-19 activity yet have had strikingly different outcomes in the student/staff population. While supporting the case for wearing masks to prevent disease transmission, one can’t ignore the adolescents who were infected and vaccine eligible (District A: 706; District B: 1,582). Their vaccination status could not be determined.
As pediatricians we have played an integral part in the elimination of diseases through educating and administering vaccinations. Adolescents are relatively healthy, thus limiting the number of encounters with them. The majority complete the 11-year visit; however, many fail to return for the 16- to 18-year visit.
So how are we doing? CDC data from 10 U.S. jurisdictions demonstrated a substantial decrease in vaccine administration between March and May of 2020, compared with the same period in 2018 and 2019. A decline was anticipated because of the nationwide lockdown. Doses of HPV administered declined almost 64% and 71% for 9- to 12-year-olds and 13- to 17-year-olds, respectively. Tdap administration declined 66% and 61% for the same respective age groups. Although administered doses increased between June and September of 2020, it was not sufficient to achieve catch-up coverage. Compared to the same period in 2018-2019, administration of the HPV vaccine declined 12.8% and 28% (ages 9-12 and ages 13-17) and for Tdap it was 21% and 30% lower (ages 9-12 and ages 13-17) (MMWR Morb Mortal Wkly Rep. 2021;70:840-5).
Now, we have another adolescent vaccine to discuss and encourage our patients to receive. We also need to address their concerns and/or to at least direct them to a reliable source to obtain accurate information. For the first time, a recommended vaccine may not be available at their medical home. Many don’t know where to go to receive it (http://www.vaccines.gov). Results of a Kaiser Family Foundation COVID-19 survey (August 2021) indicated that parents trusted their pediatricians most often (78%) for vaccine advice. The respondents voiced concern about trusting the location where the child would be immunized and long-term effects especially related to fertility. Parents who received communications regarding the benefits of vaccination were twice as likely to have their adolescents immunized. Finally, remember: Like parent, like child. An immunized parent is more likely to immunize the adolescent. (See Fig. 1.)

It is beyond the scope of this column to discuss the psychosocial aspects of this disease: children experiencing the death of teachers, classmates, family members, and those viewing the vitriol between pro- and antimask proponents often exhibited on school premises. And let’s not forget the child who wants to wear a mask but may be ostracized or bullied for doing so.
Our job is to do our very best to advocate for and to protect our patients by promoting mandatory masks at schools and encouraging vaccination of adolescents as we patiently wait for vaccines to become available for all of our children.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
I began thinking of a topic for this column weeks ago determined to discuss anything except COVID-19. Yet, news reports from all sources blasted daily reminders of rising COVID-19 cases overall and specifically in children.
In August, school resumed for many of our patients and the battle over mandating masks for school attendance was in full swing. The fact that it is a Centers for Disease Control and Prevention recommendation supported by both the American Academy of Pediatrics and the Pediatric Infectious Disease Society fell on deaf ears. One day, I heard a report that over 25,000 students attending Texas public schools were diagnosed with COVID-19 between Aug. 23 and Aug. 29. This peak in activity occurred just 2 weeks after the start of school and led to the closure of 45 school districts. Texas does not have a monopoly on these rising cases. Delta, a more contagious variant, began circulating in June 2021 and by July it was the most predominant. Emergency department visits and hospitalizations have increased nationwide. During the latter 2 weeks of August 2021, COVID-19–related ED visits and hospitalizations for persons aged 0-17 years were 3.4 and 3.7 times higher in states with the lowest vaccination coverage, compared with states with high vaccination coverage (MMWR Morb Mortal Wkly Rep. 2021;70:1249-54). Specifically, the rates of hospitalization the week ending Aug. 14, 2021, were nearly 5 times the rates for the week ending June 26, 2021, for 0- to 17-year-olds and nearly 10 times the rates for children 0-4 years of age. Hospitalization rates were 10.1 times higher for unimmunized adolescents than for fully vaccinated ones (MMWR Morb Mortal Wkly Rep. 2021;70:1255-60).
Multiple elected state leaders have opposed interventions such as mandating masks in school, and our children are paying for it. These leaders have relinquished their responsibility to local school boards. Several have reinforced the no-mask mandate while others have had the courage and insight to ignore state government leaders and have established mask mandates.
How is this lack of enforcement of national recommendations affecting our patients? Let’s look at two neighboring school districts in Texas. School districts have COVID-19 dashboards that are updated daily and accessible to the general public. School District A requires masks for school entry. It serves 196,171 students and has 27,195 teachers and staff. Since school opened in August, 1,606 cumulative cases of COVID-19 in students (0.8%) and 282 in staff (1%) have been reported. Fifty-five percent of the student cases occurred in elementary schools. In contrast, School District B located in the adjacent county serves 64,517 students and has 3,906 teachers and staff with no mask mandate. Since August, there have been 4,506 cumulative COVID-19 cases in students (6.9%) and 578 (14.7%) in staff. Information regarding the specific school type was not provided; however, the dashboard indicates that 2,924 cases (64.8%) occurred in children younger than 11 years of age. County data indicate 62% of those older than 12 years of age were fully vaccinated in District A, compared with 54% of persons older than 12 years in District B. The county COVID-19 positivity rate in District A is 17.6% and in District B it is 20%. Both counties are experiencing increased COVID-19 activity yet have had strikingly different outcomes in the student/staff population. While supporting the case for wearing masks to prevent disease transmission, one can’t ignore the adolescents who were infected and vaccine eligible (District A: 706; District B: 1,582). Their vaccination status could not be determined.
As pediatricians we have played an integral part in the elimination of diseases through educating and administering vaccinations. Adolescents are relatively healthy, thus limiting the number of encounters with them. The majority complete the 11-year visit; however, many fail to return for the 16- to 18-year visit.
So how are we doing? CDC data from 10 U.S. jurisdictions demonstrated a substantial decrease in vaccine administration between March and May of 2020, compared with the same period in 2018 and 2019. A decline was anticipated because of the nationwide lockdown. Doses of HPV administered declined almost 64% and 71% for 9- to 12-year-olds and 13- to 17-year-olds, respectively. Tdap administration declined 66% and 61% for the same respective age groups. Although administered doses increased between June and September of 2020, it was not sufficient to achieve catch-up coverage. Compared to the same period in 2018-2019, administration of the HPV vaccine declined 12.8% and 28% (ages 9-12 and ages 13-17) and for Tdap it was 21% and 30% lower (ages 9-12 and ages 13-17) (MMWR Morb Mortal Wkly Rep. 2021;70:840-5).
Now, we have another adolescent vaccine to discuss and encourage our patients to receive. We also need to address their concerns and/or to at least direct them to a reliable source to obtain accurate information. For the first time, a recommended vaccine may not be available at their medical home. Many don’t know where to go to receive it (http://www.vaccines.gov). Results of a Kaiser Family Foundation COVID-19 survey (August 2021) indicated that parents trusted their pediatricians most often (78%) for vaccine advice. The respondents voiced concern about trusting the location where the child would be immunized and long-term effects especially related to fertility. Parents who received communications regarding the benefits of vaccination were twice as likely to have their adolescents immunized. Finally, remember: Like parent, like child. An immunized parent is more likely to immunize the adolescent. (See Fig. 1.)

It is beyond the scope of this column to discuss the psychosocial aspects of this disease: children experiencing the death of teachers, classmates, family members, and those viewing the vitriol between pro- and antimask proponents often exhibited on school premises. And let’s not forget the child who wants to wear a mask but may be ostracized or bullied for doing so.
Our job is to do our very best to advocate for and to protect our patients by promoting mandatory masks at schools and encouraging vaccination of adolescents as we patiently wait for vaccines to become available for all of our children.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
New sarcoidosis treatment guideline bringing light to the darkness
Nothing about sarcoidosis is easy. First identified in 1877, it is quite common. In the United States, lifetime risk is 2.4% and 0.85% for African American persons and White persons, respectively. Still, it remains an enigma. Despite study of its genetics and immunopathology, we don’t know its cause. Diagnosis is challenging because noncaseating granulomas, the tissue finding associated with sarcoidosis, aren’t specific for the disease. With the exception of Löfgren syndrome, a well-described sarcoid presentation that portends an excellent prognosis, initial signs and symptoms are variable and disease course is unpredictable.
The inherent heterogeneity of sarcoid makes it challenging to study. In the modern era of evidence-based medicine, it’s hard to say much about it with certainty. The American Thoracic Society (ATS) is one of just a few, premier organizations that creates respiratory medicine guidelines. In 1999, they published a sarcoid consensus statement with the European Respiratory Society (ERS), another outstanding and influential respiratory medicine organization, and the World Association of Sarcoidosis and other Granulomatous Disorders (WASOG). For the past 20 years, I’ve been referring trainees to this document for guidance on managing their patients with sarcoid.
Twenty years later, sarcoid remains frustrating and mysterious, but much has changed. Our methods for evaluating evidence and creating guidelines are now based on the GRADE criteria. Now that we have easy access to advanced technologies such as endobronchial ultrasound, obtaining tissue for diagnosis is easier. Our study of sarcoid itself has advanced, with large cohorts providing data on phenotyping, new immunosuppressants being used for treatment, and an improved understanding of cardiac sarcoidosis. In short, we’re in need of a sarcoidosis guideline for the 21st century.
Within in the past 18 months, the ATS and ERS have delivered updated guidelines for diagnosis and treatment. Despite the advancements cited above, sarcoid remains difficult to study. So predictably, neither document issues earth-shattering conclusions. Truth be told, well-done guidelines rarely do. They do provide several important updates that physicians managing patients with sarcoid should note.
The guideline on diagnosis provides recommendations for routine monitoring after diagnosis. Many practicing clinicians took from the 1999 ATS/ERS/WASOG consensus statement that all patients with sarcoid needed to be seen annually. At pulmonary clinics where I’ve worked, we’ve defaulted to annual follow-up for everyone, usually with chest radiography, lab testing, electrocardiography, and referral to ophthalmology. Because a majority of patients with sarcoid will remain asymptomatic or experience spontaneous remission, this practice never really seemed cost-effective or clinically efficient. The new guidelines are far more proscriptive on what monitoring is required and grade requirements at specific levels of certainty and often advise symptom-based assessments in lieu of reflexive annual testing.
The ERS guideline on treatment provides a thoughtful discussion of corticosteroid indications and dosing, broken down by underlying disease severity (assessed by lung function abnormalities and imaging). It also recognizes that two of the most common sarcoid symptoms are fatigue and dyspnea, which are both inherently nonspecific. In practice, proving these symptoms are directly attributable to sarcoid is challenging. The treatment guideline allows for flexibility in these cases, with shared decision-making and trials of low-dose steroids recommended. This seems an excellent hedge against overtreatment with immunosuppressive medications that have harmful side effects.
The ATS and ERS guidelines are not without controversy. Their approach to cardiac sarcoid differs slightly from that recommended by a commonly cited Heart Rhythm Society consensus statement, and despite discussing treatment options, the section on fatigue is quite limited. These two facts and other limitations largely reflect differing interpretations of the limited data; they do not detract from the overall importance of the ATS and ERS guidelines. Sarcoid remains an enigma, but little by little the outstanding academic physicians at the ATS and ERS are providing clarity.
Dr. Holley is an associate professor, department of medicine, Uniformed Services University (USU); program director, pulmonary and critical care medical fellowship, department of medicine, Walter Reed National Military Medical Center, Bethesda, Maryland. He has received a research grant from Fisher-Paykel and income from the American College of Chest Physicians.
A version of this article first appeared on Medscape.com.
Nothing about sarcoidosis is easy. First identified in 1877, it is quite common. In the United States, lifetime risk is 2.4% and 0.85% for African American persons and White persons, respectively. Still, it remains an enigma. Despite study of its genetics and immunopathology, we don’t know its cause. Diagnosis is challenging because noncaseating granulomas, the tissue finding associated with sarcoidosis, aren’t specific for the disease. With the exception of Löfgren syndrome, a well-described sarcoid presentation that portends an excellent prognosis, initial signs and symptoms are variable and disease course is unpredictable.
The inherent heterogeneity of sarcoid makes it challenging to study. In the modern era of evidence-based medicine, it’s hard to say much about it with certainty. The American Thoracic Society (ATS) is one of just a few, premier organizations that creates respiratory medicine guidelines. In 1999, they published a sarcoid consensus statement with the European Respiratory Society (ERS), another outstanding and influential respiratory medicine organization, and the World Association of Sarcoidosis and other Granulomatous Disorders (WASOG). For the past 20 years, I’ve been referring trainees to this document for guidance on managing their patients with sarcoid.
Twenty years later, sarcoid remains frustrating and mysterious, but much has changed. Our methods for evaluating evidence and creating guidelines are now based on the GRADE criteria. Now that we have easy access to advanced technologies such as endobronchial ultrasound, obtaining tissue for diagnosis is easier. Our study of sarcoid itself has advanced, with large cohorts providing data on phenotyping, new immunosuppressants being used for treatment, and an improved understanding of cardiac sarcoidosis. In short, we’re in need of a sarcoidosis guideline for the 21st century.
Within in the past 18 months, the ATS and ERS have delivered updated guidelines for diagnosis and treatment. Despite the advancements cited above, sarcoid remains difficult to study. So predictably, neither document issues earth-shattering conclusions. Truth be told, well-done guidelines rarely do. They do provide several important updates that physicians managing patients with sarcoid should note.
The guideline on diagnosis provides recommendations for routine monitoring after diagnosis. Many practicing clinicians took from the 1999 ATS/ERS/WASOG consensus statement that all patients with sarcoid needed to be seen annually. At pulmonary clinics where I’ve worked, we’ve defaulted to annual follow-up for everyone, usually with chest radiography, lab testing, electrocardiography, and referral to ophthalmology. Because a majority of patients with sarcoid will remain asymptomatic or experience spontaneous remission, this practice never really seemed cost-effective or clinically efficient. The new guidelines are far more proscriptive on what monitoring is required and grade requirements at specific levels of certainty and often advise symptom-based assessments in lieu of reflexive annual testing.
The ERS guideline on treatment provides a thoughtful discussion of corticosteroid indications and dosing, broken down by underlying disease severity (assessed by lung function abnormalities and imaging). It also recognizes that two of the most common sarcoid symptoms are fatigue and dyspnea, which are both inherently nonspecific. In practice, proving these symptoms are directly attributable to sarcoid is challenging. The treatment guideline allows for flexibility in these cases, with shared decision-making and trials of low-dose steroids recommended. This seems an excellent hedge against overtreatment with immunosuppressive medications that have harmful side effects.
The ATS and ERS guidelines are not without controversy. Their approach to cardiac sarcoid differs slightly from that recommended by a commonly cited Heart Rhythm Society consensus statement, and despite discussing treatment options, the section on fatigue is quite limited. These two facts and other limitations largely reflect differing interpretations of the limited data; they do not detract from the overall importance of the ATS and ERS guidelines. Sarcoid remains an enigma, but little by little the outstanding academic physicians at the ATS and ERS are providing clarity.
Dr. Holley is an associate professor, department of medicine, Uniformed Services University (USU); program director, pulmonary and critical care medical fellowship, department of medicine, Walter Reed National Military Medical Center, Bethesda, Maryland. He has received a research grant from Fisher-Paykel and income from the American College of Chest Physicians.
A version of this article first appeared on Medscape.com.
Nothing about sarcoidosis is easy. First identified in 1877, it is quite common. In the United States, lifetime risk is 2.4% and 0.85% for African American persons and White persons, respectively. Still, it remains an enigma. Despite study of its genetics and immunopathology, we don’t know its cause. Diagnosis is challenging because noncaseating granulomas, the tissue finding associated with sarcoidosis, aren’t specific for the disease. With the exception of Löfgren syndrome, a well-described sarcoid presentation that portends an excellent prognosis, initial signs and symptoms are variable and disease course is unpredictable.
The inherent heterogeneity of sarcoid makes it challenging to study. In the modern era of evidence-based medicine, it’s hard to say much about it with certainty. The American Thoracic Society (ATS) is one of just a few, premier organizations that creates respiratory medicine guidelines. In 1999, they published a sarcoid consensus statement with the European Respiratory Society (ERS), another outstanding and influential respiratory medicine organization, and the World Association of Sarcoidosis and other Granulomatous Disorders (WASOG). For the past 20 years, I’ve been referring trainees to this document for guidance on managing their patients with sarcoid.
Twenty years later, sarcoid remains frustrating and mysterious, but much has changed. Our methods for evaluating evidence and creating guidelines are now based on the GRADE criteria. Now that we have easy access to advanced technologies such as endobronchial ultrasound, obtaining tissue for diagnosis is easier. Our study of sarcoid itself has advanced, with large cohorts providing data on phenotyping, new immunosuppressants being used for treatment, and an improved understanding of cardiac sarcoidosis. In short, we’re in need of a sarcoidosis guideline for the 21st century.
Within in the past 18 months, the ATS and ERS have delivered updated guidelines for diagnosis and treatment. Despite the advancements cited above, sarcoid remains difficult to study. So predictably, neither document issues earth-shattering conclusions. Truth be told, well-done guidelines rarely do. They do provide several important updates that physicians managing patients with sarcoid should note.
The guideline on diagnosis provides recommendations for routine monitoring after diagnosis. Many practicing clinicians took from the 1999 ATS/ERS/WASOG consensus statement that all patients with sarcoid needed to be seen annually. At pulmonary clinics where I’ve worked, we’ve defaulted to annual follow-up for everyone, usually with chest radiography, lab testing, electrocardiography, and referral to ophthalmology. Because a majority of patients with sarcoid will remain asymptomatic or experience spontaneous remission, this practice never really seemed cost-effective or clinically efficient. The new guidelines are far more proscriptive on what monitoring is required and grade requirements at specific levels of certainty and often advise symptom-based assessments in lieu of reflexive annual testing.
The ERS guideline on treatment provides a thoughtful discussion of corticosteroid indications and dosing, broken down by underlying disease severity (assessed by lung function abnormalities and imaging). It also recognizes that two of the most common sarcoid symptoms are fatigue and dyspnea, which are both inherently nonspecific. In practice, proving these symptoms are directly attributable to sarcoid is challenging. The treatment guideline allows for flexibility in these cases, with shared decision-making and trials of low-dose steroids recommended. This seems an excellent hedge against overtreatment with immunosuppressive medications that have harmful side effects.
The ATS and ERS guidelines are not without controversy. Their approach to cardiac sarcoid differs slightly from that recommended by a commonly cited Heart Rhythm Society consensus statement, and despite discussing treatment options, the section on fatigue is quite limited. These two facts and other limitations largely reflect differing interpretations of the limited data; they do not detract from the overall importance of the ATS and ERS guidelines. Sarcoid remains an enigma, but little by little the outstanding academic physicians at the ATS and ERS are providing clarity.
Dr. Holley is an associate professor, department of medicine, Uniformed Services University (USU); program director, pulmonary and critical care medical fellowship, department of medicine, Walter Reed National Military Medical Center, Bethesda, Maryland. He has received a research grant from Fisher-Paykel and income from the American College of Chest Physicians.
A version of this article first appeared on Medscape.com.
Pandemic goal deficiency disorder
In August I shared with you my observations on two opposing op-ed pieces from two major newspapers, one was in favor of masking mandates for public schools, the other against. (Masking in school: A battle of the op-eds. MDedge Pediatrics. Letters from Maine, 2021 Aug 12). Neither group of authors could offer us evidence from controlled studies to support their views. However, both agreed that returning children to school deserves a high priority. But neither the authors nor I treaded into the uncharted waters of exactly how masking fits into our national goals for managing the pandemic because ... no one in this country has articulated what these goals should be. A third op-ed appearing 3 weeks later suggests why we are floundering in this goal-deficient limbo.
Writing in the New York Times, two epidemiologists in Boston ask the simple question: “What are we actually trying to achieve in the United States?” when it comes to the pandemic. (Allen AG and Jenkins H. The Hard Covid-19 Questions We’re Not Asking. 2021 Aug 30). Is our goal zero infections? Is it hammering on the virus until we can treat it like the seasonal flu? We do seem to agree that not having kids in school has been a disaster economically, educationally, and psychologically. But, where does the goal of getting them back in school fit into a larger and as yet undefined national goal? Without that target we have little idea of what compromises and risks we should be willing to accept.
How much serious pediatric disease is acceptable? It appears that the number of fatal complications in the pediatric population is very small in comparison with other demographic groups. Although few in number, there have been and there will continue to be pediatric deaths because of COVID. Is our goal zero pediatric deaths? If it is then this dictates a level of response that ripples back upstream to every child in every classroom and could threaten our overarching goal of returning children to school. Because none of us likes the thought of a child dying, some of us may be hesitant to even consider a strategy that doesn’t include zero pediatric deaths as a goal.
Are we looking to have zero serious pediatric infections? Achieving this goal is unlikely. Even if we develop a pediatric vaccine in the near future it probably won’t be in the arms of enough children by the end of this school year to make a significant dent in the number of serious pediatric infections. Waiting until an optimal number of children are immunized doesn’t feel like it will achieve a primary goal of getting kids back in school if we continue to focus on driving the level of serious pediatric infections to zero. We have already endured a year in which many communities made decisions that seemed to have prioritized an unstated goal of no school exposure–related educator deaths. Again, a goal based on little if any evidence.
The problem we face in this country is that our response to the pandemic has been nonuniform. Here in Brunswick, Maine, 99% of the eligible adults have been vaccinated. Even with the recent surge, we may be ready for a strategy that avoids wholesale quarantining. A targeted and robust antibody testing system might work for us and make an unproven and unpopular masking mandate unnecessary. Britain seems to be moving in a similar direction to meet its goal of keeping children in school.
However, there are large population groups in regions of this country that have stumbled at taking the initial steps to get the pandemic under control. Articulating a national goal that covers both communities where the response to the pandemic has been less thoughtful and robust along with states that have been more successful is going to be difficult. But it must be done.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
In August I shared with you my observations on two opposing op-ed pieces from two major newspapers, one was in favor of masking mandates for public schools, the other against. (Masking in school: A battle of the op-eds. MDedge Pediatrics. Letters from Maine, 2021 Aug 12). Neither group of authors could offer us evidence from controlled studies to support their views. However, both agreed that returning children to school deserves a high priority. But neither the authors nor I treaded into the uncharted waters of exactly how masking fits into our national goals for managing the pandemic because ... no one in this country has articulated what these goals should be. A third op-ed appearing 3 weeks later suggests why we are floundering in this goal-deficient limbo.
Writing in the New York Times, two epidemiologists in Boston ask the simple question: “What are we actually trying to achieve in the United States?” when it comes to the pandemic. (Allen AG and Jenkins H. The Hard Covid-19 Questions We’re Not Asking. 2021 Aug 30). Is our goal zero infections? Is it hammering on the virus until we can treat it like the seasonal flu? We do seem to agree that not having kids in school has been a disaster economically, educationally, and psychologically. But, where does the goal of getting them back in school fit into a larger and as yet undefined national goal? Without that target we have little idea of what compromises and risks we should be willing to accept.
How much serious pediatric disease is acceptable? It appears that the number of fatal complications in the pediatric population is very small in comparison with other demographic groups. Although few in number, there have been and there will continue to be pediatric deaths because of COVID. Is our goal zero pediatric deaths? If it is then this dictates a level of response that ripples back upstream to every child in every classroom and could threaten our overarching goal of returning children to school. Because none of us likes the thought of a child dying, some of us may be hesitant to even consider a strategy that doesn’t include zero pediatric deaths as a goal.
Are we looking to have zero serious pediatric infections? Achieving this goal is unlikely. Even if we develop a pediatric vaccine in the near future it probably won’t be in the arms of enough children by the end of this school year to make a significant dent in the number of serious pediatric infections. Waiting until an optimal number of children are immunized doesn’t feel like it will achieve a primary goal of getting kids back in school if we continue to focus on driving the level of serious pediatric infections to zero. We have already endured a year in which many communities made decisions that seemed to have prioritized an unstated goal of no school exposure–related educator deaths. Again, a goal based on little if any evidence.
The problem we face in this country is that our response to the pandemic has been nonuniform. Here in Brunswick, Maine, 99% of the eligible adults have been vaccinated. Even with the recent surge, we may be ready for a strategy that avoids wholesale quarantining. A targeted and robust antibody testing system might work for us and make an unproven and unpopular masking mandate unnecessary. Britain seems to be moving in a similar direction to meet its goal of keeping children in school.
However, there are large population groups in regions of this country that have stumbled at taking the initial steps to get the pandemic under control. Articulating a national goal that covers both communities where the response to the pandemic has been less thoughtful and robust along with states that have been more successful is going to be difficult. But it must be done.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
In August I shared with you my observations on two opposing op-ed pieces from two major newspapers, one was in favor of masking mandates for public schools, the other against. (Masking in school: A battle of the op-eds. MDedge Pediatrics. Letters from Maine, 2021 Aug 12). Neither group of authors could offer us evidence from controlled studies to support their views. However, both agreed that returning children to school deserves a high priority. But neither the authors nor I treaded into the uncharted waters of exactly how masking fits into our national goals for managing the pandemic because ... no one in this country has articulated what these goals should be. A third op-ed appearing 3 weeks later suggests why we are floundering in this goal-deficient limbo.
Writing in the New York Times, two epidemiologists in Boston ask the simple question: “What are we actually trying to achieve in the United States?” when it comes to the pandemic. (Allen AG and Jenkins H. The Hard Covid-19 Questions We’re Not Asking. 2021 Aug 30). Is our goal zero infections? Is it hammering on the virus until we can treat it like the seasonal flu? We do seem to agree that not having kids in school has been a disaster economically, educationally, and psychologically. But, where does the goal of getting them back in school fit into a larger and as yet undefined national goal? Without that target we have little idea of what compromises and risks we should be willing to accept.
How much serious pediatric disease is acceptable? It appears that the number of fatal complications in the pediatric population is very small in comparison with other demographic groups. Although few in number, there have been and there will continue to be pediatric deaths because of COVID. Is our goal zero pediatric deaths? If it is then this dictates a level of response that ripples back upstream to every child in every classroom and could threaten our overarching goal of returning children to school. Because none of us likes the thought of a child dying, some of us may be hesitant to even consider a strategy that doesn’t include zero pediatric deaths as a goal.
Are we looking to have zero serious pediatric infections? Achieving this goal is unlikely. Even if we develop a pediatric vaccine in the near future it probably won’t be in the arms of enough children by the end of this school year to make a significant dent in the number of serious pediatric infections. Waiting until an optimal number of children are immunized doesn’t feel like it will achieve a primary goal of getting kids back in school if we continue to focus on driving the level of serious pediatric infections to zero. We have already endured a year in which many communities made decisions that seemed to have prioritized an unstated goal of no school exposure–related educator deaths. Again, a goal based on little if any evidence.
The problem we face in this country is that our response to the pandemic has been nonuniform. Here in Brunswick, Maine, 99% of the eligible adults have been vaccinated. Even with the recent surge, we may be ready for a strategy that avoids wholesale quarantining. A targeted and robust antibody testing system might work for us and make an unproven and unpopular masking mandate unnecessary. Britain seems to be moving in a similar direction to meet its goal of keeping children in school.
However, there are large population groups in regions of this country that have stumbled at taking the initial steps to get the pandemic under control. Articulating a national goal that covers both communities where the response to the pandemic has been less thoughtful and robust along with states that have been more successful is going to be difficult. But it must be done.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Online mental health treatment: Is this the answer we’ve been waiting for?
If you haven’t noticed yet, there has been an explosion of new online companies specializing in slicing off some little sliver of health care and leaving traditional medicine to take care of the rest of the patient. Lately, many of these startups involve mental health care, traditionally a difficult area to make profitable unless one caters just to the wealthy. Many pediatricians have been unsure exactly what to make of these new efforts. Are these the rescuers we’ve been waiting for to fill what seems like an enormous and growing unmet need? Are they just another means to extract money from desperate people and leave the real work to someone else? Something in-between? This article outlines some points to consider when evaluating this new frontier.
Case vignette
A 12-year-old girl presents with her parents for an annual exam. She has been struggling with her mood and anxiety over the past 2 years along with occasional superficial cutting. You have started treatment with a selective serotonin reuptake inhibitor and have recommended that she see a mental health professional but the parents report that one attempt with a therapist was a poor fit and nobody in the area seems to be accepting new patients. The parents state that they saw an advertisement on TV for a company that offers online psychotherapy by video appointments or text. They think this might be an option to pursue but are a little skeptical of the whole idea. They look for your opinion on this topic.
Most of these companies operate by having subscribers pay a monthly fee for different levels of services such as videoconference therapy sessions, supportive text messages, or even some psychopharmacological care. Many also offer the ability to switch rapidly between clinicians if you don’t like the one you have.
These arrangements sound great as the world grows increasingly comfortable with online communication and the mental health needs of children and adolescents increase with the seemingly endless COVID pandemic. Further, research generally finds that online mental health treatment is just as effective as services delivered in person, although the data on therapy by text are less robust.
Nevertheless, a lot of skepticism remains about online mental health treatment, particularly among those involved in more traditionally delivered mental health care. Some of the concerns that often get brought up include the following:
- Cost. Most of these online groups, especially the big national companies, don’t interact directly with insurance companies, leaving a lot of out-of-pocket expenses or the need for families to work things out directly with their insurance provider.
- Care fragmentation. In many ways, the online mental health care surge seems at odds with the growing “integrated care” movement that is trying to embed more behavioral care within primary care practices. From this lens, outsourcing someone’s mental health treatment to a therapist across the country that the patient has never actually met seems like a step in the wrong direction. Further, concerns arise about how much these folks will know about local resources in the community.
- The corporate model in mental health care. While being able to shop for a therapist like you would for a pillow sounds great on the surface, there are many times where a patient may need to be supportively confronted by their therapist or told no when asking about things like certain medications. The “customer is always right” principle often falls short when it comes to good mental health treatment.
- Depth and type of treatment. It is probably fair to say that most online therapy could be described as supportive psychotherapy. This type of therapy can be quite helpful for many but may lack the depth or specific techniques that some people need. For youth, some of the most effective types of psychotherapy, like cognitive-behavioral therapy (CBT), can be harder to find, and implement, online.
- Emergencies. While many online companies claim to offer round-the-clock support for paying customers, they can quickly punt to “call your doctor” or even “call 911” if there is any real mental health crisis.
Balancing these potential benefits and pitfalls of online therapy, here are a few questions your patients may want to consider before signing onto a long-term contract with an online therapy company.
- Would the online clinician have any knowledge of my community? In some cases, this may not matter that much, while for others it could be quite important.
- What happens in an emergency? Would the regular online therapist be available to help through a crisis or would things revert back to local resources?
- What about privacy and collaboration? Effective communication between a patient’s primary care clinician and their therapist can be crucial to good care, and asking the patient always to be the intermediary can be fraught with difficulty.
- How long is the contract? Just like those gym memberships, these companies bank on individuals who sign up but then don’t really use the service.
- What kind of training do the therapists at the site have? Is it possible to receive specific types of therapy, like CBT or parent training? Otherwise, pediatricians might be quite likely to hear back from the family wondering about medications after therapy “isn’t helping.”
Overall, mental health treatment delivered by telehealth is here to stay whether we like it or not. For some families, it is likely to provide new access to services not easily obtainable locally, while for others it could end up being a costly and ineffective enterprise. For families who use these services, a key challenge for pediatricians that may be important to overcome is finding a way for these clinicians to integrate into the overall medical team rather than being a detached island unto themselves.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont Larner College of Medicine, Burlington. Follow him on Twitter @PediPsych. His book, “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood” (New York: Oxford University Press, 2021). Email him at pdnews@mdedge.com.
If you haven’t noticed yet, there has been an explosion of new online companies specializing in slicing off some little sliver of health care and leaving traditional medicine to take care of the rest of the patient. Lately, many of these startups involve mental health care, traditionally a difficult area to make profitable unless one caters just to the wealthy. Many pediatricians have been unsure exactly what to make of these new efforts. Are these the rescuers we’ve been waiting for to fill what seems like an enormous and growing unmet need? Are they just another means to extract money from desperate people and leave the real work to someone else? Something in-between? This article outlines some points to consider when evaluating this new frontier.
Case vignette
A 12-year-old girl presents with her parents for an annual exam. She has been struggling with her mood and anxiety over the past 2 years along with occasional superficial cutting. You have started treatment with a selective serotonin reuptake inhibitor and have recommended that she see a mental health professional but the parents report that one attempt with a therapist was a poor fit and nobody in the area seems to be accepting new patients. The parents state that they saw an advertisement on TV for a company that offers online psychotherapy by video appointments or text. They think this might be an option to pursue but are a little skeptical of the whole idea. They look for your opinion on this topic.
Most of these companies operate by having subscribers pay a monthly fee for different levels of services such as videoconference therapy sessions, supportive text messages, or even some psychopharmacological care. Many also offer the ability to switch rapidly between clinicians if you don’t like the one you have.
These arrangements sound great as the world grows increasingly comfortable with online communication and the mental health needs of children and adolescents increase with the seemingly endless COVID pandemic. Further, research generally finds that online mental health treatment is just as effective as services delivered in person, although the data on therapy by text are less robust.
Nevertheless, a lot of skepticism remains about online mental health treatment, particularly among those involved in more traditionally delivered mental health care. Some of the concerns that often get brought up include the following:
- Cost. Most of these online groups, especially the big national companies, don’t interact directly with insurance companies, leaving a lot of out-of-pocket expenses or the need for families to work things out directly with their insurance provider.
- Care fragmentation. In many ways, the online mental health care surge seems at odds with the growing “integrated care” movement that is trying to embed more behavioral care within primary care practices. From this lens, outsourcing someone’s mental health treatment to a therapist across the country that the patient has never actually met seems like a step in the wrong direction. Further, concerns arise about how much these folks will know about local resources in the community.
- The corporate model in mental health care. While being able to shop for a therapist like you would for a pillow sounds great on the surface, there are many times where a patient may need to be supportively confronted by their therapist or told no when asking about things like certain medications. The “customer is always right” principle often falls short when it comes to good mental health treatment.
- Depth and type of treatment. It is probably fair to say that most online therapy could be described as supportive psychotherapy. This type of therapy can be quite helpful for many but may lack the depth or specific techniques that some people need. For youth, some of the most effective types of psychotherapy, like cognitive-behavioral therapy (CBT), can be harder to find, and implement, online.
- Emergencies. While many online companies claim to offer round-the-clock support for paying customers, they can quickly punt to “call your doctor” or even “call 911” if there is any real mental health crisis.
Balancing these potential benefits and pitfalls of online therapy, here are a few questions your patients may want to consider before signing onto a long-term contract with an online therapy company.
- Would the online clinician have any knowledge of my community? In some cases, this may not matter that much, while for others it could be quite important.
- What happens in an emergency? Would the regular online therapist be available to help through a crisis or would things revert back to local resources?
- What about privacy and collaboration? Effective communication between a patient’s primary care clinician and their therapist can be crucial to good care, and asking the patient always to be the intermediary can be fraught with difficulty.
- How long is the contract? Just like those gym memberships, these companies bank on individuals who sign up but then don’t really use the service.
- What kind of training do the therapists at the site have? Is it possible to receive specific types of therapy, like CBT or parent training? Otherwise, pediatricians might be quite likely to hear back from the family wondering about medications after therapy “isn’t helping.”
Overall, mental health treatment delivered by telehealth is here to stay whether we like it or not. For some families, it is likely to provide new access to services not easily obtainable locally, while for others it could end up being a costly and ineffective enterprise. For families who use these services, a key challenge for pediatricians that may be important to overcome is finding a way for these clinicians to integrate into the overall medical team rather than being a detached island unto themselves.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont Larner College of Medicine, Burlington. Follow him on Twitter @PediPsych. His book, “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood” (New York: Oxford University Press, 2021). Email him at pdnews@mdedge.com.
If you haven’t noticed yet, there has been an explosion of new online companies specializing in slicing off some little sliver of health care and leaving traditional medicine to take care of the rest of the patient. Lately, many of these startups involve mental health care, traditionally a difficult area to make profitable unless one caters just to the wealthy. Many pediatricians have been unsure exactly what to make of these new efforts. Are these the rescuers we’ve been waiting for to fill what seems like an enormous and growing unmet need? Are they just another means to extract money from desperate people and leave the real work to someone else? Something in-between? This article outlines some points to consider when evaluating this new frontier.
Case vignette
A 12-year-old girl presents with her parents for an annual exam. She has been struggling with her mood and anxiety over the past 2 years along with occasional superficial cutting. You have started treatment with a selective serotonin reuptake inhibitor and have recommended that she see a mental health professional but the parents report that one attempt with a therapist was a poor fit and nobody in the area seems to be accepting new patients. The parents state that they saw an advertisement on TV for a company that offers online psychotherapy by video appointments or text. They think this might be an option to pursue but are a little skeptical of the whole idea. They look for your opinion on this topic.
Most of these companies operate by having subscribers pay a monthly fee for different levels of services such as videoconference therapy sessions, supportive text messages, or even some psychopharmacological care. Many also offer the ability to switch rapidly between clinicians if you don’t like the one you have.
These arrangements sound great as the world grows increasingly comfortable with online communication and the mental health needs of children and adolescents increase with the seemingly endless COVID pandemic. Further, research generally finds that online mental health treatment is just as effective as services delivered in person, although the data on therapy by text are less robust.
Nevertheless, a lot of skepticism remains about online mental health treatment, particularly among those involved in more traditionally delivered mental health care. Some of the concerns that often get brought up include the following:
- Cost. Most of these online groups, especially the big national companies, don’t interact directly with insurance companies, leaving a lot of out-of-pocket expenses or the need for families to work things out directly with their insurance provider.
- Care fragmentation. In many ways, the online mental health care surge seems at odds with the growing “integrated care” movement that is trying to embed more behavioral care within primary care practices. From this lens, outsourcing someone’s mental health treatment to a therapist across the country that the patient has never actually met seems like a step in the wrong direction. Further, concerns arise about how much these folks will know about local resources in the community.
- The corporate model in mental health care. While being able to shop for a therapist like you would for a pillow sounds great on the surface, there are many times where a patient may need to be supportively confronted by their therapist or told no when asking about things like certain medications. The “customer is always right” principle often falls short when it comes to good mental health treatment.
- Depth and type of treatment. It is probably fair to say that most online therapy could be described as supportive psychotherapy. This type of therapy can be quite helpful for many but may lack the depth or specific techniques that some people need. For youth, some of the most effective types of psychotherapy, like cognitive-behavioral therapy (CBT), can be harder to find, and implement, online.
- Emergencies. While many online companies claim to offer round-the-clock support for paying customers, they can quickly punt to “call your doctor” or even “call 911” if there is any real mental health crisis.
Balancing these potential benefits and pitfalls of online therapy, here are a few questions your patients may want to consider before signing onto a long-term contract with an online therapy company.
- Would the online clinician have any knowledge of my community? In some cases, this may not matter that much, while for others it could be quite important.
- What happens in an emergency? Would the regular online therapist be available to help through a crisis or would things revert back to local resources?
- What about privacy and collaboration? Effective communication between a patient’s primary care clinician and their therapist can be crucial to good care, and asking the patient always to be the intermediary can be fraught with difficulty.
- How long is the contract? Just like those gym memberships, these companies bank on individuals who sign up but then don’t really use the service.
- What kind of training do the therapists at the site have? Is it possible to receive specific types of therapy, like CBT or parent training? Otherwise, pediatricians might be quite likely to hear back from the family wondering about medications after therapy “isn’t helping.”
Overall, mental health treatment delivered by telehealth is here to stay whether we like it or not. For some families, it is likely to provide new access to services not easily obtainable locally, while for others it could end up being a costly and ineffective enterprise. For families who use these services, a key challenge for pediatricians that may be important to overcome is finding a way for these clinicians to integrate into the overall medical team rather than being a detached island unto themselves.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont Larner College of Medicine, Burlington. Follow him on Twitter @PediPsych. His book, “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood” (New York: Oxford University Press, 2021). Email him at pdnews@mdedge.com.