User login
Six pregnancy complications flag later heart disease risk
Six pregnancy-related complications increase a woman’s risk of developing risk factors for cardiovascular disease (CVD) and subsequently developing CVD, the American Heart Association says in a new scientific statement.
They are hypertensive disorders of pregnancy, preterm delivery, gestational diabetes, small-for-gestational-age (SGA) delivery, placental abruption (abruptio placentae), and pregnancy loss.
A history of any of these adverse pregnancy outcomes should prompt “more vigorous primordial prevention of CVD risk factors and primary prevention of CVD,” the writing group says.
“Adverse pregnancy outcomes are linked to women having hypertension, diabetes, abnormal cholesterol, and cardiovascular disease events, including heart attack and stroke, long after their pregnancies,” Nisha I. Parikh, MD, MPH, chair of the writing group, said in a news release.
Adverse pregnancy outcomes can be a “powerful window” into CVD prevention “if women and their health care professionals harness the knowledge and use it for health improvement,” said Dr. Parikh, associate professor of medicine in the cardiovascular division at the University of California, San Francisco.
The statement was published online March 29 in Circulation.
For the scientific statement, the writing group reviewed the latest scientific literature on adverse pregnancy outcomes and CVD risk.
The evidence in the literature linking adverse pregnancy outcomes to later CVD is “consistent over many years and confirmed in nearly every study we examined,” Dr. Parikh said. Among their key findings:
- Gestational hypertension is associated with an increased risk of CVD later in life by 67% and the odds of stroke by 83%. Moderate and severe is associated with a more than twofold increase in the risk for CVD.
- Gestational diabetes is associated with an increase in the risk for CVD by 68% and the risk of developing after pregnancy by 10-fold.
- Preterm delivery (before 37 weeks) is associated with double the risk of developing CVD and is strongly associated with later heart disease, stroke, and CVD.
- Placental abruption is associated with an 82% increased risk for CVD.
- Stillbirth is associated with about double the risk for CVD.
“This statement should inform future prevention guidelines in terms of the important factors to consider for determining women’s risk for heart diseases and stroke,” Dr. Parikh added.
The statement emphasizes the importance of recognizing these adverse pregnancy outcomes when evaluating CVD risk in women but notes that their value in reclassifying CVD risk may not be established.
It highlights the importance of adopting a heart-healthy diet and increasing physical activity among women with any of these pregnancy-related complications, starting right after childbirth and continuing across the life span to decrease CVD risk.
Lactation and breastfeeding may lower a woman’s later cardiometabolic risk, the writing group notes.
‘Golden year of opportunity’
The statement highlights several opportunities to improve transition of care for women with adverse pregnancy outcomes and to implement strategies to reduce their long-term CVD risk.
One strategy is longer postpartum follow-up care, sometimes referred to as the “fourth trimester,” to screen for CVD risk factors and provide CVD prevention counseling.
Another strategy involves improving the transfer of health information between ob/gyns and primary care physicians to eliminate inconsistencies in electronic health record documentation, which should improve patient care.
A third strategy is obtaining a short and targeted health history for each woman to confirm if she has any of the six pregnancy-related complications.
“If a woman has had any of these adverse pregnancy outcomes, consider close blood pressure monitoring, type 2 diabetes and lipid screening, and more aggressive risk factor modification and CVD prevention recommendations,” Dr. Parikh advised.
“Our data [lend] support to the prior AHA recommendation that these important adverse pregnancy outcomes should be ‘risk enhancers’ to guide consideration for statin therapy aimed at CVD prevention in women,” Dr. Parikh added.
In a commentary in Circulation, Eliza C. Miller, MD, assistant professor of neurology at Columbia University, New York, notes that pregnancy and the postpartum period are a critical time window in a woman’s life to identify CVD risk and improve a woman’s health trajectory.
“The so-called ‘Golden Hour’ for conditions such as sepsis and acute stroke refers to a critical time window for early recognition and treatment, when we can change a patient’s clinical trajectory and prevent severe morbidity and mortality,” writes Dr. Miller.
“Pregnancy and the postpartum period can be considered a ‘Golden Year’ in a woman’s life, offering a rare opportunity for clinicians to identify young women at risk and work with them to improve their cardiovascular health trajectories,” she notes.
This scientific statement was prepared by the volunteer writing group on behalf of the AHA Council on Epidemiology and Prevention; the Council on Arteriosclerosis, Thrombosis and Vascular Biology; the Council on Cardiovascular and Stroke Nursing; and the Stroke Council.
The authors of the scientific statement have disclosed no relevant financial relationships. Dr. Miller received personal compensation from Finch McCranie and Argionis & Associates for expert testimony regarding maternal stroke; and personal compensation from Elsevier for editorial work on Handbook of Clinical Neurology, Vol. 171 and 172 (Neurology of Pregnancy).
A version of this article first appeared on Medscape.com.
Six pregnancy-related complications increase a woman’s risk of developing risk factors for cardiovascular disease (CVD) and subsequently developing CVD, the American Heart Association says in a new scientific statement.
They are hypertensive disorders of pregnancy, preterm delivery, gestational diabetes, small-for-gestational-age (SGA) delivery, placental abruption (abruptio placentae), and pregnancy loss.
A history of any of these adverse pregnancy outcomes should prompt “more vigorous primordial prevention of CVD risk factors and primary prevention of CVD,” the writing group says.
“Adverse pregnancy outcomes are linked to women having hypertension, diabetes, abnormal cholesterol, and cardiovascular disease events, including heart attack and stroke, long after their pregnancies,” Nisha I. Parikh, MD, MPH, chair of the writing group, said in a news release.
Adverse pregnancy outcomes can be a “powerful window” into CVD prevention “if women and their health care professionals harness the knowledge and use it for health improvement,” said Dr. Parikh, associate professor of medicine in the cardiovascular division at the University of California, San Francisco.
The statement was published online March 29 in Circulation.
For the scientific statement, the writing group reviewed the latest scientific literature on adverse pregnancy outcomes and CVD risk.
The evidence in the literature linking adverse pregnancy outcomes to later CVD is “consistent over many years and confirmed in nearly every study we examined,” Dr. Parikh said. Among their key findings:
- Gestational hypertension is associated with an increased risk of CVD later in life by 67% and the odds of stroke by 83%. Moderate and severe is associated with a more than twofold increase in the risk for CVD.
- Gestational diabetes is associated with an increase in the risk for CVD by 68% and the risk of developing after pregnancy by 10-fold.
- Preterm delivery (before 37 weeks) is associated with double the risk of developing CVD and is strongly associated with later heart disease, stroke, and CVD.
- Placental abruption is associated with an 82% increased risk for CVD.
- Stillbirth is associated with about double the risk for CVD.
“This statement should inform future prevention guidelines in terms of the important factors to consider for determining women’s risk for heart diseases and stroke,” Dr. Parikh added.
The statement emphasizes the importance of recognizing these adverse pregnancy outcomes when evaluating CVD risk in women but notes that their value in reclassifying CVD risk may not be established.
It highlights the importance of adopting a heart-healthy diet and increasing physical activity among women with any of these pregnancy-related complications, starting right after childbirth and continuing across the life span to decrease CVD risk.
Lactation and breastfeeding may lower a woman’s later cardiometabolic risk, the writing group notes.
‘Golden year of opportunity’
The statement highlights several opportunities to improve transition of care for women with adverse pregnancy outcomes and to implement strategies to reduce their long-term CVD risk.
One strategy is longer postpartum follow-up care, sometimes referred to as the “fourth trimester,” to screen for CVD risk factors and provide CVD prevention counseling.
Another strategy involves improving the transfer of health information between ob/gyns and primary care physicians to eliminate inconsistencies in electronic health record documentation, which should improve patient care.
A third strategy is obtaining a short and targeted health history for each woman to confirm if she has any of the six pregnancy-related complications.
“If a woman has had any of these adverse pregnancy outcomes, consider close blood pressure monitoring, type 2 diabetes and lipid screening, and more aggressive risk factor modification and CVD prevention recommendations,” Dr. Parikh advised.
“Our data [lend] support to the prior AHA recommendation that these important adverse pregnancy outcomes should be ‘risk enhancers’ to guide consideration for statin therapy aimed at CVD prevention in women,” Dr. Parikh added.
In a commentary in Circulation, Eliza C. Miller, MD, assistant professor of neurology at Columbia University, New York, notes that pregnancy and the postpartum period are a critical time window in a woman’s life to identify CVD risk and improve a woman’s health trajectory.
“The so-called ‘Golden Hour’ for conditions such as sepsis and acute stroke refers to a critical time window for early recognition and treatment, when we can change a patient’s clinical trajectory and prevent severe morbidity and mortality,” writes Dr. Miller.
“Pregnancy and the postpartum period can be considered a ‘Golden Year’ in a woman’s life, offering a rare opportunity for clinicians to identify young women at risk and work with them to improve their cardiovascular health trajectories,” she notes.
This scientific statement was prepared by the volunteer writing group on behalf of the AHA Council on Epidemiology and Prevention; the Council on Arteriosclerosis, Thrombosis and Vascular Biology; the Council on Cardiovascular and Stroke Nursing; and the Stroke Council.
The authors of the scientific statement have disclosed no relevant financial relationships. Dr. Miller received personal compensation from Finch McCranie and Argionis & Associates for expert testimony regarding maternal stroke; and personal compensation from Elsevier for editorial work on Handbook of Clinical Neurology, Vol. 171 and 172 (Neurology of Pregnancy).
A version of this article first appeared on Medscape.com.
Six pregnancy-related complications increase a woman’s risk of developing risk factors for cardiovascular disease (CVD) and subsequently developing CVD, the American Heart Association says in a new scientific statement.
They are hypertensive disorders of pregnancy, preterm delivery, gestational diabetes, small-for-gestational-age (SGA) delivery, placental abruption (abruptio placentae), and pregnancy loss.
A history of any of these adverse pregnancy outcomes should prompt “more vigorous primordial prevention of CVD risk factors and primary prevention of CVD,” the writing group says.
“Adverse pregnancy outcomes are linked to women having hypertension, diabetes, abnormal cholesterol, and cardiovascular disease events, including heart attack and stroke, long after their pregnancies,” Nisha I. Parikh, MD, MPH, chair of the writing group, said in a news release.
Adverse pregnancy outcomes can be a “powerful window” into CVD prevention “if women and their health care professionals harness the knowledge and use it for health improvement,” said Dr. Parikh, associate professor of medicine in the cardiovascular division at the University of California, San Francisco.
The statement was published online March 29 in Circulation.
For the scientific statement, the writing group reviewed the latest scientific literature on adverse pregnancy outcomes and CVD risk.
The evidence in the literature linking adverse pregnancy outcomes to later CVD is “consistent over many years and confirmed in nearly every study we examined,” Dr. Parikh said. Among their key findings:
- Gestational hypertension is associated with an increased risk of CVD later in life by 67% and the odds of stroke by 83%. Moderate and severe is associated with a more than twofold increase in the risk for CVD.
- Gestational diabetes is associated with an increase in the risk for CVD by 68% and the risk of developing after pregnancy by 10-fold.
- Preterm delivery (before 37 weeks) is associated with double the risk of developing CVD and is strongly associated with later heart disease, stroke, and CVD.
- Placental abruption is associated with an 82% increased risk for CVD.
- Stillbirth is associated with about double the risk for CVD.
“This statement should inform future prevention guidelines in terms of the important factors to consider for determining women’s risk for heart diseases and stroke,” Dr. Parikh added.
The statement emphasizes the importance of recognizing these adverse pregnancy outcomes when evaluating CVD risk in women but notes that their value in reclassifying CVD risk may not be established.
It highlights the importance of adopting a heart-healthy diet and increasing physical activity among women with any of these pregnancy-related complications, starting right after childbirth and continuing across the life span to decrease CVD risk.
Lactation and breastfeeding may lower a woman’s later cardiometabolic risk, the writing group notes.
‘Golden year of opportunity’
The statement highlights several opportunities to improve transition of care for women with adverse pregnancy outcomes and to implement strategies to reduce their long-term CVD risk.
One strategy is longer postpartum follow-up care, sometimes referred to as the “fourth trimester,” to screen for CVD risk factors and provide CVD prevention counseling.
Another strategy involves improving the transfer of health information between ob/gyns and primary care physicians to eliminate inconsistencies in electronic health record documentation, which should improve patient care.
A third strategy is obtaining a short and targeted health history for each woman to confirm if she has any of the six pregnancy-related complications.
“If a woman has had any of these adverse pregnancy outcomes, consider close blood pressure monitoring, type 2 diabetes and lipid screening, and more aggressive risk factor modification and CVD prevention recommendations,” Dr. Parikh advised.
“Our data [lend] support to the prior AHA recommendation that these important adverse pregnancy outcomes should be ‘risk enhancers’ to guide consideration for statin therapy aimed at CVD prevention in women,” Dr. Parikh added.
In a commentary in Circulation, Eliza C. Miller, MD, assistant professor of neurology at Columbia University, New York, notes that pregnancy and the postpartum period are a critical time window in a woman’s life to identify CVD risk and improve a woman’s health trajectory.
“The so-called ‘Golden Hour’ for conditions such as sepsis and acute stroke refers to a critical time window for early recognition and treatment, when we can change a patient’s clinical trajectory and prevent severe morbidity and mortality,” writes Dr. Miller.
“Pregnancy and the postpartum period can be considered a ‘Golden Year’ in a woman’s life, offering a rare opportunity for clinicians to identify young women at risk and work with them to improve their cardiovascular health trajectories,” she notes.
This scientific statement was prepared by the volunteer writing group on behalf of the AHA Council on Epidemiology and Prevention; the Council on Arteriosclerosis, Thrombosis and Vascular Biology; the Council on Cardiovascular and Stroke Nursing; and the Stroke Council.
The authors of the scientific statement have disclosed no relevant financial relationships. Dr. Miller received personal compensation from Finch McCranie and Argionis & Associates for expert testimony regarding maternal stroke; and personal compensation from Elsevier for editorial work on Handbook of Clinical Neurology, Vol. 171 and 172 (Neurology of Pregnancy).
A version of this article first appeared on Medscape.com.
Febuxostat, allopurinol real-world cardiovascular risk appears equal
Febuxostat (Uloric) was not associated with increased cardiovascular risk in patients with gout when compared to those who used allopurinol, in an analysis of new users of the drugs in Medicare fee-for-service claims data from the period of 2008-2016.
The findings, published March 25 in the Journal of the American Heart Association, update and echo the results from a similar previous study by the same Brigham and Women’s Hospital research group that covered 2008-2013 Medicare claims data. That original claims data study from 2018 sought to confirm the findings of the postmarketing surveillance CARES (Cardiovascular Safety of Febuxostat and Allopurinol in Patients With Gout and Cardiovascular Morbidities) trial that led to a boxed warning for increased risk of cardiovascular and all-cause mortality vs. allopurinol. The trial, however, did not show a higher rate of major adverse cardiovascular events (MACE) overall with febuxostat.
The recency of the new data with more febuxostat-exposed patients overall provides greater reassurance on the safety of the drug, corresponding author Seoyoung C. Kim, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, said in an interview. “We also were able to get data on cause of death, which we did not have before when we conducted our first paper.”
Dr. Kim said she was not surprised by any of the findings, which were consistent with the results of her earlier work. “Our result on CV death also was consistent and reassuring,” she noted.
The newest Medicare claims study also corroborates results from FAST (Febuxostat Versus Allopurinol Streamlined Trial), a separate postmarketing surveillance study that was ordered by the European Medicines Agency after febuxostat’s approval in 2009. It showed that the two drugs were noninferior to each other for the risk of all-cause mortality or a composite cardiovascular outcome (hospitalization for nonfatal myocardial infarction, biomarker-positive acute coronary syndrome, nonfatal stroke, or cardiovascular death).
“While CARES showed higher CV death and all-cause death rates in febuxostat compared to allopurinol, FAST did not,” Dr. Kim noted. “Our study of more than 111,000 older gout patients treated with either febuxostat or allopurinol in real-world settings also did not find a difference in the risk of MACE, CV mortality, or all-cause mortality,” she added. “Taking these data all together, I think we can be more certain about the CV safety of febuxostat when its use is clinically indicated or needed,” she said.
Study details
Dr. Kim, first author Ajinkya Pawar, PhD, of Brigham and Women’s, and colleagues identified 467,461 people with gout aged 65 years and older who had been enrolled in Medicare for at least a year. They then used propensity-score matching to compare 27,881 first-time users of febuxostat with 83,643 first-time users of allopurinol on the primary outcome of the incidence of major adverse cardiovascular events (MACE), defined as the first occurrence of myocardial infarction, stroke, or cardiovascular mortality.
In the updated study, the mean follow‐up periods for febuxostat and allopurinol were 284 days and 339 days, respectively. Overall, febuxostat was noninferior to allopurinol with regard to MACE (hazard ratio, 0.99; 95% confidence interval, 0.93-1.05), and the results were consistent among patients with baseline CVD (HR, 0.94). In addition, rates of secondary outcomes of MI, stroke, and cardiovascular mortality were not significantly different between febuxostat and allopurinol patients, except for all-cause mortality (HR, 0.92; 95% CI, 0.87-0.98).
The study findings were limited mainly by the potential bias caused by nonadherence to medications, and potential for residual confounding and misclassification bias, the researchers noted.
However, the study was strengthened by its incident new-user design that allowed only patients with no use of either medication for a year before the first dispensing and its active comparator design, and the data are generalizable to the greater population of older gout patients, they said.
Consequently, the data from this large, real-world study support the safety of febuxostat with regard to cardiovascular risk in gout patients, including those with baseline cardiovascular disease, they concluded.
The study was supported by the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital. Dr. Kim disclosed research grants to Brigham and Women’s Hospital from Roche, Pfizer, AbbVie, and Bristol‐Myers Squibb for unrelated studies. Another author reported serving as the principal investigator with research grants from Vertex, Bayer, and Novartis to Brigham and Women’s Hospital for unrelated projects.
Febuxostat (Uloric) was not associated with increased cardiovascular risk in patients with gout when compared to those who used allopurinol, in an analysis of new users of the drugs in Medicare fee-for-service claims data from the period of 2008-2016.
The findings, published March 25 in the Journal of the American Heart Association, update and echo the results from a similar previous study by the same Brigham and Women’s Hospital research group that covered 2008-2013 Medicare claims data. That original claims data study from 2018 sought to confirm the findings of the postmarketing surveillance CARES (Cardiovascular Safety of Febuxostat and Allopurinol in Patients With Gout and Cardiovascular Morbidities) trial that led to a boxed warning for increased risk of cardiovascular and all-cause mortality vs. allopurinol. The trial, however, did not show a higher rate of major adverse cardiovascular events (MACE) overall with febuxostat.
The recency of the new data with more febuxostat-exposed patients overall provides greater reassurance on the safety of the drug, corresponding author Seoyoung C. Kim, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, said in an interview. “We also were able to get data on cause of death, which we did not have before when we conducted our first paper.”
Dr. Kim said she was not surprised by any of the findings, which were consistent with the results of her earlier work. “Our result on CV death also was consistent and reassuring,” she noted.
The newest Medicare claims study also corroborates results from FAST (Febuxostat Versus Allopurinol Streamlined Trial), a separate postmarketing surveillance study that was ordered by the European Medicines Agency after febuxostat’s approval in 2009. It showed that the two drugs were noninferior to each other for the risk of all-cause mortality or a composite cardiovascular outcome (hospitalization for nonfatal myocardial infarction, biomarker-positive acute coronary syndrome, nonfatal stroke, or cardiovascular death).
“While CARES showed higher CV death and all-cause death rates in febuxostat compared to allopurinol, FAST did not,” Dr. Kim noted. “Our study of more than 111,000 older gout patients treated with either febuxostat or allopurinol in real-world settings also did not find a difference in the risk of MACE, CV mortality, or all-cause mortality,” she added. “Taking these data all together, I think we can be more certain about the CV safety of febuxostat when its use is clinically indicated or needed,” she said.
Study details
Dr. Kim, first author Ajinkya Pawar, PhD, of Brigham and Women’s, and colleagues identified 467,461 people with gout aged 65 years and older who had been enrolled in Medicare for at least a year. They then used propensity-score matching to compare 27,881 first-time users of febuxostat with 83,643 first-time users of allopurinol on the primary outcome of the incidence of major adverse cardiovascular events (MACE), defined as the first occurrence of myocardial infarction, stroke, or cardiovascular mortality.
In the updated study, the mean follow‐up periods for febuxostat and allopurinol were 284 days and 339 days, respectively. Overall, febuxostat was noninferior to allopurinol with regard to MACE (hazard ratio, 0.99; 95% confidence interval, 0.93-1.05), and the results were consistent among patients with baseline CVD (HR, 0.94). In addition, rates of secondary outcomes of MI, stroke, and cardiovascular mortality were not significantly different between febuxostat and allopurinol patients, except for all-cause mortality (HR, 0.92; 95% CI, 0.87-0.98).
The study findings were limited mainly by the potential bias caused by nonadherence to medications, and potential for residual confounding and misclassification bias, the researchers noted.
However, the study was strengthened by its incident new-user design that allowed only patients with no use of either medication for a year before the first dispensing and its active comparator design, and the data are generalizable to the greater population of older gout patients, they said.
Consequently, the data from this large, real-world study support the safety of febuxostat with regard to cardiovascular risk in gout patients, including those with baseline cardiovascular disease, they concluded.
The study was supported by the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital. Dr. Kim disclosed research grants to Brigham and Women’s Hospital from Roche, Pfizer, AbbVie, and Bristol‐Myers Squibb for unrelated studies. Another author reported serving as the principal investigator with research grants from Vertex, Bayer, and Novartis to Brigham and Women’s Hospital for unrelated projects.
Febuxostat (Uloric) was not associated with increased cardiovascular risk in patients with gout when compared to those who used allopurinol, in an analysis of new users of the drugs in Medicare fee-for-service claims data from the period of 2008-2016.
The findings, published March 25 in the Journal of the American Heart Association, update and echo the results from a similar previous study by the same Brigham and Women’s Hospital research group that covered 2008-2013 Medicare claims data. That original claims data study from 2018 sought to confirm the findings of the postmarketing surveillance CARES (Cardiovascular Safety of Febuxostat and Allopurinol in Patients With Gout and Cardiovascular Morbidities) trial that led to a boxed warning for increased risk of cardiovascular and all-cause mortality vs. allopurinol. The trial, however, did not show a higher rate of major adverse cardiovascular events (MACE) overall with febuxostat.
The recency of the new data with more febuxostat-exposed patients overall provides greater reassurance on the safety of the drug, corresponding author Seoyoung C. Kim, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, said in an interview. “We also were able to get data on cause of death, which we did not have before when we conducted our first paper.”
Dr. Kim said she was not surprised by any of the findings, which were consistent with the results of her earlier work. “Our result on CV death also was consistent and reassuring,” she noted.
The newest Medicare claims study also corroborates results from FAST (Febuxostat Versus Allopurinol Streamlined Trial), a separate postmarketing surveillance study that was ordered by the European Medicines Agency after febuxostat’s approval in 2009. It showed that the two drugs were noninferior to each other for the risk of all-cause mortality or a composite cardiovascular outcome (hospitalization for nonfatal myocardial infarction, biomarker-positive acute coronary syndrome, nonfatal stroke, or cardiovascular death).
“While CARES showed higher CV death and all-cause death rates in febuxostat compared to allopurinol, FAST did not,” Dr. Kim noted. “Our study of more than 111,000 older gout patients treated with either febuxostat or allopurinol in real-world settings also did not find a difference in the risk of MACE, CV mortality, or all-cause mortality,” she added. “Taking these data all together, I think we can be more certain about the CV safety of febuxostat when its use is clinically indicated or needed,” she said.
Study details
Dr. Kim, first author Ajinkya Pawar, PhD, of Brigham and Women’s, and colleagues identified 467,461 people with gout aged 65 years and older who had been enrolled in Medicare for at least a year. They then used propensity-score matching to compare 27,881 first-time users of febuxostat with 83,643 first-time users of allopurinol on the primary outcome of the incidence of major adverse cardiovascular events (MACE), defined as the first occurrence of myocardial infarction, stroke, or cardiovascular mortality.
In the updated study, the mean follow‐up periods for febuxostat and allopurinol were 284 days and 339 days, respectively. Overall, febuxostat was noninferior to allopurinol with regard to MACE (hazard ratio, 0.99; 95% confidence interval, 0.93-1.05), and the results were consistent among patients with baseline CVD (HR, 0.94). In addition, rates of secondary outcomes of MI, stroke, and cardiovascular mortality were not significantly different between febuxostat and allopurinol patients, except for all-cause mortality (HR, 0.92; 95% CI, 0.87-0.98).
The study findings were limited mainly by the potential bias caused by nonadherence to medications, and potential for residual confounding and misclassification bias, the researchers noted.
However, the study was strengthened by its incident new-user design that allowed only patients with no use of either medication for a year before the first dispensing and its active comparator design, and the data are generalizable to the greater population of older gout patients, they said.
Consequently, the data from this large, real-world study support the safety of febuxostat with regard to cardiovascular risk in gout patients, including those with baseline cardiovascular disease, they concluded.
The study was supported by the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital. Dr. Kim disclosed research grants to Brigham and Women’s Hospital from Roche, Pfizer, AbbVie, and Bristol‐Myers Squibb for unrelated studies. Another author reported serving as the principal investigator with research grants from Vertex, Bayer, and Novartis to Brigham and Women’s Hospital for unrelated projects.
FROM THE JOURNAL OF THE AMERICAN HEART ASSOCIATION
Arcalyst gets FDA nod as first therapy for recurrent pericarditis
The Food and Drug Administration has approved rilonacept (Arcalyst) to treat recurrent pericarditis and reduce the risk for recurrence in adults and children 12 years and older.
Approval of the weekly subcutaneous injection offers patients the first and only FDA-approved therapy for recurrent pericarditis, the agency said in a release.
Recurrent pericarditis is characterized by a remitting relapsing inflammation of the pericardium, and therapeutic options have been limited to NSAIDs, colchicine, and corticosteroids.
Rilonacept is a recombinant fusion protein that blocks interleukin-1 alpha and interleukin-1 beta signaling. It is already approved by the FDA to treat a group of rare inherited inflammatory diseases called cryopyrin-associated periodic syndromes.
The new indication is based on the pivotal phase 3 RHAPSODY trial in 86 patients with acute symptoms of recurrent pericarditis and systemic inflammation. After randomization, pericarditis recurred in 2 of 30 patients (7%) treated with rilonacept and in 23 of 31 patients (74%) treated with placebo, representing a 96% reduction in the relative risk for recurrence with rilonacept.
Patients who received rilonacept were also pain free or had minimal pain on 98% of trial days, whereas those who received placebo had minimal or no pain on 46% of trial days.
The most common adverse effects of rilonacept are injection-site reactions and upper-respiratory tract infections.
Serious, life-threatening infections have been reported in patients taking rilonacept, according to the FDA. Patients with active or chronic infections should not take the drug.
The FDA label also advises that patients should avoid live vaccines while taking rilonacept and that it should be discontinued if a hypersensitivity reaction occurs.
The commercial launch is expected in April, according to the company.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved rilonacept (Arcalyst) to treat recurrent pericarditis and reduce the risk for recurrence in adults and children 12 years and older.
Approval of the weekly subcutaneous injection offers patients the first and only FDA-approved therapy for recurrent pericarditis, the agency said in a release.
Recurrent pericarditis is characterized by a remitting relapsing inflammation of the pericardium, and therapeutic options have been limited to NSAIDs, colchicine, and corticosteroids.
Rilonacept is a recombinant fusion protein that blocks interleukin-1 alpha and interleukin-1 beta signaling. It is already approved by the FDA to treat a group of rare inherited inflammatory diseases called cryopyrin-associated periodic syndromes.
The new indication is based on the pivotal phase 3 RHAPSODY trial in 86 patients with acute symptoms of recurrent pericarditis and systemic inflammation. After randomization, pericarditis recurred in 2 of 30 patients (7%) treated with rilonacept and in 23 of 31 patients (74%) treated with placebo, representing a 96% reduction in the relative risk for recurrence with rilonacept.
Patients who received rilonacept were also pain free or had minimal pain on 98% of trial days, whereas those who received placebo had minimal or no pain on 46% of trial days.
The most common adverse effects of rilonacept are injection-site reactions and upper-respiratory tract infections.
Serious, life-threatening infections have been reported in patients taking rilonacept, according to the FDA. Patients with active or chronic infections should not take the drug.
The FDA label also advises that patients should avoid live vaccines while taking rilonacept and that it should be discontinued if a hypersensitivity reaction occurs.
The commercial launch is expected in April, according to the company.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved rilonacept (Arcalyst) to treat recurrent pericarditis and reduce the risk for recurrence in adults and children 12 years and older.
Approval of the weekly subcutaneous injection offers patients the first and only FDA-approved therapy for recurrent pericarditis, the agency said in a release.
Recurrent pericarditis is characterized by a remitting relapsing inflammation of the pericardium, and therapeutic options have been limited to NSAIDs, colchicine, and corticosteroids.
Rilonacept is a recombinant fusion protein that blocks interleukin-1 alpha and interleukin-1 beta signaling. It is already approved by the FDA to treat a group of rare inherited inflammatory diseases called cryopyrin-associated periodic syndromes.
The new indication is based on the pivotal phase 3 RHAPSODY trial in 86 patients with acute symptoms of recurrent pericarditis and systemic inflammation. After randomization, pericarditis recurred in 2 of 30 patients (7%) treated with rilonacept and in 23 of 31 patients (74%) treated with placebo, representing a 96% reduction in the relative risk for recurrence with rilonacept.
Patients who received rilonacept were also pain free or had minimal pain on 98% of trial days, whereas those who received placebo had minimal or no pain on 46% of trial days.
The most common adverse effects of rilonacept are injection-site reactions and upper-respiratory tract infections.
Serious, life-threatening infections have been reported in patients taking rilonacept, according to the FDA. Patients with active or chronic infections should not take the drug.
The FDA label also advises that patients should avoid live vaccines while taking rilonacept and that it should be discontinued if a hypersensitivity reaction occurs.
The commercial launch is expected in April, according to the company.
A version of this article first appeared on Medscape.com.
Low concordance between troponin assays for ACS
Clinicians should be aware that the discordance between high-sensitivity cardiac troponin (hs-cTn) assays is significant enough that management recommendations may change, for example, for a patient assessed for suspected acute coronary syndrome (ACS) in one hospital and transferred to another that uses a different assay, according to a team of international researchers.
When hs-cTn concentrations were measured using the three Food and Drug Administration–approved assays, only 37.4% (384 of 1,027 samples) of blood samples were classified into the same analytical benchmark category.
“We didn’t expect such low concordance, to be honest, but I have to stress that this first assessment used just one-time blood testing and serial testing is what is more commonly recommended now,” said Júlia Karády, MD, from Massachusetts General Hospital and Harvard Medical School, both in Boston.
To see if concordance improved with serial testing, the researchers looked at the 242 patients for whom serial samples were available and saw concordance of management recommendations across assays rise to 74.8%.
“We tested the 0/2-hour algorithm and found that the overall agreement almost doubled, so I think that a very important message from our study is that serial testing improves the agreement between the assays in terms of clinical management and patient stratification,” said Dr. Karády.
Dr. Karády and colleagues published their findings in the Journal of the American College of Cardiology.
The researchers tested three assays referred to clinically as high-sensitivity assays: Elecsys 2010 platform (Roche Diagnostics); ARCHITECT i2000SR (Abbott Diagnostics); and hsVista (Siemens Diagnostics). All three have received FDA approval, starting with Elecsys in 2017.
The proportion of patients with similar management recommendations differed between the assays for both “rule-out” (87.2%, 73.1%, and 78.5% for Roche, Abbott, and Siemens, respectively) and “observe” (9.5%, 24%, and 17.8%; both P < .001). For the purposes of “rule-in,” no difference was noted (3.3%, 2.9%, and 3.7%).
“It’s important to note that this was a highly selected population of patients with an intermediate likelihood for ACS, not an all-comer population. This group comprises about 20% of the [emergency department] population and actually is the group we struggle with the most, which is hardest to diagnose because it excludes the very low– and very high–risk patients,” said Dr. Karády.
The patients included in this study all had suspected ACS and were enrolled in the ROMICAT-I and II trials.
Among 1,027 samples from 624 patients (mean age, 52.8 years; 39.4% women), samples were classified as below the limit of detection (LOD) in 56.3%, 10.4%, and 41.2% (P < .001) by Roche, Abbott, and Siemens, respectively.
The proportion of sample with a troponin measurement between LOD to the 99th percentile also differed significantly between the assays at 36.5%, 83.5%, and 52.6%, respectively (P < .001).
Only the proportion classified greater than 99th percentile did not differ (7.2%, 6.0%, and 6.2%; P = .114).
When the researchers looked at sex-specific difference, no differences were seen in rule-in numbers for men, but significant differences were seen for women.
“One possible explanation for this could be differences in the representation of men and women in the various reference populations used to develop the 99th percentile values for these assays,” suggested Dr. Karády.
They estimate around 30%-40% of U.S. centers are currently using high-sensitivity troponin assays and this number is “rapidly rising.”
The diagnostic algorithms developed for use with high-sensitivity assays, such as the 0/2-h algorithm, acknowledge differences in performance characteristics and recommend that assay-specific cut points be used for clinical decision-making rather than relying on generally applicable thresholds.
Joseph S. Alpert, MD, University of Arizona, Tucson, and coauthors of an accompanying editorial said the take-home message here is caveat emptor.
“First, ‘let the buyer (i.e., the clinician) beware’ when patients are transferred from one hospital to another, where different hs-cTn assays may be used,” they wrote. This is particularly true in women and in those with troponin levels in the “observe (gray zone)” clinical management recommendation.
Dr. Karády has received grant support from the Fulbright Visiting Researcher Grant and the Rosztoczy Foundation. One of the coauthors of the editorial comment consults or has consulted for most of the major diagnostic companies, including the manufacturers of the three assays tested in this study. Dr. Alpert disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Clinicians should be aware that the discordance between high-sensitivity cardiac troponin (hs-cTn) assays is significant enough that management recommendations may change, for example, for a patient assessed for suspected acute coronary syndrome (ACS) in one hospital and transferred to another that uses a different assay, according to a team of international researchers.
When hs-cTn concentrations were measured using the three Food and Drug Administration–approved assays, only 37.4% (384 of 1,027 samples) of blood samples were classified into the same analytical benchmark category.
“We didn’t expect such low concordance, to be honest, but I have to stress that this first assessment used just one-time blood testing and serial testing is what is more commonly recommended now,” said Júlia Karády, MD, from Massachusetts General Hospital and Harvard Medical School, both in Boston.
To see if concordance improved with serial testing, the researchers looked at the 242 patients for whom serial samples were available and saw concordance of management recommendations across assays rise to 74.8%.
“We tested the 0/2-hour algorithm and found that the overall agreement almost doubled, so I think that a very important message from our study is that serial testing improves the agreement between the assays in terms of clinical management and patient stratification,” said Dr. Karády.
Dr. Karády and colleagues published their findings in the Journal of the American College of Cardiology.
The researchers tested three assays referred to clinically as high-sensitivity assays: Elecsys 2010 platform (Roche Diagnostics); ARCHITECT i2000SR (Abbott Diagnostics); and hsVista (Siemens Diagnostics). All three have received FDA approval, starting with Elecsys in 2017.
The proportion of patients with similar management recommendations differed between the assays for both “rule-out” (87.2%, 73.1%, and 78.5% for Roche, Abbott, and Siemens, respectively) and “observe” (9.5%, 24%, and 17.8%; both P < .001). For the purposes of “rule-in,” no difference was noted (3.3%, 2.9%, and 3.7%).
“It’s important to note that this was a highly selected population of patients with an intermediate likelihood for ACS, not an all-comer population. This group comprises about 20% of the [emergency department] population and actually is the group we struggle with the most, which is hardest to diagnose because it excludes the very low– and very high–risk patients,” said Dr. Karády.
The patients included in this study all had suspected ACS and were enrolled in the ROMICAT-I and II trials.
Among 1,027 samples from 624 patients (mean age, 52.8 years; 39.4% women), samples were classified as below the limit of detection (LOD) in 56.3%, 10.4%, and 41.2% (P < .001) by Roche, Abbott, and Siemens, respectively.
The proportion of sample with a troponin measurement between LOD to the 99th percentile also differed significantly between the assays at 36.5%, 83.5%, and 52.6%, respectively (P < .001).
Only the proportion classified greater than 99th percentile did not differ (7.2%, 6.0%, and 6.2%; P = .114).
When the researchers looked at sex-specific difference, no differences were seen in rule-in numbers for men, but significant differences were seen for women.
“One possible explanation for this could be differences in the representation of men and women in the various reference populations used to develop the 99th percentile values for these assays,” suggested Dr. Karády.
They estimate around 30%-40% of U.S. centers are currently using high-sensitivity troponin assays and this number is “rapidly rising.”
The diagnostic algorithms developed for use with high-sensitivity assays, such as the 0/2-h algorithm, acknowledge differences in performance characteristics and recommend that assay-specific cut points be used for clinical decision-making rather than relying on generally applicable thresholds.
Joseph S. Alpert, MD, University of Arizona, Tucson, and coauthors of an accompanying editorial said the take-home message here is caveat emptor.
“First, ‘let the buyer (i.e., the clinician) beware’ when patients are transferred from one hospital to another, where different hs-cTn assays may be used,” they wrote. This is particularly true in women and in those with troponin levels in the “observe (gray zone)” clinical management recommendation.
Dr. Karády has received grant support from the Fulbright Visiting Researcher Grant and the Rosztoczy Foundation. One of the coauthors of the editorial comment consults or has consulted for most of the major diagnostic companies, including the manufacturers of the three assays tested in this study. Dr. Alpert disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Clinicians should be aware that the discordance between high-sensitivity cardiac troponin (hs-cTn) assays is significant enough that management recommendations may change, for example, for a patient assessed for suspected acute coronary syndrome (ACS) in one hospital and transferred to another that uses a different assay, according to a team of international researchers.
When hs-cTn concentrations were measured using the three Food and Drug Administration–approved assays, only 37.4% (384 of 1,027 samples) of blood samples were classified into the same analytical benchmark category.
“We didn’t expect such low concordance, to be honest, but I have to stress that this first assessment used just one-time blood testing and serial testing is what is more commonly recommended now,” said Júlia Karády, MD, from Massachusetts General Hospital and Harvard Medical School, both in Boston.
To see if concordance improved with serial testing, the researchers looked at the 242 patients for whom serial samples were available and saw concordance of management recommendations across assays rise to 74.8%.
“We tested the 0/2-hour algorithm and found that the overall agreement almost doubled, so I think that a very important message from our study is that serial testing improves the agreement between the assays in terms of clinical management and patient stratification,” said Dr. Karády.
Dr. Karády and colleagues published their findings in the Journal of the American College of Cardiology.
The researchers tested three assays referred to clinically as high-sensitivity assays: Elecsys 2010 platform (Roche Diagnostics); ARCHITECT i2000SR (Abbott Diagnostics); and hsVista (Siemens Diagnostics). All three have received FDA approval, starting with Elecsys in 2017.
The proportion of patients with similar management recommendations differed between the assays for both “rule-out” (87.2%, 73.1%, and 78.5% for Roche, Abbott, and Siemens, respectively) and “observe” (9.5%, 24%, and 17.8%; both P < .001). For the purposes of “rule-in,” no difference was noted (3.3%, 2.9%, and 3.7%).
“It’s important to note that this was a highly selected population of patients with an intermediate likelihood for ACS, not an all-comer population. This group comprises about 20% of the [emergency department] population and actually is the group we struggle with the most, which is hardest to diagnose because it excludes the very low– and very high–risk patients,” said Dr. Karády.
The patients included in this study all had suspected ACS and were enrolled in the ROMICAT-I and II trials.
Among 1,027 samples from 624 patients (mean age, 52.8 years; 39.4% women), samples were classified as below the limit of detection (LOD) in 56.3%, 10.4%, and 41.2% (P < .001) by Roche, Abbott, and Siemens, respectively.
The proportion of sample with a troponin measurement between LOD to the 99th percentile also differed significantly between the assays at 36.5%, 83.5%, and 52.6%, respectively (P < .001).
Only the proportion classified greater than 99th percentile did not differ (7.2%, 6.0%, and 6.2%; P = .114).
When the researchers looked at sex-specific difference, no differences were seen in rule-in numbers for men, but significant differences were seen for women.
“One possible explanation for this could be differences in the representation of men and women in the various reference populations used to develop the 99th percentile values for these assays,” suggested Dr. Karády.
They estimate around 30%-40% of U.S. centers are currently using high-sensitivity troponin assays and this number is “rapidly rising.”
The diagnostic algorithms developed for use with high-sensitivity assays, such as the 0/2-h algorithm, acknowledge differences in performance characteristics and recommend that assay-specific cut points be used for clinical decision-making rather than relying on generally applicable thresholds.
Joseph S. Alpert, MD, University of Arizona, Tucson, and coauthors of an accompanying editorial said the take-home message here is caveat emptor.
“First, ‘let the buyer (i.e., the clinician) beware’ when patients are transferred from one hospital to another, where different hs-cTn assays may be used,” they wrote. This is particularly true in women and in those with troponin levels in the “observe (gray zone)” clinical management recommendation.
Dr. Karády has received grant support from the Fulbright Visiting Researcher Grant and the Rosztoczy Foundation. One of the coauthors of the editorial comment consults or has consulted for most of the major diagnostic companies, including the manufacturers of the three assays tested in this study. Dr. Alpert disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ApoB may better predict mortality risk in statin-treated patients
A new study shows apolipoprotein B (apoB) and non-HDL cholesterol – but not LDL cholesterol – are associated with increased risk for all-cause mortality and myocardial infarction in patients taking statins.
Moreover, apoB was a more accurate marker of all-cause mortality risk than non-HDL or LDL cholesterol and was more accurate at identifying MI risk than LDL cholesterol.
“Any patient that comes to a doctor for evaluation, if statin treatment is sufficient, the doctor should look not only at LDL cholesterol but HDL cholesterol and apoB, if its available – that is the take-home message,” senior author Børge Grønne Nordestgaard, MD, DMSC, University of Copenhagen, said in an interview.
The findings are very relevant to clinical practice because international guidelines focus on LDL cholesterol and “many doctors are brainwashed that that is the only thing they should look at, just to keep LDL cholesterol down,” he said. “I’ve worked for years with triglyceride lipoproteins, what I call remnant cholesterol, and I think that the risk is very high also when you have high remnant cholesterol.”
Previous work has shown that apoB and non-HDL cholesterol better reflect atherosclerotic cardiovascular disease risk than LDL cholesterol. This is the first study, however, to show that elevated apoB and non-HDL cholesterol are associated with a higher risk for all-cause death in statin-treated patients with low LDL cholesterol, Dr. Nordestgaard noted.
The investigators compared outcomes among 13,015 statin-treated participants in the Copenhagen General Population Study using median baseline values of 92 mg/dL for apoB, 3.1 mmol/L (120 mg/dL) for non-HDL cholesterol, and 2.3 mmol/L (89 mg/dL) for LDL cholesterol. Over a median follow-up of 8 years, there were 2,499 deaths and 537 MIs.
As reported in the Journal of the American College of Cardiology, discordant apoB above the median with LDL cholesterol below was associated with a 21% increased risk for all-cause mortality (hazard ratio, 1.21; 95% confidence interval, 1.07-1.36) and 49% increased risk for MI (HR, 1.49; 95% CI, 1.15-1.92), compared with concordant apoB and LDL cholesterol below the medians.
Similar results were found for discordant non-HDL cholesterol above the median with low LDL cholesterol for all-cause mortality (HR, 1.18; 95% CI, 1.02-1.36) and MI (1.78; 95% CI, 1.35-2.34).
No such associations with mortality or MI were observed when LDL cholesterol was above the median and apoB or non-HDL below.
Additional analyses showed that high apoB with low non-HDL cholesterol was associated with a higher risk for all-cause mortality (HR, 1.21; 95% CI, 1.03-1.41), whereas high non-HDL cholesterol with low apoB was associated with a lower risk (HR, 0.75; 95% CI, 0.62-0.92).
Current guidelines define apoB greater than 130 mg/dL as a risk modifier in patients not using statins but, the authors wrote, “based on our results, the threshold for apoB as a risk modifier in statin-treated patients should be closer to 92 mg/dL than to 130 mg/dL.”
In an accompanying editorial, Neil J. Stone, MD, and Donald Lloyd-Jones, MD, both from Northwestern University, Chicago, said that American and European guidelines acknowledge the usefulness of apoB and non-HDL cholesterol in their risk algorithms and as possible targets to indicate efficacy, but don’t give a strong recommendation for apoB to assess residual risk.
“This paper suggests that, in the next iteration, we’ve got to give a stronger thought to measuring apoB for residual risk in those with secondary prevention,” Dr. Stone, vice chair of the 2018 American Heart Association/ACC cholesterol guidelines, said in an interview.
“The whole part of the guidelines was not to focus on any one number but to focus on the clinical risk as a whole,” he said. “You can enlarge your understanding of the patient by looking at their non-HDL, which you have anyway, and in certain circumstances, for example, people with metabolic syndrome, diabetes, obesity, or high triglycerides, those people might very well benefit from an apoB to further understand their risk. This paper simply highlights that and, therefore, was very valuable.”
Dr. Stone and Dr. Lloyd-Jones, however, pointed out that statin use was self-reported and information was lacking on adherence, dose intensity, and the amount of LDL cholesterol lowering from baseline. LDL cholesterol levels were also above current recommendations for optimizing risk reduction. “If statin dosing and LDL [cholesterol] were not optimized already, then there may have been ‘room’ for non-HDL [cholesterol] and apoB to add value in understanding residual risk,” they wrote.
The editorialists suggested that sequential use, rather than regular use, of apoB and non-HDL cholesterol may be best and that incorporating this information may be particularly beneficial for patients with metabolic disorders and elevated triglycerides after statin therapy.
“Maybe this paper is a wake-up call that there are other markers out there that can tell you that you still have higher risk and need to tighten up lifestyle and maybe be more adherent,” Dr. Stone said. “I think this is a wonderful chance to say that preventive cardiology isn’t just ‘set it and forget it’.”
C. Noel Bairey Merz, MD, who coauthored the 2018 cholesterol guidelines, agreed there’s “an overexuberant focus on LDL [cholesterol] for residual risk” and highlighted a recent systematic review of statins, ezetimibe, and PCSK9 cardiovascular outcomes trials that showed very little gain from aggressively driving down LDL below 100 mg/dL, unless the patient is at extremely high risk.
“If I, as a treating cardiologist who spends a lot of time on lipids, had a patient on a high-intensity statin and they didn’t drop [their LDL cholesterol] 50% and I already had them going to cardiac rehab and they were already losing weight, would I measure apoB? Yeah, I might, to motivate them to do more or to take Vascepa,” she said.
“This study is a useful addition to a relatively important problem, which is residual risk, and really supports personalized or precision medicine,” added Bairey Merz, MD, Cedars-Sinai Medical Center, Los Angeles. “But now we have to do the work and do an intervention trial in these people and see whether these markers make a difference.”
The study was supported by Herlev and Gentofte Hospital’s Research Fund and the department of clinical biochemistry, Herlev and Gentofte Hospital, Copenhagen University Hospital. Dr. Nordestgaard has had consultancies or talks sponsored by AstraZeneca, Sanofi, Regeneron, Akcea, Amarin, Amgen, Esperion, Kowa, Novartis, Novo Nordisk, and Silence Therapeutics. All other authors, Dr. Stone, and Dr. Lloyd-Jones reported no conflicts. Dr. Merz reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
A new study shows apolipoprotein B (apoB) and non-HDL cholesterol – but not LDL cholesterol – are associated with increased risk for all-cause mortality and myocardial infarction in patients taking statins.
Moreover, apoB was a more accurate marker of all-cause mortality risk than non-HDL or LDL cholesterol and was more accurate at identifying MI risk than LDL cholesterol.
“Any patient that comes to a doctor for evaluation, if statin treatment is sufficient, the doctor should look not only at LDL cholesterol but HDL cholesterol and apoB, if its available – that is the take-home message,” senior author Børge Grønne Nordestgaard, MD, DMSC, University of Copenhagen, said in an interview.
The findings are very relevant to clinical practice because international guidelines focus on LDL cholesterol and “many doctors are brainwashed that that is the only thing they should look at, just to keep LDL cholesterol down,” he said. “I’ve worked for years with triglyceride lipoproteins, what I call remnant cholesterol, and I think that the risk is very high also when you have high remnant cholesterol.”
Previous work has shown that apoB and non-HDL cholesterol better reflect atherosclerotic cardiovascular disease risk than LDL cholesterol. This is the first study, however, to show that elevated apoB and non-HDL cholesterol are associated with a higher risk for all-cause death in statin-treated patients with low LDL cholesterol, Dr. Nordestgaard noted.
The investigators compared outcomes among 13,015 statin-treated participants in the Copenhagen General Population Study using median baseline values of 92 mg/dL for apoB, 3.1 mmol/L (120 mg/dL) for non-HDL cholesterol, and 2.3 mmol/L (89 mg/dL) for LDL cholesterol. Over a median follow-up of 8 years, there were 2,499 deaths and 537 MIs.
As reported in the Journal of the American College of Cardiology, discordant apoB above the median with LDL cholesterol below was associated with a 21% increased risk for all-cause mortality (hazard ratio, 1.21; 95% confidence interval, 1.07-1.36) and 49% increased risk for MI (HR, 1.49; 95% CI, 1.15-1.92), compared with concordant apoB and LDL cholesterol below the medians.
Similar results were found for discordant non-HDL cholesterol above the median with low LDL cholesterol for all-cause mortality (HR, 1.18; 95% CI, 1.02-1.36) and MI (1.78; 95% CI, 1.35-2.34).
No such associations with mortality or MI were observed when LDL cholesterol was above the median and apoB or non-HDL below.
Additional analyses showed that high apoB with low non-HDL cholesterol was associated with a higher risk for all-cause mortality (HR, 1.21; 95% CI, 1.03-1.41), whereas high non-HDL cholesterol with low apoB was associated with a lower risk (HR, 0.75; 95% CI, 0.62-0.92).
Current guidelines define apoB greater than 130 mg/dL as a risk modifier in patients not using statins but, the authors wrote, “based on our results, the threshold for apoB as a risk modifier in statin-treated patients should be closer to 92 mg/dL than to 130 mg/dL.”
In an accompanying editorial, Neil J. Stone, MD, and Donald Lloyd-Jones, MD, both from Northwestern University, Chicago, said that American and European guidelines acknowledge the usefulness of apoB and non-HDL cholesterol in their risk algorithms and as possible targets to indicate efficacy, but don’t give a strong recommendation for apoB to assess residual risk.
“This paper suggests that, in the next iteration, we’ve got to give a stronger thought to measuring apoB for residual risk in those with secondary prevention,” Dr. Stone, vice chair of the 2018 American Heart Association/ACC cholesterol guidelines, said in an interview.
“The whole part of the guidelines was not to focus on any one number but to focus on the clinical risk as a whole,” he said. “You can enlarge your understanding of the patient by looking at their non-HDL, which you have anyway, and in certain circumstances, for example, people with metabolic syndrome, diabetes, obesity, or high triglycerides, those people might very well benefit from an apoB to further understand their risk. This paper simply highlights that and, therefore, was very valuable.”
Dr. Stone and Dr. Lloyd-Jones, however, pointed out that statin use was self-reported and information was lacking on adherence, dose intensity, and the amount of LDL cholesterol lowering from baseline. LDL cholesterol levels were also above current recommendations for optimizing risk reduction. “If statin dosing and LDL [cholesterol] were not optimized already, then there may have been ‘room’ for non-HDL [cholesterol] and apoB to add value in understanding residual risk,” they wrote.
The editorialists suggested that sequential use, rather than regular use, of apoB and non-HDL cholesterol may be best and that incorporating this information may be particularly beneficial for patients with metabolic disorders and elevated triglycerides after statin therapy.
“Maybe this paper is a wake-up call that there are other markers out there that can tell you that you still have higher risk and need to tighten up lifestyle and maybe be more adherent,” Dr. Stone said. “I think this is a wonderful chance to say that preventive cardiology isn’t just ‘set it and forget it’.”
C. Noel Bairey Merz, MD, who coauthored the 2018 cholesterol guidelines, agreed there’s “an overexuberant focus on LDL [cholesterol] for residual risk” and highlighted a recent systematic review of statins, ezetimibe, and PCSK9 cardiovascular outcomes trials that showed very little gain from aggressively driving down LDL below 100 mg/dL, unless the patient is at extremely high risk.
“If I, as a treating cardiologist who spends a lot of time on lipids, had a patient on a high-intensity statin and they didn’t drop [their LDL cholesterol] 50% and I already had them going to cardiac rehab and they were already losing weight, would I measure apoB? Yeah, I might, to motivate them to do more or to take Vascepa,” she said.
“This study is a useful addition to a relatively important problem, which is residual risk, and really supports personalized or precision medicine,” added Bairey Merz, MD, Cedars-Sinai Medical Center, Los Angeles. “But now we have to do the work and do an intervention trial in these people and see whether these markers make a difference.”
The study was supported by Herlev and Gentofte Hospital’s Research Fund and the department of clinical biochemistry, Herlev and Gentofte Hospital, Copenhagen University Hospital. Dr. Nordestgaard has had consultancies or talks sponsored by AstraZeneca, Sanofi, Regeneron, Akcea, Amarin, Amgen, Esperion, Kowa, Novartis, Novo Nordisk, and Silence Therapeutics. All other authors, Dr. Stone, and Dr. Lloyd-Jones reported no conflicts. Dr. Merz reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
A new study shows apolipoprotein B (apoB) and non-HDL cholesterol – but not LDL cholesterol – are associated with increased risk for all-cause mortality and myocardial infarction in patients taking statins.
Moreover, apoB was a more accurate marker of all-cause mortality risk than non-HDL or LDL cholesterol and was more accurate at identifying MI risk than LDL cholesterol.
“Any patient that comes to a doctor for evaluation, if statin treatment is sufficient, the doctor should look not only at LDL cholesterol but HDL cholesterol and apoB, if its available – that is the take-home message,” senior author Børge Grønne Nordestgaard, MD, DMSC, University of Copenhagen, said in an interview.
The findings are very relevant to clinical practice because international guidelines focus on LDL cholesterol and “many doctors are brainwashed that that is the only thing they should look at, just to keep LDL cholesterol down,” he said. “I’ve worked for years with triglyceride lipoproteins, what I call remnant cholesterol, and I think that the risk is very high also when you have high remnant cholesterol.”
Previous work has shown that apoB and non-HDL cholesterol better reflect atherosclerotic cardiovascular disease risk than LDL cholesterol. This is the first study, however, to show that elevated apoB and non-HDL cholesterol are associated with a higher risk for all-cause death in statin-treated patients with low LDL cholesterol, Dr. Nordestgaard noted.
The investigators compared outcomes among 13,015 statin-treated participants in the Copenhagen General Population Study using median baseline values of 92 mg/dL for apoB, 3.1 mmol/L (120 mg/dL) for non-HDL cholesterol, and 2.3 mmol/L (89 mg/dL) for LDL cholesterol. Over a median follow-up of 8 years, there were 2,499 deaths and 537 MIs.
As reported in the Journal of the American College of Cardiology, discordant apoB above the median with LDL cholesterol below was associated with a 21% increased risk for all-cause mortality (hazard ratio, 1.21; 95% confidence interval, 1.07-1.36) and 49% increased risk for MI (HR, 1.49; 95% CI, 1.15-1.92), compared with concordant apoB and LDL cholesterol below the medians.
Similar results were found for discordant non-HDL cholesterol above the median with low LDL cholesterol for all-cause mortality (HR, 1.18; 95% CI, 1.02-1.36) and MI (1.78; 95% CI, 1.35-2.34).
No such associations with mortality or MI were observed when LDL cholesterol was above the median and apoB or non-HDL below.
Additional analyses showed that high apoB with low non-HDL cholesterol was associated with a higher risk for all-cause mortality (HR, 1.21; 95% CI, 1.03-1.41), whereas high non-HDL cholesterol with low apoB was associated with a lower risk (HR, 0.75; 95% CI, 0.62-0.92).
Current guidelines define apoB greater than 130 mg/dL as a risk modifier in patients not using statins but, the authors wrote, “based on our results, the threshold for apoB as a risk modifier in statin-treated patients should be closer to 92 mg/dL than to 130 mg/dL.”
In an accompanying editorial, Neil J. Stone, MD, and Donald Lloyd-Jones, MD, both from Northwestern University, Chicago, said that American and European guidelines acknowledge the usefulness of apoB and non-HDL cholesterol in their risk algorithms and as possible targets to indicate efficacy, but don’t give a strong recommendation for apoB to assess residual risk.
“This paper suggests that, in the next iteration, we’ve got to give a stronger thought to measuring apoB for residual risk in those with secondary prevention,” Dr. Stone, vice chair of the 2018 American Heart Association/ACC cholesterol guidelines, said in an interview.
“The whole part of the guidelines was not to focus on any one number but to focus on the clinical risk as a whole,” he said. “You can enlarge your understanding of the patient by looking at their non-HDL, which you have anyway, and in certain circumstances, for example, people with metabolic syndrome, diabetes, obesity, or high triglycerides, those people might very well benefit from an apoB to further understand their risk. This paper simply highlights that and, therefore, was very valuable.”
Dr. Stone and Dr. Lloyd-Jones, however, pointed out that statin use was self-reported and information was lacking on adherence, dose intensity, and the amount of LDL cholesterol lowering from baseline. LDL cholesterol levels were also above current recommendations for optimizing risk reduction. “If statin dosing and LDL [cholesterol] were not optimized already, then there may have been ‘room’ for non-HDL [cholesterol] and apoB to add value in understanding residual risk,” they wrote.
The editorialists suggested that sequential use, rather than regular use, of apoB and non-HDL cholesterol may be best and that incorporating this information may be particularly beneficial for patients with metabolic disorders and elevated triglycerides after statin therapy.
“Maybe this paper is a wake-up call that there are other markers out there that can tell you that you still have higher risk and need to tighten up lifestyle and maybe be more adherent,” Dr. Stone said. “I think this is a wonderful chance to say that preventive cardiology isn’t just ‘set it and forget it’.”
C. Noel Bairey Merz, MD, who coauthored the 2018 cholesterol guidelines, agreed there’s “an overexuberant focus on LDL [cholesterol] for residual risk” and highlighted a recent systematic review of statins, ezetimibe, and PCSK9 cardiovascular outcomes trials that showed very little gain from aggressively driving down LDL below 100 mg/dL, unless the patient is at extremely high risk.
“If I, as a treating cardiologist who spends a lot of time on lipids, had a patient on a high-intensity statin and they didn’t drop [their LDL cholesterol] 50% and I already had them going to cardiac rehab and they were already losing weight, would I measure apoB? Yeah, I might, to motivate them to do more or to take Vascepa,” she said.
“This study is a useful addition to a relatively important problem, which is residual risk, and really supports personalized or precision medicine,” added Bairey Merz, MD, Cedars-Sinai Medical Center, Los Angeles. “But now we have to do the work and do an intervention trial in these people and see whether these markers make a difference.”
The study was supported by Herlev and Gentofte Hospital’s Research Fund and the department of clinical biochemistry, Herlev and Gentofte Hospital, Copenhagen University Hospital. Dr. Nordestgaard has had consultancies or talks sponsored by AstraZeneca, Sanofi, Regeneron, Akcea, Amarin, Amgen, Esperion, Kowa, Novartis, Novo Nordisk, and Silence Therapeutics. All other authors, Dr. Stone, and Dr. Lloyd-Jones reported no conflicts. Dr. Merz reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Ultraprocessed foods, many marketed as healthy, raise CVD risk
Eating ultraprocessed foods poses a significant risk to cardiovascular and coronary heart health, according to prospective data from about 3,000 people in the Framingham Offspring Cohort, the second generation of participants in the Framingham Heart Study.
Each regular, daily serving of ultraprocessed food was linked with significant elevations of 5%-9% in the relative rates of “hard” cardiovascular disease (CVD) events, hard coronary heart disease (CHD) events, overall CVD events, and CVD death, after adjustments for numerous potential confounders including energy intake, body mass index, waist circumference, and blood pressure, Filippa Juul, PhD, and associates wrote in a report published in the Journal of the American College of Cardiology.
“Consumption of ultraprocessed foods makes up over half of the daily calories in the average American diet and are increasingly consumed worldwide. As poor diet is a major modifiable risk factor for heart disease, it represents a critical target in prevention efforts,” said Dr. Juul, a nutritional epidemiologist at New York University, in a statement released by the American College of Cardiology.
“Our findings add to a growing body of evidence suggesting cardiovascular benefits of limiting ultraprocessed foods. Ultraprocessed foods are ubiquitous and include many foods that are marketed as healthy, such as protein bars, breakfast cereals, and most industrially produced breads,” she added. Other commonplace members of the ultraprocessed food group include carbonated soft drinks, packaged snacks, candies, sausages, margarines, and energy drinks. The concept of ultraprocessed foods as a distinct, wide-ranging, and dangerous food category first appeared in 2010, and then received an update from a United Nations panel in 2019 as what’s now called the NOVA classification system.
Ultraprocessed foods fly under the radar
“Although cardiovascular guidelines emphasize consuming minimally processed foods, such as fruits, vegetables, whole grains, and nuts, they give less attention to the importance of minimizing ultraprocessed food,” wrote Robert J. Ostfeld, MD, and Kathleen E. Allen, MS, in an editorial that accompanied the new report. This reduced attention may be because of a “paucity of studies examining the association cardiovascular outcomes and ultraprocessed foods.”
The new evidence demands new policies, educational efforts, and labeling changes, suggested Dr. Ostfeld, director of preventive cardiology at Montefiore Health System in New York, and Ms. Allen, a dietitian at the Geisel School of Medicine at Dartmouth, Hanover, N.H. “The goal should be to make the unhealthy choice the hard choice and the healthy choice the easy choice.”
The new analysis used data collected from people enrolled the Framingham Offspring Cohort, with their clinical metrics and diet information collected during 1991-1995 serving as their baseline. After excluding participants with prevalent CVD at baseline and those with incomplete follow-up of CVD events, the researchers had a cohort of 3,003 adults with an average follow-up of 18 years. At baseline, the cohort averaged 54 years of age; 55% were women, their average body mass index was 27.3 kg/m2, and about 6% had diabetes. They reported eating, on average, 7.5 servings of ultraprocessed food daily.
During follow-up, the cohort tallied 648 incident CVD events, including 251 hard CVD events (coronary death, MI, or stroke) and 163 hard CHD events (coronary death or MI), and 713 total deaths including 108 CVD deaths. Other CVD events recorded but not considered hard included heart failure, intermittent claudication, and transient ischemic attack.
In a multivariate-adjusted analysis, each average daily portion of ultraprocessed food was linked with an significant 7% relative increase in the incidence of a hard CVD event, compared with participants who ate fewer ultraprocessed food portions, and a 9% relative increase in the rate of hard CHD events, the study’s two prespecified primary outcomes. The researchers also found that each ultraprocessed serving significantly was associated with a 5% relative increased rate of total CVD events, and a 9% relative rise in CVD deaths. The analysis showed no significant association between total mortality and ultraprocessed food intake. (Average follow-up for the mortality analyses was 20 years.)
The authors also reported endpoint associations with intake of specific types of ultraprocessed foods, and found significantly increased associations specifically for portions of bread, ultraprocessed meat, salty snacks, and low-calorie soft drinks.
Convenient, omnipresent, and affordable
The authors acknowledged that the associations they found need examination in ethnically diverse populations, but nonetheless the findings “suggest the need for increased efforts to implement population-wide strategies” to lower consumption of ultraprocessed foods. “Given the convenience, omnipresence, and affordability of ultraprocessed foods, careful nutrition counseling is needed to design individualized, patient-centered, heart-healthy diets,” they concluded.
“Population-wide strategies such as taxation on sugar-sweetened beverages and other ultraprocessed foods and recommendations regarding processing levels in national dietary guidelines are needed to reduce the intake of ultraprocessed foods,” added Dr. Juul in her statement. “Of course, we must also implement policies that increase the availability, accessibility, and affordability of nutritious, minimally processed foods, especially in disadvantaged populations. At the clinical level, there is a need for increased commitment to individualized nutrition counseling for adopting sustainable heart-healthy diets.”
The study had no commercial funding. Dr. Juul and coauthors, Dr. Ostfeld, and Ms. Allen had no disclosures.
Eating ultraprocessed foods poses a significant risk to cardiovascular and coronary heart health, according to prospective data from about 3,000 people in the Framingham Offspring Cohort, the second generation of participants in the Framingham Heart Study.
Each regular, daily serving of ultraprocessed food was linked with significant elevations of 5%-9% in the relative rates of “hard” cardiovascular disease (CVD) events, hard coronary heart disease (CHD) events, overall CVD events, and CVD death, after adjustments for numerous potential confounders including energy intake, body mass index, waist circumference, and blood pressure, Filippa Juul, PhD, and associates wrote in a report published in the Journal of the American College of Cardiology.
“Consumption of ultraprocessed foods makes up over half of the daily calories in the average American diet and are increasingly consumed worldwide. As poor diet is a major modifiable risk factor for heart disease, it represents a critical target in prevention efforts,” said Dr. Juul, a nutritional epidemiologist at New York University, in a statement released by the American College of Cardiology.
“Our findings add to a growing body of evidence suggesting cardiovascular benefits of limiting ultraprocessed foods. Ultraprocessed foods are ubiquitous and include many foods that are marketed as healthy, such as protein bars, breakfast cereals, and most industrially produced breads,” she added. Other commonplace members of the ultraprocessed food group include carbonated soft drinks, packaged snacks, candies, sausages, margarines, and energy drinks. The concept of ultraprocessed foods as a distinct, wide-ranging, and dangerous food category first appeared in 2010, and then received an update from a United Nations panel in 2019 as what’s now called the NOVA classification system.
Ultraprocessed foods fly under the radar
“Although cardiovascular guidelines emphasize consuming minimally processed foods, such as fruits, vegetables, whole grains, and nuts, they give less attention to the importance of minimizing ultraprocessed food,” wrote Robert J. Ostfeld, MD, and Kathleen E. Allen, MS, in an editorial that accompanied the new report. This reduced attention may be because of a “paucity of studies examining the association cardiovascular outcomes and ultraprocessed foods.”
The new evidence demands new policies, educational efforts, and labeling changes, suggested Dr. Ostfeld, director of preventive cardiology at Montefiore Health System in New York, and Ms. Allen, a dietitian at the Geisel School of Medicine at Dartmouth, Hanover, N.H. “The goal should be to make the unhealthy choice the hard choice and the healthy choice the easy choice.”
The new analysis used data collected from people enrolled the Framingham Offspring Cohort, with their clinical metrics and diet information collected during 1991-1995 serving as their baseline. After excluding participants with prevalent CVD at baseline and those with incomplete follow-up of CVD events, the researchers had a cohort of 3,003 adults with an average follow-up of 18 years. At baseline, the cohort averaged 54 years of age; 55% were women, their average body mass index was 27.3 kg/m2, and about 6% had diabetes. They reported eating, on average, 7.5 servings of ultraprocessed food daily.
During follow-up, the cohort tallied 648 incident CVD events, including 251 hard CVD events (coronary death, MI, or stroke) and 163 hard CHD events (coronary death or MI), and 713 total deaths including 108 CVD deaths. Other CVD events recorded but not considered hard included heart failure, intermittent claudication, and transient ischemic attack.
In a multivariate-adjusted analysis, each average daily portion of ultraprocessed food was linked with an significant 7% relative increase in the incidence of a hard CVD event, compared with participants who ate fewer ultraprocessed food portions, and a 9% relative increase in the rate of hard CHD events, the study’s two prespecified primary outcomes. The researchers also found that each ultraprocessed serving significantly was associated with a 5% relative increased rate of total CVD events, and a 9% relative rise in CVD deaths. The analysis showed no significant association between total mortality and ultraprocessed food intake. (Average follow-up for the mortality analyses was 20 years.)
The authors also reported endpoint associations with intake of specific types of ultraprocessed foods, and found significantly increased associations specifically for portions of bread, ultraprocessed meat, salty snacks, and low-calorie soft drinks.
Convenient, omnipresent, and affordable
The authors acknowledged that the associations they found need examination in ethnically diverse populations, but nonetheless the findings “suggest the need for increased efforts to implement population-wide strategies” to lower consumption of ultraprocessed foods. “Given the convenience, omnipresence, and affordability of ultraprocessed foods, careful nutrition counseling is needed to design individualized, patient-centered, heart-healthy diets,” they concluded.
“Population-wide strategies such as taxation on sugar-sweetened beverages and other ultraprocessed foods and recommendations regarding processing levels in national dietary guidelines are needed to reduce the intake of ultraprocessed foods,” added Dr. Juul in her statement. “Of course, we must also implement policies that increase the availability, accessibility, and affordability of nutritious, minimally processed foods, especially in disadvantaged populations. At the clinical level, there is a need for increased commitment to individualized nutrition counseling for adopting sustainable heart-healthy diets.”
The study had no commercial funding. Dr. Juul and coauthors, Dr. Ostfeld, and Ms. Allen had no disclosures.
Eating ultraprocessed foods poses a significant risk to cardiovascular and coronary heart health, according to prospective data from about 3,000 people in the Framingham Offspring Cohort, the second generation of participants in the Framingham Heart Study.
Each regular, daily serving of ultraprocessed food was linked with significant elevations of 5%-9% in the relative rates of “hard” cardiovascular disease (CVD) events, hard coronary heart disease (CHD) events, overall CVD events, and CVD death, after adjustments for numerous potential confounders including energy intake, body mass index, waist circumference, and blood pressure, Filippa Juul, PhD, and associates wrote in a report published in the Journal of the American College of Cardiology.
“Consumption of ultraprocessed foods makes up over half of the daily calories in the average American diet and are increasingly consumed worldwide. As poor diet is a major modifiable risk factor for heart disease, it represents a critical target in prevention efforts,” said Dr. Juul, a nutritional epidemiologist at New York University, in a statement released by the American College of Cardiology.
“Our findings add to a growing body of evidence suggesting cardiovascular benefits of limiting ultraprocessed foods. Ultraprocessed foods are ubiquitous and include many foods that are marketed as healthy, such as protein bars, breakfast cereals, and most industrially produced breads,” she added. Other commonplace members of the ultraprocessed food group include carbonated soft drinks, packaged snacks, candies, sausages, margarines, and energy drinks. The concept of ultraprocessed foods as a distinct, wide-ranging, and dangerous food category first appeared in 2010, and then received an update from a United Nations panel in 2019 as what’s now called the NOVA classification system.
Ultraprocessed foods fly under the radar
“Although cardiovascular guidelines emphasize consuming minimally processed foods, such as fruits, vegetables, whole grains, and nuts, they give less attention to the importance of minimizing ultraprocessed food,” wrote Robert J. Ostfeld, MD, and Kathleen E. Allen, MS, in an editorial that accompanied the new report. This reduced attention may be because of a “paucity of studies examining the association cardiovascular outcomes and ultraprocessed foods.”
The new evidence demands new policies, educational efforts, and labeling changes, suggested Dr. Ostfeld, director of preventive cardiology at Montefiore Health System in New York, and Ms. Allen, a dietitian at the Geisel School of Medicine at Dartmouth, Hanover, N.H. “The goal should be to make the unhealthy choice the hard choice and the healthy choice the easy choice.”
The new analysis used data collected from people enrolled the Framingham Offspring Cohort, with their clinical metrics and diet information collected during 1991-1995 serving as their baseline. After excluding participants with prevalent CVD at baseline and those with incomplete follow-up of CVD events, the researchers had a cohort of 3,003 adults with an average follow-up of 18 years. At baseline, the cohort averaged 54 years of age; 55% were women, their average body mass index was 27.3 kg/m2, and about 6% had diabetes. They reported eating, on average, 7.5 servings of ultraprocessed food daily.
During follow-up, the cohort tallied 648 incident CVD events, including 251 hard CVD events (coronary death, MI, or stroke) and 163 hard CHD events (coronary death or MI), and 713 total deaths including 108 CVD deaths. Other CVD events recorded but not considered hard included heart failure, intermittent claudication, and transient ischemic attack.
In a multivariate-adjusted analysis, each average daily portion of ultraprocessed food was linked with an significant 7% relative increase in the incidence of a hard CVD event, compared with participants who ate fewer ultraprocessed food portions, and a 9% relative increase in the rate of hard CHD events, the study’s two prespecified primary outcomes. The researchers also found that each ultraprocessed serving significantly was associated with a 5% relative increased rate of total CVD events, and a 9% relative rise in CVD deaths. The analysis showed no significant association between total mortality and ultraprocessed food intake. (Average follow-up for the mortality analyses was 20 years.)
The authors also reported endpoint associations with intake of specific types of ultraprocessed foods, and found significantly increased associations specifically for portions of bread, ultraprocessed meat, salty snacks, and low-calorie soft drinks.
Convenient, omnipresent, and affordable
The authors acknowledged that the associations they found need examination in ethnically diverse populations, but nonetheless the findings “suggest the need for increased efforts to implement population-wide strategies” to lower consumption of ultraprocessed foods. “Given the convenience, omnipresence, and affordability of ultraprocessed foods, careful nutrition counseling is needed to design individualized, patient-centered, heart-healthy diets,” they concluded.
“Population-wide strategies such as taxation on sugar-sweetened beverages and other ultraprocessed foods and recommendations regarding processing levels in national dietary guidelines are needed to reduce the intake of ultraprocessed foods,” added Dr. Juul in her statement. “Of course, we must also implement policies that increase the availability, accessibility, and affordability of nutritious, minimally processed foods, especially in disadvantaged populations. At the clinical level, there is a need for increased commitment to individualized nutrition counseling for adopting sustainable heart-healthy diets.”
The study had no commercial funding. Dr. Juul and coauthors, Dr. Ostfeld, and Ms. Allen had no disclosures.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Colchicine before PCI for acute MI fails to improve major outcomes
In a placebo-controlled randomized trial, a preprocedural dose of colchicine administered immediately before percutaneous coronary intervention (PCI) for an acute ST-segment elevated myocardial infarction (STEMI) did not reduce the no-reflow phenomenon or improve outcomes.
No-reflow, in which insufficient myocardial perfusion is present even though the coronary artery appears patent, was the primary outcome, and the proportion of patients experiencing this event was exactly the same (14.4%) in the colchicine and placebo groups, reported Yaser Jenab, MD, at CRT 2021 sponsored by MedStar Heart & Vascular Institute.
The hypothesis that colchicine would offer benefit in this setting was largely based on the Colchicine Cardiovascular Outcomes Trial (COLCOT). In that study, colchicine was associated with a 23% reduction in risk for major adverse cardiovascular events (MACE) relative to placebo when administered within 30 days after a myocardial infarction (hazard ratio, 0.77; P = .02).
The benefit in that trial was attributed to an anti-inflammatory effect, according to Dr. Jenab, associate professor of cardiology at Tehran (Iran) Heart Center. In particular as it relates to vascular disease, he cited experimental studies associating colchicine with a reduction in neutrophil activation and adherence to vascular endothelium.
The rationale for a preprocedural approach to colchicine was supplied by a subsequent time-to-treatment COLCOT analysis. In this study, MACE risk reduction for colchicine climbed to 48% (HR 0.52) for those treated within 3 days of the MI but largely disappeared (HR 0.96) if treatment was started at least 8 days post MI.
PodCAST-PCI trial
In the preprocedural study, called the PodCAST-PCI trial, 321 acute STEMI patients were randomized. Patients received a 1-mg dose of oral colchicine or placebo at the time PCI was scheduled. Another dose of colchicine (0.5 mg) or placebo was administered 1 hour after the procedure.
Of secondary outcomes, which included MACE at 1 month and 1 year, ST-segment resolution at 1 month, and change in inflammatory markers at 1 month, none were significant. Few even trended for significance.
For MACE, which included cardiac death, stroke, nonfatal MI, new hospitalization due to heart failure, or target vessel revascularization, the rates were lower in the colchicine group at 1 month (4.3% vs. 7.5%) and 1 year (9.3% vs. 11.2%), but neither approached significance.
For ST-segment resolution, the proportions were generally comparable among the colchicine and placebo groups, respectively, for the proportion below 50% (18.6% vs. 23.1%), between 50% and 70% (16.8% vs. 15.6%), and above 70% (64.6% vs. 61.3%).
The average troponin levels were nonsignificantly lower at 6 hours (1,847 vs. 2,883 ng/mL) in the colchicine group but higher at 48 hours (1,197 vs. 1,147 ng/mL). The average C-reactive protein (CRP) levels at 48 hours were nonsignificantly lower on colchicine (176.5 vs. 244.5 mg/L).
There were no significant differences in postprocedural perfusion, as measured with TIMI blood flow, or in the rate of stent thrombosis, which occurred in roughly 3% of each group of patients.
The small sample size was one limitation of this study, Dr. Jenab acknowledged. For this and other reasons, he cautioned that these data are not definitive and do not preclude a benefit on clinical outcomes in a study with a larger size, a different design, or different dosing.
Timing might be the issue
However, even if colchicine has a potential benefit in this setting, timing might be a major obstacle, according to Binata Shah, MD, associate director of research for the Cardiac Catheterization Laboratory at New York University.
“We have learned from our rheumatology colleagues that peak plasma levels of colchicine are not achieved for at least 1 hour after the full loading dose,” Dr. Shah said. “With us moving so quickly in a primary PCI setting, it is hard to imagine that colchicine would have had time to really kick in and exert its anti-inflammatory effect.”
Indeed, the problem might be worse than reaching the peak plasma level.
“Even though peak plasma levels occur as early as 1 hour after a full loading dose, we see that it takes about 24 hours to really see the effects translate downstream into more systemic inflammatory markers such as CRP and interleukin-6,” she added. If lowering these signals of inflammation is predictive of benefit, than this might be the biggest obstacle to benefit from colchicine in an urgent treatment setting.
Dr. Jenab and Dr. Shah reported no potential conflicts of interest.
In a placebo-controlled randomized trial, a preprocedural dose of colchicine administered immediately before percutaneous coronary intervention (PCI) for an acute ST-segment elevated myocardial infarction (STEMI) did not reduce the no-reflow phenomenon or improve outcomes.
No-reflow, in which insufficient myocardial perfusion is present even though the coronary artery appears patent, was the primary outcome, and the proportion of patients experiencing this event was exactly the same (14.4%) in the colchicine and placebo groups, reported Yaser Jenab, MD, at CRT 2021 sponsored by MedStar Heart & Vascular Institute.
The hypothesis that colchicine would offer benefit in this setting was largely based on the Colchicine Cardiovascular Outcomes Trial (COLCOT). In that study, colchicine was associated with a 23% reduction in risk for major adverse cardiovascular events (MACE) relative to placebo when administered within 30 days after a myocardial infarction (hazard ratio, 0.77; P = .02).
The benefit in that trial was attributed to an anti-inflammatory effect, according to Dr. Jenab, associate professor of cardiology at Tehran (Iran) Heart Center. In particular as it relates to vascular disease, he cited experimental studies associating colchicine with a reduction in neutrophil activation and adherence to vascular endothelium.
The rationale for a preprocedural approach to colchicine was supplied by a subsequent time-to-treatment COLCOT analysis. In this study, MACE risk reduction for colchicine climbed to 48% (HR 0.52) for those treated within 3 days of the MI but largely disappeared (HR 0.96) if treatment was started at least 8 days post MI.
PodCAST-PCI trial
In the preprocedural study, called the PodCAST-PCI trial, 321 acute STEMI patients were randomized. Patients received a 1-mg dose of oral colchicine or placebo at the time PCI was scheduled. Another dose of colchicine (0.5 mg) or placebo was administered 1 hour after the procedure.
Of secondary outcomes, which included MACE at 1 month and 1 year, ST-segment resolution at 1 month, and change in inflammatory markers at 1 month, none were significant. Few even trended for significance.
For MACE, which included cardiac death, stroke, nonfatal MI, new hospitalization due to heart failure, or target vessel revascularization, the rates were lower in the colchicine group at 1 month (4.3% vs. 7.5%) and 1 year (9.3% vs. 11.2%), but neither approached significance.
For ST-segment resolution, the proportions were generally comparable among the colchicine and placebo groups, respectively, for the proportion below 50% (18.6% vs. 23.1%), between 50% and 70% (16.8% vs. 15.6%), and above 70% (64.6% vs. 61.3%).
The average troponin levels were nonsignificantly lower at 6 hours (1,847 vs. 2,883 ng/mL) in the colchicine group but higher at 48 hours (1,197 vs. 1,147 ng/mL). The average C-reactive protein (CRP) levels at 48 hours were nonsignificantly lower on colchicine (176.5 vs. 244.5 mg/L).
There were no significant differences in postprocedural perfusion, as measured with TIMI blood flow, or in the rate of stent thrombosis, which occurred in roughly 3% of each group of patients.
The small sample size was one limitation of this study, Dr. Jenab acknowledged. For this and other reasons, he cautioned that these data are not definitive and do not preclude a benefit on clinical outcomes in a study with a larger size, a different design, or different dosing.
Timing might be the issue
However, even if colchicine has a potential benefit in this setting, timing might be a major obstacle, according to Binata Shah, MD, associate director of research for the Cardiac Catheterization Laboratory at New York University.
“We have learned from our rheumatology colleagues that peak plasma levels of colchicine are not achieved for at least 1 hour after the full loading dose,” Dr. Shah said. “With us moving so quickly in a primary PCI setting, it is hard to imagine that colchicine would have had time to really kick in and exert its anti-inflammatory effect.”
Indeed, the problem might be worse than reaching the peak plasma level.
“Even though peak plasma levels occur as early as 1 hour after a full loading dose, we see that it takes about 24 hours to really see the effects translate downstream into more systemic inflammatory markers such as CRP and interleukin-6,” she added. If lowering these signals of inflammation is predictive of benefit, than this might be the biggest obstacle to benefit from colchicine in an urgent treatment setting.
Dr. Jenab and Dr. Shah reported no potential conflicts of interest.
In a placebo-controlled randomized trial, a preprocedural dose of colchicine administered immediately before percutaneous coronary intervention (PCI) for an acute ST-segment elevated myocardial infarction (STEMI) did not reduce the no-reflow phenomenon or improve outcomes.
No-reflow, in which insufficient myocardial perfusion is present even though the coronary artery appears patent, was the primary outcome, and the proportion of patients experiencing this event was exactly the same (14.4%) in the colchicine and placebo groups, reported Yaser Jenab, MD, at CRT 2021 sponsored by MedStar Heart & Vascular Institute.
The hypothesis that colchicine would offer benefit in this setting was largely based on the Colchicine Cardiovascular Outcomes Trial (COLCOT). In that study, colchicine was associated with a 23% reduction in risk for major adverse cardiovascular events (MACE) relative to placebo when administered within 30 days after a myocardial infarction (hazard ratio, 0.77; P = .02).
The benefit in that trial was attributed to an anti-inflammatory effect, according to Dr. Jenab, associate professor of cardiology at Tehran (Iran) Heart Center. In particular as it relates to vascular disease, he cited experimental studies associating colchicine with a reduction in neutrophil activation and adherence to vascular endothelium.
The rationale for a preprocedural approach to colchicine was supplied by a subsequent time-to-treatment COLCOT analysis. In this study, MACE risk reduction for colchicine climbed to 48% (HR 0.52) for those treated within 3 days of the MI but largely disappeared (HR 0.96) if treatment was started at least 8 days post MI.
PodCAST-PCI trial
In the preprocedural study, called the PodCAST-PCI trial, 321 acute STEMI patients were randomized. Patients received a 1-mg dose of oral colchicine or placebo at the time PCI was scheduled. Another dose of colchicine (0.5 mg) or placebo was administered 1 hour after the procedure.
Of secondary outcomes, which included MACE at 1 month and 1 year, ST-segment resolution at 1 month, and change in inflammatory markers at 1 month, none were significant. Few even trended for significance.
For MACE, which included cardiac death, stroke, nonfatal MI, new hospitalization due to heart failure, or target vessel revascularization, the rates were lower in the colchicine group at 1 month (4.3% vs. 7.5%) and 1 year (9.3% vs. 11.2%), but neither approached significance.
For ST-segment resolution, the proportions were generally comparable among the colchicine and placebo groups, respectively, for the proportion below 50% (18.6% vs. 23.1%), between 50% and 70% (16.8% vs. 15.6%), and above 70% (64.6% vs. 61.3%).
The average troponin levels were nonsignificantly lower at 6 hours (1,847 vs. 2,883 ng/mL) in the colchicine group but higher at 48 hours (1,197 vs. 1,147 ng/mL). The average C-reactive protein (CRP) levels at 48 hours were nonsignificantly lower on colchicine (176.5 vs. 244.5 mg/L).
There were no significant differences in postprocedural perfusion, as measured with TIMI blood flow, or in the rate of stent thrombosis, which occurred in roughly 3% of each group of patients.
The small sample size was one limitation of this study, Dr. Jenab acknowledged. For this and other reasons, he cautioned that these data are not definitive and do not preclude a benefit on clinical outcomes in a study with a larger size, a different design, or different dosing.
Timing might be the issue
However, even if colchicine has a potential benefit in this setting, timing might be a major obstacle, according to Binata Shah, MD, associate director of research for the Cardiac Catheterization Laboratory at New York University.
“We have learned from our rheumatology colleagues that peak plasma levels of colchicine are not achieved for at least 1 hour after the full loading dose,” Dr. Shah said. “With us moving so quickly in a primary PCI setting, it is hard to imagine that colchicine would have had time to really kick in and exert its anti-inflammatory effect.”
Indeed, the problem might be worse than reaching the peak plasma level.
“Even though peak plasma levels occur as early as 1 hour after a full loading dose, we see that it takes about 24 hours to really see the effects translate downstream into more systemic inflammatory markers such as CRP and interleukin-6,” she added. If lowering these signals of inflammation is predictive of benefit, than this might be the biggest obstacle to benefit from colchicine in an urgent treatment setting.
Dr. Jenab and Dr. Shah reported no potential conflicts of interest.
FROM CRT 2021
Target-lesion failure reduced 2 years after MI with biodegradable stent
For a primary composite target-lesion failure outcome, a biodegradable polymer sirolimus-eluting stent showed superiority at 2 years over a durable polymer everolimus-eluting stent in patients undergoing percutaneous intervention (PCI) for an ST-segment elevated acute myocardial infarction (STEMI), according to a late-breaking trial presentation at CRT 2021.
As in the previously reported 1-year results from the BIOSTEMI trial, the advantage of the biodegradable device was “driven by lower rates of target-lesion revascularization,” reported Thomas Pilgrim, MD, of the University of Bern (Switzerland).
Drug-eluting stents have already been established as superior to bare-metal stents, but the question asked in this study is whether the polymer that carries antiproliferative drugs, such as sirolimus or everolimus, improves lesion-based outcomes if it is biodegradable rather than durable, Dr. Pilgrim explained.
The composite primary outcome was target-lesion failure defined by cardiac death, target-lesion MI, or clinically indicated target-lesion revascularization.
After 2 years of follow-up, the rates of target-lesion failure were 5.1% and 8.1% for the biodegradable and durable polymer stents, respectively. This 0.58 rate ratio was statistically significant, favoring the biodegradable stent.
The investigator-initiated BIOSTEMI trial randomized 1,300 patients to one of two drug-eluting stents with ultrathin struts. One was the Orsiro stent that employs a biodegradable polymer to deliver sirolimus. The other was the Xience Prime/Xpedition that uses a durable polymer stent to deliver everolimus.
The strut thicknesses of the Orsiro stent are 60 mcm for stents of 3.0 mm in diameter or smaller and 80 mcm for those with a larger diameter. The strut thickness of the Xience stent is 81 mcm regardless of diameter.
“Patients with an acute myocardial infarction are at increased risk of stent-related events due to exacerbated inflammatory response and delayed arterial healing,” Dr. Pilgrim said. The theoretical advantages of polymer that biodegrades include “mitigation of the arterial injury, facilitation of endothelialization, and reduced intimal hyperplasia,” he explained at the meeting sponsored by MedStar Heart & Vascular Institute.
The rates of cardiac death (2.9% vs. 3.2%) and target-vessel MI (2.9% vs. 3.2%) were lower for the biodegradable polymer stent, but not significantly. However, the rates of target-vessel revascularization at 2 years were 2.5% versus 5.1%. The associated rate ratio of 0.52 favoring the biodegradable stent was significant.
Similar results favoring the biodegradable polymer stent were observed at 1 year, but those earlier results factored in historical data from the BIOSCIENCE trial, using a Bayesian analysis, to improve the power of the comparison. In this 2-year analysis, the superiority of the biodegradable polymer stent to the durable polymer stent remained statistically significant even when excluding those historical controls.
The advantage of the biodegradable polymer stent was confined to “device-oriented” outcomes, according to Dr. Pilgrim. When compared for important patient-oriented outcomes at 2 years, there were no significant differences. Rather, several were numerically more common, including death (4.2% vs. 3.8%) and MI (3.7% vs. 3.1%) in those who were randomized to the biodegradable polymer stent.
But these types of clinical outcomes are not necessarily related to stent assignment because “up to one-half of all events over the 2 years of follow-up were unrelated to the stent implanted,” Dr. Pilgrim said. He noted that high rates of events unrelated to the implanted stent have also been seen in follow-up of other comparative stent trials.
The superiority of the biodegradable stent is noteworthy. Although Dr. Pilgrim described the BIOSTEMI trial as “the first head-to-head comparison of two new-generation drug-eluting stents in patients undergoing a primary percutaneous intervention for acute myocardial infarction,” there have been several studies comparing stents for other indications. Significant differences have been uncommon.
“Over the last 10 years, we have seen a number of noninferiority stent trials, but only now are we seeing some superiority differences. This is a move in the right direction,” commented Sripal Bangalore, MD, director of the cardiovascular outcomes group, New York University.
However, he, like others, questioned whether the difference in outcomes in this trial could be fully attributed to the type of polymer. He noted that all stents could be characterized by multiple small and large differences in design and composition. Any specific characteristic, such as biodegradable polymer, might be an important contributor but not an isolated factor in the outcomes observed.
On the day that the 2-year results of the BIOSTEMI trial were presented at the CRT 2021 meeting they were simultaneously published in JACC: Cardiovascular Interventions.
Dr. Pilgrim reports financial relationships with several companies that make stent devices, including Biotronik and Boston Scientific. Dr. Bangalore reports no potential conflicts of interest.
For a primary composite target-lesion failure outcome, a biodegradable polymer sirolimus-eluting stent showed superiority at 2 years over a durable polymer everolimus-eluting stent in patients undergoing percutaneous intervention (PCI) for an ST-segment elevated acute myocardial infarction (STEMI), according to a late-breaking trial presentation at CRT 2021.
As in the previously reported 1-year results from the BIOSTEMI trial, the advantage of the biodegradable device was “driven by lower rates of target-lesion revascularization,” reported Thomas Pilgrim, MD, of the University of Bern (Switzerland).
Drug-eluting stents have already been established as superior to bare-metal stents, but the question asked in this study is whether the polymer that carries antiproliferative drugs, such as sirolimus or everolimus, improves lesion-based outcomes if it is biodegradable rather than durable, Dr. Pilgrim explained.
The composite primary outcome was target-lesion failure defined by cardiac death, target-lesion MI, or clinically indicated target-lesion revascularization.
After 2 years of follow-up, the rates of target-lesion failure were 5.1% and 8.1% for the biodegradable and durable polymer stents, respectively. This 0.58 rate ratio was statistically significant, favoring the biodegradable stent.
The investigator-initiated BIOSTEMI trial randomized 1,300 patients to one of two drug-eluting stents with ultrathin struts. One was the Orsiro stent that employs a biodegradable polymer to deliver sirolimus. The other was the Xience Prime/Xpedition that uses a durable polymer stent to deliver everolimus.
The strut thicknesses of the Orsiro stent are 60 mcm for stents of 3.0 mm in diameter or smaller and 80 mcm for those with a larger diameter. The strut thickness of the Xience stent is 81 mcm regardless of diameter.
“Patients with an acute myocardial infarction are at increased risk of stent-related events due to exacerbated inflammatory response and delayed arterial healing,” Dr. Pilgrim said. The theoretical advantages of polymer that biodegrades include “mitigation of the arterial injury, facilitation of endothelialization, and reduced intimal hyperplasia,” he explained at the meeting sponsored by MedStar Heart & Vascular Institute.
The rates of cardiac death (2.9% vs. 3.2%) and target-vessel MI (2.9% vs. 3.2%) were lower for the biodegradable polymer stent, but not significantly. However, the rates of target-vessel revascularization at 2 years were 2.5% versus 5.1%. The associated rate ratio of 0.52 favoring the biodegradable stent was significant.
Similar results favoring the biodegradable polymer stent were observed at 1 year, but those earlier results factored in historical data from the BIOSCIENCE trial, using a Bayesian analysis, to improve the power of the comparison. In this 2-year analysis, the superiority of the biodegradable polymer stent to the durable polymer stent remained statistically significant even when excluding those historical controls.
The advantage of the biodegradable polymer stent was confined to “device-oriented” outcomes, according to Dr. Pilgrim. When compared for important patient-oriented outcomes at 2 years, there were no significant differences. Rather, several were numerically more common, including death (4.2% vs. 3.8%) and MI (3.7% vs. 3.1%) in those who were randomized to the biodegradable polymer stent.
But these types of clinical outcomes are not necessarily related to stent assignment because “up to one-half of all events over the 2 years of follow-up were unrelated to the stent implanted,” Dr. Pilgrim said. He noted that high rates of events unrelated to the implanted stent have also been seen in follow-up of other comparative stent trials.
The superiority of the biodegradable stent is noteworthy. Although Dr. Pilgrim described the BIOSTEMI trial as “the first head-to-head comparison of two new-generation drug-eluting stents in patients undergoing a primary percutaneous intervention for acute myocardial infarction,” there have been several studies comparing stents for other indications. Significant differences have been uncommon.
“Over the last 10 years, we have seen a number of noninferiority stent trials, but only now are we seeing some superiority differences. This is a move in the right direction,” commented Sripal Bangalore, MD, director of the cardiovascular outcomes group, New York University.
However, he, like others, questioned whether the difference in outcomes in this trial could be fully attributed to the type of polymer. He noted that all stents could be characterized by multiple small and large differences in design and composition. Any specific characteristic, such as biodegradable polymer, might be an important contributor but not an isolated factor in the outcomes observed.
On the day that the 2-year results of the BIOSTEMI trial were presented at the CRT 2021 meeting they were simultaneously published in JACC: Cardiovascular Interventions.
Dr. Pilgrim reports financial relationships with several companies that make stent devices, including Biotronik and Boston Scientific. Dr. Bangalore reports no potential conflicts of interest.
For a primary composite target-lesion failure outcome, a biodegradable polymer sirolimus-eluting stent showed superiority at 2 years over a durable polymer everolimus-eluting stent in patients undergoing percutaneous intervention (PCI) for an ST-segment elevated acute myocardial infarction (STEMI), according to a late-breaking trial presentation at CRT 2021.
As in the previously reported 1-year results from the BIOSTEMI trial, the advantage of the biodegradable device was “driven by lower rates of target-lesion revascularization,” reported Thomas Pilgrim, MD, of the University of Bern (Switzerland).
Drug-eluting stents have already been established as superior to bare-metal stents, but the question asked in this study is whether the polymer that carries antiproliferative drugs, such as sirolimus or everolimus, improves lesion-based outcomes if it is biodegradable rather than durable, Dr. Pilgrim explained.
The composite primary outcome was target-lesion failure defined by cardiac death, target-lesion MI, or clinically indicated target-lesion revascularization.
After 2 years of follow-up, the rates of target-lesion failure were 5.1% and 8.1% for the biodegradable and durable polymer stents, respectively. This 0.58 rate ratio was statistically significant, favoring the biodegradable stent.
The investigator-initiated BIOSTEMI trial randomized 1,300 patients to one of two drug-eluting stents with ultrathin struts. One was the Orsiro stent that employs a biodegradable polymer to deliver sirolimus. The other was the Xience Prime/Xpedition that uses a durable polymer stent to deliver everolimus.
The strut thicknesses of the Orsiro stent are 60 mcm for stents of 3.0 mm in diameter or smaller and 80 mcm for those with a larger diameter. The strut thickness of the Xience stent is 81 mcm regardless of diameter.
“Patients with an acute myocardial infarction are at increased risk of stent-related events due to exacerbated inflammatory response and delayed arterial healing,” Dr. Pilgrim said. The theoretical advantages of polymer that biodegrades include “mitigation of the arterial injury, facilitation of endothelialization, and reduced intimal hyperplasia,” he explained at the meeting sponsored by MedStar Heart & Vascular Institute.
The rates of cardiac death (2.9% vs. 3.2%) and target-vessel MI (2.9% vs. 3.2%) were lower for the biodegradable polymer stent, but not significantly. However, the rates of target-vessel revascularization at 2 years were 2.5% versus 5.1%. The associated rate ratio of 0.52 favoring the biodegradable stent was significant.
Similar results favoring the biodegradable polymer stent were observed at 1 year, but those earlier results factored in historical data from the BIOSCIENCE trial, using a Bayesian analysis, to improve the power of the comparison. In this 2-year analysis, the superiority of the biodegradable polymer stent to the durable polymer stent remained statistically significant even when excluding those historical controls.
The advantage of the biodegradable polymer stent was confined to “device-oriented” outcomes, according to Dr. Pilgrim. When compared for important patient-oriented outcomes at 2 years, there were no significant differences. Rather, several were numerically more common, including death (4.2% vs. 3.8%) and MI (3.7% vs. 3.1%) in those who were randomized to the biodegradable polymer stent.
But these types of clinical outcomes are not necessarily related to stent assignment because “up to one-half of all events over the 2 years of follow-up were unrelated to the stent implanted,” Dr. Pilgrim said. He noted that high rates of events unrelated to the implanted stent have also been seen in follow-up of other comparative stent trials.
The superiority of the biodegradable stent is noteworthy. Although Dr. Pilgrim described the BIOSTEMI trial as “the first head-to-head comparison of two new-generation drug-eluting stents in patients undergoing a primary percutaneous intervention for acute myocardial infarction,” there have been several studies comparing stents for other indications. Significant differences have been uncommon.
“Over the last 10 years, we have seen a number of noninferiority stent trials, but only now are we seeing some superiority differences. This is a move in the right direction,” commented Sripal Bangalore, MD, director of the cardiovascular outcomes group, New York University.
However, he, like others, questioned whether the difference in outcomes in this trial could be fully attributed to the type of polymer. He noted that all stents could be characterized by multiple small and large differences in design and composition. Any specific characteristic, such as biodegradable polymer, might be an important contributor but not an isolated factor in the outcomes observed.
On the day that the 2-year results of the BIOSTEMI trial were presented at the CRT 2021 meeting they were simultaneously published in JACC: Cardiovascular Interventions.
Dr. Pilgrim reports financial relationships with several companies that make stent devices, including Biotronik and Boston Scientific. Dr. Bangalore reports no potential conflicts of interest.
FROM CRT 2021
Eating fish tied to fewer CVD events in high-risk people
People with cardiovascular disease who regularly ate fish had significantly fewer major CVD events and there were fewer total deaths, compared with similar individuals who didn’t eat fish, but there was no beneficial link from eating fish among the general population in prospective data collected from more than 191,000 people from 58 countries.
Despite the neutral finding among people without CVD, the finding that eating fish was associated with significant benefit for those with CVD or who were at high risk for CVD confirms the public health importance of regular fish or fish oil consumption, said one expert.
A little over a quarter of those included in the new study had a history of CVD or were at high risk for CVD. In this subgroup of more than 51,000 people, those who consumed on average at least two servings of fish weekly (at least 175 g, or about 6.2 ounces per week) had a significant 16% lower rate of major CVD events during a median follow-up of about 7.5 years.
The rate of all-cause death was a significant 18% lower among people who ate two or more fish portions weekly, compared with those who didn’t, Deepa Mohan, PhD, and associates wrote in their report in JAMA Internal Medicine.
The researchers saw no additional benefit when people regularly ate greater amounts of fish.
“There is a significant protective benefit of fish consumption in people with cardiovascular disease,” said Andrew Mente, PhD, a senior investigator on the study and an epidemiologist at McMaster University, Hamilton, Ont..
“This study has important implications for guidelines on fish intake globally. It indicates that increasing fish consumption and particularly oily fish in vascular patients may produce a modest cardiovascular benefit,” he said in a statement released by McMaster.
‘A large body of evidence’ for CVD benefit
The neutral finding of no significant benefit (as well as no harm) regarding either CVD events or total mortality among people without CVD “does not alter the large body of prior observational evidence supporting the cardiac benefits of fish intake in general populations,” noted Dariush Mozaffarian, MD, DrPH, in a commentary that accompanies the report by Dr. Mohan and colleagues.
Although the new analysis failed to show a significant association between regular fish consumption and fewer CVD events for people without established CVD or CVD risk, “based on the cumulative evidence from prospective observational studies, randomized clinical trials, and mechanistic and experimental studies, modest fish consumption appears to have some cardiac benefits,” he added.
“Adults should aim to consume about two servings of fish per week, and larger benefits may accrue from nonfried oily (dark meat) fish,” wrote Dr. Mozaffarian, a professor of medicine and nutrition at Tufts University, Boston.
Oily, dark fishes include salmon, tuna steak, mackerel, herring, and sardines. Species such as these contain the highest levels of long-chain omega-3 fatty acids, eicosapentaenoic acid, and docosapentaenoic acid; these nutrients likely underlie the CVD benefits from fish, Dr. Mozaffarian said in an interview with JAMA Internal Medicine that accompanied his commentary. (Dr. Mente also participated.)
“Fish oil lowers heart rate, blood pressure, and triglycerides (at high dosages), increases adiponectin, improves endothelial function, and in some studies improves oxygen consumption in myocardium. If there is benefit from fish it’s from the omega 3s, and all in all the evidence supports this,” but because the evidence is primarily observational, it can only show linkage and cannot prove causation, he explained.
Given the potential benefit and limited risk, “I think everyone should aim to eat two servings of fish each week, preferentially oily fish. That’s very solid,” said Dr. Mozaffarian, who is also a cardiologist and dean of the Tufts Friedman School of Nutrition Science.
The investigators did not have adequate data to compare the associations between outcomes and a diet with oily fish versus less oily fish.
OTC fish oil capsules are ‘very reasonable’
For people who either can’t consume two fish meals a week or want to ensure their omega 3 intake is adequate, “it’s very reasonable for the average person to take one OTC [over-the-counter] fish oil capsule a day,” Dr. Mozaffarian added.
He acknowledged that several studies of fish oil supplements failed to show benefit, but several others have. “It’s a confusing field, but the evidence supports benefit from omega 3s,” he concluded.
He discounted the new finding that only people with established CVD or who are at high-risk benefit. “I’m not sure we should make too much of this, because many prior studies showed a lower CVD risk in fish-eating people without prevalent CVD,” he said. The new study “provides important information given its worldwide breadth.”
The new report used data regarding 191,558 people enrolled prospectively in any of four studies. The average age of the participants was 54 years, and 52% were women.
During follow-up, death from any cause occurred in 6% of those without CVD or CVD risk and in 13% of those with these factors. Major CVD events occurred in 5% and 17% of these two subgroups, respectively. To calculate the relative risks between those who ate fish and those who did not, the investigators used standard multivariate adjustment for potential confounders and adjusted for several dietary variables, Dr. Mente said.
Dr. Mohan and Dr. Mente disclosed no relevant financial relationships. Dr. Mozaffarian has received personal fees from Acasti Pharma, Amarin, America’s Test Kitchen, Barilla, Danone, GEOD, and Motif Food Works, and he has been an adviser to numerous companies.
A version of this article first appeared on Medscape.com.
People with cardiovascular disease who regularly ate fish had significantly fewer major CVD events and there were fewer total deaths, compared with similar individuals who didn’t eat fish, but there was no beneficial link from eating fish among the general population in prospective data collected from more than 191,000 people from 58 countries.
Despite the neutral finding among people without CVD, the finding that eating fish was associated with significant benefit for those with CVD or who were at high risk for CVD confirms the public health importance of regular fish or fish oil consumption, said one expert.
A little over a quarter of those included in the new study had a history of CVD or were at high risk for CVD. In this subgroup of more than 51,000 people, those who consumed on average at least two servings of fish weekly (at least 175 g, or about 6.2 ounces per week) had a significant 16% lower rate of major CVD events during a median follow-up of about 7.5 years.
The rate of all-cause death was a significant 18% lower among people who ate two or more fish portions weekly, compared with those who didn’t, Deepa Mohan, PhD, and associates wrote in their report in JAMA Internal Medicine.
The researchers saw no additional benefit when people regularly ate greater amounts of fish.
“There is a significant protective benefit of fish consumption in people with cardiovascular disease,” said Andrew Mente, PhD, a senior investigator on the study and an epidemiologist at McMaster University, Hamilton, Ont..
“This study has important implications for guidelines on fish intake globally. It indicates that increasing fish consumption and particularly oily fish in vascular patients may produce a modest cardiovascular benefit,” he said in a statement released by McMaster.
‘A large body of evidence’ for CVD benefit
The neutral finding of no significant benefit (as well as no harm) regarding either CVD events or total mortality among people without CVD “does not alter the large body of prior observational evidence supporting the cardiac benefits of fish intake in general populations,” noted Dariush Mozaffarian, MD, DrPH, in a commentary that accompanies the report by Dr. Mohan and colleagues.
Although the new analysis failed to show a significant association between regular fish consumption and fewer CVD events for people without established CVD or CVD risk, “based on the cumulative evidence from prospective observational studies, randomized clinical trials, and mechanistic and experimental studies, modest fish consumption appears to have some cardiac benefits,” he added.
“Adults should aim to consume about two servings of fish per week, and larger benefits may accrue from nonfried oily (dark meat) fish,” wrote Dr. Mozaffarian, a professor of medicine and nutrition at Tufts University, Boston.
Oily, dark fishes include salmon, tuna steak, mackerel, herring, and sardines. Species such as these contain the highest levels of long-chain omega-3 fatty acids, eicosapentaenoic acid, and docosapentaenoic acid; these nutrients likely underlie the CVD benefits from fish, Dr. Mozaffarian said in an interview with JAMA Internal Medicine that accompanied his commentary. (Dr. Mente also participated.)
“Fish oil lowers heart rate, blood pressure, and triglycerides (at high dosages), increases adiponectin, improves endothelial function, and in some studies improves oxygen consumption in myocardium. If there is benefit from fish it’s from the omega 3s, and all in all the evidence supports this,” but because the evidence is primarily observational, it can only show linkage and cannot prove causation, he explained.
Given the potential benefit and limited risk, “I think everyone should aim to eat two servings of fish each week, preferentially oily fish. That’s very solid,” said Dr. Mozaffarian, who is also a cardiologist and dean of the Tufts Friedman School of Nutrition Science.
The investigators did not have adequate data to compare the associations between outcomes and a diet with oily fish versus less oily fish.
OTC fish oil capsules are ‘very reasonable’
For people who either can’t consume two fish meals a week or want to ensure their omega 3 intake is adequate, “it’s very reasonable for the average person to take one OTC [over-the-counter] fish oil capsule a day,” Dr. Mozaffarian added.
He acknowledged that several studies of fish oil supplements failed to show benefit, but several others have. “It’s a confusing field, but the evidence supports benefit from omega 3s,” he concluded.
He discounted the new finding that only people with established CVD or who are at high-risk benefit. “I’m not sure we should make too much of this, because many prior studies showed a lower CVD risk in fish-eating people without prevalent CVD,” he said. The new study “provides important information given its worldwide breadth.”
The new report used data regarding 191,558 people enrolled prospectively in any of four studies. The average age of the participants was 54 years, and 52% were women.
During follow-up, death from any cause occurred in 6% of those without CVD or CVD risk and in 13% of those with these factors. Major CVD events occurred in 5% and 17% of these two subgroups, respectively. To calculate the relative risks between those who ate fish and those who did not, the investigators used standard multivariate adjustment for potential confounders and adjusted for several dietary variables, Dr. Mente said.
Dr. Mohan and Dr. Mente disclosed no relevant financial relationships. Dr. Mozaffarian has received personal fees from Acasti Pharma, Amarin, America’s Test Kitchen, Barilla, Danone, GEOD, and Motif Food Works, and he has been an adviser to numerous companies.
A version of this article first appeared on Medscape.com.
People with cardiovascular disease who regularly ate fish had significantly fewer major CVD events and there were fewer total deaths, compared with similar individuals who didn’t eat fish, but there was no beneficial link from eating fish among the general population in prospective data collected from more than 191,000 people from 58 countries.
Despite the neutral finding among people without CVD, the finding that eating fish was associated with significant benefit for those with CVD or who were at high risk for CVD confirms the public health importance of regular fish or fish oil consumption, said one expert.
A little over a quarter of those included in the new study had a history of CVD or were at high risk for CVD. In this subgroup of more than 51,000 people, those who consumed on average at least two servings of fish weekly (at least 175 g, or about 6.2 ounces per week) had a significant 16% lower rate of major CVD events during a median follow-up of about 7.5 years.
The rate of all-cause death was a significant 18% lower among people who ate two or more fish portions weekly, compared with those who didn’t, Deepa Mohan, PhD, and associates wrote in their report in JAMA Internal Medicine.
The researchers saw no additional benefit when people regularly ate greater amounts of fish.
“There is a significant protective benefit of fish consumption in people with cardiovascular disease,” said Andrew Mente, PhD, a senior investigator on the study and an epidemiologist at McMaster University, Hamilton, Ont..
“This study has important implications for guidelines on fish intake globally. It indicates that increasing fish consumption and particularly oily fish in vascular patients may produce a modest cardiovascular benefit,” he said in a statement released by McMaster.
‘A large body of evidence’ for CVD benefit
The neutral finding of no significant benefit (as well as no harm) regarding either CVD events or total mortality among people without CVD “does not alter the large body of prior observational evidence supporting the cardiac benefits of fish intake in general populations,” noted Dariush Mozaffarian, MD, DrPH, in a commentary that accompanies the report by Dr. Mohan and colleagues.
Although the new analysis failed to show a significant association between regular fish consumption and fewer CVD events for people without established CVD or CVD risk, “based on the cumulative evidence from prospective observational studies, randomized clinical trials, and mechanistic and experimental studies, modest fish consumption appears to have some cardiac benefits,” he added.
“Adults should aim to consume about two servings of fish per week, and larger benefits may accrue from nonfried oily (dark meat) fish,” wrote Dr. Mozaffarian, a professor of medicine and nutrition at Tufts University, Boston.
Oily, dark fishes include salmon, tuna steak, mackerel, herring, and sardines. Species such as these contain the highest levels of long-chain omega-3 fatty acids, eicosapentaenoic acid, and docosapentaenoic acid; these nutrients likely underlie the CVD benefits from fish, Dr. Mozaffarian said in an interview with JAMA Internal Medicine that accompanied his commentary. (Dr. Mente also participated.)
“Fish oil lowers heart rate, blood pressure, and triglycerides (at high dosages), increases adiponectin, improves endothelial function, and in some studies improves oxygen consumption in myocardium. If there is benefit from fish it’s from the omega 3s, and all in all the evidence supports this,” but because the evidence is primarily observational, it can only show linkage and cannot prove causation, he explained.
Given the potential benefit and limited risk, “I think everyone should aim to eat two servings of fish each week, preferentially oily fish. That’s very solid,” said Dr. Mozaffarian, who is also a cardiologist and dean of the Tufts Friedman School of Nutrition Science.
The investigators did not have adequate data to compare the associations between outcomes and a diet with oily fish versus less oily fish.
OTC fish oil capsules are ‘very reasonable’
For people who either can’t consume two fish meals a week or want to ensure their omega 3 intake is adequate, “it’s very reasonable for the average person to take one OTC [over-the-counter] fish oil capsule a day,” Dr. Mozaffarian added.
He acknowledged that several studies of fish oil supplements failed to show benefit, but several others have. “It’s a confusing field, but the evidence supports benefit from omega 3s,” he concluded.
He discounted the new finding that only people with established CVD or who are at high-risk benefit. “I’m not sure we should make too much of this, because many prior studies showed a lower CVD risk in fish-eating people without prevalent CVD,” he said. The new study “provides important information given its worldwide breadth.”
The new report used data regarding 191,558 people enrolled prospectively in any of four studies. The average age of the participants was 54 years, and 52% were women.
During follow-up, death from any cause occurred in 6% of those without CVD or CVD risk and in 13% of those with these factors. Major CVD events occurred in 5% and 17% of these two subgroups, respectively. To calculate the relative risks between those who ate fish and those who did not, the investigators used standard multivariate adjustment for potential confounders and adjusted for several dietary variables, Dr. Mente said.
Dr. Mohan and Dr. Mente disclosed no relevant financial relationships. Dr. Mozaffarian has received personal fees from Acasti Pharma, Amarin, America’s Test Kitchen, Barilla, Danone, GEOD, and Motif Food Works, and he has been an adviser to numerous companies.
A version of this article first appeared on Medscape.com.
Myocardial injury seen on MRI in 54% of recovered COVID-19 patients
About half of 148 patients hospitalized with COVID-19 infection and elevated troponin levels had at least some evidence of myocardial injury on cardiac magnetic resonance (CMR) imaging 2 months later, a new study shows.
“Our results demonstrate that in this subset of patients surviving severe COVID-19 and with troponin elevation, ongoing localized myocardial inflammation, whilst less frequent than previously reported, remains present in a proportion of patients and may represent an emerging issue of clinical relevance,” wrote Marianna Fontana, MD, PhD, of University College London, and colleagues.
The cardiac abnormalities identified were classified as nonischemic (including “myocarditis-like” late gadolinium enhancement [LGE]) in 26% of the cohort; as related to ischemic heart disease (infarction or inducible ischemia) in 22%; and as dual pathology in 6%.
Left ventricular (LV) function was normal in 89% of the 148 patients. In the 17 patients (11%) with LV dysfunction, only four had an ejection fraction below 35%. Of the nine patients whose LV dysfunction was related to myocardial infarction, six had a known history of ischemic heart disease.
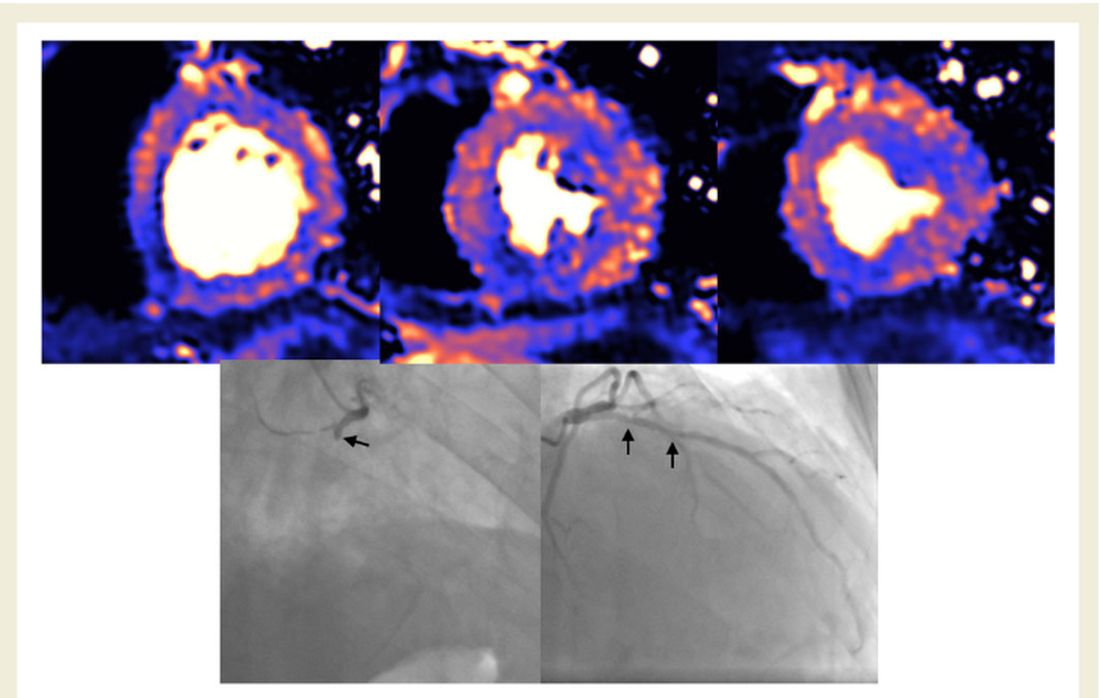
No patients with “myocarditis-pattern” LGE had regional wall motion abnormalities, and neither admission nor peak troponin values were predictive of the diagnosis of myocarditis.
The results were published online Feb. 18 in the European Heart Journal.
Glass half full
Taking a “glass half full” approach, co–senior author Graham D. Cole, MD, PhD, noted on Twitter that nearly half the patients had no major cardiac abnormalities on CMR just 2 months after a bout with troponin-positive COVID-19.
“We think this is important: Even in a group who had been very sick with raised troponin, it was common to find no evidence of heart damage,” said Dr. Cole, of the Royal Free London NHS Foundation Trust.
“We believe our data challenge the hypothesis that chronic inflammation, diffuse fibrosis, or long-term LV dysfunction is a dominant feature in those surviving COVID-19,” the investigators concluded in their report.
In an interview, Dr. Fontana explained further: “It has been reported in an early ‘pathfinder’ study that two-thirds of patients recovered from COVID-19 had CMR evidence of abnormal findings with a high incidence of elevated T1 and T2 in keeping with diffuse fibrosis and edema. Our findings with a larger, multicenter study and better controls show low rates of heart impairment and much less ongoing inflammation, which is reassuring.”
She also noted that the different patterns of injury suggest that different mechanisms are at play, including the possibility that “at least some of the found damage might have been preexisting, because people with heart damage are more likely to get severe disease.”
The investigators, including first author Tushar Kotecha, MBChB, PhD, of the Royal Free London NHS Foundation Trust, also noted that myocarditis-like injury was limited to three or fewer myocardial segments in 88% of cases with no associated ventricular dysfunction, and that biventricular function was no different than in those without myocarditis.
“We use the word ‘myocarditis-like’ but we don’t have histology,” Dr. Fontana said. “Our group actually suspects a lot of this will be microvascular clotting (microangiopathic thrombosis). This is exciting, as newer anticoagulation strategies – for example, those being tried in RECOVERY – may have benefit.”
Aloke V. Finn, MD, of the CVPath Institute in Gaithersburg, Md., wishes researchers would stop using the term myocarditis altogether to describe clinical or imaging findings in COVID-19.
“MRI can’t diagnose myocarditis. It is a specific diagnosis that requires, ideally, histology, as the investigators acknowledged,” Dr. Finn said in an interview.
His group at CVPath recently published data showing pathologic evidence of myocarditis after SARS-CoV-2 infection, as reported by theheart.org | Medscape Cardiology.
“As a clinician, when I think of myocarditis, I look at the echo and an LV gram, and I see if there is a wall motion abnormality and troponin elevation, but with normal coronary arteries. And if all that is there, then I think about myocarditis in my differential diagnosis,” he said. “But in most of these cases, as the authors rightly point out, most patients did not have what is necessary to really entertain a diagnosis of myocarditis.”
He agreed with Dr. Fontana’s suggestion that what the CMR might be picking up in these survivors is microthrombi, as his group saw in their recent autopsy study.
“It’s very possible these findings are concordant with the recent autopsy studies done by my group and others in terms of detecting the presence of microthrombi, but we don’t know this for certain because no one has ever studied this entity before in the clinic and we don’t really know how microthrombi might appear on CMR.”
Largest study to date
The 148 participants (mean age, 64 years; 70% male) in the largest study to date to investigate convalescing COVID-19 patients who had elevated troponins – something identified early in the pandemic as a risk factor for worse outcomes in COVID-19 – were treated at one of six hospitals in London.
Patients who had abnormal troponin levels were offered an MRI scan of the heart after discharge and were compared with those from a control group of patients who had not had COVID-19 and with 40 healthy volunteers.
Median length of stay was 9 days, and 32% of patients required ventilatory support in the intensive care unit.
Just over half the patients (57%) had hypertension, 7% had had a previous myocardial infarction, 34% had diabetes, 46% had hypercholesterolemia, and 24% were smokers. Mean body mass index was 28.5 kg/m2.
CMR follow-up was conducted a median of 68 days after confirmation of a COVID-19 diagnosis.
On Twitter, Dr. Cole noted that the findings are subject to both survivor bias and referral bias. “We didn’t scan frail patients where the clinician felt [CMR] was unlikely to inform management.”
The findings, said Dr. Fontana, “say nothing about what happens to people who are not hospitalized with COVID, or those who are hospitalized but without elevated troponin.”
What they do offer, particularly if replicated, is a way forward in identifying patients at higher or lower risk for long-term sequelae and inform strategies that could improve outcomes, she added.
A version of this article first appeared on Medscape.com.
About half of 148 patients hospitalized with COVID-19 infection and elevated troponin levels had at least some evidence of myocardial injury on cardiac magnetic resonance (CMR) imaging 2 months later, a new study shows.
“Our results demonstrate that in this subset of patients surviving severe COVID-19 and with troponin elevation, ongoing localized myocardial inflammation, whilst less frequent than previously reported, remains present in a proportion of patients and may represent an emerging issue of clinical relevance,” wrote Marianna Fontana, MD, PhD, of University College London, and colleagues.
The cardiac abnormalities identified were classified as nonischemic (including “myocarditis-like” late gadolinium enhancement [LGE]) in 26% of the cohort; as related to ischemic heart disease (infarction or inducible ischemia) in 22%; and as dual pathology in 6%.
Left ventricular (LV) function was normal in 89% of the 148 patients. In the 17 patients (11%) with LV dysfunction, only four had an ejection fraction below 35%. Of the nine patients whose LV dysfunction was related to myocardial infarction, six had a known history of ischemic heart disease.
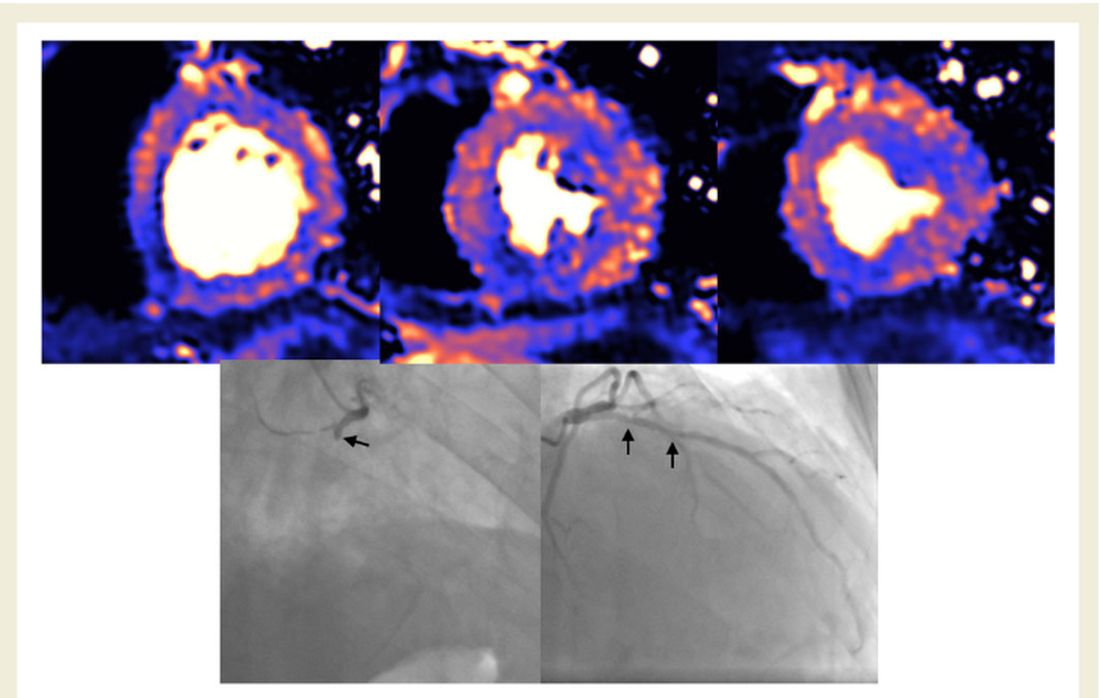
No patients with “myocarditis-pattern” LGE had regional wall motion abnormalities, and neither admission nor peak troponin values were predictive of the diagnosis of myocarditis.
The results were published online Feb. 18 in the European Heart Journal.
Glass half full
Taking a “glass half full” approach, co–senior author Graham D. Cole, MD, PhD, noted on Twitter that nearly half the patients had no major cardiac abnormalities on CMR just 2 months after a bout with troponin-positive COVID-19.
“We think this is important: Even in a group who had been very sick with raised troponin, it was common to find no evidence of heart damage,” said Dr. Cole, of the Royal Free London NHS Foundation Trust.
“We believe our data challenge the hypothesis that chronic inflammation, diffuse fibrosis, or long-term LV dysfunction is a dominant feature in those surviving COVID-19,” the investigators concluded in their report.
In an interview, Dr. Fontana explained further: “It has been reported in an early ‘pathfinder’ study that two-thirds of patients recovered from COVID-19 had CMR evidence of abnormal findings with a high incidence of elevated T1 and T2 in keeping with diffuse fibrosis and edema. Our findings with a larger, multicenter study and better controls show low rates of heart impairment and much less ongoing inflammation, which is reassuring.”
She also noted that the different patterns of injury suggest that different mechanisms are at play, including the possibility that “at least some of the found damage might have been preexisting, because people with heart damage are more likely to get severe disease.”
The investigators, including first author Tushar Kotecha, MBChB, PhD, of the Royal Free London NHS Foundation Trust, also noted that myocarditis-like injury was limited to three or fewer myocardial segments in 88% of cases with no associated ventricular dysfunction, and that biventricular function was no different than in those without myocarditis.
“We use the word ‘myocarditis-like’ but we don’t have histology,” Dr. Fontana said. “Our group actually suspects a lot of this will be microvascular clotting (microangiopathic thrombosis). This is exciting, as newer anticoagulation strategies – for example, those being tried in RECOVERY – may have benefit.”
Aloke V. Finn, MD, of the CVPath Institute in Gaithersburg, Md., wishes researchers would stop using the term myocarditis altogether to describe clinical or imaging findings in COVID-19.
“MRI can’t diagnose myocarditis. It is a specific diagnosis that requires, ideally, histology, as the investigators acknowledged,” Dr. Finn said in an interview.
His group at CVPath recently published data showing pathologic evidence of myocarditis after SARS-CoV-2 infection, as reported by theheart.org | Medscape Cardiology.
“As a clinician, when I think of myocarditis, I look at the echo and an LV gram, and I see if there is a wall motion abnormality and troponin elevation, but with normal coronary arteries. And if all that is there, then I think about myocarditis in my differential diagnosis,” he said. “But in most of these cases, as the authors rightly point out, most patients did not have what is necessary to really entertain a diagnosis of myocarditis.”
He agreed with Dr. Fontana’s suggestion that what the CMR might be picking up in these survivors is microthrombi, as his group saw in their recent autopsy study.
“It’s very possible these findings are concordant with the recent autopsy studies done by my group and others in terms of detecting the presence of microthrombi, but we don’t know this for certain because no one has ever studied this entity before in the clinic and we don’t really know how microthrombi might appear on CMR.”
Largest study to date
The 148 participants (mean age, 64 years; 70% male) in the largest study to date to investigate convalescing COVID-19 patients who had elevated troponins – something identified early in the pandemic as a risk factor for worse outcomes in COVID-19 – were treated at one of six hospitals in London.
Patients who had abnormal troponin levels were offered an MRI scan of the heart after discharge and were compared with those from a control group of patients who had not had COVID-19 and with 40 healthy volunteers.
Median length of stay was 9 days, and 32% of patients required ventilatory support in the intensive care unit.
Just over half the patients (57%) had hypertension, 7% had had a previous myocardial infarction, 34% had diabetes, 46% had hypercholesterolemia, and 24% were smokers. Mean body mass index was 28.5 kg/m2.
CMR follow-up was conducted a median of 68 days after confirmation of a COVID-19 diagnosis.
On Twitter, Dr. Cole noted that the findings are subject to both survivor bias and referral bias. “We didn’t scan frail patients where the clinician felt [CMR] was unlikely to inform management.”
The findings, said Dr. Fontana, “say nothing about what happens to people who are not hospitalized with COVID, or those who are hospitalized but without elevated troponin.”
What they do offer, particularly if replicated, is a way forward in identifying patients at higher or lower risk for long-term sequelae and inform strategies that could improve outcomes, she added.
A version of this article first appeared on Medscape.com.
About half of 148 patients hospitalized with COVID-19 infection and elevated troponin levels had at least some evidence of myocardial injury on cardiac magnetic resonance (CMR) imaging 2 months later, a new study shows.
“Our results demonstrate that in this subset of patients surviving severe COVID-19 and with troponin elevation, ongoing localized myocardial inflammation, whilst less frequent than previously reported, remains present in a proportion of patients and may represent an emerging issue of clinical relevance,” wrote Marianna Fontana, MD, PhD, of University College London, and colleagues.
The cardiac abnormalities identified were classified as nonischemic (including “myocarditis-like” late gadolinium enhancement [LGE]) in 26% of the cohort; as related to ischemic heart disease (infarction or inducible ischemia) in 22%; and as dual pathology in 6%.
Left ventricular (LV) function was normal in 89% of the 148 patients. In the 17 patients (11%) with LV dysfunction, only four had an ejection fraction below 35%. Of the nine patients whose LV dysfunction was related to myocardial infarction, six had a known history of ischemic heart disease.
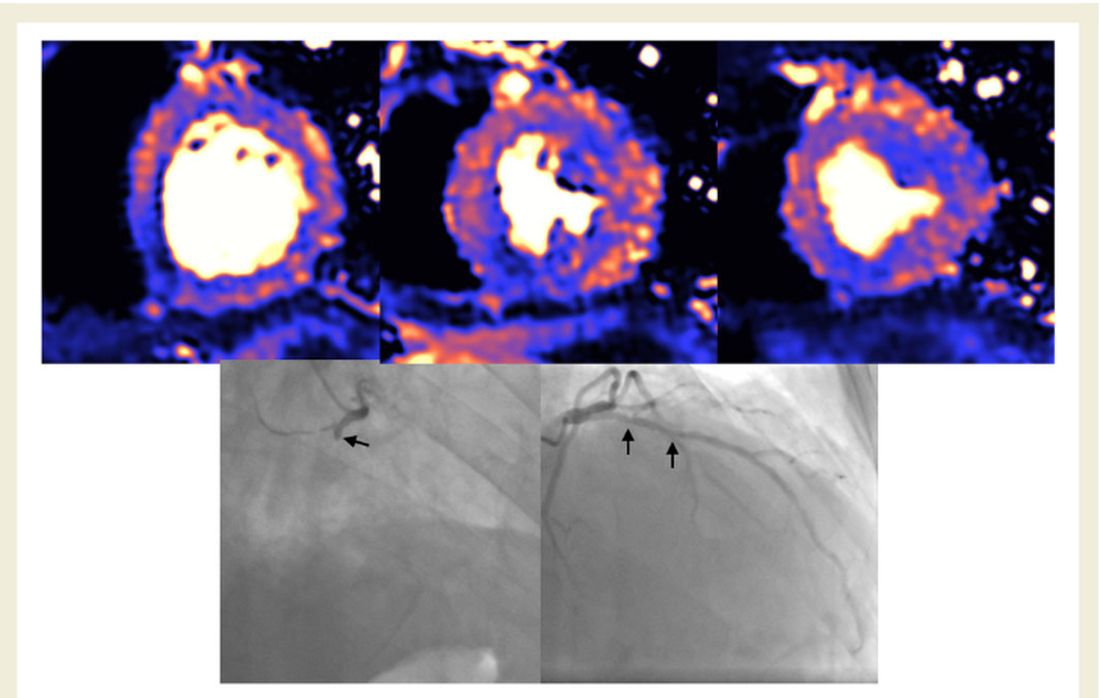
No patients with “myocarditis-pattern” LGE had regional wall motion abnormalities, and neither admission nor peak troponin values were predictive of the diagnosis of myocarditis.
The results were published online Feb. 18 in the European Heart Journal.
Glass half full
Taking a “glass half full” approach, co–senior author Graham D. Cole, MD, PhD, noted on Twitter that nearly half the patients had no major cardiac abnormalities on CMR just 2 months after a bout with troponin-positive COVID-19.
“We think this is important: Even in a group who had been very sick with raised troponin, it was common to find no evidence of heart damage,” said Dr. Cole, of the Royal Free London NHS Foundation Trust.
“We believe our data challenge the hypothesis that chronic inflammation, diffuse fibrosis, or long-term LV dysfunction is a dominant feature in those surviving COVID-19,” the investigators concluded in their report.
In an interview, Dr. Fontana explained further: “It has been reported in an early ‘pathfinder’ study that two-thirds of patients recovered from COVID-19 had CMR evidence of abnormal findings with a high incidence of elevated T1 and T2 in keeping with diffuse fibrosis and edema. Our findings with a larger, multicenter study and better controls show low rates of heart impairment and much less ongoing inflammation, which is reassuring.”
She also noted that the different patterns of injury suggest that different mechanisms are at play, including the possibility that “at least some of the found damage might have been preexisting, because people with heart damage are more likely to get severe disease.”
The investigators, including first author Tushar Kotecha, MBChB, PhD, of the Royal Free London NHS Foundation Trust, also noted that myocarditis-like injury was limited to three or fewer myocardial segments in 88% of cases with no associated ventricular dysfunction, and that biventricular function was no different than in those without myocarditis.
“We use the word ‘myocarditis-like’ but we don’t have histology,” Dr. Fontana said. “Our group actually suspects a lot of this will be microvascular clotting (microangiopathic thrombosis). This is exciting, as newer anticoagulation strategies – for example, those being tried in RECOVERY – may have benefit.”
Aloke V. Finn, MD, of the CVPath Institute in Gaithersburg, Md., wishes researchers would stop using the term myocarditis altogether to describe clinical or imaging findings in COVID-19.
“MRI can’t diagnose myocarditis. It is a specific diagnosis that requires, ideally, histology, as the investigators acknowledged,” Dr. Finn said in an interview.
His group at CVPath recently published data showing pathologic evidence of myocarditis after SARS-CoV-2 infection, as reported by theheart.org | Medscape Cardiology.
“As a clinician, when I think of myocarditis, I look at the echo and an LV gram, and I see if there is a wall motion abnormality and troponin elevation, but with normal coronary arteries. And if all that is there, then I think about myocarditis in my differential diagnosis,” he said. “But in most of these cases, as the authors rightly point out, most patients did not have what is necessary to really entertain a diagnosis of myocarditis.”
He agreed with Dr. Fontana’s suggestion that what the CMR might be picking up in these survivors is microthrombi, as his group saw in their recent autopsy study.
“It’s very possible these findings are concordant with the recent autopsy studies done by my group and others in terms of detecting the presence of microthrombi, but we don’t know this for certain because no one has ever studied this entity before in the clinic and we don’t really know how microthrombi might appear on CMR.”
Largest study to date
The 148 participants (mean age, 64 years; 70% male) in the largest study to date to investigate convalescing COVID-19 patients who had elevated troponins – something identified early in the pandemic as a risk factor for worse outcomes in COVID-19 – were treated at one of six hospitals in London.
Patients who had abnormal troponin levels were offered an MRI scan of the heart after discharge and were compared with those from a control group of patients who had not had COVID-19 and with 40 healthy volunteers.
Median length of stay was 9 days, and 32% of patients required ventilatory support in the intensive care unit.
Just over half the patients (57%) had hypertension, 7% had had a previous myocardial infarction, 34% had diabetes, 46% had hypercholesterolemia, and 24% were smokers. Mean body mass index was 28.5 kg/m2.
CMR follow-up was conducted a median of 68 days after confirmation of a COVID-19 diagnosis.
On Twitter, Dr. Cole noted that the findings are subject to both survivor bias and referral bias. “We didn’t scan frail patients where the clinician felt [CMR] was unlikely to inform management.”
The findings, said Dr. Fontana, “say nothing about what happens to people who are not hospitalized with COVID, or those who are hospitalized but without elevated troponin.”
What they do offer, particularly if replicated, is a way forward in identifying patients at higher or lower risk for long-term sequelae and inform strategies that could improve outcomes, she added.
A version of this article first appeared on Medscape.com.