User login
Hard habit to break
“I love practicing medicine.”
The speaker was one of my patients. A distinguished, friendly, gentleman in his mid-to-late 70s, here to see me for a minor problem. He still practices medicine part time.
Since his neurologic issue was simple, we spent a fair amount of the time chatting. We’d both seen changes in medicine over time, he more than I, obviously.
Some good, some bad. Fancier toys, better drugs, more paperwork (even if it’s not all on paper anymore).
But we both still like what we do, and have no plans to give it up anytime soon.
Some doctors end up hating their jobs and leave the field. I understand that, and I don’t blame them. It’s not an easy one.
But I still enjoy the job. I look forward to seeing patients each day, turning over their cases, trying to figure them out, and doing what I can to help people.
I see that it is similar with attorneys. Maybe it’s part of the time and commitment you put into getting to a job that makes it hard to walk away as you get older. Or maybe (probably more likely) it’s some intrinsic part of the personality that drove you to get there.
I’m roughly two-thirds of the way through my career, but still don’t have any plans to close down. Granted, that’s practical – I have kids in college, a mortgage, and office overhead. My colleague across the desk can stop practicing whenever he wants, but gets satisfaction, validation, and enjoyment from doing the same job. At this point in his life that’s more important than the money.
I hope to someday feel that same way. I don’t want to always work the 80-90 hours a week I do now, but I can’t imagine not doing this, either.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
“I love practicing medicine.”
The speaker was one of my patients. A distinguished, friendly, gentleman in his mid-to-late 70s, here to see me for a minor problem. He still practices medicine part time.
Since his neurologic issue was simple, we spent a fair amount of the time chatting. We’d both seen changes in medicine over time, he more than I, obviously.
Some good, some bad. Fancier toys, better drugs, more paperwork (even if it’s not all on paper anymore).
But we both still like what we do, and have no plans to give it up anytime soon.
Some doctors end up hating their jobs and leave the field. I understand that, and I don’t blame them. It’s not an easy one.
But I still enjoy the job. I look forward to seeing patients each day, turning over their cases, trying to figure them out, and doing what I can to help people.
I see that it is similar with attorneys. Maybe it’s part of the time and commitment you put into getting to a job that makes it hard to walk away as you get older. Or maybe (probably more likely) it’s some intrinsic part of the personality that drove you to get there.
I’m roughly two-thirds of the way through my career, but still don’t have any plans to close down. Granted, that’s practical – I have kids in college, a mortgage, and office overhead. My colleague across the desk can stop practicing whenever he wants, but gets satisfaction, validation, and enjoyment from doing the same job. At this point in his life that’s more important than the money.
I hope to someday feel that same way. I don’t want to always work the 80-90 hours a week I do now, but I can’t imagine not doing this, either.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
“I love practicing medicine.”
The speaker was one of my patients. A distinguished, friendly, gentleman in his mid-to-late 70s, here to see me for a minor problem. He still practices medicine part time.
Since his neurologic issue was simple, we spent a fair amount of the time chatting. We’d both seen changes in medicine over time, he more than I, obviously.
Some good, some bad. Fancier toys, better drugs, more paperwork (even if it’s not all on paper anymore).
But we both still like what we do, and have no plans to give it up anytime soon.
Some doctors end up hating their jobs and leave the field. I understand that, and I don’t blame them. It’s not an easy one.
But I still enjoy the job. I look forward to seeing patients each day, turning over their cases, trying to figure them out, and doing what I can to help people.
I see that it is similar with attorneys. Maybe it’s part of the time and commitment you put into getting to a job that makes it hard to walk away as you get older. Or maybe (probably more likely) it’s some intrinsic part of the personality that drove you to get there.
I’m roughly two-thirds of the way through my career, but still don’t have any plans to close down. Granted, that’s practical – I have kids in college, a mortgage, and office overhead. My colleague across the desk can stop practicing whenever he wants, but gets satisfaction, validation, and enjoyment from doing the same job. At this point in his life that’s more important than the money.
I hope to someday feel that same way. I don’t want to always work the 80-90 hours a week I do now, but I can’t imagine not doing this, either.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Bored? Change the world or read a book
A weekend, for most of us in solo practice, doesn’t really signify time off from work. It just means we’re not seeing patients at the office.
There’s always business stuff to do (like payroll and paying bills), legal cases to review, the never-ending forms for a million things, and all the other stuff there never seems to be enough time to do on weekdays.
So this weekend I started attacking the pile after dinner on Friday and found myself done by Saturday afternoon. Which is rare, usually I spend the better part of a weekend at my desk.
And then, unexpectedly faced with an empty desk, I found myself wondering what to do.
Boredom is one of the odder human conditions. Certainly, there are more ways to waste time now than there ever have been. TV, Netflix, phone games, TikTok, books, just to name a few.
But do we always have to be entertained? Many great scientists have said that world-changing ideas have come to them when they weren’t working, such as while showering or riding to work. Leo Szilard was crossing a London street in 1933 when he suddenly saw how a nuclear chain reaction would be self-sustaining once initiated. (Fortunately, he wasn’t hit by a car in the process.)
But I’m not Szilard. So I rationalized a reason not to exercise and sat on the couch with a book.
The remarkable human brain doesn’t shut down easily. With nothing else to do, most other mammals tend to doze off. But not us. It’s always on, trying to think of the next goal, the next move, the next whatever.
Having nothing to do sounds like a great idea, until you have nothing to do. It may be fine for a few days, but after a while you realize there’s only so long you can stare at the waves or mountains before your mind turns back to “what’s next.”
This isn’t a bad thing. Being bored is probably constructive. Without realizing it we use it to form new ideas and start new plans.
Maybe this is why we’re here. The mind that keeps working is a powerful tool, driving us forward in all walks of life. Perhaps it’s this feature that pushed the development of intelligence further and led us to form civilizations.
Perhaps it’s the real reason we keep moving forward.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
A weekend, for most of us in solo practice, doesn’t really signify time off from work. It just means we’re not seeing patients at the office.
There’s always business stuff to do (like payroll and paying bills), legal cases to review, the never-ending forms for a million things, and all the other stuff there never seems to be enough time to do on weekdays.
So this weekend I started attacking the pile after dinner on Friday and found myself done by Saturday afternoon. Which is rare, usually I spend the better part of a weekend at my desk.
And then, unexpectedly faced with an empty desk, I found myself wondering what to do.
Boredom is one of the odder human conditions. Certainly, there are more ways to waste time now than there ever have been. TV, Netflix, phone games, TikTok, books, just to name a few.
But do we always have to be entertained? Many great scientists have said that world-changing ideas have come to them when they weren’t working, such as while showering or riding to work. Leo Szilard was crossing a London street in 1933 when he suddenly saw how a nuclear chain reaction would be self-sustaining once initiated. (Fortunately, he wasn’t hit by a car in the process.)
But I’m not Szilard. So I rationalized a reason not to exercise and sat on the couch with a book.
The remarkable human brain doesn’t shut down easily. With nothing else to do, most other mammals tend to doze off. But not us. It’s always on, trying to think of the next goal, the next move, the next whatever.
Having nothing to do sounds like a great idea, until you have nothing to do. It may be fine for a few days, but after a while you realize there’s only so long you can stare at the waves or mountains before your mind turns back to “what’s next.”
This isn’t a bad thing. Being bored is probably constructive. Without realizing it we use it to form new ideas and start new plans.
Maybe this is why we’re here. The mind that keeps working is a powerful tool, driving us forward in all walks of life. Perhaps it’s this feature that pushed the development of intelligence further and led us to form civilizations.
Perhaps it’s the real reason we keep moving forward.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
A weekend, for most of us in solo practice, doesn’t really signify time off from work. It just means we’re not seeing patients at the office.
There’s always business stuff to do (like payroll and paying bills), legal cases to review, the never-ending forms for a million things, and all the other stuff there never seems to be enough time to do on weekdays.
So this weekend I started attacking the pile after dinner on Friday and found myself done by Saturday afternoon. Which is rare, usually I spend the better part of a weekend at my desk.
And then, unexpectedly faced with an empty desk, I found myself wondering what to do.
Boredom is one of the odder human conditions. Certainly, there are more ways to waste time now than there ever have been. TV, Netflix, phone games, TikTok, books, just to name a few.
But do we always have to be entertained? Many great scientists have said that world-changing ideas have come to them when they weren’t working, such as while showering or riding to work. Leo Szilard was crossing a London street in 1933 when he suddenly saw how a nuclear chain reaction would be self-sustaining once initiated. (Fortunately, he wasn’t hit by a car in the process.)
But I’m not Szilard. So I rationalized a reason not to exercise and sat on the couch with a book.
The remarkable human brain doesn’t shut down easily. With nothing else to do, most other mammals tend to doze off. But not us. It’s always on, trying to think of the next goal, the next move, the next whatever.
Having nothing to do sounds like a great idea, until you have nothing to do. It may be fine for a few days, but after a while you realize there’s only so long you can stare at the waves or mountains before your mind turns back to “what’s next.”
This isn’t a bad thing. Being bored is probably constructive. Without realizing it we use it to form new ideas and start new plans.
Maybe this is why we’re here. The mind that keeps working is a powerful tool, driving us forward in all walks of life. Perhaps it’s this feature that pushed the development of intelligence further and led us to form civilizations.
Perhaps it’s the real reason we keep moving forward.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Book Review: Quality improvement in mental health care
Sunil Khushalani and Antonio DePaolo,
“Transforming Mental Healthcare: Applying Performance Improvement Methods to Mental Healthcare”
(London: Routledge, Taylor & Francis, 2022)
Since the publication of our book, “Lean Behavioral Health: The Kings County Hospital Story” (Oxford, England: Oxford University Press, 2014) almost a decade ago, “Transforming Mental Healthcare” is the first major book published about the use of a system for quality improvement across the health care continuum. That it has taken this long is probably surprising to those of us who have spent careers on trying to improve what is universally described as a system that is “broken” and in need of a major overhaul.
Every news cycle that reports mass violence typically spends a good bit of time talking about the failures of the mental health care system. One important lesson I learned when taking over the beleaguered Kings County (N.Y.) psychiatry service in 2009 (a department that has made extraordinary improvements over the years and is now exclaimed by the U.S. Department of Justice as “a model program”), is that the employees on the front line are often erroneously blamed for such failures.
The failure is systemic and usually starts at the top of the table of organization, not at the bottom. Dr. Khushalani and Dr. DePaolo have produced an excellent volume that should be purchased by every mental health care CEO and given “with thanks” to the local leaders overseeing the direct care of some of our nation’s most vulnerable patient populations.
The first part of “Transforming Mental Healthcare” provides an excellent overview of the current state of our mental health care system and its too numerous to name problems. This section could be a primer for all our legislators so their eyes can be opened to the failures on the ground that require their help in correcting. Many of the “failures” of our mental health care are societal failures – lack of affordable housing, access to care, reimbursement for care, gun access, etc. – and cannot be “fixed” by providers of care. Such problems are societal problems that call for societal and governmental solutions, and not only at the local level but from coast to coast.
The remainder of this easy to read and follow text provides many rich resources for the deliverers of mental health care. (e.g., plan-do-act, standard work, and A3 thinking).
The closing section focuses on leadership and culture – often overlooked to the detriment of any organization that doesn’t pay close attention to supporting both. Culture is cultivated and nourished by the organization’s leaders. Culture empowers staff to become problem solvers and agents of improvement. Empowered staff support and enrich their culture. Together a workplace that brings out the best of all its people is created, and burnout is held at bay.
“Transforming Mental Healthcare: Applying Performance Improvement Methods to Mental Healthcare” is a welcome and essential addition to the current morass, which is our mental health care delivery system, an oasis in the desert from which perhaps the lotus flower can emerge.
Dr. Merlino is emeritus professor of psychiatry, SUNY Downstate College of Medicine, Rhinebeck, N.Y., and formerly director of psychiatry at Kings County Hospital Center, Brooklyn, NY. He is the coauthor of “Lean Behavioral Health: The Kings County Hospital Story.” .
Sunil Khushalani and Antonio DePaolo,
“Transforming Mental Healthcare: Applying Performance Improvement Methods to Mental Healthcare”
(London: Routledge, Taylor & Francis, 2022)
Since the publication of our book, “Lean Behavioral Health: The Kings County Hospital Story” (Oxford, England: Oxford University Press, 2014) almost a decade ago, “Transforming Mental Healthcare” is the first major book published about the use of a system for quality improvement across the health care continuum. That it has taken this long is probably surprising to those of us who have spent careers on trying to improve what is universally described as a system that is “broken” and in need of a major overhaul.
Every news cycle that reports mass violence typically spends a good bit of time talking about the failures of the mental health care system. One important lesson I learned when taking over the beleaguered Kings County (N.Y.) psychiatry service in 2009 (a department that has made extraordinary improvements over the years and is now exclaimed by the U.S. Department of Justice as “a model program”), is that the employees on the front line are often erroneously blamed for such failures.
The failure is systemic and usually starts at the top of the table of organization, not at the bottom. Dr. Khushalani and Dr. DePaolo have produced an excellent volume that should be purchased by every mental health care CEO and given “with thanks” to the local leaders overseeing the direct care of some of our nation’s most vulnerable patient populations.
The first part of “Transforming Mental Healthcare” provides an excellent overview of the current state of our mental health care system and its too numerous to name problems. This section could be a primer for all our legislators so their eyes can be opened to the failures on the ground that require their help in correcting. Many of the “failures” of our mental health care are societal failures – lack of affordable housing, access to care, reimbursement for care, gun access, etc. – and cannot be “fixed” by providers of care. Such problems are societal problems that call for societal and governmental solutions, and not only at the local level but from coast to coast.
The remainder of this easy to read and follow text provides many rich resources for the deliverers of mental health care. (e.g., plan-do-act, standard work, and A3 thinking).
The closing section focuses on leadership and culture – often overlooked to the detriment of any organization that doesn’t pay close attention to supporting both. Culture is cultivated and nourished by the organization’s leaders. Culture empowers staff to become problem solvers and agents of improvement. Empowered staff support and enrich their culture. Together a workplace that brings out the best of all its people is created, and burnout is held at bay.
“Transforming Mental Healthcare: Applying Performance Improvement Methods to Mental Healthcare” is a welcome and essential addition to the current morass, which is our mental health care delivery system, an oasis in the desert from which perhaps the lotus flower can emerge.
Dr. Merlino is emeritus professor of psychiatry, SUNY Downstate College of Medicine, Rhinebeck, N.Y., and formerly director of psychiatry at Kings County Hospital Center, Brooklyn, NY. He is the coauthor of “Lean Behavioral Health: The Kings County Hospital Story.” .
Sunil Khushalani and Antonio DePaolo,
“Transforming Mental Healthcare: Applying Performance Improvement Methods to Mental Healthcare”
(London: Routledge, Taylor & Francis, 2022)
Since the publication of our book, “Lean Behavioral Health: The Kings County Hospital Story” (Oxford, England: Oxford University Press, 2014) almost a decade ago, “Transforming Mental Healthcare” is the first major book published about the use of a system for quality improvement across the health care continuum. That it has taken this long is probably surprising to those of us who have spent careers on trying to improve what is universally described as a system that is “broken” and in need of a major overhaul.
Every news cycle that reports mass violence typically spends a good bit of time talking about the failures of the mental health care system. One important lesson I learned when taking over the beleaguered Kings County (N.Y.) psychiatry service in 2009 (a department that has made extraordinary improvements over the years and is now exclaimed by the U.S. Department of Justice as “a model program”), is that the employees on the front line are often erroneously blamed for such failures.
The failure is systemic and usually starts at the top of the table of organization, not at the bottom. Dr. Khushalani and Dr. DePaolo have produced an excellent volume that should be purchased by every mental health care CEO and given “with thanks” to the local leaders overseeing the direct care of some of our nation’s most vulnerable patient populations.
The first part of “Transforming Mental Healthcare” provides an excellent overview of the current state of our mental health care system and its too numerous to name problems. This section could be a primer for all our legislators so their eyes can be opened to the failures on the ground that require their help in correcting. Many of the “failures” of our mental health care are societal failures – lack of affordable housing, access to care, reimbursement for care, gun access, etc. – and cannot be “fixed” by providers of care. Such problems are societal problems that call for societal and governmental solutions, and not only at the local level but from coast to coast.
The remainder of this easy to read and follow text provides many rich resources for the deliverers of mental health care. (e.g., plan-do-act, standard work, and A3 thinking).
The closing section focuses on leadership and culture – often overlooked to the detriment of any organization that doesn’t pay close attention to supporting both. Culture is cultivated and nourished by the organization’s leaders. Culture empowers staff to become problem solvers and agents of improvement. Empowered staff support and enrich their culture. Together a workplace that brings out the best of all its people is created, and burnout is held at bay.
“Transforming Mental Healthcare: Applying Performance Improvement Methods to Mental Healthcare” is a welcome and essential addition to the current morass, which is our mental health care delivery system, an oasis in the desert from which perhaps the lotus flower can emerge.
Dr. Merlino is emeritus professor of psychiatry, SUNY Downstate College of Medicine, Rhinebeck, N.Y., and formerly director of psychiatry at Kings County Hospital Center, Brooklyn, NY. He is the coauthor of “Lean Behavioral Health: The Kings County Hospital Story.” .
The toll of the unwanted pregnancy
In the wake of the Supreme Court’s June decision to repeal a federal right to abortion, many women will now be faced with the prospect of carrying an unwanted pregnancy to term.
One group of researchers has studied the fate of these women and their families for the last decade. Their findings show that women who were denied an abortion are worse off physically, mentally, and economically than those who underwent the procedure.
“There has been much hypothesizing about harms from abortion without considering what the consequences are when someone wants an abortion and can’t get one,” said Diana Greene Foster, PhD, professor of obstetrics and gynecology at University of California, San Francisco.
Dr. Foster leads the Turnaway Study, one of the first efforts to examine the physical and mental health effects of receiving or being denied abortions. The ongoing research also charts the economic and social outcomes of women and their families in either circumstance.
Dr. Foster and her colleagues have followed women through childbirth, examining their well-being through phone interviews months to years after the initial interviews.
The economic consequences of carrying an unwanted pregnancy are clear. Women who did not receive a wanted abortion were more likely to live under the poverty line and struggle to cover basic living expenses like food, housing, and transportation.
The physical toll is also significant.
A 2019 analysis from the Turnaway Study found that eight out of 1,132 participants died, two after delivery, during the five-year follow up period – a far greater proportion than what would be expected among women of reproductive age. The researchers also found that women who carry unwanted pregnancies have more comorbid conditions before and after delivery than other women.
Lauren J. Ralph, PhD, MPH, an epidemiologist and member of the Turnaway Study team, examined the physical well-being of women after delivering their unwanted pregnancies.
“They reported more chronic pain, more gestational hypertension, and were more likely to rate their health as fair or poor,” Dr. Ralph said. “Somewhat to our surprise, we also found that two women denied abortions died due to pregnancy-related causes. This is my biggest concern with the loss of abortion access, as all scientific evidence indicates we will see a rise in maternal deaths as a result.”
At least one preliminary study, released as a preprint and not yet peer reviewed, estimates that the number of women who will die each year from pregnancy complications will rise by 24%. For Black women, mortality could jump from 18% to 39% in every state, according to the researchers from the University of Colorado, Boulder.
State of denial
Regulations set in place at abortion clinics in each state individually determine who is able to obtain an abortion, dictated by a “gestational age limit” – how far along a woman is in her pregnancy from the end of her menstrual cycle. Some of the women from the Turnaway Study were unable to receive an abortion because of how far along they were. Others were granted the abortion because they were just under their state’s limit.
Before the latest Supreme Court ruling, this limit was 20 weeks in most states. Now, the cutoff can be as little as 6 weeks – before many women know they are pregnant – or zero weeks, under the most restrictive laws.
Over 70% of women who are denied an abortion carry the pregnancy to term, according to Dr. Foster’s analysis.
Interviews with nearly 1,000 women – in both the first and second trimester of pregnancy – in the Turnaway Study who sought abortions at 30 abortion clinics around the country revealed the main reasons for seeking the procedure were (a) not being able to afford a child; (b) the pregnancy coming at the wrong time in life; or (c) the partner involved not being suitable.
According to the U.S. Centers for Disease Control and Prevention, 59.7% of women seeking an abortion in the United States are already mothers. Having an unplanned child results in dramatically worse economic circumstances for their other children, who become nearly four times more likely to live below the poverty line than their peers. They also experience slower physical and mental development as a result of the arrival of the new sibling.
The latest efforts by states to ban abortion could make the situation much worse, said Liza Fuentes, DrPh, senior research scientist at the Guttmacher Institute. “We will need further research on what it means for women to be denied care in the context of the new restrictions,” Dr. Fuentes told this news organization.
Researchers cannot yet predict how many women will be unable to obtain an abortion in the coming months. But John Donahue, PhD, JD, an economist and professor of law at Stanford (Calif.) University, estimated that state laws would prevent roughly one-third of the 1 million abortions per year based on 2021 figures.
Dr. Ralph and her colleagues with the Turnaway Study know that restricting access to abortions will not make the need for abortions disappear. Rather, women will be forced to travel, potentially long distances at significant cost, for the procedure or will seek medication abortion by mail through virtual clinics.
But Dr. Ralph said she’s concerned about women who live in areas where telehealth abortions are banned, or who discover their pregnancies late, as medical abortions are only recommended for women who are 10 weeks pregnant or less.
“They may look to self-source the medications online or elsewhere, potentially putting themself at legal risk,” she said. “And, as my research has shown, others may turn to self-managing an abortion with herbs, other drugs or medications, or physical methods like hitting themselves in the abdomen; with this they put themselves at both legal and potentially medical risk.”
Constance Bohon, MD, an ob.gyn. in Washington, D.C., said further research should track what happens to women if they’re forced to leave a job to care for another child.
“Many of these women live paycheck to paycheck and cannot afford the cost of an additional child,” Dr. Bohon said. “They may also need to rely on social service agencies to help them find food and housing.”
Dr. Fuentes said she hopes the Turnaway Study will inspire other researchers to examine laws that outlaw abortion and the corresponding long-term effects on women.
“From a medical and a public health standpoint, these laws are unjust,” Dr. Fuentes said in an interview. “They’re not grounded in evidence, and they incur great costs not just to pregnant people but their families and their communities as well.”
A version of this article first appeared on Medscape.com.
In the wake of the Supreme Court’s June decision to repeal a federal right to abortion, many women will now be faced with the prospect of carrying an unwanted pregnancy to term.
One group of researchers has studied the fate of these women and their families for the last decade. Their findings show that women who were denied an abortion are worse off physically, mentally, and economically than those who underwent the procedure.
“There has been much hypothesizing about harms from abortion without considering what the consequences are when someone wants an abortion and can’t get one,” said Diana Greene Foster, PhD, professor of obstetrics and gynecology at University of California, San Francisco.
Dr. Foster leads the Turnaway Study, one of the first efforts to examine the physical and mental health effects of receiving or being denied abortions. The ongoing research also charts the economic and social outcomes of women and their families in either circumstance.
Dr. Foster and her colleagues have followed women through childbirth, examining their well-being through phone interviews months to years after the initial interviews.
The economic consequences of carrying an unwanted pregnancy are clear. Women who did not receive a wanted abortion were more likely to live under the poverty line and struggle to cover basic living expenses like food, housing, and transportation.
The physical toll is also significant.
A 2019 analysis from the Turnaway Study found that eight out of 1,132 participants died, two after delivery, during the five-year follow up period – a far greater proportion than what would be expected among women of reproductive age. The researchers also found that women who carry unwanted pregnancies have more comorbid conditions before and after delivery than other women.
Lauren J. Ralph, PhD, MPH, an epidemiologist and member of the Turnaway Study team, examined the physical well-being of women after delivering their unwanted pregnancies.
“They reported more chronic pain, more gestational hypertension, and were more likely to rate their health as fair or poor,” Dr. Ralph said. “Somewhat to our surprise, we also found that two women denied abortions died due to pregnancy-related causes. This is my biggest concern with the loss of abortion access, as all scientific evidence indicates we will see a rise in maternal deaths as a result.”
At least one preliminary study, released as a preprint and not yet peer reviewed, estimates that the number of women who will die each year from pregnancy complications will rise by 24%. For Black women, mortality could jump from 18% to 39% in every state, according to the researchers from the University of Colorado, Boulder.
State of denial
Regulations set in place at abortion clinics in each state individually determine who is able to obtain an abortion, dictated by a “gestational age limit” – how far along a woman is in her pregnancy from the end of her menstrual cycle. Some of the women from the Turnaway Study were unable to receive an abortion because of how far along they were. Others were granted the abortion because they were just under their state’s limit.
Before the latest Supreme Court ruling, this limit was 20 weeks in most states. Now, the cutoff can be as little as 6 weeks – before many women know they are pregnant – or zero weeks, under the most restrictive laws.
Over 70% of women who are denied an abortion carry the pregnancy to term, according to Dr. Foster’s analysis.
Interviews with nearly 1,000 women – in both the first and second trimester of pregnancy – in the Turnaway Study who sought abortions at 30 abortion clinics around the country revealed the main reasons for seeking the procedure were (a) not being able to afford a child; (b) the pregnancy coming at the wrong time in life; or (c) the partner involved not being suitable.
According to the U.S. Centers for Disease Control and Prevention, 59.7% of women seeking an abortion in the United States are already mothers. Having an unplanned child results in dramatically worse economic circumstances for their other children, who become nearly four times more likely to live below the poverty line than their peers. They also experience slower physical and mental development as a result of the arrival of the new sibling.
The latest efforts by states to ban abortion could make the situation much worse, said Liza Fuentes, DrPh, senior research scientist at the Guttmacher Institute. “We will need further research on what it means for women to be denied care in the context of the new restrictions,” Dr. Fuentes told this news organization.
Researchers cannot yet predict how many women will be unable to obtain an abortion in the coming months. But John Donahue, PhD, JD, an economist and professor of law at Stanford (Calif.) University, estimated that state laws would prevent roughly one-third of the 1 million abortions per year based on 2021 figures.
Dr. Ralph and her colleagues with the Turnaway Study know that restricting access to abortions will not make the need for abortions disappear. Rather, women will be forced to travel, potentially long distances at significant cost, for the procedure or will seek medication abortion by mail through virtual clinics.
But Dr. Ralph said she’s concerned about women who live in areas where telehealth abortions are banned, or who discover their pregnancies late, as medical abortions are only recommended for women who are 10 weeks pregnant or less.
“They may look to self-source the medications online or elsewhere, potentially putting themself at legal risk,” she said. “And, as my research has shown, others may turn to self-managing an abortion with herbs, other drugs or medications, or physical methods like hitting themselves in the abdomen; with this they put themselves at both legal and potentially medical risk.”
Constance Bohon, MD, an ob.gyn. in Washington, D.C., said further research should track what happens to women if they’re forced to leave a job to care for another child.
“Many of these women live paycheck to paycheck and cannot afford the cost of an additional child,” Dr. Bohon said. “They may also need to rely on social service agencies to help them find food and housing.”
Dr. Fuentes said she hopes the Turnaway Study will inspire other researchers to examine laws that outlaw abortion and the corresponding long-term effects on women.
“From a medical and a public health standpoint, these laws are unjust,” Dr. Fuentes said in an interview. “They’re not grounded in evidence, and they incur great costs not just to pregnant people but their families and their communities as well.”
A version of this article first appeared on Medscape.com.
In the wake of the Supreme Court’s June decision to repeal a federal right to abortion, many women will now be faced with the prospect of carrying an unwanted pregnancy to term.
One group of researchers has studied the fate of these women and their families for the last decade. Their findings show that women who were denied an abortion are worse off physically, mentally, and economically than those who underwent the procedure.
“There has been much hypothesizing about harms from abortion without considering what the consequences are when someone wants an abortion and can’t get one,” said Diana Greene Foster, PhD, professor of obstetrics and gynecology at University of California, San Francisco.
Dr. Foster leads the Turnaway Study, one of the first efforts to examine the physical and mental health effects of receiving or being denied abortions. The ongoing research also charts the economic and social outcomes of women and their families in either circumstance.
Dr. Foster and her colleagues have followed women through childbirth, examining their well-being through phone interviews months to years after the initial interviews.
The economic consequences of carrying an unwanted pregnancy are clear. Women who did not receive a wanted abortion were more likely to live under the poverty line and struggle to cover basic living expenses like food, housing, and transportation.
The physical toll is also significant.
A 2019 analysis from the Turnaway Study found that eight out of 1,132 participants died, two after delivery, during the five-year follow up period – a far greater proportion than what would be expected among women of reproductive age. The researchers also found that women who carry unwanted pregnancies have more comorbid conditions before and after delivery than other women.
Lauren J. Ralph, PhD, MPH, an epidemiologist and member of the Turnaway Study team, examined the physical well-being of women after delivering their unwanted pregnancies.
“They reported more chronic pain, more gestational hypertension, and were more likely to rate their health as fair or poor,” Dr. Ralph said. “Somewhat to our surprise, we also found that two women denied abortions died due to pregnancy-related causes. This is my biggest concern with the loss of abortion access, as all scientific evidence indicates we will see a rise in maternal deaths as a result.”
At least one preliminary study, released as a preprint and not yet peer reviewed, estimates that the number of women who will die each year from pregnancy complications will rise by 24%. For Black women, mortality could jump from 18% to 39% in every state, according to the researchers from the University of Colorado, Boulder.
State of denial
Regulations set in place at abortion clinics in each state individually determine who is able to obtain an abortion, dictated by a “gestational age limit” – how far along a woman is in her pregnancy from the end of her menstrual cycle. Some of the women from the Turnaway Study were unable to receive an abortion because of how far along they were. Others were granted the abortion because they were just under their state’s limit.
Before the latest Supreme Court ruling, this limit was 20 weeks in most states. Now, the cutoff can be as little as 6 weeks – before many women know they are pregnant – or zero weeks, under the most restrictive laws.
Over 70% of women who are denied an abortion carry the pregnancy to term, according to Dr. Foster’s analysis.
Interviews with nearly 1,000 women – in both the first and second trimester of pregnancy – in the Turnaway Study who sought abortions at 30 abortion clinics around the country revealed the main reasons for seeking the procedure were (a) not being able to afford a child; (b) the pregnancy coming at the wrong time in life; or (c) the partner involved not being suitable.
According to the U.S. Centers for Disease Control and Prevention, 59.7% of women seeking an abortion in the United States are already mothers. Having an unplanned child results in dramatically worse economic circumstances for their other children, who become nearly four times more likely to live below the poverty line than their peers. They also experience slower physical and mental development as a result of the arrival of the new sibling.
The latest efforts by states to ban abortion could make the situation much worse, said Liza Fuentes, DrPh, senior research scientist at the Guttmacher Institute. “We will need further research on what it means for women to be denied care in the context of the new restrictions,” Dr. Fuentes told this news organization.
Researchers cannot yet predict how many women will be unable to obtain an abortion in the coming months. But John Donahue, PhD, JD, an economist and professor of law at Stanford (Calif.) University, estimated that state laws would prevent roughly one-third of the 1 million abortions per year based on 2021 figures.
Dr. Ralph and her colleagues with the Turnaway Study know that restricting access to abortions will not make the need for abortions disappear. Rather, women will be forced to travel, potentially long distances at significant cost, for the procedure or will seek medication abortion by mail through virtual clinics.
But Dr. Ralph said she’s concerned about women who live in areas where telehealth abortions are banned, or who discover their pregnancies late, as medical abortions are only recommended for women who are 10 weeks pregnant or less.
“They may look to self-source the medications online or elsewhere, potentially putting themself at legal risk,” she said. “And, as my research has shown, others may turn to self-managing an abortion with herbs, other drugs or medications, or physical methods like hitting themselves in the abdomen; with this they put themselves at both legal and potentially medical risk.”
Constance Bohon, MD, an ob.gyn. in Washington, D.C., said further research should track what happens to women if they’re forced to leave a job to care for another child.
“Many of these women live paycheck to paycheck and cannot afford the cost of an additional child,” Dr. Bohon said. “They may also need to rely on social service agencies to help them find food and housing.”
Dr. Fuentes said she hopes the Turnaway Study will inspire other researchers to examine laws that outlaw abortion and the corresponding long-term effects on women.
“From a medical and a public health standpoint, these laws are unjust,” Dr. Fuentes said in an interview. “They’re not grounded in evidence, and they incur great costs not just to pregnant people but their families and their communities as well.”
A version of this article first appeared on Medscape.com.
Physicians react: Compensation isn’t worth the hassles. What’s the solution?
How satisfied are physicians that they are fairly compensated for their dedication, skills, and time? That’s a subject that seems to steer many physicians to heated emotions and to a variety of issues with today’s medical field – not all of which directly affect their pay.
Medscape’s Physician Compensation Report 2022: “Incomes Gain, Pay Gaps Remain” generally shows encouraging trends. Physician income rose from a year earlier, when it stagnated as COVID-19 restrictions led patients to stay home and medical practices to cut hours or close. And for the first time in Medscape’s 11 years of reporting on physician compensation, average income rose for every medical specialty surveyed.
Heartening findings, right? Yet the tone of comments to the report was anything but peppy. One physician even complained his plumber earns more than he does.
A family physician lamented that he has “made less in the past 3 years, with more hassles and work” and he “can’t wait to retire next year.” Meanwhile, he complained, the U.S. health system is “the costliest, yet wasteful, with worse outcomes; reactive, not preventative; and has the costliest drugs and social issues.”
Do NPs and PAs encroach on your income?
The conversation about fair compensation launched some commenters into a discussion about competition from nurse practitioners (NPs) and physician assistants (PAs). Some physicians expressed wariness at best, and anger at worst, about NPs and PAs evolving beyond traditional doctor support roles into certain direct patient support.
One-fourth of respondents in the compensation report said their income was negatively affected by competition from NPs, PAs, and other nonphysician providers. For example, with states like Arkansas expanding independent practice for certified registered nurse anesthetists (CRNAs), one commenter complained, “we are no longer needed.”
Added another physician, “primary care, especially internal medicine, is just going away for doctors. We wasted, by all accounts, 4 full years of our working lives because NPs are ‘just as good.’ ”
Greater independence for NPs and PAs strengthens the hands of health insurers and “will end up hastening the demise of primary care as we have known it,” another reader predicted. Other physicians’ takes: “For the institution, it’s much cheaper to hire NPs than to hire doctors” and “overall, physician negotiating power will decrease in the future.”
Medicare reimbursement rates grate
Although 7 in 10 respondents in the compensation report said they would continue to accept new Medicare or Medicaid patients, comments reveal resentment about the practical need to work with Medicare and its resentment rates.
“An open question to Medicare: Are you doing the dumbest thing possible by paying low wages and giving huge administrative burdens for internal medicine on purpose?” one physician wrote. “Or are you really that short-sighted?”
Another reader cited an analysis from the American College of Surgeons of Medicare’s 1998 surgical CPT codes. If Medicare had left those codes alone beyond annual inflation adjustments, the study found, reimbursement rates by 2019 would be half of what they became.
Another way of looking at the code reimbursement increases is a 50% pay cut over 20 years for doctors and medical practices, that reader insisted. “The rising cost of employee wages, particularly of the last two-and-a-half years of COVID-19, combined with the effective pay cuts over the last 20 years, equals time to quit!”
Another commenter concurred. “In the 1990s, most full-time docs were making almost double what you see [in the report], and everything cost almost half of what it does now. So, MD purchasing power is between half and one-quarter of what it was in the early 1990s.”
Are self-pay models better?
Do physicians have a better chance at consistently fair income under a self-pay practice that avoids dealing with insurance companies?
One commenter hypothesized that psychiatrists once trailed internists in income but today earn more because many “quit working for insurance and went to a cash business 15 years ago.” Many family physicians did something similar by switching to a direct primary care model, he said.
This physician said he has done the same “with great results” for patients as well: shorter office visits, faster booking of appointments, no deductibles owed. Best of all, “I love practicing medicine again, and my patients love the great health care they receive.”
Another commenter agreed. “Two words: cash practice.” But another objected, “I guess only the very rich can afford to cover your business costs.”
Regardless of the payment model, another physician argued for private practice over employed positions. “Save on the bureaucratic expenses. Go back to private practice and get rid of electronic records.”
A version of this article first appeared on Medscape.com.
How satisfied are physicians that they are fairly compensated for their dedication, skills, and time? That’s a subject that seems to steer many physicians to heated emotions and to a variety of issues with today’s medical field – not all of which directly affect their pay.
Medscape’s Physician Compensation Report 2022: “Incomes Gain, Pay Gaps Remain” generally shows encouraging trends. Physician income rose from a year earlier, when it stagnated as COVID-19 restrictions led patients to stay home and medical practices to cut hours or close. And for the first time in Medscape’s 11 years of reporting on physician compensation, average income rose for every medical specialty surveyed.
Heartening findings, right? Yet the tone of comments to the report was anything but peppy. One physician even complained his plumber earns more than he does.
A family physician lamented that he has “made less in the past 3 years, with more hassles and work” and he “can’t wait to retire next year.” Meanwhile, he complained, the U.S. health system is “the costliest, yet wasteful, with worse outcomes; reactive, not preventative; and has the costliest drugs and social issues.”
Do NPs and PAs encroach on your income?
The conversation about fair compensation launched some commenters into a discussion about competition from nurse practitioners (NPs) and physician assistants (PAs). Some physicians expressed wariness at best, and anger at worst, about NPs and PAs evolving beyond traditional doctor support roles into certain direct patient support.
One-fourth of respondents in the compensation report said their income was negatively affected by competition from NPs, PAs, and other nonphysician providers. For example, with states like Arkansas expanding independent practice for certified registered nurse anesthetists (CRNAs), one commenter complained, “we are no longer needed.”
Added another physician, “primary care, especially internal medicine, is just going away for doctors. We wasted, by all accounts, 4 full years of our working lives because NPs are ‘just as good.’ ”
Greater independence for NPs and PAs strengthens the hands of health insurers and “will end up hastening the demise of primary care as we have known it,” another reader predicted. Other physicians’ takes: “For the institution, it’s much cheaper to hire NPs than to hire doctors” and “overall, physician negotiating power will decrease in the future.”
Medicare reimbursement rates grate
Although 7 in 10 respondents in the compensation report said they would continue to accept new Medicare or Medicaid patients, comments reveal resentment about the practical need to work with Medicare and its resentment rates.
“An open question to Medicare: Are you doing the dumbest thing possible by paying low wages and giving huge administrative burdens for internal medicine on purpose?” one physician wrote. “Or are you really that short-sighted?”
Another reader cited an analysis from the American College of Surgeons of Medicare’s 1998 surgical CPT codes. If Medicare had left those codes alone beyond annual inflation adjustments, the study found, reimbursement rates by 2019 would be half of what they became.
Another way of looking at the code reimbursement increases is a 50% pay cut over 20 years for doctors and medical practices, that reader insisted. “The rising cost of employee wages, particularly of the last two-and-a-half years of COVID-19, combined with the effective pay cuts over the last 20 years, equals time to quit!”
Another commenter concurred. “In the 1990s, most full-time docs were making almost double what you see [in the report], and everything cost almost half of what it does now. So, MD purchasing power is between half and one-quarter of what it was in the early 1990s.”
Are self-pay models better?
Do physicians have a better chance at consistently fair income under a self-pay practice that avoids dealing with insurance companies?
One commenter hypothesized that psychiatrists once trailed internists in income but today earn more because many “quit working for insurance and went to a cash business 15 years ago.” Many family physicians did something similar by switching to a direct primary care model, he said.
This physician said he has done the same “with great results” for patients as well: shorter office visits, faster booking of appointments, no deductibles owed. Best of all, “I love practicing medicine again, and my patients love the great health care they receive.”
Another commenter agreed. “Two words: cash practice.” But another objected, “I guess only the very rich can afford to cover your business costs.”
Regardless of the payment model, another physician argued for private practice over employed positions. “Save on the bureaucratic expenses. Go back to private practice and get rid of electronic records.”
A version of this article first appeared on Medscape.com.
How satisfied are physicians that they are fairly compensated for their dedication, skills, and time? That’s a subject that seems to steer many physicians to heated emotions and to a variety of issues with today’s medical field – not all of which directly affect their pay.
Medscape’s Physician Compensation Report 2022: “Incomes Gain, Pay Gaps Remain” generally shows encouraging trends. Physician income rose from a year earlier, when it stagnated as COVID-19 restrictions led patients to stay home and medical practices to cut hours or close. And for the first time in Medscape’s 11 years of reporting on physician compensation, average income rose for every medical specialty surveyed.
Heartening findings, right? Yet the tone of comments to the report was anything but peppy. One physician even complained his plumber earns more than he does.
A family physician lamented that he has “made less in the past 3 years, with more hassles and work” and he “can’t wait to retire next year.” Meanwhile, he complained, the U.S. health system is “the costliest, yet wasteful, with worse outcomes; reactive, not preventative; and has the costliest drugs and social issues.”
Do NPs and PAs encroach on your income?
The conversation about fair compensation launched some commenters into a discussion about competition from nurse practitioners (NPs) and physician assistants (PAs). Some physicians expressed wariness at best, and anger at worst, about NPs and PAs evolving beyond traditional doctor support roles into certain direct patient support.
One-fourth of respondents in the compensation report said their income was negatively affected by competition from NPs, PAs, and other nonphysician providers. For example, with states like Arkansas expanding independent practice for certified registered nurse anesthetists (CRNAs), one commenter complained, “we are no longer needed.”
Added another physician, “primary care, especially internal medicine, is just going away for doctors. We wasted, by all accounts, 4 full years of our working lives because NPs are ‘just as good.’ ”
Greater independence for NPs and PAs strengthens the hands of health insurers and “will end up hastening the demise of primary care as we have known it,” another reader predicted. Other physicians’ takes: “For the institution, it’s much cheaper to hire NPs than to hire doctors” and “overall, physician negotiating power will decrease in the future.”
Medicare reimbursement rates grate
Although 7 in 10 respondents in the compensation report said they would continue to accept new Medicare or Medicaid patients, comments reveal resentment about the practical need to work with Medicare and its resentment rates.
“An open question to Medicare: Are you doing the dumbest thing possible by paying low wages and giving huge administrative burdens for internal medicine on purpose?” one physician wrote. “Or are you really that short-sighted?”
Another reader cited an analysis from the American College of Surgeons of Medicare’s 1998 surgical CPT codes. If Medicare had left those codes alone beyond annual inflation adjustments, the study found, reimbursement rates by 2019 would be half of what they became.
Another way of looking at the code reimbursement increases is a 50% pay cut over 20 years for doctors and medical practices, that reader insisted. “The rising cost of employee wages, particularly of the last two-and-a-half years of COVID-19, combined with the effective pay cuts over the last 20 years, equals time to quit!”
Another commenter concurred. “In the 1990s, most full-time docs were making almost double what you see [in the report], and everything cost almost half of what it does now. So, MD purchasing power is between half and one-quarter of what it was in the early 1990s.”
Are self-pay models better?
Do physicians have a better chance at consistently fair income under a self-pay practice that avoids dealing with insurance companies?
One commenter hypothesized that psychiatrists once trailed internists in income but today earn more because many “quit working for insurance and went to a cash business 15 years ago.” Many family physicians did something similar by switching to a direct primary care model, he said.
This physician said he has done the same “with great results” for patients as well: shorter office visits, faster booking of appointments, no deductibles owed. Best of all, “I love practicing medicine again, and my patients love the great health care they receive.”
Another commenter agreed. “Two words: cash practice.” But another objected, “I guess only the very rich can afford to cover your business costs.”
Regardless of the payment model, another physician argued for private practice over employed positions. “Save on the bureaucratic expenses. Go back to private practice and get rid of electronic records.”
A version of this article first appeared on Medscape.com.
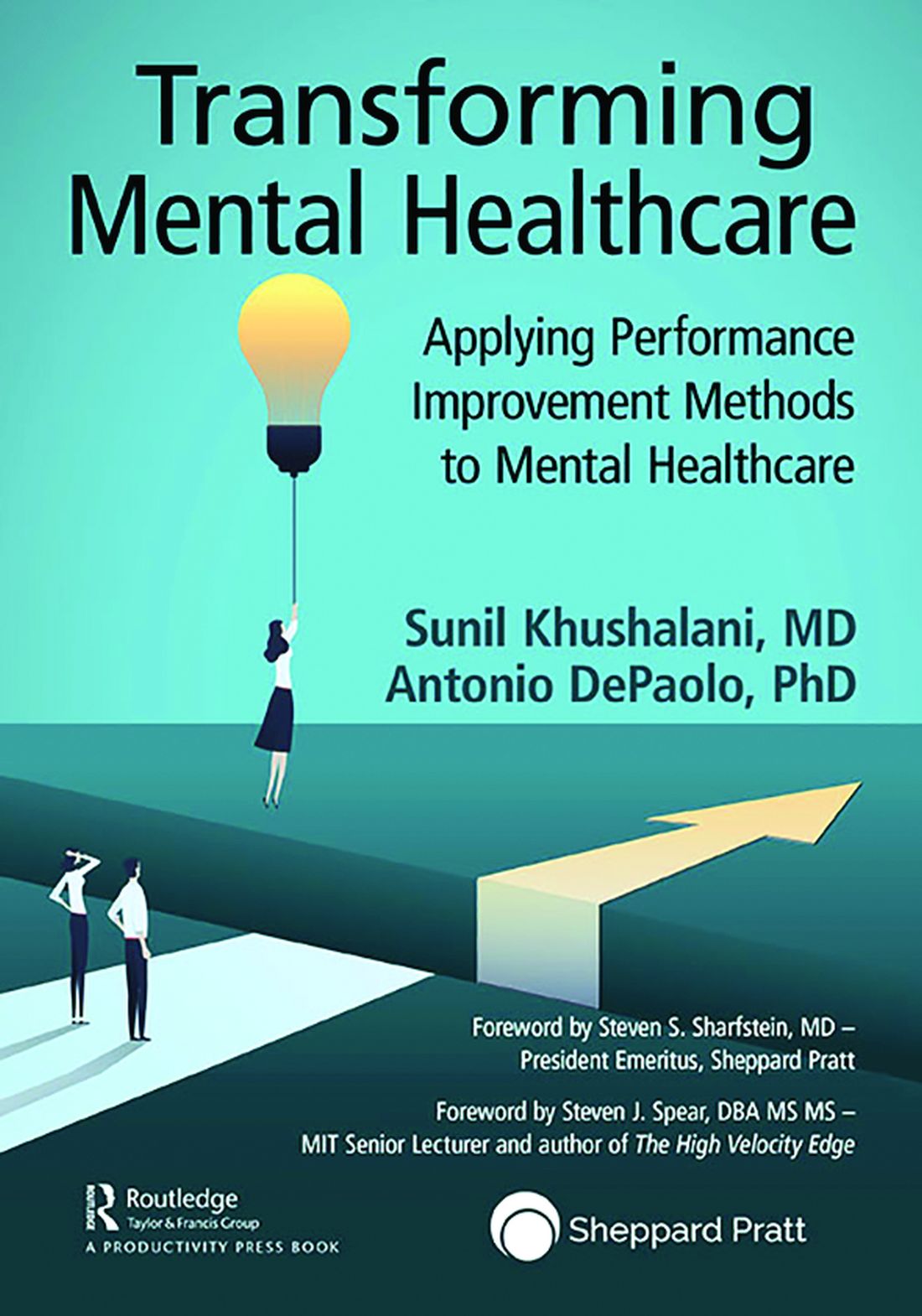
Pediatricians’ incomes rose faster than most specialties in 2021: Survey
In an unprecedented year when income increased for all specialties, pediatricians did better than most, according to a recent survey by Medscape.
. Medscape also noted that, for the first time in the 11 years it’s been conducting these physician compensation surveys, “all specialties have seen an increase in income.”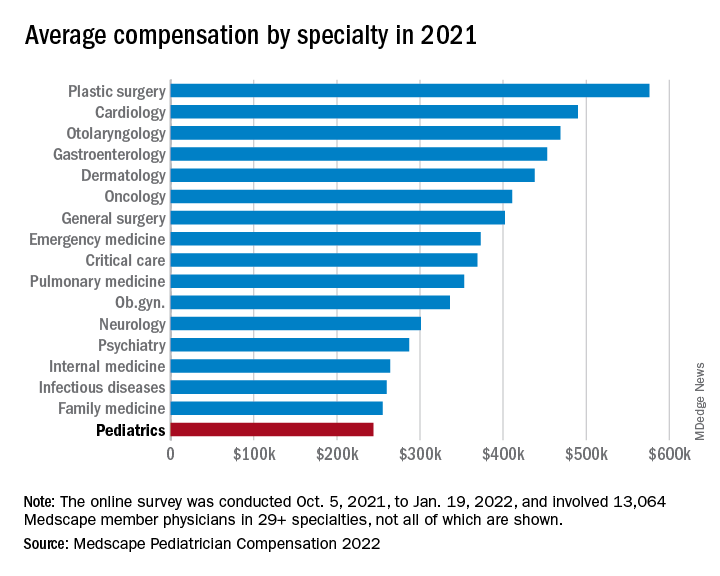
At least some of that positive news can be traced back to the reduced impact of COVID-19. “Compensation for most physicians is trending back up as demand for physicians accelerates. The market for physicians has done a complete 180 over just 7 or 8 months,” James Taylor of AMN Healthcare’s physician and leadership solutions division said in Medscape Pediatrician Compensation Report 2022.
The 10% increase in pediatricians’ income, however, was not enough to reach the average for primary care physicians, $260,000, which was up by 7.4% over 2020. It was enough, though, to move pediatricians from the bottom of the earnings-by-specialty list, where they were last year, to next-to-last this year (public health/preventive medicine, with average earnings of $243,000 in 2021, is not shown in the graph).
The gender gap in earnings left male pediatricians’ income 26% higher than their female counterparts, slightly above the gap of 25% for primary care physicians and 24% for all physicians. For specialists, the gap was 31% in favor of men, based on data from 13,064 Medscape member physicians who participated in the survey, which was conducted online from Oct. 5, 2021, to Jan. 19, 2022. For the record, 57% of the pediatricians who responded were women.
The gaps and low income averages were enough, it seems, to keep pediatricians fairly negative regarding their feelings on compensation. Only 47% think they were fairly compensated in 2021, higher only than diabetes/endocrinology and nephrology. Among the other primary care specialties, internal medicine and ob.gyn. were slightly higher at 49% and family medicine was 55% – still just middle of the pack, compared with public health/preventive medicine at 72%, Medscape said in the report.
Would you do it again?
Moving to the less-economic aspects of the survey, respondents also were asked if they would choose medicine again as a career. Once more pediatricians were low on the scale, as only 70% said that they would enter medicine again, down from 77% last year and lower than this year’s average of 73% average for all physicians.
When they were asked if they would choose pediatrics again as a specialty, the response was a bit more positive: 84% said yes. That middle-of-the-pack showing was well ahead of internal medicine (63%) and family medicine (68%), but well below dermatology (99%) and orthopedics (97%), which are “among the top groups in our survey year after year,” Medscape said.
Did the administrative challenges of medical practice have an effect on those answers? Pediatrician respondents said that they spend 14.9 hours per week on paperwork and administration, close to the average of 15.5 hours for all physicians. The internists, who are least likely to choose their original specialty again, spend 18.7 hours on paperwork each week, while dermatologists, the most likely to repeat their first choice, have just 11.9 hours of paperwork per week.
The exact number of pediatricians involved in the survey was not provided, but they made up about 8% of the total cohort, which works out to somewhere between 1,000 and 1,100 individuals. All respondents had to be practicing in the United States, and compensation was analyzed for full-time physicians only. The sampling error is ±0.86% at a 95% confidence level.
In an unprecedented year when income increased for all specialties, pediatricians did better than most, according to a recent survey by Medscape.
. Medscape also noted that, for the first time in the 11 years it’s been conducting these physician compensation surveys, “all specialties have seen an increase in income.”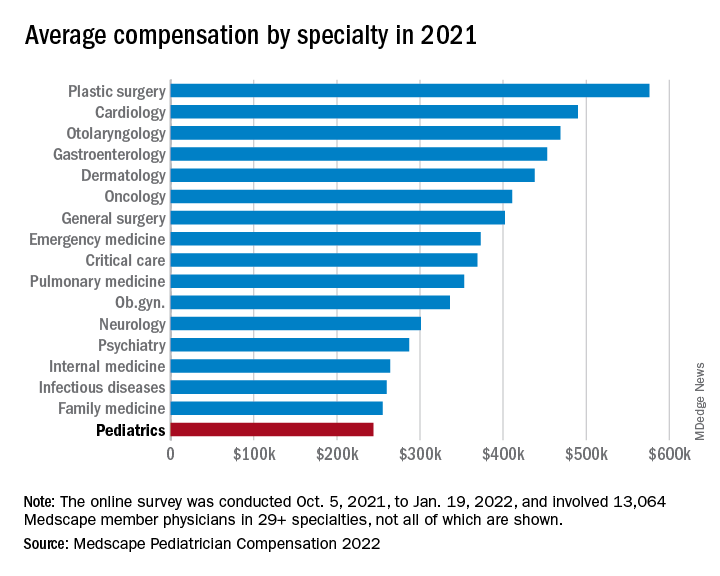
At least some of that positive news can be traced back to the reduced impact of COVID-19. “Compensation for most physicians is trending back up as demand for physicians accelerates. The market for physicians has done a complete 180 over just 7 or 8 months,” James Taylor of AMN Healthcare’s physician and leadership solutions division said in Medscape Pediatrician Compensation Report 2022.
The 10% increase in pediatricians’ income, however, was not enough to reach the average for primary care physicians, $260,000, which was up by 7.4% over 2020. It was enough, though, to move pediatricians from the bottom of the earnings-by-specialty list, where they were last year, to next-to-last this year (public health/preventive medicine, with average earnings of $243,000 in 2021, is not shown in the graph).
The gender gap in earnings left male pediatricians’ income 26% higher than their female counterparts, slightly above the gap of 25% for primary care physicians and 24% for all physicians. For specialists, the gap was 31% in favor of men, based on data from 13,064 Medscape member physicians who participated in the survey, which was conducted online from Oct. 5, 2021, to Jan. 19, 2022. For the record, 57% of the pediatricians who responded were women.
The gaps and low income averages were enough, it seems, to keep pediatricians fairly negative regarding their feelings on compensation. Only 47% think they were fairly compensated in 2021, higher only than diabetes/endocrinology and nephrology. Among the other primary care specialties, internal medicine and ob.gyn. were slightly higher at 49% and family medicine was 55% – still just middle of the pack, compared with public health/preventive medicine at 72%, Medscape said in the report.
Would you do it again?
Moving to the less-economic aspects of the survey, respondents also were asked if they would choose medicine again as a career. Once more pediatricians were low on the scale, as only 70% said that they would enter medicine again, down from 77% last year and lower than this year’s average of 73% average for all physicians.
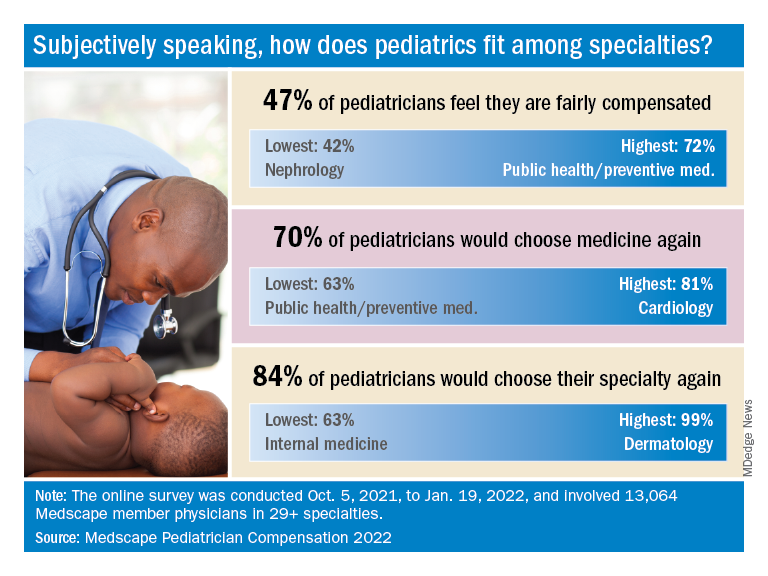
When they were asked if they would choose pediatrics again as a specialty, the response was a bit more positive: 84% said yes. That middle-of-the-pack showing was well ahead of internal medicine (63%) and family medicine (68%), but well below dermatology (99%) and orthopedics (97%), which are “among the top groups in our survey year after year,” Medscape said.
Did the administrative challenges of medical practice have an effect on those answers? Pediatrician respondents said that they spend 14.9 hours per week on paperwork and administration, close to the average of 15.5 hours for all physicians. The internists, who are least likely to choose their original specialty again, spend 18.7 hours on paperwork each week, while dermatologists, the most likely to repeat their first choice, have just 11.9 hours of paperwork per week.
The exact number of pediatricians involved in the survey was not provided, but they made up about 8% of the total cohort, which works out to somewhere between 1,000 and 1,100 individuals. All respondents had to be practicing in the United States, and compensation was analyzed for full-time physicians only. The sampling error is ±0.86% at a 95% confidence level.
In an unprecedented year when income increased for all specialties, pediatricians did better than most, according to a recent survey by Medscape.
. Medscape also noted that, for the first time in the 11 years it’s been conducting these physician compensation surveys, “all specialties have seen an increase in income.”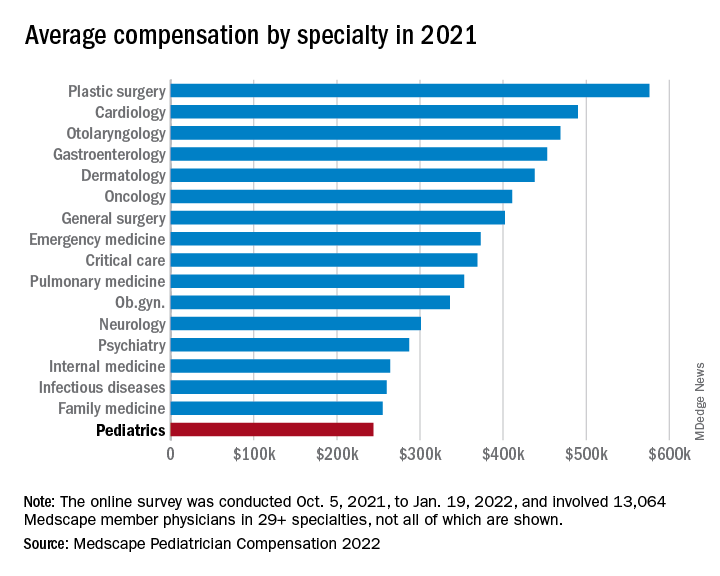
At least some of that positive news can be traced back to the reduced impact of COVID-19. “Compensation for most physicians is trending back up as demand for physicians accelerates. The market for physicians has done a complete 180 over just 7 or 8 months,” James Taylor of AMN Healthcare’s physician and leadership solutions division said in Medscape Pediatrician Compensation Report 2022.
The 10% increase in pediatricians’ income, however, was not enough to reach the average for primary care physicians, $260,000, which was up by 7.4% over 2020. It was enough, though, to move pediatricians from the bottom of the earnings-by-specialty list, where they were last year, to next-to-last this year (public health/preventive medicine, with average earnings of $243,000 in 2021, is not shown in the graph).
The gender gap in earnings left male pediatricians’ income 26% higher than their female counterparts, slightly above the gap of 25% for primary care physicians and 24% for all physicians. For specialists, the gap was 31% in favor of men, based on data from 13,064 Medscape member physicians who participated in the survey, which was conducted online from Oct. 5, 2021, to Jan. 19, 2022. For the record, 57% of the pediatricians who responded were women.
The gaps and low income averages were enough, it seems, to keep pediatricians fairly negative regarding their feelings on compensation. Only 47% think they were fairly compensated in 2021, higher only than diabetes/endocrinology and nephrology. Among the other primary care specialties, internal medicine and ob.gyn. were slightly higher at 49% and family medicine was 55% – still just middle of the pack, compared with public health/preventive medicine at 72%, Medscape said in the report.
Would you do it again?
Moving to the less-economic aspects of the survey, respondents also were asked if they would choose medicine again as a career. Once more pediatricians were low on the scale, as only 70% said that they would enter medicine again, down from 77% last year and lower than this year’s average of 73% average for all physicians.
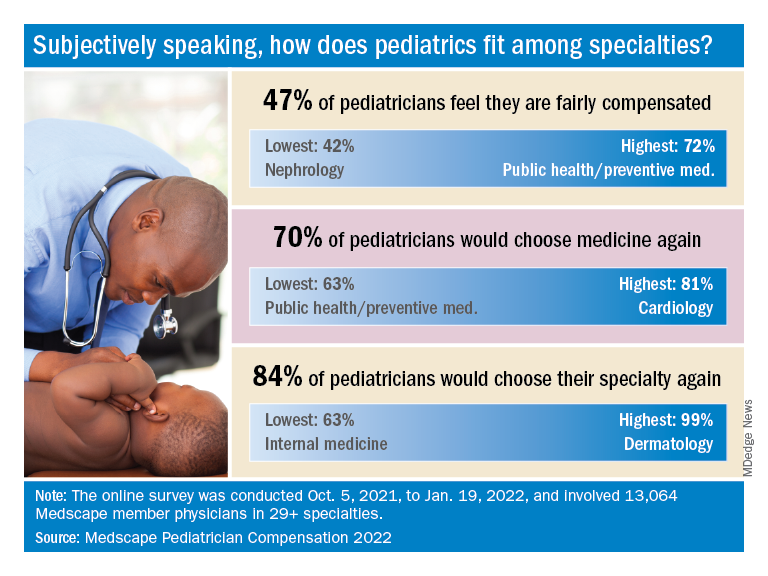
When they were asked if they would choose pediatrics again as a specialty, the response was a bit more positive: 84% said yes. That middle-of-the-pack showing was well ahead of internal medicine (63%) and family medicine (68%), but well below dermatology (99%) and orthopedics (97%), which are “among the top groups in our survey year after year,” Medscape said.
Did the administrative challenges of medical practice have an effect on those answers? Pediatrician respondents said that they spend 14.9 hours per week on paperwork and administration, close to the average of 15.5 hours for all physicians. The internists, who are least likely to choose their original specialty again, spend 18.7 hours on paperwork each week, while dermatologists, the most likely to repeat their first choice, have just 11.9 hours of paperwork per week.
The exact number of pediatricians involved in the survey was not provided, but they made up about 8% of the total cohort, which works out to somewhere between 1,000 and 1,100 individuals. All respondents had to be practicing in the United States, and compensation was analyzed for full-time physicians only. The sampling error is ±0.86% at a 95% confidence level.
How much health insurers pay for almost everything is about to go public
perhaps helping answer a question that has long dogged those who buy insurance: Are we getting the best deal we can?
As of July 1, health insurers and self-insured employers must post on websites just about every price they’ve negotiated with providers for health care services, item by item. About the only thing excluded are the prices paid for prescription drugs, except those administered in hospitals or doctors’ offices.
The federally required data release could affect future prices or even how employers contract for health care. Many will see for the first time how well their insurers are doing, compared with others.
The new rules are far broader than those that went into effect in 2021 requiring hospitals to post their negotiated rates for the public to see. Now insurers must post the amounts paid for “every physician in network, every hospital, every surgery center, every nursing facility,” said Jeffrey Leibach, a partner at the consulting firm Guidehouse.
“When you start doing the math, you’re talking trillions of records,” he said. The fines the federal government could impose for noncompliance are also heftier than the penalties that hospitals face.
Federal officials learned from the hospital experience and gave insurers more direction on what was expected, said Mr. Leibach. Insurers or self-insured employers could be fined as much as $100 a day for each violation, for each affected enrollee if they fail to provide the data.
“Get your calculator out: All of a sudden you are in the millions pretty fast,” Mr. Leibach said.
Determined consumers, especially those with high-deductible health plans, may try to dig in right away and use the data to try comparing what they will have to pay at different hospitals, clinics, or doctor offices for specific services.
But each database’s enormous size may mean that most people “will find it very hard to use the data in a nuanced way,” said Katherine Baicker, dean of the University of Chicago Harris School of Public Policy.
At least at first.
Entrepreneurs are expected to quickly translate the information into more user-friendly formats so it can be incorporated into new or existing services that estimate costs for patients. And starting Jan. 1, the rules require insurers to provide online tools that will help people get up-front cost estimates for about 500 so-called “shoppable” services, meaning medical care they can schedule ahead of time.
Once those things happen, “you’ll at least have the options in front of you,” said Chris Severn, CEO of Turquoise Health, an online company that has posted price information made available under the rules for hospitals, although many hospitals have yet to comply.
With the addition of the insurers’ data, sites like his will be able to drill down further into cost variation from one place to another or among insurers.
“If you’re going to get an x-ray, you will be able to see that you can do it for $250 at this hospital, $75 at the imaging center down the road, or your specialist can do it in office for $25,” he said.
Everyone will know everyone else’s business: for example, how much insurers Aetna and Humana pay the same surgery center for a knee replacement.
The requirements stem from the Affordable Care Act and a 2019 executive order by then-President Donald Trump.
“These plans are supposed to be acting on behalf of employers in negotiating good rates, and the little insight we have on that shows it has not happened,” said Elizabeth Mitchell, president and CEO of the Purchaser Business Group on Health, an affiliation of employers who offer job-based health benefits to workers. “I do believe the dynamics are going to change.”
Other observers are more circumspect.
“Maybe at best this will reduce the wide variance of prices out there,” said Zack Cooper, director of health policy at the Yale University Institution for Social and Policy Studies, New Haven, Conn. “But it won’t be unleashing a consumer revolution.”
Still, the biggest value of the July data release may well be to shed light on how successful insurers have been at negotiating prices. It comes on the heels of research that has shown tremendous variation in what is paid for health care. A recent study by Rand, for example, shows that employers that offer job-based insurance plans paid, on average, 224% more than Medicare for the same services.
Tens of thousands of employers who buy insurance coverage for their workers will get this more-complete pricing picture – and may not like what they see.
“What we’re learning from the hospital data is that insurers are really bad at negotiating,” said Gerard Anderson, a professor in the department of health policy at the Johns Hopkins Bloomberg, Baltimore, citing research that found that negotiated rates for hospital care can be higher than what the facilities accept from patients who are not using insurance and are paying cash.
That could add to the frustration that Ms. Mitchell and others say employers have with the current health insurance system. More might try to contract with providers directly, only using insurance companies for claims processing.
Other employers may bring their insurers back to the bargaining table.
“For the first time, an employer will be able to go to an insurance company and say: ‘You have not negotiated a good-enough deal, and we know that because we can see the same provider has negotiated a better deal with another company,’ ” said James Gelfand, president of the ERISA Industry Committee, a trade group of self-insured employers.
If that happens, he added, “patients will be able to save money.”
That’s not necessarily a given, however.
Because this kind of public release of pricing data hasn’t been tried widely in health care before, how it will affect future spending remains uncertain. If insurers are pushed back to the bargaining table or providers see where they stand relative to their peers, prices could drop. However, some providers could raise their prices if they see they are charging less than their peers.
“Downward pressure may not be a given,” said Kelley Schultz, vice president of commercial policy for AHIP, the industry’s trade lobby.
Ms. Baicker said that, even after the data is out, rates will continue to be heavily influenced by local conditions, such as the size of an insurer or employer – providers often give bigger discounts, for example, to the insurers or self-insured employers that can send them the most patients. The number of hospitals in a region also matters – if an area has only one, for instance, that usually means the facility can demand higher rates.
Another unknown: Will insurers meet the deadline and provide usable data?
Ms. Schultz, at AHIP, said the industry is well on the way, partly because the original deadline was extended by 6 months. She expects insurers to do better than the hospital industry. “We saw a lot of hospitals that just decided not to post files or make them difficult to find,” she said.
So far, more than 300 noncompliant hospitals received warning letters from the government. But they could face fines of $300 a day fines for failing to comply, which is less than what insurers potentially face, although the federal government has recently upped the ante to up to $5,500 a day for the largest facilities.
Even after the pricing data is public, “I don’t think things will change overnight,” said Mr. Leibach. “Patients are still going to make care decisions based on their doctors and referrals, a lot of reasons other than price.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
perhaps helping answer a question that has long dogged those who buy insurance: Are we getting the best deal we can?
As of July 1, health insurers and self-insured employers must post on websites just about every price they’ve negotiated with providers for health care services, item by item. About the only thing excluded are the prices paid for prescription drugs, except those administered in hospitals or doctors’ offices.
The federally required data release could affect future prices or even how employers contract for health care. Many will see for the first time how well their insurers are doing, compared with others.
The new rules are far broader than those that went into effect in 2021 requiring hospitals to post their negotiated rates for the public to see. Now insurers must post the amounts paid for “every physician in network, every hospital, every surgery center, every nursing facility,” said Jeffrey Leibach, a partner at the consulting firm Guidehouse.
“When you start doing the math, you’re talking trillions of records,” he said. The fines the federal government could impose for noncompliance are also heftier than the penalties that hospitals face.
Federal officials learned from the hospital experience and gave insurers more direction on what was expected, said Mr. Leibach. Insurers or self-insured employers could be fined as much as $100 a day for each violation, for each affected enrollee if they fail to provide the data.
“Get your calculator out: All of a sudden you are in the millions pretty fast,” Mr. Leibach said.
Determined consumers, especially those with high-deductible health plans, may try to dig in right away and use the data to try comparing what they will have to pay at different hospitals, clinics, or doctor offices for specific services.
But each database’s enormous size may mean that most people “will find it very hard to use the data in a nuanced way,” said Katherine Baicker, dean of the University of Chicago Harris School of Public Policy.
At least at first.
Entrepreneurs are expected to quickly translate the information into more user-friendly formats so it can be incorporated into new or existing services that estimate costs for patients. And starting Jan. 1, the rules require insurers to provide online tools that will help people get up-front cost estimates for about 500 so-called “shoppable” services, meaning medical care they can schedule ahead of time.
Once those things happen, “you’ll at least have the options in front of you,” said Chris Severn, CEO of Turquoise Health, an online company that has posted price information made available under the rules for hospitals, although many hospitals have yet to comply.
With the addition of the insurers’ data, sites like his will be able to drill down further into cost variation from one place to another or among insurers.
“If you’re going to get an x-ray, you will be able to see that you can do it for $250 at this hospital, $75 at the imaging center down the road, or your specialist can do it in office for $25,” he said.
Everyone will know everyone else’s business: for example, how much insurers Aetna and Humana pay the same surgery center for a knee replacement.
The requirements stem from the Affordable Care Act and a 2019 executive order by then-President Donald Trump.
“These plans are supposed to be acting on behalf of employers in negotiating good rates, and the little insight we have on that shows it has not happened,” said Elizabeth Mitchell, president and CEO of the Purchaser Business Group on Health, an affiliation of employers who offer job-based health benefits to workers. “I do believe the dynamics are going to change.”
Other observers are more circumspect.
“Maybe at best this will reduce the wide variance of prices out there,” said Zack Cooper, director of health policy at the Yale University Institution for Social and Policy Studies, New Haven, Conn. “But it won’t be unleashing a consumer revolution.”
Still, the biggest value of the July data release may well be to shed light on how successful insurers have been at negotiating prices. It comes on the heels of research that has shown tremendous variation in what is paid for health care. A recent study by Rand, for example, shows that employers that offer job-based insurance plans paid, on average, 224% more than Medicare for the same services.
Tens of thousands of employers who buy insurance coverage for their workers will get this more-complete pricing picture – and may not like what they see.
“What we’re learning from the hospital data is that insurers are really bad at negotiating,” said Gerard Anderson, a professor in the department of health policy at the Johns Hopkins Bloomberg, Baltimore, citing research that found that negotiated rates for hospital care can be higher than what the facilities accept from patients who are not using insurance and are paying cash.
That could add to the frustration that Ms. Mitchell and others say employers have with the current health insurance system. More might try to contract with providers directly, only using insurance companies for claims processing.
Other employers may bring their insurers back to the bargaining table.
“For the first time, an employer will be able to go to an insurance company and say: ‘You have not negotiated a good-enough deal, and we know that because we can see the same provider has negotiated a better deal with another company,’ ” said James Gelfand, president of the ERISA Industry Committee, a trade group of self-insured employers.
If that happens, he added, “patients will be able to save money.”
That’s not necessarily a given, however.
Because this kind of public release of pricing data hasn’t been tried widely in health care before, how it will affect future spending remains uncertain. If insurers are pushed back to the bargaining table or providers see where they stand relative to their peers, prices could drop. However, some providers could raise their prices if they see they are charging less than their peers.
“Downward pressure may not be a given,” said Kelley Schultz, vice president of commercial policy for AHIP, the industry’s trade lobby.
Ms. Baicker said that, even after the data is out, rates will continue to be heavily influenced by local conditions, such as the size of an insurer or employer – providers often give bigger discounts, for example, to the insurers or self-insured employers that can send them the most patients. The number of hospitals in a region also matters – if an area has only one, for instance, that usually means the facility can demand higher rates.
Another unknown: Will insurers meet the deadline and provide usable data?
Ms. Schultz, at AHIP, said the industry is well on the way, partly because the original deadline was extended by 6 months. She expects insurers to do better than the hospital industry. “We saw a lot of hospitals that just decided not to post files or make them difficult to find,” she said.
So far, more than 300 noncompliant hospitals received warning letters from the government. But they could face fines of $300 a day fines for failing to comply, which is less than what insurers potentially face, although the federal government has recently upped the ante to up to $5,500 a day for the largest facilities.
Even after the pricing data is public, “I don’t think things will change overnight,” said Mr. Leibach. “Patients are still going to make care decisions based on their doctors and referrals, a lot of reasons other than price.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
perhaps helping answer a question that has long dogged those who buy insurance: Are we getting the best deal we can?
As of July 1, health insurers and self-insured employers must post on websites just about every price they’ve negotiated with providers for health care services, item by item. About the only thing excluded are the prices paid for prescription drugs, except those administered in hospitals or doctors’ offices.
The federally required data release could affect future prices or even how employers contract for health care. Many will see for the first time how well their insurers are doing, compared with others.
The new rules are far broader than those that went into effect in 2021 requiring hospitals to post their negotiated rates for the public to see. Now insurers must post the amounts paid for “every physician in network, every hospital, every surgery center, every nursing facility,” said Jeffrey Leibach, a partner at the consulting firm Guidehouse.
“When you start doing the math, you’re talking trillions of records,” he said. The fines the federal government could impose for noncompliance are also heftier than the penalties that hospitals face.
Federal officials learned from the hospital experience and gave insurers more direction on what was expected, said Mr. Leibach. Insurers or self-insured employers could be fined as much as $100 a day for each violation, for each affected enrollee if they fail to provide the data.
“Get your calculator out: All of a sudden you are in the millions pretty fast,” Mr. Leibach said.
Determined consumers, especially those with high-deductible health plans, may try to dig in right away and use the data to try comparing what they will have to pay at different hospitals, clinics, or doctor offices for specific services.
But each database’s enormous size may mean that most people “will find it very hard to use the data in a nuanced way,” said Katherine Baicker, dean of the University of Chicago Harris School of Public Policy.
At least at first.
Entrepreneurs are expected to quickly translate the information into more user-friendly formats so it can be incorporated into new or existing services that estimate costs for patients. And starting Jan. 1, the rules require insurers to provide online tools that will help people get up-front cost estimates for about 500 so-called “shoppable” services, meaning medical care they can schedule ahead of time.
Once those things happen, “you’ll at least have the options in front of you,” said Chris Severn, CEO of Turquoise Health, an online company that has posted price information made available under the rules for hospitals, although many hospitals have yet to comply.
With the addition of the insurers’ data, sites like his will be able to drill down further into cost variation from one place to another or among insurers.
“If you’re going to get an x-ray, you will be able to see that you can do it for $250 at this hospital, $75 at the imaging center down the road, or your specialist can do it in office for $25,” he said.
Everyone will know everyone else’s business: for example, how much insurers Aetna and Humana pay the same surgery center for a knee replacement.
The requirements stem from the Affordable Care Act and a 2019 executive order by then-President Donald Trump.
“These plans are supposed to be acting on behalf of employers in negotiating good rates, and the little insight we have on that shows it has not happened,” said Elizabeth Mitchell, president and CEO of the Purchaser Business Group on Health, an affiliation of employers who offer job-based health benefits to workers. “I do believe the dynamics are going to change.”
Other observers are more circumspect.
“Maybe at best this will reduce the wide variance of prices out there,” said Zack Cooper, director of health policy at the Yale University Institution for Social and Policy Studies, New Haven, Conn. “But it won’t be unleashing a consumer revolution.”
Still, the biggest value of the July data release may well be to shed light on how successful insurers have been at negotiating prices. It comes on the heels of research that has shown tremendous variation in what is paid for health care. A recent study by Rand, for example, shows that employers that offer job-based insurance plans paid, on average, 224% more than Medicare for the same services.
Tens of thousands of employers who buy insurance coverage for their workers will get this more-complete pricing picture – and may not like what they see.
“What we’re learning from the hospital data is that insurers are really bad at negotiating,” said Gerard Anderson, a professor in the department of health policy at the Johns Hopkins Bloomberg, Baltimore, citing research that found that negotiated rates for hospital care can be higher than what the facilities accept from patients who are not using insurance and are paying cash.
That could add to the frustration that Ms. Mitchell and others say employers have with the current health insurance system. More might try to contract with providers directly, only using insurance companies for claims processing.
Other employers may bring their insurers back to the bargaining table.
“For the first time, an employer will be able to go to an insurance company and say: ‘You have not negotiated a good-enough deal, and we know that because we can see the same provider has negotiated a better deal with another company,’ ” said James Gelfand, president of the ERISA Industry Committee, a trade group of self-insured employers.
If that happens, he added, “patients will be able to save money.”
That’s not necessarily a given, however.
Because this kind of public release of pricing data hasn’t been tried widely in health care before, how it will affect future spending remains uncertain. If insurers are pushed back to the bargaining table or providers see where they stand relative to their peers, prices could drop. However, some providers could raise their prices if they see they are charging less than their peers.
“Downward pressure may not be a given,” said Kelley Schultz, vice president of commercial policy for AHIP, the industry’s trade lobby.
Ms. Baicker said that, even after the data is out, rates will continue to be heavily influenced by local conditions, such as the size of an insurer or employer – providers often give bigger discounts, for example, to the insurers or self-insured employers that can send them the most patients. The number of hospitals in a region also matters – if an area has only one, for instance, that usually means the facility can demand higher rates.
Another unknown: Will insurers meet the deadline and provide usable data?
Ms. Schultz, at AHIP, said the industry is well on the way, partly because the original deadline was extended by 6 months. She expects insurers to do better than the hospital industry. “We saw a lot of hospitals that just decided not to post files or make them difficult to find,” she said.
So far, more than 300 noncompliant hospitals received warning letters from the government. But they could face fines of $300 a day fines for failing to comply, which is less than what insurers potentially face, although the federal government has recently upped the ante to up to $5,500 a day for the largest facilities.
Even after the pricing data is public, “I don’t think things will change overnight,” said Mr. Leibach. “Patients are still going to make care decisions based on their doctors and referrals, a lot of reasons other than price.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Abortion opponents don’t want patients crossing state lines
Several national antiabortion advocacy groups and lawmakers in Republican-led states are pushing forward with plans to block people from crossing state lines to seek the procedure elsewhere.
Since the Supreme Court overturned Roe v. Wade last week, several states have enacted "trigger ban" laws to stop abortion, particularly across the Southeast and Midwest. As part of that, antiabortion groups are building momentum around the idea of blocking out-of-state travel as well, even discussing it at two national antiabortion conferences last weekend, according to The Washington Post.
"Just because you jump across a state line doesn't mean your home state doesn't have jurisdiction," Peter Breen, vice president and senior counsel for the Thomas More Society, told the newspaper.
"It's not a free abortion card when you drive across the state line," he said.
The Thomas More Society, a conservative legal organization, is drafting model legislation for state lawmakers to use, which would allow private citizens to sue anyone who helps a resident end a pregnancy outside of a state that has banned abortion. The draft language borrows from the recent Texas abortion ban, which allows private citizens to enforce the law through civil litigation.
The National Association of Christian Lawmakers, an antiabortion organization led by Republican state legislators, has also begun working with the authors of the Texas abortion ban, the Post reported. The group is exploring model legislation that would restrict people from crossing state lines for abortions.
Relying on private citizens to enforce civil litigation, rather than imposing a state-enforced ban on crossing state lines, could make these laws more difficult to challenge in court.
What's more, the legislation could have a chilling effect on doctors, who may stop performing abortions on people from other states while waiting on courts to intervene and overturn the laws, the newspaper reported.
Not every antiabortion group is supporting the idea. Catherine Glenn Foster, president of Americans United for Life, said that people access medical procedures across state lines often.
"I don't think you can prevent that," she said.
But some states may still propose these types of bills this year. Legislators in Arkansas and South Dakota, for instance, have already planned special sessions to discuss abortion legislation, which could include the issue. Lawmakers in Missouri have also supported the idea.
In contrast, several Democrat-led states have passed legislation this year to counteract laws that may try to restrict movement across state lines, according to the Post. Connecticut passed a law that offers protection from out-of-state subpoenas issued in cases related to abortion procedures that are legal in the state, and California passed a similar law to protect abortion providers and patients from civil suits.
The Justice Department has warned that it will fight laws that block people from crossing state lines, saying they violate the right to interstate commerce.
"The Constitution continues to restrict states' authority to ban reproductive services provided outside their borders," Attorney General Merrick Garland said in a statement after last week's ruling.
"We recognize that traveling to obtain reproductive care may not be feasible in many circumstances," he said. "But under bedrock constitutional principles, women who reside in states that have banned access to comprehensive reproductive care must remain free to seek that care in states where it is legal."
A version of this article first appeared on WebMD.com.
Several national antiabortion advocacy groups and lawmakers in Republican-led states are pushing forward with plans to block people from crossing state lines to seek the procedure elsewhere.
Since the Supreme Court overturned Roe v. Wade last week, several states have enacted "trigger ban" laws to stop abortion, particularly across the Southeast and Midwest. As part of that, antiabortion groups are building momentum around the idea of blocking out-of-state travel as well, even discussing it at two national antiabortion conferences last weekend, according to The Washington Post.
"Just because you jump across a state line doesn't mean your home state doesn't have jurisdiction," Peter Breen, vice president and senior counsel for the Thomas More Society, told the newspaper.
"It's not a free abortion card when you drive across the state line," he said.
The Thomas More Society, a conservative legal organization, is drafting model legislation for state lawmakers to use, which would allow private citizens to sue anyone who helps a resident end a pregnancy outside of a state that has banned abortion. The draft language borrows from the recent Texas abortion ban, which allows private citizens to enforce the law through civil litigation.
The National Association of Christian Lawmakers, an antiabortion organization led by Republican state legislators, has also begun working with the authors of the Texas abortion ban, the Post reported. The group is exploring model legislation that would restrict people from crossing state lines for abortions.
Relying on private citizens to enforce civil litigation, rather than imposing a state-enforced ban on crossing state lines, could make these laws more difficult to challenge in court.
What's more, the legislation could have a chilling effect on doctors, who may stop performing abortions on people from other states while waiting on courts to intervene and overturn the laws, the newspaper reported.
Not every antiabortion group is supporting the idea. Catherine Glenn Foster, president of Americans United for Life, said that people access medical procedures across state lines often.
"I don't think you can prevent that," she said.
But some states may still propose these types of bills this year. Legislators in Arkansas and South Dakota, for instance, have already planned special sessions to discuss abortion legislation, which could include the issue. Lawmakers in Missouri have also supported the idea.
In contrast, several Democrat-led states have passed legislation this year to counteract laws that may try to restrict movement across state lines, according to the Post. Connecticut passed a law that offers protection from out-of-state subpoenas issued in cases related to abortion procedures that are legal in the state, and California passed a similar law to protect abortion providers and patients from civil suits.
The Justice Department has warned that it will fight laws that block people from crossing state lines, saying they violate the right to interstate commerce.
"The Constitution continues to restrict states' authority to ban reproductive services provided outside their borders," Attorney General Merrick Garland said in a statement after last week's ruling.
"We recognize that traveling to obtain reproductive care may not be feasible in many circumstances," he said. "But under bedrock constitutional principles, women who reside in states that have banned access to comprehensive reproductive care must remain free to seek that care in states where it is legal."
A version of this article first appeared on WebMD.com.
Several national antiabortion advocacy groups and lawmakers in Republican-led states are pushing forward with plans to block people from crossing state lines to seek the procedure elsewhere.
Since the Supreme Court overturned Roe v. Wade last week, several states have enacted "trigger ban" laws to stop abortion, particularly across the Southeast and Midwest. As part of that, antiabortion groups are building momentum around the idea of blocking out-of-state travel as well, even discussing it at two national antiabortion conferences last weekend, according to The Washington Post.
"Just because you jump across a state line doesn't mean your home state doesn't have jurisdiction," Peter Breen, vice president and senior counsel for the Thomas More Society, told the newspaper.
"It's not a free abortion card when you drive across the state line," he said.
The Thomas More Society, a conservative legal organization, is drafting model legislation for state lawmakers to use, which would allow private citizens to sue anyone who helps a resident end a pregnancy outside of a state that has banned abortion. The draft language borrows from the recent Texas abortion ban, which allows private citizens to enforce the law through civil litigation.
The National Association of Christian Lawmakers, an antiabortion organization led by Republican state legislators, has also begun working with the authors of the Texas abortion ban, the Post reported. The group is exploring model legislation that would restrict people from crossing state lines for abortions.
Relying on private citizens to enforce civil litigation, rather than imposing a state-enforced ban on crossing state lines, could make these laws more difficult to challenge in court.
What's more, the legislation could have a chilling effect on doctors, who may stop performing abortions on people from other states while waiting on courts to intervene and overturn the laws, the newspaper reported.
Not every antiabortion group is supporting the idea. Catherine Glenn Foster, president of Americans United for Life, said that people access medical procedures across state lines often.
"I don't think you can prevent that," she said.
But some states may still propose these types of bills this year. Legislators in Arkansas and South Dakota, for instance, have already planned special sessions to discuss abortion legislation, which could include the issue. Lawmakers in Missouri have also supported the idea.
In contrast, several Democrat-led states have passed legislation this year to counteract laws that may try to restrict movement across state lines, according to the Post. Connecticut passed a law that offers protection from out-of-state subpoenas issued in cases related to abortion procedures that are legal in the state, and California passed a similar law to protect abortion providers and patients from civil suits.
The Justice Department has warned that it will fight laws that block people from crossing state lines, saying they violate the right to interstate commerce.
"The Constitution continues to restrict states' authority to ban reproductive services provided outside their borders," Attorney General Merrick Garland said in a statement after last week's ruling.
"We recognize that traveling to obtain reproductive care may not be feasible in many circumstances," he said. "But under bedrock constitutional principles, women who reside in states that have banned access to comprehensive reproductive care must remain free to seek that care in states where it is legal."
A version of this article first appeared on WebMD.com.
Primary care providers miss out on payments for prevention, coordination
According to the new research, primary care physicians used these codes for a median of only 2.3% of services provided to eligible patients.
“Investing in primary care is good for the health of patients, for achieving health equity, and for improving the value of health care spending, and yet the U.S. underinvests in primary care,” lead author Sumit D. Agarwal, MD, of Brigham and Women’s Hospital, Boston, said in an interview.
“One strategy to rectify this has been to add billing codes to the physician fee schedule for PCPs to use and thus raise primary care spending; Medicare has been activating new codes for the better part of 2 decades, and we wanted to investigate how successful this strategy of adding codes to the Medicare Physician Fee Schedule (MPFS) schedule has been to inform discussions on how best to finance primary care in the United States,” he said.
In a study published in Annals of Internal Medicine, Dr. Agarwal and colleagues reviewed nationally representative claims and survey data from 2019 and 2020. They analyzed 34 distinct prevention and coordination codes in 13 categories that have been added the MPFS since 2005. Of these, four involved coordination of care (cognitive impairment, behavioral health integration, chronic care management, and transitional care management). The other nine categories in prevention were wellness visits, advance care planning, shared decision making for lung cancer screening, obesity counseling, behavioral counseling for CVD, depression screening, alcohol misuse counseling, alcohol misuse screening, and smoking cessation counseling.
Overall, 8.8%-100% of older adult patients were eligible for preventive services. A range of patients (5.0%-60.6%) had codes for receiving services in their patient information.
“However, a much smaller fraction of eligible patients was billed for having received the service, ranging from less than 1% for alcohol misuse counseling or obesity counseling to 35.8% for wellness visits, with most below 10%,” the researchers wrote.
The median use of billing codes was 2.3% for eligible patients.
A PCP who provided and billed preventive services to half of all eligible patients could potentially increase revenues of $1,269 to $45,406 per code, with an annual revenue increase of $124,435 (interquartile range $30,654 to $226,813) for prevention services. Similarly, providing and billing coordination of care service to half of all eligible patients could increase revenue by $86,082 (IQR, $18,011 to $154,152).
“Importantly, all of these prevention and coordination codes involve decomposing the comprehensive care of a patient into component parts, each with multiple steps and checklists, which may be inconsistent with how PCPs practice and document care,” the researchers wrote in their discussion. “Unlike hospitals, primary care practices are typically unable to use departments of trained coders to maximize billing and ensure that documentation matches the requirements specified in billing rules,” they added.
The study findings were limited by several factors including the focus only on the Medicare segment of PCPs’ panels, which suggests conservative estimates of reimbursement, the researchers noted. Other limitations include response bias to the use of surveys, lack of survey data on specific billing requirements, and the potential underestimation of services by PCPs who delivered some, but not all, components of a service code.
However, the results reflect previous research to show the underutilization of prevention and coordination codes in primary care, and the need for ways to increase their use, the researchers said. “The discrepancies between service eligibility, provision of services regardless of billing, and actual billing suggest that attempting to codify each distinct activity done by a PCP in the MPFS may not be an effective strategy for supporting primary care,” they concluded.
Barriers to code use persist for PCPs
“What surprised us was that there were many codes; we analyzed 34 in the paper in 13 distinct categories of services, and Medicare continues to add new primary care codes to the fee schedule,” Dr. Agarwal said in an interview. Also surprising, “take-up is low virtually across the board, and this isn’t for lack of eligibility,” he said. The low use of the codes “is not for lack of counseling patients on diet, drinking, exercise, smoking, or anything else for which these codes are meant to pay PCPs ... The potential revenue from these codes in aggregate is huge,” Dr. Agarwal emphasized.
“My hope is not necessarily that physicians read this study and start using some or all of these codes more frequently,” said Dr. Agarwal. “It can be tempting to think of this as money left on the table, but it’s not; there are compliance, billing, and opportunity costs from using these codes,” he said. “For individual PCPs seeing individual patients for the breadth that is primary care, I’m not sure the juice is worth the squeeze,” he added. “My coauthors and I are all primary care physicians. We know from our research and first-hand that these codes can be cumbersome to use.” These codes also don’t reflect how PCPs practice, he said. “PCPs are not in the business of slicing and dicing a visit or patient to extract as much revenue as possible. The physician-patient interaction is more complex, and richer, than these codes imply. Instead, I hope our paper encourages Medicare and policymakers to take a harder look at other strategies for investing in primary care,” Dr. Agarwal added.
As for additional research, “Primary care spending is going in the wrong direction,” said Dr. Agarwal. “We need to figure out how best to finance primary care in the United States.”
Recent studies have examined the successes and limitations of the primary care medical home model, Medicare’s Comprehensive Primary Care Initiative, and primary care spending legislation, he said. “Our study is another piece of the puzzle: at least in its current form,” and the results suggest “that one-off codes were nice in theory but not in practice,” he noted.
New codes are cumbersome
“It’s tempting to interpret underuse of new billing codes as a simple change management problem,” Davoren Chick, MD, chief learning officer of the American College of Physicians, wrote in an accompanying editorial. However, the underuse of codes for preventive service and coordination of care likely stems from the details of the codes, he said.
The new codes require the documentation of specific components and a minimum duration of services, he explained. “Codes that reward discrete service episodes disadvantage physicians who appropriately integrate preventive services within a continuous patient care relationship,” he added.
Dr. Chick presented an example of a primary care physician who would have to deliver intensive behavioral therapy for obesity in 15-minute episodes outside of a routine office visit to meet the billing criteria for current Medicare codes.
Dr. Chick called on clinicians to educate themselves on the coding rules for the services they provide “not only to optimize current payment but also to advocate for change.”
He concluded: “Widespread underuse of new preventive service and coordination of care codes reflects system failure, not physician failure. We must stand firm with this knowledge to demand increased payment for feasible, patient-centered primary care commensurate with its value in achieving better outcomes and lower costs.”
The study was supported by the National Institute on Aging of the National Institutes of Health. Dr. Agarwal and Dr. Chick had no financial conflicts to disclose.
According to the new research, primary care physicians used these codes for a median of only 2.3% of services provided to eligible patients.
“Investing in primary care is good for the health of patients, for achieving health equity, and for improving the value of health care spending, and yet the U.S. underinvests in primary care,” lead author Sumit D. Agarwal, MD, of Brigham and Women’s Hospital, Boston, said in an interview.
“One strategy to rectify this has been to add billing codes to the physician fee schedule for PCPs to use and thus raise primary care spending; Medicare has been activating new codes for the better part of 2 decades, and we wanted to investigate how successful this strategy of adding codes to the Medicare Physician Fee Schedule (MPFS) schedule has been to inform discussions on how best to finance primary care in the United States,” he said.
In a study published in Annals of Internal Medicine, Dr. Agarwal and colleagues reviewed nationally representative claims and survey data from 2019 and 2020. They analyzed 34 distinct prevention and coordination codes in 13 categories that have been added the MPFS since 2005. Of these, four involved coordination of care (cognitive impairment, behavioral health integration, chronic care management, and transitional care management). The other nine categories in prevention were wellness visits, advance care planning, shared decision making for lung cancer screening, obesity counseling, behavioral counseling for CVD, depression screening, alcohol misuse counseling, alcohol misuse screening, and smoking cessation counseling.
Overall, 8.8%-100% of older adult patients were eligible for preventive services. A range of patients (5.0%-60.6%) had codes for receiving services in their patient information.
“However, a much smaller fraction of eligible patients was billed for having received the service, ranging from less than 1% for alcohol misuse counseling or obesity counseling to 35.8% for wellness visits, with most below 10%,” the researchers wrote.
The median use of billing codes was 2.3% for eligible patients.
A PCP who provided and billed preventive services to half of all eligible patients could potentially increase revenues of $1,269 to $45,406 per code, with an annual revenue increase of $124,435 (interquartile range $30,654 to $226,813) for prevention services. Similarly, providing and billing coordination of care service to half of all eligible patients could increase revenue by $86,082 (IQR, $18,011 to $154,152).
“Importantly, all of these prevention and coordination codes involve decomposing the comprehensive care of a patient into component parts, each with multiple steps and checklists, which may be inconsistent with how PCPs practice and document care,” the researchers wrote in their discussion. “Unlike hospitals, primary care practices are typically unable to use departments of trained coders to maximize billing and ensure that documentation matches the requirements specified in billing rules,” they added.
The study findings were limited by several factors including the focus only on the Medicare segment of PCPs’ panels, which suggests conservative estimates of reimbursement, the researchers noted. Other limitations include response bias to the use of surveys, lack of survey data on specific billing requirements, and the potential underestimation of services by PCPs who delivered some, but not all, components of a service code.
However, the results reflect previous research to show the underutilization of prevention and coordination codes in primary care, and the need for ways to increase their use, the researchers said. “The discrepancies between service eligibility, provision of services regardless of billing, and actual billing suggest that attempting to codify each distinct activity done by a PCP in the MPFS may not be an effective strategy for supporting primary care,” they concluded.
Barriers to code use persist for PCPs
“What surprised us was that there were many codes; we analyzed 34 in the paper in 13 distinct categories of services, and Medicare continues to add new primary care codes to the fee schedule,” Dr. Agarwal said in an interview. Also surprising, “take-up is low virtually across the board, and this isn’t for lack of eligibility,” he said. The low use of the codes “is not for lack of counseling patients on diet, drinking, exercise, smoking, or anything else for which these codes are meant to pay PCPs ... The potential revenue from these codes in aggregate is huge,” Dr. Agarwal emphasized.
“My hope is not necessarily that physicians read this study and start using some or all of these codes more frequently,” said Dr. Agarwal. “It can be tempting to think of this as money left on the table, but it’s not; there are compliance, billing, and opportunity costs from using these codes,” he said. “For individual PCPs seeing individual patients for the breadth that is primary care, I’m not sure the juice is worth the squeeze,” he added. “My coauthors and I are all primary care physicians. We know from our research and first-hand that these codes can be cumbersome to use.” These codes also don’t reflect how PCPs practice, he said. “PCPs are not in the business of slicing and dicing a visit or patient to extract as much revenue as possible. The physician-patient interaction is more complex, and richer, than these codes imply. Instead, I hope our paper encourages Medicare and policymakers to take a harder look at other strategies for investing in primary care,” Dr. Agarwal added.
As for additional research, “Primary care spending is going in the wrong direction,” said Dr. Agarwal. “We need to figure out how best to finance primary care in the United States.”
Recent studies have examined the successes and limitations of the primary care medical home model, Medicare’s Comprehensive Primary Care Initiative, and primary care spending legislation, he said. “Our study is another piece of the puzzle: at least in its current form,” and the results suggest “that one-off codes were nice in theory but not in practice,” he noted.
New codes are cumbersome
“It’s tempting to interpret underuse of new billing codes as a simple change management problem,” Davoren Chick, MD, chief learning officer of the American College of Physicians, wrote in an accompanying editorial. However, the underuse of codes for preventive service and coordination of care likely stems from the details of the codes, he said.
The new codes require the documentation of specific components and a minimum duration of services, he explained. “Codes that reward discrete service episodes disadvantage physicians who appropriately integrate preventive services within a continuous patient care relationship,” he added.
Dr. Chick presented an example of a primary care physician who would have to deliver intensive behavioral therapy for obesity in 15-minute episodes outside of a routine office visit to meet the billing criteria for current Medicare codes.
Dr. Chick called on clinicians to educate themselves on the coding rules for the services they provide “not only to optimize current payment but also to advocate for change.”
He concluded: “Widespread underuse of new preventive service and coordination of care codes reflects system failure, not physician failure. We must stand firm with this knowledge to demand increased payment for feasible, patient-centered primary care commensurate with its value in achieving better outcomes and lower costs.”
The study was supported by the National Institute on Aging of the National Institutes of Health. Dr. Agarwal and Dr. Chick had no financial conflicts to disclose.
According to the new research, primary care physicians used these codes for a median of only 2.3% of services provided to eligible patients.
“Investing in primary care is good for the health of patients, for achieving health equity, and for improving the value of health care spending, and yet the U.S. underinvests in primary care,” lead author Sumit D. Agarwal, MD, of Brigham and Women’s Hospital, Boston, said in an interview.
“One strategy to rectify this has been to add billing codes to the physician fee schedule for PCPs to use and thus raise primary care spending; Medicare has been activating new codes for the better part of 2 decades, and we wanted to investigate how successful this strategy of adding codes to the Medicare Physician Fee Schedule (MPFS) schedule has been to inform discussions on how best to finance primary care in the United States,” he said.
In a study published in Annals of Internal Medicine, Dr. Agarwal and colleagues reviewed nationally representative claims and survey data from 2019 and 2020. They analyzed 34 distinct prevention and coordination codes in 13 categories that have been added the MPFS since 2005. Of these, four involved coordination of care (cognitive impairment, behavioral health integration, chronic care management, and transitional care management). The other nine categories in prevention were wellness visits, advance care planning, shared decision making for lung cancer screening, obesity counseling, behavioral counseling for CVD, depression screening, alcohol misuse counseling, alcohol misuse screening, and smoking cessation counseling.
Overall, 8.8%-100% of older adult patients were eligible for preventive services. A range of patients (5.0%-60.6%) had codes for receiving services in their patient information.
“However, a much smaller fraction of eligible patients was billed for having received the service, ranging from less than 1% for alcohol misuse counseling or obesity counseling to 35.8% for wellness visits, with most below 10%,” the researchers wrote.
The median use of billing codes was 2.3% for eligible patients.
A PCP who provided and billed preventive services to half of all eligible patients could potentially increase revenues of $1,269 to $45,406 per code, with an annual revenue increase of $124,435 (interquartile range $30,654 to $226,813) for prevention services. Similarly, providing and billing coordination of care service to half of all eligible patients could increase revenue by $86,082 (IQR, $18,011 to $154,152).
“Importantly, all of these prevention and coordination codes involve decomposing the comprehensive care of a patient into component parts, each with multiple steps and checklists, which may be inconsistent with how PCPs practice and document care,” the researchers wrote in their discussion. “Unlike hospitals, primary care practices are typically unable to use departments of trained coders to maximize billing and ensure that documentation matches the requirements specified in billing rules,” they added.
The study findings were limited by several factors including the focus only on the Medicare segment of PCPs’ panels, which suggests conservative estimates of reimbursement, the researchers noted. Other limitations include response bias to the use of surveys, lack of survey data on specific billing requirements, and the potential underestimation of services by PCPs who delivered some, but not all, components of a service code.
However, the results reflect previous research to show the underutilization of prevention and coordination codes in primary care, and the need for ways to increase their use, the researchers said. “The discrepancies between service eligibility, provision of services regardless of billing, and actual billing suggest that attempting to codify each distinct activity done by a PCP in the MPFS may not be an effective strategy for supporting primary care,” they concluded.
Barriers to code use persist for PCPs
“What surprised us was that there were many codes; we analyzed 34 in the paper in 13 distinct categories of services, and Medicare continues to add new primary care codes to the fee schedule,” Dr. Agarwal said in an interview. Also surprising, “take-up is low virtually across the board, and this isn’t for lack of eligibility,” he said. The low use of the codes “is not for lack of counseling patients on diet, drinking, exercise, smoking, or anything else for which these codes are meant to pay PCPs ... The potential revenue from these codes in aggregate is huge,” Dr. Agarwal emphasized.
“My hope is not necessarily that physicians read this study and start using some or all of these codes more frequently,” said Dr. Agarwal. “It can be tempting to think of this as money left on the table, but it’s not; there are compliance, billing, and opportunity costs from using these codes,” he said. “For individual PCPs seeing individual patients for the breadth that is primary care, I’m not sure the juice is worth the squeeze,” he added. “My coauthors and I are all primary care physicians. We know from our research and first-hand that these codes can be cumbersome to use.” These codes also don’t reflect how PCPs practice, he said. “PCPs are not in the business of slicing and dicing a visit or patient to extract as much revenue as possible. The physician-patient interaction is more complex, and richer, than these codes imply. Instead, I hope our paper encourages Medicare and policymakers to take a harder look at other strategies for investing in primary care,” Dr. Agarwal added.
As for additional research, “Primary care spending is going in the wrong direction,” said Dr. Agarwal. “We need to figure out how best to finance primary care in the United States.”
Recent studies have examined the successes and limitations of the primary care medical home model, Medicare’s Comprehensive Primary Care Initiative, and primary care spending legislation, he said. “Our study is another piece of the puzzle: at least in its current form,” and the results suggest “that one-off codes were nice in theory but not in practice,” he noted.
New codes are cumbersome
“It’s tempting to interpret underuse of new billing codes as a simple change management problem,” Davoren Chick, MD, chief learning officer of the American College of Physicians, wrote in an accompanying editorial. However, the underuse of codes for preventive service and coordination of care likely stems from the details of the codes, he said.
The new codes require the documentation of specific components and a minimum duration of services, he explained. “Codes that reward discrete service episodes disadvantage physicians who appropriately integrate preventive services within a continuous patient care relationship,” he added.
Dr. Chick presented an example of a primary care physician who would have to deliver intensive behavioral therapy for obesity in 15-minute episodes outside of a routine office visit to meet the billing criteria for current Medicare codes.
Dr. Chick called on clinicians to educate themselves on the coding rules for the services they provide “not only to optimize current payment but also to advocate for change.”
He concluded: “Widespread underuse of new preventive service and coordination of care codes reflects system failure, not physician failure. We must stand firm with this knowledge to demand increased payment for feasible, patient-centered primary care commensurate with its value in achieving better outcomes and lower costs.”
The study was supported by the National Institute on Aging of the National Institutes of Health. Dr. Agarwal and Dr. Chick had no financial conflicts to disclose.
FROM ANNALS OF INTERNAL MEDICINE
Early cardiac rehab as effective as later start after sternotomy
Cardiac rehabilitation (CR) started 2 weeks after sternotomy for a cardiac procedure was noninferior to usual care, in which CR starts 6 weeks after the procedure, with a greater improvement in 6-minute walk test outcomes, a randomized study suggests.
There was no difference in adverse events between groups, although the researchers pointed out that the study was not powered specifically for safety outcomes.
“Cardiac surgical techniques have evolved significantly over the last 60 years, leading to improved survival and shorter hospital stays,” Gordon McGregor, PhD, University of Warwick, Coventry, England, told this news organization. “However, sternal precautions and rehabilitation guidelines have not changed accordingly. There has never been a guideline based on empirical evidence to support rehabilitation professionals working with cardiac surgery patients after median sternotomy.”
“By adopting a progressive individualized approach,” he added, “cardiac surgery sternotomy patients can start cardiac rehabilitation up to 4 weeks earlier than current guidance, and thus potentially complete their recovery sooner.”
Results of the Early Initiation of Poststernotomy Cardiac Rehabilitation Exercise Training study were published online in JAMA Cardiology.
In the study, Dr. McGregor and colleagues randomly assigned 158 patients (mean age, 63 years; 84% men) to 8 weeks of 1-hour, twice-weekly supervised CR exercise training starting 2 weeks (early) or 6 weeks (usual care) after sternotomy.
The primary outcome was change in the 6-minute walk test distance from baseline to 10 or 14 weeks after sternotomy, respectively, and 12 months after randomization.
For usual care, training followed British standards: a warm-up with light cardiovascular and mobility exercises; continuous moderate-intensity cardiovascular exercise; a cooldown; functional exercises using resistance machines and free weights; and upper-body exercises designed to prevent sternal and leg wound pain and complications.
There are no specific outpatient CR exercise guidelines for early CR, so study participants followed an individualized exercise program for the first 2-3 weeks after surgery, starting with light mobility and moderate-intensity cardiovascular training when they could do those exercises with minimal discomfort. They then progressed to current British standards, as per usual care.
Forty patients were lost to follow-up, largely because of the pandemic; about half the participants in each group were included in the primary analysis.
Early CR was not inferior to usual care, the authors wrote. The mean change in 6-minute walk distance from baseline to completion of CR was 28 meters greater in the early group than in the usual-care group, and was achieved 4 weeks earlier in the recovery timeline.
Secondary outcomes (functional fitness and quality of life) improved in both groups and between-group differences were not statistically significant, indicating the noninferiority of early CR, the authors noted.
Safety not proven
There were more adverse events in the early group than in the usual-care group (58 vs. 46) and more serious adverse events (18 vs. 14), but fewer deaths (1 vs. 2).
Although there was no between-group difference in the likelihood of having an adverse or serious adverse event, Dr. McGregor acknowledged that the study was “not powered specifically for safety outcomes.” He added that “there is the potential to run a very large multination definitive superiority [randomized, controlled trial] with safety as the primary outcome; however, a very large sample would be required.”
Meanwhile, he said, “we can say with some degree of certainty that early CR was likely as safe as usual-care CR. In the United Kingdom, we work closely with the British Association for Cardiovascular Prevention and Rehabilitation and the Association of Chartered Physiotherapists in Cardiovascular Rehabilitation, who will incorporate our findings in their guidelines and training courses.”
Questions remain
Asked to comment on the study, John Larry, MD, medical director of cardiology and cardiac rehabilitation at the Ohio State University Wexner Medical Center East Hospital, Columbus, said: “For those under time pressure to return to work, [early CR] could be an advantage to allow more rehab time and improved stamina prior to their return-to-work date.”
That said, he noted, “we typically delay any significant upper-body training activities for 8-10 weeks to avoid impact on healing of the sternum. Thus ... starting sooner would limit the amount of time a patient would have to engage in any upper-body resistance training. Many lose upper body strength after surgery, so this is an important part of the recovery/rehab process.”
Matthew Tomey, MD, director of the cardiac intensive care unit, Mount Sinai Morningside, New York, advised “caution” when interpreting the findings, stating that “there was no evident difference in the primary outcome measure of functional capacity by 14 weeks, and the trial was not designed to directly assess impact on either social functioning or economic productivity.”
“I would be interested to [see] more comprehensive data on safety in a larger, more diverse sample of postoperative patients,” he said, “as well as evidence to indicate clear advantage of an earlier start for patient-centered outcomes specifically after cardiac surgery.
“Perhaps the greatest challenges to full realization of the benefits of CR in practice have been gaps in referral and gaps in enrollment,” he added. “It is incumbent upon us as clinicians to counsel our patients and to provide appropriate referrals.”
The study was supported by the Medical and Life Sciences Research Fund and the Jeremy Pilcher Memorial Fund. No conflicts of interest were reported.
A version of this article first appeared on Medscape.com.
Cardiac rehabilitation (CR) started 2 weeks after sternotomy for a cardiac procedure was noninferior to usual care, in which CR starts 6 weeks after the procedure, with a greater improvement in 6-minute walk test outcomes, a randomized study suggests.
There was no difference in adverse events between groups, although the researchers pointed out that the study was not powered specifically for safety outcomes.
“Cardiac surgical techniques have evolved significantly over the last 60 years, leading to improved survival and shorter hospital stays,” Gordon McGregor, PhD, University of Warwick, Coventry, England, told this news organization. “However, sternal precautions and rehabilitation guidelines have not changed accordingly. There has never been a guideline based on empirical evidence to support rehabilitation professionals working with cardiac surgery patients after median sternotomy.”
“By adopting a progressive individualized approach,” he added, “cardiac surgery sternotomy patients can start cardiac rehabilitation up to 4 weeks earlier than current guidance, and thus potentially complete their recovery sooner.”
Results of the Early Initiation of Poststernotomy Cardiac Rehabilitation Exercise Training study were published online in JAMA Cardiology.
In the study, Dr. McGregor and colleagues randomly assigned 158 patients (mean age, 63 years; 84% men) to 8 weeks of 1-hour, twice-weekly supervised CR exercise training starting 2 weeks (early) or 6 weeks (usual care) after sternotomy.
The primary outcome was change in the 6-minute walk test distance from baseline to 10 or 14 weeks after sternotomy, respectively, and 12 months after randomization.
For usual care, training followed British standards: a warm-up with light cardiovascular and mobility exercises; continuous moderate-intensity cardiovascular exercise; a cooldown; functional exercises using resistance machines and free weights; and upper-body exercises designed to prevent sternal and leg wound pain and complications.
There are no specific outpatient CR exercise guidelines for early CR, so study participants followed an individualized exercise program for the first 2-3 weeks after surgery, starting with light mobility and moderate-intensity cardiovascular training when they could do those exercises with minimal discomfort. They then progressed to current British standards, as per usual care.
Forty patients were lost to follow-up, largely because of the pandemic; about half the participants in each group were included in the primary analysis.
Early CR was not inferior to usual care, the authors wrote. The mean change in 6-minute walk distance from baseline to completion of CR was 28 meters greater in the early group than in the usual-care group, and was achieved 4 weeks earlier in the recovery timeline.
Secondary outcomes (functional fitness and quality of life) improved in both groups and between-group differences were not statistically significant, indicating the noninferiority of early CR, the authors noted.
Safety not proven
There were more adverse events in the early group than in the usual-care group (58 vs. 46) and more serious adverse events (18 vs. 14), but fewer deaths (1 vs. 2).
Although there was no between-group difference in the likelihood of having an adverse or serious adverse event, Dr. McGregor acknowledged that the study was “not powered specifically for safety outcomes.” He added that “there is the potential to run a very large multination definitive superiority [randomized, controlled trial] with safety as the primary outcome; however, a very large sample would be required.”
Meanwhile, he said, “we can say with some degree of certainty that early CR was likely as safe as usual-care CR. In the United Kingdom, we work closely with the British Association for Cardiovascular Prevention and Rehabilitation and the Association of Chartered Physiotherapists in Cardiovascular Rehabilitation, who will incorporate our findings in their guidelines and training courses.”
Questions remain
Asked to comment on the study, John Larry, MD, medical director of cardiology and cardiac rehabilitation at the Ohio State University Wexner Medical Center East Hospital, Columbus, said: “For those under time pressure to return to work, [early CR] could be an advantage to allow more rehab time and improved stamina prior to their return-to-work date.”
That said, he noted, “we typically delay any significant upper-body training activities for 8-10 weeks to avoid impact on healing of the sternum. Thus ... starting sooner would limit the amount of time a patient would have to engage in any upper-body resistance training. Many lose upper body strength after surgery, so this is an important part of the recovery/rehab process.”
Matthew Tomey, MD, director of the cardiac intensive care unit, Mount Sinai Morningside, New York, advised “caution” when interpreting the findings, stating that “there was no evident difference in the primary outcome measure of functional capacity by 14 weeks, and the trial was not designed to directly assess impact on either social functioning or economic productivity.”
“I would be interested to [see] more comprehensive data on safety in a larger, more diverse sample of postoperative patients,” he said, “as well as evidence to indicate clear advantage of an earlier start for patient-centered outcomes specifically after cardiac surgery.
“Perhaps the greatest challenges to full realization of the benefits of CR in practice have been gaps in referral and gaps in enrollment,” he added. “It is incumbent upon us as clinicians to counsel our patients and to provide appropriate referrals.”
The study was supported by the Medical and Life Sciences Research Fund and the Jeremy Pilcher Memorial Fund. No conflicts of interest were reported.
A version of this article first appeared on Medscape.com.
Cardiac rehabilitation (CR) started 2 weeks after sternotomy for a cardiac procedure was noninferior to usual care, in which CR starts 6 weeks after the procedure, with a greater improvement in 6-minute walk test outcomes, a randomized study suggests.
There was no difference in adverse events between groups, although the researchers pointed out that the study was not powered specifically for safety outcomes.
“Cardiac surgical techniques have evolved significantly over the last 60 years, leading to improved survival and shorter hospital stays,” Gordon McGregor, PhD, University of Warwick, Coventry, England, told this news organization. “However, sternal precautions and rehabilitation guidelines have not changed accordingly. There has never been a guideline based on empirical evidence to support rehabilitation professionals working with cardiac surgery patients after median sternotomy.”
“By adopting a progressive individualized approach,” he added, “cardiac surgery sternotomy patients can start cardiac rehabilitation up to 4 weeks earlier than current guidance, and thus potentially complete their recovery sooner.”
Results of the Early Initiation of Poststernotomy Cardiac Rehabilitation Exercise Training study were published online in JAMA Cardiology.
In the study, Dr. McGregor and colleagues randomly assigned 158 patients (mean age, 63 years; 84% men) to 8 weeks of 1-hour, twice-weekly supervised CR exercise training starting 2 weeks (early) or 6 weeks (usual care) after sternotomy.
The primary outcome was change in the 6-minute walk test distance from baseline to 10 or 14 weeks after sternotomy, respectively, and 12 months after randomization.
For usual care, training followed British standards: a warm-up with light cardiovascular and mobility exercises; continuous moderate-intensity cardiovascular exercise; a cooldown; functional exercises using resistance machines and free weights; and upper-body exercises designed to prevent sternal and leg wound pain and complications.
There are no specific outpatient CR exercise guidelines for early CR, so study participants followed an individualized exercise program for the first 2-3 weeks after surgery, starting with light mobility and moderate-intensity cardiovascular training when they could do those exercises with minimal discomfort. They then progressed to current British standards, as per usual care.
Forty patients were lost to follow-up, largely because of the pandemic; about half the participants in each group were included in the primary analysis.
Early CR was not inferior to usual care, the authors wrote. The mean change in 6-minute walk distance from baseline to completion of CR was 28 meters greater in the early group than in the usual-care group, and was achieved 4 weeks earlier in the recovery timeline.
Secondary outcomes (functional fitness and quality of life) improved in both groups and between-group differences were not statistically significant, indicating the noninferiority of early CR, the authors noted.
Safety not proven
There were more adverse events in the early group than in the usual-care group (58 vs. 46) and more serious adverse events (18 vs. 14), but fewer deaths (1 vs. 2).
Although there was no between-group difference in the likelihood of having an adverse or serious adverse event, Dr. McGregor acknowledged that the study was “not powered specifically for safety outcomes.” He added that “there is the potential to run a very large multination definitive superiority [randomized, controlled trial] with safety as the primary outcome; however, a very large sample would be required.”
Meanwhile, he said, “we can say with some degree of certainty that early CR was likely as safe as usual-care CR. In the United Kingdom, we work closely with the British Association for Cardiovascular Prevention and Rehabilitation and the Association of Chartered Physiotherapists in Cardiovascular Rehabilitation, who will incorporate our findings in their guidelines and training courses.”
Questions remain
Asked to comment on the study, John Larry, MD, medical director of cardiology and cardiac rehabilitation at the Ohio State University Wexner Medical Center East Hospital, Columbus, said: “For those under time pressure to return to work, [early CR] could be an advantage to allow more rehab time and improved stamina prior to their return-to-work date.”
That said, he noted, “we typically delay any significant upper-body training activities for 8-10 weeks to avoid impact on healing of the sternum. Thus ... starting sooner would limit the amount of time a patient would have to engage in any upper-body resistance training. Many lose upper body strength after surgery, so this is an important part of the recovery/rehab process.”
Matthew Tomey, MD, director of the cardiac intensive care unit, Mount Sinai Morningside, New York, advised “caution” when interpreting the findings, stating that “there was no evident difference in the primary outcome measure of functional capacity by 14 weeks, and the trial was not designed to directly assess impact on either social functioning or economic productivity.”
“I would be interested to [see] more comprehensive data on safety in a larger, more diverse sample of postoperative patients,” he said, “as well as evidence to indicate clear advantage of an earlier start for patient-centered outcomes specifically after cardiac surgery.
“Perhaps the greatest challenges to full realization of the benefits of CR in practice have been gaps in referral and gaps in enrollment,” he added. “It is incumbent upon us as clinicians to counsel our patients and to provide appropriate referrals.”
The study was supported by the Medical and Life Sciences Research Fund and the Jeremy Pilcher Memorial Fund. No conflicts of interest were reported.
A version of this article first appeared on Medscape.com.
FROM JAMA CARDIOLOGY