User login
Medicare rule changes allow for broader CGM use
Beginning July 18, 2021, the Centers for Medicare & Medicaid Services will no longer require that beneficiaries test their blood sugar four times a day in order to qualify for CGM. In addition, the term “multiple daily injections” of insulin has been changed to multiple daily “administrations” in order to allow coverage for people who use inhaled insulin.
The changes are among those lobbied for by several organizations, including the American Diabetes Association and the Association of Diabetes Care and Education Specialists, which represents the professionals formerly known as “diabetes educators.”
The ADA tweeted on July 11 that “the removal of this criterion has been an effort long-led by the ADA, on which we have been actively engaged with CMS. People with diabetes on Medicare will now be able to more easily access this critical piece of technology, leading to better diabetes management and better health outcomes. A big win for the diabetes community!”
“After years of advocacy from the diabetes community and ADCES, Medicare has taken an important step to make [CGM] more accessible for Medicare beneficiaries with diabetes,” Kate Thomas, ADCES chief advocacy and external affairs officer, wrote in a blog post. “This updated [Local Coverage Determination] was a direct result of coordinated advocacy efforts among patient and provider groups, as well as industry partners, coalitions and other entities.”
It’s tough to test four times a day with only three strips
In a Jan. 29, 2021, letter to the Medicare Administrative Contractors, who oversee the policies for durable medical equipment, ADCES explained why the organization strongly supported removal of the four-daily fingerstick requirement, noting that “There is no evidence to suggest that requiring four or more fingerstick tests per day significantly impacts the outcomes of CGM therapy.”
Moreover, they pointed out that the requirement was particularly burdensome, considering the fact that Medicare only covers three test strips per day for insulin-using beneficiaries. “Removing this coverage requirement would allow for increased access to CGM systems and improved health outcomes for beneficiaries with diabetes by improving glycemic control. This also represents a step toward addressing the disparities that exist around diabetes technology under the Medicare program.”
As for the terminology change from “injection” to “administration,” ADCES said that, in addition to allowing CGM coverage for individuals who use rapid-acting inhaled insulin, “we also hope that updating this terminology will help to expedite coverage as future innovations in insulin delivery methods come to market.”
More changes needed, ADCES says
In that January 2021 letter, ADCES recommended several other changes, including covering CGM for anyone diagnosed with type 1 diabetes at any age and without having to meet other requirements except for twice-yearly clinician visits, and for anyone with type 2 diabetes who uses any type of insulin or who has had documented hypoglycemia regardless of therapy.
They also recommended that CGM coverage be considered for patients with chronic kidney disease, and that the required 6-month clinician visits be allowed to take place via telehealth. “ADCES believes that allowing the initiation of CGM therapy through a virtual visit will reduce barriers associated with travel and difficulty accessing a trained provider that are experienced by Medicare beneficiaries.”
In addition, ADCES requested that CMS eliminate the requirement that beneficiaries use insulin three times a day to qualify for CGM, noting that this creates a barrier for patients who can’t afford insulin at all but are at risk for hypoglycemia because they take sulfonylureas or other insulin secretagogues, or for those who use cheaper synthetic human insulins that are only taken twice a day, such as NPH.
“The existing CGM coverage criteria creates an unbalanced and disparate system that excludes from coverage beneficiaries who could greatly benefit from a CGM system, but do not qualify due to issues with insulin affordability,” ADCES wrote in the January letter.
Ms. Thomas wrote in the June 14th blog: “Our work is not done. We know there are more changes that must be made.”
Beginning July 18, 2021, the Centers for Medicare & Medicaid Services will no longer require that beneficiaries test their blood sugar four times a day in order to qualify for CGM. In addition, the term “multiple daily injections” of insulin has been changed to multiple daily “administrations” in order to allow coverage for people who use inhaled insulin.
The changes are among those lobbied for by several organizations, including the American Diabetes Association and the Association of Diabetes Care and Education Specialists, which represents the professionals formerly known as “diabetes educators.”
The ADA tweeted on July 11 that “the removal of this criterion has been an effort long-led by the ADA, on which we have been actively engaged with CMS. People with diabetes on Medicare will now be able to more easily access this critical piece of technology, leading to better diabetes management and better health outcomes. A big win for the diabetes community!”
“After years of advocacy from the diabetes community and ADCES, Medicare has taken an important step to make [CGM] more accessible for Medicare beneficiaries with diabetes,” Kate Thomas, ADCES chief advocacy and external affairs officer, wrote in a blog post. “This updated [Local Coverage Determination] was a direct result of coordinated advocacy efforts among patient and provider groups, as well as industry partners, coalitions and other entities.”
It’s tough to test four times a day with only three strips
In a Jan. 29, 2021, letter to the Medicare Administrative Contractors, who oversee the policies for durable medical equipment, ADCES explained why the organization strongly supported removal of the four-daily fingerstick requirement, noting that “There is no evidence to suggest that requiring four or more fingerstick tests per day significantly impacts the outcomes of CGM therapy.”
Moreover, they pointed out that the requirement was particularly burdensome, considering the fact that Medicare only covers three test strips per day for insulin-using beneficiaries. “Removing this coverage requirement would allow for increased access to CGM systems and improved health outcomes for beneficiaries with diabetes by improving glycemic control. This also represents a step toward addressing the disparities that exist around diabetes technology under the Medicare program.”
As for the terminology change from “injection” to “administration,” ADCES said that, in addition to allowing CGM coverage for individuals who use rapid-acting inhaled insulin, “we also hope that updating this terminology will help to expedite coverage as future innovations in insulin delivery methods come to market.”
More changes needed, ADCES says
In that January 2021 letter, ADCES recommended several other changes, including covering CGM for anyone diagnosed with type 1 diabetes at any age and without having to meet other requirements except for twice-yearly clinician visits, and for anyone with type 2 diabetes who uses any type of insulin or who has had documented hypoglycemia regardless of therapy.
They also recommended that CGM coverage be considered for patients with chronic kidney disease, and that the required 6-month clinician visits be allowed to take place via telehealth. “ADCES believes that allowing the initiation of CGM therapy through a virtual visit will reduce barriers associated with travel and difficulty accessing a trained provider that are experienced by Medicare beneficiaries.”
In addition, ADCES requested that CMS eliminate the requirement that beneficiaries use insulin three times a day to qualify for CGM, noting that this creates a barrier for patients who can’t afford insulin at all but are at risk for hypoglycemia because they take sulfonylureas or other insulin secretagogues, or for those who use cheaper synthetic human insulins that are only taken twice a day, such as NPH.
“The existing CGM coverage criteria creates an unbalanced and disparate system that excludes from coverage beneficiaries who could greatly benefit from a CGM system, but do not qualify due to issues with insulin affordability,” ADCES wrote in the January letter.
Ms. Thomas wrote in the June 14th blog: “Our work is not done. We know there are more changes that must be made.”
Beginning July 18, 2021, the Centers for Medicare & Medicaid Services will no longer require that beneficiaries test their blood sugar four times a day in order to qualify for CGM. In addition, the term “multiple daily injections” of insulin has been changed to multiple daily “administrations” in order to allow coverage for people who use inhaled insulin.
The changes are among those lobbied for by several organizations, including the American Diabetes Association and the Association of Diabetes Care and Education Specialists, which represents the professionals formerly known as “diabetes educators.”
The ADA tweeted on July 11 that “the removal of this criterion has been an effort long-led by the ADA, on which we have been actively engaged with CMS. People with diabetes on Medicare will now be able to more easily access this critical piece of technology, leading to better diabetes management and better health outcomes. A big win for the diabetes community!”
“After years of advocacy from the diabetes community and ADCES, Medicare has taken an important step to make [CGM] more accessible for Medicare beneficiaries with diabetes,” Kate Thomas, ADCES chief advocacy and external affairs officer, wrote in a blog post. “This updated [Local Coverage Determination] was a direct result of coordinated advocacy efforts among patient and provider groups, as well as industry partners, coalitions and other entities.”
It’s tough to test four times a day with only three strips
In a Jan. 29, 2021, letter to the Medicare Administrative Contractors, who oversee the policies for durable medical equipment, ADCES explained why the organization strongly supported removal of the four-daily fingerstick requirement, noting that “There is no evidence to suggest that requiring four or more fingerstick tests per day significantly impacts the outcomes of CGM therapy.”
Moreover, they pointed out that the requirement was particularly burdensome, considering the fact that Medicare only covers three test strips per day for insulin-using beneficiaries. “Removing this coverage requirement would allow for increased access to CGM systems and improved health outcomes for beneficiaries with diabetes by improving glycemic control. This also represents a step toward addressing the disparities that exist around diabetes technology under the Medicare program.”
As for the terminology change from “injection” to “administration,” ADCES said that, in addition to allowing CGM coverage for individuals who use rapid-acting inhaled insulin, “we also hope that updating this terminology will help to expedite coverage as future innovations in insulin delivery methods come to market.”
More changes needed, ADCES says
In that January 2021 letter, ADCES recommended several other changes, including covering CGM for anyone diagnosed with type 1 diabetes at any age and without having to meet other requirements except for twice-yearly clinician visits, and for anyone with type 2 diabetes who uses any type of insulin or who has had documented hypoglycemia regardless of therapy.
They also recommended that CGM coverage be considered for patients with chronic kidney disease, and that the required 6-month clinician visits be allowed to take place via telehealth. “ADCES believes that allowing the initiation of CGM therapy through a virtual visit will reduce barriers associated with travel and difficulty accessing a trained provider that are experienced by Medicare beneficiaries.”
In addition, ADCES requested that CMS eliminate the requirement that beneficiaries use insulin three times a day to qualify for CGM, noting that this creates a barrier for patients who can’t afford insulin at all but are at risk for hypoglycemia because they take sulfonylureas or other insulin secretagogues, or for those who use cheaper synthetic human insulins that are only taken twice a day, such as NPH.
“The existing CGM coverage criteria creates an unbalanced and disparate system that excludes from coverage beneficiaries who could greatly benefit from a CGM system, but do not qualify due to issues with insulin affordability,” ADCES wrote in the January letter.
Ms. Thomas wrote in the June 14th blog: “Our work is not done. We know there are more changes that must be made.”
The good old days
“It’s good to be in something from the ground floor. I came too late for that. ... But lately, I’m getting the feeling that I came in at the end. The best is over.” –Tony Soprano
For me, I’m unsure. Sometimes it feels like our best days are behind us. When I was a kid, we explored life in pond water, watching water fleas and hydra swim under our Child World toy microscopes. Today, kids learn to eat Tide Pods from TikTok. Back when I was young, a doctor’s appointment was a special occasion! My brothers and I had a bath and got dressed in our Sunday best for our appointment with Dr. Bellin, a genteel, gray-haired pediatrician who worked out of his Victorian office with wooden floors and crystal door handles. Contrast that with the appointment I had with a patient the other day, done by telephone while she was in line ordering at Starbucks. I waited patiently for her to give her order.
This ache I feel for the past is called nostalgia. At one time, it was a diagnosable condition. It was first used by Dr. Johannes Hofer in the 17th century to describe Swiss soldiers fighting in foreign lands. From the Greek, it means “homecoming pain.” Although over time nostalgia has lost its clinical meaning, the feeling of yearning for the past has dramatically gained in prevalence. The word “nostalgia” appears more in print now than at any point since 1800. We are most nostalgic during times of duress, it seems. This, no doubt, is because it’s comforting to think we’d be better off back in pastoral, idyll times, back when work ended at 5 p.m. and cotton balls were soaked in alcohol and office visits ended with a lollipop on a loop.
Of course, the good old days weren’t really better. We have a selective view of history – as many things were contemptible or bad then as now. Yes, Dr. Bellin was the consummate professional, but thank goodness, I didn’t have acute lymphocytic leukemia or Haemophilus influenzae type B or even suffocate under a pile of blankets while sleeping on my stomach. Without doubt, clinically we’re much better today. Also back then, there was hardly a consideration for atrocious racial disparities in care. We’ve not come far, but we are at least better off today than a few decades ago. And what about medicine as a profession? Although he had loads of autonomy and respect, Dr. Bellin also started every day of his 50-year career at 6 a.m. rounding in the newborn nursery before seeing patients in the office 6 days a week. Not many of us would trade our practice for his.
Yet, there’s reasons to be nostalgic. Chart notes might have been barely legible, but at least they served a purpose. The problem-oriented medical record was intended to logically capture and organize data. SOAP notes were invented to help us think better, to get diagnoses correct, to succinctly see progress. Today, notes are written for administrators and payers and patients. As a result, they’re often useless to us.
And although it may have been inconvenient to sit in the waiting room reading Highlights magazine, I’m unsure it was a worse user experience, compared with a chain pharmacy “virtual” doctor visit. (Particularly because you could always drop pennies down the large hot-air iron floor grate in the corner).
The thrumming undercurrent of progress promises artificial intelligence and genomics and wearable diagnostics in our future. But the assumption is the new things will be better suited to our needs than the old. Sometimes, they are not. Sometimes technology diminishes us instead of enhancing us.
I cannot count how many times I’ve hit my head or whacked my shin because our Tesla Model X doors open by magic and of their own accord. Back when I was young, we opened car doors by pulling on the door handle. I sometimes miss those days.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
“It’s good to be in something from the ground floor. I came too late for that. ... But lately, I’m getting the feeling that I came in at the end. The best is over.” –Tony Soprano
For me, I’m unsure. Sometimes it feels like our best days are behind us. When I was a kid, we explored life in pond water, watching water fleas and hydra swim under our Child World toy microscopes. Today, kids learn to eat Tide Pods from TikTok. Back when I was young, a doctor’s appointment was a special occasion! My brothers and I had a bath and got dressed in our Sunday best for our appointment with Dr. Bellin, a genteel, gray-haired pediatrician who worked out of his Victorian office with wooden floors and crystal door handles. Contrast that with the appointment I had with a patient the other day, done by telephone while she was in line ordering at Starbucks. I waited patiently for her to give her order.
This ache I feel for the past is called nostalgia. At one time, it was a diagnosable condition. It was first used by Dr. Johannes Hofer in the 17th century to describe Swiss soldiers fighting in foreign lands. From the Greek, it means “homecoming pain.” Although over time nostalgia has lost its clinical meaning, the feeling of yearning for the past has dramatically gained in prevalence. The word “nostalgia” appears more in print now than at any point since 1800. We are most nostalgic during times of duress, it seems. This, no doubt, is because it’s comforting to think we’d be better off back in pastoral, idyll times, back when work ended at 5 p.m. and cotton balls were soaked in alcohol and office visits ended with a lollipop on a loop.
Of course, the good old days weren’t really better. We have a selective view of history – as many things were contemptible or bad then as now. Yes, Dr. Bellin was the consummate professional, but thank goodness, I didn’t have acute lymphocytic leukemia or Haemophilus influenzae type B or even suffocate under a pile of blankets while sleeping on my stomach. Without doubt, clinically we’re much better today. Also back then, there was hardly a consideration for atrocious racial disparities in care. We’ve not come far, but we are at least better off today than a few decades ago. And what about medicine as a profession? Although he had loads of autonomy and respect, Dr. Bellin also started every day of his 50-year career at 6 a.m. rounding in the newborn nursery before seeing patients in the office 6 days a week. Not many of us would trade our practice for his.
Yet, there’s reasons to be nostalgic. Chart notes might have been barely legible, but at least they served a purpose. The problem-oriented medical record was intended to logically capture and organize data. SOAP notes were invented to help us think better, to get diagnoses correct, to succinctly see progress. Today, notes are written for administrators and payers and patients. As a result, they’re often useless to us.
And although it may have been inconvenient to sit in the waiting room reading Highlights magazine, I’m unsure it was a worse user experience, compared with a chain pharmacy “virtual” doctor visit. (Particularly because you could always drop pennies down the large hot-air iron floor grate in the corner).
The thrumming undercurrent of progress promises artificial intelligence and genomics and wearable diagnostics in our future. But the assumption is the new things will be better suited to our needs than the old. Sometimes, they are not. Sometimes technology diminishes us instead of enhancing us.
I cannot count how many times I’ve hit my head or whacked my shin because our Tesla Model X doors open by magic and of their own accord. Back when I was young, we opened car doors by pulling on the door handle. I sometimes miss those days.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
“It’s good to be in something from the ground floor. I came too late for that. ... But lately, I’m getting the feeling that I came in at the end. The best is over.” –Tony Soprano
For me, I’m unsure. Sometimes it feels like our best days are behind us. When I was a kid, we explored life in pond water, watching water fleas and hydra swim under our Child World toy microscopes. Today, kids learn to eat Tide Pods from TikTok. Back when I was young, a doctor’s appointment was a special occasion! My brothers and I had a bath and got dressed in our Sunday best for our appointment with Dr. Bellin, a genteel, gray-haired pediatrician who worked out of his Victorian office with wooden floors and crystal door handles. Contrast that with the appointment I had with a patient the other day, done by telephone while she was in line ordering at Starbucks. I waited patiently for her to give her order.
This ache I feel for the past is called nostalgia. At one time, it was a diagnosable condition. It was first used by Dr. Johannes Hofer in the 17th century to describe Swiss soldiers fighting in foreign lands. From the Greek, it means “homecoming pain.” Although over time nostalgia has lost its clinical meaning, the feeling of yearning for the past has dramatically gained in prevalence. The word “nostalgia” appears more in print now than at any point since 1800. We are most nostalgic during times of duress, it seems. This, no doubt, is because it’s comforting to think we’d be better off back in pastoral, idyll times, back when work ended at 5 p.m. and cotton balls were soaked in alcohol and office visits ended with a lollipop on a loop.
Of course, the good old days weren’t really better. We have a selective view of history – as many things were contemptible or bad then as now. Yes, Dr. Bellin was the consummate professional, but thank goodness, I didn’t have acute lymphocytic leukemia or Haemophilus influenzae type B or even suffocate under a pile of blankets while sleeping on my stomach. Without doubt, clinically we’re much better today. Also back then, there was hardly a consideration for atrocious racial disparities in care. We’ve not come far, but we are at least better off today than a few decades ago. And what about medicine as a profession? Although he had loads of autonomy and respect, Dr. Bellin also started every day of his 50-year career at 6 a.m. rounding in the newborn nursery before seeing patients in the office 6 days a week. Not many of us would trade our practice for his.
Yet, there’s reasons to be nostalgic. Chart notes might have been barely legible, but at least they served a purpose. The problem-oriented medical record was intended to logically capture and organize data. SOAP notes were invented to help us think better, to get diagnoses correct, to succinctly see progress. Today, notes are written for administrators and payers and patients. As a result, they’re often useless to us.
And although it may have been inconvenient to sit in the waiting room reading Highlights magazine, I’m unsure it was a worse user experience, compared with a chain pharmacy “virtual” doctor visit. (Particularly because you could always drop pennies down the large hot-air iron floor grate in the corner).
The thrumming undercurrent of progress promises artificial intelligence and genomics and wearable diagnostics in our future. But the assumption is the new things will be better suited to our needs than the old. Sometimes, they are not. Sometimes technology diminishes us instead of enhancing us.
I cannot count how many times I’ve hit my head or whacked my shin because our Tesla Model X doors open by magic and of their own accord. Back when I was young, we opened car doors by pulling on the door handle. I sometimes miss those days.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
Remove sex designation from public part of birth certificates, AMA advises
Requiring the designation can lead to discrimination and unnecessary burden on individuals whose current gender identity does not align with their designation at birth when they register for school or sports, adopt, get married, or request personal records.
A person’s sex designation at birth would still be submitted to the U.S. Standard Certificate of Live Birth for medical, public health, and statistical use only, report authors note.
Willie Underwood III, MD, MSc, author of Board Report 15, explained in reference committee testimony that a standard certificate of live birth is critical for uniformly collecting and processing data, but birth certificates are issued by the government to individuals.
Ten states allow gender-neutral designation
According to the report, 48 states (Tennessee and Ohio are the exceptions) and the District of Columbia allow people to amend their sex designation on their birth certificate to reflect their gender identities, but only 10 states allow for a gender-neutral designation, usually “X,” on birth certificates. The U.S. Department of State does not currently offer an option for a gender-neutral designation on U.S. passports.
“Assigning sex using binary variables in the public portion of the birth certificate fails to recognize the medical spectrum of gender identity,” Dr. Underwood said, and it can be used to discriminate.
Jeremy Toler, MD, a delegate from GLMA: Health Professionals Advancing LGBTQ Equality, testified that there is precedent for information to be removed from the public portion of the birth certificates. And much data is collected for each live birth that doesn’t show up on individuals’ birth certificates, he noted.
Dr. Toler said transgender, gender nonbinary, and individuals with differences in sex development can be placed at a disadvantage by the sex label on the birth certificate.
“We unfortunately still live in a world where it is unsafe in many cases for one’s gender to vary from the sex assigned at birth,” Dr. Toler said.
Not having this data on the widely used form will reduce unnecessary reliance on sex as a stand-in for gender, he said, and would “serve as an equalizer” since policies differ by state.
Robert Jackson, MD, an alternate delegate from the American Academy of Cosmetic Surgery, spoke against the measure.
“We as physicians need to report things accurately,” Dr. Jackson said. “All through medical school, residency, and specialty training we were supposed to delegate all of the physical findings of the patient we’re taking care of. I think when the child is born, they do have physical characteristics either male or female, and I think that probably should be on the public record. That’s just my personal opinion.”
Sarah Mae Smith, MD, delegate from California, speaking on behalf of the Women Physicians Section, said removing the sex designation is important for moving toward gender equity.
“We need to recognize [that] gender is not a binary but a spectrum,” she said. “Obligating our patients to jump through numerous administrative hoops to identify as who they are based on a sex assigned at birth primarily on genitalia is not only unnecessary but actively deleterious to their health.”
Race was once public on birth certificates
She noted that the report mentions that previously, information on the race of a person’s parents was included on the public portion of the birth certificate and that information was recognized to facilitate discrimination.
“Thankfully, a change was made to obviate at least that avenue for discriminatory practices,” she said. “Now, likewise, the information on sex assigned at birth is being used to undermine the rights of our transgender, intersex, and nonbinary patients.”
Arlene Seid, MD, MPH, an alternate delegate from the American Association of Public Health Physicians, said the resolution protects the aggregate data “without the discrimination associated with the individual data.”
Sex no longer has a role to play in the jobs people do, she noted, and the designation shouldn’t have to be evaluated for something like a job interview.
“Our society doesn’t need it on an individual basis for most of what occurs in public life,” Dr. Seid said.
Dr. Underwood, Dr. Toler, Dr. Jackson, Dr. Smith, and Dr. Seid declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Requiring the designation can lead to discrimination and unnecessary burden on individuals whose current gender identity does not align with their designation at birth when they register for school or sports, adopt, get married, or request personal records.
A person’s sex designation at birth would still be submitted to the U.S. Standard Certificate of Live Birth for medical, public health, and statistical use only, report authors note.
Willie Underwood III, MD, MSc, author of Board Report 15, explained in reference committee testimony that a standard certificate of live birth is critical for uniformly collecting and processing data, but birth certificates are issued by the government to individuals.
Ten states allow gender-neutral designation
According to the report, 48 states (Tennessee and Ohio are the exceptions) and the District of Columbia allow people to amend their sex designation on their birth certificate to reflect their gender identities, but only 10 states allow for a gender-neutral designation, usually “X,” on birth certificates. The U.S. Department of State does not currently offer an option for a gender-neutral designation on U.S. passports.
“Assigning sex using binary variables in the public portion of the birth certificate fails to recognize the medical spectrum of gender identity,” Dr. Underwood said, and it can be used to discriminate.
Jeremy Toler, MD, a delegate from GLMA: Health Professionals Advancing LGBTQ Equality, testified that there is precedent for information to be removed from the public portion of the birth certificates. And much data is collected for each live birth that doesn’t show up on individuals’ birth certificates, he noted.
Dr. Toler said transgender, gender nonbinary, and individuals with differences in sex development can be placed at a disadvantage by the sex label on the birth certificate.
“We unfortunately still live in a world where it is unsafe in many cases for one’s gender to vary from the sex assigned at birth,” Dr. Toler said.
Not having this data on the widely used form will reduce unnecessary reliance on sex as a stand-in for gender, he said, and would “serve as an equalizer” since policies differ by state.
Robert Jackson, MD, an alternate delegate from the American Academy of Cosmetic Surgery, spoke against the measure.
“We as physicians need to report things accurately,” Dr. Jackson said. “All through medical school, residency, and specialty training we were supposed to delegate all of the physical findings of the patient we’re taking care of. I think when the child is born, they do have physical characteristics either male or female, and I think that probably should be on the public record. That’s just my personal opinion.”
Sarah Mae Smith, MD, delegate from California, speaking on behalf of the Women Physicians Section, said removing the sex designation is important for moving toward gender equity.
“We need to recognize [that] gender is not a binary but a spectrum,” she said. “Obligating our patients to jump through numerous administrative hoops to identify as who they are based on a sex assigned at birth primarily on genitalia is not only unnecessary but actively deleterious to their health.”
Race was once public on birth certificates
She noted that the report mentions that previously, information on the race of a person’s parents was included on the public portion of the birth certificate and that information was recognized to facilitate discrimination.
“Thankfully, a change was made to obviate at least that avenue for discriminatory practices,” she said. “Now, likewise, the information on sex assigned at birth is being used to undermine the rights of our transgender, intersex, and nonbinary patients.”
Arlene Seid, MD, MPH, an alternate delegate from the American Association of Public Health Physicians, said the resolution protects the aggregate data “without the discrimination associated with the individual data.”
Sex no longer has a role to play in the jobs people do, she noted, and the designation shouldn’t have to be evaluated for something like a job interview.
“Our society doesn’t need it on an individual basis for most of what occurs in public life,” Dr. Seid said.
Dr. Underwood, Dr. Toler, Dr. Jackson, Dr. Smith, and Dr. Seid declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Requiring the designation can lead to discrimination and unnecessary burden on individuals whose current gender identity does not align with their designation at birth when they register for school or sports, adopt, get married, or request personal records.
A person’s sex designation at birth would still be submitted to the U.S. Standard Certificate of Live Birth for medical, public health, and statistical use only, report authors note.
Willie Underwood III, MD, MSc, author of Board Report 15, explained in reference committee testimony that a standard certificate of live birth is critical for uniformly collecting and processing data, but birth certificates are issued by the government to individuals.
Ten states allow gender-neutral designation
According to the report, 48 states (Tennessee and Ohio are the exceptions) and the District of Columbia allow people to amend their sex designation on their birth certificate to reflect their gender identities, but only 10 states allow for a gender-neutral designation, usually “X,” on birth certificates. The U.S. Department of State does not currently offer an option for a gender-neutral designation on U.S. passports.
“Assigning sex using binary variables in the public portion of the birth certificate fails to recognize the medical spectrum of gender identity,” Dr. Underwood said, and it can be used to discriminate.
Jeremy Toler, MD, a delegate from GLMA: Health Professionals Advancing LGBTQ Equality, testified that there is precedent for information to be removed from the public portion of the birth certificates. And much data is collected for each live birth that doesn’t show up on individuals’ birth certificates, he noted.
Dr. Toler said transgender, gender nonbinary, and individuals with differences in sex development can be placed at a disadvantage by the sex label on the birth certificate.
“We unfortunately still live in a world where it is unsafe in many cases for one’s gender to vary from the sex assigned at birth,” Dr. Toler said.
Not having this data on the widely used form will reduce unnecessary reliance on sex as a stand-in for gender, he said, and would “serve as an equalizer” since policies differ by state.
Robert Jackson, MD, an alternate delegate from the American Academy of Cosmetic Surgery, spoke against the measure.
“We as physicians need to report things accurately,” Dr. Jackson said. “All through medical school, residency, and specialty training we were supposed to delegate all of the physical findings of the patient we’re taking care of. I think when the child is born, they do have physical characteristics either male or female, and I think that probably should be on the public record. That’s just my personal opinion.”
Sarah Mae Smith, MD, delegate from California, speaking on behalf of the Women Physicians Section, said removing the sex designation is important for moving toward gender equity.
“We need to recognize [that] gender is not a binary but a spectrum,” she said. “Obligating our patients to jump through numerous administrative hoops to identify as who they are based on a sex assigned at birth primarily on genitalia is not only unnecessary but actively deleterious to their health.”
Race was once public on birth certificates
She noted that the report mentions that previously, information on the race of a person’s parents was included on the public portion of the birth certificate and that information was recognized to facilitate discrimination.
“Thankfully, a change was made to obviate at least that avenue for discriminatory practices,” she said. “Now, likewise, the information on sex assigned at birth is being used to undermine the rights of our transgender, intersex, and nonbinary patients.”
Arlene Seid, MD, MPH, an alternate delegate from the American Association of Public Health Physicians, said the resolution protects the aggregate data “without the discrimination associated with the individual data.”
Sex no longer has a role to play in the jobs people do, she noted, and the designation shouldn’t have to be evaluated for something like a job interview.
“Our society doesn’t need it on an individual basis for most of what occurs in public life,” Dr. Seid said.
Dr. Underwood, Dr. Toler, Dr. Jackson, Dr. Smith, and Dr. Seid declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Incorporating self-care, wellness into routines can prevent doctors’ burnout
Gradually, we are emerging from the chaos, isolation, and anxiety of COVID-19. As the Centers for Disease Control and Prevention adjusts its recommendations and vaccinations become more widely available, our communities are beginning to return to normalcy. We are encouraged to put aside our masks if vaccinated and rejoin society, to venture out with less hesitancy and anxiety. As family and friends reunite, memories of confusion, frustration, and fear are beginning to fade to black. Despite the prevailing belief that we should move on, look forward, and remember the past to safeguard our future, remnants of the pandemic remain.
Unvaccinated individuals, notably children under the age of 12, are quite significant in number. The use of telehealth is now standard practice.
For several years, we were warned about the looming “mental health crisis.” The past year has demonstrated that a crisis no longer looms – it has arrived. Our patients can reveal the vulnerability COVID-19 has wrought – from the devastation of lives lost, supply shortages, loss of employment and financial stability – to a lack of access to computers and thereby, the risk of educational decline. Those factors, coupled with isolation and uncertainty about the future, have led to an influx of individuals with anxiety, depression, and other mood disorders seeking mental health treatment.
Doctors, others suffering
As result of a medical culture guided by the sacred oath to which care, compassion, and dedication held as true in ancient Greece as it does today, the focus centers on those around us – while signs of our own weariness are waved away as “a bad day.” Even though several support groups are readily available to offer a listening ear and mental health physicians who focus on the treatment of health care professionals are becoming more ubiquitous, the vestiges of past doctrine remain.
In this modern age of medical training, there is often as much sacrifice as there is attainment of knowledge. This philosophy is so ingrained that throughout training and practice one may come across colleagues experiencing an abundance of guilt when leave is needed for personal reasons. We are quick to recommend such steps for our patients, family, and friends, but hesitant to consider such for ourselves. Yet, of all the lessons this past year has wrought, the importance of mental health and self-care cannot be overstated. This raises the question:
It is vital to accept our humanity as something not to repair, treat, or overcome but to understand. There is strength and power in vulnerability. If we do not perceive and validate this process within ourselves, how can we do so for others? In other words, the oxygen mask must be placed on us first before we can place it on anyone else – patients or otherwise.
Chiefly and above all else, the importance of identifying individual signs of stress is essential. Where do you hold tension? Are you prone to GI distress or headaches when taxed? Do you tend toward irritability, apathy, or exhaustion?
Once this is determined, it is important to assess your stress on a numerical scale, such as those used for pain. Are you a 5 or an 8? Finally, are there identifiable triggers or reliable alleviators? Is there a time of day or day of the week that is most difficult to manage? Can you anticipate potential stressors? Understanding your triggers, listening to your body, and practicing the language of self is the first step toward wellness.
Following introspection and observation, the next step is inventory. Take stock of your reserves. What replenishes? What depletes? What brings joy? What brings dread? Are there certain activities that mitigate stress? If so, how much time do they entail? Identify your number on a scale and associate that number with specific strategies or techniques. Remember that decompression for a 6 might be excessive for a 4. Furthermore, what is the duration of these feelings? Chronic stressors may incur gradual change verses sudden impact if acute. Through identifying personal signs, devising and using a scale, as well as escalating or de-escalating factors, individuals become more in tune with their bodies and therefore, more likely to intervene before burnout takes hold.
With this process well integrated, one can now consider stylized approaches for stress management. For example, those inclined toward mindfulness practices may find yoga, meditation, and relaxation exercises beneficial. Others may thrive on positive affirmations, gratitude, and thankfulness. While some might find relief in physical activity, be it strenuous or casual, the creative arts might appeal to those who find joy in painting, writing, or doing crafts. In addition, baking, reading, dancing, and/or listening to music might help lift stress.
Along with those discoveries, or in some cases, rediscoveries, basic needs such as dietary habits and nutrition, hydration, and sleep are vital toward emotional regulation, physiological homeostasis, and stress modulation. Remember HALT: Hungry, Angry, Lonely, Tired, Too hot, Too cold, Sad or Stressed. Those strategies are meant to guide self-care and highlight the importance of allowing time for self-awareness. Imagine yourself as if you are meeting a new patient. Establish rapport, identify symptoms, and explore options for treatment. When we give time to ourselves, we can give time more freely to others. With this in mind, try following the 5-minute wellness check that I formulated:
1. How am I feeling? What am I feeling?
2. Assess HALTS.
3. Identify the number on your scale.
4. Methods of quick de-escalation:
- Designate and schedule personal time.
- Write down daily goals.
- Repeat positive affirmations or write down words of gratitude.
- Use deep breathing exercises.
- Stretch or take a brief walk.
- Engage in mindfulness practices, such as meditation.
Once we develop a habit of monitoring, assessing, and practicing self-care, the process becomes more efficient and effective. Think of the way a seasoned attending can manage workflow with ease, compared with an intern. Recognizing signs and using these strategies routinely can become a quick daily measure of well-being.
Dr. Thomas is a board-certified adult psychiatrist with interests in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. Dr. Thomas has no conflicts of interest.
Gradually, we are emerging from the chaos, isolation, and anxiety of COVID-19. As the Centers for Disease Control and Prevention adjusts its recommendations and vaccinations become more widely available, our communities are beginning to return to normalcy. We are encouraged to put aside our masks if vaccinated and rejoin society, to venture out with less hesitancy and anxiety. As family and friends reunite, memories of confusion, frustration, and fear are beginning to fade to black. Despite the prevailing belief that we should move on, look forward, and remember the past to safeguard our future, remnants of the pandemic remain.
Unvaccinated individuals, notably children under the age of 12, are quite significant in number. The use of telehealth is now standard practice.
For several years, we were warned about the looming “mental health crisis.” The past year has demonstrated that a crisis no longer looms – it has arrived. Our patients can reveal the vulnerability COVID-19 has wrought – from the devastation of lives lost, supply shortages, loss of employment and financial stability – to a lack of access to computers and thereby, the risk of educational decline. Those factors, coupled with isolation and uncertainty about the future, have led to an influx of individuals with anxiety, depression, and other mood disorders seeking mental health treatment.
Doctors, others suffering
As result of a medical culture guided by the sacred oath to which care, compassion, and dedication held as true in ancient Greece as it does today, the focus centers on those around us – while signs of our own weariness are waved away as “a bad day.” Even though several support groups are readily available to offer a listening ear and mental health physicians who focus on the treatment of health care professionals are becoming more ubiquitous, the vestiges of past doctrine remain.
In this modern age of medical training, there is often as much sacrifice as there is attainment of knowledge. This philosophy is so ingrained that throughout training and practice one may come across colleagues experiencing an abundance of guilt when leave is needed for personal reasons. We are quick to recommend such steps for our patients, family, and friends, but hesitant to consider such for ourselves. Yet, of all the lessons this past year has wrought, the importance of mental health and self-care cannot be overstated. This raises the question:
It is vital to accept our humanity as something not to repair, treat, or overcome but to understand. There is strength and power in vulnerability. If we do not perceive and validate this process within ourselves, how can we do so for others? In other words, the oxygen mask must be placed on us first before we can place it on anyone else – patients or otherwise.
Chiefly and above all else, the importance of identifying individual signs of stress is essential. Where do you hold tension? Are you prone to GI distress or headaches when taxed? Do you tend toward irritability, apathy, or exhaustion?
Once this is determined, it is important to assess your stress on a numerical scale, such as those used for pain. Are you a 5 or an 8? Finally, are there identifiable triggers or reliable alleviators? Is there a time of day or day of the week that is most difficult to manage? Can you anticipate potential stressors? Understanding your triggers, listening to your body, and practicing the language of self is the first step toward wellness.
Following introspection and observation, the next step is inventory. Take stock of your reserves. What replenishes? What depletes? What brings joy? What brings dread? Are there certain activities that mitigate stress? If so, how much time do they entail? Identify your number on a scale and associate that number with specific strategies or techniques. Remember that decompression for a 6 might be excessive for a 4. Furthermore, what is the duration of these feelings? Chronic stressors may incur gradual change verses sudden impact if acute. Through identifying personal signs, devising and using a scale, as well as escalating or de-escalating factors, individuals become more in tune with their bodies and therefore, more likely to intervene before burnout takes hold.
With this process well integrated, one can now consider stylized approaches for stress management. For example, those inclined toward mindfulness practices may find yoga, meditation, and relaxation exercises beneficial. Others may thrive on positive affirmations, gratitude, and thankfulness. While some might find relief in physical activity, be it strenuous or casual, the creative arts might appeal to those who find joy in painting, writing, or doing crafts. In addition, baking, reading, dancing, and/or listening to music might help lift stress.
Along with those discoveries, or in some cases, rediscoveries, basic needs such as dietary habits and nutrition, hydration, and sleep are vital toward emotional regulation, physiological homeostasis, and stress modulation. Remember HALT: Hungry, Angry, Lonely, Tired, Too hot, Too cold, Sad or Stressed. Those strategies are meant to guide self-care and highlight the importance of allowing time for self-awareness. Imagine yourself as if you are meeting a new patient. Establish rapport, identify symptoms, and explore options for treatment. When we give time to ourselves, we can give time more freely to others. With this in mind, try following the 5-minute wellness check that I formulated:
1. How am I feeling? What am I feeling?
2. Assess HALTS.
3. Identify the number on your scale.
4. Methods of quick de-escalation:
- Designate and schedule personal time.
- Write down daily goals.
- Repeat positive affirmations or write down words of gratitude.
- Use deep breathing exercises.
- Stretch or take a brief walk.
- Engage in mindfulness practices, such as meditation.
Once we develop a habit of monitoring, assessing, and practicing self-care, the process becomes more efficient and effective. Think of the way a seasoned attending can manage workflow with ease, compared with an intern. Recognizing signs and using these strategies routinely can become a quick daily measure of well-being.
Dr. Thomas is a board-certified adult psychiatrist with interests in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. Dr. Thomas has no conflicts of interest.
Gradually, we are emerging from the chaos, isolation, and anxiety of COVID-19. As the Centers for Disease Control and Prevention adjusts its recommendations and vaccinations become more widely available, our communities are beginning to return to normalcy. We are encouraged to put aside our masks if vaccinated and rejoin society, to venture out with less hesitancy and anxiety. As family and friends reunite, memories of confusion, frustration, and fear are beginning to fade to black. Despite the prevailing belief that we should move on, look forward, and remember the past to safeguard our future, remnants of the pandemic remain.
Unvaccinated individuals, notably children under the age of 12, are quite significant in number. The use of telehealth is now standard practice.
For several years, we were warned about the looming “mental health crisis.” The past year has demonstrated that a crisis no longer looms – it has arrived. Our patients can reveal the vulnerability COVID-19 has wrought – from the devastation of lives lost, supply shortages, loss of employment and financial stability – to a lack of access to computers and thereby, the risk of educational decline. Those factors, coupled with isolation and uncertainty about the future, have led to an influx of individuals with anxiety, depression, and other mood disorders seeking mental health treatment.
Doctors, others suffering
As result of a medical culture guided by the sacred oath to which care, compassion, and dedication held as true in ancient Greece as it does today, the focus centers on those around us – while signs of our own weariness are waved away as “a bad day.” Even though several support groups are readily available to offer a listening ear and mental health physicians who focus on the treatment of health care professionals are becoming more ubiquitous, the vestiges of past doctrine remain.
In this modern age of medical training, there is often as much sacrifice as there is attainment of knowledge. This philosophy is so ingrained that throughout training and practice one may come across colleagues experiencing an abundance of guilt when leave is needed for personal reasons. We are quick to recommend such steps for our patients, family, and friends, but hesitant to consider such for ourselves. Yet, of all the lessons this past year has wrought, the importance of mental health and self-care cannot be overstated. This raises the question:
It is vital to accept our humanity as something not to repair, treat, or overcome but to understand. There is strength and power in vulnerability. If we do not perceive and validate this process within ourselves, how can we do so for others? In other words, the oxygen mask must be placed on us first before we can place it on anyone else – patients or otherwise.
Chiefly and above all else, the importance of identifying individual signs of stress is essential. Where do you hold tension? Are you prone to GI distress or headaches when taxed? Do you tend toward irritability, apathy, or exhaustion?
Once this is determined, it is important to assess your stress on a numerical scale, such as those used for pain. Are you a 5 or an 8? Finally, are there identifiable triggers or reliable alleviators? Is there a time of day or day of the week that is most difficult to manage? Can you anticipate potential stressors? Understanding your triggers, listening to your body, and practicing the language of self is the first step toward wellness.
Following introspection and observation, the next step is inventory. Take stock of your reserves. What replenishes? What depletes? What brings joy? What brings dread? Are there certain activities that mitigate stress? If so, how much time do they entail? Identify your number on a scale and associate that number with specific strategies or techniques. Remember that decompression for a 6 might be excessive for a 4. Furthermore, what is the duration of these feelings? Chronic stressors may incur gradual change verses sudden impact if acute. Through identifying personal signs, devising and using a scale, as well as escalating or de-escalating factors, individuals become more in tune with their bodies and therefore, more likely to intervene before burnout takes hold.
With this process well integrated, one can now consider stylized approaches for stress management. For example, those inclined toward mindfulness practices may find yoga, meditation, and relaxation exercises beneficial. Others may thrive on positive affirmations, gratitude, and thankfulness. While some might find relief in physical activity, be it strenuous or casual, the creative arts might appeal to those who find joy in painting, writing, or doing crafts. In addition, baking, reading, dancing, and/or listening to music might help lift stress.
Along with those discoveries, or in some cases, rediscoveries, basic needs such as dietary habits and nutrition, hydration, and sleep are vital toward emotional regulation, physiological homeostasis, and stress modulation. Remember HALT: Hungry, Angry, Lonely, Tired, Too hot, Too cold, Sad or Stressed. Those strategies are meant to guide self-care and highlight the importance of allowing time for self-awareness. Imagine yourself as if you are meeting a new patient. Establish rapport, identify symptoms, and explore options for treatment. When we give time to ourselves, we can give time more freely to others. With this in mind, try following the 5-minute wellness check that I formulated:
1. How am I feeling? What am I feeling?
2. Assess HALTS.
3. Identify the number on your scale.
4. Methods of quick de-escalation:
- Designate and schedule personal time.
- Write down daily goals.
- Repeat positive affirmations or write down words of gratitude.
- Use deep breathing exercises.
- Stretch or take a brief walk.
- Engage in mindfulness practices, such as meditation.
Once we develop a habit of monitoring, assessing, and practicing self-care, the process becomes more efficient and effective. Think of the way a seasoned attending can manage workflow with ease, compared with an intern. Recognizing signs and using these strategies routinely can become a quick daily measure of well-being.
Dr. Thomas is a board-certified adult psychiatrist with interests in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. Dr. Thomas has no conflicts of interest.
AMA: ‘Excited delirium’ not a legitimate medical diagnosis
Current evidence does not support use of “excited delirium” or “excited delirium syndrome” as a medical diagnosis, the American Medical Association said June 14, and the term should not be used unless clear diagnostic criteria are validated.
The term is disproportionately applied to people of color, “for whom inappropriate and excessive pharmacotherapy continues to be the norm instead of behavioral deescalation,” the report by the AMA’s Council on Science and Public Health stated, and is therefore indicative of systemic racism.
That conclusion was one of many included in CSAPH Report 2, which was adopted June 14 at the special meeting of the AMA House of Delegates.
The AMA also opposes “use of sedative/hypnotic and dissociative agents, including ketamine, as a pharmacologic intervention for agitated individuals in the out-of-hospital setting, when done solely for a law enforcement purpose.”
Medications typically used for restraint include dissociative ketamine, benzodiazepine sedatives such as midazolam, and antipsychotic medications including olanzapine or haloperidol, alone or in combination.
Kenneth Certa, MD, from the American Psychiatric Association, speaking on behalf of the section council on psychiatry, said in a reference committee hearing: “We have been very concerned over the years with the development of the inexact diagnosis of ‘agitated delirium’ or ‘excited delirium,’ especially after having had a number of individuals, more than what’s reported in the press, die by the use of ketamine in the field for this inexact diagnosis.”
Tamaan Osbourne-Roberts, MD, a delegate and CSAPH member, said the diagnosis lacks scientific evidence and is “disproportionately applied to otherwise healthy Black men in their mid-30s and these men are most likely to die from resulting first-responder actions.”
Dr. Osbourne-Roberts testified that deescalation training should be more widely used and that crisis intervention team models in which behavioral health specialists are first deployed to respond to behavioral health emergencies should be more prevalent.
Andrew Rudawsky, MD, an assistant medical director of two emergency departments and delegate from Ohio, speaking as an individual, testified: “I can tell you from first-hand experience that ‘excited delirium’ is very real. These acutely ill, unstable patients have an emergency medical condition best cared for by an emergency medicine physician.”
The report recognizes that drugs used outside a hospital setting by nonphysicians come with significant risks, particularly for those with underlying conditions and in terms of drug–drug interactions.
“I completely agree that medicine should not be practiced by law enforcement,” Dr. Rudawsky said. “I’m gravely concerned by the legal ramifications of stating that this condition doesn’t exist.”
He said he is optimistic that the Diagnostic and Statistical Manual of Mental Disorders (DSM) will be updated to include “excited delirium.”
in medical and mental health emergencies in local communities.
Additionally, the report urges that “administration of any pharmacologic treatments in the out-of-hospital setting be done equitably, in an evidence-based, antiracist, and stigma-free way.”
The report calls on law enforcement and frontline emergency medical service personnel, who are a part of the “dual response” in emergency situations, to engage in training overseen by EMS medical directors. “The training should minimally include deescalation techniques and the appropriate use of pharmacologic intervention for agitated individuals in the out-of-hospital setting,” the report states.
Recommendation on oversight draws controversy
Several commenters were emergency physicians and medical directors who expressed concern that investigation of potential cases of inappropriate pharmacologic intervention would be overseen by nonphysicians.
The CSAPH authors write that independent investigators are appropriate, whereas those in emergency medicine say EMS medical directors should lead oversight.
Stephen Epstein, MD, chair of the section council on emergency medicine, speaking on behalf of the section council, had moved for referral of the portion of the report that deals with oversight of EMS.
“We’re concerned that recommendation 6, by calling for independent investigators, would put nonphysicians in the position of supervising the practice of medicine of a board-approved specialty. This would set an unfortunate precedent for our AMA,” he said.
Dr. Epstein also said the American College of Emergency Physicians will soon release a report on “excited delirium,” which will add key information for debating the issue.
He added that a new report on the safety of ketamine in out-of-hospital use was published just last week in the Annals of Emergency Medicine. The authors reviewed more than 11,000 cases of the pharmacologic intervention over the past 2 years.
“We believe this information may add substantively to the recommendation in this report,” Dr. Epstein said.
Recommendation 6 was referred to the AMA Board for a decision, but the rest of the report was overwhelmingly adopted.
Dr. Certa, Dr. Osbourne-Roberts, Dr. Rudawsky, and Dr. Epstein have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Current evidence does not support use of “excited delirium” or “excited delirium syndrome” as a medical diagnosis, the American Medical Association said June 14, and the term should not be used unless clear diagnostic criteria are validated.
The term is disproportionately applied to people of color, “for whom inappropriate and excessive pharmacotherapy continues to be the norm instead of behavioral deescalation,” the report by the AMA’s Council on Science and Public Health stated, and is therefore indicative of systemic racism.
That conclusion was one of many included in CSAPH Report 2, which was adopted June 14 at the special meeting of the AMA House of Delegates.
The AMA also opposes “use of sedative/hypnotic and dissociative agents, including ketamine, as a pharmacologic intervention for agitated individuals in the out-of-hospital setting, when done solely for a law enforcement purpose.”
Medications typically used for restraint include dissociative ketamine, benzodiazepine sedatives such as midazolam, and antipsychotic medications including olanzapine or haloperidol, alone or in combination.
Kenneth Certa, MD, from the American Psychiatric Association, speaking on behalf of the section council on psychiatry, said in a reference committee hearing: “We have been very concerned over the years with the development of the inexact diagnosis of ‘agitated delirium’ or ‘excited delirium,’ especially after having had a number of individuals, more than what’s reported in the press, die by the use of ketamine in the field for this inexact diagnosis.”
Tamaan Osbourne-Roberts, MD, a delegate and CSAPH member, said the diagnosis lacks scientific evidence and is “disproportionately applied to otherwise healthy Black men in their mid-30s and these men are most likely to die from resulting first-responder actions.”
Dr. Osbourne-Roberts testified that deescalation training should be more widely used and that crisis intervention team models in which behavioral health specialists are first deployed to respond to behavioral health emergencies should be more prevalent.
Andrew Rudawsky, MD, an assistant medical director of two emergency departments and delegate from Ohio, speaking as an individual, testified: “I can tell you from first-hand experience that ‘excited delirium’ is very real. These acutely ill, unstable patients have an emergency medical condition best cared for by an emergency medicine physician.”
The report recognizes that drugs used outside a hospital setting by nonphysicians come with significant risks, particularly for those with underlying conditions and in terms of drug–drug interactions.
“I completely agree that medicine should not be practiced by law enforcement,” Dr. Rudawsky said. “I’m gravely concerned by the legal ramifications of stating that this condition doesn’t exist.”
He said he is optimistic that the Diagnostic and Statistical Manual of Mental Disorders (DSM) will be updated to include “excited delirium.”
in medical and mental health emergencies in local communities.
Additionally, the report urges that “administration of any pharmacologic treatments in the out-of-hospital setting be done equitably, in an evidence-based, antiracist, and stigma-free way.”
The report calls on law enforcement and frontline emergency medical service personnel, who are a part of the “dual response” in emergency situations, to engage in training overseen by EMS medical directors. “The training should minimally include deescalation techniques and the appropriate use of pharmacologic intervention for agitated individuals in the out-of-hospital setting,” the report states.
Recommendation on oversight draws controversy
Several commenters were emergency physicians and medical directors who expressed concern that investigation of potential cases of inappropriate pharmacologic intervention would be overseen by nonphysicians.
The CSAPH authors write that independent investigators are appropriate, whereas those in emergency medicine say EMS medical directors should lead oversight.
Stephen Epstein, MD, chair of the section council on emergency medicine, speaking on behalf of the section council, had moved for referral of the portion of the report that deals with oversight of EMS.
“We’re concerned that recommendation 6, by calling for independent investigators, would put nonphysicians in the position of supervising the practice of medicine of a board-approved specialty. This would set an unfortunate precedent for our AMA,” he said.
Dr. Epstein also said the American College of Emergency Physicians will soon release a report on “excited delirium,” which will add key information for debating the issue.
He added that a new report on the safety of ketamine in out-of-hospital use was published just last week in the Annals of Emergency Medicine. The authors reviewed more than 11,000 cases of the pharmacologic intervention over the past 2 years.
“We believe this information may add substantively to the recommendation in this report,” Dr. Epstein said.
Recommendation 6 was referred to the AMA Board for a decision, but the rest of the report was overwhelmingly adopted.
Dr. Certa, Dr. Osbourne-Roberts, Dr. Rudawsky, and Dr. Epstein have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Current evidence does not support use of “excited delirium” or “excited delirium syndrome” as a medical diagnosis, the American Medical Association said June 14, and the term should not be used unless clear diagnostic criteria are validated.
The term is disproportionately applied to people of color, “for whom inappropriate and excessive pharmacotherapy continues to be the norm instead of behavioral deescalation,” the report by the AMA’s Council on Science and Public Health stated, and is therefore indicative of systemic racism.
That conclusion was one of many included in CSAPH Report 2, which was adopted June 14 at the special meeting of the AMA House of Delegates.
The AMA also opposes “use of sedative/hypnotic and dissociative agents, including ketamine, as a pharmacologic intervention for agitated individuals in the out-of-hospital setting, when done solely for a law enforcement purpose.”
Medications typically used for restraint include dissociative ketamine, benzodiazepine sedatives such as midazolam, and antipsychotic medications including olanzapine or haloperidol, alone or in combination.
Kenneth Certa, MD, from the American Psychiatric Association, speaking on behalf of the section council on psychiatry, said in a reference committee hearing: “We have been very concerned over the years with the development of the inexact diagnosis of ‘agitated delirium’ or ‘excited delirium,’ especially after having had a number of individuals, more than what’s reported in the press, die by the use of ketamine in the field for this inexact diagnosis.”
Tamaan Osbourne-Roberts, MD, a delegate and CSAPH member, said the diagnosis lacks scientific evidence and is “disproportionately applied to otherwise healthy Black men in their mid-30s and these men are most likely to die from resulting first-responder actions.”
Dr. Osbourne-Roberts testified that deescalation training should be more widely used and that crisis intervention team models in which behavioral health specialists are first deployed to respond to behavioral health emergencies should be more prevalent.
Andrew Rudawsky, MD, an assistant medical director of two emergency departments and delegate from Ohio, speaking as an individual, testified: “I can tell you from first-hand experience that ‘excited delirium’ is very real. These acutely ill, unstable patients have an emergency medical condition best cared for by an emergency medicine physician.”
The report recognizes that drugs used outside a hospital setting by nonphysicians come with significant risks, particularly for those with underlying conditions and in terms of drug–drug interactions.
“I completely agree that medicine should not be practiced by law enforcement,” Dr. Rudawsky said. “I’m gravely concerned by the legal ramifications of stating that this condition doesn’t exist.”
He said he is optimistic that the Diagnostic and Statistical Manual of Mental Disorders (DSM) will be updated to include “excited delirium.”
in medical and mental health emergencies in local communities.
Additionally, the report urges that “administration of any pharmacologic treatments in the out-of-hospital setting be done equitably, in an evidence-based, antiracist, and stigma-free way.”
The report calls on law enforcement and frontline emergency medical service personnel, who are a part of the “dual response” in emergency situations, to engage in training overseen by EMS medical directors. “The training should minimally include deescalation techniques and the appropriate use of pharmacologic intervention for agitated individuals in the out-of-hospital setting,” the report states.
Recommendation on oversight draws controversy
Several commenters were emergency physicians and medical directors who expressed concern that investigation of potential cases of inappropriate pharmacologic intervention would be overseen by nonphysicians.
The CSAPH authors write that independent investigators are appropriate, whereas those in emergency medicine say EMS medical directors should lead oversight.
Stephen Epstein, MD, chair of the section council on emergency medicine, speaking on behalf of the section council, had moved for referral of the portion of the report that deals with oversight of EMS.
“We’re concerned that recommendation 6, by calling for independent investigators, would put nonphysicians in the position of supervising the practice of medicine of a board-approved specialty. This would set an unfortunate precedent for our AMA,” he said.
Dr. Epstein also said the American College of Emergency Physicians will soon release a report on “excited delirium,” which will add key information for debating the issue.
He added that a new report on the safety of ketamine in out-of-hospital use was published just last week in the Annals of Emergency Medicine. The authors reviewed more than 11,000 cases of the pharmacologic intervention over the past 2 years.
“We believe this information may add substantively to the recommendation in this report,” Dr. Epstein said.
Recommendation 6 was referred to the AMA Board for a decision, but the rest of the report was overwhelmingly adopted.
Dr. Certa, Dr. Osbourne-Roberts, Dr. Rudawsky, and Dr. Epstein have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AMA selects dermatologist as incoming president for 2022
Known for his advocacy efforts – promoting telemedicine and digital health and fighting rising prescription drug prices, among other issues – he has testified in Congressional hearings on all those topics and other issues crucial for a functioning U.S. health care system.
Colleagues describe him as well informed, intelligent, and an excellent listener who is skilled at understanding all sides of difficult issues.
“I am committed to relentlessly advocating for physicians and patients on issues that matter most to us, and look forward to the continued meaningful advancements our AMA will make as we strive to improve the health of the nation,” Dr. Resneck said in a statement issued by the AMA. “Now more than ever, I am proud to be part of an AMA that is dedicated to driving the future of medicine, removing obstacles to patient care, and leading the charge to prevent chronic disease and confront public health crises – all while prioritizing our goal of eliminating longstanding health inequities.”
Dr. Resneck called this a “pivotal time of learning from the COVID-19 pandemic experience as we plan for the future of medicine and public health.”
“Jack is one of the most well-informed people I know,” Barbara L. McAneny, MD, president of the AMA from 2018 to 2019 and CEO of the New Mexico Cancer Center, Albuquerque, said in an interview. “Now that the pandemic is slowly decreasing, the underlying problems in our health care system will resurface. Jack understands how the insurance industry uses prior authorization and other techniques to harm physicians and patients. He is very well positioned to be a voice of reason that is sorely needed in today’s healthcare industry.”
David O. Barbe, MD, MHA, president of the World Medical Association and president of the AMA from 2017 to 2018, calls Dr. Resneck “extremely smart, very analytical. I think one of his great strengths is, he is an excellent listener and can capture the essence of all sides of the issues. He does a remarkable job at achieving consensus.” Dr. Barbe is a family physician in Mountain Grove, Mo.
Dr. Resneck has a long history of serving the AMA, the California Medical Association, and dermatology organizations such as the American Academy of Dermatology.
“Dr. Resneck’s exemplary leadership on a number of AAD/A committees and councils and as a member of the boards of directors has made a lasting impact on the academy, and he is poised to do the same as president-elect of the American Medical Association,” AAD president Ken Tomecki, MD, said in a statement provided by the AAD. “We congratulate Dr. Resneck on his achievement, and we’re proud to have a dermatologist serving as a leading voice in the house of medicine.”
First elected to the AMA board of trustees in 2014, Dr. Resneck held the office of board chair from 2018 to 2019. He was also chair of the AMA Council on Legislation and was a delegate to the AMA House of Delegates. He has had leadership roles in the California Society of Dermatology and Dermatologic Surgery, the American Academy of Dermatology and the California Medical Association. He is vice chair and professor of dermatology at the University of California, San Francisco, with a joint appointment at the Philip R. Lee Institute for Health Policy Studies.
As a researcher, his citation list includes numerous published studies about patient access to care, telemedicine, quality metrics, prior authorization, and public health. He is on the editorial board of the Journal of the American Academy of Dermatology and the board of directors of the National Quality Forum. His undergraduate degree in public policy is from Brown University, Providence, R.I. He earned his medical degree from UCSF, where he also completed an internal medicine internship, a residency training in dermatology and a health policy fellowship.
Gerald Harmon, MD, a family practice physician in coastal South Carolina, will be inaugurated as the AMA president for 2021-2022 on June 15.
Known for his advocacy efforts – promoting telemedicine and digital health and fighting rising prescription drug prices, among other issues – he has testified in Congressional hearings on all those topics and other issues crucial for a functioning U.S. health care system.
Colleagues describe him as well informed, intelligent, and an excellent listener who is skilled at understanding all sides of difficult issues.
“I am committed to relentlessly advocating for physicians and patients on issues that matter most to us, and look forward to the continued meaningful advancements our AMA will make as we strive to improve the health of the nation,” Dr. Resneck said in a statement issued by the AMA. “Now more than ever, I am proud to be part of an AMA that is dedicated to driving the future of medicine, removing obstacles to patient care, and leading the charge to prevent chronic disease and confront public health crises – all while prioritizing our goal of eliminating longstanding health inequities.”
Dr. Resneck called this a “pivotal time of learning from the COVID-19 pandemic experience as we plan for the future of medicine and public health.”
“Jack is one of the most well-informed people I know,” Barbara L. McAneny, MD, president of the AMA from 2018 to 2019 and CEO of the New Mexico Cancer Center, Albuquerque, said in an interview. “Now that the pandemic is slowly decreasing, the underlying problems in our health care system will resurface. Jack understands how the insurance industry uses prior authorization and other techniques to harm physicians and patients. He is very well positioned to be a voice of reason that is sorely needed in today’s healthcare industry.”
David O. Barbe, MD, MHA, president of the World Medical Association and president of the AMA from 2017 to 2018, calls Dr. Resneck “extremely smart, very analytical. I think one of his great strengths is, he is an excellent listener and can capture the essence of all sides of the issues. He does a remarkable job at achieving consensus.” Dr. Barbe is a family physician in Mountain Grove, Mo.
Dr. Resneck has a long history of serving the AMA, the California Medical Association, and dermatology organizations such as the American Academy of Dermatology.
“Dr. Resneck’s exemplary leadership on a number of AAD/A committees and councils and as a member of the boards of directors has made a lasting impact on the academy, and he is poised to do the same as president-elect of the American Medical Association,” AAD president Ken Tomecki, MD, said in a statement provided by the AAD. “We congratulate Dr. Resneck on his achievement, and we’re proud to have a dermatologist serving as a leading voice in the house of medicine.”
First elected to the AMA board of trustees in 2014, Dr. Resneck held the office of board chair from 2018 to 2019. He was also chair of the AMA Council on Legislation and was a delegate to the AMA House of Delegates. He has had leadership roles in the California Society of Dermatology and Dermatologic Surgery, the American Academy of Dermatology and the California Medical Association. He is vice chair and professor of dermatology at the University of California, San Francisco, with a joint appointment at the Philip R. Lee Institute for Health Policy Studies.
As a researcher, his citation list includes numerous published studies about patient access to care, telemedicine, quality metrics, prior authorization, and public health. He is on the editorial board of the Journal of the American Academy of Dermatology and the board of directors of the National Quality Forum. His undergraduate degree in public policy is from Brown University, Providence, R.I. He earned his medical degree from UCSF, where he also completed an internal medicine internship, a residency training in dermatology and a health policy fellowship.
Gerald Harmon, MD, a family practice physician in coastal South Carolina, will be inaugurated as the AMA president for 2021-2022 on June 15.
Known for his advocacy efforts – promoting telemedicine and digital health and fighting rising prescription drug prices, among other issues – he has testified in Congressional hearings on all those topics and other issues crucial for a functioning U.S. health care system.
Colleagues describe him as well informed, intelligent, and an excellent listener who is skilled at understanding all sides of difficult issues.
“I am committed to relentlessly advocating for physicians and patients on issues that matter most to us, and look forward to the continued meaningful advancements our AMA will make as we strive to improve the health of the nation,” Dr. Resneck said in a statement issued by the AMA. “Now more than ever, I am proud to be part of an AMA that is dedicated to driving the future of medicine, removing obstacles to patient care, and leading the charge to prevent chronic disease and confront public health crises – all while prioritizing our goal of eliminating longstanding health inequities.”
Dr. Resneck called this a “pivotal time of learning from the COVID-19 pandemic experience as we plan for the future of medicine and public health.”
“Jack is one of the most well-informed people I know,” Barbara L. McAneny, MD, president of the AMA from 2018 to 2019 and CEO of the New Mexico Cancer Center, Albuquerque, said in an interview. “Now that the pandemic is slowly decreasing, the underlying problems in our health care system will resurface. Jack understands how the insurance industry uses prior authorization and other techniques to harm physicians and patients. He is very well positioned to be a voice of reason that is sorely needed in today’s healthcare industry.”
David O. Barbe, MD, MHA, president of the World Medical Association and president of the AMA from 2017 to 2018, calls Dr. Resneck “extremely smart, very analytical. I think one of his great strengths is, he is an excellent listener and can capture the essence of all sides of the issues. He does a remarkable job at achieving consensus.” Dr. Barbe is a family physician in Mountain Grove, Mo.
Dr. Resneck has a long history of serving the AMA, the California Medical Association, and dermatology organizations such as the American Academy of Dermatology.
“Dr. Resneck’s exemplary leadership on a number of AAD/A committees and councils and as a member of the boards of directors has made a lasting impact on the academy, and he is poised to do the same as president-elect of the American Medical Association,” AAD president Ken Tomecki, MD, said in a statement provided by the AAD. “We congratulate Dr. Resneck on his achievement, and we’re proud to have a dermatologist serving as a leading voice in the house of medicine.”
First elected to the AMA board of trustees in 2014, Dr. Resneck held the office of board chair from 2018 to 2019. He was also chair of the AMA Council on Legislation and was a delegate to the AMA House of Delegates. He has had leadership roles in the California Society of Dermatology and Dermatologic Surgery, the American Academy of Dermatology and the California Medical Association. He is vice chair and professor of dermatology at the University of California, San Francisco, with a joint appointment at the Philip R. Lee Institute for Health Policy Studies.
As a researcher, his citation list includes numerous published studies about patient access to care, telemedicine, quality metrics, prior authorization, and public health. He is on the editorial board of the Journal of the American Academy of Dermatology and the board of directors of the National Quality Forum. His undergraduate degree in public policy is from Brown University, Providence, R.I. He earned his medical degree from UCSF, where he also completed an internal medicine internship, a residency training in dermatology and a health policy fellowship.
Gerald Harmon, MD, a family practice physician in coastal South Carolina, will be inaugurated as the AMA president for 2021-2022 on June 15.
Minnesota named best place to practice in 2021
For physicians who are just starting out or thinking about moving, the “Land of 10,000 Lakes” could be the land of opportunity, according to a recent Medscape analysis.
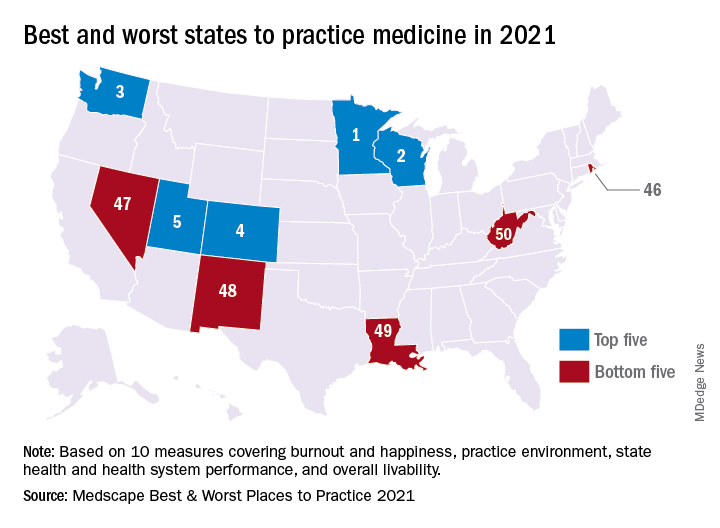
In a ranking of the 50 states, Minnesota “claimed top marks for livability, low incidence of adverse actions against doctors, and the performance of its health system,” Shelly Reese wrote in Medscape’s “Best & Worst Places to Practice 2021.”
Minnesota is below average where it’s good to be below average – share of physicians reporting burnout and/or depression – but above average in the share of physicians who say they’re “very happy” outside of work, Medscape said in the annual report.
and adverse actions and a high level of livability. Third place went to Washington (called the most livable state in the country by U.S. News and World Report), fourth to Colorado (physicians happy at and outside of work, high retention rate for residents), and fifth to Utah (low crime rate, high quality of life), Medscape said.
At the bottom of the list for 2021 is West Virginia, where physicians “may confront a bevy of challenges” in the form of low livability, a high rate of adverse actions, and relatively high malpractice payouts, Ms. Reese noted in the report.
State number 49 is Louisiana, where livability is low, malpractice payouts are high, and more than half of physicians say that they’re burned out and/or depressed. New Mexico is 48th (very high rate of adverse actions, poor resident retention), Nevada is 47th (low marks for avoidable hospital use and disparity in care), and Rhode Island is 46th (high malpractice payouts, low physician compensation), Medscape said.
Continuing with the group-of-five theme, America’s three most populous states finished in the top half of the ranking – California 16th, Texas 11th, and Florida 21st – but New York and Pennsylvania, numbers four and five by population size, did not.
The rankings are based on states’ performance in 10 different measures, three of which were sourced from Medscape surveys – happiness at work, happiness outside of work, and burnout/depression – and seven from other organizations: adverse actions against physicians, malpractice payouts, compensation (adjusted for cost of living), overall health, health system performance, overall livability, resident retention.
For physicians who are just starting out or thinking about moving, the “Land of 10,000 Lakes” could be the land of opportunity, according to a recent Medscape analysis.
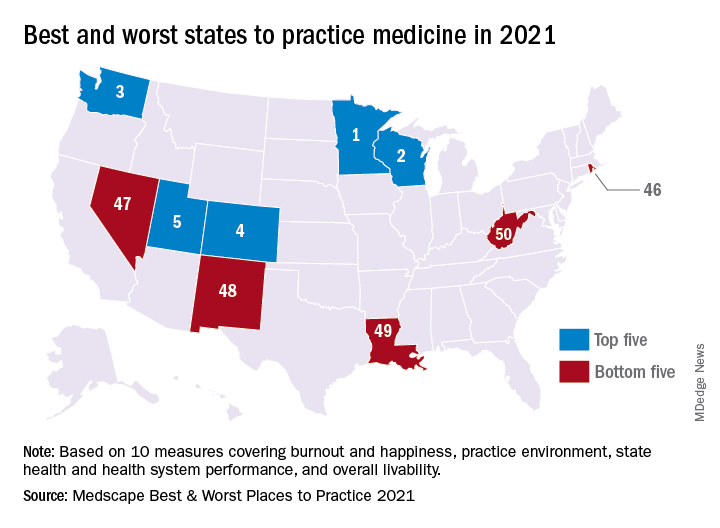
In a ranking of the 50 states, Minnesota “claimed top marks for livability, low incidence of adverse actions against doctors, and the performance of its health system,” Shelly Reese wrote in Medscape’s “Best & Worst Places to Practice 2021.”
Minnesota is below average where it’s good to be below average – share of physicians reporting burnout and/or depression – but above average in the share of physicians who say they’re “very happy” outside of work, Medscape said in the annual report.
and adverse actions and a high level of livability. Third place went to Washington (called the most livable state in the country by U.S. News and World Report), fourth to Colorado (physicians happy at and outside of work, high retention rate for residents), and fifth to Utah (low crime rate, high quality of life), Medscape said.
At the bottom of the list for 2021 is West Virginia, where physicians “may confront a bevy of challenges” in the form of low livability, a high rate of adverse actions, and relatively high malpractice payouts, Ms. Reese noted in the report.
State number 49 is Louisiana, where livability is low, malpractice payouts are high, and more than half of physicians say that they’re burned out and/or depressed. New Mexico is 48th (very high rate of adverse actions, poor resident retention), Nevada is 47th (low marks for avoidable hospital use and disparity in care), and Rhode Island is 46th (high malpractice payouts, low physician compensation), Medscape said.
Continuing with the group-of-five theme, America’s three most populous states finished in the top half of the ranking – California 16th, Texas 11th, and Florida 21st – but New York and Pennsylvania, numbers four and five by population size, did not.
The rankings are based on states’ performance in 10 different measures, three of which were sourced from Medscape surveys – happiness at work, happiness outside of work, and burnout/depression – and seven from other organizations: adverse actions against physicians, malpractice payouts, compensation (adjusted for cost of living), overall health, health system performance, overall livability, resident retention.
For physicians who are just starting out or thinking about moving, the “Land of 10,000 Lakes” could be the land of opportunity, according to a recent Medscape analysis.
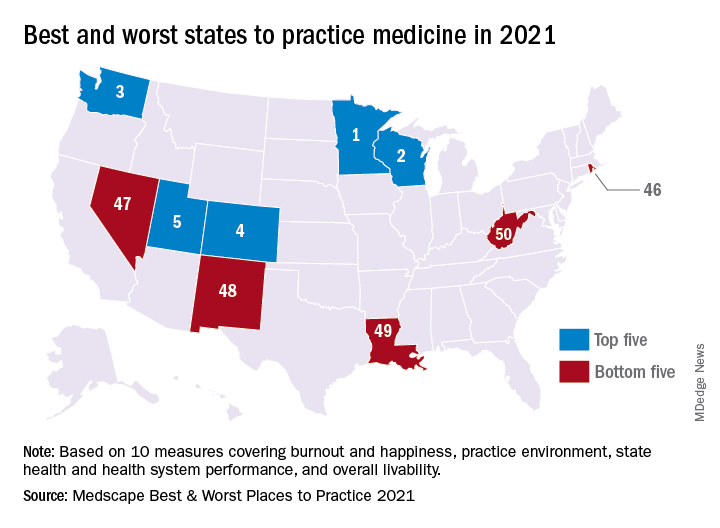
In a ranking of the 50 states, Minnesota “claimed top marks for livability, low incidence of adverse actions against doctors, and the performance of its health system,” Shelly Reese wrote in Medscape’s “Best & Worst Places to Practice 2021.”
Minnesota is below average where it’s good to be below average – share of physicians reporting burnout and/or depression – but above average in the share of physicians who say they’re “very happy” outside of work, Medscape said in the annual report.
and adverse actions and a high level of livability. Third place went to Washington (called the most livable state in the country by U.S. News and World Report), fourth to Colorado (physicians happy at and outside of work, high retention rate for residents), and fifth to Utah (low crime rate, high quality of life), Medscape said.
At the bottom of the list for 2021 is West Virginia, where physicians “may confront a bevy of challenges” in the form of low livability, a high rate of adverse actions, and relatively high malpractice payouts, Ms. Reese noted in the report.
State number 49 is Louisiana, where livability is low, malpractice payouts are high, and more than half of physicians say that they’re burned out and/or depressed. New Mexico is 48th (very high rate of adverse actions, poor resident retention), Nevada is 47th (low marks for avoidable hospital use and disparity in care), and Rhode Island is 46th (high malpractice payouts, low physician compensation), Medscape said.
Continuing with the group-of-five theme, America’s three most populous states finished in the top half of the ranking – California 16th, Texas 11th, and Florida 21st – but New York and Pennsylvania, numbers four and five by population size, did not.
The rankings are based on states’ performance in 10 different measures, three of which were sourced from Medscape surveys – happiness at work, happiness outside of work, and burnout/depression – and seven from other organizations: adverse actions against physicians, malpractice payouts, compensation (adjusted for cost of living), overall health, health system performance, overall livability, resident retention.
U.S. News releases Best Children’s Hospitals list, with changes
Released June 15, the 2021-2022 rankings, which acknowledge 50 U.S. centers for delivering exceptional care in several specialties, also give the Massachusetts hospital the top spot in 4 of 10 pediatric specialties assessed: nephrology, neurology and neurosurgery, pulmonology and lung surgery, and urology.
Children’s Hospital of Philadelphia retains second spot in the annually updated list, and Texas Children’s Hospital, in Houston, moves up a rung to third place, bumping Cincinnati Children’s Hospital Medical Center from third to fourth place. Children’s Hospital Los Angeles comes in at no. 5.
The remaining top 10 placements, in descending order, are as follows:
Children’s Hospital Colorado in Aurora; Children’s National Hospital in Washington; Nationwide Children’s Hospital in Columbus, Ohio; UPMS Children’s Hospital of Pittsburgh; and Lucile Packard Children’s Hospital Stanford (Calif.).
New regional rankings
This year’s edition offers something new, adding rankings within states and multiple-state rankings within seven regions to facilitate choice. “The Best Children’s Hospitals rankings have always highlighted hospitals that excel in specialized care,” said Ben Harder, chief of health analysis and managing editor at U.S. News, in a press release. “Now, this year’s new state and regional rankings can help families identify conveniently located hospitals capable of meeting their child’s needs. As the pandemic continues to affect travel, finding high-quality care close to home has never been more important.”
Across the seven regions, the top-ranked institutions are as follows:
- Mid-Atlantic – Children’s Hospital of Philadelphia.
- Midwest – Cincinnati Children’s Hospital Medical Center.
- New England – Boston Children’s Hospital.
- Pacific – Children’s Hospital Los Angeles.
- Rocky Mountains – Children’s Hospital Colorado.
- Southeast – Children’s Healthcare of Atlanta and Monroe Carell Jr. Children’s Hospital of Vanderbilt, in Nashville, Tenn.
- Southwest – Texas Children’s Hospital.
Specialties
Boston Children’s not only topped the overall list but also led in four specialties. For the other six specialties that were ranked, the top hospitals on the honor roll are as follows:
- Cancer – Children’s Hospital of Philadelphia.
- Cardiology and heart surgery – Texas Children’s Hospital.
- Diabetes and endocrinology – Children’s Hospital of Philadelphia.
- Gastroenterology and gastrointestinal surgery – Children’s Hospital Colorado.
- Neonatology – Children’s National Hospital.
- Orthopedics – Children’s Hospital of Philadelphia.
For the past 15 years, the objective of the rankings has been to offer a starting point for parents in making decisions about the best place to take very sick children for high-quality care. The editors of the rankings acknowledge that considerations of travel costs and insurance coverage are other factors to consider.
Helpful for families
The rankings are helpful for families, according to Joe W. St. Geme, III, MD, Children’s Hospital of Philadelphia’s physician-in-chief and chair of its department of pediatrics. “Some parents, especially those coming from outside an area, find them useful when deciding on care away from home,” he told this news organization. “Most types of pediatric care are available in the community, but sometimes a child has an unusual disease or complex disease for which local care is not available.”
Dr. St. Geme said the new regional rankings may be useful in helping parents decide where to bring a child for care that is closer to where they live.
A top ranking from U.S. News is just one indication of a hospital›s overall performance, according to Angela Lorts, MD, MBA, director of the Ventricular Assist Device Program, at Cincinnati Children’s Hospital Medical Center.
“Parents seeking care for their child should use the data to ask questions and understand the limitations,” she told this news organization. “Rankings are only based on a small subset of the children we care for. Many of the metrics may not pertain to their child and may not reflect the care they will receive.”
In her view, ranking will not give parents all the information they need about medical care and outcomes for specific conditions.
Hospital reaction
Hospitals can use the rankings to target improvements, says Dr. St. Geme. “These rankings can provide an opportunity for some benchmarking, to see what other institutions are doing and how they’re able to deliver care. They can serve as a source of ideas and can influence planning,” he said.
He cautioned that the data are not as complete as they could be. “A number of services are not included, and we try to keep that in mind,” he said.
Rankings may also affect recruitment, Dr. St. Geme added, because higher-ranked institutions may find it easier to attract sought-after clinicians and investigators in needed areas.
Another sphere of influence is philanthropy and fund raising. “People are much more likely to consider making both small and large donations to a high-ranked institution,” said J. Howard Smart, MD, chair of pediatrics at Sharp Rees-Stealy Medical Group and chair-elect of the physician leadership council at Sharp Mary Birch Hospital for Women and Newborns in San Diego.
Dr. St. Geme agrees. “Philanthropists are interested in making investments where they feel they’re a sure bet, and rankings may indicate a sure bet. But their impact on government funding and grant support is probably less.”
Ultimately, however, some families may not have lot of choice in where to go when their children are sick, Dr. Smart said. “And people probably don’t choose a location to live in based on nearby children’s hospitals the way they do for schools,” he said.
What about hospitals that continue to rank much lower on the 50-institution list – excellent though they must be to make it onto the honor roll. “To be on the list but not to have risen in rank in recent years might be a disappointment,” said Dr. St. Geme. “But it might also motivate a hospital to think about making internal investments in order to strengthen a particular service. And it may motivate nonranked hospitals to improve care in order to break into the list.”
Dr. Lorts points out that the annual survey process requires hospitals to track the clinical outcomes of a subset of patients, which may lead to improvement in these areas. It also requires data collection on structure and process, which drives needs assessments of select hospital areas. “But ideally, all hospitals would be tracking important outcomes, benchmarking to peer hospitals, and improving where needed without the U.S. News incentive,” she said.
This year’s data, compiled by research and consulting firm RTI International, derive from feedback on more than 1,200 questions provided by 118 responding institutions. Details on each hospital on the list and the methodology used in the analysis are available on U.S. News & World Report’s website.
A version of this article first appeared on Medscape.com.
Released June 15, the 2021-2022 rankings, which acknowledge 50 U.S. centers for delivering exceptional care in several specialties, also give the Massachusetts hospital the top spot in 4 of 10 pediatric specialties assessed: nephrology, neurology and neurosurgery, pulmonology and lung surgery, and urology.
Children’s Hospital of Philadelphia retains second spot in the annually updated list, and Texas Children’s Hospital, in Houston, moves up a rung to third place, bumping Cincinnati Children’s Hospital Medical Center from third to fourth place. Children’s Hospital Los Angeles comes in at no. 5.
The remaining top 10 placements, in descending order, are as follows:
Children’s Hospital Colorado in Aurora; Children’s National Hospital in Washington; Nationwide Children’s Hospital in Columbus, Ohio; UPMS Children’s Hospital of Pittsburgh; and Lucile Packard Children’s Hospital Stanford (Calif.).
New regional rankings
This year’s edition offers something new, adding rankings within states and multiple-state rankings within seven regions to facilitate choice. “The Best Children’s Hospitals rankings have always highlighted hospitals that excel in specialized care,” said Ben Harder, chief of health analysis and managing editor at U.S. News, in a press release. “Now, this year’s new state and regional rankings can help families identify conveniently located hospitals capable of meeting their child’s needs. As the pandemic continues to affect travel, finding high-quality care close to home has never been more important.”
Across the seven regions, the top-ranked institutions are as follows:
- Mid-Atlantic – Children’s Hospital of Philadelphia.
- Midwest – Cincinnati Children’s Hospital Medical Center.
- New England – Boston Children’s Hospital.
- Pacific – Children’s Hospital Los Angeles.
- Rocky Mountains – Children’s Hospital Colorado.
- Southeast – Children’s Healthcare of Atlanta and Monroe Carell Jr. Children’s Hospital of Vanderbilt, in Nashville, Tenn.
- Southwest – Texas Children’s Hospital.
Specialties
Boston Children’s not only topped the overall list but also led in four specialties. For the other six specialties that were ranked, the top hospitals on the honor roll are as follows:
- Cancer – Children’s Hospital of Philadelphia.
- Cardiology and heart surgery – Texas Children’s Hospital.
- Diabetes and endocrinology – Children’s Hospital of Philadelphia.
- Gastroenterology and gastrointestinal surgery – Children’s Hospital Colorado.
- Neonatology – Children’s National Hospital.
- Orthopedics – Children’s Hospital of Philadelphia.
For the past 15 years, the objective of the rankings has been to offer a starting point for parents in making decisions about the best place to take very sick children for high-quality care. The editors of the rankings acknowledge that considerations of travel costs and insurance coverage are other factors to consider.
Helpful for families
The rankings are helpful for families, according to Joe W. St. Geme, III, MD, Children’s Hospital of Philadelphia’s physician-in-chief and chair of its department of pediatrics. “Some parents, especially those coming from outside an area, find them useful when deciding on care away from home,” he told this news organization. “Most types of pediatric care are available in the community, but sometimes a child has an unusual disease or complex disease for which local care is not available.”
Dr. St. Geme said the new regional rankings may be useful in helping parents decide where to bring a child for care that is closer to where they live.
A top ranking from U.S. News is just one indication of a hospital›s overall performance, according to Angela Lorts, MD, MBA, director of the Ventricular Assist Device Program, at Cincinnati Children’s Hospital Medical Center.
“Parents seeking care for their child should use the data to ask questions and understand the limitations,” she told this news organization. “Rankings are only based on a small subset of the children we care for. Many of the metrics may not pertain to their child and may not reflect the care they will receive.”
In her view, ranking will not give parents all the information they need about medical care and outcomes for specific conditions.
Hospital reaction
Hospitals can use the rankings to target improvements, says Dr. St. Geme. “These rankings can provide an opportunity for some benchmarking, to see what other institutions are doing and how they’re able to deliver care. They can serve as a source of ideas and can influence planning,” he said.
He cautioned that the data are not as complete as they could be. “A number of services are not included, and we try to keep that in mind,” he said.
Rankings may also affect recruitment, Dr. St. Geme added, because higher-ranked institutions may find it easier to attract sought-after clinicians and investigators in needed areas.
Another sphere of influence is philanthropy and fund raising. “People are much more likely to consider making both small and large donations to a high-ranked institution,” said J. Howard Smart, MD, chair of pediatrics at Sharp Rees-Stealy Medical Group and chair-elect of the physician leadership council at Sharp Mary Birch Hospital for Women and Newborns in San Diego.
Dr. St. Geme agrees. “Philanthropists are interested in making investments where they feel they’re a sure bet, and rankings may indicate a sure bet. But their impact on government funding and grant support is probably less.”
Ultimately, however, some families may not have lot of choice in where to go when their children are sick, Dr. Smart said. “And people probably don’t choose a location to live in based on nearby children’s hospitals the way they do for schools,” he said.
What about hospitals that continue to rank much lower on the 50-institution list – excellent though they must be to make it onto the honor roll. “To be on the list but not to have risen in rank in recent years might be a disappointment,” said Dr. St. Geme. “But it might also motivate a hospital to think about making internal investments in order to strengthen a particular service. And it may motivate nonranked hospitals to improve care in order to break into the list.”
Dr. Lorts points out that the annual survey process requires hospitals to track the clinical outcomes of a subset of patients, which may lead to improvement in these areas. It also requires data collection on structure and process, which drives needs assessments of select hospital areas. “But ideally, all hospitals would be tracking important outcomes, benchmarking to peer hospitals, and improving where needed without the U.S. News incentive,” she said.
This year’s data, compiled by research and consulting firm RTI International, derive from feedback on more than 1,200 questions provided by 118 responding institutions. Details on each hospital on the list and the methodology used in the analysis are available on U.S. News & World Report’s website.
A version of this article first appeared on Medscape.com.
Released June 15, the 2021-2022 rankings, which acknowledge 50 U.S. centers for delivering exceptional care in several specialties, also give the Massachusetts hospital the top spot in 4 of 10 pediatric specialties assessed: nephrology, neurology and neurosurgery, pulmonology and lung surgery, and urology.
Children’s Hospital of Philadelphia retains second spot in the annually updated list, and Texas Children’s Hospital, in Houston, moves up a rung to third place, bumping Cincinnati Children’s Hospital Medical Center from third to fourth place. Children’s Hospital Los Angeles comes in at no. 5.
The remaining top 10 placements, in descending order, are as follows:
Children’s Hospital Colorado in Aurora; Children’s National Hospital in Washington; Nationwide Children’s Hospital in Columbus, Ohio; UPMS Children’s Hospital of Pittsburgh; and Lucile Packard Children’s Hospital Stanford (Calif.).
New regional rankings
This year’s edition offers something new, adding rankings within states and multiple-state rankings within seven regions to facilitate choice. “The Best Children’s Hospitals rankings have always highlighted hospitals that excel in specialized care,” said Ben Harder, chief of health analysis and managing editor at U.S. News, in a press release. “Now, this year’s new state and regional rankings can help families identify conveniently located hospitals capable of meeting their child’s needs. As the pandemic continues to affect travel, finding high-quality care close to home has never been more important.”
Across the seven regions, the top-ranked institutions are as follows:
- Mid-Atlantic – Children’s Hospital of Philadelphia.
- Midwest – Cincinnati Children’s Hospital Medical Center.
- New England – Boston Children’s Hospital.
- Pacific – Children’s Hospital Los Angeles.
- Rocky Mountains – Children’s Hospital Colorado.
- Southeast – Children’s Healthcare of Atlanta and Monroe Carell Jr. Children’s Hospital of Vanderbilt, in Nashville, Tenn.
- Southwest – Texas Children’s Hospital.
Specialties
Boston Children’s not only topped the overall list but also led in four specialties. For the other six specialties that were ranked, the top hospitals on the honor roll are as follows:
- Cancer – Children’s Hospital of Philadelphia.
- Cardiology and heart surgery – Texas Children’s Hospital.
- Diabetes and endocrinology – Children’s Hospital of Philadelphia.
- Gastroenterology and gastrointestinal surgery – Children’s Hospital Colorado.
- Neonatology – Children’s National Hospital.
- Orthopedics – Children’s Hospital of Philadelphia.
For the past 15 years, the objective of the rankings has been to offer a starting point for parents in making decisions about the best place to take very sick children for high-quality care. The editors of the rankings acknowledge that considerations of travel costs and insurance coverage are other factors to consider.
Helpful for families
The rankings are helpful for families, according to Joe W. St. Geme, III, MD, Children’s Hospital of Philadelphia’s physician-in-chief and chair of its department of pediatrics. “Some parents, especially those coming from outside an area, find them useful when deciding on care away from home,” he told this news organization. “Most types of pediatric care are available in the community, but sometimes a child has an unusual disease or complex disease for which local care is not available.”
Dr. St. Geme said the new regional rankings may be useful in helping parents decide where to bring a child for care that is closer to where they live.
A top ranking from U.S. News is just one indication of a hospital›s overall performance, according to Angela Lorts, MD, MBA, director of the Ventricular Assist Device Program, at Cincinnati Children’s Hospital Medical Center.
“Parents seeking care for their child should use the data to ask questions and understand the limitations,” she told this news organization. “Rankings are only based on a small subset of the children we care for. Many of the metrics may not pertain to their child and may not reflect the care they will receive.”
In her view, ranking will not give parents all the information they need about medical care and outcomes for specific conditions.
Hospital reaction
Hospitals can use the rankings to target improvements, says Dr. St. Geme. “These rankings can provide an opportunity for some benchmarking, to see what other institutions are doing and how they’re able to deliver care. They can serve as a source of ideas and can influence planning,” he said.
He cautioned that the data are not as complete as they could be. “A number of services are not included, and we try to keep that in mind,” he said.
Rankings may also affect recruitment, Dr. St. Geme added, because higher-ranked institutions may find it easier to attract sought-after clinicians and investigators in needed areas.
Another sphere of influence is philanthropy and fund raising. “People are much more likely to consider making both small and large donations to a high-ranked institution,” said J. Howard Smart, MD, chair of pediatrics at Sharp Rees-Stealy Medical Group and chair-elect of the physician leadership council at Sharp Mary Birch Hospital for Women and Newborns in San Diego.
Dr. St. Geme agrees. “Philanthropists are interested in making investments where they feel they’re a sure bet, and rankings may indicate a sure bet. But their impact on government funding and grant support is probably less.”
Ultimately, however, some families may not have lot of choice in where to go when their children are sick, Dr. Smart said. “And people probably don’t choose a location to live in based on nearby children’s hospitals the way they do for schools,” he said.
What about hospitals that continue to rank much lower on the 50-institution list – excellent though they must be to make it onto the honor roll. “To be on the list but not to have risen in rank in recent years might be a disappointment,” said Dr. St. Geme. “But it might also motivate a hospital to think about making internal investments in order to strengthen a particular service. And it may motivate nonranked hospitals to improve care in order to break into the list.”
Dr. Lorts points out that the annual survey process requires hospitals to track the clinical outcomes of a subset of patients, which may lead to improvement in these areas. It also requires data collection on structure and process, which drives needs assessments of select hospital areas. “But ideally, all hospitals would be tracking important outcomes, benchmarking to peer hospitals, and improving where needed without the U.S. News incentive,” she said.
This year’s data, compiled by research and consulting firm RTI International, derive from feedback on more than 1,200 questions provided by 118 responding institutions. Details on each hospital on the list and the methodology used in the analysis are available on U.S. News & World Report’s website.
A version of this article first appeared on Medscape.com.
The Cures Act: Is the “cure” worse than the disease?
There is a sudden spill of icy anxiety down your spine as you pick up your phone in your shaking hands. It’s 6 p.m.; your doctor’s office is closed. You open the message, and your worst fears are confirmed ... the cancer is back.
Or is it? You’re not sure. The biopsy sure sounds bad. But you’re an English teacher, not a doctor, and you spend the rest of the night Googling words like “tubulovillous” and “high-grade dysplasia.” You sit awake, terrified in front of the computer screen desperately trying to make sense of the possibly life-changing results. You wish you knew someone who could help you understand; you consider calling your doctor’s emergency line, or your cousin who is an ophthalmologist – anybody who can help you make sense of the results.
Or imagine another scenario: you’re a trans teen who has asked your doctor to refer to you by your preferred pronouns. You’re still presenting as your birth sex, in part because your family would disown you if they knew, and you’re not financially or emotionally ready for that step. You feel proud of yourself for advocating for your needs to your long-time physician, and excited about the resources they’ve included in your after visit summary and the referrals they’d made to gender-confirming specialists.
When you get home, you are confronted with a terrible reality that your doctor’s notes, orders, and recommendations are immediately viewable to anybody with your MyChart login – your parents knew the second your doctor signed the note. They received the notification, logged on as your guardians, and you have effectively been “outed” by the physician who took and oath to care for you and who you trusted implicitly.
How the Cures Act is affecting patients
While these examples may sound extreme, they are becoming more and more commonplace thanks to a recently enacted 21st Century Cures Act. The act was originally written to improve communication between physicians and patients. Part of the act stipulates that nearly all medical information – from notes to biopsies to lab results – must be available within 24 hours, published to a patient portal and a notification be sent to the patient by phone.
Oftentimes, this occurs before the ordering physician has even seen the results, much less interpreted them and made a plan for the patient. What happens now, not long after its enactment date, when it has become clear that the Cures Act is causing extreme harm to our patients?
Take, for example, the real example of a physician whose patient found out about her own intrauterine fetal demise by way of an EMR text message alert of “new imaging results!” sent directly to her phone. Or a physician colleague who witnessed firsthand the intrusive unhelpfulness of the Cures Act when she was informed via patient portal releasing her imaging information that she had a large, possibly malignant breast mass. “No phone call,” she said. “No human being for questions or comfort. Just a notification on my phone.”
The stories about the impact of the Cures Act across the medical community are an endless stream of anxiety, hurt, and broken trust. The relationship between a physician and a patient should be sacred, bolstered by communication and mutual respect.
In many ways, the new act feels like a third party to the patient-physician relationship – a digital imposter, oftentimes blurting out personal and life-altering medical information without any of the finesse, context, and perspective of an experienced physician.
Breaking ‘bad news’ to a patient
In training, some residents are taught how to “break bad news” to a patient. Some good practices for doing this are to have information available for the patient, provide emotional support, have a plan for their next steps already formulated, and call the appropriate specialist ahead of time if you can.
Above all, it’s most important to let the patient be the one to direct their own care. Give them time to ask questions and answer them honestly and clearly. Ask them how much they want to know and help them to understand the complex change in their usual state of health.
Now, unless physicians are keeping a very close eye on their inbox, results are slipping out to patients in a void. The bad news conversations aren’t happening at all, or if they are, they’re happening at 8 p.m. on a phone call after an exhausted physician ends their shift but has to slog through their results bin, calling all the patients who shouldn’t have to find out their results in solitude.
Reaching out to these patients immediately is an honorable, kind thing to, but for a physician, knowing they need to beat the patient to opening an email creates anxiety. Plus, making these calls at whatever hour the results are released to a patient is another burden added to doctors’ already-full plates.
Interpreting results
None of us want to harm our patients. All of us want to be there for them. But this act stands in the way of delivering quality, humanizing medical care.
It is true that patients have a right to access their own medical information. It is also true that waiting anxiously on results can cause undue harm to a patient. But the across-the-board, breakneck speed of information release mandated in this act causes irreparable harm not only to patients, but to the patient-physician relationship.
No patient should find out their cancer recurred while checking their emails at their desk. No patient should first learn of a life-altering diagnosis by way of scrolling through their smartphone in bed. The role of a physician is more than just a healer – we should also be educators, interpreters, partners and, first and foremost, advocates for our patients’ needs.
Our patients are depending on us to stand up and speak out about necessary changes to this act. Result releases should be delayed until they are viewed by a physician. Our patients deserve the dignity and opportunity of a conversation with their medical provider about their test results, and physicians deserve the chance to interpret results and frame the conversation in a way which is conducive to patient understanding and healing.
Dr. Persampiere is a first-year resident in the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece. You can contact them at fpnews@mdedge.com.
There is a sudden spill of icy anxiety down your spine as you pick up your phone in your shaking hands. It’s 6 p.m.; your doctor’s office is closed. You open the message, and your worst fears are confirmed ... the cancer is back.
Or is it? You’re not sure. The biopsy sure sounds bad. But you’re an English teacher, not a doctor, and you spend the rest of the night Googling words like “tubulovillous” and “high-grade dysplasia.” You sit awake, terrified in front of the computer screen desperately trying to make sense of the possibly life-changing results. You wish you knew someone who could help you understand; you consider calling your doctor’s emergency line, or your cousin who is an ophthalmologist – anybody who can help you make sense of the results.
Or imagine another scenario: you’re a trans teen who has asked your doctor to refer to you by your preferred pronouns. You’re still presenting as your birth sex, in part because your family would disown you if they knew, and you’re not financially or emotionally ready for that step. You feel proud of yourself for advocating for your needs to your long-time physician, and excited about the resources they’ve included in your after visit summary and the referrals they’d made to gender-confirming specialists.
When you get home, you are confronted with a terrible reality that your doctor’s notes, orders, and recommendations are immediately viewable to anybody with your MyChart login – your parents knew the second your doctor signed the note. They received the notification, logged on as your guardians, and you have effectively been “outed” by the physician who took and oath to care for you and who you trusted implicitly.
How the Cures Act is affecting patients
While these examples may sound extreme, they are becoming more and more commonplace thanks to a recently enacted 21st Century Cures Act. The act was originally written to improve communication between physicians and patients. Part of the act stipulates that nearly all medical information – from notes to biopsies to lab results – must be available within 24 hours, published to a patient portal and a notification be sent to the patient by phone.
Oftentimes, this occurs before the ordering physician has even seen the results, much less interpreted them and made a plan for the patient. What happens now, not long after its enactment date, when it has become clear that the Cures Act is causing extreme harm to our patients?
Take, for example, the real example of a physician whose patient found out about her own intrauterine fetal demise by way of an EMR text message alert of “new imaging results!” sent directly to her phone. Or a physician colleague who witnessed firsthand the intrusive unhelpfulness of the Cures Act when she was informed via patient portal releasing her imaging information that she had a large, possibly malignant breast mass. “No phone call,” she said. “No human being for questions or comfort. Just a notification on my phone.”
The stories about the impact of the Cures Act across the medical community are an endless stream of anxiety, hurt, and broken trust. The relationship between a physician and a patient should be sacred, bolstered by communication and mutual respect.
In many ways, the new act feels like a third party to the patient-physician relationship – a digital imposter, oftentimes blurting out personal and life-altering medical information without any of the finesse, context, and perspective of an experienced physician.
Breaking ‘bad news’ to a patient
In training, some residents are taught how to “break bad news” to a patient. Some good practices for doing this are to have information available for the patient, provide emotional support, have a plan for their next steps already formulated, and call the appropriate specialist ahead of time if you can.
Above all, it’s most important to let the patient be the one to direct their own care. Give them time to ask questions and answer them honestly and clearly. Ask them how much they want to know and help them to understand the complex change in their usual state of health.
Now, unless physicians are keeping a very close eye on their inbox, results are slipping out to patients in a void. The bad news conversations aren’t happening at all, or if they are, they’re happening at 8 p.m. on a phone call after an exhausted physician ends their shift but has to slog through their results bin, calling all the patients who shouldn’t have to find out their results in solitude.
Reaching out to these patients immediately is an honorable, kind thing to, but for a physician, knowing they need to beat the patient to opening an email creates anxiety. Plus, making these calls at whatever hour the results are released to a patient is another burden added to doctors’ already-full plates.
Interpreting results
None of us want to harm our patients. All of us want to be there for them. But this act stands in the way of delivering quality, humanizing medical care.
It is true that patients have a right to access their own medical information. It is also true that waiting anxiously on results can cause undue harm to a patient. But the across-the-board, breakneck speed of information release mandated in this act causes irreparable harm not only to patients, but to the patient-physician relationship.
No patient should find out their cancer recurred while checking their emails at their desk. No patient should first learn of a life-altering diagnosis by way of scrolling through their smartphone in bed. The role of a physician is more than just a healer – we should also be educators, interpreters, partners and, first and foremost, advocates for our patients’ needs.
Our patients are depending on us to stand up and speak out about necessary changes to this act. Result releases should be delayed until they are viewed by a physician. Our patients deserve the dignity and opportunity of a conversation with their medical provider about their test results, and physicians deserve the chance to interpret results and frame the conversation in a way which is conducive to patient understanding and healing.
Dr. Persampiere is a first-year resident in the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece. You can contact them at fpnews@mdedge.com.
There is a sudden spill of icy anxiety down your spine as you pick up your phone in your shaking hands. It’s 6 p.m.; your doctor’s office is closed. You open the message, and your worst fears are confirmed ... the cancer is back.
Or is it? You’re not sure. The biopsy sure sounds bad. But you’re an English teacher, not a doctor, and you spend the rest of the night Googling words like “tubulovillous” and “high-grade dysplasia.” You sit awake, terrified in front of the computer screen desperately trying to make sense of the possibly life-changing results. You wish you knew someone who could help you understand; you consider calling your doctor’s emergency line, or your cousin who is an ophthalmologist – anybody who can help you make sense of the results.
Or imagine another scenario: you’re a trans teen who has asked your doctor to refer to you by your preferred pronouns. You’re still presenting as your birth sex, in part because your family would disown you if they knew, and you’re not financially or emotionally ready for that step. You feel proud of yourself for advocating for your needs to your long-time physician, and excited about the resources they’ve included in your after visit summary and the referrals they’d made to gender-confirming specialists.
When you get home, you are confronted with a terrible reality that your doctor’s notes, orders, and recommendations are immediately viewable to anybody with your MyChart login – your parents knew the second your doctor signed the note. They received the notification, logged on as your guardians, and you have effectively been “outed” by the physician who took and oath to care for you and who you trusted implicitly.
How the Cures Act is affecting patients
While these examples may sound extreme, they are becoming more and more commonplace thanks to a recently enacted 21st Century Cures Act. The act was originally written to improve communication between physicians and patients. Part of the act stipulates that nearly all medical information – from notes to biopsies to lab results – must be available within 24 hours, published to a patient portal and a notification be sent to the patient by phone.
Oftentimes, this occurs before the ordering physician has even seen the results, much less interpreted them and made a plan for the patient. What happens now, not long after its enactment date, when it has become clear that the Cures Act is causing extreme harm to our patients?
Take, for example, the real example of a physician whose patient found out about her own intrauterine fetal demise by way of an EMR text message alert of “new imaging results!” sent directly to her phone. Or a physician colleague who witnessed firsthand the intrusive unhelpfulness of the Cures Act when she was informed via patient portal releasing her imaging information that she had a large, possibly malignant breast mass. “No phone call,” she said. “No human being for questions or comfort. Just a notification on my phone.”
The stories about the impact of the Cures Act across the medical community are an endless stream of anxiety, hurt, and broken trust. The relationship between a physician and a patient should be sacred, bolstered by communication and mutual respect.
In many ways, the new act feels like a third party to the patient-physician relationship – a digital imposter, oftentimes blurting out personal and life-altering medical information without any of the finesse, context, and perspective of an experienced physician.
Breaking ‘bad news’ to a patient
In training, some residents are taught how to “break bad news” to a patient. Some good practices for doing this are to have information available for the patient, provide emotional support, have a plan for their next steps already formulated, and call the appropriate specialist ahead of time if you can.
Above all, it’s most important to let the patient be the one to direct their own care. Give them time to ask questions and answer them honestly and clearly. Ask them how much they want to know and help them to understand the complex change in their usual state of health.
Now, unless physicians are keeping a very close eye on their inbox, results are slipping out to patients in a void. The bad news conversations aren’t happening at all, or if they are, they’re happening at 8 p.m. on a phone call after an exhausted physician ends their shift but has to slog through their results bin, calling all the patients who shouldn’t have to find out their results in solitude.
Reaching out to these patients immediately is an honorable, kind thing to, but for a physician, knowing they need to beat the patient to opening an email creates anxiety. Plus, making these calls at whatever hour the results are released to a patient is another burden added to doctors’ already-full plates.
Interpreting results
None of us want to harm our patients. All of us want to be there for them. But this act stands in the way of delivering quality, humanizing medical care.
It is true that patients have a right to access their own medical information. It is also true that waiting anxiously on results can cause undue harm to a patient. But the across-the-board, breakneck speed of information release mandated in this act causes irreparable harm not only to patients, but to the patient-physician relationship.
No patient should find out their cancer recurred while checking their emails at their desk. No patient should first learn of a life-altering diagnosis by way of scrolling through their smartphone in bed. The role of a physician is more than just a healer – we should also be educators, interpreters, partners and, first and foremost, advocates for our patients’ needs.
Our patients are depending on us to stand up and speak out about necessary changes to this act. Result releases should be delayed until they are viewed by a physician. Our patients deserve the dignity and opportunity of a conversation with their medical provider about their test results, and physicians deserve the chance to interpret results and frame the conversation in a way which is conducive to patient understanding and healing.
Dr. Persampiere is a first-year resident in the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece. You can contact them at fpnews@mdedge.com.
A high-stakes numbers game
I’m not an academic. Never will be.
I’m also a crappy statistician. Neither my university nor medical school required statistics classes, so I never really learned them. In medicine you pick up an idea of how to interpret them as part of the job, but I’m certainly not a pro with numbers.
Which brings me to the word of the day, Aduhelm, AKA aducanumab.
A lot of drugs have come and gone in the 30 years since my medical school pharmacology class, but very few with this one’s degree of uncertainty.
Clearly its mechanism works: It removes amyloid from the brain. I don’t think anyone will argue that. But the real question is whether this translates into actual clinical benefit.
The water is murky here, and even its most ardent supporters admit the evidence isn’t exactly overwhelming. To some extent the approval basically puts it in a huge open-label clinical trial, with the Food and Drug Administration saying that it will be withdrawn if success isn’t seen in follow-up studies.
I’m not a statistics person, but I understand that, when numbers are marginal, they can be spun to mean whatever someone wants them to mean. And the stakes here, both medically and financially, are pretty high.
Alzheimer’s disease, unquestionably, is a devastating illness. The best treatments we have for it are modest at best. The demand for new treatments is huge.
But “new” doesn’t mean the same as “effective.” This is where the statistics, and their supporters and detractors, come in.
Patients and their families aren’t (usually) doctors. They want a treatment that’s both effective and reasonably safe, especially for a disease where a tragic prognosis is well established. With this drug (and similar ones in development) we face a balance between uncertain benefits and a clear risk of amyloid-related imaging abnormalities. The best we can do is explain these vagaries to people so they understand the uncertainties involved.
Perhaps more troubling is the possibility lurking in the background: The amyloid comes out, but the prognosis doesn’t improve. This brings us to the possibility (already voiced in journals) that the whole amyloid theory is wrong, and we’ve spent all this time and money chasing the wrong villain. As Morpheus, in The Matrix, implies, our whole reality on this may not be real.
Regrettably, in science (and medicine is a science) the only way to find out what works and what doesn’t is through trial and error. Computer modeling can take us only so far.
But if it (and similar agents) fail in the general population, then it may be time to accept that we’re chasing the wrong bad guy.
That’s what data and statistics do.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I’m not an academic. Never will be.
I’m also a crappy statistician. Neither my university nor medical school required statistics classes, so I never really learned them. In medicine you pick up an idea of how to interpret them as part of the job, but I’m certainly not a pro with numbers.
Which brings me to the word of the day, Aduhelm, AKA aducanumab.
A lot of drugs have come and gone in the 30 years since my medical school pharmacology class, but very few with this one’s degree of uncertainty.
Clearly its mechanism works: It removes amyloid from the brain. I don’t think anyone will argue that. But the real question is whether this translates into actual clinical benefit.
The water is murky here, and even its most ardent supporters admit the evidence isn’t exactly overwhelming. To some extent the approval basically puts it in a huge open-label clinical trial, with the Food and Drug Administration saying that it will be withdrawn if success isn’t seen in follow-up studies.
I’m not a statistics person, but I understand that, when numbers are marginal, they can be spun to mean whatever someone wants them to mean. And the stakes here, both medically and financially, are pretty high.
Alzheimer’s disease, unquestionably, is a devastating illness. The best treatments we have for it are modest at best. The demand for new treatments is huge.
But “new” doesn’t mean the same as “effective.” This is where the statistics, and their supporters and detractors, come in.
Patients and their families aren’t (usually) doctors. They want a treatment that’s both effective and reasonably safe, especially for a disease where a tragic prognosis is well established. With this drug (and similar ones in development) we face a balance between uncertain benefits and a clear risk of amyloid-related imaging abnormalities. The best we can do is explain these vagaries to people so they understand the uncertainties involved.
Perhaps more troubling is the possibility lurking in the background: The amyloid comes out, but the prognosis doesn’t improve. This brings us to the possibility (already voiced in journals) that the whole amyloid theory is wrong, and we’ve spent all this time and money chasing the wrong villain. As Morpheus, in The Matrix, implies, our whole reality on this may not be real.
Regrettably, in science (and medicine is a science) the only way to find out what works and what doesn’t is through trial and error. Computer modeling can take us only so far.
But if it (and similar agents) fail in the general population, then it may be time to accept that we’re chasing the wrong bad guy.
That’s what data and statistics do.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I’m not an academic. Never will be.
I’m also a crappy statistician. Neither my university nor medical school required statistics classes, so I never really learned them. In medicine you pick up an idea of how to interpret them as part of the job, but I’m certainly not a pro with numbers.
Which brings me to the word of the day, Aduhelm, AKA aducanumab.
A lot of drugs have come and gone in the 30 years since my medical school pharmacology class, but very few with this one’s degree of uncertainty.
Clearly its mechanism works: It removes amyloid from the brain. I don’t think anyone will argue that. But the real question is whether this translates into actual clinical benefit.
The water is murky here, and even its most ardent supporters admit the evidence isn’t exactly overwhelming. To some extent the approval basically puts it in a huge open-label clinical trial, with the Food and Drug Administration saying that it will be withdrawn if success isn’t seen in follow-up studies.
I’m not a statistics person, but I understand that, when numbers are marginal, they can be spun to mean whatever someone wants them to mean. And the stakes here, both medically and financially, are pretty high.
Alzheimer’s disease, unquestionably, is a devastating illness. The best treatments we have for it are modest at best. The demand for new treatments is huge.
But “new” doesn’t mean the same as “effective.” This is where the statistics, and their supporters and detractors, come in.
Patients and their families aren’t (usually) doctors. They want a treatment that’s both effective and reasonably safe, especially for a disease where a tragic prognosis is well established. With this drug (and similar ones in development) we face a balance between uncertain benefits and a clear risk of amyloid-related imaging abnormalities. The best we can do is explain these vagaries to people so they understand the uncertainties involved.
Perhaps more troubling is the possibility lurking in the background: The amyloid comes out, but the prognosis doesn’t improve. This brings us to the possibility (already voiced in journals) that the whole amyloid theory is wrong, and we’ve spent all this time and money chasing the wrong villain. As Morpheus, in The Matrix, implies, our whole reality on this may not be real.
Regrettably, in science (and medicine is a science) the only way to find out what works and what doesn’t is through trial and error. Computer modeling can take us only so far.
But if it (and similar agents) fail in the general population, then it may be time to accept that we’re chasing the wrong bad guy.
That’s what data and statistics do.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.














