User login
Is there empathy erosion?
You learned a lot of things in medical school. But there must have been some things that you unlearned on the way to your degree. For instance, you unlearned that you could catch a cold by playing outside on a cold damp day without your jacket. You unlearned that handling a toad would give you warts.
The authors of a recent study suggest that over your 4 years in medical school you also unlearned how to be empathetic (“Does Empathy Decline in the Clinical Phase of Medical Education? A Nationwide, Multi-institutional, Cross-Sectional Study of Students at DO-Granting Medical Schools,” Acad Med. 2020 Jan 21. doi: 10.1097/ACM.0000000000003175). The researchers surveyed more than 10,000 medical students at nearly 50 DO-granting medical schools using standardized questionnaire called the Jefferson Scale of Empathy. They discovered that the students in the clinical phase (years 3 and 4) had lower “empathy scores” than the students in the preclinical phase of their education (years 1 and 2). This decline was statistically significant but “negligible” in magnitude. One wonders why they even chose to publish their results, particularly when the number of respondents to the web-based survey declined with each successive year in medical school. Having looked at the a sample of some of the questions being asked, I can understand why third- and fourth-year students couldn’t be bothered to respond. They were too busy to answer a few dozen “lame” questions.
There may be a decline in empathy over the course our medical training, but I’m not sure that this study can speak to it. An older study found that although medical students scores on a self-administered scale declined between the second and third year, the observed empathetic behavior actually increased. If I had to choose, I would lean more heavily on the results of the behavioral observations.
Certainly, we all changed over the course of our medical education. Including postgraduate training, it may have lasted a decade or more. We saw hundreds of patients, observed life and death on a scale and with an intensity that most of us previously had never experienced. Our perspective changed from being a naive observer to playing the role of an active participant. Did that change include a decline in our capacity for empathy?
Something had to change. We found quickly that we didn’t have the time or emotional energy to learn as much about the person hiding behind every complaint as we once thought we should. We had to cut corners. Sometimes we cut too many. On the other hand, as we saw more patients we may have learned more efficient ways of discovering what we needed to know about them to become an effective and caring physician. If we found ourselves in a specialty in which patients have a high mortality, we were forced to learn ways of protecting ourselves from the emotional damage.
What would you call this process? Was it empathy erosion? Was it a hardening or toughening? Or was it simply maturation? Whatever term you use, it was an obligatory process if we hoped to survive. However, not all of us have done it well. Some of us have narrowed our focus to see only the complaint and the diagnosis, and we too often fail to see the human hiding in plain sight.
For those of us who completed our training with our empathy intact, was this the result of a genetic gift or the atmosphere our parents had created at home? I suspect that in most cases our capacity for empathy as physicians was nurtured and enhanced by the role models we encountered during our training. The mentors we most revered were those who had already been through the annealing process of medical school and specialty training and become even more skilled at caring than when they left college. It is an intangible that can’t be taught. Sadly, there is no way of guaranteeing that everyone who enters medical school will be exposed to or benefit from even one of these master physicians.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
You learned a lot of things in medical school. But there must have been some things that you unlearned on the way to your degree. For instance, you unlearned that you could catch a cold by playing outside on a cold damp day without your jacket. You unlearned that handling a toad would give you warts.
The authors of a recent study suggest that over your 4 years in medical school you also unlearned how to be empathetic (“Does Empathy Decline in the Clinical Phase of Medical Education? A Nationwide, Multi-institutional, Cross-Sectional Study of Students at DO-Granting Medical Schools,” Acad Med. 2020 Jan 21. doi: 10.1097/ACM.0000000000003175). The researchers surveyed more than 10,000 medical students at nearly 50 DO-granting medical schools using standardized questionnaire called the Jefferson Scale of Empathy. They discovered that the students in the clinical phase (years 3 and 4) had lower “empathy scores” than the students in the preclinical phase of their education (years 1 and 2). This decline was statistically significant but “negligible” in magnitude. One wonders why they even chose to publish their results, particularly when the number of respondents to the web-based survey declined with each successive year in medical school. Having looked at the a sample of some of the questions being asked, I can understand why third- and fourth-year students couldn’t be bothered to respond. They were too busy to answer a few dozen “lame” questions.
There may be a decline in empathy over the course our medical training, but I’m not sure that this study can speak to it. An older study found that although medical students scores on a self-administered scale declined between the second and third year, the observed empathetic behavior actually increased. If I had to choose, I would lean more heavily on the results of the behavioral observations.
Certainly, we all changed over the course of our medical education. Including postgraduate training, it may have lasted a decade or more. We saw hundreds of patients, observed life and death on a scale and with an intensity that most of us previously had never experienced. Our perspective changed from being a naive observer to playing the role of an active participant. Did that change include a decline in our capacity for empathy?
Something had to change. We found quickly that we didn’t have the time or emotional energy to learn as much about the person hiding behind every complaint as we once thought we should. We had to cut corners. Sometimes we cut too many. On the other hand, as we saw more patients we may have learned more efficient ways of discovering what we needed to know about them to become an effective and caring physician. If we found ourselves in a specialty in which patients have a high mortality, we were forced to learn ways of protecting ourselves from the emotional damage.
What would you call this process? Was it empathy erosion? Was it a hardening or toughening? Or was it simply maturation? Whatever term you use, it was an obligatory process if we hoped to survive. However, not all of us have done it well. Some of us have narrowed our focus to see only the complaint and the diagnosis, and we too often fail to see the human hiding in plain sight.
For those of us who completed our training with our empathy intact, was this the result of a genetic gift or the atmosphere our parents had created at home? I suspect that in most cases our capacity for empathy as physicians was nurtured and enhanced by the role models we encountered during our training. The mentors we most revered were those who had already been through the annealing process of medical school and specialty training and become even more skilled at caring than when they left college. It is an intangible that can’t be taught. Sadly, there is no way of guaranteeing that everyone who enters medical school will be exposed to or benefit from even one of these master physicians.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
You learned a lot of things in medical school. But there must have been some things that you unlearned on the way to your degree. For instance, you unlearned that you could catch a cold by playing outside on a cold damp day without your jacket. You unlearned that handling a toad would give you warts.
The authors of a recent study suggest that over your 4 years in medical school you also unlearned how to be empathetic (“Does Empathy Decline in the Clinical Phase of Medical Education? A Nationwide, Multi-institutional, Cross-Sectional Study of Students at DO-Granting Medical Schools,” Acad Med. 2020 Jan 21. doi: 10.1097/ACM.0000000000003175). The researchers surveyed more than 10,000 medical students at nearly 50 DO-granting medical schools using standardized questionnaire called the Jefferson Scale of Empathy. They discovered that the students in the clinical phase (years 3 and 4) had lower “empathy scores” than the students in the preclinical phase of their education (years 1 and 2). This decline was statistically significant but “negligible” in magnitude. One wonders why they even chose to publish their results, particularly when the number of respondents to the web-based survey declined with each successive year in medical school. Having looked at the a sample of some of the questions being asked, I can understand why third- and fourth-year students couldn’t be bothered to respond. They were too busy to answer a few dozen “lame” questions.
There may be a decline in empathy over the course our medical training, but I’m not sure that this study can speak to it. An older study found that although medical students scores on a self-administered scale declined between the second and third year, the observed empathetic behavior actually increased. If I had to choose, I would lean more heavily on the results of the behavioral observations.
Certainly, we all changed over the course of our medical education. Including postgraduate training, it may have lasted a decade or more. We saw hundreds of patients, observed life and death on a scale and with an intensity that most of us previously had never experienced. Our perspective changed from being a naive observer to playing the role of an active participant. Did that change include a decline in our capacity for empathy?
Something had to change. We found quickly that we didn’t have the time or emotional energy to learn as much about the person hiding behind every complaint as we once thought we should. We had to cut corners. Sometimes we cut too many. On the other hand, as we saw more patients we may have learned more efficient ways of discovering what we needed to know about them to become an effective and caring physician. If we found ourselves in a specialty in which patients have a high mortality, we were forced to learn ways of protecting ourselves from the emotional damage.
What would you call this process? Was it empathy erosion? Was it a hardening or toughening? Or was it simply maturation? Whatever term you use, it was an obligatory process if we hoped to survive. However, not all of us have done it well. Some of us have narrowed our focus to see only the complaint and the diagnosis, and we too often fail to see the human hiding in plain sight.
For those of us who completed our training with our empathy intact, was this the result of a genetic gift or the atmosphere our parents had created at home? I suspect that in most cases our capacity for empathy as physicians was nurtured and enhanced by the role models we encountered during our training. The mentors we most revered were those who had already been through the annealing process of medical school and specialty training and become even more skilled at caring than when they left college. It is an intangible that can’t be taught. Sadly, there is no way of guaranteeing that everyone who enters medical school will be exposed to or benefit from even one of these master physicians.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
Researchers honored by ACS, IASLC
The International Association for the Study of Lung Cancer (IASLC) is naming the Translational Research Lectureship Award after Fred R. Hirsch, MD, PhD, of the Tisch Cancer Institute and Icahn School of Medicine at Mount Sinai, New York.
Dr. Hirsch was a longtime member of the IASLC and served as chief executive officer of the association from 2013 through October 2018. During this time, Dr. Hirsch grew the IASLC staff from 5 to 23 people and doubled the organization’s membership. The IASLC World Conference on Lung Cancer became an annual meeting under Dr. Hirsch’s direction and reported record attendance, according to their website.
The recipient of the Fred R. Hirsch Lectureship Award for Translational Research will be recognized at the IASLC 2020 World Conference on Lung Cancer, which is set to take place in Singapore on August 9-12, 2020.
In other news, the American Cancer Society (ACS) announced that it has awarded the 2020 Medal of Honor to three researchers. The recipients will be recognized at a black-tie ceremony in New York on Nov. 11, 2020.
Lewis C. Cantley, PhD, of Weill Cornell Medicine, New York, won the Medal of Honor for Basic Research. This award honors researchers whose work will have a “lasting impact on the cancer field” or who have made important discoveries or inventions within the field, according to the ACS.
Dr. Cantley won the award for research that has improved our understanding of cancer metabolism. He is known for his contributions to the discovery and study of phosphoinositide 3-kinase, which plays a role in many cancers and has become a target for therapies.
Leslie Bernstein, PhD, of City of Hope National Medical Center in Duarte, Calif., has won the Medal of Honor in Cancer Control. This award honors individuals who have made strides in public health, public communication, or public policy that have had an impact on cancer control.
Dr. Bernstein won the award for her work linking physical activity to a reduced risk of breast cancer. She is currently investigating links between hormone exposures, physical activity, obesity, and cancer, as well as examining how breast cancer impacts patients’ lives after treatment.
Ching-Hon Pui, MD, of St. Jude Children’s Research Hospital in Memphis, Tenn., has won the Medal of Honor in Clinical Research. This award honors researchers whose work has significantly improved cancer patients’ outcomes.
Dr. Pui won the award for his work in childhood acute lymphoblastic leukemia. Dr. Pui’s work has led to increased global treatment access, improved survival rates, and better quality of life for patients with childhood acute lymphoblastic leukemia.
The International Association for the Study of Lung Cancer (IASLC) is naming the Translational Research Lectureship Award after Fred R. Hirsch, MD, PhD, of the Tisch Cancer Institute and Icahn School of Medicine at Mount Sinai, New York.
Dr. Hirsch was a longtime member of the IASLC and served as chief executive officer of the association from 2013 through October 2018. During this time, Dr. Hirsch grew the IASLC staff from 5 to 23 people and doubled the organization’s membership. The IASLC World Conference on Lung Cancer became an annual meeting under Dr. Hirsch’s direction and reported record attendance, according to their website.
The recipient of the Fred R. Hirsch Lectureship Award for Translational Research will be recognized at the IASLC 2020 World Conference on Lung Cancer, which is set to take place in Singapore on August 9-12, 2020.
In other news, the American Cancer Society (ACS) announced that it has awarded the 2020 Medal of Honor to three researchers. The recipients will be recognized at a black-tie ceremony in New York on Nov. 11, 2020.
Lewis C. Cantley, PhD, of Weill Cornell Medicine, New York, won the Medal of Honor for Basic Research. This award honors researchers whose work will have a “lasting impact on the cancer field” or who have made important discoveries or inventions within the field, according to the ACS.
Dr. Cantley won the award for research that has improved our understanding of cancer metabolism. He is known for his contributions to the discovery and study of phosphoinositide 3-kinase, which plays a role in many cancers and has become a target for therapies.
Leslie Bernstein, PhD, of City of Hope National Medical Center in Duarte, Calif., has won the Medal of Honor in Cancer Control. This award honors individuals who have made strides in public health, public communication, or public policy that have had an impact on cancer control.
Dr. Bernstein won the award for her work linking physical activity to a reduced risk of breast cancer. She is currently investigating links between hormone exposures, physical activity, obesity, and cancer, as well as examining how breast cancer impacts patients’ lives after treatment.
Ching-Hon Pui, MD, of St. Jude Children’s Research Hospital in Memphis, Tenn., has won the Medal of Honor in Clinical Research. This award honors researchers whose work has significantly improved cancer patients’ outcomes.
Dr. Pui won the award for his work in childhood acute lymphoblastic leukemia. Dr. Pui’s work has led to increased global treatment access, improved survival rates, and better quality of life for patients with childhood acute lymphoblastic leukemia.
The International Association for the Study of Lung Cancer (IASLC) is naming the Translational Research Lectureship Award after Fred R. Hirsch, MD, PhD, of the Tisch Cancer Institute and Icahn School of Medicine at Mount Sinai, New York.
Dr. Hirsch was a longtime member of the IASLC and served as chief executive officer of the association from 2013 through October 2018. During this time, Dr. Hirsch grew the IASLC staff from 5 to 23 people and doubled the organization’s membership. The IASLC World Conference on Lung Cancer became an annual meeting under Dr. Hirsch’s direction and reported record attendance, according to their website.
The recipient of the Fred R. Hirsch Lectureship Award for Translational Research will be recognized at the IASLC 2020 World Conference on Lung Cancer, which is set to take place in Singapore on August 9-12, 2020.
In other news, the American Cancer Society (ACS) announced that it has awarded the 2020 Medal of Honor to three researchers. The recipients will be recognized at a black-tie ceremony in New York on Nov. 11, 2020.
Lewis C. Cantley, PhD, of Weill Cornell Medicine, New York, won the Medal of Honor for Basic Research. This award honors researchers whose work will have a “lasting impact on the cancer field” or who have made important discoveries or inventions within the field, according to the ACS.
Dr. Cantley won the award for research that has improved our understanding of cancer metabolism. He is known for his contributions to the discovery and study of phosphoinositide 3-kinase, which plays a role in many cancers and has become a target for therapies.
Leslie Bernstein, PhD, of City of Hope National Medical Center in Duarte, Calif., has won the Medal of Honor in Cancer Control. This award honors individuals who have made strides in public health, public communication, or public policy that have had an impact on cancer control.
Dr. Bernstein won the award for her work linking physical activity to a reduced risk of breast cancer. She is currently investigating links between hormone exposures, physical activity, obesity, and cancer, as well as examining how breast cancer impacts patients’ lives after treatment.
Ching-Hon Pui, MD, of St. Jude Children’s Research Hospital in Memphis, Tenn., has won the Medal of Honor in Clinical Research. This award honors researchers whose work has significantly improved cancer patients’ outcomes.
Dr. Pui won the award for his work in childhood acute lymphoblastic leukemia. Dr. Pui’s work has led to increased global treatment access, improved survival rates, and better quality of life for patients with childhood acute lymphoblastic leukemia.
Telehealth seen as a key tool to help fight COVID-19
Telehealth is increasingly being viewed as a key way to help fight the COVID-19 outbreak in the United States. Recognizing the potential of this technology to slow the spread of the disease, the House of Representatives included a provision in an $8.3 billion emergency response bill it approved today that would temporarily lift restrictions on Medicare telehealth coverage to assist in the efforts to contain the virus.
Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the Centers for Disease Control and Prevention (CDC), said that hospitals should be prepared to use telehealth as one of their tools in fighting the outbreak, according to a recent news release from the American Hospital Association (AHA).
Congress is responding to that need by including the service in the new coronavirus legislation now headed to the Senate, after the funding bill was approved in a 415-2 vote by the House.
The bill empowers the Secretary of Health and Human Services (HHS) to “waive or modify application of certain Medicare requirements with respect to telehealth services furnished during certain emergency periods.”
While the measure adds telehealth to the waiver authority that the HHS secretary currently has during national emergencies, it’s only for the coronavirus crisis in this case, Krista Drobac, executive director of the Alliance for Connected Care, told Medscape Medical News.
The waiver would apply to originating sites of telehealth visits, she noted. Thus Medicare coverage of telemedicine would be expanded beyond rural areas.
In addition, the waiver would allow coverage of virtual visits conducted on smartphones with audio and video capabilities. A “qualified provider,” as defined by the legislation, would be a practitioner who has an established relationship with the patient or who is in the same practice as the provider who has that relationship.
An advantage of telehealth, proponents say, is that it can enable people who believe they have COVID-19 to be seen at home rather than visit offices or emergency departments (EDs) where they might spread the disease or be in proximity to others who have it.
In an editorial published March 2 in Modern Healthcare, medical directors from Stanford Medicine, MedStar Health, and Intermountain Healthcare also noted that telehealth can give patients 24/7 access to care, allow surveillance of patients at risk while keeping them at home, ensure that treatment in hospitals is reserved for high-need patients, and enable providers to triage and screen more patients than can be handled in brick-and-mortar care settings.
However, telehealth screening would allow physicians only to judge whether a patient’s symptoms might be indicative of COVID-19, the Alliance for Connected Care, a telehealth advocacy group, noted in a letter to Congressional leaders. Patients would still have to be seen in person to be tested for the disease.
The group, which represents technology companies, health insurers, pharmacies, and other healthcare players, has been lobbying Congress to include telehealth in federal funds to combat the outbreak.
The American Telemedicine Association (ATA) also supports this goal, ATA President Joseph Kvedar, MD, told Medscape Medical News. And the authors of the Modern Healthcare editorial also advocated for this legislative solution. Because the fatality rate for COVID-19 is significantly higher for older people than for other age groups, they noted, telehealth should be an economically viable option for all seniors.
The Centers for Medicare and Medicaid Services (CMS) long covered telemedicine only in rural areas and only when initiated in healthcare settings. Recently, however, CMS loosened its approach to some extent. Virtual “check-in visits” can now be initiated from any location, including home, to determine whether a Medicare patient needs to be seen in the office. In addition, CMS allows Medicare Advantage plans to offer telemedicine as a core benefit.
Are healthcare systems prepared?
Some large healthcare systems such as Stanford, MedStar, and Intermountain are already using telehealth to diagnose and treat patients who have traditional influenza. Telehealth providers at Stanford estimate that almost 50% of these patients are being prescribed the antiviral drug Tamiflu.
It’s unclear whether other healthcare systems are this well prepared to offer telehealth on a large scale. But, according to an AHA survey, Kvedar noted, three quarters of AHA members are engaged in some form of telehealth.
Drobac said “it wouldn’t require too much effort” to ramp up a wide-scale telehealth program that could help reduce the impact of the outbreak. “The technology is there,” she noted. “You need a HIPAA-compliant telehealth platform, but there are so many out there.”
Kvedar agreed. To begin with, he said, hospitals might sequester patients who visit the ED with COVID-19 symptoms in a video-equipped “isolation room.” Staff members could then do the patient intake from a different location in the hospital.
He admitted that this approach would be infeasible if a lot of patients arrived in EDs with coronavirus symptoms. However, Kvedar noted, “All the tools are in place to go well beyond that. American Well, Teladoc, and others are all offering ways to get out in front of this. There are plenty of vendors out there, and most people have a connected cell phone that you can do a video call on.”
Hospital leaders would have to decide whether to embrace telehealth, which would mean less use of services in their institutions, he said. “But it would be for the greater good of the public.”
Kvedar recalled that there was some use of telehealth in the New York area after 9/11. Telehealth was also used in the aftermath of Hurricane Katrina in 2005. But the ATA president, who is also vice president of connected health at Partners HealthCare in Boston, noted that the COVID-19 outbreak is the first public health emergency to occur in the era of Skype and smartphones.
If Congress does ultimately authorize CMS to cover telehealth across the board during this emergency, might that lead to a permanent change in Medicare coverage policy? Kvedar wouldn’t venture an opinion. “However, the current CMS leadership has been incredibly telehealth friendly,” he said. “So it’s possible they would [embrace a lifting of restrictions]. As patients get a sense of this modality of care and how convenient it is for them, they’ll start asking for more.”
Meanwhile, he said, the telehealth opportunity goes beyond video visits with doctors to mitigate the outbreak. Telehealth data could also be used to track disease spread, similar to how researchers have studied Google searches to predict the spread of the flu, he noted.
Teladoc, a major telehealth vendor, recently told stock analysts it’s already working with the CDC on disease surveillance, according to a report in FierceHealthcare.
This article first appeared on Medscape.com.
Telehealth is increasingly being viewed as a key way to help fight the COVID-19 outbreak in the United States. Recognizing the potential of this technology to slow the spread of the disease, the House of Representatives included a provision in an $8.3 billion emergency response bill it approved today that would temporarily lift restrictions on Medicare telehealth coverage to assist in the efforts to contain the virus.
Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the Centers for Disease Control and Prevention (CDC), said that hospitals should be prepared to use telehealth as one of their tools in fighting the outbreak, according to a recent news release from the American Hospital Association (AHA).
Congress is responding to that need by including the service in the new coronavirus legislation now headed to the Senate, after the funding bill was approved in a 415-2 vote by the House.
The bill empowers the Secretary of Health and Human Services (HHS) to “waive or modify application of certain Medicare requirements with respect to telehealth services furnished during certain emergency periods.”
While the measure adds telehealth to the waiver authority that the HHS secretary currently has during national emergencies, it’s only for the coronavirus crisis in this case, Krista Drobac, executive director of the Alliance for Connected Care, told Medscape Medical News.
The waiver would apply to originating sites of telehealth visits, she noted. Thus Medicare coverage of telemedicine would be expanded beyond rural areas.
In addition, the waiver would allow coverage of virtual visits conducted on smartphones with audio and video capabilities. A “qualified provider,” as defined by the legislation, would be a practitioner who has an established relationship with the patient or who is in the same practice as the provider who has that relationship.
An advantage of telehealth, proponents say, is that it can enable people who believe they have COVID-19 to be seen at home rather than visit offices or emergency departments (EDs) where they might spread the disease or be in proximity to others who have it.
In an editorial published March 2 in Modern Healthcare, medical directors from Stanford Medicine, MedStar Health, and Intermountain Healthcare also noted that telehealth can give patients 24/7 access to care, allow surveillance of patients at risk while keeping them at home, ensure that treatment in hospitals is reserved for high-need patients, and enable providers to triage and screen more patients than can be handled in brick-and-mortar care settings.
However, telehealth screening would allow physicians only to judge whether a patient’s symptoms might be indicative of COVID-19, the Alliance for Connected Care, a telehealth advocacy group, noted in a letter to Congressional leaders. Patients would still have to be seen in person to be tested for the disease.
The group, which represents technology companies, health insurers, pharmacies, and other healthcare players, has been lobbying Congress to include telehealth in federal funds to combat the outbreak.
The American Telemedicine Association (ATA) also supports this goal, ATA President Joseph Kvedar, MD, told Medscape Medical News. And the authors of the Modern Healthcare editorial also advocated for this legislative solution. Because the fatality rate for COVID-19 is significantly higher for older people than for other age groups, they noted, telehealth should be an economically viable option for all seniors.
The Centers for Medicare and Medicaid Services (CMS) long covered telemedicine only in rural areas and only when initiated in healthcare settings. Recently, however, CMS loosened its approach to some extent. Virtual “check-in visits” can now be initiated from any location, including home, to determine whether a Medicare patient needs to be seen in the office. In addition, CMS allows Medicare Advantage plans to offer telemedicine as a core benefit.
Are healthcare systems prepared?
Some large healthcare systems such as Stanford, MedStar, and Intermountain are already using telehealth to diagnose and treat patients who have traditional influenza. Telehealth providers at Stanford estimate that almost 50% of these patients are being prescribed the antiviral drug Tamiflu.
It’s unclear whether other healthcare systems are this well prepared to offer telehealth on a large scale. But, according to an AHA survey, Kvedar noted, three quarters of AHA members are engaged in some form of telehealth.
Drobac said “it wouldn’t require too much effort” to ramp up a wide-scale telehealth program that could help reduce the impact of the outbreak. “The technology is there,” she noted. “You need a HIPAA-compliant telehealth platform, but there are so many out there.”
Kvedar agreed. To begin with, he said, hospitals might sequester patients who visit the ED with COVID-19 symptoms in a video-equipped “isolation room.” Staff members could then do the patient intake from a different location in the hospital.
He admitted that this approach would be infeasible if a lot of patients arrived in EDs with coronavirus symptoms. However, Kvedar noted, “All the tools are in place to go well beyond that. American Well, Teladoc, and others are all offering ways to get out in front of this. There are plenty of vendors out there, and most people have a connected cell phone that you can do a video call on.”
Hospital leaders would have to decide whether to embrace telehealth, which would mean less use of services in their institutions, he said. “But it would be for the greater good of the public.”
Kvedar recalled that there was some use of telehealth in the New York area after 9/11. Telehealth was also used in the aftermath of Hurricane Katrina in 2005. But the ATA president, who is also vice president of connected health at Partners HealthCare in Boston, noted that the COVID-19 outbreak is the first public health emergency to occur in the era of Skype and smartphones.
If Congress does ultimately authorize CMS to cover telehealth across the board during this emergency, might that lead to a permanent change in Medicare coverage policy? Kvedar wouldn’t venture an opinion. “However, the current CMS leadership has been incredibly telehealth friendly,” he said. “So it’s possible they would [embrace a lifting of restrictions]. As patients get a sense of this modality of care and how convenient it is for them, they’ll start asking for more.”
Meanwhile, he said, the telehealth opportunity goes beyond video visits with doctors to mitigate the outbreak. Telehealth data could also be used to track disease spread, similar to how researchers have studied Google searches to predict the spread of the flu, he noted.
Teladoc, a major telehealth vendor, recently told stock analysts it’s already working with the CDC on disease surveillance, according to a report in FierceHealthcare.
This article first appeared on Medscape.com.
Telehealth is increasingly being viewed as a key way to help fight the COVID-19 outbreak in the United States. Recognizing the potential of this technology to slow the spread of the disease, the House of Representatives included a provision in an $8.3 billion emergency response bill it approved today that would temporarily lift restrictions on Medicare telehealth coverage to assist in the efforts to contain the virus.
Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the Centers for Disease Control and Prevention (CDC), said that hospitals should be prepared to use telehealth as one of their tools in fighting the outbreak, according to a recent news release from the American Hospital Association (AHA).
Congress is responding to that need by including the service in the new coronavirus legislation now headed to the Senate, after the funding bill was approved in a 415-2 vote by the House.
The bill empowers the Secretary of Health and Human Services (HHS) to “waive or modify application of certain Medicare requirements with respect to telehealth services furnished during certain emergency periods.”
While the measure adds telehealth to the waiver authority that the HHS secretary currently has during national emergencies, it’s only for the coronavirus crisis in this case, Krista Drobac, executive director of the Alliance for Connected Care, told Medscape Medical News.
The waiver would apply to originating sites of telehealth visits, she noted. Thus Medicare coverage of telemedicine would be expanded beyond rural areas.
In addition, the waiver would allow coverage of virtual visits conducted on smartphones with audio and video capabilities. A “qualified provider,” as defined by the legislation, would be a practitioner who has an established relationship with the patient or who is in the same practice as the provider who has that relationship.
An advantage of telehealth, proponents say, is that it can enable people who believe they have COVID-19 to be seen at home rather than visit offices or emergency departments (EDs) where they might spread the disease or be in proximity to others who have it.
In an editorial published March 2 in Modern Healthcare, medical directors from Stanford Medicine, MedStar Health, and Intermountain Healthcare also noted that telehealth can give patients 24/7 access to care, allow surveillance of patients at risk while keeping them at home, ensure that treatment in hospitals is reserved for high-need patients, and enable providers to triage and screen more patients than can be handled in brick-and-mortar care settings.
However, telehealth screening would allow physicians only to judge whether a patient’s symptoms might be indicative of COVID-19, the Alliance for Connected Care, a telehealth advocacy group, noted in a letter to Congressional leaders. Patients would still have to be seen in person to be tested for the disease.
The group, which represents technology companies, health insurers, pharmacies, and other healthcare players, has been lobbying Congress to include telehealth in federal funds to combat the outbreak.
The American Telemedicine Association (ATA) also supports this goal, ATA President Joseph Kvedar, MD, told Medscape Medical News. And the authors of the Modern Healthcare editorial also advocated for this legislative solution. Because the fatality rate for COVID-19 is significantly higher for older people than for other age groups, they noted, telehealth should be an economically viable option for all seniors.
The Centers for Medicare and Medicaid Services (CMS) long covered telemedicine only in rural areas and only when initiated in healthcare settings. Recently, however, CMS loosened its approach to some extent. Virtual “check-in visits” can now be initiated from any location, including home, to determine whether a Medicare patient needs to be seen in the office. In addition, CMS allows Medicare Advantage plans to offer telemedicine as a core benefit.
Are healthcare systems prepared?
Some large healthcare systems such as Stanford, MedStar, and Intermountain are already using telehealth to diagnose and treat patients who have traditional influenza. Telehealth providers at Stanford estimate that almost 50% of these patients are being prescribed the antiviral drug Tamiflu.
It’s unclear whether other healthcare systems are this well prepared to offer telehealth on a large scale. But, according to an AHA survey, Kvedar noted, three quarters of AHA members are engaged in some form of telehealth.
Drobac said “it wouldn’t require too much effort” to ramp up a wide-scale telehealth program that could help reduce the impact of the outbreak. “The technology is there,” she noted. “You need a HIPAA-compliant telehealth platform, but there are so many out there.”
Kvedar agreed. To begin with, he said, hospitals might sequester patients who visit the ED with COVID-19 symptoms in a video-equipped “isolation room.” Staff members could then do the patient intake from a different location in the hospital.
He admitted that this approach would be infeasible if a lot of patients arrived in EDs with coronavirus symptoms. However, Kvedar noted, “All the tools are in place to go well beyond that. American Well, Teladoc, and others are all offering ways to get out in front of this. There are plenty of vendors out there, and most people have a connected cell phone that you can do a video call on.”
Hospital leaders would have to decide whether to embrace telehealth, which would mean less use of services in their institutions, he said. “But it would be for the greater good of the public.”
Kvedar recalled that there was some use of telehealth in the New York area after 9/11. Telehealth was also used in the aftermath of Hurricane Katrina in 2005. But the ATA president, who is also vice president of connected health at Partners HealthCare in Boston, noted that the COVID-19 outbreak is the first public health emergency to occur in the era of Skype and smartphones.
If Congress does ultimately authorize CMS to cover telehealth across the board during this emergency, might that lead to a permanent change in Medicare coverage policy? Kvedar wouldn’t venture an opinion. “However, the current CMS leadership has been incredibly telehealth friendly,” he said. “So it’s possible they would [embrace a lifting of restrictions]. As patients get a sense of this modality of care and how convenient it is for them, they’ll start asking for more.”
Meanwhile, he said, the telehealth opportunity goes beyond video visits with doctors to mitigate the outbreak. Telehealth data could also be used to track disease spread, similar to how researchers have studied Google searches to predict the spread of the flu, he noted.
Teladoc, a major telehealth vendor, recently told stock analysts it’s already working with the CDC on disease surveillance, according to a report in FierceHealthcare.
This article first appeared on Medscape.com.
Gender pronouns in EMR preferred by many gender nonconforming teens
Most transgender and gender nonconforming youth would like their preferred name and pronouns be recorded throughout their EMRs, but very few are ever asked for that identity information outside of gender specialty clinic settings, according to a recent research letter in JAMA Pediatrics.
The findings are not surprising, said Cora Breuner, MD, a professor of pediatrics in adolescent medicine at Seattle Children’s Hospital in Washington, because “we know that use of gender-affirming language when accessing health care is extremely important to transgender youth.”
“Use of gender-affirming language in the health care system is associated with improved mental health outcomes in this population,” Dr Breuner said in an interview.
But the authors of the study noted that EMRs often lack the functions needed to provide gender-affirming care.
“To better support this vulnerable group of youths, health systems and EMRs should allow for EMR-wide name and pronoun documentation, even when a patient has not legally changed their name,” Gina M. Sequeira, MD, of UPMC Children’s Hospital of Pittsburgh and associates wrote.
Although many providers have begun routinely asking patients for both their gender identity and their sex assigned at birth, these questions leave out a patient’s preferred name and pronouns – crucial components of respectful and affirming care, the authors explained.
At a specialty gender clinic, the authors surveyed 204 transgender youths, aged 12-26 years, regarding how their name and pronouns are recorded in their EMR files. Just over half the respondents were under age 18 years (56%), and most were white (86%). Most were transmasculine (59%), with 21% transfeminine and 20% nonbinary.
Most respondents (69%) went by a name other than their legal one, yet only 9% said they were frequently or always asked in clinical settings outside specialty gender centers whether they wanted their preferred name and pronouns noted in the EMR.
A majority (79%), however, said they wanted their name and pronouns noted throughout their EMR. The youths’ preferences varied according to their gender identity and how many people were aware of their gender identity, but not by age, race/ethnicity, or perceived amount of parental support.
Only two-thirds (67%) of 42 transfeminine patients wished their EMR to include their preferred name, compared with most (85%) of 121 transmasculine patients and nearly all (92%) of 37 nonbinary respondents (P = .007). Pronouns preferences were similar: All but one nonbinary respondent wanted their pronouns in the EMR, compared with 84% of transmasculine and 64% of transfeminine respondents (P=.0003).
“It may be that transfeminine patients have more pressure to ‘stay’ their assigned gender,” Dr Breuner said regarding these findings. “ ‘Outness’ may be challenging, and thus they remain in their traditional gender norms, but further research on this theory is warranted.”
Among those who were “out to everyone,” most (88%) wanted their preferred name and pronouns recorded in the EMR, and the proportion was similar for those “out to most.” But only 65% of those “out to few or no one” preferred their name and pronouns be noted in the EMR, a similar proportion for those “out to some.”
Of 7 youths who did not wish to include their name and pronouns throughout their EMR, all but one said they didn’t think it was necessary because they believed they already “passed” well enough as their gender. Just one person said they did not want name and pronouns recorded for confidentiality reasons.
However, confidentiality is still an important consideration particularly for minors, the authors and Dr. Breuner pointed out.
“It is essential to discuss confidentiality with the youth as parents may have access to the medical records younger than 18 years of age,” Dr. Breuner said.
The authors noted the study’s limitation in using a convenience sample but they and Dr. Breuner said that the findings still demonstrate transgender youths’ desire for EMRs to include their name and pronouns.
The research was funded by grants from the National Institutes of Health. The authors had no industry disclosures.
SOURCE: Sequeira GM et al. JAMA Pediatrics. 2020 Feb 23. doi: 10.1001/jamapediatrics.2019.6071.
Most transgender and gender nonconforming youth would like their preferred name and pronouns be recorded throughout their EMRs, but very few are ever asked for that identity information outside of gender specialty clinic settings, according to a recent research letter in JAMA Pediatrics.
The findings are not surprising, said Cora Breuner, MD, a professor of pediatrics in adolescent medicine at Seattle Children’s Hospital in Washington, because “we know that use of gender-affirming language when accessing health care is extremely important to transgender youth.”
“Use of gender-affirming language in the health care system is associated with improved mental health outcomes in this population,” Dr Breuner said in an interview.
But the authors of the study noted that EMRs often lack the functions needed to provide gender-affirming care.
“To better support this vulnerable group of youths, health systems and EMRs should allow for EMR-wide name and pronoun documentation, even when a patient has not legally changed their name,” Gina M. Sequeira, MD, of UPMC Children’s Hospital of Pittsburgh and associates wrote.
Although many providers have begun routinely asking patients for both their gender identity and their sex assigned at birth, these questions leave out a patient’s preferred name and pronouns – crucial components of respectful and affirming care, the authors explained.
At a specialty gender clinic, the authors surveyed 204 transgender youths, aged 12-26 years, regarding how their name and pronouns are recorded in their EMR files. Just over half the respondents were under age 18 years (56%), and most were white (86%). Most were transmasculine (59%), with 21% transfeminine and 20% nonbinary.
Most respondents (69%) went by a name other than their legal one, yet only 9% said they were frequently or always asked in clinical settings outside specialty gender centers whether they wanted their preferred name and pronouns noted in the EMR.
A majority (79%), however, said they wanted their name and pronouns noted throughout their EMR. The youths’ preferences varied according to their gender identity and how many people were aware of their gender identity, but not by age, race/ethnicity, or perceived amount of parental support.
Only two-thirds (67%) of 42 transfeminine patients wished their EMR to include their preferred name, compared with most (85%) of 121 transmasculine patients and nearly all (92%) of 37 nonbinary respondents (P = .007). Pronouns preferences were similar: All but one nonbinary respondent wanted their pronouns in the EMR, compared with 84% of transmasculine and 64% of transfeminine respondents (P=.0003).
“It may be that transfeminine patients have more pressure to ‘stay’ their assigned gender,” Dr Breuner said regarding these findings. “ ‘Outness’ may be challenging, and thus they remain in their traditional gender norms, but further research on this theory is warranted.”
Among those who were “out to everyone,” most (88%) wanted their preferred name and pronouns recorded in the EMR, and the proportion was similar for those “out to most.” But only 65% of those “out to few or no one” preferred their name and pronouns be noted in the EMR, a similar proportion for those “out to some.”
Of 7 youths who did not wish to include their name and pronouns throughout their EMR, all but one said they didn’t think it was necessary because they believed they already “passed” well enough as their gender. Just one person said they did not want name and pronouns recorded for confidentiality reasons.
However, confidentiality is still an important consideration particularly for minors, the authors and Dr. Breuner pointed out.
“It is essential to discuss confidentiality with the youth as parents may have access to the medical records younger than 18 years of age,” Dr. Breuner said.
The authors noted the study’s limitation in using a convenience sample but they and Dr. Breuner said that the findings still demonstrate transgender youths’ desire for EMRs to include their name and pronouns.
The research was funded by grants from the National Institutes of Health. The authors had no industry disclosures.
SOURCE: Sequeira GM et al. JAMA Pediatrics. 2020 Feb 23. doi: 10.1001/jamapediatrics.2019.6071.
Most transgender and gender nonconforming youth would like their preferred name and pronouns be recorded throughout their EMRs, but very few are ever asked for that identity information outside of gender specialty clinic settings, according to a recent research letter in JAMA Pediatrics.
The findings are not surprising, said Cora Breuner, MD, a professor of pediatrics in adolescent medicine at Seattle Children’s Hospital in Washington, because “we know that use of gender-affirming language when accessing health care is extremely important to transgender youth.”
“Use of gender-affirming language in the health care system is associated with improved mental health outcomes in this population,” Dr Breuner said in an interview.
But the authors of the study noted that EMRs often lack the functions needed to provide gender-affirming care.
“To better support this vulnerable group of youths, health systems and EMRs should allow for EMR-wide name and pronoun documentation, even when a patient has not legally changed their name,” Gina M. Sequeira, MD, of UPMC Children’s Hospital of Pittsburgh and associates wrote.
Although many providers have begun routinely asking patients for both their gender identity and their sex assigned at birth, these questions leave out a patient’s preferred name and pronouns – crucial components of respectful and affirming care, the authors explained.
At a specialty gender clinic, the authors surveyed 204 transgender youths, aged 12-26 years, regarding how their name and pronouns are recorded in their EMR files. Just over half the respondents were under age 18 years (56%), and most were white (86%). Most were transmasculine (59%), with 21% transfeminine and 20% nonbinary.
Most respondents (69%) went by a name other than their legal one, yet only 9% said they were frequently or always asked in clinical settings outside specialty gender centers whether they wanted their preferred name and pronouns noted in the EMR.
A majority (79%), however, said they wanted their name and pronouns noted throughout their EMR. The youths’ preferences varied according to their gender identity and how many people were aware of their gender identity, but not by age, race/ethnicity, or perceived amount of parental support.
Only two-thirds (67%) of 42 transfeminine patients wished their EMR to include their preferred name, compared with most (85%) of 121 transmasculine patients and nearly all (92%) of 37 nonbinary respondents (P = .007). Pronouns preferences were similar: All but one nonbinary respondent wanted their pronouns in the EMR, compared with 84% of transmasculine and 64% of transfeminine respondents (P=.0003).
“It may be that transfeminine patients have more pressure to ‘stay’ their assigned gender,” Dr Breuner said regarding these findings. “ ‘Outness’ may be challenging, and thus they remain in their traditional gender norms, but further research on this theory is warranted.”
Among those who were “out to everyone,” most (88%) wanted their preferred name and pronouns recorded in the EMR, and the proportion was similar for those “out to most.” But only 65% of those “out to few or no one” preferred their name and pronouns be noted in the EMR, a similar proportion for those “out to some.”
Of 7 youths who did not wish to include their name and pronouns throughout their EMR, all but one said they didn’t think it was necessary because they believed they already “passed” well enough as their gender. Just one person said they did not want name and pronouns recorded for confidentiality reasons.
However, confidentiality is still an important consideration particularly for minors, the authors and Dr. Breuner pointed out.
“It is essential to discuss confidentiality with the youth as parents may have access to the medical records younger than 18 years of age,” Dr. Breuner said.
The authors noted the study’s limitation in using a convenience sample but they and Dr. Breuner said that the findings still demonstrate transgender youths’ desire for EMRs to include their name and pronouns.
The research was funded by grants from the National Institutes of Health. The authors had no industry disclosures.
SOURCE: Sequeira GM et al. JAMA Pediatrics. 2020 Feb 23. doi: 10.1001/jamapediatrics.2019.6071.
FROM JAMA PEDIATRICS
More pediatricians employ developmental screening tools
Pediatricians’ reported use of developmental screening tools increased significantly to 63% from 2002 to 2016, based on survey data from more than 1,000 pediatricians at three time points.
“In 2001, an AAP [American Academy of Pediatrics] policy statement called for pediatricians to screen all children for developmental disorders during routine well-child visits,” Paul H. Lipkin, MD, of the Kennedy Krieger Institute, Baltimore, and colleagues wrote in Pediatrics. “However, only 23% of pediatricians in 2002 reported using a standardized developmental screening tool, citing lack of time, staff, and reimbursement as barriers.”
To determine trends in pediatricians’ use of recommended screening tools, the researchers reviewed data from the American Academy of Pediatrics Periodic Surveys in 2002, 2009, and 2016 that included 562, 532, and 469 respondents, respectively.
The percentage of pediatricians who reported using screening tools increased from 21% in 2002 to 63% in 2016 (P less than .001). In addition, The screening tool with the greatest increase in use was the Ages and Stages Questionnaire (ASQ), reportedly used by 48% of pediatricians in 2016, up from 9% in 2002 (P less than .001).
Most reported barriers to screening, including time constraints, inadequate reimbursement, lack of staff to perform screenings, belief that screening is not an appropriate role for pediatricians, and lack of confidence in the screening effectiveness, declined over the study period. However, the percentage of pediatricians who reported lack of available treatment options as a barrier to screening increased from 9% in 2002 to 21% in 2016, the researchers noted.
The average ages of the survey respondents at the 2002, 2009, and 2016 time points were 44, 47, and 49 years, respectively, and the majority (44%, 45%, and 49%) worked in suburban practice areas.
The study findings were limited by several factors, including the use of self-reports, the potential bias of pediatricians to overestimate some of their developmental practices, and potential over- or underreporting if autism spectrum disorder screening was mistakenly included, Dr. Lipkin and associates noted. The results suggest that use of standardized screening has increased, but more attention is needed to improve screening and referrals.
Potential improvements include adding screening tests and referrals to EHRs, and improving communication between medical practices and community-based intervention, therapy, and education programs, they concluded.
The study findings can be seen as encouraging, but one-third of pediatricians still reported not using formal screening instruments, commonly citing lack of time and suboptimal reimbursement, Mei Elansary, MD, and Michael Silverstein, MD, both of Boston University, said in an accompanying editorial.
However, “Although time and financial barriers are real, it is also likely that some of the residual gaps in guideline-concordant practice reflect variability among pediatricians in their perception of the clinical relevance of certain developmental problems that require formal instruments to identify and in the availability and effectiveness of services targeted to children with these less severe developmental issues,” they said. The path for screening children with developmental risk factors but not obviously severe delays may not be straightforward, and many pediatricians rely on their clinical judgment, they emphasized.
“As important as developing strategies to achieve more widespread developmental screening, therefore, is developing a greater understanding of the root causes of practice variation and determining the range of viable clinical practices that lead to better developmental outcomes,” Dr. Elansary and Dr. Silverstein concluded.
The study was supported by the American Academy of Pediatrics, the Department of Health & Human Services, the Health Resources and Services Administration, and the Department of Education Office of Special Education Programs. The researchers had no financial conflicts to disclose.
Editorialist Dr. Silverstein disclosed an award from the Eunice Kennedy Shriver National Institute of Child Health and Human Development; the editorial was funded by the National Institutes of Health. Dr. Silverstein is a member of the U.S. Preventive Services Task Force. Dr. Elansary had no relevant financial disclosures.
pdnews@mdedge.com
SOURCES: Lipkin PH et al. Pediatrics. 2020 Mar 2. doi: 10.1542/peds.2019-0851; Elansary M, Silverstein M. Pediatrics. 2020 Mar 2. doi: 10.1542/peds.2020-0164.
Pediatricians’ reported use of developmental screening tools increased significantly to 63% from 2002 to 2016, based on survey data from more than 1,000 pediatricians at three time points.
“In 2001, an AAP [American Academy of Pediatrics] policy statement called for pediatricians to screen all children for developmental disorders during routine well-child visits,” Paul H. Lipkin, MD, of the Kennedy Krieger Institute, Baltimore, and colleagues wrote in Pediatrics. “However, only 23% of pediatricians in 2002 reported using a standardized developmental screening tool, citing lack of time, staff, and reimbursement as barriers.”
To determine trends in pediatricians’ use of recommended screening tools, the researchers reviewed data from the American Academy of Pediatrics Periodic Surveys in 2002, 2009, and 2016 that included 562, 532, and 469 respondents, respectively.
The percentage of pediatricians who reported using screening tools increased from 21% in 2002 to 63% in 2016 (P less than .001). In addition, The screening tool with the greatest increase in use was the Ages and Stages Questionnaire (ASQ), reportedly used by 48% of pediatricians in 2016, up from 9% in 2002 (P less than .001).
Most reported barriers to screening, including time constraints, inadequate reimbursement, lack of staff to perform screenings, belief that screening is not an appropriate role for pediatricians, and lack of confidence in the screening effectiveness, declined over the study period. However, the percentage of pediatricians who reported lack of available treatment options as a barrier to screening increased from 9% in 2002 to 21% in 2016, the researchers noted.
The average ages of the survey respondents at the 2002, 2009, and 2016 time points were 44, 47, and 49 years, respectively, and the majority (44%, 45%, and 49%) worked in suburban practice areas.
The study findings were limited by several factors, including the use of self-reports, the potential bias of pediatricians to overestimate some of their developmental practices, and potential over- or underreporting if autism spectrum disorder screening was mistakenly included, Dr. Lipkin and associates noted. The results suggest that use of standardized screening has increased, but more attention is needed to improve screening and referrals.
Potential improvements include adding screening tests and referrals to EHRs, and improving communication between medical practices and community-based intervention, therapy, and education programs, they concluded.
The study findings can be seen as encouraging, but one-third of pediatricians still reported not using formal screening instruments, commonly citing lack of time and suboptimal reimbursement, Mei Elansary, MD, and Michael Silverstein, MD, both of Boston University, said in an accompanying editorial.
However, “Although time and financial barriers are real, it is also likely that some of the residual gaps in guideline-concordant practice reflect variability among pediatricians in their perception of the clinical relevance of certain developmental problems that require formal instruments to identify and in the availability and effectiveness of services targeted to children with these less severe developmental issues,” they said. The path for screening children with developmental risk factors but not obviously severe delays may not be straightforward, and many pediatricians rely on their clinical judgment, they emphasized.
“As important as developing strategies to achieve more widespread developmental screening, therefore, is developing a greater understanding of the root causes of practice variation and determining the range of viable clinical practices that lead to better developmental outcomes,” Dr. Elansary and Dr. Silverstein concluded.
The study was supported by the American Academy of Pediatrics, the Department of Health & Human Services, the Health Resources and Services Administration, and the Department of Education Office of Special Education Programs. The researchers had no financial conflicts to disclose.
Editorialist Dr. Silverstein disclosed an award from the Eunice Kennedy Shriver National Institute of Child Health and Human Development; the editorial was funded by the National Institutes of Health. Dr. Silverstein is a member of the U.S. Preventive Services Task Force. Dr. Elansary had no relevant financial disclosures.
pdnews@mdedge.com
SOURCES: Lipkin PH et al. Pediatrics. 2020 Mar 2. doi: 10.1542/peds.2019-0851; Elansary M, Silverstein M. Pediatrics. 2020 Mar 2. doi: 10.1542/peds.2020-0164.
Pediatricians’ reported use of developmental screening tools increased significantly to 63% from 2002 to 2016, based on survey data from more than 1,000 pediatricians at three time points.
“In 2001, an AAP [American Academy of Pediatrics] policy statement called for pediatricians to screen all children for developmental disorders during routine well-child visits,” Paul H. Lipkin, MD, of the Kennedy Krieger Institute, Baltimore, and colleagues wrote in Pediatrics. “However, only 23% of pediatricians in 2002 reported using a standardized developmental screening tool, citing lack of time, staff, and reimbursement as barriers.”
To determine trends in pediatricians’ use of recommended screening tools, the researchers reviewed data from the American Academy of Pediatrics Periodic Surveys in 2002, 2009, and 2016 that included 562, 532, and 469 respondents, respectively.
The percentage of pediatricians who reported using screening tools increased from 21% in 2002 to 63% in 2016 (P less than .001). In addition, The screening tool with the greatest increase in use was the Ages and Stages Questionnaire (ASQ), reportedly used by 48% of pediatricians in 2016, up from 9% in 2002 (P less than .001).
Most reported barriers to screening, including time constraints, inadequate reimbursement, lack of staff to perform screenings, belief that screening is not an appropriate role for pediatricians, and lack of confidence in the screening effectiveness, declined over the study period. However, the percentage of pediatricians who reported lack of available treatment options as a barrier to screening increased from 9% in 2002 to 21% in 2016, the researchers noted.
The average ages of the survey respondents at the 2002, 2009, and 2016 time points were 44, 47, and 49 years, respectively, and the majority (44%, 45%, and 49%) worked in suburban practice areas.
The study findings were limited by several factors, including the use of self-reports, the potential bias of pediatricians to overestimate some of their developmental practices, and potential over- or underreporting if autism spectrum disorder screening was mistakenly included, Dr. Lipkin and associates noted. The results suggest that use of standardized screening has increased, but more attention is needed to improve screening and referrals.
Potential improvements include adding screening tests and referrals to EHRs, and improving communication between medical practices and community-based intervention, therapy, and education programs, they concluded.
The study findings can be seen as encouraging, but one-third of pediatricians still reported not using formal screening instruments, commonly citing lack of time and suboptimal reimbursement, Mei Elansary, MD, and Michael Silverstein, MD, both of Boston University, said in an accompanying editorial.
However, “Although time and financial barriers are real, it is also likely that some of the residual gaps in guideline-concordant practice reflect variability among pediatricians in their perception of the clinical relevance of certain developmental problems that require formal instruments to identify and in the availability and effectiveness of services targeted to children with these less severe developmental issues,” they said. The path for screening children with developmental risk factors but not obviously severe delays may not be straightforward, and many pediatricians rely on their clinical judgment, they emphasized.
“As important as developing strategies to achieve more widespread developmental screening, therefore, is developing a greater understanding of the root causes of practice variation and determining the range of viable clinical practices that lead to better developmental outcomes,” Dr. Elansary and Dr. Silverstein concluded.
The study was supported by the American Academy of Pediatrics, the Department of Health & Human Services, the Health Resources and Services Administration, and the Department of Education Office of Special Education Programs. The researchers had no financial conflicts to disclose.
Editorialist Dr. Silverstein disclosed an award from the Eunice Kennedy Shriver National Institute of Child Health and Human Development; the editorial was funded by the National Institutes of Health. Dr. Silverstein is a member of the U.S. Preventive Services Task Force. Dr. Elansary had no relevant financial disclosures.
pdnews@mdedge.com
SOURCES: Lipkin PH et al. Pediatrics. 2020 Mar 2. doi: 10.1542/peds.2019-0851; Elansary M, Silverstein M. Pediatrics. 2020 Mar 2. doi: 10.1542/peds.2020-0164.
FROM PEDIATRICS
Breach of migrant youths’ confidentiality is unethical, unacceptable
We are in the healing profession. We practice a trade. We are doctors, therapists, counselors. We work with children, adults, and couples. We document the physical form of our patient after examination, setting the stage for interventions that heal and alleviate suffering. With those who we do not touch physically, we hold out our psychological arms to embrace them in a therapeutic relationship.
We are privileged to appreciate their deeper selves through voice, unsaid words, and body language. A trust evolves (or might not); deeper exploration where our intuition and technical skill discover what troubles the soul. Healing begins as a delicate dance: As trust is earned, our patients risk vulnerability by revealing their weakest selves.
As healers, we often find ourselves adrift with our own insecurities, our own histories that make us human; our styles may differ but training and the tenets and guidelines set by our professional societies keep us in safe waters. These guidelines are informed by the science of health care research and vetted through centuries of observation and experience of process. “Do no harm” is perhaps one of the major rules of engaging with patients. The scaffolding that our code of ethics provides healing professions trumps external pressures to deviate. If you violate these codes, the consequences are borne by the patient and the potential loss of your license.
Some of you may have read about Kevin Euceda, an adolescent who reportedly was waiting for his immigration interview and ordered to undergo mandatory therapy as part of the immigration protocol. Kevin revealed to his therapist the history of violence he experienced as a child growing up in Honduras. His subsequent initiation into a gang was the only option he had to escape a violent death. Those of us who work with youth from gang cultures know fully that allegiance to a gang is a means to find an identity and brotherhood with the payment by a lifestyle of violence. A therapist faced with this information does not judge but helps the person deal with PTSD, nightmares, and guilt that become part of an identity just as the memories of mines blowing up in the face of combat affect veterans.
But the therapist, who reportedly holds a master’s in rehabilitation counseling and was “a year away from passing her licensing exam,” according to an article published in the Washington Post, followed policy of the Office of Refugee Resettlement. The therapist betrayed Kevin by reporting the information he shared with her confidentially to Immigration and Customs Enforcement. The reason the therapist gave for the breach was that she was compelled do so because Kevin reported participating in gang activity in Honduras. Subsequently, Kevin was sent to a high-security detention center – and is now facing deportation.
Betraying a patient, profession
Therapy begins as a contract between patient and therapist. The contract stipulates that all that transpires in the process of therapy (usually a 50-minute block of time, usually weekly) is information held by the therapist and patient – and is not to be shared with anyone, including parents, guardians, legal entities, and health care agencies. This allows the gradual sharing of events, emotions, behaviors, and reactions akin to peeling an onion. Memories, reactions, and feelings assist the therapist as they start their quest of discovery of the conflict and how to resolve it. Trust is the central tenet of this journey. The patient thinks: “You will hear me; you will see me you will understand me and help me understand myself.” The doctor responds: “Even I don’t yet know fully what ails you; we will discover that together. … I will not fail your trust.”
So how does this interface with external pressures? The constitution of a free country provides some inviolable protections that prevent derailment of the codes of ethics based on science. The fine line between what are considered sacrosanct ethics of a field – be it health care, climatology, or architecture – and what could be sacrificed in the name of prevailing forces (political or otherwise) has to be under constant scrutiny by the members of the guild. In health care, when patients cannot trust the science, its implementation, or is let down by the clinician, they are unlikely to benefit from treatment. A foundation of distrust paves the way for future therapeutic relationships that are stained with distrust and noncompliance.
The ethics guidelines of the American Academy of Psychiatry and the Law specify that psychiatrists in forensic roles “should be clear about limitations on confidentiality in the treatment relationship and ensure that these limitations are communicated to the patient.” Again, the therapist in this case is not a psychiatrist, but I would argue that the same rules would apply.
It is reassuring to know that several key groups, including the American Psychiatric Association, American Academy of Child and Adolescent Psychiatry, and the American Psychological Association, have all condemned the therapist’s actions. Psychiatrists and other mental health professionals must do no harm. We must not stand idly by and allow the kind of professional breach that happened to Kevin continue. Patients who confide in mental health professionals with the promise of confidentiality must be able to do so without fear. Only with confidentiality can the therapeutic relationship thrive.
Dr. Sood is professor of psychiatry and pediatrics, and senior professor of child mental health policy, at Virginia Commonwealth University, Richmond.
We are in the healing profession. We practice a trade. We are doctors, therapists, counselors. We work with children, adults, and couples. We document the physical form of our patient after examination, setting the stage for interventions that heal and alleviate suffering. With those who we do not touch physically, we hold out our psychological arms to embrace them in a therapeutic relationship.
We are privileged to appreciate their deeper selves through voice, unsaid words, and body language. A trust evolves (or might not); deeper exploration where our intuition and technical skill discover what troubles the soul. Healing begins as a delicate dance: As trust is earned, our patients risk vulnerability by revealing their weakest selves.
As healers, we often find ourselves adrift with our own insecurities, our own histories that make us human; our styles may differ but training and the tenets and guidelines set by our professional societies keep us in safe waters. These guidelines are informed by the science of health care research and vetted through centuries of observation and experience of process. “Do no harm” is perhaps one of the major rules of engaging with patients. The scaffolding that our code of ethics provides healing professions trumps external pressures to deviate. If you violate these codes, the consequences are borne by the patient and the potential loss of your license.
Some of you may have read about Kevin Euceda, an adolescent who reportedly was waiting for his immigration interview and ordered to undergo mandatory therapy as part of the immigration protocol. Kevin revealed to his therapist the history of violence he experienced as a child growing up in Honduras. His subsequent initiation into a gang was the only option he had to escape a violent death. Those of us who work with youth from gang cultures know fully that allegiance to a gang is a means to find an identity and brotherhood with the payment by a lifestyle of violence. A therapist faced with this information does not judge but helps the person deal with PTSD, nightmares, and guilt that become part of an identity just as the memories of mines blowing up in the face of combat affect veterans.
But the therapist, who reportedly holds a master’s in rehabilitation counseling and was “a year away from passing her licensing exam,” according to an article published in the Washington Post, followed policy of the Office of Refugee Resettlement. The therapist betrayed Kevin by reporting the information he shared with her confidentially to Immigration and Customs Enforcement. The reason the therapist gave for the breach was that she was compelled do so because Kevin reported participating in gang activity in Honduras. Subsequently, Kevin was sent to a high-security detention center – and is now facing deportation.
Betraying a patient, profession
Therapy begins as a contract between patient and therapist. The contract stipulates that all that transpires in the process of therapy (usually a 50-minute block of time, usually weekly) is information held by the therapist and patient – and is not to be shared with anyone, including parents, guardians, legal entities, and health care agencies. This allows the gradual sharing of events, emotions, behaviors, and reactions akin to peeling an onion. Memories, reactions, and feelings assist the therapist as they start their quest of discovery of the conflict and how to resolve it. Trust is the central tenet of this journey. The patient thinks: “You will hear me; you will see me you will understand me and help me understand myself.” The doctor responds: “Even I don’t yet know fully what ails you; we will discover that together. … I will not fail your trust.”
So how does this interface with external pressures? The constitution of a free country provides some inviolable protections that prevent derailment of the codes of ethics based on science. The fine line between what are considered sacrosanct ethics of a field – be it health care, climatology, or architecture – and what could be sacrificed in the name of prevailing forces (political or otherwise) has to be under constant scrutiny by the members of the guild. In health care, when patients cannot trust the science, its implementation, or is let down by the clinician, they are unlikely to benefit from treatment. A foundation of distrust paves the way for future therapeutic relationships that are stained with distrust and noncompliance.
The ethics guidelines of the American Academy of Psychiatry and the Law specify that psychiatrists in forensic roles “should be clear about limitations on confidentiality in the treatment relationship and ensure that these limitations are communicated to the patient.” Again, the therapist in this case is not a psychiatrist, but I would argue that the same rules would apply.
It is reassuring to know that several key groups, including the American Psychiatric Association, American Academy of Child and Adolescent Psychiatry, and the American Psychological Association, have all condemned the therapist’s actions. Psychiatrists and other mental health professionals must do no harm. We must not stand idly by and allow the kind of professional breach that happened to Kevin continue. Patients who confide in mental health professionals with the promise of confidentiality must be able to do so without fear. Only with confidentiality can the therapeutic relationship thrive.
Dr. Sood is professor of psychiatry and pediatrics, and senior professor of child mental health policy, at Virginia Commonwealth University, Richmond.
We are in the healing profession. We practice a trade. We are doctors, therapists, counselors. We work with children, adults, and couples. We document the physical form of our patient after examination, setting the stage for interventions that heal and alleviate suffering. With those who we do not touch physically, we hold out our psychological arms to embrace them in a therapeutic relationship.
We are privileged to appreciate their deeper selves through voice, unsaid words, and body language. A trust evolves (or might not); deeper exploration where our intuition and technical skill discover what troubles the soul. Healing begins as a delicate dance: As trust is earned, our patients risk vulnerability by revealing their weakest selves.
As healers, we often find ourselves adrift with our own insecurities, our own histories that make us human; our styles may differ but training and the tenets and guidelines set by our professional societies keep us in safe waters. These guidelines are informed by the science of health care research and vetted through centuries of observation and experience of process. “Do no harm” is perhaps one of the major rules of engaging with patients. The scaffolding that our code of ethics provides healing professions trumps external pressures to deviate. If you violate these codes, the consequences are borne by the patient and the potential loss of your license.
Some of you may have read about Kevin Euceda, an adolescent who reportedly was waiting for his immigration interview and ordered to undergo mandatory therapy as part of the immigration protocol. Kevin revealed to his therapist the history of violence he experienced as a child growing up in Honduras. His subsequent initiation into a gang was the only option he had to escape a violent death. Those of us who work with youth from gang cultures know fully that allegiance to a gang is a means to find an identity and brotherhood with the payment by a lifestyle of violence. A therapist faced with this information does not judge but helps the person deal with PTSD, nightmares, and guilt that become part of an identity just as the memories of mines blowing up in the face of combat affect veterans.
But the therapist, who reportedly holds a master’s in rehabilitation counseling and was “a year away from passing her licensing exam,” according to an article published in the Washington Post, followed policy of the Office of Refugee Resettlement. The therapist betrayed Kevin by reporting the information he shared with her confidentially to Immigration and Customs Enforcement. The reason the therapist gave for the breach was that she was compelled do so because Kevin reported participating in gang activity in Honduras. Subsequently, Kevin was sent to a high-security detention center – and is now facing deportation.
Betraying a patient, profession
Therapy begins as a contract between patient and therapist. The contract stipulates that all that transpires in the process of therapy (usually a 50-minute block of time, usually weekly) is information held by the therapist and patient – and is not to be shared with anyone, including parents, guardians, legal entities, and health care agencies. This allows the gradual sharing of events, emotions, behaviors, and reactions akin to peeling an onion. Memories, reactions, and feelings assist the therapist as they start their quest of discovery of the conflict and how to resolve it. Trust is the central tenet of this journey. The patient thinks: “You will hear me; you will see me you will understand me and help me understand myself.” The doctor responds: “Even I don’t yet know fully what ails you; we will discover that together. … I will not fail your trust.”
So how does this interface with external pressures? The constitution of a free country provides some inviolable protections that prevent derailment of the codes of ethics based on science. The fine line between what are considered sacrosanct ethics of a field – be it health care, climatology, or architecture – and what could be sacrificed in the name of prevailing forces (political or otherwise) has to be under constant scrutiny by the members of the guild. In health care, when patients cannot trust the science, its implementation, or is let down by the clinician, they are unlikely to benefit from treatment. A foundation of distrust paves the way for future therapeutic relationships that are stained with distrust and noncompliance.
The ethics guidelines of the American Academy of Psychiatry and the Law specify that psychiatrists in forensic roles “should be clear about limitations on confidentiality in the treatment relationship and ensure that these limitations are communicated to the patient.” Again, the therapist in this case is not a psychiatrist, but I would argue that the same rules would apply.
It is reassuring to know that several key groups, including the American Psychiatric Association, American Academy of Child and Adolescent Psychiatry, and the American Psychological Association, have all condemned the therapist’s actions. Psychiatrists and other mental health professionals must do no harm. We must not stand idly by and allow the kind of professional breach that happened to Kevin continue. Patients who confide in mental health professionals with the promise of confidentiality must be able to do so without fear. Only with confidentiality can the therapeutic relationship thrive.
Dr. Sood is professor of psychiatry and pediatrics, and senior professor of child mental health policy, at Virginia Commonwealth University, Richmond.
Survey: 2020 will see more attacks on ACA
When physicians gaze into their crystal balls to predict what’s coming in 2020, they see continued efforts to defund the Affordable Care Act – meaning the ACA will still be around to be defunded – but they don’t see a lot of support for universal health care, according to health care market research company InCrowd.
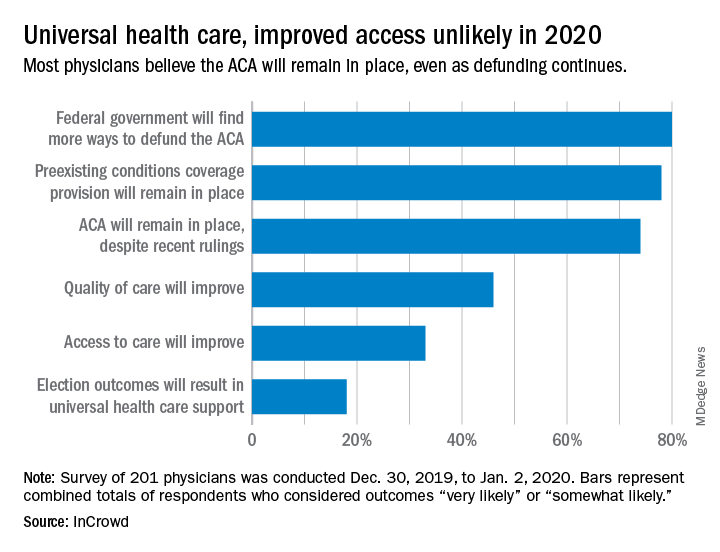
Expectations for universal health care came in at 18% of the 100 generalists and 101 specialists who responded to InCrowd’s fifth annual health care predictions survey, which left 82% who thought that “election outcomes will result in universal healthcare support” was somewhat or very unlikely in 2020.
One respondent, a specialist from California, commented that “the global data on universal healthcare for all shows that it results in overall improved population health. Unfortunately, we are so polarized in the US against universal healthcare driven by bias from health insurance companies and decision makers that are quick to ignore scientific data.”
This was the first time InCrowd asked physicians about universal health care, but ACA-related predictions have been included before, and all three scenarios presented were deemed to be increasingly likely, compared with 2019.
Respondents thought that federal government defunding was more likely to occur in 2020 (80%) than in 2019 (73%), but increased majorities also said that preexisting conditions coverage would continue (78% in 2020 vs. 70% in 2019) and that the ACA would remain in place (74% in 2020 vs. 60% in 2019), InCrowd reported after the survey, which was conducted from Dec. 30, 2019, to Jan. 2, 2020.
A respondent who thought the ACA will be eliminated said, “I have as many uninsured today as before the ACA. They are just different. Mainly younger patients who spend less in a year on healthcare than one month’s premium.” Another suggested that eliminateing it “will limit access to care and overload [emergency departments]. More people will die.”
Cost was addressed in a separate survey question that asked how physicians could help to reduce health care spending in 2020.
The leading answer, given by 37% of respondents, was for physicians to “inform themselves of costs and adapt cost-saving prescription practices.” Next came “limit use of expensive tests and scans” with 21%, followed by “prescribe generics when possible” at 20%, which was a substantial drop from the 38% it garnered in 2019, InCrowd noted.
“Participation in [shared savings] programs and risk-based incentive programs and pay-for-performance programs” would provide “better stewardship of resources,” a primary care physician from Michigan wrote.
When the survey turned to pharmaceutical industry predictions for 2020, cost was the major issue.
“What’s interesting about this year’s data is that we’re seeing less emphasis on the importance of bringing innovative, new therapies to market faster … versus expanding affordability, which was nearly a unanimous top priority for respondents,” Daniel S. Fitzgerald, InCrowd’s CEO and president, said in a separate statement.
When physicians gaze into their crystal balls to predict what’s coming in 2020, they see continued efforts to defund the Affordable Care Act – meaning the ACA will still be around to be defunded – but they don’t see a lot of support for universal health care, according to health care market research company InCrowd.
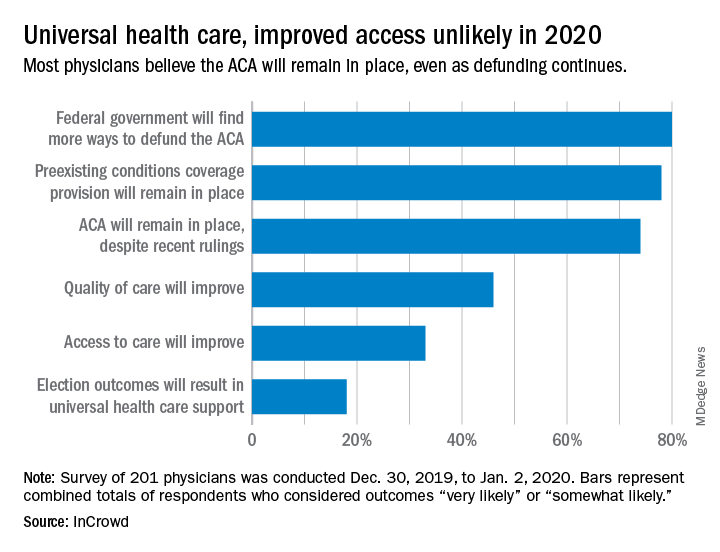
Expectations for universal health care came in at 18% of the 100 generalists and 101 specialists who responded to InCrowd’s fifth annual health care predictions survey, which left 82% who thought that “election outcomes will result in universal healthcare support” was somewhat or very unlikely in 2020.
One respondent, a specialist from California, commented that “the global data on universal healthcare for all shows that it results in overall improved population health. Unfortunately, we are so polarized in the US against universal healthcare driven by bias from health insurance companies and decision makers that are quick to ignore scientific data.”
This was the first time InCrowd asked physicians about universal health care, but ACA-related predictions have been included before, and all three scenarios presented were deemed to be increasingly likely, compared with 2019.
Respondents thought that federal government defunding was more likely to occur in 2020 (80%) than in 2019 (73%), but increased majorities also said that preexisting conditions coverage would continue (78% in 2020 vs. 70% in 2019) and that the ACA would remain in place (74% in 2020 vs. 60% in 2019), InCrowd reported after the survey, which was conducted from Dec. 30, 2019, to Jan. 2, 2020.
A respondent who thought the ACA will be eliminated said, “I have as many uninsured today as before the ACA. They are just different. Mainly younger patients who spend less in a year on healthcare than one month’s premium.” Another suggested that eliminateing it “will limit access to care and overload [emergency departments]. More people will die.”
Cost was addressed in a separate survey question that asked how physicians could help to reduce health care spending in 2020.
The leading answer, given by 37% of respondents, was for physicians to “inform themselves of costs and adapt cost-saving prescription practices.” Next came “limit use of expensive tests and scans” with 21%, followed by “prescribe generics when possible” at 20%, which was a substantial drop from the 38% it garnered in 2019, InCrowd noted.
“Participation in [shared savings] programs and risk-based incentive programs and pay-for-performance programs” would provide “better stewardship of resources,” a primary care physician from Michigan wrote.
When the survey turned to pharmaceutical industry predictions for 2020, cost was the major issue.
“What’s interesting about this year’s data is that we’re seeing less emphasis on the importance of bringing innovative, new therapies to market faster … versus expanding affordability, which was nearly a unanimous top priority for respondents,” Daniel S. Fitzgerald, InCrowd’s CEO and president, said in a separate statement.
When physicians gaze into their crystal balls to predict what’s coming in 2020, they see continued efforts to defund the Affordable Care Act – meaning the ACA will still be around to be defunded – but they don’t see a lot of support for universal health care, according to health care market research company InCrowd.
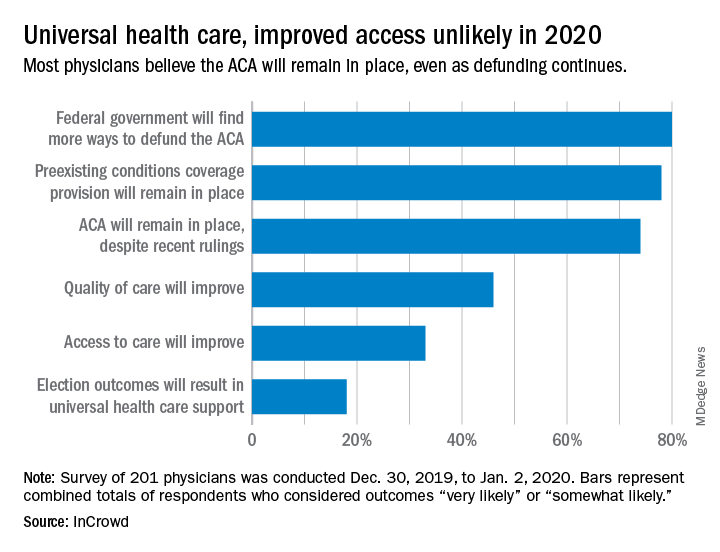
Expectations for universal health care came in at 18% of the 100 generalists and 101 specialists who responded to InCrowd’s fifth annual health care predictions survey, which left 82% who thought that “election outcomes will result in universal healthcare support” was somewhat or very unlikely in 2020.
One respondent, a specialist from California, commented that “the global data on universal healthcare for all shows that it results in overall improved population health. Unfortunately, we are so polarized in the US against universal healthcare driven by bias from health insurance companies and decision makers that are quick to ignore scientific data.”
This was the first time InCrowd asked physicians about universal health care, but ACA-related predictions have been included before, and all three scenarios presented were deemed to be increasingly likely, compared with 2019.
Respondents thought that federal government defunding was more likely to occur in 2020 (80%) than in 2019 (73%), but increased majorities also said that preexisting conditions coverage would continue (78% in 2020 vs. 70% in 2019) and that the ACA would remain in place (74% in 2020 vs. 60% in 2019), InCrowd reported after the survey, which was conducted from Dec. 30, 2019, to Jan. 2, 2020.
A respondent who thought the ACA will be eliminated said, “I have as many uninsured today as before the ACA. They are just different. Mainly younger patients who spend less in a year on healthcare than one month’s premium.” Another suggested that eliminateing it “will limit access to care and overload [emergency departments]. More people will die.”
Cost was addressed in a separate survey question that asked how physicians could help to reduce health care spending in 2020.
The leading answer, given by 37% of respondents, was for physicians to “inform themselves of costs and adapt cost-saving prescription practices.” Next came “limit use of expensive tests and scans” with 21%, followed by “prescribe generics when possible” at 20%, which was a substantial drop from the 38% it garnered in 2019, InCrowd noted.
“Participation in [shared savings] programs and risk-based incentive programs and pay-for-performance programs” would provide “better stewardship of resources,” a primary care physician from Michigan wrote.
When the survey turned to pharmaceutical industry predictions for 2020, cost was the major issue.
“What’s interesting about this year’s data is that we’re seeing less emphasis on the importance of bringing innovative, new therapies to market faster … versus expanding affordability, which was nearly a unanimous top priority for respondents,” Daniel S. Fitzgerald, InCrowd’s CEO and president, said in a separate statement.
Is telerheumatology the future of rheumatology?
MAUI, HAWAII – Alvin F. Wells, MD, PhD, believes he’s seen the future of rheumatology. So he’s taken a deep dive into telerheumatology, going all in.
“Whether you’re in academic, private, or hospital-based practice, in 2020 if you are not thinking about telerheumatology, you and your practice will not be able to compete with growing patient demands, expectations, and need for clinical monitoring. If you do not have a digital/virtual strategy, you do not have a health care strategy,” he asserted at the 2020 Rheumatology Winter Clinical Symposium.
“Begin now,” the rheumatologist advised.
In pursuit of his own telerheumatology strategy, he holds licenses to practice medicine in five states and has licensure pending in five others.
“My goal is to cover 20% of the U.S., so if the local guys can’t see the patients, I can see them virtually,” he explained. “The days of waiting 4-6 months to be seen by a rheumatologist are gone.”
Rheumatologists are already in short supply in most of the country, and a major shortage looms ahead as older practitioners retire. Telerheumatology can help fill that unmet need. But the specialty is behind the curve. In a survey that rated the medical specialties most engaged in telemedicine, the top three spots were held by radiology, psychiatry, and internal medicine. Rheumatology didn’t even crack the top 10, noted Dr. Wells, director of the Rheumatology and Immunotherapy Center in Franklin, Wisc., and a part-time faculty member at Duke University, the Medical College of Wisconsin, and the Karolinska Institute.
Yet telemedicine is primed for rheumatologic takeoff. Notably, the 2019 update of the American College of Rheumatology recommendations on rheumatoid arthritis disease activity measures incorporates the RAPID3 (Routine Assessment of Patient Index Data) as an endorsed three-question clinical assessment that doesn’t involve a physical exam or laboratory work. The ACR update is recognition that, while every rheumatology patient needs an initial physical exam along with follow-up physical exams at various rates, many patients with well-controlled disease don’t need a physical exam at every physician encounter, he said.
Telerheumatology saves time for both patient and physician. The patient saves travel time, doesn’t miss work, avoids having to arrange for child care in order to make a face-to-face clinic visit, and can schedule more frequent virtual follow-up visits. For the practitioner, telerheumatology means additional consults and – here’s the big one – “You never run behind,” according to Dr. Wells. “For a 15-minute appointment, the patient gets a 5-minute warning, then a 2-minute warning, and at 15 minutes the link is cut. If the fibromyalgia patients want 30 minutes, they pay for 30 minutes.”
He sees the strictly enforced, impersonally delivered electronic time limits as key to running an efficient practice.
“The patients with osteoarthritis who hate the nodules, the fibromyalgia patients because they’re hurting all over, the patients with back pain – you’ve really got to limit those patients because otherwise you’ll be running 30-40 minutes behind for a scheduled 15-minute visit,” he explained.
One rheumatologist’s telemedicine practice
Dr. Wells currently utilizes the Epic electronic health record integrated with a Zoom videoconferencing platform for real-time virtual patient encounters. But he noted that other virtual platforms are available, including Health Tap, American Well, MySpecialistMD, MDLIVE, and TelaDoc. The American Telemedicine Association is a valuable resource for state-by-state medicolegal, reimbursement, and how-to-do-it questions.
At present, he reserves two daily time slots for telerheumatology: one at 8:30-9:00 a.m., the other at 4:30-5:00 p.m. These can be filled with four 15-minute live consults or two 30-minute consults. His goal is to eventually make telerheumatology 20% of his patient load of about 100 patients per week.
His typical 15-minute virtual visit proceeds as follows: It begins with a 3-minute subjective patient assessment, followed by a 5-minute objective assessment which includes the RAPID3, a brief Health Assessment Questionnaire (HAQ) addressing the patient’s pain and overall satisfaction, a virtual joint inspection, the use of high-quality teleultrasound and other technology when warranted, and capture of relevant still photos. This is followed by 5 minutes to relay the treatment plan, and finally a 2-minute recap and summary.
“No niceties. We cut right to the chase,” he noted.
He documents the patient encounter as he goes, dictating his notes throughout the visit.
“When I walk out of the room, I’m done. It’s on to the next patient,” Dr. Wells said.
The reimbursement picture is improving, although major hurdles remain. At present, 48 states and the District of Columbia reimburse for live video telemedicine through Medicaid. And in January 2020, Aetna announced it covers reimbursement for telemedicine in all of its fully insured health plans via the Teladoc platform. Dr. Wells’ patients pay for their telerheumatology out of pocket if their insurance doesn’t cover it.
Telemedicine caveats
Dr. Wells shared his telerheumatology experience as the first half of a point/counterpoint session on telemedicine’s future in the specialty. His debate opponent, Orrin M. Troum, MD, announced at the outset that he is quite interested in getting into telerheumatology; however, while looking into it he has come across issues that for now give him pause and that other rheumatologists need to be aware of.
Legal risks. The telemedicine movement has gotten big enough to draw the scrutiny of federal prosecutors and regulatory enforcement officials. In April 2018, the Department of Health & Human Services Office of the Inspector General (OIG) issued a report that concluded that one-third of all examined telemedicine claims were improper.
“Just imagine who might come knocking on your door,” he said.
Among the most common offenses, according to the OIG, were claims for services outside the limited range currently covered; lack of the requisite HIPAA-compliant two-way audio and visual communication technology with fully encrypted data transmission; services billed by institutional providers not defined by Medicare as telemedicine-eligible; and claims for services received by patients who weren’t located in an officially designated Health Professional Shortage Area or in a rural county as determined by the U.S. Census Bureau.
Telemedicine is no panacea for out-of-control health care costs. A RAND study of participants in the California Public Employees’ Retirement System (CalPERS) concluded that only 12% of beneficiaries who used direct-to-consumer telemedicine did so to replace provider visits. The other 88% added on telemedicine as an additional service. So while telemedicine increased patient access to health care, it also increased the overall cost, observed Dr. Troum, a rheumatologist at the University of Southern California, Los Angeles, and in private practice in Santa Monica, Calif.
Talk to your attorney and malpractice insurer before embarking on telerheumatology. Physicians could potentially lose their medical malpractice insurance if they use telemedicine to treat patients located in states where they aren’t licensed to practice, even if through inadvertent error.
Telemedicine isn’t appropriate for all patients. Nearly a decade ago, rheumatologists at Dartmouth-Hitchcock Medical Center launched a telerheumatology service in order to bring specialty care to the largely rural populations of New Hampshire and Vermont. In a review of the experience that included interviews with both patients and providers, investigators concluded that telerheumatology successfully increased access to specialty care in underserved locations and got good satisfaction scores from both providers and beneficiaries. However, fully 19% of patients were found to be inappropriate for their telerheumatology visit, mainly because their disease was too complex or the underlying diagnosis was unclear.
“Almost one-fifth of their patients were inappropriate for telerheumatology. The question is, how are you supposed to know that ahead of time?” Dr. Troum asked.
Patient satisfaction. Dr. Troum’s reading of the literature on patient satisfaction with telerheumatology, coupled with his own extensive experience in clinical practice, makes him think that many of his younger patients with less disease activity might welcome a telerheumatology option, even with strict time boundaries. But his older patients with more disease activity are a different story.
“Typically my middle-aged and older patients won’t accept that without a lot of convincing,” he commented.
Dr. Wells and Dr. Troum had no relevant disclosures regarding their presentations.
MAUI, HAWAII – Alvin F. Wells, MD, PhD, believes he’s seen the future of rheumatology. So he’s taken a deep dive into telerheumatology, going all in.
“Whether you’re in academic, private, or hospital-based practice, in 2020 if you are not thinking about telerheumatology, you and your practice will not be able to compete with growing patient demands, expectations, and need for clinical monitoring. If you do not have a digital/virtual strategy, you do not have a health care strategy,” he asserted at the 2020 Rheumatology Winter Clinical Symposium.
“Begin now,” the rheumatologist advised.
In pursuit of his own telerheumatology strategy, he holds licenses to practice medicine in five states and has licensure pending in five others.
“My goal is to cover 20% of the U.S., so if the local guys can’t see the patients, I can see them virtually,” he explained. “The days of waiting 4-6 months to be seen by a rheumatologist are gone.”
Rheumatologists are already in short supply in most of the country, and a major shortage looms ahead as older practitioners retire. Telerheumatology can help fill that unmet need. But the specialty is behind the curve. In a survey that rated the medical specialties most engaged in telemedicine, the top three spots were held by radiology, psychiatry, and internal medicine. Rheumatology didn’t even crack the top 10, noted Dr. Wells, director of the Rheumatology and Immunotherapy Center in Franklin, Wisc., and a part-time faculty member at Duke University, the Medical College of Wisconsin, and the Karolinska Institute.
Yet telemedicine is primed for rheumatologic takeoff. Notably, the 2019 update of the American College of Rheumatology recommendations on rheumatoid arthritis disease activity measures incorporates the RAPID3 (Routine Assessment of Patient Index Data) as an endorsed three-question clinical assessment that doesn’t involve a physical exam or laboratory work. The ACR update is recognition that, while every rheumatology patient needs an initial physical exam along with follow-up physical exams at various rates, many patients with well-controlled disease don’t need a physical exam at every physician encounter, he said.
Telerheumatology saves time for both patient and physician. The patient saves travel time, doesn’t miss work, avoids having to arrange for child care in order to make a face-to-face clinic visit, and can schedule more frequent virtual follow-up visits. For the practitioner, telerheumatology means additional consults and – here’s the big one – “You never run behind,” according to Dr. Wells. “For a 15-minute appointment, the patient gets a 5-minute warning, then a 2-minute warning, and at 15 minutes the link is cut. If the fibromyalgia patients want 30 minutes, they pay for 30 minutes.”
He sees the strictly enforced, impersonally delivered electronic time limits as key to running an efficient practice.
“The patients with osteoarthritis who hate the nodules, the fibromyalgia patients because they’re hurting all over, the patients with back pain – you’ve really got to limit those patients because otherwise you’ll be running 30-40 minutes behind for a scheduled 15-minute visit,” he explained.
One rheumatologist’s telemedicine practice
Dr. Wells currently utilizes the Epic electronic health record integrated with a Zoom videoconferencing platform for real-time virtual patient encounters. But he noted that other virtual platforms are available, including Health Tap, American Well, MySpecialistMD, MDLIVE, and TelaDoc. The American Telemedicine Association is a valuable resource for state-by-state medicolegal, reimbursement, and how-to-do-it questions.
At present, he reserves two daily time slots for telerheumatology: one at 8:30-9:00 a.m., the other at 4:30-5:00 p.m. These can be filled with four 15-minute live consults or two 30-minute consults. His goal is to eventually make telerheumatology 20% of his patient load of about 100 patients per week.
His typical 15-minute virtual visit proceeds as follows: It begins with a 3-minute subjective patient assessment, followed by a 5-minute objective assessment which includes the RAPID3, a brief Health Assessment Questionnaire (HAQ) addressing the patient’s pain and overall satisfaction, a virtual joint inspection, the use of high-quality teleultrasound and other technology when warranted, and capture of relevant still photos. This is followed by 5 minutes to relay the treatment plan, and finally a 2-minute recap and summary.
“No niceties. We cut right to the chase,” he noted.
He documents the patient encounter as he goes, dictating his notes throughout the visit.
“When I walk out of the room, I’m done. It’s on to the next patient,” Dr. Wells said.
The reimbursement picture is improving, although major hurdles remain. At present, 48 states and the District of Columbia reimburse for live video telemedicine through Medicaid. And in January 2020, Aetna announced it covers reimbursement for telemedicine in all of its fully insured health plans via the Teladoc platform. Dr. Wells’ patients pay for their telerheumatology out of pocket if their insurance doesn’t cover it.
Telemedicine caveats
Dr. Wells shared his telerheumatology experience as the first half of a point/counterpoint session on telemedicine’s future in the specialty. His debate opponent, Orrin M. Troum, MD, announced at the outset that he is quite interested in getting into telerheumatology; however, while looking into it he has come across issues that for now give him pause and that other rheumatologists need to be aware of.
Legal risks. The telemedicine movement has gotten big enough to draw the scrutiny of federal prosecutors and regulatory enforcement officials. In April 2018, the Department of Health & Human Services Office of the Inspector General (OIG) issued a report that concluded that one-third of all examined telemedicine claims were improper.
“Just imagine who might come knocking on your door,” he said.
Among the most common offenses, according to the OIG, were claims for services outside the limited range currently covered; lack of the requisite HIPAA-compliant two-way audio and visual communication technology with fully encrypted data transmission; services billed by institutional providers not defined by Medicare as telemedicine-eligible; and claims for services received by patients who weren’t located in an officially designated Health Professional Shortage Area or in a rural county as determined by the U.S. Census Bureau.
Telemedicine is no panacea for out-of-control health care costs. A RAND study of participants in the California Public Employees’ Retirement System (CalPERS) concluded that only 12% of beneficiaries who used direct-to-consumer telemedicine did so to replace provider visits. The other 88% added on telemedicine as an additional service. So while telemedicine increased patient access to health care, it also increased the overall cost, observed Dr. Troum, a rheumatologist at the University of Southern California, Los Angeles, and in private practice in Santa Monica, Calif.
Talk to your attorney and malpractice insurer before embarking on telerheumatology. Physicians could potentially lose their medical malpractice insurance if they use telemedicine to treat patients located in states where they aren’t licensed to practice, even if through inadvertent error.
Telemedicine isn’t appropriate for all patients. Nearly a decade ago, rheumatologists at Dartmouth-Hitchcock Medical Center launched a telerheumatology service in order to bring specialty care to the largely rural populations of New Hampshire and Vermont. In a review of the experience that included interviews with both patients and providers, investigators concluded that telerheumatology successfully increased access to specialty care in underserved locations and got good satisfaction scores from both providers and beneficiaries. However, fully 19% of patients were found to be inappropriate for their telerheumatology visit, mainly because their disease was too complex or the underlying diagnosis was unclear.
“Almost one-fifth of their patients were inappropriate for telerheumatology. The question is, how are you supposed to know that ahead of time?” Dr. Troum asked.
Patient satisfaction. Dr. Troum’s reading of the literature on patient satisfaction with telerheumatology, coupled with his own extensive experience in clinical practice, makes him think that many of his younger patients with less disease activity might welcome a telerheumatology option, even with strict time boundaries. But his older patients with more disease activity are a different story.
“Typically my middle-aged and older patients won’t accept that without a lot of convincing,” he commented.
Dr. Wells and Dr. Troum had no relevant disclosures regarding their presentations.
MAUI, HAWAII – Alvin F. Wells, MD, PhD, believes he’s seen the future of rheumatology. So he’s taken a deep dive into telerheumatology, going all in.
“Whether you’re in academic, private, or hospital-based practice, in 2020 if you are not thinking about telerheumatology, you and your practice will not be able to compete with growing patient demands, expectations, and need for clinical monitoring. If you do not have a digital/virtual strategy, you do not have a health care strategy,” he asserted at the 2020 Rheumatology Winter Clinical Symposium.
“Begin now,” the rheumatologist advised.
In pursuit of his own telerheumatology strategy, he holds licenses to practice medicine in five states and has licensure pending in five others.
“My goal is to cover 20% of the U.S., so if the local guys can’t see the patients, I can see them virtually,” he explained. “The days of waiting 4-6 months to be seen by a rheumatologist are gone.”
Rheumatologists are already in short supply in most of the country, and a major shortage looms ahead as older practitioners retire. Telerheumatology can help fill that unmet need. But the specialty is behind the curve. In a survey that rated the medical specialties most engaged in telemedicine, the top three spots were held by radiology, psychiatry, and internal medicine. Rheumatology didn’t even crack the top 10, noted Dr. Wells, director of the Rheumatology and Immunotherapy Center in Franklin, Wisc., and a part-time faculty member at Duke University, the Medical College of Wisconsin, and the Karolinska Institute.
Yet telemedicine is primed for rheumatologic takeoff. Notably, the 2019 update of the American College of Rheumatology recommendations on rheumatoid arthritis disease activity measures incorporates the RAPID3 (Routine Assessment of Patient Index Data) as an endorsed three-question clinical assessment that doesn’t involve a physical exam or laboratory work. The ACR update is recognition that, while every rheumatology patient needs an initial physical exam along with follow-up physical exams at various rates, many patients with well-controlled disease don’t need a physical exam at every physician encounter, he said.
Telerheumatology saves time for both patient and physician. The patient saves travel time, doesn’t miss work, avoids having to arrange for child care in order to make a face-to-face clinic visit, and can schedule more frequent virtual follow-up visits. For the practitioner, telerheumatology means additional consults and – here’s the big one – “You never run behind,” according to Dr. Wells. “For a 15-minute appointment, the patient gets a 5-minute warning, then a 2-minute warning, and at 15 minutes the link is cut. If the fibromyalgia patients want 30 minutes, they pay for 30 minutes.”
He sees the strictly enforced, impersonally delivered electronic time limits as key to running an efficient practice.
“The patients with osteoarthritis who hate the nodules, the fibromyalgia patients because they’re hurting all over, the patients with back pain – you’ve really got to limit those patients because otherwise you’ll be running 30-40 minutes behind for a scheduled 15-minute visit,” he explained.
One rheumatologist’s telemedicine practice
Dr. Wells currently utilizes the Epic electronic health record integrated with a Zoom videoconferencing platform for real-time virtual patient encounters. But he noted that other virtual platforms are available, including Health Tap, American Well, MySpecialistMD, MDLIVE, and TelaDoc. The American Telemedicine Association is a valuable resource for state-by-state medicolegal, reimbursement, and how-to-do-it questions.
At present, he reserves two daily time slots for telerheumatology: one at 8:30-9:00 a.m., the other at 4:30-5:00 p.m. These can be filled with four 15-minute live consults or two 30-minute consults. His goal is to eventually make telerheumatology 20% of his patient load of about 100 patients per week.
His typical 15-minute virtual visit proceeds as follows: It begins with a 3-minute subjective patient assessment, followed by a 5-minute objective assessment which includes the RAPID3, a brief Health Assessment Questionnaire (HAQ) addressing the patient’s pain and overall satisfaction, a virtual joint inspection, the use of high-quality teleultrasound and other technology when warranted, and capture of relevant still photos. This is followed by 5 minutes to relay the treatment plan, and finally a 2-minute recap and summary.
“No niceties. We cut right to the chase,” he noted.
He documents the patient encounter as he goes, dictating his notes throughout the visit.
“When I walk out of the room, I’m done. It’s on to the next patient,” Dr. Wells said.
The reimbursement picture is improving, although major hurdles remain. At present, 48 states and the District of Columbia reimburse for live video telemedicine through Medicaid. And in January 2020, Aetna announced it covers reimbursement for telemedicine in all of its fully insured health plans via the Teladoc platform. Dr. Wells’ patients pay for their telerheumatology out of pocket if their insurance doesn’t cover it.
Telemedicine caveats
Dr. Wells shared his telerheumatology experience as the first half of a point/counterpoint session on telemedicine’s future in the specialty. His debate opponent, Orrin M. Troum, MD, announced at the outset that he is quite interested in getting into telerheumatology; however, while looking into it he has come across issues that for now give him pause and that other rheumatologists need to be aware of.
Legal risks. The telemedicine movement has gotten big enough to draw the scrutiny of federal prosecutors and regulatory enforcement officials. In April 2018, the Department of Health & Human Services Office of the Inspector General (OIG) issued a report that concluded that one-third of all examined telemedicine claims were improper.
“Just imagine who might come knocking on your door,” he said.
Among the most common offenses, according to the OIG, were claims for services outside the limited range currently covered; lack of the requisite HIPAA-compliant two-way audio and visual communication technology with fully encrypted data transmission; services billed by institutional providers not defined by Medicare as telemedicine-eligible; and claims for services received by patients who weren’t located in an officially designated Health Professional Shortage Area or in a rural county as determined by the U.S. Census Bureau.
Telemedicine is no panacea for out-of-control health care costs. A RAND study of participants in the California Public Employees’ Retirement System (CalPERS) concluded that only 12% of beneficiaries who used direct-to-consumer telemedicine did so to replace provider visits. The other 88% added on telemedicine as an additional service. So while telemedicine increased patient access to health care, it also increased the overall cost, observed Dr. Troum, a rheumatologist at the University of Southern California, Los Angeles, and in private practice in Santa Monica, Calif.
Talk to your attorney and malpractice insurer before embarking on telerheumatology. Physicians could potentially lose their medical malpractice insurance if they use telemedicine to treat patients located in states where they aren’t licensed to practice, even if through inadvertent error.
Telemedicine isn’t appropriate for all patients. Nearly a decade ago, rheumatologists at Dartmouth-Hitchcock Medical Center launched a telerheumatology service in order to bring specialty care to the largely rural populations of New Hampshire and Vermont. In a review of the experience that included interviews with both patients and providers, investigators concluded that telerheumatology successfully increased access to specialty care in underserved locations and got good satisfaction scores from both providers and beneficiaries. However, fully 19% of patients were found to be inappropriate for their telerheumatology visit, mainly because their disease was too complex or the underlying diagnosis was unclear.
“Almost one-fifth of their patients were inappropriate for telerheumatology. The question is, how are you supposed to know that ahead of time?” Dr. Troum asked.
Patient satisfaction. Dr. Troum’s reading of the literature on patient satisfaction with telerheumatology, coupled with his own extensive experience in clinical practice, makes him think that many of his younger patients with less disease activity might welcome a telerheumatology option, even with strict time boundaries. But his older patients with more disease activity are a different story.
“Typically my middle-aged and older patients won’t accept that without a lot of convincing,” he commented.
Dr. Wells and Dr. Troum had no relevant disclosures regarding their presentations.
REPORTING FROM RWCS 2020
What medical conferences are being canceled by coronavirus?
In a typical year, March marks the start of conference season, made all the more attractive by collegial gatherings and travel to warmer climes. But 2020 has already proven anything but typical as the number of novel coronavirus cases continues to increase around the globe. As a potential pandemic looms, these meetings – full of handshakes and crowded lecture halls – are also nirvana for opportunistic viruses. As are the airports, airplanes, and cabs required to get there.
So, as COVID-19 continues to spread, medical and scientific societies must make some difficult decisions. In Europe, at least a few societies have already suspended their upcoming meetings, while France has temporarily banned all gatherings over 5000 people.
In the United States, however, most medical conferences are moving forward as planned – at least for now. But one conference of 10,000 attendees, the American Physical Society annual meeting, which was scheduled for March 2-6 in Denver, was canceled the day before the meeting started. Although it’s not a medical conference, it speaks to the “rapidly escalating health concerns” that all conference organizers must grapple with.
APS Physics Meetings
@APSMeetings
Due to rapidly escalating health concerns relating to the spread of the coronavirus disease (COVID-19), the 2020 APS March Meeting in Denver, CO, has been canceled. Please do not travel to Denver to attend the March Meeting. More information will follow shortly. #apsmarch
734 9:59 PM - Feb 29, 2020
Just one smaller medical meeting, the Ataxia Conference, which was scheduled for March 6-7 in Denver, has been canceled.
Most societies hosting these meetings have put out statements to their attendees saying that they’re monitoring the situation and will adapt as necessary. The United States and Canadian Academy of Pathology, which is holding its annual meeting in Los Angeles this week, sent out an email beforehand asking international travelers to consider staying home. The Healthcare Information and Management Systems Society (HIMSS) Global Health Conference, which is slated to have about 50,000 attendees from around the world, has declared itself a “handshake-free” conference but otherwise intends to move ahead as planned.
All of these conferences will be pushing forward without at least one prominent group of attendees. New York University’s Langone Health has removed its employees from the decision-making process and instead is taking a proactive stance: The health system just declared a 60-day (minimum) ban preventing employees from attending any meetings or conferences and from all domestic and international work-related travel.
Here’s what some of the societies have said to attendees about their intent to proceed or modify their plans:
- Conference on Retroviruses and Opportunistic Infections (CROI), Boston, 3/8/20 - 3/11/20: Monitoring the situation and seeking input from local, state, and federal infectious-disease and public-health experts. Final decision expected by the evening of March 3.
- American Academy of Allergy, Asthma & Immunology (AAAAI), Philadelphia, 3/13/20 - 3/16/20: Monitoring developments but no plans to cancel or postpone at this time.
- American Academy of Orthopedic Surgeons (AAOS), Orlando, 3/24/20 - 3/28/20: Proceeding as planned.
- American Academy of Dermatology (AAD), Denver, 3/20/20 - 3/24/20: The AAD’s 2020 Annual Meeting is scheduled to take place as planned. The organization will increase the number of hand-sanitizing stations throughout the convention center, and it is adding a nursing station specifically designated for anyone with flu-like symptoms.
- American College of Cardiology (ACC), Chicago, 3/28/20 - 3/30/20: The organization is working with attendees, faculty, exhibitors, and other stakeholders in affected countries to ensure access to research and education from the meeting, but is otherwise proceeding as planned.
- Endocrine Society (ENDO), San Francisco, 3/28/20 - 3/31/20: ENDO 2020 will take place as scheduled, but this is an evolving situation worldwide. The society will continue to monitor and provide updates on its FAQ page.
- American College of Physicians Internal Medicine (ACP IM), Los Angeles, 4/23/20 - 4/25/20: ACP leadership is closely monitoring the COVID-19 situation and is actively working with the Centers for Disease Control and Prevention (CDC) to ensure authoritative communication of safety updates and recommendations as the situation evolves.
- American Association for Cancer Research (AACR), San Diego, 4/24/20 - 4/29/20: At this time, there is no plan to cancel or postpone any scheduled AACR meetings. The organization is tracking all travel restrictions as well as information and guidance from the CDC and World Health Organization.
- American Academy of Neurology (AAN), Toronto, 4/25/20 - 5/1/20: The group is continuing to closely monitor the situation in Toronto and will provide updates as the situation warrants.
This article originally appeared on Medscape.com.
In a typical year, March marks the start of conference season, made all the more attractive by collegial gatherings and travel to warmer climes. But 2020 has already proven anything but typical as the number of novel coronavirus cases continues to increase around the globe. As a potential pandemic looms, these meetings – full of handshakes and crowded lecture halls – are also nirvana for opportunistic viruses. As are the airports, airplanes, and cabs required to get there.
So, as COVID-19 continues to spread, medical and scientific societies must make some difficult decisions. In Europe, at least a few societies have already suspended their upcoming meetings, while France has temporarily banned all gatherings over 5000 people.
In the United States, however, most medical conferences are moving forward as planned – at least for now. But one conference of 10,000 attendees, the American Physical Society annual meeting, which was scheduled for March 2-6 in Denver, was canceled the day before the meeting started. Although it’s not a medical conference, it speaks to the “rapidly escalating health concerns” that all conference organizers must grapple with.
APS Physics Meetings
@APSMeetings
Due to rapidly escalating health concerns relating to the spread of the coronavirus disease (COVID-19), the 2020 APS March Meeting in Denver, CO, has been canceled. Please do not travel to Denver to attend the March Meeting. More information will follow shortly. #apsmarch
734 9:59 PM - Feb 29, 2020
Just one smaller medical meeting, the Ataxia Conference, which was scheduled for March 6-7 in Denver, has been canceled.
Most societies hosting these meetings have put out statements to their attendees saying that they’re monitoring the situation and will adapt as necessary. The United States and Canadian Academy of Pathology, which is holding its annual meeting in Los Angeles this week, sent out an email beforehand asking international travelers to consider staying home. The Healthcare Information and Management Systems Society (HIMSS) Global Health Conference, which is slated to have about 50,000 attendees from around the world, has declared itself a “handshake-free” conference but otherwise intends to move ahead as planned.
All of these conferences will be pushing forward without at least one prominent group of attendees. New York University’s Langone Health has removed its employees from the decision-making process and instead is taking a proactive stance: The health system just declared a 60-day (minimum) ban preventing employees from attending any meetings or conferences and from all domestic and international work-related travel.
Here’s what some of the societies have said to attendees about their intent to proceed or modify their plans:
- Conference on Retroviruses and Opportunistic Infections (CROI), Boston, 3/8/20 - 3/11/20: Monitoring the situation and seeking input from local, state, and federal infectious-disease and public-health experts. Final decision expected by the evening of March 3.
- American Academy of Allergy, Asthma & Immunology (AAAAI), Philadelphia, 3/13/20 - 3/16/20: Monitoring developments but no plans to cancel or postpone at this time.
- American Academy of Orthopedic Surgeons (AAOS), Orlando, 3/24/20 - 3/28/20: Proceeding as planned.
- American Academy of Dermatology (AAD), Denver, 3/20/20 - 3/24/20: The AAD’s 2020 Annual Meeting is scheduled to take place as planned. The organization will increase the number of hand-sanitizing stations throughout the convention center, and it is adding a nursing station specifically designated for anyone with flu-like symptoms.
- American College of Cardiology (ACC), Chicago, 3/28/20 - 3/30/20: The organization is working with attendees, faculty, exhibitors, and other stakeholders in affected countries to ensure access to research and education from the meeting, but is otherwise proceeding as planned.
- Endocrine Society (ENDO), San Francisco, 3/28/20 - 3/31/20: ENDO 2020 will take place as scheduled, but this is an evolving situation worldwide. The society will continue to monitor and provide updates on its FAQ page.
- American College of Physicians Internal Medicine (ACP IM), Los Angeles, 4/23/20 - 4/25/20: ACP leadership is closely monitoring the COVID-19 situation and is actively working with the Centers for Disease Control and Prevention (CDC) to ensure authoritative communication of safety updates and recommendations as the situation evolves.
- American Association for Cancer Research (AACR), San Diego, 4/24/20 - 4/29/20: At this time, there is no plan to cancel or postpone any scheduled AACR meetings. The organization is tracking all travel restrictions as well as information and guidance from the CDC and World Health Organization.
- American Academy of Neurology (AAN), Toronto, 4/25/20 - 5/1/20: The group is continuing to closely monitor the situation in Toronto and will provide updates as the situation warrants.
This article originally appeared on Medscape.com.
In a typical year, March marks the start of conference season, made all the more attractive by collegial gatherings and travel to warmer climes. But 2020 has already proven anything but typical as the number of novel coronavirus cases continues to increase around the globe. As a potential pandemic looms, these meetings – full of handshakes and crowded lecture halls – are also nirvana for opportunistic viruses. As are the airports, airplanes, and cabs required to get there.
So, as COVID-19 continues to spread, medical and scientific societies must make some difficult decisions. In Europe, at least a few societies have already suspended their upcoming meetings, while France has temporarily banned all gatherings over 5000 people.
In the United States, however, most medical conferences are moving forward as planned – at least for now. But one conference of 10,000 attendees, the American Physical Society annual meeting, which was scheduled for March 2-6 in Denver, was canceled the day before the meeting started. Although it’s not a medical conference, it speaks to the “rapidly escalating health concerns” that all conference organizers must grapple with.
APS Physics Meetings
@APSMeetings
Due to rapidly escalating health concerns relating to the spread of the coronavirus disease (COVID-19), the 2020 APS March Meeting in Denver, CO, has been canceled. Please do not travel to Denver to attend the March Meeting. More information will follow shortly. #apsmarch
734 9:59 PM - Feb 29, 2020
Just one smaller medical meeting, the Ataxia Conference, which was scheduled for March 6-7 in Denver, has been canceled.
Most societies hosting these meetings have put out statements to their attendees saying that they’re monitoring the situation and will adapt as necessary. The United States and Canadian Academy of Pathology, which is holding its annual meeting in Los Angeles this week, sent out an email beforehand asking international travelers to consider staying home. The Healthcare Information and Management Systems Society (HIMSS) Global Health Conference, which is slated to have about 50,000 attendees from around the world, has declared itself a “handshake-free” conference but otherwise intends to move ahead as planned.
All of these conferences will be pushing forward without at least one prominent group of attendees. New York University’s Langone Health has removed its employees from the decision-making process and instead is taking a proactive stance: The health system just declared a 60-day (minimum) ban preventing employees from attending any meetings or conferences and from all domestic and international work-related travel.
Here’s what some of the societies have said to attendees about their intent to proceed or modify their plans:
- Conference on Retroviruses and Opportunistic Infections (CROI), Boston, 3/8/20 - 3/11/20: Monitoring the situation and seeking input from local, state, and federal infectious-disease and public-health experts. Final decision expected by the evening of March 3.
- American Academy of Allergy, Asthma & Immunology (AAAAI), Philadelphia, 3/13/20 - 3/16/20: Monitoring developments but no plans to cancel or postpone at this time.
- American Academy of Orthopedic Surgeons (AAOS), Orlando, 3/24/20 - 3/28/20: Proceeding as planned.
- American Academy of Dermatology (AAD), Denver, 3/20/20 - 3/24/20: The AAD’s 2020 Annual Meeting is scheduled to take place as planned. The organization will increase the number of hand-sanitizing stations throughout the convention center, and it is adding a nursing station specifically designated for anyone with flu-like symptoms.
- American College of Cardiology (ACC), Chicago, 3/28/20 - 3/30/20: The organization is working with attendees, faculty, exhibitors, and other stakeholders in affected countries to ensure access to research and education from the meeting, but is otherwise proceeding as planned.
- Endocrine Society (ENDO), San Francisco, 3/28/20 - 3/31/20: ENDO 2020 will take place as scheduled, but this is an evolving situation worldwide. The society will continue to monitor and provide updates on its FAQ page.
- American College of Physicians Internal Medicine (ACP IM), Los Angeles, 4/23/20 - 4/25/20: ACP leadership is closely monitoring the COVID-19 situation and is actively working with the Centers for Disease Control and Prevention (CDC) to ensure authoritative communication of safety updates and recommendations as the situation evolves.
- American Association for Cancer Research (AACR), San Diego, 4/24/20 - 4/29/20: At this time, there is no plan to cancel or postpone any scheduled AACR meetings. The organization is tracking all travel restrictions as well as information and guidance from the CDC and World Health Organization.
- American Academy of Neurology (AAN), Toronto, 4/25/20 - 5/1/20: The group is continuing to closely monitor the situation in Toronto and will provide updates as the situation warrants.
This article originally appeared on Medscape.com.
Bad behavior by medical trainees target of new proposal
Some instances of unprofessional behavior by medical trainees are universally deemed egregious and worthy of discipline — for example, looking up a friend’s medical data after HIPAA training.
Conversely, some professionalism lapses may be widely thought of as a teaching and consoling moment, such as the human error involved in forgetting a scheduled repositioning of a patient.
But between the extremes is a vast gray area. To deal with those cases appropriately, Jason Wasserman, PhD, and colleagues propose a new framework by which to judge each infraction.
The framework draws from “just culture” concepts used to evaluate medical errors, Wasserman, associate professor of biomedical science at Oakland University William Beaumont School of Medicine in Rochester, Michigan, told Medscape Medical News. Such an approach takes into account the environment in which the error was made, the knowledge and intent of the person making the error, and the severity and consequences of the infraction so that trainees and institutions can learn from mistakes.
“Trainees by definition are not going to fully get it,” he explained. “By definition they’re not going to fully achieve professional expectations. So how can we respond to the things we need to respond to, but do it in a way that’s educational?”
Wasserman and coauthors’ framework for remediation, which they published February 20 in The New England Journal of Medicine, takes into account several questions: Was the expectation clear? Were there factors beyond the trainees› control? What were the trainees› intentions and did they understand the consequences? Did the person genuinely believe the action was inconsequential?
An example requiring discipline, the authors say, would be using a crib sheet during an exam. In that case the intent is clear, there is no defensible belief that the action is inconsequential, and there is a clear understanding the action is wrong.
But a response of “affirm, support, and advise” is more appropriate, for example, when a student’s alarm doesn’t go off after a power outage and they miss a mandatory meeting.
Wasserman points out that this framework won’t cover all situations.
“This is not an algorithm for answering your questions about what to do,” he said. “It’s an architecture for clarifying the discussion about that. It can really tease out all the threads that need to be considered to best respond to and correct the professionalism lapse, but do it in a way that is developmentally appropriate.”
A Core Competency
For two decades, professionalism has been considered a core competency of medical education. In 1999, the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties formalized it as such. In 2013, the Association of American Medical Colleges formally required related professionalism competencies.
However, identifying lapses has operated largely on an “I-know-it-when-I-see-it” basis, leading to widely varying remediation practices judged by a small number of faculty members or administrators.
The ideas outlined by Wasserman and colleagues are “a terrific application of the ‘just-culture’ framework,” according to Nicole Treadway, MD, a first-year primary care resident at Emory School of Medicine in Atlanta, Georgia.
At Emory, discussions of professionalism start from day 1 of medical school and the subject is revisited throughout training in small groups, Treadway told Medscape Medical News.
But, she said, as the authors point out, definitions of unprofessionalism are not always clear and the examples the authors put forward help put lapses in context.
The framework also allows for looking at mistakes in light of the stress trainees encounter and the greater chance of making a professionalism error in those situations, she noted.
In her own work, she says, because she is juggling both inpatient and outpatient care, she is finding it is easy to get behind on correspondence or communicating lab results or having follow-up conversations.
Those delays could be seen as lapses in professionalism, but under this framework, there may be system solutions or training opportunities to consider.
“We do need this organizational architecture, and I think it could serve us well in really helping us identify and appropriately respond to what we see regarding professionalism,” she said.
Framework Helps Standardize Thinking
She said having a universal framework also helps because while standards of professionalism are easier to monitor in a single medical school, when students scatter to other hospitals for clinical training, those hospitals may have different professionalism standards.
Wasserman agrees, saying, “This could be easily adopted in any environment where people deal with professionalism lapses. I don’t even think it’s necessarily relegated to trainees. It’s a great way to think about any kind of lapses, just as hospitals think about medical errors.”
He said the next step is presenting the framework at various medical schools for feedback and research to see whether the framework improves processes.
Potential criticism, he said, might come from those who say such a construct avoids punishing students who make errors.
“There will always be people who say we’re pandering to medical students whenever we worry about the learning environment,” he said. “There are old-school purists who say when people screw up you should punish them.”
But he adds healthcare broadly has moved past that thinking.
“People recognized 20 years ago or more from the standpoint of improving healthcare systems and safety that is a bad strategy. You’ll never get error-free humans working in your system, and what you have to do is consider how the system is functioning and think about ways to optimize the system so people can be their best within it.”
Wasserman and Treadway have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Some instances of unprofessional behavior by medical trainees are universally deemed egregious and worthy of discipline — for example, looking up a friend’s medical data after HIPAA training.
Conversely, some professionalism lapses may be widely thought of as a teaching and consoling moment, such as the human error involved in forgetting a scheduled repositioning of a patient.
But between the extremes is a vast gray area. To deal with those cases appropriately, Jason Wasserman, PhD, and colleagues propose a new framework by which to judge each infraction.
The framework draws from “just culture” concepts used to evaluate medical errors, Wasserman, associate professor of biomedical science at Oakland University William Beaumont School of Medicine in Rochester, Michigan, told Medscape Medical News. Such an approach takes into account the environment in which the error was made, the knowledge and intent of the person making the error, and the severity and consequences of the infraction so that trainees and institutions can learn from mistakes.
“Trainees by definition are not going to fully get it,” he explained. “By definition they’re not going to fully achieve professional expectations. So how can we respond to the things we need to respond to, but do it in a way that’s educational?”
Wasserman and coauthors’ framework for remediation, which they published February 20 in The New England Journal of Medicine, takes into account several questions: Was the expectation clear? Were there factors beyond the trainees› control? What were the trainees› intentions and did they understand the consequences? Did the person genuinely believe the action was inconsequential?
An example requiring discipline, the authors say, would be using a crib sheet during an exam. In that case the intent is clear, there is no defensible belief that the action is inconsequential, and there is a clear understanding the action is wrong.
But a response of “affirm, support, and advise” is more appropriate, for example, when a student’s alarm doesn’t go off after a power outage and they miss a mandatory meeting.
Wasserman points out that this framework won’t cover all situations.
“This is not an algorithm for answering your questions about what to do,” he said. “It’s an architecture for clarifying the discussion about that. It can really tease out all the threads that need to be considered to best respond to and correct the professionalism lapse, but do it in a way that is developmentally appropriate.”
A Core Competency
For two decades, professionalism has been considered a core competency of medical education. In 1999, the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties formalized it as such. In 2013, the Association of American Medical Colleges formally required related professionalism competencies.
However, identifying lapses has operated largely on an “I-know-it-when-I-see-it” basis, leading to widely varying remediation practices judged by a small number of faculty members or administrators.
The ideas outlined by Wasserman and colleagues are “a terrific application of the ‘just-culture’ framework,” according to Nicole Treadway, MD, a first-year primary care resident at Emory School of Medicine in Atlanta, Georgia.
At Emory, discussions of professionalism start from day 1 of medical school and the subject is revisited throughout training in small groups, Treadway told Medscape Medical News.
But, she said, as the authors point out, definitions of unprofessionalism are not always clear and the examples the authors put forward help put lapses in context.
The framework also allows for looking at mistakes in light of the stress trainees encounter and the greater chance of making a professionalism error in those situations, she noted.
In her own work, she says, because she is juggling both inpatient and outpatient care, she is finding it is easy to get behind on correspondence or communicating lab results or having follow-up conversations.
Those delays could be seen as lapses in professionalism, but under this framework, there may be system solutions or training opportunities to consider.
“We do need this organizational architecture, and I think it could serve us well in really helping us identify and appropriately respond to what we see regarding professionalism,” she said.
Framework Helps Standardize Thinking
She said having a universal framework also helps because while standards of professionalism are easier to monitor in a single medical school, when students scatter to other hospitals for clinical training, those hospitals may have different professionalism standards.
Wasserman agrees, saying, “This could be easily adopted in any environment where people deal with professionalism lapses. I don’t even think it’s necessarily relegated to trainees. It’s a great way to think about any kind of lapses, just as hospitals think about medical errors.”
He said the next step is presenting the framework at various medical schools for feedback and research to see whether the framework improves processes.
Potential criticism, he said, might come from those who say such a construct avoids punishing students who make errors.
“There will always be people who say we’re pandering to medical students whenever we worry about the learning environment,” he said. “There are old-school purists who say when people screw up you should punish them.”
But he adds healthcare broadly has moved past that thinking.
“People recognized 20 years ago or more from the standpoint of improving healthcare systems and safety that is a bad strategy. You’ll never get error-free humans working in your system, and what you have to do is consider how the system is functioning and think about ways to optimize the system so people can be their best within it.”
Wasserman and Treadway have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Some instances of unprofessional behavior by medical trainees are universally deemed egregious and worthy of discipline — for example, looking up a friend’s medical data after HIPAA training.
Conversely, some professionalism lapses may be widely thought of as a teaching and consoling moment, such as the human error involved in forgetting a scheduled repositioning of a patient.
But between the extremes is a vast gray area. To deal with those cases appropriately, Jason Wasserman, PhD, and colleagues propose a new framework by which to judge each infraction.
The framework draws from “just culture” concepts used to evaluate medical errors, Wasserman, associate professor of biomedical science at Oakland University William Beaumont School of Medicine in Rochester, Michigan, told Medscape Medical News. Such an approach takes into account the environment in which the error was made, the knowledge and intent of the person making the error, and the severity and consequences of the infraction so that trainees and institutions can learn from mistakes.
“Trainees by definition are not going to fully get it,” he explained. “By definition they’re not going to fully achieve professional expectations. So how can we respond to the things we need to respond to, but do it in a way that’s educational?”
Wasserman and coauthors’ framework for remediation, which they published February 20 in The New England Journal of Medicine, takes into account several questions: Was the expectation clear? Were there factors beyond the trainees› control? What were the trainees› intentions and did they understand the consequences? Did the person genuinely believe the action was inconsequential?
An example requiring discipline, the authors say, would be using a crib sheet during an exam. In that case the intent is clear, there is no defensible belief that the action is inconsequential, and there is a clear understanding the action is wrong.
But a response of “affirm, support, and advise” is more appropriate, for example, when a student’s alarm doesn’t go off after a power outage and they miss a mandatory meeting.
Wasserman points out that this framework won’t cover all situations.
“This is not an algorithm for answering your questions about what to do,” he said. “It’s an architecture for clarifying the discussion about that. It can really tease out all the threads that need to be considered to best respond to and correct the professionalism lapse, but do it in a way that is developmentally appropriate.”
A Core Competency
For two decades, professionalism has been considered a core competency of medical education. In 1999, the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties formalized it as such. In 2013, the Association of American Medical Colleges formally required related professionalism competencies.
However, identifying lapses has operated largely on an “I-know-it-when-I-see-it” basis, leading to widely varying remediation practices judged by a small number of faculty members or administrators.
The ideas outlined by Wasserman and colleagues are “a terrific application of the ‘just-culture’ framework,” according to Nicole Treadway, MD, a first-year primary care resident at Emory School of Medicine in Atlanta, Georgia.
At Emory, discussions of professionalism start from day 1 of medical school and the subject is revisited throughout training in small groups, Treadway told Medscape Medical News.
But, she said, as the authors point out, definitions of unprofessionalism are not always clear and the examples the authors put forward help put lapses in context.
The framework also allows for looking at mistakes in light of the stress trainees encounter and the greater chance of making a professionalism error in those situations, she noted.
In her own work, she says, because she is juggling both inpatient and outpatient care, she is finding it is easy to get behind on correspondence or communicating lab results or having follow-up conversations.
Those delays could be seen as lapses in professionalism, but under this framework, there may be system solutions or training opportunities to consider.
“We do need this organizational architecture, and I think it could serve us well in really helping us identify and appropriately respond to what we see regarding professionalism,” she said.
Framework Helps Standardize Thinking
She said having a universal framework also helps because while standards of professionalism are easier to monitor in a single medical school, when students scatter to other hospitals for clinical training, those hospitals may have different professionalism standards.
Wasserman agrees, saying, “This could be easily adopted in any environment where people deal with professionalism lapses. I don’t even think it’s necessarily relegated to trainees. It’s a great way to think about any kind of lapses, just as hospitals think about medical errors.”
He said the next step is presenting the framework at various medical schools for feedback and research to see whether the framework improves processes.
Potential criticism, he said, might come from those who say such a construct avoids punishing students who make errors.
“There will always be people who say we’re pandering to medical students whenever we worry about the learning environment,” he said. “There are old-school purists who say when people screw up you should punish them.”
But he adds healthcare broadly has moved past that thinking.
“People recognized 20 years ago or more from the standpoint of improving healthcare systems and safety that is a bad strategy. You’ll never get error-free humans working in your system, and what you have to do is consider how the system is functioning and think about ways to optimize the system so people can be their best within it.”
Wasserman and Treadway have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.