User login
Online resources influencing cosmetic treatment choices
Online resources are affecting most consumers’ selections of cosmetic providers, and social media are now a top-three influence on cosmetic procedure choices and skin care purchases, according to a new survey from the American Society for Dermatologic Surgery.
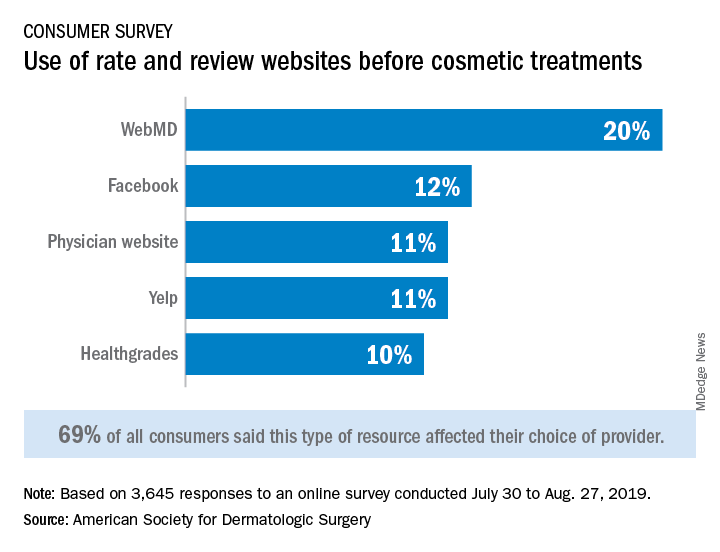
Almost 70% of respondents said that their use of rate and review websites had an impact on the choice of provider for cosmetic procedures: WebMD was the site most often visited, followed by Facebook, physician websites, and Yelp, the ASDS said based on its annual consumer survey.
For 43% of consumers, the decision to schedule an appointment was influenced by a provider’s social media presence, and 41% of patients said that they follow their current or potential provider on social media, the ASDS said.
“Online resources and social media platforms are clearly influencing consumers’ behavior and perception of skin health,” ASDS President Murad Alam, MD, MBA, chief of cutaneous and aesthetic surgery in the department of dermatology at Northwestern University, Chicago, said in a written statement.
Dermatologists, however, remain the leading influence on the decision to have a cosmetic procedure – named as a resource by 34% of respondents, who could select more than one possibility from a list of 15 – but social media moved ahead of primary care physicians into third place (24%), just behind friends (30%), the survey showed. Dermatologists, on the other hand, had polled at 50%-55% for the previous 5 years.
The dermatologists’ lead remained stronger as the top influencer for skin care purchases, selected by 45% of respondents, compared with 32% for friends and 28% for social media. In this category there were 14 factors from which respondents could choose. As for the cost of those skin care products, 48% of consumers spent $1-$50 a month, 31% said that they spent $51-$100 a month, and 12% reported spending $101-$150 a month, the ASDS said.
The society received 3,645 responses to the 2019 Consumer Survey on Cosmetic Dermatologic Procedures, which was conducted online from July 30 to Aug. 27 by Survata.
Online resources are affecting most consumers’ selections of cosmetic providers, and social media are now a top-three influence on cosmetic procedure choices and skin care purchases, according to a new survey from the American Society for Dermatologic Surgery.
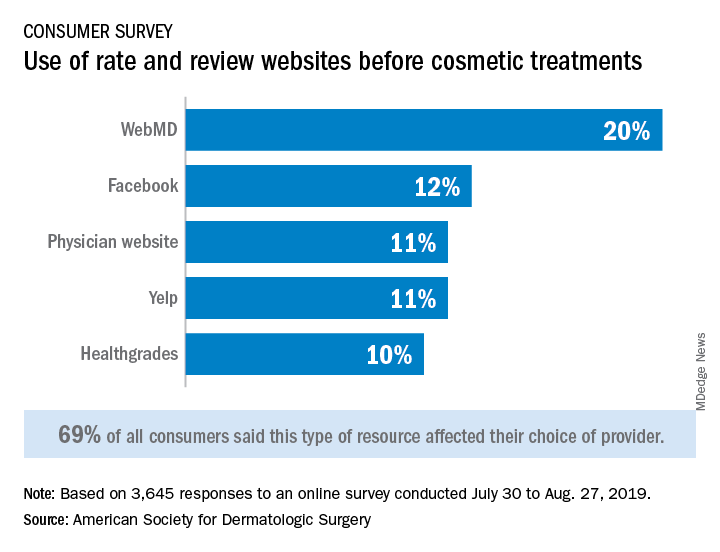
Almost 70% of respondents said that their use of rate and review websites had an impact on the choice of provider for cosmetic procedures: WebMD was the site most often visited, followed by Facebook, physician websites, and Yelp, the ASDS said based on its annual consumer survey.
For 43% of consumers, the decision to schedule an appointment was influenced by a provider’s social media presence, and 41% of patients said that they follow their current or potential provider on social media, the ASDS said.
“Online resources and social media platforms are clearly influencing consumers’ behavior and perception of skin health,” ASDS President Murad Alam, MD, MBA, chief of cutaneous and aesthetic surgery in the department of dermatology at Northwestern University, Chicago, said in a written statement.
Dermatologists, however, remain the leading influence on the decision to have a cosmetic procedure – named as a resource by 34% of respondents, who could select more than one possibility from a list of 15 – but social media moved ahead of primary care physicians into third place (24%), just behind friends (30%), the survey showed. Dermatologists, on the other hand, had polled at 50%-55% for the previous 5 years.
The dermatologists’ lead remained stronger as the top influencer for skin care purchases, selected by 45% of respondents, compared with 32% for friends and 28% for social media. In this category there were 14 factors from which respondents could choose. As for the cost of those skin care products, 48% of consumers spent $1-$50 a month, 31% said that they spent $51-$100 a month, and 12% reported spending $101-$150 a month, the ASDS said.
The society received 3,645 responses to the 2019 Consumer Survey on Cosmetic Dermatologic Procedures, which was conducted online from July 30 to Aug. 27 by Survata.
Online resources are affecting most consumers’ selections of cosmetic providers, and social media are now a top-three influence on cosmetic procedure choices and skin care purchases, according to a new survey from the American Society for Dermatologic Surgery.
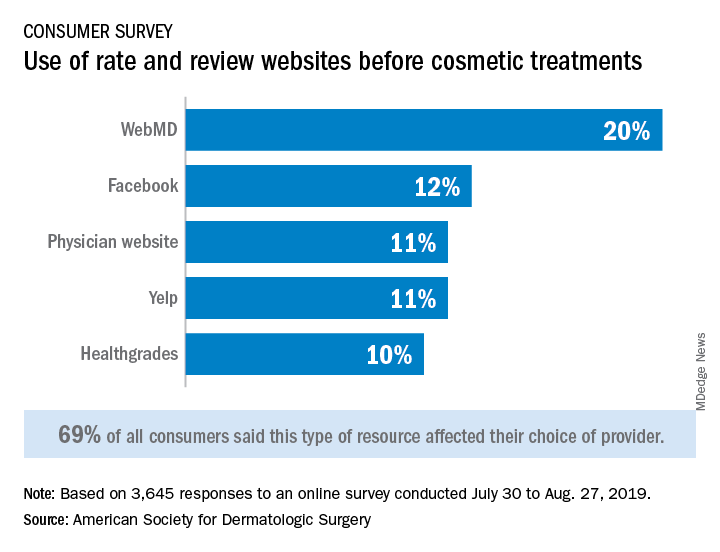
Almost 70% of respondents said that their use of rate and review websites had an impact on the choice of provider for cosmetic procedures: WebMD was the site most often visited, followed by Facebook, physician websites, and Yelp, the ASDS said based on its annual consumer survey.
For 43% of consumers, the decision to schedule an appointment was influenced by a provider’s social media presence, and 41% of patients said that they follow their current or potential provider on social media, the ASDS said.
“Online resources and social media platforms are clearly influencing consumers’ behavior and perception of skin health,” ASDS President Murad Alam, MD, MBA, chief of cutaneous and aesthetic surgery in the department of dermatology at Northwestern University, Chicago, said in a written statement.
Dermatologists, however, remain the leading influence on the decision to have a cosmetic procedure – named as a resource by 34% of respondents, who could select more than one possibility from a list of 15 – but social media moved ahead of primary care physicians into third place (24%), just behind friends (30%), the survey showed. Dermatologists, on the other hand, had polled at 50%-55% for the previous 5 years.
The dermatologists’ lead remained stronger as the top influencer for skin care purchases, selected by 45% of respondents, compared with 32% for friends and 28% for social media. In this category there were 14 factors from which respondents could choose. As for the cost of those skin care products, 48% of consumers spent $1-$50 a month, 31% said that they spent $51-$100 a month, and 12% reported spending $101-$150 a month, the ASDS said.
The society received 3,645 responses to the 2019 Consumer Survey on Cosmetic Dermatologic Procedures, which was conducted online from July 30 to Aug. 27 by Survata.
Will changing the names of psychiatric medications lead to better treatment?
Back in 1980, the American Psychiatric Association dropped the word “neurosis” from the DSM-III, so that if you had been neurotic, after 1980, you were neurotic no longer.
At the time, I discussed this on my daily radio show. For those folks who were nervous, worried, fearful, and full of anxieties about themselves, their families, welfare, health, and the environment around them, a new set of labels was introduced to more specifically describe one or more problems related to anxiety.
For codification, and at times, a clearer understanding of a specific problem, the change was made to be helpful. Certainly, for insurers and pharmacologic treatments, it worked. However, it’s interesting that the word and concept, neurosis, which still is used by some psychiatrists and psychologists – although not scientific – does offer a clear overall picture of a suffering, anxiety-ridden person who might have a combination of an anxiety disorder, panic attacks, somatic symptoms, and endless worry. This overlapping picture often is seen in clinical practice more than the multiple one-dimensional labels that are currently used. So be it.
This all leads me to what I’ve recently learned about the Neuroscience-based Nomenclature (NbN) Project. According to a recent article in the APA’s Psychiatric News, the group’s board of trustees has endorsed a proposal that would change or revise the names of psychiatric medications so that the names reflect their mechanism of action – a move seemingly focused on a pure biological model.
For example, according to the article, the medication perphenazine would be renamed a “D2 receptor antagonist” rather than an antipsychotic. For depression, we might have a serotonergic reuptake inhibitor, according to the report, and of course, the list of changes would go on – based on current knowledge of biological activity. It’s true that in general medicine, there are examples where mode of action is discussed. For example, in cardiology we have beta-blockers and alpha-blockers, which are descriptive of their actions. As doctors who have trained for years and know the mechanism of action of various medications, we will understand all this. But in patient care, both doctors and their patients often understand and feel comfortable using descriptive terms indicating the treatment modality, such as antibiotics, antivirals, antifungals, anti-inflammatory medications, as well as anti-itching, antiaging, and antispasmodic drugs.
So, I am concerned about these proposed changes. In an era focused on patient-centered care, where we seek to make it simpler for the patient/health care consumer, we might make it harder for the patient to grasp what’s going on.
It’s very important to keep in mind that we as physicians know the ins and outs of medications, and that even the most educated and bright patients who are not in medicine do not know what our education has taught us. For example, regardless of specialty, we all know the difference between left-sided and right-sided heart failure. Those outside of medicine, however, rarely know the difference. They understand heart disease as a rule. People in general might understand some general concepts, such as RBC, WBC, and platelets. A patient will speak of taking a blood thinner but rarely know or understand the differences between antiplatelets and anticoagulants. And why should they know this?
The point here is that I believe good patient care is keeping it simple and taking the time to explain what’s being treated, aiming to inform patients using down-to-earth, accessible language rather than the language of biochemistry.
It’s true that in psychiatry, wider use of certain medications than originally indicated has grown tremendously as well as off-label use. In light of that, the NbN idea is laudable. However, it would seem more practical to leave the traditional modes of action in place and expand our discussions with patients as to why we are using a specific medication. I have found a very simple and even rewarding way to explain to patients, for example, that yes, this is an antiseizure medication but it is now used in psychiatry as a mood stabilizer.
Another important point is the question of whether using nomenclature that describes the exact location of the problem is all that accurate. Currently, we know we still have a lot to learn about brain chemistry and neuronal transmission in mental disorders, just as in many medical disorders, there are gaps in our understanding of many illnesses and subsequent molecular changes.
Just as the DSM-III left behind the all-encompassing and descriptive word neurosis and the APA has changed labels in the DSM-IV and DSM-5, so the NbN project would change the nomenclature of current psychotropic medications. The intentions are good, but the idea that those changes will foster better patient understanding defies common sense. A better idea might be to continue use of both scientific names and names of commonly used actions of the medications, leaving both in place and letting clinicians decide what nomenclature best suits each patient.
It will be a sad day when psychiatrists become so medically and “scientifically” driven that we cannot explain to a patient, “I’m prescribing this antidepressant because it’s now used to treat anxiety,” or “Yes, this medicine is labeled ‘antipsychotic,’ but you’re not psychotic. It may help your mood swings and may even help you sleep better.” Now, is that hard? Is talking to a person and explaining the treatment no longer part of care? The take-home messages from the recent APA/Institute of Psychiatric Services meeting I attended seemed to suggest that human attention and care have great value. My father, a surgeon, always said that you learn a lot by simply talking to patients – and they learn from you.
Dr. London is a practicing psychiatrist and has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019).
Back in 1980, the American Psychiatric Association dropped the word “neurosis” from the DSM-III, so that if you had been neurotic, after 1980, you were neurotic no longer.
At the time, I discussed this on my daily radio show. For those folks who were nervous, worried, fearful, and full of anxieties about themselves, their families, welfare, health, and the environment around them, a new set of labels was introduced to more specifically describe one or more problems related to anxiety.
For codification, and at times, a clearer understanding of a specific problem, the change was made to be helpful. Certainly, for insurers and pharmacologic treatments, it worked. However, it’s interesting that the word and concept, neurosis, which still is used by some psychiatrists and psychologists – although not scientific – does offer a clear overall picture of a suffering, anxiety-ridden person who might have a combination of an anxiety disorder, panic attacks, somatic symptoms, and endless worry. This overlapping picture often is seen in clinical practice more than the multiple one-dimensional labels that are currently used. So be it.
This all leads me to what I’ve recently learned about the Neuroscience-based Nomenclature (NbN) Project. According to a recent article in the APA’s Psychiatric News, the group’s board of trustees has endorsed a proposal that would change or revise the names of psychiatric medications so that the names reflect their mechanism of action – a move seemingly focused on a pure biological model.
For example, according to the article, the medication perphenazine would be renamed a “D2 receptor antagonist” rather than an antipsychotic. For depression, we might have a serotonergic reuptake inhibitor, according to the report, and of course, the list of changes would go on – based on current knowledge of biological activity. It’s true that in general medicine, there are examples where mode of action is discussed. For example, in cardiology we have beta-blockers and alpha-blockers, which are descriptive of their actions. As doctors who have trained for years and know the mechanism of action of various medications, we will understand all this. But in patient care, both doctors and their patients often understand and feel comfortable using descriptive terms indicating the treatment modality, such as antibiotics, antivirals, antifungals, anti-inflammatory medications, as well as anti-itching, antiaging, and antispasmodic drugs.
So, I am concerned about these proposed changes. In an era focused on patient-centered care, where we seek to make it simpler for the patient/health care consumer, we might make it harder for the patient to grasp what’s going on.
It’s very important to keep in mind that we as physicians know the ins and outs of medications, and that even the most educated and bright patients who are not in medicine do not know what our education has taught us. For example, regardless of specialty, we all know the difference between left-sided and right-sided heart failure. Those outside of medicine, however, rarely know the difference. They understand heart disease as a rule. People in general might understand some general concepts, such as RBC, WBC, and platelets. A patient will speak of taking a blood thinner but rarely know or understand the differences between antiplatelets and anticoagulants. And why should they know this?
The point here is that I believe good patient care is keeping it simple and taking the time to explain what’s being treated, aiming to inform patients using down-to-earth, accessible language rather than the language of biochemistry.
It’s true that in psychiatry, wider use of certain medications than originally indicated has grown tremendously as well as off-label use. In light of that, the NbN idea is laudable. However, it would seem more practical to leave the traditional modes of action in place and expand our discussions with patients as to why we are using a specific medication. I have found a very simple and even rewarding way to explain to patients, for example, that yes, this is an antiseizure medication but it is now used in psychiatry as a mood stabilizer.
Another important point is the question of whether using nomenclature that describes the exact location of the problem is all that accurate. Currently, we know we still have a lot to learn about brain chemistry and neuronal transmission in mental disorders, just as in many medical disorders, there are gaps in our understanding of many illnesses and subsequent molecular changes.
Just as the DSM-III left behind the all-encompassing and descriptive word neurosis and the APA has changed labels in the DSM-IV and DSM-5, so the NbN project would change the nomenclature of current psychotropic medications. The intentions are good, but the idea that those changes will foster better patient understanding defies common sense. A better idea might be to continue use of both scientific names and names of commonly used actions of the medications, leaving both in place and letting clinicians decide what nomenclature best suits each patient.
It will be a sad day when psychiatrists become so medically and “scientifically” driven that we cannot explain to a patient, “I’m prescribing this antidepressant because it’s now used to treat anxiety,” or “Yes, this medicine is labeled ‘antipsychotic,’ but you’re not psychotic. It may help your mood swings and may even help you sleep better.” Now, is that hard? Is talking to a person and explaining the treatment no longer part of care? The take-home messages from the recent APA/Institute of Psychiatric Services meeting I attended seemed to suggest that human attention and care have great value. My father, a surgeon, always said that you learn a lot by simply talking to patients – and they learn from you.
Dr. London is a practicing psychiatrist and has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019).
Back in 1980, the American Psychiatric Association dropped the word “neurosis” from the DSM-III, so that if you had been neurotic, after 1980, you were neurotic no longer.
At the time, I discussed this on my daily radio show. For those folks who were nervous, worried, fearful, and full of anxieties about themselves, their families, welfare, health, and the environment around them, a new set of labels was introduced to more specifically describe one or more problems related to anxiety.
For codification, and at times, a clearer understanding of a specific problem, the change was made to be helpful. Certainly, for insurers and pharmacologic treatments, it worked. However, it’s interesting that the word and concept, neurosis, which still is used by some psychiatrists and psychologists – although not scientific – does offer a clear overall picture of a suffering, anxiety-ridden person who might have a combination of an anxiety disorder, panic attacks, somatic symptoms, and endless worry. This overlapping picture often is seen in clinical practice more than the multiple one-dimensional labels that are currently used. So be it.
This all leads me to what I’ve recently learned about the Neuroscience-based Nomenclature (NbN) Project. According to a recent article in the APA’s Psychiatric News, the group’s board of trustees has endorsed a proposal that would change or revise the names of psychiatric medications so that the names reflect their mechanism of action – a move seemingly focused on a pure biological model.
For example, according to the article, the medication perphenazine would be renamed a “D2 receptor antagonist” rather than an antipsychotic. For depression, we might have a serotonergic reuptake inhibitor, according to the report, and of course, the list of changes would go on – based on current knowledge of biological activity. It’s true that in general medicine, there are examples where mode of action is discussed. For example, in cardiology we have beta-blockers and alpha-blockers, which are descriptive of their actions. As doctors who have trained for years and know the mechanism of action of various medications, we will understand all this. But in patient care, both doctors and their patients often understand and feel comfortable using descriptive terms indicating the treatment modality, such as antibiotics, antivirals, antifungals, anti-inflammatory medications, as well as anti-itching, antiaging, and antispasmodic drugs.
So, I am concerned about these proposed changes. In an era focused on patient-centered care, where we seek to make it simpler for the patient/health care consumer, we might make it harder for the patient to grasp what’s going on.
It’s very important to keep in mind that we as physicians know the ins and outs of medications, and that even the most educated and bright patients who are not in medicine do not know what our education has taught us. For example, regardless of specialty, we all know the difference between left-sided and right-sided heart failure. Those outside of medicine, however, rarely know the difference. They understand heart disease as a rule. People in general might understand some general concepts, such as RBC, WBC, and platelets. A patient will speak of taking a blood thinner but rarely know or understand the differences between antiplatelets and anticoagulants. And why should they know this?
The point here is that I believe good patient care is keeping it simple and taking the time to explain what’s being treated, aiming to inform patients using down-to-earth, accessible language rather than the language of biochemistry.
It’s true that in psychiatry, wider use of certain medications than originally indicated has grown tremendously as well as off-label use. In light of that, the NbN idea is laudable. However, it would seem more practical to leave the traditional modes of action in place and expand our discussions with patients as to why we are using a specific medication. I have found a very simple and even rewarding way to explain to patients, for example, that yes, this is an antiseizure medication but it is now used in psychiatry as a mood stabilizer.
Another important point is the question of whether using nomenclature that describes the exact location of the problem is all that accurate. Currently, we know we still have a lot to learn about brain chemistry and neuronal transmission in mental disorders, just as in many medical disorders, there are gaps in our understanding of many illnesses and subsequent molecular changes.
Just as the DSM-III left behind the all-encompassing and descriptive word neurosis and the APA has changed labels in the DSM-IV and DSM-5, so the NbN project would change the nomenclature of current psychotropic medications. The intentions are good, but the idea that those changes will foster better patient understanding defies common sense. A better idea might be to continue use of both scientific names and names of commonly used actions of the medications, leaving both in place and letting clinicians decide what nomenclature best suits each patient.
It will be a sad day when psychiatrists become so medically and “scientifically” driven that we cannot explain to a patient, “I’m prescribing this antidepressant because it’s now used to treat anxiety,” or “Yes, this medicine is labeled ‘antipsychotic,’ but you’re not psychotic. It may help your mood swings and may even help you sleep better.” Now, is that hard? Is talking to a person and explaining the treatment no longer part of care? The take-home messages from the recent APA/Institute of Psychiatric Services meeting I attended seemed to suggest that human attention and care have great value. My father, a surgeon, always said that you learn a lot by simply talking to patients – and they learn from you.
Dr. London is a practicing psychiatrist and has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019).
Physician-researcher who promoted industry collaboration dies unexpectedly
Thomas Peter Stossel, MD, a physician-researcher known for his discovery of cellular proteins and advocacy for academic-industry relationships, died unexpectedly on Sept. 29 at the age of 78.
Dr. Stossel’s research was largely focused on cell motility. He is known for discovering the cellular proteins filamin and gelsolin, which regulate the assembly of actin. Dr. Stossel is also known for promoting relationships between physicians and industry. He believed these relationships accelerate medical innovation.
Dr. Stossel graduated from Princeton University and Harvard Medical School. He served as chief of the hematology-oncology unit at Massachusetts General Hospital, head of experimental medicine and codirector of the hematology and translational medicine units at Brigham and Women’s Hospital, and a professor at Harvard Medical School. When he died, Dr. Stossel was chief scientific officer of BioAegis Therapeutics, a company he cofounded.
Dr. Stossel also cofounded Options for Children in Zambia, a charity that works with Zambian partners to provide preventive dental and medical care. And he helped establish a sickle cell disease clinical and research center at University Teaching Hospital in Lusaka.
In happier news, Jeff Vacirca, MD, recently won the 2019 American Red Cross Greater New York Region’s Humanitarian Award. Dr. Vacirca received the award at the 2019 Heroes Among Us Gala on Oct. 16.
Dr. Vacirca is chief executive officer of New York Cancer & Blood Specialists. He is also a consulting physician for the Long Island Association for AIDS Care, medical director for AmerisourceBergen specialty group, a scientific advisory board member for Caris Life Sciences, director at OneOncology, director at Spectrum Pharmaceuticals, a medical board adviser for Flatiron Health, and vice-chairman of the board for Odonate Therapeutics, a company he cofounded in 2016. In 2014, Dr. Vacirca founded the New York Cancer Foundation, which provides financial assistance to patients undergoing cancer treatment.
Another award winner is Richard J. Bleicher, MD, who has won the 2020 Jamie Brooke Lieberman Remembrance Award from Susan G. Komen Philadelphia for his work related to breast cancer. Dr. Bleicher is scheduled to receive his award at the Susan G. Komen Philadelphia MORE THAN PINK Walk Kickoff event on March 18, 2020.
Dr. Bleicher is a professor, breast cancer surgeon, and clinical researcher at Fox Chase Cancer Center in Philadelphia. He is director of the breast fellowship and leader of the breast cancer program at Fox Chase. He sits on the board of the National Accreditation Program for Breast Centers and the Quality Improvement Committee, sits on the Commission for Cancer’s Operative Standards Committee, and is the vice-chair for the Society of Surgical Oncology’s breast fellowship programs for the United States and Canada.
Thomas Peter Stossel, MD, a physician-researcher known for his discovery of cellular proteins and advocacy for academic-industry relationships, died unexpectedly on Sept. 29 at the age of 78.
Dr. Stossel’s research was largely focused on cell motility. He is known for discovering the cellular proteins filamin and gelsolin, which regulate the assembly of actin. Dr. Stossel is also known for promoting relationships between physicians and industry. He believed these relationships accelerate medical innovation.
Dr. Stossel graduated from Princeton University and Harvard Medical School. He served as chief of the hematology-oncology unit at Massachusetts General Hospital, head of experimental medicine and codirector of the hematology and translational medicine units at Brigham and Women’s Hospital, and a professor at Harvard Medical School. When he died, Dr. Stossel was chief scientific officer of BioAegis Therapeutics, a company he cofounded.
Dr. Stossel also cofounded Options for Children in Zambia, a charity that works with Zambian partners to provide preventive dental and medical care. And he helped establish a sickle cell disease clinical and research center at University Teaching Hospital in Lusaka.
In happier news, Jeff Vacirca, MD, recently won the 2019 American Red Cross Greater New York Region’s Humanitarian Award. Dr. Vacirca received the award at the 2019 Heroes Among Us Gala on Oct. 16.
Dr. Vacirca is chief executive officer of New York Cancer & Blood Specialists. He is also a consulting physician for the Long Island Association for AIDS Care, medical director for AmerisourceBergen specialty group, a scientific advisory board member for Caris Life Sciences, director at OneOncology, director at Spectrum Pharmaceuticals, a medical board adviser for Flatiron Health, and vice-chairman of the board for Odonate Therapeutics, a company he cofounded in 2016. In 2014, Dr. Vacirca founded the New York Cancer Foundation, which provides financial assistance to patients undergoing cancer treatment.
Another award winner is Richard J. Bleicher, MD, who has won the 2020 Jamie Brooke Lieberman Remembrance Award from Susan G. Komen Philadelphia for his work related to breast cancer. Dr. Bleicher is scheduled to receive his award at the Susan G. Komen Philadelphia MORE THAN PINK Walk Kickoff event on March 18, 2020.
Dr. Bleicher is a professor, breast cancer surgeon, and clinical researcher at Fox Chase Cancer Center in Philadelphia. He is director of the breast fellowship and leader of the breast cancer program at Fox Chase. He sits on the board of the National Accreditation Program for Breast Centers and the Quality Improvement Committee, sits on the Commission for Cancer’s Operative Standards Committee, and is the vice-chair for the Society of Surgical Oncology’s breast fellowship programs for the United States and Canada.
Thomas Peter Stossel, MD, a physician-researcher known for his discovery of cellular proteins and advocacy for academic-industry relationships, died unexpectedly on Sept. 29 at the age of 78.
Dr. Stossel’s research was largely focused on cell motility. He is known for discovering the cellular proteins filamin and gelsolin, which regulate the assembly of actin. Dr. Stossel is also known for promoting relationships between physicians and industry. He believed these relationships accelerate medical innovation.
Dr. Stossel graduated from Princeton University and Harvard Medical School. He served as chief of the hematology-oncology unit at Massachusetts General Hospital, head of experimental medicine and codirector of the hematology and translational medicine units at Brigham and Women’s Hospital, and a professor at Harvard Medical School. When he died, Dr. Stossel was chief scientific officer of BioAegis Therapeutics, a company he cofounded.
Dr. Stossel also cofounded Options for Children in Zambia, a charity that works with Zambian partners to provide preventive dental and medical care. And he helped establish a sickle cell disease clinical and research center at University Teaching Hospital in Lusaka.
In happier news, Jeff Vacirca, MD, recently won the 2019 American Red Cross Greater New York Region’s Humanitarian Award. Dr. Vacirca received the award at the 2019 Heroes Among Us Gala on Oct. 16.
Dr. Vacirca is chief executive officer of New York Cancer & Blood Specialists. He is also a consulting physician for the Long Island Association for AIDS Care, medical director for AmerisourceBergen specialty group, a scientific advisory board member for Caris Life Sciences, director at OneOncology, director at Spectrum Pharmaceuticals, a medical board adviser for Flatiron Health, and vice-chairman of the board for Odonate Therapeutics, a company he cofounded in 2016. In 2014, Dr. Vacirca founded the New York Cancer Foundation, which provides financial assistance to patients undergoing cancer treatment.
Another award winner is Richard J. Bleicher, MD, who has won the 2020 Jamie Brooke Lieberman Remembrance Award from Susan G. Komen Philadelphia for his work related to breast cancer. Dr. Bleicher is scheduled to receive his award at the Susan G. Komen Philadelphia MORE THAN PINK Walk Kickoff event on March 18, 2020.
Dr. Bleicher is a professor, breast cancer surgeon, and clinical researcher at Fox Chase Cancer Center in Philadelphia. He is director of the breast fellowship and leader of the breast cancer program at Fox Chase. He sits on the board of the National Accreditation Program for Breast Centers and the Quality Improvement Committee, sits on the Commission for Cancer’s Operative Standards Committee, and is the vice-chair for the Society of Surgical Oncology’s breast fellowship programs for the United States and Canada.
Inspector General: NIH must improve conflict of interest reviews
the Department of Health & Human Services’ Office of Inspector General reported.
In highlighting the improvement in a September 2019 report, “NIH has made strides in reviewing financial conflicts of interest in extramural research, but could do more,” the OIG noted that, in the past 10 years, “NIH has strengthened its reporting requirements and developed an online system for collecting, reviewing, and storing financial conflicts of interest (FCOIs) that institutions report. These changes resulted in improvements in how NIH tracks and reviews FCOIs that institutions report.”
That being said, OIG also highlighted some ongoing issues with NIH’s FCOI oversight.
“Across the three NIH Institutes and Centers (ICs) that we reviewed, staff differed in the level of scrutiny they applied to their review of FCOIs,” the report states.
For example, the report notes that 15 of the 25 ICs have written procedures related to FCOI reviews and the documentation shared by the three ICs showed different levels of detail and instruction.
“Only one of the three guidance documents provided IC staff with specific criteria aimed at standardizing the review of FCOIs,” the report stated. Two of the three ICs also reported using external resources to aid in the review.
Review times also varied significantly, with two of the three ICs reporting that they spend generally 5-30 minutes per review, while the third said staff spends several hours on reviews.
The OIG also reported that “NIH lacks quality assurance procedures in its review process. Specifically, NIH central management and the three ICs that we reviewed do not perform any systematic analyses or even ad hoc checks to determine whether staff accurately and consistently review reported FCOIs, and OIG found a small number of inconsistencies in the FCOI data that institutions reported, which might highlight the need for more oversight of the review process.”
The report notes that there is a process in place to provide oversight of ICs’ review of reported FCOIs, but there is no longer sufficient staff to continue this oversight.
The “OER [Office of Extramural Research] now relies on IC staff to seek guidance when needed and does not conduct regular oversight of the ICs. Similarly, none of the three ICs we reviewed perform quality checks to ensure the thoroughness or consistency of review by program officials. Staff members from one IC stated that while they do not conduct quality checks, the IC provides new program officials more guidance during their first few reviews.”
The HHS watchdog also noted that NIH cannot identify whether FCOIs involve foreign entities even though investigators must disclose financial interests from foreign investments.
“The HHS regulations on FCOI do not require institutions to designate whether FCOIs involve foreign entities, and NIH reported that it has no plans to expand these regulations to include such a requirement,” the OIG reported.
The OIG recommended that NIH perform periodic quality assurance reviews of FCOI information to ensure adequacy of oversight and suggested it use “information regarding foreign affiliations and support that it collects during the pre-award process to decide whether to revise its FCOI review process to address concerns regarding foreign influence.”
SOURCE: Murrin S. Office of Inspector General. 2019 Sep 25. OEI-03-19-00150.
the Department of Health & Human Services’ Office of Inspector General reported.
In highlighting the improvement in a September 2019 report, “NIH has made strides in reviewing financial conflicts of interest in extramural research, but could do more,” the OIG noted that, in the past 10 years, “NIH has strengthened its reporting requirements and developed an online system for collecting, reviewing, and storing financial conflicts of interest (FCOIs) that institutions report. These changes resulted in improvements in how NIH tracks and reviews FCOIs that institutions report.”
That being said, OIG also highlighted some ongoing issues with NIH’s FCOI oversight.
“Across the three NIH Institutes and Centers (ICs) that we reviewed, staff differed in the level of scrutiny they applied to their review of FCOIs,” the report states.
For example, the report notes that 15 of the 25 ICs have written procedures related to FCOI reviews and the documentation shared by the three ICs showed different levels of detail and instruction.
“Only one of the three guidance documents provided IC staff with specific criteria aimed at standardizing the review of FCOIs,” the report stated. Two of the three ICs also reported using external resources to aid in the review.
Review times also varied significantly, with two of the three ICs reporting that they spend generally 5-30 minutes per review, while the third said staff spends several hours on reviews.
The OIG also reported that “NIH lacks quality assurance procedures in its review process. Specifically, NIH central management and the three ICs that we reviewed do not perform any systematic analyses or even ad hoc checks to determine whether staff accurately and consistently review reported FCOIs, and OIG found a small number of inconsistencies in the FCOI data that institutions reported, which might highlight the need for more oversight of the review process.”
The report notes that there is a process in place to provide oversight of ICs’ review of reported FCOIs, but there is no longer sufficient staff to continue this oversight.
The “OER [Office of Extramural Research] now relies on IC staff to seek guidance when needed and does not conduct regular oversight of the ICs. Similarly, none of the three ICs we reviewed perform quality checks to ensure the thoroughness or consistency of review by program officials. Staff members from one IC stated that while they do not conduct quality checks, the IC provides new program officials more guidance during their first few reviews.”
The HHS watchdog also noted that NIH cannot identify whether FCOIs involve foreign entities even though investigators must disclose financial interests from foreign investments.
“The HHS regulations on FCOI do not require institutions to designate whether FCOIs involve foreign entities, and NIH reported that it has no plans to expand these regulations to include such a requirement,” the OIG reported.
The OIG recommended that NIH perform periodic quality assurance reviews of FCOI information to ensure adequacy of oversight and suggested it use “information regarding foreign affiliations and support that it collects during the pre-award process to decide whether to revise its FCOI review process to address concerns regarding foreign influence.”
SOURCE: Murrin S. Office of Inspector General. 2019 Sep 25. OEI-03-19-00150.
the Department of Health & Human Services’ Office of Inspector General reported.
In highlighting the improvement in a September 2019 report, “NIH has made strides in reviewing financial conflicts of interest in extramural research, but could do more,” the OIG noted that, in the past 10 years, “NIH has strengthened its reporting requirements and developed an online system for collecting, reviewing, and storing financial conflicts of interest (FCOIs) that institutions report. These changes resulted in improvements in how NIH tracks and reviews FCOIs that institutions report.”
That being said, OIG also highlighted some ongoing issues with NIH’s FCOI oversight.
“Across the three NIH Institutes and Centers (ICs) that we reviewed, staff differed in the level of scrutiny they applied to their review of FCOIs,” the report states.
For example, the report notes that 15 of the 25 ICs have written procedures related to FCOI reviews and the documentation shared by the three ICs showed different levels of detail and instruction.
“Only one of the three guidance documents provided IC staff with specific criteria aimed at standardizing the review of FCOIs,” the report stated. Two of the three ICs also reported using external resources to aid in the review.
Review times also varied significantly, with two of the three ICs reporting that they spend generally 5-30 minutes per review, while the third said staff spends several hours on reviews.
The OIG also reported that “NIH lacks quality assurance procedures in its review process. Specifically, NIH central management and the three ICs that we reviewed do not perform any systematic analyses or even ad hoc checks to determine whether staff accurately and consistently review reported FCOIs, and OIG found a small number of inconsistencies in the FCOI data that institutions reported, which might highlight the need for more oversight of the review process.”
The report notes that there is a process in place to provide oversight of ICs’ review of reported FCOIs, but there is no longer sufficient staff to continue this oversight.
The “OER [Office of Extramural Research] now relies on IC staff to seek guidance when needed and does not conduct regular oversight of the ICs. Similarly, none of the three ICs we reviewed perform quality checks to ensure the thoroughness or consistency of review by program officials. Staff members from one IC stated that while they do not conduct quality checks, the IC provides new program officials more guidance during their first few reviews.”
The HHS watchdog also noted that NIH cannot identify whether FCOIs involve foreign entities even though investigators must disclose financial interests from foreign investments.
“The HHS regulations on FCOI do not require institutions to designate whether FCOIs involve foreign entities, and NIH reported that it has no plans to expand these regulations to include such a requirement,” the OIG reported.
The OIG recommended that NIH perform periodic quality assurance reviews of FCOI information to ensure adequacy of oversight and suggested it use “information regarding foreign affiliations and support that it collects during the pre-award process to decide whether to revise its FCOI review process to address concerns regarding foreign influence.”
SOURCE: Murrin S. Office of Inspector General. 2019 Sep 25. OEI-03-19-00150.
Sixty-five roses
Like many of you, my wife and I took the DNA plunge for fun and spit in the cup. She is genetically perfect, but I, however, am a carrier for alpha-1 anti-trypsin deficiency, hemochromatosis, and like 1 in 19 Irish people, cystic fibrosis. Plus, I was in the top 20% for Neanderthal genes.
My Y chromosome had traveled to the United States from Europe, where it had spent several hundred years in Ireland (in the house of Neal); wandering to Ireland from the Middle East, and originating in Siberia! Fascinating stuff.
away. It is hypothesized that the very-high-frequency deleterious genes have a survival advantage in the heterozygous state, coined the “heterozygote advantage.”
Alpha-1 antitrypsin deficiency allows the body to concentrate an inflammatory response in the lungs and liver, perhaps providing protection against tuberculosis (Am J Respir Crit Care Med. 2006 May 15;173[10]:1072-7).
Hemochromatosis allows for increased iron absorption attributable to decreased iron in a grain-based diet, and facilitates thyroid-stimulating hormone release in cold environments (Am J Phys Anthropol. 2016 May;160[1]:86-101).
Cystic fibrosis carriers are more resistant to diarrheal illness, particularly cholera and typhoid fever since they have only one exudative chloride channel to switch on. Their sputum is also thicker, interfering with microdroplet generation and spread of the bacilli to others.
This topic and learning of my CF carrier status bring to mind one of my patients. When doing skin exams, I sometimes ask patients about elaborate tattoos (not the obvious youthful misadventures). “Nice ink” I will say, and I wait and see if they want to elaborate. This particular patient was enthusiastic and explained that the elaborate floral design with roses on his right leg was in memory of his daughter. I asked what had happened, expecting a tragic car wreck, or perhaps cancer or a drug overdose. He cheerfully explained she had died of cystic fibrosis at age 21, a year after a lung transplant.
My eyes started to water. My patient was upbeat and said she had lived with gusto and survived long enough to buy him a triple gin and tonic at bar. She had always had a bright outlook, despite her debilitating and eventually fatal disease.
I had to ask more about the memorial tattoo. He explained that her initials were linked with his at the bottom of the bouquet of many, many roses. “Why roses?” I asked. “Well,” he said, “when she was little, she could not pronounce cystic fibrosis, so she always said, ‘My daddy says I have 65 roses.’ ”*
Oh boy. I had to go sit in my office, turn out the lights, and cry.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at dermnews@mdedge.com.
* This is in fact, what many children with the disease call it, and is the symbol of the Cystic Fibrosis Foundation, a story originating in 1965, when a 4-year-old with cystic fibrosis asked his mother about “65 Roses” after he heard her talking on the phone raising funds for research.
Like many of you, my wife and I took the DNA plunge for fun and spit in the cup. She is genetically perfect, but I, however, am a carrier for alpha-1 anti-trypsin deficiency, hemochromatosis, and like 1 in 19 Irish people, cystic fibrosis. Plus, I was in the top 20% for Neanderthal genes.
My Y chromosome had traveled to the United States from Europe, where it had spent several hundred years in Ireland (in the house of Neal); wandering to Ireland from the Middle East, and originating in Siberia! Fascinating stuff.
away. It is hypothesized that the very-high-frequency deleterious genes have a survival advantage in the heterozygous state, coined the “heterozygote advantage.”
Alpha-1 antitrypsin deficiency allows the body to concentrate an inflammatory response in the lungs and liver, perhaps providing protection against tuberculosis (Am J Respir Crit Care Med. 2006 May 15;173[10]:1072-7).
Hemochromatosis allows for increased iron absorption attributable to decreased iron in a grain-based diet, and facilitates thyroid-stimulating hormone release in cold environments (Am J Phys Anthropol. 2016 May;160[1]:86-101).
Cystic fibrosis carriers are more resistant to diarrheal illness, particularly cholera and typhoid fever since they have only one exudative chloride channel to switch on. Their sputum is also thicker, interfering with microdroplet generation and spread of the bacilli to others.
This topic and learning of my CF carrier status bring to mind one of my patients. When doing skin exams, I sometimes ask patients about elaborate tattoos (not the obvious youthful misadventures). “Nice ink” I will say, and I wait and see if they want to elaborate. This particular patient was enthusiastic and explained that the elaborate floral design with roses on his right leg was in memory of his daughter. I asked what had happened, expecting a tragic car wreck, or perhaps cancer or a drug overdose. He cheerfully explained she had died of cystic fibrosis at age 21, a year after a lung transplant.
My eyes started to water. My patient was upbeat and said she had lived with gusto and survived long enough to buy him a triple gin and tonic at bar. She had always had a bright outlook, despite her debilitating and eventually fatal disease.
I had to ask more about the memorial tattoo. He explained that her initials were linked with his at the bottom of the bouquet of many, many roses. “Why roses?” I asked. “Well,” he said, “when she was little, she could not pronounce cystic fibrosis, so she always said, ‘My daddy says I have 65 roses.’ ”*
Oh boy. I had to go sit in my office, turn out the lights, and cry.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at dermnews@mdedge.com.
* This is in fact, what many children with the disease call it, and is the symbol of the Cystic Fibrosis Foundation, a story originating in 1965, when a 4-year-old with cystic fibrosis asked his mother about “65 Roses” after he heard her talking on the phone raising funds for research.
Like many of you, my wife and I took the DNA plunge for fun and spit in the cup. She is genetically perfect, but I, however, am a carrier for alpha-1 anti-trypsin deficiency, hemochromatosis, and like 1 in 19 Irish people, cystic fibrosis. Plus, I was in the top 20% for Neanderthal genes.
My Y chromosome had traveled to the United States from Europe, where it had spent several hundred years in Ireland (in the house of Neal); wandering to Ireland from the Middle East, and originating in Siberia! Fascinating stuff.
away. It is hypothesized that the very-high-frequency deleterious genes have a survival advantage in the heterozygous state, coined the “heterozygote advantage.”
Alpha-1 antitrypsin deficiency allows the body to concentrate an inflammatory response in the lungs and liver, perhaps providing protection against tuberculosis (Am J Respir Crit Care Med. 2006 May 15;173[10]:1072-7).
Hemochromatosis allows for increased iron absorption attributable to decreased iron in a grain-based diet, and facilitates thyroid-stimulating hormone release in cold environments (Am J Phys Anthropol. 2016 May;160[1]:86-101).
Cystic fibrosis carriers are more resistant to diarrheal illness, particularly cholera and typhoid fever since they have only one exudative chloride channel to switch on. Their sputum is also thicker, interfering with microdroplet generation and spread of the bacilli to others.
This topic and learning of my CF carrier status bring to mind one of my patients. When doing skin exams, I sometimes ask patients about elaborate tattoos (not the obvious youthful misadventures). “Nice ink” I will say, and I wait and see if they want to elaborate. This particular patient was enthusiastic and explained that the elaborate floral design with roses on his right leg was in memory of his daughter. I asked what had happened, expecting a tragic car wreck, or perhaps cancer or a drug overdose. He cheerfully explained she had died of cystic fibrosis at age 21, a year after a lung transplant.
My eyes started to water. My patient was upbeat and said she had lived with gusto and survived long enough to buy him a triple gin and tonic at bar. She had always had a bright outlook, despite her debilitating and eventually fatal disease.
I had to ask more about the memorial tattoo. He explained that her initials were linked with his at the bottom of the bouquet of many, many roses. “Why roses?” I asked. “Well,” he said, “when she was little, she could not pronounce cystic fibrosis, so she always said, ‘My daddy says I have 65 roses.’ ”*
Oh boy. I had to go sit in my office, turn out the lights, and cry.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at dermnews@mdedge.com.
* This is in fact, what many children with the disease call it, and is the symbol of the Cystic Fibrosis Foundation, a story originating in 1965, when a 4-year-old with cystic fibrosis asked his mother about “65 Roses” after he heard her talking on the phone raising funds for research.
Making and using guidelines
Modern medicine increasingly relies on the adoption and use of guidelines.
Forty years ago, medicine was like free-form, rhythmic gymnastics in which physicians would develop an artisanal treatment plan for each patient. Now, medicine frequently involves recognizing when we need to do a triple-twisting, double-back somersault (the Biles II) and then performing it. The belief is that better outcomes flow from reduced variability in diagnostic and treatment plans, based on guidelines developed from evidence-based medicine from large meta-analyses. This dogma, still unproven in real life, probably works best for 95% of patients. The physician must not omit a step of deciding whether their particular patient is one of the 5% of patients to whom the guideline does not apply.
To be useful, the guidelines must be based on accurate science, produce a significantly positive cost-benefit-risk analysis, be wisely constructed, and be clearly written.
Alas, many guidelines fall far short of this ideal, and when they fail, they impugn all of medical care, they lower the credibility of the organizations that issue them, and they lower the public’s trust in medicine, which thereby impedes improving the public health. Don’t sweat the small stuff for public health guidelines.
The science matters. Nutritional guidelines have been particularly rickety, as John P.A. Ioannidis, MD, wrote in a JAMA op-ed 1 year ago.1 For instance, previous dietary recommendations to reduce cholesterol by avoiding eggs have since been shown to be wrong. The recommendation for reducing salt intake has been heavily criticized. Now the decades-long condemnation of red meat has been challenged. New “guidelines,” suggested by one group (let’s view it as a minority report that contradicts many official guidelines) in the October 1, 2019, issue of Annals of Internal Medicine, say that red meat and processed meats aren’t the boogeyman.2 The authors of the accompanying editorial are from the Center for Pediatric and Adolescent Comparative Effectiveness Research at Indiana University, Indianapolis.3 The editorial supports the new study, criticizing past recommendations because “the field of nutritional epidemiology is plagued by observational studies that have conducted inappropriate analyses, accompanied by likely erroneous conclusions.”
Clarity also matters. One factor in the current opiate epidemic was guidance in the mid-1990s making pain the “fifth vital sign.” This certainly was not the only factor nor was it necessarily the primary one. Most disasters, like most codes on the ward, proceed from multiple smaller failures and missteps. An emphasis on assessing pain in hospitalized patients did not intend to be interpreted as requiring that all pain be eliminated with strong medication, but that was the practical consequence. In response to the epidemic of overdose deaths, guidelines were promulgated in 2016 recommending reducing doses used for chronic opiate regimens. Some patients with chronic pain feared, and soon experienced, the consequences of those changes. In October 2019, those guidelines were revised telling physicians to go slower.4 In explaining the revision, one government official is quoted as saying: “Clearly we believe that there has been misinterpretation of the guidelines, which were very clear.”5 F. Scott Fitzgerald once wrote that “the test of a first-rate intelligence is the ability to hold two opposed ideas in mind at the same time and still retain the ability to function.” I reread that governmental doublespeak three times and my brain broke.
Clinical practice guidelines are an important part of modern medicine. But we need to be wiser about their creation. The science needs to be rigorous. The committees need to contain skeptics rather than just research scientists and clinicians with a vested interest in the field. The purported benefits of the guideline must be weighed against costs, risks, and unintended consequences. Humility is important. All physicians are taught the principle: “First, do no harm.” In explaining medical ethics to students, I rephrase that principle as: “Be cautious and humble. You are not as smart as you think you are.” Consider this food for thought the next time you read or create a guideline.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at pdnews@mdedge.com.
References
1. JAMA. 2018;320(10):969-70.
2. Ann Intern Med. 2019 Oct 1. doi: 10.7326/M19-1621.
3. Ann Intern Med. 2019 Oct 1. doi: 10.7326/M19-2620.
4. U.S. Department of Health & Human Services. HHS guide for clinicians on the appropriate dosage reduction or discontinuation of opioid analgesics. https://www.hhs.gov/opioids/sites/default/files/2019-10/Dosage_Reduction_Discontinuation.pdf.
5. “New guidelines on opioid tapering tell doctors to go slow.” Washington Post. 2019 Oct 10.
Modern medicine increasingly relies on the adoption and use of guidelines.
Forty years ago, medicine was like free-form, rhythmic gymnastics in which physicians would develop an artisanal treatment plan for each patient. Now, medicine frequently involves recognizing when we need to do a triple-twisting, double-back somersault (the Biles II) and then performing it. The belief is that better outcomes flow from reduced variability in diagnostic and treatment plans, based on guidelines developed from evidence-based medicine from large meta-analyses. This dogma, still unproven in real life, probably works best for 95% of patients. The physician must not omit a step of deciding whether their particular patient is one of the 5% of patients to whom the guideline does not apply.
To be useful, the guidelines must be based on accurate science, produce a significantly positive cost-benefit-risk analysis, be wisely constructed, and be clearly written.
Alas, many guidelines fall far short of this ideal, and when they fail, they impugn all of medical care, they lower the credibility of the organizations that issue them, and they lower the public’s trust in medicine, which thereby impedes improving the public health. Don’t sweat the small stuff for public health guidelines.
The science matters. Nutritional guidelines have been particularly rickety, as John P.A. Ioannidis, MD, wrote in a JAMA op-ed 1 year ago.1 For instance, previous dietary recommendations to reduce cholesterol by avoiding eggs have since been shown to be wrong. The recommendation for reducing salt intake has been heavily criticized. Now the decades-long condemnation of red meat has been challenged. New “guidelines,” suggested by one group (let’s view it as a minority report that contradicts many official guidelines) in the October 1, 2019, issue of Annals of Internal Medicine, say that red meat and processed meats aren’t the boogeyman.2 The authors of the accompanying editorial are from the Center for Pediatric and Adolescent Comparative Effectiveness Research at Indiana University, Indianapolis.3 The editorial supports the new study, criticizing past recommendations because “the field of nutritional epidemiology is plagued by observational studies that have conducted inappropriate analyses, accompanied by likely erroneous conclusions.”
Clarity also matters. One factor in the current opiate epidemic was guidance in the mid-1990s making pain the “fifth vital sign.” This certainly was not the only factor nor was it necessarily the primary one. Most disasters, like most codes on the ward, proceed from multiple smaller failures and missteps. An emphasis on assessing pain in hospitalized patients did not intend to be interpreted as requiring that all pain be eliminated with strong medication, but that was the practical consequence. In response to the epidemic of overdose deaths, guidelines were promulgated in 2016 recommending reducing doses used for chronic opiate regimens. Some patients with chronic pain feared, and soon experienced, the consequences of those changes. In October 2019, those guidelines were revised telling physicians to go slower.4 In explaining the revision, one government official is quoted as saying: “Clearly we believe that there has been misinterpretation of the guidelines, which were very clear.”5 F. Scott Fitzgerald once wrote that “the test of a first-rate intelligence is the ability to hold two opposed ideas in mind at the same time and still retain the ability to function.” I reread that governmental doublespeak three times and my brain broke.
Clinical practice guidelines are an important part of modern medicine. But we need to be wiser about their creation. The science needs to be rigorous. The committees need to contain skeptics rather than just research scientists and clinicians with a vested interest in the field. The purported benefits of the guideline must be weighed against costs, risks, and unintended consequences. Humility is important. All physicians are taught the principle: “First, do no harm.” In explaining medical ethics to students, I rephrase that principle as: “Be cautious and humble. You are not as smart as you think you are.” Consider this food for thought the next time you read or create a guideline.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at pdnews@mdedge.com.
References
1. JAMA. 2018;320(10):969-70.
2. Ann Intern Med. 2019 Oct 1. doi: 10.7326/M19-1621.
3. Ann Intern Med. 2019 Oct 1. doi: 10.7326/M19-2620.
4. U.S. Department of Health & Human Services. HHS guide for clinicians on the appropriate dosage reduction or discontinuation of opioid analgesics. https://www.hhs.gov/opioids/sites/default/files/2019-10/Dosage_Reduction_Discontinuation.pdf.
5. “New guidelines on opioid tapering tell doctors to go slow.” Washington Post. 2019 Oct 10.
Modern medicine increasingly relies on the adoption and use of guidelines.
Forty years ago, medicine was like free-form, rhythmic gymnastics in which physicians would develop an artisanal treatment plan for each patient. Now, medicine frequently involves recognizing when we need to do a triple-twisting, double-back somersault (the Biles II) and then performing it. The belief is that better outcomes flow from reduced variability in diagnostic and treatment plans, based on guidelines developed from evidence-based medicine from large meta-analyses. This dogma, still unproven in real life, probably works best for 95% of patients. The physician must not omit a step of deciding whether their particular patient is one of the 5% of patients to whom the guideline does not apply.
To be useful, the guidelines must be based on accurate science, produce a significantly positive cost-benefit-risk analysis, be wisely constructed, and be clearly written.
Alas, many guidelines fall far short of this ideal, and when they fail, they impugn all of medical care, they lower the credibility of the organizations that issue them, and they lower the public’s trust in medicine, which thereby impedes improving the public health. Don’t sweat the small stuff for public health guidelines.
The science matters. Nutritional guidelines have been particularly rickety, as John P.A. Ioannidis, MD, wrote in a JAMA op-ed 1 year ago.1 For instance, previous dietary recommendations to reduce cholesterol by avoiding eggs have since been shown to be wrong. The recommendation for reducing salt intake has been heavily criticized. Now the decades-long condemnation of red meat has been challenged. New “guidelines,” suggested by one group (let’s view it as a minority report that contradicts many official guidelines) in the October 1, 2019, issue of Annals of Internal Medicine, say that red meat and processed meats aren’t the boogeyman.2 The authors of the accompanying editorial are from the Center for Pediatric and Adolescent Comparative Effectiveness Research at Indiana University, Indianapolis.3 The editorial supports the new study, criticizing past recommendations because “the field of nutritional epidemiology is plagued by observational studies that have conducted inappropriate analyses, accompanied by likely erroneous conclusions.”
Clarity also matters. One factor in the current opiate epidemic was guidance in the mid-1990s making pain the “fifth vital sign.” This certainly was not the only factor nor was it necessarily the primary one. Most disasters, like most codes on the ward, proceed from multiple smaller failures and missteps. An emphasis on assessing pain in hospitalized patients did not intend to be interpreted as requiring that all pain be eliminated with strong medication, but that was the practical consequence. In response to the epidemic of overdose deaths, guidelines were promulgated in 2016 recommending reducing doses used for chronic opiate regimens. Some patients with chronic pain feared, and soon experienced, the consequences of those changes. In October 2019, those guidelines were revised telling physicians to go slower.4 In explaining the revision, one government official is quoted as saying: “Clearly we believe that there has been misinterpretation of the guidelines, which were very clear.”5 F. Scott Fitzgerald once wrote that “the test of a first-rate intelligence is the ability to hold two opposed ideas in mind at the same time and still retain the ability to function.” I reread that governmental doublespeak three times and my brain broke.
Clinical practice guidelines are an important part of modern medicine. But we need to be wiser about their creation. The science needs to be rigorous. The committees need to contain skeptics rather than just research scientists and clinicians with a vested interest in the field. The purported benefits of the guideline must be weighed against costs, risks, and unintended consequences. Humility is important. All physicians are taught the principle: “First, do no harm.” In explaining medical ethics to students, I rephrase that principle as: “Be cautious and humble. You are not as smart as you think you are.” Consider this food for thought the next time you read or create a guideline.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at pdnews@mdedge.com.
References
1. JAMA. 2018;320(10):969-70.
2. Ann Intern Med. 2019 Oct 1. doi: 10.7326/M19-1621.
3. Ann Intern Med. 2019 Oct 1. doi: 10.7326/M19-2620.
4. U.S. Department of Health & Human Services. HHS guide for clinicians on the appropriate dosage reduction or discontinuation of opioid analgesics. https://www.hhs.gov/opioids/sites/default/files/2019-10/Dosage_Reduction_Discontinuation.pdf.
5. “New guidelines on opioid tapering tell doctors to go slow.” Washington Post. 2019 Oct 10.
State medical boards under fire in physician suicides
SAN DIEGO – Physician suicide is “a public health crisis because of the sheer volume of people who are dying,” and many medical authorities are contributing to stigma through “invasive” questionnaires, a prevention advocate said at the annual Psych Congress.
“Physicians fear sharing their mental health struggles with the state medical health board,” said Pamela Wible, MD, a family physician who practices in Eugene, Ore., at the meeting. They “pretend, deny, and lie,” she said, and sometimes they seek care and medication hours away in order to avoid detection.
including the “very worst,” which is that of Alaska.
Dr. Wible, who speaks of suffering from suicidal feelings herself as physician in 2004, is a leading advocate for suicide prevention in the medical profession.
She told colleagues at the Psych Congress that anesthesiologists face the highest risk of suicide, followed by surgeons, ob.gyns., and psychiatrists.
“They end their lives not because they want to die but because they want to stop the pain and they can’t find any other way,” she said. “They have a great work ethic until the end: They’re smiling, doing complex surgeries, and cracking jokes to the surgical team, then they shoot themselves in the closet.”
Colleagues are often shocked, she said: “ ‘Wait a minute. He was just joking with me yesterday. What do you mean he hung himself in his office?’ ‘She just had a newborn baby and she was so happy!’ If you see the smile, you don’t see the pain.”
In 2018, she wrote a Washington Post commentary titled “What I’ve learned from my tally of 757 doctor suicides” that was based on her registry of physician suicides. In the United States, she wrote, 1 million patients lose a physician to suicide each year. Factors contributing to suicides include patient deaths, malpractice suits, “academic distress,” and overwork. “Doctors who need help don’t seek it because they fear mental health care won’t remain confidential,” she wrote. “So they drive out of town, pay cash, and use fake names to hide from state medical boards, hospitals, and insurance plans out of fear that they will lose state licensure, hospital privileges, and health plan participation.”
Dr. Wible oversaw a 2019 research project that analyzed state medical board applications. The goal was to grade the state boards by how intrusively their application questions grill applicants about their mental health history. “Physicians fear sharing their mental health struggles with the state medical health board and with each other,” she said. Some lie, and others – “the really honest physicians” – are so dedicated to telling the truth that “they’ll withhold getting care because they want to correctly check the ‘no’ box.”
Seven states – Alabama, Alaska, Delaware, Florida, Mississippi, Rhode Island, and Washington –received “F” grades for “highly invasive mental health questions unlinked to current impairment that contain confusing, punitive, or adversarial language.”
Alaska, Dr. Wible said, asks multiple 25 yes-or-no questions about mental health. One question lists 14 conditions, almost all related to mental health – including depression, “any organic mental disorder,” and “any condition requiring chronic medical or behavioral treatment” – and asks, “Have you ever been diagnosed with, treated for, or do you currently have” any of them. This is “the most invasive mental health question we found on any application,” Dr. Wible wrote on her website.
States also hurt applicants by asking peers of applicants about their mental health, she said. “I’m not against getting peer references, but can we stop getting into everyone’s business with their psych history? What we really want to know is: ‘Are you are safe with patients today?’ ”
Dr. Wible also criticizes state medical boards for asking about mental health impairment over the last 5 years: They don’t get higher than a “C.”
The 13 states with “A” grades either don’t ask about mental health or simply ask about general impairment: Connecticut, Hawaii, Indiana, Kentucky, New Jersey, Maine, Maryland, Massachusetts, Michigan, Nevada, New York, Pennsylvania, and Wyoming.
Massachusetts, for example, asks, “Do you have a medical or physical condition that currently impairs your ability to practice medicine?”
“That is a question anyone can understand,” Dr. Wible said. “I think that’s good wording.”
Going forward, she said, “we’ve got to remove these mental health questions. If we could do this, our profession would be so much better, and we’d lose so many fewer people.”
And, she added, “what we really need to do is share our stories. It’s therapeutic for you and your colleagues, it creates collegial trust and bonding, and it destigmatizes physician mental health.”
Dr. Wible reported no relevant disclosures.
SAN DIEGO – Physician suicide is “a public health crisis because of the sheer volume of people who are dying,” and many medical authorities are contributing to stigma through “invasive” questionnaires, a prevention advocate said at the annual Psych Congress.
“Physicians fear sharing their mental health struggles with the state medical health board,” said Pamela Wible, MD, a family physician who practices in Eugene, Ore., at the meeting. They “pretend, deny, and lie,” she said, and sometimes they seek care and medication hours away in order to avoid detection.
including the “very worst,” which is that of Alaska.
Dr. Wible, who speaks of suffering from suicidal feelings herself as physician in 2004, is a leading advocate for suicide prevention in the medical profession.
She told colleagues at the Psych Congress that anesthesiologists face the highest risk of suicide, followed by surgeons, ob.gyns., and psychiatrists.
“They end their lives not because they want to die but because they want to stop the pain and they can’t find any other way,” she said. “They have a great work ethic until the end: They’re smiling, doing complex surgeries, and cracking jokes to the surgical team, then they shoot themselves in the closet.”
Colleagues are often shocked, she said: “ ‘Wait a minute. He was just joking with me yesterday. What do you mean he hung himself in his office?’ ‘She just had a newborn baby and she was so happy!’ If you see the smile, you don’t see the pain.”
In 2018, she wrote a Washington Post commentary titled “What I’ve learned from my tally of 757 doctor suicides” that was based on her registry of physician suicides. In the United States, she wrote, 1 million patients lose a physician to suicide each year. Factors contributing to suicides include patient deaths, malpractice suits, “academic distress,” and overwork. “Doctors who need help don’t seek it because they fear mental health care won’t remain confidential,” she wrote. “So they drive out of town, pay cash, and use fake names to hide from state medical boards, hospitals, and insurance plans out of fear that they will lose state licensure, hospital privileges, and health plan participation.”
Dr. Wible oversaw a 2019 research project that analyzed state medical board applications. The goal was to grade the state boards by how intrusively their application questions grill applicants about their mental health history. “Physicians fear sharing their mental health struggles with the state medical health board and with each other,” she said. Some lie, and others – “the really honest physicians” – are so dedicated to telling the truth that “they’ll withhold getting care because they want to correctly check the ‘no’ box.”
Seven states – Alabama, Alaska, Delaware, Florida, Mississippi, Rhode Island, and Washington –received “F” grades for “highly invasive mental health questions unlinked to current impairment that contain confusing, punitive, or adversarial language.”
Alaska, Dr. Wible said, asks multiple 25 yes-or-no questions about mental health. One question lists 14 conditions, almost all related to mental health – including depression, “any organic mental disorder,” and “any condition requiring chronic medical or behavioral treatment” – and asks, “Have you ever been diagnosed with, treated for, or do you currently have” any of them. This is “the most invasive mental health question we found on any application,” Dr. Wible wrote on her website.
States also hurt applicants by asking peers of applicants about their mental health, she said. “I’m not against getting peer references, but can we stop getting into everyone’s business with their psych history? What we really want to know is: ‘Are you are safe with patients today?’ ”
Dr. Wible also criticizes state medical boards for asking about mental health impairment over the last 5 years: They don’t get higher than a “C.”
The 13 states with “A” grades either don’t ask about mental health or simply ask about general impairment: Connecticut, Hawaii, Indiana, Kentucky, New Jersey, Maine, Maryland, Massachusetts, Michigan, Nevada, New York, Pennsylvania, and Wyoming.
Massachusetts, for example, asks, “Do you have a medical or physical condition that currently impairs your ability to practice medicine?”
“That is a question anyone can understand,” Dr. Wible said. “I think that’s good wording.”
Going forward, she said, “we’ve got to remove these mental health questions. If we could do this, our profession would be so much better, and we’d lose so many fewer people.”
And, she added, “what we really need to do is share our stories. It’s therapeutic for you and your colleagues, it creates collegial trust and bonding, and it destigmatizes physician mental health.”
Dr. Wible reported no relevant disclosures.
SAN DIEGO – Physician suicide is “a public health crisis because of the sheer volume of people who are dying,” and many medical authorities are contributing to stigma through “invasive” questionnaires, a prevention advocate said at the annual Psych Congress.
“Physicians fear sharing their mental health struggles with the state medical health board,” said Pamela Wible, MD, a family physician who practices in Eugene, Ore., at the meeting. They “pretend, deny, and lie,” she said, and sometimes they seek care and medication hours away in order to avoid detection.
including the “very worst,” which is that of Alaska.
Dr. Wible, who speaks of suffering from suicidal feelings herself as physician in 2004, is a leading advocate for suicide prevention in the medical profession.
She told colleagues at the Psych Congress that anesthesiologists face the highest risk of suicide, followed by surgeons, ob.gyns., and psychiatrists.
“They end their lives not because they want to die but because they want to stop the pain and they can’t find any other way,” she said. “They have a great work ethic until the end: They’re smiling, doing complex surgeries, and cracking jokes to the surgical team, then they shoot themselves in the closet.”
Colleagues are often shocked, she said: “ ‘Wait a minute. He was just joking with me yesterday. What do you mean he hung himself in his office?’ ‘She just had a newborn baby and she was so happy!’ If you see the smile, you don’t see the pain.”
In 2018, she wrote a Washington Post commentary titled “What I’ve learned from my tally of 757 doctor suicides” that was based on her registry of physician suicides. In the United States, she wrote, 1 million patients lose a physician to suicide each year. Factors contributing to suicides include patient deaths, malpractice suits, “academic distress,” and overwork. “Doctors who need help don’t seek it because they fear mental health care won’t remain confidential,” she wrote. “So they drive out of town, pay cash, and use fake names to hide from state medical boards, hospitals, and insurance plans out of fear that they will lose state licensure, hospital privileges, and health plan participation.”
Dr. Wible oversaw a 2019 research project that analyzed state medical board applications. The goal was to grade the state boards by how intrusively their application questions grill applicants about their mental health history. “Physicians fear sharing their mental health struggles with the state medical health board and with each other,” she said. Some lie, and others – “the really honest physicians” – are so dedicated to telling the truth that “they’ll withhold getting care because they want to correctly check the ‘no’ box.”
Seven states – Alabama, Alaska, Delaware, Florida, Mississippi, Rhode Island, and Washington –received “F” grades for “highly invasive mental health questions unlinked to current impairment that contain confusing, punitive, or adversarial language.”
Alaska, Dr. Wible said, asks multiple 25 yes-or-no questions about mental health. One question lists 14 conditions, almost all related to mental health – including depression, “any organic mental disorder,” and “any condition requiring chronic medical or behavioral treatment” – and asks, “Have you ever been diagnosed with, treated for, or do you currently have” any of them. This is “the most invasive mental health question we found on any application,” Dr. Wible wrote on her website.
States also hurt applicants by asking peers of applicants about their mental health, she said. “I’m not against getting peer references, but can we stop getting into everyone’s business with their psych history? What we really want to know is: ‘Are you are safe with patients today?’ ”
Dr. Wible also criticizes state medical boards for asking about mental health impairment over the last 5 years: They don’t get higher than a “C.”
The 13 states with “A” grades either don’t ask about mental health or simply ask about general impairment: Connecticut, Hawaii, Indiana, Kentucky, New Jersey, Maine, Maryland, Massachusetts, Michigan, Nevada, New York, Pennsylvania, and Wyoming.
Massachusetts, for example, asks, “Do you have a medical or physical condition that currently impairs your ability to practice medicine?”
“That is a question anyone can understand,” Dr. Wible said. “I think that’s good wording.”
Going forward, she said, “we’ve got to remove these mental health questions. If we could do this, our profession would be so much better, and we’d lose so many fewer people.”
And, she added, “what we really need to do is share our stories. It’s therapeutic for you and your colleagues, it creates collegial trust and bonding, and it destigmatizes physician mental health.”
Dr. Wible reported no relevant disclosures.
EXPERT ANALYSIS FROM PSYCH CONGRESS 2019
Help wanted
In a Pediatrics article, Hsuan-hsiu Annie Chen, MD, offers a very personal and candid narrative of her struggle with depression during medical school and residency (Pediatrics. 2019 Sep 1. doi: 10.1542/peds.2019-1210). Dr. Chen knows from personal experience that she was not alone in her cohort as she faced the challenges of sleep deprivation and emotional trauma that continue to be a part of a physician’s education and training. In her discussion of how future medical trainees might be spared some of the long hours she endured, Dr. Chen suggests that this country consider expanding its physician workforce by “increasing the number of medical schools and recruiting foreign medical graduates” as some European countries have done. Dr. Chen now works in the pediatric residency office at Children’s Hospital, Los Angeles.
Ironically, or maybe it was intentionally, the editors of Pediatrics chose to open the same issue in which Dr. Chen’s personal story appears with a Pediatrics Perspective commentary that looks into the murky waters of physician workforce research (Pediatrics. 2019 Sep 1. doi: 10.1542/peds.2019-0469). Gary L. Freed, MD, MPH, at the Child Health Evaluation and Research Center at the University of Michigan, Ann Arbor, claims that, in general, the data currently being generated by workforce research must be interpreted with caution because many of the studies are flawed by one or more biases.
You may have survived the gauntlet of medical school and residency relatively unscathed. But Is part of the problem that your clinic is seeing too many patients with too few physicians? Do your colleagues share your opinion? Is the administration actively recruiting more physicians, but failing to find interested and qualified doctors? Is this a strictly local phenomenon limited to your community, or is it a regional shortage? Do you think your situation reflects a national trend that deserves attention?
Like Dr. Chen, do you think that more medical schools and active recruitment of foreign medical students would allow you to work less hours? Obviously, even if you were a teenager when you entered your residency, opening more medical schools is not going to allow you to shorten your workday. But are more medical schools the best solution for this country’s overworked physicians even in the long term? Dr. Freed’s observations should make you hesitant to even venture a guess.
You, I, and Dr. Chen only can report on how we perceive our own work environment. Your local physician shortage may be in part because the school system in your community has a poor reputation and young physicians don’t want to move there. It may be that the hospital that owns your practice is struggling and can’t afford to offer a competitive salary. Producing more physicians may not be the answer to the physician shortage in communities like yours, even in the long run.
This is a very large country with relatively porous boundaries between the states for physicians. Physician supply and demand seldom dictates where physicians choose to practice. In fact, a medically needy community is probably the least likely place a physician just finishing her training will choose to settle.
Although adding another physician to your practice may decrease your workload, can your personal finances handle the hit that might occur as you see less patients? Particularly, if the new hire turns out to be a rock star who siphons off more of your patients than you anticipated. On the other hand, there is always the chance that, despite careful vetting, your group hires a lemon who ends up creating more trouble than he is worth.
As Dr. Freed suggests, trying to determine just how many and what kind of physicians we need is complicated. It may be just a roll of the dice at best.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
In a Pediatrics article, Hsuan-hsiu Annie Chen, MD, offers a very personal and candid narrative of her struggle with depression during medical school and residency (Pediatrics. 2019 Sep 1. doi: 10.1542/peds.2019-1210). Dr. Chen knows from personal experience that she was not alone in her cohort as she faced the challenges of sleep deprivation and emotional trauma that continue to be a part of a physician’s education and training. In her discussion of how future medical trainees might be spared some of the long hours she endured, Dr. Chen suggests that this country consider expanding its physician workforce by “increasing the number of medical schools and recruiting foreign medical graduates” as some European countries have done. Dr. Chen now works in the pediatric residency office at Children’s Hospital, Los Angeles.
Ironically, or maybe it was intentionally, the editors of Pediatrics chose to open the same issue in which Dr. Chen’s personal story appears with a Pediatrics Perspective commentary that looks into the murky waters of physician workforce research (Pediatrics. 2019 Sep 1. doi: 10.1542/peds.2019-0469). Gary L. Freed, MD, MPH, at the Child Health Evaluation and Research Center at the University of Michigan, Ann Arbor, claims that, in general, the data currently being generated by workforce research must be interpreted with caution because many of the studies are flawed by one or more biases.
You may have survived the gauntlet of medical school and residency relatively unscathed. But Is part of the problem that your clinic is seeing too many patients with too few physicians? Do your colleagues share your opinion? Is the administration actively recruiting more physicians, but failing to find interested and qualified doctors? Is this a strictly local phenomenon limited to your community, or is it a regional shortage? Do you think your situation reflects a national trend that deserves attention?
Like Dr. Chen, do you think that more medical schools and active recruitment of foreign medical students would allow you to work less hours? Obviously, even if you were a teenager when you entered your residency, opening more medical schools is not going to allow you to shorten your workday. But are more medical schools the best solution for this country’s overworked physicians even in the long term? Dr. Freed’s observations should make you hesitant to even venture a guess.
You, I, and Dr. Chen only can report on how we perceive our own work environment. Your local physician shortage may be in part because the school system in your community has a poor reputation and young physicians don’t want to move there. It may be that the hospital that owns your practice is struggling and can’t afford to offer a competitive salary. Producing more physicians may not be the answer to the physician shortage in communities like yours, even in the long run.
This is a very large country with relatively porous boundaries between the states for physicians. Physician supply and demand seldom dictates where physicians choose to practice. In fact, a medically needy community is probably the least likely place a physician just finishing her training will choose to settle.
Although adding another physician to your practice may decrease your workload, can your personal finances handle the hit that might occur as you see less patients? Particularly, if the new hire turns out to be a rock star who siphons off more of your patients than you anticipated. On the other hand, there is always the chance that, despite careful vetting, your group hires a lemon who ends up creating more trouble than he is worth.
As Dr. Freed suggests, trying to determine just how many and what kind of physicians we need is complicated. It may be just a roll of the dice at best.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
In a Pediatrics article, Hsuan-hsiu Annie Chen, MD, offers a very personal and candid narrative of her struggle with depression during medical school and residency (Pediatrics. 2019 Sep 1. doi: 10.1542/peds.2019-1210). Dr. Chen knows from personal experience that she was not alone in her cohort as she faced the challenges of sleep deprivation and emotional trauma that continue to be a part of a physician’s education and training. In her discussion of how future medical trainees might be spared some of the long hours she endured, Dr. Chen suggests that this country consider expanding its physician workforce by “increasing the number of medical schools and recruiting foreign medical graduates” as some European countries have done. Dr. Chen now works in the pediatric residency office at Children’s Hospital, Los Angeles.
Ironically, or maybe it was intentionally, the editors of Pediatrics chose to open the same issue in which Dr. Chen’s personal story appears with a Pediatrics Perspective commentary that looks into the murky waters of physician workforce research (Pediatrics. 2019 Sep 1. doi: 10.1542/peds.2019-0469). Gary L. Freed, MD, MPH, at the Child Health Evaluation and Research Center at the University of Michigan, Ann Arbor, claims that, in general, the data currently being generated by workforce research must be interpreted with caution because many of the studies are flawed by one or more biases.
You may have survived the gauntlet of medical school and residency relatively unscathed. But Is part of the problem that your clinic is seeing too many patients with too few physicians? Do your colleagues share your opinion? Is the administration actively recruiting more physicians, but failing to find interested and qualified doctors? Is this a strictly local phenomenon limited to your community, or is it a regional shortage? Do you think your situation reflects a national trend that deserves attention?
Like Dr. Chen, do you think that more medical schools and active recruitment of foreign medical students would allow you to work less hours? Obviously, even if you were a teenager when you entered your residency, opening more medical schools is not going to allow you to shorten your workday. But are more medical schools the best solution for this country’s overworked physicians even in the long term? Dr. Freed’s observations should make you hesitant to even venture a guess.
You, I, and Dr. Chen only can report on how we perceive our own work environment. Your local physician shortage may be in part because the school system in your community has a poor reputation and young physicians don’t want to move there. It may be that the hospital that owns your practice is struggling and can’t afford to offer a competitive salary. Producing more physicians may not be the answer to the physician shortage in communities like yours, even in the long run.
This is a very large country with relatively porous boundaries between the states for physicians. Physician supply and demand seldom dictates where physicians choose to practice. In fact, a medically needy community is probably the least likely place a physician just finishing her training will choose to settle.
Although adding another physician to your practice may decrease your workload, can your personal finances handle the hit that might occur as you see less patients? Particularly, if the new hire turns out to be a rock star who siphons off more of your patients than you anticipated. On the other hand, there is always the chance that, despite careful vetting, your group hires a lemon who ends up creating more trouble than he is worth.
As Dr. Freed suggests, trying to determine just how many and what kind of physicians we need is complicated. It may be just a roll of the dice at best.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
Universal coverage may be possible without increases in national spending
The Commonwealth Fund and The Urban Institute looked at eight reform scenarios, including ones that build on the Affordable Care Act and expand to universal coverage or single payer. Two scenarios that continue to utilize private insurance show that, conceptually, broad coverage can be achieved without increasing spending.
“This study is important because it shows that there are several health reform approaches that have the potential to increase the number of people with health insurance, make health care more affordable, and slow cost growth,” David Blumenthal, MD, president of The Commonwealth Fund, said during an Oct. 15 conference call introducing the report.
He called the details that separate the varying models “central to the national debate on health care and health insurance coverage as the 2020 campaign season progresses.”
All the scenarios presented in the report have a foundation in various current Democratic health care reform proposals, although no one specific proposal or legislation is profiled within the eight scenarios presented.
“Our hope is that this extensive analysis will clarify for voters and policy makers the implications of the policy choices before us,” said Sara R. Collins, PhD, the vice president of health care coverage and access at The Commonwealth Fund, during the call.
The first of these scenarios, dubbed “Universal Coverage I: Private and Public Options,” includes continued use of private insurance but also involves a public option and is the first of four options presented in the report to achieve universal coverage by actively enrolling people who are not enrolled in a private plan for one year in the public option with income-scaled premiums. This option would not utilize the ACA employer mandate and would remove the “firewall” that prevents individuals with access to employer-sponsored coverage from accessing financial assistance and seeking individual coverage from the insurance marketplace.
This scenario, as with all but one of the scenarios analyzed in the report, covers all essential benefits as defined in the Affordable Care Act. The only single-payer option that does not cover all of these essential benefits still provides coverage for medically necessary care, including dental, vision, hearing, and long-term services.
The Universal Coverage I scenario does not have any penalties for not carrying insurance, but all legal residents that forgo voluntary coverage from an employer or the marketplace will be automatically enrolled in coverage for which they are responsible for a premium payment.
There would be no expanded access to short-term, limited duration plans as the automatic enrollment to those not voluntarily covered by an employer or in the marketplace would make coverage universal. Federal government spending under this plan increases government health care spending in 2020 by $122.1 billion and $1.5 trillion over 10 years. However, total national spending in this scenario would decrease by $22.6 billion or 0.6% in 2020, compared with current law.
“Universal Coverage II: Enhanced Subsidies” is similar to Universal Coverage I in all other respects other than that it includes more generous premium and cost-sharing subsidies. These additional offerings would push federal government spending up $161.8 billion more in 2020, compared with current law, and to $2 trillion more over the next 10 years, while showing a minimal decrease in total national spending of less than 1% compared with current law.
The other two options that would move toward providing everyone with health insurance include a single payer system that covers all ACA essential health benefits, features no premiums, has income-related cost sharing, and covers all legal residents. Private insurance in this scenario is prohibited, and provider payments would be similar to those received in Medicare. Federal government spending would increase in 2020 by $1.5 trillion, compared with current law, and $17.6 trillion over the next 10 years. However, total national spending would decrease by $209.5 billion, or 6%, in 2020 compared with current law. These savings would come from lower provider payments and administrative costs that outweigh increased costs associated with near universal coverage and lower cost-sharing requirements.
A second single payer scenario broadens the benefits and would cover all residents in the United States, including undocumented residents. It would have no cost-sharing requirements.
The “optimal levels at which the payments for hospitals and doctors and other providers should be paid are really unknown at this time,” said Linda Blumberg, PhD, fellow at The Urban Institute’s Health Policy Center and one of the report authors, during the call.
Providing total coverage for all people in the United States is estimated to increase federal spending by $2.8 trillion in 2020 compared with current law, and $34 trillion over 10 years, with much of this increase accounted for by the shift in existing state and private spending to the federal government. At the same time, total national spending would increase by approximately $720 billion in 2020 compared with current law. Even though employer, household, and state spending would decrease, these savings would not be enough to offset increases in federal spending as well as the increased consumption of health care that comes with more generous benefits. The offsets from lower administrative costs and lower provider payments also would not offset higher spending.
The report only looks at health care spending and does not present any suggestions on revenue to offset the spending.
SOURCE: Blumberg LJ et al. “From Incremental to Comprehensive Health Insurance Reform: How Various Reform Options Compare On Coverage and Costs.” The Commonwealth Fund and The Urban Institute. 2019 Oct 16.
The Commonwealth Fund and The Urban Institute looked at eight reform scenarios, including ones that build on the Affordable Care Act and expand to universal coverage or single payer. Two scenarios that continue to utilize private insurance show that, conceptually, broad coverage can be achieved without increasing spending.
“This study is important because it shows that there are several health reform approaches that have the potential to increase the number of people with health insurance, make health care more affordable, and slow cost growth,” David Blumenthal, MD, president of The Commonwealth Fund, said during an Oct. 15 conference call introducing the report.
He called the details that separate the varying models “central to the national debate on health care and health insurance coverage as the 2020 campaign season progresses.”
All the scenarios presented in the report have a foundation in various current Democratic health care reform proposals, although no one specific proposal or legislation is profiled within the eight scenarios presented.
“Our hope is that this extensive analysis will clarify for voters and policy makers the implications of the policy choices before us,” said Sara R. Collins, PhD, the vice president of health care coverage and access at The Commonwealth Fund, during the call.
The first of these scenarios, dubbed “Universal Coverage I: Private and Public Options,” includes continued use of private insurance but also involves a public option and is the first of four options presented in the report to achieve universal coverage by actively enrolling people who are not enrolled in a private plan for one year in the public option with income-scaled premiums. This option would not utilize the ACA employer mandate and would remove the “firewall” that prevents individuals with access to employer-sponsored coverage from accessing financial assistance and seeking individual coverage from the insurance marketplace.
This scenario, as with all but one of the scenarios analyzed in the report, covers all essential benefits as defined in the Affordable Care Act. The only single-payer option that does not cover all of these essential benefits still provides coverage for medically necessary care, including dental, vision, hearing, and long-term services.
The Universal Coverage I scenario does not have any penalties for not carrying insurance, but all legal residents that forgo voluntary coverage from an employer or the marketplace will be automatically enrolled in coverage for which they are responsible for a premium payment.
There would be no expanded access to short-term, limited duration plans as the automatic enrollment to those not voluntarily covered by an employer or in the marketplace would make coverage universal. Federal government spending under this plan increases government health care spending in 2020 by $122.1 billion and $1.5 trillion over 10 years. However, total national spending in this scenario would decrease by $22.6 billion or 0.6% in 2020, compared with current law.
“Universal Coverage II: Enhanced Subsidies” is similar to Universal Coverage I in all other respects other than that it includes more generous premium and cost-sharing subsidies. These additional offerings would push federal government spending up $161.8 billion more in 2020, compared with current law, and to $2 trillion more over the next 10 years, while showing a minimal decrease in total national spending of less than 1% compared with current law.
The other two options that would move toward providing everyone with health insurance include a single payer system that covers all ACA essential health benefits, features no premiums, has income-related cost sharing, and covers all legal residents. Private insurance in this scenario is prohibited, and provider payments would be similar to those received in Medicare. Federal government spending would increase in 2020 by $1.5 trillion, compared with current law, and $17.6 trillion over the next 10 years. However, total national spending would decrease by $209.5 billion, or 6%, in 2020 compared with current law. These savings would come from lower provider payments and administrative costs that outweigh increased costs associated with near universal coverage and lower cost-sharing requirements.
A second single payer scenario broadens the benefits and would cover all residents in the United States, including undocumented residents. It would have no cost-sharing requirements.
The “optimal levels at which the payments for hospitals and doctors and other providers should be paid are really unknown at this time,” said Linda Blumberg, PhD, fellow at The Urban Institute’s Health Policy Center and one of the report authors, during the call.
Providing total coverage for all people in the United States is estimated to increase federal spending by $2.8 trillion in 2020 compared with current law, and $34 trillion over 10 years, with much of this increase accounted for by the shift in existing state and private spending to the federal government. At the same time, total national spending would increase by approximately $720 billion in 2020 compared with current law. Even though employer, household, and state spending would decrease, these savings would not be enough to offset increases in federal spending as well as the increased consumption of health care that comes with more generous benefits. The offsets from lower administrative costs and lower provider payments also would not offset higher spending.
The report only looks at health care spending and does not present any suggestions on revenue to offset the spending.
SOURCE: Blumberg LJ et al. “From Incremental to Comprehensive Health Insurance Reform: How Various Reform Options Compare On Coverage and Costs.” The Commonwealth Fund and The Urban Institute. 2019 Oct 16.
The Commonwealth Fund and The Urban Institute looked at eight reform scenarios, including ones that build on the Affordable Care Act and expand to universal coverage or single payer. Two scenarios that continue to utilize private insurance show that, conceptually, broad coverage can be achieved without increasing spending.
“This study is important because it shows that there are several health reform approaches that have the potential to increase the number of people with health insurance, make health care more affordable, and slow cost growth,” David Blumenthal, MD, president of The Commonwealth Fund, said during an Oct. 15 conference call introducing the report.
He called the details that separate the varying models “central to the national debate on health care and health insurance coverage as the 2020 campaign season progresses.”
All the scenarios presented in the report have a foundation in various current Democratic health care reform proposals, although no one specific proposal or legislation is profiled within the eight scenarios presented.
“Our hope is that this extensive analysis will clarify for voters and policy makers the implications of the policy choices before us,” said Sara R. Collins, PhD, the vice president of health care coverage and access at The Commonwealth Fund, during the call.
The first of these scenarios, dubbed “Universal Coverage I: Private and Public Options,” includes continued use of private insurance but also involves a public option and is the first of four options presented in the report to achieve universal coverage by actively enrolling people who are not enrolled in a private plan for one year in the public option with income-scaled premiums. This option would not utilize the ACA employer mandate and would remove the “firewall” that prevents individuals with access to employer-sponsored coverage from accessing financial assistance and seeking individual coverage from the insurance marketplace.
This scenario, as with all but one of the scenarios analyzed in the report, covers all essential benefits as defined in the Affordable Care Act. The only single-payer option that does not cover all of these essential benefits still provides coverage for medically necessary care, including dental, vision, hearing, and long-term services.
The Universal Coverage I scenario does not have any penalties for not carrying insurance, but all legal residents that forgo voluntary coverage from an employer or the marketplace will be automatically enrolled in coverage for which they are responsible for a premium payment.
There would be no expanded access to short-term, limited duration plans as the automatic enrollment to those not voluntarily covered by an employer or in the marketplace would make coverage universal. Federal government spending under this plan increases government health care spending in 2020 by $122.1 billion and $1.5 trillion over 10 years. However, total national spending in this scenario would decrease by $22.6 billion or 0.6% in 2020, compared with current law.
“Universal Coverage II: Enhanced Subsidies” is similar to Universal Coverage I in all other respects other than that it includes more generous premium and cost-sharing subsidies. These additional offerings would push federal government spending up $161.8 billion more in 2020, compared with current law, and to $2 trillion more over the next 10 years, while showing a minimal decrease in total national spending of less than 1% compared with current law.
The other two options that would move toward providing everyone with health insurance include a single payer system that covers all ACA essential health benefits, features no premiums, has income-related cost sharing, and covers all legal residents. Private insurance in this scenario is prohibited, and provider payments would be similar to those received in Medicare. Federal government spending would increase in 2020 by $1.5 trillion, compared with current law, and $17.6 trillion over the next 10 years. However, total national spending would decrease by $209.5 billion, or 6%, in 2020 compared with current law. These savings would come from lower provider payments and administrative costs that outweigh increased costs associated with near universal coverage and lower cost-sharing requirements.
A second single payer scenario broadens the benefits and would cover all residents in the United States, including undocumented residents. It would have no cost-sharing requirements.
The “optimal levels at which the payments for hospitals and doctors and other providers should be paid are really unknown at this time,” said Linda Blumberg, PhD, fellow at The Urban Institute’s Health Policy Center and one of the report authors, during the call.
Providing total coverage for all people in the United States is estimated to increase federal spending by $2.8 trillion in 2020 compared with current law, and $34 trillion over 10 years, with much of this increase accounted for by the shift in existing state and private spending to the federal government. At the same time, total national spending would increase by approximately $720 billion in 2020 compared with current law. Even though employer, household, and state spending would decrease, these savings would not be enough to offset increases in federal spending as well as the increased consumption of health care that comes with more generous benefits. The offsets from lower administrative costs and lower provider payments also would not offset higher spending.
The report only looks at health care spending and does not present any suggestions on revenue to offset the spending.
SOURCE: Blumberg LJ et al. “From Incremental to Comprehensive Health Insurance Reform: How Various Reform Options Compare On Coverage and Costs.” The Commonwealth Fund and The Urban Institute. 2019 Oct 16.
Health care stayed front and center at Democratic debate
This time, it wasn’t just about Medicare-for-all.
Voters got a better look at Democrats’ health care priorities on Tuesday, as
While the debate began on the topic of impeaching President Trump, Sen. Bernie Sanders of Vermont soon steered the discussion back to kitchen-table issues.
“I think what would be a disaster, if the American people believe that all we were doing is taking on Trump,” he said. “We’re forgetting that 87 million Americans are uninsured or underinsured.”
That was only the beginning of a series of health care conversations that lasted through much of the three-hour debate.
With Sen. Elizabeth Warren of Massachusetts polling in second place before the night began, she was pressed to offer more details about what Medicare-for-all would look like under her leadership – in particular, whether she would raise taxes to pay for it.
“I have made clear what my principles are here,” she said. “That is, costs will go up for the wealthy and for big corporations, and for hardworking, middle-class families, costs will go down.”
But Mayor Pete Buttigieg of South Bend, Ind., pushed back, pointing out that, unlike Sen. Sanders – who has said taxes would increase to pay for his universal health care plan – she had not actually said whether she would raise taxes.
“Your signature is to have a plan for everything, except this,” Mr. Buttigieg said. “No plan has been laid out to explain how a multitrillion-dollar hole in this plan that Sen. Warren is putting forward is supposed to get filled in.”
Sen. Amy Klobuchar of Minnesota challenged the practicality of focusing on such a sweeping overhaul as Medicare-for-all. She pushed her support for a public option and noted the importance of issues that get less attention, like long-term care.
“The difference between a plan and a pipe dream is something that you can actually get done,” Sen. Klobuchar said.
But Sen. Warren stood her ground. When she was studying bankruptcy as a professor at Harvard Law School, she said, she noticed that two out of three families that went bankrupt after a medical problem had health insurance. The problem is cost, she said: “That is why hardworking people go broke.”
The candidates also staked their claim on two issues that are critically important to Democratic voters: strengthening gun control measures and guaranteeing access to reproductive health care.
Former Vice President Joe Biden trumpeted his role in securing the now-lapsed assault weapons ban in 1994. Among others, Sen. Kamala Harris of California called for a “comprehensive” background check requirement and a ban on the importation of assault weapons.
And one by one, the candidates vowed to codify abortion access, especially in light of recent conservative attacks in a number of states on the premise of the Supreme Court’s Roe v. Wade decision.
“It’s not an exaggeration to say women will die because these Republican legislatures in these various states who are out of touch with America are telling women what to do with their bodies,” Sen. Harris said, a reference to crackdowns on abortion access in many Republican-controlled states.
After pointing out earlier in the evening that two Planned Parenthood clinics in Ohio recently closed because of a Trump administration policy change, Sen. Cory Booker of New Jersey said he would create an office of reproductive freedom and reproductive rights in his White House.
“It’s an assault on the most fundamental ideal that human beings should control their own body,” Sen. Booker said.
And addressing the opioid crisis, blamed for lowering life expectancy in the United States, many of the candidates called outright for jailing the executives of opioid manufacturers, whom Sen. Harris called “nothing more than some high-level dope dealers.”
“The people who should pay for the treatment are the very people that got people hooked and killed them in the first place,” she said.
The evening was also Sen. Sanders’ first appearance on the debate stage since he had a heart attack and underwent heart surgery just weeks ago. Asked about his health, he seemed impatient: “I’m healthy. I’m feeling great,” Sen. Sanders said as he brought the conversation back to policy.
The debate took place in Westerville, Ohio, a traditionally conservative suburb of Columbus that had turned blue in recent years – a nod to Democrats’ hopes of winning with the support of suburban voters in 2020.
And with those 12 Democrats standing elbow-to-elbow, the debate hosted by CNN and the New York Times had an unusual distinction: the most candidates to ever appear onstage at a presidential debate.
The fifth Democratic debate is scheduled for Nov. 20. The Democratic National Committee plans to hold 12 primary debates in total.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
This time, it wasn’t just about Medicare-for-all.
Voters got a better look at Democrats’ health care priorities on Tuesday, as
While the debate began on the topic of impeaching President Trump, Sen. Bernie Sanders of Vermont soon steered the discussion back to kitchen-table issues.
“I think what would be a disaster, if the American people believe that all we were doing is taking on Trump,” he said. “We’re forgetting that 87 million Americans are uninsured or underinsured.”
That was only the beginning of a series of health care conversations that lasted through much of the three-hour debate.
With Sen. Elizabeth Warren of Massachusetts polling in second place before the night began, she was pressed to offer more details about what Medicare-for-all would look like under her leadership – in particular, whether she would raise taxes to pay for it.
“I have made clear what my principles are here,” she said. “That is, costs will go up for the wealthy and for big corporations, and for hardworking, middle-class families, costs will go down.”
But Mayor Pete Buttigieg of South Bend, Ind., pushed back, pointing out that, unlike Sen. Sanders – who has said taxes would increase to pay for his universal health care plan – she had not actually said whether she would raise taxes.
“Your signature is to have a plan for everything, except this,” Mr. Buttigieg said. “No plan has been laid out to explain how a multitrillion-dollar hole in this plan that Sen. Warren is putting forward is supposed to get filled in.”
Sen. Amy Klobuchar of Minnesota challenged the practicality of focusing on such a sweeping overhaul as Medicare-for-all. She pushed her support for a public option and noted the importance of issues that get less attention, like long-term care.
“The difference between a plan and a pipe dream is something that you can actually get done,” Sen. Klobuchar said.
But Sen. Warren stood her ground. When she was studying bankruptcy as a professor at Harvard Law School, she said, she noticed that two out of three families that went bankrupt after a medical problem had health insurance. The problem is cost, she said: “That is why hardworking people go broke.”
The candidates also staked their claim on two issues that are critically important to Democratic voters: strengthening gun control measures and guaranteeing access to reproductive health care.
Former Vice President Joe Biden trumpeted his role in securing the now-lapsed assault weapons ban in 1994. Among others, Sen. Kamala Harris of California called for a “comprehensive” background check requirement and a ban on the importation of assault weapons.
And one by one, the candidates vowed to codify abortion access, especially in light of recent conservative attacks in a number of states on the premise of the Supreme Court’s Roe v. Wade decision.
“It’s not an exaggeration to say women will die because these Republican legislatures in these various states who are out of touch with America are telling women what to do with their bodies,” Sen. Harris said, a reference to crackdowns on abortion access in many Republican-controlled states.
After pointing out earlier in the evening that two Planned Parenthood clinics in Ohio recently closed because of a Trump administration policy change, Sen. Cory Booker of New Jersey said he would create an office of reproductive freedom and reproductive rights in his White House.
“It’s an assault on the most fundamental ideal that human beings should control their own body,” Sen. Booker said.
And addressing the opioid crisis, blamed for lowering life expectancy in the United States, many of the candidates called outright for jailing the executives of opioid manufacturers, whom Sen. Harris called “nothing more than some high-level dope dealers.”
“The people who should pay for the treatment are the very people that got people hooked and killed them in the first place,” she said.
The evening was also Sen. Sanders’ first appearance on the debate stage since he had a heart attack and underwent heart surgery just weeks ago. Asked about his health, he seemed impatient: “I’m healthy. I’m feeling great,” Sen. Sanders said as he brought the conversation back to policy.
The debate took place in Westerville, Ohio, a traditionally conservative suburb of Columbus that had turned blue in recent years – a nod to Democrats’ hopes of winning with the support of suburban voters in 2020.
And with those 12 Democrats standing elbow-to-elbow, the debate hosted by CNN and the New York Times had an unusual distinction: the most candidates to ever appear onstage at a presidential debate.
The fifth Democratic debate is scheduled for Nov. 20. The Democratic National Committee plans to hold 12 primary debates in total.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
This time, it wasn’t just about Medicare-for-all.
Voters got a better look at Democrats’ health care priorities on Tuesday, as
While the debate began on the topic of impeaching President Trump, Sen. Bernie Sanders of Vermont soon steered the discussion back to kitchen-table issues.
“I think what would be a disaster, if the American people believe that all we were doing is taking on Trump,” he said. “We’re forgetting that 87 million Americans are uninsured or underinsured.”
That was only the beginning of a series of health care conversations that lasted through much of the three-hour debate.
With Sen. Elizabeth Warren of Massachusetts polling in second place before the night began, she was pressed to offer more details about what Medicare-for-all would look like under her leadership – in particular, whether she would raise taxes to pay for it.
“I have made clear what my principles are here,” she said. “That is, costs will go up for the wealthy and for big corporations, and for hardworking, middle-class families, costs will go down.”
But Mayor Pete Buttigieg of South Bend, Ind., pushed back, pointing out that, unlike Sen. Sanders – who has said taxes would increase to pay for his universal health care plan – she had not actually said whether she would raise taxes.
“Your signature is to have a plan for everything, except this,” Mr. Buttigieg said. “No plan has been laid out to explain how a multitrillion-dollar hole in this plan that Sen. Warren is putting forward is supposed to get filled in.”
Sen. Amy Klobuchar of Minnesota challenged the practicality of focusing on such a sweeping overhaul as Medicare-for-all. She pushed her support for a public option and noted the importance of issues that get less attention, like long-term care.
“The difference between a plan and a pipe dream is something that you can actually get done,” Sen. Klobuchar said.
But Sen. Warren stood her ground. When she was studying bankruptcy as a professor at Harvard Law School, she said, she noticed that two out of three families that went bankrupt after a medical problem had health insurance. The problem is cost, she said: “That is why hardworking people go broke.”
The candidates also staked their claim on two issues that are critically important to Democratic voters: strengthening gun control measures and guaranteeing access to reproductive health care.
Former Vice President Joe Biden trumpeted his role in securing the now-lapsed assault weapons ban in 1994. Among others, Sen. Kamala Harris of California called for a “comprehensive” background check requirement and a ban on the importation of assault weapons.
And one by one, the candidates vowed to codify abortion access, especially in light of recent conservative attacks in a number of states on the premise of the Supreme Court’s Roe v. Wade decision.
“It’s not an exaggeration to say women will die because these Republican legislatures in these various states who are out of touch with America are telling women what to do with their bodies,” Sen. Harris said, a reference to crackdowns on abortion access in many Republican-controlled states.
After pointing out earlier in the evening that two Planned Parenthood clinics in Ohio recently closed because of a Trump administration policy change, Sen. Cory Booker of New Jersey said he would create an office of reproductive freedom and reproductive rights in his White House.
“It’s an assault on the most fundamental ideal that human beings should control their own body,” Sen. Booker said.
And addressing the opioid crisis, blamed for lowering life expectancy in the United States, many of the candidates called outright for jailing the executives of opioid manufacturers, whom Sen. Harris called “nothing more than some high-level dope dealers.”
“The people who should pay for the treatment are the very people that got people hooked and killed them in the first place,” she said.
The evening was also Sen. Sanders’ first appearance on the debate stage since he had a heart attack and underwent heart surgery just weeks ago. Asked about his health, he seemed impatient: “I’m healthy. I’m feeling great,” Sen. Sanders said as he brought the conversation back to policy.
The debate took place in Westerville, Ohio, a traditionally conservative suburb of Columbus that had turned blue in recent years – a nod to Democrats’ hopes of winning with the support of suburban voters in 2020.
And with those 12 Democrats standing elbow-to-elbow, the debate hosted by CNN and the New York Times had an unusual distinction: the most candidates to ever appear onstage at a presidential debate.
The fifth Democratic debate is scheduled for Nov. 20. The Democratic National Committee plans to hold 12 primary debates in total.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.




















