User login
Mid-career advice
You’ve arrived at an important milestone when someone asks you to give a grand rounds titled ... “Mid-Career Advice.” Yes, I’ve been asked.
I’m flattered to be asked (although I hope I’m not halfway). Mid-career “crisis!” is what Google expected me to talk about when I searched on this topic. Apparently, I’d rather be me today than me in residency – you learn an awful lot in 40K patient visits. Here are a few notes from my journey:
1. Knowing how to care for patients is as important as knowing medicine. The bulk of work to be done in outpatient care depends on bonding, trust, and affecting change efficiently and effectively. Sometimes great diagnostic acumen and procedural skills are needed. Yet, for most, this isn’t hard. Access to differential diagnoses, recommended work-ups, and best practice treatments are easily accessible, just in time. In contrast, it’s often hard to convince patients of their diagnosis and to help them adhere to the best plan.
2. You can do everything right and still have it end up wrong. Medicine is more like poker than chess. In chess, most information is knowable, and there is always one best move. In poker, much is unknown, and a lot depends on chance. You might perform surgery with perfect sterile technique and still, the patient develops an infection. You could prescribe all the best treatments for pyoderma gangrenosum and the disease might still progress. Thinking probabilistically helps me make better choices and sleep better at night, especially when the outcome was not commensurate with the quality of care.
3. Patients are sometimes impertinent, sometimes wrong, sometimes stubborn, sometimes rude. “Restrain your indignation,” Dr. Osler advised his medical students in 1889, and remember that “offences of this kind come; expect them, and do not be vexed.” You might give the best care, the most compassionate, time-generous appointment, and still your patient files a grievance, posts a bad review, fails to follow through, chooses CBD oil instead. Remember, they are just people with all our shortcomings. Do your best to serve and know in your heart that you are enough and have done enough. Then move on; patients are waiting.
4. Adverse outcomes can be devastating, to us as well as to our patients. Any harm caused to a patient or an angry complaint against you can trigger anxiety, regret, and endless ruminating. Sometimes these thoughts become intrusive. Try setting boundaries. Take the time to absorb the discomfort, still knowing you are strong, you are not alone, and failure is sometimes inevitable. Learn what you can, then when you find you’re unable to stop your thoughts, choose an activity (like AngryBirds!) to break your thoughts. You will be a healthier human and provide better care if you can find your equanimity often and early.
5. Amor fati, or “love your fate.” You cannot know what life has planned. Small, seemingly insignificant events in my life changed my path dramatically. I could have been a store manager in Attleboro, Mass., an orthopedic surgeon in Winston-Salem, or a psychologist in Denver. I could never have known then that I’d end up here, as chief of dermatology in San Diego. Rather than depend only on a deliberate strategy with happiness at your destination being “find the job you love,” rely more on an evolving strategy. Do your job and then exploit opportunities as they develop. Forget sunk costs and move ahead. Don’t depend on fate for your happiness or search for a career to fulfill you. Close your eyes and find the happiness in you, then open your eyes and be so right there. Love your fate.
Dr. Benabio is director of healthcare transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
You’ve arrived at an important milestone when someone asks you to give a grand rounds titled ... “Mid-Career Advice.” Yes, I’ve been asked.
I’m flattered to be asked (although I hope I’m not halfway). Mid-career “crisis!” is what Google expected me to talk about when I searched on this topic. Apparently, I’d rather be me today than me in residency – you learn an awful lot in 40K patient visits. Here are a few notes from my journey:
1. Knowing how to care for patients is as important as knowing medicine. The bulk of work to be done in outpatient care depends on bonding, trust, and affecting change efficiently and effectively. Sometimes great diagnostic acumen and procedural skills are needed. Yet, for most, this isn’t hard. Access to differential diagnoses, recommended work-ups, and best practice treatments are easily accessible, just in time. In contrast, it’s often hard to convince patients of their diagnosis and to help them adhere to the best plan.
2. You can do everything right and still have it end up wrong. Medicine is more like poker than chess. In chess, most information is knowable, and there is always one best move. In poker, much is unknown, and a lot depends on chance. You might perform surgery with perfect sterile technique and still, the patient develops an infection. You could prescribe all the best treatments for pyoderma gangrenosum and the disease might still progress. Thinking probabilistically helps me make better choices and sleep better at night, especially when the outcome was not commensurate with the quality of care.
3. Patients are sometimes impertinent, sometimes wrong, sometimes stubborn, sometimes rude. “Restrain your indignation,” Dr. Osler advised his medical students in 1889, and remember that “offences of this kind come; expect them, and do not be vexed.” You might give the best care, the most compassionate, time-generous appointment, and still your patient files a grievance, posts a bad review, fails to follow through, chooses CBD oil instead. Remember, they are just people with all our shortcomings. Do your best to serve and know in your heart that you are enough and have done enough. Then move on; patients are waiting.
4. Adverse outcomes can be devastating, to us as well as to our patients. Any harm caused to a patient or an angry complaint against you can trigger anxiety, regret, and endless ruminating. Sometimes these thoughts become intrusive. Try setting boundaries. Take the time to absorb the discomfort, still knowing you are strong, you are not alone, and failure is sometimes inevitable. Learn what you can, then when you find you’re unable to stop your thoughts, choose an activity (like AngryBirds!) to break your thoughts. You will be a healthier human and provide better care if you can find your equanimity often and early.
5. Amor fati, or “love your fate.” You cannot know what life has planned. Small, seemingly insignificant events in my life changed my path dramatically. I could have been a store manager in Attleboro, Mass., an orthopedic surgeon in Winston-Salem, or a psychologist in Denver. I could never have known then that I’d end up here, as chief of dermatology in San Diego. Rather than depend only on a deliberate strategy with happiness at your destination being “find the job you love,” rely more on an evolving strategy. Do your job and then exploit opportunities as they develop. Forget sunk costs and move ahead. Don’t depend on fate for your happiness or search for a career to fulfill you. Close your eyes and find the happiness in you, then open your eyes and be so right there. Love your fate.
Dr. Benabio is director of healthcare transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
You’ve arrived at an important milestone when someone asks you to give a grand rounds titled ... “Mid-Career Advice.” Yes, I’ve been asked.
I’m flattered to be asked (although I hope I’m not halfway). Mid-career “crisis!” is what Google expected me to talk about when I searched on this topic. Apparently, I’d rather be me today than me in residency – you learn an awful lot in 40K patient visits. Here are a few notes from my journey:
1. Knowing how to care for patients is as important as knowing medicine. The bulk of work to be done in outpatient care depends on bonding, trust, and affecting change efficiently and effectively. Sometimes great diagnostic acumen and procedural skills are needed. Yet, for most, this isn’t hard. Access to differential diagnoses, recommended work-ups, and best practice treatments are easily accessible, just in time. In contrast, it’s often hard to convince patients of their diagnosis and to help them adhere to the best plan.
2. You can do everything right and still have it end up wrong. Medicine is more like poker than chess. In chess, most information is knowable, and there is always one best move. In poker, much is unknown, and a lot depends on chance. You might perform surgery with perfect sterile technique and still, the patient develops an infection. You could prescribe all the best treatments for pyoderma gangrenosum and the disease might still progress. Thinking probabilistically helps me make better choices and sleep better at night, especially when the outcome was not commensurate with the quality of care.
3. Patients are sometimes impertinent, sometimes wrong, sometimes stubborn, sometimes rude. “Restrain your indignation,” Dr. Osler advised his medical students in 1889, and remember that “offences of this kind come; expect them, and do not be vexed.” You might give the best care, the most compassionate, time-generous appointment, and still your patient files a grievance, posts a bad review, fails to follow through, chooses CBD oil instead. Remember, they are just people with all our shortcomings. Do your best to serve and know in your heart that you are enough and have done enough. Then move on; patients are waiting.
4. Adverse outcomes can be devastating, to us as well as to our patients. Any harm caused to a patient or an angry complaint against you can trigger anxiety, regret, and endless ruminating. Sometimes these thoughts become intrusive. Try setting boundaries. Take the time to absorb the discomfort, still knowing you are strong, you are not alone, and failure is sometimes inevitable. Learn what you can, then when you find you’re unable to stop your thoughts, choose an activity (like AngryBirds!) to break your thoughts. You will be a healthier human and provide better care if you can find your equanimity often and early.
5. Amor fati, or “love your fate.” You cannot know what life has planned. Small, seemingly insignificant events in my life changed my path dramatically. I could have been a store manager in Attleboro, Mass., an orthopedic surgeon in Winston-Salem, or a psychologist in Denver. I could never have known then that I’d end up here, as chief of dermatology in San Diego. Rather than depend only on a deliberate strategy with happiness at your destination being “find the job you love,” rely more on an evolving strategy. Do your job and then exploit opportunities as they develop. Forget sunk costs and move ahead. Don’t depend on fate for your happiness or search for a career to fulfill you. Close your eyes and find the happiness in you, then open your eyes and be so right there. Love your fate.
Dr. Benabio is director of healthcare transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
Most practices not screening for five social needs
that are associated with health outcomes, a study found.
Lead author Taressa K. Fraze, PhD, of the Dartmouth Institute for Health Policy and Clinical Practice in Lebanon, N.H., and colleagues conducted a cross-sectional survey analysis of responses by physician practices and hospitals that participated in the 2017-2018 National Survey of Healthcare Organizations and Systems. The investigators evaluated how many practices and hospitals reported screening of patients for five social needs: food insecurity, housing instability, utility needs, transportation needs, and experience with interpersonal violence. The final analysis included 2,190 physician practices and 739 hospitals.
Of physician practices, 56% reported screening for interpersonal violence, 35% screened for transportation needs, 30% for food insecurity, 28% for housing instability, and 23% for utility needs, according to the study published in JAMA Network Open.
Among hospitals, 75% reported screening for interpersonal violence, 74% for transportation needs, 60% for housing instability, 40% for food insecurity, and 36% for utility needs. Only 16% of physician practices and 24% of hospitals screened for all five social needs, the study found, while 33% of physician practices and 8% of hospitals reported screening for no social needs. The majority of the overall screening activity was driven by interpersonal violence screenings.
Physician practices that served more disadvantaged patients, including federally qualified health centers and those with more Medicaid revenue were more likely to screen for all five social needs. Practices in Medicaid accountable care organization contracts and those in Medicaid expansion states also had higher screening rates. Regionally, practices in the West had the highest screening rates, while practices in the Midwest had the lowest rates.
Among hospitals, the investigators found few significant screening differences based on hospital characteristics. Ownership, critical access status, delivery reform participation, rural status, region, and Medicaid expansion had no significant effects on screening rates, although academic medical centers were more likely to screen patients for all needs compared with nonacademic medical centers.
The study authors wrote that doctors and hospitals may need more resources and additional processes to screen for and/or to address the social needs of patients. They noted that practices and hospitals that did not screen for social needs were more likely to report a lack of financial resources, time, and incentives as major barriers.
To implement better screening protocols and address patients’ needs, the investigators wrote that doctors and hospitals will need financial support. For example, the Centers for Medicare & Medicaid Services should consider expanding care management billing to include managing care for patients who are both at risk or have clinically complex conditions in addition to social needs.
Dr. Fraze and three coauthors reported receiving grants from the Agency for Healthcare Research and Quality during the conduct of the study. Dr. Fraze also reported receiving grants from the Robert Wood Johnson Foundation during the conduct of the study and receiving grants as an investigator from the 6 Foundation Collaborative, Commonwealth Fund, and Centers for Disease Control and Prevention. One coauthor reported receiving grants from the National Institute on Aging/National Institutes of Health during the conduct of the study.
SOURCE: Fraze TK et al. JAMA Netw Open. 2019 Sep 18. doi: 10.1001/jamanetworkopen.2019.11514.
While momentum for social risk screening is growing nationally, the recent study by Fraze et al. illustrates that screening across multiple domains is not yet common in clinical settings, wrote Rachel Gold, PhD, of Kaiser Permanente Center for Health Research Northwest in Portland, Ore.
In an editorial accompanying the study, Dr. Gold and coauthor Laura Gottlieb, MD, an associate professor of family and community medicine at the University of California, San Francisco, wrote that a critical finding of the study is that reimbursement is associated with uptake of social risk screening (JAMA Network Open. 2019 Sep 18. doi: 10.1001/jamanetworkopen.2019.11513). Specifically, the analysis found that screening for social risks is more common in care settings that receive some form of payment to support such efforts, directly or indirectly.
“This finding aligns with other research showing that altering incentive structures may enhance the adoption of social risk screening in health care settings,” Dr. Gold and Dr. Gottlieb wrote. “But these findings are just a beginning. Disseminating and sustaining social risk screening will require a deep understanding of how best to structure financial and other incentives to optimally support social risk screening; high-quality research is needed to help design reimbursement models that reliably influence adoption.”
Further research is needed not only to explain challenges to the implementation of social risk screening, but also to reveal the best evidence-based methods for overcoming them, the authors wrote. Such methods will likely require a range of support strategies targeted to the needs of various health care settings.
“Documenting social risk data in health care settings requires identifying ways to implement such screening effectively and sustainably,” Dr. Gold and Dr. Gottlieb wrote. “These findings underscore how much we still have to learn about the types of support needed to implement and sustain these practices.”
Dr. Gold reported receiving grants from the National Institutes of Health during the conduct of the study. Dr. Gottlieb reported receiving grants from the Robert Wood Johnson Foundation, the Commonwealth Fund, Kaiser Permanente, Episcopal Health Foundation, the Agency for Healthcare Research and Quality, St. David’s Foundation, the Pritzker Family Fund, and the Harvard Research Network on Toxic Stress outside the submitted work.
While momentum for social risk screening is growing nationally, the recent study by Fraze et al. illustrates that screening across multiple domains is not yet common in clinical settings, wrote Rachel Gold, PhD, of Kaiser Permanente Center for Health Research Northwest in Portland, Ore.
In an editorial accompanying the study, Dr. Gold and coauthor Laura Gottlieb, MD, an associate professor of family and community medicine at the University of California, San Francisco, wrote that a critical finding of the study is that reimbursement is associated with uptake of social risk screening (JAMA Network Open. 2019 Sep 18. doi: 10.1001/jamanetworkopen.2019.11513). Specifically, the analysis found that screening for social risks is more common in care settings that receive some form of payment to support such efforts, directly or indirectly.
“This finding aligns with other research showing that altering incentive structures may enhance the adoption of social risk screening in health care settings,” Dr. Gold and Dr. Gottlieb wrote. “But these findings are just a beginning. Disseminating and sustaining social risk screening will require a deep understanding of how best to structure financial and other incentives to optimally support social risk screening; high-quality research is needed to help design reimbursement models that reliably influence adoption.”
Further research is needed not only to explain challenges to the implementation of social risk screening, but also to reveal the best evidence-based methods for overcoming them, the authors wrote. Such methods will likely require a range of support strategies targeted to the needs of various health care settings.
“Documenting social risk data in health care settings requires identifying ways to implement such screening effectively and sustainably,” Dr. Gold and Dr. Gottlieb wrote. “These findings underscore how much we still have to learn about the types of support needed to implement and sustain these practices.”
Dr. Gold reported receiving grants from the National Institutes of Health during the conduct of the study. Dr. Gottlieb reported receiving grants from the Robert Wood Johnson Foundation, the Commonwealth Fund, Kaiser Permanente, Episcopal Health Foundation, the Agency for Healthcare Research and Quality, St. David’s Foundation, the Pritzker Family Fund, and the Harvard Research Network on Toxic Stress outside the submitted work.
While momentum for social risk screening is growing nationally, the recent study by Fraze et al. illustrates that screening across multiple domains is not yet common in clinical settings, wrote Rachel Gold, PhD, of Kaiser Permanente Center for Health Research Northwest in Portland, Ore.
In an editorial accompanying the study, Dr. Gold and coauthor Laura Gottlieb, MD, an associate professor of family and community medicine at the University of California, San Francisco, wrote that a critical finding of the study is that reimbursement is associated with uptake of social risk screening (JAMA Network Open. 2019 Sep 18. doi: 10.1001/jamanetworkopen.2019.11513). Specifically, the analysis found that screening for social risks is more common in care settings that receive some form of payment to support such efforts, directly or indirectly.
“This finding aligns with other research showing that altering incentive structures may enhance the adoption of social risk screening in health care settings,” Dr. Gold and Dr. Gottlieb wrote. “But these findings are just a beginning. Disseminating and sustaining social risk screening will require a deep understanding of how best to structure financial and other incentives to optimally support social risk screening; high-quality research is needed to help design reimbursement models that reliably influence adoption.”
Further research is needed not only to explain challenges to the implementation of social risk screening, but also to reveal the best evidence-based methods for overcoming them, the authors wrote. Such methods will likely require a range of support strategies targeted to the needs of various health care settings.
“Documenting social risk data in health care settings requires identifying ways to implement such screening effectively and sustainably,” Dr. Gold and Dr. Gottlieb wrote. “These findings underscore how much we still have to learn about the types of support needed to implement and sustain these practices.”
Dr. Gold reported receiving grants from the National Institutes of Health during the conduct of the study. Dr. Gottlieb reported receiving grants from the Robert Wood Johnson Foundation, the Commonwealth Fund, Kaiser Permanente, Episcopal Health Foundation, the Agency for Healthcare Research and Quality, St. David’s Foundation, the Pritzker Family Fund, and the Harvard Research Network on Toxic Stress outside the submitted work.
that are associated with health outcomes, a study found.
Lead author Taressa K. Fraze, PhD, of the Dartmouth Institute for Health Policy and Clinical Practice in Lebanon, N.H., and colleagues conducted a cross-sectional survey analysis of responses by physician practices and hospitals that participated in the 2017-2018 National Survey of Healthcare Organizations and Systems. The investigators evaluated how many practices and hospitals reported screening of patients for five social needs: food insecurity, housing instability, utility needs, transportation needs, and experience with interpersonal violence. The final analysis included 2,190 physician practices and 739 hospitals.
Of physician practices, 56% reported screening for interpersonal violence, 35% screened for transportation needs, 30% for food insecurity, 28% for housing instability, and 23% for utility needs, according to the study published in JAMA Network Open.
Among hospitals, 75% reported screening for interpersonal violence, 74% for transportation needs, 60% for housing instability, 40% for food insecurity, and 36% for utility needs. Only 16% of physician practices and 24% of hospitals screened for all five social needs, the study found, while 33% of physician practices and 8% of hospitals reported screening for no social needs. The majority of the overall screening activity was driven by interpersonal violence screenings.
Physician practices that served more disadvantaged patients, including federally qualified health centers and those with more Medicaid revenue were more likely to screen for all five social needs. Practices in Medicaid accountable care organization contracts and those in Medicaid expansion states also had higher screening rates. Regionally, practices in the West had the highest screening rates, while practices in the Midwest had the lowest rates.
Among hospitals, the investigators found few significant screening differences based on hospital characteristics. Ownership, critical access status, delivery reform participation, rural status, region, and Medicaid expansion had no significant effects on screening rates, although academic medical centers were more likely to screen patients for all needs compared with nonacademic medical centers.
The study authors wrote that doctors and hospitals may need more resources and additional processes to screen for and/or to address the social needs of patients. They noted that practices and hospitals that did not screen for social needs were more likely to report a lack of financial resources, time, and incentives as major barriers.
To implement better screening protocols and address patients’ needs, the investigators wrote that doctors and hospitals will need financial support. For example, the Centers for Medicare & Medicaid Services should consider expanding care management billing to include managing care for patients who are both at risk or have clinically complex conditions in addition to social needs.
Dr. Fraze and three coauthors reported receiving grants from the Agency for Healthcare Research and Quality during the conduct of the study. Dr. Fraze also reported receiving grants from the Robert Wood Johnson Foundation during the conduct of the study and receiving grants as an investigator from the 6 Foundation Collaborative, Commonwealth Fund, and Centers for Disease Control and Prevention. One coauthor reported receiving grants from the National Institute on Aging/National Institutes of Health during the conduct of the study.
SOURCE: Fraze TK et al. JAMA Netw Open. 2019 Sep 18. doi: 10.1001/jamanetworkopen.2019.11514.
that are associated with health outcomes, a study found.
Lead author Taressa K. Fraze, PhD, of the Dartmouth Institute for Health Policy and Clinical Practice in Lebanon, N.H., and colleagues conducted a cross-sectional survey analysis of responses by physician practices and hospitals that participated in the 2017-2018 National Survey of Healthcare Organizations and Systems. The investigators evaluated how many practices and hospitals reported screening of patients for five social needs: food insecurity, housing instability, utility needs, transportation needs, and experience with interpersonal violence. The final analysis included 2,190 physician practices and 739 hospitals.
Of physician practices, 56% reported screening for interpersonal violence, 35% screened for transportation needs, 30% for food insecurity, 28% for housing instability, and 23% for utility needs, according to the study published in JAMA Network Open.
Among hospitals, 75% reported screening for interpersonal violence, 74% for transportation needs, 60% for housing instability, 40% for food insecurity, and 36% for utility needs. Only 16% of physician practices and 24% of hospitals screened for all five social needs, the study found, while 33% of physician practices and 8% of hospitals reported screening for no social needs. The majority of the overall screening activity was driven by interpersonal violence screenings.
Physician practices that served more disadvantaged patients, including federally qualified health centers and those with more Medicaid revenue were more likely to screen for all five social needs. Practices in Medicaid accountable care organization contracts and those in Medicaid expansion states also had higher screening rates. Regionally, practices in the West had the highest screening rates, while practices in the Midwest had the lowest rates.
Among hospitals, the investigators found few significant screening differences based on hospital characteristics. Ownership, critical access status, delivery reform participation, rural status, region, and Medicaid expansion had no significant effects on screening rates, although academic medical centers were more likely to screen patients for all needs compared with nonacademic medical centers.
The study authors wrote that doctors and hospitals may need more resources and additional processes to screen for and/or to address the social needs of patients. They noted that practices and hospitals that did not screen for social needs were more likely to report a lack of financial resources, time, and incentives as major barriers.
To implement better screening protocols and address patients’ needs, the investigators wrote that doctors and hospitals will need financial support. For example, the Centers for Medicare & Medicaid Services should consider expanding care management billing to include managing care for patients who are both at risk or have clinically complex conditions in addition to social needs.
Dr. Fraze and three coauthors reported receiving grants from the Agency for Healthcare Research and Quality during the conduct of the study. Dr. Fraze also reported receiving grants from the Robert Wood Johnson Foundation during the conduct of the study and receiving grants as an investigator from the 6 Foundation Collaborative, Commonwealth Fund, and Centers for Disease Control and Prevention. One coauthor reported receiving grants from the National Institute on Aging/National Institutes of Health during the conduct of the study.
SOURCE: Fraze TK et al. JAMA Netw Open. 2019 Sep 18. doi: 10.1001/jamanetworkopen.2019.11514.
FROM JAMA NETWORK OPEN
Health Policy Q&A
States pass record number of laws to reel in drug prices
Whether Congress will act this year to address the affordability of prescription drugs – a high priority among voters – remains uncertain. But states aren’t waiting.
So far this year, 33 states have enacted a record 51 laws to address drug prices, affordability, and access. That tops the previous record of 45 laws enacted in 28 states set just last year, according to the National Academy for State Health Policy, a nonprofit advocacy group that develops model legislation and promotes such laws.
Among the new measures are those that authorize importing prescription drugs, screen for excessive price increases by drug companies, and establish oversight boards to set the prices that states will pay for drugs.
“Legislative activity in this area is escalating,” said Trish Riley, NASHP’s executive director. “This year, some states moved to launch programs that directly impact what they and consumers pay for high-cost drugs.”
And more laws could be coming before year’s end. Of the handful of states still in legislative session – including California, Massachusetts, Michigan, New Jersey, Ohio, and Pennsylvania – debate continues on dozens of prescription drug bills. In New Jersey alone, some 20 proposed laws are under consideration.
“Both Democrat and Republican leaders have shown a willingness to pursue strong measures that help consumers but also protect state taxpayer dollars,” said Hemi Tewarson, director of the National Governors Association’s health programs.
Ms. Riley, Ms. Tewarson, and others note, however, that states can go only so far in addressing rising drug prices, and that federal legislation would be necessary to have a major effect on the way the marketplace works.
Federal lawmakers are keeping a close eye on the state initiatives, Ms. Tewarson said, to gauge where legislative compromise may lie – even as Congress debates more than a dozen bills that target drug costs. Political divisiveness, a packed congressional schedule and a looming election year could stall momentum at the federal level.
The pharmaceutical industry has opposed most – though not all – state bills, said Priscilla VanderVeer, a spokeswoman for the Pharmaceutical Research and Manufacturers of America, the industry’s main trade group.
“We agree that what consumers now pay for drugs out-of-pocket is a serious problem,” said Ms. VanderVeer. “Many states have passed bills that look good on paper but that we don’t believe will save consumers money.”
Limiting gag rules for pharmacists
At least 16 states have enacted 20 laws governing the behavior of pharmacy benefit managers. The so-called PBMs serve as middlemen among drugmakers, insurance companies, and pharmacies, largely with pharmaceutical industry support.
Those laws add to the 28 passed in 2018. Most of the new laws ban “gag clauses” that some PBMs impose on pharmacists. The clauses, written into pharmacy contracts, stop pharmacists from discussing with customers whether a drug’s cash price would be lower than its out-of-pocket cost under insurance.
With widespread public outrage over gag clauses pushing states to act, federal lawmakers got the message. In October, Congress passed a federal law banning such clauses in PBM-pharmacy contracts nationwide and under the Medicare Part D prescription drug benefit. The Senate passed it 98-2.
Even so, many of this year’s PBM laws contain additional gag clause limitations that go beyond the 2018 federal law.
Importing cheaper drugs
Four states – Colorado, Florida, Maine, and Vermont – this year have enacted measures to establish programs to import cheaper prescription drugs from Canada and, in Florida’s case, potentially other countries. Six other states are considering such legislation.
Medicines from Canada and other countries are less expensive because those nations negotiate directly with drugmakers to set prices.
“This is an area where states once feared to tread,” said Jane Horvath, a consultant with NASHP who has advised Maryland and Oregon, among other states, on prescription drug policy. “Now both Republicans and Democrats view it as a way to infuse more price competition into the marketplace.”
Hurdles remain, however. A 2003 law allows states to import cheaper drugs from Canada but only if the federal Health & Human Services Department approves a state’s plan and certifies its safety. During 2004-2009, the federal government halted nascent drug import efforts in five states.
Even so, momentum for importation has built in recent years in states and Congress as drug prices have continued to rise. And the Trump administration this summer threw its support behind the idea.
Florida Gov. Ron DeSantis, a Republican and close ally of President Donald Trump, signed his state’s measure into law on June 11, claiming he did so after Trump personally promised him that the White House would back the initiative.
On July 31, HHS announced an “action plan” to “lay the foundation for safe importation of certain prescription drugs.” The plan includes a process to authorize state initiatives. It also requires formal regulatory review, including establishing Food and Drug Administration safety criteria. That process could take up to 2 years.
Two big problems remain: In the weeks since the announcement, the Canadian government has opposed any plan that would rely solely on Canada as a source of imported drugs. The pharmaceutical industry also opposes the plan.
Creating drug affordability boards
Maryland and Maine enacted laws this year that establish state agencies to review the costs of drugs and take action against those whose price increases exceed a certain threshold.
New Jersey and Massachusetts are debating similar legislation this year.
Maryland’s law establishes a five-member board to review the list prices and costs of drugs purchased by the state and Maryland’s county and local governments. The board will probe drugs that increase in price by $3,000 or more per year and new medicines that enter the market costing $30,000 or more per year or over the course of treatment.
If approved by future legislation, upper payment limits on drugs with excessive price increases or annual costs would take effect in January 2022.
“My constituents have signaled loud and clear that bringing drug prices down is one of their top priorities,” said state Sen. Katherine Klausmeier, a Democrat representing Baltimore, who sponsored the legislation.
Maine’s law also establishes a five-member board. Beginning in 2021, the board will set annual spending targets for drugs purchased by the state and local governments.
Increasing price transparency
This year, four states – Colorado, Oregon, Texas, and Washington – became the latest to enact laws requiring drug companies to provide information to states and consumers on the list prices of drugs and planned price increases.
The majority of states now have such transparency laws, and most post the data on public websites. The details vary, but all states with such laws seek to identify drugs with price increases above 10% or more a year, and drugs with price increases above set dollar values.
Oregon’s new law, for example, requires manufacturers to notify the state 60 days in advance of any planned increase of 10% or more in the price of brand-name drugs, and any 25% or greater increase in the price of generic drugs.
“That 60-days’ notice was very important to us,” said state Rep. Andrea Salinas, a Democrat and chair of the Oregon House’s health committee, who represents Lake Oswego. “It gives doctors and patients advance notice and a chance to adjust and consider what to do.”
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Whether Congress will act this year to address the affordability of prescription drugs – a high priority among voters – remains uncertain. But states aren’t waiting.
So far this year, 33 states have enacted a record 51 laws to address drug prices, affordability, and access. That tops the previous record of 45 laws enacted in 28 states set just last year, according to the National Academy for State Health Policy, a nonprofit advocacy group that develops model legislation and promotes such laws.
Among the new measures are those that authorize importing prescription drugs, screen for excessive price increases by drug companies, and establish oversight boards to set the prices that states will pay for drugs.
“Legislative activity in this area is escalating,” said Trish Riley, NASHP’s executive director. “This year, some states moved to launch programs that directly impact what they and consumers pay for high-cost drugs.”
And more laws could be coming before year’s end. Of the handful of states still in legislative session – including California, Massachusetts, Michigan, New Jersey, Ohio, and Pennsylvania – debate continues on dozens of prescription drug bills. In New Jersey alone, some 20 proposed laws are under consideration.
“Both Democrat and Republican leaders have shown a willingness to pursue strong measures that help consumers but also protect state taxpayer dollars,” said Hemi Tewarson, director of the National Governors Association’s health programs.
Ms. Riley, Ms. Tewarson, and others note, however, that states can go only so far in addressing rising drug prices, and that federal legislation would be necessary to have a major effect on the way the marketplace works.
Federal lawmakers are keeping a close eye on the state initiatives, Ms. Tewarson said, to gauge where legislative compromise may lie – even as Congress debates more than a dozen bills that target drug costs. Political divisiveness, a packed congressional schedule and a looming election year could stall momentum at the federal level.
The pharmaceutical industry has opposed most – though not all – state bills, said Priscilla VanderVeer, a spokeswoman for the Pharmaceutical Research and Manufacturers of America, the industry’s main trade group.
“We agree that what consumers now pay for drugs out-of-pocket is a serious problem,” said Ms. VanderVeer. “Many states have passed bills that look good on paper but that we don’t believe will save consumers money.”
Limiting gag rules for pharmacists
At least 16 states have enacted 20 laws governing the behavior of pharmacy benefit managers. The so-called PBMs serve as middlemen among drugmakers, insurance companies, and pharmacies, largely with pharmaceutical industry support.
Those laws add to the 28 passed in 2018. Most of the new laws ban “gag clauses” that some PBMs impose on pharmacists. The clauses, written into pharmacy contracts, stop pharmacists from discussing with customers whether a drug’s cash price would be lower than its out-of-pocket cost under insurance.
With widespread public outrage over gag clauses pushing states to act, federal lawmakers got the message. In October, Congress passed a federal law banning such clauses in PBM-pharmacy contracts nationwide and under the Medicare Part D prescription drug benefit. The Senate passed it 98-2.
Even so, many of this year’s PBM laws contain additional gag clause limitations that go beyond the 2018 federal law.
Importing cheaper drugs
Four states – Colorado, Florida, Maine, and Vermont – this year have enacted measures to establish programs to import cheaper prescription drugs from Canada and, in Florida’s case, potentially other countries. Six other states are considering such legislation.
Medicines from Canada and other countries are less expensive because those nations negotiate directly with drugmakers to set prices.
“This is an area where states once feared to tread,” said Jane Horvath, a consultant with NASHP who has advised Maryland and Oregon, among other states, on prescription drug policy. “Now both Republicans and Democrats view it as a way to infuse more price competition into the marketplace.”
Hurdles remain, however. A 2003 law allows states to import cheaper drugs from Canada but only if the federal Health & Human Services Department approves a state’s plan and certifies its safety. During 2004-2009, the federal government halted nascent drug import efforts in five states.
Even so, momentum for importation has built in recent years in states and Congress as drug prices have continued to rise. And the Trump administration this summer threw its support behind the idea.
Florida Gov. Ron DeSantis, a Republican and close ally of President Donald Trump, signed his state’s measure into law on June 11, claiming he did so after Trump personally promised him that the White House would back the initiative.
On July 31, HHS announced an “action plan” to “lay the foundation for safe importation of certain prescription drugs.” The plan includes a process to authorize state initiatives. It also requires formal regulatory review, including establishing Food and Drug Administration safety criteria. That process could take up to 2 years.
Two big problems remain: In the weeks since the announcement, the Canadian government has opposed any plan that would rely solely on Canada as a source of imported drugs. The pharmaceutical industry also opposes the plan.
Creating drug affordability boards
Maryland and Maine enacted laws this year that establish state agencies to review the costs of drugs and take action against those whose price increases exceed a certain threshold.
New Jersey and Massachusetts are debating similar legislation this year.
Maryland’s law establishes a five-member board to review the list prices and costs of drugs purchased by the state and Maryland’s county and local governments. The board will probe drugs that increase in price by $3,000 or more per year and new medicines that enter the market costing $30,000 or more per year or over the course of treatment.
If approved by future legislation, upper payment limits on drugs with excessive price increases or annual costs would take effect in January 2022.
“My constituents have signaled loud and clear that bringing drug prices down is one of their top priorities,” said state Sen. Katherine Klausmeier, a Democrat representing Baltimore, who sponsored the legislation.
Maine’s law also establishes a five-member board. Beginning in 2021, the board will set annual spending targets for drugs purchased by the state and local governments.
Increasing price transparency
This year, four states – Colorado, Oregon, Texas, and Washington – became the latest to enact laws requiring drug companies to provide information to states and consumers on the list prices of drugs and planned price increases.
The majority of states now have such transparency laws, and most post the data on public websites. The details vary, but all states with such laws seek to identify drugs with price increases above 10% or more a year, and drugs with price increases above set dollar values.
Oregon’s new law, for example, requires manufacturers to notify the state 60 days in advance of any planned increase of 10% or more in the price of brand-name drugs, and any 25% or greater increase in the price of generic drugs.
“That 60-days’ notice was very important to us,” said state Rep. Andrea Salinas, a Democrat and chair of the Oregon House’s health committee, who represents Lake Oswego. “It gives doctors and patients advance notice and a chance to adjust and consider what to do.”
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Whether Congress will act this year to address the affordability of prescription drugs – a high priority among voters – remains uncertain. But states aren’t waiting.
So far this year, 33 states have enacted a record 51 laws to address drug prices, affordability, and access. That tops the previous record of 45 laws enacted in 28 states set just last year, according to the National Academy for State Health Policy, a nonprofit advocacy group that develops model legislation and promotes such laws.
Among the new measures are those that authorize importing prescription drugs, screen for excessive price increases by drug companies, and establish oversight boards to set the prices that states will pay for drugs.
“Legislative activity in this area is escalating,” said Trish Riley, NASHP’s executive director. “This year, some states moved to launch programs that directly impact what they and consumers pay for high-cost drugs.”
And more laws could be coming before year’s end. Of the handful of states still in legislative session – including California, Massachusetts, Michigan, New Jersey, Ohio, and Pennsylvania – debate continues on dozens of prescription drug bills. In New Jersey alone, some 20 proposed laws are under consideration.
“Both Democrat and Republican leaders have shown a willingness to pursue strong measures that help consumers but also protect state taxpayer dollars,” said Hemi Tewarson, director of the National Governors Association’s health programs.
Ms. Riley, Ms. Tewarson, and others note, however, that states can go only so far in addressing rising drug prices, and that federal legislation would be necessary to have a major effect on the way the marketplace works.
Federal lawmakers are keeping a close eye on the state initiatives, Ms. Tewarson said, to gauge where legislative compromise may lie – even as Congress debates more than a dozen bills that target drug costs. Political divisiveness, a packed congressional schedule and a looming election year could stall momentum at the federal level.
The pharmaceutical industry has opposed most – though not all – state bills, said Priscilla VanderVeer, a spokeswoman for the Pharmaceutical Research and Manufacturers of America, the industry’s main trade group.
“We agree that what consumers now pay for drugs out-of-pocket is a serious problem,” said Ms. VanderVeer. “Many states have passed bills that look good on paper but that we don’t believe will save consumers money.”
Limiting gag rules for pharmacists
At least 16 states have enacted 20 laws governing the behavior of pharmacy benefit managers. The so-called PBMs serve as middlemen among drugmakers, insurance companies, and pharmacies, largely with pharmaceutical industry support.
Those laws add to the 28 passed in 2018. Most of the new laws ban “gag clauses” that some PBMs impose on pharmacists. The clauses, written into pharmacy contracts, stop pharmacists from discussing with customers whether a drug’s cash price would be lower than its out-of-pocket cost under insurance.
With widespread public outrage over gag clauses pushing states to act, federal lawmakers got the message. In October, Congress passed a federal law banning such clauses in PBM-pharmacy contracts nationwide and under the Medicare Part D prescription drug benefit. The Senate passed it 98-2.
Even so, many of this year’s PBM laws contain additional gag clause limitations that go beyond the 2018 federal law.
Importing cheaper drugs
Four states – Colorado, Florida, Maine, and Vermont – this year have enacted measures to establish programs to import cheaper prescription drugs from Canada and, in Florida’s case, potentially other countries. Six other states are considering such legislation.
Medicines from Canada and other countries are less expensive because those nations negotiate directly with drugmakers to set prices.
“This is an area where states once feared to tread,” said Jane Horvath, a consultant with NASHP who has advised Maryland and Oregon, among other states, on prescription drug policy. “Now both Republicans and Democrats view it as a way to infuse more price competition into the marketplace.”
Hurdles remain, however. A 2003 law allows states to import cheaper drugs from Canada but only if the federal Health & Human Services Department approves a state’s plan and certifies its safety. During 2004-2009, the federal government halted nascent drug import efforts in five states.
Even so, momentum for importation has built in recent years in states and Congress as drug prices have continued to rise. And the Trump administration this summer threw its support behind the idea.
Florida Gov. Ron DeSantis, a Republican and close ally of President Donald Trump, signed his state’s measure into law on June 11, claiming he did so after Trump personally promised him that the White House would back the initiative.
On July 31, HHS announced an “action plan” to “lay the foundation for safe importation of certain prescription drugs.” The plan includes a process to authorize state initiatives. It also requires formal regulatory review, including establishing Food and Drug Administration safety criteria. That process could take up to 2 years.
Two big problems remain: In the weeks since the announcement, the Canadian government has opposed any plan that would rely solely on Canada as a source of imported drugs. The pharmaceutical industry also opposes the plan.
Creating drug affordability boards
Maryland and Maine enacted laws this year that establish state agencies to review the costs of drugs and take action against those whose price increases exceed a certain threshold.
New Jersey and Massachusetts are debating similar legislation this year.
Maryland’s law establishes a five-member board to review the list prices and costs of drugs purchased by the state and Maryland’s county and local governments. The board will probe drugs that increase in price by $3,000 or more per year and new medicines that enter the market costing $30,000 or more per year or over the course of treatment.
If approved by future legislation, upper payment limits on drugs with excessive price increases or annual costs would take effect in January 2022.
“My constituents have signaled loud and clear that bringing drug prices down is one of their top priorities,” said state Sen. Katherine Klausmeier, a Democrat representing Baltimore, who sponsored the legislation.
Maine’s law also establishes a five-member board. Beginning in 2021, the board will set annual spending targets for drugs purchased by the state and local governments.
Increasing price transparency
This year, four states – Colorado, Oregon, Texas, and Washington – became the latest to enact laws requiring drug companies to provide information to states and consumers on the list prices of drugs and planned price increases.
The majority of states now have such transparency laws, and most post the data on public websites. The details vary, but all states with such laws seek to identify drugs with price increases above 10% or more a year, and drugs with price increases above set dollar values.
Oregon’s new law, for example, requires manufacturers to notify the state 60 days in advance of any planned increase of 10% or more in the price of brand-name drugs, and any 25% or greater increase in the price of generic drugs.
“That 60-days’ notice was very important to us,” said state Rep. Andrea Salinas, a Democrat and chair of the Oregon House’s health committee, who represents Lake Oswego. “It gives doctors and patients advance notice and a chance to adjust and consider what to do.”
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
How do social determinants of health play out in physician practice?
Social determinants of health – access to nutritious food, safe housing, prescription drugs and transportation to medical appointments – affect a patient’s ability to adhere to a medical treatment plan. Initiatives are underway to capture and chart these data in order to connect patients with the services they need and to measure the results of those efforts.
But how can these tasks be accomplished by physicians with too little patient time and too many administrative responsibilities?
The ability to capture social factors through coding could, however, become more relevant under value-based care and population health payment models, which reward physicians and other providers for improved outcomes. They could also be used for risk adjustments to the physician’s caseload and for automatically steering community resources more precisely, such as through the EHR, by triggering referrals for social programs, said Sue Bowman, MJ, RHIA, CCS, FAHIMA, senior director for Coding Policy and Compliance at the American Health Information Management Association (AHIMA).
According to several sources interviewed for this article, documenting social determinants of health will become increasingly important for Federally Qualified Health Centers, accountable care organizations, large health systems, Medicare Advantage plans, and Centers for Medicare & Medicaid Services and Medicaid managed care pilots.
An initiative for new codes that would better document and standardize how social determinants of health data are collected, processed and integrated was unveiled earlier this year at a meeting of the U.S. ICD-10 Coordination and Maintenance Committee of the National Center for Health Statistics. The proposal came from UnitedHealthcare and has been endorsed by the American Medical Association. It includes 23 new codes that would be incorporated into the ICD-10-CM. By combining traditional medical data and social determinants of health data, the codes would trigger referrals to local and national resources in patients’ communities. A ruling on adopting the proposal is not expected until next year, with possible implementation of the codes in October 2021.
In the interim, there are 11 existing ICD-10-CM codes that can be used today to capture some of the social, nonmedical patient needs that might affect outcomes of care. These 11 “Z” codes (Z55-Z65) identify social problems related to education and literacy, employment, housing and economic circumstances, and psychosocial circumstances, but they don’t incorporate the data into a person’s overall care plan.
Mobilizing the EHR
Pablo Buitron de la Vega, MD, MSc, an internist at Boston Medical Center (BMC), has spearheaded the THRIVE social determinants initiative at BMC. THRIVE (Tool for Health and Resilience in Vulnerable Environments) is an EHR-based intervention that facilitates an automatic printout of referrals for resources in the community and in the hospital to address identified social factors.
THRIVE has been used to screen 60,000 patients at the medical center since 2017.
The patient completes the screening tool and a medical assistant enters the information into the medical record, which takes an average of one minute, he said. If patients answer that they are homeless or need help obtaining food, the EHR automatically generates a printed resource guide and a medical navigator is called. Data indicates that 85% of eligible patients at BMC have been screened, and of those who ask for help, 80%-90% are offered resources.
The THRIVE screening tool also automatically generates a code on the bill, and an accountable care organization of MassHealth, the state’s Medicaid authority which contracts with BMC’s HealthNet managed care plan, has begun recognizing the physician’s role in assessing problems like homelessness. Social factors that can be captured with ICD-10 codes, primarily homelessness, are now being included in the bill. And MassHealth is increasing its physician payment accordingly to take into account the physician’s role in addressing the issue.
More than half of the THRIVE caseload is covered under the Medicaid Accountable Care Organization (ACO). Other health plans have been slower to catch on. “Our patients have many different coverage models, and it gets very complicated,” he said. “That’s why ACOs and value-based payment models are so important to recognizing the business case that, if you address patients’ social needs, you are helping to better manage the ACO’s covered population,” he said.
Dr. Buitron de la Vega added that except for homelessness and food insecurity, existing ICD-10 codes aren’t that helpful in identifying social needs, so he looks forward to adoption of new codes such as those proposed by UnitedHealthcare. “At this time, the evidence that universal screening for [social determinants of health] will decrease cost and improve health outcomes is not there. Meanwhile, healthcare institutions need to make massive investments to help community organizations to grow and help all those patients that we are referring to them for social needs.”
Codes that spark actions
Sheila Shapiro, senior vice president of National Strategic Partnerships for UnitedHealthcare, said that “for populations covered by our plans, UnitedHealthcare has also created alternate coding methodologies, for example for transportation, as placeholder codes in lieu of an ICD-10 code, allowing us to bring this information forward.”
If identified patient needs are reported on the claim, UnitedHealthcare case managers use the information to assist members directly with referrals to social and governmental services, and then share those names and numbers with the medical providers, Ms. Shapiro said. A total of 600,000 UnitedHealthcare members have been assisted with over 760,000 such referrals.
If adopted, the new coding proposal could capture more data and trigger more referrals to service programs. The hope would be a savings in health expenditures and an improvement in patient outcomes.
Through its Integrated Health Model Initiative (IHMI), the AMA is collaborating with UnitedHealthcare on processes for incorporating social determinants of health into routine medical care, said Tom Giannulli, MD, chief medical information officer for IHMI. It’s hard to assess patients’ risks and outcomes without a rich data set to allow comparisons across populations, he added.
The proposed codes “will also help us do more research, with the idea that once we understand the risk, we can see how to mitigate it,” he said. “How do we take adjacent social resources and pull them into the medical space and create benefits – which could make the doctor’s life easier?”
Measuring efficacy
“Today we really don’t know enough about how social determinants of health are driving utilization and costs, or how to design mechanisms that will allow us eventually to change our payment systems in response,” says Bruce Chernof, MD, president and CEO of the SCAN Foundation, an independent California-based foundation devoted to transforming the health care of older adults.
The new codes proposed by UnitedHealthcare could provide powerful layers of information to make something that’s invisible more visible. “You can’t really improve what you can’t measure, but it’s not enough to just identify social factors in health. If you identify and don’t refer, or if you refer and programs are not available to respond, then what have you really accomplished?” asked Dr. Chernof, an internist,
“We were trained as internists to discuss the patient’s social history. But what has become clearer, as the population ages and we learn more about the challenges internists face today, social determinants of health are not an area where we have received enough training. And doctors already feel like they are up to their eyeballs in codes,” he said. “If we are going to start collecting this data, it is incumbent that the data actually be used to improve outcomes.”
AHIMA is advising a cautious approach. In its comments on the 23 proposed new ICD-10 codes, AHIMA recommended delaying implementation until more information is available from initiatives such as the Gravity Project of the Social Interventions Research and Evaluation Network at the University of California, San Francisco. The Gravity Project is a national collaborative to advance interoperable social risk documentation.
“There may be other, better ways to capture social factors. ... I’m not sure ICD-10-CM codes are the best way to do this because these issues are somewhat outside the scope of what ICD-10 is designed to capture,” Ms. Bowman said. There are also privacy concerns, and some of the social factors change frequently in the lives of patients.
Social determinants of health – access to nutritious food, safe housing, prescription drugs and transportation to medical appointments – affect a patient’s ability to adhere to a medical treatment plan. Initiatives are underway to capture and chart these data in order to connect patients with the services they need and to measure the results of those efforts.
But how can these tasks be accomplished by physicians with too little patient time and too many administrative responsibilities?
The ability to capture social factors through coding could, however, become more relevant under value-based care and population health payment models, which reward physicians and other providers for improved outcomes. They could also be used for risk adjustments to the physician’s caseload and for automatically steering community resources more precisely, such as through the EHR, by triggering referrals for social programs, said Sue Bowman, MJ, RHIA, CCS, FAHIMA, senior director for Coding Policy and Compliance at the American Health Information Management Association (AHIMA).
According to several sources interviewed for this article, documenting social determinants of health will become increasingly important for Federally Qualified Health Centers, accountable care organizations, large health systems, Medicare Advantage plans, and Centers for Medicare & Medicaid Services and Medicaid managed care pilots.
An initiative for new codes that would better document and standardize how social determinants of health data are collected, processed and integrated was unveiled earlier this year at a meeting of the U.S. ICD-10 Coordination and Maintenance Committee of the National Center for Health Statistics. The proposal came from UnitedHealthcare and has been endorsed by the American Medical Association. It includes 23 new codes that would be incorporated into the ICD-10-CM. By combining traditional medical data and social determinants of health data, the codes would trigger referrals to local and national resources in patients’ communities. A ruling on adopting the proposal is not expected until next year, with possible implementation of the codes in October 2021.
In the interim, there are 11 existing ICD-10-CM codes that can be used today to capture some of the social, nonmedical patient needs that might affect outcomes of care. These 11 “Z” codes (Z55-Z65) identify social problems related to education and literacy, employment, housing and economic circumstances, and psychosocial circumstances, but they don’t incorporate the data into a person’s overall care plan.
Mobilizing the EHR
Pablo Buitron de la Vega, MD, MSc, an internist at Boston Medical Center (BMC), has spearheaded the THRIVE social determinants initiative at BMC. THRIVE (Tool for Health and Resilience in Vulnerable Environments) is an EHR-based intervention that facilitates an automatic printout of referrals for resources in the community and in the hospital to address identified social factors.
THRIVE has been used to screen 60,000 patients at the medical center since 2017.
The patient completes the screening tool and a medical assistant enters the information into the medical record, which takes an average of one minute, he said. If patients answer that they are homeless or need help obtaining food, the EHR automatically generates a printed resource guide and a medical navigator is called. Data indicates that 85% of eligible patients at BMC have been screened, and of those who ask for help, 80%-90% are offered resources.
The THRIVE screening tool also automatically generates a code on the bill, and an accountable care organization of MassHealth, the state’s Medicaid authority which contracts with BMC’s HealthNet managed care plan, has begun recognizing the physician’s role in assessing problems like homelessness. Social factors that can be captured with ICD-10 codes, primarily homelessness, are now being included in the bill. And MassHealth is increasing its physician payment accordingly to take into account the physician’s role in addressing the issue.
More than half of the THRIVE caseload is covered under the Medicaid Accountable Care Organization (ACO). Other health plans have been slower to catch on. “Our patients have many different coverage models, and it gets very complicated,” he said. “That’s why ACOs and value-based payment models are so important to recognizing the business case that, if you address patients’ social needs, you are helping to better manage the ACO’s covered population,” he said.
Dr. Buitron de la Vega added that except for homelessness and food insecurity, existing ICD-10 codes aren’t that helpful in identifying social needs, so he looks forward to adoption of new codes such as those proposed by UnitedHealthcare. “At this time, the evidence that universal screening for [social determinants of health] will decrease cost and improve health outcomes is not there. Meanwhile, healthcare institutions need to make massive investments to help community organizations to grow and help all those patients that we are referring to them for social needs.”
Codes that spark actions
Sheila Shapiro, senior vice president of National Strategic Partnerships for UnitedHealthcare, said that “for populations covered by our plans, UnitedHealthcare has also created alternate coding methodologies, for example for transportation, as placeholder codes in lieu of an ICD-10 code, allowing us to bring this information forward.”
If identified patient needs are reported on the claim, UnitedHealthcare case managers use the information to assist members directly with referrals to social and governmental services, and then share those names and numbers with the medical providers, Ms. Shapiro said. A total of 600,000 UnitedHealthcare members have been assisted with over 760,000 such referrals.
If adopted, the new coding proposal could capture more data and trigger more referrals to service programs. The hope would be a savings in health expenditures and an improvement in patient outcomes.
Through its Integrated Health Model Initiative (IHMI), the AMA is collaborating with UnitedHealthcare on processes for incorporating social determinants of health into routine medical care, said Tom Giannulli, MD, chief medical information officer for IHMI. It’s hard to assess patients’ risks and outcomes without a rich data set to allow comparisons across populations, he added.
The proposed codes “will also help us do more research, with the idea that once we understand the risk, we can see how to mitigate it,” he said. “How do we take adjacent social resources and pull them into the medical space and create benefits – which could make the doctor’s life easier?”
Measuring efficacy
“Today we really don’t know enough about how social determinants of health are driving utilization and costs, or how to design mechanisms that will allow us eventually to change our payment systems in response,” says Bruce Chernof, MD, president and CEO of the SCAN Foundation, an independent California-based foundation devoted to transforming the health care of older adults.
The new codes proposed by UnitedHealthcare could provide powerful layers of information to make something that’s invisible more visible. “You can’t really improve what you can’t measure, but it’s not enough to just identify social factors in health. If you identify and don’t refer, or if you refer and programs are not available to respond, then what have you really accomplished?” asked Dr. Chernof, an internist,
“We were trained as internists to discuss the patient’s social history. But what has become clearer, as the population ages and we learn more about the challenges internists face today, social determinants of health are not an area where we have received enough training. And doctors already feel like they are up to their eyeballs in codes,” he said. “If we are going to start collecting this data, it is incumbent that the data actually be used to improve outcomes.”
AHIMA is advising a cautious approach. In its comments on the 23 proposed new ICD-10 codes, AHIMA recommended delaying implementation until more information is available from initiatives such as the Gravity Project of the Social Interventions Research and Evaluation Network at the University of California, San Francisco. The Gravity Project is a national collaborative to advance interoperable social risk documentation.
“There may be other, better ways to capture social factors. ... I’m not sure ICD-10-CM codes are the best way to do this because these issues are somewhat outside the scope of what ICD-10 is designed to capture,” Ms. Bowman said. There are also privacy concerns, and some of the social factors change frequently in the lives of patients.
Social determinants of health – access to nutritious food, safe housing, prescription drugs and transportation to medical appointments – affect a patient’s ability to adhere to a medical treatment plan. Initiatives are underway to capture and chart these data in order to connect patients with the services they need and to measure the results of those efforts.
But how can these tasks be accomplished by physicians with too little patient time and too many administrative responsibilities?
The ability to capture social factors through coding could, however, become more relevant under value-based care and population health payment models, which reward physicians and other providers for improved outcomes. They could also be used for risk adjustments to the physician’s caseload and for automatically steering community resources more precisely, such as through the EHR, by triggering referrals for social programs, said Sue Bowman, MJ, RHIA, CCS, FAHIMA, senior director for Coding Policy and Compliance at the American Health Information Management Association (AHIMA).
According to several sources interviewed for this article, documenting social determinants of health will become increasingly important for Federally Qualified Health Centers, accountable care organizations, large health systems, Medicare Advantage plans, and Centers for Medicare & Medicaid Services and Medicaid managed care pilots.
An initiative for new codes that would better document and standardize how social determinants of health data are collected, processed and integrated was unveiled earlier this year at a meeting of the U.S. ICD-10 Coordination and Maintenance Committee of the National Center for Health Statistics. The proposal came from UnitedHealthcare and has been endorsed by the American Medical Association. It includes 23 new codes that would be incorporated into the ICD-10-CM. By combining traditional medical data and social determinants of health data, the codes would trigger referrals to local and national resources in patients’ communities. A ruling on adopting the proposal is not expected until next year, with possible implementation of the codes in October 2021.
In the interim, there are 11 existing ICD-10-CM codes that can be used today to capture some of the social, nonmedical patient needs that might affect outcomes of care. These 11 “Z” codes (Z55-Z65) identify social problems related to education and literacy, employment, housing and economic circumstances, and psychosocial circumstances, but they don’t incorporate the data into a person’s overall care plan.
Mobilizing the EHR
Pablo Buitron de la Vega, MD, MSc, an internist at Boston Medical Center (BMC), has spearheaded the THRIVE social determinants initiative at BMC. THRIVE (Tool for Health and Resilience in Vulnerable Environments) is an EHR-based intervention that facilitates an automatic printout of referrals for resources in the community and in the hospital to address identified social factors.
THRIVE has been used to screen 60,000 patients at the medical center since 2017.
The patient completes the screening tool and a medical assistant enters the information into the medical record, which takes an average of one minute, he said. If patients answer that they are homeless or need help obtaining food, the EHR automatically generates a printed resource guide and a medical navigator is called. Data indicates that 85% of eligible patients at BMC have been screened, and of those who ask for help, 80%-90% are offered resources.
The THRIVE screening tool also automatically generates a code on the bill, and an accountable care organization of MassHealth, the state’s Medicaid authority which contracts with BMC’s HealthNet managed care plan, has begun recognizing the physician’s role in assessing problems like homelessness. Social factors that can be captured with ICD-10 codes, primarily homelessness, are now being included in the bill. And MassHealth is increasing its physician payment accordingly to take into account the physician’s role in addressing the issue.
More than half of the THRIVE caseload is covered under the Medicaid Accountable Care Organization (ACO). Other health plans have been slower to catch on. “Our patients have many different coverage models, and it gets very complicated,” he said. “That’s why ACOs and value-based payment models are so important to recognizing the business case that, if you address patients’ social needs, you are helping to better manage the ACO’s covered population,” he said.
Dr. Buitron de la Vega added that except for homelessness and food insecurity, existing ICD-10 codes aren’t that helpful in identifying social needs, so he looks forward to adoption of new codes such as those proposed by UnitedHealthcare. “At this time, the evidence that universal screening for [social determinants of health] will decrease cost and improve health outcomes is not there. Meanwhile, healthcare institutions need to make massive investments to help community organizations to grow and help all those patients that we are referring to them for social needs.”
Codes that spark actions
Sheila Shapiro, senior vice president of National Strategic Partnerships for UnitedHealthcare, said that “for populations covered by our plans, UnitedHealthcare has also created alternate coding methodologies, for example for transportation, as placeholder codes in lieu of an ICD-10 code, allowing us to bring this information forward.”
If identified patient needs are reported on the claim, UnitedHealthcare case managers use the information to assist members directly with referrals to social and governmental services, and then share those names and numbers with the medical providers, Ms. Shapiro said. A total of 600,000 UnitedHealthcare members have been assisted with over 760,000 such referrals.
If adopted, the new coding proposal could capture more data and trigger more referrals to service programs. The hope would be a savings in health expenditures and an improvement in patient outcomes.
Through its Integrated Health Model Initiative (IHMI), the AMA is collaborating with UnitedHealthcare on processes for incorporating social determinants of health into routine medical care, said Tom Giannulli, MD, chief medical information officer for IHMI. It’s hard to assess patients’ risks and outcomes without a rich data set to allow comparisons across populations, he added.
The proposed codes “will also help us do more research, with the idea that once we understand the risk, we can see how to mitigate it,” he said. “How do we take adjacent social resources and pull them into the medical space and create benefits – which could make the doctor’s life easier?”
Measuring efficacy
“Today we really don’t know enough about how social determinants of health are driving utilization and costs, or how to design mechanisms that will allow us eventually to change our payment systems in response,” says Bruce Chernof, MD, president and CEO of the SCAN Foundation, an independent California-based foundation devoted to transforming the health care of older adults.
The new codes proposed by UnitedHealthcare could provide powerful layers of information to make something that’s invisible more visible. “You can’t really improve what you can’t measure, but it’s not enough to just identify social factors in health. If you identify and don’t refer, or if you refer and programs are not available to respond, then what have you really accomplished?” asked Dr. Chernof, an internist,
“We were trained as internists to discuss the patient’s social history. But what has become clearer, as the population ages and we learn more about the challenges internists face today, social determinants of health are not an area where we have received enough training. And doctors already feel like they are up to their eyeballs in codes,” he said. “If we are going to start collecting this data, it is incumbent that the data actually be used to improve outcomes.”
AHIMA is advising a cautious approach. In its comments on the 23 proposed new ICD-10 codes, AHIMA recommended delaying implementation until more information is available from initiatives such as the Gravity Project of the Social Interventions Research and Evaluation Network at the University of California, San Francisco. The Gravity Project is a national collaborative to advance interoperable social risk documentation.
“There may be other, better ways to capture social factors. ... I’m not sure ICD-10-CM codes are the best way to do this because these issues are somewhat outside the scope of what ICD-10 is designed to capture,” Ms. Bowman said. There are also privacy concerns, and some of the social factors change frequently in the lives of patients.
Being the optimistic physician
Is your glass always half full? Is that because you’re so busy that you never have time to finish drinking it? Or is it because you are an optimist? Have you always been someone who could see a glimmer at the end of even the darkest, longest tunnels? Do you think your positive outlook is something you inherited? Or did you model it after continued exposure to an optimistic parent or medical school mentor?
Are you aware that your optimism makes it more likely that you will live to a ripe old age? A recent study of 69,744 women and 1,429 men initiated by researchers at the Harvard School T.H. Chan School of Public Health in Boston, Boston University Medical School, and the National Center for PTSD at Veterans Affairs Boston Health Care System found that “individuals with greater optimism are more likely to live longer and to achieve ‘exceptional longevity,’ that is, living to 85 or older” (“New Evidence that optimists live longer.” Harvard T.C. Chan School of Public Health. August 27, 2019).
Do you think your optimism has been a positive contribution to your success as a physician? Or have there been times when it has been a liability?
Because I’m not going to wait for you to answer, I’ll share my own observations. I sense that optimism is something with a strong genetic component, just as is the vulnerability to anxiety and depression. My mother was an optimist. However, I suspect that being around an individual who exudes a high degree of optimism can have a positive influence on a person who already has a partly cloudy disposition.
On the other hand, I’ve found that it is very difficult for even the most optimistic people to induce a positive outlook in individuals born with a chronically half empty glass simply by radiating their own aura of optimism. In my own experience, I have found that being an optimist has definitely been an asset in my role as a physician. – tension that may be exacerbating their ability to cope with the presenting problem. However, I have had to learn to recognize more quickly that there are situations when my optimism isn’t going to be effective and not become frustrated by its inadequacy.
Are there downsides to being an optimistic physician? Of course; there can be a fine line between being an optimist and sounding like a Pollyanna. To avoid stepping over the line, optimists must choose their words carefully. And more importantly, they must be reading the patient’s and family’s response to attempts at injecting positivity into the situation. Optimism also can be mistaken for a nonchalant attitude that signals a lack of caring and concern.
However, the most dangerous liability of optimism occurs when it slips into the swift running and turbulent waters of denial. I have almost killed myself on a couple of occasions when my “optimistic” interpretation of my symptoms has prompted me to “tough out” a potentially fatal situation instead of seeking timely advice from my physician.
My optimism sometimes has made it difficult for me to be appropriately objective when assessing the seriousness of a patient’s condition. Given a list of positives and negatives, my tendency might be focus more on the positives. As far as I know, my overly positive attitude has never killed any of my patients, but I fear a few diagnoses and remedies may have been delayed when the Prince of Optimism became the Queen of Denial.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
Is your glass always half full? Is that because you’re so busy that you never have time to finish drinking it? Or is it because you are an optimist? Have you always been someone who could see a glimmer at the end of even the darkest, longest tunnels? Do you think your positive outlook is something you inherited? Or did you model it after continued exposure to an optimistic parent or medical school mentor?
Are you aware that your optimism makes it more likely that you will live to a ripe old age? A recent study of 69,744 women and 1,429 men initiated by researchers at the Harvard School T.H. Chan School of Public Health in Boston, Boston University Medical School, and the National Center for PTSD at Veterans Affairs Boston Health Care System found that “individuals with greater optimism are more likely to live longer and to achieve ‘exceptional longevity,’ that is, living to 85 or older” (“New Evidence that optimists live longer.” Harvard T.C. Chan School of Public Health. August 27, 2019).
Do you think your optimism has been a positive contribution to your success as a physician? Or have there been times when it has been a liability?
Because I’m not going to wait for you to answer, I’ll share my own observations. I sense that optimism is something with a strong genetic component, just as is the vulnerability to anxiety and depression. My mother was an optimist. However, I suspect that being around an individual who exudes a high degree of optimism can have a positive influence on a person who already has a partly cloudy disposition.
On the other hand, I’ve found that it is very difficult for even the most optimistic people to induce a positive outlook in individuals born with a chronically half empty glass simply by radiating their own aura of optimism. In my own experience, I have found that being an optimist has definitely been an asset in my role as a physician. – tension that may be exacerbating their ability to cope with the presenting problem. However, I have had to learn to recognize more quickly that there are situations when my optimism isn’t going to be effective and not become frustrated by its inadequacy.
Are there downsides to being an optimistic physician? Of course; there can be a fine line between being an optimist and sounding like a Pollyanna. To avoid stepping over the line, optimists must choose their words carefully. And more importantly, they must be reading the patient’s and family’s response to attempts at injecting positivity into the situation. Optimism also can be mistaken for a nonchalant attitude that signals a lack of caring and concern.
However, the most dangerous liability of optimism occurs when it slips into the swift running and turbulent waters of denial. I have almost killed myself on a couple of occasions when my “optimistic” interpretation of my symptoms has prompted me to “tough out” a potentially fatal situation instead of seeking timely advice from my physician.
My optimism sometimes has made it difficult for me to be appropriately objective when assessing the seriousness of a patient’s condition. Given a list of positives and negatives, my tendency might be focus more on the positives. As far as I know, my overly positive attitude has never killed any of my patients, but I fear a few diagnoses and remedies may have been delayed when the Prince of Optimism became the Queen of Denial.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
Is your glass always half full? Is that because you’re so busy that you never have time to finish drinking it? Or is it because you are an optimist? Have you always been someone who could see a glimmer at the end of even the darkest, longest tunnels? Do you think your positive outlook is something you inherited? Or did you model it after continued exposure to an optimistic parent or medical school mentor?
Are you aware that your optimism makes it more likely that you will live to a ripe old age? A recent study of 69,744 women and 1,429 men initiated by researchers at the Harvard School T.H. Chan School of Public Health in Boston, Boston University Medical School, and the National Center for PTSD at Veterans Affairs Boston Health Care System found that “individuals with greater optimism are more likely to live longer and to achieve ‘exceptional longevity,’ that is, living to 85 or older” (“New Evidence that optimists live longer.” Harvard T.C. Chan School of Public Health. August 27, 2019).
Do you think your optimism has been a positive contribution to your success as a physician? Or have there been times when it has been a liability?
Because I’m not going to wait for you to answer, I’ll share my own observations. I sense that optimism is something with a strong genetic component, just as is the vulnerability to anxiety and depression. My mother was an optimist. However, I suspect that being around an individual who exudes a high degree of optimism can have a positive influence on a person who already has a partly cloudy disposition.
On the other hand, I’ve found that it is very difficult for even the most optimistic people to induce a positive outlook in individuals born with a chronically half empty glass simply by radiating their own aura of optimism. In my own experience, I have found that being an optimist has definitely been an asset in my role as a physician. – tension that may be exacerbating their ability to cope with the presenting problem. However, I have had to learn to recognize more quickly that there are situations when my optimism isn’t going to be effective and not become frustrated by its inadequacy.
Are there downsides to being an optimistic physician? Of course; there can be a fine line between being an optimist and sounding like a Pollyanna. To avoid stepping over the line, optimists must choose their words carefully. And more importantly, they must be reading the patient’s and family’s response to attempts at injecting positivity into the situation. Optimism also can be mistaken for a nonchalant attitude that signals a lack of caring and concern.
However, the most dangerous liability of optimism occurs when it slips into the swift running and turbulent waters of denial. I have almost killed myself on a couple of occasions when my “optimistic” interpretation of my symptoms has prompted me to “tough out” a potentially fatal situation instead of seeking timely advice from my physician.
My optimism sometimes has made it difficult for me to be appropriately objective when assessing the seriousness of a patient’s condition. Given a list of positives and negatives, my tendency might be focus more on the positives. As far as I know, my overly positive attitude has never killed any of my patients, but I fear a few diagnoses and remedies may have been delayed when the Prince of Optimism became the Queen of Denial.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
Insurers to pay record number of rebates to patients
Health insurance companies are getting ready to disburse a record $1.3 billion in medical loss ratio (MLR) rebates, according to an analysis by the Kaiser Family Foundation.
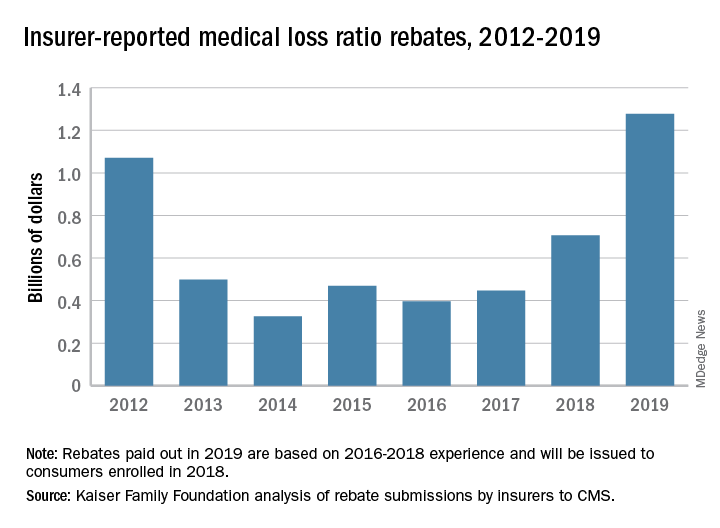
The $1.3 billion surpasses the previous rebate record of $1.1 billion, issued in 2012.
The increase is driven largely by individual market insurers who will pay $743 million in rebates this year, according to the report, which analyzed insurer data submitted to the Centers for Medicare & Medicaid Services. Rebates in the small-group and large-group insurance markets are similar to previous years, with expected paybacks of $250 million from small- and $284 million from large-group markets, according to the Kaiser report. Insurance companies have until September 30, 2019, to start issuing rebates.
The rebates stem from the MLR requirement imposed by the Affordable Care Act (ACA), which limits the amount of premium dollars that can be used for administration, marketing, and profit. Under the health law, companies are required to publicly report how much they spend on health care, quality improvement, and other activities using premium funds. Individual and small-group market insurers must spend at least 80% on health care claims and quality improvement,while large-group plans must spend at least 85%. Rebates are based on a 3-year average of financial data by each insurer.
Patients in the individual insurance market can expect their rebate in either a premium credit or a check. In the large and small group markets, rebates may be split between employee and employer depending on the plan contract.
The volume of rebates differed greatly across the states, with some states paying zero rebates and others paying millions. Virginia insurers for example, will pay the highest number of total rebates ($150 million), followed by Pennsylvania ($130 million) and Florida ($107 million), according to the report. Payments by insurers in the individual market alone ranged from zero dollars in 13 states to $111 million in Virginia. Individual market insurers in Arizona will pay $92 million in rebates to patients, while individual plans in Texas will pay $80 million. Florida insurers will pay the highest in rebates in both the small-group and large-group market at $44 million and $42 million respectively.
The largest rebates within the individual market will come from Centene, HCSC, Cigna, and Highmark. Authors of the report noted that these insurers tend to have higher enrollment and are active in multiple states.
Individual marketplace insurers will likely pay high rebates against next year, based on an individual market that remains strong and profitable, despite the recent elimination of the individual mandate penalty, according to the authors.
Health insurance companies are getting ready to disburse a record $1.3 billion in medical loss ratio (MLR) rebates, according to an analysis by the Kaiser Family Foundation.
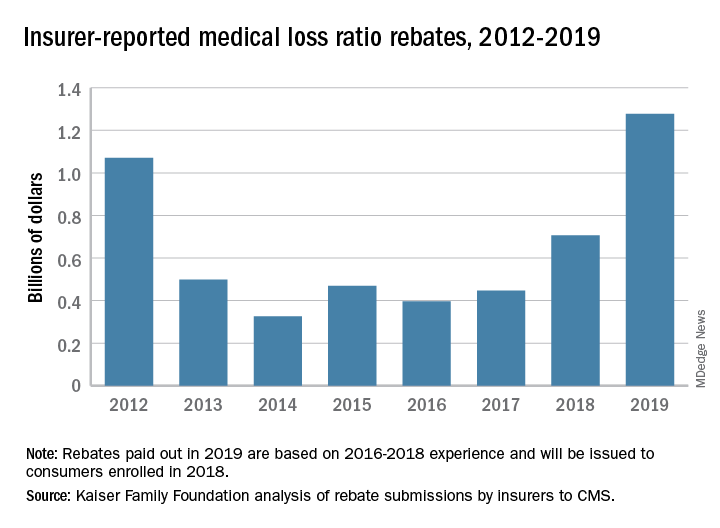
The $1.3 billion surpasses the previous rebate record of $1.1 billion, issued in 2012.
The increase is driven largely by individual market insurers who will pay $743 million in rebates this year, according to the report, which analyzed insurer data submitted to the Centers for Medicare & Medicaid Services. Rebates in the small-group and large-group insurance markets are similar to previous years, with expected paybacks of $250 million from small- and $284 million from large-group markets, according to the Kaiser report. Insurance companies have until September 30, 2019, to start issuing rebates.
The rebates stem from the MLR requirement imposed by the Affordable Care Act (ACA), which limits the amount of premium dollars that can be used for administration, marketing, and profit. Under the health law, companies are required to publicly report how much they spend on health care, quality improvement, and other activities using premium funds. Individual and small-group market insurers must spend at least 80% on health care claims and quality improvement,while large-group plans must spend at least 85%. Rebates are based on a 3-year average of financial data by each insurer.
Patients in the individual insurance market can expect their rebate in either a premium credit or a check. In the large and small group markets, rebates may be split between employee and employer depending on the plan contract.
The volume of rebates differed greatly across the states, with some states paying zero rebates and others paying millions. Virginia insurers for example, will pay the highest number of total rebates ($150 million), followed by Pennsylvania ($130 million) and Florida ($107 million), according to the report. Payments by insurers in the individual market alone ranged from zero dollars in 13 states to $111 million in Virginia. Individual market insurers in Arizona will pay $92 million in rebates to patients, while individual plans in Texas will pay $80 million. Florida insurers will pay the highest in rebates in both the small-group and large-group market at $44 million and $42 million respectively.
The largest rebates within the individual market will come from Centene, HCSC, Cigna, and Highmark. Authors of the report noted that these insurers tend to have higher enrollment and are active in multiple states.
Individual marketplace insurers will likely pay high rebates against next year, based on an individual market that remains strong and profitable, despite the recent elimination of the individual mandate penalty, according to the authors.
Health insurance companies are getting ready to disburse a record $1.3 billion in medical loss ratio (MLR) rebates, according to an analysis by the Kaiser Family Foundation.
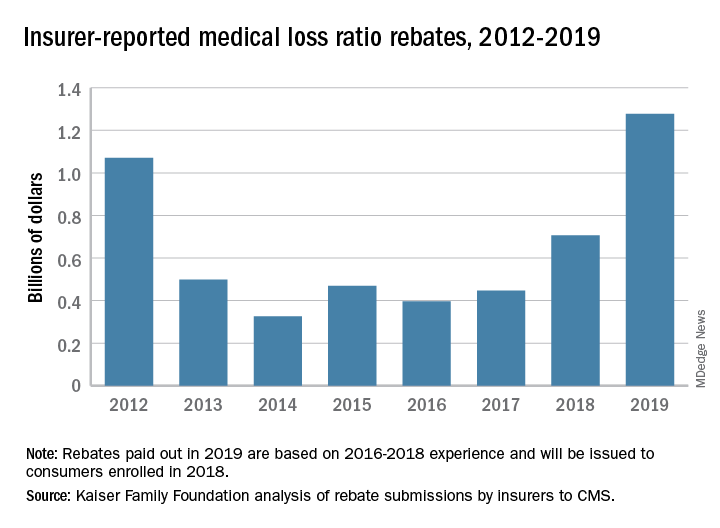
The $1.3 billion surpasses the previous rebate record of $1.1 billion, issued in 2012.
The increase is driven largely by individual market insurers who will pay $743 million in rebates this year, according to the report, which analyzed insurer data submitted to the Centers for Medicare & Medicaid Services. Rebates in the small-group and large-group insurance markets are similar to previous years, with expected paybacks of $250 million from small- and $284 million from large-group markets, according to the Kaiser report. Insurance companies have until September 30, 2019, to start issuing rebates.
The rebates stem from the MLR requirement imposed by the Affordable Care Act (ACA), which limits the amount of premium dollars that can be used for administration, marketing, and profit. Under the health law, companies are required to publicly report how much they spend on health care, quality improvement, and other activities using premium funds. Individual and small-group market insurers must spend at least 80% on health care claims and quality improvement,while large-group plans must spend at least 85%. Rebates are based on a 3-year average of financial data by each insurer.
Patients in the individual insurance market can expect their rebate in either a premium credit or a check. In the large and small group markets, rebates may be split between employee and employer depending on the plan contract.
The volume of rebates differed greatly across the states, with some states paying zero rebates and others paying millions. Virginia insurers for example, will pay the highest number of total rebates ($150 million), followed by Pennsylvania ($130 million) and Florida ($107 million), according to the report. Payments by insurers in the individual market alone ranged from zero dollars in 13 states to $111 million in Virginia. Individual market insurers in Arizona will pay $92 million in rebates to patients, while individual plans in Texas will pay $80 million. Florida insurers will pay the highest in rebates in both the small-group and large-group market at $44 million and $42 million respectively.
The largest rebates within the individual market will come from Centene, HCSC, Cigna, and Highmark. Authors of the report noted that these insurers tend to have higher enrollment and are active in multiple states.
Individual marketplace insurers will likely pay high rebates against next year, based on an individual market that remains strong and profitable, despite the recent elimination of the individual mandate penalty, according to the authors.
Review your insurance
Insurance, so goes the hoary cliché, is the one product you buy hoping never to use. While no one enjoys foreseeing unforeseeable calamities, if you haven’t reviewed your insurance coverage recently, there is no time like the present.
, but the cost has become prohibitive in many areas, when insurers are willing to write them at all. “Claims made” policies are cheaper and provide the same protection, but only while coverage is in effect. You will need “tail” coverage against belated claims after your policy lapses, but many companies provide free tail coverage if you are retiring. If you are simply switching workplaces (or policies), ask your new insurer about “nose” coverage, for claims involving acts that occurred before the new policy takes effect.
Other alternatives are gaining popularity as the demand for reasonably priced insurance increases. The most common, known as reciprocal exchanges, are very similar to traditional insurers, but require policyholders to make capital contributions in addition to payment of premiums, at least in their early stages. You get your investment back, with interest, when (if) the exchange becomes solvent.
Another option, called a captive, is a company formed by a consortium of medical practices to write their own insurance policies. All participants are shareholders, and all premiums (less administrative expenses) go toward building the security of the captive. Most captives purchase reinsurance to protect against catastrophic losses. If all goes well, individual owners sell their shares at retirement for a profit, which has grown tax-free in the interim.
Those willing to shoulder more risk might consider a risk retention group (RRG), a sort of combination of an exchange and a captive. Again, the owners are the insureds themselves, but all responsibility for management and adequate funding falls on their shoulders, and reinsurance is not usually an option. Most medical malpractice RRGs are licensed in Vermont or South Carolina, because of favorable laws in those states, but can be based in any state that allows them (36 at this writing). RRGs provide profit opportunities not available with traditional insurance, but there is risk: A few large claims could eat up all the profits, or even put owners in a financial hole.
Malpractice insurance requirements will remain fairly static throughout your career, but other insurance needs evolve over time. A good example is life insurance: As retirement savings increase, the need for life insurance decreases – especially expensive “whole life” coverage, which can often be eliminated or converted to cheaper “term” insurance.
Health insurance premiums continue to soar, but the Affordable Care Act might offer a favorable alternative for your office policy. If you are considering that, the Centers for Medicare & Medicaid Services maintains a website summarizing the various options for employers.
Worker compensation insurance is mandatory in most states and heavily regulated, so there is little wiggle room. However, some states do not require you, as the employer, to cover yourself, so eliminating that coverage could save you a substantial amount. This is only worth considering, of course, if you’re in excellent health and have very good personal health and disability coverage.
Disability insurance is not something to skimp on, but if you are approaching retirement age and have no major health issues, you may be able to decrease your coverage, or even eliminate it entirely if your retirement plan is far enough along.
Liability insurance is likewise no place to pinch pennies, but you might be able to add an “umbrella” policy providing comprehensive catastrophic coverage, which may allow you to decrease your regular coverage, or raise your deductible limits.
Two additional policies to consider are office overhead insurance, to cover the costs of keeping your office open should you be temporarily incapacitated, and employee practices liability insurance (EPLI), which protects you from lawsuits brought by militant or disgruntled employees. I covered EPLI in detail several months ago.
If you are over 50, I strongly recommend long-term-care insurance as well. It’s relatively inexpensive if you buy it while you’re still healthy, and it could save you and your heirs a load of money and aggravation on the other end. If you have shouldered the expense of caring for a chronically ill parent or grandparent, you know what I’m talking about. More about that next month.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
Insurance, so goes the hoary cliché, is the one product you buy hoping never to use. While no one enjoys foreseeing unforeseeable calamities, if you haven’t reviewed your insurance coverage recently, there is no time like the present.
, but the cost has become prohibitive in many areas, when insurers are willing to write them at all. “Claims made” policies are cheaper and provide the same protection, but only while coverage is in effect. You will need “tail” coverage against belated claims after your policy lapses, but many companies provide free tail coverage if you are retiring. If you are simply switching workplaces (or policies), ask your new insurer about “nose” coverage, for claims involving acts that occurred before the new policy takes effect.
Other alternatives are gaining popularity as the demand for reasonably priced insurance increases. The most common, known as reciprocal exchanges, are very similar to traditional insurers, but require policyholders to make capital contributions in addition to payment of premiums, at least in their early stages. You get your investment back, with interest, when (if) the exchange becomes solvent.
Another option, called a captive, is a company formed by a consortium of medical practices to write their own insurance policies. All participants are shareholders, and all premiums (less administrative expenses) go toward building the security of the captive. Most captives purchase reinsurance to protect against catastrophic losses. If all goes well, individual owners sell their shares at retirement for a profit, which has grown tax-free in the interim.
Those willing to shoulder more risk might consider a risk retention group (RRG), a sort of combination of an exchange and a captive. Again, the owners are the insureds themselves, but all responsibility for management and adequate funding falls on their shoulders, and reinsurance is not usually an option. Most medical malpractice RRGs are licensed in Vermont or South Carolina, because of favorable laws in those states, but can be based in any state that allows them (36 at this writing). RRGs provide profit opportunities not available with traditional insurance, but there is risk: A few large claims could eat up all the profits, or even put owners in a financial hole.
Malpractice insurance requirements will remain fairly static throughout your career, but other insurance needs evolve over time. A good example is life insurance: As retirement savings increase, the need for life insurance decreases – especially expensive “whole life” coverage, which can often be eliminated or converted to cheaper “term” insurance.
Health insurance premiums continue to soar, but the Affordable Care Act might offer a favorable alternative for your office policy. If you are considering that, the Centers for Medicare & Medicaid Services maintains a website summarizing the various options for employers.
Worker compensation insurance is mandatory in most states and heavily regulated, so there is little wiggle room. However, some states do not require you, as the employer, to cover yourself, so eliminating that coverage could save you a substantial amount. This is only worth considering, of course, if you’re in excellent health and have very good personal health and disability coverage.
Disability insurance is not something to skimp on, but if you are approaching retirement age and have no major health issues, you may be able to decrease your coverage, or even eliminate it entirely if your retirement plan is far enough along.
Liability insurance is likewise no place to pinch pennies, but you might be able to add an “umbrella” policy providing comprehensive catastrophic coverage, which may allow you to decrease your regular coverage, or raise your deductible limits.
Two additional policies to consider are office overhead insurance, to cover the costs of keeping your office open should you be temporarily incapacitated, and employee practices liability insurance (EPLI), which protects you from lawsuits brought by militant or disgruntled employees. I covered EPLI in detail several months ago.
If you are over 50, I strongly recommend long-term-care insurance as well. It’s relatively inexpensive if you buy it while you’re still healthy, and it could save you and your heirs a load of money and aggravation on the other end. If you have shouldered the expense of caring for a chronically ill parent or grandparent, you know what I’m talking about. More about that next month.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
Insurance, so goes the hoary cliché, is the one product you buy hoping never to use. While no one enjoys foreseeing unforeseeable calamities, if you haven’t reviewed your insurance coverage recently, there is no time like the present.
, but the cost has become prohibitive in many areas, when insurers are willing to write them at all. “Claims made” policies are cheaper and provide the same protection, but only while coverage is in effect. You will need “tail” coverage against belated claims after your policy lapses, but many companies provide free tail coverage if you are retiring. If you are simply switching workplaces (or policies), ask your new insurer about “nose” coverage, for claims involving acts that occurred before the new policy takes effect.
Other alternatives are gaining popularity as the demand for reasonably priced insurance increases. The most common, known as reciprocal exchanges, are very similar to traditional insurers, but require policyholders to make capital contributions in addition to payment of premiums, at least in their early stages. You get your investment back, with interest, when (if) the exchange becomes solvent.
Another option, called a captive, is a company formed by a consortium of medical practices to write their own insurance policies. All participants are shareholders, and all premiums (less administrative expenses) go toward building the security of the captive. Most captives purchase reinsurance to protect against catastrophic losses. If all goes well, individual owners sell their shares at retirement for a profit, which has grown tax-free in the interim.
Those willing to shoulder more risk might consider a risk retention group (RRG), a sort of combination of an exchange and a captive. Again, the owners are the insureds themselves, but all responsibility for management and adequate funding falls on their shoulders, and reinsurance is not usually an option. Most medical malpractice RRGs are licensed in Vermont or South Carolina, because of favorable laws in those states, but can be based in any state that allows them (36 at this writing). RRGs provide profit opportunities not available with traditional insurance, but there is risk: A few large claims could eat up all the profits, or even put owners in a financial hole.
Malpractice insurance requirements will remain fairly static throughout your career, but other insurance needs evolve over time. A good example is life insurance: As retirement savings increase, the need for life insurance decreases – especially expensive “whole life” coverage, which can often be eliminated or converted to cheaper “term” insurance.
Health insurance premiums continue to soar, but the Affordable Care Act might offer a favorable alternative for your office policy. If you are considering that, the Centers for Medicare & Medicaid Services maintains a website summarizing the various options for employers.
Worker compensation insurance is mandatory in most states and heavily regulated, so there is little wiggle room. However, some states do not require you, as the employer, to cover yourself, so eliminating that coverage could save you a substantial amount. This is only worth considering, of course, if you’re in excellent health and have very good personal health and disability coverage.
Disability insurance is not something to skimp on, but if you are approaching retirement age and have no major health issues, you may be able to decrease your coverage, or even eliminate it entirely if your retirement plan is far enough along.
Liability insurance is likewise no place to pinch pennies, but you might be able to add an “umbrella” policy providing comprehensive catastrophic coverage, which may allow you to decrease your regular coverage, or raise your deductible limits.
Two additional policies to consider are office overhead insurance, to cover the costs of keeping your office open should you be temporarily incapacitated, and employee practices liability insurance (EPLI), which protects you from lawsuits brought by militant or disgruntled employees. I covered EPLI in detail several months ago.
If you are over 50, I strongly recommend long-term-care insurance as well. It’s relatively inexpensive if you buy it while you’re still healthy, and it could save you and your heirs a load of money and aggravation on the other end. If you have shouldered the expense of caring for a chronically ill parent or grandparent, you know what I’m talking about. More about that next month.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
Breaking a 10-year streak, the number of uninsured Americans rises
For the first time in a decade, the number of Americans without health insurance has risen – by about 2 million people in 2018 – according to the annual U.S. Census Bureau report released Sept. 10, 2019.
The Census found that 8.5% of the U.S. population went without medical insurance for all of 2018, up from 7.9% in 2017. By contrast, in 2013, before the Affordable Care Act took full effect, 13.3% were uninsured. It was the first year-to-year increase since 2008-09, Census officials said, adding that most of the drop in health coverage was related to a 0.7% decline in Medicaid participants. The number of people with private insurance remained steady and there was a 0.4% increase in those on Medicare.
Many of those losing coverage were noncitizens, a possible fallout from the Trump administration’s tough immigration policies and rhetoric. About 574,000 noncitizens lost coverage in 2018, a drop of about 2.3%, the report found.
“Uninsured noncitizens account for almost a third of the increase in uninsured, which may reflect the administration’s more aggressive stance on immigration,” said Joseph Antos, a health economist at the American Enterprise Institute.
The increase in the number of uninsured people in 2018 was remarkable because uninsured rates typically fall or hold steady when unemployment rates drop. The U.S. unemployment rate fell slightly from about 4.3% in 2017 to 4% in 2018.
The uninsured rate continued to vary by poverty status and whether a state expanded its Medicaid program under Obamacare. Texas (17.7%), Oklahoma (14.2%), Georgia (13.7%), and Florida (13%) had the highest uninsured rates in 2018, according to the report. None of those states have expanded Medicaid under Obamacare.
The percentage of uninsured children aged under 19 years increased by 0.6 percentage points from 2017 to 2018, to 5.5%.
“The Census data are clear – the uninsured rate for kids is up sharply and it’s due to a loss of public coverage – mostly Medicaid,” Joan Alker, executive director of Georgetown University Center for Children and Families, said in a statement.
“These children are not getting private coverage as the Trump administration has suggested but rather becoming uninsured,” she said. “This serious erosion of children’s health coverage is due in large part to the Trump administration’s actions that have made health care harder to access and have deterred families from enrolling their children.”
The share of Americans without medical insurance fell steadily since 2014 but then leveled off in 2017, the year Mr. Trump became president.
Health care advocates have complained that efforts by the Trump administration and Congress are jeopardizing insurance enrollment. They point to cuts in outreach programs that aim to tell consumers about their health care options under Obamacare and the elimination of the ACA’s tax penalty for people who don’t have health coverage.
Ms. Alker complained that the administration’s policies are causing the loss of children’s coverage. “In a period of continued economic and job growth, we shouldn’t be going backwards on health coverage,” said Judy Solomon, a senior fellow for the Center on Budget and Policy Priorities, a left-leaning think tank. “This backsliding almost certainly reflects, at least in part, Trump administration policies to weaken public health coverage.”
She attributed the drop to the Trump administration making it harder for families to enroll for coverage in Medicaid by curtailing outreach efforts, allowing states to ask for more paperwork and proposing a so-called public charge rule that would make it harder for legal immigrants to get permanent resident status if they have received certain kinds of public assistance – including Medicaid.
Tom Miller, a resident fellow at the American Enterprise Institute, a conservative think tank, said the drop in Medicaid coverage “is a positive.”
“When the economy grows Medicaid eventually drops,” he said.
One reason for the drop in health coverage is that middle-income families can’t afford the rising cost of insurance in the individual market, particularly if they don’t qualify for government subsidies, he added.
“On balance, this is some short-term noise,” he said of the uptick in the uninsured rate. “I would put more stake in it if happens for several years.”
Chris Pope, a senior fellow with the conservative Manhattan Institute, also said he considered the change “fairly small” and likely caused by increasing wages “pushing people above the income eligibility cutoff in Medicaid expansion states.”
But he suggested that next year would be a better indicator of how changes in the ACA are playing out. “I expect that the mandate repeal will make next year’s increase in the uninsured more significant.”
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
For the first time in a decade, the number of Americans without health insurance has risen – by about 2 million people in 2018 – according to the annual U.S. Census Bureau report released Sept. 10, 2019.
The Census found that 8.5% of the U.S. population went without medical insurance for all of 2018, up from 7.9% in 2017. By contrast, in 2013, before the Affordable Care Act took full effect, 13.3% were uninsured. It was the first year-to-year increase since 2008-09, Census officials said, adding that most of the drop in health coverage was related to a 0.7% decline in Medicaid participants. The number of people with private insurance remained steady and there was a 0.4% increase in those on Medicare.
Many of those losing coverage were noncitizens, a possible fallout from the Trump administration’s tough immigration policies and rhetoric. About 574,000 noncitizens lost coverage in 2018, a drop of about 2.3%, the report found.
“Uninsured noncitizens account for almost a third of the increase in uninsured, which may reflect the administration’s more aggressive stance on immigration,” said Joseph Antos, a health economist at the American Enterprise Institute.
The increase in the number of uninsured people in 2018 was remarkable because uninsured rates typically fall or hold steady when unemployment rates drop. The U.S. unemployment rate fell slightly from about 4.3% in 2017 to 4% in 2018.
The uninsured rate continued to vary by poverty status and whether a state expanded its Medicaid program under Obamacare. Texas (17.7%), Oklahoma (14.2%), Georgia (13.7%), and Florida (13%) had the highest uninsured rates in 2018, according to the report. None of those states have expanded Medicaid under Obamacare.
The percentage of uninsured children aged under 19 years increased by 0.6 percentage points from 2017 to 2018, to 5.5%.
“The Census data are clear – the uninsured rate for kids is up sharply and it’s due to a loss of public coverage – mostly Medicaid,” Joan Alker, executive director of Georgetown University Center for Children and Families, said in a statement.
“These children are not getting private coverage as the Trump administration has suggested but rather becoming uninsured,” she said. “This serious erosion of children’s health coverage is due in large part to the Trump administration’s actions that have made health care harder to access and have deterred families from enrolling their children.”
The share of Americans without medical insurance fell steadily since 2014 but then leveled off in 2017, the year Mr. Trump became president.
Health care advocates have complained that efforts by the Trump administration and Congress are jeopardizing insurance enrollment. They point to cuts in outreach programs that aim to tell consumers about their health care options under Obamacare and the elimination of the ACA’s tax penalty for people who don’t have health coverage.
Ms. Alker complained that the administration’s policies are causing the loss of children’s coverage. “In a period of continued economic and job growth, we shouldn’t be going backwards on health coverage,” said Judy Solomon, a senior fellow for the Center on Budget and Policy Priorities, a left-leaning think tank. “This backsliding almost certainly reflects, at least in part, Trump administration policies to weaken public health coverage.”
She attributed the drop to the Trump administration making it harder for families to enroll for coverage in Medicaid by curtailing outreach efforts, allowing states to ask for more paperwork and proposing a so-called public charge rule that would make it harder for legal immigrants to get permanent resident status if they have received certain kinds of public assistance – including Medicaid.
Tom Miller, a resident fellow at the American Enterprise Institute, a conservative think tank, said the drop in Medicaid coverage “is a positive.”
“When the economy grows Medicaid eventually drops,” he said.
One reason for the drop in health coverage is that middle-income families can’t afford the rising cost of insurance in the individual market, particularly if they don’t qualify for government subsidies, he added.
“On balance, this is some short-term noise,” he said of the uptick in the uninsured rate. “I would put more stake in it if happens for several years.”
Chris Pope, a senior fellow with the conservative Manhattan Institute, also said he considered the change “fairly small” and likely caused by increasing wages “pushing people above the income eligibility cutoff in Medicaid expansion states.”
But he suggested that next year would be a better indicator of how changes in the ACA are playing out. “I expect that the mandate repeal will make next year’s increase in the uninsured more significant.”
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
For the first time in a decade, the number of Americans without health insurance has risen – by about 2 million people in 2018 – according to the annual U.S. Census Bureau report released Sept. 10, 2019.
The Census found that 8.5% of the U.S. population went without medical insurance for all of 2018, up from 7.9% in 2017. By contrast, in 2013, before the Affordable Care Act took full effect, 13.3% were uninsured. It was the first year-to-year increase since 2008-09, Census officials said, adding that most of the drop in health coverage was related to a 0.7% decline in Medicaid participants. The number of people with private insurance remained steady and there was a 0.4% increase in those on Medicare.
Many of those losing coverage were noncitizens, a possible fallout from the Trump administration’s tough immigration policies and rhetoric. About 574,000 noncitizens lost coverage in 2018, a drop of about 2.3%, the report found.
“Uninsured noncitizens account for almost a third of the increase in uninsured, which may reflect the administration’s more aggressive stance on immigration,” said Joseph Antos, a health economist at the American Enterprise Institute.
The increase in the number of uninsured people in 2018 was remarkable because uninsured rates typically fall or hold steady when unemployment rates drop. The U.S. unemployment rate fell slightly from about 4.3% in 2017 to 4% in 2018.
The uninsured rate continued to vary by poverty status and whether a state expanded its Medicaid program under Obamacare. Texas (17.7%), Oklahoma (14.2%), Georgia (13.7%), and Florida (13%) had the highest uninsured rates in 2018, according to the report. None of those states have expanded Medicaid under Obamacare.
The percentage of uninsured children aged under 19 years increased by 0.6 percentage points from 2017 to 2018, to 5.5%.
“The Census data are clear – the uninsured rate for kids is up sharply and it’s due to a loss of public coverage – mostly Medicaid,” Joan Alker, executive director of Georgetown University Center for Children and Families, said in a statement.
“These children are not getting private coverage as the Trump administration has suggested but rather becoming uninsured,” she said. “This serious erosion of children’s health coverage is due in large part to the Trump administration’s actions that have made health care harder to access and have deterred families from enrolling their children.”
The share of Americans without medical insurance fell steadily since 2014 but then leveled off in 2017, the year Mr. Trump became president.
Health care advocates have complained that efforts by the Trump administration and Congress are jeopardizing insurance enrollment. They point to cuts in outreach programs that aim to tell consumers about their health care options under Obamacare and the elimination of the ACA’s tax penalty for people who don’t have health coverage.
Ms. Alker complained that the administration’s policies are causing the loss of children’s coverage. “In a period of continued economic and job growth, we shouldn’t be going backwards on health coverage,” said Judy Solomon, a senior fellow for the Center on Budget and Policy Priorities, a left-leaning think tank. “This backsliding almost certainly reflects, at least in part, Trump administration policies to weaken public health coverage.”
She attributed the drop to the Trump administration making it harder for families to enroll for coverage in Medicaid by curtailing outreach efforts, allowing states to ask for more paperwork and proposing a so-called public charge rule that would make it harder for legal immigrants to get permanent resident status if they have received certain kinds of public assistance – including Medicaid.
Tom Miller, a resident fellow at the American Enterprise Institute, a conservative think tank, said the drop in Medicaid coverage “is a positive.”
“When the economy grows Medicaid eventually drops,” he said.
One reason for the drop in health coverage is that middle-income families can’t afford the rising cost of insurance in the individual market, particularly if they don’t qualify for government subsidies, he added.
“On balance, this is some short-term noise,” he said of the uptick in the uninsured rate. “I would put more stake in it if happens for several years.”
Chris Pope, a senior fellow with the conservative Manhattan Institute, also said he considered the change “fairly small” and likely caused by increasing wages “pushing people above the income eligibility cutoff in Medicaid expansion states.”
But he suggested that next year would be a better indicator of how changes in the ACA are playing out. “I expect that the mandate repeal will make next year’s increase in the uninsured more significant.”
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Judge blocks North Dakota abortion law
A district judge has temporarily blocked a North Dakota law that forces physicians to tell patients that medication abortions may be reversed, calling the measure devoid of scientific support.
In a Sept. 10 ruling, Judge Daniel Hovland of the U.S. District Court for the District of North Dakota temporarily halted enforcement of North Dakota House Bill 1336, a law that required doctors to tell women that reversing the effects of abortion-inducing drugs is possible if patients changed their minds, but that “time is of the essence.” In his 24-page decision, Judge Hovland said the North Dakota law violates a physician’s right not to speak and goes far beyond any informed consent laws addressed by the U.S. Supreme Court or other courts to date.
“Legislation which forces physicians to tell their patients, as part of informed consent, that ‘it may be possible’ to reverse or cure an ailment, disease, illness, surgical procedure, or the effects of any medication – in the absence of any medical or scientific evidence to support such a message – is unsound, misplaced, and would not survive a constitutional challenge under any level of scrutiny,” Judge Hovland wrote in his ruling. “State legislatures should not be mandating unproven medical treatments, or requiring physicians to provide patients with misleading and inaccurate information.”
North Dakota Governor Doug Burgum (R), signed HB 1336 into law in March. The measure requires that physicians inform patients at least 24 hours before a medication abortion that it may be possible to reverse the effects if they change their mind, and also mandates that doctors provide printed materials to patients with information about reversing the effects of an abortion-inducing drug.
The American Medical Association and the Red River Women’s Clinic based in Fargo, issued a joint legal challenge against North Dakota Attorney General Wayne Stenehjem in June over the law. The plaintiffs contend the North Dakota law violates physicians’ First Amendment rights that protect doctors from being compelled to speak against their will. The plaintiffs also argued that so-called abortion reversals are based on controversial, unproven theories that are rejected by major medical organizations.
The lawsuit also challenges an existing North Dakota law called the Abortion Control Act, that requires physicians to tell patients that abortion terminates “the life of a whole, separate, unique, living human being,” which the plaintiffs contend is a controversial, ideological, and nonmedical message that forces physicians to act as the mouthpiece of the state. That part of the lawsuit was not addressed in Judge Hovland’s ruling.
AMA President Patrice A. Harris, MD, said the association was pleased that the judge blocked enforcement of HB 1336 while the case advances in the court system.
“The AMA filed this lawsuit in North Dakota because we strongly believe the government should not dictate what physicians say to their patients,” Dr. Harris said in a statement. “With this ruling, physicians in North Dakota will not be forced by law to provide patients with false, misleading, non-medical information about reproductive health that contradicts reality and science.”
A spokeswoman for Mr. Stenehjem’s office said the attorney general is reviewing the order and declined to comment further.
At least seven other states have passed similar laws requiring physicians to tell patients about the possibility of medication abortion reversals, including Arkansas, Idaho, Kentucky, Nebraska, Oklahoma, South Dakota, and Utah.
A district judge has temporarily blocked a North Dakota law that forces physicians to tell patients that medication abortions may be reversed, calling the measure devoid of scientific support.
In a Sept. 10 ruling, Judge Daniel Hovland of the U.S. District Court for the District of North Dakota temporarily halted enforcement of North Dakota House Bill 1336, a law that required doctors to tell women that reversing the effects of abortion-inducing drugs is possible if patients changed their minds, but that “time is of the essence.” In his 24-page decision, Judge Hovland said the North Dakota law violates a physician’s right not to speak and goes far beyond any informed consent laws addressed by the U.S. Supreme Court or other courts to date.
“Legislation which forces physicians to tell their patients, as part of informed consent, that ‘it may be possible’ to reverse or cure an ailment, disease, illness, surgical procedure, or the effects of any medication – in the absence of any medical or scientific evidence to support such a message – is unsound, misplaced, and would not survive a constitutional challenge under any level of scrutiny,” Judge Hovland wrote in his ruling. “State legislatures should not be mandating unproven medical treatments, or requiring physicians to provide patients with misleading and inaccurate information.”
North Dakota Governor Doug Burgum (R), signed HB 1336 into law in March. The measure requires that physicians inform patients at least 24 hours before a medication abortion that it may be possible to reverse the effects if they change their mind, and also mandates that doctors provide printed materials to patients with information about reversing the effects of an abortion-inducing drug.
The American Medical Association and the Red River Women’s Clinic based in Fargo, issued a joint legal challenge against North Dakota Attorney General Wayne Stenehjem in June over the law. The plaintiffs contend the North Dakota law violates physicians’ First Amendment rights that protect doctors from being compelled to speak against their will. The plaintiffs also argued that so-called abortion reversals are based on controversial, unproven theories that are rejected by major medical organizations.
The lawsuit also challenges an existing North Dakota law called the Abortion Control Act, that requires physicians to tell patients that abortion terminates “the life of a whole, separate, unique, living human being,” which the plaintiffs contend is a controversial, ideological, and nonmedical message that forces physicians to act as the mouthpiece of the state. That part of the lawsuit was not addressed in Judge Hovland’s ruling.
AMA President Patrice A. Harris, MD, said the association was pleased that the judge blocked enforcement of HB 1336 while the case advances in the court system.
“The AMA filed this lawsuit in North Dakota because we strongly believe the government should not dictate what physicians say to their patients,” Dr. Harris said in a statement. “With this ruling, physicians in North Dakota will not be forced by law to provide patients with false, misleading, non-medical information about reproductive health that contradicts reality and science.”
A spokeswoman for Mr. Stenehjem’s office said the attorney general is reviewing the order and declined to comment further.
At least seven other states have passed similar laws requiring physicians to tell patients about the possibility of medication abortion reversals, including Arkansas, Idaho, Kentucky, Nebraska, Oklahoma, South Dakota, and Utah.
A district judge has temporarily blocked a North Dakota law that forces physicians to tell patients that medication abortions may be reversed, calling the measure devoid of scientific support.
In a Sept. 10 ruling, Judge Daniel Hovland of the U.S. District Court for the District of North Dakota temporarily halted enforcement of North Dakota House Bill 1336, a law that required doctors to tell women that reversing the effects of abortion-inducing drugs is possible if patients changed their minds, but that “time is of the essence.” In his 24-page decision, Judge Hovland said the North Dakota law violates a physician’s right not to speak and goes far beyond any informed consent laws addressed by the U.S. Supreme Court or other courts to date.
“Legislation which forces physicians to tell their patients, as part of informed consent, that ‘it may be possible’ to reverse or cure an ailment, disease, illness, surgical procedure, or the effects of any medication – in the absence of any medical or scientific evidence to support such a message – is unsound, misplaced, and would not survive a constitutional challenge under any level of scrutiny,” Judge Hovland wrote in his ruling. “State legislatures should not be mandating unproven medical treatments, or requiring physicians to provide patients with misleading and inaccurate information.”
North Dakota Governor Doug Burgum (R), signed HB 1336 into law in March. The measure requires that physicians inform patients at least 24 hours before a medication abortion that it may be possible to reverse the effects if they change their mind, and also mandates that doctors provide printed materials to patients with information about reversing the effects of an abortion-inducing drug.
The American Medical Association and the Red River Women’s Clinic based in Fargo, issued a joint legal challenge against North Dakota Attorney General Wayne Stenehjem in June over the law. The plaintiffs contend the North Dakota law violates physicians’ First Amendment rights that protect doctors from being compelled to speak against their will. The plaintiffs also argued that so-called abortion reversals are based on controversial, unproven theories that are rejected by major medical organizations.
The lawsuit also challenges an existing North Dakota law called the Abortion Control Act, that requires physicians to tell patients that abortion terminates “the life of a whole, separate, unique, living human being,” which the plaintiffs contend is a controversial, ideological, and nonmedical message that forces physicians to act as the mouthpiece of the state. That part of the lawsuit was not addressed in Judge Hovland’s ruling.
AMA President Patrice A. Harris, MD, said the association was pleased that the judge blocked enforcement of HB 1336 while the case advances in the court system.
“The AMA filed this lawsuit in North Dakota because we strongly believe the government should not dictate what physicians say to their patients,” Dr. Harris said in a statement. “With this ruling, physicians in North Dakota will not be forced by law to provide patients with false, misleading, non-medical information about reproductive health that contradicts reality and science.”
A spokeswoman for Mr. Stenehjem’s office said the attorney general is reviewing the order and declined to comment further.
At least seven other states have passed similar laws requiring physicians to tell patients about the possibility of medication abortion reversals, including Arkansas, Idaho, Kentucky, Nebraska, Oklahoma, South Dakota, and Utah.

















