User login
No Impact of Race on Cardiovascular Risk Calculations
TOPLINE:
Removing race and incorporating social determinants of health (SDOH) into the pooled cohort risk equations (PCEs) for predicting atherosclerotic cardiovascular disease (ASCVD) outcomes made no difference to patients’ risk scores.
METHODOLOGY:
- Primary prevention guidelines recommend using risk prediction algorithms to assess the 10-year ASCVD risk, with the currently recommended PCEs including race.
- Researchers evaluated the incremental value of revised risk prediction equations excluding race and introducing SDOH in 11,638 participants from the Reasons for Geographic and Racial Differences in Stroke (REGARDS) cohort.
- Participants were aged between 45 and 79 years, had no history of ASCVD, and were not taking statins.
- Participants were followed up to 10 years for incident ASCVD, including myocardial infarction, coronary heart disease death, and fatal and nonfatal stroke.
TAKEAWAY:
- Risk prediction equations performed similarly in race- and sex-stratified PCEs (C-statistic [95% CI])
- Black female: 0.71 (0.68-0.75); Black male: 0.68 (0.64-0.73); White female: 0.77 (0.74-0.80); White male: 0.68 (0.65-0.71)
- Race-free sex-specific PCEs yielded similar discrimination as race- and sex-stratified PCEs (C-statistic [95% CI]):
- Black female: 0.71 (0.67-0.75); Black male: 0.68 (0.63-0.72); White female: 0.76 (0.73-0.80); White male: 0.68 (0.65-0.71)
- The addition of SDOH to race-free sex-specific PCEs did not improve model performance (C-statistic [95% CI]):
- Black female: 0.72 (0.68-0.76); Black male: 0.68 (0.64-0.72); White female: 0.77 (0.74-0.80); White male: 0.68 (0.65-0.71)
IN PRACTICE:
“The major takeaway is we need to rethink the idea of race in cardiovascular risk prediction,” lead author Arnab Ghosh, MD, assistant professor of medicine at Weill Cornell Medical College and a hospitalist at New York-Presbyterian/Weill Cornell Medical Center, said in a press release.
“It’s essential for clinicians and scientists to consider how to appropriately address the health effects of race as a social construct, which has contributed to health disparities in cardiovascular outcomes,” Dr. Ghosh added.
SOURCE:
The study led by Dr. Ghosh was published online on December 6, 2023, in JAMA Cardiology with an Editor’s Note.
LIMITATIONS:
The study required informed consent for inclusion, which may have led to selection bias.
The REGARDS cohort’s SDOH may not have captured all social and socioeconomic influences on ASCVD outcomes.
DISCLOSURES:
The research was funded by the National Institute of Neurological Disorders and Stroke and the National Institute on Aging of the National Institutes of Health, Department of Health and Human Services, and others. Some authors declared receiving funding, grants, or personal fees from various sources.
A version of this article appeared on Medscape.com.
TOPLINE:
Removing race and incorporating social determinants of health (SDOH) into the pooled cohort risk equations (PCEs) for predicting atherosclerotic cardiovascular disease (ASCVD) outcomes made no difference to patients’ risk scores.
METHODOLOGY:
- Primary prevention guidelines recommend using risk prediction algorithms to assess the 10-year ASCVD risk, with the currently recommended PCEs including race.
- Researchers evaluated the incremental value of revised risk prediction equations excluding race and introducing SDOH in 11,638 participants from the Reasons for Geographic and Racial Differences in Stroke (REGARDS) cohort.
- Participants were aged between 45 and 79 years, had no history of ASCVD, and were not taking statins.
- Participants were followed up to 10 years for incident ASCVD, including myocardial infarction, coronary heart disease death, and fatal and nonfatal stroke.
TAKEAWAY:
- Risk prediction equations performed similarly in race- and sex-stratified PCEs (C-statistic [95% CI])
- Black female: 0.71 (0.68-0.75); Black male: 0.68 (0.64-0.73); White female: 0.77 (0.74-0.80); White male: 0.68 (0.65-0.71)
- Race-free sex-specific PCEs yielded similar discrimination as race- and sex-stratified PCEs (C-statistic [95% CI]):
- Black female: 0.71 (0.67-0.75); Black male: 0.68 (0.63-0.72); White female: 0.76 (0.73-0.80); White male: 0.68 (0.65-0.71)
- The addition of SDOH to race-free sex-specific PCEs did not improve model performance (C-statistic [95% CI]):
- Black female: 0.72 (0.68-0.76); Black male: 0.68 (0.64-0.72); White female: 0.77 (0.74-0.80); White male: 0.68 (0.65-0.71)
IN PRACTICE:
“The major takeaway is we need to rethink the idea of race in cardiovascular risk prediction,” lead author Arnab Ghosh, MD, assistant professor of medicine at Weill Cornell Medical College and a hospitalist at New York-Presbyterian/Weill Cornell Medical Center, said in a press release.
“It’s essential for clinicians and scientists to consider how to appropriately address the health effects of race as a social construct, which has contributed to health disparities in cardiovascular outcomes,” Dr. Ghosh added.
SOURCE:
The study led by Dr. Ghosh was published online on December 6, 2023, in JAMA Cardiology with an Editor’s Note.
LIMITATIONS:
The study required informed consent for inclusion, which may have led to selection bias.
The REGARDS cohort’s SDOH may not have captured all social and socioeconomic influences on ASCVD outcomes.
DISCLOSURES:
The research was funded by the National Institute of Neurological Disorders and Stroke and the National Institute on Aging of the National Institutes of Health, Department of Health and Human Services, and others. Some authors declared receiving funding, grants, or personal fees from various sources.
A version of this article appeared on Medscape.com.
TOPLINE:
Removing race and incorporating social determinants of health (SDOH) into the pooled cohort risk equations (PCEs) for predicting atherosclerotic cardiovascular disease (ASCVD) outcomes made no difference to patients’ risk scores.
METHODOLOGY:
- Primary prevention guidelines recommend using risk prediction algorithms to assess the 10-year ASCVD risk, with the currently recommended PCEs including race.
- Researchers evaluated the incremental value of revised risk prediction equations excluding race and introducing SDOH in 11,638 participants from the Reasons for Geographic and Racial Differences in Stroke (REGARDS) cohort.
- Participants were aged between 45 and 79 years, had no history of ASCVD, and were not taking statins.
- Participants were followed up to 10 years for incident ASCVD, including myocardial infarction, coronary heart disease death, and fatal and nonfatal stroke.
TAKEAWAY:
- Risk prediction equations performed similarly in race- and sex-stratified PCEs (C-statistic [95% CI])
- Black female: 0.71 (0.68-0.75); Black male: 0.68 (0.64-0.73); White female: 0.77 (0.74-0.80); White male: 0.68 (0.65-0.71)
- Race-free sex-specific PCEs yielded similar discrimination as race- and sex-stratified PCEs (C-statistic [95% CI]):
- Black female: 0.71 (0.67-0.75); Black male: 0.68 (0.63-0.72); White female: 0.76 (0.73-0.80); White male: 0.68 (0.65-0.71)
- The addition of SDOH to race-free sex-specific PCEs did not improve model performance (C-statistic [95% CI]):
- Black female: 0.72 (0.68-0.76); Black male: 0.68 (0.64-0.72); White female: 0.77 (0.74-0.80); White male: 0.68 (0.65-0.71)
IN PRACTICE:
“The major takeaway is we need to rethink the idea of race in cardiovascular risk prediction,” lead author Arnab Ghosh, MD, assistant professor of medicine at Weill Cornell Medical College and a hospitalist at New York-Presbyterian/Weill Cornell Medical Center, said in a press release.
“It’s essential for clinicians and scientists to consider how to appropriately address the health effects of race as a social construct, which has contributed to health disparities in cardiovascular outcomes,” Dr. Ghosh added.
SOURCE:
The study led by Dr. Ghosh was published online on December 6, 2023, in JAMA Cardiology with an Editor’s Note.
LIMITATIONS:
The study required informed consent for inclusion, which may have led to selection bias.
The REGARDS cohort’s SDOH may not have captured all social and socioeconomic influences on ASCVD outcomes.
DISCLOSURES:
The research was funded by the National Institute of Neurological Disorders and Stroke and the National Institute on Aging of the National Institutes of Health, Department of Health and Human Services, and others. Some authors declared receiving funding, grants, or personal fees from various sources.
A version of this article appeared on Medscape.com.
How to Reduce Cardiovascular Morbidity and Mortality in Psoriasis and PsA
Patients with psoriatic disease have significantly higher risks of myocardial infarction, stroke, and cardiovascular mortality than does the general population, yet research consistently paints what dermatologist Joel M. Gelfand, MD, calls an “abysmal” picture: Only a minority of patients with psoriatic disease know about their increased risks, only a minority of dermatologists and rheumatologists screen for cardiovascular risk factors like lipid levels and blood pressure, and only a minority of patients diagnosed with hyperlipidemia are adequately treated with statin therapy.
In the literature and at medical meetings, Dr. Gelfand and others who have studied cardiovascular disease (CVD) comorbidity and physician practices have been urging dermatologists and rheumatologists to play a more consistent and active role in primary cardiovascular prevention for patients with psoriatic disease, who are up to 50% more likely than patients without it to develop CVD and who tend to have atherosclerosis at earlier ages.
According to the 2019 joint American Academy of Dermatology (AAD)–National Psoriasis Foundation (NPF) guidelines for managing psoriasis “with awareness and attention to comorbidities,” this means not only ensuring that all patients with psoriasis receive standard CV risk assessment (screening for hypertension, diabetes, and hyperlipidemia), but also recognizing that patients who are candidates for systemic therapy or phototherapy — or who have psoriasis involving > 10% of body surface area — may benefit from earlier and more frequent screening.
CV risk and premature mortality rises with the severity of skin disease, and patients with psoriatic arthritis (PsA) are believed to have risk levels similar to patients with moderate-severe psoriasis, cardiologist Michael S. Garshick, MD, director of the cardio-rheumatology program at New York University Langone Health, said in an interview.
In a recent survey study of 100 patients seen at NYU Langone Health’s psoriasis specialty clinic, only one-third indicated they had been advised by their physicians to be screened for CV risk factors, and only one-third reported having been told of the connection between psoriasis and CVD risk. Dr. Garshick shared the unpublished findings at the annual research symposium of the NPF in October.
Similarly, data from the National Ambulatory Medical Care Survey shows that just 16% of psoriasis-related visits to dermatology providers from 2007 to 2016 involved screening for CV risk factors. Screening rates were 11% for body mass index, 7.4% for blood pressure, 2.9% for cholesterol, and 1.7% for glucose, Dr. Gelfand and coauthors reported in 2023. .
Such findings are concerning because research shows that fewer than a quarter of patients with psoriasis have a primary care visit within a year of establishing care with their physicians, and that, overall, fewer than half of commercially insured adults under age 65 visit a primary care physician each year, according to John S. Barbieri, MD, of the department of dermatology at Brigham and Women’s Hospital in Boston. He included these findings when reporting in 2022 on a survey study on CVD screening.
In many cases, dermatologists and rheumatologists may be the primary providers for patients with psoriatic disease. So, “the question is, how can the dermatologist or rheumatologist use their interactions as a touchpoint to improve the patient’s well-being?” Dr. Barbieri said in an interview.
For the dermatologist, educating patients about the higher CVD risk fits well into conversations about “how there may be inflammation inside the body as well as in the skin,” he said. “Talk about cardiovascular risk just as you talk about PsA risk.” Both specialists, he added, can incorporate blood pressure readings and look for opportunities to measure lipid levels and hemoglobin A1c (HbA1c). These labs can easily be integrated into a biologic work-up.
“The hard part — and this needs to be individualized — is how do you want to handle [abnormal readings]? Do you want to take on a lot of the ownership and calculate [10-year CVD] risk scores and then counsel patients accordingly?” Dr. Barbieri said. “Or do you want to try to refer, and encourage them to work with their PCP? There a high-touch version and a low-touch version of how you can turn screening into action, into a care plan.”
Beyond traditional risk elevation, the primary care hand-off
Rheumatologists “in general may be more apt to screen for cardiovascular disease” as a result of their internal medicine residency training, and “we’re generally more comfortable prescribing ... if we need to,” said Alexis R. Ogdie, MD, a rheumatologist at the Hospital of the University of Pennsylvania, Philadelphia, and director of the Penn Psoriatic Arthritis Clinic.
Referral to a preventive cardiologist for management of abnormal lab results or ongoing monitoring and prevention is ideal, but when hand-offs to primary care physicians are made — the more common scenario — education is important. “A common problem is that there is underrecognition of the cardiovascular risk being elevated in our patients,” she said, above and beyond risk posed by traditional risk factors such as dyslipidemia, hypertension, metabolic syndrome, and obesity, all of which have been shown to occur more frequently in patients with psoriatic disease than in the general population.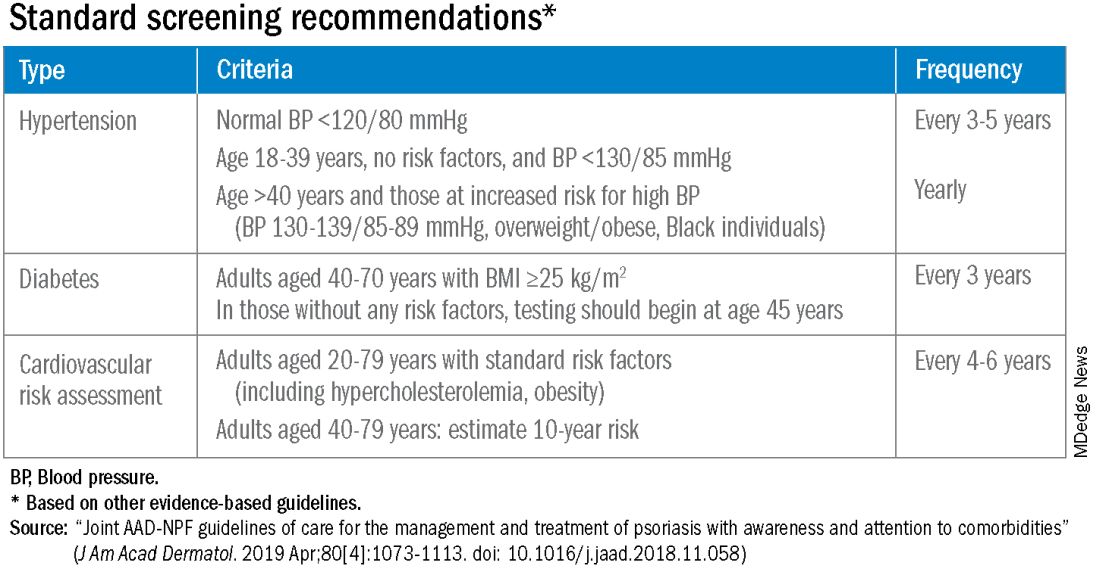
Risk stratification guides CVD prevention in the general population, and “if you use typical scores for cardiovascular risk, they may underestimate risk for our patients with PsA,” said Dr. Ogdie, who has reported on CV risk in patients with PsA. “Relative to what the patient’s perceived risk is, they may be treated similarly (to the general population). But relative to their actual risk, they’re undertreated.”
The 2019 AAD-NPF psoriasis guidelines recommend utilizing a 1.5 multiplication factor in risk score models, such as the American College of Cardiology’s Atherosclerotic Cardiovascular Disease (ASCVD) Risk Estimator, when the patient has a body surface area >10% or is a candidate for systemic therapy or phototherapy.
Similarly, the 2018 American Heart Association (AHA)-ACC Guideline on the Management of Blood Cholesterol defines psoriasis, along with RA, metabolic syndrome, HIV, and other diseases, as a “cardiovascular risk enhancer” that should be factored into assessments of ASCVD risk. (The guideline does not specify a psoriasis severity threshold.)
“It’s the first time the specialty [of cardiology] has said, ‘pay attention to a skin disease,’ ” Dr. Gelfand said at the NPF meeting.
Using the 1.5 multiplication factor, a patient who otherwise would be classified in the AHA/ACC guideline as “borderline risk,” with a 10-year ASCVD risk of 5% to <7.5%, would instead have an “intermediate” 10-year ASCVD risk of ≥7.5% to <20%. Application of the AHA-ACC “risk enhancer” would have a similar effect.
For management, the main impact of psoriasis being considered a risk enhancer is that “it lowers the threshold for treatment with standard cardiovascular prevention medications such as statins.”
In general, “we should be taking a more aggressive approach to the management of traditional cardiovascular risk factors” in patients with psoriatic disease, he said. Instead of telling a patient with mildly elevated blood pressure, ‘I’ll see you in a year or two,’ or a patient entering a prediabetic stage to “watch what you eat, and I’ll see you in a couple of years,” clinicians need to be more vigilant.
“It’s about recognizing that these traditional cardiometabolic risk factors, synergistically with psoriasis, can start enhancing CV risk at an earlier age than we might expect,” said Dr. Garshick, whose 2021 review of CV risk in psoriasis describes how the inflammatory milieu in psoriasis is linked to atherosclerosis development.
Cardiologists are aware of this, but “many primary care physicians are not. It takes time for medical knowledge to diffuse,” Dr. Gelfand said. “Tell the PCP, in notes or in a form letter, that there is a higher risk of CV disease, and reference the AHA/ACC guidelines,” he advised. “You don’t want your patient to go to their doctor and the doctor to [be uninformed].”
‘Patients trust us’
Dr. Gelfand has been at the forefront of research on psoriasis and heart disease. A study he coauthored in 2006, for instance, documented an independent risk of MI, with adjusted relative risks of 1.29 and 3.10 for a 30-year-old patient with mild or severe disease, respectively, and higher risks for a 60-year-old. In 2010, he and coinvestigators found that severe psoriasis was an independent risk factor for CV mortality (HR, 1.57) after adjusting for age, sex, smoking, diabetes, hypertension, and hyperlipidemia.
Today, along with Dr. Barbieri, Dr. Ogdie, and others, he is studying the feasibility and efficacy of a proposed national, “centralized care coordinator” model of care whereby dermatologists and rheumatologists would educate the patient, order lipid and HbA1c measurements as medically appropriate, and then refer patients as needed to a care coordinator. The care coordinator would calculate a 10-year CVD risk score and counsel the patient on possible next steps.
In a pilot study of 85 patients at four sites, 92% of patients followed through on their physician’s recommendations to have labs drawn, and 86% indicated the model was acceptable and feasible. A total of 27% of patients had “newly identified, previously undiagnosed, elevated cardiovascular disease risk,” and exploratory effectiveness results indicated a successful reduction in predicted CVD risk in patients who started statins, Dr. Gelfand reported at the NPF meeting.
With funding from the NPF, a larger, single-arm, pragmatic “CP3” trial (NCT05908240) is enrolling 525 patients with psoriasis at 10-20 academic and nonacademic dermatology sites across the United States to further test the model. The primary endpoint will be the change in LDL cholesterol measured at 6 months among people with a 10-year risk ≥5%. Secondary endpoints will cover improvement in disease severity and quality of life, behavior modification, patient experience, and other issues.
“We have only 10-15 minutes [with patients] ... a care coordinator who is empathetic and understanding and [informed] could make a big difference,” Dr. Gelfand said at the NPF meeting. If findings are positive, the model would be tested in rheumatology sites as well. The hope, he said, is that the NPF would be able to fund an in-house care coordinator(s) for the long-term.
Notably, a patient survey conducted as part of exploratory research leading up to the care coordinator project showed that patients trust their dermatologist or rheumatologist for CVD education and screening. Among 160 patients with psoriasis and 162 patients with PsA, 76% and 90% agreed that “I would like it if my dermatologist/rheumatologist educated me about my risk of heart disease,” and 60% and 75%, respectively, agree that “it would be convenient for me to have my cholesterol checked by my dermatologist/rheumatologist.”
“Patients trust us,” Dr. Gelfand said at the NPF meeting. “And the pilot study shows us that patients are motivated.”
Taking an individualized, holistic, longitudinal approach
“Sometimes you do have to triage bit,” Dr. Gelfand said in an interview. “For a young person with normal body weight who doesn’t smoke and has mild psoriasis, one could just educate and advise that they see their primary care physician” for monitoring.
“But for the same patient who is obese, maybe smokes, and doesn’t have a primary care physician, I’d order labs,” he said. “You don’t want a patient walking out the door with an [undiagnosed] LDL of 160 or hypertension.”
Age is also an important consideration, as excess CVD risk associated with autoimmune diseases like psoriasis rises with age, Dr. Gelfand said during a seminar on psoriasis and PsA held at NYU Langone in December. For a young person, typically, “I need to focus on education and lifestyle … setting them on a healthy lifestyle trajectory,” he said. “Once they get to 40, from 40 to 75 or so, that’s a sweet spot for medical intervention to lower cardiovascular risk.”
Even at older ages, however, lipid management is not the be-all and end-all, he said in the interview. “We have to be holistic.”
One advantage of having highly successful therapies for psoriasis, and to a lesser extent PsA, is the time that becomes available during follow-up visits — once disease is under control — to “focus on other things,” he said. Waiting until disease is under control to discuss diet, exercise, or smoking, for instance, makes sense anyway, he said. “You don’t want to overwhelm patients with too much to do at once.”
Indeed, said dermatologist Robert E. Kalb, MD, of the Buffalo Medical Group in Buffalo, NY, “patients have an open mind [about discussing cardiovascular disease risk], but it is not high on their radar. Most of them just want to get their skin clear.” (Dr. Kalb participated in the care coordinator pilot study, and said in an interview that since its completion, he has been more routinely ordering relevant labs.)
Rheumatologists are less fortunate with highly successful therapies, but “over the continuum of care, we do have time in office visits” to discuss issues like smoking, exercise, and lifestyle, Dr. Ogdie said. “I think of each of those pieces as part of our job.”
In the future, as researchers learn more about the impact of psoriasis and PsA treatments on CVD risk, it may be possible to tailor treatments or to prescribe treatments knowing that the therapies could reduce risk. Observational and epidemiologic data suggest that tumor necrosis factor-alpha inhibitor therapy over 3 years reduces the risk of MI, and that patients whose psoriasis is treated have reduced aortic inflammation, improved myocardial strain, and reduced coronary plaque burden, Dr. Garshick said at the NPF meeting.
“But when we look at the randomized controlled trials, they’re actually inconclusive that targeting inflammation in psoriatic disease reduces surrogates of cardiovascular disease,” he said. Dr. Garshick’s own research focuses on platelet and endothelial biology in psoriasis.
Dr. Barbieri reported he had no relevant disclosures. Dr. Garshick reported consulting fees from Bristol-Myers Squibb, Kiniksa, Horizon Therapeutics, and Agepha. Dr. Ogdie reported financial relationships with AbbVie, Amgen, Bristol-Myers Squibb, Celgene, Eli Lilly, Gilead, GlaxoSmithKline, Janssen, Novartis, Pfizer, Takeda, and UCB. Dr. Gelfand reported serving as a consultant for AbbVie, Artax, Bristol-Myers Squibb, GlaxoSmithKline, and other companies.
Patients with psoriatic disease have significantly higher risks of myocardial infarction, stroke, and cardiovascular mortality than does the general population, yet research consistently paints what dermatologist Joel M. Gelfand, MD, calls an “abysmal” picture: Only a minority of patients with psoriatic disease know about their increased risks, only a minority of dermatologists and rheumatologists screen for cardiovascular risk factors like lipid levels and blood pressure, and only a minority of patients diagnosed with hyperlipidemia are adequately treated with statin therapy.
In the literature and at medical meetings, Dr. Gelfand and others who have studied cardiovascular disease (CVD) comorbidity and physician practices have been urging dermatologists and rheumatologists to play a more consistent and active role in primary cardiovascular prevention for patients with psoriatic disease, who are up to 50% more likely than patients without it to develop CVD and who tend to have atherosclerosis at earlier ages.
According to the 2019 joint American Academy of Dermatology (AAD)–National Psoriasis Foundation (NPF) guidelines for managing psoriasis “with awareness and attention to comorbidities,” this means not only ensuring that all patients with psoriasis receive standard CV risk assessment (screening for hypertension, diabetes, and hyperlipidemia), but also recognizing that patients who are candidates for systemic therapy or phototherapy — or who have psoriasis involving > 10% of body surface area — may benefit from earlier and more frequent screening.
CV risk and premature mortality rises with the severity of skin disease, and patients with psoriatic arthritis (PsA) are believed to have risk levels similar to patients with moderate-severe psoriasis, cardiologist Michael S. Garshick, MD, director of the cardio-rheumatology program at New York University Langone Health, said in an interview.
In a recent survey study of 100 patients seen at NYU Langone Health’s psoriasis specialty clinic, only one-third indicated they had been advised by their physicians to be screened for CV risk factors, and only one-third reported having been told of the connection between psoriasis and CVD risk. Dr. Garshick shared the unpublished findings at the annual research symposium of the NPF in October.
Similarly, data from the National Ambulatory Medical Care Survey shows that just 16% of psoriasis-related visits to dermatology providers from 2007 to 2016 involved screening for CV risk factors. Screening rates were 11% for body mass index, 7.4% for blood pressure, 2.9% for cholesterol, and 1.7% for glucose, Dr. Gelfand and coauthors reported in 2023. .
Such findings are concerning because research shows that fewer than a quarter of patients with psoriasis have a primary care visit within a year of establishing care with their physicians, and that, overall, fewer than half of commercially insured adults under age 65 visit a primary care physician each year, according to John S. Barbieri, MD, of the department of dermatology at Brigham and Women’s Hospital in Boston. He included these findings when reporting in 2022 on a survey study on CVD screening.
In many cases, dermatologists and rheumatologists may be the primary providers for patients with psoriatic disease. So, “the question is, how can the dermatologist or rheumatologist use their interactions as a touchpoint to improve the patient’s well-being?” Dr. Barbieri said in an interview.
For the dermatologist, educating patients about the higher CVD risk fits well into conversations about “how there may be inflammation inside the body as well as in the skin,” he said. “Talk about cardiovascular risk just as you talk about PsA risk.” Both specialists, he added, can incorporate blood pressure readings and look for opportunities to measure lipid levels and hemoglobin A1c (HbA1c). These labs can easily be integrated into a biologic work-up.
“The hard part — and this needs to be individualized — is how do you want to handle [abnormal readings]? Do you want to take on a lot of the ownership and calculate [10-year CVD] risk scores and then counsel patients accordingly?” Dr. Barbieri said. “Or do you want to try to refer, and encourage them to work with their PCP? There a high-touch version and a low-touch version of how you can turn screening into action, into a care plan.”
Beyond traditional risk elevation, the primary care hand-off
Rheumatologists “in general may be more apt to screen for cardiovascular disease” as a result of their internal medicine residency training, and “we’re generally more comfortable prescribing ... if we need to,” said Alexis R. Ogdie, MD, a rheumatologist at the Hospital of the University of Pennsylvania, Philadelphia, and director of the Penn Psoriatic Arthritis Clinic.
Referral to a preventive cardiologist for management of abnormal lab results or ongoing monitoring and prevention is ideal, but when hand-offs to primary care physicians are made — the more common scenario — education is important. “A common problem is that there is underrecognition of the cardiovascular risk being elevated in our patients,” she said, above and beyond risk posed by traditional risk factors such as dyslipidemia, hypertension, metabolic syndrome, and obesity, all of which have been shown to occur more frequently in patients with psoriatic disease than in the general population.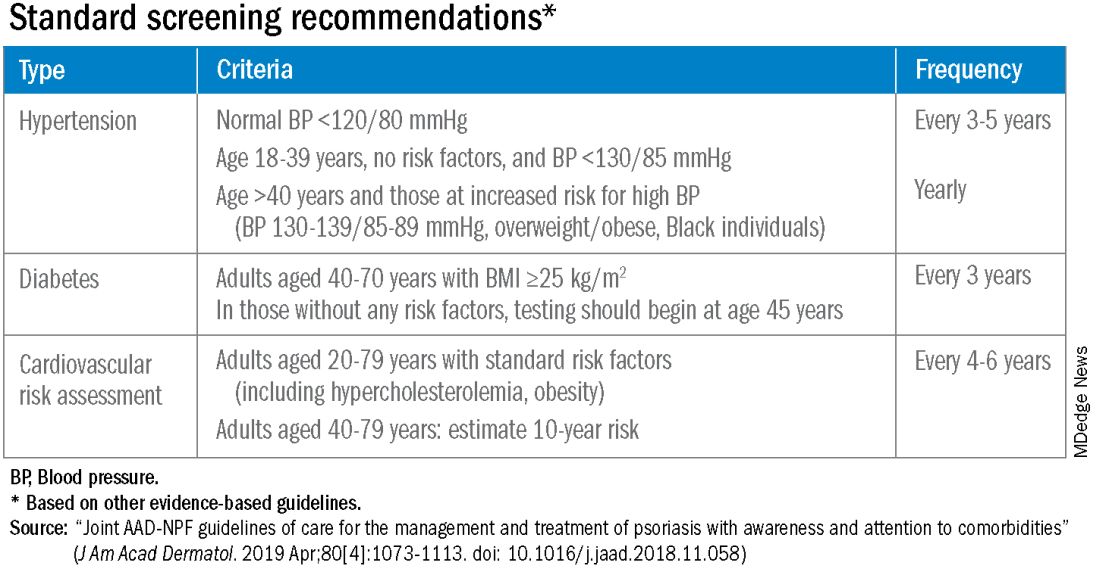
Risk stratification guides CVD prevention in the general population, and “if you use typical scores for cardiovascular risk, they may underestimate risk for our patients with PsA,” said Dr. Ogdie, who has reported on CV risk in patients with PsA. “Relative to what the patient’s perceived risk is, they may be treated similarly (to the general population). But relative to their actual risk, they’re undertreated.”
The 2019 AAD-NPF psoriasis guidelines recommend utilizing a 1.5 multiplication factor in risk score models, such as the American College of Cardiology’s Atherosclerotic Cardiovascular Disease (ASCVD) Risk Estimator, when the patient has a body surface area >10% or is a candidate for systemic therapy or phototherapy.
Similarly, the 2018 American Heart Association (AHA)-ACC Guideline on the Management of Blood Cholesterol defines psoriasis, along with RA, metabolic syndrome, HIV, and other diseases, as a “cardiovascular risk enhancer” that should be factored into assessments of ASCVD risk. (The guideline does not specify a psoriasis severity threshold.)
“It’s the first time the specialty [of cardiology] has said, ‘pay attention to a skin disease,’ ” Dr. Gelfand said at the NPF meeting.
Using the 1.5 multiplication factor, a patient who otherwise would be classified in the AHA/ACC guideline as “borderline risk,” with a 10-year ASCVD risk of 5% to <7.5%, would instead have an “intermediate” 10-year ASCVD risk of ≥7.5% to <20%. Application of the AHA-ACC “risk enhancer” would have a similar effect.
For management, the main impact of psoriasis being considered a risk enhancer is that “it lowers the threshold for treatment with standard cardiovascular prevention medications such as statins.”
In general, “we should be taking a more aggressive approach to the management of traditional cardiovascular risk factors” in patients with psoriatic disease, he said. Instead of telling a patient with mildly elevated blood pressure, ‘I’ll see you in a year or two,’ or a patient entering a prediabetic stage to “watch what you eat, and I’ll see you in a couple of years,” clinicians need to be more vigilant.
“It’s about recognizing that these traditional cardiometabolic risk factors, synergistically with psoriasis, can start enhancing CV risk at an earlier age than we might expect,” said Dr. Garshick, whose 2021 review of CV risk in psoriasis describes how the inflammatory milieu in psoriasis is linked to atherosclerosis development.
Cardiologists are aware of this, but “many primary care physicians are not. It takes time for medical knowledge to diffuse,” Dr. Gelfand said. “Tell the PCP, in notes or in a form letter, that there is a higher risk of CV disease, and reference the AHA/ACC guidelines,” he advised. “You don’t want your patient to go to their doctor and the doctor to [be uninformed].”
‘Patients trust us’
Dr. Gelfand has been at the forefront of research on psoriasis and heart disease. A study he coauthored in 2006, for instance, documented an independent risk of MI, with adjusted relative risks of 1.29 and 3.10 for a 30-year-old patient with mild or severe disease, respectively, and higher risks for a 60-year-old. In 2010, he and coinvestigators found that severe psoriasis was an independent risk factor for CV mortality (HR, 1.57) after adjusting for age, sex, smoking, diabetes, hypertension, and hyperlipidemia.
Today, along with Dr. Barbieri, Dr. Ogdie, and others, he is studying the feasibility and efficacy of a proposed national, “centralized care coordinator” model of care whereby dermatologists and rheumatologists would educate the patient, order lipid and HbA1c measurements as medically appropriate, and then refer patients as needed to a care coordinator. The care coordinator would calculate a 10-year CVD risk score and counsel the patient on possible next steps.
In a pilot study of 85 patients at four sites, 92% of patients followed through on their physician’s recommendations to have labs drawn, and 86% indicated the model was acceptable and feasible. A total of 27% of patients had “newly identified, previously undiagnosed, elevated cardiovascular disease risk,” and exploratory effectiveness results indicated a successful reduction in predicted CVD risk in patients who started statins, Dr. Gelfand reported at the NPF meeting.
With funding from the NPF, a larger, single-arm, pragmatic “CP3” trial (NCT05908240) is enrolling 525 patients with psoriasis at 10-20 academic and nonacademic dermatology sites across the United States to further test the model. The primary endpoint will be the change in LDL cholesterol measured at 6 months among people with a 10-year risk ≥5%. Secondary endpoints will cover improvement in disease severity and quality of life, behavior modification, patient experience, and other issues.
“We have only 10-15 minutes [with patients] ... a care coordinator who is empathetic and understanding and [informed] could make a big difference,” Dr. Gelfand said at the NPF meeting. If findings are positive, the model would be tested in rheumatology sites as well. The hope, he said, is that the NPF would be able to fund an in-house care coordinator(s) for the long-term.
Notably, a patient survey conducted as part of exploratory research leading up to the care coordinator project showed that patients trust their dermatologist or rheumatologist for CVD education and screening. Among 160 patients with psoriasis and 162 patients with PsA, 76% and 90% agreed that “I would like it if my dermatologist/rheumatologist educated me about my risk of heart disease,” and 60% and 75%, respectively, agree that “it would be convenient for me to have my cholesterol checked by my dermatologist/rheumatologist.”
“Patients trust us,” Dr. Gelfand said at the NPF meeting. “And the pilot study shows us that patients are motivated.”
Taking an individualized, holistic, longitudinal approach
“Sometimes you do have to triage bit,” Dr. Gelfand said in an interview. “For a young person with normal body weight who doesn’t smoke and has mild psoriasis, one could just educate and advise that they see their primary care physician” for monitoring.
“But for the same patient who is obese, maybe smokes, and doesn’t have a primary care physician, I’d order labs,” he said. “You don’t want a patient walking out the door with an [undiagnosed] LDL of 160 or hypertension.”
Age is also an important consideration, as excess CVD risk associated with autoimmune diseases like psoriasis rises with age, Dr. Gelfand said during a seminar on psoriasis and PsA held at NYU Langone in December. For a young person, typically, “I need to focus on education and lifestyle … setting them on a healthy lifestyle trajectory,” he said. “Once they get to 40, from 40 to 75 or so, that’s a sweet spot for medical intervention to lower cardiovascular risk.”
Even at older ages, however, lipid management is not the be-all and end-all, he said in the interview. “We have to be holistic.”
One advantage of having highly successful therapies for psoriasis, and to a lesser extent PsA, is the time that becomes available during follow-up visits — once disease is under control — to “focus on other things,” he said. Waiting until disease is under control to discuss diet, exercise, or smoking, for instance, makes sense anyway, he said. “You don’t want to overwhelm patients with too much to do at once.”
Indeed, said dermatologist Robert E. Kalb, MD, of the Buffalo Medical Group in Buffalo, NY, “patients have an open mind [about discussing cardiovascular disease risk], but it is not high on their radar. Most of them just want to get their skin clear.” (Dr. Kalb participated in the care coordinator pilot study, and said in an interview that since its completion, he has been more routinely ordering relevant labs.)
Rheumatologists are less fortunate with highly successful therapies, but “over the continuum of care, we do have time in office visits” to discuss issues like smoking, exercise, and lifestyle, Dr. Ogdie said. “I think of each of those pieces as part of our job.”
In the future, as researchers learn more about the impact of psoriasis and PsA treatments on CVD risk, it may be possible to tailor treatments or to prescribe treatments knowing that the therapies could reduce risk. Observational and epidemiologic data suggest that tumor necrosis factor-alpha inhibitor therapy over 3 years reduces the risk of MI, and that patients whose psoriasis is treated have reduced aortic inflammation, improved myocardial strain, and reduced coronary plaque burden, Dr. Garshick said at the NPF meeting.
“But when we look at the randomized controlled trials, they’re actually inconclusive that targeting inflammation in psoriatic disease reduces surrogates of cardiovascular disease,” he said. Dr. Garshick’s own research focuses on platelet and endothelial biology in psoriasis.
Dr. Barbieri reported he had no relevant disclosures. Dr. Garshick reported consulting fees from Bristol-Myers Squibb, Kiniksa, Horizon Therapeutics, and Agepha. Dr. Ogdie reported financial relationships with AbbVie, Amgen, Bristol-Myers Squibb, Celgene, Eli Lilly, Gilead, GlaxoSmithKline, Janssen, Novartis, Pfizer, Takeda, and UCB. Dr. Gelfand reported serving as a consultant for AbbVie, Artax, Bristol-Myers Squibb, GlaxoSmithKline, and other companies.
Patients with psoriatic disease have significantly higher risks of myocardial infarction, stroke, and cardiovascular mortality than does the general population, yet research consistently paints what dermatologist Joel M. Gelfand, MD, calls an “abysmal” picture: Only a minority of patients with psoriatic disease know about their increased risks, only a minority of dermatologists and rheumatologists screen for cardiovascular risk factors like lipid levels and blood pressure, and only a minority of patients diagnosed with hyperlipidemia are adequately treated with statin therapy.
In the literature and at medical meetings, Dr. Gelfand and others who have studied cardiovascular disease (CVD) comorbidity and physician practices have been urging dermatologists and rheumatologists to play a more consistent and active role in primary cardiovascular prevention for patients with psoriatic disease, who are up to 50% more likely than patients without it to develop CVD and who tend to have atherosclerosis at earlier ages.
According to the 2019 joint American Academy of Dermatology (AAD)–National Psoriasis Foundation (NPF) guidelines for managing psoriasis “with awareness and attention to comorbidities,” this means not only ensuring that all patients with psoriasis receive standard CV risk assessment (screening for hypertension, diabetes, and hyperlipidemia), but also recognizing that patients who are candidates for systemic therapy or phototherapy — or who have psoriasis involving > 10% of body surface area — may benefit from earlier and more frequent screening.
CV risk and premature mortality rises with the severity of skin disease, and patients with psoriatic arthritis (PsA) are believed to have risk levels similar to patients with moderate-severe psoriasis, cardiologist Michael S. Garshick, MD, director of the cardio-rheumatology program at New York University Langone Health, said in an interview.
In a recent survey study of 100 patients seen at NYU Langone Health’s psoriasis specialty clinic, only one-third indicated they had been advised by their physicians to be screened for CV risk factors, and only one-third reported having been told of the connection between psoriasis and CVD risk. Dr. Garshick shared the unpublished findings at the annual research symposium of the NPF in October.
Similarly, data from the National Ambulatory Medical Care Survey shows that just 16% of psoriasis-related visits to dermatology providers from 2007 to 2016 involved screening for CV risk factors. Screening rates were 11% for body mass index, 7.4% for blood pressure, 2.9% for cholesterol, and 1.7% for glucose, Dr. Gelfand and coauthors reported in 2023. .
Such findings are concerning because research shows that fewer than a quarter of patients with psoriasis have a primary care visit within a year of establishing care with their physicians, and that, overall, fewer than half of commercially insured adults under age 65 visit a primary care physician each year, according to John S. Barbieri, MD, of the department of dermatology at Brigham and Women’s Hospital in Boston. He included these findings when reporting in 2022 on a survey study on CVD screening.
In many cases, dermatologists and rheumatologists may be the primary providers for patients with psoriatic disease. So, “the question is, how can the dermatologist or rheumatologist use their interactions as a touchpoint to improve the patient’s well-being?” Dr. Barbieri said in an interview.
For the dermatologist, educating patients about the higher CVD risk fits well into conversations about “how there may be inflammation inside the body as well as in the skin,” he said. “Talk about cardiovascular risk just as you talk about PsA risk.” Both specialists, he added, can incorporate blood pressure readings and look for opportunities to measure lipid levels and hemoglobin A1c (HbA1c). These labs can easily be integrated into a biologic work-up.
“The hard part — and this needs to be individualized — is how do you want to handle [abnormal readings]? Do you want to take on a lot of the ownership and calculate [10-year CVD] risk scores and then counsel patients accordingly?” Dr. Barbieri said. “Or do you want to try to refer, and encourage them to work with their PCP? There a high-touch version and a low-touch version of how you can turn screening into action, into a care plan.”
Beyond traditional risk elevation, the primary care hand-off
Rheumatologists “in general may be more apt to screen for cardiovascular disease” as a result of their internal medicine residency training, and “we’re generally more comfortable prescribing ... if we need to,” said Alexis R. Ogdie, MD, a rheumatologist at the Hospital of the University of Pennsylvania, Philadelphia, and director of the Penn Psoriatic Arthritis Clinic.
Referral to a preventive cardiologist for management of abnormal lab results or ongoing monitoring and prevention is ideal, but when hand-offs to primary care physicians are made — the more common scenario — education is important. “A common problem is that there is underrecognition of the cardiovascular risk being elevated in our patients,” she said, above and beyond risk posed by traditional risk factors such as dyslipidemia, hypertension, metabolic syndrome, and obesity, all of which have been shown to occur more frequently in patients with psoriatic disease than in the general population.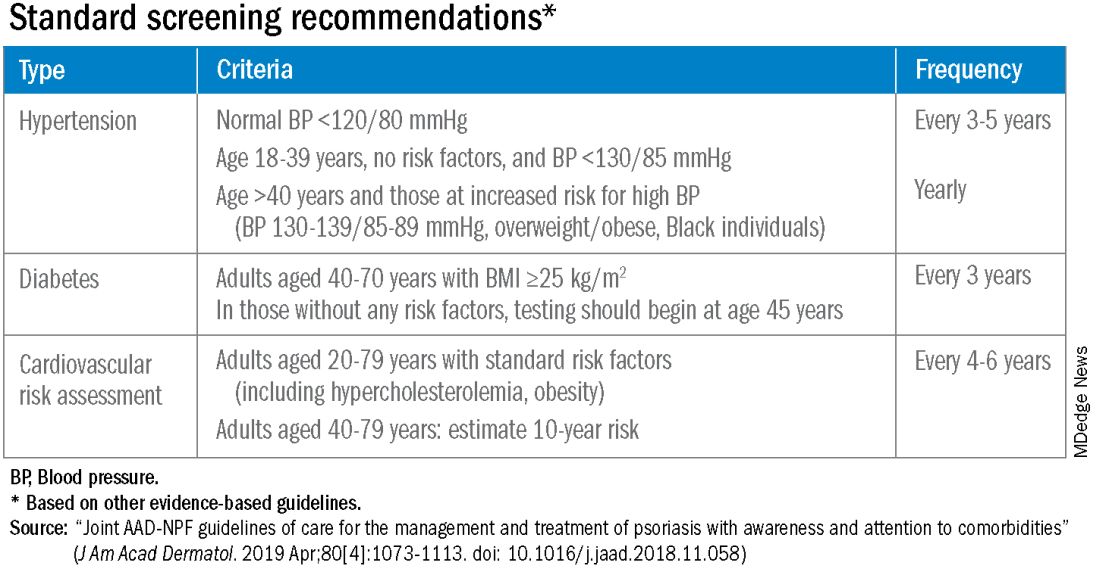
Risk stratification guides CVD prevention in the general population, and “if you use typical scores for cardiovascular risk, they may underestimate risk for our patients with PsA,” said Dr. Ogdie, who has reported on CV risk in patients with PsA. “Relative to what the patient’s perceived risk is, they may be treated similarly (to the general population). But relative to their actual risk, they’re undertreated.”
The 2019 AAD-NPF psoriasis guidelines recommend utilizing a 1.5 multiplication factor in risk score models, such as the American College of Cardiology’s Atherosclerotic Cardiovascular Disease (ASCVD) Risk Estimator, when the patient has a body surface area >10% or is a candidate for systemic therapy or phototherapy.
Similarly, the 2018 American Heart Association (AHA)-ACC Guideline on the Management of Blood Cholesterol defines psoriasis, along with RA, metabolic syndrome, HIV, and other diseases, as a “cardiovascular risk enhancer” that should be factored into assessments of ASCVD risk. (The guideline does not specify a psoriasis severity threshold.)
“It’s the first time the specialty [of cardiology] has said, ‘pay attention to a skin disease,’ ” Dr. Gelfand said at the NPF meeting.
Using the 1.5 multiplication factor, a patient who otherwise would be classified in the AHA/ACC guideline as “borderline risk,” with a 10-year ASCVD risk of 5% to <7.5%, would instead have an “intermediate” 10-year ASCVD risk of ≥7.5% to <20%. Application of the AHA-ACC “risk enhancer” would have a similar effect.
For management, the main impact of psoriasis being considered a risk enhancer is that “it lowers the threshold for treatment with standard cardiovascular prevention medications such as statins.”
In general, “we should be taking a more aggressive approach to the management of traditional cardiovascular risk factors” in patients with psoriatic disease, he said. Instead of telling a patient with mildly elevated blood pressure, ‘I’ll see you in a year or two,’ or a patient entering a prediabetic stage to “watch what you eat, and I’ll see you in a couple of years,” clinicians need to be more vigilant.
“It’s about recognizing that these traditional cardiometabolic risk factors, synergistically with psoriasis, can start enhancing CV risk at an earlier age than we might expect,” said Dr. Garshick, whose 2021 review of CV risk in psoriasis describes how the inflammatory milieu in psoriasis is linked to atherosclerosis development.
Cardiologists are aware of this, but “many primary care physicians are not. It takes time for medical knowledge to diffuse,” Dr. Gelfand said. “Tell the PCP, in notes or in a form letter, that there is a higher risk of CV disease, and reference the AHA/ACC guidelines,” he advised. “You don’t want your patient to go to their doctor and the doctor to [be uninformed].”
‘Patients trust us’
Dr. Gelfand has been at the forefront of research on psoriasis and heart disease. A study he coauthored in 2006, for instance, documented an independent risk of MI, with adjusted relative risks of 1.29 and 3.10 for a 30-year-old patient with mild or severe disease, respectively, and higher risks for a 60-year-old. In 2010, he and coinvestigators found that severe psoriasis was an independent risk factor for CV mortality (HR, 1.57) after adjusting for age, sex, smoking, diabetes, hypertension, and hyperlipidemia.
Today, along with Dr. Barbieri, Dr. Ogdie, and others, he is studying the feasibility and efficacy of a proposed national, “centralized care coordinator” model of care whereby dermatologists and rheumatologists would educate the patient, order lipid and HbA1c measurements as medically appropriate, and then refer patients as needed to a care coordinator. The care coordinator would calculate a 10-year CVD risk score and counsel the patient on possible next steps.
In a pilot study of 85 patients at four sites, 92% of patients followed through on their physician’s recommendations to have labs drawn, and 86% indicated the model was acceptable and feasible. A total of 27% of patients had “newly identified, previously undiagnosed, elevated cardiovascular disease risk,” and exploratory effectiveness results indicated a successful reduction in predicted CVD risk in patients who started statins, Dr. Gelfand reported at the NPF meeting.
With funding from the NPF, a larger, single-arm, pragmatic “CP3” trial (NCT05908240) is enrolling 525 patients with psoriasis at 10-20 academic and nonacademic dermatology sites across the United States to further test the model. The primary endpoint will be the change in LDL cholesterol measured at 6 months among people with a 10-year risk ≥5%. Secondary endpoints will cover improvement in disease severity and quality of life, behavior modification, patient experience, and other issues.
“We have only 10-15 minutes [with patients] ... a care coordinator who is empathetic and understanding and [informed] could make a big difference,” Dr. Gelfand said at the NPF meeting. If findings are positive, the model would be tested in rheumatology sites as well. The hope, he said, is that the NPF would be able to fund an in-house care coordinator(s) for the long-term.
Notably, a patient survey conducted as part of exploratory research leading up to the care coordinator project showed that patients trust their dermatologist or rheumatologist for CVD education and screening. Among 160 patients with psoriasis and 162 patients with PsA, 76% and 90% agreed that “I would like it if my dermatologist/rheumatologist educated me about my risk of heart disease,” and 60% and 75%, respectively, agree that “it would be convenient for me to have my cholesterol checked by my dermatologist/rheumatologist.”
“Patients trust us,” Dr. Gelfand said at the NPF meeting. “And the pilot study shows us that patients are motivated.”
Taking an individualized, holistic, longitudinal approach
“Sometimes you do have to triage bit,” Dr. Gelfand said in an interview. “For a young person with normal body weight who doesn’t smoke and has mild psoriasis, one could just educate and advise that they see their primary care physician” for monitoring.
“But for the same patient who is obese, maybe smokes, and doesn’t have a primary care physician, I’d order labs,” he said. “You don’t want a patient walking out the door with an [undiagnosed] LDL of 160 or hypertension.”
Age is also an important consideration, as excess CVD risk associated with autoimmune diseases like psoriasis rises with age, Dr. Gelfand said during a seminar on psoriasis and PsA held at NYU Langone in December. For a young person, typically, “I need to focus on education and lifestyle … setting them on a healthy lifestyle trajectory,” he said. “Once they get to 40, from 40 to 75 or so, that’s a sweet spot for medical intervention to lower cardiovascular risk.”
Even at older ages, however, lipid management is not the be-all and end-all, he said in the interview. “We have to be holistic.”
One advantage of having highly successful therapies for psoriasis, and to a lesser extent PsA, is the time that becomes available during follow-up visits — once disease is under control — to “focus on other things,” he said. Waiting until disease is under control to discuss diet, exercise, or smoking, for instance, makes sense anyway, he said. “You don’t want to overwhelm patients with too much to do at once.”
Indeed, said dermatologist Robert E. Kalb, MD, of the Buffalo Medical Group in Buffalo, NY, “patients have an open mind [about discussing cardiovascular disease risk], but it is not high on their radar. Most of them just want to get their skin clear.” (Dr. Kalb participated in the care coordinator pilot study, and said in an interview that since its completion, he has been more routinely ordering relevant labs.)
Rheumatologists are less fortunate with highly successful therapies, but “over the continuum of care, we do have time in office visits” to discuss issues like smoking, exercise, and lifestyle, Dr. Ogdie said. “I think of each of those pieces as part of our job.”
In the future, as researchers learn more about the impact of psoriasis and PsA treatments on CVD risk, it may be possible to tailor treatments or to prescribe treatments knowing that the therapies could reduce risk. Observational and epidemiologic data suggest that tumor necrosis factor-alpha inhibitor therapy over 3 years reduces the risk of MI, and that patients whose psoriasis is treated have reduced aortic inflammation, improved myocardial strain, and reduced coronary plaque burden, Dr. Garshick said at the NPF meeting.
“But when we look at the randomized controlled trials, they’re actually inconclusive that targeting inflammation in psoriatic disease reduces surrogates of cardiovascular disease,” he said. Dr. Garshick’s own research focuses on platelet and endothelial biology in psoriasis.
Dr. Barbieri reported he had no relevant disclosures. Dr. Garshick reported consulting fees from Bristol-Myers Squibb, Kiniksa, Horizon Therapeutics, and Agepha. Dr. Ogdie reported financial relationships with AbbVie, Amgen, Bristol-Myers Squibb, Celgene, Eli Lilly, Gilead, GlaxoSmithKline, Janssen, Novartis, Pfizer, Takeda, and UCB. Dr. Gelfand reported serving as a consultant for AbbVie, Artax, Bristol-Myers Squibb, GlaxoSmithKline, and other companies.
Alcohol and CV Risk: Both Beneficial and Harmful Effects?
with evidence emerging that alcohol use may both increase and decrease the risk for CVD.
The answer may depend on the presence of circulating metabolites of alcohol, some of which may be beneficial while others may be harmful, new research suggests.
“We adopted an association analysis, looking at 60 metabolites produced during or after alcohol has been metabolized, to see whether those metabolites can link alcohol consumption with CVD,” senior author Jiantao Ma, PhD, MBBS, assistant professor, Division of Nutrition Epidemiology and Data Science, Friedman School, Tufts University, Boston, Massachusetts, said in an interview.
“We found that the relationship is quite complex, with some metabolites showing protective effects against CVD and others showing harmful effects,” said Dr. Ma. “This opens the door for future research because we think that these molecules can help [us] understand the mechanism of the relationship between alcohol and CVD.”
The study was published online in BMC Medicine.
J-Shaped Relationship?
Previous research has painted a confusing picture of the relationship between alcohol consumption and CVD. For example, some studies have suggested that moderate levels of drinking may be hazardous to cardiac health, while others have pointed to potential cardioprotective effects.
Nevertheless, “according to the latest ACC/AHA guidelines regarding alcohol consumption and its relationship to CVD, there is no level of alcohol use that is deemed safe and considered acceptable,” Saurabh Sharma, MD, program director, Internal Medicine Residency Program, and clinical assistant professor of cardiology, Geisinger Commonwealth School of Medicine, Scranton, Pennsylvania, said in an interview.
Older observational data suggested a “J-shaped” relationship between alcohol consumption and cardiovascular risk, such that a low to moderate amount might reduce risk, while higher amounts increase it, said Dr. Sharma, a member of the American College of Cardiology (ACC) Prevention of Cardiovascular Diseases Council.
“But it’s essential to note that these findings were based on observational studies. No randomized controlled trials have provided conclusive evidence supporting the idea that moderate alcohol consumption actively reduces cardiovascular risk,” he said.
The current study is also observational, but it shines a somewhat different spotlight on the subject by examining alcohol consumption–related metabolites, said Dr. Ma — that is, small molecules that are the intermediates or end-products of metabolism in many cellular processes.
Some recent research “shows that alcohol may be harmful or at least has no beneficial effect in CVD prevention,” he said. “Our motivation was to analyze the association using metabolites, genetics, and epigenetics, because we think that these molecules may help us understand some of the mechanisms that underlie the relationship between alcohol consumption and CVD, and partially answer the question of whether alcohol may be harmful or helpful.”
Caution Warranted
Although some previous studies have looked at metabolites, most analyzed alcohol consumption measured at a single time point, “which may not represent habitual or long-term alcohol consumption,” the researchers note.
The team used data derived from 2458 Framingham Heart Study Offspring participants (mean age, 56 ± 9.3 years at the fifth examination; 52% female), calculating the cumulative average alcohol consumption from total intake of beer, wine, and liquor over an average 20-year period. Most participants were overweight, close to one fifth were current smokers, and 636 developed CVD over the study period.
Participants were assessed every 4-8 years, with metabolites measured during the fifth examination.
Linear models were used to investigate the association of alcohol consumption with 211 plasma metabolites, adjusting for a variety of potential confounders, including age, sex, batch, smoking, diet, physical activity, body mass index, and familial relationship.
Sixty metabolites associated with cumulative average alcohol consumption were identified (P < .00024), after adjustment for confounders. Of these, 40 displayed positive associations with the cumulative average alcohol consumption, with the most significant metabolite being cholesteryl palmitoleate (CE16:1), a plasma cholesteryl ester involved with cholesterol metabolism.
One gram per day of higher alcohol consumption was associated with a higher-level CE16:1 in the blood (b = .023). Several other phosphatidylcholine metabolites were also positively associated with alcohol consumption.
On the other hand, 20 metabolites were negatively associated with alcohol consumption, with triacylglycerol 54:4 (TAG 54:4) displaying the most significant association (b = –.017).
The alcoholic beverages were not equal when it came to association with metabolites: 19 metabolites were significantly associated with the cumulative average consumption of beer, 30 with wine, and 32 with liquor. Seven were significantly associated with the cumulative consumption of all three types of drinks.
The researchers conducted survival analysis that identified 10 alcohol-associated metabolites associated with differential CVD risks, after adjusting for confounders. They also built two alcohol consumption–weighted metabolite scores using these 10 metabolites. After adjustment for confounders including CVD risk factors, the two scores had “comparable but opposite” associations with incident CVD, HR 1.11 (95% CI, 1.02-1.21) vs 0.88 (0.78-0.98; both P values = .02).
“We found that seven metabolites were harmful, while three were beneficial, “ Dr. Ma reported.
Dr. Ma cautioned that association “doesn’t represent causation.” On the basis of the findings, however, “we can hypothesize that if you drink a moderate amount of alcohol, you can either increase or decrease your risk of CVD.”
For people with cardiac conditions, “it would be [wise to be] cautious in recommending alcohol consumption,” he said. “For people without cardiac conditions, I would follow the recommendations of the AHA. If people don’t already drink alcohol, we don’t recommend that you start drinking it; and if you already drink, we’d recommend keeping it minimal.”
He cautioned that this is “only one study and we need more research if we are to generate a clearer message to the patient.” At present, perhaps the best message to patients is “to be cautious and warn them that there are potentially harmful effects,” he said.
Mendelian Randomization?
Dr. Sharma, who was not involved in the study, emphasized that it’s “crucial” to recognize that the study “does not alter the established understanding that any level of alcohol consumption poses harm to the heart,” and that “any amount of alcohol consumption has the potential to elevate triglyceride levels, thereby contributing to the increased risk of cardiovascular complications.”
Previously reported cardioprotective benefits “are likely influenced by confounding factors, such as lifestyle and sociodemographic elements,” he speculated.
He noted that observational studies “encounter challenges in disentangling the influence of factors like obesity, lack of exercise, and tobacco use” as well as reverse causality.
“To overcome these limitations, Mendelian randomization emerges as a robust method,” he suggested. “This approach utilizes measured genetic variations with known functions to investigate the causal effect of a modifiable exposure on disease within the framework of observational studies.”
Notably, certain studies using this approach, including one by Larsson and colleagues, and another by Biddinger and associates, “have provided valuable insights by establishing a clear and causal relationship between alcohol consumption and CVD,” he said.
The study was funded by the National Institute of Health’s National Institute on Alcohol Abuse and Alcoholism. Data collection in the Framingham Heart Study was supported by the National Heart, Lung, and Blood Institute. Dr. Ma and coauthors and Dr. Sharma disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
with evidence emerging that alcohol use may both increase and decrease the risk for CVD.
The answer may depend on the presence of circulating metabolites of alcohol, some of which may be beneficial while others may be harmful, new research suggests.
“We adopted an association analysis, looking at 60 metabolites produced during or after alcohol has been metabolized, to see whether those metabolites can link alcohol consumption with CVD,” senior author Jiantao Ma, PhD, MBBS, assistant professor, Division of Nutrition Epidemiology and Data Science, Friedman School, Tufts University, Boston, Massachusetts, said in an interview.
“We found that the relationship is quite complex, with some metabolites showing protective effects against CVD and others showing harmful effects,” said Dr. Ma. “This opens the door for future research because we think that these molecules can help [us] understand the mechanism of the relationship between alcohol and CVD.”
The study was published online in BMC Medicine.
J-Shaped Relationship?
Previous research has painted a confusing picture of the relationship between alcohol consumption and CVD. For example, some studies have suggested that moderate levels of drinking may be hazardous to cardiac health, while others have pointed to potential cardioprotective effects.
Nevertheless, “according to the latest ACC/AHA guidelines regarding alcohol consumption and its relationship to CVD, there is no level of alcohol use that is deemed safe and considered acceptable,” Saurabh Sharma, MD, program director, Internal Medicine Residency Program, and clinical assistant professor of cardiology, Geisinger Commonwealth School of Medicine, Scranton, Pennsylvania, said in an interview.
Older observational data suggested a “J-shaped” relationship between alcohol consumption and cardiovascular risk, such that a low to moderate amount might reduce risk, while higher amounts increase it, said Dr. Sharma, a member of the American College of Cardiology (ACC) Prevention of Cardiovascular Diseases Council.
“But it’s essential to note that these findings were based on observational studies. No randomized controlled trials have provided conclusive evidence supporting the idea that moderate alcohol consumption actively reduces cardiovascular risk,” he said.
The current study is also observational, but it shines a somewhat different spotlight on the subject by examining alcohol consumption–related metabolites, said Dr. Ma — that is, small molecules that are the intermediates or end-products of metabolism in many cellular processes.
Some recent research “shows that alcohol may be harmful or at least has no beneficial effect in CVD prevention,” he said. “Our motivation was to analyze the association using metabolites, genetics, and epigenetics, because we think that these molecules may help us understand some of the mechanisms that underlie the relationship between alcohol consumption and CVD, and partially answer the question of whether alcohol may be harmful or helpful.”
Caution Warranted
Although some previous studies have looked at metabolites, most analyzed alcohol consumption measured at a single time point, “which may not represent habitual or long-term alcohol consumption,” the researchers note.
The team used data derived from 2458 Framingham Heart Study Offspring participants (mean age, 56 ± 9.3 years at the fifth examination; 52% female), calculating the cumulative average alcohol consumption from total intake of beer, wine, and liquor over an average 20-year period. Most participants were overweight, close to one fifth were current smokers, and 636 developed CVD over the study period.
Participants were assessed every 4-8 years, with metabolites measured during the fifth examination.
Linear models were used to investigate the association of alcohol consumption with 211 plasma metabolites, adjusting for a variety of potential confounders, including age, sex, batch, smoking, diet, physical activity, body mass index, and familial relationship.
Sixty metabolites associated with cumulative average alcohol consumption were identified (P < .00024), after adjustment for confounders. Of these, 40 displayed positive associations with the cumulative average alcohol consumption, with the most significant metabolite being cholesteryl palmitoleate (CE16:1), a plasma cholesteryl ester involved with cholesterol metabolism.
One gram per day of higher alcohol consumption was associated with a higher-level CE16:1 in the blood (b = .023). Several other phosphatidylcholine metabolites were also positively associated with alcohol consumption.
On the other hand, 20 metabolites were negatively associated with alcohol consumption, with triacylglycerol 54:4 (TAG 54:4) displaying the most significant association (b = –.017).
The alcoholic beverages were not equal when it came to association with metabolites: 19 metabolites were significantly associated with the cumulative average consumption of beer, 30 with wine, and 32 with liquor. Seven were significantly associated with the cumulative consumption of all three types of drinks.
The researchers conducted survival analysis that identified 10 alcohol-associated metabolites associated with differential CVD risks, after adjusting for confounders. They also built two alcohol consumption–weighted metabolite scores using these 10 metabolites. After adjustment for confounders including CVD risk factors, the two scores had “comparable but opposite” associations with incident CVD, HR 1.11 (95% CI, 1.02-1.21) vs 0.88 (0.78-0.98; both P values = .02).
“We found that seven metabolites were harmful, while three were beneficial, “ Dr. Ma reported.
Dr. Ma cautioned that association “doesn’t represent causation.” On the basis of the findings, however, “we can hypothesize that if you drink a moderate amount of alcohol, you can either increase or decrease your risk of CVD.”
For people with cardiac conditions, “it would be [wise to be] cautious in recommending alcohol consumption,” he said. “For people without cardiac conditions, I would follow the recommendations of the AHA. If people don’t already drink alcohol, we don’t recommend that you start drinking it; and if you already drink, we’d recommend keeping it minimal.”
He cautioned that this is “only one study and we need more research if we are to generate a clearer message to the patient.” At present, perhaps the best message to patients is “to be cautious and warn them that there are potentially harmful effects,” he said.
Mendelian Randomization?
Dr. Sharma, who was not involved in the study, emphasized that it’s “crucial” to recognize that the study “does not alter the established understanding that any level of alcohol consumption poses harm to the heart,” and that “any amount of alcohol consumption has the potential to elevate triglyceride levels, thereby contributing to the increased risk of cardiovascular complications.”
Previously reported cardioprotective benefits “are likely influenced by confounding factors, such as lifestyle and sociodemographic elements,” he speculated.
He noted that observational studies “encounter challenges in disentangling the influence of factors like obesity, lack of exercise, and tobacco use” as well as reverse causality.
“To overcome these limitations, Mendelian randomization emerges as a robust method,” he suggested. “This approach utilizes measured genetic variations with known functions to investigate the causal effect of a modifiable exposure on disease within the framework of observational studies.”
Notably, certain studies using this approach, including one by Larsson and colleagues, and another by Biddinger and associates, “have provided valuable insights by establishing a clear and causal relationship between alcohol consumption and CVD,” he said.
The study was funded by the National Institute of Health’s National Institute on Alcohol Abuse and Alcoholism. Data collection in the Framingham Heart Study was supported by the National Heart, Lung, and Blood Institute. Dr. Ma and coauthors and Dr. Sharma disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
with evidence emerging that alcohol use may both increase and decrease the risk for CVD.
The answer may depend on the presence of circulating metabolites of alcohol, some of which may be beneficial while others may be harmful, new research suggests.
“We adopted an association analysis, looking at 60 metabolites produced during or after alcohol has been metabolized, to see whether those metabolites can link alcohol consumption with CVD,” senior author Jiantao Ma, PhD, MBBS, assistant professor, Division of Nutrition Epidemiology and Data Science, Friedman School, Tufts University, Boston, Massachusetts, said in an interview.
“We found that the relationship is quite complex, with some metabolites showing protective effects against CVD and others showing harmful effects,” said Dr. Ma. “This opens the door for future research because we think that these molecules can help [us] understand the mechanism of the relationship between alcohol and CVD.”
The study was published online in BMC Medicine.
J-Shaped Relationship?
Previous research has painted a confusing picture of the relationship between alcohol consumption and CVD. For example, some studies have suggested that moderate levels of drinking may be hazardous to cardiac health, while others have pointed to potential cardioprotective effects.
Nevertheless, “according to the latest ACC/AHA guidelines regarding alcohol consumption and its relationship to CVD, there is no level of alcohol use that is deemed safe and considered acceptable,” Saurabh Sharma, MD, program director, Internal Medicine Residency Program, and clinical assistant professor of cardiology, Geisinger Commonwealth School of Medicine, Scranton, Pennsylvania, said in an interview.
Older observational data suggested a “J-shaped” relationship between alcohol consumption and cardiovascular risk, such that a low to moderate amount might reduce risk, while higher amounts increase it, said Dr. Sharma, a member of the American College of Cardiology (ACC) Prevention of Cardiovascular Diseases Council.
“But it’s essential to note that these findings were based on observational studies. No randomized controlled trials have provided conclusive evidence supporting the idea that moderate alcohol consumption actively reduces cardiovascular risk,” he said.
The current study is also observational, but it shines a somewhat different spotlight on the subject by examining alcohol consumption–related metabolites, said Dr. Ma — that is, small molecules that are the intermediates or end-products of metabolism in many cellular processes.
Some recent research “shows that alcohol may be harmful or at least has no beneficial effect in CVD prevention,” he said. “Our motivation was to analyze the association using metabolites, genetics, and epigenetics, because we think that these molecules may help us understand some of the mechanisms that underlie the relationship between alcohol consumption and CVD, and partially answer the question of whether alcohol may be harmful or helpful.”
Caution Warranted
Although some previous studies have looked at metabolites, most analyzed alcohol consumption measured at a single time point, “which may not represent habitual or long-term alcohol consumption,” the researchers note.
The team used data derived from 2458 Framingham Heart Study Offspring participants (mean age, 56 ± 9.3 years at the fifth examination; 52% female), calculating the cumulative average alcohol consumption from total intake of beer, wine, and liquor over an average 20-year period. Most participants were overweight, close to one fifth were current smokers, and 636 developed CVD over the study period.
Participants were assessed every 4-8 years, with metabolites measured during the fifth examination.
Linear models were used to investigate the association of alcohol consumption with 211 plasma metabolites, adjusting for a variety of potential confounders, including age, sex, batch, smoking, diet, physical activity, body mass index, and familial relationship.
Sixty metabolites associated with cumulative average alcohol consumption were identified (P < .00024), after adjustment for confounders. Of these, 40 displayed positive associations with the cumulative average alcohol consumption, with the most significant metabolite being cholesteryl palmitoleate (CE16:1), a plasma cholesteryl ester involved with cholesterol metabolism.
One gram per day of higher alcohol consumption was associated with a higher-level CE16:1 in the blood (b = .023). Several other phosphatidylcholine metabolites were also positively associated with alcohol consumption.
On the other hand, 20 metabolites were negatively associated with alcohol consumption, with triacylglycerol 54:4 (TAG 54:4) displaying the most significant association (b = –.017).
The alcoholic beverages were not equal when it came to association with metabolites: 19 metabolites were significantly associated with the cumulative average consumption of beer, 30 with wine, and 32 with liquor. Seven were significantly associated with the cumulative consumption of all three types of drinks.
The researchers conducted survival analysis that identified 10 alcohol-associated metabolites associated with differential CVD risks, after adjusting for confounders. They also built two alcohol consumption–weighted metabolite scores using these 10 metabolites. After adjustment for confounders including CVD risk factors, the two scores had “comparable but opposite” associations with incident CVD, HR 1.11 (95% CI, 1.02-1.21) vs 0.88 (0.78-0.98; both P values = .02).
“We found that seven metabolites were harmful, while three were beneficial, “ Dr. Ma reported.
Dr. Ma cautioned that association “doesn’t represent causation.” On the basis of the findings, however, “we can hypothesize that if you drink a moderate amount of alcohol, you can either increase or decrease your risk of CVD.”
For people with cardiac conditions, “it would be [wise to be] cautious in recommending alcohol consumption,” he said. “For people without cardiac conditions, I would follow the recommendations of the AHA. If people don’t already drink alcohol, we don’t recommend that you start drinking it; and if you already drink, we’d recommend keeping it minimal.”
He cautioned that this is “only one study and we need more research if we are to generate a clearer message to the patient.” At present, perhaps the best message to patients is “to be cautious and warn them that there are potentially harmful effects,” he said.
Mendelian Randomization?
Dr. Sharma, who was not involved in the study, emphasized that it’s “crucial” to recognize that the study “does not alter the established understanding that any level of alcohol consumption poses harm to the heart,” and that “any amount of alcohol consumption has the potential to elevate triglyceride levels, thereby contributing to the increased risk of cardiovascular complications.”
Previously reported cardioprotective benefits “are likely influenced by confounding factors, such as lifestyle and sociodemographic elements,” he speculated.
He noted that observational studies “encounter challenges in disentangling the influence of factors like obesity, lack of exercise, and tobacco use” as well as reverse causality.
“To overcome these limitations, Mendelian randomization emerges as a robust method,” he suggested. “This approach utilizes measured genetic variations with known functions to investigate the causal effect of a modifiable exposure on disease within the framework of observational studies.”
Notably, certain studies using this approach, including one by Larsson and colleagues, and another by Biddinger and associates, “have provided valuable insights by establishing a clear and causal relationship between alcohol consumption and CVD,” he said.
The study was funded by the National Institute of Health’s National Institute on Alcohol Abuse and Alcoholism. Data collection in the Framingham Heart Study was supported by the National Heart, Lung, and Blood Institute. Dr. Ma and coauthors and Dr. Sharma disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
FROM BMC MEDICINE
Erectile Dysfunction Rx: Give It a Shot
This transcript has been edited for clarity.
I’m Dr Rachel Rubin. I am a urologist with fellowship training in sexual medicine. Today I’m going to explain why I may recommend that your patients put a needle directly into their penises for help with erectile dysfunction (ED).
I know that sounds crazy, but in a recent video when I talked about erection hardness, I acknowledged that it may not be easy to talk with patients about their penises, but it’s important.
ED can be a marker for cardiovascular disease, with 50% of our 50-year-old patients having ED. As physicians, we must do a better job of talking to our patients about ED and letting them know that it’s a marker for overall health.
How do we treat ED? Primary care doctors can do a great deal for patients with ED, and there are other things that urologists can do when you run out of options in your own toolbox.
What’s important for a healthy erection? You need three things: healthy muscle, healthy nerves, and healthy arteries. If anything goes wrong with muscles, nerves, or arteries, this is what leads to ED. Think through the algorithm of your patient’s medical history: Do they have diabetes, which can affect their nerves? Do they have high blood pressure, which can affect their arteries? Do they have problems with testosterone, which can affect the smooth muscles of the penis? Understanding your patient’s history can be really helpful when you figure out what is the best treatment strategy for your patient.
For the penis to work, those smooth muscles have to relax; therefore, your brain has to be relaxed, along with your pelvic floor muscles. The smooth muscle of the penis has to be relaxed so it can fill with blood, increase in girth and size, and hold that erection in place.
To treat ED, we have a biopsychosocial toolbox. Biology refers to the muscles, arteries, and nerves. The psychosocial component is stress: If your brain is stressed, you have a lot of adrenaline around that can tighten those smooth muscles and cause you to lose an erection.
So, what are these treatments? I’ll start with lifestyle. A healthy heart means a healthy penis, so, all of the things you already recommend for lifestyle changes can really help with ED. Sleep is important. Does your patient need a sleep study? Do they have sleep apnea? Are they exercising? Recent data show that exercise may be just as effective, if not more effective, than Viagra. How about a good diet? The Mediterranean diet seems to be the most helpful. So, encourage your patients to make dietary, exercise, sleep, and other lifestyle changes if they want to improve erectile function.
What about sex education? Most physicians didn’t get great education about sex in medical school, but it’s very important to our patients who likewise have had inadequate sex education. Ask questions, talk to them, explain what is normal.
I can’t stress enough how important mental health is to a great sex life. Everyone would benefit from sex therapy and becoming better at sex. We need to get better at communicating and educating patients and their partners to maximize their quality of life. If you need to refer to a specialist, we recommend going to psychologytoday.com or aasect.org to find a local sex therapist. Call them and use them in your referral networks.
In the “bio” component of the biopsychosocial approach, we can do a lot to treat ED with medications and hormones. Testosterone has been shown to help with low libido and erectile function. Checking the patient’s testosterone level can be very helpful. Pills — we are familiar with Viagra, Cialis, Levitra, and Stendra. The oral PDE-5 inhibitors have been around since the late 1990s and they work quite well for many people with ED. Viagra and Cialis are generic now and patients can get them fairly inexpensively with discount coupons from GoodRx or Cost Plus Drugs. They may not even have to worry about insurance coverage.
Pills relax the smooth muscle of the penis so that it fills with blood and becomes erect, but they don’t work for everybody. If pills stop working, we often talk about synergistic treatments — combining pills and devices. Devices for ED should be discussed more often, and clinicians should consider prescribing them. We commonly discuss eyeglasses and wheelchairs, but we don’t talk about the sexual health devices that could help patients have more success and fun in the bedroom.
What are the various types of devices for ED? One common device is a vacuum pump, which can be very effective. This is how they work: The penis is lubricated and placed into the pump. A button on the pump creates suction that brings blood into the penis. The patient then applies a constriction band around the base of the penis to hold that erection in place.
“Sex tech” has really expanded to help patients with ED with devices that vibrate and hold the erection in place. Vibrating devices allow for a better orgasm. We even have devices that monitor erectile fitness (like a Fitbit for the penis), gathering data to help patients understand the firmness of their erections.
Devices are helpful adjuncts, but they don’t always do enough to achieve an erect penis that’s hard enough for penetration. In those cases, we can recommend injections that increase smooth muscle relaxation of the penis. I know it sounds crazy. If the muscles, arteries, and nerves of the penis aren’t functioning well, additional smooth muscle relaxation can be achieved by injecting alprostadil (prostaglandin E1) directly into the penis. It’s a tiny needle. It doesn’t hurt. These injections can be quite helpful for our patients, and we often recommend them.
But what happens when your patient doesn’t even respond to injections or any of the synergistic treatments? They’ve tried everything. Urologists may suggest a surgical option, the penile implant. Penile implants contain a pump inside the scrotum that fills with fluid, allowing a rigid erection. Penile implants are wonderful for patients who can no longer get erections. Talking to a urologist about the pros and the cons and the risks and benefits of surgically placed implants is very important.
Finally, ED is a marker for cardiovascular disease. These patients may need a cardiology workup. They need to improve their general health. We have to ask our patients about their goals and what they care about, and find a toolbox that makes sense for each patient and couple to maximize their sexual health and quality of life. Don’t give up. If you have questions, let us know.
Rachel S. Rubin, MD, is Assistant Clinical Professor, Department of Urology, Georgetown University, Washington, DC; Private practice, Rachel Rubin MD PLLC, North Bethesda, Maryland. She disclosed ties with Sprout, Maternal Medical, Absorption Pharmaceuticals, GSK, and Endo.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
I’m Dr Rachel Rubin. I am a urologist with fellowship training in sexual medicine. Today I’m going to explain why I may recommend that your patients put a needle directly into their penises for help with erectile dysfunction (ED).
I know that sounds crazy, but in a recent video when I talked about erection hardness, I acknowledged that it may not be easy to talk with patients about their penises, but it’s important.
ED can be a marker for cardiovascular disease, with 50% of our 50-year-old patients having ED. As physicians, we must do a better job of talking to our patients about ED and letting them know that it’s a marker for overall health.
How do we treat ED? Primary care doctors can do a great deal for patients with ED, and there are other things that urologists can do when you run out of options in your own toolbox.
What’s important for a healthy erection? You need three things: healthy muscle, healthy nerves, and healthy arteries. If anything goes wrong with muscles, nerves, or arteries, this is what leads to ED. Think through the algorithm of your patient’s medical history: Do they have diabetes, which can affect their nerves? Do they have high blood pressure, which can affect their arteries? Do they have problems with testosterone, which can affect the smooth muscles of the penis? Understanding your patient’s history can be really helpful when you figure out what is the best treatment strategy for your patient.
For the penis to work, those smooth muscles have to relax; therefore, your brain has to be relaxed, along with your pelvic floor muscles. The smooth muscle of the penis has to be relaxed so it can fill with blood, increase in girth and size, and hold that erection in place.
To treat ED, we have a biopsychosocial toolbox. Biology refers to the muscles, arteries, and nerves. The psychosocial component is stress: If your brain is stressed, you have a lot of adrenaline around that can tighten those smooth muscles and cause you to lose an erection.
So, what are these treatments? I’ll start with lifestyle. A healthy heart means a healthy penis, so, all of the things you already recommend for lifestyle changes can really help with ED. Sleep is important. Does your patient need a sleep study? Do they have sleep apnea? Are they exercising? Recent data show that exercise may be just as effective, if not more effective, than Viagra. How about a good diet? The Mediterranean diet seems to be the most helpful. So, encourage your patients to make dietary, exercise, sleep, and other lifestyle changes if they want to improve erectile function.
What about sex education? Most physicians didn’t get great education about sex in medical school, but it’s very important to our patients who likewise have had inadequate sex education. Ask questions, talk to them, explain what is normal.
I can’t stress enough how important mental health is to a great sex life. Everyone would benefit from sex therapy and becoming better at sex. We need to get better at communicating and educating patients and their partners to maximize their quality of life. If you need to refer to a specialist, we recommend going to psychologytoday.com or aasect.org to find a local sex therapist. Call them and use them in your referral networks.
In the “bio” component of the biopsychosocial approach, we can do a lot to treat ED with medications and hormones. Testosterone has been shown to help with low libido and erectile function. Checking the patient’s testosterone level can be very helpful. Pills — we are familiar with Viagra, Cialis, Levitra, and Stendra. The oral PDE-5 inhibitors have been around since the late 1990s and they work quite well for many people with ED. Viagra and Cialis are generic now and patients can get them fairly inexpensively with discount coupons from GoodRx or Cost Plus Drugs. They may not even have to worry about insurance coverage.
Pills relax the smooth muscle of the penis so that it fills with blood and becomes erect, but they don’t work for everybody. If pills stop working, we often talk about synergistic treatments — combining pills and devices. Devices for ED should be discussed more often, and clinicians should consider prescribing them. We commonly discuss eyeglasses and wheelchairs, but we don’t talk about the sexual health devices that could help patients have more success and fun in the bedroom.
What are the various types of devices for ED? One common device is a vacuum pump, which can be very effective. This is how they work: The penis is lubricated and placed into the pump. A button on the pump creates suction that brings blood into the penis. The patient then applies a constriction band around the base of the penis to hold that erection in place.
“Sex tech” has really expanded to help patients with ED with devices that vibrate and hold the erection in place. Vibrating devices allow for a better orgasm. We even have devices that monitor erectile fitness (like a Fitbit for the penis), gathering data to help patients understand the firmness of their erections.
Devices are helpful adjuncts, but they don’t always do enough to achieve an erect penis that’s hard enough for penetration. In those cases, we can recommend injections that increase smooth muscle relaxation of the penis. I know it sounds crazy. If the muscles, arteries, and nerves of the penis aren’t functioning well, additional smooth muscle relaxation can be achieved by injecting alprostadil (prostaglandin E1) directly into the penis. It’s a tiny needle. It doesn’t hurt. These injections can be quite helpful for our patients, and we often recommend them.
But what happens when your patient doesn’t even respond to injections or any of the synergistic treatments? They’ve tried everything. Urologists may suggest a surgical option, the penile implant. Penile implants contain a pump inside the scrotum that fills with fluid, allowing a rigid erection. Penile implants are wonderful for patients who can no longer get erections. Talking to a urologist about the pros and the cons and the risks and benefits of surgically placed implants is very important.
Finally, ED is a marker for cardiovascular disease. These patients may need a cardiology workup. They need to improve their general health. We have to ask our patients about their goals and what they care about, and find a toolbox that makes sense for each patient and couple to maximize their sexual health and quality of life. Don’t give up. If you have questions, let us know.
Rachel S. Rubin, MD, is Assistant Clinical Professor, Department of Urology, Georgetown University, Washington, DC; Private practice, Rachel Rubin MD PLLC, North Bethesda, Maryland. She disclosed ties with Sprout, Maternal Medical, Absorption Pharmaceuticals, GSK, and Endo.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
I’m Dr Rachel Rubin. I am a urologist with fellowship training in sexual medicine. Today I’m going to explain why I may recommend that your patients put a needle directly into their penises for help with erectile dysfunction (ED).
I know that sounds crazy, but in a recent video when I talked about erection hardness, I acknowledged that it may not be easy to talk with patients about their penises, but it’s important.
ED can be a marker for cardiovascular disease, with 50% of our 50-year-old patients having ED. As physicians, we must do a better job of talking to our patients about ED and letting them know that it’s a marker for overall health.
How do we treat ED? Primary care doctors can do a great deal for patients with ED, and there are other things that urologists can do when you run out of options in your own toolbox.
What’s important for a healthy erection? You need three things: healthy muscle, healthy nerves, and healthy arteries. If anything goes wrong with muscles, nerves, or arteries, this is what leads to ED. Think through the algorithm of your patient’s medical history: Do they have diabetes, which can affect their nerves? Do they have high blood pressure, which can affect their arteries? Do they have problems with testosterone, which can affect the smooth muscles of the penis? Understanding your patient’s history can be really helpful when you figure out what is the best treatment strategy for your patient.
For the penis to work, those smooth muscles have to relax; therefore, your brain has to be relaxed, along with your pelvic floor muscles. The smooth muscle of the penis has to be relaxed so it can fill with blood, increase in girth and size, and hold that erection in place.
To treat ED, we have a biopsychosocial toolbox. Biology refers to the muscles, arteries, and nerves. The psychosocial component is stress: If your brain is stressed, you have a lot of adrenaline around that can tighten those smooth muscles and cause you to lose an erection.
So, what are these treatments? I’ll start with lifestyle. A healthy heart means a healthy penis, so, all of the things you already recommend for lifestyle changes can really help with ED. Sleep is important. Does your patient need a sleep study? Do they have sleep apnea? Are they exercising? Recent data show that exercise may be just as effective, if not more effective, than Viagra. How about a good diet? The Mediterranean diet seems to be the most helpful. So, encourage your patients to make dietary, exercise, sleep, and other lifestyle changes if they want to improve erectile function.
What about sex education? Most physicians didn’t get great education about sex in medical school, but it’s very important to our patients who likewise have had inadequate sex education. Ask questions, talk to them, explain what is normal.
I can’t stress enough how important mental health is to a great sex life. Everyone would benefit from sex therapy and becoming better at sex. We need to get better at communicating and educating patients and their partners to maximize their quality of life. If you need to refer to a specialist, we recommend going to psychologytoday.com or aasect.org to find a local sex therapist. Call them and use them in your referral networks.
In the “bio” component of the biopsychosocial approach, we can do a lot to treat ED with medications and hormones. Testosterone has been shown to help with low libido and erectile function. Checking the patient’s testosterone level can be very helpful. Pills — we are familiar with Viagra, Cialis, Levitra, and Stendra. The oral PDE-5 inhibitors have been around since the late 1990s and they work quite well for many people with ED. Viagra and Cialis are generic now and patients can get them fairly inexpensively with discount coupons from GoodRx or Cost Plus Drugs. They may not even have to worry about insurance coverage.
Pills relax the smooth muscle of the penis so that it fills with blood and becomes erect, but they don’t work for everybody. If pills stop working, we often talk about synergistic treatments — combining pills and devices. Devices for ED should be discussed more often, and clinicians should consider prescribing them. We commonly discuss eyeglasses and wheelchairs, but we don’t talk about the sexual health devices that could help patients have more success and fun in the bedroom.
What are the various types of devices for ED? One common device is a vacuum pump, which can be very effective. This is how they work: The penis is lubricated and placed into the pump. A button on the pump creates suction that brings blood into the penis. The patient then applies a constriction band around the base of the penis to hold that erection in place.
“Sex tech” has really expanded to help patients with ED with devices that vibrate and hold the erection in place. Vibrating devices allow for a better orgasm. We even have devices that monitor erectile fitness (like a Fitbit for the penis), gathering data to help patients understand the firmness of their erections.
Devices are helpful adjuncts, but they don’t always do enough to achieve an erect penis that’s hard enough for penetration. In those cases, we can recommend injections that increase smooth muscle relaxation of the penis. I know it sounds crazy. If the muscles, arteries, and nerves of the penis aren’t functioning well, additional smooth muscle relaxation can be achieved by injecting alprostadil (prostaglandin E1) directly into the penis. It’s a tiny needle. It doesn’t hurt. These injections can be quite helpful for our patients, and we often recommend them.
But what happens when your patient doesn’t even respond to injections or any of the synergistic treatments? They’ve tried everything. Urologists may suggest a surgical option, the penile implant. Penile implants contain a pump inside the scrotum that fills with fluid, allowing a rigid erection. Penile implants are wonderful for patients who can no longer get erections. Talking to a urologist about the pros and the cons and the risks and benefits of surgically placed implants is very important.
Finally, ED is a marker for cardiovascular disease. These patients may need a cardiology workup. They need to improve their general health. We have to ask our patients about their goals and what they care about, and find a toolbox that makes sense for each patient and couple to maximize their sexual health and quality of life. Don’t give up. If you have questions, let us know.
Rachel S. Rubin, MD, is Assistant Clinical Professor, Department of Urology, Georgetown University, Washington, DC; Private practice, Rachel Rubin MD PLLC, North Bethesda, Maryland. She disclosed ties with Sprout, Maternal Medical, Absorption Pharmaceuticals, GSK, and Endo.
A version of this article appeared on Medscape.com.
GLP-1 RAs for CVD: Are cardiologists ready?
The positive results from the SELECT trial for the glucagon-like peptide-1 receptor agonists (GLP-1 RAs) were hailed as ushering in a “new era for patients with obesity.” In the trial of overweight and obese patients with cardiovascular disease (CVD), but no diabetes, semaglutide showed meaningful reductions in cardiovascular death, myocardial infarction, and stroke compared with placebo.
“I definitely see increasing adoption of GLP-1 RAs by cardiologists and expect the number to increase now that the data support its use in secondary prevention,” said Nicole L. Lohr, MD, PhD, chair of the American College of Cardiology (ACC) Board of Governors, and Mary G. Waters, chair of cardiovascular medicine at UAB, Birmingham.
But many cardiologists are more hesitant. said American Heart Association (AHA) volunteer Chiadi E. Ndumele, MD, PhD, an associate professor at Johns Hopkins Medicine in Baltimore and chair of the AHA’s recent presidential advisory on cardiovascular-kidney-metabolic health.
“Weight loss hasn’t been a central focus in our practice until recently, with the advent of these more powerful agents. There’s a need for more education around not only the use of these agents, but also around initiating weight loss discussions in a nonjudgmental way that reflects the complexity of obesity as a condition with multifactorial causes.”
The process will take time and may be similar to what happened with statins, he suggests. “Statins started in the endocrinology space, but as their cardiovascular benefits became more clear, they were increasingly adopted by cardiologists, primary care physicians, and others.”
Eugene Yang, MD, chair of the ACC Prevention of CVD Council and codirector of UW Medicine’s Cardiovascular Wellness and Prevention Program in Seattle, agrees that GLP-1 uptake by cardiologists will likely be slow. “It’s a bit premature to start prescribing right away,” he said. “Semaglutide hasn’t been approved for secondary prevention at this point, and until it’s approved specifically for that indication, I don’t think many cardiologists will prescribe it.”
Side Effects ‘Concerning’
Beyond the requisite approval, Dr. Yang is concerned about side effects such as gastroparesis, severe nausea, and vomiting. “I’m not sure cardiologists are going to feel comfortable helping patients deal with these effects.”
Because GLP-1 RAs are already being used widely in primary care, he says, “I personally would work in collaboration with either my primary care colleagues or with endocrinologists.”
Ambarish Pandey, MD, an associate professor of internal medicine (cardiology) and medical director of the heart failure with preserved ejection fraction (HFpEF) program at UT Southwestern Medical Center, Dallas, is already prescribing semaglutide to patients with HFpEF and obesity. “In terms of side effects, I just tell patients what to expect,” he says.
Dr. Pandey prepares patients for appetite reduction, early satiety and fullness, abdominal discomfort, nausea, and other gastrointestinal symptoms. “Then I start low and slowly titrate to achieve enough weight loss. If they’re having adverse effects on a higher dose, I use a lower dose.”
The approach is working well for most patients, he says. “Obviously there’s some initial getting used to the drug, but once that has happened, patients like it because they see improvements in their exercise capacity and quality of life.”
But GLP-1 RAs are also associated with increased heart rate, which “is never good news,” notes Howard Weintraub, MD, a professor of medicine at NYU Grossman School of Medicine in New York City and clinical director of the NYU Center for the Prevention of Cardiovascular Disease. At least some of the elevation may be masked by beta-blocker use, he suggests. “The mechanism is not well elucidated, but it is something we’re going to need to keep an eye on, because we don’t want to get ambushed.”
Cost, Access ‘Significant Barriers’
All the cardiologists this news organization spoke with agreed that cost and access will be significant barriers to widespread prescribing, at least for now.
“Prescribing for individuals at very high cardiovascular risk will probably give a reasonable amount of bang for your buck. But individuals with more adverse social determinants of health, who are more likely to have challenges with obesity and related complications, are also least likely to be able to pay the exorbitant costs out of pocket. So, this is also an important health equity issue,” Dr. Ndumele says.
Furthermore, he adds, where GLP-1 RAs will fit for those with a lower absolute CVD risk “is still a clear question.”
“Access comes two ways,” Dr. Weintraub says. “One is the supply, which continues to be an issue. You can’t sell the drug if you don’t have it.”
The other access route is the insurance companies. “Will they throw down a gauntlet and make cardiologists prove that a patient failed other obesity drugs before they can prescribe a GLP-1 RA? Some of the old obesity drugs are not only unpleasant to use, but they’re ineffective and may have bad cardiac signals.”
If the new drugs are approved for secondary prevention, patients will want them and doctors will want them, he says. The demand will be “huge,” and it’s not clear how it will be handled.
Dr. Pandey agrees that getting the drug without “good insurance” to cover the cost is a big challenge. “ As more of these drugs become available, hopefully the cost will come down, and hopefully access will grow as companies are able to scale up production.”
Add-On or Substitute?
Anticipating approval, Dr. Yang says it’s not yet clear where the GLP-1 RAs stand among the various available cardiovascular therapies.
“Based on the results of SELECT, one could argue that maybe it’s more important to get the weight down and reduce blood pressure versus adding another cholesterol-lowering medication, for example, especially if a patient is already on a statin and ezetimibe. But maybe their low-density lipoprotein cholesterol is not exactly below the threshold of the current guideline. And maybe they’re overweight or prediabetic, and they can lose 10% or 15% of their body weight with a GLP-1 RA. You may have to pick and choose.”
That said, he adds, “Who’s going to be able to afford all of this? Some patients would be taking a PCSK9 inhibitor, bempedoic acid because their lipids are not optimized, then a GLP-1 receptor. Right there, we’re talking about at least $2000 a month for those three medications. That’s not feasible.”
“This is one of the things I’ve worried about, given all the drugs some of our patients are on,” Dr. Weintraub says. “The data on cholesterol-lowering drugs are so monumental, it’s hard to say you can do without it. The same is true of blood pressure-lowering medication. So to my mind, a GLP-1 RA is going to have to be an add-on.”
“The only good news is that unlike in the heart failure arena, patients are not paying for other drugs on top of it,” he says. “Statins, ACE inhibitors, ARBs, and beta-blockers are all generic; they’re not going to leave a huge hole in the patient’s pocket when the donut hole [Medicare payment gap] comes around. So in this case, if the GLP-1 RAs get included, which I hope they will, the added cost may not be that horrible.”
What About Lifestyle Changes?
Everyone agreed that the drugs are not a substitute for lifestyle changes.
“I have seen many patients who take these medications reach plateaus, and when discontinued, gain back the weight. I counsel patients to view the medication as an aid and not necessarily a magic wand,” Dr. Lohr says.
Dr. Ndumele agrees. “I advocate a lifestyle-first approach,” he says. “I imagine there will be busy clinicians who will prescribe medications as a first line, but that’s not going to be our most effective approach.”
The major challenge to such an approach, he says, is that lifestyle support has to be ongoing. “It’s not the kind of thing that just happens in a yearly doctor’s visit appointment, and it’s been under-supported in most coverage and reimbursement strategies.”
In his clinical practice, which includes ongoing support for lifestyle changes, Dr. Ndumele is seeing far greater weight loss than was shown in SELECT. “I think there’s a real benefit to having the two approaches come together,” he says.
Dr. Yang also favors an emphasis on lifestyle. “The success rate of a lifestyle approach may be low, but that doesn’t change the importance of it. We need to figure out better ways to do it.” Leveraging technology is one way, he suggests, such as cellphone reminders to walk more or alerts to tell you when to sleep.
“I also encourage patients to monitor their own blood pressure, and they do.” Dr. Yang acknowledges that his patient population is highly educated with access to resources to purchase the technological devices. However, he adds, “if the clinician is negative, and doesn’t really believe these interventions will work, the patient can sense that, and then they won’t work.” It’s up to the clinician to promote the importance of these lifestyle changes in order to be successful. Is it discouraging at times? Yes. But don’t let the patient know.”
Dr. Pandey approaches the issue differently. “Our healthcare system is such that patients don’t get to see us that often, so I think we should start the lifestyle intervention, but also start the medication at the same time, in parallel, because we don’t have time to take a stepwise approach.”
“Lifestyle interventions are better received if patients see positive improvements, and the medication actually induces a positive improvement,” he says. He is concerned that if a lifestyle first approach doesn’t work “that can affect the willingness to try future therapies. And we don’t want to lose like 6 or 8 months just trying lifestyle when they could have benefited from the weight-loss medication, as well.”
Dr. Lohr, Dr. Ndumele, and Dr. Yang report no conflicts of interest. Dr. Weintraub reports being an investigator in the SELECT trial and a consultant for NovoNordisk. Dr. Pandey reports receiving research support from the National Institutes of Health; grant funding from Applied Therapeutics and Gilead Sciences; honoraria outside of the present study as an advisor/consultant for Tricog Health Inc, Lilly USA, Rivus, Cytokinetics, Roche Diagnostics, Axon therapies, Medtronic, Edwards Lifesciences, Science 37 Novo Nordisk, Bayer, Merck, Sarfez Pharmaceuticals, Emmi Solutions; and has received nonfinancial support from Pfizer and Merck; and serving as a consultant for Palomarin Inc. with stocks compensation.
A version of this article appeared on Medscape.com.
The positive results from the SELECT trial for the glucagon-like peptide-1 receptor agonists (GLP-1 RAs) were hailed as ushering in a “new era for patients with obesity.” In the trial of overweight and obese patients with cardiovascular disease (CVD), but no diabetes, semaglutide showed meaningful reductions in cardiovascular death, myocardial infarction, and stroke compared with placebo.
“I definitely see increasing adoption of GLP-1 RAs by cardiologists and expect the number to increase now that the data support its use in secondary prevention,” said Nicole L. Lohr, MD, PhD, chair of the American College of Cardiology (ACC) Board of Governors, and Mary G. Waters, chair of cardiovascular medicine at UAB, Birmingham.
But many cardiologists are more hesitant. said American Heart Association (AHA) volunteer Chiadi E. Ndumele, MD, PhD, an associate professor at Johns Hopkins Medicine in Baltimore and chair of the AHA’s recent presidential advisory on cardiovascular-kidney-metabolic health.
“Weight loss hasn’t been a central focus in our practice until recently, with the advent of these more powerful agents. There’s a need for more education around not only the use of these agents, but also around initiating weight loss discussions in a nonjudgmental way that reflects the complexity of obesity as a condition with multifactorial causes.”
The process will take time and may be similar to what happened with statins, he suggests. “Statins started in the endocrinology space, but as their cardiovascular benefits became more clear, they were increasingly adopted by cardiologists, primary care physicians, and others.”
Eugene Yang, MD, chair of the ACC Prevention of CVD Council and codirector of UW Medicine’s Cardiovascular Wellness and Prevention Program in Seattle, agrees that GLP-1 uptake by cardiologists will likely be slow. “It’s a bit premature to start prescribing right away,” he said. “Semaglutide hasn’t been approved for secondary prevention at this point, and until it’s approved specifically for that indication, I don’t think many cardiologists will prescribe it.”
Side Effects ‘Concerning’
Beyond the requisite approval, Dr. Yang is concerned about side effects such as gastroparesis, severe nausea, and vomiting. “I’m not sure cardiologists are going to feel comfortable helping patients deal with these effects.”
Because GLP-1 RAs are already being used widely in primary care, he says, “I personally would work in collaboration with either my primary care colleagues or with endocrinologists.”
Ambarish Pandey, MD, an associate professor of internal medicine (cardiology) and medical director of the heart failure with preserved ejection fraction (HFpEF) program at UT Southwestern Medical Center, Dallas, is already prescribing semaglutide to patients with HFpEF and obesity. “In terms of side effects, I just tell patients what to expect,” he says.
Dr. Pandey prepares patients for appetite reduction, early satiety and fullness, abdominal discomfort, nausea, and other gastrointestinal symptoms. “Then I start low and slowly titrate to achieve enough weight loss. If they’re having adverse effects on a higher dose, I use a lower dose.”
The approach is working well for most patients, he says. “Obviously there’s some initial getting used to the drug, but once that has happened, patients like it because they see improvements in their exercise capacity and quality of life.”
But GLP-1 RAs are also associated with increased heart rate, which “is never good news,” notes Howard Weintraub, MD, a professor of medicine at NYU Grossman School of Medicine in New York City and clinical director of the NYU Center for the Prevention of Cardiovascular Disease. At least some of the elevation may be masked by beta-blocker use, he suggests. “The mechanism is not well elucidated, but it is something we’re going to need to keep an eye on, because we don’t want to get ambushed.”
Cost, Access ‘Significant Barriers’
All the cardiologists this news organization spoke with agreed that cost and access will be significant barriers to widespread prescribing, at least for now.
“Prescribing for individuals at very high cardiovascular risk will probably give a reasonable amount of bang for your buck. But individuals with more adverse social determinants of health, who are more likely to have challenges with obesity and related complications, are also least likely to be able to pay the exorbitant costs out of pocket. So, this is also an important health equity issue,” Dr. Ndumele says.
Furthermore, he adds, where GLP-1 RAs will fit for those with a lower absolute CVD risk “is still a clear question.”
“Access comes two ways,” Dr. Weintraub says. “One is the supply, which continues to be an issue. You can’t sell the drug if you don’t have it.”
The other access route is the insurance companies. “Will they throw down a gauntlet and make cardiologists prove that a patient failed other obesity drugs before they can prescribe a GLP-1 RA? Some of the old obesity drugs are not only unpleasant to use, but they’re ineffective and may have bad cardiac signals.”
If the new drugs are approved for secondary prevention, patients will want them and doctors will want them, he says. The demand will be “huge,” and it’s not clear how it will be handled.
Dr. Pandey agrees that getting the drug without “good insurance” to cover the cost is a big challenge. “ As more of these drugs become available, hopefully the cost will come down, and hopefully access will grow as companies are able to scale up production.”
Add-On or Substitute?
Anticipating approval, Dr. Yang says it’s not yet clear where the GLP-1 RAs stand among the various available cardiovascular therapies.
“Based on the results of SELECT, one could argue that maybe it’s more important to get the weight down and reduce blood pressure versus adding another cholesterol-lowering medication, for example, especially if a patient is already on a statin and ezetimibe. But maybe their low-density lipoprotein cholesterol is not exactly below the threshold of the current guideline. And maybe they’re overweight or prediabetic, and they can lose 10% or 15% of their body weight with a GLP-1 RA. You may have to pick and choose.”
That said, he adds, “Who’s going to be able to afford all of this? Some patients would be taking a PCSK9 inhibitor, bempedoic acid because their lipids are not optimized, then a GLP-1 receptor. Right there, we’re talking about at least $2000 a month for those three medications. That’s not feasible.”
“This is one of the things I’ve worried about, given all the drugs some of our patients are on,” Dr. Weintraub says. “The data on cholesterol-lowering drugs are so monumental, it’s hard to say you can do without it. The same is true of blood pressure-lowering medication. So to my mind, a GLP-1 RA is going to have to be an add-on.”
“The only good news is that unlike in the heart failure arena, patients are not paying for other drugs on top of it,” he says. “Statins, ACE inhibitors, ARBs, and beta-blockers are all generic; they’re not going to leave a huge hole in the patient’s pocket when the donut hole [Medicare payment gap] comes around. So in this case, if the GLP-1 RAs get included, which I hope they will, the added cost may not be that horrible.”
What About Lifestyle Changes?
Everyone agreed that the drugs are not a substitute for lifestyle changes.
“I have seen many patients who take these medications reach plateaus, and when discontinued, gain back the weight. I counsel patients to view the medication as an aid and not necessarily a magic wand,” Dr. Lohr says.
Dr. Ndumele agrees. “I advocate a lifestyle-first approach,” he says. “I imagine there will be busy clinicians who will prescribe medications as a first line, but that’s not going to be our most effective approach.”
The major challenge to such an approach, he says, is that lifestyle support has to be ongoing. “It’s not the kind of thing that just happens in a yearly doctor’s visit appointment, and it’s been under-supported in most coverage and reimbursement strategies.”
In his clinical practice, which includes ongoing support for lifestyle changes, Dr. Ndumele is seeing far greater weight loss than was shown in SELECT. “I think there’s a real benefit to having the two approaches come together,” he says.
Dr. Yang also favors an emphasis on lifestyle. “The success rate of a lifestyle approach may be low, but that doesn’t change the importance of it. We need to figure out better ways to do it.” Leveraging technology is one way, he suggests, such as cellphone reminders to walk more or alerts to tell you when to sleep.
“I also encourage patients to monitor their own blood pressure, and they do.” Dr. Yang acknowledges that his patient population is highly educated with access to resources to purchase the technological devices. However, he adds, “if the clinician is negative, and doesn’t really believe these interventions will work, the patient can sense that, and then they won’t work.” It’s up to the clinician to promote the importance of these lifestyle changes in order to be successful. Is it discouraging at times? Yes. But don’t let the patient know.”
Dr. Pandey approaches the issue differently. “Our healthcare system is such that patients don’t get to see us that often, so I think we should start the lifestyle intervention, but also start the medication at the same time, in parallel, because we don’t have time to take a stepwise approach.”
“Lifestyle interventions are better received if patients see positive improvements, and the medication actually induces a positive improvement,” he says. He is concerned that if a lifestyle first approach doesn’t work “that can affect the willingness to try future therapies. And we don’t want to lose like 6 or 8 months just trying lifestyle when they could have benefited from the weight-loss medication, as well.”
Dr. Lohr, Dr. Ndumele, and Dr. Yang report no conflicts of interest. Dr. Weintraub reports being an investigator in the SELECT trial and a consultant for NovoNordisk. Dr. Pandey reports receiving research support from the National Institutes of Health; grant funding from Applied Therapeutics and Gilead Sciences; honoraria outside of the present study as an advisor/consultant for Tricog Health Inc, Lilly USA, Rivus, Cytokinetics, Roche Diagnostics, Axon therapies, Medtronic, Edwards Lifesciences, Science 37 Novo Nordisk, Bayer, Merck, Sarfez Pharmaceuticals, Emmi Solutions; and has received nonfinancial support from Pfizer and Merck; and serving as a consultant for Palomarin Inc. with stocks compensation.
A version of this article appeared on Medscape.com.
The positive results from the SELECT trial for the glucagon-like peptide-1 receptor agonists (GLP-1 RAs) were hailed as ushering in a “new era for patients with obesity.” In the trial of overweight and obese patients with cardiovascular disease (CVD), but no diabetes, semaglutide showed meaningful reductions in cardiovascular death, myocardial infarction, and stroke compared with placebo.
“I definitely see increasing adoption of GLP-1 RAs by cardiologists and expect the number to increase now that the data support its use in secondary prevention,” said Nicole L. Lohr, MD, PhD, chair of the American College of Cardiology (ACC) Board of Governors, and Mary G. Waters, chair of cardiovascular medicine at UAB, Birmingham.
But many cardiologists are more hesitant. said American Heart Association (AHA) volunteer Chiadi E. Ndumele, MD, PhD, an associate professor at Johns Hopkins Medicine in Baltimore and chair of the AHA’s recent presidential advisory on cardiovascular-kidney-metabolic health.
“Weight loss hasn’t been a central focus in our practice until recently, with the advent of these more powerful agents. There’s a need for more education around not only the use of these agents, but also around initiating weight loss discussions in a nonjudgmental way that reflects the complexity of obesity as a condition with multifactorial causes.”
The process will take time and may be similar to what happened with statins, he suggests. “Statins started in the endocrinology space, but as their cardiovascular benefits became more clear, they were increasingly adopted by cardiologists, primary care physicians, and others.”
Eugene Yang, MD, chair of the ACC Prevention of CVD Council and codirector of UW Medicine’s Cardiovascular Wellness and Prevention Program in Seattle, agrees that GLP-1 uptake by cardiologists will likely be slow. “It’s a bit premature to start prescribing right away,” he said. “Semaglutide hasn’t been approved for secondary prevention at this point, and until it’s approved specifically for that indication, I don’t think many cardiologists will prescribe it.”
Side Effects ‘Concerning’
Beyond the requisite approval, Dr. Yang is concerned about side effects such as gastroparesis, severe nausea, and vomiting. “I’m not sure cardiologists are going to feel comfortable helping patients deal with these effects.”
Because GLP-1 RAs are already being used widely in primary care, he says, “I personally would work in collaboration with either my primary care colleagues or with endocrinologists.”
Ambarish Pandey, MD, an associate professor of internal medicine (cardiology) and medical director of the heart failure with preserved ejection fraction (HFpEF) program at UT Southwestern Medical Center, Dallas, is already prescribing semaglutide to patients with HFpEF and obesity. “In terms of side effects, I just tell patients what to expect,” he says.
Dr. Pandey prepares patients for appetite reduction, early satiety and fullness, abdominal discomfort, nausea, and other gastrointestinal symptoms. “Then I start low and slowly titrate to achieve enough weight loss. If they’re having adverse effects on a higher dose, I use a lower dose.”
The approach is working well for most patients, he says. “Obviously there’s some initial getting used to the drug, but once that has happened, patients like it because they see improvements in their exercise capacity and quality of life.”
But GLP-1 RAs are also associated with increased heart rate, which “is never good news,” notes Howard Weintraub, MD, a professor of medicine at NYU Grossman School of Medicine in New York City and clinical director of the NYU Center for the Prevention of Cardiovascular Disease. At least some of the elevation may be masked by beta-blocker use, he suggests. “The mechanism is not well elucidated, but it is something we’re going to need to keep an eye on, because we don’t want to get ambushed.”
Cost, Access ‘Significant Barriers’
All the cardiologists this news organization spoke with agreed that cost and access will be significant barriers to widespread prescribing, at least for now.
“Prescribing for individuals at very high cardiovascular risk will probably give a reasonable amount of bang for your buck. But individuals with more adverse social determinants of health, who are more likely to have challenges with obesity and related complications, are also least likely to be able to pay the exorbitant costs out of pocket. So, this is also an important health equity issue,” Dr. Ndumele says.
Furthermore, he adds, where GLP-1 RAs will fit for those with a lower absolute CVD risk “is still a clear question.”
“Access comes two ways,” Dr. Weintraub says. “One is the supply, which continues to be an issue. You can’t sell the drug if you don’t have it.”
The other access route is the insurance companies. “Will they throw down a gauntlet and make cardiologists prove that a patient failed other obesity drugs before they can prescribe a GLP-1 RA? Some of the old obesity drugs are not only unpleasant to use, but they’re ineffective and may have bad cardiac signals.”
If the new drugs are approved for secondary prevention, patients will want them and doctors will want them, he says. The demand will be “huge,” and it’s not clear how it will be handled.
Dr. Pandey agrees that getting the drug without “good insurance” to cover the cost is a big challenge. “ As more of these drugs become available, hopefully the cost will come down, and hopefully access will grow as companies are able to scale up production.”
Add-On or Substitute?
Anticipating approval, Dr. Yang says it’s not yet clear where the GLP-1 RAs stand among the various available cardiovascular therapies.
“Based on the results of SELECT, one could argue that maybe it’s more important to get the weight down and reduce blood pressure versus adding another cholesterol-lowering medication, for example, especially if a patient is already on a statin and ezetimibe. But maybe their low-density lipoprotein cholesterol is not exactly below the threshold of the current guideline. And maybe they’re overweight or prediabetic, and they can lose 10% or 15% of their body weight with a GLP-1 RA. You may have to pick and choose.”
That said, he adds, “Who’s going to be able to afford all of this? Some patients would be taking a PCSK9 inhibitor, bempedoic acid because their lipids are not optimized, then a GLP-1 receptor. Right there, we’re talking about at least $2000 a month for those three medications. That’s not feasible.”
“This is one of the things I’ve worried about, given all the drugs some of our patients are on,” Dr. Weintraub says. “The data on cholesterol-lowering drugs are so monumental, it’s hard to say you can do without it. The same is true of blood pressure-lowering medication. So to my mind, a GLP-1 RA is going to have to be an add-on.”
“The only good news is that unlike in the heart failure arena, patients are not paying for other drugs on top of it,” he says. “Statins, ACE inhibitors, ARBs, and beta-blockers are all generic; they’re not going to leave a huge hole in the patient’s pocket when the donut hole [Medicare payment gap] comes around. So in this case, if the GLP-1 RAs get included, which I hope they will, the added cost may not be that horrible.”
What About Lifestyle Changes?
Everyone agreed that the drugs are not a substitute for lifestyle changes.
“I have seen many patients who take these medications reach plateaus, and when discontinued, gain back the weight. I counsel patients to view the medication as an aid and not necessarily a magic wand,” Dr. Lohr says.
Dr. Ndumele agrees. “I advocate a lifestyle-first approach,” he says. “I imagine there will be busy clinicians who will prescribe medications as a first line, but that’s not going to be our most effective approach.”
The major challenge to such an approach, he says, is that lifestyle support has to be ongoing. “It’s not the kind of thing that just happens in a yearly doctor’s visit appointment, and it’s been under-supported in most coverage and reimbursement strategies.”
In his clinical practice, which includes ongoing support for lifestyle changes, Dr. Ndumele is seeing far greater weight loss than was shown in SELECT. “I think there’s a real benefit to having the two approaches come together,” he says.
Dr. Yang also favors an emphasis on lifestyle. “The success rate of a lifestyle approach may be low, but that doesn’t change the importance of it. We need to figure out better ways to do it.” Leveraging technology is one way, he suggests, such as cellphone reminders to walk more or alerts to tell you when to sleep.
“I also encourage patients to monitor their own blood pressure, and they do.” Dr. Yang acknowledges that his patient population is highly educated with access to resources to purchase the technological devices. However, he adds, “if the clinician is negative, and doesn’t really believe these interventions will work, the patient can sense that, and then they won’t work.” It’s up to the clinician to promote the importance of these lifestyle changes in order to be successful. Is it discouraging at times? Yes. But don’t let the patient know.”
Dr. Pandey approaches the issue differently. “Our healthcare system is such that patients don’t get to see us that often, so I think we should start the lifestyle intervention, but also start the medication at the same time, in parallel, because we don’t have time to take a stepwise approach.”
“Lifestyle interventions are better received if patients see positive improvements, and the medication actually induces a positive improvement,” he says. He is concerned that if a lifestyle first approach doesn’t work “that can affect the willingness to try future therapies. And we don’t want to lose like 6 or 8 months just trying lifestyle when they could have benefited from the weight-loss medication, as well.”
Dr. Lohr, Dr. Ndumele, and Dr. Yang report no conflicts of interest. Dr. Weintraub reports being an investigator in the SELECT trial and a consultant for NovoNordisk. Dr. Pandey reports receiving research support from the National Institutes of Health; grant funding from Applied Therapeutics and Gilead Sciences; honoraria outside of the present study as an advisor/consultant for Tricog Health Inc, Lilly USA, Rivus, Cytokinetics, Roche Diagnostics, Axon therapies, Medtronic, Edwards Lifesciences, Science 37 Novo Nordisk, Bayer, Merck, Sarfez Pharmaceuticals, Emmi Solutions; and has received nonfinancial support from Pfizer and Merck; and serving as a consultant for Palomarin Inc. with stocks compensation.
A version of this article appeared on Medscape.com.
Younger heart disease onset tied to higher dementia risk
TOPLINE:
, with the risk highest — at 36% — if onset is before age 45, results of a large observational study show.
METHODOLOGY:
- The study included 432,667 of the more than 500,000 participants in the UK Biobank, with a mean age of 56.9 years, 50,685 (11.7%) of whom had CHD and 50,445 had data on age at CHD onset.
- Researchers divided participants into three groups according to age at CHD onset (below 45 years, 45-59 years, and 60 years and older), and carried out a propensity score matching analysis.
- Outcomes included all-cause dementia, AD, and VD.
- Covariates included age, sex, race, educational level, body mass index, low-density lipoprotein cholesterol, smoking status, alcohol intake, exercise, depressed mood, hypertension, diabetes, statin use, and apolipoprotein E4 status.
TAKEAWAY:
- During a median follow-up of 12.8 years, researchers identified 5876 cases of all-cause dementia, 2540 cases of AD, and 1220 cases of VD.
- Fully adjusted models showed participants with CHD had significantly higher risks than those without CHD of developing all-cause dementia (hazard ratio [HR], 1.36; 95% CI, 1.28-1.45; P < .001), AD (HR, 1.13; 95% CI, 1.02-1.24; P = .019), and VD (HR, 1.78; 95% CI, 1.56-2.02; P < .001). The higher risk for VD suggests CHD has a more profound influence on neuropathologic changes involved in this dementia type, said the authors.
- Those with CHD diagnosed at a younger age had higher risks of developing dementia (HR per 10-year decrease in age, 1.25; 95% CI, 1.20-1.30 for all-cause dementia, 1.29; 95% CI, 1.20-1.38 for AD, and 1.22; 95% CI, 1.13-1.31 for VD; P for all < .001).
- Propensity score matching analysis showed patients with CHD had significantly higher risks for dementia compared with matched controls, with the highest risk seen in patients diagnosed before age 45 (HR, 2.40; 95% CI, 1.79-3.20; P < .001), followed by those diagnosed between 45 and 59 years (HR, 1.46; 95% CI, 1.32-1.62; P < .001) and at or above 60 years (HR, 1.11; 95% CI, 1.03-1.19; P = .005), with similar results for AD and VD.
IN PRACTICE:
The findings suggest “additional attention should be paid to the cognitive status of patients with CHD, especially the ones diagnosed with CHD at a young age,” the authors conclude, noting that “timely intervention, such as cognitive training, could be implemented once signs of cognitive deteriorations are detected.”
SOURCE:
The study was conducted by Jie Liang, BS, School of Nursing, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing, and colleagues. It was published online on November 29, 2023, in the Journal of the American Heart Association.
LIMITATIONS:
As this is an observational study, it can’t conclude a causal relationship. Although the authors adjusted for many potential confounders, unknown risk factors that also contribute to CHD can’t be ruled out. As the study excluded 69,744 participants, selection bias is possible. The study included a mostly White population.
DISCLOSURES:
The study was supported by the National Natural Science Foundation of China, the Non-Profit Central Research Institute Fund of the Chinese Academy of Medical Sciences, and the China Medical Board. The authors have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
, with the risk highest — at 36% — if onset is before age 45, results of a large observational study show.
METHODOLOGY:
- The study included 432,667 of the more than 500,000 participants in the UK Biobank, with a mean age of 56.9 years, 50,685 (11.7%) of whom had CHD and 50,445 had data on age at CHD onset.
- Researchers divided participants into three groups according to age at CHD onset (below 45 years, 45-59 years, and 60 years and older), and carried out a propensity score matching analysis.
- Outcomes included all-cause dementia, AD, and VD.
- Covariates included age, sex, race, educational level, body mass index, low-density lipoprotein cholesterol, smoking status, alcohol intake, exercise, depressed mood, hypertension, diabetes, statin use, and apolipoprotein E4 status.
TAKEAWAY:
- During a median follow-up of 12.8 years, researchers identified 5876 cases of all-cause dementia, 2540 cases of AD, and 1220 cases of VD.
- Fully adjusted models showed participants with CHD had significantly higher risks than those without CHD of developing all-cause dementia (hazard ratio [HR], 1.36; 95% CI, 1.28-1.45; P < .001), AD (HR, 1.13; 95% CI, 1.02-1.24; P = .019), and VD (HR, 1.78; 95% CI, 1.56-2.02; P < .001). The higher risk for VD suggests CHD has a more profound influence on neuropathologic changes involved in this dementia type, said the authors.
- Those with CHD diagnosed at a younger age had higher risks of developing dementia (HR per 10-year decrease in age, 1.25; 95% CI, 1.20-1.30 for all-cause dementia, 1.29; 95% CI, 1.20-1.38 for AD, and 1.22; 95% CI, 1.13-1.31 for VD; P for all < .001).
- Propensity score matching analysis showed patients with CHD had significantly higher risks for dementia compared with matched controls, with the highest risk seen in patients diagnosed before age 45 (HR, 2.40; 95% CI, 1.79-3.20; P < .001), followed by those diagnosed between 45 and 59 years (HR, 1.46; 95% CI, 1.32-1.62; P < .001) and at or above 60 years (HR, 1.11; 95% CI, 1.03-1.19; P = .005), with similar results for AD and VD.
IN PRACTICE:
The findings suggest “additional attention should be paid to the cognitive status of patients with CHD, especially the ones diagnosed with CHD at a young age,” the authors conclude, noting that “timely intervention, such as cognitive training, could be implemented once signs of cognitive deteriorations are detected.”
SOURCE:
The study was conducted by Jie Liang, BS, School of Nursing, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing, and colleagues. It was published online on November 29, 2023, in the Journal of the American Heart Association.
LIMITATIONS:
As this is an observational study, it can’t conclude a causal relationship. Although the authors adjusted for many potential confounders, unknown risk factors that also contribute to CHD can’t be ruled out. As the study excluded 69,744 participants, selection bias is possible. The study included a mostly White population.
DISCLOSURES:
The study was supported by the National Natural Science Foundation of China, the Non-Profit Central Research Institute Fund of the Chinese Academy of Medical Sciences, and the China Medical Board. The authors have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
, with the risk highest — at 36% — if onset is before age 45, results of a large observational study show.
METHODOLOGY:
- The study included 432,667 of the more than 500,000 participants in the UK Biobank, with a mean age of 56.9 years, 50,685 (11.7%) of whom had CHD and 50,445 had data on age at CHD onset.
- Researchers divided participants into three groups according to age at CHD onset (below 45 years, 45-59 years, and 60 years and older), and carried out a propensity score matching analysis.
- Outcomes included all-cause dementia, AD, and VD.
- Covariates included age, sex, race, educational level, body mass index, low-density lipoprotein cholesterol, smoking status, alcohol intake, exercise, depressed mood, hypertension, diabetes, statin use, and apolipoprotein E4 status.
TAKEAWAY:
- During a median follow-up of 12.8 years, researchers identified 5876 cases of all-cause dementia, 2540 cases of AD, and 1220 cases of VD.
- Fully adjusted models showed participants with CHD had significantly higher risks than those without CHD of developing all-cause dementia (hazard ratio [HR], 1.36; 95% CI, 1.28-1.45; P < .001), AD (HR, 1.13; 95% CI, 1.02-1.24; P = .019), and VD (HR, 1.78; 95% CI, 1.56-2.02; P < .001). The higher risk for VD suggests CHD has a more profound influence on neuropathologic changes involved in this dementia type, said the authors.
- Those with CHD diagnosed at a younger age had higher risks of developing dementia (HR per 10-year decrease in age, 1.25; 95% CI, 1.20-1.30 for all-cause dementia, 1.29; 95% CI, 1.20-1.38 for AD, and 1.22; 95% CI, 1.13-1.31 for VD; P for all < .001).
- Propensity score matching analysis showed patients with CHD had significantly higher risks for dementia compared with matched controls, with the highest risk seen in patients diagnosed before age 45 (HR, 2.40; 95% CI, 1.79-3.20; P < .001), followed by those diagnosed between 45 and 59 years (HR, 1.46; 95% CI, 1.32-1.62; P < .001) and at or above 60 years (HR, 1.11; 95% CI, 1.03-1.19; P = .005), with similar results for AD and VD.
IN PRACTICE:
The findings suggest “additional attention should be paid to the cognitive status of patients with CHD, especially the ones diagnosed with CHD at a young age,” the authors conclude, noting that “timely intervention, such as cognitive training, could be implemented once signs of cognitive deteriorations are detected.”
SOURCE:
The study was conducted by Jie Liang, BS, School of Nursing, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing, and colleagues. It was published online on November 29, 2023, in the Journal of the American Heart Association.
LIMITATIONS:
As this is an observational study, it can’t conclude a causal relationship. Although the authors adjusted for many potential confounders, unknown risk factors that also contribute to CHD can’t be ruled out. As the study excluded 69,744 participants, selection bias is possible. The study included a mostly White population.
DISCLOSURES:
The study was supported by the National Natural Science Foundation of China, the Non-Profit Central Research Institute Fund of the Chinese Academy of Medical Sciences, and the China Medical Board. The authors have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Statin use remains low for at-risk patients
TOPLINE:
Changes in statin prescribing guidelines in 2013 had little effect on statin use for patients who are at risk for atherosclerotic cardiovascular disease (ASCVD), according to a study published Dec. 5 in the Annals of Internal Medicine.
METHODOLOGY:
- Statins lower cholesterol and can reduce the risk for heart and circulatory disease.
- In 2013, the American College of Cardiology and the American Heart Association (ACC/AHA) expanded indications for which clinicians could prescribe statins to adults for primary prevention, including risk scores for ASCVD above a certain threshold.
- Researchers studied trends in statin use between 1999 and 2018 using National Health and Nutrition Examination Survey data for 21,961 adults older than 20 years who did not have ASCVD.
- They analyzed data from before and after implementation of the 2013 guidelines.
TAKEAWAY:
- Statin usage increased since 1999 but peaked at 35% in 2013 despite the expanded ACC/AHA guidelines.
- No changes in usage were observed for the proportion of adults who were newly eligible for statins.
- Statin use among patients with diabetes increased by 31.1 percentage points between 1999 and 2014 but then remained stagnant from 2014 to 2018.
- Statin use among those with ASCVD risk of more than 20% increased by 23.1 percentage points between 1999 and 2013 but did not increase between 2013 and 2018.
IN PRACTICE:
“Although the ACC/AHA guidelines expanded indications for primary prevention, they also increased decision-making complexity, requiring new multistep risk calculation… Many clinicians do not routinely use cardiovascular risk calculators because of a lack of time, input availability, or buy-in. Electronic health record tools that calculate ASCVD risks show promise, but they are not routinely implemented and do not address other barriers, such as competing patient priorities and limited time for shared decision-making.“
SOURCE:
The study was led by Timothy S. Anderson, MD, MAS, Division of General Internal Medicine, at the University of Pittsburgh. The research was funded by the National Institute on Aging of the National Institutes of Health.
LIMITATIONS:
Data on whether patients had previously been offered and declined statins were not available. Risk score data for baseline ASCVD, which affects risk classification, were also not available.
DISCLOSURES:
The authors report no disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
Changes in statin prescribing guidelines in 2013 had little effect on statin use for patients who are at risk for atherosclerotic cardiovascular disease (ASCVD), according to a study published Dec. 5 in the Annals of Internal Medicine.
METHODOLOGY:
- Statins lower cholesterol and can reduce the risk for heart and circulatory disease.
- In 2013, the American College of Cardiology and the American Heart Association (ACC/AHA) expanded indications for which clinicians could prescribe statins to adults for primary prevention, including risk scores for ASCVD above a certain threshold.
- Researchers studied trends in statin use between 1999 and 2018 using National Health and Nutrition Examination Survey data for 21,961 adults older than 20 years who did not have ASCVD.
- They analyzed data from before and after implementation of the 2013 guidelines.
TAKEAWAY:
- Statin usage increased since 1999 but peaked at 35% in 2013 despite the expanded ACC/AHA guidelines.
- No changes in usage were observed for the proportion of adults who were newly eligible for statins.
- Statin use among patients with diabetes increased by 31.1 percentage points between 1999 and 2014 but then remained stagnant from 2014 to 2018.
- Statin use among those with ASCVD risk of more than 20% increased by 23.1 percentage points between 1999 and 2013 but did not increase between 2013 and 2018.
IN PRACTICE:
“Although the ACC/AHA guidelines expanded indications for primary prevention, they also increased decision-making complexity, requiring new multistep risk calculation… Many clinicians do not routinely use cardiovascular risk calculators because of a lack of time, input availability, or buy-in. Electronic health record tools that calculate ASCVD risks show promise, but they are not routinely implemented and do not address other barriers, such as competing patient priorities and limited time for shared decision-making.“
SOURCE:
The study was led by Timothy S. Anderson, MD, MAS, Division of General Internal Medicine, at the University of Pittsburgh. The research was funded by the National Institute on Aging of the National Institutes of Health.
LIMITATIONS:
Data on whether patients had previously been offered and declined statins were not available. Risk score data for baseline ASCVD, which affects risk classification, were also not available.
DISCLOSURES:
The authors report no disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
Changes in statin prescribing guidelines in 2013 had little effect on statin use for patients who are at risk for atherosclerotic cardiovascular disease (ASCVD), according to a study published Dec. 5 in the Annals of Internal Medicine.
METHODOLOGY:
- Statins lower cholesterol and can reduce the risk for heart and circulatory disease.
- In 2013, the American College of Cardiology and the American Heart Association (ACC/AHA) expanded indications for which clinicians could prescribe statins to adults for primary prevention, including risk scores for ASCVD above a certain threshold.
- Researchers studied trends in statin use between 1999 and 2018 using National Health and Nutrition Examination Survey data for 21,961 adults older than 20 years who did not have ASCVD.
- They analyzed data from before and after implementation of the 2013 guidelines.
TAKEAWAY:
- Statin usage increased since 1999 but peaked at 35% in 2013 despite the expanded ACC/AHA guidelines.
- No changes in usage were observed for the proportion of adults who were newly eligible for statins.
- Statin use among patients with diabetes increased by 31.1 percentage points between 1999 and 2014 but then remained stagnant from 2014 to 2018.
- Statin use among those with ASCVD risk of more than 20% increased by 23.1 percentage points between 1999 and 2013 but did not increase between 2013 and 2018.
IN PRACTICE:
“Although the ACC/AHA guidelines expanded indications for primary prevention, they also increased decision-making complexity, requiring new multistep risk calculation… Many clinicians do not routinely use cardiovascular risk calculators because of a lack of time, input availability, or buy-in. Electronic health record tools that calculate ASCVD risks show promise, but they are not routinely implemented and do not address other barriers, such as competing patient priorities and limited time for shared decision-making.“
SOURCE:
The study was led by Timothy S. Anderson, MD, MAS, Division of General Internal Medicine, at the University of Pittsburgh. The research was funded by the National Institute on Aging of the National Institutes of Health.
LIMITATIONS:
Data on whether patients had previously been offered and declined statins were not available. Risk score data for baseline ASCVD, which affects risk classification, were also not available.
DISCLOSURES:
The authors report no disclosures.
A version of this article appeared on Medscape.com.
Smoking alters salivary microbiota in potential path to disease risk
TOPLINE:
Salivary microbiota changes caused by cigarette smoking may affect metabolic pathways and increase disease risk.
METHODOLOGY:
The researchers analyzed health information and data on the composition of salivary microbiota from 1601 adult participants in the Cooperative Health Research in South Tyrol (CHRIS) microbiome study (CHRISMB); CHRIS is an ongoing study in Italy.
The average age of the study population was 45 years; 53% were female, and 45% were current or former smokers.
The researchers hypothesized that changes in salivary microbial composition would be associated with smoking, with more nitrate-reducing bacteria present, and that nitrate reduction pathways would be reduced in smokers.
TAKEAWAY:
The researchers identified 44 genera that differed in the salivary microbiota of current smokers and nonsmokers. In smokers, seven genera in the phylum Proteobacteria were decreased and six in the phylum Actinobacteria were increased compared with nonsmokers; these phyla contain primarily aerobic and anaerobic taxa, respectively.
Some microbiota changes were significantly associated with daily smoking intensity; genera from the classes Betaproteobacteria (Lautropia or Neisseria), Gammaproteobacteria (Cardiobacterium), and Flavobacteriia (Capnocytophaga) decreased significantly with increased grams of tobacco smoked per day, measured in 5-g increments.
Smoking was associated with changes in the salivary microbiota; the nitrate reduction pathway was significantly lower in smokers compared with nonsmokers, and these decreases were consistent with previous studies of decreased cardiovascular events in former smokers.
However, the salivary microbiota of smokers who had quit for at least 5 years resembled that of individuals who had never smoked.
IN PRACTICE:
“Decreased microbial nitrate reduction pathway abundance in smokers may provide an additional explanation for the effect of smoking on cardiovascular and periodontal diseases risk, a hypothesis which should be tested in future studies,” the researchers wrote.
SOURCE:
The lead author of the study was Giacomo Antonello, MD, of Eurac Research, Affiliated Institute of the University of Lübeck, Bolzano, Italy. The study was published online in Scientific Reports (a Nature journal) on November 2, 2023.
LIMITATIONS:
The cross-sectional design and lack of professional assessment of tooth and gum health were limiting factors, as were potential confounding factors including medication use, diet, and alcohol intake.
DISCLOSURES:
The study was supported by the Department of Innovation, Research and University of the Autonomous Province of Bolzano-South Tyrol and by the European Regional Development Fund. The CHRISMB microbiota data generation was funded by the National Institute of Dental and Craniofacial Research. The researchers had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
TOPLINE:
Salivary microbiota changes caused by cigarette smoking may affect metabolic pathways and increase disease risk.
METHODOLOGY:
The researchers analyzed health information and data on the composition of salivary microbiota from 1601 adult participants in the Cooperative Health Research in South Tyrol (CHRIS) microbiome study (CHRISMB); CHRIS is an ongoing study in Italy.
The average age of the study population was 45 years; 53% were female, and 45% were current or former smokers.
The researchers hypothesized that changes in salivary microbial composition would be associated with smoking, with more nitrate-reducing bacteria present, and that nitrate reduction pathways would be reduced in smokers.
TAKEAWAY:
The researchers identified 44 genera that differed in the salivary microbiota of current smokers and nonsmokers. In smokers, seven genera in the phylum Proteobacteria were decreased and six in the phylum Actinobacteria were increased compared with nonsmokers; these phyla contain primarily aerobic and anaerobic taxa, respectively.
Some microbiota changes were significantly associated with daily smoking intensity; genera from the classes Betaproteobacteria (Lautropia or Neisseria), Gammaproteobacteria (Cardiobacterium), and Flavobacteriia (Capnocytophaga) decreased significantly with increased grams of tobacco smoked per day, measured in 5-g increments.
Smoking was associated with changes in the salivary microbiota; the nitrate reduction pathway was significantly lower in smokers compared with nonsmokers, and these decreases were consistent with previous studies of decreased cardiovascular events in former smokers.
However, the salivary microbiota of smokers who had quit for at least 5 years resembled that of individuals who had never smoked.
IN PRACTICE:
“Decreased microbial nitrate reduction pathway abundance in smokers may provide an additional explanation for the effect of smoking on cardiovascular and periodontal diseases risk, a hypothesis which should be tested in future studies,” the researchers wrote.
SOURCE:
The lead author of the study was Giacomo Antonello, MD, of Eurac Research, Affiliated Institute of the University of Lübeck, Bolzano, Italy. The study was published online in Scientific Reports (a Nature journal) on November 2, 2023.
LIMITATIONS:
The cross-sectional design and lack of professional assessment of tooth and gum health were limiting factors, as were potential confounding factors including medication use, diet, and alcohol intake.
DISCLOSURES:
The study was supported by the Department of Innovation, Research and University of the Autonomous Province of Bolzano-South Tyrol and by the European Regional Development Fund. The CHRISMB microbiota data generation was funded by the National Institute of Dental and Craniofacial Research. The researchers had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
TOPLINE:
Salivary microbiota changes caused by cigarette smoking may affect metabolic pathways and increase disease risk.
METHODOLOGY:
The researchers analyzed health information and data on the composition of salivary microbiota from 1601 adult participants in the Cooperative Health Research in South Tyrol (CHRIS) microbiome study (CHRISMB); CHRIS is an ongoing study in Italy.
The average age of the study population was 45 years; 53% were female, and 45% were current or former smokers.
The researchers hypothesized that changes in salivary microbial composition would be associated with smoking, with more nitrate-reducing bacteria present, and that nitrate reduction pathways would be reduced in smokers.
TAKEAWAY:
The researchers identified 44 genera that differed in the salivary microbiota of current smokers and nonsmokers. In smokers, seven genera in the phylum Proteobacteria were decreased and six in the phylum Actinobacteria were increased compared with nonsmokers; these phyla contain primarily aerobic and anaerobic taxa, respectively.
Some microbiota changes were significantly associated with daily smoking intensity; genera from the classes Betaproteobacteria (Lautropia or Neisseria), Gammaproteobacteria (Cardiobacterium), and Flavobacteriia (Capnocytophaga) decreased significantly with increased grams of tobacco smoked per day, measured in 5-g increments.
Smoking was associated with changes in the salivary microbiota; the nitrate reduction pathway was significantly lower in smokers compared with nonsmokers, and these decreases were consistent with previous studies of decreased cardiovascular events in former smokers.
However, the salivary microbiota of smokers who had quit for at least 5 years resembled that of individuals who had never smoked.
IN PRACTICE:
“Decreased microbial nitrate reduction pathway abundance in smokers may provide an additional explanation for the effect of smoking on cardiovascular and periodontal diseases risk, a hypothesis which should be tested in future studies,” the researchers wrote.
SOURCE:
The lead author of the study was Giacomo Antonello, MD, of Eurac Research, Affiliated Institute of the University of Lübeck, Bolzano, Italy. The study was published online in Scientific Reports (a Nature journal) on November 2, 2023.
LIMITATIONS:
The cross-sectional design and lack of professional assessment of tooth and gum health were limiting factors, as were potential confounding factors including medication use, diet, and alcohol intake.
DISCLOSURES:
The study was supported by the Department of Innovation, Research and University of the Autonomous Province of Bolzano-South Tyrol and by the European Regional Development Fund. The CHRISMB microbiota data generation was funded by the National Institute of Dental and Craniofacial Research. The researchers had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
PTSD symptoms in women tied to worse heart, brain health
TOPLINE:
METHODOLOGY:
- Researchers conducted a cross-sectional study of 274 women (mean age, 59 years) participating in the MsBrain study of menopause and brain health.
- As part of the study, the women completed the PTSD Checklist–Civilian Version and underwent physical and neuropsychological testing, as well as carotid artery ultrasonography and brain MRI.
- Outcomes of interest were associations of PTSD symptoms with carotid intima media thickness (IMT), brain white matter hyperintensity volume (WMHV), and cognition, assessed in linear regression models.
- Interactions by APOEε4 were assessed; covariates included age, race/ethnicity, education, and CVD risk factors.
TAKEAWAY:
- Higher PTSD symptoms were associated with greater carotid IMT (P = .03); associations of PTSD symptoms with neurocognitive outcomes varied significantly by APOEε4 status.
- Among APOEε4 carriers, PTSD symptoms were associated with greater whole-brain WMHV (P = .009), periventricular WMHV (P = .02), deep WMHV (P = .01), and frontal WMHV (P = .04) in multivariable models.
- APOEε4 carriers with PTSD symptoms also had poorer cognition, specifically attention and working memory (P = .02), semantic fluency (P = .01), perceptual speed (P = .002) and processing speed (P = .002), in multivariable models.
IN PRACTICE:
“This study sheds important insight on the implications of PTSD symptoms to women’s cardiovascular and neurocognitive health. Our findings indicate that the APOEε4 genotype may identify a group of women with PTSD symptoms at particular risk for poor neurocognitive health,” the authors wrote.
SOURCE:
The study, with first author Rebecca Thurston, PhD, of the department of psychiatry, University of Pittsburgh, was published online in JAMA Network Open.
LIMITATIONS:
No diagnostic clinical interviews were conducted, and PTSD treatment was not assessed. All participants identified as cisgender, and most were non-Hispanic Black or White. The study was observational and cross-sectional, precluding assertions about directionality or causality.
DISCLOSURES:
The study was funded by the National Institutes of Health, the University of Pittsburgh Clinical and Translational Science Institute, and the University of Pittsburgh Small Molecule Biomarker Core. Dr. Thurston reported receiving personal fees from Astellas Pharma, Bayer, Hello Therapeutics, Vira Health, and Happify Health outside the submitted work.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers conducted a cross-sectional study of 274 women (mean age, 59 years) participating in the MsBrain study of menopause and brain health.
- As part of the study, the women completed the PTSD Checklist–Civilian Version and underwent physical and neuropsychological testing, as well as carotid artery ultrasonography and brain MRI.
- Outcomes of interest were associations of PTSD symptoms with carotid intima media thickness (IMT), brain white matter hyperintensity volume (WMHV), and cognition, assessed in linear regression models.
- Interactions by APOEε4 were assessed; covariates included age, race/ethnicity, education, and CVD risk factors.
TAKEAWAY:
- Higher PTSD symptoms were associated with greater carotid IMT (P = .03); associations of PTSD symptoms with neurocognitive outcomes varied significantly by APOEε4 status.
- Among APOEε4 carriers, PTSD symptoms were associated with greater whole-brain WMHV (P = .009), periventricular WMHV (P = .02), deep WMHV (P = .01), and frontal WMHV (P = .04) in multivariable models.
- APOEε4 carriers with PTSD symptoms also had poorer cognition, specifically attention and working memory (P = .02), semantic fluency (P = .01), perceptual speed (P = .002) and processing speed (P = .002), in multivariable models.
IN PRACTICE:
“This study sheds important insight on the implications of PTSD symptoms to women’s cardiovascular and neurocognitive health. Our findings indicate that the APOEε4 genotype may identify a group of women with PTSD symptoms at particular risk for poor neurocognitive health,” the authors wrote.
SOURCE:
The study, with first author Rebecca Thurston, PhD, of the department of psychiatry, University of Pittsburgh, was published online in JAMA Network Open.
LIMITATIONS:
No diagnostic clinical interviews were conducted, and PTSD treatment was not assessed. All participants identified as cisgender, and most were non-Hispanic Black or White. The study was observational and cross-sectional, precluding assertions about directionality or causality.
DISCLOSURES:
The study was funded by the National Institutes of Health, the University of Pittsburgh Clinical and Translational Science Institute, and the University of Pittsburgh Small Molecule Biomarker Core. Dr. Thurston reported receiving personal fees from Astellas Pharma, Bayer, Hello Therapeutics, Vira Health, and Happify Health outside the submitted work.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers conducted a cross-sectional study of 274 women (mean age, 59 years) participating in the MsBrain study of menopause and brain health.
- As part of the study, the women completed the PTSD Checklist–Civilian Version and underwent physical and neuropsychological testing, as well as carotid artery ultrasonography and brain MRI.
- Outcomes of interest were associations of PTSD symptoms with carotid intima media thickness (IMT), brain white matter hyperintensity volume (WMHV), and cognition, assessed in linear regression models.
- Interactions by APOEε4 were assessed; covariates included age, race/ethnicity, education, and CVD risk factors.
TAKEAWAY:
- Higher PTSD symptoms were associated with greater carotid IMT (P = .03); associations of PTSD symptoms with neurocognitive outcomes varied significantly by APOEε4 status.
- Among APOEε4 carriers, PTSD symptoms were associated with greater whole-brain WMHV (P = .009), periventricular WMHV (P = .02), deep WMHV (P = .01), and frontal WMHV (P = .04) in multivariable models.
- APOEε4 carriers with PTSD symptoms also had poorer cognition, specifically attention and working memory (P = .02), semantic fluency (P = .01), perceptual speed (P = .002) and processing speed (P = .002), in multivariable models.
IN PRACTICE:
“This study sheds important insight on the implications of PTSD symptoms to women’s cardiovascular and neurocognitive health. Our findings indicate that the APOEε4 genotype may identify a group of women with PTSD symptoms at particular risk for poor neurocognitive health,” the authors wrote.
SOURCE:
The study, with first author Rebecca Thurston, PhD, of the department of psychiatry, University of Pittsburgh, was published online in JAMA Network Open.
LIMITATIONS:
No diagnostic clinical interviews were conducted, and PTSD treatment was not assessed. All participants identified as cisgender, and most were non-Hispanic Black or White. The study was observational and cross-sectional, precluding assertions about directionality or causality.
DISCLOSURES:
The study was funded by the National Institutes of Health, the University of Pittsburgh Clinical and Translational Science Institute, and the University of Pittsburgh Small Molecule Biomarker Core. Dr. Thurston reported receiving personal fees from Astellas Pharma, Bayer, Hello Therapeutics, Vira Health, and Happify Health outside the submitted work.
A version of this article first appeared on Medscape.com.
Long-term use of ADHD meds and CVD risk: New data
results of a large Swedish nested case-control study suggest.
The increased risk was evident only for hypertension and arterial disease, was dose dependent, and was higher for stimulant than nonstimulant ADHD medications.
“Clinicians should be vigilant in monitoring signs and symptoms of cardiovascular diseases, particularly among those receiving higher doses,” Zheng Chang, PhD, principal researcher, department of medical epidemiology and biostatistics, Karolinska Institutet, Stockholm, said in an interview.
“Treatment decisions, as always, should be based on careful weighing of potential benefits and risks at individual patient level, rather than simple one-size-fits-all recommendations,” Dr. Chang added.
The study was published online in JAMA Psychiatry
Filling in the research gaps
The use of medications to treat ADHD has increased markedly over the past decades in both children and adults. The potential risk for CVD associated with long-term ADHD medication use remains unclear. Most “longitudinal” studies that have looked at the association have an average follow-up time of no more than 2 years, the authors note.
In contrast, the Swedish study assessed the association between cumulative use of ADHD medication in children and adults followed for up to 14 years and also looked at whether associations differ across types of medication and dosages, types of CVD, gender, and age.
Among 278,027 individuals aged 6-64 years diagnosed with ADHD or dispensed ADHD medication, 10,388 with CVD were identified and matched to 51,672 controls without CVD.
Longer cumulative duration of ADHD medication use was associated with a statistically significant increased risk for CVD, compared with no use.
When the risk for specific CVDs was examined, long-term use of ADHD medication (compared with no use) was associated with an increased risk for hypertension and arterial disease but not arrhythmias, heart failure, ischemic heart disease, thromboembolic disease, or cerebrovascular disease.
For hypertension, the adjusted odds ratio was 1.72 (95% confidence interval, 1.51-1.97) for 3 to ≤ 5 years and 1.80 (95% CI, 1.55-2.08) for > 5 years of medication use. For arterial disease, the AOR was 1.65 (95% CI, 1.11-2.45) for 3 to ≤ 5 years and 1.49 (95% CI, 0.96-2.32) for > 5 years of use.
Stimulants confer greatest risk
Across the 14-year follow-up period, each additional year of ADHD medication use was associated with an average 4% increased CVD risk, with a larger 8% increased risk in the first 3 years of cumulative use, followed by stable risk over the remaining follow-up.
Similar risks were observed in children and adults, as well as in females and males.
When focusing on specific ADHD medications, compared with no use, long-term use of the stimulant methylphenidate was associated with an increased risk for CVD (AOR, 1.20 [95% CI, 1.10-1.31] for 3 to ≤ 5 years and 1.19 [95% CI, 1.08-1.31] for > 5 years).
The same was true for long-term use of the stimulant lisdexamfetamine (AOR, 1.23 [95% CI, 1.05-1.44] for 2 to ≤ 3 years and 1.17 [95% CI, 0.98-1.40] for > 3 years).
In contrast, use of the nonstimulant atomoxetine was associated with elevated CVD risk only for the first year of use (AOR, 1.07; 95% CI, 1.01-1.13).
The increased risk for CVD occurred only above certain average daily doses: 45 mg for methylphenidate and lisdexamfetamine, 22.5 mg for amphetamines, and 120 mg for atomoxetine.
The authors note that, although they accounted for a wide range of potential confounding variables, considering the observational nature of the study and the possibility of residual confounding, they could not prove causality.
‘Tricky trade-offs’
The coauthors of an editorial in JAMA Psychiatry (2023 Nov 22. doi: 10.1001/jamapsychiatry.2023.4126) note that the study “should remind us that clinical decision-making is often based on tricky trade-offs that should be considered at the individual patient level.”
Given that hypertension is the leading cause of CV morbidity and mortality worldwide, the increased likelihood of hypertension with long-term use of ADHD medications “cannot be disregarded,” write Samuele Cortese, MD, PhD, and Cristiano Fava, MD, PhD, with University of Southampton (England).
“These findings are especially relevant given the reported association between ADHD and physical conditions, such as obesity, which further contribute to increased cardiovascular risk,” they add.
Dr. Cortese and Dr. Fava say that the increased CV risk – averaging 4% per year and stabilizing after 3 years of treatment – “should be carefully weighed against the established benefits, on a case-by-case basis.”
“Importantly,” they write, “large real-world self-controlled studies have shown that individuals with ADHD experience significantly fewer unintentional physical injuries, motor vehicle crashes, substance use disorders, and criminal acts, as well as improved academic functioning, during periods when they are taking, compared with periods when they are not taking, methylphenidate.”
The risk-benefit ratio, however, may be lower in people with preexisting heart conditions. However, more evidence and precise recommendations are needed in relation to the treatment of individuals with ADHD and preexisting CV conditions, the editorial writers say.
This study was supported by grants from the Swedish Research Council for Health, Working Life, and Welfare and the European Union’s Horizon 2020 research and innovation program. The authors and editorial writers have no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
results of a large Swedish nested case-control study suggest.
The increased risk was evident only for hypertension and arterial disease, was dose dependent, and was higher for stimulant than nonstimulant ADHD medications.
“Clinicians should be vigilant in monitoring signs and symptoms of cardiovascular diseases, particularly among those receiving higher doses,” Zheng Chang, PhD, principal researcher, department of medical epidemiology and biostatistics, Karolinska Institutet, Stockholm, said in an interview.
“Treatment decisions, as always, should be based on careful weighing of potential benefits and risks at individual patient level, rather than simple one-size-fits-all recommendations,” Dr. Chang added.
The study was published online in JAMA Psychiatry
Filling in the research gaps
The use of medications to treat ADHD has increased markedly over the past decades in both children and adults. The potential risk for CVD associated with long-term ADHD medication use remains unclear. Most “longitudinal” studies that have looked at the association have an average follow-up time of no more than 2 years, the authors note.
In contrast, the Swedish study assessed the association between cumulative use of ADHD medication in children and adults followed for up to 14 years and also looked at whether associations differ across types of medication and dosages, types of CVD, gender, and age.
Among 278,027 individuals aged 6-64 years diagnosed with ADHD or dispensed ADHD medication, 10,388 with CVD were identified and matched to 51,672 controls without CVD.
Longer cumulative duration of ADHD medication use was associated with a statistically significant increased risk for CVD, compared with no use.
When the risk for specific CVDs was examined, long-term use of ADHD medication (compared with no use) was associated with an increased risk for hypertension and arterial disease but not arrhythmias, heart failure, ischemic heart disease, thromboembolic disease, or cerebrovascular disease.
For hypertension, the adjusted odds ratio was 1.72 (95% confidence interval, 1.51-1.97) for 3 to ≤ 5 years and 1.80 (95% CI, 1.55-2.08) for > 5 years of medication use. For arterial disease, the AOR was 1.65 (95% CI, 1.11-2.45) for 3 to ≤ 5 years and 1.49 (95% CI, 0.96-2.32) for > 5 years of use.
Stimulants confer greatest risk
Across the 14-year follow-up period, each additional year of ADHD medication use was associated with an average 4% increased CVD risk, with a larger 8% increased risk in the first 3 years of cumulative use, followed by stable risk over the remaining follow-up.
Similar risks were observed in children and adults, as well as in females and males.
When focusing on specific ADHD medications, compared with no use, long-term use of the stimulant methylphenidate was associated with an increased risk for CVD (AOR, 1.20 [95% CI, 1.10-1.31] for 3 to ≤ 5 years and 1.19 [95% CI, 1.08-1.31] for > 5 years).
The same was true for long-term use of the stimulant lisdexamfetamine (AOR, 1.23 [95% CI, 1.05-1.44] for 2 to ≤ 3 years and 1.17 [95% CI, 0.98-1.40] for > 3 years).
In contrast, use of the nonstimulant atomoxetine was associated with elevated CVD risk only for the first year of use (AOR, 1.07; 95% CI, 1.01-1.13).
The increased risk for CVD occurred only above certain average daily doses: 45 mg for methylphenidate and lisdexamfetamine, 22.5 mg for amphetamines, and 120 mg for atomoxetine.
The authors note that, although they accounted for a wide range of potential confounding variables, considering the observational nature of the study and the possibility of residual confounding, they could not prove causality.
‘Tricky trade-offs’
The coauthors of an editorial in JAMA Psychiatry (2023 Nov 22. doi: 10.1001/jamapsychiatry.2023.4126) note that the study “should remind us that clinical decision-making is often based on tricky trade-offs that should be considered at the individual patient level.”
Given that hypertension is the leading cause of CV morbidity and mortality worldwide, the increased likelihood of hypertension with long-term use of ADHD medications “cannot be disregarded,” write Samuele Cortese, MD, PhD, and Cristiano Fava, MD, PhD, with University of Southampton (England).
“These findings are especially relevant given the reported association between ADHD and physical conditions, such as obesity, which further contribute to increased cardiovascular risk,” they add.
Dr. Cortese and Dr. Fava say that the increased CV risk – averaging 4% per year and stabilizing after 3 years of treatment – “should be carefully weighed against the established benefits, on a case-by-case basis.”
“Importantly,” they write, “large real-world self-controlled studies have shown that individuals with ADHD experience significantly fewer unintentional physical injuries, motor vehicle crashes, substance use disorders, and criminal acts, as well as improved academic functioning, during periods when they are taking, compared with periods when they are not taking, methylphenidate.”
The risk-benefit ratio, however, may be lower in people with preexisting heart conditions. However, more evidence and precise recommendations are needed in relation to the treatment of individuals with ADHD and preexisting CV conditions, the editorial writers say.
This study was supported by grants from the Swedish Research Council for Health, Working Life, and Welfare and the European Union’s Horizon 2020 research and innovation program. The authors and editorial writers have no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
results of a large Swedish nested case-control study suggest.
The increased risk was evident only for hypertension and arterial disease, was dose dependent, and was higher for stimulant than nonstimulant ADHD medications.
“Clinicians should be vigilant in monitoring signs and symptoms of cardiovascular diseases, particularly among those receiving higher doses,” Zheng Chang, PhD, principal researcher, department of medical epidemiology and biostatistics, Karolinska Institutet, Stockholm, said in an interview.
“Treatment decisions, as always, should be based on careful weighing of potential benefits and risks at individual patient level, rather than simple one-size-fits-all recommendations,” Dr. Chang added.
The study was published online in JAMA Psychiatry
Filling in the research gaps
The use of medications to treat ADHD has increased markedly over the past decades in both children and adults. The potential risk for CVD associated with long-term ADHD medication use remains unclear. Most “longitudinal” studies that have looked at the association have an average follow-up time of no more than 2 years, the authors note.
In contrast, the Swedish study assessed the association between cumulative use of ADHD medication in children and adults followed for up to 14 years and also looked at whether associations differ across types of medication and dosages, types of CVD, gender, and age.
Among 278,027 individuals aged 6-64 years diagnosed with ADHD or dispensed ADHD medication, 10,388 with CVD were identified and matched to 51,672 controls without CVD.
Longer cumulative duration of ADHD medication use was associated with a statistically significant increased risk for CVD, compared with no use.
When the risk for specific CVDs was examined, long-term use of ADHD medication (compared with no use) was associated with an increased risk for hypertension and arterial disease but not arrhythmias, heart failure, ischemic heart disease, thromboembolic disease, or cerebrovascular disease.
For hypertension, the adjusted odds ratio was 1.72 (95% confidence interval, 1.51-1.97) for 3 to ≤ 5 years and 1.80 (95% CI, 1.55-2.08) for > 5 years of medication use. For arterial disease, the AOR was 1.65 (95% CI, 1.11-2.45) for 3 to ≤ 5 years and 1.49 (95% CI, 0.96-2.32) for > 5 years of use.
Stimulants confer greatest risk
Across the 14-year follow-up period, each additional year of ADHD medication use was associated with an average 4% increased CVD risk, with a larger 8% increased risk in the first 3 years of cumulative use, followed by stable risk over the remaining follow-up.
Similar risks were observed in children and adults, as well as in females and males.
When focusing on specific ADHD medications, compared with no use, long-term use of the stimulant methylphenidate was associated with an increased risk for CVD (AOR, 1.20 [95% CI, 1.10-1.31] for 3 to ≤ 5 years and 1.19 [95% CI, 1.08-1.31] for > 5 years).
The same was true for long-term use of the stimulant lisdexamfetamine (AOR, 1.23 [95% CI, 1.05-1.44] for 2 to ≤ 3 years and 1.17 [95% CI, 0.98-1.40] for > 3 years).
In contrast, use of the nonstimulant atomoxetine was associated with elevated CVD risk only for the first year of use (AOR, 1.07; 95% CI, 1.01-1.13).
The increased risk for CVD occurred only above certain average daily doses: 45 mg for methylphenidate and lisdexamfetamine, 22.5 mg for amphetamines, and 120 mg for atomoxetine.
The authors note that, although they accounted for a wide range of potential confounding variables, considering the observational nature of the study and the possibility of residual confounding, they could not prove causality.
‘Tricky trade-offs’
The coauthors of an editorial in JAMA Psychiatry (2023 Nov 22. doi: 10.1001/jamapsychiatry.2023.4126) note that the study “should remind us that clinical decision-making is often based on tricky trade-offs that should be considered at the individual patient level.”
Given that hypertension is the leading cause of CV morbidity and mortality worldwide, the increased likelihood of hypertension with long-term use of ADHD medications “cannot be disregarded,” write Samuele Cortese, MD, PhD, and Cristiano Fava, MD, PhD, with University of Southampton (England).
“These findings are especially relevant given the reported association between ADHD and physical conditions, such as obesity, which further contribute to increased cardiovascular risk,” they add.
Dr. Cortese and Dr. Fava say that the increased CV risk – averaging 4% per year and stabilizing after 3 years of treatment – “should be carefully weighed against the established benefits, on a case-by-case basis.”
“Importantly,” they write, “large real-world self-controlled studies have shown that individuals with ADHD experience significantly fewer unintentional physical injuries, motor vehicle crashes, substance use disorders, and criminal acts, as well as improved academic functioning, during periods when they are taking, compared with periods when they are not taking, methylphenidate.”
The risk-benefit ratio, however, may be lower in people with preexisting heart conditions. However, more evidence and precise recommendations are needed in relation to the treatment of individuals with ADHD and preexisting CV conditions, the editorial writers say.
This study was supported by grants from the Swedish Research Council for Health, Working Life, and Welfare and the European Union’s Horizon 2020 research and innovation program. The authors and editorial writers have no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
FROM JAMA PSYCHIATRY






