User login
Longitudinal associations between income changes and incident CVD
Background: Low income is associated with CVD, although causality remains debated because low income is also associated with depression and negative health behaviors, which can be associated with CVD. For more robust causal inference, changes in income and their association with CVD must be observed.
Study design: Prospective observational cohort study.
Setting: Four U.S. urban centers – Jackson, Miss.; suburbs of Minneapolis; Washington County, Md.; and Forsyth County, N.C.
Synopsis: Among a large cohort of community-dwelling middle-aged adults, this study showed that negative income changes are associated with an increased incidence of CVD. Among 8,989 patients recruited from the four urban centers above, 10% experienced an income drop, 70% did not have a change in income, and 20% experienced an income increase over the first 6 years of the study. Patients were followed for a mean of 17 years, and those who experienced an income drop were found to have a 17% higher risk of incident CVD, whereas those who experienced an income increase had a 14% lower risk of CVD.
The study was limited by difficulties classifying income and its changes; the complicated nature of income, its relationship with other socioeconomic factors, and causation inferences; and the relatively short span over which income was monitored.
Bottom line: Income decrease is associated with an increased risk of incident CVD.
Citation: Wang S et al. Longitudinal associations between income changes and incident cardiovascular disease, the atherosclerosis risk in communities study. JAMA Cardiol. 2019 Oct 9;4(12):1203-12.
Dr. Rupp is a hospitalist and clinical instructor of medicine at the University of Utah, Salt Lake City.
Background: Low income is associated with CVD, although causality remains debated because low income is also associated with depression and negative health behaviors, which can be associated with CVD. For more robust causal inference, changes in income and their association with CVD must be observed.
Study design: Prospective observational cohort study.
Setting: Four U.S. urban centers – Jackson, Miss.; suburbs of Minneapolis; Washington County, Md.; and Forsyth County, N.C.
Synopsis: Among a large cohort of community-dwelling middle-aged adults, this study showed that negative income changes are associated with an increased incidence of CVD. Among 8,989 patients recruited from the four urban centers above, 10% experienced an income drop, 70% did not have a change in income, and 20% experienced an income increase over the first 6 years of the study. Patients were followed for a mean of 17 years, and those who experienced an income drop were found to have a 17% higher risk of incident CVD, whereas those who experienced an income increase had a 14% lower risk of CVD.
The study was limited by difficulties classifying income and its changes; the complicated nature of income, its relationship with other socioeconomic factors, and causation inferences; and the relatively short span over which income was monitored.
Bottom line: Income decrease is associated with an increased risk of incident CVD.
Citation: Wang S et al. Longitudinal associations between income changes and incident cardiovascular disease, the atherosclerosis risk in communities study. JAMA Cardiol. 2019 Oct 9;4(12):1203-12.
Dr. Rupp is a hospitalist and clinical instructor of medicine at the University of Utah, Salt Lake City.
Background: Low income is associated with CVD, although causality remains debated because low income is also associated with depression and negative health behaviors, which can be associated with CVD. For more robust causal inference, changes in income and their association with CVD must be observed.
Study design: Prospective observational cohort study.
Setting: Four U.S. urban centers – Jackson, Miss.; suburbs of Minneapolis; Washington County, Md.; and Forsyth County, N.C.
Synopsis: Among a large cohort of community-dwelling middle-aged adults, this study showed that negative income changes are associated with an increased incidence of CVD. Among 8,989 patients recruited from the four urban centers above, 10% experienced an income drop, 70% did not have a change in income, and 20% experienced an income increase over the first 6 years of the study. Patients were followed for a mean of 17 years, and those who experienced an income drop were found to have a 17% higher risk of incident CVD, whereas those who experienced an income increase had a 14% lower risk of CVD.
The study was limited by difficulties classifying income and its changes; the complicated nature of income, its relationship with other socioeconomic factors, and causation inferences; and the relatively short span over which income was monitored.
Bottom line: Income decrease is associated with an increased risk of incident CVD.
Citation: Wang S et al. Longitudinal associations between income changes and incident cardiovascular disease, the atherosclerosis risk in communities study. JAMA Cardiol. 2019 Oct 9;4(12):1203-12.
Dr. Rupp is a hospitalist and clinical instructor of medicine at the University of Utah, Salt Lake City.
AstraZeneca COVID vaccine: Clotting disorder mechanism revealed?
The European Medicines Agency continues to reassure the public about the safety of the AstraZeneca COVID-19 vaccine, although several countries have imposed new restrictions on the product, owing to its link to a rare clotting disorder.
Use of the vaccine has been suspended for individuals younger than 55 or 60 years in several European countries and in Canada after reports of a prothrombotic disorder and thrombocytopenia, mainly in younger individuals.
Now, more information on the prothrombotic disorder has become available. The vaccine appears to be linked to a condition that clinically resembles heparin-induced thrombocytopenia (HIT) and that occurs mainly in younger women.
Researchers have described clinical and laboratory details of nine patients from Germany and Austria who developed this condition 4-16 days after receiving the AstraZeneca vaccine in a preprint article published March 28, 2021, on Research Square.
They found that serum from four patients who were tested showed platelet-activating antibodies directed against platelet factor 4 (PF4), similar to what is seen in HIT.
They are proposing naming the condition “vaccine-induced prothrombotic immune thrombocytopenia (VIPIT)” to avoid confusion with HIT.
At a press conference March 31, the EMA said its ongoing review of the situation “has not identified any specific risk factors, such as age, gender, or a previous medical history of clotting disorders, for these very rare events. A causal link with the vaccine is not proven but is possible, and further analysis is continuing.”
A statement from the agency noted: “EMA is of the view that the benefits of the AstraZeneca vaccine in preventing COVID-19, with its associated risk of hospitalization and death, outweigh the risks of side effects.”
But it added: “Vaccinated people should be aware of the remote possibility of these very rare types of blood clots occurring. If they have symptoms suggestive of clotting problems as described in the product information, they should seek immediate medical attention and inform health care professionals of their recent vaccination.”
VIPIT study
In the Research Square preprint article, a group led by Andreas Greinacher, MD, professor of transfusion medicine at the Greifswald (Germany) University Clinic, reported on clinical and laboratory features of nine patients (eight of whom were women) in Germany and Austria who developed thrombosis and thrombocytopenia after they received the AstraZeneca vaccine.
The researchers explained that they investigated whether these patients could have a prothrombotic disorder caused by platelet-activating antibodies directed against PF4, which is known to be caused by heparin and sometimes environmental triggers.
The nine patients were aged 22-49 years and presented with thrombosis beginning 4-16 days post vaccination. Seven patients had cerebral venous thrombosis (CVT), one had pulmonary embolism, and one had splanchnic vein thrombosis and CVT. Four patients died. None had received heparin prior to symptom onset.
Serum from four patients was tested for anti-PF4/heparin antibodies, and all four tested strongly positive. All four also tested strongly positive on platelet activation assay for the presence of PF4 independently of heparin.
The authors noted that it has been recognized that triggers other than heparin, including some infections, can rarely cause a disorder that strongly resembles HIT. These cases have been referred to as spontaneous HIT syndrome.
They said that their current findings have several important clinical implications.
“Clinicians should be aware that onset of (venous or arterial) thrombosis particularly at unusual sites such as in the brain or abdomen and thrombocytopenia beginning approximately 5-14 days after vaccination can represent a rare adverse effect of preceding COVID-19 vaccination,” they wrote. To date, this has only been reported with the AstraZeneca vaccine.
They pointed out that enzyme immunoassays for HIT are widely available and can be used to investigate for potential postvaccination anti-PF4 antibody–associated thrombocytopenia/thrombosis. For such patients, referral should be made to a laboratory that performs platelet-activation assays.
Although this syndrome differs from typical HIT, the researchers noted that at least one patient showed strong platelet activation in the presence of heparin. They thus recommended therapy with nonheparin anticoagulants, such as the direct oral anticoagulants.
They also wrote that high-dose intravenous immunoglobulin has been shown to be effective for treating severe HIT and could also be an important treatment adjunct for patients who develop life-threatening thrombotic events, such as cerebral vein sinus thrombosis (CVST), after being vaccinated.
EMA data to date
Updated data, reported at the EMA press briefing on March 31, indicate that 62 cases of CVST have been reported worldwide (44 from the European Union). These data may not yet include all the German cases.
Peter Arlett, MD, head of pharmacovigilance and epidemiology at the EMA, said there were more cases than expected in the 2-week window after vaccination among patients younger than 60 and that health care professionals should be alert to features of this condition, including headache and blurred vision.
He suggested that the higher rate of the condition among younger women may reflect the population that received this vaccine, because initially, the vaccine was not recommended for older people in many countries and was targeted toward younger health care workers, who were mainly women.
The German regulatory agency, the Paul Ehrlich Institute, reported this week that it has now registered 31 cases of CVST among nearly 2.7 million people who had received the vaccine in Germany. Of these patients, 19 also were found to have a deficiency of blood platelets or thrombocytopenia. Nine of the affected patients died. All but two of the cases occurred in women aged 20-63 years. The two men were aged 36 and 57 years.
These data have prompted the German authorities to limit use of the AstraZeneca vaccine to those aged 60 years and older. Even before this decision, senior clinicians in Germany had been urging a change in the vaccination recommendations.
For example, Bernd Salzberger, MD, head of infectious diseases, University Hospital Regensburg (Germany), told the Science Media Center: “In women, a complicated course of COVID disease is less common from the start and is so rare in younger women that the chance of avoiding a fatal course through vaccination in women without comorbidities is of the same order of magnitude as the risk of this rare side effect.”
Sandra Ciesek, MD, a virologist at Goethe University, Frankfurt, Germany, told the journal Science: “The argument I keep hearing is that the risk-benefit ratio is still positive. But we do not have just one vaccine, we have several. So, restricting the AstraZeneca vaccine to older people makes sense to me, and it does not waste any doses.”
Concerns put in perspective
Commenting of the latest developments, thrombosis expert Saskia Middeldorp, MD, head of internal medicine at Radboud University Medical Center, Nijmegen, the Netherlands, said it was vitally important that these concerns be put in perspective and that the vaccination program with the AstraZeneca product continue.
“There are some concerning reports about very rare blood clotting disorders and low platelet counts possibly associated with the AstraZeneca vaccine. Groups from Germany and Norway have identified a syndrome similar to HIT, which seems to explain the cause of this very rare side effect,” Dr. Middeldorp noted.
“But with such a high pressure from the virus and many countries now going into a third wave of infection, anything that might slow down vaccination rates will cause much more harm than good,” she warned.
Dr. Middeldorp believes the incidence of this HIT-type syndrome linked to the vaccine is about 1-2 per million. “These are estimates based on the number of reports of this side effect and denominators from the U.K. and EU populations,” she explained. However, Germany has restricted the vaccine on the basis of German data, which appear to show higher rates of the condition. It is not known why the rates are higher in Germany.
“The European Medicines Agency is looking at this very closely. Their statement is quite clear. There is no foundation for changing policy on vaccination,” Dr. Middeldorp stated.
She cautioned that these reports were reducing confidence in the AstraZeneca vaccine, particularly among young people, which she said was causing “a major setback” for the vaccination program.
Noting that everything must be viewed in the context of this severe pandemic, Dr. Middeldorp emphasized that the benefit of the vaccine outweighed any risk, even among young people.
“To those who may be hesitating to have the vaccine as they don’t think they are at high risk of severe COVID infection, I would say there are a lot of young people in the ICU at present with COVID, and your chance of a severe COVID illness is far higher than the 1 or 2 in a million risk of a severe reaction to the vaccine,” she stated.
Dr. Greinacher has received grants and nonfinancial support from Aspen, Boehringer Ingelheim, Merck Sharp & Dohme, Bristol-Myers Squibb, Paringenix, Bayer Healthcare, Gore, Rovi, Sagent, and Biomarin/Prosensa; personal fees from Aspen, Boehringer Ingelheim, Merck Sharp & Dohme, Macopharma, Bristol-Myers Squibb, Chromatec, and Instrumentation Laboratory; and nonfinancial support from Boehringer Ingelheim, Portola, Ergomed, and GTH outside the submitted work.
A version of this article first appeared on Medscape.com.
The European Medicines Agency continues to reassure the public about the safety of the AstraZeneca COVID-19 vaccine, although several countries have imposed new restrictions on the product, owing to its link to a rare clotting disorder.
Use of the vaccine has been suspended for individuals younger than 55 or 60 years in several European countries and in Canada after reports of a prothrombotic disorder and thrombocytopenia, mainly in younger individuals.
Now, more information on the prothrombotic disorder has become available. The vaccine appears to be linked to a condition that clinically resembles heparin-induced thrombocytopenia (HIT) and that occurs mainly in younger women.
Researchers have described clinical and laboratory details of nine patients from Germany and Austria who developed this condition 4-16 days after receiving the AstraZeneca vaccine in a preprint article published March 28, 2021, on Research Square.
They found that serum from four patients who were tested showed platelet-activating antibodies directed against platelet factor 4 (PF4), similar to what is seen in HIT.
They are proposing naming the condition “vaccine-induced prothrombotic immune thrombocytopenia (VIPIT)” to avoid confusion with HIT.
At a press conference March 31, the EMA said its ongoing review of the situation “has not identified any specific risk factors, such as age, gender, or a previous medical history of clotting disorders, for these very rare events. A causal link with the vaccine is not proven but is possible, and further analysis is continuing.”
A statement from the agency noted: “EMA is of the view that the benefits of the AstraZeneca vaccine in preventing COVID-19, with its associated risk of hospitalization and death, outweigh the risks of side effects.”
But it added: “Vaccinated people should be aware of the remote possibility of these very rare types of blood clots occurring. If they have symptoms suggestive of clotting problems as described in the product information, they should seek immediate medical attention and inform health care professionals of their recent vaccination.”
VIPIT study
In the Research Square preprint article, a group led by Andreas Greinacher, MD, professor of transfusion medicine at the Greifswald (Germany) University Clinic, reported on clinical and laboratory features of nine patients (eight of whom were women) in Germany and Austria who developed thrombosis and thrombocytopenia after they received the AstraZeneca vaccine.
The researchers explained that they investigated whether these patients could have a prothrombotic disorder caused by platelet-activating antibodies directed against PF4, which is known to be caused by heparin and sometimes environmental triggers.
The nine patients were aged 22-49 years and presented with thrombosis beginning 4-16 days post vaccination. Seven patients had cerebral venous thrombosis (CVT), one had pulmonary embolism, and one had splanchnic vein thrombosis and CVT. Four patients died. None had received heparin prior to symptom onset.
Serum from four patients was tested for anti-PF4/heparin antibodies, and all four tested strongly positive. All four also tested strongly positive on platelet activation assay for the presence of PF4 independently of heparin.
The authors noted that it has been recognized that triggers other than heparin, including some infections, can rarely cause a disorder that strongly resembles HIT. These cases have been referred to as spontaneous HIT syndrome.
They said that their current findings have several important clinical implications.
“Clinicians should be aware that onset of (venous or arterial) thrombosis particularly at unusual sites such as in the brain or abdomen and thrombocytopenia beginning approximately 5-14 days after vaccination can represent a rare adverse effect of preceding COVID-19 vaccination,” they wrote. To date, this has only been reported with the AstraZeneca vaccine.
They pointed out that enzyme immunoassays for HIT are widely available and can be used to investigate for potential postvaccination anti-PF4 antibody–associated thrombocytopenia/thrombosis. For such patients, referral should be made to a laboratory that performs platelet-activation assays.
Although this syndrome differs from typical HIT, the researchers noted that at least one patient showed strong platelet activation in the presence of heparin. They thus recommended therapy with nonheparin anticoagulants, such as the direct oral anticoagulants.
They also wrote that high-dose intravenous immunoglobulin has been shown to be effective for treating severe HIT and could also be an important treatment adjunct for patients who develop life-threatening thrombotic events, such as cerebral vein sinus thrombosis (CVST), after being vaccinated.
EMA data to date
Updated data, reported at the EMA press briefing on March 31, indicate that 62 cases of CVST have been reported worldwide (44 from the European Union). These data may not yet include all the German cases.
Peter Arlett, MD, head of pharmacovigilance and epidemiology at the EMA, said there were more cases than expected in the 2-week window after vaccination among patients younger than 60 and that health care professionals should be alert to features of this condition, including headache and blurred vision.
He suggested that the higher rate of the condition among younger women may reflect the population that received this vaccine, because initially, the vaccine was not recommended for older people in many countries and was targeted toward younger health care workers, who were mainly women.
The German regulatory agency, the Paul Ehrlich Institute, reported this week that it has now registered 31 cases of CVST among nearly 2.7 million people who had received the vaccine in Germany. Of these patients, 19 also were found to have a deficiency of blood platelets or thrombocytopenia. Nine of the affected patients died. All but two of the cases occurred in women aged 20-63 years. The two men were aged 36 and 57 years.
These data have prompted the German authorities to limit use of the AstraZeneca vaccine to those aged 60 years and older. Even before this decision, senior clinicians in Germany had been urging a change in the vaccination recommendations.
For example, Bernd Salzberger, MD, head of infectious diseases, University Hospital Regensburg (Germany), told the Science Media Center: “In women, a complicated course of COVID disease is less common from the start and is so rare in younger women that the chance of avoiding a fatal course through vaccination in women without comorbidities is of the same order of magnitude as the risk of this rare side effect.”
Sandra Ciesek, MD, a virologist at Goethe University, Frankfurt, Germany, told the journal Science: “The argument I keep hearing is that the risk-benefit ratio is still positive. But we do not have just one vaccine, we have several. So, restricting the AstraZeneca vaccine to older people makes sense to me, and it does not waste any doses.”
Concerns put in perspective
Commenting of the latest developments, thrombosis expert Saskia Middeldorp, MD, head of internal medicine at Radboud University Medical Center, Nijmegen, the Netherlands, said it was vitally important that these concerns be put in perspective and that the vaccination program with the AstraZeneca product continue.
“There are some concerning reports about very rare blood clotting disorders and low platelet counts possibly associated with the AstraZeneca vaccine. Groups from Germany and Norway have identified a syndrome similar to HIT, which seems to explain the cause of this very rare side effect,” Dr. Middeldorp noted.
“But with such a high pressure from the virus and many countries now going into a third wave of infection, anything that might slow down vaccination rates will cause much more harm than good,” she warned.
Dr. Middeldorp believes the incidence of this HIT-type syndrome linked to the vaccine is about 1-2 per million. “These are estimates based on the number of reports of this side effect and denominators from the U.K. and EU populations,” she explained. However, Germany has restricted the vaccine on the basis of German data, which appear to show higher rates of the condition. It is not known why the rates are higher in Germany.
“The European Medicines Agency is looking at this very closely. Their statement is quite clear. There is no foundation for changing policy on vaccination,” Dr. Middeldorp stated.
She cautioned that these reports were reducing confidence in the AstraZeneca vaccine, particularly among young people, which she said was causing “a major setback” for the vaccination program.
Noting that everything must be viewed in the context of this severe pandemic, Dr. Middeldorp emphasized that the benefit of the vaccine outweighed any risk, even among young people.
“To those who may be hesitating to have the vaccine as they don’t think they are at high risk of severe COVID infection, I would say there are a lot of young people in the ICU at present with COVID, and your chance of a severe COVID illness is far higher than the 1 or 2 in a million risk of a severe reaction to the vaccine,” she stated.
Dr. Greinacher has received grants and nonfinancial support from Aspen, Boehringer Ingelheim, Merck Sharp & Dohme, Bristol-Myers Squibb, Paringenix, Bayer Healthcare, Gore, Rovi, Sagent, and Biomarin/Prosensa; personal fees from Aspen, Boehringer Ingelheim, Merck Sharp & Dohme, Macopharma, Bristol-Myers Squibb, Chromatec, and Instrumentation Laboratory; and nonfinancial support from Boehringer Ingelheim, Portola, Ergomed, and GTH outside the submitted work.
A version of this article first appeared on Medscape.com.
The European Medicines Agency continues to reassure the public about the safety of the AstraZeneca COVID-19 vaccine, although several countries have imposed new restrictions on the product, owing to its link to a rare clotting disorder.
Use of the vaccine has been suspended for individuals younger than 55 or 60 years in several European countries and in Canada after reports of a prothrombotic disorder and thrombocytopenia, mainly in younger individuals.
Now, more information on the prothrombotic disorder has become available. The vaccine appears to be linked to a condition that clinically resembles heparin-induced thrombocytopenia (HIT) and that occurs mainly in younger women.
Researchers have described clinical and laboratory details of nine patients from Germany and Austria who developed this condition 4-16 days after receiving the AstraZeneca vaccine in a preprint article published March 28, 2021, on Research Square.
They found that serum from four patients who were tested showed platelet-activating antibodies directed against platelet factor 4 (PF4), similar to what is seen in HIT.
They are proposing naming the condition “vaccine-induced prothrombotic immune thrombocytopenia (VIPIT)” to avoid confusion with HIT.
At a press conference March 31, the EMA said its ongoing review of the situation “has not identified any specific risk factors, such as age, gender, or a previous medical history of clotting disorders, for these very rare events. A causal link with the vaccine is not proven but is possible, and further analysis is continuing.”
A statement from the agency noted: “EMA is of the view that the benefits of the AstraZeneca vaccine in preventing COVID-19, with its associated risk of hospitalization and death, outweigh the risks of side effects.”
But it added: “Vaccinated people should be aware of the remote possibility of these very rare types of blood clots occurring. If they have symptoms suggestive of clotting problems as described in the product information, they should seek immediate medical attention and inform health care professionals of their recent vaccination.”
VIPIT study
In the Research Square preprint article, a group led by Andreas Greinacher, MD, professor of transfusion medicine at the Greifswald (Germany) University Clinic, reported on clinical and laboratory features of nine patients (eight of whom were women) in Germany and Austria who developed thrombosis and thrombocytopenia after they received the AstraZeneca vaccine.
The researchers explained that they investigated whether these patients could have a prothrombotic disorder caused by platelet-activating antibodies directed against PF4, which is known to be caused by heparin and sometimes environmental triggers.
The nine patients were aged 22-49 years and presented with thrombosis beginning 4-16 days post vaccination. Seven patients had cerebral venous thrombosis (CVT), one had pulmonary embolism, and one had splanchnic vein thrombosis and CVT. Four patients died. None had received heparin prior to symptom onset.
Serum from four patients was tested for anti-PF4/heparin antibodies, and all four tested strongly positive. All four also tested strongly positive on platelet activation assay for the presence of PF4 independently of heparin.
The authors noted that it has been recognized that triggers other than heparin, including some infections, can rarely cause a disorder that strongly resembles HIT. These cases have been referred to as spontaneous HIT syndrome.
They said that their current findings have several important clinical implications.
“Clinicians should be aware that onset of (venous or arterial) thrombosis particularly at unusual sites such as in the brain or abdomen and thrombocytopenia beginning approximately 5-14 days after vaccination can represent a rare adverse effect of preceding COVID-19 vaccination,” they wrote. To date, this has only been reported with the AstraZeneca vaccine.
They pointed out that enzyme immunoassays for HIT are widely available and can be used to investigate for potential postvaccination anti-PF4 antibody–associated thrombocytopenia/thrombosis. For such patients, referral should be made to a laboratory that performs platelet-activation assays.
Although this syndrome differs from typical HIT, the researchers noted that at least one patient showed strong platelet activation in the presence of heparin. They thus recommended therapy with nonheparin anticoagulants, such as the direct oral anticoagulants.
They also wrote that high-dose intravenous immunoglobulin has been shown to be effective for treating severe HIT and could also be an important treatment adjunct for patients who develop life-threatening thrombotic events, such as cerebral vein sinus thrombosis (CVST), after being vaccinated.
EMA data to date
Updated data, reported at the EMA press briefing on March 31, indicate that 62 cases of CVST have been reported worldwide (44 from the European Union). These data may not yet include all the German cases.
Peter Arlett, MD, head of pharmacovigilance and epidemiology at the EMA, said there were more cases than expected in the 2-week window after vaccination among patients younger than 60 and that health care professionals should be alert to features of this condition, including headache and blurred vision.
He suggested that the higher rate of the condition among younger women may reflect the population that received this vaccine, because initially, the vaccine was not recommended for older people in many countries and was targeted toward younger health care workers, who were mainly women.
The German regulatory agency, the Paul Ehrlich Institute, reported this week that it has now registered 31 cases of CVST among nearly 2.7 million people who had received the vaccine in Germany. Of these patients, 19 also were found to have a deficiency of blood platelets or thrombocytopenia. Nine of the affected patients died. All but two of the cases occurred in women aged 20-63 years. The two men were aged 36 and 57 years.
These data have prompted the German authorities to limit use of the AstraZeneca vaccine to those aged 60 years and older. Even before this decision, senior clinicians in Germany had been urging a change in the vaccination recommendations.
For example, Bernd Salzberger, MD, head of infectious diseases, University Hospital Regensburg (Germany), told the Science Media Center: “In women, a complicated course of COVID disease is less common from the start and is so rare in younger women that the chance of avoiding a fatal course through vaccination in women without comorbidities is of the same order of magnitude as the risk of this rare side effect.”
Sandra Ciesek, MD, a virologist at Goethe University, Frankfurt, Germany, told the journal Science: “The argument I keep hearing is that the risk-benefit ratio is still positive. But we do not have just one vaccine, we have several. So, restricting the AstraZeneca vaccine to older people makes sense to me, and it does not waste any doses.”
Concerns put in perspective
Commenting of the latest developments, thrombosis expert Saskia Middeldorp, MD, head of internal medicine at Radboud University Medical Center, Nijmegen, the Netherlands, said it was vitally important that these concerns be put in perspective and that the vaccination program with the AstraZeneca product continue.
“There are some concerning reports about very rare blood clotting disorders and low platelet counts possibly associated with the AstraZeneca vaccine. Groups from Germany and Norway have identified a syndrome similar to HIT, which seems to explain the cause of this very rare side effect,” Dr. Middeldorp noted.
“But with such a high pressure from the virus and many countries now going into a third wave of infection, anything that might slow down vaccination rates will cause much more harm than good,” she warned.
Dr. Middeldorp believes the incidence of this HIT-type syndrome linked to the vaccine is about 1-2 per million. “These are estimates based on the number of reports of this side effect and denominators from the U.K. and EU populations,” she explained. However, Germany has restricted the vaccine on the basis of German data, which appear to show higher rates of the condition. It is not known why the rates are higher in Germany.
“The European Medicines Agency is looking at this very closely. Their statement is quite clear. There is no foundation for changing policy on vaccination,” Dr. Middeldorp stated.
She cautioned that these reports were reducing confidence in the AstraZeneca vaccine, particularly among young people, which she said was causing “a major setback” for the vaccination program.
Noting that everything must be viewed in the context of this severe pandemic, Dr. Middeldorp emphasized that the benefit of the vaccine outweighed any risk, even among young people.
“To those who may be hesitating to have the vaccine as they don’t think they are at high risk of severe COVID infection, I would say there are a lot of young people in the ICU at present with COVID, and your chance of a severe COVID illness is far higher than the 1 or 2 in a million risk of a severe reaction to the vaccine,” she stated.
Dr. Greinacher has received grants and nonfinancial support from Aspen, Boehringer Ingelheim, Merck Sharp & Dohme, Bristol-Myers Squibb, Paringenix, Bayer Healthcare, Gore, Rovi, Sagent, and Biomarin/Prosensa; personal fees from Aspen, Boehringer Ingelheim, Merck Sharp & Dohme, Macopharma, Bristol-Myers Squibb, Chromatec, and Instrumentation Laboratory; and nonfinancial support from Boehringer Ingelheim, Portola, Ergomed, and GTH outside the submitted work.
A version of this article first appeared on Medscape.com.
FDA okays new indication for alirocumab in homozygous FH
The Food and Drug Administration has approved alirocumab (Praluent, Regeneron Pharmaceuticals) injection as add-on therapy for adults with homozygous familial hypercholesterolemia, the agency announced.
The proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitor was originally approved in the United States in 2015 as an adjunct to diet, alone or in combination with other lipid-lowering therapies, to reduce LDL cholesterol in adults with primary hyperlipidemia, including heterozygous familial hypercholesterolemia (FH).
Heterozygous FH is one of the most common genetic disorders, affecting 1 in every 200-500 people worldwide, whereas homozygous FH is very rare, affecting about 1 in 1 million people worldwide.
Alirocumab is also approved to reduce the risk of myocardial infarction, stroke, and unstable angina requiring hospitalization in adults with cardiovascular disease.
The new indication is based on a 12-week randomized trial in 45 adults who received 150 mg alirocumab every 2 weeks and 24 patients who received placebo, both on top of other therapies to reduce LDL cholesterol. At week 12, patients receiving alirocumab had an average 27% decrease in LDL cholesterol, compared with an average 9% increase among patients on placebo.
Common side effects of alirocumab are nasopharyngitis, injection-site reactions, and influenza. Serious hypersensitivity reactions have occurred among people taking alirocumab.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved alirocumab (Praluent, Regeneron Pharmaceuticals) injection as add-on therapy for adults with homozygous familial hypercholesterolemia, the agency announced.
The proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitor was originally approved in the United States in 2015 as an adjunct to diet, alone or in combination with other lipid-lowering therapies, to reduce LDL cholesterol in adults with primary hyperlipidemia, including heterozygous familial hypercholesterolemia (FH).
Heterozygous FH is one of the most common genetic disorders, affecting 1 in every 200-500 people worldwide, whereas homozygous FH is very rare, affecting about 1 in 1 million people worldwide.
Alirocumab is also approved to reduce the risk of myocardial infarction, stroke, and unstable angina requiring hospitalization in adults with cardiovascular disease.
The new indication is based on a 12-week randomized trial in 45 adults who received 150 mg alirocumab every 2 weeks and 24 patients who received placebo, both on top of other therapies to reduce LDL cholesterol. At week 12, patients receiving alirocumab had an average 27% decrease in LDL cholesterol, compared with an average 9% increase among patients on placebo.
Common side effects of alirocumab are nasopharyngitis, injection-site reactions, and influenza. Serious hypersensitivity reactions have occurred among people taking alirocumab.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved alirocumab (Praluent, Regeneron Pharmaceuticals) injection as add-on therapy for adults with homozygous familial hypercholesterolemia, the agency announced.
The proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitor was originally approved in the United States in 2015 as an adjunct to diet, alone or in combination with other lipid-lowering therapies, to reduce LDL cholesterol in adults with primary hyperlipidemia, including heterozygous familial hypercholesterolemia (FH).
Heterozygous FH is one of the most common genetic disorders, affecting 1 in every 200-500 people worldwide, whereas homozygous FH is very rare, affecting about 1 in 1 million people worldwide.
Alirocumab is also approved to reduce the risk of myocardial infarction, stroke, and unstable angina requiring hospitalization in adults with cardiovascular disease.
The new indication is based on a 12-week randomized trial in 45 adults who received 150 mg alirocumab every 2 weeks and 24 patients who received placebo, both on top of other therapies to reduce LDL cholesterol. At week 12, patients receiving alirocumab had an average 27% decrease in LDL cholesterol, compared with an average 9% increase among patients on placebo.
Common side effects of alirocumab are nasopharyngitis, injection-site reactions, and influenza. Serious hypersensitivity reactions have occurred among people taking alirocumab.
A version of this article first appeared on Medscape.com.
The role of aspirin in primary prevention of cardiovascular disease
Background: Previous studies have shown that aspirin reduces the relative risk of cardiovascular disease (CVD) but also increases the relative risk of bleeding. It is unclear if there are patients without known CVD in whom the absolute risk reduction of CVD outweighs the absolute risk of bleeding. Prognostic CVD and bleeding risk models allow for an assessment of absolute risks and primary preventive interventions.
Study design: Individualized risk-benefit analysis based on sex-specific risk scores and estimates from PREDICT cohort data.
Setting: Primary care practices in New Zealand.
Synopsis: Using the New Zealand–based PREDICT online tool, 245,048 patients had their CVD risk assessed and did not meet exclusion criteria. The online tool predicts CVD events avoided and bleeding events caused by aspirin. When one CVD event was equivalent to one major bleeding event, 2.5% of women and 12.1% of men were classified as benefiting from aspirin (more CVD events avoided than bleeding events caused). When one CVD event was equivalent to two major bleeding events, 21.4% of women and 40.7% of men were classified as benefiting from aspirin. The net-benefit subgroups were older, and had higher baseline 5-year CVD risk, fewer risk factors for bleeding, higher systolic blood pressure, and a higher total cholesterol to HDL cholesterol ratio. Ethnicity and socioeconomic index also influenced benefit or harm.
With use of the upper and lower limits of 95% confidence intervals for models, there were considerable ranges of benefit versus harm. Sex-specific risk scores and meta-analysis have intrinsic uncertainties and results potentially not generalizable outside New Zealand population. Ultimate decision to use aspirin requires shared decision making.
Bottom line: Some patients are likely to derive a net benefit from aspirin for primary prevention of CVD. Risk-benefit models with online tools can help providers and patients estimate these factors to inform shared decision making.
Citation: Selak V et al. Personalized prediction of cardiovascular benefits and bleeding harms for aspirin for primary prevention, a benefit-harm analysis. Ann Intern Med. 2019;71(8):529-39.
Dr. Rupp is a hospitalist and clinical instructor of medicine at the University of Utah, Salt Lake City.
Background: Previous studies have shown that aspirin reduces the relative risk of cardiovascular disease (CVD) but also increases the relative risk of bleeding. It is unclear if there are patients without known CVD in whom the absolute risk reduction of CVD outweighs the absolute risk of bleeding. Prognostic CVD and bleeding risk models allow for an assessment of absolute risks and primary preventive interventions.
Study design: Individualized risk-benefit analysis based on sex-specific risk scores and estimates from PREDICT cohort data.
Setting: Primary care practices in New Zealand.
Synopsis: Using the New Zealand–based PREDICT online tool, 245,048 patients had their CVD risk assessed and did not meet exclusion criteria. The online tool predicts CVD events avoided and bleeding events caused by aspirin. When one CVD event was equivalent to one major bleeding event, 2.5% of women and 12.1% of men were classified as benefiting from aspirin (more CVD events avoided than bleeding events caused). When one CVD event was equivalent to two major bleeding events, 21.4% of women and 40.7% of men were classified as benefiting from aspirin. The net-benefit subgroups were older, and had higher baseline 5-year CVD risk, fewer risk factors for bleeding, higher systolic blood pressure, and a higher total cholesterol to HDL cholesterol ratio. Ethnicity and socioeconomic index also influenced benefit or harm.
With use of the upper and lower limits of 95% confidence intervals for models, there were considerable ranges of benefit versus harm. Sex-specific risk scores and meta-analysis have intrinsic uncertainties and results potentially not generalizable outside New Zealand population. Ultimate decision to use aspirin requires shared decision making.
Bottom line: Some patients are likely to derive a net benefit from aspirin for primary prevention of CVD. Risk-benefit models with online tools can help providers and patients estimate these factors to inform shared decision making.
Citation: Selak V et al. Personalized prediction of cardiovascular benefits and bleeding harms for aspirin for primary prevention, a benefit-harm analysis. Ann Intern Med. 2019;71(8):529-39.
Dr. Rupp is a hospitalist and clinical instructor of medicine at the University of Utah, Salt Lake City.
Background: Previous studies have shown that aspirin reduces the relative risk of cardiovascular disease (CVD) but also increases the relative risk of bleeding. It is unclear if there are patients without known CVD in whom the absolute risk reduction of CVD outweighs the absolute risk of bleeding. Prognostic CVD and bleeding risk models allow for an assessment of absolute risks and primary preventive interventions.
Study design: Individualized risk-benefit analysis based on sex-specific risk scores and estimates from PREDICT cohort data.
Setting: Primary care practices in New Zealand.
Synopsis: Using the New Zealand–based PREDICT online tool, 245,048 patients had their CVD risk assessed and did not meet exclusion criteria. The online tool predicts CVD events avoided and bleeding events caused by aspirin. When one CVD event was equivalent to one major bleeding event, 2.5% of women and 12.1% of men were classified as benefiting from aspirin (more CVD events avoided than bleeding events caused). When one CVD event was equivalent to two major bleeding events, 21.4% of women and 40.7% of men were classified as benefiting from aspirin. The net-benefit subgroups were older, and had higher baseline 5-year CVD risk, fewer risk factors for bleeding, higher systolic blood pressure, and a higher total cholesterol to HDL cholesterol ratio. Ethnicity and socioeconomic index also influenced benefit or harm.
With use of the upper and lower limits of 95% confidence intervals for models, there were considerable ranges of benefit versus harm. Sex-specific risk scores and meta-analysis have intrinsic uncertainties and results potentially not generalizable outside New Zealand population. Ultimate decision to use aspirin requires shared decision making.
Bottom line: Some patients are likely to derive a net benefit from aspirin for primary prevention of CVD. Risk-benefit models with online tools can help providers and patients estimate these factors to inform shared decision making.
Citation: Selak V et al. Personalized prediction of cardiovascular benefits and bleeding harms for aspirin for primary prevention, a benefit-harm analysis. Ann Intern Med. 2019;71(8):529-39.
Dr. Rupp is a hospitalist and clinical instructor of medicine at the University of Utah, Salt Lake City.
Detroit cardiologists prevail in retaliation suit against Tenet
After losing at arbitration, as well as in federal court and partially on appeal, Tenet Healthcare is refusing to comment on whether it will continue to battle two Detroit-area cardiologists whom the hospital corporation fired from leadership positions in 2018.
The cardiologists were awarded $10.6 million from an arbitrator, who found that Detroit Medical Center (DMC) and its parent, Tenet, retaliated against Amir Kaki, MD, and Mahir Elder, MD, when the doctors repeatedly reported concerns about patient safety and potential fraud.
The award was made public when it was upheld in federal court in February 2021 and was partially upheld on appeal days later by the Sixth Circuit Court of Appeals.
The Sixth Circuit Court of Appeals denied Tenet’s motion to bar Dr. Kaki and Dr. Elder from returning to work with full privileges but said it would continue to consider the overall appeal. Tenet argued that it needed to keep the cardiologists out of DMC because of “behavioral issues.”
Those allegations are “complete nonsense,” said the cardiologists’ attorney, Deborah Gordon, of Bloomfield Hills, Mich. The alleged problems regarding Dr. Kaki and Dr. Elder were examined by an arbitrator, who “found that all of those complaints were unsubstantiated,” Ms. Gordon said in an interview.
In her final ruling, arbitrator Mary Beth Kelly wrote, “Both Kaki and Elder testified credibly regarding the humiliation, the emotional distress and the reputational damage they have suffered to their national reputations.”
A spokesperson for Tenet and DMC said the organizations had no further comment.
Ms. Gordon said she believes it’s unlikely Tenet will prevail in the Sixth Circuit Court of Appeals, noting that the court already had examined the merits of the case to determine whether Dr. Kaki and Dr. Elder could go back to work. In the court’s opinion, shared in an interview, nothing substantive in Tenet’s appeal prevented the doctors from returning to the hospital, she said.
As of now, both cardiologists have 1 year of privileges at the DMC-affiliated hospitals. Only Dr. Kaki has returned to work, said Ms. Gordon. Neither is speaking to the media, she said.
From respected to reviled
Both Dr. Kaki and Dr. Elder were respected at DMC, according to court filings.
Dr. Kaki was recruited from Weill Cornell Medical College by a Detroit mayor because of his expertise in interventional cardiology. He had staff privileges at DMC beginning in 2012 and was a clinical associate professor and assistant program director of the interventional cardiology fellowship program at Wayne State University in Detroit. He became director of the cardiac catheterization services unit at the new DMC Heart Hospital at Harper-Hutzel Hospital in Detroit in 2014, and 4 years later was appointed director of the facility’s anticoagulation clinic. Dr. Kaki was nominated for and completed Tenet’s Leadership Academy.
Dr. Elder was a clinical professor and assistant fellowship director at Wayne State and was a clinical professor of medicine at Michigan State University. Beginning in 2008, he held directorships at DMC’s cardiac care unit, ambulatory services program, cardiac CT angiogram program, PERT program, and carotid stenting program. Dr. Elder was voted Teacher of the Year for 10 consecutive years by DMC cardiology fellows.
The two doctors aimed high when it came to quality of care and ethics, according to legal filings. Over the years, Dr. Kaki and Dr. Elder repeatedly reported what they considered to be egregious violations of patient safety and of Medicare and Medicaid fraud laws. The clinicians complained about unsterile surgical instruments and the removal of a stat laboratory from the cardiac catheterization unit, noting that the removal would cause delays that would endanger lives.
At peer review meetings, as well as with administrators, they flagged colleagues who they said were performing unnecessary or dangerous procedures solely to generate revenue. At least one doctor falsified records of such a procedure after a patient died, alleged Dr. Kaki and Dr. Elder.
Tenet hired outside attorneys in the fall of 2018, telling Dr. Kaki and Dr. Elder that the legal team would investigate their complaints. However, the investigation was a sham: Filings allege that the investigation was used instead to build a case against Dr. Kaki and Dr. Elder and that Tenet leadership used the inquiry to pressure the cardiologists to resign.
They refused, and in October 2018, they were fired from their leadership positions. DMC and Tenet then held a press conference in which they said that Dr. Kaki and Dr. Elder had been dismissed for “violations” of the “Tenet Standards of Conduct.”
Cardiologists push back
Dr. Kaki and Dr. Elder, however, were not willing to just walk away. They sought reinstatement through an internal DMC appeals panel of their peers. The clinicians who participated on that panel ruled that neither firing was justified.
But DMC’s governing board voted in April 2020 to deny privileges to both cardiologists.
Tenet continued a campaign of retaliation, according to legal filings, by not paying the clinicians for being on call, by removing them from peer review committees, and by prohibiting them from teaching or giving lectures. DMC refused to give Dr. Kaki his personnel record, stating that he was never an employee when he was in the leadership position. Dr. Kaki sued, and a Wayne County Circuit Court judge granted his motion to get his file. DMC and Tenet appealed that ruling but lost.
Eventually, Ms. Gordon sued DMC and Tenet in federal court, alleging the hospital retaliated against the cardiologists, interfered with their ability to earn a living by disparaging them, refused to renew their privileges in 2019, and committed violations under multiple federal and state statutes, including the False Claims Act and the Fair Labor Standards Act.
Tenet successfully argued that the case should go to arbitration.
Arbitrator Mary Beth Kelly, though, ruled in December 2020 that the vast majority of the complaints compiled against the two physicians in the external investigation were not verified or supported and that Tenet and DMC had retaliated against Dr. Kaki and Dr. Elder.
For that harm, Ms. Kelly awarded each clinician $1 million, according to the final ruling shared in an interview.
In addition, she awarded Dr. Kaki $2.3 million in back pay and 2 years of front pay (slightly more than $1 million). She awarded Dr. Elder $2.3 million in back pay and $2.1 million in front pay for 4 years, noting that “his strong association with DMC may make it more difficult for him to successfully transition into the situation he enjoyed prior to termination and nonrenewal.”
The clinicians also were awarded legal fees of $623,816 and court costs of $110,673.
“Wholesale retrial”
To secure the award, Ms. Gordon had to seek a ruling from the U.S. District Court for Eastern Michigan. Tenet asked that court to overturn the arbitrator’s award and to keep it sealed from public view.
In his February ruling, Judge Arthur J. Tarnow wrote that Tenet and DMC “not only attempt to relitigate the legal issues, but also endeavor to introduce a factual counternarrative unmoored from the findings of the Arbitrator and including evidence which the Arbitrator specifically found inadmissible.
“By seeking a wholesale retrial of their case after forcing plaintiffs to arbitrate in the first place,” Tenet and DMC basically ignored the goal of arbitration, which is to relieve judicial congestion and provide a faster and cheaper alternative to litigation, he wrote.
Judge Tarnow also warned Tenet and DMC against taking too long to reinstate privileges for Dr. Kaki and Dr. Elder. If they “continue to delay the restoration of plaintiffs’ privileges in the hopes of a different result on appeal, they will be in violation of this Order,” said the judge.
Tenet, however, tried one more avenue to block the cardiologists from getting privileges, appealing to the Sixth Circuit, which again ordered the company to grant the 1-year privileges.
A version of this article first appeared on Medscape.com.
After losing at arbitration, as well as in federal court and partially on appeal, Tenet Healthcare is refusing to comment on whether it will continue to battle two Detroit-area cardiologists whom the hospital corporation fired from leadership positions in 2018.
The cardiologists were awarded $10.6 million from an arbitrator, who found that Detroit Medical Center (DMC) and its parent, Tenet, retaliated against Amir Kaki, MD, and Mahir Elder, MD, when the doctors repeatedly reported concerns about patient safety and potential fraud.
The award was made public when it was upheld in federal court in February 2021 and was partially upheld on appeal days later by the Sixth Circuit Court of Appeals.
The Sixth Circuit Court of Appeals denied Tenet’s motion to bar Dr. Kaki and Dr. Elder from returning to work with full privileges but said it would continue to consider the overall appeal. Tenet argued that it needed to keep the cardiologists out of DMC because of “behavioral issues.”
Those allegations are “complete nonsense,” said the cardiologists’ attorney, Deborah Gordon, of Bloomfield Hills, Mich. The alleged problems regarding Dr. Kaki and Dr. Elder were examined by an arbitrator, who “found that all of those complaints were unsubstantiated,” Ms. Gordon said in an interview.
In her final ruling, arbitrator Mary Beth Kelly wrote, “Both Kaki and Elder testified credibly regarding the humiliation, the emotional distress and the reputational damage they have suffered to their national reputations.”
A spokesperson for Tenet and DMC said the organizations had no further comment.
Ms. Gordon said she believes it’s unlikely Tenet will prevail in the Sixth Circuit Court of Appeals, noting that the court already had examined the merits of the case to determine whether Dr. Kaki and Dr. Elder could go back to work. In the court’s opinion, shared in an interview, nothing substantive in Tenet’s appeal prevented the doctors from returning to the hospital, she said.
As of now, both cardiologists have 1 year of privileges at the DMC-affiliated hospitals. Only Dr. Kaki has returned to work, said Ms. Gordon. Neither is speaking to the media, she said.
From respected to reviled
Both Dr. Kaki and Dr. Elder were respected at DMC, according to court filings.
Dr. Kaki was recruited from Weill Cornell Medical College by a Detroit mayor because of his expertise in interventional cardiology. He had staff privileges at DMC beginning in 2012 and was a clinical associate professor and assistant program director of the interventional cardiology fellowship program at Wayne State University in Detroit. He became director of the cardiac catheterization services unit at the new DMC Heart Hospital at Harper-Hutzel Hospital in Detroit in 2014, and 4 years later was appointed director of the facility’s anticoagulation clinic. Dr. Kaki was nominated for and completed Tenet’s Leadership Academy.
Dr. Elder was a clinical professor and assistant fellowship director at Wayne State and was a clinical professor of medicine at Michigan State University. Beginning in 2008, he held directorships at DMC’s cardiac care unit, ambulatory services program, cardiac CT angiogram program, PERT program, and carotid stenting program. Dr. Elder was voted Teacher of the Year for 10 consecutive years by DMC cardiology fellows.
The two doctors aimed high when it came to quality of care and ethics, according to legal filings. Over the years, Dr. Kaki and Dr. Elder repeatedly reported what they considered to be egregious violations of patient safety and of Medicare and Medicaid fraud laws. The clinicians complained about unsterile surgical instruments and the removal of a stat laboratory from the cardiac catheterization unit, noting that the removal would cause delays that would endanger lives.
At peer review meetings, as well as with administrators, they flagged colleagues who they said were performing unnecessary or dangerous procedures solely to generate revenue. At least one doctor falsified records of such a procedure after a patient died, alleged Dr. Kaki and Dr. Elder.
Tenet hired outside attorneys in the fall of 2018, telling Dr. Kaki and Dr. Elder that the legal team would investigate their complaints. However, the investigation was a sham: Filings allege that the investigation was used instead to build a case against Dr. Kaki and Dr. Elder and that Tenet leadership used the inquiry to pressure the cardiologists to resign.
They refused, and in October 2018, they were fired from their leadership positions. DMC and Tenet then held a press conference in which they said that Dr. Kaki and Dr. Elder had been dismissed for “violations” of the “Tenet Standards of Conduct.”
Cardiologists push back
Dr. Kaki and Dr. Elder, however, were not willing to just walk away. They sought reinstatement through an internal DMC appeals panel of their peers. The clinicians who participated on that panel ruled that neither firing was justified.
But DMC’s governing board voted in April 2020 to deny privileges to both cardiologists.
Tenet continued a campaign of retaliation, according to legal filings, by not paying the clinicians for being on call, by removing them from peer review committees, and by prohibiting them from teaching or giving lectures. DMC refused to give Dr. Kaki his personnel record, stating that he was never an employee when he was in the leadership position. Dr. Kaki sued, and a Wayne County Circuit Court judge granted his motion to get his file. DMC and Tenet appealed that ruling but lost.
Eventually, Ms. Gordon sued DMC and Tenet in federal court, alleging the hospital retaliated against the cardiologists, interfered with their ability to earn a living by disparaging them, refused to renew their privileges in 2019, and committed violations under multiple federal and state statutes, including the False Claims Act and the Fair Labor Standards Act.
Tenet successfully argued that the case should go to arbitration.
Arbitrator Mary Beth Kelly, though, ruled in December 2020 that the vast majority of the complaints compiled against the two physicians in the external investigation were not verified or supported and that Tenet and DMC had retaliated against Dr. Kaki and Dr. Elder.
For that harm, Ms. Kelly awarded each clinician $1 million, according to the final ruling shared in an interview.
In addition, she awarded Dr. Kaki $2.3 million in back pay and 2 years of front pay (slightly more than $1 million). She awarded Dr. Elder $2.3 million in back pay and $2.1 million in front pay for 4 years, noting that “his strong association with DMC may make it more difficult for him to successfully transition into the situation he enjoyed prior to termination and nonrenewal.”
The clinicians also were awarded legal fees of $623,816 and court costs of $110,673.
“Wholesale retrial”
To secure the award, Ms. Gordon had to seek a ruling from the U.S. District Court for Eastern Michigan. Tenet asked that court to overturn the arbitrator’s award and to keep it sealed from public view.
In his February ruling, Judge Arthur J. Tarnow wrote that Tenet and DMC “not only attempt to relitigate the legal issues, but also endeavor to introduce a factual counternarrative unmoored from the findings of the Arbitrator and including evidence which the Arbitrator specifically found inadmissible.
“By seeking a wholesale retrial of their case after forcing plaintiffs to arbitrate in the first place,” Tenet and DMC basically ignored the goal of arbitration, which is to relieve judicial congestion and provide a faster and cheaper alternative to litigation, he wrote.
Judge Tarnow also warned Tenet and DMC against taking too long to reinstate privileges for Dr. Kaki and Dr. Elder. If they “continue to delay the restoration of plaintiffs’ privileges in the hopes of a different result on appeal, they will be in violation of this Order,” said the judge.
Tenet, however, tried one more avenue to block the cardiologists from getting privileges, appealing to the Sixth Circuit, which again ordered the company to grant the 1-year privileges.
A version of this article first appeared on Medscape.com.
After losing at arbitration, as well as in federal court and partially on appeal, Tenet Healthcare is refusing to comment on whether it will continue to battle two Detroit-area cardiologists whom the hospital corporation fired from leadership positions in 2018.
The cardiologists were awarded $10.6 million from an arbitrator, who found that Detroit Medical Center (DMC) and its parent, Tenet, retaliated against Amir Kaki, MD, and Mahir Elder, MD, when the doctors repeatedly reported concerns about patient safety and potential fraud.
The award was made public when it was upheld in federal court in February 2021 and was partially upheld on appeal days later by the Sixth Circuit Court of Appeals.
The Sixth Circuit Court of Appeals denied Tenet’s motion to bar Dr. Kaki and Dr. Elder from returning to work with full privileges but said it would continue to consider the overall appeal. Tenet argued that it needed to keep the cardiologists out of DMC because of “behavioral issues.”
Those allegations are “complete nonsense,” said the cardiologists’ attorney, Deborah Gordon, of Bloomfield Hills, Mich. The alleged problems regarding Dr. Kaki and Dr. Elder were examined by an arbitrator, who “found that all of those complaints were unsubstantiated,” Ms. Gordon said in an interview.
In her final ruling, arbitrator Mary Beth Kelly wrote, “Both Kaki and Elder testified credibly regarding the humiliation, the emotional distress and the reputational damage they have suffered to their national reputations.”
A spokesperson for Tenet and DMC said the organizations had no further comment.
Ms. Gordon said she believes it’s unlikely Tenet will prevail in the Sixth Circuit Court of Appeals, noting that the court already had examined the merits of the case to determine whether Dr. Kaki and Dr. Elder could go back to work. In the court’s opinion, shared in an interview, nothing substantive in Tenet’s appeal prevented the doctors from returning to the hospital, she said.
As of now, both cardiologists have 1 year of privileges at the DMC-affiliated hospitals. Only Dr. Kaki has returned to work, said Ms. Gordon. Neither is speaking to the media, she said.
From respected to reviled
Both Dr. Kaki and Dr. Elder were respected at DMC, according to court filings.
Dr. Kaki was recruited from Weill Cornell Medical College by a Detroit mayor because of his expertise in interventional cardiology. He had staff privileges at DMC beginning in 2012 and was a clinical associate professor and assistant program director of the interventional cardiology fellowship program at Wayne State University in Detroit. He became director of the cardiac catheterization services unit at the new DMC Heart Hospital at Harper-Hutzel Hospital in Detroit in 2014, and 4 years later was appointed director of the facility’s anticoagulation clinic. Dr. Kaki was nominated for and completed Tenet’s Leadership Academy.
Dr. Elder was a clinical professor and assistant fellowship director at Wayne State and was a clinical professor of medicine at Michigan State University. Beginning in 2008, he held directorships at DMC’s cardiac care unit, ambulatory services program, cardiac CT angiogram program, PERT program, and carotid stenting program. Dr. Elder was voted Teacher of the Year for 10 consecutive years by DMC cardiology fellows.
The two doctors aimed high when it came to quality of care and ethics, according to legal filings. Over the years, Dr. Kaki and Dr. Elder repeatedly reported what they considered to be egregious violations of patient safety and of Medicare and Medicaid fraud laws. The clinicians complained about unsterile surgical instruments and the removal of a stat laboratory from the cardiac catheterization unit, noting that the removal would cause delays that would endanger lives.
At peer review meetings, as well as with administrators, they flagged colleagues who they said were performing unnecessary or dangerous procedures solely to generate revenue. At least one doctor falsified records of such a procedure after a patient died, alleged Dr. Kaki and Dr. Elder.
Tenet hired outside attorneys in the fall of 2018, telling Dr. Kaki and Dr. Elder that the legal team would investigate their complaints. However, the investigation was a sham: Filings allege that the investigation was used instead to build a case against Dr. Kaki and Dr. Elder and that Tenet leadership used the inquiry to pressure the cardiologists to resign.
They refused, and in October 2018, they were fired from their leadership positions. DMC and Tenet then held a press conference in which they said that Dr. Kaki and Dr. Elder had been dismissed for “violations” of the “Tenet Standards of Conduct.”
Cardiologists push back
Dr. Kaki and Dr. Elder, however, were not willing to just walk away. They sought reinstatement through an internal DMC appeals panel of their peers. The clinicians who participated on that panel ruled that neither firing was justified.
But DMC’s governing board voted in April 2020 to deny privileges to both cardiologists.
Tenet continued a campaign of retaliation, according to legal filings, by not paying the clinicians for being on call, by removing them from peer review committees, and by prohibiting them from teaching or giving lectures. DMC refused to give Dr. Kaki his personnel record, stating that he was never an employee when he was in the leadership position. Dr. Kaki sued, and a Wayne County Circuit Court judge granted his motion to get his file. DMC and Tenet appealed that ruling but lost.
Eventually, Ms. Gordon sued DMC and Tenet in federal court, alleging the hospital retaliated against the cardiologists, interfered with their ability to earn a living by disparaging them, refused to renew their privileges in 2019, and committed violations under multiple federal and state statutes, including the False Claims Act and the Fair Labor Standards Act.
Tenet successfully argued that the case should go to arbitration.
Arbitrator Mary Beth Kelly, though, ruled in December 2020 that the vast majority of the complaints compiled against the two physicians in the external investigation were not verified or supported and that Tenet and DMC had retaliated against Dr. Kaki and Dr. Elder.
For that harm, Ms. Kelly awarded each clinician $1 million, according to the final ruling shared in an interview.
In addition, she awarded Dr. Kaki $2.3 million in back pay and 2 years of front pay (slightly more than $1 million). She awarded Dr. Elder $2.3 million in back pay and $2.1 million in front pay for 4 years, noting that “his strong association with DMC may make it more difficult for him to successfully transition into the situation he enjoyed prior to termination and nonrenewal.”
The clinicians also were awarded legal fees of $623,816 and court costs of $110,673.
“Wholesale retrial”
To secure the award, Ms. Gordon had to seek a ruling from the U.S. District Court for Eastern Michigan. Tenet asked that court to overturn the arbitrator’s award and to keep it sealed from public view.
In his February ruling, Judge Arthur J. Tarnow wrote that Tenet and DMC “not only attempt to relitigate the legal issues, but also endeavor to introduce a factual counternarrative unmoored from the findings of the Arbitrator and including evidence which the Arbitrator specifically found inadmissible.
“By seeking a wholesale retrial of their case after forcing plaintiffs to arbitrate in the first place,” Tenet and DMC basically ignored the goal of arbitration, which is to relieve judicial congestion and provide a faster and cheaper alternative to litigation, he wrote.
Judge Tarnow also warned Tenet and DMC against taking too long to reinstate privileges for Dr. Kaki and Dr. Elder. If they “continue to delay the restoration of plaintiffs’ privileges in the hopes of a different result on appeal, they will be in violation of this Order,” said the judge.
Tenet, however, tried one more avenue to block the cardiologists from getting privileges, appealing to the Sixth Circuit, which again ordered the company to grant the 1-year privileges.
A version of this article first appeared on Medscape.com.
Meta-analysis supports late thrombectomy in selected stroke patients
of data from six clinical trials.
Results of the AURORA analysis showed that for every 100 patients treated with thrombectomy, 33 patients will have less disability, and 27 patients will achieve an independent level of functioning compared with patients who receive only standard medical care.
The benefit of mechanical removal of the clot for selected patients who may have salvageable brain tissue, as identified through the use of various imaging modalities, was maintained whether the patient had a “wake-up stroke” or the onset of symptoms was witnessed, regardless of the point in time within the late window. In fact, the benefit of intervention was greater for patients who presented in the latter part of the late time window.
Never too late for urgent medical care
“While the findings of this analysis do not contradict the mantra that the earlier treatment is instituted, the higher the chance of a good outcome, they highlight the fact that it is never too late to seek urgent medical care,” said lead investigator Tudor Jovin, MD, chair of neurology at Cooper University Hospital, Cherry Hill, New Jersey.
“The implications of the findings from AURORA are that they could lead to a change in guidelines from endorsement of thrombectomy as level 1a recommendation in eligible patients presenting in the 6- to 16-hour time window to a 6- to 24-hour time window,” said Dr. Jovin.
“Furthermore, there are strong signals of benefit of thrombectomy in patients who are not selected based on volumetric analysis of baseline infarct (core) or extent of tissue at risk (penumbra), such that when those imaging modalities are not available or contraindicated, selection based on noncontrast CT and clinical information only may be acceptable,” he added. “Finally, the possibility of benefit from thrombectomy performed beyond 24 hours from last seen well is real and should be explored in future studies.”
The AURORA findings were presented at the virtual International Stroke Conference (ISC) 2021.
The objective of the study was to provide a more precise estimate of the benefit of thrombectomy for patients with stroke when performed within 6-24 hours after the patient was last seen well, Dr. Jovin explained.
He said the 6-hour cutoff was chosen somewhat arbitrarily, but added, “It is highly consequential, as it marks the point of demarcation between the early and late time window, and virtually all guidelines recommend different approaches, dependent on whether patients present before or after 6 hours from symptom onset.”
The 6+ hour window
Dr. Jovin pointed out that for patients who present beyond 6 hours, treatment options are more restricted, because the data on thrombectomy in this later period come mainly from two North American trials (DEFUSE 3 and DAWN) that had very stringent imaging criteria for enrollment.
“We wanted to create a heterogeneous dataset with regard to geography and selection criteria by forming the AURORA collaboration,” he commented. Their study involved an individual-level pooled analysis of all patients who underwent randomization after 6 hours from the time that they were last seen well. Patients were randomly assigned to receive either best medical therapy alone or best medical therapy plus thrombectomy (either with stent retrievers or aspiration) for anterior circulation proximal large-vessel occlusion stroke.
The data came from six trials: DAWN (which enrolled patients 6-24 hours from stroke onset), DEFUSE 3 (6-16 hours), ESCAPE (0-12 hours), REVASCAT (0-8 hours), RESILIENT (0-8 hours), and POSITIVE (0-12 hours). In total, 505 patients were included in the meta-analysis, 266 in the intervention group, and 239 in the control group.
“By pooling data on patients presenting after 6 hours from all these trails, we achieve greater precision for treatment effect estimation and increased the power for subgroup analysis,” Dr. Jovin noted.
Although the majority of the patients were in the DAWN and DIFFUSE 3 trials (n = 388), “there are still a good number from the other four trials (n = 117),” Dr. Jovin reported.
Most of the trials used Modified Rankin Scale (mRS) ordinal or shift analysis as their primary endpoint, which was the also the endpoint chosen for this meta-analysis.
Imaging selection criteria ranged from fully automated software-generated quantitative volumetric analysis of baseline infarct (core) or tissue at risk to CT perfusion and plain CT/CTA. The minimum ASPECTS score was 5 or 6.
There were no imbalances in baseline characteristics. The median NIH Stroke Scale score was 16, and the median ASPECTS score was 8. The median time to randomization was 10.5 hours.
With regard to safety, there was no significant difference in rates of symptomatic intracerebral hemorrhage (5.3% in the intervention group vs. 3.3% in the control group; P = .23) or in mortality at 90 days (16.5% vs. 19.3%; P = .87). Jovin noted that these results are very similar to those from the HERMES meta-analysis of patients treated in the early time window.
The primary outcome – ordinal analysis of the mRS distribution – showed an adjusted odds ratio of 2.54 (P < .0001) for benefit in the intervention group. The number needed to treat to reduce disability was 3. “This is again very similar to the HERMES meta-analysis of patients in the early window,” Dr. Jovin said.
The P value for heterogeneity of treatment effect across the six studies was nonsignificant.
Secondary outcome analysis showed an “almost 27%” difference in good functional outcome (MRS, 0-2) between the two groups (45.9% in the intervention group vs. 19.3% in the control group), which translates into a number needed to treat of 3.8, Dr. Jovin reported.
Subgroup analysis showed a treatment effect favoring intervention across all prespecified subgroup factors, including age, sex, occlusion location, mode of presentation (wake-up vs. witnessed), and ASPECTS score, with the caveat that most of the patients were enrolled with ASPECTS scores of 7 or greater.
Early versus late
Surprisingly, although thrombectomy was found to be beneficial in both the 6- to 12-hour and 12- to 24-hour time window, the magnitude of benefit was significantly higher in the later rather than the earlier time window. The odds ratio of a better outcome with thrombectomy on the mRS shift analysis in those presenting in the 6- to 12-hour period was 1.78, compared with 5.86 in the 12- to 24-hour time window.
“This should not be interpreted as a higher chance of a good outcome if treated late. In fact, the rate of good outcomes were numerically higher in the earlier treated patients, but the difference comes from the control group, which did much worse in patients randomized in the later time period,” Dr. Jovin said.
“Aurora was the goddess of dawn [in ancient Roman mythology], so this is a very fitting name, as it reminds us that we are in the dawn of a new era where patients are selected based on physiological data rather than on time, and we certainly hope that this work has brought us closer to this reality,” Dr. Jovin concluded.
Commenting on the study, Michael Hill, MD, University of Calgary (Alta.), said: “The work provides pooled empiric data to support the concept that time to treatment is no longer the sole threshold variable to be used in treatment decision-making. Instead, time is now simply another variable to consider in the context of clinical and imaging factors.”
Dr. Hill, who headed up the ESCAPE trial and was also involved in the current meta-analysis, added: “This meta-analysis supports the concept of patient selection using the ‘good scan’ model, rather than using a time-based concept of patient eligibility for endovascular therapy. It will further push changes in care, because the implication is that all patients with more severe acute stroke presentations need emergency neurovascular imaging to decide if they are eligible for treatment.”
The AURORA meta-analysis was funded by Stryker Neurovascular. Dr. Jovin reports stock holdings in Anaconda, Route 92, VizAi, FreeOx, Blockade Medical, Methinks, and Corindus; personal fees from Cerenovus and Contego Medical; travel support from Fundacio Ictus; and grant support from Medtronic and Stryker Neurovascular.
A version of this article first appeared on Medscape.com.
of data from six clinical trials.
Results of the AURORA analysis showed that for every 100 patients treated with thrombectomy, 33 patients will have less disability, and 27 patients will achieve an independent level of functioning compared with patients who receive only standard medical care.
The benefit of mechanical removal of the clot for selected patients who may have salvageable brain tissue, as identified through the use of various imaging modalities, was maintained whether the patient had a “wake-up stroke” or the onset of symptoms was witnessed, regardless of the point in time within the late window. In fact, the benefit of intervention was greater for patients who presented in the latter part of the late time window.
Never too late for urgent medical care
“While the findings of this analysis do not contradict the mantra that the earlier treatment is instituted, the higher the chance of a good outcome, they highlight the fact that it is never too late to seek urgent medical care,” said lead investigator Tudor Jovin, MD, chair of neurology at Cooper University Hospital, Cherry Hill, New Jersey.
“The implications of the findings from AURORA are that they could lead to a change in guidelines from endorsement of thrombectomy as level 1a recommendation in eligible patients presenting in the 6- to 16-hour time window to a 6- to 24-hour time window,” said Dr. Jovin.
“Furthermore, there are strong signals of benefit of thrombectomy in patients who are not selected based on volumetric analysis of baseline infarct (core) or extent of tissue at risk (penumbra), such that when those imaging modalities are not available or contraindicated, selection based on noncontrast CT and clinical information only may be acceptable,” he added. “Finally, the possibility of benefit from thrombectomy performed beyond 24 hours from last seen well is real and should be explored in future studies.”
The AURORA findings were presented at the virtual International Stroke Conference (ISC) 2021.
The objective of the study was to provide a more precise estimate of the benefit of thrombectomy for patients with stroke when performed within 6-24 hours after the patient was last seen well, Dr. Jovin explained.
He said the 6-hour cutoff was chosen somewhat arbitrarily, but added, “It is highly consequential, as it marks the point of demarcation between the early and late time window, and virtually all guidelines recommend different approaches, dependent on whether patients present before or after 6 hours from symptom onset.”
The 6+ hour window
Dr. Jovin pointed out that for patients who present beyond 6 hours, treatment options are more restricted, because the data on thrombectomy in this later period come mainly from two North American trials (DEFUSE 3 and DAWN) that had very stringent imaging criteria for enrollment.
“We wanted to create a heterogeneous dataset with regard to geography and selection criteria by forming the AURORA collaboration,” he commented. Their study involved an individual-level pooled analysis of all patients who underwent randomization after 6 hours from the time that they were last seen well. Patients were randomly assigned to receive either best medical therapy alone or best medical therapy plus thrombectomy (either with stent retrievers or aspiration) for anterior circulation proximal large-vessel occlusion stroke.
The data came from six trials: DAWN (which enrolled patients 6-24 hours from stroke onset), DEFUSE 3 (6-16 hours), ESCAPE (0-12 hours), REVASCAT (0-8 hours), RESILIENT (0-8 hours), and POSITIVE (0-12 hours). In total, 505 patients were included in the meta-analysis, 266 in the intervention group, and 239 in the control group.
“By pooling data on patients presenting after 6 hours from all these trails, we achieve greater precision for treatment effect estimation and increased the power for subgroup analysis,” Dr. Jovin noted.
Although the majority of the patients were in the DAWN and DIFFUSE 3 trials (n = 388), “there are still a good number from the other four trials (n = 117),” Dr. Jovin reported.
Most of the trials used Modified Rankin Scale (mRS) ordinal or shift analysis as their primary endpoint, which was the also the endpoint chosen for this meta-analysis.
Imaging selection criteria ranged from fully automated software-generated quantitative volumetric analysis of baseline infarct (core) or tissue at risk to CT perfusion and plain CT/CTA. The minimum ASPECTS score was 5 or 6.
There were no imbalances in baseline characteristics. The median NIH Stroke Scale score was 16, and the median ASPECTS score was 8. The median time to randomization was 10.5 hours.
With regard to safety, there was no significant difference in rates of symptomatic intracerebral hemorrhage (5.3% in the intervention group vs. 3.3% in the control group; P = .23) or in mortality at 90 days (16.5% vs. 19.3%; P = .87). Jovin noted that these results are very similar to those from the HERMES meta-analysis of patients treated in the early time window.
The primary outcome – ordinal analysis of the mRS distribution – showed an adjusted odds ratio of 2.54 (P < .0001) for benefit in the intervention group. The number needed to treat to reduce disability was 3. “This is again very similar to the HERMES meta-analysis of patients in the early window,” Dr. Jovin said.
The P value for heterogeneity of treatment effect across the six studies was nonsignificant.
Secondary outcome analysis showed an “almost 27%” difference in good functional outcome (MRS, 0-2) between the two groups (45.9% in the intervention group vs. 19.3% in the control group), which translates into a number needed to treat of 3.8, Dr. Jovin reported.
Subgroup analysis showed a treatment effect favoring intervention across all prespecified subgroup factors, including age, sex, occlusion location, mode of presentation (wake-up vs. witnessed), and ASPECTS score, with the caveat that most of the patients were enrolled with ASPECTS scores of 7 or greater.
Early versus late
Surprisingly, although thrombectomy was found to be beneficial in both the 6- to 12-hour and 12- to 24-hour time window, the magnitude of benefit was significantly higher in the later rather than the earlier time window. The odds ratio of a better outcome with thrombectomy on the mRS shift analysis in those presenting in the 6- to 12-hour period was 1.78, compared with 5.86 in the 12- to 24-hour time window.
“This should not be interpreted as a higher chance of a good outcome if treated late. In fact, the rate of good outcomes were numerically higher in the earlier treated patients, but the difference comes from the control group, which did much worse in patients randomized in the later time period,” Dr. Jovin said.
“Aurora was the goddess of dawn [in ancient Roman mythology], so this is a very fitting name, as it reminds us that we are in the dawn of a new era where patients are selected based on physiological data rather than on time, and we certainly hope that this work has brought us closer to this reality,” Dr. Jovin concluded.
Commenting on the study, Michael Hill, MD, University of Calgary (Alta.), said: “The work provides pooled empiric data to support the concept that time to treatment is no longer the sole threshold variable to be used in treatment decision-making. Instead, time is now simply another variable to consider in the context of clinical and imaging factors.”
Dr. Hill, who headed up the ESCAPE trial and was also involved in the current meta-analysis, added: “This meta-analysis supports the concept of patient selection using the ‘good scan’ model, rather than using a time-based concept of patient eligibility for endovascular therapy. It will further push changes in care, because the implication is that all patients with more severe acute stroke presentations need emergency neurovascular imaging to decide if they are eligible for treatment.”
The AURORA meta-analysis was funded by Stryker Neurovascular. Dr. Jovin reports stock holdings in Anaconda, Route 92, VizAi, FreeOx, Blockade Medical, Methinks, and Corindus; personal fees from Cerenovus and Contego Medical; travel support from Fundacio Ictus; and grant support from Medtronic and Stryker Neurovascular.
A version of this article first appeared on Medscape.com.
of data from six clinical trials.
Results of the AURORA analysis showed that for every 100 patients treated with thrombectomy, 33 patients will have less disability, and 27 patients will achieve an independent level of functioning compared with patients who receive only standard medical care.
The benefit of mechanical removal of the clot for selected patients who may have salvageable brain tissue, as identified through the use of various imaging modalities, was maintained whether the patient had a “wake-up stroke” or the onset of symptoms was witnessed, regardless of the point in time within the late window. In fact, the benefit of intervention was greater for patients who presented in the latter part of the late time window.
Never too late for urgent medical care
“While the findings of this analysis do not contradict the mantra that the earlier treatment is instituted, the higher the chance of a good outcome, they highlight the fact that it is never too late to seek urgent medical care,” said lead investigator Tudor Jovin, MD, chair of neurology at Cooper University Hospital, Cherry Hill, New Jersey.
“The implications of the findings from AURORA are that they could lead to a change in guidelines from endorsement of thrombectomy as level 1a recommendation in eligible patients presenting in the 6- to 16-hour time window to a 6- to 24-hour time window,” said Dr. Jovin.
“Furthermore, there are strong signals of benefit of thrombectomy in patients who are not selected based on volumetric analysis of baseline infarct (core) or extent of tissue at risk (penumbra), such that when those imaging modalities are not available or contraindicated, selection based on noncontrast CT and clinical information only may be acceptable,” he added. “Finally, the possibility of benefit from thrombectomy performed beyond 24 hours from last seen well is real and should be explored in future studies.”
The AURORA findings were presented at the virtual International Stroke Conference (ISC) 2021.
The objective of the study was to provide a more precise estimate of the benefit of thrombectomy for patients with stroke when performed within 6-24 hours after the patient was last seen well, Dr. Jovin explained.
He said the 6-hour cutoff was chosen somewhat arbitrarily, but added, “It is highly consequential, as it marks the point of demarcation between the early and late time window, and virtually all guidelines recommend different approaches, dependent on whether patients present before or after 6 hours from symptom onset.”
The 6+ hour window
Dr. Jovin pointed out that for patients who present beyond 6 hours, treatment options are more restricted, because the data on thrombectomy in this later period come mainly from two North American trials (DEFUSE 3 and DAWN) that had very stringent imaging criteria for enrollment.
“We wanted to create a heterogeneous dataset with regard to geography and selection criteria by forming the AURORA collaboration,” he commented. Their study involved an individual-level pooled analysis of all patients who underwent randomization after 6 hours from the time that they were last seen well. Patients were randomly assigned to receive either best medical therapy alone or best medical therapy plus thrombectomy (either with stent retrievers or aspiration) for anterior circulation proximal large-vessel occlusion stroke.
The data came from six trials: DAWN (which enrolled patients 6-24 hours from stroke onset), DEFUSE 3 (6-16 hours), ESCAPE (0-12 hours), REVASCAT (0-8 hours), RESILIENT (0-8 hours), and POSITIVE (0-12 hours). In total, 505 patients were included in the meta-analysis, 266 in the intervention group, and 239 in the control group.
“By pooling data on patients presenting after 6 hours from all these trails, we achieve greater precision for treatment effect estimation and increased the power for subgroup analysis,” Dr. Jovin noted.
Although the majority of the patients were in the DAWN and DIFFUSE 3 trials (n = 388), “there are still a good number from the other four trials (n = 117),” Dr. Jovin reported.
Most of the trials used Modified Rankin Scale (mRS) ordinal or shift analysis as their primary endpoint, which was the also the endpoint chosen for this meta-analysis.
Imaging selection criteria ranged from fully automated software-generated quantitative volumetric analysis of baseline infarct (core) or tissue at risk to CT perfusion and plain CT/CTA. The minimum ASPECTS score was 5 or 6.
There were no imbalances in baseline characteristics. The median NIH Stroke Scale score was 16, and the median ASPECTS score was 8. The median time to randomization was 10.5 hours.
With regard to safety, there was no significant difference in rates of symptomatic intracerebral hemorrhage (5.3% in the intervention group vs. 3.3% in the control group; P = .23) or in mortality at 90 days (16.5% vs. 19.3%; P = .87). Jovin noted that these results are very similar to those from the HERMES meta-analysis of patients treated in the early time window.
The primary outcome – ordinal analysis of the mRS distribution – showed an adjusted odds ratio of 2.54 (P < .0001) for benefit in the intervention group. The number needed to treat to reduce disability was 3. “This is again very similar to the HERMES meta-analysis of patients in the early window,” Dr. Jovin said.
The P value for heterogeneity of treatment effect across the six studies was nonsignificant.
Secondary outcome analysis showed an “almost 27%” difference in good functional outcome (MRS, 0-2) between the two groups (45.9% in the intervention group vs. 19.3% in the control group), which translates into a number needed to treat of 3.8, Dr. Jovin reported.
Subgroup analysis showed a treatment effect favoring intervention across all prespecified subgroup factors, including age, sex, occlusion location, mode of presentation (wake-up vs. witnessed), and ASPECTS score, with the caveat that most of the patients were enrolled with ASPECTS scores of 7 or greater.
Early versus late
Surprisingly, although thrombectomy was found to be beneficial in both the 6- to 12-hour and 12- to 24-hour time window, the magnitude of benefit was significantly higher in the later rather than the earlier time window. The odds ratio of a better outcome with thrombectomy on the mRS shift analysis in those presenting in the 6- to 12-hour period was 1.78, compared with 5.86 in the 12- to 24-hour time window.
“This should not be interpreted as a higher chance of a good outcome if treated late. In fact, the rate of good outcomes were numerically higher in the earlier treated patients, but the difference comes from the control group, which did much worse in patients randomized in the later time period,” Dr. Jovin said.
“Aurora was the goddess of dawn [in ancient Roman mythology], so this is a very fitting name, as it reminds us that we are in the dawn of a new era where patients are selected based on physiological data rather than on time, and we certainly hope that this work has brought us closer to this reality,” Dr. Jovin concluded.
Commenting on the study, Michael Hill, MD, University of Calgary (Alta.), said: “The work provides pooled empiric data to support the concept that time to treatment is no longer the sole threshold variable to be used in treatment decision-making. Instead, time is now simply another variable to consider in the context of clinical and imaging factors.”
Dr. Hill, who headed up the ESCAPE trial and was also involved in the current meta-analysis, added: “This meta-analysis supports the concept of patient selection using the ‘good scan’ model, rather than using a time-based concept of patient eligibility for endovascular therapy. It will further push changes in care, because the implication is that all patients with more severe acute stroke presentations need emergency neurovascular imaging to decide if they are eligible for treatment.”
The AURORA meta-analysis was funded by Stryker Neurovascular. Dr. Jovin reports stock holdings in Anaconda, Route 92, VizAi, FreeOx, Blockade Medical, Methinks, and Corindus; personal fees from Cerenovus and Contego Medical; travel support from Fundacio Ictus; and grant support from Medtronic and Stryker Neurovascular.
A version of this article first appeared on Medscape.com.
FROM ISC 2021
PCI and CABG for left main disease have equal outcomes at 5 years
Background: While PCI with drug-eluting stents has become more accepted as treatment for some patients with left main disease, long-term outcomes from randomized control trials comparing PCI with CABG have yet to be clearly established.
Study design: International, open-label, multicenter, randomized trial.
Setting: A total of 126 sites in 17 countries.
Synopsis: Patients with low or intermediate anatomical complexity with 70% visual stenosis of the left main coronary artery or 50%-70% stenosis by noninvasive testing were randomized to either PCI (948) or CABG (957). Dual-antiplatelet therapy was given to PCI patients and aspirin to CABG patients. At 5 years there was no significant difference in the rate of the composite of death, stroke, or myocardial infarction (22.0% with PCI vs. 19.2% with CABG; difference, 2.8 percentage points; 95% CI, –0.9 to 6.5; P = .13). This was consistent across subgroups.
There were numerical differences in nonpowered secondary outcomes that may represent effects but should be interpreted cautiously: ischemia-driven revascularization (16.9% with PCI vs. 10% with CABG), transient ischemic attack plus stroke (3.3% with PCI vs. 5.2% with CABG), and death from any cause (3% with PCI vs. 9.9% with CABG). There was no significant difference in cardiovascular events, MI, or stroke.
One interesting limitation was that patients who had PCI were more commonly on dual-antiplatelet therapy and angiotensin converting–enzyme inhibitors, whereas CABG patients were more often on beta-blockers, diuretics, anticoagulants, and antiarrhythmics.
Bottom line: PCI and CABG treatments for left main disease have no significant difference in the composite outcome of death, stroke, or MI at 5 years.
Citation: Stone GW et al. Five-year outcomes after PCI or CABG for left main coronary disease. N Engl J Med. 2019;381:1820-30.
Dr. Horton is a hospitalist and clinical instructor of medicine at the University of Utah, Salt Lake City.
Background: While PCI with drug-eluting stents has become more accepted as treatment for some patients with left main disease, long-term outcomes from randomized control trials comparing PCI with CABG have yet to be clearly established.
Study design: International, open-label, multicenter, randomized trial.
Setting: A total of 126 sites in 17 countries.
Synopsis: Patients with low or intermediate anatomical complexity with 70% visual stenosis of the left main coronary artery or 50%-70% stenosis by noninvasive testing were randomized to either PCI (948) or CABG (957). Dual-antiplatelet therapy was given to PCI patients and aspirin to CABG patients. At 5 years there was no significant difference in the rate of the composite of death, stroke, or myocardial infarction (22.0% with PCI vs. 19.2% with CABG; difference, 2.8 percentage points; 95% CI, –0.9 to 6.5; P = .13). This was consistent across subgroups.
There were numerical differences in nonpowered secondary outcomes that may represent effects but should be interpreted cautiously: ischemia-driven revascularization (16.9% with PCI vs. 10% with CABG), transient ischemic attack plus stroke (3.3% with PCI vs. 5.2% with CABG), and death from any cause (3% with PCI vs. 9.9% with CABG). There was no significant difference in cardiovascular events, MI, or stroke.
One interesting limitation was that patients who had PCI were more commonly on dual-antiplatelet therapy and angiotensin converting–enzyme inhibitors, whereas CABG patients were more often on beta-blockers, diuretics, anticoagulants, and antiarrhythmics.
Bottom line: PCI and CABG treatments for left main disease have no significant difference in the composite outcome of death, stroke, or MI at 5 years.
Citation: Stone GW et al. Five-year outcomes after PCI or CABG for left main coronary disease. N Engl J Med. 2019;381:1820-30.
Dr. Horton is a hospitalist and clinical instructor of medicine at the University of Utah, Salt Lake City.
Background: While PCI with drug-eluting stents has become more accepted as treatment for some patients with left main disease, long-term outcomes from randomized control trials comparing PCI with CABG have yet to be clearly established.
Study design: International, open-label, multicenter, randomized trial.
Setting: A total of 126 sites in 17 countries.
Synopsis: Patients with low or intermediate anatomical complexity with 70% visual stenosis of the left main coronary artery or 50%-70% stenosis by noninvasive testing were randomized to either PCI (948) or CABG (957). Dual-antiplatelet therapy was given to PCI patients and aspirin to CABG patients. At 5 years there was no significant difference in the rate of the composite of death, stroke, or myocardial infarction (22.0% with PCI vs. 19.2% with CABG; difference, 2.8 percentage points; 95% CI, –0.9 to 6.5; P = .13). This was consistent across subgroups.
There were numerical differences in nonpowered secondary outcomes that may represent effects but should be interpreted cautiously: ischemia-driven revascularization (16.9% with PCI vs. 10% with CABG), transient ischemic attack plus stroke (3.3% with PCI vs. 5.2% with CABG), and death from any cause (3% with PCI vs. 9.9% with CABG). There was no significant difference in cardiovascular events, MI, or stroke.
One interesting limitation was that patients who had PCI were more commonly on dual-antiplatelet therapy and angiotensin converting–enzyme inhibitors, whereas CABG patients were more often on beta-blockers, diuretics, anticoagulants, and antiarrhythmics.
Bottom line: PCI and CABG treatments for left main disease have no significant difference in the composite outcome of death, stroke, or MI at 5 years.
Citation: Stone GW et al. Five-year outcomes after PCI or CABG for left main coronary disease. N Engl J Med. 2019;381:1820-30.
Dr. Horton is a hospitalist and clinical instructor of medicine at the University of Utah, Salt Lake City.
The best exercises for BP control? European statement sorts it out
Recommendations for prescribing exercise to control high blood pressure have been put forward by various medical organizations and expert panels, but finding the bandwidth to craft personalized exercise training for their patients poses a challenge for clinicians.
Now, European cardiology societies have issued a consensus statement that offers an algorithm of sorts for developing personalized exercise programs as part of overall management approach for patients with or at risk of high BP.
The statement, published in the European Journal of Preventive Cardiology and issued by the European Association of Preventive Cardiology and the European Society of Cardiology Council on Hypertension, claims to be the first document to focus on personalized exercise for BP.
The statement draws on a systematic review, including meta-analyses, to produce guidance on how to lower BP in three specific types of patients: Those with hypertension (>140/90 mm Hg), high-normal blood pressure (130-139/85-89 mm Hg), and normal blood pressure (<130/84 mm Hg).
By making recommendations for these three specific groups, along with providing guidance for combined exercise – that is, blending aerobic exercise with resistance training (RT) – the consensus statement goes one step further than recommendations other organizations have issued, Matthew W. Martinez, MD, said in an interview.
“What it adds is an algorithmic approach, if you will,” said Dr. Martinez, a sports medicine cardiologist at Morristown (N.J.) Medical Center. “There are some recommendations to help the clinicians to decide what they’re going to offer individuals, but what’s a challenge for us when seeing patients is finding the time to deliver the message and explain how valuable nutrition and exercise are.”
Guidelines, updates, and statements that include the role of exercise in BP control have been issued by the European Society of Cardiology, American Heart Association, and American College of Sports Medicine (Med Sci Sports Exercise. 2019;51:1314-23).
The European consensus statement includes the expected range of BP lowering for each activity. For example, aerobic exercise for patients with hypertension should lead to a reduction from –4.9 to –12 mm Hg systolic and –3.4 to –5.8 mm Hg diastolic.
The consensus statement recommends the following exercise priorities based on a patient’s blood pressure:
- Hypertension: Aerobic training (AT) as a first-line exercise therapy; and low- to moderate-intensity RT – equally using dynamic and isometric RT – as second-line therapy. In non-White patients, dynamic RT should be considered as a first-line therapy. RT can be combined with aerobic exercise on an individual basis if the clinician determines either form of RT would provide a metabolic benefit.
- High-to-normal BP: Dynamic RT as a first-line exercise, which the systematic review determined led to greater BP reduction than that of aerobic training. “Isometric RT is likely to elicit similar if not superior BP-lowering effects as [dynamic RT], but the level of evidence is low and the available data are scarce,” wrote first author Henner Hanssen, MD, of the University of Basel, Switzerland, and coauthors. Combining dynamic resistance training with aerobic training “may be preferable” to dynamic RT alone in patients with a combination of cardiovascular risk factors.
- Normal BP: Isometric RT may be indicated as a first-line intervention in individuals with a family or gestational history or obese or overweight people currently with normal BP. This advice includes a caveat: “The number of studies is limited and the 95% confidence intervals are large,” Dr. Hanssen and coauthors noted. AT is also an option in these patients, with more high-quality meta-analyses than the recommendation for isometric RT. “Hence, the BP-lowering effects of [isometric RT] as compared to AT may be overestimated and both exercise modalities may have similar BP-lowering effects in individuals with normotension,” wrote the consensus statement authors.
They note that more research is needed to validate the BP-lowering effects of combined exercise.
The statement acknowledges the difficulty clinicians face in managing patients with high blood pressure. “From a socioeconomic health perspective, it is a major challenge to develop, promote, and implement individually tailored exercise programs for patients with hypertension under consideration of sustainable costs,” wrote Dr. Hanssen and coauthors.
Dr. Martinez noted that one strength of the consensus statement is that it addresses the impact exercise can have on vascular health and metabolic function. And, it points out existing knowledge gaps.
“Are we going to see greater applicability of this as we use IT health technology?” he asked. “Are wearables and telehealth going to help deliver this message more easily, more frequently? Is there work to be done in terms of differences in gender? Do men and women respond differently, and is there a different exercise prescription based on that as well as ethnicity? We well know there’s a different treatment for African Americans compared to other ethnic groups.”
The statement also raises the stakes for using exercise as part of a multifaceted, integrated approach to hypertension management, he said.
“It’s not enough to talk just about exercise or nutrition, or to just give an antihypertension medicine,” Dr. Martinez said. “Perhaps the sweet spot is in integrating an approach that includes all three.”
Consensus statement coauthor Antonio Coca, MD, reported financial relationships with Abbott, Berlin-Chemie, Biolab, Boehringer-Ingelheim, Ferrer, Menarini, Merck, Novartis and Sanofi-Aventis. Coauthor Maria Simonenko, MD, reported financial relationships with Novartis and Sanofi-Aventis. Linda Pescatello, PhD, is lead author of the American College of Sports Medicine 2019 statement. Dr. Hanssen and all other authors have no disclosures. Dr. Martinez has no relevant relationships to disclose.
Recommendations for prescribing exercise to control high blood pressure have been put forward by various medical organizations and expert panels, but finding the bandwidth to craft personalized exercise training for their patients poses a challenge for clinicians.
Now, European cardiology societies have issued a consensus statement that offers an algorithm of sorts for developing personalized exercise programs as part of overall management approach for patients with or at risk of high BP.
The statement, published in the European Journal of Preventive Cardiology and issued by the European Association of Preventive Cardiology and the European Society of Cardiology Council on Hypertension, claims to be the first document to focus on personalized exercise for BP.
The statement draws on a systematic review, including meta-analyses, to produce guidance on how to lower BP in three specific types of patients: Those with hypertension (>140/90 mm Hg), high-normal blood pressure (130-139/85-89 mm Hg), and normal blood pressure (<130/84 mm Hg).
By making recommendations for these three specific groups, along with providing guidance for combined exercise – that is, blending aerobic exercise with resistance training (RT) – the consensus statement goes one step further than recommendations other organizations have issued, Matthew W. Martinez, MD, said in an interview.
“What it adds is an algorithmic approach, if you will,” said Dr. Martinez, a sports medicine cardiologist at Morristown (N.J.) Medical Center. “There are some recommendations to help the clinicians to decide what they’re going to offer individuals, but what’s a challenge for us when seeing patients is finding the time to deliver the message and explain how valuable nutrition and exercise are.”
Guidelines, updates, and statements that include the role of exercise in BP control have been issued by the European Society of Cardiology, American Heart Association, and American College of Sports Medicine (Med Sci Sports Exercise. 2019;51:1314-23).
The European consensus statement includes the expected range of BP lowering for each activity. For example, aerobic exercise for patients with hypertension should lead to a reduction from –4.9 to –12 mm Hg systolic and –3.4 to –5.8 mm Hg diastolic.
The consensus statement recommends the following exercise priorities based on a patient’s blood pressure:
- Hypertension: Aerobic training (AT) as a first-line exercise therapy; and low- to moderate-intensity RT – equally using dynamic and isometric RT – as second-line therapy. In non-White patients, dynamic RT should be considered as a first-line therapy. RT can be combined with aerobic exercise on an individual basis if the clinician determines either form of RT would provide a metabolic benefit.
- High-to-normal BP: Dynamic RT as a first-line exercise, which the systematic review determined led to greater BP reduction than that of aerobic training. “Isometric RT is likely to elicit similar if not superior BP-lowering effects as [dynamic RT], but the level of evidence is low and the available data are scarce,” wrote first author Henner Hanssen, MD, of the University of Basel, Switzerland, and coauthors. Combining dynamic resistance training with aerobic training “may be preferable” to dynamic RT alone in patients with a combination of cardiovascular risk factors.
- Normal BP: Isometric RT may be indicated as a first-line intervention in individuals with a family or gestational history or obese or overweight people currently with normal BP. This advice includes a caveat: “The number of studies is limited and the 95% confidence intervals are large,” Dr. Hanssen and coauthors noted. AT is also an option in these patients, with more high-quality meta-analyses than the recommendation for isometric RT. “Hence, the BP-lowering effects of [isometric RT] as compared to AT may be overestimated and both exercise modalities may have similar BP-lowering effects in individuals with normotension,” wrote the consensus statement authors.
They note that more research is needed to validate the BP-lowering effects of combined exercise.
The statement acknowledges the difficulty clinicians face in managing patients with high blood pressure. “From a socioeconomic health perspective, it is a major challenge to develop, promote, and implement individually tailored exercise programs for patients with hypertension under consideration of sustainable costs,” wrote Dr. Hanssen and coauthors.
Dr. Martinez noted that one strength of the consensus statement is that it addresses the impact exercise can have on vascular health and metabolic function. And, it points out existing knowledge gaps.
“Are we going to see greater applicability of this as we use IT health technology?” he asked. “Are wearables and telehealth going to help deliver this message more easily, more frequently? Is there work to be done in terms of differences in gender? Do men and women respond differently, and is there a different exercise prescription based on that as well as ethnicity? We well know there’s a different treatment for African Americans compared to other ethnic groups.”
The statement also raises the stakes for using exercise as part of a multifaceted, integrated approach to hypertension management, he said.
“It’s not enough to talk just about exercise or nutrition, or to just give an antihypertension medicine,” Dr. Martinez said. “Perhaps the sweet spot is in integrating an approach that includes all three.”
Consensus statement coauthor Antonio Coca, MD, reported financial relationships with Abbott, Berlin-Chemie, Biolab, Boehringer-Ingelheim, Ferrer, Menarini, Merck, Novartis and Sanofi-Aventis. Coauthor Maria Simonenko, MD, reported financial relationships with Novartis and Sanofi-Aventis. Linda Pescatello, PhD, is lead author of the American College of Sports Medicine 2019 statement. Dr. Hanssen and all other authors have no disclosures. Dr. Martinez has no relevant relationships to disclose.
Recommendations for prescribing exercise to control high blood pressure have been put forward by various medical organizations and expert panels, but finding the bandwidth to craft personalized exercise training for their patients poses a challenge for clinicians.
Now, European cardiology societies have issued a consensus statement that offers an algorithm of sorts for developing personalized exercise programs as part of overall management approach for patients with or at risk of high BP.
The statement, published in the European Journal of Preventive Cardiology and issued by the European Association of Preventive Cardiology and the European Society of Cardiology Council on Hypertension, claims to be the first document to focus on personalized exercise for BP.
The statement draws on a systematic review, including meta-analyses, to produce guidance on how to lower BP in three specific types of patients: Those with hypertension (>140/90 mm Hg), high-normal blood pressure (130-139/85-89 mm Hg), and normal blood pressure (<130/84 mm Hg).
By making recommendations for these three specific groups, along with providing guidance for combined exercise – that is, blending aerobic exercise with resistance training (RT) – the consensus statement goes one step further than recommendations other organizations have issued, Matthew W. Martinez, MD, said in an interview.
“What it adds is an algorithmic approach, if you will,” said Dr. Martinez, a sports medicine cardiologist at Morristown (N.J.) Medical Center. “There are some recommendations to help the clinicians to decide what they’re going to offer individuals, but what’s a challenge for us when seeing patients is finding the time to deliver the message and explain how valuable nutrition and exercise are.”
Guidelines, updates, and statements that include the role of exercise in BP control have been issued by the European Society of Cardiology, American Heart Association, and American College of Sports Medicine (Med Sci Sports Exercise. 2019;51:1314-23).
The European consensus statement includes the expected range of BP lowering for each activity. For example, aerobic exercise for patients with hypertension should lead to a reduction from –4.9 to –12 mm Hg systolic and –3.4 to –5.8 mm Hg diastolic.
The consensus statement recommends the following exercise priorities based on a patient’s blood pressure:
- Hypertension: Aerobic training (AT) as a first-line exercise therapy; and low- to moderate-intensity RT – equally using dynamic and isometric RT – as second-line therapy. In non-White patients, dynamic RT should be considered as a first-line therapy. RT can be combined with aerobic exercise on an individual basis if the clinician determines either form of RT would provide a metabolic benefit.
- High-to-normal BP: Dynamic RT as a first-line exercise, which the systematic review determined led to greater BP reduction than that of aerobic training. “Isometric RT is likely to elicit similar if not superior BP-lowering effects as [dynamic RT], but the level of evidence is low and the available data are scarce,” wrote first author Henner Hanssen, MD, of the University of Basel, Switzerland, and coauthors. Combining dynamic resistance training with aerobic training “may be preferable” to dynamic RT alone in patients with a combination of cardiovascular risk factors.
- Normal BP: Isometric RT may be indicated as a first-line intervention in individuals with a family or gestational history or obese or overweight people currently with normal BP. This advice includes a caveat: “The number of studies is limited and the 95% confidence intervals are large,” Dr. Hanssen and coauthors noted. AT is also an option in these patients, with more high-quality meta-analyses than the recommendation for isometric RT. “Hence, the BP-lowering effects of [isometric RT] as compared to AT may be overestimated and both exercise modalities may have similar BP-lowering effects in individuals with normotension,” wrote the consensus statement authors.
They note that more research is needed to validate the BP-lowering effects of combined exercise.
The statement acknowledges the difficulty clinicians face in managing patients with high blood pressure. “From a socioeconomic health perspective, it is a major challenge to develop, promote, and implement individually tailored exercise programs for patients with hypertension under consideration of sustainable costs,” wrote Dr. Hanssen and coauthors.
Dr. Martinez noted that one strength of the consensus statement is that it addresses the impact exercise can have on vascular health and metabolic function. And, it points out existing knowledge gaps.
“Are we going to see greater applicability of this as we use IT health technology?” he asked. “Are wearables and telehealth going to help deliver this message more easily, more frequently? Is there work to be done in terms of differences in gender? Do men and women respond differently, and is there a different exercise prescription based on that as well as ethnicity? We well know there’s a different treatment for African Americans compared to other ethnic groups.”
The statement also raises the stakes for using exercise as part of a multifaceted, integrated approach to hypertension management, he said.
“It’s not enough to talk just about exercise or nutrition, or to just give an antihypertension medicine,” Dr. Martinez said. “Perhaps the sweet spot is in integrating an approach that includes all three.”
Consensus statement coauthor Antonio Coca, MD, reported financial relationships with Abbott, Berlin-Chemie, Biolab, Boehringer-Ingelheim, Ferrer, Menarini, Merck, Novartis and Sanofi-Aventis. Coauthor Maria Simonenko, MD, reported financial relationships with Novartis and Sanofi-Aventis. Linda Pescatello, PhD, is lead author of the American College of Sports Medicine 2019 statement. Dr. Hanssen and all other authors have no disclosures. Dr. Martinez has no relevant relationships to disclose.
FROM THE EUROPEAN JOURNAL OF PREVENTIVE CARDIOLOGY
Long-haul COVID-19 brings welcome attention to POTS
Before COVID-19, postural orthostatic tachycardia syndrome (POTS) was one of those diseases that many people, including physicians, dismissed.
“They thought it was just anxious, crazy young women,” said Pam R. Taub, MD, who runs the cardiac rehabilitation program at the University of California, San Diego.
The cryptic autonomic condition was estimated to affect 1-3 million Americans before the pandemic hit. Now case reports confirm that it is a manifestation of postacute sequelae of SARS-CoV-2 infection (PASC), or so-called long-haul COVID-19.
“I’m excited that this condition that has been so often the ugly stepchild of both cardiology and neurology is getting some attention,” said Dr. Taub. She said she is hopeful that the National Institutes of Health’s commitment to PASC research will benefit patients affected by the cardiovascular dysautonomia characterized by orthostatic intolerance in the absence of orthostatic hypotension.
Postinfection POTS is not exclusive to SARS-CoV-2. It has been reported after Lyme disease and Epstein-Barr virus infections, for example. One theory is that some of the antibodies generated against the virus cross react and damage the autonomic nervous system, which regulates heart rate and blood pressure, Dr. Taub explained.
It is not known whether COVID-19 is more likely to trigger POTS than are other infections or whether the rise in cases merely reflects the fact that more than 115 million people worldwide have been infected with the novel coronavirus.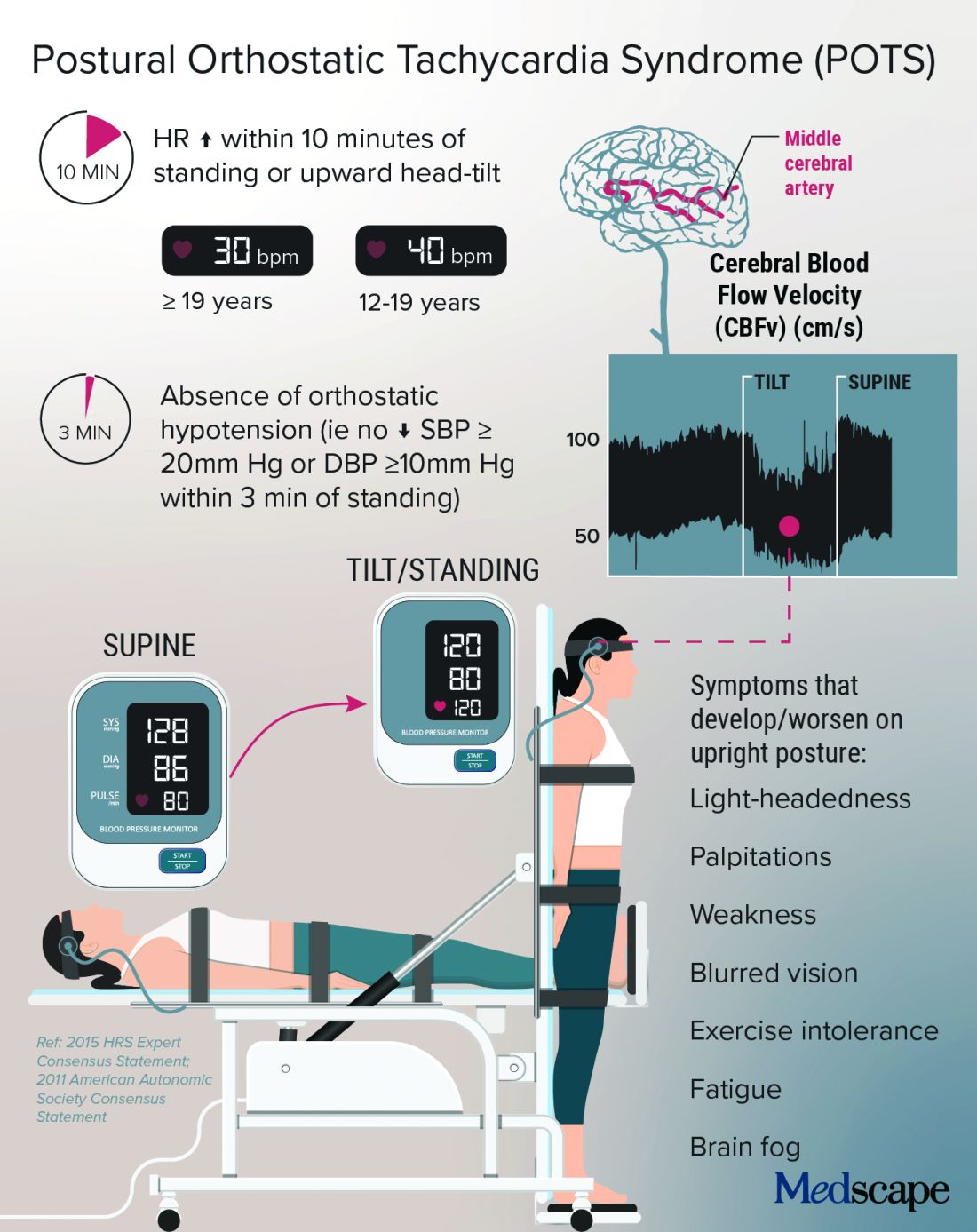
Low blood volume, dysregulation of the autonomic nervous system, and autoimmunity may all play a role in POTS, perhaps leading to distinct subtypes, according to a State of the Science document from the NIH; the National Heart, Lung, and Blood Institute; and the National Institute of Neurological Disorders and Stroke.
In Dr. Taub’s experience, “The truth is that patients actually have a mix of the subtypes.”
Kamal Shouman, MD, an autonomic neurologist at Mayo Clinic, Rochester, Minn., said in an interview that he has seen patients present with post–COVID-19 POTS in “all flavors,” including “neuropathic POTS, which is thought of as the classic postinfectious phenomenon.”
Why does it mostly affect athletic women?
The condition, which can be the result of dehydration or prolonged bed rest, leading to deconditioning, affects women disproportionately.
According to Manesh Patel, MD, if a patient with POTS who is not a young woman is presented on medical rounds, the response is, “Tell me again why you think this patient has POTS.”
Dr. Patel, chief of the division of cardiology at Duke University, Durham, N.C., has a theory for why many of the women who have POTS are athletes or are highly active: They likely have an underlying predisposition, compounded by a smaller body volume, leaving less margin for error. “If they decondition and lose 500 cc’s, it makes a bigger difference to them than, say, a 300-pound offensive lineman,” Dr. Patel explained.
That hypothesis makes sense to Dr. Taub, who added, “There are just some people metabolically that are more hyperadrenergic,” and it may be that “all their activity really helps tone down that sympathetic output,” but the infection affects these regulatory processes, and deconditioning disrupts things further.
Women also have more autoimmune disorders than do men. The driving force of the dysregulation of the autonomic nervous system is thought to be “immune mediated; we think it’s triggered by a response to a virus,” she said.
Dr. Shouman said the underlying susceptibility may predispose toward orthostatic intolerance. For example, patients will tell him, “Well, many years ago, I was prone to fainting.” He emphasized that POTS is not exclusive to women – he sees men with POTS, and one of the three recent case reports of post–COVID-19 POTS involved a 37-year-old man. So far, the male POTS patients that Dr. Patel has encountered have been deconditioned athletes.
Poor (wo)man’s tilt test and treatment options
POTS is typically diagnosed with a tilt test and transcranial Doppler. Dr. Taub described her “poor man’s tilt test” of asking the patient to lie down for 5-10 minutes and then having the patient stand up.
She likes the fact that transcranial Doppler helps validate the brain fog that patients report, which can be dismissed as “just your excuse for not wanting to work.” If blood perfusion to the brain is cut by 40%-50%, “how are you going to think clearly?” she said.
Dr. Shouman noted that overall volume expansion with salt water, compression garments, and a graduated exercise program play a major role in the rehabilitation of all POTS patients.
He likes to tailor treatments to the most likely underlying cause. But patients should first undergo a medical assessment by their internists to make sure there isn’t a primary lung or heart problem.
“Once the decision is made for them to be evaluated in the autonomic practice and [a] POTS diagnosis is made, I think it is very useful to determine what type of POTS,” he said.
With hyperadrenergic POTS, “you are looking at a standing norepinephrine level of over 600 pg/mL or so.” For these patients, drugs such as ivabradine or beta-blockers can help, he noted.
Dr. Taub recently conducted a small study that showed a benefit with the selective If channel blocker ivabradine for patients with hyperadrenergic POTS unrelated to COVID-19. She tends to favor ivabradine over beta-blockers because it lowers heart rate but not blood pressure. In addition, beta-blockers can exacerbate fatigue and brain fog.
A small crossover study will compare propranolol and ivabradine in POTS. For someone who is very hypovolemic, “you might try a salt tablet or a prescription drug like fludrocortisone,” Dr. Taub explained.
Another problem that patients with POTS experience is an inability to exercise because of orthostatic intolerance. Recumbent exercise targets deconditioning and can tamp down the hyperadrenergic effect. Dr. Shouman’s approach is to start gradually with swimming or the use of a recumbent bike or a rowing machine.
Dr. Taub recommends wearables to patients because POTS is “a very dynamic condition” that is easy to overmedicate or undermedicate. If it’s a good day, the patients are well hydrated, and the standing heart rate is only 80 bpm, she tells them they could titrate down their second dose of ivabradine, for example. The feedback from wearables also helps patients manage their exercise response.
For Dr. Shouman, wearables are not always as accurate as he would like. He tells his patients that it’s okay to use one as long as it doesn’t become a source of anxiety such that they’re constantly checking it.
POTS hope: A COVID-19 silver lining?
With increasing attention being paid to long-haul COVID-19, are there any concerns that POTS will get lost among the myriad symptoms connected to PASC?
Dr. Shouman cautioned, “Not all long COVID is POTS,” and said that clinicians at long-haul clinics should be able to recognize the different conditions “when POTS is suspected. I think it is useful for those providers to make the appropriate referral for POTS clinic autonomic assessment.”
He and his colleagues at Mayo have seen quite a few patients who have post–COVID-19 autonomic dysfunction, such as vasodepressor syncope, not just POTS. They plan to write about this soon.
“Of all the things I treat in cardiology, this is the most complex, because there’s so many different systems involved,” said Dr. Taub, who has seen patients recover fully from POTS. “There’s a spectrum, and there’s people that are definitely on one end of the spectrum where they have very severe diseases.”
For her, the important message is, “No matter where you are on the spectrum, there are things we can do to make your symptoms better.” And with grant funding for PASC research, “hopefully we will address the mechanisms of disease, and we’ll be able to cure this,” she said.
Dr. Patel has served as a consultant for Bayer, Janssen, AstraZeneca, and Heartflow and has received research grants from Bayer, Janssen, AstraZeneca, and the National Heart, Lung, and Blood Institute. Dr. Shouman reports no relevant financial relationships. Dr. Taub has served as a consultant for Amgen, Bayer, Esperion, Boehringer Ingelheim, Novo Nordisk, and Sanofi; is a shareholder in Epirium Bio; and has received research grants from the National Institutes of Health, the American Heart Association, and the Department of Homeland Security/FEMA.
A version of this article first appeared on Medscape.com.
Before COVID-19, postural orthostatic tachycardia syndrome (POTS) was one of those diseases that many people, including physicians, dismissed.
“They thought it was just anxious, crazy young women,” said Pam R. Taub, MD, who runs the cardiac rehabilitation program at the University of California, San Diego.
The cryptic autonomic condition was estimated to affect 1-3 million Americans before the pandemic hit. Now case reports confirm that it is a manifestation of postacute sequelae of SARS-CoV-2 infection (PASC), or so-called long-haul COVID-19.
“I’m excited that this condition that has been so often the ugly stepchild of both cardiology and neurology is getting some attention,” said Dr. Taub. She said she is hopeful that the National Institutes of Health’s commitment to PASC research will benefit patients affected by the cardiovascular dysautonomia characterized by orthostatic intolerance in the absence of orthostatic hypotension.
Postinfection POTS is not exclusive to SARS-CoV-2. It has been reported after Lyme disease and Epstein-Barr virus infections, for example. One theory is that some of the antibodies generated against the virus cross react and damage the autonomic nervous system, which regulates heart rate and blood pressure, Dr. Taub explained.
It is not known whether COVID-19 is more likely to trigger POTS than are other infections or whether the rise in cases merely reflects the fact that more than 115 million people worldwide have been infected with the novel coronavirus.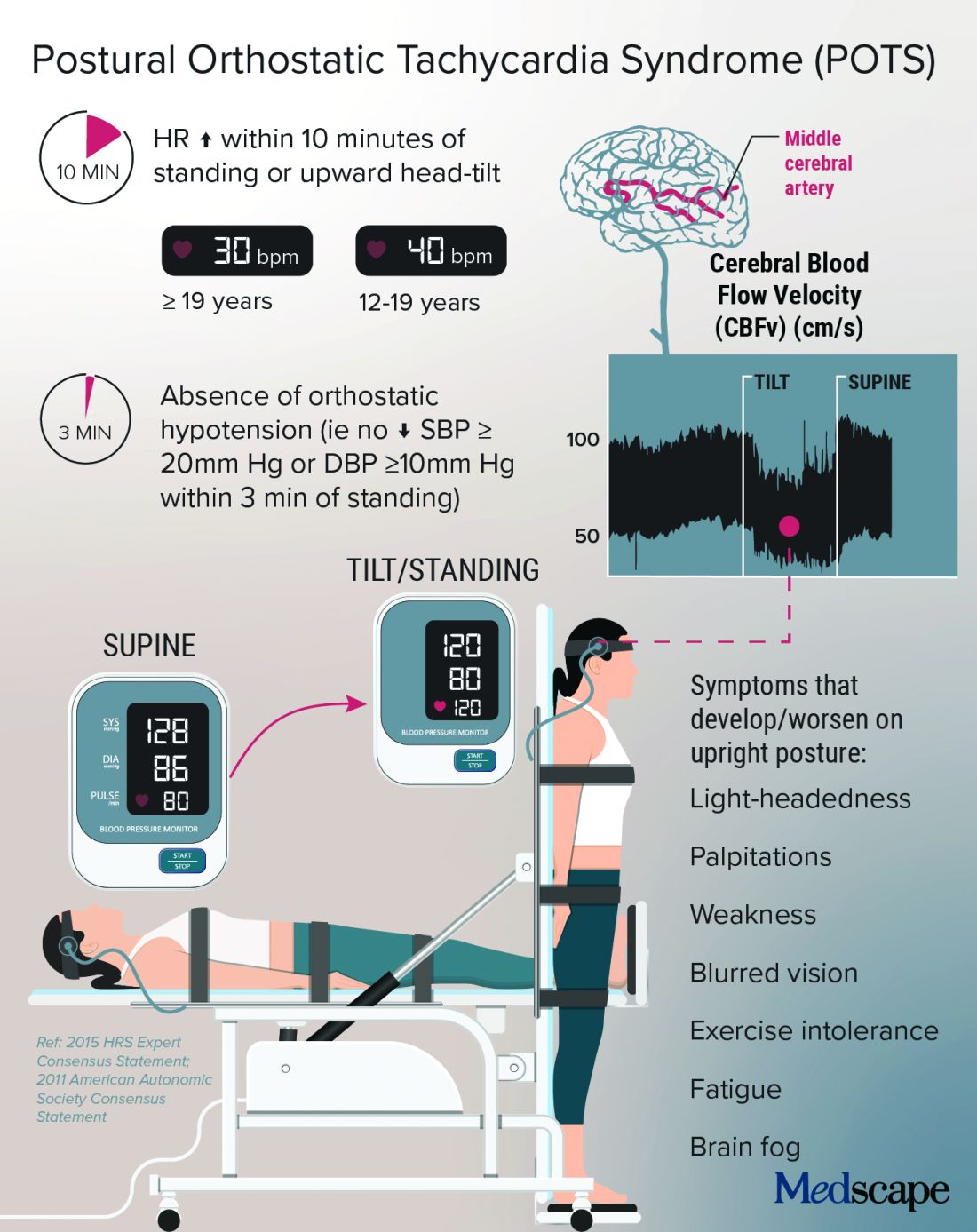
Low blood volume, dysregulation of the autonomic nervous system, and autoimmunity may all play a role in POTS, perhaps leading to distinct subtypes, according to a State of the Science document from the NIH; the National Heart, Lung, and Blood Institute; and the National Institute of Neurological Disorders and Stroke.
In Dr. Taub’s experience, “The truth is that patients actually have a mix of the subtypes.”
Kamal Shouman, MD, an autonomic neurologist at Mayo Clinic, Rochester, Minn., said in an interview that he has seen patients present with post–COVID-19 POTS in “all flavors,” including “neuropathic POTS, which is thought of as the classic postinfectious phenomenon.”
Why does it mostly affect athletic women?
The condition, which can be the result of dehydration or prolonged bed rest, leading to deconditioning, affects women disproportionately.
According to Manesh Patel, MD, if a patient with POTS who is not a young woman is presented on medical rounds, the response is, “Tell me again why you think this patient has POTS.”
Dr. Patel, chief of the division of cardiology at Duke University, Durham, N.C., has a theory for why many of the women who have POTS are athletes or are highly active: They likely have an underlying predisposition, compounded by a smaller body volume, leaving less margin for error. “If they decondition and lose 500 cc’s, it makes a bigger difference to them than, say, a 300-pound offensive lineman,” Dr. Patel explained.
That hypothesis makes sense to Dr. Taub, who added, “There are just some people metabolically that are more hyperadrenergic,” and it may be that “all their activity really helps tone down that sympathetic output,” but the infection affects these regulatory processes, and deconditioning disrupts things further.
Women also have more autoimmune disorders than do men. The driving force of the dysregulation of the autonomic nervous system is thought to be “immune mediated; we think it’s triggered by a response to a virus,” she said.
Dr. Shouman said the underlying susceptibility may predispose toward orthostatic intolerance. For example, patients will tell him, “Well, many years ago, I was prone to fainting.” He emphasized that POTS is not exclusive to women – he sees men with POTS, and one of the three recent case reports of post–COVID-19 POTS involved a 37-year-old man. So far, the male POTS patients that Dr. Patel has encountered have been deconditioned athletes.
Poor (wo)man’s tilt test and treatment options
POTS is typically diagnosed with a tilt test and transcranial Doppler. Dr. Taub described her “poor man’s tilt test” of asking the patient to lie down for 5-10 minutes and then having the patient stand up.
She likes the fact that transcranial Doppler helps validate the brain fog that patients report, which can be dismissed as “just your excuse for not wanting to work.” If blood perfusion to the brain is cut by 40%-50%, “how are you going to think clearly?” she said.
Dr. Shouman noted that overall volume expansion with salt water, compression garments, and a graduated exercise program play a major role in the rehabilitation of all POTS patients.
He likes to tailor treatments to the most likely underlying cause. But patients should first undergo a medical assessment by their internists to make sure there isn’t a primary lung or heart problem.
“Once the decision is made for them to be evaluated in the autonomic practice and [a] POTS diagnosis is made, I think it is very useful to determine what type of POTS,” he said.
With hyperadrenergic POTS, “you are looking at a standing norepinephrine level of over 600 pg/mL or so.” For these patients, drugs such as ivabradine or beta-blockers can help, he noted.
Dr. Taub recently conducted a small study that showed a benefit with the selective If channel blocker ivabradine for patients with hyperadrenergic POTS unrelated to COVID-19. She tends to favor ivabradine over beta-blockers because it lowers heart rate but not blood pressure. In addition, beta-blockers can exacerbate fatigue and brain fog.
A small crossover study will compare propranolol and ivabradine in POTS. For someone who is very hypovolemic, “you might try a salt tablet or a prescription drug like fludrocortisone,” Dr. Taub explained.
Another problem that patients with POTS experience is an inability to exercise because of orthostatic intolerance. Recumbent exercise targets deconditioning and can tamp down the hyperadrenergic effect. Dr. Shouman’s approach is to start gradually with swimming or the use of a recumbent bike or a rowing machine.
Dr. Taub recommends wearables to patients because POTS is “a very dynamic condition” that is easy to overmedicate or undermedicate. If it’s a good day, the patients are well hydrated, and the standing heart rate is only 80 bpm, she tells them they could titrate down their second dose of ivabradine, for example. The feedback from wearables also helps patients manage their exercise response.
For Dr. Shouman, wearables are not always as accurate as he would like. He tells his patients that it’s okay to use one as long as it doesn’t become a source of anxiety such that they’re constantly checking it.
POTS hope: A COVID-19 silver lining?
With increasing attention being paid to long-haul COVID-19, are there any concerns that POTS will get lost among the myriad symptoms connected to PASC?
Dr. Shouman cautioned, “Not all long COVID is POTS,” and said that clinicians at long-haul clinics should be able to recognize the different conditions “when POTS is suspected. I think it is useful for those providers to make the appropriate referral for POTS clinic autonomic assessment.”
He and his colleagues at Mayo have seen quite a few patients who have post–COVID-19 autonomic dysfunction, such as vasodepressor syncope, not just POTS. They plan to write about this soon.
“Of all the things I treat in cardiology, this is the most complex, because there’s so many different systems involved,” said Dr. Taub, who has seen patients recover fully from POTS. “There’s a spectrum, and there’s people that are definitely on one end of the spectrum where they have very severe diseases.”
For her, the important message is, “No matter where you are on the spectrum, there are things we can do to make your symptoms better.” And with grant funding for PASC research, “hopefully we will address the mechanisms of disease, and we’ll be able to cure this,” she said.
Dr. Patel has served as a consultant for Bayer, Janssen, AstraZeneca, and Heartflow and has received research grants from Bayer, Janssen, AstraZeneca, and the National Heart, Lung, and Blood Institute. Dr. Shouman reports no relevant financial relationships. Dr. Taub has served as a consultant for Amgen, Bayer, Esperion, Boehringer Ingelheim, Novo Nordisk, and Sanofi; is a shareholder in Epirium Bio; and has received research grants from the National Institutes of Health, the American Heart Association, and the Department of Homeland Security/FEMA.
A version of this article first appeared on Medscape.com.
Before COVID-19, postural orthostatic tachycardia syndrome (POTS) was one of those diseases that many people, including physicians, dismissed.
“They thought it was just anxious, crazy young women,” said Pam R. Taub, MD, who runs the cardiac rehabilitation program at the University of California, San Diego.
The cryptic autonomic condition was estimated to affect 1-3 million Americans before the pandemic hit. Now case reports confirm that it is a manifestation of postacute sequelae of SARS-CoV-2 infection (PASC), or so-called long-haul COVID-19.
“I’m excited that this condition that has been so often the ugly stepchild of both cardiology and neurology is getting some attention,” said Dr. Taub. She said she is hopeful that the National Institutes of Health’s commitment to PASC research will benefit patients affected by the cardiovascular dysautonomia characterized by orthostatic intolerance in the absence of orthostatic hypotension.
Postinfection POTS is not exclusive to SARS-CoV-2. It has been reported after Lyme disease and Epstein-Barr virus infections, for example. One theory is that some of the antibodies generated against the virus cross react and damage the autonomic nervous system, which regulates heart rate and blood pressure, Dr. Taub explained.
It is not known whether COVID-19 is more likely to trigger POTS than are other infections or whether the rise in cases merely reflects the fact that more than 115 million people worldwide have been infected with the novel coronavirus.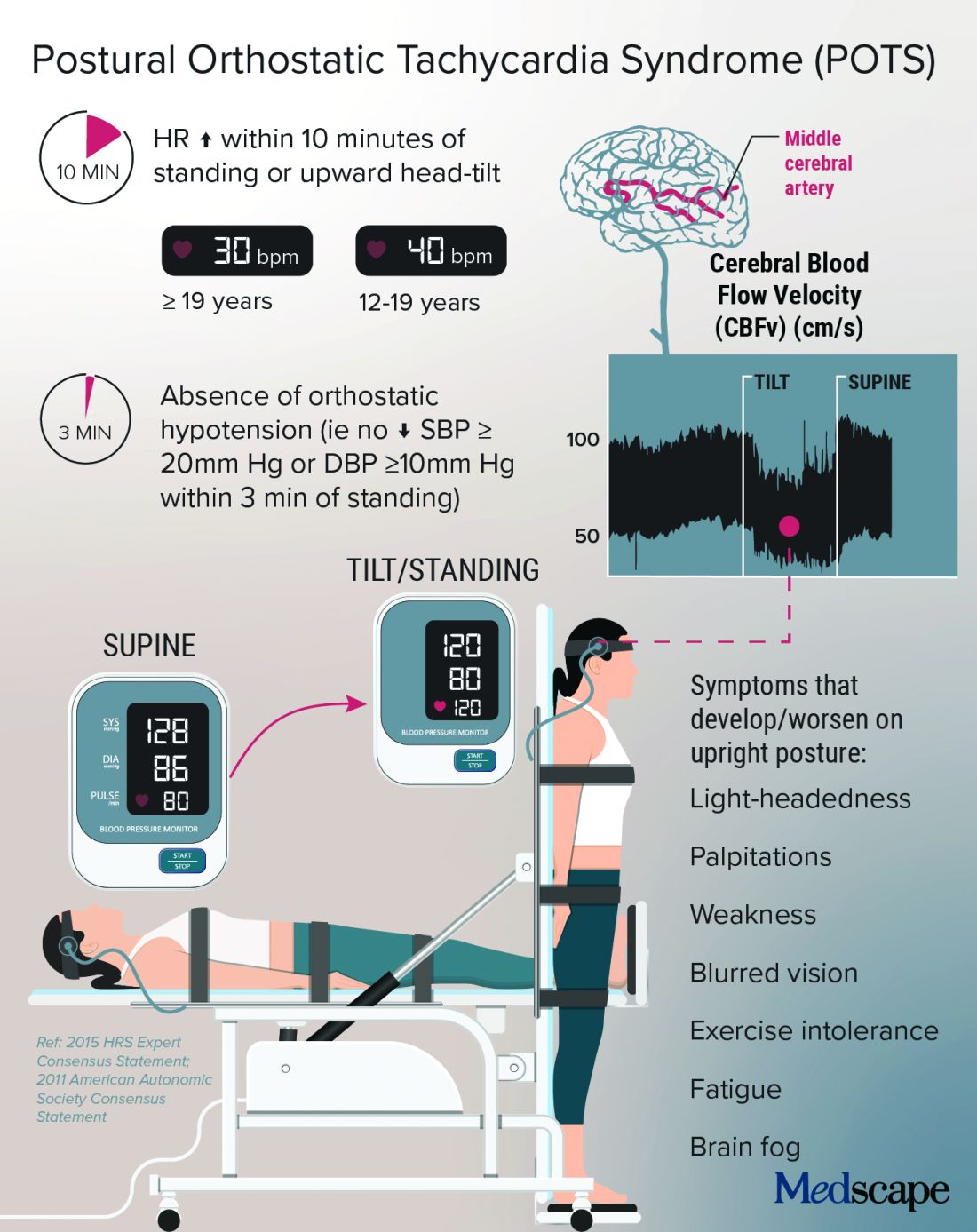
Low blood volume, dysregulation of the autonomic nervous system, and autoimmunity may all play a role in POTS, perhaps leading to distinct subtypes, according to a State of the Science document from the NIH; the National Heart, Lung, and Blood Institute; and the National Institute of Neurological Disorders and Stroke.
In Dr. Taub’s experience, “The truth is that patients actually have a mix of the subtypes.”
Kamal Shouman, MD, an autonomic neurologist at Mayo Clinic, Rochester, Minn., said in an interview that he has seen patients present with post–COVID-19 POTS in “all flavors,” including “neuropathic POTS, which is thought of as the classic postinfectious phenomenon.”
Why does it mostly affect athletic women?
The condition, which can be the result of dehydration or prolonged bed rest, leading to deconditioning, affects women disproportionately.
According to Manesh Patel, MD, if a patient with POTS who is not a young woman is presented on medical rounds, the response is, “Tell me again why you think this patient has POTS.”
Dr. Patel, chief of the division of cardiology at Duke University, Durham, N.C., has a theory for why many of the women who have POTS are athletes or are highly active: They likely have an underlying predisposition, compounded by a smaller body volume, leaving less margin for error. “If they decondition and lose 500 cc’s, it makes a bigger difference to them than, say, a 300-pound offensive lineman,” Dr. Patel explained.
That hypothesis makes sense to Dr. Taub, who added, “There are just some people metabolically that are more hyperadrenergic,” and it may be that “all their activity really helps tone down that sympathetic output,” but the infection affects these regulatory processes, and deconditioning disrupts things further.
Women also have more autoimmune disorders than do men. The driving force of the dysregulation of the autonomic nervous system is thought to be “immune mediated; we think it’s triggered by a response to a virus,” she said.
Dr. Shouman said the underlying susceptibility may predispose toward orthostatic intolerance. For example, patients will tell him, “Well, many years ago, I was prone to fainting.” He emphasized that POTS is not exclusive to women – he sees men with POTS, and one of the three recent case reports of post–COVID-19 POTS involved a 37-year-old man. So far, the male POTS patients that Dr. Patel has encountered have been deconditioned athletes.
Poor (wo)man’s tilt test and treatment options
POTS is typically diagnosed with a tilt test and transcranial Doppler. Dr. Taub described her “poor man’s tilt test” of asking the patient to lie down for 5-10 minutes and then having the patient stand up.
She likes the fact that transcranial Doppler helps validate the brain fog that patients report, which can be dismissed as “just your excuse for not wanting to work.” If blood perfusion to the brain is cut by 40%-50%, “how are you going to think clearly?” she said.
Dr. Shouman noted that overall volume expansion with salt water, compression garments, and a graduated exercise program play a major role in the rehabilitation of all POTS patients.
He likes to tailor treatments to the most likely underlying cause. But patients should first undergo a medical assessment by their internists to make sure there isn’t a primary lung or heart problem.
“Once the decision is made for them to be evaluated in the autonomic practice and [a] POTS diagnosis is made, I think it is very useful to determine what type of POTS,” he said.
With hyperadrenergic POTS, “you are looking at a standing norepinephrine level of over 600 pg/mL or so.” For these patients, drugs such as ivabradine or beta-blockers can help, he noted.
Dr. Taub recently conducted a small study that showed a benefit with the selective If channel blocker ivabradine for patients with hyperadrenergic POTS unrelated to COVID-19. She tends to favor ivabradine over beta-blockers because it lowers heart rate but not blood pressure. In addition, beta-blockers can exacerbate fatigue and brain fog.
A small crossover study will compare propranolol and ivabradine in POTS. For someone who is very hypovolemic, “you might try a salt tablet or a prescription drug like fludrocortisone,” Dr. Taub explained.
Another problem that patients with POTS experience is an inability to exercise because of orthostatic intolerance. Recumbent exercise targets deconditioning and can tamp down the hyperadrenergic effect. Dr. Shouman’s approach is to start gradually with swimming or the use of a recumbent bike or a rowing machine.
Dr. Taub recommends wearables to patients because POTS is “a very dynamic condition” that is easy to overmedicate or undermedicate. If it’s a good day, the patients are well hydrated, and the standing heart rate is only 80 bpm, she tells them they could titrate down their second dose of ivabradine, for example. The feedback from wearables also helps patients manage their exercise response.
For Dr. Shouman, wearables are not always as accurate as he would like. He tells his patients that it’s okay to use one as long as it doesn’t become a source of anxiety such that they’re constantly checking it.
POTS hope: A COVID-19 silver lining?
With increasing attention being paid to long-haul COVID-19, are there any concerns that POTS will get lost among the myriad symptoms connected to PASC?
Dr. Shouman cautioned, “Not all long COVID is POTS,” and said that clinicians at long-haul clinics should be able to recognize the different conditions “when POTS is suspected. I think it is useful for those providers to make the appropriate referral for POTS clinic autonomic assessment.”
He and his colleagues at Mayo have seen quite a few patients who have post–COVID-19 autonomic dysfunction, such as vasodepressor syncope, not just POTS. They plan to write about this soon.
“Of all the things I treat in cardiology, this is the most complex, because there’s so many different systems involved,” said Dr. Taub, who has seen patients recover fully from POTS. “There’s a spectrum, and there’s people that are definitely on one end of the spectrum where they have very severe diseases.”
For her, the important message is, “No matter where you are on the spectrum, there are things we can do to make your symptoms better.” And with grant funding for PASC research, “hopefully we will address the mechanisms of disease, and we’ll be able to cure this,” she said.
Dr. Patel has served as a consultant for Bayer, Janssen, AstraZeneca, and Heartflow and has received research grants from Bayer, Janssen, AstraZeneca, and the National Heart, Lung, and Blood Institute. Dr. Shouman reports no relevant financial relationships. Dr. Taub has served as a consultant for Amgen, Bayer, Esperion, Boehringer Ingelheim, Novo Nordisk, and Sanofi; is a shareholder in Epirium Bio; and has received research grants from the National Institutes of Health, the American Heart Association, and the Department of Homeland Security/FEMA.
A version of this article first appeared on Medscape.com.
Febuxostat, allopurinol real-world cardiovascular risk appears equal
Febuxostat (Uloric) was not associated with increased cardiovascular risk in patients with gout when compared to those who used allopurinol, in an analysis of new users of the drugs in Medicare fee-for-service claims data from the period of 2008-2016.
The findings, published March 25 in the Journal of the American Heart Association, update and echo the results from a similar previous study by the same Brigham and Women’s Hospital research group that covered 2008-2013 Medicare claims data. That original claims data study from 2018 sought to confirm the findings of the postmarketing surveillance CARES (Cardiovascular Safety of Febuxostat and Allopurinol in Patients With Gout and Cardiovascular Morbidities) trial that led to a boxed warning for increased risk of cardiovascular and all-cause mortality vs. allopurinol. The trial, however, did not show a higher rate of major adverse cardiovascular events (MACE) overall with febuxostat.
The recency of the new data with more febuxostat-exposed patients overall provides greater reassurance on the safety of the drug, corresponding author Seoyoung C. Kim, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, said in an interview. “We also were able to get data on cause of death, which we did not have before when we conducted our first paper.”
Dr. Kim said she was not surprised by any of the findings, which were consistent with the results of her earlier work. “Our result on CV death also was consistent and reassuring,” she noted.
The newest Medicare claims study also corroborates results from FAST (Febuxostat Versus Allopurinol Streamlined Trial), a separate postmarketing surveillance study that was ordered by the European Medicines Agency after febuxostat’s approval in 2009. It showed that the two drugs were noninferior to each other for the risk of all-cause mortality or a composite cardiovascular outcome (hospitalization for nonfatal myocardial infarction, biomarker-positive acute coronary syndrome, nonfatal stroke, or cardiovascular death).
“While CARES showed higher CV death and all-cause death rates in febuxostat compared to allopurinol, FAST did not,” Dr. Kim noted. “Our study of more than 111,000 older gout patients treated with either febuxostat or allopurinol in real-world settings also did not find a difference in the risk of MACE, CV mortality, or all-cause mortality,” she added. “Taking these data all together, I think we can be more certain about the CV safety of febuxostat when its use is clinically indicated or needed,” she said.
Study details
Dr. Kim, first author Ajinkya Pawar, PhD, of Brigham and Women’s, and colleagues identified 467,461 people with gout aged 65 years and older who had been enrolled in Medicare for at least a year. They then used propensity-score matching to compare 27,881 first-time users of febuxostat with 83,643 first-time users of allopurinol on the primary outcome of the incidence of major adverse cardiovascular events (MACE), defined as the first occurrence of myocardial infarction, stroke, or cardiovascular mortality.
In the updated study, the mean follow‐up periods for febuxostat and allopurinol were 284 days and 339 days, respectively. Overall, febuxostat was noninferior to allopurinol with regard to MACE (hazard ratio, 0.99; 95% confidence interval, 0.93-1.05), and the results were consistent among patients with baseline CVD (HR, 0.94). In addition, rates of secondary outcomes of MI, stroke, and cardiovascular mortality were not significantly different between febuxostat and allopurinol patients, except for all-cause mortality (HR, 0.92; 95% CI, 0.87-0.98).
The study findings were limited mainly by the potential bias caused by nonadherence to medications, and potential for residual confounding and misclassification bias, the researchers noted.
However, the study was strengthened by its incident new-user design that allowed only patients with no use of either medication for a year before the first dispensing and its active comparator design, and the data are generalizable to the greater population of older gout patients, they said.
Consequently, the data from this large, real-world study support the safety of febuxostat with regard to cardiovascular risk in gout patients, including those with baseline cardiovascular disease, they concluded.
The study was supported by the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital. Dr. Kim disclosed research grants to Brigham and Women’s Hospital from Roche, Pfizer, AbbVie, and Bristol‐Myers Squibb for unrelated studies. Another author reported serving as the principal investigator with research grants from Vertex, Bayer, and Novartis to Brigham and Women’s Hospital for unrelated projects.
Febuxostat (Uloric) was not associated with increased cardiovascular risk in patients with gout when compared to those who used allopurinol, in an analysis of new users of the drugs in Medicare fee-for-service claims data from the period of 2008-2016.
The findings, published March 25 in the Journal of the American Heart Association, update and echo the results from a similar previous study by the same Brigham and Women’s Hospital research group that covered 2008-2013 Medicare claims data. That original claims data study from 2018 sought to confirm the findings of the postmarketing surveillance CARES (Cardiovascular Safety of Febuxostat and Allopurinol in Patients With Gout and Cardiovascular Morbidities) trial that led to a boxed warning for increased risk of cardiovascular and all-cause mortality vs. allopurinol. The trial, however, did not show a higher rate of major adverse cardiovascular events (MACE) overall with febuxostat.
The recency of the new data with more febuxostat-exposed patients overall provides greater reassurance on the safety of the drug, corresponding author Seoyoung C. Kim, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, said in an interview. “We also were able to get data on cause of death, which we did not have before when we conducted our first paper.”
Dr. Kim said she was not surprised by any of the findings, which were consistent with the results of her earlier work. “Our result on CV death also was consistent and reassuring,” she noted.
The newest Medicare claims study also corroborates results from FAST (Febuxostat Versus Allopurinol Streamlined Trial), a separate postmarketing surveillance study that was ordered by the European Medicines Agency after febuxostat’s approval in 2009. It showed that the two drugs were noninferior to each other for the risk of all-cause mortality or a composite cardiovascular outcome (hospitalization for nonfatal myocardial infarction, biomarker-positive acute coronary syndrome, nonfatal stroke, or cardiovascular death).
“While CARES showed higher CV death and all-cause death rates in febuxostat compared to allopurinol, FAST did not,” Dr. Kim noted. “Our study of more than 111,000 older gout patients treated with either febuxostat or allopurinol in real-world settings also did not find a difference in the risk of MACE, CV mortality, or all-cause mortality,” she added. “Taking these data all together, I think we can be more certain about the CV safety of febuxostat when its use is clinically indicated or needed,” she said.
Study details
Dr. Kim, first author Ajinkya Pawar, PhD, of Brigham and Women’s, and colleagues identified 467,461 people with gout aged 65 years and older who had been enrolled in Medicare for at least a year. They then used propensity-score matching to compare 27,881 first-time users of febuxostat with 83,643 first-time users of allopurinol on the primary outcome of the incidence of major adverse cardiovascular events (MACE), defined as the first occurrence of myocardial infarction, stroke, or cardiovascular mortality.
In the updated study, the mean follow‐up periods for febuxostat and allopurinol were 284 days and 339 days, respectively. Overall, febuxostat was noninferior to allopurinol with regard to MACE (hazard ratio, 0.99; 95% confidence interval, 0.93-1.05), and the results were consistent among patients with baseline CVD (HR, 0.94). In addition, rates of secondary outcomes of MI, stroke, and cardiovascular mortality were not significantly different between febuxostat and allopurinol patients, except for all-cause mortality (HR, 0.92; 95% CI, 0.87-0.98).
The study findings were limited mainly by the potential bias caused by nonadherence to medications, and potential for residual confounding and misclassification bias, the researchers noted.
However, the study was strengthened by its incident new-user design that allowed only patients with no use of either medication for a year before the first dispensing and its active comparator design, and the data are generalizable to the greater population of older gout patients, they said.
Consequently, the data from this large, real-world study support the safety of febuxostat with regard to cardiovascular risk in gout patients, including those with baseline cardiovascular disease, they concluded.
The study was supported by the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital. Dr. Kim disclosed research grants to Brigham and Women’s Hospital from Roche, Pfizer, AbbVie, and Bristol‐Myers Squibb for unrelated studies. Another author reported serving as the principal investigator with research grants from Vertex, Bayer, and Novartis to Brigham and Women’s Hospital for unrelated projects.
Febuxostat (Uloric) was not associated with increased cardiovascular risk in patients with gout when compared to those who used allopurinol, in an analysis of new users of the drugs in Medicare fee-for-service claims data from the period of 2008-2016.
The findings, published March 25 in the Journal of the American Heart Association, update and echo the results from a similar previous study by the same Brigham and Women’s Hospital research group that covered 2008-2013 Medicare claims data. That original claims data study from 2018 sought to confirm the findings of the postmarketing surveillance CARES (Cardiovascular Safety of Febuxostat and Allopurinol in Patients With Gout and Cardiovascular Morbidities) trial that led to a boxed warning for increased risk of cardiovascular and all-cause mortality vs. allopurinol. The trial, however, did not show a higher rate of major adverse cardiovascular events (MACE) overall with febuxostat.
The recency of the new data with more febuxostat-exposed patients overall provides greater reassurance on the safety of the drug, corresponding author Seoyoung C. Kim, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, said in an interview. “We also were able to get data on cause of death, which we did not have before when we conducted our first paper.”
Dr. Kim said she was not surprised by any of the findings, which were consistent with the results of her earlier work. “Our result on CV death also was consistent and reassuring,” she noted.
The newest Medicare claims study also corroborates results from FAST (Febuxostat Versus Allopurinol Streamlined Trial), a separate postmarketing surveillance study that was ordered by the European Medicines Agency after febuxostat’s approval in 2009. It showed that the two drugs were noninferior to each other for the risk of all-cause mortality or a composite cardiovascular outcome (hospitalization for nonfatal myocardial infarction, biomarker-positive acute coronary syndrome, nonfatal stroke, or cardiovascular death).
“While CARES showed higher CV death and all-cause death rates in febuxostat compared to allopurinol, FAST did not,” Dr. Kim noted. “Our study of more than 111,000 older gout patients treated with either febuxostat or allopurinol in real-world settings also did not find a difference in the risk of MACE, CV mortality, or all-cause mortality,” she added. “Taking these data all together, I think we can be more certain about the CV safety of febuxostat when its use is clinically indicated or needed,” she said.
Study details
Dr. Kim, first author Ajinkya Pawar, PhD, of Brigham and Women’s, and colleagues identified 467,461 people with gout aged 65 years and older who had been enrolled in Medicare for at least a year. They then used propensity-score matching to compare 27,881 first-time users of febuxostat with 83,643 first-time users of allopurinol on the primary outcome of the incidence of major adverse cardiovascular events (MACE), defined as the first occurrence of myocardial infarction, stroke, or cardiovascular mortality.
In the updated study, the mean follow‐up periods for febuxostat and allopurinol were 284 days and 339 days, respectively. Overall, febuxostat was noninferior to allopurinol with regard to MACE (hazard ratio, 0.99; 95% confidence interval, 0.93-1.05), and the results were consistent among patients with baseline CVD (HR, 0.94). In addition, rates of secondary outcomes of MI, stroke, and cardiovascular mortality were not significantly different between febuxostat and allopurinol patients, except for all-cause mortality (HR, 0.92; 95% CI, 0.87-0.98).
The study findings were limited mainly by the potential bias caused by nonadherence to medications, and potential for residual confounding and misclassification bias, the researchers noted.
However, the study was strengthened by its incident new-user design that allowed only patients with no use of either medication for a year before the first dispensing and its active comparator design, and the data are generalizable to the greater population of older gout patients, they said.
Consequently, the data from this large, real-world study support the safety of febuxostat with regard to cardiovascular risk in gout patients, including those with baseline cardiovascular disease, they concluded.
The study was supported by the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital. Dr. Kim disclosed research grants to Brigham and Women’s Hospital from Roche, Pfizer, AbbVie, and Bristol‐Myers Squibb for unrelated studies. Another author reported serving as the principal investigator with research grants from Vertex, Bayer, and Novartis to Brigham and Women’s Hospital for unrelated projects.
FROM THE JOURNAL OF THE AMERICAN HEART ASSOCIATION