User login
Once again, no survival benefit with PCI, surgery in stable CAD
Coronary revascularization does not confer a survival advantage over initial medical therapy in patients with stable ischemic heart disease (SIHD) but reduces unstable angina, according to a new study-level meta-analysis.
Routine upfront revascularization is also associated with less spontaneous myocardial infarction but this is at the cost of increased procedural infarctions, reported lead investigator Sripal Bangalore, MD, of New York University.
“These relationships should be taken into consideration for shared decision-making for the management of patients with stable ischemic heart disease,” he said in a late-breaking trial session at PCR e-Course 2020, the virtual meeting of the Congress of European Association of Percutaneous Cardiovascular Interventions (EuroPCR).
The results, simultaneously published in Circulation, are consistent with last year’s ISCHEMIA trial and other contemporary trials, such as COURAGE, FAME 2, and BARI 2D, that have failed to show a reduction in mortality with revascularization alone in SIHD. Guidelines continue, however, to recommend revascularization to improve survival in SIHD based on trials performed in the 1980s when medical therapy was limited, Dr. Bangalore observed.
The updated meta-analysis included 14 randomized controlled trials, including the aforementioned, and 14,877 patients followed for a weighted mean of 4.5 years. Most trials enrolled patients who had preserved left ventricular function and low symptom burden (Canadian Cardiovascular Society Class I/II).
In the revascularization group, 87.5% of patients underwent any revascularization. Percutaneous coronary intervention (PCI) was the first procedure in 71.3% and bypass surgery the first choice in 16.2%. In eight trials, stents were used in at least 50% of PCI patients; drug-eluting stents were mainly used in FAME 2, ISCHEMIA, and ISCHEMIA-CKD.
In eight trials, statins were used in at least 50% of patients. Nearly 1 in 3 patients (31.9%) treated initially with medical therapy underwent revascularization during follow-up.
Results show no reduction in mortality risk with routine revascularization in the overall analysis (relative risk, 0.99; 95% confidence interval, 0.90-1.09) or when analyzed by whether studies did or did not use stents (P for interaction = .85).
Trial sequential analysis also showed that the cumulative z-curve crossed the futility boundary, “suggesting we have great data to show that there is lack of even a 10% reduction in death with revascularization,” Dr. Bangalore said.
Results were very similar for cardiovascular death (RR, 0.92; 95% CI, 0.80-1.06), including when analyzed by study stent status (P for interaction = .60).
There was no significant reduction in overall MI risk with revascularization, although a borderline significant 11% decrease in MIs was found in the contemporary stent era trials (RR, 0.89; 95% CI, 0.80-0.998).
Revascularization was associated with a 148% increase in the risk of procedural MI (RR, 2.48; 95% CI, 1.86-3.31) but reduced risk of spontaneous MI (RR, 0.76; 95% CI, 0.67-0.85).
Unstable angina was reduced in patients undergoing revascularization (RR, 0.64; 95% CI, 0.45-0.92), driven by a 55% reduction in the contemporary stent era trials. Freedom from angina was also greater with routine revascularization but the difference was modest, Dr. Bangalore said. There was no difference between the two strategies in heart failure or stroke.
“This meta-analysis is well done but really doesn’t change what we already know,” Rasha Al-Lamee, MBBS, of Imperial College, London, said in an interview. “The most important message is that intervention in stable CAD does not change survival. We don’t need to rush to intervene: We have time to plan the best strategy for each patient and to modify our plans based on their response.”
The analysis addresses some of the issues with previous meta-analyses that have included trials that were not strictly stable CAD trials such as SWISSI-2, COMPARE-ACUTE, and DANAMI-3-PRIMULTI, she noted. “However a study like this is only as good as the trials that are included. We must remember that unblinded trials really cannot be used to accurately assess endpoints that are prone to bias such as unstable angina and freedom from angina.”
Following the presentation, dedicated discussant Davide Capodanno, MD, PhD, of the University of Catania (Italy) said, “We have seen beyond any doubt that there is no difference in mortality. For cardiovascular death, it’s pretty much the same. It’s a little bit more mixed and nuanced, the story of myocardial infarction.”
“Additional science is needed to understand the prognostic implications,” he said. “Of course we know that spontaneous myocardial infarction is bad, but I’m not so sure about periprocedural MI. Is this something that is as important as spontaneous myocardial infarction?”
The meta-analysis is the largest ever performed, but there was clinical heterogeneity in the individual studies, especially in the definition of MI, Dr. Capodanno observed. Because of the use of trial-level data rather than patient-level data, the analysis also could not account for adherence to treatment or the effect of stent type or medication dosage.
The MI issue really depends on the trial definition of MI, Dr. Al-Lamee said. “We need long-term follow-up from ISCHEMIA to understand what it means for our patients. While revascularization clearly increases procedural MI rates, it also results in lower spontaneous MI rates with no impact on overall MI or death,” she said. “We will only know if these MIs are important if we see what impact they have in the long term.”
Although the meta-analysis combined data from several decades, it’s likely that the outdated revascularization techniques in the older trials are balanced out by the outdated medical therapy in the same trials, Dr. Al-Lamee observed.
The new findings can certainly be used in patient-physician discussions, with more follow-up from ISCHEMIA to provide additional insights, she said.
“We will of course hear more about the placebo-controlled efficacy of PCI in the blinded ORBITA-2 trial. And I would really like to see some of the older studies of patients and perceptions of the effect of PCI repeated,” Dr. Al-Lamee said. “Now we have more data, are we informing our patients and referrers correctly of the impact of our procedures, and do they truly choose revascularization with a true awareness of what it does and does not do?”
Dr. Bangalore reported grants from the National Heart, Lung, and Blood Institute and Abbott Vascular; and serving on the advisory boards of Abbott Vascular, Biotronik, Meril, SMT, Pfizer, Amgen, and Reata. Dr. Al-Lamee reported speaker’s honorarium from Philips Volcano and Menarini Pharmaceuticals. Dr. Capodanno has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Coronary revascularization does not confer a survival advantage over initial medical therapy in patients with stable ischemic heart disease (SIHD) but reduces unstable angina, according to a new study-level meta-analysis.
Routine upfront revascularization is also associated with less spontaneous myocardial infarction but this is at the cost of increased procedural infarctions, reported lead investigator Sripal Bangalore, MD, of New York University.
“These relationships should be taken into consideration for shared decision-making for the management of patients with stable ischemic heart disease,” he said in a late-breaking trial session at PCR e-Course 2020, the virtual meeting of the Congress of European Association of Percutaneous Cardiovascular Interventions (EuroPCR).
The results, simultaneously published in Circulation, are consistent with last year’s ISCHEMIA trial and other contemporary trials, such as COURAGE, FAME 2, and BARI 2D, that have failed to show a reduction in mortality with revascularization alone in SIHD. Guidelines continue, however, to recommend revascularization to improve survival in SIHD based on trials performed in the 1980s when medical therapy was limited, Dr. Bangalore observed.
The updated meta-analysis included 14 randomized controlled trials, including the aforementioned, and 14,877 patients followed for a weighted mean of 4.5 years. Most trials enrolled patients who had preserved left ventricular function and low symptom burden (Canadian Cardiovascular Society Class I/II).
In the revascularization group, 87.5% of patients underwent any revascularization. Percutaneous coronary intervention (PCI) was the first procedure in 71.3% and bypass surgery the first choice in 16.2%. In eight trials, stents were used in at least 50% of PCI patients; drug-eluting stents were mainly used in FAME 2, ISCHEMIA, and ISCHEMIA-CKD.
In eight trials, statins were used in at least 50% of patients. Nearly 1 in 3 patients (31.9%) treated initially with medical therapy underwent revascularization during follow-up.
Results show no reduction in mortality risk with routine revascularization in the overall analysis (relative risk, 0.99; 95% confidence interval, 0.90-1.09) or when analyzed by whether studies did or did not use stents (P for interaction = .85).
Trial sequential analysis also showed that the cumulative z-curve crossed the futility boundary, “suggesting we have great data to show that there is lack of even a 10% reduction in death with revascularization,” Dr. Bangalore said.
Results were very similar for cardiovascular death (RR, 0.92; 95% CI, 0.80-1.06), including when analyzed by study stent status (P for interaction = .60).
There was no significant reduction in overall MI risk with revascularization, although a borderline significant 11% decrease in MIs was found in the contemporary stent era trials (RR, 0.89; 95% CI, 0.80-0.998).
Revascularization was associated with a 148% increase in the risk of procedural MI (RR, 2.48; 95% CI, 1.86-3.31) but reduced risk of spontaneous MI (RR, 0.76; 95% CI, 0.67-0.85).
Unstable angina was reduced in patients undergoing revascularization (RR, 0.64; 95% CI, 0.45-0.92), driven by a 55% reduction in the contemporary stent era trials. Freedom from angina was also greater with routine revascularization but the difference was modest, Dr. Bangalore said. There was no difference between the two strategies in heart failure or stroke.
“This meta-analysis is well done but really doesn’t change what we already know,” Rasha Al-Lamee, MBBS, of Imperial College, London, said in an interview. “The most important message is that intervention in stable CAD does not change survival. We don’t need to rush to intervene: We have time to plan the best strategy for each patient and to modify our plans based on their response.”
The analysis addresses some of the issues with previous meta-analyses that have included trials that were not strictly stable CAD trials such as SWISSI-2, COMPARE-ACUTE, and DANAMI-3-PRIMULTI, she noted. “However a study like this is only as good as the trials that are included. We must remember that unblinded trials really cannot be used to accurately assess endpoints that are prone to bias such as unstable angina and freedom from angina.”
Following the presentation, dedicated discussant Davide Capodanno, MD, PhD, of the University of Catania (Italy) said, “We have seen beyond any doubt that there is no difference in mortality. For cardiovascular death, it’s pretty much the same. It’s a little bit more mixed and nuanced, the story of myocardial infarction.”
“Additional science is needed to understand the prognostic implications,” he said. “Of course we know that spontaneous myocardial infarction is bad, but I’m not so sure about periprocedural MI. Is this something that is as important as spontaneous myocardial infarction?”
The meta-analysis is the largest ever performed, but there was clinical heterogeneity in the individual studies, especially in the definition of MI, Dr. Capodanno observed. Because of the use of trial-level data rather than patient-level data, the analysis also could not account for adherence to treatment or the effect of stent type or medication dosage.
The MI issue really depends on the trial definition of MI, Dr. Al-Lamee said. “We need long-term follow-up from ISCHEMIA to understand what it means for our patients. While revascularization clearly increases procedural MI rates, it also results in lower spontaneous MI rates with no impact on overall MI or death,” she said. “We will only know if these MIs are important if we see what impact they have in the long term.”
Although the meta-analysis combined data from several decades, it’s likely that the outdated revascularization techniques in the older trials are balanced out by the outdated medical therapy in the same trials, Dr. Al-Lamee observed.
The new findings can certainly be used in patient-physician discussions, with more follow-up from ISCHEMIA to provide additional insights, she said.
“We will of course hear more about the placebo-controlled efficacy of PCI in the blinded ORBITA-2 trial. And I would really like to see some of the older studies of patients and perceptions of the effect of PCI repeated,” Dr. Al-Lamee said. “Now we have more data, are we informing our patients and referrers correctly of the impact of our procedures, and do they truly choose revascularization with a true awareness of what it does and does not do?”
Dr. Bangalore reported grants from the National Heart, Lung, and Blood Institute and Abbott Vascular; and serving on the advisory boards of Abbott Vascular, Biotronik, Meril, SMT, Pfizer, Amgen, and Reata. Dr. Al-Lamee reported speaker’s honorarium from Philips Volcano and Menarini Pharmaceuticals. Dr. Capodanno has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Coronary revascularization does not confer a survival advantage over initial medical therapy in patients with stable ischemic heart disease (SIHD) but reduces unstable angina, according to a new study-level meta-analysis.
Routine upfront revascularization is also associated with less spontaneous myocardial infarction but this is at the cost of increased procedural infarctions, reported lead investigator Sripal Bangalore, MD, of New York University.
“These relationships should be taken into consideration for shared decision-making for the management of patients with stable ischemic heart disease,” he said in a late-breaking trial session at PCR e-Course 2020, the virtual meeting of the Congress of European Association of Percutaneous Cardiovascular Interventions (EuroPCR).
The results, simultaneously published in Circulation, are consistent with last year’s ISCHEMIA trial and other contemporary trials, such as COURAGE, FAME 2, and BARI 2D, that have failed to show a reduction in mortality with revascularization alone in SIHD. Guidelines continue, however, to recommend revascularization to improve survival in SIHD based on trials performed in the 1980s when medical therapy was limited, Dr. Bangalore observed.
The updated meta-analysis included 14 randomized controlled trials, including the aforementioned, and 14,877 patients followed for a weighted mean of 4.5 years. Most trials enrolled patients who had preserved left ventricular function and low symptom burden (Canadian Cardiovascular Society Class I/II).
In the revascularization group, 87.5% of patients underwent any revascularization. Percutaneous coronary intervention (PCI) was the first procedure in 71.3% and bypass surgery the first choice in 16.2%. In eight trials, stents were used in at least 50% of PCI patients; drug-eluting stents were mainly used in FAME 2, ISCHEMIA, and ISCHEMIA-CKD.
In eight trials, statins were used in at least 50% of patients. Nearly 1 in 3 patients (31.9%) treated initially with medical therapy underwent revascularization during follow-up.
Results show no reduction in mortality risk with routine revascularization in the overall analysis (relative risk, 0.99; 95% confidence interval, 0.90-1.09) or when analyzed by whether studies did or did not use stents (P for interaction = .85).
Trial sequential analysis also showed that the cumulative z-curve crossed the futility boundary, “suggesting we have great data to show that there is lack of even a 10% reduction in death with revascularization,” Dr. Bangalore said.
Results were very similar for cardiovascular death (RR, 0.92; 95% CI, 0.80-1.06), including when analyzed by study stent status (P for interaction = .60).
There was no significant reduction in overall MI risk with revascularization, although a borderline significant 11% decrease in MIs was found in the contemporary stent era trials (RR, 0.89; 95% CI, 0.80-0.998).
Revascularization was associated with a 148% increase in the risk of procedural MI (RR, 2.48; 95% CI, 1.86-3.31) but reduced risk of spontaneous MI (RR, 0.76; 95% CI, 0.67-0.85).
Unstable angina was reduced in patients undergoing revascularization (RR, 0.64; 95% CI, 0.45-0.92), driven by a 55% reduction in the contemporary stent era trials. Freedom from angina was also greater with routine revascularization but the difference was modest, Dr. Bangalore said. There was no difference between the two strategies in heart failure or stroke.
“This meta-analysis is well done but really doesn’t change what we already know,” Rasha Al-Lamee, MBBS, of Imperial College, London, said in an interview. “The most important message is that intervention in stable CAD does not change survival. We don’t need to rush to intervene: We have time to plan the best strategy for each patient and to modify our plans based on their response.”
The analysis addresses some of the issues with previous meta-analyses that have included trials that were not strictly stable CAD trials such as SWISSI-2, COMPARE-ACUTE, and DANAMI-3-PRIMULTI, she noted. “However a study like this is only as good as the trials that are included. We must remember that unblinded trials really cannot be used to accurately assess endpoints that are prone to bias such as unstable angina and freedom from angina.”
Following the presentation, dedicated discussant Davide Capodanno, MD, PhD, of the University of Catania (Italy) said, “We have seen beyond any doubt that there is no difference in mortality. For cardiovascular death, it’s pretty much the same. It’s a little bit more mixed and nuanced, the story of myocardial infarction.”
“Additional science is needed to understand the prognostic implications,” he said. “Of course we know that spontaneous myocardial infarction is bad, but I’m not so sure about periprocedural MI. Is this something that is as important as spontaneous myocardial infarction?”
The meta-analysis is the largest ever performed, but there was clinical heterogeneity in the individual studies, especially in the definition of MI, Dr. Capodanno observed. Because of the use of trial-level data rather than patient-level data, the analysis also could not account for adherence to treatment or the effect of stent type or medication dosage.
The MI issue really depends on the trial definition of MI, Dr. Al-Lamee said. “We need long-term follow-up from ISCHEMIA to understand what it means for our patients. While revascularization clearly increases procedural MI rates, it also results in lower spontaneous MI rates with no impact on overall MI or death,” she said. “We will only know if these MIs are important if we see what impact they have in the long term.”
Although the meta-analysis combined data from several decades, it’s likely that the outdated revascularization techniques in the older trials are balanced out by the outdated medical therapy in the same trials, Dr. Al-Lamee observed.
The new findings can certainly be used in patient-physician discussions, with more follow-up from ISCHEMIA to provide additional insights, she said.
“We will of course hear more about the placebo-controlled efficacy of PCI in the blinded ORBITA-2 trial. And I would really like to see some of the older studies of patients and perceptions of the effect of PCI repeated,” Dr. Al-Lamee said. “Now we have more data, are we informing our patients and referrers correctly of the impact of our procedures, and do they truly choose revascularization with a true awareness of what it does and does not do?”
Dr. Bangalore reported grants from the National Heart, Lung, and Blood Institute and Abbott Vascular; and serving on the advisory boards of Abbott Vascular, Biotronik, Meril, SMT, Pfizer, Amgen, and Reata. Dr. Al-Lamee reported speaker’s honorarium from Philips Volcano and Menarini Pharmaceuticals. Dr. Capodanno has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Treatment developments in obstructive hypertrophic cardiomyopathy (oHCM)
Background: oHCM is characterized by mutations in sarcomeric proteins. Mavacamten is a small-molecule modulator of cardiac myosin, commonly affected in oHCM.
Study design: Open-label, nonrandomized phase 2 trial.
Setting: Five academic medical centers.
Synopsis: A total of 21 patients with oHCM were randomized to cohort A, high-dose mavacamten without additional therapy (beta-blockers, CCBs), or cohort B, low-dose mavacamten plus additional medical therapy. The LVOT gradient at 12 weeks improved in both cohorts: Cohort A had a mean change of –89.5 mm Hg (95% confidence interval, –138.3 to –40.7; P = .008) and cohort B –25.0 mm Hg (95% CI, –47.1 to –3.0, P = .020).
Bottom line: This phase 2 trial provides proof of concept and identified a plasma concentration of mavacamten needed to decrease the LVOT significantly. Phase 3 trials hold significant promise.
Citation: Heitner SB et al. Mavacamten treatment for obstructive hypertrophic cardiomyopathy: A clinical trial. Ann Intern Med. 2019 Apr 30. doi: 10.7326/M18-3016.
Dr. Blount is a hospitalist at the University of Colorado at Denver, Aurora.
Background: oHCM is characterized by mutations in sarcomeric proteins. Mavacamten is a small-molecule modulator of cardiac myosin, commonly affected in oHCM.
Study design: Open-label, nonrandomized phase 2 trial.
Setting: Five academic medical centers.
Synopsis: A total of 21 patients with oHCM were randomized to cohort A, high-dose mavacamten without additional therapy (beta-blockers, CCBs), or cohort B, low-dose mavacamten plus additional medical therapy. The LVOT gradient at 12 weeks improved in both cohorts: Cohort A had a mean change of –89.5 mm Hg (95% confidence interval, –138.3 to –40.7; P = .008) and cohort B –25.0 mm Hg (95% CI, –47.1 to –3.0, P = .020).
Bottom line: This phase 2 trial provides proof of concept and identified a plasma concentration of mavacamten needed to decrease the LVOT significantly. Phase 3 trials hold significant promise.
Citation: Heitner SB et al. Mavacamten treatment for obstructive hypertrophic cardiomyopathy: A clinical trial. Ann Intern Med. 2019 Apr 30. doi: 10.7326/M18-3016.
Dr. Blount is a hospitalist at the University of Colorado at Denver, Aurora.
Background: oHCM is characterized by mutations in sarcomeric proteins. Mavacamten is a small-molecule modulator of cardiac myosin, commonly affected in oHCM.
Study design: Open-label, nonrandomized phase 2 trial.
Setting: Five academic medical centers.
Synopsis: A total of 21 patients with oHCM were randomized to cohort A, high-dose mavacamten without additional therapy (beta-blockers, CCBs), or cohort B, low-dose mavacamten plus additional medical therapy. The LVOT gradient at 12 weeks improved in both cohorts: Cohort A had a mean change of –89.5 mm Hg (95% confidence interval, –138.3 to –40.7; P = .008) and cohort B –25.0 mm Hg (95% CI, –47.1 to –3.0, P = .020).
Bottom line: This phase 2 trial provides proof of concept and identified a plasma concentration of mavacamten needed to decrease the LVOT significantly. Phase 3 trials hold significant promise.
Citation: Heitner SB et al. Mavacamten treatment for obstructive hypertrophic cardiomyopathy: A clinical trial. Ann Intern Med. 2019 Apr 30. doi: 10.7326/M18-3016.
Dr. Blount is a hospitalist at the University of Colorado at Denver, Aurora.
Suboptimal statin response predicts future risk
Background: Rates of LDL-C reduction with statin therapy vary based on biological and genetic factors, as well as adherence. In a general primary prevention population at cardiovascular risk, little is known about the extent of this variability or its impact on outcomes.
Study design: Prospective cohort study.
Setting: Primary care practices in England and Wales.
Synopsis: Across a cohort of 183,213 patients, 51.2% had a suboptimal response, defined as a less than 40% proportional reduction in LDL-C. During more than 1 million person-years of follow-up, suboptimal statin response at 2 years was associated with a 20% higher hazard ratio for incident cardiovascular disease.Bottom line: Half of patients do not have a sufficient response to statins, with higher attendant future risk.
Citation: Akyea RK et al. Suboptimal cholesterol response to initiation of statins and future risk of cardiovascular disease. Heart. 2019 Apr 15;0:1-7. doi: 10.1136/heartjnl-2018-314253.
Dr. Anderson is chief, hospital medicine section, and deputy chief, medicine service, at the Veterans Affairs Eastern Colorado Health Care System, Aurora.
Background: Rates of LDL-C reduction with statin therapy vary based on biological and genetic factors, as well as adherence. In a general primary prevention population at cardiovascular risk, little is known about the extent of this variability or its impact on outcomes.
Study design: Prospective cohort study.
Setting: Primary care practices in England and Wales.
Synopsis: Across a cohort of 183,213 patients, 51.2% had a suboptimal response, defined as a less than 40% proportional reduction in LDL-C. During more than 1 million person-years of follow-up, suboptimal statin response at 2 years was associated with a 20% higher hazard ratio for incident cardiovascular disease.Bottom line: Half of patients do not have a sufficient response to statins, with higher attendant future risk.
Citation: Akyea RK et al. Suboptimal cholesterol response to initiation of statins and future risk of cardiovascular disease. Heart. 2019 Apr 15;0:1-7. doi: 10.1136/heartjnl-2018-314253.
Dr. Anderson is chief, hospital medicine section, and deputy chief, medicine service, at the Veterans Affairs Eastern Colorado Health Care System, Aurora.
Background: Rates of LDL-C reduction with statin therapy vary based on biological and genetic factors, as well as adherence. In a general primary prevention population at cardiovascular risk, little is known about the extent of this variability or its impact on outcomes.
Study design: Prospective cohort study.
Setting: Primary care practices in England and Wales.
Synopsis: Across a cohort of 183,213 patients, 51.2% had a suboptimal response, defined as a less than 40% proportional reduction in LDL-C. During more than 1 million person-years of follow-up, suboptimal statin response at 2 years was associated with a 20% higher hazard ratio for incident cardiovascular disease.Bottom line: Half of patients do not have a sufficient response to statins, with higher attendant future risk.
Citation: Akyea RK et al. Suboptimal cholesterol response to initiation of statins and future risk of cardiovascular disease. Heart. 2019 Apr 15;0:1-7. doi: 10.1136/heartjnl-2018-314253.
Dr. Anderson is chief, hospital medicine section, and deputy chief, medicine service, at the Veterans Affairs Eastern Colorado Health Care System, Aurora.
Findings of most heart failure trials reported late or not at all
A large proportion of results from heart failure trials registered with clinicaltrials.gov are published a year or more after completion or not at all, which violates the U.S. FDA Amendments Act (FDAAA), according to a detailed analysis of the interventional and observational trials in this database.
Of the 1,429 heart failure trials identified, 75% of which were randomized interventional studies and the remainder of which were observational, fewer than 20% met the FDAAA 1-year reporting requirement, and 44% have yet to be published at all, reported a team of collaborative investigators led by cardiologists from the Inova Heart and Vascular Institute (IHVI), Falls Church, Va.
“I believe the critical issue is that the FDAAA has thus far never been enforced,” reported Christopher M. O’Connor, MD, a cardiologist and president of IHVI. He was the senior author of the study, reported in the Journal of the American College of Cardiology.
To improve systematic reporting of clinical trials, including negative results, clinicaltrials.gov was created in 2000. In 2007, the FDAAA enacted rules to broaden the requirements for reporting and to make timely reporting of results mandatory.
Ten years later, the FDA was finally authorized to issue a penalty of $10,000 for failure to release results in a timely fashion, a provision of the 2007 amendment but not confirmed at that time, the investigators reported. In the majority of cases, timely reporting was defined as within 12 months of completion of the trial.
The new study shows that reporting of completed trials, timely or otherwise, remains low. Of the 1,243 trials completed after 2007, the proportion meeting the 1-year reporting requirement was just 20%. Although a significant improvement over the 13% reporting in this time frame before 2007, more than 80% of findings are not being released in a timely manner more than 10 years after this was made mandatory.
There are a number of reasons to consider this to be a serious issue, according to Mandeep R. Mehra, MD, of Brigham and Women’s Hospital, Boston. One of the authors of an accompanying editorial regarding this analysis, Dr. Mehra called underreporting “a public health matter because it is an impediment to medical discovery and poses plausible threats to patient safety.”
Among studies registered after 2007, publication rates were higher for trials funded by the National Institutes of Health (71%) relative to industry (49%) or the U.S. Veterans Affairs (45%).
Publication rates were also higher among interventional relative to observational trials (59% vs. 46%) and trials that enrolled more than 1,000 patients relative to those enrolling fewer than 150 (77% vs. 51%), although trial size was not a significant predictor of publication on multivariate analysis. Clinical endpoints, such as death or hospitalization, were also associated with a greater likelihood of publication relative to nonclinical endpoints.
Of the 251 trials terminated before completion, findings were published within 1 year in only 6%. Two years after completion, only 20% were published at all.
Results consistent with the primary hypothesis did not predict timely publication, but only 39% of the studies listed a primary hypothesis. Since 2017, this is another violation of the FDAAA, according to Dr. O’Connor.
The problem is not unique to heart failure trials, according to the authors who cited numerous studies showing low rates of timely publication in other therapeutic areas. Heart failure was selected for evaluation in this study mainly to keep the analysis feasible, although the authors contend this is an area with an urgent need for better treatments.
The problem needs to be fixed, according to Dr. Mehra. In his editorial, he called for rules to be “transitioned to regulations and action taken for underreporting.” Dr. O’Connor agreed.
“A combination of carrots and sticks might be needed to achieve sufficient result sharing,” Dr. O’Connor said. He suggested that stakeholders, such as investigators, sponsors, regulators, and journal editors, should collaborate to address the problem.
So far, the FDA has never levied a fine for lack of reporting or for failure to report in a timely manner. Routine imposition of large fines might not be viable, given the complex reasons that delay or inhibit publication of trial findings, but it would be a large source of revenue.
“According to the FDAAA TrialsTracker, a live tool that tracks FDAAA compliance and promotes trial transparency, the U.S. government could already have imposed more than $2.8 billion in fines for trials due after January 2018,” Dr. O’Connor reported.
The first and senior authors are among those who report financial relationships with pharmaceutical companies.
SOURCE: Psotka MA et al. J Am Coll Cardiol. 2020;75:3151-61.
A large proportion of results from heart failure trials registered with clinicaltrials.gov are published a year or more after completion or not at all, which violates the U.S. FDA Amendments Act (FDAAA), according to a detailed analysis of the interventional and observational trials in this database.
Of the 1,429 heart failure trials identified, 75% of which were randomized interventional studies and the remainder of which were observational, fewer than 20% met the FDAAA 1-year reporting requirement, and 44% have yet to be published at all, reported a team of collaborative investigators led by cardiologists from the Inova Heart and Vascular Institute (IHVI), Falls Church, Va.
“I believe the critical issue is that the FDAAA has thus far never been enforced,” reported Christopher M. O’Connor, MD, a cardiologist and president of IHVI. He was the senior author of the study, reported in the Journal of the American College of Cardiology.
To improve systematic reporting of clinical trials, including negative results, clinicaltrials.gov was created in 2000. In 2007, the FDAAA enacted rules to broaden the requirements for reporting and to make timely reporting of results mandatory.
Ten years later, the FDA was finally authorized to issue a penalty of $10,000 for failure to release results in a timely fashion, a provision of the 2007 amendment but not confirmed at that time, the investigators reported. In the majority of cases, timely reporting was defined as within 12 months of completion of the trial.
The new study shows that reporting of completed trials, timely or otherwise, remains low. Of the 1,243 trials completed after 2007, the proportion meeting the 1-year reporting requirement was just 20%. Although a significant improvement over the 13% reporting in this time frame before 2007, more than 80% of findings are not being released in a timely manner more than 10 years after this was made mandatory.
There are a number of reasons to consider this to be a serious issue, according to Mandeep R. Mehra, MD, of Brigham and Women’s Hospital, Boston. One of the authors of an accompanying editorial regarding this analysis, Dr. Mehra called underreporting “a public health matter because it is an impediment to medical discovery and poses plausible threats to patient safety.”
Among studies registered after 2007, publication rates were higher for trials funded by the National Institutes of Health (71%) relative to industry (49%) or the U.S. Veterans Affairs (45%).
Publication rates were also higher among interventional relative to observational trials (59% vs. 46%) and trials that enrolled more than 1,000 patients relative to those enrolling fewer than 150 (77% vs. 51%), although trial size was not a significant predictor of publication on multivariate analysis. Clinical endpoints, such as death or hospitalization, were also associated with a greater likelihood of publication relative to nonclinical endpoints.
Of the 251 trials terminated before completion, findings were published within 1 year in only 6%. Two years after completion, only 20% were published at all.
Results consistent with the primary hypothesis did not predict timely publication, but only 39% of the studies listed a primary hypothesis. Since 2017, this is another violation of the FDAAA, according to Dr. O’Connor.
The problem is not unique to heart failure trials, according to the authors who cited numerous studies showing low rates of timely publication in other therapeutic areas. Heart failure was selected for evaluation in this study mainly to keep the analysis feasible, although the authors contend this is an area with an urgent need for better treatments.
The problem needs to be fixed, according to Dr. Mehra. In his editorial, he called for rules to be “transitioned to regulations and action taken for underreporting.” Dr. O’Connor agreed.
“A combination of carrots and sticks might be needed to achieve sufficient result sharing,” Dr. O’Connor said. He suggested that stakeholders, such as investigators, sponsors, regulators, and journal editors, should collaborate to address the problem.
So far, the FDA has never levied a fine for lack of reporting or for failure to report in a timely manner. Routine imposition of large fines might not be viable, given the complex reasons that delay or inhibit publication of trial findings, but it would be a large source of revenue.
“According to the FDAAA TrialsTracker, a live tool that tracks FDAAA compliance and promotes trial transparency, the U.S. government could already have imposed more than $2.8 billion in fines for trials due after January 2018,” Dr. O’Connor reported.
The first and senior authors are among those who report financial relationships with pharmaceutical companies.
SOURCE: Psotka MA et al. J Am Coll Cardiol. 2020;75:3151-61.
A large proportion of results from heart failure trials registered with clinicaltrials.gov are published a year or more after completion or not at all, which violates the U.S. FDA Amendments Act (FDAAA), according to a detailed analysis of the interventional and observational trials in this database.
Of the 1,429 heart failure trials identified, 75% of which were randomized interventional studies and the remainder of which were observational, fewer than 20% met the FDAAA 1-year reporting requirement, and 44% have yet to be published at all, reported a team of collaborative investigators led by cardiologists from the Inova Heart and Vascular Institute (IHVI), Falls Church, Va.
“I believe the critical issue is that the FDAAA has thus far never been enforced,” reported Christopher M. O’Connor, MD, a cardiologist and president of IHVI. He was the senior author of the study, reported in the Journal of the American College of Cardiology.
To improve systematic reporting of clinical trials, including negative results, clinicaltrials.gov was created in 2000. In 2007, the FDAAA enacted rules to broaden the requirements for reporting and to make timely reporting of results mandatory.
Ten years later, the FDA was finally authorized to issue a penalty of $10,000 for failure to release results in a timely fashion, a provision of the 2007 amendment but not confirmed at that time, the investigators reported. In the majority of cases, timely reporting was defined as within 12 months of completion of the trial.
The new study shows that reporting of completed trials, timely or otherwise, remains low. Of the 1,243 trials completed after 2007, the proportion meeting the 1-year reporting requirement was just 20%. Although a significant improvement over the 13% reporting in this time frame before 2007, more than 80% of findings are not being released in a timely manner more than 10 years after this was made mandatory.
There are a number of reasons to consider this to be a serious issue, according to Mandeep R. Mehra, MD, of Brigham and Women’s Hospital, Boston. One of the authors of an accompanying editorial regarding this analysis, Dr. Mehra called underreporting “a public health matter because it is an impediment to medical discovery and poses plausible threats to patient safety.”
Among studies registered after 2007, publication rates were higher for trials funded by the National Institutes of Health (71%) relative to industry (49%) or the U.S. Veterans Affairs (45%).
Publication rates were also higher among interventional relative to observational trials (59% vs. 46%) and trials that enrolled more than 1,000 patients relative to those enrolling fewer than 150 (77% vs. 51%), although trial size was not a significant predictor of publication on multivariate analysis. Clinical endpoints, such as death or hospitalization, were also associated with a greater likelihood of publication relative to nonclinical endpoints.
Of the 251 trials terminated before completion, findings were published within 1 year in only 6%. Two years after completion, only 20% were published at all.
Results consistent with the primary hypothesis did not predict timely publication, but only 39% of the studies listed a primary hypothesis. Since 2017, this is another violation of the FDAAA, according to Dr. O’Connor.
The problem is not unique to heart failure trials, according to the authors who cited numerous studies showing low rates of timely publication in other therapeutic areas. Heart failure was selected for evaluation in this study mainly to keep the analysis feasible, although the authors contend this is an area with an urgent need for better treatments.
The problem needs to be fixed, according to Dr. Mehra. In his editorial, he called for rules to be “transitioned to regulations and action taken for underreporting.” Dr. O’Connor agreed.
“A combination of carrots and sticks might be needed to achieve sufficient result sharing,” Dr. O’Connor said. He suggested that stakeholders, such as investigators, sponsors, regulators, and journal editors, should collaborate to address the problem.
So far, the FDA has never levied a fine for lack of reporting or for failure to report in a timely manner. Routine imposition of large fines might not be viable, given the complex reasons that delay or inhibit publication of trial findings, but it would be a large source of revenue.
“According to the FDAAA TrialsTracker, a live tool that tracks FDAAA compliance and promotes trial transparency, the U.S. government could already have imposed more than $2.8 billion in fines for trials due after January 2018,” Dr. O’Connor reported.
The first and senior authors are among those who report financial relationships with pharmaceutical companies.
SOURCE: Psotka MA et al. J Am Coll Cardiol. 2020;75:3151-61.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
How to reboot elective CV procedures after COVID-19 lockdown
With the COVID-19 pandemic winding down in some parts of the United States, attention has turned to figuring out how to safely reboot elective cardiovascular (CV) services, which, for the most part, shut down in order to combat the virus and flatten the curve.
To aid in this effort, top cardiology societies have published a series of guidance documents. One, entitled Multimodality Cardiovascular Imaging in the Midst of the COVID-19 Pandemic: Ramping Up Safely to a New Normal, was initiated by the editors of JACC Cardiovascular Imaging and was developed in collaboration with the ACC Cardiovascular Imaging Council.
“As we enter a deceleration or indolent phase of the disease and a return to a ‘new normal’ for the foreseeable future, cardiovascular imaging laboratories will adjust to a different work flow and safety precautions for patients and staff alike,” write William Zoghbi, MD, of the department of cardiology at Houston Methodist DeBakey Heart and Vascular Center, and colleagues.
Minimize risk, maximize clinical benefit
The group outlined strategies and considerations on how to safely ramp up multimodality CV imaging laboratories in an environment of an abating but continuing pandemic.
The authors provide detailed advice on reestablishing echocardiography, transthoracic echocardiography, transesophageal echocardiography, stress testing modalities, treadmill testing, nuclear cardiology, cardiac CT, and cardiac MRI.
The advice is designed to “minimize risk, reduce resource utilization and maximize clinical benefit,” the authors wrote. They address patient and societal health; safety of healthcare professionals; choice of CV testing; and scheduling considerations.
Dr. Zoghbi and colleagues said that integrated communication among patients, referring physicians, the imaging teams, and administrative staff are key to reestablishing a more normal clinical operation.
“Recognizing that practice patterns and policies vary depending on institution and locale, the recommendations are not meant to be restrictive but rather to serve as a general framework during the COVID-19 pandemic and its recovery phase,” the writing group said.
Ultimately, the goal is to offer the necessary CV tests and information for the clinical team to provide the best care for patients, they added.
“To be successful in this new safety-driven modus operandi, innovation, coordination and adaptation among clinicians, staff and patients is necessary till herd immunity or control of COVID-19 is achieved,” they concluded.
Rebooting electrophysiology services
Uncertainty as to how to resume electrophysiology (EP) services for arrhythmia patients prompted representatives from the Heart Rhythm Society, the American Heart Association, and the ACC to develop a series of “guiding suggestions and principles” to help safely reestablish electrophysiological care.
The 28-page document is published in Circulation: Arrhythmia and Electrophysiology and the Journal of the American College of Cardiology Electrophysiology.
“Rebooting” EP services at many institutions may be more challenging than shutting down, wrote Dhanunjaya R. Lakkireddy, MD, Kansas City Heart Rhythm Institute and Research Foundation, Overland Park, Kan., and colleagues.
Topics addressed by the writing group include the role of viral screening and serologic testing, return-to-work considerations for exposed or infected health care workers, risk stratification and management strategies based on COVID-19 disease burden, institutional preparedness for resumption of elective procedures, patient preparation and communication; prioritization of procedures, and development of outpatient and periprocedural care pathways.
They suggest creating an EP COVID-19 “reboot team” made up of stakeholders involved in the EP care continuum pathway that would coordinate with institutional or hospital-level COVID-19 leadership.
The reboot team may include an electrophysiologist, an EP laboratory manager, an outpatient clinic manager, an EP nurse, advanced practice providers, a device technician, an anesthesiologist, and an imaging team to provide insights into various aspects of the work flow.
“This team can clarify, interpret, iterate and disseminate policies, and also provide the necessary operational support to plan and successfully execute the reboot process as the efforts to contain COVID-19 continue,” the writing group said.
A mandatory component of the reboot plan should be planning for a second wave of the virus.
“We will have to learn to create relatively COVID-19 safe zones within the hospitals to help isolate patients from second waves and yet be able to provide regular care for non–COVID-19 patients,” the writing group said.
“Our main goal as health care professionals, whether we serve in a clinical, teaching, research, or administrative role, is to do everything we can to create a safe environment for our patients so that they receive the excellent care they deserve,” they concluded.
Defining moment for remote arrhythmia monitoring
In a separate report, an international team of heart rhythm specialists from the Latin American Heart Rhythm Society, the HRS, the European Heart Rhythm Association, the Asia Pacific Heart Rhythm Society, the AHA, and the ACC discussed how the pandemic has fueled adoption of telehealth and remote patient management across medicine, including heart rhythm monitoring.
Their report was simultaneously published in Circulation: Arrhythmia and Electrophysiology, EP Europace, the Journal of the American College of Cardiology, the Journal of Arrhythmia, and Heart Rhythm.
The COVID-19 pandemic has “catalyzed the use of wearables and digital medical tools,” and this will likely define medicine going forward, first author Niraj Varma, MD, PhD, of the Cleveland Clinic, said in an interview.
He noted that the technology has been available for some time, but the pandemic has forced people to use it. “Necessity is the mother of invention, and this has become necessary during the pandemic when we can’t see our patients,” said Dr. Varma.
He also noted that hospitals and physicians are now realizing that telehealth and remote arrhythmia monitoring “actually work, and regulatory agencies have moved very swiftly to dissolve traditional barriers and will now reimburse for it. So it’s a win-win.”
Dr. Varma and colleagues said that the time is right to “embed and grow remote services in everyday medical practice worldwide.” In their report, they offered a list of commonly used platforms for telehealth and examples of remote electrocardiogram and heart rate monitoring devices.
Development of the three reports had no commercial funding. Complete lists of disclosures for the writing groups are available in the original articles.
A version of this article originally appeared on Medscape.com.
With the COVID-19 pandemic winding down in some parts of the United States, attention has turned to figuring out how to safely reboot elective cardiovascular (CV) services, which, for the most part, shut down in order to combat the virus and flatten the curve.
To aid in this effort, top cardiology societies have published a series of guidance documents. One, entitled Multimodality Cardiovascular Imaging in the Midst of the COVID-19 Pandemic: Ramping Up Safely to a New Normal, was initiated by the editors of JACC Cardiovascular Imaging and was developed in collaboration with the ACC Cardiovascular Imaging Council.
“As we enter a deceleration or indolent phase of the disease and a return to a ‘new normal’ for the foreseeable future, cardiovascular imaging laboratories will adjust to a different work flow and safety precautions for patients and staff alike,” write William Zoghbi, MD, of the department of cardiology at Houston Methodist DeBakey Heart and Vascular Center, and colleagues.
Minimize risk, maximize clinical benefit
The group outlined strategies and considerations on how to safely ramp up multimodality CV imaging laboratories in an environment of an abating but continuing pandemic.
The authors provide detailed advice on reestablishing echocardiography, transthoracic echocardiography, transesophageal echocardiography, stress testing modalities, treadmill testing, nuclear cardiology, cardiac CT, and cardiac MRI.
The advice is designed to “minimize risk, reduce resource utilization and maximize clinical benefit,” the authors wrote. They address patient and societal health; safety of healthcare professionals; choice of CV testing; and scheduling considerations.
Dr. Zoghbi and colleagues said that integrated communication among patients, referring physicians, the imaging teams, and administrative staff are key to reestablishing a more normal clinical operation.
“Recognizing that practice patterns and policies vary depending on institution and locale, the recommendations are not meant to be restrictive but rather to serve as a general framework during the COVID-19 pandemic and its recovery phase,” the writing group said.
Ultimately, the goal is to offer the necessary CV tests and information for the clinical team to provide the best care for patients, they added.
“To be successful in this new safety-driven modus operandi, innovation, coordination and adaptation among clinicians, staff and patients is necessary till herd immunity or control of COVID-19 is achieved,” they concluded.
Rebooting electrophysiology services
Uncertainty as to how to resume electrophysiology (EP) services for arrhythmia patients prompted representatives from the Heart Rhythm Society, the American Heart Association, and the ACC to develop a series of “guiding suggestions and principles” to help safely reestablish electrophysiological care.
The 28-page document is published in Circulation: Arrhythmia and Electrophysiology and the Journal of the American College of Cardiology Electrophysiology.
“Rebooting” EP services at many institutions may be more challenging than shutting down, wrote Dhanunjaya R. Lakkireddy, MD, Kansas City Heart Rhythm Institute and Research Foundation, Overland Park, Kan., and colleagues.
Topics addressed by the writing group include the role of viral screening and serologic testing, return-to-work considerations for exposed or infected health care workers, risk stratification and management strategies based on COVID-19 disease burden, institutional preparedness for resumption of elective procedures, patient preparation and communication; prioritization of procedures, and development of outpatient and periprocedural care pathways.
They suggest creating an EP COVID-19 “reboot team” made up of stakeholders involved in the EP care continuum pathway that would coordinate with institutional or hospital-level COVID-19 leadership.
The reboot team may include an electrophysiologist, an EP laboratory manager, an outpatient clinic manager, an EP nurse, advanced practice providers, a device technician, an anesthesiologist, and an imaging team to provide insights into various aspects of the work flow.
“This team can clarify, interpret, iterate and disseminate policies, and also provide the necessary operational support to plan and successfully execute the reboot process as the efforts to contain COVID-19 continue,” the writing group said.
A mandatory component of the reboot plan should be planning for a second wave of the virus.
“We will have to learn to create relatively COVID-19 safe zones within the hospitals to help isolate patients from second waves and yet be able to provide regular care for non–COVID-19 patients,” the writing group said.
“Our main goal as health care professionals, whether we serve in a clinical, teaching, research, or administrative role, is to do everything we can to create a safe environment for our patients so that they receive the excellent care they deserve,” they concluded.
Defining moment for remote arrhythmia monitoring
In a separate report, an international team of heart rhythm specialists from the Latin American Heart Rhythm Society, the HRS, the European Heart Rhythm Association, the Asia Pacific Heart Rhythm Society, the AHA, and the ACC discussed how the pandemic has fueled adoption of telehealth and remote patient management across medicine, including heart rhythm monitoring.
Their report was simultaneously published in Circulation: Arrhythmia and Electrophysiology, EP Europace, the Journal of the American College of Cardiology, the Journal of Arrhythmia, and Heart Rhythm.
The COVID-19 pandemic has “catalyzed the use of wearables and digital medical tools,” and this will likely define medicine going forward, first author Niraj Varma, MD, PhD, of the Cleveland Clinic, said in an interview.
He noted that the technology has been available for some time, but the pandemic has forced people to use it. “Necessity is the mother of invention, and this has become necessary during the pandemic when we can’t see our patients,” said Dr. Varma.
He also noted that hospitals and physicians are now realizing that telehealth and remote arrhythmia monitoring “actually work, and regulatory agencies have moved very swiftly to dissolve traditional barriers and will now reimburse for it. So it’s a win-win.”
Dr. Varma and colleagues said that the time is right to “embed and grow remote services in everyday medical practice worldwide.” In their report, they offered a list of commonly used platforms for telehealth and examples of remote electrocardiogram and heart rate monitoring devices.
Development of the three reports had no commercial funding. Complete lists of disclosures for the writing groups are available in the original articles.
A version of this article originally appeared on Medscape.com.
With the COVID-19 pandemic winding down in some parts of the United States, attention has turned to figuring out how to safely reboot elective cardiovascular (CV) services, which, for the most part, shut down in order to combat the virus and flatten the curve.
To aid in this effort, top cardiology societies have published a series of guidance documents. One, entitled Multimodality Cardiovascular Imaging in the Midst of the COVID-19 Pandemic: Ramping Up Safely to a New Normal, was initiated by the editors of JACC Cardiovascular Imaging and was developed in collaboration with the ACC Cardiovascular Imaging Council.
“As we enter a deceleration or indolent phase of the disease and a return to a ‘new normal’ for the foreseeable future, cardiovascular imaging laboratories will adjust to a different work flow and safety precautions for patients and staff alike,” write William Zoghbi, MD, of the department of cardiology at Houston Methodist DeBakey Heart and Vascular Center, and colleagues.
Minimize risk, maximize clinical benefit
The group outlined strategies and considerations on how to safely ramp up multimodality CV imaging laboratories in an environment of an abating but continuing pandemic.
The authors provide detailed advice on reestablishing echocardiography, transthoracic echocardiography, transesophageal echocardiography, stress testing modalities, treadmill testing, nuclear cardiology, cardiac CT, and cardiac MRI.
The advice is designed to “minimize risk, reduce resource utilization and maximize clinical benefit,” the authors wrote. They address patient and societal health; safety of healthcare professionals; choice of CV testing; and scheduling considerations.
Dr. Zoghbi and colleagues said that integrated communication among patients, referring physicians, the imaging teams, and administrative staff are key to reestablishing a more normal clinical operation.
“Recognizing that practice patterns and policies vary depending on institution and locale, the recommendations are not meant to be restrictive but rather to serve as a general framework during the COVID-19 pandemic and its recovery phase,” the writing group said.
Ultimately, the goal is to offer the necessary CV tests and information for the clinical team to provide the best care for patients, they added.
“To be successful in this new safety-driven modus operandi, innovation, coordination and adaptation among clinicians, staff and patients is necessary till herd immunity or control of COVID-19 is achieved,” they concluded.
Rebooting electrophysiology services
Uncertainty as to how to resume electrophysiology (EP) services for arrhythmia patients prompted representatives from the Heart Rhythm Society, the American Heart Association, and the ACC to develop a series of “guiding suggestions and principles” to help safely reestablish electrophysiological care.
The 28-page document is published in Circulation: Arrhythmia and Electrophysiology and the Journal of the American College of Cardiology Electrophysiology.
“Rebooting” EP services at many institutions may be more challenging than shutting down, wrote Dhanunjaya R. Lakkireddy, MD, Kansas City Heart Rhythm Institute and Research Foundation, Overland Park, Kan., and colleagues.
Topics addressed by the writing group include the role of viral screening and serologic testing, return-to-work considerations for exposed or infected health care workers, risk stratification and management strategies based on COVID-19 disease burden, institutional preparedness for resumption of elective procedures, patient preparation and communication; prioritization of procedures, and development of outpatient and periprocedural care pathways.
They suggest creating an EP COVID-19 “reboot team” made up of stakeholders involved in the EP care continuum pathway that would coordinate with institutional or hospital-level COVID-19 leadership.
The reboot team may include an electrophysiologist, an EP laboratory manager, an outpatient clinic manager, an EP nurse, advanced practice providers, a device technician, an anesthesiologist, and an imaging team to provide insights into various aspects of the work flow.
“This team can clarify, interpret, iterate and disseminate policies, and also provide the necessary operational support to plan and successfully execute the reboot process as the efforts to contain COVID-19 continue,” the writing group said.
A mandatory component of the reboot plan should be planning for a second wave of the virus.
“We will have to learn to create relatively COVID-19 safe zones within the hospitals to help isolate patients from second waves and yet be able to provide regular care for non–COVID-19 patients,” the writing group said.
“Our main goal as health care professionals, whether we serve in a clinical, teaching, research, or administrative role, is to do everything we can to create a safe environment for our patients so that they receive the excellent care they deserve,” they concluded.
Defining moment for remote arrhythmia monitoring
In a separate report, an international team of heart rhythm specialists from the Latin American Heart Rhythm Society, the HRS, the European Heart Rhythm Association, the Asia Pacific Heart Rhythm Society, the AHA, and the ACC discussed how the pandemic has fueled adoption of telehealth and remote patient management across medicine, including heart rhythm monitoring.
Their report was simultaneously published in Circulation: Arrhythmia and Electrophysiology, EP Europace, the Journal of the American College of Cardiology, the Journal of Arrhythmia, and Heart Rhythm.
The COVID-19 pandemic has “catalyzed the use of wearables and digital medical tools,” and this will likely define medicine going forward, first author Niraj Varma, MD, PhD, of the Cleveland Clinic, said in an interview.
He noted that the technology has been available for some time, but the pandemic has forced people to use it. “Necessity is the mother of invention, and this has become necessary during the pandemic when we can’t see our patients,” said Dr. Varma.
He also noted that hospitals and physicians are now realizing that telehealth and remote arrhythmia monitoring “actually work, and regulatory agencies have moved very swiftly to dissolve traditional barriers and will now reimburse for it. So it’s a win-win.”
Dr. Varma and colleagues said that the time is right to “embed and grow remote services in everyday medical practice worldwide.” In their report, they offered a list of commonly used platforms for telehealth and examples of remote electrocardiogram and heart rate monitoring devices.
Development of the three reports had no commercial funding. Complete lists of disclosures for the writing groups are available in the original articles.
A version of this article originally appeared on Medscape.com.
COVID-19: ‘dramatic’ surge in out-of-hospital cardiac arrests in NYC
The COVID-19 pandemic in New York City led to a surge in out-of-hospital cardiac arrests (OHCAs) that placed a huge burden on first responders, a new analysis shows.
During the height of the pandemic in New York, there was a “dramatic increase in cardiopulmonary arrests, nearly all presented in non-shockable cardiac rhythms (> 90% fatality rate) and vulnerable patient populations were most affected,” David J. Prezant, MD, chief medical officer, Fire Department of New York (FDNY), said in an interview.
In a news release, Dr. Prezant noted that “relatively few, if any, patients were tested to confirm the presence of COVID-19,” making it impossible to distinguish between cardiac arrests as a result of COVID-19 and those that may have resulted from other health conditions.
“We also can’t rule out the possibility that some people may have died from delays in seeking or receiving treatment for non–COVID-19-related conditions. However, the dramatic increase in cardiac arrests compared to the same period in 2019 strongly indicates that the pandemic was directly or indirectly responsible for that surge in cardiac arrests and deaths,” said Dr. Prezant.
The study was published online June 19 in JAMA Cardiology.
New York City has the largest and busiest EMS system in the United States, serving a population of more than 8.4 million people and responding to more than 1.5 million calls every year.
To gauge the impact of COVID-19 on first responders, Dr. Prezant and colleagues analyzed data for adults with OHCA who received EMS resuscitation from March 1, when the first case of COVID-19 was diagnosed in the city, through April 25, when EMS call volume had receded to pre-COVID-19 levels.
Compared with the same period in 2019, the COVID-19 period had an excess of 2,653 patients with OHCA who underwent EMS resuscitation attempts (3,989 in 2020 vs. 1,336 in 2019, P < .001), an incidence rate triple that of 2019 (47.5 vs. 15.9 per 100,000).
On the worst day – Monday, April 6 – OHCAs peaked at 305 cases, an increase of nearly 10-fold compared with the same day in 2019.
Despite the surge in cases, the median response time of available EMS units to OHCAs increased by about 1 minute over 2019, a nonsignificant difference. Although the average time varied, median response time during the COVID-19 period was less than 3 minutes.
A more vulnerable group
Compared with 2019, patients suffering OHCA during the pandemic period were older (mean age 72 vs. 68 years), less likely to be white (20% white vs. 33%) and more likely to have hypertension (54% vs. 46%), diabetes (36% vs. 26%), physical limitations (57% vs. 48%) and cardiac rhythms that don’t respond to defibrillator shocks (92% vs. 81%).
Compared with 2019, the COVID-19 period had substantial reductions in return of spontaneous circulation (ROSC) (18% vs. 35%; P < .001) and sustained ROSC (11% vs. 25%; P < .001). The case fatality rate was 90% in the COVID-19 period vs. 75% a year earlier.
“The tragedy of the COVID-19 pandemic is not just the number of patients infected, but the large increase in OHCAs and deaths,” Dr. Prezant and colleagues said.
Identifying patients with the greatest risk for OHCA and death during the COVID-19 pandemic “should allow for early, targeted interventions in the outpatient setting that could lead to reductions in out-of-hospital deaths,” they noted.
“Vulnerable patient populations need outreach, telephonic medicine, televideo medicine, home visits, not just temperature monitoring but home O2 saturation monitoring,” Dr. Prezant said in an interview. “Barriers need to be removed, not just for this pandemic but for the future – no matter what the trigger is.”
Unsung heroes
In an Editor’s Note in JAMA Cardiology, Robert O. Bonow, MD, Northwestern University, Chicago, and colleagues said the American people owe a debt of gratitude to first responders for their “heroic work” triaging, resuscitating, and transporting thousands of people affected by COVID-19.
“Although the typically bustling NYC streets remained eerily deserted, the characteristic cacophony of sounds of the ‘City that Never Sleeps’ was replaced by sirens wailing all hours of the night,” they wrote.
First responders to OHCAs in the COVID-19 era place themselves at extremely high risk, in some cases without optimal personal protective equipment, they pointed out. “Sadly,” many first responders have fallen ill to COVID-19 infection, they added.
As of June 1, 29 EMS workers and volunteers across the United States had died of COVID-19.
They are James Villecco, Gregory Hodge, Tony Thomas, Mike Field, John Redd, Idris Bey, Richard Seaberry, and Sal Mancuso of New York; Israel Tolentino, Reuven Maroth, Liana Sá, Kevin Leiva, Frank Molinari, Robert Weber, Robert Tarrant, Solomon Donald, Scott Geiger, John Farrarella, John Careccia, Bill Nauta, and David Pinto of New Jersey; Kevin Bundy, Robert Zerman, and Jeremy Emerich of Pennsylvania; Paul Cary of Colorado; Paul Novicki of Michigan; David Martin of Mississippi; Billy Birmingham of Missouri; and John “JP” Granger of South Carolina.
“We offer their families, friends, and colleagues our sincerest condolences and honor their memory with our highest respect and gratitude,” Dr. Bonow and colleagues wrote.
This study was supported by the City of New York and the Fire Department of the City of New York. The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The COVID-19 pandemic in New York City led to a surge in out-of-hospital cardiac arrests (OHCAs) that placed a huge burden on first responders, a new analysis shows.
During the height of the pandemic in New York, there was a “dramatic increase in cardiopulmonary arrests, nearly all presented in non-shockable cardiac rhythms (> 90% fatality rate) and vulnerable patient populations were most affected,” David J. Prezant, MD, chief medical officer, Fire Department of New York (FDNY), said in an interview.
In a news release, Dr. Prezant noted that “relatively few, if any, patients were tested to confirm the presence of COVID-19,” making it impossible to distinguish between cardiac arrests as a result of COVID-19 and those that may have resulted from other health conditions.
“We also can’t rule out the possibility that some people may have died from delays in seeking or receiving treatment for non–COVID-19-related conditions. However, the dramatic increase in cardiac arrests compared to the same period in 2019 strongly indicates that the pandemic was directly or indirectly responsible for that surge in cardiac arrests and deaths,” said Dr. Prezant.
The study was published online June 19 in JAMA Cardiology.
New York City has the largest and busiest EMS system in the United States, serving a population of more than 8.4 million people and responding to more than 1.5 million calls every year.
To gauge the impact of COVID-19 on first responders, Dr. Prezant and colleagues analyzed data for adults with OHCA who received EMS resuscitation from March 1, when the first case of COVID-19 was diagnosed in the city, through April 25, when EMS call volume had receded to pre-COVID-19 levels.
Compared with the same period in 2019, the COVID-19 period had an excess of 2,653 patients with OHCA who underwent EMS resuscitation attempts (3,989 in 2020 vs. 1,336 in 2019, P < .001), an incidence rate triple that of 2019 (47.5 vs. 15.9 per 100,000).
On the worst day – Monday, April 6 – OHCAs peaked at 305 cases, an increase of nearly 10-fold compared with the same day in 2019.
Despite the surge in cases, the median response time of available EMS units to OHCAs increased by about 1 minute over 2019, a nonsignificant difference. Although the average time varied, median response time during the COVID-19 period was less than 3 minutes.
A more vulnerable group
Compared with 2019, patients suffering OHCA during the pandemic period were older (mean age 72 vs. 68 years), less likely to be white (20% white vs. 33%) and more likely to have hypertension (54% vs. 46%), diabetes (36% vs. 26%), physical limitations (57% vs. 48%) and cardiac rhythms that don’t respond to defibrillator shocks (92% vs. 81%).
Compared with 2019, the COVID-19 period had substantial reductions in return of spontaneous circulation (ROSC) (18% vs. 35%; P < .001) and sustained ROSC (11% vs. 25%; P < .001). The case fatality rate was 90% in the COVID-19 period vs. 75% a year earlier.
“The tragedy of the COVID-19 pandemic is not just the number of patients infected, but the large increase in OHCAs and deaths,” Dr. Prezant and colleagues said.
Identifying patients with the greatest risk for OHCA and death during the COVID-19 pandemic “should allow for early, targeted interventions in the outpatient setting that could lead to reductions in out-of-hospital deaths,” they noted.
“Vulnerable patient populations need outreach, telephonic medicine, televideo medicine, home visits, not just temperature monitoring but home O2 saturation monitoring,” Dr. Prezant said in an interview. “Barriers need to be removed, not just for this pandemic but for the future – no matter what the trigger is.”
Unsung heroes
In an Editor’s Note in JAMA Cardiology, Robert O. Bonow, MD, Northwestern University, Chicago, and colleagues said the American people owe a debt of gratitude to first responders for their “heroic work” triaging, resuscitating, and transporting thousands of people affected by COVID-19.
“Although the typically bustling NYC streets remained eerily deserted, the characteristic cacophony of sounds of the ‘City that Never Sleeps’ was replaced by sirens wailing all hours of the night,” they wrote.
First responders to OHCAs in the COVID-19 era place themselves at extremely high risk, in some cases without optimal personal protective equipment, they pointed out. “Sadly,” many first responders have fallen ill to COVID-19 infection, they added.
As of June 1, 29 EMS workers and volunteers across the United States had died of COVID-19.
They are James Villecco, Gregory Hodge, Tony Thomas, Mike Field, John Redd, Idris Bey, Richard Seaberry, and Sal Mancuso of New York; Israel Tolentino, Reuven Maroth, Liana Sá, Kevin Leiva, Frank Molinari, Robert Weber, Robert Tarrant, Solomon Donald, Scott Geiger, John Farrarella, John Careccia, Bill Nauta, and David Pinto of New Jersey; Kevin Bundy, Robert Zerman, and Jeremy Emerich of Pennsylvania; Paul Cary of Colorado; Paul Novicki of Michigan; David Martin of Mississippi; Billy Birmingham of Missouri; and John “JP” Granger of South Carolina.
“We offer their families, friends, and colleagues our sincerest condolences and honor their memory with our highest respect and gratitude,” Dr. Bonow and colleagues wrote.
This study was supported by the City of New York and the Fire Department of the City of New York. The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The COVID-19 pandemic in New York City led to a surge in out-of-hospital cardiac arrests (OHCAs) that placed a huge burden on first responders, a new analysis shows.
During the height of the pandemic in New York, there was a “dramatic increase in cardiopulmonary arrests, nearly all presented in non-shockable cardiac rhythms (> 90% fatality rate) and vulnerable patient populations were most affected,” David J. Prezant, MD, chief medical officer, Fire Department of New York (FDNY), said in an interview.
In a news release, Dr. Prezant noted that “relatively few, if any, patients were tested to confirm the presence of COVID-19,” making it impossible to distinguish between cardiac arrests as a result of COVID-19 and those that may have resulted from other health conditions.
“We also can’t rule out the possibility that some people may have died from delays in seeking or receiving treatment for non–COVID-19-related conditions. However, the dramatic increase in cardiac arrests compared to the same period in 2019 strongly indicates that the pandemic was directly or indirectly responsible for that surge in cardiac arrests and deaths,” said Dr. Prezant.
The study was published online June 19 in JAMA Cardiology.
New York City has the largest and busiest EMS system in the United States, serving a population of more than 8.4 million people and responding to more than 1.5 million calls every year.
To gauge the impact of COVID-19 on first responders, Dr. Prezant and colleagues analyzed data for adults with OHCA who received EMS resuscitation from March 1, when the first case of COVID-19 was diagnosed in the city, through April 25, when EMS call volume had receded to pre-COVID-19 levels.
Compared with the same period in 2019, the COVID-19 period had an excess of 2,653 patients with OHCA who underwent EMS resuscitation attempts (3,989 in 2020 vs. 1,336 in 2019, P < .001), an incidence rate triple that of 2019 (47.5 vs. 15.9 per 100,000).
On the worst day – Monday, April 6 – OHCAs peaked at 305 cases, an increase of nearly 10-fold compared with the same day in 2019.
Despite the surge in cases, the median response time of available EMS units to OHCAs increased by about 1 minute over 2019, a nonsignificant difference. Although the average time varied, median response time during the COVID-19 period was less than 3 minutes.
A more vulnerable group
Compared with 2019, patients suffering OHCA during the pandemic period were older (mean age 72 vs. 68 years), less likely to be white (20% white vs. 33%) and more likely to have hypertension (54% vs. 46%), diabetes (36% vs. 26%), physical limitations (57% vs. 48%) and cardiac rhythms that don’t respond to defibrillator shocks (92% vs. 81%).
Compared with 2019, the COVID-19 period had substantial reductions in return of spontaneous circulation (ROSC) (18% vs. 35%; P < .001) and sustained ROSC (11% vs. 25%; P < .001). The case fatality rate was 90% in the COVID-19 period vs. 75% a year earlier.
“The tragedy of the COVID-19 pandemic is not just the number of patients infected, but the large increase in OHCAs and deaths,” Dr. Prezant and colleagues said.
Identifying patients with the greatest risk for OHCA and death during the COVID-19 pandemic “should allow for early, targeted interventions in the outpatient setting that could lead to reductions in out-of-hospital deaths,” they noted.
“Vulnerable patient populations need outreach, telephonic medicine, televideo medicine, home visits, not just temperature monitoring but home O2 saturation monitoring,” Dr. Prezant said in an interview. “Barriers need to be removed, not just for this pandemic but for the future – no matter what the trigger is.”
Unsung heroes
In an Editor’s Note in JAMA Cardiology, Robert O. Bonow, MD, Northwestern University, Chicago, and colleagues said the American people owe a debt of gratitude to first responders for their “heroic work” triaging, resuscitating, and transporting thousands of people affected by COVID-19.
“Although the typically bustling NYC streets remained eerily deserted, the characteristic cacophony of sounds of the ‘City that Never Sleeps’ was replaced by sirens wailing all hours of the night,” they wrote.
First responders to OHCAs in the COVID-19 era place themselves at extremely high risk, in some cases without optimal personal protective equipment, they pointed out. “Sadly,” many first responders have fallen ill to COVID-19 infection, they added.
As of June 1, 29 EMS workers and volunteers across the United States had died of COVID-19.
They are James Villecco, Gregory Hodge, Tony Thomas, Mike Field, John Redd, Idris Bey, Richard Seaberry, and Sal Mancuso of New York; Israel Tolentino, Reuven Maroth, Liana Sá, Kevin Leiva, Frank Molinari, Robert Weber, Robert Tarrant, Solomon Donald, Scott Geiger, John Farrarella, John Careccia, Bill Nauta, and David Pinto of New Jersey; Kevin Bundy, Robert Zerman, and Jeremy Emerich of Pennsylvania; Paul Cary of Colorado; Paul Novicki of Michigan; David Martin of Mississippi; Billy Birmingham of Missouri; and John “JP” Granger of South Carolina.
“We offer their families, friends, and colleagues our sincerest condolences and honor their memory with our highest respect and gratitude,” Dr. Bonow and colleagues wrote.
This study was supported by the City of New York and the Fire Department of the City of New York. The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Dapagliflozin benefits low-EF heart failure regardless of diuretic dose: DAPA-HF
The DAPA-HF trial has already changed cardiology in opening up a new class of drugs to patients with heart failure (HF), whether or not they have diabetes. Now the trial is yielding clues as to how it benefits them. For now, it’s doing so by process of elimination.
A new analysis suggests that dapagliflozin (Farxiga, AstraZeneca) didn’t need help from loop diuretics to cut the risk for clinical events in patients with HF with reduced ejection fraction (HFrEF), a benefit seen across the spectrum of glycosylated hemoglobin levels and without compromising renal function, said DAPA-HF investigators. Also, use of dapagliflozin and its clinical effects were not associated with changes in loop diuretic dosage. Those findings and others suggest the drug helps in HFrEF at least partly by some other mechanism than its own diuretic effect, the researchers say.
Such insights will likely be important to case-by-case decisions on whether to use the drug, a sodium-glucose cotransporter 2 (SGLT2) inhibitor once reserved for patients with diabetes, given the recently broader landscape of HF treatment options.
As previously reported from DAPA-HF, with more than 4,700 patients, those who received dapagliflozin showed significant reductions in the primary end point, a composite of cardiovascular (CV) death, HF hospitalization, and urgent HF visit requiring IV therapy over about 18 months. The 45% of patients with and 55% without type 2 diabetes enjoyed about equal benefit in the placebo-controlled trial for that end point, as well as for all-cause mortality.
SGLT2 inhibitors work in diabetes by promoting urinary glucose excretion. That had led some to speculate that its benefit in HFrEF comes primarily from a diuretic effect; the current findings largely put that question to rest.
“Our findings show that treatment with dapagliflozin was effective regardless of diuretic use or diuretic dose. They also show that dapagliflozin did not lead to an increase in renal adverse events or discontinuation of therapy in patients treated with a diuretic,” trialist Alice M. Jackson, MB, ChB, said in an interview.
“In fact, renal adverse events were generally less common in patients treated with dapagliflozin, across the diuretic categories,” said Dr. Jackson, from the University of Glasgow.
Dr. Jackson presented the new analysis at a Late-Breaking Science Session during the European Society of Cardiology Heart Failure Discoveries virtual meeting. The HFA sessions were conducted virtually this year due to the COVID-19 pandemic.
At baseline, 84% of patients were on conventional diuretics. The post hoc analysis broke out all patients by loop-diuretic dosage level: none; less than 40 mg furosemide equivalents (FE); 40 mg FE; or more than 40 mg FE. Clinical outcomes were similar across the four groups.
Clinicians in the trial “were not given specific advice about adjusting diuretic doses, but were encouraged to assess volume status and make changes to medical therapy based on this, if necessary,” Dr. Jackson said. “This suggests that, for most patients, starting dapagliflozin will not necessitate a change in diuretic dose.”
With the caveat that the event rate was low in the relatively few patients not prescribed loop diuretics, she said, “the magnitude of the benefit from dapagliflozin appeared to be larger in patients not treated with a diuretic.”
There was no suggestion of a diuretic dose–response effect or statistical interaction between diuretic use and clinical outcomes on dapagliflozin, Dr. Jackson observed in the interview.
Of note in the analysis, hematocrit levels shot up soon after patients started active therapy, but they didn’t rise much in the placebo group. The sustained hematocrit elevation on dapagliflozin, seen at all diuretic dosage levels, persisted even after dosage reductions at 6 months, she said.
“Dapagliflozin is effective in HFrEF irrespective of background diuretic therapy; therefore, it is almost certainly not purely acting as a diuretic,” Andrew J. Coats, MD, DSc, MBA, said in an interview.
The findings also “lessen the concern that dapagliflozin’s beneficial effects are only seen only in patients without effective diuretic dosing,” said Dr. Coats, from University of Warwick, Coventry, England.
“Altogether, these data give further reassurance that dapagliflozin can safely be used in heart failure, and has a beneficial effect independent of the use of diuretic drugs,” invited discussant Wolfram Doehner, MD, PhD, Charité-Universitätsmedizin Berlin, said after Dr. Jackson’s presentation of the analysis.
He made special mention of the sustained hematocrit elevation on dapagliflozin. “While this effect may likely relate to the mild reduction in plasma volume secondary to dapagliflozin therapy, it is noted that the increase in hematocrit was independent of any change of the diuretic dose,” Doehner said. “If additional mechanisms have a role for this observed increase in hematocrit, it may be of interest in further investigations.”
Dr. Jackson pointed to several observations that suggest the hematocrit finding isn’t explained by hemoconcentration from reduced plasma volume, at least not entirely.
For example, hematocrit levels rose “without any suggestion of a relationship between diuretic dose and degree of hematocrit elevation with dapagliflozin,” she said.
The elevations persisted even with diuretic dose reductions at 6 and 12 months, “which should have led to a decrease in hemoconcentration if it was caused by volume contraction.”
Also, she said, “among patients not taking a diuretic, volume depletion occurred less frequently in the dapagliflozin group than in the placebo group, but there was still a similar rise in hematocrit with dapagliflozin.”
Both Dr. Jackson and Dr. Coats said the sustained elevation in hematocrit on the drug is unlikely to pose a major hazard.
Dr. Coats said that, theoretically, “increased hematocrit could reduce peripheral vessel blood flow, making ischemia and thrombosis more likely. But the size of the effect is small and unlikely to be clinically important.”
A diuretic dose could not be determined for 128 of the trial’s 4,744 randomized patients with HFrEF, so the post hoc analysis was limited to the remaining 4,616. Of those, 746 were not on diuretics at baseline, 1,311 were on loop diuretics at less than 40 mg FE or on non-loop diuretics only, 1,365 were taking 40 mg FE, and 1,204 were on higher doses of loop diuretics.
The mean baseline dosage was 60 mg FE, which rose slightly throughout the trial. But the baseline dosage and the increases were both similar in the placebo and dapagliflozin groups. Dr. Jackson said 84% and 83% of patients on dapagliflozin and placebo, respectively, maintained their baseline dose at 6 months and about 77% in both groups at 12 months.
The overall trial’s significant primary endpoint reduction for dapagliflozin versus placebo applied similarly to patients not on a diuretics and to those on any dose of diuretic, with an interaction P value of .23 for the effect of diuretic use. The hazard ratios (95% confidence interval) were 0.57 (0.36-0.92) for patients not on diuretics, 0.78 (0.68-0.90) for patients on any diuretic dosage, and 0.74 (0.65-0.85) overall
Dr. Jackson said during her formal online presentation that patients on diuretics showed a “tendency toward slightly more volume depletion in those on dapagliflozin than in those on placebo, but the excess was small and not greater than approximately 3% in those taking 40 mg furosemide equivalent diuretic. And fortunately, this did not result in an increase in frequency in renal adverse events nor of discontinuation of study drug.”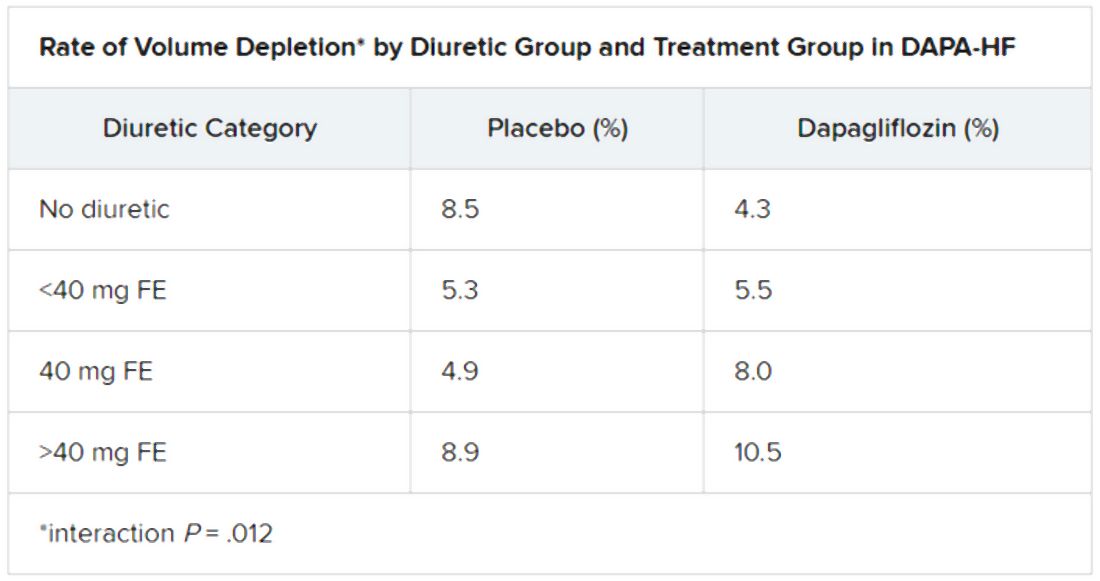
Renal adverse events were similarly prevalent in the two treatment groups, as were such events leading to treatment discontinuation. But serious renal events were less common in the dapagliflozin group (1.6% vs 2.7%; P = .009), as was investigator-reported serious acute kidney injury (1.0% vs 1.9%; P = .007).
“Overall, renal events were infrequent,” Dr. Jackson said, and “because of the small number of events, it is very difficult to draw conclusions about the impact of dapagliflozin on renal function according to diuretic-dose subgroups.”
Still, she said, worsening renal function was less common on dapagliflozin in three of the four groups by diuretic dosage; the exception was the less than 40 mg FE group, “but the absolute difference in this group was only two events.”
There seem to be dapagliflozin mechanisms “underneath the surface that need to be unraveled,” Dr. Doehner said as discussant, processes that are favorable for the treatment of HFrEF in which “diuretics play no big role.”
Dr. Jackson has no disclosures. Dr. Coats has disclosed receiving personal fees from Actimed, AstraZeneca, Faraday, WL Gore, Menarini, Novartis, Nutricia, Respicardia, Servier, Stealth Peptides, Verona, and Vifor. Dr. Doener has recently disclosed receiving grants and personal fees from Vifor, Pfizer, Boehringer Ingelheim, Sphingotec, ZS Pharma, Bayer, and Medtronic.
A version of this article originally appeared on Medscape.com.
The DAPA-HF trial has already changed cardiology in opening up a new class of drugs to patients with heart failure (HF), whether or not they have diabetes. Now the trial is yielding clues as to how it benefits them. For now, it’s doing so by process of elimination.
A new analysis suggests that dapagliflozin (Farxiga, AstraZeneca) didn’t need help from loop diuretics to cut the risk for clinical events in patients with HF with reduced ejection fraction (HFrEF), a benefit seen across the spectrum of glycosylated hemoglobin levels and without compromising renal function, said DAPA-HF investigators. Also, use of dapagliflozin and its clinical effects were not associated with changes in loop diuretic dosage. Those findings and others suggest the drug helps in HFrEF at least partly by some other mechanism than its own diuretic effect, the researchers say.
Such insights will likely be important to case-by-case decisions on whether to use the drug, a sodium-glucose cotransporter 2 (SGLT2) inhibitor once reserved for patients with diabetes, given the recently broader landscape of HF treatment options.
As previously reported from DAPA-HF, with more than 4,700 patients, those who received dapagliflozin showed significant reductions in the primary end point, a composite of cardiovascular (CV) death, HF hospitalization, and urgent HF visit requiring IV therapy over about 18 months. The 45% of patients with and 55% without type 2 diabetes enjoyed about equal benefit in the placebo-controlled trial for that end point, as well as for all-cause mortality.
SGLT2 inhibitors work in diabetes by promoting urinary glucose excretion. That had led some to speculate that its benefit in HFrEF comes primarily from a diuretic effect; the current findings largely put that question to rest.
“Our findings show that treatment with dapagliflozin was effective regardless of diuretic use or diuretic dose. They also show that dapagliflozin did not lead to an increase in renal adverse events or discontinuation of therapy in patients treated with a diuretic,” trialist Alice M. Jackson, MB, ChB, said in an interview.
“In fact, renal adverse events were generally less common in patients treated with dapagliflozin, across the diuretic categories,” said Dr. Jackson, from the University of Glasgow.
Dr. Jackson presented the new analysis at a Late-Breaking Science Session during the European Society of Cardiology Heart Failure Discoveries virtual meeting. The HFA sessions were conducted virtually this year due to the COVID-19 pandemic.
At baseline, 84% of patients were on conventional diuretics. The post hoc analysis broke out all patients by loop-diuretic dosage level: none; less than 40 mg furosemide equivalents (FE); 40 mg FE; or more than 40 mg FE. Clinical outcomes were similar across the four groups.
Clinicians in the trial “were not given specific advice about adjusting diuretic doses, but were encouraged to assess volume status and make changes to medical therapy based on this, if necessary,” Dr. Jackson said. “This suggests that, for most patients, starting dapagliflozin will not necessitate a change in diuretic dose.”
With the caveat that the event rate was low in the relatively few patients not prescribed loop diuretics, she said, “the magnitude of the benefit from dapagliflozin appeared to be larger in patients not treated with a diuretic.”
There was no suggestion of a diuretic dose–response effect or statistical interaction between diuretic use and clinical outcomes on dapagliflozin, Dr. Jackson observed in the interview.
Of note in the analysis, hematocrit levels shot up soon after patients started active therapy, but they didn’t rise much in the placebo group. The sustained hematocrit elevation on dapagliflozin, seen at all diuretic dosage levels, persisted even after dosage reductions at 6 months, she said.
“Dapagliflozin is effective in HFrEF irrespective of background diuretic therapy; therefore, it is almost certainly not purely acting as a diuretic,” Andrew J. Coats, MD, DSc, MBA, said in an interview.
The findings also “lessen the concern that dapagliflozin’s beneficial effects are only seen only in patients without effective diuretic dosing,” said Dr. Coats, from University of Warwick, Coventry, England.
“Altogether, these data give further reassurance that dapagliflozin can safely be used in heart failure, and has a beneficial effect independent of the use of diuretic drugs,” invited discussant Wolfram Doehner, MD, PhD, Charité-Universitätsmedizin Berlin, said after Dr. Jackson’s presentation of the analysis.
He made special mention of the sustained hematocrit elevation on dapagliflozin. “While this effect may likely relate to the mild reduction in plasma volume secondary to dapagliflozin therapy, it is noted that the increase in hematocrit was independent of any change of the diuretic dose,” Doehner said. “If additional mechanisms have a role for this observed increase in hematocrit, it may be of interest in further investigations.”
Dr. Jackson pointed to several observations that suggest the hematocrit finding isn’t explained by hemoconcentration from reduced plasma volume, at least not entirely.
For example, hematocrit levels rose “without any suggestion of a relationship between diuretic dose and degree of hematocrit elevation with dapagliflozin,” she said.
The elevations persisted even with diuretic dose reductions at 6 and 12 months, “which should have led to a decrease in hemoconcentration if it was caused by volume contraction.”
Also, she said, “among patients not taking a diuretic, volume depletion occurred less frequently in the dapagliflozin group than in the placebo group, but there was still a similar rise in hematocrit with dapagliflozin.”
Both Dr. Jackson and Dr. Coats said the sustained elevation in hematocrit on the drug is unlikely to pose a major hazard.
Dr. Coats said that, theoretically, “increased hematocrit could reduce peripheral vessel blood flow, making ischemia and thrombosis more likely. But the size of the effect is small and unlikely to be clinically important.”
A diuretic dose could not be determined for 128 of the trial’s 4,744 randomized patients with HFrEF, so the post hoc analysis was limited to the remaining 4,616. Of those, 746 were not on diuretics at baseline, 1,311 were on loop diuretics at less than 40 mg FE or on non-loop diuretics only, 1,365 were taking 40 mg FE, and 1,204 were on higher doses of loop diuretics.
The mean baseline dosage was 60 mg FE, which rose slightly throughout the trial. But the baseline dosage and the increases were both similar in the placebo and dapagliflozin groups. Dr. Jackson said 84% and 83% of patients on dapagliflozin and placebo, respectively, maintained their baseline dose at 6 months and about 77% in both groups at 12 months.
The overall trial’s significant primary endpoint reduction for dapagliflozin versus placebo applied similarly to patients not on a diuretics and to those on any dose of diuretic, with an interaction P value of .23 for the effect of diuretic use. The hazard ratios (95% confidence interval) were 0.57 (0.36-0.92) for patients not on diuretics, 0.78 (0.68-0.90) for patients on any diuretic dosage, and 0.74 (0.65-0.85) overall
Dr. Jackson said during her formal online presentation that patients on diuretics showed a “tendency toward slightly more volume depletion in those on dapagliflozin than in those on placebo, but the excess was small and not greater than approximately 3% in those taking 40 mg furosemide equivalent diuretic. And fortunately, this did not result in an increase in frequency in renal adverse events nor of discontinuation of study drug.”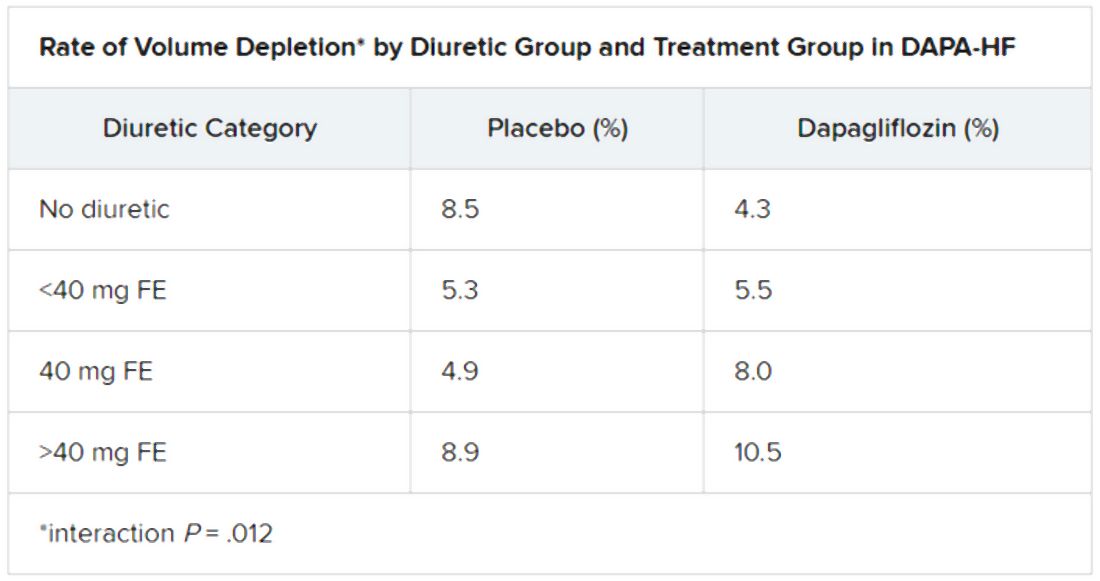
Renal adverse events were similarly prevalent in the two treatment groups, as were such events leading to treatment discontinuation. But serious renal events were less common in the dapagliflozin group (1.6% vs 2.7%; P = .009), as was investigator-reported serious acute kidney injury (1.0% vs 1.9%; P = .007).
“Overall, renal events were infrequent,” Dr. Jackson said, and “because of the small number of events, it is very difficult to draw conclusions about the impact of dapagliflozin on renal function according to diuretic-dose subgroups.”
Still, she said, worsening renal function was less common on dapagliflozin in three of the four groups by diuretic dosage; the exception was the less than 40 mg FE group, “but the absolute difference in this group was only two events.”
There seem to be dapagliflozin mechanisms “underneath the surface that need to be unraveled,” Dr. Doehner said as discussant, processes that are favorable for the treatment of HFrEF in which “diuretics play no big role.”
Dr. Jackson has no disclosures. Dr. Coats has disclosed receiving personal fees from Actimed, AstraZeneca, Faraday, WL Gore, Menarini, Novartis, Nutricia, Respicardia, Servier, Stealth Peptides, Verona, and Vifor. Dr. Doener has recently disclosed receiving grants and personal fees from Vifor, Pfizer, Boehringer Ingelheim, Sphingotec, ZS Pharma, Bayer, and Medtronic.
A version of this article originally appeared on Medscape.com.
The DAPA-HF trial has already changed cardiology in opening up a new class of drugs to patients with heart failure (HF), whether or not they have diabetes. Now the trial is yielding clues as to how it benefits them. For now, it’s doing so by process of elimination.
A new analysis suggests that dapagliflozin (Farxiga, AstraZeneca) didn’t need help from loop diuretics to cut the risk for clinical events in patients with HF with reduced ejection fraction (HFrEF), a benefit seen across the spectrum of glycosylated hemoglobin levels and without compromising renal function, said DAPA-HF investigators. Also, use of dapagliflozin and its clinical effects were not associated with changes in loop diuretic dosage. Those findings and others suggest the drug helps in HFrEF at least partly by some other mechanism than its own diuretic effect, the researchers say.
Such insights will likely be important to case-by-case decisions on whether to use the drug, a sodium-glucose cotransporter 2 (SGLT2) inhibitor once reserved for patients with diabetes, given the recently broader landscape of HF treatment options.
As previously reported from DAPA-HF, with more than 4,700 patients, those who received dapagliflozin showed significant reductions in the primary end point, a composite of cardiovascular (CV) death, HF hospitalization, and urgent HF visit requiring IV therapy over about 18 months. The 45% of patients with and 55% without type 2 diabetes enjoyed about equal benefit in the placebo-controlled trial for that end point, as well as for all-cause mortality.
SGLT2 inhibitors work in diabetes by promoting urinary glucose excretion. That had led some to speculate that its benefit in HFrEF comes primarily from a diuretic effect; the current findings largely put that question to rest.
“Our findings show that treatment with dapagliflozin was effective regardless of diuretic use or diuretic dose. They also show that dapagliflozin did not lead to an increase in renal adverse events or discontinuation of therapy in patients treated with a diuretic,” trialist Alice M. Jackson, MB, ChB, said in an interview.
“In fact, renal adverse events were generally less common in patients treated with dapagliflozin, across the diuretic categories,” said Dr. Jackson, from the University of Glasgow.
Dr. Jackson presented the new analysis at a Late-Breaking Science Session during the European Society of Cardiology Heart Failure Discoveries virtual meeting. The HFA sessions were conducted virtually this year due to the COVID-19 pandemic.
At baseline, 84% of patients were on conventional diuretics. The post hoc analysis broke out all patients by loop-diuretic dosage level: none; less than 40 mg furosemide equivalents (FE); 40 mg FE; or more than 40 mg FE. Clinical outcomes were similar across the four groups.
Clinicians in the trial “were not given specific advice about adjusting diuretic doses, but were encouraged to assess volume status and make changes to medical therapy based on this, if necessary,” Dr. Jackson said. “This suggests that, for most patients, starting dapagliflozin will not necessitate a change in diuretic dose.”
With the caveat that the event rate was low in the relatively few patients not prescribed loop diuretics, she said, “the magnitude of the benefit from dapagliflozin appeared to be larger in patients not treated with a diuretic.”
There was no suggestion of a diuretic dose–response effect or statistical interaction between diuretic use and clinical outcomes on dapagliflozin, Dr. Jackson observed in the interview.
Of note in the analysis, hematocrit levels shot up soon after patients started active therapy, but they didn’t rise much in the placebo group. The sustained hematocrit elevation on dapagliflozin, seen at all diuretic dosage levels, persisted even after dosage reductions at 6 months, she said.
“Dapagliflozin is effective in HFrEF irrespective of background diuretic therapy; therefore, it is almost certainly not purely acting as a diuretic,” Andrew J. Coats, MD, DSc, MBA, said in an interview.
The findings also “lessen the concern that dapagliflozin’s beneficial effects are only seen only in patients without effective diuretic dosing,” said Dr. Coats, from University of Warwick, Coventry, England.
“Altogether, these data give further reassurance that dapagliflozin can safely be used in heart failure, and has a beneficial effect independent of the use of diuretic drugs,” invited discussant Wolfram Doehner, MD, PhD, Charité-Universitätsmedizin Berlin, said after Dr. Jackson’s presentation of the analysis.
He made special mention of the sustained hematocrit elevation on dapagliflozin. “While this effect may likely relate to the mild reduction in plasma volume secondary to dapagliflozin therapy, it is noted that the increase in hematocrit was independent of any change of the diuretic dose,” Doehner said. “If additional mechanisms have a role for this observed increase in hematocrit, it may be of interest in further investigations.”
Dr. Jackson pointed to several observations that suggest the hematocrit finding isn’t explained by hemoconcentration from reduced plasma volume, at least not entirely.
For example, hematocrit levels rose “without any suggestion of a relationship between diuretic dose and degree of hematocrit elevation with dapagliflozin,” she said.
The elevations persisted even with diuretic dose reductions at 6 and 12 months, “which should have led to a decrease in hemoconcentration if it was caused by volume contraction.”
Also, she said, “among patients not taking a diuretic, volume depletion occurred less frequently in the dapagliflozin group than in the placebo group, but there was still a similar rise in hematocrit with dapagliflozin.”
Both Dr. Jackson and Dr. Coats said the sustained elevation in hematocrit on the drug is unlikely to pose a major hazard.
Dr. Coats said that, theoretically, “increased hematocrit could reduce peripheral vessel blood flow, making ischemia and thrombosis more likely. But the size of the effect is small and unlikely to be clinically important.”
A diuretic dose could not be determined for 128 of the trial’s 4,744 randomized patients with HFrEF, so the post hoc analysis was limited to the remaining 4,616. Of those, 746 were not on diuretics at baseline, 1,311 were on loop diuretics at less than 40 mg FE or on non-loop diuretics only, 1,365 were taking 40 mg FE, and 1,204 were on higher doses of loop diuretics.
The mean baseline dosage was 60 mg FE, which rose slightly throughout the trial. But the baseline dosage and the increases were both similar in the placebo and dapagliflozin groups. Dr. Jackson said 84% and 83% of patients on dapagliflozin and placebo, respectively, maintained their baseline dose at 6 months and about 77% in both groups at 12 months.
The overall trial’s significant primary endpoint reduction for dapagliflozin versus placebo applied similarly to patients not on a diuretics and to those on any dose of diuretic, with an interaction P value of .23 for the effect of diuretic use. The hazard ratios (95% confidence interval) were 0.57 (0.36-0.92) for patients not on diuretics, 0.78 (0.68-0.90) for patients on any diuretic dosage, and 0.74 (0.65-0.85) overall
Dr. Jackson said during her formal online presentation that patients on diuretics showed a “tendency toward slightly more volume depletion in those on dapagliflozin than in those on placebo, but the excess was small and not greater than approximately 3% in those taking 40 mg furosemide equivalent diuretic. And fortunately, this did not result in an increase in frequency in renal adverse events nor of discontinuation of study drug.”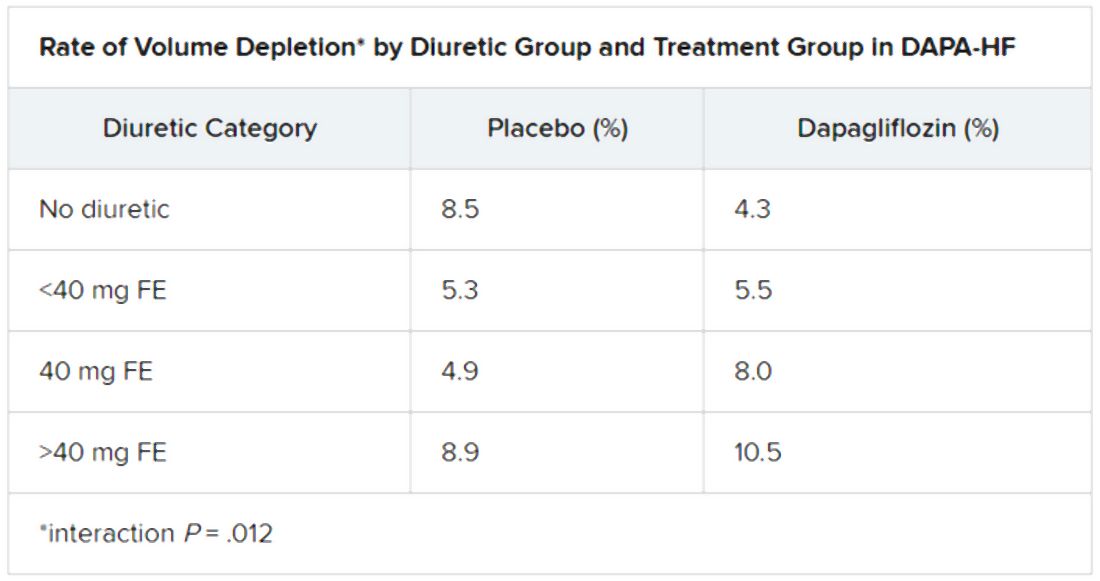
Renal adverse events were similarly prevalent in the two treatment groups, as were such events leading to treatment discontinuation. But serious renal events were less common in the dapagliflozin group (1.6% vs 2.7%; P = .009), as was investigator-reported serious acute kidney injury (1.0% vs 1.9%; P = .007).
“Overall, renal events were infrequent,” Dr. Jackson said, and “because of the small number of events, it is very difficult to draw conclusions about the impact of dapagliflozin on renal function according to diuretic-dose subgroups.”
Still, she said, worsening renal function was less common on dapagliflozin in three of the four groups by diuretic dosage; the exception was the less than 40 mg FE group, “but the absolute difference in this group was only two events.”
There seem to be dapagliflozin mechanisms “underneath the surface that need to be unraveled,” Dr. Doehner said as discussant, processes that are favorable for the treatment of HFrEF in which “diuretics play no big role.”
Dr. Jackson has no disclosures. Dr. Coats has disclosed receiving personal fees from Actimed, AstraZeneca, Faraday, WL Gore, Menarini, Novartis, Nutricia, Respicardia, Servier, Stealth Peptides, Verona, and Vifor. Dr. Doener has recently disclosed receiving grants and personal fees from Vifor, Pfizer, Boehringer Ingelheim, Sphingotec, ZS Pharma, Bayer, and Medtronic.
A version of this article originally appeared on Medscape.com.
FROM ESC HEART FAILURE 2020
VA readmissions program not linked to increased death
with no concurrent increase in 30-day mortality, a large cohort study suggests.
Unlike the Center for Medicare & Medicaid’s Hospital Readmissions Reduction Program (HRRP), whose primary objective is reducing payments to hospitals with excess readmissions, the VA’s efforts to reduce readmissions across their system did not include any financial penalties.
“The intervention focused on encouraging participation in transitions of care programs, such as the American College of Cardiology’s Hospital to Home Initiative and the creation of a heart failure provider network that included more than 900 heart failure providers throughout the VA system,” said the study’s lead author Justin T. Parizo, MD, of Stanford (Calif.) University.
The only measuring sticks the VA used were the public reporting of 30-day readmission rates (starting in 2012) and inclusion of those rates into hospitals’ overall star ratings (starting in 2014).
“The readmissions reductions we saw were similar in magnitude to those seen in patients in CMS fee-for-service categories in the HRRP,” said Dr. Parizo. “And while we had no ability to evaluate causality here, our best guess from what we can see is that there’s been no impact of the readmissions program on mortality,” he added.
Their results were published online June 17 in JAMA Cardiology.
Dr. Parizo and colleagues conducted a cohort study of 304,374 heart failure hospital admissions in 164,566 patients from January 2007 to September 2017. Importantly, he stressed, the researchers were able to do sophisticated risk adjustment for illness trends, something that has been a sticking point in some of the HRRP studies to date.
“We leveraged the robust dataset that the VA provides to adjust for illness severity. Accounting for clinical factors, like blood pressure, weight, creatinine, BNP [B-type natriuretic peptide], and other markers of heart failure severity, but also for changes in coding,” said Dr. Parizo.
Stratification according to left ventricular ejection fraction (LVEF) showed similar results both in terms of 30-day readmission and 30-day mortality for those with LVEF of 40% or greater and those with LVEF less than 40%.
In an interview, Dr. Parizo noted that they actually saw a small but significant uptick in mortality in the 2011-2012 period (compared with 2007-2008) that remains unexplained. “By the 2015-2017 period, 30-day death had returned to baseline levels,” he said.
In contrast, the HRRP, which was rolled out in 2012, has also been shown to reduce readmissions but, in most studies, 30-day mortality had gone up.
“The VA has a very robust quality infrastructure and a robust mechanism for prioritizing certain quality-improvement goals and getting them accomplished that I think they are underrecognized for,” said Leora Horwitz, MD, MHS, the director of the Center for Healthcare Innovation and Delivery Science at NYU Langone Medical Center, New York.
In an interview, she also noted some concern with the uptick seen in the 2011-2012 period, noting that the increase might be the same signal seen with the HRRP intervention.
“This is around the same time period where other people were writing the HRRP papers that showed an increase in mortality, so that’s something to consider,” she said.
Dr. Horwitz coauthored a study published in 2017 indicating that, on a hospital level (compared with a patient level, the approach most other studies took), reductions in readmissions were only weakly correlated with 30-day mortality rates after discharge.
“So, if you think that a hospital that’s behaving badly and keeping people out of the hospital inappropriately to cut down their readmissions, you’d expect to see increased mortality in that hospital, and in our study there was no correlation whatsoever. So there is still debate as to what is behind the increase in mortality on a patient level with heart failure that we’ve seen in some studies,” she said.
Dr. Horwitz doubts an intervention such as the one undertaken in the VA system – even with its fairly soft-touch “name and shame” component – would work in the non-VA hospital world.
“Those who have been in favor of financial penalties have pointed to the fact that, in general, it’s hard to get health systems to respond without financial alignment, even if it’s not an overt financial incentive,” she said.
“The VA is a unique environment,” she noted. “They have a very strong top-down command control focus where people are kind of used to being told, ‘OK, here are the measures we have to address this year.’ It’s good to see that the system that has worked for them for other outcomes also worked for them for heart failure readmissions too.”
Dr. Parizo has disclosed no relevant financial relationships. Dr. Horwitz has worked under contract to Medicare to develop readmission measures.
A version of this article originally appeared on Medscape.com.
with no concurrent increase in 30-day mortality, a large cohort study suggests.
Unlike the Center for Medicare & Medicaid’s Hospital Readmissions Reduction Program (HRRP), whose primary objective is reducing payments to hospitals with excess readmissions, the VA’s efforts to reduce readmissions across their system did not include any financial penalties.
“The intervention focused on encouraging participation in transitions of care programs, such as the American College of Cardiology’s Hospital to Home Initiative and the creation of a heart failure provider network that included more than 900 heart failure providers throughout the VA system,” said the study’s lead author Justin T. Parizo, MD, of Stanford (Calif.) University.
The only measuring sticks the VA used were the public reporting of 30-day readmission rates (starting in 2012) and inclusion of those rates into hospitals’ overall star ratings (starting in 2014).
“The readmissions reductions we saw were similar in magnitude to those seen in patients in CMS fee-for-service categories in the HRRP,” said Dr. Parizo. “And while we had no ability to evaluate causality here, our best guess from what we can see is that there’s been no impact of the readmissions program on mortality,” he added.
Their results were published online June 17 in JAMA Cardiology.
Dr. Parizo and colleagues conducted a cohort study of 304,374 heart failure hospital admissions in 164,566 patients from January 2007 to September 2017. Importantly, he stressed, the researchers were able to do sophisticated risk adjustment for illness trends, something that has been a sticking point in some of the HRRP studies to date.
“We leveraged the robust dataset that the VA provides to adjust for illness severity. Accounting for clinical factors, like blood pressure, weight, creatinine, BNP [B-type natriuretic peptide], and other markers of heart failure severity, but also for changes in coding,” said Dr. Parizo.
Stratification according to left ventricular ejection fraction (LVEF) showed similar results both in terms of 30-day readmission and 30-day mortality for those with LVEF of 40% or greater and those with LVEF less than 40%.
In an interview, Dr. Parizo noted that they actually saw a small but significant uptick in mortality in the 2011-2012 period (compared with 2007-2008) that remains unexplained. “By the 2015-2017 period, 30-day death had returned to baseline levels,” he said.
In contrast, the HRRP, which was rolled out in 2012, has also been shown to reduce readmissions but, in most studies, 30-day mortality had gone up.
“The VA has a very robust quality infrastructure and a robust mechanism for prioritizing certain quality-improvement goals and getting them accomplished that I think they are underrecognized for,” said Leora Horwitz, MD, MHS, the director of the Center for Healthcare Innovation and Delivery Science at NYU Langone Medical Center, New York.
In an interview, she also noted some concern with the uptick seen in the 2011-2012 period, noting that the increase might be the same signal seen with the HRRP intervention.
“This is around the same time period where other people were writing the HRRP papers that showed an increase in mortality, so that’s something to consider,” she said.
Dr. Horwitz coauthored a study published in 2017 indicating that, on a hospital level (compared with a patient level, the approach most other studies took), reductions in readmissions were only weakly correlated with 30-day mortality rates after discharge.
“So, if you think that a hospital that’s behaving badly and keeping people out of the hospital inappropriately to cut down their readmissions, you’d expect to see increased mortality in that hospital, and in our study there was no correlation whatsoever. So there is still debate as to what is behind the increase in mortality on a patient level with heart failure that we’ve seen in some studies,” she said.
Dr. Horwitz doubts an intervention such as the one undertaken in the VA system – even with its fairly soft-touch “name and shame” component – would work in the non-VA hospital world.
“Those who have been in favor of financial penalties have pointed to the fact that, in general, it’s hard to get health systems to respond without financial alignment, even if it’s not an overt financial incentive,” she said.
“The VA is a unique environment,” she noted. “They have a very strong top-down command control focus where people are kind of used to being told, ‘OK, here are the measures we have to address this year.’ It’s good to see that the system that has worked for them for other outcomes also worked for them for heart failure readmissions too.”
Dr. Parizo has disclosed no relevant financial relationships. Dr. Horwitz has worked under contract to Medicare to develop readmission measures.
A version of this article originally appeared on Medscape.com.
with no concurrent increase in 30-day mortality, a large cohort study suggests.
Unlike the Center for Medicare & Medicaid’s Hospital Readmissions Reduction Program (HRRP), whose primary objective is reducing payments to hospitals with excess readmissions, the VA’s efforts to reduce readmissions across their system did not include any financial penalties.
“The intervention focused on encouraging participation in transitions of care programs, such as the American College of Cardiology’s Hospital to Home Initiative and the creation of a heart failure provider network that included more than 900 heart failure providers throughout the VA system,” said the study’s lead author Justin T. Parizo, MD, of Stanford (Calif.) University.
The only measuring sticks the VA used were the public reporting of 30-day readmission rates (starting in 2012) and inclusion of those rates into hospitals’ overall star ratings (starting in 2014).
“The readmissions reductions we saw were similar in magnitude to those seen in patients in CMS fee-for-service categories in the HRRP,” said Dr. Parizo. “And while we had no ability to evaluate causality here, our best guess from what we can see is that there’s been no impact of the readmissions program on mortality,” he added.
Their results were published online June 17 in JAMA Cardiology.
Dr. Parizo and colleagues conducted a cohort study of 304,374 heart failure hospital admissions in 164,566 patients from January 2007 to September 2017. Importantly, he stressed, the researchers were able to do sophisticated risk adjustment for illness trends, something that has been a sticking point in some of the HRRP studies to date.
“We leveraged the robust dataset that the VA provides to adjust for illness severity. Accounting for clinical factors, like blood pressure, weight, creatinine, BNP [B-type natriuretic peptide], and other markers of heart failure severity, but also for changes in coding,” said Dr. Parizo.
Stratification according to left ventricular ejection fraction (LVEF) showed similar results both in terms of 30-day readmission and 30-day mortality for those with LVEF of 40% or greater and those with LVEF less than 40%.
In an interview, Dr. Parizo noted that they actually saw a small but significant uptick in mortality in the 2011-2012 period (compared with 2007-2008) that remains unexplained. “By the 2015-2017 period, 30-day death had returned to baseline levels,” he said.
In contrast, the HRRP, which was rolled out in 2012, has also been shown to reduce readmissions but, in most studies, 30-day mortality had gone up.
“The VA has a very robust quality infrastructure and a robust mechanism for prioritizing certain quality-improvement goals and getting them accomplished that I think they are underrecognized for,” said Leora Horwitz, MD, MHS, the director of the Center for Healthcare Innovation and Delivery Science at NYU Langone Medical Center, New York.
In an interview, she also noted some concern with the uptick seen in the 2011-2012 period, noting that the increase might be the same signal seen with the HRRP intervention.
“This is around the same time period where other people were writing the HRRP papers that showed an increase in mortality, so that’s something to consider,” she said.
Dr. Horwitz coauthored a study published in 2017 indicating that, on a hospital level (compared with a patient level, the approach most other studies took), reductions in readmissions were only weakly correlated with 30-day mortality rates after discharge.
“So, if you think that a hospital that’s behaving badly and keeping people out of the hospital inappropriately to cut down their readmissions, you’d expect to see increased mortality in that hospital, and in our study there was no correlation whatsoever. So there is still debate as to what is behind the increase in mortality on a patient level with heart failure that we’ve seen in some studies,” she said.
Dr. Horwitz doubts an intervention such as the one undertaken in the VA system – even with its fairly soft-touch “name and shame” component – would work in the non-VA hospital world.
“Those who have been in favor of financial penalties have pointed to the fact that, in general, it’s hard to get health systems to respond without financial alignment, even if it’s not an overt financial incentive,” she said.
“The VA is a unique environment,” she noted. “They have a very strong top-down command control focus where people are kind of used to being told, ‘OK, here are the measures we have to address this year.’ It’s good to see that the system that has worked for them for other outcomes also worked for them for heart failure readmissions too.”
Dr. Parizo has disclosed no relevant financial relationships. Dr. Horwitz has worked under contract to Medicare to develop readmission measures.
A version of this article originally appeared on Medscape.com.
Early hypertensive disorders in pregnancy linked to obesity
Rising classes of obesity are linked with progressively increased risk of early-onset hypertensive disorders in pregnant women, as has been established for late-onset hypertensive disorders, according to a U.S.-based retrospective cohort study.
Between 4% and 8% of pregnancies are impacted by hypertensive disorders, and preeclampsia is associated with a doubling of adverse neonatal events and causes 16% of maternal deaths in developed countries, previous studies have found. This study showed a clear risk of early-onset hypertensive disorders (less than 34 weeks’ gestation), which may be more deadly than late-onset disease: Compared with later-developing disorders, early hypertensive disorders are linked to a 400% increased risk of perinatal death and a 100%-300% increased risk of severe cardiovascular, renal, or hepatic maternal morbidity, according to previous studies.
The new research, led by Matthew Bicocca, MD, of the University of Texas Health Science Center, Houston, was published in Obstetrics & Gynecology. The researchers analyzed data from U.S. Vital Statistics, including over 14 million singleton births. The sample excluded women with chronic hypertension and a body mass index (BMI) below 18.5 kg/m2.
Previous studies demonstrated that obesity is a risk factor for late-onset hypertensive disorders, but studies of early-onset hypertensive disorders have yielded conflicting results. That could be because early-onset disorders are rare, representing just 5%-10% of hypertensive disorders during pregnancy, making it difficult to obtain a sufficient sample size to show a relationship.
“We know that obese pregnant women are at increased risk for adverse pregnancy outcomes, and this is of particular importance with the increasing prevalence of obesity in the United States. As this is a nationwide cohort with a large sample size, it allowed for evaluation of the rare outcome of early-onset hypertensive disorders of pregnancy,” said Iris Krishna, MD, MPH, an assistant professor of maternal-fetal medicine at Emory University, Atlanta, who was asked to comment on the study.
The researchers classified the women in the study as nonobese (BMI, 18.5-29.9 kg/m2; 46%), class I obese (BMI, 30.0-34.9; 29%), class II obese (BMI, 35.0-39.9; 15%), or class III obese (BMI, 40 or higher; 10%). About 6% of the participants developed hypertensive disorders during pregnancy (0.3% early onset), and the associated risk was greater with increasing class of obesity. Compared with nonobese women, class III obesity was associated with the highest adjusted risk ratio (2.18; 95% confidence interval, 2.12-2.24) for early-onset hypertensive disorders, followed by class II obesity (aRR, 1.57; 95% CI, 1.53-1.62) and class I (aRR, 1.13; 95% CI, 1.10-1.16). A similar pattern was observed with late-onset hypertensive disorders, with the highest risk associated with class III obese (aRR, 3.93; 95% CI, 3.91-3.96), followed by class II (aRR, 2.60; 95% CI, 2.58-2.62) and class I (aRR, 1.71; 95% CI, 1.70-1.73).
The mechanism underlying any potential link between obesity and risk of hypertensive orders of pregnancy isn’t completely understood, especially because the early-onset and late-onset hypertensive disorders have differing pathophysiology. “Early onset is the result from abnormal placentation [leading to] chronic placental insufficiency, and late onset likely [results from] placental insufficiency paired with oxidative stress from conditions such as obesity and insulin resistance,” Dr. Krishna said.
The new research reinforces the need for obese women to receive early prenatal care and counseling on nutrition and exercise “to mitigate weight gain during pregnancy in hopes of reducing their risk for adverse pregnancy outcomes, such as hypertensive disorders of pregnancy,” she concluded.
No source of funding was disclosed. The authors reported having no potential conflicts of interest.
SOURCE: Bicocca M et al. Obstet Gynecol. 2020 Jun 11. doi: 10.1097/AOG.0000000000003901.
Rising classes of obesity are linked with progressively increased risk of early-onset hypertensive disorders in pregnant women, as has been established for late-onset hypertensive disorders, according to a U.S.-based retrospective cohort study.
Between 4% and 8% of pregnancies are impacted by hypertensive disorders, and preeclampsia is associated with a doubling of adverse neonatal events and causes 16% of maternal deaths in developed countries, previous studies have found. This study showed a clear risk of early-onset hypertensive disorders (less than 34 weeks’ gestation), which may be more deadly than late-onset disease: Compared with later-developing disorders, early hypertensive disorders are linked to a 400% increased risk of perinatal death and a 100%-300% increased risk of severe cardiovascular, renal, or hepatic maternal morbidity, according to previous studies.
The new research, led by Matthew Bicocca, MD, of the University of Texas Health Science Center, Houston, was published in Obstetrics & Gynecology. The researchers analyzed data from U.S. Vital Statistics, including over 14 million singleton births. The sample excluded women with chronic hypertension and a body mass index (BMI) below 18.5 kg/m2.
Previous studies demonstrated that obesity is a risk factor for late-onset hypertensive disorders, but studies of early-onset hypertensive disorders have yielded conflicting results. That could be because early-onset disorders are rare, representing just 5%-10% of hypertensive disorders during pregnancy, making it difficult to obtain a sufficient sample size to show a relationship.
“We know that obese pregnant women are at increased risk for adverse pregnancy outcomes, and this is of particular importance with the increasing prevalence of obesity in the United States. As this is a nationwide cohort with a large sample size, it allowed for evaluation of the rare outcome of early-onset hypertensive disorders of pregnancy,” said Iris Krishna, MD, MPH, an assistant professor of maternal-fetal medicine at Emory University, Atlanta, who was asked to comment on the study.
The researchers classified the women in the study as nonobese (BMI, 18.5-29.9 kg/m2; 46%), class I obese (BMI, 30.0-34.9; 29%), class II obese (BMI, 35.0-39.9; 15%), or class III obese (BMI, 40 or higher; 10%). About 6% of the participants developed hypertensive disorders during pregnancy (0.3% early onset), and the associated risk was greater with increasing class of obesity. Compared with nonobese women, class III obesity was associated with the highest adjusted risk ratio (2.18; 95% confidence interval, 2.12-2.24) for early-onset hypertensive disorders, followed by class II obesity (aRR, 1.57; 95% CI, 1.53-1.62) and class I (aRR, 1.13; 95% CI, 1.10-1.16). A similar pattern was observed with late-onset hypertensive disorders, with the highest risk associated with class III obese (aRR, 3.93; 95% CI, 3.91-3.96), followed by class II (aRR, 2.60; 95% CI, 2.58-2.62) and class I (aRR, 1.71; 95% CI, 1.70-1.73).
The mechanism underlying any potential link between obesity and risk of hypertensive orders of pregnancy isn’t completely understood, especially because the early-onset and late-onset hypertensive disorders have differing pathophysiology. “Early onset is the result from abnormal placentation [leading to] chronic placental insufficiency, and late onset likely [results from] placental insufficiency paired with oxidative stress from conditions such as obesity and insulin resistance,” Dr. Krishna said.
The new research reinforces the need for obese women to receive early prenatal care and counseling on nutrition and exercise “to mitigate weight gain during pregnancy in hopes of reducing their risk for adverse pregnancy outcomes, such as hypertensive disorders of pregnancy,” she concluded.
No source of funding was disclosed. The authors reported having no potential conflicts of interest.
SOURCE: Bicocca M et al. Obstet Gynecol. 2020 Jun 11. doi: 10.1097/AOG.0000000000003901.
Rising classes of obesity are linked with progressively increased risk of early-onset hypertensive disorders in pregnant women, as has been established for late-onset hypertensive disorders, according to a U.S.-based retrospective cohort study.
Between 4% and 8% of pregnancies are impacted by hypertensive disorders, and preeclampsia is associated with a doubling of adverse neonatal events and causes 16% of maternal deaths in developed countries, previous studies have found. This study showed a clear risk of early-onset hypertensive disorders (less than 34 weeks’ gestation), which may be more deadly than late-onset disease: Compared with later-developing disorders, early hypertensive disorders are linked to a 400% increased risk of perinatal death and a 100%-300% increased risk of severe cardiovascular, renal, or hepatic maternal morbidity, according to previous studies.
The new research, led by Matthew Bicocca, MD, of the University of Texas Health Science Center, Houston, was published in Obstetrics & Gynecology. The researchers analyzed data from U.S. Vital Statistics, including over 14 million singleton births. The sample excluded women with chronic hypertension and a body mass index (BMI) below 18.5 kg/m2.
Previous studies demonstrated that obesity is a risk factor for late-onset hypertensive disorders, but studies of early-onset hypertensive disorders have yielded conflicting results. That could be because early-onset disorders are rare, representing just 5%-10% of hypertensive disorders during pregnancy, making it difficult to obtain a sufficient sample size to show a relationship.
“We know that obese pregnant women are at increased risk for adverse pregnancy outcomes, and this is of particular importance with the increasing prevalence of obesity in the United States. As this is a nationwide cohort with a large sample size, it allowed for evaluation of the rare outcome of early-onset hypertensive disorders of pregnancy,” said Iris Krishna, MD, MPH, an assistant professor of maternal-fetal medicine at Emory University, Atlanta, who was asked to comment on the study.
The researchers classified the women in the study as nonobese (BMI, 18.5-29.9 kg/m2; 46%), class I obese (BMI, 30.0-34.9; 29%), class II obese (BMI, 35.0-39.9; 15%), or class III obese (BMI, 40 or higher; 10%). About 6% of the participants developed hypertensive disorders during pregnancy (0.3% early onset), and the associated risk was greater with increasing class of obesity. Compared with nonobese women, class III obesity was associated with the highest adjusted risk ratio (2.18; 95% confidence interval, 2.12-2.24) for early-onset hypertensive disorders, followed by class II obesity (aRR, 1.57; 95% CI, 1.53-1.62) and class I (aRR, 1.13; 95% CI, 1.10-1.16). A similar pattern was observed with late-onset hypertensive disorders, with the highest risk associated with class III obese (aRR, 3.93; 95% CI, 3.91-3.96), followed by class II (aRR, 2.60; 95% CI, 2.58-2.62) and class I (aRR, 1.71; 95% CI, 1.70-1.73).
The mechanism underlying any potential link between obesity and risk of hypertensive orders of pregnancy isn’t completely understood, especially because the early-onset and late-onset hypertensive disorders have differing pathophysiology. “Early onset is the result from abnormal placentation [leading to] chronic placental insufficiency, and late onset likely [results from] placental insufficiency paired with oxidative stress from conditions such as obesity and insulin resistance,” Dr. Krishna said.
The new research reinforces the need for obese women to receive early prenatal care and counseling on nutrition and exercise “to mitigate weight gain during pregnancy in hopes of reducing their risk for adverse pregnancy outcomes, such as hypertensive disorders of pregnancy,” she concluded.
No source of funding was disclosed. The authors reported having no potential conflicts of interest.
SOURCE: Bicocca M et al. Obstet Gynecol. 2020 Jun 11. doi: 10.1097/AOG.0000000000003901.
FROM OBSTETRICS & GYNECOLOGY
Women thrive on baroreflex activation for heart failure
The striking gains in functional capacity and quality of life conferred by baroreflex activation therapy in patients with heart failure, as shown in the pivotal phase 3 clinical trial for this novel intervention, were at least as great in women as in men, JoAnn Lindenfeld, MD, said at the European Society of Cardiology Heart Failure Discoveries virtual meeting.
The results of the multicenter, prospective, randomized BeAT-HF trial led to marketing approval of the BaroStim Neo system for improvement in symptoms of heart failure with reduced ejection fraction (HFrEF) by the Food and Drug Administration in August 2019. Dr. Lindenfeld presented a fresh breakdown of the results by gender which showed, intriguingly, that the improvement in all study endpoints was consistently numerically greater in the women – sometimes startlingly so – although these gender differences in response didn’t achieve statistical significance. The 6-month randomized trial was underpowered for drawing definitive conclusions on that score, with a study population of only 53 women and 211 men. So the investigator remained circumspect.
“We think that what this study shows us is that women have at least equivalent improvement as men in this population. I don’t think we can conclude from this study yet that it’s better, but it’s certainly in all these parameters as least as good. And I think this is a population in which we’ve seen that improving symptoms and functional capacity is very important,” said Dr. Lindenfeld, professor of medicine and director of advanced heart failure/cardiac transplantation at Vanderbilt University, Nashville, Tenn.
The FDA approval was restricted to patients like those enrolled in BeAT-HF: that is, individuals with New York Heart Association functional class III heart failure, a left ventricular ejection fraction of 35% or less while on stable optimal medical therapy, and ineligibility for cardiac resynchronization therapy according to current guidelines. Seventy-eight percent of BeAT-HF participants had an implantable cardioverter-defibrillator.
Participants were randomized to baroreflex activation therapy (BAT) plus optimal medical therapy or to optimal medical therapy alone. The three coprimary endpoints were change from baseline to 6 months in 6-minute hall walk distance (6MHW), scores on the Minnesota Living with Heart Failure Questionnaire (MLHF), and N-terminal pro-B-type natriuretic peptide (NT-proBNP).
In the overall study population, 6MHW increased by 60 m in the BAT group and decreased by 8 m in controls; MLHF scores dropped by 14 and 6 points, respectively; and NT-proBNP fell by an average of 25% with BAT while rising by 3% in controls.
Very often, just a 5-point reduction in MLHF score is considered a clinically meaningful improvement in quality of life, the cardiologist noted.
The gender-based analysis is where things got particularly interesting.
The investigators defined a clinically relevant response as a greater than 10% increase from baseline on the 6MHW, at least a one-class improvement in NYHA class, or a reduction of 5 points or more on the MLHF. Among subjects in the BAT group, 70% of women and 60% of men met the clinically relevant response standard in terms of 6MHW, as did 70% of women and 64% of men for improvement in NYHA class, and 78% of women and 66% of men for MLHF score.
Eighty-seven percent of women and 68% of men on BAT had a clinically relevant response on at least one of these endpoints, as did about 28% of controls. Moreover, 31% of women in the BAT group were clinically relevant responders on at least two endpoints, compared with 19% of BAT men and 4% and 9% of controls.
Women dominate super-responder category
In order to be classified as a super responder, a patient had to demonstrate a greater than 20% increase in 6MHW, improvement in NYHA class I status, or at least a 10-point improvement in MLHF score. Ninety-one percent of women on BAT achieved super-responder status for at least one of these endpoints, compared with 76% of men. Forty-three percent of women and 24% of men in the BAT group were super responders in at least two domains, as were 8% and 11% of female and male controls, Dr. Lindenfeld continued.
Discussant Ewa Anita Jankowska, MD, PhD, deemed the BeAT-HF results on the therapeutic benefits of this autonomic modulation strategy “quite convincing.”
“We need to acknowledge that in recent years we have been spoiled a bit by the huge trials in heart failure where the ultimate goal was a reduction in mortality. But I think this is the time when we should think about the patients who want to live – here, now – with a better life. Patients expect symptomatic benefits. There is a substantial group of patients who are symptomatic even though they receive quite extensive neurohormonal blockage and who are not suitable for CRT. This study demonstrates that, for this group of patients, BAT can bring really significant symptomatic benefits,” she said.
“If you think about a treatment that provides patients who are NYHA class III an increase in 6MHW of 60 meters, that’s really something. And 20% of patients went from NYHA class III to class I – that’s really something, too,” added Dr. Jankowska, professor of medicine and head of the laboratory of applied research on the cardiovascular system at Wroclaw (Poland) University.
How baroreflex activation therapy works
The BaroStim system consists of a 2-mm unipolar electrode on a 7-mm backer that is placed over the carotid sinus. It is supported by a small generator with a 4- to 5-year battery life implanted under the collarbone, along with radiofrequency telemetry capability and programming flexibility.
Stimulation of the carotid baroreceptor promotes an integrated autonomic nervous system response which enhances parasympathetic activity and inhibits sympathetic nervous system activity. The result, as shown in numerous earlier proof-of-concept studies, is a reduced heart rate, decreased ventricular remodeling, enhanced diuresis, increased vasodilation, a drop in elevated blood pressure, and decreased renin secretion – all achieved nonpharmacologically.
The study was sponsored by CVRx. Dr. Lindenfeld reported serving as a consultant to CVRx, Abbott, AstraZeneca, Boehringer Ingelheim, Edwards Lifesciences, Impulse Dynamics, and VWave.
The striking gains in functional capacity and quality of life conferred by baroreflex activation therapy in patients with heart failure, as shown in the pivotal phase 3 clinical trial for this novel intervention, were at least as great in women as in men, JoAnn Lindenfeld, MD, said at the European Society of Cardiology Heart Failure Discoveries virtual meeting.
The results of the multicenter, prospective, randomized BeAT-HF trial led to marketing approval of the BaroStim Neo system for improvement in symptoms of heart failure with reduced ejection fraction (HFrEF) by the Food and Drug Administration in August 2019. Dr. Lindenfeld presented a fresh breakdown of the results by gender which showed, intriguingly, that the improvement in all study endpoints was consistently numerically greater in the women – sometimes startlingly so – although these gender differences in response didn’t achieve statistical significance. The 6-month randomized trial was underpowered for drawing definitive conclusions on that score, with a study population of only 53 women and 211 men. So the investigator remained circumspect.
“We think that what this study shows us is that women have at least equivalent improvement as men in this population. I don’t think we can conclude from this study yet that it’s better, but it’s certainly in all these parameters as least as good. And I think this is a population in which we’ve seen that improving symptoms and functional capacity is very important,” said Dr. Lindenfeld, professor of medicine and director of advanced heart failure/cardiac transplantation at Vanderbilt University, Nashville, Tenn.
The FDA approval was restricted to patients like those enrolled in BeAT-HF: that is, individuals with New York Heart Association functional class III heart failure, a left ventricular ejection fraction of 35% or less while on stable optimal medical therapy, and ineligibility for cardiac resynchronization therapy according to current guidelines. Seventy-eight percent of BeAT-HF participants had an implantable cardioverter-defibrillator.
Participants were randomized to baroreflex activation therapy (BAT) plus optimal medical therapy or to optimal medical therapy alone. The three coprimary endpoints were change from baseline to 6 months in 6-minute hall walk distance (6MHW), scores on the Minnesota Living with Heart Failure Questionnaire (MLHF), and N-terminal pro-B-type natriuretic peptide (NT-proBNP).
In the overall study population, 6MHW increased by 60 m in the BAT group and decreased by 8 m in controls; MLHF scores dropped by 14 and 6 points, respectively; and NT-proBNP fell by an average of 25% with BAT while rising by 3% in controls.
Very often, just a 5-point reduction in MLHF score is considered a clinically meaningful improvement in quality of life, the cardiologist noted.
The gender-based analysis is where things got particularly interesting.
The investigators defined a clinically relevant response as a greater than 10% increase from baseline on the 6MHW, at least a one-class improvement in NYHA class, or a reduction of 5 points or more on the MLHF. Among subjects in the BAT group, 70% of women and 60% of men met the clinically relevant response standard in terms of 6MHW, as did 70% of women and 64% of men for improvement in NYHA class, and 78% of women and 66% of men for MLHF score.
Eighty-seven percent of women and 68% of men on BAT had a clinically relevant response on at least one of these endpoints, as did about 28% of controls. Moreover, 31% of women in the BAT group were clinically relevant responders on at least two endpoints, compared with 19% of BAT men and 4% and 9% of controls.
Women dominate super-responder category
In order to be classified as a super responder, a patient had to demonstrate a greater than 20% increase in 6MHW, improvement in NYHA class I status, or at least a 10-point improvement in MLHF score. Ninety-one percent of women on BAT achieved super-responder status for at least one of these endpoints, compared with 76% of men. Forty-three percent of women and 24% of men in the BAT group were super responders in at least two domains, as were 8% and 11% of female and male controls, Dr. Lindenfeld continued.
Discussant Ewa Anita Jankowska, MD, PhD, deemed the BeAT-HF results on the therapeutic benefits of this autonomic modulation strategy “quite convincing.”
“We need to acknowledge that in recent years we have been spoiled a bit by the huge trials in heart failure where the ultimate goal was a reduction in mortality. But I think this is the time when we should think about the patients who want to live – here, now – with a better life. Patients expect symptomatic benefits. There is a substantial group of patients who are symptomatic even though they receive quite extensive neurohormonal blockage and who are not suitable for CRT. This study demonstrates that, for this group of patients, BAT can bring really significant symptomatic benefits,” she said.
“If you think about a treatment that provides patients who are NYHA class III an increase in 6MHW of 60 meters, that’s really something. And 20% of patients went from NYHA class III to class I – that’s really something, too,” added Dr. Jankowska, professor of medicine and head of the laboratory of applied research on the cardiovascular system at Wroclaw (Poland) University.
How baroreflex activation therapy works
The BaroStim system consists of a 2-mm unipolar electrode on a 7-mm backer that is placed over the carotid sinus. It is supported by a small generator with a 4- to 5-year battery life implanted under the collarbone, along with radiofrequency telemetry capability and programming flexibility.
Stimulation of the carotid baroreceptor promotes an integrated autonomic nervous system response which enhances parasympathetic activity and inhibits sympathetic nervous system activity. The result, as shown in numerous earlier proof-of-concept studies, is a reduced heart rate, decreased ventricular remodeling, enhanced diuresis, increased vasodilation, a drop in elevated blood pressure, and decreased renin secretion – all achieved nonpharmacologically.
The study was sponsored by CVRx. Dr. Lindenfeld reported serving as a consultant to CVRx, Abbott, AstraZeneca, Boehringer Ingelheim, Edwards Lifesciences, Impulse Dynamics, and VWave.
The striking gains in functional capacity and quality of life conferred by baroreflex activation therapy in patients with heart failure, as shown in the pivotal phase 3 clinical trial for this novel intervention, were at least as great in women as in men, JoAnn Lindenfeld, MD, said at the European Society of Cardiology Heart Failure Discoveries virtual meeting.
The results of the multicenter, prospective, randomized BeAT-HF trial led to marketing approval of the BaroStim Neo system for improvement in symptoms of heart failure with reduced ejection fraction (HFrEF) by the Food and Drug Administration in August 2019. Dr. Lindenfeld presented a fresh breakdown of the results by gender which showed, intriguingly, that the improvement in all study endpoints was consistently numerically greater in the women – sometimes startlingly so – although these gender differences in response didn’t achieve statistical significance. The 6-month randomized trial was underpowered for drawing definitive conclusions on that score, with a study population of only 53 women and 211 men. So the investigator remained circumspect.
“We think that what this study shows us is that women have at least equivalent improvement as men in this population. I don’t think we can conclude from this study yet that it’s better, but it’s certainly in all these parameters as least as good. And I think this is a population in which we’ve seen that improving symptoms and functional capacity is very important,” said Dr. Lindenfeld, professor of medicine and director of advanced heart failure/cardiac transplantation at Vanderbilt University, Nashville, Tenn.
The FDA approval was restricted to patients like those enrolled in BeAT-HF: that is, individuals with New York Heart Association functional class III heart failure, a left ventricular ejection fraction of 35% or less while on stable optimal medical therapy, and ineligibility for cardiac resynchronization therapy according to current guidelines. Seventy-eight percent of BeAT-HF participants had an implantable cardioverter-defibrillator.
Participants were randomized to baroreflex activation therapy (BAT) plus optimal medical therapy or to optimal medical therapy alone. The three coprimary endpoints were change from baseline to 6 months in 6-minute hall walk distance (6MHW), scores on the Minnesota Living with Heart Failure Questionnaire (MLHF), and N-terminal pro-B-type natriuretic peptide (NT-proBNP).
In the overall study population, 6MHW increased by 60 m in the BAT group and decreased by 8 m in controls; MLHF scores dropped by 14 and 6 points, respectively; and NT-proBNP fell by an average of 25% with BAT while rising by 3% in controls.
Very often, just a 5-point reduction in MLHF score is considered a clinically meaningful improvement in quality of life, the cardiologist noted.
The gender-based analysis is where things got particularly interesting.
The investigators defined a clinically relevant response as a greater than 10% increase from baseline on the 6MHW, at least a one-class improvement in NYHA class, or a reduction of 5 points or more on the MLHF. Among subjects in the BAT group, 70% of women and 60% of men met the clinically relevant response standard in terms of 6MHW, as did 70% of women and 64% of men for improvement in NYHA class, and 78% of women and 66% of men for MLHF score.
Eighty-seven percent of women and 68% of men on BAT had a clinically relevant response on at least one of these endpoints, as did about 28% of controls. Moreover, 31% of women in the BAT group were clinically relevant responders on at least two endpoints, compared with 19% of BAT men and 4% and 9% of controls.
Women dominate super-responder category
In order to be classified as a super responder, a patient had to demonstrate a greater than 20% increase in 6MHW, improvement in NYHA class I status, or at least a 10-point improvement in MLHF score. Ninety-one percent of women on BAT achieved super-responder status for at least one of these endpoints, compared with 76% of men. Forty-three percent of women and 24% of men in the BAT group were super responders in at least two domains, as were 8% and 11% of female and male controls, Dr. Lindenfeld continued.
Discussant Ewa Anita Jankowska, MD, PhD, deemed the BeAT-HF results on the therapeutic benefits of this autonomic modulation strategy “quite convincing.”
“We need to acknowledge that in recent years we have been spoiled a bit by the huge trials in heart failure where the ultimate goal was a reduction in mortality. But I think this is the time when we should think about the patients who want to live – here, now – with a better life. Patients expect symptomatic benefits. There is a substantial group of patients who are symptomatic even though they receive quite extensive neurohormonal blockage and who are not suitable for CRT. This study demonstrates that, for this group of patients, BAT can bring really significant symptomatic benefits,” she said.
“If you think about a treatment that provides patients who are NYHA class III an increase in 6MHW of 60 meters, that’s really something. And 20% of patients went from NYHA class III to class I – that’s really something, too,” added Dr. Jankowska, professor of medicine and head of the laboratory of applied research on the cardiovascular system at Wroclaw (Poland) University.
How baroreflex activation therapy works
The BaroStim system consists of a 2-mm unipolar electrode on a 7-mm backer that is placed over the carotid sinus. It is supported by a small generator with a 4- to 5-year battery life implanted under the collarbone, along with radiofrequency telemetry capability and programming flexibility.
Stimulation of the carotid baroreceptor promotes an integrated autonomic nervous system response which enhances parasympathetic activity and inhibits sympathetic nervous system activity. The result, as shown in numerous earlier proof-of-concept studies, is a reduced heart rate, decreased ventricular remodeling, enhanced diuresis, increased vasodilation, a drop in elevated blood pressure, and decreased renin secretion – all achieved nonpharmacologically.
The study was sponsored by CVRx. Dr. Lindenfeld reported serving as a consultant to CVRx, Abbott, AstraZeneca, Boehringer Ingelheim, Edwards Lifesciences, Impulse Dynamics, and VWave.
FROM ESC HEART FAILURE 2020