User login
Magnetic LES augmentation for Barrett’s regression debated
SEATTLE –
The study caught the attention of audience members – and raised a few eyebrows – at the 2018 World Congress of Endoscopic Surgery, where its results were presented, because the regression rate with the current standard operation for medically refractory gastroesophageal reflux – Nissen fundoplication – is only about 40%.
Lead investigator Evan Alicuben, MD, a general surgery resident at the university, cautioned that “longer-term follow-up is required to make a meaningful comparison with results following fundoplication.”
Fundoplication has been studied for decades, whereas the new study is likely the very first to look at the rates of Barrett’s regression after magnetic augmentation, and the 70% regression rate was based on postop endoscopies a median of 1.2 years after the procedure, not after the 5, 10, or even more years typically seen in fundoplication studies.
Magnetic sphincter augmentation (LINX Reflux Management System) was approved by the Food and Drug Administration in 2012 for reflux that persists despite maximum drug therapy. Patients have a band of magnetic titanium beads surgically placed around their LES; the band opens to let food pass, but tightens again to bolster the LES and prevent reflux.
The approach is gaining popularity. “We now know that it’s effective at controlling reflux symptoms, taking patients off proton pump inhibitors, and curing esophagitis,” at least in the short term. “One of the issues with [fundoplication] is that it may not last forever; the wrap comes undone or it slips. This device may give longer lasting” protection, Dr. Alicuben said.
“The main criticism is that it’s relatively new; people are still questioning it. The optimist in me wants to say that this is the answer we’ve been looking for; the pessimist [says] we need to wait to see what longer-term data show,” he said.
Barrett’s esophagus was confirmed by endoscopy in all 67 subjects before the magnets were placed, and each had at least one postop endoscopy.
At baseline, 29 had ultrashort-segment disease, which means there was no visible Barrett’s, but did have columnar epithelium with goblet cells on pathology. Thirty patients had short-segment disease, with up to 3 cm of visible involvement confirmed by pathology, while eight had long-segment disease, with involvement extending 3 cm or more.
Of the 67 patients, 48 had no evidence of Barrett’s after the procedure, for an overall regression rate of 71.6%. The regression rate was 82.8% in the ultrashort group (24/29); 73.3% in the short segment group (22/30); and 25% in the long segment group (2/8). Long-segment disease is notorious for persisting despite treatment; both patients had 3-cm lesions.
Among the 34 patients with two or more postop endoscopies, the regression rate was 73.5% (25).
There’s a lot of debate about whether ultrashort-segment disease is truly Barrett’s and whether it carries the same risk of malignant transformation, as one surgeon in the audience noted pointedly, worrying that including ultrashort patients oversold the results.
Dr. Alicuben countered that the regression rate remained strong even when ultrashort patients were excluded: 63% (24/38). “This is every bit as good if not better than the results of fundoplication,” another surgeon in the audience said.
The subjects were aged about 60 years, on average, with more men than women. Most had hiatal hernias, often measuring 3 cm or more. The mean body mass index was 27.3 kg/m2, but BMI ranged as high as 44.3.
Mean operative time was 66 minutes, and there were no major complications. None of the patients progressed to dysplasia or carcinoma. Median DeMeester scores fell from 35.3 to 9.2 after the operation in the 47 patients who had postop pH testing.
Surgeons have worried about esophageal erosion with the LINX system. A recent paper by Dr. Alicuben and his colleagues found 29 cases among almost 10,000 patients, which makes for an erosion rate of 0.3% at a median of about 2 years (J Gastrointest Surg. 2018 Apr 17. doi: 10.1007/s11605-018-3775-0).
About 500 LINX systems have been placed at the University of Southern California. Procedures in the study were performed between 2012 and late 2017.
Dr. Alicuben had no disclosures. Two investigators, including senior author John Lipham, MD, are paid consultants for Torax Medical, the maker of the LINX system, and Johnson & Johnson, which owns Torax through a subsidiary. There was no company funding for the review.
The World Congress of Endoscopic Surgery is hosted by the Society of American Gastrointestinal and Endoscopic Surgeons and the Canadian Association of General Surgeons
SOURCE: Alicuben E et al. WCE 2018, Abstract S095.
The enthusiasm and reservation surrounding the presented results supporting relatively high rates of regression of Barrett’s esophagus in patients undergoing LES magnetic sphincter augmentation are both well founded. Barrett’s regression, which has been observed to occur spontaneously as well as following antireflux interventions, is always a rich topic for debate. The reported rate of regression in this study being higher than that of complete fundoplication (Nissen fundoplication) is perplexing. The premise for the development of magnetic sphincter augmentation at a focal site was based on the theory that complete fundoplication is supraphysiologic, resulting in desired resolution of regurgitation with unwanted sequelae of dysphagia and bloat in a substantial number of patients. The development of magnetic sphincter augmentation was inspired by the concept that it would provide very reproducible control of regurgitation nearing that of complete fundoplication in a permanent fashion and do so at a focal point (< 1 cm) at the level of the lower esophageal sphincter, minimizing dysphagia and bloat. Since the design is one to replicate appropriate physiology without over treating the targeted reflux disease, theoretically any regression of Barrett’s esophagus should likewise approach but not exceed that of complete fundoplication.
I anticipate further studies will add to this rich debate. Any reservations about the results of this study should not overshadow the inherent advantages of magnetic sphincter augmentation. Its implantation is fairly straightforward to teach to surgeons who have a practice focused on antireflux surgery and due to the limited dissection/tissue mobilization required, most patients can return home a few hours after surgery and immediately resume a diet of solid foods.
Dr. Alicuban and colleagues discuss the small but real concern of erosion, however, another point of inherent concern is the binary function of the device. It is either implanted or not, there is no ability beyond endoscopic dilation to treat relative outflow obstruction and no means to convert the device to a “partial wrap.”
As we forge ahead with increasingly creative ways to address reflux disease the lessons we learn will contribute to the development of better medical, endoscopic and minimally invasive surgical technologies and the robust, civil debate seen here is something we can all enthusiastically anticipate.
Kevin M. Reavis, MD, FACS, is with the Division of Gastrointestinal and Minimally Invasive Surgery The Oregon Clinic; associate professor, Oregon Health & Science University, Portland, and President, Oregon Medical Society.
The enthusiasm and reservation surrounding the presented results supporting relatively high rates of regression of Barrett’s esophagus in patients undergoing LES magnetic sphincter augmentation are both well founded. Barrett’s regression, which has been observed to occur spontaneously as well as following antireflux interventions, is always a rich topic for debate. The reported rate of regression in this study being higher than that of complete fundoplication (Nissen fundoplication) is perplexing. The premise for the development of magnetic sphincter augmentation at a focal site was based on the theory that complete fundoplication is supraphysiologic, resulting in desired resolution of regurgitation with unwanted sequelae of dysphagia and bloat in a substantial number of patients. The development of magnetic sphincter augmentation was inspired by the concept that it would provide very reproducible control of regurgitation nearing that of complete fundoplication in a permanent fashion and do so at a focal point (< 1 cm) at the level of the lower esophageal sphincter, minimizing dysphagia and bloat. Since the design is one to replicate appropriate physiology without over treating the targeted reflux disease, theoretically any regression of Barrett’s esophagus should likewise approach but not exceed that of complete fundoplication.
I anticipate further studies will add to this rich debate. Any reservations about the results of this study should not overshadow the inherent advantages of magnetic sphincter augmentation. Its implantation is fairly straightforward to teach to surgeons who have a practice focused on antireflux surgery and due to the limited dissection/tissue mobilization required, most patients can return home a few hours after surgery and immediately resume a diet of solid foods.
Dr. Alicuban and colleagues discuss the small but real concern of erosion, however, another point of inherent concern is the binary function of the device. It is either implanted or not, there is no ability beyond endoscopic dilation to treat relative outflow obstruction and no means to convert the device to a “partial wrap.”
As we forge ahead with increasingly creative ways to address reflux disease the lessons we learn will contribute to the development of better medical, endoscopic and minimally invasive surgical technologies and the robust, civil debate seen here is something we can all enthusiastically anticipate.
Kevin M. Reavis, MD, FACS, is with the Division of Gastrointestinal and Minimally Invasive Surgery The Oregon Clinic; associate professor, Oregon Health & Science University, Portland, and President, Oregon Medical Society.
The enthusiasm and reservation surrounding the presented results supporting relatively high rates of regression of Barrett’s esophagus in patients undergoing LES magnetic sphincter augmentation are both well founded. Barrett’s regression, which has been observed to occur spontaneously as well as following antireflux interventions, is always a rich topic for debate. The reported rate of regression in this study being higher than that of complete fundoplication (Nissen fundoplication) is perplexing. The premise for the development of magnetic sphincter augmentation at a focal site was based on the theory that complete fundoplication is supraphysiologic, resulting in desired resolution of regurgitation with unwanted sequelae of dysphagia and bloat in a substantial number of patients. The development of magnetic sphincter augmentation was inspired by the concept that it would provide very reproducible control of regurgitation nearing that of complete fundoplication in a permanent fashion and do so at a focal point (< 1 cm) at the level of the lower esophageal sphincter, minimizing dysphagia and bloat. Since the design is one to replicate appropriate physiology without over treating the targeted reflux disease, theoretically any regression of Barrett’s esophagus should likewise approach but not exceed that of complete fundoplication.
I anticipate further studies will add to this rich debate. Any reservations about the results of this study should not overshadow the inherent advantages of magnetic sphincter augmentation. Its implantation is fairly straightforward to teach to surgeons who have a practice focused on antireflux surgery and due to the limited dissection/tissue mobilization required, most patients can return home a few hours after surgery and immediately resume a diet of solid foods.
Dr. Alicuban and colleagues discuss the small but real concern of erosion, however, another point of inherent concern is the binary function of the device. It is either implanted or not, there is no ability beyond endoscopic dilation to treat relative outflow obstruction and no means to convert the device to a “partial wrap.”
As we forge ahead with increasingly creative ways to address reflux disease the lessons we learn will contribute to the development of better medical, endoscopic and minimally invasive surgical technologies and the robust, civil debate seen here is something we can all enthusiastically anticipate.
Kevin M. Reavis, MD, FACS, is with the Division of Gastrointestinal and Minimally Invasive Surgery The Oregon Clinic; associate professor, Oregon Health & Science University, Portland, and President, Oregon Medical Society.
SEATTLE –
The study caught the attention of audience members – and raised a few eyebrows – at the 2018 World Congress of Endoscopic Surgery, where its results were presented, because the regression rate with the current standard operation for medically refractory gastroesophageal reflux – Nissen fundoplication – is only about 40%.
Lead investigator Evan Alicuben, MD, a general surgery resident at the university, cautioned that “longer-term follow-up is required to make a meaningful comparison with results following fundoplication.”
Fundoplication has been studied for decades, whereas the new study is likely the very first to look at the rates of Barrett’s regression after magnetic augmentation, and the 70% regression rate was based on postop endoscopies a median of 1.2 years after the procedure, not after the 5, 10, or even more years typically seen in fundoplication studies.
Magnetic sphincter augmentation (LINX Reflux Management System) was approved by the Food and Drug Administration in 2012 for reflux that persists despite maximum drug therapy. Patients have a band of magnetic titanium beads surgically placed around their LES; the band opens to let food pass, but tightens again to bolster the LES and prevent reflux.
The approach is gaining popularity. “We now know that it’s effective at controlling reflux symptoms, taking patients off proton pump inhibitors, and curing esophagitis,” at least in the short term. “One of the issues with [fundoplication] is that it may not last forever; the wrap comes undone or it slips. This device may give longer lasting” protection, Dr. Alicuben said.
“The main criticism is that it’s relatively new; people are still questioning it. The optimist in me wants to say that this is the answer we’ve been looking for; the pessimist [says] we need to wait to see what longer-term data show,” he said.
Barrett’s esophagus was confirmed by endoscopy in all 67 subjects before the magnets were placed, and each had at least one postop endoscopy.
At baseline, 29 had ultrashort-segment disease, which means there was no visible Barrett’s, but did have columnar epithelium with goblet cells on pathology. Thirty patients had short-segment disease, with up to 3 cm of visible involvement confirmed by pathology, while eight had long-segment disease, with involvement extending 3 cm or more.
Of the 67 patients, 48 had no evidence of Barrett’s after the procedure, for an overall regression rate of 71.6%. The regression rate was 82.8% in the ultrashort group (24/29); 73.3% in the short segment group (22/30); and 25% in the long segment group (2/8). Long-segment disease is notorious for persisting despite treatment; both patients had 3-cm lesions.
Among the 34 patients with two or more postop endoscopies, the regression rate was 73.5% (25).
There’s a lot of debate about whether ultrashort-segment disease is truly Barrett’s and whether it carries the same risk of malignant transformation, as one surgeon in the audience noted pointedly, worrying that including ultrashort patients oversold the results.
Dr. Alicuben countered that the regression rate remained strong even when ultrashort patients were excluded: 63% (24/38). “This is every bit as good if not better than the results of fundoplication,” another surgeon in the audience said.
The subjects were aged about 60 years, on average, with more men than women. Most had hiatal hernias, often measuring 3 cm or more. The mean body mass index was 27.3 kg/m2, but BMI ranged as high as 44.3.
Mean operative time was 66 minutes, and there were no major complications. None of the patients progressed to dysplasia or carcinoma. Median DeMeester scores fell from 35.3 to 9.2 after the operation in the 47 patients who had postop pH testing.
Surgeons have worried about esophageal erosion with the LINX system. A recent paper by Dr. Alicuben and his colleagues found 29 cases among almost 10,000 patients, which makes for an erosion rate of 0.3% at a median of about 2 years (J Gastrointest Surg. 2018 Apr 17. doi: 10.1007/s11605-018-3775-0).
About 500 LINX systems have been placed at the University of Southern California. Procedures in the study were performed between 2012 and late 2017.
Dr. Alicuben had no disclosures. Two investigators, including senior author John Lipham, MD, are paid consultants for Torax Medical, the maker of the LINX system, and Johnson & Johnson, which owns Torax through a subsidiary. There was no company funding for the review.
The World Congress of Endoscopic Surgery is hosted by the Society of American Gastrointestinal and Endoscopic Surgeons and the Canadian Association of General Surgeons
SOURCE: Alicuben E et al. WCE 2018, Abstract S095.
SEATTLE –
The study caught the attention of audience members – and raised a few eyebrows – at the 2018 World Congress of Endoscopic Surgery, where its results were presented, because the regression rate with the current standard operation for medically refractory gastroesophageal reflux – Nissen fundoplication – is only about 40%.
Lead investigator Evan Alicuben, MD, a general surgery resident at the university, cautioned that “longer-term follow-up is required to make a meaningful comparison with results following fundoplication.”
Fundoplication has been studied for decades, whereas the new study is likely the very first to look at the rates of Barrett’s regression after magnetic augmentation, and the 70% regression rate was based on postop endoscopies a median of 1.2 years after the procedure, not after the 5, 10, or even more years typically seen in fundoplication studies.
Magnetic sphincter augmentation (LINX Reflux Management System) was approved by the Food and Drug Administration in 2012 for reflux that persists despite maximum drug therapy. Patients have a band of magnetic titanium beads surgically placed around their LES; the band opens to let food pass, but tightens again to bolster the LES and prevent reflux.
The approach is gaining popularity. “We now know that it’s effective at controlling reflux symptoms, taking patients off proton pump inhibitors, and curing esophagitis,” at least in the short term. “One of the issues with [fundoplication] is that it may not last forever; the wrap comes undone or it slips. This device may give longer lasting” protection, Dr. Alicuben said.
“The main criticism is that it’s relatively new; people are still questioning it. The optimist in me wants to say that this is the answer we’ve been looking for; the pessimist [says] we need to wait to see what longer-term data show,” he said.
Barrett’s esophagus was confirmed by endoscopy in all 67 subjects before the magnets were placed, and each had at least one postop endoscopy.
At baseline, 29 had ultrashort-segment disease, which means there was no visible Barrett’s, but did have columnar epithelium with goblet cells on pathology. Thirty patients had short-segment disease, with up to 3 cm of visible involvement confirmed by pathology, while eight had long-segment disease, with involvement extending 3 cm or more.
Of the 67 patients, 48 had no evidence of Barrett’s after the procedure, for an overall regression rate of 71.6%. The regression rate was 82.8% in the ultrashort group (24/29); 73.3% in the short segment group (22/30); and 25% in the long segment group (2/8). Long-segment disease is notorious for persisting despite treatment; both patients had 3-cm lesions.
Among the 34 patients with two or more postop endoscopies, the regression rate was 73.5% (25).
There’s a lot of debate about whether ultrashort-segment disease is truly Barrett’s and whether it carries the same risk of malignant transformation, as one surgeon in the audience noted pointedly, worrying that including ultrashort patients oversold the results.
Dr. Alicuben countered that the regression rate remained strong even when ultrashort patients were excluded: 63% (24/38). “This is every bit as good if not better than the results of fundoplication,” another surgeon in the audience said.
The subjects were aged about 60 years, on average, with more men than women. Most had hiatal hernias, often measuring 3 cm or more. The mean body mass index was 27.3 kg/m2, but BMI ranged as high as 44.3.
Mean operative time was 66 minutes, and there were no major complications. None of the patients progressed to dysplasia or carcinoma. Median DeMeester scores fell from 35.3 to 9.2 after the operation in the 47 patients who had postop pH testing.
Surgeons have worried about esophageal erosion with the LINX system. A recent paper by Dr. Alicuben and his colleagues found 29 cases among almost 10,000 patients, which makes for an erosion rate of 0.3% at a median of about 2 years (J Gastrointest Surg. 2018 Apr 17. doi: 10.1007/s11605-018-3775-0).
About 500 LINX systems have been placed at the University of Southern California. Procedures in the study were performed between 2012 and late 2017.
Dr. Alicuben had no disclosures. Two investigators, including senior author John Lipham, MD, are paid consultants for Torax Medical, the maker of the LINX system, and Johnson & Johnson, which owns Torax through a subsidiary. There was no company funding for the review.
The World Congress of Endoscopic Surgery is hosted by the Society of American Gastrointestinal and Endoscopic Surgeons and the Canadian Association of General Surgeons
SOURCE: Alicuben E et al. WCE 2018, Abstract S095.
REPORTING FROM WCE 2018
Key clinical point: Magnetic lower esophageal sphincter augmentation might offer an easier and more effective fix for gastroesophageal reflux than the current standard, Nissen fundoplication.
Major finding: The overall regression rate of Barrett’s esophagus topped 70%.
Study details: Review of 67 patients
Disclosures: There was no industry funding, and the presenter had no disclosures. Two authors are consultants for Torax Medical, the company that makes the device.
Source: Alicuben E et al. WCE 2018, Abstract S095
Fundoplication works best for true PPI-refractory heartburn
WASHINGTON – Less than a quarter of patients with heartburn that appears refractory to proton pump inhibitor treatment truly have reflux-related, drug-refractory heartburn with a high symptom–related probability, but patients who fall into this select subgroup often have significant symptom relief from surgical fundoplication, based on results from a randomized, multicenter, Department of Veterans Affairs study with 78 patients.
Although laparoscopic Nissen fundoplication relieved the heartburn symptoms of just two-thirds of patients who met the study’s definition of having true proton pump inhibitor (PPI)–refractory heartburn, this level of efficacy far exceeded the impact of drug therapy with baclofen or desipramine, which was little better than placebo, Stuart J. Spechler, MD, said at the annual Digestive Disease Week®.
“Fundoplication fell out of favor because of the success of PPI treatment, and because of complications from the surgery, but what our results show is that there is a subgroup of patients who can benefit from fundoplication. The challenge is identifying them,” said Dr. Spechler, a gastroenterologist and professor of medicine at the University of Texas, Dallas. “If you go through a careful work-up you will find the patients who have true PPI-refractory acid reflux and heartburn, and in the end we don’t have good medical treatments for these patients,” leaving fundoplication as their best hope for symptom relief.
The study he ran included 366 patients seen at about 30 VA Medical Centers across the United States who had been referred to his center because of presumed PPI-refractory heartburn. The careful work-up that Dr. Spechler and his associates ran included a closely supervised, 2-week trial of a standardized PPI regimen with omeprazole, careful symptom scoring on this treatment with a reflux-specific, health-related quality of life questionnaire, endoscopic esophageal manometry, and esophageal pH monitoring while on omeprazole.
This process placed patients into several distinct subgroups: About 19% dropped out of the study during this assessment, and another 15% left the study because of their intolerance of various stages of the work-up. Nearly 12% of patients wound up being responsive to the PPI regimen, about 6% had organic disorders not related to gastroesophageal reflux disease, and 27% had functional heartburn with a normal level of acid reflux, which left 78 patients (21%) who demonstrated true reflux-related, PPI-refractory heartburn symptoms.
The researchers then randomized this 78-patient subgroup into three treatment arms, with one group of 27 underwent fundoplication surgery. A group of 25 underwent active medical therapy with 20 mg omeprazole b.i.d. plus baclofen, which was started at 5 mg t.i.d. and increased to 20 mg t.i.d. In baclofen-intolerant or nonresponding patients, this treatment was followed up with desipramine, increasing from a starting dosage of 25 mg/day to 100 mg/day. A third group of 26 control patients received active omeprazole at the same dosage but placebo in place of the baclofen and desipramine. These three subgroups showed no statistically significant differences at baseline for all demographic and clinical parameters recorded.
The study’s primary endpoint was the percentage of patients in each treatment arm who had a “successful” outcome, defined as at least a 50% improvement in their gastroesophageal reflux health-related quality of life score (J Gastrointest Surg. 1998 Mar-Apr;2[2]:141-5) after 1 year on treatment, which occurred in 67% of the fundoplication patients, 28% in the active medical arm, and 12% in the control arm. The fundoplication-treated patients had a significantly higher rate of a successful outcome, compared with patients in each of the other two treatment groups, while the success rates among patients in the active medical group and the control group did not differ significantly, Dr. Spechler said.
Dr. Spechler had no disclosures to report.
WASHINGTON – Less than a quarter of patients with heartburn that appears refractory to proton pump inhibitor treatment truly have reflux-related, drug-refractory heartburn with a high symptom–related probability, but patients who fall into this select subgroup often have significant symptom relief from surgical fundoplication, based on results from a randomized, multicenter, Department of Veterans Affairs study with 78 patients.
Although laparoscopic Nissen fundoplication relieved the heartburn symptoms of just two-thirds of patients who met the study’s definition of having true proton pump inhibitor (PPI)–refractory heartburn, this level of efficacy far exceeded the impact of drug therapy with baclofen or desipramine, which was little better than placebo, Stuart J. Spechler, MD, said at the annual Digestive Disease Week®.
“Fundoplication fell out of favor because of the success of PPI treatment, and because of complications from the surgery, but what our results show is that there is a subgroup of patients who can benefit from fundoplication. The challenge is identifying them,” said Dr. Spechler, a gastroenterologist and professor of medicine at the University of Texas, Dallas. “If you go through a careful work-up you will find the patients who have true PPI-refractory acid reflux and heartburn, and in the end we don’t have good medical treatments for these patients,” leaving fundoplication as their best hope for symptom relief.
The study he ran included 366 patients seen at about 30 VA Medical Centers across the United States who had been referred to his center because of presumed PPI-refractory heartburn. The careful work-up that Dr. Spechler and his associates ran included a closely supervised, 2-week trial of a standardized PPI regimen with omeprazole, careful symptom scoring on this treatment with a reflux-specific, health-related quality of life questionnaire, endoscopic esophageal manometry, and esophageal pH monitoring while on omeprazole.
This process placed patients into several distinct subgroups: About 19% dropped out of the study during this assessment, and another 15% left the study because of their intolerance of various stages of the work-up. Nearly 12% of patients wound up being responsive to the PPI regimen, about 6% had organic disorders not related to gastroesophageal reflux disease, and 27% had functional heartburn with a normal level of acid reflux, which left 78 patients (21%) who demonstrated true reflux-related, PPI-refractory heartburn symptoms.
The researchers then randomized this 78-patient subgroup into three treatment arms, with one group of 27 underwent fundoplication surgery. A group of 25 underwent active medical therapy with 20 mg omeprazole b.i.d. plus baclofen, which was started at 5 mg t.i.d. and increased to 20 mg t.i.d. In baclofen-intolerant or nonresponding patients, this treatment was followed up with desipramine, increasing from a starting dosage of 25 mg/day to 100 mg/day. A third group of 26 control patients received active omeprazole at the same dosage but placebo in place of the baclofen and desipramine. These three subgroups showed no statistically significant differences at baseline for all demographic and clinical parameters recorded.
The study’s primary endpoint was the percentage of patients in each treatment arm who had a “successful” outcome, defined as at least a 50% improvement in their gastroesophageal reflux health-related quality of life score (J Gastrointest Surg. 1998 Mar-Apr;2[2]:141-5) after 1 year on treatment, which occurred in 67% of the fundoplication patients, 28% in the active medical arm, and 12% in the control arm. The fundoplication-treated patients had a significantly higher rate of a successful outcome, compared with patients in each of the other two treatment groups, while the success rates among patients in the active medical group and the control group did not differ significantly, Dr. Spechler said.
Dr. Spechler had no disclosures to report.
WASHINGTON – Less than a quarter of patients with heartburn that appears refractory to proton pump inhibitor treatment truly have reflux-related, drug-refractory heartburn with a high symptom–related probability, but patients who fall into this select subgroup often have significant symptom relief from surgical fundoplication, based on results from a randomized, multicenter, Department of Veterans Affairs study with 78 patients.
Although laparoscopic Nissen fundoplication relieved the heartburn symptoms of just two-thirds of patients who met the study’s definition of having true proton pump inhibitor (PPI)–refractory heartburn, this level of efficacy far exceeded the impact of drug therapy with baclofen or desipramine, which was little better than placebo, Stuart J. Spechler, MD, said at the annual Digestive Disease Week®.
“Fundoplication fell out of favor because of the success of PPI treatment, and because of complications from the surgery, but what our results show is that there is a subgroup of patients who can benefit from fundoplication. The challenge is identifying them,” said Dr. Spechler, a gastroenterologist and professor of medicine at the University of Texas, Dallas. “If you go through a careful work-up you will find the patients who have true PPI-refractory acid reflux and heartburn, and in the end we don’t have good medical treatments for these patients,” leaving fundoplication as their best hope for symptom relief.
The study he ran included 366 patients seen at about 30 VA Medical Centers across the United States who had been referred to his center because of presumed PPI-refractory heartburn. The careful work-up that Dr. Spechler and his associates ran included a closely supervised, 2-week trial of a standardized PPI regimen with omeprazole, careful symptom scoring on this treatment with a reflux-specific, health-related quality of life questionnaire, endoscopic esophageal manometry, and esophageal pH monitoring while on omeprazole.
This process placed patients into several distinct subgroups: About 19% dropped out of the study during this assessment, and another 15% left the study because of their intolerance of various stages of the work-up. Nearly 12% of patients wound up being responsive to the PPI regimen, about 6% had organic disorders not related to gastroesophageal reflux disease, and 27% had functional heartburn with a normal level of acid reflux, which left 78 patients (21%) who demonstrated true reflux-related, PPI-refractory heartburn symptoms.
The researchers then randomized this 78-patient subgroup into three treatment arms, with one group of 27 underwent fundoplication surgery. A group of 25 underwent active medical therapy with 20 mg omeprazole b.i.d. plus baclofen, which was started at 5 mg t.i.d. and increased to 20 mg t.i.d. In baclofen-intolerant or nonresponding patients, this treatment was followed up with desipramine, increasing from a starting dosage of 25 mg/day to 100 mg/day. A third group of 26 control patients received active omeprazole at the same dosage but placebo in place of the baclofen and desipramine. These three subgroups showed no statistically significant differences at baseline for all demographic and clinical parameters recorded.
The study’s primary endpoint was the percentage of patients in each treatment arm who had a “successful” outcome, defined as at least a 50% improvement in their gastroesophageal reflux health-related quality of life score (J Gastrointest Surg. 1998 Mar-Apr;2[2]:141-5) after 1 year on treatment, which occurred in 67% of the fundoplication patients, 28% in the active medical arm, and 12% in the control arm. The fundoplication-treated patients had a significantly higher rate of a successful outcome, compared with patients in each of the other two treatment groups, while the success rates among patients in the active medical group and the control group did not differ significantly, Dr. Spechler said.
Dr. Spechler had no disclosures to report.
REPORTING FROM DDW 2018
Key clinical point: Fundoplication produces the best outcomes in patients with true proton pump inhibitor–refractory heartburn.
Major finding: Two-thirds of patients treated with fundoplication had successful outcomes, compared with 28% in medical controls and 12% in placebo controls.
Study details: A multicenter, randomized study with 78 patients.
Disclosures: Dr. Spechler had no disclosures to report.
Malnourished U.S. inpatients often go untreated
WASHINGTON – Hospital staffs often fail to treat .
A retrospective review of more than 150,000 patients admitted during a single year at any center within a large, multicenter U.S. hospital system found that even when patients receive oral nutritional supplementation, there is often a substantial delay to its onset.
The data also suggested potential benefits from treating malnutrition with oral nutritional supplementation (ONS). Patients who received ONS had a 10% relative reduction in their rate of 30-day readmission, compared with malnourished patients who did not receive supplements after adjusting for several baseline demographic and clinical variables, Gerard Mullin, MD, said at the annual Digestive Disease Week. His analysis also showed that every doubling of the time from hospital admission to an order for ONS significantly linked with a 6% rise in hospital length of stay.
The findings “highlight the importance of malnutrition screening on admission, starting a nutrition intervention as soon as malnutrition is confirmed, and treating with appropriate ONS,” said Dr. Mullin, a gastroenterologist at Johns Hopkins Medicine in Baltimore and director of the Celiac Disease Clinic. A standard formulation of Ensure was the ONS routinely used at the Johns Hopkins hospitals
“We’re missing malnutrition,” Dr. Mullin said in an interview. The hospital accreditation standards of the Joint Commission call for assessment of the nutritional status of hospitalized patients within 24 hours of admission (Jt Comm J Qual Patient Saf. 2015 Oct;41[10]:469-73). Screening is “not uniformly done,” and when malnutrition is identified, the finding must usually pass through several layers of a hospital’s medico-bureaucratic process before treatment actually starts, he noted. Plus, there’s often dismissal of the importance of intervention. “It’s important to treat patients with ONS sooner than later,” he said.
Dr. Mullin and his associates studied hospital records for 153,161 people admitted to any of the Baltimore-area hospitals in the Johns Hopkins system during October 2016 through the end of September 2017. The hospital staff routinely assessed nutritional status of patients after admission with a two-question screen based on the Malnutrition Screening Tool (Nutrition. 1999 June;15[6]:458-64): Have you had unplanned weight loss of 10 pounds or more during the past 6 months? Have you had decreased oral intake over the past 5 days? This identified 30,284 (20%) who qualified as possibly malnourished by either criterion. The researchers also retrospectively applied a more detailed screen to the patient records using the criteria set by an international consensus guideline committee in 2010 (J Parenter Enteraal Nutr. 2010 Mar-Apr;34[2]:156-9). This identified 8,713 of the hospitalized patients (6%) as malnourished soon after admission. Despite these numbers a scant 274 patients among these 8,713 (3%) actually received ONS, Dr. Mullin reported. In addition, it took an average of 85 hours from the time of each malnourished patient’s admission to when the ONS order appeared in their record.
Dr. Mullin conceded that both the association his group found between treatment with ONS and a reduced rate of 30-day readmission to any of the hospitals in the Johns Hopkins system, and the association between a delay in the time to the start of ONS and length of stay may have been confounded by factors not accounted for in the adjustments they applied. But he maintained that the links are consistent with results from prior studies, and warrant running prospective, randomized studies to better document the impact of ONS on newly admitted patients identified as malnourished.
“We need more of these types of studies and interventional trials to show that ONS makes a difference,” Dr. Mullin said.
The study was sponsored by Abbott, which markets the oral nutritional supplement Ensure. Dr. Mullin had no additional disclosures.
mzoler@mdedge.com
On Twitter @mitchelzoler
SOURCE: Source: Mullin G et al. DDW 2018 presentation 883.
WASHINGTON – Hospital staffs often fail to treat .
A retrospective review of more than 150,000 patients admitted during a single year at any center within a large, multicenter U.S. hospital system found that even when patients receive oral nutritional supplementation, there is often a substantial delay to its onset.
The data also suggested potential benefits from treating malnutrition with oral nutritional supplementation (ONS). Patients who received ONS had a 10% relative reduction in their rate of 30-day readmission, compared with malnourished patients who did not receive supplements after adjusting for several baseline demographic and clinical variables, Gerard Mullin, MD, said at the annual Digestive Disease Week. His analysis also showed that every doubling of the time from hospital admission to an order for ONS significantly linked with a 6% rise in hospital length of stay.
The findings “highlight the importance of malnutrition screening on admission, starting a nutrition intervention as soon as malnutrition is confirmed, and treating with appropriate ONS,” said Dr. Mullin, a gastroenterologist at Johns Hopkins Medicine in Baltimore and director of the Celiac Disease Clinic. A standard formulation of Ensure was the ONS routinely used at the Johns Hopkins hospitals
“We’re missing malnutrition,” Dr. Mullin said in an interview. The hospital accreditation standards of the Joint Commission call for assessment of the nutritional status of hospitalized patients within 24 hours of admission (Jt Comm J Qual Patient Saf. 2015 Oct;41[10]:469-73). Screening is “not uniformly done,” and when malnutrition is identified, the finding must usually pass through several layers of a hospital’s medico-bureaucratic process before treatment actually starts, he noted. Plus, there’s often dismissal of the importance of intervention. “It’s important to treat patients with ONS sooner than later,” he said.
Dr. Mullin and his associates studied hospital records for 153,161 people admitted to any of the Baltimore-area hospitals in the Johns Hopkins system during October 2016 through the end of September 2017. The hospital staff routinely assessed nutritional status of patients after admission with a two-question screen based on the Malnutrition Screening Tool (Nutrition. 1999 June;15[6]:458-64): Have you had unplanned weight loss of 10 pounds or more during the past 6 months? Have you had decreased oral intake over the past 5 days? This identified 30,284 (20%) who qualified as possibly malnourished by either criterion. The researchers also retrospectively applied a more detailed screen to the patient records using the criteria set by an international consensus guideline committee in 2010 (J Parenter Enteraal Nutr. 2010 Mar-Apr;34[2]:156-9). This identified 8,713 of the hospitalized patients (6%) as malnourished soon after admission. Despite these numbers a scant 274 patients among these 8,713 (3%) actually received ONS, Dr. Mullin reported. In addition, it took an average of 85 hours from the time of each malnourished patient’s admission to when the ONS order appeared in their record.
Dr. Mullin conceded that both the association his group found between treatment with ONS and a reduced rate of 30-day readmission to any of the hospitals in the Johns Hopkins system, and the association between a delay in the time to the start of ONS and length of stay may have been confounded by factors not accounted for in the adjustments they applied. But he maintained that the links are consistent with results from prior studies, and warrant running prospective, randomized studies to better document the impact of ONS on newly admitted patients identified as malnourished.
“We need more of these types of studies and interventional trials to show that ONS makes a difference,” Dr. Mullin said.
The study was sponsored by Abbott, which markets the oral nutritional supplement Ensure. Dr. Mullin had no additional disclosures.
mzoler@mdedge.com
On Twitter @mitchelzoler
SOURCE: Source: Mullin G et al. DDW 2018 presentation 883.
WASHINGTON – Hospital staffs often fail to treat .
A retrospective review of more than 150,000 patients admitted during a single year at any center within a large, multicenter U.S. hospital system found that even when patients receive oral nutritional supplementation, there is often a substantial delay to its onset.
The data also suggested potential benefits from treating malnutrition with oral nutritional supplementation (ONS). Patients who received ONS had a 10% relative reduction in their rate of 30-day readmission, compared with malnourished patients who did not receive supplements after adjusting for several baseline demographic and clinical variables, Gerard Mullin, MD, said at the annual Digestive Disease Week. His analysis also showed that every doubling of the time from hospital admission to an order for ONS significantly linked with a 6% rise in hospital length of stay.
The findings “highlight the importance of malnutrition screening on admission, starting a nutrition intervention as soon as malnutrition is confirmed, and treating with appropriate ONS,” said Dr. Mullin, a gastroenterologist at Johns Hopkins Medicine in Baltimore and director of the Celiac Disease Clinic. A standard formulation of Ensure was the ONS routinely used at the Johns Hopkins hospitals
“We’re missing malnutrition,” Dr. Mullin said in an interview. The hospital accreditation standards of the Joint Commission call for assessment of the nutritional status of hospitalized patients within 24 hours of admission (Jt Comm J Qual Patient Saf. 2015 Oct;41[10]:469-73). Screening is “not uniformly done,” and when malnutrition is identified, the finding must usually pass through several layers of a hospital’s medico-bureaucratic process before treatment actually starts, he noted. Plus, there’s often dismissal of the importance of intervention. “It’s important to treat patients with ONS sooner than later,” he said.
Dr. Mullin and his associates studied hospital records for 153,161 people admitted to any of the Baltimore-area hospitals in the Johns Hopkins system during October 2016 through the end of September 2017. The hospital staff routinely assessed nutritional status of patients after admission with a two-question screen based on the Malnutrition Screening Tool (Nutrition. 1999 June;15[6]:458-64): Have you had unplanned weight loss of 10 pounds or more during the past 6 months? Have you had decreased oral intake over the past 5 days? This identified 30,284 (20%) who qualified as possibly malnourished by either criterion. The researchers also retrospectively applied a more detailed screen to the patient records using the criteria set by an international consensus guideline committee in 2010 (J Parenter Enteraal Nutr. 2010 Mar-Apr;34[2]:156-9). This identified 8,713 of the hospitalized patients (6%) as malnourished soon after admission. Despite these numbers a scant 274 patients among these 8,713 (3%) actually received ONS, Dr. Mullin reported. In addition, it took an average of 85 hours from the time of each malnourished patient’s admission to when the ONS order appeared in their record.
Dr. Mullin conceded that both the association his group found between treatment with ONS and a reduced rate of 30-day readmission to any of the hospitals in the Johns Hopkins system, and the association between a delay in the time to the start of ONS and length of stay may have been confounded by factors not accounted for in the adjustments they applied. But he maintained that the links are consistent with results from prior studies, and warrant running prospective, randomized studies to better document the impact of ONS on newly admitted patients identified as malnourished.
“We need more of these types of studies and interventional trials to show that ONS makes a difference,” Dr. Mullin said.
The study was sponsored by Abbott, which markets the oral nutritional supplement Ensure. Dr. Mullin had no additional disclosures.
mzoler@mdedge.com
On Twitter @mitchelzoler
SOURCE: Source: Mullin G et al. DDW 2018 presentation 883.
REPORTING FROM DDW 2018
Key clinical point: Malnourished U.S. hospital inpatients often go untreated.
Major finding: Three percent of patients retrospectively identified as malnourished soon after hospital admission received oral nutritional supplementation.
Study details: Retrospective review of 153,161 patients admitted to a large U.S. hospital network during 2016-2017.
Disclosures: The study was sponsored by Abbott, which markets the oral nutritional supplement Ensure. Dr. Mullin had no additional disclosures.
Source: Mullin G et al. Digestive Disease Week presentation 883.
FDA issues recommendations to avoid surgical fires
The Food and Drug Administration on May 29 issued a set of recommendations to medical professionals and health care facility staff to reduce the occurrence of surgical fires on or near a patient.
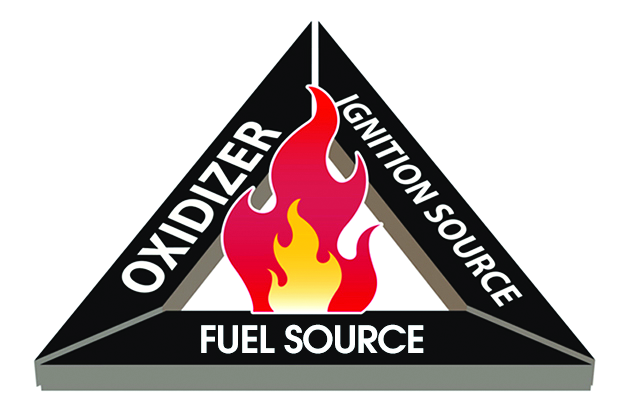
Surgical fires most often occur when there is an oxygen-enriched environment (a concentration of greater than 30%). In addition to an oxygen source, the other two necessary elements of the “fire triangle” are an ignition source and a fuel source.
The recommendations discuss the safe use of devices or items that may serve as a source of any one of those three elements.
Oxygen: Evaluate if supplemental oxygen is needed. If it is, titrate to the minimum concentration needed for adequate saturation. Closed oxygen delivery systems (such as a laryngeal mask or endotracheal tube) are safer than open oxygen delivery systems (such as a nasal cannula or mask). If you must use an open system, take additional precautions to exclude oxygen and flammable/combustible gases from the operative field, such as draping techniques that avoid accumulation of oxygen.
Ignition sources: Consider alternatives to using an ignition source for surgery of the head, neck, and upper chest if high concentrations of supplemental oxygen are being delivered. Check for insulation failure before use, and keep devices clean of char and tissue. When not in use, place the devices safely away from the patient and drapes. Devices are safer to use if you can allow time for the oxygen concentration in the room to decrease.
Fuel sources: Ensure dry conditions prior to draping, avoiding pooling of alcohol-based antiseptics during skin preparation. Use the appropriate-sized applicator for the surgical site. Be aware of products that may serve as a fuel source, such as oxygen-trapping gauze, plastic laryngeal masks, and aware of potential patient sources such as hair or gastrointestinal gases.
Training should include how to manage fires that do occur – stop the ignition source, then extinguish the fire – and evacuation procedures.
Read the full recommendations here.
The Food and Drug Administration on May 29 issued a set of recommendations to medical professionals and health care facility staff to reduce the occurrence of surgical fires on or near a patient.
Surgical fires most often occur when there is an oxygen-enriched environment (a concentration of greater than 30%). In addition to an oxygen source, the other two necessary elements of the “fire triangle” are an ignition source and a fuel source.
The recommendations discuss the safe use of devices or items that may serve as a source of any one of those three elements.
Oxygen: Evaluate if supplemental oxygen is needed. If it is, titrate to the minimum concentration needed for adequate saturation. Closed oxygen delivery systems (such as a laryngeal mask or endotracheal tube) are safer than open oxygen delivery systems (such as a nasal cannula or mask). If you must use an open system, take additional precautions to exclude oxygen and flammable/combustible gases from the operative field, such as draping techniques that avoid accumulation of oxygen.
Ignition sources: Consider alternatives to using an ignition source for surgery of the head, neck, and upper chest if high concentrations of supplemental oxygen are being delivered. Check for insulation failure before use, and keep devices clean of char and tissue. When not in use, place the devices safely away from the patient and drapes. Devices are safer to use if you can allow time for the oxygen concentration in the room to decrease.
Fuel sources: Ensure dry conditions prior to draping, avoiding pooling of alcohol-based antiseptics during skin preparation. Use the appropriate-sized applicator for the surgical site. Be aware of products that may serve as a fuel source, such as oxygen-trapping gauze, plastic laryngeal masks, and aware of potential patient sources such as hair or gastrointestinal gases.
Training should include how to manage fires that do occur – stop the ignition source, then extinguish the fire – and evacuation procedures.
Read the full recommendations here.
The Food and Drug Administration on May 29 issued a set of recommendations to medical professionals and health care facility staff to reduce the occurrence of surgical fires on or near a patient.
Surgical fires most often occur when there is an oxygen-enriched environment (a concentration of greater than 30%). In addition to an oxygen source, the other two necessary elements of the “fire triangle” are an ignition source and a fuel source.
The recommendations discuss the safe use of devices or items that may serve as a source of any one of those three elements.
Oxygen: Evaluate if supplemental oxygen is needed. If it is, titrate to the minimum concentration needed for adequate saturation. Closed oxygen delivery systems (such as a laryngeal mask or endotracheal tube) are safer than open oxygen delivery systems (such as a nasal cannula or mask). If you must use an open system, take additional precautions to exclude oxygen and flammable/combustible gases from the operative field, such as draping techniques that avoid accumulation of oxygen.
Ignition sources: Consider alternatives to using an ignition source for surgery of the head, neck, and upper chest if high concentrations of supplemental oxygen are being delivered. Check for insulation failure before use, and keep devices clean of char and tissue. When not in use, place the devices safely away from the patient and drapes. Devices are safer to use if you can allow time for the oxygen concentration in the room to decrease.
Fuel sources: Ensure dry conditions prior to draping, avoiding pooling of alcohol-based antiseptics during skin preparation. Use the appropriate-sized applicator for the surgical site. Be aware of products that may serve as a fuel source, such as oxygen-trapping gauze, plastic laryngeal masks, and aware of potential patient sources such as hair or gastrointestinal gases.
Training should include how to manage fires that do occur – stop the ignition source, then extinguish the fire – and evacuation procedures.
Read the full recommendations here.
Bezafibrate shows promise as second-line option for PBC
Nearly one-third of patients with primary biliary cholangitis treated with bezafibrate showed clinical improvement after 24 months, according to data from a randomized trial of 100 adults.
Ursodeoxycholic acid remains the standard first-line therapy for primary biliary cholangitis (PBC), but many patients have an incomplete response to the treatment, and consequently their long-term survival is limited, wrote Christophe Corpechot, MD, of Sorbonne University, Paris, and his colleagues. PBC is also known as primary biliary cirrhosis.
In the BEZURSO trial (Bezafibrate in Combination with Ursodeoxycholic Acid in Primary Biliary Cirrhosis), published in the New England Journal of Medicine, the researchers randomized 100 primary PBC patients with an inadequate response to ursodeoxycholic acid to receive 400 mg per day of bezafibrate or a placebo for 24 months. Inadequate response was defined as “a serum level of alkaline phosphatase or aspartate aminotransferase more than 1.5 times the upper limit of the normal range or an abnormal total bilirubin level, assessed after at least 6 months of treatment with ursodeoxycholic acid,” the researchers said.
Baseline demographics were not significantly different between the groups. The average age of the patients was 53 years, and 95% were white women.
After 24 months, 31% of the patients in the treatment group met the primary outcome, which was the achievement of normal levels of alkaline phosphatase, aspartate aminotransferase, alanine aminotransferase, total bilirubin, and albumin, plus a normal prothrombin index. By contrast, none of the patients in the placebo group achieved the primary outcome.
In particular, bezafibrate patients showed a 60% reduction in alkaline phosphatase levels from baseline to 3 months, and a 14% decrease in total bilirubin from baseline during the course of the study.
Clinical outcomes were similar between the groups; 20% of the bezafibrate group and 18% of the placebo group developed portal hypertension, and two patients in each group developed liver complications. No deaths occurred in either group during the study. Approximately half of the patients in each group reported adverse events. Serious adverse events occurred in 14 bezafibrate patients and 12 placebo patients.
The findings were limited by the small study population, which prevented assessment of bezafibrate on liver transplantation and death, and by the limited histologic data to look at the impact on liver fibrosis and hepatic inflammation, the researchers said.
However, the results support the use of bezafibrate as an add-on to ursodeoxycholic acid in PBC patients, and merit larger, longer studies, they noted.
The study was supported by the Programme Hospitalier de Recherche Clinique 2010, Ministry of Health, and Arrow Génériques. Dr. Corpechot disclosed relationships with companies including Intercept France, Inventiva Pharma, and GlaxoSmithKline.
SOURCE: Corpechot C et al. N Engl J Med. 2018 June 6. doi: 10.1056/NEJMoa1714519.
The BEZURSO study findings “merit cautious excitement,” Elizabeth J. Carey, MD, wrote in an editorial.
“This pivotal trial effectively doubles the limited options for second-line therapy of primary biliary cholangitis,” she said.
Approximately 40% of primary biliary cholangitis patients fail to respond adequately to ursodeoxycholic acid, the first-line therapy, and they remain at risk for progression of liver disease and liver failure, wrote Dr. Carey. Bezafibrate is the first drug to generate improvement in these patients not only in measures of biochemical markers, but also measures of fibrosis and disease symptoms, she said. Patient reports of reduced itching and lower levels of fatigue are worth noting, although they were not the primary outcomes, said Dr. Carey.
“Improvement in patient-reported outcomes prompts the question of whether there is a role for the use of bezafibrate for the management of fatigue or pruritus, even in patients who have a biochemical response to ursodeoxycholic acid,” she noted (N Engl J Med. 2018 June 6. doi: 10.1056/NEJMe1804945).
Despite the promising results, challenges remain for primary biliary cholangitis patients, as approximately 70% did not meet the primary outcome, and those with more severe disease were less likely to respond, Dr. Carey said. However, she added, any agent “that both delays disease progression and alleviates symptoms is a potential boon for patients with the debilitating symptoms of primary biliary cholangitis.”
Dr. Carey is affiliated with the Mayo Clinic in Phoenix, Ariz. Disclosure forms provided by the author are available at NEJM.org.
The BEZURSO study findings “merit cautious excitement,” Elizabeth J. Carey, MD, wrote in an editorial.
“This pivotal trial effectively doubles the limited options for second-line therapy of primary biliary cholangitis,” she said.
Approximately 40% of primary biliary cholangitis patients fail to respond adequately to ursodeoxycholic acid, the first-line therapy, and they remain at risk for progression of liver disease and liver failure, wrote Dr. Carey. Bezafibrate is the first drug to generate improvement in these patients not only in measures of biochemical markers, but also measures of fibrosis and disease symptoms, she said. Patient reports of reduced itching and lower levels of fatigue are worth noting, although they were not the primary outcomes, said Dr. Carey.
“Improvement in patient-reported outcomes prompts the question of whether there is a role for the use of bezafibrate for the management of fatigue or pruritus, even in patients who have a biochemical response to ursodeoxycholic acid,” she noted (N Engl J Med. 2018 June 6. doi: 10.1056/NEJMe1804945).
Despite the promising results, challenges remain for primary biliary cholangitis patients, as approximately 70% did not meet the primary outcome, and those with more severe disease were less likely to respond, Dr. Carey said. However, she added, any agent “that both delays disease progression and alleviates symptoms is a potential boon for patients with the debilitating symptoms of primary biliary cholangitis.”
Dr. Carey is affiliated with the Mayo Clinic in Phoenix, Ariz. Disclosure forms provided by the author are available at NEJM.org.
The BEZURSO study findings “merit cautious excitement,” Elizabeth J. Carey, MD, wrote in an editorial.
“This pivotal trial effectively doubles the limited options for second-line therapy of primary biliary cholangitis,” she said.
Approximately 40% of primary biliary cholangitis patients fail to respond adequately to ursodeoxycholic acid, the first-line therapy, and they remain at risk for progression of liver disease and liver failure, wrote Dr. Carey. Bezafibrate is the first drug to generate improvement in these patients not only in measures of biochemical markers, but also measures of fibrosis and disease symptoms, she said. Patient reports of reduced itching and lower levels of fatigue are worth noting, although they were not the primary outcomes, said Dr. Carey.
“Improvement in patient-reported outcomes prompts the question of whether there is a role for the use of bezafibrate for the management of fatigue or pruritus, even in patients who have a biochemical response to ursodeoxycholic acid,” she noted (N Engl J Med. 2018 June 6. doi: 10.1056/NEJMe1804945).
Despite the promising results, challenges remain for primary biliary cholangitis patients, as approximately 70% did not meet the primary outcome, and those with more severe disease were less likely to respond, Dr. Carey said. However, she added, any agent “that both delays disease progression and alleviates symptoms is a potential boon for patients with the debilitating symptoms of primary biliary cholangitis.”
Dr. Carey is affiliated with the Mayo Clinic in Phoenix, Ariz. Disclosure forms provided by the author are available at NEJM.org.
Nearly one-third of patients with primary biliary cholangitis treated with bezafibrate showed clinical improvement after 24 months, according to data from a randomized trial of 100 adults.
Ursodeoxycholic acid remains the standard first-line therapy for primary biliary cholangitis (PBC), but many patients have an incomplete response to the treatment, and consequently their long-term survival is limited, wrote Christophe Corpechot, MD, of Sorbonne University, Paris, and his colleagues. PBC is also known as primary biliary cirrhosis.
In the BEZURSO trial (Bezafibrate in Combination with Ursodeoxycholic Acid in Primary Biliary Cirrhosis), published in the New England Journal of Medicine, the researchers randomized 100 primary PBC patients with an inadequate response to ursodeoxycholic acid to receive 400 mg per day of bezafibrate or a placebo for 24 months. Inadequate response was defined as “a serum level of alkaline phosphatase or aspartate aminotransferase more than 1.5 times the upper limit of the normal range or an abnormal total bilirubin level, assessed after at least 6 months of treatment with ursodeoxycholic acid,” the researchers said.
Baseline demographics were not significantly different between the groups. The average age of the patients was 53 years, and 95% were white women.
After 24 months, 31% of the patients in the treatment group met the primary outcome, which was the achievement of normal levels of alkaline phosphatase, aspartate aminotransferase, alanine aminotransferase, total bilirubin, and albumin, plus a normal prothrombin index. By contrast, none of the patients in the placebo group achieved the primary outcome.
In particular, bezafibrate patients showed a 60% reduction in alkaline phosphatase levels from baseline to 3 months, and a 14% decrease in total bilirubin from baseline during the course of the study.
Clinical outcomes were similar between the groups; 20% of the bezafibrate group and 18% of the placebo group developed portal hypertension, and two patients in each group developed liver complications. No deaths occurred in either group during the study. Approximately half of the patients in each group reported adverse events. Serious adverse events occurred in 14 bezafibrate patients and 12 placebo patients.
The findings were limited by the small study population, which prevented assessment of bezafibrate on liver transplantation and death, and by the limited histologic data to look at the impact on liver fibrosis and hepatic inflammation, the researchers said.
However, the results support the use of bezafibrate as an add-on to ursodeoxycholic acid in PBC patients, and merit larger, longer studies, they noted.
The study was supported by the Programme Hospitalier de Recherche Clinique 2010, Ministry of Health, and Arrow Génériques. Dr. Corpechot disclosed relationships with companies including Intercept France, Inventiva Pharma, and GlaxoSmithKline.
SOURCE: Corpechot C et al. N Engl J Med. 2018 June 6. doi: 10.1056/NEJMoa1714519.
Nearly one-third of patients with primary biliary cholangitis treated with bezafibrate showed clinical improvement after 24 months, according to data from a randomized trial of 100 adults.
Ursodeoxycholic acid remains the standard first-line therapy for primary biliary cholangitis (PBC), but many patients have an incomplete response to the treatment, and consequently their long-term survival is limited, wrote Christophe Corpechot, MD, of Sorbonne University, Paris, and his colleagues. PBC is also known as primary biliary cirrhosis.
In the BEZURSO trial (Bezafibrate in Combination with Ursodeoxycholic Acid in Primary Biliary Cirrhosis), published in the New England Journal of Medicine, the researchers randomized 100 primary PBC patients with an inadequate response to ursodeoxycholic acid to receive 400 mg per day of bezafibrate or a placebo for 24 months. Inadequate response was defined as “a serum level of alkaline phosphatase or aspartate aminotransferase more than 1.5 times the upper limit of the normal range or an abnormal total bilirubin level, assessed after at least 6 months of treatment with ursodeoxycholic acid,” the researchers said.
Baseline demographics were not significantly different between the groups. The average age of the patients was 53 years, and 95% were white women.
After 24 months, 31% of the patients in the treatment group met the primary outcome, which was the achievement of normal levels of alkaline phosphatase, aspartate aminotransferase, alanine aminotransferase, total bilirubin, and albumin, plus a normal prothrombin index. By contrast, none of the patients in the placebo group achieved the primary outcome.
In particular, bezafibrate patients showed a 60% reduction in alkaline phosphatase levels from baseline to 3 months, and a 14% decrease in total bilirubin from baseline during the course of the study.
Clinical outcomes were similar between the groups; 20% of the bezafibrate group and 18% of the placebo group developed portal hypertension, and two patients in each group developed liver complications. No deaths occurred in either group during the study. Approximately half of the patients in each group reported adverse events. Serious adverse events occurred in 14 bezafibrate patients and 12 placebo patients.
The findings were limited by the small study population, which prevented assessment of bezafibrate on liver transplantation and death, and by the limited histologic data to look at the impact on liver fibrosis and hepatic inflammation, the researchers said.
However, the results support the use of bezafibrate as an add-on to ursodeoxycholic acid in PBC patients, and merit larger, longer studies, they noted.
The study was supported by the Programme Hospitalier de Recherche Clinique 2010, Ministry of Health, and Arrow Génériques. Dr. Corpechot disclosed relationships with companies including Intercept France, Inventiva Pharma, and GlaxoSmithKline.
SOURCE: Corpechot C et al. N Engl J Med. 2018 June 6. doi: 10.1056/NEJMoa1714519.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Primary biliary cholangitis patients who took bezafibrate showed decreases in alkaline phosphatase levels and total bilirubin.
Major finding: A total of 31% of patients who took bezafibrate achieved normal levels of disease biomarkers after 24 months compared with 0% of placebo patients.
Study details: The data come from a double-blind, placebo-controlled trial of 100 adults with primary biliary cholangitis at 21 medical centers in France.
Disclosures: Programme Hospitalier de Recherche Clinique 2010 (Ministry of Health) and Arrow Génériques supported the study. Dr. Corpechot disclosed relationships with companies including Intercept France, Inventiva Pharma, and GlaxoSmithKline.
Source: Corpechot C et al. N Engl J Med. 2018 June 6. doi: 10.1056/NEJMoa1714519.
Percutaneous procedure gives alternative to anticoagulation for portal vein thrombosis
WASHINGTON – Catheter-directed clot lysis and thrombectomy with creation of a bypass shunt is a reasonable alternative to prolonged anticoagulation for treating patients with portal vein thrombosis (PVT) based on the accumulated reported experience since 1993 using this percutaneous treatment.
” Nelson Valentin, MD, said at the annual Digestive Disease Week.® “TIPS should be considered a viable treatment option for patients with PVT,” said Dr. Valentin, a gastroenterology fellow at Mount Sinai Beth Israel hospital in New York.
“There is sufficient evidence from these reports to at least consider TIPS as an adjunct to anticoagulation or perhaps as primary therapy,” especially for patients with PVT who have a contraindication for anticoagulation, Dr. Valentin said in an interview. Standard anticoagulation for PVT would today involve acute treatment with a low-molecular-weight heparin followed by oral anticoagulation for a total treatment time of at least 6 months and continued for a year or longer in some patients. A recently published review of reported experience using anticoagulation to treat PVT found a complete recanalization rate of 41% and a complete or partial rate of 66%, which suggests that TIPS is at least as effective, although Dr. Valentin cautioned that no reported study has directly compared the two alternative approaches. A study designed to make this direct comparison is warranted by the reported results using TIPS, Dr. Valentin said. And the experience with TIPS positions it as an option for patients who do not respond to anticoagulation or would prefer an alternative to prolonged anticoagulation.
One factor currently limiting use of TIPS, which is usually performed by an interventional radiologist, is that the procedure is technically demanding, with a limited number of operators with the expertise to perform it. If TIPS became more widely accepted as an option for treating PVT, then the pool of interventionalists experienced with performing the procedure would grow, Dr. Valentin noted.
mzoler@mdedge.com
On Twitter @mitchelzoler
SOURCE: Valentin N et al. Digestive Disease Week, Presentation 361.
WASHINGTON – Catheter-directed clot lysis and thrombectomy with creation of a bypass shunt is a reasonable alternative to prolonged anticoagulation for treating patients with portal vein thrombosis (PVT) based on the accumulated reported experience since 1993 using this percutaneous treatment.
” Nelson Valentin, MD, said at the annual Digestive Disease Week.® “TIPS should be considered a viable treatment option for patients with PVT,” said Dr. Valentin, a gastroenterology fellow at Mount Sinai Beth Israel hospital in New York.
“There is sufficient evidence from these reports to at least consider TIPS as an adjunct to anticoagulation or perhaps as primary therapy,” especially for patients with PVT who have a contraindication for anticoagulation, Dr. Valentin said in an interview. Standard anticoagulation for PVT would today involve acute treatment with a low-molecular-weight heparin followed by oral anticoagulation for a total treatment time of at least 6 months and continued for a year or longer in some patients. A recently published review of reported experience using anticoagulation to treat PVT found a complete recanalization rate of 41% and a complete or partial rate of 66%, which suggests that TIPS is at least as effective, although Dr. Valentin cautioned that no reported study has directly compared the two alternative approaches. A study designed to make this direct comparison is warranted by the reported results using TIPS, Dr. Valentin said. And the experience with TIPS positions it as an option for patients who do not respond to anticoagulation or would prefer an alternative to prolonged anticoagulation.
One factor currently limiting use of TIPS, which is usually performed by an interventional radiologist, is that the procedure is technically demanding, with a limited number of operators with the expertise to perform it. If TIPS became more widely accepted as an option for treating PVT, then the pool of interventionalists experienced with performing the procedure would grow, Dr. Valentin noted.
mzoler@mdedge.com
On Twitter @mitchelzoler
SOURCE: Valentin N et al. Digestive Disease Week, Presentation 361.
WASHINGTON – Catheter-directed clot lysis and thrombectomy with creation of a bypass shunt is a reasonable alternative to prolonged anticoagulation for treating patients with portal vein thrombosis (PVT) based on the accumulated reported experience since 1993 using this percutaneous treatment.
” Nelson Valentin, MD, said at the annual Digestive Disease Week.® “TIPS should be considered a viable treatment option for patients with PVT,” said Dr. Valentin, a gastroenterology fellow at Mount Sinai Beth Israel hospital in New York.
“There is sufficient evidence from these reports to at least consider TIPS as an adjunct to anticoagulation or perhaps as primary therapy,” especially for patients with PVT who have a contraindication for anticoagulation, Dr. Valentin said in an interview. Standard anticoagulation for PVT would today involve acute treatment with a low-molecular-weight heparin followed by oral anticoagulation for a total treatment time of at least 6 months and continued for a year or longer in some patients. A recently published review of reported experience using anticoagulation to treat PVT found a complete recanalization rate of 41% and a complete or partial rate of 66%, which suggests that TIPS is at least as effective, although Dr. Valentin cautioned that no reported study has directly compared the two alternative approaches. A study designed to make this direct comparison is warranted by the reported results using TIPS, Dr. Valentin said. And the experience with TIPS positions it as an option for patients who do not respond to anticoagulation or would prefer an alternative to prolonged anticoagulation.
One factor currently limiting use of TIPS, which is usually performed by an interventional radiologist, is that the procedure is technically demanding, with a limited number of operators with the expertise to perform it. If TIPS became more widely accepted as an option for treating PVT, then the pool of interventionalists experienced with performing the procedure would grow, Dr. Valentin noted.
mzoler@mdedge.com
On Twitter @mitchelzoler
SOURCE: Valentin N et al. Digestive Disease Week, Presentation 361.
REPORTING FROM DDW 2018
Key clinical point: Reported worldwide experience with TIPS in 439 patients shows it works and is relatively safe.
Major finding: TIPS was technically successful in 87% of reported patients and achieved complete portal recanalization in 74% of patients.
Study details: Systematic review of 18 published case series from 1993 to 2016 with 439 total patients.
Disclosures: Dr. Valentin had no disclosures.
Source: Valentin N et al. Digestive Disease Week, Presentation 361.
Opioids still overprescribed for postop pain management
Most patients use far less opioids than they are prescribed after hernia and other abdominal surgery, resulting in substantial waste and potential diversion, a prospective cohort study has found.
In an evaluation of 176 narcotic-naive patients who underwent surgery in a over the 14-day postdischarge study period was 30 morphine milligram equivalents (MME) but the median prescription was 150 MME, reported Wen Hui Tan, MD, and her research team at Washington University, St. Louis. The report was published in the Journal of the American College of Surgeons.
Overall, 76.7% of patients reported being satisfied or very satisfied with their postoperative pain management. Some patients (n = 31, 17.6%) reported not filling their prescription or not taking any of their prescribed opioid pain medications at all.
Sixty-nine percent of the surgeries were laparoscopic. A variety of abdominal procedures were represented, including hiatal hernia repair, inguinal hernia repair, and cholecystectomy. The median age was 60 years. Of postoperative pain prescriptions, 67% were for hydrocodone-acetaminophen and most of the remainder were for oxycodone-acetaminophen or oxycodone alone. The median prescription was for the equivalent of 20 5-mg oxycodone pills, while the median consumption in the first 7 postoperative days was 3.7 pills. Only 4.5% of patients received a refill.
The findings are consistent with numerous studies of different types of operations showing that patients often don’t use all of the opioid medications they are prescribed for pain control after surgery.
“Now that opioid pain medications can no longer be refilled with a pharmacy via telephone, overprescription may also be partially driven by a desire to prevent future inconvenience and workload of office staff from patients requesting refills. However, the rising numbers of opioid-related unintentional deaths over the last decade point to the fact that overprescription has serious potential consequences,” the researchers wrote.
They reported having no potential conflicts of interest.
SOURCE: Tan et al. J Am Coll Surg 2018 May 7. doi: 10.1016/j.jamcollsurg.2018.04.032.
Most patients use far less opioids than they are prescribed after hernia and other abdominal surgery, resulting in substantial waste and potential diversion, a prospective cohort study has found.
In an evaluation of 176 narcotic-naive patients who underwent surgery in a over the 14-day postdischarge study period was 30 morphine milligram equivalents (MME) but the median prescription was 150 MME, reported Wen Hui Tan, MD, and her research team at Washington University, St. Louis. The report was published in the Journal of the American College of Surgeons.
Overall, 76.7% of patients reported being satisfied or very satisfied with their postoperative pain management. Some patients (n = 31, 17.6%) reported not filling their prescription or not taking any of their prescribed opioid pain medications at all.
Sixty-nine percent of the surgeries were laparoscopic. A variety of abdominal procedures were represented, including hiatal hernia repair, inguinal hernia repair, and cholecystectomy. The median age was 60 years. Of postoperative pain prescriptions, 67% were for hydrocodone-acetaminophen and most of the remainder were for oxycodone-acetaminophen or oxycodone alone. The median prescription was for the equivalent of 20 5-mg oxycodone pills, while the median consumption in the first 7 postoperative days was 3.7 pills. Only 4.5% of patients received a refill.
The findings are consistent with numerous studies of different types of operations showing that patients often don’t use all of the opioid medications they are prescribed for pain control after surgery.
“Now that opioid pain medications can no longer be refilled with a pharmacy via telephone, overprescription may also be partially driven by a desire to prevent future inconvenience and workload of office staff from patients requesting refills. However, the rising numbers of opioid-related unintentional deaths over the last decade point to the fact that overprescription has serious potential consequences,” the researchers wrote.
They reported having no potential conflicts of interest.
SOURCE: Tan et al. J Am Coll Surg 2018 May 7. doi: 10.1016/j.jamcollsurg.2018.04.032.
Most patients use far less opioids than they are prescribed after hernia and other abdominal surgery, resulting in substantial waste and potential diversion, a prospective cohort study has found.
In an evaluation of 176 narcotic-naive patients who underwent surgery in a over the 14-day postdischarge study period was 30 morphine milligram equivalents (MME) but the median prescription was 150 MME, reported Wen Hui Tan, MD, and her research team at Washington University, St. Louis. The report was published in the Journal of the American College of Surgeons.
Overall, 76.7% of patients reported being satisfied or very satisfied with their postoperative pain management. Some patients (n = 31, 17.6%) reported not filling their prescription or not taking any of their prescribed opioid pain medications at all.
Sixty-nine percent of the surgeries were laparoscopic. A variety of abdominal procedures were represented, including hiatal hernia repair, inguinal hernia repair, and cholecystectomy. The median age was 60 years. Of postoperative pain prescriptions, 67% were for hydrocodone-acetaminophen and most of the remainder were for oxycodone-acetaminophen or oxycodone alone. The median prescription was for the equivalent of 20 5-mg oxycodone pills, while the median consumption in the first 7 postoperative days was 3.7 pills. Only 4.5% of patients received a refill.
The findings are consistent with numerous studies of different types of operations showing that patients often don’t use all of the opioid medications they are prescribed for pain control after surgery.
“Now that opioid pain medications can no longer be refilled with a pharmacy via telephone, overprescription may also be partially driven by a desire to prevent future inconvenience and workload of office staff from patients requesting refills. However, the rising numbers of opioid-related unintentional deaths over the last decade point to the fact that overprescription has serious potential consequences,” the researchers wrote.
They reported having no potential conflicts of interest.
SOURCE: Tan et al. J Am Coll Surg 2018 May 7. doi: 10.1016/j.jamcollsurg.2018.04.032.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Key clinical point: For postoperative recovery, a survey showed that far more opioids are prescribed than are consumed.
Major finding: On average, surgical patients went home with opioid prescriptions of 150 MME but took a median of 30 MME.
Study details: Prospective cohort study.
Disclosures: The authors report no potential conflicts of interest.
Source: Tan et al. J Am Coll Surg 2018 May 7. doi: 10.1016/j.jamcollsurg.2018.04.032.
Postop delirium management proposed as hospital performance measure
A study suggests that outcome measures, and assessment of hospital performance.
Lead author Julia R. Berian, MD, of the University of Chicago Medical Center and her colleagues wrote, “Postoperative delirium has been associated with mortality, morbidity, prolonged length of stay, and increased costs of care. Furthermore, postoperative delirium may be associated with long-term cognitive and functional decline. However, postoperative delirium has not been incorporated as an outcome measure into major surgical quality registries. Approximately one-third of hospitalized delirium is believed to be preventable, making postoperative delirium an ideal target for surgical quality improvement efforts,” Dr. Berian and her colleagues reported in the Annals of Surgery.
The Geriatric Surgery Pilot data abstractors were instructed to assign postoperative delirium if the medical record words indicating an acute confusional stat such a mental status change, confusion, disorientation, agitation, delirium, and inappropriate behavior. Data were collected from the period 2 hours after surgery to exclude effects of the pharmacologic agents of anesthesia. Delirium status was ascertained as a binary outcome (Yes/No).
Postoperative delirium was observed in 2,427 patients for an average, unadjusted rate of 12.0%. Investigators identified 20 risk factors markedly associated with delirium. The strongest predictors included preoperative cognitive impairment, preoperative use of mobility aid, surrogate consent form, ASA class 4 or greater, age 80 years and older, preoperative sepsis, and fall history within 1 year. Patients with delirium generally were older than patients without delirium were and accounted for a greater proportion of emergency cases. Postoperative hospital length of stay was about 4 days longer on average for patients with delirium, compared with those without delirium.
By specialty, the highest rates of postoperative delirium occurred following cardiothoracic (13.7%), orthopedic (13.0%), and general surgeries (13.0%). Study authors found varied associated risk for postoperative delirium within each surgical specialty. For example, in general surgery, the risk for postoperative delirium with partial mastectomy was low, compared with a mid-level risk in the repair of a recurrent, incarcerated, or strangulated inguinal hernia and a high-level risk in Whipple operations.
The model developed to measure delirium management success in 30 hospitals found that adjusted delirium rates ranged from 3.2% to 27.5%, with eight poor- and five excellent-performing outliers. Authors noted that their model demonstrated good calibration and discrimination. Examination of changes in the Bayesian Information Criteria indicates that as few as 10-12 variables may suffice in building a parsimonious model with “an excellent fit.”
Study authors noted that screening for postoperative delirium in older adults is likely in the best interests of patients. However, they also mentioned that such screening may identify cases of postoperative delirium that were previously unrecognized, resulting in higher rates. In addition, the inclusion of only ACS NSQIP hospitals and the voluntary participation may mean a biased dataset. No one delirium prevention intervention was implemented across the hospitals and so the study doesn’t indicate why some hospitals are more successful than are others. Chart-based identification of patients who have delirium needs further study to assess validity.
Authors concluded that one solution may be to “standardize and consistently employ delirium screening in high-risk patients across hospitals, as has been advocated by a coalition of interdisciplinary experts in geriatric care.”
This project is funded in part by a grant from the John A. Hartford Foundation. The authors declare no conflict of interests.
SOURCE: Berlan JR et al. Ann Surg. 2017 July 24. doi: 10.1097/SLA.0000000000002436
A study suggests that outcome measures, and assessment of hospital performance.
Lead author Julia R. Berian, MD, of the University of Chicago Medical Center and her colleagues wrote, “Postoperative delirium has been associated with mortality, morbidity, prolonged length of stay, and increased costs of care. Furthermore, postoperative delirium may be associated with long-term cognitive and functional decline. However, postoperative delirium has not been incorporated as an outcome measure into major surgical quality registries. Approximately one-third of hospitalized delirium is believed to be preventable, making postoperative delirium an ideal target for surgical quality improvement efforts,” Dr. Berian and her colleagues reported in the Annals of Surgery.
The Geriatric Surgery Pilot data abstractors were instructed to assign postoperative delirium if the medical record words indicating an acute confusional stat such a mental status change, confusion, disorientation, agitation, delirium, and inappropriate behavior. Data were collected from the period 2 hours after surgery to exclude effects of the pharmacologic agents of anesthesia. Delirium status was ascertained as a binary outcome (Yes/No).
Postoperative delirium was observed in 2,427 patients for an average, unadjusted rate of 12.0%. Investigators identified 20 risk factors markedly associated with delirium. The strongest predictors included preoperative cognitive impairment, preoperative use of mobility aid, surrogate consent form, ASA class 4 or greater, age 80 years and older, preoperative sepsis, and fall history within 1 year. Patients with delirium generally were older than patients without delirium were and accounted for a greater proportion of emergency cases. Postoperative hospital length of stay was about 4 days longer on average for patients with delirium, compared with those without delirium.
By specialty, the highest rates of postoperative delirium occurred following cardiothoracic (13.7%), orthopedic (13.0%), and general surgeries (13.0%). Study authors found varied associated risk for postoperative delirium within each surgical specialty. For example, in general surgery, the risk for postoperative delirium with partial mastectomy was low, compared with a mid-level risk in the repair of a recurrent, incarcerated, or strangulated inguinal hernia and a high-level risk in Whipple operations.
The model developed to measure delirium management success in 30 hospitals found that adjusted delirium rates ranged from 3.2% to 27.5%, with eight poor- and five excellent-performing outliers. Authors noted that their model demonstrated good calibration and discrimination. Examination of changes in the Bayesian Information Criteria indicates that as few as 10-12 variables may suffice in building a parsimonious model with “an excellent fit.”
Study authors noted that screening for postoperative delirium in older adults is likely in the best interests of patients. However, they also mentioned that such screening may identify cases of postoperative delirium that were previously unrecognized, resulting in higher rates. In addition, the inclusion of only ACS NSQIP hospitals and the voluntary participation may mean a biased dataset. No one delirium prevention intervention was implemented across the hospitals and so the study doesn’t indicate why some hospitals are more successful than are others. Chart-based identification of patients who have delirium needs further study to assess validity.
Authors concluded that one solution may be to “standardize and consistently employ delirium screening in high-risk patients across hospitals, as has been advocated by a coalition of interdisciplinary experts in geriatric care.”
This project is funded in part by a grant from the John A. Hartford Foundation. The authors declare no conflict of interests.
SOURCE: Berlan JR et al. Ann Surg. 2017 July 24. doi: 10.1097/SLA.0000000000002436
A study suggests that outcome measures, and assessment of hospital performance.
Lead author Julia R. Berian, MD, of the University of Chicago Medical Center and her colleagues wrote, “Postoperative delirium has been associated with mortality, morbidity, prolonged length of stay, and increased costs of care. Furthermore, postoperative delirium may be associated with long-term cognitive and functional decline. However, postoperative delirium has not been incorporated as an outcome measure into major surgical quality registries. Approximately one-third of hospitalized delirium is believed to be preventable, making postoperative delirium an ideal target for surgical quality improvement efforts,” Dr. Berian and her colleagues reported in the Annals of Surgery.
The Geriatric Surgery Pilot data abstractors were instructed to assign postoperative delirium if the medical record words indicating an acute confusional stat such a mental status change, confusion, disorientation, agitation, delirium, and inappropriate behavior. Data were collected from the period 2 hours after surgery to exclude effects of the pharmacologic agents of anesthesia. Delirium status was ascertained as a binary outcome (Yes/No).
Postoperative delirium was observed in 2,427 patients for an average, unadjusted rate of 12.0%. Investigators identified 20 risk factors markedly associated with delirium. The strongest predictors included preoperative cognitive impairment, preoperative use of mobility aid, surrogate consent form, ASA class 4 or greater, age 80 years and older, preoperative sepsis, and fall history within 1 year. Patients with delirium generally were older than patients without delirium were and accounted for a greater proportion of emergency cases. Postoperative hospital length of stay was about 4 days longer on average for patients with delirium, compared with those without delirium.
By specialty, the highest rates of postoperative delirium occurred following cardiothoracic (13.7%), orthopedic (13.0%), and general surgeries (13.0%). Study authors found varied associated risk for postoperative delirium within each surgical specialty. For example, in general surgery, the risk for postoperative delirium with partial mastectomy was low, compared with a mid-level risk in the repair of a recurrent, incarcerated, or strangulated inguinal hernia and a high-level risk in Whipple operations.
The model developed to measure delirium management success in 30 hospitals found that adjusted delirium rates ranged from 3.2% to 27.5%, with eight poor- and five excellent-performing outliers. Authors noted that their model demonstrated good calibration and discrimination. Examination of changes in the Bayesian Information Criteria indicates that as few as 10-12 variables may suffice in building a parsimonious model with “an excellent fit.”
Study authors noted that screening for postoperative delirium in older adults is likely in the best interests of patients. However, they also mentioned that such screening may identify cases of postoperative delirium that were previously unrecognized, resulting in higher rates. In addition, the inclusion of only ACS NSQIP hospitals and the voluntary participation may mean a biased dataset. No one delirium prevention intervention was implemented across the hospitals and so the study doesn’t indicate why some hospitals are more successful than are others. Chart-based identification of patients who have delirium needs further study to assess validity.
Authors concluded that one solution may be to “standardize and consistently employ delirium screening in high-risk patients across hospitals, as has been advocated by a coalition of interdisciplinary experts in geriatric care.”
This project is funded in part by a grant from the John A. Hartford Foundation. The authors declare no conflict of interests.
SOURCE: Berlan JR et al. Ann Surg. 2017 July 24. doi: 10.1097/SLA.0000000000002436
FROM ANNALS OF SURGERY
Key clinical point: Through predictive modeling, the study identified 20 risk factors markedly associated with delirium that can be used to identify high-risk patients.
Major finding: Among the 2,427 patients who experienced delirium, 35% had preoperative cognitive impairment, 30 % had a surrogate sign the consent form, and 32% experienced serious postoperative complications or death.
Study details: An analysis of 2,427 elderly patients at 30 hospitals through data from the ACS NSQIP Geriatric Surgery Pilot Project.
Disclosures: This project is funded in part by a grant from the John A. Hartford Foundation. The authors declare no conflict of interests.
Source: Berian JR et al. Ann Surg. 2017Jul 24. doi: 10.1097/SLA.0000000000002436
MDR Candida auris is on the move
MADRID – The anticipated global emergence of multidrug resistant Candida auris is now an established fact, but a case study presented at the European Society of Clinical Microbiology and Infectious Diseases annual congress demonstrates just how devastating an outbreak can be to a medical facility and its surgical ICU patients.
The dangerous invasive infection is spreading through Asia, Europe, and the Americas, causing potentially fatal candidemias and proving devilishly difficult to eradicate in health care facilities once it becomes established.
Several multidrug resistant (MDR) C. auris outbreaks were reported at the ECCMID meeting. Most troubling: a continuing outbreak in a hospital in Valencia, Spain, in which 17 patients have died – a 41% fatality rate among those who developed a fulminant C. auris candidemia, Javier Pemán, MD, said at the meeting. The strain appeared to be a clonal population not previously identified in published reports.
“C. auris is hard to remove from the hospital environment,” once it becomes established, said Dr. Pemán of La Fe University and Polytechnic Hospital, Valencia. “When an outbreak lasts for months, as ours has, it is difficult, but necessary, to maintain control measures, identify it early in the lab, and isolate and treat patients early with combination therapy.”
He and his team have relied primarily on a combination of amphotericin B and echinocandin (AMB+ECN), although, he added, the optimal dosing and treatment time aren’t known, and many C. auris isolates are echinocandin resistant.
MDR C. auris first appearedin Tokyo in 2009. It then spread to South Korea around 2011, and then appeared across Asia and Western Europe. Its first appearance in Spain was the 2016 Le Fe outbreak.
According to the Centers for Disease Control and Prevention, single cases have appeared in Austria, Belgium, Malaysia, Norway, and the United Arab Emirates. Canada, Colombia, France, Germany, India, Israel, Japan, Kenya, Kuwait, Oman, Pakistan, Panama, South Korea, South Africa, Spain, the United Arab Emirates, the United Kingdom, and Venezuela have experienced multiple outbreaks.
The CDC has recorded 257 confirmed and 30 probable cases of MDR C. auris in the United States as of March 31, 2018. Most of these occurred in New York City and New Jersey; a number of patients had recent stays in hospitals in India, Pakistan, South Africa, the UAE, and Venezuela.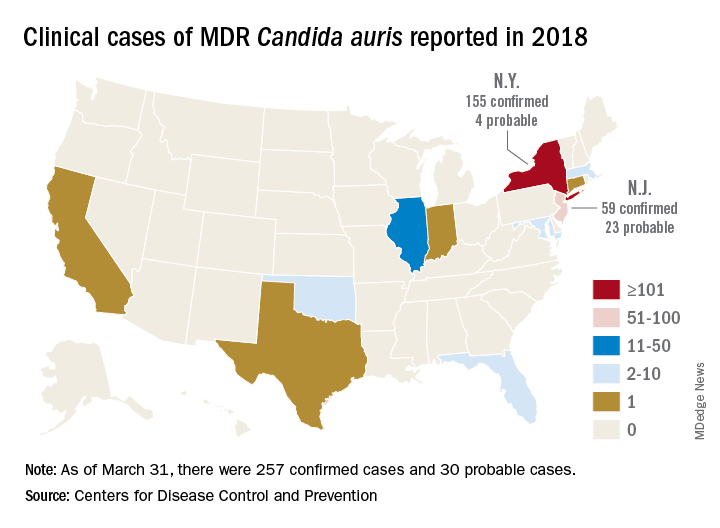
Jacques Meis, MD, of the department of medical microbiology and infectious diseases at Canisius Wilhelmina Hospital, Nijmegen, the Netherlands, set the stage for an extended discussion of C. auris at the meeting.
“This is a multidrug resistant yeast that has emerged in the last decade. Some rare isolates are resistant to all three major antifungal classes. Unlike other Candida species, it seems to persist for prolonged periods in health care environments and to colonize patients’ skin. It behaves rather like resistant bacteria.”
Once established in a health care setting – often an intensive care ward – C. auris poses major infection controls challenges and can be very hard to identify and eradicate, said Dr. Meis.
The identification problem is well known. The 2016 CDC alert noted that “commercially available biochemical-based tests, including API strips and VITEK-2, used in many U.S. laboratories to identify fungi, cannot differentiate C. auris from related species. Because of these challenges, clinical laboratories have misidentified the organism as C. haemulonii and Saccharomyces cerevisiae.”
“It’s often misidentified as other Candida species or as Saccharomyces when we investigate with biochemical methods. C. auris is best identified using Matrix Assisted Laser Desorption/Ionization time of flight mass spectrometry (MALDI-TOF),” said Dr. Meis.
Among the presentations at ECCMID were a report of a U.K. outbreak that affected 70 patients in a neuroscience ICU. It was traced to axillary skin-surface temperature probes, and eradicated only after those probes were removed. More than 90% of the isolates were resistant to fluconazole, voriconazole, and posaconazole; 18% were amphotericin resistant.
A poster described the microbiological characteristics of 50 C. auris isolates taken from 11 hospitals in Korea.
Dr. Pemán described the outbreak in Valencia, which began in April 2016; the report was simultaneously published in the online journal Mycoses (2018 Apr 14. doi: 10.1111/myc.12781).
The index case was a 66-year-old man with hepatocellular carcinoma who underwent a liver resection at Hospital Le Fe in April 2016. During his stay in the surgical ICU (SICU), he developed a fungal infection from an unknown, highly fluconazole-resistant yeast. The pathogen was twice misidentified, first as C. haemulonii and then as S. cerevisiae.
Three weeks later, the patient in the adjacent bed developed a similar infection. Sequencing of the internal transcribed spacer confirmed both as a Candida isolate – an organism previously unknown in Spain.
The SICU setup was apparently very conducive to the C. auris life cycle, Dr. Pemán said. It’s a relatively open ward divided into three rooms with 12 beds in each. There are no isolation beds, and dozens of workers have access to the ward every day, including clinical and cleaning staff.
After identifying the second isolate, Dr. Pemán said, infection control staff went into action. They instituted contact precautions in the SICU, and took regular cultures from newly admitted patients and cultures of every SICU patient every 7 days.
“We also started an intense search for more cases throughout the hospital and in 101 SICU workers. Of 305 samples from hands and ears, we found nothing.” They reviewed all the prior fluconazole-resistant Candida isolates; C. auris was not present in the hospital before the index case.
Three weeks after case 2, six new SICU patients tested positive for C. auris (two blood cultures, one vascular line, one respiratory specimen, two rectal swabs, and one urinary tract sample).
“We reinforced contact precautions in colonized and infected patients and started a twice-daily environmental cleaning practice with quaternary ammonium around them,” said Dr. Pemán. They instituted a proactive hospital-wide hand hygiene campaign and spread the word about the outbreak.
By July, there were 11 new colonized patients, 3 of whom developed candidemia. These patients were grouped in the same SICU ward and underwent daily skin treatments with 4% aqueous chlorhexidine wipes.
The environmental inspection found C. auris on beds, tables, walls, and the floor all around infected patients. The pathogen also was living on IV pumps, computer keyboards, and bedside tables. Blood pressure cuffs were a favorite haunt: 19 of 36 samples in the adjacent ICU were positive. These data were separately reported at ECCMID.
Despite all of these efforts at eradication, infections continued to rise. By November, there were 24 newly colonized patients and nine new candidemia episodes in SICU and regular ICU patients. In December, a new infection control bundle began: A surveillance nurse in the C. auris SICU ward was in charge of compliance; any patient with any yeast growth in culture was isolated, and staff used 2% alcohol chlorhexidine wipes before and after IV catheter handling. Staff also washed down all surfaces three times daily with a disinfectant.
Patients could leave isolation after three consecutive C. auris–negative cultures. After discharge, an ultraviolet light decontamination procedure disinfected each patient room.
The pathogen was almost unbelievably resilient, Dr. Pemán noted in the Mycoses article. “In some cases, C. auris was recovered from walls after cleaning with cationic surface–active products ... it was not known until very recently that these products, as well as quaternary ammonium disinfectants, cannot effectively remove C. auris from surfaces.”
As a result of the previous measures, the outbreak slowed down during December 2016, with two new candidemia cases, but by February, the outbreak resumed with 50 new cases and 18 candidemias detected. Cases continued to emerge throughout 2017.
By September 2017, 250 patients had been colonized; 116 of these were included in the Mycoses report. There were 30 episodes of candidemia (26%); of these, 17 died by 30 days (41.4%). Spondylodiscitis and endocarditis each developed in two patients and one developed ventriculitis.
A separate poster by Dr. Pemán and his colleagues gave more details:
• A 52-year-old woman with C. auris–induced endocarditis died after 4 weeks of treatment with AMB+ECN and flucytosine. She had undergone a prosthetic heart valve placement for Ebstein’s anomaly.
• A 71-year-old man with hydrocephalus developed a C. auris–induced infection of his ventriculoperitoneal shunt; he also had undergone cardiovascular surgery and had an ischemic cardiomyopathy. He died despite shunt removal and 8 weeks of AMB+ECN.
• A 71-year-old man who underwent cardiovascular surgery and received a prosthetic heart valve developed endocarditis. He is alive and at last report, on week 26 of AMB+ECN, flucytosine, and isavuconazole.
• A 68-year-old man who underwent abdominal surgery for hepatocellular carcinoma developed spondylodiscitis and is alive after 24 weeks of AMB+ECN.
• A 48-year old female multiple trauma patient developed spondylodiscitis and is alive after 48 weeks of treatment with AMB+ECN.
A multivariate analysis determined that antibacterial treatment increased the risk of candidemia by almost 30 times (odds ratio, 29.59). The next highest risk was neutropenia (OR, 20.7) and then simply being a hospital and SICU patient. Dr. Pemán’s poster said, “In the 16 months before the index case, La Fe recorded 89 candidemias, none caused by C. auris. In the 16 months afterward, there were 154 candidemias, largely C. auris. Before April 2016, C. parapsilosis accounted for the largest portion of candidemias (46%) followed by C. albicans. After the index case, C. auris accounted for 42%, followed by C. parapsilosis (21%) and C. albicans (18%).”
Because of its fluconazole resistance, patients with C. auris received a combined antifungal treatment of liposomal amphotericin B 3 mg/kg per day for 5 days, and a standard dose of echinocandin for 3 weeks. Many C. auris strains are echinocandin resistant, Dr. Pemán noted. This particular strain was clonal, different from any other previously reported, he said.
“Our results confirm those previously reported by other authors, that C. auris is grouped in different independent clusters according to its geographical origin. Although all Spanish isolates were genotypically distinct from Indian, Omani, U.K., and Venezuelan isolates, there seems to be some connection with South African isolates.”
Hospital Le Fe continues to struggle with C. auris. As of March, 335 patients have tested positive for the pathogen, and 80 have developed candidemias.
“We feel we may be approaching the end of this episode, but it’s really not possible to be sure,” he said.
Dr. Pemán had no relevant financial disclosures.
SOURCE: ECCMID 2018 Peman et al. S0067.
MADRID – The anticipated global emergence of multidrug resistant Candida auris is now an established fact, but a case study presented at the European Society of Clinical Microbiology and Infectious Diseases annual congress demonstrates just how devastating an outbreak can be to a medical facility and its surgical ICU patients.
The dangerous invasive infection is spreading through Asia, Europe, and the Americas, causing potentially fatal candidemias and proving devilishly difficult to eradicate in health care facilities once it becomes established.
Several multidrug resistant (MDR) C. auris outbreaks were reported at the ECCMID meeting. Most troubling: a continuing outbreak in a hospital in Valencia, Spain, in which 17 patients have died – a 41% fatality rate among those who developed a fulminant C. auris candidemia, Javier Pemán, MD, said at the meeting. The strain appeared to be a clonal population not previously identified in published reports.
“C. auris is hard to remove from the hospital environment,” once it becomes established, said Dr. Pemán of La Fe University and Polytechnic Hospital, Valencia. “When an outbreak lasts for months, as ours has, it is difficult, but necessary, to maintain control measures, identify it early in the lab, and isolate and treat patients early with combination therapy.”
He and his team have relied primarily on a combination of amphotericin B and echinocandin (AMB+ECN), although, he added, the optimal dosing and treatment time aren’t known, and many C. auris isolates are echinocandin resistant.
MDR C. auris first appearedin Tokyo in 2009. It then spread to South Korea around 2011, and then appeared across Asia and Western Europe. Its first appearance in Spain was the 2016 Le Fe outbreak.
According to the Centers for Disease Control and Prevention, single cases have appeared in Austria, Belgium, Malaysia, Norway, and the United Arab Emirates. Canada, Colombia, France, Germany, India, Israel, Japan, Kenya, Kuwait, Oman, Pakistan, Panama, South Korea, South Africa, Spain, the United Arab Emirates, the United Kingdom, and Venezuela have experienced multiple outbreaks.
The CDC has recorded 257 confirmed and 30 probable cases of MDR C. auris in the United States as of March 31, 2018. Most of these occurred in New York City and New Jersey; a number of patients had recent stays in hospitals in India, Pakistan, South Africa, the UAE, and Venezuela.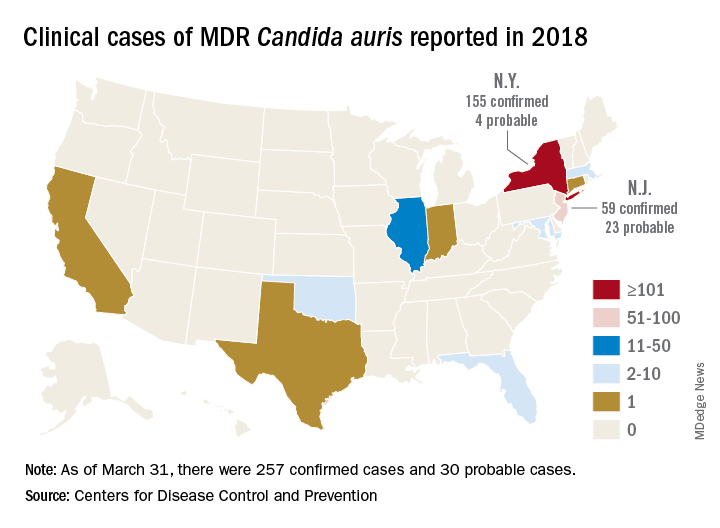
Jacques Meis, MD, of the department of medical microbiology and infectious diseases at Canisius Wilhelmina Hospital, Nijmegen, the Netherlands, set the stage for an extended discussion of C. auris at the meeting.
“This is a multidrug resistant yeast that has emerged in the last decade. Some rare isolates are resistant to all three major antifungal classes. Unlike other Candida species, it seems to persist for prolonged periods in health care environments and to colonize patients’ skin. It behaves rather like resistant bacteria.”
Once established in a health care setting – often an intensive care ward – C. auris poses major infection controls challenges and can be very hard to identify and eradicate, said Dr. Meis.
The identification problem is well known. The 2016 CDC alert noted that “commercially available biochemical-based tests, including API strips and VITEK-2, used in many U.S. laboratories to identify fungi, cannot differentiate C. auris from related species. Because of these challenges, clinical laboratories have misidentified the organism as C. haemulonii and Saccharomyces cerevisiae.”
“It’s often misidentified as other Candida species or as Saccharomyces when we investigate with biochemical methods. C. auris is best identified using Matrix Assisted Laser Desorption/Ionization time of flight mass spectrometry (MALDI-TOF),” said Dr. Meis.
Among the presentations at ECCMID were a report of a U.K. outbreak that affected 70 patients in a neuroscience ICU. It was traced to axillary skin-surface temperature probes, and eradicated only after those probes were removed. More than 90% of the isolates were resistant to fluconazole, voriconazole, and posaconazole; 18% were amphotericin resistant.
A poster described the microbiological characteristics of 50 C. auris isolates taken from 11 hospitals in Korea.
Dr. Pemán described the outbreak in Valencia, which began in April 2016; the report was simultaneously published in the online journal Mycoses (2018 Apr 14. doi: 10.1111/myc.12781).
The index case was a 66-year-old man with hepatocellular carcinoma who underwent a liver resection at Hospital Le Fe in April 2016. During his stay in the surgical ICU (SICU), he developed a fungal infection from an unknown, highly fluconazole-resistant yeast. The pathogen was twice misidentified, first as C. haemulonii and then as S. cerevisiae.
Three weeks later, the patient in the adjacent bed developed a similar infection. Sequencing of the internal transcribed spacer confirmed both as a Candida isolate – an organism previously unknown in Spain.
The SICU setup was apparently very conducive to the C. auris life cycle, Dr. Pemán said. It’s a relatively open ward divided into three rooms with 12 beds in each. There are no isolation beds, and dozens of workers have access to the ward every day, including clinical and cleaning staff.
After identifying the second isolate, Dr. Pemán said, infection control staff went into action. They instituted contact precautions in the SICU, and took regular cultures from newly admitted patients and cultures of every SICU patient every 7 days.
“We also started an intense search for more cases throughout the hospital and in 101 SICU workers. Of 305 samples from hands and ears, we found nothing.” They reviewed all the prior fluconazole-resistant Candida isolates; C. auris was not present in the hospital before the index case.
Three weeks after case 2, six new SICU patients tested positive for C. auris (two blood cultures, one vascular line, one respiratory specimen, two rectal swabs, and one urinary tract sample).
“We reinforced contact precautions in colonized and infected patients and started a twice-daily environmental cleaning practice with quaternary ammonium around them,” said Dr. Pemán. They instituted a proactive hospital-wide hand hygiene campaign and spread the word about the outbreak.
By July, there were 11 new colonized patients, 3 of whom developed candidemia. These patients were grouped in the same SICU ward and underwent daily skin treatments with 4% aqueous chlorhexidine wipes.
The environmental inspection found C. auris on beds, tables, walls, and the floor all around infected patients. The pathogen also was living on IV pumps, computer keyboards, and bedside tables. Blood pressure cuffs were a favorite haunt: 19 of 36 samples in the adjacent ICU were positive. These data were separately reported at ECCMID.
Despite all of these efforts at eradication, infections continued to rise. By November, there were 24 newly colonized patients and nine new candidemia episodes in SICU and regular ICU patients. In December, a new infection control bundle began: A surveillance nurse in the C. auris SICU ward was in charge of compliance; any patient with any yeast growth in culture was isolated, and staff used 2% alcohol chlorhexidine wipes before and after IV catheter handling. Staff also washed down all surfaces three times daily with a disinfectant.
Patients could leave isolation after three consecutive C. auris–negative cultures. After discharge, an ultraviolet light decontamination procedure disinfected each patient room.
The pathogen was almost unbelievably resilient, Dr. Pemán noted in the Mycoses article. “In some cases, C. auris was recovered from walls after cleaning with cationic surface–active products ... it was not known until very recently that these products, as well as quaternary ammonium disinfectants, cannot effectively remove C. auris from surfaces.”
As a result of the previous measures, the outbreak slowed down during December 2016, with two new candidemia cases, but by February, the outbreak resumed with 50 new cases and 18 candidemias detected. Cases continued to emerge throughout 2017.
By September 2017, 250 patients had been colonized; 116 of these were included in the Mycoses report. There were 30 episodes of candidemia (26%); of these, 17 died by 30 days (41.4%). Spondylodiscitis and endocarditis each developed in two patients and one developed ventriculitis.
A separate poster by Dr. Pemán and his colleagues gave more details:
• A 52-year-old woman with C. auris–induced endocarditis died after 4 weeks of treatment with AMB+ECN and flucytosine. She had undergone a prosthetic heart valve placement for Ebstein’s anomaly.
• A 71-year-old man with hydrocephalus developed a C. auris–induced infection of his ventriculoperitoneal shunt; he also had undergone cardiovascular surgery and had an ischemic cardiomyopathy. He died despite shunt removal and 8 weeks of AMB+ECN.
• A 71-year-old man who underwent cardiovascular surgery and received a prosthetic heart valve developed endocarditis. He is alive and at last report, on week 26 of AMB+ECN, flucytosine, and isavuconazole.
• A 68-year-old man who underwent abdominal surgery for hepatocellular carcinoma developed spondylodiscitis and is alive after 24 weeks of AMB+ECN.
• A 48-year old female multiple trauma patient developed spondylodiscitis and is alive after 48 weeks of treatment with AMB+ECN.
A multivariate analysis determined that antibacterial treatment increased the risk of candidemia by almost 30 times (odds ratio, 29.59). The next highest risk was neutropenia (OR, 20.7) and then simply being a hospital and SICU patient. Dr. Pemán’s poster said, “In the 16 months before the index case, La Fe recorded 89 candidemias, none caused by C. auris. In the 16 months afterward, there were 154 candidemias, largely C. auris. Before April 2016, C. parapsilosis accounted for the largest portion of candidemias (46%) followed by C. albicans. After the index case, C. auris accounted for 42%, followed by C. parapsilosis (21%) and C. albicans (18%).”
Because of its fluconazole resistance, patients with C. auris received a combined antifungal treatment of liposomal amphotericin B 3 mg/kg per day for 5 days, and a standard dose of echinocandin for 3 weeks. Many C. auris strains are echinocandin resistant, Dr. Pemán noted. This particular strain was clonal, different from any other previously reported, he said.
“Our results confirm those previously reported by other authors, that C. auris is grouped in different independent clusters according to its geographical origin. Although all Spanish isolates were genotypically distinct from Indian, Omani, U.K., and Venezuelan isolates, there seems to be some connection with South African isolates.”
Hospital Le Fe continues to struggle with C. auris. As of March, 335 patients have tested positive for the pathogen, and 80 have developed candidemias.
“We feel we may be approaching the end of this episode, but it’s really not possible to be sure,” he said.
Dr. Pemán had no relevant financial disclosures.
SOURCE: ECCMID 2018 Peman et al. S0067.
MADRID – The anticipated global emergence of multidrug resistant Candida auris is now an established fact, but a case study presented at the European Society of Clinical Microbiology and Infectious Diseases annual congress demonstrates just how devastating an outbreak can be to a medical facility and its surgical ICU patients.
The dangerous invasive infection is spreading through Asia, Europe, and the Americas, causing potentially fatal candidemias and proving devilishly difficult to eradicate in health care facilities once it becomes established.
Several multidrug resistant (MDR) C. auris outbreaks were reported at the ECCMID meeting. Most troubling: a continuing outbreak in a hospital in Valencia, Spain, in which 17 patients have died – a 41% fatality rate among those who developed a fulminant C. auris candidemia, Javier Pemán, MD, said at the meeting. The strain appeared to be a clonal population not previously identified in published reports.
“C. auris is hard to remove from the hospital environment,” once it becomes established, said Dr. Pemán of La Fe University and Polytechnic Hospital, Valencia. “When an outbreak lasts for months, as ours has, it is difficult, but necessary, to maintain control measures, identify it early in the lab, and isolate and treat patients early with combination therapy.”
He and his team have relied primarily on a combination of amphotericin B and echinocandin (AMB+ECN), although, he added, the optimal dosing and treatment time aren’t known, and many C. auris isolates are echinocandin resistant.
MDR C. auris first appearedin Tokyo in 2009. It then spread to South Korea around 2011, and then appeared across Asia and Western Europe. Its first appearance in Spain was the 2016 Le Fe outbreak.
According to the Centers for Disease Control and Prevention, single cases have appeared in Austria, Belgium, Malaysia, Norway, and the United Arab Emirates. Canada, Colombia, France, Germany, India, Israel, Japan, Kenya, Kuwait, Oman, Pakistan, Panama, South Korea, South Africa, Spain, the United Arab Emirates, the United Kingdom, and Venezuela have experienced multiple outbreaks.
The CDC has recorded 257 confirmed and 30 probable cases of MDR C. auris in the United States as of March 31, 2018. Most of these occurred in New York City and New Jersey; a number of patients had recent stays in hospitals in India, Pakistan, South Africa, the UAE, and Venezuela.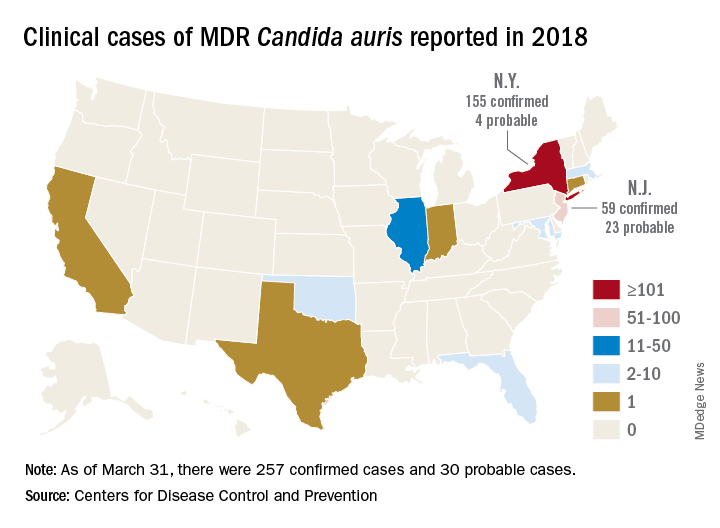
Jacques Meis, MD, of the department of medical microbiology and infectious diseases at Canisius Wilhelmina Hospital, Nijmegen, the Netherlands, set the stage for an extended discussion of C. auris at the meeting.
“This is a multidrug resistant yeast that has emerged in the last decade. Some rare isolates are resistant to all three major antifungal classes. Unlike other Candida species, it seems to persist for prolonged periods in health care environments and to colonize patients’ skin. It behaves rather like resistant bacteria.”
Once established in a health care setting – often an intensive care ward – C. auris poses major infection controls challenges and can be very hard to identify and eradicate, said Dr. Meis.
The identification problem is well known. The 2016 CDC alert noted that “commercially available biochemical-based tests, including API strips and VITEK-2, used in many U.S. laboratories to identify fungi, cannot differentiate C. auris from related species. Because of these challenges, clinical laboratories have misidentified the organism as C. haemulonii and Saccharomyces cerevisiae.”
“It’s often misidentified as other Candida species or as Saccharomyces when we investigate with biochemical methods. C. auris is best identified using Matrix Assisted Laser Desorption/Ionization time of flight mass spectrometry (MALDI-TOF),” said Dr. Meis.
Among the presentations at ECCMID were a report of a U.K. outbreak that affected 70 patients in a neuroscience ICU. It was traced to axillary skin-surface temperature probes, and eradicated only after those probes were removed. More than 90% of the isolates were resistant to fluconazole, voriconazole, and posaconazole; 18% were amphotericin resistant.
A poster described the microbiological characteristics of 50 C. auris isolates taken from 11 hospitals in Korea.
Dr. Pemán described the outbreak in Valencia, which began in April 2016; the report was simultaneously published in the online journal Mycoses (2018 Apr 14. doi: 10.1111/myc.12781).
The index case was a 66-year-old man with hepatocellular carcinoma who underwent a liver resection at Hospital Le Fe in April 2016. During his stay in the surgical ICU (SICU), he developed a fungal infection from an unknown, highly fluconazole-resistant yeast. The pathogen was twice misidentified, first as C. haemulonii and then as S. cerevisiae.
Three weeks later, the patient in the adjacent bed developed a similar infection. Sequencing of the internal transcribed spacer confirmed both as a Candida isolate – an organism previously unknown in Spain.
The SICU setup was apparently very conducive to the C. auris life cycle, Dr. Pemán said. It’s a relatively open ward divided into three rooms with 12 beds in each. There are no isolation beds, and dozens of workers have access to the ward every day, including clinical and cleaning staff.
After identifying the second isolate, Dr. Pemán said, infection control staff went into action. They instituted contact precautions in the SICU, and took regular cultures from newly admitted patients and cultures of every SICU patient every 7 days.
“We also started an intense search for more cases throughout the hospital and in 101 SICU workers. Of 305 samples from hands and ears, we found nothing.” They reviewed all the prior fluconazole-resistant Candida isolates; C. auris was not present in the hospital before the index case.
Three weeks after case 2, six new SICU patients tested positive for C. auris (two blood cultures, one vascular line, one respiratory specimen, two rectal swabs, and one urinary tract sample).
“We reinforced contact precautions in colonized and infected patients and started a twice-daily environmental cleaning practice with quaternary ammonium around them,” said Dr. Pemán. They instituted a proactive hospital-wide hand hygiene campaign and spread the word about the outbreak.
By July, there were 11 new colonized patients, 3 of whom developed candidemia. These patients were grouped in the same SICU ward and underwent daily skin treatments with 4% aqueous chlorhexidine wipes.
The environmental inspection found C. auris on beds, tables, walls, and the floor all around infected patients. The pathogen also was living on IV pumps, computer keyboards, and bedside tables. Blood pressure cuffs were a favorite haunt: 19 of 36 samples in the adjacent ICU were positive. These data were separately reported at ECCMID.
Despite all of these efforts at eradication, infections continued to rise. By November, there were 24 newly colonized patients and nine new candidemia episodes in SICU and regular ICU patients. In December, a new infection control bundle began: A surveillance nurse in the C. auris SICU ward was in charge of compliance; any patient with any yeast growth in culture was isolated, and staff used 2% alcohol chlorhexidine wipes before and after IV catheter handling. Staff also washed down all surfaces three times daily with a disinfectant.
Patients could leave isolation after three consecutive C. auris–negative cultures. After discharge, an ultraviolet light decontamination procedure disinfected each patient room.
The pathogen was almost unbelievably resilient, Dr. Pemán noted in the Mycoses article. “In some cases, C. auris was recovered from walls after cleaning with cationic surface–active products ... it was not known until very recently that these products, as well as quaternary ammonium disinfectants, cannot effectively remove C. auris from surfaces.”
As a result of the previous measures, the outbreak slowed down during December 2016, with two new candidemia cases, but by February, the outbreak resumed with 50 new cases and 18 candidemias detected. Cases continued to emerge throughout 2017.
By September 2017, 250 patients had been colonized; 116 of these were included in the Mycoses report. There were 30 episodes of candidemia (26%); of these, 17 died by 30 days (41.4%). Spondylodiscitis and endocarditis each developed in two patients and one developed ventriculitis.
A separate poster by Dr. Pemán and his colleagues gave more details:
• A 52-year-old woman with C. auris–induced endocarditis died after 4 weeks of treatment with AMB+ECN and flucytosine. She had undergone a prosthetic heart valve placement for Ebstein’s anomaly.
• A 71-year-old man with hydrocephalus developed a C. auris–induced infection of his ventriculoperitoneal shunt; he also had undergone cardiovascular surgery and had an ischemic cardiomyopathy. He died despite shunt removal and 8 weeks of AMB+ECN.
• A 71-year-old man who underwent cardiovascular surgery and received a prosthetic heart valve developed endocarditis. He is alive and at last report, on week 26 of AMB+ECN, flucytosine, and isavuconazole.
• A 68-year-old man who underwent abdominal surgery for hepatocellular carcinoma developed spondylodiscitis and is alive after 24 weeks of AMB+ECN.
• A 48-year old female multiple trauma patient developed spondylodiscitis and is alive after 48 weeks of treatment with AMB+ECN.
A multivariate analysis determined that antibacterial treatment increased the risk of candidemia by almost 30 times (odds ratio, 29.59). The next highest risk was neutropenia (OR, 20.7) and then simply being a hospital and SICU patient. Dr. Pemán’s poster said, “In the 16 months before the index case, La Fe recorded 89 candidemias, none caused by C. auris. In the 16 months afterward, there were 154 candidemias, largely C. auris. Before April 2016, C. parapsilosis accounted for the largest portion of candidemias (46%) followed by C. albicans. After the index case, C. auris accounted for 42%, followed by C. parapsilosis (21%) and C. albicans (18%).”
Because of its fluconazole resistance, patients with C. auris received a combined antifungal treatment of liposomal amphotericin B 3 mg/kg per day for 5 days, and a standard dose of echinocandin for 3 weeks. Many C. auris strains are echinocandin resistant, Dr. Pemán noted. This particular strain was clonal, different from any other previously reported, he said.
“Our results confirm those previously reported by other authors, that C. auris is grouped in different independent clusters according to its geographical origin. Although all Spanish isolates were genotypically distinct from Indian, Omani, U.K., and Venezuelan isolates, there seems to be some connection with South African isolates.”
Hospital Le Fe continues to struggle with C. auris. As of March, 335 patients have tested positive for the pathogen, and 80 have developed candidemias.
“We feel we may be approaching the end of this episode, but it’s really not possible to be sure,” he said.
Dr. Pemán had no relevant financial disclosures.
SOURCE: ECCMID 2018 Peman et al. S0067.
REPORTING FROM ECCMID 2018
FDA approves Doptelet for liver disease patients undergoing procedures
Doptelet (avatrombopag) is the first drug to be approved by the Food and Drug Administration for thrombocytopenia in adults with chronic liver disease who are scheduled to undergo a medical or dental procedure, the FDA announced in a statement.
“Patients with chronic liver disease who have low platelet counts and require a procedure are at increased risk of bleeding,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research. “Doptelet was demonstrated to safely increase the platelet count. This drug may decrease or eliminate the need for platelet transfusions, which are associated with risk of infection and other adverse reactions.”
The safety and efficacy of two different doses of Doptelet administered orally over 5 days, as compared with placebo, was studied in the ADAPT trials (ADAPT-1 and ADAPT-2) involving 435 patients with chronic liver disease and severe thrombocytopenia who were scheduled to undergo a procedure that would typically require platelet transfusion. At both dose levels of Doptelet, a higher proportion of patients had increased platelet counts and did not require platelet transfusion or any rescue therapy on the day of the procedure and up to 7 days following the procedure as compared with those treated with placebo.
The most common side effects reported by clinical trial participants who received Doptelet were fever, stomach (abdominal) pain, nausea, headache, fatigue and edema in the hands or feet. People with chronic liver disease and people with certain blood clotting conditions may have an increased risk of developing blood clots when taking Doptelet, the FDA said in a press release announcing the approval.
The FDA granted the Doptelet approval to AkaRx.
Doptelet (avatrombopag) is the first drug to be approved by the Food and Drug Administration for thrombocytopenia in adults with chronic liver disease who are scheduled to undergo a medical or dental procedure, the FDA announced in a statement.
“Patients with chronic liver disease who have low platelet counts and require a procedure are at increased risk of bleeding,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research. “Doptelet was demonstrated to safely increase the platelet count. This drug may decrease or eliminate the need for platelet transfusions, which are associated with risk of infection and other adverse reactions.”
The safety and efficacy of two different doses of Doptelet administered orally over 5 days, as compared with placebo, was studied in the ADAPT trials (ADAPT-1 and ADAPT-2) involving 435 patients with chronic liver disease and severe thrombocytopenia who were scheduled to undergo a procedure that would typically require platelet transfusion. At both dose levels of Doptelet, a higher proportion of patients had increased platelet counts and did not require platelet transfusion or any rescue therapy on the day of the procedure and up to 7 days following the procedure as compared with those treated with placebo.
The most common side effects reported by clinical trial participants who received Doptelet were fever, stomach (abdominal) pain, nausea, headache, fatigue and edema in the hands or feet. People with chronic liver disease and people with certain blood clotting conditions may have an increased risk of developing blood clots when taking Doptelet, the FDA said in a press release announcing the approval.
The FDA granted the Doptelet approval to AkaRx.
Doptelet (avatrombopag) is the first drug to be approved by the Food and Drug Administration for thrombocytopenia in adults with chronic liver disease who are scheduled to undergo a medical or dental procedure, the FDA announced in a statement.
“Patients with chronic liver disease who have low platelet counts and require a procedure are at increased risk of bleeding,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research. “Doptelet was demonstrated to safely increase the platelet count. This drug may decrease or eliminate the need for platelet transfusions, which are associated with risk of infection and other adverse reactions.”
The safety and efficacy of two different doses of Doptelet administered orally over 5 days, as compared with placebo, was studied in the ADAPT trials (ADAPT-1 and ADAPT-2) involving 435 patients with chronic liver disease and severe thrombocytopenia who were scheduled to undergo a procedure that would typically require platelet transfusion. At both dose levels of Doptelet, a higher proportion of patients had increased platelet counts and did not require platelet transfusion or any rescue therapy on the day of the procedure and up to 7 days following the procedure as compared with those treated with placebo.
The most common side effects reported by clinical trial participants who received Doptelet were fever, stomach (abdominal) pain, nausea, headache, fatigue and edema in the hands or feet. People with chronic liver disease and people with certain blood clotting conditions may have an increased risk of developing blood clots when taking Doptelet, the FDA said in a press release announcing the approval.
The FDA granted the Doptelet approval to AkaRx.