User login
FDA affirms bladder cancer warning with diabetes drug
Though a 10-year epidemiologic study did not find an increased risk of bladder cancer with pioglitazone use, the Food and Drug Administration has chosen to affirm the warning on the label of the type 2 diabetes drug following an updated review of several studies.
The FDA issued a warning about the possible risk of bladder cancer based on interim results from the 10-year epidemiologic study in 2010, and it changed the labels of pioglitazone-containing medicines in 2011 to include warnings about this risk.
There was a modest trend toward higher risk with increasing duration of use, but the trend was not statistically significant. Compared with the interim 5-year results, these final 10-year results found weaker associations that were not statistically significant.
The directions of the associations, however, remained unchanged. Based on these findings and other reviewed studies with conflicting results, the FDA has concluded that use of pioglitazone may be linked to an increased risk of bladder cancer.
The labels of pioglitazone-containing medicines already contain warnings about this risk, but the FDA has now approved label updates to describe the additional studies reviewed.
Read the FDA update and data summary here.
Though a 10-year epidemiologic study did not find an increased risk of bladder cancer with pioglitazone use, the Food and Drug Administration has chosen to affirm the warning on the label of the type 2 diabetes drug following an updated review of several studies.
The FDA issued a warning about the possible risk of bladder cancer based on interim results from the 10-year epidemiologic study in 2010, and it changed the labels of pioglitazone-containing medicines in 2011 to include warnings about this risk.
There was a modest trend toward higher risk with increasing duration of use, but the trend was not statistically significant. Compared with the interim 5-year results, these final 10-year results found weaker associations that were not statistically significant.
The directions of the associations, however, remained unchanged. Based on these findings and other reviewed studies with conflicting results, the FDA has concluded that use of pioglitazone may be linked to an increased risk of bladder cancer.
The labels of pioglitazone-containing medicines already contain warnings about this risk, but the FDA has now approved label updates to describe the additional studies reviewed.
Read the FDA update and data summary here.
Though a 10-year epidemiologic study did not find an increased risk of bladder cancer with pioglitazone use, the Food and Drug Administration has chosen to affirm the warning on the label of the type 2 diabetes drug following an updated review of several studies.
The FDA issued a warning about the possible risk of bladder cancer based on interim results from the 10-year epidemiologic study in 2010, and it changed the labels of pioglitazone-containing medicines in 2011 to include warnings about this risk.
There was a modest trend toward higher risk with increasing duration of use, but the trend was not statistically significant. Compared with the interim 5-year results, these final 10-year results found weaker associations that were not statistically significant.
The directions of the associations, however, remained unchanged. Based on these findings and other reviewed studies with conflicting results, the FDA has concluded that use of pioglitazone may be linked to an increased risk of bladder cancer.
The labels of pioglitazone-containing medicines already contain warnings about this risk, but the FDA has now approved label updates to describe the additional studies reviewed.
Read the FDA update and data summary here.
Oncolytic virus active against bladder cancer
NATIONAL HARBOR, MD – For patients with non-muscle invasive bladder cancer, intravesicular administration of an oncolytic virus was both feasible and safe, and in a small study was associated with at least one complete tumor response, investigators reported.
Instillation into the bladder of coxsackievirus A21 (CVA21; Cavatak), alone or in combination with low-dose mitomycin C, was associated with increases in immune cell filtrates and ramped-up expression of the programmed death-1 ligand (PD-L1) in the tumor microenvironment, reported Nicola Annels, PhD, a research fellow at the University of Surrey in England.
“Whilst the use of BCG [Bacille Calmette-Guerin] as an immunotherapy for non-muscle invasive bladder cancer has significantly improved disease-specific survival, the potential for serious side effects and local and systemic toxicity, together with the fact that there is a significant proportion of non-responding patients to BCG, highlights the need to develop future immune-based therapies to overcome these problems,” she said at the annual meeting of the Society for Immunotherapy of Cancer.
CVA21 is a proprietary formulation of coxsackievirus A21, a common cold virus. It targets intracellular adhesion molecule-1 (ICAM-1), and has been shown to have potent oncolytic activity against both non-muscle invasive bladder cancer (NMIBC) cell lines and ex vivo human bladder tumors. Delivering CVA21 with low-dose mitomycin C has been shown to enhance viral replication by increasing cell surface expression levels of ICAM-1, Dr. Annels noted.
In the stage I/II CANON study, the investigators studied the tolerability and safety of escalating doses of CVA21 alone or in combination with 10 mg mitomycin C in 16 patients with untreated NMIBC who were scheduled to undergo transurethral resection of bladder tumor (TURBT).
On serial cystoscopic photographs, the investigators saw evidence of anticancer activity including one complete response in one of three patients on CVA21 monotherapy at the highest of three doses, as well as virally-induced tumor inflammation.
Additional evidence of viral tumor targeting came from detection of secondary viral-load peaks in urine, and immunohistochemical analysis of tissues excised during TURBT, which tissue displayed tumor-specific viral replication and programmed cell death.
The authors also found that tissues treated with CVA21 showed upregulation of both interferon-response genes and immune checkpoint inhibitory genes compared with tissues from historical controls. This finding suggests that the antitumor effect of CVA21 might be enhanced by sequential administration of the virus followed by an immune checkpoint inhibitor, Dr. Annels said.
Patients tolerated the administration of CVA21 well, and there were no product-related adverse events greater than grade 1.
The activity observed thus “is likely to provide a strong signal in generating both a strong local and systemic anti-tumor response,” she said.
The study was funded by The Prostate Project, RingRose Foundation, Prostate Cancer UK, Topic of Cancer UK, Breast Cancer Campaign, the European Union, and Viralytics. Dr. Annels reported no conflicts of interest.
NATIONAL HARBOR, MD – For patients with non-muscle invasive bladder cancer, intravesicular administration of an oncolytic virus was both feasible and safe, and in a small study was associated with at least one complete tumor response, investigators reported.
Instillation into the bladder of coxsackievirus A21 (CVA21; Cavatak), alone or in combination with low-dose mitomycin C, was associated with increases in immune cell filtrates and ramped-up expression of the programmed death-1 ligand (PD-L1) in the tumor microenvironment, reported Nicola Annels, PhD, a research fellow at the University of Surrey in England.
“Whilst the use of BCG [Bacille Calmette-Guerin] as an immunotherapy for non-muscle invasive bladder cancer has significantly improved disease-specific survival, the potential for serious side effects and local and systemic toxicity, together with the fact that there is a significant proportion of non-responding patients to BCG, highlights the need to develop future immune-based therapies to overcome these problems,” she said at the annual meeting of the Society for Immunotherapy of Cancer.
CVA21 is a proprietary formulation of coxsackievirus A21, a common cold virus. It targets intracellular adhesion molecule-1 (ICAM-1), and has been shown to have potent oncolytic activity against both non-muscle invasive bladder cancer (NMIBC) cell lines and ex vivo human bladder tumors. Delivering CVA21 with low-dose mitomycin C has been shown to enhance viral replication by increasing cell surface expression levels of ICAM-1, Dr. Annels noted.
In the stage I/II CANON study, the investigators studied the tolerability and safety of escalating doses of CVA21 alone or in combination with 10 mg mitomycin C in 16 patients with untreated NMIBC who were scheduled to undergo transurethral resection of bladder tumor (TURBT).
On serial cystoscopic photographs, the investigators saw evidence of anticancer activity including one complete response in one of three patients on CVA21 monotherapy at the highest of three doses, as well as virally-induced tumor inflammation.
Additional evidence of viral tumor targeting came from detection of secondary viral-load peaks in urine, and immunohistochemical analysis of tissues excised during TURBT, which tissue displayed tumor-specific viral replication and programmed cell death.
The authors also found that tissues treated with CVA21 showed upregulation of both interferon-response genes and immune checkpoint inhibitory genes compared with tissues from historical controls. This finding suggests that the antitumor effect of CVA21 might be enhanced by sequential administration of the virus followed by an immune checkpoint inhibitor, Dr. Annels said.
Patients tolerated the administration of CVA21 well, and there were no product-related adverse events greater than grade 1.
The activity observed thus “is likely to provide a strong signal in generating both a strong local and systemic anti-tumor response,” she said.
The study was funded by The Prostate Project, RingRose Foundation, Prostate Cancer UK, Topic of Cancer UK, Breast Cancer Campaign, the European Union, and Viralytics. Dr. Annels reported no conflicts of interest.
NATIONAL HARBOR, MD – For patients with non-muscle invasive bladder cancer, intravesicular administration of an oncolytic virus was both feasible and safe, and in a small study was associated with at least one complete tumor response, investigators reported.
Instillation into the bladder of coxsackievirus A21 (CVA21; Cavatak), alone or in combination with low-dose mitomycin C, was associated with increases in immune cell filtrates and ramped-up expression of the programmed death-1 ligand (PD-L1) in the tumor microenvironment, reported Nicola Annels, PhD, a research fellow at the University of Surrey in England.
“Whilst the use of BCG [Bacille Calmette-Guerin] as an immunotherapy for non-muscle invasive bladder cancer has significantly improved disease-specific survival, the potential for serious side effects and local and systemic toxicity, together with the fact that there is a significant proportion of non-responding patients to BCG, highlights the need to develop future immune-based therapies to overcome these problems,” she said at the annual meeting of the Society for Immunotherapy of Cancer.
CVA21 is a proprietary formulation of coxsackievirus A21, a common cold virus. It targets intracellular adhesion molecule-1 (ICAM-1), and has been shown to have potent oncolytic activity against both non-muscle invasive bladder cancer (NMIBC) cell lines and ex vivo human bladder tumors. Delivering CVA21 with low-dose mitomycin C has been shown to enhance viral replication by increasing cell surface expression levels of ICAM-1, Dr. Annels noted.
In the stage I/II CANON study, the investigators studied the tolerability and safety of escalating doses of CVA21 alone or in combination with 10 mg mitomycin C in 16 patients with untreated NMIBC who were scheduled to undergo transurethral resection of bladder tumor (TURBT).
On serial cystoscopic photographs, the investigators saw evidence of anticancer activity including one complete response in one of three patients on CVA21 monotherapy at the highest of three doses, as well as virally-induced tumor inflammation.
Additional evidence of viral tumor targeting came from detection of secondary viral-load peaks in urine, and immunohistochemical analysis of tissues excised during TURBT, which tissue displayed tumor-specific viral replication and programmed cell death.
The authors also found that tissues treated with CVA21 showed upregulation of both interferon-response genes and immune checkpoint inhibitory genes compared with tissues from historical controls. This finding suggests that the antitumor effect of CVA21 might be enhanced by sequential administration of the virus followed by an immune checkpoint inhibitor, Dr. Annels said.
Patients tolerated the administration of CVA21 well, and there were no product-related adverse events greater than grade 1.
The activity observed thus “is likely to provide a strong signal in generating both a strong local and systemic anti-tumor response,” she said.
The study was funded by The Prostate Project, RingRose Foundation, Prostate Cancer UK, Topic of Cancer UK, Breast Cancer Campaign, the European Union, and Viralytics. Dr. Annels reported no conflicts of interest.
AT SITC 2016
Key clinical point:. Intravesicular coxsackievirus A21 (CVA21) showed good activity and safety against non-muscle invasive bladder cancer (NMIBC).
Major finding: One of three patients on the highest dose of CVA21 had a complete tumor response.
Data source: Phase I/II dose escalation and safety study in 16 patients with untreated NMIBC before surgery.
Disclosures: The study was funded by The Prostate Project, RingRose Foundation, Prostate Cancer UK, Topic of Cancer UK, Breast Cancer Campaign, the European Union, and Viralytics. Dr. Annels reported no conflicts of interest.
Vaccine/PD-1 inhibitor combo shows early promise against mCRPC
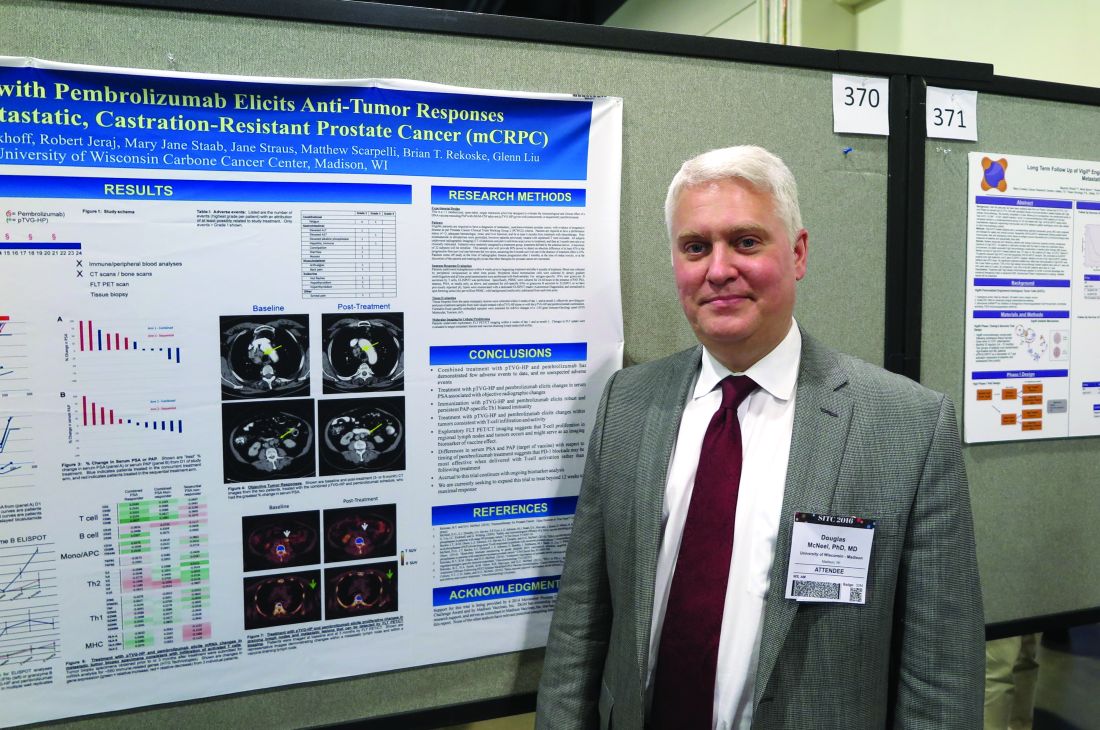
NATIONAL HARBOR, MD. – To date, checkpoint inhibitors have shown little clinical activity as single agents against metastatic, castration-resistant prostate cancer, but a combination of a DNA vaccine and a programmed-death 1 inhibitor shows promise for enhancing anti-tumor immune responses, report investigators in a phase I trial.
“If you vaccinate animals, PD-1 expression transiently goes up, and if you block it at that point you get a better anti-tumor response, and that was in models where anti PD-1 therapy alone didn’t do anything. So we thought this could be a good approach for prostate cancer,” Douglas G. McNeel, MD, PhD, of the University of Wisconsin, Madison, said in an interview at the annual meeting of the Society for Immunotherapy of Cancer.
Dr. McNeel and colleagues are exploring the therapeutic potential of combining the PD-1 inhibitor pembrolizumab (Keytruda) with an investigational DNA vaccine targeted against prostatic acid phosphatase (PAP), the same antigen targeted by sipuleucel-T (Provenge).
They presented data in a scientific poster from a pilot study of the combination in patients with metastatic, castration-resistant prostate cancer (mCRPC).
Vaccine ramps up PD-1 expression
The investigators had previously shown that patients immunized with a DNA vaccine encoding PAP (pTVG-HP; currently in phase II clinical trials) developed PD-1-regulated, PAP-specific T cells and had increased PD-L1 expression in circulating tumor cells. They also demonstrated in preclinical studies with mouse models that increased PD-1 expression on vaccine-induced CD8-positive T cells led to inferior anti-tumor immune responses, and that blocking PD-1 at the time of T-cell activation with vaccine improved anti-tumor responses.
“The current pilot trial was designed to evaluate whether delivery of PD-1 blockade after immunization (when PD-1-regulated T cells are elicited and when PD-L1 expression is induced with vaccination on tumor cells) or with immunization (when PD-1 expression increases on antigen-specific CD8+ T cells with activation) results in anti-tumor responses in patients with advanced, metastatic, castration-resistant prostate cancer,” Dr. McNeel and his colleagues wrote.
They reported preliminary impressions of the efficacy and safety of the combination in 12 patients with mCRPC. The patients all had evidence of progressive disease and were at least 6 months out from chemotherapy. Patients could have previously been treated with enzalutamide (Xtandi) or abiraterone (Zytiga), but were excluded if they had received sipuleucel-T vaccine.
Patients in the ongoing trial are randomized to receive six doses of pTVG-HP over 10 weeks with either four doses of concurrent pembrolizumab, or four doses of pembrolizumab delivered every 3 weeks beginning 2 weeks after the last vaccine dose.
The authors reported that treatment with the combination evokes changes in serum prostate-specific antigen (PSA) that are associated with objective radiographic changes, and “elicits robust and persistent PAP-specific Th1-based immunity.”
They also found evidence to suggest that concurrent administration of the vaccine and the PD-1 inhibitor may be more effective than sequential administration, based on differences in serum PSA and PAP.
Adverse events were generally mild and similar to those seen in other studies of pembrolizumab and DNA vaccine, with only three grade 3 events and no grade 4 events.
The investigators hope to expand the pilot study beyond the 12 weeks originally scheduled, and plan to explore potential biomarkers for vaccine response based on T-cell proliferation in tumors and in regional lymph nodes as seen on imaging modalities.
The study is funded by a 2014 Movember Prostate Cancer Foundation Challenge Award and Madison Vaccines Inc. Dr. McNeel reports an ownership interest and funding support from Madison Vaccines. All other coauthors reported no conflicts of interest.
NATIONAL HARBOR, MD. – To date, checkpoint inhibitors have shown little clinical activity as single agents against metastatic, castration-resistant prostate cancer, but a combination of a DNA vaccine and a programmed-death 1 inhibitor shows promise for enhancing anti-tumor immune responses, report investigators in a phase I trial.
“If you vaccinate animals, PD-1 expression transiently goes up, and if you block it at that point you get a better anti-tumor response, and that was in models where anti PD-1 therapy alone didn’t do anything. So we thought this could be a good approach for prostate cancer,” Douglas G. McNeel, MD, PhD, of the University of Wisconsin, Madison, said in an interview at the annual meeting of the Society for Immunotherapy of Cancer.
Dr. McNeel and colleagues are exploring the therapeutic potential of combining the PD-1 inhibitor pembrolizumab (Keytruda) with an investigational DNA vaccine targeted against prostatic acid phosphatase (PAP), the same antigen targeted by sipuleucel-T (Provenge).
They presented data in a scientific poster from a pilot study of the combination in patients with metastatic, castration-resistant prostate cancer (mCRPC).
Vaccine ramps up PD-1 expression
The investigators had previously shown that patients immunized with a DNA vaccine encoding PAP (pTVG-HP; currently in phase II clinical trials) developed PD-1-regulated, PAP-specific T cells and had increased PD-L1 expression in circulating tumor cells. They also demonstrated in preclinical studies with mouse models that increased PD-1 expression on vaccine-induced CD8-positive T cells led to inferior anti-tumor immune responses, and that blocking PD-1 at the time of T-cell activation with vaccine improved anti-tumor responses.
“The current pilot trial was designed to evaluate whether delivery of PD-1 blockade after immunization (when PD-1-regulated T cells are elicited and when PD-L1 expression is induced with vaccination on tumor cells) or with immunization (when PD-1 expression increases on antigen-specific CD8+ T cells with activation) results in anti-tumor responses in patients with advanced, metastatic, castration-resistant prostate cancer,” Dr. McNeel and his colleagues wrote.
They reported preliminary impressions of the efficacy and safety of the combination in 12 patients with mCRPC. The patients all had evidence of progressive disease and were at least 6 months out from chemotherapy. Patients could have previously been treated with enzalutamide (Xtandi) or abiraterone (Zytiga), but were excluded if they had received sipuleucel-T vaccine.
Patients in the ongoing trial are randomized to receive six doses of pTVG-HP over 10 weeks with either four doses of concurrent pembrolizumab, or four doses of pembrolizumab delivered every 3 weeks beginning 2 weeks after the last vaccine dose.
The authors reported that treatment with the combination evokes changes in serum prostate-specific antigen (PSA) that are associated with objective radiographic changes, and “elicits robust and persistent PAP-specific Th1-based immunity.”
They also found evidence to suggest that concurrent administration of the vaccine and the PD-1 inhibitor may be more effective than sequential administration, based on differences in serum PSA and PAP.
Adverse events were generally mild and similar to those seen in other studies of pembrolizumab and DNA vaccine, with only three grade 3 events and no grade 4 events.
The investigators hope to expand the pilot study beyond the 12 weeks originally scheduled, and plan to explore potential biomarkers for vaccine response based on T-cell proliferation in tumors and in regional lymph nodes as seen on imaging modalities.
The study is funded by a 2014 Movember Prostate Cancer Foundation Challenge Award and Madison Vaccines Inc. Dr. McNeel reports an ownership interest and funding support from Madison Vaccines. All other coauthors reported no conflicts of interest.
NATIONAL HARBOR, MD. – To date, checkpoint inhibitors have shown little clinical activity as single agents against metastatic, castration-resistant prostate cancer, but a combination of a DNA vaccine and a programmed-death 1 inhibitor shows promise for enhancing anti-tumor immune responses, report investigators in a phase I trial.
“If you vaccinate animals, PD-1 expression transiently goes up, and if you block it at that point you get a better anti-tumor response, and that was in models where anti PD-1 therapy alone didn’t do anything. So we thought this could be a good approach for prostate cancer,” Douglas G. McNeel, MD, PhD, of the University of Wisconsin, Madison, said in an interview at the annual meeting of the Society for Immunotherapy of Cancer.
Dr. McNeel and colleagues are exploring the therapeutic potential of combining the PD-1 inhibitor pembrolizumab (Keytruda) with an investigational DNA vaccine targeted against prostatic acid phosphatase (PAP), the same antigen targeted by sipuleucel-T (Provenge).
They presented data in a scientific poster from a pilot study of the combination in patients with metastatic, castration-resistant prostate cancer (mCRPC).
Vaccine ramps up PD-1 expression
The investigators had previously shown that patients immunized with a DNA vaccine encoding PAP (pTVG-HP; currently in phase II clinical trials) developed PD-1-regulated, PAP-specific T cells and had increased PD-L1 expression in circulating tumor cells. They also demonstrated in preclinical studies with mouse models that increased PD-1 expression on vaccine-induced CD8-positive T cells led to inferior anti-tumor immune responses, and that blocking PD-1 at the time of T-cell activation with vaccine improved anti-tumor responses.
“The current pilot trial was designed to evaluate whether delivery of PD-1 blockade after immunization (when PD-1-regulated T cells are elicited and when PD-L1 expression is induced with vaccination on tumor cells) or with immunization (when PD-1 expression increases on antigen-specific CD8+ T cells with activation) results in anti-tumor responses in patients with advanced, metastatic, castration-resistant prostate cancer,” Dr. McNeel and his colleagues wrote.
They reported preliminary impressions of the efficacy and safety of the combination in 12 patients with mCRPC. The patients all had evidence of progressive disease and were at least 6 months out from chemotherapy. Patients could have previously been treated with enzalutamide (Xtandi) or abiraterone (Zytiga), but were excluded if they had received sipuleucel-T vaccine.
Patients in the ongoing trial are randomized to receive six doses of pTVG-HP over 10 weeks with either four doses of concurrent pembrolizumab, or four doses of pembrolizumab delivered every 3 weeks beginning 2 weeks after the last vaccine dose.
The authors reported that treatment with the combination evokes changes in serum prostate-specific antigen (PSA) that are associated with objective radiographic changes, and “elicits robust and persistent PAP-specific Th1-based immunity.”
They also found evidence to suggest that concurrent administration of the vaccine and the PD-1 inhibitor may be more effective than sequential administration, based on differences in serum PSA and PAP.
Adverse events were generally mild and similar to those seen in other studies of pembrolizumab and DNA vaccine, with only three grade 3 events and no grade 4 events.
The investigators hope to expand the pilot study beyond the 12 weeks originally scheduled, and plan to explore potential biomarkers for vaccine response based on T-cell proliferation in tumors and in regional lymph nodes as seen on imaging modalities.
The study is funded by a 2014 Movember Prostate Cancer Foundation Challenge Award and Madison Vaccines Inc. Dr. McNeel reports an ownership interest and funding support from Madison Vaccines. All other coauthors reported no conflicts of interest.
AT SITC 2016
Key clinical point:. Adding the PD-1 inhibitor pembrolizumab to a DNA vaccine may enhance vaccine-induced immunity against metastatic castration-resistant prostate cancer (mCRPC).
Major finding: Treatment with a vaccine targeted to prostatic acid phosphatase and pembrolizumab elicited changes in PAP that are associated with objective radiographic responses.
Data source: Ongoing open-label, randomized pilot study in men with mCRPC.
Disclosures: The study is funded by a 2014 Movember Prostate Cancer Foundation Challenge Award and Madison Vaccines Inc. Dr. McNeel reports an ownership interest and funding support from Madison Vaccines. All other coauthors reported no conflicts of interest.
ADT not associated with increased risk of dementia in larger study
Treatment with androgen deprivation therapy (ADT) was not associated with an increased risk of dementia in a large, population-based study, according to investigators.
Previous studies have demonstrated that low testosterone levels are associated with cognitive impairment and Alzheimer’s disease, but the association between ADT and cognitive impairment remains controversial, with conflicting results being reported.
In the current large population-based study, compared with nonuse, treatment with ADT did not increase the risk of dementia (incidence, 7.4 vs. 4.4 per 1,000 person years, adjusted hazard ratio, 1.02; 95%CI, 0.87-1.19), reported Farzin Khosrow-Khavar, PhD, of McGill University, Montreal, and colleagues.
“Consistent with our findings, a recent meta-analysis found that although patients treated with ADT performed worse on visuomotor tasks in comparison with control subjects or their own baseline assessments, there were no significant differences in cognitive domains that are pertinent to dementia including performance on attention/working memory, executive function, language, verbal memory, visual memory, and visuospatial ability” they wrote (J Clin Oncol. 2016 Nov. 21 doi: 10.1200/JCO.2016.69.6203).
In a smaller study of 9,272 patients, recently published in JAMA Oncology, prostate cancer patients treated with ADT were more than twice as likely as were those who were not to develop dementia.
For the current study, investigators identified a cohort of 30,903 men who were newly diagnosed with nonmetastatic prostate cancer between April 1, 1988, and April 30, 2015, using the United Kingdom’s Clinical Practice Research Datalink. The patients were then observed until April 30, 2016.
Within this cohort, 799 patients were newly diagnosed with dementia, which extrapolated to a crude incidence of 6.0 per 1,000 person-years. During the follow-up period, 17,994 patients (58.2%) were treated with ADT, and the median duration of use was 2.3 years.
Men who were using ADT tended to be older and were more likely to have ever used tobacco products, and they were also more likely to have had higher prostate-specific antigen levels and a higher prevalence of comorbidities, compared with nonusers.
In the primary analysis, ADT use was not associated with an overall higher risk of developing dementia (adjusted HR, 1.02; 95% CI, 0.87-1.19).
In secondary analyses, the risk did not vary with cumulative duration of use. Findings were similar when the risk was assessed by the type of ADT used for treatment, and when the association was evaluated with Alzheimer’s disease (adjusted HR, 1.11; 95% CI, 0.85-1.44) versus other types of dementia (adjusted HR, 0.97; 95% CI, 0.80-1.18).
The authors noted that additional studies in different settings are needed to confirm these new findings.
The study was supported by a foundation grant from the Canadian Institutes of Health Research. The authors declared that there were no conflicts of interest.
Treatment with androgen deprivation therapy (ADT) was not associated with an increased risk of dementia in a large, population-based study, according to investigators.
Previous studies have demonstrated that low testosterone levels are associated with cognitive impairment and Alzheimer’s disease, but the association between ADT and cognitive impairment remains controversial, with conflicting results being reported.
In the current large population-based study, compared with nonuse, treatment with ADT did not increase the risk of dementia (incidence, 7.4 vs. 4.4 per 1,000 person years, adjusted hazard ratio, 1.02; 95%CI, 0.87-1.19), reported Farzin Khosrow-Khavar, PhD, of McGill University, Montreal, and colleagues.
“Consistent with our findings, a recent meta-analysis found that although patients treated with ADT performed worse on visuomotor tasks in comparison with control subjects or their own baseline assessments, there were no significant differences in cognitive domains that are pertinent to dementia including performance on attention/working memory, executive function, language, verbal memory, visual memory, and visuospatial ability” they wrote (J Clin Oncol. 2016 Nov. 21 doi: 10.1200/JCO.2016.69.6203).
In a smaller study of 9,272 patients, recently published in JAMA Oncology, prostate cancer patients treated with ADT were more than twice as likely as were those who were not to develop dementia.
For the current study, investigators identified a cohort of 30,903 men who were newly diagnosed with nonmetastatic prostate cancer between April 1, 1988, and April 30, 2015, using the United Kingdom’s Clinical Practice Research Datalink. The patients were then observed until April 30, 2016.
Within this cohort, 799 patients were newly diagnosed with dementia, which extrapolated to a crude incidence of 6.0 per 1,000 person-years. During the follow-up period, 17,994 patients (58.2%) were treated with ADT, and the median duration of use was 2.3 years.
Men who were using ADT tended to be older and were more likely to have ever used tobacco products, and they were also more likely to have had higher prostate-specific antigen levels and a higher prevalence of comorbidities, compared with nonusers.
In the primary analysis, ADT use was not associated with an overall higher risk of developing dementia (adjusted HR, 1.02; 95% CI, 0.87-1.19).
In secondary analyses, the risk did not vary with cumulative duration of use. Findings were similar when the risk was assessed by the type of ADT used for treatment, and when the association was evaluated with Alzheimer’s disease (adjusted HR, 1.11; 95% CI, 0.85-1.44) versus other types of dementia (adjusted HR, 0.97; 95% CI, 0.80-1.18).
The authors noted that additional studies in different settings are needed to confirm these new findings.
The study was supported by a foundation grant from the Canadian Institutes of Health Research. The authors declared that there were no conflicts of interest.
Treatment with androgen deprivation therapy (ADT) was not associated with an increased risk of dementia in a large, population-based study, according to investigators.
Previous studies have demonstrated that low testosterone levels are associated with cognitive impairment and Alzheimer’s disease, but the association between ADT and cognitive impairment remains controversial, with conflicting results being reported.
In the current large population-based study, compared with nonuse, treatment with ADT did not increase the risk of dementia (incidence, 7.4 vs. 4.4 per 1,000 person years, adjusted hazard ratio, 1.02; 95%CI, 0.87-1.19), reported Farzin Khosrow-Khavar, PhD, of McGill University, Montreal, and colleagues.
“Consistent with our findings, a recent meta-analysis found that although patients treated with ADT performed worse on visuomotor tasks in comparison with control subjects or their own baseline assessments, there were no significant differences in cognitive domains that are pertinent to dementia including performance on attention/working memory, executive function, language, verbal memory, visual memory, and visuospatial ability” they wrote (J Clin Oncol. 2016 Nov. 21 doi: 10.1200/JCO.2016.69.6203).
In a smaller study of 9,272 patients, recently published in JAMA Oncology, prostate cancer patients treated with ADT were more than twice as likely as were those who were not to develop dementia.
For the current study, investigators identified a cohort of 30,903 men who were newly diagnosed with nonmetastatic prostate cancer between April 1, 1988, and April 30, 2015, using the United Kingdom’s Clinical Practice Research Datalink. The patients were then observed until April 30, 2016.
Within this cohort, 799 patients were newly diagnosed with dementia, which extrapolated to a crude incidence of 6.0 per 1,000 person-years. During the follow-up period, 17,994 patients (58.2%) were treated with ADT, and the median duration of use was 2.3 years.
Men who were using ADT tended to be older and were more likely to have ever used tobacco products, and they were also more likely to have had higher prostate-specific antigen levels and a higher prevalence of comorbidities, compared with nonusers.
In the primary analysis, ADT use was not associated with an overall higher risk of developing dementia (adjusted HR, 1.02; 95% CI, 0.87-1.19).
In secondary analyses, the risk did not vary with cumulative duration of use. Findings were similar when the risk was assessed by the type of ADT used for treatment, and when the association was evaluated with Alzheimer’s disease (adjusted HR, 1.11; 95% CI, 0.85-1.44) versus other types of dementia (adjusted HR, 0.97; 95% CI, 0.80-1.18).
The authors noted that additional studies in different settings are needed to confirm these new findings.
The study was supported by a foundation grant from the Canadian Institutes of Health Research. The authors declared that there were no conflicts of interest.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point:
Major finding: Compared with nonuse of ADT, the use of ADT was not associated with an increased risk of dementia (incidence, 7.4 vs. 4.4 per 1,000 person-years, HR, 1.02; 95% CI, 0.87-1.19).
Data source: Population-based study that included 30,903 men newly diagnosed with nonmetastatic prostate cancer.
Disclosures: The study was supported by a foundation grant from the Canadian Institutes of Health Research. The authors declared that there were no conflicts of interest.
Expanding treatment options and ongoing challenges for urologic cancers
Urologic cancers are those that form in organs of the urinary and male reproductive systems, the most significant among them being cancers of the bladder, kidney, prostate, and testicles. Collectively, they are diagnosed in close to 400,000 Americans each year and are responsible for almost 60,000 deaths annually.1 Here, we describe the most recent developments in treating these malignancies.
Update/related article
Atezolizumab approval marks first new treatment option for bladder cancer in more than 3 decades
Click on the PDF icon at the top of this introduction to read the full article.
Urologic cancers are those that form in organs of the urinary and male reproductive systems, the most significant among them being cancers of the bladder, kidney, prostate, and testicles. Collectively, they are diagnosed in close to 400,000 Americans each year and are responsible for almost 60,000 deaths annually.1 Here, we describe the most recent developments in treating these malignancies.
Update/related article
Atezolizumab approval marks first new treatment option for bladder cancer in more than 3 decades
Click on the PDF icon at the top of this introduction to read the full article.
Urologic cancers are those that form in organs of the urinary and male reproductive systems, the most significant among them being cancers of the bladder, kidney, prostate, and testicles. Collectively, they are diagnosed in close to 400,000 Americans each year and are responsible for almost 60,000 deaths annually.1 Here, we describe the most recent developments in treating these malignancies.
Update/related article
Atezolizumab approval marks first new treatment option for bladder cancer in more than 3 decades
Click on the PDF icon at the top of this introduction to read the full article.
Renal cell carcinoma approval adds another notch to cabozantinib’s belt
In April this year, the US Food and Drug Administration awarded regulatory approval to cabozantinib for the treatment of advanced renal cell carcinoma patients previously treated with anti-angiogenic therapy.1 The small-molecule inhibitor, which targets multiple kinases, including the vascular endothelial growth factor receptors (VEGFRs) and the hepatocyte growth factor receptor (MET), had previously been approved for the treatment of medullary thyroid carcinoma in 2012.
Click on the PDF icon below for the full article.
In April this year, the US Food and Drug Administration awarded regulatory approval to cabozantinib for the treatment of advanced renal cell carcinoma patients previously treated with anti-angiogenic therapy.1 The small-molecule inhibitor, which targets multiple kinases, including the vascular endothelial growth factor receptors (VEGFRs) and the hepatocyte growth factor receptor (MET), had previously been approved for the treatment of medullary thyroid carcinoma in 2012.
Click on the PDF icon below for the full article.
In April this year, the US Food and Drug Administration awarded regulatory approval to cabozantinib for the treatment of advanced renal cell carcinoma patients previously treated with anti-angiogenic therapy.1 The small-molecule inhibitor, which targets multiple kinases, including the vascular endothelial growth factor receptors (VEGFRs) and the hepatocyte growth factor receptor (MET), had previously been approved for the treatment of medullary thyroid carcinoma in 2012.
Click on the PDF icon below for the full article.
Cabozantinib bests sunitinib against metastatic RCC
Cabozantinib showed significant improvements in progression-free survival and objective response rate over standard-of-care sunitinib in a phase II clinical trial of adults with metastatic renal cell carcinoma, according to a report published in the Journal of Clinical Oncology.
As a first-line therapy for patients with poor- to intermediate-risk renal cell carcinoma (RCC), cabozantinib improved progression-free survival by approximately 3 months, corresponding to a 34% reduction in the rate of disease progression or death. This is the first study in this patient population in which another agent demonstrated “notable and clinically meaningful” superiority over sunitinib, which has been an established standard of care for more than 10 years, wrote Toni K. Choueiri, MD, director of the Kidney Cancer Center, Dana-Farber Cancer Institute, Boston, and his associates.
In the open-label study, participants were randomly assigned to receive daily oral cabozantinib (79 patients) or daily oral sunitinib (78 patients) in 6-week cycles until disease progressed, intolerance developed, or patients withdrew from treatment. A total of 36% had bone metastases at baseline, an indicator of poor prognosis.
The primary endpoint – median duration of progression-free survival or time to death from any cause – was 8.2 months with cabozantinib and 5.6 months with sunitinib (adjusted hazard ratio, 0.66). Analyses of patient subgroups defined by disease severity consistently favored cabozantinib. Reductions in target lesion size, as measured by CT or MRI, were observed in 87% of the cabozantinib group, compared with 44% of the sunitinib group, the investigators reported (J Clin Oncol. 2016 Nov 14. doi: 10.1200/JCO.2016.70.7398).
Preliminary data showed that overall survival was 30.3 months with cabozantinib and 21.8 months with sunitinib. This represents a 20% decrease in mortality with cabozantinib.
The median number of treatment cycles was greater in the cabozantinib group (five cycles) than in the sunitinib group (two cycles), and corresponded to median treatment durations of 6.9 months and 2.8 months, respectively. Rates of treatment discontinuation due to adverse events were similar between the two study groups, as were the rates of adverse events of any grade, adverse events of grade 3 or 4, and adverse events of grade 5.
These findings indicate that cabozantinib may represent a new treatment option for previously untreated poor- or intermediate-risk metastatic RCC, Dr. Choueiri and his associates wrote.
The study was supported by the National Institutes of Health and Exelixis, which provided the cabozantinib. Dr. Choueiri and many of his associates reported ties to numerous industry sources.
Cabozantinib showed significant improvements in progression-free survival and objective response rate over standard-of-care sunitinib in a phase II clinical trial of adults with metastatic renal cell carcinoma, according to a report published in the Journal of Clinical Oncology.
As a first-line therapy for patients with poor- to intermediate-risk renal cell carcinoma (RCC), cabozantinib improved progression-free survival by approximately 3 months, corresponding to a 34% reduction in the rate of disease progression or death. This is the first study in this patient population in which another agent demonstrated “notable and clinically meaningful” superiority over sunitinib, which has been an established standard of care for more than 10 years, wrote Toni K. Choueiri, MD, director of the Kidney Cancer Center, Dana-Farber Cancer Institute, Boston, and his associates.
In the open-label study, participants were randomly assigned to receive daily oral cabozantinib (79 patients) or daily oral sunitinib (78 patients) in 6-week cycles until disease progressed, intolerance developed, or patients withdrew from treatment. A total of 36% had bone metastases at baseline, an indicator of poor prognosis.
The primary endpoint – median duration of progression-free survival or time to death from any cause – was 8.2 months with cabozantinib and 5.6 months with sunitinib (adjusted hazard ratio, 0.66). Analyses of patient subgroups defined by disease severity consistently favored cabozantinib. Reductions in target lesion size, as measured by CT or MRI, were observed in 87% of the cabozantinib group, compared with 44% of the sunitinib group, the investigators reported (J Clin Oncol. 2016 Nov 14. doi: 10.1200/JCO.2016.70.7398).
Preliminary data showed that overall survival was 30.3 months with cabozantinib and 21.8 months with sunitinib. This represents a 20% decrease in mortality with cabozantinib.
The median number of treatment cycles was greater in the cabozantinib group (five cycles) than in the sunitinib group (two cycles), and corresponded to median treatment durations of 6.9 months and 2.8 months, respectively. Rates of treatment discontinuation due to adverse events were similar between the two study groups, as were the rates of adverse events of any grade, adverse events of grade 3 or 4, and adverse events of grade 5.
These findings indicate that cabozantinib may represent a new treatment option for previously untreated poor- or intermediate-risk metastatic RCC, Dr. Choueiri and his associates wrote.
The study was supported by the National Institutes of Health and Exelixis, which provided the cabozantinib. Dr. Choueiri and many of his associates reported ties to numerous industry sources.
Cabozantinib showed significant improvements in progression-free survival and objective response rate over standard-of-care sunitinib in a phase II clinical trial of adults with metastatic renal cell carcinoma, according to a report published in the Journal of Clinical Oncology.
As a first-line therapy for patients with poor- to intermediate-risk renal cell carcinoma (RCC), cabozantinib improved progression-free survival by approximately 3 months, corresponding to a 34% reduction in the rate of disease progression or death. This is the first study in this patient population in which another agent demonstrated “notable and clinically meaningful” superiority over sunitinib, which has been an established standard of care for more than 10 years, wrote Toni K. Choueiri, MD, director of the Kidney Cancer Center, Dana-Farber Cancer Institute, Boston, and his associates.
In the open-label study, participants were randomly assigned to receive daily oral cabozantinib (79 patients) or daily oral sunitinib (78 patients) in 6-week cycles until disease progressed, intolerance developed, or patients withdrew from treatment. A total of 36% had bone metastases at baseline, an indicator of poor prognosis.
The primary endpoint – median duration of progression-free survival or time to death from any cause – was 8.2 months with cabozantinib and 5.6 months with sunitinib (adjusted hazard ratio, 0.66). Analyses of patient subgroups defined by disease severity consistently favored cabozantinib. Reductions in target lesion size, as measured by CT or MRI, were observed in 87% of the cabozantinib group, compared with 44% of the sunitinib group, the investigators reported (J Clin Oncol. 2016 Nov 14. doi: 10.1200/JCO.2016.70.7398).
Preliminary data showed that overall survival was 30.3 months with cabozantinib and 21.8 months with sunitinib. This represents a 20% decrease in mortality with cabozantinib.
The median number of treatment cycles was greater in the cabozantinib group (five cycles) than in the sunitinib group (two cycles), and corresponded to median treatment durations of 6.9 months and 2.8 months, respectively. Rates of treatment discontinuation due to adverse events were similar between the two study groups, as were the rates of adverse events of any grade, adverse events of grade 3 or 4, and adverse events of grade 5.
These findings indicate that cabozantinib may represent a new treatment option for previously untreated poor- or intermediate-risk metastatic RCC, Dr. Choueiri and his associates wrote.
The study was supported by the National Institutes of Health and Exelixis, which provided the cabozantinib. Dr. Choueiri and many of his associates reported ties to numerous industry sources.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point:
Major finding: The primary end point – median duration of progression-free survival or time to death from any cause – was 8.2 months with cabozantinib and 5.6 months with sunitinib (adjusted HR, 0.66).
Data source: A randomized, open-label phase II clinical trial of first-line treatment for 157 adults.
Disclosures: The study was supported by the National Institutes of Health and Exelixis, which provided the cabozantinib. Dr. Choueiri and many of his associates reported ties to numerous industry sources.
Targeting HER1/2 falls flat in bladder cancer trial
Patients with metastatic urothelial bladder cancer (UBC) overexpressing HER1 or HER2 did not benefit from a course of lapatinib maintenance therapy following chemotherapy, a U.K.-based research group reported.
The phase III study, led by Thomas Powles, MD, of Queen Mary University of London, randomized 232 patients (mean age 71, about 75% male) with HER1- or HER2-positive metastatic UBC who had not progressed during platinum-based chemotherapy to placebo or lapatinib (Tykerb), an oral medication that targets HER1 and HER2 and is marketed for use in some breast cancers. The lapatinib-treated group saw no significant gains in either progression-free (PFS) or overall survival (OS), Dr. Powles and associates reported (J Clin Oncol. 2016 Oct 31. doi: 10.1200/JCO.2015.66.3468).
The median PFS for patients receiving lapatinib 1,500 mg daily was 4.5 months, compared with 5.1 months for the placebo group (hazard ratio, 1.07; 95% CI, 0.81-1.43; P = .63), while OS after chemotherapy was 12.6 and 12 months, respectively (HR 0.96; 95% CI, 0.70-1.31; P = .80). A subgroup of patients strongly positive for either or both receptors did not see significant OS or PFS benefit associated with lapatinib, a finding that the investigators said reinforced a lack of benefit.
While previous studies have indicated roles for both HER1 and HER2 in bladder cancer progression, targeting them “may not be of clinical benefit in UBC,” Dr. Powles and his colleagues wrote.
Patients with metastatic UBC have short overall survival following first-line chemotherapy, and few proven second-line treatment options exist besides additional chemotherapy, whose benefit is controversial, the researchers noted.
Despite this trial’s negative result for postchemotherapy maintenance treatment with lapatinib, Dr. Powles and his colleagues said their study, which screened 446 patients with metastatic UBC before randomizing slightly more than half, nonetheless shed some light on this difficult-to-treat patient group, including identifying three prognostic factors associated with poor outcome: radiologic progression during chemotherapy, visceral metastasis, and poor performance status. Also, they noted, 61% of the screened patients received cisplatin chemotherapy, and 48% had visceral metastasis, “which gives some insight into the current population of patients who receive chemotherapy.”
GlaxoSmithKline and Cancer Research U.K. sponsored the study. Dr. Powles and several coauthors disclosed financial support from GlaxoSmithKline and other pharmaceutical firms.
Patients with metastatic urothelial bladder cancer (UBC) overexpressing HER1 or HER2 did not benefit from a course of lapatinib maintenance therapy following chemotherapy, a U.K.-based research group reported.
The phase III study, led by Thomas Powles, MD, of Queen Mary University of London, randomized 232 patients (mean age 71, about 75% male) with HER1- or HER2-positive metastatic UBC who had not progressed during platinum-based chemotherapy to placebo or lapatinib (Tykerb), an oral medication that targets HER1 and HER2 and is marketed for use in some breast cancers. The lapatinib-treated group saw no significant gains in either progression-free (PFS) or overall survival (OS), Dr. Powles and associates reported (J Clin Oncol. 2016 Oct 31. doi: 10.1200/JCO.2015.66.3468).
The median PFS for patients receiving lapatinib 1,500 mg daily was 4.5 months, compared with 5.1 months for the placebo group (hazard ratio, 1.07; 95% CI, 0.81-1.43; P = .63), while OS after chemotherapy was 12.6 and 12 months, respectively (HR 0.96; 95% CI, 0.70-1.31; P = .80). A subgroup of patients strongly positive for either or both receptors did not see significant OS or PFS benefit associated with lapatinib, a finding that the investigators said reinforced a lack of benefit.
While previous studies have indicated roles for both HER1 and HER2 in bladder cancer progression, targeting them “may not be of clinical benefit in UBC,” Dr. Powles and his colleagues wrote.
Patients with metastatic UBC have short overall survival following first-line chemotherapy, and few proven second-line treatment options exist besides additional chemotherapy, whose benefit is controversial, the researchers noted.
Despite this trial’s negative result for postchemotherapy maintenance treatment with lapatinib, Dr. Powles and his colleagues said their study, which screened 446 patients with metastatic UBC before randomizing slightly more than half, nonetheless shed some light on this difficult-to-treat patient group, including identifying three prognostic factors associated with poor outcome: radiologic progression during chemotherapy, visceral metastasis, and poor performance status. Also, they noted, 61% of the screened patients received cisplatin chemotherapy, and 48% had visceral metastasis, “which gives some insight into the current population of patients who receive chemotherapy.”
GlaxoSmithKline and Cancer Research U.K. sponsored the study. Dr. Powles and several coauthors disclosed financial support from GlaxoSmithKline and other pharmaceutical firms.
Patients with metastatic urothelial bladder cancer (UBC) overexpressing HER1 or HER2 did not benefit from a course of lapatinib maintenance therapy following chemotherapy, a U.K.-based research group reported.
The phase III study, led by Thomas Powles, MD, of Queen Mary University of London, randomized 232 patients (mean age 71, about 75% male) with HER1- or HER2-positive metastatic UBC who had not progressed during platinum-based chemotherapy to placebo or lapatinib (Tykerb), an oral medication that targets HER1 and HER2 and is marketed for use in some breast cancers. The lapatinib-treated group saw no significant gains in either progression-free (PFS) or overall survival (OS), Dr. Powles and associates reported (J Clin Oncol. 2016 Oct 31. doi: 10.1200/JCO.2015.66.3468).
The median PFS for patients receiving lapatinib 1,500 mg daily was 4.5 months, compared with 5.1 months for the placebo group (hazard ratio, 1.07; 95% CI, 0.81-1.43; P = .63), while OS after chemotherapy was 12.6 and 12 months, respectively (HR 0.96; 95% CI, 0.70-1.31; P = .80). A subgroup of patients strongly positive for either or both receptors did not see significant OS or PFS benefit associated with lapatinib, a finding that the investigators said reinforced a lack of benefit.
While previous studies have indicated roles for both HER1 and HER2 in bladder cancer progression, targeting them “may not be of clinical benefit in UBC,” Dr. Powles and his colleagues wrote.
Patients with metastatic UBC have short overall survival following first-line chemotherapy, and few proven second-line treatment options exist besides additional chemotherapy, whose benefit is controversial, the researchers noted.
Despite this trial’s negative result for postchemotherapy maintenance treatment with lapatinib, Dr. Powles and his colleagues said their study, which screened 446 patients with metastatic UBC before randomizing slightly more than half, nonetheless shed some light on this difficult-to-treat patient group, including identifying three prognostic factors associated with poor outcome: radiologic progression during chemotherapy, visceral metastasis, and poor performance status. Also, they noted, 61% of the screened patients received cisplatin chemotherapy, and 48% had visceral metastasis, “which gives some insight into the current population of patients who receive chemotherapy.”
GlaxoSmithKline and Cancer Research U.K. sponsored the study. Dr. Powles and several coauthors disclosed financial support from GlaxoSmithKline and other pharmaceutical firms.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Treatment with lapatinib after chemotherapy does not improve survival in people with HER1- or HER2-positive metastatic urothelial bladder cancer.
Major finding: Median progression-free survival for lapatinib was 4.5 months (95% CI, 2.8-5.4), compared with 5.1 (95% CI, 3.0-5.8) for placebo (HR, 1.07; 95% CI, 0.81-1.43; P = .063).
Data source: A randomized, placebo-controlled trial in which 232 patients with HER1- or HER2-positive disease were assigned treatment with lapatinib (n = 116) or placebo (n = 116) after platinum-based chemotherapy.
Disclosures: GlaxoSmithKline and Cancer Research U.K. sponsored the study. Dr. Powles and several coauthors disclosed financial support from GlaxoSmithKline and other pharmaceutical firms.
Cancer survivors report two times greater medication use for anxiety and depression
Approximately 20% of adult cancer survivors in the United States – roughly 2.5 million – take medication for anxiety or depression, a rate that is approximately twice that of the general population, according to a report published online in Journal of Clinical Oncology.
Considering that previous research reported that more than 30% of cancer survivors discuss psychosocial concerns with their medical providers, this finding suggests that “even more survivors might benefit from pharmacologic treatment than were receiving treatment at the time of this study,” said Nikki A. Hawkins, PhD, of the Centers for Disease Control and Prevention, and her associates.
“If left unaddressed and untreated, anxiety and depression have been found to negatively affect health behaviors, the body’s inflammatory response, and even survival.” Yet rates of medication use have not been examined until now, the investigators noted.
Dr. Hawkins and her associates analyzed data from the National Health Interview Surveys for 2010 through 2013 to determine population-based prevalence rates. Their study population comprised a nationally representative sample of 48,181 adults, of whom 3,184 were cancer survivors.
Compared with the general population, cancer survivors were approximately twice as likely to self-report taking medication for anxiety (16.8% vs 8.6%), depression (14.1% vs 7.8%), both conditions (11.8% vs 6.1%), and one or both conditions combined (19.1% vs 10.3%). When these results were extrapolated to the entire country, an estimated 2.5 million cancer survivors were found to currently use these medications, the investigators reported (J Clin Oncol. 2016 Oct 26. doi: 10.1200/JCO.2016.67.7690).
“Interestingly, medication use did not vary significantly by time since cancer diagnosis, which is consistent with recent research that has shown elevated rates of depression and mental disorders for cancer survivors as much as 10 years after diagnosis,” they wrote.
The highest rates (greater than 20%) of antianxiety and antidepressant use occurred among patients who were middle aged (those aged 40-64 years), had never married, had three or more chronic health conditions, expected to have a short survival time, or had ovarian or uterine cancer.
Nine types of cancer were included in this study: breast, prostate, melanoma, cervical, colorectal, hematologic, ovarian/uterine, “short survival,” and other. Of these, patients with prostate cancer were the least likely to use antianxiety or antidepressant medications, and patients with ovarian/uterine and short survival cancers were the most likely to.
“Efforts to improve the psychosocial care of cancer survivors will be aided by continued tracking of the treatment received for mental health. Good medical care requires systematic evaluation, screening for new problems, and making adjustments to the prescribed therapies as needed, and survivors’ mental health deserves the same detailed, evidence-based, and ongoing attention,” Dr. Hawkins and her associates said.
This study was supported by the Centers for Disease Control and Prevention. Dr. Hawkins and her associates reported having no relevant financial disclosures.
Approximately 20% of adult cancer survivors in the United States – roughly 2.5 million – take medication for anxiety or depression, a rate that is approximately twice that of the general population, according to a report published online in Journal of Clinical Oncology.
Considering that previous research reported that more than 30% of cancer survivors discuss psychosocial concerns with their medical providers, this finding suggests that “even more survivors might benefit from pharmacologic treatment than were receiving treatment at the time of this study,” said Nikki A. Hawkins, PhD, of the Centers for Disease Control and Prevention, and her associates.
“If left unaddressed and untreated, anxiety and depression have been found to negatively affect health behaviors, the body’s inflammatory response, and even survival.” Yet rates of medication use have not been examined until now, the investigators noted.
Dr. Hawkins and her associates analyzed data from the National Health Interview Surveys for 2010 through 2013 to determine population-based prevalence rates. Their study population comprised a nationally representative sample of 48,181 adults, of whom 3,184 were cancer survivors.
Compared with the general population, cancer survivors were approximately twice as likely to self-report taking medication for anxiety (16.8% vs 8.6%), depression (14.1% vs 7.8%), both conditions (11.8% vs 6.1%), and one or both conditions combined (19.1% vs 10.3%). When these results were extrapolated to the entire country, an estimated 2.5 million cancer survivors were found to currently use these medications, the investigators reported (J Clin Oncol. 2016 Oct 26. doi: 10.1200/JCO.2016.67.7690).
“Interestingly, medication use did not vary significantly by time since cancer diagnosis, which is consistent with recent research that has shown elevated rates of depression and mental disorders for cancer survivors as much as 10 years after diagnosis,” they wrote.
The highest rates (greater than 20%) of antianxiety and antidepressant use occurred among patients who were middle aged (those aged 40-64 years), had never married, had three or more chronic health conditions, expected to have a short survival time, or had ovarian or uterine cancer.
Nine types of cancer were included in this study: breast, prostate, melanoma, cervical, colorectal, hematologic, ovarian/uterine, “short survival,” and other. Of these, patients with prostate cancer were the least likely to use antianxiety or antidepressant medications, and patients with ovarian/uterine and short survival cancers were the most likely to.
“Efforts to improve the psychosocial care of cancer survivors will be aided by continued tracking of the treatment received for mental health. Good medical care requires systematic evaluation, screening for new problems, and making adjustments to the prescribed therapies as needed, and survivors’ mental health deserves the same detailed, evidence-based, and ongoing attention,” Dr. Hawkins and her associates said.
This study was supported by the Centers for Disease Control and Prevention. Dr. Hawkins and her associates reported having no relevant financial disclosures.
Approximately 20% of adult cancer survivors in the United States – roughly 2.5 million – take medication for anxiety or depression, a rate that is approximately twice that of the general population, according to a report published online in Journal of Clinical Oncology.
Considering that previous research reported that more than 30% of cancer survivors discuss psychosocial concerns with their medical providers, this finding suggests that “even more survivors might benefit from pharmacologic treatment than were receiving treatment at the time of this study,” said Nikki A. Hawkins, PhD, of the Centers for Disease Control and Prevention, and her associates.
“If left unaddressed and untreated, anxiety and depression have been found to negatively affect health behaviors, the body’s inflammatory response, and even survival.” Yet rates of medication use have not been examined until now, the investigators noted.
Dr. Hawkins and her associates analyzed data from the National Health Interview Surveys for 2010 through 2013 to determine population-based prevalence rates. Their study population comprised a nationally representative sample of 48,181 adults, of whom 3,184 were cancer survivors.
Compared with the general population, cancer survivors were approximately twice as likely to self-report taking medication for anxiety (16.8% vs 8.6%), depression (14.1% vs 7.8%), both conditions (11.8% vs 6.1%), and one or both conditions combined (19.1% vs 10.3%). When these results were extrapolated to the entire country, an estimated 2.5 million cancer survivors were found to currently use these medications, the investigators reported (J Clin Oncol. 2016 Oct 26. doi: 10.1200/JCO.2016.67.7690).
“Interestingly, medication use did not vary significantly by time since cancer diagnosis, which is consistent with recent research that has shown elevated rates of depression and mental disorders for cancer survivors as much as 10 years after diagnosis,” they wrote.
The highest rates (greater than 20%) of antianxiety and antidepressant use occurred among patients who were middle aged (those aged 40-64 years), had never married, had three or more chronic health conditions, expected to have a short survival time, or had ovarian or uterine cancer.
Nine types of cancer were included in this study: breast, prostate, melanoma, cervical, colorectal, hematologic, ovarian/uterine, “short survival,” and other. Of these, patients with prostate cancer were the least likely to use antianxiety or antidepressant medications, and patients with ovarian/uterine and short survival cancers were the most likely to.
“Efforts to improve the psychosocial care of cancer survivors will be aided by continued tracking of the treatment received for mental health. Good medical care requires systematic evaluation, screening for new problems, and making adjustments to the prescribed therapies as needed, and survivors’ mental health deserves the same detailed, evidence-based, and ongoing attention,” Dr. Hawkins and her associates said.
This study was supported by the Centers for Disease Control and Prevention. Dr. Hawkins and her associates reported having no relevant financial disclosures.
Key clinical point: Cancer survivors take medications for anxiety and depression at approximately double the rate in the general population.
Major finding: Compared with the general population, cancer survivors were approximately twice as likely to self-report taking medication for anxiety (16.8% vs 8.6%), depression (14.1% vs 7.8%), both conditions (11.8% vs 6.1%), and one or both conditions combined (19.1% vs 10.3%).
Data source: A cross-sectional analysis of data from nationwide surveys of 48,181 adults, including 3,184 cancer survivors, during a 4-year period.
Disclosures: This study was supported by the Centers for Disease Control and Prevention. Dr. Hawkins and her associates reported having no relevant financial disclosures.
ADT may increase dementia risk in prostate CA
Prostate cancer patients treated with androgen deprivation therapy are more than twice as likely as those who were not to develop dementia, according to a review of 9,272 prostate cancer cases at Stanford (Calif.) University.
Almost 8% of the 1,826 men treated with androgen deprivation therapy (ADT), a mainstay against prostate cancer, were diagnosed with dementia at 5 years, versus 3.5% of the 7,446 men not treated with ADT (JAMA Oncol. 2016 Oct 13. doi: 10.1001/jamaoncol.2016.3662).
“Our study extends previous work supporting an association between use of ADT and Alzheimer disease and suggests that ADT may more broadly affect neurocognitive function,” said the investigators, led by Kevin Nead, MD, formerly at Stanford but now a radiation oncology resident at the University of Pennsylvania, Philadelphia.
New-onset senile dementia, vascular dementia, frontotemporal dementia, and Alzheimer dementia were linked to ADT in both a propensity score-matched analysis (HR, 2.17; 95% CI, 1.58-2.99; P < .001) and multivariate analysis (adjusted HR, 2.21; 95% CI, 1.72-2.83; P < .001). The results held up when Alzheimer disease, just 30% of the 314 dementia cases, was excluded.
Men with at least 12 months of ADT had the greatest increased risk of dementia (HR, 2.36; 95% CI, 1.64-3.38; P < .001), suggesting a dose-response relationship; men on ADT who were at least 70 years old had the lowest cumulative probability of not developing dementia.
The link, the team said, is biologically plausible. Androgens have a role in neuron health and growth, and testosterone analogues have neuroprotective effects. Testosterone may be converted to estrogen, which is also neuroprotective. Low testosterone levels and ADT, meanwhile, have been shown to increase the risk of cardiometabolic diseases, which increase the risk of dementia.
The analyses controlled for age at prostate cancer diagnosis; race; smoking status; use of antiplatelet, anticoagulant, antihypertensive, and statin medications; and histories of cardiovascular disease, type 1 or 2 diabetes, stroke, and malignant neoplasms.
The men were treated at Stanford from 1994-2013. ADT patients tended to be older than their peers (70 versus 66 years), less likely to white (54% versus 60%), more likely to have smoked (44% versus 38%), and more likely to have other health problems.
More than 20 medications in the study were used for ADT, including leuprolide, goserelin, and triptorelin. Data were collectedd from electronic health records, and included diagnostic codes, medication lists, and clinical notes.
The work was funded by the National Institutes of Health. The senior author, Nigam Shah, PhD, has patents pending on the data-mining methods used in the study.
Prostate cancer patients treated with androgen deprivation therapy are more than twice as likely as those who were not to develop dementia, according to a review of 9,272 prostate cancer cases at Stanford (Calif.) University.
Almost 8% of the 1,826 men treated with androgen deprivation therapy (ADT), a mainstay against prostate cancer, were diagnosed with dementia at 5 years, versus 3.5% of the 7,446 men not treated with ADT (JAMA Oncol. 2016 Oct 13. doi: 10.1001/jamaoncol.2016.3662).
“Our study extends previous work supporting an association between use of ADT and Alzheimer disease and suggests that ADT may more broadly affect neurocognitive function,” said the investigators, led by Kevin Nead, MD, formerly at Stanford but now a radiation oncology resident at the University of Pennsylvania, Philadelphia.
New-onset senile dementia, vascular dementia, frontotemporal dementia, and Alzheimer dementia were linked to ADT in both a propensity score-matched analysis (HR, 2.17; 95% CI, 1.58-2.99; P < .001) and multivariate analysis (adjusted HR, 2.21; 95% CI, 1.72-2.83; P < .001). The results held up when Alzheimer disease, just 30% of the 314 dementia cases, was excluded.
Men with at least 12 months of ADT had the greatest increased risk of dementia (HR, 2.36; 95% CI, 1.64-3.38; P < .001), suggesting a dose-response relationship; men on ADT who were at least 70 years old had the lowest cumulative probability of not developing dementia.
The link, the team said, is biologically plausible. Androgens have a role in neuron health and growth, and testosterone analogues have neuroprotective effects. Testosterone may be converted to estrogen, which is also neuroprotective. Low testosterone levels and ADT, meanwhile, have been shown to increase the risk of cardiometabolic diseases, which increase the risk of dementia.
The analyses controlled for age at prostate cancer diagnosis; race; smoking status; use of antiplatelet, anticoagulant, antihypertensive, and statin medications; and histories of cardiovascular disease, type 1 or 2 diabetes, stroke, and malignant neoplasms.
The men were treated at Stanford from 1994-2013. ADT patients tended to be older than their peers (70 versus 66 years), less likely to white (54% versus 60%), more likely to have smoked (44% versus 38%), and more likely to have other health problems.
More than 20 medications in the study were used for ADT, including leuprolide, goserelin, and triptorelin. Data were collectedd from electronic health records, and included diagnostic codes, medication lists, and clinical notes.
The work was funded by the National Institutes of Health. The senior author, Nigam Shah, PhD, has patents pending on the data-mining methods used in the study.
Prostate cancer patients treated with androgen deprivation therapy are more than twice as likely as those who were not to develop dementia, according to a review of 9,272 prostate cancer cases at Stanford (Calif.) University.
Almost 8% of the 1,826 men treated with androgen deprivation therapy (ADT), a mainstay against prostate cancer, were diagnosed with dementia at 5 years, versus 3.5% of the 7,446 men not treated with ADT (JAMA Oncol. 2016 Oct 13. doi: 10.1001/jamaoncol.2016.3662).
“Our study extends previous work supporting an association between use of ADT and Alzheimer disease and suggests that ADT may more broadly affect neurocognitive function,” said the investigators, led by Kevin Nead, MD, formerly at Stanford but now a radiation oncology resident at the University of Pennsylvania, Philadelphia.
New-onset senile dementia, vascular dementia, frontotemporal dementia, and Alzheimer dementia were linked to ADT in both a propensity score-matched analysis (HR, 2.17; 95% CI, 1.58-2.99; P < .001) and multivariate analysis (adjusted HR, 2.21; 95% CI, 1.72-2.83; P < .001). The results held up when Alzheimer disease, just 30% of the 314 dementia cases, was excluded.
Men with at least 12 months of ADT had the greatest increased risk of dementia (HR, 2.36; 95% CI, 1.64-3.38; P < .001), suggesting a dose-response relationship; men on ADT who were at least 70 years old had the lowest cumulative probability of not developing dementia.
The link, the team said, is biologically plausible. Androgens have a role in neuron health and growth, and testosterone analogues have neuroprotective effects. Testosterone may be converted to estrogen, which is also neuroprotective. Low testosterone levels and ADT, meanwhile, have been shown to increase the risk of cardiometabolic diseases, which increase the risk of dementia.
The analyses controlled for age at prostate cancer diagnosis; race; smoking status; use of antiplatelet, anticoagulant, antihypertensive, and statin medications; and histories of cardiovascular disease, type 1 or 2 diabetes, stroke, and malignant neoplasms.
The men were treated at Stanford from 1994-2013. ADT patients tended to be older than their peers (70 versus 66 years), less likely to white (54% versus 60%), more likely to have smoked (44% versus 38%), and more likely to have other health problems.
More than 20 medications in the study were used for ADT, including leuprolide, goserelin, and triptorelin. Data were collectedd from electronic health records, and included diagnostic codes, medication lists, and clinical notes.
The work was funded by the National Institutes of Health. The senior author, Nigam Shah, PhD, has patents pending on the data-mining methods used in the study.
FROM JAMA ONCOLOGY
Key clinical point:
Major finding: New-onset senile dementia, vascular dementia, frontotemporal dementia, and Alzheimer dementia were linked to ADT in both a propensity score-matched analysis (HR, 2.17; 95% CI, 1.58-2.99; P < .001) and multivariate analysis (adjusted HR, 2.21; 95% CI, 1.72-2.83; P < .001).
Data source: Review of 9,272 prostate cancer cases at Stanford (Calif.) University.
Disclosures: The work was funded by the National Institutes of Health. The senior author, Nigam Shah, PhD, has patents pending on the data-mining methods used in the study.