User login
Alternative regimen reduces narcotic use after pelvic reconstructive surgery
TUCSON, ARIZ. – compared with a standard regimen, with no difference in patient satisfaction scores.
The new study extends findings from other surgical procedures to pelvic reconstructive surgery.
“This can limit both inpatient and outpatient narcotic use. It uses oral Toradol on an outpatient basis. It’s totally underutilized. People are afraid of it, people think it causes more bleeding, and maybe there’s a cost issue,” Andrey Petrikovets, MD, a urogynecologist in Los Angeles, said in an interview.
The regimen, which he calls ICE-T, relies in part on 16 tablets of Toradol sent home with the patient – 4 days’ worth. “It’s just 16 tablets, so it’s cheap, and patients do great with it. If you really use Toradol appropriately, especially on an outpatient basis, you can pretty much eliminate outpatient narcotic use,” said Dr. Petrikovets, who presented the work at the annual scientific meeting of the Society of Gynecologic Surgeons.
He believes that ICE-T is a good option for vaginal surgery. It’s a possibility for benign laparoscopic and perhaps robotic surgery, although those applications need to be studied. ICE-T should be avoided in patients with chronic pain, as well as patients with contraindications to any of the regimen’s medications, Dr. Petrikovets said.
According to the protocol, until hospital discharge, patients receive 20 minutes of ice to the perineum every 2 hours, 30 mg IV Toradol every 6 hours, 1,000 mg oral Tylenol every 6 hours, and 0.2 mg IV Dilaudid every 3 hours as needed for breakthrough pain. The constant pain management is important, said Dr. Petrikovets. “Patients don’t have an opportunity for the pain to get really high,” he said. At-home management includes 1,000 mg oral Tylenol every 6 hours, as needed (pain level 1-5, 60 tablets), and 10 mg Toradol every 6 hours as needed (pain level 6-10, 16 tablets).
The trial was conducted at two centers, where 63 patients were randomized to ICE-T or a standard regimen, which at the hospital included 600 mg ibuprofen every 6 hours as needed for pain levels 1-3, one tablet of Percocet (5/325 mg) every 4-6 hours as needed for pain levels 4-6, two tablets of Percocet for pain levels 7-10, and 0.2 mg IV Dilaudid every 3 hours as needed for breakthrough pain. At-home management consisted of 600 mg ibuprofen every 6 hours for pain levels 1-5 (60 tablets), and Percocet 5/325 mg every 6 hours for pain levels 6-10 (16 tablets).
Using the visual analog scale, researchers found that the 30 patients in the ICE-T arm of the study had less morning pain (VAS score, 20 mm vs. 40 mm; P = .03), and lower numerical pain score at 96 hours (2 vs. 3; P = .04). During the mornings and at 96 hours, the two groups had similar quality of recovery and satisfaction scores.
Narcotic use, measured as oral morphine equivalents, was significantly lower in the ICE-T arm between exit from the postanesthesia care unit (PACU) and hospital discharge (3 vs. 20; P less than .001) and through PACU all the way to discharge (17 vs. 38; P less than .001); 70% of patients in the ICE-T arm required no narcotics after PACU discharge, compared with 12% in the standard care arm (P less than .001).
At 96 hours, there was no significant difference between the two groups in the number of emergency department visits, percentage who had a bowel movement since surgery, or the number of Percocet/Toradol tablets taken. The ICE-T group took more Tylenol tablets than did the standard group took ibuprofen (11 vs. 6; P = .012).
SOURCE: Petrikovets A et al. SGS 2019, Abstract 07.
TUCSON, ARIZ. – compared with a standard regimen, with no difference in patient satisfaction scores.
The new study extends findings from other surgical procedures to pelvic reconstructive surgery.
“This can limit both inpatient and outpatient narcotic use. It uses oral Toradol on an outpatient basis. It’s totally underutilized. People are afraid of it, people think it causes more bleeding, and maybe there’s a cost issue,” Andrey Petrikovets, MD, a urogynecologist in Los Angeles, said in an interview.
The regimen, which he calls ICE-T, relies in part on 16 tablets of Toradol sent home with the patient – 4 days’ worth. “It’s just 16 tablets, so it’s cheap, and patients do great with it. If you really use Toradol appropriately, especially on an outpatient basis, you can pretty much eliminate outpatient narcotic use,” said Dr. Petrikovets, who presented the work at the annual scientific meeting of the Society of Gynecologic Surgeons.
He believes that ICE-T is a good option for vaginal surgery. It’s a possibility for benign laparoscopic and perhaps robotic surgery, although those applications need to be studied. ICE-T should be avoided in patients with chronic pain, as well as patients with contraindications to any of the regimen’s medications, Dr. Petrikovets said.
According to the protocol, until hospital discharge, patients receive 20 minutes of ice to the perineum every 2 hours, 30 mg IV Toradol every 6 hours, 1,000 mg oral Tylenol every 6 hours, and 0.2 mg IV Dilaudid every 3 hours as needed for breakthrough pain. The constant pain management is important, said Dr. Petrikovets. “Patients don’t have an opportunity for the pain to get really high,” he said. At-home management includes 1,000 mg oral Tylenol every 6 hours, as needed (pain level 1-5, 60 tablets), and 10 mg Toradol every 6 hours as needed (pain level 6-10, 16 tablets).
The trial was conducted at two centers, where 63 patients were randomized to ICE-T or a standard regimen, which at the hospital included 600 mg ibuprofen every 6 hours as needed for pain levels 1-3, one tablet of Percocet (5/325 mg) every 4-6 hours as needed for pain levels 4-6, two tablets of Percocet for pain levels 7-10, and 0.2 mg IV Dilaudid every 3 hours as needed for breakthrough pain. At-home management consisted of 600 mg ibuprofen every 6 hours for pain levels 1-5 (60 tablets), and Percocet 5/325 mg every 6 hours for pain levels 6-10 (16 tablets).
Using the visual analog scale, researchers found that the 30 patients in the ICE-T arm of the study had less morning pain (VAS score, 20 mm vs. 40 mm; P = .03), and lower numerical pain score at 96 hours (2 vs. 3; P = .04). During the mornings and at 96 hours, the two groups had similar quality of recovery and satisfaction scores.
Narcotic use, measured as oral morphine equivalents, was significantly lower in the ICE-T arm between exit from the postanesthesia care unit (PACU) and hospital discharge (3 vs. 20; P less than .001) and through PACU all the way to discharge (17 vs. 38; P less than .001); 70% of patients in the ICE-T arm required no narcotics after PACU discharge, compared with 12% in the standard care arm (P less than .001).
At 96 hours, there was no significant difference between the two groups in the number of emergency department visits, percentage who had a bowel movement since surgery, or the number of Percocet/Toradol tablets taken. The ICE-T group took more Tylenol tablets than did the standard group took ibuprofen (11 vs. 6; P = .012).
SOURCE: Petrikovets A et al. SGS 2019, Abstract 07.
TUCSON, ARIZ. – compared with a standard regimen, with no difference in patient satisfaction scores.
The new study extends findings from other surgical procedures to pelvic reconstructive surgery.
“This can limit both inpatient and outpatient narcotic use. It uses oral Toradol on an outpatient basis. It’s totally underutilized. People are afraid of it, people think it causes more bleeding, and maybe there’s a cost issue,” Andrey Petrikovets, MD, a urogynecologist in Los Angeles, said in an interview.
The regimen, which he calls ICE-T, relies in part on 16 tablets of Toradol sent home with the patient – 4 days’ worth. “It’s just 16 tablets, so it’s cheap, and patients do great with it. If you really use Toradol appropriately, especially on an outpatient basis, you can pretty much eliminate outpatient narcotic use,” said Dr. Petrikovets, who presented the work at the annual scientific meeting of the Society of Gynecologic Surgeons.
He believes that ICE-T is a good option for vaginal surgery. It’s a possibility for benign laparoscopic and perhaps robotic surgery, although those applications need to be studied. ICE-T should be avoided in patients with chronic pain, as well as patients with contraindications to any of the regimen’s medications, Dr. Petrikovets said.
According to the protocol, until hospital discharge, patients receive 20 minutes of ice to the perineum every 2 hours, 30 mg IV Toradol every 6 hours, 1,000 mg oral Tylenol every 6 hours, and 0.2 mg IV Dilaudid every 3 hours as needed for breakthrough pain. The constant pain management is important, said Dr. Petrikovets. “Patients don’t have an opportunity for the pain to get really high,” he said. At-home management includes 1,000 mg oral Tylenol every 6 hours, as needed (pain level 1-5, 60 tablets), and 10 mg Toradol every 6 hours as needed (pain level 6-10, 16 tablets).
The trial was conducted at two centers, where 63 patients were randomized to ICE-T or a standard regimen, which at the hospital included 600 mg ibuprofen every 6 hours as needed for pain levels 1-3, one tablet of Percocet (5/325 mg) every 4-6 hours as needed for pain levels 4-6, two tablets of Percocet for pain levels 7-10, and 0.2 mg IV Dilaudid every 3 hours as needed for breakthrough pain. At-home management consisted of 600 mg ibuprofen every 6 hours for pain levels 1-5 (60 tablets), and Percocet 5/325 mg every 6 hours for pain levels 6-10 (16 tablets).
Using the visual analog scale, researchers found that the 30 patients in the ICE-T arm of the study had less morning pain (VAS score, 20 mm vs. 40 mm; P = .03), and lower numerical pain score at 96 hours (2 vs. 3; P = .04). During the mornings and at 96 hours, the two groups had similar quality of recovery and satisfaction scores.
Narcotic use, measured as oral morphine equivalents, was significantly lower in the ICE-T arm between exit from the postanesthesia care unit (PACU) and hospital discharge (3 vs. 20; P less than .001) and through PACU all the way to discharge (17 vs. 38; P less than .001); 70% of patients in the ICE-T arm required no narcotics after PACU discharge, compared with 12% in the standard care arm (P less than .001).
At 96 hours, there was no significant difference between the two groups in the number of emergency department visits, percentage who had a bowel movement since surgery, or the number of Percocet/Toradol tablets taken. The ICE-T group took more Tylenol tablets than did the standard group took ibuprofen (11 vs. 6; P = .012).
SOURCE: Petrikovets A et al. SGS 2019, Abstract 07.
REPORTING FROM SGS 2019
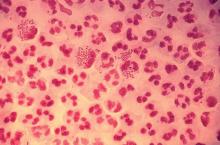
STIs pose complex challenge to HIV efforts
SEATTLE – Sexually-transmitted infections (STIs) such as gonorrhea, chlamydia, and syphilis are on the rise among HIV-infected individuals, and emerging antimicrobial resistance in these organisms is presenting serious challenges to physicians. The issue may be traceable to the introduction of preexposure prophylaxis (PrEP) in 2011, which previous studies have shown to be associated with less condom use.
In the United States, a 2017 report by the Centers for Disease Control and Prevention showed rising incidences of chlamydia (+5% from 2015 to 2017), gonorrhea (+19%), and syphilis (+18%). “We have an incidence among men who have sex with men [MSM] that is above the pre-AIDS era estimates, and we have evidence of spread into heterosexual networks, and a very scary collision with the methamphetamine and heroine using networks,” said Jeanne Marrazzo, MD, professor of infectious diseases at the University of Alabama at Birmingham.
But the numbers alone don’t tell the whole story. “It’s not just the burden of these infections. What’s characterizing these trends is that we have continuing evolution of microbial resistance, which is really a crisis,” Dr. Marrazzo added during a plenary she delivered at the Conference on Retroviruses & Opportunistic Infections.
These infections also remain intricately linked with HIV. An analysis of syphilis cases found that 88% occurred in men. Of those, 80% were MSM. Of the cases in MSM, 46% were coinfected with HIV. “Those are incredible rates,” said Dr. Marrazzo. Among women, the trends are even more alarming. There has been a greater than 150% increase in primary/secondary and congenital syphilis between 2013 and 2017.
Resistance to ceftriaxone and azithromycin remains on the rise in gonorrhea, with 24% of countries reporting at least a 5% incidence of strains that are less susceptible or resistant to ceftriaxone, and 81% of countries reporting similar trends with azithromycin.
In the absence of new drugs to overcome that resistance, or vaccines that can prevent gonorrhea and other infections, what are clinicians to do?
One option may be postexposure doxycycline. One trial in MSM showed that a 200-mg dose taken 24-72 hours after sex was associated with about a 70% increase in both time to first chlamydia and time to first syphilis infection, though no effect was seen on gonorrhea infections. “We shouldn’t be surprised. We know that gonorrhea is classically resistant to tetracyclines, and the MSM population has the highest prevalence of antimicrobial resistance in gonorrhea,” said Dr. Marrazzo.
There are pros and cons to this strategy, of course. On the one hand, doxycycline works for chlamydia and syphilis, it’s safe, and it’s easy to administer. “We’re up a tree when it comes to syphilis, so why not?” opined Dr. Marrazzo. In fact, some MSM have read the literature and are already using it prophylactically. But there are downsides, including adverse effects such as esophagitis/ulceration and photosensitivity, and it is contraindicated in pregnant women. And then there’s the potential for evolving greater resistance. “The horse is out of the barn with respect to gonorrhea, but I think it’s worth thinking about resistance to other pathogens, where we still rely on doxycycline [to treat] in rare cases,” said Dr. Marrazzo.
Finally, Dr. Marrazzo discussed the role of STI treatment in the effort to eradicate HIV. Should the Getting to 0 strategies include aggressive prevention and treatment of STIs? Despite the potentiating role of some STIs in the spread HIV, some urban areas are approaching zero new infections even as other STIs remain a problem. It could be that undetectable = untransmittable, regardless of the presence an STI. Some view targeting STIs as a regressive practice in a setting where the U=U mantra has opened up an era of sexual freedom living with or at risk of HIV.
On the other hand, there are also good arguments to target STIs while trying to eliminate HIV. Results from high-resource locales such as San Francisco and New York City are unlikely to be replicated in places like Sub-Saharan Africa. The public health burden of STIs is extensive, and antibiotic resistance and antibiotic shortages can make treatment difficult. The situation is also different for women, who may experience impacts on fertility or pregnancies, and do not have the same freedom as men in many countries. “Stigma is highly operative and I would wager that sexual pleasure and freedom remain a very elusive goal for women across the globe,” said Dr. Marrazzo.
Dr. Marrazzo has a research grant/grant pending from Cepheid, and is on the advisory panels of BioFire and Gilead.
SEATTLE – Sexually-transmitted infections (STIs) such as gonorrhea, chlamydia, and syphilis are on the rise among HIV-infected individuals, and emerging antimicrobial resistance in these organisms is presenting serious challenges to physicians. The issue may be traceable to the introduction of preexposure prophylaxis (PrEP) in 2011, which previous studies have shown to be associated with less condom use.
In the United States, a 2017 report by the Centers for Disease Control and Prevention showed rising incidences of chlamydia (+5% from 2015 to 2017), gonorrhea (+19%), and syphilis (+18%). “We have an incidence among men who have sex with men [MSM] that is above the pre-AIDS era estimates, and we have evidence of spread into heterosexual networks, and a very scary collision with the methamphetamine and heroine using networks,” said Jeanne Marrazzo, MD, professor of infectious diseases at the University of Alabama at Birmingham.
But the numbers alone don’t tell the whole story. “It’s not just the burden of these infections. What’s characterizing these trends is that we have continuing evolution of microbial resistance, which is really a crisis,” Dr. Marrazzo added during a plenary she delivered at the Conference on Retroviruses & Opportunistic Infections.
These infections also remain intricately linked with HIV. An analysis of syphilis cases found that 88% occurred in men. Of those, 80% were MSM. Of the cases in MSM, 46% were coinfected with HIV. “Those are incredible rates,” said Dr. Marrazzo. Among women, the trends are even more alarming. There has been a greater than 150% increase in primary/secondary and congenital syphilis between 2013 and 2017.
Resistance to ceftriaxone and azithromycin remains on the rise in gonorrhea, with 24% of countries reporting at least a 5% incidence of strains that are less susceptible or resistant to ceftriaxone, and 81% of countries reporting similar trends with azithromycin.
In the absence of new drugs to overcome that resistance, or vaccines that can prevent gonorrhea and other infections, what are clinicians to do?
One option may be postexposure doxycycline. One trial in MSM showed that a 200-mg dose taken 24-72 hours after sex was associated with about a 70% increase in both time to first chlamydia and time to first syphilis infection, though no effect was seen on gonorrhea infections. “We shouldn’t be surprised. We know that gonorrhea is classically resistant to tetracyclines, and the MSM population has the highest prevalence of antimicrobial resistance in gonorrhea,” said Dr. Marrazzo.
There are pros and cons to this strategy, of course. On the one hand, doxycycline works for chlamydia and syphilis, it’s safe, and it’s easy to administer. “We’re up a tree when it comes to syphilis, so why not?” opined Dr. Marrazzo. In fact, some MSM have read the literature and are already using it prophylactically. But there are downsides, including adverse effects such as esophagitis/ulceration and photosensitivity, and it is contraindicated in pregnant women. And then there’s the potential for evolving greater resistance. “The horse is out of the barn with respect to gonorrhea, but I think it’s worth thinking about resistance to other pathogens, where we still rely on doxycycline [to treat] in rare cases,” said Dr. Marrazzo.
Finally, Dr. Marrazzo discussed the role of STI treatment in the effort to eradicate HIV. Should the Getting to 0 strategies include aggressive prevention and treatment of STIs? Despite the potentiating role of some STIs in the spread HIV, some urban areas are approaching zero new infections even as other STIs remain a problem. It could be that undetectable = untransmittable, regardless of the presence an STI. Some view targeting STIs as a regressive practice in a setting where the U=U mantra has opened up an era of sexual freedom living with or at risk of HIV.
On the other hand, there are also good arguments to target STIs while trying to eliminate HIV. Results from high-resource locales such as San Francisco and New York City are unlikely to be replicated in places like Sub-Saharan Africa. The public health burden of STIs is extensive, and antibiotic resistance and antibiotic shortages can make treatment difficult. The situation is also different for women, who may experience impacts on fertility or pregnancies, and do not have the same freedom as men in many countries. “Stigma is highly operative and I would wager that sexual pleasure and freedom remain a very elusive goal for women across the globe,” said Dr. Marrazzo.
Dr. Marrazzo has a research grant/grant pending from Cepheid, and is on the advisory panels of BioFire and Gilead.
SEATTLE – Sexually-transmitted infections (STIs) such as gonorrhea, chlamydia, and syphilis are on the rise among HIV-infected individuals, and emerging antimicrobial resistance in these organisms is presenting serious challenges to physicians. The issue may be traceable to the introduction of preexposure prophylaxis (PrEP) in 2011, which previous studies have shown to be associated with less condom use.
In the United States, a 2017 report by the Centers for Disease Control and Prevention showed rising incidences of chlamydia (+5% from 2015 to 2017), gonorrhea (+19%), and syphilis (+18%). “We have an incidence among men who have sex with men [MSM] that is above the pre-AIDS era estimates, and we have evidence of spread into heterosexual networks, and a very scary collision with the methamphetamine and heroine using networks,” said Jeanne Marrazzo, MD, professor of infectious diseases at the University of Alabama at Birmingham.
But the numbers alone don’t tell the whole story. “It’s not just the burden of these infections. What’s characterizing these trends is that we have continuing evolution of microbial resistance, which is really a crisis,” Dr. Marrazzo added during a plenary she delivered at the Conference on Retroviruses & Opportunistic Infections.
These infections also remain intricately linked with HIV. An analysis of syphilis cases found that 88% occurred in men. Of those, 80% were MSM. Of the cases in MSM, 46% were coinfected with HIV. “Those are incredible rates,” said Dr. Marrazzo. Among women, the trends are even more alarming. There has been a greater than 150% increase in primary/secondary and congenital syphilis between 2013 and 2017.
Resistance to ceftriaxone and azithromycin remains on the rise in gonorrhea, with 24% of countries reporting at least a 5% incidence of strains that are less susceptible or resistant to ceftriaxone, and 81% of countries reporting similar trends with azithromycin.
In the absence of new drugs to overcome that resistance, or vaccines that can prevent gonorrhea and other infections, what are clinicians to do?
One option may be postexposure doxycycline. One trial in MSM showed that a 200-mg dose taken 24-72 hours after sex was associated with about a 70% increase in both time to first chlamydia and time to first syphilis infection, though no effect was seen on gonorrhea infections. “We shouldn’t be surprised. We know that gonorrhea is classically resistant to tetracyclines, and the MSM population has the highest prevalence of antimicrobial resistance in gonorrhea,” said Dr. Marrazzo.
There are pros and cons to this strategy, of course. On the one hand, doxycycline works for chlamydia and syphilis, it’s safe, and it’s easy to administer. “We’re up a tree when it comes to syphilis, so why not?” opined Dr. Marrazzo. In fact, some MSM have read the literature and are already using it prophylactically. But there are downsides, including adverse effects such as esophagitis/ulceration and photosensitivity, and it is contraindicated in pregnant women. And then there’s the potential for evolving greater resistance. “The horse is out of the barn with respect to gonorrhea, but I think it’s worth thinking about resistance to other pathogens, where we still rely on doxycycline [to treat] in rare cases,” said Dr. Marrazzo.
Finally, Dr. Marrazzo discussed the role of STI treatment in the effort to eradicate HIV. Should the Getting to 0 strategies include aggressive prevention and treatment of STIs? Despite the potentiating role of some STIs in the spread HIV, some urban areas are approaching zero new infections even as other STIs remain a problem. It could be that undetectable = untransmittable, regardless of the presence an STI. Some view targeting STIs as a regressive practice in a setting where the U=U mantra has opened up an era of sexual freedom living with or at risk of HIV.
On the other hand, there are also good arguments to target STIs while trying to eliminate HIV. Results from high-resource locales such as San Francisco and New York City are unlikely to be replicated in places like Sub-Saharan Africa. The public health burden of STIs is extensive, and antibiotic resistance and antibiotic shortages can make treatment difficult. The situation is also different for women, who may experience impacts on fertility or pregnancies, and do not have the same freedom as men in many countries. “Stigma is highly operative and I would wager that sexual pleasure and freedom remain a very elusive goal for women across the globe,” said Dr. Marrazzo.
Dr. Marrazzo has a research grant/grant pending from Cepheid, and is on the advisory panels of BioFire and Gilead.
EXPERT ANALYSIS FROM CROI 2019
Anterior, apical, posterior: Vaginal anatomy for the gynecologic surgeon
CASE 1 Defining anatomic structures to assure surgical precision
A 44-year-old woman is scheduled for a vaginal hysterectomy and bilateral salpingectomy for abnormal uterine bleeding. In your academic practice, a resident routinely operates with you and is accompanied by a medical student. As this is your first case with each learner, you review the steps of the procedure along with pertinent anatomy. During this discussion, numerous anatomic terms are used to describe anterior cul-de-sac entry, including pubocervical fascia, vesicouterine fold, and vesicovaginal space. Which of these terms, if any, are correct? Is there a preferred term that should be used to teach future learners so we can all “speak” the same language?
What’s in a name?
ObGyns must thoroughly understand pelvic anatomy, since much of our patient care relates to structures in that region. We also must understand the terminology that most appropriately describes each pelvic structure so that we can communicate effectively with colleagues and other providers. The case described above lists several terms that are commonly found in gynecologic textbooks and surgical atlases to describe dissection for vaginal hysterectomy. Lack of a standardized vocabulary, however, often confuses teachers and learners alike, and it highlights the importance of having a universal language to ensure the safe, effective performance of surgical procedures.1
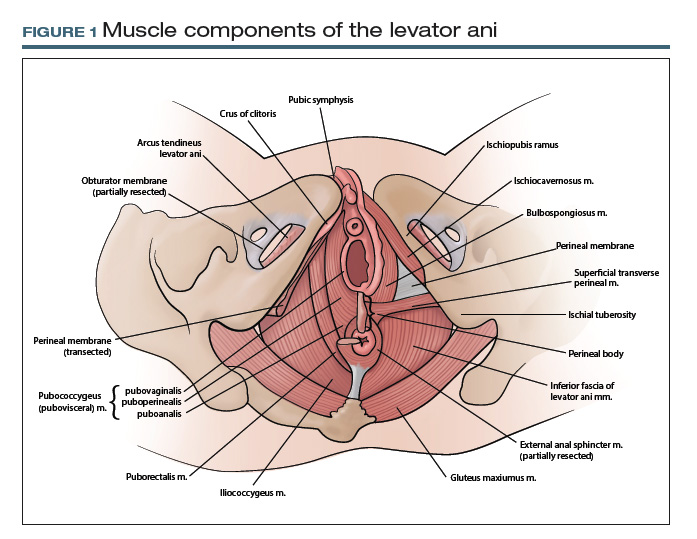
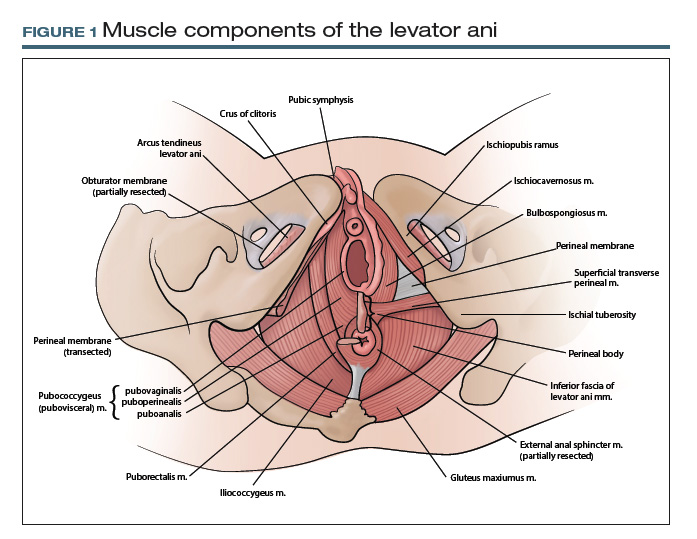
At first glance, it may seem that anatomic terms are inherently descriptive of the structure they represent; for example, the terms uterus and vagina seem rather obvious. However, many anatomic terms convey ambiguity. Which muscles, for example, constitute the levator ani: pubococcygeus, pubovisceral, pubovisceralis, puboperinealis, puboanalis, pubovaginalis, puborectalis, puborectal, iliococcygeus, ischiococcygeus? Do any of these terms redundantly describe the same structure, or does each term refer to an independent structure?
Standard terminology is essential
Anatomists long have recognized the need for standardized terminology to facilitate clear communication. To provide historical background, the term anatomy is derived from the Greek word for “dissection” or “to cut open.”2 Records on the scientific study of human anatomy date back thousands of years.
A brief review of current standardized terminology can be traced back to 1895, with the publication of Basle Terminologia Anatomica.3 That work was intended to provide a consolidated reference with clear direction regarding which anatomic terms should be used. It was updated several times during the ensuing century and was later published as Nomina Anatomica.
In 1990, an international committee was formed with representatives from many anatomical organizations, again with the intention of providing standardized anatomic terminology. Those efforts resulted in the publication of Terminologia Anatomica: International Anatomical Terminology, commonly referred to as TA, in 1998. TA continues to be the referent standard for human anatomic terminology; it was most recently updated in 2011.4
CASE 2 Conveying details of mesh erosion
A 52-year-old woman presents to the general gynecology clinic with a 10-year history of pelvic pain and dyspareunia after undergoing vaginal mesh surgery for prolapse and urinary incontinence. On examination, there is a visible ridge of mesh extending from the left side of the midurethra along the anterior and lateral vagina for a length of 1.5 cm. There also is a palpable tight band on the right vaginal wall near the ischial spine that reproduces her pain and causes spasm of the levator ani. You believe the patient needs a urogynecology referral for complications of vaginal mesh. How do you best describe your findings to your urogynecology colleague?
Continue to: Pelvic anatomy from the SGS perspective...
Pelvic anatomy from the SGS perspective
The Society of Gynecologic Surgeons (SGS) recognized the importance of standardizing terminology specific to the pelvis. The SGS Pelvic Anatomy Group thus was organized in 2016. The Pelvic Anatomy Group’s purpose is to help educate physicians about pelvic anatomy, with the overarching goal of compiling instructional materials, primarily from dissections (surgical or cadaveric), and radiologic imaging for all pelvic structures. Throughout the discussions on this initiative, it became clear that standardized terms needed to be established and used for pelvic structures.
While TA is an excellent reference work, it does not include all of the clinically relevant structures for gynecologic surgeons. As physicians, surgeons, and women’s health care providers, we read about and discuss pelvic anatomy structures in medical textbooks, medical literature, and clinical settings that are not necessarily included in TA. In addition, advances in information technology have facilitated the creation of clinically oriented computer-based anatomy programs and expanded the number and availability of electronic publications on surgical and clinical anatomy.5 As a result, there is a need not only to standardize nomenclature but also to continually revise and update terminology and integrate new terms, both from an anatomic and a clinical perspective.
The Pelvic Anatomy Group developed a novel approach to anatomic terminology. We decided to review the medical literature, identify the terms used, adjudicate the terms with current TA terms, and provide consensus for the terms and structures in the pelvis. Because of the volume of literature available and the existing number of terms, we divided the pelvis into 4 regions—anterior, apical, posterior, and vulvar—to improve the feasibility of reviewing the medical literature for the entire female pelvis.
Our process for tackling terminology
Our literature review started with the anterior compartment. (For complete details, see our prior publication.3) Modeled on a systematic review, we searched the MEDLINE database for terms related to the anterior pelvis, screened all associated abstracts, and then extracted terms from appropriate papers. We also identified several book chapters from various disciplines (anatomy, gynecology, urology, and radiology) to ensure wide representation of disciplines. We then extracted all terms pertinent to the anterior pelvis.
We organized the terms, with terms that referred to the same anatomic structure grouped together. Whenever possible, we used TA terms as the preferred terms. In this process, however, we identified several clinically relevant terms that were not included in TA: pelvic sidewall, pelvic bones, anterior compartment, pubourethral ligament, vaginal sulcus, and levator hiatus, among others. The new terms were then proposed and agreed on by members of the SGS Pelvic Anatomy Group and accepted by SGS members. We currently are completing a similar process for the apical pelvis, posterior pelvis, and vulvar regions.
TA code numbers pinpoint the nomenclature
As we move forward, we suggest that physicians use TA or other approved terms for patient and research communication. Such use will help standardize anatomic terms and also will improve communication between providers and education for learners.
Continue to: TA includes approved options...
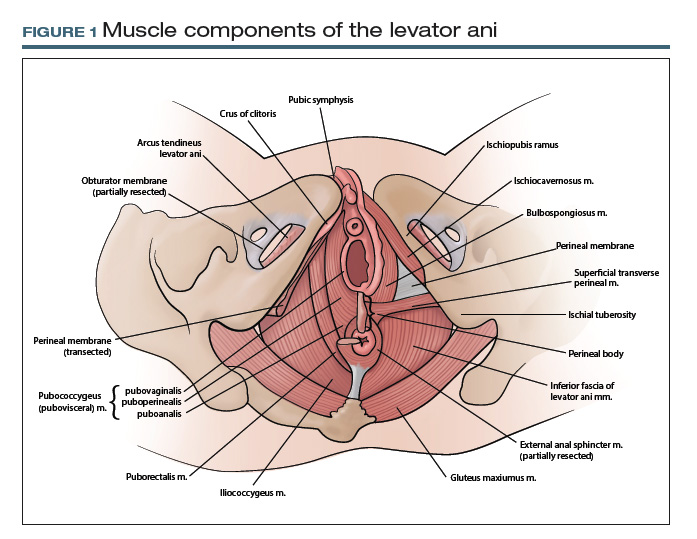
TA includes approved options in English and Latin and lists a unique identification number for each term (shown in parentheses in the examples that follow). For instance, to answer the question posed earlier, the levator ani (A04.5.04.002) is comprised of the pubococcygeus (A04.5.04.003), puborectalis (A04.5.04.007), and iliococcygeus (A04.5.04.008) muscles (FIGURE 1).The terms pubovisceral and pubovisceralis are used synonymously in the literature with pubococcygeus (A04.5.04.003).3 The additional terms puboperinealis (A04.5.04.004), pubovaginalis (A04.5.04.005), and puboanalis (A04.5.04.006) are subcomponents of the pubococcygeus (A04.5.04.003), and this relationship is indicated in TA by indentation formatting.4 Finally, the ischiococcygeus (A04.5.04.011) muscle is not considered part of the levator ani (A04.5.04.002).
Revisiting the mesh erosion case: Reporting your findings
After reviewing the recommended terminology for the anterior pelvis,3,4 you might draft a report as follows: “A mesh erosion was visualized in anterior vaginal wall (A09.1.04.006) at the level of the mid-urethra extending into ‘anterior and lateral vaginal sulci’ (proposed term). In addition, there is a painful tight band in the ‘lateral vaginal wall’ (proposed term) near the ischial spine (A02.5.01.205). Palpation of this band reproduces the patient’s pain and causes secondary spasm of the levator ani (A04.5.04.002).” Certainly, TA identification numbers would not be expected to be included in medical communication; they are included here for reference.
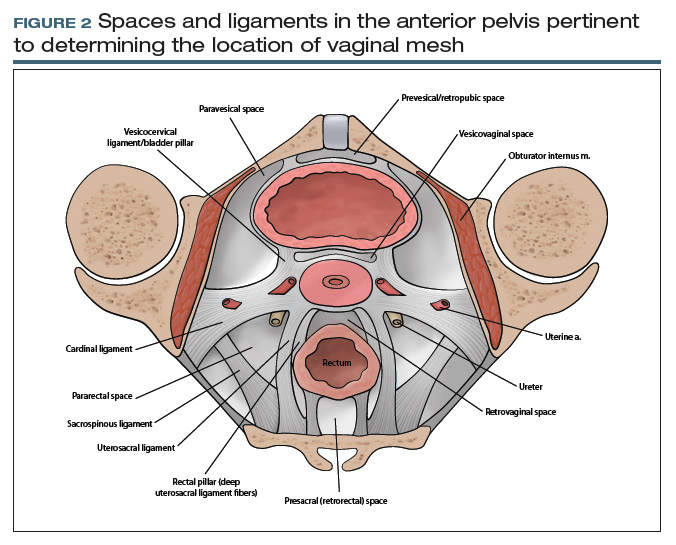
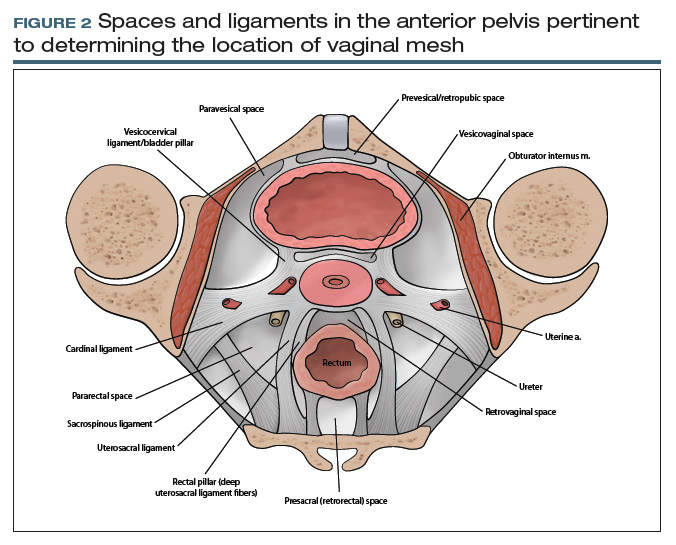
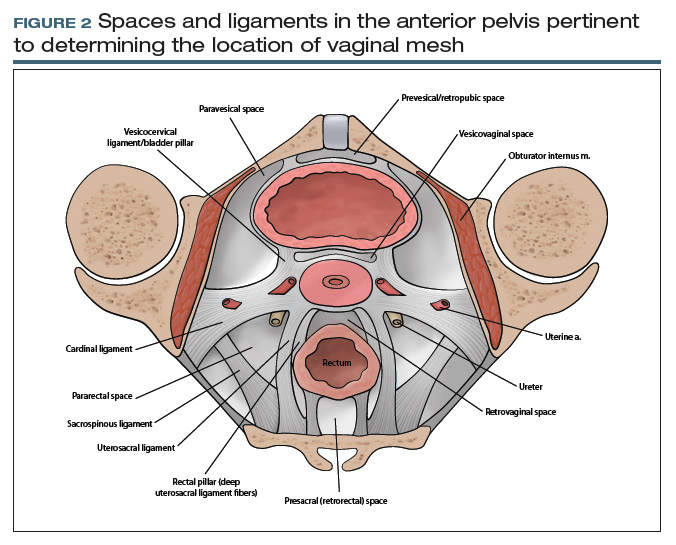
From your description, your urogynecology colleague has a better understanding of the location of your patient’s vaginal mesh and requests her operative report from an outside facility. In the operative report, the surgeon described “placement of mesh into the vagina, dissection through the rectal spaces, and anchoring of the mesh into the levator/pelvic muscles, the cervix, and lastly to the paraurethral ligaments,” and “passage of trocars through the cave of Retzius at the level of the midurethra” (FIGURE 2).
Based on this description, the urogynecologist ascertains that the mesh is located in the anterior vaginal wall (A09.1.04.006), with passage of anchoring arms through the bilateral sacrospinous ligaments (A03.6.03.007) and retropubic space (A10.1.01.003). Exposed mesh is visible, extending from the midurethra to the “anterior and lateral vaginal sulci” (proposed term).
This case clearly demonstrates the importance of communication between providers for patient care, since understanding the patient’s anatomy and the location of the vaginal mesh is important for planning surgical excision of the exposed mesh.
Additional initiatives
Outlining standardized terminology is just the first step toward improving the anatomic “language” used among providers. Ongoing efforts from the SGS Pelvic Anatomy Group include a special imaging group’s review of imaging modalities (ultrasonography, magnetic resonance imaging, computerized tomography) to improve standardization on reporting clinical anatomy. In addition, SGS has developed a group to create educational content related to the structures identified by the terminology group from cadaveric or surgical dissections. Educational materials will be compiled to help physicians and learners expand their anatomic understanding and improve their communication.
Further details of the Pelvic Anatomy Group’s efforts can be found on the SGS website at https://www.sgsonline.org.
- American Association of Clinical Anatomists, Educational Affairs Committee. The clinical anatomy of several invasive procedures. Clin Anat. 1999;12:43-54.
- Venes D, ed. Taber's Cyclopedic Medical Dictionary. 23rd ed. Philadelphia, PA: FA Davis Company; 2017.
- Jeppson PC, Balgobin S, Washington BB, et al; for the Society of Gynecologic Surgeons Pelvic Anatomy Group. Recommended standardized terminology of the anterior female pelvis based on a structured medical literature review. Am J Obstet Gynecol. 2018;219:26-39.
- Federative Committee on Anatomical Terminologies (FCAT). Terminologia Anatomica: International Anatomical Terminology. 2nd ed. Stuttgart, Germany: Thieme; 2011.
- Rosse C. Terminologia Anatomica: considered from the perspective of next-generation knowledge sources. Clin Anat. 2001;14:120-133.
CASE 1 Defining anatomic structures to assure surgical precision
A 44-year-old woman is scheduled for a vaginal hysterectomy and bilateral salpingectomy for abnormal uterine bleeding. In your academic practice, a resident routinely operates with you and is accompanied by a medical student. As this is your first case with each learner, you review the steps of the procedure along with pertinent anatomy. During this discussion, numerous anatomic terms are used to describe anterior cul-de-sac entry, including pubocervical fascia, vesicouterine fold, and vesicovaginal space. Which of these terms, if any, are correct? Is there a preferred term that should be used to teach future learners so we can all “speak” the same language?
What’s in a name?
ObGyns must thoroughly understand pelvic anatomy, since much of our patient care relates to structures in that region. We also must understand the terminology that most appropriately describes each pelvic structure so that we can communicate effectively with colleagues and other providers. The case described above lists several terms that are commonly found in gynecologic textbooks and surgical atlases to describe dissection for vaginal hysterectomy. Lack of a standardized vocabulary, however, often confuses teachers and learners alike, and it highlights the importance of having a universal language to ensure the safe, effective performance of surgical procedures.1
At first glance, it may seem that anatomic terms are inherently descriptive of the structure they represent; for example, the terms uterus and vagina seem rather obvious. However, many anatomic terms convey ambiguity. Which muscles, for example, constitute the levator ani: pubococcygeus, pubovisceral, pubovisceralis, puboperinealis, puboanalis, pubovaginalis, puborectalis, puborectal, iliococcygeus, ischiococcygeus? Do any of these terms redundantly describe the same structure, or does each term refer to an independent structure?
Standard terminology is essential
Anatomists long have recognized the need for standardized terminology to facilitate clear communication. To provide historical background, the term anatomy is derived from the Greek word for “dissection” or “to cut open.”2 Records on the scientific study of human anatomy date back thousands of years.
A brief review of current standardized terminology can be traced back to 1895, with the publication of Basle Terminologia Anatomica.3 That work was intended to provide a consolidated reference with clear direction regarding which anatomic terms should be used. It was updated several times during the ensuing century and was later published as Nomina Anatomica.
In 1990, an international committee was formed with representatives from many anatomical organizations, again with the intention of providing standardized anatomic terminology. Those efforts resulted in the publication of Terminologia Anatomica: International Anatomical Terminology, commonly referred to as TA, in 1998. TA continues to be the referent standard for human anatomic terminology; it was most recently updated in 2011.4
CASE 2 Conveying details of mesh erosion
A 52-year-old woman presents to the general gynecology clinic with a 10-year history of pelvic pain and dyspareunia after undergoing vaginal mesh surgery for prolapse and urinary incontinence. On examination, there is a visible ridge of mesh extending from the left side of the midurethra along the anterior and lateral vagina for a length of 1.5 cm. There also is a palpable tight band on the right vaginal wall near the ischial spine that reproduces her pain and causes spasm of the levator ani. You believe the patient needs a urogynecology referral for complications of vaginal mesh. How do you best describe your findings to your urogynecology colleague?
Continue to: Pelvic anatomy from the SGS perspective...
Pelvic anatomy from the SGS perspective
The Society of Gynecologic Surgeons (SGS) recognized the importance of standardizing terminology specific to the pelvis. The SGS Pelvic Anatomy Group thus was organized in 2016. The Pelvic Anatomy Group’s purpose is to help educate physicians about pelvic anatomy, with the overarching goal of compiling instructional materials, primarily from dissections (surgical or cadaveric), and radiologic imaging for all pelvic structures. Throughout the discussions on this initiative, it became clear that standardized terms needed to be established and used for pelvic structures.
While TA is an excellent reference work, it does not include all of the clinically relevant structures for gynecologic surgeons. As physicians, surgeons, and women’s health care providers, we read about and discuss pelvic anatomy structures in medical textbooks, medical literature, and clinical settings that are not necessarily included in TA. In addition, advances in information technology have facilitated the creation of clinically oriented computer-based anatomy programs and expanded the number and availability of electronic publications on surgical and clinical anatomy.5 As a result, there is a need not only to standardize nomenclature but also to continually revise and update terminology and integrate new terms, both from an anatomic and a clinical perspective.
The Pelvic Anatomy Group developed a novel approach to anatomic terminology. We decided to review the medical literature, identify the terms used, adjudicate the terms with current TA terms, and provide consensus for the terms and structures in the pelvis. Because of the volume of literature available and the existing number of terms, we divided the pelvis into 4 regions—anterior, apical, posterior, and vulvar—to improve the feasibility of reviewing the medical literature for the entire female pelvis.
Our process for tackling terminology
Our literature review started with the anterior compartment. (For complete details, see our prior publication.3) Modeled on a systematic review, we searched the MEDLINE database for terms related to the anterior pelvis, screened all associated abstracts, and then extracted terms from appropriate papers. We also identified several book chapters from various disciplines (anatomy, gynecology, urology, and radiology) to ensure wide representation of disciplines. We then extracted all terms pertinent to the anterior pelvis.
We organized the terms, with terms that referred to the same anatomic structure grouped together. Whenever possible, we used TA terms as the preferred terms. In this process, however, we identified several clinically relevant terms that were not included in TA: pelvic sidewall, pelvic bones, anterior compartment, pubourethral ligament, vaginal sulcus, and levator hiatus, among others. The new terms were then proposed and agreed on by members of the SGS Pelvic Anatomy Group and accepted by SGS members. We currently are completing a similar process for the apical pelvis, posterior pelvis, and vulvar regions.
TA code numbers pinpoint the nomenclature
As we move forward, we suggest that physicians use TA or other approved terms for patient and research communication. Such use will help standardize anatomic terms and also will improve communication between providers and education for learners.
Continue to: TA includes approved options...
TA includes approved options in English and Latin and lists a unique identification number for each term (shown in parentheses in the examples that follow). For instance, to answer the question posed earlier, the levator ani (A04.5.04.002) is comprised of the pubococcygeus (A04.5.04.003), puborectalis (A04.5.04.007), and iliococcygeus (A04.5.04.008) muscles (FIGURE 1).The terms pubovisceral and pubovisceralis are used synonymously in the literature with pubococcygeus (A04.5.04.003).3 The additional terms puboperinealis (A04.5.04.004), pubovaginalis (A04.5.04.005), and puboanalis (A04.5.04.006) are subcomponents of the pubococcygeus (A04.5.04.003), and this relationship is indicated in TA by indentation formatting.4 Finally, the ischiococcygeus (A04.5.04.011) muscle is not considered part of the levator ani (A04.5.04.002).
Revisiting the mesh erosion case: Reporting your findings
After reviewing the recommended terminology for the anterior pelvis,3,4 you might draft a report as follows: “A mesh erosion was visualized in anterior vaginal wall (A09.1.04.006) at the level of the mid-urethra extending into ‘anterior and lateral vaginal sulci’ (proposed term). In addition, there is a painful tight band in the ‘lateral vaginal wall’ (proposed term) near the ischial spine (A02.5.01.205). Palpation of this band reproduces the patient’s pain and causes secondary spasm of the levator ani (A04.5.04.002).” Certainly, TA identification numbers would not be expected to be included in medical communication; they are included here for reference.
From your description, your urogynecology colleague has a better understanding of the location of your patient’s vaginal mesh and requests her operative report from an outside facility. In the operative report, the surgeon described “placement of mesh into the vagina, dissection through the rectal spaces, and anchoring of the mesh into the levator/pelvic muscles, the cervix, and lastly to the paraurethral ligaments,” and “passage of trocars through the cave of Retzius at the level of the midurethra” (FIGURE 2).
Based on this description, the urogynecologist ascertains that the mesh is located in the anterior vaginal wall (A09.1.04.006), with passage of anchoring arms through the bilateral sacrospinous ligaments (A03.6.03.007) and retropubic space (A10.1.01.003). Exposed mesh is visible, extending from the midurethra to the “anterior and lateral vaginal sulci” (proposed term).
This case clearly demonstrates the importance of communication between providers for patient care, since understanding the patient’s anatomy and the location of the vaginal mesh is important for planning surgical excision of the exposed mesh.
Additional initiatives
Outlining standardized terminology is just the first step toward improving the anatomic “language” used among providers. Ongoing efforts from the SGS Pelvic Anatomy Group include a special imaging group’s review of imaging modalities (ultrasonography, magnetic resonance imaging, computerized tomography) to improve standardization on reporting clinical anatomy. In addition, SGS has developed a group to create educational content related to the structures identified by the terminology group from cadaveric or surgical dissections. Educational materials will be compiled to help physicians and learners expand their anatomic understanding and improve their communication.
Further details of the Pelvic Anatomy Group’s efforts can be found on the SGS website at https://www.sgsonline.org.
CASE 1 Defining anatomic structures to assure surgical precision
A 44-year-old woman is scheduled for a vaginal hysterectomy and bilateral salpingectomy for abnormal uterine bleeding. In your academic practice, a resident routinely operates with you and is accompanied by a medical student. As this is your first case with each learner, you review the steps of the procedure along with pertinent anatomy. During this discussion, numerous anatomic terms are used to describe anterior cul-de-sac entry, including pubocervical fascia, vesicouterine fold, and vesicovaginal space. Which of these terms, if any, are correct? Is there a preferred term that should be used to teach future learners so we can all “speak” the same language?
What’s in a name?
ObGyns must thoroughly understand pelvic anatomy, since much of our patient care relates to structures in that region. We also must understand the terminology that most appropriately describes each pelvic structure so that we can communicate effectively with colleagues and other providers. The case described above lists several terms that are commonly found in gynecologic textbooks and surgical atlases to describe dissection for vaginal hysterectomy. Lack of a standardized vocabulary, however, often confuses teachers and learners alike, and it highlights the importance of having a universal language to ensure the safe, effective performance of surgical procedures.1
At first glance, it may seem that anatomic terms are inherently descriptive of the structure they represent; for example, the terms uterus and vagina seem rather obvious. However, many anatomic terms convey ambiguity. Which muscles, for example, constitute the levator ani: pubococcygeus, pubovisceral, pubovisceralis, puboperinealis, puboanalis, pubovaginalis, puborectalis, puborectal, iliococcygeus, ischiococcygeus? Do any of these terms redundantly describe the same structure, or does each term refer to an independent structure?
Standard terminology is essential
Anatomists long have recognized the need for standardized terminology to facilitate clear communication. To provide historical background, the term anatomy is derived from the Greek word for “dissection” or “to cut open.”2 Records on the scientific study of human anatomy date back thousands of years.
A brief review of current standardized terminology can be traced back to 1895, with the publication of Basle Terminologia Anatomica.3 That work was intended to provide a consolidated reference with clear direction regarding which anatomic terms should be used. It was updated several times during the ensuing century and was later published as Nomina Anatomica.
In 1990, an international committee was formed with representatives from many anatomical organizations, again with the intention of providing standardized anatomic terminology. Those efforts resulted in the publication of Terminologia Anatomica: International Anatomical Terminology, commonly referred to as TA, in 1998. TA continues to be the referent standard for human anatomic terminology; it was most recently updated in 2011.4
CASE 2 Conveying details of mesh erosion
A 52-year-old woman presents to the general gynecology clinic with a 10-year history of pelvic pain and dyspareunia after undergoing vaginal mesh surgery for prolapse and urinary incontinence. On examination, there is a visible ridge of mesh extending from the left side of the midurethra along the anterior and lateral vagina for a length of 1.5 cm. There also is a palpable tight band on the right vaginal wall near the ischial spine that reproduces her pain and causes spasm of the levator ani. You believe the patient needs a urogynecology referral for complications of vaginal mesh. How do you best describe your findings to your urogynecology colleague?
Continue to: Pelvic anatomy from the SGS perspective...
Pelvic anatomy from the SGS perspective
The Society of Gynecologic Surgeons (SGS) recognized the importance of standardizing terminology specific to the pelvis. The SGS Pelvic Anatomy Group thus was organized in 2016. The Pelvic Anatomy Group’s purpose is to help educate physicians about pelvic anatomy, with the overarching goal of compiling instructional materials, primarily from dissections (surgical or cadaveric), and radiologic imaging for all pelvic structures. Throughout the discussions on this initiative, it became clear that standardized terms needed to be established and used for pelvic structures.
While TA is an excellent reference work, it does not include all of the clinically relevant structures for gynecologic surgeons. As physicians, surgeons, and women’s health care providers, we read about and discuss pelvic anatomy structures in medical textbooks, medical literature, and clinical settings that are not necessarily included in TA. In addition, advances in information technology have facilitated the creation of clinically oriented computer-based anatomy programs and expanded the number and availability of electronic publications on surgical and clinical anatomy.5 As a result, there is a need not only to standardize nomenclature but also to continually revise and update terminology and integrate new terms, both from an anatomic and a clinical perspective.
The Pelvic Anatomy Group developed a novel approach to anatomic terminology. We decided to review the medical literature, identify the terms used, adjudicate the terms with current TA terms, and provide consensus for the terms and structures in the pelvis. Because of the volume of literature available and the existing number of terms, we divided the pelvis into 4 regions—anterior, apical, posterior, and vulvar—to improve the feasibility of reviewing the medical literature for the entire female pelvis.
Our process for tackling terminology
Our literature review started with the anterior compartment. (For complete details, see our prior publication.3) Modeled on a systematic review, we searched the MEDLINE database for terms related to the anterior pelvis, screened all associated abstracts, and then extracted terms from appropriate papers. We also identified several book chapters from various disciplines (anatomy, gynecology, urology, and radiology) to ensure wide representation of disciplines. We then extracted all terms pertinent to the anterior pelvis.
We organized the terms, with terms that referred to the same anatomic structure grouped together. Whenever possible, we used TA terms as the preferred terms. In this process, however, we identified several clinically relevant terms that were not included in TA: pelvic sidewall, pelvic bones, anterior compartment, pubourethral ligament, vaginal sulcus, and levator hiatus, among others. The new terms were then proposed and agreed on by members of the SGS Pelvic Anatomy Group and accepted by SGS members. We currently are completing a similar process for the apical pelvis, posterior pelvis, and vulvar regions.
TA code numbers pinpoint the nomenclature
As we move forward, we suggest that physicians use TA or other approved terms for patient and research communication. Such use will help standardize anatomic terms and also will improve communication between providers and education for learners.
Continue to: TA includes approved options...
TA includes approved options in English and Latin and lists a unique identification number for each term (shown in parentheses in the examples that follow). For instance, to answer the question posed earlier, the levator ani (A04.5.04.002) is comprised of the pubococcygeus (A04.5.04.003), puborectalis (A04.5.04.007), and iliococcygeus (A04.5.04.008) muscles (FIGURE 1).The terms pubovisceral and pubovisceralis are used synonymously in the literature with pubococcygeus (A04.5.04.003).3 The additional terms puboperinealis (A04.5.04.004), pubovaginalis (A04.5.04.005), and puboanalis (A04.5.04.006) are subcomponents of the pubococcygeus (A04.5.04.003), and this relationship is indicated in TA by indentation formatting.4 Finally, the ischiococcygeus (A04.5.04.011) muscle is not considered part of the levator ani (A04.5.04.002).
Revisiting the mesh erosion case: Reporting your findings
After reviewing the recommended terminology for the anterior pelvis,3,4 you might draft a report as follows: “A mesh erosion was visualized in anterior vaginal wall (A09.1.04.006) at the level of the mid-urethra extending into ‘anterior and lateral vaginal sulci’ (proposed term). In addition, there is a painful tight band in the ‘lateral vaginal wall’ (proposed term) near the ischial spine (A02.5.01.205). Palpation of this band reproduces the patient’s pain and causes secondary spasm of the levator ani (A04.5.04.002).” Certainly, TA identification numbers would not be expected to be included in medical communication; they are included here for reference.
From your description, your urogynecology colleague has a better understanding of the location of your patient’s vaginal mesh and requests her operative report from an outside facility. In the operative report, the surgeon described “placement of mesh into the vagina, dissection through the rectal spaces, and anchoring of the mesh into the levator/pelvic muscles, the cervix, and lastly to the paraurethral ligaments,” and “passage of trocars through the cave of Retzius at the level of the midurethra” (FIGURE 2).
Based on this description, the urogynecologist ascertains that the mesh is located in the anterior vaginal wall (A09.1.04.006), with passage of anchoring arms through the bilateral sacrospinous ligaments (A03.6.03.007) and retropubic space (A10.1.01.003). Exposed mesh is visible, extending from the midurethra to the “anterior and lateral vaginal sulci” (proposed term).
This case clearly demonstrates the importance of communication between providers for patient care, since understanding the patient’s anatomy and the location of the vaginal mesh is important for planning surgical excision of the exposed mesh.
Additional initiatives
Outlining standardized terminology is just the first step toward improving the anatomic “language” used among providers. Ongoing efforts from the SGS Pelvic Anatomy Group include a special imaging group’s review of imaging modalities (ultrasonography, magnetic resonance imaging, computerized tomography) to improve standardization on reporting clinical anatomy. In addition, SGS has developed a group to create educational content related to the structures identified by the terminology group from cadaveric or surgical dissections. Educational materials will be compiled to help physicians and learners expand their anatomic understanding and improve their communication.
Further details of the Pelvic Anatomy Group’s efforts can be found on the SGS website at https://www.sgsonline.org.
- American Association of Clinical Anatomists, Educational Affairs Committee. The clinical anatomy of several invasive procedures. Clin Anat. 1999;12:43-54.
- Venes D, ed. Taber's Cyclopedic Medical Dictionary. 23rd ed. Philadelphia, PA: FA Davis Company; 2017.
- Jeppson PC, Balgobin S, Washington BB, et al; for the Society of Gynecologic Surgeons Pelvic Anatomy Group. Recommended standardized terminology of the anterior female pelvis based on a structured medical literature review. Am J Obstet Gynecol. 2018;219:26-39.
- Federative Committee on Anatomical Terminologies (FCAT). Terminologia Anatomica: International Anatomical Terminology. 2nd ed. Stuttgart, Germany: Thieme; 2011.
- Rosse C. Terminologia Anatomica: considered from the perspective of next-generation knowledge sources. Clin Anat. 2001;14:120-133.
- American Association of Clinical Anatomists, Educational Affairs Committee. The clinical anatomy of several invasive procedures. Clin Anat. 1999;12:43-54.
- Venes D, ed. Taber's Cyclopedic Medical Dictionary. 23rd ed. Philadelphia, PA: FA Davis Company; 2017.
- Jeppson PC, Balgobin S, Washington BB, et al; for the Society of Gynecologic Surgeons Pelvic Anatomy Group. Recommended standardized terminology of the anterior female pelvis based on a structured medical literature review. Am J Obstet Gynecol. 2018;219:26-39.
- Federative Committee on Anatomical Terminologies (FCAT). Terminologia Anatomica: International Anatomical Terminology. 2nd ed. Stuttgart, Germany: Thieme; 2011.
- Rosse C. Terminologia Anatomica: considered from the perspective of next-generation knowledge sources. Clin Anat. 2001;14:120-133.
Pre-exposure prophylaxis for the prevention of HIV infection: Ready for prime time
The first cases of HIV infection in the United States were reported in 1981. Since that time, more than 700,000 individuals in our country have died of AIDS. Slightly more than 1 million persons in the United States are currently living with HIV infection; approximately 15% of them are unaware of their infection. Men who have sex with men (MSM) and African American and Hispanic/Latino men and women are disproportionately affected by HIV infection.1 Among men, MSM is the most common method of infection transmission, accounting for 83% of infections. Heterosexual contact accounts for 9.4% of new infections and injection drug use for 4.0%. Among women in the United States, heterosexual contact is the most common mechanism of transmission, accounting for about 87% of cases; injection drug use accounts for about 12%.1 Perinatal transmission rates are extremely low—less than 1%—when women receive effective treatment during pregnancy and their infants are treated in the neonatal period.1,2
The prognosis for HIV-infected patients has improved dramatically in recent years with the availability of many new and exceptionally effective highly-active antiretroviral treatment regimens. Nevertheless, the disease is not yet completely curable. Therefore, preventive measures are of great importance in reducing the enormous toll imposed by this condition.2
Evaluating effectiveness of PrEP
At the request of the US Preventive Services Task Force, Chou and colleagues recently conducted a systematic review to determine the effectiveness of pre-exposure prophylaxis (PrEP) in preventing the horizontal transmission of HIV infection.1 The authors’ secondary objectives included assessing the relationship between degree of adherence to the prophylactic regimen and degree of effectiveness and evaluating the accuracy of various screening systems for identifying patients at high risk for acquiring HIV infection.
The authors reviewed prospective, randomized controlled trials (treatment versus no treatment or treatment versus placebo) published through 2018. Pregnant women were excluded from the studies, as were women who became pregnant after enrollment.
Two different prophylactic regimens were used in the reviewed studies: 1) the combination of tenofovir disoproxil fumarate 300 mg or 245 mg plus emtricitabine 200 mg and 2) tenofovir 300 mg alone. Most trials used the combination regimen. With the exception of one trial, the medications were given daily to uninfected patients at high risk of acquiring HIV infection. In one investigation, the administration of prophylaxis was event driven (administered after a specific high-risk exposure).
Key study findings
PrEP decreased HIV transmission in high-risk patients. Chou and colleagues found that high-risk patients included primarily MSM who did not use condoms consistently or who had a high number of sex partners, individuals in an HIV-serodiscordant relationship, and intravenous drug users who shared injection equipment.
In these high-risk patients, PrEP was associated with a significantly decreased risk of HIV transmission. Observations from 11 trials demonstrated a relative risk (RR) of 0.46 (95% confidence interval [CI], 0.33–0.66). The absolute risk reduction was -2.0% (95% CI, -2.8% to -1.2%). The duration of follow up ranged from 4 months to 4 years.
Continue to: Better medication adherence = greater prophylaxis effectiveness...
Better medication adherence = greater prophylaxis effectiveness. When adherence was ≥70%, the RR was 0.27 (95% CI, 0.19–0.39). When adherence was 40% to 70%, the RR was 0.51 (95% CI, 0.38–0.70). When adherence was ≤40%, the relative risk was 0.93 (95% CI, 0.72–1.20). Adherence was better with daily administration, as opposed to event-driven administration.
Although the combination prophylactic regimen (tenofovir plus emtricitabine) was most frequently used in the clinical trials, tenofovir alone was comparable in effectiveness.
PrEP resulted in more mild adverse effects. Patients who received PrEP were more likely to develop gastrointestinal adverse effects and renal function abnormalities when compared with patients in the control arms of the studies. These adverse effects were virtually always mild and did not necessitate discontinuation of treatment.
No increase in promiscuous sexual behavior with PrEP. Specifically, investigators did not document an increased incidence of new sexually transmitted infections (STIs) in treated patients.
PrEP did not increase adverse pregnancy outcomes. In women who became pregnant while on PrEP, and who then discontinued treatment, there was no increase in the frequency of spontaneous abortion, congenital anomalies, or other adverse pregnancy outcomes.
In addition, PrEP posed a low risk for causing drug resistance in patients who became infected despite prophylaxis. Finally, the authors found that screening instruments for identifying patients at highest risk for acquiring HIV infection had low to modest sensitivity.
My recommendations for practice
Based on the study by Chou and colleagues, and on a recent commentary by Marcus et al, I believe that the following actions are justified1–3:
- For prophylaxis to be effective, we must identify all infected patients. Therefore, screening of asymptomatic individuals during routine health encounters is essential.
- All patients should have access to easy-to-understand information related to risk factors for HIV infection.
- Every effort should be made to promote safe sex practices, such as use of latex condoms, avoidance of sex during menses and in the presence of ulcerative genital lesions, and avoidance of use of contaminated drug-injection needles.
- All high-risk patients, as defined above, should be offered PrEP.
- To the greatest extent possible, financial barriers to PrEP should be eliminated.
- Patients receiving PrEP should be monitored for evidence of renal dysfunction. Should they become infected despite prophylaxis, they should be evaluated carefully to detect drug-resistant viral strains.
- Although PrEP is definitely effective in reducing the risk of transmission of HIV infection, it does not prevent the transmission of other STIs, such as syphilis, gonorrhea, and chlamydia.
In my practice, I administer prophyaxis on a daily basis rather than just before, or after, a high-risk exposure. This approach enhances patient adherence and, hopefully, will lead to maximum effectiveness over time. I also use the combination of tenofovir disoproxil fumarate plus emtricitabine rather than tenofovir alone because there is more published information regarding the effectiveness of the combination regimen.
- Chou R, Evans C, Hoverman A, et al. Pre-exposure Prophylaxis for the Prevention of HIV Infection: A Systematic Review for the U.S. Preventive Services Task Force. AHRQ Publication No. 18-05247-EF-1; November 2018.
- Duff P. Maternal and fetal infections. In: Resnik R, Lockwood CJ, Moore TR, Green MF, Copel JA, Silver RM (eds). Creasy & Resnik's Maternal-Fetal Medicine. Principles and Practice (8th ed). Philadelphia, PA: Elsevier; 2019.
- Marcus JL, Katz KA, Krakower DS, et al. Risk compensation and clinical decision making--the case of HIV preexposure prophylaxis. N Engl J Med. 2019;380:510-512.
The first cases of HIV infection in the United States were reported in 1981. Since that time, more than 700,000 individuals in our country have died of AIDS. Slightly more than 1 million persons in the United States are currently living with HIV infection; approximately 15% of them are unaware of their infection. Men who have sex with men (MSM) and African American and Hispanic/Latino men and women are disproportionately affected by HIV infection.1 Among men, MSM is the most common method of infection transmission, accounting for 83% of infections. Heterosexual contact accounts for 9.4% of new infections and injection drug use for 4.0%. Among women in the United States, heterosexual contact is the most common mechanism of transmission, accounting for about 87% of cases; injection drug use accounts for about 12%.1 Perinatal transmission rates are extremely low—less than 1%—when women receive effective treatment during pregnancy and their infants are treated in the neonatal period.1,2
The prognosis for HIV-infected patients has improved dramatically in recent years with the availability of many new and exceptionally effective highly-active antiretroviral treatment regimens. Nevertheless, the disease is not yet completely curable. Therefore, preventive measures are of great importance in reducing the enormous toll imposed by this condition.2
Evaluating effectiveness of PrEP
At the request of the US Preventive Services Task Force, Chou and colleagues recently conducted a systematic review to determine the effectiveness of pre-exposure prophylaxis (PrEP) in preventing the horizontal transmission of HIV infection.1 The authors’ secondary objectives included assessing the relationship between degree of adherence to the prophylactic regimen and degree of effectiveness and evaluating the accuracy of various screening systems for identifying patients at high risk for acquiring HIV infection.
The authors reviewed prospective, randomized controlled trials (treatment versus no treatment or treatment versus placebo) published through 2018. Pregnant women were excluded from the studies, as were women who became pregnant after enrollment.
Two different prophylactic regimens were used in the reviewed studies: 1) the combination of tenofovir disoproxil fumarate 300 mg or 245 mg plus emtricitabine 200 mg and 2) tenofovir 300 mg alone. Most trials used the combination regimen. With the exception of one trial, the medications were given daily to uninfected patients at high risk of acquiring HIV infection. In one investigation, the administration of prophylaxis was event driven (administered after a specific high-risk exposure).
Key study findings
PrEP decreased HIV transmission in high-risk patients. Chou and colleagues found that high-risk patients included primarily MSM who did not use condoms consistently or who had a high number of sex partners, individuals in an HIV-serodiscordant relationship, and intravenous drug users who shared injection equipment.
In these high-risk patients, PrEP was associated with a significantly decreased risk of HIV transmission. Observations from 11 trials demonstrated a relative risk (RR) of 0.46 (95% confidence interval [CI], 0.33–0.66). The absolute risk reduction was -2.0% (95% CI, -2.8% to -1.2%). The duration of follow up ranged from 4 months to 4 years.
Continue to: Better medication adherence = greater prophylaxis effectiveness...
Better medication adherence = greater prophylaxis effectiveness. When adherence was ≥70%, the RR was 0.27 (95% CI, 0.19–0.39). When adherence was 40% to 70%, the RR was 0.51 (95% CI, 0.38–0.70). When adherence was ≤40%, the relative risk was 0.93 (95% CI, 0.72–1.20). Adherence was better with daily administration, as opposed to event-driven administration.
Although the combination prophylactic regimen (tenofovir plus emtricitabine) was most frequently used in the clinical trials, tenofovir alone was comparable in effectiveness.
PrEP resulted in more mild adverse effects. Patients who received PrEP were more likely to develop gastrointestinal adverse effects and renal function abnormalities when compared with patients in the control arms of the studies. These adverse effects were virtually always mild and did not necessitate discontinuation of treatment.
No increase in promiscuous sexual behavior with PrEP. Specifically, investigators did not document an increased incidence of new sexually transmitted infections (STIs) in treated patients.
PrEP did not increase adverse pregnancy outcomes. In women who became pregnant while on PrEP, and who then discontinued treatment, there was no increase in the frequency of spontaneous abortion, congenital anomalies, or other adverse pregnancy outcomes.
In addition, PrEP posed a low risk for causing drug resistance in patients who became infected despite prophylaxis. Finally, the authors found that screening instruments for identifying patients at highest risk for acquiring HIV infection had low to modest sensitivity.
My recommendations for practice
Based on the study by Chou and colleagues, and on a recent commentary by Marcus et al, I believe that the following actions are justified1–3:
- For prophylaxis to be effective, we must identify all infected patients. Therefore, screening of asymptomatic individuals during routine health encounters is essential.
- All patients should have access to easy-to-understand information related to risk factors for HIV infection.
- Every effort should be made to promote safe sex practices, such as use of latex condoms, avoidance of sex during menses and in the presence of ulcerative genital lesions, and avoidance of use of contaminated drug-injection needles.
- All high-risk patients, as defined above, should be offered PrEP.
- To the greatest extent possible, financial barriers to PrEP should be eliminated.
- Patients receiving PrEP should be monitored for evidence of renal dysfunction. Should they become infected despite prophylaxis, they should be evaluated carefully to detect drug-resistant viral strains.
- Although PrEP is definitely effective in reducing the risk of transmission of HIV infection, it does not prevent the transmission of other STIs, such as syphilis, gonorrhea, and chlamydia.
In my practice, I administer prophyaxis on a daily basis rather than just before, or after, a high-risk exposure. This approach enhances patient adherence and, hopefully, will lead to maximum effectiveness over time. I also use the combination of tenofovir disoproxil fumarate plus emtricitabine rather than tenofovir alone because there is more published information regarding the effectiveness of the combination regimen.
The first cases of HIV infection in the United States were reported in 1981. Since that time, more than 700,000 individuals in our country have died of AIDS. Slightly more than 1 million persons in the United States are currently living with HIV infection; approximately 15% of them are unaware of their infection. Men who have sex with men (MSM) and African American and Hispanic/Latino men and women are disproportionately affected by HIV infection.1 Among men, MSM is the most common method of infection transmission, accounting for 83% of infections. Heterosexual contact accounts for 9.4% of new infections and injection drug use for 4.0%. Among women in the United States, heterosexual contact is the most common mechanism of transmission, accounting for about 87% of cases; injection drug use accounts for about 12%.1 Perinatal transmission rates are extremely low—less than 1%—when women receive effective treatment during pregnancy and their infants are treated in the neonatal period.1,2
The prognosis for HIV-infected patients has improved dramatically in recent years with the availability of many new and exceptionally effective highly-active antiretroviral treatment regimens. Nevertheless, the disease is not yet completely curable. Therefore, preventive measures are of great importance in reducing the enormous toll imposed by this condition.2
Evaluating effectiveness of PrEP
At the request of the US Preventive Services Task Force, Chou and colleagues recently conducted a systematic review to determine the effectiveness of pre-exposure prophylaxis (PrEP) in preventing the horizontal transmission of HIV infection.1 The authors’ secondary objectives included assessing the relationship between degree of adherence to the prophylactic regimen and degree of effectiveness and evaluating the accuracy of various screening systems for identifying patients at high risk for acquiring HIV infection.
The authors reviewed prospective, randomized controlled trials (treatment versus no treatment or treatment versus placebo) published through 2018. Pregnant women were excluded from the studies, as were women who became pregnant after enrollment.
Two different prophylactic regimens were used in the reviewed studies: 1) the combination of tenofovir disoproxil fumarate 300 mg or 245 mg plus emtricitabine 200 mg and 2) tenofovir 300 mg alone. Most trials used the combination regimen. With the exception of one trial, the medications were given daily to uninfected patients at high risk of acquiring HIV infection. In one investigation, the administration of prophylaxis was event driven (administered after a specific high-risk exposure).
Key study findings
PrEP decreased HIV transmission in high-risk patients. Chou and colleagues found that high-risk patients included primarily MSM who did not use condoms consistently or who had a high number of sex partners, individuals in an HIV-serodiscordant relationship, and intravenous drug users who shared injection equipment.
In these high-risk patients, PrEP was associated with a significantly decreased risk of HIV transmission. Observations from 11 trials demonstrated a relative risk (RR) of 0.46 (95% confidence interval [CI], 0.33–0.66). The absolute risk reduction was -2.0% (95% CI, -2.8% to -1.2%). The duration of follow up ranged from 4 months to 4 years.
Continue to: Better medication adherence = greater prophylaxis effectiveness...
Better medication adherence = greater prophylaxis effectiveness. When adherence was ≥70%, the RR was 0.27 (95% CI, 0.19–0.39). When adherence was 40% to 70%, the RR was 0.51 (95% CI, 0.38–0.70). When adherence was ≤40%, the relative risk was 0.93 (95% CI, 0.72–1.20). Adherence was better with daily administration, as opposed to event-driven administration.
Although the combination prophylactic regimen (tenofovir plus emtricitabine) was most frequently used in the clinical trials, tenofovir alone was comparable in effectiveness.
PrEP resulted in more mild adverse effects. Patients who received PrEP were more likely to develop gastrointestinal adverse effects and renal function abnormalities when compared with patients in the control arms of the studies. These adverse effects were virtually always mild and did not necessitate discontinuation of treatment.
No increase in promiscuous sexual behavior with PrEP. Specifically, investigators did not document an increased incidence of new sexually transmitted infections (STIs) in treated patients.
PrEP did not increase adverse pregnancy outcomes. In women who became pregnant while on PrEP, and who then discontinued treatment, there was no increase in the frequency of spontaneous abortion, congenital anomalies, or other adverse pregnancy outcomes.
In addition, PrEP posed a low risk for causing drug resistance in patients who became infected despite prophylaxis. Finally, the authors found that screening instruments for identifying patients at highest risk for acquiring HIV infection had low to modest sensitivity.
My recommendations for practice
Based on the study by Chou and colleagues, and on a recent commentary by Marcus et al, I believe that the following actions are justified1–3:
- For prophylaxis to be effective, we must identify all infected patients. Therefore, screening of asymptomatic individuals during routine health encounters is essential.
- All patients should have access to easy-to-understand information related to risk factors for HIV infection.
- Every effort should be made to promote safe sex practices, such as use of latex condoms, avoidance of sex during menses and in the presence of ulcerative genital lesions, and avoidance of use of contaminated drug-injection needles.
- All high-risk patients, as defined above, should be offered PrEP.
- To the greatest extent possible, financial barriers to PrEP should be eliminated.
- Patients receiving PrEP should be monitored for evidence of renal dysfunction. Should they become infected despite prophylaxis, they should be evaluated carefully to detect drug-resistant viral strains.
- Although PrEP is definitely effective in reducing the risk of transmission of HIV infection, it does not prevent the transmission of other STIs, such as syphilis, gonorrhea, and chlamydia.
In my practice, I administer prophyaxis on a daily basis rather than just before, or after, a high-risk exposure. This approach enhances patient adherence and, hopefully, will lead to maximum effectiveness over time. I also use the combination of tenofovir disoproxil fumarate plus emtricitabine rather than tenofovir alone because there is more published information regarding the effectiveness of the combination regimen.
- Chou R, Evans C, Hoverman A, et al. Pre-exposure Prophylaxis for the Prevention of HIV Infection: A Systematic Review for the U.S. Preventive Services Task Force. AHRQ Publication No. 18-05247-EF-1; November 2018.
- Duff P. Maternal and fetal infections. In: Resnik R, Lockwood CJ, Moore TR, Green MF, Copel JA, Silver RM (eds). Creasy & Resnik's Maternal-Fetal Medicine. Principles and Practice (8th ed). Philadelphia, PA: Elsevier; 2019.
- Marcus JL, Katz KA, Krakower DS, et al. Risk compensation and clinical decision making--the case of HIV preexposure prophylaxis. N Engl J Med. 2019;380:510-512.
- Chou R, Evans C, Hoverman A, et al. Pre-exposure Prophylaxis for the Prevention of HIV Infection: A Systematic Review for the U.S. Preventive Services Task Force. AHRQ Publication No. 18-05247-EF-1; November 2018.
- Duff P. Maternal and fetal infections. In: Resnik R, Lockwood CJ, Moore TR, Green MF, Copel JA, Silver RM (eds). Creasy & Resnik's Maternal-Fetal Medicine. Principles and Practice (8th ed). Philadelphia, PA: Elsevier; 2019.
- Marcus JL, Katz KA, Krakower DS, et al. Risk compensation and clinical decision making--the case of HIV preexposure prophylaxis. N Engl J Med. 2019;380:510-512.
Following pelvic floor surgery, patients value functional goals
TUCSON, ARIZ. – according to results of a new study. Such negative reactions occur more frequently as time passes and may be related to incongruent patient expectations, which may in turn affect physician-patient communication.
“We must bridge the gap between expectations and the occurrence of an unanticipated problem. What this study highlights is a need for counseling beyond the traditional complications, and more discussion about the possibility of failure in terms of the things that the patients identify as important,” Brenna McGuire, MD, a resident at the University of New Mexico, Albuquerque, said while presenting the results at the annual scientific meeting of the Society of Gynecologic Surgeons.
The work highlights the need to look at outcomes in a different way, said Vivian Sung, MD, who was not involved in the research and was a discussant following the presentation. “Most of our studies are designed with methodology to emphasize efficacy and often secondary outcomes to capture complications and adverse events. But there is a gray area. It’s something that’s evolving, and we’re getting better at,” Dr. Sung, professor of obstetrics and gynecology at Brown University and a urogynecologist at Women and Infants Hospital, both in Providence, R.I., said in an interview.
The success of a procedure is typically evaluated by determining incontinence during an office visit, but the problem may not be occurring at that particular moment, and the patient may not be happy with the overall outcome. “Sometimes you can fix one problem, and the other problems become more prominent, or new problems develop. [Incontinence alone is] not a perfect picture or what the patient was envisioning her outcome to be,” Dr. Sung said.
Expectations can potentially be better managed through better patient counseling, but that’s not a simple fix either, she noted. Most surgeons counsel patients on negative outcomes, but adverse events with a 5%-10% probability may fail to make an impression. “Really, the rate is zero or 100%. It’s not that it doesn’t seem like a meaningful complication, it’s just that it doesn’t seem like it will happen to you. And then when it does, it can be very devastating depending on what it is and what your expectation was.”
Dr. McGuire and her associates followed 20 women (mean age, 55 years; 50% non-Hispanic white, 25% Hispanic, 25% Native American) at a single institution in New Mexico who underwent surgeries for pelvic floor disorders. They interviewed each participant before and after surgery, at 4-6 weeks, and 6 months after surgery, asking them to rank adverse events at each time point.
Before surgery, patients expressed concerns about postoperative pain, injury, and catheter issues. At 6-8 weeks, the chief concerns were daily activities, sexual activity, and symptom reduction. At 6 months, incontinence, sexual dysfunction, and mental health issues predominated. In other words, concerns migrated from traditional complications to functional outcomes over time.
At the 6-8 week interview, a representative quote was: “It’s the fact that it didn’t work. It’s the fact that I’m still suffering from all the same symptoms.” At 6 months, another quote was: “I hate this so much. It really does impact my life negatively. It affects my work, it affects everything, and makes me very angry.”
Traditional adverse events such as pain and infection dropped in frequency between the preoperative interview and the 6-month interview from 7.5%-10.0% to 2.5%-5.0% by 6 months. However, functional outcomes were a different matter: Concerns about a failed surgery increased from 10% to 25%, sexual dysfunction from 4% to 8%, and effect on daily function from 4% to 11%.
The study was funded by the University of New Mexico. Dr. McGuire and Dr. Sung reported no relevant financial disclosures.
SOURCE: McGuire B et al. SGS 2019, Abstract 01.
TUCSON, ARIZ. – according to results of a new study. Such negative reactions occur more frequently as time passes and may be related to incongruent patient expectations, which may in turn affect physician-patient communication.
“We must bridge the gap between expectations and the occurrence of an unanticipated problem. What this study highlights is a need for counseling beyond the traditional complications, and more discussion about the possibility of failure in terms of the things that the patients identify as important,” Brenna McGuire, MD, a resident at the University of New Mexico, Albuquerque, said while presenting the results at the annual scientific meeting of the Society of Gynecologic Surgeons.
The work highlights the need to look at outcomes in a different way, said Vivian Sung, MD, who was not involved in the research and was a discussant following the presentation. “Most of our studies are designed with methodology to emphasize efficacy and often secondary outcomes to capture complications and adverse events. But there is a gray area. It’s something that’s evolving, and we’re getting better at,” Dr. Sung, professor of obstetrics and gynecology at Brown University and a urogynecologist at Women and Infants Hospital, both in Providence, R.I., said in an interview.
The success of a procedure is typically evaluated by determining incontinence during an office visit, but the problem may not be occurring at that particular moment, and the patient may not be happy with the overall outcome. “Sometimes you can fix one problem, and the other problems become more prominent, or new problems develop. [Incontinence alone is] not a perfect picture or what the patient was envisioning her outcome to be,” Dr. Sung said.
Expectations can potentially be better managed through better patient counseling, but that’s not a simple fix either, she noted. Most surgeons counsel patients on negative outcomes, but adverse events with a 5%-10% probability may fail to make an impression. “Really, the rate is zero or 100%. It’s not that it doesn’t seem like a meaningful complication, it’s just that it doesn’t seem like it will happen to you. And then when it does, it can be very devastating depending on what it is and what your expectation was.”
Dr. McGuire and her associates followed 20 women (mean age, 55 years; 50% non-Hispanic white, 25% Hispanic, 25% Native American) at a single institution in New Mexico who underwent surgeries for pelvic floor disorders. They interviewed each participant before and after surgery, at 4-6 weeks, and 6 months after surgery, asking them to rank adverse events at each time point.
Before surgery, patients expressed concerns about postoperative pain, injury, and catheter issues. At 6-8 weeks, the chief concerns were daily activities, sexual activity, and symptom reduction. At 6 months, incontinence, sexual dysfunction, and mental health issues predominated. In other words, concerns migrated from traditional complications to functional outcomes over time.
At the 6-8 week interview, a representative quote was: “It’s the fact that it didn’t work. It’s the fact that I’m still suffering from all the same symptoms.” At 6 months, another quote was: “I hate this so much. It really does impact my life negatively. It affects my work, it affects everything, and makes me very angry.”
Traditional adverse events such as pain and infection dropped in frequency between the preoperative interview and the 6-month interview from 7.5%-10.0% to 2.5%-5.0% by 6 months. However, functional outcomes were a different matter: Concerns about a failed surgery increased from 10% to 25%, sexual dysfunction from 4% to 8%, and effect on daily function from 4% to 11%.
The study was funded by the University of New Mexico. Dr. McGuire and Dr. Sung reported no relevant financial disclosures.
SOURCE: McGuire B et al. SGS 2019, Abstract 01.
TUCSON, ARIZ. – according to results of a new study. Such negative reactions occur more frequently as time passes and may be related to incongruent patient expectations, which may in turn affect physician-patient communication.
“We must bridge the gap between expectations and the occurrence of an unanticipated problem. What this study highlights is a need for counseling beyond the traditional complications, and more discussion about the possibility of failure in terms of the things that the patients identify as important,” Brenna McGuire, MD, a resident at the University of New Mexico, Albuquerque, said while presenting the results at the annual scientific meeting of the Society of Gynecologic Surgeons.
The work highlights the need to look at outcomes in a different way, said Vivian Sung, MD, who was not involved in the research and was a discussant following the presentation. “Most of our studies are designed with methodology to emphasize efficacy and often secondary outcomes to capture complications and adverse events. But there is a gray area. It’s something that’s evolving, and we’re getting better at,” Dr. Sung, professor of obstetrics and gynecology at Brown University and a urogynecologist at Women and Infants Hospital, both in Providence, R.I., said in an interview.
The success of a procedure is typically evaluated by determining incontinence during an office visit, but the problem may not be occurring at that particular moment, and the patient may not be happy with the overall outcome. “Sometimes you can fix one problem, and the other problems become more prominent, or new problems develop. [Incontinence alone is] not a perfect picture or what the patient was envisioning her outcome to be,” Dr. Sung said.
Expectations can potentially be better managed through better patient counseling, but that’s not a simple fix either, she noted. Most surgeons counsel patients on negative outcomes, but adverse events with a 5%-10% probability may fail to make an impression. “Really, the rate is zero or 100%. It’s not that it doesn’t seem like a meaningful complication, it’s just that it doesn’t seem like it will happen to you. And then when it does, it can be very devastating depending on what it is and what your expectation was.”
Dr. McGuire and her associates followed 20 women (mean age, 55 years; 50% non-Hispanic white, 25% Hispanic, 25% Native American) at a single institution in New Mexico who underwent surgeries for pelvic floor disorders. They interviewed each participant before and after surgery, at 4-6 weeks, and 6 months after surgery, asking them to rank adverse events at each time point.
Before surgery, patients expressed concerns about postoperative pain, injury, and catheter issues. At 6-8 weeks, the chief concerns were daily activities, sexual activity, and symptom reduction. At 6 months, incontinence, sexual dysfunction, and mental health issues predominated. In other words, concerns migrated from traditional complications to functional outcomes over time.
At the 6-8 week interview, a representative quote was: “It’s the fact that it didn’t work. It’s the fact that I’m still suffering from all the same symptoms.” At 6 months, another quote was: “I hate this so much. It really does impact my life negatively. It affects my work, it affects everything, and makes me very angry.”
Traditional adverse events such as pain and infection dropped in frequency between the preoperative interview and the 6-month interview from 7.5%-10.0% to 2.5%-5.0% by 6 months. However, functional outcomes were a different matter: Concerns about a failed surgery increased from 10% to 25%, sexual dysfunction from 4% to 8%, and effect on daily function from 4% to 11%.
The study was funded by the University of New Mexico. Dr. McGuire and Dr. Sung reported no relevant financial disclosures.
SOURCE: McGuire B et al. SGS 2019, Abstract 01.
REPORTING FROM SGS 2019
New postmenopausal osteoporosis guidelines emphasize patient priorities
NEW ORLEANS – In new guidelines for the pharmacologic management of osteoporosis, bisphosphonates have been identified as the first-line therapy with denosumab (Prolia) listed as an acceptable alternative that is particularly well suited for high-risk patients, according to a presentation at the annual meeting of the Endocrine Society.
“We hope our guideline will not only improve patient care but provide confidence in treatment,” reported guideline writing committee member Clifford J. Rosen, MD, director of the Center for Clinical and Translational Research at Maine Medical Center Research Institute, Scarborough.
The new guidelines are evidence based, relying on randomized, controlled trials to evaluate the data quality of treatment options with GRADE methodology, but Dr. Rosen said that the guideline writing committee also considered patient preferences because of concerns about the abundant evidence that adherence to pharmacologic therapies for osteoporosis is poor.
“There is a considerable gap in the treatment of osteoporosis. Most women will not take anti-osteoporosis therapies despite their efficacy, and those who do often stop,” Dr. Rosen observed. He said it was the intention of the writing committee to provide acceptable recommendations with a clear outline of benefits and risks in order to enlist patients more successfully in understanding and participating in fracture prevention.
The Endocrine Society guidelines, which are available online and will soon appear in print (J Clin Endocrinol Metab. 2019;104:1-28), are focused on pharmacologic management and therefore differ from guidelines on diagnosis and treatment published previously by the American Association of Clinical Endocrinologists (AACE) (Endocr Pract. 2016;22[Suppl 4]:1-42).
The AACE guidelines, which devote considerable space to prevention, indicated that bisphosphonates should “be generally considered as initial options for most patients who are candidates for treatment.” The AACE guidelines identify denosumab as the “treatment of choice” in patients with renal insufficiency (although not in those on dialysis or with end-stage renal disease).
In outlining some of the key features of the new guidelines at ENDO 2019, Dr. Rosen drew attention to a call for reevaluation of the need for bisphosphonates after patients have been on this therapy for 3 or more years. For those found at this time to be at low or moderate risk of fracture, a drug holiday is recommended based on guideline-cited evidence that bisphosphonates offer a residual therapeutic effect after stopping.
However, stopping is not recommended in those who remain at high risk. In these patients, bone density should be monitored at regular intervals for the goal of switching or intensifying therapy if needed. This includes use of teriparatide (Forteo) or abaloparatide (Tymlos) for periods of up to 2 years in patients with a history of severe or multiple fractures. These and other choices are included in a detailed algorithm covering both low- and high-risk patients.
Although many postmenopausal women hope to avoid pharmacologic therapy with high dietary intake of calcium and vitamin D, Dr. Rosen stressed the limited benefit of these nutrients in preventing fracture for those with established osteoporosis. While acknowledging that calcium and vitamin D enhance mineralization and maintenance of bone mass, he characterized them as “supplements” once pharmacologic therapies are indicated.
Unsurprisingly, patients prefer oral therapies that are effective but with a low burden of adverse events, according to a review of evidence undertaken by the guideline committee. Cost was a less important consideration. Dr. Rosen indicated that recognizing patient goals and priorities while explaining relative risks might engage patients in selecting a therapy to which they are willing to adhere.
He reported having no relevant financial relationships.
NEW ORLEANS – In new guidelines for the pharmacologic management of osteoporosis, bisphosphonates have been identified as the first-line therapy with denosumab (Prolia) listed as an acceptable alternative that is particularly well suited for high-risk patients, according to a presentation at the annual meeting of the Endocrine Society.
“We hope our guideline will not only improve patient care but provide confidence in treatment,” reported guideline writing committee member Clifford J. Rosen, MD, director of the Center for Clinical and Translational Research at Maine Medical Center Research Institute, Scarborough.
The new guidelines are evidence based, relying on randomized, controlled trials to evaluate the data quality of treatment options with GRADE methodology, but Dr. Rosen said that the guideline writing committee also considered patient preferences because of concerns about the abundant evidence that adherence to pharmacologic therapies for osteoporosis is poor.
“There is a considerable gap in the treatment of osteoporosis. Most women will not take anti-osteoporosis therapies despite their efficacy, and those who do often stop,” Dr. Rosen observed. He said it was the intention of the writing committee to provide acceptable recommendations with a clear outline of benefits and risks in order to enlist patients more successfully in understanding and participating in fracture prevention.
The Endocrine Society guidelines, which are available online and will soon appear in print (J Clin Endocrinol Metab. 2019;104:1-28), are focused on pharmacologic management and therefore differ from guidelines on diagnosis and treatment published previously by the American Association of Clinical Endocrinologists (AACE) (Endocr Pract. 2016;22[Suppl 4]:1-42).
The AACE guidelines, which devote considerable space to prevention, indicated that bisphosphonates should “be generally considered as initial options for most patients who are candidates for treatment.” The AACE guidelines identify denosumab as the “treatment of choice” in patients with renal insufficiency (although not in those on dialysis or with end-stage renal disease).
In outlining some of the key features of the new guidelines at ENDO 2019, Dr. Rosen drew attention to a call for reevaluation of the need for bisphosphonates after patients have been on this therapy for 3 or more years. For those found at this time to be at low or moderate risk of fracture, a drug holiday is recommended based on guideline-cited evidence that bisphosphonates offer a residual therapeutic effect after stopping.
However, stopping is not recommended in those who remain at high risk. In these patients, bone density should be monitored at regular intervals for the goal of switching or intensifying therapy if needed. This includes use of teriparatide (Forteo) or abaloparatide (Tymlos) for periods of up to 2 years in patients with a history of severe or multiple fractures. These and other choices are included in a detailed algorithm covering both low- and high-risk patients.
Although many postmenopausal women hope to avoid pharmacologic therapy with high dietary intake of calcium and vitamin D, Dr. Rosen stressed the limited benefit of these nutrients in preventing fracture for those with established osteoporosis. While acknowledging that calcium and vitamin D enhance mineralization and maintenance of bone mass, he characterized them as “supplements” once pharmacologic therapies are indicated.
Unsurprisingly, patients prefer oral therapies that are effective but with a low burden of adverse events, according to a review of evidence undertaken by the guideline committee. Cost was a less important consideration. Dr. Rosen indicated that recognizing patient goals and priorities while explaining relative risks might engage patients in selecting a therapy to which they are willing to adhere.
He reported having no relevant financial relationships.
NEW ORLEANS – In new guidelines for the pharmacologic management of osteoporosis, bisphosphonates have been identified as the first-line therapy with denosumab (Prolia) listed as an acceptable alternative that is particularly well suited for high-risk patients, according to a presentation at the annual meeting of the Endocrine Society.
“We hope our guideline will not only improve patient care but provide confidence in treatment,” reported guideline writing committee member Clifford J. Rosen, MD, director of the Center for Clinical and Translational Research at Maine Medical Center Research Institute, Scarborough.
The new guidelines are evidence based, relying on randomized, controlled trials to evaluate the data quality of treatment options with GRADE methodology, but Dr. Rosen said that the guideline writing committee also considered patient preferences because of concerns about the abundant evidence that adherence to pharmacologic therapies for osteoporosis is poor.
“There is a considerable gap in the treatment of osteoporosis. Most women will not take anti-osteoporosis therapies despite their efficacy, and those who do often stop,” Dr. Rosen observed. He said it was the intention of the writing committee to provide acceptable recommendations with a clear outline of benefits and risks in order to enlist patients more successfully in understanding and participating in fracture prevention.
The Endocrine Society guidelines, which are available online and will soon appear in print (J Clin Endocrinol Metab. 2019;104:1-28), are focused on pharmacologic management and therefore differ from guidelines on diagnosis and treatment published previously by the American Association of Clinical Endocrinologists (AACE) (Endocr Pract. 2016;22[Suppl 4]:1-42).
The AACE guidelines, which devote considerable space to prevention, indicated that bisphosphonates should “be generally considered as initial options for most patients who are candidates for treatment.” The AACE guidelines identify denosumab as the “treatment of choice” in patients with renal insufficiency (although not in those on dialysis or with end-stage renal disease).
In outlining some of the key features of the new guidelines at ENDO 2019, Dr. Rosen drew attention to a call for reevaluation of the need for bisphosphonates after patients have been on this therapy for 3 or more years. For those found at this time to be at low or moderate risk of fracture, a drug holiday is recommended based on guideline-cited evidence that bisphosphonates offer a residual therapeutic effect after stopping.
However, stopping is not recommended in those who remain at high risk. In these patients, bone density should be monitored at regular intervals for the goal of switching or intensifying therapy if needed. This includes use of teriparatide (Forteo) or abaloparatide (Tymlos) for periods of up to 2 years in patients with a history of severe or multiple fractures. These and other choices are included in a detailed algorithm covering both low- and high-risk patients.
Although many postmenopausal women hope to avoid pharmacologic therapy with high dietary intake of calcium and vitamin D, Dr. Rosen stressed the limited benefit of these nutrients in preventing fracture for those with established osteoporosis. While acknowledging that calcium and vitamin D enhance mineralization and maintenance of bone mass, he characterized them as “supplements” once pharmacologic therapies are indicated.
Unsurprisingly, patients prefer oral therapies that are effective but with a low burden of adverse events, according to a review of evidence undertaken by the guideline committee. Cost was a less important consideration. Dr. Rosen indicated that recognizing patient goals and priorities while explaining relative risks might engage patients in selecting a therapy to which they are willing to adhere.
He reported having no relevant financial relationships.
REPORTING FROM ENDO 2019
Opportunistic salpingectomy appears to reduce risk of ovarian cancer
Women at high risk of ovarian cancer secondary to genetic predisposition (BRCA gene mutation, Lynch syndrome) still are recommended to undergo bilateral salpingo-oophorectomy after completion of child bearing or by age 40-45 years depending on the specific mutation and family history. For a woman not at risk of hereditary-related ovarian cancer, opportunistic salpingectomy would appear to reduce the risk of ovarian cancer.
Unlike bilateral tubal ligation, which has a greater protective risk of endometrioid and clear-cell carcinoma of the ovary, as well. A Swedish population-based cohort study involving over a quarter of a million women undergoing benign surgery noted a statistically significant decrease in ovarian cancer risk with salpingectomy. The degree of risk reduction was greater when bilateral salpingectomy was performed.1 Moreover, a Danish case-control study of over 13,000 women with ovarian cancer demonstrated a 42% decrease in epithelial carcinoma risk following bilateral salpingectomy.2
Bilateral salpingectomy does not appear to decrease ovarian function. A study by Venturella et al. that compared 91 women undergoing bilateral salpingectomy with 95 women with mesosalpinx removal within the tubes during salpingectomy observed no significant difference in change of ovarian reserve.3 Moreover, Kotlyar et al. performed a literature review and noted similar findings.4 Finally, in another study by Venturella et al. no effects were noted 3-5 years following prophylactic bilateral salpingectomy on ovarian reserve in women undergoing total laparoscopic hysterectomy in their late reproductive years, compared with healthy women with intact uterus and adnexa.5
Introduction of opportunistic salpingectomy secondary to potential ovarian cancer reduction has seen increased adoption over the years. A U.S. study of 400,000 hysterectomies performed for benign indications from 1998 to 2011 showed an increased annual rate of bilateral salpingectomy of 8% (1998-2008) and a 24% annual increase (2008-2011).6 A retrospective study of 12,143 hysterectomies performed within a large U.S. health care system reported an increased rate of salpingectomy from 15% in 2011 to 45% in 2012 to 73% in 2014.7
Given the fact that the American College of Obstetricians and Gynecologists and the AAGL recommend vaginal hysterectomy as the approach of choice when feasible, tips and tricks on opportunistic salpingectomy form an important topic.
For this edition of the Master Class in Gynecologic Surgery, I have enlisted the assistance of Rosanne M. Kho, MD. Dr. Kho’s academic and clinical work focuses on advancing vaginal and minimally invasive surgery. Dr. Kho is a strong advocate of the vaginal approach for benign hysterectomy and is recognized for her passion for bringing vaginal surgery back into the armamentarium of the gynecologic surgeon. Dr. Kho is published in the field of gynecologic surgery, having authored many peer-reviewed manuscripts and book chapters. She is currently an associate editor for the Journal of Minimally Invasive Gynecology (JMIG).
It is truly a pleasure to welcome Dr. Kho to this edition of the Master Class in Gynecologic Surgery.
Dr. Miller is a clinical associate professor at the University of Illinois in Chicago and past president of the AAGL. He is a reproductive endocrinologist and minimally invasive gynecologic surgeon in metropolitan Chicago and the director of minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, Ill. He has no disclosures relevant to this Master Class.
References
1. J Natl Cancer Inst. 2015 Jan 27. doi: 10.1093/jnci/dju410.
2. Acta Obstet Gynecol Scand. 2015 Jan;94(1):86-94.
3. Fertil Steril. 2015 Nov;104(5):1332-9.
4. J Minim Invasive Gynecol. 2017 May-Jun;24(4):563-78.
5. J Minim Invasive Gynecol. 2017 Jan 1;24(1):145-50.
6. Am J Obstet Gynecol. 2015 Nov;213(5):713.e1-13.
7. Obstet Gynecol. 2016 Aug;128(2):277-83.
Women at high risk of ovarian cancer secondary to genetic predisposition (BRCA gene mutation, Lynch syndrome) still are recommended to undergo bilateral salpingo-oophorectomy after completion of child bearing or by age 40-45 years depending on the specific mutation and family history. For a woman not at risk of hereditary-related ovarian cancer, opportunistic salpingectomy would appear to reduce the risk of ovarian cancer.
Unlike bilateral tubal ligation, which has a greater protective risk of endometrioid and clear-cell carcinoma of the ovary, as well. A Swedish population-based cohort study involving over a quarter of a million women undergoing benign surgery noted a statistically significant decrease in ovarian cancer risk with salpingectomy. The degree of risk reduction was greater when bilateral salpingectomy was performed.1 Moreover, a Danish case-control study of over 13,000 women with ovarian cancer demonstrated a 42% decrease in epithelial carcinoma risk following bilateral salpingectomy.2
Bilateral salpingectomy does not appear to decrease ovarian function. A study by Venturella et al. that compared 91 women undergoing bilateral salpingectomy with 95 women with mesosalpinx removal within the tubes during salpingectomy observed no significant difference in change of ovarian reserve.3 Moreover, Kotlyar et al. performed a literature review and noted similar findings.4 Finally, in another study by Venturella et al. no effects were noted 3-5 years following prophylactic bilateral salpingectomy on ovarian reserve in women undergoing total laparoscopic hysterectomy in their late reproductive years, compared with healthy women with intact uterus and adnexa.5
Introduction of opportunistic salpingectomy secondary to potential ovarian cancer reduction has seen increased adoption over the years. A U.S. study of 400,000 hysterectomies performed for benign indications from 1998 to 2011 showed an increased annual rate of bilateral salpingectomy of 8% (1998-2008) and a 24% annual increase (2008-2011).6 A retrospective study of 12,143 hysterectomies performed within a large U.S. health care system reported an increased rate of salpingectomy from 15% in 2011 to 45% in 2012 to 73% in 2014.7
Given the fact that the American College of Obstetricians and Gynecologists and the AAGL recommend vaginal hysterectomy as the approach of choice when feasible, tips and tricks on opportunistic salpingectomy form an important topic.
For this edition of the Master Class in Gynecologic Surgery, I have enlisted the assistance of Rosanne M. Kho, MD. Dr. Kho’s academic and clinical work focuses on advancing vaginal and minimally invasive surgery. Dr. Kho is a strong advocate of the vaginal approach for benign hysterectomy and is recognized for her passion for bringing vaginal surgery back into the armamentarium of the gynecologic surgeon. Dr. Kho is published in the field of gynecologic surgery, having authored many peer-reviewed manuscripts and book chapters. She is currently an associate editor for the Journal of Minimally Invasive Gynecology (JMIG).
It is truly a pleasure to welcome Dr. Kho to this edition of the Master Class in Gynecologic Surgery.
Dr. Miller is a clinical associate professor at the University of Illinois in Chicago and past president of the AAGL. He is a reproductive endocrinologist and minimally invasive gynecologic surgeon in metropolitan Chicago and the director of minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, Ill. He has no disclosures relevant to this Master Class.
References
1. J Natl Cancer Inst. 2015 Jan 27. doi: 10.1093/jnci/dju410.
2. Acta Obstet Gynecol Scand. 2015 Jan;94(1):86-94.
3. Fertil Steril. 2015 Nov;104(5):1332-9.
4. J Minim Invasive Gynecol. 2017 May-Jun;24(4):563-78.
5. J Minim Invasive Gynecol. 2017 Jan 1;24(1):145-50.
6. Am J Obstet Gynecol. 2015 Nov;213(5):713.e1-13.
7. Obstet Gynecol. 2016 Aug;128(2):277-83.
Women at high risk of ovarian cancer secondary to genetic predisposition (BRCA gene mutation, Lynch syndrome) still are recommended to undergo bilateral salpingo-oophorectomy after completion of child bearing or by age 40-45 years depending on the specific mutation and family history. For a woman not at risk of hereditary-related ovarian cancer, opportunistic salpingectomy would appear to reduce the risk of ovarian cancer.
Unlike bilateral tubal ligation, which has a greater protective risk of endometrioid and clear-cell carcinoma of the ovary, as well. A Swedish population-based cohort study involving over a quarter of a million women undergoing benign surgery noted a statistically significant decrease in ovarian cancer risk with salpingectomy. The degree of risk reduction was greater when bilateral salpingectomy was performed.1 Moreover, a Danish case-control study of over 13,000 women with ovarian cancer demonstrated a 42% decrease in epithelial carcinoma risk following bilateral salpingectomy.2
Bilateral salpingectomy does not appear to decrease ovarian function. A study by Venturella et al. that compared 91 women undergoing bilateral salpingectomy with 95 women with mesosalpinx removal within the tubes during salpingectomy observed no significant difference in change of ovarian reserve.3 Moreover, Kotlyar et al. performed a literature review and noted similar findings.4 Finally, in another study by Venturella et al. no effects were noted 3-5 years following prophylactic bilateral salpingectomy on ovarian reserve in women undergoing total laparoscopic hysterectomy in their late reproductive years, compared with healthy women with intact uterus and adnexa.5
Introduction of opportunistic salpingectomy secondary to potential ovarian cancer reduction has seen increased adoption over the years. A U.S. study of 400,000 hysterectomies performed for benign indications from 1998 to 2011 showed an increased annual rate of bilateral salpingectomy of 8% (1998-2008) and a 24% annual increase (2008-2011).6 A retrospective study of 12,143 hysterectomies performed within a large U.S. health care system reported an increased rate of salpingectomy from 15% in 2011 to 45% in 2012 to 73% in 2014.7
Given the fact that the American College of Obstetricians and Gynecologists and the AAGL recommend vaginal hysterectomy as the approach of choice when feasible, tips and tricks on opportunistic salpingectomy form an important topic.
For this edition of the Master Class in Gynecologic Surgery, I have enlisted the assistance of Rosanne M. Kho, MD. Dr. Kho’s academic and clinical work focuses on advancing vaginal and minimally invasive surgery. Dr. Kho is a strong advocate of the vaginal approach for benign hysterectomy and is recognized for her passion for bringing vaginal surgery back into the armamentarium of the gynecologic surgeon. Dr. Kho is published in the field of gynecologic surgery, having authored many peer-reviewed manuscripts and book chapters. She is currently an associate editor for the Journal of Minimally Invasive Gynecology (JMIG).
It is truly a pleasure to welcome Dr. Kho to this edition of the Master Class in Gynecologic Surgery.
Dr. Miller is a clinical associate professor at the University of Illinois in Chicago and past president of the AAGL. He is a reproductive endocrinologist and minimally invasive gynecologic surgeon in metropolitan Chicago and the director of minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, Ill. He has no disclosures relevant to this Master Class.
References
1. J Natl Cancer Inst. 2015 Jan 27. doi: 10.1093/jnci/dju410.
2. Acta Obstet Gynecol Scand. 2015 Jan;94(1):86-94.
3. Fertil Steril. 2015 Nov;104(5):1332-9.
4. J Minim Invasive Gynecol. 2017 May-Jun;24(4):563-78.
5. J Minim Invasive Gynecol. 2017 Jan 1;24(1):145-50.
6. Am J Obstet Gynecol. 2015 Nov;213(5):713.e1-13.
7. Obstet Gynecol. 2016 Aug;128(2):277-83.
FDA approves brexanolone for postpartum depression
The Food and Drug Administration on March 19 approved the first medication specifically for the treatment of postpartum depression.
The drug, brexanolone (Zulresso), is to be administered as a single continuous 60-hour infusion for each episode of postpartum depression. . By binding to GABA A receptors, brexanolone increases receptor functionality. The recommended maximum dose of brexanolone is 90 µg/kg/h, and the infusion includes three dosing phases.
Brexanolone provides “an important new treatment option,” said Tiffany Farchione, MD, acting director of the division of psychiatry products in the FDA’s Center for Drug Evaluation and Research, in a press release. “Because of concerns about serious risks, including excessive sedation or sudden loss of consciousness during administration, Zulresso has been approved with a Risk Evaluation and Mitigation Strategy (REMS) and is only available to patients through a restricted distribution program at certified health care facilities where the health care provider can carefully monitor the patient.”
The approval was based on results of three phase 3 trials, which were double-blind, randomized, and placebo-controlled studies in which the primary efficacy endpoint was a change in baseline 60 hours after the start of the infusion on the Hamilton Depression Rating Scale (HAM-D). In all two of the trials, known as Hummingbird 202B and 202C, brexanolone’s impact on the patients’ HAM-D scores was greater than that of placebo, the FDA reported in briefing document released late last year. In addition, the impact of brexanolone on postpartum depression proved both rapid and durable.
Side effects observed in about 3% of the brexanolone patients included dizziness, dry mouth, fatigue, headache, infusion site pain, somnolence, and loss of consciousness. The FDA’s concern about loss of consciousness led the agency to recommend a REMS protocol before a hearing of its Psychopharmacologic Drugs Advisory and Drug Safety and Risk Management Advisory panels late last year. The Zulresso REMS Program will require that the drug be administered by a clinician in a health care facility that is certified. Patients will have to be monitored for excessive sedation and “sudden loss of consciousness and have continuous pulse oximetry monitoring (monitors oxygen levels in the blood),” the FDA said. Another requirement is that patients who receive the infusion will have to be accompanied while interacting with their children. Patients will be advised not to drive, operate machinery or engage in other dangerous activities until they feel totally alert. Those requirements will be addressed in a boxed warning.
The drug should be either adjusted or discontinued for patients whose postpartum depression becomes worse or for those experience suicidal thoughts and behaviors after taking brexanolone, the agency said.
Some physicians use antidepressants to treat postpartum depression, but their effectiveness is limited, according to the FDA. Interventions such as electroconvulsive therapy and psychotherapy also are used, but getting results can several weeks.
The symptoms of postpartum depression are indistinguishable from major depressive disorder, but “the timing of its onset has led to its recognition as potentially unique illness,” the FDA said. Postpartum depression in the United States affects up to 12% of births. In the developed world, suicide is the most common cause of maternal death after childbirth. This suicide risk makes postpartum depression a condition that is life-threatening. In addition, the condition has “profound negative effects on the maternal-infant bond and later infant development,” the FDA said.
SAGE Therapeutics, developer of brexanolone, secured the approval through the FDA’s breakthrough therapy designation process.
Heidi Splete contributed to this article.
The Food and Drug Administration on March 19 approved the first medication specifically for the treatment of postpartum depression.
The drug, brexanolone (Zulresso), is to be administered as a single continuous 60-hour infusion for each episode of postpartum depression. . By binding to GABA A receptors, brexanolone increases receptor functionality. The recommended maximum dose of brexanolone is 90 µg/kg/h, and the infusion includes three dosing phases.
Brexanolone provides “an important new treatment option,” said Tiffany Farchione, MD, acting director of the division of psychiatry products in the FDA’s Center for Drug Evaluation and Research, in a press release. “Because of concerns about serious risks, including excessive sedation or sudden loss of consciousness during administration, Zulresso has been approved with a Risk Evaluation and Mitigation Strategy (REMS) and is only available to patients through a restricted distribution program at certified health care facilities where the health care provider can carefully monitor the patient.”
The approval was based on results of three phase 3 trials, which were double-blind, randomized, and placebo-controlled studies in which the primary efficacy endpoint was a change in baseline 60 hours after the start of the infusion on the Hamilton Depression Rating Scale (HAM-D). In all two of the trials, known as Hummingbird 202B and 202C, brexanolone’s impact on the patients’ HAM-D scores was greater than that of placebo, the FDA reported in briefing document released late last year. In addition, the impact of brexanolone on postpartum depression proved both rapid and durable.
Side effects observed in about 3% of the brexanolone patients included dizziness, dry mouth, fatigue, headache, infusion site pain, somnolence, and loss of consciousness. The FDA’s concern about loss of consciousness led the agency to recommend a REMS protocol before a hearing of its Psychopharmacologic Drugs Advisory and Drug Safety and Risk Management Advisory panels late last year. The Zulresso REMS Program will require that the drug be administered by a clinician in a health care facility that is certified. Patients will have to be monitored for excessive sedation and “sudden loss of consciousness and have continuous pulse oximetry monitoring (monitors oxygen levels in the blood),” the FDA said. Another requirement is that patients who receive the infusion will have to be accompanied while interacting with their children. Patients will be advised not to drive, operate machinery or engage in other dangerous activities until they feel totally alert. Those requirements will be addressed in a boxed warning.
The drug should be either adjusted or discontinued for patients whose postpartum depression becomes worse or for those experience suicidal thoughts and behaviors after taking brexanolone, the agency said.
Some physicians use antidepressants to treat postpartum depression, but their effectiveness is limited, according to the FDA. Interventions such as electroconvulsive therapy and psychotherapy also are used, but getting results can several weeks.
The symptoms of postpartum depression are indistinguishable from major depressive disorder, but “the timing of its onset has led to its recognition as potentially unique illness,” the FDA said. Postpartum depression in the United States affects up to 12% of births. In the developed world, suicide is the most common cause of maternal death after childbirth. This suicide risk makes postpartum depression a condition that is life-threatening. In addition, the condition has “profound negative effects on the maternal-infant bond and later infant development,” the FDA said.
SAGE Therapeutics, developer of brexanolone, secured the approval through the FDA’s breakthrough therapy designation process.
Heidi Splete contributed to this article.
The Food and Drug Administration on March 19 approved the first medication specifically for the treatment of postpartum depression.
The drug, brexanolone (Zulresso), is to be administered as a single continuous 60-hour infusion for each episode of postpartum depression. . By binding to GABA A receptors, brexanolone increases receptor functionality. The recommended maximum dose of brexanolone is 90 µg/kg/h, and the infusion includes three dosing phases.
Brexanolone provides “an important new treatment option,” said Tiffany Farchione, MD, acting director of the division of psychiatry products in the FDA’s Center for Drug Evaluation and Research, in a press release. “Because of concerns about serious risks, including excessive sedation or sudden loss of consciousness during administration, Zulresso has been approved with a Risk Evaluation and Mitigation Strategy (REMS) and is only available to patients through a restricted distribution program at certified health care facilities where the health care provider can carefully monitor the patient.”
The approval was based on results of three phase 3 trials, which were double-blind, randomized, and placebo-controlled studies in which the primary efficacy endpoint was a change in baseline 60 hours after the start of the infusion on the Hamilton Depression Rating Scale (HAM-D). In all two of the trials, known as Hummingbird 202B and 202C, brexanolone’s impact on the patients’ HAM-D scores was greater than that of placebo, the FDA reported in briefing document released late last year. In addition, the impact of brexanolone on postpartum depression proved both rapid and durable.
Side effects observed in about 3% of the brexanolone patients included dizziness, dry mouth, fatigue, headache, infusion site pain, somnolence, and loss of consciousness. The FDA’s concern about loss of consciousness led the agency to recommend a REMS protocol before a hearing of its Psychopharmacologic Drugs Advisory and Drug Safety and Risk Management Advisory panels late last year. The Zulresso REMS Program will require that the drug be administered by a clinician in a health care facility that is certified. Patients will have to be monitored for excessive sedation and “sudden loss of consciousness and have continuous pulse oximetry monitoring (monitors oxygen levels in the blood),” the FDA said. Another requirement is that patients who receive the infusion will have to be accompanied while interacting with their children. Patients will be advised not to drive, operate machinery or engage in other dangerous activities until they feel totally alert. Those requirements will be addressed in a boxed warning.
The drug should be either adjusted or discontinued for patients whose postpartum depression becomes worse or for those experience suicidal thoughts and behaviors after taking brexanolone, the agency said.
Some physicians use antidepressants to treat postpartum depression, but their effectiveness is limited, according to the FDA. Interventions such as electroconvulsive therapy and psychotherapy also are used, but getting results can several weeks.
The symptoms of postpartum depression are indistinguishable from major depressive disorder, but “the timing of its onset has led to its recognition as potentially unique illness,” the FDA said. Postpartum depression in the United States affects up to 12% of births. In the developed world, suicide is the most common cause of maternal death after childbirth. This suicide risk makes postpartum depression a condition that is life-threatening. In addition, the condition has “profound negative effects on the maternal-infant bond and later infant development,” the FDA said.
SAGE Therapeutics, developer of brexanolone, secured the approval through the FDA’s breakthrough therapy designation process.
Heidi Splete contributed to this article.
Access to abortion care: Facts matter
In 1973, the Supreme Court of the United States recognized a constitutional right to abortion in the landmark case of Roe v Wade. The Court held that states may regulate, but not ban, abortion after the first trimester, for the purpose of protecting the woman’s health. The Court further indicated that states’ interest in “potential life” could be the basis for abortion regulations only after the point of viability, at which point states may ban abortion except when necessary to preserve the life or health of the woman.1 In 1992, the Court decided Planned Parenthood v Casey and eliminated the trimester framework while upholding women’s right to abortion.2 As with Roe v Wade, the Casey decision held that there must be an exception for the woman’s health and life.
Fast forward to 2019
New York passed a law in 2019,3 and Virginia had a proposed law that was recently tabled by the House of Delegates,4 both related to abortions performed past the first trimester.
New York. The New York law supports legal abortion by a licensed practitioner within 24 weeks of pregnancy commencement. After 24 weeks’ gestation, if there is “an absence of fetal viability, or the abortion is necessary to protect the patient’s life or health” then termination is permissible.3
Virginia. Previously, Virginia had abortion laws that required significant measures to approve a third-trimester abortion, including certification by 3 physicians that the procedure is necessary to “save mother’s life or [prevent] substantial and irremediable impairment of mental or physical health of the mother.”5 Violation included potential for jail time and a significant monetary fine.
The proposed bill, now tabled, was introduced by delegate Kathy Tran (House Bill 2491) and would have rolled back many requirements of the old law, including the 24-hour waiting period and mandate for second-trimester abortions to occur in a hospital.
The controversy centered on a provision concerning third-trimester abortions. Specifically, the proposed bill would only have required 1 doctor to deem the abortion necessary and would have removed the “substantially and irremediably” qualifier. Thus, abortions would be allowed in cases in which the woman’s mental or physical health was threatened, even in cases in which the potential damage may be reversible.5
The facts
Misconceptions about abortion care can be dangerous and work to further stigmatize our patients who may need an abortion or who have had an abortion in the past. The American College of Obstetricians and Gynecologists (ACOG) recently published a document discussing facts regarding abortion care later in pregnancy. The document (aptly named “Facts are Important”) enforces that policy be based on medical science and facts, and not simply driven by political beliefs.6
Fact. The majority of abortions occur prior to 21 weeks, before viability:
- 91.1% of abortions occur at or before 13 weeks’ gestation7
- only 1.3% of abortions occur at or after 21 weeks’ gestation7
- abortions occurring later in the second trimester or in the third trimester are very uncommon.
Fact. The language “late-term abortion” has no medical definition, is not used in a clinical setting or to describe the delivery of abortion care later in pregnancy in any medical institution.6
Fact. Many of the abortions occurring later in pregnancy are due to fetal anomalies incompatible with life. Anomalies can include lack of a major portion of the brain (anencephaly), bilateral renal agenesis, some skeletal dysplasias, and other chromosomal abnormalities. These are cases in which death is likely before or shortly after birth, with great potential for suffering of both the fetus and the family.
Fact. The need for abortion also may be due to serious complications that will likely cause significant morbidity or mortality to the woman. These complications, in turn, reduce the likelihood of survival of the fetus.
It is thus vital for women to have the freedom to evaluate their medical circumstance with their provider and, using evidence, make informed health care decisions—which may include abortion, induction of labor, or cesarean delivery in some circumstances. Access to accurate, complete information and care is a right bestowed amongst all women and “must never be constrained by politicians.”6 We must focus on medically appropriate and compassionate care for both the family and the fetus.
Use your voice
As clinicians, we are trusted members of our communities. The New York law and the prior proposed Virginia law emphasize important access to care for women and their families. Abortions at a later gestational age are a rare event but are most often performed when the health or life of the mother is at risk or the fetus has an anomaly incompatible with life.
We urge you to use your voice to correct misconceptions, whether in your office with your patients or colleagues or in your communities, locally and nationally. Email your friends and colleagues about ACOG’s “Facts are Important” document, organize a grand rounds on the topic, and utilize social media to share facts about abortion care. These actions support our patients and can make an impact by spreading factual information.
For more facts and figures about abortion laws, visit the website of the Guttmacher Institute.
- Roe v Wade, 410 US 113 (1973).
- Planned Parenthood v Casey, 505 US 833 (1992).
- New York abortion laws. FindLaw website. https://statelaws.findlaw.com/new-york-law/new-york-abortion-laws.html. Accessed March 7, 2019.
- North A. The controversy around Virginia’s new abortion bill, explained. https://www.vox.com/2019/2/1/18205428/virginia-abortion-bill-kathy-tran-ralph-northam Accessed March 13, 2019.
- Virginia abortion laws. FindLaw website. https://statelaws.findlaw.com/virginia-law/virginia-abortion-laws.html. Accessed March 7, 2019.
- Facts are important. The American College of Obstetricians and Gynecologists website. https://www.acog.org/-/media/Departments/Government-Relations-and-Outreach/Facts-Are-Important_Abortion-Care-Later-In-Pregnancy-February-2019-College.pdf?dmc=1&ts=20190214T2242210541. Accessed March 7, 2019.
- Jatlaoui TC, Boutot ME, Mandel MG, et al. Abortion surveillance—United States, 2015. MMWR Surveill Summ. 2018;67(13):1-45.
In 1973, the Supreme Court of the United States recognized a constitutional right to abortion in the landmark case of Roe v Wade. The Court held that states may regulate, but not ban, abortion after the first trimester, for the purpose of protecting the woman’s health. The Court further indicated that states’ interest in “potential life” could be the basis for abortion regulations only after the point of viability, at which point states may ban abortion except when necessary to preserve the life or health of the woman.1 In 1992, the Court decided Planned Parenthood v Casey and eliminated the trimester framework while upholding women’s right to abortion.2 As with Roe v Wade, the Casey decision held that there must be an exception for the woman’s health and life.
Fast forward to 2019
New York passed a law in 2019,3 and Virginia had a proposed law that was recently tabled by the House of Delegates,4 both related to abortions performed past the first trimester.
New York. The New York law supports legal abortion by a licensed practitioner within 24 weeks of pregnancy commencement. After 24 weeks’ gestation, if there is “an absence of fetal viability, or the abortion is necessary to protect the patient’s life or health” then termination is permissible.3
Virginia. Previously, Virginia had abortion laws that required significant measures to approve a third-trimester abortion, including certification by 3 physicians that the procedure is necessary to “save mother’s life or [prevent] substantial and irremediable impairment of mental or physical health of the mother.”5 Violation included potential for jail time and a significant monetary fine.
The proposed bill, now tabled, was introduced by delegate Kathy Tran (House Bill 2491) and would have rolled back many requirements of the old law, including the 24-hour waiting period and mandate for second-trimester abortions to occur in a hospital.
The controversy centered on a provision concerning third-trimester abortions. Specifically, the proposed bill would only have required 1 doctor to deem the abortion necessary and would have removed the “substantially and irremediably” qualifier. Thus, abortions would be allowed in cases in which the woman’s mental or physical health was threatened, even in cases in which the potential damage may be reversible.5
The facts
Misconceptions about abortion care can be dangerous and work to further stigmatize our patients who may need an abortion or who have had an abortion in the past. The American College of Obstetricians and Gynecologists (ACOG) recently published a document discussing facts regarding abortion care later in pregnancy. The document (aptly named “Facts are Important”) enforces that policy be based on medical science and facts, and not simply driven by political beliefs.6
Fact. The majority of abortions occur prior to 21 weeks, before viability:
- 91.1% of abortions occur at or before 13 weeks’ gestation7
- only 1.3% of abortions occur at or after 21 weeks’ gestation7
- abortions occurring later in the second trimester or in the third trimester are very uncommon.
Fact. The language “late-term abortion” has no medical definition, is not used in a clinical setting or to describe the delivery of abortion care later in pregnancy in any medical institution.6
Fact. Many of the abortions occurring later in pregnancy are due to fetal anomalies incompatible with life. Anomalies can include lack of a major portion of the brain (anencephaly), bilateral renal agenesis, some skeletal dysplasias, and other chromosomal abnormalities. These are cases in which death is likely before or shortly after birth, with great potential for suffering of both the fetus and the family.
Fact. The need for abortion also may be due to serious complications that will likely cause significant morbidity or mortality to the woman. These complications, in turn, reduce the likelihood of survival of the fetus.
It is thus vital for women to have the freedom to evaluate their medical circumstance with their provider and, using evidence, make informed health care decisions—which may include abortion, induction of labor, or cesarean delivery in some circumstances. Access to accurate, complete information and care is a right bestowed amongst all women and “must never be constrained by politicians.”6 We must focus on medically appropriate and compassionate care for both the family and the fetus.
Use your voice
As clinicians, we are trusted members of our communities. The New York law and the prior proposed Virginia law emphasize important access to care for women and their families. Abortions at a later gestational age are a rare event but are most often performed when the health or life of the mother is at risk or the fetus has an anomaly incompatible with life.
We urge you to use your voice to correct misconceptions, whether in your office with your patients or colleagues or in your communities, locally and nationally. Email your friends and colleagues about ACOG’s “Facts are Important” document, organize a grand rounds on the topic, and utilize social media to share facts about abortion care. These actions support our patients and can make an impact by spreading factual information.
For more facts and figures about abortion laws, visit the website of the Guttmacher Institute.
In 1973, the Supreme Court of the United States recognized a constitutional right to abortion in the landmark case of Roe v Wade. The Court held that states may regulate, but not ban, abortion after the first trimester, for the purpose of protecting the woman’s health. The Court further indicated that states’ interest in “potential life” could be the basis for abortion regulations only after the point of viability, at which point states may ban abortion except when necessary to preserve the life or health of the woman.1 In 1992, the Court decided Planned Parenthood v Casey and eliminated the trimester framework while upholding women’s right to abortion.2 As with Roe v Wade, the Casey decision held that there must be an exception for the woman’s health and life.
Fast forward to 2019
New York passed a law in 2019,3 and Virginia had a proposed law that was recently tabled by the House of Delegates,4 both related to abortions performed past the first trimester.
New York. The New York law supports legal abortion by a licensed practitioner within 24 weeks of pregnancy commencement. After 24 weeks’ gestation, if there is “an absence of fetal viability, or the abortion is necessary to protect the patient’s life or health” then termination is permissible.3
Virginia. Previously, Virginia had abortion laws that required significant measures to approve a third-trimester abortion, including certification by 3 physicians that the procedure is necessary to “save mother’s life or [prevent] substantial and irremediable impairment of mental or physical health of the mother.”5 Violation included potential for jail time and a significant monetary fine.
The proposed bill, now tabled, was introduced by delegate Kathy Tran (House Bill 2491) and would have rolled back many requirements of the old law, including the 24-hour waiting period and mandate for second-trimester abortions to occur in a hospital.
The controversy centered on a provision concerning third-trimester abortions. Specifically, the proposed bill would only have required 1 doctor to deem the abortion necessary and would have removed the “substantially and irremediably” qualifier. Thus, abortions would be allowed in cases in which the woman’s mental or physical health was threatened, even in cases in which the potential damage may be reversible.5
The facts
Misconceptions about abortion care can be dangerous and work to further stigmatize our patients who may need an abortion or who have had an abortion in the past. The American College of Obstetricians and Gynecologists (ACOG) recently published a document discussing facts regarding abortion care later in pregnancy. The document (aptly named “Facts are Important”) enforces that policy be based on medical science and facts, and not simply driven by political beliefs.6
Fact. The majority of abortions occur prior to 21 weeks, before viability:
- 91.1% of abortions occur at or before 13 weeks’ gestation7
- only 1.3% of abortions occur at or after 21 weeks’ gestation7
- abortions occurring later in the second trimester or in the third trimester are very uncommon.
Fact. The language “late-term abortion” has no medical definition, is not used in a clinical setting or to describe the delivery of abortion care later in pregnancy in any medical institution.6
Fact. Many of the abortions occurring later in pregnancy are due to fetal anomalies incompatible with life. Anomalies can include lack of a major portion of the brain (anencephaly), bilateral renal agenesis, some skeletal dysplasias, and other chromosomal abnormalities. These are cases in which death is likely before or shortly after birth, with great potential for suffering of both the fetus and the family.
Fact. The need for abortion also may be due to serious complications that will likely cause significant morbidity or mortality to the woman. These complications, in turn, reduce the likelihood of survival of the fetus.
It is thus vital for women to have the freedom to evaluate their medical circumstance with their provider and, using evidence, make informed health care decisions—which may include abortion, induction of labor, or cesarean delivery in some circumstances. Access to accurate, complete information and care is a right bestowed amongst all women and “must never be constrained by politicians.”6 We must focus on medically appropriate and compassionate care for both the family and the fetus.
Use your voice
As clinicians, we are trusted members of our communities. The New York law and the prior proposed Virginia law emphasize important access to care for women and their families. Abortions at a later gestational age are a rare event but are most often performed when the health or life of the mother is at risk or the fetus has an anomaly incompatible with life.
We urge you to use your voice to correct misconceptions, whether in your office with your patients or colleagues or in your communities, locally and nationally. Email your friends and colleagues about ACOG’s “Facts are Important” document, organize a grand rounds on the topic, and utilize social media to share facts about abortion care. These actions support our patients and can make an impact by spreading factual information.
For more facts and figures about abortion laws, visit the website of the Guttmacher Institute.
- Roe v Wade, 410 US 113 (1973).
- Planned Parenthood v Casey, 505 US 833 (1992).
- New York abortion laws. FindLaw website. https://statelaws.findlaw.com/new-york-law/new-york-abortion-laws.html. Accessed March 7, 2019.
- North A. The controversy around Virginia’s new abortion bill, explained. https://www.vox.com/2019/2/1/18205428/virginia-abortion-bill-kathy-tran-ralph-northam Accessed March 13, 2019.
- Virginia abortion laws. FindLaw website. https://statelaws.findlaw.com/virginia-law/virginia-abortion-laws.html. Accessed March 7, 2019.
- Facts are important. The American College of Obstetricians and Gynecologists website. https://www.acog.org/-/media/Departments/Government-Relations-and-Outreach/Facts-Are-Important_Abortion-Care-Later-In-Pregnancy-February-2019-College.pdf?dmc=1&ts=20190214T2242210541. Accessed March 7, 2019.
- Jatlaoui TC, Boutot ME, Mandel MG, et al. Abortion surveillance—United States, 2015. MMWR Surveill Summ. 2018;67(13):1-45.
- Roe v Wade, 410 US 113 (1973).
- Planned Parenthood v Casey, 505 US 833 (1992).
- New York abortion laws. FindLaw website. https://statelaws.findlaw.com/new-york-law/new-york-abortion-laws.html. Accessed March 7, 2019.
- North A. The controversy around Virginia’s new abortion bill, explained. https://www.vox.com/2019/2/1/18205428/virginia-abortion-bill-kathy-tran-ralph-northam Accessed March 13, 2019.
- Virginia abortion laws. FindLaw website. https://statelaws.findlaw.com/virginia-law/virginia-abortion-laws.html. Accessed March 7, 2019.
- Facts are important. The American College of Obstetricians and Gynecologists website. https://www.acog.org/-/media/Departments/Government-Relations-and-Outreach/Facts-Are-Important_Abortion-Care-Later-In-Pregnancy-February-2019-College.pdf?dmc=1&ts=20190214T2242210541. Accessed March 7, 2019.
- Jatlaoui TC, Boutot ME, Mandel MG, et al. Abortion surveillance—United States, 2015. MMWR Surveill Summ. 2018;67(13):1-45.
‘The birth of a mother is a complex process’
Softening the blow to women and families of severe perinatal, postpartum psychiatric disorders
Editor’s Note: Alison M. Heru, MD, the Families in Psychiatry columnist, invited Dr. Reinstein to address this topic.
“But this was not what I expected!” That’s a statement I have heard from countless new mothers.
Women often envision pregnancy and the postpartum period as a time of pure joy. The glow of an expectant woman and the excitement of the arrival of a new baby masks the reality that many women struggle emotionally when transitioning to motherhood. Like the birth of a child, the birth of a mother is a complex process. Upholding the myth that all women seamlessly transform into mothers can have devastating effects and hinder access to mental health care.
As a psychiatrist working on a women’s inpatient unit with a perinatal program, I treat women at times of crisis. What may have begun as mild anxiety or depression sometimes quickly spirals into severe psychiatric illness. The sheer force of these severe perinatal and postpartum psychiatric disorders often leaves women and families shocked and confused, wondering what happened to their crumbled dreams of early motherhood.
What must general psychiatrists know about perinatal and postpartum psychiatric disorders? Why is maternal mental health so important? What are the barriers to treatment for these women? How can general psychiatrists best support and treat these new mothers and their families?
What data show
Maternal depression is now known to be one of the most common complications of pregnancy. Studies have suggested that about 11% of women experience depression during pregnancy1 and approximately 17% of women are depressed in the postpartum period.2 Perinatal generalized anxiety disorder has been shown to have a prevalence of 8.5%-10.5% during pregnancy with a wider variance post partum.3 Approximately 3% of women in the general community develop PTSD symptoms following childbirth.4 Research suggests that about 2% of women develop obsessive-compulsive disorder symptoms in the postpartum period.5 Postpartum psychosis, a rare but potentially devastating illness, occurs after 0.1%-0.2% of births.6
Importance of maternal mental health
There is a growing body of literature supporting both obstetric and pediatric adverse outcomes related to untreated psychiatric illness. Untreated maternal depression has been associated with obstetric complications, such as preterm delivery, preeclampsia, low birth weight, as well as the child’s developing cognitive function.7 Anxiety during pregnancy has been associated with both a shorter gestational period and adverse implications for fetal neurodevelopment.
These adverse effects were found to be even more potent in “pregnancy anxiety,” or anxiety specifically focused on the pregnancy, the birth experience, and the transition to motherhood.8 The psychotic symptoms occurring during postpartum psychosis can jeopardize the lives of both a woman and her child and carries a 4% risk of infanticide.9 Although there are limited data about the long-term effects of postpartum obsessive-compulsive disorders and PTSD, it is reasonable to assume that they might carry negative long-term implications for the mother and possibly her child.
Barriers to treatment
Despite the significant rates of mental illness, pregnant and new mothers often face barriers to receiving treatment. Many psychiatrists are hesitant to prescribe psychiatric medication to pregnant women because of concerns about teratogenic potential of psychiatric medications; similar concerns exist for newborn babies when prescribing medications to lactating mothers. In addition, the field of reproductive psychiatry is evolving at a rapid pace, making it difficult for busy psychiatrists to keep up with the ever-growing literature.
Also, it is hard to imagine a population that has more barriers to attending outpatient appointments. For many new mothers, the exhaustion and all-consuming work involved with taking care of a newborn are insurmountable barriers to obtaining mental health care. In addition, despite the awareness that new mothers often are more emotional, families can be slow to recognize the developing severity of a psychiatric illness during the peripartum and postpartum periods.
Supporting and treating new mothers
As general psychiatrists, there are several ways to directly help these women.
1. Expect the expected. Even in women with no prior psychiatric history, a significant percentage of expectant and postpartum women will develop acute psychiatric symptoms. Learn about the different presentations and treatments of perinatal and postpartum psychiatric disorders. For example, a woman might have thoughts of harming her baby in both postpartum psychosis and obsessive-compulsive disorder. However, the acuity and treatment of these two conditions drastically differ.
2. Learn more about psychiatric medications. Several apps and websites are available to psychiatrists to learn about the safety profile of psychiatric medications, such as Reprotox.org, mothertobaby.org, lactmed, and womensmentalhealth.org. Many medications are considered to be relatively safe during pregnancy and breastfeeding. It is important for psychiatrists to appreciate the risks when choosing not to prescribe to pregnant and postpartum women. Sometimes a known risk of a specific medication may be preferable to the unknown risk of leaving a woman susceptible to a severe psychiatric decompensation.
3. Involve all members of the family. A mother’s mental health has significant implications for the entire family. Psychoeducation for the family as well as frequent family sessions are key tools when treating this population. In addition, prescribing to pregnant women provides the opportunity for a psychiatrist to refine skills in joint decision making; it is crucial to involve both a patient and her spouse when discussing psychiatric medications.
4. Provide ready access and collaborate care. It is important to understand the potential rapid onset of psychiatric symptoms during the pregnancy and postpartum period. Psychiatrists should be prepared to collaborate care with other specialties. It is important to establish relationships with community psychotherapists specializing in maternal mental health, pediatricians, as well as obstetricians.
5. Learn when to seek a higher level of care. Although many women with perinatal and postpartum psychiatric symptoms can be managed as outpatients, women at times need a higher level of care. Similar to general psychiatry, women who are acutely suicidal or homicidal or have a sudden onset of psychotic and manic symptoms all should be evaluated immediately for inpatient hospitalization. Women with less severe symptoms but who require a higher level of care than typically offered in standard outpatient treatment should be candidates for partial hospitalization programs.
General intensive programs usually can accommodate these women, but it is ideal to refer this population to perinatal intensive programs. Postpartum Support International (postpartum.net) lists the nationwide inpatient and partial perinatal programs as well as regional and local services. An example of inpatient perinatal care is the women’s unit at Zucker Hillside Hospital (Northwell Health System, Glen Oaks, N.Y.), which houses an inpatient perinatal program. As a psychiatrist on the unit, I treat acute symptoms such as depression, anxiety, psychosis, mania, and catatonia that occur during the perinatal and postpartum periods. Given the severity of symptoms, I use a wide range of psychiatric medications with the possibility of electroconvulsive therapy when indicated. Psychotherapy staff on the unit offer specialized perinatal, mothers, and dialectical behavioral therapy groups. Breast pumps are available for women who wish to breastfeed. Accommodations are made for babies and children to visit their mother when clinically appropriate. Once discharged, women often are referred to Zucker Hillside’s own perinatal outpatient clinic for continued treatment. Similar models exist in select inpatient units as well as an increasing number of partial programs across the United States.
Conclusion
Psychiatric care for pregnant and new mothers can be challenging, but it is also immensely rewarding. Restoring a mother’s mental health usually leads to increased emotional stability for her entire family. Given the prevalence of maternal mental health disorders, psychiatrists in nearly every setting will encounter this population of women. With dedicated time devoted to reviewing the literature and learning about local resources, psychiatrists can feel comfortable treating women throughout the childbearing experience.
References
1. J Affect Disord. 2017 Sep;219:86-92.
2. J Psychiatr Res. 2018 Sep;104:235-48.
3. J Womens Health. (Larchmt). 2015 Sep;24(9):762-70.
4. Clin Psychol Rev. 2014 Jul;34(5):389-401.
5. Compr Psychiatry. 2009 Nov-Dec;50(6):503-9.
6. Int Rev Psychiatry. 2003 Aug;15(3):231-42.
7. Clin Obstet Gynecol. 2018 Sep;61(3):533-43.
8. Curr Opinion Psychiatry. 2012 Mar;25(2):141-8.
9. Am J Psychiatry. 2009 Apr;166(4):405-8.
Dr. Reinstein is a psychiatry attending at Zucker Hillside Hospital. Her clinical interests include reproductive psychiatry and family therapy, with a specific focus on maternal mental health. Dr. Reinstein completed her adult psychiatry residency training at Montefiore Hospital/Albert Einstein College of Medicine, New York, after graduating from the Albert Einstein College of Medicine and Yeshiva University, New York, with a BA in biology. She is one of the recipients of the 4th Annual Resident Recognition Award for Excellence in Family Oriented Care.
Softening the blow to women and families of severe perinatal, postpartum psychiatric disorders
Softening the blow to women and families of severe perinatal, postpartum psychiatric disorders
Editor’s Note: Alison M. Heru, MD, the Families in Psychiatry columnist, invited Dr. Reinstein to address this topic.
“But this was not what I expected!” That’s a statement I have heard from countless new mothers.
Women often envision pregnancy and the postpartum period as a time of pure joy. The glow of an expectant woman and the excitement of the arrival of a new baby masks the reality that many women struggle emotionally when transitioning to motherhood. Like the birth of a child, the birth of a mother is a complex process. Upholding the myth that all women seamlessly transform into mothers can have devastating effects and hinder access to mental health care.
As a psychiatrist working on a women’s inpatient unit with a perinatal program, I treat women at times of crisis. What may have begun as mild anxiety or depression sometimes quickly spirals into severe psychiatric illness. The sheer force of these severe perinatal and postpartum psychiatric disorders often leaves women and families shocked and confused, wondering what happened to their crumbled dreams of early motherhood.
What must general psychiatrists know about perinatal and postpartum psychiatric disorders? Why is maternal mental health so important? What are the barriers to treatment for these women? How can general psychiatrists best support and treat these new mothers and their families?
What data show
Maternal depression is now known to be one of the most common complications of pregnancy. Studies have suggested that about 11% of women experience depression during pregnancy1 and approximately 17% of women are depressed in the postpartum period.2 Perinatal generalized anxiety disorder has been shown to have a prevalence of 8.5%-10.5% during pregnancy with a wider variance post partum.3 Approximately 3% of women in the general community develop PTSD symptoms following childbirth.4 Research suggests that about 2% of women develop obsessive-compulsive disorder symptoms in the postpartum period.5 Postpartum psychosis, a rare but potentially devastating illness, occurs after 0.1%-0.2% of births.6
Importance of maternal mental health
There is a growing body of literature supporting both obstetric and pediatric adverse outcomes related to untreated psychiatric illness. Untreated maternal depression has been associated with obstetric complications, such as preterm delivery, preeclampsia, low birth weight, as well as the child’s developing cognitive function.7 Anxiety during pregnancy has been associated with both a shorter gestational period and adverse implications for fetal neurodevelopment.
These adverse effects were found to be even more potent in “pregnancy anxiety,” or anxiety specifically focused on the pregnancy, the birth experience, and the transition to motherhood.8 The psychotic symptoms occurring during postpartum psychosis can jeopardize the lives of both a woman and her child and carries a 4% risk of infanticide.9 Although there are limited data about the long-term effects of postpartum obsessive-compulsive disorders and PTSD, it is reasonable to assume that they might carry negative long-term implications for the mother and possibly her child.
Barriers to treatment
Despite the significant rates of mental illness, pregnant and new mothers often face barriers to receiving treatment. Many psychiatrists are hesitant to prescribe psychiatric medication to pregnant women because of concerns about teratogenic potential of psychiatric medications; similar concerns exist for newborn babies when prescribing medications to lactating mothers. In addition, the field of reproductive psychiatry is evolving at a rapid pace, making it difficult for busy psychiatrists to keep up with the ever-growing literature.
Also, it is hard to imagine a population that has more barriers to attending outpatient appointments. For many new mothers, the exhaustion and all-consuming work involved with taking care of a newborn are insurmountable barriers to obtaining mental health care. In addition, despite the awareness that new mothers often are more emotional, families can be slow to recognize the developing severity of a psychiatric illness during the peripartum and postpartum periods.
Supporting and treating new mothers
As general psychiatrists, there are several ways to directly help these women.
1. Expect the expected. Even in women with no prior psychiatric history, a significant percentage of expectant and postpartum women will develop acute psychiatric symptoms. Learn about the different presentations and treatments of perinatal and postpartum psychiatric disorders. For example, a woman might have thoughts of harming her baby in both postpartum psychosis and obsessive-compulsive disorder. However, the acuity and treatment of these two conditions drastically differ.
2. Learn more about psychiatric medications. Several apps and websites are available to psychiatrists to learn about the safety profile of psychiatric medications, such as Reprotox.org, mothertobaby.org, lactmed, and womensmentalhealth.org. Many medications are considered to be relatively safe during pregnancy and breastfeeding. It is important for psychiatrists to appreciate the risks when choosing not to prescribe to pregnant and postpartum women. Sometimes a known risk of a specific medication may be preferable to the unknown risk of leaving a woman susceptible to a severe psychiatric decompensation.
3. Involve all members of the family. A mother’s mental health has significant implications for the entire family. Psychoeducation for the family as well as frequent family sessions are key tools when treating this population. In addition, prescribing to pregnant women provides the opportunity for a psychiatrist to refine skills in joint decision making; it is crucial to involve both a patient and her spouse when discussing psychiatric medications.
4. Provide ready access and collaborate care. It is important to understand the potential rapid onset of psychiatric symptoms during the pregnancy and postpartum period. Psychiatrists should be prepared to collaborate care with other specialties. It is important to establish relationships with community psychotherapists specializing in maternal mental health, pediatricians, as well as obstetricians.
5. Learn when to seek a higher level of care. Although many women with perinatal and postpartum psychiatric symptoms can be managed as outpatients, women at times need a higher level of care. Similar to general psychiatry, women who are acutely suicidal or homicidal or have a sudden onset of psychotic and manic symptoms all should be evaluated immediately for inpatient hospitalization. Women with less severe symptoms but who require a higher level of care than typically offered in standard outpatient treatment should be candidates for partial hospitalization programs.
General intensive programs usually can accommodate these women, but it is ideal to refer this population to perinatal intensive programs. Postpartum Support International (postpartum.net) lists the nationwide inpatient and partial perinatal programs as well as regional and local services. An example of inpatient perinatal care is the women’s unit at Zucker Hillside Hospital (Northwell Health System, Glen Oaks, N.Y.), which houses an inpatient perinatal program. As a psychiatrist on the unit, I treat acute symptoms such as depression, anxiety, psychosis, mania, and catatonia that occur during the perinatal and postpartum periods. Given the severity of symptoms, I use a wide range of psychiatric medications with the possibility of electroconvulsive therapy when indicated. Psychotherapy staff on the unit offer specialized perinatal, mothers, and dialectical behavioral therapy groups. Breast pumps are available for women who wish to breastfeed. Accommodations are made for babies and children to visit their mother when clinically appropriate. Once discharged, women often are referred to Zucker Hillside’s own perinatal outpatient clinic for continued treatment. Similar models exist in select inpatient units as well as an increasing number of partial programs across the United States.
Conclusion
Psychiatric care for pregnant and new mothers can be challenging, but it is also immensely rewarding. Restoring a mother’s mental health usually leads to increased emotional stability for her entire family. Given the prevalence of maternal mental health disorders, psychiatrists in nearly every setting will encounter this population of women. With dedicated time devoted to reviewing the literature and learning about local resources, psychiatrists can feel comfortable treating women throughout the childbearing experience.
References
1. J Affect Disord. 2017 Sep;219:86-92.
2. J Psychiatr Res. 2018 Sep;104:235-48.
3. J Womens Health. (Larchmt). 2015 Sep;24(9):762-70.
4. Clin Psychol Rev. 2014 Jul;34(5):389-401.
5. Compr Psychiatry. 2009 Nov-Dec;50(6):503-9.
6. Int Rev Psychiatry. 2003 Aug;15(3):231-42.
7. Clin Obstet Gynecol. 2018 Sep;61(3):533-43.
8. Curr Opinion Psychiatry. 2012 Mar;25(2):141-8.
9. Am J Psychiatry. 2009 Apr;166(4):405-8.
Dr. Reinstein is a psychiatry attending at Zucker Hillside Hospital. Her clinical interests include reproductive psychiatry and family therapy, with a specific focus on maternal mental health. Dr. Reinstein completed her adult psychiatry residency training at Montefiore Hospital/Albert Einstein College of Medicine, New York, after graduating from the Albert Einstein College of Medicine and Yeshiva University, New York, with a BA in biology. She is one of the recipients of the 4th Annual Resident Recognition Award for Excellence in Family Oriented Care.
Editor’s Note: Alison M. Heru, MD, the Families in Psychiatry columnist, invited Dr. Reinstein to address this topic.
“But this was not what I expected!” That’s a statement I have heard from countless new mothers.
Women often envision pregnancy and the postpartum period as a time of pure joy. The glow of an expectant woman and the excitement of the arrival of a new baby masks the reality that many women struggle emotionally when transitioning to motherhood. Like the birth of a child, the birth of a mother is a complex process. Upholding the myth that all women seamlessly transform into mothers can have devastating effects and hinder access to mental health care.
As a psychiatrist working on a women’s inpatient unit with a perinatal program, I treat women at times of crisis. What may have begun as mild anxiety or depression sometimes quickly spirals into severe psychiatric illness. The sheer force of these severe perinatal and postpartum psychiatric disorders often leaves women and families shocked and confused, wondering what happened to their crumbled dreams of early motherhood.
What must general psychiatrists know about perinatal and postpartum psychiatric disorders? Why is maternal mental health so important? What are the barriers to treatment for these women? How can general psychiatrists best support and treat these new mothers and their families?
What data show
Maternal depression is now known to be one of the most common complications of pregnancy. Studies have suggested that about 11% of women experience depression during pregnancy1 and approximately 17% of women are depressed in the postpartum period.2 Perinatal generalized anxiety disorder has been shown to have a prevalence of 8.5%-10.5% during pregnancy with a wider variance post partum.3 Approximately 3% of women in the general community develop PTSD symptoms following childbirth.4 Research suggests that about 2% of women develop obsessive-compulsive disorder symptoms in the postpartum period.5 Postpartum psychosis, a rare but potentially devastating illness, occurs after 0.1%-0.2% of births.6
Importance of maternal mental health
There is a growing body of literature supporting both obstetric and pediatric adverse outcomes related to untreated psychiatric illness. Untreated maternal depression has been associated with obstetric complications, such as preterm delivery, preeclampsia, low birth weight, as well as the child’s developing cognitive function.7 Anxiety during pregnancy has been associated with both a shorter gestational period and adverse implications for fetal neurodevelopment.
These adverse effects were found to be even more potent in “pregnancy anxiety,” or anxiety specifically focused on the pregnancy, the birth experience, and the transition to motherhood.8 The psychotic symptoms occurring during postpartum psychosis can jeopardize the lives of both a woman and her child and carries a 4% risk of infanticide.9 Although there are limited data about the long-term effects of postpartum obsessive-compulsive disorders and PTSD, it is reasonable to assume that they might carry negative long-term implications for the mother and possibly her child.
Barriers to treatment
Despite the significant rates of mental illness, pregnant and new mothers often face barriers to receiving treatment. Many psychiatrists are hesitant to prescribe psychiatric medication to pregnant women because of concerns about teratogenic potential of psychiatric medications; similar concerns exist for newborn babies when prescribing medications to lactating mothers. In addition, the field of reproductive psychiatry is evolving at a rapid pace, making it difficult for busy psychiatrists to keep up with the ever-growing literature.
Also, it is hard to imagine a population that has more barriers to attending outpatient appointments. For many new mothers, the exhaustion and all-consuming work involved with taking care of a newborn are insurmountable barriers to obtaining mental health care. In addition, despite the awareness that new mothers often are more emotional, families can be slow to recognize the developing severity of a psychiatric illness during the peripartum and postpartum periods.
Supporting and treating new mothers
As general psychiatrists, there are several ways to directly help these women.
1. Expect the expected. Even in women with no prior psychiatric history, a significant percentage of expectant and postpartum women will develop acute psychiatric symptoms. Learn about the different presentations and treatments of perinatal and postpartum psychiatric disorders. For example, a woman might have thoughts of harming her baby in both postpartum psychosis and obsessive-compulsive disorder. However, the acuity and treatment of these two conditions drastically differ.
2. Learn more about psychiatric medications. Several apps and websites are available to psychiatrists to learn about the safety profile of psychiatric medications, such as Reprotox.org, mothertobaby.org, lactmed, and womensmentalhealth.org. Many medications are considered to be relatively safe during pregnancy and breastfeeding. It is important for psychiatrists to appreciate the risks when choosing not to prescribe to pregnant and postpartum women. Sometimes a known risk of a specific medication may be preferable to the unknown risk of leaving a woman susceptible to a severe psychiatric decompensation.
3. Involve all members of the family. A mother’s mental health has significant implications for the entire family. Psychoeducation for the family as well as frequent family sessions are key tools when treating this population. In addition, prescribing to pregnant women provides the opportunity for a psychiatrist to refine skills in joint decision making; it is crucial to involve both a patient and her spouse when discussing psychiatric medications.
4. Provide ready access and collaborate care. It is important to understand the potential rapid onset of psychiatric symptoms during the pregnancy and postpartum period. Psychiatrists should be prepared to collaborate care with other specialties. It is important to establish relationships with community psychotherapists specializing in maternal mental health, pediatricians, as well as obstetricians.
5. Learn when to seek a higher level of care. Although many women with perinatal and postpartum psychiatric symptoms can be managed as outpatients, women at times need a higher level of care. Similar to general psychiatry, women who are acutely suicidal or homicidal or have a sudden onset of psychotic and manic symptoms all should be evaluated immediately for inpatient hospitalization. Women with less severe symptoms but who require a higher level of care than typically offered in standard outpatient treatment should be candidates for partial hospitalization programs.
General intensive programs usually can accommodate these women, but it is ideal to refer this population to perinatal intensive programs. Postpartum Support International (postpartum.net) lists the nationwide inpatient and partial perinatal programs as well as regional and local services. An example of inpatient perinatal care is the women’s unit at Zucker Hillside Hospital (Northwell Health System, Glen Oaks, N.Y.), which houses an inpatient perinatal program. As a psychiatrist on the unit, I treat acute symptoms such as depression, anxiety, psychosis, mania, and catatonia that occur during the perinatal and postpartum periods. Given the severity of symptoms, I use a wide range of psychiatric medications with the possibility of electroconvulsive therapy when indicated. Psychotherapy staff on the unit offer specialized perinatal, mothers, and dialectical behavioral therapy groups. Breast pumps are available for women who wish to breastfeed. Accommodations are made for babies and children to visit their mother when clinically appropriate. Once discharged, women often are referred to Zucker Hillside’s own perinatal outpatient clinic for continued treatment. Similar models exist in select inpatient units as well as an increasing number of partial programs across the United States.
Conclusion
Psychiatric care for pregnant and new mothers can be challenging, but it is also immensely rewarding. Restoring a mother’s mental health usually leads to increased emotional stability for her entire family. Given the prevalence of maternal mental health disorders, psychiatrists in nearly every setting will encounter this population of women. With dedicated time devoted to reviewing the literature and learning about local resources, psychiatrists can feel comfortable treating women throughout the childbearing experience.
References
1. J Affect Disord. 2017 Sep;219:86-92.
2. J Psychiatr Res. 2018 Sep;104:235-48.
3. J Womens Health. (Larchmt). 2015 Sep;24(9):762-70.
4. Clin Psychol Rev. 2014 Jul;34(5):389-401.
5. Compr Psychiatry. 2009 Nov-Dec;50(6):503-9.
6. Int Rev Psychiatry. 2003 Aug;15(3):231-42.
7. Clin Obstet Gynecol. 2018 Sep;61(3):533-43.
8. Curr Opinion Psychiatry. 2012 Mar;25(2):141-8.
9. Am J Psychiatry. 2009 Apr;166(4):405-8.
Dr. Reinstein is a psychiatry attending at Zucker Hillside Hospital. Her clinical interests include reproductive psychiatry and family therapy, with a specific focus on maternal mental health. Dr. Reinstein completed her adult psychiatry residency training at Montefiore Hospital/Albert Einstein College of Medicine, New York, after graduating from the Albert Einstein College of Medicine and Yeshiva University, New York, with a BA in biology. She is one of the recipients of the 4th Annual Resident Recognition Award for Excellence in Family Oriented Care.