User login
Syphilis Treatment Falls Short for Pregnant Patients
Approximately one third of pregnant individuals with syphilis were inadequately treated or not treated for syphilis despite receiving timely prenatal care, based on data from nearly 1500 patients.
Although congenital syphilis is preventable with treatment before or early in pregnancy, data from the Centers for Disease Control and Prevention (CDC) show a doubling of syphilis rates in the United States between 2018 and 2021 wrote Ayzsa Tannis, MPH, of the Centers for Disease Control and Prevention, Atlanta, and colleagues.
To better understand factors contributing to inadequate syphilis treatment during pregnancy, the researchers examined data from 1476 individuals with syphilis during pregnancy. The study population came from six jurisdictions that participated in the Surveillance for Emerging Threats to Pregnant People and Infants Network, and sources included case investigations, medical records, and links between laboratory data and vital records.
The researchers characterized the status of syphilis during pregnancy as adequate, inadequate, or not treated based on the CDC’s Sexually Transmitted Infections Treatment Guidelines, 2021. Prenatal care was defined as timely (at least 30 days prior to pregnancy outcome), nontimely (less than 30 days before pregnancy outcome), and no prenatal care. The findings were published in Obstetrics & Gynecology.
Of the 1476 individuals studied, 855 (57.9%) were adequately treated for syphilis and 621 (42.1%) were inadequately or not treated.
Overall, 82% of the study population received timely prenatal care. However, 32.1% of those who received timely prenatal care were inadequately treated, including 14.8% who received no syphilis treatment. Individuals with nontimely or no prenatal care were significantly more likely to receive inadequate or no treatment for syphilis than those who received timely care (risk ratio, 2.50 and 2.73, respectively).
The findings were consistent with previous studies of missed opportunities for prevention and treatment, the researchers noted. Factors behind nontimely treatment (less than 30 days before pregnancy outcome) may include intermittent shortages of benzathine penicillin G, the standard treatment for syphilis, as well as the lack of time and administrative support for clinicians to communicate with patients and health departments, and to expedite treatment, the researchers wrote.
The results were limited by several factors including the use of data from six US jurisdictions that may not generalize to other areas, the variations in reporting years for the different jurisdictions, and variation in mandates for syphilis screening during pregnancy, the researchers noted.
More research is needed to improve syphilis testing itself, and to develop more treatment options, the researchers concluded. Partnerships among public health, patient advocacy groups, prenatal care clinicians, and other clinicians outside the prenatal care setting also are needed for effective intervention in pregnant individuals with syphilis, they said.
The study was carried out as part of the regular work of the CDC, supported by the Epidemiology and Laboratory Capacity for Prevention and Control of Emerging Infectious Diseases Cooperative Agreement and through contractual mechanisms including the Local Health Department Initiative to Chickasaw Health Consulting. The researchers had no financial conflicts to disclose.
Approximately one third of pregnant individuals with syphilis were inadequately treated or not treated for syphilis despite receiving timely prenatal care, based on data from nearly 1500 patients.
Although congenital syphilis is preventable with treatment before or early in pregnancy, data from the Centers for Disease Control and Prevention (CDC) show a doubling of syphilis rates in the United States between 2018 and 2021 wrote Ayzsa Tannis, MPH, of the Centers for Disease Control and Prevention, Atlanta, and colleagues.
To better understand factors contributing to inadequate syphilis treatment during pregnancy, the researchers examined data from 1476 individuals with syphilis during pregnancy. The study population came from six jurisdictions that participated in the Surveillance for Emerging Threats to Pregnant People and Infants Network, and sources included case investigations, medical records, and links between laboratory data and vital records.
The researchers characterized the status of syphilis during pregnancy as adequate, inadequate, or not treated based on the CDC’s Sexually Transmitted Infections Treatment Guidelines, 2021. Prenatal care was defined as timely (at least 30 days prior to pregnancy outcome), nontimely (less than 30 days before pregnancy outcome), and no prenatal care. The findings were published in Obstetrics & Gynecology.
Of the 1476 individuals studied, 855 (57.9%) were adequately treated for syphilis and 621 (42.1%) were inadequately or not treated.
Overall, 82% of the study population received timely prenatal care. However, 32.1% of those who received timely prenatal care were inadequately treated, including 14.8% who received no syphilis treatment. Individuals with nontimely or no prenatal care were significantly more likely to receive inadequate or no treatment for syphilis than those who received timely care (risk ratio, 2.50 and 2.73, respectively).
The findings were consistent with previous studies of missed opportunities for prevention and treatment, the researchers noted. Factors behind nontimely treatment (less than 30 days before pregnancy outcome) may include intermittent shortages of benzathine penicillin G, the standard treatment for syphilis, as well as the lack of time and administrative support for clinicians to communicate with patients and health departments, and to expedite treatment, the researchers wrote.
The results were limited by several factors including the use of data from six US jurisdictions that may not generalize to other areas, the variations in reporting years for the different jurisdictions, and variation in mandates for syphilis screening during pregnancy, the researchers noted.
More research is needed to improve syphilis testing itself, and to develop more treatment options, the researchers concluded. Partnerships among public health, patient advocacy groups, prenatal care clinicians, and other clinicians outside the prenatal care setting also are needed for effective intervention in pregnant individuals with syphilis, they said.
The study was carried out as part of the regular work of the CDC, supported by the Epidemiology and Laboratory Capacity for Prevention and Control of Emerging Infectious Diseases Cooperative Agreement and through contractual mechanisms including the Local Health Department Initiative to Chickasaw Health Consulting. The researchers had no financial conflicts to disclose.
Approximately one third of pregnant individuals with syphilis were inadequately treated or not treated for syphilis despite receiving timely prenatal care, based on data from nearly 1500 patients.
Although congenital syphilis is preventable with treatment before or early in pregnancy, data from the Centers for Disease Control and Prevention (CDC) show a doubling of syphilis rates in the United States between 2018 and 2021 wrote Ayzsa Tannis, MPH, of the Centers for Disease Control and Prevention, Atlanta, and colleagues.
To better understand factors contributing to inadequate syphilis treatment during pregnancy, the researchers examined data from 1476 individuals with syphilis during pregnancy. The study population came from six jurisdictions that participated in the Surveillance for Emerging Threats to Pregnant People and Infants Network, and sources included case investigations, medical records, and links between laboratory data and vital records.
The researchers characterized the status of syphilis during pregnancy as adequate, inadequate, or not treated based on the CDC’s Sexually Transmitted Infections Treatment Guidelines, 2021. Prenatal care was defined as timely (at least 30 days prior to pregnancy outcome), nontimely (less than 30 days before pregnancy outcome), and no prenatal care. The findings were published in Obstetrics & Gynecology.
Of the 1476 individuals studied, 855 (57.9%) were adequately treated for syphilis and 621 (42.1%) were inadequately or not treated.
Overall, 82% of the study population received timely prenatal care. However, 32.1% of those who received timely prenatal care were inadequately treated, including 14.8% who received no syphilis treatment. Individuals with nontimely or no prenatal care were significantly more likely to receive inadequate or no treatment for syphilis than those who received timely care (risk ratio, 2.50 and 2.73, respectively).
The findings were consistent with previous studies of missed opportunities for prevention and treatment, the researchers noted. Factors behind nontimely treatment (less than 30 days before pregnancy outcome) may include intermittent shortages of benzathine penicillin G, the standard treatment for syphilis, as well as the lack of time and administrative support for clinicians to communicate with patients and health departments, and to expedite treatment, the researchers wrote.
The results were limited by several factors including the use of data from six US jurisdictions that may not generalize to other areas, the variations in reporting years for the different jurisdictions, and variation in mandates for syphilis screening during pregnancy, the researchers noted.
More research is needed to improve syphilis testing itself, and to develop more treatment options, the researchers concluded. Partnerships among public health, patient advocacy groups, prenatal care clinicians, and other clinicians outside the prenatal care setting also are needed for effective intervention in pregnant individuals with syphilis, they said.
The study was carried out as part of the regular work of the CDC, supported by the Epidemiology and Laboratory Capacity for Prevention and Control of Emerging Infectious Diseases Cooperative Agreement and through contractual mechanisms including the Local Health Department Initiative to Chickasaw Health Consulting. The researchers had no financial conflicts to disclose.
FROM OBSTETRICS & GYNECOLOGY
Menopause, RSV, and More: 4 New Meds to Know
BOSTON — The US Food and Drug Administration (FDA) approved 55 new medications in 2023 and 11 more in 2024 to date.
A New First-Line for GERD?
Vonoprazan, an oral potassium-competitive acid blocker — which received FDA approval in November 2023 — may be a good alternative for patients whose symptoms continue to linger despite taking medications designated to treat gastroesophageal reflux disease (GERD).
GERD is the most common gastrointestinal symptom encountered by primary care physicians. Proton-pump inhibitors (PPIs) are the first-line treatment for the condition but can have long-term side effects such as Clostridioides difficile infection and kidney lesions.
“We know that not all patients are going to have symptom relief with H2 blockers and PPIs, so there’s an opportunity for patients who don’t get full symptom relief,” Dr. Smetana told attendees.
Vonoprazan blocks potassium binding to ATPase proton pumps and inhibits the secretion of gastric acid.
The approval of vonoprazan for erosive GERD was based on results from the phase 3 PHALCON-EE study, a randomized, double-blind, multicenter study that found the drug to be more effective than lansoprazole in treating erosive esophagitis.
Vonoprazan “has more rapid absorption than PPIs [and a] longer half-life and is more potent than PPIs, so theoretically it could be more effective in certain settings,” Dr. Smetana said.
Vonoprazan is FDA approved for only 6 months of use. Despite its efficacy, cost may be a barrier to many patients. H2 blockers generally cost patients less than $10 for 1 month’s supply, whereas vonoprazan can cost up to $650.
Nonhormonal Drug for Menopause
Fezolinetant, the first neurokinin receptor antagonist to receive approval from the FDA to treat vasomotor symptoms, may be an option for women concerned about hormone-based therapy for menopausal hot flashes.
“[Fezolinetant] specifically works in the area of the brain that’s involved in body temperature regulation and sweating,” Dr. Smetana said.
Results from the SKYLIGHT 1 randomized controlled trial of fezolinetant found the medication reduced the frequency and severity of hot flashes. Some of the side effects include abdominal pain, diarrhea, and insomnia.
Other nonestrogen treatments, including selective serotonin reuptake inhibitors (SSRIs), gabapentin, cognitive-behavioral therapy, and hypnosis, are modestly effective, according to the North American Menopause Society.
“[Fezolinetant] offers a different option that physicians may be more comfortable prescribing,” Dr. Smetana said. “And I think this will be an important addition to nonhormonal therapy.”
RSV Vaccine for Everyone
Once considered an illness that is more prevalent in young children, respiratory syncytial virus (RSV) has become more prevalent and severe among older adults. Between 60,000 and 120,000 older adults are hospitalized and 6000-10,000 die of RSV infection each year, according to the US Centers for Disease Control and Prevention.
The FDA has approved two RSV vaccines approved for older adults, but clinicians may find it challenging to get older patients vaccinated for this and other preventable illnesses.
Patients who received the RSV vaccine had an 83% relative risk reduction for the illness, according to a recent study, and an overall lower risk for hospitalization.
Moderna is developing an mRNA vaccine for RSV that is similar to many COVID-19 vaccines. A study published in 2023 in The New England Journal of Medicine found no cases of neuroinflammatory disorders among patients who received the mRNA RSV vaccine, with a median follow-up of 112 days.
“This is important given ongoing concerns of neurological safety,” among older adults who receive the RSV vaccine, Dr. Smetana said.
As of March 2024, the CDC recommends shared decision-making for adults older than 60 years and for healthcare providers to “consider” rather than “recommend” the vaccine for their patients. The agency’s Adult RSV Work Group plans to meet at June 2024 to reconsider whether shared clinical decision-making remains the preferred policy option.
New Antidepressants
A medication thrice rejected by the FDA is now heading a new class of drugs to treat major depressive disorder.
Gepirone, a 5-HT1A receptor agonist, has a different mechanism of action from that of SSRIs, which are currently considered the first-line treatment for depression.
Gepirone was rejected by the FDA in 2002, 2004, and 2007, with concerns that the efficacy studies were too small. In 2015, an FDA advisory committee agreed that the evidence to date did not support approval of an extended-release form of the drug. But the agency decided to approve the medication in September 2023.
“So why is this medication worth discussing now?” Dr. Smetana said. “It’s because the side effect profile is different from existing antidepressants.”
Many patients may stop using SSRIs because of side effects such as insomnia and loss of libido, Dr. Smetana said. Gepirone has the potential to avoid activation of other 5-HT receptors that mediate side effects, he said.
Studies suggest that gepirone reduces both anxiety and depression scores on the Hamilton Depression Rating Scale in patients who have both conditions and decreases rates of depression relapse compared with placebo through at least 48 weeks. The drug also may be less likely than SSRIs to cause sexual dysfunction in men, Dr. Smetana said.
Gepirone will be available to prescribe to patients in fall 2024.
Dr. Smetana reported no relevant financial conflicts of interest.
A version of this article appeared on Medscape.com.
BOSTON — The US Food and Drug Administration (FDA) approved 55 new medications in 2023 and 11 more in 2024 to date.
A New First-Line for GERD?
Vonoprazan, an oral potassium-competitive acid blocker — which received FDA approval in November 2023 — may be a good alternative for patients whose symptoms continue to linger despite taking medications designated to treat gastroesophageal reflux disease (GERD).
GERD is the most common gastrointestinal symptom encountered by primary care physicians. Proton-pump inhibitors (PPIs) are the first-line treatment for the condition but can have long-term side effects such as Clostridioides difficile infection and kidney lesions.
“We know that not all patients are going to have symptom relief with H2 blockers and PPIs, so there’s an opportunity for patients who don’t get full symptom relief,” Dr. Smetana told attendees.
Vonoprazan blocks potassium binding to ATPase proton pumps and inhibits the secretion of gastric acid.
The approval of vonoprazan for erosive GERD was based on results from the phase 3 PHALCON-EE study, a randomized, double-blind, multicenter study that found the drug to be more effective than lansoprazole in treating erosive esophagitis.
Vonoprazan “has more rapid absorption than PPIs [and a] longer half-life and is more potent than PPIs, so theoretically it could be more effective in certain settings,” Dr. Smetana said.
Vonoprazan is FDA approved for only 6 months of use. Despite its efficacy, cost may be a barrier to many patients. H2 blockers generally cost patients less than $10 for 1 month’s supply, whereas vonoprazan can cost up to $650.
Nonhormonal Drug for Menopause
Fezolinetant, the first neurokinin receptor antagonist to receive approval from the FDA to treat vasomotor symptoms, may be an option for women concerned about hormone-based therapy for menopausal hot flashes.
“[Fezolinetant] specifically works in the area of the brain that’s involved in body temperature regulation and sweating,” Dr. Smetana said.
Results from the SKYLIGHT 1 randomized controlled trial of fezolinetant found the medication reduced the frequency and severity of hot flashes. Some of the side effects include abdominal pain, diarrhea, and insomnia.
Other nonestrogen treatments, including selective serotonin reuptake inhibitors (SSRIs), gabapentin, cognitive-behavioral therapy, and hypnosis, are modestly effective, according to the North American Menopause Society.
“[Fezolinetant] offers a different option that physicians may be more comfortable prescribing,” Dr. Smetana said. “And I think this will be an important addition to nonhormonal therapy.”
RSV Vaccine for Everyone
Once considered an illness that is more prevalent in young children, respiratory syncytial virus (RSV) has become more prevalent and severe among older adults. Between 60,000 and 120,000 older adults are hospitalized and 6000-10,000 die of RSV infection each year, according to the US Centers for Disease Control and Prevention.
The FDA has approved two RSV vaccines approved for older adults, but clinicians may find it challenging to get older patients vaccinated for this and other preventable illnesses.
Patients who received the RSV vaccine had an 83% relative risk reduction for the illness, according to a recent study, and an overall lower risk for hospitalization.
Moderna is developing an mRNA vaccine for RSV that is similar to many COVID-19 vaccines. A study published in 2023 in The New England Journal of Medicine found no cases of neuroinflammatory disorders among patients who received the mRNA RSV vaccine, with a median follow-up of 112 days.
“This is important given ongoing concerns of neurological safety,” among older adults who receive the RSV vaccine, Dr. Smetana said.
As of March 2024, the CDC recommends shared decision-making for adults older than 60 years and for healthcare providers to “consider” rather than “recommend” the vaccine for their patients. The agency’s Adult RSV Work Group plans to meet at June 2024 to reconsider whether shared clinical decision-making remains the preferred policy option.
New Antidepressants
A medication thrice rejected by the FDA is now heading a new class of drugs to treat major depressive disorder.
Gepirone, a 5-HT1A receptor agonist, has a different mechanism of action from that of SSRIs, which are currently considered the first-line treatment for depression.
Gepirone was rejected by the FDA in 2002, 2004, and 2007, with concerns that the efficacy studies were too small. In 2015, an FDA advisory committee agreed that the evidence to date did not support approval of an extended-release form of the drug. But the agency decided to approve the medication in September 2023.
“So why is this medication worth discussing now?” Dr. Smetana said. “It’s because the side effect profile is different from existing antidepressants.”
Many patients may stop using SSRIs because of side effects such as insomnia and loss of libido, Dr. Smetana said. Gepirone has the potential to avoid activation of other 5-HT receptors that mediate side effects, he said.
Studies suggest that gepirone reduces both anxiety and depression scores on the Hamilton Depression Rating Scale in patients who have both conditions and decreases rates of depression relapse compared with placebo through at least 48 weeks. The drug also may be less likely than SSRIs to cause sexual dysfunction in men, Dr. Smetana said.
Gepirone will be available to prescribe to patients in fall 2024.
Dr. Smetana reported no relevant financial conflicts of interest.
A version of this article appeared on Medscape.com.
BOSTON — The US Food and Drug Administration (FDA) approved 55 new medications in 2023 and 11 more in 2024 to date.
A New First-Line for GERD?
Vonoprazan, an oral potassium-competitive acid blocker — which received FDA approval in November 2023 — may be a good alternative for patients whose symptoms continue to linger despite taking medications designated to treat gastroesophageal reflux disease (GERD).
GERD is the most common gastrointestinal symptom encountered by primary care physicians. Proton-pump inhibitors (PPIs) are the first-line treatment for the condition but can have long-term side effects such as Clostridioides difficile infection and kidney lesions.
“We know that not all patients are going to have symptom relief with H2 blockers and PPIs, so there’s an opportunity for patients who don’t get full symptom relief,” Dr. Smetana told attendees.
Vonoprazan blocks potassium binding to ATPase proton pumps and inhibits the secretion of gastric acid.
The approval of vonoprazan for erosive GERD was based on results from the phase 3 PHALCON-EE study, a randomized, double-blind, multicenter study that found the drug to be more effective than lansoprazole in treating erosive esophagitis.
Vonoprazan “has more rapid absorption than PPIs [and a] longer half-life and is more potent than PPIs, so theoretically it could be more effective in certain settings,” Dr. Smetana said.
Vonoprazan is FDA approved for only 6 months of use. Despite its efficacy, cost may be a barrier to many patients. H2 blockers generally cost patients less than $10 for 1 month’s supply, whereas vonoprazan can cost up to $650.
Nonhormonal Drug for Menopause
Fezolinetant, the first neurokinin receptor antagonist to receive approval from the FDA to treat vasomotor symptoms, may be an option for women concerned about hormone-based therapy for menopausal hot flashes.
“[Fezolinetant] specifically works in the area of the brain that’s involved in body temperature regulation and sweating,” Dr. Smetana said.
Results from the SKYLIGHT 1 randomized controlled trial of fezolinetant found the medication reduced the frequency and severity of hot flashes. Some of the side effects include abdominal pain, diarrhea, and insomnia.
Other nonestrogen treatments, including selective serotonin reuptake inhibitors (SSRIs), gabapentin, cognitive-behavioral therapy, and hypnosis, are modestly effective, according to the North American Menopause Society.
“[Fezolinetant] offers a different option that physicians may be more comfortable prescribing,” Dr. Smetana said. “And I think this will be an important addition to nonhormonal therapy.”
RSV Vaccine for Everyone
Once considered an illness that is more prevalent in young children, respiratory syncytial virus (RSV) has become more prevalent and severe among older adults. Between 60,000 and 120,000 older adults are hospitalized and 6000-10,000 die of RSV infection each year, according to the US Centers for Disease Control and Prevention.
The FDA has approved two RSV vaccines approved for older adults, but clinicians may find it challenging to get older patients vaccinated for this and other preventable illnesses.
Patients who received the RSV vaccine had an 83% relative risk reduction for the illness, according to a recent study, and an overall lower risk for hospitalization.
Moderna is developing an mRNA vaccine for RSV that is similar to many COVID-19 vaccines. A study published in 2023 in The New England Journal of Medicine found no cases of neuroinflammatory disorders among patients who received the mRNA RSV vaccine, with a median follow-up of 112 days.
“This is important given ongoing concerns of neurological safety,” among older adults who receive the RSV vaccine, Dr. Smetana said.
As of March 2024, the CDC recommends shared decision-making for adults older than 60 years and for healthcare providers to “consider” rather than “recommend” the vaccine for their patients. The agency’s Adult RSV Work Group plans to meet at June 2024 to reconsider whether shared clinical decision-making remains the preferred policy option.
New Antidepressants
A medication thrice rejected by the FDA is now heading a new class of drugs to treat major depressive disorder.
Gepirone, a 5-HT1A receptor agonist, has a different mechanism of action from that of SSRIs, which are currently considered the first-line treatment for depression.
Gepirone was rejected by the FDA in 2002, 2004, and 2007, with concerns that the efficacy studies were too small. In 2015, an FDA advisory committee agreed that the evidence to date did not support approval of an extended-release form of the drug. But the agency decided to approve the medication in September 2023.
“So why is this medication worth discussing now?” Dr. Smetana said. “It’s because the side effect profile is different from existing antidepressants.”
Many patients may stop using SSRIs because of side effects such as insomnia and loss of libido, Dr. Smetana said. Gepirone has the potential to avoid activation of other 5-HT receptors that mediate side effects, he said.
Studies suggest that gepirone reduces both anxiety and depression scores on the Hamilton Depression Rating Scale in patients who have both conditions and decreases rates of depression relapse compared with placebo through at least 48 weeks. The drug also may be less likely than SSRIs to cause sexual dysfunction in men, Dr. Smetana said.
Gepirone will be available to prescribe to patients in fall 2024.
Dr. Smetana reported no relevant financial conflicts of interest.
A version of this article appeared on Medscape.com.
Ocular Microbiome May Be Dry Eye Culprit
A mix of microbes may help explain why some people develop dry eye disease, new research showed.
This finding suggests that bacteria may cause dry eye and could someday point to new treatments for the condition and related disorders, which affect an estimated 27 million Americans, according to researchers.
Current treatments aim to preserve and enhance tears and tear production to ease the grittiness and itchiness that accompany dry eye disease.
To examine the role of the ocular microbiome in dry eye disease, scientists in Texas analyzed swab samples from 30 men and women, nine of whom had dry eye.
They found Streptococcus and Pedobacter species were the most common bacteria in healthy eyes.
In people with dry eye, however, more Acinetobacter species were detected.
“We think the metabolites produced by these bacteria are responsible for dry eye conditions,” study coauthor Pallavi Sharma said in a news release about the findings.
Sharma, a graduate student at Stephen F. Austin State University in Nacogdoches, Texas, presented this research last month at the annual meeting of the American Society for Biochemistry and Molecular Biology. The research team was led by Alexandra Van Kley, PhD, a professor of biology at the university.
“Once we understand the eye microbiota properly, it will improve disease diagnosis at an early stage,” Van Kley predicted in the news release. “This knowledge can also serve as a catalyst for developing innovative therapies aimed at preventing and treating ocular disease as well as those that affect the central microbiome site: The gut.”
Investigators in Australia have conducted similar experiments in patients with meibomian gland dysfunction, a condition marked by underproduction of key oils in the eye.
One group reported in August 2023 the finding of “detectable differences in the bacterial richness, diversity, and community structure of the conjunctiva and eyelid margin between individuals with meibomian gland dysfunction with and without lacrimal dysfunction, as well as to healthy controls.”
More research is needed to confirm and understand the findings, though, and “to determine if manipulating the microbiome could be a potential treatment for the condition,” they wrote.
A version of this article appeared on Medscape.com.
A mix of microbes may help explain why some people develop dry eye disease, new research showed.
This finding suggests that bacteria may cause dry eye and could someday point to new treatments for the condition and related disorders, which affect an estimated 27 million Americans, according to researchers.
Current treatments aim to preserve and enhance tears and tear production to ease the grittiness and itchiness that accompany dry eye disease.
To examine the role of the ocular microbiome in dry eye disease, scientists in Texas analyzed swab samples from 30 men and women, nine of whom had dry eye.
They found Streptococcus and Pedobacter species were the most common bacteria in healthy eyes.
In people with dry eye, however, more Acinetobacter species were detected.
“We think the metabolites produced by these bacteria are responsible for dry eye conditions,” study coauthor Pallavi Sharma said in a news release about the findings.
Sharma, a graduate student at Stephen F. Austin State University in Nacogdoches, Texas, presented this research last month at the annual meeting of the American Society for Biochemistry and Molecular Biology. The research team was led by Alexandra Van Kley, PhD, a professor of biology at the university.
“Once we understand the eye microbiota properly, it will improve disease diagnosis at an early stage,” Van Kley predicted in the news release. “This knowledge can also serve as a catalyst for developing innovative therapies aimed at preventing and treating ocular disease as well as those that affect the central microbiome site: The gut.”
Investigators in Australia have conducted similar experiments in patients with meibomian gland dysfunction, a condition marked by underproduction of key oils in the eye.
One group reported in August 2023 the finding of “detectable differences in the bacterial richness, diversity, and community structure of the conjunctiva and eyelid margin between individuals with meibomian gland dysfunction with and without lacrimal dysfunction, as well as to healthy controls.”
More research is needed to confirm and understand the findings, though, and “to determine if manipulating the microbiome could be a potential treatment for the condition,” they wrote.
A version of this article appeared on Medscape.com.
A mix of microbes may help explain why some people develop dry eye disease, new research showed.
This finding suggests that bacteria may cause dry eye and could someday point to new treatments for the condition and related disorders, which affect an estimated 27 million Americans, according to researchers.
Current treatments aim to preserve and enhance tears and tear production to ease the grittiness and itchiness that accompany dry eye disease.
To examine the role of the ocular microbiome in dry eye disease, scientists in Texas analyzed swab samples from 30 men and women, nine of whom had dry eye.
They found Streptococcus and Pedobacter species were the most common bacteria in healthy eyes.
In people with dry eye, however, more Acinetobacter species were detected.
“We think the metabolites produced by these bacteria are responsible for dry eye conditions,” study coauthor Pallavi Sharma said in a news release about the findings.
Sharma, a graduate student at Stephen F. Austin State University in Nacogdoches, Texas, presented this research last month at the annual meeting of the American Society for Biochemistry and Molecular Biology. The research team was led by Alexandra Van Kley, PhD, a professor of biology at the university.
“Once we understand the eye microbiota properly, it will improve disease diagnosis at an early stage,” Van Kley predicted in the news release. “This knowledge can also serve as a catalyst for developing innovative therapies aimed at preventing and treating ocular disease as well as those that affect the central microbiome site: The gut.”
Investigators in Australia have conducted similar experiments in patients with meibomian gland dysfunction, a condition marked by underproduction of key oils in the eye.
One group reported in August 2023 the finding of “detectable differences in the bacterial richness, diversity, and community structure of the conjunctiva and eyelid margin between individuals with meibomian gland dysfunction with and without lacrimal dysfunction, as well as to healthy controls.”
More research is needed to confirm and understand the findings, though, and “to determine if manipulating the microbiome could be a potential treatment for the condition,” they wrote.
A version of this article appeared on Medscape.com.
Vaccine ‘Will Not Curb’ Dengue Epidemic, Says PAHO
The current tetravalent dengue vaccine TAK-003, from the Japanese laboratory Takeda, is not likely to control the ongoing epidemic, according to the Pan American Health Organization (PAHO). The organization emphasized the need to better understand the vaccine’s effectiveness against different serotypes and its safety under real-world clinical conditions.
The Americas are experiencing a record increase in dengue cases. Three times as many cases have been identified during 2024 (3.5 million) than were reported for the same period in 2023.
“The vaccine we have available will not curb the dengue epidemic; it should be used complementarily with other actions. The most important actions are field operations, vector control, prevention, and education,” said Daniel Salas, MD, executive manager of the PAHO Comprehensive Immunization Program, during a press conference on March 28.
“The vaccines we currently have are not the best response to reduce transmission and prevent deaths,” added Jarbas Barbosa, MD, PhD, PAHO’s director. The fatality rate remains below 0.05%, but this figure could be hard to maintain if the situation becomes more uncontrolled.
The TAK-003 regimen consists of two doses with a 3-month interval between applications, so “it is not a tool to control transmission at this moment. Studies have shown that only 8 years of [population-level] vaccination would have a significant impact on dengue transmission,” said Dr. Barbosa.
A new vaccine developed in Brazil in partnership with the company MSD, Butantan-DV, is in phase 3 trials and has the advantage of being a single-dose application, which could facilitate its use in situations with accelerated transmission. “But this vaccine will likely only be available in 2025,” said Dr. Barbosa.
PAHO officials also highlighted the need to better characterize the vaccine’s effectiveness and safety in the real world. They observed, for example, that when TAK-003 was investigated, the circulation of dengue serotype 3 was almost nonexistent, so the efficacy data against that serotype “are very limited.”
“The producer, Takeda, has very limited production capacity. Brazil is the country that uses this vaccine the most, followed by Argentina. Given that these countries have a good epidemiological surveillance system and adverse effect registration, they can conduct studies on how the vaccine performs in real life, which will greatly increase our knowledge about it. For example, we will see its effectiveness against serotype 3,” said Dr. Barbosa.
The PAHO Technical Advisory Group (TAG) on vaccine-preventable diseases recommended that any country using these vaccines have surveillance systems in place because it is important to promptly report and investigate any adverse events, said Dr. Salas. The organization also suggested that vaccination should ideally be administered in a “more controlled environment,” a phase 4 study, “to complete the safety and efficacy profile, especially in those who have not had dengue before and for dengue 3 and 4,” said Dr. Salas in response to a question from this news organization.
“People cannot expect that just because they were vaccinated, they will not get dengue. The vaccine has limited reach,” he emphasized.
Other research strategies for vector control, such as the use of the Wolbachia bacteria and mosquito sterilization, are future strategies and “not tools to control this outbreak,” noted Sylvain Aldighieri, MD, director of the Department of Prevention, Control, and Elimination of Transmissible Diseases at PAHO.
In his opening remarks, Dr. Barbosa urged the intensification of efforts with tools that are already available. These approaches include eliminating mosquito breeding sites (“80% are in or near homes”) and protecting against mosquito bites, preparing health services for early diagnosis and timely clinical management, and educating the population about dengue symptoms so they seek medical attention immediately.
Although dengue is increasing throughout Latin America and the Caribbean, the most affected countries are Brazil (83%), Paraguay (5.3%), and Argentina (3.7%), which account for 92% of the cases and 87% of the deaths, PAHO reported.
This story was translated from the Medscape Spanish edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com .
The current tetravalent dengue vaccine TAK-003, from the Japanese laboratory Takeda, is not likely to control the ongoing epidemic, according to the Pan American Health Organization (PAHO). The organization emphasized the need to better understand the vaccine’s effectiveness against different serotypes and its safety under real-world clinical conditions.
The Americas are experiencing a record increase in dengue cases. Three times as many cases have been identified during 2024 (3.5 million) than were reported for the same period in 2023.
“The vaccine we have available will not curb the dengue epidemic; it should be used complementarily with other actions. The most important actions are field operations, vector control, prevention, and education,” said Daniel Salas, MD, executive manager of the PAHO Comprehensive Immunization Program, during a press conference on March 28.
“The vaccines we currently have are not the best response to reduce transmission and prevent deaths,” added Jarbas Barbosa, MD, PhD, PAHO’s director. The fatality rate remains below 0.05%, but this figure could be hard to maintain if the situation becomes more uncontrolled.
The TAK-003 regimen consists of two doses with a 3-month interval between applications, so “it is not a tool to control transmission at this moment. Studies have shown that only 8 years of [population-level] vaccination would have a significant impact on dengue transmission,” said Dr. Barbosa.
A new vaccine developed in Brazil in partnership with the company MSD, Butantan-DV, is in phase 3 trials and has the advantage of being a single-dose application, which could facilitate its use in situations with accelerated transmission. “But this vaccine will likely only be available in 2025,” said Dr. Barbosa.
PAHO officials also highlighted the need to better characterize the vaccine’s effectiveness and safety in the real world. They observed, for example, that when TAK-003 was investigated, the circulation of dengue serotype 3 was almost nonexistent, so the efficacy data against that serotype “are very limited.”
“The producer, Takeda, has very limited production capacity. Brazil is the country that uses this vaccine the most, followed by Argentina. Given that these countries have a good epidemiological surveillance system and adverse effect registration, they can conduct studies on how the vaccine performs in real life, which will greatly increase our knowledge about it. For example, we will see its effectiveness against serotype 3,” said Dr. Barbosa.
The PAHO Technical Advisory Group (TAG) on vaccine-preventable diseases recommended that any country using these vaccines have surveillance systems in place because it is important to promptly report and investigate any adverse events, said Dr. Salas. The organization also suggested that vaccination should ideally be administered in a “more controlled environment,” a phase 4 study, “to complete the safety and efficacy profile, especially in those who have not had dengue before and for dengue 3 and 4,” said Dr. Salas in response to a question from this news organization.
“People cannot expect that just because they were vaccinated, they will not get dengue. The vaccine has limited reach,” he emphasized.
Other research strategies for vector control, such as the use of the Wolbachia bacteria and mosquito sterilization, are future strategies and “not tools to control this outbreak,” noted Sylvain Aldighieri, MD, director of the Department of Prevention, Control, and Elimination of Transmissible Diseases at PAHO.
In his opening remarks, Dr. Barbosa urged the intensification of efforts with tools that are already available. These approaches include eliminating mosquito breeding sites (“80% are in or near homes”) and protecting against mosquito bites, preparing health services for early diagnosis and timely clinical management, and educating the population about dengue symptoms so they seek medical attention immediately.
Although dengue is increasing throughout Latin America and the Caribbean, the most affected countries are Brazil (83%), Paraguay (5.3%), and Argentina (3.7%), which account for 92% of the cases and 87% of the deaths, PAHO reported.
This story was translated from the Medscape Spanish edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com .
The current tetravalent dengue vaccine TAK-003, from the Japanese laboratory Takeda, is not likely to control the ongoing epidemic, according to the Pan American Health Organization (PAHO). The organization emphasized the need to better understand the vaccine’s effectiveness against different serotypes and its safety under real-world clinical conditions.
The Americas are experiencing a record increase in dengue cases. Three times as many cases have been identified during 2024 (3.5 million) than were reported for the same period in 2023.
“The vaccine we have available will not curb the dengue epidemic; it should be used complementarily with other actions. The most important actions are field operations, vector control, prevention, and education,” said Daniel Salas, MD, executive manager of the PAHO Comprehensive Immunization Program, during a press conference on March 28.
“The vaccines we currently have are not the best response to reduce transmission and prevent deaths,” added Jarbas Barbosa, MD, PhD, PAHO’s director. The fatality rate remains below 0.05%, but this figure could be hard to maintain if the situation becomes more uncontrolled.
The TAK-003 regimen consists of two doses with a 3-month interval between applications, so “it is not a tool to control transmission at this moment. Studies have shown that only 8 years of [population-level] vaccination would have a significant impact on dengue transmission,” said Dr. Barbosa.
A new vaccine developed in Brazil in partnership with the company MSD, Butantan-DV, is in phase 3 trials and has the advantage of being a single-dose application, which could facilitate its use in situations with accelerated transmission. “But this vaccine will likely only be available in 2025,” said Dr. Barbosa.
PAHO officials also highlighted the need to better characterize the vaccine’s effectiveness and safety in the real world. They observed, for example, that when TAK-003 was investigated, the circulation of dengue serotype 3 was almost nonexistent, so the efficacy data against that serotype “are very limited.”
“The producer, Takeda, has very limited production capacity. Brazil is the country that uses this vaccine the most, followed by Argentina. Given that these countries have a good epidemiological surveillance system and adverse effect registration, they can conduct studies on how the vaccine performs in real life, which will greatly increase our knowledge about it. For example, we will see its effectiveness against serotype 3,” said Dr. Barbosa.
The PAHO Technical Advisory Group (TAG) on vaccine-preventable diseases recommended that any country using these vaccines have surveillance systems in place because it is important to promptly report and investigate any adverse events, said Dr. Salas. The organization also suggested that vaccination should ideally be administered in a “more controlled environment,” a phase 4 study, “to complete the safety and efficacy profile, especially in those who have not had dengue before and for dengue 3 and 4,” said Dr. Salas in response to a question from this news organization.
“People cannot expect that just because they were vaccinated, they will not get dengue. The vaccine has limited reach,” he emphasized.
Other research strategies for vector control, such as the use of the Wolbachia bacteria and mosquito sterilization, are future strategies and “not tools to control this outbreak,” noted Sylvain Aldighieri, MD, director of the Department of Prevention, Control, and Elimination of Transmissible Diseases at PAHO.
In his opening remarks, Dr. Barbosa urged the intensification of efforts with tools that are already available. These approaches include eliminating mosquito breeding sites (“80% are in or near homes”) and protecting against mosquito bites, preparing health services for early diagnosis and timely clinical management, and educating the population about dengue symptoms so they seek medical attention immediately.
Although dengue is increasing throughout Latin America and the Caribbean, the most affected countries are Brazil (83%), Paraguay (5.3%), and Argentina (3.7%), which account for 92% of the cases and 87% of the deaths, PAHO reported.
This story was translated from the Medscape Spanish edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com .
FDA Approves AI Diagnostic Tool for Early Sepsis Detection
The US Food and Drug Administration (FDA) has approved a medical device named the Sepsis ImmunoScore, which is an artificial intelligence/machine learning software, to guide rapid diagnosis and prediction of sepsis. The authorization was granted through the FDA’s De Novo pathway.
Sepsis is a complex condition, so diagnosing it early is difficult and has been a decades-long challenge for the US healthcare system.
Using both biomarkers and clinical data with the assistance of AI, the Sepsis ImmunoScore helps assess the risk for the presence of or progression to sepsis within 24 hours of patient evaluation in the emergency department or hospital. By considering 22 diverse parameters, the AI-powered tool provides a comprehensive evaluation of the patient’s biological condition, resulting in a risk score and categorization into four distinct risk levels.
It’s important to note that this system is not an alert mechanism. These risk categories are correlated with the risk for patient deterioration, including length of hospital stay, in-hospital mortality, and the need for escalated care within 24 hours (such as intensive care unit admission, mechanical ventilation, or vasopressor use). The diagnostic software is integrated directly into hospital electronic medical records.
This is the first AI diagnostic tool for sepsis to receive marketing authorization from the FDA.
A version of this article appeared on Medscape.com.
The US Food and Drug Administration (FDA) has approved a medical device named the Sepsis ImmunoScore, which is an artificial intelligence/machine learning software, to guide rapid diagnosis and prediction of sepsis. The authorization was granted through the FDA’s De Novo pathway.
Sepsis is a complex condition, so diagnosing it early is difficult and has been a decades-long challenge for the US healthcare system.
Using both biomarkers and clinical data with the assistance of AI, the Sepsis ImmunoScore helps assess the risk for the presence of or progression to sepsis within 24 hours of patient evaluation in the emergency department or hospital. By considering 22 diverse parameters, the AI-powered tool provides a comprehensive evaluation of the patient’s biological condition, resulting in a risk score and categorization into four distinct risk levels.
It’s important to note that this system is not an alert mechanism. These risk categories are correlated with the risk for patient deterioration, including length of hospital stay, in-hospital mortality, and the need for escalated care within 24 hours (such as intensive care unit admission, mechanical ventilation, or vasopressor use). The diagnostic software is integrated directly into hospital electronic medical records.
This is the first AI diagnostic tool for sepsis to receive marketing authorization from the FDA.
A version of this article appeared on Medscape.com.
The US Food and Drug Administration (FDA) has approved a medical device named the Sepsis ImmunoScore, which is an artificial intelligence/machine learning software, to guide rapid diagnosis and prediction of sepsis. The authorization was granted through the FDA’s De Novo pathway.
Sepsis is a complex condition, so diagnosing it early is difficult and has been a decades-long challenge for the US healthcare system.
Using both biomarkers and clinical data with the assistance of AI, the Sepsis ImmunoScore helps assess the risk for the presence of or progression to sepsis within 24 hours of patient evaluation in the emergency department or hospital. By considering 22 diverse parameters, the AI-powered tool provides a comprehensive evaluation of the patient’s biological condition, resulting in a risk score and categorization into four distinct risk levels.
It’s important to note that this system is not an alert mechanism. These risk categories are correlated with the risk for patient deterioration, including length of hospital stay, in-hospital mortality, and the need for escalated care within 24 hours (such as intensive care unit admission, mechanical ventilation, or vasopressor use). The diagnostic software is integrated directly into hospital electronic medical records.
This is the first AI diagnostic tool for sepsis to receive marketing authorization from the FDA.
A version of this article appeared on Medscape.com.
Diabetic Foot Ulcers: Life-Threatening Issue in Need of Help
The photo of the patient’s foot, sent from his campsite, included a cheeky note: “I remember you telling me that getting in trouble doing something was better than getting in trouble doing nothing. This lets me get out there and know that I have feedback.”
The “this” was the patient’s “foot selfie,” an approach that allows patients at a risk for diabetic foot ulcers (DFUs) to snap a picture and send it to their healthcare providers for evaluation.
This particular patient had an extensive history of previous wounds. Some had essentially kept him house-bound in the past, as he was afraid to get another one.
This time, however, he got an all-clear to keep on camping, “and we scheduled him in on the following Tuesday [for follow-up],” said the camper’s physician David G. Armstrong, DPM, MD, PhD, professor of surgery and neurological surgery, USC Keck School of Medicine, Los Angeles.
Dr. Armstrong is one of the researchers evaluating the concept of foot selfies. It’s a welcome advance, he and others said, and has been shown to help heal wounds and reverse pre-ulcer lesions. Research on foot selfies continues, but much more is needed to solve the issue of DFUs, diabetic foot infections (DFIs), and the high rates of reinfection, experts know.
Worldwide, about 18.6 million people have a DFU each year, including 1.6 million in the United States. About 50%-60% of ulcers become infected, with 20% of moderate to severe infections requiring amputation of the limb. The 5-year mortality rate for DFUs is 30%, but it climbs to 70% after amputation. While about 40% of ulcers heal within 12 weeks, 42% recur at the 1-year mark, setting up a vicious and costly cycle. Healthcare costs for patients with diabetes and DFUs are five times as high as costs for patients with diabetes but no DFUs. The per capita cost to treat a DFU in America is $17,500.
While the statistics paint a grim picture, progress is being made on several fronts:
- US Food and Drug Administration (FDA) guidance on the development of drugs for DFUs, under evaluation, is forthcoming.
- New treatments are under study.
- A multidisciplinary team approach is known to improve outcomes.
Anatomy of a DFU
When neuropathy develops in those with diabetes, they no longer have what Dr. Armstrong calls the “gift” of pain perception. “They can wear a hole in their foot like you and I wear a hole in our sock or shoe,” he said. “That hole is called a diabetic foot ulcer.”
A DFU is an open wound on the foot, often occurring when bleeding develops beneath a callus and then the callus wears away. Deeper tissues of the foot are then exposed.
About half of the DFUs get infected, hence the FDA guidance, said Dr. Armstrong, who is also founding president of the American Limb Preservation Society, which aims to eliminate preventable amputations within the next generation. Every 20 seconds, Dr. Armstrong said, someone in the world loses a leg due to diabetes.
FDA Guidance on Drug Development for DFIs
In October, the FDA issued draft guidance for industry to articulate the design of clinical trials for developing antibacterial drugs to treat DFIs without concomitant bone and joint involvement. Comments closed on December 18. Among the points in the guidance, which is nonbinding, are to include DFIs of varying depths and extent in phase 3 trials and ideally to include only those patients who have not had prior antibacterial treatment for the current DFI.
According to an FDA spokesperson, “The agency is working to finalize the guidance. However, a timeline for its release has not yet been established.”
The good news about the upcoming FDA guidance, Dr. Armstrong said, is that the agency has realized the importance of treating the infections. Fully one third of direct costs of care for diabetes are spent on the lower extremities, he said. Keeping patients out of the hospital, uninfected, and “keeping legs on bodies” are all important goals, he said.
Pharmaceutical firms need to understand that “you aren’t dealing with a normal ulcer,” said Andrew J.M. Boulton, MD, professor of medicine at the University of Manchester and physician consultant at the Manchester Royal Infirmary, Manchester, England, and a visiting professor at the University of Miami. For research, “the most important thing is to take account of off-loading the ulcers,” he said. “Most ulcers will heal if put in a boot.”
Dr. Boulton, like Dr. Armstrong, a long-time expert in the field, contended that pharma has not understood this concept and has wasted millions over the last three decades doing studies that were poorly designed and controlled.
Treatments: Current, Under Study
Currently, DFIs are treated with antimicrobial therapy, without or without debridement, along with a clinical assessment for ischemia. If ischemia is found, care progresses to wound care and off-loading devices, such as healing sandals. Clinicians then assess the likelihood of improved outcomes with revascularization based on operative risks and distribution of lower extremity artery disease and proceed depending on the likelihood. If osteomyelitis testing shows it is present, providers proceed to wound debridement, limb-sparing amputation, and prolonged antimicrobials, as needed.
More options are needed, Dr. Armstrong said.
Among the many approaches under study:
- DFUs can be accurately detected by applying artificial intelligence to the “foot selfie” images taken by patients on smartphones, research by Dr. and has found.
- After a phase 3 study of for DFUs originally intending to enroll 300 subjects was discontinued because of slow patient recruitment, an interim analysis was conducted on 44 participants. It showed a positive trend toward wound closure in the group receiving the injected gene therapy, VM202 (ENGENSIS), in their calf muscles. VM202 is a plasmid DNA-encoding human hepatocyte growth factor. While those in both the intervention and placebo groups showed wound-closing effects at month 6, in 23 patients with neuro-ischemic ulcers, the percentage of those reaching complete closure of the DFU was significantly higher in the treated group at months 3, 4, and 5 (P = .0391, .0391, and .0361, respectively). After excluding two outliers, the difference in months 3-6 became more significant (P = .03).
- An closed more DFUs than standard care after 12 weeks — 70% vs 34% (P = .00032). Of the 100 participants randomized, 50 per group, 42% of the treatment group and 56% of the control group experienced adverse events, with eight withdrawn due to serious adverse events (such as osteomyelitis).
- A closed more refractory DFUs over a 16-week study than standard sharp debridement, with 65% of water-treated ulcers healed but just 42% of the standard care group (P = .021, unadjusted).
- Researchers from UC Davis and VA Northern California Healthcare are evaluating timolol, a beta adrenergic receptor blocker already approved for topical administration for glaucoma, as a way to heal chronic DFUs faster. After demonstrating that the medication worked in animal models, researchers then launched a study to use it off-label for DFUs. While data are still being analyzed, researcher Roslyn (Rivkah) Isseroff, MD, of UC Davis and VA, said that data so far demonstrate that the timolol reduced transepidermal water loss in the healed wounds, and that is linked with a decrease in re-ulceration.
The Power of a Team
Multidisciplinary approaches to treatment are effective in reducing amputation, with one review of 33 studies finding the approach worked to decrease amputation in 94% of them. “The American Limb Preservation Society (ALPS) lists 30 programs,” said Dr. Armstrong, the founding president of the organization. “There may be as many as 100.”
Team compositions vary but usually include at least one medical specialty clinician, such as infectious disease, primary care, or endocrinology, and two or more specialty clinicians, such as vascular, podiatric, orthopedic, or plastic surgery. A shoe specialist is needed to prescribe and manage footwear. Other important team members include nutrition experts and behavioral health professionals to deal with associated depression.
Johns Hopkins’ Multidisciplinary Diabetic Foot and Wound Service launched in 2012 and includes vascular surgeons, surgical podiatrists, endocrinologists, wound care nurses, advanced practice staff, board-certified wound care specialists, orthopedic surgeons, infection disease experts, physical therapists, and certified orthotists.
“This interdisciplinary care model has been repeatedly validated by research as superior for limb salvage and wound healing,” said Nestoras Mathioudakis, MD, codirector of the service. “For instance, endocrinologists and diabetes educators are crucial for managing uncontrolled diabetes — a key factor in infection and delayed wound healing. Similarly, vascular surgeons play a vital role in addressing peripheral arterial disease to improve blood flow to the affected area.”
“Diabetic foot ulcers might require prolonged periods of specialized care, including meticulous wound management and off-loading, overseen by surgical podiatrists and wound care experts,” he said. “In cases where infection is present, particularly with multidrug resistant organisms or when standard antibiotics are contraindicated, the insight of an infectious disease specialist is invaluable.”
While the makeup of teams varies from location to location, he said “the hallmark of effective teams is their ability to comprehensively manage glycemic control, foot wounds, vascular disease, and infections.”
The power of teams, Dr. Armstrong said, is very much evident after his weekly “foot selfie rounds” conducted Mondays at 7 AM, with an “all feet on deck” approach. “Not a week goes by when we don’t stop a hospitalization,” he said of the team evaluating the photos, due to detecting issues early, while still in the manageable state.
Teams can trump technology, Dr. Armstrong said. A team of just a primary care doctor and a podiatrist can make a significant reduction in amputations, he said, just by a “Knock your socks off” approach. He reminds primary care doctors that observing the feet of their patients with diabetes can go a long way to reducing DFUs and the hospitalizations and amputations that can result.
Dr. Mathioudakis and Dr. Isseroff reported no disclosures. Dr. Boulton consults for Urgo Medical, Nevro Corporation, and AOT, Inc. Dr. Armstrong reported receiving consulting fees from Podimetrics; Molnlycke; Cardiovascular Systems, Inc.; Endo Pharmaceuticals; and Averitas Pharma (GRT US).
A version of this article first appeared on Medscape.com.
The photo of the patient’s foot, sent from his campsite, included a cheeky note: “I remember you telling me that getting in trouble doing something was better than getting in trouble doing nothing. This lets me get out there and know that I have feedback.”
The “this” was the patient’s “foot selfie,” an approach that allows patients at a risk for diabetic foot ulcers (DFUs) to snap a picture and send it to their healthcare providers for evaluation.
This particular patient had an extensive history of previous wounds. Some had essentially kept him house-bound in the past, as he was afraid to get another one.
This time, however, he got an all-clear to keep on camping, “and we scheduled him in on the following Tuesday [for follow-up],” said the camper’s physician David G. Armstrong, DPM, MD, PhD, professor of surgery and neurological surgery, USC Keck School of Medicine, Los Angeles.
Dr. Armstrong is one of the researchers evaluating the concept of foot selfies. It’s a welcome advance, he and others said, and has been shown to help heal wounds and reverse pre-ulcer lesions. Research on foot selfies continues, but much more is needed to solve the issue of DFUs, diabetic foot infections (DFIs), and the high rates of reinfection, experts know.
Worldwide, about 18.6 million people have a DFU each year, including 1.6 million in the United States. About 50%-60% of ulcers become infected, with 20% of moderate to severe infections requiring amputation of the limb. The 5-year mortality rate for DFUs is 30%, but it climbs to 70% after amputation. While about 40% of ulcers heal within 12 weeks, 42% recur at the 1-year mark, setting up a vicious and costly cycle. Healthcare costs for patients with diabetes and DFUs are five times as high as costs for patients with diabetes but no DFUs. The per capita cost to treat a DFU in America is $17,500.
While the statistics paint a grim picture, progress is being made on several fronts:
- US Food and Drug Administration (FDA) guidance on the development of drugs for DFUs, under evaluation, is forthcoming.
- New treatments are under study.
- A multidisciplinary team approach is known to improve outcomes.
Anatomy of a DFU
When neuropathy develops in those with diabetes, they no longer have what Dr. Armstrong calls the “gift” of pain perception. “They can wear a hole in their foot like you and I wear a hole in our sock or shoe,” he said. “That hole is called a diabetic foot ulcer.”
A DFU is an open wound on the foot, often occurring when bleeding develops beneath a callus and then the callus wears away. Deeper tissues of the foot are then exposed.
About half of the DFUs get infected, hence the FDA guidance, said Dr. Armstrong, who is also founding president of the American Limb Preservation Society, which aims to eliminate preventable amputations within the next generation. Every 20 seconds, Dr. Armstrong said, someone in the world loses a leg due to diabetes.
FDA Guidance on Drug Development for DFIs
In October, the FDA issued draft guidance for industry to articulate the design of clinical trials for developing antibacterial drugs to treat DFIs without concomitant bone and joint involvement. Comments closed on December 18. Among the points in the guidance, which is nonbinding, are to include DFIs of varying depths and extent in phase 3 trials and ideally to include only those patients who have not had prior antibacterial treatment for the current DFI.
According to an FDA spokesperson, “The agency is working to finalize the guidance. However, a timeline for its release has not yet been established.”
The good news about the upcoming FDA guidance, Dr. Armstrong said, is that the agency has realized the importance of treating the infections. Fully one third of direct costs of care for diabetes are spent on the lower extremities, he said. Keeping patients out of the hospital, uninfected, and “keeping legs on bodies” are all important goals, he said.
Pharmaceutical firms need to understand that “you aren’t dealing with a normal ulcer,” said Andrew J.M. Boulton, MD, professor of medicine at the University of Manchester and physician consultant at the Manchester Royal Infirmary, Manchester, England, and a visiting professor at the University of Miami. For research, “the most important thing is to take account of off-loading the ulcers,” he said. “Most ulcers will heal if put in a boot.”
Dr. Boulton, like Dr. Armstrong, a long-time expert in the field, contended that pharma has not understood this concept and has wasted millions over the last three decades doing studies that were poorly designed and controlled.
Treatments: Current, Under Study
Currently, DFIs are treated with antimicrobial therapy, without or without debridement, along with a clinical assessment for ischemia. If ischemia is found, care progresses to wound care and off-loading devices, such as healing sandals. Clinicians then assess the likelihood of improved outcomes with revascularization based on operative risks and distribution of lower extremity artery disease and proceed depending on the likelihood. If osteomyelitis testing shows it is present, providers proceed to wound debridement, limb-sparing amputation, and prolonged antimicrobials, as needed.
More options are needed, Dr. Armstrong said.
Among the many approaches under study:
- DFUs can be accurately detected by applying artificial intelligence to the “foot selfie” images taken by patients on smartphones, research by Dr. and has found.
- After a phase 3 study of for DFUs originally intending to enroll 300 subjects was discontinued because of slow patient recruitment, an interim analysis was conducted on 44 participants. It showed a positive trend toward wound closure in the group receiving the injected gene therapy, VM202 (ENGENSIS), in their calf muscles. VM202 is a plasmid DNA-encoding human hepatocyte growth factor. While those in both the intervention and placebo groups showed wound-closing effects at month 6, in 23 patients with neuro-ischemic ulcers, the percentage of those reaching complete closure of the DFU was significantly higher in the treated group at months 3, 4, and 5 (P = .0391, .0391, and .0361, respectively). After excluding two outliers, the difference in months 3-6 became more significant (P = .03).
- An closed more DFUs than standard care after 12 weeks — 70% vs 34% (P = .00032). Of the 100 participants randomized, 50 per group, 42% of the treatment group and 56% of the control group experienced adverse events, with eight withdrawn due to serious adverse events (such as osteomyelitis).
- A closed more refractory DFUs over a 16-week study than standard sharp debridement, with 65% of water-treated ulcers healed but just 42% of the standard care group (P = .021, unadjusted).
- Researchers from UC Davis and VA Northern California Healthcare are evaluating timolol, a beta adrenergic receptor blocker already approved for topical administration for glaucoma, as a way to heal chronic DFUs faster. After demonstrating that the medication worked in animal models, researchers then launched a study to use it off-label for DFUs. While data are still being analyzed, researcher Roslyn (Rivkah) Isseroff, MD, of UC Davis and VA, said that data so far demonstrate that the timolol reduced transepidermal water loss in the healed wounds, and that is linked with a decrease in re-ulceration.
The Power of a Team
Multidisciplinary approaches to treatment are effective in reducing amputation, with one review of 33 studies finding the approach worked to decrease amputation in 94% of them. “The American Limb Preservation Society (ALPS) lists 30 programs,” said Dr. Armstrong, the founding president of the organization. “There may be as many as 100.”
Team compositions vary but usually include at least one medical specialty clinician, such as infectious disease, primary care, or endocrinology, and two or more specialty clinicians, such as vascular, podiatric, orthopedic, or plastic surgery. A shoe specialist is needed to prescribe and manage footwear. Other important team members include nutrition experts and behavioral health professionals to deal with associated depression.
Johns Hopkins’ Multidisciplinary Diabetic Foot and Wound Service launched in 2012 and includes vascular surgeons, surgical podiatrists, endocrinologists, wound care nurses, advanced practice staff, board-certified wound care specialists, orthopedic surgeons, infection disease experts, physical therapists, and certified orthotists.
“This interdisciplinary care model has been repeatedly validated by research as superior for limb salvage and wound healing,” said Nestoras Mathioudakis, MD, codirector of the service. “For instance, endocrinologists and diabetes educators are crucial for managing uncontrolled diabetes — a key factor in infection and delayed wound healing. Similarly, vascular surgeons play a vital role in addressing peripheral arterial disease to improve blood flow to the affected area.”
“Diabetic foot ulcers might require prolonged periods of specialized care, including meticulous wound management and off-loading, overseen by surgical podiatrists and wound care experts,” he said. “In cases where infection is present, particularly with multidrug resistant organisms or when standard antibiotics are contraindicated, the insight of an infectious disease specialist is invaluable.”
While the makeup of teams varies from location to location, he said “the hallmark of effective teams is their ability to comprehensively manage glycemic control, foot wounds, vascular disease, and infections.”
The power of teams, Dr. Armstrong said, is very much evident after his weekly “foot selfie rounds” conducted Mondays at 7 AM, with an “all feet on deck” approach. “Not a week goes by when we don’t stop a hospitalization,” he said of the team evaluating the photos, due to detecting issues early, while still in the manageable state.
Teams can trump technology, Dr. Armstrong said. A team of just a primary care doctor and a podiatrist can make a significant reduction in amputations, he said, just by a “Knock your socks off” approach. He reminds primary care doctors that observing the feet of their patients with diabetes can go a long way to reducing DFUs and the hospitalizations and amputations that can result.
Dr. Mathioudakis and Dr. Isseroff reported no disclosures. Dr. Boulton consults for Urgo Medical, Nevro Corporation, and AOT, Inc. Dr. Armstrong reported receiving consulting fees from Podimetrics; Molnlycke; Cardiovascular Systems, Inc.; Endo Pharmaceuticals; and Averitas Pharma (GRT US).
A version of this article first appeared on Medscape.com.
The photo of the patient’s foot, sent from his campsite, included a cheeky note: “I remember you telling me that getting in trouble doing something was better than getting in trouble doing nothing. This lets me get out there and know that I have feedback.”
The “this” was the patient’s “foot selfie,” an approach that allows patients at a risk for diabetic foot ulcers (DFUs) to snap a picture and send it to their healthcare providers for evaluation.
This particular patient had an extensive history of previous wounds. Some had essentially kept him house-bound in the past, as he was afraid to get another one.
This time, however, he got an all-clear to keep on camping, “and we scheduled him in on the following Tuesday [for follow-up],” said the camper’s physician David G. Armstrong, DPM, MD, PhD, professor of surgery and neurological surgery, USC Keck School of Medicine, Los Angeles.
Dr. Armstrong is one of the researchers evaluating the concept of foot selfies. It’s a welcome advance, he and others said, and has been shown to help heal wounds and reverse pre-ulcer lesions. Research on foot selfies continues, but much more is needed to solve the issue of DFUs, diabetic foot infections (DFIs), and the high rates of reinfection, experts know.
Worldwide, about 18.6 million people have a DFU each year, including 1.6 million in the United States. About 50%-60% of ulcers become infected, with 20% of moderate to severe infections requiring amputation of the limb. The 5-year mortality rate for DFUs is 30%, but it climbs to 70% after amputation. While about 40% of ulcers heal within 12 weeks, 42% recur at the 1-year mark, setting up a vicious and costly cycle. Healthcare costs for patients with diabetes and DFUs are five times as high as costs for patients with diabetes but no DFUs. The per capita cost to treat a DFU in America is $17,500.
While the statistics paint a grim picture, progress is being made on several fronts:
- US Food and Drug Administration (FDA) guidance on the development of drugs for DFUs, under evaluation, is forthcoming.
- New treatments are under study.
- A multidisciplinary team approach is known to improve outcomes.
Anatomy of a DFU
When neuropathy develops in those with diabetes, they no longer have what Dr. Armstrong calls the “gift” of pain perception. “They can wear a hole in their foot like you and I wear a hole in our sock or shoe,” he said. “That hole is called a diabetic foot ulcer.”
A DFU is an open wound on the foot, often occurring when bleeding develops beneath a callus and then the callus wears away. Deeper tissues of the foot are then exposed.
About half of the DFUs get infected, hence the FDA guidance, said Dr. Armstrong, who is also founding president of the American Limb Preservation Society, which aims to eliminate preventable amputations within the next generation. Every 20 seconds, Dr. Armstrong said, someone in the world loses a leg due to diabetes.
FDA Guidance on Drug Development for DFIs
In October, the FDA issued draft guidance for industry to articulate the design of clinical trials for developing antibacterial drugs to treat DFIs without concomitant bone and joint involvement. Comments closed on December 18. Among the points in the guidance, which is nonbinding, are to include DFIs of varying depths and extent in phase 3 trials and ideally to include only those patients who have not had prior antibacterial treatment for the current DFI.
According to an FDA spokesperson, “The agency is working to finalize the guidance. However, a timeline for its release has not yet been established.”
The good news about the upcoming FDA guidance, Dr. Armstrong said, is that the agency has realized the importance of treating the infections. Fully one third of direct costs of care for diabetes are spent on the lower extremities, he said. Keeping patients out of the hospital, uninfected, and “keeping legs on bodies” are all important goals, he said.
Pharmaceutical firms need to understand that “you aren’t dealing with a normal ulcer,” said Andrew J.M. Boulton, MD, professor of medicine at the University of Manchester and physician consultant at the Manchester Royal Infirmary, Manchester, England, and a visiting professor at the University of Miami. For research, “the most important thing is to take account of off-loading the ulcers,” he said. “Most ulcers will heal if put in a boot.”
Dr. Boulton, like Dr. Armstrong, a long-time expert in the field, contended that pharma has not understood this concept and has wasted millions over the last three decades doing studies that were poorly designed and controlled.
Treatments: Current, Under Study
Currently, DFIs are treated with antimicrobial therapy, without or without debridement, along with a clinical assessment for ischemia. If ischemia is found, care progresses to wound care and off-loading devices, such as healing sandals. Clinicians then assess the likelihood of improved outcomes with revascularization based on operative risks and distribution of lower extremity artery disease and proceed depending on the likelihood. If osteomyelitis testing shows it is present, providers proceed to wound debridement, limb-sparing amputation, and prolonged antimicrobials, as needed.
More options are needed, Dr. Armstrong said.
Among the many approaches under study:
- DFUs can be accurately detected by applying artificial intelligence to the “foot selfie” images taken by patients on smartphones, research by Dr. and has found.
- After a phase 3 study of for DFUs originally intending to enroll 300 subjects was discontinued because of slow patient recruitment, an interim analysis was conducted on 44 participants. It showed a positive trend toward wound closure in the group receiving the injected gene therapy, VM202 (ENGENSIS), in their calf muscles. VM202 is a plasmid DNA-encoding human hepatocyte growth factor. While those in both the intervention and placebo groups showed wound-closing effects at month 6, in 23 patients with neuro-ischemic ulcers, the percentage of those reaching complete closure of the DFU was significantly higher in the treated group at months 3, 4, and 5 (P = .0391, .0391, and .0361, respectively). After excluding two outliers, the difference in months 3-6 became more significant (P = .03).
- An closed more DFUs than standard care after 12 weeks — 70% vs 34% (P = .00032). Of the 100 participants randomized, 50 per group, 42% of the treatment group and 56% of the control group experienced adverse events, with eight withdrawn due to serious adverse events (such as osteomyelitis).
- A closed more refractory DFUs over a 16-week study than standard sharp debridement, with 65% of water-treated ulcers healed but just 42% of the standard care group (P = .021, unadjusted).
- Researchers from UC Davis and VA Northern California Healthcare are evaluating timolol, a beta adrenergic receptor blocker already approved for topical administration for glaucoma, as a way to heal chronic DFUs faster. After demonstrating that the medication worked in animal models, researchers then launched a study to use it off-label for DFUs. While data are still being analyzed, researcher Roslyn (Rivkah) Isseroff, MD, of UC Davis and VA, said that data so far demonstrate that the timolol reduced transepidermal water loss in the healed wounds, and that is linked with a decrease in re-ulceration.
The Power of a Team
Multidisciplinary approaches to treatment are effective in reducing amputation, with one review of 33 studies finding the approach worked to decrease amputation in 94% of them. “The American Limb Preservation Society (ALPS) lists 30 programs,” said Dr. Armstrong, the founding president of the organization. “There may be as many as 100.”
Team compositions vary but usually include at least one medical specialty clinician, such as infectious disease, primary care, or endocrinology, and two or more specialty clinicians, such as vascular, podiatric, orthopedic, or plastic surgery. A shoe specialist is needed to prescribe and manage footwear. Other important team members include nutrition experts and behavioral health professionals to deal with associated depression.
Johns Hopkins’ Multidisciplinary Diabetic Foot and Wound Service launched in 2012 and includes vascular surgeons, surgical podiatrists, endocrinologists, wound care nurses, advanced practice staff, board-certified wound care specialists, orthopedic surgeons, infection disease experts, physical therapists, and certified orthotists.
“This interdisciplinary care model has been repeatedly validated by research as superior for limb salvage and wound healing,” said Nestoras Mathioudakis, MD, codirector of the service. “For instance, endocrinologists and diabetes educators are crucial for managing uncontrolled diabetes — a key factor in infection and delayed wound healing. Similarly, vascular surgeons play a vital role in addressing peripheral arterial disease to improve blood flow to the affected area.”
“Diabetic foot ulcers might require prolonged periods of specialized care, including meticulous wound management and off-loading, overseen by surgical podiatrists and wound care experts,” he said. “In cases where infection is present, particularly with multidrug resistant organisms or when standard antibiotics are contraindicated, the insight of an infectious disease specialist is invaluable.”
While the makeup of teams varies from location to location, he said “the hallmark of effective teams is their ability to comprehensively manage glycemic control, foot wounds, vascular disease, and infections.”
The power of teams, Dr. Armstrong said, is very much evident after his weekly “foot selfie rounds” conducted Mondays at 7 AM, with an “all feet on deck” approach. “Not a week goes by when we don’t stop a hospitalization,” he said of the team evaluating the photos, due to detecting issues early, while still in the manageable state.
Teams can trump technology, Dr. Armstrong said. A team of just a primary care doctor and a podiatrist can make a significant reduction in amputations, he said, just by a “Knock your socks off” approach. He reminds primary care doctors that observing the feet of their patients with diabetes can go a long way to reducing DFUs and the hospitalizations and amputations that can result.
Dr. Mathioudakis and Dr. Isseroff reported no disclosures. Dr. Boulton consults for Urgo Medical, Nevro Corporation, and AOT, Inc. Dr. Armstrong reported receiving consulting fees from Podimetrics; Molnlycke; Cardiovascular Systems, Inc.; Endo Pharmaceuticals; and Averitas Pharma (GRT US).
A version of this article first appeared on Medscape.com.
4 Years In, a Sobering Look at Long COVID Progress
Four years ago in the spring of 2020, physicians and patients coined the term “long COVID” to describe a form of the viral infection from which recovery seemed impossible. (And the old nickname “long-haulers” seems so quaint now.)
What started as a pandemic that killed nearly 3 million people globally in 2020 alone would turn into a chronic disease causing a long list of symptoms — from extreme fatigue, to brain fog, tremors, nausea, headaches, rapid heartbeat, and more.
Today, 6.4% of Americans report symptoms of long COVID, and many have never recovered.
Still, we’ve come a long way, although there’s much we don’t understand about the condition. At the very least, physicians have a greater understanding that long COVID exists and can cause serious long-term symptoms.
While physicians may not have a blanket diagnostic tool that works for all patients with long COVID, they have refined existing tests for more accurate results, said Nisha Viswanathan, MD, director of the University of California Los Angeles Long COVID Program at UCLA Health.
Also, a range of new treatments, now undergoing clinical trials, have emerged that have proved effective in managing long COVID symptoms.
Catecholamine testing, for example, is now commonly used to diagnose long COVID, particularly in those who have dysautonomia, a condition caused by dysfunction of the autonomic nervous system and marked by dizziness, low blood pressure, nausea, and brain fog.
Very high levels of the neurotransmitter, for example, were shown to indicate long COVID in a January 2021 study published in the journal Clinical Medicine.
Certain biomarkers have also been shown indicative of the condition, including low serotonin levels. A study published this year in Cell found lower serotonin levels in patients with long COVID driven by low levels of circulating SARS-CoV-2, the virus that causes the condition.
Still, said Dr. Viswanathan, long COVID is a disease diagnosed by figuring out what a patient does not have — by ruling out other causes — rather than what they do. “It’s still a moving target,” she said, meaning that the disease is always changing based on the variant of acute COVID.
Promising Treatments Have Emerged
Dysautonomia, and especially the associated brain fog, fatigue, and dizziness, are now common conditions. As a result, physicians have gotten better at treating them. The vagus nerve is the main nerve of the parasympathetic nervous system that controls everything from digestion to mental health. A February 2022 pilot study suggested a link between vagus nerve dysfunction and some long COVID symptoms.
Vagus nerve stimulation is one form of treatment which involves using a device to stimulate the vagus nerve with electrical impulses. Dr. Viswanathan has been using the treatment in patients with fatigue, brain fog, anxiety, and depression — results, she contends, have been positive.
“This is something tangible that we can offer to patients,” she said.
Curative treatments for long COVID remain elusive, but doctors have many more tools for symptom management than before, said Ziyad Al-Aly, MD, a global expert on long COVID and chief of research and development at the Veterans Affairs St. Louis Health Care System.
For example, physicians are using beta-blockers to treat postural tachycardia syndrome (POTS), a symptom of long COVID that happens when the heart rate increases rapidly after someone stands up or lies down. Beta-blockers, such as the off-label medication ivabradine, have been used clinically to control heart rate, according to a March 2022 study published in the journal HeartRhythm Case Reports.
“It’s not a cure, but beta-blockers can help patients manage their symptoms,” said Dr. Al-Aly.
Additionally, some patients respond well to low-dose naltrexone for the treatment of extreme fatigue associated with long COVID. A January 2024 article in the journal Clinical Therapeutics found that fatigue symptoms improved in patients taking the medication.
Dr. Al-Aly said doctors treating patients with long COVID are getting better at pinpointing the phenotype or manifestation of the condition and diagnosing a treatment accordingly. Treating long COVID fatigue is not the same as treating POTS or symptoms of headache and joint pain.
It’s still all about the management of symptoms and doctors lack any US Food and Drug Administration–approved medications specifically for the condition.
Clinical Trials Exploring New Therapies
Still, a number of large clinical trials currently underway may change that, said David F. Putrino, PhD, who runs the long COVID clinic at Mount Sinai Health System in New York City.
Two clinical trials headed by Dr. Putrino’s lab are looking into repurposing two HIV antivirals to see whether they affect the levels of circulating SARS-CoV-2 virus in the body that may cause long COVID. The hope is that the antivirals Truvada and maraviroc can reduce the «reactivation of latent virus» that, said Dr. Putrino, causes lingering long COVID symptoms.
Ongoing trials are looking into the promise of SARS-CoV-2 monoclonal antibodies, produced from cells made by cloning a unique white blood cell, as a treatment option. The trials are investigating whether these antibodies may similarly target viral reservoirs that are causing persistence of symptoms in some patients.
Other trials are underway through the National Institutes of Health (NIH) RECOVER initiative in which more than 17,000 patients are enrolled, the largest study of its kind, said Grace McComsey, MD.
Dr. McComsey, who leads the study at University Hospitals Health System in Cleveland, said that after following patients for up to 4 years researchers have gathered “a massive repository of information” they hope will help scientists crack the code of this very complex disease.
She and other RECOVER researchers have recently published studies on a variety of findings, reporting in February, for example, that COVID infections may trigger other autoimmune diseases such as rheumatoid arthritis and type 2 diabetes. Another recent finding showed that people with HIV are at a higher risk for complications due to acute COVID-19.
Lack of Urgency Holds Back Progress
Still, others like Dr. Al-Aly and Dr. Putrino felt that the initiative isn’t moving fast enough. Dr. Al-Aly said that the NIH needs to “get its act together” and do more for long COVID. In the future, he said that we need to double down on our efforts to expand funding and increase urgency to better understand the mechanism of disease, risk factors, and treatments, as well as societal and economic implications.
“We did trials for COVID-19 vaccines at warp speed, but we’re doing trials for long COVID at a snail’s pace,” he said.
Dr. Al-Aly is concerned about the chronic nature of the disease and how it affects patients down the line. His large-scale study published last month in the journal Science looked specifically at chronic fatigue syndrome triggered by the infection and its long-term impact on patients.
He’s concerned about the practical implications for people who are weighted down with symptoms for multiple years.
“Being fatigued and ill for a few months is one thing, but being at home for 5 years is a totally different ballgame.”
A version of this article first appeared on Medscape.com.
Four years ago in the spring of 2020, physicians and patients coined the term “long COVID” to describe a form of the viral infection from which recovery seemed impossible. (And the old nickname “long-haulers” seems so quaint now.)
What started as a pandemic that killed nearly 3 million people globally in 2020 alone would turn into a chronic disease causing a long list of symptoms — from extreme fatigue, to brain fog, tremors, nausea, headaches, rapid heartbeat, and more.
Today, 6.4% of Americans report symptoms of long COVID, and many have never recovered.
Still, we’ve come a long way, although there’s much we don’t understand about the condition. At the very least, physicians have a greater understanding that long COVID exists and can cause serious long-term symptoms.
While physicians may not have a blanket diagnostic tool that works for all patients with long COVID, they have refined existing tests for more accurate results, said Nisha Viswanathan, MD, director of the University of California Los Angeles Long COVID Program at UCLA Health.
Also, a range of new treatments, now undergoing clinical trials, have emerged that have proved effective in managing long COVID symptoms.
Catecholamine testing, for example, is now commonly used to diagnose long COVID, particularly in those who have dysautonomia, a condition caused by dysfunction of the autonomic nervous system and marked by dizziness, low blood pressure, nausea, and brain fog.
Very high levels of the neurotransmitter, for example, were shown to indicate long COVID in a January 2021 study published in the journal Clinical Medicine.
Certain biomarkers have also been shown indicative of the condition, including low serotonin levels. A study published this year in Cell found lower serotonin levels in patients with long COVID driven by low levels of circulating SARS-CoV-2, the virus that causes the condition.
Still, said Dr. Viswanathan, long COVID is a disease diagnosed by figuring out what a patient does not have — by ruling out other causes — rather than what they do. “It’s still a moving target,” she said, meaning that the disease is always changing based on the variant of acute COVID.
Promising Treatments Have Emerged
Dysautonomia, and especially the associated brain fog, fatigue, and dizziness, are now common conditions. As a result, physicians have gotten better at treating them. The vagus nerve is the main nerve of the parasympathetic nervous system that controls everything from digestion to mental health. A February 2022 pilot study suggested a link between vagus nerve dysfunction and some long COVID symptoms.
Vagus nerve stimulation is one form of treatment which involves using a device to stimulate the vagus nerve with electrical impulses. Dr. Viswanathan has been using the treatment in patients with fatigue, brain fog, anxiety, and depression — results, she contends, have been positive.
“This is something tangible that we can offer to patients,” she said.
Curative treatments for long COVID remain elusive, but doctors have many more tools for symptom management than before, said Ziyad Al-Aly, MD, a global expert on long COVID and chief of research and development at the Veterans Affairs St. Louis Health Care System.
For example, physicians are using beta-blockers to treat postural tachycardia syndrome (POTS), a symptom of long COVID that happens when the heart rate increases rapidly after someone stands up or lies down. Beta-blockers, such as the off-label medication ivabradine, have been used clinically to control heart rate, according to a March 2022 study published in the journal HeartRhythm Case Reports.
“It’s not a cure, but beta-blockers can help patients manage their symptoms,” said Dr. Al-Aly.
Additionally, some patients respond well to low-dose naltrexone for the treatment of extreme fatigue associated with long COVID. A January 2024 article in the journal Clinical Therapeutics found that fatigue symptoms improved in patients taking the medication.
Dr. Al-Aly said doctors treating patients with long COVID are getting better at pinpointing the phenotype or manifestation of the condition and diagnosing a treatment accordingly. Treating long COVID fatigue is not the same as treating POTS or symptoms of headache and joint pain.
It’s still all about the management of symptoms and doctors lack any US Food and Drug Administration–approved medications specifically for the condition.
Clinical Trials Exploring New Therapies
Still, a number of large clinical trials currently underway may change that, said David F. Putrino, PhD, who runs the long COVID clinic at Mount Sinai Health System in New York City.
Two clinical trials headed by Dr. Putrino’s lab are looking into repurposing two HIV antivirals to see whether they affect the levels of circulating SARS-CoV-2 virus in the body that may cause long COVID. The hope is that the antivirals Truvada and maraviroc can reduce the «reactivation of latent virus» that, said Dr. Putrino, causes lingering long COVID symptoms.
Ongoing trials are looking into the promise of SARS-CoV-2 monoclonal antibodies, produced from cells made by cloning a unique white blood cell, as a treatment option. The trials are investigating whether these antibodies may similarly target viral reservoirs that are causing persistence of symptoms in some patients.
Other trials are underway through the National Institutes of Health (NIH) RECOVER initiative in which more than 17,000 patients are enrolled, the largest study of its kind, said Grace McComsey, MD.
Dr. McComsey, who leads the study at University Hospitals Health System in Cleveland, said that after following patients for up to 4 years researchers have gathered “a massive repository of information” they hope will help scientists crack the code of this very complex disease.
She and other RECOVER researchers have recently published studies on a variety of findings, reporting in February, for example, that COVID infections may trigger other autoimmune diseases such as rheumatoid arthritis and type 2 diabetes. Another recent finding showed that people with HIV are at a higher risk for complications due to acute COVID-19.
Lack of Urgency Holds Back Progress
Still, others like Dr. Al-Aly and Dr. Putrino felt that the initiative isn’t moving fast enough. Dr. Al-Aly said that the NIH needs to “get its act together” and do more for long COVID. In the future, he said that we need to double down on our efforts to expand funding and increase urgency to better understand the mechanism of disease, risk factors, and treatments, as well as societal and economic implications.
“We did trials for COVID-19 vaccines at warp speed, but we’re doing trials for long COVID at a snail’s pace,” he said.
Dr. Al-Aly is concerned about the chronic nature of the disease and how it affects patients down the line. His large-scale study published last month in the journal Science looked specifically at chronic fatigue syndrome triggered by the infection and its long-term impact on patients.
He’s concerned about the practical implications for people who are weighted down with symptoms for multiple years.
“Being fatigued and ill for a few months is one thing, but being at home for 5 years is a totally different ballgame.”
A version of this article first appeared on Medscape.com.
Four years ago in the spring of 2020, physicians and patients coined the term “long COVID” to describe a form of the viral infection from which recovery seemed impossible. (And the old nickname “long-haulers” seems so quaint now.)
What started as a pandemic that killed nearly 3 million people globally in 2020 alone would turn into a chronic disease causing a long list of symptoms — from extreme fatigue, to brain fog, tremors, nausea, headaches, rapid heartbeat, and more.
Today, 6.4% of Americans report symptoms of long COVID, and many have never recovered.
Still, we’ve come a long way, although there’s much we don’t understand about the condition. At the very least, physicians have a greater understanding that long COVID exists and can cause serious long-term symptoms.
While physicians may not have a blanket diagnostic tool that works for all patients with long COVID, they have refined existing tests for more accurate results, said Nisha Viswanathan, MD, director of the University of California Los Angeles Long COVID Program at UCLA Health.
Also, a range of new treatments, now undergoing clinical trials, have emerged that have proved effective in managing long COVID symptoms.
Catecholamine testing, for example, is now commonly used to diagnose long COVID, particularly in those who have dysautonomia, a condition caused by dysfunction of the autonomic nervous system and marked by dizziness, low blood pressure, nausea, and brain fog.
Very high levels of the neurotransmitter, for example, were shown to indicate long COVID in a January 2021 study published in the journal Clinical Medicine.
Certain biomarkers have also been shown indicative of the condition, including low serotonin levels. A study published this year in Cell found lower serotonin levels in patients with long COVID driven by low levels of circulating SARS-CoV-2, the virus that causes the condition.
Still, said Dr. Viswanathan, long COVID is a disease diagnosed by figuring out what a patient does not have — by ruling out other causes — rather than what they do. “It’s still a moving target,” she said, meaning that the disease is always changing based on the variant of acute COVID.
Promising Treatments Have Emerged
Dysautonomia, and especially the associated brain fog, fatigue, and dizziness, are now common conditions. As a result, physicians have gotten better at treating them. The vagus nerve is the main nerve of the parasympathetic nervous system that controls everything from digestion to mental health. A February 2022 pilot study suggested a link between vagus nerve dysfunction and some long COVID symptoms.
Vagus nerve stimulation is one form of treatment which involves using a device to stimulate the vagus nerve with electrical impulses. Dr. Viswanathan has been using the treatment in patients with fatigue, brain fog, anxiety, and depression — results, she contends, have been positive.
“This is something tangible that we can offer to patients,” she said.
Curative treatments for long COVID remain elusive, but doctors have many more tools for symptom management than before, said Ziyad Al-Aly, MD, a global expert on long COVID and chief of research and development at the Veterans Affairs St. Louis Health Care System.
For example, physicians are using beta-blockers to treat postural tachycardia syndrome (POTS), a symptom of long COVID that happens when the heart rate increases rapidly after someone stands up or lies down. Beta-blockers, such as the off-label medication ivabradine, have been used clinically to control heart rate, according to a March 2022 study published in the journal HeartRhythm Case Reports.
“It’s not a cure, but beta-blockers can help patients manage their symptoms,” said Dr. Al-Aly.
Additionally, some patients respond well to low-dose naltrexone for the treatment of extreme fatigue associated with long COVID. A January 2024 article in the journal Clinical Therapeutics found that fatigue symptoms improved in patients taking the medication.
Dr. Al-Aly said doctors treating patients with long COVID are getting better at pinpointing the phenotype or manifestation of the condition and diagnosing a treatment accordingly. Treating long COVID fatigue is not the same as treating POTS or symptoms of headache and joint pain.
It’s still all about the management of symptoms and doctors lack any US Food and Drug Administration–approved medications specifically for the condition.
Clinical Trials Exploring New Therapies
Still, a number of large clinical trials currently underway may change that, said David F. Putrino, PhD, who runs the long COVID clinic at Mount Sinai Health System in New York City.
Two clinical trials headed by Dr. Putrino’s lab are looking into repurposing two HIV antivirals to see whether they affect the levels of circulating SARS-CoV-2 virus in the body that may cause long COVID. The hope is that the antivirals Truvada and maraviroc can reduce the «reactivation of latent virus» that, said Dr. Putrino, causes lingering long COVID symptoms.
Ongoing trials are looking into the promise of SARS-CoV-2 monoclonal antibodies, produced from cells made by cloning a unique white blood cell, as a treatment option. The trials are investigating whether these antibodies may similarly target viral reservoirs that are causing persistence of symptoms in some patients.
Other trials are underway through the National Institutes of Health (NIH) RECOVER initiative in which more than 17,000 patients are enrolled, the largest study of its kind, said Grace McComsey, MD.
Dr. McComsey, who leads the study at University Hospitals Health System in Cleveland, said that after following patients for up to 4 years researchers have gathered “a massive repository of information” they hope will help scientists crack the code of this very complex disease.
She and other RECOVER researchers have recently published studies on a variety of findings, reporting in February, for example, that COVID infections may trigger other autoimmune diseases such as rheumatoid arthritis and type 2 diabetes. Another recent finding showed that people with HIV are at a higher risk for complications due to acute COVID-19.
Lack of Urgency Holds Back Progress
Still, others like Dr. Al-Aly and Dr. Putrino felt that the initiative isn’t moving fast enough. Dr. Al-Aly said that the NIH needs to “get its act together” and do more for long COVID. In the future, he said that we need to double down on our efforts to expand funding and increase urgency to better understand the mechanism of disease, risk factors, and treatments, as well as societal and economic implications.
“We did trials for COVID-19 vaccines at warp speed, but we’re doing trials for long COVID at a snail’s pace,” he said.
Dr. Al-Aly is concerned about the chronic nature of the disease and how it affects patients down the line. His large-scale study published last month in the journal Science looked specifically at chronic fatigue syndrome triggered by the infection and its long-term impact on patients.
He’s concerned about the practical implications for people who are weighted down with symptoms for multiple years.
“Being fatigued and ill for a few months is one thing, but being at home for 5 years is a totally different ballgame.”
A version of this article first appeared on Medscape.com.
Recently Immunized Febrile Infants Have Low Infection Risk
TOPLINE:
METHODOLOGY:
- Researchers evaluated 508 infants aged 6-12 weeks who presented with a fever of 38 °C or greater at two US military academic emergency departments (EDs) over a span of 4 years.
- The infants were categorized as “recently immunized” if they had received immunizations within 72 hours before ED presentation and “not recently immunized” if they had not. Among the 508 infants, 114 were immunized recently.
- The primary outcome was the prevalence of a serious bacterial infection (SBI), categorized into IBI and non-IBI on the basis of culture and radiography findings.
TAKEAWAY:
- The prevalence of SBI was 3.5% in the recently immunized febrile infants and 13.7% in not recently immunized febrile infants.
- Among the recently immunized infants, the prevalence of SBI was lower in those immunized within the first 24 hours than those immunized more than 24 hours before ED presentation (2% vs 14.3%, respectively).
- Almost all identified SBI cases were of urinary tract infection (UTI), with the only non-UTI case being pneumonia in an infant who exhibited respiratory symptoms within 24 hours of receiving immunization.
IN PRACTICE:
Physicians should discuss the possibilities of a less invasive approach for evaluating recently immunized febrile infants. The study findings support the general recommendation to obtain a urinalysis for all recently immunized infants over 60 days presenting with fever, including those presenting less than 24 hours post immunization.
SOURCE:
This study, led by Kyla Casey, MD, Department of Emergency Medicine, Naval Medical Center San Diego, was published online in The American Journal of Emergency Medicine.
LIMITATIONS:
The small sample size and retrospective design might have resulted in an overestimation of outcomes like IBIs within 24 hours after immunization. As the study was conducted in a specific clinical setting with febrile infants from military medical centers, the findings may have limited generalizability. Moreover, the inclusion of premature infants without age correction for prematurity could have impacted the prevalence of IBIs. Factors like missing vaccination history, healthcare referral patterns, and immunization practices in the military system may have introduced bias.
DISCLOSURE:
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors. The authors had no conflicts of interest to disclose.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers evaluated 508 infants aged 6-12 weeks who presented with a fever of 38 °C or greater at two US military academic emergency departments (EDs) over a span of 4 years.
- The infants were categorized as “recently immunized” if they had received immunizations within 72 hours before ED presentation and “not recently immunized” if they had not. Among the 508 infants, 114 were immunized recently.
- The primary outcome was the prevalence of a serious bacterial infection (SBI), categorized into IBI and non-IBI on the basis of culture and radiography findings.
TAKEAWAY:
- The prevalence of SBI was 3.5% in the recently immunized febrile infants and 13.7% in not recently immunized febrile infants.
- Among the recently immunized infants, the prevalence of SBI was lower in those immunized within the first 24 hours than those immunized more than 24 hours before ED presentation (2% vs 14.3%, respectively).
- Almost all identified SBI cases were of urinary tract infection (UTI), with the only non-UTI case being pneumonia in an infant who exhibited respiratory symptoms within 24 hours of receiving immunization.
IN PRACTICE:
Physicians should discuss the possibilities of a less invasive approach for evaluating recently immunized febrile infants. The study findings support the general recommendation to obtain a urinalysis for all recently immunized infants over 60 days presenting with fever, including those presenting less than 24 hours post immunization.
SOURCE:
This study, led by Kyla Casey, MD, Department of Emergency Medicine, Naval Medical Center San Diego, was published online in The American Journal of Emergency Medicine.
LIMITATIONS:
The small sample size and retrospective design might have resulted in an overestimation of outcomes like IBIs within 24 hours after immunization. As the study was conducted in a specific clinical setting with febrile infants from military medical centers, the findings may have limited generalizability. Moreover, the inclusion of premature infants without age correction for prematurity could have impacted the prevalence of IBIs. Factors like missing vaccination history, healthcare referral patterns, and immunization practices in the military system may have introduced bias.
DISCLOSURE:
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors. The authors had no conflicts of interest to disclose.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers evaluated 508 infants aged 6-12 weeks who presented with a fever of 38 °C or greater at two US military academic emergency departments (EDs) over a span of 4 years.
- The infants were categorized as “recently immunized” if they had received immunizations within 72 hours before ED presentation and “not recently immunized” if they had not. Among the 508 infants, 114 were immunized recently.
- The primary outcome was the prevalence of a serious bacterial infection (SBI), categorized into IBI and non-IBI on the basis of culture and radiography findings.
TAKEAWAY:
- The prevalence of SBI was 3.5% in the recently immunized febrile infants and 13.7% in not recently immunized febrile infants.
- Among the recently immunized infants, the prevalence of SBI was lower in those immunized within the first 24 hours than those immunized more than 24 hours before ED presentation (2% vs 14.3%, respectively).
- Almost all identified SBI cases were of urinary tract infection (UTI), with the only non-UTI case being pneumonia in an infant who exhibited respiratory symptoms within 24 hours of receiving immunization.
IN PRACTICE:
Physicians should discuss the possibilities of a less invasive approach for evaluating recently immunized febrile infants. The study findings support the general recommendation to obtain a urinalysis for all recently immunized infants over 60 days presenting with fever, including those presenting less than 24 hours post immunization.
SOURCE:
This study, led by Kyla Casey, MD, Department of Emergency Medicine, Naval Medical Center San Diego, was published online in The American Journal of Emergency Medicine.
LIMITATIONS:
The small sample size and retrospective design might have resulted in an overestimation of outcomes like IBIs within 24 hours after immunization. As the study was conducted in a specific clinical setting with febrile infants from military medical centers, the findings may have limited generalizability. Moreover, the inclusion of premature infants without age correction for prematurity could have impacted the prevalence of IBIs. Factors like missing vaccination history, healthcare referral patterns, and immunization practices in the military system may have introduced bias.
DISCLOSURE:
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors. The authors had no conflicts of interest to disclose.
A version of this article appeared on Medscape.com.
D-Mannose as UTI Treatment Offers No Benefit
TOPLINE:
A natural sugar used to treat recurring urinary tract infections (rUTIs) did not reduce future episodes, outpatient visits, the use of antibiotics, or symptoms compared with a placebo, according to a new study.
METHODOLOGY:
- D-Mannose is recommended as a natural alternative to antibiotics and sold as a dietary supplement; research showing the efficacy of D-mannose in treating UTIs is mixed.
- The double-blind, randomized controlled trial followed 598 women older than 18 years (median age, 61.3; range 18.2-93.5 years) with a history of rUTIs over 6 months from nearly 100 primary care clinics in the United Kingdom.
- Patients took 2 g of D-mannose or placebo powder daily and recorded their symptoms using a daily diary or through responses to health surveys, weekly questionnaires, and phone calls.
- Researchers checked medical records for urine culture results, antibiotic prescriptions, hospitalizations, and outpatient visits for UTIs.
TAKEAWAY:
- Approximately 51% of participants who took D-mannose and 55.7% of those who took a placebo contacted a healthcare professional reporting a UTI (relative risk, 0.92; 95% CI, 0.80-1.05; P = .22).
- Women in both groups reported similar durations of “moderately bad” or “worse” symptoms, and the number of antibiotic courses, instances of clinically suspected UTIs, and hospital admissions were similar between the two groups.
- Some studies have reported that synthetic mannosides are promising alternatives to D-mannose.
IN PRACTICE:
“D-Mannose should not be recommended to prevent future episodes of medically attended UTI in women with recurrent UTI in primary care,” the study authors wrote.
SOURCE:
The study was led by Gail Hayward, DPhil, associate professor at the Nuffield Department of Primary Care Health Sciences at the University of Oxford in England, and was published online in JAMA Internal Medicine.
LIMITATIONS:
Some participants may have taken less than 2 mg/d or skipped days. Because researchers used powder rather than capsules, dosing could have been inconsistent. Researchers did not obtain a microbiologic confirmation for each rUTI. A small percentage of women were taking antibiotics.
DISCLOSURES:
The study was funded by the National Institute for Health and Care Research (NIHR) School for Primary Care Research and the NIHR Oxford Biomedical Research Centre. Various authors reported receiving support from the NIHR Health Protection Research Unit on Healthcare-Associated Infections and Antimicrobial Resistance and were NIHR investigators.
A version of this article first appeared on Medscape.com.
TOPLINE:
A natural sugar used to treat recurring urinary tract infections (rUTIs) did not reduce future episodes, outpatient visits, the use of antibiotics, or symptoms compared with a placebo, according to a new study.
METHODOLOGY:
- D-Mannose is recommended as a natural alternative to antibiotics and sold as a dietary supplement; research showing the efficacy of D-mannose in treating UTIs is mixed.
- The double-blind, randomized controlled trial followed 598 women older than 18 years (median age, 61.3; range 18.2-93.5 years) with a history of rUTIs over 6 months from nearly 100 primary care clinics in the United Kingdom.
- Patients took 2 g of D-mannose or placebo powder daily and recorded their symptoms using a daily diary or through responses to health surveys, weekly questionnaires, and phone calls.
- Researchers checked medical records for urine culture results, antibiotic prescriptions, hospitalizations, and outpatient visits for UTIs.
TAKEAWAY:
- Approximately 51% of participants who took D-mannose and 55.7% of those who took a placebo contacted a healthcare professional reporting a UTI (relative risk, 0.92; 95% CI, 0.80-1.05; P = .22).
- Women in both groups reported similar durations of “moderately bad” or “worse” symptoms, and the number of antibiotic courses, instances of clinically suspected UTIs, and hospital admissions were similar between the two groups.
- Some studies have reported that synthetic mannosides are promising alternatives to D-mannose.
IN PRACTICE:
“D-Mannose should not be recommended to prevent future episodes of medically attended UTI in women with recurrent UTI in primary care,” the study authors wrote.
SOURCE:
The study was led by Gail Hayward, DPhil, associate professor at the Nuffield Department of Primary Care Health Sciences at the University of Oxford in England, and was published online in JAMA Internal Medicine.
LIMITATIONS:
Some participants may have taken less than 2 mg/d or skipped days. Because researchers used powder rather than capsules, dosing could have been inconsistent. Researchers did not obtain a microbiologic confirmation for each rUTI. A small percentage of women were taking antibiotics.
DISCLOSURES:
The study was funded by the National Institute for Health and Care Research (NIHR) School for Primary Care Research and the NIHR Oxford Biomedical Research Centre. Various authors reported receiving support from the NIHR Health Protection Research Unit on Healthcare-Associated Infections and Antimicrobial Resistance and were NIHR investigators.
A version of this article first appeared on Medscape.com.
TOPLINE:
A natural sugar used to treat recurring urinary tract infections (rUTIs) did not reduce future episodes, outpatient visits, the use of antibiotics, or symptoms compared with a placebo, according to a new study.
METHODOLOGY:
- D-Mannose is recommended as a natural alternative to antibiotics and sold as a dietary supplement; research showing the efficacy of D-mannose in treating UTIs is mixed.
- The double-blind, randomized controlled trial followed 598 women older than 18 years (median age, 61.3; range 18.2-93.5 years) with a history of rUTIs over 6 months from nearly 100 primary care clinics in the United Kingdom.
- Patients took 2 g of D-mannose or placebo powder daily and recorded their symptoms using a daily diary or through responses to health surveys, weekly questionnaires, and phone calls.
- Researchers checked medical records for urine culture results, antibiotic prescriptions, hospitalizations, and outpatient visits for UTIs.
TAKEAWAY:
- Approximately 51% of participants who took D-mannose and 55.7% of those who took a placebo contacted a healthcare professional reporting a UTI (relative risk, 0.92; 95% CI, 0.80-1.05; P = .22).
- Women in both groups reported similar durations of “moderately bad” or “worse” symptoms, and the number of antibiotic courses, instances of clinically suspected UTIs, and hospital admissions were similar between the two groups.
- Some studies have reported that synthetic mannosides are promising alternatives to D-mannose.
IN PRACTICE:
“D-Mannose should not be recommended to prevent future episodes of medically attended UTI in women with recurrent UTI in primary care,” the study authors wrote.
SOURCE:
The study was led by Gail Hayward, DPhil, associate professor at the Nuffield Department of Primary Care Health Sciences at the University of Oxford in England, and was published online in JAMA Internal Medicine.
LIMITATIONS:
Some participants may have taken less than 2 mg/d or skipped days. Because researchers used powder rather than capsules, dosing could have been inconsistent. Researchers did not obtain a microbiologic confirmation for each rUTI. A small percentage of women were taking antibiotics.
DISCLOSURES:
The study was funded by the National Institute for Health and Care Research (NIHR) School for Primary Care Research and the NIHR Oxford Biomedical Research Centre. Various authors reported receiving support from the NIHR Health Protection Research Unit on Healthcare-Associated Infections and Antimicrobial Resistance and were NIHR investigators.
A version of this article first appeared on Medscape.com.
Worldwide Uptick in Invasive Group A Streptococcus Disease Post Pandemic — What Should We Know?
Invasive group A streptococcus (iGAS) infections are rare (4-9 cases/100,000 US population annually) but potentially devastating (approximately 2,300 deaths annually in US), and affect all ages. Cases increase in winter-spring, paralleling the “season” of increased noninvasive GAS, e.g., pharyngitis and scarlet fever. iGAS case rates are lower in children than adults. That said, one well-known pediatric iGAS scenario has been deep cellulitis and necrotizing fasciitis during the healing phase of varicella. Other forms of iGAS include bacteremia, pneumonia (particularly when empyema is present), lymphangitis, erysipelas, and toxic shock syndrome. iGAS can occur with/after influenza but has also occurred concurrently with other viral respiratory infections.
Persons with underlying conditions (cancer or immune compromised status; chronic diseases of the heart, kidney or lung; diabetes mellitus) are at higher risk. Other subpopulations at risk for iGAS are illicit drug users, the elderly, homeless persons, nursing home residents, American Indian persons, and Alaska Native persons. Most experts feel that highly toxigenic strains of GAS are responsible for most iGAS. Indeed, most iGAS isolates produce (sometimes hyper-produce) superantigens that cause exaggerated innate immune responses, higher levels of inflammation, and often times tissue destruction, e.g., “flesh eating bacteria.” And who can forget that Jim Henson, creator of the Muppets, died of iGAS?
But why discuss iGAS in 2024? The pattern for iGAS has fluctuated more than usual in the last decade. So much so that the recent upsurge has caught the collective eye of the lay press. So, patients and friends may have questions about why and how iGAS is increasing lately. The bottom line is that no one knows for sure. However, the most recent 2 years of uptick may reflect GAS circulating at relatively high levels even when taking into account that GAS season occurs in winter-spring most years. Yet it seems likely that additional factors may have played a role in the fluctuations noted this past decade, e.g., temporary changes in societal behavior, a new GAS strain with over two dozen mutations, and possibly rapid waning of protection against GAS exotoxins.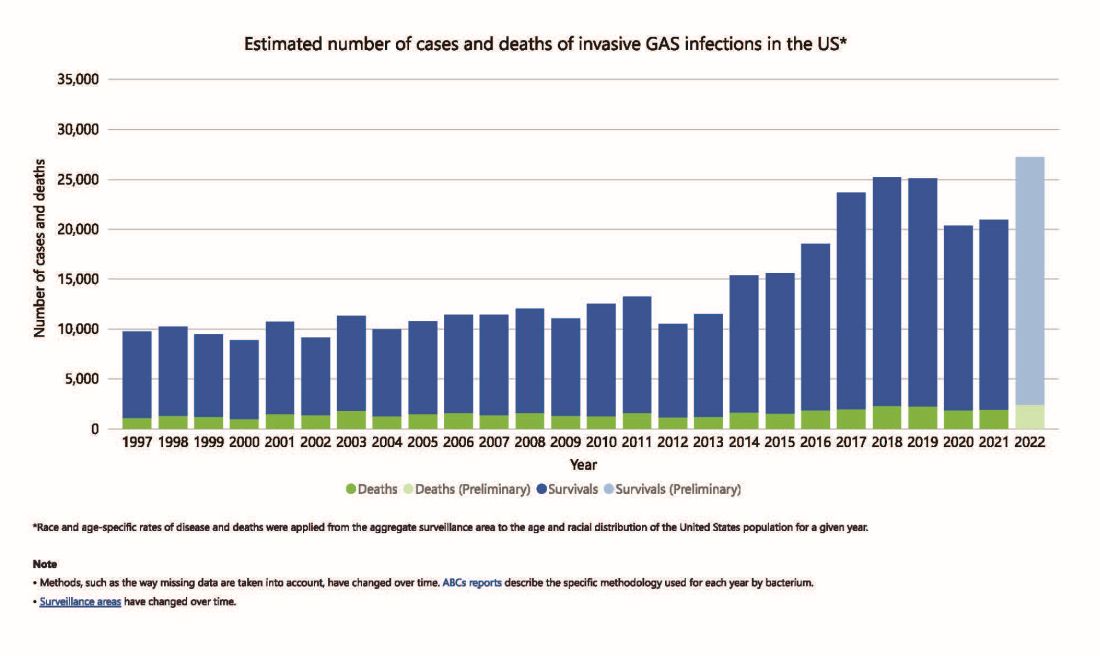
Social Behavior Factor
The SARS-CoV-2 pandemic brought extremes of disease and death to the world and dramatic changes in social behavior. A byproduct was dramatic decreases in nearly all infectious diseases, with numerous reports of near absence of many respiratory and gastrointestinal viruses in the 2020-2021 seasons. Interestingly, we did not see a drop in human rhinovirus infections, justifying its nickname as the cockroach of viruses. Reports also emerged about drops in bacterial diseases during 2020-2021 (although not so much for STIs), including noninvasive and invasive GAS disease, and also GAS-associated deaths (lowest since 2016).1 The drop in iGAS during social restrictions makes sense because GAS is spread by direct contact with infected persons or their secretions, and social contact had dramatically decreased particularly in the first 6 months of the pandemic.
However, since 2022 and the return to “normal” social behaviors, both viral diseases (e.g., RSV, influenza, and Norovirus), and some bacterial diseases have rebounded. That said, something else must be contributing, because iGAS rates had increased 4-5 years pre pandemic. In fact, the fluctuating pattern included “normal” annual rates in the early 2000s rising in ~2015 followed by the explainable pandemic drop (by nearly 25%), and not-too-unexpected 2-year postpandemic rise. But interestingly enough, the rebound is higher than might be expected for iGAS and children were overrepresented in first year’s rise (2022 rate for pediatric iGAS was the highest since 1997) while those older than 65 were overrepresented in second year (2023).1
Emergence of M1UK
One potential factor for the prepandemic rise in iGAS infections worldwide is the emergence and worldwide spread of a new GAS emm type variant designated M1UK.2 GAS isolates can be typed into categories designated as emm types based on DNA sequence. There are more than 240 emm types, with 6 being most common — M1, M3, and M28 (each up to 20% of GAS isolates) and M12, M82, and M89 (each up to 10%). M1, M3 and M28 have also been particularly associated with invasive disease. While emm types vary year to year and region by region, the overall emm type distribution among iGAS isolates in the United States had not been unusual since the turn of the century and the US M1 strain was the same as that which had been predominant worldwide (designated M1GLOBAL). This new M1UK sublineage had emerged around 2010 and had been increasing pre pandemic. The M1UK sequence contained a specific set of 27 SNPs (single nucleoside polymorphisms, i.e., single base mutations) and was associated with an uptick in scarlet fever in the United Kingdom starting around 2010. Its prevalence increased up to around 2015 while spreading internationally. It also had enhanced expression of SpeA, a phage-encoded superantigen. Some of the M1UK mutations also appear to alter GAS metabolic processes to allow better survival (better “fitness”) compared with other GAS. So, a more virulent hardier GAS had arisen and seems a reasonable candidate for contributing to the increased iGAS rates.
Waning Antibody to GAS As Potential Factor in Rebound
No consensus exists on correlates of protection from iGAS. However, adults seem to have less noninvasive GAS than children. One potential reason is that frequent GAS re-exposure, regardless of whether disease results, likely boosts anti-GAS antibodies. Pandemic social restrictions temporarily prevented such boosts. In children with developing antibody repertoires, anti-GAS antibodies may have waned below protective levels faster during a year without frequent boosting. Thus, children were iGAS susceptible soon after pandemic restrictions were dropped (2022). Increased iGAS rates in the elderly in 2023 may have occurred because of diminished GAS exposures accelerating immune senescence with anti-GAS antibodies dropping, but less quickly than in children. These speculations are simply hypotheses until future studies can test them.
All that said, how do we use information on increased iGAS in our daily practices? In addition to standard preventive strategies for viral coinfections (e.g., varicella and influenza vaccine), reminding families about rigorous attention to wound care is the one high-risk scenario we have not yet discussed. During 2024, a time of expected increased prevalence of iGAS, early wound care needs to be fastidious. Further, share warning signs with families (e.g., rapidly expanding painful erythema), “streaks” ascending from extremity wounds, fever and a highly painful wound, darkening almost purple color within cellulitis or soft tissue infection, or loss of sensation in the middle of an otherwise painful soft tissue infection. These presentations require immediate medical attention.
If such a patient presents, the Centers for Disease Control and Prevention (CDC) recommends admission along with blood and, where possible, wound cultures. If in the context of pneumonia with pleural effusion, culturing pleural fluid is also important. Remember, leading edge cultures are not often positive for GAS, seemingly because GAS exotoxins are found at erythema’s leading edge, not the bacteria. The bacteria are somewhere more central in the inflammatory process. Despite not being prominent among recent iGAS cases, another scenario that could sneak up on you is the infected surgical wound as nascent iGAS.
Finally, remember that nationally increasing numbers of iGAS isolates are resistant to erythromycin and clindamycin, the latter usually recommended to reduce tissue damage in iGAS.3 So, it is important to be aware of susceptibility patterns in your locale and consider an ID consultation. My hope is that you do not see an iGAS case this year, but we all need to remain alert. With a high index of suspicion and rapid diagnosis, you can minimize long-term sequelae and potential fatalities.
While it is too early to tell how the rest of 2024 will turn out, preliminary indications are that GAS is circulating at higher than usual levels (30%-35% GAS positive throat swabs in early April 2024 in Kansas City area) and iGAS rates will likely also be relatively high, particularly if Ontario, Canada, data are any indication.4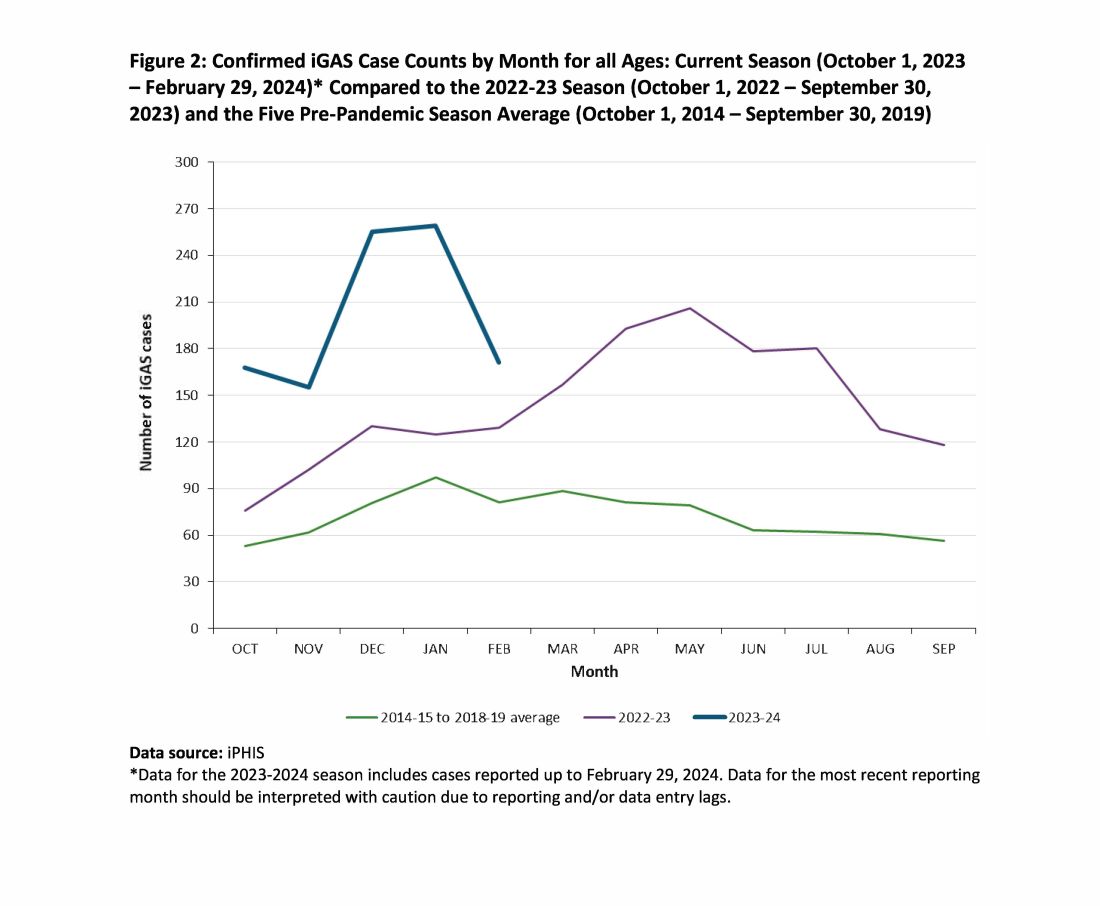
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics, Kansas City, Mo. He said he had no relevant financial disclosures. Email him at pdnews@mdedge.com.
References
1. Current Group A Strep Activity, Centers for Disease Control and Prevention. April 2024. CDC webpage on current invasive GAS disease. April 2024.
2. Li Y et al. Expansion of Invasive Group A Streptococcus M1UK Lineage in Active Bacterial Core Surveillance, United States, 2019-2021 Emerg Infect Dis. 2023;29(10):2116-2120. doi: 10.3201/eid2910.230675.
3. Andreoni F et al. Clindamycin Affects Group A Streptococcus Virulence Factors and Improves Clinical Outcome. J Infect Dis. 2017 Jan 15;215(2):269-277. doi: 10.1093/infdis/jiw229.
4. Group A Streptococcal Disease, Invasive (iGAS), Public Health Ontario.
Invasive group A streptococcus (iGAS) infections are rare (4-9 cases/100,000 US population annually) but potentially devastating (approximately 2,300 deaths annually in US), and affect all ages. Cases increase in winter-spring, paralleling the “season” of increased noninvasive GAS, e.g., pharyngitis and scarlet fever. iGAS case rates are lower in children than adults. That said, one well-known pediatric iGAS scenario has been deep cellulitis and necrotizing fasciitis during the healing phase of varicella. Other forms of iGAS include bacteremia, pneumonia (particularly when empyema is present), lymphangitis, erysipelas, and toxic shock syndrome. iGAS can occur with/after influenza but has also occurred concurrently with other viral respiratory infections.
Persons with underlying conditions (cancer or immune compromised status; chronic diseases of the heart, kidney or lung; diabetes mellitus) are at higher risk. Other subpopulations at risk for iGAS are illicit drug users, the elderly, homeless persons, nursing home residents, American Indian persons, and Alaska Native persons. Most experts feel that highly toxigenic strains of GAS are responsible for most iGAS. Indeed, most iGAS isolates produce (sometimes hyper-produce) superantigens that cause exaggerated innate immune responses, higher levels of inflammation, and often times tissue destruction, e.g., “flesh eating bacteria.” And who can forget that Jim Henson, creator of the Muppets, died of iGAS?
But why discuss iGAS in 2024? The pattern for iGAS has fluctuated more than usual in the last decade. So much so that the recent upsurge has caught the collective eye of the lay press. So, patients and friends may have questions about why and how iGAS is increasing lately. The bottom line is that no one knows for sure. However, the most recent 2 years of uptick may reflect GAS circulating at relatively high levels even when taking into account that GAS season occurs in winter-spring most years. Yet it seems likely that additional factors may have played a role in the fluctuations noted this past decade, e.g., temporary changes in societal behavior, a new GAS strain with over two dozen mutations, and possibly rapid waning of protection against GAS exotoxins.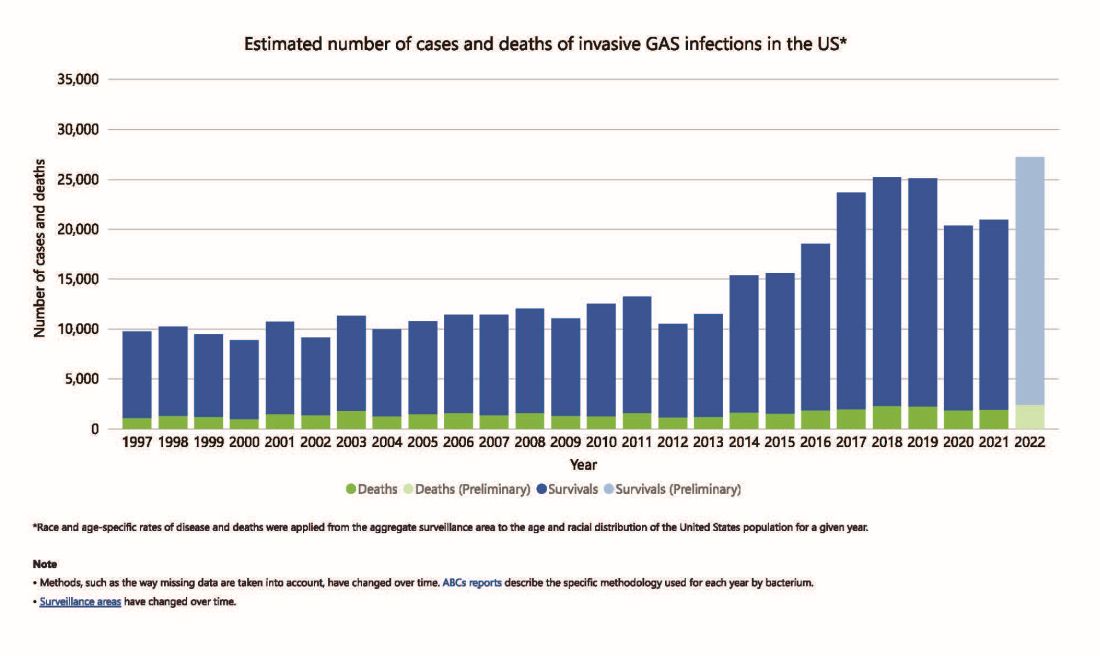
Social Behavior Factor
The SARS-CoV-2 pandemic brought extremes of disease and death to the world and dramatic changes in social behavior. A byproduct was dramatic decreases in nearly all infectious diseases, with numerous reports of near absence of many respiratory and gastrointestinal viruses in the 2020-2021 seasons. Interestingly, we did not see a drop in human rhinovirus infections, justifying its nickname as the cockroach of viruses. Reports also emerged about drops in bacterial diseases during 2020-2021 (although not so much for STIs), including noninvasive and invasive GAS disease, and also GAS-associated deaths (lowest since 2016).1 The drop in iGAS during social restrictions makes sense because GAS is spread by direct contact with infected persons or their secretions, and social contact had dramatically decreased particularly in the first 6 months of the pandemic.
However, since 2022 and the return to “normal” social behaviors, both viral diseases (e.g., RSV, influenza, and Norovirus), and some bacterial diseases have rebounded. That said, something else must be contributing, because iGAS rates had increased 4-5 years pre pandemic. In fact, the fluctuating pattern included “normal” annual rates in the early 2000s rising in ~2015 followed by the explainable pandemic drop (by nearly 25%), and not-too-unexpected 2-year postpandemic rise. But interestingly enough, the rebound is higher than might be expected for iGAS and children were overrepresented in first year’s rise (2022 rate for pediatric iGAS was the highest since 1997) while those older than 65 were overrepresented in second year (2023).1
Emergence of M1UK
One potential factor for the prepandemic rise in iGAS infections worldwide is the emergence and worldwide spread of a new GAS emm type variant designated M1UK.2 GAS isolates can be typed into categories designated as emm types based on DNA sequence. There are more than 240 emm types, with 6 being most common — M1, M3, and M28 (each up to 20% of GAS isolates) and M12, M82, and M89 (each up to 10%). M1, M3 and M28 have also been particularly associated with invasive disease. While emm types vary year to year and region by region, the overall emm type distribution among iGAS isolates in the United States had not been unusual since the turn of the century and the US M1 strain was the same as that which had been predominant worldwide (designated M1GLOBAL). This new M1UK sublineage had emerged around 2010 and had been increasing pre pandemic. The M1UK sequence contained a specific set of 27 SNPs (single nucleoside polymorphisms, i.e., single base mutations) and was associated with an uptick in scarlet fever in the United Kingdom starting around 2010. Its prevalence increased up to around 2015 while spreading internationally. It also had enhanced expression of SpeA, a phage-encoded superantigen. Some of the M1UK mutations also appear to alter GAS metabolic processes to allow better survival (better “fitness”) compared with other GAS. So, a more virulent hardier GAS had arisen and seems a reasonable candidate for contributing to the increased iGAS rates.
Waning Antibody to GAS As Potential Factor in Rebound
No consensus exists on correlates of protection from iGAS. However, adults seem to have less noninvasive GAS than children. One potential reason is that frequent GAS re-exposure, regardless of whether disease results, likely boosts anti-GAS antibodies. Pandemic social restrictions temporarily prevented such boosts. In children with developing antibody repertoires, anti-GAS antibodies may have waned below protective levels faster during a year without frequent boosting. Thus, children were iGAS susceptible soon after pandemic restrictions were dropped (2022). Increased iGAS rates in the elderly in 2023 may have occurred because of diminished GAS exposures accelerating immune senescence with anti-GAS antibodies dropping, but less quickly than in children. These speculations are simply hypotheses until future studies can test them.
All that said, how do we use information on increased iGAS in our daily practices? In addition to standard preventive strategies for viral coinfections (e.g., varicella and influenza vaccine), reminding families about rigorous attention to wound care is the one high-risk scenario we have not yet discussed. During 2024, a time of expected increased prevalence of iGAS, early wound care needs to be fastidious. Further, share warning signs with families (e.g., rapidly expanding painful erythema), “streaks” ascending from extremity wounds, fever and a highly painful wound, darkening almost purple color within cellulitis or soft tissue infection, or loss of sensation in the middle of an otherwise painful soft tissue infection. These presentations require immediate medical attention.
If such a patient presents, the Centers for Disease Control and Prevention (CDC) recommends admission along with blood and, where possible, wound cultures. If in the context of pneumonia with pleural effusion, culturing pleural fluid is also important. Remember, leading edge cultures are not often positive for GAS, seemingly because GAS exotoxins are found at erythema’s leading edge, not the bacteria. The bacteria are somewhere more central in the inflammatory process. Despite not being prominent among recent iGAS cases, another scenario that could sneak up on you is the infected surgical wound as nascent iGAS.
Finally, remember that nationally increasing numbers of iGAS isolates are resistant to erythromycin and clindamycin, the latter usually recommended to reduce tissue damage in iGAS.3 So, it is important to be aware of susceptibility patterns in your locale and consider an ID consultation. My hope is that you do not see an iGAS case this year, but we all need to remain alert. With a high index of suspicion and rapid diagnosis, you can minimize long-term sequelae and potential fatalities.
While it is too early to tell how the rest of 2024 will turn out, preliminary indications are that GAS is circulating at higher than usual levels (30%-35% GAS positive throat swabs in early April 2024 in Kansas City area) and iGAS rates will likely also be relatively high, particularly if Ontario, Canada, data are any indication.4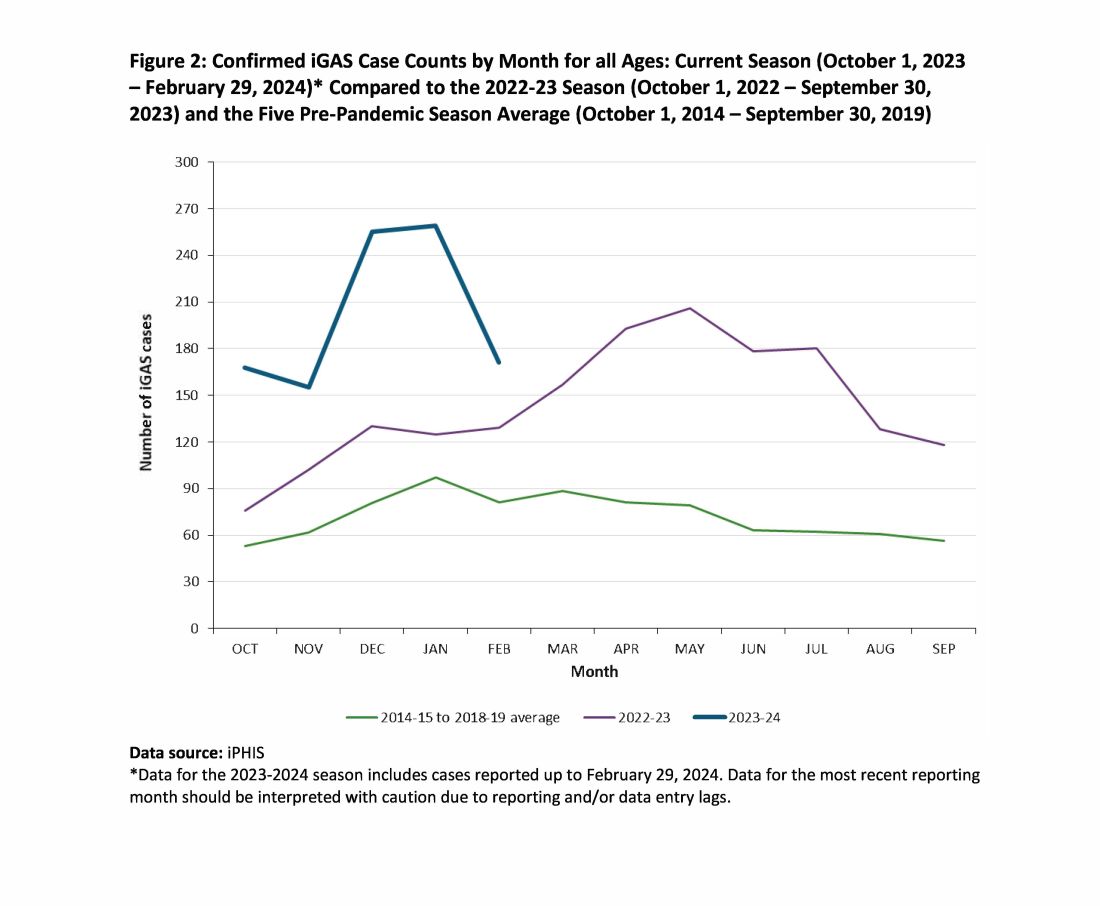
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics, Kansas City, Mo. He said he had no relevant financial disclosures. Email him at pdnews@mdedge.com.
References
1. Current Group A Strep Activity, Centers for Disease Control and Prevention. April 2024. CDC webpage on current invasive GAS disease. April 2024.
2. Li Y et al. Expansion of Invasive Group A Streptococcus M1UK Lineage in Active Bacterial Core Surveillance, United States, 2019-2021 Emerg Infect Dis. 2023;29(10):2116-2120. doi: 10.3201/eid2910.230675.
3. Andreoni F et al. Clindamycin Affects Group A Streptococcus Virulence Factors and Improves Clinical Outcome. J Infect Dis. 2017 Jan 15;215(2):269-277. doi: 10.1093/infdis/jiw229.
4. Group A Streptococcal Disease, Invasive (iGAS), Public Health Ontario.
Invasive group A streptococcus (iGAS) infections are rare (4-9 cases/100,000 US population annually) but potentially devastating (approximately 2,300 deaths annually in US), and affect all ages. Cases increase in winter-spring, paralleling the “season” of increased noninvasive GAS, e.g., pharyngitis and scarlet fever. iGAS case rates are lower in children than adults. That said, one well-known pediatric iGAS scenario has been deep cellulitis and necrotizing fasciitis during the healing phase of varicella. Other forms of iGAS include bacteremia, pneumonia (particularly when empyema is present), lymphangitis, erysipelas, and toxic shock syndrome. iGAS can occur with/after influenza but has also occurred concurrently with other viral respiratory infections.
Persons with underlying conditions (cancer or immune compromised status; chronic diseases of the heart, kidney or lung; diabetes mellitus) are at higher risk. Other subpopulations at risk for iGAS are illicit drug users, the elderly, homeless persons, nursing home residents, American Indian persons, and Alaska Native persons. Most experts feel that highly toxigenic strains of GAS are responsible for most iGAS. Indeed, most iGAS isolates produce (sometimes hyper-produce) superantigens that cause exaggerated innate immune responses, higher levels of inflammation, and often times tissue destruction, e.g., “flesh eating bacteria.” And who can forget that Jim Henson, creator of the Muppets, died of iGAS?
But why discuss iGAS in 2024? The pattern for iGAS has fluctuated more than usual in the last decade. So much so that the recent upsurge has caught the collective eye of the lay press. So, patients and friends may have questions about why and how iGAS is increasing lately. The bottom line is that no one knows for sure. However, the most recent 2 years of uptick may reflect GAS circulating at relatively high levels even when taking into account that GAS season occurs in winter-spring most years. Yet it seems likely that additional factors may have played a role in the fluctuations noted this past decade, e.g., temporary changes in societal behavior, a new GAS strain with over two dozen mutations, and possibly rapid waning of protection against GAS exotoxins.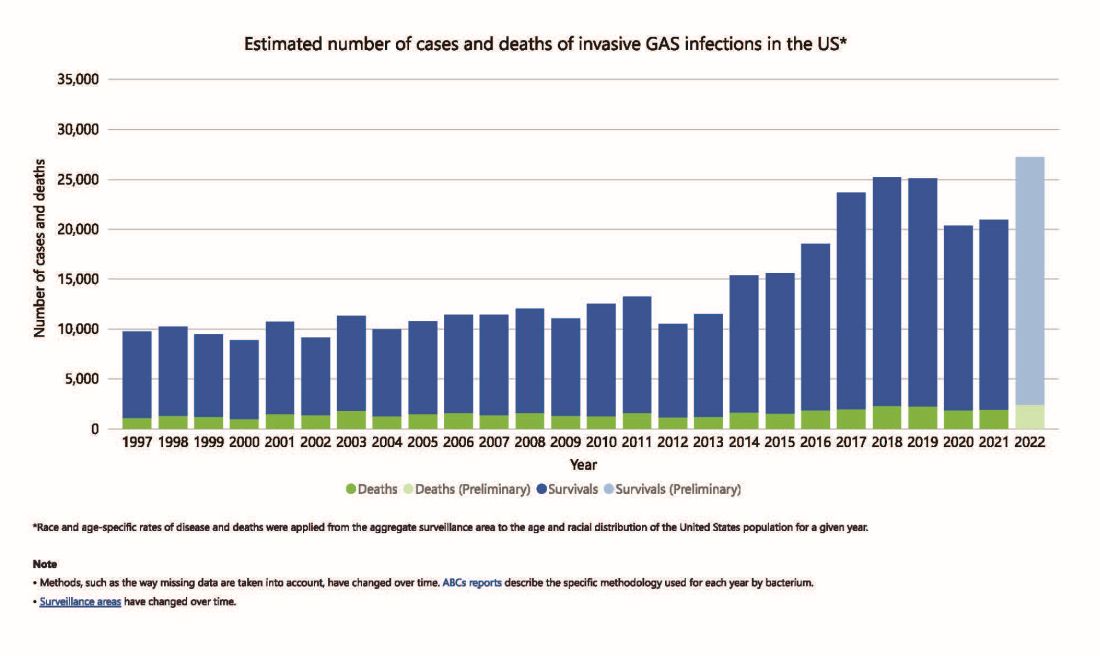
Social Behavior Factor
The SARS-CoV-2 pandemic brought extremes of disease and death to the world and dramatic changes in social behavior. A byproduct was dramatic decreases in nearly all infectious diseases, with numerous reports of near absence of many respiratory and gastrointestinal viruses in the 2020-2021 seasons. Interestingly, we did not see a drop in human rhinovirus infections, justifying its nickname as the cockroach of viruses. Reports also emerged about drops in bacterial diseases during 2020-2021 (although not so much for STIs), including noninvasive and invasive GAS disease, and also GAS-associated deaths (lowest since 2016).1 The drop in iGAS during social restrictions makes sense because GAS is spread by direct contact with infected persons or their secretions, and social contact had dramatically decreased particularly in the first 6 months of the pandemic.
However, since 2022 and the return to “normal” social behaviors, both viral diseases (e.g., RSV, influenza, and Norovirus), and some bacterial diseases have rebounded. That said, something else must be contributing, because iGAS rates had increased 4-5 years pre pandemic. In fact, the fluctuating pattern included “normal” annual rates in the early 2000s rising in ~2015 followed by the explainable pandemic drop (by nearly 25%), and not-too-unexpected 2-year postpandemic rise. But interestingly enough, the rebound is higher than might be expected for iGAS and children were overrepresented in first year’s rise (2022 rate for pediatric iGAS was the highest since 1997) while those older than 65 were overrepresented in second year (2023).1
Emergence of M1UK
One potential factor for the prepandemic rise in iGAS infections worldwide is the emergence and worldwide spread of a new GAS emm type variant designated M1UK.2 GAS isolates can be typed into categories designated as emm types based on DNA sequence. There are more than 240 emm types, with 6 being most common — M1, M3, and M28 (each up to 20% of GAS isolates) and M12, M82, and M89 (each up to 10%). M1, M3 and M28 have also been particularly associated with invasive disease. While emm types vary year to year and region by region, the overall emm type distribution among iGAS isolates in the United States had not been unusual since the turn of the century and the US M1 strain was the same as that which had been predominant worldwide (designated M1GLOBAL). This new M1UK sublineage had emerged around 2010 and had been increasing pre pandemic. The M1UK sequence contained a specific set of 27 SNPs (single nucleoside polymorphisms, i.e., single base mutations) and was associated with an uptick in scarlet fever in the United Kingdom starting around 2010. Its prevalence increased up to around 2015 while spreading internationally. It also had enhanced expression of SpeA, a phage-encoded superantigen. Some of the M1UK mutations also appear to alter GAS metabolic processes to allow better survival (better “fitness”) compared with other GAS. So, a more virulent hardier GAS had arisen and seems a reasonable candidate for contributing to the increased iGAS rates.
Waning Antibody to GAS As Potential Factor in Rebound
No consensus exists on correlates of protection from iGAS. However, adults seem to have less noninvasive GAS than children. One potential reason is that frequent GAS re-exposure, regardless of whether disease results, likely boosts anti-GAS antibodies. Pandemic social restrictions temporarily prevented such boosts. In children with developing antibody repertoires, anti-GAS antibodies may have waned below protective levels faster during a year without frequent boosting. Thus, children were iGAS susceptible soon after pandemic restrictions were dropped (2022). Increased iGAS rates in the elderly in 2023 may have occurred because of diminished GAS exposures accelerating immune senescence with anti-GAS antibodies dropping, but less quickly than in children. These speculations are simply hypotheses until future studies can test them.
All that said, how do we use information on increased iGAS in our daily practices? In addition to standard preventive strategies for viral coinfections (e.g., varicella and influenza vaccine), reminding families about rigorous attention to wound care is the one high-risk scenario we have not yet discussed. During 2024, a time of expected increased prevalence of iGAS, early wound care needs to be fastidious. Further, share warning signs with families (e.g., rapidly expanding painful erythema), “streaks” ascending from extremity wounds, fever and a highly painful wound, darkening almost purple color within cellulitis or soft tissue infection, or loss of sensation in the middle of an otherwise painful soft tissue infection. These presentations require immediate medical attention.
If such a patient presents, the Centers for Disease Control and Prevention (CDC) recommends admission along with blood and, where possible, wound cultures. If in the context of pneumonia with pleural effusion, culturing pleural fluid is also important. Remember, leading edge cultures are not often positive for GAS, seemingly because GAS exotoxins are found at erythema’s leading edge, not the bacteria. The bacteria are somewhere more central in the inflammatory process. Despite not being prominent among recent iGAS cases, another scenario that could sneak up on you is the infected surgical wound as nascent iGAS.
Finally, remember that nationally increasing numbers of iGAS isolates are resistant to erythromycin and clindamycin, the latter usually recommended to reduce tissue damage in iGAS.3 So, it is important to be aware of susceptibility patterns in your locale and consider an ID consultation. My hope is that you do not see an iGAS case this year, but we all need to remain alert. With a high index of suspicion and rapid diagnosis, you can minimize long-term sequelae and potential fatalities.
While it is too early to tell how the rest of 2024 will turn out, preliminary indications are that GAS is circulating at higher than usual levels (30%-35% GAS positive throat swabs in early April 2024 in Kansas City area) and iGAS rates will likely also be relatively high, particularly if Ontario, Canada, data are any indication.4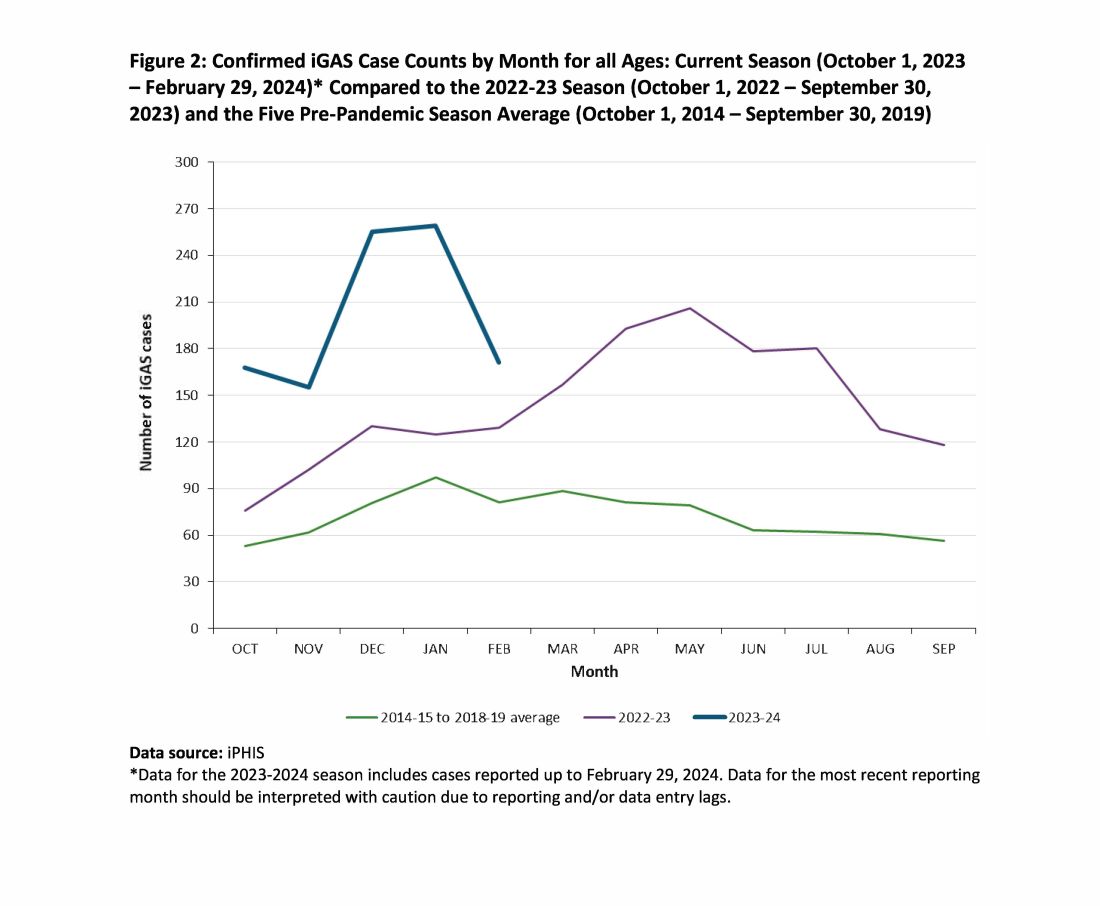
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics, Kansas City, Mo. He said he had no relevant financial disclosures. Email him at pdnews@mdedge.com.
References
1. Current Group A Strep Activity, Centers for Disease Control and Prevention. April 2024. CDC webpage on current invasive GAS disease. April 2024.
2. Li Y et al. Expansion of Invasive Group A Streptococcus M1UK Lineage in Active Bacterial Core Surveillance, United States, 2019-2021 Emerg Infect Dis. 2023;29(10):2116-2120. doi: 10.3201/eid2910.230675.
3. Andreoni F et al. Clindamycin Affects Group A Streptococcus Virulence Factors and Improves Clinical Outcome. J Infect Dis. 2017 Jan 15;215(2):269-277. doi: 10.1093/infdis/jiw229.
4. Group A Streptococcal Disease, Invasive (iGAS), Public Health Ontario.
