User login
Aspirin may accelerate cancer progression in older adults
Aspirin may accelerate the progression of advanced cancers and lead to an earlier death as a result, new data from the ASPREE study suggest.
The results showed that patients 65 years and older who started taking daily low-dose aspirin had a 19% higher chance of being diagnosed with metastatic cancer, a 22% higher chance of being diagnosed with a stage 4 tumor, and a 31% increased risk of death from stage 4 cancer, when compared with patients who took a placebo.
John J. McNeil, MBBS, PhD, of Monash University in Melbourne, Australia, and colleagues detailed these findings in the Journal of the National Cancer Institute.
“If confirmed, the clinical implications of these findings could be important for the use of aspirin in an older population,” the authors wrote.
When results of the ASPREE study were first reported in 2018, they “raised important concerns,” Ernest Hawk, MD, and Karen Colbert Maresso wrote in an editorial related to the current publication.
“Unlike ARRIVE, ASCEND, and nearly all prior primary prevention CVD [cardiovascular disease] trials of aspirin, ASPREE surprisingly demonstrated increased all-cause mortality in the aspirin group, which appeared to be driven largely by an increase in cancer-related deaths,” wrote the editorialists, who are both from the University of Texas MD Anderson Cancer Center in Houston.
Even though the ASPREE investigators have now taken a deeper dive into their data, the findings “neither explain nor alleviate the concerns raised by the initial ASPREE report,” the editorialists noted.
ASPREE design and results
ASPREE is a multicenter, double-blind trial of 19,114 older adults living in Australia (n = 16,703) or the United States (n = 2,411). Most patients were 70 years or older at baseline. However, the U.S. group also included patients 65 years and older who were racial/ethnic minorities (n = 564).
Patients were randomized to receive 100 mg of enteric-coated aspirin daily (n = 9,525) or matching placebo (n = 9,589) from March 2010 through December 2014.
At inclusion, all participants were free from cardiovascular disease, dementia, or physical disability. A previous history of cancer was not used to exclude participants, and 19.1% of patients had cancer at randomization. Most patients (89%) had not used aspirin regularly before entering the trial.
At a median follow-up of 4.7 years, there were 981 incident cancer events in the aspirin-treated group and 952 in the placebo-treated group, with an overall incident cancer rate of 10.1%.
Of the 1,933 patients with newly diagnosed cancer, 65.7% had a localized cancer, 18.8% had a new metastatic cancer, 5.8% had metastatic disease from an existing cancer, and 9.7% had a new hematologic or lymphatic cancer.
A quarter of cancer patients (n = 495) died as a result of their malignancy, with 52 dying from a cancer they already had at randomization.
Aspirin was not associated with the risk of first incident cancer diagnosis or incident localized cancer diagnosis. The hazard ratios were 1.04 for all incident cancers (95% confidence interval, 0.95-1.14) and 0.99 for incident localized cancers (95% CI, 0.89-1.11).
However, aspirin was associated with an increased risk of metastatic cancer and cancer presenting at stage 4. The HR for metastatic cancer was 1.19 (95% CI, 1.00-1.43), and the HR for newly diagnosed stage 4 cancer was 1.22 (95% CI, 1.02-1.45).
Furthermore, “an increased progression to death was observed amongst those randomized to aspirin, regardless of whether the initial cancer presentation had been localized or metastatic,” the investigators wrote.
The HRs for death were 1.35 for all cancers (95% CI, 1.13-1.61), 1.47 for localized cancers (95% CI, 1.07-2.02), and 1.30 for metastatic cancers (95% CI, 1.03-1.63).
“Deaths were particularly high among those on aspirin who were diagnosed with advanced solid cancers,” study author Andrew Chan, MD, of Massachusetts General Hospital in Boston, said in a press statement.
Indeed, HRs for death in patients with solid tumors presenting at stage 3 and 4 were a respective 2.11 (95% CI, 1.03-4.33) and 1.31 (95% CI, 1.04-1.64). This suggests a possible adverse effect of aspirin on the growth of cancers once they have already developed in older adults, Dr. Chan said.
Where does that leave aspirin for cancer prevention?
“Although these results suggest that we should be cautious about starting aspirin therapy in otherwise healthy older adults, this does not mean that individuals who are already taking aspirin – particularly if they began taking it at a younger age – should stop their aspirin regimen,” Dr. Chan said.
There are decades of data supporting the use of daily aspirin to prevent multiple cancer types, particularly colorectal cancer, in individuals under the age of 70 years. In a recent meta-analysis, for example, regular aspirin use was linked to a 27% reduced risk for colorectal cancer, a 33% reduced risk for squamous cell esophageal cancer, a 39% decreased risk for adenocarcinoma of the esophagus and gastric cardia, a 36% decreased risk for stomach cancer, a 38% decreased risk for hepatobiliary tract cancer, and a 22% decreased risk for pancreatic cancer.
While these figures are mostly based on observational and case-control studies, it “reaffirms the fact that, overall, when you look at all of the ages, that there is still a benefit of aspirin for cancer,” John Cuzick, PhD, of Queen Mary University of London (England), said in an interview.
In fact, the meta-analysis goes as far as suggesting that perhaps the dose of aspirin being used is too low, with the authors noting that there was a 35% risk reduction in colorectal cancer with a dose of 325 mg daily. That’s a new finding, Dr. Cuzick said.
He noted that the ASPREE study largely consists of patients 70 years of age or older, and the authors “draw some conclusions which we can’t ignore about potential safety.”
One of the safety concerns is the increased risk for gastrointestinal bleeding, which is why Dr. Cuzick and colleagues previously recommended caution in the use of aspirin to prevent cancer in elderly patients. The group published a study in 2015 that suggested a benefit of taking aspirin daily for 5-10 years in patients aged 50-65 years, but the risk/benefit ratio was unclear for patients 70 years and older.
The ASPREE data now add to those uncertainties and suggest “there may be some side effects that we do not understand,” Dr. Cuzick said.
“I’m still optimistic that aspirin is going to be important for cancer prevention, but probably focusing on ages 50-70,” he added. “[The ASPREE data] reinforce the caution that we have to take in terms of trying to understand what the side effects are and what’s going on at these older ages.”
Dr. Cuzick is currently leading the AsCaP Project, an international effort to better understand why aspirin might work in preventing some cancer types but not others. AsCaP is supported by Cancer Research UK and also includes Dr. Chan among the researchers attempting to find out which patients may benefit the most from aspirin and which may be at greater risk of adverse effects.
The ASPREE trial was funded by grants from the National Institute on Aging, the National Cancer Institute, the National Health and Medical Research Council of Australia, Monash University, and the Victorian Cancer Agency. Several ASPREE investigators disclosed financial relationships with Bayer Pharma. The editorialists had no conflicts of interest. Dr. Cuzick has been an advisory board member for Bayer in the past.
SOURCE: McNeil J et al. J Natl Cancer Inst. 2020 Aug 11. doi: 10.1093/jnci/djaa114.
Aspirin may accelerate the progression of advanced cancers and lead to an earlier death as a result, new data from the ASPREE study suggest.
The results showed that patients 65 years and older who started taking daily low-dose aspirin had a 19% higher chance of being diagnosed with metastatic cancer, a 22% higher chance of being diagnosed with a stage 4 tumor, and a 31% increased risk of death from stage 4 cancer, when compared with patients who took a placebo.
John J. McNeil, MBBS, PhD, of Monash University in Melbourne, Australia, and colleagues detailed these findings in the Journal of the National Cancer Institute.
“If confirmed, the clinical implications of these findings could be important for the use of aspirin in an older population,” the authors wrote.
When results of the ASPREE study were first reported in 2018, they “raised important concerns,” Ernest Hawk, MD, and Karen Colbert Maresso wrote in an editorial related to the current publication.
“Unlike ARRIVE, ASCEND, and nearly all prior primary prevention CVD [cardiovascular disease] trials of aspirin, ASPREE surprisingly demonstrated increased all-cause mortality in the aspirin group, which appeared to be driven largely by an increase in cancer-related deaths,” wrote the editorialists, who are both from the University of Texas MD Anderson Cancer Center in Houston.
Even though the ASPREE investigators have now taken a deeper dive into their data, the findings “neither explain nor alleviate the concerns raised by the initial ASPREE report,” the editorialists noted.
ASPREE design and results
ASPREE is a multicenter, double-blind trial of 19,114 older adults living in Australia (n = 16,703) or the United States (n = 2,411). Most patients were 70 years or older at baseline. However, the U.S. group also included patients 65 years and older who were racial/ethnic minorities (n = 564).
Patients were randomized to receive 100 mg of enteric-coated aspirin daily (n = 9,525) or matching placebo (n = 9,589) from March 2010 through December 2014.
At inclusion, all participants were free from cardiovascular disease, dementia, or physical disability. A previous history of cancer was not used to exclude participants, and 19.1% of patients had cancer at randomization. Most patients (89%) had not used aspirin regularly before entering the trial.
At a median follow-up of 4.7 years, there were 981 incident cancer events in the aspirin-treated group and 952 in the placebo-treated group, with an overall incident cancer rate of 10.1%.
Of the 1,933 patients with newly diagnosed cancer, 65.7% had a localized cancer, 18.8% had a new metastatic cancer, 5.8% had metastatic disease from an existing cancer, and 9.7% had a new hematologic or lymphatic cancer.
A quarter of cancer patients (n = 495) died as a result of their malignancy, with 52 dying from a cancer they already had at randomization.
Aspirin was not associated with the risk of first incident cancer diagnosis or incident localized cancer diagnosis. The hazard ratios were 1.04 for all incident cancers (95% confidence interval, 0.95-1.14) and 0.99 for incident localized cancers (95% CI, 0.89-1.11).
However, aspirin was associated with an increased risk of metastatic cancer and cancer presenting at stage 4. The HR for metastatic cancer was 1.19 (95% CI, 1.00-1.43), and the HR for newly diagnosed stage 4 cancer was 1.22 (95% CI, 1.02-1.45).
Furthermore, “an increased progression to death was observed amongst those randomized to aspirin, regardless of whether the initial cancer presentation had been localized or metastatic,” the investigators wrote.
The HRs for death were 1.35 for all cancers (95% CI, 1.13-1.61), 1.47 for localized cancers (95% CI, 1.07-2.02), and 1.30 for metastatic cancers (95% CI, 1.03-1.63).
“Deaths were particularly high among those on aspirin who were diagnosed with advanced solid cancers,” study author Andrew Chan, MD, of Massachusetts General Hospital in Boston, said in a press statement.
Indeed, HRs for death in patients with solid tumors presenting at stage 3 and 4 were a respective 2.11 (95% CI, 1.03-4.33) and 1.31 (95% CI, 1.04-1.64). This suggests a possible adverse effect of aspirin on the growth of cancers once they have already developed in older adults, Dr. Chan said.
Where does that leave aspirin for cancer prevention?
“Although these results suggest that we should be cautious about starting aspirin therapy in otherwise healthy older adults, this does not mean that individuals who are already taking aspirin – particularly if they began taking it at a younger age – should stop their aspirin regimen,” Dr. Chan said.
There are decades of data supporting the use of daily aspirin to prevent multiple cancer types, particularly colorectal cancer, in individuals under the age of 70 years. In a recent meta-analysis, for example, regular aspirin use was linked to a 27% reduced risk for colorectal cancer, a 33% reduced risk for squamous cell esophageal cancer, a 39% decreased risk for adenocarcinoma of the esophagus and gastric cardia, a 36% decreased risk for stomach cancer, a 38% decreased risk for hepatobiliary tract cancer, and a 22% decreased risk for pancreatic cancer.
While these figures are mostly based on observational and case-control studies, it “reaffirms the fact that, overall, when you look at all of the ages, that there is still a benefit of aspirin for cancer,” John Cuzick, PhD, of Queen Mary University of London (England), said in an interview.
In fact, the meta-analysis goes as far as suggesting that perhaps the dose of aspirin being used is too low, with the authors noting that there was a 35% risk reduction in colorectal cancer with a dose of 325 mg daily. That’s a new finding, Dr. Cuzick said.
He noted that the ASPREE study largely consists of patients 70 years of age or older, and the authors “draw some conclusions which we can’t ignore about potential safety.”
One of the safety concerns is the increased risk for gastrointestinal bleeding, which is why Dr. Cuzick and colleagues previously recommended caution in the use of aspirin to prevent cancer in elderly patients. The group published a study in 2015 that suggested a benefit of taking aspirin daily for 5-10 years in patients aged 50-65 years, but the risk/benefit ratio was unclear for patients 70 years and older.
The ASPREE data now add to those uncertainties and suggest “there may be some side effects that we do not understand,” Dr. Cuzick said.
“I’m still optimistic that aspirin is going to be important for cancer prevention, but probably focusing on ages 50-70,” he added. “[The ASPREE data] reinforce the caution that we have to take in terms of trying to understand what the side effects are and what’s going on at these older ages.”
Dr. Cuzick is currently leading the AsCaP Project, an international effort to better understand why aspirin might work in preventing some cancer types but not others. AsCaP is supported by Cancer Research UK and also includes Dr. Chan among the researchers attempting to find out which patients may benefit the most from aspirin and which may be at greater risk of adverse effects.
The ASPREE trial was funded by grants from the National Institute on Aging, the National Cancer Institute, the National Health and Medical Research Council of Australia, Monash University, and the Victorian Cancer Agency. Several ASPREE investigators disclosed financial relationships with Bayer Pharma. The editorialists had no conflicts of interest. Dr. Cuzick has been an advisory board member for Bayer in the past.
SOURCE: McNeil J et al. J Natl Cancer Inst. 2020 Aug 11. doi: 10.1093/jnci/djaa114.
Aspirin may accelerate the progression of advanced cancers and lead to an earlier death as a result, new data from the ASPREE study suggest.
The results showed that patients 65 years and older who started taking daily low-dose aspirin had a 19% higher chance of being diagnosed with metastatic cancer, a 22% higher chance of being diagnosed with a stage 4 tumor, and a 31% increased risk of death from stage 4 cancer, when compared with patients who took a placebo.
John J. McNeil, MBBS, PhD, of Monash University in Melbourne, Australia, and colleagues detailed these findings in the Journal of the National Cancer Institute.
“If confirmed, the clinical implications of these findings could be important for the use of aspirin in an older population,” the authors wrote.
When results of the ASPREE study were first reported in 2018, they “raised important concerns,” Ernest Hawk, MD, and Karen Colbert Maresso wrote in an editorial related to the current publication.
“Unlike ARRIVE, ASCEND, and nearly all prior primary prevention CVD [cardiovascular disease] trials of aspirin, ASPREE surprisingly demonstrated increased all-cause mortality in the aspirin group, which appeared to be driven largely by an increase in cancer-related deaths,” wrote the editorialists, who are both from the University of Texas MD Anderson Cancer Center in Houston.
Even though the ASPREE investigators have now taken a deeper dive into their data, the findings “neither explain nor alleviate the concerns raised by the initial ASPREE report,” the editorialists noted.
ASPREE design and results
ASPREE is a multicenter, double-blind trial of 19,114 older adults living in Australia (n = 16,703) or the United States (n = 2,411). Most patients were 70 years or older at baseline. However, the U.S. group also included patients 65 years and older who were racial/ethnic minorities (n = 564).
Patients were randomized to receive 100 mg of enteric-coated aspirin daily (n = 9,525) or matching placebo (n = 9,589) from March 2010 through December 2014.
At inclusion, all participants were free from cardiovascular disease, dementia, or physical disability. A previous history of cancer was not used to exclude participants, and 19.1% of patients had cancer at randomization. Most patients (89%) had not used aspirin regularly before entering the trial.
At a median follow-up of 4.7 years, there were 981 incident cancer events in the aspirin-treated group and 952 in the placebo-treated group, with an overall incident cancer rate of 10.1%.
Of the 1,933 patients with newly diagnosed cancer, 65.7% had a localized cancer, 18.8% had a new metastatic cancer, 5.8% had metastatic disease from an existing cancer, and 9.7% had a new hematologic or lymphatic cancer.
A quarter of cancer patients (n = 495) died as a result of their malignancy, with 52 dying from a cancer they already had at randomization.
Aspirin was not associated with the risk of first incident cancer diagnosis or incident localized cancer diagnosis. The hazard ratios were 1.04 for all incident cancers (95% confidence interval, 0.95-1.14) and 0.99 for incident localized cancers (95% CI, 0.89-1.11).
However, aspirin was associated with an increased risk of metastatic cancer and cancer presenting at stage 4. The HR for metastatic cancer was 1.19 (95% CI, 1.00-1.43), and the HR for newly diagnosed stage 4 cancer was 1.22 (95% CI, 1.02-1.45).
Furthermore, “an increased progression to death was observed amongst those randomized to aspirin, regardless of whether the initial cancer presentation had been localized or metastatic,” the investigators wrote.
The HRs for death were 1.35 for all cancers (95% CI, 1.13-1.61), 1.47 for localized cancers (95% CI, 1.07-2.02), and 1.30 for metastatic cancers (95% CI, 1.03-1.63).
“Deaths were particularly high among those on aspirin who were diagnosed with advanced solid cancers,” study author Andrew Chan, MD, of Massachusetts General Hospital in Boston, said in a press statement.
Indeed, HRs for death in patients with solid tumors presenting at stage 3 and 4 were a respective 2.11 (95% CI, 1.03-4.33) and 1.31 (95% CI, 1.04-1.64). This suggests a possible adverse effect of aspirin on the growth of cancers once they have already developed in older adults, Dr. Chan said.
Where does that leave aspirin for cancer prevention?
“Although these results suggest that we should be cautious about starting aspirin therapy in otherwise healthy older adults, this does not mean that individuals who are already taking aspirin – particularly if they began taking it at a younger age – should stop their aspirin regimen,” Dr. Chan said.
There are decades of data supporting the use of daily aspirin to prevent multiple cancer types, particularly colorectal cancer, in individuals under the age of 70 years. In a recent meta-analysis, for example, regular aspirin use was linked to a 27% reduced risk for colorectal cancer, a 33% reduced risk for squamous cell esophageal cancer, a 39% decreased risk for adenocarcinoma of the esophagus and gastric cardia, a 36% decreased risk for stomach cancer, a 38% decreased risk for hepatobiliary tract cancer, and a 22% decreased risk for pancreatic cancer.
While these figures are mostly based on observational and case-control studies, it “reaffirms the fact that, overall, when you look at all of the ages, that there is still a benefit of aspirin for cancer,” John Cuzick, PhD, of Queen Mary University of London (England), said in an interview.
In fact, the meta-analysis goes as far as suggesting that perhaps the dose of aspirin being used is too low, with the authors noting that there was a 35% risk reduction in colorectal cancer with a dose of 325 mg daily. That’s a new finding, Dr. Cuzick said.
He noted that the ASPREE study largely consists of patients 70 years of age or older, and the authors “draw some conclusions which we can’t ignore about potential safety.”
One of the safety concerns is the increased risk for gastrointestinal bleeding, which is why Dr. Cuzick and colleagues previously recommended caution in the use of aspirin to prevent cancer in elderly patients. The group published a study in 2015 that suggested a benefit of taking aspirin daily for 5-10 years in patients aged 50-65 years, but the risk/benefit ratio was unclear for patients 70 years and older.
The ASPREE data now add to those uncertainties and suggest “there may be some side effects that we do not understand,” Dr. Cuzick said.
“I’m still optimistic that aspirin is going to be important for cancer prevention, but probably focusing on ages 50-70,” he added. “[The ASPREE data] reinforce the caution that we have to take in terms of trying to understand what the side effects are and what’s going on at these older ages.”
Dr. Cuzick is currently leading the AsCaP Project, an international effort to better understand why aspirin might work in preventing some cancer types but not others. AsCaP is supported by Cancer Research UK and also includes Dr. Chan among the researchers attempting to find out which patients may benefit the most from aspirin and which may be at greater risk of adverse effects.
The ASPREE trial was funded by grants from the National Institute on Aging, the National Cancer Institute, the National Health and Medical Research Council of Australia, Monash University, and the Victorian Cancer Agency. Several ASPREE investigators disclosed financial relationships with Bayer Pharma. The editorialists had no conflicts of interest. Dr. Cuzick has been an advisory board member for Bayer in the past.
SOURCE: McNeil J et al. J Natl Cancer Inst. 2020 Aug 11. doi: 10.1093/jnci/djaa114.
FROM JOURNAL OF THE NATIONAL CANCER INSTITUTE
Black/White gap gone: ‘The only cancer where this has happened’
The historically higher incidence rates of lung cancer among Black men, compared with White men, in the United States have all but been eliminated, at least among most men in the younger age groups, a new analysis from the American Cancer Society (ACS) indicates.
Among women, the trend is even more impressive, as the Black/White gap in lung cancer incidence rates has actually reversed in younger women. Black women in certain age groups are now less likely to develop lung cancer than White women, the same study indicates.
These trends reflect the steeper declines in smoking rates among Blacks in the US, compared with comparably-aged Whites, say the authors.
“This is the only cancer where this has happened,” lead author Ahmedin Jemal, DVM, PhD, senior vice president for Data Science at the American Cancer Society, told Medscape Medical News.
“If you look at cancers that are affected by access to screening and treatment, the disparity between the Blacks and the Whites has been increasing over the years because tests and treatment require access to insurance, so the Whites are getting more of them than the Blacks,” Jemal explained.
“But for smoking, all you have to do for prevention is just don’t smoke, so this is a success story that really should be highlighted,” he emphasized.
The study was published online Aug. 20 in JNCI Cancer: Spectrum.
Nationwide Incidence Data
For this study, Jemal and colleagues collected nationwide incidence data on individuals between ages 30 and 54 who had been diagnosed with lung cancer between 1997 and 2016.
“We categorized age at diagnosis by 5-year age intervals (from 30-34 to 50-54 years) and year of diagnosis by 5-year calendar period (from 1997-2001 to 2012-2016),” the investigators explain.
Analyses showed that lung cancer incidence rates generally decreased among both Black and White men during the study interval but the decline in incidence rates was steeper in Black men than in White men. As a consequence, the Black-to-White incidence rate ratios (IRRs) became similar in men born between 1967 and 1972 and reversed in women born since about 1967. For example, the Black-to-White IRRs in men between the ages of 40 and 44 who were born between 1957 and 1972 declined from 1.92 to 1.03.
Similarly, lung cancer incidence rates during the study interval declined among both Black and White women between the ages of 30 and 49 but, again, the decline was “considerably larger” among Black women. As a consequence, the Black-to-White IRR in women age 45 to 49 dropped from 1.25 during the period 1997-2001 down to 0.83 during the period 2012-2016.
This is in stark contrast to historical trends in lung cancer incidence rates, which were over 30% higher among similarly aged Black women born in the late 1950s. Now, lung cancer incidence rates are about 30% lower for similarly aged Black women born in 1972, compared with White women.
For Black and White women between age 50 and 54, lung cancer incidence rates either declined only slightly or remained stable during the study interval, the investigators reported.
The one exception to the diminishing gap in lung cancer incidence rates between Black and White men was an observed increase in IRRs in men born around the period 1977-1982
Among this group of men, who were between age 30 and 39 in the years 2012-2016, lung cancer incidence rates were higher in Black men than in White men.
As the authors point out, this increase in lung cancer rates among young Black men likely reflects a rapid rise in smoking seen among Black youth in the 1990s.
This trend coincided with an R.J. Reynolds tobacco ad campaign in which African Americans were targeted; between 1991 and 1997, the prevalence of smoking among Black high school students doubled from 14.1% to 28.2%, the investigators point out, citing a 2008 Centers for Disease Control and Prevention report on cigarette use among US high school students.
Smoking Prevalence Rates
Smoking prevalence rates were derived from National Health Interview Survey data from 1970 to 2016.
Mirroring findings in the racial patterns of lung cancer incidence rates, smoking prevalence rates declined in successive birth cohorts in both Black and White males and females, but the decline was again steeper in Black men and women than it was in White men and women.
As a result, the historically higher sex-specific smoking prevalence rates seen historically in Blacks disappeared in men born around 1960, and reversed in women born at the same time, Jemal and colleagues point out.
As the authors explain, the more rapid decline in smoking prevalence after 1960 is likely a reflection of the “precipitous” drop in smoking initiation rates among Black teenagers starting about the late 1970s through to the early 1990s.
For example, among 12th graders, smoking prevalence rates between 1977 and 1992 dropped from 36.7% to 8.1% among Black teens. In stark contrast, they hardly changed at all among White teens, dropping only from 38.3% in 1977 to 31.8% in 1992.
Jemal suggested that steeper decline in smoking initiation rates seen between the late 1970s and early 90s reflects the fact that Black teenagers were deterred from smoking because the cost of cigarettes kept going up.
He also suggested that smoking is less acceptable in the Black community than it is in the White community, especially among churchgoers, where smoking is severely frowned upon and nonsmoking is the community “norm.”
Additionally, Black youth may simply be heeding government antismoking messages to a greater extent than White youth, Jemal suggested.
He wondered if there are parallels now in the current pandemic. “When I go to a store here in Georgia, I would say almost all Blacks are wearing a mask [even though masks are not mandatory in Georgia] whereas it’s amazing the number of Whites who don’t wear a mask,” he recounts.
“So it would seem that Whites feel that government is simply interfering with their lives, while Blacks have a better perspective of the harms of smoking, so they are listening to the government’s antismoking campaigns,” he speculated.
Some Isolated Areas
Asked to comment on the study’s findings, Otis Brawley, MD, Bloomberg, distinguished professor of oncology and epidemiology at Johns Hopkins University in Baltimore, said that, while overall Black smoking rates are declining, there are some isolated areas where they are still very high.
For example, in his hometown of Baltimore, recent prevalence rates indicate that over 30% of Blacks are still smoking, “so these areas with high usage are still areas to focus on,” he told Medscape Medical News.
On the other hand, the study also supports the benefits of local, state, and federal government efforts to promote antismoking messages and tobacco-control activities over the past number of years.
“It proves that tactics used to control tobacco use have had some effect [even though] the study also shows that the tobacco industry’s advertising tactics such as the R.J. Reynolds targeted ads in the 90s can have deleterious effects,” Brawley noted.
Lung cancer has traditionally been one of the biggest drivers in the Black/White cancer mortality gap, Brawley said, adding that steeper declines in smoking initiation rates among Blacks compared with Whites are the main reason why this disparity is decreasing.
The study was supported by the Intramural Research Department of the American Cancer Society. The study authors have disclosed no relevant financial relationships. Brawley declares he does some consulting work for pharmaceutical company Genentech.
This article first appeared on Medscape.com.
The historically higher incidence rates of lung cancer among Black men, compared with White men, in the United States have all but been eliminated, at least among most men in the younger age groups, a new analysis from the American Cancer Society (ACS) indicates.
Among women, the trend is even more impressive, as the Black/White gap in lung cancer incidence rates has actually reversed in younger women. Black women in certain age groups are now less likely to develop lung cancer than White women, the same study indicates.
These trends reflect the steeper declines in smoking rates among Blacks in the US, compared with comparably-aged Whites, say the authors.
“This is the only cancer where this has happened,” lead author Ahmedin Jemal, DVM, PhD, senior vice president for Data Science at the American Cancer Society, told Medscape Medical News.
“If you look at cancers that are affected by access to screening and treatment, the disparity between the Blacks and the Whites has been increasing over the years because tests and treatment require access to insurance, so the Whites are getting more of them than the Blacks,” Jemal explained.
“But for smoking, all you have to do for prevention is just don’t smoke, so this is a success story that really should be highlighted,” he emphasized.
The study was published online Aug. 20 in JNCI Cancer: Spectrum.
Nationwide Incidence Data
For this study, Jemal and colleagues collected nationwide incidence data on individuals between ages 30 and 54 who had been diagnosed with lung cancer between 1997 and 2016.
“We categorized age at diagnosis by 5-year age intervals (from 30-34 to 50-54 years) and year of diagnosis by 5-year calendar period (from 1997-2001 to 2012-2016),” the investigators explain.
Analyses showed that lung cancer incidence rates generally decreased among both Black and White men during the study interval but the decline in incidence rates was steeper in Black men than in White men. As a consequence, the Black-to-White incidence rate ratios (IRRs) became similar in men born between 1967 and 1972 and reversed in women born since about 1967. For example, the Black-to-White IRRs in men between the ages of 40 and 44 who were born between 1957 and 1972 declined from 1.92 to 1.03.
Similarly, lung cancer incidence rates during the study interval declined among both Black and White women between the ages of 30 and 49 but, again, the decline was “considerably larger” among Black women. As a consequence, the Black-to-White IRR in women age 45 to 49 dropped from 1.25 during the period 1997-2001 down to 0.83 during the period 2012-2016.
This is in stark contrast to historical trends in lung cancer incidence rates, which were over 30% higher among similarly aged Black women born in the late 1950s. Now, lung cancer incidence rates are about 30% lower for similarly aged Black women born in 1972, compared with White women.
For Black and White women between age 50 and 54, lung cancer incidence rates either declined only slightly or remained stable during the study interval, the investigators reported.
The one exception to the diminishing gap in lung cancer incidence rates between Black and White men was an observed increase in IRRs in men born around the period 1977-1982
Among this group of men, who were between age 30 and 39 in the years 2012-2016, lung cancer incidence rates were higher in Black men than in White men.
As the authors point out, this increase in lung cancer rates among young Black men likely reflects a rapid rise in smoking seen among Black youth in the 1990s.
This trend coincided with an R.J. Reynolds tobacco ad campaign in which African Americans were targeted; between 1991 and 1997, the prevalence of smoking among Black high school students doubled from 14.1% to 28.2%, the investigators point out, citing a 2008 Centers for Disease Control and Prevention report on cigarette use among US high school students.
Smoking Prevalence Rates
Smoking prevalence rates were derived from National Health Interview Survey data from 1970 to 2016.
Mirroring findings in the racial patterns of lung cancer incidence rates, smoking prevalence rates declined in successive birth cohorts in both Black and White males and females, but the decline was again steeper in Black men and women than it was in White men and women.
As a result, the historically higher sex-specific smoking prevalence rates seen historically in Blacks disappeared in men born around 1960, and reversed in women born at the same time, Jemal and colleagues point out.
As the authors explain, the more rapid decline in smoking prevalence after 1960 is likely a reflection of the “precipitous” drop in smoking initiation rates among Black teenagers starting about the late 1970s through to the early 1990s.
For example, among 12th graders, smoking prevalence rates between 1977 and 1992 dropped from 36.7% to 8.1% among Black teens. In stark contrast, they hardly changed at all among White teens, dropping only from 38.3% in 1977 to 31.8% in 1992.
Jemal suggested that steeper decline in smoking initiation rates seen between the late 1970s and early 90s reflects the fact that Black teenagers were deterred from smoking because the cost of cigarettes kept going up.
He also suggested that smoking is less acceptable in the Black community than it is in the White community, especially among churchgoers, where smoking is severely frowned upon and nonsmoking is the community “norm.”
Additionally, Black youth may simply be heeding government antismoking messages to a greater extent than White youth, Jemal suggested.
He wondered if there are parallels now in the current pandemic. “When I go to a store here in Georgia, I would say almost all Blacks are wearing a mask [even though masks are not mandatory in Georgia] whereas it’s amazing the number of Whites who don’t wear a mask,” he recounts.
“So it would seem that Whites feel that government is simply interfering with their lives, while Blacks have a better perspective of the harms of smoking, so they are listening to the government’s antismoking campaigns,” he speculated.
Some Isolated Areas
Asked to comment on the study’s findings, Otis Brawley, MD, Bloomberg, distinguished professor of oncology and epidemiology at Johns Hopkins University in Baltimore, said that, while overall Black smoking rates are declining, there are some isolated areas where they are still very high.
For example, in his hometown of Baltimore, recent prevalence rates indicate that over 30% of Blacks are still smoking, “so these areas with high usage are still areas to focus on,” he told Medscape Medical News.
On the other hand, the study also supports the benefits of local, state, and federal government efforts to promote antismoking messages and tobacco-control activities over the past number of years.
“It proves that tactics used to control tobacco use have had some effect [even though] the study also shows that the tobacco industry’s advertising tactics such as the R.J. Reynolds targeted ads in the 90s can have deleterious effects,” Brawley noted.
Lung cancer has traditionally been one of the biggest drivers in the Black/White cancer mortality gap, Brawley said, adding that steeper declines in smoking initiation rates among Blacks compared with Whites are the main reason why this disparity is decreasing.
The study was supported by the Intramural Research Department of the American Cancer Society. The study authors have disclosed no relevant financial relationships. Brawley declares he does some consulting work for pharmaceutical company Genentech.
This article first appeared on Medscape.com.
The historically higher incidence rates of lung cancer among Black men, compared with White men, in the United States have all but been eliminated, at least among most men in the younger age groups, a new analysis from the American Cancer Society (ACS) indicates.
Among women, the trend is even more impressive, as the Black/White gap in lung cancer incidence rates has actually reversed in younger women. Black women in certain age groups are now less likely to develop lung cancer than White women, the same study indicates.
These trends reflect the steeper declines in smoking rates among Blacks in the US, compared with comparably-aged Whites, say the authors.
“This is the only cancer where this has happened,” lead author Ahmedin Jemal, DVM, PhD, senior vice president for Data Science at the American Cancer Society, told Medscape Medical News.
“If you look at cancers that are affected by access to screening and treatment, the disparity between the Blacks and the Whites has been increasing over the years because tests and treatment require access to insurance, so the Whites are getting more of them than the Blacks,” Jemal explained.
“But for smoking, all you have to do for prevention is just don’t smoke, so this is a success story that really should be highlighted,” he emphasized.
The study was published online Aug. 20 in JNCI Cancer: Spectrum.
Nationwide Incidence Data
For this study, Jemal and colleagues collected nationwide incidence data on individuals between ages 30 and 54 who had been diagnosed with lung cancer between 1997 and 2016.
“We categorized age at diagnosis by 5-year age intervals (from 30-34 to 50-54 years) and year of diagnosis by 5-year calendar period (from 1997-2001 to 2012-2016),” the investigators explain.
Analyses showed that lung cancer incidence rates generally decreased among both Black and White men during the study interval but the decline in incidence rates was steeper in Black men than in White men. As a consequence, the Black-to-White incidence rate ratios (IRRs) became similar in men born between 1967 and 1972 and reversed in women born since about 1967. For example, the Black-to-White IRRs in men between the ages of 40 and 44 who were born between 1957 and 1972 declined from 1.92 to 1.03.
Similarly, lung cancer incidence rates during the study interval declined among both Black and White women between the ages of 30 and 49 but, again, the decline was “considerably larger” among Black women. As a consequence, the Black-to-White IRR in women age 45 to 49 dropped from 1.25 during the period 1997-2001 down to 0.83 during the period 2012-2016.
This is in stark contrast to historical trends in lung cancer incidence rates, which were over 30% higher among similarly aged Black women born in the late 1950s. Now, lung cancer incidence rates are about 30% lower for similarly aged Black women born in 1972, compared with White women.
For Black and White women between age 50 and 54, lung cancer incidence rates either declined only slightly or remained stable during the study interval, the investigators reported.
The one exception to the diminishing gap in lung cancer incidence rates between Black and White men was an observed increase in IRRs in men born around the period 1977-1982
Among this group of men, who were between age 30 and 39 in the years 2012-2016, lung cancer incidence rates were higher in Black men than in White men.
As the authors point out, this increase in lung cancer rates among young Black men likely reflects a rapid rise in smoking seen among Black youth in the 1990s.
This trend coincided with an R.J. Reynolds tobacco ad campaign in which African Americans were targeted; between 1991 and 1997, the prevalence of smoking among Black high school students doubled from 14.1% to 28.2%, the investigators point out, citing a 2008 Centers for Disease Control and Prevention report on cigarette use among US high school students.
Smoking Prevalence Rates
Smoking prevalence rates were derived from National Health Interview Survey data from 1970 to 2016.
Mirroring findings in the racial patterns of lung cancer incidence rates, smoking prevalence rates declined in successive birth cohorts in both Black and White males and females, but the decline was again steeper in Black men and women than it was in White men and women.
As a result, the historically higher sex-specific smoking prevalence rates seen historically in Blacks disappeared in men born around 1960, and reversed in women born at the same time, Jemal and colleagues point out.
As the authors explain, the more rapid decline in smoking prevalence after 1960 is likely a reflection of the “precipitous” drop in smoking initiation rates among Black teenagers starting about the late 1970s through to the early 1990s.
For example, among 12th graders, smoking prevalence rates between 1977 and 1992 dropped from 36.7% to 8.1% among Black teens. In stark contrast, they hardly changed at all among White teens, dropping only from 38.3% in 1977 to 31.8% in 1992.
Jemal suggested that steeper decline in smoking initiation rates seen between the late 1970s and early 90s reflects the fact that Black teenagers were deterred from smoking because the cost of cigarettes kept going up.
He also suggested that smoking is less acceptable in the Black community than it is in the White community, especially among churchgoers, where smoking is severely frowned upon and nonsmoking is the community “norm.”
Additionally, Black youth may simply be heeding government antismoking messages to a greater extent than White youth, Jemal suggested.
He wondered if there are parallels now in the current pandemic. “When I go to a store here in Georgia, I would say almost all Blacks are wearing a mask [even though masks are not mandatory in Georgia] whereas it’s amazing the number of Whites who don’t wear a mask,” he recounts.
“So it would seem that Whites feel that government is simply interfering with their lives, while Blacks have a better perspective of the harms of smoking, so they are listening to the government’s antismoking campaigns,” he speculated.
Some Isolated Areas
Asked to comment on the study’s findings, Otis Brawley, MD, Bloomberg, distinguished professor of oncology and epidemiology at Johns Hopkins University in Baltimore, said that, while overall Black smoking rates are declining, there are some isolated areas where they are still very high.
For example, in his hometown of Baltimore, recent prevalence rates indicate that over 30% of Blacks are still smoking, “so these areas with high usage are still areas to focus on,” he told Medscape Medical News.
On the other hand, the study also supports the benefits of local, state, and federal government efforts to promote antismoking messages and tobacco-control activities over the past number of years.
“It proves that tactics used to control tobacco use have had some effect [even though] the study also shows that the tobacco industry’s advertising tactics such as the R.J. Reynolds targeted ads in the 90s can have deleterious effects,” Brawley noted.
Lung cancer has traditionally been one of the biggest drivers in the Black/White cancer mortality gap, Brawley said, adding that steeper declines in smoking initiation rates among Blacks compared with Whites are the main reason why this disparity is decreasing.
The study was supported by the Intramural Research Department of the American Cancer Society. The study authors have disclosed no relevant financial relationships. Brawley declares he does some consulting work for pharmaceutical company Genentech.
This article first appeared on Medscape.com.
Age, smoking among leading cancer risk factors for SLE patients
A new study has quantified cancer risk factors in patients with systemic lupus erythematosus, including smoking and the use of certain medications.
“As expected, older age was associated with cancer overall, as well as with the most common cancer subtypes,” wrote Sasha Bernatsky, MD, PhD, of McGill University, Montreal, and coauthors. The study was published in Arthritis Care & Research.
To determine the risk of cancer in people with clinically confirmed incident systemic lupus erythematosus (SLE), the researchers analyzed data from 1,668 newly diagnosed lupus patients with at least one follow-up visit. All patients were enrolled in the Systemic Lupus International Collaborating Clinics inception cohort from across 33 different centers in North America, Europe, and Asia. A total of 89% (n = 1,480) were women, and 49% (n = 824) were white. The average follow-up period was 9 years.
Of the 1,668 SLE patients, 65 developed some type of cancer. The cancers included 15 breast;, 10 nonmelanoma skin; 7 lung; 6 hematologic, 6 prostate; 5 melanoma; 3 cervical; 3 renal; 2 gastric; 2 head and neck; 2 thyroid; and 1 rectal, sarcoma, thymoma, or uterine. No patient had more than one type, and the mean age of the cancer patients at time of SLE diagnosis was 45.6 (standard deviation, 14.5).
Almost half of the 65 cancers occurred in past or current smokers, including all of the lung cancers, while only 33% of patients without cancers smoked prior to baseline. After univariate analysis, characteristics associated with a higher risk of all cancers included older age at SLE diagnosis (adjusted hazard ratio, 1.05; 95% confidence interval, 1.03-1.06), White race/ethnicity (aHR 1.34; 95% CI, 0.76-2.37), and smoking (aHR 1.21; 95% CI, 0.73-2.01).
After multivariate analysis, the two characteristics most associated with increased cancer risk were older age at SLE diagnosis and being male. The analyses also confirmed that older age was a risk factor for breast cancer (aHR 1.06; 95% CI, 1.02-1.10) and nonmelanoma skin cancer (aHR, 1.06; 95% CI, 1.02-1.11), while use of antimalarial drugs was associated with a lower risk of both breast (aHR, 0.28; 95% CI, 0.09-0.90) and nonmelanoma skin (aHR, 0.23; 95% CI, 0.05-0.95) cancers. For lung cancer, the highest risk factor was smoking 15 or more cigarettes a day (aHR, 6.64; 95% CI, 1.43-30.9); for hematologic cancers, it was being in the top quartile of SLE disease activity (aHR, 7.14; 95% CI, 1.13-45.3).
The authors acknowledged their study’s limitations, including the small number of cancers overall and purposefully not comparing cancer risk in SLE patients with risk in the general population. Although their methods – “physicians recording events at annual visits, confirmed by review of charts” – were recognized as very suitable for the current analysis, they noted that a broader comparison would “potentially be problematic due to differential misclassification error” in cancer registry data.
Two of the study’s authors reported potential conflicts of interest, including receiving grants and consulting and personal fees from various pharmaceutical companies. No other potential conflicts were reported.
SOURCE: Bernatsky S et al. Arthritis Care Res. 2020 Aug 19. doi: 10.1002/acr.24425.
A new study has quantified cancer risk factors in patients with systemic lupus erythematosus, including smoking and the use of certain medications.
“As expected, older age was associated with cancer overall, as well as with the most common cancer subtypes,” wrote Sasha Bernatsky, MD, PhD, of McGill University, Montreal, and coauthors. The study was published in Arthritis Care & Research.
To determine the risk of cancer in people with clinically confirmed incident systemic lupus erythematosus (SLE), the researchers analyzed data from 1,668 newly diagnosed lupus patients with at least one follow-up visit. All patients were enrolled in the Systemic Lupus International Collaborating Clinics inception cohort from across 33 different centers in North America, Europe, and Asia. A total of 89% (n = 1,480) were women, and 49% (n = 824) were white. The average follow-up period was 9 years.
Of the 1,668 SLE patients, 65 developed some type of cancer. The cancers included 15 breast;, 10 nonmelanoma skin; 7 lung; 6 hematologic, 6 prostate; 5 melanoma; 3 cervical; 3 renal; 2 gastric; 2 head and neck; 2 thyroid; and 1 rectal, sarcoma, thymoma, or uterine. No patient had more than one type, and the mean age of the cancer patients at time of SLE diagnosis was 45.6 (standard deviation, 14.5).
Almost half of the 65 cancers occurred in past or current smokers, including all of the lung cancers, while only 33% of patients without cancers smoked prior to baseline. After univariate analysis, characteristics associated with a higher risk of all cancers included older age at SLE diagnosis (adjusted hazard ratio, 1.05; 95% confidence interval, 1.03-1.06), White race/ethnicity (aHR 1.34; 95% CI, 0.76-2.37), and smoking (aHR 1.21; 95% CI, 0.73-2.01).
After multivariate analysis, the two characteristics most associated with increased cancer risk were older age at SLE diagnosis and being male. The analyses also confirmed that older age was a risk factor for breast cancer (aHR 1.06; 95% CI, 1.02-1.10) and nonmelanoma skin cancer (aHR, 1.06; 95% CI, 1.02-1.11), while use of antimalarial drugs was associated with a lower risk of both breast (aHR, 0.28; 95% CI, 0.09-0.90) and nonmelanoma skin (aHR, 0.23; 95% CI, 0.05-0.95) cancers. For lung cancer, the highest risk factor was smoking 15 or more cigarettes a day (aHR, 6.64; 95% CI, 1.43-30.9); for hematologic cancers, it was being in the top quartile of SLE disease activity (aHR, 7.14; 95% CI, 1.13-45.3).
The authors acknowledged their study’s limitations, including the small number of cancers overall and purposefully not comparing cancer risk in SLE patients with risk in the general population. Although their methods – “physicians recording events at annual visits, confirmed by review of charts” – were recognized as very suitable for the current analysis, they noted that a broader comparison would “potentially be problematic due to differential misclassification error” in cancer registry data.
Two of the study’s authors reported potential conflicts of interest, including receiving grants and consulting and personal fees from various pharmaceutical companies. No other potential conflicts were reported.
SOURCE: Bernatsky S et al. Arthritis Care Res. 2020 Aug 19. doi: 10.1002/acr.24425.
A new study has quantified cancer risk factors in patients with systemic lupus erythematosus, including smoking and the use of certain medications.
“As expected, older age was associated with cancer overall, as well as with the most common cancer subtypes,” wrote Sasha Bernatsky, MD, PhD, of McGill University, Montreal, and coauthors. The study was published in Arthritis Care & Research.
To determine the risk of cancer in people with clinically confirmed incident systemic lupus erythematosus (SLE), the researchers analyzed data from 1,668 newly diagnosed lupus patients with at least one follow-up visit. All patients were enrolled in the Systemic Lupus International Collaborating Clinics inception cohort from across 33 different centers in North America, Europe, and Asia. A total of 89% (n = 1,480) were women, and 49% (n = 824) were white. The average follow-up period was 9 years.
Of the 1,668 SLE patients, 65 developed some type of cancer. The cancers included 15 breast;, 10 nonmelanoma skin; 7 lung; 6 hematologic, 6 prostate; 5 melanoma; 3 cervical; 3 renal; 2 gastric; 2 head and neck; 2 thyroid; and 1 rectal, sarcoma, thymoma, or uterine. No patient had more than one type, and the mean age of the cancer patients at time of SLE diagnosis was 45.6 (standard deviation, 14.5).
Almost half of the 65 cancers occurred in past or current smokers, including all of the lung cancers, while only 33% of patients without cancers smoked prior to baseline. After univariate analysis, characteristics associated with a higher risk of all cancers included older age at SLE diagnosis (adjusted hazard ratio, 1.05; 95% confidence interval, 1.03-1.06), White race/ethnicity (aHR 1.34; 95% CI, 0.76-2.37), and smoking (aHR 1.21; 95% CI, 0.73-2.01).
After multivariate analysis, the two characteristics most associated with increased cancer risk were older age at SLE diagnosis and being male. The analyses also confirmed that older age was a risk factor for breast cancer (aHR 1.06; 95% CI, 1.02-1.10) and nonmelanoma skin cancer (aHR, 1.06; 95% CI, 1.02-1.11), while use of antimalarial drugs was associated with a lower risk of both breast (aHR, 0.28; 95% CI, 0.09-0.90) and nonmelanoma skin (aHR, 0.23; 95% CI, 0.05-0.95) cancers. For lung cancer, the highest risk factor was smoking 15 or more cigarettes a day (aHR, 6.64; 95% CI, 1.43-30.9); for hematologic cancers, it was being in the top quartile of SLE disease activity (aHR, 7.14; 95% CI, 1.13-45.3).
The authors acknowledged their study’s limitations, including the small number of cancers overall and purposefully not comparing cancer risk in SLE patients with risk in the general population. Although their methods – “physicians recording events at annual visits, confirmed by review of charts” – were recognized as very suitable for the current analysis, they noted that a broader comparison would “potentially be problematic due to differential misclassification error” in cancer registry data.
Two of the study’s authors reported potential conflicts of interest, including receiving grants and consulting and personal fees from various pharmaceutical companies. No other potential conflicts were reported.
SOURCE: Bernatsky S et al. Arthritis Care Res. 2020 Aug 19. doi: 10.1002/acr.24425.
FROM ARTHRITIS CARE & RESEARCH
Treatment for a tobacco-dependent adult
Applying American Thoracic Society’s new clinical practice guideline
Complications from tobacco use are the most common preventable cause of death, disability, and disease in the United States. Tobacco use causes 480,000 premature deaths every year. In pregnancy, tobacco use causes complications such as premature birth, intrauterine growth restriction, and placental abruption. In the perinatal period, it is associated with sudden infant death syndrome. While cigarette smoking is decreasing in adolescents, e-cigarette use in on the rise. Approximately 1,600 children aged 12-17 smoke their first cigarette every day and it is estimated that 5.6 million children and adolescents will die of a tobacco use–related death.1 For these reasons it is important to address tobacco use and cessation with patients whenever it is possible.
Case
A forty-five-year-old male who rarely comes to the office is here today for a physical exam at the urging of his partner. He has been smoking a pack a day since age 17. You have tried at past visits to discuss quitting, but he had been in the precontemplative stage and had been unwilling to consider any change. This visit, however, he is ready to try to quit. What can you offer him?
Core recommendations from ATS guidelines
This patient can be offered varenicline plus nicotine replacement therapy rather than nicotine replacement therapy, bupropion, e-cigarettes, or varenicline alone. His course of therapy should extend beyond 12 weeks instead of the standard 6- to 12-week therapy. Alternatively, he could be offered varenicline alone, rather than nicotine replacement.2
A change from previous guidelines
What makes this recommendation so interesting and new is the emphasis it places on varenicline. The United States Preventive Services Task Force released a recommendation statement in 2015 that stressed a combination of pharmacological and behavioral interventions. It discussed nicotine replacement therapy, bupropion, and varenicline, but did not recommend any one over any of the others.3 The new recommendation from the American Thoracic Society favors varenicline over other pharmacologic interventions. It is based on an independent systematic review of the literature that showed higher rates of tobacco use abstinence at the 6-month follow-up with varenicline alone versus nicotine replacement therapy alone, bupropion alone, or e-cigarette use only.
A review of 14 randomized controlled trials showed that varenicline improves abstinence rates during treatment by approximately 40% compared with nicotine replacement, and by 20% at the end of 6 months of treatment. The review found that varenicline plus nicotine replacement therapy is more effective than varenicline alone. In this comparison, based on three trials, there was a 36% higher abstinence rate at 6 months using varenicline plus nicotine replacement. When varenicline use was compared with use of a nicotine patch, bupropion, or e-cigarettes, there was a reduction in serious adverse events – changes in mood, suicidal ideation, and neurological side effects such as seizures.2 Clinicians may remember a black box warning on the varenicline label citing neuropsychiatric effects and it is important to note that the Food and Drug Administration removed this boxed warning in 2016.4
Opinion
This recommendation represents an important, evidence-based change from previous guidelines. It presents the opportunity for better outcomes, but will likely take a while to filter into practice, as clinicians need to become more comfortable with the use of varenicline and insurance supports the cost of varenicline.
The average cost of varenicline for 12 weeks is between $1,220 and $1,584. For comparison, nicotine replacement therapy costs $170 to $240 for the same number of weeks. To put those costs in perspective, the 12-week cost of cigarettes for a two-pack-a-day smoker is approximately $1,000.
For some patients, the motivation to quit smoking comes from the realization of how much they are spending on cigarettes each month. That said, if a patient does not have insurance or their insurance does not cover the cost of varenicline, nicotine replacement therapy might be more appealing. It should be noted that better abstinence rates have been seen in patients taking varenicline plus nicotine replacement therapy versus varenicline alone.
Suggested treatment
Based on a systematic review of randomized controlled trials, the American Thoracic Society’s guideline on pharmacological treatment in tobacco-dependent adults concludes that varenicline plus nicotine patch is the preferred pharmacological treatment for tobacco cessation when compared with varenicline alone, bupropion alone, nicotine replacement therapy alone, and e-cigarettes alone. If the patient does not want to start two medicines at once, then varenicline alone would be the preferred choice.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. Dr. Sprogell is a third-year resident in the family medicine residency program at Abington Jefferson Health. They have no conflicts related to the content of this piece. For questions or comments, feel free to contact Dr. Skolnik on Twitter @NeilSkolnik.
References
1. U.S. Preventive Services Task Force. Primary care interventions for prevention and cessation of tobacco use in children and adolescents: U.S. Preventive Services Task Force Recommendation Statement. JAMA.2020;323(16):1590-8. doi: 10.1001/jama.2020.4679.
2. Leone FT et al. Initiating pharmacologic treatment in tobacco-dependent adults: An official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med. 2020;202(2):e5–e31.
3. Tobacco smoking cessation in adults, including pregnant women: Behavioral and pharmacotherapy interventions. U.S. Preventive Services Task Force 2015 Sep 21.
4. FDA Drug Safety Communication: FDA revises description of mental health side effects of the stop-smoking medicines Chantix (varenicline) and Zyban (bupropion) to reflect clinical trial findings. 2016 Dec. 16.
Applying American Thoracic Society’s new clinical practice guideline
Applying American Thoracic Society’s new clinical practice guideline
Complications from tobacco use are the most common preventable cause of death, disability, and disease in the United States. Tobacco use causes 480,000 premature deaths every year. In pregnancy, tobacco use causes complications such as premature birth, intrauterine growth restriction, and placental abruption. In the perinatal period, it is associated with sudden infant death syndrome. While cigarette smoking is decreasing in adolescents, e-cigarette use in on the rise. Approximately 1,600 children aged 12-17 smoke their first cigarette every day and it is estimated that 5.6 million children and adolescents will die of a tobacco use–related death.1 For these reasons it is important to address tobacco use and cessation with patients whenever it is possible.
Case
A forty-five-year-old male who rarely comes to the office is here today for a physical exam at the urging of his partner. He has been smoking a pack a day since age 17. You have tried at past visits to discuss quitting, but he had been in the precontemplative stage and had been unwilling to consider any change. This visit, however, he is ready to try to quit. What can you offer him?
Core recommendations from ATS guidelines
This patient can be offered varenicline plus nicotine replacement therapy rather than nicotine replacement therapy, bupropion, e-cigarettes, or varenicline alone. His course of therapy should extend beyond 12 weeks instead of the standard 6- to 12-week therapy. Alternatively, he could be offered varenicline alone, rather than nicotine replacement.2
A change from previous guidelines
What makes this recommendation so interesting and new is the emphasis it places on varenicline. The United States Preventive Services Task Force released a recommendation statement in 2015 that stressed a combination of pharmacological and behavioral interventions. It discussed nicotine replacement therapy, bupropion, and varenicline, but did not recommend any one over any of the others.3 The new recommendation from the American Thoracic Society favors varenicline over other pharmacologic interventions. It is based on an independent systematic review of the literature that showed higher rates of tobacco use abstinence at the 6-month follow-up with varenicline alone versus nicotine replacement therapy alone, bupropion alone, or e-cigarette use only.
A review of 14 randomized controlled trials showed that varenicline improves abstinence rates during treatment by approximately 40% compared with nicotine replacement, and by 20% at the end of 6 months of treatment. The review found that varenicline plus nicotine replacement therapy is more effective than varenicline alone. In this comparison, based on three trials, there was a 36% higher abstinence rate at 6 months using varenicline plus nicotine replacement. When varenicline use was compared with use of a nicotine patch, bupropion, or e-cigarettes, there was a reduction in serious adverse events – changes in mood, suicidal ideation, and neurological side effects such as seizures.2 Clinicians may remember a black box warning on the varenicline label citing neuropsychiatric effects and it is important to note that the Food and Drug Administration removed this boxed warning in 2016.4
Opinion
This recommendation represents an important, evidence-based change from previous guidelines. It presents the opportunity for better outcomes, but will likely take a while to filter into practice, as clinicians need to become more comfortable with the use of varenicline and insurance supports the cost of varenicline.
The average cost of varenicline for 12 weeks is between $1,220 and $1,584. For comparison, nicotine replacement therapy costs $170 to $240 for the same number of weeks. To put those costs in perspective, the 12-week cost of cigarettes for a two-pack-a-day smoker is approximately $1,000.
For some patients, the motivation to quit smoking comes from the realization of how much they are spending on cigarettes each month. That said, if a patient does not have insurance or their insurance does not cover the cost of varenicline, nicotine replacement therapy might be more appealing. It should be noted that better abstinence rates have been seen in patients taking varenicline plus nicotine replacement therapy versus varenicline alone.
Suggested treatment
Based on a systematic review of randomized controlled trials, the American Thoracic Society’s guideline on pharmacological treatment in tobacco-dependent adults concludes that varenicline plus nicotine patch is the preferred pharmacological treatment for tobacco cessation when compared with varenicline alone, bupropion alone, nicotine replacement therapy alone, and e-cigarettes alone. If the patient does not want to start two medicines at once, then varenicline alone would be the preferred choice.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. Dr. Sprogell is a third-year resident in the family medicine residency program at Abington Jefferson Health. They have no conflicts related to the content of this piece. For questions or comments, feel free to contact Dr. Skolnik on Twitter @NeilSkolnik.
References
1. U.S. Preventive Services Task Force. Primary care interventions for prevention and cessation of tobacco use in children and adolescents: U.S. Preventive Services Task Force Recommendation Statement. JAMA.2020;323(16):1590-8. doi: 10.1001/jama.2020.4679.
2. Leone FT et al. Initiating pharmacologic treatment in tobacco-dependent adults: An official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med. 2020;202(2):e5–e31.
3. Tobacco smoking cessation in adults, including pregnant women: Behavioral and pharmacotherapy interventions. U.S. Preventive Services Task Force 2015 Sep 21.
4. FDA Drug Safety Communication: FDA revises description of mental health side effects of the stop-smoking medicines Chantix (varenicline) and Zyban (bupropion) to reflect clinical trial findings. 2016 Dec. 16.
Complications from tobacco use are the most common preventable cause of death, disability, and disease in the United States. Tobacco use causes 480,000 premature deaths every year. In pregnancy, tobacco use causes complications such as premature birth, intrauterine growth restriction, and placental abruption. In the perinatal period, it is associated with sudden infant death syndrome. While cigarette smoking is decreasing in adolescents, e-cigarette use in on the rise. Approximately 1,600 children aged 12-17 smoke their first cigarette every day and it is estimated that 5.6 million children and adolescents will die of a tobacco use–related death.1 For these reasons it is important to address tobacco use and cessation with patients whenever it is possible.
Case
A forty-five-year-old male who rarely comes to the office is here today for a physical exam at the urging of his partner. He has been smoking a pack a day since age 17. You have tried at past visits to discuss quitting, but he had been in the precontemplative stage and had been unwilling to consider any change. This visit, however, he is ready to try to quit. What can you offer him?
Core recommendations from ATS guidelines
This patient can be offered varenicline plus nicotine replacement therapy rather than nicotine replacement therapy, bupropion, e-cigarettes, or varenicline alone. His course of therapy should extend beyond 12 weeks instead of the standard 6- to 12-week therapy. Alternatively, he could be offered varenicline alone, rather than nicotine replacement.2
A change from previous guidelines
What makes this recommendation so interesting and new is the emphasis it places on varenicline. The United States Preventive Services Task Force released a recommendation statement in 2015 that stressed a combination of pharmacological and behavioral interventions. It discussed nicotine replacement therapy, bupropion, and varenicline, but did not recommend any one over any of the others.3 The new recommendation from the American Thoracic Society favors varenicline over other pharmacologic interventions. It is based on an independent systematic review of the literature that showed higher rates of tobacco use abstinence at the 6-month follow-up with varenicline alone versus nicotine replacement therapy alone, bupropion alone, or e-cigarette use only.
A review of 14 randomized controlled trials showed that varenicline improves abstinence rates during treatment by approximately 40% compared with nicotine replacement, and by 20% at the end of 6 months of treatment. The review found that varenicline plus nicotine replacement therapy is more effective than varenicline alone. In this comparison, based on three trials, there was a 36% higher abstinence rate at 6 months using varenicline plus nicotine replacement. When varenicline use was compared with use of a nicotine patch, bupropion, or e-cigarettes, there was a reduction in serious adverse events – changes in mood, suicidal ideation, and neurological side effects such as seizures.2 Clinicians may remember a black box warning on the varenicline label citing neuropsychiatric effects and it is important to note that the Food and Drug Administration removed this boxed warning in 2016.4
Opinion
This recommendation represents an important, evidence-based change from previous guidelines. It presents the opportunity for better outcomes, but will likely take a while to filter into practice, as clinicians need to become more comfortable with the use of varenicline and insurance supports the cost of varenicline.
The average cost of varenicline for 12 weeks is between $1,220 and $1,584. For comparison, nicotine replacement therapy costs $170 to $240 for the same number of weeks. To put those costs in perspective, the 12-week cost of cigarettes for a two-pack-a-day smoker is approximately $1,000.
For some patients, the motivation to quit smoking comes from the realization of how much they are spending on cigarettes each month. That said, if a patient does not have insurance or their insurance does not cover the cost of varenicline, nicotine replacement therapy might be more appealing. It should be noted that better abstinence rates have been seen in patients taking varenicline plus nicotine replacement therapy versus varenicline alone.
Suggested treatment
Based on a systematic review of randomized controlled trials, the American Thoracic Society’s guideline on pharmacological treatment in tobacco-dependent adults concludes that varenicline plus nicotine patch is the preferred pharmacological treatment for tobacco cessation when compared with varenicline alone, bupropion alone, nicotine replacement therapy alone, and e-cigarettes alone. If the patient does not want to start two medicines at once, then varenicline alone would be the preferred choice.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. Dr. Sprogell is a third-year resident in the family medicine residency program at Abington Jefferson Health. They have no conflicts related to the content of this piece. For questions or comments, feel free to contact Dr. Skolnik on Twitter @NeilSkolnik.
References
1. U.S. Preventive Services Task Force. Primary care interventions for prevention and cessation of tobacco use in children and adolescents: U.S. Preventive Services Task Force Recommendation Statement. JAMA.2020;323(16):1590-8. doi: 10.1001/jama.2020.4679.
2. Leone FT et al. Initiating pharmacologic treatment in tobacco-dependent adults: An official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med. 2020;202(2):e5–e31.
3. Tobacco smoking cessation in adults, including pregnant women: Behavioral and pharmacotherapy interventions. U.S. Preventive Services Task Force 2015 Sep 21.
4. FDA Drug Safety Communication: FDA revises description of mental health side effects of the stop-smoking medicines Chantix (varenicline) and Zyban (bupropion) to reflect clinical trial findings. 2016 Dec. 16.
Performance status, molecular testing key to metastatic cancer prognosis
according to Sam Brondfield, MD, MA, an inpatient medical oncologist at the University of California, San Francisco.
Oncologists have at their fingertips a voluminous and ever-growing body of clinical trials data to draw on for prognostication. Yet many hospitalists will be surprised to learn that this wealth of information is of little value in the inpatient settings where they work, he said at HM20 Virtual, hosted by the Society of Hospital Medicine.
“The applicability of clinical trials data to hospitalized patients is generally poor. That’s an important caveat to keep in mind,” Dr. Brondfield said.
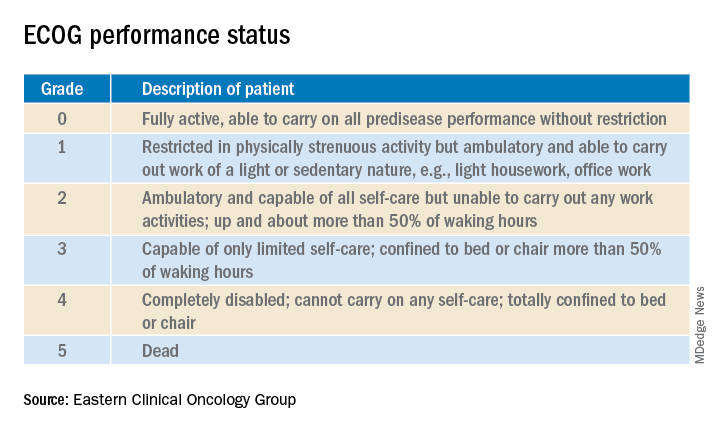
Enrollment in clinical trials is usually restricted to patients with a score of 0 or 1 on the Eastern Clinical Oncology Group Performance Status, meaning their cancer is causing minimal or no disruption to their life (see graphic). Sometimes trials will include patients with a performance status of 2 on the ECOG scale, a tool developed nearly 40 years ago, but clinical trials virtually never enroll those with an ECOG status of 3 or 4. Yet most hospitalized patients with metastatic cancer have an ECOG performance status of 3 or worse. Thus, the clinical trials outcome data are of little relevance.
“In oncology the distinction between ECOG 2 and 3 is very important,” Dr. Brondfield emphasized.
When he talks about treatment options with hospitalized patients who have metastatic cancer and poor performance status – that is, ECOG 3 or 4 – he’ll often say: “Assuming you feel better and can go home, that’s when these clinical trial data may apply better to you.”
Dr. Brondfield cautioned against quoting the National Cancer Institute’s Surveillance, Epidemiology and End Results (SEER) 5-year overall survival data when hospitalized patients with advanced cancer ask how long they have to live. For one thing, the national average 5-year overall survival figure is hardly an individualized assessment. Plus, oncology is a fast-moving field in which important treatment advances occur all the time, and the SEER data lag far behind. For example, when Dr. Brondfield recently looked up the current SEER 5-year survival for patients diagnosed with metastatic non–small cell lung cancer (NSCLC), the figure quoted was less than 6%, and it was drawn from data accrued in 2009-2015. That simply doesn’t reflect contemporary practice.
Indeed, it’s no longer true that the average survival of patients with metastatic NSCLC is less than a year. In the practice-changing KEYNOTE-189 randomized trial, which accrued participants in 2016-2017, the median overall survival of patients randomized to pembrolizumab (Keytruda) plus standard cytotoxic chemotherapy was 22 months, compared with 11 months with chemotherapy plus placebo (J Clin Oncol. 2020 May 10. doi: 10.1200/JCO.19.03136). As a result, immunotherapy with a programmed death–1 inhibitor such as pembrolizumab in combination with chemotherapy is now standard practice in patients with metastatic NSCLC without targetable mutations.
Performance status guides treatment decision-making
Hospitalists can help oncologists in decision-making regarding whether to offer palliative systemic therapy to patients with advanced metastatic cancer and poor performance status by determining whether that status is caused by the cancer itself or some other cause that’s not easily reversible, such as liver failure.
Take, for example, the inpatient with advanced SCLC. This is an aggressive and chemosensitive cancer. Dr. Brondfield said he is among many medical oncologists who are convinced that, if poor performance status in a patient with advanced SCLC is caused by the cancer itself, prompt initiation of inpatient chemotherapy should be recommended to elicit a response that improves quality of life and performance status in the short term. If, on the other hand, the poor performance status is caused by organ failure or some other issue that can’t easily be improved, hospice may be more appropriate.
“The contour of SCLC over time is that despite its treatment responsiveness it inevitably recurs. But with chemotherapy you can give people in this situation months of quality time, so we generally try to treat these sorts of patients,” Dr. Brondfield explained.
The National Comprehensive Cancer Network guidelines upon which oncologists rely leave lots of room for interpretation regarding the appropriateness of inpatient chemotherapy in patients with advanced cancer and poor patient performance status. Citing “knowledge that’s been passed down across oncology generations,” Dr. Brondfield said he and many of his colleagues believe early palliative supportive care rather than systemic cytotoxic cancer-directed therapy is appropriate for patients with poor performance status who have one of several specific relatively nonchemoresponsive types of metastatic cancer. These include esophageal, gastric, and head and neck cancers.
On the other hand, advanced SCLC isn’t the only type of metastatic cancer that’s so chemosensitive that he and many other oncologists believe aggressive chemotherapy should be offered even in the face of poor patient performance status attributable to the cancer itself.
Take, for example, colorectal cancer with no more than five metastases to the lung or liver, provided those metastases are treatable with resection or radiation. “Those patients are actually curable at a high rate. They have about a 30%-40% cure rate. So those patients, even if they have poor performance status, if we can get them up for surgery or radiation, we usually do try to treat them aggressively,” Dr. Brondfield said.
There are other often chemoresponsive metastatic cancers for which oncologists frequently recommend aggressive treatment to improve quality of life in patients with poor performance status. These cancers include aggressive lymphomas, which are actually often curable; multiple myeloma; testicular and germ cell cancers; NSCLC with a targetable mutation, which is often responsive to oral medications; and prostate and well-differentiated thyroid cancers, which can usually be treated with hormone- or iodine-based therapies rather than more toxic intravenous cytotoxic chemotherapy.
The impact of inpatient palliative chemotherapy in patients with poor performance status and advanced solid cancers not on the short list of highly chemosensitive cancers has not been well studied. A recent retrospective study of 228 such patients who received inpatient palliative chemotherapy at a large Brazilian academic medical center provided little reason for enthusiasm regarding the practice. Survival was short, with 30- and 60-day survival rates of 56% and 39%, respectively. Plus, 30% of patients were admitted to the ICU, where they received aggressive and costly end-of-life care. The investigators found these results suggestive of overprescribing of inpatient palliative chemotherapy (BMC Palliat Care. 2019 May 20;18[1]:42. doi: 10.1186/s12904-019-0427-4).
Of note, the investigators found in a multivariate analysis that an elevated bilirubin was associated with a 217% increased risk of 30-day mortality, and hypercalcemia was associated with a 119% increased risk.
“That’s something to take into account when these decisions are being made,” Dr. Brondfield advised.
In response to an audience comment that oncologists often seem overly optimistic about prognosis, Dr. Brondfield observed, “I think it’s very common for there to be a disagreement between the oncologist wanting to be aggressive for a sick inpatient and the hospitalist or generalist provider thinking: ‘This person looks way too sick for chemotherapy.’ ”
For this reason he is a firm believer in having multidisciplinary conversations regarding prognosis in challenging situations involving hospitalized patients with advanced cancer. An oncologist can bring to such discussions a detailed understanding of clinical trial and molecular data as well as information about the patient’s response to the first round of therapy. But lots of other factors are relevant to prognosis, including nutritional status, comorbidities, and the intuitive eyeball test of how a patient might do. The patient’s family, primary care provider, oncologist, the hospitalist, and the palliative care team will have perspectives of their own.
Molecular testing is now the norm in metastatic cancers
These days oncologists order molecular testing for most patients with metastatic carcinomas to determine eligibility for targeted therapy, suitability for participation in clinical trials, prognostication, and/or assistance in determining the site of origin if that’s unclear.
A single-pass fine needle aspiration biopsy doesn’t provide enough tissue for molecular testing. It’s therefore important to order initially a multipass fine needle aspiration to avoid the need for a repeat biopsy, which is uncomfortable for the patient and can delay diagnosis and treatment.
Dr. Brondfield advised waiting for molecular testing results to come in before trying to prognosticate in patients with a metastatic cancer for which targetable mutations might be present. Survival rates can vary substantially depending upon those test results. Take, for example, metastatic NSCLC: Just within the past year, clinical trials have been published reporting overall survival rates of 39 months in patients with treatable mutations in epidermal growth factor receptor, 42 months with anaplastic lymphoma kinase mutations, and 51 months in patients whose tumor signature features mutations in c-ros oncogene 1, as compared with 22 months with no targetable mutations in the KEYNOTE-189 trial.
“There’s a lot of heterogeneity around how metastatic tumors behave and respond to therapy. Not all metastatic cancers are the same,” the oncologist emphasized.
according to Sam Brondfield, MD, MA, an inpatient medical oncologist at the University of California, San Francisco.
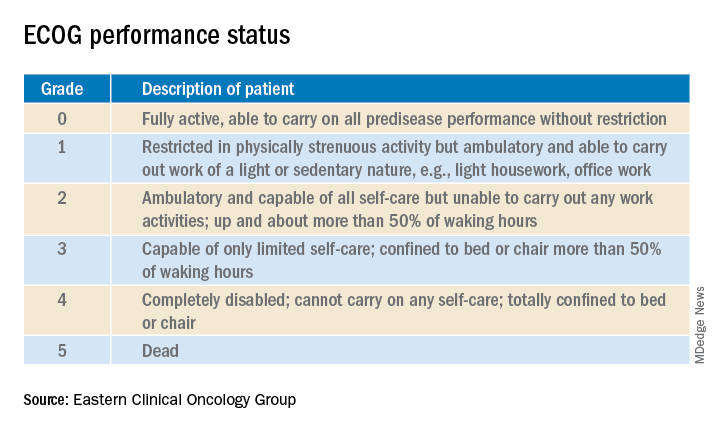
Oncologists have at their fingertips a voluminous and ever-growing body of clinical trials data to draw on for prognostication. Yet many hospitalists will be surprised to learn that this wealth of information is of little value in the inpatient settings where they work, he said at HM20 Virtual, hosted by the Society of Hospital Medicine.
“The applicability of clinical trials data to hospitalized patients is generally poor. That’s an important caveat to keep in mind,” Dr. Brondfield said.
Enrollment in clinical trials is usually restricted to patients with a score of 0 or 1 on the Eastern Clinical Oncology Group Performance Status, meaning their cancer is causing minimal or no disruption to their life (see graphic). Sometimes trials will include patients with a performance status of 2 on the ECOG scale, a tool developed nearly 40 years ago, but clinical trials virtually never enroll those with an ECOG status of 3 or 4. Yet most hospitalized patients with metastatic cancer have an ECOG performance status of 3 or worse. Thus, the clinical trials outcome data are of little relevance.
“In oncology the distinction between ECOG 2 and 3 is very important,” Dr. Brondfield emphasized.
When he talks about treatment options with hospitalized patients who have metastatic cancer and poor performance status – that is, ECOG 3 or 4 – he’ll often say: “Assuming you feel better and can go home, that’s when these clinical trial data may apply better to you.”
Dr. Brondfield cautioned against quoting the National Cancer Institute’s Surveillance, Epidemiology and End Results (SEER) 5-year overall survival data when hospitalized patients with advanced cancer ask how long they have to live. For one thing, the national average 5-year overall survival figure is hardly an individualized assessment. Plus, oncology is a fast-moving field in which important treatment advances occur all the time, and the SEER data lag far behind. For example, when Dr. Brondfield recently looked up the current SEER 5-year survival for patients diagnosed with metastatic non–small cell lung cancer (NSCLC), the figure quoted was less than 6%, and it was drawn from data accrued in 2009-2015. That simply doesn’t reflect contemporary practice.
Indeed, it’s no longer true that the average survival of patients with metastatic NSCLC is less than a year. In the practice-changing KEYNOTE-189 randomized trial, which accrued participants in 2016-2017, the median overall survival of patients randomized to pembrolizumab (Keytruda) plus standard cytotoxic chemotherapy was 22 months, compared with 11 months with chemotherapy plus placebo (J Clin Oncol. 2020 May 10. doi: 10.1200/JCO.19.03136). As a result, immunotherapy with a programmed death–1 inhibitor such as pembrolizumab in combination with chemotherapy is now standard practice in patients with metastatic NSCLC without targetable mutations.
Performance status guides treatment decision-making
Hospitalists can help oncologists in decision-making regarding whether to offer palliative systemic therapy to patients with advanced metastatic cancer and poor performance status by determining whether that status is caused by the cancer itself or some other cause that’s not easily reversible, such as liver failure.
Take, for example, the inpatient with advanced SCLC. This is an aggressive and chemosensitive cancer. Dr. Brondfield said he is among many medical oncologists who are convinced that, if poor performance status in a patient with advanced SCLC is caused by the cancer itself, prompt initiation of inpatient chemotherapy should be recommended to elicit a response that improves quality of life and performance status in the short term. If, on the other hand, the poor performance status is caused by organ failure or some other issue that can’t easily be improved, hospice may be more appropriate.
“The contour of SCLC over time is that despite its treatment responsiveness it inevitably recurs. But with chemotherapy you can give people in this situation months of quality time, so we generally try to treat these sorts of patients,” Dr. Brondfield explained.
The National Comprehensive Cancer Network guidelines upon which oncologists rely leave lots of room for interpretation regarding the appropriateness of inpatient chemotherapy in patients with advanced cancer and poor patient performance status. Citing “knowledge that’s been passed down across oncology generations,” Dr. Brondfield said he and many of his colleagues believe early palliative supportive care rather than systemic cytotoxic cancer-directed therapy is appropriate for patients with poor performance status who have one of several specific relatively nonchemoresponsive types of metastatic cancer. These include esophageal, gastric, and head and neck cancers.
On the other hand, advanced SCLC isn’t the only type of metastatic cancer that’s so chemosensitive that he and many other oncologists believe aggressive chemotherapy should be offered even in the face of poor patient performance status attributable to the cancer itself.
Take, for example, colorectal cancer with no more than five metastases to the lung or liver, provided those metastases are treatable with resection or radiation. “Those patients are actually curable at a high rate. They have about a 30%-40% cure rate. So those patients, even if they have poor performance status, if we can get them up for surgery or radiation, we usually do try to treat them aggressively,” Dr. Brondfield said.
There are other often chemoresponsive metastatic cancers for which oncologists frequently recommend aggressive treatment to improve quality of life in patients with poor performance status. These cancers include aggressive lymphomas, which are actually often curable; multiple myeloma; testicular and germ cell cancers; NSCLC with a targetable mutation, which is often responsive to oral medications; and prostate and well-differentiated thyroid cancers, which can usually be treated with hormone- or iodine-based therapies rather than more toxic intravenous cytotoxic chemotherapy.
The impact of inpatient palliative chemotherapy in patients with poor performance status and advanced solid cancers not on the short list of highly chemosensitive cancers has not been well studied. A recent retrospective study of 228 such patients who received inpatient palliative chemotherapy at a large Brazilian academic medical center provided little reason for enthusiasm regarding the practice. Survival was short, with 30- and 60-day survival rates of 56% and 39%, respectively. Plus, 30% of patients were admitted to the ICU, where they received aggressive and costly end-of-life care. The investigators found these results suggestive of overprescribing of inpatient palliative chemotherapy (BMC Palliat Care. 2019 May 20;18[1]:42. doi: 10.1186/s12904-019-0427-4).
Of note, the investigators found in a multivariate analysis that an elevated bilirubin was associated with a 217% increased risk of 30-day mortality, and hypercalcemia was associated with a 119% increased risk.
“That’s something to take into account when these decisions are being made,” Dr. Brondfield advised.
In response to an audience comment that oncologists often seem overly optimistic about prognosis, Dr. Brondfield observed, “I think it’s very common for there to be a disagreement between the oncologist wanting to be aggressive for a sick inpatient and the hospitalist or generalist provider thinking: ‘This person looks way too sick for chemotherapy.’ ”
For this reason he is a firm believer in having multidisciplinary conversations regarding prognosis in challenging situations involving hospitalized patients with advanced cancer. An oncologist can bring to such discussions a detailed understanding of clinical trial and molecular data as well as information about the patient’s response to the first round of therapy. But lots of other factors are relevant to prognosis, including nutritional status, comorbidities, and the intuitive eyeball test of how a patient might do. The patient’s family, primary care provider, oncologist, the hospitalist, and the palliative care team will have perspectives of their own.
Molecular testing is now the norm in metastatic cancers
These days oncologists order molecular testing for most patients with metastatic carcinomas to determine eligibility for targeted therapy, suitability for participation in clinical trials, prognostication, and/or assistance in determining the site of origin if that’s unclear.
A single-pass fine needle aspiration biopsy doesn’t provide enough tissue for molecular testing. It’s therefore important to order initially a multipass fine needle aspiration to avoid the need for a repeat biopsy, which is uncomfortable for the patient and can delay diagnosis and treatment.
Dr. Brondfield advised waiting for molecular testing results to come in before trying to prognosticate in patients with a metastatic cancer for which targetable mutations might be present. Survival rates can vary substantially depending upon those test results. Take, for example, metastatic NSCLC: Just within the past year, clinical trials have been published reporting overall survival rates of 39 months in patients with treatable mutations in epidermal growth factor receptor, 42 months with anaplastic lymphoma kinase mutations, and 51 months in patients whose tumor signature features mutations in c-ros oncogene 1, as compared with 22 months with no targetable mutations in the KEYNOTE-189 trial.
“There’s a lot of heterogeneity around how metastatic tumors behave and respond to therapy. Not all metastatic cancers are the same,” the oncologist emphasized.
according to Sam Brondfield, MD, MA, an inpatient medical oncologist at the University of California, San Francisco.
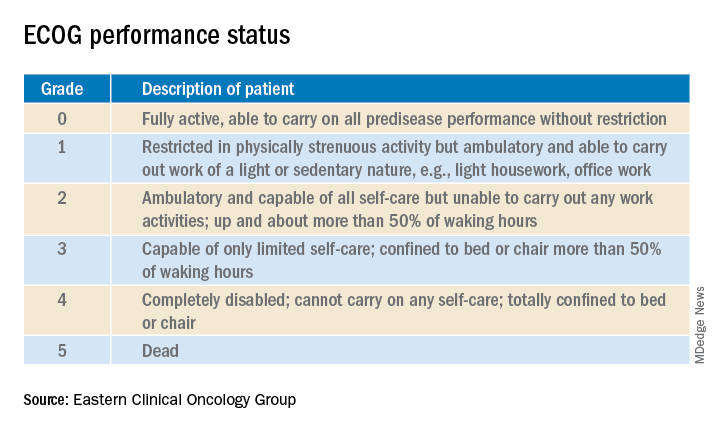
Oncologists have at their fingertips a voluminous and ever-growing body of clinical trials data to draw on for prognostication. Yet many hospitalists will be surprised to learn that this wealth of information is of little value in the inpatient settings where they work, he said at HM20 Virtual, hosted by the Society of Hospital Medicine.
“The applicability of clinical trials data to hospitalized patients is generally poor. That’s an important caveat to keep in mind,” Dr. Brondfield said.
Enrollment in clinical trials is usually restricted to patients with a score of 0 or 1 on the Eastern Clinical Oncology Group Performance Status, meaning their cancer is causing minimal or no disruption to their life (see graphic). Sometimes trials will include patients with a performance status of 2 on the ECOG scale, a tool developed nearly 40 years ago, but clinical trials virtually never enroll those with an ECOG status of 3 or 4. Yet most hospitalized patients with metastatic cancer have an ECOG performance status of 3 or worse. Thus, the clinical trials outcome data are of little relevance.
“In oncology the distinction between ECOG 2 and 3 is very important,” Dr. Brondfield emphasized.
When he talks about treatment options with hospitalized patients who have metastatic cancer and poor performance status – that is, ECOG 3 or 4 – he’ll often say: “Assuming you feel better and can go home, that’s when these clinical trial data may apply better to you.”
Dr. Brondfield cautioned against quoting the National Cancer Institute’s Surveillance, Epidemiology and End Results (SEER) 5-year overall survival data when hospitalized patients with advanced cancer ask how long they have to live. For one thing, the national average 5-year overall survival figure is hardly an individualized assessment. Plus, oncology is a fast-moving field in which important treatment advances occur all the time, and the SEER data lag far behind. For example, when Dr. Brondfield recently looked up the current SEER 5-year survival for patients diagnosed with metastatic non–small cell lung cancer (NSCLC), the figure quoted was less than 6%, and it was drawn from data accrued in 2009-2015. That simply doesn’t reflect contemporary practice.
Indeed, it’s no longer true that the average survival of patients with metastatic NSCLC is less than a year. In the practice-changing KEYNOTE-189 randomized trial, which accrued participants in 2016-2017, the median overall survival of patients randomized to pembrolizumab (Keytruda) plus standard cytotoxic chemotherapy was 22 months, compared with 11 months with chemotherapy plus placebo (J Clin Oncol. 2020 May 10. doi: 10.1200/JCO.19.03136). As a result, immunotherapy with a programmed death–1 inhibitor such as pembrolizumab in combination with chemotherapy is now standard practice in patients with metastatic NSCLC without targetable mutations.
Performance status guides treatment decision-making
Hospitalists can help oncologists in decision-making regarding whether to offer palliative systemic therapy to patients with advanced metastatic cancer and poor performance status by determining whether that status is caused by the cancer itself or some other cause that’s not easily reversible, such as liver failure.
Take, for example, the inpatient with advanced SCLC. This is an aggressive and chemosensitive cancer. Dr. Brondfield said he is among many medical oncologists who are convinced that, if poor performance status in a patient with advanced SCLC is caused by the cancer itself, prompt initiation of inpatient chemotherapy should be recommended to elicit a response that improves quality of life and performance status in the short term. If, on the other hand, the poor performance status is caused by organ failure or some other issue that can’t easily be improved, hospice may be more appropriate.
“The contour of SCLC over time is that despite its treatment responsiveness it inevitably recurs. But with chemotherapy you can give people in this situation months of quality time, so we generally try to treat these sorts of patients,” Dr. Brondfield explained.
The National Comprehensive Cancer Network guidelines upon which oncologists rely leave lots of room for interpretation regarding the appropriateness of inpatient chemotherapy in patients with advanced cancer and poor patient performance status. Citing “knowledge that’s been passed down across oncology generations,” Dr. Brondfield said he and many of his colleagues believe early palliative supportive care rather than systemic cytotoxic cancer-directed therapy is appropriate for patients with poor performance status who have one of several specific relatively nonchemoresponsive types of metastatic cancer. These include esophageal, gastric, and head and neck cancers.
On the other hand, advanced SCLC isn’t the only type of metastatic cancer that’s so chemosensitive that he and many other oncologists believe aggressive chemotherapy should be offered even in the face of poor patient performance status attributable to the cancer itself.
Take, for example, colorectal cancer with no more than five metastases to the lung or liver, provided those metastases are treatable with resection or radiation. “Those patients are actually curable at a high rate. They have about a 30%-40% cure rate. So those patients, even if they have poor performance status, if we can get them up for surgery or radiation, we usually do try to treat them aggressively,” Dr. Brondfield said.
There are other often chemoresponsive metastatic cancers for which oncologists frequently recommend aggressive treatment to improve quality of life in patients with poor performance status. These cancers include aggressive lymphomas, which are actually often curable; multiple myeloma; testicular and germ cell cancers; NSCLC with a targetable mutation, which is often responsive to oral medications; and prostate and well-differentiated thyroid cancers, which can usually be treated with hormone- or iodine-based therapies rather than more toxic intravenous cytotoxic chemotherapy.
The impact of inpatient palliative chemotherapy in patients with poor performance status and advanced solid cancers not on the short list of highly chemosensitive cancers has not been well studied. A recent retrospective study of 228 such patients who received inpatient palliative chemotherapy at a large Brazilian academic medical center provided little reason for enthusiasm regarding the practice. Survival was short, with 30- and 60-day survival rates of 56% and 39%, respectively. Plus, 30% of patients were admitted to the ICU, where they received aggressive and costly end-of-life care. The investigators found these results suggestive of overprescribing of inpatient palliative chemotherapy (BMC Palliat Care. 2019 May 20;18[1]:42. doi: 10.1186/s12904-019-0427-4).
Of note, the investigators found in a multivariate analysis that an elevated bilirubin was associated with a 217% increased risk of 30-day mortality, and hypercalcemia was associated with a 119% increased risk.
“That’s something to take into account when these decisions are being made,” Dr. Brondfield advised.
In response to an audience comment that oncologists often seem overly optimistic about prognosis, Dr. Brondfield observed, “I think it’s very common for there to be a disagreement between the oncologist wanting to be aggressive for a sick inpatient and the hospitalist or generalist provider thinking: ‘This person looks way too sick for chemotherapy.’ ”
For this reason he is a firm believer in having multidisciplinary conversations regarding prognosis in challenging situations involving hospitalized patients with advanced cancer. An oncologist can bring to such discussions a detailed understanding of clinical trial and molecular data as well as information about the patient’s response to the first round of therapy. But lots of other factors are relevant to prognosis, including nutritional status, comorbidities, and the intuitive eyeball test of how a patient might do. The patient’s family, primary care provider, oncologist, the hospitalist, and the palliative care team will have perspectives of their own.
Molecular testing is now the norm in metastatic cancers
These days oncologists order molecular testing for most patients with metastatic carcinomas to determine eligibility for targeted therapy, suitability for participation in clinical trials, prognostication, and/or assistance in determining the site of origin if that’s unclear.
A single-pass fine needle aspiration biopsy doesn’t provide enough tissue for molecular testing. It’s therefore important to order initially a multipass fine needle aspiration to avoid the need for a repeat biopsy, which is uncomfortable for the patient and can delay diagnosis and treatment.
Dr. Brondfield advised waiting for molecular testing results to come in before trying to prognosticate in patients with a metastatic cancer for which targetable mutations might be present. Survival rates can vary substantially depending upon those test results. Take, for example, metastatic NSCLC: Just within the past year, clinical trials have been published reporting overall survival rates of 39 months in patients with treatable mutations in epidermal growth factor receptor, 42 months with anaplastic lymphoma kinase mutations, and 51 months in patients whose tumor signature features mutations in c-ros oncogene 1, as compared with 22 months with no targetable mutations in the KEYNOTE-189 trial.
“There’s a lot of heterogeneity around how metastatic tumors behave and respond to therapy. Not all metastatic cancers are the same,” the oncologist emphasized.
FROM HM20 VIRTUAL
Incidence, prognosis of second lung cancers support long-term surveillance
Second lung cancers occurring up to a decade after the first are on the rise, but their prognosis is similar – especially when detected early – which supports long-term surveillance in survivors, finds a large population-based study.
Although guidelines recommend continued annual low-dose CT scan surveillance extending beyond 4 years for this population based on expert consensus, long-term evidence of benefit is lacking.
Investigators led by John M. Varlotto, MD, a radiation oncologist at the University of Massachusetts Medical Center, Worcester, analyzed Surveillance, Epidemiology & End Results (SEER) data for more than 58,000 patients with first and sometimes second non–small cell lung cancers initially treated by surgical resection.
Study results reported in Lung Cancer showed that the age-adjusted incidence of second lung cancers occurring 4-10 years after the first lung cancer rose sharply during the 1985-2014 study period, driven by a large uptick in women patients.
Among all patients, second lung cancers had similar overall survival as first lung cancers, but poorer lung cancer–specific survival. However, among the subset of patients having early-stage resectable disease (tumors measuring less than 4 cm with negative nodes), both outcomes were statistically indistinguishable.
“Because our investigation noted that the overall survival of patients undergoing a second lung cancer operation was similar to those patients undergoing a first operation, and because there is a rising rate of second lung cancer in lung cancer survivors, we feel that continued surveillance beyond the 4-year interval as recommended by the American Association for Thoracic Surgery as well as the [National Comprehensive Cancer Network] guidelines would be beneficial to long-term survivors of early-stage lung cancer,” Dr. Varlotto and coinvestigators wrote.
“The recent results from recent lung cancer screening studies demonstrate that females may benefit preferentially from screening … and our study suggests that these preferential benefits of increased CT scan surveillance may extend to females who are long-term survivors of lung cancer as well,” they added.
Findings in context
“As this is an observational study, it is challenging to understand what is driving the rise in prevalence of second lung cancers,” Mara Antonoff, MD, of The University of Texas MD Anderson Cancer Center in Houston commented in an interview.
“Overall, the findings are very important, as they suggest that we should continue to perform surveillance imaging for patients beyond recommended guidelines, which may allow us to achieve better survival outcomes for those individuals who develop a second lung cancer years after the first lung cancer,” she agreed.
“Just as lung cancer screening is important to identifying lung cancers at an earlier stage when they are more easily treatable and more likely to be cured, surveillance after an initial treatment for lung cancer would allow a diagnosis of second lung cancers at an earlier stage, so the patients can again achieve durable cure,” Dr. Antonoff concluded.
Study details
For the study, Dr. Varlotto and coinvestigators used data from SEER-13 and SEER-18 to identify patients with a lung cancer diagnosis during 1998-2013, and data from SEER-9, covering the years 1985-2014, to calculate rates of second cancers occurring 4-10 years after a first lung cancer.
Analyses were based on 58,758 patients with a surgically resected first primary lung cancer (55.9% with early-stage disease) and 384 patients with a surgically resected second primary lung cancer (77.6% with early-stage disease). Median follow-up was 76 months for the former and 46 months for the latter.
Results showed that in the 4-10 years after a first lung cancer diagnosis, the age-adjusted incidence of second lung cancers rose by study year but remained less than that of all other second cancers combined until the mid-2000s. Among women, incidence started rising sharply in 2001 and significantly exceeded that of all other second cancers starting in 2005.
In the entire population of study patients, propensity-adjusted analyses showed that second lung cancers were similar to first lung cancers on overall survival (P = .1726) but had worse lung cancer–specific survival (P = .0143). However, in the subset of patients with early-stage resectable disease, second and first lung cancers were similar on both overall survival (P = .3872) and lung cancer–specific survival (P = .1276).
Dr. Varlotto disclosed that he had no conflicts of interest. The study was funded by the Department of Radiation Oncology, University of Massachusetts. Dr. Antonoff disclosed that she had no relevant conflicts of interest.
SOURCE: Varlotto JM et al. Lung Cancer. 2020;147:115-122.
Second lung cancers occurring up to a decade after the first are on the rise, but their prognosis is similar – especially when detected early – which supports long-term surveillance in survivors, finds a large population-based study.
Although guidelines recommend continued annual low-dose CT scan surveillance extending beyond 4 years for this population based on expert consensus, long-term evidence of benefit is lacking.
Investigators led by John M. Varlotto, MD, a radiation oncologist at the University of Massachusetts Medical Center, Worcester, analyzed Surveillance, Epidemiology & End Results (SEER) data for more than 58,000 patients with first and sometimes second non–small cell lung cancers initially treated by surgical resection.
Study results reported in Lung Cancer showed that the age-adjusted incidence of second lung cancers occurring 4-10 years after the first lung cancer rose sharply during the 1985-2014 study period, driven by a large uptick in women patients.
Among all patients, second lung cancers had similar overall survival as first lung cancers, but poorer lung cancer–specific survival. However, among the subset of patients having early-stage resectable disease (tumors measuring less than 4 cm with negative nodes), both outcomes were statistically indistinguishable.
“Because our investigation noted that the overall survival of patients undergoing a second lung cancer operation was similar to those patients undergoing a first operation, and because there is a rising rate of second lung cancer in lung cancer survivors, we feel that continued surveillance beyond the 4-year interval as recommended by the American Association for Thoracic Surgery as well as the [National Comprehensive Cancer Network] guidelines would be beneficial to long-term survivors of early-stage lung cancer,” Dr. Varlotto and coinvestigators wrote.
“The recent results from recent lung cancer screening studies demonstrate that females may benefit preferentially from screening … and our study suggests that these preferential benefits of increased CT scan surveillance may extend to females who are long-term survivors of lung cancer as well,” they added.
Findings in context
“As this is an observational study, it is challenging to understand what is driving the rise in prevalence of second lung cancers,” Mara Antonoff, MD, of The University of Texas MD Anderson Cancer Center in Houston commented in an interview.
“Overall, the findings are very important, as they suggest that we should continue to perform surveillance imaging for patients beyond recommended guidelines, which may allow us to achieve better survival outcomes for those individuals who develop a second lung cancer years after the first lung cancer,” she agreed.
“Just as lung cancer screening is important to identifying lung cancers at an earlier stage when they are more easily treatable and more likely to be cured, surveillance after an initial treatment for lung cancer would allow a diagnosis of second lung cancers at an earlier stage, so the patients can again achieve durable cure,” Dr. Antonoff concluded.
Study details
For the study, Dr. Varlotto and coinvestigators used data from SEER-13 and SEER-18 to identify patients with a lung cancer diagnosis during 1998-2013, and data from SEER-9, covering the years 1985-2014, to calculate rates of second cancers occurring 4-10 years after a first lung cancer.
Analyses were based on 58,758 patients with a surgically resected first primary lung cancer (55.9% with early-stage disease) and 384 patients with a surgically resected second primary lung cancer (77.6% with early-stage disease). Median follow-up was 76 months for the former and 46 months for the latter.
Results showed that in the 4-10 years after a first lung cancer diagnosis, the age-adjusted incidence of second lung cancers rose by study year but remained less than that of all other second cancers combined until the mid-2000s. Among women, incidence started rising sharply in 2001 and significantly exceeded that of all other second cancers starting in 2005.
In the entire population of study patients, propensity-adjusted analyses showed that second lung cancers were similar to first lung cancers on overall survival (P = .1726) but had worse lung cancer–specific survival (P = .0143). However, in the subset of patients with early-stage resectable disease, second and first lung cancers were similar on both overall survival (P = .3872) and lung cancer–specific survival (P = .1276).
Dr. Varlotto disclosed that he had no conflicts of interest. The study was funded by the Department of Radiation Oncology, University of Massachusetts. Dr. Antonoff disclosed that she had no relevant conflicts of interest.
SOURCE: Varlotto JM et al. Lung Cancer. 2020;147:115-122.
Second lung cancers occurring up to a decade after the first are on the rise, but their prognosis is similar – especially when detected early – which supports long-term surveillance in survivors, finds a large population-based study.
Although guidelines recommend continued annual low-dose CT scan surveillance extending beyond 4 years for this population based on expert consensus, long-term evidence of benefit is lacking.
Investigators led by John M. Varlotto, MD, a radiation oncologist at the University of Massachusetts Medical Center, Worcester, analyzed Surveillance, Epidemiology & End Results (SEER) data for more than 58,000 patients with first and sometimes second non–small cell lung cancers initially treated by surgical resection.
Study results reported in Lung Cancer showed that the age-adjusted incidence of second lung cancers occurring 4-10 years after the first lung cancer rose sharply during the 1985-2014 study period, driven by a large uptick in women patients.
Among all patients, second lung cancers had similar overall survival as first lung cancers, but poorer lung cancer–specific survival. However, among the subset of patients having early-stage resectable disease (tumors measuring less than 4 cm with negative nodes), both outcomes were statistically indistinguishable.
“Because our investigation noted that the overall survival of patients undergoing a second lung cancer operation was similar to those patients undergoing a first operation, and because there is a rising rate of second lung cancer in lung cancer survivors, we feel that continued surveillance beyond the 4-year interval as recommended by the American Association for Thoracic Surgery as well as the [National Comprehensive Cancer Network] guidelines would be beneficial to long-term survivors of early-stage lung cancer,” Dr. Varlotto and coinvestigators wrote.
“The recent results from recent lung cancer screening studies demonstrate that females may benefit preferentially from screening … and our study suggests that these preferential benefits of increased CT scan surveillance may extend to females who are long-term survivors of lung cancer as well,” they added.
Findings in context
“As this is an observational study, it is challenging to understand what is driving the rise in prevalence of second lung cancers,” Mara Antonoff, MD, of The University of Texas MD Anderson Cancer Center in Houston commented in an interview.
“Overall, the findings are very important, as they suggest that we should continue to perform surveillance imaging for patients beyond recommended guidelines, which may allow us to achieve better survival outcomes for those individuals who develop a second lung cancer years after the first lung cancer,” she agreed.
“Just as lung cancer screening is important to identifying lung cancers at an earlier stage when they are more easily treatable and more likely to be cured, surveillance after an initial treatment for lung cancer would allow a diagnosis of second lung cancers at an earlier stage, so the patients can again achieve durable cure,” Dr. Antonoff concluded.
Study details
For the study, Dr. Varlotto and coinvestigators used data from SEER-13 and SEER-18 to identify patients with a lung cancer diagnosis during 1998-2013, and data from SEER-9, covering the years 1985-2014, to calculate rates of second cancers occurring 4-10 years after a first lung cancer.
Analyses were based on 58,758 patients with a surgically resected first primary lung cancer (55.9% with early-stage disease) and 384 patients with a surgically resected second primary lung cancer (77.6% with early-stage disease). Median follow-up was 76 months for the former and 46 months for the latter.
Results showed that in the 4-10 years after a first lung cancer diagnosis, the age-adjusted incidence of second lung cancers rose by study year but remained less than that of all other second cancers combined until the mid-2000s. Among women, incidence started rising sharply in 2001 and significantly exceeded that of all other second cancers starting in 2005.
In the entire population of study patients, propensity-adjusted analyses showed that second lung cancers were similar to first lung cancers on overall survival (P = .1726) but had worse lung cancer–specific survival (P = .0143). However, in the subset of patients with early-stage resectable disease, second and first lung cancers were similar on both overall survival (P = .3872) and lung cancer–specific survival (P = .1276).
Dr. Varlotto disclosed that he had no conflicts of interest. The study was funded by the Department of Radiation Oncology, University of Massachusetts. Dr. Antonoff disclosed that she had no relevant conflicts of interest.
SOURCE: Varlotto JM et al. Lung Cancer. 2020;147:115-122.
FROM LUNG CANCER
COVID-19 impact: Less chemo, immune checkpoint inhibitors, and steroids
While neoadjuvant treatment recommendations were not strongly affected by the pandemic, about half of oncologists reported increased hesitancy over recommending frontline chemotherapy for metastatic disease, and a vast majority said they would recommend second- or third-line chemotherapy less often in the metastatic setting.
Most oncologists said they did not perform routine COVID-19 testing via reverse transcriptase–polymerase chain reaction (RT-PCR) before treating cancer patients. In fact, only 3% said they performed COVID-19 RT-PCR testing routinely.
Yüksel Ürün, MD, of Ankara (Turkey) University, and colleagues reported these findings in JCO Global Oncology.
The goal of the survey was to “understand readiness measures taken by oncologists to protect patients and health care workers from the novel coronavirus (COVID-19) and how their clinical decision-making was influenced by the pandemic,” the authors wrote.
The online survey was conducted among 343 oncologists from 28 countries. Responses were collected anonymously, a majority (71%) from university or academic centers, with 95% received between April 1 and April 29, 2020.
Use of telemedicine was common (80%) among respondents, as was use of surgical masks (90%) and personal protective equipment in general.
Only 33% of respondents described using N95 masks. However, the proportion of oncologists who had access to N95 masks while caring for patients known to have COVID-19, especially while doing invasive procedures such as intubation, bronchoscopy, and any airway-related manipulations, was not captured by the survey.
COVID testing and cancer treatment
Most respondents (58%) said they did not perform routine COVID-19 RT-PCR testing prior to administering systemic cancer treatment, with 39% stating they performed RT-PCR tests in selected patients, and 3% saying they performed such testing in all patients.
The survey indicated that hormonal treatments, tyrosine kinase inhibitors, and bone-modifying agents were considered relatively safe, but cytotoxic chemotherapy and immune therapies were not.
Nearly all oncologists said the pandemic would cause them to make no change to their recommendations regarding hormone therapy, and nearly 80% said they would make no changes regarding tyrosine kinase inhibitors or bone-modifying agents.
However, more than 90% of respondents said they would recommend cytotoxic chemotherapy less often, about 70% said they would recommend corticosteroids less often, and around 50% said they would recommend anti–programmed death-1/PD-ligand 1 or anti–cytotoxic T-lymphocyte–associated protein 4 antibodies less often.
The pandemic made most respondents more reluctant to recommend second- or third-line chemotherapy in the metastatic setting. About 80% and 70% of respondents, respectively, would recommend second- or third-line chemotherapy less often.
However, first-line chemotherapy for metastatic disease, as well as adjuvant and neoadjuvant therapy, were less affected. About 30% of respondents said they would recommend neoadjuvant therapy less often, and 50%-55% would recommend adjuvant therapy or frontline chemotherapy for metastatic disease less often.
Most respondents (78%) said they would use granulocyte colony–stimulating factor (G-CSF) more frequently during the pandemic.
The factors most likely to affect oncologists’ treatment decisions were patient age (81%) and concomitant disease (92%). Additionally, 80% of respondents’ treatment decisions were influenced by Eastern Cooperative Oncology Group performance status of 2 or higher, or the presence of chronic obstructive pulmonary disease.
Interpretation and implications
“These results highlight that, even in the early phases of COVID-19 – during which there was considerable uncertainty – basic core principles were guideposts for oncologists,” observed Aly-Khan Lalani, MD, of Juravinski Cancer Centre and McMaster University, Hamilton, Ont., who was not involved in this study.
“For example, [oncologists were] prioritizing strategies for treatments with the largest expected impact and carefully tailoring treatment according to patient comorbidities and performance status,” Dr. Lalani said.
Another oncologist who was not involved in the study expressed concern over reductions in adjuvant therapy supported by half of oncologists surveyed.
“Although benefits may be marginal in some cases, these are curative settings and especially warrant careful individual-level risk/benefit discussions,” said Kartik Sehgal, MD, of Dana-Farber Cancer Institute/Brigham and Women’s Hospital in Boston.
His concern extended as well to the small proportion (3%) of oncologists testing for COVID-19 in all patients. “Systematic testing is the need of the hour,” Dr. Sehgal said.
In their discussion of the findings, Dr. Ürün and colleagues noted a lack of consensus on monoclonal antibody and immunotherapy safety among surveyed oncologists. The steroids needed to manage severe immune-mediated toxicity with immune checkpoint inhibitors has led to some prescribing reluctance during the pandemic.
Immunosuppressive properties of immune checkpoint inhibitors also raise concern that they can increase COVID-19 severity. Studies are few, and findings to date are inconsistent with respect to the effect of immune checkpoint inhibitors on COVID-19 clinical course. However, a recently presented study suggested that immune checkpoint inhibitors do not increase the risk of death among cancer patients with COVID-19 (AACR: COVID-19 and Cancer, Abstract S02-01).
Dr. Ürün and colleagues noted that greater COVID-19 severity has been shown in patients with performance status greater than 1, hematologic malignancies, lung cancer, stage IV metastatic disease, chemotherapy within the prior 3 months, cancer treatment in the last 14 days, and the presence of chronic obstructive pulmonary disease. Nonmetastatic cancer has not been shown to affect COVID-19 severity, however.
Dr. Ürün and colleagues also underscored the need for research evidence to balance potential reductions in neutropenic complications with G-CSF (and therefore, reduced hospitalizations) with a theoretical risk of G-CSF–mediated pulmonary injury through its stimulation of an excessive immune response.
Finally, the authors urged oncologists to evaluate each proposed therapy’s risk/benefit ratio on an individual patient basis, and the team tasked the oncology community with gathering comprehensive, rigorous data.
There was no funding source declared for this study. Dr. Ürün and colleagues disclosed various relationships with many pharmaceutical companies, which included receiving research funding. Dr. Sehgal and Dr. Lalani reported no relevant conflicts.
SOURCE: Ürün Y et al. JCO Glob Oncol. 2020 Aug;6:1248-57.
While neoadjuvant treatment recommendations were not strongly affected by the pandemic, about half of oncologists reported increased hesitancy over recommending frontline chemotherapy for metastatic disease, and a vast majority said they would recommend second- or third-line chemotherapy less often in the metastatic setting.
Most oncologists said they did not perform routine COVID-19 testing via reverse transcriptase–polymerase chain reaction (RT-PCR) before treating cancer patients. In fact, only 3% said they performed COVID-19 RT-PCR testing routinely.
Yüksel Ürün, MD, of Ankara (Turkey) University, and colleagues reported these findings in JCO Global Oncology.
The goal of the survey was to “understand readiness measures taken by oncologists to protect patients and health care workers from the novel coronavirus (COVID-19) and how their clinical decision-making was influenced by the pandemic,” the authors wrote.
The online survey was conducted among 343 oncologists from 28 countries. Responses were collected anonymously, a majority (71%) from university or academic centers, with 95% received between April 1 and April 29, 2020.
Use of telemedicine was common (80%) among respondents, as was use of surgical masks (90%) and personal protective equipment in general.
Only 33% of respondents described using N95 masks. However, the proportion of oncologists who had access to N95 masks while caring for patients known to have COVID-19, especially while doing invasive procedures such as intubation, bronchoscopy, and any airway-related manipulations, was not captured by the survey.
COVID testing and cancer treatment
Most respondents (58%) said they did not perform routine COVID-19 RT-PCR testing prior to administering systemic cancer treatment, with 39% stating they performed RT-PCR tests in selected patients, and 3% saying they performed such testing in all patients.
The survey indicated that hormonal treatments, tyrosine kinase inhibitors, and bone-modifying agents were considered relatively safe, but cytotoxic chemotherapy and immune therapies were not.
Nearly all oncologists said the pandemic would cause them to make no change to their recommendations regarding hormone therapy, and nearly 80% said they would make no changes regarding tyrosine kinase inhibitors or bone-modifying agents.
However, more than 90% of respondents said they would recommend cytotoxic chemotherapy less often, about 70% said they would recommend corticosteroids less often, and around 50% said they would recommend anti–programmed death-1/PD-ligand 1 or anti–cytotoxic T-lymphocyte–associated protein 4 antibodies less often.
The pandemic made most respondents more reluctant to recommend second- or third-line chemotherapy in the metastatic setting. About 80% and 70% of respondents, respectively, would recommend second- or third-line chemotherapy less often.
However, first-line chemotherapy for metastatic disease, as well as adjuvant and neoadjuvant therapy, were less affected. About 30% of respondents said they would recommend neoadjuvant therapy less often, and 50%-55% would recommend adjuvant therapy or frontline chemotherapy for metastatic disease less often.
Most respondents (78%) said they would use granulocyte colony–stimulating factor (G-CSF) more frequently during the pandemic.
The factors most likely to affect oncologists’ treatment decisions were patient age (81%) and concomitant disease (92%). Additionally, 80% of respondents’ treatment decisions were influenced by Eastern Cooperative Oncology Group performance status of 2 or higher, or the presence of chronic obstructive pulmonary disease.
Interpretation and implications
“These results highlight that, even in the early phases of COVID-19 – during which there was considerable uncertainty – basic core principles were guideposts for oncologists,” observed Aly-Khan Lalani, MD, of Juravinski Cancer Centre and McMaster University, Hamilton, Ont., who was not involved in this study.
“For example, [oncologists were] prioritizing strategies for treatments with the largest expected impact and carefully tailoring treatment according to patient comorbidities and performance status,” Dr. Lalani said.
Another oncologist who was not involved in the study expressed concern over reductions in adjuvant therapy supported by half of oncologists surveyed.
“Although benefits may be marginal in some cases, these are curative settings and especially warrant careful individual-level risk/benefit discussions,” said Kartik Sehgal, MD, of Dana-Farber Cancer Institute/Brigham and Women’s Hospital in Boston.
His concern extended as well to the small proportion (3%) of oncologists testing for COVID-19 in all patients. “Systematic testing is the need of the hour,” Dr. Sehgal said.
In their discussion of the findings, Dr. Ürün and colleagues noted a lack of consensus on monoclonal antibody and immunotherapy safety among surveyed oncologists. The steroids needed to manage severe immune-mediated toxicity with immune checkpoint inhibitors has led to some prescribing reluctance during the pandemic.
Immunosuppressive properties of immune checkpoint inhibitors also raise concern that they can increase COVID-19 severity. Studies are few, and findings to date are inconsistent with respect to the effect of immune checkpoint inhibitors on COVID-19 clinical course. However, a recently presented study suggested that immune checkpoint inhibitors do not increase the risk of death among cancer patients with COVID-19 (AACR: COVID-19 and Cancer, Abstract S02-01).
Dr. Ürün and colleagues noted that greater COVID-19 severity has been shown in patients with performance status greater than 1, hematologic malignancies, lung cancer, stage IV metastatic disease, chemotherapy within the prior 3 months, cancer treatment in the last 14 days, and the presence of chronic obstructive pulmonary disease. Nonmetastatic cancer has not been shown to affect COVID-19 severity, however.
Dr. Ürün and colleagues also underscored the need for research evidence to balance potential reductions in neutropenic complications with G-CSF (and therefore, reduced hospitalizations) with a theoretical risk of G-CSF–mediated pulmonary injury through its stimulation of an excessive immune response.
Finally, the authors urged oncologists to evaluate each proposed therapy’s risk/benefit ratio on an individual patient basis, and the team tasked the oncology community with gathering comprehensive, rigorous data.
There was no funding source declared for this study. Dr. Ürün and colleagues disclosed various relationships with many pharmaceutical companies, which included receiving research funding. Dr. Sehgal and Dr. Lalani reported no relevant conflicts.
SOURCE: Ürün Y et al. JCO Glob Oncol. 2020 Aug;6:1248-57.
While neoadjuvant treatment recommendations were not strongly affected by the pandemic, about half of oncologists reported increased hesitancy over recommending frontline chemotherapy for metastatic disease, and a vast majority said they would recommend second- or third-line chemotherapy less often in the metastatic setting.
Most oncologists said they did not perform routine COVID-19 testing via reverse transcriptase–polymerase chain reaction (RT-PCR) before treating cancer patients. In fact, only 3% said they performed COVID-19 RT-PCR testing routinely.
Yüksel Ürün, MD, of Ankara (Turkey) University, and colleagues reported these findings in JCO Global Oncology.
The goal of the survey was to “understand readiness measures taken by oncologists to protect patients and health care workers from the novel coronavirus (COVID-19) and how their clinical decision-making was influenced by the pandemic,” the authors wrote.
The online survey was conducted among 343 oncologists from 28 countries. Responses were collected anonymously, a majority (71%) from university or academic centers, with 95% received between April 1 and April 29, 2020.
Use of telemedicine was common (80%) among respondents, as was use of surgical masks (90%) and personal protective equipment in general.
Only 33% of respondents described using N95 masks. However, the proportion of oncologists who had access to N95 masks while caring for patients known to have COVID-19, especially while doing invasive procedures such as intubation, bronchoscopy, and any airway-related manipulations, was not captured by the survey.
COVID testing and cancer treatment
Most respondents (58%) said they did not perform routine COVID-19 RT-PCR testing prior to administering systemic cancer treatment, with 39% stating they performed RT-PCR tests in selected patients, and 3% saying they performed such testing in all patients.
The survey indicated that hormonal treatments, tyrosine kinase inhibitors, and bone-modifying agents were considered relatively safe, but cytotoxic chemotherapy and immune therapies were not.
Nearly all oncologists said the pandemic would cause them to make no change to their recommendations regarding hormone therapy, and nearly 80% said they would make no changes regarding tyrosine kinase inhibitors or bone-modifying agents.
However, more than 90% of respondents said they would recommend cytotoxic chemotherapy less often, about 70% said they would recommend corticosteroids less often, and around 50% said they would recommend anti–programmed death-1/PD-ligand 1 or anti–cytotoxic T-lymphocyte–associated protein 4 antibodies less often.
The pandemic made most respondents more reluctant to recommend second- or third-line chemotherapy in the metastatic setting. About 80% and 70% of respondents, respectively, would recommend second- or third-line chemotherapy less often.
However, first-line chemotherapy for metastatic disease, as well as adjuvant and neoadjuvant therapy, were less affected. About 30% of respondents said they would recommend neoadjuvant therapy less often, and 50%-55% would recommend adjuvant therapy or frontline chemotherapy for metastatic disease less often.
Most respondents (78%) said they would use granulocyte colony–stimulating factor (G-CSF) more frequently during the pandemic.
The factors most likely to affect oncologists’ treatment decisions were patient age (81%) and concomitant disease (92%). Additionally, 80% of respondents’ treatment decisions were influenced by Eastern Cooperative Oncology Group performance status of 2 or higher, or the presence of chronic obstructive pulmonary disease.
Interpretation and implications
“These results highlight that, even in the early phases of COVID-19 – during which there was considerable uncertainty – basic core principles were guideposts for oncologists,” observed Aly-Khan Lalani, MD, of Juravinski Cancer Centre and McMaster University, Hamilton, Ont., who was not involved in this study.
“For example, [oncologists were] prioritizing strategies for treatments with the largest expected impact and carefully tailoring treatment according to patient comorbidities and performance status,” Dr. Lalani said.
Another oncologist who was not involved in the study expressed concern over reductions in adjuvant therapy supported by half of oncologists surveyed.
“Although benefits may be marginal in some cases, these are curative settings and especially warrant careful individual-level risk/benefit discussions,” said Kartik Sehgal, MD, of Dana-Farber Cancer Institute/Brigham and Women’s Hospital in Boston.
His concern extended as well to the small proportion (3%) of oncologists testing for COVID-19 in all patients. “Systematic testing is the need of the hour,” Dr. Sehgal said.
In their discussion of the findings, Dr. Ürün and colleagues noted a lack of consensus on monoclonal antibody and immunotherapy safety among surveyed oncologists. The steroids needed to manage severe immune-mediated toxicity with immune checkpoint inhibitors has led to some prescribing reluctance during the pandemic.
Immunosuppressive properties of immune checkpoint inhibitors also raise concern that they can increase COVID-19 severity. Studies are few, and findings to date are inconsistent with respect to the effect of immune checkpoint inhibitors on COVID-19 clinical course. However, a recently presented study suggested that immune checkpoint inhibitors do not increase the risk of death among cancer patients with COVID-19 (AACR: COVID-19 and Cancer, Abstract S02-01).
Dr. Ürün and colleagues noted that greater COVID-19 severity has been shown in patients with performance status greater than 1, hematologic malignancies, lung cancer, stage IV metastatic disease, chemotherapy within the prior 3 months, cancer treatment in the last 14 days, and the presence of chronic obstructive pulmonary disease. Nonmetastatic cancer has not been shown to affect COVID-19 severity, however.
Dr. Ürün and colleagues also underscored the need for research evidence to balance potential reductions in neutropenic complications with G-CSF (and therefore, reduced hospitalizations) with a theoretical risk of G-CSF–mediated pulmonary injury through its stimulation of an excessive immune response.
Finally, the authors urged oncologists to evaluate each proposed therapy’s risk/benefit ratio on an individual patient basis, and the team tasked the oncology community with gathering comprehensive, rigorous data.
There was no funding source declared for this study. Dr. Ürün and colleagues disclosed various relationships with many pharmaceutical companies, which included receiving research funding. Dr. Sehgal and Dr. Lalani reported no relevant conflicts.
SOURCE: Ürün Y et al. JCO Glob Oncol. 2020 Aug;6:1248-57.
FROM JCO GLOBAL ONCOLOGY
NSCLC success story: Mortality down, survival improved
“This analysis shows for the first time that nationwide mortality rates for the most common category of lung cancer, NSCLC, are declining faster than its incidence, an advance that correlates with the [FDA] approval of several targeted therapies for this cancer in recent years,” coauthor Douglas Lowy, MD, deputy director, National Cancer Institute, Bethesda, Md., said in a statement.
“Major improvements have been made in NSCLC treatment with the advent of targeted therapies and immunotherapies,” lead author Nadia Howlander, PhD, National Cancer Institute, and colleagues observed.
“The survival benefit for patients with NSCLC treated with targeted therapy has been shown in clinical trials, but our study highlights their possible effect at the population level,” they added.
In contrast, mortality from SCLC has dropped only in tandem with a decline in the incidence of SCLC, and survival has remained largely unchanged, the same analysis showed.
NSCLC is by far the most common type of lung cancer, accounting for more than 75% of all lung cancer cases in the United States. SCLC accounts for about 13%.
The study was published online Aug. 12 in the New England Journal of Medicine.
“Although overall mortality from lung cancer has been declining in the United States, little is known about mortality trends according to cancer subtype at the population level because death certificates do not record subtype information,” the authors commented.
“To address this data limitation, the U.S. Surveillance, Epidemiology and End Results (SEER) program has linked mortality records to incidence cancer cases,” the authors explained. This allowed them to calculate incidence-based mortality among men and women in the United States.
The incidence-based mortality method that the researchers used was applied to the SEER data to describe population-level mortality trends in the United States that were attributable to each subtype of lung cancer as well as gender from 2001 to 2016.
Among men, the incidence of NSCLC decreased gradually by 1.9% a year from 2001 to 2008, then more dramatically by 3.1% a year from 2008 to 2016.
Corresponding incidence-based mortality rates among men dropped by 3.2% a year from 2006 to 2013, then again more dramatically by 6.3% a year from 2013 to 2016.
“The 2-year relative survival among patients with lung cancer improved substantially from 26% among men with NSCLC diagnosed in 2001 to 35% among those with NSCLC diagnosed in 2014,” the researchers added.
Among women, the incidence of NSCLC remained unchanged between 2001 and 2006, after which it began to drop by 1.5% a year from 2006 to 2016.
“In contrast, incidence-based mortality decreased slowly [among women] by 2.3% annually ... from 2006 through 2014 and then at a faster rate of 5.9% annually ... from 2014 through 2016,” the authors noted.
The 2-year relative survival rate for patients with NSCLC was higher among women than among men, improving from 35% in 2001 to 44% in 2014.
Improvements in survival were also observed for all races and ethnicities, despite concerns that new cancer treatments might increase treatment disparities between races, because they are all so expensive, the authors commented.
Mortality from SCLC declined by 4.3% a year among men, but that decline was entirely due to a similar decrease in the incidence of SCLC. Survival at 2 years for patients with this subtype of lung cancer remained largely unchanged over the same interval.
Genetic testing
The accelerating decline in NSCLC mortality starting in 2013 corresponds to the period in which clinicians began to routinely test for molecular alterations in epidermal growth factor receptor (EGFR) and anaplastic lymphoma kinase (ALK), the authors pointed out.
In 2012, the National Comprehensive Cancer Network recommended that all patients with nonsquamous NSCLC undergo genetic testing for EGFR mutations and ALK rearrangements.
At about the same time, the FDA approved a number of targeted therapies for tumors that are sensitive to targeted tyrosine kinase inhibition.
More recently, immunotherapies that act as programmed cell death inhibitors have substantially improved NSCLC outcomes, the authors noted.
The first of these was approved for NSCLC in 2015 (pembrolizumab). It was followed by a number of similar agents. It is unlikely that their approval contributed to the observed decline in NSCLC mortality, which started to accelerate in 2013 in the United States, the authors commented.
Nevertheless, the effect that the immune checkpoint inhibitors has had on the survival of patients with NSCLC can be expected to continue and to extend improvement in survival beyond the current study endpoint in 2016, they suggest.
Another contributing factor is the decline in smoking that has occurred in the United States since the 1960s. This has led to the decrease in the incidence of lung cancer. The faster decrease in the incidence of SCLC, compared with NSCLC can be explained by the higher relative risk of smoking with regard to SCLC compared to NSCLC, they commented.
Similarly, the faster decrease in lung cancer incidence in men compared to women can be explained by the relative difference in the prevalence of smoking between men and women, they added.
The authors disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
“This analysis shows for the first time that nationwide mortality rates for the most common category of lung cancer, NSCLC, are declining faster than its incidence, an advance that correlates with the [FDA] approval of several targeted therapies for this cancer in recent years,” coauthor Douglas Lowy, MD, deputy director, National Cancer Institute, Bethesda, Md., said in a statement.
“Major improvements have been made in NSCLC treatment with the advent of targeted therapies and immunotherapies,” lead author Nadia Howlander, PhD, National Cancer Institute, and colleagues observed.
“The survival benefit for patients with NSCLC treated with targeted therapy has been shown in clinical trials, but our study highlights their possible effect at the population level,” they added.
In contrast, mortality from SCLC has dropped only in tandem with a decline in the incidence of SCLC, and survival has remained largely unchanged, the same analysis showed.
NSCLC is by far the most common type of lung cancer, accounting for more than 75% of all lung cancer cases in the United States. SCLC accounts for about 13%.
The study was published online Aug. 12 in the New England Journal of Medicine.
“Although overall mortality from lung cancer has been declining in the United States, little is known about mortality trends according to cancer subtype at the population level because death certificates do not record subtype information,” the authors commented.
“To address this data limitation, the U.S. Surveillance, Epidemiology and End Results (SEER) program has linked mortality records to incidence cancer cases,” the authors explained. This allowed them to calculate incidence-based mortality among men and women in the United States.
The incidence-based mortality method that the researchers used was applied to the SEER data to describe population-level mortality trends in the United States that were attributable to each subtype of lung cancer as well as gender from 2001 to 2016.
Among men, the incidence of NSCLC decreased gradually by 1.9% a year from 2001 to 2008, then more dramatically by 3.1% a year from 2008 to 2016.
Corresponding incidence-based mortality rates among men dropped by 3.2% a year from 2006 to 2013, then again more dramatically by 6.3% a year from 2013 to 2016.
“The 2-year relative survival among patients with lung cancer improved substantially from 26% among men with NSCLC diagnosed in 2001 to 35% among those with NSCLC diagnosed in 2014,” the researchers added.
Among women, the incidence of NSCLC remained unchanged between 2001 and 2006, after which it began to drop by 1.5% a year from 2006 to 2016.
“In contrast, incidence-based mortality decreased slowly [among women] by 2.3% annually ... from 2006 through 2014 and then at a faster rate of 5.9% annually ... from 2014 through 2016,” the authors noted.
The 2-year relative survival rate for patients with NSCLC was higher among women than among men, improving from 35% in 2001 to 44% in 2014.
Improvements in survival were also observed for all races and ethnicities, despite concerns that new cancer treatments might increase treatment disparities between races, because they are all so expensive, the authors commented.
Mortality from SCLC declined by 4.3% a year among men, but that decline was entirely due to a similar decrease in the incidence of SCLC. Survival at 2 years for patients with this subtype of lung cancer remained largely unchanged over the same interval.
Genetic testing
The accelerating decline in NSCLC mortality starting in 2013 corresponds to the period in which clinicians began to routinely test for molecular alterations in epidermal growth factor receptor (EGFR) and anaplastic lymphoma kinase (ALK), the authors pointed out.
In 2012, the National Comprehensive Cancer Network recommended that all patients with nonsquamous NSCLC undergo genetic testing for EGFR mutations and ALK rearrangements.
At about the same time, the FDA approved a number of targeted therapies for tumors that are sensitive to targeted tyrosine kinase inhibition.
More recently, immunotherapies that act as programmed cell death inhibitors have substantially improved NSCLC outcomes, the authors noted.
The first of these was approved for NSCLC in 2015 (pembrolizumab). It was followed by a number of similar agents. It is unlikely that their approval contributed to the observed decline in NSCLC mortality, which started to accelerate in 2013 in the United States, the authors commented.
Nevertheless, the effect that the immune checkpoint inhibitors has had on the survival of patients with NSCLC can be expected to continue and to extend improvement in survival beyond the current study endpoint in 2016, they suggest.
Another contributing factor is the decline in smoking that has occurred in the United States since the 1960s. This has led to the decrease in the incidence of lung cancer. The faster decrease in the incidence of SCLC, compared with NSCLC can be explained by the higher relative risk of smoking with regard to SCLC compared to NSCLC, they commented.
Similarly, the faster decrease in lung cancer incidence in men compared to women can be explained by the relative difference in the prevalence of smoking between men and women, they added.
The authors disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
“This analysis shows for the first time that nationwide mortality rates for the most common category of lung cancer, NSCLC, are declining faster than its incidence, an advance that correlates with the [FDA] approval of several targeted therapies for this cancer in recent years,” coauthor Douglas Lowy, MD, deputy director, National Cancer Institute, Bethesda, Md., said in a statement.
“Major improvements have been made in NSCLC treatment with the advent of targeted therapies and immunotherapies,” lead author Nadia Howlander, PhD, National Cancer Institute, and colleagues observed.
“The survival benefit for patients with NSCLC treated with targeted therapy has been shown in clinical trials, but our study highlights their possible effect at the population level,” they added.
In contrast, mortality from SCLC has dropped only in tandem with a decline in the incidence of SCLC, and survival has remained largely unchanged, the same analysis showed.
NSCLC is by far the most common type of lung cancer, accounting for more than 75% of all lung cancer cases in the United States. SCLC accounts for about 13%.
The study was published online Aug. 12 in the New England Journal of Medicine.
“Although overall mortality from lung cancer has been declining in the United States, little is known about mortality trends according to cancer subtype at the population level because death certificates do not record subtype information,” the authors commented.
“To address this data limitation, the U.S. Surveillance, Epidemiology and End Results (SEER) program has linked mortality records to incidence cancer cases,” the authors explained. This allowed them to calculate incidence-based mortality among men and women in the United States.
The incidence-based mortality method that the researchers used was applied to the SEER data to describe population-level mortality trends in the United States that were attributable to each subtype of lung cancer as well as gender from 2001 to 2016.
Among men, the incidence of NSCLC decreased gradually by 1.9% a year from 2001 to 2008, then more dramatically by 3.1% a year from 2008 to 2016.
Corresponding incidence-based mortality rates among men dropped by 3.2% a year from 2006 to 2013, then again more dramatically by 6.3% a year from 2013 to 2016.
“The 2-year relative survival among patients with lung cancer improved substantially from 26% among men with NSCLC diagnosed in 2001 to 35% among those with NSCLC diagnosed in 2014,” the researchers added.
Among women, the incidence of NSCLC remained unchanged between 2001 and 2006, after which it began to drop by 1.5% a year from 2006 to 2016.
“In contrast, incidence-based mortality decreased slowly [among women] by 2.3% annually ... from 2006 through 2014 and then at a faster rate of 5.9% annually ... from 2014 through 2016,” the authors noted.
The 2-year relative survival rate for patients with NSCLC was higher among women than among men, improving from 35% in 2001 to 44% in 2014.
Improvements in survival were also observed for all races and ethnicities, despite concerns that new cancer treatments might increase treatment disparities between races, because they are all so expensive, the authors commented.
Mortality from SCLC declined by 4.3% a year among men, but that decline was entirely due to a similar decrease in the incidence of SCLC. Survival at 2 years for patients with this subtype of lung cancer remained largely unchanged over the same interval.
Genetic testing
The accelerating decline in NSCLC mortality starting in 2013 corresponds to the period in which clinicians began to routinely test for molecular alterations in epidermal growth factor receptor (EGFR) and anaplastic lymphoma kinase (ALK), the authors pointed out.
In 2012, the National Comprehensive Cancer Network recommended that all patients with nonsquamous NSCLC undergo genetic testing for EGFR mutations and ALK rearrangements.
At about the same time, the FDA approved a number of targeted therapies for tumors that are sensitive to targeted tyrosine kinase inhibition.
More recently, immunotherapies that act as programmed cell death inhibitors have substantially improved NSCLC outcomes, the authors noted.
The first of these was approved for NSCLC in 2015 (pembrolizumab). It was followed by a number of similar agents. It is unlikely that their approval contributed to the observed decline in NSCLC mortality, which started to accelerate in 2013 in the United States, the authors commented.
Nevertheless, the effect that the immune checkpoint inhibitors has had on the survival of patients with NSCLC can be expected to continue and to extend improvement in survival beyond the current study endpoint in 2016, they suggest.
Another contributing factor is the decline in smoking that has occurred in the United States since the 1960s. This has led to the decrease in the incidence of lung cancer. The faster decrease in the incidence of SCLC, compared with NSCLC can be explained by the higher relative risk of smoking with regard to SCLC compared to NSCLC, they commented.
Similarly, the faster decrease in lung cancer incidence in men compared to women can be explained by the relative difference in the prevalence of smoking between men and women, they added.
The authors disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Sintilimab scintillates in first-line nonsquamous NSCLC
The investigational anti-PD-1 antibody sintilimab (Tyvyt, Innovent Biologics and Eli Lilly) has shown that it improves the efficacy of platinum-based chemotherapy in the first-line treatment of patients with advanced nonsquamous non–small cell lung cancer (NSCLC) in a phase 3 trial dubbed ORIENT-11.
The study was presented at the World Congress on Lung Cancer 2020 Virtual Presidential Symposium, held virtually due to the COVID-19 pandemic, on August 8. It was also published simultaneously in the Journal of Thoracic Oncology.
Sintilimab is a fully human IgG4 monoclonal antibody that blocks the binding of programmed death (PD)-1 to PD-ligand 1 (PD-L1) or PD-L2 with high affinity, and has received market authorization in China for the treatment of Hodgkin lymphoma.
For ORIENT-11, almost 400 patients with advanced nonsquamous NSCLC were randomly assigned to sintilimab or placebo plus pemetrexed and platinum-based chemotherapy in a 2:1 ratio.
“The addition of sintilimab to pemetrexed and platinum significantly improved PFS [progression-free survival], compared to placebo,” reducing progression rates by 52%, noted lead investigator Li Zhang, MD, professor of medical oncology, Sun Yat-Sen University Cancer Center, Guangzhou, China.
Crucially, this benefit “was seen across key clinical subgroups,” he added.
He noted that the overall response rate “was also improved, with a durable response,” while the results, which are not yet mature, suggest the experimental arm was associated with an overall survival (OS) benefit.
Study discussant Misako Nagasaka, MD, a thoracic oncologist and clinical investigator at Karmanos Cancer Institute, Detroit, said that the PFS benefit seen in the study is “certainly encouraging.”
Adding a note of caution, she continued: “But we have seen studies with PFS improvement which did not translate into OS improvement.
“Longer follow-up would allow events to mature and we will ultimately see if there would be a significant OS benefit,” she said.
Dr. Nagasaka also pointed out that the greater benefit with sintilimab seen in patients with high PD-L1 begs the question as to what would be the preferred regimen in those with higher or lower expression.
And, she said, this is not just about what regimen to choose but “more importantly, why?”
“Perhaps you’d like to use something with the best response rate, perhaps you’re sticking to a single agent immunotherapy because the toxicity profile is more favorable, or perhaps you [are] convinced with a certain regimen because of the robust PFS and OS data,” she said.
“Whatever you chose, there was a reason for your choice,” she said, adding that the sintilimab combination would have to “fulfill those reasons for you to consider choosing this regimen.”
Study details
Dr. Zhang began his presentation by noting that previous phase 1b studies have shown that sintilimab plus pemetrexed and platinum-based chemotherapy has a “tolerable safety profile and promising efficacy” in previously untreated non-squamous NSCLC.
They therefore conducted ORIENT-11, a randomized, double-blind, phase 3 study involving 397 patients with untreated stage IIIB/C or IV nonsquamous NSCLC who had neither EGFR nor ALK gene alterations.
The patients were randomly assigned in a 2:1 fashion to sintilimab plus pemetrexed and platinum-based chemotherapy (n = 266) or placebo plus pemetrexed and chemo (n = 131) for four cycles, followed by sintilimab or placebo plus pemetrexed for up to 24 months.
Thirty-five patients in the placebo arm crossed over to sintilimab monotherapy, representing 31.3% of the intention-to-treat population.
At the data cutoff of Nov. 15, 2019, 198 events had occurred, at a median follow-up of 8.9 months.
The team found that median PFS was significantly higher with sintilimab than placebo combination therapy, at 8.9 months vs. 5.0 months, or a hazard ratio of 0.482 (P < .00001).
Dr. Zhang noted that the benefit with sintilimab plus pemetrexed and platinum-based chemotherapy was seen across all subgroups.
However, it was notable that the impact of adding sintilimab on PFS was greater in patients with a tumor proportion score (TPS) ≥50%.
The HR for progression vs. the placebo treatment arm was 0.310, with median PFS not reached, which decreased to 0.503 in patients with a TPS of 1%-49% and 0.664 among those with a TPS <1%.
The results also showed that there was a “nominally significant improvement” in overall survival with sintilimab versus placebo, at a HR of 0.609 (P = 0.01921).
The ORR was markedly different between the sintilimab and placebo groups, at 51.9% vs. 29.8%, with the duration of response not reached in the sintilimab arm compared with 5.5 months in the placebo arm.
The sintilimab arm included three (1.1%) complete responses, which was not observed with pemetrexed and platinum-based chemotherapy alone.
Finally, Dr. Zhang observed that the safety profiles of the sintilimab and placebo arms were similar, with comparable rates of any, grade 3-5, and serious adverse events largely driven by high rates of chemotherapy-related events.
While there were fewer adverse events that led to death with sintilimab, at 2.3% vs. 6.9% with placebo, there were, as expected, more immune-related adverse events, at 43.2% vs. 36.6%, respectively.
Comparison with pembrolizumab
In her discussion, Dr. Nagasaka said that the first question that came to mind when she saw the results was: “How does the ORIENT-11 data compare with KEYNOTE-189?”
For that study, pembrolizumab (Keytruda, Merck) was added to pemetrexed plus carboplatin chemotherapy and compared with standard of care alone in patients with untreated metastatic nonsquamous NSCLC.
As reported by Medscape Medical News, pembrolizumab was associated with a 48% reduced risk of disease progression, as well as improved overall survival.
Dr. Nagasaka said that ORIENT-11 “had patients that tended to be younger, there were more males, more with performance status 1, and those who had never smoked” than those in KEYNOTE-189.
“But most importantly, KEYNOTE-189 had a very small number of patients from East Asia, only 1% in the pembro arm and 2.9% in the placebo arm.”
In contrast, all the patients included in ORIENT-11 were from East Asia, making the study of “high importance.”
She added that, “while across-trial comparisons must be taken with caution, the medium PFS of ORIENT-11 ... appears comparable to those of KEYNOTE-189,” while the HR “appears identical.”
This is despite median follow-up time in ORIENT-11 of “only” 8.9 months vs. a median of 23.1 months in the updated KEYNOTE-189 data.
There are plans to register the sintilimab combination therapy in China for the treatment of nonsquamous NSCLC, where it will go up against pembrolizumab as well as, potentially, tislelizumab (BeiGene).
The study was sponsored by Innovent Biologics and Eli Lilly. Dr. Zhang disclosed research grants from Eli Lilly and Pfizer. Dr. Nagasaka disclosed serving on the advisory boards of AstraZeneca, Daiichi Sankyo, Takeda, Novartis, and EMD Serono; as a consultant for Caris Life Sciences; and receiving travel support from An Hearts Therapeutics.
This article first appeared on Medscape.com.
The investigational anti-PD-1 antibody sintilimab (Tyvyt, Innovent Biologics and Eli Lilly) has shown that it improves the efficacy of platinum-based chemotherapy in the first-line treatment of patients with advanced nonsquamous non–small cell lung cancer (NSCLC) in a phase 3 trial dubbed ORIENT-11.
The study was presented at the World Congress on Lung Cancer 2020 Virtual Presidential Symposium, held virtually due to the COVID-19 pandemic, on August 8. It was also published simultaneously in the Journal of Thoracic Oncology.
Sintilimab is a fully human IgG4 monoclonal antibody that blocks the binding of programmed death (PD)-1 to PD-ligand 1 (PD-L1) or PD-L2 with high affinity, and has received market authorization in China for the treatment of Hodgkin lymphoma.
For ORIENT-11, almost 400 patients with advanced nonsquamous NSCLC were randomly assigned to sintilimab or placebo plus pemetrexed and platinum-based chemotherapy in a 2:1 ratio.
“The addition of sintilimab to pemetrexed and platinum significantly improved PFS [progression-free survival], compared to placebo,” reducing progression rates by 52%, noted lead investigator Li Zhang, MD, professor of medical oncology, Sun Yat-Sen University Cancer Center, Guangzhou, China.
Crucially, this benefit “was seen across key clinical subgroups,” he added.
He noted that the overall response rate “was also improved, with a durable response,” while the results, which are not yet mature, suggest the experimental arm was associated with an overall survival (OS) benefit.
Study discussant Misako Nagasaka, MD, a thoracic oncologist and clinical investigator at Karmanos Cancer Institute, Detroit, said that the PFS benefit seen in the study is “certainly encouraging.”
Adding a note of caution, she continued: “But we have seen studies with PFS improvement which did not translate into OS improvement.
“Longer follow-up would allow events to mature and we will ultimately see if there would be a significant OS benefit,” she said.
Dr. Nagasaka also pointed out that the greater benefit with sintilimab seen in patients with high PD-L1 begs the question as to what would be the preferred regimen in those with higher or lower expression.
And, she said, this is not just about what regimen to choose but “more importantly, why?”
“Perhaps you’d like to use something with the best response rate, perhaps you’re sticking to a single agent immunotherapy because the toxicity profile is more favorable, or perhaps you [are] convinced with a certain regimen because of the robust PFS and OS data,” she said.
“Whatever you chose, there was a reason for your choice,” she said, adding that the sintilimab combination would have to “fulfill those reasons for you to consider choosing this regimen.”
Study details
Dr. Zhang began his presentation by noting that previous phase 1b studies have shown that sintilimab plus pemetrexed and platinum-based chemotherapy has a “tolerable safety profile and promising efficacy” in previously untreated non-squamous NSCLC.
They therefore conducted ORIENT-11, a randomized, double-blind, phase 3 study involving 397 patients with untreated stage IIIB/C or IV nonsquamous NSCLC who had neither EGFR nor ALK gene alterations.
The patients were randomly assigned in a 2:1 fashion to sintilimab plus pemetrexed and platinum-based chemotherapy (n = 266) or placebo plus pemetrexed and chemo (n = 131) for four cycles, followed by sintilimab or placebo plus pemetrexed for up to 24 months.
Thirty-five patients in the placebo arm crossed over to sintilimab monotherapy, representing 31.3% of the intention-to-treat population.
At the data cutoff of Nov. 15, 2019, 198 events had occurred, at a median follow-up of 8.9 months.
The team found that median PFS was significantly higher with sintilimab than placebo combination therapy, at 8.9 months vs. 5.0 months, or a hazard ratio of 0.482 (P < .00001).
Dr. Zhang noted that the benefit with sintilimab plus pemetrexed and platinum-based chemotherapy was seen across all subgroups.
However, it was notable that the impact of adding sintilimab on PFS was greater in patients with a tumor proportion score (TPS) ≥50%.
The HR for progression vs. the placebo treatment arm was 0.310, with median PFS not reached, which decreased to 0.503 in patients with a TPS of 1%-49% and 0.664 among those with a TPS <1%.
The results also showed that there was a “nominally significant improvement” in overall survival with sintilimab versus placebo, at a HR of 0.609 (P = 0.01921).
The ORR was markedly different between the sintilimab and placebo groups, at 51.9% vs. 29.8%, with the duration of response not reached in the sintilimab arm compared with 5.5 months in the placebo arm.
The sintilimab arm included three (1.1%) complete responses, which was not observed with pemetrexed and platinum-based chemotherapy alone.
Finally, Dr. Zhang observed that the safety profiles of the sintilimab and placebo arms were similar, with comparable rates of any, grade 3-5, and serious adverse events largely driven by high rates of chemotherapy-related events.
While there were fewer adverse events that led to death with sintilimab, at 2.3% vs. 6.9% with placebo, there were, as expected, more immune-related adverse events, at 43.2% vs. 36.6%, respectively.
Comparison with pembrolizumab
In her discussion, Dr. Nagasaka said that the first question that came to mind when she saw the results was: “How does the ORIENT-11 data compare with KEYNOTE-189?”
For that study, pembrolizumab (Keytruda, Merck) was added to pemetrexed plus carboplatin chemotherapy and compared with standard of care alone in patients with untreated metastatic nonsquamous NSCLC.
As reported by Medscape Medical News, pembrolizumab was associated with a 48% reduced risk of disease progression, as well as improved overall survival.
Dr. Nagasaka said that ORIENT-11 “had patients that tended to be younger, there were more males, more with performance status 1, and those who had never smoked” than those in KEYNOTE-189.
“But most importantly, KEYNOTE-189 had a very small number of patients from East Asia, only 1% in the pembro arm and 2.9% in the placebo arm.”
In contrast, all the patients included in ORIENT-11 were from East Asia, making the study of “high importance.”
She added that, “while across-trial comparisons must be taken with caution, the medium PFS of ORIENT-11 ... appears comparable to those of KEYNOTE-189,” while the HR “appears identical.”
This is despite median follow-up time in ORIENT-11 of “only” 8.9 months vs. a median of 23.1 months in the updated KEYNOTE-189 data.
There are plans to register the sintilimab combination therapy in China for the treatment of nonsquamous NSCLC, where it will go up against pembrolizumab as well as, potentially, tislelizumab (BeiGene).
The study was sponsored by Innovent Biologics and Eli Lilly. Dr. Zhang disclosed research grants from Eli Lilly and Pfizer. Dr. Nagasaka disclosed serving on the advisory boards of AstraZeneca, Daiichi Sankyo, Takeda, Novartis, and EMD Serono; as a consultant for Caris Life Sciences; and receiving travel support from An Hearts Therapeutics.
This article first appeared on Medscape.com.
The investigational anti-PD-1 antibody sintilimab (Tyvyt, Innovent Biologics and Eli Lilly) has shown that it improves the efficacy of platinum-based chemotherapy in the first-line treatment of patients with advanced nonsquamous non–small cell lung cancer (NSCLC) in a phase 3 trial dubbed ORIENT-11.
The study was presented at the World Congress on Lung Cancer 2020 Virtual Presidential Symposium, held virtually due to the COVID-19 pandemic, on August 8. It was also published simultaneously in the Journal of Thoracic Oncology.
Sintilimab is a fully human IgG4 monoclonal antibody that blocks the binding of programmed death (PD)-1 to PD-ligand 1 (PD-L1) or PD-L2 with high affinity, and has received market authorization in China for the treatment of Hodgkin lymphoma.
For ORIENT-11, almost 400 patients with advanced nonsquamous NSCLC were randomly assigned to sintilimab or placebo plus pemetrexed and platinum-based chemotherapy in a 2:1 ratio.
“The addition of sintilimab to pemetrexed and platinum significantly improved PFS [progression-free survival], compared to placebo,” reducing progression rates by 52%, noted lead investigator Li Zhang, MD, professor of medical oncology, Sun Yat-Sen University Cancer Center, Guangzhou, China.
Crucially, this benefit “was seen across key clinical subgroups,” he added.
He noted that the overall response rate “was also improved, with a durable response,” while the results, which are not yet mature, suggest the experimental arm was associated with an overall survival (OS) benefit.
Study discussant Misako Nagasaka, MD, a thoracic oncologist and clinical investigator at Karmanos Cancer Institute, Detroit, said that the PFS benefit seen in the study is “certainly encouraging.”
Adding a note of caution, she continued: “But we have seen studies with PFS improvement which did not translate into OS improvement.
“Longer follow-up would allow events to mature and we will ultimately see if there would be a significant OS benefit,” she said.
Dr. Nagasaka also pointed out that the greater benefit with sintilimab seen in patients with high PD-L1 begs the question as to what would be the preferred regimen in those with higher or lower expression.
And, she said, this is not just about what regimen to choose but “more importantly, why?”
“Perhaps you’d like to use something with the best response rate, perhaps you’re sticking to a single agent immunotherapy because the toxicity profile is more favorable, or perhaps you [are] convinced with a certain regimen because of the robust PFS and OS data,” she said.
“Whatever you chose, there was a reason for your choice,” she said, adding that the sintilimab combination would have to “fulfill those reasons for you to consider choosing this regimen.”
Study details
Dr. Zhang began his presentation by noting that previous phase 1b studies have shown that sintilimab plus pemetrexed and platinum-based chemotherapy has a “tolerable safety profile and promising efficacy” in previously untreated non-squamous NSCLC.
They therefore conducted ORIENT-11, a randomized, double-blind, phase 3 study involving 397 patients with untreated stage IIIB/C or IV nonsquamous NSCLC who had neither EGFR nor ALK gene alterations.
The patients were randomly assigned in a 2:1 fashion to sintilimab plus pemetrexed and platinum-based chemotherapy (n = 266) or placebo plus pemetrexed and chemo (n = 131) for four cycles, followed by sintilimab or placebo plus pemetrexed for up to 24 months.
Thirty-five patients in the placebo arm crossed over to sintilimab monotherapy, representing 31.3% of the intention-to-treat population.
At the data cutoff of Nov. 15, 2019, 198 events had occurred, at a median follow-up of 8.9 months.
The team found that median PFS was significantly higher with sintilimab than placebo combination therapy, at 8.9 months vs. 5.0 months, or a hazard ratio of 0.482 (P < .00001).
Dr. Zhang noted that the benefit with sintilimab plus pemetrexed and platinum-based chemotherapy was seen across all subgroups.
However, it was notable that the impact of adding sintilimab on PFS was greater in patients with a tumor proportion score (TPS) ≥50%.
The HR for progression vs. the placebo treatment arm was 0.310, with median PFS not reached, which decreased to 0.503 in patients with a TPS of 1%-49% and 0.664 among those with a TPS <1%.
The results also showed that there was a “nominally significant improvement” in overall survival with sintilimab versus placebo, at a HR of 0.609 (P = 0.01921).
The ORR was markedly different between the sintilimab and placebo groups, at 51.9% vs. 29.8%, with the duration of response not reached in the sintilimab arm compared with 5.5 months in the placebo arm.
The sintilimab arm included three (1.1%) complete responses, which was not observed with pemetrexed and platinum-based chemotherapy alone.
Finally, Dr. Zhang observed that the safety profiles of the sintilimab and placebo arms were similar, with comparable rates of any, grade 3-5, and serious adverse events largely driven by high rates of chemotherapy-related events.
While there were fewer adverse events that led to death with sintilimab, at 2.3% vs. 6.9% with placebo, there were, as expected, more immune-related adverse events, at 43.2% vs. 36.6%, respectively.
Comparison with pembrolizumab
In her discussion, Dr. Nagasaka said that the first question that came to mind when she saw the results was: “How does the ORIENT-11 data compare with KEYNOTE-189?”
For that study, pembrolizumab (Keytruda, Merck) was added to pemetrexed plus carboplatin chemotherapy and compared with standard of care alone in patients with untreated metastatic nonsquamous NSCLC.
As reported by Medscape Medical News, pembrolizumab was associated with a 48% reduced risk of disease progression, as well as improved overall survival.
Dr. Nagasaka said that ORIENT-11 “had patients that tended to be younger, there were more males, more with performance status 1, and those who had never smoked” than those in KEYNOTE-189.
“But most importantly, KEYNOTE-189 had a very small number of patients from East Asia, only 1% in the pembro arm and 2.9% in the placebo arm.”
In contrast, all the patients included in ORIENT-11 were from East Asia, making the study of “high importance.”
She added that, “while across-trial comparisons must be taken with caution, the medium PFS of ORIENT-11 ... appears comparable to those of KEYNOTE-189,” while the HR “appears identical.”
This is despite median follow-up time in ORIENT-11 of “only” 8.9 months vs. a median of 23.1 months in the updated KEYNOTE-189 data.
There are plans to register the sintilimab combination therapy in China for the treatment of nonsquamous NSCLC, where it will go up against pembrolizumab as well as, potentially, tislelizumab (BeiGene).
The study was sponsored by Innovent Biologics and Eli Lilly. Dr. Zhang disclosed research grants from Eli Lilly and Pfizer. Dr. Nagasaka disclosed serving on the advisory boards of AstraZeneca, Daiichi Sankyo, Takeda, Novartis, and EMD Serono; as a consultant for Caris Life Sciences; and receiving travel support from An Hearts Therapeutics.
This article first appeared on Medscape.com.
Chemo-free management of mesothelioma on horizon
Patients with untreated mesothelioma may be able to avoid chemotherapy, say researchers reporting new survival data with the immunotherapy combination of nivolumab (Opdivo) and ipilimumab (Yervoy).
The two approaches were compared in more than 600 patients with treatment-naive mesothelioma in the phase 3 CheckMate 743 trial, which was supported by the manufacturer of both immunotherapies, Bristol-Myers Squibb.
The trial “met its primary endpoint of statistically improving overall survival for the experimental arm vs chemotherapy in a prespecified interim analysis,” reported Paul Baas, MD, PhD, Netherlands Cancer Institute, Amsterdam, The Netherlands,
The combined nivo+ipi immunotherapy regimen was associated with a 26% improvement in overall survival. At 2 years, 41% of patients in the immunotherapy arm were still alive, vs 27% in the chemotherapy group.
“This is the first positive randomized trial of dual immunotherapy in the first-line treatment of patients with mesothelioma,” he said. He suggested that it should therefore “be considered as a new standard of care.”
The data were presented on August 8 in the presidential symposium of the World Congress on Lung Cancer 2020, which was held online because of the COVID-19 pandemic.
A key analysis for the study was by histologic subgroup. It is known that standard-of-care chemotherapy performs better in patients with epithelioid as opposed to nonepithelioid tumor subtypes.
Bass highlighted that the performance of nivo+ipi was “almost the same” in patients with epithelioid and nonepithelioid tumors, at a median overall survival of 18.7 months and 18.1 months, respectively.
In contrast, overall survival in the chemotherapy arm was markedly lower in patients with nonepithelioid tumors, at 8.8 months vs 16.5 months among those with epithelioid tumors.
This was reflected in the hazard ratios for overall survival vs nivo+ipi, at 0.46 and 0.86, respectively, the latter nonsignificantly different from combination immunotherapy.
For study discussant Dean A. Fennell, MD, PhD, professor and consultant in thoracic medical oncology, University of Leicester, United Kingdom, the epithet of a “new standard of care” for nivo+ipi should be reserved for nonepithelioid disease.
In this setting, he described the overall survival improvement as “transformative,” considering the “marked chemo resistance” of nonepithelioid tumors, which is “almost certainly” associated with epithelial-to-mesenchymal transition (EMT).
In the future, he suggested, combinations of chemotherapy and immunotherapy involving all histologies or selective targeting of nonepithelioid mesothelioma “could further extend the benefit for patients.”
Improving survival in mesothelioma
“We have been trying to improve the overall survival of patients with mesothelioma now for many decades,” Bass commented. Platinum-based chemotherapy plus pemetrexed is a standard of care, although the 5-year survival rate «is still below 10%,” he noted.
Randomized trials of single-agent immune checkpoint inhibitor therapy in the second-line treatment of patients with mesothelioma have not shown any significant benefits.
However, nivolumab and ipilimumab have a “complementary mechanism of action,” and two previous reports have indicated that together, they have clinical activity in the second-line setting.
The team conducted CheckMate 743 to determine the efficacy of the combination in the first-line setting.
The study involved 605 patients with pleural mesothelioma who had received no prior systemic therapy and had good performance status.
They were randomly assigned in a 1:1 ratio to receive nivo+ipi for up to 2 years or six cycles of pemetrexed plus cisplatin or carboplatin until disease progression or unacceptable toxicity occurred.
“Patients could have a subsequent therapy,” Bass noted; 44.0% of patients in the experimental arm received subsequent therapy, vs 44.1% of those in the chemotherapy arm.
Of the latter, 20% received an immune checkpoint inhibitor as subsequent therapy.
The minimum follow-up for overall survival was 22.1 months; the median follow-up was 29.7 months.
Nivo+ipi was associated with a significant improvement in overall survival vs standard-of-care chemotherapy, at a median overall survival of 18.1 months vs 14.1 months, with a hazard ratio of 0.74 (P = .0020).
The results indicated that overall survival was similar across key subgroups, which suggests that “no subgroup was harmed” by nivo+ipi, Bass said.
Stratification by PD-LI expression
Stratifying the patients by the absence or presence of programmed cell death–ligand-1 (PD-L1) expression, the team found that the performance of nivo+ipi was “the same” as that of chemotherapy, Bass said.
“But in cases where there is any expression of PD-L1, the experimental arm performs better,” at an overall survival 18.0 months vs 13.3 months for chemotherapy and a hazard ratio of 0.69, he said.
There was no difference between the two treatment arms in progression-free survival. Chemotherapy performed better in the first 6 months of treatment, after which the nivo+ipi arm had lower event rates.
Nivo+ipi was also associated with a greater duration of response, at a median of 11.0 months vs 6.7 months for standard-of-care chemotherapy.
Moreover, at 24 months, 32% of nivo+ipi patients were still experiencing a response, whereas 8% of those in the chemotherapy arm were.
Treatment-related adverse events rates were almost identical between the two treatment groups, although treatment with nivo+ipi was associated with more grade 3/4 serious treatment-related adverse events, at 15 vs six for chemotherapy.
Choosing immunotherapy vs. chemotherapy
In his discussion of the new study, Fennell compared the current results with those from two studies, INITIATE and MAPS2. “What’s very clear is the response rate is slightly higher,” as is the disease control rate, he said.
This, he explained, “is perhaps not surprising, given that these two previous trials were in the relapse setting.”
He pointed out, however, that the progression-free survival data from those previous trials were “not a million miles away” from results seen in CheckMate 743, “suggesting that this immunotherapy does have significant activity in the relapse setting.”
For Fennell, the “pivotal data” are in patients with nonepithelioid tumors, particularly inasmuch as chemotherapy performed “poorly” in this setting, whereas it performs “as expected” in epithelioid mesothelioma.
He believes that the driver for this is the poor prognosis associated with sarcomatoid biphasic disease, a subtype characterized by increased expression of vimentin and ZEB1, proteins both associated with EMT.
“What does this mean?” Fennell asked.
“If you have have enrichment of EMT, what you see is increased drug resistance, increased invasiveness, something we know well with sarcomatoid mesotheliomas in particular, and this drug-resistance phenotype may account for the drug resistance that we see in CheckMate 743 with chemotherapy.
“This does not appear, however, to impact in any way the efficacy of the immunotherapy,” he noted.
Fennell believes that, with regard to both efficacy and safety, the balance is “very much in favor” of nivo+ipi in epithelioid mesothelioma, although there is less to choose between immunotherapy and chemotherapy in the nonepithelioid setting.
Indeed, the choice is “possible tilting slightly towards chemotherapy” in patients with the nonepithelioid tumors, owing to the lower rates of grade 3/4 serious treatment-related adverse events in comparison with combination immunotherapy.
The study was supported by Bristol-Myers Squibb. Bass has served on the advisory boards of MSD, AstraZeneca, and Takeda. Fennell has received research support from AstraZeneca, Bristol-Myers Squibb, Clovis Oncology, Eli Lilly, MSD, and Roche; research funding from Astex Therapeutics, Bayer, and Boehringer Ingelheim; has served on the speaker bureau of AstraZeneca, Boehringer Ingelheim, and Roche; has acted as a consultant for Bayer and Lab 21; and has served on the advisory board of Atara Biotherapeutics, Boehringer Ingelheim, and Inventiva.
This article first appeared on Medscape.com.
Patients with untreated mesothelioma may be able to avoid chemotherapy, say researchers reporting new survival data with the immunotherapy combination of nivolumab (Opdivo) and ipilimumab (Yervoy).
The two approaches were compared in more than 600 patients with treatment-naive mesothelioma in the phase 3 CheckMate 743 trial, which was supported by the manufacturer of both immunotherapies, Bristol-Myers Squibb.
The trial “met its primary endpoint of statistically improving overall survival for the experimental arm vs chemotherapy in a prespecified interim analysis,” reported Paul Baas, MD, PhD, Netherlands Cancer Institute, Amsterdam, The Netherlands,
The combined nivo+ipi immunotherapy regimen was associated with a 26% improvement in overall survival. At 2 years, 41% of patients in the immunotherapy arm were still alive, vs 27% in the chemotherapy group.
“This is the first positive randomized trial of dual immunotherapy in the first-line treatment of patients with mesothelioma,” he said. He suggested that it should therefore “be considered as a new standard of care.”
The data were presented on August 8 in the presidential symposium of the World Congress on Lung Cancer 2020, which was held online because of the COVID-19 pandemic.
A key analysis for the study was by histologic subgroup. It is known that standard-of-care chemotherapy performs better in patients with epithelioid as opposed to nonepithelioid tumor subtypes.
Bass highlighted that the performance of nivo+ipi was “almost the same” in patients with epithelioid and nonepithelioid tumors, at a median overall survival of 18.7 months and 18.1 months, respectively.
In contrast, overall survival in the chemotherapy arm was markedly lower in patients with nonepithelioid tumors, at 8.8 months vs 16.5 months among those with epithelioid tumors.
This was reflected in the hazard ratios for overall survival vs nivo+ipi, at 0.46 and 0.86, respectively, the latter nonsignificantly different from combination immunotherapy.
For study discussant Dean A. Fennell, MD, PhD, professor and consultant in thoracic medical oncology, University of Leicester, United Kingdom, the epithet of a “new standard of care” for nivo+ipi should be reserved for nonepithelioid disease.
In this setting, he described the overall survival improvement as “transformative,” considering the “marked chemo resistance” of nonepithelioid tumors, which is “almost certainly” associated with epithelial-to-mesenchymal transition (EMT).
In the future, he suggested, combinations of chemotherapy and immunotherapy involving all histologies or selective targeting of nonepithelioid mesothelioma “could further extend the benefit for patients.”
Improving survival in mesothelioma
“We have been trying to improve the overall survival of patients with mesothelioma now for many decades,” Bass commented. Platinum-based chemotherapy plus pemetrexed is a standard of care, although the 5-year survival rate «is still below 10%,” he noted.
Randomized trials of single-agent immune checkpoint inhibitor therapy in the second-line treatment of patients with mesothelioma have not shown any significant benefits.
However, nivolumab and ipilimumab have a “complementary mechanism of action,” and two previous reports have indicated that together, they have clinical activity in the second-line setting.
The team conducted CheckMate 743 to determine the efficacy of the combination in the first-line setting.
The study involved 605 patients with pleural mesothelioma who had received no prior systemic therapy and had good performance status.
They were randomly assigned in a 1:1 ratio to receive nivo+ipi for up to 2 years or six cycles of pemetrexed plus cisplatin or carboplatin until disease progression or unacceptable toxicity occurred.
“Patients could have a subsequent therapy,” Bass noted; 44.0% of patients in the experimental arm received subsequent therapy, vs 44.1% of those in the chemotherapy arm.
Of the latter, 20% received an immune checkpoint inhibitor as subsequent therapy.
The minimum follow-up for overall survival was 22.1 months; the median follow-up was 29.7 months.
Nivo+ipi was associated with a significant improvement in overall survival vs standard-of-care chemotherapy, at a median overall survival of 18.1 months vs 14.1 months, with a hazard ratio of 0.74 (P = .0020).
The results indicated that overall survival was similar across key subgroups, which suggests that “no subgroup was harmed” by nivo+ipi, Bass said.
Stratification by PD-LI expression
Stratifying the patients by the absence or presence of programmed cell death–ligand-1 (PD-L1) expression, the team found that the performance of nivo+ipi was “the same” as that of chemotherapy, Bass said.
“But in cases where there is any expression of PD-L1, the experimental arm performs better,” at an overall survival 18.0 months vs 13.3 months for chemotherapy and a hazard ratio of 0.69, he said.
There was no difference between the two treatment arms in progression-free survival. Chemotherapy performed better in the first 6 months of treatment, after which the nivo+ipi arm had lower event rates.
Nivo+ipi was also associated with a greater duration of response, at a median of 11.0 months vs 6.7 months for standard-of-care chemotherapy.
Moreover, at 24 months, 32% of nivo+ipi patients were still experiencing a response, whereas 8% of those in the chemotherapy arm were.
Treatment-related adverse events rates were almost identical between the two treatment groups, although treatment with nivo+ipi was associated with more grade 3/4 serious treatment-related adverse events, at 15 vs six for chemotherapy.
Choosing immunotherapy vs. chemotherapy
In his discussion of the new study, Fennell compared the current results with those from two studies, INITIATE and MAPS2. “What’s very clear is the response rate is slightly higher,” as is the disease control rate, he said.
This, he explained, “is perhaps not surprising, given that these two previous trials were in the relapse setting.”
He pointed out, however, that the progression-free survival data from those previous trials were “not a million miles away” from results seen in CheckMate 743, “suggesting that this immunotherapy does have significant activity in the relapse setting.”
For Fennell, the “pivotal data” are in patients with nonepithelioid tumors, particularly inasmuch as chemotherapy performed “poorly” in this setting, whereas it performs “as expected” in epithelioid mesothelioma.
He believes that the driver for this is the poor prognosis associated with sarcomatoid biphasic disease, a subtype characterized by increased expression of vimentin and ZEB1, proteins both associated with EMT.
“What does this mean?” Fennell asked.
“If you have have enrichment of EMT, what you see is increased drug resistance, increased invasiveness, something we know well with sarcomatoid mesotheliomas in particular, and this drug-resistance phenotype may account for the drug resistance that we see in CheckMate 743 with chemotherapy.
“This does not appear, however, to impact in any way the efficacy of the immunotherapy,” he noted.
Fennell believes that, with regard to both efficacy and safety, the balance is “very much in favor” of nivo+ipi in epithelioid mesothelioma, although there is less to choose between immunotherapy and chemotherapy in the nonepithelioid setting.
Indeed, the choice is “possible tilting slightly towards chemotherapy” in patients with the nonepithelioid tumors, owing to the lower rates of grade 3/4 serious treatment-related adverse events in comparison with combination immunotherapy.
The study was supported by Bristol-Myers Squibb. Bass has served on the advisory boards of MSD, AstraZeneca, and Takeda. Fennell has received research support from AstraZeneca, Bristol-Myers Squibb, Clovis Oncology, Eli Lilly, MSD, and Roche; research funding from Astex Therapeutics, Bayer, and Boehringer Ingelheim; has served on the speaker bureau of AstraZeneca, Boehringer Ingelheim, and Roche; has acted as a consultant for Bayer and Lab 21; and has served on the advisory board of Atara Biotherapeutics, Boehringer Ingelheim, and Inventiva.
This article first appeared on Medscape.com.
Patients with untreated mesothelioma may be able to avoid chemotherapy, say researchers reporting new survival data with the immunotherapy combination of nivolumab (Opdivo) and ipilimumab (Yervoy).
The two approaches were compared in more than 600 patients with treatment-naive mesothelioma in the phase 3 CheckMate 743 trial, which was supported by the manufacturer of both immunotherapies, Bristol-Myers Squibb.
The trial “met its primary endpoint of statistically improving overall survival for the experimental arm vs chemotherapy in a prespecified interim analysis,” reported Paul Baas, MD, PhD, Netherlands Cancer Institute, Amsterdam, The Netherlands,
The combined nivo+ipi immunotherapy regimen was associated with a 26% improvement in overall survival. At 2 years, 41% of patients in the immunotherapy arm were still alive, vs 27% in the chemotherapy group.
“This is the first positive randomized trial of dual immunotherapy in the first-line treatment of patients with mesothelioma,” he said. He suggested that it should therefore “be considered as a new standard of care.”
The data were presented on August 8 in the presidential symposium of the World Congress on Lung Cancer 2020, which was held online because of the COVID-19 pandemic.
A key analysis for the study was by histologic subgroup. It is known that standard-of-care chemotherapy performs better in patients with epithelioid as opposed to nonepithelioid tumor subtypes.
Bass highlighted that the performance of nivo+ipi was “almost the same” in patients with epithelioid and nonepithelioid tumors, at a median overall survival of 18.7 months and 18.1 months, respectively.
In contrast, overall survival in the chemotherapy arm was markedly lower in patients with nonepithelioid tumors, at 8.8 months vs 16.5 months among those with epithelioid tumors.
This was reflected in the hazard ratios for overall survival vs nivo+ipi, at 0.46 and 0.86, respectively, the latter nonsignificantly different from combination immunotherapy.
For study discussant Dean A. Fennell, MD, PhD, professor and consultant in thoracic medical oncology, University of Leicester, United Kingdom, the epithet of a “new standard of care” for nivo+ipi should be reserved for nonepithelioid disease.
In this setting, he described the overall survival improvement as “transformative,” considering the “marked chemo resistance” of nonepithelioid tumors, which is “almost certainly” associated with epithelial-to-mesenchymal transition (EMT).
In the future, he suggested, combinations of chemotherapy and immunotherapy involving all histologies or selective targeting of nonepithelioid mesothelioma “could further extend the benefit for patients.”
Improving survival in mesothelioma
“We have been trying to improve the overall survival of patients with mesothelioma now for many decades,” Bass commented. Platinum-based chemotherapy plus pemetrexed is a standard of care, although the 5-year survival rate «is still below 10%,” he noted.
Randomized trials of single-agent immune checkpoint inhibitor therapy in the second-line treatment of patients with mesothelioma have not shown any significant benefits.
However, nivolumab and ipilimumab have a “complementary mechanism of action,” and two previous reports have indicated that together, they have clinical activity in the second-line setting.
The team conducted CheckMate 743 to determine the efficacy of the combination in the first-line setting.
The study involved 605 patients with pleural mesothelioma who had received no prior systemic therapy and had good performance status.
They were randomly assigned in a 1:1 ratio to receive nivo+ipi for up to 2 years or six cycles of pemetrexed plus cisplatin or carboplatin until disease progression or unacceptable toxicity occurred.
“Patients could have a subsequent therapy,” Bass noted; 44.0% of patients in the experimental arm received subsequent therapy, vs 44.1% of those in the chemotherapy arm.
Of the latter, 20% received an immune checkpoint inhibitor as subsequent therapy.
The minimum follow-up for overall survival was 22.1 months; the median follow-up was 29.7 months.
Nivo+ipi was associated with a significant improvement in overall survival vs standard-of-care chemotherapy, at a median overall survival of 18.1 months vs 14.1 months, with a hazard ratio of 0.74 (P = .0020).
The results indicated that overall survival was similar across key subgroups, which suggests that “no subgroup was harmed” by nivo+ipi, Bass said.
Stratification by PD-LI expression
Stratifying the patients by the absence or presence of programmed cell death–ligand-1 (PD-L1) expression, the team found that the performance of nivo+ipi was “the same” as that of chemotherapy, Bass said.
“But in cases where there is any expression of PD-L1, the experimental arm performs better,” at an overall survival 18.0 months vs 13.3 months for chemotherapy and a hazard ratio of 0.69, he said.
There was no difference between the two treatment arms in progression-free survival. Chemotherapy performed better in the first 6 months of treatment, after which the nivo+ipi arm had lower event rates.
Nivo+ipi was also associated with a greater duration of response, at a median of 11.0 months vs 6.7 months for standard-of-care chemotherapy.
Moreover, at 24 months, 32% of nivo+ipi patients were still experiencing a response, whereas 8% of those in the chemotherapy arm were.
Treatment-related adverse events rates were almost identical between the two treatment groups, although treatment with nivo+ipi was associated with more grade 3/4 serious treatment-related adverse events, at 15 vs six for chemotherapy.
Choosing immunotherapy vs. chemotherapy
In his discussion of the new study, Fennell compared the current results with those from two studies, INITIATE and MAPS2. “What’s very clear is the response rate is slightly higher,” as is the disease control rate, he said.
This, he explained, “is perhaps not surprising, given that these two previous trials were in the relapse setting.”
He pointed out, however, that the progression-free survival data from those previous trials were “not a million miles away” from results seen in CheckMate 743, “suggesting that this immunotherapy does have significant activity in the relapse setting.”
For Fennell, the “pivotal data” are in patients with nonepithelioid tumors, particularly inasmuch as chemotherapy performed “poorly” in this setting, whereas it performs “as expected” in epithelioid mesothelioma.
He believes that the driver for this is the poor prognosis associated with sarcomatoid biphasic disease, a subtype characterized by increased expression of vimentin and ZEB1, proteins both associated with EMT.
“What does this mean?” Fennell asked.
“If you have have enrichment of EMT, what you see is increased drug resistance, increased invasiveness, something we know well with sarcomatoid mesotheliomas in particular, and this drug-resistance phenotype may account for the drug resistance that we see in CheckMate 743 with chemotherapy.
“This does not appear, however, to impact in any way the efficacy of the immunotherapy,” he noted.
Fennell believes that, with regard to both efficacy and safety, the balance is “very much in favor” of nivo+ipi in epithelioid mesothelioma, although there is less to choose between immunotherapy and chemotherapy in the nonepithelioid setting.
Indeed, the choice is “possible tilting slightly towards chemotherapy” in patients with the nonepithelioid tumors, owing to the lower rates of grade 3/4 serious treatment-related adverse events in comparison with combination immunotherapy.
The study was supported by Bristol-Myers Squibb. Bass has served on the advisory boards of MSD, AstraZeneca, and Takeda. Fennell has received research support from AstraZeneca, Bristol-Myers Squibb, Clovis Oncology, Eli Lilly, MSD, and Roche; research funding from Astex Therapeutics, Bayer, and Boehringer Ingelheim; has served on the speaker bureau of AstraZeneca, Boehringer Ingelheim, and Roche; has acted as a consultant for Bayer and Lab 21; and has served on the advisory board of Atara Biotherapeutics, Boehringer Ingelheim, and Inventiva.
This article first appeared on Medscape.com.






