User login
For MD-IQ use only
Productivity-based salary structure not associated with value-based culture
Background: Although new payment models have been implemented by the Centers for Medicare & Medicaid Services (CMS) for hospital reimbursement, little is known about the effects of reimbursement models on the culture of providing value-based care among individual hospitalists. The concern is that productivity-based models increase pressure on hospitalists to maximize volume and billing, as opposed to focusing on value.
Study design: Observational, cross-sectional, survey-based study.
Setting: A total of 12 hospitals in California, which represented university, community, and safety-net settings.
Synopsis: Hospitalists were asked to complete the High-Value Care Culture Survey (HVCCS), a validated tool that assesses value-based decision making. Components of the survey assessed leadership and health system messaging, data transparency and access, comfort with cost conversations, and blame-free environments. Hospitalists were also asked to self-report their reimbursement structure: salary alone, salary plus productivity, or salary plus value-based adjustments.
A total of 255 hospitalists completed the survey. The mean HVCCS score was 50.2 on a 0-100 scale. Hospitalists who reported reimbursement with salary plus productivity adjustments had a lower mean HVCCS score (beta = –6.2; 95% confidence interval, –9.9 to –2.5) when compared with hospitalists paid with salary alone. An association was not found between HVCCS score and reimbursement with salary plus value-based adjustments when compared with salary alone, though this finding may have been limited by sample size.
Bottom line: A hospitalist reimbursement model of salary plus productivity was associated with lower measures of value-based care culture.
Citation: Gupta R et al. Association between hospitalist productivity payments and high-value care culture. J Hosp Med. 2019;14(1):16-21.
Dr. Huang is a physician adviser and associate clinical professor in the division of hospital medicine at the University of California, San Diego.
Background: Although new payment models have been implemented by the Centers for Medicare & Medicaid Services (CMS) for hospital reimbursement, little is known about the effects of reimbursement models on the culture of providing value-based care among individual hospitalists. The concern is that productivity-based models increase pressure on hospitalists to maximize volume and billing, as opposed to focusing on value.
Study design: Observational, cross-sectional, survey-based study.
Setting: A total of 12 hospitals in California, which represented university, community, and safety-net settings.
Synopsis: Hospitalists were asked to complete the High-Value Care Culture Survey (HVCCS), a validated tool that assesses value-based decision making. Components of the survey assessed leadership and health system messaging, data transparency and access, comfort with cost conversations, and blame-free environments. Hospitalists were also asked to self-report their reimbursement structure: salary alone, salary plus productivity, or salary plus value-based adjustments.
A total of 255 hospitalists completed the survey. The mean HVCCS score was 50.2 on a 0-100 scale. Hospitalists who reported reimbursement with salary plus productivity adjustments had a lower mean HVCCS score (beta = –6.2; 95% confidence interval, –9.9 to –2.5) when compared with hospitalists paid with salary alone. An association was not found between HVCCS score and reimbursement with salary plus value-based adjustments when compared with salary alone, though this finding may have been limited by sample size.
Bottom line: A hospitalist reimbursement model of salary plus productivity was associated with lower measures of value-based care culture.
Citation: Gupta R et al. Association between hospitalist productivity payments and high-value care culture. J Hosp Med. 2019;14(1):16-21.
Dr. Huang is a physician adviser and associate clinical professor in the division of hospital medicine at the University of California, San Diego.
Background: Although new payment models have been implemented by the Centers for Medicare & Medicaid Services (CMS) for hospital reimbursement, little is known about the effects of reimbursement models on the culture of providing value-based care among individual hospitalists. The concern is that productivity-based models increase pressure on hospitalists to maximize volume and billing, as opposed to focusing on value.
Study design: Observational, cross-sectional, survey-based study.
Setting: A total of 12 hospitals in California, which represented university, community, and safety-net settings.
Synopsis: Hospitalists were asked to complete the High-Value Care Culture Survey (HVCCS), a validated tool that assesses value-based decision making. Components of the survey assessed leadership and health system messaging, data transparency and access, comfort with cost conversations, and blame-free environments. Hospitalists were also asked to self-report their reimbursement structure: salary alone, salary plus productivity, or salary plus value-based adjustments.
A total of 255 hospitalists completed the survey. The mean HVCCS score was 50.2 on a 0-100 scale. Hospitalists who reported reimbursement with salary plus productivity adjustments had a lower mean HVCCS score (beta = –6.2; 95% confidence interval, –9.9 to –2.5) when compared with hospitalists paid with salary alone. An association was not found between HVCCS score and reimbursement with salary plus value-based adjustments when compared with salary alone, though this finding may have been limited by sample size.
Bottom line: A hospitalist reimbursement model of salary plus productivity was associated with lower measures of value-based care culture.
Citation: Gupta R et al. Association between hospitalist productivity payments and high-value care culture. J Hosp Med. 2019;14(1):16-21.
Dr. Huang is a physician adviser and associate clinical professor in the division of hospital medicine at the University of California, San Diego.
IHS Launches Pilot to Redress Racial Misclassification in Records
American Indians and Alaska Natives (AI/AN) are often misidentified as other races in public health administrative records. In the Northwest, for instance, the Northwest Tribal Epidemiology Center (NTEC) has found that about 10% of AI/AN birth and death records and up to 60% of hospitalization records are misclassified.
Racial misclassification makes it difficult to accurately assess the health of Native people: The numbers affected by a disease may appear lower or higher than they actually are. It can muddle and misrepresent information in birth certificates, cancer registries, death certificates, emergency department records, hospitalization records, injury reports. Without accurate health data, says Lisa Neel, director of the Indian Health Service (IHS) Tribal Epidemiology Center Program, tribes cannot make informed decisions about how best to serve their people.
That is why the IHS and the Center recently signed an agreement supporting a new information-sharing project. The agreement will allow the IHS to provide the NTEC with a list of people who have received health services at IHS, tribal, and urban Indian health programs in the Portland Area. The list will include no information about patients’ medical histories and will not be shared outside the NTEC. The center will then compare the list with outside information sources, such as state cancer registries, to check for racial misclassification.
The NTEC is 1 of 13 national “EpiCenters” charged with collecting tribal health status data, evaluating data monitoring and delivery systems, and helping tribes identify local priorities for health care delivery and health education. NTEC serves the 43 federally recognized tribes in Idaho, Oregon, and Washington. The center is housed in the Northwest Portland Area Indian Health Board (NPAIHB), whose delegates, representing the member tribes, direct and oversee activities, including health promotion, disease prevention, training and technical assistance.
The IHS plans for this to be a pilot project, possibly pointing the way for other tribal EpiCenters to launch similar projects.
American Indians and Alaska Natives (AI/AN) are often misidentified as other races in public health administrative records. In the Northwest, for instance, the Northwest Tribal Epidemiology Center (NTEC) has found that about 10% of AI/AN birth and death records and up to 60% of hospitalization records are misclassified.
Racial misclassification makes it difficult to accurately assess the health of Native people: The numbers affected by a disease may appear lower or higher than they actually are. It can muddle and misrepresent information in birth certificates, cancer registries, death certificates, emergency department records, hospitalization records, injury reports. Without accurate health data, says Lisa Neel, director of the Indian Health Service (IHS) Tribal Epidemiology Center Program, tribes cannot make informed decisions about how best to serve their people.
That is why the IHS and the Center recently signed an agreement supporting a new information-sharing project. The agreement will allow the IHS to provide the NTEC with a list of people who have received health services at IHS, tribal, and urban Indian health programs in the Portland Area. The list will include no information about patients’ medical histories and will not be shared outside the NTEC. The center will then compare the list with outside information sources, such as state cancer registries, to check for racial misclassification.
The NTEC is 1 of 13 national “EpiCenters” charged with collecting tribal health status data, evaluating data monitoring and delivery systems, and helping tribes identify local priorities for health care delivery and health education. NTEC serves the 43 federally recognized tribes in Idaho, Oregon, and Washington. The center is housed in the Northwest Portland Area Indian Health Board (NPAIHB), whose delegates, representing the member tribes, direct and oversee activities, including health promotion, disease prevention, training and technical assistance.
The IHS plans for this to be a pilot project, possibly pointing the way for other tribal EpiCenters to launch similar projects.
American Indians and Alaska Natives (AI/AN) are often misidentified as other races in public health administrative records. In the Northwest, for instance, the Northwest Tribal Epidemiology Center (NTEC) has found that about 10% of AI/AN birth and death records and up to 60% of hospitalization records are misclassified.
Racial misclassification makes it difficult to accurately assess the health of Native people: The numbers affected by a disease may appear lower or higher than they actually are. It can muddle and misrepresent information in birth certificates, cancer registries, death certificates, emergency department records, hospitalization records, injury reports. Without accurate health data, says Lisa Neel, director of the Indian Health Service (IHS) Tribal Epidemiology Center Program, tribes cannot make informed decisions about how best to serve their people.
That is why the IHS and the Center recently signed an agreement supporting a new information-sharing project. The agreement will allow the IHS to provide the NTEC with a list of people who have received health services at IHS, tribal, and urban Indian health programs in the Portland Area. The list will include no information about patients’ medical histories and will not be shared outside the NTEC. The center will then compare the list with outside information sources, such as state cancer registries, to check for racial misclassification.
The NTEC is 1 of 13 national “EpiCenters” charged with collecting tribal health status data, evaluating data monitoring and delivery systems, and helping tribes identify local priorities for health care delivery and health education. NTEC serves the 43 federally recognized tribes in Idaho, Oregon, and Washington. The center is housed in the Northwest Portland Area Indian Health Board (NPAIHB), whose delegates, representing the member tribes, direct and oversee activities, including health promotion, disease prevention, training and technical assistance.
The IHS plans for this to be a pilot project, possibly pointing the way for other tribal EpiCenters to launch similar projects.
Five genetic variations associated with same-sex sexual behavior
There is no single “gay gene.”
There are, however, signals that nonheterosexual behavior has at least some genetic component, according to Andrea Ganna, PhD, and colleagues.
Five candidate genes found in a half-million subject genetic study each account for less than 1% of the variance in same-sex sexual behavior, the scientists found. Over the entire genome, genetic variants accounted for less than a quarter of such behavior.
None of the genetic signals can reliably predict sexual behavior, Benjamin Neale, PhD, director of genetics in the Stanley Center for Psychiatric Research at the Broad Institute of the Massachusetts Institute of Technology and Harvard Medical School, both in Boston, said in a telebriefing that included Dr. Ganna, a postdoctoral researcher in his lab. Instead, the variability of human sexuality is an entirely natural continuum of human behavior.
“Whether we are attracted exclusively to the opposite sex, the same sex, or both sexes falls along a spectrum that is an integral, and entirely normal, part of the human experience,” said Dr. Neale. “The choice of a sexual partner and the fraction of partners that are of the same sex are all consistent with this diversity being a key feature of our sexual behavior as a species and this diversity is a natural part of being human.”
The study, published in Science, clarifies findings of smaller, previous studies, which determined that sexual behavior is a combination of genetics and environment – although environment is a much more difficult association to assess.
“[Environment] can range from anything in utero, all the way all the way through who you happen to stand next to on the tube in the morning, right? That’s all potentially environmental factors that can have some influence on complex traits and so we don’t really understand,” Dr. Neale said.
However, he added, the concept of individual choice in sexual behaviors was beyond the scope of the study, which strictly centered on genetic associations with sexual behavior.
The study combined genetic information from three extant databases (the U.K. Biobank, National Longitudinal Study of Adolescent to Adult Health, the Molecular Genetic Study of Sexual Orientation, and the Child and Adolescent Twin Study in Sweden) with newly collected data from 23andMe, the technology company that provides at-home genetics tests largely used to determine ethnic origin.
The primary phenotype investigated was a binary measure: self-reported sexual behavior with someone of the same sex (nonheterosexuality) or someone of the opposite sex (heterosexuality).
“The binary variable also collapses rich and multifaceted diversity among nonheterosexuality individuals, wrote Dr. Ganna and his coauthors. Therefore, “we explored finer-scaled measurements and some of the complexities of the phenotype, although intricacies of the social and cultural influences on sexuality made it impossible to fully explore this complexity.”
The team also performed replication analyses on three smaller datasets: the Molecular Genetic Study of Sexual Orientation (2,308 U.S. adult males), Add Health (4,755 U.S. young adults), and the Child and Adolescent Twin Study in Sweden (8,093 Swedish adolescents). Data were available for 188,825 males and 220,170 females overall. When broken down by sexual behavior, data were available for 1,766 homosexual and 180,431 heterosexual males, and 693 homosexual and 214,062 heterosexual females.
The team identified two genes that significantly predicted same-sex sexual behavior (rs11114975-12q21.31 and rs10261857-7q31.2). Two more genes predicted same-sex sexual behavior in males only (rs28371400-15q21.3 and rs34730029-11q12.1), and one additional gene predicted the behavior in females only (rs13135637-4p14).
Three of the single nucleotide polymorphisms (SNPs) nominally replicated those in some of the other datasets, despite the much smaller sample sizes.
“The SNPs that reached genome-wide significance had very small effects (odds ratio, 1.1),” the authors wrote. “For example, in the U.K. Biobank, males with a GT genotype at the rs34730029 locus had 0.4% higher prevalence of same-sex sexual behavior than those with a TT genotype. Nevertheless, the contribution of all measured common SNPs in aggregate was estimated to [account for] 8%-25% of variation in female and male same-sex sexual behavior. … The discrepancy between the variance captured by the significant SNPs and all common SNPs suggests that same-sex sexual behavior, like most complex human traits, is influenced by the small, additive effects of very many genetic variants, most of which cannot be detected at the current sample size.”
The Child and Adolescent Twin Study in Sweden contained the youngest subjects. The polygenic scores in this dataset were significantly associated with sexual attraction at age 15 years, “suggesting that at least some of the genetic influences on same-sex sexual behavior manifest early in sexual development.”
The team also investigated the biological pathways associated with the SNPs. Among the male variants, rs34730029-11q12.1 contains numerous olfactory receptor genes.
“Second, rs28371400-15q21.3 had several indications of being involved in sex hormone regulation. The allele positively associated with same-sex sexual behavior is associated with higher rate of male pattern balding, in which sex-hormone sensitivity is implicated,” they wrote.
This is located near the TCF12 gene, related to a normal gonadal development in mice.
Among women, there were inverse associations with the level of sex hormone–binding globulin, which regulates the balance between testosterone and estrogen.
There were significant associations with some mental health traits, including loneliness, openness to experience, and risky behaviors such as smoking and using cannabis. There were also associations with depression and schizophrenia. The genetic correlations for bipolar disorder, cannabis use, and number of sexual partners were significantly higher in females than in males.
“We emphasize that the causal processes underlying these genetic correlations are unclear and could be generated by environmental factors relating to prejudice against individuals engaging in same-sex sexual behavior,” the authors wrote.
In an interview, Jack Drescher, MD, said he was not surprised by the findings and cited the results a twin study by J. Michael Bailey, PhD, and Richard C. Pillard, MD, as evidence of the complexities surrounding sexual orientation. The study examined the likelihood of one twin having a gay twin (Arch Gen Psychiatry. 1991 Dec;48[12]:1089-96).
“If you were a gay identical twin, you had a 52% chance of having a gay twin, he said. “If you were a gay fraternal twin, you only had a 22% chance of having a gay twin. The chance of an adoptive brother being gay was 11%. If homosexuality were simply a result of simple genetic transmission, then one would expect closer to 100% gay identical twins, since they both have the same genes.”
Dr. Drescher, clinical professor of psychiatry at the Center for Psychoanalytic Training and Research at Columbia University, New York, has written extensively about human sexuality, gender-conversion therapies, and gender.
The study by Dr. Ganna and associates as a whole invalidates several commonly used sexual behavior scales, including the Kinsey Scale, which is solely predicated upon self-reported attraction. The Klein Sexual Orientation Grid, which measures sexual behavior, fantasies, and sexual identification, is similarly problematic, the authors noted.
“Overall, our findings suggest that the most popular measures are based on a misconception of the underlying structure of sexual orientation and may need to be rethought. In particular, using separate measures of attraction to the opposite sex and attraction to the same sex, such as in the Sell Assessment of Sexual Orientation, would remove the assumption that these variables are perfectly inversely related and would enable more nuanced exploration of the full diversity of sexual orientation, including bisexuality and asexuality,” they wrote.
During the telebriefing discussion, Dr. Neale said the study supports the nuances in sexuality espoused by self-identified sexual orientation communities. “I think those things that we’ve learned include the idea that there is more diversity out there in the world. We see that diversity in the genetic analysis. And we reinforce that sort of message that the expanding acronyms in the LGBTQIA+ [lesbian, gay, bisexual, transgender, queer, intersex, asexual, and other] is justified.”
The study “underscores that there is an element of biology and it underscores that there’s an element of the environment,” he said. “And it underscores that this is a natural part of our species and so these are the things that both matter and there’s no way to get away from that idea.”
Several entities funded the study, including the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Dr. Ganna reported no financial conflicts. Two of the researchers and members of the 23andMe research team are 23andMe employees or hold stock options in the company. Another researcher is affiliated with Deep Genomics as a member of its scientific advisory board.
SOURCE: Ganna A et al. Science. 2019 Aug 30. doi: 10.1126/science.aat769.
A large study that reliably shows a genetic component to nonheterosexuality could have far-reaching societal and legal impact, Melinda C. Mills, PhD, wrote in an accompanying editorial (Science. 2019 Aug 30. doi: 10.1126/science.aay2726).
“Studies have indicated that same-sex orientation and behavior has a genetic basis and runs in families, yet specific genetic variants have not been isolated,” Dr. Mills wrote. “Evidence that sexual orientation has a biological component could shape acceptance and legal protection: 4%-10% of individuals report ever engaging in same-sex behavior in the United States, so this could affect a sizable proportion of the population.”
The half-million subject genome-wide association study by Ganna et al. could go a long way toward achieving that goal – much farther than prior studies, all of which were smaller and unreplicated.
“The genetic basis of same-sex orientation and sexual behavior has evaded discovery, largely because of the challenges of using small and nonrepresentative cohorts,” Dr. Mills wrote. “Initial evidence focused mostly on gay men, providing indirect and often speculative evidence of a relationship with fraternal birth order, prenatal exposure to sex hormones, neurodevelopmental traits, or maternal immunization to sex-specific proteins. Work in the 1990s isolated a relationship with the Xq28 region on the X chromosome. Subsequent studies found similarity in the sexual orientation of identical twins, with genetics explaining 18% (for women) and 37% (for men), with the remainder accounted for by directly shared environments (such as family or school) and nonshared environments (such as legalization or norms regarding same-sex behavior).”
Despite these findings, and others hinting at a heritable genetic cause, specific variants have not been identified – until now. The finding of five predictive genes, including two specific to males and one specific to females, is novel and exciting.
Attributing same-sex orientation to genetics could enhance civil rights or reduce stigma, she wrote. “Conversely, there are fears it provides a tool for intervention or ‘cure.’ Same-sex orientation has been classified as pathological and illegal, and remains criminalized in more than 70 countries, some with the death penalty.”
By calculating the overall potential genetic contribution of 8%-25% along with the identification of specific genetic loci, Ganna et al. showed “the potential magnitude of genetic effects that we may eventually measure and a sign that complex behaviors continue to have small, likely polygenic, influences.”
Dr. Mills is the Nuffield Professor of Sociology at the University of Oxford (England). She had no relevant financial disclosures.
A large study that reliably shows a genetic component to nonheterosexuality could have far-reaching societal and legal impact, Melinda C. Mills, PhD, wrote in an accompanying editorial (Science. 2019 Aug 30. doi: 10.1126/science.aay2726).
“Studies have indicated that same-sex orientation and behavior has a genetic basis and runs in families, yet specific genetic variants have not been isolated,” Dr. Mills wrote. “Evidence that sexual orientation has a biological component could shape acceptance and legal protection: 4%-10% of individuals report ever engaging in same-sex behavior in the United States, so this could affect a sizable proportion of the population.”
The half-million subject genome-wide association study by Ganna et al. could go a long way toward achieving that goal – much farther than prior studies, all of which were smaller and unreplicated.
“The genetic basis of same-sex orientation and sexual behavior has evaded discovery, largely because of the challenges of using small and nonrepresentative cohorts,” Dr. Mills wrote. “Initial evidence focused mostly on gay men, providing indirect and often speculative evidence of a relationship with fraternal birth order, prenatal exposure to sex hormones, neurodevelopmental traits, or maternal immunization to sex-specific proteins. Work in the 1990s isolated a relationship with the Xq28 region on the X chromosome. Subsequent studies found similarity in the sexual orientation of identical twins, with genetics explaining 18% (for women) and 37% (for men), with the remainder accounted for by directly shared environments (such as family or school) and nonshared environments (such as legalization or norms regarding same-sex behavior).”
Despite these findings, and others hinting at a heritable genetic cause, specific variants have not been identified – until now. The finding of five predictive genes, including two specific to males and one specific to females, is novel and exciting.
Attributing same-sex orientation to genetics could enhance civil rights or reduce stigma, she wrote. “Conversely, there are fears it provides a tool for intervention or ‘cure.’ Same-sex orientation has been classified as pathological and illegal, and remains criminalized in more than 70 countries, some with the death penalty.”
By calculating the overall potential genetic contribution of 8%-25% along with the identification of specific genetic loci, Ganna et al. showed “the potential magnitude of genetic effects that we may eventually measure and a sign that complex behaviors continue to have small, likely polygenic, influences.”
Dr. Mills is the Nuffield Professor of Sociology at the University of Oxford (England). She had no relevant financial disclosures.
A large study that reliably shows a genetic component to nonheterosexuality could have far-reaching societal and legal impact, Melinda C. Mills, PhD, wrote in an accompanying editorial (Science. 2019 Aug 30. doi: 10.1126/science.aay2726).
“Studies have indicated that same-sex orientation and behavior has a genetic basis and runs in families, yet specific genetic variants have not been isolated,” Dr. Mills wrote. “Evidence that sexual orientation has a biological component could shape acceptance and legal protection: 4%-10% of individuals report ever engaging in same-sex behavior in the United States, so this could affect a sizable proportion of the population.”
The half-million subject genome-wide association study by Ganna et al. could go a long way toward achieving that goal – much farther than prior studies, all of which were smaller and unreplicated.
“The genetic basis of same-sex orientation and sexual behavior has evaded discovery, largely because of the challenges of using small and nonrepresentative cohorts,” Dr. Mills wrote. “Initial evidence focused mostly on gay men, providing indirect and often speculative evidence of a relationship with fraternal birth order, prenatal exposure to sex hormones, neurodevelopmental traits, or maternal immunization to sex-specific proteins. Work in the 1990s isolated a relationship with the Xq28 region on the X chromosome. Subsequent studies found similarity in the sexual orientation of identical twins, with genetics explaining 18% (for women) and 37% (for men), with the remainder accounted for by directly shared environments (such as family or school) and nonshared environments (such as legalization or norms regarding same-sex behavior).”
Despite these findings, and others hinting at a heritable genetic cause, specific variants have not been identified – until now. The finding of five predictive genes, including two specific to males and one specific to females, is novel and exciting.
Attributing same-sex orientation to genetics could enhance civil rights or reduce stigma, she wrote. “Conversely, there are fears it provides a tool for intervention or ‘cure.’ Same-sex orientation has been classified as pathological and illegal, and remains criminalized in more than 70 countries, some with the death penalty.”
By calculating the overall potential genetic contribution of 8%-25% along with the identification of specific genetic loci, Ganna et al. showed “the potential magnitude of genetic effects that we may eventually measure and a sign that complex behaviors continue to have small, likely polygenic, influences.”
Dr. Mills is the Nuffield Professor of Sociology at the University of Oxford (England). She had no relevant financial disclosures.
There is no single “gay gene.”
There are, however, signals that nonheterosexual behavior has at least some genetic component, according to Andrea Ganna, PhD, and colleagues.
Five candidate genes found in a half-million subject genetic study each account for less than 1% of the variance in same-sex sexual behavior, the scientists found. Over the entire genome, genetic variants accounted for less than a quarter of such behavior.
None of the genetic signals can reliably predict sexual behavior, Benjamin Neale, PhD, director of genetics in the Stanley Center for Psychiatric Research at the Broad Institute of the Massachusetts Institute of Technology and Harvard Medical School, both in Boston, said in a telebriefing that included Dr. Ganna, a postdoctoral researcher in his lab. Instead, the variability of human sexuality is an entirely natural continuum of human behavior.
“Whether we are attracted exclusively to the opposite sex, the same sex, or both sexes falls along a spectrum that is an integral, and entirely normal, part of the human experience,” said Dr. Neale. “The choice of a sexual partner and the fraction of partners that are of the same sex are all consistent with this diversity being a key feature of our sexual behavior as a species and this diversity is a natural part of being human.”
The study, published in Science, clarifies findings of smaller, previous studies, which determined that sexual behavior is a combination of genetics and environment – although environment is a much more difficult association to assess.
“[Environment] can range from anything in utero, all the way all the way through who you happen to stand next to on the tube in the morning, right? That’s all potentially environmental factors that can have some influence on complex traits and so we don’t really understand,” Dr. Neale said.
However, he added, the concept of individual choice in sexual behaviors was beyond the scope of the study, which strictly centered on genetic associations with sexual behavior.
The study combined genetic information from three extant databases (the U.K. Biobank, National Longitudinal Study of Adolescent to Adult Health, the Molecular Genetic Study of Sexual Orientation, and the Child and Adolescent Twin Study in Sweden) with newly collected data from 23andMe, the technology company that provides at-home genetics tests largely used to determine ethnic origin.
The primary phenotype investigated was a binary measure: self-reported sexual behavior with someone of the same sex (nonheterosexuality) or someone of the opposite sex (heterosexuality).
“The binary variable also collapses rich and multifaceted diversity among nonheterosexuality individuals, wrote Dr. Ganna and his coauthors. Therefore, “we explored finer-scaled measurements and some of the complexities of the phenotype, although intricacies of the social and cultural influences on sexuality made it impossible to fully explore this complexity.”
The team also performed replication analyses on three smaller datasets: the Molecular Genetic Study of Sexual Orientation (2,308 U.S. adult males), Add Health (4,755 U.S. young adults), and the Child and Adolescent Twin Study in Sweden (8,093 Swedish adolescents). Data were available for 188,825 males and 220,170 females overall. When broken down by sexual behavior, data were available for 1,766 homosexual and 180,431 heterosexual males, and 693 homosexual and 214,062 heterosexual females.
The team identified two genes that significantly predicted same-sex sexual behavior (rs11114975-12q21.31 and rs10261857-7q31.2). Two more genes predicted same-sex sexual behavior in males only (rs28371400-15q21.3 and rs34730029-11q12.1), and one additional gene predicted the behavior in females only (rs13135637-4p14).
Three of the single nucleotide polymorphisms (SNPs) nominally replicated those in some of the other datasets, despite the much smaller sample sizes.
“The SNPs that reached genome-wide significance had very small effects (odds ratio, 1.1),” the authors wrote. “For example, in the U.K. Biobank, males with a GT genotype at the rs34730029 locus had 0.4% higher prevalence of same-sex sexual behavior than those with a TT genotype. Nevertheless, the contribution of all measured common SNPs in aggregate was estimated to [account for] 8%-25% of variation in female and male same-sex sexual behavior. … The discrepancy between the variance captured by the significant SNPs and all common SNPs suggests that same-sex sexual behavior, like most complex human traits, is influenced by the small, additive effects of very many genetic variants, most of which cannot be detected at the current sample size.”
The Child and Adolescent Twin Study in Sweden contained the youngest subjects. The polygenic scores in this dataset were significantly associated with sexual attraction at age 15 years, “suggesting that at least some of the genetic influences on same-sex sexual behavior manifest early in sexual development.”
The team also investigated the biological pathways associated with the SNPs. Among the male variants, rs34730029-11q12.1 contains numerous olfactory receptor genes.
“Second, rs28371400-15q21.3 had several indications of being involved in sex hormone regulation. The allele positively associated with same-sex sexual behavior is associated with higher rate of male pattern balding, in which sex-hormone sensitivity is implicated,” they wrote.
This is located near the TCF12 gene, related to a normal gonadal development in mice.
Among women, there were inverse associations with the level of sex hormone–binding globulin, which regulates the balance between testosterone and estrogen.
There were significant associations with some mental health traits, including loneliness, openness to experience, and risky behaviors such as smoking and using cannabis. There were also associations with depression and schizophrenia. The genetic correlations for bipolar disorder, cannabis use, and number of sexual partners were significantly higher in females than in males.
“We emphasize that the causal processes underlying these genetic correlations are unclear and could be generated by environmental factors relating to prejudice against individuals engaging in same-sex sexual behavior,” the authors wrote.
In an interview, Jack Drescher, MD, said he was not surprised by the findings and cited the results a twin study by J. Michael Bailey, PhD, and Richard C. Pillard, MD, as evidence of the complexities surrounding sexual orientation. The study examined the likelihood of one twin having a gay twin (Arch Gen Psychiatry. 1991 Dec;48[12]:1089-96).
“If you were a gay identical twin, you had a 52% chance of having a gay twin, he said. “If you were a gay fraternal twin, you only had a 22% chance of having a gay twin. The chance of an adoptive brother being gay was 11%. If homosexuality were simply a result of simple genetic transmission, then one would expect closer to 100% gay identical twins, since they both have the same genes.”
Dr. Drescher, clinical professor of psychiatry at the Center for Psychoanalytic Training and Research at Columbia University, New York, has written extensively about human sexuality, gender-conversion therapies, and gender.
The study by Dr. Ganna and associates as a whole invalidates several commonly used sexual behavior scales, including the Kinsey Scale, which is solely predicated upon self-reported attraction. The Klein Sexual Orientation Grid, which measures sexual behavior, fantasies, and sexual identification, is similarly problematic, the authors noted.
“Overall, our findings suggest that the most popular measures are based on a misconception of the underlying structure of sexual orientation and may need to be rethought. In particular, using separate measures of attraction to the opposite sex and attraction to the same sex, such as in the Sell Assessment of Sexual Orientation, would remove the assumption that these variables are perfectly inversely related and would enable more nuanced exploration of the full diversity of sexual orientation, including bisexuality and asexuality,” they wrote.
During the telebriefing discussion, Dr. Neale said the study supports the nuances in sexuality espoused by self-identified sexual orientation communities. “I think those things that we’ve learned include the idea that there is more diversity out there in the world. We see that diversity in the genetic analysis. And we reinforce that sort of message that the expanding acronyms in the LGBTQIA+ [lesbian, gay, bisexual, transgender, queer, intersex, asexual, and other] is justified.”
The study “underscores that there is an element of biology and it underscores that there’s an element of the environment,” he said. “And it underscores that this is a natural part of our species and so these are the things that both matter and there’s no way to get away from that idea.”
Several entities funded the study, including the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Dr. Ganna reported no financial conflicts. Two of the researchers and members of the 23andMe research team are 23andMe employees or hold stock options in the company. Another researcher is affiliated with Deep Genomics as a member of its scientific advisory board.
SOURCE: Ganna A et al. Science. 2019 Aug 30. doi: 10.1126/science.aat769.
There is no single “gay gene.”
There are, however, signals that nonheterosexual behavior has at least some genetic component, according to Andrea Ganna, PhD, and colleagues.
Five candidate genes found in a half-million subject genetic study each account for less than 1% of the variance in same-sex sexual behavior, the scientists found. Over the entire genome, genetic variants accounted for less than a quarter of such behavior.
None of the genetic signals can reliably predict sexual behavior, Benjamin Neale, PhD, director of genetics in the Stanley Center for Psychiatric Research at the Broad Institute of the Massachusetts Institute of Technology and Harvard Medical School, both in Boston, said in a telebriefing that included Dr. Ganna, a postdoctoral researcher in his lab. Instead, the variability of human sexuality is an entirely natural continuum of human behavior.
“Whether we are attracted exclusively to the opposite sex, the same sex, or both sexes falls along a spectrum that is an integral, and entirely normal, part of the human experience,” said Dr. Neale. “The choice of a sexual partner and the fraction of partners that are of the same sex are all consistent with this diversity being a key feature of our sexual behavior as a species and this diversity is a natural part of being human.”
The study, published in Science, clarifies findings of smaller, previous studies, which determined that sexual behavior is a combination of genetics and environment – although environment is a much more difficult association to assess.
“[Environment] can range from anything in utero, all the way all the way through who you happen to stand next to on the tube in the morning, right? That’s all potentially environmental factors that can have some influence on complex traits and so we don’t really understand,” Dr. Neale said.
However, he added, the concept of individual choice in sexual behaviors was beyond the scope of the study, which strictly centered on genetic associations with sexual behavior.
The study combined genetic information from three extant databases (the U.K. Biobank, National Longitudinal Study of Adolescent to Adult Health, the Molecular Genetic Study of Sexual Orientation, and the Child and Adolescent Twin Study in Sweden) with newly collected data from 23andMe, the technology company that provides at-home genetics tests largely used to determine ethnic origin.
The primary phenotype investigated was a binary measure: self-reported sexual behavior with someone of the same sex (nonheterosexuality) or someone of the opposite sex (heterosexuality).
“The binary variable also collapses rich and multifaceted diversity among nonheterosexuality individuals, wrote Dr. Ganna and his coauthors. Therefore, “we explored finer-scaled measurements and some of the complexities of the phenotype, although intricacies of the social and cultural influences on sexuality made it impossible to fully explore this complexity.”
The team also performed replication analyses on three smaller datasets: the Molecular Genetic Study of Sexual Orientation (2,308 U.S. adult males), Add Health (4,755 U.S. young adults), and the Child and Adolescent Twin Study in Sweden (8,093 Swedish adolescents). Data were available for 188,825 males and 220,170 females overall. When broken down by sexual behavior, data were available for 1,766 homosexual and 180,431 heterosexual males, and 693 homosexual and 214,062 heterosexual females.
The team identified two genes that significantly predicted same-sex sexual behavior (rs11114975-12q21.31 and rs10261857-7q31.2). Two more genes predicted same-sex sexual behavior in males only (rs28371400-15q21.3 and rs34730029-11q12.1), and one additional gene predicted the behavior in females only (rs13135637-4p14).
Three of the single nucleotide polymorphisms (SNPs) nominally replicated those in some of the other datasets, despite the much smaller sample sizes.
“The SNPs that reached genome-wide significance had very small effects (odds ratio, 1.1),” the authors wrote. “For example, in the U.K. Biobank, males with a GT genotype at the rs34730029 locus had 0.4% higher prevalence of same-sex sexual behavior than those with a TT genotype. Nevertheless, the contribution of all measured common SNPs in aggregate was estimated to [account for] 8%-25% of variation in female and male same-sex sexual behavior. … The discrepancy between the variance captured by the significant SNPs and all common SNPs suggests that same-sex sexual behavior, like most complex human traits, is influenced by the small, additive effects of very many genetic variants, most of which cannot be detected at the current sample size.”
The Child and Adolescent Twin Study in Sweden contained the youngest subjects. The polygenic scores in this dataset were significantly associated with sexual attraction at age 15 years, “suggesting that at least some of the genetic influences on same-sex sexual behavior manifest early in sexual development.”
The team also investigated the biological pathways associated with the SNPs. Among the male variants, rs34730029-11q12.1 contains numerous olfactory receptor genes.
“Second, rs28371400-15q21.3 had several indications of being involved in sex hormone regulation. The allele positively associated with same-sex sexual behavior is associated with higher rate of male pattern balding, in which sex-hormone sensitivity is implicated,” they wrote.
This is located near the TCF12 gene, related to a normal gonadal development in mice.
Among women, there were inverse associations with the level of sex hormone–binding globulin, which regulates the balance between testosterone and estrogen.
There were significant associations with some mental health traits, including loneliness, openness to experience, and risky behaviors such as smoking and using cannabis. There were also associations with depression and schizophrenia. The genetic correlations for bipolar disorder, cannabis use, and number of sexual partners were significantly higher in females than in males.
“We emphasize that the causal processes underlying these genetic correlations are unclear and could be generated by environmental factors relating to prejudice against individuals engaging in same-sex sexual behavior,” the authors wrote.
In an interview, Jack Drescher, MD, said he was not surprised by the findings and cited the results a twin study by J. Michael Bailey, PhD, and Richard C. Pillard, MD, as evidence of the complexities surrounding sexual orientation. The study examined the likelihood of one twin having a gay twin (Arch Gen Psychiatry. 1991 Dec;48[12]:1089-96).
“If you were a gay identical twin, you had a 52% chance of having a gay twin, he said. “If you were a gay fraternal twin, you only had a 22% chance of having a gay twin. The chance of an adoptive brother being gay was 11%. If homosexuality were simply a result of simple genetic transmission, then one would expect closer to 100% gay identical twins, since they both have the same genes.”
Dr. Drescher, clinical professor of psychiatry at the Center for Psychoanalytic Training and Research at Columbia University, New York, has written extensively about human sexuality, gender-conversion therapies, and gender.
The study by Dr. Ganna and associates as a whole invalidates several commonly used sexual behavior scales, including the Kinsey Scale, which is solely predicated upon self-reported attraction. The Klein Sexual Orientation Grid, which measures sexual behavior, fantasies, and sexual identification, is similarly problematic, the authors noted.
“Overall, our findings suggest that the most popular measures are based on a misconception of the underlying structure of sexual orientation and may need to be rethought. In particular, using separate measures of attraction to the opposite sex and attraction to the same sex, such as in the Sell Assessment of Sexual Orientation, would remove the assumption that these variables are perfectly inversely related and would enable more nuanced exploration of the full diversity of sexual orientation, including bisexuality and asexuality,” they wrote.
During the telebriefing discussion, Dr. Neale said the study supports the nuances in sexuality espoused by self-identified sexual orientation communities. “I think those things that we’ve learned include the idea that there is more diversity out there in the world. We see that diversity in the genetic analysis. And we reinforce that sort of message that the expanding acronyms in the LGBTQIA+ [lesbian, gay, bisexual, transgender, queer, intersex, asexual, and other] is justified.”
The study “underscores that there is an element of biology and it underscores that there’s an element of the environment,” he said. “And it underscores that this is a natural part of our species and so these are the things that both matter and there’s no way to get away from that idea.”
Several entities funded the study, including the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Dr. Ganna reported no financial conflicts. Two of the researchers and members of the 23andMe research team are 23andMe employees or hold stock options in the company. Another researcher is affiliated with Deep Genomics as a member of its scientific advisory board.
SOURCE: Ganna A et al. Science. 2019 Aug 30. doi: 10.1126/science.aat769.
FROM SCIENCE
Key clinical point: Genetic variants do appear to contribute to same-sex sexual behaviors.
Major finding: Five single nucleotide polymorphisms each account for about 1% of the variability in sexual behavior, while across a large population, genetic variants account for 8%-25% of the variation.
Study details: The genome-wide association study was made up of about 500,000 subjects.
Disclosures: The study was funded by several entities, including the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Dr. Ganna reported no financial conflicts. Two of the researchers and members of the 23andMe research team are 23andMe employees or hold stock options in the company. Another researcher is affiliated with Deep Genomics as a member of its scientific advisory board.
Source: Ganna A et al. Science. 2019 Aug 30. doi: 10.1126/science.aat769.
Successful Treatment of Refractory Epidermolysis Bullosa Acquisita With Intravenous Immunoglobulin and Dapsone
To the Editor:
Evidence-based recommendations for optimal medical management of patients with immunobullous diseases prior to elective surgery are sparse.1,2 There is an uncertain balance between the use of immunomodulators and immunosuppressants, and implementation of these agents is heavily weighted against an increased infection risk from both active disease with denuded skin and suboptimal wound healing due to iatrogenic immunosuppression.1-5 Historically, clinical management of epidermolysis bullosa acquisita (EBA) seldomly has resulted in substantial disease resolution.1,3,4 Herein, we describe a case of recalcitrant EBA that was treated with a combination of intravenous immunoglobulin (IVIG) and dapsone, which resulted in a favorable clinical response and successful hip arthroplasty without cutaneous complications.
A 66-year-old man presented to an outside clinic with nonhealing ulcers on the oral mucosa, hands, groin, and feet. He was treated with systemic steroids after a histologic examination suggested bullous pemphigoid, but the lesions did not exhibit any appreciable improvement after several months of treatment. Despite the lack of improvement, the patient was continued on systemic steroids with a waxing and waning disease course.
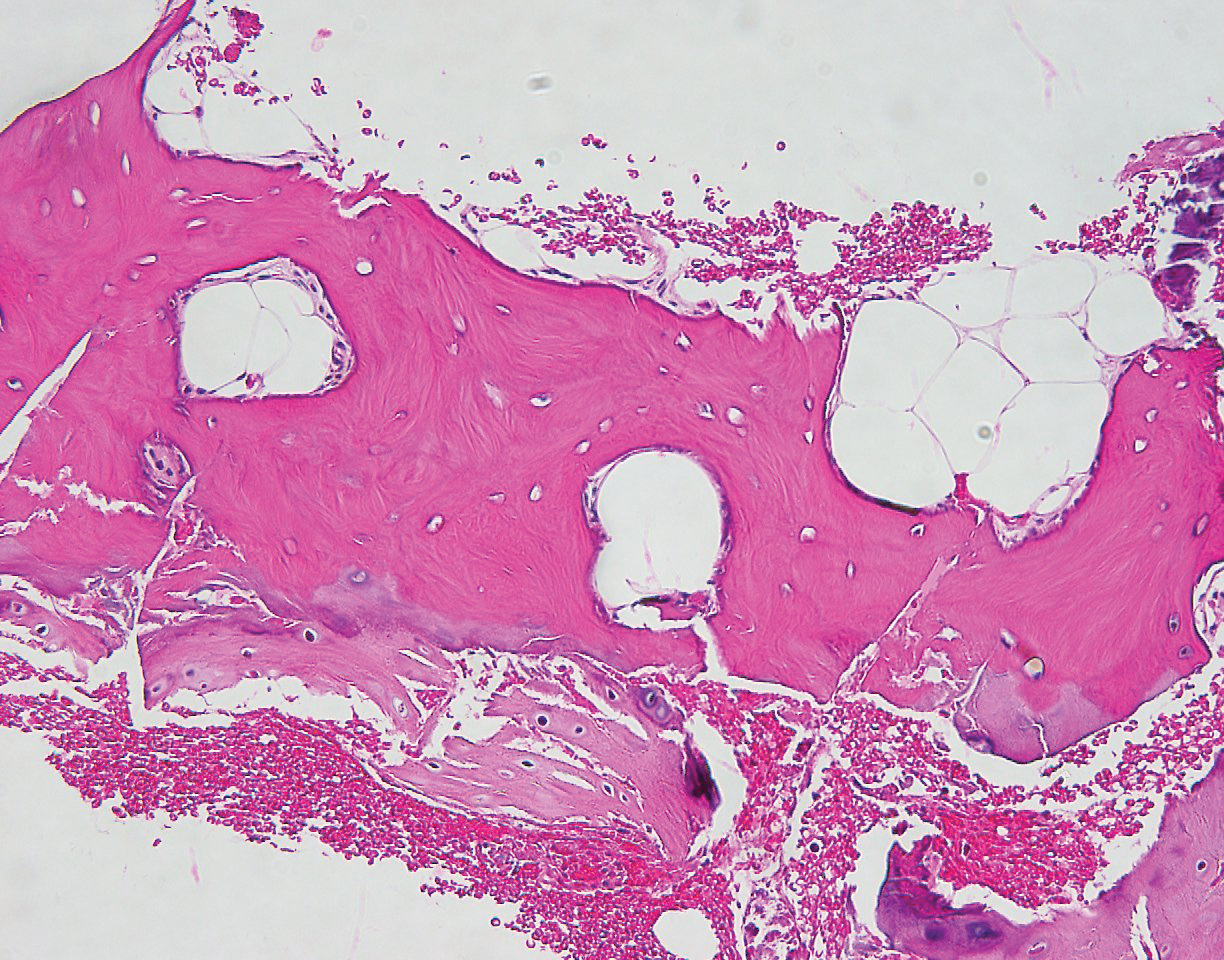
Within a year, the patient presented to an orthopedist at our institution with severe left hip pain that had been limiting his mobility and had become unresponsive to conservative therapy. Radiologic investigations suggested advanced osteoarthritis and avascular necrosis of the left hip. Surgical intervention was delayed, as his orthopedist expressed concern that the extent of the body surface area affected by cutaneous denudation placed him at an unacceptable risk for infection. The orthopedic surgeon then referred the patient to our clinic for evaluation of the lesions. Physical examination revealed numerous crusted erosions in various stages of healing on the oral mucosa, palms, groin, and soles. Repeat biopsy of a denuded ulcer on the patient’s arm was obtained by our providers (nearly 1 year after the first biopsy by the outside physician). Histologic examination showed a pauci-immune subepidermal blister without acantholysis, which in combination with the clinical presentation of tense bullae on trauma-prone surfaces led to a favored diagnosis of EBA.
The patient began trials of several immunomodulatory and immunosuppressive agents, both in isolation and in combination, including systemic steroids, mycophenolate mofetil, four 1000-mg infusions of rituximab, and dapsone. Although results were suboptimal, dapsone 150 mg once daily for 3 months yielded the greatest clinical improvement with subsequent granulation and/or re-epithelialization of the chronic ulcers. After discussion during our department’s Grand Rounds, it was determined that the patient should undergo a trial of IVIG infusions, which were initiated with a loading dose of 2000 mg/kg over 5 consecutive days, followed by once-monthly maintenance infusion doses of 1200 mg/kg for 4 consecutive months. While receiving IVIG, he was maintained on a once-daily dose of dapsone 150 mg
Following this treatment regimen, he was noted to have marked improvement with only few scattered healing erosions. Upon completion of his last IVIG infusion, his cutaneous and mucosal manifestations of EBA were greatly minimized, demonstrating the best level of control that had been achieved during the disease course (Figure 1). This therapy completely cleared the cutaneous and mucosal ulcerations, thus permitting the patient to undergo a total left hip arthroplasty without complications (Figure 2).
Our report is novel in that it supports a combination of IVIG and dapsone as a viable presurgical therapy for patients with EBA, and this treatment also may be applicable for other primary immunobullous disorders.2,5 Our case was particularly challenging in that the severity of the patient’s bullous disease precluded him from an elective orthopedic joint replacement due to the risk for wound dehiscence and surgical site infection.2 We determined that IVIG and dapsone would be the most optimal combination therapy to facilitate superior disease control and concurrently allow for appropriate wound healing without impairing the host immune response. This report is unique from a clinical perspective in that a balance was successfully achieved between immune suppression, with avoidance of associated side effects, and disease activity.
- Ahmed AR, Gürcan HM. Treatment of epidermolysis bullosa acquisita with intravenous immunoglobulin in patients non-responsive to conventional therapy: clinical outcome and post-treatment long-term follow-up [published online August 8, 2011]. J Eur Acad Dermatol Venereol. 2012;26:1074-1083.
- Rubin J, Touloei K, Favreau T, et al. Mohs surgery in patients immunobullous diseases: should prednisone be increased prior to surgery? J Clin Aesthet Dermatol. 2014;7:45-46.
- Ishii N, Hamada T, Dainichi T, et al. Epidermolysis bullosa acquisita: what’s new? J Dermatol. 2010;37:220-230.
- Mosqueira CB, Furlani Lde A, Xavier AF, et al. Intravenous immunoglobulin for treatment of severe acquired bullous epidermolysis refractory to conventional immunosuppressive therapy. An Bras Dermatol. 2010;85:521-524.
- Ludwig RJ. Clinical presentation, pathogenesis, diagnosis, and treatment of EBA. ISRN Dermatology. 2013;2013:812029.
To the Editor:
Evidence-based recommendations for optimal medical management of patients with immunobullous diseases prior to elective surgery are sparse.1,2 There is an uncertain balance between the use of immunomodulators and immunosuppressants, and implementation of these agents is heavily weighted against an increased infection risk from both active disease with denuded skin and suboptimal wound healing due to iatrogenic immunosuppression.1-5 Historically, clinical management of epidermolysis bullosa acquisita (EBA) seldomly has resulted in substantial disease resolution.1,3,4 Herein, we describe a case of recalcitrant EBA that was treated with a combination of intravenous immunoglobulin (IVIG) and dapsone, which resulted in a favorable clinical response and successful hip arthroplasty without cutaneous complications.
A 66-year-old man presented to an outside clinic with nonhealing ulcers on the oral mucosa, hands, groin, and feet. He was treated with systemic steroids after a histologic examination suggested bullous pemphigoid, but the lesions did not exhibit any appreciable improvement after several months of treatment. Despite the lack of improvement, the patient was continued on systemic steroids with a waxing and waning disease course.
Within a year, the patient presented to an orthopedist at our institution with severe left hip pain that had been limiting his mobility and had become unresponsive to conservative therapy. Radiologic investigations suggested advanced osteoarthritis and avascular necrosis of the left hip. Surgical intervention was delayed, as his orthopedist expressed concern that the extent of the body surface area affected by cutaneous denudation placed him at an unacceptable risk for infection. The orthopedic surgeon then referred the patient to our clinic for evaluation of the lesions. Physical examination revealed numerous crusted erosions in various stages of healing on the oral mucosa, palms, groin, and soles. Repeat biopsy of a denuded ulcer on the patient’s arm was obtained by our providers (nearly 1 year after the first biopsy by the outside physician). Histologic examination showed a pauci-immune subepidermal blister without acantholysis, which in combination with the clinical presentation of tense bullae on trauma-prone surfaces led to a favored diagnosis of EBA.
The patient began trials of several immunomodulatory and immunosuppressive agents, both in isolation and in combination, including systemic steroids, mycophenolate mofetil, four 1000-mg infusions of rituximab, and dapsone. Although results were suboptimal, dapsone 150 mg once daily for 3 months yielded the greatest clinical improvement with subsequent granulation and/or re-epithelialization of the chronic ulcers. After discussion during our department’s Grand Rounds, it was determined that the patient should undergo a trial of IVIG infusions, which were initiated with a loading dose of 2000 mg/kg over 5 consecutive days, followed by once-monthly maintenance infusion doses of 1200 mg/kg for 4 consecutive months. While receiving IVIG, he was maintained on a once-daily dose of dapsone 150 mg
Following this treatment regimen, he was noted to have marked improvement with only few scattered healing erosions. Upon completion of his last IVIG infusion, his cutaneous and mucosal manifestations of EBA were greatly minimized, demonstrating the best level of control that had been achieved during the disease course (Figure 1). This therapy completely cleared the cutaneous and mucosal ulcerations, thus permitting the patient to undergo a total left hip arthroplasty without complications (Figure 2).
Our report is novel in that it supports a combination of IVIG and dapsone as a viable presurgical therapy for patients with EBA, and this treatment also may be applicable for other primary immunobullous disorders.2,5 Our case was particularly challenging in that the severity of the patient’s bullous disease precluded him from an elective orthopedic joint replacement due to the risk for wound dehiscence and surgical site infection.2 We determined that IVIG and dapsone would be the most optimal combination therapy to facilitate superior disease control and concurrently allow for appropriate wound healing without impairing the host immune response. This report is unique from a clinical perspective in that a balance was successfully achieved between immune suppression, with avoidance of associated side effects, and disease activity.
To the Editor:
Evidence-based recommendations for optimal medical management of patients with immunobullous diseases prior to elective surgery are sparse.1,2 There is an uncertain balance between the use of immunomodulators and immunosuppressants, and implementation of these agents is heavily weighted against an increased infection risk from both active disease with denuded skin and suboptimal wound healing due to iatrogenic immunosuppression.1-5 Historically, clinical management of epidermolysis bullosa acquisita (EBA) seldomly has resulted in substantial disease resolution.1,3,4 Herein, we describe a case of recalcitrant EBA that was treated with a combination of intravenous immunoglobulin (IVIG) and dapsone, which resulted in a favorable clinical response and successful hip arthroplasty without cutaneous complications.
A 66-year-old man presented to an outside clinic with nonhealing ulcers on the oral mucosa, hands, groin, and feet. He was treated with systemic steroids after a histologic examination suggested bullous pemphigoid, but the lesions did not exhibit any appreciable improvement after several months of treatment. Despite the lack of improvement, the patient was continued on systemic steroids with a waxing and waning disease course.
Within a year, the patient presented to an orthopedist at our institution with severe left hip pain that had been limiting his mobility and had become unresponsive to conservative therapy. Radiologic investigations suggested advanced osteoarthritis and avascular necrosis of the left hip. Surgical intervention was delayed, as his orthopedist expressed concern that the extent of the body surface area affected by cutaneous denudation placed him at an unacceptable risk for infection. The orthopedic surgeon then referred the patient to our clinic for evaluation of the lesions. Physical examination revealed numerous crusted erosions in various stages of healing on the oral mucosa, palms, groin, and soles. Repeat biopsy of a denuded ulcer on the patient’s arm was obtained by our providers (nearly 1 year after the first biopsy by the outside physician). Histologic examination showed a pauci-immune subepidermal blister without acantholysis, which in combination with the clinical presentation of tense bullae on trauma-prone surfaces led to a favored diagnosis of EBA.
The patient began trials of several immunomodulatory and immunosuppressive agents, both in isolation and in combination, including systemic steroids, mycophenolate mofetil, four 1000-mg infusions of rituximab, and dapsone. Although results were suboptimal, dapsone 150 mg once daily for 3 months yielded the greatest clinical improvement with subsequent granulation and/or re-epithelialization of the chronic ulcers. After discussion during our department’s Grand Rounds, it was determined that the patient should undergo a trial of IVIG infusions, which were initiated with a loading dose of 2000 mg/kg over 5 consecutive days, followed by once-monthly maintenance infusion doses of 1200 mg/kg for 4 consecutive months. While receiving IVIG, he was maintained on a once-daily dose of dapsone 150 mg
Following this treatment regimen, he was noted to have marked improvement with only few scattered healing erosions. Upon completion of his last IVIG infusion, his cutaneous and mucosal manifestations of EBA were greatly minimized, demonstrating the best level of control that had been achieved during the disease course (Figure 1). This therapy completely cleared the cutaneous and mucosal ulcerations, thus permitting the patient to undergo a total left hip arthroplasty without complications (Figure 2).
Our report is novel in that it supports a combination of IVIG and dapsone as a viable presurgical therapy for patients with EBA, and this treatment also may be applicable for other primary immunobullous disorders.2,5 Our case was particularly challenging in that the severity of the patient’s bullous disease precluded him from an elective orthopedic joint replacement due to the risk for wound dehiscence and surgical site infection.2 We determined that IVIG and dapsone would be the most optimal combination therapy to facilitate superior disease control and concurrently allow for appropriate wound healing without impairing the host immune response. This report is unique from a clinical perspective in that a balance was successfully achieved between immune suppression, with avoidance of associated side effects, and disease activity.
- Ahmed AR, Gürcan HM. Treatment of epidermolysis bullosa acquisita with intravenous immunoglobulin in patients non-responsive to conventional therapy: clinical outcome and post-treatment long-term follow-up [published online August 8, 2011]. J Eur Acad Dermatol Venereol. 2012;26:1074-1083.
- Rubin J, Touloei K, Favreau T, et al. Mohs surgery in patients immunobullous diseases: should prednisone be increased prior to surgery? J Clin Aesthet Dermatol. 2014;7:45-46.
- Ishii N, Hamada T, Dainichi T, et al. Epidermolysis bullosa acquisita: what’s new? J Dermatol. 2010;37:220-230.
- Mosqueira CB, Furlani Lde A, Xavier AF, et al. Intravenous immunoglobulin for treatment of severe acquired bullous epidermolysis refractory to conventional immunosuppressive therapy. An Bras Dermatol. 2010;85:521-524.
- Ludwig RJ. Clinical presentation, pathogenesis, diagnosis, and treatment of EBA. ISRN Dermatology. 2013;2013:812029.
- Ahmed AR, Gürcan HM. Treatment of epidermolysis bullosa acquisita with intravenous immunoglobulin in patients non-responsive to conventional therapy: clinical outcome and post-treatment long-term follow-up [published online August 8, 2011]. J Eur Acad Dermatol Venereol. 2012;26:1074-1083.
- Rubin J, Touloei K, Favreau T, et al. Mohs surgery in patients immunobullous diseases: should prednisone be increased prior to surgery? J Clin Aesthet Dermatol. 2014;7:45-46.
- Ishii N, Hamada T, Dainichi T, et al. Epidermolysis bullosa acquisita: what’s new? J Dermatol. 2010;37:220-230.
- Mosqueira CB, Furlani Lde A, Xavier AF, et al. Intravenous immunoglobulin for treatment of severe acquired bullous epidermolysis refractory to conventional immunosuppressive therapy. An Bras Dermatol. 2010;85:521-524.
- Ludwig RJ. Clinical presentation, pathogenesis, diagnosis, and treatment of EBA. ISRN Dermatology. 2013;2013:812029.
Practice Points
- Treatment of epidermolysis bullosa acquisita (EBA) is difficult, and most treatment regimens are based on anecdotal reports.
- Systemic corticosteroids have been the mainstay of therapy for severe or extensive disease but impose an increased risk for postoperative complications including surgical site infections.
- A steroid-sparing regimen of intravenous immunoglobulin and systemic dapsone may be used when rapid clearance of EBA is needed prior to elective surgery.
What is your diagnosis? - September 2019
Erosive protein-losing enteropathy secondary to disseminated histoplasmosis
This patient was treated with amphotericin B and transitioned to oral itraconazole with frequent blood level monitoring to ensure absorption. His symptoms improved gradually. Small-bowel enteroscopy 3 weeks after presentation showed a normal duodenum and healing, superficial ulcers in the proximal jejunum (Figure F, G). Blood albumin levels had recovered to 3.1 g/dL (normal, 3.5–5.0 g/dL).
Protein-losing enteropathy (PLE) is a rare syndrome characterized by loss of serum proteins in the gastrointestinal (GI) tract, resulting in significant hypoproteinemia and consequent edema.1 PLE can also result in ascites, pleural and pericardial effusions, and, in prolonged cases, malnutrition. There are a variety of causes of PLE that can be broadly grouped into erosive GI disorders, disorders of increased GI mucosal permeability, and disorders of increased interstitial pressure. The clinical presentation depends on the underlying etiology, but commonly includes generalized edema owing to hypoproteinemia and resulting reduced oncotic pressure. GI symptoms are not frequently observed. The initial step in evaluating a patient with symptoms concerning for PLE is to rule out more common causes of hypoproteinemia, such as renal or hepatic disease, and malnutrition. To confirm enteric protein loss, alpha 1-antitrypsin clearance with a 24-hour stool collection is commonly and reliably used. Treatment of PLE is centered on treating the underlying cause while monitoring and treating malnutrition, including micronutrient deficiencies.
Fungal infections are a rare cause of PLE, but important to recognize as a potential complication of tumor necrosis factor–therapy, because these medications are commonly used for a variety of autoimmune diseases.2 Although histoplasmosis is an uncommon cause of GI inflammation, disseminated histoplasmosis causing PLE has been previously reported.3 In our patient, Histoplasma capsulatum infection caused diffuse GI ulcers, which allowed protein loss in the GI tract (erosive PLE). Antifungal treatment resulted in healing of intestinal ulcers and correction of hypoalbuminemia, thereby confirming the diagnosis of PLE and obviating the need for a confirmatory alpha 1-antitrypsin clearance study.
References
1. Umar SB, DiBaise JK. Protein-losing enteropathy: case illustrations and clinical review. Am J Gastroenterol. 2010;105:43-9.
2. Tsiodras S, Samonis G, Boumpas DT. et al. Fungal infections complicating tumor necrosis factor alpha blockade therapy. Mayo Clin Proc. 2008;83:181-94.
3. Kok J, Chen SC, Anderson L, et al. Protein-losing enteropathy and hypogammaglobulinaemia as first manifestations of disseminated histoplasmosis coincident with Nocardia infection. J Med Microbiol. 2010;59:610-3.
Erosive protein-losing enteropathy secondary to disseminated histoplasmosis
This patient was treated with amphotericin B and transitioned to oral itraconazole with frequent blood level monitoring to ensure absorption. His symptoms improved gradually. Small-bowel enteroscopy 3 weeks after presentation showed a normal duodenum and healing, superficial ulcers in the proximal jejunum (Figure F, G). Blood albumin levels had recovered to 3.1 g/dL (normal, 3.5–5.0 g/dL).
Protein-losing enteropathy (PLE) is a rare syndrome characterized by loss of serum proteins in the gastrointestinal (GI) tract, resulting in significant hypoproteinemia and consequent edema.1 PLE can also result in ascites, pleural and pericardial effusions, and, in prolonged cases, malnutrition. There are a variety of causes of PLE that can be broadly grouped into erosive GI disorders, disorders of increased GI mucosal permeability, and disorders of increased interstitial pressure. The clinical presentation depends on the underlying etiology, but commonly includes generalized edema owing to hypoproteinemia and resulting reduced oncotic pressure. GI symptoms are not frequently observed. The initial step in evaluating a patient with symptoms concerning for PLE is to rule out more common causes of hypoproteinemia, such as renal or hepatic disease, and malnutrition. To confirm enteric protein loss, alpha 1-antitrypsin clearance with a 24-hour stool collection is commonly and reliably used. Treatment of PLE is centered on treating the underlying cause while monitoring and treating malnutrition, including micronutrient deficiencies.
Fungal infections are a rare cause of PLE, but important to recognize as a potential complication of tumor necrosis factor–therapy, because these medications are commonly used for a variety of autoimmune diseases.2 Although histoplasmosis is an uncommon cause of GI inflammation, disseminated histoplasmosis causing PLE has been previously reported.3 In our patient, Histoplasma capsulatum infection caused diffuse GI ulcers, which allowed protein loss in the GI tract (erosive PLE). Antifungal treatment resulted in healing of intestinal ulcers and correction of hypoalbuminemia, thereby confirming the diagnosis of PLE and obviating the need for a confirmatory alpha 1-antitrypsin clearance study.
References
1. Umar SB, DiBaise JK. Protein-losing enteropathy: case illustrations and clinical review. Am J Gastroenterol. 2010;105:43-9.
2. Tsiodras S, Samonis G, Boumpas DT. et al. Fungal infections complicating tumor necrosis factor alpha blockade therapy. Mayo Clin Proc. 2008;83:181-94.
3. Kok J, Chen SC, Anderson L, et al. Protein-losing enteropathy and hypogammaglobulinaemia as first manifestations of disseminated histoplasmosis coincident with Nocardia infection. J Med Microbiol. 2010;59:610-3.
Erosive protein-losing enteropathy secondary to disseminated histoplasmosis
This patient was treated with amphotericin B and transitioned to oral itraconazole with frequent blood level monitoring to ensure absorption. His symptoms improved gradually. Small-bowel enteroscopy 3 weeks after presentation showed a normal duodenum and healing, superficial ulcers in the proximal jejunum (Figure F, G). Blood albumin levels had recovered to 3.1 g/dL (normal, 3.5–5.0 g/dL).
Protein-losing enteropathy (PLE) is a rare syndrome characterized by loss of serum proteins in the gastrointestinal (GI) tract, resulting in significant hypoproteinemia and consequent edema.1 PLE can also result in ascites, pleural and pericardial effusions, and, in prolonged cases, malnutrition. There are a variety of causes of PLE that can be broadly grouped into erosive GI disorders, disorders of increased GI mucosal permeability, and disorders of increased interstitial pressure. The clinical presentation depends on the underlying etiology, but commonly includes generalized edema owing to hypoproteinemia and resulting reduced oncotic pressure. GI symptoms are not frequently observed. The initial step in evaluating a patient with symptoms concerning for PLE is to rule out more common causes of hypoproteinemia, such as renal or hepatic disease, and malnutrition. To confirm enteric protein loss, alpha 1-antitrypsin clearance with a 24-hour stool collection is commonly and reliably used. Treatment of PLE is centered on treating the underlying cause while monitoring and treating malnutrition, including micronutrient deficiencies.
Fungal infections are a rare cause of PLE, but important to recognize as a potential complication of tumor necrosis factor–therapy, because these medications are commonly used for a variety of autoimmune diseases.2 Although histoplasmosis is an uncommon cause of GI inflammation, disseminated histoplasmosis causing PLE has been previously reported.3 In our patient, Histoplasma capsulatum infection caused diffuse GI ulcers, which allowed protein loss in the GI tract (erosive PLE). Antifungal treatment resulted in healing of intestinal ulcers and correction of hypoalbuminemia, thereby confirming the diagnosis of PLE and obviating the need for a confirmatory alpha 1-antitrypsin clearance study.
References
1. Umar SB, DiBaise JK. Protein-losing enteropathy: case illustrations and clinical review. Am J Gastroenterol. 2010;105:43-9.
2. Tsiodras S, Samonis G, Boumpas DT. et al. Fungal infections complicating tumor necrosis factor alpha blockade therapy. Mayo Clin Proc. 2008;83:181-94.
3. Kok J, Chen SC, Anderson L, et al. Protein-losing enteropathy and hypogammaglobulinaemia as first manifestations of disseminated histoplasmosis coincident with Nocardia infection. J Med Microbiol. 2010;59:610-3.
A 34-year-old man with a medical history of psoriasis, on adalimumab, presented with a 2-week history of progressively worsening abdominal pain, nausea, vomiting, melenic diarrhea, subjective fevers, and generalized weakness. One week into the illness, he developed progressive bilateral extremity and scrotal swelling.
His vital signs included a temperature of 36.8°C, heart rate of 104 beats per minute, respiratory rate of 18 breaths per minute, and a blood pressure of 114/71 mm Hg. The physical examination was notable for a well-nourished appearance, diffuse abdominal tenderness to palpation without distension, organomegaly, or rigidity, and pitting lower extremity edema.
Laboratory evaluation showed hemoglobin 10.3 g/dL (normal, 13.5–17.5 g/dL), leukocytes 10 × 109/L (normal, 3.5–10.5 × 109/L), platelets 212 × 109/L (normal, 150–450 × 109/L), sodium 131 mmol/L (normal, 135–145 mmol/L), creatinine 1 mg/dL (normal, 0.8–1.3 mg/dL), albumin 1.8 g/dL (normal, 3.5–5.0 g/dL), and C-reactive protein 53 mg/L (normal, less than 8 mg/L). Liver chemistries were all normal.
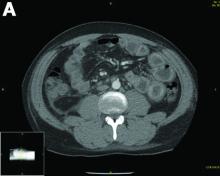
Urinalysis was unremarkable with normal urine protein levels. The enteric pathogen panel by polymerase chain reaction was negative. Computed tomography (CT) of the abdomen and pelvis showed marked circumferential wall thickening with mural enhancement of multiple loops of jejunum (Figure A).
Small-bowel enteroscopy showed diffuse erosions in the entire duodenum and many oozing superficial ulcers with edematous and erythematous mucosa in the proximal jejunum (Figures B, C).
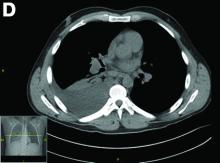
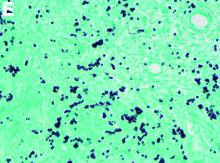
CT scan of the chest showed right lower lobe consolidation associated with a large right pleural effusion, and mediastinal, bilateral, hilar and abdominal lymphadenopathy (Figure D). Endobronchial ultrasound-guided transbronchial biopsy of lymph nodes was positive for oval-shaped organisms exhibiting narrow-based budding on GMS stain (Figure E).
Based on the clinical scenario and images, what is the most likely diagnosis?
Idiopathic Bilateral Auricular Ossificans
To the Editor:
A 60-year-old man with a history of basal cell carcinoma, rosacea, and seborrheic dermatitis presented for a routine skin examination. The patient mentioned incidentally that both of his ears were “rock hard” and had been so for the last 10 to 20 years. He was not experiencing hearing abnormalities and denied any history of external ear trauma, frostbite injury of the ears, or history of endocrinopathy. Physical examination revealed normal-appearing skin on the bilateral ears (Figure 1), and palpation confirmed a bonelike consistency of the auricles with sparing of the earlobes. The differential diagnosis included osteoma cutis, ectopic calcification, tophaceous gout, localized scleroderma, and relapsing polychondritis. Incisional biopsy of the left posterior auricle to the level of cartilage revealed a histologically normal epidermis and dermis, with small fragments of cartilage calcification and lacunar bone formation (Figure 2). A radiograph of the skull showed faint calcification of the auricular cartilage, but no other osseous abnormalities were observed (Figure 3). Further laboratory workup including a comprehensive metabolic panel; complete blood cell count; and thyroid stimulating hormone, parathyroid hormone, and cortisol levels were normal. Based on these findings, a diagnosis of bilateral idiopathic auricular ossificans was made. Therapy was not pursued because the patient was asymptomatic, but referral to otolaryngology would have been considered if hearing impairment had occurred.
with auricular ossificans. Palpation of the auricle revealed a
bonelike consistency.
Auricular ossificans, which is characterized by the replacement of external ear cartilage by bone, is a rare condition with as few as 22 histologically proven cases documented in the literature.1,2 One case was reported in 2012 with consistent clinical and radiographic findings, but the patient declined biopsy.3 Similar to our patient, many pathologically documented cases have been determined to be idiopathic after workup, with identifiable triggering factors including cold injury, trauma, perichondritis, Addison disease, diabetes, and postpartum hypopituitarism.1 The male-to-female ratio is 18 to 5, the average age at diagnosis is 57 years, and as many as 70% of cases have demonstrated bilateral involvement.1,2
The majority of cases of auricular ossificans are asymptomatic at presentation with an insidious onset of the disease process over several years. Physical examination of the ear generally reveals a petrified auricle with sparing of the lobule and an otherwise normal clinical appearance. Radiographs demonstrate calcification, sometimes exactly mimicking the pattern seen in normal bone. Biopsy and histologic analysis show not only calcified cartilage but also actual lamellar bone formation.4 Depending on the precipitating factors, laboratory workup may uncover underlying metabolic abnormalities but often is unremarkable. Expert opinion generally recommends against extensive workup, which should be guided by the clinical presentation and the physician’s judgement.5 An insufficient number of patients with auricular ossificans have been definitively identified to provide clearer evidence-based recommendations.
Most patients present without pain or hearing abnormalities and do not require treatment. In one case, involvement of both the auricle and external ear canal resulted in intractable cerumen impaction that caused conductive hearing loss, eventually requiring resection of the ossified external ear cartilage and tragus.6 The most common reason for treatment has been discomfort impairing sleep, with surgical intervention including conchal reduction or wedge resection.5 A combined paucity of cases and poor understanding of the pathophysiologic mechanisms behind auricular ossificans limits current therapeutic options. Fortunately, this process appears to be benign in the majority of patients and generally represents a phenomenon that is much more interesting to the clinician than it is vexing to the patient.
- Calderon-Komaromy A, Cordoba S, Tardio JC, et al. Bilateral ossification of the auricular cartilage [published online November 28, 2014]. Actas Dermosifiliogr. 2015;106:433-435.
- Chang KH, Kim DK, Kim JH, et al. Idiopathic acquired ectopic auricular ossification: a case report and review of the literature. Ear Nose Throat J. 2011;90:424-427.
- Buikema KE, Adams EG. A rare case of petrified ear [published online October 15, 2012]. Case Rep Dermatol Med. 2012;2012:410601.
- Mastronikolis NS, Zampakis P, Kalogeropoulou C, et al. Bilateral ossification of the auricles: an unusual entity and review of the literature. Head Face Med. 2009;5:17.
- High WA, Larson MJ, Hoang MP. Idiopathic bilateral auricular ossificans: a case report and review of the literature. Arch Pathol Lab Med. 2004;128:1432-1434.
- Manni JJ, Berénos-Riley LC. Ossification of the external ear: a case report and review of the literature [published online June 18, 2005]. Eur Arch Otorhinolaryngol. 2005;262:961-964.
To the Editor:
A 60-year-old man with a history of basal cell carcinoma, rosacea, and seborrheic dermatitis presented for a routine skin examination. The patient mentioned incidentally that both of his ears were “rock hard” and had been so for the last 10 to 20 years. He was not experiencing hearing abnormalities and denied any history of external ear trauma, frostbite injury of the ears, or history of endocrinopathy. Physical examination revealed normal-appearing skin on the bilateral ears (Figure 1), and palpation confirmed a bonelike consistency of the auricles with sparing of the earlobes. The differential diagnosis included osteoma cutis, ectopic calcification, tophaceous gout, localized scleroderma, and relapsing polychondritis. Incisional biopsy of the left posterior auricle to the level of cartilage revealed a histologically normal epidermis and dermis, with small fragments of cartilage calcification and lacunar bone formation (Figure 2). A radiograph of the skull showed faint calcification of the auricular cartilage, but no other osseous abnormalities were observed (Figure 3). Further laboratory workup including a comprehensive metabolic panel; complete blood cell count; and thyroid stimulating hormone, parathyroid hormone, and cortisol levels were normal. Based on these findings, a diagnosis of bilateral idiopathic auricular ossificans was made. Therapy was not pursued because the patient was asymptomatic, but referral to otolaryngology would have been considered if hearing impairment had occurred.
with auricular ossificans. Palpation of the auricle revealed a
bonelike consistency.
Auricular ossificans, which is characterized by the replacement of external ear cartilage by bone, is a rare condition with as few as 22 histologically proven cases documented in the literature.1,2 One case was reported in 2012 with consistent clinical and radiographic findings, but the patient declined biopsy.3 Similar to our patient, many pathologically documented cases have been determined to be idiopathic after workup, with identifiable triggering factors including cold injury, trauma, perichondritis, Addison disease, diabetes, and postpartum hypopituitarism.1 The male-to-female ratio is 18 to 5, the average age at diagnosis is 57 years, and as many as 70% of cases have demonstrated bilateral involvement.1,2
The majority of cases of auricular ossificans are asymptomatic at presentation with an insidious onset of the disease process over several years. Physical examination of the ear generally reveals a petrified auricle with sparing of the lobule and an otherwise normal clinical appearance. Radiographs demonstrate calcification, sometimes exactly mimicking the pattern seen in normal bone. Biopsy and histologic analysis show not only calcified cartilage but also actual lamellar bone formation.4 Depending on the precipitating factors, laboratory workup may uncover underlying metabolic abnormalities but often is unremarkable. Expert opinion generally recommends against extensive workup, which should be guided by the clinical presentation and the physician’s judgement.5 An insufficient number of patients with auricular ossificans have been definitively identified to provide clearer evidence-based recommendations.
Most patients present without pain or hearing abnormalities and do not require treatment. In one case, involvement of both the auricle and external ear canal resulted in intractable cerumen impaction that caused conductive hearing loss, eventually requiring resection of the ossified external ear cartilage and tragus.6 The most common reason for treatment has been discomfort impairing sleep, with surgical intervention including conchal reduction or wedge resection.5 A combined paucity of cases and poor understanding of the pathophysiologic mechanisms behind auricular ossificans limits current therapeutic options. Fortunately, this process appears to be benign in the majority of patients and generally represents a phenomenon that is much more interesting to the clinician than it is vexing to the patient.
To the Editor:
A 60-year-old man with a history of basal cell carcinoma, rosacea, and seborrheic dermatitis presented for a routine skin examination. The patient mentioned incidentally that both of his ears were “rock hard” and had been so for the last 10 to 20 years. He was not experiencing hearing abnormalities and denied any history of external ear trauma, frostbite injury of the ears, or history of endocrinopathy. Physical examination revealed normal-appearing skin on the bilateral ears (Figure 1), and palpation confirmed a bonelike consistency of the auricles with sparing of the earlobes. The differential diagnosis included osteoma cutis, ectopic calcification, tophaceous gout, localized scleroderma, and relapsing polychondritis. Incisional biopsy of the left posterior auricle to the level of cartilage revealed a histologically normal epidermis and dermis, with small fragments of cartilage calcification and lacunar bone formation (Figure 2). A radiograph of the skull showed faint calcification of the auricular cartilage, but no other osseous abnormalities were observed (Figure 3). Further laboratory workup including a comprehensive metabolic panel; complete blood cell count; and thyroid stimulating hormone, parathyroid hormone, and cortisol levels were normal. Based on these findings, a diagnosis of bilateral idiopathic auricular ossificans was made. Therapy was not pursued because the patient was asymptomatic, but referral to otolaryngology would have been considered if hearing impairment had occurred.
with auricular ossificans. Palpation of the auricle revealed a
bonelike consistency.
Auricular ossificans, which is characterized by the replacement of external ear cartilage by bone, is a rare condition with as few as 22 histologically proven cases documented in the literature.1,2 One case was reported in 2012 with consistent clinical and radiographic findings, but the patient declined biopsy.3 Similar to our patient, many pathologically documented cases have been determined to be idiopathic after workup, with identifiable triggering factors including cold injury, trauma, perichondritis, Addison disease, diabetes, and postpartum hypopituitarism.1 The male-to-female ratio is 18 to 5, the average age at diagnosis is 57 years, and as many as 70% of cases have demonstrated bilateral involvement.1,2
The majority of cases of auricular ossificans are asymptomatic at presentation with an insidious onset of the disease process over several years. Physical examination of the ear generally reveals a petrified auricle with sparing of the lobule and an otherwise normal clinical appearance. Radiographs demonstrate calcification, sometimes exactly mimicking the pattern seen in normal bone. Biopsy and histologic analysis show not only calcified cartilage but also actual lamellar bone formation.4 Depending on the precipitating factors, laboratory workup may uncover underlying metabolic abnormalities but often is unremarkable. Expert opinion generally recommends against extensive workup, which should be guided by the clinical presentation and the physician’s judgement.5 An insufficient number of patients with auricular ossificans have been definitively identified to provide clearer evidence-based recommendations.
Most patients present without pain or hearing abnormalities and do not require treatment. In one case, involvement of both the auricle and external ear canal resulted in intractable cerumen impaction that caused conductive hearing loss, eventually requiring resection of the ossified external ear cartilage and tragus.6 The most common reason for treatment has been discomfort impairing sleep, with surgical intervention including conchal reduction or wedge resection.5 A combined paucity of cases and poor understanding of the pathophysiologic mechanisms behind auricular ossificans limits current therapeutic options. Fortunately, this process appears to be benign in the majority of patients and generally represents a phenomenon that is much more interesting to the clinician than it is vexing to the patient.
- Calderon-Komaromy A, Cordoba S, Tardio JC, et al. Bilateral ossification of the auricular cartilage [published online November 28, 2014]. Actas Dermosifiliogr. 2015;106:433-435.
- Chang KH, Kim DK, Kim JH, et al. Idiopathic acquired ectopic auricular ossification: a case report and review of the literature. Ear Nose Throat J. 2011;90:424-427.
- Buikema KE, Adams EG. A rare case of petrified ear [published online October 15, 2012]. Case Rep Dermatol Med. 2012;2012:410601.
- Mastronikolis NS, Zampakis P, Kalogeropoulou C, et al. Bilateral ossification of the auricles: an unusual entity and review of the literature. Head Face Med. 2009;5:17.
- High WA, Larson MJ, Hoang MP. Idiopathic bilateral auricular ossificans: a case report and review of the literature. Arch Pathol Lab Med. 2004;128:1432-1434.
- Manni JJ, Berénos-Riley LC. Ossification of the external ear: a case report and review of the literature [published online June 18, 2005]. Eur Arch Otorhinolaryngol. 2005;262:961-964.
- Calderon-Komaromy A, Cordoba S, Tardio JC, et al. Bilateral ossification of the auricular cartilage [published online November 28, 2014]. Actas Dermosifiliogr. 2015;106:433-435.
- Chang KH, Kim DK, Kim JH, et al. Idiopathic acquired ectopic auricular ossification: a case report and review of the literature. Ear Nose Throat J. 2011;90:424-427.
- Buikema KE, Adams EG. A rare case of petrified ear [published online October 15, 2012]. Case Rep Dermatol Med. 2012;2012:410601.
- Mastronikolis NS, Zampakis P, Kalogeropoulou C, et al. Bilateral ossification of the auricles: an unusual entity and review of the literature. Head Face Med. 2009;5:17.
- High WA, Larson MJ, Hoang MP. Idiopathic bilateral auricular ossificans: a case report and review of the literature. Arch Pathol Lab Med. 2004;128:1432-1434.
- Manni JJ, Berénos-Riley LC. Ossification of the external ear: a case report and review of the literature [published online June 18, 2005]. Eur Arch Otorhinolaryngol. 2005;262:961-964.
Practice Points
- Auricular ossificans is a rare condition characterized by the replacement of external ear cartilage by bone.
- The majority of cases are asymptomatic at presentation with an insidious onset of the disease process over several years.
- Most patients present without pain or hearing abnormalities and do not require treatment.
Severe lipodystrophy linked to pembrolizumab
according to a case study.
A 47-year-old woman received pembrolizumab to treat metastatic melanoma and developed immune-related generalized acquired lipodystrophy. The condition has persisted 12 months after she stopped taking pembrolizumab.
Julie Delyon, MD, PhD, of Saint-Louis Hospital in Paris, and colleagues described this case in the British Journal of Dermatology.
The patient was diagnosed with BRAF-mutated, stage IV melanoma with bone and lymph node metastases. She received pembrolizumab at 2 mg/kg every 3 weeks as first-line treatment. She achieved a complete response and was still in remission at last follow-up.
The patient was obese at baseline, with a body mass index of 40 kg/m2, but she did not have diabetes, hepatic steatosis, or dyslipidemia.
Within 2 months of starting pembrolizumab, the patient observed “some major changes to her physical appearance,” according to Dr. Delyon and colleagues. At 10 months, the patient had severe lipodystrophy.
The patient experienced a change in fat distribution – namely, severe peripheral lipoatrophy and an accumulation of trunk fat. Imaging revealed a decrease in subcutaneous adipose tissue, which contrasted with an increase in visceral fat observed from baseline.
The patient also developed “moderate hirsutism, facial and limb atrophy, and prominent forearm and leg muscles and veins,” according to the authors. She had impaired glucose tolerance with insulin resistance, reduced concentrations of leptin and adiponectin, hypertriglyceridemia, a low level of HDL cholesterol, and hepatic steatosis.
Analyses of subcutaneous fat revealed adipose tissue atrophy with edema, lipophages, and CD3+/CD4+ T-cell infiltration of the fat and vessel walls. This suggested that the lipodystrophy had an autoimmune origin, according to the authors.
The patient had no family history of autoimmune disease or lipodystrophy. She tested negative for mutations in 23 genes associated with generalized lipodystrophy.
The patient also tested negative for HIV, antinuclear antibodies, native anti-DNA, and anti-insulin receptor antibodies. There were no signs of panniculitis, and the authors noted that “there were no arguments in favor of hyperthyroidism, Cushing syndrome, or acromegaly.”
In an attempt to reverse the lipodystrophy, the researchers stopped pembrolizumab treatment. The patient was treated for diabetes and hypertriglyceridemia as well. She could not receive corticosteroids because of the risk of severe metabolic complications, and she didn’t receive metreleptin because it wasn’t available. The patient still had lipodystrophy 12 months after stopping pembrolizumab.
Dr. Delyon and colleagues wrote that this case suggests pembrolizumab, and perhaps other anti–programmed death 1 therapies, may cause lipodystrophy with severe metabolic complications. “The long-term side effects of such metabolic adverse events, although rare, are unknown and will probably become a topic of utmost importance, considering the increasing rate of remission following ICIs and their use in the adjuvant setting.”
Two coauthors reported relationships with Merck, which markets pembrolizumab as Keytruda. The authors also reported relationships with Bristol-Myers Squibb, Pierre Fabre, Takeda, Innate Pharma, LEO Pharma, Roche, GlaxoSmithKline, Novartis, and Amgen.
SOURCE: Delyon J et al. Br J Dermatol. 2019 May 11. doi: 10.1111/bjd.18124.
according to a case study.
A 47-year-old woman received pembrolizumab to treat metastatic melanoma and developed immune-related generalized acquired lipodystrophy. The condition has persisted 12 months after she stopped taking pembrolizumab.
Julie Delyon, MD, PhD, of Saint-Louis Hospital in Paris, and colleagues described this case in the British Journal of Dermatology.
The patient was diagnosed with BRAF-mutated, stage IV melanoma with bone and lymph node metastases. She received pembrolizumab at 2 mg/kg every 3 weeks as first-line treatment. She achieved a complete response and was still in remission at last follow-up.
The patient was obese at baseline, with a body mass index of 40 kg/m2, but she did not have diabetes, hepatic steatosis, or dyslipidemia.
Within 2 months of starting pembrolizumab, the patient observed “some major changes to her physical appearance,” according to Dr. Delyon and colleagues. At 10 months, the patient had severe lipodystrophy.
The patient experienced a change in fat distribution – namely, severe peripheral lipoatrophy and an accumulation of trunk fat. Imaging revealed a decrease in subcutaneous adipose tissue, which contrasted with an increase in visceral fat observed from baseline.
The patient also developed “moderate hirsutism, facial and limb atrophy, and prominent forearm and leg muscles and veins,” according to the authors. She had impaired glucose tolerance with insulin resistance, reduced concentrations of leptin and adiponectin, hypertriglyceridemia, a low level of HDL cholesterol, and hepatic steatosis.
Analyses of subcutaneous fat revealed adipose tissue atrophy with edema, lipophages, and CD3+/CD4+ T-cell infiltration of the fat and vessel walls. This suggested that the lipodystrophy had an autoimmune origin, according to the authors.
The patient had no family history of autoimmune disease or lipodystrophy. She tested negative for mutations in 23 genes associated with generalized lipodystrophy.
The patient also tested negative for HIV, antinuclear antibodies, native anti-DNA, and anti-insulin receptor antibodies. There were no signs of panniculitis, and the authors noted that “there were no arguments in favor of hyperthyroidism, Cushing syndrome, or acromegaly.”
In an attempt to reverse the lipodystrophy, the researchers stopped pembrolizumab treatment. The patient was treated for diabetes and hypertriglyceridemia as well. She could not receive corticosteroids because of the risk of severe metabolic complications, and she didn’t receive metreleptin because it wasn’t available. The patient still had lipodystrophy 12 months after stopping pembrolizumab.
Dr. Delyon and colleagues wrote that this case suggests pembrolizumab, and perhaps other anti–programmed death 1 therapies, may cause lipodystrophy with severe metabolic complications. “The long-term side effects of such metabolic adverse events, although rare, are unknown and will probably become a topic of utmost importance, considering the increasing rate of remission following ICIs and their use in the adjuvant setting.”
Two coauthors reported relationships with Merck, which markets pembrolizumab as Keytruda. The authors also reported relationships with Bristol-Myers Squibb, Pierre Fabre, Takeda, Innate Pharma, LEO Pharma, Roche, GlaxoSmithKline, Novartis, and Amgen.
SOURCE: Delyon J et al. Br J Dermatol. 2019 May 11. doi: 10.1111/bjd.18124.
according to a case study.
A 47-year-old woman received pembrolizumab to treat metastatic melanoma and developed immune-related generalized acquired lipodystrophy. The condition has persisted 12 months after she stopped taking pembrolizumab.
Julie Delyon, MD, PhD, of Saint-Louis Hospital in Paris, and colleagues described this case in the British Journal of Dermatology.
The patient was diagnosed with BRAF-mutated, stage IV melanoma with bone and lymph node metastases. She received pembrolizumab at 2 mg/kg every 3 weeks as first-line treatment. She achieved a complete response and was still in remission at last follow-up.
The patient was obese at baseline, with a body mass index of 40 kg/m2, but she did not have diabetes, hepatic steatosis, or dyslipidemia.
Within 2 months of starting pembrolizumab, the patient observed “some major changes to her physical appearance,” according to Dr. Delyon and colleagues. At 10 months, the patient had severe lipodystrophy.
The patient experienced a change in fat distribution – namely, severe peripheral lipoatrophy and an accumulation of trunk fat. Imaging revealed a decrease in subcutaneous adipose tissue, which contrasted with an increase in visceral fat observed from baseline.
The patient also developed “moderate hirsutism, facial and limb atrophy, and prominent forearm and leg muscles and veins,” according to the authors. She had impaired glucose tolerance with insulin resistance, reduced concentrations of leptin and adiponectin, hypertriglyceridemia, a low level of HDL cholesterol, and hepatic steatosis.
Analyses of subcutaneous fat revealed adipose tissue atrophy with edema, lipophages, and CD3+/CD4+ T-cell infiltration of the fat and vessel walls. This suggested that the lipodystrophy had an autoimmune origin, according to the authors.
The patient had no family history of autoimmune disease or lipodystrophy. She tested negative for mutations in 23 genes associated with generalized lipodystrophy.
The patient also tested negative for HIV, antinuclear antibodies, native anti-DNA, and anti-insulin receptor antibodies. There were no signs of panniculitis, and the authors noted that “there were no arguments in favor of hyperthyroidism, Cushing syndrome, or acromegaly.”
In an attempt to reverse the lipodystrophy, the researchers stopped pembrolizumab treatment. The patient was treated for diabetes and hypertriglyceridemia as well. She could not receive corticosteroids because of the risk of severe metabolic complications, and she didn’t receive metreleptin because it wasn’t available. The patient still had lipodystrophy 12 months after stopping pembrolizumab.
Dr. Delyon and colleagues wrote that this case suggests pembrolizumab, and perhaps other anti–programmed death 1 therapies, may cause lipodystrophy with severe metabolic complications. “The long-term side effects of such metabolic adverse events, although rare, are unknown and will probably become a topic of utmost importance, considering the increasing rate of remission following ICIs and their use in the adjuvant setting.”
Two coauthors reported relationships with Merck, which markets pembrolizumab as Keytruda. The authors also reported relationships with Bristol-Myers Squibb, Pierre Fabre, Takeda, Innate Pharma, LEO Pharma, Roche, GlaxoSmithKline, Novartis, and Amgen.
SOURCE: Delyon J et al. Br J Dermatol. 2019 May 11. doi: 10.1111/bjd.18124.
FROM THE BRITISH JOURNAL OF DERMATOLOGY
Two rheumatologists join MDedge Rheumatology editorial advisory board
.
Dr. Oliver is an assistant professor of clinical pediatrics in the department of pediatric rheumatology at Indiana University and practices at Riley Hospital for Children, both in Indianapolis. She completed her training in pediatrics at New Jersey Medical School, Newark, and Pediatric Rheumatology at Stanford (Calif.) University.
Her research interests include improving patient outcomes in the juvenile spondyloarthropathy and chronic nonbacterial osteomyelitis populations. She is an active member of the Childhood Arthritis & Rheumatology Research Alliance.
Dr. Kwoh is director of the University of Arizona Arthritis Center, Tucson. He holds the Charles A.L. and Suzanne M. Stephens Endowed Chair in Rheumatology and is the chief of the division of rheumatology and professor of medicine and medical imaging at the university.
His current major research interests focus on the identification of biomarkers – most notably MRI imaging biomarkers for the development and/or progression of knee OA and the characterization of knee pain patterns in OA. He also has a major interest in the reduction and ultimately the elimination of disparities in the management of arthritis and musculoskeletal diseases.
.
Dr. Oliver is an assistant professor of clinical pediatrics in the department of pediatric rheumatology at Indiana University and practices at Riley Hospital for Children, both in Indianapolis. She completed her training in pediatrics at New Jersey Medical School, Newark, and Pediatric Rheumatology at Stanford (Calif.) University.
Her research interests include improving patient outcomes in the juvenile spondyloarthropathy and chronic nonbacterial osteomyelitis populations. She is an active member of the Childhood Arthritis & Rheumatology Research Alliance.
Dr. Kwoh is director of the University of Arizona Arthritis Center, Tucson. He holds the Charles A.L. and Suzanne M. Stephens Endowed Chair in Rheumatology and is the chief of the division of rheumatology and professor of medicine and medical imaging at the university.
His current major research interests focus on the identification of biomarkers – most notably MRI imaging biomarkers for the development and/or progression of knee OA and the characterization of knee pain patterns in OA. He also has a major interest in the reduction and ultimately the elimination of disparities in the management of arthritis and musculoskeletal diseases.
.
Dr. Oliver is an assistant professor of clinical pediatrics in the department of pediatric rheumatology at Indiana University and practices at Riley Hospital for Children, both in Indianapolis. She completed her training in pediatrics at New Jersey Medical School, Newark, and Pediatric Rheumatology at Stanford (Calif.) University.
Her research interests include improving patient outcomes in the juvenile spondyloarthropathy and chronic nonbacterial osteomyelitis populations. She is an active member of the Childhood Arthritis & Rheumatology Research Alliance.
Dr. Kwoh is director of the University of Arizona Arthritis Center, Tucson. He holds the Charles A.L. and Suzanne M. Stephens Endowed Chair in Rheumatology and is the chief of the division of rheumatology and professor of medicine and medical imaging at the university.
His current major research interests focus on the identification of biomarkers – most notably MRI imaging biomarkers for the development and/or progression of knee OA and the characterization of knee pain patterns in OA. He also has a major interest in the reduction and ultimately the elimination of disparities in the management of arthritis and musculoskeletal diseases.
Criminals in the psychiatric ED
Despite popular belief, the absence of a strong link between mental illness and violence has been well studied and established. In summary, in a small subset of patients, mental illness provides a minor increase in the risk of committing violence.1
In part as a result of this research, police departments across the country have established programs and protocols to divert patients with mental illness out of the legal system and into mental hospitals. Instead of accepting the common refrain that mental illness is the explanation and best predictor of all atrocious behaviors, police departments have correctly referred patients with mental illness to mental hospitals. We commend those initiatives and encourage their adoption in all locales. Yet, to safeguard such programs, we would like to warn of a potential pitfall and offer possible remedies.
Having worked in both correctional and clinical settings, we are saddened by the similar nature of the work with respect to the management of mental illness. It should defy logic to assume the need for mental health care in our jails is in any way comparable to the one in mental hospitals. However, we have grown accustomed to seeing large numbers of our most vulnerable patients with severe mental illness accumulating in our jails and correctional facilities, which often are the largest employers of mental health clinicians. The reasons correctional institutions have become so reliant on psychiatric clinicians are vast and complex. Incarceration is tremendously destabilizing and can lead to the onset or relapse of mental illness – even in the most resilient patients. In addition, mental illness is undertreated in our communities yet inescapable in the confined settings of our jails. Furthermore, our mass incarceration problems have resulted in the most disenfranchised populations, including our patients with mental illness, becoming the targets of policies criminalizing poverty.2
To prevent furthering the process by which our correctional facilities have become the new asylums,3 law enforcement agencies have enacted a vast array of initiatives. Some include the placement of mental health staff within emergency response teams. Some include training police officers in how to talk to patients with mental illness as well as how to deescalate mental health crises. Most of the initiatives have one common goal: diverting patients with mental illness who are better treated in mental hospitals from going to jail. However, herein lies the problem: If mental illness is an explanation for only a small subset of criminal behavior, why is there a large need to divert patients with mental illness from jails to mental hospitals?
Over the past few years, psychiatrists in emergency departments have noted a concerning trend: an increase in referrals to mental hospitals by law enforcement for what appears to be a crime with only a vague or obscure link to mental illness. Most psychiatrists who regularly work in emergency departments will witness many examples. Some might be fairly benign: “They were going to arrest me for trespassing; I was yelling at a coffee shop. But when I told them that I had run out of meds, they brought me here instead.”
However, some stories are more chilling, including the case of an older male who had made threats while shooting his gun in the air and was brought to the emergency department because, as the police officer told us, “I think that he is just depressed; you guys can keep him safe till he is better.”
We applaud society’s desire to reduce the criminalization of mental illness. We think that psychiatry should be deeply involved in the attempts to resolve this problem. Furthermore, we are cognizant that the number of patients with mental illness unnecessarily imprisoned as a result of prosecutorial zealousness is a larger problem than criminals inappropriately brought to mental hospitals. However, we also are aware of the limitation of psychiatric hospitals in solving nonpsychiatric problems.
Recent studies have demonstrated the need to examine criminogenic needs before psychiatric ones when attempting to reduce recidivism in all offenders, including those with mental illnesses.4 The emphasis on addressing psychiatric needs over criminogenic ones is misguided and not based on evidence. Yet, we appreciate the complexity of those questions and of individual cases.
Substance use disorders are emblematic of this problem. Psychiatry has now communicated the position that substance use disorders are mental illness and not a moral failing. However, are the crimes committed by individuals with substance use disorders, whether in a state of intoxication or driven by the cycles of addiction, the blameless result of mental illness? The legal system struggles with this question, trying to determine when addiction-related crimes should be referred to a diversion program or treated as a straightforward criminal prosecution. Those who favor diversion for addiction can point out that many criminal acts are associated with mitigating factors that are no less valid than is addiction.
However, those mitigating factors, such as poverty, childhood deprivation, or a violence-infused sociological milieu, cannot be found in the Diagnostic and Statistical Manual of Mental Disorders. As such, if those factors alone were considered, no diversion would be offered by the courts. There also can be unforeseen consequences to this bias for diversion or criminal prosecution. Violent outbursts are a recognized part of PTSD in veterans. Psychiatrists who work at Veterans Affairs can be faced with the diagnosis of PTSD being used as an excuse for violent behavior, which may, at some level be valid, but which can be dangerous in that labeling a patient with that diagnosis might lower the barriers to violent behavior by providing a ready-made explanation already internalized by the patient through unspoken, sociocultural norms.
With the awareness of the complex nature of the intersectionality of mental illness and criminality, we recommend improvements to current diversion programs. As diversion programs rightfully continue to expand across the country, we likely will see an increase in the number of referrals by police officers to our emergency departments. Some of the referrals will be considered “inappropriate” after thorough and thoughtful clinical evaluation by emergency psychiatrists. The inappropriateness might be secondary to an absence of active symptoms, an absence of correlation between the illness and the offense, or a more urgent criminogenic need.
When faced with someone who will not benefit from diversion to a psychiatric emergency department, psychiatrists should have the tools to revert the person back into the legal system. Those tools could come in many forms – law enforcement liaison, prosecution liaison, or simply the presence of officers who are mandated to wait for the approval of the clinician prior to dismissing legal charges. Whatever the solution might be for any particular locale, policy makers should not wait for adverse events to realize the potential pitfalls of the important work being done in developing our country’s diversion programs.
References
1. Swanson JW et al. Mental illness and reduction of gun violence and suicide: Bringing epidemiologic research to policy. Ann Epidemiol. 2015 May;25(5):366-76.
2. Ehrenreich B. “How America criminalized poverty.” The Guardian. 2011 Aug 10.
3. Roth A. “Prisons are the new asylums.” The Atlantic. 2018 April.
4. Latessa EJ et al. “What works (and doesn’t) in reducing recidivism.” New York: Routledge, 2015.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. Dr. Badre can be reached at his website, BadreMD.com. Dr. Lehman is an associate professor of psychiatry at the University of California, San Diego. He is codirector of all acute and intensive psychiatric treatment at the Veterans Affairs Medical Center in San Diego, where he practices clinical psychiatry. He also is the course director for the UCSD third-year medical student psychiatry clerkship.
Despite popular belief, the absence of a strong link between mental illness and violence has been well studied and established. In summary, in a small subset of patients, mental illness provides a minor increase in the risk of committing violence.1
In part as a result of this research, police departments across the country have established programs and protocols to divert patients with mental illness out of the legal system and into mental hospitals. Instead of accepting the common refrain that mental illness is the explanation and best predictor of all atrocious behaviors, police departments have correctly referred patients with mental illness to mental hospitals. We commend those initiatives and encourage their adoption in all locales. Yet, to safeguard such programs, we would like to warn of a potential pitfall and offer possible remedies.
Having worked in both correctional and clinical settings, we are saddened by the similar nature of the work with respect to the management of mental illness. It should defy logic to assume the need for mental health care in our jails is in any way comparable to the one in mental hospitals. However, we have grown accustomed to seeing large numbers of our most vulnerable patients with severe mental illness accumulating in our jails and correctional facilities, which often are the largest employers of mental health clinicians. The reasons correctional institutions have become so reliant on psychiatric clinicians are vast and complex. Incarceration is tremendously destabilizing and can lead to the onset or relapse of mental illness – even in the most resilient patients. In addition, mental illness is undertreated in our communities yet inescapable in the confined settings of our jails. Furthermore, our mass incarceration problems have resulted in the most disenfranchised populations, including our patients with mental illness, becoming the targets of policies criminalizing poverty.2
To prevent furthering the process by which our correctional facilities have become the new asylums,3 law enforcement agencies have enacted a vast array of initiatives. Some include the placement of mental health staff within emergency response teams. Some include training police officers in how to talk to patients with mental illness as well as how to deescalate mental health crises. Most of the initiatives have one common goal: diverting patients with mental illness who are better treated in mental hospitals from going to jail. However, herein lies the problem: If mental illness is an explanation for only a small subset of criminal behavior, why is there a large need to divert patients with mental illness from jails to mental hospitals?
Over the past few years, psychiatrists in emergency departments have noted a concerning trend: an increase in referrals to mental hospitals by law enforcement for what appears to be a crime with only a vague or obscure link to mental illness. Most psychiatrists who regularly work in emergency departments will witness many examples. Some might be fairly benign: “They were going to arrest me for trespassing; I was yelling at a coffee shop. But when I told them that I had run out of meds, they brought me here instead.”
However, some stories are more chilling, including the case of an older male who had made threats while shooting his gun in the air and was brought to the emergency department because, as the police officer told us, “I think that he is just depressed; you guys can keep him safe till he is better.”
We applaud society’s desire to reduce the criminalization of mental illness. We think that psychiatry should be deeply involved in the attempts to resolve this problem. Furthermore, we are cognizant that the number of patients with mental illness unnecessarily imprisoned as a result of prosecutorial zealousness is a larger problem than criminals inappropriately brought to mental hospitals. However, we also are aware of the limitation of psychiatric hospitals in solving nonpsychiatric problems.
Recent studies have demonstrated the need to examine criminogenic needs before psychiatric ones when attempting to reduce recidivism in all offenders, including those with mental illnesses.4 The emphasis on addressing psychiatric needs over criminogenic ones is misguided and not based on evidence. Yet, we appreciate the complexity of those questions and of individual cases.
Substance use disorders are emblematic of this problem. Psychiatry has now communicated the position that substance use disorders are mental illness and not a moral failing. However, are the crimes committed by individuals with substance use disorders, whether in a state of intoxication or driven by the cycles of addiction, the blameless result of mental illness? The legal system struggles with this question, trying to determine when addiction-related crimes should be referred to a diversion program or treated as a straightforward criminal prosecution. Those who favor diversion for addiction can point out that many criminal acts are associated with mitigating factors that are no less valid than is addiction.
However, those mitigating factors, such as poverty, childhood deprivation, or a violence-infused sociological milieu, cannot be found in the Diagnostic and Statistical Manual of Mental Disorders. As such, if those factors alone were considered, no diversion would be offered by the courts. There also can be unforeseen consequences to this bias for diversion or criminal prosecution. Violent outbursts are a recognized part of PTSD in veterans. Psychiatrists who work at Veterans Affairs can be faced with the diagnosis of PTSD being used as an excuse for violent behavior, which may, at some level be valid, but which can be dangerous in that labeling a patient with that diagnosis might lower the barriers to violent behavior by providing a ready-made explanation already internalized by the patient through unspoken, sociocultural norms.
With the awareness of the complex nature of the intersectionality of mental illness and criminality, we recommend improvements to current diversion programs. As diversion programs rightfully continue to expand across the country, we likely will see an increase in the number of referrals by police officers to our emergency departments. Some of the referrals will be considered “inappropriate” after thorough and thoughtful clinical evaluation by emergency psychiatrists. The inappropriateness might be secondary to an absence of active symptoms, an absence of correlation between the illness and the offense, or a more urgent criminogenic need.
When faced with someone who will not benefit from diversion to a psychiatric emergency department, psychiatrists should have the tools to revert the person back into the legal system. Those tools could come in many forms – law enforcement liaison, prosecution liaison, or simply the presence of officers who are mandated to wait for the approval of the clinician prior to dismissing legal charges. Whatever the solution might be for any particular locale, policy makers should not wait for adverse events to realize the potential pitfalls of the important work being done in developing our country’s diversion programs.
References
1. Swanson JW et al. Mental illness and reduction of gun violence and suicide: Bringing epidemiologic research to policy. Ann Epidemiol. 2015 May;25(5):366-76.
2. Ehrenreich B. “How America criminalized poverty.” The Guardian. 2011 Aug 10.
3. Roth A. “Prisons are the new asylums.” The Atlantic. 2018 April.
4. Latessa EJ et al. “What works (and doesn’t) in reducing recidivism.” New York: Routledge, 2015.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. Dr. Badre can be reached at his website, BadreMD.com. Dr. Lehman is an associate professor of psychiatry at the University of California, San Diego. He is codirector of all acute and intensive psychiatric treatment at the Veterans Affairs Medical Center in San Diego, where he practices clinical psychiatry. He also is the course director for the UCSD third-year medical student psychiatry clerkship.
Despite popular belief, the absence of a strong link between mental illness and violence has been well studied and established. In summary, in a small subset of patients, mental illness provides a minor increase in the risk of committing violence.1
In part as a result of this research, police departments across the country have established programs and protocols to divert patients with mental illness out of the legal system and into mental hospitals. Instead of accepting the common refrain that mental illness is the explanation and best predictor of all atrocious behaviors, police departments have correctly referred patients with mental illness to mental hospitals. We commend those initiatives and encourage their adoption in all locales. Yet, to safeguard such programs, we would like to warn of a potential pitfall and offer possible remedies.
Having worked in both correctional and clinical settings, we are saddened by the similar nature of the work with respect to the management of mental illness. It should defy logic to assume the need for mental health care in our jails is in any way comparable to the one in mental hospitals. However, we have grown accustomed to seeing large numbers of our most vulnerable patients with severe mental illness accumulating in our jails and correctional facilities, which often are the largest employers of mental health clinicians. The reasons correctional institutions have become so reliant on psychiatric clinicians are vast and complex. Incarceration is tremendously destabilizing and can lead to the onset or relapse of mental illness – even in the most resilient patients. In addition, mental illness is undertreated in our communities yet inescapable in the confined settings of our jails. Furthermore, our mass incarceration problems have resulted in the most disenfranchised populations, including our patients with mental illness, becoming the targets of policies criminalizing poverty.2
To prevent furthering the process by which our correctional facilities have become the new asylums,3 law enforcement agencies have enacted a vast array of initiatives. Some include the placement of mental health staff within emergency response teams. Some include training police officers in how to talk to patients with mental illness as well as how to deescalate mental health crises. Most of the initiatives have one common goal: diverting patients with mental illness who are better treated in mental hospitals from going to jail. However, herein lies the problem: If mental illness is an explanation for only a small subset of criminal behavior, why is there a large need to divert patients with mental illness from jails to mental hospitals?
Over the past few years, psychiatrists in emergency departments have noted a concerning trend: an increase in referrals to mental hospitals by law enforcement for what appears to be a crime with only a vague or obscure link to mental illness. Most psychiatrists who regularly work in emergency departments will witness many examples. Some might be fairly benign: “They were going to arrest me for trespassing; I was yelling at a coffee shop. But when I told them that I had run out of meds, they brought me here instead.”
However, some stories are more chilling, including the case of an older male who had made threats while shooting his gun in the air and was brought to the emergency department because, as the police officer told us, “I think that he is just depressed; you guys can keep him safe till he is better.”
We applaud society’s desire to reduce the criminalization of mental illness. We think that psychiatry should be deeply involved in the attempts to resolve this problem. Furthermore, we are cognizant that the number of patients with mental illness unnecessarily imprisoned as a result of prosecutorial zealousness is a larger problem than criminals inappropriately brought to mental hospitals. However, we also are aware of the limitation of psychiatric hospitals in solving nonpsychiatric problems.
Recent studies have demonstrated the need to examine criminogenic needs before psychiatric ones when attempting to reduce recidivism in all offenders, including those with mental illnesses.4 The emphasis on addressing psychiatric needs over criminogenic ones is misguided and not based on evidence. Yet, we appreciate the complexity of those questions and of individual cases.
Substance use disorders are emblematic of this problem. Psychiatry has now communicated the position that substance use disorders are mental illness and not a moral failing. However, are the crimes committed by individuals with substance use disorders, whether in a state of intoxication or driven by the cycles of addiction, the blameless result of mental illness? The legal system struggles with this question, trying to determine when addiction-related crimes should be referred to a diversion program or treated as a straightforward criminal prosecution. Those who favor diversion for addiction can point out that many criminal acts are associated with mitigating factors that are no less valid than is addiction.
However, those mitigating factors, such as poverty, childhood deprivation, or a violence-infused sociological milieu, cannot be found in the Diagnostic and Statistical Manual of Mental Disorders. As such, if those factors alone were considered, no diversion would be offered by the courts. There also can be unforeseen consequences to this bias for diversion or criminal prosecution. Violent outbursts are a recognized part of PTSD in veterans. Psychiatrists who work at Veterans Affairs can be faced with the diagnosis of PTSD being used as an excuse for violent behavior, which may, at some level be valid, but which can be dangerous in that labeling a patient with that diagnosis might lower the barriers to violent behavior by providing a ready-made explanation already internalized by the patient through unspoken, sociocultural norms.
With the awareness of the complex nature of the intersectionality of mental illness and criminality, we recommend improvements to current diversion programs. As diversion programs rightfully continue to expand across the country, we likely will see an increase in the number of referrals by police officers to our emergency departments. Some of the referrals will be considered “inappropriate” after thorough and thoughtful clinical evaluation by emergency psychiatrists. The inappropriateness might be secondary to an absence of active symptoms, an absence of correlation between the illness and the offense, or a more urgent criminogenic need.
When faced with someone who will not benefit from diversion to a psychiatric emergency department, psychiatrists should have the tools to revert the person back into the legal system. Those tools could come in many forms – law enforcement liaison, prosecution liaison, or simply the presence of officers who are mandated to wait for the approval of the clinician prior to dismissing legal charges. Whatever the solution might be for any particular locale, policy makers should not wait for adverse events to realize the potential pitfalls of the important work being done in developing our country’s diversion programs.
References
1. Swanson JW et al. Mental illness and reduction of gun violence and suicide: Bringing epidemiologic research to policy. Ann Epidemiol. 2015 May;25(5):366-76.
2. Ehrenreich B. “How America criminalized poverty.” The Guardian. 2011 Aug 10.
3. Roth A. “Prisons are the new asylums.” The Atlantic. 2018 April.
4. Latessa EJ et al. “What works (and doesn’t) in reducing recidivism.” New York: Routledge, 2015.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. Dr. Badre can be reached at his website, BadreMD.com. Dr. Lehman is an associate professor of psychiatry at the University of California, San Diego. He is codirector of all acute and intensive psychiatric treatment at the Veterans Affairs Medical Center in San Diego, where he practices clinical psychiatry. He also is the course director for the UCSD third-year medical student psychiatry clerkship.
False links between violence, mental illness fast-tracked report release
Stigmatizing language in the public domain that falsely links U.S. gun violence to mental illness led the National Council for Behavioral Health to move up release of a report analyzing causes, impacts, and solutions of mass violence, according to Jack Rozel, MD.
“We were planning to release it in October but released it early to push back,” Dr. Rozel, a member of the report’s expert panel and medical director of resolve Crisis Services, said on the Aug. 21 MDedge Psychcast.
The 82-page report examines behavior-based motives and solutions related to mass violence in the United States (Parks J et al. National Council for Behavioral Health. 2019 Aug 6. “Mass Violence in America: Causes, Impacts and Solutions”). It was created by the Medical Director Institute, which advises the National Council on current issues affecting clinical practice.
Policy makers and the public often leap to conclusions about the role of mental illness in the actions of individuals responsible for mass violence, wrote the panel convened by the institute. The panel included not only clinicians such as Dr. Rozel with expertise in treating mental illness, but also researchers, educators, law enforcement personnel, FBI members, judges, policy makers, and parents.
According to the report’s executive summary, perpetrators of mass violence share certain traits independent of cultural, demographic, socioeconomic, and occupational factors. The most common perpetrators of mass violence are “males, often hopeless and harboring grievances that are frequently related to work, school, finances, or interpersonal relationships; feeling victimized and sympathizing with others whom they perceive to be similarly mistreated; indifference to life; and often subsequently dying by suicide.”
, according to the report. In fact, many perpetrators do not suffer from any major psychiatric disorder, and most individuals who do suffer from mental illness are not violent.
“Lumping all mental illness together, and then assuming that acts that seem incomprehensible to the average person are due to mental illness, results in millions of harmless, nonviolent individuals recovering from treatable mental health conditions being subjected to stigma, rejection, discrimination and even unwarranted legal restrictions and social control,” the panel wrote. Recent episodes of mass violence in the United States can contribute to a generalized fear of individuals with mental illness, they added.
More research and strategies are needed to explore and address the root causes that contribute to acts of mass violence, including social problems and insufficient mental health care, the report said.
The panelists also offered recommendations for stakeholders, including health care organizations, schools, law enforcement, and community groups.
Recommendations for health care organizations in particular include establishing multidisciplinary teams for threat assessment and management that include not only security personnel, but also human resources, legal, and law enforcement. In addition, the panel recommended that health care staff be trained in lethal means reduction. “This is a rational strategy for lethal violence reduction and very helpful in combating suicide,” they said. However, staff also should be prepared for compassion fatigue and vicarious trauma, and health care organizations should develop resources for self-care and staff support.
Other recommendations include enacting state red flag laws that would remove guns from high-risk individuals for the short term, and reassessing the value of school safety protocols, such as bulletproof glass, zero tolerance policies, and active shooter drills.
The panel also offered recommendations for additional research on mass violence, including studies on “the nature and factors that contribute to mass violence, including neurobiological, psychological and sociological factors,” as well as research on methods of intervention and prevention of mass violence and the creation of a standardized analysis for mass violence incidence led by the Department of Justice with a multidisciplinary team.
Working with the media is important for engaging and educating the public about mental illness and mass violence, the panel members wrote. They recommended that all stakeholders in mental health develop messages in advance and protocols about how to respond to media requests for information about behavioral health.
“Talk about the role of treatment in helping people at risk of violence. Highlight the fact that most people with mental illnesses will never become violent. Speak to untreated or undertreated mental illness in combination with other risk factors,” they said.
Finally, they emphasized the need to remind the public to be aware of risk factors for mass violence, and the value of the “see something, say something” message.
In the Psychcast interview, Dr. Rozel said he and several colleagues will be conducting talks and training on these issues over the next few months, including at the Institute on Psychiatric Services conference (IPS 2019) in October in New York; at the National Council’s preconference (NatCon20) in April in Austin, Tex.; and at the American College of Emergency Physicians (ACEP 2019) meeting in October in Denver.
The National Council’s expert panel was led by Joe Parks, MD, medical director of the National Council; Donald W. Bechtold, MD, of the Colorado-based Jefferson Center for Mental Health; Sara Coffey, DO, of Oklahoma State University, Tulsa; Jeffrey A. Lieberman, MD, of Columbia University, New York; and Frank Shelp, MD, MPH, of Envolve Health, Atlanta.
Stigmatizing language in the public domain that falsely links U.S. gun violence to mental illness led the National Council for Behavioral Health to move up release of a report analyzing causes, impacts, and solutions of mass violence, according to Jack Rozel, MD.
“We were planning to release it in October but released it early to push back,” Dr. Rozel, a member of the report’s expert panel and medical director of resolve Crisis Services, said on the Aug. 21 MDedge Psychcast.
The 82-page report examines behavior-based motives and solutions related to mass violence in the United States (Parks J et al. National Council for Behavioral Health. 2019 Aug 6. “Mass Violence in America: Causes, Impacts and Solutions”). It was created by the Medical Director Institute, which advises the National Council on current issues affecting clinical practice.
Policy makers and the public often leap to conclusions about the role of mental illness in the actions of individuals responsible for mass violence, wrote the panel convened by the institute. The panel included not only clinicians such as Dr. Rozel with expertise in treating mental illness, but also researchers, educators, law enforcement personnel, FBI members, judges, policy makers, and parents.
According to the report’s executive summary, perpetrators of mass violence share certain traits independent of cultural, demographic, socioeconomic, and occupational factors. The most common perpetrators of mass violence are “males, often hopeless and harboring grievances that are frequently related to work, school, finances, or interpersonal relationships; feeling victimized and sympathizing with others whom they perceive to be similarly mistreated; indifference to life; and often subsequently dying by suicide.”
, according to the report. In fact, many perpetrators do not suffer from any major psychiatric disorder, and most individuals who do suffer from mental illness are not violent.
“Lumping all mental illness together, and then assuming that acts that seem incomprehensible to the average person are due to mental illness, results in millions of harmless, nonviolent individuals recovering from treatable mental health conditions being subjected to stigma, rejection, discrimination and even unwarranted legal restrictions and social control,” the panel wrote. Recent episodes of mass violence in the United States can contribute to a generalized fear of individuals with mental illness, they added.
More research and strategies are needed to explore and address the root causes that contribute to acts of mass violence, including social problems and insufficient mental health care, the report said.
The panelists also offered recommendations for stakeholders, including health care organizations, schools, law enforcement, and community groups.
Recommendations for health care organizations in particular include establishing multidisciplinary teams for threat assessment and management that include not only security personnel, but also human resources, legal, and law enforcement. In addition, the panel recommended that health care staff be trained in lethal means reduction. “This is a rational strategy for lethal violence reduction and very helpful in combating suicide,” they said. However, staff also should be prepared for compassion fatigue and vicarious trauma, and health care organizations should develop resources for self-care and staff support.
Other recommendations include enacting state red flag laws that would remove guns from high-risk individuals for the short term, and reassessing the value of school safety protocols, such as bulletproof glass, zero tolerance policies, and active shooter drills.
The panel also offered recommendations for additional research on mass violence, including studies on “the nature and factors that contribute to mass violence, including neurobiological, psychological and sociological factors,” as well as research on methods of intervention and prevention of mass violence and the creation of a standardized analysis for mass violence incidence led by the Department of Justice with a multidisciplinary team.
Working with the media is important for engaging and educating the public about mental illness and mass violence, the panel members wrote. They recommended that all stakeholders in mental health develop messages in advance and protocols about how to respond to media requests for information about behavioral health.
“Talk about the role of treatment in helping people at risk of violence. Highlight the fact that most people with mental illnesses will never become violent. Speak to untreated or undertreated mental illness in combination with other risk factors,” they said.
Finally, they emphasized the need to remind the public to be aware of risk factors for mass violence, and the value of the “see something, say something” message.
In the Psychcast interview, Dr. Rozel said he and several colleagues will be conducting talks and training on these issues over the next few months, including at the Institute on Psychiatric Services conference (IPS 2019) in October in New York; at the National Council’s preconference (NatCon20) in April in Austin, Tex.; and at the American College of Emergency Physicians (ACEP 2019) meeting in October in Denver.
The National Council’s expert panel was led by Joe Parks, MD, medical director of the National Council; Donald W. Bechtold, MD, of the Colorado-based Jefferson Center for Mental Health; Sara Coffey, DO, of Oklahoma State University, Tulsa; Jeffrey A. Lieberman, MD, of Columbia University, New York; and Frank Shelp, MD, MPH, of Envolve Health, Atlanta.
Stigmatizing language in the public domain that falsely links U.S. gun violence to mental illness led the National Council for Behavioral Health to move up release of a report analyzing causes, impacts, and solutions of mass violence, according to Jack Rozel, MD.
“We were planning to release it in October but released it early to push back,” Dr. Rozel, a member of the report’s expert panel and medical director of resolve Crisis Services, said on the Aug. 21 MDedge Psychcast.
The 82-page report examines behavior-based motives and solutions related to mass violence in the United States (Parks J et al. National Council for Behavioral Health. 2019 Aug 6. “Mass Violence in America: Causes, Impacts and Solutions”). It was created by the Medical Director Institute, which advises the National Council on current issues affecting clinical practice.
Policy makers and the public often leap to conclusions about the role of mental illness in the actions of individuals responsible for mass violence, wrote the panel convened by the institute. The panel included not only clinicians such as Dr. Rozel with expertise in treating mental illness, but also researchers, educators, law enforcement personnel, FBI members, judges, policy makers, and parents.
According to the report’s executive summary, perpetrators of mass violence share certain traits independent of cultural, demographic, socioeconomic, and occupational factors. The most common perpetrators of mass violence are “males, often hopeless and harboring grievances that are frequently related to work, school, finances, or interpersonal relationships; feeling victimized and sympathizing with others whom they perceive to be similarly mistreated; indifference to life; and often subsequently dying by suicide.”
, according to the report. In fact, many perpetrators do not suffer from any major psychiatric disorder, and most individuals who do suffer from mental illness are not violent.
“Lumping all mental illness together, and then assuming that acts that seem incomprehensible to the average person are due to mental illness, results in millions of harmless, nonviolent individuals recovering from treatable mental health conditions being subjected to stigma, rejection, discrimination and even unwarranted legal restrictions and social control,” the panel wrote. Recent episodes of mass violence in the United States can contribute to a generalized fear of individuals with mental illness, they added.
More research and strategies are needed to explore and address the root causes that contribute to acts of mass violence, including social problems and insufficient mental health care, the report said.
The panelists also offered recommendations for stakeholders, including health care organizations, schools, law enforcement, and community groups.
Recommendations for health care organizations in particular include establishing multidisciplinary teams for threat assessment and management that include not only security personnel, but also human resources, legal, and law enforcement. In addition, the panel recommended that health care staff be trained in lethal means reduction. “This is a rational strategy for lethal violence reduction and very helpful in combating suicide,” they said. However, staff also should be prepared for compassion fatigue and vicarious trauma, and health care organizations should develop resources for self-care and staff support.
Other recommendations include enacting state red flag laws that would remove guns from high-risk individuals for the short term, and reassessing the value of school safety protocols, such as bulletproof glass, zero tolerance policies, and active shooter drills.
The panel also offered recommendations for additional research on mass violence, including studies on “the nature and factors that contribute to mass violence, including neurobiological, psychological and sociological factors,” as well as research on methods of intervention and prevention of mass violence and the creation of a standardized analysis for mass violence incidence led by the Department of Justice with a multidisciplinary team.
Working with the media is important for engaging and educating the public about mental illness and mass violence, the panel members wrote. They recommended that all stakeholders in mental health develop messages in advance and protocols about how to respond to media requests for information about behavioral health.
“Talk about the role of treatment in helping people at risk of violence. Highlight the fact that most people with mental illnesses will never become violent. Speak to untreated or undertreated mental illness in combination with other risk factors,” they said.
Finally, they emphasized the need to remind the public to be aware of risk factors for mass violence, and the value of the “see something, say something” message.
In the Psychcast interview, Dr. Rozel said he and several colleagues will be conducting talks and training on these issues over the next few months, including at the Institute on Psychiatric Services conference (IPS 2019) in October in New York; at the National Council’s preconference (NatCon20) in April in Austin, Tex.; and at the American College of Emergency Physicians (ACEP 2019) meeting in October in Denver.
The National Council’s expert panel was led by Joe Parks, MD, medical director of the National Council; Donald W. Bechtold, MD, of the Colorado-based Jefferson Center for Mental Health; Sara Coffey, DO, of Oklahoma State University, Tulsa; Jeffrey A. Lieberman, MD, of Columbia University, New York; and Frank Shelp, MD, MPH, of Envolve Health, Atlanta.