User login
Bariatric surgery found to be effective in IBD patients
SAN DIEGO – In carefully selected patients with well-controlled inflammatory bowel disease (IBD), bariatric surgery results in sustained weight loss over a 2-year period, results from a retrospective study suggest.
“Obesity is increasing in patients with inflammatory bowel disease at a rate similar to that seen in the general population,” the study’s primary author, Nicholas P. McKenna, MD, said in an interview in advance of the annual Digestive Disease Week. “While bariatric surgery is a well-accepted therapy for obesity in patients without IBD, its use in patients with IBD is less well studied.”
For the current study, Dr. McKenna, a resident in the department of surgery at the Mayo Clinic in Rochester, Minn., and colleagues collected data on 33 patients who underwent bariatric surgery with a pre- or postoperative diagnosis of IBD across three academic centers between August 2006 and December 2017. They evaluated IBD characteristics and medications; postoperative complications; the need for future IBD-related surgery; and weight loss at 6, 12, and 24 months.
The patients underwent 34 bariatric operations. Their median age was 51 years and their median duration of IBD was 13 years. Of the 33 patients, 16 underwent a Roux-en-Y gastric bypass procedure: 9 who had ulcerative colitis, 6 who had Crohn’s disease, and 1 who had indeterminate colitis. A total of 14 patients underwent sleeve gastrectomy: 7 who had ulcerative colitis and 7 who had Crohn’s disease. Four patients underwent a gastric band procedure, all of whom had ulcerative colitis. The mean body mass index of patients prior to their bariatric procedures was 42.7 kg/m2. A total of 31 patients had an existing diagnosis of IBD, and 2 were diagnosed with Crohn’s disease after Roux-en-Y gastric bypass. In addition, 9 patients were on preoperative immunosuppression for IBD, and 11 had undergone prior intestinal resection for IBD.
Dr. McKenna reported that the average hospitalization for all patients was 3.6 days and that only four 30-day infectious complications occurred: two superficial surgical site infections, one infected intra-abdominal hematoma, and one hepatic abscess. In the long term, seven patients required reoperation: three for failed gastric band, two for reduction of internal hernia, and two for cholelithiasis. The researchers found that the mean percentage of overall excess weight loss was 57.5% at 6 months, 63.3% at 12 months, and 58.6% at 24 months. During a mean follow-up of 3.4 years, no IBD flares requiring surgery were observed.
“Our hypothesis based on the existing literature was that bariatric surgery would be safe in carefully selected patients with IBD and result in sustained weight loss, so we were not surprised with these results,” Dr. McKenna said. “We were not sure if medication requirements would change after surgery as the literature is conflicted on this. We observed that most patients continued to require no immunosuppression for control of their IBD after surgery. Further, we did not observe that any patients required future surgery at the time of last follow-up for an IBD flare.”
He acknowledged certain limitations of the study, including its retrospective design. “Additionally, though it is a relatively large sample, compared to the existing literature on bariatric surgery in IBD, it is still only 33 patients. This limits the comparisons that can be performed between patients with ulcerative colitis and Crohn’s disease and between the operation choices.”
The study’s secondary author, Alaa Sada, MD, a surgery resident at Mayo, presented the findings at the meeting. The researchers reported having no financial disclosures.
SAN DIEGO – In carefully selected patients with well-controlled inflammatory bowel disease (IBD), bariatric surgery results in sustained weight loss over a 2-year period, results from a retrospective study suggest.
“Obesity is increasing in patients with inflammatory bowel disease at a rate similar to that seen in the general population,” the study’s primary author, Nicholas P. McKenna, MD, said in an interview in advance of the annual Digestive Disease Week. “While bariatric surgery is a well-accepted therapy for obesity in patients without IBD, its use in patients with IBD is less well studied.”
For the current study, Dr. McKenna, a resident in the department of surgery at the Mayo Clinic in Rochester, Minn., and colleagues collected data on 33 patients who underwent bariatric surgery with a pre- or postoperative diagnosis of IBD across three academic centers between August 2006 and December 2017. They evaluated IBD characteristics and medications; postoperative complications; the need for future IBD-related surgery; and weight loss at 6, 12, and 24 months.
The patients underwent 34 bariatric operations. Their median age was 51 years and their median duration of IBD was 13 years. Of the 33 patients, 16 underwent a Roux-en-Y gastric bypass procedure: 9 who had ulcerative colitis, 6 who had Crohn’s disease, and 1 who had indeterminate colitis. A total of 14 patients underwent sleeve gastrectomy: 7 who had ulcerative colitis and 7 who had Crohn’s disease. Four patients underwent a gastric band procedure, all of whom had ulcerative colitis. The mean body mass index of patients prior to their bariatric procedures was 42.7 kg/m2. A total of 31 patients had an existing diagnosis of IBD, and 2 were diagnosed with Crohn’s disease after Roux-en-Y gastric bypass. In addition, 9 patients were on preoperative immunosuppression for IBD, and 11 had undergone prior intestinal resection for IBD.
Dr. McKenna reported that the average hospitalization for all patients was 3.6 days and that only four 30-day infectious complications occurred: two superficial surgical site infections, one infected intra-abdominal hematoma, and one hepatic abscess. In the long term, seven patients required reoperation: three for failed gastric band, two for reduction of internal hernia, and two for cholelithiasis. The researchers found that the mean percentage of overall excess weight loss was 57.5% at 6 months, 63.3% at 12 months, and 58.6% at 24 months. During a mean follow-up of 3.4 years, no IBD flares requiring surgery were observed.
“Our hypothesis based on the existing literature was that bariatric surgery would be safe in carefully selected patients with IBD and result in sustained weight loss, so we were not surprised with these results,” Dr. McKenna said. “We were not sure if medication requirements would change after surgery as the literature is conflicted on this. We observed that most patients continued to require no immunosuppression for control of their IBD after surgery. Further, we did not observe that any patients required future surgery at the time of last follow-up for an IBD flare.”
He acknowledged certain limitations of the study, including its retrospective design. “Additionally, though it is a relatively large sample, compared to the existing literature on bariatric surgery in IBD, it is still only 33 patients. This limits the comparisons that can be performed between patients with ulcerative colitis and Crohn’s disease and between the operation choices.”
The study’s secondary author, Alaa Sada, MD, a surgery resident at Mayo, presented the findings at the meeting. The researchers reported having no financial disclosures.
SAN DIEGO – In carefully selected patients with well-controlled inflammatory bowel disease (IBD), bariatric surgery results in sustained weight loss over a 2-year period, results from a retrospective study suggest.
“Obesity is increasing in patients with inflammatory bowel disease at a rate similar to that seen in the general population,” the study’s primary author, Nicholas P. McKenna, MD, said in an interview in advance of the annual Digestive Disease Week. “While bariatric surgery is a well-accepted therapy for obesity in patients without IBD, its use in patients with IBD is less well studied.”
For the current study, Dr. McKenna, a resident in the department of surgery at the Mayo Clinic in Rochester, Minn., and colleagues collected data on 33 patients who underwent bariatric surgery with a pre- or postoperative diagnosis of IBD across three academic centers between August 2006 and December 2017. They evaluated IBD characteristics and medications; postoperative complications; the need for future IBD-related surgery; and weight loss at 6, 12, and 24 months.
The patients underwent 34 bariatric operations. Their median age was 51 years and their median duration of IBD was 13 years. Of the 33 patients, 16 underwent a Roux-en-Y gastric bypass procedure: 9 who had ulcerative colitis, 6 who had Crohn’s disease, and 1 who had indeterminate colitis. A total of 14 patients underwent sleeve gastrectomy: 7 who had ulcerative colitis and 7 who had Crohn’s disease. Four patients underwent a gastric band procedure, all of whom had ulcerative colitis. The mean body mass index of patients prior to their bariatric procedures was 42.7 kg/m2. A total of 31 patients had an existing diagnosis of IBD, and 2 were diagnosed with Crohn’s disease after Roux-en-Y gastric bypass. In addition, 9 patients were on preoperative immunosuppression for IBD, and 11 had undergone prior intestinal resection for IBD.
Dr. McKenna reported that the average hospitalization for all patients was 3.6 days and that only four 30-day infectious complications occurred: two superficial surgical site infections, one infected intra-abdominal hematoma, and one hepatic abscess. In the long term, seven patients required reoperation: three for failed gastric band, two for reduction of internal hernia, and two for cholelithiasis. The researchers found that the mean percentage of overall excess weight loss was 57.5% at 6 months, 63.3% at 12 months, and 58.6% at 24 months. During a mean follow-up of 3.4 years, no IBD flares requiring surgery were observed.
“Our hypothesis based on the existing literature was that bariatric surgery would be safe in carefully selected patients with IBD and result in sustained weight loss, so we were not surprised with these results,” Dr. McKenna said. “We were not sure if medication requirements would change after surgery as the literature is conflicted on this. We observed that most patients continued to require no immunosuppression for control of their IBD after surgery. Further, we did not observe that any patients required future surgery at the time of last follow-up for an IBD flare.”
He acknowledged certain limitations of the study, including its retrospective design. “Additionally, though it is a relatively large sample, compared to the existing literature on bariatric surgery in IBD, it is still only 33 patients. This limits the comparisons that can be performed between patients with ulcerative colitis and Crohn’s disease and between the operation choices.”
The study’s secondary author, Alaa Sada, MD, a surgery resident at Mayo, presented the findings at the meeting. The researchers reported having no financial disclosures.
REPORTING FROM DDW 2019
Weight can block psychiatric facility admission
SAN FRANCISCO – Not too long ago, a 42-year-old homeless man could not leave the Los Angeles County Hospital because he was too heavy.
He had been admitted on a 72-hour involuntary psychiatric hold because he was suicidal; he had a history of severe depression and had made several attempts in the past. He had few social connections and had come in covered in lice after sleeping outdoors for months. He was mobile, but barely so, with the help of a walker.
He was cleaned up and medically stabilized at the hospital, but when it came time to transfer him to a psychiatric facility, no one would take him because he was morbidly obese, with a body mass index (BMI) of 53 mg/m2.
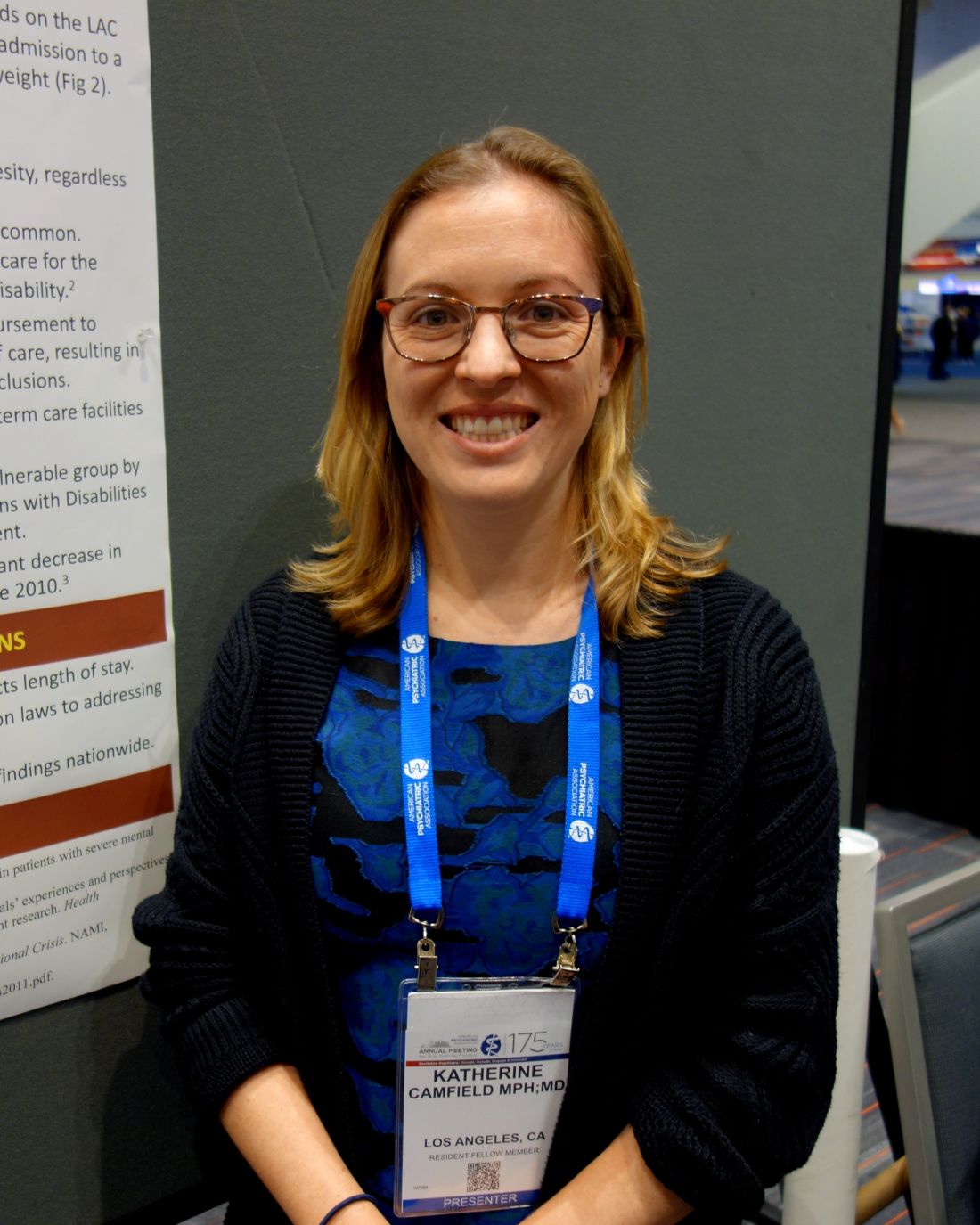
“We noticed this had happened with other patients. It wasn’t just this one case, so we” decided to take a closer look, said Katherine Camfield, MD, a psychiatric resident at Los Angeles County Hospital.
She and her colleagues called 43 inpatient psychiatric facilities in L.A. County. It turned out that 41, more than 60% of the total and including both public and private facilities, had weight restrictions. Staff members at the remaining two facilities were unsure.
For 2 hospitals, it was a BMI above 50; for 17, a weight above 350 pounds; and for 6, a weight above 300 pounds. Three had a limit of just 250 pounds. Others decided on a case-by-case basis. About 10% of the people put on psychiatric holds at the L.A. County Hospital weigh 250 pounds or more and therefore would not meet the weight limits at many facilities.
Some hospitals cited concerns about staff injuries from moving – or trying to calm – a large patient. Others said they did not have lifts and other specialized equipment or that their beds could not handle the weight. Others did not really give a reason.
County hospitals “are not a very therapeutic milieu; staff and nursing aren’t necessarily trained for unstable psychiatric patients,” Dr. Camfield said at the American Psychiatric Association annual meeting.
“Honestly, having a mental illness alone increases your risk of obesity, and then we give a lot of medications that increase the risk” even more. “It’s a vicious cycle,” and one that raises the issue of discrimination, although “whether these routine denials to access psychiatric hospitalization violate antidiscrimination laws is unclear,” she said.
She and her colleagues plan to take a deeper dive into the issue, to find out how widespread the problem is, and the reasons behind it. They are also interested in cost; “a county facility has limited resources; are they being misallocated because these patients are stuck in the hospital?” Dr. Camfield wondered.
The homeless man never made to a psychiatric facility. He was put on antidepressants and stayed in the county hospital for 20 days, until he was no longer suicidal. He then was transferred to skilled nursing facility.
There was no external funding, and Dr. Camfield had no disclosures.
SAN FRANCISCO – Not too long ago, a 42-year-old homeless man could not leave the Los Angeles County Hospital because he was too heavy.
He had been admitted on a 72-hour involuntary psychiatric hold because he was suicidal; he had a history of severe depression and had made several attempts in the past. He had few social connections and had come in covered in lice after sleeping outdoors for months. He was mobile, but barely so, with the help of a walker.
He was cleaned up and medically stabilized at the hospital, but when it came time to transfer him to a psychiatric facility, no one would take him because he was morbidly obese, with a body mass index (BMI) of 53 mg/m2.
“We noticed this had happened with other patients. It wasn’t just this one case, so we” decided to take a closer look, said Katherine Camfield, MD, a psychiatric resident at Los Angeles County Hospital.
She and her colleagues called 43 inpatient psychiatric facilities in L.A. County. It turned out that 41, more than 60% of the total and including both public and private facilities, had weight restrictions. Staff members at the remaining two facilities were unsure.
For 2 hospitals, it was a BMI above 50; for 17, a weight above 350 pounds; and for 6, a weight above 300 pounds. Three had a limit of just 250 pounds. Others decided on a case-by-case basis. About 10% of the people put on psychiatric holds at the L.A. County Hospital weigh 250 pounds or more and therefore would not meet the weight limits at many facilities.
Some hospitals cited concerns about staff injuries from moving – or trying to calm – a large patient. Others said they did not have lifts and other specialized equipment or that their beds could not handle the weight. Others did not really give a reason.
County hospitals “are not a very therapeutic milieu; staff and nursing aren’t necessarily trained for unstable psychiatric patients,” Dr. Camfield said at the American Psychiatric Association annual meeting.
“Honestly, having a mental illness alone increases your risk of obesity, and then we give a lot of medications that increase the risk” even more. “It’s a vicious cycle,” and one that raises the issue of discrimination, although “whether these routine denials to access psychiatric hospitalization violate antidiscrimination laws is unclear,” she said.
She and her colleagues plan to take a deeper dive into the issue, to find out how widespread the problem is, and the reasons behind it. They are also interested in cost; “a county facility has limited resources; are they being misallocated because these patients are stuck in the hospital?” Dr. Camfield wondered.
The homeless man never made to a psychiatric facility. He was put on antidepressants and stayed in the county hospital for 20 days, until he was no longer suicidal. He then was transferred to skilled nursing facility.
There was no external funding, and Dr. Camfield had no disclosures.
SAN FRANCISCO – Not too long ago, a 42-year-old homeless man could not leave the Los Angeles County Hospital because he was too heavy.
He had been admitted on a 72-hour involuntary psychiatric hold because he was suicidal; he had a history of severe depression and had made several attempts in the past. He had few social connections and had come in covered in lice after sleeping outdoors for months. He was mobile, but barely so, with the help of a walker.
He was cleaned up and medically stabilized at the hospital, but when it came time to transfer him to a psychiatric facility, no one would take him because he was morbidly obese, with a body mass index (BMI) of 53 mg/m2.
“We noticed this had happened with other patients. It wasn’t just this one case, so we” decided to take a closer look, said Katherine Camfield, MD, a psychiatric resident at Los Angeles County Hospital.
She and her colleagues called 43 inpatient psychiatric facilities in L.A. County. It turned out that 41, more than 60% of the total and including both public and private facilities, had weight restrictions. Staff members at the remaining two facilities were unsure.
For 2 hospitals, it was a BMI above 50; for 17, a weight above 350 pounds; and for 6, a weight above 300 pounds. Three had a limit of just 250 pounds. Others decided on a case-by-case basis. About 10% of the people put on psychiatric holds at the L.A. County Hospital weigh 250 pounds or more and therefore would not meet the weight limits at many facilities.
Some hospitals cited concerns about staff injuries from moving – or trying to calm – a large patient. Others said they did not have lifts and other specialized equipment or that their beds could not handle the weight. Others did not really give a reason.
County hospitals “are not a very therapeutic milieu; staff and nursing aren’t necessarily trained for unstable psychiatric patients,” Dr. Camfield said at the American Psychiatric Association annual meeting.
“Honestly, having a mental illness alone increases your risk of obesity, and then we give a lot of medications that increase the risk” even more. “It’s a vicious cycle,” and one that raises the issue of discrimination, although “whether these routine denials to access psychiatric hospitalization violate antidiscrimination laws is unclear,” she said.
She and her colleagues plan to take a deeper dive into the issue, to find out how widespread the problem is, and the reasons behind it. They are also interested in cost; “a county facility has limited resources; are they being misallocated because these patients are stuck in the hospital?” Dr. Camfield wondered.
The homeless man never made to a psychiatric facility. He was put on antidepressants and stayed in the county hospital for 20 days, until he was no longer suicidal. He then was transferred to skilled nursing facility.
There was no external funding, and Dr. Camfield had no disclosures.
REPORTING FROM APA 2019
Keep sports fun, keep kids playing
according to a clinical report from the American Academy of Pediatrics’ Council on Sports Medicine and Fitness.
In the report, “Organized Sports for Children, Preadolescents, and Adolescents,” published online in Pediatrics, the authors addressed the risks and benefits of organized sports for children and teens and offered guidance for how clinicians, schools, and communities can involve more children in sports programs.
The authors emphasized the role of free play and the development of skills for children younger than 6 years. However, they wrote that you and parents should encourage organized sports – with emphasis on physical activity enjoyment – for children older than 6 years at a range of skill levels.
“Aspects of readiness to consider are motor skill acquisition, ability to combine those skills, and attention span,” according to the authors, who noted that most children younger than 6 years may not yet have the skills and attention for organized sports.
You also can remind parents to step back from pushing children into particular sports. Allowing children to choose which activities to try helps keep the focus on fun, even if the child’s idea of fun may differ from parental ideas. “Forcing children to participate in organized sports (or any physical activity) is likely to decrease fun in the activity and discourage future participation,” according to the authors.
They recognize barriers to organized sports for children from low socioeconomic backgrounds and advise communities to try to reduce them; other recommendations include having more options for organized sports at a range of skill levels to encourage participation and long-term involvement, and promoting physical activity.
“If we offer children a variety of sports for all skill levels, they are more likely to try new activities and stick with the ones they enjoy,” Kelsey Logan, MD, a coauthor of the report, said in a statement. “The interest should start with the child, not the parent.”
“Families can help by encouraging children to ‘sample’ sports, so they can figure out what they find enjoyable,” he said. “Ideally, there is an activity for everyone, with the focus on having fun.”
“Given the epidemic of obesity and all of its accompanying medical conditions, it is important to find ways to keep kids physically active. Organized sports participation is one tactic to accomplish this,” the authors said.
They acknowledge the potential risks involved in organized sports such as sports injuries, bullying, and burnout, but also advise empowering parents to support a positive coaching environment with playing time for all participants so they can enjoy the physical and mental benefits of being on a team.
“Young athletes typically learn skills and values that they can use in everyday life,” Steven Cuff, MD, coauthor of the report, said in a statement. “The camaraderie and teamwork needed on a playing field offers lasting lessons on personal responsibility, sportsmanship, goal-setting, and emotional control.”
Children with developmental and neurologic disabilities also can benefit from organized sports participation in programs such as Special Olympics, the authors said.
The report authors had no financial conflicts to disclose.
SOURCE: Logan K et al. Pediatrics. 2019 May 20. doi: 10.1542/peds.2019-0997.
“I think it is quite timely with the obesity epidemic and lack of PE in schools to highlight how important physical activity is for children, and organized sports is one of the ways to accomplish that,” Andrew Gregory, MD, said in an interview.
“I think the summary of both benefits and risks is well informed and complete,” he said.
However, “I think most pediatricians and parents are aware of the physical benefits of exercise, but many may be unaware of the psychological and social benefits,” Dr. Gregory noted. “It is also important that parents and coaches understand that bullying and hazing have no place in organized sports and should not be tolerated.”
“I think the most important thing for clinicians to pass on is that the benefits of organized sports far outweigh the risks,” he said. The challenge is, “How do we better incorporate organized sports into schools and community organizations so that more children have access?”
Dr. Gregory is an associate professor of orthopaedics, neurosurgery & pediatrics at Vanderbilt University in Nashville, Tenn., and serves as codirector of the Vanderbilt Sports Concussion Center. He had no financial conflicts to disclose.
“I think it is quite timely with the obesity epidemic and lack of PE in schools to highlight how important physical activity is for children, and organized sports is one of the ways to accomplish that,” Andrew Gregory, MD, said in an interview.
“I think the summary of both benefits and risks is well informed and complete,” he said.
However, “I think most pediatricians and parents are aware of the physical benefits of exercise, but many may be unaware of the psychological and social benefits,” Dr. Gregory noted. “It is also important that parents and coaches understand that bullying and hazing have no place in organized sports and should not be tolerated.”
“I think the most important thing for clinicians to pass on is that the benefits of organized sports far outweigh the risks,” he said. The challenge is, “How do we better incorporate organized sports into schools and community organizations so that more children have access?”
Dr. Gregory is an associate professor of orthopaedics, neurosurgery & pediatrics at Vanderbilt University in Nashville, Tenn., and serves as codirector of the Vanderbilt Sports Concussion Center. He had no financial conflicts to disclose.
“I think it is quite timely with the obesity epidemic and lack of PE in schools to highlight how important physical activity is for children, and organized sports is one of the ways to accomplish that,” Andrew Gregory, MD, said in an interview.
“I think the summary of both benefits and risks is well informed and complete,” he said.
However, “I think most pediatricians and parents are aware of the physical benefits of exercise, but many may be unaware of the psychological and social benefits,” Dr. Gregory noted. “It is also important that parents and coaches understand that bullying and hazing have no place in organized sports and should not be tolerated.”
“I think the most important thing for clinicians to pass on is that the benefits of organized sports far outweigh the risks,” he said. The challenge is, “How do we better incorporate organized sports into schools and community organizations so that more children have access?”
Dr. Gregory is an associate professor of orthopaedics, neurosurgery & pediatrics at Vanderbilt University in Nashville, Tenn., and serves as codirector of the Vanderbilt Sports Concussion Center. He had no financial conflicts to disclose.
according to a clinical report from the American Academy of Pediatrics’ Council on Sports Medicine and Fitness.
In the report, “Organized Sports for Children, Preadolescents, and Adolescents,” published online in Pediatrics, the authors addressed the risks and benefits of organized sports for children and teens and offered guidance for how clinicians, schools, and communities can involve more children in sports programs.
The authors emphasized the role of free play and the development of skills for children younger than 6 years. However, they wrote that you and parents should encourage organized sports – with emphasis on physical activity enjoyment – for children older than 6 years at a range of skill levels.
“Aspects of readiness to consider are motor skill acquisition, ability to combine those skills, and attention span,” according to the authors, who noted that most children younger than 6 years may not yet have the skills and attention for organized sports.
You also can remind parents to step back from pushing children into particular sports. Allowing children to choose which activities to try helps keep the focus on fun, even if the child’s idea of fun may differ from parental ideas. “Forcing children to participate in organized sports (or any physical activity) is likely to decrease fun in the activity and discourage future participation,” according to the authors.
They recognize barriers to organized sports for children from low socioeconomic backgrounds and advise communities to try to reduce them; other recommendations include having more options for organized sports at a range of skill levels to encourage participation and long-term involvement, and promoting physical activity.
“If we offer children a variety of sports for all skill levels, they are more likely to try new activities and stick with the ones they enjoy,” Kelsey Logan, MD, a coauthor of the report, said in a statement. “The interest should start with the child, not the parent.”
“Families can help by encouraging children to ‘sample’ sports, so they can figure out what they find enjoyable,” he said. “Ideally, there is an activity for everyone, with the focus on having fun.”
“Given the epidemic of obesity and all of its accompanying medical conditions, it is important to find ways to keep kids physically active. Organized sports participation is one tactic to accomplish this,” the authors said.
They acknowledge the potential risks involved in organized sports such as sports injuries, bullying, and burnout, but also advise empowering parents to support a positive coaching environment with playing time for all participants so they can enjoy the physical and mental benefits of being on a team.
“Young athletes typically learn skills and values that they can use in everyday life,” Steven Cuff, MD, coauthor of the report, said in a statement. “The camaraderie and teamwork needed on a playing field offers lasting lessons on personal responsibility, sportsmanship, goal-setting, and emotional control.”
Children with developmental and neurologic disabilities also can benefit from organized sports participation in programs such as Special Olympics, the authors said.
The report authors had no financial conflicts to disclose.
SOURCE: Logan K et al. Pediatrics. 2019 May 20. doi: 10.1542/peds.2019-0997.
according to a clinical report from the American Academy of Pediatrics’ Council on Sports Medicine and Fitness.
In the report, “Organized Sports for Children, Preadolescents, and Adolescents,” published online in Pediatrics, the authors addressed the risks and benefits of organized sports for children and teens and offered guidance for how clinicians, schools, and communities can involve more children in sports programs.
The authors emphasized the role of free play and the development of skills for children younger than 6 years. However, they wrote that you and parents should encourage organized sports – with emphasis on physical activity enjoyment – for children older than 6 years at a range of skill levels.
“Aspects of readiness to consider are motor skill acquisition, ability to combine those skills, and attention span,” according to the authors, who noted that most children younger than 6 years may not yet have the skills and attention for organized sports.
You also can remind parents to step back from pushing children into particular sports. Allowing children to choose which activities to try helps keep the focus on fun, even if the child’s idea of fun may differ from parental ideas. “Forcing children to participate in organized sports (or any physical activity) is likely to decrease fun in the activity and discourage future participation,” according to the authors.
They recognize barriers to organized sports for children from low socioeconomic backgrounds and advise communities to try to reduce them; other recommendations include having more options for organized sports at a range of skill levels to encourage participation and long-term involvement, and promoting physical activity.
“If we offer children a variety of sports for all skill levels, they are more likely to try new activities and stick with the ones they enjoy,” Kelsey Logan, MD, a coauthor of the report, said in a statement. “The interest should start with the child, not the parent.”
“Families can help by encouraging children to ‘sample’ sports, so they can figure out what they find enjoyable,” he said. “Ideally, there is an activity for everyone, with the focus on having fun.”
“Given the epidemic of obesity and all of its accompanying medical conditions, it is important to find ways to keep kids physically active. Organized sports participation is one tactic to accomplish this,” the authors said.
They acknowledge the potential risks involved in organized sports such as sports injuries, bullying, and burnout, but also advise empowering parents to support a positive coaching environment with playing time for all participants so they can enjoy the physical and mental benefits of being on a team.
“Young athletes typically learn skills and values that they can use in everyday life,” Steven Cuff, MD, coauthor of the report, said in a statement. “The camaraderie and teamwork needed on a playing field offers lasting lessons on personal responsibility, sportsmanship, goal-setting, and emotional control.”
Children with developmental and neurologic disabilities also can benefit from organized sports participation in programs such as Special Olympics, the authors said.
The report authors had no financial conflicts to disclose.
SOURCE: Logan K et al. Pediatrics. 2019 May 20. doi: 10.1542/peds.2019-0997.
FROM PEDIATRICS
BMI in male teens predicts cardiomyopathy risk
and their risk increased as body mass index increased, according to the results of a nationwide, prospective, registry-based cohort study from Sweden.
The association was strongest for dilated cardiomyopathy, wrote Josefina Robertson, MD, and associates at the University of Gothenburg (Sweden). Over a median of 27 years of follow-up, the risk for dilated cardiomyopathy in adulthood was approximately 38% greater when adolescent body mass index was 22.5-25.0 kg/m2, using a lean but not underweight BMI (18.5-20.0 kg/m2) as the reference group. The increase in risk for dilated cardiomyopathy continued to rise with adolescent BMI and exceeded 700% at a BMI over 35.
The rate of hospitalizations for heart failure caused by cardiomyopathy more than doubled in Sweden from 1987 to 2006, the researchers noted. Adolescent obesity is strongly linked to early heart failure, but few studies have assessed whether adiposity as measured by BMI is associated with cardiomyopathy, and none have confirmed diagnostic validity or looked at subtypes of cardiomyopathy.
“The already marked importance of weight control in youth is further strengthened by [our] findings,” the researchers wrote, “as well as greater evidence for obesity as a potential important cause of adverse cardiac remodeling independent of clinically evident ischemic heart disease.”
The study included 1,668,893 male adolescents who had enlisted for military service in Sweden between 1969 and 2005, when compulsory enlistment ended. It excluded women and the small proportion of men lacking weight or height data. A total of 4,477 cases of cardiomyopathy were diagnosed during follow-up, 59% were dilated cardiomyopathy, 15% were hypertrophic cardiomyopathy, and 11% were alcohol or drug-related cardiomyopathy.
The link between even slightly elevated BMI and dilated cardiomyopathy did not depend on age, year, location, or baseline comorbidities. For each unit increase in BMI, the adjusted risk of dilated cardiomyopathy rose by approximately 15%, the risk of hypertrophic cardiomyopathy rose by 9%, and the risk for drug- or alcohol-related cardiomyopathy rose by 10%. Estimated risks were generally similar after controlling for blood pressure, cardiorespiratory fitness, muscle strength, parents’ level of education, and alcohol or substance use disorders.
Funders included the Swedish government; Swedish Research Council; Swedish Heart and Lung Foundation; and Swedish Council for Health, Working Life, and Welfare. The researchers reported having no conflicts of interest.
SOURCE: Robertson J et al. Circulation. 2019 May 20.
and their risk increased as body mass index increased, according to the results of a nationwide, prospective, registry-based cohort study from Sweden.
The association was strongest for dilated cardiomyopathy, wrote Josefina Robertson, MD, and associates at the University of Gothenburg (Sweden). Over a median of 27 years of follow-up, the risk for dilated cardiomyopathy in adulthood was approximately 38% greater when adolescent body mass index was 22.5-25.0 kg/m2, using a lean but not underweight BMI (18.5-20.0 kg/m2) as the reference group. The increase in risk for dilated cardiomyopathy continued to rise with adolescent BMI and exceeded 700% at a BMI over 35.
The rate of hospitalizations for heart failure caused by cardiomyopathy more than doubled in Sweden from 1987 to 2006, the researchers noted. Adolescent obesity is strongly linked to early heart failure, but few studies have assessed whether adiposity as measured by BMI is associated with cardiomyopathy, and none have confirmed diagnostic validity or looked at subtypes of cardiomyopathy.
“The already marked importance of weight control in youth is further strengthened by [our] findings,” the researchers wrote, “as well as greater evidence for obesity as a potential important cause of adverse cardiac remodeling independent of clinically evident ischemic heart disease.”
The study included 1,668,893 male adolescents who had enlisted for military service in Sweden between 1969 and 2005, when compulsory enlistment ended. It excluded women and the small proportion of men lacking weight or height data. A total of 4,477 cases of cardiomyopathy were diagnosed during follow-up, 59% were dilated cardiomyopathy, 15% were hypertrophic cardiomyopathy, and 11% were alcohol or drug-related cardiomyopathy.
The link between even slightly elevated BMI and dilated cardiomyopathy did not depend on age, year, location, or baseline comorbidities. For each unit increase in BMI, the adjusted risk of dilated cardiomyopathy rose by approximately 15%, the risk of hypertrophic cardiomyopathy rose by 9%, and the risk for drug- or alcohol-related cardiomyopathy rose by 10%. Estimated risks were generally similar after controlling for blood pressure, cardiorespiratory fitness, muscle strength, parents’ level of education, and alcohol or substance use disorders.
Funders included the Swedish government; Swedish Research Council; Swedish Heart and Lung Foundation; and Swedish Council for Health, Working Life, and Welfare. The researchers reported having no conflicts of interest.
SOURCE: Robertson J et al. Circulation. 2019 May 20.
and their risk increased as body mass index increased, according to the results of a nationwide, prospective, registry-based cohort study from Sweden.
The association was strongest for dilated cardiomyopathy, wrote Josefina Robertson, MD, and associates at the University of Gothenburg (Sweden). Over a median of 27 years of follow-up, the risk for dilated cardiomyopathy in adulthood was approximately 38% greater when adolescent body mass index was 22.5-25.0 kg/m2, using a lean but not underweight BMI (18.5-20.0 kg/m2) as the reference group. The increase in risk for dilated cardiomyopathy continued to rise with adolescent BMI and exceeded 700% at a BMI over 35.
The rate of hospitalizations for heart failure caused by cardiomyopathy more than doubled in Sweden from 1987 to 2006, the researchers noted. Adolescent obesity is strongly linked to early heart failure, but few studies have assessed whether adiposity as measured by BMI is associated with cardiomyopathy, and none have confirmed diagnostic validity or looked at subtypes of cardiomyopathy.
“The already marked importance of weight control in youth is further strengthened by [our] findings,” the researchers wrote, “as well as greater evidence for obesity as a potential important cause of adverse cardiac remodeling independent of clinically evident ischemic heart disease.”
The study included 1,668,893 male adolescents who had enlisted for military service in Sweden between 1969 and 2005, when compulsory enlistment ended. It excluded women and the small proportion of men lacking weight or height data. A total of 4,477 cases of cardiomyopathy were diagnosed during follow-up, 59% were dilated cardiomyopathy, 15% were hypertrophic cardiomyopathy, and 11% were alcohol or drug-related cardiomyopathy.
The link between even slightly elevated BMI and dilated cardiomyopathy did not depend on age, year, location, or baseline comorbidities. For each unit increase in BMI, the adjusted risk of dilated cardiomyopathy rose by approximately 15%, the risk of hypertrophic cardiomyopathy rose by 9%, and the risk for drug- or alcohol-related cardiomyopathy rose by 10%. Estimated risks were generally similar after controlling for blood pressure, cardiorespiratory fitness, muscle strength, parents’ level of education, and alcohol or substance use disorders.
Funders included the Swedish government; Swedish Research Council; Swedish Heart and Lung Foundation; and Swedish Council for Health, Working Life, and Welfare. The researchers reported having no conflicts of interest.
SOURCE: Robertson J et al. Circulation. 2019 May 20.
FROM CIRCULATION
Key clinical point: Overweight in male teens predicts subsequent cardiomyopathy. The association increases with BMI and is strongest for dilated cardiomyopathy.
Major finding: Over a median of 27 years of follow-up, the hazard ratio for dilated cardiomyopathy in adulthood was 1.38 when adolescent body mass index was 22.5-25.0 kg/m2, using a BMI of 18.5-20.0 as the reference group. At a BMI over 35, the hazard ratio reached 8.11.
Study details: A nationwide, prospective registry cohort study of 1.67 million adolescent males in Sweden.
Disclosures: Funders included the Swedish government; Swedish Research Council; Swedish Heart and Lung Foundation; and Swedish Council for Health, Working Life and Welfare. The researchers reported having no conflicts of interest.
More empathy for women
At the risk of too much personal self-disclosure, I feel the need to write about my having developed more empathy for women. Having been described as a “manly man,” by a woman who feels she knows me, it has always been difficult for me to understand women. Fortunately, an experience I’ve had has given me more insight into women – shallow though it may still be.
About a year ago, I had learned I had prostate carcinoma, which is now in remission – thanks to a proctectomy, radiation, and hormone therapy. The antitestosterone hormones I need to take for 2 years are turning me into an old woman, thus my newfound empathy.
After the surgery, I found myself leaking – something that I probably only experienced as a child and of which I have little memory. I now have some more empathy for the problems women have with leaking each month or in general – it is a constant preoccupation. The leuprolide shots I am taking are giving me hot flashes, causing me to be more emotional about things I really don’t understand, and apparently I am at risk for getting osteoporosis – all things that happen to women that have been mildly on my radar for years but for which I lacked direct and personal experience.
Since having my testosterone turned off by the leuprolide, my joints are more prone to aches and pains from various injuries over the years. Because I understand that “motion is lotion,” I have some control of this problem. However, the hormone therapy has greatly reduced my endurance, so my exercise tolerance is far more limited – I understand fatigue now. When I was telling another woman who feels she knows me about my experience, she told me it was hormones that made it more difficult to lose weight. And, I am gaining weight.
All in all, I believe my experience has given me more empathy for women, but I realize I still have a very long way to go. Nonetheless, I will continue in my quest to understand the opposite sex, as I am told “women hold up half the sky,” and I have always believed that to be true.
Fortunately, women are ascending in psychiatry and, with some serious dedication, the dearth of scientific understanding of women’s issues will be a thing of the past. and fill that void of knowledge that we men psychiatrists have in our testosterone-bathed brains.
Dr. Bell is a staff psychiatrist at Jackson Park Hospital’s Medical/Surgical-Psychiatry Inpatient Unit in Chicago, clinical psychiatrist emeritus in the department of psychiatry at the University of Illinois at Chicago, former president/CEO of Community Mental Health Council, and former director of the Institute for Juvenile Research (birthplace of child psychiatry), also in Chicago.
At the risk of too much personal self-disclosure, I feel the need to write about my having developed more empathy for women. Having been described as a “manly man,” by a woman who feels she knows me, it has always been difficult for me to understand women. Fortunately, an experience I’ve had has given me more insight into women – shallow though it may still be.
About a year ago, I had learned I had prostate carcinoma, which is now in remission – thanks to a proctectomy, radiation, and hormone therapy. The antitestosterone hormones I need to take for 2 years are turning me into an old woman, thus my newfound empathy.
After the surgery, I found myself leaking – something that I probably only experienced as a child and of which I have little memory. I now have some more empathy for the problems women have with leaking each month or in general – it is a constant preoccupation. The leuprolide shots I am taking are giving me hot flashes, causing me to be more emotional about things I really don’t understand, and apparently I am at risk for getting osteoporosis – all things that happen to women that have been mildly on my radar for years but for which I lacked direct and personal experience.
Since having my testosterone turned off by the leuprolide, my joints are more prone to aches and pains from various injuries over the years. Because I understand that “motion is lotion,” I have some control of this problem. However, the hormone therapy has greatly reduced my endurance, so my exercise tolerance is far more limited – I understand fatigue now. When I was telling another woman who feels she knows me about my experience, she told me it was hormones that made it more difficult to lose weight. And, I am gaining weight.
All in all, I believe my experience has given me more empathy for women, but I realize I still have a very long way to go. Nonetheless, I will continue in my quest to understand the opposite sex, as I am told “women hold up half the sky,” and I have always believed that to be true.
Fortunately, women are ascending in psychiatry and, with some serious dedication, the dearth of scientific understanding of women’s issues will be a thing of the past. and fill that void of knowledge that we men psychiatrists have in our testosterone-bathed brains.
Dr. Bell is a staff psychiatrist at Jackson Park Hospital’s Medical/Surgical-Psychiatry Inpatient Unit in Chicago, clinical psychiatrist emeritus in the department of psychiatry at the University of Illinois at Chicago, former president/CEO of Community Mental Health Council, and former director of the Institute for Juvenile Research (birthplace of child psychiatry), also in Chicago.
At the risk of too much personal self-disclosure, I feel the need to write about my having developed more empathy for women. Having been described as a “manly man,” by a woman who feels she knows me, it has always been difficult for me to understand women. Fortunately, an experience I’ve had has given me more insight into women – shallow though it may still be.
About a year ago, I had learned I had prostate carcinoma, which is now in remission – thanks to a proctectomy, radiation, and hormone therapy. The antitestosterone hormones I need to take for 2 years are turning me into an old woman, thus my newfound empathy.
After the surgery, I found myself leaking – something that I probably only experienced as a child and of which I have little memory. I now have some more empathy for the problems women have with leaking each month or in general – it is a constant preoccupation. The leuprolide shots I am taking are giving me hot flashes, causing me to be more emotional about things I really don’t understand, and apparently I am at risk for getting osteoporosis – all things that happen to women that have been mildly on my radar for years but for which I lacked direct and personal experience.
Since having my testosterone turned off by the leuprolide, my joints are more prone to aches and pains from various injuries over the years. Because I understand that “motion is lotion,” I have some control of this problem. However, the hormone therapy has greatly reduced my endurance, so my exercise tolerance is far more limited – I understand fatigue now. When I was telling another woman who feels she knows me about my experience, she told me it was hormones that made it more difficult to lose weight. And, I am gaining weight.
All in all, I believe my experience has given me more empathy for women, but I realize I still have a very long way to go. Nonetheless, I will continue in my quest to understand the opposite sex, as I am told “women hold up half the sky,” and I have always believed that to be true.
Fortunately, women are ascending in psychiatry and, with some serious dedication, the dearth of scientific understanding of women’s issues will be a thing of the past. and fill that void of knowledge that we men psychiatrists have in our testosterone-bathed brains.
Dr. Bell is a staff psychiatrist at Jackson Park Hospital’s Medical/Surgical-Psychiatry Inpatient Unit in Chicago, clinical psychiatrist emeritus in the department of psychiatry at the University of Illinois at Chicago, former president/CEO of Community Mental Health Council, and former director of the Institute for Juvenile Research (birthplace of child psychiatry), also in Chicago.
PPI metabolism may be altered in about one-third of bariatric surgery candidates
SAN DIEGO – Rapid proton pump inhibitor (PPI) metabolism was present in nearly one-third of patients who underwent bariatric surgery, results from a small, single-center study showed. Patients who were fast metabolizers also exhibited a higher, although not significant, incidence of early marginal ulceration following Roux-en-Y gastric bypass.
“Roux-en-Y gastric bypass [RYGB] is one of the most effective surgical approaches to mitigating obesity and its attendant comorbidities including diabetes, hypertension, hyperlipidemia, reflux, and sleep apnea,” lead study author Sabrena F. Noria, MD, PhD, said in an interview at the annual Digestive Disease Week. “However, as with all surgeries, there are associated risks, the more common of which is marginal ulceration, or ulcer formation at the gastrojejunostomy, which occurs at a rate of 1%-16%.”
Dr. Noria, surgical research director of the comprehensive weight management, metabolic/bariatric surgery program at the Ohio State University’s Wexner Medical Center, noted that marginal ulcers (MUs) are divided into early (within 90 days) and late (more than 90 days), based on their time of onset after surgery, and are usually diagnosed during upper endoscopy on postoperative patients who complain of epigastric pain, dysphagia, nausea/vomiting, and/or dehydration.
“Given that MUs are associated with multiple hospital readmissions for pain and dehydration, multiple diagnostic and therapeutic endoscopic procedures, and escalation in both antiulcer and analgesic medication, their clinical impact cannot be overstated, especially since RYGB is the second most commonly performed bariatric procedure in the U.S.,” she said. “Given that the majority of marginal ulcers occur early after surgery, bariatric surgery programs have adopted the prophylactic use of proton pump inhibitors for up to 90 days postoperatively. While studies have demonstrated up to a two-fold decrease in ulcer formation, sample heterogeneity, in terms of combining both early and late ulcers, make it difficult to determine the effect on early ulcer formation.”
In an effort to compare preoperative endoscopic findings and MU formation in patients with and without altered PPI metabolism, the researchers prospectively enrolled 94 bariatric patients to undergo genetic testing pertinent to drug metabolism for a comprehensive panel of medications using a commercially available pharmacogenetic testing kit for the activity of cytochrome P450 in drug metabolism. They grouped patients by whether they were fast or normal metabolizers, and compared preoperative endoscopic findings for patients on PPIs at baseline and rates of early (within 90 days) and late ulceration (between 90 and 180 days).
Dr. Noria reported that 28 patients (30%) in the entire cohort met criteria for being fast metabolizers. The researchers observed no differences in baseline body mass index, age, gender, or former smoking status between both groups. Among those treated with a PPI at baseline, fast metabolizers demonstrated a trend toward a higher incidence of gastritis on preoperative endoscopy, compared with controls (89% vs. 65%, respectively; P = .12), while detection of Helicobacter pylori and Barrett’s esophagus were nonsignificant between groups. Eight patients (17%) who underwent RYGB developed marginal ulcers within 6 months of the index operation, of which four (50%) were diagnosed within 90 days and categorized as early ulcers. Development of early ulceration was higher among fast metabolizers, compared with controls (13% vs. 6%), but this did not reach statistical significance (P = .60). All late ulcerations occurred within the control group.
“While none of our findings are statistically significant given the small sample size, there were two findings I found clinically compelling,” Dr. Noria said. “First, in the group of patients who were on PPIs preoperatively, we found a 24% increase in the presence of pathologically diagnosed gastritis in the rapid-metabolizer group, during screening endoscopy. This suggests that either these patients were undertreated or were not treated with the appropriate medication. The second interesting finding was an over doubling of early ulcer formation in the RYGB group who were rapid metabolizers. However, again I would caution against drawing any real conclusions as our sample size was not powered to detect any difference.”
She also acknowledged that the study was limited by the inability to determine the effect of confounders such as surgical approach and the lack of randomization.
Anahita D. Jalilvand, MD, a general surgery resident, postdoctoral research fellow, and PhD candidate, was instrumental to this study, Dr. Noria said.
The trial was sponsored by Pathnostics, a pharmacogenetic testing company, who covered the cost of the tests. The researchers reported having no financial disclosures.
SAN DIEGO – Rapid proton pump inhibitor (PPI) metabolism was present in nearly one-third of patients who underwent bariatric surgery, results from a small, single-center study showed. Patients who were fast metabolizers also exhibited a higher, although not significant, incidence of early marginal ulceration following Roux-en-Y gastric bypass.
“Roux-en-Y gastric bypass [RYGB] is one of the most effective surgical approaches to mitigating obesity and its attendant comorbidities including diabetes, hypertension, hyperlipidemia, reflux, and sleep apnea,” lead study author Sabrena F. Noria, MD, PhD, said in an interview at the annual Digestive Disease Week. “However, as with all surgeries, there are associated risks, the more common of which is marginal ulceration, or ulcer formation at the gastrojejunostomy, which occurs at a rate of 1%-16%.”
Dr. Noria, surgical research director of the comprehensive weight management, metabolic/bariatric surgery program at the Ohio State University’s Wexner Medical Center, noted that marginal ulcers (MUs) are divided into early (within 90 days) and late (more than 90 days), based on their time of onset after surgery, and are usually diagnosed during upper endoscopy on postoperative patients who complain of epigastric pain, dysphagia, nausea/vomiting, and/or dehydration.
“Given that MUs are associated with multiple hospital readmissions for pain and dehydration, multiple diagnostic and therapeutic endoscopic procedures, and escalation in both antiulcer and analgesic medication, their clinical impact cannot be overstated, especially since RYGB is the second most commonly performed bariatric procedure in the U.S.,” she said. “Given that the majority of marginal ulcers occur early after surgery, bariatric surgery programs have adopted the prophylactic use of proton pump inhibitors for up to 90 days postoperatively. While studies have demonstrated up to a two-fold decrease in ulcer formation, sample heterogeneity, in terms of combining both early and late ulcers, make it difficult to determine the effect on early ulcer formation.”
In an effort to compare preoperative endoscopic findings and MU formation in patients with and without altered PPI metabolism, the researchers prospectively enrolled 94 bariatric patients to undergo genetic testing pertinent to drug metabolism for a comprehensive panel of medications using a commercially available pharmacogenetic testing kit for the activity of cytochrome P450 in drug metabolism. They grouped patients by whether they were fast or normal metabolizers, and compared preoperative endoscopic findings for patients on PPIs at baseline and rates of early (within 90 days) and late ulceration (between 90 and 180 days).
Dr. Noria reported that 28 patients (30%) in the entire cohort met criteria for being fast metabolizers. The researchers observed no differences in baseline body mass index, age, gender, or former smoking status between both groups. Among those treated with a PPI at baseline, fast metabolizers demonstrated a trend toward a higher incidence of gastritis on preoperative endoscopy, compared with controls (89% vs. 65%, respectively; P = .12), while detection of Helicobacter pylori and Barrett’s esophagus were nonsignificant between groups. Eight patients (17%) who underwent RYGB developed marginal ulcers within 6 months of the index operation, of which four (50%) were diagnosed within 90 days and categorized as early ulcers. Development of early ulceration was higher among fast metabolizers, compared with controls (13% vs. 6%), but this did not reach statistical significance (P = .60). All late ulcerations occurred within the control group.
“While none of our findings are statistically significant given the small sample size, there were two findings I found clinically compelling,” Dr. Noria said. “First, in the group of patients who were on PPIs preoperatively, we found a 24% increase in the presence of pathologically diagnosed gastritis in the rapid-metabolizer group, during screening endoscopy. This suggests that either these patients were undertreated or were not treated with the appropriate medication. The second interesting finding was an over doubling of early ulcer formation in the RYGB group who were rapid metabolizers. However, again I would caution against drawing any real conclusions as our sample size was not powered to detect any difference.”
She also acknowledged that the study was limited by the inability to determine the effect of confounders such as surgical approach and the lack of randomization.
Anahita D. Jalilvand, MD, a general surgery resident, postdoctoral research fellow, and PhD candidate, was instrumental to this study, Dr. Noria said.
The trial was sponsored by Pathnostics, a pharmacogenetic testing company, who covered the cost of the tests. The researchers reported having no financial disclosures.
SAN DIEGO – Rapid proton pump inhibitor (PPI) metabolism was present in nearly one-third of patients who underwent bariatric surgery, results from a small, single-center study showed. Patients who were fast metabolizers also exhibited a higher, although not significant, incidence of early marginal ulceration following Roux-en-Y gastric bypass.
“Roux-en-Y gastric bypass [RYGB] is one of the most effective surgical approaches to mitigating obesity and its attendant comorbidities including diabetes, hypertension, hyperlipidemia, reflux, and sleep apnea,” lead study author Sabrena F. Noria, MD, PhD, said in an interview at the annual Digestive Disease Week. “However, as with all surgeries, there are associated risks, the more common of which is marginal ulceration, or ulcer formation at the gastrojejunostomy, which occurs at a rate of 1%-16%.”
Dr. Noria, surgical research director of the comprehensive weight management, metabolic/bariatric surgery program at the Ohio State University’s Wexner Medical Center, noted that marginal ulcers (MUs) are divided into early (within 90 days) and late (more than 90 days), based on their time of onset after surgery, and are usually diagnosed during upper endoscopy on postoperative patients who complain of epigastric pain, dysphagia, nausea/vomiting, and/or dehydration.
“Given that MUs are associated with multiple hospital readmissions for pain and dehydration, multiple diagnostic and therapeutic endoscopic procedures, and escalation in both antiulcer and analgesic medication, their clinical impact cannot be overstated, especially since RYGB is the second most commonly performed bariatric procedure in the U.S.,” she said. “Given that the majority of marginal ulcers occur early after surgery, bariatric surgery programs have adopted the prophylactic use of proton pump inhibitors for up to 90 days postoperatively. While studies have demonstrated up to a two-fold decrease in ulcer formation, sample heterogeneity, in terms of combining both early and late ulcers, make it difficult to determine the effect on early ulcer formation.”
In an effort to compare preoperative endoscopic findings and MU formation in patients with and without altered PPI metabolism, the researchers prospectively enrolled 94 bariatric patients to undergo genetic testing pertinent to drug metabolism for a comprehensive panel of medications using a commercially available pharmacogenetic testing kit for the activity of cytochrome P450 in drug metabolism. They grouped patients by whether they were fast or normal metabolizers, and compared preoperative endoscopic findings for patients on PPIs at baseline and rates of early (within 90 days) and late ulceration (between 90 and 180 days).
Dr. Noria reported that 28 patients (30%) in the entire cohort met criteria for being fast metabolizers. The researchers observed no differences in baseline body mass index, age, gender, or former smoking status between both groups. Among those treated with a PPI at baseline, fast metabolizers demonstrated a trend toward a higher incidence of gastritis on preoperative endoscopy, compared with controls (89% vs. 65%, respectively; P = .12), while detection of Helicobacter pylori and Barrett’s esophagus were nonsignificant between groups. Eight patients (17%) who underwent RYGB developed marginal ulcers within 6 months of the index operation, of which four (50%) were diagnosed within 90 days and categorized as early ulcers. Development of early ulceration was higher among fast metabolizers, compared with controls (13% vs. 6%), but this did not reach statistical significance (P = .60). All late ulcerations occurred within the control group.
“While none of our findings are statistically significant given the small sample size, there were two findings I found clinically compelling,” Dr. Noria said. “First, in the group of patients who were on PPIs preoperatively, we found a 24% increase in the presence of pathologically diagnosed gastritis in the rapid-metabolizer group, during screening endoscopy. This suggests that either these patients were undertreated or were not treated with the appropriate medication. The second interesting finding was an over doubling of early ulcer formation in the RYGB group who were rapid metabolizers. However, again I would caution against drawing any real conclusions as our sample size was not powered to detect any difference.”
She also acknowledged that the study was limited by the inability to determine the effect of confounders such as surgical approach and the lack of randomization.
Anahita D. Jalilvand, MD, a general surgery resident, postdoctoral research fellow, and PhD candidate, was instrumental to this study, Dr. Noria said.
The trial was sponsored by Pathnostics, a pharmacogenetic testing company, who covered the cost of the tests. The researchers reported having no financial disclosures.
REPORTING FROM DDW 2019
Sustainable weight loss seen 5 years after endoscopic sleeve gastroplasty

The finding comes from the first long-term analysis of outcomes following endoscopic sleeve gastroplasty, a relatively new, minimally invasive weight-loss procedure that offers patients an alternative to bariatric surgery.
“Endoscopic sleeve gastrectomy is a 1-day outpatient procedure that uses a suturing device attached to an endoscope to create a series of sutures that cinch the stomach like an accordion down to roughly the size of a banana, and leaves no scars,” lead study author Reem Z. Sharaiha, MD, MSc, said during a media briefing in advance of the annual Digestive Disease Week®. “The procedure causes patients to eat less because they feel full faster. This results in weight loss.”
Digestive Disease Week is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
While previous studies have tracked ESG results for 1-2 years, her research team followed 203 patients who underwent the procedure between August 2013 and October 2018. “We felt that a longer-term study was needed to make sure weight loss was sustainable with this method of treatment, because research shows that if you keep weight loss for an extended period of time, you’re more likely to keep it off permanently, which is ultimately what we want for these patients,” said Dr. Sharaiha, who is an attending physician at New York–Presbyterian/Weill Cornell Medicine, New York.
At baseline, the mean age of the 203 patients was 46 years, 67% were female, and their mean body mass index was 39 kg/m2. Dr. Sharaiha and colleagues observed that maximum weight loss was generally achieved by 24 months after the procedure, after which patients tended to regain a small amount of their lost weight. For example, at 1 year, the mean weight loss was 18.1 kg, with a total body weight loss of 15.2% (P less than .0001 for both associations). At 2 years, the mean weight loss was 17.3 kg, with a total body weight loss of 14.5% (P less than .0001 for both associations). At 3 years, the mean weight loss was 20.8 kg, with a total body weight loss of 14.5% (P less than .0001 for both associations). At 5 years, the mean weight loss was 18.7 kg (P = .0003) and the total body weight loss was 14.5% (P = .0002).
Overall, patients gained an average 2.4 kg of weight after achieving their minimum weight after ESG until the end of follow-up. The researchers also found that failure to lose at least 10% of total body weight within the first 3 months after ESG decreased the chance of subsequent significant weight loss by 80%. Fewer than 1% of patients experienced complications, an improvement over surgical procedures.
“Our study showed very sustainable, significant weight loss for our patients between the 1 and 5 year mark,” Dr. Sharaiha said. “Out to 5 years, there was an average 15% total body weight loss. This is significant, because studies have shown that when people lose at least 10% of their body weight, they see improvement in blood pressure, diabetes, and heart outcomes, which are the comorbidities associated with obesity. We hope these findings will help persuade insurance companies that ESG is not experimental, but has value over patients’ lifespans.”
Dr. Sharaiha and colleagues plan to follow the current cohort for the next 10-20 years. “It’s important to show the value of these endoscopic procedures, so we’ll be looking at improvement in comorbidities such as diabetes, high blood pressure, and cholesterol,” she said. “We’re also part of a randomized study that’s currently under way looking at ESG in combination with diet and exercise.”
She reported having no financial disclosures.

The finding comes from the first long-term analysis of outcomes following endoscopic sleeve gastroplasty, a relatively new, minimally invasive weight-loss procedure that offers patients an alternative to bariatric surgery.
“Endoscopic sleeve gastrectomy is a 1-day outpatient procedure that uses a suturing device attached to an endoscope to create a series of sutures that cinch the stomach like an accordion down to roughly the size of a banana, and leaves no scars,” lead study author Reem Z. Sharaiha, MD, MSc, said during a media briefing in advance of the annual Digestive Disease Week®. “The procedure causes patients to eat less because they feel full faster. This results in weight loss.”
Digestive Disease Week is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
While previous studies have tracked ESG results for 1-2 years, her research team followed 203 patients who underwent the procedure between August 2013 and October 2018. “We felt that a longer-term study was needed to make sure weight loss was sustainable with this method of treatment, because research shows that if you keep weight loss for an extended period of time, you’re more likely to keep it off permanently, which is ultimately what we want for these patients,” said Dr. Sharaiha, who is an attending physician at New York–Presbyterian/Weill Cornell Medicine, New York.
At baseline, the mean age of the 203 patients was 46 years, 67% were female, and their mean body mass index was 39 kg/m2. Dr. Sharaiha and colleagues observed that maximum weight loss was generally achieved by 24 months after the procedure, after which patients tended to regain a small amount of their lost weight. For example, at 1 year, the mean weight loss was 18.1 kg, with a total body weight loss of 15.2% (P less than .0001 for both associations). At 2 years, the mean weight loss was 17.3 kg, with a total body weight loss of 14.5% (P less than .0001 for both associations). At 3 years, the mean weight loss was 20.8 kg, with a total body weight loss of 14.5% (P less than .0001 for both associations). At 5 years, the mean weight loss was 18.7 kg (P = .0003) and the total body weight loss was 14.5% (P = .0002).
Overall, patients gained an average 2.4 kg of weight after achieving their minimum weight after ESG until the end of follow-up. The researchers also found that failure to lose at least 10% of total body weight within the first 3 months after ESG decreased the chance of subsequent significant weight loss by 80%. Fewer than 1% of patients experienced complications, an improvement over surgical procedures.
“Our study showed very sustainable, significant weight loss for our patients between the 1 and 5 year mark,” Dr. Sharaiha said. “Out to 5 years, there was an average 15% total body weight loss. This is significant, because studies have shown that when people lose at least 10% of their body weight, they see improvement in blood pressure, diabetes, and heart outcomes, which are the comorbidities associated with obesity. We hope these findings will help persuade insurance companies that ESG is not experimental, but has value over patients’ lifespans.”
Dr. Sharaiha and colleagues plan to follow the current cohort for the next 10-20 years. “It’s important to show the value of these endoscopic procedures, so we’ll be looking at improvement in comorbidities such as diabetes, high blood pressure, and cholesterol,” she said. “We’re also part of a randomized study that’s currently under way looking at ESG in combination with diet and exercise.”
She reported having no financial disclosures.

The finding comes from the first long-term analysis of outcomes following endoscopic sleeve gastroplasty, a relatively new, minimally invasive weight-loss procedure that offers patients an alternative to bariatric surgery.
“Endoscopic sleeve gastrectomy is a 1-day outpatient procedure that uses a suturing device attached to an endoscope to create a series of sutures that cinch the stomach like an accordion down to roughly the size of a banana, and leaves no scars,” lead study author Reem Z. Sharaiha, MD, MSc, said during a media briefing in advance of the annual Digestive Disease Week®. “The procedure causes patients to eat less because they feel full faster. This results in weight loss.”
Digestive Disease Week is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
While previous studies have tracked ESG results for 1-2 years, her research team followed 203 patients who underwent the procedure between August 2013 and October 2018. “We felt that a longer-term study was needed to make sure weight loss was sustainable with this method of treatment, because research shows that if you keep weight loss for an extended period of time, you’re more likely to keep it off permanently, which is ultimately what we want for these patients,” said Dr. Sharaiha, who is an attending physician at New York–Presbyterian/Weill Cornell Medicine, New York.
At baseline, the mean age of the 203 patients was 46 years, 67% were female, and their mean body mass index was 39 kg/m2. Dr. Sharaiha and colleagues observed that maximum weight loss was generally achieved by 24 months after the procedure, after which patients tended to regain a small amount of their lost weight. For example, at 1 year, the mean weight loss was 18.1 kg, with a total body weight loss of 15.2% (P less than .0001 for both associations). At 2 years, the mean weight loss was 17.3 kg, with a total body weight loss of 14.5% (P less than .0001 for both associations). At 3 years, the mean weight loss was 20.8 kg, with a total body weight loss of 14.5% (P less than .0001 for both associations). At 5 years, the mean weight loss was 18.7 kg (P = .0003) and the total body weight loss was 14.5% (P = .0002).
Overall, patients gained an average 2.4 kg of weight after achieving their minimum weight after ESG until the end of follow-up. The researchers also found that failure to lose at least 10% of total body weight within the first 3 months after ESG decreased the chance of subsequent significant weight loss by 80%. Fewer than 1% of patients experienced complications, an improvement over surgical procedures.
“Our study showed very sustainable, significant weight loss for our patients between the 1 and 5 year mark,” Dr. Sharaiha said. “Out to 5 years, there was an average 15% total body weight loss. This is significant, because studies have shown that when people lose at least 10% of their body weight, they see improvement in blood pressure, diabetes, and heart outcomes, which are the comorbidities associated with obesity. We hope these findings will help persuade insurance companies that ESG is not experimental, but has value over patients’ lifespans.”
Dr. Sharaiha and colleagues plan to follow the current cohort for the next 10-20 years. “It’s important to show the value of these endoscopic procedures, so we’ll be looking at improvement in comorbidities such as diabetes, high blood pressure, and cholesterol,” she said. “We’re also part of a randomized study that’s currently under way looking at ESG in combination with diet and exercise.”
She reported having no financial disclosures.
FROM DDW 2019
Key clinical point: Endoscopic sleeve gastroplasty is an effective, minimally invasive weight-loss procedure that results in significant total body weight loss.
Major finding: Between 1 and 5 years after endoscopic sleeve gastroplasty, patients lost 15%-20% of their total body weight.
Study details: A retrospective study of prospectively collected data on 203 patients.
Disclosures: Dr. Sharaiha reported having no financial disclosures.
Study identifies predictors of bariatric surgery attrition
BALTIMORE – Even in a public health system like Canada’s, almost and researchers have identified patient characteristics that could be predictive of dropout risk that would potentially have implications in a nonuniversal system, such as that of the United States, according to a study of almost 18,000 patients reported at the annual meeting Society of American Gastrointestinal and Endoscopic Surgeons.
“Even in a universal health care system, clear disparities exist among patient populations having bariatric surgery,” said Aristithes Doumouras, MD, of McMaster University in Hamilton, Ont. “Extensive work-ups and long wait times can have an impact on the delivery of bariatric care.”
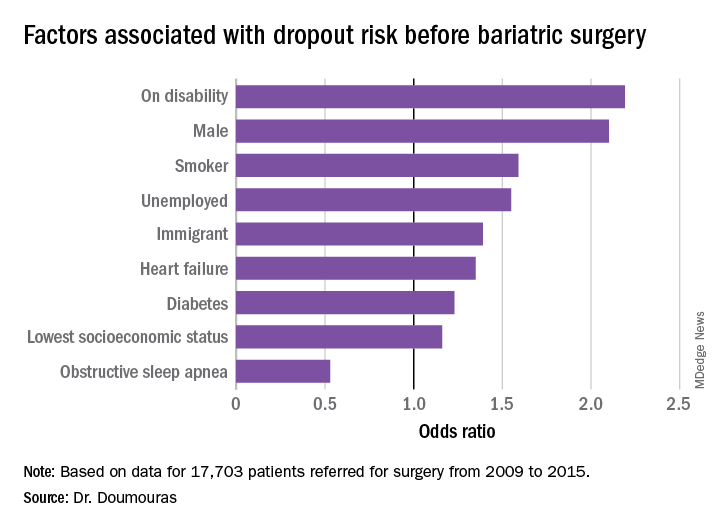
Dr. Doumouras reported on results of a retrospective, population-based study of 17,703 patients referred for surgery during 2009-2015 in the Ontario Bariatric Network, a province-wide network of 11 hospitals credentialed to perform bariatric surgery. The study found that 23.2% of patients referred for bariatric surgery did not go through with it and that overall average wait times between referral and the operation were just short of a year – 362.2 days to be precise.
The goal of the study was to identify any factors associated with attrition, Dr. Doumouras said.
“Predictors of interest included patient demographics – age, sex, income quintile, immigration status, employment status, smoking status – and comorbidities, such as diabetes, heart failure, hypertension, sleep apnea, and renal disease,” he said. “The study also evaluated health services factors, such as overall wait time to bariatric surgery, presence of centers of excellence, and health care utilization.”
The study found that demographics with more than twice the odds of attrition were male gender and presence of a disability (P less than .01). Smokers were 60% more likely to drop out (P less than .01), he said. “To receive bariatric surgery in Ontario, smokers must go through a smoking cessation program.”
Unemployed individuals and immigrants also had higher rates of attrition, at 55% and 39%, respectively, and were more likely to not go through with the operation (P less than .01). Health factors associated with attrition, but to a lesser extent, were diabetes (odds ratio, 1.23) and heart failure (OR, 1.35; P less than .01).
“Low socioeconomic status actually had a very low impact in our system on attrition after adjustment for other demographic factors such as disability and unemployment,” Dr. Doumouras said, noting a 16% greater risk of attrition in this group (P = .02).
“Interestingly,” he noted, “there was one factor associated with less dropout – obstructive sleep apnea – probably because people hate using the CPAP machines every single night.” People with OSA were 47% less likely to drop out than were people without the disease (P less than .001).
When asked if the findings would be applicable in the United States, Dr. Doumouras said they would to an extent.
“I think we can say confidently that they would apply to most universal health care systems,” he said. “In nonuniversal health care systems, the interplay between insurance status, socioeconomic status, and the like makes it more of a complex relationship, but if you were to take any kind of health care system, even in the United States, you would probably see very similar trends in terms of who can get bariatric surgery.”
He added, “I think also the length of work-up matters. Only a 3- or 4-week work-up probably affects attrition as well. These are relatively universal things.”
Dr. Doumouras has no financial relationships to disclose.
SOURCE: Doumouras A et al. SAGES 2019, Abstract S118.
BALTIMORE – Even in a public health system like Canada’s, almost and researchers have identified patient characteristics that could be predictive of dropout risk that would potentially have implications in a nonuniversal system, such as that of the United States, according to a study of almost 18,000 patients reported at the annual meeting Society of American Gastrointestinal and Endoscopic Surgeons.
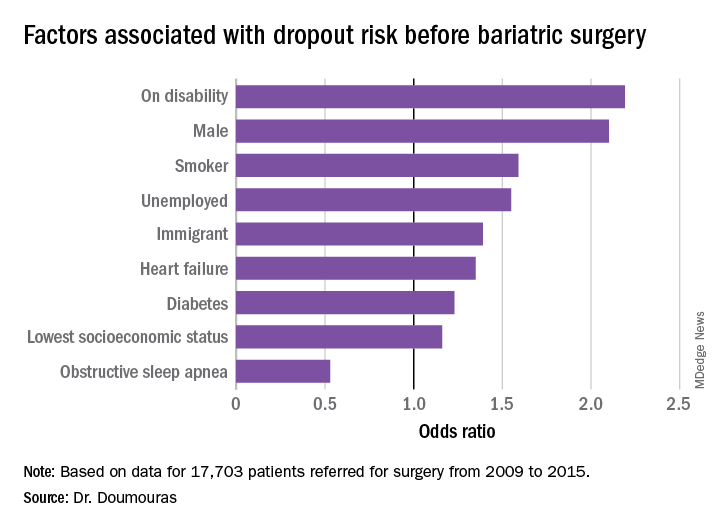
“Even in a universal health care system, clear disparities exist among patient populations having bariatric surgery,” said Aristithes Doumouras, MD, of McMaster University in Hamilton, Ont. “Extensive work-ups and long wait times can have an impact on the delivery of bariatric care.”
Dr. Doumouras reported on results of a retrospective, population-based study of 17,703 patients referred for surgery during 2009-2015 in the Ontario Bariatric Network, a province-wide network of 11 hospitals credentialed to perform bariatric surgery. The study found that 23.2% of patients referred for bariatric surgery did not go through with it and that overall average wait times between referral and the operation were just short of a year – 362.2 days to be precise.
The goal of the study was to identify any factors associated with attrition, Dr. Doumouras said.
“Predictors of interest included patient demographics – age, sex, income quintile, immigration status, employment status, smoking status – and comorbidities, such as diabetes, heart failure, hypertension, sleep apnea, and renal disease,” he said. “The study also evaluated health services factors, such as overall wait time to bariatric surgery, presence of centers of excellence, and health care utilization.”
The study found that demographics with more than twice the odds of attrition were male gender and presence of a disability (P less than .01). Smokers were 60% more likely to drop out (P less than .01), he said. “To receive bariatric surgery in Ontario, smokers must go through a smoking cessation program.”
Unemployed individuals and immigrants also had higher rates of attrition, at 55% and 39%, respectively, and were more likely to not go through with the operation (P less than .01). Health factors associated with attrition, but to a lesser extent, were diabetes (odds ratio, 1.23) and heart failure (OR, 1.35; P less than .01).
“Low socioeconomic status actually had a very low impact in our system on attrition after adjustment for other demographic factors such as disability and unemployment,” Dr. Doumouras said, noting a 16% greater risk of attrition in this group (P = .02).
“Interestingly,” he noted, “there was one factor associated with less dropout – obstructive sleep apnea – probably because people hate using the CPAP machines every single night.” People with OSA were 47% less likely to drop out than were people without the disease (P less than .001).
When asked if the findings would be applicable in the United States, Dr. Doumouras said they would to an extent.
“I think we can say confidently that they would apply to most universal health care systems,” he said. “In nonuniversal health care systems, the interplay between insurance status, socioeconomic status, and the like makes it more of a complex relationship, but if you were to take any kind of health care system, even in the United States, you would probably see very similar trends in terms of who can get bariatric surgery.”
He added, “I think also the length of work-up matters. Only a 3- or 4-week work-up probably affects attrition as well. These are relatively universal things.”
Dr. Doumouras has no financial relationships to disclose.
SOURCE: Doumouras A et al. SAGES 2019, Abstract S118.
BALTIMORE – Even in a public health system like Canada’s, almost and researchers have identified patient characteristics that could be predictive of dropout risk that would potentially have implications in a nonuniversal system, such as that of the United States, according to a study of almost 18,000 patients reported at the annual meeting Society of American Gastrointestinal and Endoscopic Surgeons.
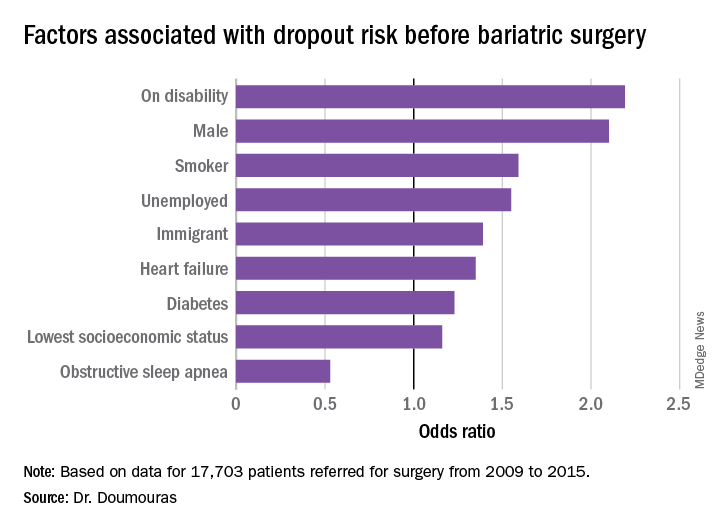
“Even in a universal health care system, clear disparities exist among patient populations having bariatric surgery,” said Aristithes Doumouras, MD, of McMaster University in Hamilton, Ont. “Extensive work-ups and long wait times can have an impact on the delivery of bariatric care.”
Dr. Doumouras reported on results of a retrospective, population-based study of 17,703 patients referred for surgery during 2009-2015 in the Ontario Bariatric Network, a province-wide network of 11 hospitals credentialed to perform bariatric surgery. The study found that 23.2% of patients referred for bariatric surgery did not go through with it and that overall average wait times between referral and the operation were just short of a year – 362.2 days to be precise.
The goal of the study was to identify any factors associated with attrition, Dr. Doumouras said.
“Predictors of interest included patient demographics – age, sex, income quintile, immigration status, employment status, smoking status – and comorbidities, such as diabetes, heart failure, hypertension, sleep apnea, and renal disease,” he said. “The study also evaluated health services factors, such as overall wait time to bariatric surgery, presence of centers of excellence, and health care utilization.”
The study found that demographics with more than twice the odds of attrition were male gender and presence of a disability (P less than .01). Smokers were 60% more likely to drop out (P less than .01), he said. “To receive bariatric surgery in Ontario, smokers must go through a smoking cessation program.”
Unemployed individuals and immigrants also had higher rates of attrition, at 55% and 39%, respectively, and were more likely to not go through with the operation (P less than .01). Health factors associated with attrition, but to a lesser extent, were diabetes (odds ratio, 1.23) and heart failure (OR, 1.35; P less than .01).
“Low socioeconomic status actually had a very low impact in our system on attrition after adjustment for other demographic factors such as disability and unemployment,” Dr. Doumouras said, noting a 16% greater risk of attrition in this group (P = .02).
“Interestingly,” he noted, “there was one factor associated with less dropout – obstructive sleep apnea – probably because people hate using the CPAP machines every single night.” People with OSA were 47% less likely to drop out than were people without the disease (P less than .001).
When asked if the findings would be applicable in the United States, Dr. Doumouras said they would to an extent.
“I think we can say confidently that they would apply to most universal health care systems,” he said. “In nonuniversal health care systems, the interplay between insurance status, socioeconomic status, and the like makes it more of a complex relationship, but if you were to take any kind of health care system, even in the United States, you would probably see very similar trends in terms of who can get bariatric surgery.”
He added, “I think also the length of work-up matters. Only a 3- or 4-week work-up probably affects attrition as well. These are relatively universal things.”
Dr. Doumouras has no financial relationships to disclose.
SOURCE: Doumouras A et al. SAGES 2019, Abstract S118.
REPORTING FROM SAGES 2019
Study finds inconsistencies in MBSAQIP database
BALTIMORE – A which could be misleading for clinicians and investigators who used the data, according to an analysis presented at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons. The researchers recommended ways to improve data-gathering techniques to better identify the nature of these inconsistencies.
“Our original enthusiasm about the availability of data from MBASQIP turned into a cautious optimism about potential usefulness of these data,” Katia Noyes, PhD, of the State University of New York at Buffalo, said in presenting the study. She noted her research team’s analysis of 168,093 cases in the 2015 MBASQIP Participant Use Data File found that 20% of the cases (n = 33,868) had missing or unusable information for at least one key variable, such as age, race, ethnicity, body mass index (BMI) before and after surgery, and American Society of Anesthesiologists classification. Specifically, preoperative and postoperative BMI data were missing or zero in 6.7% of cases (n = 11,211).
The researchers developed a single flat file for patient-level outcomes evaluation using five files (main, BMI, readmission, intervention, and reoperation). They used logic and validity tests that included individual profiles of patient BMI changes over time, individual patient care pathways (chronologic record of patient admission, discharge and procedure history), and correlation tests between pairs of variables associated with the same clinical encounters (emergency intervention vs. procedure type; related admission with intervention vs. planned intervention).
“Weight reduction at the first postoperative visit ranged from –71% to a gain of 132% of preoperative weight,” she said. “We also found inconsistency in the sequence of events. Seven percent of readmissions and 12.5% of postoperative interventions were categorized as planned, which is not a problem, but when you look at the reported reasons for planned procedures, they could not all have been possibly planned before discharge.”
Based on 2015 MBASQIP data, “planned” readmissions and postoperative procedures included admissions for nonspecific abdominal pain, band erosion, slippage or prolapse, bleeding, gastrogastric fistula, incisional hernia, infection and/or fever, pneumonia, and wound infection, among other reasons.
“Our analysis found inconsistent quality of data for key parameters, missing and miscoded values and lack of clarity for coding and definitions,” Dr. Noyes said.
The study made four recommendations to improve the quality of data submitted to MASQIP.
- Use health IT applications to provide automated data checks to validate completeness of submitted data – by utilizing a no-skip pattern for core variables – and accuracy of data– by flagging values outside predefined acceptable ranges.
- Perform data audits for consistency, using multiple variables to conduct logic checks, such as by not allowing “readmission” before discharge for the index admission.
- Give data auditors specific recommendations for definitions of registry variables, standardization of algorithms for abstracting values based on commonly used clinical data systems, such as Allscripts and Epic, and standardized use of diagnostic and procedure codes to link with payers’ reimbursement schedules.
- Provide ongoing education to stakeholders such as researchers and hospital administrators on best data management practices and how to best use the data for quality improvement.
Dr. Noyes had no financial relationships to disclose. Coauthor Steven Schwaitzberg, MD, disclosed consulting arrangements with New View Surgical, AcuityBio, Activ Surgical, Human Extensions, Levita Magnetics, and Arch Therapeutics. Aaron Hoffman, MD, disclosed a consulting arrangement with Ethicon.
SOURCE: Noyes K et al. SAGES 2019, Abstract 21
BALTIMORE – A which could be misleading for clinicians and investigators who used the data, according to an analysis presented at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons. The researchers recommended ways to improve data-gathering techniques to better identify the nature of these inconsistencies.
“Our original enthusiasm about the availability of data from MBASQIP turned into a cautious optimism about potential usefulness of these data,” Katia Noyes, PhD, of the State University of New York at Buffalo, said in presenting the study. She noted her research team’s analysis of 168,093 cases in the 2015 MBASQIP Participant Use Data File found that 20% of the cases (n = 33,868) had missing or unusable information for at least one key variable, such as age, race, ethnicity, body mass index (BMI) before and after surgery, and American Society of Anesthesiologists classification. Specifically, preoperative and postoperative BMI data were missing or zero in 6.7% of cases (n = 11,211).
The researchers developed a single flat file for patient-level outcomes evaluation using five files (main, BMI, readmission, intervention, and reoperation). They used logic and validity tests that included individual profiles of patient BMI changes over time, individual patient care pathways (chronologic record of patient admission, discharge and procedure history), and correlation tests between pairs of variables associated with the same clinical encounters (emergency intervention vs. procedure type; related admission with intervention vs. planned intervention).
“Weight reduction at the first postoperative visit ranged from –71% to a gain of 132% of preoperative weight,” she said. “We also found inconsistency in the sequence of events. Seven percent of readmissions and 12.5% of postoperative interventions were categorized as planned, which is not a problem, but when you look at the reported reasons for planned procedures, they could not all have been possibly planned before discharge.”
Based on 2015 MBASQIP data, “planned” readmissions and postoperative procedures included admissions for nonspecific abdominal pain, band erosion, slippage or prolapse, bleeding, gastrogastric fistula, incisional hernia, infection and/or fever, pneumonia, and wound infection, among other reasons.
“Our analysis found inconsistent quality of data for key parameters, missing and miscoded values and lack of clarity for coding and definitions,” Dr. Noyes said.
The study made four recommendations to improve the quality of data submitted to MASQIP.
- Use health IT applications to provide automated data checks to validate completeness of submitted data – by utilizing a no-skip pattern for core variables – and accuracy of data– by flagging values outside predefined acceptable ranges.
- Perform data audits for consistency, using multiple variables to conduct logic checks, such as by not allowing “readmission” before discharge for the index admission.
- Give data auditors specific recommendations for definitions of registry variables, standardization of algorithms for abstracting values based on commonly used clinical data systems, such as Allscripts and Epic, and standardized use of diagnostic and procedure codes to link with payers’ reimbursement schedules.
- Provide ongoing education to stakeholders such as researchers and hospital administrators on best data management practices and how to best use the data for quality improvement.
Dr. Noyes had no financial relationships to disclose. Coauthor Steven Schwaitzberg, MD, disclosed consulting arrangements with New View Surgical, AcuityBio, Activ Surgical, Human Extensions, Levita Magnetics, and Arch Therapeutics. Aaron Hoffman, MD, disclosed a consulting arrangement with Ethicon.
SOURCE: Noyes K et al. SAGES 2019, Abstract 21
BALTIMORE – A which could be misleading for clinicians and investigators who used the data, according to an analysis presented at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons. The researchers recommended ways to improve data-gathering techniques to better identify the nature of these inconsistencies.
“Our original enthusiasm about the availability of data from MBASQIP turned into a cautious optimism about potential usefulness of these data,” Katia Noyes, PhD, of the State University of New York at Buffalo, said in presenting the study. She noted her research team’s analysis of 168,093 cases in the 2015 MBASQIP Participant Use Data File found that 20% of the cases (n = 33,868) had missing or unusable information for at least one key variable, such as age, race, ethnicity, body mass index (BMI) before and after surgery, and American Society of Anesthesiologists classification. Specifically, preoperative and postoperative BMI data were missing or zero in 6.7% of cases (n = 11,211).
The researchers developed a single flat file for patient-level outcomes evaluation using five files (main, BMI, readmission, intervention, and reoperation). They used logic and validity tests that included individual profiles of patient BMI changes over time, individual patient care pathways (chronologic record of patient admission, discharge and procedure history), and correlation tests between pairs of variables associated with the same clinical encounters (emergency intervention vs. procedure type; related admission with intervention vs. planned intervention).
“Weight reduction at the first postoperative visit ranged from –71% to a gain of 132% of preoperative weight,” she said. “We also found inconsistency in the sequence of events. Seven percent of readmissions and 12.5% of postoperative interventions were categorized as planned, which is not a problem, but when you look at the reported reasons for planned procedures, they could not all have been possibly planned before discharge.”
Based on 2015 MBASQIP data, “planned” readmissions and postoperative procedures included admissions for nonspecific abdominal pain, band erosion, slippage or prolapse, bleeding, gastrogastric fistula, incisional hernia, infection and/or fever, pneumonia, and wound infection, among other reasons.
“Our analysis found inconsistent quality of data for key parameters, missing and miscoded values and lack of clarity for coding and definitions,” Dr. Noyes said.
The study made four recommendations to improve the quality of data submitted to MASQIP.
- Use health IT applications to provide automated data checks to validate completeness of submitted data – by utilizing a no-skip pattern for core variables – and accuracy of data– by flagging values outside predefined acceptable ranges.
- Perform data audits for consistency, using multiple variables to conduct logic checks, such as by not allowing “readmission” before discharge for the index admission.
- Give data auditors specific recommendations for definitions of registry variables, standardization of algorithms for abstracting values based on commonly used clinical data systems, such as Allscripts and Epic, and standardized use of diagnostic and procedure codes to link with payers’ reimbursement schedules.
- Provide ongoing education to stakeholders such as researchers and hospital administrators on best data management practices and how to best use the data for quality improvement.
Dr. Noyes had no financial relationships to disclose. Coauthor Steven Schwaitzberg, MD, disclosed consulting arrangements with New View Surgical, AcuityBio, Activ Surgical, Human Extensions, Levita Magnetics, and Arch Therapeutics. Aaron Hoffman, MD, disclosed a consulting arrangement with Ethicon.
SOURCE: Noyes K et al. SAGES 2019, Abstract 21
REPORTING FROM SAGES 2019
Study: Surgeon post-SG reflux rates vary widely
BALTIMORE – An analysis ofamong surgeons despite similarities in surgeon training, experience, skills, technique, and complication rates, according to findings presented at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
“We found that about a third of patients undergoing sleeve gastrectomy within this data registry developed worsening symptoms after sleeve gastrectomy, and the severity of these symptoms actually varied considerably, from 1 to 13.8 increase in their [GERD–Health Related Quality of Life Questionnaire (HRQL)] score,” said Oliver Varban, MD, of the University of Michigan, Ann Arbor. “Among the surgeons themselves, the rates of severe symptoms varied despite the surgeon’s experience and rate of hiatal hernia repair being similar between the groups.”
This study involved 7,358 patients in the Michigan Bariatric Surgery Collaborative (MBSC) registry who had SG from 2013 to 2017 and 52 surgeons who performed 25 or more SG cases per year. The patients completed the GERD-HRQL survey at baseline and 1 year after SG. The two scores were compared and patients were divided into terciles – mild, moderate, and severe – for worsening of symptoms, then matched with the surgeons who performed the operation. In all, 31.2% of patients (n = 2,294) reported worsening symptoms a year after SG, divided into the following terciles: mild with a 1.4-point increase in GERD-HRQL score (11.7%, n = 866); moderate, a 4.2-point increase (9.7%, n = 716); and severe, 13.8-point increase (9.7%, n = 712).
Among surgeons, the highest rate of patients with severe worsening of GERD was 44.7%, the lowest rate, 18.7%. So the researchers compared characteristics among the surgeons with the highest and lowest rates. “We found that they’re quite similar, actually, in terms of years of bariatric fellowship training, annual sleeve gastrectomy volume, total bariatric annual volume, as well as operative time,” Dr. Varban said. “Interestingly, the rate of concurrent hiatal hernia repair within these two groups is similar as well, which is about one-third for each group” (34.3% for the highest-rate group and 27% for the lowest-rate surgeons).
Likewise, 30-day risk adjusted complication rates were similar between both groups, 3.7% for the high group and 4.3% for the low group.
“Total–body weight loss or excess–body weight loss was actually fairly similar clinically between the two groups, but there was a statistical significance with more weight loss in the GERD patients who had higher severe worsening of symptoms,” Dr. Varban noted.
Surgeons with the highest rates of severe reflux symptoms in their patients tended to operate on more patients with diabetes, hypertension, and cardiovascular disease, whereas the surgeons with the lowest rate of severe symptoms had a higher proportion of patients who were male, white, and had hyperlipidemia and sleep apnea.
Dr. Varban has no financial relationships to disclose. Blue Cross Blue Shield of Michigan provided salary support through the MBSC.
SOURCE: Varban O et al. SAGES 2019; Session SS29, Abstract S139.
BALTIMORE – An analysis ofamong surgeons despite similarities in surgeon training, experience, skills, technique, and complication rates, according to findings presented at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
“We found that about a third of patients undergoing sleeve gastrectomy within this data registry developed worsening symptoms after sleeve gastrectomy, and the severity of these symptoms actually varied considerably, from 1 to 13.8 increase in their [GERD–Health Related Quality of Life Questionnaire (HRQL)] score,” said Oliver Varban, MD, of the University of Michigan, Ann Arbor. “Among the surgeons themselves, the rates of severe symptoms varied despite the surgeon’s experience and rate of hiatal hernia repair being similar between the groups.”
This study involved 7,358 patients in the Michigan Bariatric Surgery Collaborative (MBSC) registry who had SG from 2013 to 2017 and 52 surgeons who performed 25 or more SG cases per year. The patients completed the GERD-HRQL survey at baseline and 1 year after SG. The two scores were compared and patients were divided into terciles – mild, moderate, and severe – for worsening of symptoms, then matched with the surgeons who performed the operation. In all, 31.2% of patients (n = 2,294) reported worsening symptoms a year after SG, divided into the following terciles: mild with a 1.4-point increase in GERD-HRQL score (11.7%, n = 866); moderate, a 4.2-point increase (9.7%, n = 716); and severe, 13.8-point increase (9.7%, n = 712).
Among surgeons, the highest rate of patients with severe worsening of GERD was 44.7%, the lowest rate, 18.7%. So the researchers compared characteristics among the surgeons with the highest and lowest rates. “We found that they’re quite similar, actually, in terms of years of bariatric fellowship training, annual sleeve gastrectomy volume, total bariatric annual volume, as well as operative time,” Dr. Varban said. “Interestingly, the rate of concurrent hiatal hernia repair within these two groups is similar as well, which is about one-third for each group” (34.3% for the highest-rate group and 27% for the lowest-rate surgeons).
Likewise, 30-day risk adjusted complication rates were similar between both groups, 3.7% for the high group and 4.3% for the low group.
“Total–body weight loss or excess–body weight loss was actually fairly similar clinically between the two groups, but there was a statistical significance with more weight loss in the GERD patients who had higher severe worsening of symptoms,” Dr. Varban noted.
Surgeons with the highest rates of severe reflux symptoms in their patients tended to operate on more patients with diabetes, hypertension, and cardiovascular disease, whereas the surgeons with the lowest rate of severe symptoms had a higher proportion of patients who were male, white, and had hyperlipidemia and sleep apnea.
Dr. Varban has no financial relationships to disclose. Blue Cross Blue Shield of Michigan provided salary support through the MBSC.
SOURCE: Varban O et al. SAGES 2019; Session SS29, Abstract S139.
BALTIMORE – An analysis ofamong surgeons despite similarities in surgeon training, experience, skills, technique, and complication rates, according to findings presented at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
“We found that about a third of patients undergoing sleeve gastrectomy within this data registry developed worsening symptoms after sleeve gastrectomy, and the severity of these symptoms actually varied considerably, from 1 to 13.8 increase in their [GERD–Health Related Quality of Life Questionnaire (HRQL)] score,” said Oliver Varban, MD, of the University of Michigan, Ann Arbor. “Among the surgeons themselves, the rates of severe symptoms varied despite the surgeon’s experience and rate of hiatal hernia repair being similar between the groups.”
This study involved 7,358 patients in the Michigan Bariatric Surgery Collaborative (MBSC) registry who had SG from 2013 to 2017 and 52 surgeons who performed 25 or more SG cases per year. The patients completed the GERD-HRQL survey at baseline and 1 year after SG. The two scores were compared and patients were divided into terciles – mild, moderate, and severe – for worsening of symptoms, then matched with the surgeons who performed the operation. In all, 31.2% of patients (n = 2,294) reported worsening symptoms a year after SG, divided into the following terciles: mild with a 1.4-point increase in GERD-HRQL score (11.7%, n = 866); moderate, a 4.2-point increase (9.7%, n = 716); and severe, 13.8-point increase (9.7%, n = 712).
Among surgeons, the highest rate of patients with severe worsening of GERD was 44.7%, the lowest rate, 18.7%. So the researchers compared characteristics among the surgeons with the highest and lowest rates. “We found that they’re quite similar, actually, in terms of years of bariatric fellowship training, annual sleeve gastrectomy volume, total bariatric annual volume, as well as operative time,” Dr. Varban said. “Interestingly, the rate of concurrent hiatal hernia repair within these two groups is similar as well, which is about one-third for each group” (34.3% for the highest-rate group and 27% for the lowest-rate surgeons).
Likewise, 30-day risk adjusted complication rates were similar between both groups, 3.7% for the high group and 4.3% for the low group.
“Total–body weight loss or excess–body weight loss was actually fairly similar clinically between the two groups, but there was a statistical significance with more weight loss in the GERD patients who had higher severe worsening of symptoms,” Dr. Varban noted.
Surgeons with the highest rates of severe reflux symptoms in their patients tended to operate on more patients with diabetes, hypertension, and cardiovascular disease, whereas the surgeons with the lowest rate of severe symptoms had a higher proportion of patients who were male, white, and had hyperlipidemia and sleep apnea.
Dr. Varban has no financial relationships to disclose. Blue Cross Blue Shield of Michigan provided salary support through the MBSC.
SOURCE: Varban O et al. SAGES 2019; Session SS29, Abstract S139.
REPORTING FROM SAGES 2019