User login
FDA: More metformin extended-release tablets recalled
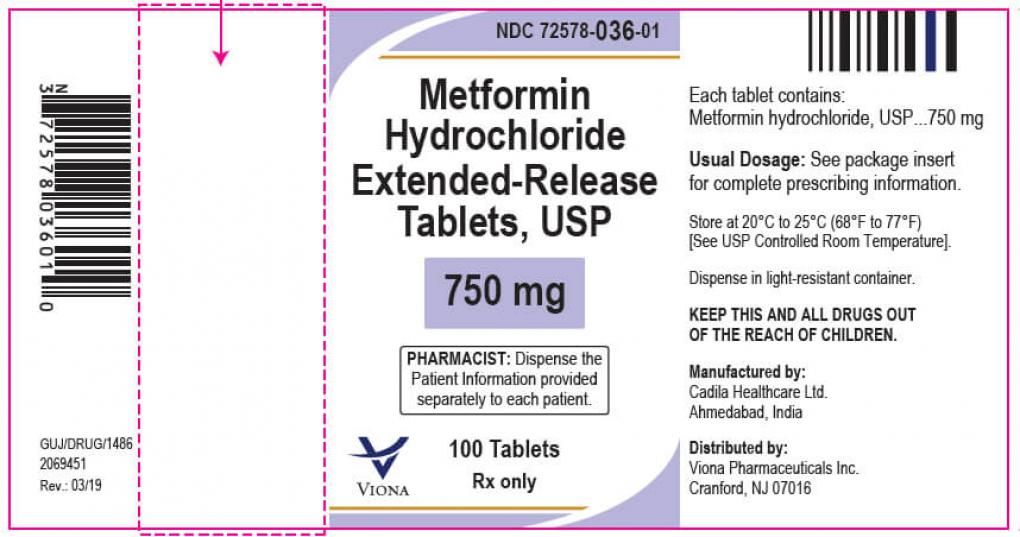
Two lots of metformin HCl extended-release tablets have been recalled by Viona Pharmaceuticals because unacceptable levels of nitrosodimethylamine (NDMA), a likely carcinogen, were found in the 750-mg tablets.
According to a June 11 alert from the Food and Drug Administration, the affected lot numbers are M915601 and M915602.
This generic product was made by Cadila Healthcare, Ahmedabad, India, in November 2019 with an expiration date of October 2021, and distributed throughout the United States. The pill is white to off-white, capsule-shaped, uncoated tablets, debossed with “Z”, “C” on one side and “20” on the other side.
No adverse events related to the lots involved in the recall have been reported, the FDA said. It also recommends that clinicians continue to prescribe metformin when clinically appropriate.
In late 2019, the FDA announced it had become aware of NDMA in some metformin products in other countries. The agency immediately began testing to determine whether the metformin in the U.S. supply was at risk, as part of the ongoing investigation into nitrosamine impurities across medication types, which included recalls of hypertension and heartburn medications within the past 3 years.
In February 2020, the FDA reported that they hadn’t found NDMA levels that exceeded the acceptable daily intake. But starting in May 2020, voluntary recalls by, numerous manufacturers have been announced as levels of the compound exceeded that cutoff.
Two lots of metformin HCl extended-release tablets have been recalled by Viona Pharmaceuticals because unacceptable levels of nitrosodimethylamine (NDMA), a likely carcinogen, were found in the 750-mg tablets.
According to a June 11 alert from the Food and Drug Administration, the affected lot numbers are M915601 and M915602.
This generic product was made by Cadila Healthcare, Ahmedabad, India, in November 2019 with an expiration date of October 2021, and distributed throughout the United States. The pill is white to off-white, capsule-shaped, uncoated tablets, debossed with “Z”, “C” on one side and “20” on the other side.
No adverse events related to the lots involved in the recall have been reported, the FDA said. It also recommends that clinicians continue to prescribe metformin when clinically appropriate.
In late 2019, the FDA announced it had become aware of NDMA in some metformin products in other countries. The agency immediately began testing to determine whether the metformin in the U.S. supply was at risk, as part of the ongoing investigation into nitrosamine impurities across medication types, which included recalls of hypertension and heartburn medications within the past 3 years.
In February 2020, the FDA reported that they hadn’t found NDMA levels that exceeded the acceptable daily intake. But starting in May 2020, voluntary recalls by, numerous manufacturers have been announced as levels of the compound exceeded that cutoff.
Two lots of metformin HCl extended-release tablets have been recalled by Viona Pharmaceuticals because unacceptable levels of nitrosodimethylamine (NDMA), a likely carcinogen, were found in the 750-mg tablets.
According to a June 11 alert from the Food and Drug Administration, the affected lot numbers are M915601 and M915602.
This generic product was made by Cadila Healthcare, Ahmedabad, India, in November 2019 with an expiration date of October 2021, and distributed throughout the United States. The pill is white to off-white, capsule-shaped, uncoated tablets, debossed with “Z”, “C” on one side and “20” on the other side.
No adverse events related to the lots involved in the recall have been reported, the FDA said. It also recommends that clinicians continue to prescribe metformin when clinically appropriate.
In late 2019, the FDA announced it had become aware of NDMA in some metformin products in other countries. The agency immediately began testing to determine whether the metformin in the U.S. supply was at risk, as part of the ongoing investigation into nitrosamine impurities across medication types, which included recalls of hypertension and heartburn medications within the past 3 years.
In February 2020, the FDA reported that they hadn’t found NDMA levels that exceeded the acceptable daily intake. But starting in May 2020, voluntary recalls by, numerous manufacturers have been announced as levels of the compound exceeded that cutoff.
FROM THE FOOD AND DRUG ADMINISTRATION
Screaming for screens: Digital well-being in the 2020s
Charlie is a 15-year-old male whose medical history includes overweight and autism spectrum disorder. While his autism symptoms are stable and he is doing fairly well in school, your sense is that he is underperforming and unhappy. His screening for anxiety and depression is not outstanding and you wonder whether to leave well enough alone.
Historically, pediatrician queries about media use happen in a minority of visits,1 overcrowded by the multitude of screening and acute care needs, let alone the pressures of electronic health record prompts, billing, and documentation. Yet the COVID-19 pandemic has emphasized what was already getting louder: screen life is becoming a ubiquitous, increasing, and normative function of child development. Digital well-being exhibits bidirectional interactions with most of the core indicators of child health: sleep, nutrition, safety, mood, relationships, and many other aspects of physical and mental health.1
The pandemic unveiled the blessings and curses of digital life by shifting many into remote work and school situations where screen time became both necessary and uncontrollable. Reeling with changes in employment, health, finances, and more, families struggled to forge a new screen-life balance that could bridge academic, professional, and recreational use.
Research has wavered in producing a verdict on the effects of screen time, in part because of limitations in methodology and follow-up time,2 and exacerbated by the quickly changing nature of screen use. Screen time may put youth at risk for obesity and behavior problems,3 but the latter may be mediated in part by loss of sleep because of late-night digital activity.4 While survey data at the population level show little link between screen time and well-being impairments,5 zooming in on individuals may tell a different story. Twenge and Campbell show light use of digital media (compared with nonuse) is associated with greater well-being while heavy use is associated with lower well-being and a higher risk for depression and suicidal behavior – especially in girls.6,7 Largely cross-sectional data show a small detriment to psychological well-being associated with digital technology, though this may be bidirectional and does not clearly differentiate types of technology.2
Recent neuroscience suggests that, compared with active play, sedentary screen time after school reduced impulse control and increased brain activity in regions associated with craving.8 This may explain some of the link between screen time and obesity. Brain imaging of preschoolers showed that greater screen time correlated with lower reading readiness as well as less integrity of white-matter tracts involved in language and executive function,9 whereas nurturing home reading practices were protective for language development and white matter integrity.10
Returning to the care of Charlie, providers may benefit from taking time to reflect on their own digital environment. What does the patient-side view of your office look like? Many offices use telephone reminders and patient portals, fill prescriptions electronically, and have waiting rooms with WiFi or devices for children’s use. Office visits share space with providers’ desktops, laptops, and smartphones, with EMRs guiding the visit. EMRs may come home for evening documentation. How does this affect provider digital well-being? How do you start the conversation with families about digital well-being?
The American Academy of Pediatrics recommends media screening be incorporated into routine pediatric care, with several tools available to support this. Adapting the HEADSSS model for psychosocial check-ins, Clark and colleagues propose an additional “S” to capture screen time.11 Their model queries which apps and social media are used, quantity of use, effects on self-confidence, and whether cyberbullying or sexting are occurring. Smartphones themselves provide an eye-opening and accessible dataset, with built-in features (for example, Screen Time for iOS) tracking not just daily duration of use, but also how frequently the phone is picked up and which apps get more use. Screening may be followed by motivational coaching, emphasizing nonjudgment, curiosity, empathy, and flexibility — for patient and provider.12
In Charlie’s case, screening reveals heavy use of social Internet games that connect him with like-minded peers. While he describes an inclusiveness and level of socialization that he has not found outside the home, the quantity of use is interfering with sleep, schoolwork, and physical activity.
Significant problematic Internet use may lead to intervention or referral – addictive behaviors and mental health symptoms may warrant connection with mental health providers. Cyberbullying or unsafe behaviors may additionally benefit from parental and school-based support. There is early and limited evidence that psychological and educational interventions may be of benefit for problematic Internet use.13
When digital life is not so dramatically affecting well-being, providers may begin by working with families on a media use plan. The AAP offers its own website to support this. Other well-researched and well-designed sites include Digital Wellness Lab For Parents, with developmentally staged information and plentiful research, and Common Sense Media, which reviews apps, movies, and more; plus they have a knowledge/advice section under “Parents Need to Know.” Keep in mind that digital media can also support youth in managing psychiatric problems, e.g., a digital intervention promoting positive psychology practices looked very helpful for young people with psychosis.14
For Charlie, a health coaching approach is adopted. Using Gabrielli’s TECH parenting rubric,15 Charlie’s parents are coached to make space to talk about and coview media and apps, as well as creating a Family Media Use Plan for everyone – parents included. Alongside setting limits on screen time; health promotion activities like exercise, reading, and schoolwork are also rewarded with extra screen time. When Charlie returns 3 months later, the family reports that, in recognition of their collective digital overload, they preserved dinnertime and after 10 p.m. as screen-free downtime. While they still have concerns about Charlie’s gaming and social life, his sleep is somewhat improved and family tension is lower.
Attention to digital well-being stands to benefit provider and patient alike, and over time may gain from the scaffolding of handouts, standardized assessments, and health coaching providers that may be in place to support other important domains like sleep hygiene, food security, and parenting.
Dr. Rosenfeld is assistant professor, University of Vermont, Vermont Center for Children, Youth, and Families, Burlington. He has no relevant disclosures.
References
1. Chassiakos YR et al. Pediatrics. 2016;138(5)e20162593.
2. Orben A. Soc Psychiatry Psych Epi. 2020;55(4):407.
3. Fang K et al. Child Care Health Dev. 2019;45(5):744-53.
4. Janssen X et al. Sleep Med Rev. 2020;49:101226.
5. George MJ et al. J Ped. 2020;219:180.
6. Twenge JM and Campbell WK. Psychiatry Q. 2019;90(2):311-31.
7. Twenge JM and Martin GN. J Adolesc. 2020;79:91.
8. Efraim M et al. Brain Imaging Behav. 2021;15(1):177-89.
9. Hutton JS et al. JAMA Pediatr. 2020;174(1):e193869.
10. Hutton JS et al. Acta Paediatr. 2020;109(7):1376-86.
11. Clark DL et al. Pediatrics. 2018;141(6).
12. Jericho M and Elliot A. Clin Child Psychol Psychiatry. 2020;25(3):662.
13. Malinauskas R and Malinauskine V. J Behav Addict. 2019;8(4):613.
14. Lim MH et al. Soc Psychiatry Psychiatr Epi. 2020;55(7):877-89.
15. Gabrielli J et al. Pediatrics. 2018;142(1)e20173718.
Charlie is a 15-year-old male whose medical history includes overweight and autism spectrum disorder. While his autism symptoms are stable and he is doing fairly well in school, your sense is that he is underperforming and unhappy. His screening for anxiety and depression is not outstanding and you wonder whether to leave well enough alone.
Historically, pediatrician queries about media use happen in a minority of visits,1 overcrowded by the multitude of screening and acute care needs, let alone the pressures of electronic health record prompts, billing, and documentation. Yet the COVID-19 pandemic has emphasized what was already getting louder: screen life is becoming a ubiquitous, increasing, and normative function of child development. Digital well-being exhibits bidirectional interactions with most of the core indicators of child health: sleep, nutrition, safety, mood, relationships, and many other aspects of physical and mental health.1
The pandemic unveiled the blessings and curses of digital life by shifting many into remote work and school situations where screen time became both necessary and uncontrollable. Reeling with changes in employment, health, finances, and more, families struggled to forge a new screen-life balance that could bridge academic, professional, and recreational use.
Research has wavered in producing a verdict on the effects of screen time, in part because of limitations in methodology and follow-up time,2 and exacerbated by the quickly changing nature of screen use. Screen time may put youth at risk for obesity and behavior problems,3 but the latter may be mediated in part by loss of sleep because of late-night digital activity.4 While survey data at the population level show little link between screen time and well-being impairments,5 zooming in on individuals may tell a different story. Twenge and Campbell show light use of digital media (compared with nonuse) is associated with greater well-being while heavy use is associated with lower well-being and a higher risk for depression and suicidal behavior – especially in girls.6,7 Largely cross-sectional data show a small detriment to psychological well-being associated with digital technology, though this may be bidirectional and does not clearly differentiate types of technology.2
Recent neuroscience suggests that, compared with active play, sedentary screen time after school reduced impulse control and increased brain activity in regions associated with craving.8 This may explain some of the link between screen time and obesity. Brain imaging of preschoolers showed that greater screen time correlated with lower reading readiness as well as less integrity of white-matter tracts involved in language and executive function,9 whereas nurturing home reading practices were protective for language development and white matter integrity.10
Returning to the care of Charlie, providers may benefit from taking time to reflect on their own digital environment. What does the patient-side view of your office look like? Many offices use telephone reminders and patient portals, fill prescriptions electronically, and have waiting rooms with WiFi or devices for children’s use. Office visits share space with providers’ desktops, laptops, and smartphones, with EMRs guiding the visit. EMRs may come home for evening documentation. How does this affect provider digital well-being? How do you start the conversation with families about digital well-being?
The American Academy of Pediatrics recommends media screening be incorporated into routine pediatric care, with several tools available to support this. Adapting the HEADSSS model for psychosocial check-ins, Clark and colleagues propose an additional “S” to capture screen time.11 Their model queries which apps and social media are used, quantity of use, effects on self-confidence, and whether cyberbullying or sexting are occurring. Smartphones themselves provide an eye-opening and accessible dataset, with built-in features (for example, Screen Time for iOS) tracking not just daily duration of use, but also how frequently the phone is picked up and which apps get more use. Screening may be followed by motivational coaching, emphasizing nonjudgment, curiosity, empathy, and flexibility — for patient and provider.12
In Charlie’s case, screening reveals heavy use of social Internet games that connect him with like-minded peers. While he describes an inclusiveness and level of socialization that he has not found outside the home, the quantity of use is interfering with sleep, schoolwork, and physical activity.
Significant problematic Internet use may lead to intervention or referral – addictive behaviors and mental health symptoms may warrant connection with mental health providers. Cyberbullying or unsafe behaviors may additionally benefit from parental and school-based support. There is early and limited evidence that psychological and educational interventions may be of benefit for problematic Internet use.13
When digital life is not so dramatically affecting well-being, providers may begin by working with families on a media use plan. The AAP offers its own website to support this. Other well-researched and well-designed sites include Digital Wellness Lab For Parents, with developmentally staged information and plentiful research, and Common Sense Media, which reviews apps, movies, and more; plus they have a knowledge/advice section under “Parents Need to Know.” Keep in mind that digital media can also support youth in managing psychiatric problems, e.g., a digital intervention promoting positive psychology practices looked very helpful for young people with psychosis.14
For Charlie, a health coaching approach is adopted. Using Gabrielli’s TECH parenting rubric,15 Charlie’s parents are coached to make space to talk about and coview media and apps, as well as creating a Family Media Use Plan for everyone – parents included. Alongside setting limits on screen time; health promotion activities like exercise, reading, and schoolwork are also rewarded with extra screen time. When Charlie returns 3 months later, the family reports that, in recognition of their collective digital overload, they preserved dinnertime and after 10 p.m. as screen-free downtime. While they still have concerns about Charlie’s gaming and social life, his sleep is somewhat improved and family tension is lower.
Attention to digital well-being stands to benefit provider and patient alike, and over time may gain from the scaffolding of handouts, standardized assessments, and health coaching providers that may be in place to support other important domains like sleep hygiene, food security, and parenting.
Dr. Rosenfeld is assistant professor, University of Vermont, Vermont Center for Children, Youth, and Families, Burlington. He has no relevant disclosures.
References
1. Chassiakos YR et al. Pediatrics. 2016;138(5)e20162593.
2. Orben A. Soc Psychiatry Psych Epi. 2020;55(4):407.
3. Fang K et al. Child Care Health Dev. 2019;45(5):744-53.
4. Janssen X et al. Sleep Med Rev. 2020;49:101226.
5. George MJ et al. J Ped. 2020;219:180.
6. Twenge JM and Campbell WK. Psychiatry Q. 2019;90(2):311-31.
7. Twenge JM and Martin GN. J Adolesc. 2020;79:91.
8. Efraim M et al. Brain Imaging Behav. 2021;15(1):177-89.
9. Hutton JS et al. JAMA Pediatr. 2020;174(1):e193869.
10. Hutton JS et al. Acta Paediatr. 2020;109(7):1376-86.
11. Clark DL et al. Pediatrics. 2018;141(6).
12. Jericho M and Elliot A. Clin Child Psychol Psychiatry. 2020;25(3):662.
13. Malinauskas R and Malinauskine V. J Behav Addict. 2019;8(4):613.
14. Lim MH et al. Soc Psychiatry Psychiatr Epi. 2020;55(7):877-89.
15. Gabrielli J et al. Pediatrics. 2018;142(1)e20173718.
Charlie is a 15-year-old male whose medical history includes overweight and autism spectrum disorder. While his autism symptoms are stable and he is doing fairly well in school, your sense is that he is underperforming and unhappy. His screening for anxiety and depression is not outstanding and you wonder whether to leave well enough alone.
Historically, pediatrician queries about media use happen in a minority of visits,1 overcrowded by the multitude of screening and acute care needs, let alone the pressures of electronic health record prompts, billing, and documentation. Yet the COVID-19 pandemic has emphasized what was already getting louder: screen life is becoming a ubiquitous, increasing, and normative function of child development. Digital well-being exhibits bidirectional interactions with most of the core indicators of child health: sleep, nutrition, safety, mood, relationships, and many other aspects of physical and mental health.1
The pandemic unveiled the blessings and curses of digital life by shifting many into remote work and school situations where screen time became both necessary and uncontrollable. Reeling with changes in employment, health, finances, and more, families struggled to forge a new screen-life balance that could bridge academic, professional, and recreational use.
Research has wavered in producing a verdict on the effects of screen time, in part because of limitations in methodology and follow-up time,2 and exacerbated by the quickly changing nature of screen use. Screen time may put youth at risk for obesity and behavior problems,3 but the latter may be mediated in part by loss of sleep because of late-night digital activity.4 While survey data at the population level show little link between screen time and well-being impairments,5 zooming in on individuals may tell a different story. Twenge and Campbell show light use of digital media (compared with nonuse) is associated with greater well-being while heavy use is associated with lower well-being and a higher risk for depression and suicidal behavior – especially in girls.6,7 Largely cross-sectional data show a small detriment to psychological well-being associated with digital technology, though this may be bidirectional and does not clearly differentiate types of technology.2
Recent neuroscience suggests that, compared with active play, sedentary screen time after school reduced impulse control and increased brain activity in regions associated with craving.8 This may explain some of the link between screen time and obesity. Brain imaging of preschoolers showed that greater screen time correlated with lower reading readiness as well as less integrity of white-matter tracts involved in language and executive function,9 whereas nurturing home reading practices were protective for language development and white matter integrity.10
Returning to the care of Charlie, providers may benefit from taking time to reflect on their own digital environment. What does the patient-side view of your office look like? Many offices use telephone reminders and patient portals, fill prescriptions electronically, and have waiting rooms with WiFi or devices for children’s use. Office visits share space with providers’ desktops, laptops, and smartphones, with EMRs guiding the visit. EMRs may come home for evening documentation. How does this affect provider digital well-being? How do you start the conversation with families about digital well-being?
The American Academy of Pediatrics recommends media screening be incorporated into routine pediatric care, with several tools available to support this. Adapting the HEADSSS model for psychosocial check-ins, Clark and colleagues propose an additional “S” to capture screen time.11 Their model queries which apps and social media are used, quantity of use, effects on self-confidence, and whether cyberbullying or sexting are occurring. Smartphones themselves provide an eye-opening and accessible dataset, with built-in features (for example, Screen Time for iOS) tracking not just daily duration of use, but also how frequently the phone is picked up and which apps get more use. Screening may be followed by motivational coaching, emphasizing nonjudgment, curiosity, empathy, and flexibility — for patient and provider.12
In Charlie’s case, screening reveals heavy use of social Internet games that connect him with like-minded peers. While he describes an inclusiveness and level of socialization that he has not found outside the home, the quantity of use is interfering with sleep, schoolwork, and physical activity.
Significant problematic Internet use may lead to intervention or referral – addictive behaviors and mental health symptoms may warrant connection with mental health providers. Cyberbullying or unsafe behaviors may additionally benefit from parental and school-based support. There is early and limited evidence that psychological and educational interventions may be of benefit for problematic Internet use.13
When digital life is not so dramatically affecting well-being, providers may begin by working with families on a media use plan. The AAP offers its own website to support this. Other well-researched and well-designed sites include Digital Wellness Lab For Parents, with developmentally staged information and plentiful research, and Common Sense Media, which reviews apps, movies, and more; plus they have a knowledge/advice section under “Parents Need to Know.” Keep in mind that digital media can also support youth in managing psychiatric problems, e.g., a digital intervention promoting positive psychology practices looked very helpful for young people with psychosis.14
For Charlie, a health coaching approach is adopted. Using Gabrielli’s TECH parenting rubric,15 Charlie’s parents are coached to make space to talk about and coview media and apps, as well as creating a Family Media Use Plan for everyone – parents included. Alongside setting limits on screen time; health promotion activities like exercise, reading, and schoolwork are also rewarded with extra screen time. When Charlie returns 3 months later, the family reports that, in recognition of their collective digital overload, they preserved dinnertime and after 10 p.m. as screen-free downtime. While they still have concerns about Charlie’s gaming and social life, his sleep is somewhat improved and family tension is lower.
Attention to digital well-being stands to benefit provider and patient alike, and over time may gain from the scaffolding of handouts, standardized assessments, and health coaching providers that may be in place to support other important domains like sleep hygiene, food security, and parenting.
Dr. Rosenfeld is assistant professor, University of Vermont, Vermont Center for Children, Youth, and Families, Burlington. He has no relevant disclosures.
References
1. Chassiakos YR et al. Pediatrics. 2016;138(5)e20162593.
2. Orben A. Soc Psychiatry Psych Epi. 2020;55(4):407.
3. Fang K et al. Child Care Health Dev. 2019;45(5):744-53.
4. Janssen X et al. Sleep Med Rev. 2020;49:101226.
5. George MJ et al. J Ped. 2020;219:180.
6. Twenge JM and Campbell WK. Psychiatry Q. 2019;90(2):311-31.
7. Twenge JM and Martin GN. J Adolesc. 2020;79:91.
8. Efraim M et al. Brain Imaging Behav. 2021;15(1):177-89.
9. Hutton JS et al. JAMA Pediatr. 2020;174(1):e193869.
10. Hutton JS et al. Acta Paediatr. 2020;109(7):1376-86.
11. Clark DL et al. Pediatrics. 2018;141(6).
12. Jericho M and Elliot A. Clin Child Psychol Psychiatry. 2020;25(3):662.
13. Malinauskas R and Malinauskine V. J Behav Addict. 2019;8(4):613.
14. Lim MH et al. Soc Psychiatry Psychiatr Epi. 2020;55(7):877-89.
15. Gabrielli J et al. Pediatrics. 2018;142(1)e20173718.
‘Twincretin’ meets primary endpoints in five pivotal diabetes trials
The investigational, novel, injected once-weekly “twincretin” tirzepatide met its primary efficacy endpoint of significantly cutting hemoglobin A1c as well as its secondary weight-loss endpoint in patients with type 2 diabetes when compared with control patients in top-line results from each of five discrete pivotal trials.
The company developing tirzepatide, Lilly, announced these results in a series of four press releases issued during December 2020–May 2021. Scientific reports on the outcomes from four of these trials are scheduled during the American Diabetes Association’s Scientific Sessions being held virtually in late June 2021, with results from the fifth on track for a report during the annual meeting of the European Association for the Study of Diabetes in September 2021.
Tirzepatide is a “twincretin” because it combines in a single molecule two different gut-hormone activities. It works as both a glucagonlike peptide–1 receptor agonist (GLP-1 RA) and as an agent that mimics the glucose-dependent insulinotropic polypeptide (GIP).
While diabetologists qualified their comments on these results because of the limited scope and format of the five reports to date, they also expressed enthusiasm over what the press releases said.
Results give hope
“It’s quite exciting, but of course we would like to go by the data that’s presented” at upcoming meetings, commented Robert A. Gabbay, MD, PhD, chief science and medical officer of the American Diabetes Association in Arlington, Va. “The idea of GLP-1 and GIP activities working together has been out there for a while, but without any therapeutic options that leverage this,” he said in an interview.
“The preliminary results give us hope that tirzepatide will be a very effective glucose-lowering agent, perhaps the most effective among all options currently available, including insulin,” commented Ildiko Lingvay, MD, a diabetologist and professor at the University of Texas Southwestern Medical Center, Dallas. “Tirzepatide might have the added benefit of clinically meaningful weight loss,” and “the adverse event profile seems to be in line with what we are accustomed to with the GLP-1 RA class. I look forward to seeing the full results. Tirzepatide promises to be a great addition for type 2 diabetes,” Dr. Lingvay said in an interview.
A rare head-to-head against semaglutide
The five phase 3, randomized controlled trials described by Lilly in its four press releases all belong to the SURPASS series of studies for this agent. Perhaps the most intriguing of the five were results from SURPASS-2, announced in a release on March 4. This trial randomized 1,879 patients from the United States or any of seven other countries to 40 weeks of open-label treatment with one of three different dosages of tirzepatide administered by injection once weekly, or to the control group that received a weekly 1-mg injection of semaglutide (Ozempic), the highest dosage approved for controlling glycemia in patients with type 2 diabetes at the time the study launched.
In SURPASS-2 all three tested dosages of tirzepatide led to a significantly larger reduction, from baseline in A1c, compared with semaglutide, after 40 weeks, according to the Lilly release. Each of the three tirzepatide dosages also led to significantly greater weight loss from baseline, compared with semaglutide, and significantly greater percentages of patients who achieved an A1c of less than 7%, compared with semaglutide.
As an example, the highest tested tirzepatide dosage of 15 mg weekly led to an average A1c reduction from baseline of 2.46% and an average weight loss from baseline of 12.4 kg; 92% of patients achieved an A1c of less than 7%, and 51% had their A1c fall below 5.7% which indicates completely normalization of glycemic control. By comparison, the patients randomized to treatment with semaglutide had an average 1.86% reduction in their A1c level from baseline and a 6.2-kg average cut in body weight from baseline; 81% achieved an A1c of less than 7%, and 20% reached an A1c of less than 5.7%.
There are caveats
While these findings are notable as a rare example of an industry-sponsored head-to-head comparison of two new agents, the study comes with a few important asterisks.
First, it was open label, a curious limitation given that both agents are delivered by the same delivery method and schedule. “I cannot conclude based on this study that tirzepatide is superior because it was open label,” commented Anastassia Amaro, MD, medical director of Penn Metabolic Medicine at the University of Pennsylvania, Philadelphia.
“The gold standard is the double-blind study. An open-label design is a limitation,” agreed Dr. Gabbay.
A second caveat is that the Food and Drug Administration recently approved a higher dosage of semaglutide (2.4 g once/week) for treating overweight or obesity in patients with type 2 diabetes and in those without diabetes but a different weight-related condition such as hypertension of hypercholesterolemia. This means that the tested comparator dosage of 1 mg/week is no longer the maximum that most patients treated with semaglutide for glycemic control can receive.
“The inevitable question” about this comparison study is “what about a higher semaglutide dose,” and how might tirzepatide perform relative to that, said Dr. Gabbay. The recently approved higher dosage of semaglutide “adds an interesting wrinkle.”
Lilly has launched a series of studies testing tirzepatide as a treatment for overweight or obesity in people without diabetes, but the results are not expected until sometime in 2022 or 2023.
And there’s a third caveat: Semaglutide has already shown its value for cardiovascular risk reduction in patients with type 2 diabetes in the SUSTAIN 6 trial with nearly 3,300 randomized patients followed for 2 years and reported in 2016. The cardiovascular outcomes trial for tirzepatide, SURPASS-CVOT with more than 12,000 patients with type 2 diabetes, is underway but its results are not expected until 2024.
Despite these important limitations, a blinded comparison of tirzepatide and higher-dose semaglutide is unlikely, Dr. Amaro predicted. “It’s not worth the expense,” she said in an interview. A more likely scenario will be that, if tirzepatide enters the U.S. market, decisions on whether to treat patients with it or semaglutide will pivot on factors like the cost for treatment to individual patients based on their insurance coverage and tolerability, suggested both Dr. Amaro and Dr. Gabbay. “Physicians will need to develop a sense for tirzepatide: Do patients tolerate it and are they happy using it?” Dr. Amaro said.
Tirzepatide versus insulin, or on top of insulin
The other four trials in patients with type 2 diabetes reported by Lilly in releases included SURPASS-1, which randomized 478 patients to treatment with tirzepatide or placebo as monotherapy; SURPASS-3, which randomized 1,444 patients to tirzepatide or insulin degludec (Tresiba) on top of background treatment with metformin; SURPASS-4, which randomized 2,002 patients with high cardiovascular disease risk to treatment with tirzepatide or insulin glargine (Lantus) on top of background treatment with one to three different oral drugs; and SURPASS-5, which randomized 475 patients to treatment with tirzepatide or placebo on top of background treatment with insulin glargine and optional addition of metformin. Altogether, the five trials randomized nearly 6,300 patients.
The studies that compared tirzepatide against two different types of insulin, and the third that tested tirzepatide on top of insulin glargine, are especially notable. “It’s good to see that the combination [of tirzepatide and insulin glargine] works without causing major adverse events,” said Dr. Amaro.
“These are fair and helpful comparisons. I applaud Lilly for doing the right kind of comparisons,” said Dr. Gabbay.
In total, the five studies “provide evidence that tirzepatide will be effective at all stages of type 2 diabetes and can safely be used in combination with other glucose-lowering agents, including insulin,” said Dr. Lingvay. The studies with active comparator agents “allow us to compare tirzepatide’s efficacy against established therapies.”
The SURPASS trials were sponsored by Lilly, which is developing tirzepatide. Dr. Gabbay had no relevant disclosures. Dr. Lingvay has received research funds, consulting and advisory fees, or other support from Lilly as well as from several other companies including Novo Nordisk, which markets semaglutide (Ozempic) and insulin degludec (Tresiba), and Sanofi, which markets insulin glargine (Lantus). Dr. Amaro has received research funding from Lilly and from Fractyl, and has been a consultant to and received research funding from Novo Nordisk.
The investigational, novel, injected once-weekly “twincretin” tirzepatide met its primary efficacy endpoint of significantly cutting hemoglobin A1c as well as its secondary weight-loss endpoint in patients with type 2 diabetes when compared with control patients in top-line results from each of five discrete pivotal trials.
The company developing tirzepatide, Lilly, announced these results in a series of four press releases issued during December 2020–May 2021. Scientific reports on the outcomes from four of these trials are scheduled during the American Diabetes Association’s Scientific Sessions being held virtually in late June 2021, with results from the fifth on track for a report during the annual meeting of the European Association for the Study of Diabetes in September 2021.
Tirzepatide is a “twincretin” because it combines in a single molecule two different gut-hormone activities. It works as both a glucagonlike peptide–1 receptor agonist (GLP-1 RA) and as an agent that mimics the glucose-dependent insulinotropic polypeptide (GIP).
While diabetologists qualified their comments on these results because of the limited scope and format of the five reports to date, they also expressed enthusiasm over what the press releases said.
Results give hope
“It’s quite exciting, but of course we would like to go by the data that’s presented” at upcoming meetings, commented Robert A. Gabbay, MD, PhD, chief science and medical officer of the American Diabetes Association in Arlington, Va. “The idea of GLP-1 and GIP activities working together has been out there for a while, but without any therapeutic options that leverage this,” he said in an interview.
“The preliminary results give us hope that tirzepatide will be a very effective glucose-lowering agent, perhaps the most effective among all options currently available, including insulin,” commented Ildiko Lingvay, MD, a diabetologist and professor at the University of Texas Southwestern Medical Center, Dallas. “Tirzepatide might have the added benefit of clinically meaningful weight loss,” and “the adverse event profile seems to be in line with what we are accustomed to with the GLP-1 RA class. I look forward to seeing the full results. Tirzepatide promises to be a great addition for type 2 diabetes,” Dr. Lingvay said in an interview.
A rare head-to-head against semaglutide
The five phase 3, randomized controlled trials described by Lilly in its four press releases all belong to the SURPASS series of studies for this agent. Perhaps the most intriguing of the five were results from SURPASS-2, announced in a release on March 4. This trial randomized 1,879 patients from the United States or any of seven other countries to 40 weeks of open-label treatment with one of three different dosages of tirzepatide administered by injection once weekly, or to the control group that received a weekly 1-mg injection of semaglutide (Ozempic), the highest dosage approved for controlling glycemia in patients with type 2 diabetes at the time the study launched.
In SURPASS-2 all three tested dosages of tirzepatide led to a significantly larger reduction, from baseline in A1c, compared with semaglutide, after 40 weeks, according to the Lilly release. Each of the three tirzepatide dosages also led to significantly greater weight loss from baseline, compared with semaglutide, and significantly greater percentages of patients who achieved an A1c of less than 7%, compared with semaglutide.
As an example, the highest tested tirzepatide dosage of 15 mg weekly led to an average A1c reduction from baseline of 2.46% and an average weight loss from baseline of 12.4 kg; 92% of patients achieved an A1c of less than 7%, and 51% had their A1c fall below 5.7% which indicates completely normalization of glycemic control. By comparison, the patients randomized to treatment with semaglutide had an average 1.86% reduction in their A1c level from baseline and a 6.2-kg average cut in body weight from baseline; 81% achieved an A1c of less than 7%, and 20% reached an A1c of less than 5.7%.
There are caveats
While these findings are notable as a rare example of an industry-sponsored head-to-head comparison of two new agents, the study comes with a few important asterisks.
First, it was open label, a curious limitation given that both agents are delivered by the same delivery method and schedule. “I cannot conclude based on this study that tirzepatide is superior because it was open label,” commented Anastassia Amaro, MD, medical director of Penn Metabolic Medicine at the University of Pennsylvania, Philadelphia.
“The gold standard is the double-blind study. An open-label design is a limitation,” agreed Dr. Gabbay.
A second caveat is that the Food and Drug Administration recently approved a higher dosage of semaglutide (2.4 g once/week) for treating overweight or obesity in patients with type 2 diabetes and in those without diabetes but a different weight-related condition such as hypertension of hypercholesterolemia. This means that the tested comparator dosage of 1 mg/week is no longer the maximum that most patients treated with semaglutide for glycemic control can receive.
“The inevitable question” about this comparison study is “what about a higher semaglutide dose,” and how might tirzepatide perform relative to that, said Dr. Gabbay. The recently approved higher dosage of semaglutide “adds an interesting wrinkle.”
Lilly has launched a series of studies testing tirzepatide as a treatment for overweight or obesity in people without diabetes, but the results are not expected until sometime in 2022 or 2023.
And there’s a third caveat: Semaglutide has already shown its value for cardiovascular risk reduction in patients with type 2 diabetes in the SUSTAIN 6 trial with nearly 3,300 randomized patients followed for 2 years and reported in 2016. The cardiovascular outcomes trial for tirzepatide, SURPASS-CVOT with more than 12,000 patients with type 2 diabetes, is underway but its results are not expected until 2024.
Despite these important limitations, a blinded comparison of tirzepatide and higher-dose semaglutide is unlikely, Dr. Amaro predicted. “It’s not worth the expense,” she said in an interview. A more likely scenario will be that, if tirzepatide enters the U.S. market, decisions on whether to treat patients with it or semaglutide will pivot on factors like the cost for treatment to individual patients based on their insurance coverage and tolerability, suggested both Dr. Amaro and Dr. Gabbay. “Physicians will need to develop a sense for tirzepatide: Do patients tolerate it and are they happy using it?” Dr. Amaro said.
Tirzepatide versus insulin, or on top of insulin
The other four trials in patients with type 2 diabetes reported by Lilly in releases included SURPASS-1, which randomized 478 patients to treatment with tirzepatide or placebo as monotherapy; SURPASS-3, which randomized 1,444 patients to tirzepatide or insulin degludec (Tresiba) on top of background treatment with metformin; SURPASS-4, which randomized 2,002 patients with high cardiovascular disease risk to treatment with tirzepatide or insulin glargine (Lantus) on top of background treatment with one to three different oral drugs; and SURPASS-5, which randomized 475 patients to treatment with tirzepatide or placebo on top of background treatment with insulin glargine and optional addition of metformin. Altogether, the five trials randomized nearly 6,300 patients.
The studies that compared tirzepatide against two different types of insulin, and the third that tested tirzepatide on top of insulin glargine, are especially notable. “It’s good to see that the combination [of tirzepatide and insulin glargine] works without causing major adverse events,” said Dr. Amaro.
“These are fair and helpful comparisons. I applaud Lilly for doing the right kind of comparisons,” said Dr. Gabbay.
In total, the five studies “provide evidence that tirzepatide will be effective at all stages of type 2 diabetes and can safely be used in combination with other glucose-lowering agents, including insulin,” said Dr. Lingvay. The studies with active comparator agents “allow us to compare tirzepatide’s efficacy against established therapies.”
The SURPASS trials were sponsored by Lilly, which is developing tirzepatide. Dr. Gabbay had no relevant disclosures. Dr. Lingvay has received research funds, consulting and advisory fees, or other support from Lilly as well as from several other companies including Novo Nordisk, which markets semaglutide (Ozempic) and insulin degludec (Tresiba), and Sanofi, which markets insulin glargine (Lantus). Dr. Amaro has received research funding from Lilly and from Fractyl, and has been a consultant to and received research funding from Novo Nordisk.
The investigational, novel, injected once-weekly “twincretin” tirzepatide met its primary efficacy endpoint of significantly cutting hemoglobin A1c as well as its secondary weight-loss endpoint in patients with type 2 diabetes when compared with control patients in top-line results from each of five discrete pivotal trials.
The company developing tirzepatide, Lilly, announced these results in a series of four press releases issued during December 2020–May 2021. Scientific reports on the outcomes from four of these trials are scheduled during the American Diabetes Association’s Scientific Sessions being held virtually in late June 2021, with results from the fifth on track for a report during the annual meeting of the European Association for the Study of Diabetes in September 2021.
Tirzepatide is a “twincretin” because it combines in a single molecule two different gut-hormone activities. It works as both a glucagonlike peptide–1 receptor agonist (GLP-1 RA) and as an agent that mimics the glucose-dependent insulinotropic polypeptide (GIP).
While diabetologists qualified their comments on these results because of the limited scope and format of the five reports to date, they also expressed enthusiasm over what the press releases said.
Results give hope
“It’s quite exciting, but of course we would like to go by the data that’s presented” at upcoming meetings, commented Robert A. Gabbay, MD, PhD, chief science and medical officer of the American Diabetes Association in Arlington, Va. “The idea of GLP-1 and GIP activities working together has been out there for a while, but without any therapeutic options that leverage this,” he said in an interview.
“The preliminary results give us hope that tirzepatide will be a very effective glucose-lowering agent, perhaps the most effective among all options currently available, including insulin,” commented Ildiko Lingvay, MD, a diabetologist and professor at the University of Texas Southwestern Medical Center, Dallas. “Tirzepatide might have the added benefit of clinically meaningful weight loss,” and “the adverse event profile seems to be in line with what we are accustomed to with the GLP-1 RA class. I look forward to seeing the full results. Tirzepatide promises to be a great addition for type 2 diabetes,” Dr. Lingvay said in an interview.
A rare head-to-head against semaglutide
The five phase 3, randomized controlled trials described by Lilly in its four press releases all belong to the SURPASS series of studies for this agent. Perhaps the most intriguing of the five were results from SURPASS-2, announced in a release on March 4. This trial randomized 1,879 patients from the United States or any of seven other countries to 40 weeks of open-label treatment with one of three different dosages of tirzepatide administered by injection once weekly, or to the control group that received a weekly 1-mg injection of semaglutide (Ozempic), the highest dosage approved for controlling glycemia in patients with type 2 diabetes at the time the study launched.
In SURPASS-2 all three tested dosages of tirzepatide led to a significantly larger reduction, from baseline in A1c, compared with semaglutide, after 40 weeks, according to the Lilly release. Each of the three tirzepatide dosages also led to significantly greater weight loss from baseline, compared with semaglutide, and significantly greater percentages of patients who achieved an A1c of less than 7%, compared with semaglutide.
As an example, the highest tested tirzepatide dosage of 15 mg weekly led to an average A1c reduction from baseline of 2.46% and an average weight loss from baseline of 12.4 kg; 92% of patients achieved an A1c of less than 7%, and 51% had their A1c fall below 5.7% which indicates completely normalization of glycemic control. By comparison, the patients randomized to treatment with semaglutide had an average 1.86% reduction in their A1c level from baseline and a 6.2-kg average cut in body weight from baseline; 81% achieved an A1c of less than 7%, and 20% reached an A1c of less than 5.7%.
There are caveats
While these findings are notable as a rare example of an industry-sponsored head-to-head comparison of two new agents, the study comes with a few important asterisks.
First, it was open label, a curious limitation given that both agents are delivered by the same delivery method and schedule. “I cannot conclude based on this study that tirzepatide is superior because it was open label,” commented Anastassia Amaro, MD, medical director of Penn Metabolic Medicine at the University of Pennsylvania, Philadelphia.
“The gold standard is the double-blind study. An open-label design is a limitation,” agreed Dr. Gabbay.
A second caveat is that the Food and Drug Administration recently approved a higher dosage of semaglutide (2.4 g once/week) for treating overweight or obesity in patients with type 2 diabetes and in those without diabetes but a different weight-related condition such as hypertension of hypercholesterolemia. This means that the tested comparator dosage of 1 mg/week is no longer the maximum that most patients treated with semaglutide for glycemic control can receive.
“The inevitable question” about this comparison study is “what about a higher semaglutide dose,” and how might tirzepatide perform relative to that, said Dr. Gabbay. The recently approved higher dosage of semaglutide “adds an interesting wrinkle.”
Lilly has launched a series of studies testing tirzepatide as a treatment for overweight or obesity in people without diabetes, but the results are not expected until sometime in 2022 or 2023.
And there’s a third caveat: Semaglutide has already shown its value for cardiovascular risk reduction in patients with type 2 diabetes in the SUSTAIN 6 trial with nearly 3,300 randomized patients followed for 2 years and reported in 2016. The cardiovascular outcomes trial for tirzepatide, SURPASS-CVOT with more than 12,000 patients with type 2 diabetes, is underway but its results are not expected until 2024.
Despite these important limitations, a blinded comparison of tirzepatide and higher-dose semaglutide is unlikely, Dr. Amaro predicted. “It’s not worth the expense,” she said in an interview. A more likely scenario will be that, if tirzepatide enters the U.S. market, decisions on whether to treat patients with it or semaglutide will pivot on factors like the cost for treatment to individual patients based on their insurance coverage and tolerability, suggested both Dr. Amaro and Dr. Gabbay. “Physicians will need to develop a sense for tirzepatide: Do patients tolerate it and are they happy using it?” Dr. Amaro said.
Tirzepatide versus insulin, or on top of insulin
The other four trials in patients with type 2 diabetes reported by Lilly in releases included SURPASS-1, which randomized 478 patients to treatment with tirzepatide or placebo as monotherapy; SURPASS-3, which randomized 1,444 patients to tirzepatide or insulin degludec (Tresiba) on top of background treatment with metformin; SURPASS-4, which randomized 2,002 patients with high cardiovascular disease risk to treatment with tirzepatide or insulin glargine (Lantus) on top of background treatment with one to three different oral drugs; and SURPASS-5, which randomized 475 patients to treatment with tirzepatide or placebo on top of background treatment with insulin glargine and optional addition of metformin. Altogether, the five trials randomized nearly 6,300 patients.
The studies that compared tirzepatide against two different types of insulin, and the third that tested tirzepatide on top of insulin glargine, are especially notable. “It’s good to see that the combination [of tirzepatide and insulin glargine] works without causing major adverse events,” said Dr. Amaro.
“These are fair and helpful comparisons. I applaud Lilly for doing the right kind of comparisons,” said Dr. Gabbay.
In total, the five studies “provide evidence that tirzepatide will be effective at all stages of type 2 diabetes and can safely be used in combination with other glucose-lowering agents, including insulin,” said Dr. Lingvay. The studies with active comparator agents “allow us to compare tirzepatide’s efficacy against established therapies.”
The SURPASS trials were sponsored by Lilly, which is developing tirzepatide. Dr. Gabbay had no relevant disclosures. Dr. Lingvay has received research funds, consulting and advisory fees, or other support from Lilly as well as from several other companies including Novo Nordisk, which markets semaglutide (Ozempic) and insulin degludec (Tresiba), and Sanofi, which markets insulin glargine (Lantus). Dr. Amaro has received research funding from Lilly and from Fractyl, and has been a consultant to and received research funding from Novo Nordisk.
Obesity amplifies harmful effects of alcohol on the liver
Being overweight or having obesity significantly increases the risk for liver disease and the likelihood of dying from it compared with being of normal weight, regardless of level of alcohol consumption, new research shows.
"People in the overweight or obese range who drank were found to be at greater risk of liver diseases compared with participants within a healthy weight range who consumed alcohol at the same level," senior author Emmanuel Stamatakis, PhD, of the Charles Perkins Centre and the Faculty of Medicine and Health, Sydney, said in a press statement.
"Even for people who drank within alcohol guidelines, participants classified as obese were at over 50% greater risk of liver disease," he said.
"Obesity is an independent risk factor for steatosis, acute alcoholic hepatitis, and cirrhosis in alcoholic liver disease (ALD), which may increase the risk of mortality in ALD patients," the study's first author, Elif Inan-Eroglu, PhD, a postdoctoral research fellow at the Charles Perkins Centre, said in an interview.
Further prospective studies are needed to better understand the underlying mechanisms behind the association between alcohol consumption and liver disease across different adiposity levels, the authors say.
Meanwhile, the take-home message from the findings should be that "clinicians should consider the presence of overweight and obesity when they discuss defining safe alcohol levels for their patients, keeping in mind that there is no 'safe' level of alcohol," Dr. Inan-Eroglu said.
"Alcohol drinking guidelines need to acknowledge that two-thirds of the adult population are overweight or obese and consider specific recommendations for this majority population group," he said.
First and largest study of its kind
Obesity, well-known to be an independent risk factor for nonalcoholic fatty liver disease (NAFLD), is also known to worsen outcomes in ALD. And likewise, alcohol consumption, the cause of ALD, can promote obesity and therefore increase the risk of NAFLD.
Dr. Stamatakis and colleagues sought to evaluate the roles of the combined factors in terms of incidence and mortality in both ALD and NAFLD.
For the study, published online May 31 in the European Journal of Clinical Nutrition, they evaluated data from 465,437 participants in the U.K. Biobank. The study is said to be the first and largest of its kind.
In the cohort, a total of 1,090 liver disease deaths were recorded, including 230 deaths from ALD and 192 from NAFLD over an average follow-up of 10.5 years.
After a multivariate adjustment, the overall risk of ALD, NAFLD, and liver disease incidence and mortality were significantly higher in participants who were overweight or had obesity, compared with those of normal weight, at all levels of alcohol consumption.
For instance, among those with alcohol use exceeding guidelines, the risk of ALD was significantly increased in normal weight individuals versus never-drinkers (hazard ratio [HR], 5.38), and the risk was even higher among those who were also overweight or had obesity (HR, 8.58).
In terms of the risk of death related to ALD, among those reporting alcohol consumption above guidelines, the risk was nearly double among those who were overweight or had obesity (HR, 10.29) versus those with normal weight (HR, 5.84), when each group was compared to those drinking within guidelines.
Regarding NAFLD, consistent with evidence that low to moderate alcohol consumption is, in fact, linked to a reduced risk, those in the study who reported alcohol consumption within guidelines and normal weight did show a reduced risk of NAFLD compared with an index group of never-drinkers (HR, 0.85).
However, being overweight or having obesity increased the risk of NAFLD in those participants (HR, 1.51).
Furthermore, even those reporting alcohol consumption above guidelines who were of normal weight had a reduced risk of NAFLD compared with never drinkers of normal weight (HR, 0.89).
Regarding the risk of liver disease among those reporting alcohol consumption above guidelines compared with never-drinkers, the risk was again lower among those of normal weight versus those who were overweight or had obesity (HR, 0.95 vs. 1.52), as were the risks of mortality (HR, 1.24 vs. 2.20).
Overall, "we found evidence that being overweight/[having obesity] amplified the harmful effect of alcohol on the liver disease incidence and mortality," the authors conclude.
The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com
Being overweight or having obesity significantly increases the risk for liver disease and the likelihood of dying from it compared with being of normal weight, regardless of level of alcohol consumption, new research shows.
"People in the overweight or obese range who drank were found to be at greater risk of liver diseases compared with participants within a healthy weight range who consumed alcohol at the same level," senior author Emmanuel Stamatakis, PhD, of the Charles Perkins Centre and the Faculty of Medicine and Health, Sydney, said in a press statement.
"Even for people who drank within alcohol guidelines, participants classified as obese were at over 50% greater risk of liver disease," he said.
"Obesity is an independent risk factor for steatosis, acute alcoholic hepatitis, and cirrhosis in alcoholic liver disease (ALD), which may increase the risk of mortality in ALD patients," the study's first author, Elif Inan-Eroglu, PhD, a postdoctoral research fellow at the Charles Perkins Centre, said in an interview.
Further prospective studies are needed to better understand the underlying mechanisms behind the association between alcohol consumption and liver disease across different adiposity levels, the authors say.
Meanwhile, the take-home message from the findings should be that "clinicians should consider the presence of overweight and obesity when they discuss defining safe alcohol levels for their patients, keeping in mind that there is no 'safe' level of alcohol," Dr. Inan-Eroglu said.
"Alcohol drinking guidelines need to acknowledge that two-thirds of the adult population are overweight or obese and consider specific recommendations for this majority population group," he said.
First and largest study of its kind
Obesity, well-known to be an independent risk factor for nonalcoholic fatty liver disease (NAFLD), is also known to worsen outcomes in ALD. And likewise, alcohol consumption, the cause of ALD, can promote obesity and therefore increase the risk of NAFLD.
Dr. Stamatakis and colleagues sought to evaluate the roles of the combined factors in terms of incidence and mortality in both ALD and NAFLD.
For the study, published online May 31 in the European Journal of Clinical Nutrition, they evaluated data from 465,437 participants in the U.K. Biobank. The study is said to be the first and largest of its kind.
In the cohort, a total of 1,090 liver disease deaths were recorded, including 230 deaths from ALD and 192 from NAFLD over an average follow-up of 10.5 years.
After a multivariate adjustment, the overall risk of ALD, NAFLD, and liver disease incidence and mortality were significantly higher in participants who were overweight or had obesity, compared with those of normal weight, at all levels of alcohol consumption.
For instance, among those with alcohol use exceeding guidelines, the risk of ALD was significantly increased in normal weight individuals versus never-drinkers (hazard ratio [HR], 5.38), and the risk was even higher among those who were also overweight or had obesity (HR, 8.58).
In terms of the risk of death related to ALD, among those reporting alcohol consumption above guidelines, the risk was nearly double among those who were overweight or had obesity (HR, 10.29) versus those with normal weight (HR, 5.84), when each group was compared to those drinking within guidelines.
Regarding NAFLD, consistent with evidence that low to moderate alcohol consumption is, in fact, linked to a reduced risk, those in the study who reported alcohol consumption within guidelines and normal weight did show a reduced risk of NAFLD compared with an index group of never-drinkers (HR, 0.85).
However, being overweight or having obesity increased the risk of NAFLD in those participants (HR, 1.51).
Furthermore, even those reporting alcohol consumption above guidelines who were of normal weight had a reduced risk of NAFLD compared with never drinkers of normal weight (HR, 0.89).
Regarding the risk of liver disease among those reporting alcohol consumption above guidelines compared with never-drinkers, the risk was again lower among those of normal weight versus those who were overweight or had obesity (HR, 0.95 vs. 1.52), as were the risks of mortality (HR, 1.24 vs. 2.20).
Overall, "we found evidence that being overweight/[having obesity] amplified the harmful effect of alcohol on the liver disease incidence and mortality," the authors conclude.
The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com
Being overweight or having obesity significantly increases the risk for liver disease and the likelihood of dying from it compared with being of normal weight, regardless of level of alcohol consumption, new research shows.
"People in the overweight or obese range who drank were found to be at greater risk of liver diseases compared with participants within a healthy weight range who consumed alcohol at the same level," senior author Emmanuel Stamatakis, PhD, of the Charles Perkins Centre and the Faculty of Medicine and Health, Sydney, said in a press statement.
"Even for people who drank within alcohol guidelines, participants classified as obese were at over 50% greater risk of liver disease," he said.
"Obesity is an independent risk factor for steatosis, acute alcoholic hepatitis, and cirrhosis in alcoholic liver disease (ALD), which may increase the risk of mortality in ALD patients," the study's first author, Elif Inan-Eroglu, PhD, a postdoctoral research fellow at the Charles Perkins Centre, said in an interview.
Further prospective studies are needed to better understand the underlying mechanisms behind the association between alcohol consumption and liver disease across different adiposity levels, the authors say.
Meanwhile, the take-home message from the findings should be that "clinicians should consider the presence of overweight and obesity when they discuss defining safe alcohol levels for their patients, keeping in mind that there is no 'safe' level of alcohol," Dr. Inan-Eroglu said.
"Alcohol drinking guidelines need to acknowledge that two-thirds of the adult population are overweight or obese and consider specific recommendations for this majority population group," he said.
First and largest study of its kind
Obesity, well-known to be an independent risk factor for nonalcoholic fatty liver disease (NAFLD), is also known to worsen outcomes in ALD. And likewise, alcohol consumption, the cause of ALD, can promote obesity and therefore increase the risk of NAFLD.
Dr. Stamatakis and colleagues sought to evaluate the roles of the combined factors in terms of incidence and mortality in both ALD and NAFLD.
For the study, published online May 31 in the European Journal of Clinical Nutrition, they evaluated data from 465,437 participants in the U.K. Biobank. The study is said to be the first and largest of its kind.
In the cohort, a total of 1,090 liver disease deaths were recorded, including 230 deaths from ALD and 192 from NAFLD over an average follow-up of 10.5 years.
After a multivariate adjustment, the overall risk of ALD, NAFLD, and liver disease incidence and mortality were significantly higher in participants who were overweight or had obesity, compared with those of normal weight, at all levels of alcohol consumption.
For instance, among those with alcohol use exceeding guidelines, the risk of ALD was significantly increased in normal weight individuals versus never-drinkers (hazard ratio [HR], 5.38), and the risk was even higher among those who were also overweight or had obesity (HR, 8.58).
In terms of the risk of death related to ALD, among those reporting alcohol consumption above guidelines, the risk was nearly double among those who were overweight or had obesity (HR, 10.29) versus those with normal weight (HR, 5.84), when each group was compared to those drinking within guidelines.
Regarding NAFLD, consistent with evidence that low to moderate alcohol consumption is, in fact, linked to a reduced risk, those in the study who reported alcohol consumption within guidelines and normal weight did show a reduced risk of NAFLD compared with an index group of never-drinkers (HR, 0.85).
However, being overweight or having obesity increased the risk of NAFLD in those participants (HR, 1.51).
Furthermore, even those reporting alcohol consumption above guidelines who were of normal weight had a reduced risk of NAFLD compared with never drinkers of normal weight (HR, 0.89).
Regarding the risk of liver disease among those reporting alcohol consumption above guidelines compared with never-drinkers, the risk was again lower among those of normal weight versus those who were overweight or had obesity (HR, 0.95 vs. 1.52), as were the risks of mortality (HR, 1.24 vs. 2.20).
Overall, "we found evidence that being overweight/[having obesity] amplified the harmful effect of alcohol on the liver disease incidence and mortality," the authors conclude.
The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com
Waist circumference a marker for NAFL in type 1 diabetes
It follows that, as the prevalence of obesity among people with type 1 diabetes mellitus (T1DM) increases, so would the incidence of nonalcoholic fatty liver (NAFL), as it does in type 2 diabetes.
However, researchers in Finland report that the incidence of NAFL in T1DM is much lower, and that the use of the waist-to-height ratio to calculate midsection girth could be a low-cost alternative to MRI and computed tomography to more precisely diagnose NAFL in T1DM.
In a cross-sectional analysis of 121 adults with T1DM in the Finnish Diabetic Nephropathy study, known as FinnDiane, researchers from the University of Helsinki report in Diabetes Care that a waist-to-height ratio of 0.5 showed a relatively high rate of accuracy for identifying NAFL that was statistically significant (P = .04).
Lead author Erika B. Parente, MD, PhD, a researcher at the Folkhälsän Research Center in Helsinki, noted that the findings do not identify any causality between what the researchers called visceral adiposity and NAFL. “As long as they have accumulation of fat in the center of body and they can develop this low-grade inflammation that also goes to insulin-load sensitivity, people with T1DM can accumulate fat in the liver as do people with T2DM and the general population,” she said in an interview.
These findings build on her group’s previous work published in Scientific Reports showing a strong relationship between waist-to-height ratio and visceral fat percentage in adults with T1DM. The most recent FinnDiane analysis found no similar relationship between NAFL and fat tissue in the hips, arms and legs, and total adipose tissue.
Better than BMI as a measure
“We also found that waist-to-height ratio is better than body mass index to identify those individuals at higher risk of having NAFL,” Dr. Parente said. However, it’s not possible to predict which patients referred to imaging evaluation after being screened by waist-to-height ratio of 0.5 will surely have NAFL, she added.
That answer, she said, would require a longitudinal and cost-effectiveness study with larger population.
The waist-to-height ratio cutoff of 0.5 showed an 86% sensitivity and 55% specificity for NAFL, whereas BMI of 26.6 kg/m2 showed an 79% sensitivity and 57% specificity.
“The most important message from our research is that health care professionals should be aware that individuals with T1DM can have NAFL, and waist-to-height ratio may help to identify those at higher risk,” she said.
The prevalence of NAFL among the adults with T1DM in the study was 11.6%, which is lower than the prevalence other studies reported in T2DM – 76% in a U.S. study – and in the general population – ranging from 19% to 46%. This underscores, Dr. Parente noted, the importance of using waist-to-height ratio in T1DM patients to determine the status of NAFL.
She said that few studies have investigated the consequences of NAFL in T1DM, pointing to two that linked NAFL with chronic kidney disease and cardiovascular disease in T1DM (Diabetes Care. 2014;37:1729-36; J Hepatol. 2010;53:713-8). “Most of the studies about the consequences of NAFL included people with T2DM,” she said. “From our research, we cannot conclude about the impact of NAFL in cardiovascular or kidney complications in our population because this is a cross-sectional study.”
That question may be answered by a future follow-up study of the ongoing FinnDiane study, she said.
The study is a “good reminder” that people with central adiposity and metabolic syndrome can develop NAFL disease, said Jeanne Marie Clark, MD, MPH, of Johns Hopkins University, Baltimore. “Even patients we may not think of having insulin resistance, such as those with T1DM.”
However, Dr. Clark added, “I do not think we can really determine which measure of central adiposity is best.” She noted that the study was “pretty small” with only 14 patients who had NAFL disease. “Waist-to-height ratio is certainly a reasonable option,” she added. “Waist circumference alone is known to be a strong predictor. I would say some measure is better than none, and it should be more routine in clinical practice.”
Dr. Parente disclosed financial relationships with Eli Lilly, Abbott, AstraZeneca, Sanofi, and Boehringer Ingelheim. Two of eight coauthors disclosed financial relationships with AbbVie, Astellas, AstraZeneca, Bayer, Boehringer Ingelheim, Eli Lilly, Elo Water, Fresenius, GE Healthcare, Medscape, Merck Sharpe and Dohme, Mundipharma, Novo Nordisk, Peer-Voice, Sanofi, and Sciarc. The remaining coauthors had no disclosures.
Dr. Clark had no disclosures.
It follows that, as the prevalence of obesity among people with type 1 diabetes mellitus (T1DM) increases, so would the incidence of nonalcoholic fatty liver (NAFL), as it does in type 2 diabetes.
However, researchers in Finland report that the incidence of NAFL in T1DM is much lower, and that the use of the waist-to-height ratio to calculate midsection girth could be a low-cost alternative to MRI and computed tomography to more precisely diagnose NAFL in T1DM.
In a cross-sectional analysis of 121 adults with T1DM in the Finnish Diabetic Nephropathy study, known as FinnDiane, researchers from the University of Helsinki report in Diabetes Care that a waist-to-height ratio of 0.5 showed a relatively high rate of accuracy for identifying NAFL that was statistically significant (P = .04).
Lead author Erika B. Parente, MD, PhD, a researcher at the Folkhälsän Research Center in Helsinki, noted that the findings do not identify any causality between what the researchers called visceral adiposity and NAFL. “As long as they have accumulation of fat in the center of body and they can develop this low-grade inflammation that also goes to insulin-load sensitivity, people with T1DM can accumulate fat in the liver as do people with T2DM and the general population,” she said in an interview.
These findings build on her group’s previous work published in Scientific Reports showing a strong relationship between waist-to-height ratio and visceral fat percentage in adults with T1DM. The most recent FinnDiane analysis found no similar relationship between NAFL and fat tissue in the hips, arms and legs, and total adipose tissue.
Better than BMI as a measure
“We also found that waist-to-height ratio is better than body mass index to identify those individuals at higher risk of having NAFL,” Dr. Parente said. However, it’s not possible to predict which patients referred to imaging evaluation after being screened by waist-to-height ratio of 0.5 will surely have NAFL, she added.
That answer, she said, would require a longitudinal and cost-effectiveness study with larger population.
The waist-to-height ratio cutoff of 0.5 showed an 86% sensitivity and 55% specificity for NAFL, whereas BMI of 26.6 kg/m2 showed an 79% sensitivity and 57% specificity.
“The most important message from our research is that health care professionals should be aware that individuals with T1DM can have NAFL, and waist-to-height ratio may help to identify those at higher risk,” she said.
The prevalence of NAFL among the adults with T1DM in the study was 11.6%, which is lower than the prevalence other studies reported in T2DM – 76% in a U.S. study – and in the general population – ranging from 19% to 46%. This underscores, Dr. Parente noted, the importance of using waist-to-height ratio in T1DM patients to determine the status of NAFL.
She said that few studies have investigated the consequences of NAFL in T1DM, pointing to two that linked NAFL with chronic kidney disease and cardiovascular disease in T1DM (Diabetes Care. 2014;37:1729-36; J Hepatol. 2010;53:713-8). “Most of the studies about the consequences of NAFL included people with T2DM,” she said. “From our research, we cannot conclude about the impact of NAFL in cardiovascular or kidney complications in our population because this is a cross-sectional study.”
That question may be answered by a future follow-up study of the ongoing FinnDiane study, she said.
The study is a “good reminder” that people with central adiposity and metabolic syndrome can develop NAFL disease, said Jeanne Marie Clark, MD, MPH, of Johns Hopkins University, Baltimore. “Even patients we may not think of having insulin resistance, such as those with T1DM.”
However, Dr. Clark added, “I do not think we can really determine which measure of central adiposity is best.” She noted that the study was “pretty small” with only 14 patients who had NAFL disease. “Waist-to-height ratio is certainly a reasonable option,” she added. “Waist circumference alone is known to be a strong predictor. I would say some measure is better than none, and it should be more routine in clinical practice.”
Dr. Parente disclosed financial relationships with Eli Lilly, Abbott, AstraZeneca, Sanofi, and Boehringer Ingelheim. Two of eight coauthors disclosed financial relationships with AbbVie, Astellas, AstraZeneca, Bayer, Boehringer Ingelheim, Eli Lilly, Elo Water, Fresenius, GE Healthcare, Medscape, Merck Sharpe and Dohme, Mundipharma, Novo Nordisk, Peer-Voice, Sanofi, and Sciarc. The remaining coauthors had no disclosures.
Dr. Clark had no disclosures.
It follows that, as the prevalence of obesity among people with type 1 diabetes mellitus (T1DM) increases, so would the incidence of nonalcoholic fatty liver (NAFL), as it does in type 2 diabetes.
However, researchers in Finland report that the incidence of NAFL in T1DM is much lower, and that the use of the waist-to-height ratio to calculate midsection girth could be a low-cost alternative to MRI and computed tomography to more precisely diagnose NAFL in T1DM.
In a cross-sectional analysis of 121 adults with T1DM in the Finnish Diabetic Nephropathy study, known as FinnDiane, researchers from the University of Helsinki report in Diabetes Care that a waist-to-height ratio of 0.5 showed a relatively high rate of accuracy for identifying NAFL that was statistically significant (P = .04).
Lead author Erika B. Parente, MD, PhD, a researcher at the Folkhälsän Research Center in Helsinki, noted that the findings do not identify any causality between what the researchers called visceral adiposity and NAFL. “As long as they have accumulation of fat in the center of body and they can develop this low-grade inflammation that also goes to insulin-load sensitivity, people with T1DM can accumulate fat in the liver as do people with T2DM and the general population,” she said in an interview.
These findings build on her group’s previous work published in Scientific Reports showing a strong relationship between waist-to-height ratio and visceral fat percentage in adults with T1DM. The most recent FinnDiane analysis found no similar relationship between NAFL and fat tissue in the hips, arms and legs, and total adipose tissue.
Better than BMI as a measure
“We also found that waist-to-height ratio is better than body mass index to identify those individuals at higher risk of having NAFL,” Dr. Parente said. However, it’s not possible to predict which patients referred to imaging evaluation after being screened by waist-to-height ratio of 0.5 will surely have NAFL, she added.
That answer, she said, would require a longitudinal and cost-effectiveness study with larger population.
The waist-to-height ratio cutoff of 0.5 showed an 86% sensitivity and 55% specificity for NAFL, whereas BMI of 26.6 kg/m2 showed an 79% sensitivity and 57% specificity.
“The most important message from our research is that health care professionals should be aware that individuals with T1DM can have NAFL, and waist-to-height ratio may help to identify those at higher risk,” she said.
The prevalence of NAFL among the adults with T1DM in the study was 11.6%, which is lower than the prevalence other studies reported in T2DM – 76% in a U.S. study – and in the general population – ranging from 19% to 46%. This underscores, Dr. Parente noted, the importance of using waist-to-height ratio in T1DM patients to determine the status of NAFL.
She said that few studies have investigated the consequences of NAFL in T1DM, pointing to two that linked NAFL with chronic kidney disease and cardiovascular disease in T1DM (Diabetes Care. 2014;37:1729-36; J Hepatol. 2010;53:713-8). “Most of the studies about the consequences of NAFL included people with T2DM,” she said. “From our research, we cannot conclude about the impact of NAFL in cardiovascular or kidney complications in our population because this is a cross-sectional study.”
That question may be answered by a future follow-up study of the ongoing FinnDiane study, she said.
The study is a “good reminder” that people with central adiposity and metabolic syndrome can develop NAFL disease, said Jeanne Marie Clark, MD, MPH, of Johns Hopkins University, Baltimore. “Even patients we may not think of having insulin resistance, such as those with T1DM.”
However, Dr. Clark added, “I do not think we can really determine which measure of central adiposity is best.” She noted that the study was “pretty small” with only 14 patients who had NAFL disease. “Waist-to-height ratio is certainly a reasonable option,” she added. “Waist circumference alone is known to be a strong predictor. I would say some measure is better than none, and it should be more routine in clinical practice.”
Dr. Parente disclosed financial relationships with Eli Lilly, Abbott, AstraZeneca, Sanofi, and Boehringer Ingelheim. Two of eight coauthors disclosed financial relationships with AbbVie, Astellas, AstraZeneca, Bayer, Boehringer Ingelheim, Eli Lilly, Elo Water, Fresenius, GE Healthcare, Medscape, Merck Sharpe and Dohme, Mundipharma, Novo Nordisk, Peer-Voice, Sanofi, and Sciarc. The remaining coauthors had no disclosures.
Dr. Clark had no disclosures.
FROM DIABETES CARE
New obesity target? Dopamine circuit in brainstem affects satiety
Researchers have discovered a new dopaminergic neural circuit leading to the hindbrain that is involved in satiety (feeling full and eating cessation) in mice, which may eventually lead to new ways to treat obesity.
Moreover, when mice were given methylphenidate (Ritalin, Concerta) – a stimulant approved to treat attention deficit hyperactivity disorder (ADHD) with a well-known side effect of decreasing appetite – signals in this dopaminergic pathway were enhanced and the mice ate less.
The study by Yong Han, PhD, a postdoctoral associate at Baylor College of Medicine, Houston, and colleagues was published online May 27 in Science Advances.
“We identified a new dopamine neural circuit from the midbrain to the hindbrain (brainstem) that regulates feeding behavior through an enhanced satiation response,” senior author Qi Wu, PhD, assistant professor in pediatrics-nutrition at Baylor College of Medicine, summarized in an interview.
The findings suggest that “people with obesity have a compromised dopaminergic neural pathway, presumably in ways that delay the satiation response, which makes them eat more, have a larger meal,” he explained.
Newly identified brain circuit plays a key role in satiety response
The study is about a circuit in the brain that helps precisely regulate the size of food portion consumed, Dr. Wu emphasized in a statement from the university, adding that the satiation response is as important as appetite.
Importantly, the results also provide clues about how methylphenidate can lead to weight loss.
Regulators have deemed that methylphenidate, a controlled substance with other side effects such as anxiety and a fast heart rate, is safe and effective for ADHD, Dr. Wu noted.
He speculated that, “If researchers want to do clinical trials of methylphenidate for obesity, it ultimately could evolve to be an anti-obesity drug, alone or combined with other drugs, or possibly derivatives of methylphenidate could be tested.”
The brain circuit “we discovered is the first to be fully described to regulate portion size via dopamine signaling,” Dr. Han stressed in the statement.
“Our new study shows that a circuit connecting neurons that produce dopamine, a chemical messenger previously known for the regulation of motivation and pleasure, has a new [critical] role in the control of feeding through dynamically regulating the satiety response,” he explained.
Brain signals that control portion size
Earlier studies that investigated how the dopaminergic system may regulate food intake, appetite, and body weight, have produced conflicting results, Dr. Wu said.
The researchers performed several experiments in mice that included the use of cell-specific circuitry mapping, optogenetics, and real-time recordings of brain activity.
They identified a new dopaminergic neural circuit comprised of dopaminergic neurons in the caudal ventral tegmental area (DA-VTA neurons) in the midbrain that directly innervate dopamine receptor D1-expressing neurons within the lateral parabrachial nucleus (DRD1-LPBN neurons) in the hindbrain.
There were four main findings:
- DA-VTA neurons were activated immediately before the cessation of each feeding bout.
- Actively inhibiting DA-VTA neurons before the end of each feeding bout prolonged the feeding.
- Activating DRD1-LPBN neurons inhibited feeding.
- Mice that lacked the DRD1 gene ate much more and gained weight.
“Our study illuminates a hindbrain dopaminergic circuit that controls feeding through dynamic regulation in satiety response and meal structure,” the researchers reiterate.
The study was supported by grants from the National Institutes of Health, NIH Digestive Diseases Center, Pew Charitable Trust, American Diabetes Association, Baylor Collaborative Faculty Research Investment Program, USDA/CRIS, USDA/ARS, American Heart Association, and NIH Centers of Biomedical Research Excellence, and by Pew and Kavli scholarships. The researchers have reported no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
Researchers have discovered a new dopaminergic neural circuit leading to the hindbrain that is involved in satiety (feeling full and eating cessation) in mice, which may eventually lead to new ways to treat obesity.
Moreover, when mice were given methylphenidate (Ritalin, Concerta) – a stimulant approved to treat attention deficit hyperactivity disorder (ADHD) with a well-known side effect of decreasing appetite – signals in this dopaminergic pathway were enhanced and the mice ate less.
The study by Yong Han, PhD, a postdoctoral associate at Baylor College of Medicine, Houston, and colleagues was published online May 27 in Science Advances.
“We identified a new dopamine neural circuit from the midbrain to the hindbrain (brainstem) that regulates feeding behavior through an enhanced satiation response,” senior author Qi Wu, PhD, assistant professor in pediatrics-nutrition at Baylor College of Medicine, summarized in an interview.
The findings suggest that “people with obesity have a compromised dopaminergic neural pathway, presumably in ways that delay the satiation response, which makes them eat more, have a larger meal,” he explained.
Newly identified brain circuit plays a key role in satiety response
The study is about a circuit in the brain that helps precisely regulate the size of food portion consumed, Dr. Wu emphasized in a statement from the university, adding that the satiation response is as important as appetite.
Importantly, the results also provide clues about how methylphenidate can lead to weight loss.
Regulators have deemed that methylphenidate, a controlled substance with other side effects such as anxiety and a fast heart rate, is safe and effective for ADHD, Dr. Wu noted.
He speculated that, “If researchers want to do clinical trials of methylphenidate for obesity, it ultimately could evolve to be an anti-obesity drug, alone or combined with other drugs, or possibly derivatives of methylphenidate could be tested.”
The brain circuit “we discovered is the first to be fully described to regulate portion size via dopamine signaling,” Dr. Han stressed in the statement.
“Our new study shows that a circuit connecting neurons that produce dopamine, a chemical messenger previously known for the regulation of motivation and pleasure, has a new [critical] role in the control of feeding through dynamically regulating the satiety response,” he explained.
Brain signals that control portion size
Earlier studies that investigated how the dopaminergic system may regulate food intake, appetite, and body weight, have produced conflicting results, Dr. Wu said.
The researchers performed several experiments in mice that included the use of cell-specific circuitry mapping, optogenetics, and real-time recordings of brain activity.
They identified a new dopaminergic neural circuit comprised of dopaminergic neurons in the caudal ventral tegmental area (DA-VTA neurons) in the midbrain that directly innervate dopamine receptor D1-expressing neurons within the lateral parabrachial nucleus (DRD1-LPBN neurons) in the hindbrain.
There were four main findings:
- DA-VTA neurons were activated immediately before the cessation of each feeding bout.
- Actively inhibiting DA-VTA neurons before the end of each feeding bout prolonged the feeding.
- Activating DRD1-LPBN neurons inhibited feeding.
- Mice that lacked the DRD1 gene ate much more and gained weight.
“Our study illuminates a hindbrain dopaminergic circuit that controls feeding through dynamic regulation in satiety response and meal structure,” the researchers reiterate.
The study was supported by grants from the National Institutes of Health, NIH Digestive Diseases Center, Pew Charitable Trust, American Diabetes Association, Baylor Collaborative Faculty Research Investment Program, USDA/CRIS, USDA/ARS, American Heart Association, and NIH Centers of Biomedical Research Excellence, and by Pew and Kavli scholarships. The researchers have reported no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
Researchers have discovered a new dopaminergic neural circuit leading to the hindbrain that is involved in satiety (feeling full and eating cessation) in mice, which may eventually lead to new ways to treat obesity.
Moreover, when mice were given methylphenidate (Ritalin, Concerta) – a stimulant approved to treat attention deficit hyperactivity disorder (ADHD) with a well-known side effect of decreasing appetite – signals in this dopaminergic pathway were enhanced and the mice ate less.
The study by Yong Han, PhD, a postdoctoral associate at Baylor College of Medicine, Houston, and colleagues was published online May 27 in Science Advances.
“We identified a new dopamine neural circuit from the midbrain to the hindbrain (brainstem) that regulates feeding behavior through an enhanced satiation response,” senior author Qi Wu, PhD, assistant professor in pediatrics-nutrition at Baylor College of Medicine, summarized in an interview.
The findings suggest that “people with obesity have a compromised dopaminergic neural pathway, presumably in ways that delay the satiation response, which makes them eat more, have a larger meal,” he explained.
Newly identified brain circuit plays a key role in satiety response
The study is about a circuit in the brain that helps precisely regulate the size of food portion consumed, Dr. Wu emphasized in a statement from the university, adding that the satiation response is as important as appetite.
Importantly, the results also provide clues about how methylphenidate can lead to weight loss.
Regulators have deemed that methylphenidate, a controlled substance with other side effects such as anxiety and a fast heart rate, is safe and effective for ADHD, Dr. Wu noted.
He speculated that, “If researchers want to do clinical trials of methylphenidate for obesity, it ultimately could evolve to be an anti-obesity drug, alone or combined with other drugs, or possibly derivatives of methylphenidate could be tested.”
The brain circuit “we discovered is the first to be fully described to regulate portion size via dopamine signaling,” Dr. Han stressed in the statement.
“Our new study shows that a circuit connecting neurons that produce dopamine, a chemical messenger previously known for the regulation of motivation and pleasure, has a new [critical] role in the control of feeding through dynamically regulating the satiety response,” he explained.
Brain signals that control portion size
Earlier studies that investigated how the dopaminergic system may regulate food intake, appetite, and body weight, have produced conflicting results, Dr. Wu said.
The researchers performed several experiments in mice that included the use of cell-specific circuitry mapping, optogenetics, and real-time recordings of brain activity.
They identified a new dopaminergic neural circuit comprised of dopaminergic neurons in the caudal ventral tegmental area (DA-VTA neurons) in the midbrain that directly innervate dopamine receptor D1-expressing neurons within the lateral parabrachial nucleus (DRD1-LPBN neurons) in the hindbrain.
There were four main findings:
- DA-VTA neurons were activated immediately before the cessation of each feeding bout.
- Actively inhibiting DA-VTA neurons before the end of each feeding bout prolonged the feeding.
- Activating DRD1-LPBN neurons inhibited feeding.
- Mice that lacked the DRD1 gene ate much more and gained weight.
“Our study illuminates a hindbrain dopaminergic circuit that controls feeding through dynamic regulation in satiety response and meal structure,” the researchers reiterate.
The study was supported by grants from the National Institutes of Health, NIH Digestive Diseases Center, Pew Charitable Trust, American Diabetes Association, Baylor Collaborative Faculty Research Investment Program, USDA/CRIS, USDA/ARS, American Heart Association, and NIH Centers of Biomedical Research Excellence, and by Pew and Kavli scholarships. The researchers have reported no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
FDA approves ‘game changer’ semaglutide for weight loss
The U.S. Food and Drug Administration has approved a 2.4 mg/week subcutaneous dose of the glucagonlike peptide–1 (GLP-1) receptor agonist semaglutide (Wegovy, Novo Nordisk) for weight loss.
Specifically, this drug format and dosage are approved as an adjunct to a reduced-calorie diet and increased physical activity to treat adults who have obesity (body mass index [BMI] ≥ 30 kg/m2) or are overweight (BMI ≥ 27 kg/m2) with at least one weight-related comorbidity.
Semaglutide “induces weight loss by reducing hunger, increasing feelings of fullness, and thereby helping people eat less and reduce their calorie intake,” according to a company statement.
Novo Nordisk plans to launch Wegovy later this month in the United States. The prescribing information can be found here.
This weight-loss drug is currently under review by the European Medicines Agency.
Several experts told Medscape that they believe the approval of this drug – as long as it is reimbursed – has the potential to change the paradigm of care when it comes to weight loss.
‘Game changer’ drug tested in STEP clinical trial program
The favorable FDA ruling is based on results from the Semaglutide Treatment Effect in People With Obesity (STEP) program of four phase 3 clinical trials that tested the drug’s safety and efficacy in more than 4,500 adults with overweight or obesity obesity who were randomized to receive a reduced a calorie meal plan and increased physical activity (placebo) or this lifestyle intervention plus semaglutide.
The four 68-week trials of subcutaneous semaglutide 2.4 mg/week versus placebo were published in February and March 2021.
As previously reported by this news organization, all trials were in adults with overweight or obesity:
- was in 1,961 adults (N Engl J Med. 2021 March 18;384:989-1002).
- was in 1,210 adults who also had diabetes (Lancet. 2021 Mar 13;397;971-84).
- was in 611 adults, where those in the treatment group also underwent an intensive lifestyle intervention (JAMA. 2021 Feb 24;325:1403-13.
- was in 803 adults who had reached a target dose of 2.4 mg semaglutide after a 20-week run-in (and the trial examined further weight loss in the subsequent 48 weeks) (JAMA 2021 Mar 23;325:1414-25).
In the STEP 1, 2, and 4 trials of individuals with overweight and obesity, those in the semaglutide groups attained a 15%-18% weight loss over 68 weeks.
The dosage was well-tolerated. The most common side effects were gastrointestinal, and they were transient and mild or moderate in severity.
The side effects, contraindications, and a black box warning about thyroid C-cell tumors are spelled out in the prescribing information.
A coauthor of the STEP 1 trial, Rachel Batterham, MBBS, PhD, of the Centre for Obesity Research at University College London, said at the time of publication: “The findings of this study represent a major breakthrough for improving the health of people with obesity.”
“No other drug has come close to producing this level of weight loss – this really is a gamechanger. For the first time, people can achieve through drugs what was only possible through weight-loss surgery,” she added.
Welcome Addition, But Will Insurance Coverage, Price Thwart Access?
Thomas A. Wadden, PhD, from the Perelman School of Medicine at the University of Pennsylvania, Philadelphia, and lead author of STEP 3, commented in an email to this news organization that “semaglutide 2.4 mg appears to be the breakthrough in weight management that healthcare providers and their patients with obesity have been waiting for.”
The mean 15% weight loss at 68 weeks is nearly twice what is seen with other FDA-approved anti-obesity medications, he noted, and moreover, 70% of patients taking semaglutide lost at least 10% of their initial weight, which is associated with clinically meaningful improvements in obesity-related type 2 diabetes, hypertension, obstructive sleep apnea, and impaired quality of life.
And “nearly one-third of users are likely to lose 20% or more of their starting weight, an outcome which eludes traditional diet and exercise interventions and which approaches weight losses produced by the most widely performed bariatric surgery, sleeve gastrectomy (with mean losses of 25% of initial weight at 1 year).” Dr. Wadden stressed.
Thus “the efficacy of semaglutide 2.4 mg, combined with its favorable safety profile, makes this medication a potential game changer,” he summarized, echoing Dr. Batterham.
However, insurance coverage and price could block uptake.
“I hope that the millions of people – in the U.S. and worldwide – who could benefit from this medication eventually will have access to it,” said Dr. Wadden. “In the U.S., the coverage of anti-obesity medications by insurers and employers will need to improve to ensure this happens, and the medication must be reasonably priced. These changes are critical to making this medication the game changer it could be.”
“This approval is an important development,” Scott Kahan, MD, director of the National Center for Weight and Wellness, Washington, who was not involved in the clinical trials of this drug, similarly wrote in an email.
“In a field with relatively few medication options, the availability of additional obesity pharmacotherapy agents is welcome,” he said. “In particular, semaglutide has shown impressive efficacy and safety data; as such it should be a valuable clinical option for many patients.”
However, it is concerning that “access to obesity treatments has traditionally been a challenge,” Dr. Kahan warned. “Novo Nordisk’s other obesity medication, Saxenda, has been a valuable tool, but one that exceedingly few patients are able to utilize due to minimal insurance reimbursement and very high cost.”
“It remains to be seen how accessible semaglutide will be for patients,” according to Dr. Kahan, “Still, if the challenge of limited coverage and high cost can be mitigated, this medication has a chance to significantly change the current paradigm of care, which until till now has included minimal use of pharmacotherapy outside specialty clinics,” he maintains.
Lower-dose injectable and pill already approved for diabetes
Subcutaneous semaglutide at doses up to 1 mg/week (Ozempic, Novo Nordisk), which comes as prefilled pens at doses of 0.5 mg or 1.0 mg, is already approved for the treatment of type 2 diabetes.
The company is also applying for approval for a higher dose of semaglutide, 2 mg/week, for use in type 2 diabetes, and has just resubmitted its label expansion application to the FDA, after the agency issued a refusal to file letter in March.
And in September 2019, the FDA approved oral semaglutide (Rybelsus, Novo Nordisk), in doses of 7 and 14 mg/day, to improve glycemic control in type 2 diabetes, making it the first GLP-1 receptor agonist available in tablet form.
CVOT and oral format trials for obesity on the horizon
The ongoing Semaglutide Effects on Heart Disease and Stroke in Patients With Overweight or Obesity (SELECT) trial will shed light on cardiovascular outcomes after 2.5-5 years in patients with cardiovascular disease and overweight or obesity but without type 2 diabetes. Participants will receive semaglutide in doses up to a maximum of 2.4 mg/week, or placebo, as an adjunct to lifestyle recommendations focused on cardiovascular risk reduction. The study is expected to complete in 2023.
And Novo Nordisk plans to initiate a global 68-week phase 3 trial in the second half of 2021 on the efficacy and safety of oral semaglutide 50 mg compared with placebo in 1000 people with obesity or overweight and comorbidities.
A version of this article first appeared on Medscape.com.
This article was updated 6/7/21.
The U.S. Food and Drug Administration has approved a 2.4 mg/week subcutaneous dose of the glucagonlike peptide–1 (GLP-1) receptor agonist semaglutide (Wegovy, Novo Nordisk) for weight loss.
Specifically, this drug format and dosage are approved as an adjunct to a reduced-calorie diet and increased physical activity to treat adults who have obesity (body mass index [BMI] ≥ 30 kg/m2) or are overweight (BMI ≥ 27 kg/m2) with at least one weight-related comorbidity.
Semaglutide “induces weight loss by reducing hunger, increasing feelings of fullness, and thereby helping people eat less and reduce their calorie intake,” according to a company statement.
Novo Nordisk plans to launch Wegovy later this month in the United States. The prescribing information can be found here.
This weight-loss drug is currently under review by the European Medicines Agency.
Several experts told Medscape that they believe the approval of this drug – as long as it is reimbursed – has the potential to change the paradigm of care when it comes to weight loss.
‘Game changer’ drug tested in STEP clinical trial program
The favorable FDA ruling is based on results from the Semaglutide Treatment Effect in People With Obesity (STEP) program of four phase 3 clinical trials that tested the drug’s safety and efficacy in more than 4,500 adults with overweight or obesity obesity who were randomized to receive a reduced a calorie meal plan and increased physical activity (placebo) or this lifestyle intervention plus semaglutide.
The four 68-week trials of subcutaneous semaglutide 2.4 mg/week versus placebo were published in February and March 2021.
As previously reported by this news organization, all trials were in adults with overweight or obesity:
- was in 1,961 adults (N Engl J Med. 2021 March 18;384:989-1002).
- was in 1,210 adults who also had diabetes (Lancet. 2021 Mar 13;397;971-84).
- was in 611 adults, where those in the treatment group also underwent an intensive lifestyle intervention (JAMA. 2021 Feb 24;325:1403-13.
- was in 803 adults who had reached a target dose of 2.4 mg semaglutide after a 20-week run-in (and the trial examined further weight loss in the subsequent 48 weeks) (JAMA 2021 Mar 23;325:1414-25).
In the STEP 1, 2, and 4 trials of individuals with overweight and obesity, those in the semaglutide groups attained a 15%-18% weight loss over 68 weeks.
The dosage was well-tolerated. The most common side effects were gastrointestinal, and they were transient and mild or moderate in severity.
The side effects, contraindications, and a black box warning about thyroid C-cell tumors are spelled out in the prescribing information.
A coauthor of the STEP 1 trial, Rachel Batterham, MBBS, PhD, of the Centre for Obesity Research at University College London, said at the time of publication: “The findings of this study represent a major breakthrough for improving the health of people with obesity.”
“No other drug has come close to producing this level of weight loss – this really is a gamechanger. For the first time, people can achieve through drugs what was only possible through weight-loss surgery,” she added.
Welcome Addition, But Will Insurance Coverage, Price Thwart Access?
Thomas A. Wadden, PhD, from the Perelman School of Medicine at the University of Pennsylvania, Philadelphia, and lead author of STEP 3, commented in an email to this news organization that “semaglutide 2.4 mg appears to be the breakthrough in weight management that healthcare providers and their patients with obesity have been waiting for.”
The mean 15% weight loss at 68 weeks is nearly twice what is seen with other FDA-approved anti-obesity medications, he noted, and moreover, 70% of patients taking semaglutide lost at least 10% of their initial weight, which is associated with clinically meaningful improvements in obesity-related type 2 diabetes, hypertension, obstructive sleep apnea, and impaired quality of life.
And “nearly one-third of users are likely to lose 20% or more of their starting weight, an outcome which eludes traditional diet and exercise interventions and which approaches weight losses produced by the most widely performed bariatric surgery, sleeve gastrectomy (with mean losses of 25% of initial weight at 1 year).” Dr. Wadden stressed.
Thus “the efficacy of semaglutide 2.4 mg, combined with its favorable safety profile, makes this medication a potential game changer,” he summarized, echoing Dr. Batterham.
However, insurance coverage and price could block uptake.
“I hope that the millions of people – in the U.S. and worldwide – who could benefit from this medication eventually will have access to it,” said Dr. Wadden. “In the U.S., the coverage of anti-obesity medications by insurers and employers will need to improve to ensure this happens, and the medication must be reasonably priced. These changes are critical to making this medication the game changer it could be.”
“This approval is an important development,” Scott Kahan, MD, director of the National Center for Weight and Wellness, Washington, who was not involved in the clinical trials of this drug, similarly wrote in an email.
“In a field with relatively few medication options, the availability of additional obesity pharmacotherapy agents is welcome,” he said. “In particular, semaglutide has shown impressive efficacy and safety data; as such it should be a valuable clinical option for many patients.”
However, it is concerning that “access to obesity treatments has traditionally been a challenge,” Dr. Kahan warned. “Novo Nordisk’s other obesity medication, Saxenda, has been a valuable tool, but one that exceedingly few patients are able to utilize due to minimal insurance reimbursement and very high cost.”
“It remains to be seen how accessible semaglutide will be for patients,” according to Dr. Kahan, “Still, if the challenge of limited coverage and high cost can be mitigated, this medication has a chance to significantly change the current paradigm of care, which until till now has included minimal use of pharmacotherapy outside specialty clinics,” he maintains.
Lower-dose injectable and pill already approved for diabetes
Subcutaneous semaglutide at doses up to 1 mg/week (Ozempic, Novo Nordisk), which comes as prefilled pens at doses of 0.5 mg or 1.0 mg, is already approved for the treatment of type 2 diabetes.
The company is also applying for approval for a higher dose of semaglutide, 2 mg/week, for use in type 2 diabetes, and has just resubmitted its label expansion application to the FDA, after the agency issued a refusal to file letter in March.
And in September 2019, the FDA approved oral semaglutide (Rybelsus, Novo Nordisk), in doses of 7 and 14 mg/day, to improve glycemic control in type 2 diabetes, making it the first GLP-1 receptor agonist available in tablet form.
CVOT and oral format trials for obesity on the horizon
The ongoing Semaglutide Effects on Heart Disease and Stroke in Patients With Overweight or Obesity (SELECT) trial will shed light on cardiovascular outcomes after 2.5-5 years in patients with cardiovascular disease and overweight or obesity but without type 2 diabetes. Participants will receive semaglutide in doses up to a maximum of 2.4 mg/week, or placebo, as an adjunct to lifestyle recommendations focused on cardiovascular risk reduction. The study is expected to complete in 2023.
And Novo Nordisk plans to initiate a global 68-week phase 3 trial in the second half of 2021 on the efficacy and safety of oral semaglutide 50 mg compared with placebo in 1000 people with obesity or overweight and comorbidities.
A version of this article first appeared on Medscape.com.
This article was updated 6/7/21.
The U.S. Food and Drug Administration has approved a 2.4 mg/week subcutaneous dose of the glucagonlike peptide–1 (GLP-1) receptor agonist semaglutide (Wegovy, Novo Nordisk) for weight loss.
Specifically, this drug format and dosage are approved as an adjunct to a reduced-calorie diet and increased physical activity to treat adults who have obesity (body mass index [BMI] ≥ 30 kg/m2) or are overweight (BMI ≥ 27 kg/m2) with at least one weight-related comorbidity.
Semaglutide “induces weight loss by reducing hunger, increasing feelings of fullness, and thereby helping people eat less and reduce their calorie intake,” according to a company statement.
Novo Nordisk plans to launch Wegovy later this month in the United States. The prescribing information can be found here.
This weight-loss drug is currently under review by the European Medicines Agency.
Several experts told Medscape that they believe the approval of this drug – as long as it is reimbursed – has the potential to change the paradigm of care when it comes to weight loss.
‘Game changer’ drug tested in STEP clinical trial program
The favorable FDA ruling is based on results from the Semaglutide Treatment Effect in People With Obesity (STEP) program of four phase 3 clinical trials that tested the drug’s safety and efficacy in more than 4,500 adults with overweight or obesity obesity who were randomized to receive a reduced a calorie meal plan and increased physical activity (placebo) or this lifestyle intervention plus semaglutide.
The four 68-week trials of subcutaneous semaglutide 2.4 mg/week versus placebo were published in February and March 2021.
As previously reported by this news organization, all trials were in adults with overweight or obesity:
- was in 1,961 adults (N Engl J Med. 2021 March 18;384:989-1002).
- was in 1,210 adults who also had diabetes (Lancet. 2021 Mar 13;397;971-84).
- was in 611 adults, where those in the treatment group also underwent an intensive lifestyle intervention (JAMA. 2021 Feb 24;325:1403-13.
- was in 803 adults who had reached a target dose of 2.4 mg semaglutide after a 20-week run-in (and the trial examined further weight loss in the subsequent 48 weeks) (JAMA 2021 Mar 23;325:1414-25).
In the STEP 1, 2, and 4 trials of individuals with overweight and obesity, those in the semaglutide groups attained a 15%-18% weight loss over 68 weeks.
The dosage was well-tolerated. The most common side effects were gastrointestinal, and they were transient and mild or moderate in severity.
The side effects, contraindications, and a black box warning about thyroid C-cell tumors are spelled out in the prescribing information.
A coauthor of the STEP 1 trial, Rachel Batterham, MBBS, PhD, of the Centre for Obesity Research at University College London, said at the time of publication: “The findings of this study represent a major breakthrough for improving the health of people with obesity.”
“No other drug has come close to producing this level of weight loss – this really is a gamechanger. For the first time, people can achieve through drugs what was only possible through weight-loss surgery,” she added.
Welcome Addition, But Will Insurance Coverage, Price Thwart Access?
Thomas A. Wadden, PhD, from the Perelman School of Medicine at the University of Pennsylvania, Philadelphia, and lead author of STEP 3, commented in an email to this news organization that “semaglutide 2.4 mg appears to be the breakthrough in weight management that healthcare providers and their patients with obesity have been waiting for.”
The mean 15% weight loss at 68 weeks is nearly twice what is seen with other FDA-approved anti-obesity medications, he noted, and moreover, 70% of patients taking semaglutide lost at least 10% of their initial weight, which is associated with clinically meaningful improvements in obesity-related type 2 diabetes, hypertension, obstructive sleep apnea, and impaired quality of life.
And “nearly one-third of users are likely to lose 20% or more of their starting weight, an outcome which eludes traditional diet and exercise interventions and which approaches weight losses produced by the most widely performed bariatric surgery, sleeve gastrectomy (with mean losses of 25% of initial weight at 1 year).” Dr. Wadden stressed.
Thus “the efficacy of semaglutide 2.4 mg, combined with its favorable safety profile, makes this medication a potential game changer,” he summarized, echoing Dr. Batterham.
However, insurance coverage and price could block uptake.
“I hope that the millions of people – in the U.S. and worldwide – who could benefit from this medication eventually will have access to it,” said Dr. Wadden. “In the U.S., the coverage of anti-obesity medications by insurers and employers will need to improve to ensure this happens, and the medication must be reasonably priced. These changes are critical to making this medication the game changer it could be.”
“This approval is an important development,” Scott Kahan, MD, director of the National Center for Weight and Wellness, Washington, who was not involved in the clinical trials of this drug, similarly wrote in an email.
“In a field with relatively few medication options, the availability of additional obesity pharmacotherapy agents is welcome,” he said. “In particular, semaglutide has shown impressive efficacy and safety data; as such it should be a valuable clinical option for many patients.”
However, it is concerning that “access to obesity treatments has traditionally been a challenge,” Dr. Kahan warned. “Novo Nordisk’s other obesity medication, Saxenda, has been a valuable tool, but one that exceedingly few patients are able to utilize due to minimal insurance reimbursement and very high cost.”
“It remains to be seen how accessible semaglutide will be for patients,” according to Dr. Kahan, “Still, if the challenge of limited coverage and high cost can be mitigated, this medication has a chance to significantly change the current paradigm of care, which until till now has included minimal use of pharmacotherapy outside specialty clinics,” he maintains.
Lower-dose injectable and pill already approved for diabetes
Subcutaneous semaglutide at doses up to 1 mg/week (Ozempic, Novo Nordisk), which comes as prefilled pens at doses of 0.5 mg or 1.0 mg, is already approved for the treatment of type 2 diabetes.
The company is also applying for approval for a higher dose of semaglutide, 2 mg/week, for use in type 2 diabetes, and has just resubmitted its label expansion application to the FDA, after the agency issued a refusal to file letter in March.
And in September 2019, the FDA approved oral semaglutide (Rybelsus, Novo Nordisk), in doses of 7 and 14 mg/day, to improve glycemic control in type 2 diabetes, making it the first GLP-1 receptor agonist available in tablet form.
CVOT and oral format trials for obesity on the horizon
The ongoing Semaglutide Effects on Heart Disease and Stroke in Patients With Overweight or Obesity (SELECT) trial will shed light on cardiovascular outcomes after 2.5-5 years in patients with cardiovascular disease and overweight or obesity but without type 2 diabetes. Participants will receive semaglutide in doses up to a maximum of 2.4 mg/week, or placebo, as an adjunct to lifestyle recommendations focused on cardiovascular risk reduction. The study is expected to complete in 2023.
And Novo Nordisk plans to initiate a global 68-week phase 3 trial in the second half of 2021 on the efficacy and safety of oral semaglutide 50 mg compared with placebo in 1000 people with obesity or overweight and comorbidities.
A version of this article first appeared on Medscape.com.
This article was updated 6/7/21.
Tai chi as good as working out to shrink waistline
Results of a randomized controlled trial published online May 31 in Annals of Internal Medicine show that people who have a tough time with some kinds of aerobic exercise may gain similar benefits from tai chi.
The study is “very impressive,” said Bavani Nadeswaran, MD, of the University of California Irvine’s Susan Samueli Integrative Health Institute, who was not involved in the study.
Many people have arthritis or back pain, “and aerobic exercise can be hard on them,” she said. “The good thing about exercises like tai chi and yoga is that they are low-impact.” That means that people who can’t run or get access to a pool for swimming have a viable alternative.
The study included nearly 550 adults ages 50 and up in Hong Kong who were randomly assigned to engage in tai chi, aerobic exercise with strength training, or no exercise program for 12 weeks. All had waistlines greater than 35.4 inches for men and 31.5 inches for women.
The tai chi program involved three 1-hour weekly sessions of the practice, led by an instructor. Those who took part in the aerobic exercise group engaged three times each week in an exercise program of brisk tai chi and strength training, also led by an instructor.
The researchers measured changes in waistline size, cholesterol levels, and weight for about 9 months. Those who didn’t exercise had little change in their average waistline. Compared to the group that didn’t exercise, the average waistline of people in the two exercise groups declined more: by 0.7 inches more with tai chi, and 0.5 inches more with brisk walking and strength training.
Both exercise groups also had greater drops in body weight and triglyceride (a type of fat found in the blood) levels, and larger increases in high-density lipoprotein cholesterol, the “good” cholesterol, compared to the no-exercise group. All of these improvements lasted about 9 months with tai chi. But improvements in cholesterol levels did not last as long in those in the brisk-walking program.
The researchers also looked at the effects on blood pressure and blood sugar, but they found no differences between the groups.
The findings don’t necessarily mean that people with larger waistlines should dispense with their current exercise programs and turn to tai chi, said study author Parco Siu, PhD, head of the Division of Kinesiology at the University of Hong Kong’s School of Public Health. They show that tai chi is a good option if a person prefers it.
“This is good news for middle-aged and older adults who may be averse to conventional exercise,” he said in an email. But “certainly it is no problem for people to keep regularly participating in conventional exercise.”
Tai chi may also be a good choice for people without larger waistlines because practicing this form of exercise is a way to follow advice from the World Health Organization on physical activity, said Dr. Siu, though the study did not address this question.
Dr. Siu and the other researchers noted several limits to the study, including that all the people who took part were in China, so how the practice would affect people in different regions is not clear. Also, almost a third of those who began the study dropped out before it ended, and they tended to have a higher body weight than those who remained to the end. The authors said this high dropout rate could mean that some people had negative experiences during their exercise programs.
Next steps, said Dr. Siu, include further assessing how tai chi affects things such as blood sugar and blood pressure. Other, early-stage studies also show tai chi having some positive effects on mood and cognition, he said, pointing to a need for more research.
UC Irvine’s Dr. Nadeswaran agreed. The work opens the door, she said, to taking a long-term look at how practicing tai chi might affect a person’s risk of dying from heart disease or another cause. Her team’s work involves evaluating tai chi’s effects on several conditions, including metabolic syndrome and even the aftermath of COVID-19.
While researchers pursue these questions, tai chi is accessible in many ways. Dr. Siu noted the availability of classes in this “meditation in motion” practice at community centers and fitness clubs. For people who can’t yet rejoin activities in the real world, Dr. Nadeswaran said virtual tai chi classes also are available.
A version of this article first appeared on WebMD.com.
Results of a randomized controlled trial published online May 31 in Annals of Internal Medicine show that people who have a tough time with some kinds of aerobic exercise may gain similar benefits from tai chi.
The study is “very impressive,” said Bavani Nadeswaran, MD, of the University of California Irvine’s Susan Samueli Integrative Health Institute, who was not involved in the study.
Many people have arthritis or back pain, “and aerobic exercise can be hard on them,” she said. “The good thing about exercises like tai chi and yoga is that they are low-impact.” That means that people who can’t run or get access to a pool for swimming have a viable alternative.
The study included nearly 550 adults ages 50 and up in Hong Kong who were randomly assigned to engage in tai chi, aerobic exercise with strength training, or no exercise program for 12 weeks. All had waistlines greater than 35.4 inches for men and 31.5 inches for women.
The tai chi program involved three 1-hour weekly sessions of the practice, led by an instructor. Those who took part in the aerobic exercise group engaged three times each week in an exercise program of brisk tai chi and strength training, also led by an instructor.
The researchers measured changes in waistline size, cholesterol levels, and weight for about 9 months. Those who didn’t exercise had little change in their average waistline. Compared to the group that didn’t exercise, the average waistline of people in the two exercise groups declined more: by 0.7 inches more with tai chi, and 0.5 inches more with brisk walking and strength training.
Both exercise groups also had greater drops in body weight and triglyceride (a type of fat found in the blood) levels, and larger increases in high-density lipoprotein cholesterol, the “good” cholesterol, compared to the no-exercise group. All of these improvements lasted about 9 months with tai chi. But improvements in cholesterol levels did not last as long in those in the brisk-walking program.
The researchers also looked at the effects on blood pressure and blood sugar, but they found no differences between the groups.
The findings don’t necessarily mean that people with larger waistlines should dispense with their current exercise programs and turn to tai chi, said study author Parco Siu, PhD, head of the Division of Kinesiology at the University of Hong Kong’s School of Public Health. They show that tai chi is a good option if a person prefers it.
“This is good news for middle-aged and older adults who may be averse to conventional exercise,” he said in an email. But “certainly it is no problem for people to keep regularly participating in conventional exercise.”
Tai chi may also be a good choice for people without larger waistlines because practicing this form of exercise is a way to follow advice from the World Health Organization on physical activity, said Dr. Siu, though the study did not address this question.
Dr. Siu and the other researchers noted several limits to the study, including that all the people who took part were in China, so how the practice would affect people in different regions is not clear. Also, almost a third of those who began the study dropped out before it ended, and they tended to have a higher body weight than those who remained to the end. The authors said this high dropout rate could mean that some people had negative experiences during their exercise programs.
Next steps, said Dr. Siu, include further assessing how tai chi affects things such as blood sugar and blood pressure. Other, early-stage studies also show tai chi having some positive effects on mood and cognition, he said, pointing to a need for more research.
UC Irvine’s Dr. Nadeswaran agreed. The work opens the door, she said, to taking a long-term look at how practicing tai chi might affect a person’s risk of dying from heart disease or another cause. Her team’s work involves evaluating tai chi’s effects on several conditions, including metabolic syndrome and even the aftermath of COVID-19.
While researchers pursue these questions, tai chi is accessible in many ways. Dr. Siu noted the availability of classes in this “meditation in motion” practice at community centers and fitness clubs. For people who can’t yet rejoin activities in the real world, Dr. Nadeswaran said virtual tai chi classes also are available.
A version of this article first appeared on WebMD.com.
Results of a randomized controlled trial published online May 31 in Annals of Internal Medicine show that people who have a tough time with some kinds of aerobic exercise may gain similar benefits from tai chi.
The study is “very impressive,” said Bavani Nadeswaran, MD, of the University of California Irvine’s Susan Samueli Integrative Health Institute, who was not involved in the study.
Many people have arthritis or back pain, “and aerobic exercise can be hard on them,” she said. “The good thing about exercises like tai chi and yoga is that they are low-impact.” That means that people who can’t run or get access to a pool for swimming have a viable alternative.
The study included nearly 550 adults ages 50 and up in Hong Kong who were randomly assigned to engage in tai chi, aerobic exercise with strength training, or no exercise program for 12 weeks. All had waistlines greater than 35.4 inches for men and 31.5 inches for women.
The tai chi program involved three 1-hour weekly sessions of the practice, led by an instructor. Those who took part in the aerobic exercise group engaged three times each week in an exercise program of brisk tai chi and strength training, also led by an instructor.
The researchers measured changes in waistline size, cholesterol levels, and weight for about 9 months. Those who didn’t exercise had little change in their average waistline. Compared to the group that didn’t exercise, the average waistline of people in the two exercise groups declined more: by 0.7 inches more with tai chi, and 0.5 inches more with brisk walking and strength training.
Both exercise groups also had greater drops in body weight and triglyceride (a type of fat found in the blood) levels, and larger increases in high-density lipoprotein cholesterol, the “good” cholesterol, compared to the no-exercise group. All of these improvements lasted about 9 months with tai chi. But improvements in cholesterol levels did not last as long in those in the brisk-walking program.
The researchers also looked at the effects on blood pressure and blood sugar, but they found no differences between the groups.
The findings don’t necessarily mean that people with larger waistlines should dispense with their current exercise programs and turn to tai chi, said study author Parco Siu, PhD, head of the Division of Kinesiology at the University of Hong Kong’s School of Public Health. They show that tai chi is a good option if a person prefers it.
“This is good news for middle-aged and older adults who may be averse to conventional exercise,” he said in an email. But “certainly it is no problem for people to keep regularly participating in conventional exercise.”
Tai chi may also be a good choice for people without larger waistlines because practicing this form of exercise is a way to follow advice from the World Health Organization on physical activity, said Dr. Siu, though the study did not address this question.
Dr. Siu and the other researchers noted several limits to the study, including that all the people who took part were in China, so how the practice would affect people in different regions is not clear. Also, almost a third of those who began the study dropped out before it ended, and they tended to have a higher body weight than those who remained to the end. The authors said this high dropout rate could mean that some people had negative experiences during their exercise programs.
Next steps, said Dr. Siu, include further assessing how tai chi affects things such as blood sugar and blood pressure. Other, early-stage studies also show tai chi having some positive effects on mood and cognition, he said, pointing to a need for more research.
UC Irvine’s Dr. Nadeswaran agreed. The work opens the door, she said, to taking a long-term look at how practicing tai chi might affect a person’s risk of dying from heart disease or another cause. Her team’s work involves evaluating tai chi’s effects on several conditions, including metabolic syndrome and even the aftermath of COVID-19.
While researchers pursue these questions, tai chi is accessible in many ways. Dr. Siu noted the availability of classes in this “meditation in motion” practice at community centers and fitness clubs. For people who can’t yet rejoin activities in the real world, Dr. Nadeswaran said virtual tai chi classes also are available.
A version of this article first appeared on WebMD.com.
Adding daily steps linked to longer life
Taking more steps each day, in short spurts or longer bouts, was associated with a longer life in women older than 60 years, according to data from more than 16,000 participants in the ongoing Women’s Health Study.
The American Heart Association recommends at least 150 minutes per week of moderate physical activity, 75 minutes of vigorous physical activity, or a combination of both as fitness guidelines for adults. Walking is a safe and easy way for many adults to follow these guidelines, according to Christopher C. Moore, MS, a PhD candidate at the University of North Carolina at Chapel Hill.
The popularity of step counts reflect that they are simple and objective, and “focusing on steps can help promote an active lifestyle,” he said. Data on the impact of sporadic steps accumulated outside of longer bouts of activity on health outcomes are limited; however, technology advances in the form of fitness apps and wearable devices make it possible for researchers to track and measure the benefits of short periods of activity as well as longer periods.
In a study presented at the Epidemiology and Prevention/Lifestyle and Cardiometabolic Health meeting, sponsored by the AHA, Mr. Moore and colleagues assessed data from women older than 60 years who used wearable step-counting devices to measure their daily steps and walking patterns.
The study population included 16,732 women enrolled in the Women’s Health Study, a longstanding study of heart disease, cancer, and disease prevention among women in the United States. The participants wore waist step counters 4-7 days a week during 2011-2015. The average of the women was 72 years; 96% were non-Hispanic White, and the average BMI was 26 kg/m2.
The researchers divided the total number of steps for each study participant into two groups: “bouted” steps, defined as 10 minutes or longer bouts of walking with few interruptions; and “sporadic” steps, defined as short spurts of walking during regular daily activities such as housework, taking the stairs, or walking to or from a car.
A total of 804 deaths occurred during an average of 6 years of follow-up. Each initial increase of 1,000 steps including sporadic or bouted steps was associated with a 28% decrease in death, compared with no daily steps (hazard ratio, 0.72).
Each increasing quartile of sporadic steps was linked with higher total steps per day, Mr. Moore said. “Initial increase in sporadic steps corresponded to the greatest reductions in mortality,” with a HR of 0.69 per additional sporadic steps below 3,200 per day, and the impact on reduced mortality plateaued at about 4,500 sporadic steps per day.
In further analysis, the researchers also found a roughly 32% decrease in death in participants who took more than 2,000 steps daily in uninterrupted bouts (HR, 0.69).
The study findings were limited by several factors, including the relatively short follow-up period and number of events, the assessment of steps at a single time point, and the mostly homogeneous population, Mr. Moore noted. Additional research is needed to assess whether the results are generalizable to men, younger women, and diverse racial and ethnic groups.
However, the results may have implications for public health messaging, he emphasized. The message is that, to impact longevity, the total volume of steps is more important than the type of activity through which they are accumulated.
“You can accumulate your steps through longer bouts of purposeful activity or through everyday behaviors such as walking to your car, taking the stairs, and doing housework,” Mr. Moore concluded.
Find a friend, both of you benefit
On the basis of this study and other available evidence, more steps daily are recommended for everyone, Nieca Goldberg, MD, a cardiologist at New York University Langone Health, said in an interview.
“You can increase minutes of walking and frequency of walking,” she said.
Dr. Goldberg emphasized that you don’t need a fancy app or wearable device to up your steps. She offered some tips to help overcome barriers to putting one foot in front of the other. “Take the steps instead of the elevator. Park your car farther from your destination so you can walk.” Also, you can help yourself and help a friend to better health. “Get a walking buddy so you can encourage each other to walk,” Dr. Goldberg added.
Mr. Moore and Dr. Goldberg had no financial conflicts to disclose. The Women’s Health Study is funded by Brigham and Women’s Hospital; the National Heart, Lung, and Blood Institute; and the National Cancer Institute. Mr. Moore was funded by a grant from the NHLBI but had no other financial conflicts to disclose.
Taking more steps each day, in short spurts or longer bouts, was associated with a longer life in women older than 60 years, according to data from more than 16,000 participants in the ongoing Women’s Health Study.
The American Heart Association recommends at least 150 minutes per week of moderate physical activity, 75 minutes of vigorous physical activity, or a combination of both as fitness guidelines for adults. Walking is a safe and easy way for many adults to follow these guidelines, according to Christopher C. Moore, MS, a PhD candidate at the University of North Carolina at Chapel Hill.
The popularity of step counts reflect that they are simple and objective, and “focusing on steps can help promote an active lifestyle,” he said. Data on the impact of sporadic steps accumulated outside of longer bouts of activity on health outcomes are limited; however, technology advances in the form of fitness apps and wearable devices make it possible for researchers to track and measure the benefits of short periods of activity as well as longer periods.
In a study presented at the Epidemiology and Prevention/Lifestyle and Cardiometabolic Health meeting, sponsored by the AHA, Mr. Moore and colleagues assessed data from women older than 60 years who used wearable step-counting devices to measure their daily steps and walking patterns.
The study population included 16,732 women enrolled in the Women’s Health Study, a longstanding study of heart disease, cancer, and disease prevention among women in the United States. The participants wore waist step counters 4-7 days a week during 2011-2015. The average of the women was 72 years; 96% were non-Hispanic White, and the average BMI was 26 kg/m2.
The researchers divided the total number of steps for each study participant into two groups: “bouted” steps, defined as 10 minutes or longer bouts of walking with few interruptions; and “sporadic” steps, defined as short spurts of walking during regular daily activities such as housework, taking the stairs, or walking to or from a car.
A total of 804 deaths occurred during an average of 6 years of follow-up. Each initial increase of 1,000 steps including sporadic or bouted steps was associated with a 28% decrease in death, compared with no daily steps (hazard ratio, 0.72).
Each increasing quartile of sporadic steps was linked with higher total steps per day, Mr. Moore said. “Initial increase in sporadic steps corresponded to the greatest reductions in mortality,” with a HR of 0.69 per additional sporadic steps below 3,200 per day, and the impact on reduced mortality plateaued at about 4,500 sporadic steps per day.
In further analysis, the researchers also found a roughly 32% decrease in death in participants who took more than 2,000 steps daily in uninterrupted bouts (HR, 0.69).
The study findings were limited by several factors, including the relatively short follow-up period and number of events, the assessment of steps at a single time point, and the mostly homogeneous population, Mr. Moore noted. Additional research is needed to assess whether the results are generalizable to men, younger women, and diverse racial and ethnic groups.
However, the results may have implications for public health messaging, he emphasized. The message is that, to impact longevity, the total volume of steps is more important than the type of activity through which they are accumulated.
“You can accumulate your steps through longer bouts of purposeful activity or through everyday behaviors such as walking to your car, taking the stairs, and doing housework,” Mr. Moore concluded.
Find a friend, both of you benefit
On the basis of this study and other available evidence, more steps daily are recommended for everyone, Nieca Goldberg, MD, a cardiologist at New York University Langone Health, said in an interview.
“You can increase minutes of walking and frequency of walking,” she said.
Dr. Goldberg emphasized that you don’t need a fancy app or wearable device to up your steps. She offered some tips to help overcome barriers to putting one foot in front of the other. “Take the steps instead of the elevator. Park your car farther from your destination so you can walk.” Also, you can help yourself and help a friend to better health. “Get a walking buddy so you can encourage each other to walk,” Dr. Goldberg added.
Mr. Moore and Dr. Goldberg had no financial conflicts to disclose. The Women’s Health Study is funded by Brigham and Women’s Hospital; the National Heart, Lung, and Blood Institute; and the National Cancer Institute. Mr. Moore was funded by a grant from the NHLBI but had no other financial conflicts to disclose.
Taking more steps each day, in short spurts or longer bouts, was associated with a longer life in women older than 60 years, according to data from more than 16,000 participants in the ongoing Women’s Health Study.
The American Heart Association recommends at least 150 minutes per week of moderate physical activity, 75 minutes of vigorous physical activity, or a combination of both as fitness guidelines for adults. Walking is a safe and easy way for many adults to follow these guidelines, according to Christopher C. Moore, MS, a PhD candidate at the University of North Carolina at Chapel Hill.
The popularity of step counts reflect that they are simple and objective, and “focusing on steps can help promote an active lifestyle,” he said. Data on the impact of sporadic steps accumulated outside of longer bouts of activity on health outcomes are limited; however, technology advances in the form of fitness apps and wearable devices make it possible for researchers to track and measure the benefits of short periods of activity as well as longer periods.
In a study presented at the Epidemiology and Prevention/Lifestyle and Cardiometabolic Health meeting, sponsored by the AHA, Mr. Moore and colleagues assessed data from women older than 60 years who used wearable step-counting devices to measure their daily steps and walking patterns.
The study population included 16,732 women enrolled in the Women’s Health Study, a longstanding study of heart disease, cancer, and disease prevention among women in the United States. The participants wore waist step counters 4-7 days a week during 2011-2015. The average of the women was 72 years; 96% were non-Hispanic White, and the average BMI was 26 kg/m2.
The researchers divided the total number of steps for each study participant into two groups: “bouted” steps, defined as 10 minutes or longer bouts of walking with few interruptions; and “sporadic” steps, defined as short spurts of walking during regular daily activities such as housework, taking the stairs, or walking to or from a car.
A total of 804 deaths occurred during an average of 6 years of follow-up. Each initial increase of 1,000 steps including sporadic or bouted steps was associated with a 28% decrease in death, compared with no daily steps (hazard ratio, 0.72).
Each increasing quartile of sporadic steps was linked with higher total steps per day, Mr. Moore said. “Initial increase in sporadic steps corresponded to the greatest reductions in mortality,” with a HR of 0.69 per additional sporadic steps below 3,200 per day, and the impact on reduced mortality plateaued at about 4,500 sporadic steps per day.
In further analysis, the researchers also found a roughly 32% decrease in death in participants who took more than 2,000 steps daily in uninterrupted bouts (HR, 0.69).
The study findings were limited by several factors, including the relatively short follow-up period and number of events, the assessment of steps at a single time point, and the mostly homogeneous population, Mr. Moore noted. Additional research is needed to assess whether the results are generalizable to men, younger women, and diverse racial and ethnic groups.
However, the results may have implications for public health messaging, he emphasized. The message is that, to impact longevity, the total volume of steps is more important than the type of activity through which they are accumulated.
“You can accumulate your steps through longer bouts of purposeful activity or through everyday behaviors such as walking to your car, taking the stairs, and doing housework,” Mr. Moore concluded.
Find a friend, both of you benefit
On the basis of this study and other available evidence, more steps daily are recommended for everyone, Nieca Goldberg, MD, a cardiologist at New York University Langone Health, said in an interview.
“You can increase minutes of walking and frequency of walking,” she said.
Dr. Goldberg emphasized that you don’t need a fancy app or wearable device to up your steps. She offered some tips to help overcome barriers to putting one foot in front of the other. “Take the steps instead of the elevator. Park your car farther from your destination so you can walk.” Also, you can help yourself and help a friend to better health. “Get a walking buddy so you can encourage each other to walk,” Dr. Goldberg added.
Mr. Moore and Dr. Goldberg had no financial conflicts to disclose. The Women’s Health Study is funded by Brigham and Women’s Hospital; the National Heart, Lung, and Blood Institute; and the National Cancer Institute. Mr. Moore was funded by a grant from the NHLBI but had no other financial conflicts to disclose.
FROM EPI LIFESTYLE 2021
Do anti–apo A-I antibodies link fatty liver disease and CVD?
Anti–apolipoprotein A-I (apo A-I) antibodies are common in nonalcoholic fatty liver disease and may not only drive its development but also underlie the link between NAFLD and cardiovascular disease, suggests a novel analysis.
Conducting a clinical analysis and a series of experiments, Sabrina Pagano, PhD, diagnostic department, Geneva University Hospital, and colleagues looked for anti–apo A-I antibodies in patients with NAFLD and then examined their impact on hepatic cells and inflammatory markers.
They found that nearly half of 137 patients with NAFLD were seropositive, and that the antibodies were associated with increased lipid accumulation in the liver, altered triglyceride metabolism, and proinflammatory effects on liver cells.
“We hypothesize that anti–apo A-I IgG may be a potential driver in the development of NAFLD, and further studies are needed to support anti–apo A-I IgG as a possible link between NAFLD and cardiovascular disease,” Dr. Pagano said.
The research was presented at the European Atherosclerosis Society 2021 Virtual Congress.
Asked whether anti–apo A-I antibodies could represent a potential treatment target for NAFLD, Dr. Pagano said in an interview that they have “already developed a peptide that is recognized by the antibodies in order to try to reverse the anti–apo A-I deleterious effect.”
While this was successful in vitro, “unfortunately we didn’t observe ... the peptide reverse of these anti–apo A-I effects in mice, so ... for the moment it’s a little early,” to say whether it represents a promising target.
Approached for comment, Maciej Banach, MD, PhD, full professor of cardiology, Polish Mother’s Memorial Hospital Research Institute, Lodz, said that the results are “very interesting and encouraging.”
He said that his own global burden of disease analysis, which is set to be published soon, showed that the worldwide prevalence of NAFLD is 11%, “representing almost 900 million cases,” and a more than 33% increase in prevalence in the past 30 years.
Consequently, any “attempt to have effective, especially early, diagnosis and treatment,” is highly anticipated.
Dr. Banach said the findings from the experimental analyses are “very interesting and promising,” especially regarding the proinflammatory effects of anti–apo A-I antibodies.
However, he underlined that the clinical part, looking at antibody seropositivity in patients with NAFLD, was limited by the lack of a control group, and there was no indication as to what treatment the patients received, despite it being clear that many were obese.
Dr. Banach also believes that, taking into account the patient characteristics, it is likely that most of the patients had the more severe nonalcoholic steatohepatitis, and “it would be additionally useful to see the autoantibodies levels both in NASH and NAFLD.”
Nevertheless, the clinical utility of measuring anti–apo A-I antibodies is limited at this stage.
He said that the lack of “good, easy, and cheap diagnostic methods based on both laboratory and imaging data” for NAFLD means it would be difficult to determine whether assessing antibody seropositivity “might be indeed an added value.”
Independent predictors
Dr. Pagano explained that anti–apo A-I antibodies, which target the major protein fraction of HDL cholesterol, are independent predictors of cardiovascular events in high-risk populations.
They are also independently associated with cardiovascular disease in the general population, as well as atherosclerotic plaque vulnerability in both mice and humans.
She said that apo A-I antibodies have a metabolic role in vivo, and have been shown in vitro to disrupt cholesterol metabolism, promoting foam cell formation.
Studies have also indicated they play a role in hepatic fibrosis, predicting the development of cirrhosis in individuals with chronic hepatitis C infection.
The team therefore set out to determine the presence of anti–apo A-I antibodies in individuals with NAFLD, defined here as fatty acid levels greater than 5% of liver weight, as well as their effect on hepatic cells.
Working with colleagues at Magna Græcia University of Catanzaro (Italy), they obtained serum samples from 137 patients with NAFLD confirmed on ultrasound.
The patients had an average age of 49 years, and 48.9% were male. The median body mass index was 31.8 kg/m2. Cholesterol levels were typically in the intermediate range.
They found that 46% of the participants had anti–apo A-I IgG antibodies, “which is quite high when compared with the 15%-20% positivity that we retrieved from the general population,” Dr. Pagano said.
To explore the link between high anti–apo A-I antibodies and NAFLD, the team studied hepatic cells, treating them with anti–apo A-I IgG antibodies or control IgG antibodies, or leaving them untreated, for 24 hours.
This revealed that anti–apo A-I IgG antibodies were associated with a significant increase in liquid droplet content in hepatic cells, compared with both cells treated with control IgG (P = .0008), and untreated cells (P = .0002).
Next, the team immunized apo E knockout mice with anti–apo A-I or control IgG antibodies. After 16 weeks, they found there was a significant increase in liver lipid content in mice given anti–apo A-I antibodies versus those treated with controls (P = .03).
They then asked whether anti–apo A-I antibodies could affect triglyceride metabolism. They examined the expression of the transcription factor sterol regulatory element binding protein (SREBP) and regulation of the triglyceride and cholesterol pathways.
Treating hepatic cells again for 24 hours with anti–apo A-I IgG antibodies or control IgG antibodies, or leaving them untreated, showed that anti–apo A-I antibodies were associated with “dramatic” increases in the active form of SREBP.
They also found that expression of two key enzymes in the triglyceride pathway, fatty acid synthetase and glycerol phosphate acyltransferase, was substantially decreased in the presence anti–apo A-I antibodies.
In both experiments, the untreated hepatic cells and those exposed to control IgG antibodies showed no significant changes.
“These results suggest that negative feedback ... turns off these enzymes, probably due to the lipid overload that is found in the cells after 24 hours of anti–apo A-I treatment,” Dr. Pagano said.
Finally, the researchers observed that anti–apo A-I, but not control antibodies, were associated with increases in inflammatory markers in liver cells.
Specifically, exposure to the antibodies was linked to an approximately 10-fold increase in interleukin-6 levels, as well as an approximate 25-fold increase in IL-8, and around a 7-fold increase in tumor necrosis factor–alpha.
Dr. Pagano suggested that the inflammatory effects are “probably mediated by binding anti–apo A-I antibodies to toll-like receptor 2, which has been previously described in macrophages.”
No funding was declared. The study authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Anti–apolipoprotein A-I (apo A-I) antibodies are common in nonalcoholic fatty liver disease and may not only drive its development but also underlie the link between NAFLD and cardiovascular disease, suggests a novel analysis.
Conducting a clinical analysis and a series of experiments, Sabrina Pagano, PhD, diagnostic department, Geneva University Hospital, and colleagues looked for anti–apo A-I antibodies in patients with NAFLD and then examined their impact on hepatic cells and inflammatory markers.
They found that nearly half of 137 patients with NAFLD were seropositive, and that the antibodies were associated with increased lipid accumulation in the liver, altered triglyceride metabolism, and proinflammatory effects on liver cells.
“We hypothesize that anti–apo A-I IgG may be a potential driver in the development of NAFLD, and further studies are needed to support anti–apo A-I IgG as a possible link between NAFLD and cardiovascular disease,” Dr. Pagano said.
The research was presented at the European Atherosclerosis Society 2021 Virtual Congress.
Asked whether anti–apo A-I antibodies could represent a potential treatment target for NAFLD, Dr. Pagano said in an interview that they have “already developed a peptide that is recognized by the antibodies in order to try to reverse the anti–apo A-I deleterious effect.”
While this was successful in vitro, “unfortunately we didn’t observe ... the peptide reverse of these anti–apo A-I effects in mice, so ... for the moment it’s a little early,” to say whether it represents a promising target.
Approached for comment, Maciej Banach, MD, PhD, full professor of cardiology, Polish Mother’s Memorial Hospital Research Institute, Lodz, said that the results are “very interesting and encouraging.”
He said that his own global burden of disease analysis, which is set to be published soon, showed that the worldwide prevalence of NAFLD is 11%, “representing almost 900 million cases,” and a more than 33% increase in prevalence in the past 30 years.
Consequently, any “attempt to have effective, especially early, diagnosis and treatment,” is highly anticipated.
Dr. Banach said the findings from the experimental analyses are “very interesting and promising,” especially regarding the proinflammatory effects of anti–apo A-I antibodies.
However, he underlined that the clinical part, looking at antibody seropositivity in patients with NAFLD, was limited by the lack of a control group, and there was no indication as to what treatment the patients received, despite it being clear that many were obese.
Dr. Banach also believes that, taking into account the patient characteristics, it is likely that most of the patients had the more severe nonalcoholic steatohepatitis, and “it would be additionally useful to see the autoantibodies levels both in NASH and NAFLD.”
Nevertheless, the clinical utility of measuring anti–apo A-I antibodies is limited at this stage.
He said that the lack of “good, easy, and cheap diagnostic methods based on both laboratory and imaging data” for NAFLD means it would be difficult to determine whether assessing antibody seropositivity “might be indeed an added value.”
Independent predictors
Dr. Pagano explained that anti–apo A-I antibodies, which target the major protein fraction of HDL cholesterol, are independent predictors of cardiovascular events in high-risk populations.
They are also independently associated with cardiovascular disease in the general population, as well as atherosclerotic plaque vulnerability in both mice and humans.
She said that apo A-I antibodies have a metabolic role in vivo, and have been shown in vitro to disrupt cholesterol metabolism, promoting foam cell formation.
Studies have also indicated they play a role in hepatic fibrosis, predicting the development of cirrhosis in individuals with chronic hepatitis C infection.
The team therefore set out to determine the presence of anti–apo A-I antibodies in individuals with NAFLD, defined here as fatty acid levels greater than 5% of liver weight, as well as their effect on hepatic cells.
Working with colleagues at Magna Græcia University of Catanzaro (Italy), they obtained serum samples from 137 patients with NAFLD confirmed on ultrasound.
The patients had an average age of 49 years, and 48.9% were male. The median body mass index was 31.8 kg/m2. Cholesterol levels were typically in the intermediate range.
They found that 46% of the participants had anti–apo A-I IgG antibodies, “which is quite high when compared with the 15%-20% positivity that we retrieved from the general population,” Dr. Pagano said.
To explore the link between high anti–apo A-I antibodies and NAFLD, the team studied hepatic cells, treating them with anti–apo A-I IgG antibodies or control IgG antibodies, or leaving them untreated, for 24 hours.
This revealed that anti–apo A-I IgG antibodies were associated with a significant increase in liquid droplet content in hepatic cells, compared with both cells treated with control IgG (P = .0008), and untreated cells (P = .0002).
Next, the team immunized apo E knockout mice with anti–apo A-I or control IgG antibodies. After 16 weeks, they found there was a significant increase in liver lipid content in mice given anti–apo A-I antibodies versus those treated with controls (P = .03).
They then asked whether anti–apo A-I antibodies could affect triglyceride metabolism. They examined the expression of the transcription factor sterol regulatory element binding protein (SREBP) and regulation of the triglyceride and cholesterol pathways.
Treating hepatic cells again for 24 hours with anti–apo A-I IgG antibodies or control IgG antibodies, or leaving them untreated, showed that anti–apo A-I antibodies were associated with “dramatic” increases in the active form of SREBP.
They also found that expression of two key enzymes in the triglyceride pathway, fatty acid synthetase and glycerol phosphate acyltransferase, was substantially decreased in the presence anti–apo A-I antibodies.
In both experiments, the untreated hepatic cells and those exposed to control IgG antibodies showed no significant changes.
“These results suggest that negative feedback ... turns off these enzymes, probably due to the lipid overload that is found in the cells after 24 hours of anti–apo A-I treatment,” Dr. Pagano said.
Finally, the researchers observed that anti–apo A-I, but not control antibodies, were associated with increases in inflammatory markers in liver cells.
Specifically, exposure to the antibodies was linked to an approximately 10-fold increase in interleukin-6 levels, as well as an approximate 25-fold increase in IL-8, and around a 7-fold increase in tumor necrosis factor–alpha.
Dr. Pagano suggested that the inflammatory effects are “probably mediated by binding anti–apo A-I antibodies to toll-like receptor 2, which has been previously described in macrophages.”
No funding was declared. The study authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Anti–apolipoprotein A-I (apo A-I) antibodies are common in nonalcoholic fatty liver disease and may not only drive its development but also underlie the link between NAFLD and cardiovascular disease, suggests a novel analysis.
Conducting a clinical analysis and a series of experiments, Sabrina Pagano, PhD, diagnostic department, Geneva University Hospital, and colleagues looked for anti–apo A-I antibodies in patients with NAFLD and then examined their impact on hepatic cells and inflammatory markers.
They found that nearly half of 137 patients with NAFLD were seropositive, and that the antibodies were associated with increased lipid accumulation in the liver, altered triglyceride metabolism, and proinflammatory effects on liver cells.
“We hypothesize that anti–apo A-I IgG may be a potential driver in the development of NAFLD, and further studies are needed to support anti–apo A-I IgG as a possible link between NAFLD and cardiovascular disease,” Dr. Pagano said.
The research was presented at the European Atherosclerosis Society 2021 Virtual Congress.
Asked whether anti–apo A-I antibodies could represent a potential treatment target for NAFLD, Dr. Pagano said in an interview that they have “already developed a peptide that is recognized by the antibodies in order to try to reverse the anti–apo A-I deleterious effect.”
While this was successful in vitro, “unfortunately we didn’t observe ... the peptide reverse of these anti–apo A-I effects in mice, so ... for the moment it’s a little early,” to say whether it represents a promising target.
Approached for comment, Maciej Banach, MD, PhD, full professor of cardiology, Polish Mother’s Memorial Hospital Research Institute, Lodz, said that the results are “very interesting and encouraging.”
He said that his own global burden of disease analysis, which is set to be published soon, showed that the worldwide prevalence of NAFLD is 11%, “representing almost 900 million cases,” and a more than 33% increase in prevalence in the past 30 years.
Consequently, any “attempt to have effective, especially early, diagnosis and treatment,” is highly anticipated.
Dr. Banach said the findings from the experimental analyses are “very interesting and promising,” especially regarding the proinflammatory effects of anti–apo A-I antibodies.
However, he underlined that the clinical part, looking at antibody seropositivity in patients with NAFLD, was limited by the lack of a control group, and there was no indication as to what treatment the patients received, despite it being clear that many were obese.
Dr. Banach also believes that, taking into account the patient characteristics, it is likely that most of the patients had the more severe nonalcoholic steatohepatitis, and “it would be additionally useful to see the autoantibodies levels both in NASH and NAFLD.”
Nevertheless, the clinical utility of measuring anti–apo A-I antibodies is limited at this stage.
He said that the lack of “good, easy, and cheap diagnostic methods based on both laboratory and imaging data” for NAFLD means it would be difficult to determine whether assessing antibody seropositivity “might be indeed an added value.”
Independent predictors
Dr. Pagano explained that anti–apo A-I antibodies, which target the major protein fraction of HDL cholesterol, are independent predictors of cardiovascular events in high-risk populations.
They are also independently associated with cardiovascular disease in the general population, as well as atherosclerotic plaque vulnerability in both mice and humans.
She said that apo A-I antibodies have a metabolic role in vivo, and have been shown in vitro to disrupt cholesterol metabolism, promoting foam cell formation.
Studies have also indicated they play a role in hepatic fibrosis, predicting the development of cirrhosis in individuals with chronic hepatitis C infection.
The team therefore set out to determine the presence of anti–apo A-I antibodies in individuals with NAFLD, defined here as fatty acid levels greater than 5% of liver weight, as well as their effect on hepatic cells.
Working with colleagues at Magna Græcia University of Catanzaro (Italy), they obtained serum samples from 137 patients with NAFLD confirmed on ultrasound.
The patients had an average age of 49 years, and 48.9% were male. The median body mass index was 31.8 kg/m2. Cholesterol levels were typically in the intermediate range.
They found that 46% of the participants had anti–apo A-I IgG antibodies, “which is quite high when compared with the 15%-20% positivity that we retrieved from the general population,” Dr. Pagano said.
To explore the link between high anti–apo A-I antibodies and NAFLD, the team studied hepatic cells, treating them with anti–apo A-I IgG antibodies or control IgG antibodies, or leaving them untreated, for 24 hours.
This revealed that anti–apo A-I IgG antibodies were associated with a significant increase in liquid droplet content in hepatic cells, compared with both cells treated with control IgG (P = .0008), and untreated cells (P = .0002).
Next, the team immunized apo E knockout mice with anti–apo A-I or control IgG antibodies. After 16 weeks, they found there was a significant increase in liver lipid content in mice given anti–apo A-I antibodies versus those treated with controls (P = .03).
They then asked whether anti–apo A-I antibodies could affect triglyceride metabolism. They examined the expression of the transcription factor sterol regulatory element binding protein (SREBP) and regulation of the triglyceride and cholesterol pathways.
Treating hepatic cells again for 24 hours with anti–apo A-I IgG antibodies or control IgG antibodies, or leaving them untreated, showed that anti–apo A-I antibodies were associated with “dramatic” increases in the active form of SREBP.
They also found that expression of two key enzymes in the triglyceride pathway, fatty acid synthetase and glycerol phosphate acyltransferase, was substantially decreased in the presence anti–apo A-I antibodies.
In both experiments, the untreated hepatic cells and those exposed to control IgG antibodies showed no significant changes.
“These results suggest that negative feedback ... turns off these enzymes, probably due to the lipid overload that is found in the cells after 24 hours of anti–apo A-I treatment,” Dr. Pagano said.
Finally, the researchers observed that anti–apo A-I, but not control antibodies, were associated with increases in inflammatory markers in liver cells.
Specifically, exposure to the antibodies was linked to an approximately 10-fold increase in interleukin-6 levels, as well as an approximate 25-fold increase in IL-8, and around a 7-fold increase in tumor necrosis factor–alpha.
Dr. Pagano suggested that the inflammatory effects are “probably mediated by binding anti–apo A-I antibodies to toll-like receptor 2, which has been previously described in macrophages.”
No funding was declared. The study authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.