User login
Femoral nerve blocks delay recovery after ACL reconstruction
SEATTLE – Postoperative femoral nerve blocks prolong quadricep and hamstring weakness after anterior cruciate ligament reconstruction in young athletes, and delay recovery, according to investigators from the Mayo Clinic in Rochester, Minn.
Because of that, "I’ve stopped using them," said investigator Dr. Amy McIntosh, a pediatric orthopedic surgeon in Rochester.
In a retrospective study of patients no older than 18 years, her team found that 68% (42 of 62 patients) who got the block – weight-based bupivacaine HCl in all cases – were cleared for sports at 6 months, meaning that their operated knee was at least 85% as strong as their uninjured knee, and at least 90% as functional. Among children who didn’t get the blocks after anterior cruciate ligament reconstruction (ACL), 90% (56 of 62) were ready to return to sports, a significant difference. Overall, unblocked kids were 4.4 times more likely to be cleared at 6 months.
"Kids who didn’t clear at 6 months usually took another 3-4 months. At a year, everybody looked about the same," Dr. McIntosh said at the American Orthopaedic Society for Sports Medicine annual meeting.
Also at 6 months, kids who got the nerve block had significantly greater mean deficits in fast isokinetic knee extensions, a measure of quadricep strength (17.6% in the operated knee vs. 11.2% in the uninjured knee), and fast (9.9% vs. 5.7%) and slow (13.0% vs. 8.5%) isokinetic flexion, a measure of hamstring strength. It didn’t seem to matter if they got a one-shot femoral nerve block or a continuous pump infusion.
Dr. McIntosh initially lobbied Mayo anesthesiologists to use femoral blocks in kids, opting first for the pump. "Then I saw that those kids had a lot of quad atrophy and were taking a longer time to get off their crutches, so I started going to the one-shot block, but they still had quad atrophy, and took a little longer to get off their crutches and get their normal gait back. Now, after seeing this data, I’m done with it," she said.
She’s not alone. Long considered a benign and effective method for short-term pain control, surgeons have been reconsidering the blocks because of similar findings in adults.
"I tell patients [and parents] that they have to decide if they want great pain control up front, or a little more pain in the first few days after surgery," but a quicker return to sports. When offered the choice, young athletes opt against the block because it will likely mean missing an entire season. "That’s what matters to these kids," Dr. McIntosh said.
The nerve block group and control groups were evenly matched; children in both were about 16 years old, on average, with a mean body mass index of about 24 kg/m2. There were slightly more girls in the study than boys.
Most of the kids in both groups had patellar tendon autografts, and the rest had hamstring autografts. Those who got nerve blocks had shorter tourniquet (82 vs. 93 minutes), operative (134 vs. 155 minutes.), and anesthesia times (177 vs. 200 minutes).
Dr. McIntosh said he had no relevant financial disclosures. The project was funded internally.
SEATTLE – Postoperative femoral nerve blocks prolong quadricep and hamstring weakness after anterior cruciate ligament reconstruction in young athletes, and delay recovery, according to investigators from the Mayo Clinic in Rochester, Minn.
Because of that, "I’ve stopped using them," said investigator Dr. Amy McIntosh, a pediatric orthopedic surgeon in Rochester.
In a retrospective study of patients no older than 18 years, her team found that 68% (42 of 62 patients) who got the block – weight-based bupivacaine HCl in all cases – were cleared for sports at 6 months, meaning that their operated knee was at least 85% as strong as their uninjured knee, and at least 90% as functional. Among children who didn’t get the blocks after anterior cruciate ligament reconstruction (ACL), 90% (56 of 62) were ready to return to sports, a significant difference. Overall, unblocked kids were 4.4 times more likely to be cleared at 6 months.
"Kids who didn’t clear at 6 months usually took another 3-4 months. At a year, everybody looked about the same," Dr. McIntosh said at the American Orthopaedic Society for Sports Medicine annual meeting.
Also at 6 months, kids who got the nerve block had significantly greater mean deficits in fast isokinetic knee extensions, a measure of quadricep strength (17.6% in the operated knee vs. 11.2% in the uninjured knee), and fast (9.9% vs. 5.7%) and slow (13.0% vs. 8.5%) isokinetic flexion, a measure of hamstring strength. It didn’t seem to matter if they got a one-shot femoral nerve block or a continuous pump infusion.
Dr. McIntosh initially lobbied Mayo anesthesiologists to use femoral blocks in kids, opting first for the pump. "Then I saw that those kids had a lot of quad atrophy and were taking a longer time to get off their crutches, so I started going to the one-shot block, but they still had quad atrophy, and took a little longer to get off their crutches and get their normal gait back. Now, after seeing this data, I’m done with it," she said.
She’s not alone. Long considered a benign and effective method for short-term pain control, surgeons have been reconsidering the blocks because of similar findings in adults.
"I tell patients [and parents] that they have to decide if they want great pain control up front, or a little more pain in the first few days after surgery," but a quicker return to sports. When offered the choice, young athletes opt against the block because it will likely mean missing an entire season. "That’s what matters to these kids," Dr. McIntosh said.
The nerve block group and control groups were evenly matched; children in both were about 16 years old, on average, with a mean body mass index of about 24 kg/m2. There were slightly more girls in the study than boys.
Most of the kids in both groups had patellar tendon autografts, and the rest had hamstring autografts. Those who got nerve blocks had shorter tourniquet (82 vs. 93 minutes), operative (134 vs. 155 minutes.), and anesthesia times (177 vs. 200 minutes).
Dr. McIntosh said he had no relevant financial disclosures. The project was funded internally.
SEATTLE – Postoperative femoral nerve blocks prolong quadricep and hamstring weakness after anterior cruciate ligament reconstruction in young athletes, and delay recovery, according to investigators from the Mayo Clinic in Rochester, Minn.
Because of that, "I’ve stopped using them," said investigator Dr. Amy McIntosh, a pediatric orthopedic surgeon in Rochester.
In a retrospective study of patients no older than 18 years, her team found that 68% (42 of 62 patients) who got the block – weight-based bupivacaine HCl in all cases – were cleared for sports at 6 months, meaning that their operated knee was at least 85% as strong as their uninjured knee, and at least 90% as functional. Among children who didn’t get the blocks after anterior cruciate ligament reconstruction (ACL), 90% (56 of 62) were ready to return to sports, a significant difference. Overall, unblocked kids were 4.4 times more likely to be cleared at 6 months.
"Kids who didn’t clear at 6 months usually took another 3-4 months. At a year, everybody looked about the same," Dr. McIntosh said at the American Orthopaedic Society for Sports Medicine annual meeting.
Also at 6 months, kids who got the nerve block had significantly greater mean deficits in fast isokinetic knee extensions, a measure of quadricep strength (17.6% in the operated knee vs. 11.2% in the uninjured knee), and fast (9.9% vs. 5.7%) and slow (13.0% vs. 8.5%) isokinetic flexion, a measure of hamstring strength. It didn’t seem to matter if they got a one-shot femoral nerve block or a continuous pump infusion.
Dr. McIntosh initially lobbied Mayo anesthesiologists to use femoral blocks in kids, opting first for the pump. "Then I saw that those kids had a lot of quad atrophy and were taking a longer time to get off their crutches, so I started going to the one-shot block, but they still had quad atrophy, and took a little longer to get off their crutches and get their normal gait back. Now, after seeing this data, I’m done with it," she said.
She’s not alone. Long considered a benign and effective method for short-term pain control, surgeons have been reconsidering the blocks because of similar findings in adults.
"I tell patients [and parents] that they have to decide if they want great pain control up front, or a little more pain in the first few days after surgery," but a quicker return to sports. When offered the choice, young athletes opt against the block because it will likely mean missing an entire season. "That’s what matters to these kids," Dr. McIntosh said.
The nerve block group and control groups were evenly matched; children in both were about 16 years old, on average, with a mean body mass index of about 24 kg/m2. There were slightly more girls in the study than boys.
Most of the kids in both groups had patellar tendon autografts, and the rest had hamstring autografts. Those who got nerve blocks had shorter tourniquet (82 vs. 93 minutes), operative (134 vs. 155 minutes.), and anesthesia times (177 vs. 200 minutes).
Dr. McIntosh said he had no relevant financial disclosures. The project was funded internally.
AT THE AOSSM 2014 ANNUAL MEETING
Key clinical point: When young athletes want to be back in the game at 6 months, skip femoral nerve blocks after ACL surgery.
Major finding: Ninety percent of young athletes are ready to return to sports at 6 months if they don’t get a femoral nerve block following anterior cruciate ligament reconstruction; among those who get the block, 68% are ready to get back into the game.
Data Source: A retrospective matched cohort study.
Disclosures: The work was funded internally, and the presenter said he had no disclosures.
Bone Loss Continues Two Years After Weight Loss Surgery
Patients who have had bariatric surgery continue to lose bone for at least two years, even after their weight stabilizes, according to study results presented at the 2014 joint meeting of the International Society of Endocrinology and the Endocrine Society. “The long-term consequences of this substantial bone loss are unclear, but it might put them at increased risk of fracture, or breaking a bone,” said lead study author Elaine Yu, MD, MSc, an endocrinologist at Massachusetts General Hospital in Boston and her research colleagues.
Dr. Yu’s team previously found that patients who have gastric bypass surgery lose bone mineral density within the first year after the surgery. Because the rate of bone loss was high, they researchers continued to monitor the patients in this study.
Since the standard imaging method for bone mineral density, dual-energy x-ray absorptiometry (DXA), can sometimes give inaccurate results in obese individuals, the investigators also measured bone density using quantitative computed tomography (QCT). They compared bone density at the lower spine and the hip in 50 obese adults (30 who had bariatric surgery and 20 who lost weight through nonsurgical ways but were similar to surgical patients in baseline age, sex, and body mass index). After surgery, nearly all patients received calcium and high-dose vitamin D supplementation.
Two years later, bone density was 5% to 7% lower at the spine and 7% to 10% lower at the hip in the surgical group compared with the nonsurgical control group, as shown by both DXA and QCT. In addition, the surgical patients had substantial and persistent increases in markers of bone resorption.
The bone loss in the surgical patients occurred despite the fact that the patients were not losing any more weight in the second post-surgical year and had stable blood levels of calcium and vitamin D. “Therefore, the cause of the bone loss is probably not related to weight loss itself,” Dr. Yu said.
None of the gastric bypass patients have required osteoporosis treatment, according to Dr. Yu. “The question is when is the bone loss going to stop? Over time this could be a problem in terms of fracture,” she said. Dr. Yu recommended that bariatric surgery candidates who have risk factors for osteoporosis receive bone density tests.
Patients who have had bariatric surgery continue to lose bone for at least two years, even after their weight stabilizes, according to study results presented at the 2014 joint meeting of the International Society of Endocrinology and the Endocrine Society. “The long-term consequences of this substantial bone loss are unclear, but it might put them at increased risk of fracture, or breaking a bone,” said lead study author Elaine Yu, MD, MSc, an endocrinologist at Massachusetts General Hospital in Boston and her research colleagues.
Dr. Yu’s team previously found that patients who have gastric bypass surgery lose bone mineral density within the first year after the surgery. Because the rate of bone loss was high, they researchers continued to monitor the patients in this study.
Since the standard imaging method for bone mineral density, dual-energy x-ray absorptiometry (DXA), can sometimes give inaccurate results in obese individuals, the investigators also measured bone density using quantitative computed tomography (QCT). They compared bone density at the lower spine and the hip in 50 obese adults (30 who had bariatric surgery and 20 who lost weight through nonsurgical ways but were similar to surgical patients in baseline age, sex, and body mass index). After surgery, nearly all patients received calcium and high-dose vitamin D supplementation.
Two years later, bone density was 5% to 7% lower at the spine and 7% to 10% lower at the hip in the surgical group compared with the nonsurgical control group, as shown by both DXA and QCT. In addition, the surgical patients had substantial and persistent increases in markers of bone resorption.
The bone loss in the surgical patients occurred despite the fact that the patients were not losing any more weight in the second post-surgical year and had stable blood levels of calcium and vitamin D. “Therefore, the cause of the bone loss is probably not related to weight loss itself,” Dr. Yu said.
None of the gastric bypass patients have required osteoporosis treatment, according to Dr. Yu. “The question is when is the bone loss going to stop? Over time this could be a problem in terms of fracture,” she said. Dr. Yu recommended that bariatric surgery candidates who have risk factors for osteoporosis receive bone density tests.
Patients who have had bariatric surgery continue to lose bone for at least two years, even after their weight stabilizes, according to study results presented at the 2014 joint meeting of the International Society of Endocrinology and the Endocrine Society. “The long-term consequences of this substantial bone loss are unclear, but it might put them at increased risk of fracture, or breaking a bone,” said lead study author Elaine Yu, MD, MSc, an endocrinologist at Massachusetts General Hospital in Boston and her research colleagues.
Dr. Yu’s team previously found that patients who have gastric bypass surgery lose bone mineral density within the first year after the surgery. Because the rate of bone loss was high, they researchers continued to monitor the patients in this study.
Since the standard imaging method for bone mineral density, dual-energy x-ray absorptiometry (DXA), can sometimes give inaccurate results in obese individuals, the investigators also measured bone density using quantitative computed tomography (QCT). They compared bone density at the lower spine and the hip in 50 obese adults (30 who had bariatric surgery and 20 who lost weight through nonsurgical ways but were similar to surgical patients in baseline age, sex, and body mass index). After surgery, nearly all patients received calcium and high-dose vitamin D supplementation.
Two years later, bone density was 5% to 7% lower at the spine and 7% to 10% lower at the hip in the surgical group compared with the nonsurgical control group, as shown by both DXA and QCT. In addition, the surgical patients had substantial and persistent increases in markers of bone resorption.
The bone loss in the surgical patients occurred despite the fact that the patients were not losing any more weight in the second post-surgical year and had stable blood levels of calcium and vitamin D. “Therefore, the cause of the bone loss is probably not related to weight loss itself,” Dr. Yu said.
None of the gastric bypass patients have required osteoporosis treatment, according to Dr. Yu. “The question is when is the bone loss going to stop? Over time this could be a problem in terms of fracture,” she said. Dr. Yu recommended that bariatric surgery candidates who have risk factors for osteoporosis receive bone density tests.
Denosumab Increases Bone Density in Postmenopausal Women With Osteoporosis
Postmenopausal women with osteoporosis who take denosumab long-term have increased bone density and a sustained low rate of fractures, according to study results presented at the 2014 joint meeting of the International Society of Endocrinology and the Endocrine Society. Lead study author E. Michael Lewiecki, MD, Clinical Assistant Professor of Medicine at the University of New Mexico School of Medicine in Albuquerque and research colleagues reported that long-term treatment with denosumab was safe and resulted in continuing increases in bone density over the eight years of treatment with persistently low fracture rates.
“This study provides reassurance to physicians and their patients that long-term treatment with denosumab for at least eight years leads to significant increases in bone density and is safe for appropriately selected women with postmenopausal osteoporosis.” He also noted that the overall risk of side effects did not increase over time.
Among the almost 8,000 women originally enrolled in the FREEDOM trial, denosumab reduced their risk of vertebral fractures by 68%, reduced their risk of nonvertebral fractures by 20%, and reduced their risk of hip fractures by 40%, compared with placebo. Women taking the drug had no increase in their overall risk for cancer, infection, cardiovascular disease, delayed fracture healing, or hypocalcemia.
All of the roughly 3,000 women in the long-term extension of the trial took denosumab for up to eight years. Overall, they showed a continued increase in their mean bone mineral density, with a cumulative eight-year gain of 18.4% at the lumbar spine and 8.3% at the total hip, with few fractures and a good safety profile. The tolerability profile of denosumab during this extension phase was consistent with that observed during the initial 3-year FREEDOM trial. At 12 months, denosumab treatment increased bone mineral density (BMD) at the total hip, lumbar spine and/or femoral neck and reduced markers of bone turnover to a significantly greater extent than oral bisphosphonates in women who were essentially bisphosphonate-naive and in those who had switched from alendronate to denosumab treatment.
Postmenopausal women with osteoporosis who take denosumab long-term have increased bone density and a sustained low rate of fractures, according to study results presented at the 2014 joint meeting of the International Society of Endocrinology and the Endocrine Society. Lead study author E. Michael Lewiecki, MD, Clinical Assistant Professor of Medicine at the University of New Mexico School of Medicine in Albuquerque and research colleagues reported that long-term treatment with denosumab was safe and resulted in continuing increases in bone density over the eight years of treatment with persistently low fracture rates.
“This study provides reassurance to physicians and their patients that long-term treatment with denosumab for at least eight years leads to significant increases in bone density and is safe for appropriately selected women with postmenopausal osteoporosis.” He also noted that the overall risk of side effects did not increase over time.
Among the almost 8,000 women originally enrolled in the FREEDOM trial, denosumab reduced their risk of vertebral fractures by 68%, reduced their risk of nonvertebral fractures by 20%, and reduced their risk of hip fractures by 40%, compared with placebo. Women taking the drug had no increase in their overall risk for cancer, infection, cardiovascular disease, delayed fracture healing, or hypocalcemia.
All of the roughly 3,000 women in the long-term extension of the trial took denosumab for up to eight years. Overall, they showed a continued increase in their mean bone mineral density, with a cumulative eight-year gain of 18.4% at the lumbar spine and 8.3% at the total hip, with few fractures and a good safety profile. The tolerability profile of denosumab during this extension phase was consistent with that observed during the initial 3-year FREEDOM trial. At 12 months, denosumab treatment increased bone mineral density (BMD) at the total hip, lumbar spine and/or femoral neck and reduced markers of bone turnover to a significantly greater extent than oral bisphosphonates in women who were essentially bisphosphonate-naive and in those who had switched from alendronate to denosumab treatment.
Postmenopausal women with osteoporosis who take denosumab long-term have increased bone density and a sustained low rate of fractures, according to study results presented at the 2014 joint meeting of the International Society of Endocrinology and the Endocrine Society. Lead study author E. Michael Lewiecki, MD, Clinical Assistant Professor of Medicine at the University of New Mexico School of Medicine in Albuquerque and research colleagues reported that long-term treatment with denosumab was safe and resulted in continuing increases in bone density over the eight years of treatment with persistently low fracture rates.
“This study provides reassurance to physicians and their patients that long-term treatment with denosumab for at least eight years leads to significant increases in bone density and is safe for appropriately selected women with postmenopausal osteoporosis.” He also noted that the overall risk of side effects did not increase over time.
Among the almost 8,000 women originally enrolled in the FREEDOM trial, denosumab reduced their risk of vertebral fractures by 68%, reduced their risk of nonvertebral fractures by 20%, and reduced their risk of hip fractures by 40%, compared with placebo. Women taking the drug had no increase in their overall risk for cancer, infection, cardiovascular disease, delayed fracture healing, or hypocalcemia.
All of the roughly 3,000 women in the long-term extension of the trial took denosumab for up to eight years. Overall, they showed a continued increase in their mean bone mineral density, with a cumulative eight-year gain of 18.4% at the lumbar spine and 8.3% at the total hip, with few fractures and a good safety profile. The tolerability profile of denosumab during this extension phase was consistent with that observed during the initial 3-year FREEDOM trial. At 12 months, denosumab treatment increased bone mineral density (BMD) at the total hip, lumbar spine and/or femoral neck and reduced markers of bone turnover to a significantly greater extent than oral bisphosphonates in women who were essentially bisphosphonate-naive and in those who had switched from alendronate to denosumab treatment.
Medical consultation rates for surgical cases vary
The use of inpatient medical consultations for hospitalized surgical patients was found to vary by hospital, but consultations didn’t appear to have much of an impact on risk-adjusted 30-day mortality rates, a study found.
Rates of medical consultations varied from 50% to 91% among 91,684 patients undergoing colectomy and from 36% to 90% among 339,319 patients undergoing total hip replacements, a retrospective study found.
The variation was most dramatic for patients undergoing colectomy who did not have complications, among whom rates of inpatient medical consultation ranged from 47% to 79% between hospitals, Dr. Lena M. Chen and her associates reported. For patients undergoing colectomy who did have complications, 90%-95% received medical consultations.
Similarly, variation in the use of medical consultation for patients getting total hip replacement was wider for those without complications (36%-87%), compared with patients with complications (89%-94%).
The results highlight the fact that there’s no consensus on when and how to best provide medical consultation for hospitalized surgical patients. "Wide variation in medical consultation use – particularly among patients without complications – suggests that understanding when medical consultations provide value will be important as hospitals seek to increase their efficiency under bundled payments," wrote Dr. Chen of the University of Michigan, Ann Arbor (JAMA Intern. Med. 2014 Aug. 4 [doi:10.1001/jamainternmed.2014.3376]).
She and her associates analyzed Medicare claims data and American Hospital Association data on patients aged 65-99 years who underwent colectomy at 930 hospitals or total hip replacement at 1,589 hospitals in 2007-2010. These are 2 of the top 10 procedures performed on Medicare patients, and total hip replacement is included in the Centers for Medicare & Medicaid Services bundled payment demonstration project, the authors noted.
At least one medical consultant saw 69% of patients undergoing colectomy and 63% of patients getting a total hip replacement. Among patients who got consultations, colectomy patients saw consultants a median of nine times, and hip replacement patients saw consultants a median of three times.
Colectomy patients most often saw general medicine consultants (50%), followed by cardiologists (28%), oncologists (25%), or gastroenterologists (22%). Among patients receiving total hip replacement, 53% had a general medicine consultation, and the most common specialist consultations were for physical medicine and rehabilitation (11%) or cardiology (8%).
Approximately a third of hip replacement patients were "comanaged" by surgeons and medical consultants, defined by records of a claim for evaluation and management by a medicine physician on at least 70% of inpatient days.
It seems logical to assume that extra care from nonsurgical physicians should improve outcomes for some surgical patients, but an exploratory analysis of the data found that risk-adjusted 30-day mortality rates were not significantly different between hospitals with the greatest or least use of medical consultations, Dr. Chen reported. The 30-day mortality rate for colectomy patients was 5% at hospitals in the lowest quintile of medical consultations and 6% at hospitals in the highest quintile. The results for total hip replacement were similar.
Greater use of medical consultation was associated with a significantly greater likelihood of having at least one postoperative complication, affecting 24% of colectomy patients at hospitals in the lowest quintile of consultations and 28% at hospitals in the highest quintile. The results for total hip replacement were similar.
The National Institute of Aging and a University of Michigan McCubed grant funded the study. Dr. Chen reported having no relevant financial disclosures. One of her coinvestigators owns stock in ArborMetrix, a company that analyzes hospital quality and cost efficiency.
On Twitter @sherryboschert
Dr. Chen’s findings that rates of medical consultation varied widely for surgical patients without complications complement a 2010 study by Dr. Gulshan Sharma and his associates that found 35% of patients hospitalized for a common surgical procedure were comanaged by medicine physicians (Arch. Intern. Med. 2010;170:363-8).
"I agree [with Dr. Chen] that understanding the ‘value’ of medical consultation is an important next step, especially in low-risk patients undergoing elective surgery," Dr. Sharma commented in an article accompanying Dr. Chen’s study (JAMA Intern. Med. 2014 Aug. 4 [doi:10.1001/jamainternmed.2014.1499]).
Comanagement may benefit patients by increasing the use of evidence-based treatments or reducing the time to surgery, postoperative complications, the need for ICU care, the length of stay, and readmission rates, among other possibilities. But there are possible downsides, too, including potential confusion among caregivers, more complicated decision making, lack of "ownership" of problems, or added costs, he noted.
Hospitals with the greatest use of medical consultation in Dr. Chen’s study had higher risk-adjusted rates of 30-day mortality and complications, compared with hospitals with the least use of medical consultation (though the difference in mortality was not statistically significant). "Is there a potential harm associated with medical consultation?" Dr. Sharma asked.
"There is no one fit for all" hospitals, he wrote. Institutional data on quality and cost should drive decisions on the routine use of medical consultation. The practice of mandating comanagement of all surgical patients "should be discouraged," Dr. Sharma said. "During preoperative evaluation, patients with comorbid conditions and those at significant risk of postoperative complications should be considered for medical comanagement."
Dr. Sharma is director of the division of pulmonary critical care and sleep medicine at the University of Texas Medical Branch, Galveston. He reported having no relevant financial disclosures.
Dr. Chen’s findings that rates of medical consultation varied widely for surgical patients without complications complement a 2010 study by Dr. Gulshan Sharma and his associates that found 35% of patients hospitalized for a common surgical procedure were comanaged by medicine physicians (Arch. Intern. Med. 2010;170:363-8).
"I agree [with Dr. Chen] that understanding the ‘value’ of medical consultation is an important next step, especially in low-risk patients undergoing elective surgery," Dr. Sharma commented in an article accompanying Dr. Chen’s study (JAMA Intern. Med. 2014 Aug. 4 [doi:10.1001/jamainternmed.2014.1499]).
Comanagement may benefit patients by increasing the use of evidence-based treatments or reducing the time to surgery, postoperative complications, the need for ICU care, the length of stay, and readmission rates, among other possibilities. But there are possible downsides, too, including potential confusion among caregivers, more complicated decision making, lack of "ownership" of problems, or added costs, he noted.
Hospitals with the greatest use of medical consultation in Dr. Chen’s study had higher risk-adjusted rates of 30-day mortality and complications, compared with hospitals with the least use of medical consultation (though the difference in mortality was not statistically significant). "Is there a potential harm associated with medical consultation?" Dr. Sharma asked.
"There is no one fit for all" hospitals, he wrote. Institutional data on quality and cost should drive decisions on the routine use of medical consultation. The practice of mandating comanagement of all surgical patients "should be discouraged," Dr. Sharma said. "During preoperative evaluation, patients with comorbid conditions and those at significant risk of postoperative complications should be considered for medical comanagement."
Dr. Sharma is director of the division of pulmonary critical care and sleep medicine at the University of Texas Medical Branch, Galveston. He reported having no relevant financial disclosures.
Dr. Chen’s findings that rates of medical consultation varied widely for surgical patients without complications complement a 2010 study by Dr. Gulshan Sharma and his associates that found 35% of patients hospitalized for a common surgical procedure were comanaged by medicine physicians (Arch. Intern. Med. 2010;170:363-8).
"I agree [with Dr. Chen] that understanding the ‘value’ of medical consultation is an important next step, especially in low-risk patients undergoing elective surgery," Dr. Sharma commented in an article accompanying Dr. Chen’s study (JAMA Intern. Med. 2014 Aug. 4 [doi:10.1001/jamainternmed.2014.1499]).
Comanagement may benefit patients by increasing the use of evidence-based treatments or reducing the time to surgery, postoperative complications, the need for ICU care, the length of stay, and readmission rates, among other possibilities. But there are possible downsides, too, including potential confusion among caregivers, more complicated decision making, lack of "ownership" of problems, or added costs, he noted.
Hospitals with the greatest use of medical consultation in Dr. Chen’s study had higher risk-adjusted rates of 30-day mortality and complications, compared with hospitals with the least use of medical consultation (though the difference in mortality was not statistically significant). "Is there a potential harm associated with medical consultation?" Dr. Sharma asked.
"There is no one fit for all" hospitals, he wrote. Institutional data on quality and cost should drive decisions on the routine use of medical consultation. The practice of mandating comanagement of all surgical patients "should be discouraged," Dr. Sharma said. "During preoperative evaluation, patients with comorbid conditions and those at significant risk of postoperative complications should be considered for medical comanagement."
Dr. Sharma is director of the division of pulmonary critical care and sleep medicine at the University of Texas Medical Branch, Galveston. He reported having no relevant financial disclosures.
The use of inpatient medical consultations for hospitalized surgical patients was found to vary by hospital, but consultations didn’t appear to have much of an impact on risk-adjusted 30-day mortality rates, a study found.
Rates of medical consultations varied from 50% to 91% among 91,684 patients undergoing colectomy and from 36% to 90% among 339,319 patients undergoing total hip replacements, a retrospective study found.
The variation was most dramatic for patients undergoing colectomy who did not have complications, among whom rates of inpatient medical consultation ranged from 47% to 79% between hospitals, Dr. Lena M. Chen and her associates reported. For patients undergoing colectomy who did have complications, 90%-95% received medical consultations.
Similarly, variation in the use of medical consultation for patients getting total hip replacement was wider for those without complications (36%-87%), compared with patients with complications (89%-94%).
The results highlight the fact that there’s no consensus on when and how to best provide medical consultation for hospitalized surgical patients. "Wide variation in medical consultation use – particularly among patients without complications – suggests that understanding when medical consultations provide value will be important as hospitals seek to increase their efficiency under bundled payments," wrote Dr. Chen of the University of Michigan, Ann Arbor (JAMA Intern. Med. 2014 Aug. 4 [doi:10.1001/jamainternmed.2014.3376]).
She and her associates analyzed Medicare claims data and American Hospital Association data on patients aged 65-99 years who underwent colectomy at 930 hospitals or total hip replacement at 1,589 hospitals in 2007-2010. These are 2 of the top 10 procedures performed on Medicare patients, and total hip replacement is included in the Centers for Medicare & Medicaid Services bundled payment demonstration project, the authors noted.
At least one medical consultant saw 69% of patients undergoing colectomy and 63% of patients getting a total hip replacement. Among patients who got consultations, colectomy patients saw consultants a median of nine times, and hip replacement patients saw consultants a median of three times.
Colectomy patients most often saw general medicine consultants (50%), followed by cardiologists (28%), oncologists (25%), or gastroenterologists (22%). Among patients receiving total hip replacement, 53% had a general medicine consultation, and the most common specialist consultations were for physical medicine and rehabilitation (11%) or cardiology (8%).
Approximately a third of hip replacement patients were "comanaged" by surgeons and medical consultants, defined by records of a claim for evaluation and management by a medicine physician on at least 70% of inpatient days.
It seems logical to assume that extra care from nonsurgical physicians should improve outcomes for some surgical patients, but an exploratory analysis of the data found that risk-adjusted 30-day mortality rates were not significantly different between hospitals with the greatest or least use of medical consultations, Dr. Chen reported. The 30-day mortality rate for colectomy patients was 5% at hospitals in the lowest quintile of medical consultations and 6% at hospitals in the highest quintile. The results for total hip replacement were similar.
Greater use of medical consultation was associated with a significantly greater likelihood of having at least one postoperative complication, affecting 24% of colectomy patients at hospitals in the lowest quintile of consultations and 28% at hospitals in the highest quintile. The results for total hip replacement were similar.
The National Institute of Aging and a University of Michigan McCubed grant funded the study. Dr. Chen reported having no relevant financial disclosures. One of her coinvestigators owns stock in ArborMetrix, a company that analyzes hospital quality and cost efficiency.
On Twitter @sherryboschert
The use of inpatient medical consultations for hospitalized surgical patients was found to vary by hospital, but consultations didn’t appear to have much of an impact on risk-adjusted 30-day mortality rates, a study found.
Rates of medical consultations varied from 50% to 91% among 91,684 patients undergoing colectomy and from 36% to 90% among 339,319 patients undergoing total hip replacements, a retrospective study found.
The variation was most dramatic for patients undergoing colectomy who did not have complications, among whom rates of inpatient medical consultation ranged from 47% to 79% between hospitals, Dr. Lena M. Chen and her associates reported. For patients undergoing colectomy who did have complications, 90%-95% received medical consultations.
Similarly, variation in the use of medical consultation for patients getting total hip replacement was wider for those without complications (36%-87%), compared with patients with complications (89%-94%).
The results highlight the fact that there’s no consensus on when and how to best provide medical consultation for hospitalized surgical patients. "Wide variation in medical consultation use – particularly among patients without complications – suggests that understanding when medical consultations provide value will be important as hospitals seek to increase their efficiency under bundled payments," wrote Dr. Chen of the University of Michigan, Ann Arbor (JAMA Intern. Med. 2014 Aug. 4 [doi:10.1001/jamainternmed.2014.3376]).
She and her associates analyzed Medicare claims data and American Hospital Association data on patients aged 65-99 years who underwent colectomy at 930 hospitals or total hip replacement at 1,589 hospitals in 2007-2010. These are 2 of the top 10 procedures performed on Medicare patients, and total hip replacement is included in the Centers for Medicare & Medicaid Services bundled payment demonstration project, the authors noted.
At least one medical consultant saw 69% of patients undergoing colectomy and 63% of patients getting a total hip replacement. Among patients who got consultations, colectomy patients saw consultants a median of nine times, and hip replacement patients saw consultants a median of three times.
Colectomy patients most often saw general medicine consultants (50%), followed by cardiologists (28%), oncologists (25%), or gastroenterologists (22%). Among patients receiving total hip replacement, 53% had a general medicine consultation, and the most common specialist consultations were for physical medicine and rehabilitation (11%) or cardiology (8%).
Approximately a third of hip replacement patients were "comanaged" by surgeons and medical consultants, defined by records of a claim for evaluation and management by a medicine physician on at least 70% of inpatient days.
It seems logical to assume that extra care from nonsurgical physicians should improve outcomes for some surgical patients, but an exploratory analysis of the data found that risk-adjusted 30-day mortality rates were not significantly different between hospitals with the greatest or least use of medical consultations, Dr. Chen reported. The 30-day mortality rate for colectomy patients was 5% at hospitals in the lowest quintile of medical consultations and 6% at hospitals in the highest quintile. The results for total hip replacement were similar.
Greater use of medical consultation was associated with a significantly greater likelihood of having at least one postoperative complication, affecting 24% of colectomy patients at hospitals in the lowest quintile of consultations and 28% at hospitals in the highest quintile. The results for total hip replacement were similar.
The National Institute of Aging and a University of Michigan McCubed grant funded the study. Dr. Chen reported having no relevant financial disclosures. One of her coinvestigators owns stock in ArborMetrix, a company that analyzes hospital quality and cost efficiency.
On Twitter @sherryboschert
FROM JAMA INTERNAL MEDICINE
Key clinical point: In the era of bundled payments for episodes of care, consider when and how medical consultation for surgical patients is helpful.
Major finding: Use of medical consultations ranged from 50%-91% for colectomies and 36%-90% for total hip replacements.
Data source: A retrospective study of Medicare data on 431,003 older adults undergoing colectomy or total hip replacement in 2007-2010.
Disclosures: Dr. Chen reported having no financial disclosures. One of her associates owns stock in ArborMetrix, a company that analyzes hospital quality and cost efficiency.
MicroRNA Provides New Therapeutic Target for Bone Metastases and Osteoporosis
Researchers have identified miR-34a as a promising molecule that blocks bone destruction, according to a study published online ahead of print June 25 in Nature. Lead study author Yihong Wan, PhD, Assistant Professor of Pharmacology and member of the UT Southwestern Harold C. Simmons Cancer Center, and her research colleagues reported that mice with higher than normal levels of miR-34a had increased bone mass and reduced bone breakdown. According to the researchers, this is because miR-34a blocks osteoclasts, which make the bone less dense and prone to fracture.
“This new finding may lead to the development of miR-34a mimics as a new and better treatment for osteoporosis and cancers that metastasize to the bone,” said Dr. Wan.
Investigators found that injecting nanoparticles containing a mimic, or artificial version of miR-34a, into a mouse with post-menopausal osteoporosis decreased bone loss. miR-34a could also offer protection from bone metastases in a variety of cancers, Dr. Wan noted. Injecting the miR-34a mimic in the mice could prevent the metastasis of skin and breast cancer because it can disarm the metastatic niche in bone.
Study findings also suggest:
• MicroRNAs play important roles in physiology and disease, and present tremendous therapeutic potential.
• miR-34a is downregulated during osteoclast differentiation.
• Osteoclastic miR-34a-overexpressing transgenic mice exhibit lower bone resorption and higher bone mass.
• miR-34a knockout and heterozygous mice exhibit elevated bone resorption and reduced bone mass.
• Ovariectomy-induced osteoporosis, as well as bone metastasis of breast and skin cancers, are diminished in osteoclastic miR-34a transgenic mice, and can be effectively attenuated by miR-34a nanoparticle treatment.
• Transforming growth factor-β-induced factor 2 (Tgif2) as an essential direct miR-34a target that is pro-osteoclastogenic.
• Tgif2 deletion reduces bone resorption and abolishes miR-34a regulation.
Commenting on the study findings Dr. Wan said, “The mouse miR-34a is identical to that in humans, which means that our findings may apply to humans as well.”
Suggested Reading
Krzeszinski JY, Wei W, Huynh H, et al. miR-34a blocks osteoporosis and bone metastasis by inhibiting osteoclastogenesis and Tgif2. Nature. 2014 Jun 25. doi: 10.1038/nature13375. [Epub ahead of print]
Researchers have identified miR-34a as a promising molecule that blocks bone destruction, according to a study published online ahead of print June 25 in Nature. Lead study author Yihong Wan, PhD, Assistant Professor of Pharmacology and member of the UT Southwestern Harold C. Simmons Cancer Center, and her research colleagues reported that mice with higher than normal levels of miR-34a had increased bone mass and reduced bone breakdown. According to the researchers, this is because miR-34a blocks osteoclasts, which make the bone less dense and prone to fracture.
“This new finding may lead to the development of miR-34a mimics as a new and better treatment for osteoporosis and cancers that metastasize to the bone,” said Dr. Wan.
Investigators found that injecting nanoparticles containing a mimic, or artificial version of miR-34a, into a mouse with post-menopausal osteoporosis decreased bone loss. miR-34a could also offer protection from bone metastases in a variety of cancers, Dr. Wan noted. Injecting the miR-34a mimic in the mice could prevent the metastasis of skin and breast cancer because it can disarm the metastatic niche in bone.
Study findings also suggest:
• MicroRNAs play important roles in physiology and disease, and present tremendous therapeutic potential.
• miR-34a is downregulated during osteoclast differentiation.
• Osteoclastic miR-34a-overexpressing transgenic mice exhibit lower bone resorption and higher bone mass.
• miR-34a knockout and heterozygous mice exhibit elevated bone resorption and reduced bone mass.
• Ovariectomy-induced osteoporosis, as well as bone metastasis of breast and skin cancers, are diminished in osteoclastic miR-34a transgenic mice, and can be effectively attenuated by miR-34a nanoparticle treatment.
• Transforming growth factor-β-induced factor 2 (Tgif2) as an essential direct miR-34a target that is pro-osteoclastogenic.
• Tgif2 deletion reduces bone resorption and abolishes miR-34a regulation.
Commenting on the study findings Dr. Wan said, “The mouse miR-34a is identical to that in humans, which means that our findings may apply to humans as well.”
Researchers have identified miR-34a as a promising molecule that blocks bone destruction, according to a study published online ahead of print June 25 in Nature. Lead study author Yihong Wan, PhD, Assistant Professor of Pharmacology and member of the UT Southwestern Harold C. Simmons Cancer Center, and her research colleagues reported that mice with higher than normal levels of miR-34a had increased bone mass and reduced bone breakdown. According to the researchers, this is because miR-34a blocks osteoclasts, which make the bone less dense and prone to fracture.
“This new finding may lead to the development of miR-34a mimics as a new and better treatment for osteoporosis and cancers that metastasize to the bone,” said Dr. Wan.
Investigators found that injecting nanoparticles containing a mimic, or artificial version of miR-34a, into a mouse with post-menopausal osteoporosis decreased bone loss. miR-34a could also offer protection from bone metastases in a variety of cancers, Dr. Wan noted. Injecting the miR-34a mimic in the mice could prevent the metastasis of skin and breast cancer because it can disarm the metastatic niche in bone.
Study findings also suggest:
• MicroRNAs play important roles in physiology and disease, and present tremendous therapeutic potential.
• miR-34a is downregulated during osteoclast differentiation.
• Osteoclastic miR-34a-overexpressing transgenic mice exhibit lower bone resorption and higher bone mass.
• miR-34a knockout and heterozygous mice exhibit elevated bone resorption and reduced bone mass.
• Ovariectomy-induced osteoporosis, as well as bone metastasis of breast and skin cancers, are diminished in osteoclastic miR-34a transgenic mice, and can be effectively attenuated by miR-34a nanoparticle treatment.
• Transforming growth factor-β-induced factor 2 (Tgif2) as an essential direct miR-34a target that is pro-osteoclastogenic.
• Tgif2 deletion reduces bone resorption and abolishes miR-34a regulation.
Commenting on the study findings Dr. Wan said, “The mouse miR-34a is identical to that in humans, which means that our findings may apply to humans as well.”
Suggested Reading
Krzeszinski JY, Wei W, Huynh H, et al. miR-34a blocks osteoporosis and bone metastasis by inhibiting osteoclastogenesis and Tgif2. Nature. 2014 Jun 25. doi: 10.1038/nature13375. [Epub ahead of print]
Suggested Reading
Krzeszinski JY, Wei W, Huynh H, et al. miR-34a blocks osteoporosis and bone metastasis by inhibiting osteoclastogenesis and Tgif2. Nature. 2014 Jun 25. doi: 10.1038/nature13375. [Epub ahead of print]
Glenoid fossa loss can make Bankart shoulder repair less effective
SEATTLE – Arthroscopic Bankart lesion repairs don’t seem to work well in patients who have lost more than 13.5% of their glenoid fossa after dislocating their shoulders; an open inferior capsular shift or Latarjet procedure is likely to be a better bet, according to a review of 72 consecutive soldiers at Tripler Army Medical Center in Honolulu, who had an arthroscopic Bankart repair after shoulder dislocation.
Seven of the 29 patients (24%) who went into the operation with greater levels of bone loss redislocated over an average of about 4 years of follow-up, versus 2 of 37 (5%) who had less than 13.5% of their glenoid fossa missing. When patients who redislocated were excluded, the mean Western Ontario Shoulder Instability (WOSI) score was 43% of normal in the 13.5% or more bone loss group, but about 80% of normal in those who had lost less bone.
In short, bone loss of 13.5% led to "unacceptable clinical outcomes. Patients with bone loss beyond this threshold should be counseled accordingly with consideration for alternative surgical procedures," the investigators concluded.
Surgeons "have to pay a lot more attention to how much bone loss is there. We have traditionally defined the level of bone loss" that triggers an open procedure at 20%. "In today’s world, everybody agrees that 20% is too high, but the" question has been by how much. At 13.5% – judged by preoperative MRI or CT – "two things become clear. They redislocate at too high a level, and they" report too much instability on the WOSI," said lead investigator Dr. John Tokish, now an orthopedic surgeon at the Greenville (S.C.) Health System.
"If you are just evaluating your results based on whether or not the person redislocates, you missed the point. When we evaluate function in these patients with well below 20% bone loss, they have pain and apprehension. Even if their shoulders don’t come out again, these patients are self-limiting," he said.
When arthroscopic Bankart repair is ruled out, Dr. Tokish cautioned, it "doesn’t necessarily mean we should jump right away to a Latarjet," in which the tip of the coracoid process is repositioned to increase glenoid surface area. "Some would argue that a Latarjet is too big a step. An open inferior capsular shift" may be enough, or even superior.
There were 73 operated shoulders in the 72 patients, 68 of whom were men. The average age at surgery was 26.3 years. Glenoid bone loss was calculated by overlaying a circle onto preop images of the fossa. Patients were excluded if they had a previous shoulder operation.
Dr. Tokish had no disclosures. The work was funded internally.
SEATTLE – Arthroscopic Bankart lesion repairs don’t seem to work well in patients who have lost more than 13.5% of their glenoid fossa after dislocating their shoulders; an open inferior capsular shift or Latarjet procedure is likely to be a better bet, according to a review of 72 consecutive soldiers at Tripler Army Medical Center in Honolulu, who had an arthroscopic Bankart repair after shoulder dislocation.
Seven of the 29 patients (24%) who went into the operation with greater levels of bone loss redislocated over an average of about 4 years of follow-up, versus 2 of 37 (5%) who had less than 13.5% of their glenoid fossa missing. When patients who redislocated were excluded, the mean Western Ontario Shoulder Instability (WOSI) score was 43% of normal in the 13.5% or more bone loss group, but about 80% of normal in those who had lost less bone.
In short, bone loss of 13.5% led to "unacceptable clinical outcomes. Patients with bone loss beyond this threshold should be counseled accordingly with consideration for alternative surgical procedures," the investigators concluded.
Surgeons "have to pay a lot more attention to how much bone loss is there. We have traditionally defined the level of bone loss" that triggers an open procedure at 20%. "In today’s world, everybody agrees that 20% is too high, but the" question has been by how much. At 13.5% – judged by preoperative MRI or CT – "two things become clear. They redislocate at too high a level, and they" report too much instability on the WOSI," said lead investigator Dr. John Tokish, now an orthopedic surgeon at the Greenville (S.C.) Health System.
"If you are just evaluating your results based on whether or not the person redislocates, you missed the point. When we evaluate function in these patients with well below 20% bone loss, they have pain and apprehension. Even if their shoulders don’t come out again, these patients are self-limiting," he said.
When arthroscopic Bankart repair is ruled out, Dr. Tokish cautioned, it "doesn’t necessarily mean we should jump right away to a Latarjet," in which the tip of the coracoid process is repositioned to increase glenoid surface area. "Some would argue that a Latarjet is too big a step. An open inferior capsular shift" may be enough, or even superior.
There were 73 operated shoulders in the 72 patients, 68 of whom were men. The average age at surgery was 26.3 years. Glenoid bone loss was calculated by overlaying a circle onto preop images of the fossa. Patients were excluded if they had a previous shoulder operation.
Dr. Tokish had no disclosures. The work was funded internally.
SEATTLE – Arthroscopic Bankart lesion repairs don’t seem to work well in patients who have lost more than 13.5% of their glenoid fossa after dislocating their shoulders; an open inferior capsular shift or Latarjet procedure is likely to be a better bet, according to a review of 72 consecutive soldiers at Tripler Army Medical Center in Honolulu, who had an arthroscopic Bankart repair after shoulder dislocation.
Seven of the 29 patients (24%) who went into the operation with greater levels of bone loss redislocated over an average of about 4 years of follow-up, versus 2 of 37 (5%) who had less than 13.5% of their glenoid fossa missing. When patients who redislocated were excluded, the mean Western Ontario Shoulder Instability (WOSI) score was 43% of normal in the 13.5% or more bone loss group, but about 80% of normal in those who had lost less bone.
In short, bone loss of 13.5% led to "unacceptable clinical outcomes. Patients with bone loss beyond this threshold should be counseled accordingly with consideration for alternative surgical procedures," the investigators concluded.
Surgeons "have to pay a lot more attention to how much bone loss is there. We have traditionally defined the level of bone loss" that triggers an open procedure at 20%. "In today’s world, everybody agrees that 20% is too high, but the" question has been by how much. At 13.5% – judged by preoperative MRI or CT – "two things become clear. They redislocate at too high a level, and they" report too much instability on the WOSI," said lead investigator Dr. John Tokish, now an orthopedic surgeon at the Greenville (S.C.) Health System.
"If you are just evaluating your results based on whether or not the person redislocates, you missed the point. When we evaluate function in these patients with well below 20% bone loss, they have pain and apprehension. Even if their shoulders don’t come out again, these patients are self-limiting," he said.
When arthroscopic Bankart repair is ruled out, Dr. Tokish cautioned, it "doesn’t necessarily mean we should jump right away to a Latarjet," in which the tip of the coracoid process is repositioned to increase glenoid surface area. "Some would argue that a Latarjet is too big a step. An open inferior capsular shift" may be enough, or even superior.
There were 73 operated shoulders in the 72 patients, 68 of whom were men. The average age at surgery was 26.3 years. Glenoid bone loss was calculated by overlaying a circle onto preop images of the fossa. Patients were excluded if they had a previous shoulder operation.
Dr. Tokish had no disclosures. The work was funded internally.
AT AOSSM 2014
Key clinical point: When dislocated shoulders need to be fixed surgically, pick an open procedure if more than 13.5% of the glenoid fossa has been destroyed.
Major finding: About a quarter of patients will redislocate if they have an arthroscopic Bankart lesion repair with more than 13.5% of the glenoid fossa missing; at 4 years, their Western Ontario Shoulder Instability scores will be 43% of normal.
Data source: Retrospective study of 72 consecutive cases.
Disclosures: Dr. Tokish had no disclosures. The work was funded internally.
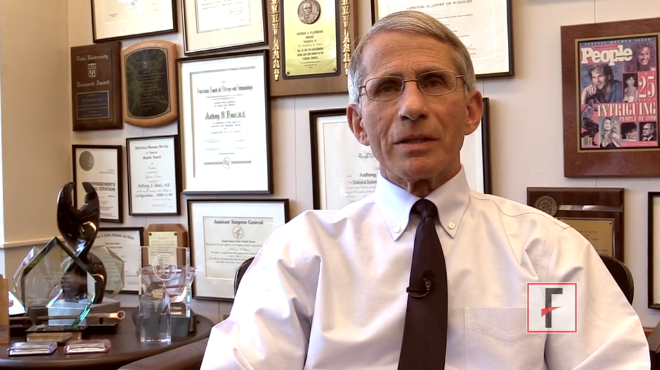
VIDEO: Dr. Fauci: What you need to know about chikungunya
The Centers for Disease Control and Prevention on July 17 reported the first two cases in the United States of locally acquired chikungunya –but the announcement wasn’t a big surprise to researchers who follow the patterns of emerging and reemerging diseases.
In an article in the New England Journal of Medicine, Dr. Anthony S. Fauci, director of the National Institute of Allergy and Infectious Diseases, predicted the arrival of the mosquito-borne illness in the United States just 2 days before the CDC announcement.
In a video interview in his office at NIAID, Dr. Fauci talks about the epidemiology and pathogenesis of the disease and shares his advice on diagnosis and treatment.
On Twitter @naseemmiller
The Centers for Disease Control and Prevention on July 17 reported the first two cases in the United States of locally acquired chikungunya –but the announcement wasn’t a big surprise to researchers who follow the patterns of emerging and reemerging diseases.
In an article in the New England Journal of Medicine, Dr. Anthony S. Fauci, director of the National Institute of Allergy and Infectious Diseases, predicted the arrival of the mosquito-borne illness in the United States just 2 days before the CDC announcement.
In a video interview in his office at NIAID, Dr. Fauci talks about the epidemiology and pathogenesis of the disease and shares his advice on diagnosis and treatment.
On Twitter @naseemmiller
The Centers for Disease Control and Prevention on July 17 reported the first two cases in the United States of locally acquired chikungunya –but the announcement wasn’t a big surprise to researchers who follow the patterns of emerging and reemerging diseases.
In an article in the New England Journal of Medicine, Dr. Anthony S. Fauci, director of the National Institute of Allergy and Infectious Diseases, predicted the arrival of the mosquito-borne illness in the United States just 2 days before the CDC announcement.
In a video interview in his office at NIAID, Dr. Fauci talks about the epidemiology and pathogenesis of the disease and shares his advice on diagnosis and treatment.
On Twitter @naseemmiller