User login
Biosimilar infliximab gains FDA Advisory Committee endorsement
A biosimilar agent to Remicade, the brand-name and reference form of infliximab, stayed on track to become the second biosimilar drug to enter the U.S. market when the Arthritis Advisory Committee of the Food and Drug Administration voted overwhelmingly in favor of licensure of the biosimilar at a meeting on Feb. 9.
The vote was 21 in favor and 3 against, with no abstentions.
Because of the way the FDA staff worded the question that the Advisory Committee voted on, the panel not only was in favor of approving biosimilar licensure but also recommended that license for six of the seven diverse indications that Remicade currently has: treatment of rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, plaque psoriasis, adult and pediatric Crohn’s disease, and adult ulcerative colitis. The panel did not vote on licensing the biosimilar for treatment of pediatric ulcerative colitis because that specific indication for Remicade remains on patent for a few more years.
The broad range of indications for which the Committee recommended approval was notable because the formulation of biosimilar infliximab under review, manufactured by Celltrion and known in the United States as CT-P13, had been clinically studied only in patients with rheumatoid arthritis or ankylosing spondylitis. The other four recommended indications represented extrapolations, based on the totality of biosimilar evidence presented at the meeting by both Celltrion staffers and consultants as well as analyses presented by FDA staff members.
The overall thrust of the extrapolation issue was that if biosimilarity to Remicade was proven by a range of preclinical and clinical testing, and if safety and efficacy similar to Remicade was shown in trials that enrolled only patients with rheumatoid arthritis or ankylosing spondylitis, then the safety and efficacy previously proven for Remicade for the other indications could be reasonably extrapolated to apply to CT-P13 also, even though CT-P13 was never tested on patients with those conditions. This turned out to often be the key issue that panel members grappled with as they decided whether to vote in favor of the question the FDA asked them to address.
“Many of us are uncomfortable with this new pathway” of extrapolation, said panel member Dr. Beth L. Jonas, a rheumatologist at the University of North Carolina at Chapel Hill.
“I feel we’re taking a risk” with the extrapolations, said Dr. Mary E. Maloney, professor of medicine and chief of dermatology at the University of Massachusetts in Worcester. “We have a responsibility to take a risk to provide biosimilars to patients and to reduce their cost” for needed treatments, she said during the Committee’s discussion of their votes.
“Biosimilar is a new concept, but it’s the future of how we will look at drugs,” explained panel member Dr. Wilma Bergfeld, professor of dermatology at the Cleveland Clinic.
CT-P13 is currently marketed in many other countries worldwide under the brand names Remsima or Inflectra.
The FDA’s staff was clearly behind this application. After summarizing the agency’s internal analysis of the data submitted by Celltrion, Dr. Nikolay Nikolov, clinical team leader for the FDA’s Division of Pulmonary, Allergy and Rheumatology Products, concluded that “the totality of evidence provided by the applicant supports a conclusion that CT-P13 is biosimilar to U.S.-licensed Remicade,” and that “scientific justification for extrapolating the clinical data supports a finding of biosimilarity for all indications for which U.S.-licensed Remicade is licensed.” The FDA’s position makes it seem very likely that the agency will accept the Advisory Committee’s vote and grant CT-P13 license for U.S. marketing in the near future.
CT-P13 also received support during the public comment period of the Committee’s deliberations. At that time, Dr. Gideon P. Smith, a dermatologist at Massachusetts General Hospital in Boston spoke on behalf of the American Academy of Dermatology Association. “Biologics are some of the most important recent developments in treating plaque psoriasis, but cost is an important issue. We hope that biosimilars will decrease the cost of this treatment,” Dr. Smith said. “Infliximab is a complex molecule with a complex production process. We are concerned about the safety and efficacy of treatment. The AADA supports approval based on reducing cost and improving patient access. However, we strongly recommend caution through long-term postmarketing surveillance and using registry data to identify issues of immunogenicity, efficacy, and safety that were not seen in the clinical trials.”
The drug also received support from Dr. Angus B. Worthing, who represented the American College of Rheumatology. “Biosimilars may be the only tool to keep prices of biologics within reason,” said Dr. Worthing, a rheumatologist in Washington. But he also stressed that “extrapolation should be done with caution and not routinely granted.”
CT-P13 has the potential to make a fairly widely used biologic significantly more affordable. In countries where it has come onto the market, it’s been priced at roughly 30% below the prevailing cost of Remicade prior to this competition.
“Infliximab is an extremely important tool in our armamentarium for treatment of both ulcerative colitis and Crohn’s disease,” commented Dr. Stephen B. Hanauer, professor of gastroenterology and hepatology at Northwestern University in Chicago. “Biologic therapies account for an increasing proportion of health care costs for chronic diseases such as inflammatory bowel disease and reducing these costs will be important as increasing numbers of patients are benefiting from long-term biologic therapies. Having reviewed the extensive preclinical and clinical data with CT-P13, I am comfortable with potential substitution or switching as long as physicians are aware of the change and can track any potential reactions to the administered product,” he said in an interview.
“Infliximab is currently used by U.S. rheumatologists to treat certain patients with rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis. It is not the most-widely used tumor necrosis factor inhibitor, which is adalimumab, but it is often used. After FDA approval, biosimilar infliximab is anticipated to be priced lower than Remicade and that would likely increase use of infliximab for rheumatologic conditions,” said Dr. Jonathan Kay, a rheumatologist and professor of medicine at the University of Massachusetts in Worcester. “The clinical experience with CT-P13 in trials and in routine use in other countries show no significant loss of efficacy or any other major problem when changing patients from Remicade to CT-P13. All the data suggest that CT-P13 is highly similar to the reference product. It’s almost akin to comparing one lot of Remicade to another lot of Remicade. I personally would not have a problem initiating a patient on CT-P13 if infliximab was the appropriate drug to use,” Dr. Kay said in an interview.
Dr. Hanauer has been a consultant to Celltrion. Dr. Kay has been a consultant to several drug companies.
On Twitter @mitchelzoler
A biosimilar agent to Remicade, the brand-name and reference form of infliximab, stayed on track to become the second biosimilar drug to enter the U.S. market when the Arthritis Advisory Committee of the Food and Drug Administration voted overwhelmingly in favor of licensure of the biosimilar at a meeting on Feb. 9.
The vote was 21 in favor and 3 against, with no abstentions.
Because of the way the FDA staff worded the question that the Advisory Committee voted on, the panel not only was in favor of approving biosimilar licensure but also recommended that license for six of the seven diverse indications that Remicade currently has: treatment of rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, plaque psoriasis, adult and pediatric Crohn’s disease, and adult ulcerative colitis. The panel did not vote on licensing the biosimilar for treatment of pediatric ulcerative colitis because that specific indication for Remicade remains on patent for a few more years.
The broad range of indications for which the Committee recommended approval was notable because the formulation of biosimilar infliximab under review, manufactured by Celltrion and known in the United States as CT-P13, had been clinically studied only in patients with rheumatoid arthritis or ankylosing spondylitis. The other four recommended indications represented extrapolations, based on the totality of biosimilar evidence presented at the meeting by both Celltrion staffers and consultants as well as analyses presented by FDA staff members.
The overall thrust of the extrapolation issue was that if biosimilarity to Remicade was proven by a range of preclinical and clinical testing, and if safety and efficacy similar to Remicade was shown in trials that enrolled only patients with rheumatoid arthritis or ankylosing spondylitis, then the safety and efficacy previously proven for Remicade for the other indications could be reasonably extrapolated to apply to CT-P13 also, even though CT-P13 was never tested on patients with those conditions. This turned out to often be the key issue that panel members grappled with as they decided whether to vote in favor of the question the FDA asked them to address.
“Many of us are uncomfortable with this new pathway” of extrapolation, said panel member Dr. Beth L. Jonas, a rheumatologist at the University of North Carolina at Chapel Hill.
“I feel we’re taking a risk” with the extrapolations, said Dr. Mary E. Maloney, professor of medicine and chief of dermatology at the University of Massachusetts in Worcester. “We have a responsibility to take a risk to provide biosimilars to patients and to reduce their cost” for needed treatments, she said during the Committee’s discussion of their votes.
“Biosimilar is a new concept, but it’s the future of how we will look at drugs,” explained panel member Dr. Wilma Bergfeld, professor of dermatology at the Cleveland Clinic.
CT-P13 is currently marketed in many other countries worldwide under the brand names Remsima or Inflectra.
The FDA’s staff was clearly behind this application. After summarizing the agency’s internal analysis of the data submitted by Celltrion, Dr. Nikolay Nikolov, clinical team leader for the FDA’s Division of Pulmonary, Allergy and Rheumatology Products, concluded that “the totality of evidence provided by the applicant supports a conclusion that CT-P13 is biosimilar to U.S.-licensed Remicade,” and that “scientific justification for extrapolating the clinical data supports a finding of biosimilarity for all indications for which U.S.-licensed Remicade is licensed.” The FDA’s position makes it seem very likely that the agency will accept the Advisory Committee’s vote and grant CT-P13 license for U.S. marketing in the near future.
CT-P13 also received support during the public comment period of the Committee’s deliberations. At that time, Dr. Gideon P. Smith, a dermatologist at Massachusetts General Hospital in Boston spoke on behalf of the American Academy of Dermatology Association. “Biologics are some of the most important recent developments in treating plaque psoriasis, but cost is an important issue. We hope that biosimilars will decrease the cost of this treatment,” Dr. Smith said. “Infliximab is a complex molecule with a complex production process. We are concerned about the safety and efficacy of treatment. The AADA supports approval based on reducing cost and improving patient access. However, we strongly recommend caution through long-term postmarketing surveillance and using registry data to identify issues of immunogenicity, efficacy, and safety that were not seen in the clinical trials.”
The drug also received support from Dr. Angus B. Worthing, who represented the American College of Rheumatology. “Biosimilars may be the only tool to keep prices of biologics within reason,” said Dr. Worthing, a rheumatologist in Washington. But he also stressed that “extrapolation should be done with caution and not routinely granted.”
CT-P13 has the potential to make a fairly widely used biologic significantly more affordable. In countries where it has come onto the market, it’s been priced at roughly 30% below the prevailing cost of Remicade prior to this competition.
“Infliximab is an extremely important tool in our armamentarium for treatment of both ulcerative colitis and Crohn’s disease,” commented Dr. Stephen B. Hanauer, professor of gastroenterology and hepatology at Northwestern University in Chicago. “Biologic therapies account for an increasing proportion of health care costs for chronic diseases such as inflammatory bowel disease and reducing these costs will be important as increasing numbers of patients are benefiting from long-term biologic therapies. Having reviewed the extensive preclinical and clinical data with CT-P13, I am comfortable with potential substitution or switching as long as physicians are aware of the change and can track any potential reactions to the administered product,” he said in an interview.
“Infliximab is currently used by U.S. rheumatologists to treat certain patients with rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis. It is not the most-widely used tumor necrosis factor inhibitor, which is adalimumab, but it is often used. After FDA approval, biosimilar infliximab is anticipated to be priced lower than Remicade and that would likely increase use of infliximab for rheumatologic conditions,” said Dr. Jonathan Kay, a rheumatologist and professor of medicine at the University of Massachusetts in Worcester. “The clinical experience with CT-P13 in trials and in routine use in other countries show no significant loss of efficacy or any other major problem when changing patients from Remicade to CT-P13. All the data suggest that CT-P13 is highly similar to the reference product. It’s almost akin to comparing one lot of Remicade to another lot of Remicade. I personally would not have a problem initiating a patient on CT-P13 if infliximab was the appropriate drug to use,” Dr. Kay said in an interview.
Dr. Hanauer has been a consultant to Celltrion. Dr. Kay has been a consultant to several drug companies.
On Twitter @mitchelzoler
A biosimilar agent to Remicade, the brand-name and reference form of infliximab, stayed on track to become the second biosimilar drug to enter the U.S. market when the Arthritis Advisory Committee of the Food and Drug Administration voted overwhelmingly in favor of licensure of the biosimilar at a meeting on Feb. 9.
The vote was 21 in favor and 3 against, with no abstentions.
Because of the way the FDA staff worded the question that the Advisory Committee voted on, the panel not only was in favor of approving biosimilar licensure but also recommended that license for six of the seven diverse indications that Remicade currently has: treatment of rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, plaque psoriasis, adult and pediatric Crohn’s disease, and adult ulcerative colitis. The panel did not vote on licensing the biosimilar for treatment of pediatric ulcerative colitis because that specific indication for Remicade remains on patent for a few more years.
The broad range of indications for which the Committee recommended approval was notable because the formulation of biosimilar infliximab under review, manufactured by Celltrion and known in the United States as CT-P13, had been clinically studied only in patients with rheumatoid arthritis or ankylosing spondylitis. The other four recommended indications represented extrapolations, based on the totality of biosimilar evidence presented at the meeting by both Celltrion staffers and consultants as well as analyses presented by FDA staff members.
The overall thrust of the extrapolation issue was that if biosimilarity to Remicade was proven by a range of preclinical and clinical testing, and if safety and efficacy similar to Remicade was shown in trials that enrolled only patients with rheumatoid arthritis or ankylosing spondylitis, then the safety and efficacy previously proven for Remicade for the other indications could be reasonably extrapolated to apply to CT-P13 also, even though CT-P13 was never tested on patients with those conditions. This turned out to often be the key issue that panel members grappled with as they decided whether to vote in favor of the question the FDA asked them to address.
“Many of us are uncomfortable with this new pathway” of extrapolation, said panel member Dr. Beth L. Jonas, a rheumatologist at the University of North Carolina at Chapel Hill.
“I feel we’re taking a risk” with the extrapolations, said Dr. Mary E. Maloney, professor of medicine and chief of dermatology at the University of Massachusetts in Worcester. “We have a responsibility to take a risk to provide biosimilars to patients and to reduce their cost” for needed treatments, she said during the Committee’s discussion of their votes.
“Biosimilar is a new concept, but it’s the future of how we will look at drugs,” explained panel member Dr. Wilma Bergfeld, professor of dermatology at the Cleveland Clinic.
CT-P13 is currently marketed in many other countries worldwide under the brand names Remsima or Inflectra.
The FDA’s staff was clearly behind this application. After summarizing the agency’s internal analysis of the data submitted by Celltrion, Dr. Nikolay Nikolov, clinical team leader for the FDA’s Division of Pulmonary, Allergy and Rheumatology Products, concluded that “the totality of evidence provided by the applicant supports a conclusion that CT-P13 is biosimilar to U.S.-licensed Remicade,” and that “scientific justification for extrapolating the clinical data supports a finding of biosimilarity for all indications for which U.S.-licensed Remicade is licensed.” The FDA’s position makes it seem very likely that the agency will accept the Advisory Committee’s vote and grant CT-P13 license for U.S. marketing in the near future.
CT-P13 also received support during the public comment period of the Committee’s deliberations. At that time, Dr. Gideon P. Smith, a dermatologist at Massachusetts General Hospital in Boston spoke on behalf of the American Academy of Dermatology Association. “Biologics are some of the most important recent developments in treating plaque psoriasis, but cost is an important issue. We hope that biosimilars will decrease the cost of this treatment,” Dr. Smith said. “Infliximab is a complex molecule with a complex production process. We are concerned about the safety and efficacy of treatment. The AADA supports approval based on reducing cost and improving patient access. However, we strongly recommend caution through long-term postmarketing surveillance and using registry data to identify issues of immunogenicity, efficacy, and safety that were not seen in the clinical trials.”
The drug also received support from Dr. Angus B. Worthing, who represented the American College of Rheumatology. “Biosimilars may be the only tool to keep prices of biologics within reason,” said Dr. Worthing, a rheumatologist in Washington. But he also stressed that “extrapolation should be done with caution and not routinely granted.”
CT-P13 has the potential to make a fairly widely used biologic significantly more affordable. In countries where it has come onto the market, it’s been priced at roughly 30% below the prevailing cost of Remicade prior to this competition.
“Infliximab is an extremely important tool in our armamentarium for treatment of both ulcerative colitis and Crohn’s disease,” commented Dr. Stephen B. Hanauer, professor of gastroenterology and hepatology at Northwestern University in Chicago. “Biologic therapies account for an increasing proportion of health care costs for chronic diseases such as inflammatory bowel disease and reducing these costs will be important as increasing numbers of patients are benefiting from long-term biologic therapies. Having reviewed the extensive preclinical and clinical data with CT-P13, I am comfortable with potential substitution or switching as long as physicians are aware of the change and can track any potential reactions to the administered product,” he said in an interview.
“Infliximab is currently used by U.S. rheumatologists to treat certain patients with rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis. It is not the most-widely used tumor necrosis factor inhibitor, which is adalimumab, but it is often used. After FDA approval, biosimilar infliximab is anticipated to be priced lower than Remicade and that would likely increase use of infliximab for rheumatologic conditions,” said Dr. Jonathan Kay, a rheumatologist and professor of medicine at the University of Massachusetts in Worcester. “The clinical experience with CT-P13 in trials and in routine use in other countries show no significant loss of efficacy or any other major problem when changing patients from Remicade to CT-P13. All the data suggest that CT-P13 is highly similar to the reference product. It’s almost akin to comparing one lot of Remicade to another lot of Remicade. I personally would not have a problem initiating a patient on CT-P13 if infliximab was the appropriate drug to use,” Dr. Kay said in an interview.
Dr. Hanauer has been a consultant to Celltrion. Dr. Kay has been a consultant to several drug companies.
On Twitter @mitchelzoler
SCCA2: Potential biomarker for psoriasis severity and treatment efficacy
The level of serum squamous cell carcinoma antigen 2 – an isoform of SCCA that is widely used as a tumor marker for SCC – was significantly higher in both skin and serum of patients with psoriasis, compared with healthy volunteers in a recent study, correlating with psoriasis severity score and reflecting treatment efficacy.
The intensity of skin and serum levels of SCCA2 was correlated in patients with psoriasis, and the study results also suggest that Th17 cytokines (IL-17 and IL-22) induce SCCA 2 elevation in serum and skin. “Significant elevation of SCCA2 is associated with disease severity and reflects treatment efficacy. SCCA2 may be a useful biomarker in psoriasis, reflecting Th17-type inflammation – the main determinant of the severity of psoriasis,” wrote Dr. Yuko Watanabe of Yokohama (Japan) City University and associates (Br J Derm. 2016 Jan 29. doi: 10.1111/bjd.14426).
According to the investigators, the commonly used psoriasis area severity index (PASI) is suboptimal because it is not truly quantitative and varies among clinicians. Since there are several new treatment options for psoriasis, including biologics, the authors believe that a new serum marker for psoriasis is needed to evaluate disease activity and manage treatment.
The prospective, cross-sectional study included 123 patients with psoriasis and 25 healthy controls. Serum SCCA2 levels were significantly higher in patients with psoriasis, compared with controls: a median of 2.7 ng/mL versus 0.70 ng/mL, respectively (P <.0001). Serum SCCA2 levels were positively correlated with PASI for all patients with psoriasis, regardless of subtype. In 38 patients on monotherapy or combination therapy with drugs to treat psoriasis, SCCA2 levels decreased in the 35 patients whose PASI improved on treatment (P <.0001) and increased in the three cases of clinical deterioration.
The study was supported by a grant from Japan’s Ministry of Education, Culture, Sports, Science and Technology. The investigators declared that they had no conflicts of interest.
The level of serum squamous cell carcinoma antigen 2 – an isoform of SCCA that is widely used as a tumor marker for SCC – was significantly higher in both skin and serum of patients with psoriasis, compared with healthy volunteers in a recent study, correlating with psoriasis severity score and reflecting treatment efficacy.
The intensity of skin and serum levels of SCCA2 was correlated in patients with psoriasis, and the study results also suggest that Th17 cytokines (IL-17 and IL-22) induce SCCA 2 elevation in serum and skin. “Significant elevation of SCCA2 is associated with disease severity and reflects treatment efficacy. SCCA2 may be a useful biomarker in psoriasis, reflecting Th17-type inflammation – the main determinant of the severity of psoriasis,” wrote Dr. Yuko Watanabe of Yokohama (Japan) City University and associates (Br J Derm. 2016 Jan 29. doi: 10.1111/bjd.14426).
According to the investigators, the commonly used psoriasis area severity index (PASI) is suboptimal because it is not truly quantitative and varies among clinicians. Since there are several new treatment options for psoriasis, including biologics, the authors believe that a new serum marker for psoriasis is needed to evaluate disease activity and manage treatment.
The prospective, cross-sectional study included 123 patients with psoriasis and 25 healthy controls. Serum SCCA2 levels were significantly higher in patients with psoriasis, compared with controls: a median of 2.7 ng/mL versus 0.70 ng/mL, respectively (P <.0001). Serum SCCA2 levels were positively correlated with PASI for all patients with psoriasis, regardless of subtype. In 38 patients on monotherapy or combination therapy with drugs to treat psoriasis, SCCA2 levels decreased in the 35 patients whose PASI improved on treatment (P <.0001) and increased in the three cases of clinical deterioration.
The study was supported by a grant from Japan’s Ministry of Education, Culture, Sports, Science and Technology. The investigators declared that they had no conflicts of interest.
The level of serum squamous cell carcinoma antigen 2 – an isoform of SCCA that is widely used as a tumor marker for SCC – was significantly higher in both skin and serum of patients with psoriasis, compared with healthy volunteers in a recent study, correlating with psoriasis severity score and reflecting treatment efficacy.
The intensity of skin and serum levels of SCCA2 was correlated in patients with psoriasis, and the study results also suggest that Th17 cytokines (IL-17 and IL-22) induce SCCA 2 elevation in serum and skin. “Significant elevation of SCCA2 is associated with disease severity and reflects treatment efficacy. SCCA2 may be a useful biomarker in psoriasis, reflecting Th17-type inflammation – the main determinant of the severity of psoriasis,” wrote Dr. Yuko Watanabe of Yokohama (Japan) City University and associates (Br J Derm. 2016 Jan 29. doi: 10.1111/bjd.14426).
According to the investigators, the commonly used psoriasis area severity index (PASI) is suboptimal because it is not truly quantitative and varies among clinicians. Since there are several new treatment options for psoriasis, including biologics, the authors believe that a new serum marker for psoriasis is needed to evaluate disease activity and manage treatment.
The prospective, cross-sectional study included 123 patients with psoriasis and 25 healthy controls. Serum SCCA2 levels were significantly higher in patients with psoriasis, compared with controls: a median of 2.7 ng/mL versus 0.70 ng/mL, respectively (P <.0001). Serum SCCA2 levels were positively correlated with PASI for all patients with psoriasis, regardless of subtype. In 38 patients on monotherapy or combination therapy with drugs to treat psoriasis, SCCA2 levels decreased in the 35 patients whose PASI improved on treatment (P <.0001) and increased in the three cases of clinical deterioration.
The study was supported by a grant from Japan’s Ministry of Education, Culture, Sports, Science and Technology. The investigators declared that they had no conflicts of interest.
FROM THE BRITISH JOURNAL OF DERMATOLOGY
VIDEO: Humor, psychology turn noncompliance into better outcomes
GRAND CAYMAN – “Why say ‘noncompliant patient’? It’s redundant!”
That’s what Dr. Steven R. Feldman jokingly told an audience at this year’s Caribbean Dermatology Symposium, provided by the Global Academy for Medical Education.
In this video interview, Dr. Feldman, the director of the Psoriasis Treatment Center at Wake Forest University, Winston-Salem, N.C., recounts anecdotes that led him to understand what it takes to get patients to comply with treatment, also shares his tips for getting patients to take a more active role in healing what ails them, whether it be psoriasis or any other illness.
Global Academy and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
GRAND CAYMAN – “Why say ‘noncompliant patient’? It’s redundant!”
That’s what Dr. Steven R. Feldman jokingly told an audience at this year’s Caribbean Dermatology Symposium, provided by the Global Academy for Medical Education.
In this video interview, Dr. Feldman, the director of the Psoriasis Treatment Center at Wake Forest University, Winston-Salem, N.C., recounts anecdotes that led him to understand what it takes to get patients to comply with treatment, also shares his tips for getting patients to take a more active role in healing what ails them, whether it be psoriasis or any other illness.
Global Academy and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
GRAND CAYMAN – “Why say ‘noncompliant patient’? It’s redundant!”
That’s what Dr. Steven R. Feldman jokingly told an audience at this year’s Caribbean Dermatology Symposium, provided by the Global Academy for Medical Education.
In this video interview, Dr. Feldman, the director of the Psoriasis Treatment Center at Wake Forest University, Winston-Salem, N.C., recounts anecdotes that led him to understand what it takes to get patients to comply with treatment, also shares his tips for getting patients to take a more active role in healing what ails them, whether it be psoriasis or any other illness.
Global Academy and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
AT THE CARIBBEAN DERMATOLOGY SYMPOSIUM
VIDEO: Ken Gordon’s pro tips on using biologics in psoriasis
GRAND CAYMAN – When considering the use of biologic therapy for psoriasis patients who are at greater risk of cancer or of serious infection, Dr. Kenneth B. Gordon advises clinicians to “look at the patient in front of you” and the impact the disease is having on them.
In an interview at the annual Caribbean Dermatology Symposium, Dr. Gordon, professor of dermatology at Northwestern University, Chicago, discusses the use of biologics to treat psoriasis in patients with a history of cancer, patients at an increased risk for serious infections (such as those with chronic renal disease or diabetes), as well as patients with HIV, who can have significant psoriasis.
He also provides some recommendations on counseling patients and discusses the use of biologics in children with psoriasis.
The meeting is provided by Global Academy for Medical Education. Global Academy and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
This article was updated 1/31/2016.
GRAND CAYMAN – When considering the use of biologic therapy for psoriasis patients who are at greater risk of cancer or of serious infection, Dr. Kenneth B. Gordon advises clinicians to “look at the patient in front of you” and the impact the disease is having on them.
In an interview at the annual Caribbean Dermatology Symposium, Dr. Gordon, professor of dermatology at Northwestern University, Chicago, discusses the use of biologics to treat psoriasis in patients with a history of cancer, patients at an increased risk for serious infections (such as those with chronic renal disease or diabetes), as well as patients with HIV, who can have significant psoriasis.
He also provides some recommendations on counseling patients and discusses the use of biologics in children with psoriasis.
The meeting is provided by Global Academy for Medical Education. Global Academy and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
This article was updated 1/31/2016.
GRAND CAYMAN – When considering the use of biologic therapy for psoriasis patients who are at greater risk of cancer or of serious infection, Dr. Kenneth B. Gordon advises clinicians to “look at the patient in front of you” and the impact the disease is having on them.
In an interview at the annual Caribbean Dermatology Symposium, Dr. Gordon, professor of dermatology at Northwestern University, Chicago, discusses the use of biologics to treat psoriasis in patients with a history of cancer, patients at an increased risk for serious infections (such as those with chronic renal disease or diabetes), as well as patients with HIV, who can have significant psoriasis.
He also provides some recommendations on counseling patients and discusses the use of biologics in children with psoriasis.
The meeting is provided by Global Academy for Medical Education. Global Academy and this news organization are owned by the same parent company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
This article was updated 1/31/2016.
AT THE CARIBBEAN DERMATOLOGY SYMPOSIUM
Step therapy and biologics: An easier road ahead?
Laws recently passed or under consideration in state legislatures may offer some relief to physicians and patients dogged by the “step” or “fail-first” therapy protocols mandated by insurers, but until better clinical evidence is available to support treatment decisions and biosimilars reduce costs, clinicians must strategize to get patients through the step pathways as fast as possible.
Rheumatologists, gastroenterologists, and dermatologists all confront fail-first policies in their practices, particularly when prescribing the biologic agents that have been game changers in treating rheumatoid arthritis (RA), inflammatory bowel disease (IBD), and psoriasis, among other diseases.
In RA, for example, a patient might be required to fail a series of disease-modifying antirheumatic drugs (DMARDs), including methotrexate, before starting a biologic. In Crohn’s disease, patients might have to first fail on steroids and immunosuppressants.
Most clinicians consider cost concerns fair as a basis for insurance decisions. But they can also have strong rationales for making exceptions. This may mean starting patients on a biologic early, particularly those they deem unlikely to respond to first- or second-line treatments – which may be cheaper but are not necessarily safer.
In egregious cases, a patient already stable on a biologic who has changed insurance plans may be forced to go backwards in the treatment pathway, and fail first- and second-line therapies all over again before resuming – a process unlikely to be cost-effective in the long term, and also rife with ethical concerns, say clinicians.
“Making a patient fail to get a less toxic drug sort of violates our ‘do no harm’ principle,” Dr. Stephen B. Hanauer, medical director of the Digestive Health Center at Northwestern University, Chicago, said in an interview.
“I always say that if biologics cost a dollar, we’d be using them for everybody. If you take away the steroids and the immunosuppressants, these are very safe drugs for IBD, far safer than steroids – but steroids are cheap,” Dr. Hanauer said.
And with some debilitating disease presentations, such as severe Crohn’s, “being told that we have to try conventional therapies and the patient has to fail them can mean putting the patient through progression of their disease, and suffering,” Dr. David T. Rubin, codirector of the Digestive Diseases Center at the University of Chicago, said in an interview. “We really struggle with this.”
Dr. Joseph S. Eastern, a dermatologist practicing in Belleville, N.J., said his specialty faces similar challenges with step therapy. “Dermatologists as a group are pretty risk averse. When given the opportunity, we do an excellent job of prescribing conventional medications, ultraviolet therapy, and biologics in the most cost-efficient possible way,” he said in an email.
Yet “third-party payers tell us, for example, that a patient must fail methotrexate before we can use a biologic, when the whole advantage of biologic therapy for many of these patients is the avoidance of organotoxicity and other serious risks.”
As a result, Dr. Eastern said, “I write a lot more vehement letters to payers about the biologics these days.”
Choice vs. cost
Rheumatologists are among the clinicians most affected by fail-first and step therapy mandates, as the diseases they treat – particularly RA – are the most established indications for biologic therapies, and for which the largest number of these are approved.
Though Medicare and Medicaid allow physicians considerable leeway, private insurers often tightly circumscribe the timing and choice of biologics in RA. As insurers’ first-choice biologic drug changes frequently, and varies from plan to plan, a patient who is stable on one agent might be asked to switch to another, a phenomenon known as nonmedical switching.
Insurers are seldom transparent about their reasons for establishing certain biologic drugs as their go-to agents, clinicians say, while making it difficult for physicians to prescribe others. “There’s a tremendous amount of discounting going on that we are oblivious to as physicians. I’ve seen situations where drug A is the first one you have to use this month and the next month, drug C,” said Dr. Norman Gaylis, a rheumatologist practicing in Aventura, Fla.
Attempting to start a patient on a nonpreferential biologic will generate paperwork and delays, Dr. Gaylis said, which can cost patients valuable time. “There’s a window of opportunity to treat these diseases, and by creating a step therapy pathway we’re closing the window at least partially.”
“As an example, rituximab in most payer plans is not tiered as a first-line biologic treatment option despite the fact that there are frequent scenarios where the clinical and serological presentation of a patient would suggest it to be preferable as a first-line treatment choice over an anti-TNF [tumor necrosis factor],” Dr. Gaylis said.
“There is no room for clinical decision making based upon the unique presentation of each different patient when choosing the best treatment option,” he said.
Rheumatologists often become overwhelmed with authorization paperwork, “and still in many instances end up with a denial of their request.”
Dr. Karen Kolba, a rheumatologist in private practice in Santa Maria, Calif., said that she agreed in principle with the way step therapy protocols have been established, and that some of the frustration with step therapy amounts to a tendency among specialist clinicians to bristle at being told what to do.
“Physicians hate protocol,” Dr. Kolba said. “But comparing one protocol to another is the only way we are going to make advances.” It took the rheumatology community about 30 years to come to terms with the use of methotrexate in RA, she noted, and the stepped approach grew naturally from the treatment of methotrexate failures with biologic agents when these first emerged in the late 1990s.
A majority of RA patients started on a stepped approach using DMARDs will respond, Dr. Kolba said, and for those who must move into the biologic realm, the vast majority will succeed on the first anti-TNF agent prescribed. And there is little science to establish that one TNF inhibitor is superior – only that patients can sometimes succeed with one and fail another.
“As far as which biologic to initiate, my personal opinion is I don’t care, and I tell the patients that I don’t mind if the insurer picks out of this category because I’m flipping a coin as well,” she said.
Step mandates become objectionable, Dr. Kolba said, when they are purportedly based in science that doesn’t exist, or when they seem to exist only to wear down the provider.
“With private insurance not only do they have the drug of the year, they’re going to make me battle for every single prescription. When I say I have tried this patient on maximal tolerable doses of all these DMARDs, they ought to believe me. Yet I get six-page forms back saying, ‘Give me the start and stop dates of all the drugs you’ve used.’”
States constrain fail first
For many specialists treating patients with biologics, some of these hurdles are already getting lowered.
Concerns about physician choice, a lack of transparency in insurer decision making, and the ethics of forcing patients to fail have led advocacy groups to press hard in recent years for legislation limiting step therapy – with successes in a dozen states.
While the state legislation is not disease or drug specific, it has important implications for clinicians treating with biologics. “Step therapy in its genesis was a good idea – it’s OK to try to reduce costs in the health care system,” said Patrick Stone, state government relations manager at the National Psoriasis Foundation in Annapolis, Md., a group that works extensively on step therapy issues. “But when these protocols were first crafted, medications like biologics weren’t in use.”
Jeff Okazaki, associate director of the Coalition of State Rheumatology Organizations, a group based in Schaumberg, Ill., said lawmakers are starting to accept that in terms of cost of care, “somebody not being treated appropriately and down the line has organ damage or comorbidity because of incorrect treatment decisions due to step therapy is a higher burden.”
Moreover, he said, “we’d seen protocols requiring five or more steps, and for each step you have to try it at least 90 days.” For a patient with rheumatic or autoimmune disease, “getting through something like that can just be devastating.”
In 2011, Connecticut, Mississippi, and Arkansas became the first states to pass legislation limiting some aspect of step therapy. Since then, nine additional states have passed legislation varying in focus and scope.
In Kentucky, for example, patients cannot be forced by their insurer to remain on an ineffective therapy for more than 30 days, and insurers must respond to physician requests for an override within 2 days. Mississippi allows physicians to override insurer decisions with proof of clinical evidence. In California, legislation passed last year aims to reduce bureaucracy and speed up response to physician requests for overrides.
Mr. Stone and Mr. Okazaki are working in a coalition with other dermatology, rheumatology, and GI groups to push bills in seven more states, including New York, North Carolina, and Ohio.
While all the bills differ in what they attempt to limit, the model legislation has three basic objectives, Mr. Okazaki said. “We want a clear set of clinical guidelines, a quick review process, and overrides that allow for exceptions in cases where patients shouldn’t have to go through step therapy.”
Clinical strategies and research gaps
New legislation undoubtedly will help providers and patients get access to their choice of treatment agents. But so long as biologics are expensive – and it will be a while before the first biosimilar drugs, which will have efficacy and safety similar to their reference biologics, reduce prices in any meaningful way – step therapy will likely remain the norm.
One of the key difficulties providers face when pushing back on an insurer in favor of a biologic drug is insufficient clinical evidence.
With IBD, Dr. Rubin said, “we need a need more longitudinal understanding” and better prognostic indicators “in order to justify spending the extra money or going to one of these therapies.”
Dr. Hanauer said one of the limitations he faces in practice is insufficient clinical evidence for biologics early in the treatment pathway for IBD.
RA “is much more common than Crohn’s disease is. In trials, it’s much easier to recruit hundreds of patients [for an RA trial], while with Crohn’s it’s very hard to enroll more than a couple a year at most sites,” he said. “And as you move earlier in the treatment pathway that becomes somewhat more difficult as well.”
His solution for now, he said, is to follow established step pathways in an accelerated way, for “a rapid transition toward highly effective therapies” without having to face extensive pushback from insurers.
“The idea is to initiate immunosuppressants for any patients with sufficient disease activity to justify steroids,” Dr. Hanauer said. “Their steroids are then tapered, and while on immunosuppressants, patients are in a perfect setup to get combination therapy with an immunosuppressive and a biologic – and that’s a 2- to 3-month transition, not 2-3 years.”
Dr. Kolba said that despite the wide array of options for treating RA, the specialty suffers from a dearth of understanding as to why some patients fail drugs while others succeed, even within the same drug class.
Rheumatologists’ prescribing choices would be highly influenced by better biomarkers, were they to become available, she said. And they’d have far better arguments when confronted with payer pushback.
“We’re all looking for that magic biologic marker to tell me which drug to use,” Dr. Kolba said, “because God knows if I had a blood test that said ‘this is the drug,’ I would go to the mat with the insurer.”
Laws recently passed or under consideration in state legislatures may offer some relief to physicians and patients dogged by the “step” or “fail-first” therapy protocols mandated by insurers, but until better clinical evidence is available to support treatment decisions and biosimilars reduce costs, clinicians must strategize to get patients through the step pathways as fast as possible.
Rheumatologists, gastroenterologists, and dermatologists all confront fail-first policies in their practices, particularly when prescribing the biologic agents that have been game changers in treating rheumatoid arthritis (RA), inflammatory bowel disease (IBD), and psoriasis, among other diseases.
In RA, for example, a patient might be required to fail a series of disease-modifying antirheumatic drugs (DMARDs), including methotrexate, before starting a biologic. In Crohn’s disease, patients might have to first fail on steroids and immunosuppressants.
Most clinicians consider cost concerns fair as a basis for insurance decisions. But they can also have strong rationales for making exceptions. This may mean starting patients on a biologic early, particularly those they deem unlikely to respond to first- or second-line treatments – which may be cheaper but are not necessarily safer.
In egregious cases, a patient already stable on a biologic who has changed insurance plans may be forced to go backwards in the treatment pathway, and fail first- and second-line therapies all over again before resuming – a process unlikely to be cost-effective in the long term, and also rife with ethical concerns, say clinicians.
“Making a patient fail to get a less toxic drug sort of violates our ‘do no harm’ principle,” Dr. Stephen B. Hanauer, medical director of the Digestive Health Center at Northwestern University, Chicago, said in an interview.
“I always say that if biologics cost a dollar, we’d be using them for everybody. If you take away the steroids and the immunosuppressants, these are very safe drugs for IBD, far safer than steroids – but steroids are cheap,” Dr. Hanauer said.
And with some debilitating disease presentations, such as severe Crohn’s, “being told that we have to try conventional therapies and the patient has to fail them can mean putting the patient through progression of their disease, and suffering,” Dr. David T. Rubin, codirector of the Digestive Diseases Center at the University of Chicago, said in an interview. “We really struggle with this.”
Dr. Joseph S. Eastern, a dermatologist practicing in Belleville, N.J., said his specialty faces similar challenges with step therapy. “Dermatologists as a group are pretty risk averse. When given the opportunity, we do an excellent job of prescribing conventional medications, ultraviolet therapy, and biologics in the most cost-efficient possible way,” he said in an email.
Yet “third-party payers tell us, for example, that a patient must fail methotrexate before we can use a biologic, when the whole advantage of biologic therapy for many of these patients is the avoidance of organotoxicity and other serious risks.”
As a result, Dr. Eastern said, “I write a lot more vehement letters to payers about the biologics these days.”
Choice vs. cost
Rheumatologists are among the clinicians most affected by fail-first and step therapy mandates, as the diseases they treat – particularly RA – are the most established indications for biologic therapies, and for which the largest number of these are approved.
Though Medicare and Medicaid allow physicians considerable leeway, private insurers often tightly circumscribe the timing and choice of biologics in RA. As insurers’ first-choice biologic drug changes frequently, and varies from plan to plan, a patient who is stable on one agent might be asked to switch to another, a phenomenon known as nonmedical switching.
Insurers are seldom transparent about their reasons for establishing certain biologic drugs as their go-to agents, clinicians say, while making it difficult for physicians to prescribe others. “There’s a tremendous amount of discounting going on that we are oblivious to as physicians. I’ve seen situations where drug A is the first one you have to use this month and the next month, drug C,” said Dr. Norman Gaylis, a rheumatologist practicing in Aventura, Fla.
Attempting to start a patient on a nonpreferential biologic will generate paperwork and delays, Dr. Gaylis said, which can cost patients valuable time. “There’s a window of opportunity to treat these diseases, and by creating a step therapy pathway we’re closing the window at least partially.”
“As an example, rituximab in most payer plans is not tiered as a first-line biologic treatment option despite the fact that there are frequent scenarios where the clinical and serological presentation of a patient would suggest it to be preferable as a first-line treatment choice over an anti-TNF [tumor necrosis factor],” Dr. Gaylis said.
“There is no room for clinical decision making based upon the unique presentation of each different patient when choosing the best treatment option,” he said.
Rheumatologists often become overwhelmed with authorization paperwork, “and still in many instances end up with a denial of their request.”
Dr. Karen Kolba, a rheumatologist in private practice in Santa Maria, Calif., said that she agreed in principle with the way step therapy protocols have been established, and that some of the frustration with step therapy amounts to a tendency among specialist clinicians to bristle at being told what to do.
“Physicians hate protocol,” Dr. Kolba said. “But comparing one protocol to another is the only way we are going to make advances.” It took the rheumatology community about 30 years to come to terms with the use of methotrexate in RA, she noted, and the stepped approach grew naturally from the treatment of methotrexate failures with biologic agents when these first emerged in the late 1990s.
A majority of RA patients started on a stepped approach using DMARDs will respond, Dr. Kolba said, and for those who must move into the biologic realm, the vast majority will succeed on the first anti-TNF agent prescribed. And there is little science to establish that one TNF inhibitor is superior – only that patients can sometimes succeed with one and fail another.
“As far as which biologic to initiate, my personal opinion is I don’t care, and I tell the patients that I don’t mind if the insurer picks out of this category because I’m flipping a coin as well,” she said.
Step mandates become objectionable, Dr. Kolba said, when they are purportedly based in science that doesn’t exist, or when they seem to exist only to wear down the provider.
“With private insurance not only do they have the drug of the year, they’re going to make me battle for every single prescription. When I say I have tried this patient on maximal tolerable doses of all these DMARDs, they ought to believe me. Yet I get six-page forms back saying, ‘Give me the start and stop dates of all the drugs you’ve used.’”
States constrain fail first
For many specialists treating patients with biologics, some of these hurdles are already getting lowered.
Concerns about physician choice, a lack of transparency in insurer decision making, and the ethics of forcing patients to fail have led advocacy groups to press hard in recent years for legislation limiting step therapy – with successes in a dozen states.
While the state legislation is not disease or drug specific, it has important implications for clinicians treating with biologics. “Step therapy in its genesis was a good idea – it’s OK to try to reduce costs in the health care system,” said Patrick Stone, state government relations manager at the National Psoriasis Foundation in Annapolis, Md., a group that works extensively on step therapy issues. “But when these protocols were first crafted, medications like biologics weren’t in use.”
Jeff Okazaki, associate director of the Coalition of State Rheumatology Organizations, a group based in Schaumberg, Ill., said lawmakers are starting to accept that in terms of cost of care, “somebody not being treated appropriately and down the line has organ damage or comorbidity because of incorrect treatment decisions due to step therapy is a higher burden.”
Moreover, he said, “we’d seen protocols requiring five or more steps, and for each step you have to try it at least 90 days.” For a patient with rheumatic or autoimmune disease, “getting through something like that can just be devastating.”
In 2011, Connecticut, Mississippi, and Arkansas became the first states to pass legislation limiting some aspect of step therapy. Since then, nine additional states have passed legislation varying in focus and scope.
In Kentucky, for example, patients cannot be forced by their insurer to remain on an ineffective therapy for more than 30 days, and insurers must respond to physician requests for an override within 2 days. Mississippi allows physicians to override insurer decisions with proof of clinical evidence. In California, legislation passed last year aims to reduce bureaucracy and speed up response to physician requests for overrides.
Mr. Stone and Mr. Okazaki are working in a coalition with other dermatology, rheumatology, and GI groups to push bills in seven more states, including New York, North Carolina, and Ohio.
While all the bills differ in what they attempt to limit, the model legislation has three basic objectives, Mr. Okazaki said. “We want a clear set of clinical guidelines, a quick review process, and overrides that allow for exceptions in cases where patients shouldn’t have to go through step therapy.”
Clinical strategies and research gaps
New legislation undoubtedly will help providers and patients get access to their choice of treatment agents. But so long as biologics are expensive – and it will be a while before the first biosimilar drugs, which will have efficacy and safety similar to their reference biologics, reduce prices in any meaningful way – step therapy will likely remain the norm.
One of the key difficulties providers face when pushing back on an insurer in favor of a biologic drug is insufficient clinical evidence.
With IBD, Dr. Rubin said, “we need a need more longitudinal understanding” and better prognostic indicators “in order to justify spending the extra money or going to one of these therapies.”
Dr. Hanauer said one of the limitations he faces in practice is insufficient clinical evidence for biologics early in the treatment pathway for IBD.
RA “is much more common than Crohn’s disease is. In trials, it’s much easier to recruit hundreds of patients [for an RA trial], while with Crohn’s it’s very hard to enroll more than a couple a year at most sites,” he said. “And as you move earlier in the treatment pathway that becomes somewhat more difficult as well.”
His solution for now, he said, is to follow established step pathways in an accelerated way, for “a rapid transition toward highly effective therapies” without having to face extensive pushback from insurers.
“The idea is to initiate immunosuppressants for any patients with sufficient disease activity to justify steroids,” Dr. Hanauer said. “Their steroids are then tapered, and while on immunosuppressants, patients are in a perfect setup to get combination therapy with an immunosuppressive and a biologic – and that’s a 2- to 3-month transition, not 2-3 years.”
Dr. Kolba said that despite the wide array of options for treating RA, the specialty suffers from a dearth of understanding as to why some patients fail drugs while others succeed, even within the same drug class.
Rheumatologists’ prescribing choices would be highly influenced by better biomarkers, were they to become available, she said. And they’d have far better arguments when confronted with payer pushback.
“We’re all looking for that magic biologic marker to tell me which drug to use,” Dr. Kolba said, “because God knows if I had a blood test that said ‘this is the drug,’ I would go to the mat with the insurer.”
Laws recently passed or under consideration in state legislatures may offer some relief to physicians and patients dogged by the “step” or “fail-first” therapy protocols mandated by insurers, but until better clinical evidence is available to support treatment decisions and biosimilars reduce costs, clinicians must strategize to get patients through the step pathways as fast as possible.
Rheumatologists, gastroenterologists, and dermatologists all confront fail-first policies in their practices, particularly when prescribing the biologic agents that have been game changers in treating rheumatoid arthritis (RA), inflammatory bowel disease (IBD), and psoriasis, among other diseases.
In RA, for example, a patient might be required to fail a series of disease-modifying antirheumatic drugs (DMARDs), including methotrexate, before starting a biologic. In Crohn’s disease, patients might have to first fail on steroids and immunosuppressants.
Most clinicians consider cost concerns fair as a basis for insurance decisions. But they can also have strong rationales for making exceptions. This may mean starting patients on a biologic early, particularly those they deem unlikely to respond to first- or second-line treatments – which may be cheaper but are not necessarily safer.
In egregious cases, a patient already stable on a biologic who has changed insurance plans may be forced to go backwards in the treatment pathway, and fail first- and second-line therapies all over again before resuming – a process unlikely to be cost-effective in the long term, and also rife with ethical concerns, say clinicians.
“Making a patient fail to get a less toxic drug sort of violates our ‘do no harm’ principle,” Dr. Stephen B. Hanauer, medical director of the Digestive Health Center at Northwestern University, Chicago, said in an interview.
“I always say that if biologics cost a dollar, we’d be using them for everybody. If you take away the steroids and the immunosuppressants, these are very safe drugs for IBD, far safer than steroids – but steroids are cheap,” Dr. Hanauer said.
And with some debilitating disease presentations, such as severe Crohn’s, “being told that we have to try conventional therapies and the patient has to fail them can mean putting the patient through progression of their disease, and suffering,” Dr. David T. Rubin, codirector of the Digestive Diseases Center at the University of Chicago, said in an interview. “We really struggle with this.”
Dr. Joseph S. Eastern, a dermatologist practicing in Belleville, N.J., said his specialty faces similar challenges with step therapy. “Dermatologists as a group are pretty risk averse. When given the opportunity, we do an excellent job of prescribing conventional medications, ultraviolet therapy, and biologics in the most cost-efficient possible way,” he said in an email.
Yet “third-party payers tell us, for example, that a patient must fail methotrexate before we can use a biologic, when the whole advantage of biologic therapy for many of these patients is the avoidance of organotoxicity and other serious risks.”
As a result, Dr. Eastern said, “I write a lot more vehement letters to payers about the biologics these days.”
Choice vs. cost
Rheumatologists are among the clinicians most affected by fail-first and step therapy mandates, as the diseases they treat – particularly RA – are the most established indications for biologic therapies, and for which the largest number of these are approved.
Though Medicare and Medicaid allow physicians considerable leeway, private insurers often tightly circumscribe the timing and choice of biologics in RA. As insurers’ first-choice biologic drug changes frequently, and varies from plan to plan, a patient who is stable on one agent might be asked to switch to another, a phenomenon known as nonmedical switching.
Insurers are seldom transparent about their reasons for establishing certain biologic drugs as their go-to agents, clinicians say, while making it difficult for physicians to prescribe others. “There’s a tremendous amount of discounting going on that we are oblivious to as physicians. I’ve seen situations where drug A is the first one you have to use this month and the next month, drug C,” said Dr. Norman Gaylis, a rheumatologist practicing in Aventura, Fla.
Attempting to start a patient on a nonpreferential biologic will generate paperwork and delays, Dr. Gaylis said, which can cost patients valuable time. “There’s a window of opportunity to treat these diseases, and by creating a step therapy pathway we’re closing the window at least partially.”
“As an example, rituximab in most payer plans is not tiered as a first-line biologic treatment option despite the fact that there are frequent scenarios where the clinical and serological presentation of a patient would suggest it to be preferable as a first-line treatment choice over an anti-TNF [tumor necrosis factor],” Dr. Gaylis said.
“There is no room for clinical decision making based upon the unique presentation of each different patient when choosing the best treatment option,” he said.
Rheumatologists often become overwhelmed with authorization paperwork, “and still in many instances end up with a denial of their request.”
Dr. Karen Kolba, a rheumatologist in private practice in Santa Maria, Calif., said that she agreed in principle with the way step therapy protocols have been established, and that some of the frustration with step therapy amounts to a tendency among specialist clinicians to bristle at being told what to do.
“Physicians hate protocol,” Dr. Kolba said. “But comparing one protocol to another is the only way we are going to make advances.” It took the rheumatology community about 30 years to come to terms with the use of methotrexate in RA, she noted, and the stepped approach grew naturally from the treatment of methotrexate failures with biologic agents when these first emerged in the late 1990s.
A majority of RA patients started on a stepped approach using DMARDs will respond, Dr. Kolba said, and for those who must move into the biologic realm, the vast majority will succeed on the first anti-TNF agent prescribed. And there is little science to establish that one TNF inhibitor is superior – only that patients can sometimes succeed with one and fail another.
“As far as which biologic to initiate, my personal opinion is I don’t care, and I tell the patients that I don’t mind if the insurer picks out of this category because I’m flipping a coin as well,” she said.
Step mandates become objectionable, Dr. Kolba said, when they are purportedly based in science that doesn’t exist, or when they seem to exist only to wear down the provider.
“With private insurance not only do they have the drug of the year, they’re going to make me battle for every single prescription. When I say I have tried this patient on maximal tolerable doses of all these DMARDs, they ought to believe me. Yet I get six-page forms back saying, ‘Give me the start and stop dates of all the drugs you’ve used.’”
States constrain fail first
For many specialists treating patients with biologics, some of these hurdles are already getting lowered.
Concerns about physician choice, a lack of transparency in insurer decision making, and the ethics of forcing patients to fail have led advocacy groups to press hard in recent years for legislation limiting step therapy – with successes in a dozen states.
While the state legislation is not disease or drug specific, it has important implications for clinicians treating with biologics. “Step therapy in its genesis was a good idea – it’s OK to try to reduce costs in the health care system,” said Patrick Stone, state government relations manager at the National Psoriasis Foundation in Annapolis, Md., a group that works extensively on step therapy issues. “But when these protocols were first crafted, medications like biologics weren’t in use.”
Jeff Okazaki, associate director of the Coalition of State Rheumatology Organizations, a group based in Schaumberg, Ill., said lawmakers are starting to accept that in terms of cost of care, “somebody not being treated appropriately and down the line has organ damage or comorbidity because of incorrect treatment decisions due to step therapy is a higher burden.”
Moreover, he said, “we’d seen protocols requiring five or more steps, and for each step you have to try it at least 90 days.” For a patient with rheumatic or autoimmune disease, “getting through something like that can just be devastating.”
In 2011, Connecticut, Mississippi, and Arkansas became the first states to pass legislation limiting some aspect of step therapy. Since then, nine additional states have passed legislation varying in focus and scope.
In Kentucky, for example, patients cannot be forced by their insurer to remain on an ineffective therapy for more than 30 days, and insurers must respond to physician requests for an override within 2 days. Mississippi allows physicians to override insurer decisions with proof of clinical evidence. In California, legislation passed last year aims to reduce bureaucracy and speed up response to physician requests for overrides.
Mr. Stone and Mr. Okazaki are working in a coalition with other dermatology, rheumatology, and GI groups to push bills in seven more states, including New York, North Carolina, and Ohio.
While all the bills differ in what they attempt to limit, the model legislation has three basic objectives, Mr. Okazaki said. “We want a clear set of clinical guidelines, a quick review process, and overrides that allow for exceptions in cases where patients shouldn’t have to go through step therapy.”
Clinical strategies and research gaps
New legislation undoubtedly will help providers and patients get access to their choice of treatment agents. But so long as biologics are expensive – and it will be a while before the first biosimilar drugs, which will have efficacy and safety similar to their reference biologics, reduce prices in any meaningful way – step therapy will likely remain the norm.
One of the key difficulties providers face when pushing back on an insurer in favor of a biologic drug is insufficient clinical evidence.
With IBD, Dr. Rubin said, “we need a need more longitudinal understanding” and better prognostic indicators “in order to justify spending the extra money or going to one of these therapies.”
Dr. Hanauer said one of the limitations he faces in practice is insufficient clinical evidence for biologics early in the treatment pathway for IBD.
RA “is much more common than Crohn’s disease is. In trials, it’s much easier to recruit hundreds of patients [for an RA trial], while with Crohn’s it’s very hard to enroll more than a couple a year at most sites,” he said. “And as you move earlier in the treatment pathway that becomes somewhat more difficult as well.”
His solution for now, he said, is to follow established step pathways in an accelerated way, for “a rapid transition toward highly effective therapies” without having to face extensive pushback from insurers.
“The idea is to initiate immunosuppressants for any patients with sufficient disease activity to justify steroids,” Dr. Hanauer said. “Their steroids are then tapered, and while on immunosuppressants, patients are in a perfect setup to get combination therapy with an immunosuppressive and a biologic – and that’s a 2- to 3-month transition, not 2-3 years.”
Dr. Kolba said that despite the wide array of options for treating RA, the specialty suffers from a dearth of understanding as to why some patients fail drugs while others succeed, even within the same drug class.
Rheumatologists’ prescribing choices would be highly influenced by better biomarkers, were they to become available, she said. And they’d have far better arguments when confronted with payer pushback.
“We’re all looking for that magic biologic marker to tell me which drug to use,” Dr. Kolba said, “because God knows if I had a blood test that said ‘this is the drug,’ I would go to the mat with the insurer.”
Price Explosion

One of the biggest burdens of modern clinical dermatology practice is the ability to obtain appropriate drug therapy for patients. In the current health care environment, insurance formularies have become increasingly restrictive and more individuals have to deal with high-deductible insurance plans.
In a JAMA Dermatology study published online on November 25, Rosenberg and Rosenberg sought to determine changes in the prices of commonly prescribed dermatologic medications since 2009 and identify trends in price increases for different classes of drugs. To perform this analysis, they sent surveys to 4 national chain pharmacies requesting price information for commonly prescribed dermatologic therapies in 2009, 2011, 2014, and 2015. The initial survey requested information on 72 brand-name drugs.
The findings of the analysis were staggering. Of the 19 brand-name drugs analyzed, the retail prices of 7 drugs more than quadrupled over the study period. The mean price increase for this group of drugs was 401% during the entire survey period.
Rosenberg and Rosenberg grouped the price increase by therapeutic class. Prices of topical antineoplastic therapies had the largest mean absolute and percentage increase ($10,926.58 [1240%]). Prices of drugs in the anti-infective class had the smallest mean absolute increase ($333.99); prices of psoriasis medications had the smallest mean percentage increase (180%). Prices of acne and rosacea medications had a mean increase of 195%, and prices of topical corticosteroids experienced a mean increase of 290%. Selected generic drugs examined in 2011 and 2014 also increased a mean of 279% during the 3-year period.
Rosenberg and Rosenberg noted that the increases for commonly prescribed medications greatly outpaced inflation, national health expenditure growth, and increases in reimbursements for physician services. They did not detect any specific trend to explain the substantial increase in the costs of dermatologic prescription drugs and they did not investigate reasons for the price increases.
What’s the issue?
Price increases for psoriatic and other therapies are creating barriers to both our appropriate treatment of patients and our ability to effectively practice medicine. How are you coping with this challenge in your practice?

One of the biggest burdens of modern clinical dermatology practice is the ability to obtain appropriate drug therapy for patients. In the current health care environment, insurance formularies have become increasingly restrictive and more individuals have to deal with high-deductible insurance plans.
In a JAMA Dermatology study published online on November 25, Rosenberg and Rosenberg sought to determine changes in the prices of commonly prescribed dermatologic medications since 2009 and identify trends in price increases for different classes of drugs. To perform this analysis, they sent surveys to 4 national chain pharmacies requesting price information for commonly prescribed dermatologic therapies in 2009, 2011, 2014, and 2015. The initial survey requested information on 72 brand-name drugs.
The findings of the analysis were staggering. Of the 19 brand-name drugs analyzed, the retail prices of 7 drugs more than quadrupled over the study period. The mean price increase for this group of drugs was 401% during the entire survey period.
Rosenberg and Rosenberg grouped the price increase by therapeutic class. Prices of topical antineoplastic therapies had the largest mean absolute and percentage increase ($10,926.58 [1240%]). Prices of drugs in the anti-infective class had the smallest mean absolute increase ($333.99); prices of psoriasis medications had the smallest mean percentage increase (180%). Prices of acne and rosacea medications had a mean increase of 195%, and prices of topical corticosteroids experienced a mean increase of 290%. Selected generic drugs examined in 2011 and 2014 also increased a mean of 279% during the 3-year period.
Rosenberg and Rosenberg noted that the increases for commonly prescribed medications greatly outpaced inflation, national health expenditure growth, and increases in reimbursements for physician services. They did not detect any specific trend to explain the substantial increase in the costs of dermatologic prescription drugs and they did not investigate reasons for the price increases.
What’s the issue?
Price increases for psoriatic and other therapies are creating barriers to both our appropriate treatment of patients and our ability to effectively practice medicine. How are you coping with this challenge in your practice?

One of the biggest burdens of modern clinical dermatology practice is the ability to obtain appropriate drug therapy for patients. In the current health care environment, insurance formularies have become increasingly restrictive and more individuals have to deal with high-deductible insurance plans.
In a JAMA Dermatology study published online on November 25, Rosenberg and Rosenberg sought to determine changes in the prices of commonly prescribed dermatologic medications since 2009 and identify trends in price increases for different classes of drugs. To perform this analysis, they sent surveys to 4 national chain pharmacies requesting price information for commonly prescribed dermatologic therapies in 2009, 2011, 2014, and 2015. The initial survey requested information on 72 brand-name drugs.
The findings of the analysis were staggering. Of the 19 brand-name drugs analyzed, the retail prices of 7 drugs more than quadrupled over the study period. The mean price increase for this group of drugs was 401% during the entire survey period.
Rosenberg and Rosenberg grouped the price increase by therapeutic class. Prices of topical antineoplastic therapies had the largest mean absolute and percentage increase ($10,926.58 [1240%]). Prices of drugs in the anti-infective class had the smallest mean absolute increase ($333.99); prices of psoriasis medications had the smallest mean percentage increase (180%). Prices of acne and rosacea medications had a mean increase of 195%, and prices of topical corticosteroids experienced a mean increase of 290%. Selected generic drugs examined in 2011 and 2014 also increased a mean of 279% during the 3-year period.
Rosenberg and Rosenberg noted that the increases for commonly prescribed medications greatly outpaced inflation, national health expenditure growth, and increases in reimbursements for physician services. They did not detect any specific trend to explain the substantial increase in the costs of dermatologic prescription drugs and they did not investigate reasons for the price increases.
What’s the issue?
Price increases for psoriatic and other therapies are creating barriers to both our appropriate treatment of patients and our ability to effectively practice medicine. How are you coping with this challenge in your practice?
Secukinumab receives FDA approval for psoriatic arthritis, ankylosing spondylitis
The Food and Drug Administration approved two new indications for the interleukin-17A inhibitor secukinumab (Cosentyx) – psoriatic arthritis in adults and ankylosing spondylitis in adults – on Jan. 15. These join the approval for moderate to severe plaque psoriasis in adults it received in January 2015, according to an announcement from the drug’s manufacturer, Novartis.
The approvals are based on the efficacy and safety outcomes from four placebo-controlled, phase III studies, which included more than 1,500 adult patients with ankylosing spondylitis (AS) or psoriatic arthritis (PsA) who were biologic treatment naive or had an inadequate response or were intolerant to anti-TNF agents.
Pivotal phase III studies in the secukinumab clinical trial program, which provided key data for the submission, were MEASURE 1 and MEASURE 2 involving 590 patients with AS, and FUTURE 1 and FUTURE 2 involving 1,003 patients with PsA. Novartis continues to investigate the fully human monoclonal antibody against IL-17A for its potential in preventing radiographic progression of spinal and joint structural damage in AS and PsA patients, respectively.
The European Medicines Agency approved secukinumab for PsA and AS in November 2015.
The Food and Drug Administration approved two new indications for the interleukin-17A inhibitor secukinumab (Cosentyx) – psoriatic arthritis in adults and ankylosing spondylitis in adults – on Jan. 15. These join the approval for moderate to severe plaque psoriasis in adults it received in January 2015, according to an announcement from the drug’s manufacturer, Novartis.
The approvals are based on the efficacy and safety outcomes from four placebo-controlled, phase III studies, which included more than 1,500 adult patients with ankylosing spondylitis (AS) or psoriatic arthritis (PsA) who were biologic treatment naive or had an inadequate response or were intolerant to anti-TNF agents.
Pivotal phase III studies in the secukinumab clinical trial program, which provided key data for the submission, were MEASURE 1 and MEASURE 2 involving 590 patients with AS, and FUTURE 1 and FUTURE 2 involving 1,003 patients with PsA. Novartis continues to investigate the fully human monoclonal antibody against IL-17A for its potential in preventing radiographic progression of spinal and joint structural damage in AS and PsA patients, respectively.
The European Medicines Agency approved secukinumab for PsA and AS in November 2015.
The Food and Drug Administration approved two new indications for the interleukin-17A inhibitor secukinumab (Cosentyx) – psoriatic arthritis in adults and ankylosing spondylitis in adults – on Jan. 15. These join the approval for moderate to severe plaque psoriasis in adults it received in January 2015, according to an announcement from the drug’s manufacturer, Novartis.
The approvals are based on the efficacy and safety outcomes from four placebo-controlled, phase III studies, which included more than 1,500 adult patients with ankylosing spondylitis (AS) or psoriatic arthritis (PsA) who were biologic treatment naive or had an inadequate response or were intolerant to anti-TNF agents.
Pivotal phase III studies in the secukinumab clinical trial program, which provided key data for the submission, were MEASURE 1 and MEASURE 2 involving 590 patients with AS, and FUTURE 1 and FUTURE 2 involving 1,003 patients with PsA. Novartis continues to investigate the fully human monoclonal antibody against IL-17A for its potential in preventing radiographic progression of spinal and joint structural damage in AS and PsA patients, respectively.
The European Medicines Agency approved secukinumab for PsA and AS in November 2015.
EADV: Family history of cardiovascular disease is key in psoriasis patients
COPENHAGEN – The increased risk of MI and stroke in patients who develop psoriasis as young adults is essentially confined to those having a positive family history of cardiovascular disease, according to a Danish national study presented at the annual congress of the European Academy of Dermatology and Venereology.
“We found a significantly increased risk of MACE [major adverse cardiovascular events] in patients with psoriasis only when a family history of cardiovascular disease was present. This just highlights why it’s important that future studies of cardiovascular risk in psoriasis should include family history. Also, an increased focus on cardiovascular disease in relatives may be appropriate in the cardiovascular risk assessment of patients with psoriasis,” said Dr. Alexander Egeberg of the University of Copenhagen.
He presented a population-based study involving 15 years of follow-up of 30,278 Danes diagnosed with psoriasis in their 20s and a control group consisting of nearly 2.7 million of their Danish contemporaries who were not. None had personal history of acute MI or stroke at baseline. Family medical history, including whether cardiovascular disease occurred in first-degree relatives, was available for all subjects.
Dr. Egeberg and coinvestigators mapped the incidence of acute MI, ischemic stroke, or cardiovascular death in psoriasis patients and the general population controls during follow-up.
“When you look at the patients who developed psoriasis and didn’t have a positive family history of cardiovascular disease, there are almost no cardiovascular events for the entire country,” Dr. Egeberg observed.
In contrast, in a multivariate analysis adjusted for age, gender, socioeconomic status, comorbid cardiovascular disease, smoking, and the use of cardiovascular medications, patients with mild psoriasis and a positive family history for cardiovascular disease had a 28% greater risk of a premature cardiovascular event than the general population during follow-up out to roughly age 40. Those with a positive family history and severe psoriasis as defined by the use of systemic therapies had a 62% increase in risk. Both of these elevated risks were statistically significant.
Among young adult Danes with a positive family history for cardiovascular disease, there were 222 MACE events during 62,225 person-years of follow-up in the mild psoriasis group and 31 events during 6,848 person-years in the 4,504 subjects with severe psoriasis. The resultant incidence rates in both groups were significantly higher than in the control group, who experienced 28,846 MACE events during 16.1 million person-years of follow-up.
In contrast, fewer than 10 MACE events occurred in Danish psoriasis patients without a family history of cardiovascular disease.
A positive family history was also associated with increased MACE in the nonpsoriatic general population, although it didn’t confer as great a risk as in the Danes with psoriasis.
A point worthy of consideration, Dr. Egeberg noted, is that the epidemiology of psoriasis in Denmark apparently differs in several important ways from psoriasis in the United States and some other countries. For one, the prevalence is higher in Scandinavian countries – 7.1% in a Danish national cross-sectional study (Int J Dermatol. 2013 Jun;52[6]:681-3) and 8% in neighboring Norway – as compared with 2%-3% in much of the rest of the world.
Moreover, according to the same cross-sectional study, the prevalence of traditional cardiovascular risk factors, such as smoking and the components of the metabolic syndrome, isn’t higher in Danish psoriasis patients than in the country’s general population. That’s in contrast to the situation in the United Kingdom, where Dr. Joel M. Gelfand of the University of Pennsylvania and associates reported a decade ago in a landmark study that the prevalence of hypertension, obesity, hyperlipidemia, diabetes, and smoking were all higher in persons with psoriasis than in the general population (J Am Acad Dermatol. 2006 Nov;55[5]:829-35). Similar findings were subsequently reported in U.S. psoriasis patients.
Despite their absence of elevated levels of the standard cardiovascular risk factors, Danish psoriasis patients as a group do face a clinically significant increase in cardiovascular risk, compared with the general population, as shown in yet another Danish national cohort study in which the rate ratios for cardiovascular death for mild and severe psoriasis were 1.14 and 1.57, respectively, compared with controls (J Intern Med. 2011 Aug;270[2]:147-57).
In an even more recent Danish nationwide study, the overall death rate was found to be 25.4 per 1,000 person-years in patients with severe psoriasis, 17.0 in those with mild psoriasis, and 13.8 per 1,000 person-years in the general population (J Eur Acad Dermatol Venereol. 2015 May;29[5]:1002-5).
Dr. Egeberg said his new Danish findings suggest that even in psoriasis patients with a greater burden of systemic inflammation as expressed in severe disease, that burden alone doesn’t translate into increased cardiovascular risk. Rather, elevated cardiovascular risk appears to be a consequence of heritable factors, Dr. Egeberg said.
An important caveat regarding this study, he continued, is that the mean age at which participants were diagnosed with psoriasis was 26.6 years. It’s unclear whether the study findings extend to individuals who develop the dermatologic disease later in life.
Dr. Egeberg reported having no financial conflicts regarding this study, supported by Danish national research funding.
COPENHAGEN – The increased risk of MI and stroke in patients who develop psoriasis as young adults is essentially confined to those having a positive family history of cardiovascular disease, according to a Danish national study presented at the annual congress of the European Academy of Dermatology and Venereology.
“We found a significantly increased risk of MACE [major adverse cardiovascular events] in patients with psoriasis only when a family history of cardiovascular disease was present. This just highlights why it’s important that future studies of cardiovascular risk in psoriasis should include family history. Also, an increased focus on cardiovascular disease in relatives may be appropriate in the cardiovascular risk assessment of patients with psoriasis,” said Dr. Alexander Egeberg of the University of Copenhagen.
He presented a population-based study involving 15 years of follow-up of 30,278 Danes diagnosed with psoriasis in their 20s and a control group consisting of nearly 2.7 million of their Danish contemporaries who were not. None had personal history of acute MI or stroke at baseline. Family medical history, including whether cardiovascular disease occurred in first-degree relatives, was available for all subjects.
Dr. Egeberg and coinvestigators mapped the incidence of acute MI, ischemic stroke, or cardiovascular death in psoriasis patients and the general population controls during follow-up.
“When you look at the patients who developed psoriasis and didn’t have a positive family history of cardiovascular disease, there are almost no cardiovascular events for the entire country,” Dr. Egeberg observed.
In contrast, in a multivariate analysis adjusted for age, gender, socioeconomic status, comorbid cardiovascular disease, smoking, and the use of cardiovascular medications, patients with mild psoriasis and a positive family history for cardiovascular disease had a 28% greater risk of a premature cardiovascular event than the general population during follow-up out to roughly age 40. Those with a positive family history and severe psoriasis as defined by the use of systemic therapies had a 62% increase in risk. Both of these elevated risks were statistically significant.
Among young adult Danes with a positive family history for cardiovascular disease, there were 222 MACE events during 62,225 person-years of follow-up in the mild psoriasis group and 31 events during 6,848 person-years in the 4,504 subjects with severe psoriasis. The resultant incidence rates in both groups were significantly higher than in the control group, who experienced 28,846 MACE events during 16.1 million person-years of follow-up.
In contrast, fewer than 10 MACE events occurred in Danish psoriasis patients without a family history of cardiovascular disease.
A positive family history was also associated with increased MACE in the nonpsoriatic general population, although it didn’t confer as great a risk as in the Danes with psoriasis.
A point worthy of consideration, Dr. Egeberg noted, is that the epidemiology of psoriasis in Denmark apparently differs in several important ways from psoriasis in the United States and some other countries. For one, the prevalence is higher in Scandinavian countries – 7.1% in a Danish national cross-sectional study (Int J Dermatol. 2013 Jun;52[6]:681-3) and 8% in neighboring Norway – as compared with 2%-3% in much of the rest of the world.
Moreover, according to the same cross-sectional study, the prevalence of traditional cardiovascular risk factors, such as smoking and the components of the metabolic syndrome, isn’t higher in Danish psoriasis patients than in the country’s general population. That’s in contrast to the situation in the United Kingdom, where Dr. Joel M. Gelfand of the University of Pennsylvania and associates reported a decade ago in a landmark study that the prevalence of hypertension, obesity, hyperlipidemia, diabetes, and smoking were all higher in persons with psoriasis than in the general population (J Am Acad Dermatol. 2006 Nov;55[5]:829-35). Similar findings were subsequently reported in U.S. psoriasis patients.
Despite their absence of elevated levels of the standard cardiovascular risk factors, Danish psoriasis patients as a group do face a clinically significant increase in cardiovascular risk, compared with the general population, as shown in yet another Danish national cohort study in which the rate ratios for cardiovascular death for mild and severe psoriasis were 1.14 and 1.57, respectively, compared with controls (J Intern Med. 2011 Aug;270[2]:147-57).
In an even more recent Danish nationwide study, the overall death rate was found to be 25.4 per 1,000 person-years in patients with severe psoriasis, 17.0 in those with mild psoriasis, and 13.8 per 1,000 person-years in the general population (J Eur Acad Dermatol Venereol. 2015 May;29[5]:1002-5).
Dr. Egeberg said his new Danish findings suggest that even in psoriasis patients with a greater burden of systemic inflammation as expressed in severe disease, that burden alone doesn’t translate into increased cardiovascular risk. Rather, elevated cardiovascular risk appears to be a consequence of heritable factors, Dr. Egeberg said.
An important caveat regarding this study, he continued, is that the mean age at which participants were diagnosed with psoriasis was 26.6 years. It’s unclear whether the study findings extend to individuals who develop the dermatologic disease later in life.
Dr. Egeberg reported having no financial conflicts regarding this study, supported by Danish national research funding.
COPENHAGEN – The increased risk of MI and stroke in patients who develop psoriasis as young adults is essentially confined to those having a positive family history of cardiovascular disease, according to a Danish national study presented at the annual congress of the European Academy of Dermatology and Venereology.
“We found a significantly increased risk of MACE [major adverse cardiovascular events] in patients with psoriasis only when a family history of cardiovascular disease was present. This just highlights why it’s important that future studies of cardiovascular risk in psoriasis should include family history. Also, an increased focus on cardiovascular disease in relatives may be appropriate in the cardiovascular risk assessment of patients with psoriasis,” said Dr. Alexander Egeberg of the University of Copenhagen.
He presented a population-based study involving 15 years of follow-up of 30,278 Danes diagnosed with psoriasis in their 20s and a control group consisting of nearly 2.7 million of their Danish contemporaries who were not. None had personal history of acute MI or stroke at baseline. Family medical history, including whether cardiovascular disease occurred in first-degree relatives, was available for all subjects.
Dr. Egeberg and coinvestigators mapped the incidence of acute MI, ischemic stroke, or cardiovascular death in psoriasis patients and the general population controls during follow-up.
“When you look at the patients who developed psoriasis and didn’t have a positive family history of cardiovascular disease, there are almost no cardiovascular events for the entire country,” Dr. Egeberg observed.
In contrast, in a multivariate analysis adjusted for age, gender, socioeconomic status, comorbid cardiovascular disease, smoking, and the use of cardiovascular medications, patients with mild psoriasis and a positive family history for cardiovascular disease had a 28% greater risk of a premature cardiovascular event than the general population during follow-up out to roughly age 40. Those with a positive family history and severe psoriasis as defined by the use of systemic therapies had a 62% increase in risk. Both of these elevated risks were statistically significant.
Among young adult Danes with a positive family history for cardiovascular disease, there were 222 MACE events during 62,225 person-years of follow-up in the mild psoriasis group and 31 events during 6,848 person-years in the 4,504 subjects with severe psoriasis. The resultant incidence rates in both groups were significantly higher than in the control group, who experienced 28,846 MACE events during 16.1 million person-years of follow-up.
In contrast, fewer than 10 MACE events occurred in Danish psoriasis patients without a family history of cardiovascular disease.
A positive family history was also associated with increased MACE in the nonpsoriatic general population, although it didn’t confer as great a risk as in the Danes with psoriasis.
A point worthy of consideration, Dr. Egeberg noted, is that the epidemiology of psoriasis in Denmark apparently differs in several important ways from psoriasis in the United States and some other countries. For one, the prevalence is higher in Scandinavian countries – 7.1% in a Danish national cross-sectional study (Int J Dermatol. 2013 Jun;52[6]:681-3) and 8% in neighboring Norway – as compared with 2%-3% in much of the rest of the world.
Moreover, according to the same cross-sectional study, the prevalence of traditional cardiovascular risk factors, such as smoking and the components of the metabolic syndrome, isn’t higher in Danish psoriasis patients than in the country’s general population. That’s in contrast to the situation in the United Kingdom, where Dr. Joel M. Gelfand of the University of Pennsylvania and associates reported a decade ago in a landmark study that the prevalence of hypertension, obesity, hyperlipidemia, diabetes, and smoking were all higher in persons with psoriasis than in the general population (J Am Acad Dermatol. 2006 Nov;55[5]:829-35). Similar findings were subsequently reported in U.S. psoriasis patients.
Despite their absence of elevated levels of the standard cardiovascular risk factors, Danish psoriasis patients as a group do face a clinically significant increase in cardiovascular risk, compared with the general population, as shown in yet another Danish national cohort study in which the rate ratios for cardiovascular death for mild and severe psoriasis were 1.14 and 1.57, respectively, compared with controls (J Intern Med. 2011 Aug;270[2]:147-57).
In an even more recent Danish nationwide study, the overall death rate was found to be 25.4 per 1,000 person-years in patients with severe psoriasis, 17.0 in those with mild psoriasis, and 13.8 per 1,000 person-years in the general population (J Eur Acad Dermatol Venereol. 2015 May;29[5]:1002-5).
Dr. Egeberg said his new Danish findings suggest that even in psoriasis patients with a greater burden of systemic inflammation as expressed in severe disease, that burden alone doesn’t translate into increased cardiovascular risk. Rather, elevated cardiovascular risk appears to be a consequence of heritable factors, Dr. Egeberg said.
An important caveat regarding this study, he continued, is that the mean age at which participants were diagnosed with psoriasis was 26.6 years. It’s unclear whether the study findings extend to individuals who develop the dermatologic disease later in life.
Dr. Egeberg reported having no financial conflicts regarding this study, supported by Danish national research funding.
AT THE EADV CONGRESS
Key clinical point: A family history of cardiovascular disease takes on extra importance in assessing cardiovascular risk in young adult psoriasis patients.
Major finding: Danes with mild or severe psoriasis plus a family history of cardiovascular disease were respectively 28% and 62% more likely to have an early cardiovascular event than the general population. In contrast, Danish psoriasis patients without a positive family history were not at increased risk of a cardiovascular event.
Data source: A population-based study of 2.7 million Danish young adults, including more than 30,000 diagnosed with psoriasis in their 20s, who were followed for 15 years.
Disclosures: The presenter reported having no financial conflicts regarding this study, which was supported by Danish national research funding.
EADV: New oral psoriasis drug shows excellent safety
COPENHAGEN – An oral small molecule with a novel mechanism of action for treatment of moderate to severe plaque psoriasis is being developed as a potential first-line systemic treatment in view of its highly favorable safety profile.
The investigational drug, known for now as CF101, is a first-in-class agonist of the A3 adenosine receptor. This cell surface receptor is upregulated in the pathologic cells of certain inflammatory diseases, but has little or no expression in normal cells. This high degree of specificity accounts for its safety, which in a recent phase II/III trial was essentially indistinguishable from placebo, making it an attractive potential alternative to methotrexate or biologics as a starting point in systemic therapy, Pnina Fishman, Ph.D., said at the annual congress of the European Academy of Dermatology and Venereology.
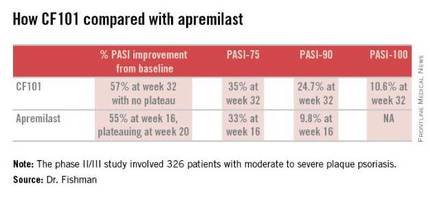
Planning is underway for a pivotal phase III trial of CF101 in psoriasis, which is also being organized for CF101 in rheumatoid arthritis on the strength of favorable phase II findings, according to Dr. Fishman, CEO of Can-Fite BioPharma, an Israeli biotech company that is developing the drug.
The phase II/III psoriasis trial was a 326-patient, double-blind, placebo-controlled study. It showed efficacy comparable to and in some respects better than that reported in the phase III ESTEEM-1 study of the oral phosphodiesterase 4 inhibitor apremilast (J Am Acad Dermatol. 2015 Jul;73:37-49).
Moreover, it appears that the twice-daily 2-mg dosing of CF101 studied in the phase II/III trial was suboptimal in light of the observed linear increase in Psoriasis Area and Severity Index (PASI)-75, -90, and -100 response rates over time. Those response rates rose steadily until the study’s end at week 32 with no evidence of a plateau. In contrast, in ESTEEM-1, the improvement with apremilast (Otezla) leveled off starting at about week 20, she observed.
In the recent phase II/III trial, the PASI-75 rate for CF101 at week 12 – the prespecified primary endpoint – was not significantly better than placebo was. However, the PASI-75 response rate continued to climb such that by week 32, it was 35.3%, similar to the 33.1% PASI-75 response seen at 16 weeks in ESTEEM-1. PASI improved by an average of 57% from baseline to week 32 with CF101 with no plateau in sight, and by 55% with apremilast at week 16, with a leveling off at week 20. This is why the upcoming phase III trial will employ a higher dose of CF101 than twice-daily 2-mg dose used in the phase II/III study and will run longer. The goal is to achieve higher PASI response rates faster than obtainable with 2 mg BID, Dr. Fishman explained.
She added that the PASI-90 response data in the phase II/III trial bode particularly well for the future of CF101 as a first-line systemic agent. At week 32, this stringent outcome measure was achieved by 26.9% of participants who hadn’t previously been on methotrexate or a biologic and by 13.7% of those who had. And as was the case for the PASI-75 results, the PASI-90 response increased in linear fashion out to 32 weeks with no plateau. In ESTEEM-1, the PASI-90 rate was 9.8% at week 16.
No treatment-related adverse events were seen in the phase II/III CF101 study, Dr. Fishman reported.
The study was sponsored by Can-Fite BioPharma and presented by Dr. Fishman, who is the company’s CEO.
COPENHAGEN – An oral small molecule with a novel mechanism of action for treatment of moderate to severe plaque psoriasis is being developed as a potential first-line systemic treatment in view of its highly favorable safety profile.
The investigational drug, known for now as CF101, is a first-in-class agonist of the A3 adenosine receptor. This cell surface receptor is upregulated in the pathologic cells of certain inflammatory diseases, but has little or no expression in normal cells. This high degree of specificity accounts for its safety, which in a recent phase II/III trial was essentially indistinguishable from placebo, making it an attractive potential alternative to methotrexate or biologics as a starting point in systemic therapy, Pnina Fishman, Ph.D., said at the annual congress of the European Academy of Dermatology and Venereology.
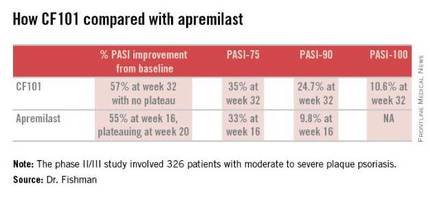
Planning is underway for a pivotal phase III trial of CF101 in psoriasis, which is also being organized for CF101 in rheumatoid arthritis on the strength of favorable phase II findings, according to Dr. Fishman, CEO of Can-Fite BioPharma, an Israeli biotech company that is developing the drug.
The phase II/III psoriasis trial was a 326-patient, double-blind, placebo-controlled study. It showed efficacy comparable to and in some respects better than that reported in the phase III ESTEEM-1 study of the oral phosphodiesterase 4 inhibitor apremilast (J Am Acad Dermatol. 2015 Jul;73:37-49).
Moreover, it appears that the twice-daily 2-mg dosing of CF101 studied in the phase II/III trial was suboptimal in light of the observed linear increase in Psoriasis Area and Severity Index (PASI)-75, -90, and -100 response rates over time. Those response rates rose steadily until the study’s end at week 32 with no evidence of a plateau. In contrast, in ESTEEM-1, the improvement with apremilast (Otezla) leveled off starting at about week 20, she observed.
In the recent phase II/III trial, the PASI-75 rate for CF101 at week 12 – the prespecified primary endpoint – was not significantly better than placebo was. However, the PASI-75 response rate continued to climb such that by week 32, it was 35.3%, similar to the 33.1% PASI-75 response seen at 16 weeks in ESTEEM-1. PASI improved by an average of 57% from baseline to week 32 with CF101 with no plateau in sight, and by 55% with apremilast at week 16, with a leveling off at week 20. This is why the upcoming phase III trial will employ a higher dose of CF101 than twice-daily 2-mg dose used in the phase II/III study and will run longer. The goal is to achieve higher PASI response rates faster than obtainable with 2 mg BID, Dr. Fishman explained.
She added that the PASI-90 response data in the phase II/III trial bode particularly well for the future of CF101 as a first-line systemic agent. At week 32, this stringent outcome measure was achieved by 26.9% of participants who hadn’t previously been on methotrexate or a biologic and by 13.7% of those who had. And as was the case for the PASI-75 results, the PASI-90 response increased in linear fashion out to 32 weeks with no plateau. In ESTEEM-1, the PASI-90 rate was 9.8% at week 16.
No treatment-related adverse events were seen in the phase II/III CF101 study, Dr. Fishman reported.
The study was sponsored by Can-Fite BioPharma and presented by Dr. Fishman, who is the company’s CEO.
COPENHAGEN – An oral small molecule with a novel mechanism of action for treatment of moderate to severe plaque psoriasis is being developed as a potential first-line systemic treatment in view of its highly favorable safety profile.
The investigational drug, known for now as CF101, is a first-in-class agonist of the A3 adenosine receptor. This cell surface receptor is upregulated in the pathologic cells of certain inflammatory diseases, but has little or no expression in normal cells. This high degree of specificity accounts for its safety, which in a recent phase II/III trial was essentially indistinguishable from placebo, making it an attractive potential alternative to methotrexate or biologics as a starting point in systemic therapy, Pnina Fishman, Ph.D., said at the annual congress of the European Academy of Dermatology and Venereology.
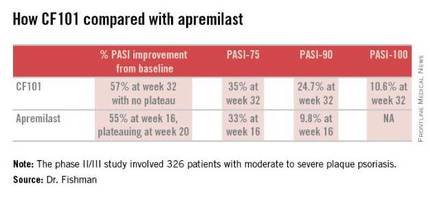
Planning is underway for a pivotal phase III trial of CF101 in psoriasis, which is also being organized for CF101 in rheumatoid arthritis on the strength of favorable phase II findings, according to Dr. Fishman, CEO of Can-Fite BioPharma, an Israeli biotech company that is developing the drug.
The phase II/III psoriasis trial was a 326-patient, double-blind, placebo-controlled study. It showed efficacy comparable to and in some respects better than that reported in the phase III ESTEEM-1 study of the oral phosphodiesterase 4 inhibitor apremilast (J Am Acad Dermatol. 2015 Jul;73:37-49).
Moreover, it appears that the twice-daily 2-mg dosing of CF101 studied in the phase II/III trial was suboptimal in light of the observed linear increase in Psoriasis Area and Severity Index (PASI)-75, -90, and -100 response rates over time. Those response rates rose steadily until the study’s end at week 32 with no evidence of a plateau. In contrast, in ESTEEM-1, the improvement with apremilast (Otezla) leveled off starting at about week 20, she observed.
In the recent phase II/III trial, the PASI-75 rate for CF101 at week 12 – the prespecified primary endpoint – was not significantly better than placebo was. However, the PASI-75 response rate continued to climb such that by week 32, it was 35.3%, similar to the 33.1% PASI-75 response seen at 16 weeks in ESTEEM-1. PASI improved by an average of 57% from baseline to week 32 with CF101 with no plateau in sight, and by 55% with apremilast at week 16, with a leveling off at week 20. This is why the upcoming phase III trial will employ a higher dose of CF101 than twice-daily 2-mg dose used in the phase II/III study and will run longer. The goal is to achieve higher PASI response rates faster than obtainable with 2 mg BID, Dr. Fishman explained.
She added that the PASI-90 response data in the phase II/III trial bode particularly well for the future of CF101 as a first-line systemic agent. At week 32, this stringent outcome measure was achieved by 26.9% of participants who hadn’t previously been on methotrexate or a biologic and by 13.7% of those who had. And as was the case for the PASI-75 results, the PASI-90 response increased in linear fashion out to 32 weeks with no plateau. In ESTEEM-1, the PASI-90 rate was 9.8% at week 16.
No treatment-related adverse events were seen in the phase II/III CF101 study, Dr. Fishman reported.
The study was sponsored by Can-Fite BioPharma and presented by Dr. Fishman, who is the company’s CEO.
AT THE EADV CONGRESS
Key clinical point: The oral A3 adenosine receptor agonist CF1-1 shows promise as a potential first-line systemic therapy for moderate to severe plaque psoriasis.
Major finding: The PASI-75 response rate with the twice-daily 2-mg dose of oral CF101 was 35.3% at 32 weeks in a phase II/III study.
Data source: This was a randomized, double-blind, placebo-controlled, 32-week phase II/III study including 326 patients with moderate-to-severe plaque psoriasis.
Disclosures: The study was sponsored by Can-Fite BioPharma of Israel and presented by the Dr. Fishman, the company’s CEO.
Topical Psoriasis Therapies and Unmet Patient Needs: The Importance of Optimizing Methotrexate
Although a wide variety of treatment modalities exist for the management of psoriasis, nontreatment, undertreatment, and treatment dissatisfaction represent key clinical challenges. Careful tailoring of therapeutic regimens to meet individual patient needs and priorities may therefore be critical to improving treatment adherence and clinical outcomes. Importantly, systemic therapies such as methotrexate (MTX) may be particularly useful for individualizing patient treatment regimens and appear to be underutilized components of treatment optimization.
A majority of psoriasis patients have mild to moderate disease and many are treated primarily with topical medications. Although these treatments generally are safe and effective, practical limitations (eg, formulation, ease of application) may affect patients’ treatment adherence and satisfaction even in the context of high efficacy. Systemic therapies, although associated with a distinct set of risks and treatment challenges, may enable patients to overcome many of these limitations, particularly in patients with moderate to severe disease or impaired quality of life as well as those with an inadequate response to or dissatisfaction with topical treatments.
Systemic Treatment Options
Among the systemic treatment options for psoriasis, biologic therapies often are most highly regarded due to their strong efficacy, although traditional systemic therapies such as MTX, cyclosporine, and acitretin remain important treatment options and have an extensive history in the treatment of psoriasis. In addition to typically being required by insurance companies prior to the initiation of biologic therapies, traditional systemic therapies also may be preferred by patients because of the options for oral and subcutaneous administration and their relatively low costs. Furthermore, systemic therapies may be critical in patients for whom biologic therapies are relatively contraindicated, such as those with an increased risk of infection, history of malignancy, or hypersensitivity to any of the product’s ingredients.
Among traditional systemic therapies, MTX is one of the most frequently used psoriasis treatment worldwide and can be highly effective for even severe cases. Importantly, MTX is a valuable component of combination treatments for psoriasis and is frequently coadministered with topical and biologic agents and phototherapy, suggesting that MTX may be a particularly useful option to consider when adjusting a patient’s treatment regimen.
Benefits of Subcutaneous Methotrexate Administration
Methotrexate can be delivered either orally or parenterally, contributing to its compatibility with a wide variety of psoriasis treatment regimens and patient preferences. Administration is predominantly oral in the United States, but parenteral MTX (most commonly delivered subcutaneously) can confer important benefits and is used regularly in countries outside of the United States.
An important advantage of subcutaneous versus oral MTX is greater bioavailability, particularly at higher doses. In studies of healthy volunteers or patients with rheumatoid arthritis, the bioavailability of MTX following oral administration appears to plateau at doses of 15 mg or higher,1 whereas that of subcutaneous MTX appears to increase linearly at a wide range of doses and exceeds that of oral MTX at each dose examined.1,2 A switch from oral to subcutaneous MTX may therefore benefit patients experiencing suboptimal disease control.
Another important benefit of subcutanoues versus oral MTX is the potential for reduced intensity of gastrointestinal adverse events.2,3 In a study of patients with rheumatoid arthritis, those who received subcutaneous MTX reported less severe nausea, vomiting, abdominal pain, and diarrhea than those who received oral MTX,3 which may improve treatment adherence and potentially enable patients to tolerate higher doses. Because gastrointestinal adverse events are a common cause of MTX treatment discontinuation, a switch from oral to subcutaneous MTX may be an important strategy to enable more patients to benefit from this treatment option.
Subcutaneous MTX presents some potential challenges, including patients’ fear of needles and difficulties with drawing and administering an accurate drug dose using a vial, needle, and syringe. However, recent developments in autoinjector technology have produced MTX injection devices that largely mitigate many of these challenges. Methotrexate autoinjectors allow for the accurate administration of prespecified doses, and patients generally find them easy to use.4 Furthermore, MTX autoinjectors have been associated with low levels of adminsitration-site pain (median pain score on a visual analog scale, 1.0/100 mm in one study4), and the concealment of a needle from view may potentially lessen needle phobia.
Role of Subcutaneous Methotrexate in Patient Care
The types of patients expected to benefit most from subcutaneous MTX include those with moderate to severe psoriasis and those who have experienced dissatisfaction with topical medications or phototherapy. The increased bioavailability of subcutaneous MTX as well as the reduced intensity of gastrointestinal adverse events compared with oral MTX may enable patients to achieve a greater clinical response, and the systemic route of administration may improve treatment adherence and patient satisfaction among those who are dissatisfied with topical treatment regimens. Notably, an additional benefit of optimizing MTX treatment may be the potential to prevent or delay progression to biologic therapies, which may be an important goal of both patients and physicians to prevent higher health care costs.
Another principal role of subcutaneous MTX is as a component of combination therapy with topicals or other systemic therapies for either long-term care or periodic treatment of disease flares. Methotrexate is a frequent component of combination therapies, and subcutaneous administration may be preferable for many patients, particularly those who are already accustomed to injectable therapies (eg, biologic agents) and those who regularly visit a physician who can perform the injections (eg, for regular phototherapy treatments). Interestingly, the coadministration of MTX may be especially valuable in the context of biologic therapies, as concomitant MTX is associated with a reduced incidence of antidrug antibodies and may therefore enhance or prolong responses to biologic agents.
Final Thoughts
Because subcutaneous MTX is infrequently used for the treatment of psoriasis in the United States, increased awareness of its unique advantages may provide new opportunities for patients to tailor treatment regimens to meet individual needs and preferences. Treatment optimization across a broad range of patient characteristics may be critical to improving adherence and satisfaction in psoriasis patients and may be considered a major therapeutic goal.
Acknowledgment
Medical writing assistance was provided by Anna Abt, PhD, of ETHOS Health Communications in Newtown, Pennsylvania, with financial support from LEO Pharma.
- Schiff MH, Jaffe JS, Freundlich B. Head-to-head, randomised, crossover study of oral versus subcutaneous methotrexate in patients with rheumatoid arthritis: drug-exposure limitations of oral methotrexate at doses ≥15 mg may be overcome with subcutaneous administration. Ann Rheum Dis. 2014;73:1549-1551.
- Pichlmeier U, Heuer KU. Subcutaneous administration of methotrexate with a prefilled autoinjector pen results in a higher relative bioavailability compared with oral administration of methotrexate. Clin Exp Rheumatol. 2014;32:563-571.
- Rutkowska-Sak L, Rell-Bakalarska M, Lisowska B. Oral vs. subcutaneous low-dose methotrexate treatment in reducing gastrointestinal side effects. Reumatologia. 2009;47:207-211.
- Freundlich B, Kivitz A, Jaffe JS. Nearly pain-free self-administration of subcutaneous methotrexate with an autoinjector: results of a phase 2 clinical trial in patients with rheumatoid arthritis who have functional limitations. J Clin Rheumatol. 2014;20:256-260.
Although a wide variety of treatment modalities exist for the management of psoriasis, nontreatment, undertreatment, and treatment dissatisfaction represent key clinical challenges. Careful tailoring of therapeutic regimens to meet individual patient needs and priorities may therefore be critical to improving treatment adherence and clinical outcomes. Importantly, systemic therapies such as methotrexate (MTX) may be particularly useful for individualizing patient treatment regimens and appear to be underutilized components of treatment optimization.
A majority of psoriasis patients have mild to moderate disease and many are treated primarily with topical medications. Although these treatments generally are safe and effective, practical limitations (eg, formulation, ease of application) may affect patients’ treatment adherence and satisfaction even in the context of high efficacy. Systemic therapies, although associated with a distinct set of risks and treatment challenges, may enable patients to overcome many of these limitations, particularly in patients with moderate to severe disease or impaired quality of life as well as those with an inadequate response to or dissatisfaction with topical treatments.
Systemic Treatment Options
Among the systemic treatment options for psoriasis, biologic therapies often are most highly regarded due to their strong efficacy, although traditional systemic therapies such as MTX, cyclosporine, and acitretin remain important treatment options and have an extensive history in the treatment of psoriasis. In addition to typically being required by insurance companies prior to the initiation of biologic therapies, traditional systemic therapies also may be preferred by patients because of the options for oral and subcutaneous administration and their relatively low costs. Furthermore, systemic therapies may be critical in patients for whom biologic therapies are relatively contraindicated, such as those with an increased risk of infection, history of malignancy, or hypersensitivity to any of the product’s ingredients.
Among traditional systemic therapies, MTX is one of the most frequently used psoriasis treatment worldwide and can be highly effective for even severe cases. Importantly, MTX is a valuable component of combination treatments for psoriasis and is frequently coadministered with topical and biologic agents and phototherapy, suggesting that MTX may be a particularly useful option to consider when adjusting a patient’s treatment regimen.
Benefits of Subcutaneous Methotrexate Administration
Methotrexate can be delivered either orally or parenterally, contributing to its compatibility with a wide variety of psoriasis treatment regimens and patient preferences. Administration is predominantly oral in the United States, but parenteral MTX (most commonly delivered subcutaneously) can confer important benefits and is used regularly in countries outside of the United States.
An important advantage of subcutaneous versus oral MTX is greater bioavailability, particularly at higher doses. In studies of healthy volunteers or patients with rheumatoid arthritis, the bioavailability of MTX following oral administration appears to plateau at doses of 15 mg or higher,1 whereas that of subcutaneous MTX appears to increase linearly at a wide range of doses and exceeds that of oral MTX at each dose examined.1,2 A switch from oral to subcutaneous MTX may therefore benefit patients experiencing suboptimal disease control.
Another important benefit of subcutanoues versus oral MTX is the potential for reduced intensity of gastrointestinal adverse events.2,3 In a study of patients with rheumatoid arthritis, those who received subcutaneous MTX reported less severe nausea, vomiting, abdominal pain, and diarrhea than those who received oral MTX,3 which may improve treatment adherence and potentially enable patients to tolerate higher doses. Because gastrointestinal adverse events are a common cause of MTX treatment discontinuation, a switch from oral to subcutaneous MTX may be an important strategy to enable more patients to benefit from this treatment option.
Subcutaneous MTX presents some potential challenges, including patients’ fear of needles and difficulties with drawing and administering an accurate drug dose using a vial, needle, and syringe. However, recent developments in autoinjector technology have produced MTX injection devices that largely mitigate many of these challenges. Methotrexate autoinjectors allow for the accurate administration of prespecified doses, and patients generally find them easy to use.4 Furthermore, MTX autoinjectors have been associated with low levels of adminsitration-site pain (median pain score on a visual analog scale, 1.0/100 mm in one study4), and the concealment of a needle from view may potentially lessen needle phobia.
Role of Subcutaneous Methotrexate in Patient Care
The types of patients expected to benefit most from subcutaneous MTX include those with moderate to severe psoriasis and those who have experienced dissatisfaction with topical medications or phototherapy. The increased bioavailability of subcutaneous MTX as well as the reduced intensity of gastrointestinal adverse events compared with oral MTX may enable patients to achieve a greater clinical response, and the systemic route of administration may improve treatment adherence and patient satisfaction among those who are dissatisfied with topical treatment regimens. Notably, an additional benefit of optimizing MTX treatment may be the potential to prevent or delay progression to biologic therapies, which may be an important goal of both patients and physicians to prevent higher health care costs.
Another principal role of subcutaneous MTX is as a component of combination therapy with topicals or other systemic therapies for either long-term care or periodic treatment of disease flares. Methotrexate is a frequent component of combination therapies, and subcutaneous administration may be preferable for many patients, particularly those who are already accustomed to injectable therapies (eg, biologic agents) and those who regularly visit a physician who can perform the injections (eg, for regular phototherapy treatments). Interestingly, the coadministration of MTX may be especially valuable in the context of biologic therapies, as concomitant MTX is associated with a reduced incidence of antidrug antibodies and may therefore enhance or prolong responses to biologic agents.
Final Thoughts
Because subcutaneous MTX is infrequently used for the treatment of psoriasis in the United States, increased awareness of its unique advantages may provide new opportunities for patients to tailor treatment regimens to meet individual needs and preferences. Treatment optimization across a broad range of patient characteristics may be critical to improving adherence and satisfaction in psoriasis patients and may be considered a major therapeutic goal.
Acknowledgment
Medical writing assistance was provided by Anna Abt, PhD, of ETHOS Health Communications in Newtown, Pennsylvania, with financial support from LEO Pharma.
Although a wide variety of treatment modalities exist for the management of psoriasis, nontreatment, undertreatment, and treatment dissatisfaction represent key clinical challenges. Careful tailoring of therapeutic regimens to meet individual patient needs and priorities may therefore be critical to improving treatment adherence and clinical outcomes. Importantly, systemic therapies such as methotrexate (MTX) may be particularly useful for individualizing patient treatment regimens and appear to be underutilized components of treatment optimization.
A majority of psoriasis patients have mild to moderate disease and many are treated primarily with topical medications. Although these treatments generally are safe and effective, practical limitations (eg, formulation, ease of application) may affect patients’ treatment adherence and satisfaction even in the context of high efficacy. Systemic therapies, although associated with a distinct set of risks and treatment challenges, may enable patients to overcome many of these limitations, particularly in patients with moderate to severe disease or impaired quality of life as well as those with an inadequate response to or dissatisfaction with topical treatments.
Systemic Treatment Options
Among the systemic treatment options for psoriasis, biologic therapies often are most highly regarded due to their strong efficacy, although traditional systemic therapies such as MTX, cyclosporine, and acitretin remain important treatment options and have an extensive history in the treatment of psoriasis. In addition to typically being required by insurance companies prior to the initiation of biologic therapies, traditional systemic therapies also may be preferred by patients because of the options for oral and subcutaneous administration and their relatively low costs. Furthermore, systemic therapies may be critical in patients for whom biologic therapies are relatively contraindicated, such as those with an increased risk of infection, history of malignancy, or hypersensitivity to any of the product’s ingredients.
Among traditional systemic therapies, MTX is one of the most frequently used psoriasis treatment worldwide and can be highly effective for even severe cases. Importantly, MTX is a valuable component of combination treatments for psoriasis and is frequently coadministered with topical and biologic agents and phototherapy, suggesting that MTX may be a particularly useful option to consider when adjusting a patient’s treatment regimen.
Benefits of Subcutaneous Methotrexate Administration
Methotrexate can be delivered either orally or parenterally, contributing to its compatibility with a wide variety of psoriasis treatment regimens and patient preferences. Administration is predominantly oral in the United States, but parenteral MTX (most commonly delivered subcutaneously) can confer important benefits and is used regularly in countries outside of the United States.
An important advantage of subcutaneous versus oral MTX is greater bioavailability, particularly at higher doses. In studies of healthy volunteers or patients with rheumatoid arthritis, the bioavailability of MTX following oral administration appears to plateau at doses of 15 mg or higher,1 whereas that of subcutaneous MTX appears to increase linearly at a wide range of doses and exceeds that of oral MTX at each dose examined.1,2 A switch from oral to subcutaneous MTX may therefore benefit patients experiencing suboptimal disease control.
Another important benefit of subcutanoues versus oral MTX is the potential for reduced intensity of gastrointestinal adverse events.2,3 In a study of patients with rheumatoid arthritis, those who received subcutaneous MTX reported less severe nausea, vomiting, abdominal pain, and diarrhea than those who received oral MTX,3 which may improve treatment adherence and potentially enable patients to tolerate higher doses. Because gastrointestinal adverse events are a common cause of MTX treatment discontinuation, a switch from oral to subcutaneous MTX may be an important strategy to enable more patients to benefit from this treatment option.
Subcutaneous MTX presents some potential challenges, including patients’ fear of needles and difficulties with drawing and administering an accurate drug dose using a vial, needle, and syringe. However, recent developments in autoinjector technology have produced MTX injection devices that largely mitigate many of these challenges. Methotrexate autoinjectors allow for the accurate administration of prespecified doses, and patients generally find them easy to use.4 Furthermore, MTX autoinjectors have been associated with low levels of adminsitration-site pain (median pain score on a visual analog scale, 1.0/100 mm in one study4), and the concealment of a needle from view may potentially lessen needle phobia.
Role of Subcutaneous Methotrexate in Patient Care
The types of patients expected to benefit most from subcutaneous MTX include those with moderate to severe psoriasis and those who have experienced dissatisfaction with topical medications or phototherapy. The increased bioavailability of subcutaneous MTX as well as the reduced intensity of gastrointestinal adverse events compared with oral MTX may enable patients to achieve a greater clinical response, and the systemic route of administration may improve treatment adherence and patient satisfaction among those who are dissatisfied with topical treatment regimens. Notably, an additional benefit of optimizing MTX treatment may be the potential to prevent or delay progression to biologic therapies, which may be an important goal of both patients and physicians to prevent higher health care costs.
Another principal role of subcutaneous MTX is as a component of combination therapy with topicals or other systemic therapies for either long-term care or periodic treatment of disease flares. Methotrexate is a frequent component of combination therapies, and subcutaneous administration may be preferable for many patients, particularly those who are already accustomed to injectable therapies (eg, biologic agents) and those who regularly visit a physician who can perform the injections (eg, for regular phototherapy treatments). Interestingly, the coadministration of MTX may be especially valuable in the context of biologic therapies, as concomitant MTX is associated with a reduced incidence of antidrug antibodies and may therefore enhance or prolong responses to biologic agents.
Final Thoughts
Because subcutaneous MTX is infrequently used for the treatment of psoriasis in the United States, increased awareness of its unique advantages may provide new opportunities for patients to tailor treatment regimens to meet individual needs and preferences. Treatment optimization across a broad range of patient characteristics may be critical to improving adherence and satisfaction in psoriasis patients and may be considered a major therapeutic goal.
Acknowledgment
Medical writing assistance was provided by Anna Abt, PhD, of ETHOS Health Communications in Newtown, Pennsylvania, with financial support from LEO Pharma.
- Schiff MH, Jaffe JS, Freundlich B. Head-to-head, randomised, crossover study of oral versus subcutaneous methotrexate in patients with rheumatoid arthritis: drug-exposure limitations of oral methotrexate at doses ≥15 mg may be overcome with subcutaneous administration. Ann Rheum Dis. 2014;73:1549-1551.
- Pichlmeier U, Heuer KU. Subcutaneous administration of methotrexate with a prefilled autoinjector pen results in a higher relative bioavailability compared with oral administration of methotrexate. Clin Exp Rheumatol. 2014;32:563-571.
- Rutkowska-Sak L, Rell-Bakalarska M, Lisowska B. Oral vs. subcutaneous low-dose methotrexate treatment in reducing gastrointestinal side effects. Reumatologia. 2009;47:207-211.
- Freundlich B, Kivitz A, Jaffe JS. Nearly pain-free self-administration of subcutaneous methotrexate with an autoinjector: results of a phase 2 clinical trial in patients with rheumatoid arthritis who have functional limitations. J Clin Rheumatol. 2014;20:256-260.
- Schiff MH, Jaffe JS, Freundlich B. Head-to-head, randomised, crossover study of oral versus subcutaneous methotrexate in patients with rheumatoid arthritis: drug-exposure limitations of oral methotrexate at doses ≥15 mg may be overcome with subcutaneous administration. Ann Rheum Dis. 2014;73:1549-1551.
- Pichlmeier U, Heuer KU. Subcutaneous administration of methotrexate with a prefilled autoinjector pen results in a higher relative bioavailability compared with oral administration of methotrexate. Clin Exp Rheumatol. 2014;32:563-571.
- Rutkowska-Sak L, Rell-Bakalarska M, Lisowska B. Oral vs. subcutaneous low-dose methotrexate treatment in reducing gastrointestinal side effects. Reumatologia. 2009;47:207-211.
- Freundlich B, Kivitz A, Jaffe JS. Nearly pain-free self-administration of subcutaneous methotrexate with an autoinjector: results of a phase 2 clinical trial in patients with rheumatoid arthritis who have functional limitations. J Clin Rheumatol. 2014;20:256-260.