User login
TNF inhibitor–induced psoriasis treatment algorithm maintains TNF inhibitor if possible
In a single-center retrospective analysis of 102 patients with psoriasis induced by tumor necrosis factor (TNF) inhibitors, most cases improved or resolved with use of topical medications or with discontinuation of the inciting TNF inhibitor, with or without other interventions. All patients were treated and diagnosed by dermatologists.
While TNF inhibitors have revolutionized management of numerous debilitating chronic inflammatory diseases, they are associated with mild and potentially serious adverse reactions, including de novo psoriasiform eruptions, noted Sean E. Mazloom, MD, and colleagues, at the Cleveland Clinic, Cleveland, Ohio, in the Journal of the American Academy of Dermatology. Despite the fact that it has been more than 15 years since the first reports of TNF inhibitor-induced psoriasis, optimal treatment strategies still remain poorly understood.
IBD and RA most common
Dr. Mazloom and colleagues identified 102 patients (median onset, 41 years; 72.5% female) with TNF inhibitor-induced psoriasis seen at a single tertiary care institution (the Cleveland Clinic) over a 10-year period. The authors proposed a treatment algorithm based on their findings.
Inciting TNF inhibitors were prescribed most commonly for inflammatory bowel disease (IBD) (52%) and rheumatoid arthritis (RA) (24.5%). The most common inciting TNF inhibitor was infliximab (52%). TNF inhibitor-induced psoriasis improved or resolved with topical medications alone in 63.5% of patients, and cyclosporine and methotrexate (10 mg weekly) were often effective (cyclosporine in five of five patients; methotrexate in 7 of 13) if topicals failed.
Noting that the success with topicals in this cohort exceeded that of earlier reports, the authors suggested that more accurate diagnoses and optimal strategies attributable to the involvement of dermatologists may be explanatory.
In 67% of refractory cases, discontinuation of the inciting TNF inhibitor with or without other interventions improved or resolved TNF inhibitor-induced psoriasis. With switching of TNF inhibitors, persistence or worsening of TNF inhibitor-induced psoriasis was reported in 16 of 25 patients (64%).
Algorithm aims at balancing control
The treatment algorithm proposed by Dr. Mazloom and colleagues aims at balancing control of the primary disease with minimization of skin symptom discomfort and continuation of the inciting TNF inhibitor if possible. Only with cyclosporine or methotrexate failure amid severe symptoms and less-than-optimal primary disease control should TNF inhibitors be discontinued and biologics and/or small-molecule inhibitors with alternative mechanisms of action be introduced. Transitioning to other TNF inhibitors may be tried before alternative strategies when the underlying disease is well-controlled but TNF inhibitor-induced psoriasis remains severe.
“Most dermatologists who see TNF-induced psoriasis often are likely already using strategies like the one proposed in the algorithm,” commented senior author Anthony Fernandez, MD, PhD, of the Cleveland (Ohio) Clinic, in an interview. “The concern is over those who may not see TNF inhibitor-induced psoriasis very often, and who may, as a knee-jerk response to TNF-induced psoriasis, stop the inciting medication. When strong side effects occur in IBD and RA, it’s critical to know how well the TNF inhibitor is controlling the underlying disease because lack of control can lead to permanent damage.”
Risk to benefit ratio favors retaining TNF inhibitors
The dermatologist’s goal, if the TNF inhibitor is working well, should be to exhaust all reasonable options to control the psoriasiform eruption and keep the patient on the TNF inhibitor rather than turn to potentially less effective alternatives, Dr. Fernandez added. “The risk:benefit ratio still usually favors adding more immune therapies to treat these reactions in order to enable patients to stay” on their TNF inhibitors.
Study authors disclosed no direct funding for the study. Dr Fernandez, the senior author, receives research funding from Pfizer, Mallinckrodt, and Novartis, consults for AbbVie and Celgene, and is a speaker for AbbVie and Mallinckrodt.
SOURCE: Mazloom SE et al. J Am Acad Dermatol. 2020 Dec;83(6):1590-8.
In a single-center retrospective analysis of 102 patients with psoriasis induced by tumor necrosis factor (TNF) inhibitors, most cases improved or resolved with use of topical medications or with discontinuation of the inciting TNF inhibitor, with or without other interventions. All patients were treated and diagnosed by dermatologists.
While TNF inhibitors have revolutionized management of numerous debilitating chronic inflammatory diseases, they are associated with mild and potentially serious adverse reactions, including de novo psoriasiform eruptions, noted Sean E. Mazloom, MD, and colleagues, at the Cleveland Clinic, Cleveland, Ohio, in the Journal of the American Academy of Dermatology. Despite the fact that it has been more than 15 years since the first reports of TNF inhibitor-induced psoriasis, optimal treatment strategies still remain poorly understood.
IBD and RA most common
Dr. Mazloom and colleagues identified 102 patients (median onset, 41 years; 72.5% female) with TNF inhibitor-induced psoriasis seen at a single tertiary care institution (the Cleveland Clinic) over a 10-year period. The authors proposed a treatment algorithm based on their findings.
Inciting TNF inhibitors were prescribed most commonly for inflammatory bowel disease (IBD) (52%) and rheumatoid arthritis (RA) (24.5%). The most common inciting TNF inhibitor was infliximab (52%). TNF inhibitor-induced psoriasis improved or resolved with topical medications alone in 63.5% of patients, and cyclosporine and methotrexate (10 mg weekly) were often effective (cyclosporine in five of five patients; methotrexate in 7 of 13) if topicals failed.
Noting that the success with topicals in this cohort exceeded that of earlier reports, the authors suggested that more accurate diagnoses and optimal strategies attributable to the involvement of dermatologists may be explanatory.
In 67% of refractory cases, discontinuation of the inciting TNF inhibitor with or without other interventions improved or resolved TNF inhibitor-induced psoriasis. With switching of TNF inhibitors, persistence or worsening of TNF inhibitor-induced psoriasis was reported in 16 of 25 patients (64%).
Algorithm aims at balancing control
The treatment algorithm proposed by Dr. Mazloom and colleagues aims at balancing control of the primary disease with minimization of skin symptom discomfort and continuation of the inciting TNF inhibitor if possible. Only with cyclosporine or methotrexate failure amid severe symptoms and less-than-optimal primary disease control should TNF inhibitors be discontinued and biologics and/or small-molecule inhibitors with alternative mechanisms of action be introduced. Transitioning to other TNF inhibitors may be tried before alternative strategies when the underlying disease is well-controlled but TNF inhibitor-induced psoriasis remains severe.
“Most dermatologists who see TNF-induced psoriasis often are likely already using strategies like the one proposed in the algorithm,” commented senior author Anthony Fernandez, MD, PhD, of the Cleveland (Ohio) Clinic, in an interview. “The concern is over those who may not see TNF inhibitor-induced psoriasis very often, and who may, as a knee-jerk response to TNF-induced psoriasis, stop the inciting medication. When strong side effects occur in IBD and RA, it’s critical to know how well the TNF inhibitor is controlling the underlying disease because lack of control can lead to permanent damage.”
Risk to benefit ratio favors retaining TNF inhibitors
The dermatologist’s goal, if the TNF inhibitor is working well, should be to exhaust all reasonable options to control the psoriasiform eruption and keep the patient on the TNF inhibitor rather than turn to potentially less effective alternatives, Dr. Fernandez added. “The risk:benefit ratio still usually favors adding more immune therapies to treat these reactions in order to enable patients to stay” on their TNF inhibitors.
Study authors disclosed no direct funding for the study. Dr Fernandez, the senior author, receives research funding from Pfizer, Mallinckrodt, and Novartis, consults for AbbVie and Celgene, and is a speaker for AbbVie and Mallinckrodt.
SOURCE: Mazloom SE et al. J Am Acad Dermatol. 2020 Dec;83(6):1590-8.
In a single-center retrospective analysis of 102 patients with psoriasis induced by tumor necrosis factor (TNF) inhibitors, most cases improved or resolved with use of topical medications or with discontinuation of the inciting TNF inhibitor, with or without other interventions. All patients were treated and diagnosed by dermatologists.
While TNF inhibitors have revolutionized management of numerous debilitating chronic inflammatory diseases, they are associated with mild and potentially serious adverse reactions, including de novo psoriasiform eruptions, noted Sean E. Mazloom, MD, and colleagues, at the Cleveland Clinic, Cleveland, Ohio, in the Journal of the American Academy of Dermatology. Despite the fact that it has been more than 15 years since the first reports of TNF inhibitor-induced psoriasis, optimal treatment strategies still remain poorly understood.
IBD and RA most common
Dr. Mazloom and colleagues identified 102 patients (median onset, 41 years; 72.5% female) with TNF inhibitor-induced psoriasis seen at a single tertiary care institution (the Cleveland Clinic) over a 10-year period. The authors proposed a treatment algorithm based on their findings.
Inciting TNF inhibitors were prescribed most commonly for inflammatory bowel disease (IBD) (52%) and rheumatoid arthritis (RA) (24.5%). The most common inciting TNF inhibitor was infliximab (52%). TNF inhibitor-induced psoriasis improved or resolved with topical medications alone in 63.5% of patients, and cyclosporine and methotrexate (10 mg weekly) were often effective (cyclosporine in five of five patients; methotrexate in 7 of 13) if topicals failed.
Noting that the success with topicals in this cohort exceeded that of earlier reports, the authors suggested that more accurate diagnoses and optimal strategies attributable to the involvement of dermatologists may be explanatory.
In 67% of refractory cases, discontinuation of the inciting TNF inhibitor with or without other interventions improved or resolved TNF inhibitor-induced psoriasis. With switching of TNF inhibitors, persistence or worsening of TNF inhibitor-induced psoriasis was reported in 16 of 25 patients (64%).
Algorithm aims at balancing control
The treatment algorithm proposed by Dr. Mazloom and colleagues aims at balancing control of the primary disease with minimization of skin symptom discomfort and continuation of the inciting TNF inhibitor if possible. Only with cyclosporine or methotrexate failure amid severe symptoms and less-than-optimal primary disease control should TNF inhibitors be discontinued and biologics and/or small-molecule inhibitors with alternative mechanisms of action be introduced. Transitioning to other TNF inhibitors may be tried before alternative strategies when the underlying disease is well-controlled but TNF inhibitor-induced psoriasis remains severe.
“Most dermatologists who see TNF-induced psoriasis often are likely already using strategies like the one proposed in the algorithm,” commented senior author Anthony Fernandez, MD, PhD, of the Cleveland (Ohio) Clinic, in an interview. “The concern is over those who may not see TNF inhibitor-induced psoriasis very often, and who may, as a knee-jerk response to TNF-induced psoriasis, stop the inciting medication. When strong side effects occur in IBD and RA, it’s critical to know how well the TNF inhibitor is controlling the underlying disease because lack of control can lead to permanent damage.”
Risk to benefit ratio favors retaining TNF inhibitors
The dermatologist’s goal, if the TNF inhibitor is working well, should be to exhaust all reasonable options to control the psoriasiform eruption and keep the patient on the TNF inhibitor rather than turn to potentially less effective alternatives, Dr. Fernandez added. “The risk:benefit ratio still usually favors adding more immune therapies to treat these reactions in order to enable patients to stay” on their TNF inhibitors.
Study authors disclosed no direct funding for the study. Dr Fernandez, the senior author, receives research funding from Pfizer, Mallinckrodt, and Novartis, consults for AbbVie and Celgene, and is a speaker for AbbVie and Mallinckrodt.
SOURCE: Mazloom SE et al. J Am Acad Dermatol. 2020 Dec;83(6):1590-8.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Golimumab preserves insulin production in type 1 diabetes
The human monoclonal antibody golimumab (Simponi) preserved endogenous insulin secretion in patients with new-onset type 1 diabetes and reduced their exogenous insulin requirements at 1 year, newly published phase 2 data indicate.
Results from the multicenter, double-blind, placebo-controlled trial were first reported as a poster at the virtual American Diabetes Association 80th Scientific Sessions in June. They were published online Nov. 18 in the New England Journal of Medicine.
In the 52-week study of 84 children and adults with new-onset type 1 diabetes, those given golimumab injections every 2 weeks had significantly higher levels of C-peptide, a marker of insulin secretion, and required less injected or infused insulin than did those who received placebo injections. There were no treatment-associated serious adverse events.
Golimumab is a human monoclonal antibody specific for tumor necrosis factor–alpha. It is approved for the treatment of several autoimmune diseases, including rheumatoid arthritis and ulcerative colitis, in the United States, Europe, and elsewhere.
An intermediate step toward a cure
Although none of the patients were able to stop taking insulin entirely, the results have important clinical implications, lead author Teresa Quattrin, MD, said in an interview.
“People want a cure, but the fact is, a cure is not available yet. So, this is an intermediate step towards a cure.... There are advantages to being on a small insulin dose,” including lower rates of hypoglycemia and maintenance of intraportal insulin, said Dr. Quattrin, of the State University of New York at Buffalo.
But in an accompanying editorial, Domenico Accili, MD, points to potential risks from immunotherapy and from attempting additional interventions at an “emotionally fraught” time when patients and families are coping with the new diabetes diagnosis.
He said of golimumab, “the effect is actually very small. ... There’s nothing wrong in and of itself with improving those outcomes. I just wouldn’t assign them as game changers.”
If this or a similar immunotherapeutic intervention were approved for this indication, “I would tell patients it exists and let them make the decision whether they want to try it. I wouldn’t say you must try it,” said Dr. Accili, of the Columbia University Diabetes and Endocrinology Research Center, New York.
With golimumab, higher C-peptide, lower insulin requirement
Of the 84 patients, who ranged in age from 6 to 21 years, 56 were randomly assigned within 100 days of being diagnosed with type 1 diabetes to receive golimumab, and 28 were assigned to receive placebo injections, given every 2 weeks.
The drug resulted in lower insulin use (0.51U/Kg per day vs. 0.69 U/kg per day), and the increase in insulin use over 52 weeks was less with golimumab than with placebo (0.07 vs. 0.24 U/kg per day; P = .001).
The mean percent decrease of C-peptide production from baseline was 12% with golimumab versus 56% with placebo.
Although the mean number of overall hypoglycemic events was similar, the mean number of level 2 hypoglycemic events (<54 mg/dL) was 36% lower with golimumab (11.5 vs. 17.6). There were no severe cases of hypoglycemia in either group.
No severe or serious infections occurred in either group, although mild to moderate infections were reported in 71% with golimumab versus 61% with placebo. More patients in the golimumab group experienced a decrease in neutrophils (29% vs. 19%).
Immunotherapy: Which one, and when should it start?
These findings come on the heels of the 2019 landmark results with another monoclonal antibody, the investigational anti-CD3 teplizumab (PRV-031). Among patients at risk, a diagnosis of type 1 diabetes was delayed by 2 years, and continued benefit was seen at 3 years.
However, Dr. Quattrin said teplizumab is limited by the fact that it must be administered via a 14-day infusion, whereas golimumab can be injected by patients themselves at home.
Moreover, the phase 2 teplizumab study was conducted in people who had antibodies that placed them at high risk for type 1 diabetes, but those patients did not yet have the condition. They were identified because they had close relatives with type 1 diabetes and were enrolled in the federally funded TrialNet screening program.
Dr. Quattrin is now participating in an ongoing phase 3 study of teplizumab that involves patients newly diagnosed with type 1 diabetes.
A Janssen spokesperson said in an interview that the company isn’t planning to further develop golimumab for use in type 1 diabetes.
“Our focus is to apply insights from the phase 2 ... proof-of-concept study to progress what we believe are novel, immunologically targeted pipeline candidates in stage 2 disease or presymptomatic stages of type 1 diabetes, which is consistent with our mission to intercept and prevent type 1 diabetes,” the spokesperson said.
To identify more individuals at risk for type 1 diabetes beyond the close relatives of those who already have it, so as to be able to intervene at a presymptomatic stage, Janssen is organizing a public-private effort to advocate for routine population screening for type 1 diabetes–related autoantibodies.
Dr. Quattrin said: “Preserving some insulin is key. Having somebody with beta cell functioning still is an intermediate step to a cure and will make their life easier, and that’s what people should care about.”
Dr. Accili, who cofounded and leads a company working on a novel approach to type 1 diabetes treatment, writes in his editorial: “We should also be mindful that this treatment debate is first world–centric.
“Current treatments for type 1 diabetes require resources not readily available in most parts of the world, where something as simple as refrigeration of insulin can become a logistic nightmare. While combinations of [approaches] tailored to individual risk and potential benefits are likely to make inroads in clinical practice, the need for a simpler, safer, and equally effective alternative to insulin remains,” he wrote.
Dr. Quattrin is a researcher and consultant for Janssen and conducts clinical trials for Provention Bio, Opko, and Ascendis. Dr. Accili is founder and director of Forkhead Therapeutics.
A version of this article originally appeared on Medscape.com.
The human monoclonal antibody golimumab (Simponi) preserved endogenous insulin secretion in patients with new-onset type 1 diabetes and reduced their exogenous insulin requirements at 1 year, newly published phase 2 data indicate.
Results from the multicenter, double-blind, placebo-controlled trial were first reported as a poster at the virtual American Diabetes Association 80th Scientific Sessions in June. They were published online Nov. 18 in the New England Journal of Medicine.
In the 52-week study of 84 children and adults with new-onset type 1 diabetes, those given golimumab injections every 2 weeks had significantly higher levels of C-peptide, a marker of insulin secretion, and required less injected or infused insulin than did those who received placebo injections. There were no treatment-associated serious adverse events.
Golimumab is a human monoclonal antibody specific for tumor necrosis factor–alpha. It is approved for the treatment of several autoimmune diseases, including rheumatoid arthritis and ulcerative colitis, in the United States, Europe, and elsewhere.
An intermediate step toward a cure
Although none of the patients were able to stop taking insulin entirely, the results have important clinical implications, lead author Teresa Quattrin, MD, said in an interview.
“People want a cure, but the fact is, a cure is not available yet. So, this is an intermediate step towards a cure.... There are advantages to being on a small insulin dose,” including lower rates of hypoglycemia and maintenance of intraportal insulin, said Dr. Quattrin, of the State University of New York at Buffalo.
But in an accompanying editorial, Domenico Accili, MD, points to potential risks from immunotherapy and from attempting additional interventions at an “emotionally fraught” time when patients and families are coping with the new diabetes diagnosis.
He said of golimumab, “the effect is actually very small. ... There’s nothing wrong in and of itself with improving those outcomes. I just wouldn’t assign them as game changers.”
If this or a similar immunotherapeutic intervention were approved for this indication, “I would tell patients it exists and let them make the decision whether they want to try it. I wouldn’t say you must try it,” said Dr. Accili, of the Columbia University Diabetes and Endocrinology Research Center, New York.
With golimumab, higher C-peptide, lower insulin requirement
Of the 84 patients, who ranged in age from 6 to 21 years, 56 were randomly assigned within 100 days of being diagnosed with type 1 diabetes to receive golimumab, and 28 were assigned to receive placebo injections, given every 2 weeks.
The drug resulted in lower insulin use (0.51U/Kg per day vs. 0.69 U/kg per day), and the increase in insulin use over 52 weeks was less with golimumab than with placebo (0.07 vs. 0.24 U/kg per day; P = .001).
The mean percent decrease of C-peptide production from baseline was 12% with golimumab versus 56% with placebo.
Although the mean number of overall hypoglycemic events was similar, the mean number of level 2 hypoglycemic events (<54 mg/dL) was 36% lower with golimumab (11.5 vs. 17.6). There were no severe cases of hypoglycemia in either group.
No severe or serious infections occurred in either group, although mild to moderate infections were reported in 71% with golimumab versus 61% with placebo. More patients in the golimumab group experienced a decrease in neutrophils (29% vs. 19%).
Immunotherapy: Which one, and when should it start?
These findings come on the heels of the 2019 landmark results with another monoclonal antibody, the investigational anti-CD3 teplizumab (PRV-031). Among patients at risk, a diagnosis of type 1 diabetes was delayed by 2 years, and continued benefit was seen at 3 years.
However, Dr. Quattrin said teplizumab is limited by the fact that it must be administered via a 14-day infusion, whereas golimumab can be injected by patients themselves at home.
Moreover, the phase 2 teplizumab study was conducted in people who had antibodies that placed them at high risk for type 1 diabetes, but those patients did not yet have the condition. They were identified because they had close relatives with type 1 diabetes and were enrolled in the federally funded TrialNet screening program.
Dr. Quattrin is now participating in an ongoing phase 3 study of teplizumab that involves patients newly diagnosed with type 1 diabetes.
A Janssen spokesperson said in an interview that the company isn’t planning to further develop golimumab for use in type 1 diabetes.
“Our focus is to apply insights from the phase 2 ... proof-of-concept study to progress what we believe are novel, immunologically targeted pipeline candidates in stage 2 disease or presymptomatic stages of type 1 diabetes, which is consistent with our mission to intercept and prevent type 1 diabetes,” the spokesperson said.
To identify more individuals at risk for type 1 diabetes beyond the close relatives of those who already have it, so as to be able to intervene at a presymptomatic stage, Janssen is organizing a public-private effort to advocate for routine population screening for type 1 diabetes–related autoantibodies.
Dr. Quattrin said: “Preserving some insulin is key. Having somebody with beta cell functioning still is an intermediate step to a cure and will make their life easier, and that’s what people should care about.”
Dr. Accili, who cofounded and leads a company working on a novel approach to type 1 diabetes treatment, writes in his editorial: “We should also be mindful that this treatment debate is first world–centric.
“Current treatments for type 1 diabetes require resources not readily available in most parts of the world, where something as simple as refrigeration of insulin can become a logistic nightmare. While combinations of [approaches] tailored to individual risk and potential benefits are likely to make inroads in clinical practice, the need for a simpler, safer, and equally effective alternative to insulin remains,” he wrote.
Dr. Quattrin is a researcher and consultant for Janssen and conducts clinical trials for Provention Bio, Opko, and Ascendis. Dr. Accili is founder and director of Forkhead Therapeutics.
A version of this article originally appeared on Medscape.com.
The human monoclonal antibody golimumab (Simponi) preserved endogenous insulin secretion in patients with new-onset type 1 diabetes and reduced their exogenous insulin requirements at 1 year, newly published phase 2 data indicate.
Results from the multicenter, double-blind, placebo-controlled trial were first reported as a poster at the virtual American Diabetes Association 80th Scientific Sessions in June. They were published online Nov. 18 in the New England Journal of Medicine.
In the 52-week study of 84 children and adults with new-onset type 1 diabetes, those given golimumab injections every 2 weeks had significantly higher levels of C-peptide, a marker of insulin secretion, and required less injected or infused insulin than did those who received placebo injections. There were no treatment-associated serious adverse events.
Golimumab is a human monoclonal antibody specific for tumor necrosis factor–alpha. It is approved for the treatment of several autoimmune diseases, including rheumatoid arthritis and ulcerative colitis, in the United States, Europe, and elsewhere.
An intermediate step toward a cure
Although none of the patients were able to stop taking insulin entirely, the results have important clinical implications, lead author Teresa Quattrin, MD, said in an interview.
“People want a cure, but the fact is, a cure is not available yet. So, this is an intermediate step towards a cure.... There are advantages to being on a small insulin dose,” including lower rates of hypoglycemia and maintenance of intraportal insulin, said Dr. Quattrin, of the State University of New York at Buffalo.
But in an accompanying editorial, Domenico Accili, MD, points to potential risks from immunotherapy and from attempting additional interventions at an “emotionally fraught” time when patients and families are coping with the new diabetes diagnosis.
He said of golimumab, “the effect is actually very small. ... There’s nothing wrong in and of itself with improving those outcomes. I just wouldn’t assign them as game changers.”
If this or a similar immunotherapeutic intervention were approved for this indication, “I would tell patients it exists and let them make the decision whether they want to try it. I wouldn’t say you must try it,” said Dr. Accili, of the Columbia University Diabetes and Endocrinology Research Center, New York.
With golimumab, higher C-peptide, lower insulin requirement
Of the 84 patients, who ranged in age from 6 to 21 years, 56 were randomly assigned within 100 days of being diagnosed with type 1 diabetes to receive golimumab, and 28 were assigned to receive placebo injections, given every 2 weeks.
The drug resulted in lower insulin use (0.51U/Kg per day vs. 0.69 U/kg per day), and the increase in insulin use over 52 weeks was less with golimumab than with placebo (0.07 vs. 0.24 U/kg per day; P = .001).
The mean percent decrease of C-peptide production from baseline was 12% with golimumab versus 56% with placebo.
Although the mean number of overall hypoglycemic events was similar, the mean number of level 2 hypoglycemic events (<54 mg/dL) was 36% lower with golimumab (11.5 vs. 17.6). There were no severe cases of hypoglycemia in either group.
No severe or serious infections occurred in either group, although mild to moderate infections were reported in 71% with golimumab versus 61% with placebo. More patients in the golimumab group experienced a decrease in neutrophils (29% vs. 19%).
Immunotherapy: Which one, and when should it start?
These findings come on the heels of the 2019 landmark results with another monoclonal antibody, the investigational anti-CD3 teplizumab (PRV-031). Among patients at risk, a diagnosis of type 1 diabetes was delayed by 2 years, and continued benefit was seen at 3 years.
However, Dr. Quattrin said teplizumab is limited by the fact that it must be administered via a 14-day infusion, whereas golimumab can be injected by patients themselves at home.
Moreover, the phase 2 teplizumab study was conducted in people who had antibodies that placed them at high risk for type 1 diabetes, but those patients did not yet have the condition. They were identified because they had close relatives with type 1 diabetes and were enrolled in the federally funded TrialNet screening program.
Dr. Quattrin is now participating in an ongoing phase 3 study of teplizumab that involves patients newly diagnosed with type 1 diabetes.
A Janssen spokesperson said in an interview that the company isn’t planning to further develop golimumab for use in type 1 diabetes.
“Our focus is to apply insights from the phase 2 ... proof-of-concept study to progress what we believe are novel, immunologically targeted pipeline candidates in stage 2 disease or presymptomatic stages of type 1 diabetes, which is consistent with our mission to intercept and prevent type 1 diabetes,” the spokesperson said.
To identify more individuals at risk for type 1 diabetes beyond the close relatives of those who already have it, so as to be able to intervene at a presymptomatic stage, Janssen is organizing a public-private effort to advocate for routine population screening for type 1 diabetes–related autoantibodies.
Dr. Quattrin said: “Preserving some insulin is key. Having somebody with beta cell functioning still is an intermediate step to a cure and will make their life easier, and that’s what people should care about.”
Dr. Accili, who cofounded and leads a company working on a novel approach to type 1 diabetes treatment, writes in his editorial: “We should also be mindful that this treatment debate is first world–centric.
“Current treatments for type 1 diabetes require resources not readily available in most parts of the world, where something as simple as refrigeration of insulin can become a logistic nightmare. While combinations of [approaches] tailored to individual risk and potential benefits are likely to make inroads in clinical practice, the need for a simpler, safer, and equally effective alternative to insulin remains,” he wrote.
Dr. Quattrin is a researcher and consultant for Janssen and conducts clinical trials for Provention Bio, Opko, and Ascendis. Dr. Accili is founder and director of Forkhead Therapeutics.
A version of this article originally appeared on Medscape.com.
Stopping methotrexate, staying on etanercept provides best RA outcomes after remission
In patients with RA whose disease is well controlled by methotrexate combined with etanercept, withdrawal of methotrexate led to long-term outcomes that were nearly as good as continuation of combination therapy. The finding comes from the randomized, controlled SEAM-RA trial that sought to address weaknesses of previous studies. It included a long lead-in time with stringent criteria to ensure that participants had very good disease control.
Both the American College of Rheumatology and the European League Against Rheumatism recommend tapering medication in RA patients who are in long-term remission, but there is no established optimal strategy.
“There have been some prior RA trials that have looked at therapy reduction or withdrawal, but most did not use a very stringent definition of how well people were when they began. Were they in remission, or only in low disease activity?” said Jeffrey R. Curtis, MD, during a presentation of the results at the virtual annual meeting of the ACR. The study was also published online Nov. 18 in Arthritis & Rheumatology.
Stringent remission criteria
The key feature of the trial was the 6-month run-in period, when subjects were taking 50 mg etanercept once per week and 10-25 mg of oral methotrexate once per week, and had to complete at least three visits. They were excluded from the ensuing randomization if they had a Simplified Disease Activity Index (SDAI) score >3.3 and ≤11 at two or more visits, had an SDAI >11 at any time during the run-in period, or had an SDAI >3.3 at the third run-in visit.
“We [wanted them] to be doing quite well for a long period of time. That was empirically confirmed under observation as part of the lead-in period, and even before that, the clinical investigator had to affirm that they believed the patient was doing well for 6 or more months even before they were screened to enter the trial,” said Dr. Curtis, professor of medicine in the division of clinical immunology and rheumatology at the University of Alabama at Birmingham.
Once enrolled in the trial, patients were randomized 2:2:1 to continuing etanercept only (n = 101), continuing methotrexate only (n = 101), or continuing both medications (n = 51). Patients were eligible for rescue after randomization if they had an SDAI score >11 at any time, SDAI between 3.3 and 11 on three separate visits, or between 3.3 and 11 at two consecutive visits at least 2 weeks apart. About three-quarters of patients in each treatment arm were female, with a mean age of about 55 years, and 82%-91% were White.
Good remission recovery with rescue therapy
At week 48, 28.7% of the methotrexate-only group were in remission (SDAI ≤3.3), compared with 49.5% of the etanercept-only group (P = .004) and 52.9% of the combination group (P = .006). Time to disease worsening was shorter in the methotrexate-only group (median, 198 days) than in the etanercept-only group (median, not estimable; P < .001) and the combined therapy group (median, not estimable; P < .001).
The researchers also found that most patients who underwent rescue therapy once again achieved remission, including 71% of the methotrexate-only group, 75% of the etanercept-only group, and 80% of the combination therapy group. There was no between-group differences in the time required to reattain remission.
The high rate of remission recovery was a good sign, Dr. Curtis said. “To me as a clinician, the risk to try [withdrawing a medication] is quite low because the likelihood you can regain where you were before is quite good. It’s obviously more successful if you stop methotrexate and continue etanercept than if you do the reverse, but to me, this is quite a practical trial, and in fact the rigor of the inclusion criteria are much more like the patients I’m talking to about stopping therapy than some of the past studies in this regard. I think it’s quite useful in terms of generalizability. We want people that are doing this well or close to it before we take away medication.”
Positive reactions from rheumatologists
The reaction from the viewing audience was also positive. “I think this study fills a big data gap for what we do in clinical practice,” wrote Janet Pope, MD, in comments during the session.
Dr. Pope, who is a professor of medicine at the University of Western Ontario and head of rheumatology at St. Joseph’s Health Centre, both in London, said that the results build on previous work, including the CAMEO study, which showed that discontinuation of methotrexate in patients taking methotrexate and etanercept failed to achieve noninferiority to continuation of both medications, and the PRIZE study, which showed that continuing combination therapy at a reduced dose led to better outcomes than did switching to methotrexate alone or placebo. “This may be for some patients what they prefer if they don’t tolerate methotrexate,” she added.
“It’s wonderful to have these data to counsel patients. This is something we face every day,” wrote Elizabeth Wahl, MD, who is an acting assistant professor at the University of Washington, Seattle, and acting chief of rheumatology at the VA Puget Sound Healthcare System.
The study was funded by Amgen. Dr. Curtis has received grants or research support from AbbVie, Amgen, Bristol-Myers Squibb, Corrona, Janssen, Lilly, Myriad, Pfizer, Regeneron, Roche, and UCB. Dr. Pope consults for a variety of pharmaceutical companies. Dr. Wahl has no relevant financial disclosures.
SOURCE: Curtis JR et al. Arthritis Rheumatol. 2020;72(suppl 10), Abstract 0939.
In patients with RA whose disease is well controlled by methotrexate combined with etanercept, withdrawal of methotrexate led to long-term outcomes that were nearly as good as continuation of combination therapy. The finding comes from the randomized, controlled SEAM-RA trial that sought to address weaknesses of previous studies. It included a long lead-in time with stringent criteria to ensure that participants had very good disease control.
Both the American College of Rheumatology and the European League Against Rheumatism recommend tapering medication in RA patients who are in long-term remission, but there is no established optimal strategy.
“There have been some prior RA trials that have looked at therapy reduction or withdrawal, but most did not use a very stringent definition of how well people were when they began. Were they in remission, or only in low disease activity?” said Jeffrey R. Curtis, MD, during a presentation of the results at the virtual annual meeting of the ACR. The study was also published online Nov. 18 in Arthritis & Rheumatology.
Stringent remission criteria
The key feature of the trial was the 6-month run-in period, when subjects were taking 50 mg etanercept once per week and 10-25 mg of oral methotrexate once per week, and had to complete at least three visits. They were excluded from the ensuing randomization if they had a Simplified Disease Activity Index (SDAI) score >3.3 and ≤11 at two or more visits, had an SDAI >11 at any time during the run-in period, or had an SDAI >3.3 at the third run-in visit.
“We [wanted them] to be doing quite well for a long period of time. That was empirically confirmed under observation as part of the lead-in period, and even before that, the clinical investigator had to affirm that they believed the patient was doing well for 6 or more months even before they were screened to enter the trial,” said Dr. Curtis, professor of medicine in the division of clinical immunology and rheumatology at the University of Alabama at Birmingham.
Once enrolled in the trial, patients were randomized 2:2:1 to continuing etanercept only (n = 101), continuing methotrexate only (n = 101), or continuing both medications (n = 51). Patients were eligible for rescue after randomization if they had an SDAI score >11 at any time, SDAI between 3.3 and 11 on three separate visits, or between 3.3 and 11 at two consecutive visits at least 2 weeks apart. About three-quarters of patients in each treatment arm were female, with a mean age of about 55 years, and 82%-91% were White.
Good remission recovery with rescue therapy
At week 48, 28.7% of the methotrexate-only group were in remission (SDAI ≤3.3), compared with 49.5% of the etanercept-only group (P = .004) and 52.9% of the combination group (P = .006). Time to disease worsening was shorter in the methotrexate-only group (median, 198 days) than in the etanercept-only group (median, not estimable; P < .001) and the combined therapy group (median, not estimable; P < .001).
The researchers also found that most patients who underwent rescue therapy once again achieved remission, including 71% of the methotrexate-only group, 75% of the etanercept-only group, and 80% of the combination therapy group. There was no between-group differences in the time required to reattain remission.
The high rate of remission recovery was a good sign, Dr. Curtis said. “To me as a clinician, the risk to try [withdrawing a medication] is quite low because the likelihood you can regain where you were before is quite good. It’s obviously more successful if you stop methotrexate and continue etanercept than if you do the reverse, but to me, this is quite a practical trial, and in fact the rigor of the inclusion criteria are much more like the patients I’m talking to about stopping therapy than some of the past studies in this regard. I think it’s quite useful in terms of generalizability. We want people that are doing this well or close to it before we take away medication.”
Positive reactions from rheumatologists
The reaction from the viewing audience was also positive. “I think this study fills a big data gap for what we do in clinical practice,” wrote Janet Pope, MD, in comments during the session.
Dr. Pope, who is a professor of medicine at the University of Western Ontario and head of rheumatology at St. Joseph’s Health Centre, both in London, said that the results build on previous work, including the CAMEO study, which showed that discontinuation of methotrexate in patients taking methotrexate and etanercept failed to achieve noninferiority to continuation of both medications, and the PRIZE study, which showed that continuing combination therapy at a reduced dose led to better outcomes than did switching to methotrexate alone or placebo. “This may be for some patients what they prefer if they don’t tolerate methotrexate,” she added.
“It’s wonderful to have these data to counsel patients. This is something we face every day,” wrote Elizabeth Wahl, MD, who is an acting assistant professor at the University of Washington, Seattle, and acting chief of rheumatology at the VA Puget Sound Healthcare System.
The study was funded by Amgen. Dr. Curtis has received grants or research support from AbbVie, Amgen, Bristol-Myers Squibb, Corrona, Janssen, Lilly, Myriad, Pfizer, Regeneron, Roche, and UCB. Dr. Pope consults for a variety of pharmaceutical companies. Dr. Wahl has no relevant financial disclosures.
SOURCE: Curtis JR et al. Arthritis Rheumatol. 2020;72(suppl 10), Abstract 0939.
In patients with RA whose disease is well controlled by methotrexate combined with etanercept, withdrawal of methotrexate led to long-term outcomes that were nearly as good as continuation of combination therapy. The finding comes from the randomized, controlled SEAM-RA trial that sought to address weaknesses of previous studies. It included a long lead-in time with stringent criteria to ensure that participants had very good disease control.
Both the American College of Rheumatology and the European League Against Rheumatism recommend tapering medication in RA patients who are in long-term remission, but there is no established optimal strategy.
“There have been some prior RA trials that have looked at therapy reduction or withdrawal, but most did not use a very stringent definition of how well people were when they began. Were they in remission, or only in low disease activity?” said Jeffrey R. Curtis, MD, during a presentation of the results at the virtual annual meeting of the ACR. The study was also published online Nov. 18 in Arthritis & Rheumatology.
Stringent remission criteria
The key feature of the trial was the 6-month run-in period, when subjects were taking 50 mg etanercept once per week and 10-25 mg of oral methotrexate once per week, and had to complete at least three visits. They were excluded from the ensuing randomization if they had a Simplified Disease Activity Index (SDAI) score >3.3 and ≤11 at two or more visits, had an SDAI >11 at any time during the run-in period, or had an SDAI >3.3 at the third run-in visit.
“We [wanted them] to be doing quite well for a long period of time. That was empirically confirmed under observation as part of the lead-in period, and even before that, the clinical investigator had to affirm that they believed the patient was doing well for 6 or more months even before they were screened to enter the trial,” said Dr. Curtis, professor of medicine in the division of clinical immunology and rheumatology at the University of Alabama at Birmingham.
Once enrolled in the trial, patients were randomized 2:2:1 to continuing etanercept only (n = 101), continuing methotrexate only (n = 101), or continuing both medications (n = 51). Patients were eligible for rescue after randomization if they had an SDAI score >11 at any time, SDAI between 3.3 and 11 on three separate visits, or between 3.3 and 11 at two consecutive visits at least 2 weeks apart. About three-quarters of patients in each treatment arm were female, with a mean age of about 55 years, and 82%-91% were White.
Good remission recovery with rescue therapy
At week 48, 28.7% of the methotrexate-only group were in remission (SDAI ≤3.3), compared with 49.5% of the etanercept-only group (P = .004) and 52.9% of the combination group (P = .006). Time to disease worsening was shorter in the methotrexate-only group (median, 198 days) than in the etanercept-only group (median, not estimable; P < .001) and the combined therapy group (median, not estimable; P < .001).
The researchers also found that most patients who underwent rescue therapy once again achieved remission, including 71% of the methotrexate-only group, 75% of the etanercept-only group, and 80% of the combination therapy group. There was no between-group differences in the time required to reattain remission.
The high rate of remission recovery was a good sign, Dr. Curtis said. “To me as a clinician, the risk to try [withdrawing a medication] is quite low because the likelihood you can regain where you were before is quite good. It’s obviously more successful if you stop methotrexate and continue etanercept than if you do the reverse, but to me, this is quite a practical trial, and in fact the rigor of the inclusion criteria are much more like the patients I’m talking to about stopping therapy than some of the past studies in this regard. I think it’s quite useful in terms of generalizability. We want people that are doing this well or close to it before we take away medication.”
Positive reactions from rheumatologists
The reaction from the viewing audience was also positive. “I think this study fills a big data gap for what we do in clinical practice,” wrote Janet Pope, MD, in comments during the session.
Dr. Pope, who is a professor of medicine at the University of Western Ontario and head of rheumatology at St. Joseph’s Health Centre, both in London, said that the results build on previous work, including the CAMEO study, which showed that discontinuation of methotrexate in patients taking methotrexate and etanercept failed to achieve noninferiority to continuation of both medications, and the PRIZE study, which showed that continuing combination therapy at a reduced dose led to better outcomes than did switching to methotrexate alone or placebo. “This may be for some patients what they prefer if they don’t tolerate methotrexate,” she added.
“It’s wonderful to have these data to counsel patients. This is something we face every day,” wrote Elizabeth Wahl, MD, who is an acting assistant professor at the University of Washington, Seattle, and acting chief of rheumatology at the VA Puget Sound Healthcare System.
The study was funded by Amgen. Dr. Curtis has received grants or research support from AbbVie, Amgen, Bristol-Myers Squibb, Corrona, Janssen, Lilly, Myriad, Pfizer, Regeneron, Roche, and UCB. Dr. Pope consults for a variety of pharmaceutical companies. Dr. Wahl has no relevant financial disclosures.
SOURCE: Curtis JR et al. Arthritis Rheumatol. 2020;72(suppl 10), Abstract 0939.
FROM ACR 2020
Debate: After methotrexate failure, is JAK inhibitor or biologic next?
What is the next step in treatment after a person with rheumatoid arthritis fails to adequately respond to methotrexate – a Janus kinase (JAK) inhibitor or a biologic? That was the focus of a lively debate at the virtual annual meeting of the American College of Rheumatology.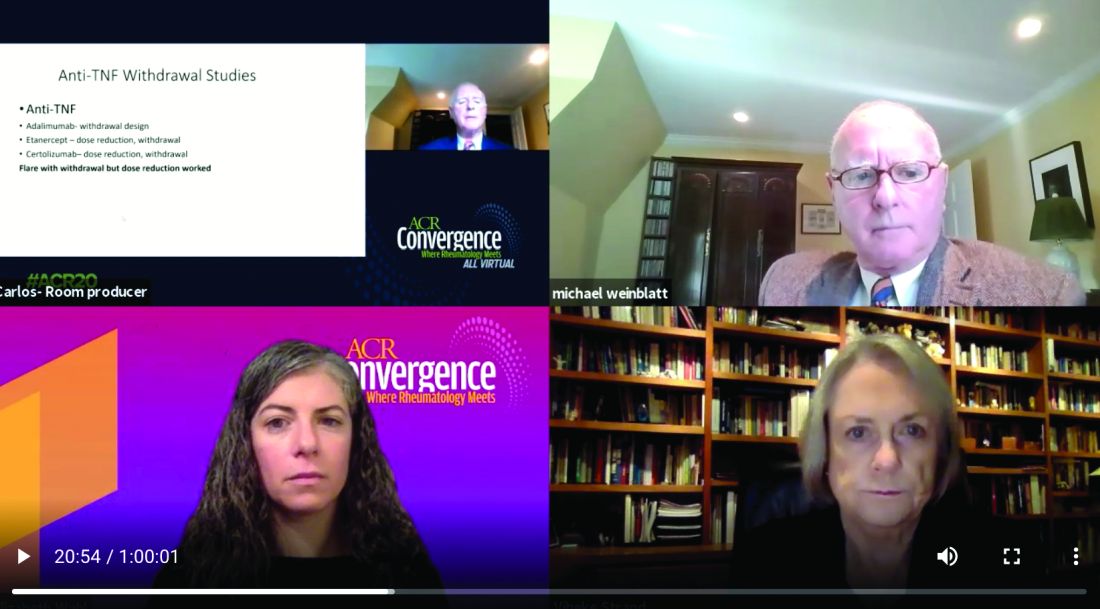
Vibeke Strand, MD, argued that JAK inhibitors offer the distinct advantage of a faster clinical response than biologics, meaning that decisions to change therapy based on nonresponse or adverse effects can be made earlier in a treatment plan.
Michael Weinblatt, MD, countered that the faster-response advantage is offset by potential adverse events associated with the JAK inhibitors, including increased risk of herpes zoster infection, venous thromboembolism (VTE), and arterial thromboembolism (ATE). He suggested switching patients to a biologic instead.
In addition, the debate was held just days before the ACR released a proposed guideline for the management of RA. This update to the 2015 guidance is the first to prioritize the order of RA treatments, emphasizing that clinicians should maximize methotrexate therapy before switching RA patients to a JAK inhibitor or a biologic. Release of the full guidelines is pending, and it remains unclear if the ACR provides any guidance regarding the “jakinib” versus biologic decision.
Interestingly, the debate did not hinge on any differences in efficacy. Both speakers pointed to similar efficacy between anti–tumor necrosis factor (TNF) agents and JAK inhibitors, and despite working on different pathways, among the individual JAK inhibitors as well.
Is timing of the essence?
Knowing whether a person with RA responds to a JAK inhibitor more quickly than to a biologic is a major advantage, said Dr. Strand, of the division of immunology and rheumatology at Stanford (Calif.) University. “The argument that I am making is that patients are more responsive if treated earlier in the disease process and they are less treatment-experienced.”
Dr. Strand said the advantages extend to remission as well. “When patients are aware of early improvements, their adherence is increased. Remission is more likely because it occurs earlier.”
“I will certainly grant it to Vibeke that jakinibs work much faster,” said Dr. Weinblatt, chair of rheumatology at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School in Boston. However, he added, “my bias is that you give patients an anti-TNF therapy first, and if they are not responding by 12 weeks, you move on to another class of drugs, perhaps even the jakinibs.”
Herpes zoster risk
Dr. Strand and Dr. Weinblatt addressed potential adverse events associated with both classes of agents. For the JAK inhibitors, concerns include herpes zoster infections, increased VTE and ATE incidence, and largely unknown risks during pregnancy and lactation. For the anti-TNF agents, safety concerns include reactivation of tuberculosis, fungal infections, demyelinating syndrome, and skin cancer.
With the shortest half-life of any therapeutic class in rheumatology, adverse events with JAK inhibitors often can resolve quickly, Dr. Strand said.
The increased risk of herpes zoster is important, she added, “but we have a recombinant vaccination that works. It’s quite effective.”
Dr. Weinblatt pointed out that all the JAK inhibitors carry this increase herpes zoster risk, which is related to their mechanism of action. There is a catch with the vaccine, however, he added. The vaccine is approved for treatment of patients 50 years and older. For younger people with RA starting a JAK inhibitor, the cost is out-of-pocket.
Evaluating risk of emboli
The incidence of VTE is about two times higher among people with RA, compared with the general population, Dr. Strand said, with research suggesting the majority of risk resides among people with a previous event. However, she added, an emerging profile of thromboembolic events associated with JAK inhibitors is “considered a class effect by the FDA.”
One exception in the JAK inhibitor class could be tofacitinib (Xeljanz), which might carry less risk because “most of the data with tofacitinib are quite good,” Dr. Weinblatt said. One study presented at ACR 2018, for example, showed a similar VTE rate between tofacitinib and TNF inhibitors.
Nevertheless, the FDA issued a boxed warning in July 2019 about elevated risks of blood clots and death at a higher dose of tofacitinib. The concerns stem from an open-label, endpoint-driven study mandated by the FDA to explore major adverse cardiac events. “There was a clinically important and statistically significant occurrence of pulmonary embolism and VTE, and an increase in mortality in the 10-mg dose group as opposed to the anti-TNF therapies,” Dr. Weinblatt said. As a result, the FDA requested patients on the 10-mg twice-daily dose be transitioned to the 5-mg twice-daily dose.
The package labeling for the JAK inhibitors baricitinib (Olumiant) and upadacitinib (Rinvoq) feature warnings about increased risk for thromboembolic events. Furthermore, the labeling for filgotinib, a JAK inhibitor in development that received a complete response letter from the FDA in August 2020, is expected to carry the same warning.An unanswered question remains on why this class of agents potentially increases risk of thromboembolism. “We’re all uncomfortable because there is no known mechanism of JAK inhibition that should lead to this,” he added. Another unresolved issue is whether or not patients prescribed a JAK inhibitor should also be prescribed an anticoagulant.
Anti-TNF adverse events
Infections, primarily reactivation of tuberculosis and an increased risk for fungal disease, are concerns with the anti-TNF agents. However, the risk is not restricted to this class. “Greater risk of infection is seen with all our immune-modulating therapies,” Dr. Weinblatt said.
Rare adverse events include demyelinating syndromes, hematologic toxicity, and a worsening of heart failure in some cases.
“Despite a concern about malignancy, the only defined cancer reported over 22 years of use was skin cancer,” he said. “It took more than a decade of ongoing registry data for skin cancer to be identified. It was not noted in randomized, placebo-controlled trials.”
Potential pregnancy concerns
When it comes to risk during reproduction, “there is a clear difference,” Dr. Weinblatt said. “We know anti-TNF therapy can be used safely in pregnant women. We know they can conceive on them and maintain them during pregnancy. They can also breastfeed on them.”
“Frankly, I’m not so ‘gung ho’ on TNF inhibitor safety in pregnancy and lactation with exception of certolizumab, which doesn’t result in high levels of antibody in the placenta or the mother’s milk,” Dr. Strand said.
The 2020 ACR Guideline for the Management of Reproductive Health in Rheumatic and Musculoskeletal Diseases states that all anti-TNF therapies can be used during pregnancy and lactation, Dr. Weinblatt said. “Although I agree certolizumab has the best safety profile, all of them can be used.”
“The same is not true with the jakinibs,” he added, pointing to warnings that women of reproductive age should use contraception while on JAK inhibitors and for 4 weeks after stopping treatment.
However, Dr. Strand defended the pregnancy risk with JAK inhibitors. She cited two publications, including a 2016 study where researchers evaluated the safety of tofacitinib during pregnancy in women with rheumatoid arthritis and psoriasis. “There was only one possible deformity, a pulmonary stenosis,” Dr. Strand said. “Essentially, the majority of patients delivered healthy babies. There was very little difference from what we know occurs in RA otherwise.”
A 2018 study assessed pregnancy outcomes with tofacitinib among people with ulcerative colitis, “again showing the majority of patients had normal deliveries.”
“There just aren’t enough data,” Dr. Weinblatt said. “Perhaps in 5 years, we will reach same conclusion with the jakinibs.”
Differences in cost?
“We have not benefited yet from the biosimilar costs. But in Europe, the cost of an adalimumab or etanercept biosimilar is about $5,000, versus about $50,000 to $60,000 in the U.S. for the JAK inhibitors,” Dr. Weinblatt said. “So there are major cost savings with biosimilars.”
“I can’t understand cost at all for our drugs,” he continued. “They’re not rational, and the price increases are clearly not rational. Potentially, a small molecule is going to be a lot easier to produce than a biologic, so you could argue that generic jakinibs ought to be less. But in the United States we have a distorted pricing model.”
“Until that changes, I don’t think we can predict [future costs]. One could predict that generics and biosimilars will be less than the orginators,” Dr. Weinblatt said.
“It is really criminal we don’t have biosimilars for most of our TNFs, but that is the way it is,” Dr. Strand said.
Summary statements
“The JAK-inhibitor class is an exciting development for rheumatology and a broad variety of autoimmune diseases,” Dr. Strand said.
“In rheumatoid arthritis, they should be used early,” she added. “Based on phase 3 trials, responses are better in progressively earlier disease with less treatment-experienced patients.”
She pointed out that many patients like the convenience of the oral JAK inhibitors.
Dr. Weinblatt stated the 22 years of clinical experience with the anti-TNF class versus about 8 years with jakinibs favors the biologics. “Virtually every approved drug has been tested versus methotrexate, in early studies, long-term studies, and most importantly, in reduction and withdrawal studies, which are not available with the JAK inhibitors.”
Anti-TNFs have impressive effects on clinical disease activity, functional outcomes, and radiographic progression, Dr. Weinblatt said. They work in early and longstanding disease among patients who are disease-modifying antirheumatic drug naive and after multiple DMARD failures, he added.
Adding up the vote
The question was: Should JAK inhibitors be used before TNF inhibitors? The results showed 69%-31% in favor of anti-TNF agents.
“So the majority are more comfortable using TNFs,” said debate moderator Elizabeth Wahl, MD, of the department of rheumatology at VA Puget Sound Healthcare System and the University of Washington in Seattle. Regarding a switch to JAK inhibitors, she interpreted the poll numbers to mean, “we are not there yet, it takes years and years of safety data.”
Both Dr. Strand and Dr. Weinblatt disclosed numerous financial relationships with pharmaceutical companies that market RA drugs.
What is the next step in treatment after a person with rheumatoid arthritis fails to adequately respond to methotrexate – a Janus kinase (JAK) inhibitor or a biologic? That was the focus of a lively debate at the virtual annual meeting of the American College of Rheumatology.
Vibeke Strand, MD, argued that JAK inhibitors offer the distinct advantage of a faster clinical response than biologics, meaning that decisions to change therapy based on nonresponse or adverse effects can be made earlier in a treatment plan.
Michael Weinblatt, MD, countered that the faster-response advantage is offset by potential adverse events associated with the JAK inhibitors, including increased risk of herpes zoster infection, venous thromboembolism (VTE), and arterial thromboembolism (ATE). He suggested switching patients to a biologic instead.
In addition, the debate was held just days before the ACR released a proposed guideline for the management of RA. This update to the 2015 guidance is the first to prioritize the order of RA treatments, emphasizing that clinicians should maximize methotrexate therapy before switching RA patients to a JAK inhibitor or a biologic. Release of the full guidelines is pending, and it remains unclear if the ACR provides any guidance regarding the “jakinib” versus biologic decision.
Interestingly, the debate did not hinge on any differences in efficacy. Both speakers pointed to similar efficacy between anti–tumor necrosis factor (TNF) agents and JAK inhibitors, and despite working on different pathways, among the individual JAK inhibitors as well.
Is timing of the essence?
Knowing whether a person with RA responds to a JAK inhibitor more quickly than to a biologic is a major advantage, said Dr. Strand, of the division of immunology and rheumatology at Stanford (Calif.) University. “The argument that I am making is that patients are more responsive if treated earlier in the disease process and they are less treatment-experienced.”
Dr. Strand said the advantages extend to remission as well. “When patients are aware of early improvements, their adherence is increased. Remission is more likely because it occurs earlier.”
“I will certainly grant it to Vibeke that jakinibs work much faster,” said Dr. Weinblatt, chair of rheumatology at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School in Boston. However, he added, “my bias is that you give patients an anti-TNF therapy first, and if they are not responding by 12 weeks, you move on to another class of drugs, perhaps even the jakinibs.”
Herpes zoster risk
Dr. Strand and Dr. Weinblatt addressed potential adverse events associated with both classes of agents. For the JAK inhibitors, concerns include herpes zoster infections, increased VTE and ATE incidence, and largely unknown risks during pregnancy and lactation. For the anti-TNF agents, safety concerns include reactivation of tuberculosis, fungal infections, demyelinating syndrome, and skin cancer.
With the shortest half-life of any therapeutic class in rheumatology, adverse events with JAK inhibitors often can resolve quickly, Dr. Strand said.
The increased risk of herpes zoster is important, she added, “but we have a recombinant vaccination that works. It’s quite effective.”
Dr. Weinblatt pointed out that all the JAK inhibitors carry this increase herpes zoster risk, which is related to their mechanism of action. There is a catch with the vaccine, however, he added. The vaccine is approved for treatment of patients 50 years and older. For younger people with RA starting a JAK inhibitor, the cost is out-of-pocket.
Evaluating risk of emboli
The incidence of VTE is about two times higher among people with RA, compared with the general population, Dr. Strand said, with research suggesting the majority of risk resides among people with a previous event. However, she added, an emerging profile of thromboembolic events associated with JAK inhibitors is “considered a class effect by the FDA.”
One exception in the JAK inhibitor class could be tofacitinib (Xeljanz), which might carry less risk because “most of the data with tofacitinib are quite good,” Dr. Weinblatt said. One study presented at ACR 2018, for example, showed a similar VTE rate between tofacitinib and TNF inhibitors.
Nevertheless, the FDA issued a boxed warning in July 2019 about elevated risks of blood clots and death at a higher dose of tofacitinib. The concerns stem from an open-label, endpoint-driven study mandated by the FDA to explore major adverse cardiac events. “There was a clinically important and statistically significant occurrence of pulmonary embolism and VTE, and an increase in mortality in the 10-mg dose group as opposed to the anti-TNF therapies,” Dr. Weinblatt said. As a result, the FDA requested patients on the 10-mg twice-daily dose be transitioned to the 5-mg twice-daily dose.
The package labeling for the JAK inhibitors baricitinib (Olumiant) and upadacitinib (Rinvoq) feature warnings about increased risk for thromboembolic events. Furthermore, the labeling for filgotinib, a JAK inhibitor in development that received a complete response letter from the FDA in August 2020, is expected to carry the same warning.An unanswered question remains on why this class of agents potentially increases risk of thromboembolism. “We’re all uncomfortable because there is no known mechanism of JAK inhibition that should lead to this,” he added. Another unresolved issue is whether or not patients prescribed a JAK inhibitor should also be prescribed an anticoagulant.
Anti-TNF adverse events
Infections, primarily reactivation of tuberculosis and an increased risk for fungal disease, are concerns with the anti-TNF agents. However, the risk is not restricted to this class. “Greater risk of infection is seen with all our immune-modulating therapies,” Dr. Weinblatt said.
Rare adverse events include demyelinating syndromes, hematologic toxicity, and a worsening of heart failure in some cases.
“Despite a concern about malignancy, the only defined cancer reported over 22 years of use was skin cancer,” he said. “It took more than a decade of ongoing registry data for skin cancer to be identified. It was not noted in randomized, placebo-controlled trials.”
Potential pregnancy concerns
When it comes to risk during reproduction, “there is a clear difference,” Dr. Weinblatt said. “We know anti-TNF therapy can be used safely in pregnant women. We know they can conceive on them and maintain them during pregnancy. They can also breastfeed on them.”
“Frankly, I’m not so ‘gung ho’ on TNF inhibitor safety in pregnancy and lactation with exception of certolizumab, which doesn’t result in high levels of antibody in the placenta or the mother’s milk,” Dr. Strand said.
The 2020 ACR Guideline for the Management of Reproductive Health in Rheumatic and Musculoskeletal Diseases states that all anti-TNF therapies can be used during pregnancy and lactation, Dr. Weinblatt said. “Although I agree certolizumab has the best safety profile, all of them can be used.”
“The same is not true with the jakinibs,” he added, pointing to warnings that women of reproductive age should use contraception while on JAK inhibitors and for 4 weeks after stopping treatment.
However, Dr. Strand defended the pregnancy risk with JAK inhibitors. She cited two publications, including a 2016 study where researchers evaluated the safety of tofacitinib during pregnancy in women with rheumatoid arthritis and psoriasis. “There was only one possible deformity, a pulmonary stenosis,” Dr. Strand said. “Essentially, the majority of patients delivered healthy babies. There was very little difference from what we know occurs in RA otherwise.”
A 2018 study assessed pregnancy outcomes with tofacitinib among people with ulcerative colitis, “again showing the majority of patients had normal deliveries.”
“There just aren’t enough data,” Dr. Weinblatt said. “Perhaps in 5 years, we will reach same conclusion with the jakinibs.”
Differences in cost?
“We have not benefited yet from the biosimilar costs. But in Europe, the cost of an adalimumab or etanercept biosimilar is about $5,000, versus about $50,000 to $60,000 in the U.S. for the JAK inhibitors,” Dr. Weinblatt said. “So there are major cost savings with biosimilars.”
“I can’t understand cost at all for our drugs,” he continued. “They’re not rational, and the price increases are clearly not rational. Potentially, a small molecule is going to be a lot easier to produce than a biologic, so you could argue that generic jakinibs ought to be less. But in the United States we have a distorted pricing model.”
“Until that changes, I don’t think we can predict [future costs]. One could predict that generics and biosimilars will be less than the orginators,” Dr. Weinblatt said.
“It is really criminal we don’t have biosimilars for most of our TNFs, but that is the way it is,” Dr. Strand said.
Summary statements
“The JAK-inhibitor class is an exciting development for rheumatology and a broad variety of autoimmune diseases,” Dr. Strand said.
“In rheumatoid arthritis, they should be used early,” she added. “Based on phase 3 trials, responses are better in progressively earlier disease with less treatment-experienced patients.”
She pointed out that many patients like the convenience of the oral JAK inhibitors.
Dr. Weinblatt stated the 22 years of clinical experience with the anti-TNF class versus about 8 years with jakinibs favors the biologics. “Virtually every approved drug has been tested versus methotrexate, in early studies, long-term studies, and most importantly, in reduction and withdrawal studies, which are not available with the JAK inhibitors.”
Anti-TNFs have impressive effects on clinical disease activity, functional outcomes, and radiographic progression, Dr. Weinblatt said. They work in early and longstanding disease among patients who are disease-modifying antirheumatic drug naive and after multiple DMARD failures, he added.
Adding up the vote
The question was: Should JAK inhibitors be used before TNF inhibitors? The results showed 69%-31% in favor of anti-TNF agents.
“So the majority are more comfortable using TNFs,” said debate moderator Elizabeth Wahl, MD, of the department of rheumatology at VA Puget Sound Healthcare System and the University of Washington in Seattle. Regarding a switch to JAK inhibitors, she interpreted the poll numbers to mean, “we are not there yet, it takes years and years of safety data.”
Both Dr. Strand and Dr. Weinblatt disclosed numerous financial relationships with pharmaceutical companies that market RA drugs.
What is the next step in treatment after a person with rheumatoid arthritis fails to adequately respond to methotrexate – a Janus kinase (JAK) inhibitor or a biologic? That was the focus of a lively debate at the virtual annual meeting of the American College of Rheumatology.
Vibeke Strand, MD, argued that JAK inhibitors offer the distinct advantage of a faster clinical response than biologics, meaning that decisions to change therapy based on nonresponse or adverse effects can be made earlier in a treatment plan.
Michael Weinblatt, MD, countered that the faster-response advantage is offset by potential adverse events associated with the JAK inhibitors, including increased risk of herpes zoster infection, venous thromboembolism (VTE), and arterial thromboembolism (ATE). He suggested switching patients to a biologic instead.
In addition, the debate was held just days before the ACR released a proposed guideline for the management of RA. This update to the 2015 guidance is the first to prioritize the order of RA treatments, emphasizing that clinicians should maximize methotrexate therapy before switching RA patients to a JAK inhibitor or a biologic. Release of the full guidelines is pending, and it remains unclear if the ACR provides any guidance regarding the “jakinib” versus biologic decision.
Interestingly, the debate did not hinge on any differences in efficacy. Both speakers pointed to similar efficacy between anti–tumor necrosis factor (TNF) agents and JAK inhibitors, and despite working on different pathways, among the individual JAK inhibitors as well.
Is timing of the essence?
Knowing whether a person with RA responds to a JAK inhibitor more quickly than to a biologic is a major advantage, said Dr. Strand, of the division of immunology and rheumatology at Stanford (Calif.) University. “The argument that I am making is that patients are more responsive if treated earlier in the disease process and they are less treatment-experienced.”
Dr. Strand said the advantages extend to remission as well. “When patients are aware of early improvements, their adherence is increased. Remission is more likely because it occurs earlier.”
“I will certainly grant it to Vibeke that jakinibs work much faster,” said Dr. Weinblatt, chair of rheumatology at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School in Boston. However, he added, “my bias is that you give patients an anti-TNF therapy first, and if they are not responding by 12 weeks, you move on to another class of drugs, perhaps even the jakinibs.”
Herpes zoster risk
Dr. Strand and Dr. Weinblatt addressed potential adverse events associated with both classes of agents. For the JAK inhibitors, concerns include herpes zoster infections, increased VTE and ATE incidence, and largely unknown risks during pregnancy and lactation. For the anti-TNF agents, safety concerns include reactivation of tuberculosis, fungal infections, demyelinating syndrome, and skin cancer.
With the shortest half-life of any therapeutic class in rheumatology, adverse events with JAK inhibitors often can resolve quickly, Dr. Strand said.
The increased risk of herpes zoster is important, she added, “but we have a recombinant vaccination that works. It’s quite effective.”
Dr. Weinblatt pointed out that all the JAK inhibitors carry this increase herpes zoster risk, which is related to their mechanism of action. There is a catch with the vaccine, however, he added. The vaccine is approved for treatment of patients 50 years and older. For younger people with RA starting a JAK inhibitor, the cost is out-of-pocket.
Evaluating risk of emboli
The incidence of VTE is about two times higher among people with RA, compared with the general population, Dr. Strand said, with research suggesting the majority of risk resides among people with a previous event. However, she added, an emerging profile of thromboembolic events associated with JAK inhibitors is “considered a class effect by the FDA.”
One exception in the JAK inhibitor class could be tofacitinib (Xeljanz), which might carry less risk because “most of the data with tofacitinib are quite good,” Dr. Weinblatt said. One study presented at ACR 2018, for example, showed a similar VTE rate between tofacitinib and TNF inhibitors.
Nevertheless, the FDA issued a boxed warning in July 2019 about elevated risks of blood clots and death at a higher dose of tofacitinib. The concerns stem from an open-label, endpoint-driven study mandated by the FDA to explore major adverse cardiac events. “There was a clinically important and statistically significant occurrence of pulmonary embolism and VTE, and an increase in mortality in the 10-mg dose group as opposed to the anti-TNF therapies,” Dr. Weinblatt said. As a result, the FDA requested patients on the 10-mg twice-daily dose be transitioned to the 5-mg twice-daily dose.
The package labeling for the JAK inhibitors baricitinib (Olumiant) and upadacitinib (Rinvoq) feature warnings about increased risk for thromboembolic events. Furthermore, the labeling for filgotinib, a JAK inhibitor in development that received a complete response letter from the FDA in August 2020, is expected to carry the same warning.An unanswered question remains on why this class of agents potentially increases risk of thromboembolism. “We’re all uncomfortable because there is no known mechanism of JAK inhibition that should lead to this,” he added. Another unresolved issue is whether or not patients prescribed a JAK inhibitor should also be prescribed an anticoagulant.
Anti-TNF adverse events
Infections, primarily reactivation of tuberculosis and an increased risk for fungal disease, are concerns with the anti-TNF agents. However, the risk is not restricted to this class. “Greater risk of infection is seen with all our immune-modulating therapies,” Dr. Weinblatt said.
Rare adverse events include demyelinating syndromes, hematologic toxicity, and a worsening of heart failure in some cases.
“Despite a concern about malignancy, the only defined cancer reported over 22 years of use was skin cancer,” he said. “It took more than a decade of ongoing registry data for skin cancer to be identified. It was not noted in randomized, placebo-controlled trials.”
Potential pregnancy concerns
When it comes to risk during reproduction, “there is a clear difference,” Dr. Weinblatt said. “We know anti-TNF therapy can be used safely in pregnant women. We know they can conceive on them and maintain them during pregnancy. They can also breastfeed on them.”
“Frankly, I’m not so ‘gung ho’ on TNF inhibitor safety in pregnancy and lactation with exception of certolizumab, which doesn’t result in high levels of antibody in the placenta or the mother’s milk,” Dr. Strand said.
The 2020 ACR Guideline for the Management of Reproductive Health in Rheumatic and Musculoskeletal Diseases states that all anti-TNF therapies can be used during pregnancy and lactation, Dr. Weinblatt said. “Although I agree certolizumab has the best safety profile, all of them can be used.”
“The same is not true with the jakinibs,” he added, pointing to warnings that women of reproductive age should use contraception while on JAK inhibitors and for 4 weeks after stopping treatment.
However, Dr. Strand defended the pregnancy risk with JAK inhibitors. She cited two publications, including a 2016 study where researchers evaluated the safety of tofacitinib during pregnancy in women with rheumatoid arthritis and psoriasis. “There was only one possible deformity, a pulmonary stenosis,” Dr. Strand said. “Essentially, the majority of patients delivered healthy babies. There was very little difference from what we know occurs in RA otherwise.”
A 2018 study assessed pregnancy outcomes with tofacitinib among people with ulcerative colitis, “again showing the majority of patients had normal deliveries.”
“There just aren’t enough data,” Dr. Weinblatt said. “Perhaps in 5 years, we will reach same conclusion with the jakinibs.”
Differences in cost?
“We have not benefited yet from the biosimilar costs. But in Europe, the cost of an adalimumab or etanercept biosimilar is about $5,000, versus about $50,000 to $60,000 in the U.S. for the JAK inhibitors,” Dr. Weinblatt said. “So there are major cost savings with biosimilars.”
“I can’t understand cost at all for our drugs,” he continued. “They’re not rational, and the price increases are clearly not rational. Potentially, a small molecule is going to be a lot easier to produce than a biologic, so you could argue that generic jakinibs ought to be less. But in the United States we have a distorted pricing model.”
“Until that changes, I don’t think we can predict [future costs]. One could predict that generics and biosimilars will be less than the orginators,” Dr. Weinblatt said.
“It is really criminal we don’t have biosimilars for most of our TNFs, but that is the way it is,” Dr. Strand said.
Summary statements
“The JAK-inhibitor class is an exciting development for rheumatology and a broad variety of autoimmune diseases,” Dr. Strand said.
“In rheumatoid arthritis, they should be used early,” she added. “Based on phase 3 trials, responses are better in progressively earlier disease with less treatment-experienced patients.”
She pointed out that many patients like the convenience of the oral JAK inhibitors.
Dr. Weinblatt stated the 22 years of clinical experience with the anti-TNF class versus about 8 years with jakinibs favors the biologics. “Virtually every approved drug has been tested versus methotrexate, in early studies, long-term studies, and most importantly, in reduction and withdrawal studies, which are not available with the JAK inhibitors.”
Anti-TNFs have impressive effects on clinical disease activity, functional outcomes, and radiographic progression, Dr. Weinblatt said. They work in early and longstanding disease among patients who are disease-modifying antirheumatic drug naive and after multiple DMARD failures, he added.
Adding up the vote
The question was: Should JAK inhibitors be used before TNF inhibitors? The results showed 69%-31% in favor of anti-TNF agents.
“So the majority are more comfortable using TNFs,” said debate moderator Elizabeth Wahl, MD, of the department of rheumatology at VA Puget Sound Healthcare System and the University of Washington in Seattle. Regarding a switch to JAK inhibitors, she interpreted the poll numbers to mean, “we are not there yet, it takes years and years of safety data.”
Both Dr. Strand and Dr. Weinblatt disclosed numerous financial relationships with pharmaceutical companies that market RA drugs.
FROM ACR 2020
Chronic inflammatory diseases vary widely in CHD risk
Not all chronic systemic inflammatory diseases are equal enhancers of atherosclerotic cardiovascular disease risk, according to a large case-control study.
Current AHA/American College of Cardiology guidelines cite three chronic inflammatory diseases as atherosclerotic cardiovascular disease risk enhancers: rheumatoid arthritis, psoriasis, and HIV infection. But this study of those three diseases, along with three others marked by elevated high sensitivity C-reactive protein (systemic sclerosis, inflammatory bowel disease, and systemic lupus erythematosus [SLE]), showed that chronic inflammatory diseases are not monolithic in terms of their associated risk of incident coronary heart disease (CHD).
Indeed, two of the six inflammatory diseases – psoriasis and inflammatory bowel disease – turned out to be not at all associated with increased cardiovascular risk in the 37,117-patient study. The highest-risk disease was SLE, not specifically mentioned in the guidelines, Arjun Sinha, MD, a cardiology fellow at Northwestern University, Chicago, noted in his presentation at the virtual American Heart Association scientific sessions.
The study included 18,129 patients with one of the six chronic inflammatory diseases and 18,988 matched controls, none with CHD at baseline. All regularly received outpatient care at Northwestern during 2000-2019. There were 1,011 incident CHD events during a median of 3.5 years of follow-up.
In a Cox proportional hazards analysis adjusted for demographics, insurance status, hypertension, diabetes, current smoking, total cholesterol, and estimated glomerular filtration rate, here’s how the chronic inflammatory diseases stacked up in terms of incident CHD and MI risks:
- SLE: hazard ratio for CHD, 2.85; for MI, 4.76.
- Systemic sclerosis: HR for CHD, 2.14; for MI, 3.19.
- HIV: HR for CHD, 1.38; for MI, 1.69.
- Rheumatoid arthritis: HR for CHD, 1.22; for MI, 1.45.
- Psoriasis: no significant increase.
- Inflammatory bowel disease: no significant increase.
In an exploratory analysis, Dr. Sinha and coinvestigators evaluated the risk of incident CHD stratified by disease severity. For lack of standardized disease severity scales, the investigators relied upon tertiles of CD4 T cell count in the HIV group and CRP in the others. The HR for new-onset CHD in the more than 5,000 patients with psoriasis didn’t vary by CRP tertile. However, there was a nonsignificant trend for greater disease severity, as reflected by CRP tertile, to be associated with increased incident CHD risk in the HIV and inflammatory bowel disease groups.
In contrast, patients with rheumatoid arthritis or systemic sclerosis who were in the top CRP tertile had a significantly greater risk of developing CHD than that of controls, with HRs of 2.11 in the rheumatoid arthritis group and 4.59 with systemic sclerosis, although patients in the other two tertiles weren’t at significantly increased risk. But all three tertiles of CRP in patients with SLE were associated with significantly increased CHD risk: 3.17-fold in the lowest tertile of lupus severity, 5.38-fold in the middle tertile, and 4.04-fold in the top tertile for inflammation.
These findings could be used in clinical practice to fine-tune atherosclerotic cardiovascular disease risk assessment based upon chronic inflammatory disease type and severity. That’s information which in turn can help guide the timing and intensity of preventive therapy for patients with each disease type.
But studying the association between chronic systemic inflammatory diseases and CHD risk can be useful in additional ways, according to Dr. Sinha. These inflammatory diseases can serve as models of atherosclerosis that shed light on the non–lipid-related mechanisms involved in cardiovascular disease.
“The gradient in risk may be hypothesis-generating with respect to which specific inflammatory pathways may contribute to CHD,” he explained.
Each of these six chronic inflammatory diseases is characterized by a different form of major immune dysfunction, Dr. Sinha continued. A case in point is SLE, the inflammatory disease associated with the highest risk of CHD and MI. Lupus is characterized by a form of neutrophil dysfunction marked by increased formation and reduced degradation of neutrophil extracellular traps, or NETs, as well as by an increase in autoreactive B cells and dysfunctional CD4+ T helper cells. The increase in NETs of of particular interest because NETs have also been shown to contribute to the development of atherosclerosis, endothelial dysfunction, plaque erosion, and thrombosis.
In another exploratory analysis, Dr. Sinha and coworkers found that SLE patients with a neutrophil count above the median level were twice as likely to develop CHD than were those with a neutrophil count below the median.
A better understanding of the upstream pathways linking NET formation in SLE and atherosclerosis could lead to development of new or repurposed medications that target immune dysfunction in order to curb atherosclerosis, said Dr. Sinha, whose study won the AHA’s Samuel A. Levine Early Career Clinical Investigator Award.
He reported having no financial conflicts regarding his study.
Not all chronic systemic inflammatory diseases are equal enhancers of atherosclerotic cardiovascular disease risk, according to a large case-control study.
Current AHA/American College of Cardiology guidelines cite three chronic inflammatory diseases as atherosclerotic cardiovascular disease risk enhancers: rheumatoid arthritis, psoriasis, and HIV infection. But this study of those three diseases, along with three others marked by elevated high sensitivity C-reactive protein (systemic sclerosis, inflammatory bowel disease, and systemic lupus erythematosus [SLE]), showed that chronic inflammatory diseases are not monolithic in terms of their associated risk of incident coronary heart disease (CHD).
Indeed, two of the six inflammatory diseases – psoriasis and inflammatory bowel disease – turned out to be not at all associated with increased cardiovascular risk in the 37,117-patient study. The highest-risk disease was SLE, not specifically mentioned in the guidelines, Arjun Sinha, MD, a cardiology fellow at Northwestern University, Chicago, noted in his presentation at the virtual American Heart Association scientific sessions.
The study included 18,129 patients with one of the six chronic inflammatory diseases and 18,988 matched controls, none with CHD at baseline. All regularly received outpatient care at Northwestern during 2000-2019. There were 1,011 incident CHD events during a median of 3.5 years of follow-up.
In a Cox proportional hazards analysis adjusted for demographics, insurance status, hypertension, diabetes, current smoking, total cholesterol, and estimated glomerular filtration rate, here’s how the chronic inflammatory diseases stacked up in terms of incident CHD and MI risks:
- SLE: hazard ratio for CHD, 2.85; for MI, 4.76.
- Systemic sclerosis: HR for CHD, 2.14; for MI, 3.19.
- HIV: HR for CHD, 1.38; for MI, 1.69.
- Rheumatoid arthritis: HR for CHD, 1.22; for MI, 1.45.
- Psoriasis: no significant increase.
- Inflammatory bowel disease: no significant increase.
In an exploratory analysis, Dr. Sinha and coinvestigators evaluated the risk of incident CHD stratified by disease severity. For lack of standardized disease severity scales, the investigators relied upon tertiles of CD4 T cell count in the HIV group and CRP in the others. The HR for new-onset CHD in the more than 5,000 patients with psoriasis didn’t vary by CRP tertile. However, there was a nonsignificant trend for greater disease severity, as reflected by CRP tertile, to be associated with increased incident CHD risk in the HIV and inflammatory bowel disease groups.
In contrast, patients with rheumatoid arthritis or systemic sclerosis who were in the top CRP tertile had a significantly greater risk of developing CHD than that of controls, with HRs of 2.11 in the rheumatoid arthritis group and 4.59 with systemic sclerosis, although patients in the other two tertiles weren’t at significantly increased risk. But all three tertiles of CRP in patients with SLE were associated with significantly increased CHD risk: 3.17-fold in the lowest tertile of lupus severity, 5.38-fold in the middle tertile, and 4.04-fold in the top tertile for inflammation.
These findings could be used in clinical practice to fine-tune atherosclerotic cardiovascular disease risk assessment based upon chronic inflammatory disease type and severity. That’s information which in turn can help guide the timing and intensity of preventive therapy for patients with each disease type.
But studying the association between chronic systemic inflammatory diseases and CHD risk can be useful in additional ways, according to Dr. Sinha. These inflammatory diseases can serve as models of atherosclerosis that shed light on the non–lipid-related mechanisms involved in cardiovascular disease.
“The gradient in risk may be hypothesis-generating with respect to which specific inflammatory pathways may contribute to CHD,” he explained.
Each of these six chronic inflammatory diseases is characterized by a different form of major immune dysfunction, Dr. Sinha continued. A case in point is SLE, the inflammatory disease associated with the highest risk of CHD and MI. Lupus is characterized by a form of neutrophil dysfunction marked by increased formation and reduced degradation of neutrophil extracellular traps, or NETs, as well as by an increase in autoreactive B cells and dysfunctional CD4+ T helper cells. The increase in NETs of of particular interest because NETs have also been shown to contribute to the development of atherosclerosis, endothelial dysfunction, plaque erosion, and thrombosis.
In another exploratory analysis, Dr. Sinha and coworkers found that SLE patients with a neutrophil count above the median level were twice as likely to develop CHD than were those with a neutrophil count below the median.
A better understanding of the upstream pathways linking NET formation in SLE and atherosclerosis could lead to development of new or repurposed medications that target immune dysfunction in order to curb atherosclerosis, said Dr. Sinha, whose study won the AHA’s Samuel A. Levine Early Career Clinical Investigator Award.
He reported having no financial conflicts regarding his study.
Not all chronic systemic inflammatory diseases are equal enhancers of atherosclerotic cardiovascular disease risk, according to a large case-control study.
Current AHA/American College of Cardiology guidelines cite three chronic inflammatory diseases as atherosclerotic cardiovascular disease risk enhancers: rheumatoid arthritis, psoriasis, and HIV infection. But this study of those three diseases, along with three others marked by elevated high sensitivity C-reactive protein (systemic sclerosis, inflammatory bowel disease, and systemic lupus erythematosus [SLE]), showed that chronic inflammatory diseases are not monolithic in terms of their associated risk of incident coronary heart disease (CHD).
Indeed, two of the six inflammatory diseases – psoriasis and inflammatory bowel disease – turned out to be not at all associated with increased cardiovascular risk in the 37,117-patient study. The highest-risk disease was SLE, not specifically mentioned in the guidelines, Arjun Sinha, MD, a cardiology fellow at Northwestern University, Chicago, noted in his presentation at the virtual American Heart Association scientific sessions.
The study included 18,129 patients with one of the six chronic inflammatory diseases and 18,988 matched controls, none with CHD at baseline. All regularly received outpatient care at Northwestern during 2000-2019. There were 1,011 incident CHD events during a median of 3.5 years of follow-up.
In a Cox proportional hazards analysis adjusted for demographics, insurance status, hypertension, diabetes, current smoking, total cholesterol, and estimated glomerular filtration rate, here’s how the chronic inflammatory diseases stacked up in terms of incident CHD and MI risks:
- SLE: hazard ratio for CHD, 2.85; for MI, 4.76.
- Systemic sclerosis: HR for CHD, 2.14; for MI, 3.19.
- HIV: HR for CHD, 1.38; for MI, 1.69.
- Rheumatoid arthritis: HR for CHD, 1.22; for MI, 1.45.
- Psoriasis: no significant increase.
- Inflammatory bowel disease: no significant increase.
In an exploratory analysis, Dr. Sinha and coinvestigators evaluated the risk of incident CHD stratified by disease severity. For lack of standardized disease severity scales, the investigators relied upon tertiles of CD4 T cell count in the HIV group and CRP in the others. The HR for new-onset CHD in the more than 5,000 patients with psoriasis didn’t vary by CRP tertile. However, there was a nonsignificant trend for greater disease severity, as reflected by CRP tertile, to be associated with increased incident CHD risk in the HIV and inflammatory bowel disease groups.
In contrast, patients with rheumatoid arthritis or systemic sclerosis who were in the top CRP tertile had a significantly greater risk of developing CHD than that of controls, with HRs of 2.11 in the rheumatoid arthritis group and 4.59 with systemic sclerosis, although patients in the other two tertiles weren’t at significantly increased risk. But all three tertiles of CRP in patients with SLE were associated with significantly increased CHD risk: 3.17-fold in the lowest tertile of lupus severity, 5.38-fold in the middle tertile, and 4.04-fold in the top tertile for inflammation.
These findings could be used in clinical practice to fine-tune atherosclerotic cardiovascular disease risk assessment based upon chronic inflammatory disease type and severity. That’s information which in turn can help guide the timing and intensity of preventive therapy for patients with each disease type.
But studying the association between chronic systemic inflammatory diseases and CHD risk can be useful in additional ways, according to Dr. Sinha. These inflammatory diseases can serve as models of atherosclerosis that shed light on the non–lipid-related mechanisms involved in cardiovascular disease.
“The gradient in risk may be hypothesis-generating with respect to which specific inflammatory pathways may contribute to CHD,” he explained.
Each of these six chronic inflammatory diseases is characterized by a different form of major immune dysfunction, Dr. Sinha continued. A case in point is SLE, the inflammatory disease associated with the highest risk of CHD and MI. Lupus is characterized by a form of neutrophil dysfunction marked by increased formation and reduced degradation of neutrophil extracellular traps, or NETs, as well as by an increase in autoreactive B cells and dysfunctional CD4+ T helper cells. The increase in NETs of of particular interest because NETs have also been shown to contribute to the development of atherosclerosis, endothelial dysfunction, plaque erosion, and thrombosis.
In another exploratory analysis, Dr. Sinha and coworkers found that SLE patients with a neutrophil count above the median level were twice as likely to develop CHD than were those with a neutrophil count below the median.
A better understanding of the upstream pathways linking NET formation in SLE and atherosclerosis could lead to development of new or repurposed medications that target immune dysfunction in order to curb atherosclerosis, said Dr. Sinha, whose study won the AHA’s Samuel A. Levine Early Career Clinical Investigator Award.
He reported having no financial conflicts regarding his study.
FROM AHA 2020
Methotrexate and hydroxychloroquine split on cardiovascular outcomes in RA
No significant differences in major adverse cardiovascular events (MACE) emerged between methotrexate and hydroxychloroquine (HCQ) treatment in a comparison of adults 65 years or older with rheumatoid arthritis. However, researchers reported some elevation in risk for stroke in the methotrexate group and for myocardial infarction and heart failure in the HCQ group.
The primary outcome, a composite of MI, stroke, or cardiovascular death, had an incidence of 23.39 per 1,000 person-years in the methotrexate group versus 24.33 in the HCQ group in this observational study of nearly 60,000 people.
“These results suggest an importance of looking at different individual events of cardiovascular disease rather than the whole ‘CV’ disease only,” Seoyoung Kim, MD, said in an interview. “The other important thing is that the mortality was not significantly different between the two groups.”
For example, the researchers reported 256 cardiovascular-related deaths in the methotrexate group and 263 such deaths in the HCQ cohort.
Addressing a recognized risk
“It is well known that patients with rheumatoid arthritis have excessive morbidity and mortality,” Dr. Kim, of the division of rheumatology at Brigham and Women’s Hospital and associate professor of medicine at Harvard Medical School in Boston, said at the virtual annual meeting of the American College of Rheumatology.
Among prior studies in this area, the Cardiovascular Inflammation Reduction Trial (CIRT) found no significant reduction in cardiovascular events among people taking methotrexate versus placebo. However, the study of 4,786 people was not specific to RA, Dr. Kim said. The lack of efficacy on this endpoint prompted researchers to stop CIRT early.
“So what does the conclusion of the CIRT trial mean for rheumatoid arthritis patients?” Dr. Kim asked.
To find out, she and colleagues compared risk of MACE among participants newly starting either methotrexate or HCQ. The study included 59,329 people aged 65 and older who were identified through Medicare claims data from 2008 to 2016. Mean age was 74 years, and 80% were women.
The investigators used propensity score matching to control for multiple covariates for demographics, other medications, and comorbidities. Use of other medications was similar between groups, including glucocorticoids, NSAIDs, and statins. Baseline cardiovascular morbidities likewise were well balanced, Dr. Kim said.
The hazard ratio for the primary MACE outcome was 0.96 (95% confidence interval, 0.86-1.08).
Secondary outcomes
MI was less common in the methotrexate group, for example, with an incidence of 8.49 per 1,000 person-years versus 10.68 per 1,000 person-years in the HCQ cohort. This finding was statically significant, Dr. Kim said, with a hazard ratio of 0.80 favoring methotrexate.
Heart failure also occurred less often in the methotrexate cohort, with an incidence rate of 8.57 per 1,000 person-years versus a rate of 14.24 in the HCQ group. The hazard ratio again favored methotrexate at 0.60.
In contrast, strokes were more common with methotrexate than with (incidence of 7.94 vs. 6.01 per 1,000 person-years).
Another secondary outcome, all-cause mortality, was not significantly different between groups. There were 821 deaths in the methotrexate group (28.65 per 1,000 person-years) and 796 deaths in the HCQ group (31.33 per 1,000 person-years).
Studying causality next?
Session moderator Maya Buch, MD, PhD, professor of rheumatology at the University of Manchester (England), asked Dr. Kim why she found significant differences in some secondary outcomes but not the primary composite endpoint.
“When we think of cardiovascular diseases, we tend to think of them all developing through the same mechanism. But perhaps the exact mechanism might not be identical,” Dr. Kim replied. The findings do not suggest causality because the study was observational, she added, “but maybe this will lead to a randomized, controlled trial.”
When asked for comment, Dr. Buch said that the study was “interesting” and “suggestive of differences in type of MACE between the two drugs evaluated,” but that there should be caution in interpreting the findings because of the lack of detailed information on RA disease and activity in claims databases, in addition to other factors, even though the investigators made adjustments for known differences through propensity score matching.
The division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital supported the study. Dr. Kim has received support for Brigham and Women’s Hospital for unrelated research from Pfizer, AbbVie, Roche, and Bristol-Myers Squibb. Several other coauthors reported having financial relationships with pharmaceutical companies that make drugs for RA. Dr. Buch had no relevant disclosures.
SOURCE: He M et al. Arthritis Rheumatol. 2020;72(suppl 10): Abstract 1993.
No significant differences in major adverse cardiovascular events (MACE) emerged between methotrexate and hydroxychloroquine (HCQ) treatment in a comparison of adults 65 years or older with rheumatoid arthritis. However, researchers reported some elevation in risk for stroke in the methotrexate group and for myocardial infarction and heart failure in the HCQ group.
The primary outcome, a composite of MI, stroke, or cardiovascular death, had an incidence of 23.39 per 1,000 person-years in the methotrexate group versus 24.33 in the HCQ group in this observational study of nearly 60,000 people.
“These results suggest an importance of looking at different individual events of cardiovascular disease rather than the whole ‘CV’ disease only,” Seoyoung Kim, MD, said in an interview. “The other important thing is that the mortality was not significantly different between the two groups.”
For example, the researchers reported 256 cardiovascular-related deaths in the methotrexate group and 263 such deaths in the HCQ cohort.
Addressing a recognized risk
“It is well known that patients with rheumatoid arthritis have excessive morbidity and mortality,” Dr. Kim, of the division of rheumatology at Brigham and Women’s Hospital and associate professor of medicine at Harvard Medical School in Boston, said at the virtual annual meeting of the American College of Rheumatology.
Among prior studies in this area, the Cardiovascular Inflammation Reduction Trial (CIRT) found no significant reduction in cardiovascular events among people taking methotrexate versus placebo. However, the study of 4,786 people was not specific to RA, Dr. Kim said. The lack of efficacy on this endpoint prompted researchers to stop CIRT early.
“So what does the conclusion of the CIRT trial mean for rheumatoid arthritis patients?” Dr. Kim asked.
To find out, she and colleagues compared risk of MACE among participants newly starting either methotrexate or HCQ. The study included 59,329 people aged 65 and older who were identified through Medicare claims data from 2008 to 2016. Mean age was 74 years, and 80% were women.
The investigators used propensity score matching to control for multiple covariates for demographics, other medications, and comorbidities. Use of other medications was similar between groups, including glucocorticoids, NSAIDs, and statins. Baseline cardiovascular morbidities likewise were well balanced, Dr. Kim said.
The hazard ratio for the primary MACE outcome was 0.96 (95% confidence interval, 0.86-1.08).
Secondary outcomes
MI was less common in the methotrexate group, for example, with an incidence of 8.49 per 1,000 person-years versus 10.68 per 1,000 person-years in the HCQ cohort. This finding was statically significant, Dr. Kim said, with a hazard ratio of 0.80 favoring methotrexate.
Heart failure also occurred less often in the methotrexate cohort, with an incidence rate of 8.57 per 1,000 person-years versus a rate of 14.24 in the HCQ group. The hazard ratio again favored methotrexate at 0.60.
In contrast, strokes were more common with methotrexate than with (incidence of 7.94 vs. 6.01 per 1,000 person-years).
Another secondary outcome, all-cause mortality, was not significantly different between groups. There were 821 deaths in the methotrexate group (28.65 per 1,000 person-years) and 796 deaths in the HCQ group (31.33 per 1,000 person-years).
Studying causality next?
Session moderator Maya Buch, MD, PhD, professor of rheumatology at the University of Manchester (England), asked Dr. Kim why she found significant differences in some secondary outcomes but not the primary composite endpoint.
“When we think of cardiovascular diseases, we tend to think of them all developing through the same mechanism. But perhaps the exact mechanism might not be identical,” Dr. Kim replied. The findings do not suggest causality because the study was observational, she added, “but maybe this will lead to a randomized, controlled trial.”
When asked for comment, Dr. Buch said that the study was “interesting” and “suggestive of differences in type of MACE between the two drugs evaluated,” but that there should be caution in interpreting the findings because of the lack of detailed information on RA disease and activity in claims databases, in addition to other factors, even though the investigators made adjustments for known differences through propensity score matching.
The division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital supported the study. Dr. Kim has received support for Brigham and Women’s Hospital for unrelated research from Pfizer, AbbVie, Roche, and Bristol-Myers Squibb. Several other coauthors reported having financial relationships with pharmaceutical companies that make drugs for RA. Dr. Buch had no relevant disclosures.
SOURCE: He M et al. Arthritis Rheumatol. 2020;72(suppl 10): Abstract 1993.
No significant differences in major adverse cardiovascular events (MACE) emerged between methotrexate and hydroxychloroquine (HCQ) treatment in a comparison of adults 65 years or older with rheumatoid arthritis. However, researchers reported some elevation in risk for stroke in the methotrexate group and for myocardial infarction and heart failure in the HCQ group.
The primary outcome, a composite of MI, stroke, or cardiovascular death, had an incidence of 23.39 per 1,000 person-years in the methotrexate group versus 24.33 in the HCQ group in this observational study of nearly 60,000 people.
“These results suggest an importance of looking at different individual events of cardiovascular disease rather than the whole ‘CV’ disease only,” Seoyoung Kim, MD, said in an interview. “The other important thing is that the mortality was not significantly different between the two groups.”
For example, the researchers reported 256 cardiovascular-related deaths in the methotrexate group and 263 such deaths in the HCQ cohort.
Addressing a recognized risk
“It is well known that patients with rheumatoid arthritis have excessive morbidity and mortality,” Dr. Kim, of the division of rheumatology at Brigham and Women’s Hospital and associate professor of medicine at Harvard Medical School in Boston, said at the virtual annual meeting of the American College of Rheumatology.
Among prior studies in this area, the Cardiovascular Inflammation Reduction Trial (CIRT) found no significant reduction in cardiovascular events among people taking methotrexate versus placebo. However, the study of 4,786 people was not specific to RA, Dr. Kim said. The lack of efficacy on this endpoint prompted researchers to stop CIRT early.
“So what does the conclusion of the CIRT trial mean for rheumatoid arthritis patients?” Dr. Kim asked.
To find out, she and colleagues compared risk of MACE among participants newly starting either methotrexate or HCQ. The study included 59,329 people aged 65 and older who were identified through Medicare claims data from 2008 to 2016. Mean age was 74 years, and 80% were women.
The investigators used propensity score matching to control for multiple covariates for demographics, other medications, and comorbidities. Use of other medications was similar between groups, including glucocorticoids, NSAIDs, and statins. Baseline cardiovascular morbidities likewise were well balanced, Dr. Kim said.
The hazard ratio for the primary MACE outcome was 0.96 (95% confidence interval, 0.86-1.08).
Secondary outcomes
MI was less common in the methotrexate group, for example, with an incidence of 8.49 per 1,000 person-years versus 10.68 per 1,000 person-years in the HCQ cohort. This finding was statically significant, Dr. Kim said, with a hazard ratio of 0.80 favoring methotrexate.
Heart failure also occurred less often in the methotrexate cohort, with an incidence rate of 8.57 per 1,000 person-years versus a rate of 14.24 in the HCQ group. The hazard ratio again favored methotrexate at 0.60.
In contrast, strokes were more common with methotrexate than with (incidence of 7.94 vs. 6.01 per 1,000 person-years).
Another secondary outcome, all-cause mortality, was not significantly different between groups. There were 821 deaths in the methotrexate group (28.65 per 1,000 person-years) and 796 deaths in the HCQ group (31.33 per 1,000 person-years).
Studying causality next?
Session moderator Maya Buch, MD, PhD, professor of rheumatology at the University of Manchester (England), asked Dr. Kim why she found significant differences in some secondary outcomes but not the primary composite endpoint.
“When we think of cardiovascular diseases, we tend to think of them all developing through the same mechanism. But perhaps the exact mechanism might not be identical,” Dr. Kim replied. The findings do not suggest causality because the study was observational, she added, “but maybe this will lead to a randomized, controlled trial.”
When asked for comment, Dr. Buch said that the study was “interesting” and “suggestive of differences in type of MACE between the two drugs evaluated,” but that there should be caution in interpreting the findings because of the lack of detailed information on RA disease and activity in claims databases, in addition to other factors, even though the investigators made adjustments for known differences through propensity score matching.
The division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital supported the study. Dr. Kim has received support for Brigham and Women’s Hospital for unrelated research from Pfizer, AbbVie, Roche, and Bristol-Myers Squibb. Several other coauthors reported having financial relationships with pharmaceutical companies that make drugs for RA. Dr. Buch had no relevant disclosures.
SOURCE: He M et al. Arthritis Rheumatol. 2020;72(suppl 10): Abstract 1993.
FROM ACR 2020
Proposed RA guidelines: Maximize methotrexate before switching
New proposed guidelines for managing rheumatoid arthritis (RA) recommend that methotrexate (MTX) be used aggressively before other treatment options.
Previous guidelines, last updated in 2015, had not ranked the order of the treatments, said Liana Fraenkel, MD, MPH, principal investigator for the American College of Rheumatology’s treatment guidelines.
“There’s a strong emphasis on maximizing methotrexate using various means before switching to a biologic or JAK [Janus kinase] inhibitor,” she said in a press conference at the virtual annual meeting of the American College of Rheumatology. The guidelines draft was developed collaboratively with clinicians, researchers, and patients. In addition, the authors conducted a comprehensive review of the literature.
Dr. Fraenkel, of Yale University in New Haven, Conn., said the exception for maximizing MTX would be for patients with low disease activity for whom treatments with other medications, such as hydroxychloroquine (HCQ) and sulfasalazine, are feasible, she said.
Stop defaulting to prednisone
Another recommendation urges against the use of prednisone as a default treatment.
“We should really be trying to maximize disease-modifying antirheumatic drugs [DMARDs] and try to push the needle away from using prednisone as frequently as we do,” she said.
Dr. Fraenkel said the panel wanted to emphasize that “even lower doses of prednisone can be harmful.”
She noted that patients on the guidelines panel said it’s hard to taper off prednisone.
Don Thomas, MD, who is in private rheumatology practice in Greenbelt, Md., said in an interview he loves the guidelines.
“Most of my patients are not on steroids,” he said, “which is a godsend because of the great therapies we have.”
He said he was glad to see support for exhausting methotrexate options first before trying new treatments.
“Too many of us are not as aggressive as we should be with using methotrexate initially,” he said.
Specific recommendations
In the proposed guidelines, MTX alone is strongly recommended over HCQ or sulfasalazine and is conditionally recommended over a conventional synthetic DMARD dual or triple combination. MTX alone is also conditionally recommended over MTX in combination with a tumor necrosis factor (TNF) inhibitor and is strongly recommended over MTX in combination with a non-TNF inhibitor, a biologic, or a targeted synthetic DMARD.
For patients with low disease activity who have not taken DMARDs, HCQ is recommended over other conventional synthetic DMARDs. Sulfasalazine is recommended over MTX, and MTX is recommended over leflunomide.
For initial treatment, oral MTX is conditionally recommended over subcutaneous administration. For patients who are not tolerating the oral version, “recommend split-dose or subcutaneous or increasing folic acid over switching to a new DMARD,” she said.
Dr. Fraenkel said the oral recommendation was based largely on patient preference.
Use of glucocorticoids
For patients who need glucocorticoids to remain at target, adding or switching DMARDs is recommended over continuing glucocorticoids, the guidelines indicate.
“For patients on DMARDs and not at target, adding or switching DMARDs with or without the use of intraarticular glucocorticoids is conditionally recommended over the use of intraarticular glucocorticoids alone,” the proposed guidelines advise.
Tapering
Tapering should only be considered for patients “who have been at target for at least 6 months,” she said. “In these patients, continuation of all DMARDs at their current dose is conditionally recommended over any dose reduction.”
Dose reduction is recommended over gradual discontinuation, and gradual discontinuation is recommended over abruptly stopping.
Dr. Fraenkel acknowledged that the level of evidence is low to very low for many of the recommendations (only 7 of 44 recommendations were classified as strong), which, she said, underscores the importance of shared decision making for RA.
She added, “We really need trials to address clinically important questions driven by patients and not simply driven by [having] a new molecule to test.”
ACR says the final version of the proposed guidelines is expected to be simultaneously published in Arthritis Care and Research and Arthritis and Rheumatology by the end of the year.
These guidelines are focused on pharmacologic agents. Separate ACR guidelines will address nonpharmacologic management of RA and vaccine recommendations for inflammatory disease.
Dr. Fraenkel and Dr. Thomas have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
New proposed guidelines for managing rheumatoid arthritis (RA) recommend that methotrexate (MTX) be used aggressively before other treatment options.
Previous guidelines, last updated in 2015, had not ranked the order of the treatments, said Liana Fraenkel, MD, MPH, principal investigator for the American College of Rheumatology’s treatment guidelines.
“There’s a strong emphasis on maximizing methotrexate using various means before switching to a biologic or JAK [Janus kinase] inhibitor,” she said in a press conference at the virtual annual meeting of the American College of Rheumatology. The guidelines draft was developed collaboratively with clinicians, researchers, and patients. In addition, the authors conducted a comprehensive review of the literature.
Dr. Fraenkel, of Yale University in New Haven, Conn., said the exception for maximizing MTX would be for patients with low disease activity for whom treatments with other medications, such as hydroxychloroquine (HCQ) and sulfasalazine, are feasible, she said.
Stop defaulting to prednisone
Another recommendation urges against the use of prednisone as a default treatment.
“We should really be trying to maximize disease-modifying antirheumatic drugs [DMARDs] and try to push the needle away from using prednisone as frequently as we do,” she said.
Dr. Fraenkel said the panel wanted to emphasize that “even lower doses of prednisone can be harmful.”
She noted that patients on the guidelines panel said it’s hard to taper off prednisone.
Don Thomas, MD, who is in private rheumatology practice in Greenbelt, Md., said in an interview he loves the guidelines.
“Most of my patients are not on steroids,” he said, “which is a godsend because of the great therapies we have.”
He said he was glad to see support for exhausting methotrexate options first before trying new treatments.
“Too many of us are not as aggressive as we should be with using methotrexate initially,” he said.
Specific recommendations
In the proposed guidelines, MTX alone is strongly recommended over HCQ or sulfasalazine and is conditionally recommended over a conventional synthetic DMARD dual or triple combination. MTX alone is also conditionally recommended over MTX in combination with a tumor necrosis factor (TNF) inhibitor and is strongly recommended over MTX in combination with a non-TNF inhibitor, a biologic, or a targeted synthetic DMARD.
For patients with low disease activity who have not taken DMARDs, HCQ is recommended over other conventional synthetic DMARDs. Sulfasalazine is recommended over MTX, and MTX is recommended over leflunomide.
For initial treatment, oral MTX is conditionally recommended over subcutaneous administration. For patients who are not tolerating the oral version, “recommend split-dose or subcutaneous or increasing folic acid over switching to a new DMARD,” she said.
Dr. Fraenkel said the oral recommendation was based largely on patient preference.
Use of glucocorticoids
For patients who need glucocorticoids to remain at target, adding or switching DMARDs is recommended over continuing glucocorticoids, the guidelines indicate.
“For patients on DMARDs and not at target, adding or switching DMARDs with or without the use of intraarticular glucocorticoids is conditionally recommended over the use of intraarticular glucocorticoids alone,” the proposed guidelines advise.
Tapering
Tapering should only be considered for patients “who have been at target for at least 6 months,” she said. “In these patients, continuation of all DMARDs at their current dose is conditionally recommended over any dose reduction.”
Dose reduction is recommended over gradual discontinuation, and gradual discontinuation is recommended over abruptly stopping.
Dr. Fraenkel acknowledged that the level of evidence is low to very low for many of the recommendations (only 7 of 44 recommendations were classified as strong), which, she said, underscores the importance of shared decision making for RA.
She added, “We really need trials to address clinically important questions driven by patients and not simply driven by [having] a new molecule to test.”
ACR says the final version of the proposed guidelines is expected to be simultaneously published in Arthritis Care and Research and Arthritis and Rheumatology by the end of the year.
These guidelines are focused on pharmacologic agents. Separate ACR guidelines will address nonpharmacologic management of RA and vaccine recommendations for inflammatory disease.
Dr. Fraenkel and Dr. Thomas have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
New proposed guidelines for managing rheumatoid arthritis (RA) recommend that methotrexate (MTX) be used aggressively before other treatment options.
Previous guidelines, last updated in 2015, had not ranked the order of the treatments, said Liana Fraenkel, MD, MPH, principal investigator for the American College of Rheumatology’s treatment guidelines.
“There’s a strong emphasis on maximizing methotrexate using various means before switching to a biologic or JAK [Janus kinase] inhibitor,” she said in a press conference at the virtual annual meeting of the American College of Rheumatology. The guidelines draft was developed collaboratively with clinicians, researchers, and patients. In addition, the authors conducted a comprehensive review of the literature.
Dr. Fraenkel, of Yale University in New Haven, Conn., said the exception for maximizing MTX would be for patients with low disease activity for whom treatments with other medications, such as hydroxychloroquine (HCQ) and sulfasalazine, are feasible, she said.
Stop defaulting to prednisone
Another recommendation urges against the use of prednisone as a default treatment.
“We should really be trying to maximize disease-modifying antirheumatic drugs [DMARDs] and try to push the needle away from using prednisone as frequently as we do,” she said.
Dr. Fraenkel said the panel wanted to emphasize that “even lower doses of prednisone can be harmful.”
She noted that patients on the guidelines panel said it’s hard to taper off prednisone.
Don Thomas, MD, who is in private rheumatology practice in Greenbelt, Md., said in an interview he loves the guidelines.
“Most of my patients are not on steroids,” he said, “which is a godsend because of the great therapies we have.”
He said he was glad to see support for exhausting methotrexate options first before trying new treatments.
“Too many of us are not as aggressive as we should be with using methotrexate initially,” he said.
Specific recommendations
In the proposed guidelines, MTX alone is strongly recommended over HCQ or sulfasalazine and is conditionally recommended over a conventional synthetic DMARD dual or triple combination. MTX alone is also conditionally recommended over MTX in combination with a tumor necrosis factor (TNF) inhibitor and is strongly recommended over MTX in combination with a non-TNF inhibitor, a biologic, or a targeted synthetic DMARD.
For patients with low disease activity who have not taken DMARDs, HCQ is recommended over other conventional synthetic DMARDs. Sulfasalazine is recommended over MTX, and MTX is recommended over leflunomide.
For initial treatment, oral MTX is conditionally recommended over subcutaneous administration. For patients who are not tolerating the oral version, “recommend split-dose or subcutaneous or increasing folic acid over switching to a new DMARD,” she said.
Dr. Fraenkel said the oral recommendation was based largely on patient preference.
Use of glucocorticoids
For patients who need glucocorticoids to remain at target, adding or switching DMARDs is recommended over continuing glucocorticoids, the guidelines indicate.
“For patients on DMARDs and not at target, adding or switching DMARDs with or without the use of intraarticular glucocorticoids is conditionally recommended over the use of intraarticular glucocorticoids alone,” the proposed guidelines advise.
Tapering
Tapering should only be considered for patients “who have been at target for at least 6 months,” she said. “In these patients, continuation of all DMARDs at their current dose is conditionally recommended over any dose reduction.”
Dose reduction is recommended over gradual discontinuation, and gradual discontinuation is recommended over abruptly stopping.
Dr. Fraenkel acknowledged that the level of evidence is low to very low for many of the recommendations (only 7 of 44 recommendations were classified as strong), which, she said, underscores the importance of shared decision making for RA.
She added, “We really need trials to address clinically important questions driven by patients and not simply driven by [having] a new molecule to test.”
ACR says the final version of the proposed guidelines is expected to be simultaneously published in Arthritis Care and Research and Arthritis and Rheumatology by the end of the year.
These guidelines are focused on pharmacologic agents. Separate ACR guidelines will address nonpharmacologic management of RA and vaccine recommendations for inflammatory disease.
Dr. Fraenkel and Dr. Thomas have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM ACR 2020
Methotrexate users need tuberculosis tests in high-TB areas
People taking even low-dose methotrexate need tuberculosis screening and ongoing clinical care if they live in areas where TB is common, results of a study presented at the virtual annual meeting of the American College of Rheumatology suggest.
Coauthor Carol Hitchon, MD, MSc, a rheumatologist with the University of Manitoba in Winnipeg, who presented the findings, warned that methotrexate (MTX) users who also take corticosteroids or other immunosuppressants are at particular risk and need TB screening.
Current management guidelines for rheumatic disease address TB in relation to biologics, but not in relation to methotrexate, Dr. Hitchon said.
“We know that methotrexate is the foundational DMARD [disease-modifying antirheumatic drug] for many rheumatic diseases, especially rheumatoid arthritis,” Dr. Hitchon noted at a press conference. “It’s safe and effective when dosed properly. However, methotrexate does have the potential for significant liver toxicity as well as infection, particularly for infectious organisms that are targeted by cell-mediated immunity, and TB is one of those agents.”
Using multiple databases, researchers conducted a systematic review of the literature published from 1990 to 2018 on TB rates among people who take less than 30 mg of methotrexate a week. Of the 4,700 studies they examined, 31 fit the criteria for this analysis.
They collected data on tuberculosis incidence or new TB diagnoses vs. reactivation of latent TB infection as well as TB outcomes, such as pulmonary symptoms, dissemination, and mortality.
They found a modest increase in the risk of TB infections in the setting of low-dose methotrexate. In addition, rates of TB in people with rheumatic disease who are treated with either methotrexate or biologics are generally higher than in the general population.
They also found that methotrexate users had higher rates of the type of TB that spreads beyond a patient’s lungs, compared with the general population.
Safety of INH with methotrexate
Researchers also looked at the safety of isoniazid (INH), the antibiotic used to treat TB, and found that isoniazid-related liver toxicity and neutropenia were more common when people took the antibiotic along with methotrexate, but those effects were usually reversible.
TB is endemic in various regions around the world. Historically there hasn’t been much rheumatology capacity in many of these areas, but as that capacity increases more people who are at high risk for developing or reactivating TB will be receiving methotrexate for rheumatic diseases, Dr. Hitchon said.
“It’s prudent for people managing patients who may be at higher risk for TB either from where they live or from where they travel that we should have a high suspicion for TB and consider screening as part of our workup in the course of initiating treatment like methotrexate,” she said.
Narender Annapureddy, MD, a rheumatologist at Vanderbilt University, Nashville, Tenn., who was not involved in the research, pointed out that a limitation of the work is that only 27% of the studies are from developing countries, which are more likely to have endemic TB, and those studies had very few cases.
“This finding needs to be studied in larger populations in TB-endemic areas and in high-risk populations,” he said in an interview.
As for practice implications in the United States, Dr. Annapureddy noted that TB is rare in the United States and most of the cases occur in people born in other countries.
“This population may be at risk for TB and should probably be screened for TB before initiating methotrexate,” he said. “Since biologics are usually the next step, especially in RA after patients fail methotrexate, having information on TB status may also help guide management options after MTX failure.
“Since high-dose steroids are another important risk factor for TB activation,” Dr. Annapureddy continued, “rheumatologists should likely consider screening patients who are going to be on moderate to high doses of steroids with MTX.”
A version of this article originally appeared on Medscape.com.
People taking even low-dose methotrexate need tuberculosis screening and ongoing clinical care if they live in areas where TB is common, results of a study presented at the virtual annual meeting of the American College of Rheumatology suggest.
Coauthor Carol Hitchon, MD, MSc, a rheumatologist with the University of Manitoba in Winnipeg, who presented the findings, warned that methotrexate (MTX) users who also take corticosteroids or other immunosuppressants are at particular risk and need TB screening.
Current management guidelines for rheumatic disease address TB in relation to biologics, but not in relation to methotrexate, Dr. Hitchon said.
“We know that methotrexate is the foundational DMARD [disease-modifying antirheumatic drug] for many rheumatic diseases, especially rheumatoid arthritis,” Dr. Hitchon noted at a press conference. “It’s safe and effective when dosed properly. However, methotrexate does have the potential for significant liver toxicity as well as infection, particularly for infectious organisms that are targeted by cell-mediated immunity, and TB is one of those agents.”
Using multiple databases, researchers conducted a systematic review of the literature published from 1990 to 2018 on TB rates among people who take less than 30 mg of methotrexate a week. Of the 4,700 studies they examined, 31 fit the criteria for this analysis.
They collected data on tuberculosis incidence or new TB diagnoses vs. reactivation of latent TB infection as well as TB outcomes, such as pulmonary symptoms, dissemination, and mortality.
They found a modest increase in the risk of TB infections in the setting of low-dose methotrexate. In addition, rates of TB in people with rheumatic disease who are treated with either methotrexate or biologics are generally higher than in the general population.
They also found that methotrexate users had higher rates of the type of TB that spreads beyond a patient’s lungs, compared with the general population.
Safety of INH with methotrexate
Researchers also looked at the safety of isoniazid (INH), the antibiotic used to treat TB, and found that isoniazid-related liver toxicity and neutropenia were more common when people took the antibiotic along with methotrexate, but those effects were usually reversible.
TB is endemic in various regions around the world. Historically there hasn’t been much rheumatology capacity in many of these areas, but as that capacity increases more people who are at high risk for developing or reactivating TB will be receiving methotrexate for rheumatic diseases, Dr. Hitchon said.
“It’s prudent for people managing patients who may be at higher risk for TB either from where they live or from where they travel that we should have a high suspicion for TB and consider screening as part of our workup in the course of initiating treatment like methotrexate,” she said.
Narender Annapureddy, MD, a rheumatologist at Vanderbilt University, Nashville, Tenn., who was not involved in the research, pointed out that a limitation of the work is that only 27% of the studies are from developing countries, which are more likely to have endemic TB, and those studies had very few cases.
“This finding needs to be studied in larger populations in TB-endemic areas and in high-risk populations,” he said in an interview.
As for practice implications in the United States, Dr. Annapureddy noted that TB is rare in the United States and most of the cases occur in people born in other countries.
“This population may be at risk for TB and should probably be screened for TB before initiating methotrexate,” he said. “Since biologics are usually the next step, especially in RA after patients fail methotrexate, having information on TB status may also help guide management options after MTX failure.
“Since high-dose steroids are another important risk factor for TB activation,” Dr. Annapureddy continued, “rheumatologists should likely consider screening patients who are going to be on moderate to high doses of steroids with MTX.”
A version of this article originally appeared on Medscape.com.
People taking even low-dose methotrexate need tuberculosis screening and ongoing clinical care if they live in areas where TB is common, results of a study presented at the virtual annual meeting of the American College of Rheumatology suggest.
Coauthor Carol Hitchon, MD, MSc, a rheumatologist with the University of Manitoba in Winnipeg, who presented the findings, warned that methotrexate (MTX) users who also take corticosteroids or other immunosuppressants are at particular risk and need TB screening.
Current management guidelines for rheumatic disease address TB in relation to biologics, but not in relation to methotrexate, Dr. Hitchon said.
“We know that methotrexate is the foundational DMARD [disease-modifying antirheumatic drug] for many rheumatic diseases, especially rheumatoid arthritis,” Dr. Hitchon noted at a press conference. “It’s safe and effective when dosed properly. However, methotrexate does have the potential for significant liver toxicity as well as infection, particularly for infectious organisms that are targeted by cell-mediated immunity, and TB is one of those agents.”
Using multiple databases, researchers conducted a systematic review of the literature published from 1990 to 2018 on TB rates among people who take less than 30 mg of methotrexate a week. Of the 4,700 studies they examined, 31 fit the criteria for this analysis.
They collected data on tuberculosis incidence or new TB diagnoses vs. reactivation of latent TB infection as well as TB outcomes, such as pulmonary symptoms, dissemination, and mortality.
They found a modest increase in the risk of TB infections in the setting of low-dose methotrexate. In addition, rates of TB in people with rheumatic disease who are treated with either methotrexate or biologics are generally higher than in the general population.
They also found that methotrexate users had higher rates of the type of TB that spreads beyond a patient’s lungs, compared with the general population.
Safety of INH with methotrexate
Researchers also looked at the safety of isoniazid (INH), the antibiotic used to treat TB, and found that isoniazid-related liver toxicity and neutropenia were more common when people took the antibiotic along with methotrexate, but those effects were usually reversible.
TB is endemic in various regions around the world. Historically there hasn’t been much rheumatology capacity in many of these areas, but as that capacity increases more people who are at high risk for developing or reactivating TB will be receiving methotrexate for rheumatic diseases, Dr. Hitchon said.
“It’s prudent for people managing patients who may be at higher risk for TB either from where they live or from where they travel that we should have a high suspicion for TB and consider screening as part of our workup in the course of initiating treatment like methotrexate,” she said.
Narender Annapureddy, MD, a rheumatologist at Vanderbilt University, Nashville, Tenn., who was not involved in the research, pointed out that a limitation of the work is that only 27% of the studies are from developing countries, which are more likely to have endemic TB, and those studies had very few cases.
“This finding needs to be studied in larger populations in TB-endemic areas and in high-risk populations,” he said in an interview.
As for practice implications in the United States, Dr. Annapureddy noted that TB is rare in the United States and most of the cases occur in people born in other countries.
“This population may be at risk for TB and should probably be screened for TB before initiating methotrexate,” he said. “Since biologics are usually the next step, especially in RA after patients fail methotrexate, having information on TB status may also help guide management options after MTX failure.
“Since high-dose steroids are another important risk factor for TB activation,” Dr. Annapureddy continued, “rheumatologists should likely consider screening patients who are going to be on moderate to high doses of steroids with MTX.”
A version of this article originally appeared on Medscape.com.
Pregnancy can be safe with interstitial lung disease
Pregnant women with interstitial lung disease (ILD) related to autoimmune disease may not need to terminate their pregnancies if they have close monitoring before, during, and after pregnancy with a multidisciplinary team of physicians, new research suggests.
Senior author Megan Clowse, MD, MPH, associate professor of medicine in the division of rheumatology at Duke University, Durham, N.C., explained during a press conference at the virtual annual meeting of the American College of Rheumatology that women with ILD are often advised by obstetricians or rheumatologists to avoid conception or terminate their pregnancies, though evidence for that has been based on small studies of 9-15 patients that have had mixed results.
“Many of these pregnancies were delivered 20-30 years ago, definitely with different rheumatic and obstetric care than we can provide now,” she said. “It’s really time to rethink our approach to interstitial lung disease and pregnancy.”
This study showed that while adverse pregnancy outcomes are common in these women, overall maternal morbidity and mortality are low.
ILD may be a secondary disease in people who have scleroderma, lupus, and sarcoidosis.
Largest study to date
This Pfizer-sponsored retrospective study of 67 pregnant women is the largest to date, and it analyzed 94 pregnancies (including five sets of twins).
Sarah Rae Easter, MD, maternal-fetal medicine doctor in the department of obstetrics and gynecology at Brigham and Women’s Hospital, Boston, called the work “exciting” as the researchers were able to look back at a large number of cases for a rare condition for more than 20 years.
“Their data provides much-needed evidence to provide some reassurance for women affected by this type of pulmonary disease regarding the relative safety of pregnancy,” she said in an interview.
Study spanned 23 years
The researchers reviewed pregnancy records in patients diagnosed with ILD secondary to autoimmune disease at Duke University Health System from January 1996 to July 2019.
They classified the severity of ILD based on two standard breathing tests – forced vital capacity and diffusion capacity for carbon monoxide.
Overall, 69% of the women were diagnosed with sarcoidosis and the remaining 31% had a connective tissue disease associated with ILD (CTD-ILD). Of those measured for ILD severity, 11% were severe, 25% were moderate, 50% were mild, and 14% were normal. Their average maternal age was 32.1 and 83% were Black.
While 70% of the pregnancies resulted in live births, 9% were terminated. The remainder resulted in miscarriage or stillbirth.
Researchers reported a 15% rate of preeclampsia, a 34% rate of the composite measure PROMISSE-Adverse Pregnancy Outcome (APO), and a 15% rate of PROMISSE-APO SEVERE. Patients with severe disease had the highest rates of PROMISSE-APO (P = .03 across groups).
(PROMISSE stands for the Predictors of Pregnancy Outcome: Biomarkers in Antiphospholipid Antibody Syndrome and Systemic Lupus Erythematosus study.)
None of the women died
Dr. Clowse said it was a pleasant surprise to find that none of the women died, though patients with severe ILD had more adverse outcomes. Only 2.1% were treated in an intensive care unit during or soon after delivery. In 4.2%, ILD patients had significant shortness of breath due to fluid volume overload around the time of delivery.
For the women who had normal-to-moderate lung disease, Dr. Clowse said, “they really had remarkably good outcomes, really pretty comparable to the general population. About 15% delivered preterm and about 20% suffered a pregnancy loss.”
Dr. Easter, who was not involved with the study, noted the large number of Black women in the cohort.
“Focusing in on improving outcomes for Black and Brown women related to pregnancy in our country is a much-needed undertaking,” Dr. Easter said.
Being able to quote percentages from this research, based on a good-sized study “at least gives people a benchmark about what kind of risk they are willing to assume for themselves,” she said.
For providers, being able to place this rare disease within the spectrum of other diseases where there is more data is also very helpful, she said.
Dr. Clowse said in an interview that the preponderance of Black women in the study was a surprise but may be explained by two factors: Sarcoidosis is seen more frequently in Black women and in the study area in North Carolina there is a large population of Black women.
“Also, our patients with more severe lupus, the ones who are more likely to have interstitial lung disease, are often Black and that’s likely contributing as well,” she said.
Multidisciplinary teams advised
Dr. Clowse emphasized that women with ILD need multidisciplinary teams in pregnancy and should be managed at tertiary care centers where there is a full complement of obstetric and internal medicine experts.
“We do recommend evaluating the severity of their lungs and their heart disease around the time of pregnancy and during pregnancy if they have shortness of breath,” she said.
“We currently recommend that these patients with moderate or severe disease stay in the hospital for up to a week, just for monitoring,” she said.
Dr. Easter said having that kind of access to a large academic healthcare center should be an important part of the decision-making.
Patients need to think about whether they would have access to care similar to what the researchers are describing when they are making the decision to pursue or continue pregnancy, she said.
The study was sponsored by Pfizer Inc. Dr. Clowse reported relationships with UCB, GlaxoSmithKline, AstraZeneca, and Pfizer. Dr. Easter has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Pregnant women with interstitial lung disease (ILD) related to autoimmune disease may not need to terminate their pregnancies if they have close monitoring before, during, and after pregnancy with a multidisciplinary team of physicians, new research suggests.
Senior author Megan Clowse, MD, MPH, associate professor of medicine in the division of rheumatology at Duke University, Durham, N.C., explained during a press conference at the virtual annual meeting of the American College of Rheumatology that women with ILD are often advised by obstetricians or rheumatologists to avoid conception or terminate their pregnancies, though evidence for that has been based on small studies of 9-15 patients that have had mixed results.
“Many of these pregnancies were delivered 20-30 years ago, definitely with different rheumatic and obstetric care than we can provide now,” she said. “It’s really time to rethink our approach to interstitial lung disease and pregnancy.”
This study showed that while adverse pregnancy outcomes are common in these women, overall maternal morbidity and mortality are low.
ILD may be a secondary disease in people who have scleroderma, lupus, and sarcoidosis.
Largest study to date
This Pfizer-sponsored retrospective study of 67 pregnant women is the largest to date, and it analyzed 94 pregnancies (including five sets of twins).
Sarah Rae Easter, MD, maternal-fetal medicine doctor in the department of obstetrics and gynecology at Brigham and Women’s Hospital, Boston, called the work “exciting” as the researchers were able to look back at a large number of cases for a rare condition for more than 20 years.
“Their data provides much-needed evidence to provide some reassurance for women affected by this type of pulmonary disease regarding the relative safety of pregnancy,” she said in an interview.
Study spanned 23 years
The researchers reviewed pregnancy records in patients diagnosed with ILD secondary to autoimmune disease at Duke University Health System from January 1996 to July 2019.
They classified the severity of ILD based on two standard breathing tests – forced vital capacity and diffusion capacity for carbon monoxide.
Overall, 69% of the women were diagnosed with sarcoidosis and the remaining 31% had a connective tissue disease associated with ILD (CTD-ILD). Of those measured for ILD severity, 11% were severe, 25% were moderate, 50% were mild, and 14% were normal. Their average maternal age was 32.1 and 83% were Black.
While 70% of the pregnancies resulted in live births, 9% were terminated. The remainder resulted in miscarriage or stillbirth.
Researchers reported a 15% rate of preeclampsia, a 34% rate of the composite measure PROMISSE-Adverse Pregnancy Outcome (APO), and a 15% rate of PROMISSE-APO SEVERE. Patients with severe disease had the highest rates of PROMISSE-APO (P = .03 across groups).
(PROMISSE stands for the Predictors of Pregnancy Outcome: Biomarkers in Antiphospholipid Antibody Syndrome and Systemic Lupus Erythematosus study.)
None of the women died
Dr. Clowse said it was a pleasant surprise to find that none of the women died, though patients with severe ILD had more adverse outcomes. Only 2.1% were treated in an intensive care unit during or soon after delivery. In 4.2%, ILD patients had significant shortness of breath due to fluid volume overload around the time of delivery.
For the women who had normal-to-moderate lung disease, Dr. Clowse said, “they really had remarkably good outcomes, really pretty comparable to the general population. About 15% delivered preterm and about 20% suffered a pregnancy loss.”
Dr. Easter, who was not involved with the study, noted the large number of Black women in the cohort.
“Focusing in on improving outcomes for Black and Brown women related to pregnancy in our country is a much-needed undertaking,” Dr. Easter said.
Being able to quote percentages from this research, based on a good-sized study “at least gives people a benchmark about what kind of risk they are willing to assume for themselves,” she said.
For providers, being able to place this rare disease within the spectrum of other diseases where there is more data is also very helpful, she said.
Dr. Clowse said in an interview that the preponderance of Black women in the study was a surprise but may be explained by two factors: Sarcoidosis is seen more frequently in Black women and in the study area in North Carolina there is a large population of Black women.
“Also, our patients with more severe lupus, the ones who are more likely to have interstitial lung disease, are often Black and that’s likely contributing as well,” she said.
Multidisciplinary teams advised
Dr. Clowse emphasized that women with ILD need multidisciplinary teams in pregnancy and should be managed at tertiary care centers where there is a full complement of obstetric and internal medicine experts.
“We do recommend evaluating the severity of their lungs and their heart disease around the time of pregnancy and during pregnancy if they have shortness of breath,” she said.
“We currently recommend that these patients with moderate or severe disease stay in the hospital for up to a week, just for monitoring,” she said.
Dr. Easter said having that kind of access to a large academic healthcare center should be an important part of the decision-making.
Patients need to think about whether they would have access to care similar to what the researchers are describing when they are making the decision to pursue or continue pregnancy, she said.
The study was sponsored by Pfizer Inc. Dr. Clowse reported relationships with UCB, GlaxoSmithKline, AstraZeneca, and Pfizer. Dr. Easter has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Pregnant women with interstitial lung disease (ILD) related to autoimmune disease may not need to terminate their pregnancies if they have close monitoring before, during, and after pregnancy with a multidisciplinary team of physicians, new research suggests.
Senior author Megan Clowse, MD, MPH, associate professor of medicine in the division of rheumatology at Duke University, Durham, N.C., explained during a press conference at the virtual annual meeting of the American College of Rheumatology that women with ILD are often advised by obstetricians or rheumatologists to avoid conception or terminate their pregnancies, though evidence for that has been based on small studies of 9-15 patients that have had mixed results.
“Many of these pregnancies were delivered 20-30 years ago, definitely with different rheumatic and obstetric care than we can provide now,” she said. “It’s really time to rethink our approach to interstitial lung disease and pregnancy.”
This study showed that while adverse pregnancy outcomes are common in these women, overall maternal morbidity and mortality are low.
ILD may be a secondary disease in people who have scleroderma, lupus, and sarcoidosis.
Largest study to date
This Pfizer-sponsored retrospective study of 67 pregnant women is the largest to date, and it analyzed 94 pregnancies (including five sets of twins).
Sarah Rae Easter, MD, maternal-fetal medicine doctor in the department of obstetrics and gynecology at Brigham and Women’s Hospital, Boston, called the work “exciting” as the researchers were able to look back at a large number of cases for a rare condition for more than 20 years.
“Their data provides much-needed evidence to provide some reassurance for women affected by this type of pulmonary disease regarding the relative safety of pregnancy,” she said in an interview.
Study spanned 23 years
The researchers reviewed pregnancy records in patients diagnosed with ILD secondary to autoimmune disease at Duke University Health System from January 1996 to July 2019.
They classified the severity of ILD based on two standard breathing tests – forced vital capacity and diffusion capacity for carbon monoxide.
Overall, 69% of the women were diagnosed with sarcoidosis and the remaining 31% had a connective tissue disease associated with ILD (CTD-ILD). Of those measured for ILD severity, 11% were severe, 25% were moderate, 50% were mild, and 14% were normal. Their average maternal age was 32.1 and 83% were Black.
While 70% of the pregnancies resulted in live births, 9% were terminated. The remainder resulted in miscarriage or stillbirth.
Researchers reported a 15% rate of preeclampsia, a 34% rate of the composite measure PROMISSE-Adverse Pregnancy Outcome (APO), and a 15% rate of PROMISSE-APO SEVERE. Patients with severe disease had the highest rates of PROMISSE-APO (P = .03 across groups).
(PROMISSE stands for the Predictors of Pregnancy Outcome: Biomarkers in Antiphospholipid Antibody Syndrome and Systemic Lupus Erythematosus study.)
None of the women died
Dr. Clowse said it was a pleasant surprise to find that none of the women died, though patients with severe ILD had more adverse outcomes. Only 2.1% were treated in an intensive care unit during or soon after delivery. In 4.2%, ILD patients had significant shortness of breath due to fluid volume overload around the time of delivery.
For the women who had normal-to-moderate lung disease, Dr. Clowse said, “they really had remarkably good outcomes, really pretty comparable to the general population. About 15% delivered preterm and about 20% suffered a pregnancy loss.”
Dr. Easter, who was not involved with the study, noted the large number of Black women in the cohort.
“Focusing in on improving outcomes for Black and Brown women related to pregnancy in our country is a much-needed undertaking,” Dr. Easter said.
Being able to quote percentages from this research, based on a good-sized study “at least gives people a benchmark about what kind of risk they are willing to assume for themselves,” she said.
For providers, being able to place this rare disease within the spectrum of other diseases where there is more data is also very helpful, she said.
Dr. Clowse said in an interview that the preponderance of Black women in the study was a surprise but may be explained by two factors: Sarcoidosis is seen more frequently in Black women and in the study area in North Carolina there is a large population of Black women.
“Also, our patients with more severe lupus, the ones who are more likely to have interstitial lung disease, are often Black and that’s likely contributing as well,” she said.
Multidisciplinary teams advised
Dr. Clowse emphasized that women with ILD need multidisciplinary teams in pregnancy and should be managed at tertiary care centers where there is a full complement of obstetric and internal medicine experts.
“We do recommend evaluating the severity of their lungs and their heart disease around the time of pregnancy and during pregnancy if they have shortness of breath,” she said.
“We currently recommend that these patients with moderate or severe disease stay in the hospital for up to a week, just for monitoring,” she said.
Dr. Easter said having that kind of access to a large academic healthcare center should be an important part of the decision-making.
Patients need to think about whether they would have access to care similar to what the researchers are describing when they are making the decision to pursue or continue pregnancy, she said.
The study was sponsored by Pfizer Inc. Dr. Clowse reported relationships with UCB, GlaxoSmithKline, AstraZeneca, and Pfizer. Dr. Easter has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
COVID-19 risks in rheumatic disease remain unclear
ACR 2020 studies offer conflicting findings.
Among people with COVID-19, those with systemic autoimmune rheumatic diseases had an elevated 30-day risk of hospitalization, ICU admission, need for mechanical ventilation, and acute kidney injury, compared to a group without rheumatic diseases at 4 months in a match-controlled study.
When investigators expanded the study to 6 months, the difference in need for mechanical ventilation disappeared. However, relative risk for venous thromboembolism (VTE) emerged as 74% higher among people with COVID-19 and with rheumatic disease, said Kristin D’Silva, MD, who presented the findings during a plenary session at the virtual annual meeting of the American College of Rheumatology. She noted that rheumatic disease itself could contribute to VTE risk.
Comorbidities including hypertension, diabetes, and asthma were more common among people with systemic autoimmune rheumatic diseases (SARDs). After adjustment for comorbidities, “the risks of hospitalization and ICU admission were attenuated, suggesting comorbidities are likely key mediators of the increased risk of severe COVID-19 outcomes observed in SARDs patients versus comparators,” Dr. D’Silva, a rheumatology fellow at Massachusetts General Hospital in Boston, said in an interview.
“The risk of venous thromboembolism persisted even after adjusting for comorbidities,” Dr. D’Silva said. Patients with SARDs should be closely monitored for VTE during COVID-19 infection, she added. “Patients with significant cardiovascular, pulmonary, and metabolic comorbidities should be closely monitored for severe COVID-19.”
At the same time, a systematic review of 15 published studies revealed a low incidence of COVID-19 infection among people with rheumatic disease. Furthermore, most experienced a mild clinical course and low mortality, Akhil Sood, MD, said when presenting results of his poster at the meeting.
Underlying immunosuppression, chronic inflammation, comorbidities, and disparities based on racial, ethnic, and socioeconomic status could predispose people with rheumatic disease to poorer COVID-19 outcomes. However, the risks and outcomes of COVID-19 infection among this population “are not well understood,” said Dr. Sood, a second-year resident in internal medicine at the University of Texas Medical Branch in Galveston.
Elevated risks in match-controlled study
Dr. D’Silva and colleagues examined a COVID-19 population and compared 716 people with SARDs and another 716 people from the general public at 4 months, as well as 2,379 people each in similar groups at 6 months. They used real-time electronic medical record data from the TriNetX research network to identify ICD-10 codes for inflammatory arthritis, connective tissue diseases, and systemic vasculitis. They also used ICD-10 codes and positive PCR tests to identify people with COVID-19.
Mean age was 57 years and women accounted for 79% of both groups evaluated at 4 months. Those with SARDs were 23% more likely to be hospitalized (relative risk, 1.23; 95% confidence interval, 1.01-1.50). This group was 75% more likely to be admitted to the ICU (RR, 1.75; 95% CI, 1.11-2.75), 77% more likely to require mechanical ventilation (RR, 1.77; 95% CI, 1.06-2.96), and 83% more likely to experience acute kidney injury (RR, 1.83; 95% CI, 1.11-3.00).
Risk of death was not significantly higher in the SARDs group (RR, 1.16; 95% CI, 0.73-1.86).
When Dr. D’Silva expanded the study to more people at 6 months, they added additional 30-day outcomes of interest: renal replacement therapy, VTE, and ischemic stroke. Risk of need for renal replacement therapy, for example, was 81% higher in the SARDs group (RR, 1.81; 95% CI, 1.07-3.07). Risk of stroke was not significantly different between groups.The improvement in mechanical ventilation risk between 4 and 6 months was not completely unexpected, Dr. D’Silva said. The relative risk dropped from 1.77 to 1.05. “This is not particularly surprising given national trends in the general population reporting decreased severe outcomes of COVID-19 including mortality as the pandemic progresses. This is likely multifactorial including changes in COVID-19 management (such as increasing use of nonintubated prone positioning rather than early intubation and treatments such as dexamethasone and remdesivir), decreased strain on hospitals and staffing compared to the early crisis phase of the pandemic, and higher testing capacity leading to detection of milder cases.”
When the 6-month analysis was further adjusted for comorbidities and a history of prior hospitalization within 1 year, only risk for acute kidney injury and VTE remained significant with relative risks of 1.33 and 1.60, respectively, likely because comorbidities are causal intermediates of COVID-19 30-day outcomes rather than confounders.
When asked to comment on the results, session comoderator Victoria K. Shanmugam, MD, said in an interview that the study “is of great interest both to rheumatologists and to patients with rheumatic disease.”
The higher risk of hospitalization, ICU admission, mechanical ventilation, acute kidney injury, and heart failure “is an important finding with implications for how our patients navigate risk during this pandemic,” said Dr. Shanmugam, director of the division of rheumatology at George Washington University in Washington.
Lower risks emerge in systematic review
The 15 observational studies in the systematic review included 11,815 participants. A total of 179, or 1.5%, tested positive for COVID-19.
“The incidence of COVID-19 infection among patients with rheumatic disease was low,” Dr. Sood said.
Within the COVID-19-positive group, almost 50% required hospitalization, 10% required ICU admission, and 8% died. The pooled event rate for hospitalization was 0.440 (95% CI, 0.296-0.596), while for ICU admission it was 0.132 (95% CI, 0.087-0.194) and for death it was 0.125 (95% CI, 0.082-0.182).
Different calculations of risk
The two studies seem to offer contradictory findings, but the disparities could be explained by study design differences. For example, Dr. D’Silva’s study evaluated a population with COVID-19 and compared those with SARDs versus a matched group from the general public. Dr. Sood and colleagues assessed study populations with rheumatic disease and assessed incidence of SARS-CoV-2 infection and difference in outcomes.
“We are asking very different questions,” Dr. D’Silva said.
“The study by D’Silva et al. was able to account for different factors to reduce confounding,” Dr. Sood said, adding that Dr. D’Silva and colleagues included a high proportion of minorities, compared with a less diverse population in the systematic review, which featured a large number of studies from Italy.
The authors of the two studies had no relevant financial disclosures to report.
SOURCES: D’Silva K et al. Arthritis Rheumatol. 2020;72(suppl 10): Abstract 0430, and Sood A et al. Arthritis Rheumatol. 2020;72(suppl 10): Abstract 0008.
ACR 2020 studies offer conflicting findings.
ACR 2020 studies offer conflicting findings.
Among people with COVID-19, those with systemic autoimmune rheumatic diseases had an elevated 30-day risk of hospitalization, ICU admission, need for mechanical ventilation, and acute kidney injury, compared to a group without rheumatic diseases at 4 months in a match-controlled study.
When investigators expanded the study to 6 months, the difference in need for mechanical ventilation disappeared. However, relative risk for venous thromboembolism (VTE) emerged as 74% higher among people with COVID-19 and with rheumatic disease, said Kristin D’Silva, MD, who presented the findings during a plenary session at the virtual annual meeting of the American College of Rheumatology. She noted that rheumatic disease itself could contribute to VTE risk.
Comorbidities including hypertension, diabetes, and asthma were more common among people with systemic autoimmune rheumatic diseases (SARDs). After adjustment for comorbidities, “the risks of hospitalization and ICU admission were attenuated, suggesting comorbidities are likely key mediators of the increased risk of severe COVID-19 outcomes observed in SARDs patients versus comparators,” Dr. D’Silva, a rheumatology fellow at Massachusetts General Hospital in Boston, said in an interview.
“The risk of venous thromboembolism persisted even after adjusting for comorbidities,” Dr. D’Silva said. Patients with SARDs should be closely monitored for VTE during COVID-19 infection, she added. “Patients with significant cardiovascular, pulmonary, and metabolic comorbidities should be closely monitored for severe COVID-19.”
At the same time, a systematic review of 15 published studies revealed a low incidence of COVID-19 infection among people with rheumatic disease. Furthermore, most experienced a mild clinical course and low mortality, Akhil Sood, MD, said when presenting results of his poster at the meeting.
Underlying immunosuppression, chronic inflammation, comorbidities, and disparities based on racial, ethnic, and socioeconomic status could predispose people with rheumatic disease to poorer COVID-19 outcomes. However, the risks and outcomes of COVID-19 infection among this population “are not well understood,” said Dr. Sood, a second-year resident in internal medicine at the University of Texas Medical Branch in Galveston.
Elevated risks in match-controlled study
Dr. D’Silva and colleagues examined a COVID-19 population and compared 716 people with SARDs and another 716 people from the general public at 4 months, as well as 2,379 people each in similar groups at 6 months. They used real-time electronic medical record data from the TriNetX research network to identify ICD-10 codes for inflammatory arthritis, connective tissue diseases, and systemic vasculitis. They also used ICD-10 codes and positive PCR tests to identify people with COVID-19.
Mean age was 57 years and women accounted for 79% of both groups evaluated at 4 months. Those with SARDs were 23% more likely to be hospitalized (relative risk, 1.23; 95% confidence interval, 1.01-1.50). This group was 75% more likely to be admitted to the ICU (RR, 1.75; 95% CI, 1.11-2.75), 77% more likely to require mechanical ventilation (RR, 1.77; 95% CI, 1.06-2.96), and 83% more likely to experience acute kidney injury (RR, 1.83; 95% CI, 1.11-3.00).
Risk of death was not significantly higher in the SARDs group (RR, 1.16; 95% CI, 0.73-1.86).
When Dr. D’Silva expanded the study to more people at 6 months, they added additional 30-day outcomes of interest: renal replacement therapy, VTE, and ischemic stroke. Risk of need for renal replacement therapy, for example, was 81% higher in the SARDs group (RR, 1.81; 95% CI, 1.07-3.07). Risk of stroke was not significantly different between groups.The improvement in mechanical ventilation risk between 4 and 6 months was not completely unexpected, Dr. D’Silva said. The relative risk dropped from 1.77 to 1.05. “This is not particularly surprising given national trends in the general population reporting decreased severe outcomes of COVID-19 including mortality as the pandemic progresses. This is likely multifactorial including changes in COVID-19 management (such as increasing use of nonintubated prone positioning rather than early intubation and treatments such as dexamethasone and remdesivir), decreased strain on hospitals and staffing compared to the early crisis phase of the pandemic, and higher testing capacity leading to detection of milder cases.”
When the 6-month analysis was further adjusted for comorbidities and a history of prior hospitalization within 1 year, only risk for acute kidney injury and VTE remained significant with relative risks of 1.33 and 1.60, respectively, likely because comorbidities are causal intermediates of COVID-19 30-day outcomes rather than confounders.
When asked to comment on the results, session comoderator Victoria K. Shanmugam, MD, said in an interview that the study “is of great interest both to rheumatologists and to patients with rheumatic disease.”
The higher risk of hospitalization, ICU admission, mechanical ventilation, acute kidney injury, and heart failure “is an important finding with implications for how our patients navigate risk during this pandemic,” said Dr. Shanmugam, director of the division of rheumatology at George Washington University in Washington.
Lower risks emerge in systematic review
The 15 observational studies in the systematic review included 11,815 participants. A total of 179, or 1.5%, tested positive for COVID-19.
“The incidence of COVID-19 infection among patients with rheumatic disease was low,” Dr. Sood said.
Within the COVID-19-positive group, almost 50% required hospitalization, 10% required ICU admission, and 8% died. The pooled event rate for hospitalization was 0.440 (95% CI, 0.296-0.596), while for ICU admission it was 0.132 (95% CI, 0.087-0.194) and for death it was 0.125 (95% CI, 0.082-0.182).
Different calculations of risk
The two studies seem to offer contradictory findings, but the disparities could be explained by study design differences. For example, Dr. D’Silva’s study evaluated a population with COVID-19 and compared those with SARDs versus a matched group from the general public. Dr. Sood and colleagues assessed study populations with rheumatic disease and assessed incidence of SARS-CoV-2 infection and difference in outcomes.
“We are asking very different questions,” Dr. D’Silva said.
“The study by D’Silva et al. was able to account for different factors to reduce confounding,” Dr. Sood said, adding that Dr. D’Silva and colleagues included a high proportion of minorities, compared with a less diverse population in the systematic review, which featured a large number of studies from Italy.
The authors of the two studies had no relevant financial disclosures to report.
SOURCES: D’Silva K et al. Arthritis Rheumatol. 2020;72(suppl 10): Abstract 0430, and Sood A et al. Arthritis Rheumatol. 2020;72(suppl 10): Abstract 0008.
Among people with COVID-19, those with systemic autoimmune rheumatic diseases had an elevated 30-day risk of hospitalization, ICU admission, need for mechanical ventilation, and acute kidney injury, compared to a group without rheumatic diseases at 4 months in a match-controlled study.
When investigators expanded the study to 6 months, the difference in need for mechanical ventilation disappeared. However, relative risk for venous thromboembolism (VTE) emerged as 74% higher among people with COVID-19 and with rheumatic disease, said Kristin D’Silva, MD, who presented the findings during a plenary session at the virtual annual meeting of the American College of Rheumatology. She noted that rheumatic disease itself could contribute to VTE risk.
Comorbidities including hypertension, diabetes, and asthma were more common among people with systemic autoimmune rheumatic diseases (SARDs). After adjustment for comorbidities, “the risks of hospitalization and ICU admission were attenuated, suggesting comorbidities are likely key mediators of the increased risk of severe COVID-19 outcomes observed in SARDs patients versus comparators,” Dr. D’Silva, a rheumatology fellow at Massachusetts General Hospital in Boston, said in an interview.
“The risk of venous thromboembolism persisted even after adjusting for comorbidities,” Dr. D’Silva said. Patients with SARDs should be closely monitored for VTE during COVID-19 infection, she added. “Patients with significant cardiovascular, pulmonary, and metabolic comorbidities should be closely monitored for severe COVID-19.”
At the same time, a systematic review of 15 published studies revealed a low incidence of COVID-19 infection among people with rheumatic disease. Furthermore, most experienced a mild clinical course and low mortality, Akhil Sood, MD, said when presenting results of his poster at the meeting.
Underlying immunosuppression, chronic inflammation, comorbidities, and disparities based on racial, ethnic, and socioeconomic status could predispose people with rheumatic disease to poorer COVID-19 outcomes. However, the risks and outcomes of COVID-19 infection among this population “are not well understood,” said Dr. Sood, a second-year resident in internal medicine at the University of Texas Medical Branch in Galveston.
Elevated risks in match-controlled study
Dr. D’Silva and colleagues examined a COVID-19 population and compared 716 people with SARDs and another 716 people from the general public at 4 months, as well as 2,379 people each in similar groups at 6 months. They used real-time electronic medical record data from the TriNetX research network to identify ICD-10 codes for inflammatory arthritis, connective tissue diseases, and systemic vasculitis. They also used ICD-10 codes and positive PCR tests to identify people with COVID-19.
Mean age was 57 years and women accounted for 79% of both groups evaluated at 4 months. Those with SARDs were 23% more likely to be hospitalized (relative risk, 1.23; 95% confidence interval, 1.01-1.50). This group was 75% more likely to be admitted to the ICU (RR, 1.75; 95% CI, 1.11-2.75), 77% more likely to require mechanical ventilation (RR, 1.77; 95% CI, 1.06-2.96), and 83% more likely to experience acute kidney injury (RR, 1.83; 95% CI, 1.11-3.00).
Risk of death was not significantly higher in the SARDs group (RR, 1.16; 95% CI, 0.73-1.86).
When Dr. D’Silva expanded the study to more people at 6 months, they added additional 30-day outcomes of interest: renal replacement therapy, VTE, and ischemic stroke. Risk of need for renal replacement therapy, for example, was 81% higher in the SARDs group (RR, 1.81; 95% CI, 1.07-3.07). Risk of stroke was not significantly different between groups.The improvement in mechanical ventilation risk between 4 and 6 months was not completely unexpected, Dr. D’Silva said. The relative risk dropped from 1.77 to 1.05. “This is not particularly surprising given national trends in the general population reporting decreased severe outcomes of COVID-19 including mortality as the pandemic progresses. This is likely multifactorial including changes in COVID-19 management (such as increasing use of nonintubated prone positioning rather than early intubation and treatments such as dexamethasone and remdesivir), decreased strain on hospitals and staffing compared to the early crisis phase of the pandemic, and higher testing capacity leading to detection of milder cases.”
When the 6-month analysis was further adjusted for comorbidities and a history of prior hospitalization within 1 year, only risk for acute kidney injury and VTE remained significant with relative risks of 1.33 and 1.60, respectively, likely because comorbidities are causal intermediates of COVID-19 30-day outcomes rather than confounders.
When asked to comment on the results, session comoderator Victoria K. Shanmugam, MD, said in an interview that the study “is of great interest both to rheumatologists and to patients with rheumatic disease.”
The higher risk of hospitalization, ICU admission, mechanical ventilation, acute kidney injury, and heart failure “is an important finding with implications for how our patients navigate risk during this pandemic,” said Dr. Shanmugam, director of the division of rheumatology at George Washington University in Washington.
Lower risks emerge in systematic review
The 15 observational studies in the systematic review included 11,815 participants. A total of 179, or 1.5%, tested positive for COVID-19.
“The incidence of COVID-19 infection among patients with rheumatic disease was low,” Dr. Sood said.
Within the COVID-19-positive group, almost 50% required hospitalization, 10% required ICU admission, and 8% died. The pooled event rate for hospitalization was 0.440 (95% CI, 0.296-0.596), while for ICU admission it was 0.132 (95% CI, 0.087-0.194) and for death it was 0.125 (95% CI, 0.082-0.182).
Different calculations of risk
The two studies seem to offer contradictory findings, but the disparities could be explained by study design differences. For example, Dr. D’Silva’s study evaluated a population with COVID-19 and compared those with SARDs versus a matched group from the general public. Dr. Sood and colleagues assessed study populations with rheumatic disease and assessed incidence of SARS-CoV-2 infection and difference in outcomes.
“We are asking very different questions,” Dr. D’Silva said.
“The study by D’Silva et al. was able to account for different factors to reduce confounding,” Dr. Sood said, adding that Dr. D’Silva and colleagues included a high proportion of minorities, compared with a less diverse population in the systematic review, which featured a large number of studies from Italy.
The authors of the two studies had no relevant financial disclosures to report.
SOURCES: D’Silva K et al. Arthritis Rheumatol. 2020;72(suppl 10): Abstract 0430, and Sood A et al. Arthritis Rheumatol. 2020;72(suppl 10): Abstract 0008.
FROM ACR 2020