User login
Outcomes After Endoscopic Dilation of Laryngotracheal Stenosis: An Analysis of ACS-NSQIP
From the Northwestern University, Feinberg School of Medicine, Chicago, IL (Mr. Bavishi, Dr. Lavin), the Johns Hopkins University, Baltimore, MD (Dr. Boss), Children’s National Medical Center, Washington, DC (Dr. Shah), and Ann & Robert H. Lurie Children’s Hospital of Chicago, Chicago, IL (Dr. Lavin).
Abstract
- Background: Endoscopic management of pediatric subglottic stenosis is common; however, no multiinstitutional studies have assessed its perioperative outcomes. The American College of Surgeon’s National Surgical Quality Improvement Program – Pediatric (ACS-NSQIP-P) represents a source of such data.
- Objective: To investigate 30-day outcomes of endoscopic dilation of the pediatric airway and to compare these outcomes to those seen with open reconstruction techniques.
- Methods: Current procedural terminology (CPT) codes were queried for endoscopic or open airway reconstruction in the 2015 ACS-NSQIP-P Public Use File (PUF). Demographics and 30-day events were abstracted to compare open to endoscopic techniques and to assess for risk factors for varied outcomes after endoscopic dilation. Outcome measures included length of stay (LOS), 30-day rates of reintubation, readmission, and reoperation.
- Results: 171 endoscopic and 116 open procedures were identified. Mean age at endoscopic and open procedures was 4.1 (SEM = 0.37) and 5.4 years (SEM = 0.40). Mean LOS was shorter after endoscopic procedures (5.5 days, SEM = 1.13 vs. 11.3 days SEM = 1.01, P < 0.001). Open procedures had higher rates of reintubation (OR = 7.41, P = 0.026) and reoperation (OR = 3.09, P = 0.009). In patients undergoing endoscopic dilation, children < 1 year were more likely to require readmission (OR = 4.21, P = 0.03) and reoperation (OR = 4.39, P = 0.03) when compared with older children.
- Conclusion: Open airway reconstruction is associated with longer LOS and increased reintubations and reoperations, suggesting a possible opportunity to improve value in health care in the appropriately selected patient. Reoperations and readmissions following endoscopic dilation are more prevalent in children younger than 1 year.
Keywords: airway stenosis; subglottic stenosis; endoscopic dilation; pediatrics; outcomes.
Historically, pediatric laryngotracheal stenosis was managed using open reconstruction techniques, including laryngoplasty, tracheal resection, and cervical tracheoplasty. Initial reports of endoscopic dilation were described in the 1980s as a means to salvage re-stenosis after open reconstruction [1]. Currently, primary endoscopic dilation has become commonplace in otolaryngology due to its less invasive nature as well as—in cases of balloon dilation—minimization of tissue damage [2]. The advancements made in endoscopic balloon dilation have reduced the frequency with which open reconstruction is performed.
Systematic reviews and case series investigating endoscopic dilation indicate a 70% to 80% success rate in preventing future open surgery or tracheostomy [2–5]. While increased severity of stenosis has been associated with poorer outcomes in endoscopic procedures, few other risk factors that influence surgical success have been identified [4,5]. In a single study in the adult literature, open surgical management of idiopathic subglottic stenosis was associated with improved outcomes when compared to endoscopic techniques [5]. Such findings suggest a need to identify these factors for the purpose of optimizing clinical decision-making.
As laryngotracheal stenosis is rare, postoperative outcomes and risk factors are best identified on a multiinstitutional level. Due to its participation from 80 hospitals and its accurate and reliable reporting of both demographic and risk-stratified 30-day outcomes data, the American College of Surgeon’s National Surgical Quality Improvement Program – Pediatric (ACS NSQIP-P) provides such a platform [6–8]. Thirty-day outcomes and risk factors for open reconstruction utilizing the ACS NSQIP-P database have previously been reported; however, no such outcomes for endoscopic dilation have been described, and no comparison between endoscopic and open procedures has been made [9]. The purpose of this study was to utilize the 2015 ACS-NSQIP-P database to investigate 30-day outcomes of endoscopic dilation of the pediatric airway and to compare these outcomes to open reconstruction techniques. Secondarily, we aimed to determine if any demographic factors or medical comorbidities are associated with varied outcomes in endoscopic reconstruction. While these data reflect safety and quality of this procedure in the United States, findings may potentially be applied across international settings.
Methods
Data Source
Data was obtained from the 2015 ACS-NSQIP-P Public Use File (PUF). Due to the de-identified and public nature of these data, this research was exempt from review by the Ann & Robert H. Lurie Children’s Hospital of Chicago review board. Data collection methods for ACS-NSQIP-P have previously been described [10]. In brief, data was collected from 80 hospitals on approximately 120 preoperative, intraoperative, and postoperative variables. Cases are systematically sampled on an 8-day cycle basis, where the first 35 cases meeting the inclusion criteria in each hospital in each cycle are submitted to ACS-NSQIP-P.
Variables and Outcomes
Airway procedures for endoscopic dilations and open reconstructions were obtained by CPT code. Endoscopic dilations (CPT 31528) were compared to open reconstructions, which included laryngoplasty (31580, 31582), cervical tracheoplasty (31750), cricoid split (31587), and tracheal resection (31780). Demographic variables included age, sex, race, and history of prematurity. Presence of specific comorbid diseases were also collected and tested for significance.
Dependent outcomes of interest were unplanned 30-day postoperative events grouped as reoperation, unplanned readmission, and postoperative reintubation. In the case of endoscopic procedures, the presence of salvage open reconstruction or tracheostomy within 30 days of surgery was also recorded. Length of stay (LOS) after the procedure was collected. Specific postoperative complications and reasons for readmission were recorded within the limitations of data available in the PUF.
Analysis
Analysis was performed using descriptive statistics and frequency analysis where appropriate. Chi-square analysis was used to compare adverse events between open and endoscopic procedures. Logistic regression with calculation of odds ratio (OR) was performed to determine predictive factors for reoperation, readmission, and reintubation in all pediatric airway reconstructive procedures in adjusted and unadjusted models. T-test and linear regression was performed on the continuous outcome of length of stay. For all analyses, a p value of < 0.05 was considered statistically significant. All variable recoding and statistical analyses were performed in SAS/STAT software (Cary, NC).
Results
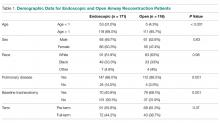
A total of 84,056 pediatric procedures were extracted from the 2015 NSQIP-P PUFs. Using the above CPT codes, 171 endoscopic dilations and 116 open airway reconstructions were identified, with patient age ranging from 0 days to 17.6 years. Average age of patients undergoing endoscopic dilation and open reconstruction was 4.1 and 5.4 years, respectively (Table 1).
Potential confounders were tested with univariate logistic regression to determine if they had a significant impact on readmission, reintubation, or reoperation rates. These variables (Table 2)
In patients undergoing endoscopic dilation, average length of stay was 5.5 days (SEM = 1.13), with 79 (48.5%) patients having a length of stay of zero days. Of all patients who had endoscopic dilations, 70 (40.1%) had a pre-existing tracheostomy and these accounted for the majority (73%) of patients who had zero days as their LOS. LOS after endoscopic management was significantly shorter than the mean of 11.3 days (SEM = 1.01) reported in those undergoing open reconstruction (P < 0.001).
With respect to 30-day adverse events, 2 patients in the endoscopic group (1.1%) required reintubation. Thirteen endoscopic dilation cases (7.6%) had an unplanned readmission, four (2.3%) of which were associated with reoperation within 30 days of the primary surgical procedure. There were 9 other reoperations unassociated with unplanned readmission. Three of these reoperations were due to failed endoscopic dilations, resulting in 2 tracheostomies and one open airway reconstruction. There was one patient death, in a 0-day old with tetralogy of Fallot, trachea-esophageal fistula, and ventilator dependence who underwent emergent endoscopic dilation and died the same day.
Open procedures were associated with 11 unplanned readmissions (9.5%), 7 re-intubations (6%) and 18 reoperations (15.5%). Of patents undergoing reoperation, one patient undergoing open reconstruction underwent tracheostomy within 30 days of surgery.
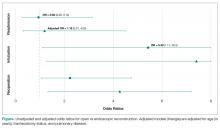
When comparing open reconstruction to endoscopic dilation, there was a significant increase in reintubation (OR = 7.41, P = 0.026) and reoperation (OR = 3.09, P = 0.009) for open procedures, even with adjustment for age, tracheostomy status, and pulmonary disease. There was no significant difference between the two for unplanned readmissions (OR = 1.19, P = 0.79) (Figure
Younger age was also found to be significantly associated with reoperation rates, in an adjusted logistic model that accounted for tracheostomy status, type of surgery, and pulmonary disease. Per year of life, younger children had higher reoperation rates than older children (OR = 1.91, P = 0.017). When endoscopic dilation was individually examined, children younger than 1 year of age were more likely to undergo reoperation after an endoscopic dilation than children older than 1 (OR = 4.39, P = 0.03). Children under age 1 were also more likely to have an unplanned readmission after an endoscopic dilation (OR = 4.21, P = 0.03). The relationship between age and re-intubation was not significant (OR = 0, P = 0.95). For open reconstruction, this age dichotomization was not associated with any increased reoperation (OR = 2.3, P = 0.52), readmission (OR = 0, P = 0.97), or reintubation (OR = 0, P = 0.94).
T-test analysis was performed to determine if children < 1 year old also had significantly longer hospital stays after endoscopic dilation than older children (mean 14.1 days vs 1.9 days, P < 0.001). This relationship held true in a linear regression after adjustment for pulmonary disease and tracheostomy, with length of stay decreasing by 0.48 days per year of life (P = 0.03). For endoscopic dilations, the same relationship held true, where length of stay decreased by 0.75 days per year of life.
Discussion
Endoscopic dilation for primary management of pediatric laryngotracheal stenosis has become commonplace. Despite this, outcomes of this procedure have only been described in case series and meta-analyses [2–5]. The relative rarity of pediatric laryngotracheal stenosis suggests the need for large, multi-institutional data for purposes of patient selection and medical decision-making.
This study utilized the ACS-NSQIP-Pediatric database to highlight 30-day outcomes of endoscopic dilation and to compare these outcomes to those of open airway reconstruction procedures. The ACS-NSQIP database has been endorsed by multiple organizations, including the Center for Medicare and Medicaid Services, the Joint Commission, and the American Medical Association. It has been shown to have higher sensitivity and a lower false-positive rate when compared to administrative data, in part due to data collection from trained personnel [11]. Furthermore, ACS-NSQIP use has the additional benefit of reporting an unplanned admission—a feature unavailable in review of claims data [12].
With respect to adverse events, our study demonstrates that endoscopic dilation is associated with an equally high rate of unplanned readmission when compared to open reconstruction. The high prevalence of comorbid disease such as chronic lung disease (32% of endoscopic dilation and 43% of open reconstruction) can account for some of the morbidity associated with any airway procedures.
Despite high rates of unplanned readmission, patients undergoing endoscopic dilation were less likely to have reoperations within 30 days of initial surgery when compared to those undergoing open reconstruction. While differences in disease severity may be partially responsible for this difference in the reoperation rate, this finding is notable given the health care costs associated with multiple operations as well as safety concerns with multiple anesthetics in the very young [13,14].
The ACS-NSQIP platform does not distinguish unplanned from planned reoperations. In the setting of airway surgery, where multiple planned reoperations are commonplace, this metric is a suboptimal stand-alone indicator of adverse outcomes. Other markers available in the database—such as reintubations and performance of tracheostomy or open airway reconstruction within 30-days of surgery—are more indicative of surgical outcome in the setting of airway surgery. We found that both reintubations and salvage open reconstruction within 30-days were rare. It should be noted that the ACS-NSQIP data does not report any events occurring outside of the 30-day postoperative period, representing potential limitation of the use of this database. As was previously advocated by Roxbury and colleagues, procedure/subspecialty specific outcome data collection would also improve outcome analysis of airway and other otolaryngologic procedures [9]. In the setting of airway reconstruction, this would include data pertaining to Cotton-Meyer grading systems well as postoperative voice and swallow outcomes.
In addition to safety profile, endoscopic procedures were associated with shorter LOS when compared with open reconstruction, representing another potential source of cost savings with this less invasive method. This is especially significant given that open reconstruction patients spend much of their inpatient stay in an ICU setting. In patients who are candidates for endoscopic procedures, this lower-risk, lower-cost profile of endoscopic dilation has the opportunity to improve value in health care and may be the source of future improvement initiatives.
In addition to comparing overall outcomes between endoscopic and open management of laryngotracheal stenosis, our study aimed to identify factors that were associated with varied outcomes in patients undergoing primary endoscopic dilation. We found that children younger than 1 year of age were 5.8 times more likely to undergo an unplanned reoperation after an endoscopic dilation than children over 1 year. A similar finding was reported in open airway surgeries, with increased reoperation rates in children < 3 years old [9]. The justification of a dichotomization at 1 year was made as expert opinion recognizes that the infant airway is less forgiving to intervention given its small size. Young age was also a factor in prolonged LOS as was determined by linear regression. It is likely that this increased LOS may be in part due to associations of young age and the neonatal ICU population. One must balance the increased risk of surgery in the young with that of tracheostomy, which has a published complication rate of 18% to 50% and direct mortality rate of 1% to 2% in the pediatric population [15–18]. Understanding these relative risks may help guide the airway surgeon in preoperative counseling with families and medical decision-making.
As discussed above, the limitation of data to a 30-day period is a relative weakness of ACS-NSQIP database use for studies of airway reconstruction, as the ultimate outcome—a stable, decannulated airway—may occur outside of this time period. As many quality metrics utilize data from the 30-day postoperative period, knowledge of these outcomes remains valuable in surgical decision-making. Ultimately, collection of data in a large, long-term dataset would allow broader generalizations to be made about the differences between open and endoscopic procedures and would also give a more comprehensive picture of the outcomes of endoscopic dilation.
In conclusion, this study is the first to analyze 30-day postoperative outcomes in pediatric endoscopic airway dilations using data aggregated by ACS-NSQIP from institutions across the United States. This data indicates that endoscopic airway dilation is a relatively safe procedure, especially compared with open reconstruction; however, additional data on disease severity and other outcomes is necessary to draw final conclusions of superiority of technique. Future improvement initiatives could be aimed at the impact of this lower-risk, lower-cost procedure in the appropriately selected patient. Outcomes of endoscopic dilation are poorer in those less than 1 year of age, as they are associated with increased reoperation rates and increased length of stay compared to older children. One must balance these risks in the very young with the risks associated with tracheostomy and other alternative airway management modalities.
Note: This work was presented in a paper at the AAO-HNS 2017 meeting, Chicago, IL, 10 Sep 2017.
Corresponding author: Jennifer Lavin, MD, MS, 225 E Chicago Ave., Box 25, Chicago, IL 60611, JLavin@luriechildrens.org.
Financial disclosures: None.
1. Cohen MD, Weber TR, Rao CC. Balloon dilatation of tracheal and bronchial stenosis. AJR Am J Roentgenol 1984;142:477–8.
2. Chueng K, Chadha NK. Primary dilatation as a treatment for pediatric laryngotracheal stenosis: a systematic review. Int J Pediatr Otorhinolaryngol 2013;77:623–8.
3. Hautefort C, Teissier N, Viala P, Van Den Abbeele T. Balloon dilation laryngoplasty for subglottic stenosis in children: eight years’ experience. Arch Otolaryngol Head Neck Surg 2012;138:235–40.
4. Lang M, Brietzke SE. A systematic review and meta-analysis of endoscopic balloon dilation of pediatric subglottic stenosis. Otolaryngol Head Neck Surg 2014;150:174–9.
5. Maresh A, Preciado DA, O’Connell AP, Zalzal GH. A comparative analysis of open surgery vs endoscopic balloon dilation for pediatric subglottic stenosis. JAMA Otolaryngol Head Neck Surg 2014;140:901–5.
6. Gelbard A, Donovan DT, Ongkasuwan J, et al. Disease homogeneity and treatment heterogeneity in idiopathic subglottic stenosis. Laryngoscope 2016;126:1390–6.
7. ACS-NSQIP. ACS National Surgical Quality Improvement Program® (ACS NSQIP®). 2017. Available at: http://site.acsnsqip.org/program-specifics/scr-training-and-resources. Accessed June 2 2017.
8. Shiloach M, Frencher SK Jr, Steeger JE, et al. Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg 2010;210:6–16.
9. Roxbury CR, Jatana KR, Shah RK, Boss EF. Safety and postoperative adverse events in pediatric airway reconstruction: Analysis of ACS-NSQIP-P 30-day outcomes. Laryngoscope 2017;127:504–8.
10. Raval MV, Dillon PW, Bruny JL, et al. Pediatric American College of Surgeons National Surgical Quality Improvement Program: feasibility of a novel, prospective assessment of surgical outcomes. J Pediatr Surg 2011;46:115–21.
11. Lawson EH, Louie R, Zingmond DS, et al. A comparison of clinical registry versus administrative claims data for reporting of 30-day surgical complications. Ann Surg 2012;256:973–81.
12. Sellers MM, Merkow RP, Halverson A, et al. Validation of new readmission data in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg 2013;216:420–7.
13. Jevtovic-Todorovic V, Hartman RE, Izumi Y, et al. Early exposure to common anesthetic agents causes widespread neurodegeneration in the developing rat brain and persistent learning deficits. J Neurosci 2003;23:876–82.
14. Patel P, Sun L. Update on neonatal anesthetic neurotoxicity: insight into molecular mechanisms and relevance to humans. Anesthesiology 2009;110:703–8.
15. Crysdale WS, Feldman RI, Naito K. Tracheotomies: a 10-year experience in 319 children. Ann Otol Rhinol Laryngol 1988;97(5 Pt 1):439–43.
16. Goldenberg D, Ari EG, Golz A, et al. Tracheotomy complications: a retrospective study of 1130 cases. Otolaryngol Head Neck Surg 2000;123:495–500.
17. Mahadevan M, Barber C, Salkeld L, et al N. Pediatric tracheotomy: 17 year review. Int J Pediatr Otorhinolaryngol 2007;71:1829–35.
18. Ozmen S, Ozmen OA, Unal OF. Pediatric tracheotomies: a 37-year experience in 282 children. Int J Pediatr Otorhinolaryngol 2009;73:959–61.
From the Northwestern University, Feinberg School of Medicine, Chicago, IL (Mr. Bavishi, Dr. Lavin), the Johns Hopkins University, Baltimore, MD (Dr. Boss), Children’s National Medical Center, Washington, DC (Dr. Shah), and Ann & Robert H. Lurie Children’s Hospital of Chicago, Chicago, IL (Dr. Lavin).
Abstract
- Background: Endoscopic management of pediatric subglottic stenosis is common; however, no multiinstitutional studies have assessed its perioperative outcomes. The American College of Surgeon’s National Surgical Quality Improvement Program – Pediatric (ACS-NSQIP-P) represents a source of such data.
- Objective: To investigate 30-day outcomes of endoscopic dilation of the pediatric airway and to compare these outcomes to those seen with open reconstruction techniques.
- Methods: Current procedural terminology (CPT) codes were queried for endoscopic or open airway reconstruction in the 2015 ACS-NSQIP-P Public Use File (PUF). Demographics and 30-day events were abstracted to compare open to endoscopic techniques and to assess for risk factors for varied outcomes after endoscopic dilation. Outcome measures included length of stay (LOS), 30-day rates of reintubation, readmission, and reoperation.
- Results: 171 endoscopic and 116 open procedures were identified. Mean age at endoscopic and open procedures was 4.1 (SEM = 0.37) and 5.4 years (SEM = 0.40). Mean LOS was shorter after endoscopic procedures (5.5 days, SEM = 1.13 vs. 11.3 days SEM = 1.01, P < 0.001). Open procedures had higher rates of reintubation (OR = 7.41, P = 0.026) and reoperation (OR = 3.09, P = 0.009). In patients undergoing endoscopic dilation, children < 1 year were more likely to require readmission (OR = 4.21, P = 0.03) and reoperation (OR = 4.39, P = 0.03) when compared with older children.
- Conclusion: Open airway reconstruction is associated with longer LOS and increased reintubations and reoperations, suggesting a possible opportunity to improve value in health care in the appropriately selected patient. Reoperations and readmissions following endoscopic dilation are more prevalent in children younger than 1 year.
Keywords: airway stenosis; subglottic stenosis; endoscopic dilation; pediatrics; outcomes.
Historically, pediatric laryngotracheal stenosis was managed using open reconstruction techniques, including laryngoplasty, tracheal resection, and cervical tracheoplasty. Initial reports of endoscopic dilation were described in the 1980s as a means to salvage re-stenosis after open reconstruction [1]. Currently, primary endoscopic dilation has become commonplace in otolaryngology due to its less invasive nature as well as—in cases of balloon dilation—minimization of tissue damage [2]. The advancements made in endoscopic balloon dilation have reduced the frequency with which open reconstruction is performed.
Systematic reviews and case series investigating endoscopic dilation indicate a 70% to 80% success rate in preventing future open surgery or tracheostomy [2–5]. While increased severity of stenosis has been associated with poorer outcomes in endoscopic procedures, few other risk factors that influence surgical success have been identified [4,5]. In a single study in the adult literature, open surgical management of idiopathic subglottic stenosis was associated with improved outcomes when compared to endoscopic techniques [5]. Such findings suggest a need to identify these factors for the purpose of optimizing clinical decision-making.
As laryngotracheal stenosis is rare, postoperative outcomes and risk factors are best identified on a multiinstitutional level. Due to its participation from 80 hospitals and its accurate and reliable reporting of both demographic and risk-stratified 30-day outcomes data, the American College of Surgeon’s National Surgical Quality Improvement Program – Pediatric (ACS NSQIP-P) provides such a platform [6–8]. Thirty-day outcomes and risk factors for open reconstruction utilizing the ACS NSQIP-P database have previously been reported; however, no such outcomes for endoscopic dilation have been described, and no comparison between endoscopic and open procedures has been made [9]. The purpose of this study was to utilize the 2015 ACS-NSQIP-P database to investigate 30-day outcomes of endoscopic dilation of the pediatric airway and to compare these outcomes to open reconstruction techniques. Secondarily, we aimed to determine if any demographic factors or medical comorbidities are associated with varied outcomes in endoscopic reconstruction. While these data reflect safety and quality of this procedure in the United States, findings may potentially be applied across international settings.
Methods
Data Source
Data was obtained from the 2015 ACS-NSQIP-P Public Use File (PUF). Due to the de-identified and public nature of these data, this research was exempt from review by the Ann & Robert H. Lurie Children’s Hospital of Chicago review board. Data collection methods for ACS-NSQIP-P have previously been described [10]. In brief, data was collected from 80 hospitals on approximately 120 preoperative, intraoperative, and postoperative variables. Cases are systematically sampled on an 8-day cycle basis, where the first 35 cases meeting the inclusion criteria in each hospital in each cycle are submitted to ACS-NSQIP-P.
Variables and Outcomes
Airway procedures for endoscopic dilations and open reconstructions were obtained by CPT code. Endoscopic dilations (CPT 31528) were compared to open reconstructions, which included laryngoplasty (31580, 31582), cervical tracheoplasty (31750), cricoid split (31587), and tracheal resection (31780). Demographic variables included age, sex, race, and history of prematurity. Presence of specific comorbid diseases were also collected and tested for significance.
Dependent outcomes of interest were unplanned 30-day postoperative events grouped as reoperation, unplanned readmission, and postoperative reintubation. In the case of endoscopic procedures, the presence of salvage open reconstruction or tracheostomy within 30 days of surgery was also recorded. Length of stay (LOS) after the procedure was collected. Specific postoperative complications and reasons for readmission were recorded within the limitations of data available in the PUF.
Analysis
Analysis was performed using descriptive statistics and frequency analysis where appropriate. Chi-square analysis was used to compare adverse events between open and endoscopic procedures. Logistic regression with calculation of odds ratio (OR) was performed to determine predictive factors for reoperation, readmission, and reintubation in all pediatric airway reconstructive procedures in adjusted and unadjusted models. T-test and linear regression was performed on the continuous outcome of length of stay. For all analyses, a p value of < 0.05 was considered statistically significant. All variable recoding and statistical analyses were performed in SAS/STAT software (Cary, NC).
Results
A total of 84,056 pediatric procedures were extracted from the 2015 NSQIP-P PUFs. Using the above CPT codes, 171 endoscopic dilations and 116 open airway reconstructions were identified, with patient age ranging from 0 days to 17.6 years. Average age of patients undergoing endoscopic dilation and open reconstruction was 4.1 and 5.4 years, respectively (Table 1).
Potential confounders were tested with univariate logistic regression to determine if they had a significant impact on readmission, reintubation, or reoperation rates. These variables (Table 2)
In patients undergoing endoscopic dilation, average length of stay was 5.5 days (SEM = 1.13), with 79 (48.5%) patients having a length of stay of zero days. Of all patients who had endoscopic dilations, 70 (40.1%) had a pre-existing tracheostomy and these accounted for the majority (73%) of patients who had zero days as their LOS. LOS after endoscopic management was significantly shorter than the mean of 11.3 days (SEM = 1.01) reported in those undergoing open reconstruction (P < 0.001).
With respect to 30-day adverse events, 2 patients in the endoscopic group (1.1%) required reintubation. Thirteen endoscopic dilation cases (7.6%) had an unplanned readmission, four (2.3%) of which were associated with reoperation within 30 days of the primary surgical procedure. There were 9 other reoperations unassociated with unplanned readmission. Three of these reoperations were due to failed endoscopic dilations, resulting in 2 tracheostomies and one open airway reconstruction. There was one patient death, in a 0-day old with tetralogy of Fallot, trachea-esophageal fistula, and ventilator dependence who underwent emergent endoscopic dilation and died the same day.
Open procedures were associated with 11 unplanned readmissions (9.5%), 7 re-intubations (6%) and 18 reoperations (15.5%). Of patents undergoing reoperation, one patient undergoing open reconstruction underwent tracheostomy within 30 days of surgery.
When comparing open reconstruction to endoscopic dilation, there was a significant increase in reintubation (OR = 7.41, P = 0.026) and reoperation (OR = 3.09, P = 0.009) for open procedures, even with adjustment for age, tracheostomy status, and pulmonary disease. There was no significant difference between the two for unplanned readmissions (OR = 1.19, P = 0.79) (Figure
Younger age was also found to be significantly associated with reoperation rates, in an adjusted logistic model that accounted for tracheostomy status, type of surgery, and pulmonary disease. Per year of life, younger children had higher reoperation rates than older children (OR = 1.91, P = 0.017). When endoscopic dilation was individually examined, children younger than 1 year of age were more likely to undergo reoperation after an endoscopic dilation than children older than 1 (OR = 4.39, P = 0.03). Children under age 1 were also more likely to have an unplanned readmission after an endoscopic dilation (OR = 4.21, P = 0.03). The relationship between age and re-intubation was not significant (OR = 0, P = 0.95). For open reconstruction, this age dichotomization was not associated with any increased reoperation (OR = 2.3, P = 0.52), readmission (OR = 0, P = 0.97), or reintubation (OR = 0, P = 0.94).
T-test analysis was performed to determine if children < 1 year old also had significantly longer hospital stays after endoscopic dilation than older children (mean 14.1 days vs 1.9 days, P < 0.001). This relationship held true in a linear regression after adjustment for pulmonary disease and tracheostomy, with length of stay decreasing by 0.48 days per year of life (P = 0.03). For endoscopic dilations, the same relationship held true, where length of stay decreased by 0.75 days per year of life.
Discussion
Endoscopic dilation for primary management of pediatric laryngotracheal stenosis has become commonplace. Despite this, outcomes of this procedure have only been described in case series and meta-analyses [2–5]. The relative rarity of pediatric laryngotracheal stenosis suggests the need for large, multi-institutional data for purposes of patient selection and medical decision-making.
This study utilized the ACS-NSQIP-Pediatric database to highlight 30-day outcomes of endoscopic dilation and to compare these outcomes to those of open airway reconstruction procedures. The ACS-NSQIP database has been endorsed by multiple organizations, including the Center for Medicare and Medicaid Services, the Joint Commission, and the American Medical Association. It has been shown to have higher sensitivity and a lower false-positive rate when compared to administrative data, in part due to data collection from trained personnel [11]. Furthermore, ACS-NSQIP use has the additional benefit of reporting an unplanned admission—a feature unavailable in review of claims data [12].
With respect to adverse events, our study demonstrates that endoscopic dilation is associated with an equally high rate of unplanned readmission when compared to open reconstruction. The high prevalence of comorbid disease such as chronic lung disease (32% of endoscopic dilation and 43% of open reconstruction) can account for some of the morbidity associated with any airway procedures.
Despite high rates of unplanned readmission, patients undergoing endoscopic dilation were less likely to have reoperations within 30 days of initial surgery when compared to those undergoing open reconstruction. While differences in disease severity may be partially responsible for this difference in the reoperation rate, this finding is notable given the health care costs associated with multiple operations as well as safety concerns with multiple anesthetics in the very young [13,14].
The ACS-NSQIP platform does not distinguish unplanned from planned reoperations. In the setting of airway surgery, where multiple planned reoperations are commonplace, this metric is a suboptimal stand-alone indicator of adverse outcomes. Other markers available in the database—such as reintubations and performance of tracheostomy or open airway reconstruction within 30-days of surgery—are more indicative of surgical outcome in the setting of airway surgery. We found that both reintubations and salvage open reconstruction within 30-days were rare. It should be noted that the ACS-NSQIP data does not report any events occurring outside of the 30-day postoperative period, representing potential limitation of the use of this database. As was previously advocated by Roxbury and colleagues, procedure/subspecialty specific outcome data collection would also improve outcome analysis of airway and other otolaryngologic procedures [9]. In the setting of airway reconstruction, this would include data pertaining to Cotton-Meyer grading systems well as postoperative voice and swallow outcomes.
In addition to safety profile, endoscopic procedures were associated with shorter LOS when compared with open reconstruction, representing another potential source of cost savings with this less invasive method. This is especially significant given that open reconstruction patients spend much of their inpatient stay in an ICU setting. In patients who are candidates for endoscopic procedures, this lower-risk, lower-cost profile of endoscopic dilation has the opportunity to improve value in health care and may be the source of future improvement initiatives.
In addition to comparing overall outcomes between endoscopic and open management of laryngotracheal stenosis, our study aimed to identify factors that were associated with varied outcomes in patients undergoing primary endoscopic dilation. We found that children younger than 1 year of age were 5.8 times more likely to undergo an unplanned reoperation after an endoscopic dilation than children over 1 year. A similar finding was reported in open airway surgeries, with increased reoperation rates in children < 3 years old [9]. The justification of a dichotomization at 1 year was made as expert opinion recognizes that the infant airway is less forgiving to intervention given its small size. Young age was also a factor in prolonged LOS as was determined by linear regression. It is likely that this increased LOS may be in part due to associations of young age and the neonatal ICU population. One must balance the increased risk of surgery in the young with that of tracheostomy, which has a published complication rate of 18% to 50% and direct mortality rate of 1% to 2% in the pediatric population [15–18]. Understanding these relative risks may help guide the airway surgeon in preoperative counseling with families and medical decision-making.
As discussed above, the limitation of data to a 30-day period is a relative weakness of ACS-NSQIP database use for studies of airway reconstruction, as the ultimate outcome—a stable, decannulated airway—may occur outside of this time period. As many quality metrics utilize data from the 30-day postoperative period, knowledge of these outcomes remains valuable in surgical decision-making. Ultimately, collection of data in a large, long-term dataset would allow broader generalizations to be made about the differences between open and endoscopic procedures and would also give a more comprehensive picture of the outcomes of endoscopic dilation.
In conclusion, this study is the first to analyze 30-day postoperative outcomes in pediatric endoscopic airway dilations using data aggregated by ACS-NSQIP from institutions across the United States. This data indicates that endoscopic airway dilation is a relatively safe procedure, especially compared with open reconstruction; however, additional data on disease severity and other outcomes is necessary to draw final conclusions of superiority of technique. Future improvement initiatives could be aimed at the impact of this lower-risk, lower-cost procedure in the appropriately selected patient. Outcomes of endoscopic dilation are poorer in those less than 1 year of age, as they are associated with increased reoperation rates and increased length of stay compared to older children. One must balance these risks in the very young with the risks associated with tracheostomy and other alternative airway management modalities.
Note: This work was presented in a paper at the AAO-HNS 2017 meeting, Chicago, IL, 10 Sep 2017.
Corresponding author: Jennifer Lavin, MD, MS, 225 E Chicago Ave., Box 25, Chicago, IL 60611, JLavin@luriechildrens.org.
Financial disclosures: None.
From the Northwestern University, Feinberg School of Medicine, Chicago, IL (Mr. Bavishi, Dr. Lavin), the Johns Hopkins University, Baltimore, MD (Dr. Boss), Children’s National Medical Center, Washington, DC (Dr. Shah), and Ann & Robert H. Lurie Children’s Hospital of Chicago, Chicago, IL (Dr. Lavin).
Abstract
- Background: Endoscopic management of pediatric subglottic stenosis is common; however, no multiinstitutional studies have assessed its perioperative outcomes. The American College of Surgeon’s National Surgical Quality Improvement Program – Pediatric (ACS-NSQIP-P) represents a source of such data.
- Objective: To investigate 30-day outcomes of endoscopic dilation of the pediatric airway and to compare these outcomes to those seen with open reconstruction techniques.
- Methods: Current procedural terminology (CPT) codes were queried for endoscopic or open airway reconstruction in the 2015 ACS-NSQIP-P Public Use File (PUF). Demographics and 30-day events were abstracted to compare open to endoscopic techniques and to assess for risk factors for varied outcomes after endoscopic dilation. Outcome measures included length of stay (LOS), 30-day rates of reintubation, readmission, and reoperation.
- Results: 171 endoscopic and 116 open procedures were identified. Mean age at endoscopic and open procedures was 4.1 (SEM = 0.37) and 5.4 years (SEM = 0.40). Mean LOS was shorter after endoscopic procedures (5.5 days, SEM = 1.13 vs. 11.3 days SEM = 1.01, P < 0.001). Open procedures had higher rates of reintubation (OR = 7.41, P = 0.026) and reoperation (OR = 3.09, P = 0.009). In patients undergoing endoscopic dilation, children < 1 year were more likely to require readmission (OR = 4.21, P = 0.03) and reoperation (OR = 4.39, P = 0.03) when compared with older children.
- Conclusion: Open airway reconstruction is associated with longer LOS and increased reintubations and reoperations, suggesting a possible opportunity to improve value in health care in the appropriately selected patient. Reoperations and readmissions following endoscopic dilation are more prevalent in children younger than 1 year.
Keywords: airway stenosis; subglottic stenosis; endoscopic dilation; pediatrics; outcomes.
Historically, pediatric laryngotracheal stenosis was managed using open reconstruction techniques, including laryngoplasty, tracheal resection, and cervical tracheoplasty. Initial reports of endoscopic dilation were described in the 1980s as a means to salvage re-stenosis after open reconstruction [1]. Currently, primary endoscopic dilation has become commonplace in otolaryngology due to its less invasive nature as well as—in cases of balloon dilation—minimization of tissue damage [2]. The advancements made in endoscopic balloon dilation have reduced the frequency with which open reconstruction is performed.
Systematic reviews and case series investigating endoscopic dilation indicate a 70% to 80% success rate in preventing future open surgery or tracheostomy [2–5]. While increased severity of stenosis has been associated with poorer outcomes in endoscopic procedures, few other risk factors that influence surgical success have been identified [4,5]. In a single study in the adult literature, open surgical management of idiopathic subglottic stenosis was associated with improved outcomes when compared to endoscopic techniques [5]. Such findings suggest a need to identify these factors for the purpose of optimizing clinical decision-making.
As laryngotracheal stenosis is rare, postoperative outcomes and risk factors are best identified on a multiinstitutional level. Due to its participation from 80 hospitals and its accurate and reliable reporting of both demographic and risk-stratified 30-day outcomes data, the American College of Surgeon’s National Surgical Quality Improvement Program – Pediatric (ACS NSQIP-P) provides such a platform [6–8]. Thirty-day outcomes and risk factors for open reconstruction utilizing the ACS NSQIP-P database have previously been reported; however, no such outcomes for endoscopic dilation have been described, and no comparison between endoscopic and open procedures has been made [9]. The purpose of this study was to utilize the 2015 ACS-NSQIP-P database to investigate 30-day outcomes of endoscopic dilation of the pediatric airway and to compare these outcomes to open reconstruction techniques. Secondarily, we aimed to determine if any demographic factors or medical comorbidities are associated with varied outcomes in endoscopic reconstruction. While these data reflect safety and quality of this procedure in the United States, findings may potentially be applied across international settings.
Methods
Data Source
Data was obtained from the 2015 ACS-NSQIP-P Public Use File (PUF). Due to the de-identified and public nature of these data, this research was exempt from review by the Ann & Robert H. Lurie Children’s Hospital of Chicago review board. Data collection methods for ACS-NSQIP-P have previously been described [10]. In brief, data was collected from 80 hospitals on approximately 120 preoperative, intraoperative, and postoperative variables. Cases are systematically sampled on an 8-day cycle basis, where the first 35 cases meeting the inclusion criteria in each hospital in each cycle are submitted to ACS-NSQIP-P.
Variables and Outcomes
Airway procedures for endoscopic dilations and open reconstructions were obtained by CPT code. Endoscopic dilations (CPT 31528) were compared to open reconstructions, which included laryngoplasty (31580, 31582), cervical tracheoplasty (31750), cricoid split (31587), and tracheal resection (31780). Demographic variables included age, sex, race, and history of prematurity. Presence of specific comorbid diseases were also collected and tested for significance.
Dependent outcomes of interest were unplanned 30-day postoperative events grouped as reoperation, unplanned readmission, and postoperative reintubation. In the case of endoscopic procedures, the presence of salvage open reconstruction or tracheostomy within 30 days of surgery was also recorded. Length of stay (LOS) after the procedure was collected. Specific postoperative complications and reasons for readmission were recorded within the limitations of data available in the PUF.
Analysis
Analysis was performed using descriptive statistics and frequency analysis where appropriate. Chi-square analysis was used to compare adverse events between open and endoscopic procedures. Logistic regression with calculation of odds ratio (OR) was performed to determine predictive factors for reoperation, readmission, and reintubation in all pediatric airway reconstructive procedures in adjusted and unadjusted models. T-test and linear regression was performed on the continuous outcome of length of stay. For all analyses, a p value of < 0.05 was considered statistically significant. All variable recoding and statistical analyses were performed in SAS/STAT software (Cary, NC).
Results
A total of 84,056 pediatric procedures were extracted from the 2015 NSQIP-P PUFs. Using the above CPT codes, 171 endoscopic dilations and 116 open airway reconstructions were identified, with patient age ranging from 0 days to 17.6 years. Average age of patients undergoing endoscopic dilation and open reconstruction was 4.1 and 5.4 years, respectively (Table 1).
Potential confounders were tested with univariate logistic regression to determine if they had a significant impact on readmission, reintubation, or reoperation rates. These variables (Table 2)
In patients undergoing endoscopic dilation, average length of stay was 5.5 days (SEM = 1.13), with 79 (48.5%) patients having a length of stay of zero days. Of all patients who had endoscopic dilations, 70 (40.1%) had a pre-existing tracheostomy and these accounted for the majority (73%) of patients who had zero days as their LOS. LOS after endoscopic management was significantly shorter than the mean of 11.3 days (SEM = 1.01) reported in those undergoing open reconstruction (P < 0.001).
With respect to 30-day adverse events, 2 patients in the endoscopic group (1.1%) required reintubation. Thirteen endoscopic dilation cases (7.6%) had an unplanned readmission, four (2.3%) of which were associated with reoperation within 30 days of the primary surgical procedure. There were 9 other reoperations unassociated with unplanned readmission. Three of these reoperations were due to failed endoscopic dilations, resulting in 2 tracheostomies and one open airway reconstruction. There was one patient death, in a 0-day old with tetralogy of Fallot, trachea-esophageal fistula, and ventilator dependence who underwent emergent endoscopic dilation and died the same day.
Open procedures were associated with 11 unplanned readmissions (9.5%), 7 re-intubations (6%) and 18 reoperations (15.5%). Of patents undergoing reoperation, one patient undergoing open reconstruction underwent tracheostomy within 30 days of surgery.
When comparing open reconstruction to endoscopic dilation, there was a significant increase in reintubation (OR = 7.41, P = 0.026) and reoperation (OR = 3.09, P = 0.009) for open procedures, even with adjustment for age, tracheostomy status, and pulmonary disease. There was no significant difference between the two for unplanned readmissions (OR = 1.19, P = 0.79) (Figure
Younger age was also found to be significantly associated with reoperation rates, in an adjusted logistic model that accounted for tracheostomy status, type of surgery, and pulmonary disease. Per year of life, younger children had higher reoperation rates than older children (OR = 1.91, P = 0.017). When endoscopic dilation was individually examined, children younger than 1 year of age were more likely to undergo reoperation after an endoscopic dilation than children older than 1 (OR = 4.39, P = 0.03). Children under age 1 were also more likely to have an unplanned readmission after an endoscopic dilation (OR = 4.21, P = 0.03). The relationship between age and re-intubation was not significant (OR = 0, P = 0.95). For open reconstruction, this age dichotomization was not associated with any increased reoperation (OR = 2.3, P = 0.52), readmission (OR = 0, P = 0.97), or reintubation (OR = 0, P = 0.94).
T-test analysis was performed to determine if children < 1 year old also had significantly longer hospital stays after endoscopic dilation than older children (mean 14.1 days vs 1.9 days, P < 0.001). This relationship held true in a linear regression after adjustment for pulmonary disease and tracheostomy, with length of stay decreasing by 0.48 days per year of life (P = 0.03). For endoscopic dilations, the same relationship held true, where length of stay decreased by 0.75 days per year of life.
Discussion
Endoscopic dilation for primary management of pediatric laryngotracheal stenosis has become commonplace. Despite this, outcomes of this procedure have only been described in case series and meta-analyses [2–5]. The relative rarity of pediatric laryngotracheal stenosis suggests the need for large, multi-institutional data for purposes of patient selection and medical decision-making.
This study utilized the ACS-NSQIP-Pediatric database to highlight 30-day outcomes of endoscopic dilation and to compare these outcomes to those of open airway reconstruction procedures. The ACS-NSQIP database has been endorsed by multiple organizations, including the Center for Medicare and Medicaid Services, the Joint Commission, and the American Medical Association. It has been shown to have higher sensitivity and a lower false-positive rate when compared to administrative data, in part due to data collection from trained personnel [11]. Furthermore, ACS-NSQIP use has the additional benefit of reporting an unplanned admission—a feature unavailable in review of claims data [12].
With respect to adverse events, our study demonstrates that endoscopic dilation is associated with an equally high rate of unplanned readmission when compared to open reconstruction. The high prevalence of comorbid disease such as chronic lung disease (32% of endoscopic dilation and 43% of open reconstruction) can account for some of the morbidity associated with any airway procedures.
Despite high rates of unplanned readmission, patients undergoing endoscopic dilation were less likely to have reoperations within 30 days of initial surgery when compared to those undergoing open reconstruction. While differences in disease severity may be partially responsible for this difference in the reoperation rate, this finding is notable given the health care costs associated with multiple operations as well as safety concerns with multiple anesthetics in the very young [13,14].
The ACS-NSQIP platform does not distinguish unplanned from planned reoperations. In the setting of airway surgery, where multiple planned reoperations are commonplace, this metric is a suboptimal stand-alone indicator of adverse outcomes. Other markers available in the database—such as reintubations and performance of tracheostomy or open airway reconstruction within 30-days of surgery—are more indicative of surgical outcome in the setting of airway surgery. We found that both reintubations and salvage open reconstruction within 30-days were rare. It should be noted that the ACS-NSQIP data does not report any events occurring outside of the 30-day postoperative period, representing potential limitation of the use of this database. As was previously advocated by Roxbury and colleagues, procedure/subspecialty specific outcome data collection would also improve outcome analysis of airway and other otolaryngologic procedures [9]. In the setting of airway reconstruction, this would include data pertaining to Cotton-Meyer grading systems well as postoperative voice and swallow outcomes.
In addition to safety profile, endoscopic procedures were associated with shorter LOS when compared with open reconstruction, representing another potential source of cost savings with this less invasive method. This is especially significant given that open reconstruction patients spend much of their inpatient stay in an ICU setting. In patients who are candidates for endoscopic procedures, this lower-risk, lower-cost profile of endoscopic dilation has the opportunity to improve value in health care and may be the source of future improvement initiatives.
In addition to comparing overall outcomes between endoscopic and open management of laryngotracheal stenosis, our study aimed to identify factors that were associated with varied outcomes in patients undergoing primary endoscopic dilation. We found that children younger than 1 year of age were 5.8 times more likely to undergo an unplanned reoperation after an endoscopic dilation than children over 1 year. A similar finding was reported in open airway surgeries, with increased reoperation rates in children < 3 years old [9]. The justification of a dichotomization at 1 year was made as expert opinion recognizes that the infant airway is less forgiving to intervention given its small size. Young age was also a factor in prolonged LOS as was determined by linear regression. It is likely that this increased LOS may be in part due to associations of young age and the neonatal ICU population. One must balance the increased risk of surgery in the young with that of tracheostomy, which has a published complication rate of 18% to 50% and direct mortality rate of 1% to 2% in the pediatric population [15–18]. Understanding these relative risks may help guide the airway surgeon in preoperative counseling with families and medical decision-making.
As discussed above, the limitation of data to a 30-day period is a relative weakness of ACS-NSQIP database use for studies of airway reconstruction, as the ultimate outcome—a stable, decannulated airway—may occur outside of this time period. As many quality metrics utilize data from the 30-day postoperative period, knowledge of these outcomes remains valuable in surgical decision-making. Ultimately, collection of data in a large, long-term dataset would allow broader generalizations to be made about the differences between open and endoscopic procedures and would also give a more comprehensive picture of the outcomes of endoscopic dilation.
In conclusion, this study is the first to analyze 30-day postoperative outcomes in pediatric endoscopic airway dilations using data aggregated by ACS-NSQIP from institutions across the United States. This data indicates that endoscopic airway dilation is a relatively safe procedure, especially compared with open reconstruction; however, additional data on disease severity and other outcomes is necessary to draw final conclusions of superiority of technique. Future improvement initiatives could be aimed at the impact of this lower-risk, lower-cost procedure in the appropriately selected patient. Outcomes of endoscopic dilation are poorer in those less than 1 year of age, as they are associated with increased reoperation rates and increased length of stay compared to older children. One must balance these risks in the very young with the risks associated with tracheostomy and other alternative airway management modalities.
Note: This work was presented in a paper at the AAO-HNS 2017 meeting, Chicago, IL, 10 Sep 2017.
Corresponding author: Jennifer Lavin, MD, MS, 225 E Chicago Ave., Box 25, Chicago, IL 60611, JLavin@luriechildrens.org.
Financial disclosures: None.
1. Cohen MD, Weber TR, Rao CC. Balloon dilatation of tracheal and bronchial stenosis. AJR Am J Roentgenol 1984;142:477–8.
2. Chueng K, Chadha NK. Primary dilatation as a treatment for pediatric laryngotracheal stenosis: a systematic review. Int J Pediatr Otorhinolaryngol 2013;77:623–8.
3. Hautefort C, Teissier N, Viala P, Van Den Abbeele T. Balloon dilation laryngoplasty for subglottic stenosis in children: eight years’ experience. Arch Otolaryngol Head Neck Surg 2012;138:235–40.
4. Lang M, Brietzke SE. A systematic review and meta-analysis of endoscopic balloon dilation of pediatric subglottic stenosis. Otolaryngol Head Neck Surg 2014;150:174–9.
5. Maresh A, Preciado DA, O’Connell AP, Zalzal GH. A comparative analysis of open surgery vs endoscopic balloon dilation for pediatric subglottic stenosis. JAMA Otolaryngol Head Neck Surg 2014;140:901–5.
6. Gelbard A, Donovan DT, Ongkasuwan J, et al. Disease homogeneity and treatment heterogeneity in idiopathic subglottic stenosis. Laryngoscope 2016;126:1390–6.
7. ACS-NSQIP. ACS National Surgical Quality Improvement Program® (ACS NSQIP®). 2017. Available at: http://site.acsnsqip.org/program-specifics/scr-training-and-resources. Accessed June 2 2017.
8. Shiloach M, Frencher SK Jr, Steeger JE, et al. Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg 2010;210:6–16.
9. Roxbury CR, Jatana KR, Shah RK, Boss EF. Safety and postoperative adverse events in pediatric airway reconstruction: Analysis of ACS-NSQIP-P 30-day outcomes. Laryngoscope 2017;127:504–8.
10. Raval MV, Dillon PW, Bruny JL, et al. Pediatric American College of Surgeons National Surgical Quality Improvement Program: feasibility of a novel, prospective assessment of surgical outcomes. J Pediatr Surg 2011;46:115–21.
11. Lawson EH, Louie R, Zingmond DS, et al. A comparison of clinical registry versus administrative claims data for reporting of 30-day surgical complications. Ann Surg 2012;256:973–81.
12. Sellers MM, Merkow RP, Halverson A, et al. Validation of new readmission data in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg 2013;216:420–7.
13. Jevtovic-Todorovic V, Hartman RE, Izumi Y, et al. Early exposure to common anesthetic agents causes widespread neurodegeneration in the developing rat brain and persistent learning deficits. J Neurosci 2003;23:876–82.
14. Patel P, Sun L. Update on neonatal anesthetic neurotoxicity: insight into molecular mechanisms and relevance to humans. Anesthesiology 2009;110:703–8.
15. Crysdale WS, Feldman RI, Naito K. Tracheotomies: a 10-year experience in 319 children. Ann Otol Rhinol Laryngol 1988;97(5 Pt 1):439–43.
16. Goldenberg D, Ari EG, Golz A, et al. Tracheotomy complications: a retrospective study of 1130 cases. Otolaryngol Head Neck Surg 2000;123:495–500.
17. Mahadevan M, Barber C, Salkeld L, et al N. Pediatric tracheotomy: 17 year review. Int J Pediatr Otorhinolaryngol 2007;71:1829–35.
18. Ozmen S, Ozmen OA, Unal OF. Pediatric tracheotomies: a 37-year experience in 282 children. Int J Pediatr Otorhinolaryngol 2009;73:959–61.
1. Cohen MD, Weber TR, Rao CC. Balloon dilatation of tracheal and bronchial stenosis. AJR Am J Roentgenol 1984;142:477–8.
2. Chueng K, Chadha NK. Primary dilatation as a treatment for pediatric laryngotracheal stenosis: a systematic review. Int J Pediatr Otorhinolaryngol 2013;77:623–8.
3. Hautefort C, Teissier N, Viala P, Van Den Abbeele T. Balloon dilation laryngoplasty for subglottic stenosis in children: eight years’ experience. Arch Otolaryngol Head Neck Surg 2012;138:235–40.
4. Lang M, Brietzke SE. A systematic review and meta-analysis of endoscopic balloon dilation of pediatric subglottic stenosis. Otolaryngol Head Neck Surg 2014;150:174–9.
5. Maresh A, Preciado DA, O’Connell AP, Zalzal GH. A comparative analysis of open surgery vs endoscopic balloon dilation for pediatric subglottic stenosis. JAMA Otolaryngol Head Neck Surg 2014;140:901–5.
6. Gelbard A, Donovan DT, Ongkasuwan J, et al. Disease homogeneity and treatment heterogeneity in idiopathic subglottic stenosis. Laryngoscope 2016;126:1390–6.
7. ACS-NSQIP. ACS National Surgical Quality Improvement Program® (ACS NSQIP®). 2017. Available at: http://site.acsnsqip.org/program-specifics/scr-training-and-resources. Accessed June 2 2017.
8. Shiloach M, Frencher SK Jr, Steeger JE, et al. Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg 2010;210:6–16.
9. Roxbury CR, Jatana KR, Shah RK, Boss EF. Safety and postoperative adverse events in pediatric airway reconstruction: Analysis of ACS-NSQIP-P 30-day outcomes. Laryngoscope 2017;127:504–8.
10. Raval MV, Dillon PW, Bruny JL, et al. Pediatric American College of Surgeons National Surgical Quality Improvement Program: feasibility of a novel, prospective assessment of surgical outcomes. J Pediatr Surg 2011;46:115–21.
11. Lawson EH, Louie R, Zingmond DS, et al. A comparison of clinical registry versus administrative claims data for reporting of 30-day surgical complications. Ann Surg 2012;256:973–81.
12. Sellers MM, Merkow RP, Halverson A, et al. Validation of new readmission data in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg 2013;216:420–7.
13. Jevtovic-Todorovic V, Hartman RE, Izumi Y, et al. Early exposure to common anesthetic agents causes widespread neurodegeneration in the developing rat brain and persistent learning deficits. J Neurosci 2003;23:876–82.
14. Patel P, Sun L. Update on neonatal anesthetic neurotoxicity: insight into molecular mechanisms and relevance to humans. Anesthesiology 2009;110:703–8.
15. Crysdale WS, Feldman RI, Naito K. Tracheotomies: a 10-year experience in 319 children. Ann Otol Rhinol Laryngol 1988;97(5 Pt 1):439–43.
16. Goldenberg D, Ari EG, Golz A, et al. Tracheotomy complications: a retrospective study of 1130 cases. Otolaryngol Head Neck Surg 2000;123:495–500.
17. Mahadevan M, Barber C, Salkeld L, et al N. Pediatric tracheotomy: 17 year review. Int J Pediatr Otorhinolaryngol 2007;71:1829–35.
18. Ozmen S, Ozmen OA, Unal OF. Pediatric tracheotomies: a 37-year experience in 282 children. Int J Pediatr Otorhinolaryngol 2009;73:959–61.
No clear winner in Pfannenstiel vs. vertical incision for high BMI cesareans
DALLAS – though enrollment difficulties limited study numbers, with almost two-thirds of eligible women declining to participate in the surgical trial.
At 6 weeks postdelivery, 21.1% of women who had a vertical incision experienced wound complications, compared with 18.6% of those who had a Pfannenstiel incision, a nonsignificant difference. This was a smaller difference than was seen at 2 weeks postpartum, when 20% of the vertical incision group had wound complications, compared with 10.4% of those who had a Pfannenstiel, also a nonsignificant difference. Maternal and fetal outcomes didn’t differ significantly with the two surgical approaches.
Though there had been several observational studies comparing vertical with Pfannenstiel incisions for cesarean delivery in women with obesity, no randomized, controlled trials had been conducted, and observational study results were mixed, said Dr. Marrs.
Each approach comes with theoretical pros and cons: For women who have a large pannus, the incision site may lie in a moist environment with a low transverse incision, and oxygen tension may be low. However, a Pfannenstiel incision usually will have better cosmesis than will a vertical incision, and generally will result in less postoperative pain.
On the other hand, said Dr. Marrs, vertical incisions can provide improved exposure of the uterus during delivery, and the moist environment underlying the pannus is avoided. However, wound tension may be higher, and subcutaneous thickness is likely to be higher than at the Pfannenstiel incision site.
The study, conducted at two academic medical centers, enrolled women with a body mass index (BMI) of at least 40 kg/m2 at a gestational age of 24 weeks or greater who required cesarean delivery. Consenting women were then randomized to receive Pfannenstiel or vertical incisions.
Women who had clinical chorioamnionitis, whose amniotic membranes had been ruptured for 18 hours or more, or who had placenta accreta were excluded. Also excluded were women with a private physician and those desiring vaginal delivery, said Dr. Marrs, a maternal-fetal medicine fellow at the University of Texas Medical Branch, Galveston.
The study’s primary outcome measure was a composite of wound complications seen within 6 weeks of delivery, including surgical site infection, whether superficial, deep, or involving an organ or tissue space; cellulitis; seroma or hematoma; and wound separation. Other maternal outcomes tracked in the study included postoperative length of stay, transfusion requirement, sepsis, readmission, and death.
Cesarean-specific secondary outcomes included operative time and time from skin incision to delivery, estimated blood loss, and any incidence of hysterectomy through a low transverse incision. Neonatal outcomes included a 5-minute Apgar score of less than 7, umbilical cord pH of less than 7, and neonatal ICU admissions.
Dr. Mars said that the goal enrollment for the study was 300 patients, to ensure adequate statistical power. However, they found enrollment a challenge, with low consent rates during the defined time period from October 2013 to May 2017. They shifted their statistical technique to a Bayesian analysis, taking into account the estimated probability of treatment benefit.
Using this approach, they found a 59% probability that a Pfannenstiel incision would lead to a lower primary outcome rate – a better result – than would a vertical incision. This result just missed the predetermined threshold of 60%, said Dr. Marrs.
Of the 789 women who met the BMI threshold for eligibility assessment, 420 (65%) who passed the screening declined to participate. Of those who consented to participation, an additional 137 women either withdrew consent or failed further screening, leaving 50 women who were randomized to the Pfannenstiel arm and 41 who were randomized to the vertical incision arm.
Baseline characteristics were similar between groups, with a mean maternal age of 30 years in the Pfannenstiel group and 28 years in the vertical incision group. Gestational age at delivery was a mean of 37 weeks in both groups, and mean BMI was 48-50 kg/m2.
Most patients (80%-90%) had public insurance. Diabetes was more common in the Pfannenstiel group (48%) than in the vertical incision cohort (32%). Just over 40% of patients were African American.
Two women in the Pfannenstiel group and three in the vertical incision group did not receive the intended incision. After accounting for patients lost to follow-up by 6 weeks, 43 women who received Pfannenstiel and 38 women who received vertical incisions were available for full evaluation.
Dr. Marrs said that the study, the first randomized trial to address this issue, had several strengths, including its being conducted at two sites with appropriate stratification for the sites. Also, an independent data safety monitoring board and two chart reviewers helped overcome some of the limitations of a surgical study, where complete blinding is impossible.
The Bayesian analysis allowed ascertainment of the probability of treatment benefit despite the lower-than-hoped-for enrollment numbers. The primary weakness of the study, said Dr. Marrs, centered around the low consent rate, which led to a small study that was prematurely terminated.
“It’s difficult to enroll women in a trial that requires random allocation of skin incision, due to their preference to choose their own incision. A larger trial would likewise be challenging, and unlikely to yield different results,” said Dr. Marrs.
Dr. Marrs reported no conflicts of interest.
SOURCE: Marrs CC et al. Am J Obstet Gynecol. 2018 Jan;218:S29.
DALLAS – though enrollment difficulties limited study numbers, with almost two-thirds of eligible women declining to participate in the surgical trial.
At 6 weeks postdelivery, 21.1% of women who had a vertical incision experienced wound complications, compared with 18.6% of those who had a Pfannenstiel incision, a nonsignificant difference. This was a smaller difference than was seen at 2 weeks postpartum, when 20% of the vertical incision group had wound complications, compared with 10.4% of those who had a Pfannenstiel, also a nonsignificant difference. Maternal and fetal outcomes didn’t differ significantly with the two surgical approaches.
Though there had been several observational studies comparing vertical with Pfannenstiel incisions for cesarean delivery in women with obesity, no randomized, controlled trials had been conducted, and observational study results were mixed, said Dr. Marrs.
Each approach comes with theoretical pros and cons: For women who have a large pannus, the incision site may lie in a moist environment with a low transverse incision, and oxygen tension may be low. However, a Pfannenstiel incision usually will have better cosmesis than will a vertical incision, and generally will result in less postoperative pain.
On the other hand, said Dr. Marrs, vertical incisions can provide improved exposure of the uterus during delivery, and the moist environment underlying the pannus is avoided. However, wound tension may be higher, and subcutaneous thickness is likely to be higher than at the Pfannenstiel incision site.
The study, conducted at two academic medical centers, enrolled women with a body mass index (BMI) of at least 40 kg/m2 at a gestational age of 24 weeks or greater who required cesarean delivery. Consenting women were then randomized to receive Pfannenstiel or vertical incisions.
Women who had clinical chorioamnionitis, whose amniotic membranes had been ruptured for 18 hours or more, or who had placenta accreta were excluded. Also excluded were women with a private physician and those desiring vaginal delivery, said Dr. Marrs, a maternal-fetal medicine fellow at the University of Texas Medical Branch, Galveston.
The study’s primary outcome measure was a composite of wound complications seen within 6 weeks of delivery, including surgical site infection, whether superficial, deep, or involving an organ or tissue space; cellulitis; seroma or hematoma; and wound separation. Other maternal outcomes tracked in the study included postoperative length of stay, transfusion requirement, sepsis, readmission, and death.
Cesarean-specific secondary outcomes included operative time and time from skin incision to delivery, estimated blood loss, and any incidence of hysterectomy through a low transverse incision. Neonatal outcomes included a 5-minute Apgar score of less than 7, umbilical cord pH of less than 7, and neonatal ICU admissions.
Dr. Mars said that the goal enrollment for the study was 300 patients, to ensure adequate statistical power. However, they found enrollment a challenge, with low consent rates during the defined time period from October 2013 to May 2017. They shifted their statistical technique to a Bayesian analysis, taking into account the estimated probability of treatment benefit.
Using this approach, they found a 59% probability that a Pfannenstiel incision would lead to a lower primary outcome rate – a better result – than would a vertical incision. This result just missed the predetermined threshold of 60%, said Dr. Marrs.
Of the 789 women who met the BMI threshold for eligibility assessment, 420 (65%) who passed the screening declined to participate. Of those who consented to participation, an additional 137 women either withdrew consent or failed further screening, leaving 50 women who were randomized to the Pfannenstiel arm and 41 who were randomized to the vertical incision arm.
Baseline characteristics were similar between groups, with a mean maternal age of 30 years in the Pfannenstiel group and 28 years in the vertical incision group. Gestational age at delivery was a mean of 37 weeks in both groups, and mean BMI was 48-50 kg/m2.
Most patients (80%-90%) had public insurance. Diabetes was more common in the Pfannenstiel group (48%) than in the vertical incision cohort (32%). Just over 40% of patients were African American.
Two women in the Pfannenstiel group and three in the vertical incision group did not receive the intended incision. After accounting for patients lost to follow-up by 6 weeks, 43 women who received Pfannenstiel and 38 women who received vertical incisions were available for full evaluation.
Dr. Marrs said that the study, the first randomized trial to address this issue, had several strengths, including its being conducted at two sites with appropriate stratification for the sites. Also, an independent data safety monitoring board and two chart reviewers helped overcome some of the limitations of a surgical study, where complete blinding is impossible.
The Bayesian analysis allowed ascertainment of the probability of treatment benefit despite the lower-than-hoped-for enrollment numbers. The primary weakness of the study, said Dr. Marrs, centered around the low consent rate, which led to a small study that was prematurely terminated.
“It’s difficult to enroll women in a trial that requires random allocation of skin incision, due to their preference to choose their own incision. A larger trial would likewise be challenging, and unlikely to yield different results,” said Dr. Marrs.
Dr. Marrs reported no conflicts of interest.
SOURCE: Marrs CC et al. Am J Obstet Gynecol. 2018 Jan;218:S29.
DALLAS – though enrollment difficulties limited study numbers, with almost two-thirds of eligible women declining to participate in the surgical trial.
At 6 weeks postdelivery, 21.1% of women who had a vertical incision experienced wound complications, compared with 18.6% of those who had a Pfannenstiel incision, a nonsignificant difference. This was a smaller difference than was seen at 2 weeks postpartum, when 20% of the vertical incision group had wound complications, compared with 10.4% of those who had a Pfannenstiel, also a nonsignificant difference. Maternal and fetal outcomes didn’t differ significantly with the two surgical approaches.
Though there had been several observational studies comparing vertical with Pfannenstiel incisions for cesarean delivery in women with obesity, no randomized, controlled trials had been conducted, and observational study results were mixed, said Dr. Marrs.
Each approach comes with theoretical pros and cons: For women who have a large pannus, the incision site may lie in a moist environment with a low transverse incision, and oxygen tension may be low. However, a Pfannenstiel incision usually will have better cosmesis than will a vertical incision, and generally will result in less postoperative pain.
On the other hand, said Dr. Marrs, vertical incisions can provide improved exposure of the uterus during delivery, and the moist environment underlying the pannus is avoided. However, wound tension may be higher, and subcutaneous thickness is likely to be higher than at the Pfannenstiel incision site.
The study, conducted at two academic medical centers, enrolled women with a body mass index (BMI) of at least 40 kg/m2 at a gestational age of 24 weeks or greater who required cesarean delivery. Consenting women were then randomized to receive Pfannenstiel or vertical incisions.
Women who had clinical chorioamnionitis, whose amniotic membranes had been ruptured for 18 hours or more, or who had placenta accreta were excluded. Also excluded were women with a private physician and those desiring vaginal delivery, said Dr. Marrs, a maternal-fetal medicine fellow at the University of Texas Medical Branch, Galveston.
The study’s primary outcome measure was a composite of wound complications seen within 6 weeks of delivery, including surgical site infection, whether superficial, deep, or involving an organ or tissue space; cellulitis; seroma or hematoma; and wound separation. Other maternal outcomes tracked in the study included postoperative length of stay, transfusion requirement, sepsis, readmission, and death.
Cesarean-specific secondary outcomes included operative time and time from skin incision to delivery, estimated blood loss, and any incidence of hysterectomy through a low transverse incision. Neonatal outcomes included a 5-minute Apgar score of less than 7, umbilical cord pH of less than 7, and neonatal ICU admissions.
Dr. Mars said that the goal enrollment for the study was 300 patients, to ensure adequate statistical power. However, they found enrollment a challenge, with low consent rates during the defined time period from October 2013 to May 2017. They shifted their statistical technique to a Bayesian analysis, taking into account the estimated probability of treatment benefit.
Using this approach, they found a 59% probability that a Pfannenstiel incision would lead to a lower primary outcome rate – a better result – than would a vertical incision. This result just missed the predetermined threshold of 60%, said Dr. Marrs.
Of the 789 women who met the BMI threshold for eligibility assessment, 420 (65%) who passed the screening declined to participate. Of those who consented to participation, an additional 137 women either withdrew consent or failed further screening, leaving 50 women who were randomized to the Pfannenstiel arm and 41 who were randomized to the vertical incision arm.
Baseline characteristics were similar between groups, with a mean maternal age of 30 years in the Pfannenstiel group and 28 years in the vertical incision group. Gestational age at delivery was a mean of 37 weeks in both groups, and mean BMI was 48-50 kg/m2.
Most patients (80%-90%) had public insurance. Diabetes was more common in the Pfannenstiel group (48%) than in the vertical incision cohort (32%). Just over 40% of patients were African American.
Two women in the Pfannenstiel group and three in the vertical incision group did not receive the intended incision. After accounting for patients lost to follow-up by 6 weeks, 43 women who received Pfannenstiel and 38 women who received vertical incisions were available for full evaluation.
Dr. Marrs said that the study, the first randomized trial to address this issue, had several strengths, including its being conducted at two sites with appropriate stratification for the sites. Also, an independent data safety monitoring board and two chart reviewers helped overcome some of the limitations of a surgical study, where complete blinding is impossible.
The Bayesian analysis allowed ascertainment of the probability of treatment benefit despite the lower-than-hoped-for enrollment numbers. The primary weakness of the study, said Dr. Marrs, centered around the low consent rate, which led to a small study that was prematurely terminated.
“It’s difficult to enroll women in a trial that requires random allocation of skin incision, due to their preference to choose their own incision. A larger trial would likewise be challenging, and unlikely to yield different results,” said Dr. Marrs.
Dr. Marrs reported no conflicts of interest.
SOURCE: Marrs CC et al. Am J Obstet Gynecol. 2018 Jan;218:S29.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: Wound complication rates were similar with Pfannenstiel and vertical incisions in women with obesity.
Major finding: At 6 weeks, 21.1% of vertical incision recipients and 18.6% of Pfannenstiel recipients had wound complications.
Study details: Randomized controlled trial of 91 women with obesity receiving cesarean section.
Disclosures: Dr. Marrs reported no conflicts of interest.
Source: Marrs CC et al. Am J Obstet Gynecol. 2018 Jan;218:S29.
Enhanced recovery after surgery for the patient with chronic pain
CASE Chronic pelvic pain from endometriosis
A 40-year-old woman (G0) has a 20-year history of chronic pelvic pain. Stage III endometriosis is diagnosed on laparoscopic excision of endometriotic tissue. Postoperative pain symptoms include dysmenorrhea and deep dyspareunia, and the patient is feeling anxious. Physical examination reveals a retroverted uterus, right adnexal fullness and tenderness, and tenderness on palpation of the right levator ani and right obturator internus; rectovaginal examination findings are unremarkable. The patient, though now engaged in a pelvic floor physical therapy program, has yet to achieve the pain control she desires. After reviewing the treatment strategies for endometriosis with the patient, she elects definitive surgical management with minimally invasive hysterectomy and salpingo-oophorectomy. What pre-, intra-, and postoperative pain management plan do you devise for this patient?
Chronic pelvic pain presents a unique clinical challenge, as pain typically is multifactorial, and several peripheral pain generators may be involved. Although surgery can be performed to manage anatomically based disease processes, it does not address pain from musculoskeletal or neuropathic sources. A complete medical history and a physical examination are of utmost importance in developing a comprehensive multimodal management plan that may include surgery as treatment for the pain.
The standard of care for surgery is a minimally invasive approach (vaginal, laparoscopic, or robot-assisted laparoscopic), as it causes the least amount of trauma. Benefits of minimally invasive surgery include shorter hospitalization and faster recovery, likely owing to improved perioperative pain control, decreased blood loss, and fewer infections. Although this approach minimizes surgical trauma and thereby helps decrease the surgical stress response, the patient experience can be optimized with use of enhanced recovery pathways (ERPs), a multimodal approach to perioperative care.
ERPs were initially proposed as a means of reducing the degree of surgical injury and the subsequent physiologic stress response.1 This multimodal approach begins in the outpatient setting, includes preoperative and intraoperative modalities, and continues postoperatively. In patients with chronic pain, ERPs are even more important. Assigning “prehabilitation” and setting expectations for surgery goals are the first step in improving the patient experience. Intraoperative use of opioid-sparing anesthetics or regional anesthesia can improve recovery. After surgery, patients with chronic pain and/or opioid dependence receive medications on a schedule, along with short-interval follow-up. Ultimately, reducing acute postoperative pain may lower the risk of developing chronic pain.
In this article on patients with chronic pelvic pain, we highlight elements of ERPs within the framework of enhanced recovery after surgery. Many of the interventions proposed here also can be used to improve the surgical experience of patients without chronic pain.
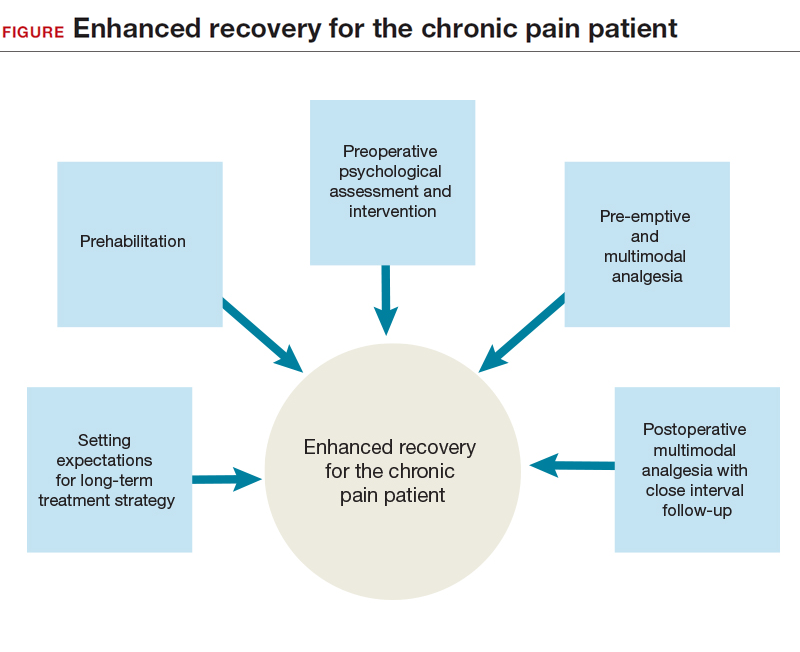
Preadmission education, expectations, and optimization
Preoperative counseling for elective procedures generally occurs in the outpatient setting. Although discussion traditionally has covered the type of procedure and its associated risks, benefits, and alternatives, new guidelines suggest a more mindful and comprehensive approach is warranted. Individualized patient-centered education programs have a positive impact on the perioperative course, effecting reductions in preoperative anxiety, opioid requirements, and hospital length of stay.2 From a pain management perspective, the clinician can take some time during preoperative counseling to inform the patient about the pain to be expected from surgery, the ways the pain will be managed intraoperatively and postoperatively, and the multimodal strategies that will be used throughout the patient’s stay2 and that may allow for early discharge. Although preadmission counseling still should address expectations for the surgery, it also presents an opportunity both to assess the patient’s ability to cope with the physical and psychological stress of surgery and to offer the patient appropriate need-based interventions, such as prehabilitation and cognitive-behavioral therapy (CBT).
Prehabilitation is the process of increasing functional capacity before surgery in order to mitigate the stress of the surgery. Prehabilitation may involve aerobic exercise, strength training, or functional task training. The gynecologic surgery literature lacks prehabilitation data, but data in the colorectal literature support use of a prehabilitation program for patients having a scheduled colectomy, with improved postoperative recovery.3 Although the colectomy cohort predominantly included older men, the principle that guides program implementation is the same: improve recovery after the stress of abdominal surgery. Indeed, a patient who opts for an elective surgery may have to wait several weeks before undergoing the procedure, and during this period behavioral interventions can take effect. With postoperative complications occurring more often in patients with reduced functional capacity, the data support using prehabilitation to decrease the incidence of postoperative complications, particularly among the most vulnerable patients.4 However, a definitive recommendation on use of pelvic floor exercises as an adjunct to prehabilitation cannot be made.4 Successful prehabilitation takes at least 4 weeks and should be part of a multimodal program that addresses other behavioral risk factors that may negatively affect recovery.5 For example, current tobacco users have compromised pulmonary status and wound healing immediately after surgery, and use more opioids.6 Conversely, smoking cessation for as little as 4 weeks before surgery is associated with fewer complications.7 In addition, given that alcohol abuse may compromise the surgical stress response and increase the risk of opioid misuse, addressing alcohol abuse preoperatively may improve postoperative recovery.8
Treating mood disorders that coexist with chronic pain disorders is an important part of outpatient multimodal management—psychological intervention is a useful adjunct to prehabilitation in reducing perioperative anxiety and improving postoperative functional capacity.9 For patients who have chronic pain and are undergoing surgery, it is important to address any anxiety, depression, or poor coping skills (eg, pain catastrophizing) to try to reduce the postoperative pain experience and decrease the risk of chronic postsurgical pain (CPSP).10,11
Before surgery, patients with chronic pain syndromes should be evaluated for emotional distress and pain coping ability. When possible, they should be referred to a pain psychologist, who can initiate CBT and other interventions. In addition, pain coping skills can be developed or reinforced to address preoperative anxiety and pain catastrophizing. These interventions, which may include use of visual imagery, breathing exercises, and other relaxation techniques, are applicable to the management of postoperative anxiety as well.
Read about preoperative multimodal analgesia and intra- and postoperative management.
Preoperative multimodal analgesia
Multimodal analgesia has several benefits. Simultaneous effects can be generated on multiple pain-related neurotransmitters, and a synergistic effect (eg, of acetaminophen and a nonsteroidal anti-inflammatory drug [NSAID]) can improve pain management. In addition, small doses of multiple medications can be given, instead of a large dose of a single medication. Of course, this strategy must be modified in elderly and patients with impaired renal function, who are at high risk for polypharmacy.
Preoperative administration of 3 medications—a selective cyclooxygenase 2 (COX-2) inhibitor, acetaminophen, and a gabapentinoid—is increasingly accepted as part of multimodal analgesia. The selective COX-2 inhibitor targets inflammatory prostaglandins and has anti-inflammatory and analgesic effects; acetaminophen, an effective analgesic with an unclear mechanism of action, can reduce postoperative opioid consumption12 and works synergistically with NSAIDs13; and the gabapentinoid gabapentin has an analgesic effect likely contributing to decreased movement-related pain and subsequent improved functional recovery (data are mixed on whether continuing gabapentin after surgery prevents CPSP).14−16
Although serotonin and norepinephrine reuptake inhibitors (SNRIs) are commonly used in outpatient management of chronic pelvic pain, data suggest that their role in perioperative pain management is evolving. As SNRIs may reduce central nervous system (CNS) sensitization,17 their analgesic effect is thought to result from increased descending inhibitory tone in the CNS, which makes this class of medication ideal for patients with chronic neuropathic pain.15
Limited data also suggest a role for SNRIs in decreasing immediate postoperative pain and CPSP in high-risk patients. Studies of duloxetine use in the immediate perioperative period have found reduced postoperative acute pain and opioid use.18,19 In addition, a short course of low-dose (37.5 mg) venlafaxine both before and after surgery has demonstrated a reduction in postoperative opioid use and a reduction in movement-related pain 6 months after surgery.20
Intraoperative management
The surgical and anesthesia teams share the goal of optimizing both pain control and postoperative recovery. Surgical team members, who want longer-acting anesthetics for infiltration of incision sites, discuss with the anesthesiologist the appropriateness of using peripheral nerve blocks or neuraxial anesthesia, given the patient’s history and planned procedure. Anesthesia team members can improve anesthesia and minimize intraoperative opioid use through several methods, including total intravenous anesthesia,21 dexamethasone,22 ketorolac,23 and intravenous ketamine. Ketamine, in particular, has a wide range of surgical applications and has been found to reduce postoperative pain, postoperative pain medication use, and the risk of CPSP.2
Incision sites should be infiltrated before and after surgery. Lidocaine traditionally is used for its rapid onset of action in reducing surgical site pain, but its short half-life may limit its applicability to postoperative pain. Recently, bupivacaine (half-life, 3.5 hours) and liposomal bupivacaine (24–34 hours) have gained more attention. Both of these medications appear to be as effective as lidocaine in reducing surgical site pain.24
Transversus abdominis plane (TAP) blocks have been used as an adjunct in pain management during abdominopelvic surgery. Although initial data on postoperative pain and opioid use reductions with TAP blocks were inconclusive,25 more recent data showed a role for TAP blocks in a multimodal approach for reducing opioid use during laparoscopic and open surgery.26,27 Given the small number of studies on using liposomal bupivacaine for peripheral nerve blocks (eg, TAP blocks) in postoperative pain management, current data are inconclusive.28
Postoperative management
The ERP approach calls for continuing multimodal analgesia after surgery—in most cases, scheduling early use of oral acetaminophen and ibuprofen, and providing short-acting, low-dose opioid analgesia as needed. All patients should be given a bowel regimen. Similar to undergoing prehabilitation for surgery, patients should prepare themselves for recovery. They should be encouraged to engage in early ambulation and oral intake and, when clinically appropriate, be given same-day discharge for minimally invasive surgical procedures.
Patients with chronic pain before surgery are at increased risk for suboptimal postoperative pain management, and those who are dependent on opioids require additional perioperative measures for adequate postoperative pain control. In these complicated cases, it is appropriate to enlist a pain specialist, potentially before surgery, to help plan perioperative and postoperative pain management.2 Postoperative pain management for opioid-dependent patients should include pharmacologic and nonpharmacologic interventions, such as use of nonopioid medications (eg, gabapentin) and continuation of CBT. Patients with chronic pain should be closely followed up for assessment of postoperative pain control and recovery.
CASE Resolved
Surgical management is one aspect of the longer term multimodal pain management strategy for this patient. After preoperative pelvic floor physical therapy, she is receptive to starting a trial of an SNRI for her pain and mood symptoms. Both interventions allow for optimization of her preoperative physical and psychological status. Expectations are set that she will be discharged the day of surgery and that the surgery is but one component of her multimodal treatment plan. In addition, before surgery, she takes oral acetaminophen, gabapentin, and celecoxib—previously having had no contraindications to these medications. During surgery, bupivacaine is used for infiltration of all incision sites, and the anesthesia team administers ketamine and a TAP block. After surgery, the patient is prepared for same-day discharge and given the NSAIDs and acetaminophen she is scheduled to take over the next 72 hours. She is also given a limited prescription for oxycodone for breakthrough pain. An office visit 1 to 2 weeks after surgery is scheduled.
ERP strategies for surgical management of endometriosis have not only improved this patient’s postoperative recovery but also reduced her surgical stress response and subsequent transition to chronic postoperative pain. Many of the strategies used in this case are applicable to patients without chronic pain.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. 1997;78(5):606−617.
- Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17(2):131−157.
- Mayo NE, Feldman L, Scott S, et al. Impact of preoperative change in physical function on postoperative recovery: argument supporting prehabilitation for colorectal surgery. Surgery. 2011;150(3):505−514.
- Moran J, Guinan E, McCormick P, et al. The ability of prehabilitation to influence postoperative outcome after intra-abdominal operation: a systematic review and meta-analysis. Surgery. 2016;160(5):1189−1201.
- Tew GA, Ayyash R, Durrand J, Danjoux GR. Clinical guideline and recommendations on pre-operative exercise training in patients awaiting major non-cardiac surgery [published online ahead of print January 13, 2018]. Anaesthesia. doi:10.1111/anae.14177.
- Chiang HL, Chia YY, Lin HS, Chen CH. The implications of tobacco smoking on acute postoperative pain: a prospective observational study. Pain Res Manag. 2016;2016:9432493.
- Mastracci TM, Carli F, Finley RJ, Muccio S, Warner DO; Members of the Evidence-Based Reviews in Surgery Group. Effect of preoperative smoking cessation interventions on postoperative complications. J Am Coll Surg. 2011;212(6):1094−1096.
- Tonnesen H, Kehlet H. Preoperative alcoholism and postoperative morbidity. Br J Surg. 1999;86(7):869−874.
- Gillis C, Li C, Lee L, et al. Prehabilitation versus rehabilitation: a randomized control trial in patients undergoing colorectal resection for cancer. Anesthesiology. 2014;121(5):937−947.
- Khan RS, Ahmed K, Blakeway E, et al. Catastrophizing: a predictive factor for postoperative pain. Am J Surg. 2011;201(1):122−131.
- Pinto PR, McIntyre T, Nogueira-Silva C, Almeida A, Araujo-Soares V. Risk factors for persistent postsurgical pain in women undergoing hysterectomy due to benign causes: a prospective predictive study. J Pain. 2012;13(11):1045−1057.
- Moon YE, Lee YK, Lee J, Moon DE. The effects of preoperative intravenous acetaminophen in patients undergoing abdominal hysterectomy. Arch Gynecol Obstet. 2011;284(6):1455−1460.
- Ong CK, Seymour RA, Lirk P, Merry AF. Combining paracetamol (acetaminophen) with nonsteroidal antiinflammatory drugs: a qualitative systematic review of analgesic efficacy for acute postoperative pain. Anesth Analg. 2010;110(4):1170−1179.
- Clarke H, Bonin RP, Orser BA, Englesakis M, Wijeysundera DN, Katz J. The prevention of chronic postsurgical pain using gabapentin and pregabalin: a combined systematic review and meta-analysis. Anesth Analg. 2012;115(2):428−442.
- Gilron I. Gabapentin and pregabalin for chronic neuropathic and early postsurgical pain: current evidence and future directions. Curr Opin Anaesthesiol. 2007;20(5):456−472.
- Chaparro LE, Smith SA, Moore RA, Wiffen PJ, Gilron I. Pharmacotherapy for the prevention of chronic pain after surgery in adults. Cochrane Database Syst Rev. 2013;(7):CD008307.
- Woolf CJ. Central sensitization: implications for the diagnosis and treatment of pain. Pain. 2011;152(3 suppl):S2−S15.
- Castro-Alves LJ, Oliveira de Medeiros AC, Neves SP, et al. Perioperative duloxetine to improve postoperative recovery after abdominal hysterectomy: a prospective, randomized, double-blinded, placebo-controlled study. Anesth Analg. 2016;122(1):98−104.
- Bedin A, Caldart Bedin RA, Vieira JE, Ashmawi HA. Duloxetine as an analgesic reduces opioid consumption after spine surgery: a randomized, double-blind, controlled study. Clin J Pain. 2017;33(10):865−869.
- Amr YM, Yousef AA. Evaluation of efficacy of the perioperative administration of venlafaxine or gabapentin on acute and chronic postmastectomy pain. Clin J Pain. 2010;26(5):381–385.
- Marret E, Rolin M, Beaussier M, Bonnet F. Meta-analysis of intravenous lidocaine and postoperative recovery after abdominal surgery. Br J Surg. 2008;95(11):1331–1338.
- De Oliveira GS Jr, Almeida MD, Benzon HT, McCarthy RJ. Perioperative single dose systemic dexamethasone for postoperative pain: a meta-analysis of randomized controlled trials. Anesthesiology. 2011;115(3):575–588.
- De Oliveira GS Jr, Agarwal D, Benzon HT. Perioperative single dose ketorolac to prevent postoperative pain: a meta-analysis of randomized trials. Anesth Analg. 2012;114(2):424–433.
- Hamilton TW, Athanassoglou V, Mellon S, et al. Liposomal bupivacaine infiltration at the surgical site for the management of postoperative pain. Cochrane Database Syst Rev. 2017;(2):CD011419.
- Charlton S, Cyna AM, Middleton P, Griffiths JD. Perioperative transversus abdominis plane (TAP) blocks for analgesia after abdominal surgery. Cochrane Database Syst Rev. 2010;(12):CD007705.
- Hain E, Maggiori L, Prost À la Denise J, Panis Y. Transversus abdominis plane (TAP) block in laparoscopic colorectal surgery improves postoperative pain management: a meta-analysis [published online ahead of print January 30, 2018]. Colorectal Dis. doi:10.1111/codi.14037.
- Staker JJ, Liu D, Church R, et al. A triple-blind, placebo-controlled randomised trial of the ilioinguinal-transversus abdominis plane (I-TAP) nerve block for elective caesarean section [published online ahead of print January 29, 2018]. Anaesthesia. doi:10.1111/anae.14222.
- Hamilton TW, Athanassoglou V, Trivella M, et al. Liposomal bupivacaine peripheral nerve block for the management of postoperative pain. Cochrane Database Syst Rev. 2016;(8):CD011476.
CASE Chronic pelvic pain from endometriosis
A 40-year-old woman (G0) has a 20-year history of chronic pelvic pain. Stage III endometriosis is diagnosed on laparoscopic excision of endometriotic tissue. Postoperative pain symptoms include dysmenorrhea and deep dyspareunia, and the patient is feeling anxious. Physical examination reveals a retroverted uterus, right adnexal fullness and tenderness, and tenderness on palpation of the right levator ani and right obturator internus; rectovaginal examination findings are unremarkable. The patient, though now engaged in a pelvic floor physical therapy program, has yet to achieve the pain control she desires. After reviewing the treatment strategies for endometriosis with the patient, she elects definitive surgical management with minimally invasive hysterectomy and salpingo-oophorectomy. What pre-, intra-, and postoperative pain management plan do you devise for this patient?
Chronic pelvic pain presents a unique clinical challenge, as pain typically is multifactorial, and several peripheral pain generators may be involved. Although surgery can be performed to manage anatomically based disease processes, it does not address pain from musculoskeletal or neuropathic sources. A complete medical history and a physical examination are of utmost importance in developing a comprehensive multimodal management plan that may include surgery as treatment for the pain.
The standard of care for surgery is a minimally invasive approach (vaginal, laparoscopic, or robot-assisted laparoscopic), as it causes the least amount of trauma. Benefits of minimally invasive surgery include shorter hospitalization and faster recovery, likely owing to improved perioperative pain control, decreased blood loss, and fewer infections. Although this approach minimizes surgical trauma and thereby helps decrease the surgical stress response, the patient experience can be optimized with use of enhanced recovery pathways (ERPs), a multimodal approach to perioperative care.
ERPs were initially proposed as a means of reducing the degree of surgical injury and the subsequent physiologic stress response.1 This multimodal approach begins in the outpatient setting, includes preoperative and intraoperative modalities, and continues postoperatively. In patients with chronic pain, ERPs are even more important. Assigning “prehabilitation” and setting expectations for surgery goals are the first step in improving the patient experience. Intraoperative use of opioid-sparing anesthetics or regional anesthesia can improve recovery. After surgery, patients with chronic pain and/or opioid dependence receive medications on a schedule, along with short-interval follow-up. Ultimately, reducing acute postoperative pain may lower the risk of developing chronic pain.
In this article on patients with chronic pelvic pain, we highlight elements of ERPs within the framework of enhanced recovery after surgery. Many of the interventions proposed here also can be used to improve the surgical experience of patients without chronic pain.
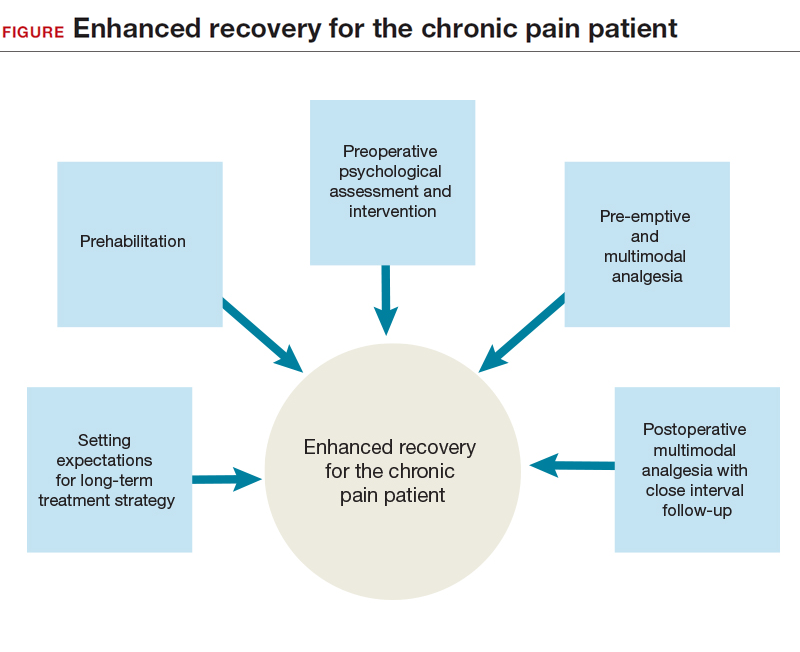
Preadmission education, expectations, and optimization
Preoperative counseling for elective procedures generally occurs in the outpatient setting. Although discussion traditionally has covered the type of procedure and its associated risks, benefits, and alternatives, new guidelines suggest a more mindful and comprehensive approach is warranted. Individualized patient-centered education programs have a positive impact on the perioperative course, effecting reductions in preoperative anxiety, opioid requirements, and hospital length of stay.2 From a pain management perspective, the clinician can take some time during preoperative counseling to inform the patient about the pain to be expected from surgery, the ways the pain will be managed intraoperatively and postoperatively, and the multimodal strategies that will be used throughout the patient’s stay2 and that may allow for early discharge. Although preadmission counseling still should address expectations for the surgery, it also presents an opportunity both to assess the patient’s ability to cope with the physical and psychological stress of surgery and to offer the patient appropriate need-based interventions, such as prehabilitation and cognitive-behavioral therapy (CBT).
Prehabilitation is the process of increasing functional capacity before surgery in order to mitigate the stress of the surgery. Prehabilitation may involve aerobic exercise, strength training, or functional task training. The gynecologic surgery literature lacks prehabilitation data, but data in the colorectal literature support use of a prehabilitation program for patients having a scheduled colectomy, with improved postoperative recovery.3 Although the colectomy cohort predominantly included older men, the principle that guides program implementation is the same: improve recovery after the stress of abdominal surgery. Indeed, a patient who opts for an elective surgery may have to wait several weeks before undergoing the procedure, and during this period behavioral interventions can take effect. With postoperative complications occurring more often in patients with reduced functional capacity, the data support using prehabilitation to decrease the incidence of postoperative complications, particularly among the most vulnerable patients.4 However, a definitive recommendation on use of pelvic floor exercises as an adjunct to prehabilitation cannot be made.4 Successful prehabilitation takes at least 4 weeks and should be part of a multimodal program that addresses other behavioral risk factors that may negatively affect recovery.5 For example, current tobacco users have compromised pulmonary status and wound healing immediately after surgery, and use more opioids.6 Conversely, smoking cessation for as little as 4 weeks before surgery is associated with fewer complications.7 In addition, given that alcohol abuse may compromise the surgical stress response and increase the risk of opioid misuse, addressing alcohol abuse preoperatively may improve postoperative recovery.8
Treating mood disorders that coexist with chronic pain disorders is an important part of outpatient multimodal management—psychological intervention is a useful adjunct to prehabilitation in reducing perioperative anxiety and improving postoperative functional capacity.9 For patients who have chronic pain and are undergoing surgery, it is important to address any anxiety, depression, or poor coping skills (eg, pain catastrophizing) to try to reduce the postoperative pain experience and decrease the risk of chronic postsurgical pain (CPSP).10,11
Before surgery, patients with chronic pain syndromes should be evaluated for emotional distress and pain coping ability. When possible, they should be referred to a pain psychologist, who can initiate CBT and other interventions. In addition, pain coping skills can be developed or reinforced to address preoperative anxiety and pain catastrophizing. These interventions, which may include use of visual imagery, breathing exercises, and other relaxation techniques, are applicable to the management of postoperative anxiety as well.
Read about preoperative multimodal analgesia and intra- and postoperative management.
Preoperative multimodal analgesia
Multimodal analgesia has several benefits. Simultaneous effects can be generated on multiple pain-related neurotransmitters, and a synergistic effect (eg, of acetaminophen and a nonsteroidal anti-inflammatory drug [NSAID]) can improve pain management. In addition, small doses of multiple medications can be given, instead of a large dose of a single medication. Of course, this strategy must be modified in elderly and patients with impaired renal function, who are at high risk for polypharmacy.
Preoperative administration of 3 medications—a selective cyclooxygenase 2 (COX-2) inhibitor, acetaminophen, and a gabapentinoid—is increasingly accepted as part of multimodal analgesia. The selective COX-2 inhibitor targets inflammatory prostaglandins and has anti-inflammatory and analgesic effects; acetaminophen, an effective analgesic with an unclear mechanism of action, can reduce postoperative opioid consumption12 and works synergistically with NSAIDs13; and the gabapentinoid gabapentin has an analgesic effect likely contributing to decreased movement-related pain and subsequent improved functional recovery (data are mixed on whether continuing gabapentin after surgery prevents CPSP).14−16
Although serotonin and norepinephrine reuptake inhibitors (SNRIs) are commonly used in outpatient management of chronic pelvic pain, data suggest that their role in perioperative pain management is evolving. As SNRIs may reduce central nervous system (CNS) sensitization,17 their analgesic effect is thought to result from increased descending inhibitory tone in the CNS, which makes this class of medication ideal for patients with chronic neuropathic pain.15
Limited data also suggest a role for SNRIs in decreasing immediate postoperative pain and CPSP in high-risk patients. Studies of duloxetine use in the immediate perioperative period have found reduced postoperative acute pain and opioid use.18,19 In addition, a short course of low-dose (37.5 mg) venlafaxine both before and after surgery has demonstrated a reduction in postoperative opioid use and a reduction in movement-related pain 6 months after surgery.20
Intraoperative management
The surgical and anesthesia teams share the goal of optimizing both pain control and postoperative recovery. Surgical team members, who want longer-acting anesthetics for infiltration of incision sites, discuss with the anesthesiologist the appropriateness of using peripheral nerve blocks or neuraxial anesthesia, given the patient’s history and planned procedure. Anesthesia team members can improve anesthesia and minimize intraoperative opioid use through several methods, including total intravenous anesthesia,21 dexamethasone,22 ketorolac,23 and intravenous ketamine. Ketamine, in particular, has a wide range of surgical applications and has been found to reduce postoperative pain, postoperative pain medication use, and the risk of CPSP.2
Incision sites should be infiltrated before and after surgery. Lidocaine traditionally is used for its rapid onset of action in reducing surgical site pain, but its short half-life may limit its applicability to postoperative pain. Recently, bupivacaine (half-life, 3.5 hours) and liposomal bupivacaine (24–34 hours) have gained more attention. Both of these medications appear to be as effective as lidocaine in reducing surgical site pain.24
Transversus abdominis plane (TAP) blocks have been used as an adjunct in pain management during abdominopelvic surgery. Although initial data on postoperative pain and opioid use reductions with TAP blocks were inconclusive,25 more recent data showed a role for TAP blocks in a multimodal approach for reducing opioid use during laparoscopic and open surgery.26,27 Given the small number of studies on using liposomal bupivacaine for peripheral nerve blocks (eg, TAP blocks) in postoperative pain management, current data are inconclusive.28
Postoperative management
The ERP approach calls for continuing multimodal analgesia after surgery—in most cases, scheduling early use of oral acetaminophen and ibuprofen, and providing short-acting, low-dose opioid analgesia as needed. All patients should be given a bowel regimen. Similar to undergoing prehabilitation for surgery, patients should prepare themselves for recovery. They should be encouraged to engage in early ambulation and oral intake and, when clinically appropriate, be given same-day discharge for minimally invasive surgical procedures.
Patients with chronic pain before surgery are at increased risk for suboptimal postoperative pain management, and those who are dependent on opioids require additional perioperative measures for adequate postoperative pain control. In these complicated cases, it is appropriate to enlist a pain specialist, potentially before surgery, to help plan perioperative and postoperative pain management.2 Postoperative pain management for opioid-dependent patients should include pharmacologic and nonpharmacologic interventions, such as use of nonopioid medications (eg, gabapentin) and continuation of CBT. Patients with chronic pain should be closely followed up for assessment of postoperative pain control and recovery.
CASE Resolved
Surgical management is one aspect of the longer term multimodal pain management strategy for this patient. After preoperative pelvic floor physical therapy, she is receptive to starting a trial of an SNRI for her pain and mood symptoms. Both interventions allow for optimization of her preoperative physical and psychological status. Expectations are set that she will be discharged the day of surgery and that the surgery is but one component of her multimodal treatment plan. In addition, before surgery, she takes oral acetaminophen, gabapentin, and celecoxib—previously having had no contraindications to these medications. During surgery, bupivacaine is used for infiltration of all incision sites, and the anesthesia team administers ketamine and a TAP block. After surgery, the patient is prepared for same-day discharge and given the NSAIDs and acetaminophen she is scheduled to take over the next 72 hours. She is also given a limited prescription for oxycodone for breakthrough pain. An office visit 1 to 2 weeks after surgery is scheduled.
ERP strategies for surgical management of endometriosis have not only improved this patient’s postoperative recovery but also reduced her surgical stress response and subsequent transition to chronic postoperative pain. Many of the strategies used in this case are applicable to patients without chronic pain.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
CASE Chronic pelvic pain from endometriosis
A 40-year-old woman (G0) has a 20-year history of chronic pelvic pain. Stage III endometriosis is diagnosed on laparoscopic excision of endometriotic tissue. Postoperative pain symptoms include dysmenorrhea and deep dyspareunia, and the patient is feeling anxious. Physical examination reveals a retroverted uterus, right adnexal fullness and tenderness, and tenderness on palpation of the right levator ani and right obturator internus; rectovaginal examination findings are unremarkable. The patient, though now engaged in a pelvic floor physical therapy program, has yet to achieve the pain control she desires. After reviewing the treatment strategies for endometriosis with the patient, she elects definitive surgical management with minimally invasive hysterectomy and salpingo-oophorectomy. What pre-, intra-, and postoperative pain management plan do you devise for this patient?
Chronic pelvic pain presents a unique clinical challenge, as pain typically is multifactorial, and several peripheral pain generators may be involved. Although surgery can be performed to manage anatomically based disease processes, it does not address pain from musculoskeletal or neuropathic sources. A complete medical history and a physical examination are of utmost importance in developing a comprehensive multimodal management plan that may include surgery as treatment for the pain.
The standard of care for surgery is a minimally invasive approach (vaginal, laparoscopic, or robot-assisted laparoscopic), as it causes the least amount of trauma. Benefits of minimally invasive surgery include shorter hospitalization and faster recovery, likely owing to improved perioperative pain control, decreased blood loss, and fewer infections. Although this approach minimizes surgical trauma and thereby helps decrease the surgical stress response, the patient experience can be optimized with use of enhanced recovery pathways (ERPs), a multimodal approach to perioperative care.
ERPs were initially proposed as a means of reducing the degree of surgical injury and the subsequent physiologic stress response.1 This multimodal approach begins in the outpatient setting, includes preoperative and intraoperative modalities, and continues postoperatively. In patients with chronic pain, ERPs are even more important. Assigning “prehabilitation” and setting expectations for surgery goals are the first step in improving the patient experience. Intraoperative use of opioid-sparing anesthetics or regional anesthesia can improve recovery. After surgery, patients with chronic pain and/or opioid dependence receive medications on a schedule, along with short-interval follow-up. Ultimately, reducing acute postoperative pain may lower the risk of developing chronic pain.
In this article on patients with chronic pelvic pain, we highlight elements of ERPs within the framework of enhanced recovery after surgery. Many of the interventions proposed here also can be used to improve the surgical experience of patients without chronic pain.
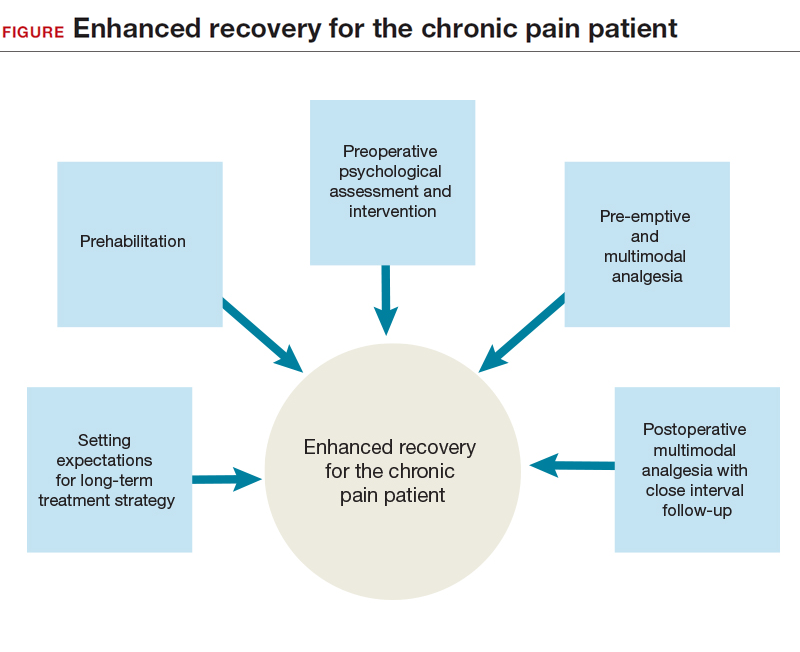
Preadmission education, expectations, and optimization
Preoperative counseling for elective procedures generally occurs in the outpatient setting. Although discussion traditionally has covered the type of procedure and its associated risks, benefits, and alternatives, new guidelines suggest a more mindful and comprehensive approach is warranted. Individualized patient-centered education programs have a positive impact on the perioperative course, effecting reductions in preoperative anxiety, opioid requirements, and hospital length of stay.2 From a pain management perspective, the clinician can take some time during preoperative counseling to inform the patient about the pain to be expected from surgery, the ways the pain will be managed intraoperatively and postoperatively, and the multimodal strategies that will be used throughout the patient’s stay2 and that may allow for early discharge. Although preadmission counseling still should address expectations for the surgery, it also presents an opportunity both to assess the patient’s ability to cope with the physical and psychological stress of surgery and to offer the patient appropriate need-based interventions, such as prehabilitation and cognitive-behavioral therapy (CBT).
Prehabilitation is the process of increasing functional capacity before surgery in order to mitigate the stress of the surgery. Prehabilitation may involve aerobic exercise, strength training, or functional task training. The gynecologic surgery literature lacks prehabilitation data, but data in the colorectal literature support use of a prehabilitation program for patients having a scheduled colectomy, with improved postoperative recovery.3 Although the colectomy cohort predominantly included older men, the principle that guides program implementation is the same: improve recovery after the stress of abdominal surgery. Indeed, a patient who opts for an elective surgery may have to wait several weeks before undergoing the procedure, and during this period behavioral interventions can take effect. With postoperative complications occurring more often in patients with reduced functional capacity, the data support using prehabilitation to decrease the incidence of postoperative complications, particularly among the most vulnerable patients.4 However, a definitive recommendation on use of pelvic floor exercises as an adjunct to prehabilitation cannot be made.4 Successful prehabilitation takes at least 4 weeks and should be part of a multimodal program that addresses other behavioral risk factors that may negatively affect recovery.5 For example, current tobacco users have compromised pulmonary status and wound healing immediately after surgery, and use more opioids.6 Conversely, smoking cessation for as little as 4 weeks before surgery is associated with fewer complications.7 In addition, given that alcohol abuse may compromise the surgical stress response and increase the risk of opioid misuse, addressing alcohol abuse preoperatively may improve postoperative recovery.8
Treating mood disorders that coexist with chronic pain disorders is an important part of outpatient multimodal management—psychological intervention is a useful adjunct to prehabilitation in reducing perioperative anxiety and improving postoperative functional capacity.9 For patients who have chronic pain and are undergoing surgery, it is important to address any anxiety, depression, or poor coping skills (eg, pain catastrophizing) to try to reduce the postoperative pain experience and decrease the risk of chronic postsurgical pain (CPSP).10,11
Before surgery, patients with chronic pain syndromes should be evaluated for emotional distress and pain coping ability. When possible, they should be referred to a pain psychologist, who can initiate CBT and other interventions. In addition, pain coping skills can be developed or reinforced to address preoperative anxiety and pain catastrophizing. These interventions, which may include use of visual imagery, breathing exercises, and other relaxation techniques, are applicable to the management of postoperative anxiety as well.
Read about preoperative multimodal analgesia and intra- and postoperative management.
Preoperative multimodal analgesia
Multimodal analgesia has several benefits. Simultaneous effects can be generated on multiple pain-related neurotransmitters, and a synergistic effect (eg, of acetaminophen and a nonsteroidal anti-inflammatory drug [NSAID]) can improve pain management. In addition, small doses of multiple medications can be given, instead of a large dose of a single medication. Of course, this strategy must be modified in elderly and patients with impaired renal function, who are at high risk for polypharmacy.
Preoperative administration of 3 medications—a selective cyclooxygenase 2 (COX-2) inhibitor, acetaminophen, and a gabapentinoid—is increasingly accepted as part of multimodal analgesia. The selective COX-2 inhibitor targets inflammatory prostaglandins and has anti-inflammatory and analgesic effects; acetaminophen, an effective analgesic with an unclear mechanism of action, can reduce postoperative opioid consumption12 and works synergistically with NSAIDs13; and the gabapentinoid gabapentin has an analgesic effect likely contributing to decreased movement-related pain and subsequent improved functional recovery (data are mixed on whether continuing gabapentin after surgery prevents CPSP).14−16
Although serotonin and norepinephrine reuptake inhibitors (SNRIs) are commonly used in outpatient management of chronic pelvic pain, data suggest that their role in perioperative pain management is evolving. As SNRIs may reduce central nervous system (CNS) sensitization,17 their analgesic effect is thought to result from increased descending inhibitory tone in the CNS, which makes this class of medication ideal for patients with chronic neuropathic pain.15
Limited data also suggest a role for SNRIs in decreasing immediate postoperative pain and CPSP in high-risk patients. Studies of duloxetine use in the immediate perioperative period have found reduced postoperative acute pain and opioid use.18,19 In addition, a short course of low-dose (37.5 mg) venlafaxine both before and after surgery has demonstrated a reduction in postoperative opioid use and a reduction in movement-related pain 6 months after surgery.20
Intraoperative management
The surgical and anesthesia teams share the goal of optimizing both pain control and postoperative recovery. Surgical team members, who want longer-acting anesthetics for infiltration of incision sites, discuss with the anesthesiologist the appropriateness of using peripheral nerve blocks or neuraxial anesthesia, given the patient’s history and planned procedure. Anesthesia team members can improve anesthesia and minimize intraoperative opioid use through several methods, including total intravenous anesthesia,21 dexamethasone,22 ketorolac,23 and intravenous ketamine. Ketamine, in particular, has a wide range of surgical applications and has been found to reduce postoperative pain, postoperative pain medication use, and the risk of CPSP.2
Incision sites should be infiltrated before and after surgery. Lidocaine traditionally is used for its rapid onset of action in reducing surgical site pain, but its short half-life may limit its applicability to postoperative pain. Recently, bupivacaine (half-life, 3.5 hours) and liposomal bupivacaine (24–34 hours) have gained more attention. Both of these medications appear to be as effective as lidocaine in reducing surgical site pain.24
Transversus abdominis plane (TAP) blocks have been used as an adjunct in pain management during abdominopelvic surgery. Although initial data on postoperative pain and opioid use reductions with TAP blocks were inconclusive,25 more recent data showed a role for TAP blocks in a multimodal approach for reducing opioid use during laparoscopic and open surgery.26,27 Given the small number of studies on using liposomal bupivacaine for peripheral nerve blocks (eg, TAP blocks) in postoperative pain management, current data are inconclusive.28
Postoperative management
The ERP approach calls for continuing multimodal analgesia after surgery—in most cases, scheduling early use of oral acetaminophen and ibuprofen, and providing short-acting, low-dose opioid analgesia as needed. All patients should be given a bowel regimen. Similar to undergoing prehabilitation for surgery, patients should prepare themselves for recovery. They should be encouraged to engage in early ambulation and oral intake and, when clinically appropriate, be given same-day discharge for minimally invasive surgical procedures.
Patients with chronic pain before surgery are at increased risk for suboptimal postoperative pain management, and those who are dependent on opioids require additional perioperative measures for adequate postoperative pain control. In these complicated cases, it is appropriate to enlist a pain specialist, potentially before surgery, to help plan perioperative and postoperative pain management.2 Postoperative pain management for opioid-dependent patients should include pharmacologic and nonpharmacologic interventions, such as use of nonopioid medications (eg, gabapentin) and continuation of CBT. Patients with chronic pain should be closely followed up for assessment of postoperative pain control and recovery.
CASE Resolved
Surgical management is one aspect of the longer term multimodal pain management strategy for this patient. After preoperative pelvic floor physical therapy, she is receptive to starting a trial of an SNRI for her pain and mood symptoms. Both interventions allow for optimization of her preoperative physical and psychological status. Expectations are set that she will be discharged the day of surgery and that the surgery is but one component of her multimodal treatment plan. In addition, before surgery, she takes oral acetaminophen, gabapentin, and celecoxib—previously having had no contraindications to these medications. During surgery, bupivacaine is used for infiltration of all incision sites, and the anesthesia team administers ketamine and a TAP block. After surgery, the patient is prepared for same-day discharge and given the NSAIDs and acetaminophen she is scheduled to take over the next 72 hours. She is also given a limited prescription for oxycodone for breakthrough pain. An office visit 1 to 2 weeks after surgery is scheduled.
ERP strategies for surgical management of endometriosis have not only improved this patient’s postoperative recovery but also reduced her surgical stress response and subsequent transition to chronic postoperative pain. Many of the strategies used in this case are applicable to patients without chronic pain.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. 1997;78(5):606−617.
- Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17(2):131−157.
- Mayo NE, Feldman L, Scott S, et al. Impact of preoperative change in physical function on postoperative recovery: argument supporting prehabilitation for colorectal surgery. Surgery. 2011;150(3):505−514.
- Moran J, Guinan E, McCormick P, et al. The ability of prehabilitation to influence postoperative outcome after intra-abdominal operation: a systematic review and meta-analysis. Surgery. 2016;160(5):1189−1201.
- Tew GA, Ayyash R, Durrand J, Danjoux GR. Clinical guideline and recommendations on pre-operative exercise training in patients awaiting major non-cardiac surgery [published online ahead of print January 13, 2018]. Anaesthesia. doi:10.1111/anae.14177.
- Chiang HL, Chia YY, Lin HS, Chen CH. The implications of tobacco smoking on acute postoperative pain: a prospective observational study. Pain Res Manag. 2016;2016:9432493.
- Mastracci TM, Carli F, Finley RJ, Muccio S, Warner DO; Members of the Evidence-Based Reviews in Surgery Group. Effect of preoperative smoking cessation interventions on postoperative complications. J Am Coll Surg. 2011;212(6):1094−1096.
- Tonnesen H, Kehlet H. Preoperative alcoholism and postoperative morbidity. Br J Surg. 1999;86(7):869−874.
- Gillis C, Li C, Lee L, et al. Prehabilitation versus rehabilitation: a randomized control trial in patients undergoing colorectal resection for cancer. Anesthesiology. 2014;121(5):937−947.
- Khan RS, Ahmed K, Blakeway E, et al. Catastrophizing: a predictive factor for postoperative pain. Am J Surg. 2011;201(1):122−131.
- Pinto PR, McIntyre T, Nogueira-Silva C, Almeida A, Araujo-Soares V. Risk factors for persistent postsurgical pain in women undergoing hysterectomy due to benign causes: a prospective predictive study. J Pain. 2012;13(11):1045−1057.
- Moon YE, Lee YK, Lee J, Moon DE. The effects of preoperative intravenous acetaminophen in patients undergoing abdominal hysterectomy. Arch Gynecol Obstet. 2011;284(6):1455−1460.
- Ong CK, Seymour RA, Lirk P, Merry AF. Combining paracetamol (acetaminophen) with nonsteroidal antiinflammatory drugs: a qualitative systematic review of analgesic efficacy for acute postoperative pain. Anesth Analg. 2010;110(4):1170−1179.
- Clarke H, Bonin RP, Orser BA, Englesakis M, Wijeysundera DN, Katz J. The prevention of chronic postsurgical pain using gabapentin and pregabalin: a combined systematic review and meta-analysis. Anesth Analg. 2012;115(2):428−442.
- Gilron I. Gabapentin and pregabalin for chronic neuropathic and early postsurgical pain: current evidence and future directions. Curr Opin Anaesthesiol. 2007;20(5):456−472.
- Chaparro LE, Smith SA, Moore RA, Wiffen PJ, Gilron I. Pharmacotherapy for the prevention of chronic pain after surgery in adults. Cochrane Database Syst Rev. 2013;(7):CD008307.
- Woolf CJ. Central sensitization: implications for the diagnosis and treatment of pain. Pain. 2011;152(3 suppl):S2−S15.
- Castro-Alves LJ, Oliveira de Medeiros AC, Neves SP, et al. Perioperative duloxetine to improve postoperative recovery after abdominal hysterectomy: a prospective, randomized, double-blinded, placebo-controlled study. Anesth Analg. 2016;122(1):98−104.
- Bedin A, Caldart Bedin RA, Vieira JE, Ashmawi HA. Duloxetine as an analgesic reduces opioid consumption after spine surgery: a randomized, double-blind, controlled study. Clin J Pain. 2017;33(10):865−869.
- Amr YM, Yousef AA. Evaluation of efficacy of the perioperative administration of venlafaxine or gabapentin on acute and chronic postmastectomy pain. Clin J Pain. 2010;26(5):381–385.
- Marret E, Rolin M, Beaussier M, Bonnet F. Meta-analysis of intravenous lidocaine and postoperative recovery after abdominal surgery. Br J Surg. 2008;95(11):1331–1338.
- De Oliveira GS Jr, Almeida MD, Benzon HT, McCarthy RJ. Perioperative single dose systemic dexamethasone for postoperative pain: a meta-analysis of randomized controlled trials. Anesthesiology. 2011;115(3):575–588.
- De Oliveira GS Jr, Agarwal D, Benzon HT. Perioperative single dose ketorolac to prevent postoperative pain: a meta-analysis of randomized trials. Anesth Analg. 2012;114(2):424–433.
- Hamilton TW, Athanassoglou V, Mellon S, et al. Liposomal bupivacaine infiltration at the surgical site for the management of postoperative pain. Cochrane Database Syst Rev. 2017;(2):CD011419.
- Charlton S, Cyna AM, Middleton P, Griffiths JD. Perioperative transversus abdominis plane (TAP) blocks for analgesia after abdominal surgery. Cochrane Database Syst Rev. 2010;(12):CD007705.
- Hain E, Maggiori L, Prost À la Denise J, Panis Y. Transversus abdominis plane (TAP) block in laparoscopic colorectal surgery improves postoperative pain management: a meta-analysis [published online ahead of print January 30, 2018]. Colorectal Dis. doi:10.1111/codi.14037.
- Staker JJ, Liu D, Church R, et al. A triple-blind, placebo-controlled randomised trial of the ilioinguinal-transversus abdominis plane (I-TAP) nerve block for elective caesarean section [published online ahead of print January 29, 2018]. Anaesthesia. doi:10.1111/anae.14222.
- Hamilton TW, Athanassoglou V, Trivella M, et al. Liposomal bupivacaine peripheral nerve block for the management of postoperative pain. Cochrane Database Syst Rev. 2016;(8):CD011476.
- Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. 1997;78(5):606−617.
- Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17(2):131−157.
- Mayo NE, Feldman L, Scott S, et al. Impact of preoperative change in physical function on postoperative recovery: argument supporting prehabilitation for colorectal surgery. Surgery. 2011;150(3):505−514.
- Moran J, Guinan E, McCormick P, et al. The ability of prehabilitation to influence postoperative outcome after intra-abdominal operation: a systematic review and meta-analysis. Surgery. 2016;160(5):1189−1201.
- Tew GA, Ayyash R, Durrand J, Danjoux GR. Clinical guideline and recommendations on pre-operative exercise training in patients awaiting major non-cardiac surgery [published online ahead of print January 13, 2018]. Anaesthesia. doi:10.1111/anae.14177.
- Chiang HL, Chia YY, Lin HS, Chen CH. The implications of tobacco smoking on acute postoperative pain: a prospective observational study. Pain Res Manag. 2016;2016:9432493.
- Mastracci TM, Carli F, Finley RJ, Muccio S, Warner DO; Members of the Evidence-Based Reviews in Surgery Group. Effect of preoperative smoking cessation interventions on postoperative complications. J Am Coll Surg. 2011;212(6):1094−1096.
- Tonnesen H, Kehlet H. Preoperative alcoholism and postoperative morbidity. Br J Surg. 1999;86(7):869−874.
- Gillis C, Li C, Lee L, et al. Prehabilitation versus rehabilitation: a randomized control trial in patients undergoing colorectal resection for cancer. Anesthesiology. 2014;121(5):937−947.
- Khan RS, Ahmed K, Blakeway E, et al. Catastrophizing: a predictive factor for postoperative pain. Am J Surg. 2011;201(1):122−131.
- Pinto PR, McIntyre T, Nogueira-Silva C, Almeida A, Araujo-Soares V. Risk factors for persistent postsurgical pain in women undergoing hysterectomy due to benign causes: a prospective predictive study. J Pain. 2012;13(11):1045−1057.
- Moon YE, Lee YK, Lee J, Moon DE. The effects of preoperative intravenous acetaminophen in patients undergoing abdominal hysterectomy. Arch Gynecol Obstet. 2011;284(6):1455−1460.
- Ong CK, Seymour RA, Lirk P, Merry AF. Combining paracetamol (acetaminophen) with nonsteroidal antiinflammatory drugs: a qualitative systematic review of analgesic efficacy for acute postoperative pain. Anesth Analg. 2010;110(4):1170−1179.
- Clarke H, Bonin RP, Orser BA, Englesakis M, Wijeysundera DN, Katz J. The prevention of chronic postsurgical pain using gabapentin and pregabalin: a combined systematic review and meta-analysis. Anesth Analg. 2012;115(2):428−442.
- Gilron I. Gabapentin and pregabalin for chronic neuropathic and early postsurgical pain: current evidence and future directions. Curr Opin Anaesthesiol. 2007;20(5):456−472.
- Chaparro LE, Smith SA, Moore RA, Wiffen PJ, Gilron I. Pharmacotherapy for the prevention of chronic pain after surgery in adults. Cochrane Database Syst Rev. 2013;(7):CD008307.
- Woolf CJ. Central sensitization: implications for the diagnosis and treatment of pain. Pain. 2011;152(3 suppl):S2−S15.
- Castro-Alves LJ, Oliveira de Medeiros AC, Neves SP, et al. Perioperative duloxetine to improve postoperative recovery after abdominal hysterectomy: a prospective, randomized, double-blinded, placebo-controlled study. Anesth Analg. 2016;122(1):98−104.
- Bedin A, Caldart Bedin RA, Vieira JE, Ashmawi HA. Duloxetine as an analgesic reduces opioid consumption after spine surgery: a randomized, double-blind, controlled study. Clin J Pain. 2017;33(10):865−869.
- Amr YM, Yousef AA. Evaluation of efficacy of the perioperative administration of venlafaxine or gabapentin on acute and chronic postmastectomy pain. Clin J Pain. 2010;26(5):381–385.
- Marret E, Rolin M, Beaussier M, Bonnet F. Meta-analysis of intravenous lidocaine and postoperative recovery after abdominal surgery. Br J Surg. 2008;95(11):1331–1338.
- De Oliveira GS Jr, Almeida MD, Benzon HT, McCarthy RJ. Perioperative single dose systemic dexamethasone for postoperative pain: a meta-analysis of randomized controlled trials. Anesthesiology. 2011;115(3):575–588.
- De Oliveira GS Jr, Agarwal D, Benzon HT. Perioperative single dose ketorolac to prevent postoperative pain: a meta-analysis of randomized trials. Anesth Analg. 2012;114(2):424–433.
- Hamilton TW, Athanassoglou V, Mellon S, et al. Liposomal bupivacaine infiltration at the surgical site for the management of postoperative pain. Cochrane Database Syst Rev. 2017;(2):CD011419.
- Charlton S, Cyna AM, Middleton P, Griffiths JD. Perioperative transversus abdominis plane (TAP) blocks for analgesia after abdominal surgery. Cochrane Database Syst Rev. 2010;(12):CD007705.
- Hain E, Maggiori L, Prost À la Denise J, Panis Y. Transversus abdominis plane (TAP) block in laparoscopic colorectal surgery improves postoperative pain management: a meta-analysis [published online ahead of print January 30, 2018]. Colorectal Dis. doi:10.1111/codi.14037.
- Staker JJ, Liu D, Church R, et al. A triple-blind, placebo-controlled randomised trial of the ilioinguinal-transversus abdominis plane (I-TAP) nerve block for elective caesarean section [published online ahead of print January 29, 2018]. Anaesthesia. doi:10.1111/anae.14222.
- Hamilton TW, Athanassoglou V, Trivella M, et al. Liposomal bupivacaine peripheral nerve block for the management of postoperative pain. Cochrane Database Syst Rev. 2016;(8):CD011476.
Product Update: Vistara; Ultravision trocar; CompuFlo Epidural; and Philips ultrasound
PRENATAL SCREENING FOR SINGLE-GENE DISORDERS
Vistara®, a non-invasive prenatal test (NIPT) from Natera, Inc, screens for single-gene disorders after 9 weeks’ gestation. Complementing the Panorama® NIPT, Vistara tests for major anatomic abnormalities and chromosome imbalances that have a combined incidence rate of 1 in 600 (higher than Down syndrome). These mutations can cause severe conditions affecting skeletal, cardiac, and neurologic systems, such as Noonan syndrome, osteogenesis imperfecta, craniosynostosis syndromes, achondroplasia, and Rett syndrome. Standard NIPT commonly cannot detect these de novo (not inherited) mutations. Ultrasound exams may either completely miss the disorders or identify nonspecific findings later in pregnancy.
Natera says that Vistara has a combined analytical sensitivity of >99% and a combined analytical specificity of >99% in validation studies.
FOR MORE INFORMATION, VISIT: https://www.natera.com/vistara
ELECTROSTATIC SURGICAL SMOKE REMOVAL
The UltravisionTM Trocar device from Alesi Surgical Technologies uses a low-energy electrostatic charge to eliminate the surgical smoke generated by cutting instruments during laparoscopic surgery. Electrostatic precipitation accelerates the natural process of sedimentation; Ultravision creates negatively charged gas ions that draw water vapor and particulate matter away from the surgical site toward “positive” patient tissue.
Alesi says that bench studies comparing Ultravision with a vacuum-system when using monopolar, bipolar, and ultrasonic instruments show that its device is faster and more efficient than smoke evacuation. When switched on before cutting, Ultravision precipitates 99% of particles within 30 seconds. After 1 minute of continuous use, Ultravision precipitates 99.9% of particles, independent of particle size, from 7 nm to 10 µm. Smoke evacuation removes 30.2% of particles after 1 minute, according to Alesi.
FOR MORE INFORMATION, VISIT: http://www.alesi-surgical.com
PRESSURE-SENSING TECHNOLOGY FOR EPIDURALS
The CompuFlo®Epidural from Milestone Scientific uses pressure-sensing technology to identify the epidural space, and provides a computer-controlled drug delivery system.
Knowing the precise needle location during an epidural injection procedure provides a measure of safety not available to physicians who use conventional syringes. Milestone says that its CompuFlo Epidural allows anesthesiologists to use both hands to advance and direct the needle, and to confirm the epidural space with 99% accuracy on the first attempt.
CompuFlo Epidural differentiates tissue types for the medical professional via visual and audio feedback, leading to precise location guidance as the needle advances toward the intended area. It also allows for controlled needle exit pressure, precise flow rate and drug volumes, and patient treatment documentation.
FOR MORE INFORMATION, VISIT: https://www.milestonescientific.com/products/compuflo-epidural
OBGYN ULTRASOUND INNOVATIONS
Philips recently announced enhancements to its EPIQ 7 and 5 and Affiniti 70 ultrasound systems. According to Philips, the eL18-4 transducer provides high-detail resolution and image uniformity with penetration for enhanced diagnostic quality in 1st- and 2nd-trimester obstetric exams. aBiometry AssistAI, with anatomical intelligence of fetal anatomy, streamlines fetal measurement by preplacing measurement cursors on selected structures. The new TouchVue control-panel interface on TrueVue allows practitioners to interact with finger gestures and to direct 3D-volume rotation and internal light-source position. The 2D Tilt feature offered on the 3D9-v3 transducer provides lateral scanning of anatomic structures that are off-axis without having to manually angle the transducer.
These new features complement the existing suite of Philips ObGyn ultrasound visualization tools: TrueVue, GlassVue, aRevealAI, and MaxVue.
FOR MORE INFORMATION, VISIT: https://www.usa.philips.com/healthcare/resources/feature-detail/ultrasound-truevue-imaging
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
PRENATAL SCREENING FOR SINGLE-GENE DISORDERS
Vistara®, a non-invasive prenatal test (NIPT) from Natera, Inc, screens for single-gene disorders after 9 weeks’ gestation. Complementing the Panorama® NIPT, Vistara tests for major anatomic abnormalities and chromosome imbalances that have a combined incidence rate of 1 in 600 (higher than Down syndrome). These mutations can cause severe conditions affecting skeletal, cardiac, and neurologic systems, such as Noonan syndrome, osteogenesis imperfecta, craniosynostosis syndromes, achondroplasia, and Rett syndrome. Standard NIPT commonly cannot detect these de novo (not inherited) mutations. Ultrasound exams may either completely miss the disorders or identify nonspecific findings later in pregnancy.
Natera says that Vistara has a combined analytical sensitivity of >99% and a combined analytical specificity of >99% in validation studies.
FOR MORE INFORMATION, VISIT: https://www.natera.com/vistara
ELECTROSTATIC SURGICAL SMOKE REMOVAL
The UltravisionTM Trocar device from Alesi Surgical Technologies uses a low-energy electrostatic charge to eliminate the surgical smoke generated by cutting instruments during laparoscopic surgery. Electrostatic precipitation accelerates the natural process of sedimentation; Ultravision creates negatively charged gas ions that draw water vapor and particulate matter away from the surgical site toward “positive” patient tissue.
Alesi says that bench studies comparing Ultravision with a vacuum-system when using monopolar, bipolar, and ultrasonic instruments show that its device is faster and more efficient than smoke evacuation. When switched on before cutting, Ultravision precipitates 99% of particles within 30 seconds. After 1 minute of continuous use, Ultravision precipitates 99.9% of particles, independent of particle size, from 7 nm to 10 µm. Smoke evacuation removes 30.2% of particles after 1 minute, according to Alesi.
FOR MORE INFORMATION, VISIT: http://www.alesi-surgical.com
PRESSURE-SENSING TECHNOLOGY FOR EPIDURALS
The CompuFlo®Epidural from Milestone Scientific uses pressure-sensing technology to identify the epidural space, and provides a computer-controlled drug delivery system.
Knowing the precise needle location during an epidural injection procedure provides a measure of safety not available to physicians who use conventional syringes. Milestone says that its CompuFlo Epidural allows anesthesiologists to use both hands to advance and direct the needle, and to confirm the epidural space with 99% accuracy on the first attempt.
CompuFlo Epidural differentiates tissue types for the medical professional via visual and audio feedback, leading to precise location guidance as the needle advances toward the intended area. It also allows for controlled needle exit pressure, precise flow rate and drug volumes, and patient treatment documentation.
FOR MORE INFORMATION, VISIT: https://www.milestonescientific.com/products/compuflo-epidural
OBGYN ULTRASOUND INNOVATIONS
Philips recently announced enhancements to its EPIQ 7 and 5 and Affiniti 70 ultrasound systems. According to Philips, the eL18-4 transducer provides high-detail resolution and image uniformity with penetration for enhanced diagnostic quality in 1st- and 2nd-trimester obstetric exams. aBiometry AssistAI, with anatomical intelligence of fetal anatomy, streamlines fetal measurement by preplacing measurement cursors on selected structures. The new TouchVue control-panel interface on TrueVue allows practitioners to interact with finger gestures and to direct 3D-volume rotation and internal light-source position. The 2D Tilt feature offered on the 3D9-v3 transducer provides lateral scanning of anatomic structures that are off-axis without having to manually angle the transducer.
These new features complement the existing suite of Philips ObGyn ultrasound visualization tools: TrueVue, GlassVue, aRevealAI, and MaxVue.
FOR MORE INFORMATION, VISIT: https://www.usa.philips.com/healthcare/resources/feature-detail/ultrasound-truevue-imaging
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
PRENATAL SCREENING FOR SINGLE-GENE DISORDERS
Vistara®, a non-invasive prenatal test (NIPT) from Natera, Inc, screens for single-gene disorders after 9 weeks’ gestation. Complementing the Panorama® NIPT, Vistara tests for major anatomic abnormalities and chromosome imbalances that have a combined incidence rate of 1 in 600 (higher than Down syndrome). These mutations can cause severe conditions affecting skeletal, cardiac, and neurologic systems, such as Noonan syndrome, osteogenesis imperfecta, craniosynostosis syndromes, achondroplasia, and Rett syndrome. Standard NIPT commonly cannot detect these de novo (not inherited) mutations. Ultrasound exams may either completely miss the disorders or identify nonspecific findings later in pregnancy.
Natera says that Vistara has a combined analytical sensitivity of >99% and a combined analytical specificity of >99% in validation studies.
FOR MORE INFORMATION, VISIT: https://www.natera.com/vistara
ELECTROSTATIC SURGICAL SMOKE REMOVAL
The UltravisionTM Trocar device from Alesi Surgical Technologies uses a low-energy electrostatic charge to eliminate the surgical smoke generated by cutting instruments during laparoscopic surgery. Electrostatic precipitation accelerates the natural process of sedimentation; Ultravision creates negatively charged gas ions that draw water vapor and particulate matter away from the surgical site toward “positive” patient tissue.
Alesi says that bench studies comparing Ultravision with a vacuum-system when using monopolar, bipolar, and ultrasonic instruments show that its device is faster and more efficient than smoke evacuation. When switched on before cutting, Ultravision precipitates 99% of particles within 30 seconds. After 1 minute of continuous use, Ultravision precipitates 99.9% of particles, independent of particle size, from 7 nm to 10 µm. Smoke evacuation removes 30.2% of particles after 1 minute, according to Alesi.
FOR MORE INFORMATION, VISIT: http://www.alesi-surgical.com
PRESSURE-SENSING TECHNOLOGY FOR EPIDURALS
The CompuFlo®Epidural from Milestone Scientific uses pressure-sensing technology to identify the epidural space, and provides a computer-controlled drug delivery system.
Knowing the precise needle location during an epidural injection procedure provides a measure of safety not available to physicians who use conventional syringes. Milestone says that its CompuFlo Epidural allows anesthesiologists to use both hands to advance and direct the needle, and to confirm the epidural space with 99% accuracy on the first attempt.
CompuFlo Epidural differentiates tissue types for the medical professional via visual and audio feedback, leading to precise location guidance as the needle advances toward the intended area. It also allows for controlled needle exit pressure, precise flow rate and drug volumes, and patient treatment documentation.
FOR MORE INFORMATION, VISIT: https://www.milestonescientific.com/products/compuflo-epidural
OBGYN ULTRASOUND INNOVATIONS
Philips recently announced enhancements to its EPIQ 7 and 5 and Affiniti 70 ultrasound systems. According to Philips, the eL18-4 transducer provides high-detail resolution and image uniformity with penetration for enhanced diagnostic quality in 1st- and 2nd-trimester obstetric exams. aBiometry AssistAI, with anatomical intelligence of fetal anatomy, streamlines fetal measurement by preplacing measurement cursors on selected structures. The new TouchVue control-panel interface on TrueVue allows practitioners to interact with finger gestures and to direct 3D-volume rotation and internal light-source position. The 2D Tilt feature offered on the 3D9-v3 transducer provides lateral scanning of anatomic structures that are off-axis without having to manually angle the transducer.
These new features complement the existing suite of Philips ObGyn ultrasound visualization tools: TrueVue, GlassVue, aRevealAI, and MaxVue.
FOR MORE INFORMATION, VISIT: https://www.usa.philips.com/healthcare/resources/feature-detail/ultrasound-truevue-imaging
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
2018 Update on gynecologic cancer
In this Update, I report on the latest US Preventive Services Task Force (USPSTF) cervical cancer screening recommendations. In addition, I describe the results of 2 studies, a large prospective multicenter study of the accuracy of sentinel lymph node (SLN) biopsy in endometrial cancer, and a proof-of-concept review of use of checkpoint blockade to increase immune response and of its possible role in endometrial cancer.
hrHPV testing used alone as primary screening for cervical cancer: USPSTF recommendations
US Preventive Services Task Force. Draft recommendation statement: cervical cancer: screening. https://www.uspreventiveservicestaskforce.org/Page/Document/draft-recommendation-statement/cervical-cancer-screening2. Published October 2017. Accessed February 5, 2018.
Despite our rapid advances in understanding the molecular underpinnings of cancer, gynecologic malignancies are still a major cause of morbidity and mortality among women. Cervical cancer stands as an example of how a cancer screening test can be implemented to reduce mortality. In this section, I report on the USPSTF cervical cancer screening recommendations, which were updated in October 2017.
Even with the widespread implementation of screening programs for cervical cancer in the United States, 13,240 women will be diagnosed with the disease in 2018, and 4,170 will die from cervical cancer.1 Most often, cervical cancer occurs in women who have not been adequately screened. It is now recognized that the human papillomavirus (HPV) is the cause of cervical cancer.2
While cervical cytology has long been used as a screening test for cervical cancer, testing for high-risk HPV subtypes (hrHPV testing) also has been used as a screening modality. Traditionally, hrHPV testing is used in combination with cervical cytology, so called cotesting. There is convincing evidence that cervical cytology, as well as strategies that use hrHPV testing, can detect high-grade cervical precancers and cancers and thereby reduce mortality. However, cervical cancer screening is also associated with frequent follow-ups, invasive procedures performed to assess abnormal results, psychological distress, and adverse pregnancy outcomes of treatment for precancerous lesions.
The USPSTF based its new cervical cancer screening recommendations on clinical trial data and decision modeling of various screening strategies, and weighed the benefits and harms of each strategy.
Recommendations from the USPSTF
hrHPV screening for cervical cancer. TheUSPSTF recommends screening with cervical cytology every 3 years for women 21 to 29 years of age. For women 30 to 65 years of age, screening with cytology every 3 years, or hrHPV testing alone used every 5 years, is recommended.
Data from large randomized trials suggest cytologic screening is slightly less sensitive than hrHPV testing in detecting high-grade (grade 2 or 3) cervical intraepithelial neoplasia (CIN). However, hrHPV testing results in more follow-up tests and colposcopies. In a decision model, the USPSTF found that cotesting increased the number of follow-up tests but did not increase detection of grade 3 CIN or invasive cancer. This is the first clinical guideline to recommend hrHPV testing used alone for screening. The American College of Obstetricians and Gynecologists (ACOG) continues to recommend cotesting (cytology in combination with hrHPV) as a primary screening modality in this population.3
Exceptions. According to the USPSTF, 3 populations should not be screened: women over 65 years of age with adequate prior screening who are not otherwise at high risk for cervical cancer; women under 21 years of age; and women who have had a hysterectomy and do not have a history of grade 2 or 3 CIN or cancer.
Summary. The USPSTF recommendations are intended for the general population and are not applicable to women with a history of high-grade CIN or cervical cancer, women with in utero exposure to diethylstilbestrol, and women who are immunocompromised. The remaining USPSTF recommendations are largely in line with guidelines published by ACOG and other groups.3,4
Testing for high-risk HPV alone is a reasonable screening option for cervical cancer. This modality can be used in women 30 to 65 years of age but should not be repeated more frequently than every 5 years in those with a negative result.
Read about SLN biopsy to stage endometrial cancer
SLN biopsy for staging endometrial cancer
Rossi EC, Kowalski LD, Scalici J, et al. A comparison of sentinel lymph node biopsy to lymphadenectomy for endometrial cancer staging (FIRES trial): a multicentre, prospective, cohort study. Lancet Oncol. 2017;18(3):384-392.
Surgery is the cornerstone of treatment for most gynecologic cancers. The widespread use of minimally invasive surgical techniques and the introduction of less radical procedures for gynecologic cancers have helped reduce surgical morbidity.
For endometrial cancer, the role of lymphadenectomy is controversial. Data from prospective trials of this procedure suggest an association with increased morbidity and long-term sequelae, such as lymphedema, and no association with improved survival.5,6
SLN biopsy is an important advance and a potential alternative nodal evaluation method that may be associated with decreased morbidity. In this more limited assessment technique, the first nodal drainage basins of a tumor are identified and removed for pathologic evaluation.
Accuracy of SLN biopsy in endometrial cancer was the subject of Rossi and colleagues' recent large prospective multicenter study, the Fluorescence Imaging for Robotic Endometrial Sentinel lymph node biopsy (FIRES) trial.
Details of the study
Rossi and colleagues conducted the FIRES trial to estimate the sensitivity of SLN biopsy in detecting nodal metastases in women with stage I endometrial cancer. Patients (N = 385) from 10 US sites were enrolled in the study. SLN evaluation was performed after cervical injection of indocyanine green followed by robotic-assisted hysterectomy. After identification of the SLN, participants underwent pelvic lymphadenectomy. Performance of para-aortic lymphadenectomy was optional.
Mapping of the SLN was feasible in 86% of patients, including bilateral mapping in 52%. Twelve percent of the participants had nodal metastases. SLN biopsy had a sensitivity of 97% in women who had identification of the SLNs. Similarly, the negative predictive value was high, 99.6%. The procedure was associated with acceptable short-term toxicity with adverse events in 9% of study participants. Common complications included neurologic complications, respiratory distress, nausea and vomiting, and, in 3 patients, bowel injury.
Accurate detection of nodal metastases. Results of the study suggest SLN biopsy is accurate in detecting nodal metastases in women with endometrial cancer. Although long-term toxicity was not examined, other work suggests the lymphedema rates associated with SLN biopsy may be lower than those of lymphadenectomy. While the study described impressive performance characteristics, there remain technical challenges. Even among skilled surgeons trained for the protocol, there was no nodal mapping in nearly half of the women with endometrial cancer. Women without node mapping require full lymphadenectomy thus negating the possible benefits of the procedure.
Given the high accuracy of SLN mapping in endometrial cancer, the procedure likely will become the standard of care for nodal evaluation by gynecologic oncologists.
Read about immunotherapy for gynecologic cancers
Immunotherapy for gynecologic cancers
Le DT, Durham JN, Smith KN, et al. Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science. 2017;357(6349):409-413.
In oncology, precision medicine is rapidly becoming a standard treatment approach. Therapies are being used to target specific genetic alterations in tumors. In cancer immunotherapy, the immune system is being used to facilitate clearance of cancer cells.
The most common mechanism of action of clinically used immunotherapeutic agents is blockade of programmed cell death protein 1 (PD-1), a lymphocyte receptor that prevents the immune system from targeting the body's own cells.7 Cancers that have mutations in the DNA mismatch repair (MMR) proteins display microsatellite instability (MSI) and produce high levels of abnormal proteins.8 These abnormal proteins serve as tumor antigens that can be targeted by the body's normal immune system.
In May 2017, the US Food and Drug Administration (FDA) granted accelerated approval of the PD-1 blocking antibody pembrolizumab for the treatment of unresectable or metastatic MSI-high (MSI-H) or MMR-deficient solid tumors.9 The approval was based on data from 149 patients treated in 5 studies that demonstrated a response rate of 39.6%, including responses that lasted at least 6 months in 78% of participants. This was the first ever cancer drug that received FDA approval based on a tumor's biomarker profile without regard to the site of origin. I describe the results of a study by Le and colleagues that examines the possible role of immunotherapy in a variety of solid tumors in this section.
Details of the study
This study examined the clinical efficacy of PD-1 blockade in 86 patients with advanced, MMR-deficient tumors from 12 different sites. Endometrial cancer was the second most frequent primary tumor site in 17% of patients. Within the cohort, the overall objective response rate was 53%, which included 21% of patients with complete radiographic response (no imaging evidence of cancer). Disease control, either complete or partial response or stable disease, was achieved in 77% of patients. After a median follow-up of 12.5 months, neither the median progression-free survival (PFS) nor median overall survival had been reached. The authors estimated that 2-year overall survival was 64%, substantially higher than expected for patients with advanced solid tumors.
Le and colleagues also performed several in vivo laboratory experiments to explore the mechanisms by which patients responded. In addition, they used sequencing to determine the prevalence of MMR deficiency in 12,019 cancer samples that included 32 distinct tumor types (FIGURE). Endometrial cancer had the highest frequency of MMR deficiency (17%). Four percent of cervical cancers and less than 2% of ovarian cancers were MMR-deficient.
The promise of immunotherapy for endometrial cancer. This study's data and other emerging data have important implications for women with gynecologic cancer, particularly endometrial cancer. First, given the frequency of MMR mutations among women with endometrial cancer, MMR testing should be strongly considered for these patients. Many institutions have protocols for reflex testing with immunohistochemistry for women with endometrial cancer. For women with positive test results, germline sequencing can be performed to determine if they have an inherited MMR deficiency, Lynch syndrome. Presence of an MMR deficiency is an important factor in cancer screening and potential treatment.
Second, the impressive results of PD-1 blockade in patients with MMR-deficient tumors suggest that this treatment strategy may be important for women with recurrent or metastatic endometrial cancer. The ideal timing of immunotherapy for women with endometrial cancer is an area of active ongoing study.
Immunotherapy with PD-1 blockade is an important treatment strategy for women with MMR-deficient or MSI-H gynecologic cancers.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- American Cancer Society. Cancer Facts & Figures 2018. Atlanta, GA: American Cancer Society; 2018.
- Walboomers JM, Jacobs MV, Manos MM, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189(1):12–19.
- American College of Obstetricians and Gynecologists Committee on Practice Bulletins-Gynecology. ACOG Practice Bulletin No. 168: Cervical cancer screening and prevention. Obstet Gynecol. 2016;128(4):e111–e130.
- Saslow D, Solomon D, Lawson HW, et al; ACS-ASCCP-ASCP Cervical Cancer Guideline Committee. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. CA Cancer J Clin. 2012;62(3):147–172.
- Benedetti Panici P, Basile S, Maneschi F, et al. Systematic pelvic lymphadenectomy vs. no lymphadenectomy in early-stage endometrial carcinoma: randomized clinical trial. J Natl Cancer Inst. 2008;100(23):1707–1716.
- ASTEC Study Group, Kitchener H, Swart AM, Qian Q, Amos C, Parmar MK. Efficacy of systematic pelvic lymphadenectomy in endometrial cancer (MRC ASTEC trial): a randomised study. Lancet. 2009;373(9658):125–136.
- Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer. 2012;12(4):252–264.
- Buza N, Ziai J, Hui P. Mismatch repair deficiency testing in clinical practice. Expert Rev Mol Diagn. 2016;16(5):591–604.
- FDA approves first cancer treatment for any solid tumor with a specific genetic feature [news release]. Silver Spring, MD: US Food and Drug Administration. https://www.fda.gov/newsevents/newsroom/pressannouncements/ucm560167.htm. Published May 23, 2017. Accessed February 5, 2018.
In this Update, I report on the latest US Preventive Services Task Force (USPSTF) cervical cancer screening recommendations. In addition, I describe the results of 2 studies, a large prospective multicenter study of the accuracy of sentinel lymph node (SLN) biopsy in endometrial cancer, and a proof-of-concept review of use of checkpoint blockade to increase immune response and of its possible role in endometrial cancer.
hrHPV testing used alone as primary screening for cervical cancer: USPSTF recommendations
US Preventive Services Task Force. Draft recommendation statement: cervical cancer: screening. https://www.uspreventiveservicestaskforce.org/Page/Document/draft-recommendation-statement/cervical-cancer-screening2. Published October 2017. Accessed February 5, 2018.
Despite our rapid advances in understanding the molecular underpinnings of cancer, gynecologic malignancies are still a major cause of morbidity and mortality among women. Cervical cancer stands as an example of how a cancer screening test can be implemented to reduce mortality. In this section, I report on the USPSTF cervical cancer screening recommendations, which were updated in October 2017.
Even with the widespread implementation of screening programs for cervical cancer in the United States, 13,240 women will be diagnosed with the disease in 2018, and 4,170 will die from cervical cancer.1 Most often, cervical cancer occurs in women who have not been adequately screened. It is now recognized that the human papillomavirus (HPV) is the cause of cervical cancer.2
While cervical cytology has long been used as a screening test for cervical cancer, testing for high-risk HPV subtypes (hrHPV testing) also has been used as a screening modality. Traditionally, hrHPV testing is used in combination with cervical cytology, so called cotesting. There is convincing evidence that cervical cytology, as well as strategies that use hrHPV testing, can detect high-grade cervical precancers and cancers and thereby reduce mortality. However, cervical cancer screening is also associated with frequent follow-ups, invasive procedures performed to assess abnormal results, psychological distress, and adverse pregnancy outcomes of treatment for precancerous lesions.
The USPSTF based its new cervical cancer screening recommendations on clinical trial data and decision modeling of various screening strategies, and weighed the benefits and harms of each strategy.
Recommendations from the USPSTF
hrHPV screening for cervical cancer. TheUSPSTF recommends screening with cervical cytology every 3 years for women 21 to 29 years of age. For women 30 to 65 years of age, screening with cytology every 3 years, or hrHPV testing alone used every 5 years, is recommended.
Data from large randomized trials suggest cytologic screening is slightly less sensitive than hrHPV testing in detecting high-grade (grade 2 or 3) cervical intraepithelial neoplasia (CIN). However, hrHPV testing results in more follow-up tests and colposcopies. In a decision model, the USPSTF found that cotesting increased the number of follow-up tests but did not increase detection of grade 3 CIN or invasive cancer. This is the first clinical guideline to recommend hrHPV testing used alone for screening. The American College of Obstetricians and Gynecologists (ACOG) continues to recommend cotesting (cytology in combination with hrHPV) as a primary screening modality in this population.3
Exceptions. According to the USPSTF, 3 populations should not be screened: women over 65 years of age with adequate prior screening who are not otherwise at high risk for cervical cancer; women under 21 years of age; and women who have had a hysterectomy and do not have a history of grade 2 or 3 CIN or cancer.
Summary. The USPSTF recommendations are intended for the general population and are not applicable to women with a history of high-grade CIN or cervical cancer, women with in utero exposure to diethylstilbestrol, and women who are immunocompromised. The remaining USPSTF recommendations are largely in line with guidelines published by ACOG and other groups.3,4
Testing for high-risk HPV alone is a reasonable screening option for cervical cancer. This modality can be used in women 30 to 65 years of age but should not be repeated more frequently than every 5 years in those with a negative result.
Read about SLN biopsy to stage endometrial cancer
SLN biopsy for staging endometrial cancer
Rossi EC, Kowalski LD, Scalici J, et al. A comparison of sentinel lymph node biopsy to lymphadenectomy for endometrial cancer staging (FIRES trial): a multicentre, prospective, cohort study. Lancet Oncol. 2017;18(3):384-392.
Surgery is the cornerstone of treatment for most gynecologic cancers. The widespread use of minimally invasive surgical techniques and the introduction of less radical procedures for gynecologic cancers have helped reduce surgical morbidity.
For endometrial cancer, the role of lymphadenectomy is controversial. Data from prospective trials of this procedure suggest an association with increased morbidity and long-term sequelae, such as lymphedema, and no association with improved survival.5,6
SLN biopsy is an important advance and a potential alternative nodal evaluation method that may be associated with decreased morbidity. In this more limited assessment technique, the first nodal drainage basins of a tumor are identified and removed for pathologic evaluation.
Accuracy of SLN biopsy in endometrial cancer was the subject of Rossi and colleagues' recent large prospective multicenter study, the Fluorescence Imaging for Robotic Endometrial Sentinel lymph node biopsy (FIRES) trial.
Details of the study
Rossi and colleagues conducted the FIRES trial to estimate the sensitivity of SLN biopsy in detecting nodal metastases in women with stage I endometrial cancer. Patients (N = 385) from 10 US sites were enrolled in the study. SLN evaluation was performed after cervical injection of indocyanine green followed by robotic-assisted hysterectomy. After identification of the SLN, participants underwent pelvic lymphadenectomy. Performance of para-aortic lymphadenectomy was optional.
Mapping of the SLN was feasible in 86% of patients, including bilateral mapping in 52%. Twelve percent of the participants had nodal metastases. SLN biopsy had a sensitivity of 97% in women who had identification of the SLNs. Similarly, the negative predictive value was high, 99.6%. The procedure was associated with acceptable short-term toxicity with adverse events in 9% of study participants. Common complications included neurologic complications, respiratory distress, nausea and vomiting, and, in 3 patients, bowel injury.
Accurate detection of nodal metastases. Results of the study suggest SLN biopsy is accurate in detecting nodal metastases in women with endometrial cancer. Although long-term toxicity was not examined, other work suggests the lymphedema rates associated with SLN biopsy may be lower than those of lymphadenectomy. While the study described impressive performance characteristics, there remain technical challenges. Even among skilled surgeons trained for the protocol, there was no nodal mapping in nearly half of the women with endometrial cancer. Women without node mapping require full lymphadenectomy thus negating the possible benefits of the procedure.
Given the high accuracy of SLN mapping in endometrial cancer, the procedure likely will become the standard of care for nodal evaluation by gynecologic oncologists.
Read about immunotherapy for gynecologic cancers
Immunotherapy for gynecologic cancers
Le DT, Durham JN, Smith KN, et al. Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science. 2017;357(6349):409-413.
In oncology, precision medicine is rapidly becoming a standard treatment approach. Therapies are being used to target specific genetic alterations in tumors. In cancer immunotherapy, the immune system is being used to facilitate clearance of cancer cells.
The most common mechanism of action of clinically used immunotherapeutic agents is blockade of programmed cell death protein 1 (PD-1), a lymphocyte receptor that prevents the immune system from targeting the body's own cells.7 Cancers that have mutations in the DNA mismatch repair (MMR) proteins display microsatellite instability (MSI) and produce high levels of abnormal proteins.8 These abnormal proteins serve as tumor antigens that can be targeted by the body's normal immune system.
In May 2017, the US Food and Drug Administration (FDA) granted accelerated approval of the PD-1 blocking antibody pembrolizumab for the treatment of unresectable or metastatic MSI-high (MSI-H) or MMR-deficient solid tumors.9 The approval was based on data from 149 patients treated in 5 studies that demonstrated a response rate of 39.6%, including responses that lasted at least 6 months in 78% of participants. This was the first ever cancer drug that received FDA approval based on a tumor's biomarker profile without regard to the site of origin. I describe the results of a study by Le and colleagues that examines the possible role of immunotherapy in a variety of solid tumors in this section.
Details of the study
This study examined the clinical efficacy of PD-1 blockade in 86 patients with advanced, MMR-deficient tumors from 12 different sites. Endometrial cancer was the second most frequent primary tumor site in 17% of patients. Within the cohort, the overall objective response rate was 53%, which included 21% of patients with complete radiographic response (no imaging evidence of cancer). Disease control, either complete or partial response or stable disease, was achieved in 77% of patients. After a median follow-up of 12.5 months, neither the median progression-free survival (PFS) nor median overall survival had been reached. The authors estimated that 2-year overall survival was 64%, substantially higher than expected for patients with advanced solid tumors.
Le and colleagues also performed several in vivo laboratory experiments to explore the mechanisms by which patients responded. In addition, they used sequencing to determine the prevalence of MMR deficiency in 12,019 cancer samples that included 32 distinct tumor types (FIGURE). Endometrial cancer had the highest frequency of MMR deficiency (17%). Four percent of cervical cancers and less than 2% of ovarian cancers were MMR-deficient.
The promise of immunotherapy for endometrial cancer. This study's data and other emerging data have important implications for women with gynecologic cancer, particularly endometrial cancer. First, given the frequency of MMR mutations among women with endometrial cancer, MMR testing should be strongly considered for these patients. Many institutions have protocols for reflex testing with immunohistochemistry for women with endometrial cancer. For women with positive test results, germline sequencing can be performed to determine if they have an inherited MMR deficiency, Lynch syndrome. Presence of an MMR deficiency is an important factor in cancer screening and potential treatment.
Second, the impressive results of PD-1 blockade in patients with MMR-deficient tumors suggest that this treatment strategy may be important for women with recurrent or metastatic endometrial cancer. The ideal timing of immunotherapy for women with endometrial cancer is an area of active ongoing study.
Immunotherapy with PD-1 blockade is an important treatment strategy for women with MMR-deficient or MSI-H gynecologic cancers.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
In this Update, I report on the latest US Preventive Services Task Force (USPSTF) cervical cancer screening recommendations. In addition, I describe the results of 2 studies, a large prospective multicenter study of the accuracy of sentinel lymph node (SLN) biopsy in endometrial cancer, and a proof-of-concept review of use of checkpoint blockade to increase immune response and of its possible role in endometrial cancer.
hrHPV testing used alone as primary screening for cervical cancer: USPSTF recommendations
US Preventive Services Task Force. Draft recommendation statement: cervical cancer: screening. https://www.uspreventiveservicestaskforce.org/Page/Document/draft-recommendation-statement/cervical-cancer-screening2. Published October 2017. Accessed February 5, 2018.
Despite our rapid advances in understanding the molecular underpinnings of cancer, gynecologic malignancies are still a major cause of morbidity and mortality among women. Cervical cancer stands as an example of how a cancer screening test can be implemented to reduce mortality. In this section, I report on the USPSTF cervical cancer screening recommendations, which were updated in October 2017.
Even with the widespread implementation of screening programs for cervical cancer in the United States, 13,240 women will be diagnosed with the disease in 2018, and 4,170 will die from cervical cancer.1 Most often, cervical cancer occurs in women who have not been adequately screened. It is now recognized that the human papillomavirus (HPV) is the cause of cervical cancer.2
While cervical cytology has long been used as a screening test for cervical cancer, testing for high-risk HPV subtypes (hrHPV testing) also has been used as a screening modality. Traditionally, hrHPV testing is used in combination with cervical cytology, so called cotesting. There is convincing evidence that cervical cytology, as well as strategies that use hrHPV testing, can detect high-grade cervical precancers and cancers and thereby reduce mortality. However, cervical cancer screening is also associated with frequent follow-ups, invasive procedures performed to assess abnormal results, psychological distress, and adverse pregnancy outcomes of treatment for precancerous lesions.
The USPSTF based its new cervical cancer screening recommendations on clinical trial data and decision modeling of various screening strategies, and weighed the benefits and harms of each strategy.
Recommendations from the USPSTF
hrHPV screening for cervical cancer. TheUSPSTF recommends screening with cervical cytology every 3 years for women 21 to 29 years of age. For women 30 to 65 years of age, screening with cytology every 3 years, or hrHPV testing alone used every 5 years, is recommended.
Data from large randomized trials suggest cytologic screening is slightly less sensitive than hrHPV testing in detecting high-grade (grade 2 or 3) cervical intraepithelial neoplasia (CIN). However, hrHPV testing results in more follow-up tests and colposcopies. In a decision model, the USPSTF found that cotesting increased the number of follow-up tests but did not increase detection of grade 3 CIN or invasive cancer. This is the first clinical guideline to recommend hrHPV testing used alone for screening. The American College of Obstetricians and Gynecologists (ACOG) continues to recommend cotesting (cytology in combination with hrHPV) as a primary screening modality in this population.3
Exceptions. According to the USPSTF, 3 populations should not be screened: women over 65 years of age with adequate prior screening who are not otherwise at high risk for cervical cancer; women under 21 years of age; and women who have had a hysterectomy and do not have a history of grade 2 or 3 CIN or cancer.
Summary. The USPSTF recommendations are intended for the general population and are not applicable to women with a history of high-grade CIN or cervical cancer, women with in utero exposure to diethylstilbestrol, and women who are immunocompromised. The remaining USPSTF recommendations are largely in line with guidelines published by ACOG and other groups.3,4
Testing for high-risk HPV alone is a reasonable screening option for cervical cancer. This modality can be used in women 30 to 65 years of age but should not be repeated more frequently than every 5 years in those with a negative result.
Read about SLN biopsy to stage endometrial cancer
SLN biopsy for staging endometrial cancer
Rossi EC, Kowalski LD, Scalici J, et al. A comparison of sentinel lymph node biopsy to lymphadenectomy for endometrial cancer staging (FIRES trial): a multicentre, prospective, cohort study. Lancet Oncol. 2017;18(3):384-392.
Surgery is the cornerstone of treatment for most gynecologic cancers. The widespread use of minimally invasive surgical techniques and the introduction of less radical procedures for gynecologic cancers have helped reduce surgical morbidity.
For endometrial cancer, the role of lymphadenectomy is controversial. Data from prospective trials of this procedure suggest an association with increased morbidity and long-term sequelae, such as lymphedema, and no association with improved survival.5,6
SLN biopsy is an important advance and a potential alternative nodal evaluation method that may be associated with decreased morbidity. In this more limited assessment technique, the first nodal drainage basins of a tumor are identified and removed for pathologic evaluation.
Accuracy of SLN biopsy in endometrial cancer was the subject of Rossi and colleagues' recent large prospective multicenter study, the Fluorescence Imaging for Robotic Endometrial Sentinel lymph node biopsy (FIRES) trial.
Details of the study
Rossi and colleagues conducted the FIRES trial to estimate the sensitivity of SLN biopsy in detecting nodal metastases in women with stage I endometrial cancer. Patients (N = 385) from 10 US sites were enrolled in the study. SLN evaluation was performed after cervical injection of indocyanine green followed by robotic-assisted hysterectomy. After identification of the SLN, participants underwent pelvic lymphadenectomy. Performance of para-aortic lymphadenectomy was optional.
Mapping of the SLN was feasible in 86% of patients, including bilateral mapping in 52%. Twelve percent of the participants had nodal metastases. SLN biopsy had a sensitivity of 97% in women who had identification of the SLNs. Similarly, the negative predictive value was high, 99.6%. The procedure was associated with acceptable short-term toxicity with adverse events in 9% of study participants. Common complications included neurologic complications, respiratory distress, nausea and vomiting, and, in 3 patients, bowel injury.
Accurate detection of nodal metastases. Results of the study suggest SLN biopsy is accurate in detecting nodal metastases in women with endometrial cancer. Although long-term toxicity was not examined, other work suggests the lymphedema rates associated with SLN biopsy may be lower than those of lymphadenectomy. While the study described impressive performance characteristics, there remain technical challenges. Even among skilled surgeons trained for the protocol, there was no nodal mapping in nearly half of the women with endometrial cancer. Women without node mapping require full lymphadenectomy thus negating the possible benefits of the procedure.
Given the high accuracy of SLN mapping in endometrial cancer, the procedure likely will become the standard of care for nodal evaluation by gynecologic oncologists.
Read about immunotherapy for gynecologic cancers
Immunotherapy for gynecologic cancers
Le DT, Durham JN, Smith KN, et al. Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science. 2017;357(6349):409-413.
In oncology, precision medicine is rapidly becoming a standard treatment approach. Therapies are being used to target specific genetic alterations in tumors. In cancer immunotherapy, the immune system is being used to facilitate clearance of cancer cells.
The most common mechanism of action of clinically used immunotherapeutic agents is blockade of programmed cell death protein 1 (PD-1), a lymphocyte receptor that prevents the immune system from targeting the body's own cells.7 Cancers that have mutations in the DNA mismatch repair (MMR) proteins display microsatellite instability (MSI) and produce high levels of abnormal proteins.8 These abnormal proteins serve as tumor antigens that can be targeted by the body's normal immune system.
In May 2017, the US Food and Drug Administration (FDA) granted accelerated approval of the PD-1 blocking antibody pembrolizumab for the treatment of unresectable or metastatic MSI-high (MSI-H) or MMR-deficient solid tumors.9 The approval was based on data from 149 patients treated in 5 studies that demonstrated a response rate of 39.6%, including responses that lasted at least 6 months in 78% of participants. This was the first ever cancer drug that received FDA approval based on a tumor's biomarker profile without regard to the site of origin. I describe the results of a study by Le and colleagues that examines the possible role of immunotherapy in a variety of solid tumors in this section.
Details of the study
This study examined the clinical efficacy of PD-1 blockade in 86 patients with advanced, MMR-deficient tumors from 12 different sites. Endometrial cancer was the second most frequent primary tumor site in 17% of patients. Within the cohort, the overall objective response rate was 53%, which included 21% of patients with complete radiographic response (no imaging evidence of cancer). Disease control, either complete or partial response or stable disease, was achieved in 77% of patients. After a median follow-up of 12.5 months, neither the median progression-free survival (PFS) nor median overall survival had been reached. The authors estimated that 2-year overall survival was 64%, substantially higher than expected for patients with advanced solid tumors.
Le and colleagues also performed several in vivo laboratory experiments to explore the mechanisms by which patients responded. In addition, they used sequencing to determine the prevalence of MMR deficiency in 12,019 cancer samples that included 32 distinct tumor types (FIGURE). Endometrial cancer had the highest frequency of MMR deficiency (17%). Four percent of cervical cancers and less than 2% of ovarian cancers were MMR-deficient.
The promise of immunotherapy for endometrial cancer. This study's data and other emerging data have important implications for women with gynecologic cancer, particularly endometrial cancer. First, given the frequency of MMR mutations among women with endometrial cancer, MMR testing should be strongly considered for these patients. Many institutions have protocols for reflex testing with immunohistochemistry for women with endometrial cancer. For women with positive test results, germline sequencing can be performed to determine if they have an inherited MMR deficiency, Lynch syndrome. Presence of an MMR deficiency is an important factor in cancer screening and potential treatment.
Second, the impressive results of PD-1 blockade in patients with MMR-deficient tumors suggest that this treatment strategy may be important for women with recurrent or metastatic endometrial cancer. The ideal timing of immunotherapy for women with endometrial cancer is an area of active ongoing study.
Immunotherapy with PD-1 blockade is an important treatment strategy for women with MMR-deficient or MSI-H gynecologic cancers.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- American Cancer Society. Cancer Facts & Figures 2018. Atlanta, GA: American Cancer Society; 2018.
- Walboomers JM, Jacobs MV, Manos MM, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189(1):12–19.
- American College of Obstetricians and Gynecologists Committee on Practice Bulletins-Gynecology. ACOG Practice Bulletin No. 168: Cervical cancer screening and prevention. Obstet Gynecol. 2016;128(4):e111–e130.
- Saslow D, Solomon D, Lawson HW, et al; ACS-ASCCP-ASCP Cervical Cancer Guideline Committee. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. CA Cancer J Clin. 2012;62(3):147–172.
- Benedetti Panici P, Basile S, Maneschi F, et al. Systematic pelvic lymphadenectomy vs. no lymphadenectomy in early-stage endometrial carcinoma: randomized clinical trial. J Natl Cancer Inst. 2008;100(23):1707–1716.
- ASTEC Study Group, Kitchener H, Swart AM, Qian Q, Amos C, Parmar MK. Efficacy of systematic pelvic lymphadenectomy in endometrial cancer (MRC ASTEC trial): a randomised study. Lancet. 2009;373(9658):125–136.
- Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer. 2012;12(4):252–264.
- Buza N, Ziai J, Hui P. Mismatch repair deficiency testing in clinical practice. Expert Rev Mol Diagn. 2016;16(5):591–604.
- FDA approves first cancer treatment for any solid tumor with a specific genetic feature [news release]. Silver Spring, MD: US Food and Drug Administration. https://www.fda.gov/newsevents/newsroom/pressannouncements/ucm560167.htm. Published May 23, 2017. Accessed February 5, 2018.
- American Cancer Society. Cancer Facts & Figures 2018. Atlanta, GA: American Cancer Society; 2018.
- Walboomers JM, Jacobs MV, Manos MM, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189(1):12–19.
- American College of Obstetricians and Gynecologists Committee on Practice Bulletins-Gynecology. ACOG Practice Bulletin No. 168: Cervical cancer screening and prevention. Obstet Gynecol. 2016;128(4):e111–e130.
- Saslow D, Solomon D, Lawson HW, et al; ACS-ASCCP-ASCP Cervical Cancer Guideline Committee. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. CA Cancer J Clin. 2012;62(3):147–172.
- Benedetti Panici P, Basile S, Maneschi F, et al. Systematic pelvic lymphadenectomy vs. no lymphadenectomy in early-stage endometrial carcinoma: randomized clinical trial. J Natl Cancer Inst. 2008;100(23):1707–1716.
- ASTEC Study Group, Kitchener H, Swart AM, Qian Q, Amos C, Parmar MK. Efficacy of systematic pelvic lymphadenectomy in endometrial cancer (MRC ASTEC trial): a randomised study. Lancet. 2009;373(9658):125–136.
- Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer. 2012;12(4):252–264.
- Buza N, Ziai J, Hui P. Mismatch repair deficiency testing in clinical practice. Expert Rev Mol Diagn. 2016;16(5):591–604.
- FDA approves first cancer treatment for any solid tumor with a specific genetic feature [news release]. Silver Spring, MD: US Food and Drug Administration. https://www.fda.gov/newsevents/newsroom/pressannouncements/ucm560167.htm. Published May 23, 2017. Accessed February 5, 2018.
New device cuts postoperative pulmonary complications
SAN ANTONIO – according to results of a nonrandomized study including high-risk patients undergoing elective surgical procedures.
“For certain types of surgical procedures, this therapy (MetaNeb, Hill-Rom) may provide a benefit for high-risk patients in terms of reducing their pulmonary complications and their hospital stay,” said Toan Huynh, MD, lead investigator and director of trauma research at Carolinas HealthCare System, Charlotte, N.C., at the Critical Care Congress sponsored by the Society for Critical Care Medicine.
Currently, aggressive management of high-risk patients with strategies such as optimal analgesia, early ambulation, secretion mobilization, and lung expansion are used to try to reduce the incidence of postoperative pulmonary complications, noted Dr. Huynh, in an interview.
In this study, Dr. Huynh and his colleagues from the University of Pennsylvania, Philadelphia, and the Lahey Hospital & Medical Center, Burlington, Mass., sought to evaluate the efficacy of the MetaNeb system, which delivers continuous high-frequency oscillation, continuous positive expiratory pressure, and in-line aerosol flow in one combined unit. To estimate usual postoperative pulmonary complication rates, they first queried CPT and ICD-9-CM codes to identify a total of 210 patients who had undergone thoracic, upper-abdominal, or aortic open surgical procedures. Then, in the second stage of the study, the investigators prospectively enrolled 209 subjects who underwent those types of surgery with the MetaNeb system in addition to a standard postoperative respiratory regimen. All patients were high risk as defined by having either an American Society of Anesthesiologists classification of at least 3 or an ASA classification of 2 along with one or more comorbidities, such as COPD or recent smoking history.
Among the patients managed with MetaNeb, 33 (15.8%) experienced one or more pulmonary complications, compared with 48 (22.9%) in the retrospective cohort (P = 0.06). For intubated patients, at least one complication was seen in 22 patients (36.7%) in the MetaNeb group, compared with 37 (69.8%) in the comparison group (P less than .05). Time on mechanical ventilation was 8.5 hours in the MetaNeb group versus 23.7 hours in the comparison group (P less than .05).
Use of the device was also associated with decreased length of hospital stay, but the difference between lengths of stay was not statistically significant. Hospital length of stay was 6.8 days in the MetaNeb versus 8.4 days in the comparison groups.“In the current day and age of value-based health care, I think any kind of reduction in expenditure related to health care costs would be compelling for clinicians,” Dr. Huynh said in the interview.
Further study may be needed to better define the role of the combined modality system in clinical practice, according to Dr. Huynh.
“This is sort of a ‘before and after’ nonrandomized trial,” Dr. Huynh explained. “I think, ideally, if we can do a truly controlled, randomized trial, that will be much more powerful.”
The study was sponsored by Hill-Rom, which manufactures the device under study. Dr. Huynh said he and coinvestigators had no financial conflicts related to the research.
SOURCE: Huynh T et al. Critical Care Congress, Abstract 17.
SAN ANTONIO – according to results of a nonrandomized study including high-risk patients undergoing elective surgical procedures.
“For certain types of surgical procedures, this therapy (MetaNeb, Hill-Rom) may provide a benefit for high-risk patients in terms of reducing their pulmonary complications and their hospital stay,” said Toan Huynh, MD, lead investigator and director of trauma research at Carolinas HealthCare System, Charlotte, N.C., at the Critical Care Congress sponsored by the Society for Critical Care Medicine.
Currently, aggressive management of high-risk patients with strategies such as optimal analgesia, early ambulation, secretion mobilization, and lung expansion are used to try to reduce the incidence of postoperative pulmonary complications, noted Dr. Huynh, in an interview.
In this study, Dr. Huynh and his colleagues from the University of Pennsylvania, Philadelphia, and the Lahey Hospital & Medical Center, Burlington, Mass., sought to evaluate the efficacy of the MetaNeb system, which delivers continuous high-frequency oscillation, continuous positive expiratory pressure, and in-line aerosol flow in one combined unit. To estimate usual postoperative pulmonary complication rates, they first queried CPT and ICD-9-CM codes to identify a total of 210 patients who had undergone thoracic, upper-abdominal, or aortic open surgical procedures. Then, in the second stage of the study, the investigators prospectively enrolled 209 subjects who underwent those types of surgery with the MetaNeb system in addition to a standard postoperative respiratory regimen. All patients were high risk as defined by having either an American Society of Anesthesiologists classification of at least 3 or an ASA classification of 2 along with one or more comorbidities, such as COPD or recent smoking history.
Among the patients managed with MetaNeb, 33 (15.8%) experienced one or more pulmonary complications, compared with 48 (22.9%) in the retrospective cohort (P = 0.06). For intubated patients, at least one complication was seen in 22 patients (36.7%) in the MetaNeb group, compared with 37 (69.8%) in the comparison group (P less than .05). Time on mechanical ventilation was 8.5 hours in the MetaNeb group versus 23.7 hours in the comparison group (P less than .05).
Use of the device was also associated with decreased length of hospital stay, but the difference between lengths of stay was not statistically significant. Hospital length of stay was 6.8 days in the MetaNeb versus 8.4 days in the comparison groups.“In the current day and age of value-based health care, I think any kind of reduction in expenditure related to health care costs would be compelling for clinicians,” Dr. Huynh said in the interview.
Further study may be needed to better define the role of the combined modality system in clinical practice, according to Dr. Huynh.
“This is sort of a ‘before and after’ nonrandomized trial,” Dr. Huynh explained. “I think, ideally, if we can do a truly controlled, randomized trial, that will be much more powerful.”
The study was sponsored by Hill-Rom, which manufactures the device under study. Dr. Huynh said he and coinvestigators had no financial conflicts related to the research.
SOURCE: Huynh T et al. Critical Care Congress, Abstract 17.
SAN ANTONIO – according to results of a nonrandomized study including high-risk patients undergoing elective surgical procedures.
“For certain types of surgical procedures, this therapy (MetaNeb, Hill-Rom) may provide a benefit for high-risk patients in terms of reducing their pulmonary complications and their hospital stay,” said Toan Huynh, MD, lead investigator and director of trauma research at Carolinas HealthCare System, Charlotte, N.C., at the Critical Care Congress sponsored by the Society for Critical Care Medicine.
Currently, aggressive management of high-risk patients with strategies such as optimal analgesia, early ambulation, secretion mobilization, and lung expansion are used to try to reduce the incidence of postoperative pulmonary complications, noted Dr. Huynh, in an interview.
In this study, Dr. Huynh and his colleagues from the University of Pennsylvania, Philadelphia, and the Lahey Hospital & Medical Center, Burlington, Mass., sought to evaluate the efficacy of the MetaNeb system, which delivers continuous high-frequency oscillation, continuous positive expiratory pressure, and in-line aerosol flow in one combined unit. To estimate usual postoperative pulmonary complication rates, they first queried CPT and ICD-9-CM codes to identify a total of 210 patients who had undergone thoracic, upper-abdominal, or aortic open surgical procedures. Then, in the second stage of the study, the investigators prospectively enrolled 209 subjects who underwent those types of surgery with the MetaNeb system in addition to a standard postoperative respiratory regimen. All patients were high risk as defined by having either an American Society of Anesthesiologists classification of at least 3 or an ASA classification of 2 along with one or more comorbidities, such as COPD or recent smoking history.
Among the patients managed with MetaNeb, 33 (15.8%) experienced one or more pulmonary complications, compared with 48 (22.9%) in the retrospective cohort (P = 0.06). For intubated patients, at least one complication was seen in 22 patients (36.7%) in the MetaNeb group, compared with 37 (69.8%) in the comparison group (P less than .05). Time on mechanical ventilation was 8.5 hours in the MetaNeb group versus 23.7 hours in the comparison group (P less than .05).
Use of the device was also associated with decreased length of hospital stay, but the difference between lengths of stay was not statistically significant. Hospital length of stay was 6.8 days in the MetaNeb versus 8.4 days in the comparison groups.“In the current day and age of value-based health care, I think any kind of reduction in expenditure related to health care costs would be compelling for clinicians,” Dr. Huynh said in the interview.
Further study may be needed to better define the role of the combined modality system in clinical practice, according to Dr. Huynh.
“This is sort of a ‘before and after’ nonrandomized trial,” Dr. Huynh explained. “I think, ideally, if we can do a truly controlled, randomized trial, that will be much more powerful.”
The study was sponsored by Hill-Rom, which manufactures the device under study. Dr. Huynh said he and coinvestigators had no financial conflicts related to the research.
SOURCE: Huynh T et al. Critical Care Congress, Abstract 17.
AT THE CRITICAL CARE CONGRESS
Key clinical point: A device that combines lung expansion, secretion clearance, and aerosol delivery (MetaNeb) appears to reduce postoperative pulmonary complications and resource use.Major finding: Pulmonary complications occurred in 36.7% of intubated patients, compared with 69.8% for a prospectively evaluated reference population (P less than 0.05).
Data source: A prospective, nonrandomized, two-stage study including 417 subjects who underwent thoracic, upper-abdominal, or aortic open surgical procedure at one of three centers.
Disclosures: The study was sponsored by Hill-Rom, which manufactures the MetaNeb device. Investigators had no financial conflicts related to the study.
Source: Huynh T et al. Critical Care Congress, Abstract 17.
Adenotonsillectomy reduced hypertension in OSA subgroup
after surgery, according to a retrospective analysis.
This is one of the few studies to have ever examined whether adenotonsillectomy for children with OSA had any effects on blood pressure (BP) and was based on “one of the largest cohorts for evaluating postoperative BP changes in nonobese children with OSA,” noted Cho-Hsueh Lee, MD, and colleagues. The report was published in JAMA Otolaryngology–Head & Neck Surgery. Among the previous studies that evaluated BP in children with OSA before and after having this surgery, the results varied, they added.
The researchers analyzed the medical records of 240 nonobese children with clinical symptoms and polysomnography-confirmed OSA (having an apnea-hypopnea index of greater than 1) who underwent adenotonsillectomy. Prior to surgery, 169 patients (70.4%) of the patients were classified as nonhypertensive, while 71 (29.6%) were classified as hypertensive. The children had a mean age of 7.3 years, and 160 were males.
Patients participated in full-night polysomnography (PSG) before surgery and at 3-6 months after adenotonsillectomy in the National Taiwan University Hospital Sleep Center. Apnea episodes were defined as a 90% decrease in airflow for two consecutive breaths. Sleep center staff measured the study participants’ systolic and diastolic BP in a sleep center using an electronic sphygmomanometer, in the evening, prior to the PSG study, and in the morning. Pediatric hypertension was based on the nocturnal BP measurement and was defined as having mean systolic and diastolic BP greater or equal to the 95th percentile for age, sex, and height.
“Postoperatively, hypertensive children had a significant decrease in all BP measures, including nocturnal and morning [systolic] BP ... A total of 47 hypertensive patients (66.2%) became nonhypertensive after surgery,” the researchers said.
For patients who were hypertensive before surgery, the average nocturnal (before PSG) preop systolic BP was 114.3 mm Hg, versus 107.5 mm Hg after surgery. The mean nocturnal diastolic BP for this same group of patients decreased to 65.1 mm Hg from 74.3 mm Hg. Similarly, the average morning (after PSG) systolic BP and diastolic BP were 106.0 mm Hg and 64.4 mm Hg after these patients underwent adenotonsillectomy, compared with 111.8 mm Hg and 71.7 mm Hg prior to surgery, respectively.
The adenotonsillectomy didn’t improve all patients’ BP. For some who were nonhypertensive before surgery, blood pressure increased, with 36 (21.3%) of this group having become hypersensitive after surgery, the researchers acknowledged.
Overall, the cohort experienced significant improvements in several PSG measures, including the average apnea-hypopnea index, which decreased from 12.1 events per hour to 1.7. The total arousal index also declined, going from 6.1 events per hour to 4.2. In addition, the mean oxygen saturation improved from 96.8% to 97.7%.
The investigators described several limitations of the study, including their inability to collect patients’ arterial stiffness, carotid intima thickness, and other cardiovascular measures beyond BP.
They recommended a follow-up study. “Although we observed improvements in BP measures within 6 months after surgery for hypertensive children with OSA, the long-term effects of surgery on BP remain uncertain,” they explained.
The study was supported by grants from the Ministry of Science and Technology, Republic of China (Taiwan). The researchers disclosed no potential conflicts of interest.
SOURCE: Lee, C-H et al. JAMA Otolaryngol Head Neck Surg. 2018 Feb 15. doi: 10.1001/jamaoto.2017.3127.
after surgery, according to a retrospective analysis.
This is one of the few studies to have ever examined whether adenotonsillectomy for children with OSA had any effects on blood pressure (BP) and was based on “one of the largest cohorts for evaluating postoperative BP changes in nonobese children with OSA,” noted Cho-Hsueh Lee, MD, and colleagues. The report was published in JAMA Otolaryngology–Head & Neck Surgery. Among the previous studies that evaluated BP in children with OSA before and after having this surgery, the results varied, they added.
The researchers analyzed the medical records of 240 nonobese children with clinical symptoms and polysomnography-confirmed OSA (having an apnea-hypopnea index of greater than 1) who underwent adenotonsillectomy. Prior to surgery, 169 patients (70.4%) of the patients were classified as nonhypertensive, while 71 (29.6%) were classified as hypertensive. The children had a mean age of 7.3 years, and 160 were males.
Patients participated in full-night polysomnography (PSG) before surgery and at 3-6 months after adenotonsillectomy in the National Taiwan University Hospital Sleep Center. Apnea episodes were defined as a 90% decrease in airflow for two consecutive breaths. Sleep center staff measured the study participants’ systolic and diastolic BP in a sleep center using an electronic sphygmomanometer, in the evening, prior to the PSG study, and in the morning. Pediatric hypertension was based on the nocturnal BP measurement and was defined as having mean systolic and diastolic BP greater or equal to the 95th percentile for age, sex, and height.
“Postoperatively, hypertensive children had a significant decrease in all BP measures, including nocturnal and morning [systolic] BP ... A total of 47 hypertensive patients (66.2%) became nonhypertensive after surgery,” the researchers said.
For patients who were hypertensive before surgery, the average nocturnal (before PSG) preop systolic BP was 114.3 mm Hg, versus 107.5 mm Hg after surgery. The mean nocturnal diastolic BP for this same group of patients decreased to 65.1 mm Hg from 74.3 mm Hg. Similarly, the average morning (after PSG) systolic BP and diastolic BP were 106.0 mm Hg and 64.4 mm Hg after these patients underwent adenotonsillectomy, compared with 111.8 mm Hg and 71.7 mm Hg prior to surgery, respectively.
The adenotonsillectomy didn’t improve all patients’ BP. For some who were nonhypertensive before surgery, blood pressure increased, with 36 (21.3%) of this group having become hypersensitive after surgery, the researchers acknowledged.
Overall, the cohort experienced significant improvements in several PSG measures, including the average apnea-hypopnea index, which decreased from 12.1 events per hour to 1.7. The total arousal index also declined, going from 6.1 events per hour to 4.2. In addition, the mean oxygen saturation improved from 96.8% to 97.7%.
The investigators described several limitations of the study, including their inability to collect patients’ arterial stiffness, carotid intima thickness, and other cardiovascular measures beyond BP.
They recommended a follow-up study. “Although we observed improvements in BP measures within 6 months after surgery for hypertensive children with OSA, the long-term effects of surgery on BP remain uncertain,” they explained.
The study was supported by grants from the Ministry of Science and Technology, Republic of China (Taiwan). The researchers disclosed no potential conflicts of interest.
SOURCE: Lee, C-H et al. JAMA Otolaryngol Head Neck Surg. 2018 Feb 15. doi: 10.1001/jamaoto.2017.3127.
after surgery, according to a retrospective analysis.
This is one of the few studies to have ever examined whether adenotonsillectomy for children with OSA had any effects on blood pressure (BP) and was based on “one of the largest cohorts for evaluating postoperative BP changes in nonobese children with OSA,” noted Cho-Hsueh Lee, MD, and colleagues. The report was published in JAMA Otolaryngology–Head & Neck Surgery. Among the previous studies that evaluated BP in children with OSA before and after having this surgery, the results varied, they added.
The researchers analyzed the medical records of 240 nonobese children with clinical symptoms and polysomnography-confirmed OSA (having an apnea-hypopnea index of greater than 1) who underwent adenotonsillectomy. Prior to surgery, 169 patients (70.4%) of the patients were classified as nonhypertensive, while 71 (29.6%) were classified as hypertensive. The children had a mean age of 7.3 years, and 160 were males.
Patients participated in full-night polysomnography (PSG) before surgery and at 3-6 months after adenotonsillectomy in the National Taiwan University Hospital Sleep Center. Apnea episodes were defined as a 90% decrease in airflow for two consecutive breaths. Sleep center staff measured the study participants’ systolic and diastolic BP in a sleep center using an electronic sphygmomanometer, in the evening, prior to the PSG study, and in the morning. Pediatric hypertension was based on the nocturnal BP measurement and was defined as having mean systolic and diastolic BP greater or equal to the 95th percentile for age, sex, and height.
“Postoperatively, hypertensive children had a significant decrease in all BP measures, including nocturnal and morning [systolic] BP ... A total of 47 hypertensive patients (66.2%) became nonhypertensive after surgery,” the researchers said.
For patients who were hypertensive before surgery, the average nocturnal (before PSG) preop systolic BP was 114.3 mm Hg, versus 107.5 mm Hg after surgery. The mean nocturnal diastolic BP for this same group of patients decreased to 65.1 mm Hg from 74.3 mm Hg. Similarly, the average morning (after PSG) systolic BP and diastolic BP were 106.0 mm Hg and 64.4 mm Hg after these patients underwent adenotonsillectomy, compared with 111.8 mm Hg and 71.7 mm Hg prior to surgery, respectively.
The adenotonsillectomy didn’t improve all patients’ BP. For some who were nonhypertensive before surgery, blood pressure increased, with 36 (21.3%) of this group having become hypersensitive after surgery, the researchers acknowledged.
Overall, the cohort experienced significant improvements in several PSG measures, including the average apnea-hypopnea index, which decreased from 12.1 events per hour to 1.7. The total arousal index also declined, going from 6.1 events per hour to 4.2. In addition, the mean oxygen saturation improved from 96.8% to 97.7%.
The investigators described several limitations of the study, including their inability to collect patients’ arterial stiffness, carotid intima thickness, and other cardiovascular measures beyond BP.
They recommended a follow-up study. “Although we observed improvements in BP measures within 6 months after surgery for hypertensive children with OSA, the long-term effects of surgery on BP remain uncertain,” they explained.
The study was supported by grants from the Ministry of Science and Technology, Republic of China (Taiwan). The researchers disclosed no potential conflicts of interest.
SOURCE: Lee, C-H et al. JAMA Otolaryngol Head Neck Surg. 2018 Feb 15. doi: 10.1001/jamaoto.2017.3127.
FROM JAMA OTOLARYNGOLOGY-HEAD & NECK SURGERY
Key clinical point: Hypertensive children with obstructive sleep apnea (OSA) who had an adenotonsillectomy experienced significant improvements in their blood pressure after surgery.
Major finding: Sixty-six percent of hypertensive patients with OSA became nonhypertensive after adenotonsillectomy.
Study details: A retrospective analysis of 240 nonobese children with OSA who underwent adenotonsillectomy.
Disclosures: The study was supported by grants from the Ministry of Science and Technology, Republic of China (Taiwan). The researchers disclosed no potential conflicts of interest.
Source: Lee, C-H et al. JAMA Otolaryngol Head Neck Surg. 2018 Feb 15. doi: 10.1001/jamaoto.2017.3127.
Telling her she has cancer: A patient-centered approach to breaking bad news
Hearing a diagnosis of cancer is one of the most significant moments of a patient’s life and informing a patient of her diagnosis is an emotionally and technically challenging task for an obstetrician gynecologist who is frequently on the front line of making this diagnosis. In this column, we will explore some patient-centered strategies to perform this difficult task well so that patients come away informed but with the highest chance for positive emotional adjustment.
Fewer than 10% of physicians report receiving formal training in techniques of breaking bad news. For the majority of clinicians concerns are centered on being honest and not taking away hope, and in responding to a patient’s emotions.1 The SPIKES approach was developed to arm physicians with strategies to discuss a cancer diagnosis with their patients. This approach includes six key elements to incorporate during the encounter. These strategies are not meant to be formulaic but rather consistent principles that can be adjusted for individual patient needs.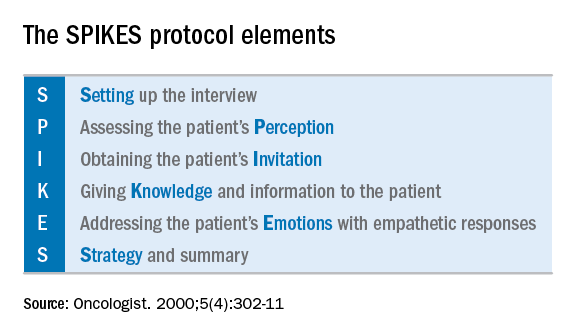
Setting up the discussion
Breaking bad news should not be a one-size-fits-all approach. Age, educational level, culture, religion, race and ethnicity, and socioeconomic opportunities each affects what and how patients may want to have this kind of information communicated to them. So how do you know how best to deliver a patient-centered approach for your patient? I recommend this simple strategy: Ask her. When ordering a test or performing a biopsy, let the patient know then why you are ordering the test and inform her of the possibility that the results may show cancer. Ask her how she would like for you to communicate that result. Would she like to be called by phone, the benefit of which is quick dissemination of information? Or would she like to receive the information face to face in the office? Research supports that most patients prefer to learn the result in the office.2 If so, I recommend scheduling a follow-up appointment in advance to prevent delays. Ask her if she would like a family member or a supportive friend to be present for the conveying of results so that she will have time to make these arrangements. Ask her if she would prefer for an alternate person to be provided with the results on her behalf.
When preparing to speak with the patient, it is valuable to mentally rehearse the words that you’ll use. Arrange for privacy and manage time constraints and interruptions (silence pagers and phones, ensure there is adequate time allocated in the schedule). Sit down to deliver the news and make a connection with eye contact and, if appropriate, touch.
Assessing the patient’s perception. Before you tell, ask. For example, “what is your understanding about why we did the biopsy?” This will guide you in where her head and heart are and can ensure you meet her wherever she is.
Obtaining the patient’s invitation. Ask the patient what she would like to be told and how much information. What would she like you to focus on? What does she not want to hear?
Giving knowledge and information to the patient. Especially now, it is important to avoid jargon and use nontechnical terms. However, do not shy away from using specific words like “cancer” by substituting them for more vague and confusing terms such as “malignancy” or “tumor.” It is important to find the balance between expressing information without being overly emotive, while avoiding excessive bluntness. Word choice is critical. Communication styles in the breaking of bad news can be separated broadly into three styles: disease centered, emotion centered, and patient-centered.3 The patient-centered approach is achieved by balancing emotional connection, information sharing, nondominance, and conveying hope. (For example, “I have some disappointing news to share. Shall we talk about the next steps in treatment? I understand this is that this is difficult for you.”) In general, this approach is most valued by patients and is associated with better information recall.
Addressing the patient’s emotions with empathetic responses. It is important that physicians take a moment to pause after communicating the test result. Even if prepared, most patients will still have a moment of shock, and their minds will likely spin through a multitude of thoughts preventing them from being able to “hear” and focus on the subsequent information. This is a moment to reflect on her reactions, her body language, and nonverbal communications to guide you on how to approach the rest of the encounter. Offer her your comfort and condolence in whichever way feels appropriate for you and her.
Beware of your own inclinations to “soften the blow.” It is a natural, compassionate instinct to follow-up giving a bad piece of information by balancing a good piece of information. For example, after just telling a woman that she has endometrial cancer, following with a statement such as “but it’s just stage 1 and is curable with surgery.” While this certainly may have immediate comforting effects, it has a couple of unintended consequences. First, it can result in difficulties later adjusting to a change in diagnosis when more information comes in (for example, upstaging after surgery or imaging). It is better to be honest and tell patients only what you know for sure in these immediate first moments of diagnosis when complete information is lacking. A more general statement such as “for most women, this is found at an early stage and is highly treatable” may be more appropriate and still provide some comfort. Second, attempts to soften the blow with a qualifying statement of positivity, such as “this is a good kind of cancer to have” might be interpreted by some patients as failing to acknowledge their devastation. She may feel that you are minimizing her condition and not allowing her to grieve or be distressed.
Strategy and summary. Patients who leave the encounter with some kind of plan for the future feel less distressed and anxious. The direction at this point of the encounter should be led by the patient. What are her greatest concerns (such as mortality, loss of fertility, time off work for treatment), and what does she want to know right now? Most patients express a desire to know more about treatment or prognosis.2,4 Unfortunately, it often is not possible to furnish this yet, particularly if this falls into the realm of a subspecialist, and prognostication typically requires more information than a provider has at initial diagnosis. However, leaving these questions unanswered is likely to result in a patient feeling helpless. For example, if an ob.gyn. discovers an apparent advanced ovarian cancer on a CT scan, tell her that, despite its apparent advanced case, it is usually treatable and that a gynecologic oncologist will discuss those best treatment options with her. Assure her that you will expeditiously refer her to a specialist who will provide her with those specifics.
The aftermath
That interval between initial diagnosis and specialist consultation is extraordinarily difficult and a high anxiety time. It is not unreasonable, in such cases, to recommend the patient to reputable online information sources, such as the Society of Gynecologic Oncology or American Cancer Society websites so that she and her family can do some research prior to that visit in order to prepare them better and give them a sense of understanding in their disease.
It is a particularly compassionate touch to reach out to the patient in the days following her cancer diagnosis, even if she has moved on to a specialist. Patients often tell me that they felt enormous reassurance and appreciation when their ob.gyn. reached out to them to “check on how they are doing.” This can usually reasonably be done by phone. This second contact serves another critical purpose: it allows for repetition of the diagnosis and initial plan, and the ability to fill in the blanks of what the patient may have missed during the prior visit, if her mind was, naturally, elsewhere. It also, quite simply, shows that you care.
Ultimately, none of us can break bad news perfectly every time. We all need to be insightful with each of these encounters as to what we did well, what we did not, and how we can adjust in the future. With respect to the SPIKES approach, patients report that physicians struggle most with the “perception,” “invitation,” and “strategy and summary” components.5 Our objective should be keeping the patient’s needs in mind, rather than our own, to maximize the chance of doing a good job. If this task is done well, not only are patients more likely to have positive emotional adjustments to their diagnosis but also more adherence with future therapies.4 In the end, it is the patient who has the final say on whether it was done well or not.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She reports no relevant financial disclosures.
References
1. Baile WF et al. Oncologist. 2000;5(4):302-11.
2. Girgis A et al. Behav Med. 1999 Summer;25(2):69-77.
3. Schmid MM et al. Patient Educ Couns. 2005 Sep;58(3):244-51.
4. Girgis A et al. J Clin Oncol. 1995 Sep;13(9):2449-56.
5. Marscholiek P et al. J Cancer Educ. 2018 Feb 5. doi: 10.1007/s13187-017-1315-3.
Hearing a diagnosis of cancer is one of the most significant moments of a patient’s life and informing a patient of her diagnosis is an emotionally and technically challenging task for an obstetrician gynecologist who is frequently on the front line of making this diagnosis. In this column, we will explore some patient-centered strategies to perform this difficult task well so that patients come away informed but with the highest chance for positive emotional adjustment.
Fewer than 10% of physicians report receiving formal training in techniques of breaking bad news. For the majority of clinicians concerns are centered on being honest and not taking away hope, and in responding to a patient’s emotions.1 The SPIKES approach was developed to arm physicians with strategies to discuss a cancer diagnosis with their patients. This approach includes six key elements to incorporate during the encounter. These strategies are not meant to be formulaic but rather consistent principles that can be adjusted for individual patient needs.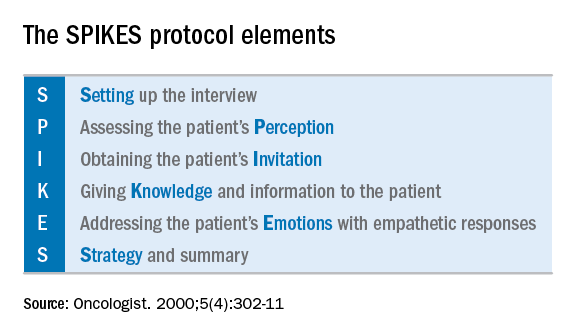
Setting up the discussion
Breaking bad news should not be a one-size-fits-all approach. Age, educational level, culture, religion, race and ethnicity, and socioeconomic opportunities each affects what and how patients may want to have this kind of information communicated to them. So how do you know how best to deliver a patient-centered approach for your patient? I recommend this simple strategy: Ask her. When ordering a test or performing a biopsy, let the patient know then why you are ordering the test and inform her of the possibility that the results may show cancer. Ask her how she would like for you to communicate that result. Would she like to be called by phone, the benefit of which is quick dissemination of information? Or would she like to receive the information face to face in the office? Research supports that most patients prefer to learn the result in the office.2 If so, I recommend scheduling a follow-up appointment in advance to prevent delays. Ask her if she would like a family member or a supportive friend to be present for the conveying of results so that she will have time to make these arrangements. Ask her if she would prefer for an alternate person to be provided with the results on her behalf.
When preparing to speak with the patient, it is valuable to mentally rehearse the words that you’ll use. Arrange for privacy and manage time constraints and interruptions (silence pagers and phones, ensure there is adequate time allocated in the schedule). Sit down to deliver the news and make a connection with eye contact and, if appropriate, touch.
Assessing the patient’s perception. Before you tell, ask. For example, “what is your understanding about why we did the biopsy?” This will guide you in where her head and heart are and can ensure you meet her wherever she is.
Obtaining the patient’s invitation. Ask the patient what she would like to be told and how much information. What would she like you to focus on? What does she not want to hear?
Giving knowledge and information to the patient. Especially now, it is important to avoid jargon and use nontechnical terms. However, do not shy away from using specific words like “cancer” by substituting them for more vague and confusing terms such as “malignancy” or “tumor.” It is important to find the balance between expressing information without being overly emotive, while avoiding excessive bluntness. Word choice is critical. Communication styles in the breaking of bad news can be separated broadly into three styles: disease centered, emotion centered, and patient-centered.3 The patient-centered approach is achieved by balancing emotional connection, information sharing, nondominance, and conveying hope. (For example, “I have some disappointing news to share. Shall we talk about the next steps in treatment? I understand this is that this is difficult for you.”) In general, this approach is most valued by patients and is associated with better information recall.
Addressing the patient’s emotions with empathetic responses. It is important that physicians take a moment to pause after communicating the test result. Even if prepared, most patients will still have a moment of shock, and their minds will likely spin through a multitude of thoughts preventing them from being able to “hear” and focus on the subsequent information. This is a moment to reflect on her reactions, her body language, and nonverbal communications to guide you on how to approach the rest of the encounter. Offer her your comfort and condolence in whichever way feels appropriate for you and her.
Beware of your own inclinations to “soften the blow.” It is a natural, compassionate instinct to follow-up giving a bad piece of information by balancing a good piece of information. For example, after just telling a woman that she has endometrial cancer, following with a statement such as “but it’s just stage 1 and is curable with surgery.” While this certainly may have immediate comforting effects, it has a couple of unintended consequences. First, it can result in difficulties later adjusting to a change in diagnosis when more information comes in (for example, upstaging after surgery or imaging). It is better to be honest and tell patients only what you know for sure in these immediate first moments of diagnosis when complete information is lacking. A more general statement such as “for most women, this is found at an early stage and is highly treatable” may be more appropriate and still provide some comfort. Second, attempts to soften the blow with a qualifying statement of positivity, such as “this is a good kind of cancer to have” might be interpreted by some patients as failing to acknowledge their devastation. She may feel that you are minimizing her condition and not allowing her to grieve or be distressed.
Strategy and summary. Patients who leave the encounter with some kind of plan for the future feel less distressed and anxious. The direction at this point of the encounter should be led by the patient. What are her greatest concerns (such as mortality, loss of fertility, time off work for treatment), and what does she want to know right now? Most patients express a desire to know more about treatment or prognosis.2,4 Unfortunately, it often is not possible to furnish this yet, particularly if this falls into the realm of a subspecialist, and prognostication typically requires more information than a provider has at initial diagnosis. However, leaving these questions unanswered is likely to result in a patient feeling helpless. For example, if an ob.gyn. discovers an apparent advanced ovarian cancer on a CT scan, tell her that, despite its apparent advanced case, it is usually treatable and that a gynecologic oncologist will discuss those best treatment options with her. Assure her that you will expeditiously refer her to a specialist who will provide her with those specifics.
The aftermath
That interval between initial diagnosis and specialist consultation is extraordinarily difficult and a high anxiety time. It is not unreasonable, in such cases, to recommend the patient to reputable online information sources, such as the Society of Gynecologic Oncology or American Cancer Society websites so that she and her family can do some research prior to that visit in order to prepare them better and give them a sense of understanding in their disease.
It is a particularly compassionate touch to reach out to the patient in the days following her cancer diagnosis, even if she has moved on to a specialist. Patients often tell me that they felt enormous reassurance and appreciation when their ob.gyn. reached out to them to “check on how they are doing.” This can usually reasonably be done by phone. This second contact serves another critical purpose: it allows for repetition of the diagnosis and initial plan, and the ability to fill in the blanks of what the patient may have missed during the prior visit, if her mind was, naturally, elsewhere. It also, quite simply, shows that you care.
Ultimately, none of us can break bad news perfectly every time. We all need to be insightful with each of these encounters as to what we did well, what we did not, and how we can adjust in the future. With respect to the SPIKES approach, patients report that physicians struggle most with the “perception,” “invitation,” and “strategy and summary” components.5 Our objective should be keeping the patient’s needs in mind, rather than our own, to maximize the chance of doing a good job. If this task is done well, not only are patients more likely to have positive emotional adjustments to their diagnosis but also more adherence with future therapies.4 In the end, it is the patient who has the final say on whether it was done well or not.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She reports no relevant financial disclosures.
References
1. Baile WF et al. Oncologist. 2000;5(4):302-11.
2. Girgis A et al. Behav Med. 1999 Summer;25(2):69-77.
3. Schmid MM et al. Patient Educ Couns. 2005 Sep;58(3):244-51.
4. Girgis A et al. J Clin Oncol. 1995 Sep;13(9):2449-56.
5. Marscholiek P et al. J Cancer Educ. 2018 Feb 5. doi: 10.1007/s13187-017-1315-3.
Hearing a diagnosis of cancer is one of the most significant moments of a patient’s life and informing a patient of her diagnosis is an emotionally and technically challenging task for an obstetrician gynecologist who is frequently on the front line of making this diagnosis. In this column, we will explore some patient-centered strategies to perform this difficult task well so that patients come away informed but with the highest chance for positive emotional adjustment.
Fewer than 10% of physicians report receiving formal training in techniques of breaking bad news. For the majority of clinicians concerns are centered on being honest and not taking away hope, and in responding to a patient’s emotions.1 The SPIKES approach was developed to arm physicians with strategies to discuss a cancer diagnosis with their patients. This approach includes six key elements to incorporate during the encounter. These strategies are not meant to be formulaic but rather consistent principles that can be adjusted for individual patient needs.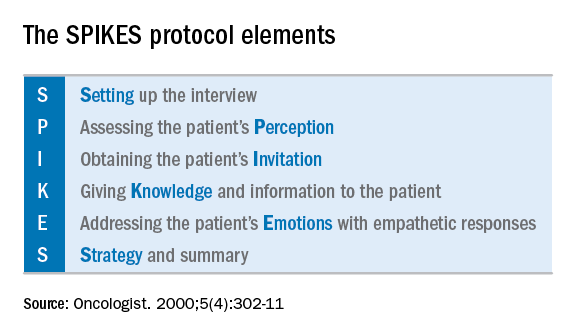
Setting up the discussion
Breaking bad news should not be a one-size-fits-all approach. Age, educational level, culture, religion, race and ethnicity, and socioeconomic opportunities each affects what and how patients may want to have this kind of information communicated to them. So how do you know how best to deliver a patient-centered approach for your patient? I recommend this simple strategy: Ask her. When ordering a test or performing a biopsy, let the patient know then why you are ordering the test and inform her of the possibility that the results may show cancer. Ask her how she would like for you to communicate that result. Would she like to be called by phone, the benefit of which is quick dissemination of information? Or would she like to receive the information face to face in the office? Research supports that most patients prefer to learn the result in the office.2 If so, I recommend scheduling a follow-up appointment in advance to prevent delays. Ask her if she would like a family member or a supportive friend to be present for the conveying of results so that she will have time to make these arrangements. Ask her if she would prefer for an alternate person to be provided with the results on her behalf.
When preparing to speak with the patient, it is valuable to mentally rehearse the words that you’ll use. Arrange for privacy and manage time constraints and interruptions (silence pagers and phones, ensure there is adequate time allocated in the schedule). Sit down to deliver the news and make a connection with eye contact and, if appropriate, touch.
Assessing the patient’s perception. Before you tell, ask. For example, “what is your understanding about why we did the biopsy?” This will guide you in where her head and heart are and can ensure you meet her wherever she is.
Obtaining the patient’s invitation. Ask the patient what she would like to be told and how much information. What would she like you to focus on? What does she not want to hear?
Giving knowledge and information to the patient. Especially now, it is important to avoid jargon and use nontechnical terms. However, do not shy away from using specific words like “cancer” by substituting them for more vague and confusing terms such as “malignancy” or “tumor.” It is important to find the balance between expressing information without being overly emotive, while avoiding excessive bluntness. Word choice is critical. Communication styles in the breaking of bad news can be separated broadly into three styles: disease centered, emotion centered, and patient-centered.3 The patient-centered approach is achieved by balancing emotional connection, information sharing, nondominance, and conveying hope. (For example, “I have some disappointing news to share. Shall we talk about the next steps in treatment? I understand this is that this is difficult for you.”) In general, this approach is most valued by patients and is associated with better information recall.
Addressing the patient’s emotions with empathetic responses. It is important that physicians take a moment to pause after communicating the test result. Even if prepared, most patients will still have a moment of shock, and their minds will likely spin through a multitude of thoughts preventing them from being able to “hear” and focus on the subsequent information. This is a moment to reflect on her reactions, her body language, and nonverbal communications to guide you on how to approach the rest of the encounter. Offer her your comfort and condolence in whichever way feels appropriate for you and her.
Beware of your own inclinations to “soften the blow.” It is a natural, compassionate instinct to follow-up giving a bad piece of information by balancing a good piece of information. For example, after just telling a woman that she has endometrial cancer, following with a statement such as “but it’s just stage 1 and is curable with surgery.” While this certainly may have immediate comforting effects, it has a couple of unintended consequences. First, it can result in difficulties later adjusting to a change in diagnosis when more information comes in (for example, upstaging after surgery or imaging). It is better to be honest and tell patients only what you know for sure in these immediate first moments of diagnosis when complete information is lacking. A more general statement such as “for most women, this is found at an early stage and is highly treatable” may be more appropriate and still provide some comfort. Second, attempts to soften the blow with a qualifying statement of positivity, such as “this is a good kind of cancer to have” might be interpreted by some patients as failing to acknowledge their devastation. She may feel that you are minimizing her condition and not allowing her to grieve or be distressed.
Strategy and summary. Patients who leave the encounter with some kind of plan for the future feel less distressed and anxious. The direction at this point of the encounter should be led by the patient. What are her greatest concerns (such as mortality, loss of fertility, time off work for treatment), and what does she want to know right now? Most patients express a desire to know more about treatment or prognosis.2,4 Unfortunately, it often is not possible to furnish this yet, particularly if this falls into the realm of a subspecialist, and prognostication typically requires more information than a provider has at initial diagnosis. However, leaving these questions unanswered is likely to result in a patient feeling helpless. For example, if an ob.gyn. discovers an apparent advanced ovarian cancer on a CT scan, tell her that, despite its apparent advanced case, it is usually treatable and that a gynecologic oncologist will discuss those best treatment options with her. Assure her that you will expeditiously refer her to a specialist who will provide her with those specifics.
The aftermath
That interval between initial diagnosis and specialist consultation is extraordinarily difficult and a high anxiety time. It is not unreasonable, in such cases, to recommend the patient to reputable online information sources, such as the Society of Gynecologic Oncology or American Cancer Society websites so that she and her family can do some research prior to that visit in order to prepare them better and give them a sense of understanding in their disease.
It is a particularly compassionate touch to reach out to the patient in the days following her cancer diagnosis, even if she has moved on to a specialist. Patients often tell me that they felt enormous reassurance and appreciation when their ob.gyn. reached out to them to “check on how they are doing.” This can usually reasonably be done by phone. This second contact serves another critical purpose: it allows for repetition of the diagnosis and initial plan, and the ability to fill in the blanks of what the patient may have missed during the prior visit, if her mind was, naturally, elsewhere. It also, quite simply, shows that you care.
Ultimately, none of us can break bad news perfectly every time. We all need to be insightful with each of these encounters as to what we did well, what we did not, and how we can adjust in the future. With respect to the SPIKES approach, patients report that physicians struggle most with the “perception,” “invitation,” and “strategy and summary” components.5 Our objective should be keeping the patient’s needs in mind, rather than our own, to maximize the chance of doing a good job. If this task is done well, not only are patients more likely to have positive emotional adjustments to their diagnosis but also more adherence with future therapies.4 In the end, it is the patient who has the final say on whether it was done well or not.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She reports no relevant financial disclosures.
References
1. Baile WF et al. Oncologist. 2000;5(4):302-11.
2. Girgis A et al. Behav Med. 1999 Summer;25(2):69-77.
3. Schmid MM et al. Patient Educ Couns. 2005 Sep;58(3):244-51.
4. Girgis A et al. J Clin Oncol. 1995 Sep;13(9):2449-56.
5. Marscholiek P et al. J Cancer Educ. 2018 Feb 5. doi: 10.1007/s13187-017-1315-3.
Parental leave not available to all academic surgeons
Paid parental leave policies have been unevenly adopted among academic medical centers, according to a study published in the Journal of Surgical Research. These policies, or their lack, may have important ramifications for recruiting and specialty selection by surgeons, and for women of child-rearing age in particular.
Parental leave for surgeons has been championed by the American College of Surgeons, among other professional societies, in formal statements and supportive policies in recent years.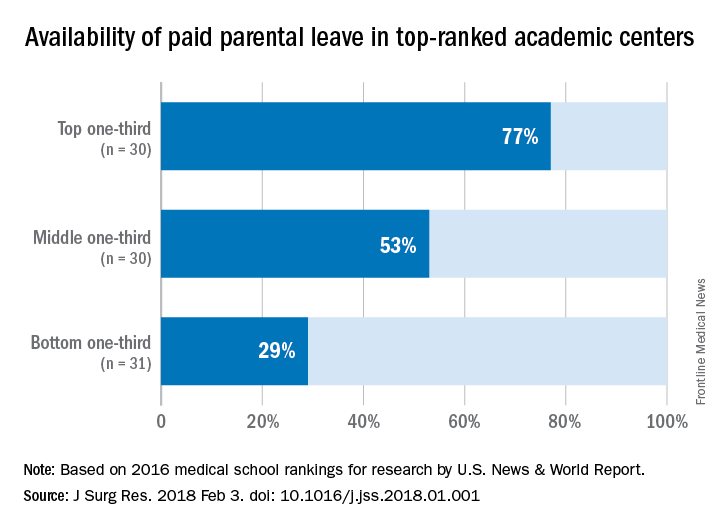
Dina S. Itum, MD, a fifth-year resident in the department of surgery, University of Texas Southwestern Medical Center, Houston, and a research team looked into how widespread parental leave is for surgeons in US medical centers. Their sample was the 91 top-ranked academic medical centers identified by U.S. News & World Report in 2016. The method used by U.S. News & World Report for ranking medical centers is based on student selectivity, dean and residency directors’ peer assessment of national institutions, faculty to student ratio, and the dollar amount in NIH research grants received.
“Parental leave” was defined by the research team as any leave dedicated to new mothers, fathers and/or primary caregivers after childbirth or adoption. “Paid leave” was defined as some protected leave with salary without mandated use of sick leave or vacation leave.
The study found that among the top-ranked 91 institutions, 48 (53%) offered some form of paid parental leave to faculty surgeons. The higher the rating, the more likely the institution offered paid parental leave: 77% of those in the top third of rankings vs. 53% in the middle third and 29% in the bottom third. Private institutions were more likely to offer paid leave of 6 weeks or longer; 67% vs. 33% of public institutions.
The investigators posed a question: Did these institutions implement the policy to attract the top talent, or did the policy improve faculty morale and productivity leading to a higher ranking? The study does not answer the question, but the investigators consider it an important issue for further study.
The investigators also suggested that surgeons of child-rearing age use parental leave information their in their own employment negotiations. “As physicians, we are aware of the health care benefits associated with parental leave, and as leaders within our communities, we should be at the forefront of supporting further advancement of this benefit,” the investigators wrote.
The investigators reported having no financial disclosures.
SOURCE: Itum DS et al. J Surg Res. 2018 Feb 3. doi. org/10.1016/j.jss.2018.01.001.
Paid parental leave policies have been unevenly adopted among academic medical centers, according to a study published in the Journal of Surgical Research. These policies, or their lack, may have important ramifications for recruiting and specialty selection by surgeons, and for women of child-rearing age in particular.
Parental leave for surgeons has been championed by the American College of Surgeons, among other professional societies, in formal statements and supportive policies in recent years.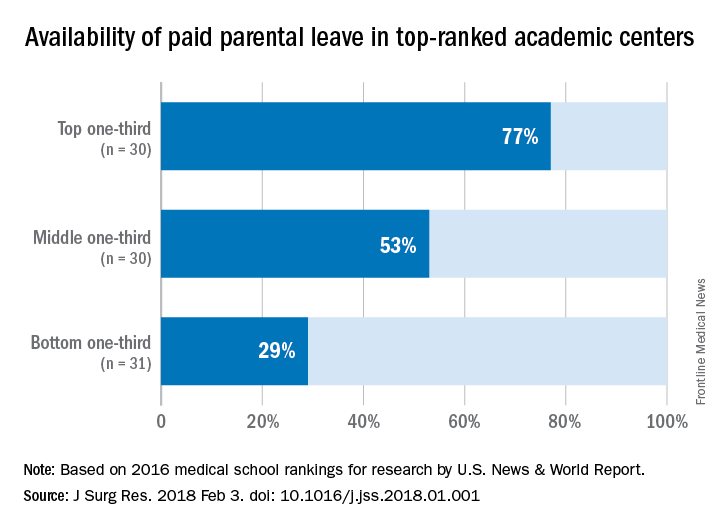
Dina S. Itum, MD, a fifth-year resident in the department of surgery, University of Texas Southwestern Medical Center, Houston, and a research team looked into how widespread parental leave is for surgeons in US medical centers. Their sample was the 91 top-ranked academic medical centers identified by U.S. News & World Report in 2016. The method used by U.S. News & World Report for ranking medical centers is based on student selectivity, dean and residency directors’ peer assessment of national institutions, faculty to student ratio, and the dollar amount in NIH research grants received.
“Parental leave” was defined by the research team as any leave dedicated to new mothers, fathers and/or primary caregivers after childbirth or adoption. “Paid leave” was defined as some protected leave with salary without mandated use of sick leave or vacation leave.
The study found that among the top-ranked 91 institutions, 48 (53%) offered some form of paid parental leave to faculty surgeons. The higher the rating, the more likely the institution offered paid parental leave: 77% of those in the top third of rankings vs. 53% in the middle third and 29% in the bottom third. Private institutions were more likely to offer paid leave of 6 weeks or longer; 67% vs. 33% of public institutions.
The investigators posed a question: Did these institutions implement the policy to attract the top talent, or did the policy improve faculty morale and productivity leading to a higher ranking? The study does not answer the question, but the investigators consider it an important issue for further study.
The investigators also suggested that surgeons of child-rearing age use parental leave information their in their own employment negotiations. “As physicians, we are aware of the health care benefits associated with parental leave, and as leaders within our communities, we should be at the forefront of supporting further advancement of this benefit,” the investigators wrote.
The investigators reported having no financial disclosures.
SOURCE: Itum DS et al. J Surg Res. 2018 Feb 3. doi. org/10.1016/j.jss.2018.01.001.
Paid parental leave policies have been unevenly adopted among academic medical centers, according to a study published in the Journal of Surgical Research. These policies, or their lack, may have important ramifications for recruiting and specialty selection by surgeons, and for women of child-rearing age in particular.
Parental leave for surgeons has been championed by the American College of Surgeons, among other professional societies, in formal statements and supportive policies in recent years.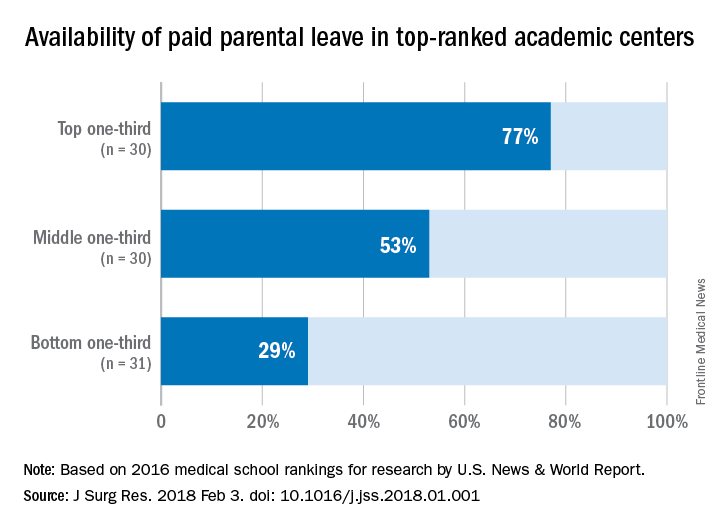
Dina S. Itum, MD, a fifth-year resident in the department of surgery, University of Texas Southwestern Medical Center, Houston, and a research team looked into how widespread parental leave is for surgeons in US medical centers. Their sample was the 91 top-ranked academic medical centers identified by U.S. News & World Report in 2016. The method used by U.S. News & World Report for ranking medical centers is based on student selectivity, dean and residency directors’ peer assessment of national institutions, faculty to student ratio, and the dollar amount in NIH research grants received.
“Parental leave” was defined by the research team as any leave dedicated to new mothers, fathers and/or primary caregivers after childbirth or adoption. “Paid leave” was defined as some protected leave with salary without mandated use of sick leave or vacation leave.
The study found that among the top-ranked 91 institutions, 48 (53%) offered some form of paid parental leave to faculty surgeons. The higher the rating, the more likely the institution offered paid parental leave: 77% of those in the top third of rankings vs. 53% in the middle third and 29% in the bottom third. Private institutions were more likely to offer paid leave of 6 weeks or longer; 67% vs. 33% of public institutions.
The investigators posed a question: Did these institutions implement the policy to attract the top talent, or did the policy improve faculty morale and productivity leading to a higher ranking? The study does not answer the question, but the investigators consider it an important issue for further study.
The investigators also suggested that surgeons of child-rearing age use parental leave information their in their own employment negotiations. “As physicians, we are aware of the health care benefits associated with parental leave, and as leaders within our communities, we should be at the forefront of supporting further advancement of this benefit,” the investigators wrote.
The investigators reported having no financial disclosures.
SOURCE: Itum DS et al. J Surg Res. 2018 Feb 3. doi. org/10.1016/j.jss.2018.01.001.
FROM THE JOURNAL OF SURGICAL RESEARCH
Key clinical point: Parental leave policies have been unevenly adopted by U.S. medical schools.
Major finding: Among the top 91 ranked medical schools, 53% offer paid parental leave.
Data source: Survey of 91 top academic medical centers identified in U.S. News & World Report 2016 listing.
Disclosures: The investigators reported having no financial disclosures.
SOURCE: Itum DS et al. J Surg Res. 2018 Feb 3. doi. org/10.1016/j.jss.2018.01.001.
Salpingectomy at cesarean feasible, but adds to operative time
DALLAS – Salpingectomy – which can reduce the risk for later ovarian cancer – was completed successfully in about two-thirds of women who desired permanent contraception at cesarean delivery and were randomized to receive this procedure rather than simple tubal ligation.
In a study of 80 patients, operative times were longer by 15 minutes for those who received salpingectomy, and neither group had adverse outcomes or serious complications, according to Akila Subramaniam, MD, who presented the findings of the single-site Salpingectomy at Cesarean Delivery for Ovarian Cancer Reduction (SCORE) trial at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The strategy to perform salpingectomy during cesarean delivery may be one way to reduce the incidence of ovarian cancer, “the most lethal gynecologic malignancy in the United States,” said Dr. Subramaniam, a maternal-fetal medicine specialist at the University of Alabama at Birmingham. “Primary prevention is the focus to reduce the ovarian cancer burden.”
However, Dr. Subramaniam said, there had been limited prospective data on salpingectomy performed at the time of cesarean delivery. One theoretical concern is an increased risk of bleeding; another is the additional operative time required for a potentially difficult dissection of the entire fallopian tube.
Dr. Subramaniam and her colleagues constructed a clinical trial that asked patients who were receiving cesarean delivery and who desired surgical sterilization to agree to randomization to complete salpingectomy or standard tubal ligation. Patient allocation was determined by computer-generated numbers, placed in a sealed envelope, and revealed to the surgeon only at the time of the opening incision for the cesarean procedure. Patients were unaware of the allocation until hospital discharge.
The single-center trial enrolled women undergoing a planned cesarean delivery at 35 or more weeks’ gestation, including those who had previous cesareans and women with multiple gestations or fetal malpresentations. Women who went on to cesarean after a trial of labor after prior cesarean were also eligible.
Patients younger than 25 years and patients with known fetal anomalies or fetal demise were excluded, as were women with previous tubal surgery and those who were anticoagulated or had immunodeficiency. The study did not enroll women who were known to carry the BRCA mutation.
Patients who were randomized to the intervention arm received a complete salpingectomy involving excision from the fimbriae to within 1 cm of the cornua, when technically feasible. The control arm participants received a standard bilateral tubal ligation using either the modified Pomeroy technique or the Parkland technique.
All study participants received routine pre- and postoperative care and instructions, and had study follow-up visits at 1 and 6 weeks post partum.
The study had two primary endpoints: rate of bilateral completion of the randomized procedure, and mean total operative time measured from skin incision to closure. Secondary outcomes included assessments of blood loss and surgical complications, followed through the 6-week postpartum visit.
The study just met the predetermined statistical power needed to detect a 10-minute difference in operative time, enrolling 80 patients and randomizing 40 to each arm.
Of the 40 patients randomized to salpingectomy, 27 (67.5%) received the intended complete salpingectomy. Three had a unilateral salpingectomy, with a tubal ligation contralaterally. Eight patients received bilateral tubal ligations, and in two patients, the surgeon was unable to perform any sterilization procedure at all.
In the tubal ligation arm, 38 patients (95%) received bilateral tubal ligation, 1 patient received a unilateral tubal ligation and a unilateral salpingectomy, and 1 patient received no procedure. The difference in success of completing the intended procedures between the two study arms was statistically significant (P = .002); in both groups, adhesions and scarring were the primary impediments to successful completion of the intended procedure, Dr. Subramaniam said.
Operative times were longer by about 15 minutes in the salpingectomy arm, with the difference accounted for by the longer duration of the sterilization procedure. No significant differences were seen in estimated blood loss or decrease in hematocrit between the two groups, and pain scores were similar.
The study, which successfully recruited 80 women from 221 approached, “may be underpowered for safety outcomes,” said Dr. Subramaniam. She also pointed out that there was no assessment of ovarian reserve, and that it’s not possible to assess the true risk reduction of salpingectomy in this study design.
Still, “It’s reasonable to consider this surgical sterilization method during cesarean as an ovarian cancer risk-reducing strategy.” One impediment to study recruitment, she said, was that after receiving education about salpingectomy, many patients desired salpingectomy and were not willing to risk randomization to simple tubal ligation.
Dr. Subramaniam reported receiving research funding for the study from the Debra Kogan Lyda Memorial Ovarian Cancer Fund.
SOURCE: Subramaniam A et al. Am J Obstet Gynecol. 2018 Jan;218:S27-8.
DALLAS – Salpingectomy – which can reduce the risk for later ovarian cancer – was completed successfully in about two-thirds of women who desired permanent contraception at cesarean delivery and were randomized to receive this procedure rather than simple tubal ligation.
In a study of 80 patients, operative times were longer by 15 minutes for those who received salpingectomy, and neither group had adverse outcomes or serious complications, according to Akila Subramaniam, MD, who presented the findings of the single-site Salpingectomy at Cesarean Delivery for Ovarian Cancer Reduction (SCORE) trial at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The strategy to perform salpingectomy during cesarean delivery may be one way to reduce the incidence of ovarian cancer, “the most lethal gynecologic malignancy in the United States,” said Dr. Subramaniam, a maternal-fetal medicine specialist at the University of Alabama at Birmingham. “Primary prevention is the focus to reduce the ovarian cancer burden.”
However, Dr. Subramaniam said, there had been limited prospective data on salpingectomy performed at the time of cesarean delivery. One theoretical concern is an increased risk of bleeding; another is the additional operative time required for a potentially difficult dissection of the entire fallopian tube.
Dr. Subramaniam and her colleagues constructed a clinical trial that asked patients who were receiving cesarean delivery and who desired surgical sterilization to agree to randomization to complete salpingectomy or standard tubal ligation. Patient allocation was determined by computer-generated numbers, placed in a sealed envelope, and revealed to the surgeon only at the time of the opening incision for the cesarean procedure. Patients were unaware of the allocation until hospital discharge.
The single-center trial enrolled women undergoing a planned cesarean delivery at 35 or more weeks’ gestation, including those who had previous cesareans and women with multiple gestations or fetal malpresentations. Women who went on to cesarean after a trial of labor after prior cesarean were also eligible.
Patients younger than 25 years and patients with known fetal anomalies or fetal demise were excluded, as were women with previous tubal surgery and those who were anticoagulated or had immunodeficiency. The study did not enroll women who were known to carry the BRCA mutation.
Patients who were randomized to the intervention arm received a complete salpingectomy involving excision from the fimbriae to within 1 cm of the cornua, when technically feasible. The control arm participants received a standard bilateral tubal ligation using either the modified Pomeroy technique or the Parkland technique.
All study participants received routine pre- and postoperative care and instructions, and had study follow-up visits at 1 and 6 weeks post partum.
The study had two primary endpoints: rate of bilateral completion of the randomized procedure, and mean total operative time measured from skin incision to closure. Secondary outcomes included assessments of blood loss and surgical complications, followed through the 6-week postpartum visit.
The study just met the predetermined statistical power needed to detect a 10-minute difference in operative time, enrolling 80 patients and randomizing 40 to each arm.
Of the 40 patients randomized to salpingectomy, 27 (67.5%) received the intended complete salpingectomy. Three had a unilateral salpingectomy, with a tubal ligation contralaterally. Eight patients received bilateral tubal ligations, and in two patients, the surgeon was unable to perform any sterilization procedure at all.
In the tubal ligation arm, 38 patients (95%) received bilateral tubal ligation, 1 patient received a unilateral tubal ligation and a unilateral salpingectomy, and 1 patient received no procedure. The difference in success of completing the intended procedures between the two study arms was statistically significant (P = .002); in both groups, adhesions and scarring were the primary impediments to successful completion of the intended procedure, Dr. Subramaniam said.
Operative times were longer by about 15 minutes in the salpingectomy arm, with the difference accounted for by the longer duration of the sterilization procedure. No significant differences were seen in estimated blood loss or decrease in hematocrit between the two groups, and pain scores were similar.
The study, which successfully recruited 80 women from 221 approached, “may be underpowered for safety outcomes,” said Dr. Subramaniam. She also pointed out that there was no assessment of ovarian reserve, and that it’s not possible to assess the true risk reduction of salpingectomy in this study design.
Still, “It’s reasonable to consider this surgical sterilization method during cesarean as an ovarian cancer risk-reducing strategy.” One impediment to study recruitment, she said, was that after receiving education about salpingectomy, many patients desired salpingectomy and were not willing to risk randomization to simple tubal ligation.
Dr. Subramaniam reported receiving research funding for the study from the Debra Kogan Lyda Memorial Ovarian Cancer Fund.
SOURCE: Subramaniam A et al. Am J Obstet Gynecol. 2018 Jan;218:S27-8.
DALLAS – Salpingectomy – which can reduce the risk for later ovarian cancer – was completed successfully in about two-thirds of women who desired permanent contraception at cesarean delivery and were randomized to receive this procedure rather than simple tubal ligation.
In a study of 80 patients, operative times were longer by 15 minutes for those who received salpingectomy, and neither group had adverse outcomes or serious complications, according to Akila Subramaniam, MD, who presented the findings of the single-site Salpingectomy at Cesarean Delivery for Ovarian Cancer Reduction (SCORE) trial at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The strategy to perform salpingectomy during cesarean delivery may be one way to reduce the incidence of ovarian cancer, “the most lethal gynecologic malignancy in the United States,” said Dr. Subramaniam, a maternal-fetal medicine specialist at the University of Alabama at Birmingham. “Primary prevention is the focus to reduce the ovarian cancer burden.”
However, Dr. Subramaniam said, there had been limited prospective data on salpingectomy performed at the time of cesarean delivery. One theoretical concern is an increased risk of bleeding; another is the additional operative time required for a potentially difficult dissection of the entire fallopian tube.
Dr. Subramaniam and her colleagues constructed a clinical trial that asked patients who were receiving cesarean delivery and who desired surgical sterilization to agree to randomization to complete salpingectomy or standard tubal ligation. Patient allocation was determined by computer-generated numbers, placed in a sealed envelope, and revealed to the surgeon only at the time of the opening incision for the cesarean procedure. Patients were unaware of the allocation until hospital discharge.
The single-center trial enrolled women undergoing a planned cesarean delivery at 35 or more weeks’ gestation, including those who had previous cesareans and women with multiple gestations or fetal malpresentations. Women who went on to cesarean after a trial of labor after prior cesarean were also eligible.
Patients younger than 25 years and patients with known fetal anomalies or fetal demise were excluded, as were women with previous tubal surgery and those who were anticoagulated or had immunodeficiency. The study did not enroll women who were known to carry the BRCA mutation.
Patients who were randomized to the intervention arm received a complete salpingectomy involving excision from the fimbriae to within 1 cm of the cornua, when technically feasible. The control arm participants received a standard bilateral tubal ligation using either the modified Pomeroy technique or the Parkland technique.
All study participants received routine pre- and postoperative care and instructions, and had study follow-up visits at 1 and 6 weeks post partum.
The study had two primary endpoints: rate of bilateral completion of the randomized procedure, and mean total operative time measured from skin incision to closure. Secondary outcomes included assessments of blood loss and surgical complications, followed through the 6-week postpartum visit.
The study just met the predetermined statistical power needed to detect a 10-minute difference in operative time, enrolling 80 patients and randomizing 40 to each arm.
Of the 40 patients randomized to salpingectomy, 27 (67.5%) received the intended complete salpingectomy. Three had a unilateral salpingectomy, with a tubal ligation contralaterally. Eight patients received bilateral tubal ligations, and in two patients, the surgeon was unable to perform any sterilization procedure at all.
In the tubal ligation arm, 38 patients (95%) received bilateral tubal ligation, 1 patient received a unilateral tubal ligation and a unilateral salpingectomy, and 1 patient received no procedure. The difference in success of completing the intended procedures between the two study arms was statistically significant (P = .002); in both groups, adhesions and scarring were the primary impediments to successful completion of the intended procedure, Dr. Subramaniam said.
Operative times were longer by about 15 minutes in the salpingectomy arm, with the difference accounted for by the longer duration of the sterilization procedure. No significant differences were seen in estimated blood loss or decrease in hematocrit between the two groups, and pain scores were similar.
The study, which successfully recruited 80 women from 221 approached, “may be underpowered for safety outcomes,” said Dr. Subramaniam. She also pointed out that there was no assessment of ovarian reserve, and that it’s not possible to assess the true risk reduction of salpingectomy in this study design.
Still, “It’s reasonable to consider this surgical sterilization method during cesarean as an ovarian cancer risk-reducing strategy.” One impediment to study recruitment, she said, was that after receiving education about salpingectomy, many patients desired salpingectomy and were not willing to risk randomization to simple tubal ligation.
Dr. Subramaniam reported receiving research funding for the study from the Debra Kogan Lyda Memorial Ovarian Cancer Fund.
SOURCE: Subramaniam A et al. Am J Obstet Gynecol. 2018 Jan;218:S27-8.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: Salpingectomy was successful in two-thirds of patients but added 15 minutes to operative time.
Major finding: The intended procedure was successful in 27 of 40 salpingectomy patients (67.5%) and 38 of 40 tubal ligation patients (95%; P = .02).
Study details: Randomized controlled trial of 80 women receiving bilateral salpingectomy or tubal ligation at cesarean delivery.
Disclosures: Study funding was received from the Debra Kogan Lyda Memorial Ovarian Cancer Fund.
Source: Subramaniam A et al. Am J Obstet Gynecol. 2018 Jan;218:S27-8.