User login
Infliximab safe for recently vaccinated Kawasaki patients
Infliximab is safe to use in infants and young children with Kawasaki disease (KD) who have recently received live viral vaccinations, reported Aaron M. Lee, MS, and his associates at Rady Children’s Hospital-San Diego.
The study included 38 children, aged either less than 18 months or 4-6 years, who received either a 5 mg/kg or a 10 mg/kg dose of infliximab within 90 days of receiving a live vaccination of MMR, varicella-zoster virus, or rotavirus. During a 90-day follow-up period, no serious infections requiring antimicrobial therapy or hospitalization were reported. A single patient who received an MMR/VZV vaccine 42 days before infliximab treatment developed urticaria 15 minutes after the infliximab transfusion began, which was resolved with hydroxyzine.
“The data presented here suggest that a single dose of infliximab can be safely administered to acute KD patients regardless of recent live virus vaccination,” the investigators concluded.
Find the full report in the Pediatric Infectious Disease Journal (2017 Apr;36(4):435-7).
Infliximab is safe to use in infants and young children with Kawasaki disease (KD) who have recently received live viral vaccinations, reported Aaron M. Lee, MS, and his associates at Rady Children’s Hospital-San Diego.
The study included 38 children, aged either less than 18 months or 4-6 years, who received either a 5 mg/kg or a 10 mg/kg dose of infliximab within 90 days of receiving a live vaccination of MMR, varicella-zoster virus, or rotavirus. During a 90-day follow-up period, no serious infections requiring antimicrobial therapy or hospitalization were reported. A single patient who received an MMR/VZV vaccine 42 days before infliximab treatment developed urticaria 15 minutes after the infliximab transfusion began, which was resolved with hydroxyzine.
“The data presented here suggest that a single dose of infliximab can be safely administered to acute KD patients regardless of recent live virus vaccination,” the investigators concluded.
Find the full report in the Pediatric Infectious Disease Journal (2017 Apr;36(4):435-7).
Infliximab is safe to use in infants and young children with Kawasaki disease (KD) who have recently received live viral vaccinations, reported Aaron M. Lee, MS, and his associates at Rady Children’s Hospital-San Diego.
The study included 38 children, aged either less than 18 months or 4-6 years, who received either a 5 mg/kg or a 10 mg/kg dose of infliximab within 90 days of receiving a live vaccination of MMR, varicella-zoster virus, or rotavirus. During a 90-day follow-up period, no serious infections requiring antimicrobial therapy or hospitalization were reported. A single patient who received an MMR/VZV vaccine 42 days before infliximab treatment developed urticaria 15 minutes after the infliximab transfusion began, which was resolved with hydroxyzine.
“The data presented here suggest that a single dose of infliximab can be safely administered to acute KD patients regardless of recent live virus vaccination,” the investigators concluded.
Find the full report in the Pediatric Infectious Disease Journal (2017 Apr;36(4):435-7).
FROM THE PEDIATRIC INFECTIOUS DISEASE JOURNAL
Maternal Tdap vaccination highly protective against infant pertussis
, results of a study show.
From 2010 to 2015, researchers collected data from a cohort study of full-term infants born at Kaiser Permanente of Northern California. “We estimated the effectiveness of maternal pertussis vaccination for protecting newborns against pertussis in the first 2 months of life and in the first year of life, accounting for each infant DTaP dose,” said Roger Baxter, MD, and his associates at Kaiser Permanente Vaccine Study Center, Oakland, Calif.
The vaccine effectiveness was an estimated 88% before infants had any DTaP vaccine doses, 81% between doses 1 and 2, 6% between doses 2 and 3, and 66% after infants had 3 DTaP doses.
“This result is consistent with 2 earlier studies in the United Kingdom” showing protection in infants less than 3 months of age, and a U.S. study showing maternal Tdap vaccination conferring protection to infants in the first 8 weeks of life, the researchers said.
In conclusion, even after infant DTaP dosing, there was evidence of additional protection from maternal Tdap vaccination for the first year of life (Pediatrics. 2017 Apr 3. doi: 10.1542/peds.2016-4091).
, results of a study show.
From 2010 to 2015, researchers collected data from a cohort study of full-term infants born at Kaiser Permanente of Northern California. “We estimated the effectiveness of maternal pertussis vaccination for protecting newborns against pertussis in the first 2 months of life and in the first year of life, accounting for each infant DTaP dose,” said Roger Baxter, MD, and his associates at Kaiser Permanente Vaccine Study Center, Oakland, Calif.
The vaccine effectiveness was an estimated 88% before infants had any DTaP vaccine doses, 81% between doses 1 and 2, 6% between doses 2 and 3, and 66% after infants had 3 DTaP doses.
“This result is consistent with 2 earlier studies in the United Kingdom” showing protection in infants less than 3 months of age, and a U.S. study showing maternal Tdap vaccination conferring protection to infants in the first 8 weeks of life, the researchers said.
In conclusion, even after infant DTaP dosing, there was evidence of additional protection from maternal Tdap vaccination for the first year of life (Pediatrics. 2017 Apr 3. doi: 10.1542/peds.2016-4091).
, results of a study show.
From 2010 to 2015, researchers collected data from a cohort study of full-term infants born at Kaiser Permanente of Northern California. “We estimated the effectiveness of maternal pertussis vaccination for protecting newborns against pertussis in the first 2 months of life and in the first year of life, accounting for each infant DTaP dose,” said Roger Baxter, MD, and his associates at Kaiser Permanente Vaccine Study Center, Oakland, Calif.
The vaccine effectiveness was an estimated 88% before infants had any DTaP vaccine doses, 81% between doses 1 and 2, 6% between doses 2 and 3, and 66% after infants had 3 DTaP doses.
“This result is consistent with 2 earlier studies in the United Kingdom” showing protection in infants less than 3 months of age, and a U.S. study showing maternal Tdap vaccination conferring protection to infants in the first 8 weeks of life, the researchers said.
In conclusion, even after infant DTaP dosing, there was evidence of additional protection from maternal Tdap vaccination for the first year of life (Pediatrics. 2017 Apr 3. doi: 10.1542/peds.2016-4091).
In ‘stealth move,’ Mich. refines vaccine waivers, improves rate among kids
Just 3 years ago, Michigan had the fourth-highest rate of unvaccinated kindergartners in the nation. But, when a charter school in northwestern Traverse City reported nearly two dozen cases of whooping cough and several cases of measles that November, state officials were jolted to action.
Without much fanfare – or time for opponents to respond – they abandoned the state’s relatively loose rules for getting an exemption and issued a regulation requiring families to consult personally with local public health departments before obtaining an immunization waiver.
The new rule sidestepped potential ideological firefights in the state legislature, which have plagued lawmakers in other states who are trying to crack down on vaccination waivers. The regulation had a dramatic effect. In the first year, the Michigan Department of Health & Human Services reported that the number of statewide waivers issued had plunged 35%. Today, Michigan is in the middle of the pack among vaccination rates.
“The idea was to make the process more burdensome,” said Michigan State University health policy specialist Mark Largent, PhD, who has written extensively about vaccines. “Research has shown that, if you make it more inconvenient to apply for a waiver, fewer people get them.”
Michigan’s experience demonstrates a way for governments to increase immunization rates without having to address religious or philosophical opposition to vaccines.
For many years, opposition to mandatory childhood vaccines has served as a frequent rallying point for those who see immunizations as interference with nature’s intentions, rebel against them as government meddling in family affairs, or raise concerns about their safety.
Vaccine advocates and health professionals regard these views as dangerous, noting that the drugs have dramatically lowered the number of serious childhood illnesses and that studies suggesting they are not safe have been debunked. They also note that vaccines’ proven effectiveness lies in “herd immunity” – the higher the participation rate, the greater the community’s protection against outbreaks of infectious disease.
Many states adopt strategies to curb exemptions “by making applications complicated to fill out or complete,” according to University of Georgia public policy expert W. David Bradford, PhD, who studies immunization. Some states require parents to notarize applications or have them certified by a physician before sending them in, and, “generally speaking, anything that raises the opportunity cost [of exemptions] works to some degree,” Bradford said. “Michigan took it a step further.”
Increasing the number of vaccinated kids in Michigan, which has a Republican governor and Republican majorities in both legislative houses, took a degree of political finesse.
“Health & Human Services wanted to do something, but the legislative option wasn’t there,” Dr. Largent said. Instead, Michigan decided to use a strategy he calls “inconvenience.”
Since 1978, Michigan had required schoolchildren entering kindergarten and middle school to obtain vaccination waiver certificates from county officials. “Some counties allowed you to do it over the phone; in others you mailed in a form and some even let you do it online,” Dr. Largent said. But, in studying vaccine policy across the country, he noted, “One thing is really clear – health departments that require you to go in and get the waiver have much lower rates.”
Michigan offered the perfect vehicle for introducing inconvenience into the process. The Joint Committee on Administrative Rules reviews state agency regulations and, if it takes no action, allows them to go into effect after 15 legislative days. The committee is composed of lawmakers, giving it a legislative imprimatur, but it is not the legislature itself, thus avoiding the political rancor that can accompany debate on controversial issues.
During the 2013-14 school year, the federal Centers for Disease Control and Prevention found that Michigan had the fourth-highest rate of children entering kindergarten who had been exempted from vaccinations. The state Health & Human Services officials proposed a simple requirement: Parents seeking vaccine waivers must be briefed in person by a county health educator before a waiver would be granted. The joint committee approved the rule Dec. 11, 2014. It took effect Jan. 1, 2015.
“We were not aware of the rule until the day it happened,” said Suzanne Waltman, president of Michigan for Vaccine Choice, an antivaccine organization. “We thought it was a stealth move.”
The office of Gov. Rick Snyder did not respond directly to requests for comment on the political hazards of vaccine policy. Retired Republican state Sen. John Pappageorge, cochair of the administrative rules committee in 2014, voted to adopt the rule and described the procedure as a simple one designed to ensure “that implementation is in concurrence with the law.” Republican Rep. Tom McMillin, who was cochair of the committee at the time and voted against the rule, did not respond to requests for an interview.
In a look at one key metric, before 2015, about 22% of Michigan children did not get the fourth round of immunizations for diphtheria, tetanus, and pertussis that is required by the state. That had fallen to 15% 1 year later, slightly better than the national average.
The Traverse City outbreaks were overshadowed in the national media by a more dramatic measles outbreak in Southern California’s Disneyland, which also occurred over the 2014-15 holidays and ultimately led to 150 cases of the disease. But the states’ responses were quite different.
California’s solution was what Dr. Largent calls “eliminationism.” The state Legislature, with Democratic supermajorities, passed a measure doing away with religious and philosophical vaccine exemptions. Passage of the law triggered widespread protests among opponents of vaccines. Besides California, only West Virginia and Mississippi disallow nonmedical waivers.
Dr. Largent said a small number of children need waivers for medical reasons, usually because of allergies or immune deficiencies. Much larger numbers seek waivers for religious or philosophical reasons.
“The idea was to bring the waiver rate down,” Michigan Health & Human Services spokeswoman Angela Minicuci said. “From the perspective of the general population, vaccinations are recommended. This doesn’t take away choice. It simply ensures that people have education.”
But, Dr. Largent said most vaccine opponents are not necessarily swayed by arguments in favor of immunization. Instead, “by heightening the burden, you change some of the incentives” for obtaining waivers. “Moral claims and ideology don’t matter as much when it’s inconvenient.”
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Just 3 years ago, Michigan had the fourth-highest rate of unvaccinated kindergartners in the nation. But, when a charter school in northwestern Traverse City reported nearly two dozen cases of whooping cough and several cases of measles that November, state officials were jolted to action.
Without much fanfare – or time for opponents to respond – they abandoned the state’s relatively loose rules for getting an exemption and issued a regulation requiring families to consult personally with local public health departments before obtaining an immunization waiver.
The new rule sidestepped potential ideological firefights in the state legislature, which have plagued lawmakers in other states who are trying to crack down on vaccination waivers. The regulation had a dramatic effect. In the first year, the Michigan Department of Health & Human Services reported that the number of statewide waivers issued had plunged 35%. Today, Michigan is in the middle of the pack among vaccination rates.
“The idea was to make the process more burdensome,” said Michigan State University health policy specialist Mark Largent, PhD, who has written extensively about vaccines. “Research has shown that, if you make it more inconvenient to apply for a waiver, fewer people get them.”
Michigan’s experience demonstrates a way for governments to increase immunization rates without having to address religious or philosophical opposition to vaccines.
For many years, opposition to mandatory childhood vaccines has served as a frequent rallying point for those who see immunizations as interference with nature’s intentions, rebel against them as government meddling in family affairs, or raise concerns about their safety.
Vaccine advocates and health professionals regard these views as dangerous, noting that the drugs have dramatically lowered the number of serious childhood illnesses and that studies suggesting they are not safe have been debunked. They also note that vaccines’ proven effectiveness lies in “herd immunity” – the higher the participation rate, the greater the community’s protection against outbreaks of infectious disease.
Many states adopt strategies to curb exemptions “by making applications complicated to fill out or complete,” according to University of Georgia public policy expert W. David Bradford, PhD, who studies immunization. Some states require parents to notarize applications or have them certified by a physician before sending them in, and, “generally speaking, anything that raises the opportunity cost [of exemptions] works to some degree,” Bradford said. “Michigan took it a step further.”
Increasing the number of vaccinated kids in Michigan, which has a Republican governor and Republican majorities in both legislative houses, took a degree of political finesse.
“Health & Human Services wanted to do something, but the legislative option wasn’t there,” Dr. Largent said. Instead, Michigan decided to use a strategy he calls “inconvenience.”
Since 1978, Michigan had required schoolchildren entering kindergarten and middle school to obtain vaccination waiver certificates from county officials. “Some counties allowed you to do it over the phone; in others you mailed in a form and some even let you do it online,” Dr. Largent said. But, in studying vaccine policy across the country, he noted, “One thing is really clear – health departments that require you to go in and get the waiver have much lower rates.”
Michigan offered the perfect vehicle for introducing inconvenience into the process. The Joint Committee on Administrative Rules reviews state agency regulations and, if it takes no action, allows them to go into effect after 15 legislative days. The committee is composed of lawmakers, giving it a legislative imprimatur, but it is not the legislature itself, thus avoiding the political rancor that can accompany debate on controversial issues.
During the 2013-14 school year, the federal Centers for Disease Control and Prevention found that Michigan had the fourth-highest rate of children entering kindergarten who had been exempted from vaccinations. The state Health & Human Services officials proposed a simple requirement: Parents seeking vaccine waivers must be briefed in person by a county health educator before a waiver would be granted. The joint committee approved the rule Dec. 11, 2014. It took effect Jan. 1, 2015.
“We were not aware of the rule until the day it happened,” said Suzanne Waltman, president of Michigan for Vaccine Choice, an antivaccine organization. “We thought it was a stealth move.”
The office of Gov. Rick Snyder did not respond directly to requests for comment on the political hazards of vaccine policy. Retired Republican state Sen. John Pappageorge, cochair of the administrative rules committee in 2014, voted to adopt the rule and described the procedure as a simple one designed to ensure “that implementation is in concurrence with the law.” Republican Rep. Tom McMillin, who was cochair of the committee at the time and voted against the rule, did not respond to requests for an interview.
In a look at one key metric, before 2015, about 22% of Michigan children did not get the fourth round of immunizations for diphtheria, tetanus, and pertussis that is required by the state. That had fallen to 15% 1 year later, slightly better than the national average.
The Traverse City outbreaks were overshadowed in the national media by a more dramatic measles outbreak in Southern California’s Disneyland, which also occurred over the 2014-15 holidays and ultimately led to 150 cases of the disease. But the states’ responses were quite different.
California’s solution was what Dr. Largent calls “eliminationism.” The state Legislature, with Democratic supermajorities, passed a measure doing away with religious and philosophical vaccine exemptions. Passage of the law triggered widespread protests among opponents of vaccines. Besides California, only West Virginia and Mississippi disallow nonmedical waivers.
Dr. Largent said a small number of children need waivers for medical reasons, usually because of allergies or immune deficiencies. Much larger numbers seek waivers for religious or philosophical reasons.
“The idea was to bring the waiver rate down,” Michigan Health & Human Services spokeswoman Angela Minicuci said. “From the perspective of the general population, vaccinations are recommended. This doesn’t take away choice. It simply ensures that people have education.”
But, Dr. Largent said most vaccine opponents are not necessarily swayed by arguments in favor of immunization. Instead, “by heightening the burden, you change some of the incentives” for obtaining waivers. “Moral claims and ideology don’t matter as much when it’s inconvenient.”
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Just 3 years ago, Michigan had the fourth-highest rate of unvaccinated kindergartners in the nation. But, when a charter school in northwestern Traverse City reported nearly two dozen cases of whooping cough and several cases of measles that November, state officials were jolted to action.
Without much fanfare – or time for opponents to respond – they abandoned the state’s relatively loose rules for getting an exemption and issued a regulation requiring families to consult personally with local public health departments before obtaining an immunization waiver.
The new rule sidestepped potential ideological firefights in the state legislature, which have plagued lawmakers in other states who are trying to crack down on vaccination waivers. The regulation had a dramatic effect. In the first year, the Michigan Department of Health & Human Services reported that the number of statewide waivers issued had plunged 35%. Today, Michigan is in the middle of the pack among vaccination rates.
“The idea was to make the process more burdensome,” said Michigan State University health policy specialist Mark Largent, PhD, who has written extensively about vaccines. “Research has shown that, if you make it more inconvenient to apply for a waiver, fewer people get them.”
Michigan’s experience demonstrates a way for governments to increase immunization rates without having to address religious or philosophical opposition to vaccines.
For many years, opposition to mandatory childhood vaccines has served as a frequent rallying point for those who see immunizations as interference with nature’s intentions, rebel against them as government meddling in family affairs, or raise concerns about their safety.
Vaccine advocates and health professionals regard these views as dangerous, noting that the drugs have dramatically lowered the number of serious childhood illnesses and that studies suggesting they are not safe have been debunked. They also note that vaccines’ proven effectiveness lies in “herd immunity” – the higher the participation rate, the greater the community’s protection against outbreaks of infectious disease.
Many states adopt strategies to curb exemptions “by making applications complicated to fill out or complete,” according to University of Georgia public policy expert W. David Bradford, PhD, who studies immunization. Some states require parents to notarize applications or have them certified by a physician before sending them in, and, “generally speaking, anything that raises the opportunity cost [of exemptions] works to some degree,” Bradford said. “Michigan took it a step further.”
Increasing the number of vaccinated kids in Michigan, which has a Republican governor and Republican majorities in both legislative houses, took a degree of political finesse.
“Health & Human Services wanted to do something, but the legislative option wasn’t there,” Dr. Largent said. Instead, Michigan decided to use a strategy he calls “inconvenience.”
Since 1978, Michigan had required schoolchildren entering kindergarten and middle school to obtain vaccination waiver certificates from county officials. “Some counties allowed you to do it over the phone; in others you mailed in a form and some even let you do it online,” Dr. Largent said. But, in studying vaccine policy across the country, he noted, “One thing is really clear – health departments that require you to go in and get the waiver have much lower rates.”
Michigan offered the perfect vehicle for introducing inconvenience into the process. The Joint Committee on Administrative Rules reviews state agency regulations and, if it takes no action, allows them to go into effect after 15 legislative days. The committee is composed of lawmakers, giving it a legislative imprimatur, but it is not the legislature itself, thus avoiding the political rancor that can accompany debate on controversial issues.
During the 2013-14 school year, the federal Centers for Disease Control and Prevention found that Michigan had the fourth-highest rate of children entering kindergarten who had been exempted from vaccinations. The state Health & Human Services officials proposed a simple requirement: Parents seeking vaccine waivers must be briefed in person by a county health educator before a waiver would be granted. The joint committee approved the rule Dec. 11, 2014. It took effect Jan. 1, 2015.
“We were not aware of the rule until the day it happened,” said Suzanne Waltman, president of Michigan for Vaccine Choice, an antivaccine organization. “We thought it was a stealth move.”
The office of Gov. Rick Snyder did not respond directly to requests for comment on the political hazards of vaccine policy. Retired Republican state Sen. John Pappageorge, cochair of the administrative rules committee in 2014, voted to adopt the rule and described the procedure as a simple one designed to ensure “that implementation is in concurrence with the law.” Republican Rep. Tom McMillin, who was cochair of the committee at the time and voted against the rule, did not respond to requests for an interview.
In a look at one key metric, before 2015, about 22% of Michigan children did not get the fourth round of immunizations for diphtheria, tetanus, and pertussis that is required by the state. That had fallen to 15% 1 year later, slightly better than the national average.
The Traverse City outbreaks were overshadowed in the national media by a more dramatic measles outbreak in Southern California’s Disneyland, which also occurred over the 2014-15 holidays and ultimately led to 150 cases of the disease. But the states’ responses were quite different.
California’s solution was what Dr. Largent calls “eliminationism.” The state Legislature, with Democratic supermajorities, passed a measure doing away with religious and philosophical vaccine exemptions. Passage of the law triggered widespread protests among opponents of vaccines. Besides California, only West Virginia and Mississippi disallow nonmedical waivers.
Dr. Largent said a small number of children need waivers for medical reasons, usually because of allergies or immune deficiencies. Much larger numbers seek waivers for religious or philosophical reasons.
“The idea was to bring the waiver rate down,” Michigan Health & Human Services spokeswoman Angela Minicuci said. “From the perspective of the general population, vaccinations are recommended. This doesn’t take away choice. It simply ensures that people have education.”
But, Dr. Largent said most vaccine opponents are not necessarily swayed by arguments in favor of immunization. Instead, “by heightening the burden, you change some of the incentives” for obtaining waivers. “Moral claims and ideology don’t matter as much when it’s inconvenient.”
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Vaccination reduces risk of flu-associated pediatric deaths
.
“These results support current recommendations for annual influenza vaccination for all children 6 months of age” and older, wrote Brendan Flannery, PhD, and his coauthors at the Centers for Disease Control and Prevention, Atlanta. “To our knowledge, this is the first study to use laboratory-confirmed outcomes to investigate influenza vaccine effectiveness against influenza-associated deaths.”
“Best estimates based on [National Health Interview Survey] data suggested that vaccination reduced the risk of influenza-associated death by half among children with high-risk conditions and by nearly two-thirds among children without high-risk conditions,” Dr. Flannery and his coauthors reported.
Of 358 cases of pediatric death (aged 6 months to 17 years) confirmed to be associated with influenza, 75 (26%) had been vaccinated prior to their disease onset. The case-cohort analysis compared the 358 cases against three cohorts of U.S. children and adolescents: a telephone survey, a household survey, and a health insurance claims database.
The researchers had examined cases that were reported to the U.S. Influenza-Associated Pediatric Mortality Surveillance System from July 2010 to June 2014. They excluded cases of children not yet eligible to be vaccinated or whose disease onset may have occurred before their vaccine had 14 days to take full effect (Pediatrics. 2017 Apr. doi: 10.1542/peds.2016-4244).
.
“These results support current recommendations for annual influenza vaccination for all children 6 months of age” and older, wrote Brendan Flannery, PhD, and his coauthors at the Centers for Disease Control and Prevention, Atlanta. “To our knowledge, this is the first study to use laboratory-confirmed outcomes to investigate influenza vaccine effectiveness against influenza-associated deaths.”
“Best estimates based on [National Health Interview Survey] data suggested that vaccination reduced the risk of influenza-associated death by half among children with high-risk conditions and by nearly two-thirds among children without high-risk conditions,” Dr. Flannery and his coauthors reported.
Of 358 cases of pediatric death (aged 6 months to 17 years) confirmed to be associated with influenza, 75 (26%) had been vaccinated prior to their disease onset. The case-cohort analysis compared the 358 cases against three cohorts of U.S. children and adolescents: a telephone survey, a household survey, and a health insurance claims database.
The researchers had examined cases that were reported to the U.S. Influenza-Associated Pediatric Mortality Surveillance System from July 2010 to June 2014. They excluded cases of children not yet eligible to be vaccinated or whose disease onset may have occurred before their vaccine had 14 days to take full effect (Pediatrics. 2017 Apr. doi: 10.1542/peds.2016-4244).
.
“These results support current recommendations for annual influenza vaccination for all children 6 months of age” and older, wrote Brendan Flannery, PhD, and his coauthors at the Centers for Disease Control and Prevention, Atlanta. “To our knowledge, this is the first study to use laboratory-confirmed outcomes to investigate influenza vaccine effectiveness against influenza-associated deaths.”
“Best estimates based on [National Health Interview Survey] data suggested that vaccination reduced the risk of influenza-associated death by half among children with high-risk conditions and by nearly two-thirds among children without high-risk conditions,” Dr. Flannery and his coauthors reported.
Of 358 cases of pediatric death (aged 6 months to 17 years) confirmed to be associated with influenza, 75 (26%) had been vaccinated prior to their disease onset. The case-cohort analysis compared the 358 cases against three cohorts of U.S. children and adolescents: a telephone survey, a household survey, and a health insurance claims database.
The researchers had examined cases that were reported to the U.S. Influenza-Associated Pediatric Mortality Surveillance System from July 2010 to June 2014. They excluded cases of children not yet eligible to be vaccinated or whose disease onset may have occurred before their vaccine had 14 days to take full effect (Pediatrics. 2017 Apr. doi: 10.1542/peds.2016-4244).
FROM PEDIATRICS
Ebola vaccine maintains immune response after 1 year
People who received an Ebola virus vaccine maintained immune response one year after vaccination, according to a research letter from Rebecca L.Winslow, MRCGP, of the University of Oxford (UK) and her associates.
The immune response of 64 vaccine recipients of European descent 360 days after receiving either adenovirus type 26 vector vaccine encoding Ebolavirus glycoprotein (Ad26.ZEBOV) followed by modified vaccinia virus Ankara vector vaccine (MVA-BN-Filo), or MVA-BN-Filo followed by Ad26.ZEBOV. The 360 day follow-up occurred 120 days after the previous follow-up, during which time no significant adverse events were reported.
“Immune responses may differ in a sub-Saharan African population; these vaccine candidates are being assessed in this region. Additional research is also warranted to explore the persistence of immunity beyond 1 year following immunization and response to booster doses of vaccine,” the investigators concluded.
Find the full research letter in JAMA (doi: 10.1001/jama.2016.20644)
People who received an Ebola virus vaccine maintained immune response one year after vaccination, according to a research letter from Rebecca L.Winslow, MRCGP, of the University of Oxford (UK) and her associates.
The immune response of 64 vaccine recipients of European descent 360 days after receiving either adenovirus type 26 vector vaccine encoding Ebolavirus glycoprotein (Ad26.ZEBOV) followed by modified vaccinia virus Ankara vector vaccine (MVA-BN-Filo), or MVA-BN-Filo followed by Ad26.ZEBOV. The 360 day follow-up occurred 120 days after the previous follow-up, during which time no significant adverse events were reported.
“Immune responses may differ in a sub-Saharan African population; these vaccine candidates are being assessed in this region. Additional research is also warranted to explore the persistence of immunity beyond 1 year following immunization and response to booster doses of vaccine,” the investigators concluded.
Find the full research letter in JAMA (doi: 10.1001/jama.2016.20644)
People who received an Ebola virus vaccine maintained immune response one year after vaccination, according to a research letter from Rebecca L.Winslow, MRCGP, of the University of Oxford (UK) and her associates.
The immune response of 64 vaccine recipients of European descent 360 days after receiving either adenovirus type 26 vector vaccine encoding Ebolavirus glycoprotein (Ad26.ZEBOV) followed by modified vaccinia virus Ankara vector vaccine (MVA-BN-Filo), or MVA-BN-Filo followed by Ad26.ZEBOV. The 360 day follow-up occurred 120 days after the previous follow-up, during which time no significant adverse events were reported.
“Immune responses may differ in a sub-Saharan African population; these vaccine candidates are being assessed in this region. Additional research is also warranted to explore the persistence of immunity beyond 1 year following immunization and response to booster doses of vaccine,” the investigators concluded.
Find the full research letter in JAMA (doi: 10.1001/jama.2016.20644)
FROM JAMA
Make assessment of immunization status of older adults routine
ATLANTA – In the opinion of John M. Kelso, MD, assessment of immunization status in older adults should be a routine part of all visits.
“Don’t assume that your patients are getting their vaccines someplace else,” he said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. “We should be taking advantage of the fact that these patients are in our offices.”
Inactivated influenza vaccine (IIV3)
For adults aged 65 and older, the high-dose, trivalent version of the flu vaccine (60 micrograms of hemagglutinin per strain, or IIV3-HD) may be preferable to the standard dose of 15 micrograms of hemagglutinin per strain (IIV3-SD). A study of nearly 32,000 patients found that IIV3-HD induced significantly higher antibody responses and provided better protection against laboratory-confirmed influenza, compared with IIV3-SD (N Engl J Med. 2014;371:635-45). The relative efficacy of high dose vs. standard dose was 24.2%. “That means that one-quarter of all breakthrough influenza illnesses could be prevented if IIV3HD were used instead of IIV3-SD,” Dr. Kelso said.
Another approach is to use an adjuvanted influenza vaccine, which contains the standard 15 micrograms of influenza antigen but the adjuvant is MF59, a squalene-based oil-in-water emulsion. One small study of 282 patients aged 65 and older showed the adjuvanted vaccine to be more effective than the unadjuvanted vaccine (Vaccine. 2013;51:1622-8).
The Centers for Disease Control and Prevention does not express a preference for the high-dose or adjuvanted vaccine, but rather stresses the importance of influenza vaccination with whatever age-appropriate IIV formulation is available at the time of the patient’s visit.
The 13-valent pneumococcal conjugate vaccine (PCV13) and the 23-valent pneumococcal polysaccharide vaccine (PPSV23)
All adults who turn 65 years of age should receive the PCV13, followed 1 year later by the PPSV23. For those who already received the PPSV23 after age 65 years of age, they should receive the PCV13 at least 1 year later. “The real bulk of hospitalizations and fatalities from invasive pneumococcal disease are happening to people over 65 year of age,” said Dr. Kelso, who is also a clinical professor of pediatrics and internal medicine at the University of California, San Diego “So there’s a real need here for vaccination.”
Tdap
This should be administered to all adolescents and adults regardless of interval since their last tetanus-diphtheria vaccine. “This includes those age 65 years of age and older in whom the vaccine has been found to be equally safe and immunogenic,” Dr. Kelso said. “This is important not only to prevent pertussis in older adults, but also to prevent them from spreading the disease to infants where it can be fatal.”
Zoster vaccine
One in three adults will develop zoster during their lifetime, he said, and one million episodes occur in the United States each year. Common complications include postherpetic neuralgia and eye involvement that can result in loss of vision. The CDC recommends routine vaccination of all immunocompetent persons over age 60 with one dose of zoster vaccine. “Persons who report a previous episode of zoster can be vaccinated but it is not indicated to treat acute zoster, to prevent persons with acute zoster from developing postherpetic neuralgia, or to treat ongoing postherpetic neuralgia,” Dr. Kelso said.
He reported having no relevant financial disclosures.
ATLANTA – In the opinion of John M. Kelso, MD, assessment of immunization status in older adults should be a routine part of all visits.
“Don’t assume that your patients are getting their vaccines someplace else,” he said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. “We should be taking advantage of the fact that these patients are in our offices.”
Inactivated influenza vaccine (IIV3)
For adults aged 65 and older, the high-dose, trivalent version of the flu vaccine (60 micrograms of hemagglutinin per strain, or IIV3-HD) may be preferable to the standard dose of 15 micrograms of hemagglutinin per strain (IIV3-SD). A study of nearly 32,000 patients found that IIV3-HD induced significantly higher antibody responses and provided better protection against laboratory-confirmed influenza, compared with IIV3-SD (N Engl J Med. 2014;371:635-45). The relative efficacy of high dose vs. standard dose was 24.2%. “That means that one-quarter of all breakthrough influenza illnesses could be prevented if IIV3HD were used instead of IIV3-SD,” Dr. Kelso said.
Another approach is to use an adjuvanted influenza vaccine, which contains the standard 15 micrograms of influenza antigen but the adjuvant is MF59, a squalene-based oil-in-water emulsion. One small study of 282 patients aged 65 and older showed the adjuvanted vaccine to be more effective than the unadjuvanted vaccine (Vaccine. 2013;51:1622-8).
The Centers for Disease Control and Prevention does not express a preference for the high-dose or adjuvanted vaccine, but rather stresses the importance of influenza vaccination with whatever age-appropriate IIV formulation is available at the time of the patient’s visit.
The 13-valent pneumococcal conjugate vaccine (PCV13) and the 23-valent pneumococcal polysaccharide vaccine (PPSV23)
All adults who turn 65 years of age should receive the PCV13, followed 1 year later by the PPSV23. For those who already received the PPSV23 after age 65 years of age, they should receive the PCV13 at least 1 year later. “The real bulk of hospitalizations and fatalities from invasive pneumococcal disease are happening to people over 65 year of age,” said Dr. Kelso, who is also a clinical professor of pediatrics and internal medicine at the University of California, San Diego “So there’s a real need here for vaccination.”
Tdap
This should be administered to all adolescents and adults regardless of interval since their last tetanus-diphtheria vaccine. “This includes those age 65 years of age and older in whom the vaccine has been found to be equally safe and immunogenic,” Dr. Kelso said. “This is important not only to prevent pertussis in older adults, but also to prevent them from spreading the disease to infants where it can be fatal.”
Zoster vaccine
One in three adults will develop zoster during their lifetime, he said, and one million episodes occur in the United States each year. Common complications include postherpetic neuralgia and eye involvement that can result in loss of vision. The CDC recommends routine vaccination of all immunocompetent persons over age 60 with one dose of zoster vaccine. “Persons who report a previous episode of zoster can be vaccinated but it is not indicated to treat acute zoster, to prevent persons with acute zoster from developing postherpetic neuralgia, or to treat ongoing postherpetic neuralgia,” Dr. Kelso said.
He reported having no relevant financial disclosures.
ATLANTA – In the opinion of John M. Kelso, MD, assessment of immunization status in older adults should be a routine part of all visits.
“Don’t assume that your patients are getting their vaccines someplace else,” he said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology. “We should be taking advantage of the fact that these patients are in our offices.”
Inactivated influenza vaccine (IIV3)
For adults aged 65 and older, the high-dose, trivalent version of the flu vaccine (60 micrograms of hemagglutinin per strain, or IIV3-HD) may be preferable to the standard dose of 15 micrograms of hemagglutinin per strain (IIV3-SD). A study of nearly 32,000 patients found that IIV3-HD induced significantly higher antibody responses and provided better protection against laboratory-confirmed influenza, compared with IIV3-SD (N Engl J Med. 2014;371:635-45). The relative efficacy of high dose vs. standard dose was 24.2%. “That means that one-quarter of all breakthrough influenza illnesses could be prevented if IIV3HD were used instead of IIV3-SD,” Dr. Kelso said.
Another approach is to use an adjuvanted influenza vaccine, which contains the standard 15 micrograms of influenza antigen but the adjuvant is MF59, a squalene-based oil-in-water emulsion. One small study of 282 patients aged 65 and older showed the adjuvanted vaccine to be more effective than the unadjuvanted vaccine (Vaccine. 2013;51:1622-8).
The Centers for Disease Control and Prevention does not express a preference for the high-dose or adjuvanted vaccine, but rather stresses the importance of influenza vaccination with whatever age-appropriate IIV formulation is available at the time of the patient’s visit.
The 13-valent pneumococcal conjugate vaccine (PCV13) and the 23-valent pneumococcal polysaccharide vaccine (PPSV23)
All adults who turn 65 years of age should receive the PCV13, followed 1 year later by the PPSV23. For those who already received the PPSV23 after age 65 years of age, they should receive the PCV13 at least 1 year later. “The real bulk of hospitalizations and fatalities from invasive pneumococcal disease are happening to people over 65 year of age,” said Dr. Kelso, who is also a clinical professor of pediatrics and internal medicine at the University of California, San Diego “So there’s a real need here for vaccination.”
Tdap
This should be administered to all adolescents and adults regardless of interval since their last tetanus-diphtheria vaccine. “This includes those age 65 years of age and older in whom the vaccine has been found to be equally safe and immunogenic,” Dr. Kelso said. “This is important not only to prevent pertussis in older adults, but also to prevent them from spreading the disease to infants where it can be fatal.”
Zoster vaccine
One in three adults will develop zoster during their lifetime, he said, and one million episodes occur in the United States each year. Common complications include postherpetic neuralgia and eye involvement that can result in loss of vision. The CDC recommends routine vaccination of all immunocompetent persons over age 60 with one dose of zoster vaccine. “Persons who report a previous episode of zoster can be vaccinated but it is not indicated to treat acute zoster, to prevent persons with acute zoster from developing postherpetic neuralgia, or to treat ongoing postherpetic neuralgia,” Dr. Kelso said.
He reported having no relevant financial disclosures.
EXPERT ANALYSIS AT THE 2017 AAAAI ANNUAL MEETING
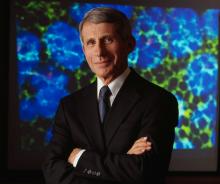
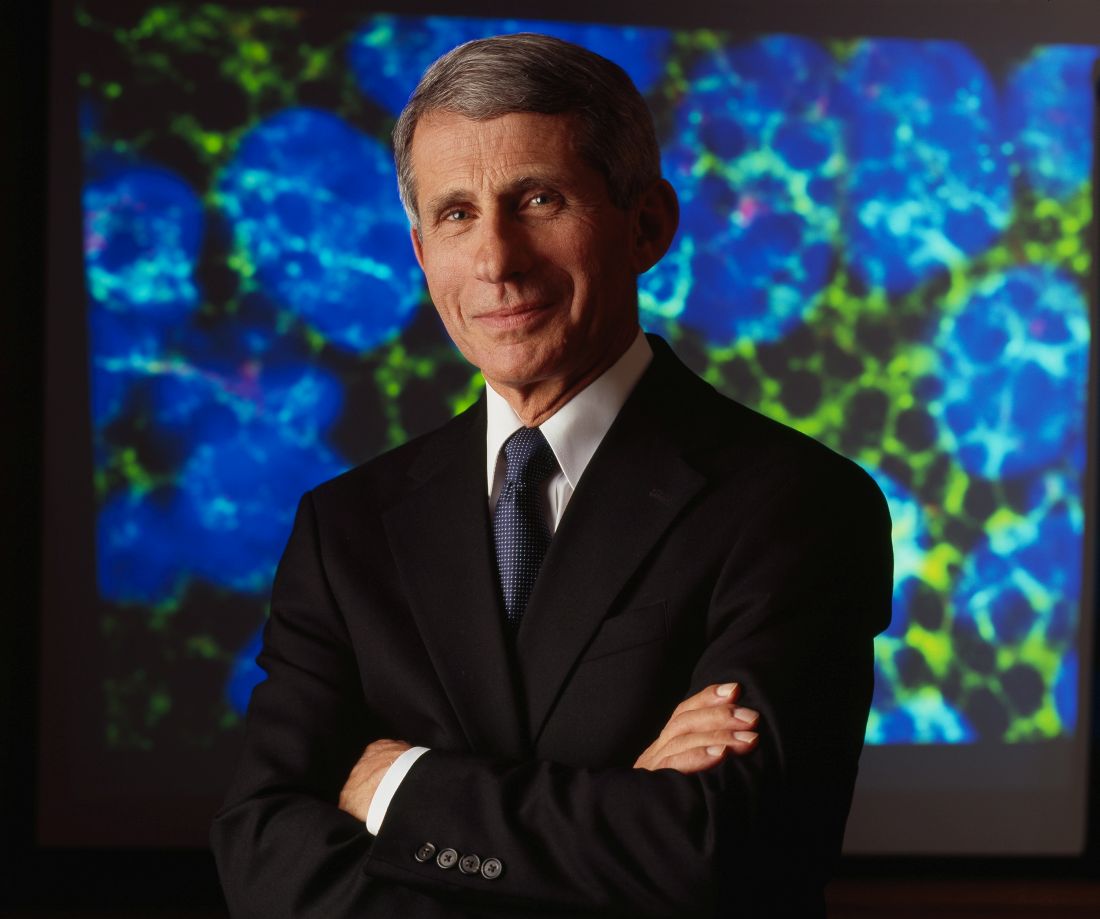
Anthony Fauci faces the ‘perpetual challenge’ of emerging infections
SAN DIEGO – Reflecting on his 33-year career as director of the National Institute of Allergy and Infectious Diseases, Anthony S. Fauci, MD, can say one thing for certain: Emerging and re-emerging infectious diseases in the continental United States are here to stay.
In an article that he and his colleagues published in the Lancet in 2008, they used the term “perpetual challenge” to describe emerging infections, a descriptor that resonates with him to this day.
Global examples of emerging and re-emerging infectious diseases he discussed include dengue, West Nile virus, chikungunya, and carbapenem-resistant Enterobacteriaceae, “which is becoming a progressively more serious problem in hospitalized patients,” said Dr. Fauci, who is also chief of the NIAID Laboratory of Immunoregulation.
“We had a serious challenge with that at our own clinical center in Bethesda just a few years ago,” he noted. Numerous cases of antimicrobial resistance in methicillin-resistant Staphylococcus aureus, Clostridium difficile, and Neisseria gonorrhoeae have been reported.
Dr. Fauci described the Ebola outbreak as “a globally important disease that had ripple effects in the United States that were unpredicted,” referring to the case of the infected man who traveled from Monrovia to Dallas on Sept. 19, 2014, and developed Ebola symptoms 5 days later. Between 2014 and 2016, there were 28,616 cases and 11,310 deaths combined in the countries of Guinea, Sierra Leone, and Liberia.
“There is virtually no health care system in those three countries,” he said. “There’s a distrust in authority, and anything we tried to do as a global health [effort] made things worse. What we’re trying to do now is built sustainable health care issues in countries that don’t have it.”
Of particular concern to public health officials worldwide is getting a lid on Zika virus, a mosquito-borne illness that can be passed from a pregnant woman to her fetus and cause an increased risk of microcephaly, particularly during the first trimester.
“Not only is there microcephaly, there’s a whole host of abnormalities that involve hearing loss, visual abnormalities, and a variety of other issues,” Dr. Fauci said. “There are about 50 countries in the Americas and the Caribbean that have Zika virus transmission.”
According to data from the Centers for Disease Control and Prevention, from Jan. 1, 2015, to March 29, 2017, there were 5,182 reported cases of Zika virus disease in the 50 states and the District of Columbia. The majority of those (4,886) were travel associated, 222 were locally acquired mosquito-borne, 45 were sexually transmitted, 27 congenital, 1 was laboratory acquired, and 1 was unknown.
At the same time, there have been 38,303 cases in the U.S. territories. Of those, 38,156 were locally acquired, and 147 were travel associated. “That’s why there’s such an intense effort to develop a Zika vaccine,” he said.
According to the CDC, as of March 15, 2017, there are 265 cases of locally transmitted cases in Florida: 216 by mosquito and the rest by sexual transmission. “Talk about surprises,” Dr. Fauci said. “Zika is the first mosquito-borne infection that can result in a congenital abnormality, the first mosquito-borne infection that can be sexually transmitted, and now we’re learning more about this problem, which is the reason why it’s very important for us to develop a vaccine.”
A phase I trial of a DNA vaccine developed by the NIH Vaccine Research Center has reached its enrollment goal of 80 patients age 18-35 years. Initial results are expected sometime in the first quarter of 2017. A phase II trial in the United States and Puerto Rico is expected to launch soon.
Dr. Fauci closed his presentation by sharing lessons learned from previous pandemics.
The first lesson is that global surveillance is required. “Namely, know what’s going on in real time,” he said. “That has to be linked to transparency and communication. So that if something happens in China, we don’t find out about it months later, but we know about it in real time.”
Infrastructure and capacity building are also important. “The lack of capacity in West Africa can ultimately have an indirect impact on us here in the United States,” he said.
“Finally, we need to coordinate and collaborate; we need adaptable platforms for vaccines,” Dr. Fauci cautioned. “Importantly, we need a stable funding mechanism such as a public health emergency fund so that we do not have to go scrambling before the Congress when we need emergency funds.”
SAN DIEGO – Reflecting on his 33-year career as director of the National Institute of Allergy and Infectious Diseases, Anthony S. Fauci, MD, can say one thing for certain: Emerging and re-emerging infectious diseases in the continental United States are here to stay.
In an article that he and his colleagues published in the Lancet in 2008, they used the term “perpetual challenge” to describe emerging infections, a descriptor that resonates with him to this day.
Global examples of emerging and re-emerging infectious diseases he discussed include dengue, West Nile virus, chikungunya, and carbapenem-resistant Enterobacteriaceae, “which is becoming a progressively more serious problem in hospitalized patients,” said Dr. Fauci, who is also chief of the NIAID Laboratory of Immunoregulation.
“We had a serious challenge with that at our own clinical center in Bethesda just a few years ago,” he noted. Numerous cases of antimicrobial resistance in methicillin-resistant Staphylococcus aureus, Clostridium difficile, and Neisseria gonorrhoeae have been reported.
Dr. Fauci described the Ebola outbreak as “a globally important disease that had ripple effects in the United States that were unpredicted,” referring to the case of the infected man who traveled from Monrovia to Dallas on Sept. 19, 2014, and developed Ebola symptoms 5 days later. Between 2014 and 2016, there were 28,616 cases and 11,310 deaths combined in the countries of Guinea, Sierra Leone, and Liberia.
“There is virtually no health care system in those three countries,” he said. “There’s a distrust in authority, and anything we tried to do as a global health [effort] made things worse. What we’re trying to do now is built sustainable health care issues in countries that don’t have it.”
Of particular concern to public health officials worldwide is getting a lid on Zika virus, a mosquito-borne illness that can be passed from a pregnant woman to her fetus and cause an increased risk of microcephaly, particularly during the first trimester.
“Not only is there microcephaly, there’s a whole host of abnormalities that involve hearing loss, visual abnormalities, and a variety of other issues,” Dr. Fauci said. “There are about 50 countries in the Americas and the Caribbean that have Zika virus transmission.”
According to data from the Centers for Disease Control and Prevention, from Jan. 1, 2015, to March 29, 2017, there were 5,182 reported cases of Zika virus disease in the 50 states and the District of Columbia. The majority of those (4,886) were travel associated, 222 were locally acquired mosquito-borne, 45 were sexually transmitted, 27 congenital, 1 was laboratory acquired, and 1 was unknown.
At the same time, there have been 38,303 cases in the U.S. territories. Of those, 38,156 were locally acquired, and 147 were travel associated. “That’s why there’s such an intense effort to develop a Zika vaccine,” he said.
According to the CDC, as of March 15, 2017, there are 265 cases of locally transmitted cases in Florida: 216 by mosquito and the rest by sexual transmission. “Talk about surprises,” Dr. Fauci said. “Zika is the first mosquito-borne infection that can result in a congenital abnormality, the first mosquito-borne infection that can be sexually transmitted, and now we’re learning more about this problem, which is the reason why it’s very important for us to develop a vaccine.”
A phase I trial of a DNA vaccine developed by the NIH Vaccine Research Center has reached its enrollment goal of 80 patients age 18-35 years. Initial results are expected sometime in the first quarter of 2017. A phase II trial in the United States and Puerto Rico is expected to launch soon.
Dr. Fauci closed his presentation by sharing lessons learned from previous pandemics.
The first lesson is that global surveillance is required. “Namely, know what’s going on in real time,” he said. “That has to be linked to transparency and communication. So that if something happens in China, we don’t find out about it months later, but we know about it in real time.”
Infrastructure and capacity building are also important. “The lack of capacity in West Africa can ultimately have an indirect impact on us here in the United States,” he said.
“Finally, we need to coordinate and collaborate; we need adaptable platforms for vaccines,” Dr. Fauci cautioned. “Importantly, we need a stable funding mechanism such as a public health emergency fund so that we do not have to go scrambling before the Congress when we need emergency funds.”
SAN DIEGO – Reflecting on his 33-year career as director of the National Institute of Allergy and Infectious Diseases, Anthony S. Fauci, MD, can say one thing for certain: Emerging and re-emerging infectious diseases in the continental United States are here to stay.
In an article that he and his colleagues published in the Lancet in 2008, they used the term “perpetual challenge” to describe emerging infections, a descriptor that resonates with him to this day.
Global examples of emerging and re-emerging infectious diseases he discussed include dengue, West Nile virus, chikungunya, and carbapenem-resistant Enterobacteriaceae, “which is becoming a progressively more serious problem in hospitalized patients,” said Dr. Fauci, who is also chief of the NIAID Laboratory of Immunoregulation.
“We had a serious challenge with that at our own clinical center in Bethesda just a few years ago,” he noted. Numerous cases of antimicrobial resistance in methicillin-resistant Staphylococcus aureus, Clostridium difficile, and Neisseria gonorrhoeae have been reported.
Dr. Fauci described the Ebola outbreak as “a globally important disease that had ripple effects in the United States that were unpredicted,” referring to the case of the infected man who traveled from Monrovia to Dallas on Sept. 19, 2014, and developed Ebola symptoms 5 days later. Between 2014 and 2016, there were 28,616 cases and 11,310 deaths combined in the countries of Guinea, Sierra Leone, and Liberia.
“There is virtually no health care system in those three countries,” he said. “There’s a distrust in authority, and anything we tried to do as a global health [effort] made things worse. What we’re trying to do now is built sustainable health care issues in countries that don’t have it.”
Of particular concern to public health officials worldwide is getting a lid on Zika virus, a mosquito-borne illness that can be passed from a pregnant woman to her fetus and cause an increased risk of microcephaly, particularly during the first trimester.
“Not only is there microcephaly, there’s a whole host of abnormalities that involve hearing loss, visual abnormalities, and a variety of other issues,” Dr. Fauci said. “There are about 50 countries in the Americas and the Caribbean that have Zika virus transmission.”
According to data from the Centers for Disease Control and Prevention, from Jan. 1, 2015, to March 29, 2017, there were 5,182 reported cases of Zika virus disease in the 50 states and the District of Columbia. The majority of those (4,886) were travel associated, 222 were locally acquired mosquito-borne, 45 were sexually transmitted, 27 congenital, 1 was laboratory acquired, and 1 was unknown.
At the same time, there have been 38,303 cases in the U.S. territories. Of those, 38,156 were locally acquired, and 147 were travel associated. “That’s why there’s such an intense effort to develop a Zika vaccine,” he said.
According to the CDC, as of March 15, 2017, there are 265 cases of locally transmitted cases in Florida: 216 by mosquito and the rest by sexual transmission. “Talk about surprises,” Dr. Fauci said. “Zika is the first mosquito-borne infection that can result in a congenital abnormality, the first mosquito-borne infection that can be sexually transmitted, and now we’re learning more about this problem, which is the reason why it’s very important for us to develop a vaccine.”
A phase I trial of a DNA vaccine developed by the NIH Vaccine Research Center has reached its enrollment goal of 80 patients age 18-35 years. Initial results are expected sometime in the first quarter of 2017. A phase II trial in the United States and Puerto Rico is expected to launch soon.
Dr. Fauci closed his presentation by sharing lessons learned from previous pandemics.
The first lesson is that global surveillance is required. “Namely, know what’s going on in real time,” he said. “That has to be linked to transparency and communication. So that if something happens in China, we don’t find out about it months later, but we know about it in real time.”
Infrastructure and capacity building are also important. “The lack of capacity in West Africa can ultimately have an indirect impact on us here in the United States,” he said.
“Finally, we need to coordinate and collaborate; we need adaptable platforms for vaccines,” Dr. Fauci cautioned. “Importantly, we need a stable funding mechanism such as a public health emergency fund so that we do not have to go scrambling before the Congress when we need emergency funds.”
EXPERT ANALYSIS FROM ACP INTERNAL MEDICINE
Heat-stable rotavirus vaccine shows promising results
A new low-cost rotavirus gastroenteritis vaccine that does not require cold storage showed a vaccine efficacy of 67% in a per-protocol test of 3,508 Nigerien infants, according to a study by Sheila Isanaka of the department of research at Epicentre, Paris, and her associates.
In a double blind, placebo-controlled test of the oral bovine rotavirus pentavalent vaccine (BRV-PV), 31 severe cases of rotavirus were found in the vaccinated group of 1,780, while 87 cases were found in the placebo group of 1,728 (2.14 vs. 6.44 cases per 100 person-years, respectively), according to Ms. Isanaka and her colleagues (N Engl J Med. 2017 Mar 23;376[12]:1121-30).
Researchers gathered infants with severe symptoms and administered three injections of either BRV-PV or the placebo from August 2014 through November 2015. The BRV-PV vaccine, manufactured by Serum Institute of India, contains the rotavirus serotypes G1, G2, G3, G4, and G9.
With regard to adverse events, there was no distinction between the two groups (P greater than .15). According to medical investigators, the most common cause of deaths – 27 and 22 in the vaccine and placebo groups, respectively – was infections and infestations (in 37 infants) and metabolism and nutrition disorders (in 6).
Part of what makes this vaccine unique is its shelf life of 2 years when kept at 37° C, or 6 months at 40° C, a key point for Ms. Isanaka and her colleagues.
“The global supply of the vaccines is constrained, and unreliable transportation and storage systems make delivery of vaccines that require refrigeration difficult,” Ms. Isanaka and her colleagues reported. “The introduction of BRV-PV may help to minimize the burden on already strained immunization programs.” The vaccine is also “for sale at or below the current price of the two WHO prequalified vaccines that are supported by the Gavi alliance,” making it possibly more financially accessible as well.
While the per-protocol test found efficacy at 67%, the intention-to-treat population reported a higher efficacy of 73%. Ms. Isanaka and her colleagues believe this number “may more closely represent the efficacy under real-world conditions,” due to the more flexible vaccination schedule.
This study was limited by a short time frame, which did not allow researchers to gather genotyping data pertaining to the efficacy against changing serotypes. BRV-PV also was not given consistently with the oral polio vaccine.
The study was supported by Médecins sans Frontières Operational Center in Geneva and the Kavli Foundation. Ms. Isanaka’s institution, Epicentre, receives core funding from Médecins sans Frontières. Ms. McNeal reports grant support from Epicentre for the study, and other support from Merck and GlaxoSmithKline outside the submitted work. None of the other researchers had relevant financial disclosures.
ezimmerman@frontlinemedcom.com
On Twitter @EAZTweets
Rotavirus is the leading cause of diarrhea-associated death in children aged under 5 years, and with 85% of all deaths occurring in Africa and Asia, proper channels of vaccine dissemination are critical. There is no question to the positive influence of rotavirus vaccines, as research suggests they could save 2.46 million children’s lives and prevent another 83 million from living with a disability between 2011 and 2030.
While two vaccines, Rotarix and RotaTeq, are already being introduced to patients in 48 countries, diminishing vaccine uptake is standing in the way of these interventions reaching their full potential. Despite subsidies from Gavi (the vaccine alliance) and the World Health Organization, costs are still too high and the necessity for cold storage poses a financial and logistical problem for a majority of high risk countries. The BRV-PV vaccine developed by Serum Institute of India seems to be a step in the right direction in helping to ease this burden.
While its efficacy is modest, BRV-PV has shown promise through its heat stability as well as its cost, which falls between the prices of the two already available vaccines.
It is not perfect; as a freeze-dried vaccine, it may pose problems in areas where oral liquid, all-in-one vaccinations are preferred. Yet, there is no doubt that an increase in affordable, programmatically suitable options will help achieve the goal of ending rotavirus related deaths globally.
Mathuram Santosham, MD, is professor of pediatrics and pediatric infectious diseases at Johns Hopkins University, Baltimore. Duncan Steele, PhD, is a microbiologist and deputy director and strategic lead for enteric vaccines and enteric and diarrheal diseases for the Bill & Melinda Gates Foundation, Seattle. They coauthored the editorial regarding the article by Isanaka et al. (N Engl J Med. 2017 March 23;376[12]:1170-2). Dr. Santosham reported no relevant financial disclosures. Dr. Steele reports that he is employed at the Bill & Melinda Gates Foundation, which has supported through funding, the development of multiple rotavirus vaccine candidates including the lyophilized rotavirus vaccine produced by Serum Institute.
Rotavirus is the leading cause of diarrhea-associated death in children aged under 5 years, and with 85% of all deaths occurring in Africa and Asia, proper channels of vaccine dissemination are critical. There is no question to the positive influence of rotavirus vaccines, as research suggests they could save 2.46 million children’s lives and prevent another 83 million from living with a disability between 2011 and 2030.
While two vaccines, Rotarix and RotaTeq, are already being introduced to patients in 48 countries, diminishing vaccine uptake is standing in the way of these interventions reaching their full potential. Despite subsidies from Gavi (the vaccine alliance) and the World Health Organization, costs are still too high and the necessity for cold storage poses a financial and logistical problem for a majority of high risk countries. The BRV-PV vaccine developed by Serum Institute of India seems to be a step in the right direction in helping to ease this burden.
While its efficacy is modest, BRV-PV has shown promise through its heat stability as well as its cost, which falls between the prices of the two already available vaccines.
It is not perfect; as a freeze-dried vaccine, it may pose problems in areas where oral liquid, all-in-one vaccinations are preferred. Yet, there is no doubt that an increase in affordable, programmatically suitable options will help achieve the goal of ending rotavirus related deaths globally.
Mathuram Santosham, MD, is professor of pediatrics and pediatric infectious diseases at Johns Hopkins University, Baltimore. Duncan Steele, PhD, is a microbiologist and deputy director and strategic lead for enteric vaccines and enteric and diarrheal diseases for the Bill & Melinda Gates Foundation, Seattle. They coauthored the editorial regarding the article by Isanaka et al. (N Engl J Med. 2017 March 23;376[12]:1170-2). Dr. Santosham reported no relevant financial disclosures. Dr. Steele reports that he is employed at the Bill & Melinda Gates Foundation, which has supported through funding, the development of multiple rotavirus vaccine candidates including the lyophilized rotavirus vaccine produced by Serum Institute.
Rotavirus is the leading cause of diarrhea-associated death in children aged under 5 years, and with 85% of all deaths occurring in Africa and Asia, proper channels of vaccine dissemination are critical. There is no question to the positive influence of rotavirus vaccines, as research suggests they could save 2.46 million children’s lives and prevent another 83 million from living with a disability between 2011 and 2030.
While two vaccines, Rotarix and RotaTeq, are already being introduced to patients in 48 countries, diminishing vaccine uptake is standing in the way of these interventions reaching their full potential. Despite subsidies from Gavi (the vaccine alliance) and the World Health Organization, costs are still too high and the necessity for cold storage poses a financial and logistical problem for a majority of high risk countries. The BRV-PV vaccine developed by Serum Institute of India seems to be a step in the right direction in helping to ease this burden.
While its efficacy is modest, BRV-PV has shown promise through its heat stability as well as its cost, which falls between the prices of the two already available vaccines.
It is not perfect; as a freeze-dried vaccine, it may pose problems in areas where oral liquid, all-in-one vaccinations are preferred. Yet, there is no doubt that an increase in affordable, programmatically suitable options will help achieve the goal of ending rotavirus related deaths globally.
Mathuram Santosham, MD, is professor of pediatrics and pediatric infectious diseases at Johns Hopkins University, Baltimore. Duncan Steele, PhD, is a microbiologist and deputy director and strategic lead for enteric vaccines and enteric and diarrheal diseases for the Bill & Melinda Gates Foundation, Seattle. They coauthored the editorial regarding the article by Isanaka et al. (N Engl J Med. 2017 March 23;376[12]:1170-2). Dr. Santosham reported no relevant financial disclosures. Dr. Steele reports that he is employed at the Bill & Melinda Gates Foundation, which has supported through funding, the development of multiple rotavirus vaccine candidates including the lyophilized rotavirus vaccine produced by Serum Institute.
A new low-cost rotavirus gastroenteritis vaccine that does not require cold storage showed a vaccine efficacy of 67% in a per-protocol test of 3,508 Nigerien infants, according to a study by Sheila Isanaka of the department of research at Epicentre, Paris, and her associates.
In a double blind, placebo-controlled test of the oral bovine rotavirus pentavalent vaccine (BRV-PV), 31 severe cases of rotavirus were found in the vaccinated group of 1,780, while 87 cases were found in the placebo group of 1,728 (2.14 vs. 6.44 cases per 100 person-years, respectively), according to Ms. Isanaka and her colleagues (N Engl J Med. 2017 Mar 23;376[12]:1121-30).
Researchers gathered infants with severe symptoms and administered three injections of either BRV-PV or the placebo from August 2014 through November 2015. The BRV-PV vaccine, manufactured by Serum Institute of India, contains the rotavirus serotypes G1, G2, G3, G4, and G9.
With regard to adverse events, there was no distinction between the two groups (P greater than .15). According to medical investigators, the most common cause of deaths – 27 and 22 in the vaccine and placebo groups, respectively – was infections and infestations (in 37 infants) and metabolism and nutrition disorders (in 6).
Part of what makes this vaccine unique is its shelf life of 2 years when kept at 37° C, or 6 months at 40° C, a key point for Ms. Isanaka and her colleagues.
“The global supply of the vaccines is constrained, and unreliable transportation and storage systems make delivery of vaccines that require refrigeration difficult,” Ms. Isanaka and her colleagues reported. “The introduction of BRV-PV may help to minimize the burden on already strained immunization programs.” The vaccine is also “for sale at or below the current price of the two WHO prequalified vaccines that are supported by the Gavi alliance,” making it possibly more financially accessible as well.
While the per-protocol test found efficacy at 67%, the intention-to-treat population reported a higher efficacy of 73%. Ms. Isanaka and her colleagues believe this number “may more closely represent the efficacy under real-world conditions,” due to the more flexible vaccination schedule.
This study was limited by a short time frame, which did not allow researchers to gather genotyping data pertaining to the efficacy against changing serotypes. BRV-PV also was not given consistently with the oral polio vaccine.
The study was supported by Médecins sans Frontières Operational Center in Geneva and the Kavli Foundation. Ms. Isanaka’s institution, Epicentre, receives core funding from Médecins sans Frontières. Ms. McNeal reports grant support from Epicentre for the study, and other support from Merck and GlaxoSmithKline outside the submitted work. None of the other researchers had relevant financial disclosures.
ezimmerman@frontlinemedcom.com
On Twitter @EAZTweets
A new low-cost rotavirus gastroenteritis vaccine that does not require cold storage showed a vaccine efficacy of 67% in a per-protocol test of 3,508 Nigerien infants, according to a study by Sheila Isanaka of the department of research at Epicentre, Paris, and her associates.
In a double blind, placebo-controlled test of the oral bovine rotavirus pentavalent vaccine (BRV-PV), 31 severe cases of rotavirus were found in the vaccinated group of 1,780, while 87 cases were found in the placebo group of 1,728 (2.14 vs. 6.44 cases per 100 person-years, respectively), according to Ms. Isanaka and her colleagues (N Engl J Med. 2017 Mar 23;376[12]:1121-30).
Researchers gathered infants with severe symptoms and administered three injections of either BRV-PV or the placebo from August 2014 through November 2015. The BRV-PV vaccine, manufactured by Serum Institute of India, contains the rotavirus serotypes G1, G2, G3, G4, and G9.
With regard to adverse events, there was no distinction between the two groups (P greater than .15). According to medical investigators, the most common cause of deaths – 27 and 22 in the vaccine and placebo groups, respectively – was infections and infestations (in 37 infants) and metabolism and nutrition disorders (in 6).
Part of what makes this vaccine unique is its shelf life of 2 years when kept at 37° C, or 6 months at 40° C, a key point for Ms. Isanaka and her colleagues.
“The global supply of the vaccines is constrained, and unreliable transportation and storage systems make delivery of vaccines that require refrigeration difficult,” Ms. Isanaka and her colleagues reported. “The introduction of BRV-PV may help to minimize the burden on already strained immunization programs.” The vaccine is also “for sale at or below the current price of the two WHO prequalified vaccines that are supported by the Gavi alliance,” making it possibly more financially accessible as well.
While the per-protocol test found efficacy at 67%, the intention-to-treat population reported a higher efficacy of 73%. Ms. Isanaka and her colleagues believe this number “may more closely represent the efficacy under real-world conditions,” due to the more flexible vaccination schedule.
This study was limited by a short time frame, which did not allow researchers to gather genotyping data pertaining to the efficacy against changing serotypes. BRV-PV also was not given consistently with the oral polio vaccine.
The study was supported by Médecins sans Frontières Operational Center in Geneva and the Kavli Foundation. Ms. Isanaka’s institution, Epicentre, receives core funding from Médecins sans Frontières. Ms. McNeal reports grant support from Epicentre for the study, and other support from Merck and GlaxoSmithKline outside the submitted work. None of the other researchers had relevant financial disclosures.
ezimmerman@frontlinemedcom.com
On Twitter @EAZTweets
Key clinical point:
Major finding: Of 3,508 infants studied, 31 cases of severe rotavirus gastroenteritis were found in the vaccine group, and 87 cases in the placebo group, putting efficacy at 67%.
Data source: Double blind, placebo-controlled test of 3,508 Nigerian infants whose symptoms were measured via 20-point Vesikari scoring.
Disclosures: The study was supported by Médecins sans Frontières Operational Center in Geneva and the Kavli Foundation. Ms. Isanaka’s institution, Epicentre, receives core funding from Médecins sans Frontières. Ms. McNeal reports grant support from Epicentre for the study, and other support from Merck and GlaxoSmithKline outside the submitted work. None of the other researchers had relevant financial disclosures.
Exposure to HPV vaccine in pregnancy not linked to birth defects
The quadrivalent human papillomavirus (HPV) vaccine was not associated with any adverse pregnancy outcomes when inadvertently given during pregnancy, according to the findings from a nationwide Danish study.
“Our results are consistent with other evidence that does not indicate that the vaccination of pregnant women with inactivated virus, bacterial, or toxoid vaccines generally confers a higher risk of adverse pregnancy outcomes than no such vaccination. Our results also confirm and considerably expand on results from previous studies of the quadrivalent HPV vaccine,” wrote Nikolai M. Scheller, MD, of the Statens Serum Institut, Copenhagen, and his colleagues.
Quadrivalent HPV vaccination was not associated with any increase in risk for major birth defects (prevalence odds ratio, 1.19), spontaneous abortion (hazard ratio, 0.71), preterm birth (prevalence OR, 1.15), small size for gestational age (prevalence OR, 0.86), or low birth weight (prevalence OR, 1.10). It also was not associated with increased risk for stillbirth, but this outcome occurred in only two case patients and four controls, making it “impossible to draw clinically meaningful conclusions” regarding the risk for stillbirth, Dr. Scheller and his colleagues reported (N Engl J Med. 2017;376[13]:1223-33).
“Because many [adverse] pregnancy outcomes are rare, our study did not have the statistical power to assess the risks of stillbirth and specific major birth defects associated with quadrivalent HPV vaccination. Larger studies would be needed to address these outcomes,” they added.
Novo Nordisk and the Danish Medical Research Council funded the study. Dr. Scheller reported having no relevant financial disclosures; two of his coauthors reported receiving research grants from the Novo Nordisk Foundation and the Danish Medical Research Council.
Although a large number of women (1,665) were immunized in the first trimester of pregnancy, when organogenesis occurs, their offspring did not have a significantly higher rate of major birth defects compared with offspring born to unvaccinated women. The numbers of spontaneous abortions, preterm births, infants with low birth weight, infants who were small for gestational age, and stillbirths were not higher in the vaccinated cohorts than in the unvaccinated cohorts, although the number of stillbirths was small.
These data are very encouraging and strongly support the safety of HPV vaccines if they are inadvertently given in pregnancy, a finding that complements previous safety reports of HPV vaccine in nonpregnant women. These data also show that adverse outcomes occur at a baseline rate in pregnancy and that when no control group is included in studies, these outcomes may be inappropriately attributed to the vaccine.
Kathryn M. Edwards, MD, is in the division of infectious diseases and the department of pediatrics at Vanderbilt University, Nashville, Tenn. She reported receiving grants from Novartis for research on group B strep vaccines in pregnancy. These comments are excerpted from an accompanying editorial (N Engl J Med. 2017;376[13]:1280-2).
Although a large number of women (1,665) were immunized in the first trimester of pregnancy, when organogenesis occurs, their offspring did not have a significantly higher rate of major birth defects compared with offspring born to unvaccinated women. The numbers of spontaneous abortions, preterm births, infants with low birth weight, infants who were small for gestational age, and stillbirths were not higher in the vaccinated cohorts than in the unvaccinated cohorts, although the number of stillbirths was small.
These data are very encouraging and strongly support the safety of HPV vaccines if they are inadvertently given in pregnancy, a finding that complements previous safety reports of HPV vaccine in nonpregnant women. These data also show that adverse outcomes occur at a baseline rate in pregnancy and that when no control group is included in studies, these outcomes may be inappropriately attributed to the vaccine.
Kathryn M. Edwards, MD, is in the division of infectious diseases and the department of pediatrics at Vanderbilt University, Nashville, Tenn. She reported receiving grants from Novartis for research on group B strep vaccines in pregnancy. These comments are excerpted from an accompanying editorial (N Engl J Med. 2017;376[13]:1280-2).
Although a large number of women (1,665) were immunized in the first trimester of pregnancy, when organogenesis occurs, their offspring did not have a significantly higher rate of major birth defects compared with offspring born to unvaccinated women. The numbers of spontaneous abortions, preterm births, infants with low birth weight, infants who were small for gestational age, and stillbirths were not higher in the vaccinated cohorts than in the unvaccinated cohorts, although the number of stillbirths was small.
These data are very encouraging and strongly support the safety of HPV vaccines if they are inadvertently given in pregnancy, a finding that complements previous safety reports of HPV vaccine in nonpregnant women. These data also show that adverse outcomes occur at a baseline rate in pregnancy and that when no control group is included in studies, these outcomes may be inappropriately attributed to the vaccine.
Kathryn M. Edwards, MD, is in the division of infectious diseases and the department of pediatrics at Vanderbilt University, Nashville, Tenn. She reported receiving grants from Novartis for research on group B strep vaccines in pregnancy. These comments are excerpted from an accompanying editorial (N Engl J Med. 2017;376[13]:1280-2).
The quadrivalent human papillomavirus (HPV) vaccine was not associated with any adverse pregnancy outcomes when inadvertently given during pregnancy, according to the findings from a nationwide Danish study.
“Our results are consistent with other evidence that does not indicate that the vaccination of pregnant women with inactivated virus, bacterial, or toxoid vaccines generally confers a higher risk of adverse pregnancy outcomes than no such vaccination. Our results also confirm and considerably expand on results from previous studies of the quadrivalent HPV vaccine,” wrote Nikolai M. Scheller, MD, of the Statens Serum Institut, Copenhagen, and his colleagues.
Quadrivalent HPV vaccination was not associated with any increase in risk for major birth defects (prevalence odds ratio, 1.19), spontaneous abortion (hazard ratio, 0.71), preterm birth (prevalence OR, 1.15), small size for gestational age (prevalence OR, 0.86), or low birth weight (prevalence OR, 1.10). It also was not associated with increased risk for stillbirth, but this outcome occurred in only two case patients and four controls, making it “impossible to draw clinically meaningful conclusions” regarding the risk for stillbirth, Dr. Scheller and his colleagues reported (N Engl J Med. 2017;376[13]:1223-33).
“Because many [adverse] pregnancy outcomes are rare, our study did not have the statistical power to assess the risks of stillbirth and specific major birth defects associated with quadrivalent HPV vaccination. Larger studies would be needed to address these outcomes,” they added.
Novo Nordisk and the Danish Medical Research Council funded the study. Dr. Scheller reported having no relevant financial disclosures; two of his coauthors reported receiving research grants from the Novo Nordisk Foundation and the Danish Medical Research Council.
The quadrivalent human papillomavirus (HPV) vaccine was not associated with any adverse pregnancy outcomes when inadvertently given during pregnancy, according to the findings from a nationwide Danish study.
“Our results are consistent with other evidence that does not indicate that the vaccination of pregnant women with inactivated virus, bacterial, or toxoid vaccines generally confers a higher risk of adverse pregnancy outcomes than no such vaccination. Our results also confirm and considerably expand on results from previous studies of the quadrivalent HPV vaccine,” wrote Nikolai M. Scheller, MD, of the Statens Serum Institut, Copenhagen, and his colleagues.
Quadrivalent HPV vaccination was not associated with any increase in risk for major birth defects (prevalence odds ratio, 1.19), spontaneous abortion (hazard ratio, 0.71), preterm birth (prevalence OR, 1.15), small size for gestational age (prevalence OR, 0.86), or low birth weight (prevalence OR, 1.10). It also was not associated with increased risk for stillbirth, but this outcome occurred in only two case patients and four controls, making it “impossible to draw clinically meaningful conclusions” regarding the risk for stillbirth, Dr. Scheller and his colleagues reported (N Engl J Med. 2017;376[13]:1223-33).
“Because many [adverse] pregnancy outcomes are rare, our study did not have the statistical power to assess the risks of stillbirth and specific major birth defects associated with quadrivalent HPV vaccination. Larger studies would be needed to address these outcomes,” they added.
Novo Nordisk and the Danish Medical Research Council funded the study. Dr. Scheller reported having no relevant financial disclosures; two of his coauthors reported receiving research grants from the Novo Nordisk Foundation and the Danish Medical Research Council.
Key clinical point:
Major finding: Quadrivalent HPV vaccination was not associated with any increase in risk for major birth defects (prevalence odds ratio, 1.19).
Data source: A population-based cohort study involving 581,550 pregnancies across Denmark during a 7-year period, including 1,665 in which the mother inadvertently received the HPV vaccine.
Disclosures: Novo Nordisk and the Danish Medical Research Council funded the study. Dr. Scheller reported having no relevant financial disclosures; two of his coauthors reported receiving research grants from the Novo Nordisk Foundation and the Danish Medical Research Council.
New self-persuasion app to promote HPV vaccine appears effective
A new tablet application using a self-persuasion method has been successful in convincing parents in underserved communities to have their children vaccinated for human papillomavirus (HPV), according to a study.
Of 45 participating parents, 27 of the 33 (82%) parents whose adolescents were not vaccinated reported that they decided to get their children vaccinated after completing the application. The remaining 12 already had an HPV-vaccinated adolescent. Children of participating parents were aged 11-17 years (Patient Educ Couns. 2016. doi: 10.1016/j.pec.2016.11.014).
Of the 45 parents, 31 (69%) were Hispanic and 29 (64%) held a high school education or less, according to the study.
To test the effectiveness of self-persuasion, researchers developed a tablet application which started with a 5 minute video on HPV and vaccine efficacy, and then asked parents to complete two tasks: answer questions about the HPV vaccine that prompt thought on its benefits and come up with personal reasons for why having their child vaccinated is important.
Parents then participated in a 45-60 minute interview with one of six research assistants, who prompted participants to address four research points: Did they like the application? Which questions generated interest in the HPV vaccine without raising concerns? Were they able to communicate reasons for vaccination? Were they convinced to have their children vaccinated?
After watching the video, 18 (55%) of the 33 parents whose children were not vaccinated changed their minds, and, after participating in the self-persuasion questionnaire, an additional 9 parents decided to vaccinate their children, according to the study. Five parents remained undecided, and one decided against HPV vaccination.
Overall, participants reported that the application questions were helpful in their decision to vaccinate their children, with question ratings ranging from 4.33 to 4.98 on a scale of 1 to 5.
Mr. Baldwin and his colleagues said that, while the initial test showed promise, further research must be done on actual vaccine behavior, as these tests only studied verbally reported decisions by parents.
One of the limitations to the study was that the research was primarily conducted at a research facility. While some was conducted in local clinics, Mr. Baldwin and his colleagues consider that further studies should be conducted in more public areas. All but one of the participants were female, which may make it hard to generalize about the effects of this application with male parents.
The researchers reported no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
On Twitter @EAZTweets
The media has not been kind when it comes to HPV vaccinations. When most parents are approached with the option to have their children vaccinated, they are hesitant because of what they have heard from television, news articles, or online mom chat rooms about the dangerous side effects of the vaccine. When a mother hears about other mothers’ daughters fainting or being subjected to pain, she usually wonders if it is really worth the risk.
The same goes for parents who expect their daughters to practice celibacy until marriage. After all, why expose a child to negative side effects when she won’t be having sex anyway? The problem with this thinking, however, is that, often, it is not based in reality. When I approach families about HPV vaccine, or any other vaccine for that matter, I make sure to present studies that explain the lack of evidence on negative vaccine side effects, as well as information pertaining to how common HPV is.
However, simply handing out a fact sheet is not enough. Parents who are convinced that their children do not need to be vaccinated will not be persuaded through statistics but through personal anecdotes. I like to tell mothers to ask their girlfriends about being vaccinated, to not only see how common HPV is but to break the stigma as well. I explain to parents who do not want their child having sex now that, at some point, they might want their child to grow their family, and, when that time comes, don’t they want their child to be safe? Even if it is just one time, shouldn’t their child be protected? From that point on, the language of conversation has changed, and the channels of communication are more open.
As pediatricians, we are the medical advocates for our patients and their families, not just someone to prescribe medication for them. Establish that role through knowledge and conversation, and persuasion will soon follow.
Francine Pearce, MD, is a pediatrician in Frankfort, Ill. She writes the Pediatric News teen column, Pearce-ings .
The media has not been kind when it comes to HPV vaccinations. When most parents are approached with the option to have their children vaccinated, they are hesitant because of what they have heard from television, news articles, or online mom chat rooms about the dangerous side effects of the vaccine. When a mother hears about other mothers’ daughters fainting or being subjected to pain, she usually wonders if it is really worth the risk.
The same goes for parents who expect their daughters to practice celibacy until marriage. After all, why expose a child to negative side effects when she won’t be having sex anyway? The problem with this thinking, however, is that, often, it is not based in reality. When I approach families about HPV vaccine, or any other vaccine for that matter, I make sure to present studies that explain the lack of evidence on negative vaccine side effects, as well as information pertaining to how common HPV is.
However, simply handing out a fact sheet is not enough. Parents who are convinced that their children do not need to be vaccinated will not be persuaded through statistics but through personal anecdotes. I like to tell mothers to ask their girlfriends about being vaccinated, to not only see how common HPV is but to break the stigma as well. I explain to parents who do not want their child having sex now that, at some point, they might want their child to grow their family, and, when that time comes, don’t they want their child to be safe? Even if it is just one time, shouldn’t their child be protected? From that point on, the language of conversation has changed, and the channels of communication are more open.
As pediatricians, we are the medical advocates for our patients and their families, not just someone to prescribe medication for them. Establish that role through knowledge and conversation, and persuasion will soon follow.
Francine Pearce, MD, is a pediatrician in Frankfort, Ill. She writes the Pediatric News teen column, Pearce-ings .
The media has not been kind when it comes to HPV vaccinations. When most parents are approached with the option to have their children vaccinated, they are hesitant because of what they have heard from television, news articles, or online mom chat rooms about the dangerous side effects of the vaccine. When a mother hears about other mothers’ daughters fainting or being subjected to pain, she usually wonders if it is really worth the risk.
The same goes for parents who expect their daughters to practice celibacy until marriage. After all, why expose a child to negative side effects when she won’t be having sex anyway? The problem with this thinking, however, is that, often, it is not based in reality. When I approach families about HPV vaccine, or any other vaccine for that matter, I make sure to present studies that explain the lack of evidence on negative vaccine side effects, as well as information pertaining to how common HPV is.
However, simply handing out a fact sheet is not enough. Parents who are convinced that their children do not need to be vaccinated will not be persuaded through statistics but through personal anecdotes. I like to tell mothers to ask their girlfriends about being vaccinated, to not only see how common HPV is but to break the stigma as well. I explain to parents who do not want their child having sex now that, at some point, they might want their child to grow their family, and, when that time comes, don’t they want their child to be safe? Even if it is just one time, shouldn’t their child be protected? From that point on, the language of conversation has changed, and the channels of communication are more open.
As pediatricians, we are the medical advocates for our patients and their families, not just someone to prescribe medication for them. Establish that role through knowledge and conversation, and persuasion will soon follow.
Francine Pearce, MD, is a pediatrician in Frankfort, Ill. She writes the Pediatric News teen column, Pearce-ings .
A new tablet application using a self-persuasion method has been successful in convincing parents in underserved communities to have their children vaccinated for human papillomavirus (HPV), according to a study.
Of 45 participating parents, 27 of the 33 (82%) parents whose adolescents were not vaccinated reported that they decided to get their children vaccinated after completing the application. The remaining 12 already had an HPV-vaccinated adolescent. Children of participating parents were aged 11-17 years (Patient Educ Couns. 2016. doi: 10.1016/j.pec.2016.11.014).
Of the 45 parents, 31 (69%) were Hispanic and 29 (64%) held a high school education or less, according to the study.
To test the effectiveness of self-persuasion, researchers developed a tablet application which started with a 5 minute video on HPV and vaccine efficacy, and then asked parents to complete two tasks: answer questions about the HPV vaccine that prompt thought on its benefits and come up with personal reasons for why having their child vaccinated is important.
Parents then participated in a 45-60 minute interview with one of six research assistants, who prompted participants to address four research points: Did they like the application? Which questions generated interest in the HPV vaccine without raising concerns? Were they able to communicate reasons for vaccination? Were they convinced to have their children vaccinated?
After watching the video, 18 (55%) of the 33 parents whose children were not vaccinated changed their minds, and, after participating in the self-persuasion questionnaire, an additional 9 parents decided to vaccinate their children, according to the study. Five parents remained undecided, and one decided against HPV vaccination.
Overall, participants reported that the application questions were helpful in their decision to vaccinate their children, with question ratings ranging from 4.33 to 4.98 on a scale of 1 to 5.
Mr. Baldwin and his colleagues said that, while the initial test showed promise, further research must be done on actual vaccine behavior, as these tests only studied verbally reported decisions by parents.
One of the limitations to the study was that the research was primarily conducted at a research facility. While some was conducted in local clinics, Mr. Baldwin and his colleagues consider that further studies should be conducted in more public areas. All but one of the participants were female, which may make it hard to generalize about the effects of this application with male parents.
The researchers reported no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
On Twitter @EAZTweets
A new tablet application using a self-persuasion method has been successful in convincing parents in underserved communities to have their children vaccinated for human papillomavirus (HPV), according to a study.
Of 45 participating parents, 27 of the 33 (82%) parents whose adolescents were not vaccinated reported that they decided to get their children vaccinated after completing the application. The remaining 12 already had an HPV-vaccinated adolescent. Children of participating parents were aged 11-17 years (Patient Educ Couns. 2016. doi: 10.1016/j.pec.2016.11.014).
Of the 45 parents, 31 (69%) were Hispanic and 29 (64%) held a high school education or less, according to the study.
To test the effectiveness of self-persuasion, researchers developed a tablet application which started with a 5 minute video on HPV and vaccine efficacy, and then asked parents to complete two tasks: answer questions about the HPV vaccine that prompt thought on its benefits and come up with personal reasons for why having their child vaccinated is important.
Parents then participated in a 45-60 minute interview with one of six research assistants, who prompted participants to address four research points: Did they like the application? Which questions generated interest in the HPV vaccine without raising concerns? Were they able to communicate reasons for vaccination? Were they convinced to have their children vaccinated?
After watching the video, 18 (55%) of the 33 parents whose children were not vaccinated changed their minds, and, after participating in the self-persuasion questionnaire, an additional 9 parents decided to vaccinate their children, according to the study. Five parents remained undecided, and one decided against HPV vaccination.
Overall, participants reported that the application questions were helpful in their decision to vaccinate their children, with question ratings ranging from 4.33 to 4.98 on a scale of 1 to 5.
Mr. Baldwin and his colleagues said that, while the initial test showed promise, further research must be done on actual vaccine behavior, as these tests only studied verbally reported decisions by parents.
One of the limitations to the study was that the research was primarily conducted at a research facility. While some was conducted in local clinics, Mr. Baldwin and his colleagues consider that further studies should be conducted in more public areas. All but one of the participants were female, which may make it hard to generalize about the effects of this application with male parents.
The researchers reported no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
On Twitter @EAZTweets
FROM PATIENT EDUCATION & COUNSELING
Key clinical point:
Major finding: Of the 33 parents whose children were not vaccinated, 27 (818%) decided to have their children vaccinated after using the application.
Data source: A study of 45 parents in low-income communities, evaluated through self-reporting questionnaires and in-person interviews conducted by research assistants.
Disclosures: Researchers reported no relevant financial disclosures.